User login
An integrated response to Surfside: Lessons learned
The catastrophic collapse of the Surfside, Fla., Champlain Towers South left ambiguous loss, trauma, grief, and other psychiatric and psychological sequelae in its wake.
Now that a few months have passed since the tragedy, which took the lives of 98 residents, it is helpful to examine the psychiatric and psychological support efforts that emerged.
We can think of those support efforts as operating on two tracks: one was pursued by mental health professionals representing numerous organizations; the other was pursued by local, regional, and international first responders – specifically, by Israeli Defense Force (IDF) members who came to our community at the request of Surfside families.
Those efforts were guided by existing frameworks for crisis response designed to provide containment amid the naturally disorganizing effects of the trauma and ambiguous loss. In retrospect, it was clear that the mechanisms by which those frameworks coalesced and functioned were more implicit and organically synchronous than explicitly coordinated and agreed upon. key themes emerged and revealed intrinsic links between the first-responder/search and rescue and psychological strategies.
In this article, we discuss relevant themes and parallels between the psychological intervention/strategies and the first-responder disaster response and the practical utility of implementing an integrated strategy. Our hope is that a better understanding of these strategies will help future therapists and responders who respond to crises.
Setting the frame
The importance of setting a psychotherapeutic frame is indisputable regardless of theoretical orientation or therapeutic modality. Predictable, consistent conditions under which therapy takes place support a patient’s capacity to tolerate the ambiguous and unpredictable aspects of the process. Those “rules of engagement” provide a structure where subjective experiences can be formulated, organized, understood, and integrated. Twice-daily briefs held in a centralized location (dubbed the Surfside “family center”) paralleled this frame and served that same containing function by offering structure, order, and predictability amid the palpable chaos of ambiguous loss and traumatic grief. Those briefs provided key information on the status of the operation and described the rescue strategy. These were led by the Miami-Dade assistant fire chief and IDF colonel (E.E.), who presented a unified front and consistent presence.
It is essential that briefings such as these be coordinated (and unified) with clear expectations about ground rules, much like what is involved in therapeutic informed consent. In this context, rules included permissions related to documentation of meetings, information sharing, and rules of communication with the media in an effort to protect the vulnerable.
The centralized meeting location served as an important center of gravity and unified place of waiting and information receipt. It provided a dedicated space to meet with humanitarian aid organizations and government officials, and symbolized continuity, consistency, ease of information transmission, and a place where practical needs could be addressed. Meals, toiletries, and other supplies were provided to simplify and maintain daily routines. Those are otherwise unremarkable practices that seemed impossible to manage amid a crisis, yet can be inherently grounding and emotionally organizing when facing deep psychological fragmentation.
Meeting in person allowed the IDF to offer operational visuals to allow those affected to feel less helpless and cultivate a sense of purpose by being part of the strategy/mission. Their strategy included “population intelligence,” which was aimed at both information gathering to practically facilitate the rescue/recovery process (for example, locating victims, property, and recreating a visual of how the building fell), and inspiring people to participate. This engagement helped many transition from a place of denial/repression to acknowledging loss/grief, and from a passive to active part of the effort, in a way that was safe and realistic – as opposed to going to the site and aiding themselves, as some had requested.
Naturally, a central location made it possible to offer immediate psychological assistance and support. Clinicians responding to crisis should be carefully selected in light of the immense suffering, emotional vulnerability, and heightened reactivity of those affected. People were overwhelmed by deep sorrow, fear, anger, and uncertainty, vacillating between hope and despair, and mobilized by a desire to help. Those providing support need to be interpersonally skilled and able to regulate their own emotions. They must be able to formulate – in real time – an understanding of what is needed, and implement a strategic plan. Like first responders, it is also key for providers to be easily accessible and identifiable in uniform so that people in the grip of a survival response can easily identify and elicit support.
The power of strategy
The Israeli delegation and mental health approaches were aligned with respect to cultivating a team identity and keeping the team spirit elevated. The delegation’s approach was to deemphasize rank during the mission in that everyone was responsible for anything that was needed and no task was below anyone’s rank. The same was true for the mental health support response: Early interventions were focused on addressing practical needs – providing blankets, water, chargers, food, and a calming presence to counter the initial chaos. No task was too small, regardless of title or role. As more structure and order ensued, it was possible to offer more traditional crisis-related interventions aimed at grounding those affected.
Both teams worked to ensure 24-hour coverage, which was crucial given the need for consistency and continuity. Our commitment was to support the victims’ families and survivors by fully embracing the chaos and the situational demands, offering attunement and support, and satisfying both basic and higher-level needs. We divided and conquered work, observed signals of need, offered immediate support where necessary, and coordinated longer-term care plans when possible. The importance of ongoing self-care, consultation, and debriefing while doing this work cannot be overstated. Time to address basic needs and the impact of vicarious trauma as a team must be built in.
Importance of flexibility
This tragedy came with unique complexities and sensitivities that needed to be identified expediently and addressed with a concrete, comprehensive plan. This was true for both the rescue and psychological support efforts, and flexibility was key. There was nothing traditional about our work from a therapeutic perspective – we found quiet corners and empty offices, went for walks, met in lobbies, and checked in by phone. The interventions were brief.
Roles shifted often between aiding in addressing practical needs, advocating for victims and connecting them to appropriate resources, supporting the police in making death notifications, providing support and space for processing during and after briefings, and more.
Similarly, the rescue team constantly reevaluated their strategy because of what they discovered as they dismantled the collapsed building, in addition to managing external impacting factors (heat, rain, lightning, and the threat of the remaining structure falling).
Language matters
The iteration of commitment to the families/victims/mission and to work speedily and efficiently was important for both rescuers and therapists. It was key during the briefings for the chief and colonel (E.E.) to share information in a manner that was professional, discreet, honest and explicit. Their willingness and ability to be vulnerable and to share their personal feelings as active rescuers humanized them. Their approach was matter of fact, yet warm, loving, and containing, all of which conveyed dignity and respect.
Word choice mattered, and the IDF’s intentional choice to refer to recovered victims as “souls,” rather than “bodies,” conveyed their sensitivity to the intensity of anguish, depth of loss, and gravity of the situation. From a psychological perspective, the transition between “rescue” efforts signifying the potential saving of lives to “recovery” of bodies or remains was significant and demarcated a dramatic shift. The weeks-long efforts, once painfully slow, then felt too abrupt to process.
One extraordinary moment was the chief’s response to the families’ discomfort at the news of the switch from rescue to recovery. The families were anxious about losing the structure that the briefings provided and were apprehensive about the handoff from fire to the police department. With great compassion and attunement, he assured them that he would stay with them, and they together, as a family, would decide when to conclude the in-person briefings. The colonel (E.E.), too, provided assurance that neither procedure nor the urgency of the recovery would change. It was both heart-warming and containing that information related to the operation was shared in a clear manner, and that the thought process and rationale behind major decisions (e.g., demolishing the remaining building, decision to pause operations, switch from rescue to recovery) was shared. It was useful for the clinicians to be aware of this rationale in helping individuals metabolize the information and process the associated trauma and grief.
Unification is key
Surfside has left an indelible impact on us. We saw and experienced unity in many respects – clinicians from various backgrounds collaborating, families bonding and caring for one another, community support and solidarity, and the cooperation and coordination of the search and rescue teams. The diverse groups providing support came to feel like a family, and the importance of inter- and intrateam integration cannot be overstated. We were transformed both by our professional collaborations and authentic connections with those affected, and will forever cherish the experience, one another, the families, and the souls lost.
Dr. Feldman is a licensed clinical psychologist in private practice in Miami. She is an adjunct professor in the college of psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she teaches clinical psychology doctoral students. She also serves on the board of directors of The Southeast Florida Association for Psychoanalytic Psychology. Dr. Feldman has no disclosures. Col. Edri is the Israeli Defense Forces District Commander of the Home Front Command Haifa District. He served as the deputy commander for the Israeli Defense Forces Search and Rescue Delegation, which was brought in to provide international aid to the local and domestic forces responding to the Surfside, Fla., building collapse. Col. Edri has no disclosures. Dr. Davidtz is a licensed psychologist and associate professor in the College of Psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she is director of internship training for the Psychology Services Center and director of psychological services for the emotionally distressed, a specialty clinic that serves people with serious mental illness and personality disorders. She also maintains a part-time private practice specializing in the treatment of complex posttraumatic conditions and personality disorders. Dr. Davidtz has no disclosures.
The catastrophic collapse of the Surfside, Fla., Champlain Towers South left ambiguous loss, trauma, grief, and other psychiatric and psychological sequelae in its wake.
Now that a few months have passed since the tragedy, which took the lives of 98 residents, it is helpful to examine the psychiatric and psychological support efforts that emerged.
We can think of those support efforts as operating on two tracks: one was pursued by mental health professionals representing numerous organizations; the other was pursued by local, regional, and international first responders – specifically, by Israeli Defense Force (IDF) members who came to our community at the request of Surfside families.
Those efforts were guided by existing frameworks for crisis response designed to provide containment amid the naturally disorganizing effects of the trauma and ambiguous loss. In retrospect, it was clear that the mechanisms by which those frameworks coalesced and functioned were more implicit and organically synchronous than explicitly coordinated and agreed upon. key themes emerged and revealed intrinsic links between the first-responder/search and rescue and psychological strategies.
In this article, we discuss relevant themes and parallels between the psychological intervention/strategies and the first-responder disaster response and the practical utility of implementing an integrated strategy. Our hope is that a better understanding of these strategies will help future therapists and responders who respond to crises.
Setting the frame
The importance of setting a psychotherapeutic frame is indisputable regardless of theoretical orientation or therapeutic modality. Predictable, consistent conditions under which therapy takes place support a patient’s capacity to tolerate the ambiguous and unpredictable aspects of the process. Those “rules of engagement” provide a structure where subjective experiences can be formulated, organized, understood, and integrated. Twice-daily briefs held in a centralized location (dubbed the Surfside “family center”) paralleled this frame and served that same containing function by offering structure, order, and predictability amid the palpable chaos of ambiguous loss and traumatic grief. Those briefs provided key information on the status of the operation and described the rescue strategy. These were led by the Miami-Dade assistant fire chief and IDF colonel (E.E.), who presented a unified front and consistent presence.
It is essential that briefings such as these be coordinated (and unified) with clear expectations about ground rules, much like what is involved in therapeutic informed consent. In this context, rules included permissions related to documentation of meetings, information sharing, and rules of communication with the media in an effort to protect the vulnerable.
The centralized meeting location served as an important center of gravity and unified place of waiting and information receipt. It provided a dedicated space to meet with humanitarian aid organizations and government officials, and symbolized continuity, consistency, ease of information transmission, and a place where practical needs could be addressed. Meals, toiletries, and other supplies were provided to simplify and maintain daily routines. Those are otherwise unremarkable practices that seemed impossible to manage amid a crisis, yet can be inherently grounding and emotionally organizing when facing deep psychological fragmentation.
Meeting in person allowed the IDF to offer operational visuals to allow those affected to feel less helpless and cultivate a sense of purpose by being part of the strategy/mission. Their strategy included “population intelligence,” which was aimed at both information gathering to practically facilitate the rescue/recovery process (for example, locating victims, property, and recreating a visual of how the building fell), and inspiring people to participate. This engagement helped many transition from a place of denial/repression to acknowledging loss/grief, and from a passive to active part of the effort, in a way that was safe and realistic – as opposed to going to the site and aiding themselves, as some had requested.
Naturally, a central location made it possible to offer immediate psychological assistance and support. Clinicians responding to crisis should be carefully selected in light of the immense suffering, emotional vulnerability, and heightened reactivity of those affected. People were overwhelmed by deep sorrow, fear, anger, and uncertainty, vacillating between hope and despair, and mobilized by a desire to help. Those providing support need to be interpersonally skilled and able to regulate their own emotions. They must be able to formulate – in real time – an understanding of what is needed, and implement a strategic plan. Like first responders, it is also key for providers to be easily accessible and identifiable in uniform so that people in the grip of a survival response can easily identify and elicit support.
The power of strategy
The Israeli delegation and mental health approaches were aligned with respect to cultivating a team identity and keeping the team spirit elevated. The delegation’s approach was to deemphasize rank during the mission in that everyone was responsible for anything that was needed and no task was below anyone’s rank. The same was true for the mental health support response: Early interventions were focused on addressing practical needs – providing blankets, water, chargers, food, and a calming presence to counter the initial chaos. No task was too small, regardless of title or role. As more structure and order ensued, it was possible to offer more traditional crisis-related interventions aimed at grounding those affected.
Both teams worked to ensure 24-hour coverage, which was crucial given the need for consistency and continuity. Our commitment was to support the victims’ families and survivors by fully embracing the chaos and the situational demands, offering attunement and support, and satisfying both basic and higher-level needs. We divided and conquered work, observed signals of need, offered immediate support where necessary, and coordinated longer-term care plans when possible. The importance of ongoing self-care, consultation, and debriefing while doing this work cannot be overstated. Time to address basic needs and the impact of vicarious trauma as a team must be built in.
Importance of flexibility
This tragedy came with unique complexities and sensitivities that needed to be identified expediently and addressed with a concrete, comprehensive plan. This was true for both the rescue and psychological support efforts, and flexibility was key. There was nothing traditional about our work from a therapeutic perspective – we found quiet corners and empty offices, went for walks, met in lobbies, and checked in by phone. The interventions were brief.
Roles shifted often between aiding in addressing practical needs, advocating for victims and connecting them to appropriate resources, supporting the police in making death notifications, providing support and space for processing during and after briefings, and more.
Similarly, the rescue team constantly reevaluated their strategy because of what they discovered as they dismantled the collapsed building, in addition to managing external impacting factors (heat, rain, lightning, and the threat of the remaining structure falling).
Language matters
The iteration of commitment to the families/victims/mission and to work speedily and efficiently was important for both rescuers and therapists. It was key during the briefings for the chief and colonel (E.E.) to share information in a manner that was professional, discreet, honest and explicit. Their willingness and ability to be vulnerable and to share their personal feelings as active rescuers humanized them. Their approach was matter of fact, yet warm, loving, and containing, all of which conveyed dignity and respect.
Word choice mattered, and the IDF’s intentional choice to refer to recovered victims as “souls,” rather than “bodies,” conveyed their sensitivity to the intensity of anguish, depth of loss, and gravity of the situation. From a psychological perspective, the transition between “rescue” efforts signifying the potential saving of lives to “recovery” of bodies or remains was significant and demarcated a dramatic shift. The weeks-long efforts, once painfully slow, then felt too abrupt to process.
One extraordinary moment was the chief’s response to the families’ discomfort at the news of the switch from rescue to recovery. The families were anxious about losing the structure that the briefings provided and were apprehensive about the handoff from fire to the police department. With great compassion and attunement, he assured them that he would stay with them, and they together, as a family, would decide when to conclude the in-person briefings. The colonel (E.E.), too, provided assurance that neither procedure nor the urgency of the recovery would change. It was both heart-warming and containing that information related to the operation was shared in a clear manner, and that the thought process and rationale behind major decisions (e.g., demolishing the remaining building, decision to pause operations, switch from rescue to recovery) was shared. It was useful for the clinicians to be aware of this rationale in helping individuals metabolize the information and process the associated trauma and grief.
Unification is key
Surfside has left an indelible impact on us. We saw and experienced unity in many respects – clinicians from various backgrounds collaborating, families bonding and caring for one another, community support and solidarity, and the cooperation and coordination of the search and rescue teams. The diverse groups providing support came to feel like a family, and the importance of inter- and intrateam integration cannot be overstated. We were transformed both by our professional collaborations and authentic connections with those affected, and will forever cherish the experience, one another, the families, and the souls lost.
Dr. Feldman is a licensed clinical psychologist in private practice in Miami. She is an adjunct professor in the college of psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she teaches clinical psychology doctoral students. She also serves on the board of directors of The Southeast Florida Association for Psychoanalytic Psychology. Dr. Feldman has no disclosures. Col. Edri is the Israeli Defense Forces District Commander of the Home Front Command Haifa District. He served as the deputy commander for the Israeli Defense Forces Search and Rescue Delegation, which was brought in to provide international aid to the local and domestic forces responding to the Surfside, Fla., building collapse. Col. Edri has no disclosures. Dr. Davidtz is a licensed psychologist and associate professor in the College of Psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she is director of internship training for the Psychology Services Center and director of psychological services for the emotionally distressed, a specialty clinic that serves people with serious mental illness and personality disorders. She also maintains a part-time private practice specializing in the treatment of complex posttraumatic conditions and personality disorders. Dr. Davidtz has no disclosures.
The catastrophic collapse of the Surfside, Fla., Champlain Towers South left ambiguous loss, trauma, grief, and other psychiatric and psychological sequelae in its wake.
Now that a few months have passed since the tragedy, which took the lives of 98 residents, it is helpful to examine the psychiatric and psychological support efforts that emerged.
We can think of those support efforts as operating on two tracks: one was pursued by mental health professionals representing numerous organizations; the other was pursued by local, regional, and international first responders – specifically, by Israeli Defense Force (IDF) members who came to our community at the request of Surfside families.
Those efforts were guided by existing frameworks for crisis response designed to provide containment amid the naturally disorganizing effects of the trauma and ambiguous loss. In retrospect, it was clear that the mechanisms by which those frameworks coalesced and functioned were more implicit and organically synchronous than explicitly coordinated and agreed upon. key themes emerged and revealed intrinsic links between the first-responder/search and rescue and psychological strategies.
In this article, we discuss relevant themes and parallels between the psychological intervention/strategies and the first-responder disaster response and the practical utility of implementing an integrated strategy. Our hope is that a better understanding of these strategies will help future therapists and responders who respond to crises.
Setting the frame
The importance of setting a psychotherapeutic frame is indisputable regardless of theoretical orientation or therapeutic modality. Predictable, consistent conditions under which therapy takes place support a patient’s capacity to tolerate the ambiguous and unpredictable aspects of the process. Those “rules of engagement” provide a structure where subjective experiences can be formulated, organized, understood, and integrated. Twice-daily briefs held in a centralized location (dubbed the Surfside “family center”) paralleled this frame and served that same containing function by offering structure, order, and predictability amid the palpable chaos of ambiguous loss and traumatic grief. Those briefs provided key information on the status of the operation and described the rescue strategy. These were led by the Miami-Dade assistant fire chief and IDF colonel (E.E.), who presented a unified front and consistent presence.
It is essential that briefings such as these be coordinated (and unified) with clear expectations about ground rules, much like what is involved in therapeutic informed consent. In this context, rules included permissions related to documentation of meetings, information sharing, and rules of communication with the media in an effort to protect the vulnerable.
The centralized meeting location served as an important center of gravity and unified place of waiting and information receipt. It provided a dedicated space to meet with humanitarian aid organizations and government officials, and symbolized continuity, consistency, ease of information transmission, and a place where practical needs could be addressed. Meals, toiletries, and other supplies were provided to simplify and maintain daily routines. Those are otherwise unremarkable practices that seemed impossible to manage amid a crisis, yet can be inherently grounding and emotionally organizing when facing deep psychological fragmentation.
Meeting in person allowed the IDF to offer operational visuals to allow those affected to feel less helpless and cultivate a sense of purpose by being part of the strategy/mission. Their strategy included “population intelligence,” which was aimed at both information gathering to practically facilitate the rescue/recovery process (for example, locating victims, property, and recreating a visual of how the building fell), and inspiring people to participate. This engagement helped many transition from a place of denial/repression to acknowledging loss/grief, and from a passive to active part of the effort, in a way that was safe and realistic – as opposed to going to the site and aiding themselves, as some had requested.
Naturally, a central location made it possible to offer immediate psychological assistance and support. Clinicians responding to crisis should be carefully selected in light of the immense suffering, emotional vulnerability, and heightened reactivity of those affected. People were overwhelmed by deep sorrow, fear, anger, and uncertainty, vacillating between hope and despair, and mobilized by a desire to help. Those providing support need to be interpersonally skilled and able to regulate their own emotions. They must be able to formulate – in real time – an understanding of what is needed, and implement a strategic plan. Like first responders, it is also key for providers to be easily accessible and identifiable in uniform so that people in the grip of a survival response can easily identify and elicit support.
The power of strategy
The Israeli delegation and mental health approaches were aligned with respect to cultivating a team identity and keeping the team spirit elevated. The delegation’s approach was to deemphasize rank during the mission in that everyone was responsible for anything that was needed and no task was below anyone’s rank. The same was true for the mental health support response: Early interventions were focused on addressing practical needs – providing blankets, water, chargers, food, and a calming presence to counter the initial chaos. No task was too small, regardless of title or role. As more structure and order ensued, it was possible to offer more traditional crisis-related interventions aimed at grounding those affected.
Both teams worked to ensure 24-hour coverage, which was crucial given the need for consistency and continuity. Our commitment was to support the victims’ families and survivors by fully embracing the chaos and the situational demands, offering attunement and support, and satisfying both basic and higher-level needs. We divided and conquered work, observed signals of need, offered immediate support where necessary, and coordinated longer-term care plans when possible. The importance of ongoing self-care, consultation, and debriefing while doing this work cannot be overstated. Time to address basic needs and the impact of vicarious trauma as a team must be built in.
Importance of flexibility
This tragedy came with unique complexities and sensitivities that needed to be identified expediently and addressed with a concrete, comprehensive plan. This was true for both the rescue and psychological support efforts, and flexibility was key. There was nothing traditional about our work from a therapeutic perspective – we found quiet corners and empty offices, went for walks, met in lobbies, and checked in by phone. The interventions were brief.
Roles shifted often between aiding in addressing practical needs, advocating for victims and connecting them to appropriate resources, supporting the police in making death notifications, providing support and space for processing during and after briefings, and more.
Similarly, the rescue team constantly reevaluated their strategy because of what they discovered as they dismantled the collapsed building, in addition to managing external impacting factors (heat, rain, lightning, and the threat of the remaining structure falling).
Language matters
The iteration of commitment to the families/victims/mission and to work speedily and efficiently was important for both rescuers and therapists. It was key during the briefings for the chief and colonel (E.E.) to share information in a manner that was professional, discreet, honest and explicit. Their willingness and ability to be vulnerable and to share their personal feelings as active rescuers humanized them. Their approach was matter of fact, yet warm, loving, and containing, all of which conveyed dignity and respect.
Word choice mattered, and the IDF’s intentional choice to refer to recovered victims as “souls,” rather than “bodies,” conveyed their sensitivity to the intensity of anguish, depth of loss, and gravity of the situation. From a psychological perspective, the transition between “rescue” efforts signifying the potential saving of lives to “recovery” of bodies or remains was significant and demarcated a dramatic shift. The weeks-long efforts, once painfully slow, then felt too abrupt to process.
One extraordinary moment was the chief’s response to the families’ discomfort at the news of the switch from rescue to recovery. The families were anxious about losing the structure that the briefings provided and were apprehensive about the handoff from fire to the police department. With great compassion and attunement, he assured them that he would stay with them, and they together, as a family, would decide when to conclude the in-person briefings. The colonel (E.E.), too, provided assurance that neither procedure nor the urgency of the recovery would change. It was both heart-warming and containing that information related to the operation was shared in a clear manner, and that the thought process and rationale behind major decisions (e.g., demolishing the remaining building, decision to pause operations, switch from rescue to recovery) was shared. It was useful for the clinicians to be aware of this rationale in helping individuals metabolize the information and process the associated trauma and grief.
Unification is key
Surfside has left an indelible impact on us. We saw and experienced unity in many respects – clinicians from various backgrounds collaborating, families bonding and caring for one another, community support and solidarity, and the cooperation and coordination of the search and rescue teams. The diverse groups providing support came to feel like a family, and the importance of inter- and intrateam integration cannot be overstated. We were transformed both by our professional collaborations and authentic connections with those affected, and will forever cherish the experience, one another, the families, and the souls lost.
Dr. Feldman is a licensed clinical psychologist in private practice in Miami. She is an adjunct professor in the college of psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she teaches clinical psychology doctoral students. She also serves on the board of directors of The Southeast Florida Association for Psychoanalytic Psychology. Dr. Feldman has no disclosures. Col. Edri is the Israeli Defense Forces District Commander of the Home Front Command Haifa District. He served as the deputy commander for the Israeli Defense Forces Search and Rescue Delegation, which was brought in to provide international aid to the local and domestic forces responding to the Surfside, Fla., building collapse. Col. Edri has no disclosures. Dr. Davidtz is a licensed psychologist and associate professor in the College of Psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she is director of internship training for the Psychology Services Center and director of psychological services for the emotionally distressed, a specialty clinic that serves people with serious mental illness and personality disorders. She also maintains a part-time private practice specializing in the treatment of complex posttraumatic conditions and personality disorders. Dr. Davidtz has no disclosures.
Sleep problems in mental illness highly pervasive
An inpatient psychiatric diagnosis at some point over a lifetime is significantly associated with a range of sleep problems, results from the largest study of its kind show.
A prior diagnosis of major depression, schizophrenia, anxiety, or bipolar disorder was associated with a later bedtime, earlier waking time, and significantly poorer sleep quality that included frequent awakenings during the night and shorter sleep bouts.
“We were struck by the pervasiveness of sleep problems across all the diagnoses of mental illness and sleep parameters we looked at,” study investigator Michael Wainberg, PhD, a postdoctoral fellow at the Krembil Centre for Neuroinformatics at the Center for Addiction and Mental Health (CAMH), Toronto, told this news organization. “This suggests there may need to be even more of an emphasis on sleep in these patients than there already is.”
The study, which includes data from nearly 90,000 adults in the United Kingdom, was published online October 12 in PLoS Medicine.
Trove of data
Data for the analysis comes from the UK Biobank, a large-scale biomedical database launched in 2006 that has collected biological and medical data on more than 500,000 individuals who consented to provide blood, urine, and saliva samples and detailed lifestyle information that is matched to their medical records.
Between 2013 and 2015, more than 103,000 of these participants agreed to wear accelerometers on their wrists for 24 hours a day for 7 days, collecting a trove of data for researchers to mine.
“This allows us to get at objectively derived sleep measures and to measure them in greater numbers of people who have experienced mental illness,” said senior author Shreejoy Tripathy, PhD, assistant professor at the University of Toronto and independent scientist for CAMH. “You can study multiple disorders at once and the influence of other variables that might not be possible in the context of other studies.”
The research is the first known large-scale transdiagnostic study of objectively measured sleep and mental health. Insomnia and other sleep disorders are common among people with mental illness, as shown in prior research, including at least one study that used the same dataset the team employed for this project.
The new findings add to that body of work, Dr. Wainberg said, and look beyond just how long a person sleeps to the quality of the sleep they get.
“We found that the metrics of sleep quality seem to be affected more than mere sleep duration,” he said.
Unexpected finding
After excluding participants with faulty accelerometers and those who didn’t wear them for the entire 7-day study period, data from 89,205 participants (aged 43-79, 56% female, 97% self-reported White) was included. Lifetime inpatient psychiatric diagnoses were reported in 2.5% of the entire cohort.
Researchers looked at 10 sleep measures: bedtime, wake-up time, sleep duration, wake after sleep onset, sleep efficiency, number of awakenings, duration of longest sleep bout, number of naps, and variability in bedtime and sleep duration.
Although the effect sizes were small, having any psychiatric diagnosis was associated with significantly lower scores on every sleep measure except sleep duration.
Compared with those with no inpatient psychiatric diagnosis, those with any psychiatric diagnosis were significantly more likely to:
- have a later bedtime (beta = 0.07; 95% confidence interval, 0.06-0.09)
- have later wake-up time (beta = 0.10; 95% CI, 0.09-0.11)
- wake after sleep onset (beta = 0.10; 95% CI, 0.09-0.12)
- have poorer sleep efficiency (beta = –0.12; 95% CI, −0.14 to −0.11)
- have more awakenings (beta = 0.10; 95% CI, 0.09-0.11)
- have shorter duration of their longest sleep bout (beta = –0.09; 95% CI, −0.11 to −0.08)
- take more naps (beta = 0.11; 95% CI, 0.09-0.12)
- have greater variability in their bedtime (beta = 0.08; 95% CI, 0.06-0.09)
- have greater variability in their sleep duration (beta = 0.10; 95% CI, 0.09-0.12)
The only significant differences in sleep duration were found in those with lifetime major depressive disorder, who slept significantly less (beta = −0.02; P = .003), and in those with lifetime schizophrenia, who slept significantly longer (beta = 0.02; P = .0008).
Researchers found similar results when they examined patient-reported sleep measures collected when participants enrolled in the biobank, long before they agreed to wear an accelerometer.
“Everyone with a lifetime mental illness diagnosis trended toward worse sleep quality, regardless of their diagnosis,” Dr. Tripathy said. “We didn’t expect to see that.”
Limitations of the biobank data prohibited analysis by age and past or current use of psychiatric medications. In addition, investigators were unable to determine whether mental illness was active or controlled at the time of the study. Information on these, and other factors, is needed to truly begin to understand the real-world status of sleep patterns in people with mental illness, the researchers note.
However, the biobank data demonstrates how this type of information can be collected, helping Dr. Tripathy and others to design a new study that will launch next year with patients at CAMH. This effort is part of the BrainHealth Databank, a project that aims to develop a patient data bank similar to the one in the UK that was used for this study.
“We’ve shown that you can use wearable devices to measure correlates of sleep and derive insights about the objective measurements of sleep and associate them with mental illness diagnosis,” Dr. Tripathy said.
The study received no outside funding. Dr. Wainberg and Dr. Tripathy report receiving funding from Kavli Foundation, Krembil Foundation, CAMH Discovery Fund, the McLaughlin Foundation, NSERC, and CIHR. Disclosures for other authors are fully listed in the original article.
A version of this article first appeared on Medscape.com.
An inpatient psychiatric diagnosis at some point over a lifetime is significantly associated with a range of sleep problems, results from the largest study of its kind show.
A prior diagnosis of major depression, schizophrenia, anxiety, or bipolar disorder was associated with a later bedtime, earlier waking time, and significantly poorer sleep quality that included frequent awakenings during the night and shorter sleep bouts.
“We were struck by the pervasiveness of sleep problems across all the diagnoses of mental illness and sleep parameters we looked at,” study investigator Michael Wainberg, PhD, a postdoctoral fellow at the Krembil Centre for Neuroinformatics at the Center for Addiction and Mental Health (CAMH), Toronto, told this news organization. “This suggests there may need to be even more of an emphasis on sleep in these patients than there already is.”
The study, which includes data from nearly 90,000 adults in the United Kingdom, was published online October 12 in PLoS Medicine.
Trove of data
Data for the analysis comes from the UK Biobank, a large-scale biomedical database launched in 2006 that has collected biological and medical data on more than 500,000 individuals who consented to provide blood, urine, and saliva samples and detailed lifestyle information that is matched to their medical records.
Between 2013 and 2015, more than 103,000 of these participants agreed to wear accelerometers on their wrists for 24 hours a day for 7 days, collecting a trove of data for researchers to mine.
“This allows us to get at objectively derived sleep measures and to measure them in greater numbers of people who have experienced mental illness,” said senior author Shreejoy Tripathy, PhD, assistant professor at the University of Toronto and independent scientist for CAMH. “You can study multiple disorders at once and the influence of other variables that might not be possible in the context of other studies.”
The research is the first known large-scale transdiagnostic study of objectively measured sleep and mental health. Insomnia and other sleep disorders are common among people with mental illness, as shown in prior research, including at least one study that used the same dataset the team employed for this project.
The new findings add to that body of work, Dr. Wainberg said, and look beyond just how long a person sleeps to the quality of the sleep they get.
“We found that the metrics of sleep quality seem to be affected more than mere sleep duration,” he said.
Unexpected finding
After excluding participants with faulty accelerometers and those who didn’t wear them for the entire 7-day study period, data from 89,205 participants (aged 43-79, 56% female, 97% self-reported White) was included. Lifetime inpatient psychiatric diagnoses were reported in 2.5% of the entire cohort.
Researchers looked at 10 sleep measures: bedtime, wake-up time, sleep duration, wake after sleep onset, sleep efficiency, number of awakenings, duration of longest sleep bout, number of naps, and variability in bedtime and sleep duration.
Although the effect sizes were small, having any psychiatric diagnosis was associated with significantly lower scores on every sleep measure except sleep duration.
Compared with those with no inpatient psychiatric diagnosis, those with any psychiatric diagnosis were significantly more likely to:
- have a later bedtime (beta = 0.07; 95% confidence interval, 0.06-0.09)
- have later wake-up time (beta = 0.10; 95% CI, 0.09-0.11)
- wake after sleep onset (beta = 0.10; 95% CI, 0.09-0.12)
- have poorer sleep efficiency (beta = –0.12; 95% CI, −0.14 to −0.11)
- have more awakenings (beta = 0.10; 95% CI, 0.09-0.11)
- have shorter duration of their longest sleep bout (beta = –0.09; 95% CI, −0.11 to −0.08)
- take more naps (beta = 0.11; 95% CI, 0.09-0.12)
- have greater variability in their bedtime (beta = 0.08; 95% CI, 0.06-0.09)
- have greater variability in their sleep duration (beta = 0.10; 95% CI, 0.09-0.12)
The only significant differences in sleep duration were found in those with lifetime major depressive disorder, who slept significantly less (beta = −0.02; P = .003), and in those with lifetime schizophrenia, who slept significantly longer (beta = 0.02; P = .0008).
Researchers found similar results when they examined patient-reported sleep measures collected when participants enrolled in the biobank, long before they agreed to wear an accelerometer.
“Everyone with a lifetime mental illness diagnosis trended toward worse sleep quality, regardless of their diagnosis,” Dr. Tripathy said. “We didn’t expect to see that.”
Limitations of the biobank data prohibited analysis by age and past or current use of psychiatric medications. In addition, investigators were unable to determine whether mental illness was active or controlled at the time of the study. Information on these, and other factors, is needed to truly begin to understand the real-world status of sleep patterns in people with mental illness, the researchers note.
However, the biobank data demonstrates how this type of information can be collected, helping Dr. Tripathy and others to design a new study that will launch next year with patients at CAMH. This effort is part of the BrainHealth Databank, a project that aims to develop a patient data bank similar to the one in the UK that was used for this study.
“We’ve shown that you can use wearable devices to measure correlates of sleep and derive insights about the objective measurements of sleep and associate them with mental illness diagnosis,” Dr. Tripathy said.
The study received no outside funding. Dr. Wainberg and Dr. Tripathy report receiving funding from Kavli Foundation, Krembil Foundation, CAMH Discovery Fund, the McLaughlin Foundation, NSERC, and CIHR. Disclosures for other authors are fully listed in the original article.
A version of this article first appeared on Medscape.com.
An inpatient psychiatric diagnosis at some point over a lifetime is significantly associated with a range of sleep problems, results from the largest study of its kind show.
A prior diagnosis of major depression, schizophrenia, anxiety, or bipolar disorder was associated with a later bedtime, earlier waking time, and significantly poorer sleep quality that included frequent awakenings during the night and shorter sleep bouts.
“We were struck by the pervasiveness of sleep problems across all the diagnoses of mental illness and sleep parameters we looked at,” study investigator Michael Wainberg, PhD, a postdoctoral fellow at the Krembil Centre for Neuroinformatics at the Center for Addiction and Mental Health (CAMH), Toronto, told this news organization. “This suggests there may need to be even more of an emphasis on sleep in these patients than there already is.”
The study, which includes data from nearly 90,000 adults in the United Kingdom, was published online October 12 in PLoS Medicine.
Trove of data
Data for the analysis comes from the UK Biobank, a large-scale biomedical database launched in 2006 that has collected biological and medical data on more than 500,000 individuals who consented to provide blood, urine, and saliva samples and detailed lifestyle information that is matched to their medical records.
Between 2013 and 2015, more than 103,000 of these participants agreed to wear accelerometers on their wrists for 24 hours a day for 7 days, collecting a trove of data for researchers to mine.
“This allows us to get at objectively derived sleep measures and to measure them in greater numbers of people who have experienced mental illness,” said senior author Shreejoy Tripathy, PhD, assistant professor at the University of Toronto and independent scientist for CAMH. “You can study multiple disorders at once and the influence of other variables that might not be possible in the context of other studies.”
The research is the first known large-scale transdiagnostic study of objectively measured sleep and mental health. Insomnia and other sleep disorders are common among people with mental illness, as shown in prior research, including at least one study that used the same dataset the team employed for this project.
The new findings add to that body of work, Dr. Wainberg said, and look beyond just how long a person sleeps to the quality of the sleep they get.
“We found that the metrics of sleep quality seem to be affected more than mere sleep duration,” he said.
Unexpected finding
After excluding participants with faulty accelerometers and those who didn’t wear them for the entire 7-day study period, data from 89,205 participants (aged 43-79, 56% female, 97% self-reported White) was included. Lifetime inpatient psychiatric diagnoses were reported in 2.5% of the entire cohort.
Researchers looked at 10 sleep measures: bedtime, wake-up time, sleep duration, wake after sleep onset, sleep efficiency, number of awakenings, duration of longest sleep bout, number of naps, and variability in bedtime and sleep duration.
Although the effect sizes were small, having any psychiatric diagnosis was associated with significantly lower scores on every sleep measure except sleep duration.
Compared with those with no inpatient psychiatric diagnosis, those with any psychiatric diagnosis were significantly more likely to:
- have a later bedtime (beta = 0.07; 95% confidence interval, 0.06-0.09)
- have later wake-up time (beta = 0.10; 95% CI, 0.09-0.11)
- wake after sleep onset (beta = 0.10; 95% CI, 0.09-0.12)
- have poorer sleep efficiency (beta = –0.12; 95% CI, −0.14 to −0.11)
- have more awakenings (beta = 0.10; 95% CI, 0.09-0.11)
- have shorter duration of their longest sleep bout (beta = –0.09; 95% CI, −0.11 to −0.08)
- take more naps (beta = 0.11; 95% CI, 0.09-0.12)
- have greater variability in their bedtime (beta = 0.08; 95% CI, 0.06-0.09)
- have greater variability in their sleep duration (beta = 0.10; 95% CI, 0.09-0.12)
The only significant differences in sleep duration were found in those with lifetime major depressive disorder, who slept significantly less (beta = −0.02; P = .003), and in those with lifetime schizophrenia, who slept significantly longer (beta = 0.02; P = .0008).
Researchers found similar results when they examined patient-reported sleep measures collected when participants enrolled in the biobank, long before they agreed to wear an accelerometer.
“Everyone with a lifetime mental illness diagnosis trended toward worse sleep quality, regardless of their diagnosis,” Dr. Tripathy said. “We didn’t expect to see that.”
Limitations of the biobank data prohibited analysis by age and past or current use of psychiatric medications. In addition, investigators were unable to determine whether mental illness was active or controlled at the time of the study. Information on these, and other factors, is needed to truly begin to understand the real-world status of sleep patterns in people with mental illness, the researchers note.
However, the biobank data demonstrates how this type of information can be collected, helping Dr. Tripathy and others to design a new study that will launch next year with patients at CAMH. This effort is part of the BrainHealth Databank, a project that aims to develop a patient data bank similar to the one in the UK that was used for this study.
“We’ve shown that you can use wearable devices to measure correlates of sleep and derive insights about the objective measurements of sleep and associate them with mental illness diagnosis,” Dr. Tripathy said.
The study received no outside funding. Dr. Wainberg and Dr. Tripathy report receiving funding from Kavli Foundation, Krembil Foundation, CAMH Discovery Fund, the McLaughlin Foundation, NSERC, and CIHR. Disclosures for other authors are fully listed in the original article.
A version of this article first appeared on Medscape.com.
Avoidant attachment style may drive mood in movement disorders
Patients with functional neurological disorders demonstrate higher levels of depression and alexithymia – in addition to signs of an avoidant attachment style – compared with those with other neurological disorders and healthy controls, investigators report.
The pathological mechanism of functional neurological disorders (FND) remains poorly understood, but current models include both psychological and environmental factors, Sofia Cuoco, PhD, and colleagues wrote in a study published in the Journal of Psychosomatic Research.
Previous studies have suggested a relationship between attachment styles (AS) and psychiatric symptoms in FND patients but most have been limited to the FND population, noted Dr. Cuoco, of the University of Salerno, Italy, and colleagues. In FND, “it is unclear to what extent psychiatric features are explained by AS per se or are part of the FND spectrum,” they said.
To conduct the study, the investigators recruited 46 patients with FND, 34 patients with neurological disorders (ND) and 30 healthy controls. Demographic characteristics, including age, education, and gender, were similar among the groups. Overall, depression and alexithymia were significantly more prevalent in the FND group, compared with the other groups. Anxiety was more common in the FND group, compared with healthy controls, but similar compared with the ND group. Patients in the FND group reported significantly lower quality of life, compared with those in the other groups.
In a multivariate analysis aimed at examining AS and psychiatric features, the researchers found that the Experiences in Close Relationships–Revised questionnaire avoidance, Beck Depression Inventory, Somatic Affective, and the 20-item Toronto Alexithymia Scale Difficulty Identifying Feelings scale (TAS-20 Difficulty Identifying Feelings) were significant predictors of FND and accounted for about half of the variance.
The researchers also compared FND to functional seizures, and found that the TAS-20 Difficulty Identifying Feelings scale, the Hamilton Anxiety Scale–Anxiety, and female gender were significant predictors of functional seizures.
The results were mainly in line with those from previous studies, the researchers said. However, than ND, which might suggest that these psychiatric features would not be merely reactive to physical symptoms,” they noted.
The study findings were limited by several factors, including the absence of systematic interviews for personality disorders or traits, monitoring psychotropic medications, and conducting formal psychiatric assessments, the researchers noted. Other limitations include the heterogenous study population and absence of data on symptom severity, history of trauma, or other factors that might contributed to FND, they said.
However, the results suggest that avoidant AS might play an important role in the occurrence of psychiatric features in FND patients and should be considered in managing these conditions. More research is needed to explore the impact of attachment on pathophysiology with more complex instruments, such as the Adult Attachment Interview, Dr. Cuoco and colleagues said.
The study received no outside funding, and the researchers disclosed no financial conflicts.
Patients with functional neurological disorders demonstrate higher levels of depression and alexithymia – in addition to signs of an avoidant attachment style – compared with those with other neurological disorders and healthy controls, investigators report.
The pathological mechanism of functional neurological disorders (FND) remains poorly understood, but current models include both psychological and environmental factors, Sofia Cuoco, PhD, and colleagues wrote in a study published in the Journal of Psychosomatic Research.
Previous studies have suggested a relationship between attachment styles (AS) and psychiatric symptoms in FND patients but most have been limited to the FND population, noted Dr. Cuoco, of the University of Salerno, Italy, and colleagues. In FND, “it is unclear to what extent psychiatric features are explained by AS per se or are part of the FND spectrum,” they said.
To conduct the study, the investigators recruited 46 patients with FND, 34 patients with neurological disorders (ND) and 30 healthy controls. Demographic characteristics, including age, education, and gender, were similar among the groups. Overall, depression and alexithymia were significantly more prevalent in the FND group, compared with the other groups. Anxiety was more common in the FND group, compared with healthy controls, but similar compared with the ND group. Patients in the FND group reported significantly lower quality of life, compared with those in the other groups.
In a multivariate analysis aimed at examining AS and psychiatric features, the researchers found that the Experiences in Close Relationships–Revised questionnaire avoidance, Beck Depression Inventory, Somatic Affective, and the 20-item Toronto Alexithymia Scale Difficulty Identifying Feelings scale (TAS-20 Difficulty Identifying Feelings) were significant predictors of FND and accounted for about half of the variance.
The researchers also compared FND to functional seizures, and found that the TAS-20 Difficulty Identifying Feelings scale, the Hamilton Anxiety Scale–Anxiety, and female gender were significant predictors of functional seizures.
The results were mainly in line with those from previous studies, the researchers said. However, than ND, which might suggest that these psychiatric features would not be merely reactive to physical symptoms,” they noted.
The study findings were limited by several factors, including the absence of systematic interviews for personality disorders or traits, monitoring psychotropic medications, and conducting formal psychiatric assessments, the researchers noted. Other limitations include the heterogenous study population and absence of data on symptom severity, history of trauma, or other factors that might contributed to FND, they said.
However, the results suggest that avoidant AS might play an important role in the occurrence of psychiatric features in FND patients and should be considered in managing these conditions. More research is needed to explore the impact of attachment on pathophysiology with more complex instruments, such as the Adult Attachment Interview, Dr. Cuoco and colleagues said.
The study received no outside funding, and the researchers disclosed no financial conflicts.
Patients with functional neurological disorders demonstrate higher levels of depression and alexithymia – in addition to signs of an avoidant attachment style – compared with those with other neurological disorders and healthy controls, investigators report.
The pathological mechanism of functional neurological disorders (FND) remains poorly understood, but current models include both psychological and environmental factors, Sofia Cuoco, PhD, and colleagues wrote in a study published in the Journal of Psychosomatic Research.
Previous studies have suggested a relationship between attachment styles (AS) and psychiatric symptoms in FND patients but most have been limited to the FND population, noted Dr. Cuoco, of the University of Salerno, Italy, and colleagues. In FND, “it is unclear to what extent psychiatric features are explained by AS per se or are part of the FND spectrum,” they said.
To conduct the study, the investigators recruited 46 patients with FND, 34 patients with neurological disorders (ND) and 30 healthy controls. Demographic characteristics, including age, education, and gender, were similar among the groups. Overall, depression and alexithymia were significantly more prevalent in the FND group, compared with the other groups. Anxiety was more common in the FND group, compared with healthy controls, but similar compared with the ND group. Patients in the FND group reported significantly lower quality of life, compared with those in the other groups.
In a multivariate analysis aimed at examining AS and psychiatric features, the researchers found that the Experiences in Close Relationships–Revised questionnaire avoidance, Beck Depression Inventory, Somatic Affective, and the 20-item Toronto Alexithymia Scale Difficulty Identifying Feelings scale (TAS-20 Difficulty Identifying Feelings) were significant predictors of FND and accounted for about half of the variance.
The researchers also compared FND to functional seizures, and found that the TAS-20 Difficulty Identifying Feelings scale, the Hamilton Anxiety Scale–Anxiety, and female gender were significant predictors of functional seizures.
The results were mainly in line with those from previous studies, the researchers said. However, than ND, which might suggest that these psychiatric features would not be merely reactive to physical symptoms,” they noted.
The study findings were limited by several factors, including the absence of systematic interviews for personality disorders or traits, monitoring psychotropic medications, and conducting formal psychiatric assessments, the researchers noted. Other limitations include the heterogenous study population and absence of data on symptom severity, history of trauma, or other factors that might contributed to FND, they said.
However, the results suggest that avoidant AS might play an important role in the occurrence of psychiatric features in FND patients and should be considered in managing these conditions. More research is needed to explore the impact of attachment on pathophysiology with more complex instruments, such as the Adult Attachment Interview, Dr. Cuoco and colleagues said.
The study received no outside funding, and the researchers disclosed no financial conflicts.
FROM THE JOURNAL OF PSYCHOSOMATIC RESEARCH
Therapeutic homework adherence improves tics in Tourette’s disorder
Homework adherence between behavior therapy sessions is a significant predictor of therapeutic improvement in patients with Tourette’s disorder (TD), a study of 119 youth and adults suggests.
The assigning of “homework” to be completed between sessions – often used in cognitive-behavioral therapy – has been shown to reinforce learning but has not been well studied in TD.
“Understanding the relationship between homework adherence and therapeutic improvement from behavior therapy for TD may offer new insights for enhancing tic severity reductions achieved during this evidence-based treatment,” wrote Joey Ka-Yee Essoe, PhD, of the department of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, and colleagues.
To conduct the study, published in Behaviour Research and Therapy, the researchers recruited 70 youth and 49 adults with TD, ranging in age from 9 to 67 years, who underwent treatment at a single center. The average age was 21 years, and 80 participants were male. Treatment response was based on the Clinical Global Impressions of Improvement scale (CGI-I). Participants were assessed at baseline for tic severity and received eight sessions over 10 weeks. During those sessions, they were taught to perform a competing response to inhibit the expression of a tic when the tic or urge was detected.
Participants received homework at each weekly therapy session; most consisted of three to four practice sessions of about 30 minutes per week. Therapists reviewed the homework at the following session and adapted as needed to improve tic reduction skills.
After eight sessions of behavior therapy, overall greater homework adherence significantly predicted reduced tic severity and therapeutic improvement. However, early homework adherence predicted therapeutic improvement in youth, while late homework adherence predicted it in adults.
Overall,
However, homework adherence dipped midway through treatment in youth and showed a linear decline in adults, the researchers noted.
Among youth, baseline predictors of early homework adherence included lower levels of hyperactivity/impulsivity and caregiver strain. Among adults, baseline predictors of early homework adherence included lower anger scores, less social disability, and greater work disability.
The study findings were limited by several factors, including the absence of complete data on baseline predictors of homework adherence, reliance on a single measure of tic severity and improvement, and reliance on therapists’ reports of homework adherence, the researchers noted.
Future research should include objective measures of homework adherence, such as time-stamped videos, and different strategies may be needed for youth vs. adults, they added.
“Strategies that optimize homework adherence may enhance the efficacy of behavioral therapy, lead to greater tic severity reductions, and higher treatment response rates,” Dr. Essoe and colleagues wrote.
The study was supported by the Tourette Association of America, the National Institute of Mental Health, the American Academy of Neurology, and the American Psychological Foundation.
Homework adherence between behavior therapy sessions is a significant predictor of therapeutic improvement in patients with Tourette’s disorder (TD), a study of 119 youth and adults suggests.
The assigning of “homework” to be completed between sessions – often used in cognitive-behavioral therapy – has been shown to reinforce learning but has not been well studied in TD.
“Understanding the relationship between homework adherence and therapeutic improvement from behavior therapy for TD may offer new insights for enhancing tic severity reductions achieved during this evidence-based treatment,” wrote Joey Ka-Yee Essoe, PhD, of the department of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, and colleagues.
To conduct the study, published in Behaviour Research and Therapy, the researchers recruited 70 youth and 49 adults with TD, ranging in age from 9 to 67 years, who underwent treatment at a single center. The average age was 21 years, and 80 participants were male. Treatment response was based on the Clinical Global Impressions of Improvement scale (CGI-I). Participants were assessed at baseline for tic severity and received eight sessions over 10 weeks. During those sessions, they were taught to perform a competing response to inhibit the expression of a tic when the tic or urge was detected.
Participants received homework at each weekly therapy session; most consisted of three to four practice sessions of about 30 minutes per week. Therapists reviewed the homework at the following session and adapted as needed to improve tic reduction skills.
After eight sessions of behavior therapy, overall greater homework adherence significantly predicted reduced tic severity and therapeutic improvement. However, early homework adherence predicted therapeutic improvement in youth, while late homework adherence predicted it in adults.
Overall,
However, homework adherence dipped midway through treatment in youth and showed a linear decline in adults, the researchers noted.
Among youth, baseline predictors of early homework adherence included lower levels of hyperactivity/impulsivity and caregiver strain. Among adults, baseline predictors of early homework adherence included lower anger scores, less social disability, and greater work disability.
The study findings were limited by several factors, including the absence of complete data on baseline predictors of homework adherence, reliance on a single measure of tic severity and improvement, and reliance on therapists’ reports of homework adherence, the researchers noted.
Future research should include objective measures of homework adherence, such as time-stamped videos, and different strategies may be needed for youth vs. adults, they added.
“Strategies that optimize homework adherence may enhance the efficacy of behavioral therapy, lead to greater tic severity reductions, and higher treatment response rates,” Dr. Essoe and colleagues wrote.
The study was supported by the Tourette Association of America, the National Institute of Mental Health, the American Academy of Neurology, and the American Psychological Foundation.
Homework adherence between behavior therapy sessions is a significant predictor of therapeutic improvement in patients with Tourette’s disorder (TD), a study of 119 youth and adults suggests.
The assigning of “homework” to be completed between sessions – often used in cognitive-behavioral therapy – has been shown to reinforce learning but has not been well studied in TD.
“Understanding the relationship between homework adherence and therapeutic improvement from behavior therapy for TD may offer new insights for enhancing tic severity reductions achieved during this evidence-based treatment,” wrote Joey Ka-Yee Essoe, PhD, of the department of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, and colleagues.
To conduct the study, published in Behaviour Research and Therapy, the researchers recruited 70 youth and 49 adults with TD, ranging in age from 9 to 67 years, who underwent treatment at a single center. The average age was 21 years, and 80 participants were male. Treatment response was based on the Clinical Global Impressions of Improvement scale (CGI-I). Participants were assessed at baseline for tic severity and received eight sessions over 10 weeks. During those sessions, they were taught to perform a competing response to inhibit the expression of a tic when the tic or urge was detected.
Participants received homework at each weekly therapy session; most consisted of three to four practice sessions of about 30 minutes per week. Therapists reviewed the homework at the following session and adapted as needed to improve tic reduction skills.
After eight sessions of behavior therapy, overall greater homework adherence significantly predicted reduced tic severity and therapeutic improvement. However, early homework adherence predicted therapeutic improvement in youth, while late homework adherence predicted it in adults.
Overall,
However, homework adherence dipped midway through treatment in youth and showed a linear decline in adults, the researchers noted.
Among youth, baseline predictors of early homework adherence included lower levels of hyperactivity/impulsivity and caregiver strain. Among adults, baseline predictors of early homework adherence included lower anger scores, less social disability, and greater work disability.
The study findings were limited by several factors, including the absence of complete data on baseline predictors of homework adherence, reliance on a single measure of tic severity and improvement, and reliance on therapists’ reports of homework adherence, the researchers noted.
Future research should include objective measures of homework adherence, such as time-stamped videos, and different strategies may be needed for youth vs. adults, they added.
“Strategies that optimize homework adherence may enhance the efficacy of behavioral therapy, lead to greater tic severity reductions, and higher treatment response rates,” Dr. Essoe and colleagues wrote.
The study was supported by the Tourette Association of America, the National Institute of Mental Health, the American Academy of Neurology, and the American Psychological Foundation.
FROM BEHAVIOUR RESEARCH & THERAPY
Lower thyroid hormone levels a red flag for elevated suicide risk?
Patients with comorbid anxiety and mood disorders who have reduced, albeit “normal” serum levels of thyroid-stimulating hormone (TSH) may be at increased risk for suicidal ideation, new research suggests.
In a cross-sectional study, clinical data on diagnosis, medication use, and symptom scores were gathered, along with assessments of blood levels of thyroid axis hormones, in patients with both anxiety and mood disorders.
After investigators accounted for age, gender, symptoms, medication use, and other potential confounders, patients with suicidal ideation were 54% less likely to have higher TSH levels. There was no association found with other thyroid hormones.
Based on the results, the assessment of thyroid hormone levels “may be important for suicide prevention and might allow clinicians to evaluate the potential of the suicidal ideation risk in individuals with [anxiety and mood disorders],” co-investigator Vilma Liaugaudaite, PhD student, Neuroscience Institute of the Lithuanian University of Health Sciences, Palanga, and colleagues note.
The findings were presented at the 34th European College of Neuropsychopharmacology (ECNP) Congress.
‘Complex mechanism’
Ms. Liaugaudaite told this news organization that thyroid hormones are known to have a “profound” effect on mood and behavior.
Recent studies show “various degrees of hypothalamic-pituitary-thyroid axis dysregulation are associated with suicidal behavior” in patients with depression, she added.
Noting that disturbances in the serotonin system “constitute the most common biochemical abnormality associated with suicidal behavior,” Ms. Liaugaudaite said it is thought thyroid hormones “are involved in a complex compensatory mechanism to correct reduced central 5-hydroxytryptamine activity” via lower TSH levels.
In addition, hypersecretion of thyrotropin-releasing hormone, which stimulates the release of TSH, “has been considered a compensatory mechanism to maintain normal thyroid hormone secretion and normalize serotonin activity in depressed patients,” she said.
To investigate associations between thyroid axis hormones and suicidality in individuals with comorbid anxiety and mood disorders, the researchers assessed consecutive patients attending a stress disorders clinic.
Sociodemographic and clinical information was gathered, and patients completed the Mini International Neuropsychiatric Interview, the Patient Health Questionnaire-9 (PHQ-9), and the General Anxiety Disorder-7 (GAD-7) scale.
Fasting blood samples were also tested for free thyroxine (FT4), free triiodothyronine (FT3), and TSH levels.
Significant association
Suicidal ideation was identified in 42 participants. Serum FT4, FT3, and TSH levels were within the normal range.
There were no significant differences between patients with and without suicidal ideation in terms of age, gender, education, obesity, smoking, and medication use.
Suicidal ideation was associated with higher scores on the PHQ-9 (15.5 vs. 13.3; P = .085), and with lower TSH levels (1.54 IU/L vs. 2.04 IU/L; P = .092).
The association between serum TSH levels and suicidal ideation was significant after multivariate logistic regression analysis accounted for age, gender, PHQ-9 and GAD-7 scores, education, body mass index, smoking, and use of antidepressants, tranquilizers, mood stabilizers, and neuroleptics.
Specifically, patients with suicidal ideation were significantly less likely to have higher TSH levels than those without, at an odds ratio of 0.46 (P = .027).
There were no significant associations between serum FT4 and FT3 levels and suicidal ideation.
Interesting, but preliminary
Commenting on the findings, Sanjeev Sockalingam, MD, vice chair and professor of psychiatry at the University of Toronto, said it is an “interesting study” because the literature on trying to identify individuals at risk for suicidal ideation or behaviors is “quite mixed, in terms of the results.”
However, it was a cross-sectional study with a relatively small sample size, and studies of this nature typically include patients with hypothyroidism “who end up having suicidal thoughts,” said Dr. Sockalingam, who was not involved with the research.
“I do wonder, given the sample size and patient population, if there may be other factors that may have been related to this,” he added.
Dr. Sockalingam noted that he would like to see more data on the medications the patients were taking, and he underlined that the thyroid levels were in the normal range, “so it’s a bit difficult to untangle what that means in terms of these subtle changes in thyroid levels.”
Robert Levitan, MD, Cameron Wilson Chair in Depression Research at the Centre for Addiction and Mental Health, Toronto, also emphasized that the thyroid levels were in the normal range.
He commented that it therefore “seems unlikely that there’s going to be some biological effect that’s going to affect the brain in a significant enough way” to influence suicidal ideation.
Dr. Levitan continued, “What’s probably happening is there’s some other clinical issue here that they just haven’t picked up on that’s leading in one direction to the suicidal ideation and perhaps affecting the TSH to some extent.”
Although the study is, therefore, “preliminary,” the findings are nevertheless “interesting,” he concluded.
The study received no funding. Ms. Liaugaudaite, Dr. Sockalingam, and Dr. Levitan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with comorbid anxiety and mood disorders who have reduced, albeit “normal” serum levels of thyroid-stimulating hormone (TSH) may be at increased risk for suicidal ideation, new research suggests.
In a cross-sectional study, clinical data on diagnosis, medication use, and symptom scores were gathered, along with assessments of blood levels of thyroid axis hormones, in patients with both anxiety and mood disorders.
After investigators accounted for age, gender, symptoms, medication use, and other potential confounders, patients with suicidal ideation were 54% less likely to have higher TSH levels. There was no association found with other thyroid hormones.
Based on the results, the assessment of thyroid hormone levels “may be important for suicide prevention and might allow clinicians to evaluate the potential of the suicidal ideation risk in individuals with [anxiety and mood disorders],” co-investigator Vilma Liaugaudaite, PhD student, Neuroscience Institute of the Lithuanian University of Health Sciences, Palanga, and colleagues note.
The findings were presented at the 34th European College of Neuropsychopharmacology (ECNP) Congress.
‘Complex mechanism’
Ms. Liaugaudaite told this news organization that thyroid hormones are known to have a “profound” effect on mood and behavior.
Recent studies show “various degrees of hypothalamic-pituitary-thyroid axis dysregulation are associated with suicidal behavior” in patients with depression, she added.
Noting that disturbances in the serotonin system “constitute the most common biochemical abnormality associated with suicidal behavior,” Ms. Liaugaudaite said it is thought thyroid hormones “are involved in a complex compensatory mechanism to correct reduced central 5-hydroxytryptamine activity” via lower TSH levels.
In addition, hypersecretion of thyrotropin-releasing hormone, which stimulates the release of TSH, “has been considered a compensatory mechanism to maintain normal thyroid hormone secretion and normalize serotonin activity in depressed patients,” she said.
To investigate associations between thyroid axis hormones and suicidality in individuals with comorbid anxiety and mood disorders, the researchers assessed consecutive patients attending a stress disorders clinic.
Sociodemographic and clinical information was gathered, and patients completed the Mini International Neuropsychiatric Interview, the Patient Health Questionnaire-9 (PHQ-9), and the General Anxiety Disorder-7 (GAD-7) scale.
Fasting blood samples were also tested for free thyroxine (FT4), free triiodothyronine (FT3), and TSH levels.
Significant association
Suicidal ideation was identified in 42 participants. Serum FT4, FT3, and TSH levels were within the normal range.
There were no significant differences between patients with and without suicidal ideation in terms of age, gender, education, obesity, smoking, and medication use.
Suicidal ideation was associated with higher scores on the PHQ-9 (15.5 vs. 13.3; P = .085), and with lower TSH levels (1.54 IU/L vs. 2.04 IU/L; P = .092).
The association between serum TSH levels and suicidal ideation was significant after multivariate logistic regression analysis accounted for age, gender, PHQ-9 and GAD-7 scores, education, body mass index, smoking, and use of antidepressants, tranquilizers, mood stabilizers, and neuroleptics.
Specifically, patients with suicidal ideation were significantly less likely to have higher TSH levels than those without, at an odds ratio of 0.46 (P = .027).
There were no significant associations between serum FT4 and FT3 levels and suicidal ideation.
Interesting, but preliminary
Commenting on the findings, Sanjeev Sockalingam, MD, vice chair and professor of psychiatry at the University of Toronto, said it is an “interesting study” because the literature on trying to identify individuals at risk for suicidal ideation or behaviors is “quite mixed, in terms of the results.”
However, it was a cross-sectional study with a relatively small sample size, and studies of this nature typically include patients with hypothyroidism “who end up having suicidal thoughts,” said Dr. Sockalingam, who was not involved with the research.
“I do wonder, given the sample size and patient population, if there may be other factors that may have been related to this,” he added.
Dr. Sockalingam noted that he would like to see more data on the medications the patients were taking, and he underlined that the thyroid levels were in the normal range, “so it’s a bit difficult to untangle what that means in terms of these subtle changes in thyroid levels.”
Robert Levitan, MD, Cameron Wilson Chair in Depression Research at the Centre for Addiction and Mental Health, Toronto, also emphasized that the thyroid levels were in the normal range.
He commented that it therefore “seems unlikely that there’s going to be some biological effect that’s going to affect the brain in a significant enough way” to influence suicidal ideation.
Dr. Levitan continued, “What’s probably happening is there’s some other clinical issue here that they just haven’t picked up on that’s leading in one direction to the suicidal ideation and perhaps affecting the TSH to some extent.”
Although the study is, therefore, “preliminary,” the findings are nevertheless “interesting,” he concluded.
The study received no funding. Ms. Liaugaudaite, Dr. Sockalingam, and Dr. Levitan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with comorbid anxiety and mood disorders who have reduced, albeit “normal” serum levels of thyroid-stimulating hormone (TSH) may be at increased risk for suicidal ideation, new research suggests.
In a cross-sectional study, clinical data on diagnosis, medication use, and symptom scores were gathered, along with assessments of blood levels of thyroid axis hormones, in patients with both anxiety and mood disorders.
After investigators accounted for age, gender, symptoms, medication use, and other potential confounders, patients with suicidal ideation were 54% less likely to have higher TSH levels. There was no association found with other thyroid hormones.
Based on the results, the assessment of thyroid hormone levels “may be important for suicide prevention and might allow clinicians to evaluate the potential of the suicidal ideation risk in individuals with [anxiety and mood disorders],” co-investigator Vilma Liaugaudaite, PhD student, Neuroscience Institute of the Lithuanian University of Health Sciences, Palanga, and colleagues note.
The findings were presented at the 34th European College of Neuropsychopharmacology (ECNP) Congress.
‘Complex mechanism’
Ms. Liaugaudaite told this news organization that thyroid hormones are known to have a “profound” effect on mood and behavior.
Recent studies show “various degrees of hypothalamic-pituitary-thyroid axis dysregulation are associated with suicidal behavior” in patients with depression, she added.
Noting that disturbances in the serotonin system “constitute the most common biochemical abnormality associated with suicidal behavior,” Ms. Liaugaudaite said it is thought thyroid hormones “are involved in a complex compensatory mechanism to correct reduced central 5-hydroxytryptamine activity” via lower TSH levels.
In addition, hypersecretion of thyrotropin-releasing hormone, which stimulates the release of TSH, “has been considered a compensatory mechanism to maintain normal thyroid hormone secretion and normalize serotonin activity in depressed patients,” she said.
To investigate associations between thyroid axis hormones and suicidality in individuals with comorbid anxiety and mood disorders, the researchers assessed consecutive patients attending a stress disorders clinic.
Sociodemographic and clinical information was gathered, and patients completed the Mini International Neuropsychiatric Interview, the Patient Health Questionnaire-9 (PHQ-9), and the General Anxiety Disorder-7 (GAD-7) scale.
Fasting blood samples were also tested for free thyroxine (FT4), free triiodothyronine (FT3), and TSH levels.
Significant association
Suicidal ideation was identified in 42 participants. Serum FT4, FT3, and TSH levels were within the normal range.
There were no significant differences between patients with and without suicidal ideation in terms of age, gender, education, obesity, smoking, and medication use.
Suicidal ideation was associated with higher scores on the PHQ-9 (15.5 vs. 13.3; P = .085), and with lower TSH levels (1.54 IU/L vs. 2.04 IU/L; P = .092).
The association between serum TSH levels and suicidal ideation was significant after multivariate logistic regression analysis accounted for age, gender, PHQ-9 and GAD-7 scores, education, body mass index, smoking, and use of antidepressants, tranquilizers, mood stabilizers, and neuroleptics.
Specifically, patients with suicidal ideation were significantly less likely to have higher TSH levels than those without, at an odds ratio of 0.46 (P = .027).
There were no significant associations between serum FT4 and FT3 levels and suicidal ideation.
Interesting, but preliminary
Commenting on the findings, Sanjeev Sockalingam, MD, vice chair and professor of psychiatry at the University of Toronto, said it is an “interesting study” because the literature on trying to identify individuals at risk for suicidal ideation or behaviors is “quite mixed, in terms of the results.”
However, it was a cross-sectional study with a relatively small sample size, and studies of this nature typically include patients with hypothyroidism “who end up having suicidal thoughts,” said Dr. Sockalingam, who was not involved with the research.
“I do wonder, given the sample size and patient population, if there may be other factors that may have been related to this,” he added.
Dr. Sockalingam noted that he would like to see more data on the medications the patients were taking, and he underlined that the thyroid levels were in the normal range, “so it’s a bit difficult to untangle what that means in terms of these subtle changes in thyroid levels.”
Robert Levitan, MD, Cameron Wilson Chair in Depression Research at the Centre for Addiction and Mental Health, Toronto, also emphasized that the thyroid levels were in the normal range.
He commented that it therefore “seems unlikely that there’s going to be some biological effect that’s going to affect the brain in a significant enough way” to influence suicidal ideation.
Dr. Levitan continued, “What’s probably happening is there’s some other clinical issue here that they just haven’t picked up on that’s leading in one direction to the suicidal ideation and perhaps affecting the TSH to some extent.”
Although the study is, therefore, “preliminary,” the findings are nevertheless “interesting,” he concluded.
The study received no funding. Ms. Liaugaudaite, Dr. Sockalingam, and Dr. Levitan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ECNP 2021
What turns wandering thoughts into something worse?
With all the lockdowns and social distancing of the pandemic, millions of people have had a lot of time to themselves. Many may have filled that time with baking, long walks, or video games, but minds wandering during these periods was inevitable. Coincident with these experiences were increases in depression and anxiety, which could be linked to the same brain network that is thought to support a meandering mind, called the default mode network.
Scientists interested in this network wanted to understand how wandering thoughts can lead some people to a state of brooding in which the same negative thoughts resurface repeatedly. To gain some insight into these patterns, they recorded more than 2,000 thoughts spoken aloud by 78 study participants who did nothing but let their minds wander for 10 minutes.
Senior researcher Jessica Andrews-Hanna, PhD, assistant professor of psychology, University of Arizona, Tucson, and colleagues hoped that analyzing these stream-of-consciousness thoughts could yield insights into how people become stuck in negative mental spirals.
They found that most participants thought about the present or future in words that were neither particularly negative nor positive. Almost three-quarters of the thoughts were focused inward on the person or were imaginative.
Negativity breeds negativity
But the investigators found an interesting pattern with regard to negative thoughts. The more negative someone’s thoughts became, the more likely that their next idea would be related to their previous one. In other words, negative thoughts created a chain reaction of more negative thoughts.
, indicating true mental meandering. The pattern suggested that negativity tends to narrow the range of thoughts, whereas positivity tends to expand it during periods in which the mind wanders.
The researchers also found, unsurprisingly, that negative thoughts that were focused on the self and on the past were more likely to result in brooding and that positive thoughts were less likely to arise.
Most study participants were young and educated and may have only said things that they were comfortable allowing the researchers to hear. And because the authors didn’t ask participants about their moods, the investigators could not associate specific patterns of thought with any mental health conditions.
Although the findings, published in Scientific Reports, do not on their own point to solutions for depression or anxiety, they may offer a starting point for future research into how negative trains of thoughts begin – and perhaps how to derail them.
A version of this article first appeared on Medscape.com.
With all the lockdowns and social distancing of the pandemic, millions of people have had a lot of time to themselves. Many may have filled that time with baking, long walks, or video games, but minds wandering during these periods was inevitable. Coincident with these experiences were increases in depression and anxiety, which could be linked to the same brain network that is thought to support a meandering mind, called the default mode network.
Scientists interested in this network wanted to understand how wandering thoughts can lead some people to a state of brooding in which the same negative thoughts resurface repeatedly. To gain some insight into these patterns, they recorded more than 2,000 thoughts spoken aloud by 78 study participants who did nothing but let their minds wander for 10 minutes.
Senior researcher Jessica Andrews-Hanna, PhD, assistant professor of psychology, University of Arizona, Tucson, and colleagues hoped that analyzing these stream-of-consciousness thoughts could yield insights into how people become stuck in negative mental spirals.
They found that most participants thought about the present or future in words that were neither particularly negative nor positive. Almost three-quarters of the thoughts were focused inward on the person or were imaginative.
Negativity breeds negativity
But the investigators found an interesting pattern with regard to negative thoughts. The more negative someone’s thoughts became, the more likely that their next idea would be related to their previous one. In other words, negative thoughts created a chain reaction of more negative thoughts.
, indicating true mental meandering. The pattern suggested that negativity tends to narrow the range of thoughts, whereas positivity tends to expand it during periods in which the mind wanders.
The researchers also found, unsurprisingly, that negative thoughts that were focused on the self and on the past were more likely to result in brooding and that positive thoughts were less likely to arise.
Most study participants were young and educated and may have only said things that they were comfortable allowing the researchers to hear. And because the authors didn’t ask participants about their moods, the investigators could not associate specific patterns of thought with any mental health conditions.
Although the findings, published in Scientific Reports, do not on their own point to solutions for depression or anxiety, they may offer a starting point for future research into how negative trains of thoughts begin – and perhaps how to derail them.
A version of this article first appeared on Medscape.com.
With all the lockdowns and social distancing of the pandemic, millions of people have had a lot of time to themselves. Many may have filled that time with baking, long walks, or video games, but minds wandering during these periods was inevitable. Coincident with these experiences were increases in depression and anxiety, which could be linked to the same brain network that is thought to support a meandering mind, called the default mode network.
Scientists interested in this network wanted to understand how wandering thoughts can lead some people to a state of brooding in which the same negative thoughts resurface repeatedly. To gain some insight into these patterns, they recorded more than 2,000 thoughts spoken aloud by 78 study participants who did nothing but let their minds wander for 10 minutes.
Senior researcher Jessica Andrews-Hanna, PhD, assistant professor of psychology, University of Arizona, Tucson, and colleagues hoped that analyzing these stream-of-consciousness thoughts could yield insights into how people become stuck in negative mental spirals.
They found that most participants thought about the present or future in words that were neither particularly negative nor positive. Almost three-quarters of the thoughts were focused inward on the person or were imaginative.
Negativity breeds negativity
But the investigators found an interesting pattern with regard to negative thoughts. The more negative someone’s thoughts became, the more likely that their next idea would be related to their previous one. In other words, negative thoughts created a chain reaction of more negative thoughts.
, indicating true mental meandering. The pattern suggested that negativity tends to narrow the range of thoughts, whereas positivity tends to expand it during periods in which the mind wanders.
The researchers also found, unsurprisingly, that negative thoughts that were focused on the self and on the past were more likely to result in brooding and that positive thoughts were less likely to arise.
Most study participants were young and educated and may have only said things that they were comfortable allowing the researchers to hear. And because the authors didn’t ask participants about their moods, the investigators could not associate specific patterns of thought with any mental health conditions.
Although the findings, published in Scientific Reports, do not on their own point to solutions for depression or anxiety, they may offer a starting point for future research into how negative trains of thoughts begin – and perhaps how to derail them.
A version of this article first appeared on Medscape.com.
Anxiety, depression symptoms rose and fell with new COVID cases
Anxiety and depression symptoms increased in adults last winter as COVID-19 surged in the United States but declined in the spring as COVID activity approached its nadir, according to an analysis from the Centers for Disease Control and Prevention.
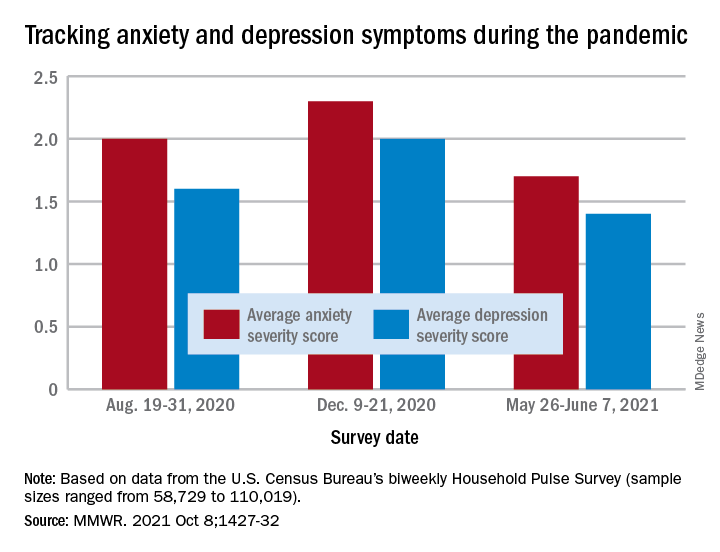
“The relative increases and decreases in frequency of reported symptoms of anxiety and depression at both the national and state levels mirrored the national weekly number of new COVID-19 cases during the same period,” Haomiao Jia, PhD, and associates wrote in the Morbidity and Mortality Weekly Report.
In a national survey conducted Aug. 19-31, 2020, the average anxiety severity score was 2.0 and the average depression score was 1.6 among adults in all 50 states. Those scores rose to 2.3 (+13.0%) and 2.0 (+14.8%), respectively, by Dec. 9-21, but then fell to 1.7 (–26.8%) and 1.4 (–24.8%) during the survey conducted from May 26 to June 7, 2021, the investigators reported.
Despite that decrease in the spring, however, “the frequency of symptoms ... in June 2021 remained elevated compared with estimates from” 2019, said Dr. Jia of Columbia University, New York, and associates. Data from the National Health Interview Survey put the prepandemic severity scores at 0.63 for anxiety and 0.51 for depression.
Weekly symptom frequency in the Household Pulse Survey, which began in April 2020, was assessed with the four-item Patient Health Questionnaire, which includes two questions on anxiety and two on depression. Each answer scored on a scale from 0 (no symptoms at all) to 3 (symptoms nearly every day), making a total of 6 possible for each severity score, they explained. Sample sizes for the biweekly surveys ranged from 58,729 to 110,019.
Among the states, there was something of a pattern involving the drop in scores during the fall and the rise over the winter and spring months. “States with larger increases in severity scores during August–December 2020 also tended to have larger decreases during January–June 2021,” the researchers noted.
That group includes Minnesota, Mississippi, South Dakota, and Utah for anxiety and Idaho, Michigan, Minnesota, and Wisconsin for depression, the survey data show.
Florida and New York had the smallest increases in depression and anxiety scores, respectively, from August to December, and New York had the smallest decrease in both anxiety and depression from January to June, Dr. Jia and associates said.
“ during national emergencies. The observed differences in severity score magnitude and peaks across states in this study indicate that these efforts are important at both the national and state levels,” they wrote.
Anxiety and depression symptoms increased in adults last winter as COVID-19 surged in the United States but declined in the spring as COVID activity approached its nadir, according to an analysis from the Centers for Disease Control and Prevention.
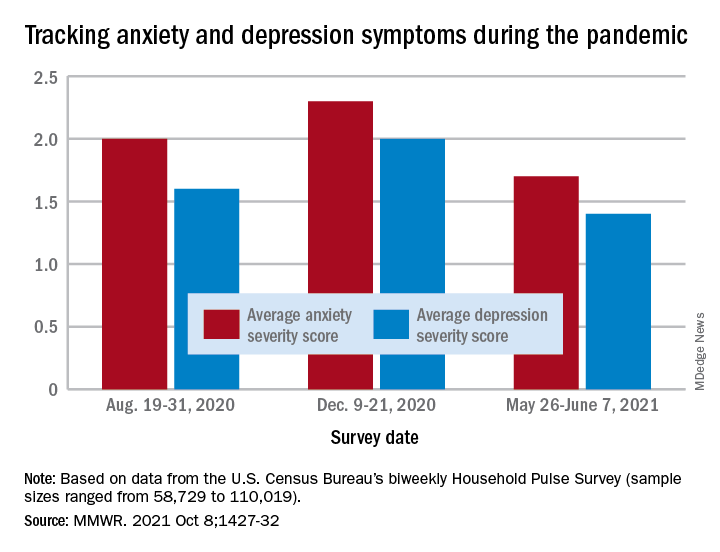
“The relative increases and decreases in frequency of reported symptoms of anxiety and depression at both the national and state levels mirrored the national weekly number of new COVID-19 cases during the same period,” Haomiao Jia, PhD, and associates wrote in the Morbidity and Mortality Weekly Report.
In a national survey conducted Aug. 19-31, 2020, the average anxiety severity score was 2.0 and the average depression score was 1.6 among adults in all 50 states. Those scores rose to 2.3 (+13.0%) and 2.0 (+14.8%), respectively, by Dec. 9-21, but then fell to 1.7 (–26.8%) and 1.4 (–24.8%) during the survey conducted from May 26 to June 7, 2021, the investigators reported.
Despite that decrease in the spring, however, “the frequency of symptoms ... in June 2021 remained elevated compared with estimates from” 2019, said Dr. Jia of Columbia University, New York, and associates. Data from the National Health Interview Survey put the prepandemic severity scores at 0.63 for anxiety and 0.51 for depression.
Weekly symptom frequency in the Household Pulse Survey, which began in April 2020, was assessed with the four-item Patient Health Questionnaire, which includes two questions on anxiety and two on depression. Each answer scored on a scale from 0 (no symptoms at all) to 3 (symptoms nearly every day), making a total of 6 possible for each severity score, they explained. Sample sizes for the biweekly surveys ranged from 58,729 to 110,019.
Among the states, there was something of a pattern involving the drop in scores during the fall and the rise over the winter and spring months. “States with larger increases in severity scores during August–December 2020 also tended to have larger decreases during January–June 2021,” the researchers noted.
That group includes Minnesota, Mississippi, South Dakota, and Utah for anxiety and Idaho, Michigan, Minnesota, and Wisconsin for depression, the survey data show.
Florida and New York had the smallest increases in depression and anxiety scores, respectively, from August to December, and New York had the smallest decrease in both anxiety and depression from January to June, Dr. Jia and associates said.
“ during national emergencies. The observed differences in severity score magnitude and peaks across states in this study indicate that these efforts are important at both the national and state levels,” they wrote.
Anxiety and depression symptoms increased in adults last winter as COVID-19 surged in the United States but declined in the spring as COVID activity approached its nadir, according to an analysis from the Centers for Disease Control and Prevention.
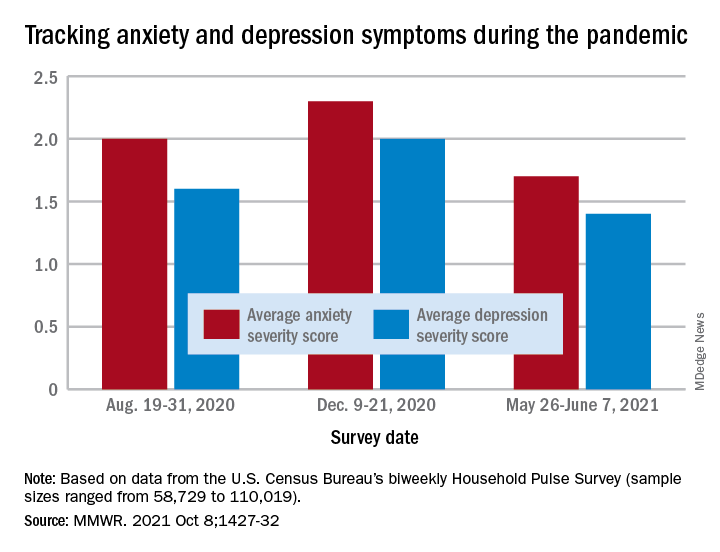
“The relative increases and decreases in frequency of reported symptoms of anxiety and depression at both the national and state levels mirrored the national weekly number of new COVID-19 cases during the same period,” Haomiao Jia, PhD, and associates wrote in the Morbidity and Mortality Weekly Report.
In a national survey conducted Aug. 19-31, 2020, the average anxiety severity score was 2.0 and the average depression score was 1.6 among adults in all 50 states. Those scores rose to 2.3 (+13.0%) and 2.0 (+14.8%), respectively, by Dec. 9-21, but then fell to 1.7 (–26.8%) and 1.4 (–24.8%) during the survey conducted from May 26 to June 7, 2021, the investigators reported.
Despite that decrease in the spring, however, “the frequency of symptoms ... in June 2021 remained elevated compared with estimates from” 2019, said Dr. Jia of Columbia University, New York, and associates. Data from the National Health Interview Survey put the prepandemic severity scores at 0.63 for anxiety and 0.51 for depression.
Weekly symptom frequency in the Household Pulse Survey, which began in April 2020, was assessed with the four-item Patient Health Questionnaire, which includes two questions on anxiety and two on depression. Each answer scored on a scale from 0 (no symptoms at all) to 3 (symptoms nearly every day), making a total of 6 possible for each severity score, they explained. Sample sizes for the biweekly surveys ranged from 58,729 to 110,019.
Among the states, there was something of a pattern involving the drop in scores during the fall and the rise over the winter and spring months. “States with larger increases in severity scores during August–December 2020 also tended to have larger decreases during January–June 2021,” the researchers noted.
That group includes Minnesota, Mississippi, South Dakota, and Utah for anxiety and Idaho, Michigan, Minnesota, and Wisconsin for depression, the survey data show.
Florida and New York had the smallest increases in depression and anxiety scores, respectively, from August to December, and New York had the smallest decrease in both anxiety and depression from January to June, Dr. Jia and associates said.
“ during national emergencies. The observed differences in severity score magnitude and peaks across states in this study indicate that these efforts are important at both the national and state levels,” they wrote.
FROM THE MMWR
Web of antimicrobials doesn’t hold water
Music plus mushrooms equals therapy
Magic mushrooms have been used recreationally and medicinally for thousands of years, but researchers have found adding music could be a game changer in antidepressant treatment.
The ingredient that makes these mushrooms so magical is psilocybin. It works well for the clinical treatment of mental health conditions and some forms of depression because the “trip” can be contained to one work day, making it easy to administer under supervision. With the accompaniment of music, scientists have found that psilocybin evokes emotion.
This recent study, presented at the European College of Neuropsychopharmacology Congress in Lisbon, tested participants’ emotional response to music before and after the psilocybin. Ketanserin, an antihypertensive drug, was used to test against the effects of psilocybin. The scientist played Mozart and Elgar and found that participants on psilocybin had an emotional response increase of 60%. That response was even greater, compared with ketanserin, which actually lessened the emotional response to music.
“This shows that combination of psilocybin and music has a strong emotional effect, and we believe that this will be important for the therapeutic application of psychedelics if they are approved for clinical use,” said lead researcher Dea Siggaard Stenbæk of the University of Copenhagen.
Professor David J. Nutt of Imperial College in London, who was not involved in the study, said that it supports the use of music for treatment efficacy with psychedelics and suggested that the next step is to “optimise this approach probably through individualising and personalising music tracks in therapy.”
Cue the 1960s LSD music montage.
Chicken ‘white striping is not a disease’
Have you ever sliced open a new pack of chicken breasts to start dinner and noticed white fatty lines running through the chicken? Maybe you thought it was just some extra fat to trim off, but the Humane League calls it “white striping disease.”
Chicken is the No. 1 meat consumed by Americans, so it’s not surprising that chickens are factory farmed and raised to be ready for slaughter quickly, according to CBSNews.com, which reported that the Humane League claims white striping is found in 70% of the chicken in popular grocery stores. The league expressed concern for the chickens’ welfare as they are bred to grow bigger quickly, which is causing the white striping and increasing the fat content of the meat by as much as 224%.
The National Chicken Council told CBS that the league’s findings were unscientific. A spokesperson said, “White striping is not a disease. It is a quality factor in chicken breast meat caused by deposits of fat in the muscle during the bird’s growth and development.” He went on to say that severe white striping happens in 3%-6% of birds, which are mostly used in further processed products, not in chicken breast packages.
Somehow, that’s not making us feel any better.
The itsy bitsy spider lets us all down
Most people do not like spiders. That’s too bad, because spiders are generally nothing but helpful little creatures that prey upon annoying flies and other pests. Then there’s the silk they produce. The ancient Romans used it to treat conditions such as warts and skin lesions. Spiders wrap their eggs in silk to protect them from harmful bacteria.
Of course, we can hardly trust the medical opinions of people from 2,000 years ago, but modern-day studies have not definitively proved whether or not spider silk has any antimicrobial properties.
To settle the matter once and for all, researchers from Denmark built a silk-harvesting machine using the most famous of Danish inventions: Legos. The contraption, sort of a paddle wheel, pulled the silk from several different species of spider pinned down by the researchers. The silk was then tested against three different bacteria species, including good old Escherichia coli.
Unfortunately for our spider friends, their silk has no antimicrobial activity. The researchers suspected that any such activity seen in previous studies was actually caused by improper control for the solvents used to extract the silk; those solvents can have antimicrobial properties on their own. As for protecting their eggs, rather than killing bacteria, the silk likely provides a physical barrier alone.
It is bad news for spiders on the benefit-to-humanity front, but look at the bright side: If their silk had antimicrobial activity, we’d have to start farming them to acquire more silk. And that’s no good. Spiders deserve to roam free, hunt as they please, and drop down on your head from the ceiling.
Anxiety and allergies: Cause, effect, confusion
We’re big fans of science, but as longtime, totally impartial (Science rules!) observers of science’s medical realm, we can see that the day-to-day process of practicing the scientific method occasionally gets a bit messy. And no, we’re not talking about COVID-19.
We’re talking allergies. We’re talking mental health. We’re talking allergic disease and mental health.
We’re talking about a pair of press releases we came across during our never-ending search for material to educate, entertain, and astound our fabulously wonderful and loyal readers. (We say that, of course, in the most impartial way possible.)
The first release was titled, “Allergies including asthma and hay fever not linked to mental health traits” and covered research from the University of Bristol (England). The investigators were trying to determine if “allergic diseases actually causes mental health traits including anxiety, depression, bipolar disorder, and schizophrenia, or vice versa,” according to the release.
What they found, however, was “little evidence of a causal relationship between the onset of allergic disease and mental health.” Again, this is the press release talking.
The second release seemed to suggest the exact opposite: “Study uncovers link between allergies and mental health conditions.” That got our attention. A little more reading revealed that “people with asthma, atopic dermatitis, and hay fever also had a higher likelihood of having depression, anxiety, bipolar disorder, or neuroticism.”
One of the investigators was quoted as saying, “Establishing whether allergic disease causes mental health problems, or vice versa, is important to ensure that resources and treatment strategies are targeted appropriately.”
Did you notice the “vice versa”? Did you notice that it appeared in quotes from both releases? We did, so we took a closer look at the source. The second release covered a group of investigators from the University of Bristol – the same group, and the same study, in fact, as the first one.
So there you have it. One study, two press releases, and one confused journalist. Thank you, science.
Music plus mushrooms equals therapy
Magic mushrooms have been used recreationally and medicinally for thousands of years, but researchers have found adding music could be a game changer in antidepressant treatment.
The ingredient that makes these mushrooms so magical is psilocybin. It works well for the clinical treatment of mental health conditions and some forms of depression because the “trip” can be contained to one work day, making it easy to administer under supervision. With the accompaniment of music, scientists have found that psilocybin evokes emotion.
This recent study, presented at the European College of Neuropsychopharmacology Congress in Lisbon, tested participants’ emotional response to music before and after the psilocybin. Ketanserin, an antihypertensive drug, was used to test against the effects of psilocybin. The scientist played Mozart and Elgar and found that participants on psilocybin had an emotional response increase of 60%. That response was even greater, compared with ketanserin, which actually lessened the emotional response to music.
“This shows that combination of psilocybin and music has a strong emotional effect, and we believe that this will be important for the therapeutic application of psychedelics if they are approved for clinical use,” said lead researcher Dea Siggaard Stenbæk of the University of Copenhagen.
Professor David J. Nutt of Imperial College in London, who was not involved in the study, said that it supports the use of music for treatment efficacy with psychedelics and suggested that the next step is to “optimise this approach probably through individualising and personalising music tracks in therapy.”
Cue the 1960s LSD music montage.
Chicken ‘white striping is not a disease’
Have you ever sliced open a new pack of chicken breasts to start dinner and noticed white fatty lines running through the chicken? Maybe you thought it was just some extra fat to trim off, but the Humane League calls it “white striping disease.”
Chicken is the No. 1 meat consumed by Americans, so it’s not surprising that chickens are factory farmed and raised to be ready for slaughter quickly, according to CBSNews.com, which reported that the Humane League claims white striping is found in 70% of the chicken in popular grocery stores. The league expressed concern for the chickens’ welfare as they are bred to grow bigger quickly, which is causing the white striping and increasing the fat content of the meat by as much as 224%.
The National Chicken Council told CBS that the league’s findings were unscientific. A spokesperson said, “White striping is not a disease. It is a quality factor in chicken breast meat caused by deposits of fat in the muscle during the bird’s growth and development.” He went on to say that severe white striping happens in 3%-6% of birds, which are mostly used in further processed products, not in chicken breast packages.
Somehow, that’s not making us feel any better.
The itsy bitsy spider lets us all down
Most people do not like spiders. That’s too bad, because spiders are generally nothing but helpful little creatures that prey upon annoying flies and other pests. Then there’s the silk they produce. The ancient Romans used it to treat conditions such as warts and skin lesions. Spiders wrap their eggs in silk to protect them from harmful bacteria.
Of course, we can hardly trust the medical opinions of people from 2,000 years ago, but modern-day studies have not definitively proved whether or not spider silk has any antimicrobial properties.
To settle the matter once and for all, researchers from Denmark built a silk-harvesting machine using the most famous of Danish inventions: Legos. The contraption, sort of a paddle wheel, pulled the silk from several different species of spider pinned down by the researchers. The silk was then tested against three different bacteria species, including good old Escherichia coli.
Unfortunately for our spider friends, their silk has no antimicrobial activity. The researchers suspected that any such activity seen in previous studies was actually caused by improper control for the solvents used to extract the silk; those solvents can have antimicrobial properties on their own. As for protecting their eggs, rather than killing bacteria, the silk likely provides a physical barrier alone.
It is bad news for spiders on the benefit-to-humanity front, but look at the bright side: If their silk had antimicrobial activity, we’d have to start farming them to acquire more silk. And that’s no good. Spiders deserve to roam free, hunt as they please, and drop down on your head from the ceiling.
Anxiety and allergies: Cause, effect, confusion
We’re big fans of science, but as longtime, totally impartial (Science rules!) observers of science’s medical realm, we can see that the day-to-day process of practicing the scientific method occasionally gets a bit messy. And no, we’re not talking about COVID-19.
We’re talking allergies. We’re talking mental health. We’re talking allergic disease and mental health.
We’re talking about a pair of press releases we came across during our never-ending search for material to educate, entertain, and astound our fabulously wonderful and loyal readers. (We say that, of course, in the most impartial way possible.)
The first release was titled, “Allergies including asthma and hay fever not linked to mental health traits” and covered research from the University of Bristol (England). The investigators were trying to determine if “allergic diseases actually causes mental health traits including anxiety, depression, bipolar disorder, and schizophrenia, or vice versa,” according to the release.
What they found, however, was “little evidence of a causal relationship between the onset of allergic disease and mental health.” Again, this is the press release talking.
The second release seemed to suggest the exact opposite: “Study uncovers link between allergies and mental health conditions.” That got our attention. A little more reading revealed that “people with asthma, atopic dermatitis, and hay fever also had a higher likelihood of having depression, anxiety, bipolar disorder, or neuroticism.”
One of the investigators was quoted as saying, “Establishing whether allergic disease causes mental health problems, or vice versa, is important to ensure that resources and treatment strategies are targeted appropriately.”
Did you notice the “vice versa”? Did you notice that it appeared in quotes from both releases? We did, so we took a closer look at the source. The second release covered a group of investigators from the University of Bristol – the same group, and the same study, in fact, as the first one.
So there you have it. One study, two press releases, and one confused journalist. Thank you, science.
Music plus mushrooms equals therapy
Magic mushrooms have been used recreationally and medicinally for thousands of years, but researchers have found adding music could be a game changer in antidepressant treatment.
The ingredient that makes these mushrooms so magical is psilocybin. It works well for the clinical treatment of mental health conditions and some forms of depression because the “trip” can be contained to one work day, making it easy to administer under supervision. With the accompaniment of music, scientists have found that psilocybin evokes emotion.
This recent study, presented at the European College of Neuropsychopharmacology Congress in Lisbon, tested participants’ emotional response to music before and after the psilocybin. Ketanserin, an antihypertensive drug, was used to test against the effects of psilocybin. The scientist played Mozart and Elgar and found that participants on psilocybin had an emotional response increase of 60%. That response was even greater, compared with ketanserin, which actually lessened the emotional response to music.
“This shows that combination of psilocybin and music has a strong emotional effect, and we believe that this will be important for the therapeutic application of psychedelics if they are approved for clinical use,” said lead researcher Dea Siggaard Stenbæk of the University of Copenhagen.
Professor David J. Nutt of Imperial College in London, who was not involved in the study, said that it supports the use of music for treatment efficacy with psychedelics and suggested that the next step is to “optimise this approach probably through individualising and personalising music tracks in therapy.”
Cue the 1960s LSD music montage.
Chicken ‘white striping is not a disease’
Have you ever sliced open a new pack of chicken breasts to start dinner and noticed white fatty lines running through the chicken? Maybe you thought it was just some extra fat to trim off, but the Humane League calls it “white striping disease.”
Chicken is the No. 1 meat consumed by Americans, so it’s not surprising that chickens are factory farmed and raised to be ready for slaughter quickly, according to CBSNews.com, which reported that the Humane League claims white striping is found in 70% of the chicken in popular grocery stores. The league expressed concern for the chickens’ welfare as they are bred to grow bigger quickly, which is causing the white striping and increasing the fat content of the meat by as much as 224%.
The National Chicken Council told CBS that the league’s findings were unscientific. A spokesperson said, “White striping is not a disease. It is a quality factor in chicken breast meat caused by deposits of fat in the muscle during the bird’s growth and development.” He went on to say that severe white striping happens in 3%-6% of birds, which are mostly used in further processed products, not in chicken breast packages.
Somehow, that’s not making us feel any better.
The itsy bitsy spider lets us all down
Most people do not like spiders. That’s too bad, because spiders are generally nothing but helpful little creatures that prey upon annoying flies and other pests. Then there’s the silk they produce. The ancient Romans used it to treat conditions such as warts and skin lesions. Spiders wrap their eggs in silk to protect them from harmful bacteria.
Of course, we can hardly trust the medical opinions of people from 2,000 years ago, but modern-day studies have not definitively proved whether or not spider silk has any antimicrobial properties.
To settle the matter once and for all, researchers from Denmark built a silk-harvesting machine using the most famous of Danish inventions: Legos. The contraption, sort of a paddle wheel, pulled the silk from several different species of spider pinned down by the researchers. The silk was then tested against three different bacteria species, including good old Escherichia coli.
Unfortunately for our spider friends, their silk has no antimicrobial activity. The researchers suspected that any such activity seen in previous studies was actually caused by improper control for the solvents used to extract the silk; those solvents can have antimicrobial properties on their own. As for protecting their eggs, rather than killing bacteria, the silk likely provides a physical barrier alone.
It is bad news for spiders on the benefit-to-humanity front, but look at the bright side: If their silk had antimicrobial activity, we’d have to start farming them to acquire more silk. And that’s no good. Spiders deserve to roam free, hunt as they please, and drop down on your head from the ceiling.
Anxiety and allergies: Cause, effect, confusion
We’re big fans of science, but as longtime, totally impartial (Science rules!) observers of science’s medical realm, we can see that the day-to-day process of practicing the scientific method occasionally gets a bit messy. And no, we’re not talking about COVID-19.
We’re talking allergies. We’re talking mental health. We’re talking allergic disease and mental health.
We’re talking about a pair of press releases we came across during our never-ending search for material to educate, entertain, and astound our fabulously wonderful and loyal readers. (We say that, of course, in the most impartial way possible.)
The first release was titled, “Allergies including asthma and hay fever not linked to mental health traits” and covered research from the University of Bristol (England). The investigators were trying to determine if “allergic diseases actually causes mental health traits including anxiety, depression, bipolar disorder, and schizophrenia, or vice versa,” according to the release.
What they found, however, was “little evidence of a causal relationship between the onset of allergic disease and mental health.” Again, this is the press release talking.
The second release seemed to suggest the exact opposite: “Study uncovers link between allergies and mental health conditions.” That got our attention. A little more reading revealed that “people with asthma, atopic dermatitis, and hay fever also had a higher likelihood of having depression, anxiety, bipolar disorder, or neuroticism.”
One of the investigators was quoted as saying, “Establishing whether allergic disease causes mental health problems, or vice versa, is important to ensure that resources and treatment strategies are targeted appropriately.”
Did you notice the “vice versa”? Did you notice that it appeared in quotes from both releases? We did, so we took a closer look at the source. The second release covered a group of investigators from the University of Bristol – the same group, and the same study, in fact, as the first one.
So there you have it. One study, two press releases, and one confused journalist. Thank you, science.
Dopamine and reward: The story of social media
How often do you find yourself on social media? The first thing I do when I wake up is check my email and text messages, as well as my Facebook, Snapchat, and Instagram notifications.
Some 150,000 messages are shared on Facebook each minute; 293 million daily active users worldwide were recorded on Snapchat during the second quarter of 2021; 127.2 million monthly active users in the United States are projected to be on Instagram by 2023.
Social media has gained the hearts and wonder of many around the world. It’s absolutely incredible how ingrained it has become in our lives as a medium for creativity, outlet for communication, and platform for information. In fact, these online network tools have now become essential during COVID-19 to ensure productive workflow, keep in touch with our loved ones, and, overall, maintain social capital. Social media has truly emerged as a powerful form of living beyond our physical selves.
Yet, increased (and addictive) social media use is associated with negative health outcomes, especially among adolescents. For example, in a study reporting parent and adolescent accounts of social media use, it was reported that social media use was associated with hyperactivity/impulsivity, depression, anxiety, loneliness, and a fear of missing out. Furthermore, a meta-analysis investigating the relationship between social media use and depressive symptoms among adolescents found a small but significant and positive relationship between the two. However, additional research is required to elucidate this association.
Notwithstanding, the addictive nature of social media has previously been called out as analogous to the addictive nature of gambling. Let’s think about it. Whether you’re on Instagram, TikTok, or a similar platform, you can’t help but scroll from one video to the next. It’s one 5- to 10-second video after the next, and before you know it, you’ve spent the past hour going through random videos – but you can’t stop. Why is that so?
Social media actually “rewires” our brain such that we expect instant gratification. In other words, when we get a notification, message, like, or share, we expect fast and short-term pleasure/reward because the brain will produce a “hit of dopamine.” However, it is important to note that the reward system is not delimited to the dopaminergic pathway and, in fact, should be understood as a complex network system (i.e., governed by changes in brain morphology through addiction and excessive behavior). Given the quick pace of the social media world, the reward pathways in our brain change and there’s an increasing demand for attention, perpetuating an addictive mindset.
When we refresh our page, we expect instant gratification. But what happens when we don’t get a like, or a message, or some sort of “reward”? Recounts of social media use by adolescents have likened online attention to popularity. Accordingly, a lack of constant attention on social media has created a vicious cycle of anxiety, loneliness, and depression because of a failure to receive “virtual” reward. Taken together, social media may be harmful because it distorts our self-image, and while social media platforms help connect us, they can also ironically make us feel isolated, lower our self-confidence, and diminish our overall sense of well-being.
As the platforms for communication and information have evolved so rapidly over the past decade, there is a need to establish boundaries between what is beneficial and what is potentially detrimental to our mental health. While social media companies should play a role in mitigating addictive social network behavior, it would also seem counterintuitive to the general business model. In that case, who takes charge? This multifaceted problem requires a multidisciplinary approach.
Leanna M.W. Lui is an MSc candidate at the University of Toronto.
A version of this article first appeared on Medscape.com.
How often do you find yourself on social media? The first thing I do when I wake up is check my email and text messages, as well as my Facebook, Snapchat, and Instagram notifications.
Some 150,000 messages are shared on Facebook each minute; 293 million daily active users worldwide were recorded on Snapchat during the second quarter of 2021; 127.2 million monthly active users in the United States are projected to be on Instagram by 2023.
Social media has gained the hearts and wonder of many around the world. It’s absolutely incredible how ingrained it has become in our lives as a medium for creativity, outlet for communication, and platform for information. In fact, these online network tools have now become essential during COVID-19 to ensure productive workflow, keep in touch with our loved ones, and, overall, maintain social capital. Social media has truly emerged as a powerful form of living beyond our physical selves.
Yet, increased (and addictive) social media use is associated with negative health outcomes, especially among adolescents. For example, in a study reporting parent and adolescent accounts of social media use, it was reported that social media use was associated with hyperactivity/impulsivity, depression, anxiety, loneliness, and a fear of missing out. Furthermore, a meta-analysis investigating the relationship between social media use and depressive symptoms among adolescents found a small but significant and positive relationship between the two. However, additional research is required to elucidate this association.
Notwithstanding, the addictive nature of social media has previously been called out as analogous to the addictive nature of gambling. Let’s think about it. Whether you’re on Instagram, TikTok, or a similar platform, you can’t help but scroll from one video to the next. It’s one 5- to 10-second video after the next, and before you know it, you’ve spent the past hour going through random videos – but you can’t stop. Why is that so?
Social media actually “rewires” our brain such that we expect instant gratification. In other words, when we get a notification, message, like, or share, we expect fast and short-term pleasure/reward because the brain will produce a “hit of dopamine.” However, it is important to note that the reward system is not delimited to the dopaminergic pathway and, in fact, should be understood as a complex network system (i.e., governed by changes in brain morphology through addiction and excessive behavior). Given the quick pace of the social media world, the reward pathways in our brain change and there’s an increasing demand for attention, perpetuating an addictive mindset.
When we refresh our page, we expect instant gratification. But what happens when we don’t get a like, or a message, or some sort of “reward”? Recounts of social media use by adolescents have likened online attention to popularity. Accordingly, a lack of constant attention on social media has created a vicious cycle of anxiety, loneliness, and depression because of a failure to receive “virtual” reward. Taken together, social media may be harmful because it distorts our self-image, and while social media platforms help connect us, they can also ironically make us feel isolated, lower our self-confidence, and diminish our overall sense of well-being.
As the platforms for communication and information have evolved so rapidly over the past decade, there is a need to establish boundaries between what is beneficial and what is potentially detrimental to our mental health. While social media companies should play a role in mitigating addictive social network behavior, it would also seem counterintuitive to the general business model. In that case, who takes charge? This multifaceted problem requires a multidisciplinary approach.
Leanna M.W. Lui is an MSc candidate at the University of Toronto.
A version of this article first appeared on Medscape.com.
How often do you find yourself on social media? The first thing I do when I wake up is check my email and text messages, as well as my Facebook, Snapchat, and Instagram notifications.
Some 150,000 messages are shared on Facebook each minute; 293 million daily active users worldwide were recorded on Snapchat during the second quarter of 2021; 127.2 million monthly active users in the United States are projected to be on Instagram by 2023.
Social media has gained the hearts and wonder of many around the world. It’s absolutely incredible how ingrained it has become in our lives as a medium for creativity, outlet for communication, and platform for information. In fact, these online network tools have now become essential during COVID-19 to ensure productive workflow, keep in touch with our loved ones, and, overall, maintain social capital. Social media has truly emerged as a powerful form of living beyond our physical selves.
Yet, increased (and addictive) social media use is associated with negative health outcomes, especially among adolescents. For example, in a study reporting parent and adolescent accounts of social media use, it was reported that social media use was associated with hyperactivity/impulsivity, depression, anxiety, loneliness, and a fear of missing out. Furthermore, a meta-analysis investigating the relationship between social media use and depressive symptoms among adolescents found a small but significant and positive relationship between the two. However, additional research is required to elucidate this association.
Notwithstanding, the addictive nature of social media has previously been called out as analogous to the addictive nature of gambling. Let’s think about it. Whether you’re on Instagram, TikTok, or a similar platform, you can’t help but scroll from one video to the next. It’s one 5- to 10-second video after the next, and before you know it, you’ve spent the past hour going through random videos – but you can’t stop. Why is that so?
Social media actually “rewires” our brain such that we expect instant gratification. In other words, when we get a notification, message, like, or share, we expect fast and short-term pleasure/reward because the brain will produce a “hit of dopamine.” However, it is important to note that the reward system is not delimited to the dopaminergic pathway and, in fact, should be understood as a complex network system (i.e., governed by changes in brain morphology through addiction and excessive behavior). Given the quick pace of the social media world, the reward pathways in our brain change and there’s an increasing demand for attention, perpetuating an addictive mindset.
When we refresh our page, we expect instant gratification. But what happens when we don’t get a like, or a message, or some sort of “reward”? Recounts of social media use by adolescents have likened online attention to popularity. Accordingly, a lack of constant attention on social media has created a vicious cycle of anxiety, loneliness, and depression because of a failure to receive “virtual” reward. Taken together, social media may be harmful because it distorts our self-image, and while social media platforms help connect us, they can also ironically make us feel isolated, lower our self-confidence, and diminish our overall sense of well-being.
As the platforms for communication and information have evolved so rapidly over the past decade, there is a need to establish boundaries between what is beneficial and what is potentially detrimental to our mental health. While social media companies should play a role in mitigating addictive social network behavior, it would also seem counterintuitive to the general business model. In that case, who takes charge? This multifaceted problem requires a multidisciplinary approach.
Leanna M.W. Lui is an MSc candidate at the University of Toronto.
A version of this article first appeared on Medscape.com.
Gut health ‘vitally important’ for mental health
Disturbances in gut microbiota are associated with depletion of anti-inflammatory bacteria and proliferation of proinflammatory bacteria, a pattern tied to several major psychiatric disorders including depression, bipolar disorder (BD), schizophrenia, and anxiety, new research shows.
A meta-analysis of 59 studies, encompassing roughly 2,600 patients with psychiatric conditions, showed a decrease in microbial richness in patients with psychiatric conditions versus controls.
In addition, those with depression, anxiety, BD, and psychosis had a similar set of abnormalities in the microbiota, particularly lower levels of Faecalibacterium and Coprococcus – two types of bacteria that have an anti-inflammatory effect in gut – and higher levels of Eggerthella, a bacterium with proinflammatory effects.
“The wealth of evidence we have summarized clearly demonstrates that the gut microbiota is vitally important to the wider mental health of individuals,” lead author Viktoriya Nikolova, MRes, Centre for Affective Disorders, King’s College London, said in an interview.
“While it is still too early to recommend specific interventions, it’s clear that clinicians need to place a greater awareness of gut health when considering the treatment of certain psychiatric disorders,” she said.
The study was published online Sept. 15, 2021, in JAMA Psychiatry.
Reliable biomarkers
“Evidence of gut microbiota perturbations has accumulated for multiple psychiatric disorders, with microbiota signatures proposed as potential biomarkers,” the authors wrote.
However, “while there is a wealth of evidence to suggest that abnormalities within the composition of the gut microbiota are connected to a number of psychiatric disorders, there haven’t been any attempts to evaluate the specificity of this evidence – that is, if these changes are unique to specific disorders or shared across many,” Ms. Nikolova said.
Previous research in individual disorders has identified “patterns that may be promising biomarker targets,” with the potential to “improve diagnostic accuracy, guide treatment, and assist the monitoring of treatment response,” the authors noted.
“We wanted to see if we could reliably establish biomarkers for individual conditions in an effort to further our understanding of the relationship between mental illness and gut microbiota,” said Ms. Nikolova.
The researchers wanted to “evaluate the specificity and reproducibility of gut microbiota alterations and delineate those with potential to become biomarkers.”
They identified 59 studies (64 case-control comparisons; n = 2,643 patients, 2,336 controls). Most (54.2%) were conducted in East Asia, followed by Westernized populations (40.7%) and Africa (1.7%).
These studies evaluated diversity or abundance of gut microbes in adult populations encompassing an array of psychiatric disorders: major depressive disorder (MDD), BD, psychosis and schizophrenia, eating disorders (anorexia nervosa and bulimia nervosa), anxiety, obsessive-compulsive disorder (OCD), PTSD, and ADHD.
Although studies were similar in exclusion criteria, few attempted to minimize dietary changes or control dietary intake. In addition, use of psychiatric medication also “varied substantially.”
The researchers conducted several analyses, with primary outcomes consisting of “community-level measures of gut microbiota composition (alpha and beta diversity) as well as taxonomic findings at the phylum, family, and genus levels (relative abundance).”
Alpha diversity provides a “summary of the microbial community in individual samples,” which “can be compared across groups to evaluate the role of a particular factor (in this case psychiatric diagnosis) on the richness (number of species) and evenness (how well each species is represented) in the sample.”
Beta diversity, on the other hand, “measures interindividual (between samples) diversity that assesses similarity of communities, compared with the other samples analyzed.”
Control samples consisted of participants without the relevant condition.
Biological overlap?
The alpha-diversity meta-analysis encompassed 34 studies (n = 1,519 patients, 1,429 controls). The researchers found significant decreases in microbial richness in patients, compared with controls (observed species standardized mean difference, −0.26; 95% CI, −0.47 to −0.06; Chao1 SMD, −0.5; 95% CI, −0.79 to −0.21). On the other hand, when they examined each diagnosis separately, they found consistent decreases only in bipolar disorder. There was a small, nonsignificant decrease in phylogenetic diversity between groups.
MDD, psychosis, and schizophrenia were the only conditions in which differences in beta diversity were consistently observed.
“These findings suggest there is reliable evidence for differences in the shared phylogenetic structure in MDD and psychosis and schizophrenia compared with controls,” the authors write.
However, “method of measurement and method of patient classification (symptom vs. diagnosis based) may affect findings,” they added.
When they focused on relative abundance, they found “little evidence” of disorder specificity, but rather a “transdiagnostic pattern of microbiota signatures.”
In particular, depleted levels of Faecalibacterium and Coprococcus and enriched levels of Eggerthella were “consistently shared” between MDD, BD, psychosis and schizophrenia, and anxiety, “suggesting these disorders are characterized by a reduction of anti-inflammatory butyrate-producing bacteria, while proinflammatory genera are enriched.”
“The finding that these perturbations do not appear to be disorder-specific suggests that the microbiota is affected in a similar manner by conditions such as depression, anxiety, bipolar disorder, and psychosis,” said Ms. Nikolova.
“We have seen similar findings from previous meta-analyses of inflammatory marker studies and genetic studies, for example, suggesting that there is a biological overlap between these conditions, which we have now also seen in the microbiota.”
The authors highlighted potential confounders, including study region and medication use.
Conditions such as MDD, psychosis, and schizophrenia were “largely investigated in the East,” while anorexia nervosa and OCD were primarily investigated in the West.
Moreover, comparing results from medication-free studies with those in which 80% or more of patients were taking psychiatric medication showed increases in bacterial families Lactobacillaceae, Klebsiella, Streptococcus, and Megasphaera only in medicated groups, and decreases in Dialister.
In light of these confounders, the findings should be considered “preliminary,” the investigators noted.
Greater standardization needed
Commenting on the study, Emeran Mayer, MD, director of the Oppenheimer Center for Neurobiology of Stress and Resilience at the University of California, Los Angeles, said it is “intriguing to speculate that low-grade immune activation due to reduced production of butyrate may be such a generalized factor affecting microbial composition shared similarly in several brain disorders. However, such a mechanism has not been confirmed in mechanistic studies to date.”
In addition, the study “lumps together a large number of studies and heterogeneous patient populations, with and without centrally acting medication, without adequate dietary history, studied in different ethnic populations, studied with highly variable collection and analysis methods, including highly variable sample and study sizes for different diseases, and using only measures of microbial composition but not function,” cautioned Dr. Mayer, who was not involved in the research.
Future studies “with much greater standardization of subject populations and clinical and biological analyses techniques should be performed to reevaluate the results of the current study and confirm or reject the main hypotheses,” asserted Dr. Mayer, who is also the founding director of the UCLA Brain Gut Microbiome Center.
Ms. Nikolova is funded by a Medical Research Council PhD Studentship. Other sources of funding include the National Institute for Health Research Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. Ms. Nikolova has disclosed no relevant financial relationships. Dr. Mayer is a scientific advisory board member of Danone, Axial Therapeutics, Viome, Amare, Mahana Therapeutics, Pendulum, Bloom Biosciences, and APC Microbiome Ireland.
A version of this article first appeared on Medscape.com .
Disturbances in gut microbiota are associated with depletion of anti-inflammatory bacteria and proliferation of proinflammatory bacteria, a pattern tied to several major psychiatric disorders including depression, bipolar disorder (BD), schizophrenia, and anxiety, new research shows.
A meta-analysis of 59 studies, encompassing roughly 2,600 patients with psychiatric conditions, showed a decrease in microbial richness in patients with psychiatric conditions versus controls.
In addition, those with depression, anxiety, BD, and psychosis had a similar set of abnormalities in the microbiota, particularly lower levels of Faecalibacterium and Coprococcus – two types of bacteria that have an anti-inflammatory effect in gut – and higher levels of Eggerthella, a bacterium with proinflammatory effects.
“The wealth of evidence we have summarized clearly demonstrates that the gut microbiota is vitally important to the wider mental health of individuals,” lead author Viktoriya Nikolova, MRes, Centre for Affective Disorders, King’s College London, said in an interview.
“While it is still too early to recommend specific interventions, it’s clear that clinicians need to place a greater awareness of gut health when considering the treatment of certain psychiatric disorders,” she said.
The study was published online Sept. 15, 2021, in JAMA Psychiatry.
Reliable biomarkers
“Evidence of gut microbiota perturbations has accumulated for multiple psychiatric disorders, with microbiota signatures proposed as potential biomarkers,” the authors wrote.
However, “while there is a wealth of evidence to suggest that abnormalities within the composition of the gut microbiota are connected to a number of psychiatric disorders, there haven’t been any attempts to evaluate the specificity of this evidence – that is, if these changes are unique to specific disorders or shared across many,” Ms. Nikolova said.
Previous research in individual disorders has identified “patterns that may be promising biomarker targets,” with the potential to “improve diagnostic accuracy, guide treatment, and assist the monitoring of treatment response,” the authors noted.
“We wanted to see if we could reliably establish biomarkers for individual conditions in an effort to further our understanding of the relationship between mental illness and gut microbiota,” said Ms. Nikolova.
The researchers wanted to “evaluate the specificity and reproducibility of gut microbiota alterations and delineate those with potential to become biomarkers.”
They identified 59 studies (64 case-control comparisons; n = 2,643 patients, 2,336 controls). Most (54.2%) were conducted in East Asia, followed by Westernized populations (40.7%) and Africa (1.7%).
These studies evaluated diversity or abundance of gut microbes in adult populations encompassing an array of psychiatric disorders: major depressive disorder (MDD), BD, psychosis and schizophrenia, eating disorders (anorexia nervosa and bulimia nervosa), anxiety, obsessive-compulsive disorder (OCD), PTSD, and ADHD.
Although studies were similar in exclusion criteria, few attempted to minimize dietary changes or control dietary intake. In addition, use of psychiatric medication also “varied substantially.”
The researchers conducted several analyses, with primary outcomes consisting of “community-level measures of gut microbiota composition (alpha and beta diversity) as well as taxonomic findings at the phylum, family, and genus levels (relative abundance).”
Alpha diversity provides a “summary of the microbial community in individual samples,” which “can be compared across groups to evaluate the role of a particular factor (in this case psychiatric diagnosis) on the richness (number of species) and evenness (how well each species is represented) in the sample.”
Beta diversity, on the other hand, “measures interindividual (between samples) diversity that assesses similarity of communities, compared with the other samples analyzed.”
Control samples consisted of participants without the relevant condition.
Biological overlap?
The alpha-diversity meta-analysis encompassed 34 studies (n = 1,519 patients, 1,429 controls). The researchers found significant decreases in microbial richness in patients, compared with controls (observed species standardized mean difference, −0.26; 95% CI, −0.47 to −0.06; Chao1 SMD, −0.5; 95% CI, −0.79 to −0.21). On the other hand, when they examined each diagnosis separately, they found consistent decreases only in bipolar disorder. There was a small, nonsignificant decrease in phylogenetic diversity between groups.
MDD, psychosis, and schizophrenia were the only conditions in which differences in beta diversity were consistently observed.
“These findings suggest there is reliable evidence for differences in the shared phylogenetic structure in MDD and psychosis and schizophrenia compared with controls,” the authors write.
However, “method of measurement and method of patient classification (symptom vs. diagnosis based) may affect findings,” they added.
When they focused on relative abundance, they found “little evidence” of disorder specificity, but rather a “transdiagnostic pattern of microbiota signatures.”
In particular, depleted levels of Faecalibacterium and Coprococcus and enriched levels of Eggerthella were “consistently shared” between MDD, BD, psychosis and schizophrenia, and anxiety, “suggesting these disorders are characterized by a reduction of anti-inflammatory butyrate-producing bacteria, while proinflammatory genera are enriched.”
“The finding that these perturbations do not appear to be disorder-specific suggests that the microbiota is affected in a similar manner by conditions such as depression, anxiety, bipolar disorder, and psychosis,” said Ms. Nikolova.
“We have seen similar findings from previous meta-analyses of inflammatory marker studies and genetic studies, for example, suggesting that there is a biological overlap between these conditions, which we have now also seen in the microbiota.”
The authors highlighted potential confounders, including study region and medication use.
Conditions such as MDD, psychosis, and schizophrenia were “largely investigated in the East,” while anorexia nervosa and OCD were primarily investigated in the West.
Moreover, comparing results from medication-free studies with those in which 80% or more of patients were taking psychiatric medication showed increases in bacterial families Lactobacillaceae, Klebsiella, Streptococcus, and Megasphaera only in medicated groups, and decreases in Dialister.
In light of these confounders, the findings should be considered “preliminary,” the investigators noted.
Greater standardization needed
Commenting on the study, Emeran Mayer, MD, director of the Oppenheimer Center for Neurobiology of Stress and Resilience at the University of California, Los Angeles, said it is “intriguing to speculate that low-grade immune activation due to reduced production of butyrate may be such a generalized factor affecting microbial composition shared similarly in several brain disorders. However, such a mechanism has not been confirmed in mechanistic studies to date.”
In addition, the study “lumps together a large number of studies and heterogeneous patient populations, with and without centrally acting medication, without adequate dietary history, studied in different ethnic populations, studied with highly variable collection and analysis methods, including highly variable sample and study sizes for different diseases, and using only measures of microbial composition but not function,” cautioned Dr. Mayer, who was not involved in the research.
Future studies “with much greater standardization of subject populations and clinical and biological analyses techniques should be performed to reevaluate the results of the current study and confirm or reject the main hypotheses,” asserted Dr. Mayer, who is also the founding director of the UCLA Brain Gut Microbiome Center.
Ms. Nikolova is funded by a Medical Research Council PhD Studentship. Other sources of funding include the National Institute for Health Research Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. Ms. Nikolova has disclosed no relevant financial relationships. Dr. Mayer is a scientific advisory board member of Danone, Axial Therapeutics, Viome, Amare, Mahana Therapeutics, Pendulum, Bloom Biosciences, and APC Microbiome Ireland.
A version of this article first appeared on Medscape.com .
Disturbances in gut microbiota are associated with depletion of anti-inflammatory bacteria and proliferation of proinflammatory bacteria, a pattern tied to several major psychiatric disorders including depression, bipolar disorder (BD), schizophrenia, and anxiety, new research shows.
A meta-analysis of 59 studies, encompassing roughly 2,600 patients with psychiatric conditions, showed a decrease in microbial richness in patients with psychiatric conditions versus controls.
In addition, those with depression, anxiety, BD, and psychosis had a similar set of abnormalities in the microbiota, particularly lower levels of Faecalibacterium and Coprococcus – two types of bacteria that have an anti-inflammatory effect in gut – and higher levels of Eggerthella, a bacterium with proinflammatory effects.
“The wealth of evidence we have summarized clearly demonstrates that the gut microbiota is vitally important to the wider mental health of individuals,” lead author Viktoriya Nikolova, MRes, Centre for Affective Disorders, King’s College London, said in an interview.
“While it is still too early to recommend specific interventions, it’s clear that clinicians need to place a greater awareness of gut health when considering the treatment of certain psychiatric disorders,” she said.
The study was published online Sept. 15, 2021, in JAMA Psychiatry.
Reliable biomarkers
“Evidence of gut microbiota perturbations has accumulated for multiple psychiatric disorders, with microbiota signatures proposed as potential biomarkers,” the authors wrote.
However, “while there is a wealth of evidence to suggest that abnormalities within the composition of the gut microbiota are connected to a number of psychiatric disorders, there haven’t been any attempts to evaluate the specificity of this evidence – that is, if these changes are unique to specific disorders or shared across many,” Ms. Nikolova said.
Previous research in individual disorders has identified “patterns that may be promising biomarker targets,” with the potential to “improve diagnostic accuracy, guide treatment, and assist the monitoring of treatment response,” the authors noted.
“We wanted to see if we could reliably establish biomarkers for individual conditions in an effort to further our understanding of the relationship between mental illness and gut microbiota,” said Ms. Nikolova.
The researchers wanted to “evaluate the specificity and reproducibility of gut microbiota alterations and delineate those with potential to become biomarkers.”
They identified 59 studies (64 case-control comparisons; n = 2,643 patients, 2,336 controls). Most (54.2%) were conducted in East Asia, followed by Westernized populations (40.7%) and Africa (1.7%).
These studies evaluated diversity or abundance of gut microbes in adult populations encompassing an array of psychiatric disorders: major depressive disorder (MDD), BD, psychosis and schizophrenia, eating disorders (anorexia nervosa and bulimia nervosa), anxiety, obsessive-compulsive disorder (OCD), PTSD, and ADHD.
Although studies were similar in exclusion criteria, few attempted to minimize dietary changes or control dietary intake. In addition, use of psychiatric medication also “varied substantially.”
The researchers conducted several analyses, with primary outcomes consisting of “community-level measures of gut microbiota composition (alpha and beta diversity) as well as taxonomic findings at the phylum, family, and genus levels (relative abundance).”
Alpha diversity provides a “summary of the microbial community in individual samples,” which “can be compared across groups to evaluate the role of a particular factor (in this case psychiatric diagnosis) on the richness (number of species) and evenness (how well each species is represented) in the sample.”
Beta diversity, on the other hand, “measures interindividual (between samples) diversity that assesses similarity of communities, compared with the other samples analyzed.”
Control samples consisted of participants without the relevant condition.
Biological overlap?
The alpha-diversity meta-analysis encompassed 34 studies (n = 1,519 patients, 1,429 controls). The researchers found significant decreases in microbial richness in patients, compared with controls (observed species standardized mean difference, −0.26; 95% CI, −0.47 to −0.06; Chao1 SMD, −0.5; 95% CI, −0.79 to −0.21). On the other hand, when they examined each diagnosis separately, they found consistent decreases only in bipolar disorder. There was a small, nonsignificant decrease in phylogenetic diversity between groups.
MDD, psychosis, and schizophrenia were the only conditions in which differences in beta diversity were consistently observed.
“These findings suggest there is reliable evidence for differences in the shared phylogenetic structure in MDD and psychosis and schizophrenia compared with controls,” the authors write.
However, “method of measurement and method of patient classification (symptom vs. diagnosis based) may affect findings,” they added.
When they focused on relative abundance, they found “little evidence” of disorder specificity, but rather a “transdiagnostic pattern of microbiota signatures.”
In particular, depleted levels of Faecalibacterium and Coprococcus and enriched levels of Eggerthella were “consistently shared” between MDD, BD, psychosis and schizophrenia, and anxiety, “suggesting these disorders are characterized by a reduction of anti-inflammatory butyrate-producing bacteria, while proinflammatory genera are enriched.”
“The finding that these perturbations do not appear to be disorder-specific suggests that the microbiota is affected in a similar manner by conditions such as depression, anxiety, bipolar disorder, and psychosis,” said Ms. Nikolova.
“We have seen similar findings from previous meta-analyses of inflammatory marker studies and genetic studies, for example, suggesting that there is a biological overlap between these conditions, which we have now also seen in the microbiota.”
The authors highlighted potential confounders, including study region and medication use.
Conditions such as MDD, psychosis, and schizophrenia were “largely investigated in the East,” while anorexia nervosa and OCD were primarily investigated in the West.
Moreover, comparing results from medication-free studies with those in which 80% or more of patients were taking psychiatric medication showed increases in bacterial families Lactobacillaceae, Klebsiella, Streptococcus, and Megasphaera only in medicated groups, and decreases in Dialister.
In light of these confounders, the findings should be considered “preliminary,” the investigators noted.
Greater standardization needed
Commenting on the study, Emeran Mayer, MD, director of the Oppenheimer Center for Neurobiology of Stress and Resilience at the University of California, Los Angeles, said it is “intriguing to speculate that low-grade immune activation due to reduced production of butyrate may be such a generalized factor affecting microbial composition shared similarly in several brain disorders. However, such a mechanism has not been confirmed in mechanistic studies to date.”
In addition, the study “lumps together a large number of studies and heterogeneous patient populations, with and without centrally acting medication, without adequate dietary history, studied in different ethnic populations, studied with highly variable collection and analysis methods, including highly variable sample and study sizes for different diseases, and using only measures of microbial composition but not function,” cautioned Dr. Mayer, who was not involved in the research.
Future studies “with much greater standardization of subject populations and clinical and biological analyses techniques should be performed to reevaluate the results of the current study and confirm or reject the main hypotheses,” asserted Dr. Mayer, who is also the founding director of the UCLA Brain Gut Microbiome Center.
Ms. Nikolova is funded by a Medical Research Council PhD Studentship. Other sources of funding include the National Institute for Health Research Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. Ms. Nikolova has disclosed no relevant financial relationships. Dr. Mayer is a scientific advisory board member of Danone, Axial Therapeutics, Viome, Amare, Mahana Therapeutics, Pendulum, Bloom Biosciences, and APC Microbiome Ireland.
A version of this article first appeared on Medscape.com .