User login
Are aging physicians a burden?
The evaluation of physicians with alleged cognitive decline
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
The evaluation of physicians with alleged cognitive decline
The evaluation of physicians with alleged cognitive decline
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
CDC data confirm mental health is suffering during COVID-19
The ongoing COVID-19 pandemic continues to exact a huge toll on mental health in the United States, according to results of a survey released Aug. 13 by the Centers for Disease Control and Prevention.
During late June, about two in five U.S. adults surveyed said they were struggling with mental health or substance use. Younger adults, racial/ethnic minorities, essential workers, and those with preexisting psychiatric conditions were suffering the most.
“Addressing mental health disparities and preparing support systems to mitigate mental health consequences as the pandemic evolves will continue to be needed urgently,” write Rashon Lane, with the CDC COVID-19 Response Team, and colleagues in an article published online in the CDC’s Morbidity and Mortality Weekly Report.
During the period of June 24-30, 2020, 5,412 U.S. adults aged 18 and older completed online surveys that gauged mental health, substance use, and suicidal ideation.
Overall, 40.9% of respondents reported having at least one adverse mental or behavioral health condition; 31% reported symptoms of anxiety or depressive disorder; and 26% reported symptoms of a trauma- and stressor-related disorder related to the pandemic.
The prevalence of symptoms of anxiety disorder alone was roughly three times that reported in the second quarter of 2019, the authors noted.
In addition, , and nearly 11% reported having seriously considered suicide in the preceding 30 days.
Approximately twice as many respondents reported seriously considering suicide in the prior month compared with adults in the United States in 2018 (referring to the previous 12 months), the authors noted.
Suicidal ideation was significantly higher among younger respondents (aged 18-24 years, 26%), Hispanic persons (19%), non-Hispanic Black persons (15%), unpaid caregivers for adults (31%), and essential workers (22%).
The survey results are in line with recent data from Mental Health America, which indicate dramatic increases in depression, anxiety, and suicidality since the start of the COVID-19 pandemic.
The “markedly elevated” prevalence of adverse mental and behavioral health conditions associated with the COVID-19 pandemic highlights the “broad impact of the pandemic and the need to prevent and treat these conditions,” the researchers wrote.
The survey also highlights populations at increased risk for psychological distress and unhealthy coping.
“Future studies should identify drivers of adverse mental and behavioral health during the COVID-19 pandemic and whether factors such as social isolation, absence of school structure, unemployment and other financial worries, and various forms of violence (e.g., physical, emotional, mental, or sexual abuse) serve as additional stressors,” they suggested.
A version of this article originally appeared on Medscape.com.
The ongoing COVID-19 pandemic continues to exact a huge toll on mental health in the United States, according to results of a survey released Aug. 13 by the Centers for Disease Control and Prevention.
During late June, about two in five U.S. adults surveyed said they were struggling with mental health or substance use. Younger adults, racial/ethnic minorities, essential workers, and those with preexisting psychiatric conditions were suffering the most.
“Addressing mental health disparities and preparing support systems to mitigate mental health consequences as the pandemic evolves will continue to be needed urgently,” write Rashon Lane, with the CDC COVID-19 Response Team, and colleagues in an article published online in the CDC’s Morbidity and Mortality Weekly Report.
During the period of June 24-30, 2020, 5,412 U.S. adults aged 18 and older completed online surveys that gauged mental health, substance use, and suicidal ideation.
Overall, 40.9% of respondents reported having at least one adverse mental or behavioral health condition; 31% reported symptoms of anxiety or depressive disorder; and 26% reported symptoms of a trauma- and stressor-related disorder related to the pandemic.
The prevalence of symptoms of anxiety disorder alone was roughly three times that reported in the second quarter of 2019, the authors noted.
In addition, , and nearly 11% reported having seriously considered suicide in the preceding 30 days.
Approximately twice as many respondents reported seriously considering suicide in the prior month compared with adults in the United States in 2018 (referring to the previous 12 months), the authors noted.
Suicidal ideation was significantly higher among younger respondents (aged 18-24 years, 26%), Hispanic persons (19%), non-Hispanic Black persons (15%), unpaid caregivers for adults (31%), and essential workers (22%).
The survey results are in line with recent data from Mental Health America, which indicate dramatic increases in depression, anxiety, and suicidality since the start of the COVID-19 pandemic.
The “markedly elevated” prevalence of adverse mental and behavioral health conditions associated with the COVID-19 pandemic highlights the “broad impact of the pandemic and the need to prevent and treat these conditions,” the researchers wrote.
The survey also highlights populations at increased risk for psychological distress and unhealthy coping.
“Future studies should identify drivers of adverse mental and behavioral health during the COVID-19 pandemic and whether factors such as social isolation, absence of school structure, unemployment and other financial worries, and various forms of violence (e.g., physical, emotional, mental, or sexual abuse) serve as additional stressors,” they suggested.
A version of this article originally appeared on Medscape.com.
The ongoing COVID-19 pandemic continues to exact a huge toll on mental health in the United States, according to results of a survey released Aug. 13 by the Centers for Disease Control and Prevention.
During late June, about two in five U.S. adults surveyed said they were struggling with mental health or substance use. Younger adults, racial/ethnic minorities, essential workers, and those with preexisting psychiatric conditions were suffering the most.
“Addressing mental health disparities and preparing support systems to mitigate mental health consequences as the pandemic evolves will continue to be needed urgently,” write Rashon Lane, with the CDC COVID-19 Response Team, and colleagues in an article published online in the CDC’s Morbidity and Mortality Weekly Report.
During the period of June 24-30, 2020, 5,412 U.S. adults aged 18 and older completed online surveys that gauged mental health, substance use, and suicidal ideation.
Overall, 40.9% of respondents reported having at least one adverse mental or behavioral health condition; 31% reported symptoms of anxiety or depressive disorder; and 26% reported symptoms of a trauma- and stressor-related disorder related to the pandemic.
The prevalence of symptoms of anxiety disorder alone was roughly three times that reported in the second quarter of 2019, the authors noted.
In addition, , and nearly 11% reported having seriously considered suicide in the preceding 30 days.
Approximately twice as many respondents reported seriously considering suicide in the prior month compared with adults in the United States in 2018 (referring to the previous 12 months), the authors noted.
Suicidal ideation was significantly higher among younger respondents (aged 18-24 years, 26%), Hispanic persons (19%), non-Hispanic Black persons (15%), unpaid caregivers for adults (31%), and essential workers (22%).
The survey results are in line with recent data from Mental Health America, which indicate dramatic increases in depression, anxiety, and suicidality since the start of the COVID-19 pandemic.
The “markedly elevated” prevalence of adverse mental and behavioral health conditions associated with the COVID-19 pandemic highlights the “broad impact of the pandemic and the need to prevent and treat these conditions,” the researchers wrote.
The survey also highlights populations at increased risk for psychological distress and unhealthy coping.
“Future studies should identify drivers of adverse mental and behavioral health during the COVID-19 pandemic and whether factors such as social isolation, absence of school structure, unemployment and other financial worries, and various forms of violence (e.g., physical, emotional, mental, or sexual abuse) serve as additional stressors,” they suggested.
A version of this article originally appeared on Medscape.com.
Chloroquine linked to serious psychiatric side effects
Chloroquine may be associated with serious psychiatric side effects, even in patients with no family or personal history of psychiatric disorders, a new review suggests.
In a letter to the editor published online July 28 in The Journal of Clinical Psychiatry, the authors summarize data from several studies published as far back as 1993 and as recently as May 2020.
“In addition to previously reported side effects, chloroquine could also induce psychiatric side effects which are polymorphic and can persist even after stopping the drug,” lead author Florence Gressier, MD, PhD, CESP, Inserm, department of psychiatry, Le Kremlin Bicêtre, France, said in an interview.
“In COVID-19 patients who may still be [undergoing treatment] with chloroquine, close psychiatric assessment and monitoring should be performed,” she said.
Heated controversy
Following findings of a small French study that suggested efficacy in lowering the viral load in patients with COVID-19, President Donald Trump expressed optimism regarding the role of hydroxychloroquine in treating COVID-19, calling it a “game changer”.
Other studies, however, have called into question both the efficacy and the safety of hydroxychloroquine in treating COVID-19. On June 15, the Food and Drug Administration revoked the emergency use authorization it had given in March to chloroquine and hydroxychloroquine for the treatment of COVID-19.
Nevertheless, hydroxychloroquine continues to be prescribed for COVID-19. For example, an article that appeared in Click2Houston on June 15 quoted the chief medical officer of Houston’s United Memorial Center as saying he plans to continue prescribing hydroxychloroquine for patients with COVID-19 until he finds a better alternative.
As discussed in a Medscape expert commentary, a group of physicians who held a “white coat summit” in front of the U.S. Supreme Court building promoted the use of hydroxychloroquine for the treatment of COVID-19. The video of their summit was retweeted by President Trump and garnered millions of views before it was taken down by Twitter, Facebook, and YouTube.
Sudden onset
For the new review, “we wanted to alert the public and practitioners on the potentially psychiatric risks induced by chloroquine, as it could be taken as self-medication or potentially still prescribed,” Dr. Gressier said.
“We think the format of the letter to the editor allows information to be provided in a concise and clear manner,” she added.
According to the FDA’s Adverse Event Reporting System database, 12% of reported adverse events (520 of 4,336) following the use of chloroquine that occurred between the fourth quarter of 2012 and the fourth quarter of 2019 were neuropsychiatric. These events included amnesia, delirium, hallucinations, depression, and loss of consciousness, the authors write.
The researchers acknowledged that the incidence of psychiatric adverse effects associated with the use of chloroquine is “unclear in the absence of high-quality, randomized placebo-controlled trials of its safety.” Nevertheless, they pointed out that there have been reports of insomnia and depression when the drug was used as prophylaxis against malaria .
Moreover, some case series or case reports describe symptoms such as depression, anxiety, agitation, violent outburst, suicidal ideation, and psychosis in patients who have been treated with chloroquine for malaria, lupus erythematosus, and rheumatoid arthritis .
“In contrast to many other psychoses, chloroquine psychosis may be more affective and include prominent visual hallucinations, symptoms of derealization, and disorders of thought, with preserved insight,” the authors wrote.
They noted that the frequency of symptoms does not appear to be connected to the cumulative dose or the duration of treatment, and the onset of psychosis or other adverse effects is usually “sudden.”
In addition, they warn that the drug’s psychiatric effects may go unnoticed, especially because COVID-19 itself has been associated with neuropsychiatric symptoms, making it hard to distinguish between symptoms caused by the illness and those caused by the drug.
Although the psychiatric symptoms typically occur early after treatment initiation, some “subtle” symptoms might persist after stopping the drug, possibly owing to its “extremely long” half-life, the authors stated.
Dr. Gressier noted that practicing clinicians should look up reports about self-medication with chloroquine “and warn their patients about the risk induced by chloroquine.”
Safe but ‘not benign’
Nilanjana Bose, MD, MBA, a rheumatologist at the Rheumatology Center of Houston, said she uses hydroxychloroquine “all the time” in clinical practice to treat patients with rheumatic conditions.
“I cannot comment on whether it [hydroxychloroquine or chloroquine] is a potential prophylactic or treatment for COVID-19, but I can say that, from a safety point of view, as a rheumatologist who uses hydroxychloroquine at a dose of 400 mg/day, I do not think we need to worry about serious [psychiatric] side effects,” Dr. Bose said in an interview.
Because clinicians are trying all types of possible treatments for COVID-19, “if this medication has possible efficacy, it is a great medicine from a rheumatologic perspective and is safe,” she added.
Nevertheless, the drug is “not benign, and regular side effects will be there, and of course, higher doses will cause more side effects,” said Dr. Bose, who was not involved in authoring the letter.
She counsels patients about potential psychiatric side effects of hydroxychloroquine because some of her patients have complained about irritability, worsening anxiety and depression, and difficulty sleeping.
Be wary
James “Jimmy” Potash, MD, MPH, Henry Phipps Professor of Psychiatry and Behavioral Sciences, Johns Hopkins Medicine, Baltimore, said in an interview that the “take-home message of this letter is that serious psychiatric effects, psychotic illness in particular,” can occur in individuals who take chloroquine and hydroxychloroquine.
In addition, “these are potentially very concerning side effects that psychiatrists should be aware of,” noted Dr. Potash, department director and psychiatrist-in-chief at Johns Hopkins.
He said that one of his patients who had been “completely psychiatrically healthy” took chloroquine prophylactically prior to traveling overseas. After she began taking the drug, she had an episode of mania that resolved once she discontinued the medication and received treatment for the mania.
“If you add potential psychiatric side effects to the other side effects that can result from these medications, that adds up to a pretty important reason to be wary of taking them, particularly for the indication of COVID-19, where the level of evidence that it helps in any way is still quite weak,” Dr. Potash said.
In an interview, Remington Nevin, MD, MPH, DrPH, executive director at the Quinism Foundation, White River Junction, Vt., a nonprofit organization that supports and promotes education and research on disorders caused by poisoning by quinoline drugs; and faculty associate in the department of mental health at Johns Hopkins Bloomberg School of Public Health, said that the authors of the letter “are to be commended for their efforts in raising awareness of the potentially lasting and disabling psychiatric effects of chloroquine and hydroxychloroquine, which, as with similar effects from other synthetic quinoline antimalarials, have occasionally been overlooked or misattributed to other conditions.”
He added: “I have proposed that the chronic neuropsychiatric effects of this class of drug are best considered not as side effects but as signs and symptoms of a disorder known as chronic quinoline encephalopathy caused by poisoning of the central nervous system.”
Dr. Gressier and the other letter authors, Dr. Bose, and Dr. Potash have reported no relevant financial relationships. Dr. Nevin has been retained as a consultant and expert witness in legal cases involving claims of adverse effects from quinoline antimalarial drugs.
A version of this article originally appeared on Medscape.com.
Chloroquine may be associated with serious psychiatric side effects, even in patients with no family or personal history of psychiatric disorders, a new review suggests.
In a letter to the editor published online July 28 in The Journal of Clinical Psychiatry, the authors summarize data from several studies published as far back as 1993 and as recently as May 2020.
“In addition to previously reported side effects, chloroquine could also induce psychiatric side effects which are polymorphic and can persist even after stopping the drug,” lead author Florence Gressier, MD, PhD, CESP, Inserm, department of psychiatry, Le Kremlin Bicêtre, France, said in an interview.
“In COVID-19 patients who may still be [undergoing treatment] with chloroquine, close psychiatric assessment and monitoring should be performed,” she said.
Heated controversy
Following findings of a small French study that suggested efficacy in lowering the viral load in patients with COVID-19, President Donald Trump expressed optimism regarding the role of hydroxychloroquine in treating COVID-19, calling it a “game changer”.
Other studies, however, have called into question both the efficacy and the safety of hydroxychloroquine in treating COVID-19. On June 15, the Food and Drug Administration revoked the emergency use authorization it had given in March to chloroquine and hydroxychloroquine for the treatment of COVID-19.
Nevertheless, hydroxychloroquine continues to be prescribed for COVID-19. For example, an article that appeared in Click2Houston on June 15 quoted the chief medical officer of Houston’s United Memorial Center as saying he plans to continue prescribing hydroxychloroquine for patients with COVID-19 until he finds a better alternative.
As discussed in a Medscape expert commentary, a group of physicians who held a “white coat summit” in front of the U.S. Supreme Court building promoted the use of hydroxychloroquine for the treatment of COVID-19. The video of their summit was retweeted by President Trump and garnered millions of views before it was taken down by Twitter, Facebook, and YouTube.
Sudden onset
For the new review, “we wanted to alert the public and practitioners on the potentially psychiatric risks induced by chloroquine, as it could be taken as self-medication or potentially still prescribed,” Dr. Gressier said.
“We think the format of the letter to the editor allows information to be provided in a concise and clear manner,” she added.
According to the FDA’s Adverse Event Reporting System database, 12% of reported adverse events (520 of 4,336) following the use of chloroquine that occurred between the fourth quarter of 2012 and the fourth quarter of 2019 were neuropsychiatric. These events included amnesia, delirium, hallucinations, depression, and loss of consciousness, the authors write.
The researchers acknowledged that the incidence of psychiatric adverse effects associated with the use of chloroquine is “unclear in the absence of high-quality, randomized placebo-controlled trials of its safety.” Nevertheless, they pointed out that there have been reports of insomnia and depression when the drug was used as prophylaxis against malaria .
Moreover, some case series or case reports describe symptoms such as depression, anxiety, agitation, violent outburst, suicidal ideation, and psychosis in patients who have been treated with chloroquine for malaria, lupus erythematosus, and rheumatoid arthritis .
“In contrast to many other psychoses, chloroquine psychosis may be more affective and include prominent visual hallucinations, symptoms of derealization, and disorders of thought, with preserved insight,” the authors wrote.
They noted that the frequency of symptoms does not appear to be connected to the cumulative dose or the duration of treatment, and the onset of psychosis or other adverse effects is usually “sudden.”
In addition, they warn that the drug’s psychiatric effects may go unnoticed, especially because COVID-19 itself has been associated with neuropsychiatric symptoms, making it hard to distinguish between symptoms caused by the illness and those caused by the drug.
Although the psychiatric symptoms typically occur early after treatment initiation, some “subtle” symptoms might persist after stopping the drug, possibly owing to its “extremely long” half-life, the authors stated.
Dr. Gressier noted that practicing clinicians should look up reports about self-medication with chloroquine “and warn their patients about the risk induced by chloroquine.”
Safe but ‘not benign’
Nilanjana Bose, MD, MBA, a rheumatologist at the Rheumatology Center of Houston, said she uses hydroxychloroquine “all the time” in clinical practice to treat patients with rheumatic conditions.
“I cannot comment on whether it [hydroxychloroquine or chloroquine] is a potential prophylactic or treatment for COVID-19, but I can say that, from a safety point of view, as a rheumatologist who uses hydroxychloroquine at a dose of 400 mg/day, I do not think we need to worry about serious [psychiatric] side effects,” Dr. Bose said in an interview.
Because clinicians are trying all types of possible treatments for COVID-19, “if this medication has possible efficacy, it is a great medicine from a rheumatologic perspective and is safe,” she added.
Nevertheless, the drug is “not benign, and regular side effects will be there, and of course, higher doses will cause more side effects,” said Dr. Bose, who was not involved in authoring the letter.
She counsels patients about potential psychiatric side effects of hydroxychloroquine because some of her patients have complained about irritability, worsening anxiety and depression, and difficulty sleeping.
Be wary
James “Jimmy” Potash, MD, MPH, Henry Phipps Professor of Psychiatry and Behavioral Sciences, Johns Hopkins Medicine, Baltimore, said in an interview that the “take-home message of this letter is that serious psychiatric effects, psychotic illness in particular,” can occur in individuals who take chloroquine and hydroxychloroquine.
In addition, “these are potentially very concerning side effects that psychiatrists should be aware of,” noted Dr. Potash, department director and psychiatrist-in-chief at Johns Hopkins.
He said that one of his patients who had been “completely psychiatrically healthy” took chloroquine prophylactically prior to traveling overseas. After she began taking the drug, she had an episode of mania that resolved once she discontinued the medication and received treatment for the mania.
“If you add potential psychiatric side effects to the other side effects that can result from these medications, that adds up to a pretty important reason to be wary of taking them, particularly for the indication of COVID-19, where the level of evidence that it helps in any way is still quite weak,” Dr. Potash said.
In an interview, Remington Nevin, MD, MPH, DrPH, executive director at the Quinism Foundation, White River Junction, Vt., a nonprofit organization that supports and promotes education and research on disorders caused by poisoning by quinoline drugs; and faculty associate in the department of mental health at Johns Hopkins Bloomberg School of Public Health, said that the authors of the letter “are to be commended for their efforts in raising awareness of the potentially lasting and disabling psychiatric effects of chloroquine and hydroxychloroquine, which, as with similar effects from other synthetic quinoline antimalarials, have occasionally been overlooked or misattributed to other conditions.”
He added: “I have proposed that the chronic neuropsychiatric effects of this class of drug are best considered not as side effects but as signs and symptoms of a disorder known as chronic quinoline encephalopathy caused by poisoning of the central nervous system.”
Dr. Gressier and the other letter authors, Dr. Bose, and Dr. Potash have reported no relevant financial relationships. Dr. Nevin has been retained as a consultant and expert witness in legal cases involving claims of adverse effects from quinoline antimalarial drugs.
A version of this article originally appeared on Medscape.com.
Chloroquine may be associated with serious psychiatric side effects, even in patients with no family or personal history of psychiatric disorders, a new review suggests.
In a letter to the editor published online July 28 in The Journal of Clinical Psychiatry, the authors summarize data from several studies published as far back as 1993 and as recently as May 2020.
“In addition to previously reported side effects, chloroquine could also induce psychiatric side effects which are polymorphic and can persist even after stopping the drug,” lead author Florence Gressier, MD, PhD, CESP, Inserm, department of psychiatry, Le Kremlin Bicêtre, France, said in an interview.
“In COVID-19 patients who may still be [undergoing treatment] with chloroquine, close psychiatric assessment and monitoring should be performed,” she said.
Heated controversy
Following findings of a small French study that suggested efficacy in lowering the viral load in patients with COVID-19, President Donald Trump expressed optimism regarding the role of hydroxychloroquine in treating COVID-19, calling it a “game changer”.
Other studies, however, have called into question both the efficacy and the safety of hydroxychloroquine in treating COVID-19. On June 15, the Food and Drug Administration revoked the emergency use authorization it had given in March to chloroquine and hydroxychloroquine for the treatment of COVID-19.
Nevertheless, hydroxychloroquine continues to be prescribed for COVID-19. For example, an article that appeared in Click2Houston on June 15 quoted the chief medical officer of Houston’s United Memorial Center as saying he plans to continue prescribing hydroxychloroquine for patients with COVID-19 until he finds a better alternative.
As discussed in a Medscape expert commentary, a group of physicians who held a “white coat summit” in front of the U.S. Supreme Court building promoted the use of hydroxychloroquine for the treatment of COVID-19. The video of their summit was retweeted by President Trump and garnered millions of views before it was taken down by Twitter, Facebook, and YouTube.
Sudden onset
For the new review, “we wanted to alert the public and practitioners on the potentially psychiatric risks induced by chloroquine, as it could be taken as self-medication or potentially still prescribed,” Dr. Gressier said.
“We think the format of the letter to the editor allows information to be provided in a concise and clear manner,” she added.
According to the FDA’s Adverse Event Reporting System database, 12% of reported adverse events (520 of 4,336) following the use of chloroquine that occurred between the fourth quarter of 2012 and the fourth quarter of 2019 were neuropsychiatric. These events included amnesia, delirium, hallucinations, depression, and loss of consciousness, the authors write.
The researchers acknowledged that the incidence of psychiatric adverse effects associated with the use of chloroquine is “unclear in the absence of high-quality, randomized placebo-controlled trials of its safety.” Nevertheless, they pointed out that there have been reports of insomnia and depression when the drug was used as prophylaxis against malaria .
Moreover, some case series or case reports describe symptoms such as depression, anxiety, agitation, violent outburst, suicidal ideation, and psychosis in patients who have been treated with chloroquine for malaria, lupus erythematosus, and rheumatoid arthritis .
“In contrast to many other psychoses, chloroquine psychosis may be more affective and include prominent visual hallucinations, symptoms of derealization, and disorders of thought, with preserved insight,” the authors wrote.
They noted that the frequency of symptoms does not appear to be connected to the cumulative dose or the duration of treatment, and the onset of psychosis or other adverse effects is usually “sudden.”
In addition, they warn that the drug’s psychiatric effects may go unnoticed, especially because COVID-19 itself has been associated with neuropsychiatric symptoms, making it hard to distinguish between symptoms caused by the illness and those caused by the drug.
Although the psychiatric symptoms typically occur early after treatment initiation, some “subtle” symptoms might persist after stopping the drug, possibly owing to its “extremely long” half-life, the authors stated.
Dr. Gressier noted that practicing clinicians should look up reports about self-medication with chloroquine “and warn their patients about the risk induced by chloroquine.”
Safe but ‘not benign’
Nilanjana Bose, MD, MBA, a rheumatologist at the Rheumatology Center of Houston, said she uses hydroxychloroquine “all the time” in clinical practice to treat patients with rheumatic conditions.
“I cannot comment on whether it [hydroxychloroquine or chloroquine] is a potential prophylactic or treatment for COVID-19, but I can say that, from a safety point of view, as a rheumatologist who uses hydroxychloroquine at a dose of 400 mg/day, I do not think we need to worry about serious [psychiatric] side effects,” Dr. Bose said in an interview.
Because clinicians are trying all types of possible treatments for COVID-19, “if this medication has possible efficacy, it is a great medicine from a rheumatologic perspective and is safe,” she added.
Nevertheless, the drug is “not benign, and regular side effects will be there, and of course, higher doses will cause more side effects,” said Dr. Bose, who was not involved in authoring the letter.
She counsels patients about potential psychiatric side effects of hydroxychloroquine because some of her patients have complained about irritability, worsening anxiety and depression, and difficulty sleeping.
Be wary
James “Jimmy” Potash, MD, MPH, Henry Phipps Professor of Psychiatry and Behavioral Sciences, Johns Hopkins Medicine, Baltimore, said in an interview that the “take-home message of this letter is that serious psychiatric effects, psychotic illness in particular,” can occur in individuals who take chloroquine and hydroxychloroquine.
In addition, “these are potentially very concerning side effects that psychiatrists should be aware of,” noted Dr. Potash, department director and psychiatrist-in-chief at Johns Hopkins.
He said that one of his patients who had been “completely psychiatrically healthy” took chloroquine prophylactically prior to traveling overseas. After she began taking the drug, she had an episode of mania that resolved once she discontinued the medication and received treatment for the mania.
“If you add potential psychiatric side effects to the other side effects that can result from these medications, that adds up to a pretty important reason to be wary of taking them, particularly for the indication of COVID-19, where the level of evidence that it helps in any way is still quite weak,” Dr. Potash said.
In an interview, Remington Nevin, MD, MPH, DrPH, executive director at the Quinism Foundation, White River Junction, Vt., a nonprofit organization that supports and promotes education and research on disorders caused by poisoning by quinoline drugs; and faculty associate in the department of mental health at Johns Hopkins Bloomberg School of Public Health, said that the authors of the letter “are to be commended for their efforts in raising awareness of the potentially lasting and disabling psychiatric effects of chloroquine and hydroxychloroquine, which, as with similar effects from other synthetic quinoline antimalarials, have occasionally been overlooked or misattributed to other conditions.”
He added: “I have proposed that the chronic neuropsychiatric effects of this class of drug are best considered not as side effects but as signs and symptoms of a disorder known as chronic quinoline encephalopathy caused by poisoning of the central nervous system.”
Dr. Gressier and the other letter authors, Dr. Bose, and Dr. Potash have reported no relevant financial relationships. Dr. Nevin has been retained as a consultant and expert witness in legal cases involving claims of adverse effects from quinoline antimalarial drugs.
A version of this article originally appeared on Medscape.com.
Exploring cannabis use by older adults
Older Americans – people aged 65 or older – make up 15% of the U.S. population, according to the Census Bureau. By the end of this decade, or the year 2030, this proportion will increase to 21% – and all “baby boomers,” those born between 1946 and 1964, will be older than 65.1 Those demographic developments are occurring alongside a change in societal, legal, and public attitudes on cannabis.
Liberalization of cannabis laws across the United States allows for ever easier access to medicinal and recreational cannabis. Traditionally, cannabis use, its effects, and related considerations in the adolescent and young adult populations have commanded significant research attention. Cannabis use in older adults, however, is not as well studied.2 An exploration of trends in cannabis use by older adults and potential impact in terms of health is timely and important.
According to data from the National Survey on Drug Use and Health, cannabis use in adults aged 65 years and older appears to have been increasing steadily over the past 2 decades. Use among this group rose from 0.4% in 2006 and 2007, to 2.9% in 2015 and 2016.2 And, most recently, use climbed from 3.7% in 2017 to 4.2% in 2018.2
Cannabis use also has risen among other adults. For those aged 50-64, cannabis use increased from 2.8% in 2006-2007 to 4.8% in 2012-2013.2,3 Meanwhile, from 2015 to 2016, that number increased to 9.0%.3,4
Past-year cannabis use in the groups of those aged 50-64 and those aged 65 and older appears to be higher in individuals with mental health problems, alcohol use disorder, and nicotine dependence.5,6 Being male and being unmarried appear to be correlated with past-year cannabis use. Multimorbidity does not appear to be associated with past-year cannabis use. Those using cannabis tend to be long-term users and have first use at a much younger age, typically before age 21.
Older adults use cannabis for both recreational and perceived medical benefits. Arthritis, chronic back pain, anxiety, depression, relaxation, stress reduction, and enhancement in terms of creativity are all purported reasons for use. However, there is limited to no evidence for the efficacy of cannabis in helping with those conditions and purposes. Clinical trials have shown that cannabis can be beneficial in managing pain and nausea, but those trials have not been conducted in older adults.7,8
There is a real risk of cannabis use having a negative impact on the health of older adults. To begin with, the cannabis consumed today is significantly higher in potency than the cannabis that baby boomers were introduced to in their youth. The higher potency, combined with an age-related decline in function experienced by some older adults, makes them vulnerable to its known side effects, such as anxiety, dry mouth, tachycardia, high blood pressure, palpitations, wheezing, confusion, and dizziness.
Cannabis use is reported to bring a fourfold increase in cardiac events within the first hour of ingestion.9 Cognitive decline and memory impairment are well known adverse effects of cannabis use. Research has shown significant self-reported cognitive decline in older adults in relation to cannabis use.Cannabis metabolites are known to have an effect on cytochrome P450 enzymes, affecting the metabolism of medication, and increasing the susceptibility of older adults who use cannabis to adverse effects of polypharmacy. Finally, as research on emergency department visits by older adults shows, cannabis use can increase the risk of injury among this cohort.
As in the United States, cannabis use among older adults in Canada has increased significantly. The percentage of older adults who use cannabis in the Canadian province of Ontario, for example, reportedly doubled from 2005 to 2015. In response to this increase, and in anticipation of a rise in problematic use of cannabis and cannabis use disorder in older adults, the Canadian Coalition for Seniors’ Mental Health (through financial support from Substance Use and Addictions Program of Health Canada) has created guidelines on the prevention, assessment, and management of cannabis use disorder in older adults.
In the absence of a set of guidelines specific to the United States, the recommendations made by the coalition should be helpful in the care of older Americans. Among other recommendations, the guidelines highlight the needs for primary care physicians to build a better knowledge base around the use of cannabis in older adults, to screen older adults for cannabis use, and to educate older adults and their families about the risk of cannabis use.9
Cannabis use is increasingly popular among older adults10 for both medicinal and recreational purposes. Research and data supporting its medical benefits are limited, and the potential of harm from its use among older adults is present and significant. Importantly, many older adults who use marijuana have co-occurring mental health issues and substance use disorder(s).
Often, our older patients learn about benefits and harms of cannabis from friends and the Internet rather than from physicians and other clinicians.9 We must do our part to make sure that older patients understand the potential negative health impact that cannabis can have on their health. Physicians should screen older adults for marijuana use. Building a better knowledge base around changing trends and views in/on the use and accessibility of cannabis will help physicians better address cannabis use in older adults.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University College of Medicine, Mount Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in vulnerable populations.
References
1. Vespa J et al. Demographic turning points for the United States: Population projections for 2020 to 2060. Current Population Reports. Washington: U.S. Census Bureau. 2020 Feb.
2. Han BH et al. Addiction. 2016 Oct 21. doi: 10.1111/add.13670.
3. Han BH and Palamar JJ. Drug Alcohol Depend. 2018 Oct;191:374-81.
4. Han BH and Palamar JJ. JAMA Intern Med. 2020 Feb 4;180(4):609-11.
5. Choi NG et al. Drug Alcohol Abuse. 2018;44(2):215-23.
6. Reynolds IR et al. J Am Griatr Soc. 2018 Nov;66(11):2167-71.
7. Ahmed AIA et al. J Am Geriatr Soc. 2014 Feb;62(2):410-1.
8. Lum HD et al. Gerontol Geriatr Med. 2019 Jan-Dec;5:2333721419843707.
9. Bertram JR et al. Can Geriatr J. 2020 Mar;23(1):135-42.
10. Baumbusch J and Yip IS. Clin Gerontol. 2020 Mar 29;1-7.
Older Americans – people aged 65 or older – make up 15% of the U.S. population, according to the Census Bureau. By the end of this decade, or the year 2030, this proportion will increase to 21% – and all “baby boomers,” those born between 1946 and 1964, will be older than 65.1 Those demographic developments are occurring alongside a change in societal, legal, and public attitudes on cannabis.
Liberalization of cannabis laws across the United States allows for ever easier access to medicinal and recreational cannabis. Traditionally, cannabis use, its effects, and related considerations in the adolescent and young adult populations have commanded significant research attention. Cannabis use in older adults, however, is not as well studied.2 An exploration of trends in cannabis use by older adults and potential impact in terms of health is timely and important.
According to data from the National Survey on Drug Use and Health, cannabis use in adults aged 65 years and older appears to have been increasing steadily over the past 2 decades. Use among this group rose from 0.4% in 2006 and 2007, to 2.9% in 2015 and 2016.2 And, most recently, use climbed from 3.7% in 2017 to 4.2% in 2018.2
Cannabis use also has risen among other adults. For those aged 50-64, cannabis use increased from 2.8% in 2006-2007 to 4.8% in 2012-2013.2,3 Meanwhile, from 2015 to 2016, that number increased to 9.0%.3,4
Past-year cannabis use in the groups of those aged 50-64 and those aged 65 and older appears to be higher in individuals with mental health problems, alcohol use disorder, and nicotine dependence.5,6 Being male and being unmarried appear to be correlated with past-year cannabis use. Multimorbidity does not appear to be associated with past-year cannabis use. Those using cannabis tend to be long-term users and have first use at a much younger age, typically before age 21.
Older adults use cannabis for both recreational and perceived medical benefits. Arthritis, chronic back pain, anxiety, depression, relaxation, stress reduction, and enhancement in terms of creativity are all purported reasons for use. However, there is limited to no evidence for the efficacy of cannabis in helping with those conditions and purposes. Clinical trials have shown that cannabis can be beneficial in managing pain and nausea, but those trials have not been conducted in older adults.7,8
There is a real risk of cannabis use having a negative impact on the health of older adults. To begin with, the cannabis consumed today is significantly higher in potency than the cannabis that baby boomers were introduced to in their youth. The higher potency, combined with an age-related decline in function experienced by some older adults, makes them vulnerable to its known side effects, such as anxiety, dry mouth, tachycardia, high blood pressure, palpitations, wheezing, confusion, and dizziness.
Cannabis use is reported to bring a fourfold increase in cardiac events within the first hour of ingestion.9 Cognitive decline and memory impairment are well known adverse effects of cannabis use. Research has shown significant self-reported cognitive decline in older adults in relation to cannabis use.Cannabis metabolites are known to have an effect on cytochrome P450 enzymes, affecting the metabolism of medication, and increasing the susceptibility of older adults who use cannabis to adverse effects of polypharmacy. Finally, as research on emergency department visits by older adults shows, cannabis use can increase the risk of injury among this cohort.
As in the United States, cannabis use among older adults in Canada has increased significantly. The percentage of older adults who use cannabis in the Canadian province of Ontario, for example, reportedly doubled from 2005 to 2015. In response to this increase, and in anticipation of a rise in problematic use of cannabis and cannabis use disorder in older adults, the Canadian Coalition for Seniors’ Mental Health (through financial support from Substance Use and Addictions Program of Health Canada) has created guidelines on the prevention, assessment, and management of cannabis use disorder in older adults.
In the absence of a set of guidelines specific to the United States, the recommendations made by the coalition should be helpful in the care of older Americans. Among other recommendations, the guidelines highlight the needs for primary care physicians to build a better knowledge base around the use of cannabis in older adults, to screen older adults for cannabis use, and to educate older adults and their families about the risk of cannabis use.9
Cannabis use is increasingly popular among older adults10 for both medicinal and recreational purposes. Research and data supporting its medical benefits are limited, and the potential of harm from its use among older adults is present and significant. Importantly, many older adults who use marijuana have co-occurring mental health issues and substance use disorder(s).
Often, our older patients learn about benefits and harms of cannabis from friends and the Internet rather than from physicians and other clinicians.9 We must do our part to make sure that older patients understand the potential negative health impact that cannabis can have on their health. Physicians should screen older adults for marijuana use. Building a better knowledge base around changing trends and views in/on the use and accessibility of cannabis will help physicians better address cannabis use in older adults.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University College of Medicine, Mount Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in vulnerable populations.
References
1. Vespa J et al. Demographic turning points for the United States: Population projections for 2020 to 2060. Current Population Reports. Washington: U.S. Census Bureau. 2020 Feb.
2. Han BH et al. Addiction. 2016 Oct 21. doi: 10.1111/add.13670.
3. Han BH and Palamar JJ. Drug Alcohol Depend. 2018 Oct;191:374-81.
4. Han BH and Palamar JJ. JAMA Intern Med. 2020 Feb 4;180(4):609-11.
5. Choi NG et al. Drug Alcohol Abuse. 2018;44(2):215-23.
6. Reynolds IR et al. J Am Griatr Soc. 2018 Nov;66(11):2167-71.
7. Ahmed AIA et al. J Am Geriatr Soc. 2014 Feb;62(2):410-1.
8. Lum HD et al. Gerontol Geriatr Med. 2019 Jan-Dec;5:2333721419843707.
9. Bertram JR et al. Can Geriatr J. 2020 Mar;23(1):135-42.
10. Baumbusch J and Yip IS. Clin Gerontol. 2020 Mar 29;1-7.
Older Americans – people aged 65 or older – make up 15% of the U.S. population, according to the Census Bureau. By the end of this decade, or the year 2030, this proportion will increase to 21% – and all “baby boomers,” those born between 1946 and 1964, will be older than 65.1 Those demographic developments are occurring alongside a change in societal, legal, and public attitudes on cannabis.
Liberalization of cannabis laws across the United States allows for ever easier access to medicinal and recreational cannabis. Traditionally, cannabis use, its effects, and related considerations in the adolescent and young adult populations have commanded significant research attention. Cannabis use in older adults, however, is not as well studied.2 An exploration of trends in cannabis use by older adults and potential impact in terms of health is timely and important.
According to data from the National Survey on Drug Use and Health, cannabis use in adults aged 65 years and older appears to have been increasing steadily over the past 2 decades. Use among this group rose from 0.4% in 2006 and 2007, to 2.9% in 2015 and 2016.2 And, most recently, use climbed from 3.7% in 2017 to 4.2% in 2018.2
Cannabis use also has risen among other adults. For those aged 50-64, cannabis use increased from 2.8% in 2006-2007 to 4.8% in 2012-2013.2,3 Meanwhile, from 2015 to 2016, that number increased to 9.0%.3,4
Past-year cannabis use in the groups of those aged 50-64 and those aged 65 and older appears to be higher in individuals with mental health problems, alcohol use disorder, and nicotine dependence.5,6 Being male and being unmarried appear to be correlated with past-year cannabis use. Multimorbidity does not appear to be associated with past-year cannabis use. Those using cannabis tend to be long-term users and have first use at a much younger age, typically before age 21.
Older adults use cannabis for both recreational and perceived medical benefits. Arthritis, chronic back pain, anxiety, depression, relaxation, stress reduction, and enhancement in terms of creativity are all purported reasons for use. However, there is limited to no evidence for the efficacy of cannabis in helping with those conditions and purposes. Clinical trials have shown that cannabis can be beneficial in managing pain and nausea, but those trials have not been conducted in older adults.7,8
There is a real risk of cannabis use having a negative impact on the health of older adults. To begin with, the cannabis consumed today is significantly higher in potency than the cannabis that baby boomers were introduced to in their youth. The higher potency, combined with an age-related decline in function experienced by some older adults, makes them vulnerable to its known side effects, such as anxiety, dry mouth, tachycardia, high blood pressure, palpitations, wheezing, confusion, and dizziness.
Cannabis use is reported to bring a fourfold increase in cardiac events within the first hour of ingestion.9 Cognitive decline and memory impairment are well known adverse effects of cannabis use. Research has shown significant self-reported cognitive decline in older adults in relation to cannabis use.Cannabis metabolites are known to have an effect on cytochrome P450 enzymes, affecting the metabolism of medication, and increasing the susceptibility of older adults who use cannabis to adverse effects of polypharmacy. Finally, as research on emergency department visits by older adults shows, cannabis use can increase the risk of injury among this cohort.
As in the United States, cannabis use among older adults in Canada has increased significantly. The percentage of older adults who use cannabis in the Canadian province of Ontario, for example, reportedly doubled from 2005 to 2015. In response to this increase, and in anticipation of a rise in problematic use of cannabis and cannabis use disorder in older adults, the Canadian Coalition for Seniors’ Mental Health (through financial support from Substance Use and Addictions Program of Health Canada) has created guidelines on the prevention, assessment, and management of cannabis use disorder in older adults.
In the absence of a set of guidelines specific to the United States, the recommendations made by the coalition should be helpful in the care of older Americans. Among other recommendations, the guidelines highlight the needs for primary care physicians to build a better knowledge base around the use of cannabis in older adults, to screen older adults for cannabis use, and to educate older adults and their families about the risk of cannabis use.9
Cannabis use is increasingly popular among older adults10 for both medicinal and recreational purposes. Research and data supporting its medical benefits are limited, and the potential of harm from its use among older adults is present and significant. Importantly, many older adults who use marijuana have co-occurring mental health issues and substance use disorder(s).
Often, our older patients learn about benefits and harms of cannabis from friends and the Internet rather than from physicians and other clinicians.9 We must do our part to make sure that older patients understand the potential negative health impact that cannabis can have on their health. Physicians should screen older adults for marijuana use. Building a better knowledge base around changing trends and views in/on the use and accessibility of cannabis will help physicians better address cannabis use in older adults.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University College of Medicine, Mount Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in vulnerable populations.
References
1. Vespa J et al. Demographic turning points for the United States: Population projections for 2020 to 2060. Current Population Reports. Washington: U.S. Census Bureau. 2020 Feb.
2. Han BH et al. Addiction. 2016 Oct 21. doi: 10.1111/add.13670.
3. Han BH and Palamar JJ. Drug Alcohol Depend. 2018 Oct;191:374-81.
4. Han BH and Palamar JJ. JAMA Intern Med. 2020 Feb 4;180(4):609-11.
5. Choi NG et al. Drug Alcohol Abuse. 2018;44(2):215-23.
6. Reynolds IR et al. J Am Griatr Soc. 2018 Nov;66(11):2167-71.
7. Ahmed AIA et al. J Am Geriatr Soc. 2014 Feb;62(2):410-1.
8. Lum HD et al. Gerontol Geriatr Med. 2019 Jan-Dec;5:2333721419843707.
9. Bertram JR et al. Can Geriatr J. 2020 Mar;23(1):135-42.
10. Baumbusch J and Yip IS. Clin Gerontol. 2020 Mar 29;1-7.
PANS may be more prevalent than thought
Pediatric acute-onset neuropsychiatric syndrome (PANS), a rare acute onset of psychiatric symptoms, might be more common than initially thought, according to Kiki D. Chang, MD.
PANS is characterized by the National Center for Advancing Translational Sciences Genetic and Rare Diseases Information Center as a “sudden onset of obsessive-compulsive symptoms and/or severe eating restrictions, along with at least two other cognitive, behavioral, or neurological symptoms.” These symptoms can include anxiety, depression, oppositional behavior, difficulty concentrating, abnormalities in motor and sensory skills, and other somatic symptoms. The condition develops as a result of an infection that causes an autoimmune or inflammatory response in the brain, and patients tend to respond well to treatment from antibiotics, anti-inflammatory medication, and immunomodulatory therapy.
Both PANS and a subtype condition, pediatric autoimmune neuropsychiatric disorders associated with Streptococcus infections (PANDAS), are underrecognized, Dr. Chang said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. It is often misdiagnosed as Tourette syndrome or obsessive-compulsive disorder (OCD) because tics are present in about half of cases, he said, but more severe associated symptoms, such as psychosis, can be misdiagnosed as psychotic disorders or mood disorders. Currently, neither PANS nor PANDAS are officially recognized by the American Academy of Pediatrics or the DSM-5.
“We’re hoping that it is soon because it clearly exists,” Dr. Chang said at the meeting, presented by Global Academy for Medical Education. “If you’ve ever treated a child with PANS or PANDAS and you have seen antibiotics totally reverse OCD and tic-like behavior, if you’ve seen prednisone actually treat symptoms of mania or even psychosis and actually make those things better rather than worse, it’s really eye-opening and it makes a believer out of you.”
Anxiety is the most common psychiatric symptom in youth, and anxiety disorders are also common, said Dr. Chang. According to the National Comorbidity Survey: Adolescent Supplement, 2001-2004, 31.9% adolescents overall reported an anxiety disorder, and 8.3% said their anxiety disorder caused severe impairment. The COVID-19 pandemic has increased the level of anxiety for children and adolescents, which can lead to other disorders, such as separation anxiety disorder, panic disorder, specific phobia, social anxiety disorder, acute stress disorder, generalized anxiety disorder, OCD, or posttraumatic stress disorder. Psychiatrists should be suspicious of any sudden onset of symptoms that overlap with PANS, said Dr. Chang, who is now in private practice in Palo Alto, Calif.
“Anxiety disorders are incredibly common. Remember that you’ve got to carefully screen for other anxiety disorders, because they’re highly comorbid,” Dr. Chang said. “You’ve got to do a full workup. If there are other things going on, you’ve got to think PANS. If it’s acute onset, you’ve really got to think [PANS], and you should do that workup or refer to someone who does.”
The prevalence of PANS and PANDAS is not known, but it may be more common than psychiatrists realize, Dr. Chang said. “I’ve been doing this for about 10 years now in the PANS and PANDAS field, and it’s very clear to me that this is something that is prevalent,” he said.
Together with Jennifer Frankovich, MD, Dr. Chang founded a clinic at the Lucile Packard Children’s Hospital Stanford, and also helped to develop treatment guidelines for youth with PANS. At the clinic, patients are approximately 7.7 years old when developing the first symptoms, and are 10.7 years old when presenting for treatment. Most patients at the clinic are male (78%), and 40% are acute onset cases. Nearly all patients have symptoms of anxiety (92%), mood disorder (88%), OCD (86%), sensory/motor abnormalities (88%), irritability/aggression (82%), somatic symptoms, deterioration in school (76%), and behavioral regression (59%). More than one-third present with suicidal ideation (38%) and violence to themselves (29%), others (38%), or objects. About one-fourth have symptoms of psychosis (24%).
“These can be really sick kids,” Dr. Chang said. not able to eat because they’re afraid of things, not able to take care of their body or daily living. These were sometimes highly functional people beforehand, sometimes they weren’t, but it was still an acute change.”
Treatment for PANS
Treatment guidelines released by the PANS/PANDAS Consortium in 2017 recommend a first course of antistreptococcal treatment for new PANS cases. Psychiatrists should look for evidence of strep or other infection and use antibiotics to eradicate any underlying acute or residual infection.
“Very commonly, we’ll use things like azithromycin, or Augmentin, or amoxicillin, and you’ll see suddenly the OCD go away or at least diminish, the sleep return to normal, the mood come back down,” Dr. Chang said. “It’s pretty amazing when you see it.”
In other cases, ongoing treatment is needed for longer than the normal 5-day or 10-day course of antibiotics. “We’re not exactly sure how long: sometimes it’s 3 weeks, sometimes it’s 4 weeks, but you have to give it more than a week. Sometimes it’s the anti-inflammatory properties that are helping.” While concerns about haphazardly prescribing antibiotics are valid, “if you can cure this stuff on antibiotics, it’s low-hanging fruit,” Dr. Chang said.
There is evidence in the literature that prescribing antibiotics for PANS is beneficial. A randomized controlled trial published in 2017 showed that patients with PANS prescribed azithromycin for 4 weeks had greater reductions in severity of OCD, compared with placebo.
“We need more studies, but clearly, antibiotics do have the potential to help with certain kids. And certainly, in my practice, I see sometimes a slam-dunk response,” Dr. Chang said. “Unfortunately, sometimes you don’t see a slam-dunk response or you can’t find an infection. That’s when it might be more of an inflammation from some other reason. It could be a leftover infection, or it could be an anti-inflammatory situation.”
Immunomodulatory treatment for PANS includes use of NSAIDs, such as ibuprofen or naproxen sodium; steroids, such as prednisone or intravenous corticosteroids; intravenous immunoglobulin; or plasma exchange. Other therapies to consider are rituximab, mycophenolate mofetil, and cyclophosphamide.
Some psychiatric treatments may help patients with PANS. While there is no empirical evidence that psychotropics are effective in treating PANS, some SSRIs might help if patients are able to handle any adverse events. Psychotherapy and education of the family are also important for patients with PANS and their caregivers.
“Basically, [PANS] has as high a caregiver burden as having someone in the household with Alzheimer’s disease or cancer. It’s a huge burden, it’s very stressful, and the family needs support for this,” Dr. Chang said.
Global Academy and this news organization are owned by the same parent company. Dr. Chang reports he is a consultant for Allergan, Impel NeuroPharma, and Sunovion. He is also on the speaker’s bureau for Sunovion.
Pediatric acute-onset neuropsychiatric syndrome (PANS), a rare acute onset of psychiatric symptoms, might be more common than initially thought, according to Kiki D. Chang, MD.
PANS is characterized by the National Center for Advancing Translational Sciences Genetic and Rare Diseases Information Center as a “sudden onset of obsessive-compulsive symptoms and/or severe eating restrictions, along with at least two other cognitive, behavioral, or neurological symptoms.” These symptoms can include anxiety, depression, oppositional behavior, difficulty concentrating, abnormalities in motor and sensory skills, and other somatic symptoms. The condition develops as a result of an infection that causes an autoimmune or inflammatory response in the brain, and patients tend to respond well to treatment from antibiotics, anti-inflammatory medication, and immunomodulatory therapy.
Both PANS and a subtype condition, pediatric autoimmune neuropsychiatric disorders associated with Streptococcus infections (PANDAS), are underrecognized, Dr. Chang said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. It is often misdiagnosed as Tourette syndrome or obsessive-compulsive disorder (OCD) because tics are present in about half of cases, he said, but more severe associated symptoms, such as psychosis, can be misdiagnosed as psychotic disorders or mood disorders. Currently, neither PANS nor PANDAS are officially recognized by the American Academy of Pediatrics or the DSM-5.
“We’re hoping that it is soon because it clearly exists,” Dr. Chang said at the meeting, presented by Global Academy for Medical Education. “If you’ve ever treated a child with PANS or PANDAS and you have seen antibiotics totally reverse OCD and tic-like behavior, if you’ve seen prednisone actually treat symptoms of mania or even psychosis and actually make those things better rather than worse, it’s really eye-opening and it makes a believer out of you.”
Anxiety is the most common psychiatric symptom in youth, and anxiety disorders are also common, said Dr. Chang. According to the National Comorbidity Survey: Adolescent Supplement, 2001-2004, 31.9% adolescents overall reported an anxiety disorder, and 8.3% said their anxiety disorder caused severe impairment. The COVID-19 pandemic has increased the level of anxiety for children and adolescents, which can lead to other disorders, such as separation anxiety disorder, panic disorder, specific phobia, social anxiety disorder, acute stress disorder, generalized anxiety disorder, OCD, or posttraumatic stress disorder. Psychiatrists should be suspicious of any sudden onset of symptoms that overlap with PANS, said Dr. Chang, who is now in private practice in Palo Alto, Calif.
“Anxiety disorders are incredibly common. Remember that you’ve got to carefully screen for other anxiety disorders, because they’re highly comorbid,” Dr. Chang said. “You’ve got to do a full workup. If there are other things going on, you’ve got to think PANS. If it’s acute onset, you’ve really got to think [PANS], and you should do that workup or refer to someone who does.”
The prevalence of PANS and PANDAS is not known, but it may be more common than psychiatrists realize, Dr. Chang said. “I’ve been doing this for about 10 years now in the PANS and PANDAS field, and it’s very clear to me that this is something that is prevalent,” he said.
Together with Jennifer Frankovich, MD, Dr. Chang founded a clinic at the Lucile Packard Children’s Hospital Stanford, and also helped to develop treatment guidelines for youth with PANS. At the clinic, patients are approximately 7.7 years old when developing the first symptoms, and are 10.7 years old when presenting for treatment. Most patients at the clinic are male (78%), and 40% are acute onset cases. Nearly all patients have symptoms of anxiety (92%), mood disorder (88%), OCD (86%), sensory/motor abnormalities (88%), irritability/aggression (82%), somatic symptoms, deterioration in school (76%), and behavioral regression (59%). More than one-third present with suicidal ideation (38%) and violence to themselves (29%), others (38%), or objects. About one-fourth have symptoms of psychosis (24%).
“These can be really sick kids,” Dr. Chang said. not able to eat because they’re afraid of things, not able to take care of their body or daily living. These were sometimes highly functional people beforehand, sometimes they weren’t, but it was still an acute change.”
Treatment for PANS
Treatment guidelines released by the PANS/PANDAS Consortium in 2017 recommend a first course of antistreptococcal treatment for new PANS cases. Psychiatrists should look for evidence of strep or other infection and use antibiotics to eradicate any underlying acute or residual infection.
“Very commonly, we’ll use things like azithromycin, or Augmentin, or amoxicillin, and you’ll see suddenly the OCD go away or at least diminish, the sleep return to normal, the mood come back down,” Dr. Chang said. “It’s pretty amazing when you see it.”
In other cases, ongoing treatment is needed for longer than the normal 5-day or 10-day course of antibiotics. “We’re not exactly sure how long: sometimes it’s 3 weeks, sometimes it’s 4 weeks, but you have to give it more than a week. Sometimes it’s the anti-inflammatory properties that are helping.” While concerns about haphazardly prescribing antibiotics are valid, “if you can cure this stuff on antibiotics, it’s low-hanging fruit,” Dr. Chang said.
There is evidence in the literature that prescribing antibiotics for PANS is beneficial. A randomized controlled trial published in 2017 showed that patients with PANS prescribed azithromycin for 4 weeks had greater reductions in severity of OCD, compared with placebo.
“We need more studies, but clearly, antibiotics do have the potential to help with certain kids. And certainly, in my practice, I see sometimes a slam-dunk response,” Dr. Chang said. “Unfortunately, sometimes you don’t see a slam-dunk response or you can’t find an infection. That’s when it might be more of an inflammation from some other reason. It could be a leftover infection, or it could be an anti-inflammatory situation.”
Immunomodulatory treatment for PANS includes use of NSAIDs, such as ibuprofen or naproxen sodium; steroids, such as prednisone or intravenous corticosteroids; intravenous immunoglobulin; or plasma exchange. Other therapies to consider are rituximab, mycophenolate mofetil, and cyclophosphamide.
Some psychiatric treatments may help patients with PANS. While there is no empirical evidence that psychotropics are effective in treating PANS, some SSRIs might help if patients are able to handle any adverse events. Psychotherapy and education of the family are also important for patients with PANS and their caregivers.
“Basically, [PANS] has as high a caregiver burden as having someone in the household with Alzheimer’s disease or cancer. It’s a huge burden, it’s very stressful, and the family needs support for this,” Dr. Chang said.
Global Academy and this news organization are owned by the same parent company. Dr. Chang reports he is a consultant for Allergan, Impel NeuroPharma, and Sunovion. He is also on the speaker’s bureau for Sunovion.
Pediatric acute-onset neuropsychiatric syndrome (PANS), a rare acute onset of psychiatric symptoms, might be more common than initially thought, according to Kiki D. Chang, MD.
PANS is characterized by the National Center for Advancing Translational Sciences Genetic and Rare Diseases Information Center as a “sudden onset of obsessive-compulsive symptoms and/or severe eating restrictions, along with at least two other cognitive, behavioral, or neurological symptoms.” These symptoms can include anxiety, depression, oppositional behavior, difficulty concentrating, abnormalities in motor and sensory skills, and other somatic symptoms. The condition develops as a result of an infection that causes an autoimmune or inflammatory response in the brain, and patients tend to respond well to treatment from antibiotics, anti-inflammatory medication, and immunomodulatory therapy.
Both PANS and a subtype condition, pediatric autoimmune neuropsychiatric disorders associated with Streptococcus infections (PANDAS), are underrecognized, Dr. Chang said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. It is often misdiagnosed as Tourette syndrome or obsessive-compulsive disorder (OCD) because tics are present in about half of cases, he said, but more severe associated symptoms, such as psychosis, can be misdiagnosed as psychotic disorders or mood disorders. Currently, neither PANS nor PANDAS are officially recognized by the American Academy of Pediatrics or the DSM-5.
“We’re hoping that it is soon because it clearly exists,” Dr. Chang said at the meeting, presented by Global Academy for Medical Education. “If you’ve ever treated a child with PANS or PANDAS and you have seen antibiotics totally reverse OCD and tic-like behavior, if you’ve seen prednisone actually treat symptoms of mania or even psychosis and actually make those things better rather than worse, it’s really eye-opening and it makes a believer out of you.”
Anxiety is the most common psychiatric symptom in youth, and anxiety disorders are also common, said Dr. Chang. According to the National Comorbidity Survey: Adolescent Supplement, 2001-2004, 31.9% adolescents overall reported an anxiety disorder, and 8.3% said their anxiety disorder caused severe impairment. The COVID-19 pandemic has increased the level of anxiety for children and adolescents, which can lead to other disorders, such as separation anxiety disorder, panic disorder, specific phobia, social anxiety disorder, acute stress disorder, generalized anxiety disorder, OCD, or posttraumatic stress disorder. Psychiatrists should be suspicious of any sudden onset of symptoms that overlap with PANS, said Dr. Chang, who is now in private practice in Palo Alto, Calif.
“Anxiety disorders are incredibly common. Remember that you’ve got to carefully screen for other anxiety disorders, because they’re highly comorbid,” Dr. Chang said. “You’ve got to do a full workup. If there are other things going on, you’ve got to think PANS. If it’s acute onset, you’ve really got to think [PANS], and you should do that workup or refer to someone who does.”
The prevalence of PANS and PANDAS is not known, but it may be more common than psychiatrists realize, Dr. Chang said. “I’ve been doing this for about 10 years now in the PANS and PANDAS field, and it’s very clear to me that this is something that is prevalent,” he said.
Together with Jennifer Frankovich, MD, Dr. Chang founded a clinic at the Lucile Packard Children’s Hospital Stanford, and also helped to develop treatment guidelines for youth with PANS. At the clinic, patients are approximately 7.7 years old when developing the first symptoms, and are 10.7 years old when presenting for treatment. Most patients at the clinic are male (78%), and 40% are acute onset cases. Nearly all patients have symptoms of anxiety (92%), mood disorder (88%), OCD (86%), sensory/motor abnormalities (88%), irritability/aggression (82%), somatic symptoms, deterioration in school (76%), and behavioral regression (59%). More than one-third present with suicidal ideation (38%) and violence to themselves (29%), others (38%), or objects. About one-fourth have symptoms of psychosis (24%).
“These can be really sick kids,” Dr. Chang said. not able to eat because they’re afraid of things, not able to take care of their body or daily living. These were sometimes highly functional people beforehand, sometimes they weren’t, but it was still an acute change.”
Treatment for PANS
Treatment guidelines released by the PANS/PANDAS Consortium in 2017 recommend a first course of antistreptococcal treatment for new PANS cases. Psychiatrists should look for evidence of strep or other infection and use antibiotics to eradicate any underlying acute or residual infection.
“Very commonly, we’ll use things like azithromycin, or Augmentin, or amoxicillin, and you’ll see suddenly the OCD go away or at least diminish, the sleep return to normal, the mood come back down,” Dr. Chang said. “It’s pretty amazing when you see it.”
In other cases, ongoing treatment is needed for longer than the normal 5-day or 10-day course of antibiotics. “We’re not exactly sure how long: sometimes it’s 3 weeks, sometimes it’s 4 weeks, but you have to give it more than a week. Sometimes it’s the anti-inflammatory properties that are helping.” While concerns about haphazardly prescribing antibiotics are valid, “if you can cure this stuff on antibiotics, it’s low-hanging fruit,” Dr. Chang said.
There is evidence in the literature that prescribing antibiotics for PANS is beneficial. A randomized controlled trial published in 2017 showed that patients with PANS prescribed azithromycin for 4 weeks had greater reductions in severity of OCD, compared with placebo.
“We need more studies, but clearly, antibiotics do have the potential to help with certain kids. And certainly, in my practice, I see sometimes a slam-dunk response,” Dr. Chang said. “Unfortunately, sometimes you don’t see a slam-dunk response or you can’t find an infection. That’s when it might be more of an inflammation from some other reason. It could be a leftover infection, or it could be an anti-inflammatory situation.”
Immunomodulatory treatment for PANS includes use of NSAIDs, such as ibuprofen or naproxen sodium; steroids, such as prednisone or intravenous corticosteroids; intravenous immunoglobulin; or plasma exchange. Other therapies to consider are rituximab, mycophenolate mofetil, and cyclophosphamide.
Some psychiatric treatments may help patients with PANS. While there is no empirical evidence that psychotropics are effective in treating PANS, some SSRIs might help if patients are able to handle any adverse events. Psychotherapy and education of the family are also important for patients with PANS and their caregivers.
“Basically, [PANS] has as high a caregiver burden as having someone in the household with Alzheimer’s disease or cancer. It’s a huge burden, it’s very stressful, and the family needs support for this,” Dr. Chang said.
Global Academy and this news organization are owned by the same parent company. Dr. Chang reports he is a consultant for Allergan, Impel NeuroPharma, and Sunovion. He is also on the speaker’s bureau for Sunovion.
FROM CP/AACP PSYCHIATRY UPDATE
‘Staggering’ increase in COVID-linked depression, anxiety
Since the start of the COVID-19 pandemic, there has been a dramatic increase in depression, anxiety, psychosis, and suicidality, new research shows.
The new data, released by Mental Health America (MHA), came from individuals who completed a voluntary online mental health screen.
As of the end of June, over 169,000 additional participants reported having moderate to severe depression or anxiety, compared with participants who completed the screen prior to the pandemic.
In June alone, 18,000 additional participants were found to be at risk for psychosis, continuing a rising pattern that began in May, when 16,000 reported psychosis risk.
“We continue to see staggering numbers that indicate increased rates in depression and anxiety because of COVID-19,” Paul Gionfriddo, president and CEO of MHA, said in a release.
“In fact, the problem is bigger than anyone imagined, making it clear how the pandemic is affecting people now and will continue to affect people who mourn loved ones and whose serious mental conditions are left untreated. So we need to take this very seriously,” Mr. Gionfriddo said in an interview.
Real-time data
MHA has been conducting online screenings for 6 years. To date, nearly 5.5 million screenings have been completed, making it the largest screening program of its kind in the United States, Mr. Gionfriddo reported.
“At the beginning of the pandemic, we were asked by a member of the media if we could offer any insight about how anxiety in particular was affecting people during the pandemic since we were the only ones with a database that could give quantitative detail,” he said.
The results of their screen could also help find that information “in real time,” he added.
More people are now undergoing mental health screenings, Mr. Gionfriddo noted.
At roughly 7,000 per day in May and June, the number of anxiety and depression screenings that were completed per day were 406% and 457% higher, respectively, than the number completed in January.
The youngest group of participants were those aged 11-17 years; the oldest age group consisted of individuals 65 years and older.
The Patient Health Questionnaire–9 was used to identify those at risk for depression, the General Anxiety Disorder–7 was used to identify those at risk for anxiety, and the Prodromal Questionnaire Brief Version was used to identify those at high risk for psychosis.
Current events
Roughly 90% screened positive for moderate to severe depression, and 80% screened positive for moderate to severe anxiety.
“Kids between the ages of 11 and 17 years have been the most stressed, but it seems to be easier to bear as you get older,” Mr. Gionfriddo said.
Loneliness and isolation were cited as contributors to depression and anxiety by the largest percentage of individuals with these conditions (74% and 65%, respectively).
In June, roughly one quarter of participants also cited grief or loss and financial concerns as contributors to anxiety (25.31% and 24.18%, respectively) and to depression (26.53% and 23.36%).
Current events were cited as an important contributor, leading to more mental health problems in June, compared with May (36.11% vs 29.41 for anxiety; 29.13% vs 21.77% for depression).
The June screen added the category of racism as a potential contributor. Close to 8% reported it as a reason for anxiety, and roughly 5% considered it a reason for depression.
“We will be releasing more data at the end of July, and it will be interesting to see how the racism category compares to data we collected at the end of June,” Mr. Gionfriddo noted.
Dramatic increase
The screen also showed a “dramatic increase” in the number of people who reported being at risk for psychosis, with 18,000 participants screening positive. This represented more than four times the baseline figures recorded through March.
“We were not surprised to see a spike in depression and anxiety, but why were we seeing a spike in psychosis in May/June?” Mr. Gionfriddo asked. He suggested that stress may play a role in driving this increased risk.
“These data, we hope, will get policymakers to pay attention, take it seriously, and intervene to prevent psychosis at an earlier stage before signs and symptoms emerge,” said Mr. Gionfriddo.
One of the most alarming findings was that in June, 25,498 participants who screened positive for depression reported thinking of suicide or self-harm on “more than half of days to nearly every day.” A total of 14,607 participants said they had these thoughts every day.
Overall, the results should reinforce the recommendations of the US Preventive Services Task Force to routinely screen for depression in any clinical setting on a regular basis, Mr. Gionfriddo said.
In addition, policymakers “need to balance reopening vs. quarantining and isolating, and we need to think about what the next 2-4 years look like in terms of balancing physical health risks and mental health risks,” he noted.
“We’ve been treating the pandemic like a sprint and now, 4 or 5 months into it, perhaps as a middle-distance run, when in fact it’s a marathon,” he added.
Advocates needed
The increase in anxiety and depression often centers on the changes and uncertainties in the college experience, such as whether classes will be held in person, online, or a hybrid of the two, said Dr. Ritchie, who was not involved with the research.
Additionally, some college students who have “left the nest” have been forced to “return to the nest,” which compounds stress, she said.
LGBTQ youngsters may be particularly affected because some have “come out of the closet” while away from home and now must negotiate going back to their home of record. They are uncertain whether or not “to go back into the closet,” added Dr. Ritchie, who is also vice chair of psychiatry at Georgetown University, Washington.
Psychiatrists and other mental health professionals should be advocates for “getting services to more people for the greatest good,” she noted.
For example, the MHA data “might be useful in advocating for keeping telehealth accessible and even promoting it,” she said.
The full report is available on MHA’s website.
Mr. Gionfriddo and Dr. Ritchie report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Since the start of the COVID-19 pandemic, there has been a dramatic increase in depression, anxiety, psychosis, and suicidality, new research shows.
The new data, released by Mental Health America (MHA), came from individuals who completed a voluntary online mental health screen.
As of the end of June, over 169,000 additional participants reported having moderate to severe depression or anxiety, compared with participants who completed the screen prior to the pandemic.
In June alone, 18,000 additional participants were found to be at risk for psychosis, continuing a rising pattern that began in May, when 16,000 reported psychosis risk.
“We continue to see staggering numbers that indicate increased rates in depression and anxiety because of COVID-19,” Paul Gionfriddo, president and CEO of MHA, said in a release.
“In fact, the problem is bigger than anyone imagined, making it clear how the pandemic is affecting people now and will continue to affect people who mourn loved ones and whose serious mental conditions are left untreated. So we need to take this very seriously,” Mr. Gionfriddo said in an interview.
Real-time data
MHA has been conducting online screenings for 6 years. To date, nearly 5.5 million screenings have been completed, making it the largest screening program of its kind in the United States, Mr. Gionfriddo reported.
“At the beginning of the pandemic, we were asked by a member of the media if we could offer any insight about how anxiety in particular was affecting people during the pandemic since we were the only ones with a database that could give quantitative detail,” he said.
The results of their screen could also help find that information “in real time,” he added.
More people are now undergoing mental health screenings, Mr. Gionfriddo noted.
At roughly 7,000 per day in May and June, the number of anxiety and depression screenings that were completed per day were 406% and 457% higher, respectively, than the number completed in January.
The youngest group of participants were those aged 11-17 years; the oldest age group consisted of individuals 65 years and older.
The Patient Health Questionnaire–9 was used to identify those at risk for depression, the General Anxiety Disorder–7 was used to identify those at risk for anxiety, and the Prodromal Questionnaire Brief Version was used to identify those at high risk for psychosis.
Current events
Roughly 90% screened positive for moderate to severe depression, and 80% screened positive for moderate to severe anxiety.
“Kids between the ages of 11 and 17 years have been the most stressed, but it seems to be easier to bear as you get older,” Mr. Gionfriddo said.
Loneliness and isolation were cited as contributors to depression and anxiety by the largest percentage of individuals with these conditions (74% and 65%, respectively).
In June, roughly one quarter of participants also cited grief or loss and financial concerns as contributors to anxiety (25.31% and 24.18%, respectively) and to depression (26.53% and 23.36%).
Current events were cited as an important contributor, leading to more mental health problems in June, compared with May (36.11% vs 29.41 for anxiety; 29.13% vs 21.77% for depression).
The June screen added the category of racism as a potential contributor. Close to 8% reported it as a reason for anxiety, and roughly 5% considered it a reason for depression.
“We will be releasing more data at the end of July, and it will be interesting to see how the racism category compares to data we collected at the end of June,” Mr. Gionfriddo noted.
Dramatic increase
The screen also showed a “dramatic increase” in the number of people who reported being at risk for psychosis, with 18,000 participants screening positive. This represented more than four times the baseline figures recorded through March.
“We were not surprised to see a spike in depression and anxiety, but why were we seeing a spike in psychosis in May/June?” Mr. Gionfriddo asked. He suggested that stress may play a role in driving this increased risk.
“These data, we hope, will get policymakers to pay attention, take it seriously, and intervene to prevent psychosis at an earlier stage before signs and symptoms emerge,” said Mr. Gionfriddo.
One of the most alarming findings was that in June, 25,498 participants who screened positive for depression reported thinking of suicide or self-harm on “more than half of days to nearly every day.” A total of 14,607 participants said they had these thoughts every day.
Overall, the results should reinforce the recommendations of the US Preventive Services Task Force to routinely screen for depression in any clinical setting on a regular basis, Mr. Gionfriddo said.
In addition, policymakers “need to balance reopening vs. quarantining and isolating, and we need to think about what the next 2-4 years look like in terms of balancing physical health risks and mental health risks,” he noted.
“We’ve been treating the pandemic like a sprint and now, 4 or 5 months into it, perhaps as a middle-distance run, when in fact it’s a marathon,” he added.
Advocates needed
The increase in anxiety and depression often centers on the changes and uncertainties in the college experience, such as whether classes will be held in person, online, or a hybrid of the two, said Dr. Ritchie, who was not involved with the research.
Additionally, some college students who have “left the nest” have been forced to “return to the nest,” which compounds stress, she said.
LGBTQ youngsters may be particularly affected because some have “come out of the closet” while away from home and now must negotiate going back to their home of record. They are uncertain whether or not “to go back into the closet,” added Dr. Ritchie, who is also vice chair of psychiatry at Georgetown University, Washington.
Psychiatrists and other mental health professionals should be advocates for “getting services to more people for the greatest good,” she noted.
For example, the MHA data “might be useful in advocating for keeping telehealth accessible and even promoting it,” she said.
The full report is available on MHA’s website.
Mr. Gionfriddo and Dr. Ritchie report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Since the start of the COVID-19 pandemic, there has been a dramatic increase in depression, anxiety, psychosis, and suicidality, new research shows.
The new data, released by Mental Health America (MHA), came from individuals who completed a voluntary online mental health screen.
As of the end of June, over 169,000 additional participants reported having moderate to severe depression or anxiety, compared with participants who completed the screen prior to the pandemic.
In June alone, 18,000 additional participants were found to be at risk for psychosis, continuing a rising pattern that began in May, when 16,000 reported psychosis risk.
“We continue to see staggering numbers that indicate increased rates in depression and anxiety because of COVID-19,” Paul Gionfriddo, president and CEO of MHA, said in a release.
“In fact, the problem is bigger than anyone imagined, making it clear how the pandemic is affecting people now and will continue to affect people who mourn loved ones and whose serious mental conditions are left untreated. So we need to take this very seriously,” Mr. Gionfriddo said in an interview.
Real-time data
MHA has been conducting online screenings for 6 years. To date, nearly 5.5 million screenings have been completed, making it the largest screening program of its kind in the United States, Mr. Gionfriddo reported.
“At the beginning of the pandemic, we were asked by a member of the media if we could offer any insight about how anxiety in particular was affecting people during the pandemic since we were the only ones with a database that could give quantitative detail,” he said.
The results of their screen could also help find that information “in real time,” he added.
More people are now undergoing mental health screenings, Mr. Gionfriddo noted.
At roughly 7,000 per day in May and June, the number of anxiety and depression screenings that were completed per day were 406% and 457% higher, respectively, than the number completed in January.
The youngest group of participants were those aged 11-17 years; the oldest age group consisted of individuals 65 years and older.
The Patient Health Questionnaire–9 was used to identify those at risk for depression, the General Anxiety Disorder–7 was used to identify those at risk for anxiety, and the Prodromal Questionnaire Brief Version was used to identify those at high risk for psychosis.
Current events
Roughly 90% screened positive for moderate to severe depression, and 80% screened positive for moderate to severe anxiety.
“Kids between the ages of 11 and 17 years have been the most stressed, but it seems to be easier to bear as you get older,” Mr. Gionfriddo said.
Loneliness and isolation were cited as contributors to depression and anxiety by the largest percentage of individuals with these conditions (74% and 65%, respectively).
In June, roughly one quarter of participants also cited grief or loss and financial concerns as contributors to anxiety (25.31% and 24.18%, respectively) and to depression (26.53% and 23.36%).
Current events were cited as an important contributor, leading to more mental health problems in June, compared with May (36.11% vs 29.41 for anxiety; 29.13% vs 21.77% for depression).
The June screen added the category of racism as a potential contributor. Close to 8% reported it as a reason for anxiety, and roughly 5% considered it a reason for depression.
“We will be releasing more data at the end of July, and it will be interesting to see how the racism category compares to data we collected at the end of June,” Mr. Gionfriddo noted.
Dramatic increase
The screen also showed a “dramatic increase” in the number of people who reported being at risk for psychosis, with 18,000 participants screening positive. This represented more than four times the baseline figures recorded through March.
“We were not surprised to see a spike in depression and anxiety, but why were we seeing a spike in psychosis in May/June?” Mr. Gionfriddo asked. He suggested that stress may play a role in driving this increased risk.
“These data, we hope, will get policymakers to pay attention, take it seriously, and intervene to prevent psychosis at an earlier stage before signs and symptoms emerge,” said Mr. Gionfriddo.
One of the most alarming findings was that in June, 25,498 participants who screened positive for depression reported thinking of suicide or self-harm on “more than half of days to nearly every day.” A total of 14,607 participants said they had these thoughts every day.
Overall, the results should reinforce the recommendations of the US Preventive Services Task Force to routinely screen for depression in any clinical setting on a regular basis, Mr. Gionfriddo said.
In addition, policymakers “need to balance reopening vs. quarantining and isolating, and we need to think about what the next 2-4 years look like in terms of balancing physical health risks and mental health risks,” he noted.
“We’ve been treating the pandemic like a sprint and now, 4 or 5 months into it, perhaps as a middle-distance run, when in fact it’s a marathon,” he added.
Advocates needed
The increase in anxiety and depression often centers on the changes and uncertainties in the college experience, such as whether classes will be held in person, online, or a hybrid of the two, said Dr. Ritchie, who was not involved with the research.
Additionally, some college students who have “left the nest” have been forced to “return to the nest,” which compounds stress, she said.
LGBTQ youngsters may be particularly affected because some have “come out of the closet” while away from home and now must negotiate going back to their home of record. They are uncertain whether or not “to go back into the closet,” added Dr. Ritchie, who is also vice chair of psychiatry at Georgetown University, Washington.
Psychiatrists and other mental health professionals should be advocates for “getting services to more people for the greatest good,” she noted.
For example, the MHA data “might be useful in advocating for keeping telehealth accessible and even promoting it,” she said.
The full report is available on MHA’s website.
Mr. Gionfriddo and Dr. Ritchie report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Pandemic-related stress causing health issues in many Americans
Over the last 2 months, more than half of Americans have experienced some sort of adverse effect caused by stress related to the COVID-19 pandemic, according to a survey from the Kaiser Family Foundation (KFF).
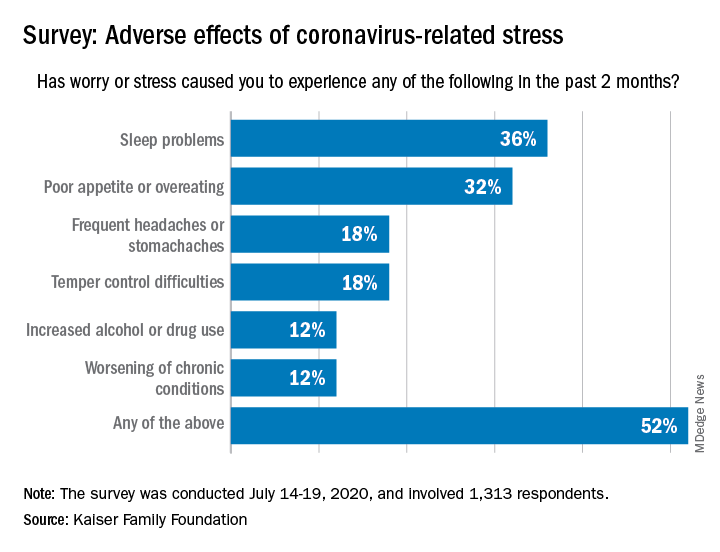
More than a third (36%) of the 1,313 respondents said they either had difficulty sleeping, falling asleep, or sleeping too much, KFF said in its latest Health Tracking Poll, conducted July 14-19, 2020. That was followed by poor appetite or overeating, which was mentioned by 32% of those surveyed.
Other adverse effects included frequent headaches or stomachaches (18%), temper-control issues (18%), increased drug or alcohol use (12%), and worsening of chronic conditions such as diabetes or hypertension (12%). Altogether, 52% of Americans have had at least one of these issues in the past 2 months, Liz Hamel and associates at KFF reported.
breaking down to 26% reporting a major impact and 28% reporting a minor impact (figures have been rounded), they said.
“As life with the coronavirus pandemic wears on, Americans increasingly say it is taking a negative toll on their mental health,” the investigators wrote. Earlier polls showed that pandemic-related stress was having an impact on mental health for 39% of respondents in May, compared with 45% in early April and 32% in March.
In the July poll, Black adults were much more likely to report a negative mental health impact (68%) than were Hispanics or Whites, who were both at 51%. Age was also a factor: The youngest group of respondents (ages 18-29 years) had the highest negative-impact rate (62%), and the oldest group (65 years and older) had the lowest (47%), they said.
When it came to reporting the adverse effects of stress or worry, however, the situation was somewhat different. Hispanics had the highest rate of such effects at 63%, while Blacks had a rate of 57% and 47% of Whites reported issues with sleep, eating, temper, and other problems, Ms. Hamel and associates reported.
Over the last 2 months, more than half of Americans have experienced some sort of adverse effect caused by stress related to the COVID-19 pandemic, according to a survey from the Kaiser Family Foundation (KFF).
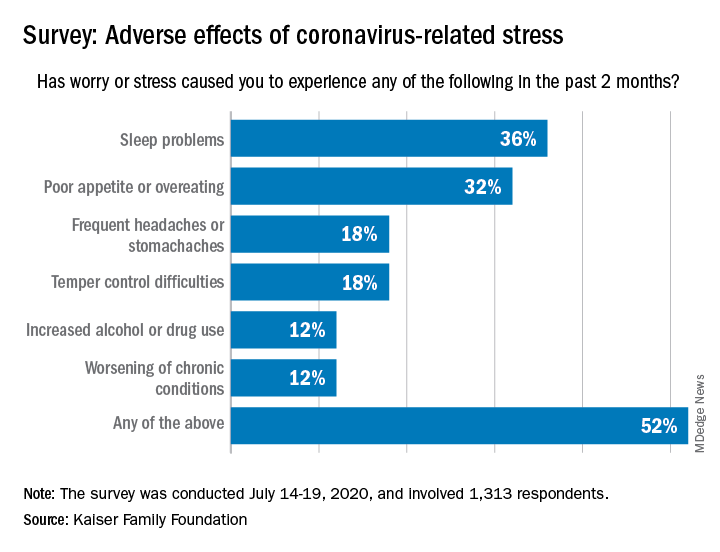
More than a third (36%) of the 1,313 respondents said they either had difficulty sleeping, falling asleep, or sleeping too much, KFF said in its latest Health Tracking Poll, conducted July 14-19, 2020. That was followed by poor appetite or overeating, which was mentioned by 32% of those surveyed.
Other adverse effects included frequent headaches or stomachaches (18%), temper-control issues (18%), increased drug or alcohol use (12%), and worsening of chronic conditions such as diabetes or hypertension (12%). Altogether, 52% of Americans have had at least one of these issues in the past 2 months, Liz Hamel and associates at KFF reported.
breaking down to 26% reporting a major impact and 28% reporting a minor impact (figures have been rounded), they said.
“As life with the coronavirus pandemic wears on, Americans increasingly say it is taking a negative toll on their mental health,” the investigators wrote. Earlier polls showed that pandemic-related stress was having an impact on mental health for 39% of respondents in May, compared with 45% in early April and 32% in March.
In the July poll, Black adults were much more likely to report a negative mental health impact (68%) than were Hispanics or Whites, who were both at 51%. Age was also a factor: The youngest group of respondents (ages 18-29 years) had the highest negative-impact rate (62%), and the oldest group (65 years and older) had the lowest (47%), they said.
When it came to reporting the adverse effects of stress or worry, however, the situation was somewhat different. Hispanics had the highest rate of such effects at 63%, while Blacks had a rate of 57% and 47% of Whites reported issues with sleep, eating, temper, and other problems, Ms. Hamel and associates reported.
Over the last 2 months, more than half of Americans have experienced some sort of adverse effect caused by stress related to the COVID-19 pandemic, according to a survey from the Kaiser Family Foundation (KFF).
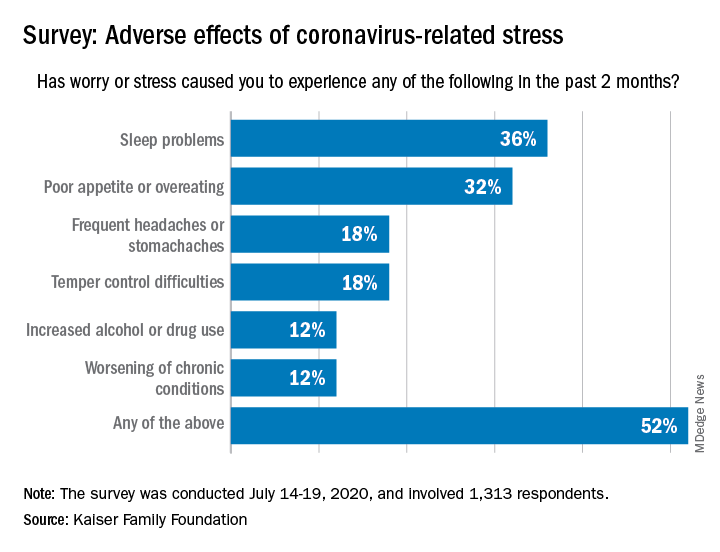
More than a third (36%) of the 1,313 respondents said they either had difficulty sleeping, falling asleep, or sleeping too much, KFF said in its latest Health Tracking Poll, conducted July 14-19, 2020. That was followed by poor appetite or overeating, which was mentioned by 32% of those surveyed.
Other adverse effects included frequent headaches or stomachaches (18%), temper-control issues (18%), increased drug or alcohol use (12%), and worsening of chronic conditions such as diabetes or hypertension (12%). Altogether, 52% of Americans have had at least one of these issues in the past 2 months, Liz Hamel and associates at KFF reported.
breaking down to 26% reporting a major impact and 28% reporting a minor impact (figures have been rounded), they said.
“As life with the coronavirus pandemic wears on, Americans increasingly say it is taking a negative toll on their mental health,” the investigators wrote. Earlier polls showed that pandemic-related stress was having an impact on mental health for 39% of respondents in May, compared with 45% in early April and 32% in March.
In the July poll, Black adults were much more likely to report a negative mental health impact (68%) than were Hispanics or Whites, who were both at 51%. Age was also a factor: The youngest group of respondents (ages 18-29 years) had the highest negative-impact rate (62%), and the oldest group (65 years and older) had the lowest (47%), they said.
When it came to reporting the adverse effects of stress or worry, however, the situation was somewhat different. Hispanics had the highest rate of such effects at 63%, while Blacks had a rate of 57% and 47% of Whites reported issues with sleep, eating, temper, and other problems, Ms. Hamel and associates reported.
Learn to anticipate, resolve difficult interactions with patients
Every physician encounters difficult or challenging patients during their career, but learning how to anticipate and handle these interactions is not something taught in medical school or residency, according to Donald W. Black, MD, MS.
Difficult or challenging encounters with patients are not only unavoidable, they should be expected, Dr. Black said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Every doctor I know has had challenging interactions,” he said. About 15% of encounters were deemed “difficult” in a prospective study of patients by Jeffrey L. Jackson, MD, MPH, and Kurt Kroenke, MD. A depressive or anxiety disorder was present in 29% of patients, with 11% experiencing two or more disorders. Major depression was present in 8.4%, other depressive disorders in 17.4%, panic disorder in 1.4%, and other anxiety disorders in 14.2% of patients. Dr. Jackson and Dr. Kroenke found that difficult patients demonstrated disrespect and anger, made threats, and locked themselves in rooms (Arch Intern Med. 1999 May 24;159[10]:1069-75). “Rest assured, you are not the only psychiatrist to face this type of issue,” Dr. Black said at the meeting, presented by Global Academy for Medical Education.
Common scenarios can include patients who want certain tests performed after researching symptoms online, threats of legal or social media action after feeling like they are not being listened to, a demand for a second opinion after not agreeing with a physician’s diagnosis, mistrust of doctors after presenting with symptoms and not being diagnosed, patients who focus on negative outcomes, and those who do not comply with treatment. These patients can often appear angry, defensive, frightened or resistant, or manipulative; may provide vague or exaggerated symptoms; or may inappropriately rely on hospital or clinic staff for emotional and physical support.
To complicate matters, the patients’ condition also might contribute to difficult interactions, such as in patients who have conditions like chronic pain or fibromyalgia.
“These often contribute because patients never feel that their problems are being appropriately addressed,” said Dr. Black, professor of psychiatry at the University of Iowa in Iowa City. Patients with psychiatric disorders can also present unique challenges that may result in difficult encounters. Patients with anxiety might not be able to be reassured by their doctor, for example, or patients with eating disorders might refuse treatment recommendations, he said.
Difficult encounters can lead to physicians feeling angry, upset, stressed, disrespected, abused, or fearful. But “it’s not just about the patient,” Dr. Black said. Physicians can become angry or defensive because of burnout, stress, or frustration, which can lead to them snapping at patients. Physicians are also overworked, sleep-deprived, and busier than they’d like to be, he added. Personal problems can contribute, and a physician’s belief system can cause a bad interaction with a patient. If physicians “label” one of their patients, that might end up becoming a “self-fulfilling prophecy” for that patient, Dr. Black said. Poor communication, such as not conveying bad news appropriately or with empathy, seeing a patient but never making eye contact, and using medical jargon that could be confusing to the patient, also can contribute to a challenging encounter, he added.
Situational issues also might create a bad experience for the patient. For example, a patient might find it hard to make an appointment, or the clinic might be busy or have a lack of privacy or encounter administrative issues. For patients who do not speak English as their native language, not having access to an interpreter can lead to frustration on the part of both the physician and the patient. “Bad interactions are not good for patient care,” Dr. Black said.
The key to resolving these issues is to focus on the goal, Dr. Black said. “We all want the same thing. We want to help the patient get better; we want to keep patients healthy; we want to keep them happy; we want to be fulfilled; [and] we want to manage our time and make a living – and meet our professional expectations.”
Begin by recognizing the difficult situation and assessing how the patient, the environment, or you might be contributing to the problem. “You have to step back and say what’s going on with this, and what are the factors that are combining to create this situation,” Dr. Black said. It is important to be calm and professional and not argue or talk over the patient. The goal is to work with the patient to find a solution.
One technique is to verbalize the problem without blaming the patient, the physician, or the environment (“We both have very different views about how your symptoms should be investigated, and that’s causing some difficulty between us. Do you agree?”).
There also might be alternative explanations for a patient’s behavior. For example, anger could be misdirected at a physician because of anxiety surrounding an unrelated event. In this case, it is important to listen to the patient and empathize, which will help the patient feel supported and build a rapport that can aid in resolving the problem encounter, Dr. Black said. Finding common ground when patients and physicians have different ideas on treatment or diagnosis is another way to help resolve a difficult encounter.
However, setting boundaries also is important, he noted. If, after remediation or if patients demonstrate signs of threatening or abusive behavior, initiate sexual advances, refuse to follow a treatment plan, fail to pay their bills, or are potentially putting themselves in harm’s way through noncompliance, a physician might consider terminating the relationship. Terminating the patient relationship should be done after attempting to work with the patient through a case manager and team members, and clearly advising a patient about behavior that could lead to termination of the patient-provider relationship.
Global Academy and this news organization are owned by the same parent company. Dr. Black reported that he is a consultant for Otsuka and receives royalties from American Psychiatric Publishing, Oxford University Press, and UpToDate. In addition, he receives funding from Nellie Ball Trust, the National Institute on Drug Abuse, the National Institute on Aging, and the National Center for Responsible Gaming.
Every physician encounters difficult or challenging patients during their career, but learning how to anticipate and handle these interactions is not something taught in medical school or residency, according to Donald W. Black, MD, MS.
Difficult or challenging encounters with patients are not only unavoidable, they should be expected, Dr. Black said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Every doctor I know has had challenging interactions,” he said. About 15% of encounters were deemed “difficult” in a prospective study of patients by Jeffrey L. Jackson, MD, MPH, and Kurt Kroenke, MD. A depressive or anxiety disorder was present in 29% of patients, with 11% experiencing two or more disorders. Major depression was present in 8.4%, other depressive disorders in 17.4%, panic disorder in 1.4%, and other anxiety disorders in 14.2% of patients. Dr. Jackson and Dr. Kroenke found that difficult patients demonstrated disrespect and anger, made threats, and locked themselves in rooms (Arch Intern Med. 1999 May 24;159[10]:1069-75). “Rest assured, you are not the only psychiatrist to face this type of issue,” Dr. Black said at the meeting, presented by Global Academy for Medical Education.
Common scenarios can include patients who want certain tests performed after researching symptoms online, threats of legal or social media action after feeling like they are not being listened to, a demand for a second opinion after not agreeing with a physician’s diagnosis, mistrust of doctors after presenting with symptoms and not being diagnosed, patients who focus on negative outcomes, and those who do not comply with treatment. These patients can often appear angry, defensive, frightened or resistant, or manipulative; may provide vague or exaggerated symptoms; or may inappropriately rely on hospital or clinic staff for emotional and physical support.
To complicate matters, the patients’ condition also might contribute to difficult interactions, such as in patients who have conditions like chronic pain or fibromyalgia.
“These often contribute because patients never feel that their problems are being appropriately addressed,” said Dr. Black, professor of psychiatry at the University of Iowa in Iowa City. Patients with psychiatric disorders can also present unique challenges that may result in difficult encounters. Patients with anxiety might not be able to be reassured by their doctor, for example, or patients with eating disorders might refuse treatment recommendations, he said.
Difficult encounters can lead to physicians feeling angry, upset, stressed, disrespected, abused, or fearful. But “it’s not just about the patient,” Dr. Black said. Physicians can become angry or defensive because of burnout, stress, or frustration, which can lead to them snapping at patients. Physicians are also overworked, sleep-deprived, and busier than they’d like to be, he added. Personal problems can contribute, and a physician’s belief system can cause a bad interaction with a patient. If physicians “label” one of their patients, that might end up becoming a “self-fulfilling prophecy” for that patient, Dr. Black said. Poor communication, such as not conveying bad news appropriately or with empathy, seeing a patient but never making eye contact, and using medical jargon that could be confusing to the patient, also can contribute to a challenging encounter, he added.
Situational issues also might create a bad experience for the patient. For example, a patient might find it hard to make an appointment, or the clinic might be busy or have a lack of privacy or encounter administrative issues. For patients who do not speak English as their native language, not having access to an interpreter can lead to frustration on the part of both the physician and the patient. “Bad interactions are not good for patient care,” Dr. Black said.
The key to resolving these issues is to focus on the goal, Dr. Black said. “We all want the same thing. We want to help the patient get better; we want to keep patients healthy; we want to keep them happy; we want to be fulfilled; [and] we want to manage our time and make a living – and meet our professional expectations.”
Begin by recognizing the difficult situation and assessing how the patient, the environment, or you might be contributing to the problem. “You have to step back and say what’s going on with this, and what are the factors that are combining to create this situation,” Dr. Black said. It is important to be calm and professional and not argue or talk over the patient. The goal is to work with the patient to find a solution.
One technique is to verbalize the problem without blaming the patient, the physician, or the environment (“We both have very different views about how your symptoms should be investigated, and that’s causing some difficulty between us. Do you agree?”).
There also might be alternative explanations for a patient’s behavior. For example, anger could be misdirected at a physician because of anxiety surrounding an unrelated event. In this case, it is important to listen to the patient and empathize, which will help the patient feel supported and build a rapport that can aid in resolving the problem encounter, Dr. Black said. Finding common ground when patients and physicians have different ideas on treatment or diagnosis is another way to help resolve a difficult encounter.
However, setting boundaries also is important, he noted. If, after remediation or if patients demonstrate signs of threatening or abusive behavior, initiate sexual advances, refuse to follow a treatment plan, fail to pay their bills, or are potentially putting themselves in harm’s way through noncompliance, a physician might consider terminating the relationship. Terminating the patient relationship should be done after attempting to work with the patient through a case manager and team members, and clearly advising a patient about behavior that could lead to termination of the patient-provider relationship.
Global Academy and this news organization are owned by the same parent company. Dr. Black reported that he is a consultant for Otsuka and receives royalties from American Psychiatric Publishing, Oxford University Press, and UpToDate. In addition, he receives funding from Nellie Ball Trust, the National Institute on Drug Abuse, the National Institute on Aging, and the National Center for Responsible Gaming.
Every physician encounters difficult or challenging patients during their career, but learning how to anticipate and handle these interactions is not something taught in medical school or residency, according to Donald W. Black, MD, MS.
Difficult or challenging encounters with patients are not only unavoidable, they should be expected, Dr. Black said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Every doctor I know has had challenging interactions,” he said. About 15% of encounters were deemed “difficult” in a prospective study of patients by Jeffrey L. Jackson, MD, MPH, and Kurt Kroenke, MD. A depressive or anxiety disorder was present in 29% of patients, with 11% experiencing two or more disorders. Major depression was present in 8.4%, other depressive disorders in 17.4%, panic disorder in 1.4%, and other anxiety disorders in 14.2% of patients. Dr. Jackson and Dr. Kroenke found that difficult patients demonstrated disrespect and anger, made threats, and locked themselves in rooms (Arch Intern Med. 1999 May 24;159[10]:1069-75). “Rest assured, you are not the only psychiatrist to face this type of issue,” Dr. Black said at the meeting, presented by Global Academy for Medical Education.
Common scenarios can include patients who want certain tests performed after researching symptoms online, threats of legal or social media action after feeling like they are not being listened to, a demand for a second opinion after not agreeing with a physician’s diagnosis, mistrust of doctors after presenting with symptoms and not being diagnosed, patients who focus on negative outcomes, and those who do not comply with treatment. These patients can often appear angry, defensive, frightened or resistant, or manipulative; may provide vague or exaggerated symptoms; or may inappropriately rely on hospital or clinic staff for emotional and physical support.
To complicate matters, the patients’ condition also might contribute to difficult interactions, such as in patients who have conditions like chronic pain or fibromyalgia.
“These often contribute because patients never feel that their problems are being appropriately addressed,” said Dr. Black, professor of psychiatry at the University of Iowa in Iowa City. Patients with psychiatric disorders can also present unique challenges that may result in difficult encounters. Patients with anxiety might not be able to be reassured by their doctor, for example, or patients with eating disorders might refuse treatment recommendations, he said.
Difficult encounters can lead to physicians feeling angry, upset, stressed, disrespected, abused, or fearful. But “it’s not just about the patient,” Dr. Black said. Physicians can become angry or defensive because of burnout, stress, or frustration, which can lead to them snapping at patients. Physicians are also overworked, sleep-deprived, and busier than they’d like to be, he added. Personal problems can contribute, and a physician’s belief system can cause a bad interaction with a patient. If physicians “label” one of their patients, that might end up becoming a “self-fulfilling prophecy” for that patient, Dr. Black said. Poor communication, such as not conveying bad news appropriately or with empathy, seeing a patient but never making eye contact, and using medical jargon that could be confusing to the patient, also can contribute to a challenging encounter, he added.
Situational issues also might create a bad experience for the patient. For example, a patient might find it hard to make an appointment, or the clinic might be busy or have a lack of privacy or encounter administrative issues. For patients who do not speak English as their native language, not having access to an interpreter can lead to frustration on the part of both the physician and the patient. “Bad interactions are not good for patient care,” Dr. Black said.
The key to resolving these issues is to focus on the goal, Dr. Black said. “We all want the same thing. We want to help the patient get better; we want to keep patients healthy; we want to keep them happy; we want to be fulfilled; [and] we want to manage our time and make a living – and meet our professional expectations.”
Begin by recognizing the difficult situation and assessing how the patient, the environment, or you might be contributing to the problem. “You have to step back and say what’s going on with this, and what are the factors that are combining to create this situation,” Dr. Black said. It is important to be calm and professional and not argue or talk over the patient. The goal is to work with the patient to find a solution.
One technique is to verbalize the problem without blaming the patient, the physician, or the environment (“We both have very different views about how your symptoms should be investigated, and that’s causing some difficulty between us. Do you agree?”).
There also might be alternative explanations for a patient’s behavior. For example, anger could be misdirected at a physician because of anxiety surrounding an unrelated event. In this case, it is important to listen to the patient and empathize, which will help the patient feel supported and build a rapport that can aid in resolving the problem encounter, Dr. Black said. Finding common ground when patients and physicians have different ideas on treatment or diagnosis is another way to help resolve a difficult encounter.
However, setting boundaries also is important, he noted. If, after remediation or if patients demonstrate signs of threatening or abusive behavior, initiate sexual advances, refuse to follow a treatment plan, fail to pay their bills, or are potentially putting themselves in harm’s way through noncompliance, a physician might consider terminating the relationship. Terminating the patient relationship should be done after attempting to work with the patient through a case manager and team members, and clearly advising a patient about behavior that could lead to termination of the patient-provider relationship.
Global Academy and this news organization are owned by the same parent company. Dr. Black reported that he is a consultant for Otsuka and receives royalties from American Psychiatric Publishing, Oxford University Press, and UpToDate. In addition, he receives funding from Nellie Ball Trust, the National Institute on Drug Abuse, the National Institute on Aging, and the National Center for Responsible Gaming.
FROM CP/AACP PSYCHIATRY UPDATE
Stress, COVID-19 contribute to mental health concerns in college students
Socioeconomic, technological, cultural, and historical conditions are contributing to a mental health crisis among college students in the United States, according to Anthony L. Rostain, MD, MA, in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
A recent National College Health Assessment published in fall of 2018 by the American College Health Association found that one in four college students had some kind of diagnosable mental illness, and 44% had symptoms of depression within the past year.
The assessment also found that college students felt overwhelmed (86%), felt sad (68%), felt very lonely (63%), had overwhelming anxiety (62%), experienced feelings of hopelessness (53%), or were depressed to the point where functioning was difficult (41%), all of which was higher than in previous years. Students also were more likely than in previous years to engage in interpersonal violence (17%), seriously consider suicide (11%), intentionally hurt themselves (7.4%), and attempt suicide (1.9%). According to the organization Active Minds, suicide is a leading cause of death in college students.
This shift in mental health for individuals in Generation Z, those born between the mid-1990s and early 2010s, can be attributed to historical events since the turn of the century, Dr. Rostain said at the meeting, presented by Global Academy for Medical Education. The Sept. 11, 2001, attacks, wars in Iraq and Afghanistan, the financial crisis of 2007-2008, school shootings, globalization leading to economic uncertainty, the 24-hour news cycle and continuous media exposure, and the influence of the Internet have all influenced Gen Z’s identity.
“Growing up immersed in the Internet certainly has its advantages, but also maybe created some vulnerabilities in our young people,” he said.
Concerns about climate change, the burden of higher education and student debt, and the COVID-19 pandemic also have contributed to anxiety in this group. In a spring survey of students published by Active Minds about COVID-19 and its impact on mental health, 91% of students reported having stress or anxiety, 81% were disappointed or sad, 80% said they felt lonely or isolated, 56% had relocated as a result of the pandemic, and 48% reported financial setbacks tied to COVID-19.
“Anxiety seems to have become a feature of modern life,” said Dr. Rostain, who is director of education at the department of psychiatry and professor of psychiatry at the Hospital of the University of Pennsylvania in Philadelphia.
“Our culture, which often has a prominent emotional tone of fear, tends to promote cognitive distortions in which everyone is perceiving danger at every turn.” in this group, he noted. While people should be washing their hands and staying safe through social distancing during the pandemic, “we don’t want people to stop functioning, planning the future, and really in college students’ case, studying and getting ready for their careers,” he said. Parents can hinder those goals through intensively parenting or “overparenting” their children, which can result in destructive perfectionism, anxiety and depression, abject fear of failure and risk avoidance, and a focus on the external aspects of life rather than internal feelings.
Heavier alcohol use and amphetamine use also is on the rise in college students, Dr. Rostain said. Increased stimulant use in young adults is attributed to greater access to prescription drugs prior to college, greater prevalence of attention-deficit/hyperactivity disorder (ADHD), peer pressure, and influence from marketing and media messaging, he said. Another important change is the rise of smartphones and the Internet, which might drive the need to be constantly connected and compete for attention.
“This is the first generation who had constant access to the Internet. Smartphones in particular are everywhere, and we think this is another important factor in considering what might be happening to young people,” Dr. Rostain said.
Developing problem-solving and conflict resolution skills, developing coping mechanisms, being able to regulate emotions, finding optimism toward the future, having access to mental health services, and having cultural or religious beliefs with a negative view of suicide are all protective factors that promote resiliency in young people, Dr. Rostain said. Other protective factors include the development of socio-emotional readiness skills, such as conscientiousness, self-management, interpersonal skills, self-control, task persistence, risk management, self-acceptance, and having an open mindset or seeking help when needed. However, he noted, family is one area that can be both a help or a risk to mental health.
“Family attachments and supportive relationships in the family are really critical in predicting good outcomes. By the same token, families that are conflicted, where there’s a lot of stress or there’s a lot of turmoil and/or where resources are not available, that may be a risk factor to coping in young adulthood,” he said.
Individual resilience can be developed through learning from mistakes and overcoming mindset barriers, such as feelings of not belonging, concerns about disappointing one’s parents, worries about not making it, or fears of being different.
On campus, best practices and emerging trends include wellness and resiliency programs, reducing stigma, engagement from students, training of faculty and staff, crisis management plans, telehealth counseling, substance abuse programs, postvention support after suicide, collaboration with mental health providers, and support for diverse populations.
“The best schools are the ones that promote communication and that invite families to be involved early on because parents and families can be and need to be educated about what to do to prevent adverse outcomes of young people who are really at risk,” Dr. Rostain said. “It takes a village to raise a child, and it takes the same village to bring someone from adolescence to young adulthood.”
Family-based intervention has also shown promise, he said, but clinicians should watch for signs that a family is not willing to undergo therapy, is scapegoating a college student, or there are signs of boundary violations, violence, or sexual abuse in the family – or attempts to undermine treatment.
Specific to COVID-19, campus mental health services should focus on routine, self-care, physical activity, and connections with other people while also space for grieving lost experiences, facing uncertainty, developing resilience, and finding meaning. In the family, challenges around COVID-19 can include issues of physical distancing and quarantine, anxiety about becoming infected with the virus, economic insecurity, managing conflicts, setting and enforcing boundaries in addition to providing mutual support, and finding new meaning during the pandemic.
“I think these are the challenges, but we think this whole process of people living together and handling life in a way they’ve never expected to may hold some silver linings,” Dr. Rostain said. “It may be a way of addressing many issues that were never addressed before the young person went off to college.”
Global Academy and this news organization are owned by the same parent company. Dr. Rostain reported receiving royalties from Routledge/Taylor Francis Group and St. Martin’s Press, scientific advisory board honoraria from Arbor and Shire/Takeda, consulting fees from the National Football League and Tris Pharmaceuticals, and has presented CME sessions for American Psychiatric Publishing, Global Medical Education, Shire/Takeda, and the U.S. Psychiatric Congress.
Socioeconomic, technological, cultural, and historical conditions are contributing to a mental health crisis among college students in the United States, according to Anthony L. Rostain, MD, MA, in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
A recent National College Health Assessment published in fall of 2018 by the American College Health Association found that one in four college students had some kind of diagnosable mental illness, and 44% had symptoms of depression within the past year.
The assessment also found that college students felt overwhelmed (86%), felt sad (68%), felt very lonely (63%), had overwhelming anxiety (62%), experienced feelings of hopelessness (53%), or were depressed to the point where functioning was difficult (41%), all of which was higher than in previous years. Students also were more likely than in previous years to engage in interpersonal violence (17%), seriously consider suicide (11%), intentionally hurt themselves (7.4%), and attempt suicide (1.9%). According to the organization Active Minds, suicide is a leading cause of death in college students.
This shift in mental health for individuals in Generation Z, those born between the mid-1990s and early 2010s, can be attributed to historical events since the turn of the century, Dr. Rostain said at the meeting, presented by Global Academy for Medical Education. The Sept. 11, 2001, attacks, wars in Iraq and Afghanistan, the financial crisis of 2007-2008, school shootings, globalization leading to economic uncertainty, the 24-hour news cycle and continuous media exposure, and the influence of the Internet have all influenced Gen Z’s identity.
“Growing up immersed in the Internet certainly has its advantages, but also maybe created some vulnerabilities in our young people,” he said.
Concerns about climate change, the burden of higher education and student debt, and the COVID-19 pandemic also have contributed to anxiety in this group. In a spring survey of students published by Active Minds about COVID-19 and its impact on mental health, 91% of students reported having stress or anxiety, 81% were disappointed or sad, 80% said they felt lonely or isolated, 56% had relocated as a result of the pandemic, and 48% reported financial setbacks tied to COVID-19.
“Anxiety seems to have become a feature of modern life,” said Dr. Rostain, who is director of education at the department of psychiatry and professor of psychiatry at the Hospital of the University of Pennsylvania in Philadelphia.
“Our culture, which often has a prominent emotional tone of fear, tends to promote cognitive distortions in which everyone is perceiving danger at every turn.” in this group, he noted. While people should be washing their hands and staying safe through social distancing during the pandemic, “we don’t want people to stop functioning, planning the future, and really in college students’ case, studying and getting ready for their careers,” he said. Parents can hinder those goals through intensively parenting or “overparenting” their children, which can result in destructive perfectionism, anxiety and depression, abject fear of failure and risk avoidance, and a focus on the external aspects of life rather than internal feelings.
Heavier alcohol use and amphetamine use also is on the rise in college students, Dr. Rostain said. Increased stimulant use in young adults is attributed to greater access to prescription drugs prior to college, greater prevalence of attention-deficit/hyperactivity disorder (ADHD), peer pressure, and influence from marketing and media messaging, he said. Another important change is the rise of smartphones and the Internet, which might drive the need to be constantly connected and compete for attention.
“This is the first generation who had constant access to the Internet. Smartphones in particular are everywhere, and we think this is another important factor in considering what might be happening to young people,” Dr. Rostain said.
Developing problem-solving and conflict resolution skills, developing coping mechanisms, being able to regulate emotions, finding optimism toward the future, having access to mental health services, and having cultural or religious beliefs with a negative view of suicide are all protective factors that promote resiliency in young people, Dr. Rostain said. Other protective factors include the development of socio-emotional readiness skills, such as conscientiousness, self-management, interpersonal skills, self-control, task persistence, risk management, self-acceptance, and having an open mindset or seeking help when needed. However, he noted, family is one area that can be both a help or a risk to mental health.
“Family attachments and supportive relationships in the family are really critical in predicting good outcomes. By the same token, families that are conflicted, where there’s a lot of stress or there’s a lot of turmoil and/or where resources are not available, that may be a risk factor to coping in young adulthood,” he said.
Individual resilience can be developed through learning from mistakes and overcoming mindset barriers, such as feelings of not belonging, concerns about disappointing one’s parents, worries about not making it, or fears of being different.
On campus, best practices and emerging trends include wellness and resiliency programs, reducing stigma, engagement from students, training of faculty and staff, crisis management plans, telehealth counseling, substance abuse programs, postvention support after suicide, collaboration with mental health providers, and support for diverse populations.
“The best schools are the ones that promote communication and that invite families to be involved early on because parents and families can be and need to be educated about what to do to prevent adverse outcomes of young people who are really at risk,” Dr. Rostain said. “It takes a village to raise a child, and it takes the same village to bring someone from adolescence to young adulthood.”
Family-based intervention has also shown promise, he said, but clinicians should watch for signs that a family is not willing to undergo therapy, is scapegoating a college student, or there are signs of boundary violations, violence, or sexual abuse in the family – or attempts to undermine treatment.
Specific to COVID-19, campus mental health services should focus on routine, self-care, physical activity, and connections with other people while also space for grieving lost experiences, facing uncertainty, developing resilience, and finding meaning. In the family, challenges around COVID-19 can include issues of physical distancing and quarantine, anxiety about becoming infected with the virus, economic insecurity, managing conflicts, setting and enforcing boundaries in addition to providing mutual support, and finding new meaning during the pandemic.
“I think these are the challenges, but we think this whole process of people living together and handling life in a way they’ve never expected to may hold some silver linings,” Dr. Rostain said. “It may be a way of addressing many issues that were never addressed before the young person went off to college.”
Global Academy and this news organization are owned by the same parent company. Dr. Rostain reported receiving royalties from Routledge/Taylor Francis Group and St. Martin’s Press, scientific advisory board honoraria from Arbor and Shire/Takeda, consulting fees from the National Football League and Tris Pharmaceuticals, and has presented CME sessions for American Psychiatric Publishing, Global Medical Education, Shire/Takeda, and the U.S. Psychiatric Congress.
Socioeconomic, technological, cultural, and historical conditions are contributing to a mental health crisis among college students in the United States, according to Anthony L. Rostain, MD, MA, in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
A recent National College Health Assessment published in fall of 2018 by the American College Health Association found that one in four college students had some kind of diagnosable mental illness, and 44% had symptoms of depression within the past year.
The assessment also found that college students felt overwhelmed (86%), felt sad (68%), felt very lonely (63%), had overwhelming anxiety (62%), experienced feelings of hopelessness (53%), or were depressed to the point where functioning was difficult (41%), all of which was higher than in previous years. Students also were more likely than in previous years to engage in interpersonal violence (17%), seriously consider suicide (11%), intentionally hurt themselves (7.4%), and attempt suicide (1.9%). According to the organization Active Minds, suicide is a leading cause of death in college students.
This shift in mental health for individuals in Generation Z, those born between the mid-1990s and early 2010s, can be attributed to historical events since the turn of the century, Dr. Rostain said at the meeting, presented by Global Academy for Medical Education. The Sept. 11, 2001, attacks, wars in Iraq and Afghanistan, the financial crisis of 2007-2008, school shootings, globalization leading to economic uncertainty, the 24-hour news cycle and continuous media exposure, and the influence of the Internet have all influenced Gen Z’s identity.
“Growing up immersed in the Internet certainly has its advantages, but also maybe created some vulnerabilities in our young people,” he said.
Concerns about climate change, the burden of higher education and student debt, and the COVID-19 pandemic also have contributed to anxiety in this group. In a spring survey of students published by Active Minds about COVID-19 and its impact on mental health, 91% of students reported having stress or anxiety, 81% were disappointed or sad, 80% said they felt lonely or isolated, 56% had relocated as a result of the pandemic, and 48% reported financial setbacks tied to COVID-19.
“Anxiety seems to have become a feature of modern life,” said Dr. Rostain, who is director of education at the department of psychiatry and professor of psychiatry at the Hospital of the University of Pennsylvania in Philadelphia.
“Our culture, which often has a prominent emotional tone of fear, tends to promote cognitive distortions in which everyone is perceiving danger at every turn.” in this group, he noted. While people should be washing their hands and staying safe through social distancing during the pandemic, “we don’t want people to stop functioning, planning the future, and really in college students’ case, studying and getting ready for their careers,” he said. Parents can hinder those goals through intensively parenting or “overparenting” their children, which can result in destructive perfectionism, anxiety and depression, abject fear of failure and risk avoidance, and a focus on the external aspects of life rather than internal feelings.
Heavier alcohol use and amphetamine use also is on the rise in college students, Dr. Rostain said. Increased stimulant use in young adults is attributed to greater access to prescription drugs prior to college, greater prevalence of attention-deficit/hyperactivity disorder (ADHD), peer pressure, and influence from marketing and media messaging, he said. Another important change is the rise of smartphones and the Internet, which might drive the need to be constantly connected and compete for attention.
“This is the first generation who had constant access to the Internet. Smartphones in particular are everywhere, and we think this is another important factor in considering what might be happening to young people,” Dr. Rostain said.
Developing problem-solving and conflict resolution skills, developing coping mechanisms, being able to regulate emotions, finding optimism toward the future, having access to mental health services, and having cultural or religious beliefs with a negative view of suicide are all protective factors that promote resiliency in young people, Dr. Rostain said. Other protective factors include the development of socio-emotional readiness skills, such as conscientiousness, self-management, interpersonal skills, self-control, task persistence, risk management, self-acceptance, and having an open mindset or seeking help when needed. However, he noted, family is one area that can be both a help or a risk to mental health.
“Family attachments and supportive relationships in the family are really critical in predicting good outcomes. By the same token, families that are conflicted, where there’s a lot of stress or there’s a lot of turmoil and/or where resources are not available, that may be a risk factor to coping in young adulthood,” he said.
Individual resilience can be developed through learning from mistakes and overcoming mindset barriers, such as feelings of not belonging, concerns about disappointing one’s parents, worries about not making it, or fears of being different.
On campus, best practices and emerging trends include wellness and resiliency programs, reducing stigma, engagement from students, training of faculty and staff, crisis management plans, telehealth counseling, substance abuse programs, postvention support after suicide, collaboration with mental health providers, and support for diverse populations.
“The best schools are the ones that promote communication and that invite families to be involved early on because parents and families can be and need to be educated about what to do to prevent adverse outcomes of young people who are really at risk,” Dr. Rostain said. “It takes a village to raise a child, and it takes the same village to bring someone from adolescence to young adulthood.”
Family-based intervention has also shown promise, he said, but clinicians should watch for signs that a family is not willing to undergo therapy, is scapegoating a college student, or there are signs of boundary violations, violence, or sexual abuse in the family – or attempts to undermine treatment.
Specific to COVID-19, campus mental health services should focus on routine, self-care, physical activity, and connections with other people while also space for grieving lost experiences, facing uncertainty, developing resilience, and finding meaning. In the family, challenges around COVID-19 can include issues of physical distancing and quarantine, anxiety about becoming infected with the virus, economic insecurity, managing conflicts, setting and enforcing boundaries in addition to providing mutual support, and finding new meaning during the pandemic.
“I think these are the challenges, but we think this whole process of people living together and handling life in a way they’ve never expected to may hold some silver linings,” Dr. Rostain said. “It may be a way of addressing many issues that were never addressed before the young person went off to college.”
Global Academy and this news organization are owned by the same parent company. Dr. Rostain reported receiving royalties from Routledge/Taylor Francis Group and St. Martin’s Press, scientific advisory board honoraria from Arbor and Shire/Takeda, consulting fees from the National Football League and Tris Pharmaceuticals, and has presented CME sessions for American Psychiatric Publishing, Global Medical Education, Shire/Takeda, and the U.S. Psychiatric Congress.
EXPERT ANALYSIS FROM CP/AACP 2020 PSYCHIATRY UPDATE
Revisiting Xanax amid the coronavirus crisis
One of the more alarming trends that has emerged during the coronavirus crisis is the concomitant rise in the use of benzodiazepines, such as Xanax. It has been reported that at-risk individuals began seeking prescription anxiolytics as early as mid-February with a consequent peak of 34% the following month, coinciding with the World Health Organization’s declaration of a global pandemic.1
Consistent with the available literature indicating that women are twice as likely to be affected by anxiety disorders, the prescription spikes were almost double when compared with those of their male counterparts.2 The pandemic has instilled a sense of fear in people, leading to social repercussions, such as estrangement, insomnia, and paranoia for at-risk populations.3,4
“Benzos” are commonly prescribed to help people sleep or to assist them in overcoming a host of anxiety disorders. The rapid onset of effects make Xanax a desirable and efficacious benzodiazepine.5 The use of these medications might not be an immediate cause for concern because patients might be taking it as intended. Nevertheless, clinicians are shying away from medical management in favor of counseling or therapy.
Dangerous trends
Numerous factors might contribute to this grim scenario, including patient dependence on benzodiazepines, paranoia about engaging with health care professionals because of fear tied to potential COVID-19 exposure, and/or increased access to illicit counterfeit pills from drug dealers or the dark web markets.
Lessons can be gleaned from the most extensive dark web drug busts in Britain’s history, in which a deluge of “pharmaceutical grade” Xanax pills made it to the hands of drug dealers and consumers between 2015 and 2017.6 A similar phenomenon emerged stateside.7 Virtually indistinguishable from recognized 2-mg Xanax pills, these fake pills posed a serious challenge to forensic scientists.8 The threat of overdose is very real for users targeted by the counterfeit Xanax trade, especially since those at risk often bypass professional health care guidelines.
In broad daylight, the drug dealers ran their operations revolving around two fake Xanax products: a primary knockoff and a limited edition – and vastly more potent “Red Devil” variant that was intentionally dyed for branding purposes. Because the “Red Devil” formulations contained 2.5 times the dose of the 2-mg pill, it had even more pronounced tolerance, dependence, and withdrawal effects (for example, panic attacks, anxiety, and/or hallucinations) – fatal consequences for users involved in consuming other drugs, such as alcohol or opioids. Preexisting drug users tend to gravitate toward benzodiazepines, such as alprazolam (Xanax), perhaps in part, because of its relatively rapid onset of action. Xanax also is known for inducing proeuphoric states at higher doses, hence the appeal of the “Red Devil” pills.
Benzodiazepines, as a class of drugs, facilitate the neurotransmitter gamma-aminobutryric acid’s (GABA) effect on the brain, producing anxiolytic, hypnotic, and/or anticonvulsant states within the user.9 Unbeknownst to numerous users is the fact that drugs such as alcohol and opioids, like Xanax, also serve as respiratory depressants, overriding the brain’s governance of the breathing mechanism. This, in turn, leads to unintended overdose deaths, even among seasoned drug seekers.
Overdose deaths have been steadily climbing over the years because it is common for some users to consume alcohol while being on Xanax therapy – without realizing that both substances are depressants and that taking them together can lead to side effects such as respiratory depression.
Forensic cases also have revealed that preexisting opioid consumers were drawn to Xanax; the drug’s potent mechanism of action would likely appeal to habituated users. A typical behavioral pattern has emerged among users and must be addressed. According to Australian Professor Shane Darke: “So they take their Xanax, they take their painkiller, then they get drunk, that could be enough to kill them.”
Fatalities are more likely when benzodiazepines are combined with other drug classes or if the existing supply is contaminated or laced (for example, with fentanyl).8
As far as deaths by accidental benzodiazepine overdose are concerned, a similar epidemic has been recorded in the United States. In 2013, almost one-third of all prescription overdose deaths can be attributed to the use of benzodiazepines (for example, Xanax, Valium, and Ativan). However, media attention has been considerably muted, especially when compared with that of narcotic abuse. This is even more puzzling when taking into account that three-quarters of benzodiazepine mortalities co-occur within the context of narcotic consumption. Substance Abuse and Mental Health Services Administration data confirm the ubiquitous nature of benzodiazepine (such as alprazolam) coprescriptions, accounting for roughly half of the 176,000 emergency department cases for 2011. The Centers for Disease Control and Prevention noted that there was a 67% increase in benzodiazepine prescriptions between 1996 and 2013, which warranted more stringent regulations for this particular class of drugs.
In 2016, the CDC issued new guidelines for opioid use acknowledging the danger of benzodiazepine coprescriptions. Food and Drug Administration “black box” warnings now grace the prescriptions of both of these drug classes.10 This trend remains on an upward trajectory, even more so during the pandemic, as there are 9.7 million prescriptions of anxiolytics/hypnotics such as Xanax, Ativan, and Klonopin in the United States as of March 2020, which represents a 10% increase over the previous year. , as well as the implementation of urine drug screening monitoring for drug adherence/compliance and diversion in those with suspected benzodiazepine addiction or a history of polysubstance abuse.11,12
Clinical correlates
For patients who present acutely with Xanax toxicity in the emergency room setting, we will need to initially stabilize the vital signs and address the ongoing symptoms. It is advisable to arrange health care accommodations for patients with physical dependence to monitor and treat their withdrawal symptoms. The patient should be enrolled in a comprehensive addiction facility after undergoing formal detoxification; a tapered treatment protocol will need to be implemented because quitting “cold turkey” can lead to convulsions and, in some cases, death. Patient education, talk therapy, and alternatives to benzodiazepines should be discussed with the clinician.13,145
However, to truly address the elephant in the room, we will need to consider institutional reforms to prevent a similar situation from arising in the future. Primary care physician shortages are compounded by changes in insurance policies. Nurses and physician assistants will need to be trained to manage benzodiazepine prescriptions. If there are community shortages in physicians, patients might turn to illegal means to secure their benzodiazepine supply, and it is imperative that we have the necessary fellowship and education programs to educate nonphysician health care clinicians with benzodiazepine management. Because physicians were prescribing benzodiazepines liberally, the Prescription Drug Monitoring Programs (PDMP) was enacted to monitor physician practices. Unfortunately, this ultimately intimidated physicians and effectively curbed reasonable physician prescribing patterns. It might be necessary to revisit existing prescription monitoring programs, encourage drug evaluations and guidelines based on evidence-based medicine and embrace telemedicine in order to facilitate patient-physician communication.
As of now, it is too early to prescribe Xanax routinely for ongoing anxiety experienced during the coronavirus crisis, and several physicians are cautious about prescribing antianxiety medications for more than a few months.17 Surprisingly, researchers in Barcelona have even explored the role of Xanax as potentially inhibiting Mpro, the primary protease of coronavirus, thereby forestalling the virus’s ability to replicate.16 However, it is worth noting that, given the preliminary nature of the results, any attempts at conclusively integrating Xanax within the context of coronavirus therapy would be premature.
References
1. Luhby T. Anti-anxiety medication prescriptions up 34% since coronavirus. CNN. 2020 Apr 16.
2. Women and Anxiety. Anxiety and Depression Association of America.
3. Shigemura J et al. Psychiatry Clin Neurosci. 2012 Apr 7;74(4):281-2.
4. Petersen A. More people are taking drugs for anxiety and insomnia, and doctors are worried. The Wall Street Journal. 2020 May 25.
5. Downey M. Xanax overdose and related deaths. National Drug & Alcohol Research Centre. UNSW Sydney.
6. Bryant B. Fake Xanax: The UK’s biggest ever dark net drugs bust. BBC. 2018 Mar 10.
7. Reinberg S. Fatal overdoses rising from sedatives like Valium, Xanax. HealthDay. 2016 Feb.
8. Is counterfeit Xanax dangerous? American Addiction Centers. Updated 2018 Nov 14.
9. McLaren E. Xanax history and statistics. Drugabuse.com.
10. Benzodiazepines and opioids. National Institute on Drug Abuse. 2018 Mar 15.
11. Choudhry Z et al. J Psychiatry. 2015;18(5). doi: 10.4172/2378-5756.1000319.
12. Islam FA et al. Current Psychiatry. 2018 Dec 17(12):43-4.
13. Adams M. Xanax death rate on the rise. White Sands Treatment. 2017 Sept.NEED LINK
14. Storrs C. Benzodiazepine overdose deaths soared in recent years, study finds. CNN. 2016 Feb. 18.
15. Hanscom DA. Plan A – Thrive and survive COVID-19. Back in Control. 2020.
16. Smith C. Xanax, a common anxiety medication, might actually block coronavirus. BGR. 2020 May 29.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Mr. Choudhry is a research assistant at the IMCHF. He has no disclosures.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. He has no disclosures.
One of the more alarming trends that has emerged during the coronavirus crisis is the concomitant rise in the use of benzodiazepines, such as Xanax. It has been reported that at-risk individuals began seeking prescription anxiolytics as early as mid-February with a consequent peak of 34% the following month, coinciding with the World Health Organization’s declaration of a global pandemic.1
Consistent with the available literature indicating that women are twice as likely to be affected by anxiety disorders, the prescription spikes were almost double when compared with those of their male counterparts.2 The pandemic has instilled a sense of fear in people, leading to social repercussions, such as estrangement, insomnia, and paranoia for at-risk populations.3,4
“Benzos” are commonly prescribed to help people sleep or to assist them in overcoming a host of anxiety disorders. The rapid onset of effects make Xanax a desirable and efficacious benzodiazepine.5 The use of these medications might not be an immediate cause for concern because patients might be taking it as intended. Nevertheless, clinicians are shying away from medical management in favor of counseling or therapy.
Dangerous trends
Numerous factors might contribute to this grim scenario, including patient dependence on benzodiazepines, paranoia about engaging with health care professionals because of fear tied to potential COVID-19 exposure, and/or increased access to illicit counterfeit pills from drug dealers or the dark web markets.
Lessons can be gleaned from the most extensive dark web drug busts in Britain’s history, in which a deluge of “pharmaceutical grade” Xanax pills made it to the hands of drug dealers and consumers between 2015 and 2017.6 A similar phenomenon emerged stateside.7 Virtually indistinguishable from recognized 2-mg Xanax pills, these fake pills posed a serious challenge to forensic scientists.8 The threat of overdose is very real for users targeted by the counterfeit Xanax trade, especially since those at risk often bypass professional health care guidelines.
In broad daylight, the drug dealers ran their operations revolving around two fake Xanax products: a primary knockoff and a limited edition – and vastly more potent “Red Devil” variant that was intentionally dyed for branding purposes. Because the “Red Devil” formulations contained 2.5 times the dose of the 2-mg pill, it had even more pronounced tolerance, dependence, and withdrawal effects (for example, panic attacks, anxiety, and/or hallucinations) – fatal consequences for users involved in consuming other drugs, such as alcohol or opioids. Preexisting drug users tend to gravitate toward benzodiazepines, such as alprazolam (Xanax), perhaps in part, because of its relatively rapid onset of action. Xanax also is known for inducing proeuphoric states at higher doses, hence the appeal of the “Red Devil” pills.
Benzodiazepines, as a class of drugs, facilitate the neurotransmitter gamma-aminobutryric acid’s (GABA) effect on the brain, producing anxiolytic, hypnotic, and/or anticonvulsant states within the user.9 Unbeknownst to numerous users is the fact that drugs such as alcohol and opioids, like Xanax, also serve as respiratory depressants, overriding the brain’s governance of the breathing mechanism. This, in turn, leads to unintended overdose deaths, even among seasoned drug seekers.
Overdose deaths have been steadily climbing over the years because it is common for some users to consume alcohol while being on Xanax therapy – without realizing that both substances are depressants and that taking them together can lead to side effects such as respiratory depression.
Forensic cases also have revealed that preexisting opioid consumers were drawn to Xanax; the drug’s potent mechanism of action would likely appeal to habituated users. A typical behavioral pattern has emerged among users and must be addressed. According to Australian Professor Shane Darke: “So they take their Xanax, they take their painkiller, then they get drunk, that could be enough to kill them.”
Fatalities are more likely when benzodiazepines are combined with other drug classes or if the existing supply is contaminated or laced (for example, with fentanyl).8
As far as deaths by accidental benzodiazepine overdose are concerned, a similar epidemic has been recorded in the United States. In 2013, almost one-third of all prescription overdose deaths can be attributed to the use of benzodiazepines (for example, Xanax, Valium, and Ativan). However, media attention has been considerably muted, especially when compared with that of narcotic abuse. This is even more puzzling when taking into account that three-quarters of benzodiazepine mortalities co-occur within the context of narcotic consumption. Substance Abuse and Mental Health Services Administration data confirm the ubiquitous nature of benzodiazepine (such as alprazolam) coprescriptions, accounting for roughly half of the 176,000 emergency department cases for 2011. The Centers for Disease Control and Prevention noted that there was a 67% increase in benzodiazepine prescriptions between 1996 and 2013, which warranted more stringent regulations for this particular class of drugs.
In 2016, the CDC issued new guidelines for opioid use acknowledging the danger of benzodiazepine coprescriptions. Food and Drug Administration “black box” warnings now grace the prescriptions of both of these drug classes.10 This trend remains on an upward trajectory, even more so during the pandemic, as there are 9.7 million prescriptions of anxiolytics/hypnotics such as Xanax, Ativan, and Klonopin in the United States as of March 2020, which represents a 10% increase over the previous year. , as well as the implementation of urine drug screening monitoring for drug adherence/compliance and diversion in those with suspected benzodiazepine addiction or a history of polysubstance abuse.11,12
Clinical correlates
For patients who present acutely with Xanax toxicity in the emergency room setting, we will need to initially stabilize the vital signs and address the ongoing symptoms. It is advisable to arrange health care accommodations for patients with physical dependence to monitor and treat their withdrawal symptoms. The patient should be enrolled in a comprehensive addiction facility after undergoing formal detoxification; a tapered treatment protocol will need to be implemented because quitting “cold turkey” can lead to convulsions and, in some cases, death. Patient education, talk therapy, and alternatives to benzodiazepines should be discussed with the clinician.13,145
However, to truly address the elephant in the room, we will need to consider institutional reforms to prevent a similar situation from arising in the future. Primary care physician shortages are compounded by changes in insurance policies. Nurses and physician assistants will need to be trained to manage benzodiazepine prescriptions. If there are community shortages in physicians, patients might turn to illegal means to secure their benzodiazepine supply, and it is imperative that we have the necessary fellowship and education programs to educate nonphysician health care clinicians with benzodiazepine management. Because physicians were prescribing benzodiazepines liberally, the Prescription Drug Monitoring Programs (PDMP) was enacted to monitor physician practices. Unfortunately, this ultimately intimidated physicians and effectively curbed reasonable physician prescribing patterns. It might be necessary to revisit existing prescription monitoring programs, encourage drug evaluations and guidelines based on evidence-based medicine and embrace telemedicine in order to facilitate patient-physician communication.
As of now, it is too early to prescribe Xanax routinely for ongoing anxiety experienced during the coronavirus crisis, and several physicians are cautious about prescribing antianxiety medications for more than a few months.17 Surprisingly, researchers in Barcelona have even explored the role of Xanax as potentially inhibiting Mpro, the primary protease of coronavirus, thereby forestalling the virus’s ability to replicate.16 However, it is worth noting that, given the preliminary nature of the results, any attempts at conclusively integrating Xanax within the context of coronavirus therapy would be premature.
References
1. Luhby T. Anti-anxiety medication prescriptions up 34% since coronavirus. CNN. 2020 Apr 16.
2. Women and Anxiety. Anxiety and Depression Association of America.
3. Shigemura J et al. Psychiatry Clin Neurosci. 2012 Apr 7;74(4):281-2.
4. Petersen A. More people are taking drugs for anxiety and insomnia, and doctors are worried. The Wall Street Journal. 2020 May 25.
5. Downey M. Xanax overdose and related deaths. National Drug & Alcohol Research Centre. UNSW Sydney.
6. Bryant B. Fake Xanax: The UK’s biggest ever dark net drugs bust. BBC. 2018 Mar 10.
7. Reinberg S. Fatal overdoses rising from sedatives like Valium, Xanax. HealthDay. 2016 Feb.
8. Is counterfeit Xanax dangerous? American Addiction Centers. Updated 2018 Nov 14.
9. McLaren E. Xanax history and statistics. Drugabuse.com.
10. Benzodiazepines and opioids. National Institute on Drug Abuse. 2018 Mar 15.
11. Choudhry Z et al. J Psychiatry. 2015;18(5). doi: 10.4172/2378-5756.1000319.
12. Islam FA et al. Current Psychiatry. 2018 Dec 17(12):43-4.
13. Adams M. Xanax death rate on the rise. White Sands Treatment. 2017 Sept.NEED LINK
14. Storrs C. Benzodiazepine overdose deaths soared in recent years, study finds. CNN. 2016 Feb. 18.
15. Hanscom DA. Plan A – Thrive and survive COVID-19. Back in Control. 2020.
16. Smith C. Xanax, a common anxiety medication, might actually block coronavirus. BGR. 2020 May 29.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Mr. Choudhry is a research assistant at the IMCHF. He has no disclosures.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. He has no disclosures.
One of the more alarming trends that has emerged during the coronavirus crisis is the concomitant rise in the use of benzodiazepines, such as Xanax. It has been reported that at-risk individuals began seeking prescription anxiolytics as early as mid-February with a consequent peak of 34% the following month, coinciding with the World Health Organization’s declaration of a global pandemic.1
Consistent with the available literature indicating that women are twice as likely to be affected by anxiety disorders, the prescription spikes were almost double when compared with those of their male counterparts.2 The pandemic has instilled a sense of fear in people, leading to social repercussions, such as estrangement, insomnia, and paranoia for at-risk populations.3,4
“Benzos” are commonly prescribed to help people sleep or to assist them in overcoming a host of anxiety disorders. The rapid onset of effects make Xanax a desirable and efficacious benzodiazepine.5 The use of these medications might not be an immediate cause for concern because patients might be taking it as intended. Nevertheless, clinicians are shying away from medical management in favor of counseling or therapy.
Dangerous trends
Numerous factors might contribute to this grim scenario, including patient dependence on benzodiazepines, paranoia about engaging with health care professionals because of fear tied to potential COVID-19 exposure, and/or increased access to illicit counterfeit pills from drug dealers or the dark web markets.
Lessons can be gleaned from the most extensive dark web drug busts in Britain’s history, in which a deluge of “pharmaceutical grade” Xanax pills made it to the hands of drug dealers and consumers between 2015 and 2017.6 A similar phenomenon emerged stateside.7 Virtually indistinguishable from recognized 2-mg Xanax pills, these fake pills posed a serious challenge to forensic scientists.8 The threat of overdose is very real for users targeted by the counterfeit Xanax trade, especially since those at risk often bypass professional health care guidelines.
In broad daylight, the drug dealers ran their operations revolving around two fake Xanax products: a primary knockoff and a limited edition – and vastly more potent “Red Devil” variant that was intentionally dyed for branding purposes. Because the “Red Devil” formulations contained 2.5 times the dose of the 2-mg pill, it had even more pronounced tolerance, dependence, and withdrawal effects (for example, panic attacks, anxiety, and/or hallucinations) – fatal consequences for users involved in consuming other drugs, such as alcohol or opioids. Preexisting drug users tend to gravitate toward benzodiazepines, such as alprazolam (Xanax), perhaps in part, because of its relatively rapid onset of action. Xanax also is known for inducing proeuphoric states at higher doses, hence the appeal of the “Red Devil” pills.
Benzodiazepines, as a class of drugs, facilitate the neurotransmitter gamma-aminobutryric acid’s (GABA) effect on the brain, producing anxiolytic, hypnotic, and/or anticonvulsant states within the user.9 Unbeknownst to numerous users is the fact that drugs such as alcohol and opioids, like Xanax, also serve as respiratory depressants, overriding the brain’s governance of the breathing mechanism. This, in turn, leads to unintended overdose deaths, even among seasoned drug seekers.
Overdose deaths have been steadily climbing over the years because it is common for some users to consume alcohol while being on Xanax therapy – without realizing that both substances are depressants and that taking them together can lead to side effects such as respiratory depression.
Forensic cases also have revealed that preexisting opioid consumers were drawn to Xanax; the drug’s potent mechanism of action would likely appeal to habituated users. A typical behavioral pattern has emerged among users and must be addressed. According to Australian Professor Shane Darke: “So they take their Xanax, they take their painkiller, then they get drunk, that could be enough to kill them.”
Fatalities are more likely when benzodiazepines are combined with other drug classes or if the existing supply is contaminated or laced (for example, with fentanyl).8
As far as deaths by accidental benzodiazepine overdose are concerned, a similar epidemic has been recorded in the United States. In 2013, almost one-third of all prescription overdose deaths can be attributed to the use of benzodiazepines (for example, Xanax, Valium, and Ativan). However, media attention has been considerably muted, especially when compared with that of narcotic abuse. This is even more puzzling when taking into account that three-quarters of benzodiazepine mortalities co-occur within the context of narcotic consumption. Substance Abuse and Mental Health Services Administration data confirm the ubiquitous nature of benzodiazepine (such as alprazolam) coprescriptions, accounting for roughly half of the 176,000 emergency department cases for 2011. The Centers for Disease Control and Prevention noted that there was a 67% increase in benzodiazepine prescriptions between 1996 and 2013, which warranted more stringent regulations for this particular class of drugs.
In 2016, the CDC issued new guidelines for opioid use acknowledging the danger of benzodiazepine coprescriptions. Food and Drug Administration “black box” warnings now grace the prescriptions of both of these drug classes.10 This trend remains on an upward trajectory, even more so during the pandemic, as there are 9.7 million prescriptions of anxiolytics/hypnotics such as Xanax, Ativan, and Klonopin in the United States as of March 2020, which represents a 10% increase over the previous year. , as well as the implementation of urine drug screening monitoring for drug adherence/compliance and diversion in those with suspected benzodiazepine addiction or a history of polysubstance abuse.11,12
Clinical correlates
For patients who present acutely with Xanax toxicity in the emergency room setting, we will need to initially stabilize the vital signs and address the ongoing symptoms. It is advisable to arrange health care accommodations for patients with physical dependence to monitor and treat their withdrawal symptoms. The patient should be enrolled in a comprehensive addiction facility after undergoing formal detoxification; a tapered treatment protocol will need to be implemented because quitting “cold turkey” can lead to convulsions and, in some cases, death. Patient education, talk therapy, and alternatives to benzodiazepines should be discussed with the clinician.13,145
However, to truly address the elephant in the room, we will need to consider institutional reforms to prevent a similar situation from arising in the future. Primary care physician shortages are compounded by changes in insurance policies. Nurses and physician assistants will need to be trained to manage benzodiazepine prescriptions. If there are community shortages in physicians, patients might turn to illegal means to secure their benzodiazepine supply, and it is imperative that we have the necessary fellowship and education programs to educate nonphysician health care clinicians with benzodiazepine management. Because physicians were prescribing benzodiazepines liberally, the Prescription Drug Monitoring Programs (PDMP) was enacted to monitor physician practices. Unfortunately, this ultimately intimidated physicians and effectively curbed reasonable physician prescribing patterns. It might be necessary to revisit existing prescription monitoring programs, encourage drug evaluations and guidelines based on evidence-based medicine and embrace telemedicine in order to facilitate patient-physician communication.
As of now, it is too early to prescribe Xanax routinely for ongoing anxiety experienced during the coronavirus crisis, and several physicians are cautious about prescribing antianxiety medications for more than a few months.17 Surprisingly, researchers in Barcelona have even explored the role of Xanax as potentially inhibiting Mpro, the primary protease of coronavirus, thereby forestalling the virus’s ability to replicate.16 However, it is worth noting that, given the preliminary nature of the results, any attempts at conclusively integrating Xanax within the context of coronavirus therapy would be premature.
References
1. Luhby T. Anti-anxiety medication prescriptions up 34% since coronavirus. CNN. 2020 Apr 16.
2. Women and Anxiety. Anxiety and Depression Association of America.
3. Shigemura J et al. Psychiatry Clin Neurosci. 2012 Apr 7;74(4):281-2.
4. Petersen A. More people are taking drugs for anxiety and insomnia, and doctors are worried. The Wall Street Journal. 2020 May 25.
5. Downey M. Xanax overdose and related deaths. National Drug & Alcohol Research Centre. UNSW Sydney.
6. Bryant B. Fake Xanax: The UK’s biggest ever dark net drugs bust. BBC. 2018 Mar 10.
7. Reinberg S. Fatal overdoses rising from sedatives like Valium, Xanax. HealthDay. 2016 Feb.
8. Is counterfeit Xanax dangerous? American Addiction Centers. Updated 2018 Nov 14.
9. McLaren E. Xanax history and statistics. Drugabuse.com.
10. Benzodiazepines and opioids. National Institute on Drug Abuse. 2018 Mar 15.
11. Choudhry Z et al. J Psychiatry. 2015;18(5). doi: 10.4172/2378-5756.1000319.
12. Islam FA et al. Current Psychiatry. 2018 Dec 17(12):43-4.
13. Adams M. Xanax death rate on the rise. White Sands Treatment. 2017 Sept.NEED LINK
14. Storrs C. Benzodiazepine overdose deaths soared in recent years, study finds. CNN. 2016 Feb. 18.
15. Hanscom DA. Plan A – Thrive and survive COVID-19. Back in Control. 2020.
16. Smith C. Xanax, a common anxiety medication, might actually block coronavirus. BGR. 2020 May 29.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Mr. Choudhry is a research assistant at the IMCHF. He has no disclosures.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. He has no disclosures.