User login
Air pollution tied to ventricular arrhythmias in those with ICDs
Ventricular arrhythmias more commonly occur on days when there are higher levels of air pollution, especially with fine particulate matter (PM), a new study suggests.
The investigators studied the relationship between air pollution and ventricular arrhythmias in Piacenza, Italy by examining 5-year data on patients who received an implantable cardioverter defibrillator (ICD).
They found a significant association between PM2.5 levels and ventricular arrhythmias, especially those treated with direct current shock. Moreover, higher levels of PM2.5 and PM10 were associated with increased risk of all ventricular arrhythmias.
“These data confirm that environmental pollution is not only a climate emergency but also a public health problem,” lead author Alessia Zanni, currently at Maggiore Hospital, Bologna, Italy, and previously at Piacenza Hospital, said in an interview.
“The study suggests that the survival of patients with heart disease is affected not only by pharmacological therapies and advances in cardiology, but also by the air that they breathe,” she said.
The results were presented at European Society of Cardiology Heart Failure 2022.
More ED visits
The World Health Organization estimates around 7 million people die every year from exposure to polluted air, “as 91% of the world’s population lives in areas where air contaminants exceed safety levels,” Dr. Zanni said. Furthermore, “air pollution has been defined as the fourth-highest ranking risk factor for mortality – more important than LDL cholesterol, obesity, physical activity, or alcohol use.”
She noted that Piacenza has “historically been very attentive to the issues of early defibrillation and cardiac arrest.” Her group had previously found a correlation between out-of-hospital cardiac arrests and air pollution in the general population.
Moreover, her group recently observed that ED visits for patients with ICDs “tended to cluster; on some special days, many patients with ICDs had cardiac arrhythmias, and during those days, air pollution levels were particularly high.”
Her group therefore decided to compare the concentration of air pollutants on days when patients suffered from an arrhythmia event versus pollution levels on days without an arrhythmia, she said.
Further piece in a complex puzzle
The researchers studied 146 patients with ICDs between January 2013 and December 2017, assigning exposures (short, mid, and long term) to these patients based on their residential addresses.
They extracted day-by-day urban PM10, PM2.5, CO, NO2, and O3 levels from the Environmental Protection Agency monitoring stations and then, using time-stratified case-crossover analysis methodology, they calculated the association of ventricular arrhythmia onset with 0- to 7-day moving averages of the various air pollutants prior to the event.
Patients had received their ICD to control cardiac dysfunction brought on by previous myocardial infarction (n = 93), genetic or inflammatory conditions (n = 53), secondary prevention after a lethal arrhythmia (n = 67), and primary prevention (n = 79).
Of the 440 ventricular arrhythmias recorded, 322 were treated with antitachycardia pacing, while the remaining 118 were treated with direct current shock.
The researchers found a significant association between PM2.5 levels and ventricular arrhythmia treated with shock, corresponding to a 15% increased risk or every additional 10mg/m3 (P < .019).
They also found that, when PM2.5 concentrations were elevated by 1 mg/m3 for an entire week, compared with average levels, there was a 2.4% higher likelihood of ventricular arrhythmias, regardless of the temperature, and when PM10 was 1 mg/m3 above average for a week, there was a 2.1% increased risk for arrhythmias (odds ratio, 1,024; 95% confidence interval, 1,009-1,040] and OR, 1,021; 95% CI, 1,009-1,033, respectively), Dr. Zanni reported.
“Since the majority of out-of-hospital cardiac arrest causes still remain unclear, our data add a further piece to the complex puzzle of cardiac arrest triggers,” Dr. Zanni commented. “We think that particulate matter can cause acute inflammation of the heart muscle and potentially act as a trigger for lethal cardiac arrhythmias.
“As these toxic particles are emitted from power plants, industries, and cars, we think that cardiovascular research should highlight these new findings to promote green projects among the general population, clarifying the risks to the health of the human being, and we think strategies to prevent air pollutant exposure in high-risk patients [with previous cardiac disease] should be developed,” she added.
Further, “we advise patients at risk, during days with high PM2.5 (> 35 mg/m3) and PM10 (> 50 mg/m3) to use a mask of the N95 type outdoors, to reduce time spent outdoors – particularly in traffic – and to improve home air filtration,” Dr. Zanni said.
Entering the mainstream
In a comment, Joel Kaufman, MD, MPH, professor of internal medicine and environmental health, University of Washington, Seattle, said the study “adds to a fairly substantial literature already on this topic of short-term exposure to air pollution.”
The evidence that air pollutants “can be a trigger of worsening of cardiovascular disease is fairly consistent at this time, and although the effect sizes are small, they are consistent,” said Dr. Kaufman, who was the chair of the writing group for the American Heart Association’s 2020 policy statement, “Guidance to Reduce Cardiovascular Burden of Ambient Air Pollutants.”
“The research into this issue has become clearer during the past 10 years but still is not in the mainstream of most cardiologists’ awareness. They tend to focus more on controlling cholesterol and performing procedures, etc., but there are modifiable risk factors like air pollution that are increasingly recognized as being part of the picture,” said Dr. Kaufman, who was not involved with the current study.
Dr. Zanni added: “It is important that politics work hand in hand with the scientific community in order to win the battle against global warming, which will reduce the number of cardiovascular deaths – the leading cause of death worldwide – as well as environmental integrity.”
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Dr. Zanni and coauthors and Dr. Kaufman reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Ventricular arrhythmias more commonly occur on days when there are higher levels of air pollution, especially with fine particulate matter (PM), a new study suggests.
The investigators studied the relationship between air pollution and ventricular arrhythmias in Piacenza, Italy by examining 5-year data on patients who received an implantable cardioverter defibrillator (ICD).
They found a significant association between PM2.5 levels and ventricular arrhythmias, especially those treated with direct current shock. Moreover, higher levels of PM2.5 and PM10 were associated with increased risk of all ventricular arrhythmias.
“These data confirm that environmental pollution is not only a climate emergency but also a public health problem,” lead author Alessia Zanni, currently at Maggiore Hospital, Bologna, Italy, and previously at Piacenza Hospital, said in an interview.
“The study suggests that the survival of patients with heart disease is affected not only by pharmacological therapies and advances in cardiology, but also by the air that they breathe,” she said.
The results were presented at European Society of Cardiology Heart Failure 2022.
More ED visits
The World Health Organization estimates around 7 million people die every year from exposure to polluted air, “as 91% of the world’s population lives in areas where air contaminants exceed safety levels,” Dr. Zanni said. Furthermore, “air pollution has been defined as the fourth-highest ranking risk factor for mortality – more important than LDL cholesterol, obesity, physical activity, or alcohol use.”
She noted that Piacenza has “historically been very attentive to the issues of early defibrillation and cardiac arrest.” Her group had previously found a correlation between out-of-hospital cardiac arrests and air pollution in the general population.
Moreover, her group recently observed that ED visits for patients with ICDs “tended to cluster; on some special days, many patients with ICDs had cardiac arrhythmias, and during those days, air pollution levels were particularly high.”
Her group therefore decided to compare the concentration of air pollutants on days when patients suffered from an arrhythmia event versus pollution levels on days without an arrhythmia, she said.
Further piece in a complex puzzle
The researchers studied 146 patients with ICDs between January 2013 and December 2017, assigning exposures (short, mid, and long term) to these patients based on their residential addresses.
They extracted day-by-day urban PM10, PM2.5, CO, NO2, and O3 levels from the Environmental Protection Agency monitoring stations and then, using time-stratified case-crossover analysis methodology, they calculated the association of ventricular arrhythmia onset with 0- to 7-day moving averages of the various air pollutants prior to the event.
Patients had received their ICD to control cardiac dysfunction brought on by previous myocardial infarction (n = 93), genetic or inflammatory conditions (n = 53), secondary prevention after a lethal arrhythmia (n = 67), and primary prevention (n = 79).
Of the 440 ventricular arrhythmias recorded, 322 were treated with antitachycardia pacing, while the remaining 118 were treated with direct current shock.
The researchers found a significant association between PM2.5 levels and ventricular arrhythmia treated with shock, corresponding to a 15% increased risk or every additional 10mg/m3 (P < .019).
They also found that, when PM2.5 concentrations were elevated by 1 mg/m3 for an entire week, compared with average levels, there was a 2.4% higher likelihood of ventricular arrhythmias, regardless of the temperature, and when PM10 was 1 mg/m3 above average for a week, there was a 2.1% increased risk for arrhythmias (odds ratio, 1,024; 95% confidence interval, 1,009-1,040] and OR, 1,021; 95% CI, 1,009-1,033, respectively), Dr. Zanni reported.
“Since the majority of out-of-hospital cardiac arrest causes still remain unclear, our data add a further piece to the complex puzzle of cardiac arrest triggers,” Dr. Zanni commented. “We think that particulate matter can cause acute inflammation of the heart muscle and potentially act as a trigger for lethal cardiac arrhythmias.
“As these toxic particles are emitted from power plants, industries, and cars, we think that cardiovascular research should highlight these new findings to promote green projects among the general population, clarifying the risks to the health of the human being, and we think strategies to prevent air pollutant exposure in high-risk patients [with previous cardiac disease] should be developed,” she added.
Further, “we advise patients at risk, during days with high PM2.5 (> 35 mg/m3) and PM10 (> 50 mg/m3) to use a mask of the N95 type outdoors, to reduce time spent outdoors – particularly in traffic – and to improve home air filtration,” Dr. Zanni said.
Entering the mainstream
In a comment, Joel Kaufman, MD, MPH, professor of internal medicine and environmental health, University of Washington, Seattle, said the study “adds to a fairly substantial literature already on this topic of short-term exposure to air pollution.”
The evidence that air pollutants “can be a trigger of worsening of cardiovascular disease is fairly consistent at this time, and although the effect sizes are small, they are consistent,” said Dr. Kaufman, who was the chair of the writing group for the American Heart Association’s 2020 policy statement, “Guidance to Reduce Cardiovascular Burden of Ambient Air Pollutants.”
“The research into this issue has become clearer during the past 10 years but still is not in the mainstream of most cardiologists’ awareness. They tend to focus more on controlling cholesterol and performing procedures, etc., but there are modifiable risk factors like air pollution that are increasingly recognized as being part of the picture,” said Dr. Kaufman, who was not involved with the current study.
Dr. Zanni added: “It is important that politics work hand in hand with the scientific community in order to win the battle against global warming, which will reduce the number of cardiovascular deaths – the leading cause of death worldwide – as well as environmental integrity.”
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Dr. Zanni and coauthors and Dr. Kaufman reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Ventricular arrhythmias more commonly occur on days when there are higher levels of air pollution, especially with fine particulate matter (PM), a new study suggests.
The investigators studied the relationship between air pollution and ventricular arrhythmias in Piacenza, Italy by examining 5-year data on patients who received an implantable cardioverter defibrillator (ICD).
They found a significant association between PM2.5 levels and ventricular arrhythmias, especially those treated with direct current shock. Moreover, higher levels of PM2.5 and PM10 were associated with increased risk of all ventricular arrhythmias.
“These data confirm that environmental pollution is not only a climate emergency but also a public health problem,” lead author Alessia Zanni, currently at Maggiore Hospital, Bologna, Italy, and previously at Piacenza Hospital, said in an interview.
“The study suggests that the survival of patients with heart disease is affected not only by pharmacological therapies and advances in cardiology, but also by the air that they breathe,” she said.
The results were presented at European Society of Cardiology Heart Failure 2022.
More ED visits
The World Health Organization estimates around 7 million people die every year from exposure to polluted air, “as 91% of the world’s population lives in areas where air contaminants exceed safety levels,” Dr. Zanni said. Furthermore, “air pollution has been defined as the fourth-highest ranking risk factor for mortality – more important than LDL cholesterol, obesity, physical activity, or alcohol use.”
She noted that Piacenza has “historically been very attentive to the issues of early defibrillation and cardiac arrest.” Her group had previously found a correlation between out-of-hospital cardiac arrests and air pollution in the general population.
Moreover, her group recently observed that ED visits for patients with ICDs “tended to cluster; on some special days, many patients with ICDs had cardiac arrhythmias, and during those days, air pollution levels were particularly high.”
Her group therefore decided to compare the concentration of air pollutants on days when patients suffered from an arrhythmia event versus pollution levels on days without an arrhythmia, she said.
Further piece in a complex puzzle
The researchers studied 146 patients with ICDs between January 2013 and December 2017, assigning exposures (short, mid, and long term) to these patients based on their residential addresses.
They extracted day-by-day urban PM10, PM2.5, CO, NO2, and O3 levels from the Environmental Protection Agency monitoring stations and then, using time-stratified case-crossover analysis methodology, they calculated the association of ventricular arrhythmia onset with 0- to 7-day moving averages of the various air pollutants prior to the event.
Patients had received their ICD to control cardiac dysfunction brought on by previous myocardial infarction (n = 93), genetic or inflammatory conditions (n = 53), secondary prevention after a lethal arrhythmia (n = 67), and primary prevention (n = 79).
Of the 440 ventricular arrhythmias recorded, 322 were treated with antitachycardia pacing, while the remaining 118 were treated with direct current shock.
The researchers found a significant association between PM2.5 levels and ventricular arrhythmia treated with shock, corresponding to a 15% increased risk or every additional 10mg/m3 (P < .019).
They also found that, when PM2.5 concentrations were elevated by 1 mg/m3 for an entire week, compared with average levels, there was a 2.4% higher likelihood of ventricular arrhythmias, regardless of the temperature, and when PM10 was 1 mg/m3 above average for a week, there was a 2.1% increased risk for arrhythmias (odds ratio, 1,024; 95% confidence interval, 1,009-1,040] and OR, 1,021; 95% CI, 1,009-1,033, respectively), Dr. Zanni reported.
“Since the majority of out-of-hospital cardiac arrest causes still remain unclear, our data add a further piece to the complex puzzle of cardiac arrest triggers,” Dr. Zanni commented. “We think that particulate matter can cause acute inflammation of the heart muscle and potentially act as a trigger for lethal cardiac arrhythmias.
“As these toxic particles are emitted from power plants, industries, and cars, we think that cardiovascular research should highlight these new findings to promote green projects among the general population, clarifying the risks to the health of the human being, and we think strategies to prevent air pollutant exposure in high-risk patients [with previous cardiac disease] should be developed,” she added.
Further, “we advise patients at risk, during days with high PM2.5 (> 35 mg/m3) and PM10 (> 50 mg/m3) to use a mask of the N95 type outdoors, to reduce time spent outdoors – particularly in traffic – and to improve home air filtration,” Dr. Zanni said.
Entering the mainstream
In a comment, Joel Kaufman, MD, MPH, professor of internal medicine and environmental health, University of Washington, Seattle, said the study “adds to a fairly substantial literature already on this topic of short-term exposure to air pollution.”
The evidence that air pollutants “can be a trigger of worsening of cardiovascular disease is fairly consistent at this time, and although the effect sizes are small, they are consistent,” said Dr. Kaufman, who was the chair of the writing group for the American Heart Association’s 2020 policy statement, “Guidance to Reduce Cardiovascular Burden of Ambient Air Pollutants.”
“The research into this issue has become clearer during the past 10 years but still is not in the mainstream of most cardiologists’ awareness. They tend to focus more on controlling cholesterol and performing procedures, etc., but there are modifiable risk factors like air pollution that are increasingly recognized as being part of the picture,” said Dr. Kaufman, who was not involved with the current study.
Dr. Zanni added: “It is important that politics work hand in hand with the scientific community in order to win the battle against global warming, which will reduce the number of cardiovascular deaths – the leading cause of death worldwide – as well as environmental integrity.”
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Dr. Zanni and coauthors and Dr. Kaufman reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ESC HEART FAILURE 2022
SGLT2 inhibitors cut AFib risk in real-word analysis
NEW ORLEANS – The case continues to grow for prioritizing a sodium-glucose transporter 2 (SGLT2) inhibitor in patients with type 2 diabetes, as real-world evidence of benefit and safety accumulates on top of the data from randomized trials that first established this class as a management pillar.
Another important effect of these agents gaining increasing currency, on top of their well-established benefits in patients with type 2 diabetes for preventing acute heart failure exacerbations and slowing progression of diabetic kidney disease, is that they cut the incidence of new-onset atrial fibrillation (AFib). That effect was confirmed in an analysis of data from about 300,000 U.S. patients included in recent Medicare records, Elisabetta Patorno, MD, reported at the annual scientific sessions of the American Diabetes Association.
But despite documentation like this, real-world evidence also continues to show limited uptake of SGLT2 inhibitors in U.S. patients with type 2 diabetes. Records from more than 1.3 million patients with type 2 diabetes managed in the Veterans Affairs Healthcare System during 2019 or 2022 documented that just 10% of these patients received an agent from this class, even though all were eligible to receive it, according to findings in a separate report at the meeting.
The AFib analysis analyzed two sets of propensity score–matched Medicare patients during 2013-2018 aged 65 years or older with type 2 diabetes and no history of AFib. One analysis focused on 80,475 matched patients who started on treatment with either an SGLT2 inhibitor or a glucagonlike peptide–1 (GLP-1) receptor agonist, and a second on 74,868 matched patients who began either an SGTL2 inhibitor or a dipeptidyl peptidase–4 (DPP4) inhibitor. In both analyses, matching involved more than 130 variables. In both pair sets, patients at baseline averaged about 72 years old, nearly two-thirds were women, about 8%-9% had heart failure, 77%-80% were on metformin, and 20%-25% were using insulin.
The study’s primary endpoint was the incidence of hospitalization for AFib, which occurred a significant 18% less often in the patients who started on an SGLT2, compared with those who started a DPP4 inhibitor during median follow-up of 6.7 months, and a significant 10% less often, compared with those starting a GLP-1 receptor agonist during a median follow-up of 6.0 months, Elisabetta Patorno, MD, DrPH, reported at the meeting. This worked out to 3.7 fewer hospitalizations for AFib per 1,000 patient-years of follow-up among the people who received an SGLT2 inhibitor, compared with a DPP4 inhibitor, and a decrease of 1.8 hospitalizations/1,000 patient-years when compared against patients in a GLP-1 receptor agonist.
Two secondary outcomes showed significantly fewer episodes of newly diagnosed AFib, and significantly fewer patients initiating AFib treatment among those who received an SGLT2 inhibitor relative to the comparator groups. In addition, these associations were consistent across subgroup analyses that divided patients by their age, sex, history of heart failure, and history of atherosclerotic cardiovascular disease.
AFib effects add to benefits
The findings “suggest that initiation of an SGLT2 inhibitor may be beneficial in older adults with type 2 diabetes who are at risk for AFib,” said Dr. Patorno, a researcher in the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston. “These new findings on AFib may be helpful when weighing the potential risks and benefits of various glucose-lowering drugs in older patients with type 2 diabetes.”
This new evidence follows several prior reports from other research groups of data supporting an AFib benefit from SGLT2 inhibitors. The earlier reports include a post hoc analysis of more than 17,000 patients enrolled in the DECLARE-TIMI 58 cardiovascular outcome trial of dapagliflozin (Farxiga), which showed a 19% relative decrease in the rate of incident AFib or atrial flutter events during a median 4.2 year follow-up.
Other prior reports that found a reduced incidence of AFib events linked with SGLT2 inhibitor treatment include a 2020 meta-analysis based on data from more than 38,000 patients with type 2 diabetes enrolled in any of 16 randomized, controlled trials, which found a 24% relative risk reduction. And an as-yet unpublished report from researchers at the University of Rochester (N.Y.) and their associates presented in November 2021 at the annual scientific sessions of the American Heart Association that documented a significant 24% relative risk reduction in incident AFib events linked to SGLT2 inhibitor treatment in a prospective study of 13,890 patients at several hospitals in Israel or the United States.
Evidence ‘convincing’ in totality
The accumulated evidence for a reduced incidence of AFib when patients were on treatment with an SGLT2 inhibitor are “convincing because it’s real world data that complements what we know from clinical trials,” commented Silvio E. Inzucchi, MD, professor of medicine at Yale University and director of the Yale Medicine Diabetes Center in New Haven, Conn., who was not involved with the study.
“If these drugs reduce heart failure, they may also reduce AFib. Heart failure patients easily slip into AFib,” he noted in an interview, but added that “I don’t think this explains all cases” of the reduced AFib incidence.
Dr. Patorno offered a few other possible mechanisms for the observed effect. The class may work by reducing blood pressure, weight, inflammation, and oxidative stress, mitochondrial dysfunction, atrial remodeling, and AFib susceptibility. These agents are also known to cause natriuresis and diuresis, which could reduce atrial dilation, a mechanism that again relates the AFib effect to the better documented reduction in acute heart failure exacerbations.
“With the diuretic effect, we’d expect less overload at the atrium and less dilation, and the same mechanism would reduce heart failure,” she said in an interview.
“If you reduce preload and afterload you may reduce stress on the ventricle and reduce atrial stretch, and that might have a significant effect on atrial arrhythmia,” agreed Dr. Inzucchi.
EMPRISE produces more real-world evidence
A pair of additional reports at the meeting that Dr. Patorno coauthored provided real-world evidence supporting the dramatic heart failure benefit of the SGLT2 inhibitor empagliflozin (Jardiance) in U.S. patients with type 2 diabetes, compared with alternative drug classes. The EMPRISE study used data from the Medicare, Optum Clinformatics, and MarketScan databases during the period from August 2014, when empagliflozin became available, to September 2019. The study used more than 140 variables to match patients treated with either empagliflozin or a comparator agent.
The results showed that, in an analysis of more than 130,000 matched pairs, treatment with empagliflozin was linked to a significant 30% reduction in the incidence of hospitalization for heart failure, compared with patients treated with a GLP-1 receptor agonist. Analysis of more than 116,000 matched pairs of patients showed that treatment with empagliflozin linked with a significant 29%-50% reduced rate of hospitalization for heart failure, compared with matched patients treated with a DPP4 inhibitor.
These findings “add to the pool of information” on the efficacy of agents from the SGLT2 inhibitor class, Dr. Patorno said in an interview. “We wanted to look at the full range of patients with type 2 diabetes who we see in practice,” rather than the more selected group of patients enrolled in randomized trials.
SGLT2 inhibitor use lags even when cost isn’t an issue
Despite all the accumulated evidence for efficacy and safety of the class, usage remains low, Julio A. Lamprea-Montealegre, MD, PhD, a cardiologist at the University of California, San Francisco, reported in a separate talk at the meeting. The study he presented examined records for 1,319,500 adults with type 2 diabetes managed in the VA Healthcare System during 2019 and 2020. Despite being in a system that “removes the influence of cost,” just 10% of these patients received treatment with an SGLT2 inhibitor, and 7% received treatment with a GLP-1 receptor agonist.
Notably, his analysis further showed that treatment with an SGLT2 inhibitor was especially depressed among patients with an estimated glomerular filtration rate (eGFR) of 30-44 mL/min per 1.73m2. In this subgroup, usage of a drug from this class was at two-thirds of the rate, compared with patients with an eGFR of at least 90 mL/min per 1.73m2. His findings also documented lower rates of use in patients with higher risk for atherosclerotic cardiovascular disease. Dr. Lamprea-Montealegre called this a “treatment paradox,” in which patients likely to get the most benefit from an SGLT2 inhibitor were also less likely to actually receive it.
While his findings from the VA System suggest that drug cost is not the only factor driving underuse, the high price set for the SGLT2 inhibitor drugs that all currently remain on U.S. patents is widely considered an important factor.
“There is a big problem of affordability,” said Dr. Patorno.
“SGLT2 inhibitors should probably be first-line therapy” for many patients with type 2 diabetes, said Dr. Inzucchi. “The only thing holding it back is cost,” a situation that he hopes will dramatically shift once agents from this class become generic and have substantially lower price tags.
The EMPRISE study received funding from Boehringer Ingelheim, the company that markets empagliflozin (Jardiance). Dr. Patorno had no relevant commercial disclosures. Dr. Inzucchi is an adviser to Abbott Diagnostics, Esperion Therapeutics, and vTv Therapeutics, a consultant to Merck and Pfizer, and has other relationships with AstraZeneca, Boehringer Ingelheim, Lexicon, and Novo Nordisk. Dr. Lamprea-Montealegre had received research funding from Bayer.
NEW ORLEANS – The case continues to grow for prioritizing a sodium-glucose transporter 2 (SGLT2) inhibitor in patients with type 2 diabetes, as real-world evidence of benefit and safety accumulates on top of the data from randomized trials that first established this class as a management pillar.
Another important effect of these agents gaining increasing currency, on top of their well-established benefits in patients with type 2 diabetes for preventing acute heart failure exacerbations and slowing progression of diabetic kidney disease, is that they cut the incidence of new-onset atrial fibrillation (AFib). That effect was confirmed in an analysis of data from about 300,000 U.S. patients included in recent Medicare records, Elisabetta Patorno, MD, reported at the annual scientific sessions of the American Diabetes Association.
But despite documentation like this, real-world evidence also continues to show limited uptake of SGLT2 inhibitors in U.S. patients with type 2 diabetes. Records from more than 1.3 million patients with type 2 diabetes managed in the Veterans Affairs Healthcare System during 2019 or 2022 documented that just 10% of these patients received an agent from this class, even though all were eligible to receive it, according to findings in a separate report at the meeting.
The AFib analysis analyzed two sets of propensity score–matched Medicare patients during 2013-2018 aged 65 years or older with type 2 diabetes and no history of AFib. One analysis focused on 80,475 matched patients who started on treatment with either an SGLT2 inhibitor or a glucagonlike peptide–1 (GLP-1) receptor agonist, and a second on 74,868 matched patients who began either an SGTL2 inhibitor or a dipeptidyl peptidase–4 (DPP4) inhibitor. In both analyses, matching involved more than 130 variables. In both pair sets, patients at baseline averaged about 72 years old, nearly two-thirds were women, about 8%-9% had heart failure, 77%-80% were on metformin, and 20%-25% were using insulin.
The study’s primary endpoint was the incidence of hospitalization for AFib, which occurred a significant 18% less often in the patients who started on an SGLT2, compared with those who started a DPP4 inhibitor during median follow-up of 6.7 months, and a significant 10% less often, compared with those starting a GLP-1 receptor agonist during a median follow-up of 6.0 months, Elisabetta Patorno, MD, DrPH, reported at the meeting. This worked out to 3.7 fewer hospitalizations for AFib per 1,000 patient-years of follow-up among the people who received an SGLT2 inhibitor, compared with a DPP4 inhibitor, and a decrease of 1.8 hospitalizations/1,000 patient-years when compared against patients in a GLP-1 receptor agonist.
Two secondary outcomes showed significantly fewer episodes of newly diagnosed AFib, and significantly fewer patients initiating AFib treatment among those who received an SGLT2 inhibitor relative to the comparator groups. In addition, these associations were consistent across subgroup analyses that divided patients by their age, sex, history of heart failure, and history of atherosclerotic cardiovascular disease.
AFib effects add to benefits
The findings “suggest that initiation of an SGLT2 inhibitor may be beneficial in older adults with type 2 diabetes who are at risk for AFib,” said Dr. Patorno, a researcher in the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston. “These new findings on AFib may be helpful when weighing the potential risks and benefits of various glucose-lowering drugs in older patients with type 2 diabetes.”
This new evidence follows several prior reports from other research groups of data supporting an AFib benefit from SGLT2 inhibitors. The earlier reports include a post hoc analysis of more than 17,000 patients enrolled in the DECLARE-TIMI 58 cardiovascular outcome trial of dapagliflozin (Farxiga), which showed a 19% relative decrease in the rate of incident AFib or atrial flutter events during a median 4.2 year follow-up.
Other prior reports that found a reduced incidence of AFib events linked with SGLT2 inhibitor treatment include a 2020 meta-analysis based on data from more than 38,000 patients with type 2 diabetes enrolled in any of 16 randomized, controlled trials, which found a 24% relative risk reduction. And an as-yet unpublished report from researchers at the University of Rochester (N.Y.) and their associates presented in November 2021 at the annual scientific sessions of the American Heart Association that documented a significant 24% relative risk reduction in incident AFib events linked to SGLT2 inhibitor treatment in a prospective study of 13,890 patients at several hospitals in Israel or the United States.
Evidence ‘convincing’ in totality
The accumulated evidence for a reduced incidence of AFib when patients were on treatment with an SGLT2 inhibitor are “convincing because it’s real world data that complements what we know from clinical trials,” commented Silvio E. Inzucchi, MD, professor of medicine at Yale University and director of the Yale Medicine Diabetes Center in New Haven, Conn., who was not involved with the study.
“If these drugs reduce heart failure, they may also reduce AFib. Heart failure patients easily slip into AFib,” he noted in an interview, but added that “I don’t think this explains all cases” of the reduced AFib incidence.
Dr. Patorno offered a few other possible mechanisms for the observed effect. The class may work by reducing blood pressure, weight, inflammation, and oxidative stress, mitochondrial dysfunction, atrial remodeling, and AFib susceptibility. These agents are also known to cause natriuresis and diuresis, which could reduce atrial dilation, a mechanism that again relates the AFib effect to the better documented reduction in acute heart failure exacerbations.
“With the diuretic effect, we’d expect less overload at the atrium and less dilation, and the same mechanism would reduce heart failure,” she said in an interview.
“If you reduce preload and afterload you may reduce stress on the ventricle and reduce atrial stretch, and that might have a significant effect on atrial arrhythmia,” agreed Dr. Inzucchi.
EMPRISE produces more real-world evidence
A pair of additional reports at the meeting that Dr. Patorno coauthored provided real-world evidence supporting the dramatic heart failure benefit of the SGLT2 inhibitor empagliflozin (Jardiance) in U.S. patients with type 2 diabetes, compared with alternative drug classes. The EMPRISE study used data from the Medicare, Optum Clinformatics, and MarketScan databases during the period from August 2014, when empagliflozin became available, to September 2019. The study used more than 140 variables to match patients treated with either empagliflozin or a comparator agent.
The results showed that, in an analysis of more than 130,000 matched pairs, treatment with empagliflozin was linked to a significant 30% reduction in the incidence of hospitalization for heart failure, compared with patients treated with a GLP-1 receptor agonist. Analysis of more than 116,000 matched pairs of patients showed that treatment with empagliflozin linked with a significant 29%-50% reduced rate of hospitalization for heart failure, compared with matched patients treated with a DPP4 inhibitor.
These findings “add to the pool of information” on the efficacy of agents from the SGLT2 inhibitor class, Dr. Patorno said in an interview. “We wanted to look at the full range of patients with type 2 diabetes who we see in practice,” rather than the more selected group of patients enrolled in randomized trials.
SGLT2 inhibitor use lags even when cost isn’t an issue
Despite all the accumulated evidence for efficacy and safety of the class, usage remains low, Julio A. Lamprea-Montealegre, MD, PhD, a cardiologist at the University of California, San Francisco, reported in a separate talk at the meeting. The study he presented examined records for 1,319,500 adults with type 2 diabetes managed in the VA Healthcare System during 2019 and 2020. Despite being in a system that “removes the influence of cost,” just 10% of these patients received treatment with an SGLT2 inhibitor, and 7% received treatment with a GLP-1 receptor agonist.
Notably, his analysis further showed that treatment with an SGLT2 inhibitor was especially depressed among patients with an estimated glomerular filtration rate (eGFR) of 30-44 mL/min per 1.73m2. In this subgroup, usage of a drug from this class was at two-thirds of the rate, compared with patients with an eGFR of at least 90 mL/min per 1.73m2. His findings also documented lower rates of use in patients with higher risk for atherosclerotic cardiovascular disease. Dr. Lamprea-Montealegre called this a “treatment paradox,” in which patients likely to get the most benefit from an SGLT2 inhibitor were also less likely to actually receive it.
While his findings from the VA System suggest that drug cost is not the only factor driving underuse, the high price set for the SGLT2 inhibitor drugs that all currently remain on U.S. patents is widely considered an important factor.
“There is a big problem of affordability,” said Dr. Patorno.
“SGLT2 inhibitors should probably be first-line therapy” for many patients with type 2 diabetes, said Dr. Inzucchi. “The only thing holding it back is cost,” a situation that he hopes will dramatically shift once agents from this class become generic and have substantially lower price tags.
The EMPRISE study received funding from Boehringer Ingelheim, the company that markets empagliflozin (Jardiance). Dr. Patorno had no relevant commercial disclosures. Dr. Inzucchi is an adviser to Abbott Diagnostics, Esperion Therapeutics, and vTv Therapeutics, a consultant to Merck and Pfizer, and has other relationships with AstraZeneca, Boehringer Ingelheim, Lexicon, and Novo Nordisk. Dr. Lamprea-Montealegre had received research funding from Bayer.
NEW ORLEANS – The case continues to grow for prioritizing a sodium-glucose transporter 2 (SGLT2) inhibitor in patients with type 2 diabetes, as real-world evidence of benefit and safety accumulates on top of the data from randomized trials that first established this class as a management pillar.
Another important effect of these agents gaining increasing currency, on top of their well-established benefits in patients with type 2 diabetes for preventing acute heart failure exacerbations and slowing progression of diabetic kidney disease, is that they cut the incidence of new-onset atrial fibrillation (AFib). That effect was confirmed in an analysis of data from about 300,000 U.S. patients included in recent Medicare records, Elisabetta Patorno, MD, reported at the annual scientific sessions of the American Diabetes Association.
But despite documentation like this, real-world evidence also continues to show limited uptake of SGLT2 inhibitors in U.S. patients with type 2 diabetes. Records from more than 1.3 million patients with type 2 diabetes managed in the Veterans Affairs Healthcare System during 2019 or 2022 documented that just 10% of these patients received an agent from this class, even though all were eligible to receive it, according to findings in a separate report at the meeting.
The AFib analysis analyzed two sets of propensity score–matched Medicare patients during 2013-2018 aged 65 years or older with type 2 diabetes and no history of AFib. One analysis focused on 80,475 matched patients who started on treatment with either an SGLT2 inhibitor or a glucagonlike peptide–1 (GLP-1) receptor agonist, and a second on 74,868 matched patients who began either an SGTL2 inhibitor or a dipeptidyl peptidase–4 (DPP4) inhibitor. In both analyses, matching involved more than 130 variables. In both pair sets, patients at baseline averaged about 72 years old, nearly two-thirds were women, about 8%-9% had heart failure, 77%-80% were on metformin, and 20%-25% were using insulin.
The study’s primary endpoint was the incidence of hospitalization for AFib, which occurred a significant 18% less often in the patients who started on an SGLT2, compared with those who started a DPP4 inhibitor during median follow-up of 6.7 months, and a significant 10% less often, compared with those starting a GLP-1 receptor agonist during a median follow-up of 6.0 months, Elisabetta Patorno, MD, DrPH, reported at the meeting. This worked out to 3.7 fewer hospitalizations for AFib per 1,000 patient-years of follow-up among the people who received an SGLT2 inhibitor, compared with a DPP4 inhibitor, and a decrease of 1.8 hospitalizations/1,000 patient-years when compared against patients in a GLP-1 receptor agonist.
Two secondary outcomes showed significantly fewer episodes of newly diagnosed AFib, and significantly fewer patients initiating AFib treatment among those who received an SGLT2 inhibitor relative to the comparator groups. In addition, these associations were consistent across subgroup analyses that divided patients by their age, sex, history of heart failure, and history of atherosclerotic cardiovascular disease.
AFib effects add to benefits
The findings “suggest that initiation of an SGLT2 inhibitor may be beneficial in older adults with type 2 diabetes who are at risk for AFib,” said Dr. Patorno, a researcher in the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital, Boston. “These new findings on AFib may be helpful when weighing the potential risks and benefits of various glucose-lowering drugs in older patients with type 2 diabetes.”
This new evidence follows several prior reports from other research groups of data supporting an AFib benefit from SGLT2 inhibitors. The earlier reports include a post hoc analysis of more than 17,000 patients enrolled in the DECLARE-TIMI 58 cardiovascular outcome trial of dapagliflozin (Farxiga), which showed a 19% relative decrease in the rate of incident AFib or atrial flutter events during a median 4.2 year follow-up.
Other prior reports that found a reduced incidence of AFib events linked with SGLT2 inhibitor treatment include a 2020 meta-analysis based on data from more than 38,000 patients with type 2 diabetes enrolled in any of 16 randomized, controlled trials, which found a 24% relative risk reduction. And an as-yet unpublished report from researchers at the University of Rochester (N.Y.) and their associates presented in November 2021 at the annual scientific sessions of the American Heart Association that documented a significant 24% relative risk reduction in incident AFib events linked to SGLT2 inhibitor treatment in a prospective study of 13,890 patients at several hospitals in Israel or the United States.
Evidence ‘convincing’ in totality
The accumulated evidence for a reduced incidence of AFib when patients were on treatment with an SGLT2 inhibitor are “convincing because it’s real world data that complements what we know from clinical trials,” commented Silvio E. Inzucchi, MD, professor of medicine at Yale University and director of the Yale Medicine Diabetes Center in New Haven, Conn., who was not involved with the study.
“If these drugs reduce heart failure, they may also reduce AFib. Heart failure patients easily slip into AFib,” he noted in an interview, but added that “I don’t think this explains all cases” of the reduced AFib incidence.
Dr. Patorno offered a few other possible mechanisms for the observed effect. The class may work by reducing blood pressure, weight, inflammation, and oxidative stress, mitochondrial dysfunction, atrial remodeling, and AFib susceptibility. These agents are also known to cause natriuresis and diuresis, which could reduce atrial dilation, a mechanism that again relates the AFib effect to the better documented reduction in acute heart failure exacerbations.
“With the diuretic effect, we’d expect less overload at the atrium and less dilation, and the same mechanism would reduce heart failure,” she said in an interview.
“If you reduce preload and afterload you may reduce stress on the ventricle and reduce atrial stretch, and that might have a significant effect on atrial arrhythmia,” agreed Dr. Inzucchi.
EMPRISE produces more real-world evidence
A pair of additional reports at the meeting that Dr. Patorno coauthored provided real-world evidence supporting the dramatic heart failure benefit of the SGLT2 inhibitor empagliflozin (Jardiance) in U.S. patients with type 2 diabetes, compared with alternative drug classes. The EMPRISE study used data from the Medicare, Optum Clinformatics, and MarketScan databases during the period from August 2014, when empagliflozin became available, to September 2019. The study used more than 140 variables to match patients treated with either empagliflozin or a comparator agent.
The results showed that, in an analysis of more than 130,000 matched pairs, treatment with empagliflozin was linked to a significant 30% reduction in the incidence of hospitalization for heart failure, compared with patients treated with a GLP-1 receptor agonist. Analysis of more than 116,000 matched pairs of patients showed that treatment with empagliflozin linked with a significant 29%-50% reduced rate of hospitalization for heart failure, compared with matched patients treated with a DPP4 inhibitor.
These findings “add to the pool of information” on the efficacy of agents from the SGLT2 inhibitor class, Dr. Patorno said in an interview. “We wanted to look at the full range of patients with type 2 diabetes who we see in practice,” rather than the more selected group of patients enrolled in randomized trials.
SGLT2 inhibitor use lags even when cost isn’t an issue
Despite all the accumulated evidence for efficacy and safety of the class, usage remains low, Julio A. Lamprea-Montealegre, MD, PhD, a cardiologist at the University of California, San Francisco, reported in a separate talk at the meeting. The study he presented examined records for 1,319,500 adults with type 2 diabetes managed in the VA Healthcare System during 2019 and 2020. Despite being in a system that “removes the influence of cost,” just 10% of these patients received treatment with an SGLT2 inhibitor, and 7% received treatment with a GLP-1 receptor agonist.
Notably, his analysis further showed that treatment with an SGLT2 inhibitor was especially depressed among patients with an estimated glomerular filtration rate (eGFR) of 30-44 mL/min per 1.73m2. In this subgroup, usage of a drug from this class was at two-thirds of the rate, compared with patients with an eGFR of at least 90 mL/min per 1.73m2. His findings also documented lower rates of use in patients with higher risk for atherosclerotic cardiovascular disease. Dr. Lamprea-Montealegre called this a “treatment paradox,” in which patients likely to get the most benefit from an SGLT2 inhibitor were also less likely to actually receive it.
While his findings from the VA System suggest that drug cost is not the only factor driving underuse, the high price set for the SGLT2 inhibitor drugs that all currently remain on U.S. patents is widely considered an important factor.
“There is a big problem of affordability,” said Dr. Patorno.
“SGLT2 inhibitors should probably be first-line therapy” for many patients with type 2 diabetes, said Dr. Inzucchi. “The only thing holding it back is cost,” a situation that he hopes will dramatically shift once agents from this class become generic and have substantially lower price tags.
The EMPRISE study received funding from Boehringer Ingelheim, the company that markets empagliflozin (Jardiance). Dr. Patorno had no relevant commercial disclosures. Dr. Inzucchi is an adviser to Abbott Diagnostics, Esperion Therapeutics, and vTv Therapeutics, a consultant to Merck and Pfizer, and has other relationships with AstraZeneca, Boehringer Ingelheim, Lexicon, and Novo Nordisk. Dr. Lamprea-Montealegre had received research funding from Bayer.
AT ADA 2022
Emergency angiography for cardiac arrest without ST elevation?
Patients successfully resuscitated after an out-of-hospital cardiac arrest who did not have ST-segment elevation on their electrocardiogram did not benefit from emergency coronary angiography in a new randomized clinical trial.
In the EMERGE trial, a strategy of emergency coronary angiography was not found to be better than a strategy of delayed coronary angiography with respect to the 180-day survival rate with no or minimal neurologic sequelae.
The authors note that, although the study was underpowered, the results are consistent with previously published studies and do not support routine emergency coronary angiography in survivors of out-of-hospital cardiac arrest without ST elevation.
But senior author, Christian Spaulding, MD, PhD, European Hospital Georges Pompidou, Paris, believes some such patients may still benefit from emergency angiography.
“Most patients who have been resuscitated after out of hospital cardiac arrest will have neurological damage, which will be the primary cause of death,” Dr. Spaulding told this news organization. “It will not make any difference to these patients if they have a coronary lesion treated. So, going forward, I think we need to look for patients who are likely not to have a high degree of neurological damage and who could still benefit from early angiography.”
The EMERGE study was published online in JAMA Cardiology.
In patients who have suffered an out-of-hospital cardiac arrest with no obvious noncardiac cause such as trauma, it is believed that the cardiac arrest is caused by coronary occlusions, and emergency angiography may be able to improve survival in these patients, Dr. Spaulding explained.
In about one-third of such patients, the ECG before hospitalization shows ST elevation, and in this group, there is a high probability (around 70%-80%) that there is going to be a coronary occlusion, so these patients are usually taken directly to emergency angiography.
But, in the other two-thirds of patients, there is no ST elevation on the ECG, and in these patients the chances of finding a coronary occlusion are lower (around 25%-35%).
The EMERGE trial was conducted in this latter group without ST elevation.
For the study, which was conducted in 22 French centers, 279 such patients (mean age, 64 years) were randomized to either emergency or delayed (48-96 hours) coronary angiography. The mean time delay between randomization and coronary angiography was 0.6 hours in the emergency group and 55.1 hours in the delayed group.
The primary outcome was the 180-day survival rate with minimal neurological damage, defined as Cerebral Performance Category of 2 or less. This occurred in 34.1% of the emergency angiography group and 30.7% of the delayed angiography group (hazard ratio, 0.87; 95% confidence interval, 0.65-1.15; P = .32).
There was also no difference in the overall survival rate at 180 days (36.2% vs. 33.3%; HR, 0.86; P = .31) and in secondary outcomes between the two groups.
Dr. Spaulding noted that three other randomized trials in a similar patient population have all shown similar results, with no difference in survival found between patients who have emergency coronary angiography as soon as they are admitted to hospital and those in whom angiography was not performed until a couple of days later.
However, several registry studies in a total of more than 6,000 patients have suggested a benefit of immediate angiography in these patients. “So, there is some disconnect here,” he said.
Dr. Spaulding believes the reason for this disconnect may be that the registry studies may have included patients with less neurological damage so more likely to survive and to benefit from having coronary lesions treated promptly.
“Paramedics sometimes make a judgment on which patients may have minimal neurological damage, and this may affect the choice of hospital a patient is taken to, and then the emergency department doctor may again assess whether a patient should go for immediate angiography or not. So, patients in these registry studies who received emergency angiography were likely already preselected to some extent,” he suggested.
In contrast, the randomized trials have accepted all patients, so there were probably more with neurological damage. “In our trial, almost 70% of patients were in asystole. These are the ones who [are] the most likely to have neurological damage,” he pointed out.
“Because there was such a striking difference in the registry studies, I think there is a group of patients [who] will benefit from immediate emergency coronary angiography, but we have to work out how to select these patients,” he commented.
Dr. Spaulding noted that a recent registry study published in JACC: Cardiovascular Interventions used a score known as MIRACLE2, (which takes into account various factors including age of patient and type of rhythm on ECG) and the degree of cardiogenic shock on arrival at hospital as measured by the SCAI shock score to define a potential cohort of patients at low risk for neurologic injury who benefit most from immediate coronary angiography.
“In my practice at present, I would advise the emergency team that a young patient who had had resuscitation started quickly, had been defibrillated early, and got to hospital quickly should go for an immediate coronary angiogram. It can’t do any harm, and there may be a benefit in such patients,” Dr. Spaulding added.The EMERGE study was supported in part by Assistance Publique–Hôpitaux de Paris and the French Ministry of Health, through the national Programme Hospitalier de Recherche Clinique. Dr. Spaulding reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients successfully resuscitated after an out-of-hospital cardiac arrest who did not have ST-segment elevation on their electrocardiogram did not benefit from emergency coronary angiography in a new randomized clinical trial.
In the EMERGE trial, a strategy of emergency coronary angiography was not found to be better than a strategy of delayed coronary angiography with respect to the 180-day survival rate with no or minimal neurologic sequelae.
The authors note that, although the study was underpowered, the results are consistent with previously published studies and do not support routine emergency coronary angiography in survivors of out-of-hospital cardiac arrest without ST elevation.
But senior author, Christian Spaulding, MD, PhD, European Hospital Georges Pompidou, Paris, believes some such patients may still benefit from emergency angiography.
“Most patients who have been resuscitated after out of hospital cardiac arrest will have neurological damage, which will be the primary cause of death,” Dr. Spaulding told this news organization. “It will not make any difference to these patients if they have a coronary lesion treated. So, going forward, I think we need to look for patients who are likely not to have a high degree of neurological damage and who could still benefit from early angiography.”
The EMERGE study was published online in JAMA Cardiology.
In patients who have suffered an out-of-hospital cardiac arrest with no obvious noncardiac cause such as trauma, it is believed that the cardiac arrest is caused by coronary occlusions, and emergency angiography may be able to improve survival in these patients, Dr. Spaulding explained.
In about one-third of such patients, the ECG before hospitalization shows ST elevation, and in this group, there is a high probability (around 70%-80%) that there is going to be a coronary occlusion, so these patients are usually taken directly to emergency angiography.
But, in the other two-thirds of patients, there is no ST elevation on the ECG, and in these patients the chances of finding a coronary occlusion are lower (around 25%-35%).
The EMERGE trial was conducted in this latter group without ST elevation.
For the study, which was conducted in 22 French centers, 279 such patients (mean age, 64 years) were randomized to either emergency or delayed (48-96 hours) coronary angiography. The mean time delay between randomization and coronary angiography was 0.6 hours in the emergency group and 55.1 hours in the delayed group.
The primary outcome was the 180-day survival rate with minimal neurological damage, defined as Cerebral Performance Category of 2 or less. This occurred in 34.1% of the emergency angiography group and 30.7% of the delayed angiography group (hazard ratio, 0.87; 95% confidence interval, 0.65-1.15; P = .32).
There was also no difference in the overall survival rate at 180 days (36.2% vs. 33.3%; HR, 0.86; P = .31) and in secondary outcomes between the two groups.
Dr. Spaulding noted that three other randomized trials in a similar patient population have all shown similar results, with no difference in survival found between patients who have emergency coronary angiography as soon as they are admitted to hospital and those in whom angiography was not performed until a couple of days later.
However, several registry studies in a total of more than 6,000 patients have suggested a benefit of immediate angiography in these patients. “So, there is some disconnect here,” he said.
Dr. Spaulding believes the reason for this disconnect may be that the registry studies may have included patients with less neurological damage so more likely to survive and to benefit from having coronary lesions treated promptly.
“Paramedics sometimes make a judgment on which patients may have minimal neurological damage, and this may affect the choice of hospital a patient is taken to, and then the emergency department doctor may again assess whether a patient should go for immediate angiography or not. So, patients in these registry studies who received emergency angiography were likely already preselected to some extent,” he suggested.
In contrast, the randomized trials have accepted all patients, so there were probably more with neurological damage. “In our trial, almost 70% of patients were in asystole. These are the ones who [are] the most likely to have neurological damage,” he pointed out.
“Because there was such a striking difference in the registry studies, I think there is a group of patients [who] will benefit from immediate emergency coronary angiography, but we have to work out how to select these patients,” he commented.
Dr. Spaulding noted that a recent registry study published in JACC: Cardiovascular Interventions used a score known as MIRACLE2, (which takes into account various factors including age of patient and type of rhythm on ECG) and the degree of cardiogenic shock on arrival at hospital as measured by the SCAI shock score to define a potential cohort of patients at low risk for neurologic injury who benefit most from immediate coronary angiography.
“In my practice at present, I would advise the emergency team that a young patient who had had resuscitation started quickly, had been defibrillated early, and got to hospital quickly should go for an immediate coronary angiogram. It can’t do any harm, and there may be a benefit in such patients,” Dr. Spaulding added.The EMERGE study was supported in part by Assistance Publique–Hôpitaux de Paris and the French Ministry of Health, through the national Programme Hospitalier de Recherche Clinique. Dr. Spaulding reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients successfully resuscitated after an out-of-hospital cardiac arrest who did not have ST-segment elevation on their electrocardiogram did not benefit from emergency coronary angiography in a new randomized clinical trial.
In the EMERGE trial, a strategy of emergency coronary angiography was not found to be better than a strategy of delayed coronary angiography with respect to the 180-day survival rate with no or minimal neurologic sequelae.
The authors note that, although the study was underpowered, the results are consistent with previously published studies and do not support routine emergency coronary angiography in survivors of out-of-hospital cardiac arrest without ST elevation.
But senior author, Christian Spaulding, MD, PhD, European Hospital Georges Pompidou, Paris, believes some such patients may still benefit from emergency angiography.
“Most patients who have been resuscitated after out of hospital cardiac arrest will have neurological damage, which will be the primary cause of death,” Dr. Spaulding told this news organization. “It will not make any difference to these patients if they have a coronary lesion treated. So, going forward, I think we need to look for patients who are likely not to have a high degree of neurological damage and who could still benefit from early angiography.”
The EMERGE study was published online in JAMA Cardiology.
In patients who have suffered an out-of-hospital cardiac arrest with no obvious noncardiac cause such as trauma, it is believed that the cardiac arrest is caused by coronary occlusions, and emergency angiography may be able to improve survival in these patients, Dr. Spaulding explained.
In about one-third of such patients, the ECG before hospitalization shows ST elevation, and in this group, there is a high probability (around 70%-80%) that there is going to be a coronary occlusion, so these patients are usually taken directly to emergency angiography.
But, in the other two-thirds of patients, there is no ST elevation on the ECG, and in these patients the chances of finding a coronary occlusion are lower (around 25%-35%).
The EMERGE trial was conducted in this latter group without ST elevation.
For the study, which was conducted in 22 French centers, 279 such patients (mean age, 64 years) were randomized to either emergency or delayed (48-96 hours) coronary angiography. The mean time delay between randomization and coronary angiography was 0.6 hours in the emergency group and 55.1 hours in the delayed group.
The primary outcome was the 180-day survival rate with minimal neurological damage, defined as Cerebral Performance Category of 2 or less. This occurred in 34.1% of the emergency angiography group and 30.7% of the delayed angiography group (hazard ratio, 0.87; 95% confidence interval, 0.65-1.15; P = .32).
There was also no difference in the overall survival rate at 180 days (36.2% vs. 33.3%; HR, 0.86; P = .31) and in secondary outcomes between the two groups.
Dr. Spaulding noted that three other randomized trials in a similar patient population have all shown similar results, with no difference in survival found between patients who have emergency coronary angiography as soon as they are admitted to hospital and those in whom angiography was not performed until a couple of days later.
However, several registry studies in a total of more than 6,000 patients have suggested a benefit of immediate angiography in these patients. “So, there is some disconnect here,” he said.
Dr. Spaulding believes the reason for this disconnect may be that the registry studies may have included patients with less neurological damage so more likely to survive and to benefit from having coronary lesions treated promptly.
“Paramedics sometimes make a judgment on which patients may have minimal neurological damage, and this may affect the choice of hospital a patient is taken to, and then the emergency department doctor may again assess whether a patient should go for immediate angiography or not. So, patients in these registry studies who received emergency angiography were likely already preselected to some extent,” he suggested.
In contrast, the randomized trials have accepted all patients, so there were probably more with neurological damage. “In our trial, almost 70% of patients were in asystole. These are the ones who [are] the most likely to have neurological damage,” he pointed out.
“Because there was such a striking difference in the registry studies, I think there is a group of patients [who] will benefit from immediate emergency coronary angiography, but we have to work out how to select these patients,” he commented.
Dr. Spaulding noted that a recent registry study published in JACC: Cardiovascular Interventions used a score known as MIRACLE2, (which takes into account various factors including age of patient and type of rhythm on ECG) and the degree of cardiogenic shock on arrival at hospital as measured by the SCAI shock score to define a potential cohort of patients at low risk for neurologic injury who benefit most from immediate coronary angiography.
“In my practice at present, I would advise the emergency team that a young patient who had had resuscitation started quickly, had been defibrillated early, and got to hospital quickly should go for an immediate coronary angiogram. It can’t do any harm, and there may be a benefit in such patients,” Dr. Spaulding added.The EMERGE study was supported in part by Assistance Publique–Hôpitaux de Paris and the French Ministry of Health, through the national Programme Hospitalier de Recherche Clinique. Dr. Spaulding reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Takotsubo syndrome more deadly in men
Takotsubo syndrome occurs much more frequently in women than it does in men, but men are much more likely to die from it, according to the results of a new study.
In an analysis of almost 2,500 patients with Takotsubo syndrome (TSS) who were enrolled in an international registry, men, who made up just 11% of the sample, had significantly higher rates of cardiogenic shock and were more than twice as likely to die in the hospital than their female counterparts.
The authors concluded that TSS in males requires close in-hospital monitoring and long-term follow-up. Their study was published in the Journal of the American College of Cardiology.
Takotsubo syndrome is a condition characterized by acute heart failure and transient ventricular contractile dysfunction that can be precipitated by acute emotional or physical stress. It affects mostly women, particularly postmenopausal women, although the reasons for this are still not fully clear, Luca Arcari, MD, from the Institute of Cardiology, Madre Giuseppina Vannini Hospital, Rome, and colleagues wrote.
The syndrome also affects men, and recent data have identified that male sex is associated with worse outcomes. But, because it occurs relatively uncommonly in men, information about outcomes in men is limited.
To shed more light on the influence of gender on TTS, the investigators looked at 2,492 TTS patients (286 men, 2,206 women) who were participants in the GEIST (German Italian Spanish Takotsubo) registry and compared the clinical features and short- and long-term outcomes between the two.
Male patients were significantly younger (69 years) than women (71 years; P = .005) and had a higher prevalence of comorbid conditions, including diabetes (25% vs. 19%; P = .01); pulmonary diseases (21% vs. 15%; P = .006); malignancies (25% vs. 13%; P < .001).
In addition, TTS in men was more likely to be caused by physical triggers (55% vs. 32%; P < .01), whereas emotional triggers were more common in females (39% vs. 19%; P < 0.001).
The investigators then performed a propensity score analysis by matching men and women 1:1; this yielded 207 patients from each group.
After propensity matching, male patients had higher rates of cardiogenic shock (16% vs 6%), and in-hospital mortality (8% vs. 3%; both P < .05).
Men also had a higher mortality rate during the acute and long-term follow up. Male sex remained independently associated with both in-hospital mortality (odds ratio, 2.26; 95% confidence interval, 1.16-4.40) and long-term mortality (hazard ratio, 1.83; 95% CI, 1.32-2.52).
The study by Dr. Arcari and colleagues “shows convincingly that although men are far less likely to develop TTS than women, they have more serious complications and are more likely to die than women presenting with the syndrome, Ilan S. Wittstein, MD, of Johns Hopkins University, Baltimore, wrote in an accompanying editorial.
In an interview, Dr. Wittstein said one of the strengths of the study was its size.
“Over the years, there have been a lot of smaller, single center studies. This large registry had over 2,000 patients. So when the researchers say the rate of TTS is 10% in men and 90% in women, this is not necessarily surprising because that’s about the breakdown we’ve had since the very beginning, but it certainly validates that in a cohort that is large,” he said.
“I think what was novel about the paper is that the size of the cohort allowed the researchers to do propensity matching, so they were able not only to compare men versus women, they could do a 1:1 comparison. And they found even when you match men and women for various comorbidities, the men were much sicker
“What makes this a fascinating syndrome and different from most types of heart muscle problems is that, in the majority of patients, the condition is precipitated by an acute stressor,” said Dr. Wittstein.
“It can either be an emotional trigger, so for instance, getting some bad news that a loved one just died. That’s why we nicknamed the syndrome ‘broken heart syndrome’ many years ago. Or it can be a physical trigger, which can be a wide variety of things, such infection, a stroke, bad pneumonia, anything that stresses the body and causes a stress response. Regular heart attacks are not triggered in this way,” he said.
Dr. Arcari and Dr. Wittstein reported no relevant financial relationships.
Takotsubo syndrome occurs much more frequently in women than it does in men, but men are much more likely to die from it, according to the results of a new study.
In an analysis of almost 2,500 patients with Takotsubo syndrome (TSS) who were enrolled in an international registry, men, who made up just 11% of the sample, had significantly higher rates of cardiogenic shock and were more than twice as likely to die in the hospital than their female counterparts.
The authors concluded that TSS in males requires close in-hospital monitoring and long-term follow-up. Their study was published in the Journal of the American College of Cardiology.
Takotsubo syndrome is a condition characterized by acute heart failure and transient ventricular contractile dysfunction that can be precipitated by acute emotional or physical stress. It affects mostly women, particularly postmenopausal women, although the reasons for this are still not fully clear, Luca Arcari, MD, from the Institute of Cardiology, Madre Giuseppina Vannini Hospital, Rome, and colleagues wrote.
The syndrome also affects men, and recent data have identified that male sex is associated with worse outcomes. But, because it occurs relatively uncommonly in men, information about outcomes in men is limited.
To shed more light on the influence of gender on TTS, the investigators looked at 2,492 TTS patients (286 men, 2,206 women) who were participants in the GEIST (German Italian Spanish Takotsubo) registry and compared the clinical features and short- and long-term outcomes between the two.
Male patients were significantly younger (69 years) than women (71 years; P = .005) and had a higher prevalence of comorbid conditions, including diabetes (25% vs. 19%; P = .01); pulmonary diseases (21% vs. 15%; P = .006); malignancies (25% vs. 13%; P < .001).
In addition, TTS in men was more likely to be caused by physical triggers (55% vs. 32%; P < .01), whereas emotional triggers were more common in females (39% vs. 19%; P < 0.001).
The investigators then performed a propensity score analysis by matching men and women 1:1; this yielded 207 patients from each group.
After propensity matching, male patients had higher rates of cardiogenic shock (16% vs 6%), and in-hospital mortality (8% vs. 3%; both P < .05).
Men also had a higher mortality rate during the acute and long-term follow up. Male sex remained independently associated with both in-hospital mortality (odds ratio, 2.26; 95% confidence interval, 1.16-4.40) and long-term mortality (hazard ratio, 1.83; 95% CI, 1.32-2.52).
The study by Dr. Arcari and colleagues “shows convincingly that although men are far less likely to develop TTS than women, they have more serious complications and are more likely to die than women presenting with the syndrome, Ilan S. Wittstein, MD, of Johns Hopkins University, Baltimore, wrote in an accompanying editorial.
In an interview, Dr. Wittstein said one of the strengths of the study was its size.
“Over the years, there have been a lot of smaller, single center studies. This large registry had over 2,000 patients. So when the researchers say the rate of TTS is 10% in men and 90% in women, this is not necessarily surprising because that’s about the breakdown we’ve had since the very beginning, but it certainly validates that in a cohort that is large,” he said.
“I think what was novel about the paper is that the size of the cohort allowed the researchers to do propensity matching, so they were able not only to compare men versus women, they could do a 1:1 comparison. And they found even when you match men and women for various comorbidities, the men were much sicker
“What makes this a fascinating syndrome and different from most types of heart muscle problems is that, in the majority of patients, the condition is precipitated by an acute stressor,” said Dr. Wittstein.
“It can either be an emotional trigger, so for instance, getting some bad news that a loved one just died. That’s why we nicknamed the syndrome ‘broken heart syndrome’ many years ago. Or it can be a physical trigger, which can be a wide variety of things, such infection, a stroke, bad pneumonia, anything that stresses the body and causes a stress response. Regular heart attacks are not triggered in this way,” he said.
Dr. Arcari and Dr. Wittstein reported no relevant financial relationships.
Takotsubo syndrome occurs much more frequently in women than it does in men, but men are much more likely to die from it, according to the results of a new study.
In an analysis of almost 2,500 patients with Takotsubo syndrome (TSS) who were enrolled in an international registry, men, who made up just 11% of the sample, had significantly higher rates of cardiogenic shock and were more than twice as likely to die in the hospital than their female counterparts.
The authors concluded that TSS in males requires close in-hospital monitoring and long-term follow-up. Their study was published in the Journal of the American College of Cardiology.
Takotsubo syndrome is a condition characterized by acute heart failure and transient ventricular contractile dysfunction that can be precipitated by acute emotional or physical stress. It affects mostly women, particularly postmenopausal women, although the reasons for this are still not fully clear, Luca Arcari, MD, from the Institute of Cardiology, Madre Giuseppina Vannini Hospital, Rome, and colleagues wrote.
The syndrome also affects men, and recent data have identified that male sex is associated with worse outcomes. But, because it occurs relatively uncommonly in men, information about outcomes in men is limited.
To shed more light on the influence of gender on TTS, the investigators looked at 2,492 TTS patients (286 men, 2,206 women) who were participants in the GEIST (German Italian Spanish Takotsubo) registry and compared the clinical features and short- and long-term outcomes between the two.
Male patients were significantly younger (69 years) than women (71 years; P = .005) and had a higher prevalence of comorbid conditions, including diabetes (25% vs. 19%; P = .01); pulmonary diseases (21% vs. 15%; P = .006); malignancies (25% vs. 13%; P < .001).
In addition, TTS in men was more likely to be caused by physical triggers (55% vs. 32%; P < .01), whereas emotional triggers were more common in females (39% vs. 19%; P < 0.001).
The investigators then performed a propensity score analysis by matching men and women 1:1; this yielded 207 patients from each group.
After propensity matching, male patients had higher rates of cardiogenic shock (16% vs 6%), and in-hospital mortality (8% vs. 3%; both P < .05).
Men also had a higher mortality rate during the acute and long-term follow up. Male sex remained independently associated with both in-hospital mortality (odds ratio, 2.26; 95% confidence interval, 1.16-4.40) and long-term mortality (hazard ratio, 1.83; 95% CI, 1.32-2.52).
The study by Dr. Arcari and colleagues “shows convincingly that although men are far less likely to develop TTS than women, they have more serious complications and are more likely to die than women presenting with the syndrome, Ilan S. Wittstein, MD, of Johns Hopkins University, Baltimore, wrote in an accompanying editorial.
In an interview, Dr. Wittstein said one of the strengths of the study was its size.
“Over the years, there have been a lot of smaller, single center studies. This large registry had over 2,000 patients. So when the researchers say the rate of TTS is 10% in men and 90% in women, this is not necessarily surprising because that’s about the breakdown we’ve had since the very beginning, but it certainly validates that in a cohort that is large,” he said.
“I think what was novel about the paper is that the size of the cohort allowed the researchers to do propensity matching, so they were able not only to compare men versus women, they could do a 1:1 comparison. And they found even when you match men and women for various comorbidities, the men were much sicker
“What makes this a fascinating syndrome and different from most types of heart muscle problems is that, in the majority of patients, the condition is precipitated by an acute stressor,” said Dr. Wittstein.
“It can either be an emotional trigger, so for instance, getting some bad news that a loved one just died. That’s why we nicknamed the syndrome ‘broken heart syndrome’ many years ago. Or it can be a physical trigger, which can be a wide variety of things, such infection, a stroke, bad pneumonia, anything that stresses the body and causes a stress response. Regular heart attacks are not triggered in this way,” he said.
Dr. Arcari and Dr. Wittstein reported no relevant financial relationships.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
SCAI issues guidelines for PFO management, makes case for expansion
The first-ever guidelines for interventional cardiologists using percutaneous patent foramen ovale closure recommend expanding the use of the procedure beyond the Food and Drug Administration–approved indication following PFO-associated ischemic stroke, adding clarification about the use of PFO with anticoagulation and hedging against abuse and overuse of the procedure, said the chair of the guideline writing committee.
“The most important things surrounding these guidelines are to help clinicians and policymakers – third-party payers – to address PFO in patient subsets that were not included in the large randomized clinical trials that led to FDA approval,” said writing group chair Clifford J. Kavinsky, MD, PhD, chief of structural and interventional cardiology at Rush University Medical Center, Chicago.
The Society for Cardiovascular Angiography & Interventions issued the guidelines at its annual scientific sessions meeting in Atlanta and published them simultaneously in the society’s journal.
The guidelines issue strong and conditional recommendations. The former means clinicians should order the intervention for most patients; the latter means decisionmaking is more nuanced and should consider contributing factors.
The guidelines clarify patient selection for PFO closure outside the “pretty narrow” indication the FDA approved, Dr. Kavinsky said, which is for PFO-associated ischemic stroke in patients aged 18-60 years.
“So what about patients who are older than 60? What about patients who had their stroke 10 years ago?” Dr. Kavinsky asked. “Those are issues that were unanswered in the randomized clinical trials.”
The guidelines also refine recommendations about anticoagulation in these patients, including its use after PFO closure in selected patients, Dr. Kavinsky noted. “It’s the opinion of the panel that although anticoagulants may be effective, because of issues of noncompliance, because of issues of interruption of therapy by physicians for a variety of reasons, including surgery or noncompliance, that it is preferable to do a PFO device closure to giving anticoagulant therapy.”
Many of the recommendations cover PFO closure alongside antiplatelet or anticoagulation therapy. Key conditional recommendations for patients who haven’t had a PFO-related stroke are:
- Avoiding its routine use in patients with chronic migraines, prior decompression illness (DCI), thrombophilia, atrial septal aneurysm, transient ischemic attack (TIA), or deep vein thrombosis (DVT).
- Considering PFO closure in patients with platypnea-orthodeoxia syndrome (POS) with no other discernible cause of hypoxia or systemic embolism in whom other embolic causes have been ruled out.
In patients who’ve had a PFO-related stroke, the guidelines strongly recommend PFO closure versus antiplatelet therapy alone, but conditionally, not in patients with atrial fibrillation who’ve had an ischemic stroke. They also conditionally suggest PFO closure rather than long-term antiplatelet therapy alone in PFO stroke patients aged 60 and older, as well as those with thrombophilia already on antiplatelet therapy but not anticoagulation. However, the guidelines make no recommendation on PFO closure based on how much time has passed since the previous stroke.
“Furthermore,” Dr. Kavinsky said, “in patients who require lifelong anticoagulation because of recurrent DVT or recurrent pulmonary emboli or thrombopenia, if they’ve had a PFO-mediated stroke, then it’s our opinion that they should have their PFO closed in addition to taking lifelong anticoagulation because of the same issues of noncompliance and interruption of therapy.” Those are conditional recommendations.
The guideline also checks a box in the FDA labeling that mandated agreement between cardiology and neurology in patient selection. The American Academy of Neurology (AAN) issued its own guideline in 2020 for patients with stroke and PFO. In Europe, the European Society of Cardiology issued two position papers on expanded applications of PFO closure.
The recommendations on when PFO closure shouldn’t be done are noteworthy, Dr. Kavinsky said. “PFOs are present in 25% of the adult population, so the number of patients with PFO is huge and the indication for the FDA is really narrow: to reduce the risk of recurrent stroke in patients with PFO-mediated stroke. So, there’s the tremendous potential for abuse out there, of excessive procedures, of doing unnecessary procedures.”
The guidelines are a follow-up to the operator institutional requirements document SCAI issued in 2019 that set requirements for hospital offering and physicians performing PFO closure, Dr. Kavinsky added.
In an editorial accompanying the published guideline, Robert J. Sommer, MD, and Jamil A. Aboulhosn, MD, wrote that they support the recommendations “which help spotlight and clarify the growing list of potential indications for PFO closure.” They noted that the guidelines panel’s “strong” recommendations were for indications validated by randomized trials and that “conditional” recommendations were based on panelists’ experience and observational data.
“It is critical to recognize that most of these guidelines represent consensus opinion only,” wrote Dr. Sommer, who specializes in adult congenital and pediatric cardiology at Columbia University Irving Medical Center, New York, and Dr. Aboulhosn, an interventional cardiologist at Ronald Reagan University of California, Los Angeles, Medical Center. They emphasized the guidelines’ “heavy emphasis” on shared decisionmaking with patients.
Dr. Kavinsky is a principal investigator for Edwards Lifesciences, W.L. Gore and Associates, Medtronic, and Abbott. Dr. Sommer is a principal investigator and investigator in studies sponsored by W.L. Gore & Associates. Dr. Aboulhosn is a consultant to Abbott Medical.
The first-ever guidelines for interventional cardiologists using percutaneous patent foramen ovale closure recommend expanding the use of the procedure beyond the Food and Drug Administration–approved indication following PFO-associated ischemic stroke, adding clarification about the use of PFO with anticoagulation and hedging against abuse and overuse of the procedure, said the chair of the guideline writing committee.
“The most important things surrounding these guidelines are to help clinicians and policymakers – third-party payers – to address PFO in patient subsets that were not included in the large randomized clinical trials that led to FDA approval,” said writing group chair Clifford J. Kavinsky, MD, PhD, chief of structural and interventional cardiology at Rush University Medical Center, Chicago.
The Society for Cardiovascular Angiography & Interventions issued the guidelines at its annual scientific sessions meeting in Atlanta and published them simultaneously in the society’s journal.
The guidelines issue strong and conditional recommendations. The former means clinicians should order the intervention for most patients; the latter means decisionmaking is more nuanced and should consider contributing factors.
The guidelines clarify patient selection for PFO closure outside the “pretty narrow” indication the FDA approved, Dr. Kavinsky said, which is for PFO-associated ischemic stroke in patients aged 18-60 years.
“So what about patients who are older than 60? What about patients who had their stroke 10 years ago?” Dr. Kavinsky asked. “Those are issues that were unanswered in the randomized clinical trials.”
The guidelines also refine recommendations about anticoagulation in these patients, including its use after PFO closure in selected patients, Dr. Kavinsky noted. “It’s the opinion of the panel that although anticoagulants may be effective, because of issues of noncompliance, because of issues of interruption of therapy by physicians for a variety of reasons, including surgery or noncompliance, that it is preferable to do a PFO device closure to giving anticoagulant therapy.”
Many of the recommendations cover PFO closure alongside antiplatelet or anticoagulation therapy. Key conditional recommendations for patients who haven’t had a PFO-related stroke are:
- Avoiding its routine use in patients with chronic migraines, prior decompression illness (DCI), thrombophilia, atrial septal aneurysm, transient ischemic attack (TIA), or deep vein thrombosis (DVT).
- Considering PFO closure in patients with platypnea-orthodeoxia syndrome (POS) with no other discernible cause of hypoxia or systemic embolism in whom other embolic causes have been ruled out.
In patients who’ve had a PFO-related stroke, the guidelines strongly recommend PFO closure versus antiplatelet therapy alone, but conditionally, not in patients with atrial fibrillation who’ve had an ischemic stroke. They also conditionally suggest PFO closure rather than long-term antiplatelet therapy alone in PFO stroke patients aged 60 and older, as well as those with thrombophilia already on antiplatelet therapy but not anticoagulation. However, the guidelines make no recommendation on PFO closure based on how much time has passed since the previous stroke.
“Furthermore,” Dr. Kavinsky said, “in patients who require lifelong anticoagulation because of recurrent DVT or recurrent pulmonary emboli or thrombopenia, if they’ve had a PFO-mediated stroke, then it’s our opinion that they should have their PFO closed in addition to taking lifelong anticoagulation because of the same issues of noncompliance and interruption of therapy.” Those are conditional recommendations.
The guideline also checks a box in the FDA labeling that mandated agreement between cardiology and neurology in patient selection. The American Academy of Neurology (AAN) issued its own guideline in 2020 for patients with stroke and PFO. In Europe, the European Society of Cardiology issued two position papers on expanded applications of PFO closure.
The recommendations on when PFO closure shouldn’t be done are noteworthy, Dr. Kavinsky said. “PFOs are present in 25% of the adult population, so the number of patients with PFO is huge and the indication for the FDA is really narrow: to reduce the risk of recurrent stroke in patients with PFO-mediated stroke. So, there’s the tremendous potential for abuse out there, of excessive procedures, of doing unnecessary procedures.”
The guidelines are a follow-up to the operator institutional requirements document SCAI issued in 2019 that set requirements for hospital offering and physicians performing PFO closure, Dr. Kavinsky added.
In an editorial accompanying the published guideline, Robert J. Sommer, MD, and Jamil A. Aboulhosn, MD, wrote that they support the recommendations “which help spotlight and clarify the growing list of potential indications for PFO closure.” They noted that the guidelines panel’s “strong” recommendations were for indications validated by randomized trials and that “conditional” recommendations were based on panelists’ experience and observational data.
“It is critical to recognize that most of these guidelines represent consensus opinion only,” wrote Dr. Sommer, who specializes in adult congenital and pediatric cardiology at Columbia University Irving Medical Center, New York, and Dr. Aboulhosn, an interventional cardiologist at Ronald Reagan University of California, Los Angeles, Medical Center. They emphasized the guidelines’ “heavy emphasis” on shared decisionmaking with patients.
Dr. Kavinsky is a principal investigator for Edwards Lifesciences, W.L. Gore and Associates, Medtronic, and Abbott. Dr. Sommer is a principal investigator and investigator in studies sponsored by W.L. Gore & Associates. Dr. Aboulhosn is a consultant to Abbott Medical.
The first-ever guidelines for interventional cardiologists using percutaneous patent foramen ovale closure recommend expanding the use of the procedure beyond the Food and Drug Administration–approved indication following PFO-associated ischemic stroke, adding clarification about the use of PFO with anticoagulation and hedging against abuse and overuse of the procedure, said the chair of the guideline writing committee.
“The most important things surrounding these guidelines are to help clinicians and policymakers – third-party payers – to address PFO in patient subsets that were not included in the large randomized clinical trials that led to FDA approval,” said writing group chair Clifford J. Kavinsky, MD, PhD, chief of structural and interventional cardiology at Rush University Medical Center, Chicago.
The Society for Cardiovascular Angiography & Interventions issued the guidelines at its annual scientific sessions meeting in Atlanta and published them simultaneously in the society’s journal.
The guidelines issue strong and conditional recommendations. The former means clinicians should order the intervention for most patients; the latter means decisionmaking is more nuanced and should consider contributing factors.
The guidelines clarify patient selection for PFO closure outside the “pretty narrow” indication the FDA approved, Dr. Kavinsky said, which is for PFO-associated ischemic stroke in patients aged 18-60 years.
“So what about patients who are older than 60? What about patients who had their stroke 10 years ago?” Dr. Kavinsky asked. “Those are issues that were unanswered in the randomized clinical trials.”
The guidelines also refine recommendations about anticoagulation in these patients, including its use after PFO closure in selected patients, Dr. Kavinsky noted. “It’s the opinion of the panel that although anticoagulants may be effective, because of issues of noncompliance, because of issues of interruption of therapy by physicians for a variety of reasons, including surgery or noncompliance, that it is preferable to do a PFO device closure to giving anticoagulant therapy.”
Many of the recommendations cover PFO closure alongside antiplatelet or anticoagulation therapy. Key conditional recommendations for patients who haven’t had a PFO-related stroke are:
- Avoiding its routine use in patients with chronic migraines, prior decompression illness (DCI), thrombophilia, atrial septal aneurysm, transient ischemic attack (TIA), or deep vein thrombosis (DVT).
- Considering PFO closure in patients with platypnea-orthodeoxia syndrome (POS) with no other discernible cause of hypoxia or systemic embolism in whom other embolic causes have been ruled out.
In patients who’ve had a PFO-related stroke, the guidelines strongly recommend PFO closure versus antiplatelet therapy alone, but conditionally, not in patients with atrial fibrillation who’ve had an ischemic stroke. They also conditionally suggest PFO closure rather than long-term antiplatelet therapy alone in PFO stroke patients aged 60 and older, as well as those with thrombophilia already on antiplatelet therapy but not anticoagulation. However, the guidelines make no recommendation on PFO closure based on how much time has passed since the previous stroke.
“Furthermore,” Dr. Kavinsky said, “in patients who require lifelong anticoagulation because of recurrent DVT or recurrent pulmonary emboli or thrombopenia, if they’ve had a PFO-mediated stroke, then it’s our opinion that they should have their PFO closed in addition to taking lifelong anticoagulation because of the same issues of noncompliance and interruption of therapy.” Those are conditional recommendations.
The guideline also checks a box in the FDA labeling that mandated agreement between cardiology and neurology in patient selection. The American Academy of Neurology (AAN) issued its own guideline in 2020 for patients with stroke and PFO. In Europe, the European Society of Cardiology issued two position papers on expanded applications of PFO closure.
The recommendations on when PFO closure shouldn’t be done are noteworthy, Dr. Kavinsky said. “PFOs are present in 25% of the adult population, so the number of patients with PFO is huge and the indication for the FDA is really narrow: to reduce the risk of recurrent stroke in patients with PFO-mediated stroke. So, there’s the tremendous potential for abuse out there, of excessive procedures, of doing unnecessary procedures.”
The guidelines are a follow-up to the operator institutional requirements document SCAI issued in 2019 that set requirements for hospital offering and physicians performing PFO closure, Dr. Kavinsky added.
In an editorial accompanying the published guideline, Robert J. Sommer, MD, and Jamil A. Aboulhosn, MD, wrote that they support the recommendations “which help spotlight and clarify the growing list of potential indications for PFO closure.” They noted that the guidelines panel’s “strong” recommendations were for indications validated by randomized trials and that “conditional” recommendations were based on panelists’ experience and observational data.
“It is critical to recognize that most of these guidelines represent consensus opinion only,” wrote Dr. Sommer, who specializes in adult congenital and pediatric cardiology at Columbia University Irving Medical Center, New York, and Dr. Aboulhosn, an interventional cardiologist at Ronald Reagan University of California, Los Angeles, Medical Center. They emphasized the guidelines’ “heavy emphasis” on shared decisionmaking with patients.
Dr. Kavinsky is a principal investigator for Edwards Lifesciences, W.L. Gore and Associates, Medtronic, and Abbott. Dr. Sommer is a principal investigator and investigator in studies sponsored by W.L. Gore & Associates. Dr. Aboulhosn is a consultant to Abbott Medical.
FROM SCAI 2022
Keeping thyroid hormone treatment on target is key for the heart
A new study highlights the importance of avoiding both exogenous hyperthyroidism and exogenous hypothyroidism to decrease cardiovascular risk and death among patients receiving thyroid hormone treatment.
“Our findings suggest that clinicians should make every effort to maintain euthyroidism in patients on thyroid hormone treatment, regardless of underlying cardiovascular risk, particularly in vulnerable populations, such as older adults,” senior author Maria Papaleontiou, MD, said in an interview.
Commenting on the study, David S. Cooper, MD, of Johns Hopkins University School of Medicine, Baltimore, agreed that the findings are significant.
“Both undertreatment and overtreatment were associated with adverse cardiovascular outcomes, meaning that patients’ thyroid function needs to be monitored, and levothyroxine adjusted if need be, on an ongoing basis,” he told this news organization.
Getting the balance right: a tricky task
Variations in thyroid hormone levels falling above or below target ranges are common with thyroid hormone therapy, as a wide array of factors can prompt the need to regularly adjust dosing to maintain “index” levels. And while guidelines from the American Thyroid Association (ATA) recommend maintaining serum thyroid stimulating hormone (TSH) levels in the normal ranges during treatment, the task is tricky.
“Despite these [ATA] guidelines, prior studies in adults with hypothyroidism have shown that up to 30% are undertreated and up to 48% are overtreated,” said Dr. Papaleontiou, an assistant professor in the Division of Metabolism, Endocrinology at the University of Michigan, Ann Arbor.
In a previous study, Dr. Papaleontiou and colleagues showed that the intensity of thyroid hormone treatment is a modifiable risk factor for incident atrial fibrillation and stroke, however, less is understood about the association with cardiovascular mortality.
For the new study, published in JAMA Network Open, Josh M. Evron, MD, of the University of North Carolina, Chapel Hill, and colleagues further investigated the issue in a large, retrospective cohort of 705,307 adults in the Veterans Health Administration Corporate Data Warehouse treated with thyroid hormone during 2004-2017 who had a median follow-up of 4 years.
They investigated the roles of TSH as well as free thyroxine (FT4) levels among 701,929 adults in the group with data on TSH and 373,981 patients with FT4 measurements.
The mean age of participants was 67 years and 88.7% were male.
Over the course of the study, 10.8% of patients (75,963) died of cardiovascular causes.
Compared with patients with normal thyroid levels, those with exogenous hyperthyroidism related to thyroid hormone treatment had an increased risk of cardiovascular mortality, specifically including when TSH levels were below 0.1 mIU/L (adjusted hazard ratio, 1.39) and when FT4 levels were above 1.9 ng/dL (AHR, 1.29), independent of factors including age, sex, and traditional cardiovascular risk factors, including hypertension, smoking, and previous cardiovascular disease or arrhythmia.
In addition, the increased risk of cardiovascular mortality was observed with exogenous hypothyroidism, specifically among those with TSH levels above 20 mIU/L (AHR, 2.67) and FT4 levels below 0.7 ng/dL (AHR, 1.56), after multivariate adjustment.
Of note, the risk of cardiovascular mortality was dose-dependent, with the risk increasing progressively with the lower and higher TSH levels, compared with normal levels.
The increased mortality risk in relation to TSH levels was more pronounced among older patients, compared with FT4 associations, the authors note.
“From a clinical perspective, older adults, and particularly the oldest old (aged 85 years), appear to be the most vulnerable, with increased risk of cardiovascular mortality with both exogenous hyperthyroidism and hypothyroidism,” they report.
Among key limitations is that women, who make up the majority of patients with thyroid disease, are under-represented in the predominantly male population of the Veterans Health Administration.
Nevertheless, “because the risk of cardiovascular disease is higher for men than for women, and because more than 70,000 women were included in this cohort, the results of this study are highly clinically relevant,” the authors note.
Addressing over- and under-treatment will avoid harm
The results are also important considering the status of levothyroxine (for hypothyroidism) as consistently ranking among the top three prescription medications in the United States.
And with the common occurrence of exogenous hyperthyroidism or hypothyroidism, the findings have important implications.
“Addressing over- and under-treatment of hypothyroidism promptly will help reduce patient harm, particularly in vulnerable populations such as older adults who are at higher risk for adverse effects,” Dr. Papaleontiou said.
Dr. Cooper further commented that the findings underscore the need to be aware of treatment adjustments and targets that may vary according to patient age.
“In older persons, over 65-70, the target TSH may be higher [for example, 2-4 mIU/L] than in younger persons, and in patients above ages 70 or 80, serum TSH levels may be allowed to rise even further into the 4-6 mIU/L range,” he explained.
“The older the patient, the higher the chance for an adverse cardiovascular outcome if the TSH is subnormal due to iatrogenic thyrotoxicosis,” Dr. Cooper explained.
“In contrast, in younger individuals, an elevated TSH, indicating mild [subclinical] hypothyroidism may be associated with increased cardiovascular risk, especially with serum TSH levels greater than 7 mIU/L.”
The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study highlights the importance of avoiding both exogenous hyperthyroidism and exogenous hypothyroidism to decrease cardiovascular risk and death among patients receiving thyroid hormone treatment.
“Our findings suggest that clinicians should make every effort to maintain euthyroidism in patients on thyroid hormone treatment, regardless of underlying cardiovascular risk, particularly in vulnerable populations, such as older adults,” senior author Maria Papaleontiou, MD, said in an interview.
Commenting on the study, David S. Cooper, MD, of Johns Hopkins University School of Medicine, Baltimore, agreed that the findings are significant.
“Both undertreatment and overtreatment were associated with adverse cardiovascular outcomes, meaning that patients’ thyroid function needs to be monitored, and levothyroxine adjusted if need be, on an ongoing basis,” he told this news organization.
Getting the balance right: a tricky task
Variations in thyroid hormone levels falling above or below target ranges are common with thyroid hormone therapy, as a wide array of factors can prompt the need to regularly adjust dosing to maintain “index” levels. And while guidelines from the American Thyroid Association (ATA) recommend maintaining serum thyroid stimulating hormone (TSH) levels in the normal ranges during treatment, the task is tricky.
“Despite these [ATA] guidelines, prior studies in adults with hypothyroidism have shown that up to 30% are undertreated and up to 48% are overtreated,” said Dr. Papaleontiou, an assistant professor in the Division of Metabolism, Endocrinology at the University of Michigan, Ann Arbor.
In a previous study, Dr. Papaleontiou and colleagues showed that the intensity of thyroid hormone treatment is a modifiable risk factor for incident atrial fibrillation and stroke, however, less is understood about the association with cardiovascular mortality.
For the new study, published in JAMA Network Open, Josh M. Evron, MD, of the University of North Carolina, Chapel Hill, and colleagues further investigated the issue in a large, retrospective cohort of 705,307 adults in the Veterans Health Administration Corporate Data Warehouse treated with thyroid hormone during 2004-2017 who had a median follow-up of 4 years.
They investigated the roles of TSH as well as free thyroxine (FT4) levels among 701,929 adults in the group with data on TSH and 373,981 patients with FT4 measurements.
The mean age of participants was 67 years and 88.7% were male.
Over the course of the study, 10.8% of patients (75,963) died of cardiovascular causes.
Compared with patients with normal thyroid levels, those with exogenous hyperthyroidism related to thyroid hormone treatment had an increased risk of cardiovascular mortality, specifically including when TSH levels were below 0.1 mIU/L (adjusted hazard ratio, 1.39) and when FT4 levels were above 1.9 ng/dL (AHR, 1.29), independent of factors including age, sex, and traditional cardiovascular risk factors, including hypertension, smoking, and previous cardiovascular disease or arrhythmia.
In addition, the increased risk of cardiovascular mortality was observed with exogenous hypothyroidism, specifically among those with TSH levels above 20 mIU/L (AHR, 2.67) and FT4 levels below 0.7 ng/dL (AHR, 1.56), after multivariate adjustment.
Of note, the risk of cardiovascular mortality was dose-dependent, with the risk increasing progressively with the lower and higher TSH levels, compared with normal levels.
The increased mortality risk in relation to TSH levels was more pronounced among older patients, compared with FT4 associations, the authors note.
“From a clinical perspective, older adults, and particularly the oldest old (aged 85 years), appear to be the most vulnerable, with increased risk of cardiovascular mortality with both exogenous hyperthyroidism and hypothyroidism,” they report.
Among key limitations is that women, who make up the majority of patients with thyroid disease, are under-represented in the predominantly male population of the Veterans Health Administration.
Nevertheless, “because the risk of cardiovascular disease is higher for men than for women, and because more than 70,000 women were included in this cohort, the results of this study are highly clinically relevant,” the authors note.
Addressing over- and under-treatment will avoid harm
The results are also important considering the status of levothyroxine (for hypothyroidism) as consistently ranking among the top three prescription medications in the United States.
And with the common occurrence of exogenous hyperthyroidism or hypothyroidism, the findings have important implications.
“Addressing over- and under-treatment of hypothyroidism promptly will help reduce patient harm, particularly in vulnerable populations such as older adults who are at higher risk for adverse effects,” Dr. Papaleontiou said.
Dr. Cooper further commented that the findings underscore the need to be aware of treatment adjustments and targets that may vary according to patient age.
“In older persons, over 65-70, the target TSH may be higher [for example, 2-4 mIU/L] than in younger persons, and in patients above ages 70 or 80, serum TSH levels may be allowed to rise even further into the 4-6 mIU/L range,” he explained.
“The older the patient, the higher the chance for an adverse cardiovascular outcome if the TSH is subnormal due to iatrogenic thyrotoxicosis,” Dr. Cooper explained.
“In contrast, in younger individuals, an elevated TSH, indicating mild [subclinical] hypothyroidism may be associated with increased cardiovascular risk, especially with serum TSH levels greater than 7 mIU/L.”
The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study highlights the importance of avoiding both exogenous hyperthyroidism and exogenous hypothyroidism to decrease cardiovascular risk and death among patients receiving thyroid hormone treatment.
“Our findings suggest that clinicians should make every effort to maintain euthyroidism in patients on thyroid hormone treatment, regardless of underlying cardiovascular risk, particularly in vulnerable populations, such as older adults,” senior author Maria Papaleontiou, MD, said in an interview.
Commenting on the study, David S. Cooper, MD, of Johns Hopkins University School of Medicine, Baltimore, agreed that the findings are significant.
“Both undertreatment and overtreatment were associated with adverse cardiovascular outcomes, meaning that patients’ thyroid function needs to be monitored, and levothyroxine adjusted if need be, on an ongoing basis,” he told this news organization.
Getting the balance right: a tricky task
Variations in thyroid hormone levels falling above or below target ranges are common with thyroid hormone therapy, as a wide array of factors can prompt the need to regularly adjust dosing to maintain “index” levels. And while guidelines from the American Thyroid Association (ATA) recommend maintaining serum thyroid stimulating hormone (TSH) levels in the normal ranges during treatment, the task is tricky.
“Despite these [ATA] guidelines, prior studies in adults with hypothyroidism have shown that up to 30% are undertreated and up to 48% are overtreated,” said Dr. Papaleontiou, an assistant professor in the Division of Metabolism, Endocrinology at the University of Michigan, Ann Arbor.
In a previous study, Dr. Papaleontiou and colleagues showed that the intensity of thyroid hormone treatment is a modifiable risk factor for incident atrial fibrillation and stroke, however, less is understood about the association with cardiovascular mortality.
For the new study, published in JAMA Network Open, Josh M. Evron, MD, of the University of North Carolina, Chapel Hill, and colleagues further investigated the issue in a large, retrospective cohort of 705,307 adults in the Veterans Health Administration Corporate Data Warehouse treated with thyroid hormone during 2004-2017 who had a median follow-up of 4 years.
They investigated the roles of TSH as well as free thyroxine (FT4) levels among 701,929 adults in the group with data on TSH and 373,981 patients with FT4 measurements.
The mean age of participants was 67 years and 88.7% were male.
Over the course of the study, 10.8% of patients (75,963) died of cardiovascular causes.
Compared with patients with normal thyroid levels, those with exogenous hyperthyroidism related to thyroid hormone treatment had an increased risk of cardiovascular mortality, specifically including when TSH levels were below 0.1 mIU/L (adjusted hazard ratio, 1.39) and when FT4 levels were above 1.9 ng/dL (AHR, 1.29), independent of factors including age, sex, and traditional cardiovascular risk factors, including hypertension, smoking, and previous cardiovascular disease or arrhythmia.
In addition, the increased risk of cardiovascular mortality was observed with exogenous hypothyroidism, specifically among those with TSH levels above 20 mIU/L (AHR, 2.67) and FT4 levels below 0.7 ng/dL (AHR, 1.56), after multivariate adjustment.
Of note, the risk of cardiovascular mortality was dose-dependent, with the risk increasing progressively with the lower and higher TSH levels, compared with normal levels.
The increased mortality risk in relation to TSH levels was more pronounced among older patients, compared with FT4 associations, the authors note.
“From a clinical perspective, older adults, and particularly the oldest old (aged 85 years), appear to be the most vulnerable, with increased risk of cardiovascular mortality with both exogenous hyperthyroidism and hypothyroidism,” they report.
Among key limitations is that women, who make up the majority of patients with thyroid disease, are under-represented in the predominantly male population of the Veterans Health Administration.
Nevertheless, “because the risk of cardiovascular disease is higher for men than for women, and because more than 70,000 women were included in this cohort, the results of this study are highly clinically relevant,” the authors note.
Addressing over- and under-treatment will avoid harm
The results are also important considering the status of levothyroxine (for hypothyroidism) as consistently ranking among the top three prescription medications in the United States.
And with the common occurrence of exogenous hyperthyroidism or hypothyroidism, the findings have important implications.
“Addressing over- and under-treatment of hypothyroidism promptly will help reduce patient harm, particularly in vulnerable populations such as older adults who are at higher risk for adverse effects,” Dr. Papaleontiou said.
Dr. Cooper further commented that the findings underscore the need to be aware of treatment adjustments and targets that may vary according to patient age.
“In older persons, over 65-70, the target TSH may be higher [for example, 2-4 mIU/L] than in younger persons, and in patients above ages 70 or 80, serum TSH levels may be allowed to rise even further into the 4-6 mIU/L range,” he explained.
“The older the patient, the higher the chance for an adverse cardiovascular outcome if the TSH is subnormal due to iatrogenic thyrotoxicosis,” Dr. Cooper explained.
“In contrast, in younger individuals, an elevated TSH, indicating mild [subclinical] hypothyroidism may be associated with increased cardiovascular risk, especially with serum TSH levels greater than 7 mIU/L.”
The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Taking cardiac pacing from boring to super cool
For the past 2 decades, catheter ablation stole most of the excitement in electrophysiology. Cardiac pacing was seen as necessary but boring. His-bundle pacing earned only modest attention.
But at the annual scientific sessions of the Heart Rhythm Society, cardiac pacing consolidated its comeback and entered the super-cool category.
Not one but three late-breaking clinical trials considered the role of pacing the heart’s conduction system for both preventive and therapeutic purposes. Conduction system pacing, or CSP as we call it, includes pacing the His bundle or the left bundle branch. Left bundle–branch pacing has now largely replaced His-bundle pacing.
Before I tell you about the studies, let’s review why CSP disrupts the status quo.
The core idea goes back to basic physiology: After the impulse leaves the atrioventricular node, the heart’s specialized conduction system allows rapid and synchronous conduction to both the right and left ventricles.
Standard cardiac pacing means fixing a pacing lead into the muscle of the right ventricle. From that spot, conduction spreads via slower muscle-to-muscle conduction, which leads to a wide QRS complex and the right ventricle contracts before the left ventricle.
While such dyssynchronous contraction is better than no contraction, this approach leads to a pacing-induced cardiomyopathy in a substantial number of cases. (The incidence reported in many studies varies widely.)
The most disruptive effect of conduction system pacing is that it is a form of cardiac resynchronization therapy (CRT). And that is nifty because, until recently, resynchronizing the ventricles required placing two ventricular leads: one in the right ventricle and the other in the coronary sinus to pace the left ventricle.
Left bundle-branch pacing vs. biventricular pacing
The first of the three HRS studies is the LBBP-RESYNC randomized controlled trial led by Jiangang Zou, MD, PhD, and performed in multiple centers in China. It compared the efficacy of left bundle–branch pacing (LBBP) with that of conventional biventricular pacing in 40 patients with heart failure who were eligible for CRT. The primary endpoint was the change in left ventricular ejection fraction (LVEF) from baseline to 6-month follow-up.
The results favored LBBP. Although both pacing techniques improved LVEF from baseline, the between-group difference in LVEF was greater in the LBBP arm than the biventricular pacing arm by a statistically significant 5.6% (95% confidence interval, 0.3%-10.9%). Secondary endpoints, such as reductions in left ventricular end-systolic volume, N-terminal of the prohormone brain natriuretic peptide, and QRS duration, also favored LBBP.
Conduction system pacing vs. biventricular pacing
A second late-breaking study, from the Geisinger group, led by Pugazhendhi Vijayaraman, MD, was simultaneously published in Heart Rhythm.
This nonrandomized observational study compared nearly 500 patients eligible for CRT treated at two health systems. One group favors conduction system pacing and the other does traditional biventricular pacing, which set up a two-armed comparison.
CSP was accomplished by LBBP (65%) and His-bundle pacing (35%).
The primary endpoint of death or first hospitalization for heart failure occurred in 28.3% of patients in the CSP arm versus 38.4% of the biventricular arm (hazard ratio, 1.52; 95% CI, 1.08-2.09). QRS duration and LVEF also improved from baseline in both groups.
LBB area pacing as a bailout for failed CRT
The Geisinger group also presented and published an international multicenter study that assessed the feasibility of LBBP as a bailout when standard biventricular pacing did not work – because of inadequate coronary sinus anatomy or CRT nonresponse, defined as lack of clinical or echocardiographic improvement.
This series included 212 patients in whom CRT failed and who underwent attempted LBBP pacing. The bailout was successful in 200 patients (91%). The primary endpoint was defined as an increase in LVEF above 5% on echocardiography.
During 12-month follow-up, 61% of patients had an improvement in LVEF above 5% and nearly 30% had a “super-response,” defined as a 20% or greater increase or normalization of LVEF. Similar to the previous studies, LBBP resulted in shorter QRS duration and improved echocardiography parameters.
Am I persuaded?
I was an early adopter of His-bundle pacing. When successful, it delivered both aesthetically pleasing QRS complexes and clinical efficacy. But there were many challenges: it is technically difficult, and capture thresholds are often high at implant and get higher over time, which leads to shorter battery life.
Pacing the left bundle branch mitigates these challenges. Here, the operator approaches from the right side and screws the lead a few millimeters into the septum, so the tip of the lead can capture the left bundle or one of its branches. This allows activation of the heart’s specialized conduction system and thus synchronizes right and left ventricle contraction.
Although there is a learning curve, LBBP is technically easier than His-bundle pacing and ultimately results in far better pacing and sensing parameters. What’s more, the preferred lead for LBBP has a stellar efficacy record – over years.
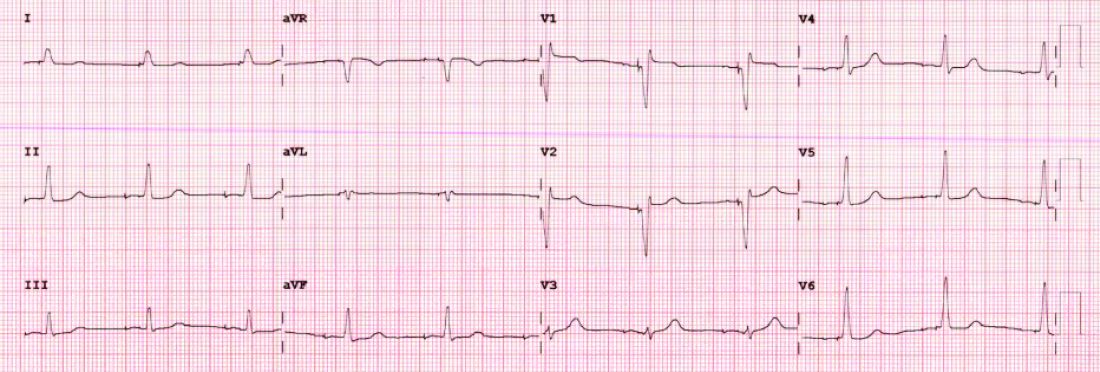
I have become enthralled by the gorgeous QRS complexes from LBBP. The ability to pace the heart without creating dyssynchrony infuses me with joy. I chose cardiology largely because of the beauty of the ECG.
But as a medical conservative who is cautious about unproven therapies, I have questions. How is LBBP defined? Is left septal pacing good enough, or do you need actual left bundle capture? What about long-term performance of a lead in the septum?
Biventricular pacing has set a high bar because it has been proven effective for reducing hard clinical outcomes in large randomized controlled trials.
The studies at HRS begin to answer these questions. The randomized controlled trial from China supports the notion that effective LBBP (the investigators rigorously defined left bundle capture) leads to favorable effects on cardiac contraction. The two observational studies reported similarly encouraging findings on cardiac function.
The three studies therefore tentatively support the notion that LBBP actually produces favorable cardiac performance.
Whether LBBP leads to better clinical outcomes remains uncertain. The nonrandomized comparison study, which found better hard outcomes in the CSP arm, cannot be used to infer causality. There is too much risk for selection bias.
But the LBBP bailout study does suggest that this strategy is reasonable when coronary sinus leads fail – especially since the alternative is surgical placement of an epicardial lead on the left ventricle.
At minimum, the HRS studies persuade me that LBBP will likely prevent pacing-induced cardiomyopathy. If I or a family member required a pacemaker, I’d surely want the operator to be skilled at placing a left bundle lead.
While I am confident that conduction system pacing will become a transformative advance in cardiac pacing, aesthetically pleasing ECG patterns are not enough. There remains much to learn with this nascent approach.
The barriers to getting more CSP trials
The challenge going forward will be funding new trials. CSP stands to prevent pacing-induced cardiomyopathy and offer less costly alternatives to standard biventricular pacing for CRT. This is great for patients, but it would mean that fewer higher-cost CRT devices will be sold.
Heart rhythm research is largely industry-funded because in most cases better therapies for patients mean more profits for industry. In the case of CSP, there is no such confluence of interests.
Conduction system pacing has come about because of the efforts of a few tireless champions who not only published extensively but were also skilled at using social media to spread the excitement. Trials have been small and often self-funded.
The data presented at HRS provides enough equipoise to support a large outcomes-based randomized controlled trial. Imagine if our CSP champions were able to find public-funding sources for such future trials.
Now that would be super cool.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
For the past 2 decades, catheter ablation stole most of the excitement in electrophysiology. Cardiac pacing was seen as necessary but boring. His-bundle pacing earned only modest attention.
But at the annual scientific sessions of the Heart Rhythm Society, cardiac pacing consolidated its comeback and entered the super-cool category.
Not one but three late-breaking clinical trials considered the role of pacing the heart’s conduction system for both preventive and therapeutic purposes. Conduction system pacing, or CSP as we call it, includes pacing the His bundle or the left bundle branch. Left bundle–branch pacing has now largely replaced His-bundle pacing.
Before I tell you about the studies, let’s review why CSP disrupts the status quo.
The core idea goes back to basic physiology: After the impulse leaves the atrioventricular node, the heart’s specialized conduction system allows rapid and synchronous conduction to both the right and left ventricles.
Standard cardiac pacing means fixing a pacing lead into the muscle of the right ventricle. From that spot, conduction spreads via slower muscle-to-muscle conduction, which leads to a wide QRS complex and the right ventricle contracts before the left ventricle.
While such dyssynchronous contraction is better than no contraction, this approach leads to a pacing-induced cardiomyopathy in a substantial number of cases. (The incidence reported in many studies varies widely.)
The most disruptive effect of conduction system pacing is that it is a form of cardiac resynchronization therapy (CRT). And that is nifty because, until recently, resynchronizing the ventricles required placing two ventricular leads: one in the right ventricle and the other in the coronary sinus to pace the left ventricle.
Left bundle-branch pacing vs. biventricular pacing
The first of the three HRS studies is the LBBP-RESYNC randomized controlled trial led by Jiangang Zou, MD, PhD, and performed in multiple centers in China. It compared the efficacy of left bundle–branch pacing (LBBP) with that of conventional biventricular pacing in 40 patients with heart failure who were eligible for CRT. The primary endpoint was the change in left ventricular ejection fraction (LVEF) from baseline to 6-month follow-up.
The results favored LBBP. Although both pacing techniques improved LVEF from baseline, the between-group difference in LVEF was greater in the LBBP arm than the biventricular pacing arm by a statistically significant 5.6% (95% confidence interval, 0.3%-10.9%). Secondary endpoints, such as reductions in left ventricular end-systolic volume, N-terminal of the prohormone brain natriuretic peptide, and QRS duration, also favored LBBP.
Conduction system pacing vs. biventricular pacing
A second late-breaking study, from the Geisinger group, led by Pugazhendhi Vijayaraman, MD, was simultaneously published in Heart Rhythm.
This nonrandomized observational study compared nearly 500 patients eligible for CRT treated at two health systems. One group favors conduction system pacing and the other does traditional biventricular pacing, which set up a two-armed comparison.
CSP was accomplished by LBBP (65%) and His-bundle pacing (35%).
The primary endpoint of death or first hospitalization for heart failure occurred in 28.3% of patients in the CSP arm versus 38.4% of the biventricular arm (hazard ratio, 1.52; 95% CI, 1.08-2.09). QRS duration and LVEF also improved from baseline in both groups.
LBB area pacing as a bailout for failed CRT
The Geisinger group also presented and published an international multicenter study that assessed the feasibility of LBBP as a bailout when standard biventricular pacing did not work – because of inadequate coronary sinus anatomy or CRT nonresponse, defined as lack of clinical or echocardiographic improvement.
This series included 212 patients in whom CRT failed and who underwent attempted LBBP pacing. The bailout was successful in 200 patients (91%). The primary endpoint was defined as an increase in LVEF above 5% on echocardiography.
During 12-month follow-up, 61% of patients had an improvement in LVEF above 5% and nearly 30% had a “super-response,” defined as a 20% or greater increase or normalization of LVEF. Similar to the previous studies, LBBP resulted in shorter QRS duration and improved echocardiography parameters.
Am I persuaded?
I was an early adopter of His-bundle pacing. When successful, it delivered both aesthetically pleasing QRS complexes and clinical efficacy. But there were many challenges: it is technically difficult, and capture thresholds are often high at implant and get higher over time, which leads to shorter battery life.
Pacing the left bundle branch mitigates these challenges. Here, the operator approaches from the right side and screws the lead a few millimeters into the septum, so the tip of the lead can capture the left bundle or one of its branches. This allows activation of the heart’s specialized conduction system and thus synchronizes right and left ventricle contraction.
Although there is a learning curve, LBBP is technically easier than His-bundle pacing and ultimately results in far better pacing and sensing parameters. What’s more, the preferred lead for LBBP has a stellar efficacy record – over years.
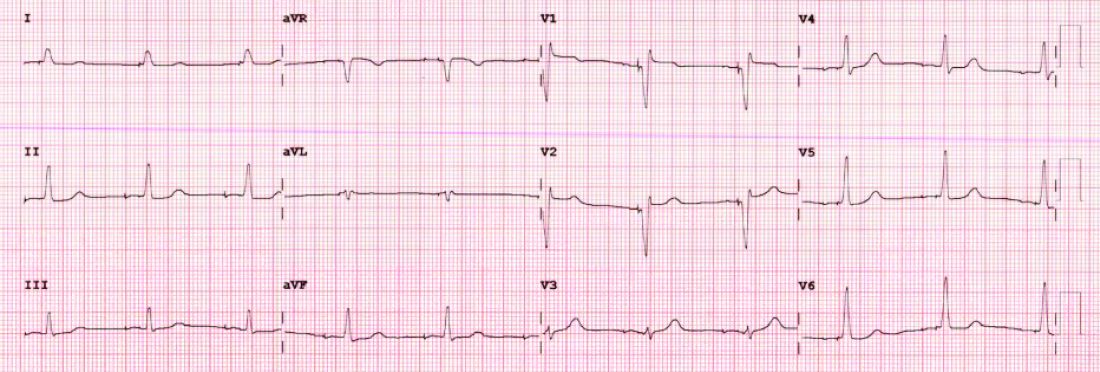
I have become enthralled by the gorgeous QRS complexes from LBBP. The ability to pace the heart without creating dyssynchrony infuses me with joy. I chose cardiology largely because of the beauty of the ECG.
But as a medical conservative who is cautious about unproven therapies, I have questions. How is LBBP defined? Is left septal pacing good enough, or do you need actual left bundle capture? What about long-term performance of a lead in the septum?
Biventricular pacing has set a high bar because it has been proven effective for reducing hard clinical outcomes in large randomized controlled trials.
The studies at HRS begin to answer these questions. The randomized controlled trial from China supports the notion that effective LBBP (the investigators rigorously defined left bundle capture) leads to favorable effects on cardiac contraction. The two observational studies reported similarly encouraging findings on cardiac function.
The three studies therefore tentatively support the notion that LBBP actually produces favorable cardiac performance.
Whether LBBP leads to better clinical outcomes remains uncertain. The nonrandomized comparison study, which found better hard outcomes in the CSP arm, cannot be used to infer causality. There is too much risk for selection bias.
But the LBBP bailout study does suggest that this strategy is reasonable when coronary sinus leads fail – especially since the alternative is surgical placement of an epicardial lead on the left ventricle.
At minimum, the HRS studies persuade me that LBBP will likely prevent pacing-induced cardiomyopathy. If I or a family member required a pacemaker, I’d surely want the operator to be skilled at placing a left bundle lead.
While I am confident that conduction system pacing will become a transformative advance in cardiac pacing, aesthetically pleasing ECG patterns are not enough. There remains much to learn with this nascent approach.
The barriers to getting more CSP trials
The challenge going forward will be funding new trials. CSP stands to prevent pacing-induced cardiomyopathy and offer less costly alternatives to standard biventricular pacing for CRT. This is great for patients, but it would mean that fewer higher-cost CRT devices will be sold.
Heart rhythm research is largely industry-funded because in most cases better therapies for patients mean more profits for industry. In the case of CSP, there is no such confluence of interests.
Conduction system pacing has come about because of the efforts of a few tireless champions who not only published extensively but were also skilled at using social media to spread the excitement. Trials have been small and often self-funded.
The data presented at HRS provides enough equipoise to support a large outcomes-based randomized controlled trial. Imagine if our CSP champions were able to find public-funding sources for such future trials.
Now that would be super cool.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
For the past 2 decades, catheter ablation stole most of the excitement in electrophysiology. Cardiac pacing was seen as necessary but boring. His-bundle pacing earned only modest attention.
But at the annual scientific sessions of the Heart Rhythm Society, cardiac pacing consolidated its comeback and entered the super-cool category.
Not one but three late-breaking clinical trials considered the role of pacing the heart’s conduction system for both preventive and therapeutic purposes. Conduction system pacing, or CSP as we call it, includes pacing the His bundle or the left bundle branch. Left bundle–branch pacing has now largely replaced His-bundle pacing.
Before I tell you about the studies, let’s review why CSP disrupts the status quo.
The core idea goes back to basic physiology: After the impulse leaves the atrioventricular node, the heart’s specialized conduction system allows rapid and synchronous conduction to both the right and left ventricles.
Standard cardiac pacing means fixing a pacing lead into the muscle of the right ventricle. From that spot, conduction spreads via slower muscle-to-muscle conduction, which leads to a wide QRS complex and the right ventricle contracts before the left ventricle.
While such dyssynchronous contraction is better than no contraction, this approach leads to a pacing-induced cardiomyopathy in a substantial number of cases. (The incidence reported in many studies varies widely.)
The most disruptive effect of conduction system pacing is that it is a form of cardiac resynchronization therapy (CRT). And that is nifty because, until recently, resynchronizing the ventricles required placing two ventricular leads: one in the right ventricle and the other in the coronary sinus to pace the left ventricle.
Left bundle-branch pacing vs. biventricular pacing
The first of the three HRS studies is the LBBP-RESYNC randomized controlled trial led by Jiangang Zou, MD, PhD, and performed in multiple centers in China. It compared the efficacy of left bundle–branch pacing (LBBP) with that of conventional biventricular pacing in 40 patients with heart failure who were eligible for CRT. The primary endpoint was the change in left ventricular ejection fraction (LVEF) from baseline to 6-month follow-up.
The results favored LBBP. Although both pacing techniques improved LVEF from baseline, the between-group difference in LVEF was greater in the LBBP arm than the biventricular pacing arm by a statistically significant 5.6% (95% confidence interval, 0.3%-10.9%). Secondary endpoints, such as reductions in left ventricular end-systolic volume, N-terminal of the prohormone brain natriuretic peptide, and QRS duration, also favored LBBP.
Conduction system pacing vs. biventricular pacing
A second late-breaking study, from the Geisinger group, led by Pugazhendhi Vijayaraman, MD, was simultaneously published in Heart Rhythm.
This nonrandomized observational study compared nearly 500 patients eligible for CRT treated at two health systems. One group favors conduction system pacing and the other does traditional biventricular pacing, which set up a two-armed comparison.
CSP was accomplished by LBBP (65%) and His-bundle pacing (35%).
The primary endpoint of death or first hospitalization for heart failure occurred in 28.3% of patients in the CSP arm versus 38.4% of the biventricular arm (hazard ratio, 1.52; 95% CI, 1.08-2.09). QRS duration and LVEF also improved from baseline in both groups.
LBB area pacing as a bailout for failed CRT
The Geisinger group also presented and published an international multicenter study that assessed the feasibility of LBBP as a bailout when standard biventricular pacing did not work – because of inadequate coronary sinus anatomy or CRT nonresponse, defined as lack of clinical or echocardiographic improvement.
This series included 212 patients in whom CRT failed and who underwent attempted LBBP pacing. The bailout was successful in 200 patients (91%). The primary endpoint was defined as an increase in LVEF above 5% on echocardiography.
During 12-month follow-up, 61% of patients had an improvement in LVEF above 5% and nearly 30% had a “super-response,” defined as a 20% or greater increase or normalization of LVEF. Similar to the previous studies, LBBP resulted in shorter QRS duration and improved echocardiography parameters.
Am I persuaded?
I was an early adopter of His-bundle pacing. When successful, it delivered both aesthetically pleasing QRS complexes and clinical efficacy. But there were many challenges: it is technically difficult, and capture thresholds are often high at implant and get higher over time, which leads to shorter battery life.
Pacing the left bundle branch mitigates these challenges. Here, the operator approaches from the right side and screws the lead a few millimeters into the septum, so the tip of the lead can capture the left bundle or one of its branches. This allows activation of the heart’s specialized conduction system and thus synchronizes right and left ventricle contraction.
Although there is a learning curve, LBBP is technically easier than His-bundle pacing and ultimately results in far better pacing and sensing parameters. What’s more, the preferred lead for LBBP has a stellar efficacy record – over years.
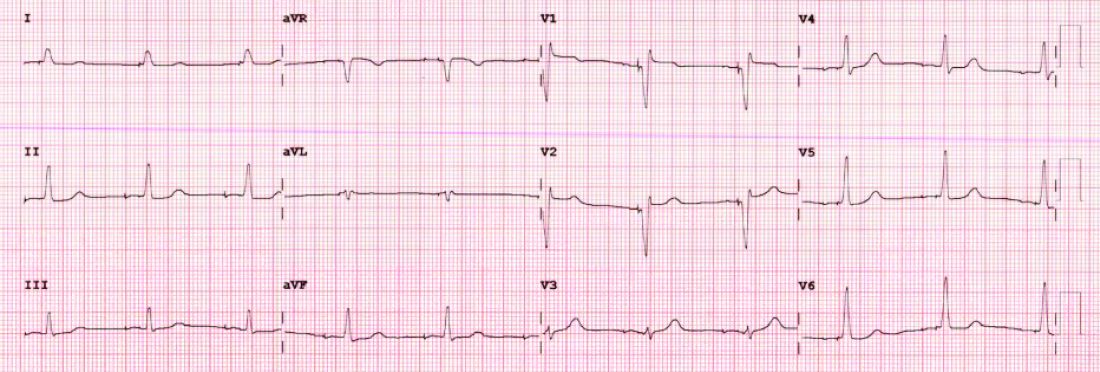
I have become enthralled by the gorgeous QRS complexes from LBBP. The ability to pace the heart without creating dyssynchrony infuses me with joy. I chose cardiology largely because of the beauty of the ECG.
But as a medical conservative who is cautious about unproven therapies, I have questions. How is LBBP defined? Is left septal pacing good enough, or do you need actual left bundle capture? What about long-term performance of a lead in the septum?
Biventricular pacing has set a high bar because it has been proven effective for reducing hard clinical outcomes in large randomized controlled trials.
The studies at HRS begin to answer these questions. The randomized controlled trial from China supports the notion that effective LBBP (the investigators rigorously defined left bundle capture) leads to favorable effects on cardiac contraction. The two observational studies reported similarly encouraging findings on cardiac function.
The three studies therefore tentatively support the notion that LBBP actually produces favorable cardiac performance.
Whether LBBP leads to better clinical outcomes remains uncertain. The nonrandomized comparison study, which found better hard outcomes in the CSP arm, cannot be used to infer causality. There is too much risk for selection bias.
But the LBBP bailout study does suggest that this strategy is reasonable when coronary sinus leads fail – especially since the alternative is surgical placement of an epicardial lead on the left ventricle.
At minimum, the HRS studies persuade me that LBBP will likely prevent pacing-induced cardiomyopathy. If I or a family member required a pacemaker, I’d surely want the operator to be skilled at placing a left bundle lead.
While I am confident that conduction system pacing will become a transformative advance in cardiac pacing, aesthetically pleasing ECG patterns are not enough. There remains much to learn with this nascent approach.
The barriers to getting more CSP trials
The challenge going forward will be funding new trials. CSP stands to prevent pacing-induced cardiomyopathy and offer less costly alternatives to standard biventricular pacing for CRT. This is great for patients, but it would mean that fewer higher-cost CRT devices will be sold.
Heart rhythm research is largely industry-funded because in most cases better therapies for patients mean more profits for industry. In the case of CSP, there is no such confluence of interests.
Conduction system pacing has come about because of the efforts of a few tireless champions who not only published extensively but were also skilled at using social media to spread the excitement. Trials have been small and often self-funded.
The data presented at HRS provides enough equipoise to support a large outcomes-based randomized controlled trial. Imagine if our CSP champions were able to find public-funding sources for such future trials.
Now that would be super cool.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Antithrombotic therapies shifting for Watchman LAA occlusion
A new study finds clinicians are shifting away from the U.S. Food and Drug Administration–approved combination of warfarin and aspirin after left atrial appendage occlusion (LAAO) with the Watchman device and that adverse events, particularly bleeding, are lower when aspirin is dropped.
Of 31,994 patients successfully implanted with the Watchman 2.5 device in the 3 years after its March 2015 approval, only 1 in 10 received the full postprocedure protocol studied in pivotal trials and codified into the FDA-device approval.
The protocol consisted of aspirin (81-325 mg) indefinitely and warfarin for 45 days. Following transesophageal echocardiography, patients were then maintained on warfarin and aspirin if there was a peridevice leak greater than 5 mm or switched to clopidogrel 75 mg for 6 months if a peridevice leak was ruled out or was 5 mm or less.
Based on the results, drawn from the National Cardiovascular Data Registry (NCDR) LAAO Registry, the most common discharge medications were warfarin and aspirin in 36.9% of patients, followed by a direct oral anticoagulant (DOAC) and aspirin (20.8%), warfarin alone (13.5%), DOAC only (12.3%), and dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor (5%).
“There’s a little bit of practice leading the science in this space,” lead author James V. Freeman, MD, MPH, Yale School of Medicine, New Haven, Conn., told this news organization.
Patients who couldn’t tolerate long-term anticoagulation were excluded from the pivotal trials but are now the patients in whom the device is most often used, because of the Centers for Medicare & Medicaid reimbursement mandate for a relative or absolute contraindication to long-term anticoagulation, he noted.
Not surprisingly, 70% of patients in the registry had history of clinically relevant bleeding, the mean CHA2DS2-VASc score was 4.6, and mean HAS-BLED score was 3. At an average age of 76, they were also older, by years, than those in the clinical trials.
Secular trends at the time also saw the ascendancy of the DOACs relative to warfarin, observed Dr. Freeman. “So I think it’s pretty reasonable for physicians to be considering DOACs rather than warfarin in this context.”
Aspirin takes another hit
Results, published May 2 in the Journal of the American College of Cardiology, showed that any adverse event occurred at 45 days in 5.7% of patients discharged on warfarin and aspirin, 4% on warfarin alone, 5.2% on DOAC and aspirin, 3.8% on DOAC only, and 5.5% on DAPT.
Rates of any major adverse event were 4.4%, 3.3%, 4.3%, 3.1%, and 4.2% respectively, and for major bleeding were 3%, 1.8%, 2.8%, 1.7%, and 2.2% respectively. Although patients were similar across treatment groups, those treated with DAPT were slightly older and had more comorbidities, Dr. Freeman said.
In Cox frailty regression, the adjusted risk of any adverse event at 45 days was significantly lower when patients were discharged on warfarin alone (hazard ratio, 0.692; 95% confidence interval, 0.56-0.84) and a DOAC alone (HR, 0.731; 95% CI, 0.57-0.93), compared with warfarin and aspirin. There were no differences among the other groups.
The risk of any major adverse event was also significantly lower with warfarin alone (HR, 0.658; 95% CI, 0.53-0.80) and DOAC alone (HR, 0.767; 95% CI, 0.59-0.98).
At 6 months, rates of any adverse event (HR, 0.814; 95% CI, 0.72-0.93) and any major adverse event (HR, 0.840; 95% CI, 0.73-0.95) were significantly lower only in patients treated with warfarin alone.
“I think if there’s a take-home [message] here, it’s that for a lot of patients there’s good data now to suggest getting rid of the aspirin is a very reasonable thing to do,” Dr. Freeman said.
Further studies are needed in the space, but the results are consistent with those from transcatheter aortic valve replacement studies showing discharge on warfarin or DOAC anticoagulation alone reduces major adverse events without increasing thrombotic events, he said.
“I do think if there’s a strong indication for aspirin – someone has terrible coronary disease – there may be a role for using it,” Dr. Freeman said. But for a lot of these patients, anticoagulation alone without aspirin “may present a big opportunity to mitigate morbidity associated with this procedure.”
Dr. Freeman said he doesn’t expect the findings would be dramatically different with the second-generation Watchman FLX device but noted that randomized data will be forthcoming, as Boston Scientific changed the CHAMPION-AF trial protocol to include DOAC alone without aspirin.
Commenting for this news organization, Domenico Della Rocca, MD, Texas Cardiac Arrhythmia Institute at St. David’s Medical Center, Austin, said the study is a useful overview of post-LAAO therapies in a large population – but not surprising.
“Practice has changed over the years. More and more we are adopting and trusting the DOACs,” he said. “And, we are realizing that dual antiplatelet therapy is so aggressive and antiplatelet therapy alone maybe is not the best choice based on data on activation of coagulation.”
Commenting further, he said “I think it’s too early to suggest being too keen to completely drop aspirin,” noting that 20%-25% of patients have clopidogrel resistance and that the combination of two antiplatelets may be too aggressive a strategy for others.
Dr. Della Rocca and colleagues recently reported favorable long-term results with half-dose DOAC therapy after Watchman implantation and said the team is launching a randomized trial in more than 500 LAAO patients in the United States and Europe later this year. The trial will be comparing a DOAC-based strategy with low-dose apixaban long-term versus clopidogrel and aspirin initially and then switching to 100 mg aspirin long-term.
“We hope that in the next 2-3 years we will have some better answers, but at this point I would say that clopidogrel is kind of an obsolete strategy for appendage closure,” Dr. Della Rocca said.
In an accompanying editorial, David R. Holmes Jr., MD, Mayo Clinic, Rochester, Minn., says “the cornucopia of these specific strategies can be expected to change as practices evolve, as instructions for use broaden and, hopefully, with the results of well-done, scientifically performed trials. This current LAAO Registry report, however, serves as a useful benchmark.”
He cautioned that this is an observational cohort study and that unmeasured imbalances still may affect the ability to identify an unbiased treatment signal. The use of DAPT was also infrequent during the study and “conclusions based on this information are soft.”
The study was funded by the American College of Cardiology National Cardiovascular Data Registry (NCDR), and the National Heart, Lung, and Blood Institute (NHLBI) grants. Dr. Freeman has received salary support from the ACC NCDR and the NHLBI and has received consulting/advisory board fees from Boston Scientific, Medtronic, Janssen Pharmaceuticals, and Biosense Webster.
A version of this article first appeared on Medscape.com.
A new study finds clinicians are shifting away from the U.S. Food and Drug Administration–approved combination of warfarin and aspirin after left atrial appendage occlusion (LAAO) with the Watchman device and that adverse events, particularly bleeding, are lower when aspirin is dropped.
Of 31,994 patients successfully implanted with the Watchman 2.5 device in the 3 years after its March 2015 approval, only 1 in 10 received the full postprocedure protocol studied in pivotal trials and codified into the FDA-device approval.
The protocol consisted of aspirin (81-325 mg) indefinitely and warfarin for 45 days. Following transesophageal echocardiography, patients were then maintained on warfarin and aspirin if there was a peridevice leak greater than 5 mm or switched to clopidogrel 75 mg for 6 months if a peridevice leak was ruled out or was 5 mm or less.
Based on the results, drawn from the National Cardiovascular Data Registry (NCDR) LAAO Registry, the most common discharge medications were warfarin and aspirin in 36.9% of patients, followed by a direct oral anticoagulant (DOAC) and aspirin (20.8%), warfarin alone (13.5%), DOAC only (12.3%), and dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor (5%).
“There’s a little bit of practice leading the science in this space,” lead author James V. Freeman, MD, MPH, Yale School of Medicine, New Haven, Conn., told this news organization.
Patients who couldn’t tolerate long-term anticoagulation were excluded from the pivotal trials but are now the patients in whom the device is most often used, because of the Centers for Medicare & Medicaid reimbursement mandate for a relative or absolute contraindication to long-term anticoagulation, he noted.
Not surprisingly, 70% of patients in the registry had history of clinically relevant bleeding, the mean CHA2DS2-VASc score was 4.6, and mean HAS-BLED score was 3. At an average age of 76, they were also older, by years, than those in the clinical trials.
Secular trends at the time also saw the ascendancy of the DOACs relative to warfarin, observed Dr. Freeman. “So I think it’s pretty reasonable for physicians to be considering DOACs rather than warfarin in this context.”
Aspirin takes another hit
Results, published May 2 in the Journal of the American College of Cardiology, showed that any adverse event occurred at 45 days in 5.7% of patients discharged on warfarin and aspirin, 4% on warfarin alone, 5.2% on DOAC and aspirin, 3.8% on DOAC only, and 5.5% on DAPT.
Rates of any major adverse event were 4.4%, 3.3%, 4.3%, 3.1%, and 4.2% respectively, and for major bleeding were 3%, 1.8%, 2.8%, 1.7%, and 2.2% respectively. Although patients were similar across treatment groups, those treated with DAPT were slightly older and had more comorbidities, Dr. Freeman said.
In Cox frailty regression, the adjusted risk of any adverse event at 45 days was significantly lower when patients were discharged on warfarin alone (hazard ratio, 0.692; 95% confidence interval, 0.56-0.84) and a DOAC alone (HR, 0.731; 95% CI, 0.57-0.93), compared with warfarin and aspirin. There were no differences among the other groups.
The risk of any major adverse event was also significantly lower with warfarin alone (HR, 0.658; 95% CI, 0.53-0.80) and DOAC alone (HR, 0.767; 95% CI, 0.59-0.98).
At 6 months, rates of any adverse event (HR, 0.814; 95% CI, 0.72-0.93) and any major adverse event (HR, 0.840; 95% CI, 0.73-0.95) were significantly lower only in patients treated with warfarin alone.
“I think if there’s a take-home [message] here, it’s that for a lot of patients there’s good data now to suggest getting rid of the aspirin is a very reasonable thing to do,” Dr. Freeman said.
Further studies are needed in the space, but the results are consistent with those from transcatheter aortic valve replacement studies showing discharge on warfarin or DOAC anticoagulation alone reduces major adverse events without increasing thrombotic events, he said.
“I do think if there’s a strong indication for aspirin – someone has terrible coronary disease – there may be a role for using it,” Dr. Freeman said. But for a lot of these patients, anticoagulation alone without aspirin “may present a big opportunity to mitigate morbidity associated with this procedure.”
Dr. Freeman said he doesn’t expect the findings would be dramatically different with the second-generation Watchman FLX device but noted that randomized data will be forthcoming, as Boston Scientific changed the CHAMPION-AF trial protocol to include DOAC alone without aspirin.
Commenting for this news organization, Domenico Della Rocca, MD, Texas Cardiac Arrhythmia Institute at St. David’s Medical Center, Austin, said the study is a useful overview of post-LAAO therapies in a large population – but not surprising.
“Practice has changed over the years. More and more we are adopting and trusting the DOACs,” he said. “And, we are realizing that dual antiplatelet therapy is so aggressive and antiplatelet therapy alone maybe is not the best choice based on data on activation of coagulation.”
Commenting further, he said “I think it’s too early to suggest being too keen to completely drop aspirin,” noting that 20%-25% of patients have clopidogrel resistance and that the combination of two antiplatelets may be too aggressive a strategy for others.
Dr. Della Rocca and colleagues recently reported favorable long-term results with half-dose DOAC therapy after Watchman implantation and said the team is launching a randomized trial in more than 500 LAAO patients in the United States and Europe later this year. The trial will be comparing a DOAC-based strategy with low-dose apixaban long-term versus clopidogrel and aspirin initially and then switching to 100 mg aspirin long-term.
“We hope that in the next 2-3 years we will have some better answers, but at this point I would say that clopidogrel is kind of an obsolete strategy for appendage closure,” Dr. Della Rocca said.
In an accompanying editorial, David R. Holmes Jr., MD, Mayo Clinic, Rochester, Minn., says “the cornucopia of these specific strategies can be expected to change as practices evolve, as instructions for use broaden and, hopefully, with the results of well-done, scientifically performed trials. This current LAAO Registry report, however, serves as a useful benchmark.”
He cautioned that this is an observational cohort study and that unmeasured imbalances still may affect the ability to identify an unbiased treatment signal. The use of DAPT was also infrequent during the study and “conclusions based on this information are soft.”
The study was funded by the American College of Cardiology National Cardiovascular Data Registry (NCDR), and the National Heart, Lung, and Blood Institute (NHLBI) grants. Dr. Freeman has received salary support from the ACC NCDR and the NHLBI and has received consulting/advisory board fees from Boston Scientific, Medtronic, Janssen Pharmaceuticals, and Biosense Webster.
A version of this article first appeared on Medscape.com.
A new study finds clinicians are shifting away from the U.S. Food and Drug Administration–approved combination of warfarin and aspirin after left atrial appendage occlusion (LAAO) with the Watchman device and that adverse events, particularly bleeding, are lower when aspirin is dropped.
Of 31,994 patients successfully implanted with the Watchman 2.5 device in the 3 years after its March 2015 approval, only 1 in 10 received the full postprocedure protocol studied in pivotal trials and codified into the FDA-device approval.
The protocol consisted of aspirin (81-325 mg) indefinitely and warfarin for 45 days. Following transesophageal echocardiography, patients were then maintained on warfarin and aspirin if there was a peridevice leak greater than 5 mm or switched to clopidogrel 75 mg for 6 months if a peridevice leak was ruled out or was 5 mm or less.
Based on the results, drawn from the National Cardiovascular Data Registry (NCDR) LAAO Registry, the most common discharge medications were warfarin and aspirin in 36.9% of patients, followed by a direct oral anticoagulant (DOAC) and aspirin (20.8%), warfarin alone (13.5%), DOAC only (12.3%), and dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor (5%).
“There’s a little bit of practice leading the science in this space,” lead author James V. Freeman, MD, MPH, Yale School of Medicine, New Haven, Conn., told this news organization.
Patients who couldn’t tolerate long-term anticoagulation were excluded from the pivotal trials but are now the patients in whom the device is most often used, because of the Centers for Medicare & Medicaid reimbursement mandate for a relative or absolute contraindication to long-term anticoagulation, he noted.
Not surprisingly, 70% of patients in the registry had history of clinically relevant bleeding, the mean CHA2DS2-VASc score was 4.6, and mean HAS-BLED score was 3. At an average age of 76, they were also older, by years, than those in the clinical trials.
Secular trends at the time also saw the ascendancy of the DOACs relative to warfarin, observed Dr. Freeman. “So I think it’s pretty reasonable for physicians to be considering DOACs rather than warfarin in this context.”
Aspirin takes another hit
Results, published May 2 in the Journal of the American College of Cardiology, showed that any adverse event occurred at 45 days in 5.7% of patients discharged on warfarin and aspirin, 4% on warfarin alone, 5.2% on DOAC and aspirin, 3.8% on DOAC only, and 5.5% on DAPT.
Rates of any major adverse event were 4.4%, 3.3%, 4.3%, 3.1%, and 4.2% respectively, and for major bleeding were 3%, 1.8%, 2.8%, 1.7%, and 2.2% respectively. Although patients were similar across treatment groups, those treated with DAPT were slightly older and had more comorbidities, Dr. Freeman said.
In Cox frailty regression, the adjusted risk of any adverse event at 45 days was significantly lower when patients were discharged on warfarin alone (hazard ratio, 0.692; 95% confidence interval, 0.56-0.84) and a DOAC alone (HR, 0.731; 95% CI, 0.57-0.93), compared with warfarin and aspirin. There were no differences among the other groups.
The risk of any major adverse event was also significantly lower with warfarin alone (HR, 0.658; 95% CI, 0.53-0.80) and DOAC alone (HR, 0.767; 95% CI, 0.59-0.98).
At 6 months, rates of any adverse event (HR, 0.814; 95% CI, 0.72-0.93) and any major adverse event (HR, 0.840; 95% CI, 0.73-0.95) were significantly lower only in patients treated with warfarin alone.
“I think if there’s a take-home [message] here, it’s that for a lot of patients there’s good data now to suggest getting rid of the aspirin is a very reasonable thing to do,” Dr. Freeman said.
Further studies are needed in the space, but the results are consistent with those from transcatheter aortic valve replacement studies showing discharge on warfarin or DOAC anticoagulation alone reduces major adverse events without increasing thrombotic events, he said.
“I do think if there’s a strong indication for aspirin – someone has terrible coronary disease – there may be a role for using it,” Dr. Freeman said. But for a lot of these patients, anticoagulation alone without aspirin “may present a big opportunity to mitigate morbidity associated with this procedure.”
Dr. Freeman said he doesn’t expect the findings would be dramatically different with the second-generation Watchman FLX device but noted that randomized data will be forthcoming, as Boston Scientific changed the CHAMPION-AF trial protocol to include DOAC alone without aspirin.
Commenting for this news organization, Domenico Della Rocca, MD, Texas Cardiac Arrhythmia Institute at St. David’s Medical Center, Austin, said the study is a useful overview of post-LAAO therapies in a large population – but not surprising.
“Practice has changed over the years. More and more we are adopting and trusting the DOACs,” he said. “And, we are realizing that dual antiplatelet therapy is so aggressive and antiplatelet therapy alone maybe is not the best choice based on data on activation of coagulation.”
Commenting further, he said “I think it’s too early to suggest being too keen to completely drop aspirin,” noting that 20%-25% of patients have clopidogrel resistance and that the combination of two antiplatelets may be too aggressive a strategy for others.
Dr. Della Rocca and colleagues recently reported favorable long-term results with half-dose DOAC therapy after Watchman implantation and said the team is launching a randomized trial in more than 500 LAAO patients in the United States and Europe later this year. The trial will be comparing a DOAC-based strategy with low-dose apixaban long-term versus clopidogrel and aspirin initially and then switching to 100 mg aspirin long-term.
“We hope that in the next 2-3 years we will have some better answers, but at this point I would say that clopidogrel is kind of an obsolete strategy for appendage closure,” Dr. Della Rocca said.
In an accompanying editorial, David R. Holmes Jr., MD, Mayo Clinic, Rochester, Minn., says “the cornucopia of these specific strategies can be expected to change as practices evolve, as instructions for use broaden and, hopefully, with the results of well-done, scientifically performed trials. This current LAAO Registry report, however, serves as a useful benchmark.”
He cautioned that this is an observational cohort study and that unmeasured imbalances still may affect the ability to identify an unbiased treatment signal. The use of DAPT was also infrequent during the study and “conclusions based on this information are soft.”
The study was funded by the American College of Cardiology National Cardiovascular Data Registry (NCDR), and the National Heart, Lung, and Blood Institute (NHLBI) grants. Dr. Freeman has received salary support from the ACC NCDR and the NHLBI and has received consulting/advisory board fees from Boston Scientific, Medtronic, Janssen Pharmaceuticals, and Biosense Webster.
A version of this article first appeared on Medscape.com.
Cutting dementia risk in AFib: Does rhythm control strategy matter?
The risk for dementia goes up in patients with atrial fibrillation (AFib), but some evidence suggests that risk can be blunted with therapies that restore sinus rhythm. However, a new cohort study suggests that the treatment effect’s magnitude might depend on the rhythm control strategy. It hinted that AFib catheter ablation might be more effective than pharmacologic rhythm control alone at cutting the risk for dementia.
The case-matched study of more than 38,000 adults with AFib saw a 41% reduction (P < .0001) in risk for dementia among those who underwent catheter ablation after attempted rhythm control with antiarrhythmic drugs (AAD), compared with those managed with pharmacologic rhythm control therapy alone.
The observational study comprising 20 years of data comes with big limitations and can’t say for sure whether catheter ablation is better than AAD-only at cutting the dementia risk in AFib. But it and other evidence support the idea, which has yet to be explored in a randomized fashion.
In a secondary finding, the analysis showed a similar reduction in dementia risk from catheter ablation, compared with AAD, in women and in men by 40% and 45%, respectively (P < .0001 for both). The findings are particularly relevant “given the higher life-long risk of dementia among women and the lower likelihood that women will be offered ablation, which has been demonstrated repeatedly,” Emily P. Zeitler, MD, MHS, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, told this news organization. “I think this is another reason to try to be more generous in offering ablation to women.”
Management of AFib certainly evolved in important ways from 2000 to 2021, the period covered by the study. But a sensitivity analysis based on data from 2010 to 2021 showed “no meaningful differences” in the results, said Dr. Zeitler, who is slated to present the findings April 30 at the Heart Rhythm Society 2022 Scientific Sessions, conducted virtually and live in San Francisco.
Dr. Zeitler acknowledged that the observational study, even with its propensity-matched ablation and AAD cohorts, can only hint at a preference for ablation over AAD for lowering risk for AFib-associated dementia. “We know there’s unmeasured and unfixable confounding between those two groups, so we see this really as hypothesis-generating.”
It was “a well-done analysis,” and the conclusion that the dementia risk was lower with catheter ablation is “absolutely correct,” but only as far as the study and its limitations allow, agreed David Conen, MD, MPH, McMaster University, Hamilton, Ontario, who is not a coauthor.
“Even with propensity matching, you can get rid of some sorts of confounding, but you can never get rid of all selection bias issues.” That, he said when interviewed, takes randomized trials.
Dr. Conen, who is studying cognitive decline in AFib as a SWISS-AF trial principal investigator, pointed to a secondary finding of the analysis as evidence for such confounding. He said the ablation group’s nearly 50% drop (P < .0001) in competing risk for death, compared with patients managed with AAD, isn’t plausible.
The finding “strongly suggests these people were healthier and that there’s some sort of selection bias. They were at lower risk of death, they were at lower risk of dementia, and they were probably also at lower risk of stroke, myocardial infarction, thrombosis, and cancer because they were just probably a little healthier than the others,” Dr. Conen said. The ablation and AAD groups “were two very different populations from the get-go.”
The analysis was based on U.S. insurance and Medicare claims data from AFib patients who either underwent catheter ablation after at least one AAD trial or filled prescriptions for at least two different antiarrhythmic agents in the year after AFib diagnosis. Patients with history of dementia, catheter or surgical AFib ablation, or a valve procedure were excluded.
The ablation and AAD-only groups each consisted of 19,066 patients after propensity matching, and the groups were balanced with respect to age, sex, type of insurance, CHA2DS2-VASc scores, and use of renin-angiotensin-system inhibitors, oral anticoagulants, and antiplatelets.
The overall risk for dementia was 1.9% for the ablation group and 3.3% for AAD-only patients (hazard ratio, 0.59; 95% confidence interval, 0.52-0.67). Corresponding HRs by sex were 0.55 (95% CI, 0.46-0.66) for men and 0.60 (95% CI, 0.50-0.72) for women.
The competing risk for death was also significantly decreased in the ablation group (HR, 0.51; 95% CI, 0.46-0.55).
Dr. Zeitler pointed to a randomized trial now in the early stages called Neurocognition and Greater Maintenance of Sinus Rhythm in Atrial Fibrillation, or NOGGIN-AF, which will explore relationships between rhythm control therapy and dementia in patients with AFib, whether catheter ablation or AAD can mitigate that risk, and whether either strategy works better than the other, among other goals.
“I’m optimistic,” she said, “and I think it’s going to add to the growing motivations to get patients ablated more quickly and more broadly.”
The analysis was funded by Biosense-Webster. Dr. Zeitler discloses consulting for Biosense-Webster and Arena Pharmaceuticals (now Pfizer); fees for speaking from Medtronic; and receiving research support from Boston Scientific, Sanofi, and Biosense-Webster. Dr. Conen has previously reported receiving speaker fees from Servier Canada.
A version of this article first appeared on Medscape.com.
The risk for dementia goes up in patients with atrial fibrillation (AFib), but some evidence suggests that risk can be blunted with therapies that restore sinus rhythm. However, a new cohort study suggests that the treatment effect’s magnitude might depend on the rhythm control strategy. It hinted that AFib catheter ablation might be more effective than pharmacologic rhythm control alone at cutting the risk for dementia.
The case-matched study of more than 38,000 adults with AFib saw a 41% reduction (P < .0001) in risk for dementia among those who underwent catheter ablation after attempted rhythm control with antiarrhythmic drugs (AAD), compared with those managed with pharmacologic rhythm control therapy alone.
The observational study comprising 20 years of data comes with big limitations and can’t say for sure whether catheter ablation is better than AAD-only at cutting the dementia risk in AFib. But it and other evidence support the idea, which has yet to be explored in a randomized fashion.
In a secondary finding, the analysis showed a similar reduction in dementia risk from catheter ablation, compared with AAD, in women and in men by 40% and 45%, respectively (P < .0001 for both). The findings are particularly relevant “given the higher life-long risk of dementia among women and the lower likelihood that women will be offered ablation, which has been demonstrated repeatedly,” Emily P. Zeitler, MD, MHS, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, told this news organization. “I think this is another reason to try to be more generous in offering ablation to women.”
Management of AFib certainly evolved in important ways from 2000 to 2021, the period covered by the study. But a sensitivity analysis based on data from 2010 to 2021 showed “no meaningful differences” in the results, said Dr. Zeitler, who is slated to present the findings April 30 at the Heart Rhythm Society 2022 Scientific Sessions, conducted virtually and live in San Francisco.
Dr. Zeitler acknowledged that the observational study, even with its propensity-matched ablation and AAD cohorts, can only hint at a preference for ablation over AAD for lowering risk for AFib-associated dementia. “We know there’s unmeasured and unfixable confounding between those two groups, so we see this really as hypothesis-generating.”
It was “a well-done analysis,” and the conclusion that the dementia risk was lower with catheter ablation is “absolutely correct,” but only as far as the study and its limitations allow, agreed David Conen, MD, MPH, McMaster University, Hamilton, Ontario, who is not a coauthor.
“Even with propensity matching, you can get rid of some sorts of confounding, but you can never get rid of all selection bias issues.” That, he said when interviewed, takes randomized trials.
Dr. Conen, who is studying cognitive decline in AFib as a SWISS-AF trial principal investigator, pointed to a secondary finding of the analysis as evidence for such confounding. He said the ablation group’s nearly 50% drop (P < .0001) in competing risk for death, compared with patients managed with AAD, isn’t plausible.
The finding “strongly suggests these people were healthier and that there’s some sort of selection bias. They were at lower risk of death, they were at lower risk of dementia, and they were probably also at lower risk of stroke, myocardial infarction, thrombosis, and cancer because they were just probably a little healthier than the others,” Dr. Conen said. The ablation and AAD groups “were two very different populations from the get-go.”
The analysis was based on U.S. insurance and Medicare claims data from AFib patients who either underwent catheter ablation after at least one AAD trial or filled prescriptions for at least two different antiarrhythmic agents in the year after AFib diagnosis. Patients with history of dementia, catheter or surgical AFib ablation, or a valve procedure were excluded.
The ablation and AAD-only groups each consisted of 19,066 patients after propensity matching, and the groups were balanced with respect to age, sex, type of insurance, CHA2DS2-VASc scores, and use of renin-angiotensin-system inhibitors, oral anticoagulants, and antiplatelets.
The overall risk for dementia was 1.9% for the ablation group and 3.3% for AAD-only patients (hazard ratio, 0.59; 95% confidence interval, 0.52-0.67). Corresponding HRs by sex were 0.55 (95% CI, 0.46-0.66) for men and 0.60 (95% CI, 0.50-0.72) for women.
The competing risk for death was also significantly decreased in the ablation group (HR, 0.51; 95% CI, 0.46-0.55).
Dr. Zeitler pointed to a randomized trial now in the early stages called Neurocognition and Greater Maintenance of Sinus Rhythm in Atrial Fibrillation, or NOGGIN-AF, which will explore relationships between rhythm control therapy and dementia in patients with AFib, whether catheter ablation or AAD can mitigate that risk, and whether either strategy works better than the other, among other goals.
“I’m optimistic,” she said, “and I think it’s going to add to the growing motivations to get patients ablated more quickly and more broadly.”
The analysis was funded by Biosense-Webster. Dr. Zeitler discloses consulting for Biosense-Webster and Arena Pharmaceuticals (now Pfizer); fees for speaking from Medtronic; and receiving research support from Boston Scientific, Sanofi, and Biosense-Webster. Dr. Conen has previously reported receiving speaker fees from Servier Canada.
A version of this article first appeared on Medscape.com.
The risk for dementia goes up in patients with atrial fibrillation (AFib), but some evidence suggests that risk can be blunted with therapies that restore sinus rhythm. However, a new cohort study suggests that the treatment effect’s magnitude might depend on the rhythm control strategy. It hinted that AFib catheter ablation might be more effective than pharmacologic rhythm control alone at cutting the risk for dementia.
The case-matched study of more than 38,000 adults with AFib saw a 41% reduction (P < .0001) in risk for dementia among those who underwent catheter ablation after attempted rhythm control with antiarrhythmic drugs (AAD), compared with those managed with pharmacologic rhythm control therapy alone.
The observational study comprising 20 years of data comes with big limitations and can’t say for sure whether catheter ablation is better than AAD-only at cutting the dementia risk in AFib. But it and other evidence support the idea, which has yet to be explored in a randomized fashion.
In a secondary finding, the analysis showed a similar reduction in dementia risk from catheter ablation, compared with AAD, in women and in men by 40% and 45%, respectively (P < .0001 for both). The findings are particularly relevant “given the higher life-long risk of dementia among women and the lower likelihood that women will be offered ablation, which has been demonstrated repeatedly,” Emily P. Zeitler, MD, MHS, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, told this news organization. “I think this is another reason to try to be more generous in offering ablation to women.”
Management of AFib certainly evolved in important ways from 2000 to 2021, the period covered by the study. But a sensitivity analysis based on data from 2010 to 2021 showed “no meaningful differences” in the results, said Dr. Zeitler, who is slated to present the findings April 30 at the Heart Rhythm Society 2022 Scientific Sessions, conducted virtually and live in San Francisco.
Dr. Zeitler acknowledged that the observational study, even with its propensity-matched ablation and AAD cohorts, can only hint at a preference for ablation over AAD for lowering risk for AFib-associated dementia. “We know there’s unmeasured and unfixable confounding between those two groups, so we see this really as hypothesis-generating.”
It was “a well-done analysis,” and the conclusion that the dementia risk was lower with catheter ablation is “absolutely correct,” but only as far as the study and its limitations allow, agreed David Conen, MD, MPH, McMaster University, Hamilton, Ontario, who is not a coauthor.
“Even with propensity matching, you can get rid of some sorts of confounding, but you can never get rid of all selection bias issues.” That, he said when interviewed, takes randomized trials.
Dr. Conen, who is studying cognitive decline in AFib as a SWISS-AF trial principal investigator, pointed to a secondary finding of the analysis as evidence for such confounding. He said the ablation group’s nearly 50% drop (P < .0001) in competing risk for death, compared with patients managed with AAD, isn’t plausible.
The finding “strongly suggests these people were healthier and that there’s some sort of selection bias. They were at lower risk of death, they were at lower risk of dementia, and they were probably also at lower risk of stroke, myocardial infarction, thrombosis, and cancer because they were just probably a little healthier than the others,” Dr. Conen said. The ablation and AAD groups “were two very different populations from the get-go.”
The analysis was based on U.S. insurance and Medicare claims data from AFib patients who either underwent catheter ablation after at least one AAD trial or filled prescriptions for at least two different antiarrhythmic agents in the year after AFib diagnosis. Patients with history of dementia, catheter or surgical AFib ablation, or a valve procedure were excluded.
The ablation and AAD-only groups each consisted of 19,066 patients after propensity matching, and the groups were balanced with respect to age, sex, type of insurance, CHA2DS2-VASc scores, and use of renin-angiotensin-system inhibitors, oral anticoagulants, and antiplatelets.
The overall risk for dementia was 1.9% for the ablation group and 3.3% for AAD-only patients (hazard ratio, 0.59; 95% confidence interval, 0.52-0.67). Corresponding HRs by sex were 0.55 (95% CI, 0.46-0.66) for men and 0.60 (95% CI, 0.50-0.72) for women.
The competing risk for death was also significantly decreased in the ablation group (HR, 0.51; 95% CI, 0.46-0.55).
Dr. Zeitler pointed to a randomized trial now in the early stages called Neurocognition and Greater Maintenance of Sinus Rhythm in Atrial Fibrillation, or NOGGIN-AF, which will explore relationships between rhythm control therapy and dementia in patients with AFib, whether catheter ablation or AAD can mitigate that risk, and whether either strategy works better than the other, among other goals.
“I’m optimistic,” she said, “and I think it’s going to add to the growing motivations to get patients ablated more quickly and more broadly.”
The analysis was funded by Biosense-Webster. Dr. Zeitler discloses consulting for Biosense-Webster and Arena Pharmaceuticals (now Pfizer); fees for speaking from Medtronic; and receiving research support from Boston Scientific, Sanofi, and Biosense-Webster. Dr. Conen has previously reported receiving speaker fees from Servier Canada.
A version of this article first appeared on Medscape.com.
Cutting dementia risk in atrial fibrillation: Does rhythm control strategy matter?
The risk for dementia goes up in patients with atrial fibrillation (AFib), but some evidence suggests that risk can be blunted with therapies that restore sinus rhythm. But a new cohort study suggests that the treatment effect’s magnitude might depend on the rhythm control strategy. It hinted that AFib catheter ablation might be more effective than pharmacologic rhythm control alone at cutting the risk for dementia.
The case-matched study of more than 38,000 adults with AFib saw a 41% reduction (P < .0001) in risk for dementia among those who underwent catheter ablation after attempted rhythm control with antiarrhythmic drugs (AAD), compared with those managed with pharmacologic rhythm control therapy alone.
The observational study comprising 20 years of data comes with big limitations and can’t say for sure whether catheter ablation is better than AAD alone at cutting the dementia risk in AFib. But it and other evidence support the idea, which has yet to be explored in a randomized fashion.
In a secondary finding, the analysis showed a similar reduction in dementia risk from catheter ablation, compared with AAD, in women and in men by 40% and 45%, respectively (P < .0001 for both). The findings are particularly relevant “given the higher life-long risk of dementia among women and the lower likelihood that women will be offered ablation, which has been demonstrated repeatedly,” Emily P. Zeitler, MD, MHS, Dartmouth-Hitchcock Medical Center, Lebanon, N.H., said in an interview. “I think this is another reason to try to be more generous in offering ablation to women.”
Management of AFib certainly evolved in important ways from 2000 to 2021, the period covered by the study. But a sensitivity analysis based on data from 2010 to 2021 showed “no meaningful differences” in the results, said Dr. Zeitler, who is slated to present the findings at the annual scientific sessions of the Heart Rhythm Society.
Dr. Zeitler acknowledged that the observational study, even with its propensity-matched ablation and AAD cohorts, can only hint at a preference for ablation over AAD for lowering risk for AFib-associated dementia. “We know there’s unmeasured and unfixable confounding between those two groups, so we see this really as hypothesis-generating.”
It was “a well-done analysis,” and the conclusion that the dementia risk was lower with catheter ablation is “absolutely correct,” but only as far as the study and its limitations allow, agreed David Conen, MD, MPH, McMaster University, Hamilton, Ont., who is not a coauthor.
“Even with propensity matching, you can get rid of some sorts of confounding, but you can never get rid of all selection bias issues.” That, he said when interviewed, takes randomized trials.
Dr. Conen, who is studying cognitive decline in AFib as a SWISS-AF trial principal investigator, pointed to a secondary finding of the analysis as evidence for such confounding. He said the ablation group’s nearly 50% drop (P < .0001) in competing risk for death, compared with patients managed with AAD, isn’t plausible.
The finding “strongly suggests these people were healthier and that there’s some sort of selection bias. They were at lower risk of death, they were at lower risk of dementia, and they were probably also at lower risk of stroke, myocardial infarction, thrombosis, and cancer because they were just probably a little healthier than the others,” Dr. Conen said. The ablation and AAD groups “were two very different populations from the get-go.”
The analysis was based on U.S. insurance and Medicare claims data from AFib patients who either underwent catheter ablation after at least one AAD trial or filled prescriptions for at least two different antiarrhythmic agents in the year after AFib diagnosis. Patients with history of dementia, catheter or surgical AFib ablation, or a valve procedure were excluded.
The ablation and AAD-only groups each consisted of 19,066 patients after propensity matching, and the groups were balanced with respect to age, sex, type of insurance, CHA2DS2-VASc scores, and use of renin-angiotensin system inhibitors, oral anticoagulants, and antiplatelets.
The overall risk for dementia was 1.9% for the ablation group and 3.3% for AAD-only patients (hazard ratio, 0.59; 95% confidence interval, 0.52-0.67). Corresponding HRs by sex were 0.55 (95% CI, 0.46-0.66) for men and 0.60 (95% CI, 0.50-0.72) for women.
The competing risk for death was also significantly decreased in the ablation group (HR, 0.51; 95% CI, 0.46-0.55).
Dr. Zeitler pointed to a randomized trial now in the early stages called Neurocognition and Greater Maintenance of Sinus Rhythm in Atrial Fibrillation, or NOGGIN-AF, which will explore relationships between rhythm control therapy and dementia in patients with AFib, whether catheter ablation or AAD can mitigate that risk, and whether either strategy works better than the other, among other goals.
“I’m optimistic,” she said, “and I think it’s going to add to the growing motivations to get patients ablated more quickly and more broadly.”
The analysis was funded by Biosense-Webster. Dr. Zeitler disclosed consulting for Biosense-Webster and Arena Pharmaceuticals (now Pfizer); fees for speaking from Medtronic; and receiving research support from Boston Scientific, Sanofi, and Biosense-Webster. Dr. Conen has previously reported receiving speaker fees from Servier Canada.
A version of this article first appeared on Medscape.com.
The risk for dementia goes up in patients with atrial fibrillation (AFib), but some evidence suggests that risk can be blunted with therapies that restore sinus rhythm. But a new cohort study suggests that the treatment effect’s magnitude might depend on the rhythm control strategy. It hinted that AFib catheter ablation might be more effective than pharmacologic rhythm control alone at cutting the risk for dementia.
The case-matched study of more than 38,000 adults with AFib saw a 41% reduction (P < .0001) in risk for dementia among those who underwent catheter ablation after attempted rhythm control with antiarrhythmic drugs (AAD), compared with those managed with pharmacologic rhythm control therapy alone.
The observational study comprising 20 years of data comes with big limitations and can’t say for sure whether catheter ablation is better than AAD alone at cutting the dementia risk in AFib. But it and other evidence support the idea, which has yet to be explored in a randomized fashion.
In a secondary finding, the analysis showed a similar reduction in dementia risk from catheter ablation, compared with AAD, in women and in men by 40% and 45%, respectively (P < .0001 for both). The findings are particularly relevant “given the higher life-long risk of dementia among women and the lower likelihood that women will be offered ablation, which has been demonstrated repeatedly,” Emily P. Zeitler, MD, MHS, Dartmouth-Hitchcock Medical Center, Lebanon, N.H., said in an interview. “I think this is another reason to try to be more generous in offering ablation to women.”
Management of AFib certainly evolved in important ways from 2000 to 2021, the period covered by the study. But a sensitivity analysis based on data from 2010 to 2021 showed “no meaningful differences” in the results, said Dr. Zeitler, who is slated to present the findings at the annual scientific sessions of the Heart Rhythm Society.
Dr. Zeitler acknowledged that the observational study, even with its propensity-matched ablation and AAD cohorts, can only hint at a preference for ablation over AAD for lowering risk for AFib-associated dementia. “We know there’s unmeasured and unfixable confounding between those two groups, so we see this really as hypothesis-generating.”
It was “a well-done analysis,” and the conclusion that the dementia risk was lower with catheter ablation is “absolutely correct,” but only as far as the study and its limitations allow, agreed David Conen, MD, MPH, McMaster University, Hamilton, Ont., who is not a coauthor.
“Even with propensity matching, you can get rid of some sorts of confounding, but you can never get rid of all selection bias issues.” That, he said when interviewed, takes randomized trials.
Dr. Conen, who is studying cognitive decline in AFib as a SWISS-AF trial principal investigator, pointed to a secondary finding of the analysis as evidence for such confounding. He said the ablation group’s nearly 50% drop (P < .0001) in competing risk for death, compared with patients managed with AAD, isn’t plausible.
The finding “strongly suggests these people were healthier and that there’s some sort of selection bias. They were at lower risk of death, they were at lower risk of dementia, and they were probably also at lower risk of stroke, myocardial infarction, thrombosis, and cancer because they were just probably a little healthier than the others,” Dr. Conen said. The ablation and AAD groups “were two very different populations from the get-go.”
The analysis was based on U.S. insurance and Medicare claims data from AFib patients who either underwent catheter ablation after at least one AAD trial or filled prescriptions for at least two different antiarrhythmic agents in the year after AFib diagnosis. Patients with history of dementia, catheter or surgical AFib ablation, or a valve procedure were excluded.
The ablation and AAD-only groups each consisted of 19,066 patients after propensity matching, and the groups were balanced with respect to age, sex, type of insurance, CHA2DS2-VASc scores, and use of renin-angiotensin system inhibitors, oral anticoagulants, and antiplatelets.
The overall risk for dementia was 1.9% for the ablation group and 3.3% for AAD-only patients (hazard ratio, 0.59; 95% confidence interval, 0.52-0.67). Corresponding HRs by sex were 0.55 (95% CI, 0.46-0.66) for men and 0.60 (95% CI, 0.50-0.72) for women.
The competing risk for death was also significantly decreased in the ablation group (HR, 0.51; 95% CI, 0.46-0.55).
Dr. Zeitler pointed to a randomized trial now in the early stages called Neurocognition and Greater Maintenance of Sinus Rhythm in Atrial Fibrillation, or NOGGIN-AF, which will explore relationships between rhythm control therapy and dementia in patients with AFib, whether catheter ablation or AAD can mitigate that risk, and whether either strategy works better than the other, among other goals.
“I’m optimistic,” she said, “and I think it’s going to add to the growing motivations to get patients ablated more quickly and more broadly.”
The analysis was funded by Biosense-Webster. Dr. Zeitler disclosed consulting for Biosense-Webster and Arena Pharmaceuticals (now Pfizer); fees for speaking from Medtronic; and receiving research support from Boston Scientific, Sanofi, and Biosense-Webster. Dr. Conen has previously reported receiving speaker fees from Servier Canada.
A version of this article first appeared on Medscape.com.
The risk for dementia goes up in patients with atrial fibrillation (AFib), but some evidence suggests that risk can be blunted with therapies that restore sinus rhythm. But a new cohort study suggests that the treatment effect’s magnitude might depend on the rhythm control strategy. It hinted that AFib catheter ablation might be more effective than pharmacologic rhythm control alone at cutting the risk for dementia.
The case-matched study of more than 38,000 adults with AFib saw a 41% reduction (P < .0001) in risk for dementia among those who underwent catheter ablation after attempted rhythm control with antiarrhythmic drugs (AAD), compared with those managed with pharmacologic rhythm control therapy alone.
The observational study comprising 20 years of data comes with big limitations and can’t say for sure whether catheter ablation is better than AAD alone at cutting the dementia risk in AFib. But it and other evidence support the idea, which has yet to be explored in a randomized fashion.
In a secondary finding, the analysis showed a similar reduction in dementia risk from catheter ablation, compared with AAD, in women and in men by 40% and 45%, respectively (P < .0001 for both). The findings are particularly relevant “given the higher life-long risk of dementia among women and the lower likelihood that women will be offered ablation, which has been demonstrated repeatedly,” Emily P. Zeitler, MD, MHS, Dartmouth-Hitchcock Medical Center, Lebanon, N.H., said in an interview. “I think this is another reason to try to be more generous in offering ablation to women.”
Management of AFib certainly evolved in important ways from 2000 to 2021, the period covered by the study. But a sensitivity analysis based on data from 2010 to 2021 showed “no meaningful differences” in the results, said Dr. Zeitler, who is slated to present the findings at the annual scientific sessions of the Heart Rhythm Society.
Dr. Zeitler acknowledged that the observational study, even with its propensity-matched ablation and AAD cohorts, can only hint at a preference for ablation over AAD for lowering risk for AFib-associated dementia. “We know there’s unmeasured and unfixable confounding between those two groups, so we see this really as hypothesis-generating.”
It was “a well-done analysis,” and the conclusion that the dementia risk was lower with catheter ablation is “absolutely correct,” but only as far as the study and its limitations allow, agreed David Conen, MD, MPH, McMaster University, Hamilton, Ont., who is not a coauthor.
“Even with propensity matching, you can get rid of some sorts of confounding, but you can never get rid of all selection bias issues.” That, he said when interviewed, takes randomized trials.
Dr. Conen, who is studying cognitive decline in AFib as a SWISS-AF trial principal investigator, pointed to a secondary finding of the analysis as evidence for such confounding. He said the ablation group’s nearly 50% drop (P < .0001) in competing risk for death, compared with patients managed with AAD, isn’t plausible.
The finding “strongly suggests these people were healthier and that there’s some sort of selection bias. They were at lower risk of death, they were at lower risk of dementia, and they were probably also at lower risk of stroke, myocardial infarction, thrombosis, and cancer because they were just probably a little healthier than the others,” Dr. Conen said. The ablation and AAD groups “were two very different populations from the get-go.”
The analysis was based on U.S. insurance and Medicare claims data from AFib patients who either underwent catheter ablation after at least one AAD trial or filled prescriptions for at least two different antiarrhythmic agents in the year after AFib diagnosis. Patients with history of dementia, catheter or surgical AFib ablation, or a valve procedure were excluded.
The ablation and AAD-only groups each consisted of 19,066 patients after propensity matching, and the groups were balanced with respect to age, sex, type of insurance, CHA2DS2-VASc scores, and use of renin-angiotensin system inhibitors, oral anticoagulants, and antiplatelets.
The overall risk for dementia was 1.9% for the ablation group and 3.3% for AAD-only patients (hazard ratio, 0.59; 95% confidence interval, 0.52-0.67). Corresponding HRs by sex were 0.55 (95% CI, 0.46-0.66) for men and 0.60 (95% CI, 0.50-0.72) for women.
The competing risk for death was also significantly decreased in the ablation group (HR, 0.51; 95% CI, 0.46-0.55).
Dr. Zeitler pointed to a randomized trial now in the early stages called Neurocognition and Greater Maintenance of Sinus Rhythm in Atrial Fibrillation, or NOGGIN-AF, which will explore relationships between rhythm control therapy and dementia in patients with AFib, whether catheter ablation or AAD can mitigate that risk, and whether either strategy works better than the other, among other goals.
“I’m optimistic,” she said, “and I think it’s going to add to the growing motivations to get patients ablated more quickly and more broadly.”
The analysis was funded by Biosense-Webster. Dr. Zeitler disclosed consulting for Biosense-Webster and Arena Pharmaceuticals (now Pfizer); fees for speaking from Medtronic; and receiving research support from Boston Scientific, Sanofi, and Biosense-Webster. Dr. Conen has previously reported receiving speaker fees from Servier Canada.
A version of this article first appeared on Medscape.com.
HEART RHYTHM 2022








