User login
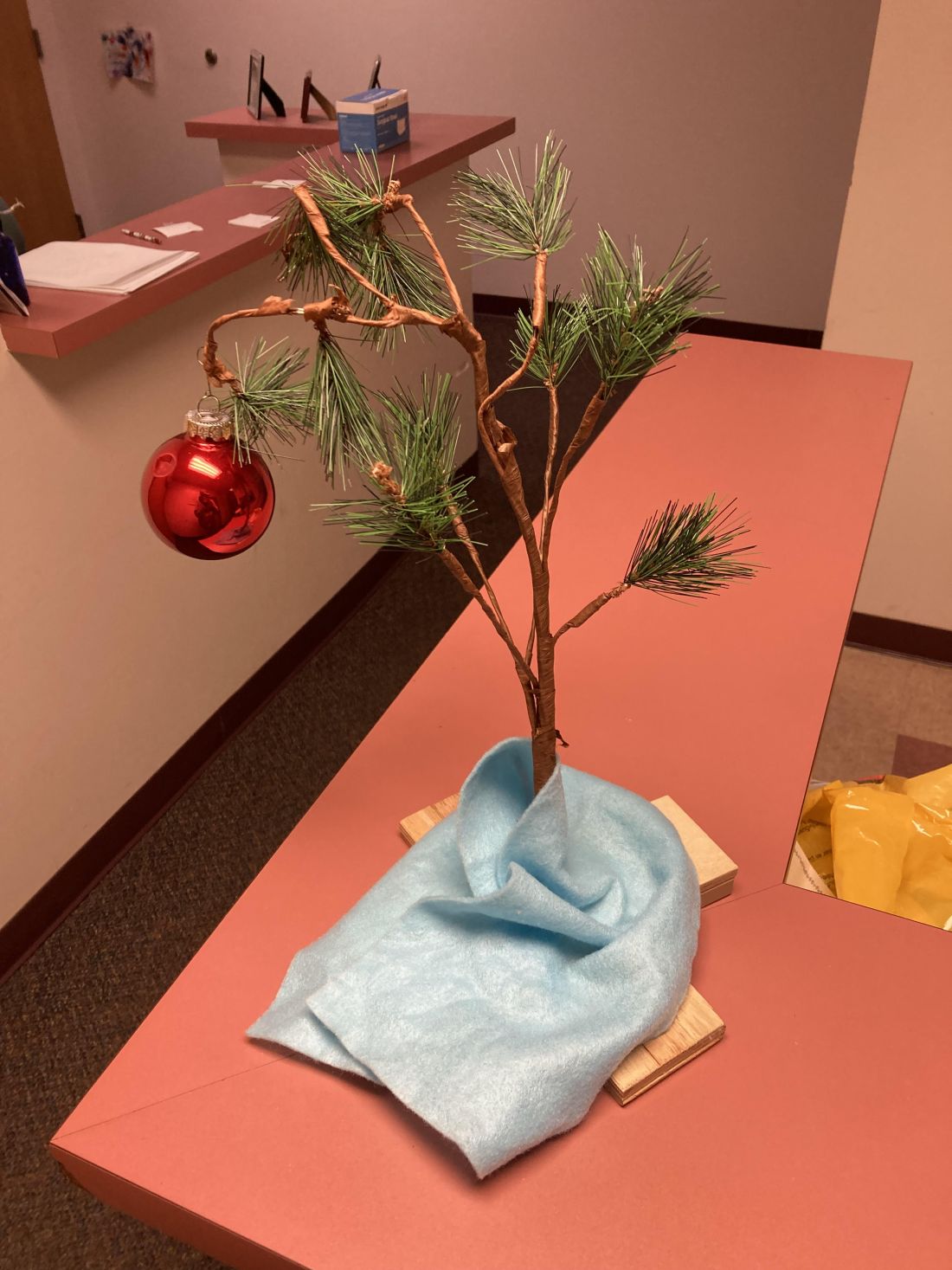
The Charlie Brown tree
I put a Christmas tree up early in November.
It’s not like it’s a real tree, or even a fancy one. For that matter, I’m Jewish.
Growing up in the 1970s one thing that could be relied on every year was the Charlie Brown Christmas special. It never changed. By age 5 you knew most of the lines, and loved the highlight when Charlie Brown brings home the saddest-looking tree ever, which collapses when he puts a single bauble on it.
Years ago, my kids gave me a Charlie Brown tree as a gift. It even plays the late Vince Guaraldi’s immortal Peanuts theme when you push a button. I forgot about it for a few years, then discovered it, and immediately brought it to my office.
I’m not a fan of holiday creep, where they move up earlier in the year, so I used to put it up after Thanksgiving. But we close the office 2-3 weeks later for the rest of the year. I like the tree, my staff likes the tree, and my patients like the tree, so I just started putting it up in early November so we can enjoy it for a month.
It’s whimsical and brings back memories of innocence, childhood, and (of course) Peanuts. It sets a cheerful tone when you see it there. Very few of my patients can resist pressing the button and playing the music as they go by.
The start of a new year is a relatively arbitrary date, chosen long ago. But its approach is always a reminder that life goes on. We continue our trips around the sun. Good times and bad times come and go, but time never stops.
In bad years the tree reminds me that it’s coming to an end, and to look toward the next. In good years it reminds me that it’s time to be ready for the surprises of the coming one.
In mid-December, after the patients are done for the last day of the year, I quietly put it away. It’s a vaguely somber moment, but at the same time I’m glad to know I now have 2-3 weeks of home time. It mostly involves working at my desk and returning phone calls, but there’s also time to relax with my kids, do jigsaw puzzles, and enjoy the Phoenix winter weather as a break before the next round starts.
To those who disagree with my choice of decoration or its timing, I simply respond: “Good grief!”
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I put a Christmas tree up early in November.
It’s not like it’s a real tree, or even a fancy one. For that matter, I’m Jewish.
Growing up in the 1970s one thing that could be relied on every year was the Charlie Brown Christmas special. It never changed. By age 5 you knew most of the lines, and loved the highlight when Charlie Brown brings home the saddest-looking tree ever, which collapses when he puts a single bauble on it.
Years ago, my kids gave me a Charlie Brown tree as a gift. It even plays the late Vince Guaraldi’s immortal Peanuts theme when you push a button. I forgot about it for a few years, then discovered it, and immediately brought it to my office.
I’m not a fan of holiday creep, where they move up earlier in the year, so I used to put it up after Thanksgiving. But we close the office 2-3 weeks later for the rest of the year. I like the tree, my staff likes the tree, and my patients like the tree, so I just started putting it up in early November so we can enjoy it for a month.
It’s whimsical and brings back memories of innocence, childhood, and (of course) Peanuts. It sets a cheerful tone when you see it there. Very few of my patients can resist pressing the button and playing the music as they go by.
The start of a new year is a relatively arbitrary date, chosen long ago. But its approach is always a reminder that life goes on. We continue our trips around the sun. Good times and bad times come and go, but time never stops.
In bad years the tree reminds me that it’s coming to an end, and to look toward the next. In good years it reminds me that it’s time to be ready for the surprises of the coming one.
In mid-December, after the patients are done for the last day of the year, I quietly put it away. It’s a vaguely somber moment, but at the same time I’m glad to know I now have 2-3 weeks of home time. It mostly involves working at my desk and returning phone calls, but there’s also time to relax with my kids, do jigsaw puzzles, and enjoy the Phoenix winter weather as a break before the next round starts.
To those who disagree with my choice of decoration or its timing, I simply respond: “Good grief!”
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I put a Christmas tree up early in November.
It’s not like it’s a real tree, or even a fancy one. For that matter, I’m Jewish.
Growing up in the 1970s one thing that could be relied on every year was the Charlie Brown Christmas special. It never changed. By age 5 you knew most of the lines, and loved the highlight when Charlie Brown brings home the saddest-looking tree ever, which collapses when he puts a single bauble on it.
Years ago, my kids gave me a Charlie Brown tree as a gift. It even plays the late Vince Guaraldi’s immortal Peanuts theme when you push a button. I forgot about it for a few years, then discovered it, and immediately brought it to my office.
I’m not a fan of holiday creep, where they move up earlier in the year, so I used to put it up after Thanksgiving. But we close the office 2-3 weeks later for the rest of the year. I like the tree, my staff likes the tree, and my patients like the tree, so I just started putting it up in early November so we can enjoy it for a month.
It’s whimsical and brings back memories of innocence, childhood, and (of course) Peanuts. It sets a cheerful tone when you see it there. Very few of my patients can resist pressing the button and playing the music as they go by.
The start of a new year is a relatively arbitrary date, chosen long ago. But its approach is always a reminder that life goes on. We continue our trips around the sun. Good times and bad times come and go, but time never stops.
In bad years the tree reminds me that it’s coming to an end, and to look toward the next. In good years it reminds me that it’s time to be ready for the surprises of the coming one.
In mid-December, after the patients are done for the last day of the year, I quietly put it away. It’s a vaguely somber moment, but at the same time I’m glad to know I now have 2-3 weeks of home time. It mostly involves working at my desk and returning phone calls, but there’s also time to relax with my kids, do jigsaw puzzles, and enjoy the Phoenix winter weather as a break before the next round starts.
To those who disagree with my choice of decoration or its timing, I simply respond: “Good grief!”
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Use 2022’s advocacy successes and frustrations as a catalyst for the new year
As we come to a close on 2022, let’s take a look at the celebrations and frustrations of the past year’s health policies so that they may act as a catalyst, encouraging us to engage with our representatives. Some of these policies include actions by major companies that rule our health care system, as well as the regulations and legislation passed (or not passed) by our governmental entities. And of course, we must consider how profits and politics influence these policies and often rule the roost!
Insurance
Once again, we are facing increased nonmedical switching of stable patients to different medications through ever-increasing formulary exclusions and higher tiering of less profitable drugs. There are some reports of patients being whipsawed back and forth yearly between reference infliximab and various biosimilars, depending on which is the most profitable to the health plan at the time. And now it’s not just the copay accumulator or maximizer programs that are abusing patient assistance programs, there are new “alternative funding companies” that are carving out expensive and specialty drugs from coverage of employers’ funded health plans. These alternative funding companies then obtain medications – sometimes from other countries – and other forms of assistance from manufacturers and foundations. There have been reports that they make the patient assign power of attorney to them and even pretend to be the patient to obtain the drug, assistance, and copay cards and then bill the employer for getting the free drug or assistance. This abuse of the system, along with copay maximizers, are causing drug manufacturers to rethink their assistance policies, with middlemen reaping the advantages of the assistance plans and not the truly needy patient.
Legislation and regulation
Substantive progress continues to be made on access issues in the states. A total of 5 states signed step-therapy legislation into law, 3 states have new copay accumulator program bans, 13 states began to debate the issue of white bagging, and 16 states began to consider the next stage of pharmacy benefit manager (PBM) reform with rebate-pass-through legislation.
At the federal level, the Inflation Reduction Act (IRA; H.R. 5376) was enacted in August and, like all major pieces of legislation, there are pros and cons. On the positive side, the legislation reforms Medicare Part D cost-sharing, including – for the first time – the creation of an annual cap on cost-sharing by beneficiaries. That will especially help patients with high, ongoing prescription drug needs. On the negative side, despite its extensive drug-pricing provisions, the IRA did not include any reform of PBM practices. In fact, Congress has delayed implementation of the so-called “rebate rule” for 10 years. That rule would have essentially ended payments from drug companies to PBMs in exchange for formulary placement by removing safe harbor protection from antikickback law for these payments, allowing patients to benefit from these payments.
Finally, the IRA included extensive provisions applicable to drug manufacturers, including a mechanism for Medicare to set prices directly for medications that have been on the market for a certain number of years but are still without a biosimilar or generic. This will apply fully to selected Part B drugs as of 2028. The key for rheumatologists and our patients in the next few years will be to engage with the Centers for Medicare & Medicaid Services as it implements this provision to ensure that rheumatologists are not underwater financially on the acquisition of medications subject to the new pricing mechanism.
With regard to utilization management reform at the federal level, the Ensuring Seniors’ Timely Access to Care Act (H.R. 3173) would reform prior authorization in Medicare Advantage, but after passing in the House on Sept. 14, the bill has slowed down in the Senate. In some part, that may be because of a surprising score from the Congressional Budget Office, which projected that the bill would cost $16 billion. However, this is not insurmountable: The legislation enjoys broad bipartisan support in the Senate, and its sponsors remain committed to enactment before the end of the year. Additionally, the Safe Step Act (S. 464) would reform step therapy practices in employer-based coverage, but that legislation has not passed either chamber of Congress despite bipartisan support and is unlikely to be enacted before the end of this congressional session.
As noted above, PBMs escaped meaningful scrutiny or reform in the IRA, but the Federal Trade Commission took a different approach when it announced earlier in 2022 that it would conduct an investigation into the business practices of several major PBMs. That study is ongoing and, when finished, will likely result in some additional ideas for meaningful legislative reform.
Finally, there’s the frustration of the egregious Medicare Physician Fee Schedule that has decreased physicians’ reimbursement in a time of accelerated inflation in the cost of running a practice. At the same time, Medicare Advantage plans and everyone else in the government-reimbursed health system are getting at least an inflationary raise. This has created an ire among all physicians that we have not seen in quite a while and which we are leveraging into grassroots outreach.
The problems in the Fee Schedule result from a combination of factors, but one overarching issue is the concept of “budget neutrality,” which essentially requires CMS to make up for any new spending over a certain amount by a commensurate reduction across the whole Fee Schedule. This has the effect of turning the Fee Schedule into a fixed pie: If someone’s slice gets bigger, someone else’s slice must get smaller, but the pie itself never gets bigger. To make matters worse, the Medicare Access and CHIP Reauthorization Act of 2015 has not resulted in advancing value-driven care as the Congress had envisioned when it enacted that legislation. The good news is that there is widespread recognition in Congress that a system built on temporary legislative “patches” to avoid deep payment reductions is unsustainable and must be fixed. The Supporting Medicare Providers Act of 2022 (H.R. 8800) that’s currently pending in the House to offset the looming 2023 Fee Schedule cuts also includes a Sense of the Congress, or nonbinding resolution, establishing the need for administrative and legislative actions for long-term, meaningful reform of Medicare physician payment, along three principles: ensuring financial stability and predictability, promoting and rewarding value-based care innovation, and safeguarding timely access to high-quality care by advancing health equity and reducing disparities.
Turning frustration into action
Much of the frustration for those of us who take care of patients is that many actions and policies are based on profits and politics and not on patient care.
It is unfortunate that money plays such an important role in politics. We are all aware of the power of the well-heeled lobbyist and how money can lead to legislation that is more beneficial to one for-profit company versus another in the health care sector. But then there is the party politics of health care legislation. We see examples of great legislation offered by one party being buried because it might be beneficial to the “other side” in the next election, in spite of the fact that both sides agree on the issue. Here is where we must fight our cynicism and remember our patients. Building and maintaining a relationship with our representatives, whether we agree with them are not, is a very important part of advocacy.
As we come off the recent elections, it is important that we acquaint ourselves with our newly elected representatives and reacquaint ourselves with our re-elected officials. Recently, the Coalition of State Rheumatology Organizations had an advocacy day asking rheumatologists to invite their legislator (city, state, or federal) to their office to witness first-hand the practice of rheumatology. The importance of asking your representative to visit your office cannot be overemphasized. First, you get to know the staffer who arranges these visits. Having a good relationship with your representative’s staff is important in maintaining future communications. Having your legislator tour your office, while you share the daily challenges of getting the right medication for patients, is invaluable to their understanding of how the delay in care that utilization management tools such as prior authorizations and step therapy can cause. It is also helpful for you or your office manager to highlight how independent practices are small businesses that must be run efficiently to ensure they can stay open. Building a relationship with and educating your representatives on issues they may not be familiar with will encourage them to use you as a resource in the future.
CSRO has a legislator invitation template, and we can provide talking points if the invitation is accepted. Many state legislative sessions begin in January, so now is the time to get to know your legislator.
Let’s celebrate the wins of 2022 and not let the frustrations with the system diminish our passion – that’s the hard part! Onward to 2023 as “Rheums for Action!”
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
As we come to a close on 2022, let’s take a look at the celebrations and frustrations of the past year’s health policies so that they may act as a catalyst, encouraging us to engage with our representatives. Some of these policies include actions by major companies that rule our health care system, as well as the regulations and legislation passed (or not passed) by our governmental entities. And of course, we must consider how profits and politics influence these policies and often rule the roost!
Insurance
Once again, we are facing increased nonmedical switching of stable patients to different medications through ever-increasing formulary exclusions and higher tiering of less profitable drugs. There are some reports of patients being whipsawed back and forth yearly between reference infliximab and various biosimilars, depending on which is the most profitable to the health plan at the time. And now it’s not just the copay accumulator or maximizer programs that are abusing patient assistance programs, there are new “alternative funding companies” that are carving out expensive and specialty drugs from coverage of employers’ funded health plans. These alternative funding companies then obtain medications – sometimes from other countries – and other forms of assistance from manufacturers and foundations. There have been reports that they make the patient assign power of attorney to them and even pretend to be the patient to obtain the drug, assistance, and copay cards and then bill the employer for getting the free drug or assistance. This abuse of the system, along with copay maximizers, are causing drug manufacturers to rethink their assistance policies, with middlemen reaping the advantages of the assistance plans and not the truly needy patient.
Legislation and regulation
Substantive progress continues to be made on access issues in the states. A total of 5 states signed step-therapy legislation into law, 3 states have new copay accumulator program bans, 13 states began to debate the issue of white bagging, and 16 states began to consider the next stage of pharmacy benefit manager (PBM) reform with rebate-pass-through legislation.
At the federal level, the Inflation Reduction Act (IRA; H.R. 5376) was enacted in August and, like all major pieces of legislation, there are pros and cons. On the positive side, the legislation reforms Medicare Part D cost-sharing, including – for the first time – the creation of an annual cap on cost-sharing by beneficiaries. That will especially help patients with high, ongoing prescription drug needs. On the negative side, despite its extensive drug-pricing provisions, the IRA did not include any reform of PBM practices. In fact, Congress has delayed implementation of the so-called “rebate rule” for 10 years. That rule would have essentially ended payments from drug companies to PBMs in exchange for formulary placement by removing safe harbor protection from antikickback law for these payments, allowing patients to benefit from these payments.
Finally, the IRA included extensive provisions applicable to drug manufacturers, including a mechanism for Medicare to set prices directly for medications that have been on the market for a certain number of years but are still without a biosimilar or generic. This will apply fully to selected Part B drugs as of 2028. The key for rheumatologists and our patients in the next few years will be to engage with the Centers for Medicare & Medicaid Services as it implements this provision to ensure that rheumatologists are not underwater financially on the acquisition of medications subject to the new pricing mechanism.
With regard to utilization management reform at the federal level, the Ensuring Seniors’ Timely Access to Care Act (H.R. 3173) would reform prior authorization in Medicare Advantage, but after passing in the House on Sept. 14, the bill has slowed down in the Senate. In some part, that may be because of a surprising score from the Congressional Budget Office, which projected that the bill would cost $16 billion. However, this is not insurmountable: The legislation enjoys broad bipartisan support in the Senate, and its sponsors remain committed to enactment before the end of the year. Additionally, the Safe Step Act (S. 464) would reform step therapy practices in employer-based coverage, but that legislation has not passed either chamber of Congress despite bipartisan support and is unlikely to be enacted before the end of this congressional session.
As noted above, PBMs escaped meaningful scrutiny or reform in the IRA, but the Federal Trade Commission took a different approach when it announced earlier in 2022 that it would conduct an investigation into the business practices of several major PBMs. That study is ongoing and, when finished, will likely result in some additional ideas for meaningful legislative reform.
Finally, there’s the frustration of the egregious Medicare Physician Fee Schedule that has decreased physicians’ reimbursement in a time of accelerated inflation in the cost of running a practice. At the same time, Medicare Advantage plans and everyone else in the government-reimbursed health system are getting at least an inflationary raise. This has created an ire among all physicians that we have not seen in quite a while and which we are leveraging into grassroots outreach.
The problems in the Fee Schedule result from a combination of factors, but one overarching issue is the concept of “budget neutrality,” which essentially requires CMS to make up for any new spending over a certain amount by a commensurate reduction across the whole Fee Schedule. This has the effect of turning the Fee Schedule into a fixed pie: If someone’s slice gets bigger, someone else’s slice must get smaller, but the pie itself never gets bigger. To make matters worse, the Medicare Access and CHIP Reauthorization Act of 2015 has not resulted in advancing value-driven care as the Congress had envisioned when it enacted that legislation. The good news is that there is widespread recognition in Congress that a system built on temporary legislative “patches” to avoid deep payment reductions is unsustainable and must be fixed. The Supporting Medicare Providers Act of 2022 (H.R. 8800) that’s currently pending in the House to offset the looming 2023 Fee Schedule cuts also includes a Sense of the Congress, or nonbinding resolution, establishing the need for administrative and legislative actions for long-term, meaningful reform of Medicare physician payment, along three principles: ensuring financial stability and predictability, promoting and rewarding value-based care innovation, and safeguarding timely access to high-quality care by advancing health equity and reducing disparities.
Turning frustration into action
Much of the frustration for those of us who take care of patients is that many actions and policies are based on profits and politics and not on patient care.
It is unfortunate that money plays such an important role in politics. We are all aware of the power of the well-heeled lobbyist and how money can lead to legislation that is more beneficial to one for-profit company versus another in the health care sector. But then there is the party politics of health care legislation. We see examples of great legislation offered by one party being buried because it might be beneficial to the “other side” in the next election, in spite of the fact that both sides agree on the issue. Here is where we must fight our cynicism and remember our patients. Building and maintaining a relationship with our representatives, whether we agree with them are not, is a very important part of advocacy.
As we come off the recent elections, it is important that we acquaint ourselves with our newly elected representatives and reacquaint ourselves with our re-elected officials. Recently, the Coalition of State Rheumatology Organizations had an advocacy day asking rheumatologists to invite their legislator (city, state, or federal) to their office to witness first-hand the practice of rheumatology. The importance of asking your representative to visit your office cannot be overemphasized. First, you get to know the staffer who arranges these visits. Having a good relationship with your representative’s staff is important in maintaining future communications. Having your legislator tour your office, while you share the daily challenges of getting the right medication for patients, is invaluable to their understanding of how the delay in care that utilization management tools such as prior authorizations and step therapy can cause. It is also helpful for you or your office manager to highlight how independent practices are small businesses that must be run efficiently to ensure they can stay open. Building a relationship with and educating your representatives on issues they may not be familiar with will encourage them to use you as a resource in the future.
CSRO has a legislator invitation template, and we can provide talking points if the invitation is accepted. Many state legislative sessions begin in January, so now is the time to get to know your legislator.
Let’s celebrate the wins of 2022 and not let the frustrations with the system diminish our passion – that’s the hard part! Onward to 2023 as “Rheums for Action!”
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
As we come to a close on 2022, let’s take a look at the celebrations and frustrations of the past year’s health policies so that they may act as a catalyst, encouraging us to engage with our representatives. Some of these policies include actions by major companies that rule our health care system, as well as the regulations and legislation passed (or not passed) by our governmental entities. And of course, we must consider how profits and politics influence these policies and often rule the roost!
Insurance
Once again, we are facing increased nonmedical switching of stable patients to different medications through ever-increasing formulary exclusions and higher tiering of less profitable drugs. There are some reports of patients being whipsawed back and forth yearly between reference infliximab and various biosimilars, depending on which is the most profitable to the health plan at the time. And now it’s not just the copay accumulator or maximizer programs that are abusing patient assistance programs, there are new “alternative funding companies” that are carving out expensive and specialty drugs from coverage of employers’ funded health plans. These alternative funding companies then obtain medications – sometimes from other countries – and other forms of assistance from manufacturers and foundations. There have been reports that they make the patient assign power of attorney to them and even pretend to be the patient to obtain the drug, assistance, and copay cards and then bill the employer for getting the free drug or assistance. This abuse of the system, along with copay maximizers, are causing drug manufacturers to rethink their assistance policies, with middlemen reaping the advantages of the assistance plans and not the truly needy patient.
Legislation and regulation
Substantive progress continues to be made on access issues in the states. A total of 5 states signed step-therapy legislation into law, 3 states have new copay accumulator program bans, 13 states began to debate the issue of white bagging, and 16 states began to consider the next stage of pharmacy benefit manager (PBM) reform with rebate-pass-through legislation.
At the federal level, the Inflation Reduction Act (IRA; H.R. 5376) was enacted in August and, like all major pieces of legislation, there are pros and cons. On the positive side, the legislation reforms Medicare Part D cost-sharing, including – for the first time – the creation of an annual cap on cost-sharing by beneficiaries. That will especially help patients with high, ongoing prescription drug needs. On the negative side, despite its extensive drug-pricing provisions, the IRA did not include any reform of PBM practices. In fact, Congress has delayed implementation of the so-called “rebate rule” for 10 years. That rule would have essentially ended payments from drug companies to PBMs in exchange for formulary placement by removing safe harbor protection from antikickback law for these payments, allowing patients to benefit from these payments.
Finally, the IRA included extensive provisions applicable to drug manufacturers, including a mechanism for Medicare to set prices directly for medications that have been on the market for a certain number of years but are still without a biosimilar or generic. This will apply fully to selected Part B drugs as of 2028. The key for rheumatologists and our patients in the next few years will be to engage with the Centers for Medicare & Medicaid Services as it implements this provision to ensure that rheumatologists are not underwater financially on the acquisition of medications subject to the new pricing mechanism.
With regard to utilization management reform at the federal level, the Ensuring Seniors’ Timely Access to Care Act (H.R. 3173) would reform prior authorization in Medicare Advantage, but after passing in the House on Sept. 14, the bill has slowed down in the Senate. In some part, that may be because of a surprising score from the Congressional Budget Office, which projected that the bill would cost $16 billion. However, this is not insurmountable: The legislation enjoys broad bipartisan support in the Senate, and its sponsors remain committed to enactment before the end of the year. Additionally, the Safe Step Act (S. 464) would reform step therapy practices in employer-based coverage, but that legislation has not passed either chamber of Congress despite bipartisan support and is unlikely to be enacted before the end of this congressional session.
As noted above, PBMs escaped meaningful scrutiny or reform in the IRA, but the Federal Trade Commission took a different approach when it announced earlier in 2022 that it would conduct an investigation into the business practices of several major PBMs. That study is ongoing and, when finished, will likely result in some additional ideas for meaningful legislative reform.
Finally, there’s the frustration of the egregious Medicare Physician Fee Schedule that has decreased physicians’ reimbursement in a time of accelerated inflation in the cost of running a practice. At the same time, Medicare Advantage plans and everyone else in the government-reimbursed health system are getting at least an inflationary raise. This has created an ire among all physicians that we have not seen in quite a while and which we are leveraging into grassroots outreach.
The problems in the Fee Schedule result from a combination of factors, but one overarching issue is the concept of “budget neutrality,” which essentially requires CMS to make up for any new spending over a certain amount by a commensurate reduction across the whole Fee Schedule. This has the effect of turning the Fee Schedule into a fixed pie: If someone’s slice gets bigger, someone else’s slice must get smaller, but the pie itself never gets bigger. To make matters worse, the Medicare Access and CHIP Reauthorization Act of 2015 has not resulted in advancing value-driven care as the Congress had envisioned when it enacted that legislation. The good news is that there is widespread recognition in Congress that a system built on temporary legislative “patches” to avoid deep payment reductions is unsustainable and must be fixed. The Supporting Medicare Providers Act of 2022 (H.R. 8800) that’s currently pending in the House to offset the looming 2023 Fee Schedule cuts also includes a Sense of the Congress, or nonbinding resolution, establishing the need for administrative and legislative actions for long-term, meaningful reform of Medicare physician payment, along three principles: ensuring financial stability and predictability, promoting and rewarding value-based care innovation, and safeguarding timely access to high-quality care by advancing health equity and reducing disparities.
Turning frustration into action
Much of the frustration for those of us who take care of patients is that many actions and policies are based on profits and politics and not on patient care.
It is unfortunate that money plays such an important role in politics. We are all aware of the power of the well-heeled lobbyist and how money can lead to legislation that is more beneficial to one for-profit company versus another in the health care sector. But then there is the party politics of health care legislation. We see examples of great legislation offered by one party being buried because it might be beneficial to the “other side” in the next election, in spite of the fact that both sides agree on the issue. Here is where we must fight our cynicism and remember our patients. Building and maintaining a relationship with our representatives, whether we agree with them are not, is a very important part of advocacy.
As we come off the recent elections, it is important that we acquaint ourselves with our newly elected representatives and reacquaint ourselves with our re-elected officials. Recently, the Coalition of State Rheumatology Organizations had an advocacy day asking rheumatologists to invite their legislator (city, state, or federal) to their office to witness first-hand the practice of rheumatology. The importance of asking your representative to visit your office cannot be overemphasized. First, you get to know the staffer who arranges these visits. Having a good relationship with your representative’s staff is important in maintaining future communications. Having your legislator tour your office, while you share the daily challenges of getting the right medication for patients, is invaluable to their understanding of how the delay in care that utilization management tools such as prior authorizations and step therapy can cause. It is also helpful for you or your office manager to highlight how independent practices are small businesses that must be run efficiently to ensure they can stay open. Building a relationship with and educating your representatives on issues they may not be familiar with will encourage them to use you as a resource in the future.
CSRO has a legislator invitation template, and we can provide talking points if the invitation is accepted. Many state legislative sessions begin in January, so now is the time to get to know your legislator.
Let’s celebrate the wins of 2022 and not let the frustrations with the system diminish our passion – that’s the hard part! Onward to 2023 as “Rheums for Action!”
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
Telepsychiatry tips: Etiquette and ethics
From providing virtual therapy sessions to patients in the front seats of their cars, to sessions with patients who turn out to be in another state,
But key practice tips are emerging for the optimization of virtual sessions, said Sanjay Gupta, MD, chief medical officer of the BryLin Behavioral Health System in Buffalo, N.Y., during a presentation on the subject at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists in Cincinnati, Ohio.
Dr. Gupta noted that while “many pitfalls [may] occur,” an overriding rule that should be emphasized with telepsychiatry is that “[virtual visits] are held to the same standard of care as an in-person visit.” This “rule” needs to be followed diligently, he said, as the key difference in virtual visits is a reduced sense of the formality of a psychotherapy session.
With virtual sessions, the therapeutic experience “can feel kind of trivialized,” said Dr. Gupta, who is also a clinical professor in the department of psychiatry, State University of New York at Buffalo. He noted that it is crucial that “the sacredness of a private setting should not be diluted.”
Challenges in finding that privacy for some, however, lead to the issue of the “patients in cars” scenario, Dr. Gupta said. Still, he added, while psychiatric sessions should never be conducted when a patient is driving, the front seat of a parked car may, for some, be the most private setting available.
“For many patients, their car may be the only private place from which they can take a video call,” Dr. Gupta noted. “Perhaps they are at work and the only way they could fit in the appointment is by going out to their car on their break. Or patients may even be at home, but they’re not alone and need to go out to their car for privacy.”
If the car isn’t being driven, sitting inside it should be fine for virtual therapy, but even there, clinicians should retain a focus on the consistency of care regardless of the setting.
Meanwhile, psychiatrists can take key measures to keep things professional, at least on their end of the session.
Before starting, for instance, keep in mind the patient’s viewing experience, Dr. Gupta suggested. Tips he offered include:
- Keep the background of your video image subtle, with no distractions, such as windows looking out to an ocean or other distracting background elements.
- The camera should be above eye level to suggest a face-to-face conversation more effectively.
- Try not to have other browser windows open and look directly into the camera lens so that the patient knows they have your full attention.
- Try not to take notes or document in the electronic health record during the session, which also can give the impression of being distracted and not listening to the patient.
Psychiatrists should remember that older patients – who may be uncomfortable with email, much less video conferencing – may still struggle with video-calling technology. In such cases, consider:
- Sending the patient instructions in advance of the appointment.
- Have your office hold a “tech check” prior to the appointment to ensure the patient is ready.
- Be prepared to provide troubleshooting.
Whether the patient is tech savvy or not, make sure communication is clear:
- Speak in short sentences on teleconferencing sessions.
- Speak slowly and use a lower frequency.
- Recognize that non-native English speakers may struggle with comprehension, and explore interpreter options.
Dr. Gupta noted that the first minute of the virtual therapy session is crucial in setting the tone.
“The patient wants to hear a professional, confident tone on the other end at the beginning of the session,” he said. “Be warm and respectful throughout the visit, and make sure to explain to the patient how the session will be reconnected if the call is interrupted.”
Clinicians should also make sure to identify the patient’s physical location during the session in case of an emergency, such as the patient becoming suicidal.
Impending ‘telehealth cliff’
Many laws and licensing requirements for telehealth are still relatively loose, falling under the COVID-19 public health emergency (PHE) policies. These policies allow practitioners who are eligible to bill Medicare for telehealth services regardless of where the patient or provider is located, and providers can also deliver telehealth services across state lines, depending on state and federal rules.
However, Dr. Gupta warns that practitioners should be prepared for the potential “telehealth cliff” that is anticipated when those PHE policies are lifted, as barriers in licensing, billing, and other factors, such as HIPAA, are reinstated.
“HIPAA is [flexible] now as long as the public emergency policies exist,” Dr. Gupta said. “However, in noncrisis times, technology will be required to be HIPAA compliant. If you are a solo provider, for instance, you really need to choose a telepsychiatry platform that is HIPAA compliant before that happens.”
While the timing of the “telehealth cliff” is still uncertain, providers have been promised a 60-day advance notice of the PHE end, and at that time, there will be an additional 151-day grace period before the waivers lift.
A key federal measure that could protect more favorable telemedicine policies across state lines, the Temporary Reciprocity to Ensure Access to Treatment Act, currently remains stalled in Congress.
Regardless of those developments, Dr. Gupta underscored that “telepsychiatry is here to stay because the patients and their families like it, and they will be the driving factors.”
He noted that “the future is likely going to be a hybrid model of in-person and virtual visits,” to accommodate the various scenarios in which in-person visits may be preferred or necessary, but many will still likely choose the convenience and greater flexibility of virtual sessions.
Dr. Gupta serves or has served as a speaker or member of a speaker’s bureau for AbbVie, Acadia, Alkermes, Intra-Cellular Therapies, Janssen, Neurocrine, and Otsuka, and serves as a consultant/on an advisory board for Intra-Cellular Therapies.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
From providing virtual therapy sessions to patients in the front seats of their cars, to sessions with patients who turn out to be in another state,
But key practice tips are emerging for the optimization of virtual sessions, said Sanjay Gupta, MD, chief medical officer of the BryLin Behavioral Health System in Buffalo, N.Y., during a presentation on the subject at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists in Cincinnati, Ohio.
Dr. Gupta noted that while “many pitfalls [may] occur,” an overriding rule that should be emphasized with telepsychiatry is that “[virtual visits] are held to the same standard of care as an in-person visit.” This “rule” needs to be followed diligently, he said, as the key difference in virtual visits is a reduced sense of the formality of a psychotherapy session.
With virtual sessions, the therapeutic experience “can feel kind of trivialized,” said Dr. Gupta, who is also a clinical professor in the department of psychiatry, State University of New York at Buffalo. He noted that it is crucial that “the sacredness of a private setting should not be diluted.”
Challenges in finding that privacy for some, however, lead to the issue of the “patients in cars” scenario, Dr. Gupta said. Still, he added, while psychiatric sessions should never be conducted when a patient is driving, the front seat of a parked car may, for some, be the most private setting available.
“For many patients, their car may be the only private place from which they can take a video call,” Dr. Gupta noted. “Perhaps they are at work and the only way they could fit in the appointment is by going out to their car on their break. Or patients may even be at home, but they’re not alone and need to go out to their car for privacy.”
If the car isn’t being driven, sitting inside it should be fine for virtual therapy, but even there, clinicians should retain a focus on the consistency of care regardless of the setting.
Meanwhile, psychiatrists can take key measures to keep things professional, at least on their end of the session.
Before starting, for instance, keep in mind the patient’s viewing experience, Dr. Gupta suggested. Tips he offered include:
- Keep the background of your video image subtle, with no distractions, such as windows looking out to an ocean or other distracting background elements.
- The camera should be above eye level to suggest a face-to-face conversation more effectively.
- Try not to have other browser windows open and look directly into the camera lens so that the patient knows they have your full attention.
- Try not to take notes or document in the electronic health record during the session, which also can give the impression of being distracted and not listening to the patient.
Psychiatrists should remember that older patients – who may be uncomfortable with email, much less video conferencing – may still struggle with video-calling technology. In such cases, consider:
- Sending the patient instructions in advance of the appointment.
- Have your office hold a “tech check” prior to the appointment to ensure the patient is ready.
- Be prepared to provide troubleshooting.
Whether the patient is tech savvy or not, make sure communication is clear:
- Speak in short sentences on teleconferencing sessions.
- Speak slowly and use a lower frequency.
- Recognize that non-native English speakers may struggle with comprehension, and explore interpreter options.
Dr. Gupta noted that the first minute of the virtual therapy session is crucial in setting the tone.
“The patient wants to hear a professional, confident tone on the other end at the beginning of the session,” he said. “Be warm and respectful throughout the visit, and make sure to explain to the patient how the session will be reconnected if the call is interrupted.”
Clinicians should also make sure to identify the patient’s physical location during the session in case of an emergency, such as the patient becoming suicidal.
Impending ‘telehealth cliff’
Many laws and licensing requirements for telehealth are still relatively loose, falling under the COVID-19 public health emergency (PHE) policies. These policies allow practitioners who are eligible to bill Medicare for telehealth services regardless of where the patient or provider is located, and providers can also deliver telehealth services across state lines, depending on state and federal rules.
However, Dr. Gupta warns that practitioners should be prepared for the potential “telehealth cliff” that is anticipated when those PHE policies are lifted, as barriers in licensing, billing, and other factors, such as HIPAA, are reinstated.
“HIPAA is [flexible] now as long as the public emergency policies exist,” Dr. Gupta said. “However, in noncrisis times, technology will be required to be HIPAA compliant. If you are a solo provider, for instance, you really need to choose a telepsychiatry platform that is HIPAA compliant before that happens.”
While the timing of the “telehealth cliff” is still uncertain, providers have been promised a 60-day advance notice of the PHE end, and at that time, there will be an additional 151-day grace period before the waivers lift.
A key federal measure that could protect more favorable telemedicine policies across state lines, the Temporary Reciprocity to Ensure Access to Treatment Act, currently remains stalled in Congress.
Regardless of those developments, Dr. Gupta underscored that “telepsychiatry is here to stay because the patients and their families like it, and they will be the driving factors.”
He noted that “the future is likely going to be a hybrid model of in-person and virtual visits,” to accommodate the various scenarios in which in-person visits may be preferred or necessary, but many will still likely choose the convenience and greater flexibility of virtual sessions.
Dr. Gupta serves or has served as a speaker or member of a speaker’s bureau for AbbVie, Acadia, Alkermes, Intra-Cellular Therapies, Janssen, Neurocrine, and Otsuka, and serves as a consultant/on an advisory board for Intra-Cellular Therapies.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
From providing virtual therapy sessions to patients in the front seats of their cars, to sessions with patients who turn out to be in another state,
But key practice tips are emerging for the optimization of virtual sessions, said Sanjay Gupta, MD, chief medical officer of the BryLin Behavioral Health System in Buffalo, N.Y., during a presentation on the subject at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists in Cincinnati, Ohio.
Dr. Gupta noted that while “many pitfalls [may] occur,” an overriding rule that should be emphasized with telepsychiatry is that “[virtual visits] are held to the same standard of care as an in-person visit.” This “rule” needs to be followed diligently, he said, as the key difference in virtual visits is a reduced sense of the formality of a psychotherapy session.
With virtual sessions, the therapeutic experience “can feel kind of trivialized,” said Dr. Gupta, who is also a clinical professor in the department of psychiatry, State University of New York at Buffalo. He noted that it is crucial that “the sacredness of a private setting should not be diluted.”
Challenges in finding that privacy for some, however, lead to the issue of the “patients in cars” scenario, Dr. Gupta said. Still, he added, while psychiatric sessions should never be conducted when a patient is driving, the front seat of a parked car may, for some, be the most private setting available.
“For many patients, their car may be the only private place from which they can take a video call,” Dr. Gupta noted. “Perhaps they are at work and the only way they could fit in the appointment is by going out to their car on their break. Or patients may even be at home, but they’re not alone and need to go out to their car for privacy.”
If the car isn’t being driven, sitting inside it should be fine for virtual therapy, but even there, clinicians should retain a focus on the consistency of care regardless of the setting.
Meanwhile, psychiatrists can take key measures to keep things professional, at least on their end of the session.
Before starting, for instance, keep in mind the patient’s viewing experience, Dr. Gupta suggested. Tips he offered include:
- Keep the background of your video image subtle, with no distractions, such as windows looking out to an ocean or other distracting background elements.
- The camera should be above eye level to suggest a face-to-face conversation more effectively.
- Try not to have other browser windows open and look directly into the camera lens so that the patient knows they have your full attention.
- Try not to take notes or document in the electronic health record during the session, which also can give the impression of being distracted and not listening to the patient.
Psychiatrists should remember that older patients – who may be uncomfortable with email, much less video conferencing – may still struggle with video-calling technology. In such cases, consider:
- Sending the patient instructions in advance of the appointment.
- Have your office hold a “tech check” prior to the appointment to ensure the patient is ready.
- Be prepared to provide troubleshooting.
Whether the patient is tech savvy or not, make sure communication is clear:
- Speak in short sentences on teleconferencing sessions.
- Speak slowly and use a lower frequency.
- Recognize that non-native English speakers may struggle with comprehension, and explore interpreter options.
Dr. Gupta noted that the first minute of the virtual therapy session is crucial in setting the tone.
“The patient wants to hear a professional, confident tone on the other end at the beginning of the session,” he said. “Be warm and respectful throughout the visit, and make sure to explain to the patient how the session will be reconnected if the call is interrupted.”
Clinicians should also make sure to identify the patient’s physical location during the session in case of an emergency, such as the patient becoming suicidal.
Impending ‘telehealth cliff’
Many laws and licensing requirements for telehealth are still relatively loose, falling under the COVID-19 public health emergency (PHE) policies. These policies allow practitioners who are eligible to bill Medicare for telehealth services regardless of where the patient or provider is located, and providers can also deliver telehealth services across state lines, depending on state and federal rules.
However, Dr. Gupta warns that practitioners should be prepared for the potential “telehealth cliff” that is anticipated when those PHE policies are lifted, as barriers in licensing, billing, and other factors, such as HIPAA, are reinstated.
“HIPAA is [flexible] now as long as the public emergency policies exist,” Dr. Gupta said. “However, in noncrisis times, technology will be required to be HIPAA compliant. If you are a solo provider, for instance, you really need to choose a telepsychiatry platform that is HIPAA compliant before that happens.”
While the timing of the “telehealth cliff” is still uncertain, providers have been promised a 60-day advance notice of the PHE end, and at that time, there will be an additional 151-day grace period before the waivers lift.
A key federal measure that could protect more favorable telemedicine policies across state lines, the Temporary Reciprocity to Ensure Access to Treatment Act, currently remains stalled in Congress.
Regardless of those developments, Dr. Gupta underscored that “telepsychiatry is here to stay because the patients and their families like it, and they will be the driving factors.”
He noted that “the future is likely going to be a hybrid model of in-person and virtual visits,” to accommodate the various scenarios in which in-person visits may be preferred or necessary, but many will still likely choose the convenience and greater flexibility of virtual sessions.
Dr. Gupta serves or has served as a speaker or member of a speaker’s bureau for AbbVie, Acadia, Alkermes, Intra-Cellular Therapies, Janssen, Neurocrine, and Otsuka, and serves as a consultant/on an advisory board for Intra-Cellular Therapies.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
FROM PSYCHOPHARMACOLOGY UPDATE
Will Congress step up to save primary care?
Primary care and family physicians operate on the front lines of health care, working tirelessly to serve patients and their families. However, many primary care practices are operating on tight margins and cannot sustain additional financial hits. As we continue to navigate a pandemic that has altered our health care landscape, we traveled to Capitol Hill to urge Congress to act on two critical issues: Medicare payment reform and streamlining administrative burden for physicians.
The current Medicare system for compensating physicians jeopardizes access to primary care. Family physicians, along with other primary care clinicians, are facing significant cuts in payments and rising inflation that threaten our ability to care for patients.
Each of us has experienced the effects of this pincer in devastating ways – from the independent clinicians who have been forced to sell their practices to hospitals or large health systems, to the physicians who are retiring early, leaving their practices, or even closing them because they can’t afford to keep their doors open.
Practices also struggle to cover the rising costs of staff wages, leasing space, and purchasing supplies and equipment, leaving little room for innovation or investments to transition into new payment models. Meanwhile, hospitals, skilled nursing facilities, ambulatory surgery centers, and other Medicare providers receive annual payment increases to account for rising costs.
Insufficient Medicare payments also challenge practices that serve many publicly insured patients. If practices cannot cover their expenses, they may be forced to turn away new Medicare and Medicaid patients – something that goes against the core tenets of our health care system.
Fortunately, we have some solutions. We’re asking Congress to pass the Supporting Medicare Providers Act of 2022, which calls for a 4.42% positive adjustment to the Medicare Physician Fee Schedule (MPFS) conversion factor for 2023 to offset the statutory reduction triggered by budget neutrality rules.
We also are calling on lawmakers to end the statutory freeze on annual updates to the MPFS and enact a positive annual update to the conversion factor based on the Medicare Economic Index. This critical relief would stave off the most immediate cuts while giving us more time to work with Congress on comprehensive reforms to the Medicare physician payment system.
As many practices struggle to operate, burnout among primary care physicians has also increased, with research showing that 66% of primary care physicians reported frequent burnout symptoms in 2021. Streamlining prior authorizations – a cumbersome process that requires physicians to obtain preapproval for treatments or tests before providing care to patients, and can risk patients’ access to timely care – is one way to reduce burden and alleviate burnout.
According to the American Medical Association, 82% of physicians report that prior authorization can lead to patients abandoning care, and 93% believe that prior authorization delays access to necessary care.
All of us have had patients whose care has been affected by these delays, including difficulty in getting necessary medications filled or having medical procedures postponed. Moreover, primary care physicians and their staff spend hours each week completing paperwork and communicating with insurers to ensure that their patients can access the treatments and services they need.
That is why we’re urging the Senate to pass the Improving Seniors’ Timely Access to Care Act, which would streamline the prior authorization process in the Medicare Advantage program.
As family physicians, we are in a unique position to help improve our patients’ health and their quality of life. But we can’t do this alone. We need the support of policy makers to make patient health and primary care a national priority.
Dr. Iroku-Malize is a family physician in Long Island, New York, and President of the American Academy of Family Physicians. Dr. Ransone is a family physician in Deltaville, Va., and board chair, immediate past president of the AAFP. Dr. Furr is a family physician in Jackson, Ala., and President-elect of the AAFP. They reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Primary care and family physicians operate on the front lines of health care, working tirelessly to serve patients and their families. However, many primary care practices are operating on tight margins and cannot sustain additional financial hits. As we continue to navigate a pandemic that has altered our health care landscape, we traveled to Capitol Hill to urge Congress to act on two critical issues: Medicare payment reform and streamlining administrative burden for physicians.
The current Medicare system for compensating physicians jeopardizes access to primary care. Family physicians, along with other primary care clinicians, are facing significant cuts in payments and rising inflation that threaten our ability to care for patients.
Each of us has experienced the effects of this pincer in devastating ways – from the independent clinicians who have been forced to sell their practices to hospitals or large health systems, to the physicians who are retiring early, leaving their practices, or even closing them because they can’t afford to keep their doors open.
Practices also struggle to cover the rising costs of staff wages, leasing space, and purchasing supplies and equipment, leaving little room for innovation or investments to transition into new payment models. Meanwhile, hospitals, skilled nursing facilities, ambulatory surgery centers, and other Medicare providers receive annual payment increases to account for rising costs.
Insufficient Medicare payments also challenge practices that serve many publicly insured patients. If practices cannot cover their expenses, they may be forced to turn away new Medicare and Medicaid patients – something that goes against the core tenets of our health care system.
Fortunately, we have some solutions. We’re asking Congress to pass the Supporting Medicare Providers Act of 2022, which calls for a 4.42% positive adjustment to the Medicare Physician Fee Schedule (MPFS) conversion factor for 2023 to offset the statutory reduction triggered by budget neutrality rules.
We also are calling on lawmakers to end the statutory freeze on annual updates to the MPFS and enact a positive annual update to the conversion factor based on the Medicare Economic Index. This critical relief would stave off the most immediate cuts while giving us more time to work with Congress on comprehensive reforms to the Medicare physician payment system.
As many practices struggle to operate, burnout among primary care physicians has also increased, with research showing that 66% of primary care physicians reported frequent burnout symptoms in 2021. Streamlining prior authorizations – a cumbersome process that requires physicians to obtain preapproval for treatments or tests before providing care to patients, and can risk patients’ access to timely care – is one way to reduce burden and alleviate burnout.
According to the American Medical Association, 82% of physicians report that prior authorization can lead to patients abandoning care, and 93% believe that prior authorization delays access to necessary care.
All of us have had patients whose care has been affected by these delays, including difficulty in getting necessary medications filled or having medical procedures postponed. Moreover, primary care physicians and their staff spend hours each week completing paperwork and communicating with insurers to ensure that their patients can access the treatments and services they need.
That is why we’re urging the Senate to pass the Improving Seniors’ Timely Access to Care Act, which would streamline the prior authorization process in the Medicare Advantage program.
As family physicians, we are in a unique position to help improve our patients’ health and their quality of life. But we can’t do this alone. We need the support of policy makers to make patient health and primary care a national priority.
Dr. Iroku-Malize is a family physician in Long Island, New York, and President of the American Academy of Family Physicians. Dr. Ransone is a family physician in Deltaville, Va., and board chair, immediate past president of the AAFP. Dr. Furr is a family physician in Jackson, Ala., and President-elect of the AAFP. They reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Primary care and family physicians operate on the front lines of health care, working tirelessly to serve patients and their families. However, many primary care practices are operating on tight margins and cannot sustain additional financial hits. As we continue to navigate a pandemic that has altered our health care landscape, we traveled to Capitol Hill to urge Congress to act on two critical issues: Medicare payment reform and streamlining administrative burden for physicians.
The current Medicare system for compensating physicians jeopardizes access to primary care. Family physicians, along with other primary care clinicians, are facing significant cuts in payments and rising inflation that threaten our ability to care for patients.
Each of us has experienced the effects of this pincer in devastating ways – from the independent clinicians who have been forced to sell their practices to hospitals or large health systems, to the physicians who are retiring early, leaving their practices, or even closing them because they can’t afford to keep their doors open.
Practices also struggle to cover the rising costs of staff wages, leasing space, and purchasing supplies and equipment, leaving little room for innovation or investments to transition into new payment models. Meanwhile, hospitals, skilled nursing facilities, ambulatory surgery centers, and other Medicare providers receive annual payment increases to account for rising costs.
Insufficient Medicare payments also challenge practices that serve many publicly insured patients. If practices cannot cover their expenses, they may be forced to turn away new Medicare and Medicaid patients – something that goes against the core tenets of our health care system.
Fortunately, we have some solutions. We’re asking Congress to pass the Supporting Medicare Providers Act of 2022, which calls for a 4.42% positive adjustment to the Medicare Physician Fee Schedule (MPFS) conversion factor for 2023 to offset the statutory reduction triggered by budget neutrality rules.
We also are calling on lawmakers to end the statutory freeze on annual updates to the MPFS and enact a positive annual update to the conversion factor based on the Medicare Economic Index. This critical relief would stave off the most immediate cuts while giving us more time to work with Congress on comprehensive reforms to the Medicare physician payment system.
As many practices struggle to operate, burnout among primary care physicians has also increased, with research showing that 66% of primary care physicians reported frequent burnout symptoms in 2021. Streamlining prior authorizations – a cumbersome process that requires physicians to obtain preapproval for treatments or tests before providing care to patients, and can risk patients’ access to timely care – is one way to reduce burden and alleviate burnout.
According to the American Medical Association, 82% of physicians report that prior authorization can lead to patients abandoning care, and 93% believe that prior authorization delays access to necessary care.
All of us have had patients whose care has been affected by these delays, including difficulty in getting necessary medications filled or having medical procedures postponed. Moreover, primary care physicians and their staff spend hours each week completing paperwork and communicating with insurers to ensure that their patients can access the treatments and services they need.
That is why we’re urging the Senate to pass the Improving Seniors’ Timely Access to Care Act, which would streamline the prior authorization process in the Medicare Advantage program.
As family physicians, we are in a unique position to help improve our patients’ health and their quality of life. But we can’t do this alone. We need the support of policy makers to make patient health and primary care a national priority.
Dr. Iroku-Malize is a family physician in Long Island, New York, and President of the American Academy of Family Physicians. Dr. Ransone is a family physician in Deltaville, Va., and board chair, immediate past president of the AAFP. Dr. Furr is a family physician in Jackson, Ala., and President-elect of the AAFP. They reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
U.K. doctor found guilty of trying to conceal cause of child’s death
The parents of Claire Roberts were told at the time that a viral infection had spread from her stomach to her brain and that medics had done everything possible to save her. But a television documentary, UTV’s “When Hospitals Kill” (broadcast in October 2004), raised concerns about the treatment of a number of children who died from hyponatremia, which occurs when there is a shortage of sodium in the bloodstream.
After the screening, a public inquiry was announced as Alan and Jennifer Roberts sought answers from the Royal Belfast Hospital for Sick Children, Northern Ireland, about the care of their daughter, who died in October 1996.
On Nov. 7, a Medical Practitioners Tribunal Service (MPTS) panel found that Dr. Heather Steen was not aware of the risks of “dilutional hyponatraemia” at the time, but there was “far more awareness” of the issue after the UTV documentary.
Doctor ‘persisted’ with ‘misrepresentation’ of a viral cause to ‘avoid scrutiny’
Tribunal chairman Sean Ell said: “The tribunal accepted that Dr. Steen was not attempting to conceal details of, or failings in, Patient A’s care in 1996/97, when she believed there was a viral cause of death.
“However, once dilutional hyponatraemia as a result of fluid and electrolyte mismanagement became a live issue from 2004, Dr. Steen persisted with her focus on a viral cause and continued to emphasise this aspect whilst seeking to downplay, qualify, and minimise or ignore findings to the contrary.”
He said this “misrepresentation” continued through the consultant pediatrician’s involvement with Claire’s parents, at a coroner’s inquest, which was ordered after the documentary screening, and the public inquiry.
Mr. Ell said: “It was done in order to conceal the true circumstances of Patient A’s death, and in particular, the possible failings in Patient A’s care.
“Dr. Steen had many opportunities to reconsider and be open and transparent, but chose to maintain her dishonesty over the course of events after 2004.
“Whilst the failings may not have changed the tragic outcome of Patient A’s death, her parents were seeking answers to what happened and were entitled to full transparency.”
Dr. Steen denied the allegations but did not give evidence.
The General Medical Council had argued Dr. Steen tried to cover up the circumstances of Claire’s death to “avoid scrutiny.” The MPTS panel, sitting remotely, will next consider whether Dr. Steen’s fitness to practice is impaired by reason of misconduct.
The hyponatremia public inquiry concluded in 2018 that Claire’s death was the result of “negligent care” from an overdose of fluids and medication. A fresh inquest in 2019 ruled her death was “caused by the treatment she received in hospital.”
This article contains information from PA Media. A version of this article appeared on MedscapeUK.
The parents of Claire Roberts were told at the time that a viral infection had spread from her stomach to her brain and that medics had done everything possible to save her. But a television documentary, UTV’s “When Hospitals Kill” (broadcast in October 2004), raised concerns about the treatment of a number of children who died from hyponatremia, which occurs when there is a shortage of sodium in the bloodstream.
After the screening, a public inquiry was announced as Alan and Jennifer Roberts sought answers from the Royal Belfast Hospital for Sick Children, Northern Ireland, about the care of their daughter, who died in October 1996.
On Nov. 7, a Medical Practitioners Tribunal Service (MPTS) panel found that Dr. Heather Steen was not aware of the risks of “dilutional hyponatraemia” at the time, but there was “far more awareness” of the issue after the UTV documentary.
Doctor ‘persisted’ with ‘misrepresentation’ of a viral cause to ‘avoid scrutiny’
Tribunal chairman Sean Ell said: “The tribunal accepted that Dr. Steen was not attempting to conceal details of, or failings in, Patient A’s care in 1996/97, when she believed there was a viral cause of death.
“However, once dilutional hyponatraemia as a result of fluid and electrolyte mismanagement became a live issue from 2004, Dr. Steen persisted with her focus on a viral cause and continued to emphasise this aspect whilst seeking to downplay, qualify, and minimise or ignore findings to the contrary.”
He said this “misrepresentation” continued through the consultant pediatrician’s involvement with Claire’s parents, at a coroner’s inquest, which was ordered after the documentary screening, and the public inquiry.
Mr. Ell said: “It was done in order to conceal the true circumstances of Patient A’s death, and in particular, the possible failings in Patient A’s care.
“Dr. Steen had many opportunities to reconsider and be open and transparent, but chose to maintain her dishonesty over the course of events after 2004.
“Whilst the failings may not have changed the tragic outcome of Patient A’s death, her parents were seeking answers to what happened and were entitled to full transparency.”
Dr. Steen denied the allegations but did not give evidence.
The General Medical Council had argued Dr. Steen tried to cover up the circumstances of Claire’s death to “avoid scrutiny.” The MPTS panel, sitting remotely, will next consider whether Dr. Steen’s fitness to practice is impaired by reason of misconduct.
The hyponatremia public inquiry concluded in 2018 that Claire’s death was the result of “negligent care” from an overdose of fluids and medication. A fresh inquest in 2019 ruled her death was “caused by the treatment she received in hospital.”
This article contains information from PA Media. A version of this article appeared on MedscapeUK.
The parents of Claire Roberts were told at the time that a viral infection had spread from her stomach to her brain and that medics had done everything possible to save her. But a television documentary, UTV’s “When Hospitals Kill” (broadcast in October 2004), raised concerns about the treatment of a number of children who died from hyponatremia, which occurs when there is a shortage of sodium in the bloodstream.
After the screening, a public inquiry was announced as Alan and Jennifer Roberts sought answers from the Royal Belfast Hospital for Sick Children, Northern Ireland, about the care of their daughter, who died in October 1996.
On Nov. 7, a Medical Practitioners Tribunal Service (MPTS) panel found that Dr. Heather Steen was not aware of the risks of “dilutional hyponatraemia” at the time, but there was “far more awareness” of the issue after the UTV documentary.
Doctor ‘persisted’ with ‘misrepresentation’ of a viral cause to ‘avoid scrutiny’
Tribunal chairman Sean Ell said: “The tribunal accepted that Dr. Steen was not attempting to conceal details of, or failings in, Patient A’s care in 1996/97, when she believed there was a viral cause of death.
“However, once dilutional hyponatraemia as a result of fluid and electrolyte mismanagement became a live issue from 2004, Dr. Steen persisted with her focus on a viral cause and continued to emphasise this aspect whilst seeking to downplay, qualify, and minimise or ignore findings to the contrary.”
He said this “misrepresentation” continued through the consultant pediatrician’s involvement with Claire’s parents, at a coroner’s inquest, which was ordered after the documentary screening, and the public inquiry.
Mr. Ell said: “It was done in order to conceal the true circumstances of Patient A’s death, and in particular, the possible failings in Patient A’s care.
“Dr. Steen had many opportunities to reconsider and be open and transparent, but chose to maintain her dishonesty over the course of events after 2004.
“Whilst the failings may not have changed the tragic outcome of Patient A’s death, her parents were seeking answers to what happened and were entitled to full transparency.”
Dr. Steen denied the allegations but did not give evidence.
The General Medical Council had argued Dr. Steen tried to cover up the circumstances of Claire’s death to “avoid scrutiny.” The MPTS panel, sitting remotely, will next consider whether Dr. Steen’s fitness to practice is impaired by reason of misconduct.
The hyponatremia public inquiry concluded in 2018 that Claire’s death was the result of “negligent care” from an overdose of fluids and medication. A fresh inquest in 2019 ruled her death was “caused by the treatment she received in hospital.”
This article contains information from PA Media. A version of this article appeared on MedscapeUK.
Florida medical boards ban transgender care for minors
Florida’s two main medical bodies have voted to stop gender-affirming treatment of children, including the use of puberty blockers, cross-sex hormones, and surgery, other than in minors who are already receiving such care.
The move, which is unprecedented, makes Florida one of several U.S. states to restrict gender-affirming care for adolescents, but the first to do so via an administrative process, through the actions of its Board of Medicine and Board of Osteopathic Medicine.
“I appreciate the integrity of the Boards for ruling in the best interest of children in Florida despite facing tremendous pressure to permit these unproven and risky treatments,” Florida Surgeon General Joseph Ladapo, MD, PhD, said in a statement.
In a statement, The Endocrine Society criticizes the decision as “blatantly discriminatory” and not based on medical evidence.
During a meeting on Oct. 28 that involved testimonies from doctors, parents of transgender children, detransitioners, and patients, board members referred to similar changes in Europe, where some countries have pushed psychotherapy instead of surgery or hormone treatment.
Then, on Nov. 4, the boards each set slightly different instructions, with the Board of Osteopathic Medicine voting to restrict care for new patients but allowing an exception for children enrolled in clinical studies, which “must include long-term longitudinal assessments of the patients’ physiologic and psychologic outcomes,” according to the Florida Department of Health.
The Board of Medicine did not allow the latter.
The proposed rules are open to public comment before finalization.
Arkansas was the first state to enact such a ban on gender-affirming care, with Republican lawmakers in 2021 overriding GOP Gov. Asa Hutchinson’s veto of the legislation. Alabama Republicans in 2022 approved legislation to outlaw gender-affirming medications for transgender youths. Both laws have been paused amid unfolding legal battles, according to Associated Press.
Oklahoma Gov. Kevin Stitt, a Republican, signed a bill in October that bars federal funds earmarked for the University of Oklahoma Medical Center from being used for gender reassignment treatments for minors. Gov. Stitt also called for the legislature to ban some of those gender reassignment treatments statewide when it returns in February.
Top Tennessee Republicans also have vowed to push for strict antitransgender policies. The state already bans doctors from providing gender-confirming hormone treatment to prepubescent minors. To date, no one has legally challenged the law as medical experts maintain no doctor in Tennessee does so.
A version of this article first appeared on Medscape.com.
Florida’s two main medical bodies have voted to stop gender-affirming treatment of children, including the use of puberty blockers, cross-sex hormones, and surgery, other than in minors who are already receiving such care.
The move, which is unprecedented, makes Florida one of several U.S. states to restrict gender-affirming care for adolescents, but the first to do so via an administrative process, through the actions of its Board of Medicine and Board of Osteopathic Medicine.
“I appreciate the integrity of the Boards for ruling in the best interest of children in Florida despite facing tremendous pressure to permit these unproven and risky treatments,” Florida Surgeon General Joseph Ladapo, MD, PhD, said in a statement.
In a statement, The Endocrine Society criticizes the decision as “blatantly discriminatory” and not based on medical evidence.
During a meeting on Oct. 28 that involved testimonies from doctors, parents of transgender children, detransitioners, and patients, board members referred to similar changes in Europe, where some countries have pushed psychotherapy instead of surgery or hormone treatment.
Then, on Nov. 4, the boards each set slightly different instructions, with the Board of Osteopathic Medicine voting to restrict care for new patients but allowing an exception for children enrolled in clinical studies, which “must include long-term longitudinal assessments of the patients’ physiologic and psychologic outcomes,” according to the Florida Department of Health.
The Board of Medicine did not allow the latter.
The proposed rules are open to public comment before finalization.
Arkansas was the first state to enact such a ban on gender-affirming care, with Republican lawmakers in 2021 overriding GOP Gov. Asa Hutchinson’s veto of the legislation. Alabama Republicans in 2022 approved legislation to outlaw gender-affirming medications for transgender youths. Both laws have been paused amid unfolding legal battles, according to Associated Press.
Oklahoma Gov. Kevin Stitt, a Republican, signed a bill in October that bars federal funds earmarked for the University of Oklahoma Medical Center from being used for gender reassignment treatments for minors. Gov. Stitt also called for the legislature to ban some of those gender reassignment treatments statewide when it returns in February.
Top Tennessee Republicans also have vowed to push for strict antitransgender policies. The state already bans doctors from providing gender-confirming hormone treatment to prepubescent minors. To date, no one has legally challenged the law as medical experts maintain no doctor in Tennessee does so.
A version of this article first appeared on Medscape.com.
Florida’s two main medical bodies have voted to stop gender-affirming treatment of children, including the use of puberty blockers, cross-sex hormones, and surgery, other than in minors who are already receiving such care.
The move, which is unprecedented, makes Florida one of several U.S. states to restrict gender-affirming care for adolescents, but the first to do so via an administrative process, through the actions of its Board of Medicine and Board of Osteopathic Medicine.
“I appreciate the integrity of the Boards for ruling in the best interest of children in Florida despite facing tremendous pressure to permit these unproven and risky treatments,” Florida Surgeon General Joseph Ladapo, MD, PhD, said in a statement.
In a statement, The Endocrine Society criticizes the decision as “blatantly discriminatory” and not based on medical evidence.
During a meeting on Oct. 28 that involved testimonies from doctors, parents of transgender children, detransitioners, and patients, board members referred to similar changes in Europe, where some countries have pushed psychotherapy instead of surgery or hormone treatment.
Then, on Nov. 4, the boards each set slightly different instructions, with the Board of Osteopathic Medicine voting to restrict care for new patients but allowing an exception for children enrolled in clinical studies, which “must include long-term longitudinal assessments of the patients’ physiologic and psychologic outcomes,” according to the Florida Department of Health.
The Board of Medicine did not allow the latter.
The proposed rules are open to public comment before finalization.
Arkansas was the first state to enact such a ban on gender-affirming care, with Republican lawmakers in 2021 overriding GOP Gov. Asa Hutchinson’s veto of the legislation. Alabama Republicans in 2022 approved legislation to outlaw gender-affirming medications for transgender youths. Both laws have been paused amid unfolding legal battles, according to Associated Press.
Oklahoma Gov. Kevin Stitt, a Republican, signed a bill in October that bars federal funds earmarked for the University of Oklahoma Medical Center from being used for gender reassignment treatments for minors. Gov. Stitt also called for the legislature to ban some of those gender reassignment treatments statewide when it returns in February.
Top Tennessee Republicans also have vowed to push for strict antitransgender policies. The state already bans doctors from providing gender-confirming hormone treatment to prepubescent minors. To date, no one has legally challenged the law as medical experts maintain no doctor in Tennessee does so.
A version of this article first appeared on Medscape.com.
Physicians react: Climate change and other social issues
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
Med students dismayed that residency match process won’t change
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
FDA puts REMS requirements on hold to ensure continuity of care
In a Nov. 2 notice on its website, the FDA said it is aware that health care professionals and patients continue to experience ongoing difficulties with the clozapine REMS program, including issues with patient access to clozapine following discharge from inpatient care.
A chief concern is that inpatient pharmacies are only allowed to dispense a 7-days’ supply of clozapine to the patient upon discharge.
To address this issue, the FDA said it will now (temporarily) not object if inpatient pharmacies dispense a days’ supply of clozapine that aligns with the patient’s monitoring frequency.
For example, a 7-days’ supply for weekly monitoring, a 14-days’ supply for twice-monthly monitoring, and a 30-days’ supply for monthly monitoring upon discharge from an inpatient facility.
Clozapine is a second-generation (atypical) antipsychotic used to treat schizophrenia that is not well controlled with standard antipsychotics.
While clozapine can be highly effective in some patients, it also carries serious risks, including a decrease in neutrophil count, which can lead to severe neutropenia, serious infections, and death.
As a result, those taking the drug must undergo regular absolute neutrophil count monitoring. Clozapine REMS is intended to maximize the benefits of the drug and minimize risk.
The FDA says it will continue to exercise earlier enforcement discretion regarding the clozapine REMS program announced back in November 2021. This includes allowing pharmacists to dispense clozapine without a REMS dispense authorization and allowing wholesalers to ship clozapine to pharmacies and health care settings without confirming enrollment in the REMS.
“We understand that difficulties with the clozapine REMS program have caused frustration and have led to problems with patient access to clozapine. FDA takes these concerns seriously. Continuity of care, patient access to clozapine, and patient safety are our highest priorities,” the FDA says.
The agency is working closely with the clozapine REMS program administrators to address these challenges and avoid interruptions in patient care.
The FDA encourages pharmacists and prescribers to continue working with the clozapine REMS to complete certification and prescribers to enroll patients in the program.
A version of this article first appeared on Medscape.com.
In a Nov. 2 notice on its website, the FDA said it is aware that health care professionals and patients continue to experience ongoing difficulties with the clozapine REMS program, including issues with patient access to clozapine following discharge from inpatient care.
A chief concern is that inpatient pharmacies are only allowed to dispense a 7-days’ supply of clozapine to the patient upon discharge.
To address this issue, the FDA said it will now (temporarily) not object if inpatient pharmacies dispense a days’ supply of clozapine that aligns with the patient’s monitoring frequency.
For example, a 7-days’ supply for weekly monitoring, a 14-days’ supply for twice-monthly monitoring, and a 30-days’ supply for monthly monitoring upon discharge from an inpatient facility.
Clozapine is a second-generation (atypical) antipsychotic used to treat schizophrenia that is not well controlled with standard antipsychotics.
While clozapine can be highly effective in some patients, it also carries serious risks, including a decrease in neutrophil count, which can lead to severe neutropenia, serious infections, and death.
As a result, those taking the drug must undergo regular absolute neutrophil count monitoring. Clozapine REMS is intended to maximize the benefits of the drug and minimize risk.
The FDA says it will continue to exercise earlier enforcement discretion regarding the clozapine REMS program announced back in November 2021. This includes allowing pharmacists to dispense clozapine without a REMS dispense authorization and allowing wholesalers to ship clozapine to pharmacies and health care settings without confirming enrollment in the REMS.
“We understand that difficulties with the clozapine REMS program have caused frustration and have led to problems with patient access to clozapine. FDA takes these concerns seriously. Continuity of care, patient access to clozapine, and patient safety are our highest priorities,” the FDA says.
The agency is working closely with the clozapine REMS program administrators to address these challenges and avoid interruptions in patient care.
The FDA encourages pharmacists and prescribers to continue working with the clozapine REMS to complete certification and prescribers to enroll patients in the program.
A version of this article first appeared on Medscape.com.
In a Nov. 2 notice on its website, the FDA said it is aware that health care professionals and patients continue to experience ongoing difficulties with the clozapine REMS program, including issues with patient access to clozapine following discharge from inpatient care.
A chief concern is that inpatient pharmacies are only allowed to dispense a 7-days’ supply of clozapine to the patient upon discharge.
To address this issue, the FDA said it will now (temporarily) not object if inpatient pharmacies dispense a days’ supply of clozapine that aligns with the patient’s monitoring frequency.
For example, a 7-days’ supply for weekly monitoring, a 14-days’ supply for twice-monthly monitoring, and a 30-days’ supply for monthly monitoring upon discharge from an inpatient facility.
Clozapine is a second-generation (atypical) antipsychotic used to treat schizophrenia that is not well controlled with standard antipsychotics.
While clozapine can be highly effective in some patients, it also carries serious risks, including a decrease in neutrophil count, which can lead to severe neutropenia, serious infections, and death.
As a result, those taking the drug must undergo regular absolute neutrophil count monitoring. Clozapine REMS is intended to maximize the benefits of the drug and minimize risk.
The FDA says it will continue to exercise earlier enforcement discretion regarding the clozapine REMS program announced back in November 2021. This includes allowing pharmacists to dispense clozapine without a REMS dispense authorization and allowing wholesalers to ship clozapine to pharmacies and health care settings without confirming enrollment in the REMS.
“We understand that difficulties with the clozapine REMS program have caused frustration and have led to problems with patient access to clozapine. FDA takes these concerns seriously. Continuity of care, patient access to clozapine, and patient safety are our highest priorities,” the FDA says.
The agency is working closely with the clozapine REMS program administrators to address these challenges and avoid interruptions in patient care.
The FDA encourages pharmacists and prescribers to continue working with the clozapine REMS to complete certification and prescribers to enroll patients in the program.
A version of this article first appeared on Medscape.com.
What does it take for men to embrace cosmetic treatments?
with the same gusto as women.
However, this could be changing as millennials – who tend to be more proactive about efforts to prevent skin aging – are getting older.
At a virtual course on laser and aesthetic skin therapy, Dr. Carruthers referred to the results of an online survey of 600 men aged 30-65 years conducted by Jared Jagdeo, MD, and colleagues in 2016, to gauge attitudes toward age-related changes of their facial features and their preferences for prioritizing treatment. The top five barriers to treatment cited by the respondents were: “I don’t think I need it yet” (47%); “concerned about safety/side effects” (46%); “concerned about injecting a foreign substance into my body” (45%); “cost” (42%), and “concerned my face won’t look natural” (41%).
“Since then, millennials took over as the largest portion of our workforce in North America,” said Dr. Carruthers who, with her husband, Alastair Carruthers, MD, pioneered the cosmetic use of onabotulinumtoxinA (Botox). “Millennials are interested in how they look and how to keep their aesthetic the best it can possibly be,” she said, so there may be “a generational aspect to this.”
Another factor that may affect the uptake of cosmetic procedures among men is the number of hours they spend gazing at their own image on a computer screen. Since the beginning of the COVID-19 pandemic, men have spent an increasing number of hours on video-conferencing calls via Zoom and other platforms, causing them to rethink how they view their appearance, Dr. Carruthers added. “Zoom dysmorphia” is the term that describes the phenomenon that developed during the pandemic where more patients expressed a desire to make changes to their appearance, including nose jobs and smoothing out forehead wrinkles.
“When we’re on a Zoom call, we’re spending 40% of our time looking at ourselves,” said Dr. Carruthers, clinical professor of ophthalmology and visual sciences at the University of British Columbia in Vancouver. “This would hint that the looking glass is not as powerful as the computer screen to motivate men” to pursue aesthetic treatments.
According to data from the American Society of Plastic Surgeons, the top 5 cosmetic surgical procedures performed in men in 2020 were nose shaping, eyelid surgery, cheek implants, liposuction, and ear surgery. The top 5 minimally-invasive procedures in men were botulinum toxin type A, followed by laser skin resurfacing, laser hair removal, soft tissue fillers, and microdermabrasion.
Why might men consider an injectable instead of surgery? Dr. Carruthers asked. “According to the 2016 survey by Dr. Jagdeo and colleagues, it’s to appear more youthful and to appear good for their age.”
From a clinical standpoint, success comes from understanding the subtle differences between treating men and women, she added.
In a 2022 article about optimizing skin tightening in aesthetics in men, Christian A. Albornoz, MD, and colleagues noted that in contrast to women, men “tend to have higher levels of collagen density and greater skin thickness, but these begin to decrease earlier on. They can also more frequently have severe photodamage”.
In another article published in 2018, Terrence Keaney, MD, and colleagues reviewed the objective data available on male aging and aesthetics. They stated that a “communication gap exists for men, as evidenced by the lack of information available online or by word of mouth about injectable treatments” and concluded that “educating men about available aesthetic treatments and about the safety and side effects associated with each treatment, as well as addressing concerns about their treatment results looking natural, are key considerations.”
That sentiment resonates with Dr. Carruthers. Part of the reason why men have not sought cosmetic treatments along with their female partners and friends seeking cosmetic treatments “is that they haven’t had anything in their cup,” she said. “Maybe this is something we need to think about, to try and help men come in and enjoy the positive benefits of aesthetic, noninvasive cosmetic treatments.”
The course was sponsored by Harvard Medical School, Massachusetts General Hospital, and Wellman Center for Photomedicine.
Dr. Carruthers disclosed that she is a consultant and researcher for Alastin, Appiell, Allergan Aesthetics, Avari Medical, Bonti, Evolus, Fount Bio, Jeune Aesthetics, Merz, and Revance Biopharma.
with the same gusto as women.
However, this could be changing as millennials – who tend to be more proactive about efforts to prevent skin aging – are getting older.
At a virtual course on laser and aesthetic skin therapy, Dr. Carruthers referred to the results of an online survey of 600 men aged 30-65 years conducted by Jared Jagdeo, MD, and colleagues in 2016, to gauge attitudes toward age-related changes of their facial features and their preferences for prioritizing treatment. The top five barriers to treatment cited by the respondents were: “I don’t think I need it yet” (47%); “concerned about safety/side effects” (46%); “concerned about injecting a foreign substance into my body” (45%); “cost” (42%), and “concerned my face won’t look natural” (41%).
“Since then, millennials took over as the largest portion of our workforce in North America,” said Dr. Carruthers who, with her husband, Alastair Carruthers, MD, pioneered the cosmetic use of onabotulinumtoxinA (Botox). “Millennials are interested in how they look and how to keep their aesthetic the best it can possibly be,” she said, so there may be “a generational aspect to this.”
Another factor that may affect the uptake of cosmetic procedures among men is the number of hours they spend gazing at their own image on a computer screen. Since the beginning of the COVID-19 pandemic, men have spent an increasing number of hours on video-conferencing calls via Zoom and other platforms, causing them to rethink how they view their appearance, Dr. Carruthers added. “Zoom dysmorphia” is the term that describes the phenomenon that developed during the pandemic where more patients expressed a desire to make changes to their appearance, including nose jobs and smoothing out forehead wrinkles.
“When we’re on a Zoom call, we’re spending 40% of our time looking at ourselves,” said Dr. Carruthers, clinical professor of ophthalmology and visual sciences at the University of British Columbia in Vancouver. “This would hint that the looking glass is not as powerful as the computer screen to motivate men” to pursue aesthetic treatments.
According to data from the American Society of Plastic Surgeons, the top 5 cosmetic surgical procedures performed in men in 2020 were nose shaping, eyelid surgery, cheek implants, liposuction, and ear surgery. The top 5 minimally-invasive procedures in men were botulinum toxin type A, followed by laser skin resurfacing, laser hair removal, soft tissue fillers, and microdermabrasion.
Why might men consider an injectable instead of surgery? Dr. Carruthers asked. “According to the 2016 survey by Dr. Jagdeo and colleagues, it’s to appear more youthful and to appear good for their age.”
From a clinical standpoint, success comes from understanding the subtle differences between treating men and women, she added.
In a 2022 article about optimizing skin tightening in aesthetics in men, Christian A. Albornoz, MD, and colleagues noted that in contrast to women, men “tend to have higher levels of collagen density and greater skin thickness, but these begin to decrease earlier on. They can also more frequently have severe photodamage”.
In another article published in 2018, Terrence Keaney, MD, and colleagues reviewed the objective data available on male aging and aesthetics. They stated that a “communication gap exists for men, as evidenced by the lack of information available online or by word of mouth about injectable treatments” and concluded that “educating men about available aesthetic treatments and about the safety and side effects associated with each treatment, as well as addressing concerns about their treatment results looking natural, are key considerations.”
That sentiment resonates with Dr. Carruthers. Part of the reason why men have not sought cosmetic treatments along with their female partners and friends seeking cosmetic treatments “is that they haven’t had anything in their cup,” she said. “Maybe this is something we need to think about, to try and help men come in and enjoy the positive benefits of aesthetic, noninvasive cosmetic treatments.”
The course was sponsored by Harvard Medical School, Massachusetts General Hospital, and Wellman Center for Photomedicine.
Dr. Carruthers disclosed that she is a consultant and researcher for Alastin, Appiell, Allergan Aesthetics, Avari Medical, Bonti, Evolus, Fount Bio, Jeune Aesthetics, Merz, and Revance Biopharma.
with the same gusto as women.
However, this could be changing as millennials – who tend to be more proactive about efforts to prevent skin aging – are getting older.
At a virtual course on laser and aesthetic skin therapy, Dr. Carruthers referred to the results of an online survey of 600 men aged 30-65 years conducted by Jared Jagdeo, MD, and colleagues in 2016, to gauge attitudes toward age-related changes of their facial features and their preferences for prioritizing treatment. The top five barriers to treatment cited by the respondents were: “I don’t think I need it yet” (47%); “concerned about safety/side effects” (46%); “concerned about injecting a foreign substance into my body” (45%); “cost” (42%), and “concerned my face won’t look natural” (41%).
“Since then, millennials took over as the largest portion of our workforce in North America,” said Dr. Carruthers who, with her husband, Alastair Carruthers, MD, pioneered the cosmetic use of onabotulinumtoxinA (Botox). “Millennials are interested in how they look and how to keep their aesthetic the best it can possibly be,” she said, so there may be “a generational aspect to this.”
Another factor that may affect the uptake of cosmetic procedures among men is the number of hours they spend gazing at their own image on a computer screen. Since the beginning of the COVID-19 pandemic, men have spent an increasing number of hours on video-conferencing calls via Zoom and other platforms, causing them to rethink how they view their appearance, Dr. Carruthers added. “Zoom dysmorphia” is the term that describes the phenomenon that developed during the pandemic where more patients expressed a desire to make changes to their appearance, including nose jobs and smoothing out forehead wrinkles.
“When we’re on a Zoom call, we’re spending 40% of our time looking at ourselves,” said Dr. Carruthers, clinical professor of ophthalmology and visual sciences at the University of British Columbia in Vancouver. “This would hint that the looking glass is not as powerful as the computer screen to motivate men” to pursue aesthetic treatments.
According to data from the American Society of Plastic Surgeons, the top 5 cosmetic surgical procedures performed in men in 2020 were nose shaping, eyelid surgery, cheek implants, liposuction, and ear surgery. The top 5 minimally-invasive procedures in men were botulinum toxin type A, followed by laser skin resurfacing, laser hair removal, soft tissue fillers, and microdermabrasion.
Why might men consider an injectable instead of surgery? Dr. Carruthers asked. “According to the 2016 survey by Dr. Jagdeo and colleagues, it’s to appear more youthful and to appear good for their age.”
From a clinical standpoint, success comes from understanding the subtle differences between treating men and women, she added.
In a 2022 article about optimizing skin tightening in aesthetics in men, Christian A. Albornoz, MD, and colleagues noted that in contrast to women, men “tend to have higher levels of collagen density and greater skin thickness, but these begin to decrease earlier on. They can also more frequently have severe photodamage”.
In another article published in 2018, Terrence Keaney, MD, and colleagues reviewed the objective data available on male aging and aesthetics. They stated that a “communication gap exists for men, as evidenced by the lack of information available online or by word of mouth about injectable treatments” and concluded that “educating men about available aesthetic treatments and about the safety and side effects associated with each treatment, as well as addressing concerns about their treatment results looking natural, are key considerations.”
That sentiment resonates with Dr. Carruthers. Part of the reason why men have not sought cosmetic treatments along with their female partners and friends seeking cosmetic treatments “is that they haven’t had anything in their cup,” she said. “Maybe this is something we need to think about, to try and help men come in and enjoy the positive benefits of aesthetic, noninvasive cosmetic treatments.”
The course was sponsored by Harvard Medical School, Massachusetts General Hospital, and Wellman Center for Photomedicine.
Dr. Carruthers disclosed that she is a consultant and researcher for Alastin, Appiell, Allergan Aesthetics, Avari Medical, Bonti, Evolus, Fount Bio, Jeune Aesthetics, Merz, and Revance Biopharma.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE