User login
A Practical and Cost-Effective Approach to the Diagnosis of Heparin-Induced Thrombocytopenia: A Single-Center Quality Improvement Study
From the Veterans Affairs Ann Arbor Healthcare System Medicine Service (Dr. Cusick), University of Michigan College of Pharmacy, Clinical Pharmacy Service, Michigan Medicine (Dr. Hanigan), Department of Internal Medicine Clinical Experience and Quality, Michigan Medicine (Linda Bashaw), Department of Internal Medicine, University of Michigan Medical School, Ann Arbor, MI (Dr. Heidemann), and the Operational Excellence Department, Sparrow Health System, Lansing, MI (Matthew Johnson).
Abstract
Background: Diagnosis of heparin-induced thrombocytopenia (HIT) requires completion of an enzyme-linked immunosorbent assay (ELISA)–based heparin-platelet factor 4 (PF4) antibody test. If this test is negative, HIT is excluded. If positive, a serotonin-release assay (SRA) test is indicated. The SRA is expensive and sometimes inappropriately ordered despite negative PF4 results, leading to unnecessary treatment with argatroban while awaiting SRA results.
Objectives: The primary objectives of this project were to reduce unnecessary SRA testing and argatroban utilization in patients with suspected HIT.
Methods: The authors implemented an intervention at a tertiary care academic hospital in November 2017 targeting patients hospitalized with suspected HIT. The intervention was controlled at the level of the laboratory and prevented ordering of SRA tests in the absence of a positive PF4 test. The number of SRA tests performed and argatroban bags administered were identified retrospectively via chart review before the intervention (January 2016 to November 2017) and post intervention (December 2017 to March 2020). Associated costs were calculated based on institutional SRA testing cost as well as the average wholesale price of argatroban.
Results: SRA testing decreased from an average of 3.7 SRA results per 1000 admissions before the intervention to an average of 0.6 results per 1000 admissions post intervention. The number of 50-mL argatroban bags used per 1000 admissions decreased from 18.8 prior to the intervention to 14.3 post intervention. Total estimated cost savings per 1000 admissions was $2361.20.
Conclusion: An evidence-based testing strategy for HIT can be effectively implemented at the level of the laboratory. This approach led to reductions in SRA testing and argatroban utilization with resultant cost savings.
Keywords: HIT, argatroban, anticoagulation, serotonin-release assay.
Thrombocytopenia is a common finding in hospitalized patients.1,2 Heparin-induced thrombocytopenia (HIT) is one of the many potential causes of thrombocytopenia in hospitalized patients and occurs when antibodies to the heparin-platelet factor 4 (PF4) complex develop after heparin exposure. This triggers a cascade of events, leading to platelet activation, platelet consumption, and thrombosis. While HIT is relatively rare, occurring in 0.3% to 0.5% of critically ill patients, many patients will be tested to rule out this potentially life-threatening cause of thrombocytopenia.3
The diagnosis of HIT utilizes a combination of both clinical suspicion and laboratory testing.4 The 4T score (Table) was developed to evaluate the clinical probability of HIT and involves assessing the degree and timing of thrombocytopenia, the presence or absence of thrombosis, and other potential causes of the thrombocytopenia.5 The 4T score is designed to be utilized to identify patients who require laboratory testing for HIT; however, it has low inter-rater agreement in patients undergoing evaluation for HIT,6 and, in our experience, completion of this scoring is time-consuming.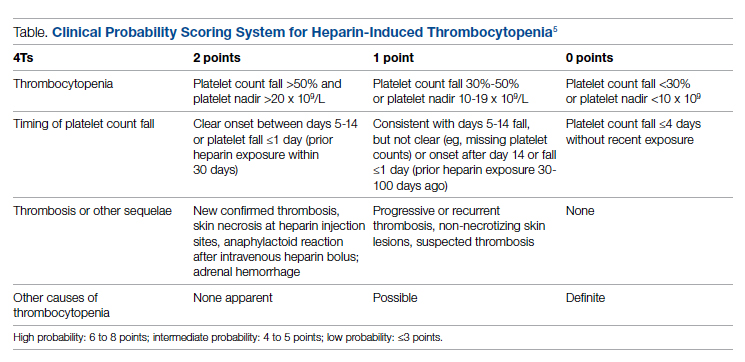
The enzyme-linked immunosorbent assay (ELISA) is a commonly used laboratory test to diagnose HIT that detects antibodies to the heparin-PF4 complex utilizing optical density (OD) units. When using an OD cutoff of 0.400, ELISA PF4 (PF4) tests have a sensitivity of 99.6%, but poor specificity at 69.3%.7 When the PF4 antibody test is positive with an OD ≥0.400, then a functional test is used to determine whether the antibodies detected will activate platelets. The serotonin-release assay (SRA) is a functional test that measures 14C-labeled serotonin release from donor platelets when mixed with patient serum or plasma containing HIT antibodies. In the correct clinical context, a positive ELISA PF4 antibody test along with a positive SRA is diagnostic of HIT.8
The process of diagnosing HIT in a timely and cost-effective manner is dependent on the clinician’s experience in diagnosing HIT as well as access to the laboratory testing necessary to confirm the diagnosis. PF4 antibody tests are time-consuming and not always available daily and/or are not available onsite. The SRA requires access to donor platelets and specialized radioactivity counting equipment, making it available only at particular centers.
The treatment of HIT is more straightforward and involves stopping all heparin products and starting a nonheparin anticoagulant. The direct thrombin inhibitor argatroban is one of the standard nonheparin anticoagulants used in patients with suspected HIT.4 While it is expensive, its short half-life and lack of renal clearance make it ideal for treatment of hospitalized patients with suspected HIT, many of whom need frequent procedures and/or have renal disease.
At our academic tertiary care center, we performed a retrospective analysis that showed inappropriate ordering of diagnostic HIT testing as well as unnecessary use of argatroban even when there was low suspicion for HIT based on laboratory findings. The aim of our project was to reduce unnecessary HIT testing and argatroban utilization without overburdening providers or interfering with established workflows.
Methods
Setting
The University of Michigan (UM) hospital is a 1000-bed tertiary care center in Ann Arbor, Michigan. The UM guidelines reflect evidence-based guidelines for the diagnosis and treatment of HIT.4 In 2016 the UM guidelines for laboratory testing included sending the PF4 antibody test first when there was clinical suspicion of HIT. The SRA was to be sent separately only when the PF4 returned positive (OD ≥ 0.400). Standard guidelines at UM also included switching patients with suspected HIT from heparin to a nonheparin anticoagulant and stopping all heparin products while awaiting the SRA results. The direct thrombin inhibitor argatroban is utilized at UM and monitored with anti-IIa levels. University of Michigan Hospital utilizes the Immucor PF4 IgG ELISA for detecting heparin-associated antibodies.9 In 2016, this PF4 test was performed in the UM onsite laboratory Monday through Friday. At UM the SRA is performed off site, with a turnaround time of 3 to 5 business days.
Baseline Data
We retrospectively reviewed PF4 and SRA testing as well as argatroban usage from December 2016 to May 2017. Despite the institutional guidelines, providers were sending PF4 and SRA simultaneously as soon as HIT was suspected; 62% of PF4 tests were ordered simultaneously with the SRA, but only 8% of these PF4 tests were positive with an OD ≥0.400. Of those patients with negative PF4 testing, argatroban was continued until the SRA returned negative, leading to many days of unnecessary argatroban usage. An informal survey of the anticoagulation pharmacists revealed that many recommended discontinuing argatroban when the PF4 test was negative, but providers routinely did not feel comfortable with this approach. This suggested many providers misunderstood the performance characteristics of the PF4 test.
Intervention
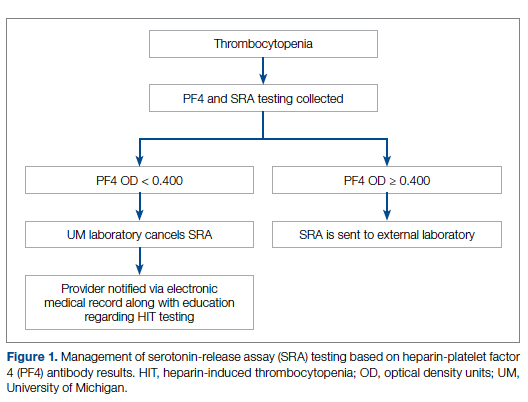
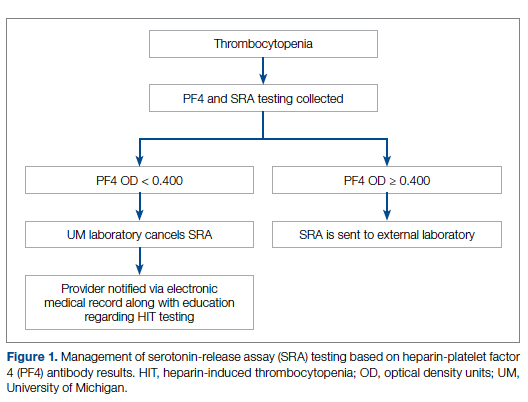
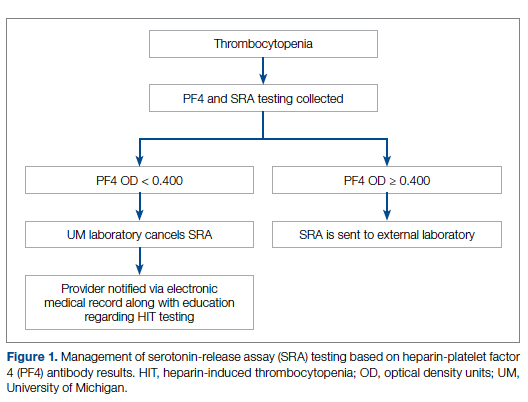
Our team consisted of hematology and internal medicine faculty, pharmacists, coagulation laboratory personnel, and quality improvement specialists. We designed and implemented an intervention in November 2017 focused on controlling the ordering of the SRA test. We chose to focus on this step due to the excellent sensitivity of the PF4 test with a cutoff of OD <0.400 and the significant expense of the SRA test. Under direction of the Coagulation Laboratory Director, a standard operating procedure was developed where the coagulation laboratory personnel did not send out the SRA until a positive PF4 test (OD ≥ 0.400) was reported. If the PF4 was negative, the SRA was canceled and the ordering provider received notification of the cancelled test via the electronic medical record, accompanied by education about HIT testing (Figure 1). In addition, the lab increased the availability of PF4 testing from 5 days to 7 days a week so there were no delays in tests ordered on Fridays or weekends.
Outcomes
Our primary goals were to decrease both SRA testing and argatroban use. Secondarily, we examined the cost-effectiveness of this intervention. We hypothesized that controlling the SRA testing at the laboratory level would decrease both SRA testing and argatroban use.
Data Collection
Pre- and postintervention data were collected retrospectively. Pre-intervention data were from January 2016 through November 2017, and postintervention data were from December 2017 through March 2020. The number of SRA tests performed were identified retrospectively via review of electronic ordering records. All patients who had a hospital admission after January 1, 2016, were included. These patients were filtered to include only those who had a result for an SRA test. In order to calculate cost-savings, we identified both the number of SRA tests ordered retrospectively as well as patients who had both an SRA resulted and had been administered argatroban. Cost-savings were calculated based on our institutional cost of $357 per SRA test.
At our institution, argatroban is supplied in 50-mL bags; therefore, we utilized the number of bags to identify argatroban usage. Savings were calculated using the average wholesale price (AWP) of $292.50 per 50-mL bag. The amounts billed or collected for the SRA testing or argatroban treatment were not collected. Costs were estimated using only direct costs to the institution. Safety data were not collected. As the intent of our project was a quality improvement activity, this project did not require institutional review board regulation per our institutional guidance.
Results
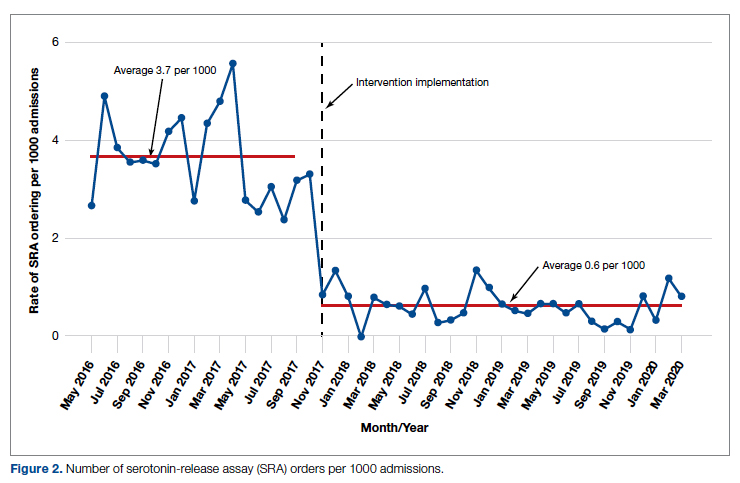
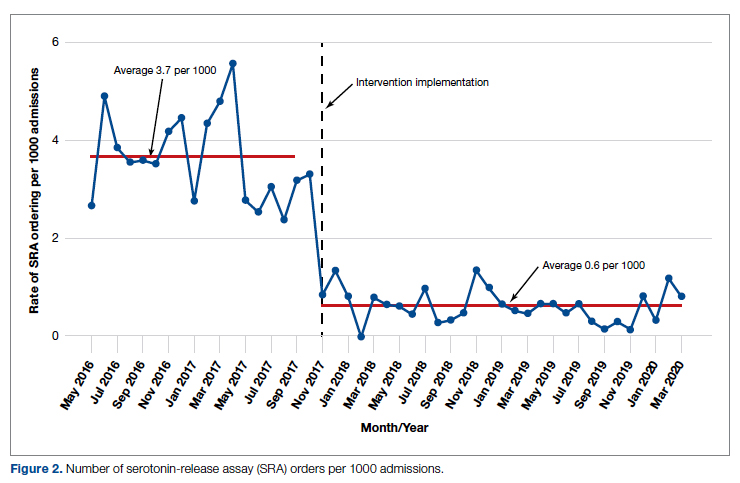
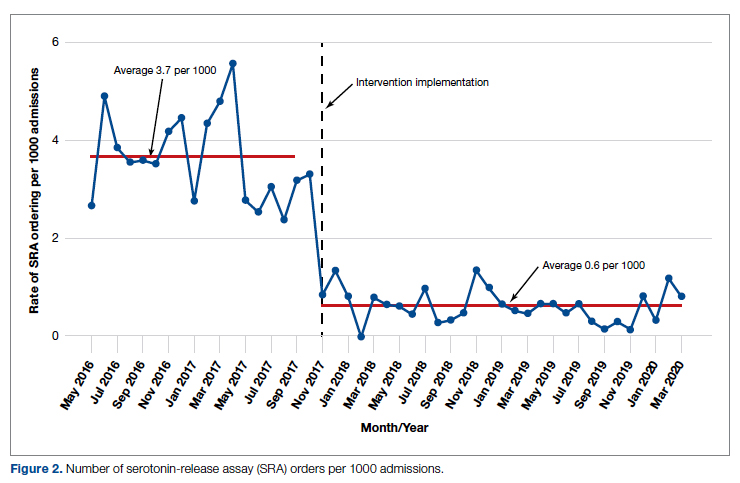
During the pre-intervention period, the average number of admissions (adults and children) at UM was 5863 per month. Post intervention there was an average of 5842 admissions per month. A total of 1192 PF4 tests were ordered before the intervention and 1148 were ordered post intervention. Prior to the intervention, 481 SRA tests were completed, while post intervention 105 were completed. Serotonin-release testing decreased from an average of 3.7 SRA results per 1000 admissions during the pre-intervention period to an average of 0.6 per 1000 admissions post intervention (Figure 2). Cost-savings were $1045 per 1000 admissions.
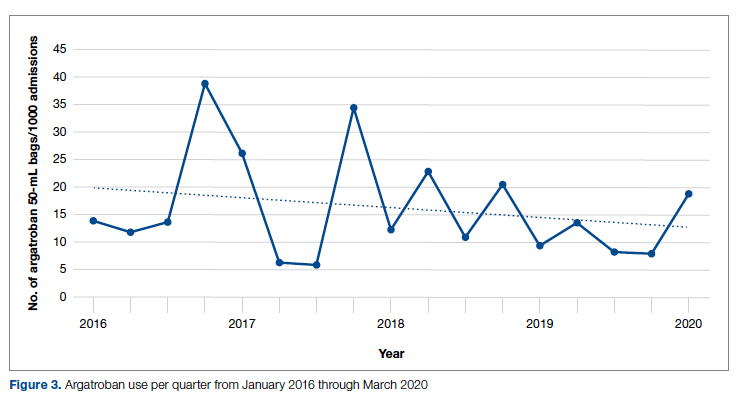
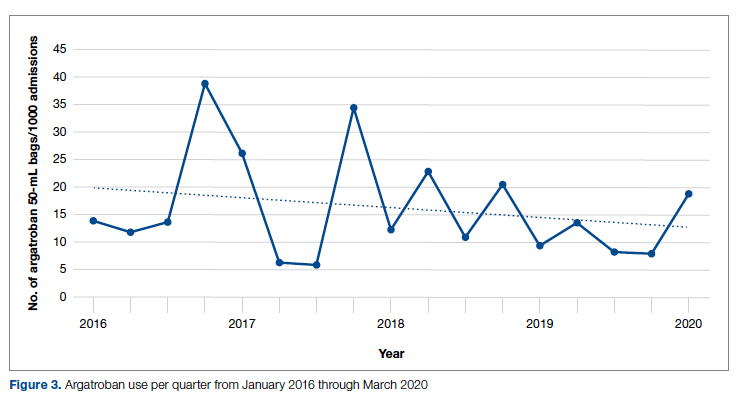
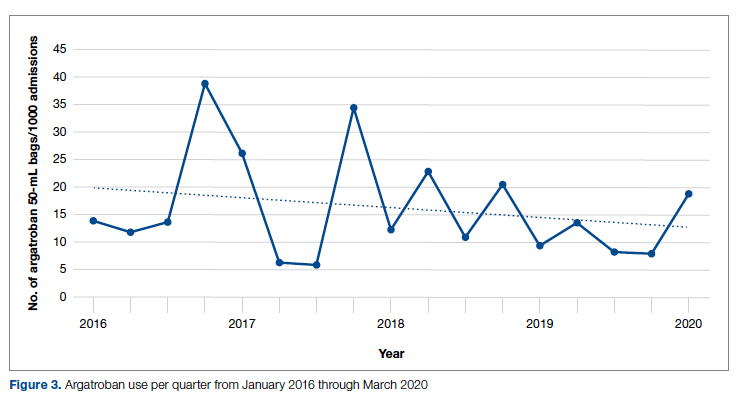
During the pre-intervention period, 2539 bags of argatroban were used, while 2337 bags were used post intervention. The number of 50-mL argatroban bags used per 1000 admissions decreased from 18.8 before the intervention to 14.3 post intervention. Cost-savings were $1316.20 per 1000 admissions. Figure 3 illustrates the monthly argatroban utilization per 1000 admissions during each quarter from January 2016 through March 2020.
Discussion
We designed and implemented an evidence-based strategy for HIT at our academic institution which led to a decrease in unnecessary SRA testing and argatroban utilization, with associated cost savings. By focusing on a single point of intervention at the laboratory level where SRA tests were held and canceled if the PF4 test was negative, we helped offload the decision-making from the provider while simultaneously providing just-in-time education to the provider. This intervention was designed with input from multiple stakeholders, including physicians, quality improvement specialists, pharmacists, and coagulation laboratory personnel.
Serotonin-release testing dramatically decreased post intervention even though a similar number of PF4 tests were performed before and after the intervention. This suggests that the decrease in SRA testing was a direct consequence of our intervention. Post intervention the number of completed SRA tests was 9% of the number of PF4 tests sent. This is consistent with our baseline pre-intervention data showing that only 8% of all PF4 tests sent were positive.
While the absolute number of argatroban bags utilized did not dramatically decrease after the intervention, the quarterly rate did, particularly after 2018. Given that argatroban data were only drawn from patients with a concurrent SRA test, this decrease is clearly from decreased usage in patients with suspected HIT. We suspect the decrease occurred because argatroban was not being continued while awaiting an SRA test in patients with a negative PF4 test. Decreasing the utilization of argatroban not only saved money but also reduced days of exposure to argatroban. While we do not have data regarding adverse events related to argatroban prior to the intervention, it is logical to conclude that reducing unnecessary exposure to argatroban reduces the risk of adverse events related to bleeding. Future studies would ideally address specific safety outcome metrics such as adverse events, bleeding risk, or missed diagnoses of HIT.
Our institutional guidelines for the diagnosis of HIT are evidence-based and helpful but are rarely followed by busy inpatient providers. Controlling the utilization of the SRA at the laboratory level had several advantages. First, removing SRA decision-making from providers who are not experts in the diagnosis of HIT guaranteed adherence to evidence-based guidelines. Second, pharmacists could safely recommend discontinuing argatroban when the PF4 test was negative as there was no SRA pending. Third, with cancellation at the laboratory level there was no need to further burden providers with yet another alert in the electronic health record. Fourth, just-in-time education was provided to the providers with justification for why the SRA test was canceled. Last, ruling out HIT within 24 hours with the PF4 test alone allowed providers to evaluate patients for other causes of thrombocytopenia much earlier than the 3 to 5 business days before the SRA results returned.
A limitation of this study is that it was conducted at a single center. Our approach is also limited by the lack of universal applicability. At our institution we are fortunate to have PF4 testing available in our coagulation laboratory 7 days a week. In addition, the coagulation laboratory controls sending the SRA to the reference laboratory. The specific intervention of controlling the SRA testing is therefore applicable only to institutions similar to ours; however, the concept of removing control of specialized testing from the provider is not unique. Inpatient thrombophilia testing has been a successful target of this approach.11-13 While electronic alerts and education of individual providers can also be effective initially, the effectiveness of these interventions has been repeatedly shown to wane over time.14-16
Conclusion
At our institution we were able to implement practical, evidence-based testing for HIT by implementing control over SRA testing at the level of the laboratory. This approach led to decreased argatroban utilization and cost savings.
Corresponding author: Alice Cusick, MD; LTC Charles S Kettles VA Medical Center, 2215 Fuller Road, Ann Arbor, MI 48105; [email protected]
Disclosures: None reported.
doi: 10.12788/jcom.0087
1. Fountain E, Arepally GM. Thrombocytopenia in hospitalized non-ICU patients. Blood. 2015;126(23):1060. doi:10.1182/blood.v126.23.1060.1060
2. Hui P, Cook DJ, Lim W, Fraser GA, Arnold DM. The frequency and clinical significance of thrombocytopenia complicating critical illness: a systematic review. Chest. 2011;139(2):271-278. doi:10.1378/chest.10-2243
3. Warkentin TE. Heparin-induced thrombocytopenia. Curr Opin Crit Care. 2015;21(6):576-585. doi:10.1097/MCC.0000000000000259
4. Cuker A, Arepally GM, Chong BH, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: heparin-induced thrombocytopenia. Blood Adv. 2018;2(22):3360-3392. doi:10.1182/bloodadvances.2018024489
5. Cuker A, Gimotty PA, Crowther MA, Warkentin TE. Predictive value of the 4Ts scoring system for heparin-induced thrombocytopenia: a systematic review and meta-analysis. Blood. 2012;120(20):4160-4167. doi:10.1182/blood-2012-07-443051
6. Northam KA, Parker WF, Chen S-L, et al. Evaluation of 4Ts score inter-rater agreement in patients undergoing evaluation for heparin-induced thrombocytopenia. Blood Coagul Fibrinolysis. 2021;32(5):328-334. doi:10.1097/MBC.0000000000001042
7. Raschke RA, Curry SC, Warkentin TE, Gerkin RD. Improving clinical interpretation of the anti-platelet factor 4/heparin enzyme-linked immunosorbent assay for the diagnosis of heparin-induced thrombocytopenia through the use of receiver operating characteristic analysis, stratum-specific likelihood ratios, and Bayes theorem. Chest. 2013;144(4):1269-1275. doi:10.1378/chest.12-2712
8. Warkentin TE, Arnold DM, Nazi I, Kelton JG. The platelet serotonin-release assay. Am J Hematol. 2015;90(6):564-572. doi:10.1002/ajh.24006
9. Use IFOR, Contents TOF. LIFECODES ® PF4 IgG assay:1-9.
10. Ancker JS, Edwards A, Nosal S, Hauser D, Mauer E, Kaushal R. Effects of workload, work complexity, and repeated alerts on alert fatigue in a clinical decision support system. BMC Med Inform Decis Mak. 2017;17(1):1-9. doi:10.1186/s12911-017-0430-8
11. O’Connor N, Carter-Johnson R. Effective screening of pathology tests controls costs: thrombophilia testing. J Clin Pathol. 2006;59(5):556. doi:10.1136/jcp.2005.030700
12. Lim MY, Greenberg CS. Inpatient thrombophilia testing: Impact of healthcare system technology and targeted clinician education on changing practice patterns. Vasc Med (United Kingdom). 2018;23(1):78-79. doi:10.1177/1358863X17742509
13. Cox JL, Shunkwiler SM, Koepsell SA. Requirement for a pathologist’s second signature limits inappropriate inpatient thrombophilia testing. Lab Med. 2017;48(4):367-371. doi:10.1093/labmed/lmx040
14. Kwang H, Mou E, Richman I, et al. Thrombophilia testing in the inpatient setting: impact of an educational intervention. BMC Med Inform Decis Mak. 2019;19(1):167. doi:10.1186/s12911-019-0889-6
15. Shah T, Patel-Teague S, Kroupa L, Meyer AND, Singh H. Impact of a national QI programme on reducing electronic health record notifications to clinicians. BMJ Qual Saf. 2019;28(1):10-14. doi:10.1136/bmjqs-2017-007447
16. Singh H, Spitzmueller C, Petersen NJ, Sawhney MK, Sittig DF. Information overload and missed test results in electronic health record-based settings. JAMA Intern Med. 2013;173(8):702-704. doi:10.1001/2013.jamainternmed.61
From the Veterans Affairs Ann Arbor Healthcare System Medicine Service (Dr. Cusick), University of Michigan College of Pharmacy, Clinical Pharmacy Service, Michigan Medicine (Dr. Hanigan), Department of Internal Medicine Clinical Experience and Quality, Michigan Medicine (Linda Bashaw), Department of Internal Medicine, University of Michigan Medical School, Ann Arbor, MI (Dr. Heidemann), and the Operational Excellence Department, Sparrow Health System, Lansing, MI (Matthew Johnson).
Abstract
Background: Diagnosis of heparin-induced thrombocytopenia (HIT) requires completion of an enzyme-linked immunosorbent assay (ELISA)–based heparin-platelet factor 4 (PF4) antibody test. If this test is negative, HIT is excluded. If positive, a serotonin-release assay (SRA) test is indicated. The SRA is expensive and sometimes inappropriately ordered despite negative PF4 results, leading to unnecessary treatment with argatroban while awaiting SRA results.
Objectives: The primary objectives of this project were to reduce unnecessary SRA testing and argatroban utilization in patients with suspected HIT.
Methods: The authors implemented an intervention at a tertiary care academic hospital in November 2017 targeting patients hospitalized with suspected HIT. The intervention was controlled at the level of the laboratory and prevented ordering of SRA tests in the absence of a positive PF4 test. The number of SRA tests performed and argatroban bags administered were identified retrospectively via chart review before the intervention (January 2016 to November 2017) and post intervention (December 2017 to March 2020). Associated costs were calculated based on institutional SRA testing cost as well as the average wholesale price of argatroban.
Results: SRA testing decreased from an average of 3.7 SRA results per 1000 admissions before the intervention to an average of 0.6 results per 1000 admissions post intervention. The number of 50-mL argatroban bags used per 1000 admissions decreased from 18.8 prior to the intervention to 14.3 post intervention. Total estimated cost savings per 1000 admissions was $2361.20.
Conclusion: An evidence-based testing strategy for HIT can be effectively implemented at the level of the laboratory. This approach led to reductions in SRA testing and argatroban utilization with resultant cost savings.
Keywords: HIT, argatroban, anticoagulation, serotonin-release assay.
Thrombocytopenia is a common finding in hospitalized patients.1,2 Heparin-induced thrombocytopenia (HIT) is one of the many potential causes of thrombocytopenia in hospitalized patients and occurs when antibodies to the heparin-platelet factor 4 (PF4) complex develop after heparin exposure. This triggers a cascade of events, leading to platelet activation, platelet consumption, and thrombosis. While HIT is relatively rare, occurring in 0.3% to 0.5% of critically ill patients, many patients will be tested to rule out this potentially life-threatening cause of thrombocytopenia.3
The diagnosis of HIT utilizes a combination of both clinical suspicion and laboratory testing.4 The 4T score (Table) was developed to evaluate the clinical probability of HIT and involves assessing the degree and timing of thrombocytopenia, the presence or absence of thrombosis, and other potential causes of the thrombocytopenia.5 The 4T score is designed to be utilized to identify patients who require laboratory testing for HIT; however, it has low inter-rater agreement in patients undergoing evaluation for HIT,6 and, in our experience, completion of this scoring is time-consuming.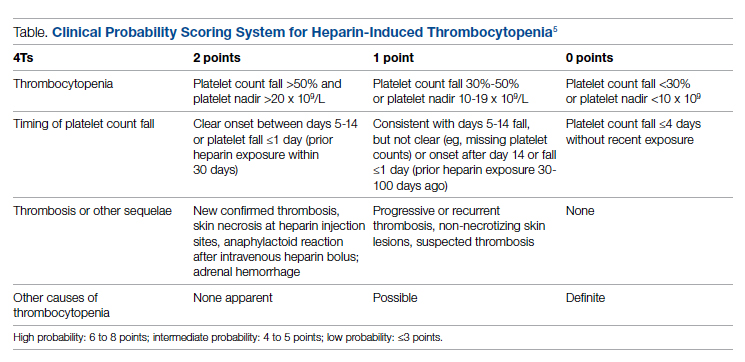
The enzyme-linked immunosorbent assay (ELISA) is a commonly used laboratory test to diagnose HIT that detects antibodies to the heparin-PF4 complex utilizing optical density (OD) units. When using an OD cutoff of 0.400, ELISA PF4 (PF4) tests have a sensitivity of 99.6%, but poor specificity at 69.3%.7 When the PF4 antibody test is positive with an OD ≥0.400, then a functional test is used to determine whether the antibodies detected will activate platelets. The serotonin-release assay (SRA) is a functional test that measures 14C-labeled serotonin release from donor platelets when mixed with patient serum or plasma containing HIT antibodies. In the correct clinical context, a positive ELISA PF4 antibody test along with a positive SRA is diagnostic of HIT.8
The process of diagnosing HIT in a timely and cost-effective manner is dependent on the clinician’s experience in diagnosing HIT as well as access to the laboratory testing necessary to confirm the diagnosis. PF4 antibody tests are time-consuming and not always available daily and/or are not available onsite. The SRA requires access to donor platelets and specialized radioactivity counting equipment, making it available only at particular centers.
The treatment of HIT is more straightforward and involves stopping all heparin products and starting a nonheparin anticoagulant. The direct thrombin inhibitor argatroban is one of the standard nonheparin anticoagulants used in patients with suspected HIT.4 While it is expensive, its short half-life and lack of renal clearance make it ideal for treatment of hospitalized patients with suspected HIT, many of whom need frequent procedures and/or have renal disease.
At our academic tertiary care center, we performed a retrospective analysis that showed inappropriate ordering of diagnostic HIT testing as well as unnecessary use of argatroban even when there was low suspicion for HIT based on laboratory findings. The aim of our project was to reduce unnecessary HIT testing and argatroban utilization without overburdening providers or interfering with established workflows.
Methods
Setting
The University of Michigan (UM) hospital is a 1000-bed tertiary care center in Ann Arbor, Michigan. The UM guidelines reflect evidence-based guidelines for the diagnosis and treatment of HIT.4 In 2016 the UM guidelines for laboratory testing included sending the PF4 antibody test first when there was clinical suspicion of HIT. The SRA was to be sent separately only when the PF4 returned positive (OD ≥ 0.400). Standard guidelines at UM also included switching patients with suspected HIT from heparin to a nonheparin anticoagulant and stopping all heparin products while awaiting the SRA results. The direct thrombin inhibitor argatroban is utilized at UM and monitored with anti-IIa levels. University of Michigan Hospital utilizes the Immucor PF4 IgG ELISA for detecting heparin-associated antibodies.9 In 2016, this PF4 test was performed in the UM onsite laboratory Monday through Friday. At UM the SRA is performed off site, with a turnaround time of 3 to 5 business days.
Baseline Data
We retrospectively reviewed PF4 and SRA testing as well as argatroban usage from December 2016 to May 2017. Despite the institutional guidelines, providers were sending PF4 and SRA simultaneously as soon as HIT was suspected; 62% of PF4 tests were ordered simultaneously with the SRA, but only 8% of these PF4 tests were positive with an OD ≥0.400. Of those patients with negative PF4 testing, argatroban was continued until the SRA returned negative, leading to many days of unnecessary argatroban usage. An informal survey of the anticoagulation pharmacists revealed that many recommended discontinuing argatroban when the PF4 test was negative, but providers routinely did not feel comfortable with this approach. This suggested many providers misunderstood the performance characteristics of the PF4 test.
Intervention
Our team consisted of hematology and internal medicine faculty, pharmacists, coagulation laboratory personnel, and quality improvement specialists. We designed and implemented an intervention in November 2017 focused on controlling the ordering of the SRA test. We chose to focus on this step due to the excellent sensitivity of the PF4 test with a cutoff of OD <0.400 and the significant expense of the SRA test. Under direction of the Coagulation Laboratory Director, a standard operating procedure was developed where the coagulation laboratory personnel did not send out the SRA until a positive PF4 test (OD ≥ 0.400) was reported. If the PF4 was negative, the SRA was canceled and the ordering provider received notification of the cancelled test via the electronic medical record, accompanied by education about HIT testing (Figure 1). In addition, the lab increased the availability of PF4 testing from 5 days to 7 days a week so there were no delays in tests ordered on Fridays or weekends.
Outcomes
Our primary goals were to decrease both SRA testing and argatroban use. Secondarily, we examined the cost-effectiveness of this intervention. We hypothesized that controlling the SRA testing at the laboratory level would decrease both SRA testing and argatroban use.
Data Collection
Pre- and postintervention data were collected retrospectively. Pre-intervention data were from January 2016 through November 2017, and postintervention data were from December 2017 through March 2020. The number of SRA tests performed were identified retrospectively via review of electronic ordering records. All patients who had a hospital admission after January 1, 2016, were included. These patients were filtered to include only those who had a result for an SRA test. In order to calculate cost-savings, we identified both the number of SRA tests ordered retrospectively as well as patients who had both an SRA resulted and had been administered argatroban. Cost-savings were calculated based on our institutional cost of $357 per SRA test.
At our institution, argatroban is supplied in 50-mL bags; therefore, we utilized the number of bags to identify argatroban usage. Savings were calculated using the average wholesale price (AWP) of $292.50 per 50-mL bag. The amounts billed or collected for the SRA testing or argatroban treatment were not collected. Costs were estimated using only direct costs to the institution. Safety data were not collected. As the intent of our project was a quality improvement activity, this project did not require institutional review board regulation per our institutional guidance.
Results
During the pre-intervention period, the average number of admissions (adults and children) at UM was 5863 per month. Post intervention there was an average of 5842 admissions per month. A total of 1192 PF4 tests were ordered before the intervention and 1148 were ordered post intervention. Prior to the intervention, 481 SRA tests were completed, while post intervention 105 were completed. Serotonin-release testing decreased from an average of 3.7 SRA results per 1000 admissions during the pre-intervention period to an average of 0.6 per 1000 admissions post intervention (Figure 2). Cost-savings were $1045 per 1000 admissions.
During the pre-intervention period, 2539 bags of argatroban were used, while 2337 bags were used post intervention. The number of 50-mL argatroban bags used per 1000 admissions decreased from 18.8 before the intervention to 14.3 post intervention. Cost-savings were $1316.20 per 1000 admissions. Figure 3 illustrates the monthly argatroban utilization per 1000 admissions during each quarter from January 2016 through March 2020.
Discussion
We designed and implemented an evidence-based strategy for HIT at our academic institution which led to a decrease in unnecessary SRA testing and argatroban utilization, with associated cost savings. By focusing on a single point of intervention at the laboratory level where SRA tests were held and canceled if the PF4 test was negative, we helped offload the decision-making from the provider while simultaneously providing just-in-time education to the provider. This intervention was designed with input from multiple stakeholders, including physicians, quality improvement specialists, pharmacists, and coagulation laboratory personnel.
Serotonin-release testing dramatically decreased post intervention even though a similar number of PF4 tests were performed before and after the intervention. This suggests that the decrease in SRA testing was a direct consequence of our intervention. Post intervention the number of completed SRA tests was 9% of the number of PF4 tests sent. This is consistent with our baseline pre-intervention data showing that only 8% of all PF4 tests sent were positive.
While the absolute number of argatroban bags utilized did not dramatically decrease after the intervention, the quarterly rate did, particularly after 2018. Given that argatroban data were only drawn from patients with a concurrent SRA test, this decrease is clearly from decreased usage in patients with suspected HIT. We suspect the decrease occurred because argatroban was not being continued while awaiting an SRA test in patients with a negative PF4 test. Decreasing the utilization of argatroban not only saved money but also reduced days of exposure to argatroban. While we do not have data regarding adverse events related to argatroban prior to the intervention, it is logical to conclude that reducing unnecessary exposure to argatroban reduces the risk of adverse events related to bleeding. Future studies would ideally address specific safety outcome metrics such as adverse events, bleeding risk, or missed diagnoses of HIT.
Our institutional guidelines for the diagnosis of HIT are evidence-based and helpful but are rarely followed by busy inpatient providers. Controlling the utilization of the SRA at the laboratory level had several advantages. First, removing SRA decision-making from providers who are not experts in the diagnosis of HIT guaranteed adherence to evidence-based guidelines. Second, pharmacists could safely recommend discontinuing argatroban when the PF4 test was negative as there was no SRA pending. Third, with cancellation at the laboratory level there was no need to further burden providers with yet another alert in the electronic health record. Fourth, just-in-time education was provided to the providers with justification for why the SRA test was canceled. Last, ruling out HIT within 24 hours with the PF4 test alone allowed providers to evaluate patients for other causes of thrombocytopenia much earlier than the 3 to 5 business days before the SRA results returned.
A limitation of this study is that it was conducted at a single center. Our approach is also limited by the lack of universal applicability. At our institution we are fortunate to have PF4 testing available in our coagulation laboratory 7 days a week. In addition, the coagulation laboratory controls sending the SRA to the reference laboratory. The specific intervention of controlling the SRA testing is therefore applicable only to institutions similar to ours; however, the concept of removing control of specialized testing from the provider is not unique. Inpatient thrombophilia testing has been a successful target of this approach.11-13 While electronic alerts and education of individual providers can also be effective initially, the effectiveness of these interventions has been repeatedly shown to wane over time.14-16
Conclusion
At our institution we were able to implement practical, evidence-based testing for HIT by implementing control over SRA testing at the level of the laboratory. This approach led to decreased argatroban utilization and cost savings.
Corresponding author: Alice Cusick, MD; LTC Charles S Kettles VA Medical Center, 2215 Fuller Road, Ann Arbor, MI 48105; [email protected]
Disclosures: None reported.
doi: 10.12788/jcom.0087
From the Veterans Affairs Ann Arbor Healthcare System Medicine Service (Dr. Cusick), University of Michigan College of Pharmacy, Clinical Pharmacy Service, Michigan Medicine (Dr. Hanigan), Department of Internal Medicine Clinical Experience and Quality, Michigan Medicine (Linda Bashaw), Department of Internal Medicine, University of Michigan Medical School, Ann Arbor, MI (Dr. Heidemann), and the Operational Excellence Department, Sparrow Health System, Lansing, MI (Matthew Johnson).
Abstract
Background: Diagnosis of heparin-induced thrombocytopenia (HIT) requires completion of an enzyme-linked immunosorbent assay (ELISA)–based heparin-platelet factor 4 (PF4) antibody test. If this test is negative, HIT is excluded. If positive, a serotonin-release assay (SRA) test is indicated. The SRA is expensive and sometimes inappropriately ordered despite negative PF4 results, leading to unnecessary treatment with argatroban while awaiting SRA results.
Objectives: The primary objectives of this project were to reduce unnecessary SRA testing and argatroban utilization in patients with suspected HIT.
Methods: The authors implemented an intervention at a tertiary care academic hospital in November 2017 targeting patients hospitalized with suspected HIT. The intervention was controlled at the level of the laboratory and prevented ordering of SRA tests in the absence of a positive PF4 test. The number of SRA tests performed and argatroban bags administered were identified retrospectively via chart review before the intervention (January 2016 to November 2017) and post intervention (December 2017 to March 2020). Associated costs were calculated based on institutional SRA testing cost as well as the average wholesale price of argatroban.
Results: SRA testing decreased from an average of 3.7 SRA results per 1000 admissions before the intervention to an average of 0.6 results per 1000 admissions post intervention. The number of 50-mL argatroban bags used per 1000 admissions decreased from 18.8 prior to the intervention to 14.3 post intervention. Total estimated cost savings per 1000 admissions was $2361.20.
Conclusion: An evidence-based testing strategy for HIT can be effectively implemented at the level of the laboratory. This approach led to reductions in SRA testing and argatroban utilization with resultant cost savings.
Keywords: HIT, argatroban, anticoagulation, serotonin-release assay.
Thrombocytopenia is a common finding in hospitalized patients.1,2 Heparin-induced thrombocytopenia (HIT) is one of the many potential causes of thrombocytopenia in hospitalized patients and occurs when antibodies to the heparin-platelet factor 4 (PF4) complex develop after heparin exposure. This triggers a cascade of events, leading to platelet activation, platelet consumption, and thrombosis. While HIT is relatively rare, occurring in 0.3% to 0.5% of critically ill patients, many patients will be tested to rule out this potentially life-threatening cause of thrombocytopenia.3
The diagnosis of HIT utilizes a combination of both clinical suspicion and laboratory testing.4 The 4T score (Table) was developed to evaluate the clinical probability of HIT and involves assessing the degree and timing of thrombocytopenia, the presence or absence of thrombosis, and other potential causes of the thrombocytopenia.5 The 4T score is designed to be utilized to identify patients who require laboratory testing for HIT; however, it has low inter-rater agreement in patients undergoing evaluation for HIT,6 and, in our experience, completion of this scoring is time-consuming.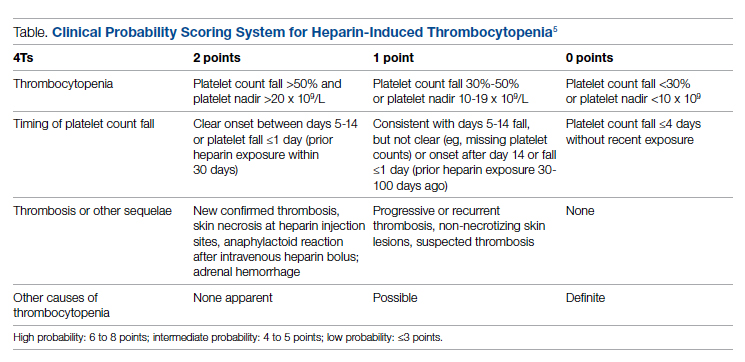
The enzyme-linked immunosorbent assay (ELISA) is a commonly used laboratory test to diagnose HIT that detects antibodies to the heparin-PF4 complex utilizing optical density (OD) units. When using an OD cutoff of 0.400, ELISA PF4 (PF4) tests have a sensitivity of 99.6%, but poor specificity at 69.3%.7 When the PF4 antibody test is positive with an OD ≥0.400, then a functional test is used to determine whether the antibodies detected will activate platelets. The serotonin-release assay (SRA) is a functional test that measures 14C-labeled serotonin release from donor platelets when mixed with patient serum or plasma containing HIT antibodies. In the correct clinical context, a positive ELISA PF4 antibody test along with a positive SRA is diagnostic of HIT.8
The process of diagnosing HIT in a timely and cost-effective manner is dependent on the clinician’s experience in diagnosing HIT as well as access to the laboratory testing necessary to confirm the diagnosis. PF4 antibody tests are time-consuming and not always available daily and/or are not available onsite. The SRA requires access to donor platelets and specialized radioactivity counting equipment, making it available only at particular centers.
The treatment of HIT is more straightforward and involves stopping all heparin products and starting a nonheparin anticoagulant. The direct thrombin inhibitor argatroban is one of the standard nonheparin anticoagulants used in patients with suspected HIT.4 While it is expensive, its short half-life and lack of renal clearance make it ideal for treatment of hospitalized patients with suspected HIT, many of whom need frequent procedures and/or have renal disease.
At our academic tertiary care center, we performed a retrospective analysis that showed inappropriate ordering of diagnostic HIT testing as well as unnecessary use of argatroban even when there was low suspicion for HIT based on laboratory findings. The aim of our project was to reduce unnecessary HIT testing and argatroban utilization without overburdening providers or interfering with established workflows.
Methods
Setting
The University of Michigan (UM) hospital is a 1000-bed tertiary care center in Ann Arbor, Michigan. The UM guidelines reflect evidence-based guidelines for the diagnosis and treatment of HIT.4 In 2016 the UM guidelines for laboratory testing included sending the PF4 antibody test first when there was clinical suspicion of HIT. The SRA was to be sent separately only when the PF4 returned positive (OD ≥ 0.400). Standard guidelines at UM also included switching patients with suspected HIT from heparin to a nonheparin anticoagulant and stopping all heparin products while awaiting the SRA results. The direct thrombin inhibitor argatroban is utilized at UM and monitored with anti-IIa levels. University of Michigan Hospital utilizes the Immucor PF4 IgG ELISA for detecting heparin-associated antibodies.9 In 2016, this PF4 test was performed in the UM onsite laboratory Monday through Friday. At UM the SRA is performed off site, with a turnaround time of 3 to 5 business days.
Baseline Data
We retrospectively reviewed PF4 and SRA testing as well as argatroban usage from December 2016 to May 2017. Despite the institutional guidelines, providers were sending PF4 and SRA simultaneously as soon as HIT was suspected; 62% of PF4 tests were ordered simultaneously with the SRA, but only 8% of these PF4 tests were positive with an OD ≥0.400. Of those patients with negative PF4 testing, argatroban was continued until the SRA returned negative, leading to many days of unnecessary argatroban usage. An informal survey of the anticoagulation pharmacists revealed that many recommended discontinuing argatroban when the PF4 test was negative, but providers routinely did not feel comfortable with this approach. This suggested many providers misunderstood the performance characteristics of the PF4 test.
Intervention
Our team consisted of hematology and internal medicine faculty, pharmacists, coagulation laboratory personnel, and quality improvement specialists. We designed and implemented an intervention in November 2017 focused on controlling the ordering of the SRA test. We chose to focus on this step due to the excellent sensitivity of the PF4 test with a cutoff of OD <0.400 and the significant expense of the SRA test. Under direction of the Coagulation Laboratory Director, a standard operating procedure was developed where the coagulation laboratory personnel did not send out the SRA until a positive PF4 test (OD ≥ 0.400) was reported. If the PF4 was negative, the SRA was canceled and the ordering provider received notification of the cancelled test via the electronic medical record, accompanied by education about HIT testing (Figure 1). In addition, the lab increased the availability of PF4 testing from 5 days to 7 days a week so there were no delays in tests ordered on Fridays or weekends.
Outcomes
Our primary goals were to decrease both SRA testing and argatroban use. Secondarily, we examined the cost-effectiveness of this intervention. We hypothesized that controlling the SRA testing at the laboratory level would decrease both SRA testing and argatroban use.
Data Collection
Pre- and postintervention data were collected retrospectively. Pre-intervention data were from January 2016 through November 2017, and postintervention data were from December 2017 through March 2020. The number of SRA tests performed were identified retrospectively via review of electronic ordering records. All patients who had a hospital admission after January 1, 2016, were included. These patients were filtered to include only those who had a result for an SRA test. In order to calculate cost-savings, we identified both the number of SRA tests ordered retrospectively as well as patients who had both an SRA resulted and had been administered argatroban. Cost-savings were calculated based on our institutional cost of $357 per SRA test.
At our institution, argatroban is supplied in 50-mL bags; therefore, we utilized the number of bags to identify argatroban usage. Savings were calculated using the average wholesale price (AWP) of $292.50 per 50-mL bag. The amounts billed or collected for the SRA testing or argatroban treatment were not collected. Costs were estimated using only direct costs to the institution. Safety data were not collected. As the intent of our project was a quality improvement activity, this project did not require institutional review board regulation per our institutional guidance.
Results
During the pre-intervention period, the average number of admissions (adults and children) at UM was 5863 per month. Post intervention there was an average of 5842 admissions per month. A total of 1192 PF4 tests were ordered before the intervention and 1148 were ordered post intervention. Prior to the intervention, 481 SRA tests were completed, while post intervention 105 were completed. Serotonin-release testing decreased from an average of 3.7 SRA results per 1000 admissions during the pre-intervention period to an average of 0.6 per 1000 admissions post intervention (Figure 2). Cost-savings were $1045 per 1000 admissions.
During the pre-intervention period, 2539 bags of argatroban were used, while 2337 bags were used post intervention. The number of 50-mL argatroban bags used per 1000 admissions decreased from 18.8 before the intervention to 14.3 post intervention. Cost-savings were $1316.20 per 1000 admissions. Figure 3 illustrates the monthly argatroban utilization per 1000 admissions during each quarter from January 2016 through March 2020.
Discussion
We designed and implemented an evidence-based strategy for HIT at our academic institution which led to a decrease in unnecessary SRA testing and argatroban utilization, with associated cost savings. By focusing on a single point of intervention at the laboratory level where SRA tests were held and canceled if the PF4 test was negative, we helped offload the decision-making from the provider while simultaneously providing just-in-time education to the provider. This intervention was designed with input from multiple stakeholders, including physicians, quality improvement specialists, pharmacists, and coagulation laboratory personnel.
Serotonin-release testing dramatically decreased post intervention even though a similar number of PF4 tests were performed before and after the intervention. This suggests that the decrease in SRA testing was a direct consequence of our intervention. Post intervention the number of completed SRA tests was 9% of the number of PF4 tests sent. This is consistent with our baseline pre-intervention data showing that only 8% of all PF4 tests sent were positive.
While the absolute number of argatroban bags utilized did not dramatically decrease after the intervention, the quarterly rate did, particularly after 2018. Given that argatroban data were only drawn from patients with a concurrent SRA test, this decrease is clearly from decreased usage in patients with suspected HIT. We suspect the decrease occurred because argatroban was not being continued while awaiting an SRA test in patients with a negative PF4 test. Decreasing the utilization of argatroban not only saved money but also reduced days of exposure to argatroban. While we do not have data regarding adverse events related to argatroban prior to the intervention, it is logical to conclude that reducing unnecessary exposure to argatroban reduces the risk of adverse events related to bleeding. Future studies would ideally address specific safety outcome metrics such as adverse events, bleeding risk, or missed diagnoses of HIT.
Our institutional guidelines for the diagnosis of HIT are evidence-based and helpful but are rarely followed by busy inpatient providers. Controlling the utilization of the SRA at the laboratory level had several advantages. First, removing SRA decision-making from providers who are not experts in the diagnosis of HIT guaranteed adherence to evidence-based guidelines. Second, pharmacists could safely recommend discontinuing argatroban when the PF4 test was negative as there was no SRA pending. Third, with cancellation at the laboratory level there was no need to further burden providers with yet another alert in the electronic health record. Fourth, just-in-time education was provided to the providers with justification for why the SRA test was canceled. Last, ruling out HIT within 24 hours with the PF4 test alone allowed providers to evaluate patients for other causes of thrombocytopenia much earlier than the 3 to 5 business days before the SRA results returned.
A limitation of this study is that it was conducted at a single center. Our approach is also limited by the lack of universal applicability. At our institution we are fortunate to have PF4 testing available in our coagulation laboratory 7 days a week. In addition, the coagulation laboratory controls sending the SRA to the reference laboratory. The specific intervention of controlling the SRA testing is therefore applicable only to institutions similar to ours; however, the concept of removing control of specialized testing from the provider is not unique. Inpatient thrombophilia testing has been a successful target of this approach.11-13 While electronic alerts and education of individual providers can also be effective initially, the effectiveness of these interventions has been repeatedly shown to wane over time.14-16
Conclusion
At our institution we were able to implement practical, evidence-based testing for HIT by implementing control over SRA testing at the level of the laboratory. This approach led to decreased argatroban utilization and cost savings.
Corresponding author: Alice Cusick, MD; LTC Charles S Kettles VA Medical Center, 2215 Fuller Road, Ann Arbor, MI 48105; [email protected]
Disclosures: None reported.
doi: 10.12788/jcom.0087
1. Fountain E, Arepally GM. Thrombocytopenia in hospitalized non-ICU patients. Blood. 2015;126(23):1060. doi:10.1182/blood.v126.23.1060.1060
2. Hui P, Cook DJ, Lim W, Fraser GA, Arnold DM. The frequency and clinical significance of thrombocytopenia complicating critical illness: a systematic review. Chest. 2011;139(2):271-278. doi:10.1378/chest.10-2243
3. Warkentin TE. Heparin-induced thrombocytopenia. Curr Opin Crit Care. 2015;21(6):576-585. doi:10.1097/MCC.0000000000000259
4. Cuker A, Arepally GM, Chong BH, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: heparin-induced thrombocytopenia. Blood Adv. 2018;2(22):3360-3392. doi:10.1182/bloodadvances.2018024489
5. Cuker A, Gimotty PA, Crowther MA, Warkentin TE. Predictive value of the 4Ts scoring system for heparin-induced thrombocytopenia: a systematic review and meta-analysis. Blood. 2012;120(20):4160-4167. doi:10.1182/blood-2012-07-443051
6. Northam KA, Parker WF, Chen S-L, et al. Evaluation of 4Ts score inter-rater agreement in patients undergoing evaluation for heparin-induced thrombocytopenia. Blood Coagul Fibrinolysis. 2021;32(5):328-334. doi:10.1097/MBC.0000000000001042
7. Raschke RA, Curry SC, Warkentin TE, Gerkin RD. Improving clinical interpretation of the anti-platelet factor 4/heparin enzyme-linked immunosorbent assay for the diagnosis of heparin-induced thrombocytopenia through the use of receiver operating characteristic analysis, stratum-specific likelihood ratios, and Bayes theorem. Chest. 2013;144(4):1269-1275. doi:10.1378/chest.12-2712
8. Warkentin TE, Arnold DM, Nazi I, Kelton JG. The platelet serotonin-release assay. Am J Hematol. 2015;90(6):564-572. doi:10.1002/ajh.24006
9. Use IFOR, Contents TOF. LIFECODES ® PF4 IgG assay:1-9.
10. Ancker JS, Edwards A, Nosal S, Hauser D, Mauer E, Kaushal R. Effects of workload, work complexity, and repeated alerts on alert fatigue in a clinical decision support system. BMC Med Inform Decis Mak. 2017;17(1):1-9. doi:10.1186/s12911-017-0430-8
11. O’Connor N, Carter-Johnson R. Effective screening of pathology tests controls costs: thrombophilia testing. J Clin Pathol. 2006;59(5):556. doi:10.1136/jcp.2005.030700
12. Lim MY, Greenberg CS. Inpatient thrombophilia testing: Impact of healthcare system technology and targeted clinician education on changing practice patterns. Vasc Med (United Kingdom). 2018;23(1):78-79. doi:10.1177/1358863X17742509
13. Cox JL, Shunkwiler SM, Koepsell SA. Requirement for a pathologist’s second signature limits inappropriate inpatient thrombophilia testing. Lab Med. 2017;48(4):367-371. doi:10.1093/labmed/lmx040
14. Kwang H, Mou E, Richman I, et al. Thrombophilia testing in the inpatient setting: impact of an educational intervention. BMC Med Inform Decis Mak. 2019;19(1):167. doi:10.1186/s12911-019-0889-6
15. Shah T, Patel-Teague S, Kroupa L, Meyer AND, Singh H. Impact of a national QI programme on reducing electronic health record notifications to clinicians. BMJ Qual Saf. 2019;28(1):10-14. doi:10.1136/bmjqs-2017-007447
16. Singh H, Spitzmueller C, Petersen NJ, Sawhney MK, Sittig DF. Information overload and missed test results in electronic health record-based settings. JAMA Intern Med. 2013;173(8):702-704. doi:10.1001/2013.jamainternmed.61
1. Fountain E, Arepally GM. Thrombocytopenia in hospitalized non-ICU patients. Blood. 2015;126(23):1060. doi:10.1182/blood.v126.23.1060.1060
2. Hui P, Cook DJ, Lim W, Fraser GA, Arnold DM. The frequency and clinical significance of thrombocytopenia complicating critical illness: a systematic review. Chest. 2011;139(2):271-278. doi:10.1378/chest.10-2243
3. Warkentin TE. Heparin-induced thrombocytopenia. Curr Opin Crit Care. 2015;21(6):576-585. doi:10.1097/MCC.0000000000000259
4. Cuker A, Arepally GM, Chong BH, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: heparin-induced thrombocytopenia. Blood Adv. 2018;2(22):3360-3392. doi:10.1182/bloodadvances.2018024489
5. Cuker A, Gimotty PA, Crowther MA, Warkentin TE. Predictive value of the 4Ts scoring system for heparin-induced thrombocytopenia: a systematic review and meta-analysis. Blood. 2012;120(20):4160-4167. doi:10.1182/blood-2012-07-443051
6. Northam KA, Parker WF, Chen S-L, et al. Evaluation of 4Ts score inter-rater agreement in patients undergoing evaluation for heparin-induced thrombocytopenia. Blood Coagul Fibrinolysis. 2021;32(5):328-334. doi:10.1097/MBC.0000000000001042
7. Raschke RA, Curry SC, Warkentin TE, Gerkin RD. Improving clinical interpretation of the anti-platelet factor 4/heparin enzyme-linked immunosorbent assay for the diagnosis of heparin-induced thrombocytopenia through the use of receiver operating characteristic analysis, stratum-specific likelihood ratios, and Bayes theorem. Chest. 2013;144(4):1269-1275. doi:10.1378/chest.12-2712
8. Warkentin TE, Arnold DM, Nazi I, Kelton JG. The platelet serotonin-release assay. Am J Hematol. 2015;90(6):564-572. doi:10.1002/ajh.24006
9. Use IFOR, Contents TOF. LIFECODES ® PF4 IgG assay:1-9.
10. Ancker JS, Edwards A, Nosal S, Hauser D, Mauer E, Kaushal R. Effects of workload, work complexity, and repeated alerts on alert fatigue in a clinical decision support system. BMC Med Inform Decis Mak. 2017;17(1):1-9. doi:10.1186/s12911-017-0430-8
11. O’Connor N, Carter-Johnson R. Effective screening of pathology tests controls costs: thrombophilia testing. J Clin Pathol. 2006;59(5):556. doi:10.1136/jcp.2005.030700
12. Lim MY, Greenberg CS. Inpatient thrombophilia testing: Impact of healthcare system technology and targeted clinician education on changing practice patterns. Vasc Med (United Kingdom). 2018;23(1):78-79. doi:10.1177/1358863X17742509
13. Cox JL, Shunkwiler SM, Koepsell SA. Requirement for a pathologist’s second signature limits inappropriate inpatient thrombophilia testing. Lab Med. 2017;48(4):367-371. doi:10.1093/labmed/lmx040
14. Kwang H, Mou E, Richman I, et al. Thrombophilia testing in the inpatient setting: impact of an educational intervention. BMC Med Inform Decis Mak. 2019;19(1):167. doi:10.1186/s12911-019-0889-6
15. Shah T, Patel-Teague S, Kroupa L, Meyer AND, Singh H. Impact of a national QI programme on reducing electronic health record notifications to clinicians. BMJ Qual Saf. 2019;28(1):10-14. doi:10.1136/bmjqs-2017-007447
16. Singh H, Spitzmueller C, Petersen NJ, Sawhney MK, Sittig DF. Information overload and missed test results in electronic health record-based settings. JAMA Intern Med. 2013;173(8):702-704. doi:10.1001/2013.jamainternmed.61
Using a Real-Time Prediction Algorithm to Improve Sleep in the Hospital
Study Overview
Objective: This study evaluated whether a clinical-decision-support (CDS) tool that utilizes a real-time algorithm incorporating patient vital sign data can identify hospitalized patients who can forgo overnight vital sign checks and thus reduce delirium incidence.
Design: This was a parallel randomized clinical trial of adult inpatients admitted to the general medical service of a tertiary care academic medical center in the United States. The trial intervention consisted of a CDS notification in the electronic health record (EHR) that informed the physician if a patient had a high likelihood of nighttime vital signs within the reference ranges based on a logistic regression model of real-time patient data input. This notification provided the physician an opportunity to discontinue nighttime vital sign checks, dismiss the notification for 1 hour, or dismiss the notification until the next day.
Setting and participants: This clinical trial was conducted at the University of California, San Francisco Medical Center from March 11 to November 24, 2019. Participants included physicians who served on the primary team (eg, attending, resident) of 1699 patients on the general medical service who were outside of the intensive care unit (ICU). The hospital encounters were randomized (allocation ratio of 1:1) to sleep promotion vitals CDS (SPV CDS) intervention or usual care.
Main outcome and measures: The primary outcome was delirium as determined by bedside nurse assessment using the Nursing Delirium Screening Scale (Nu-DESC) recorded once per nursing shift. The Nu-DESC is a standardized delirium screening tool that defines delirium with a score ≥2. Secondary outcomes included sleep opportunity (ie, EHR-based sleep metrics that reflected the maximum time between iatrogenic interruptions, such as nighttime vital sign checks) and patient satisfaction (ie, patient satisfaction measured by standardized Hospital Consumer Assessment of Healthcare Providers and Systems [HCAHPS] survey). Potential balancing outcomes were assessed to ensure that reduced vital sign checks were not causing harms; these included ICU transfers, rapid response calls, and code blue alarms. All analyses were conducted on the basis of intention-to-treat.
Main results: A total of 3025 inpatient encounters were screened and 1930 encounters were randomized (966 SPV CDS intervention; 964 usual care). The randomized encounters consisted of 1699 patients; demographic factors between the 2 trial arms were similar. Specifically, the intervention arm included 566 men (59%) and mean (SD) age was 53 (15) years. The incidence of delirium was similar between the intervention and usual care arms: 108 (11%) vs 123 (13%) (P = .32). Compared to the usual care arm, the intervention arm had a higher mean (SD) number of sleep opportunity hours per night (4.95 [1.45] vs 4.57 [1.30], P < .001) and fewer nighttime vital sign checks (0.97 [0.95] vs 1.41 [0.86], P < .001). The post-discharge HCAHPS survey measuring patient satisfaction was completed by only 5% of patients (53 intervention, 49 usual care), and survey results were similar between the 2 arms (P = .86). In addition, safety outcomes including ICU transfers (49 [5%] vs 47 [5%], P = .92), rapid response calls (68 [7%] vs 55 [6%], P = .27), and code blue alarms (2 [0.2%] vs 9 [0.9%], P = .07) were similar between the study arms.
Conclusion: In this randomized clinical trial, a CDS tool utilizing a real-time prediction algorithm embedded in EHR did not reduce the incidence of delirium in hospitalized patients. However, this SPV CDS intervention helped physicians identify clinically stable patients who can forgo routine nighttime vital sign checks and facilitated greater opportunity for patients to sleep. These findings suggest that augmenting physician judgment using a real-time prediction algorithm can help to improve sleep opportunity without an accompanying increased risk of clinical decompensation during acute care.
Commentary
High-quality sleep is fundamental to health and well-being. Sleep deprivation and disorders are associated with many adverse health outcomes, including increased risks for obesity, diabetes, hypertension, myocardial infarction, and depression.1 In hospitalized patients who are acutely ill, restorative sleep is critical to facilitating recovery. However, poor sleep is exceedingly common in hospitalized patients and is associated with deleterious outcomes, such as high blood pressure, hyperglycemia, and delirium.2,3 Moreover, some of these adverse sleep-induced cardiometabolic outcomes, as well as sleep disruption itself, may persist after hospital discharge.4 Factors that precipitate interrupted sleep during hospitalization include iatrogenic causes such as frequent vital sign checks, nighttime procedures or early morning blood draws, and environmental factors such as loud ambient noise.3 Thus, a potential intervention to improve sleep quality in the hospital is to reduce nighttime interruptions such as frequent vital sign checks.
In the current study, Najafi and colleagues conducted a randomized trial to evaluate whether a CDS tool embedded in EHR, powered by a real-time prediction algorithm of patient data, can be utilized to identify patients in whom vital sign checks can be safely discontinued at nighttime. The authors found a modest but statistically significant reduction in the number of nighttime vital sign checks in patients who underwent the SPV CDS intervention, and a corresponding higher sleep opportunity per night in those who received the intervention. Importantly, this reduction in nighttime vital sign checks did not cause a higher risk of clinical decompensation as measured by ICU transfers, rapid response calls, or code blue alarms. Thus, the results demonstrated the feasibility of using a real-time, patient data-driven CDS tool to augment physician judgment in managing sleep disruption, an important hospital-associated stressor and a common hazard of hospitalization in older patients.
Delirium is a common clinical problem in hospitalized older patients that is associated with prolonged hospitalization, functional and cognitive decline, institutionalization, death, and increased health care costs.5 Despite a potential benefit of SPV CDS intervention in reducing vital sign checks and increasing sleep opportunity, this intervention did not reduce the incidence of delirium in hospitalized patients. This finding is not surprising given that delirium has a multifactorial etiology (eg, metabolic derangements, infections, medication side effects and drug toxicity, hospital environment). A small modification in nighttime vital sign checks and sleep opportunity may have limited impact on optimizing sleep quality and does not address other risk factors for delirium. As such, a multicomponent nonpharmacologic approach that includes sleep enhancement, early mobilization, feeding assistance, fluid repletion, infection prevention, and other interventions should guide delirium prevention in the hospital setting. The SPV CDS intervention may play a role in the delivery of a multifaceted, nonpharmacologic delirium prevention intervention in high-risk individuals.
Sleep disruption is one of the multiple hazards of hospitalization frequently experience by hospitalized older patients. Other hazards, or hospital-associated stressors, include mobility restriction (eg, physical restraints such as urinary catheters and intravenous lines, bed elevation and rails), malnourishment and dehydration (eg, frequent use of no-food-by-mouth order, lack of easy access to hydration), and pain (eg, poor pain control). Extended exposures to these stressors may lead to a maladaptive state called allostatic overload that transiently increases vulnerability to post-hospitalization adverse events, including emergency department use, hospital readmission, or death (ie, post-hospital syndrome).6 Thus, the optimization of sleep during hospitalization in vulnerable patients may have benefits that extend beyond delirium prevention. It is perceivable that a CDS tool embedded in EHR, powered by a real-time prediction algorithm of patient data, may be applied to reduce some of these hazards of hospitalization in addition to improving sleep opportunity.
Applications for Clinical Practice
Findings from the current study indicate that a CDS tool embedded in EHR that utilizes a real-time prediction algorithm of patient data may help to safely improve sleep opportunity in hospitalized patients. The participants in the current study were relatively young (53 [15] years). Given that age is a risk factor for delirium, the effects of this intervention on delirium prevention in the most susceptible population (ie, those over the age of 65) remain unknown and further investigation is warranted. Additional studies are needed to determine whether this approach yields similar results in geriatric patients and improves clinical outcomes.
—Fred Ko, MD
1. Institute of Medicine (US) Committee on Sleep Medicine and Research. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Colten HR, Altevogt BM, editors. National Academies Press (US); 2006.
2. Pilkington S. Causes and consequences of sleep deprivation in hospitalised patients. Nurs Stand. 2013;27(49):350-342. doi:10.7748/ns2013.08.27.49.35.e7649
3. Stewart NH, Arora VM. Sleep in hospitalized older adults. Sleep Med Clin. 2018;13(1):127-135. doi:10.1016/j.jsmc.2017.09.012
4. Altman MT, Knauert MP, Pisani MA. Sleep disturbance after hospitalization and critical illness: a systematic review. Ann Am Thorac Soc. 2017;14(9):1457-1468. doi:10.1513/AnnalsATS.201702-148SR
5. Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318(12):1161-1174. doi:10.1001/jama.2017.12067
6. Goldwater DS, Dharmarajan K, McEwan BS, Krumholz HM. Is posthospital syndrome a result of hospitalization-induced allostatic overload? J Hosp Med. 2018;13(5). doi:10.12788/jhm.2986
Study Overview
Objective: This study evaluated whether a clinical-decision-support (CDS) tool that utilizes a real-time algorithm incorporating patient vital sign data can identify hospitalized patients who can forgo overnight vital sign checks and thus reduce delirium incidence.
Design: This was a parallel randomized clinical trial of adult inpatients admitted to the general medical service of a tertiary care academic medical center in the United States. The trial intervention consisted of a CDS notification in the electronic health record (EHR) that informed the physician if a patient had a high likelihood of nighttime vital signs within the reference ranges based on a logistic regression model of real-time patient data input. This notification provided the physician an opportunity to discontinue nighttime vital sign checks, dismiss the notification for 1 hour, or dismiss the notification until the next day.
Setting and participants: This clinical trial was conducted at the University of California, San Francisco Medical Center from March 11 to November 24, 2019. Participants included physicians who served on the primary team (eg, attending, resident) of 1699 patients on the general medical service who were outside of the intensive care unit (ICU). The hospital encounters were randomized (allocation ratio of 1:1) to sleep promotion vitals CDS (SPV CDS) intervention or usual care.
Main outcome and measures: The primary outcome was delirium as determined by bedside nurse assessment using the Nursing Delirium Screening Scale (Nu-DESC) recorded once per nursing shift. The Nu-DESC is a standardized delirium screening tool that defines delirium with a score ≥2. Secondary outcomes included sleep opportunity (ie, EHR-based sleep metrics that reflected the maximum time between iatrogenic interruptions, such as nighttime vital sign checks) and patient satisfaction (ie, patient satisfaction measured by standardized Hospital Consumer Assessment of Healthcare Providers and Systems [HCAHPS] survey). Potential balancing outcomes were assessed to ensure that reduced vital sign checks were not causing harms; these included ICU transfers, rapid response calls, and code blue alarms. All analyses were conducted on the basis of intention-to-treat.
Main results: A total of 3025 inpatient encounters were screened and 1930 encounters were randomized (966 SPV CDS intervention; 964 usual care). The randomized encounters consisted of 1699 patients; demographic factors between the 2 trial arms were similar. Specifically, the intervention arm included 566 men (59%) and mean (SD) age was 53 (15) years. The incidence of delirium was similar between the intervention and usual care arms: 108 (11%) vs 123 (13%) (P = .32). Compared to the usual care arm, the intervention arm had a higher mean (SD) number of sleep opportunity hours per night (4.95 [1.45] vs 4.57 [1.30], P < .001) and fewer nighttime vital sign checks (0.97 [0.95] vs 1.41 [0.86], P < .001). The post-discharge HCAHPS survey measuring patient satisfaction was completed by only 5% of patients (53 intervention, 49 usual care), and survey results were similar between the 2 arms (P = .86). In addition, safety outcomes including ICU transfers (49 [5%] vs 47 [5%], P = .92), rapid response calls (68 [7%] vs 55 [6%], P = .27), and code blue alarms (2 [0.2%] vs 9 [0.9%], P = .07) were similar between the study arms.
Conclusion: In this randomized clinical trial, a CDS tool utilizing a real-time prediction algorithm embedded in EHR did not reduce the incidence of delirium in hospitalized patients. However, this SPV CDS intervention helped physicians identify clinically stable patients who can forgo routine nighttime vital sign checks and facilitated greater opportunity for patients to sleep. These findings suggest that augmenting physician judgment using a real-time prediction algorithm can help to improve sleep opportunity without an accompanying increased risk of clinical decompensation during acute care.
Commentary
High-quality sleep is fundamental to health and well-being. Sleep deprivation and disorders are associated with many adverse health outcomes, including increased risks for obesity, diabetes, hypertension, myocardial infarction, and depression.1 In hospitalized patients who are acutely ill, restorative sleep is critical to facilitating recovery. However, poor sleep is exceedingly common in hospitalized patients and is associated with deleterious outcomes, such as high blood pressure, hyperglycemia, and delirium.2,3 Moreover, some of these adverse sleep-induced cardiometabolic outcomes, as well as sleep disruption itself, may persist after hospital discharge.4 Factors that precipitate interrupted sleep during hospitalization include iatrogenic causes such as frequent vital sign checks, nighttime procedures or early morning blood draws, and environmental factors such as loud ambient noise.3 Thus, a potential intervention to improve sleep quality in the hospital is to reduce nighttime interruptions such as frequent vital sign checks.
In the current study, Najafi and colleagues conducted a randomized trial to evaluate whether a CDS tool embedded in EHR, powered by a real-time prediction algorithm of patient data, can be utilized to identify patients in whom vital sign checks can be safely discontinued at nighttime. The authors found a modest but statistically significant reduction in the number of nighttime vital sign checks in patients who underwent the SPV CDS intervention, and a corresponding higher sleep opportunity per night in those who received the intervention. Importantly, this reduction in nighttime vital sign checks did not cause a higher risk of clinical decompensation as measured by ICU transfers, rapid response calls, or code blue alarms. Thus, the results demonstrated the feasibility of using a real-time, patient data-driven CDS tool to augment physician judgment in managing sleep disruption, an important hospital-associated stressor and a common hazard of hospitalization in older patients.
Delirium is a common clinical problem in hospitalized older patients that is associated with prolonged hospitalization, functional and cognitive decline, institutionalization, death, and increased health care costs.5 Despite a potential benefit of SPV CDS intervention in reducing vital sign checks and increasing sleep opportunity, this intervention did not reduce the incidence of delirium in hospitalized patients. This finding is not surprising given that delirium has a multifactorial etiology (eg, metabolic derangements, infections, medication side effects and drug toxicity, hospital environment). A small modification in nighttime vital sign checks and sleep opportunity may have limited impact on optimizing sleep quality and does not address other risk factors for delirium. As such, a multicomponent nonpharmacologic approach that includes sleep enhancement, early mobilization, feeding assistance, fluid repletion, infection prevention, and other interventions should guide delirium prevention in the hospital setting. The SPV CDS intervention may play a role in the delivery of a multifaceted, nonpharmacologic delirium prevention intervention in high-risk individuals.
Sleep disruption is one of the multiple hazards of hospitalization frequently experience by hospitalized older patients. Other hazards, or hospital-associated stressors, include mobility restriction (eg, physical restraints such as urinary catheters and intravenous lines, bed elevation and rails), malnourishment and dehydration (eg, frequent use of no-food-by-mouth order, lack of easy access to hydration), and pain (eg, poor pain control). Extended exposures to these stressors may lead to a maladaptive state called allostatic overload that transiently increases vulnerability to post-hospitalization adverse events, including emergency department use, hospital readmission, or death (ie, post-hospital syndrome).6 Thus, the optimization of sleep during hospitalization in vulnerable patients may have benefits that extend beyond delirium prevention. It is perceivable that a CDS tool embedded in EHR, powered by a real-time prediction algorithm of patient data, may be applied to reduce some of these hazards of hospitalization in addition to improving sleep opportunity.
Applications for Clinical Practice
Findings from the current study indicate that a CDS tool embedded in EHR that utilizes a real-time prediction algorithm of patient data may help to safely improve sleep opportunity in hospitalized patients. The participants in the current study were relatively young (53 [15] years). Given that age is a risk factor for delirium, the effects of this intervention on delirium prevention in the most susceptible population (ie, those over the age of 65) remain unknown and further investigation is warranted. Additional studies are needed to determine whether this approach yields similar results in geriatric patients and improves clinical outcomes.
—Fred Ko, MD
Study Overview
Objective: This study evaluated whether a clinical-decision-support (CDS) tool that utilizes a real-time algorithm incorporating patient vital sign data can identify hospitalized patients who can forgo overnight vital sign checks and thus reduce delirium incidence.
Design: This was a parallel randomized clinical trial of adult inpatients admitted to the general medical service of a tertiary care academic medical center in the United States. The trial intervention consisted of a CDS notification in the electronic health record (EHR) that informed the physician if a patient had a high likelihood of nighttime vital signs within the reference ranges based on a logistic regression model of real-time patient data input. This notification provided the physician an opportunity to discontinue nighttime vital sign checks, dismiss the notification for 1 hour, or dismiss the notification until the next day.
Setting and participants: This clinical trial was conducted at the University of California, San Francisco Medical Center from March 11 to November 24, 2019. Participants included physicians who served on the primary team (eg, attending, resident) of 1699 patients on the general medical service who were outside of the intensive care unit (ICU). The hospital encounters were randomized (allocation ratio of 1:1) to sleep promotion vitals CDS (SPV CDS) intervention or usual care.
Main outcome and measures: The primary outcome was delirium as determined by bedside nurse assessment using the Nursing Delirium Screening Scale (Nu-DESC) recorded once per nursing shift. The Nu-DESC is a standardized delirium screening tool that defines delirium with a score ≥2. Secondary outcomes included sleep opportunity (ie, EHR-based sleep metrics that reflected the maximum time between iatrogenic interruptions, such as nighttime vital sign checks) and patient satisfaction (ie, patient satisfaction measured by standardized Hospital Consumer Assessment of Healthcare Providers and Systems [HCAHPS] survey). Potential balancing outcomes were assessed to ensure that reduced vital sign checks were not causing harms; these included ICU transfers, rapid response calls, and code blue alarms. All analyses were conducted on the basis of intention-to-treat.
Main results: A total of 3025 inpatient encounters were screened and 1930 encounters were randomized (966 SPV CDS intervention; 964 usual care). The randomized encounters consisted of 1699 patients; demographic factors between the 2 trial arms were similar. Specifically, the intervention arm included 566 men (59%) and mean (SD) age was 53 (15) years. The incidence of delirium was similar between the intervention and usual care arms: 108 (11%) vs 123 (13%) (P = .32). Compared to the usual care arm, the intervention arm had a higher mean (SD) number of sleep opportunity hours per night (4.95 [1.45] vs 4.57 [1.30], P < .001) and fewer nighttime vital sign checks (0.97 [0.95] vs 1.41 [0.86], P < .001). The post-discharge HCAHPS survey measuring patient satisfaction was completed by only 5% of patients (53 intervention, 49 usual care), and survey results were similar between the 2 arms (P = .86). In addition, safety outcomes including ICU transfers (49 [5%] vs 47 [5%], P = .92), rapid response calls (68 [7%] vs 55 [6%], P = .27), and code blue alarms (2 [0.2%] vs 9 [0.9%], P = .07) were similar between the study arms.
Conclusion: In this randomized clinical trial, a CDS tool utilizing a real-time prediction algorithm embedded in EHR did not reduce the incidence of delirium in hospitalized patients. However, this SPV CDS intervention helped physicians identify clinically stable patients who can forgo routine nighttime vital sign checks and facilitated greater opportunity for patients to sleep. These findings suggest that augmenting physician judgment using a real-time prediction algorithm can help to improve sleep opportunity without an accompanying increased risk of clinical decompensation during acute care.
Commentary
High-quality sleep is fundamental to health and well-being. Sleep deprivation and disorders are associated with many adverse health outcomes, including increased risks for obesity, diabetes, hypertension, myocardial infarction, and depression.1 In hospitalized patients who are acutely ill, restorative sleep is critical to facilitating recovery. However, poor sleep is exceedingly common in hospitalized patients and is associated with deleterious outcomes, such as high blood pressure, hyperglycemia, and delirium.2,3 Moreover, some of these adverse sleep-induced cardiometabolic outcomes, as well as sleep disruption itself, may persist after hospital discharge.4 Factors that precipitate interrupted sleep during hospitalization include iatrogenic causes such as frequent vital sign checks, nighttime procedures or early morning blood draws, and environmental factors such as loud ambient noise.3 Thus, a potential intervention to improve sleep quality in the hospital is to reduce nighttime interruptions such as frequent vital sign checks.
In the current study, Najafi and colleagues conducted a randomized trial to evaluate whether a CDS tool embedded in EHR, powered by a real-time prediction algorithm of patient data, can be utilized to identify patients in whom vital sign checks can be safely discontinued at nighttime. The authors found a modest but statistically significant reduction in the number of nighttime vital sign checks in patients who underwent the SPV CDS intervention, and a corresponding higher sleep opportunity per night in those who received the intervention. Importantly, this reduction in nighttime vital sign checks did not cause a higher risk of clinical decompensation as measured by ICU transfers, rapid response calls, or code blue alarms. Thus, the results demonstrated the feasibility of using a real-time, patient data-driven CDS tool to augment physician judgment in managing sleep disruption, an important hospital-associated stressor and a common hazard of hospitalization in older patients.
Delirium is a common clinical problem in hospitalized older patients that is associated with prolonged hospitalization, functional and cognitive decline, institutionalization, death, and increased health care costs.5 Despite a potential benefit of SPV CDS intervention in reducing vital sign checks and increasing sleep opportunity, this intervention did not reduce the incidence of delirium in hospitalized patients. This finding is not surprising given that delirium has a multifactorial etiology (eg, metabolic derangements, infections, medication side effects and drug toxicity, hospital environment). A small modification in nighttime vital sign checks and sleep opportunity may have limited impact on optimizing sleep quality and does not address other risk factors for delirium. As such, a multicomponent nonpharmacologic approach that includes sleep enhancement, early mobilization, feeding assistance, fluid repletion, infection prevention, and other interventions should guide delirium prevention in the hospital setting. The SPV CDS intervention may play a role in the delivery of a multifaceted, nonpharmacologic delirium prevention intervention in high-risk individuals.
Sleep disruption is one of the multiple hazards of hospitalization frequently experience by hospitalized older patients. Other hazards, or hospital-associated stressors, include mobility restriction (eg, physical restraints such as urinary catheters and intravenous lines, bed elevation and rails), malnourishment and dehydration (eg, frequent use of no-food-by-mouth order, lack of easy access to hydration), and pain (eg, poor pain control). Extended exposures to these stressors may lead to a maladaptive state called allostatic overload that transiently increases vulnerability to post-hospitalization adverse events, including emergency department use, hospital readmission, or death (ie, post-hospital syndrome).6 Thus, the optimization of sleep during hospitalization in vulnerable patients may have benefits that extend beyond delirium prevention. It is perceivable that a CDS tool embedded in EHR, powered by a real-time prediction algorithm of patient data, may be applied to reduce some of these hazards of hospitalization in addition to improving sleep opportunity.
Applications for Clinical Practice
Findings from the current study indicate that a CDS tool embedded in EHR that utilizes a real-time prediction algorithm of patient data may help to safely improve sleep opportunity in hospitalized patients. The participants in the current study were relatively young (53 [15] years). Given that age is a risk factor for delirium, the effects of this intervention on delirium prevention in the most susceptible population (ie, those over the age of 65) remain unknown and further investigation is warranted. Additional studies are needed to determine whether this approach yields similar results in geriatric patients and improves clinical outcomes.
—Fred Ko, MD
1. Institute of Medicine (US) Committee on Sleep Medicine and Research. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Colten HR, Altevogt BM, editors. National Academies Press (US); 2006.
2. Pilkington S. Causes and consequences of sleep deprivation in hospitalised patients. Nurs Stand. 2013;27(49):350-342. doi:10.7748/ns2013.08.27.49.35.e7649
3. Stewart NH, Arora VM. Sleep in hospitalized older adults. Sleep Med Clin. 2018;13(1):127-135. doi:10.1016/j.jsmc.2017.09.012
4. Altman MT, Knauert MP, Pisani MA. Sleep disturbance after hospitalization and critical illness: a systematic review. Ann Am Thorac Soc. 2017;14(9):1457-1468. doi:10.1513/AnnalsATS.201702-148SR
5. Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318(12):1161-1174. doi:10.1001/jama.2017.12067
6. Goldwater DS, Dharmarajan K, McEwan BS, Krumholz HM. Is posthospital syndrome a result of hospitalization-induced allostatic overload? J Hosp Med. 2018;13(5). doi:10.12788/jhm.2986
1. Institute of Medicine (US) Committee on Sleep Medicine and Research. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Colten HR, Altevogt BM, editors. National Academies Press (US); 2006.
2. Pilkington S. Causes and consequences of sleep deprivation in hospitalised patients. Nurs Stand. 2013;27(49):350-342. doi:10.7748/ns2013.08.27.49.35.e7649
3. Stewart NH, Arora VM. Sleep in hospitalized older adults. Sleep Med Clin. 2018;13(1):127-135. doi:10.1016/j.jsmc.2017.09.012
4. Altman MT, Knauert MP, Pisani MA. Sleep disturbance after hospitalization and critical illness: a systematic review. Ann Am Thorac Soc. 2017;14(9):1457-1468. doi:10.1513/AnnalsATS.201702-148SR
5. Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318(12):1161-1174. doi:10.1001/jama.2017.12067
6. Goldwater DS, Dharmarajan K, McEwan BS, Krumholz HM. Is posthospital syndrome a result of hospitalization-induced allostatic overload? J Hosp Med. 2018;13(5). doi:10.12788/jhm.2986
Get the science right
Get the science right. I have spent years researching and reflecting on what makes the best physicians, the best medicine, the optimal organized medical system, and the best medical ethics and law to support all of it. I have traveled to almost innumerable conferences to discuss these topics with colleagues who have similar goals. Time and time again, I come back to the conclusion that, in the modern era, the second-most important thing to do is to get the science right.
The practice of medicine in my Western world can be traced back to Hippocrates and earlier. The practice of nursing has other milestones. The healing arts have different points of origin in other cultures, such as China. In a modern world of mass communication, these various historical paths are converging on scientific evidence. The science to support medicine has always had flaws, but it has fared better than the other options. Sometimes, the science was so sketchy that the key was to believe in whatever the shaman was providing. But for the past 100 years, science, rather than tradition and hierarchy, has been relied upon to guide policy and action. For the past 50 years, evidence-based medicine has ascended. Have we become better than the snake oil salesmen of the late 19th century?
Modern health care is far from perfect. The pandemic has been a major stressor to the health care system. The pandemic has revealed flaws and weaknesses, including inequity in access to care, health illiteracy, and a shaky moral compass balancing individual liberty and social good. Overall, despite multiple mistakes dealing with a novel threat, I think the institutions promoting science have performed well during the pandemic, especially when compared with the moral and governmental institutions encouraging ethical behavior and making policies to promote justice.
My highest praise would be for the professionalism of health care workers. Nurses and physicians have staffed the hospitals and clinics caring for people when the hallways were overflowing for days without end. Without the commitment, the teamwork, and the courage to provide that care, the death toll would have been much higher and the suffering unimaginable. My observation is that these people were not motivated by an abstract primum non nocere, first do no harm. It was the commitment to love one’s neighbor and care for the sick. This dedication is the first most important thing in professionalism.
Part of what fuels that commitment is a belief that what they are doing makes a difference. The belief is stronger when there is measurable, scientific evidence that a difference is being made. The scientific decisions have not been perfect, but at this point the evidence is clear that the shutdown flattened the curve. Vaccines saved lives and will continue to do so. Masks saved lives. Nursing care, particularly intensive care, reduced the case fatality rate and assuaged suffering and grief.
What lessons about training new providers can be gleaned from the past 2 years? Those who teach professionalism for physicians, nurses, and other health care workers should strengthen the common value systems that undergird the commitment people have to the patients and the professions. In the face of postmodern nihilism and relativism, virtues need to be clarified and reinforced. In the face of political polarization which seeks to make a political affiliation the locus of loyalty and commitment, emphasize the fellowship of the health care professions.
To me as a scientist, a key lesson is that we need to be better at getting the science right. Two years ago I was wiping some groceries with alcohol and quarantining cans in shopping bags in the corner of the kitchen for 24 hours before shelving them. I still push elevator buttons with my knuckles. The Centers for Disease Control and Prevention needs to revamp their policy making procedures.
Institutions must work to reestablish the public trust in science. That is a challenge because while many amazing scientific advances have occurred (i.e., my MRI last week showed far more going on than my orthopedist and physical therapist detected based on clinical exam). Imaging such as MR and ultrasound have been major advances in diagnostic medicine, but there are also repeated examples demonstrating where medicine has been wrong. In the past 6 months I have read new guidelines for ear tubes, for neonatal jaundice, for newborn sepsis, and for newborn hypoglycemia. All indicate to me that my training 30 years ago was on target and the interval “improvements” in practice have been worthless Brownian motion based on false scientific discoveries. My recommendation would be that pediatrics do one-third as much research but do that research three times better and get it right.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
Get the science right. I have spent years researching and reflecting on what makes the best physicians, the best medicine, the optimal organized medical system, and the best medical ethics and law to support all of it. I have traveled to almost innumerable conferences to discuss these topics with colleagues who have similar goals. Time and time again, I come back to the conclusion that, in the modern era, the second-most important thing to do is to get the science right.
The practice of medicine in my Western world can be traced back to Hippocrates and earlier. The practice of nursing has other milestones. The healing arts have different points of origin in other cultures, such as China. In a modern world of mass communication, these various historical paths are converging on scientific evidence. The science to support medicine has always had flaws, but it has fared better than the other options. Sometimes, the science was so sketchy that the key was to believe in whatever the shaman was providing. But for the past 100 years, science, rather than tradition and hierarchy, has been relied upon to guide policy and action. For the past 50 years, evidence-based medicine has ascended. Have we become better than the snake oil salesmen of the late 19th century?
Modern health care is far from perfect. The pandemic has been a major stressor to the health care system. The pandemic has revealed flaws and weaknesses, including inequity in access to care, health illiteracy, and a shaky moral compass balancing individual liberty and social good. Overall, despite multiple mistakes dealing with a novel threat, I think the institutions promoting science have performed well during the pandemic, especially when compared with the moral and governmental institutions encouraging ethical behavior and making policies to promote justice.
My highest praise would be for the professionalism of health care workers. Nurses and physicians have staffed the hospitals and clinics caring for people when the hallways were overflowing for days without end. Without the commitment, the teamwork, and the courage to provide that care, the death toll would have been much higher and the suffering unimaginable. My observation is that these people were not motivated by an abstract primum non nocere, first do no harm. It was the commitment to love one’s neighbor and care for the sick. This dedication is the first most important thing in professionalism.
Part of what fuels that commitment is a belief that what they are doing makes a difference. The belief is stronger when there is measurable, scientific evidence that a difference is being made. The scientific decisions have not been perfect, but at this point the evidence is clear that the shutdown flattened the curve. Vaccines saved lives and will continue to do so. Masks saved lives. Nursing care, particularly intensive care, reduced the case fatality rate and assuaged suffering and grief.
What lessons about training new providers can be gleaned from the past 2 years? Those who teach professionalism for physicians, nurses, and other health care workers should strengthen the common value systems that undergird the commitment people have to the patients and the professions. In the face of postmodern nihilism and relativism, virtues need to be clarified and reinforced. In the face of political polarization which seeks to make a political affiliation the locus of loyalty and commitment, emphasize the fellowship of the health care professions.
To me as a scientist, a key lesson is that we need to be better at getting the science right. Two years ago I was wiping some groceries with alcohol and quarantining cans in shopping bags in the corner of the kitchen for 24 hours before shelving them. I still push elevator buttons with my knuckles. The Centers for Disease Control and Prevention needs to revamp their policy making procedures.
Institutions must work to reestablish the public trust in science. That is a challenge because while many amazing scientific advances have occurred (i.e., my MRI last week showed far more going on than my orthopedist and physical therapist detected based on clinical exam). Imaging such as MR and ultrasound have been major advances in diagnostic medicine, but there are also repeated examples demonstrating where medicine has been wrong. In the past 6 months I have read new guidelines for ear tubes, for neonatal jaundice, for newborn sepsis, and for newborn hypoglycemia. All indicate to me that my training 30 years ago was on target and the interval “improvements” in practice have been worthless Brownian motion based on false scientific discoveries. My recommendation would be that pediatrics do one-third as much research but do that research three times better and get it right.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
Get the science right. I have spent years researching and reflecting on what makes the best physicians, the best medicine, the optimal organized medical system, and the best medical ethics and law to support all of it. I have traveled to almost innumerable conferences to discuss these topics with colleagues who have similar goals. Time and time again, I come back to the conclusion that, in the modern era, the second-most important thing to do is to get the science right.
The practice of medicine in my Western world can be traced back to Hippocrates and earlier. The practice of nursing has other milestones. The healing arts have different points of origin in other cultures, such as China. In a modern world of mass communication, these various historical paths are converging on scientific evidence. The science to support medicine has always had flaws, but it has fared better than the other options. Sometimes, the science was so sketchy that the key was to believe in whatever the shaman was providing. But for the past 100 years, science, rather than tradition and hierarchy, has been relied upon to guide policy and action. For the past 50 years, evidence-based medicine has ascended. Have we become better than the snake oil salesmen of the late 19th century?
Modern health care is far from perfect. The pandemic has been a major stressor to the health care system. The pandemic has revealed flaws and weaknesses, including inequity in access to care, health illiteracy, and a shaky moral compass balancing individual liberty and social good. Overall, despite multiple mistakes dealing with a novel threat, I think the institutions promoting science have performed well during the pandemic, especially when compared with the moral and governmental institutions encouraging ethical behavior and making policies to promote justice.
My highest praise would be for the professionalism of health care workers. Nurses and physicians have staffed the hospitals and clinics caring for people when the hallways were overflowing for days without end. Without the commitment, the teamwork, and the courage to provide that care, the death toll would have been much higher and the suffering unimaginable. My observation is that these people were not motivated by an abstract primum non nocere, first do no harm. It was the commitment to love one’s neighbor and care for the sick. This dedication is the first most important thing in professionalism.
Part of what fuels that commitment is a belief that what they are doing makes a difference. The belief is stronger when there is measurable, scientific evidence that a difference is being made. The scientific decisions have not been perfect, but at this point the evidence is clear that the shutdown flattened the curve. Vaccines saved lives and will continue to do so. Masks saved lives. Nursing care, particularly intensive care, reduced the case fatality rate and assuaged suffering and grief.
What lessons about training new providers can be gleaned from the past 2 years? Those who teach professionalism for physicians, nurses, and other health care workers should strengthen the common value systems that undergird the commitment people have to the patients and the professions. In the face of postmodern nihilism and relativism, virtues need to be clarified and reinforced. In the face of political polarization which seeks to make a political affiliation the locus of loyalty and commitment, emphasize the fellowship of the health care professions.
To me as a scientist, a key lesson is that we need to be better at getting the science right. Two years ago I was wiping some groceries with alcohol and quarantining cans in shopping bags in the corner of the kitchen for 24 hours before shelving them. I still push elevator buttons with my knuckles. The Centers for Disease Control and Prevention needs to revamp their policy making procedures.
Institutions must work to reestablish the public trust in science. That is a challenge because while many amazing scientific advances have occurred (i.e., my MRI last week showed far more going on than my orthopedist and physical therapist detected based on clinical exam). Imaging such as MR and ultrasound have been major advances in diagnostic medicine, but there are also repeated examples demonstrating where medicine has been wrong. In the past 6 months I have read new guidelines for ear tubes, for neonatal jaundice, for newborn sepsis, and for newborn hypoglycemia. All indicate to me that my training 30 years ago was on target and the interval “improvements” in practice have been worthless Brownian motion based on false scientific discoveries. My recommendation would be that pediatrics do one-third as much research but do that research three times better and get it right.
Dr. Powell is a retired pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
Doc sues patient and wins
Urologist Arnaldo Trabucco, MD, was outraged when he learned of a legal claim filed by a patient’s family blaming him for the patient’s death.
Dr. Trabucco had performed a successful laparoscopic left radical nephrectomy on Gerald Scharf, but he died 3 days later from an unrelated condition, said Dr. Trabucco, who now practices in California. The claims alleged not only wrongful death, but also that Dr. Trabucco “committed willful and malicious actions upon” the patient, eventually resulting in his death, and that Dr. Trabucco’s actions constituted “extreme and outrageous behavior.”
The accusations were levied on behalf of the patient’s family by a bankruptcy attorney who admittedly had no experience in medical malpractice litigation.
“It was a vicious allegation that I intentionally tried to kill my own patient,” said Dr. Trabucco, 66. “It’s an allegation that was outlandish. Those were fighting words.”
As the case dragged on, Dr. Trabucco filed a complaint against the Scharfs and bankruptcy attorney Jeffrey Cogan for malicious prosecution and abuse of process. In 2018, Dr. Trabucco prevailed when a jury awarded him $6,232,000 in compensatory damages and $1,768,000 in punitive damages against Mr. Cogan. (No damages were assessed against the patient’s family.)
“This was a principle issue more than anything else,” Dr. Trabucco said. “My name was tarnished and thrown through the mud. I’m very proud of my name and my reputation.”
Mr. Cogan, a bankruptcy attorney licensed in Nevada and California, disputes that his actions were malicious and disagrees with the jury’s verdict.
“I don’t think I did anything wrong with filing the lawsuit,” he said.
Despite the $8 million award, the legal fight between Dr. Trabucco and Mr. Cogan has continued – and is not over yet.
Not your ordinary legal journey
Dr. Trabucco completed his medical training in Rome before moving back to the United States to begin his residency in Brooklyn, New York.
He quietly practiced urology in New York for years before moving to Columbus, Ind., to work at a urology clinic. In 2005, Dr. Trabucco made headlines when the Bartholomew County, Ind., sheriff’s deputies found marijuana plants growing in his home. His medical license was suspended, and he pled guilty to a misdemeanor.
Dr. Trabucco said he was unaware that a family member was growing the plants in the home and that he was not responsible for the operation. The misdemeanor has since been expunged from his record, according to Dr. Trabucco. Bartholomew County records do not list the offense. He later moved to Arizona, where he opened a medical practice.
Before the Scharfs filed their malpractice case in 2013, Dr. Trabucco had been embroiled in a series of unrelated legal disputes, including postdivorce proceedings and a complaint against him by another physician, alleging defamation. In that case, the physician claimed Dr. Trabucco published false and defamatory communications about him, including that the physician committed intentional fraud.
Dr. Trabucco filed his own suit for defamation and infliction of emotional distress against the same physician for alleged threats and harassment and making false reports about him to several Arizona state entities. The defamation suit against Dr. Trabucco ended in a settlement, the terms of which are confidential, according to Mr. Cogan. Dr. Trabucco’s defamation case against the physician was dismissed, according to court records, but they do not specify the reason. Dr. Trabucco said he dropped the defamation case because of the other relentless litigation he was facing.
In November 2012, Dr. Trabucco filed for Chapter 7 bankruptcy protection.
Mr. Cogan was representing Dr. Trabucco’s ex-wife’s interests as a creditor in the bankruptcy proceeding and eventually represented the physician who sued Dr. Trabucco, according to court documents. In all, Mr. Cogan represented six creditors in connection to Dr. Trabucco’s bankruptcy, including the Scharfs. He also took over the Scharfs’ malpractice case in Arizona’s Mohave County Superior Court after their attorney died.
As part of a filing in Nevada bankruptcy court called a “Complaint to Determine Nondischargeabiliy of Debts,” Mr. Cogan alleged that Dr. Trabucco knew he lacked sufficient expertise regarding the laparoscopic nephrectomy, that an intraoperative complication occurred because of his error, and that Dr. Trabucco hid the complication and did not attempt to remedy the situation, among other claims.
In addition to the Mohave County filing and the bankruptcy filing, Mr. Cogan filed a similar medical malpractice case against Dr. Trabucco in Arizona district court.
“I believe, based upon the statements by [a retired medical malpractice attorney], that Dr Trabucco squeezed the abdominal aorta,” Mr. Cogan said. “When he did so, plaque from Mr Scharf blocked blood from going to his remaining his kidney, causing his death. My lawsuit said that Dr Trabucco knew he made a mistake and went home rather than fixing the mistake.”
Dr. Trabucco said the laparoscopic nephrectomy went smoothly. A few hours after the surgery, however, Mr. Scharf was transferred to a Las Vegas hospital with a diagnosis of potential occlusion of the abdominal aorta. Surgery was performed, and while the operative report noted the presence of severe atherosclerosis of the abdominal aorta, there was no indication of an intraoperative injury to the aorta from Dr. Trabucco’s surgery, according to court documents filed in U.S. District Court for the District of Arizona. An autopsy performed on Mr. Scharf reported “severe calcific aortic atherosclerosis, primarily at the aortic arch and abdominal aorta at the level of the branching of the renal arteries with small adherent thrombus.” The autopsy did not include any indication or suggestion of an intraoperative injury to the abdominal aorta.
A federal jury found unanimously in favor of Dr. Trabucco, concluding that he did nothing wrong. The original medical malpractice case in Mohave County court was ultimately dismissed and in 2014, the bankruptcy court entered an order discharging Dr. Trabucco from all prepetition debts, according to court records.
Meanwhile, as the malicious prosecution case against Mr. Cogan continued, Dr. Trabucco’s name again drew media attention. His former girlfriend was arrested for plotting to kidnap and kill an attorney who was representing Dr. Trabucco’s ex-wife in a divorce proceeding. Renee Perillo was sentenced to 27 years in prison for conspiracy to commit kidnapping and murder for hire for trying to kill Noblesville, Ind., attorney Rebecca Eimerman. Ms. Eimerman was pursuing divorce settlement money from Dr. Trabucco on behalf of his ex-wife. Ms. Perillo’s son was also charged in the crime.
No charges related to the crime were filed against Dr. Trabucco, according to the Hamilton County Prosecutor’s Office and federal charging records. Dr. Trabucco said he was not involved in the incident and had no knowledge of Perillo’s plans.
A hard fought – and still continuing – legal battle
After a 3-day trial, jurors in 2018 found that Mr. Cogan owed Dr. Trabucco $8 million for the harm caused by the unfounded claims.
“This has had a tremendous impact on my life,” Dr. Trabucco said. “It’s cost me a lot of time, money, and anguish.”
Mr. Cogan appealed the verdict. An Arizona appeals court in 2020 upheld the finding of liability for malicious prosecution against Mr. Cogan, but it vacated the finding of liability for abuse of process. Because of the partial reversal, the appellate court vacated the $8 million and sent the case back to the Superior Court in Mohave County, Ariz., for a new trial on damages.
But shortly before the December 2021 retrial, both parties agreed to settle for $8 million.
The settlement, however, is not the end of the litigation between the parties.
Late last year, Mr. Cogan filed a new case in the U.S. District Court for the District of Nevada against Dr. Trabucco alleging the Arizona court that tried the malicious prosecution case never had jurisdiction. Mr. Cogan contends that per federal case law, any damages resulting from a bankruptcy court pleading give the federal court exclusive jurisdiction over the matter.
“I believe that I will win the federal court case,” Mr. Cogan said. “If Judge Andrew P. Gordon finds for me, Dr. Trabucco’s judgment in Arizona is void as Arizona did not have subject-matter jurisdiction.”
Dr. Trabucco says the new federal case has no merit.
“The federal courts have no jurisdiction over civil matters, and this should be thrown out,” he said. “However, my attorney is fully prepared to take this to the Supreme Court [if it moves forward].”
At this article’s deadline, the judge had not yet ruled on Dr. Trabucco’s motion to dismiss the federal complaint.
Should a physician sue for malicious prosecution?
Dr. Trabucco’s case raises the question of whether physicians should consider suing a patient after winning their malpractice case. As many doctors know, a successful case outcome doesn’t necessarily undo the time spent, income lost, and reputation harm that often comes with a negligence lawsuit. Is suing for malicious prosecution a reasonable route to recoup some of the damages caused by the claim?
“It’s an uphill struggle to prevail,” said Jeffrey Segal, MD, JD. “Have people done it? Yes, they have. Is it easy? No.”
A physician must hit the marks of a distinct checklist to pursue a malicious prosecution case, said Dr. Segal, CEO and founder of Medical Justice, a company that aids and advises physicians on legal matters. One necessary element is that the malpractice case against the physician must have been adjudicated on the merits, he said. For example, the doctor won the case at trial or the case was dismissed on summary judgment. Summary judgment refers to a court tossing the claim because there was no genuine dispute as to any material fact and because the defendant is entitled to judgment as a matter of law.
If the case was dismissed for another reason, such as a technicality, or dropped by the plaintiff, the case would not meet the threshold for a malicious prosecution claim, Dr. Segal explains.
The physician must also show that the lawsuit was instituted with “malice,” meaning with an intent to hurt the physician, and that the lawsuit was brought without “probable cause,” adds J. Richard Moore, JD, a medical malpractice defense attorney based in Indianapolis.
“The courts are still pretty good at weeding out cases with no merit whatsoever, so even if a physician takes a case to trial and wins, it is exceedingly rare that a case that makes it that far, has no merit whatsoever,” Mr. Moore said.
In addition, a plaintiffs’ attorney may be protected from a malicious prosecution claim because they relied on a medical expert’s opinion that reasonable cause existed to file a lawsuit, notes William Sullivan, DO, JD, an emergency physician and attorney based in Frankfort, Ill.
Dr. Sullivan has personal experience with such a challenge. He filed a malicious prosecution claim against a plaintiffs’ attorney after being dismissed from a medical malpractice case. The claim stemmed from Dr. Sullivan inserting an emergency central line into a trauma patient who was taken to surgery and later died. The suit alleged Dr. Sullivan failed to diagnose internal bleeding and failed to perform surgery, although surgeons at the hospital knew internal bleeding was present and Dr. Sullivan had no privileges to perform surgery, he said.
However, Dr. Sullivan was unable to identify the medical expert involved in the claim. Illinois law allows a malpractice plaintiff to withhold the identity of a medical expert who certifies a malpractice lawsuit. Because Dr. Sullivan couldn’t identify the expert, he could not depose the physician, and the law firm claimed there was no malicious prosecution because it relied on the trauma surgeon’s opinion that Dr. Sullivan was liable.
The trial court agreed with the law firm’s argument and dismissed them from the case, Dr. Sullivan said. The trial court also agreed that the expert trauma surgeon should be allowed to remain anonymous in accordance with Illinois law.
Alternative options for doctors to recover damages
For physicians who want to recoup after a frivolous claim, but don’t want to dive into another lawsuit, there are other options, say legal experts.
One alternative is filing a motion for sanctions, Dr. Sullivan said. If an attorney files a lawsuit that does not have a reasonable basis in fact or law, that attorney could be subject to sanctions, including paying for the physician’s attorney’s fees and costs, he explained. If a motion for sanctions is granted against an opposing attorney, that fact may be reportable to the attorney’s insurance carrier and also reportable to the attorney’s state licensing board. A motion for sanctions does not require filing of a separate lawsuit and filing a motion for sanctions may allow the defendant physician or the defense attorney to depose the plaintiff attorney regarding the reasonable basis that attorney had for filing a lawsuit, Dr. Sullivan said.
Dr. Sullivan recently represented a physician who won a motion for sanctions. During the legal action against him, Dr. Sullivan presented the plaintiff’s attorney with information showing why his lawsuit did not have a reasonable basis, but the attorney repeatedly ignored the information.
“Eventually, I filed a motion to dismiss the physician from the lawsuit and that motion was granted,” he said. “I also filed a motion for sanctions so that the physician could recover the costs involved in defending the claim. The trial court granted our motion for sanctions against the plaintiff and her law firm and awarded my client more than $10,000.”
Physicians who believe a plaintiffs’ attorney is acting unprofessionally can also file a complaint with the attorney’s bar, Dr. Segal said. And expert witnesses acting in bad faith can be reported to professional societies, medical licensing boards, and/or specialty boards.
“There are a number of avenues to address the sense of justice,” he said. “But if you’re looking for a payday, the only way to do that is by going to court.”
A version of this article first appeared on Medscape.com.
Urologist Arnaldo Trabucco, MD, was outraged when he learned of a legal claim filed by a patient’s family blaming him for the patient’s death.
Dr. Trabucco had performed a successful laparoscopic left radical nephrectomy on Gerald Scharf, but he died 3 days later from an unrelated condition, said Dr. Trabucco, who now practices in California. The claims alleged not only wrongful death, but also that Dr. Trabucco “committed willful and malicious actions upon” the patient, eventually resulting in his death, and that Dr. Trabucco’s actions constituted “extreme and outrageous behavior.”
The accusations were levied on behalf of the patient’s family by a bankruptcy attorney who admittedly had no experience in medical malpractice litigation.
“It was a vicious allegation that I intentionally tried to kill my own patient,” said Dr. Trabucco, 66. “It’s an allegation that was outlandish. Those were fighting words.”
As the case dragged on, Dr. Trabucco filed a complaint against the Scharfs and bankruptcy attorney Jeffrey Cogan for malicious prosecution and abuse of process. In 2018, Dr. Trabucco prevailed when a jury awarded him $6,232,000 in compensatory damages and $1,768,000 in punitive damages against Mr. Cogan. (No damages were assessed against the patient’s family.)
“This was a principle issue more than anything else,” Dr. Trabucco said. “My name was tarnished and thrown through the mud. I’m very proud of my name and my reputation.”
Mr. Cogan, a bankruptcy attorney licensed in Nevada and California, disputes that his actions were malicious and disagrees with the jury’s verdict.
“I don’t think I did anything wrong with filing the lawsuit,” he said.
Despite the $8 million award, the legal fight between Dr. Trabucco and Mr. Cogan has continued – and is not over yet.
Not your ordinary legal journey
Dr. Trabucco completed his medical training in Rome before moving back to the United States to begin his residency in Brooklyn, New York.
He quietly practiced urology in New York for years before moving to Columbus, Ind., to work at a urology clinic. In 2005, Dr. Trabucco made headlines when the Bartholomew County, Ind., sheriff’s deputies found marijuana plants growing in his home. His medical license was suspended, and he pled guilty to a misdemeanor.
Dr. Trabucco said he was unaware that a family member was growing the plants in the home and that he was not responsible for the operation. The misdemeanor has since been expunged from his record, according to Dr. Trabucco. Bartholomew County records do not list the offense. He later moved to Arizona, where he opened a medical practice.
Before the Scharfs filed their malpractice case in 2013, Dr. Trabucco had been embroiled in a series of unrelated legal disputes, including postdivorce proceedings and a complaint against him by another physician, alleging defamation. In that case, the physician claimed Dr. Trabucco published false and defamatory communications about him, including that the physician committed intentional fraud.
Dr. Trabucco filed his own suit for defamation and infliction of emotional distress against the same physician for alleged threats and harassment and making false reports about him to several Arizona state entities. The defamation suit against Dr. Trabucco ended in a settlement, the terms of which are confidential, according to Mr. Cogan. Dr. Trabucco’s defamation case against the physician was dismissed, according to court records, but they do not specify the reason. Dr. Trabucco said he dropped the defamation case because of the other relentless litigation he was facing.
In November 2012, Dr. Trabucco filed for Chapter 7 bankruptcy protection.
Mr. Cogan was representing Dr. Trabucco’s ex-wife’s interests as a creditor in the bankruptcy proceeding and eventually represented the physician who sued Dr. Trabucco, according to court documents. In all, Mr. Cogan represented six creditors in connection to Dr. Trabucco’s bankruptcy, including the Scharfs. He also took over the Scharfs’ malpractice case in Arizona’s Mohave County Superior Court after their attorney died.
As part of a filing in Nevada bankruptcy court called a “Complaint to Determine Nondischargeabiliy of Debts,” Mr. Cogan alleged that Dr. Trabucco knew he lacked sufficient expertise regarding the laparoscopic nephrectomy, that an intraoperative complication occurred because of his error, and that Dr. Trabucco hid the complication and did not attempt to remedy the situation, among other claims.
In addition to the Mohave County filing and the bankruptcy filing, Mr. Cogan filed a similar medical malpractice case against Dr. Trabucco in Arizona district court.
“I believe, based upon the statements by [a retired medical malpractice attorney], that Dr Trabucco squeezed the abdominal aorta,” Mr. Cogan said. “When he did so, plaque from Mr Scharf blocked blood from going to his remaining his kidney, causing his death. My lawsuit said that Dr Trabucco knew he made a mistake and went home rather than fixing the mistake.”
Dr. Trabucco said the laparoscopic nephrectomy went smoothly. A few hours after the surgery, however, Mr. Scharf was transferred to a Las Vegas hospital with a diagnosis of potential occlusion of the abdominal aorta. Surgery was performed, and while the operative report noted the presence of severe atherosclerosis of the abdominal aorta, there was no indication of an intraoperative injury to the aorta from Dr. Trabucco’s surgery, according to court documents filed in U.S. District Court for the District of Arizona. An autopsy performed on Mr. Scharf reported “severe calcific aortic atherosclerosis, primarily at the aortic arch and abdominal aorta at the level of the branching of the renal arteries with small adherent thrombus.” The autopsy did not include any indication or suggestion of an intraoperative injury to the abdominal aorta.
A federal jury found unanimously in favor of Dr. Trabucco, concluding that he did nothing wrong. The original medical malpractice case in Mohave County court was ultimately dismissed and in 2014, the bankruptcy court entered an order discharging Dr. Trabucco from all prepetition debts, according to court records.
Meanwhile, as the malicious prosecution case against Mr. Cogan continued, Dr. Trabucco’s name again drew media attention. His former girlfriend was arrested for plotting to kidnap and kill an attorney who was representing Dr. Trabucco’s ex-wife in a divorce proceeding. Renee Perillo was sentenced to 27 years in prison for conspiracy to commit kidnapping and murder for hire for trying to kill Noblesville, Ind., attorney Rebecca Eimerman. Ms. Eimerman was pursuing divorce settlement money from Dr. Trabucco on behalf of his ex-wife. Ms. Perillo’s son was also charged in the crime.
No charges related to the crime were filed against Dr. Trabucco, according to the Hamilton County Prosecutor’s Office and federal charging records. Dr. Trabucco said he was not involved in the incident and had no knowledge of Perillo’s plans.
A hard fought – and still continuing – legal battle
After a 3-day trial, jurors in 2018 found that Mr. Cogan owed Dr. Trabucco $8 million for the harm caused by the unfounded claims.
“This has had a tremendous impact on my life,” Dr. Trabucco said. “It’s cost me a lot of time, money, and anguish.”
Mr. Cogan appealed the verdict. An Arizona appeals court in 2020 upheld the finding of liability for malicious prosecution against Mr. Cogan, but it vacated the finding of liability for abuse of process. Because of the partial reversal, the appellate court vacated the $8 million and sent the case back to the Superior Court in Mohave County, Ariz., for a new trial on damages.
But shortly before the December 2021 retrial, both parties agreed to settle for $8 million.
The settlement, however, is not the end of the litigation between the parties.
Late last year, Mr. Cogan filed a new case in the U.S. District Court for the District of Nevada against Dr. Trabucco alleging the Arizona court that tried the malicious prosecution case never had jurisdiction. Mr. Cogan contends that per federal case law, any damages resulting from a bankruptcy court pleading give the federal court exclusive jurisdiction over the matter.
“I believe that I will win the federal court case,” Mr. Cogan said. “If Judge Andrew P. Gordon finds for me, Dr. Trabucco’s judgment in Arizona is void as Arizona did not have subject-matter jurisdiction.”
Dr. Trabucco says the new federal case has no merit.
“The federal courts have no jurisdiction over civil matters, and this should be thrown out,” he said. “However, my attorney is fully prepared to take this to the Supreme Court [if it moves forward].”
At this article’s deadline, the judge had not yet ruled on Dr. Trabucco’s motion to dismiss the federal complaint.
Should a physician sue for malicious prosecution?
Dr. Trabucco’s case raises the question of whether physicians should consider suing a patient after winning their malpractice case. As many doctors know, a successful case outcome doesn’t necessarily undo the time spent, income lost, and reputation harm that often comes with a negligence lawsuit. Is suing for malicious prosecution a reasonable route to recoup some of the damages caused by the claim?
“It’s an uphill struggle to prevail,” said Jeffrey Segal, MD, JD. “Have people done it? Yes, they have. Is it easy? No.”
A physician must hit the marks of a distinct checklist to pursue a malicious prosecution case, said Dr. Segal, CEO and founder of Medical Justice, a company that aids and advises physicians on legal matters. One necessary element is that the malpractice case against the physician must have been adjudicated on the merits, he said. For example, the doctor won the case at trial or the case was dismissed on summary judgment. Summary judgment refers to a court tossing the claim because there was no genuine dispute as to any material fact and because the defendant is entitled to judgment as a matter of law.
If the case was dismissed for another reason, such as a technicality, or dropped by the plaintiff, the case would not meet the threshold for a malicious prosecution claim, Dr. Segal explains.
The physician must also show that the lawsuit was instituted with “malice,” meaning with an intent to hurt the physician, and that the lawsuit was brought without “probable cause,” adds J. Richard Moore, JD, a medical malpractice defense attorney based in Indianapolis.
“The courts are still pretty good at weeding out cases with no merit whatsoever, so even if a physician takes a case to trial and wins, it is exceedingly rare that a case that makes it that far, has no merit whatsoever,” Mr. Moore said.
In addition, a plaintiffs’ attorney may be protected from a malicious prosecution claim because they relied on a medical expert’s opinion that reasonable cause existed to file a lawsuit, notes William Sullivan, DO, JD, an emergency physician and attorney based in Frankfort, Ill.
Dr. Sullivan has personal experience with such a challenge. He filed a malicious prosecution claim against a plaintiffs’ attorney after being dismissed from a medical malpractice case. The claim stemmed from Dr. Sullivan inserting an emergency central line into a trauma patient who was taken to surgery and later died. The suit alleged Dr. Sullivan failed to diagnose internal bleeding and failed to perform surgery, although surgeons at the hospital knew internal bleeding was present and Dr. Sullivan had no privileges to perform surgery, he said.
However, Dr. Sullivan was unable to identify the medical expert involved in the claim. Illinois law allows a malpractice plaintiff to withhold the identity of a medical expert who certifies a malpractice lawsuit. Because Dr. Sullivan couldn’t identify the expert, he could not depose the physician, and the law firm claimed there was no malicious prosecution because it relied on the trauma surgeon’s opinion that Dr. Sullivan was liable.
The trial court agreed with the law firm’s argument and dismissed them from the case, Dr. Sullivan said. The trial court also agreed that the expert trauma surgeon should be allowed to remain anonymous in accordance with Illinois law.
Alternative options for doctors to recover damages
For physicians who want to recoup after a frivolous claim, but don’t want to dive into another lawsuit, there are other options, say legal experts.
One alternative is filing a motion for sanctions, Dr. Sullivan said. If an attorney files a lawsuit that does not have a reasonable basis in fact or law, that attorney could be subject to sanctions, including paying for the physician’s attorney’s fees and costs, he explained. If a motion for sanctions is granted against an opposing attorney, that fact may be reportable to the attorney’s insurance carrier and also reportable to the attorney’s state licensing board. A motion for sanctions does not require filing of a separate lawsuit and filing a motion for sanctions may allow the defendant physician or the defense attorney to depose the plaintiff attorney regarding the reasonable basis that attorney had for filing a lawsuit, Dr. Sullivan said.
Dr. Sullivan recently represented a physician who won a motion for sanctions. During the legal action against him, Dr. Sullivan presented the plaintiff’s attorney with information showing why his lawsuit did not have a reasonable basis, but the attorney repeatedly ignored the information.
“Eventually, I filed a motion to dismiss the physician from the lawsuit and that motion was granted,” he said. “I also filed a motion for sanctions so that the physician could recover the costs involved in defending the claim. The trial court granted our motion for sanctions against the plaintiff and her law firm and awarded my client more than $10,000.”
Physicians who believe a plaintiffs’ attorney is acting unprofessionally can also file a complaint with the attorney’s bar, Dr. Segal said. And expert witnesses acting in bad faith can be reported to professional societies, medical licensing boards, and/or specialty boards.
“There are a number of avenues to address the sense of justice,” he said. “But if you’re looking for a payday, the only way to do that is by going to court.”
A version of this article first appeared on Medscape.com.
Urologist Arnaldo Trabucco, MD, was outraged when he learned of a legal claim filed by a patient’s family blaming him for the patient’s death.
Dr. Trabucco had performed a successful laparoscopic left radical nephrectomy on Gerald Scharf, but he died 3 days later from an unrelated condition, said Dr. Trabucco, who now practices in California. The claims alleged not only wrongful death, but also that Dr. Trabucco “committed willful and malicious actions upon” the patient, eventually resulting in his death, and that Dr. Trabucco’s actions constituted “extreme and outrageous behavior.”
The accusations were levied on behalf of the patient’s family by a bankruptcy attorney who admittedly had no experience in medical malpractice litigation.
“It was a vicious allegation that I intentionally tried to kill my own patient,” said Dr. Trabucco, 66. “It’s an allegation that was outlandish. Those were fighting words.”
As the case dragged on, Dr. Trabucco filed a complaint against the Scharfs and bankruptcy attorney Jeffrey Cogan for malicious prosecution and abuse of process. In 2018, Dr. Trabucco prevailed when a jury awarded him $6,232,000 in compensatory damages and $1,768,000 in punitive damages against Mr. Cogan. (No damages were assessed against the patient’s family.)
“This was a principle issue more than anything else,” Dr. Trabucco said. “My name was tarnished and thrown through the mud. I’m very proud of my name and my reputation.”
Mr. Cogan, a bankruptcy attorney licensed in Nevada and California, disputes that his actions were malicious and disagrees with the jury’s verdict.
“I don’t think I did anything wrong with filing the lawsuit,” he said.
Despite the $8 million award, the legal fight between Dr. Trabucco and Mr. Cogan has continued – and is not over yet.
Not your ordinary legal journey
Dr. Trabucco completed his medical training in Rome before moving back to the United States to begin his residency in Brooklyn, New York.
He quietly practiced urology in New York for years before moving to Columbus, Ind., to work at a urology clinic. In 2005, Dr. Trabucco made headlines when the Bartholomew County, Ind., sheriff’s deputies found marijuana plants growing in his home. His medical license was suspended, and he pled guilty to a misdemeanor.
Dr. Trabucco said he was unaware that a family member was growing the plants in the home and that he was not responsible for the operation. The misdemeanor has since been expunged from his record, according to Dr. Trabucco. Bartholomew County records do not list the offense. He later moved to Arizona, where he opened a medical practice.
Before the Scharfs filed their malpractice case in 2013, Dr. Trabucco had been embroiled in a series of unrelated legal disputes, including postdivorce proceedings and a complaint against him by another physician, alleging defamation. In that case, the physician claimed Dr. Trabucco published false and defamatory communications about him, including that the physician committed intentional fraud.
Dr. Trabucco filed his own suit for defamation and infliction of emotional distress against the same physician for alleged threats and harassment and making false reports about him to several Arizona state entities. The defamation suit against Dr. Trabucco ended in a settlement, the terms of which are confidential, according to Mr. Cogan. Dr. Trabucco’s defamation case against the physician was dismissed, according to court records, but they do not specify the reason. Dr. Trabucco said he dropped the defamation case because of the other relentless litigation he was facing.
In November 2012, Dr. Trabucco filed for Chapter 7 bankruptcy protection.
Mr. Cogan was representing Dr. Trabucco’s ex-wife’s interests as a creditor in the bankruptcy proceeding and eventually represented the physician who sued Dr. Trabucco, according to court documents. In all, Mr. Cogan represented six creditors in connection to Dr. Trabucco’s bankruptcy, including the Scharfs. He also took over the Scharfs’ malpractice case in Arizona’s Mohave County Superior Court after their attorney died.
As part of a filing in Nevada bankruptcy court called a “Complaint to Determine Nondischargeabiliy of Debts,” Mr. Cogan alleged that Dr. Trabucco knew he lacked sufficient expertise regarding the laparoscopic nephrectomy, that an intraoperative complication occurred because of his error, and that Dr. Trabucco hid the complication and did not attempt to remedy the situation, among other claims.
In addition to the Mohave County filing and the bankruptcy filing, Mr. Cogan filed a similar medical malpractice case against Dr. Trabucco in Arizona district court.
“I believe, based upon the statements by [a retired medical malpractice attorney], that Dr Trabucco squeezed the abdominal aorta,” Mr. Cogan said. “When he did so, plaque from Mr Scharf blocked blood from going to his remaining his kidney, causing his death. My lawsuit said that Dr Trabucco knew he made a mistake and went home rather than fixing the mistake.”
Dr. Trabucco said the laparoscopic nephrectomy went smoothly. A few hours after the surgery, however, Mr. Scharf was transferred to a Las Vegas hospital with a diagnosis of potential occlusion of the abdominal aorta. Surgery was performed, and while the operative report noted the presence of severe atherosclerosis of the abdominal aorta, there was no indication of an intraoperative injury to the aorta from Dr. Trabucco’s surgery, according to court documents filed in U.S. District Court for the District of Arizona. An autopsy performed on Mr. Scharf reported “severe calcific aortic atherosclerosis, primarily at the aortic arch and abdominal aorta at the level of the branching of the renal arteries with small adherent thrombus.” The autopsy did not include any indication or suggestion of an intraoperative injury to the abdominal aorta.
A federal jury found unanimously in favor of Dr. Trabucco, concluding that he did nothing wrong. The original medical malpractice case in Mohave County court was ultimately dismissed and in 2014, the bankruptcy court entered an order discharging Dr. Trabucco from all prepetition debts, according to court records.
Meanwhile, as the malicious prosecution case against Mr. Cogan continued, Dr. Trabucco’s name again drew media attention. His former girlfriend was arrested for plotting to kidnap and kill an attorney who was representing Dr. Trabucco’s ex-wife in a divorce proceeding. Renee Perillo was sentenced to 27 years in prison for conspiracy to commit kidnapping and murder for hire for trying to kill Noblesville, Ind., attorney Rebecca Eimerman. Ms. Eimerman was pursuing divorce settlement money from Dr. Trabucco on behalf of his ex-wife. Ms. Perillo’s son was also charged in the crime.
No charges related to the crime were filed against Dr. Trabucco, according to the Hamilton County Prosecutor’s Office and federal charging records. Dr. Trabucco said he was not involved in the incident and had no knowledge of Perillo’s plans.
A hard fought – and still continuing – legal battle
After a 3-day trial, jurors in 2018 found that Mr. Cogan owed Dr. Trabucco $8 million for the harm caused by the unfounded claims.
“This has had a tremendous impact on my life,” Dr. Trabucco said. “It’s cost me a lot of time, money, and anguish.”
Mr. Cogan appealed the verdict. An Arizona appeals court in 2020 upheld the finding of liability for malicious prosecution against Mr. Cogan, but it vacated the finding of liability for abuse of process. Because of the partial reversal, the appellate court vacated the $8 million and sent the case back to the Superior Court in Mohave County, Ariz., for a new trial on damages.
But shortly before the December 2021 retrial, both parties agreed to settle for $8 million.
The settlement, however, is not the end of the litigation between the parties.
Late last year, Mr. Cogan filed a new case in the U.S. District Court for the District of Nevada against Dr. Trabucco alleging the Arizona court that tried the malicious prosecution case never had jurisdiction. Mr. Cogan contends that per federal case law, any damages resulting from a bankruptcy court pleading give the federal court exclusive jurisdiction over the matter.
“I believe that I will win the federal court case,” Mr. Cogan said. “If Judge Andrew P. Gordon finds for me, Dr. Trabucco’s judgment in Arizona is void as Arizona did not have subject-matter jurisdiction.”
Dr. Trabucco says the new federal case has no merit.
“The federal courts have no jurisdiction over civil matters, and this should be thrown out,” he said. “However, my attorney is fully prepared to take this to the Supreme Court [if it moves forward].”
At this article’s deadline, the judge had not yet ruled on Dr. Trabucco’s motion to dismiss the federal complaint.
Should a physician sue for malicious prosecution?
Dr. Trabucco’s case raises the question of whether physicians should consider suing a patient after winning their malpractice case. As many doctors know, a successful case outcome doesn’t necessarily undo the time spent, income lost, and reputation harm that often comes with a negligence lawsuit. Is suing for malicious prosecution a reasonable route to recoup some of the damages caused by the claim?
“It’s an uphill struggle to prevail,” said Jeffrey Segal, MD, JD. “Have people done it? Yes, they have. Is it easy? No.”
A physician must hit the marks of a distinct checklist to pursue a malicious prosecution case, said Dr. Segal, CEO and founder of Medical Justice, a company that aids and advises physicians on legal matters. One necessary element is that the malpractice case against the physician must have been adjudicated on the merits, he said. For example, the doctor won the case at trial or the case was dismissed on summary judgment. Summary judgment refers to a court tossing the claim because there was no genuine dispute as to any material fact and because the defendant is entitled to judgment as a matter of law.
If the case was dismissed for another reason, such as a technicality, or dropped by the plaintiff, the case would not meet the threshold for a malicious prosecution claim, Dr. Segal explains.
The physician must also show that the lawsuit was instituted with “malice,” meaning with an intent to hurt the physician, and that the lawsuit was brought without “probable cause,” adds J. Richard Moore, JD, a medical malpractice defense attorney based in Indianapolis.
“The courts are still pretty good at weeding out cases with no merit whatsoever, so even if a physician takes a case to trial and wins, it is exceedingly rare that a case that makes it that far, has no merit whatsoever,” Mr. Moore said.
In addition, a plaintiffs’ attorney may be protected from a malicious prosecution claim because they relied on a medical expert’s opinion that reasonable cause existed to file a lawsuit, notes William Sullivan, DO, JD, an emergency physician and attorney based in Frankfort, Ill.
Dr. Sullivan has personal experience with such a challenge. He filed a malicious prosecution claim against a plaintiffs’ attorney after being dismissed from a medical malpractice case. The claim stemmed from Dr. Sullivan inserting an emergency central line into a trauma patient who was taken to surgery and later died. The suit alleged Dr. Sullivan failed to diagnose internal bleeding and failed to perform surgery, although surgeons at the hospital knew internal bleeding was present and Dr. Sullivan had no privileges to perform surgery, he said.
However, Dr. Sullivan was unable to identify the medical expert involved in the claim. Illinois law allows a malpractice plaintiff to withhold the identity of a medical expert who certifies a malpractice lawsuit. Because Dr. Sullivan couldn’t identify the expert, he could not depose the physician, and the law firm claimed there was no malicious prosecution because it relied on the trauma surgeon’s opinion that Dr. Sullivan was liable.
The trial court agreed with the law firm’s argument and dismissed them from the case, Dr. Sullivan said. The trial court also agreed that the expert trauma surgeon should be allowed to remain anonymous in accordance with Illinois law.
Alternative options for doctors to recover damages
For physicians who want to recoup after a frivolous claim, but don’t want to dive into another lawsuit, there are other options, say legal experts.
One alternative is filing a motion for sanctions, Dr. Sullivan said. If an attorney files a lawsuit that does not have a reasonable basis in fact or law, that attorney could be subject to sanctions, including paying for the physician’s attorney’s fees and costs, he explained. If a motion for sanctions is granted against an opposing attorney, that fact may be reportable to the attorney’s insurance carrier and also reportable to the attorney’s state licensing board. A motion for sanctions does not require filing of a separate lawsuit and filing a motion for sanctions may allow the defendant physician or the defense attorney to depose the plaintiff attorney regarding the reasonable basis that attorney had for filing a lawsuit, Dr. Sullivan said.
Dr. Sullivan recently represented a physician who won a motion for sanctions. During the legal action against him, Dr. Sullivan presented the plaintiff’s attorney with information showing why his lawsuit did not have a reasonable basis, but the attorney repeatedly ignored the information.
“Eventually, I filed a motion to dismiss the physician from the lawsuit and that motion was granted,” he said. “I also filed a motion for sanctions so that the physician could recover the costs involved in defending the claim. The trial court granted our motion for sanctions against the plaintiff and her law firm and awarded my client more than $10,000.”
Physicians who believe a plaintiffs’ attorney is acting unprofessionally can also file a complaint with the attorney’s bar, Dr. Segal said. And expert witnesses acting in bad faith can be reported to professional societies, medical licensing boards, and/or specialty boards.
“There are a number of avenues to address the sense of justice,” he said. “But if you’re looking for a payday, the only way to do that is by going to court.”
A version of this article first appeared on Medscape.com.
U.S. primary care seen lagging in key markers
In delivery of primary care, including access and coordination, the U.S. trails well behind 10 other wealthy countries, according to a new report from the Commonwealth Fund.
The document, released March 15, concludes that the shortcomings in the U.S. system – from a lack of a relationship with a primary care physician to unequal access to after-hours care – “disproportionately affect Black and Latinx communities and rural areas, exacerbating disparities that have widened during the COVID-19 pandemic.”
“This report really shows that the U.S. is falling behind. We know that a strong primary care system yields better health outcomes. We have a lot to learn from other high-income countries,” coauthor Munira Z. Gunja, MPH, a senior researcher for the Commonwealth Fund’s International Program in Health Policy and Practice Innovations, told this news organization. “At baseline, we really need to make sure that everyone has health insurance in this country so they can actually use primary care services, and we need to increase the supply of those services.”
The report draws from the Commonwealth Fund’s 2019 and 2020 International Health Policy Surveys and the 2020 International Profiles of Health Care Systems. Among the main points:
- U.S. adults are the least likely to have a regular physician or place of care or a long-standing relationship with a primary care provider: 43% of American adults have a long-term relationship with a primary care doctor, compared with highs of 71% in Germany and the Netherlands.
- Access to home visits or after-hours care – excluding emergency department visits – is lowest in the United States (45%). In the Netherlands, Norway, New Zealand, and Germany, the rate is 90% to 96%.
- Half of primary care providers in the United States report adequate coordination with specialists and hospitals – around the average for the 11 countries studied.
‘Dismal mess’
Experts reacted to the report with a mix of concern and frustration – but not surprise.
“The results in this report are not surprising, and we have known them all for a number of years now,” Timothy Hoff, PhD, a health policy expert at Northeastern University, Boston, said. “Primary care doctors remain the backbone of our primary care system. But there are too few of them in the United States, and there likely will remain too few of them in the future. This opens the door to other and more diverse forms of innovation that will be required to help complement the work they do.”
Dr. Hoff, author of Searching for the Family Doctor: Primary Care on the Brink, added that comparing the United States to smaller countries like Norway or the United Kingdom is “somewhat problematic.”
“Our system has to take care of several hundred million people, trapped in a fragmented and market-based delivery system focused on specialty care, each of whom may have a different insurance plan,” he said. “Doing some of the things very small countries with government-funded insurance and a history of strong primary care delivery do in taking care of far fewer citizens is not realistic.”
Jeffrey Borkan, MD, PhD, chair and professor in the department of family medicine at the Alpert Medical School of Brown University, Providence, R.I., said the most shocking finding in the report is that despite spending far more on health care than any other country, “we cannot manage to provide one of the least expensive and most efficacious services: a relationship with a primary care doctor.”
Arthur Caplan, PhD, director of the Division of Medical Ethics at New York University Langone Medical Center, called primary care in this country “a dismal mess. It has been for many years. This is especially so in mental health. Access in many counties is nonexistent, and many primary care physicians are opting into boutique care.”
R. Shawn Martin, CEO of the 133,000-member American Academy of Family Physicians, said, “None of this surprises me. I think these are trendlines; we have been following this for many, many years here at the Academy.”
Mr. Martin added that he was disappointed that the recent, large investments in sharing and digitizing information have not closed the gaps that hinder the efficient and widespread delivery of primary care.
The findings in the report weren’t all bad. More primary care providers in the United States (30%) screen their patients for social needs such as housing, food security, and transportation – the highest among all 11 nations studied.
Also, Commonwealth Fund said the proportion of patients who said they received information on meeting their social needs and screening for domestic violence or social isolation was low everywhere. However, the percentage in the United States, Canada, and Norway was the highest, at 9%. Sweden had the lowest rate for such screenings, at 1%.
The researchers noted that social determinants of health account for as much as 55% of health outcomes. “In some countries, like the United States, the higher rates of receiving such information may be a response to the higher rates of material hardship, along with a weaker safety net,” the report states.
Ms. Gunja and her colleagues suggested several options for changes in policies, including narrowing the wage gap between primary care providers and higher-paid specialists; subsidizing medical school tuition to give students incentives to enter primary care; investing in telehealth to make primary care more accessible; and rewarding and holding providers accountable for continuity of care.
“The U.S. had the largest wage gap and highest tuition fees among the countries we studied,” Ms. Gunja told this news organization..
Researchers noted that U.S. patients could benefit from the introduction of incentives such as those paid in New Zealand to primary health organizations, which receive additional funding per capita to promote health and coordinate care.
But Dr. Caplan was skeptical that those measures would do much to correct the problems.
“We have no will to fix this ongoing, scandalous situation,” he said. “Specialist care still pays inordinately large salaries. Nurses and physician extenders are underused. Academic prestige does little to reward primary care. Plus, patients are not pressing for better access. Sorry, but I see no solutions pending in the current climate. Obamacare barely survived.”
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In delivery of primary care, including access and coordination, the U.S. trails well behind 10 other wealthy countries, according to a new report from the Commonwealth Fund.
The document, released March 15, concludes that the shortcomings in the U.S. system – from a lack of a relationship with a primary care physician to unequal access to after-hours care – “disproportionately affect Black and Latinx communities and rural areas, exacerbating disparities that have widened during the COVID-19 pandemic.”
“This report really shows that the U.S. is falling behind. We know that a strong primary care system yields better health outcomes. We have a lot to learn from other high-income countries,” coauthor Munira Z. Gunja, MPH, a senior researcher for the Commonwealth Fund’s International Program in Health Policy and Practice Innovations, told this news organization. “At baseline, we really need to make sure that everyone has health insurance in this country so they can actually use primary care services, and we need to increase the supply of those services.”
The report draws from the Commonwealth Fund’s 2019 and 2020 International Health Policy Surveys and the 2020 International Profiles of Health Care Systems. Among the main points:
- U.S. adults are the least likely to have a regular physician or place of care or a long-standing relationship with a primary care provider: 43% of American adults have a long-term relationship with a primary care doctor, compared with highs of 71% in Germany and the Netherlands.
- Access to home visits or after-hours care – excluding emergency department visits – is lowest in the United States (45%). In the Netherlands, Norway, New Zealand, and Germany, the rate is 90% to 96%.
- Half of primary care providers in the United States report adequate coordination with specialists and hospitals – around the average for the 11 countries studied.
‘Dismal mess’
Experts reacted to the report with a mix of concern and frustration – but not surprise.
“The results in this report are not surprising, and we have known them all for a number of years now,” Timothy Hoff, PhD, a health policy expert at Northeastern University, Boston, said. “Primary care doctors remain the backbone of our primary care system. But there are too few of them in the United States, and there likely will remain too few of them in the future. This opens the door to other and more diverse forms of innovation that will be required to help complement the work they do.”
Dr. Hoff, author of Searching for the Family Doctor: Primary Care on the Brink, added that comparing the United States to smaller countries like Norway or the United Kingdom is “somewhat problematic.”
“Our system has to take care of several hundred million people, trapped in a fragmented and market-based delivery system focused on specialty care, each of whom may have a different insurance plan,” he said. “Doing some of the things very small countries with government-funded insurance and a history of strong primary care delivery do in taking care of far fewer citizens is not realistic.”
Jeffrey Borkan, MD, PhD, chair and professor in the department of family medicine at the Alpert Medical School of Brown University, Providence, R.I., said the most shocking finding in the report is that despite spending far more on health care than any other country, “we cannot manage to provide one of the least expensive and most efficacious services: a relationship with a primary care doctor.”
Arthur Caplan, PhD, director of the Division of Medical Ethics at New York University Langone Medical Center, called primary care in this country “a dismal mess. It has been for many years. This is especially so in mental health. Access in many counties is nonexistent, and many primary care physicians are opting into boutique care.”
R. Shawn Martin, CEO of the 133,000-member American Academy of Family Physicians, said, “None of this surprises me. I think these are trendlines; we have been following this for many, many years here at the Academy.”
Mr. Martin added that he was disappointed that the recent, large investments in sharing and digitizing information have not closed the gaps that hinder the efficient and widespread delivery of primary care.
The findings in the report weren’t all bad. More primary care providers in the United States (30%) screen their patients for social needs such as housing, food security, and transportation – the highest among all 11 nations studied.
Also, Commonwealth Fund said the proportion of patients who said they received information on meeting their social needs and screening for domestic violence or social isolation was low everywhere. However, the percentage in the United States, Canada, and Norway was the highest, at 9%. Sweden had the lowest rate for such screenings, at 1%.
The researchers noted that social determinants of health account for as much as 55% of health outcomes. “In some countries, like the United States, the higher rates of receiving such information may be a response to the higher rates of material hardship, along with a weaker safety net,” the report states.
Ms. Gunja and her colleagues suggested several options for changes in policies, including narrowing the wage gap between primary care providers and higher-paid specialists; subsidizing medical school tuition to give students incentives to enter primary care; investing in telehealth to make primary care more accessible; and rewarding and holding providers accountable for continuity of care.
“The U.S. had the largest wage gap and highest tuition fees among the countries we studied,” Ms. Gunja told this news organization..
Researchers noted that U.S. patients could benefit from the introduction of incentives such as those paid in New Zealand to primary health organizations, which receive additional funding per capita to promote health and coordinate care.
But Dr. Caplan was skeptical that those measures would do much to correct the problems.
“We have no will to fix this ongoing, scandalous situation,” he said. “Specialist care still pays inordinately large salaries. Nurses and physician extenders are underused. Academic prestige does little to reward primary care. Plus, patients are not pressing for better access. Sorry, but I see no solutions pending in the current climate. Obamacare barely survived.”
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In delivery of primary care, including access and coordination, the U.S. trails well behind 10 other wealthy countries, according to a new report from the Commonwealth Fund.
The document, released March 15, concludes that the shortcomings in the U.S. system – from a lack of a relationship with a primary care physician to unequal access to after-hours care – “disproportionately affect Black and Latinx communities and rural areas, exacerbating disparities that have widened during the COVID-19 pandemic.”
“This report really shows that the U.S. is falling behind. We know that a strong primary care system yields better health outcomes. We have a lot to learn from other high-income countries,” coauthor Munira Z. Gunja, MPH, a senior researcher for the Commonwealth Fund’s International Program in Health Policy and Practice Innovations, told this news organization. “At baseline, we really need to make sure that everyone has health insurance in this country so they can actually use primary care services, and we need to increase the supply of those services.”
The report draws from the Commonwealth Fund’s 2019 and 2020 International Health Policy Surveys and the 2020 International Profiles of Health Care Systems. Among the main points:
- U.S. adults are the least likely to have a regular physician or place of care or a long-standing relationship with a primary care provider: 43% of American adults have a long-term relationship with a primary care doctor, compared with highs of 71% in Germany and the Netherlands.
- Access to home visits or after-hours care – excluding emergency department visits – is lowest in the United States (45%). In the Netherlands, Norway, New Zealand, and Germany, the rate is 90% to 96%.
- Half of primary care providers in the United States report adequate coordination with specialists and hospitals – around the average for the 11 countries studied.
‘Dismal mess’
Experts reacted to the report with a mix of concern and frustration – but not surprise.
“The results in this report are not surprising, and we have known them all for a number of years now,” Timothy Hoff, PhD, a health policy expert at Northeastern University, Boston, said. “Primary care doctors remain the backbone of our primary care system. But there are too few of them in the United States, and there likely will remain too few of them in the future. This opens the door to other and more diverse forms of innovation that will be required to help complement the work they do.”
Dr. Hoff, author of Searching for the Family Doctor: Primary Care on the Brink, added that comparing the United States to smaller countries like Norway or the United Kingdom is “somewhat problematic.”
“Our system has to take care of several hundred million people, trapped in a fragmented and market-based delivery system focused on specialty care, each of whom may have a different insurance plan,” he said. “Doing some of the things very small countries with government-funded insurance and a history of strong primary care delivery do in taking care of far fewer citizens is not realistic.”
Jeffrey Borkan, MD, PhD, chair and professor in the department of family medicine at the Alpert Medical School of Brown University, Providence, R.I., said the most shocking finding in the report is that despite spending far more on health care than any other country, “we cannot manage to provide one of the least expensive and most efficacious services: a relationship with a primary care doctor.”
Arthur Caplan, PhD, director of the Division of Medical Ethics at New York University Langone Medical Center, called primary care in this country “a dismal mess. It has been for many years. This is especially so in mental health. Access in many counties is nonexistent, and many primary care physicians are opting into boutique care.”
R. Shawn Martin, CEO of the 133,000-member American Academy of Family Physicians, said, “None of this surprises me. I think these are trendlines; we have been following this for many, many years here at the Academy.”
Mr. Martin added that he was disappointed that the recent, large investments in sharing and digitizing information have not closed the gaps that hinder the efficient and widespread delivery of primary care.
The findings in the report weren’t all bad. More primary care providers in the United States (30%) screen their patients for social needs such as housing, food security, and transportation – the highest among all 11 nations studied.
Also, Commonwealth Fund said the proportion of patients who said they received information on meeting their social needs and screening for domestic violence or social isolation was low everywhere. However, the percentage in the United States, Canada, and Norway was the highest, at 9%. Sweden had the lowest rate for such screenings, at 1%.
The researchers noted that social determinants of health account for as much as 55% of health outcomes. “In some countries, like the United States, the higher rates of receiving such information may be a response to the higher rates of material hardship, along with a weaker safety net,” the report states.
Ms. Gunja and her colleagues suggested several options for changes in policies, including narrowing the wage gap between primary care providers and higher-paid specialists; subsidizing medical school tuition to give students incentives to enter primary care; investing in telehealth to make primary care more accessible; and rewarding and holding providers accountable for continuity of care.
“The U.S. had the largest wage gap and highest tuition fees among the countries we studied,” Ms. Gunja told this news organization..
Researchers noted that U.S. patients could benefit from the introduction of incentives such as those paid in New Zealand to primary health organizations, which receive additional funding per capita to promote health and coordinate care.
But Dr. Caplan was skeptical that those measures would do much to correct the problems.
“We have no will to fix this ongoing, scandalous situation,” he said. “Specialist care still pays inordinately large salaries. Nurses and physician extenders are underused. Academic prestige does little to reward primary care. Plus, patients are not pressing for better access. Sorry, but I see no solutions pending in the current climate. Obamacare barely survived.”
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
‘We don’t want to be an inspiration’
Over 2.5 million people have fled the ghastly war in Ukraine for safety. But, not everyone is trying to leave. Shockingly, hundreds of thousands are actually flocking toward the danger in Ukraine right now. Many of them are women.
I was commuting to work when I first heard this story on a podcast. In astonishing numbers, women have chosen to return to or stay in Ukraine because they’re needed to fight and to protect their families. My reaction, like yours, was to be inspired. What amazing courage! Twitter and Instagram will swell with images of their balaclava masked faces standing in the breach once more. Like the women in medicine who armed themselves with surgical masks and face shields and babies on their backs to join the fight against COVID-19. They will be poster girls, blue sleeves rolled up and red polka dotted bandanas covering their hair.
But that’s not what they want. “We don’t want to be an inspiration,” said one fearless Ukrainian fighter in the story, “we want to be alive.”
At the time of this writing as we celebrate the brilliant accomplishments of women on March 8, International Women’s Day, I wonder if we don’t have it slightly wrong.
Although acknowledgment is appreciated, the women I work alongside don’t need me to be inspired by them. They need me to stand with them, to help them. . The “she-session” it’s been called, refers to the million women who have not rejoined the workforce since COVID-19. This is especially acute for us in medicine where women are significantly more likely than are men to report not working full time, or not working at all.
The truth is that even in 2022, the burdens of family life are still not borne equally. Bias against mothers in particular can be insidious. Take academia, where there is little sympathy for not publishing on schedule. Perhaps there are unexplained gaps, but where exactly on a CV does one put “recurrent pregnancy loss?” Do you know how many clinics or ORs a woman must cancel to attempt maddeningly unpredictable egg retrievals and embryo transfers? A lot. Not to mention the financial burden of doing so.
During the pandemic, female physicians were more likely to manage child care, schooling, and household duties, compared to male physicians.
And yet (perhaps even because of that?) women in medicine make less money. How much? About $80,000 less on average in dermatology. Inspired? Indeed. No thanks. Let’s #BreakTheBias rather.
I’m not a policy expert nor a sociologist. I don’t know what advice might be helpful here. I’d say raising our collective consciousness of the unfairness, highlighting discrepancies, and advocating for equality are good starts. But, International Women’s Day isn’t new. It’s old. Like over a hundred years old (since 1909 to be exact). We don’t just need a better hashtag, we need to do something. Give equity in pay. Offer opportunities for leadership that accommodate the extra duty women might have outside work. Create flexibility in schedules and without the penalty of having to pump at work or leave early to pick up a child. Not to mention all the opportunities we men have to do more of the household work that women currently do.
The gallant women of Ukraine don’t need our approbation. They need our aid and our prayers. Like the women in my department, at my medical center, in my community, they aren’t posing to be made into posters. There’s work to be done and they are flocking toward it right now.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Over 2.5 million people have fled the ghastly war in Ukraine for safety. But, not everyone is trying to leave. Shockingly, hundreds of thousands are actually flocking toward the danger in Ukraine right now. Many of them are women.
I was commuting to work when I first heard this story on a podcast. In astonishing numbers, women have chosen to return to or stay in Ukraine because they’re needed to fight and to protect their families. My reaction, like yours, was to be inspired. What amazing courage! Twitter and Instagram will swell with images of their balaclava masked faces standing in the breach once more. Like the women in medicine who armed themselves with surgical masks and face shields and babies on their backs to join the fight against COVID-19. They will be poster girls, blue sleeves rolled up and red polka dotted bandanas covering their hair.
But that’s not what they want. “We don’t want to be an inspiration,” said one fearless Ukrainian fighter in the story, “we want to be alive.”
At the time of this writing as we celebrate the brilliant accomplishments of women on March 8, International Women’s Day, I wonder if we don’t have it slightly wrong.
Although acknowledgment is appreciated, the women I work alongside don’t need me to be inspired by them. They need me to stand with them, to help them. . The “she-session” it’s been called, refers to the million women who have not rejoined the workforce since COVID-19. This is especially acute for us in medicine where women are significantly more likely than are men to report not working full time, or not working at all.
The truth is that even in 2022, the burdens of family life are still not borne equally. Bias against mothers in particular can be insidious. Take academia, where there is little sympathy for not publishing on schedule. Perhaps there are unexplained gaps, but where exactly on a CV does one put “recurrent pregnancy loss?” Do you know how many clinics or ORs a woman must cancel to attempt maddeningly unpredictable egg retrievals and embryo transfers? A lot. Not to mention the financial burden of doing so.
During the pandemic, female physicians were more likely to manage child care, schooling, and household duties, compared to male physicians.
And yet (perhaps even because of that?) women in medicine make less money. How much? About $80,000 less on average in dermatology. Inspired? Indeed. No thanks. Let’s #BreakTheBias rather.
I’m not a policy expert nor a sociologist. I don’t know what advice might be helpful here. I’d say raising our collective consciousness of the unfairness, highlighting discrepancies, and advocating for equality are good starts. But, International Women’s Day isn’t new. It’s old. Like over a hundred years old (since 1909 to be exact). We don’t just need a better hashtag, we need to do something. Give equity in pay. Offer opportunities for leadership that accommodate the extra duty women might have outside work. Create flexibility in schedules and without the penalty of having to pump at work or leave early to pick up a child. Not to mention all the opportunities we men have to do more of the household work that women currently do.
The gallant women of Ukraine don’t need our approbation. They need our aid and our prayers. Like the women in my department, at my medical center, in my community, they aren’t posing to be made into posters. There’s work to be done and they are flocking toward it right now.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Over 2.5 million people have fled the ghastly war in Ukraine for safety. But, not everyone is trying to leave. Shockingly, hundreds of thousands are actually flocking toward the danger in Ukraine right now. Many of them are women.
I was commuting to work when I first heard this story on a podcast. In astonishing numbers, women have chosen to return to or stay in Ukraine because they’re needed to fight and to protect their families. My reaction, like yours, was to be inspired. What amazing courage! Twitter and Instagram will swell with images of their balaclava masked faces standing in the breach once more. Like the women in medicine who armed themselves with surgical masks and face shields and babies on their backs to join the fight against COVID-19. They will be poster girls, blue sleeves rolled up and red polka dotted bandanas covering their hair.
But that’s not what they want. “We don’t want to be an inspiration,” said one fearless Ukrainian fighter in the story, “we want to be alive.”
At the time of this writing as we celebrate the brilliant accomplishments of women on March 8, International Women’s Day, I wonder if we don’t have it slightly wrong.
Although acknowledgment is appreciated, the women I work alongside don’t need me to be inspired by them. They need me to stand with them, to help them. . The “she-session” it’s been called, refers to the million women who have not rejoined the workforce since COVID-19. This is especially acute for us in medicine where women are significantly more likely than are men to report not working full time, or not working at all.
The truth is that even in 2022, the burdens of family life are still not borne equally. Bias against mothers in particular can be insidious. Take academia, where there is little sympathy for not publishing on schedule. Perhaps there are unexplained gaps, but where exactly on a CV does one put “recurrent pregnancy loss?” Do you know how many clinics or ORs a woman must cancel to attempt maddeningly unpredictable egg retrievals and embryo transfers? A lot. Not to mention the financial burden of doing so.
During the pandemic, female physicians were more likely to manage child care, schooling, and household duties, compared to male physicians.
And yet (perhaps even because of that?) women in medicine make less money. How much? About $80,000 less on average in dermatology. Inspired? Indeed. No thanks. Let’s #BreakTheBias rather.
I’m not a policy expert nor a sociologist. I don’t know what advice might be helpful here. I’d say raising our collective consciousness of the unfairness, highlighting discrepancies, and advocating for equality are good starts. But, International Women’s Day isn’t new. It’s old. Like over a hundred years old (since 1909 to be exact). We don’t just need a better hashtag, we need to do something. Give equity in pay. Offer opportunities for leadership that accommodate the extra duty women might have outside work. Create flexibility in schedules and without the penalty of having to pump at work or leave early to pick up a child. Not to mention all the opportunities we men have to do more of the household work that women currently do.
The gallant women of Ukraine don’t need our approbation. They need our aid and our prayers. Like the women in my department, at my medical center, in my community, they aren’t posing to be made into posters. There’s work to be done and they are flocking toward it right now.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Physician loses right leg, sues podiatrist; more
, as a story in the Pennsylvania Record, among other news sites, reports.
In December 2020, Mario Adajar, MD, 59, an internist in Wyoming, Penn., sought treatment for his foot calluses and the chronic ulceration of his right foot.
Dr. Adajar consulted a podiatrist, who has surgical privileges at Wilkes-Barre Commonwealth Hospital. According to his complaint, Dr. Adajar made the podiatrist aware that he had type 2 diabetes and had recently undergone a kidney transplant.
Over the next several months, Adajar continued to be treated by the podiatrist who, among other things, debrided and cleaned his patient’s ulcerated right foot on multiple occasions. In June 2021, working out of the hospital’s Wound Healing Center, the podiatrist placed Dr. Adajar’s right leg in a total contact cast.
By the following day, the patient experienced what he later described as “excruciating” pain around the cast. He was also running a fever of 102.3. Taken to a local emergency department, Dr. Adajar soon went into septic shock, accompanied by both atrial fibrillation and acute hypoxic respiratory failure.
Doctors soon had a diagnosis: a gram-negative bacilli infection. Meanwhile, his right leg had become severely gangrenous, of the gas gangrene type. Nevertheless, after treatment, Dr. Adajar was discharged on June 15, 2021, and advised to continue with his follow-up, which included a referral to physical therapy. However, on July 27, 2021, doctors at Wilkes-Barre Commonwealth were forced to amputate Dr. Adajar’s right leg through the fibula and tibia.
In his suit, Dr. Adajar claims that the decision by the podiatrist and his associates to place him in a total contact cast was the direct and immediate cause of his injuries, most catastrophically the amputation of his right leg. He and his legal team are seeking damages “in excess of $50,000,” the standard language in Pennsylvania for cases likely to involve much larger awards.
Dr. Adajar, despite the loss of his right leg, continues to practice internal medicine.
Doctor wins forceps-delivery suit
Last month, a Virginia jury decided in favor of a physician accused of damaging a baby’s eye during delivery, a story in The Winchester Star reports.
In December 2015, Melissa Clements went to Winchester Medical Center, part of Valley Health, to have her baby delivered. Her doctor was ob.gyn. George F. Craft II, at the time a member of Winchester Women’s Specialists. At one point during the roughly 30-minute delivery, Dr. Craft used forceps to remove Ms. Clements’s baby, who in the process sustained facial fractures and left-eye damage.
At trial, Craft argued that a forceps delivery was justified because the baby was stuck and his patient had refused a C-section.
The attorney for the plaintiffs — which included Ms. Clements’s husband — claimed that the use of forceps was premature, as professional guidelines require that a woman in labor be allowed at least 3 hours to push on her own before forceps are employed. (The suit, initially filed in 2019, also accused Dr. Craft of failing to properly inform his patient about the risks of, and alternatives to, this form of delivery. That part of the complaint was dropped, however, prior to the recent trial.)
The jury debated just 50 minutes before deciding Dr. Craft wasn’t medically negligent in the birth of William, Ms. Clements’s now 6-year-old son, who will be forced to wear contact lenses or glasses for life, or undergo corrective surgery.
As Dr. Craft’s attorney explained at trial: “He [Dr. Craft] hoped to give her [Ms. Clements] what she wanted: a vaginal delivery. But forceps techniques can and will cause injuries, even when properly placed.”
Unsupervised PAs subject to med-mal cap, state says
The California Supreme Court ruled late last month that even unsupervised physician assistants (PAs) are protected under the state’s $250,000 cap on noneconomic damages, according to a posting on the website of the Claims Journal, among other news sites.
The ruling stems from a 2013 suit filed by Marisol Lopez, who claimed that a dermatologist, a plastic surgeon, and two PAs had misdiagnosed her child’s skin cancer. Ms. Lopez’s child, Olivia Sarinana, died in February 2014, causing her mother to amend her original claim to a wrongful-death suit.
A trial court found both the doctors and the PAs liable for negligence, awarding the plaintiff $11,200 in economic damages and $4.25 million in noneconomic damages. The court subsequently reduced that amount, however, referencing the state’s $250,000 limit on noneconomic damages, which is part of the Medical Injury Compensation Reform Act of 1975, known as MICRA.
Ms. Lopez appealed the decision, arguing that the cap shouldn’t apply to the two PAs, because neither was under a physician’s direct supervision and therefore not acting within the proper scope of practice, as defined by state law. Despite agreeing with the factual basis of Ms. Lopez’s claim — that neither PA was being supervised during the period in question — the trial court refused to wave the state cap. Ms. Lopez again appealed, and, in a split decision, the Second District Court of Appeal upheld the trial court’s decision.
At this point, attorneys for Ms. Lopez applied for, and obtained, a review before the state’s highest court. Last month, the justices weighed in, ruling that the PAs were still entitled to protection under MICRA because they “had valid delegation-of-service agreements in place.” In other words, while the two PAs had not been directly supervised by a physician, their services had been properly delegated by one.
Said Associate Justice Goodwin Liu, who wrote the opinion: “To be sure, there are reasonable policy arguments for excluding physician assistants who perform medical services without actual supervision from a cap on non-economic damages, and the Legislature is well equipped to weigh and reweigh the competing policy considerations. But our role is confined to interpreting the statute before us in the manner that comports most closely with the Legislature’s purpose in enacting MICRA.”
Despite the high-court ruling, voters may soon get a chance to amend the nearly 5-decades-old MICRA legislation. A November ballot initiative would not only adjust the cap for inflation, raising it to more than $1.2 million, but would also permit “judges and juries to waive the cap entirely for cases involving death and permanent disability.”
Medical groups have said that if either or both of these changes happen the cost of healthcare in the Golden State will surely go up.
The content contained in this article is for informational purposes only and does not constitute legal advice. Reliance on any information provided in this article is solely at your own risk.
A version of this article first appeared on Medscape.com.
, as a story in the Pennsylvania Record, among other news sites, reports.
In December 2020, Mario Adajar, MD, 59, an internist in Wyoming, Penn., sought treatment for his foot calluses and the chronic ulceration of his right foot.
Dr. Adajar consulted a podiatrist, who has surgical privileges at Wilkes-Barre Commonwealth Hospital. According to his complaint, Dr. Adajar made the podiatrist aware that he had type 2 diabetes and had recently undergone a kidney transplant.
Over the next several months, Adajar continued to be treated by the podiatrist who, among other things, debrided and cleaned his patient’s ulcerated right foot on multiple occasions. In June 2021, working out of the hospital’s Wound Healing Center, the podiatrist placed Dr. Adajar’s right leg in a total contact cast.
By the following day, the patient experienced what he later described as “excruciating” pain around the cast. He was also running a fever of 102.3. Taken to a local emergency department, Dr. Adajar soon went into septic shock, accompanied by both atrial fibrillation and acute hypoxic respiratory failure.
Doctors soon had a diagnosis: a gram-negative bacilli infection. Meanwhile, his right leg had become severely gangrenous, of the gas gangrene type. Nevertheless, after treatment, Dr. Adajar was discharged on June 15, 2021, and advised to continue with his follow-up, which included a referral to physical therapy. However, on July 27, 2021, doctors at Wilkes-Barre Commonwealth were forced to amputate Dr. Adajar’s right leg through the fibula and tibia.
In his suit, Dr. Adajar claims that the decision by the podiatrist and his associates to place him in a total contact cast was the direct and immediate cause of his injuries, most catastrophically the amputation of his right leg. He and his legal team are seeking damages “in excess of $50,000,” the standard language in Pennsylvania for cases likely to involve much larger awards.
Dr. Adajar, despite the loss of his right leg, continues to practice internal medicine.
Doctor wins forceps-delivery suit
Last month, a Virginia jury decided in favor of a physician accused of damaging a baby’s eye during delivery, a story in The Winchester Star reports.
In December 2015, Melissa Clements went to Winchester Medical Center, part of Valley Health, to have her baby delivered. Her doctor was ob.gyn. George F. Craft II, at the time a member of Winchester Women’s Specialists. At one point during the roughly 30-minute delivery, Dr. Craft used forceps to remove Ms. Clements’s baby, who in the process sustained facial fractures and left-eye damage.
At trial, Craft argued that a forceps delivery was justified because the baby was stuck and his patient had refused a C-section.
The attorney for the plaintiffs — which included Ms. Clements’s husband — claimed that the use of forceps was premature, as professional guidelines require that a woman in labor be allowed at least 3 hours to push on her own before forceps are employed. (The suit, initially filed in 2019, also accused Dr. Craft of failing to properly inform his patient about the risks of, and alternatives to, this form of delivery. That part of the complaint was dropped, however, prior to the recent trial.)
The jury debated just 50 minutes before deciding Dr. Craft wasn’t medically negligent in the birth of William, Ms. Clements’s now 6-year-old son, who will be forced to wear contact lenses or glasses for life, or undergo corrective surgery.
As Dr. Craft’s attorney explained at trial: “He [Dr. Craft] hoped to give her [Ms. Clements] what she wanted: a vaginal delivery. But forceps techniques can and will cause injuries, even when properly placed.”
Unsupervised PAs subject to med-mal cap, state says
The California Supreme Court ruled late last month that even unsupervised physician assistants (PAs) are protected under the state’s $250,000 cap on noneconomic damages, according to a posting on the website of the Claims Journal, among other news sites.
The ruling stems from a 2013 suit filed by Marisol Lopez, who claimed that a dermatologist, a plastic surgeon, and two PAs had misdiagnosed her child’s skin cancer. Ms. Lopez’s child, Olivia Sarinana, died in February 2014, causing her mother to amend her original claim to a wrongful-death suit.
A trial court found both the doctors and the PAs liable for negligence, awarding the plaintiff $11,200 in economic damages and $4.25 million in noneconomic damages. The court subsequently reduced that amount, however, referencing the state’s $250,000 limit on noneconomic damages, which is part of the Medical Injury Compensation Reform Act of 1975, known as MICRA.
Ms. Lopez appealed the decision, arguing that the cap shouldn’t apply to the two PAs, because neither was under a physician’s direct supervision and therefore not acting within the proper scope of practice, as defined by state law. Despite agreeing with the factual basis of Ms. Lopez’s claim — that neither PA was being supervised during the period in question — the trial court refused to wave the state cap. Ms. Lopez again appealed, and, in a split decision, the Second District Court of Appeal upheld the trial court’s decision.
At this point, attorneys for Ms. Lopez applied for, and obtained, a review before the state’s highest court. Last month, the justices weighed in, ruling that the PAs were still entitled to protection under MICRA because they “had valid delegation-of-service agreements in place.” In other words, while the two PAs had not been directly supervised by a physician, their services had been properly delegated by one.
Said Associate Justice Goodwin Liu, who wrote the opinion: “To be sure, there are reasonable policy arguments for excluding physician assistants who perform medical services without actual supervision from a cap on non-economic damages, and the Legislature is well equipped to weigh and reweigh the competing policy considerations. But our role is confined to interpreting the statute before us in the manner that comports most closely with the Legislature’s purpose in enacting MICRA.”
Despite the high-court ruling, voters may soon get a chance to amend the nearly 5-decades-old MICRA legislation. A November ballot initiative would not only adjust the cap for inflation, raising it to more than $1.2 million, but would also permit “judges and juries to waive the cap entirely for cases involving death and permanent disability.”
Medical groups have said that if either or both of these changes happen the cost of healthcare in the Golden State will surely go up.
The content contained in this article is for informational purposes only and does not constitute legal advice. Reliance on any information provided in this article is solely at your own risk.
A version of this article first appeared on Medscape.com.
, as a story in the Pennsylvania Record, among other news sites, reports.
In December 2020, Mario Adajar, MD, 59, an internist in Wyoming, Penn., sought treatment for his foot calluses and the chronic ulceration of his right foot.
Dr. Adajar consulted a podiatrist, who has surgical privileges at Wilkes-Barre Commonwealth Hospital. According to his complaint, Dr. Adajar made the podiatrist aware that he had type 2 diabetes and had recently undergone a kidney transplant.
Over the next several months, Adajar continued to be treated by the podiatrist who, among other things, debrided and cleaned his patient’s ulcerated right foot on multiple occasions. In June 2021, working out of the hospital’s Wound Healing Center, the podiatrist placed Dr. Adajar’s right leg in a total contact cast.
By the following day, the patient experienced what he later described as “excruciating” pain around the cast. He was also running a fever of 102.3. Taken to a local emergency department, Dr. Adajar soon went into septic shock, accompanied by both atrial fibrillation and acute hypoxic respiratory failure.
Doctors soon had a diagnosis: a gram-negative bacilli infection. Meanwhile, his right leg had become severely gangrenous, of the gas gangrene type. Nevertheless, after treatment, Dr. Adajar was discharged on June 15, 2021, and advised to continue with his follow-up, which included a referral to physical therapy. However, on July 27, 2021, doctors at Wilkes-Barre Commonwealth were forced to amputate Dr. Adajar’s right leg through the fibula and tibia.
In his suit, Dr. Adajar claims that the decision by the podiatrist and his associates to place him in a total contact cast was the direct and immediate cause of his injuries, most catastrophically the amputation of his right leg. He and his legal team are seeking damages “in excess of $50,000,” the standard language in Pennsylvania for cases likely to involve much larger awards.
Dr. Adajar, despite the loss of his right leg, continues to practice internal medicine.
Doctor wins forceps-delivery suit
Last month, a Virginia jury decided in favor of a physician accused of damaging a baby’s eye during delivery, a story in The Winchester Star reports.
In December 2015, Melissa Clements went to Winchester Medical Center, part of Valley Health, to have her baby delivered. Her doctor was ob.gyn. George F. Craft II, at the time a member of Winchester Women’s Specialists. At one point during the roughly 30-minute delivery, Dr. Craft used forceps to remove Ms. Clements’s baby, who in the process sustained facial fractures and left-eye damage.
At trial, Craft argued that a forceps delivery was justified because the baby was stuck and his patient had refused a C-section.
The attorney for the plaintiffs — which included Ms. Clements’s husband — claimed that the use of forceps was premature, as professional guidelines require that a woman in labor be allowed at least 3 hours to push on her own before forceps are employed. (The suit, initially filed in 2019, also accused Dr. Craft of failing to properly inform his patient about the risks of, and alternatives to, this form of delivery. That part of the complaint was dropped, however, prior to the recent trial.)
The jury debated just 50 minutes before deciding Dr. Craft wasn’t medically negligent in the birth of William, Ms. Clements’s now 6-year-old son, who will be forced to wear contact lenses or glasses for life, or undergo corrective surgery.
As Dr. Craft’s attorney explained at trial: “He [Dr. Craft] hoped to give her [Ms. Clements] what she wanted: a vaginal delivery. But forceps techniques can and will cause injuries, even when properly placed.”
Unsupervised PAs subject to med-mal cap, state says
The California Supreme Court ruled late last month that even unsupervised physician assistants (PAs) are protected under the state’s $250,000 cap on noneconomic damages, according to a posting on the website of the Claims Journal, among other news sites.
The ruling stems from a 2013 suit filed by Marisol Lopez, who claimed that a dermatologist, a plastic surgeon, and two PAs had misdiagnosed her child’s skin cancer. Ms. Lopez’s child, Olivia Sarinana, died in February 2014, causing her mother to amend her original claim to a wrongful-death suit.
A trial court found both the doctors and the PAs liable for negligence, awarding the plaintiff $11,200 in economic damages and $4.25 million in noneconomic damages. The court subsequently reduced that amount, however, referencing the state’s $250,000 limit on noneconomic damages, which is part of the Medical Injury Compensation Reform Act of 1975, known as MICRA.
Ms. Lopez appealed the decision, arguing that the cap shouldn’t apply to the two PAs, because neither was under a physician’s direct supervision and therefore not acting within the proper scope of practice, as defined by state law. Despite agreeing with the factual basis of Ms. Lopez’s claim — that neither PA was being supervised during the period in question — the trial court refused to wave the state cap. Ms. Lopez again appealed, and, in a split decision, the Second District Court of Appeal upheld the trial court’s decision.
At this point, attorneys for Ms. Lopez applied for, and obtained, a review before the state’s highest court. Last month, the justices weighed in, ruling that the PAs were still entitled to protection under MICRA because they “had valid delegation-of-service agreements in place.” In other words, while the two PAs had not been directly supervised by a physician, their services had been properly delegated by one.
Said Associate Justice Goodwin Liu, who wrote the opinion: “To be sure, there are reasonable policy arguments for excluding physician assistants who perform medical services without actual supervision from a cap on non-economic damages, and the Legislature is well equipped to weigh and reweigh the competing policy considerations. But our role is confined to interpreting the statute before us in the manner that comports most closely with the Legislature’s purpose in enacting MICRA.”
Despite the high-court ruling, voters may soon get a chance to amend the nearly 5-decades-old MICRA legislation. A November ballot initiative would not only adjust the cap for inflation, raising it to more than $1.2 million, but would also permit “judges and juries to waive the cap entirely for cases involving death and permanent disability.”
Medical groups have said that if either or both of these changes happen the cost of healthcare in the Golden State will surely go up.
The content contained in this article is for informational purposes only and does not constitute legal advice. Reliance on any information provided in this article is solely at your own risk.
A version of this article first appeared on Medscape.com.
Cardiologists say rights to maternity leave violated
A survey of 323 women cardiologists who were working while they were pregnant showed that nearly 75% experienced discriminatory maternity-leave practices, some of which were likely violations of the Family and Medical Leave Act (FMLA).
More than 40% saw their salaries decreased during their year of pregnancy, 38% were required to perform extra service or call before taking maternity leave, exposing them to occupational hazards such as radiation, and 40% experienced a pregnancy complication, significantly higher than the general population and other medical specialties.
Additionally, of those who performed extra service or call, 18% were placed on bedrest before delivery, compared with 7.4% who did not perform extra service or call.
More than half of respondents reported that pregnancy negatively impacted their careers, and 42.4% said they experienced pressure to return to work and a delay in promotions, both illegal practices under the FMLA.
The survey is published in the Journal of the American College of Cardiology.
“Childbearing is difficult for women in cardiology with more than double the rate of gestational complications of the U.S. population, frequent income loss out of proportion to reduced productivity, and for nearly half, has an adverse impact on their career,” lead author Martha Gulati, MD, University of Arizona, Phoenix, said in a statement.
“While many professions struggle to create environments supportive of pregnancy and child-rearing, the prevalence of illegal behavior in cardiology is quite high and presents substantial legal risk for employers,” Dr. Gulati added.
C. Noel Bairey Merz, MD, professor of cardiology at Cedars-Sinai Smidt Heart Institute, Los Angeles, and a coauthor of the survey, told this news organization that it’s not surprising that such a situation exists, even “in this day and age.”
“I’m not surprised as a woman in cardiology myself. I was told by my training director that if I took off more than my allowed sick leave when I had my first and second children, I would have to repeat the year of training, so not surprised at all. I hear this from colleagues all the time,” Dr. Bairey Merz said.
The exchange left her feeling fearful for her career.
“Who wants to repeat a year? It pushes you back from a career standpoint, financially, everything. It also made me angry. I had a colleague who busted his leg in a motorcycle accident. He was unable to do any procedures for 16 weeks, and he didn’t have to repeat the year,” she pointed out.
The challenge that pregnancy represents is frequently cited by women as a deterrent for applying for a cardiology fellowship, Laxmi S. Mehta, MD, Ohio State University, Columbus, and colleagues wrote in an accompanying editorial.
The findings from the survey “reveal restrictive maternity leave data in a profession that has historically and currently continues to have a diversity problem,” they wrote.
“Maternity and pregnancy issues are a thing in cardiology,” Dr. Mehta said in an interview. “It’s one of the reasons why women get deterred from going into the field. It makes it challenging to choose cardiology if you perceive that the culture is negative, that it’s hard to be pregnant, or to bear children, or to take care of them post partum. It is problematic and it should not be occurring now.”
Leadership that condones such restrictive policies or even promotes them through ignorance and inaction needs to be held accountable, she added.
“We need to move forward from this negativity and make it more warm and welcoming to have families, whether you are a trainee or a practicing cardiologist, male or female. We need transparent and consistent parental leave policies and things like lactation support when a woman returns to work. That is a big issue,” Dr. Mehta said.
Having cardiovascular leaders champion the cause of adequate maternity and paternity leave are crucial to creating a newer, inclusive environment in cardiology.
As an example, Dr. Mehta recounted her own experience when she was in training 17 years ago.
“When I interviewed for a cardiology fellowship, one of the female program directors asked me if I was planning to have children, because if I did, the other fellows wouldn’t like it if they had to cover for me,” she said. “I ended up doing my fellowship where the chief of cardiology encouraged me to have children. He said: ‘Have your children during training, we will support you.’ And he did. I still had to do all of the call make-up and that stuff, but I worked in a supportive environment, and it made all the difference.”
“It’s about allyship,” she added. “You will have some people who are supportive and some who are not, but when you have the chief supporting you, you have a strong ally.”
The researchers suggest that one strategy is to temporarily replace cardiologists on maternity leave with locums, or “deepen the bench of coverage for clinical work, as is done for other absences. Given the expanding coverage of parental and family medical leaves, and awareness of these issues nationally, the need for this is likely to become less of an exception and more the rule.”
For example, nine states and Washington, D.C. now provide paid parental leave, they wrote, “and there is pending legislation in others.”
Dr. Bairey Merz and Dr. Mehta reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A survey of 323 women cardiologists who were working while they were pregnant showed that nearly 75% experienced discriminatory maternity-leave practices, some of which were likely violations of the Family and Medical Leave Act (FMLA).
More than 40% saw their salaries decreased during their year of pregnancy, 38% were required to perform extra service or call before taking maternity leave, exposing them to occupational hazards such as radiation, and 40% experienced a pregnancy complication, significantly higher than the general population and other medical specialties.
Additionally, of those who performed extra service or call, 18% were placed on bedrest before delivery, compared with 7.4% who did not perform extra service or call.
More than half of respondents reported that pregnancy negatively impacted their careers, and 42.4% said they experienced pressure to return to work and a delay in promotions, both illegal practices under the FMLA.
The survey is published in the Journal of the American College of Cardiology.
“Childbearing is difficult for women in cardiology with more than double the rate of gestational complications of the U.S. population, frequent income loss out of proportion to reduced productivity, and for nearly half, has an adverse impact on their career,” lead author Martha Gulati, MD, University of Arizona, Phoenix, said in a statement.
“While many professions struggle to create environments supportive of pregnancy and child-rearing, the prevalence of illegal behavior in cardiology is quite high and presents substantial legal risk for employers,” Dr. Gulati added.
C. Noel Bairey Merz, MD, professor of cardiology at Cedars-Sinai Smidt Heart Institute, Los Angeles, and a coauthor of the survey, told this news organization that it’s not surprising that such a situation exists, even “in this day and age.”
“I’m not surprised as a woman in cardiology myself. I was told by my training director that if I took off more than my allowed sick leave when I had my first and second children, I would have to repeat the year of training, so not surprised at all. I hear this from colleagues all the time,” Dr. Bairey Merz said.
The exchange left her feeling fearful for her career.
“Who wants to repeat a year? It pushes you back from a career standpoint, financially, everything. It also made me angry. I had a colleague who busted his leg in a motorcycle accident. He was unable to do any procedures for 16 weeks, and he didn’t have to repeat the year,” she pointed out.
The challenge that pregnancy represents is frequently cited by women as a deterrent for applying for a cardiology fellowship, Laxmi S. Mehta, MD, Ohio State University, Columbus, and colleagues wrote in an accompanying editorial.
The findings from the survey “reveal restrictive maternity leave data in a profession that has historically and currently continues to have a diversity problem,” they wrote.
“Maternity and pregnancy issues are a thing in cardiology,” Dr. Mehta said in an interview. “It’s one of the reasons why women get deterred from going into the field. It makes it challenging to choose cardiology if you perceive that the culture is negative, that it’s hard to be pregnant, or to bear children, or to take care of them post partum. It is problematic and it should not be occurring now.”
Leadership that condones such restrictive policies or even promotes them through ignorance and inaction needs to be held accountable, she added.
“We need to move forward from this negativity and make it more warm and welcoming to have families, whether you are a trainee or a practicing cardiologist, male or female. We need transparent and consistent parental leave policies and things like lactation support when a woman returns to work. That is a big issue,” Dr. Mehta said.
Having cardiovascular leaders champion the cause of adequate maternity and paternity leave are crucial to creating a newer, inclusive environment in cardiology.
As an example, Dr. Mehta recounted her own experience when she was in training 17 years ago.
“When I interviewed for a cardiology fellowship, one of the female program directors asked me if I was planning to have children, because if I did, the other fellows wouldn’t like it if they had to cover for me,” she said. “I ended up doing my fellowship where the chief of cardiology encouraged me to have children. He said: ‘Have your children during training, we will support you.’ And he did. I still had to do all of the call make-up and that stuff, but I worked in a supportive environment, and it made all the difference.”
“It’s about allyship,” she added. “You will have some people who are supportive and some who are not, but when you have the chief supporting you, you have a strong ally.”
The researchers suggest that one strategy is to temporarily replace cardiologists on maternity leave with locums, or “deepen the bench of coverage for clinical work, as is done for other absences. Given the expanding coverage of parental and family medical leaves, and awareness of these issues nationally, the need for this is likely to become less of an exception and more the rule.”
For example, nine states and Washington, D.C. now provide paid parental leave, they wrote, “and there is pending legislation in others.”
Dr. Bairey Merz and Dr. Mehta reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A survey of 323 women cardiologists who were working while they were pregnant showed that nearly 75% experienced discriminatory maternity-leave practices, some of which were likely violations of the Family and Medical Leave Act (FMLA).
More than 40% saw their salaries decreased during their year of pregnancy, 38% were required to perform extra service or call before taking maternity leave, exposing them to occupational hazards such as radiation, and 40% experienced a pregnancy complication, significantly higher than the general population and other medical specialties.
Additionally, of those who performed extra service or call, 18% were placed on bedrest before delivery, compared with 7.4% who did not perform extra service or call.
More than half of respondents reported that pregnancy negatively impacted their careers, and 42.4% said they experienced pressure to return to work and a delay in promotions, both illegal practices under the FMLA.
The survey is published in the Journal of the American College of Cardiology.
“Childbearing is difficult for women in cardiology with more than double the rate of gestational complications of the U.S. population, frequent income loss out of proportion to reduced productivity, and for nearly half, has an adverse impact on their career,” lead author Martha Gulati, MD, University of Arizona, Phoenix, said in a statement.
“While many professions struggle to create environments supportive of pregnancy and child-rearing, the prevalence of illegal behavior in cardiology is quite high and presents substantial legal risk for employers,” Dr. Gulati added.
C. Noel Bairey Merz, MD, professor of cardiology at Cedars-Sinai Smidt Heart Institute, Los Angeles, and a coauthor of the survey, told this news organization that it’s not surprising that such a situation exists, even “in this day and age.”
“I’m not surprised as a woman in cardiology myself. I was told by my training director that if I took off more than my allowed sick leave when I had my first and second children, I would have to repeat the year of training, so not surprised at all. I hear this from colleagues all the time,” Dr. Bairey Merz said.
The exchange left her feeling fearful for her career.
“Who wants to repeat a year? It pushes you back from a career standpoint, financially, everything. It also made me angry. I had a colleague who busted his leg in a motorcycle accident. He was unable to do any procedures for 16 weeks, and he didn’t have to repeat the year,” she pointed out.
The challenge that pregnancy represents is frequently cited by women as a deterrent for applying for a cardiology fellowship, Laxmi S. Mehta, MD, Ohio State University, Columbus, and colleagues wrote in an accompanying editorial.
The findings from the survey “reveal restrictive maternity leave data in a profession that has historically and currently continues to have a diversity problem,” they wrote.
“Maternity and pregnancy issues are a thing in cardiology,” Dr. Mehta said in an interview. “It’s one of the reasons why women get deterred from going into the field. It makes it challenging to choose cardiology if you perceive that the culture is negative, that it’s hard to be pregnant, or to bear children, or to take care of them post partum. It is problematic and it should not be occurring now.”
Leadership that condones such restrictive policies or even promotes them through ignorance and inaction needs to be held accountable, she added.
“We need to move forward from this negativity and make it more warm and welcoming to have families, whether you are a trainee or a practicing cardiologist, male or female. We need transparent and consistent parental leave policies and things like lactation support when a woman returns to work. That is a big issue,” Dr. Mehta said.
Having cardiovascular leaders champion the cause of adequate maternity and paternity leave are crucial to creating a newer, inclusive environment in cardiology.
As an example, Dr. Mehta recounted her own experience when she was in training 17 years ago.
“When I interviewed for a cardiology fellowship, one of the female program directors asked me if I was planning to have children, because if I did, the other fellows wouldn’t like it if they had to cover for me,” she said. “I ended up doing my fellowship where the chief of cardiology encouraged me to have children. He said: ‘Have your children during training, we will support you.’ And he did. I still had to do all of the call make-up and that stuff, but I worked in a supportive environment, and it made all the difference.”
“It’s about allyship,” she added. “You will have some people who are supportive and some who are not, but when you have the chief supporting you, you have a strong ally.”
The researchers suggest that one strategy is to temporarily replace cardiologists on maternity leave with locums, or “deepen the bench of coverage for clinical work, as is done for other absences. Given the expanding coverage of parental and family medical leaves, and awareness of these issues nationally, the need for this is likely to become less of an exception and more the rule.”
For example, nine states and Washington, D.C. now provide paid parental leave, they wrote, “and there is pending legislation in others.”
Dr. Bairey Merz and Dr. Mehta reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Insurance mandates drive genetic testing and sex selection in IVF
The use of preimplantation genetic tests (PGT) in in vitro fertilization cycles, including tests for nonmedical sex selection, increased significantly in states without mandated insurance coverage, based on data from a study of 300,000 IVF cycles.
Previous studies have shown associations between IVF insurance coverage and various IVF practice patterns, but trends in genetic testing according to state-mandated insurance have not been explored, Bronwyn S. Bedrick, MD, of Johns Hopkins University, Baltimore, and colleagues wrote.
“Preimplantation genetic testing was introduced into clinical practice to prevent transmission of genetic disease and to improve uptake of single embryo transfer, but in the real world there are many potential applications,” corresponding author Emily Jungheim, MD, of Northwestern University, Chicago, said in an interview. “We wanted to know how PGT is being applied given that its use is on the rise.”
In a study published in Obstetrics & Gynecology, the researchers analyzed genetic testing in deidentified autologous, nonbanking IVF cycles from 2014 to 2016 obtained through the Society for Assisted Reproductive Technology Clinic Outcome Reporting System (SART CORS). The data set included 301,465 IVF cycles and 224,235 unique patients over the 3-year study period. Of these, 78,578 cycles (26%) used PGT, and overall, the proportion of IVF cycles using PGT approximately doubled, from 17% in 2014 to 34% in 2016 – a significant increase over time (risk ratio, 1.37). As of 2021, 13 states had mandates that health insurance include IVF costs.
In states with insurance mandates versus nonmandated states, the proportion of any PGT was 28.8% vs. 19.6%, and the probability was 32% lower in states with mandates (RR. 0.68; P < .001).
Aneuploidy was the most common indication for PGT, and accounted for 60% of the cycles; however, the number of cycles using PGT for elective sex selection increased from 1,314 cycles in 2014 to 2,184 in 2016 (approximately 66% increase).
In a multivariate analysis, IVF cycles for elective sex selection was 56% lower in states with mandates, compared with those without (RR, 0.44; P < .001).
In addition, cycles involving nonmedical sex selection were significantly more likely to result in male offspring, the researchers said.
“The increase in the number of cycles using elective sex selection seen in this study may reflect the growing number of clinics offering [PGT] for nonmedical sex selection as well as increasing public awareness of preimplantation genetic testing,” the researchers wrote.
However, the socioeconomic characteristics of women may play a role in the use of PGT, as those living in states with no mandate must be able pay the cost of IVF procedures, as well as the cost of PGT if desired, they noted.
“Because fertility centers may offer patients the choice to select the sex of their embryo after preimplantation genetic testing, this may in effect permit elective sex selection,” the researchers said. The shift in the male-female sex ratio in these cases “is concerning given the implications for future social demographics as IVF and preimplantation genetic testing utilization increase, and the negative effect outcomes could have on medical insurance policy and allocation of resources for medically indicated IVF and preimplantation genetic testing.”
The study findings were limited by several factors including the lack of clinic identifiers and lack of data characteristics including, race, ethnicity, and previous live births, the researchers noted. Other limitations included a lack of data on the sex preferences of the couple, and whether the sex of the embryo was known, and whether male and female embryos were transferred. Also, no states have mandates to cover PGT, and the limited study period may not generalize to current practices.
However, the study strengths include the large size and comprehensive database, and have implications for future policies and expansion of insurance coverage for infertility treatment and for preventing transmission of genetic diseases, they said.
Be mindful of consequences of testing
In an interview, Dr. Jungheim said she was surprised by some of the findings. “I thought we would see that PGT-A utilization was lower in states without mandates given the already high cost of IVF for patients paying out of pocket. I was also surprised to see that more males were born after PGT-A; it suggests that overall, patients using PGT-A favor males.
“For clinicians, we need to be mindful of the long-term impact of our practices,” she emphasized. “Shifting the sex ratio in favor of one sex or the other is an unintended consequence of IVF with PGT-A that can have negative implications for future generations.”
In the study, the researchers proposed a revision to the American Society for Reproductive Medicine Ethics Committee opinion on sex selection to provide guidance in keeping with ASRM’s mission of “accessible, ethical, and quality reproductive care for every person.”
However, “even if the ASRM Ethics Committee Opinion was revised, it’s up to clinicians to decide what they are comfortable with,” said Dr. Jungheim. “When patients are paying out of pocket for expensive treatments that require emotional investment and time, it can be difficult to keep medical decision making strictly evidence based.” Improved insurance coverage and access to fertility care may help with some of these decisions, but more real-world evidence is needed.
Let’s talk about sex (selection)
The study findings are both “novel and sobering,” and enhance the current body of evidence of associations between state insurance mandates and IVF outcomes, Jennifer Eaton, MD, of Brown University, Providence, R.I., wrote in an accompanying editorial.
“The association between mandate status and elective sex selection is particularly eye-opening,” said Dr. Eaton. The overall increased use of PGT for sex selection does not account for sex selection as part of testing for aneuploidy. In fact, “patients with euploid embryos of both sexes are frequently given the opportunity to select which embryo to transfer.”
The current study provides “compelling evidence that it is time to revisit the ethical dilemma of elective sex selection in the United States,” Dr. Eaton emphasized. The current ASRM guidance states that IVF clinics are not obligated to provide or refuse to provide nonmedically indicated methods of sex selection, but in light of the current study and other studies, a revision to the existing ASRM Ethics Committee opinion is needed.
The study received no outside funding. Neither the researchers nor Dr. Eaton had any financial conflicts to disclose.
The use of preimplantation genetic tests (PGT) in in vitro fertilization cycles, including tests for nonmedical sex selection, increased significantly in states without mandated insurance coverage, based on data from a study of 300,000 IVF cycles.
Previous studies have shown associations between IVF insurance coverage and various IVF practice patterns, but trends in genetic testing according to state-mandated insurance have not been explored, Bronwyn S. Bedrick, MD, of Johns Hopkins University, Baltimore, and colleagues wrote.
“Preimplantation genetic testing was introduced into clinical practice to prevent transmission of genetic disease and to improve uptake of single embryo transfer, but in the real world there are many potential applications,” corresponding author Emily Jungheim, MD, of Northwestern University, Chicago, said in an interview. “We wanted to know how PGT is being applied given that its use is on the rise.”
In a study published in Obstetrics & Gynecology, the researchers analyzed genetic testing in deidentified autologous, nonbanking IVF cycles from 2014 to 2016 obtained through the Society for Assisted Reproductive Technology Clinic Outcome Reporting System (SART CORS). The data set included 301,465 IVF cycles and 224,235 unique patients over the 3-year study period. Of these, 78,578 cycles (26%) used PGT, and overall, the proportion of IVF cycles using PGT approximately doubled, from 17% in 2014 to 34% in 2016 – a significant increase over time (risk ratio, 1.37). As of 2021, 13 states had mandates that health insurance include IVF costs.
In states with insurance mandates versus nonmandated states, the proportion of any PGT was 28.8% vs. 19.6%, and the probability was 32% lower in states with mandates (RR. 0.68; P < .001).
Aneuploidy was the most common indication for PGT, and accounted for 60% of the cycles; however, the number of cycles using PGT for elective sex selection increased from 1,314 cycles in 2014 to 2,184 in 2016 (approximately 66% increase).
In a multivariate analysis, IVF cycles for elective sex selection was 56% lower in states with mandates, compared with those without (RR, 0.44; P < .001).
In addition, cycles involving nonmedical sex selection were significantly more likely to result in male offspring, the researchers said.
“The increase in the number of cycles using elective sex selection seen in this study may reflect the growing number of clinics offering [PGT] for nonmedical sex selection as well as increasing public awareness of preimplantation genetic testing,” the researchers wrote.
However, the socioeconomic characteristics of women may play a role in the use of PGT, as those living in states with no mandate must be able pay the cost of IVF procedures, as well as the cost of PGT if desired, they noted.
“Because fertility centers may offer patients the choice to select the sex of their embryo after preimplantation genetic testing, this may in effect permit elective sex selection,” the researchers said. The shift in the male-female sex ratio in these cases “is concerning given the implications for future social demographics as IVF and preimplantation genetic testing utilization increase, and the negative effect outcomes could have on medical insurance policy and allocation of resources for medically indicated IVF and preimplantation genetic testing.”
The study findings were limited by several factors including the lack of clinic identifiers and lack of data characteristics including, race, ethnicity, and previous live births, the researchers noted. Other limitations included a lack of data on the sex preferences of the couple, and whether the sex of the embryo was known, and whether male and female embryos were transferred. Also, no states have mandates to cover PGT, and the limited study period may not generalize to current practices.
However, the study strengths include the large size and comprehensive database, and have implications for future policies and expansion of insurance coverage for infertility treatment and for preventing transmission of genetic diseases, they said.
Be mindful of consequences of testing
In an interview, Dr. Jungheim said she was surprised by some of the findings. “I thought we would see that PGT-A utilization was lower in states without mandates given the already high cost of IVF for patients paying out of pocket. I was also surprised to see that more males were born after PGT-A; it suggests that overall, patients using PGT-A favor males.
“For clinicians, we need to be mindful of the long-term impact of our practices,” she emphasized. “Shifting the sex ratio in favor of one sex or the other is an unintended consequence of IVF with PGT-A that can have negative implications for future generations.”
In the study, the researchers proposed a revision to the American Society for Reproductive Medicine Ethics Committee opinion on sex selection to provide guidance in keeping with ASRM’s mission of “accessible, ethical, and quality reproductive care for every person.”
However, “even if the ASRM Ethics Committee Opinion was revised, it’s up to clinicians to decide what they are comfortable with,” said Dr. Jungheim. “When patients are paying out of pocket for expensive treatments that require emotional investment and time, it can be difficult to keep medical decision making strictly evidence based.” Improved insurance coverage and access to fertility care may help with some of these decisions, but more real-world evidence is needed.
Let’s talk about sex (selection)
The study findings are both “novel and sobering,” and enhance the current body of evidence of associations between state insurance mandates and IVF outcomes, Jennifer Eaton, MD, of Brown University, Providence, R.I., wrote in an accompanying editorial.
“The association between mandate status and elective sex selection is particularly eye-opening,” said Dr. Eaton. The overall increased use of PGT for sex selection does not account for sex selection as part of testing for aneuploidy. In fact, “patients with euploid embryos of both sexes are frequently given the opportunity to select which embryo to transfer.”
The current study provides “compelling evidence that it is time to revisit the ethical dilemma of elective sex selection in the United States,” Dr. Eaton emphasized. The current ASRM guidance states that IVF clinics are not obligated to provide or refuse to provide nonmedically indicated methods of sex selection, but in light of the current study and other studies, a revision to the existing ASRM Ethics Committee opinion is needed.
The study received no outside funding. Neither the researchers nor Dr. Eaton had any financial conflicts to disclose.
The use of preimplantation genetic tests (PGT) in in vitro fertilization cycles, including tests for nonmedical sex selection, increased significantly in states without mandated insurance coverage, based on data from a study of 300,000 IVF cycles.
Previous studies have shown associations between IVF insurance coverage and various IVF practice patterns, but trends in genetic testing according to state-mandated insurance have not been explored, Bronwyn S. Bedrick, MD, of Johns Hopkins University, Baltimore, and colleagues wrote.
“Preimplantation genetic testing was introduced into clinical practice to prevent transmission of genetic disease and to improve uptake of single embryo transfer, but in the real world there are many potential applications,” corresponding author Emily Jungheim, MD, of Northwestern University, Chicago, said in an interview. “We wanted to know how PGT is being applied given that its use is on the rise.”
In a study published in Obstetrics & Gynecology, the researchers analyzed genetic testing in deidentified autologous, nonbanking IVF cycles from 2014 to 2016 obtained through the Society for Assisted Reproductive Technology Clinic Outcome Reporting System (SART CORS). The data set included 301,465 IVF cycles and 224,235 unique patients over the 3-year study period. Of these, 78,578 cycles (26%) used PGT, and overall, the proportion of IVF cycles using PGT approximately doubled, from 17% in 2014 to 34% in 2016 – a significant increase over time (risk ratio, 1.37). As of 2021, 13 states had mandates that health insurance include IVF costs.
In states with insurance mandates versus nonmandated states, the proportion of any PGT was 28.8% vs. 19.6%, and the probability was 32% lower in states with mandates (RR. 0.68; P < .001).
Aneuploidy was the most common indication for PGT, and accounted for 60% of the cycles; however, the number of cycles using PGT for elective sex selection increased from 1,314 cycles in 2014 to 2,184 in 2016 (approximately 66% increase).
In a multivariate analysis, IVF cycles for elective sex selection was 56% lower in states with mandates, compared with those without (RR, 0.44; P < .001).
In addition, cycles involving nonmedical sex selection were significantly more likely to result in male offspring, the researchers said.
“The increase in the number of cycles using elective sex selection seen in this study may reflect the growing number of clinics offering [PGT] for nonmedical sex selection as well as increasing public awareness of preimplantation genetic testing,” the researchers wrote.
However, the socioeconomic characteristics of women may play a role in the use of PGT, as those living in states with no mandate must be able pay the cost of IVF procedures, as well as the cost of PGT if desired, they noted.
“Because fertility centers may offer patients the choice to select the sex of their embryo after preimplantation genetic testing, this may in effect permit elective sex selection,” the researchers said. The shift in the male-female sex ratio in these cases “is concerning given the implications for future social demographics as IVF and preimplantation genetic testing utilization increase, and the negative effect outcomes could have on medical insurance policy and allocation of resources for medically indicated IVF and preimplantation genetic testing.”
The study findings were limited by several factors including the lack of clinic identifiers and lack of data characteristics including, race, ethnicity, and previous live births, the researchers noted. Other limitations included a lack of data on the sex preferences of the couple, and whether the sex of the embryo was known, and whether male and female embryos were transferred. Also, no states have mandates to cover PGT, and the limited study period may not generalize to current practices.
However, the study strengths include the large size and comprehensive database, and have implications for future policies and expansion of insurance coverage for infertility treatment and for preventing transmission of genetic diseases, they said.
Be mindful of consequences of testing
In an interview, Dr. Jungheim said she was surprised by some of the findings. “I thought we would see that PGT-A utilization was lower in states without mandates given the already high cost of IVF for patients paying out of pocket. I was also surprised to see that more males were born after PGT-A; it suggests that overall, patients using PGT-A favor males.
“For clinicians, we need to be mindful of the long-term impact of our practices,” she emphasized. “Shifting the sex ratio in favor of one sex or the other is an unintended consequence of IVF with PGT-A that can have negative implications for future generations.”
In the study, the researchers proposed a revision to the American Society for Reproductive Medicine Ethics Committee opinion on sex selection to provide guidance in keeping with ASRM’s mission of “accessible, ethical, and quality reproductive care for every person.”
However, “even if the ASRM Ethics Committee Opinion was revised, it’s up to clinicians to decide what they are comfortable with,” said Dr. Jungheim. “When patients are paying out of pocket for expensive treatments that require emotional investment and time, it can be difficult to keep medical decision making strictly evidence based.” Improved insurance coverage and access to fertility care may help with some of these decisions, but more real-world evidence is needed.
Let’s talk about sex (selection)
The study findings are both “novel and sobering,” and enhance the current body of evidence of associations between state insurance mandates and IVF outcomes, Jennifer Eaton, MD, of Brown University, Providence, R.I., wrote in an accompanying editorial.
“The association between mandate status and elective sex selection is particularly eye-opening,” said Dr. Eaton. The overall increased use of PGT for sex selection does not account for sex selection as part of testing for aneuploidy. In fact, “patients with euploid embryos of both sexes are frequently given the opportunity to select which embryo to transfer.”
The current study provides “compelling evidence that it is time to revisit the ethical dilemma of elective sex selection in the United States,” Dr. Eaton emphasized. The current ASRM guidance states that IVF clinics are not obligated to provide or refuse to provide nonmedically indicated methods of sex selection, but in light of the current study and other studies, a revision to the existing ASRM Ethics Committee opinion is needed.
The study received no outside funding. Neither the researchers nor Dr. Eaton had any financial conflicts to disclose.
FROM OBSTETRICS & GYNECOLOGY
Study: Majority of research on homeopathic remedies unpublished or unregistered
Homeopathy is a form of alternative medicine based on the concept that increasing dilution of a substance leads to a stronger treatment effect.
The authors of the new paper, published in BMJ Evidence-Based Medicine, also found that a quarter of the 90 randomized published trials on homeopathic remedies they analyzed changed their results before publication.
The benefits of homeopathy touted in studies may be greatly exaggerated, suggest the authors, Gerald Gartlehner, MD, of Danube University, Krems, Austria, and colleagues.
The results raise awareness that published homeopathy trials represent a limited proportion of research, skewed toward favorable results, they wrote.
“This likely affects the validity of the body of evidence of homeopathic literature and may substantially overestimate the true treatment effect of homeopathic remedies,” they concluded.
Homeopathy as practiced today was developed approximately 200 years ago in Germany, and despite ongoing debate about its effectiveness, it remains a popular alternative to conventional medicine in many developed countries, the authors noted.
According to the National Institutes of Health, homeopathy is based on the idea of “like cures like,” meaning that a disease can be cured with a substance that produces similar symptoms in healthy people, and the “law of minimum dose,” meaning that a lower dose of medication will be more effective. “Many homeopathic products are so diluted that no molecules of the original substance remain,” according to the NIH.
Homeopathy is not subject to most regulatory requirements, so assessment of effectiveness of homeopathic remedies is limited to published data, the researchers said. “When no information is publicly available about the majority of homeopathic trials, sound conclusions about the efficacy and the risks of using homeopathic medicinal products for treating health conditions are impossible,” they wrote.
Study methods and findings
The researchers examined 17 trial registries for studies involving homeopathic remedies conducted since 2002.
The registries included clinicaltrials.gov, the EU Clinical Trials Register, and the International Clinical Trials Registry Platform up to April 2019 to identify registered homeopathy trials.
To determine whether registered trials were published and to identify trials that were published but unregistered, the researchers examined PubMed, the Allied and Complementary Medicine Database, Embase, and Google Scholar up to April 2021.
They found that approximately 38% of registered trials of homeopathy were never published, and 53% of the published randomized, controlled trials (RCTs) were not registered. Notably, 25% of the trials that were registered and published showed primary outcomes that were changed compared with the registry.
The number of registered homeopathy trials increased significantly over the past 5 years, but approximately one-third (30%) of trials published during the last 5 years were not registered, they said. In a meta-analysis, unregistered RCTs showed significantly greater treatment effects than registered RCTs, with standardized mean differences of –0.53 and –0.14, respectively.
The study findings were limited by several factors including the potential for missed records of studies not covered by the registries searched. Other limitations include the analysis of pooled data from homeopathic treatments that may not generalize to personalized homeopathy, and the exclusion of trials labeled as terminated or suspended.
Proceed with caution before recommending use of homeopathic remedies, says expert
Linda Girgis, MD, noted that prior to reading this report she had known that most homeopathic remedies didn’t have any evidence of being effective, and that, therefore, the results validated her understanding of the findings of studies of homeopathy.
The study is especially important at this time in the wake of the COVID-19 pandemic, Dr. Girgis, a family physician in private practice in South River, N.J., said in an interview.
“Many people are promoting treatments that don’t have any evidence that they are effective, and more people are turning to homeopathic treatments not knowing the risks and assuming they are safe,” she continued. “Many people are taking advantage of this and trying to cash in on this with ill-proven remedies.”
Homeopathic remedies become especially harmful when patients think they can use them instead of traditional medicine, she added.
Noting that some homeopathic remedies have been studied and show some evidence that they work, Dr. Girgis said there may be a role for certain ones in primary care.
“An example would be black cohosh or primrose oil for perimenopausal hot flashes. This could be a good alternative when you want to avoid hormonal supplements,” she said.
At the same time, Dr. Girgis advised clinicians to be cautious about suggesting homeopathic remedies to patients.
“Homeopathy seems to be a good money maker if you sell these products. However, you are not protected from liability and can be found more liable for prescribing off-label treatments or those not [Food and Drug Administration] approved,” Dr. Girgis said. Her general message to clinicians: Stick with evidence-based medicine.
Her message to patients who might want to pursue homeopathic remedies is that just because something is “homeopathic” or natural doesn’t mean that it is safe.
“There are some [homeopathic] products that have caused liver damage or other problems,” she explained. “Also, these remedies can interact with other medications.”
The study received no outside funding. The researchers and Dr. Girgis had no financial conflicts to disclose.
Homeopathy is a form of alternative medicine based on the concept that increasing dilution of a substance leads to a stronger treatment effect.
The authors of the new paper, published in BMJ Evidence-Based Medicine, also found that a quarter of the 90 randomized published trials on homeopathic remedies they analyzed changed their results before publication.
The benefits of homeopathy touted in studies may be greatly exaggerated, suggest the authors, Gerald Gartlehner, MD, of Danube University, Krems, Austria, and colleagues.
The results raise awareness that published homeopathy trials represent a limited proportion of research, skewed toward favorable results, they wrote.
“This likely affects the validity of the body of evidence of homeopathic literature and may substantially overestimate the true treatment effect of homeopathic remedies,” they concluded.
Homeopathy as practiced today was developed approximately 200 years ago in Germany, and despite ongoing debate about its effectiveness, it remains a popular alternative to conventional medicine in many developed countries, the authors noted.
According to the National Institutes of Health, homeopathy is based on the idea of “like cures like,” meaning that a disease can be cured with a substance that produces similar symptoms in healthy people, and the “law of minimum dose,” meaning that a lower dose of medication will be more effective. “Many homeopathic products are so diluted that no molecules of the original substance remain,” according to the NIH.
Homeopathy is not subject to most regulatory requirements, so assessment of effectiveness of homeopathic remedies is limited to published data, the researchers said. “When no information is publicly available about the majority of homeopathic trials, sound conclusions about the efficacy and the risks of using homeopathic medicinal products for treating health conditions are impossible,” they wrote.
Study methods and findings
The researchers examined 17 trial registries for studies involving homeopathic remedies conducted since 2002.
The registries included clinicaltrials.gov, the EU Clinical Trials Register, and the International Clinical Trials Registry Platform up to April 2019 to identify registered homeopathy trials.
To determine whether registered trials were published and to identify trials that were published but unregistered, the researchers examined PubMed, the Allied and Complementary Medicine Database, Embase, and Google Scholar up to April 2021.
They found that approximately 38% of registered trials of homeopathy were never published, and 53% of the published randomized, controlled trials (RCTs) were not registered. Notably, 25% of the trials that were registered and published showed primary outcomes that were changed compared with the registry.
The number of registered homeopathy trials increased significantly over the past 5 years, but approximately one-third (30%) of trials published during the last 5 years were not registered, they said. In a meta-analysis, unregistered RCTs showed significantly greater treatment effects than registered RCTs, with standardized mean differences of –0.53 and –0.14, respectively.
The study findings were limited by several factors including the potential for missed records of studies not covered by the registries searched. Other limitations include the analysis of pooled data from homeopathic treatments that may not generalize to personalized homeopathy, and the exclusion of trials labeled as terminated or suspended.
Proceed with caution before recommending use of homeopathic remedies, says expert
Linda Girgis, MD, noted that prior to reading this report she had known that most homeopathic remedies didn’t have any evidence of being effective, and that, therefore, the results validated her understanding of the findings of studies of homeopathy.
The study is especially important at this time in the wake of the COVID-19 pandemic, Dr. Girgis, a family physician in private practice in South River, N.J., said in an interview.
“Many people are promoting treatments that don’t have any evidence that they are effective, and more people are turning to homeopathic treatments not knowing the risks and assuming they are safe,” she continued. “Many people are taking advantage of this and trying to cash in on this with ill-proven remedies.”
Homeopathic remedies become especially harmful when patients think they can use them instead of traditional medicine, she added.
Noting that some homeopathic remedies have been studied and show some evidence that they work, Dr. Girgis said there may be a role for certain ones in primary care.
“An example would be black cohosh or primrose oil for perimenopausal hot flashes. This could be a good alternative when you want to avoid hormonal supplements,” she said.
At the same time, Dr. Girgis advised clinicians to be cautious about suggesting homeopathic remedies to patients.
“Homeopathy seems to be a good money maker if you sell these products. However, you are not protected from liability and can be found more liable for prescribing off-label treatments or those not [Food and Drug Administration] approved,” Dr. Girgis said. Her general message to clinicians: Stick with evidence-based medicine.
Her message to patients who might want to pursue homeopathic remedies is that just because something is “homeopathic” or natural doesn’t mean that it is safe.
“There are some [homeopathic] products that have caused liver damage or other problems,” she explained. “Also, these remedies can interact with other medications.”
The study received no outside funding. The researchers and Dr. Girgis had no financial conflicts to disclose.
Homeopathy is a form of alternative medicine based on the concept that increasing dilution of a substance leads to a stronger treatment effect.
The authors of the new paper, published in BMJ Evidence-Based Medicine, also found that a quarter of the 90 randomized published trials on homeopathic remedies they analyzed changed their results before publication.
The benefits of homeopathy touted in studies may be greatly exaggerated, suggest the authors, Gerald Gartlehner, MD, of Danube University, Krems, Austria, and colleagues.
The results raise awareness that published homeopathy trials represent a limited proportion of research, skewed toward favorable results, they wrote.
“This likely affects the validity of the body of evidence of homeopathic literature and may substantially overestimate the true treatment effect of homeopathic remedies,” they concluded.
Homeopathy as practiced today was developed approximately 200 years ago in Germany, and despite ongoing debate about its effectiveness, it remains a popular alternative to conventional medicine in many developed countries, the authors noted.
According to the National Institutes of Health, homeopathy is based on the idea of “like cures like,” meaning that a disease can be cured with a substance that produces similar symptoms in healthy people, and the “law of minimum dose,” meaning that a lower dose of medication will be more effective. “Many homeopathic products are so diluted that no molecules of the original substance remain,” according to the NIH.
Homeopathy is not subject to most regulatory requirements, so assessment of effectiveness of homeopathic remedies is limited to published data, the researchers said. “When no information is publicly available about the majority of homeopathic trials, sound conclusions about the efficacy and the risks of using homeopathic medicinal products for treating health conditions are impossible,” they wrote.
Study methods and findings
The researchers examined 17 trial registries for studies involving homeopathic remedies conducted since 2002.
The registries included clinicaltrials.gov, the EU Clinical Trials Register, and the International Clinical Trials Registry Platform up to April 2019 to identify registered homeopathy trials.
To determine whether registered trials were published and to identify trials that were published but unregistered, the researchers examined PubMed, the Allied and Complementary Medicine Database, Embase, and Google Scholar up to April 2021.
They found that approximately 38% of registered trials of homeopathy were never published, and 53% of the published randomized, controlled trials (RCTs) were not registered. Notably, 25% of the trials that were registered and published showed primary outcomes that were changed compared with the registry.
The number of registered homeopathy trials increased significantly over the past 5 years, but approximately one-third (30%) of trials published during the last 5 years were not registered, they said. In a meta-analysis, unregistered RCTs showed significantly greater treatment effects than registered RCTs, with standardized mean differences of –0.53 and –0.14, respectively.
The study findings were limited by several factors including the potential for missed records of studies not covered by the registries searched. Other limitations include the analysis of pooled data from homeopathic treatments that may not generalize to personalized homeopathy, and the exclusion of trials labeled as terminated or suspended.
Proceed with caution before recommending use of homeopathic remedies, says expert
Linda Girgis, MD, noted that prior to reading this report she had known that most homeopathic remedies didn’t have any evidence of being effective, and that, therefore, the results validated her understanding of the findings of studies of homeopathy.
The study is especially important at this time in the wake of the COVID-19 pandemic, Dr. Girgis, a family physician in private practice in South River, N.J., said in an interview.
“Many people are promoting treatments that don’t have any evidence that they are effective, and more people are turning to homeopathic treatments not knowing the risks and assuming they are safe,” she continued. “Many people are taking advantage of this and trying to cash in on this with ill-proven remedies.”
Homeopathic remedies become especially harmful when patients think they can use them instead of traditional medicine, she added.
Noting that some homeopathic remedies have been studied and show some evidence that they work, Dr. Girgis said there may be a role for certain ones in primary care.
“An example would be black cohosh or primrose oil for perimenopausal hot flashes. This could be a good alternative when you want to avoid hormonal supplements,” she said.
At the same time, Dr. Girgis advised clinicians to be cautious about suggesting homeopathic remedies to patients.
“Homeopathy seems to be a good money maker if you sell these products. However, you are not protected from liability and can be found more liable for prescribing off-label treatments or those not [Food and Drug Administration] approved,” Dr. Girgis said. Her general message to clinicians: Stick with evidence-based medicine.
Her message to patients who might want to pursue homeopathic remedies is that just because something is “homeopathic” or natural doesn’t mean that it is safe.
“There are some [homeopathic] products that have caused liver damage or other problems,” she explained. “Also, these remedies can interact with other medications.”
The study received no outside funding. The researchers and Dr. Girgis had no financial conflicts to disclose.
FROM BMJ EVIDENCE BASED MEDICINE









