User login
How much would you bet on a diagnosis?
“You have psoriasis,” I say all the time. I mean it when I say it, of course. But I don’t always to the same degree. Sometimes I’m trying to say, “You probably have psoriasis.” Other times I mean, “You most definitely have psoriasis.” I rarely use those terms though.
One 36-year-old man with a flaky scalp and scaly elbows wasn’t satisfied with my assessment. His dad has psoriasis. So does his older brother. He was in to see me to find out if he had psoriasis too. “Probably” was what I gave him. He pushed back, “What percent chance?” That’s a good question — must be an engineer. I’m unsure.
With the exception of the poker players, our species is notoriously bad at probabilities. We’re wired to notice the significance of events, but terrible at understanding their likelihood. This is salient in lottery ticket holders and some NFL offensive coordinators who persist despite very long odds of things working out. It’s also reflected in the language we use. Rarely do we say, there’s a sixty percent chance something will happen. Rather, we say, “it’s likely.” There are two problems here. One, we often misjudge the actual probability of something occurring and two, the terms we use are subjective and differences in interpretation can lead to misunderstandings.
Let’s take a look. A 55-year-old man with a chronic eczematous rash on his trunk and extremities is getting worse despite dupilumab. He recently had night sweats. Do you think he has atopic dermatitis or cutaneous T-cell lymphoma? If you had to place a $100 bet, would you change your answer? Immanuel Kant thinks you would. In his “Critique of Pure Reason,” the German philosopher proposes that betting helps clarify the mind, an antidote to brashness. The example Kant uses is of a physician who observes a patient and concludes he has phthisis (tuberculosis), but we really don’t know if the physician is confident. Kant proposes that if he had to bet on his conclusion, then we’d have insight into just how convinced he is of phthisis. So, what’s your bet?
If you’re a bad poker player, then you might bet he has cutaneous T-cell lymphoma. However, not having any additional information, the smart call is atopic dermatitis, which has a base rate 1000-fold higher than CTCL. It is therefore more probable to be eczema even in a case that worsens despite dupilumab or with recent night sweats, both of which could be a result of common variables such as weather and COVID. Failure to account for the base rate is a mistake we physicians sometimes make. Economists rarely do. Try to think like one before answering a likelihood question.
If you think about it, “probably” means something different even to me, depending on the situation. I might say I’ll probably go to Montana this summer and I’ll probably retire at 65. The actual likelihoods might be 95% and 70%. That’s a big difference. What about between probably and likely? Or possibly and maybe? Do they mean the same to you as to the person you’re speaking with? For much of the work we do, precise likelihoods aren’t critical. Yet, it can be important in decision making and in discussing probabilities, such as the risk of hepatitis on terbinafine or of melanoma recurrence after Mohs.
I told my patient “I say about a 70% chance you have psoriasis. I could do a biopsy today to confirm.” He thought for a second and asked, “What is the chance it’s psoriasis if the biopsy shows it?” “Eighty six percent,” I replied.
Seemed like a good bet to me.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at [email protected].
“You have psoriasis,” I say all the time. I mean it when I say it, of course. But I don’t always to the same degree. Sometimes I’m trying to say, “You probably have psoriasis.” Other times I mean, “You most definitely have psoriasis.” I rarely use those terms though.
One 36-year-old man with a flaky scalp and scaly elbows wasn’t satisfied with my assessment. His dad has psoriasis. So does his older brother. He was in to see me to find out if he had psoriasis too. “Probably” was what I gave him. He pushed back, “What percent chance?” That’s a good question — must be an engineer. I’m unsure.
With the exception of the poker players, our species is notoriously bad at probabilities. We’re wired to notice the significance of events, but terrible at understanding their likelihood. This is salient in lottery ticket holders and some NFL offensive coordinators who persist despite very long odds of things working out. It’s also reflected in the language we use. Rarely do we say, there’s a sixty percent chance something will happen. Rather, we say, “it’s likely.” There are two problems here. One, we often misjudge the actual probability of something occurring and two, the terms we use are subjective and differences in interpretation can lead to misunderstandings.
Let’s take a look. A 55-year-old man with a chronic eczematous rash on his trunk and extremities is getting worse despite dupilumab. He recently had night sweats. Do you think he has atopic dermatitis or cutaneous T-cell lymphoma? If you had to place a $100 bet, would you change your answer? Immanuel Kant thinks you would. In his “Critique of Pure Reason,” the German philosopher proposes that betting helps clarify the mind, an antidote to brashness. The example Kant uses is of a physician who observes a patient and concludes he has phthisis (tuberculosis), but we really don’t know if the physician is confident. Kant proposes that if he had to bet on his conclusion, then we’d have insight into just how convinced he is of phthisis. So, what’s your bet?
If you’re a bad poker player, then you might bet he has cutaneous T-cell lymphoma. However, not having any additional information, the smart call is atopic dermatitis, which has a base rate 1000-fold higher than CTCL. It is therefore more probable to be eczema even in a case that worsens despite dupilumab or with recent night sweats, both of which could be a result of common variables such as weather and COVID. Failure to account for the base rate is a mistake we physicians sometimes make. Economists rarely do. Try to think like one before answering a likelihood question.
If you think about it, “probably” means something different even to me, depending on the situation. I might say I’ll probably go to Montana this summer and I’ll probably retire at 65. The actual likelihoods might be 95% and 70%. That’s a big difference. What about between probably and likely? Or possibly and maybe? Do they mean the same to you as to the person you’re speaking with? For much of the work we do, precise likelihoods aren’t critical. Yet, it can be important in decision making and in discussing probabilities, such as the risk of hepatitis on terbinafine or of melanoma recurrence after Mohs.
I told my patient “I say about a 70% chance you have psoriasis. I could do a biopsy today to confirm.” He thought for a second and asked, “What is the chance it’s psoriasis if the biopsy shows it?” “Eighty six percent,” I replied.
Seemed like a good bet to me.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at [email protected].
“You have psoriasis,” I say all the time. I mean it when I say it, of course. But I don’t always to the same degree. Sometimes I’m trying to say, “You probably have psoriasis.” Other times I mean, “You most definitely have psoriasis.” I rarely use those terms though.
One 36-year-old man with a flaky scalp and scaly elbows wasn’t satisfied with my assessment. His dad has psoriasis. So does his older brother. He was in to see me to find out if he had psoriasis too. “Probably” was what I gave him. He pushed back, “What percent chance?” That’s a good question — must be an engineer. I’m unsure.
With the exception of the poker players, our species is notoriously bad at probabilities. We’re wired to notice the significance of events, but terrible at understanding their likelihood. This is salient in lottery ticket holders and some NFL offensive coordinators who persist despite very long odds of things working out. It’s also reflected in the language we use. Rarely do we say, there’s a sixty percent chance something will happen. Rather, we say, “it’s likely.” There are two problems here. One, we often misjudge the actual probability of something occurring and two, the terms we use are subjective and differences in interpretation can lead to misunderstandings.
Let’s take a look. A 55-year-old man with a chronic eczematous rash on his trunk and extremities is getting worse despite dupilumab. He recently had night sweats. Do you think he has atopic dermatitis or cutaneous T-cell lymphoma? If you had to place a $100 bet, would you change your answer? Immanuel Kant thinks you would. In his “Critique of Pure Reason,” the German philosopher proposes that betting helps clarify the mind, an antidote to brashness. The example Kant uses is of a physician who observes a patient and concludes he has phthisis (tuberculosis), but we really don’t know if the physician is confident. Kant proposes that if he had to bet on his conclusion, then we’d have insight into just how convinced he is of phthisis. So, what’s your bet?
If you’re a bad poker player, then you might bet he has cutaneous T-cell lymphoma. However, not having any additional information, the smart call is atopic dermatitis, which has a base rate 1000-fold higher than CTCL. It is therefore more probable to be eczema even in a case that worsens despite dupilumab or with recent night sweats, both of which could be a result of common variables such as weather and COVID. Failure to account for the base rate is a mistake we physicians sometimes make. Economists rarely do. Try to think like one before answering a likelihood question.
If you think about it, “probably” means something different even to me, depending on the situation. I might say I’ll probably go to Montana this summer and I’ll probably retire at 65. The actual likelihoods might be 95% and 70%. That’s a big difference. What about between probably and likely? Or possibly and maybe? Do they mean the same to you as to the person you’re speaking with? For much of the work we do, precise likelihoods aren’t critical. Yet, it can be important in decision making and in discussing probabilities, such as the risk of hepatitis on terbinafine or of melanoma recurrence after Mohs.
I told my patient “I say about a 70% chance you have psoriasis. I could do a biopsy today to confirm.” He thought for a second and asked, “What is the chance it’s psoriasis if the biopsy shows it?” “Eighty six percent,” I replied.
Seemed like a good bet to me.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at [email protected].
Cutting Across the Bias
On a recent rainy afternoon I was speed skimming through the pile of publications sitting on the floor next to my Grampy’s chair. A bright patch of color jumped off the gray background of the printed page forcing me to pause and consider the content.
In the right upper corner was a photograph of an attractive Black woman nursing her baby. Her bare arms suggested she might be slightly overweight. She wore a simple off-white head wrap and smiled broadly as she played with her infant’s fingers. The image was a reproduction of a WIC poster encouraging women to take advantage of the program’s breastfeeding support services. The accompanying article from American Academy of Pediatrics offered ten strategies for achieving breastfeeding equity.
I must admit that I tend to shy away from discussions of equity because I’ve seldom found them very informative. However, the engaging image of this Black woman breastfeeding led me to read beyond the title.
The first of the strategies listed was “Check you biases.” I will certainly admit to having biases. We all have biases and see and interpret the world through lenses ground and tinted by our experiences and the environment we have inhabited. In the case of breastfeeding, I wasn’t sure where my biases lay. Maybe one of mine is reflected in a hesitancy to actively promote exclusive breastfeeding for the first 6 months. I prefer a more nuanced approach adjusted to the unique needs and limitations of each family. But I decided to chase down the Implicit Association Test (IAT) suggested in the article. I couldn’t make that link work, but found a long list of subjects on the Harvard Implicit Association Test website. None dealt with breastfeeding, so I chose the one described as Black/White.
If, like me, you have never had your implicit biases assessed by taking an IAT, you might find it interesting. Probably took me about 15 minutes using my laptop. There are a lot of demographic questions then some rapid-fire exercises in which you must provide your first response to a barrage of photos of faces and words. At times I sensed that the test makers were trying to trick me into making associations that I didn’t want to make by the order in which the exercises were presented. At the end I was told that I was a little slow in associating Black faces with positive words.
I’m not sure what this means. After doing a little internet searching I learned that one of the criticisms of the IAT is that, while it may hint at a bias, it is really more important whether you cut with or across that bias. If I acknowledge that where and how I grew up may have left me with some implicit biases, it is more important that I make a strong and honest effort to act independently of those biases.
In full disclosure I must tell you that there was one Black girl in my high school of a thousand students. I have lived and practiced in Maine for 50 years. At less than 2%, we are sixth from the bottom in Black population among other states. However, in the last 5 or 6 years here in Brunswick we have welcomed a large infusion of asylum seekers who come predominantly from Black African countries.
Skimming through the rest of the article, I found it hard to argue with the remaining nine recommendations for promoting breastfeeding, although most of them we not terribly applicable to small community practices. The photo of the Black woman nursing her baby at the top of the page remains as the primary message. The fact that I was drawn to that image is a testament to several of my biases and another example of a picture being worth far more than a thousand words.
I suspect that I’m not alone in appreciating the uniqueness of that image. Until recently, the standard photos of a mother breastfeeding have used trim White women as their models. I suspect and hope this poster will be effective in encouraging Black women to nurse. I urge you all to hang it in your office as a reminder to you and your staff of your biases and assumptions. Don’t bother to take the Implicit Association Test unless you’re retired and have 15 minutes to burn on a rainy afternoon.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
On a recent rainy afternoon I was speed skimming through the pile of publications sitting on the floor next to my Grampy’s chair. A bright patch of color jumped off the gray background of the printed page forcing me to pause and consider the content.
In the right upper corner was a photograph of an attractive Black woman nursing her baby. Her bare arms suggested she might be slightly overweight. She wore a simple off-white head wrap and smiled broadly as she played with her infant’s fingers. The image was a reproduction of a WIC poster encouraging women to take advantage of the program’s breastfeeding support services. The accompanying article from American Academy of Pediatrics offered ten strategies for achieving breastfeeding equity.
I must admit that I tend to shy away from discussions of equity because I’ve seldom found them very informative. However, the engaging image of this Black woman breastfeeding led me to read beyond the title.
The first of the strategies listed was “Check you biases.” I will certainly admit to having biases. We all have biases and see and interpret the world through lenses ground and tinted by our experiences and the environment we have inhabited. In the case of breastfeeding, I wasn’t sure where my biases lay. Maybe one of mine is reflected in a hesitancy to actively promote exclusive breastfeeding for the first 6 months. I prefer a more nuanced approach adjusted to the unique needs and limitations of each family. But I decided to chase down the Implicit Association Test (IAT) suggested in the article. I couldn’t make that link work, but found a long list of subjects on the Harvard Implicit Association Test website. None dealt with breastfeeding, so I chose the one described as Black/White.
If, like me, you have never had your implicit biases assessed by taking an IAT, you might find it interesting. Probably took me about 15 minutes using my laptop. There are a lot of demographic questions then some rapid-fire exercises in which you must provide your first response to a barrage of photos of faces and words. At times I sensed that the test makers were trying to trick me into making associations that I didn’t want to make by the order in which the exercises were presented. At the end I was told that I was a little slow in associating Black faces with positive words.
I’m not sure what this means. After doing a little internet searching I learned that one of the criticisms of the IAT is that, while it may hint at a bias, it is really more important whether you cut with or across that bias. If I acknowledge that where and how I grew up may have left me with some implicit biases, it is more important that I make a strong and honest effort to act independently of those biases.
In full disclosure I must tell you that there was one Black girl in my high school of a thousand students. I have lived and practiced in Maine for 50 years. At less than 2%, we are sixth from the bottom in Black population among other states. However, in the last 5 or 6 years here in Brunswick we have welcomed a large infusion of asylum seekers who come predominantly from Black African countries.
Skimming through the rest of the article, I found it hard to argue with the remaining nine recommendations for promoting breastfeeding, although most of them we not terribly applicable to small community practices. The photo of the Black woman nursing her baby at the top of the page remains as the primary message. The fact that I was drawn to that image is a testament to several of my biases and another example of a picture being worth far more than a thousand words.
I suspect that I’m not alone in appreciating the uniqueness of that image. Until recently, the standard photos of a mother breastfeeding have used trim White women as their models. I suspect and hope this poster will be effective in encouraging Black women to nurse. I urge you all to hang it in your office as a reminder to you and your staff of your biases and assumptions. Don’t bother to take the Implicit Association Test unless you’re retired and have 15 minutes to burn on a rainy afternoon.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
On a recent rainy afternoon I was speed skimming through the pile of publications sitting on the floor next to my Grampy’s chair. A bright patch of color jumped off the gray background of the printed page forcing me to pause and consider the content.
In the right upper corner was a photograph of an attractive Black woman nursing her baby. Her bare arms suggested she might be slightly overweight. She wore a simple off-white head wrap and smiled broadly as she played with her infant’s fingers. The image was a reproduction of a WIC poster encouraging women to take advantage of the program’s breastfeeding support services. The accompanying article from American Academy of Pediatrics offered ten strategies for achieving breastfeeding equity.
I must admit that I tend to shy away from discussions of equity because I’ve seldom found them very informative. However, the engaging image of this Black woman breastfeeding led me to read beyond the title.
The first of the strategies listed was “Check you biases.” I will certainly admit to having biases. We all have biases and see and interpret the world through lenses ground and tinted by our experiences and the environment we have inhabited. In the case of breastfeeding, I wasn’t sure where my biases lay. Maybe one of mine is reflected in a hesitancy to actively promote exclusive breastfeeding for the first 6 months. I prefer a more nuanced approach adjusted to the unique needs and limitations of each family. But I decided to chase down the Implicit Association Test (IAT) suggested in the article. I couldn’t make that link work, but found a long list of subjects on the Harvard Implicit Association Test website. None dealt with breastfeeding, so I chose the one described as Black/White.
If, like me, you have never had your implicit biases assessed by taking an IAT, you might find it interesting. Probably took me about 15 minutes using my laptop. There are a lot of demographic questions then some rapid-fire exercises in which you must provide your first response to a barrage of photos of faces and words. At times I sensed that the test makers were trying to trick me into making associations that I didn’t want to make by the order in which the exercises were presented. At the end I was told that I was a little slow in associating Black faces with positive words.
I’m not sure what this means. After doing a little internet searching I learned that one of the criticisms of the IAT is that, while it may hint at a bias, it is really more important whether you cut with or across that bias. If I acknowledge that where and how I grew up may have left me with some implicit biases, it is more important that I make a strong and honest effort to act independently of those biases.
In full disclosure I must tell you that there was one Black girl in my high school of a thousand students. I have lived and practiced in Maine for 50 years. At less than 2%, we are sixth from the bottom in Black population among other states. However, in the last 5 or 6 years here in Brunswick we have welcomed a large infusion of asylum seekers who come predominantly from Black African countries.
Skimming through the rest of the article, I found it hard to argue with the remaining nine recommendations for promoting breastfeeding, although most of them we not terribly applicable to small community practices. The photo of the Black woman nursing her baby at the top of the page remains as the primary message. The fact that I was drawn to that image is a testament to several of my biases and another example of a picture being worth far more than a thousand words.
I suspect that I’m not alone in appreciating the uniqueness of that image. Until recently, the standard photos of a mother breastfeeding have used trim White women as their models. I suspect and hope this poster will be effective in encouraging Black women to nurse. I urge you all to hang it in your office as a reminder to you and your staff of your biases and assumptions. Don’t bother to take the Implicit Association Test unless you’re retired and have 15 minutes to burn on a rainy afternoon.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Oncologists Sound the Alarm About Rise of White Bagging
For years, oncologist John DiPersio, MD, PhD, had faced frustrating encounters with insurers that only cover medications through a process called white bagging.
Instead of the traditional buy-and-bill pathway where oncologists purchase specialty drugs, such as infusion medications, directly from the distributor or manufacturer, white bagging requires physicians to receive these drugs from a specialty pharmacy.
On its face, the differences may seem minor. However, as Dr. DiPersio knows well, the consequences for oncologists and patients are not.
That is why Dr. DiPersio’s cancer center does not allow white bagging.
And when insurers refuse to reconsider the white bagging policy, his cancer team is left with few options.
“Sometimes, we have to redirect patients to other places,” said Dr. DiPersio, a bone marrow transplant specialist at Siteman Cancer Center, Washington University, St. Louis.
In emergency instances where patients cannot wait, Dr. DiPersio’s team will administer their own stock of a drug. In such cases, “we accept the fact that by not allowing white bagging, there may be nonpayment. We take the hit as far as cost.”
Increasingly, white bagging mandates are becoming harder for practices to avoid.
In a 2021 survey, 87% of Association of Community Cancer Centers members said white bagging has become an insurer mandate for some of their patients.
A 2023 analysis from Adam J. Fein, PhD, of Drug Channels Institute, Philadelphia, found that white bagging accounted for 17% of infused oncology product sourcing from clinics and 38% from hospital outpatient departments, up from 15% to 28% in 2019. Another practice called brown bagging, where specialty pharmacies send drugs directly to patients, creates many of the same issues but is much less prevalent than white bagging.
This change reflects “the broader battle over oncology margins” and insurers’ “attempts to shift costs to providers, patients, and manufacturers,” Dr. Fein wrote in his 2023 report.
White Bagging: Who Benefits?
At its core, white bagging changes how drugs are covered and reimbursed. Under buy and bill, drugs fall under a patient’s medical benefit. Oncologists purchase drugs directly from the manufacturer or distributor and receive reimbursement from the insurance company for both the cost of the drug as well as for administering it to patients.
Under white bagging, drugs fall under a patient’s pharmacy benefit. In these instances, a specialty pharmacy prepares the infusion ahead of time and ships it directly to the physician’s office or clinic. Because oncologists do not purchase the drug directly, they cannot bill insurers for it; instead, the pharmacy receives reimbursement for the drug and the provider is reimbursed for administering it.
Insurance companies argue that white bagging reduces patients’ out-of-pocket costs “by preventing hospitals and physicians from charging exorbitant fees to buy and store specialty medicines themselves,” according to advocacy group America’s Health Insurance Plans (AHIP).
Data from AHIP suggested that hospitals mark up the price of cancer drugs considerably, charging about twice as much as a specialty pharmacy, and that physician’s offices also charge about 23% more. However, these figures highlight how much insurers are billed, not necessarily how much patients ultimately pay.
Other evidence shows that white bagging raises costs for patients while reducing reimbursement for oncologists and saving insurance companies money.
A recent analysis in JAMA Network Open, which looked at 50 cancer drugs associated with the highest total spending from the 2020 Medicare Part B, found that mean insurance payments to providers were more than $2000 lower for drugs distributed under bagging than traditional buy and bill: $7405 vs $9547 per patient per month. Investigators found the same pattern in median insurance payments: $5746 vs $6681. Patients also paid more out-of-pocket each month with bagging vs buy and bill: $315 vs $145.
For patients with private insurance, “out-of-pocket costs were higher under bagging practice than the traditional buy-and-bill practice,” said lead author Ya-Chen Tina Shih, PhD, a professor in the department of radiation oncology at UCLA Health, Los Angeles.
White bagging is entirely for the profit of health insurers, specialty pharmacies, and pharmacy benefit managers, the middlemen who negotiate drug prices on behalf of payers.
Many people may not realize the underlying money-making strategies behind white bagging, explained Ted Okon, executive director for Community Oncology Alliance, which opposes the practice. Often, an insurer, pharmacy benefit manager, and mail order pharmacy involved in the process are all affiliated with the same corporation. In such cases, an insurer has a financial motive to control the source of medications and steer business to its affiliated pharmacies, Mr. Okon said.
When a single corporation owns numerous parts of the drug supply chain, insurers end up having “sway over what drug to use and then how the patient is going to get it,” Mr. Okon said. If the specialty pharmacy is a 340B contract pharmacy, it likely also receives a sizable discount on the drug and can make more money through white bagging.
Dangerous to Patients?
On the safety front, proponents of white bagging say the process is safe and efficient.
Specialty pharmacies are used only for prescription drugs that can be safely delivered, said AHIP spokesman David Allen.
In addition to having the same supply chain safety requirements as any other dispensing pharmacy, “specialty pharmacies also must meet additional safety requirements for specialty drugs” to ensure “the safe storage, handling, and dispensing of the drugs,” Mr. Allen explained.
However, oncologists argue that white bagging can be dangerous.
With white bagging, specialty pharmacies send a specified dose to practices, which does not allow practices to source and mix the drug themselves or make essential last-minute dose-related changes — something that happens every day in the clinic, said Debra Patt, MD, PhD, MBA, executive vice president for policy and strategy for Texas Oncology, Dallas.
White bagging also increases the risk for drug contamination, results in drug waste if the medication can’t be used, and can create delays in care.
Essentially, white bagging takes control away from oncologists and makes patient care more unpredictable and complex, explained Dr. Patt, president of the Texas Society of Clinical Oncology, Rockville, Maryland.
Dr. Patt, who does not allow white bagging in her practice, recalled a recent patient with metastatic breast cancer who came to the clinic for trastuzumab deruxtecan. The patient had been experiencing acute abdominal pain. After an exam and CT, Dr. Patt found the breast cancer had grown and moved into the patient’s liver.
“I had to discontinue that plan and change to a different chemotherapy,” she said. “If we had white bagged, that would have been a waste of several thousand dollars. Also, the patient would have to wait for the new medication to be white bagged, a delay that would be at least a week and the patient would have to come back at another time.”
When asked about the safety concerns associated with white bagging, Lemrey “Al” Carter, MS, PharmD, RPh, executive director of the National Association of Boards of Pharmacy (NABP), said the NABP “acknowledges that all these issues exist.
“It is unfortunate if patient care or costs are negatively impacted,” Dr. Carter said, adding that “boards of pharmacy can investigate if they are made aware of safety concerns at the pharmacy level. If a violation of the pharmacy laws or rules is found, boards can take action.”
More Legislation to Prevent Bagging
As white bagging mandates from insurance companies ramp up, more practices and states are banning it.
In the Association of Community Cancer Centers’ 2021 survey, 59% of members said their cancer program or practice does not allow white bagging.
At least 15 states have introduced legislation that restricts and/or prohibits white and brown bagging practices, according to a 2023 report by the Institute for Clinical and Economic Review. Some of the proposed laws would restrict mandates by stipulating that physicians are reimbursed at the contracted amount for clinician-administered drugs, whether obtained from a pharmacy or the manufacturer.
Louisiana, Vermont, and Minnesota were the first to enact anti–white bagging laws. Louisiana’s law, for example, enacted in 2021, bans white bagging and requires insurers to reimburse providers for physician-administered drugs if obtained from out-of-network pharmacies.
When the legislation passed, white bagging was just starting to enter the healthcare market in Louisiana, and the state wanted to act proactively, said Kathy W. Oubre, MS, CEO of the Pontchartrain Cancer Center, Covington, Louisiana, and president of the Coalition of Hematology and Oncology Practices, Mountain View, California.
“We recognized the growing concern around it,” Ms. Oubre said. The state legislature at the time included physicians and pharmacists who “really understood from a practice and patient perspective, the harm that policy could do.”
Ms. Oubre would like to see more legislation in other states and believes Louisiana’s law is a good model.
At the federal level, the American Hospital Association and American Society of Health-System Pharmacists have also urged the US Food and Drug Administration to take appropriate enforcement action to protect patients from white bagging.
Legislation that bars white bagging mandates is the most reasonable way to support timely and appropriate access to cancer care, Dr. Patt said. In the absence of such legislation, she said oncologists can only opt out of insurance contracts that may require the practice.
“That is a difficult position to put oncologists in,” she said.
A version of this article appeared on Medscape.com.
For years, oncologist John DiPersio, MD, PhD, had faced frustrating encounters with insurers that only cover medications through a process called white bagging.
Instead of the traditional buy-and-bill pathway where oncologists purchase specialty drugs, such as infusion medications, directly from the distributor or manufacturer, white bagging requires physicians to receive these drugs from a specialty pharmacy.
On its face, the differences may seem minor. However, as Dr. DiPersio knows well, the consequences for oncologists and patients are not.
That is why Dr. DiPersio’s cancer center does not allow white bagging.
And when insurers refuse to reconsider the white bagging policy, his cancer team is left with few options.
“Sometimes, we have to redirect patients to other places,” said Dr. DiPersio, a bone marrow transplant specialist at Siteman Cancer Center, Washington University, St. Louis.
In emergency instances where patients cannot wait, Dr. DiPersio’s team will administer their own stock of a drug. In such cases, “we accept the fact that by not allowing white bagging, there may be nonpayment. We take the hit as far as cost.”
Increasingly, white bagging mandates are becoming harder for practices to avoid.
In a 2021 survey, 87% of Association of Community Cancer Centers members said white bagging has become an insurer mandate for some of their patients.
A 2023 analysis from Adam J. Fein, PhD, of Drug Channels Institute, Philadelphia, found that white bagging accounted for 17% of infused oncology product sourcing from clinics and 38% from hospital outpatient departments, up from 15% to 28% in 2019. Another practice called brown bagging, where specialty pharmacies send drugs directly to patients, creates many of the same issues but is much less prevalent than white bagging.
This change reflects “the broader battle over oncology margins” and insurers’ “attempts to shift costs to providers, patients, and manufacturers,” Dr. Fein wrote in his 2023 report.
White Bagging: Who Benefits?
At its core, white bagging changes how drugs are covered and reimbursed. Under buy and bill, drugs fall under a patient’s medical benefit. Oncologists purchase drugs directly from the manufacturer or distributor and receive reimbursement from the insurance company for both the cost of the drug as well as for administering it to patients.
Under white bagging, drugs fall under a patient’s pharmacy benefit. In these instances, a specialty pharmacy prepares the infusion ahead of time and ships it directly to the physician’s office or clinic. Because oncologists do not purchase the drug directly, they cannot bill insurers for it; instead, the pharmacy receives reimbursement for the drug and the provider is reimbursed for administering it.
Insurance companies argue that white bagging reduces patients’ out-of-pocket costs “by preventing hospitals and physicians from charging exorbitant fees to buy and store specialty medicines themselves,” according to advocacy group America’s Health Insurance Plans (AHIP).
Data from AHIP suggested that hospitals mark up the price of cancer drugs considerably, charging about twice as much as a specialty pharmacy, and that physician’s offices also charge about 23% more. However, these figures highlight how much insurers are billed, not necessarily how much patients ultimately pay.
Other evidence shows that white bagging raises costs for patients while reducing reimbursement for oncologists and saving insurance companies money.
A recent analysis in JAMA Network Open, which looked at 50 cancer drugs associated with the highest total spending from the 2020 Medicare Part B, found that mean insurance payments to providers were more than $2000 lower for drugs distributed under bagging than traditional buy and bill: $7405 vs $9547 per patient per month. Investigators found the same pattern in median insurance payments: $5746 vs $6681. Patients also paid more out-of-pocket each month with bagging vs buy and bill: $315 vs $145.
For patients with private insurance, “out-of-pocket costs were higher under bagging practice than the traditional buy-and-bill practice,” said lead author Ya-Chen Tina Shih, PhD, a professor in the department of radiation oncology at UCLA Health, Los Angeles.
White bagging is entirely for the profit of health insurers, specialty pharmacies, and pharmacy benefit managers, the middlemen who negotiate drug prices on behalf of payers.
Many people may not realize the underlying money-making strategies behind white bagging, explained Ted Okon, executive director for Community Oncology Alliance, which opposes the practice. Often, an insurer, pharmacy benefit manager, and mail order pharmacy involved in the process are all affiliated with the same corporation. In such cases, an insurer has a financial motive to control the source of medications and steer business to its affiliated pharmacies, Mr. Okon said.
When a single corporation owns numerous parts of the drug supply chain, insurers end up having “sway over what drug to use and then how the patient is going to get it,” Mr. Okon said. If the specialty pharmacy is a 340B contract pharmacy, it likely also receives a sizable discount on the drug and can make more money through white bagging.
Dangerous to Patients?
On the safety front, proponents of white bagging say the process is safe and efficient.
Specialty pharmacies are used only for prescription drugs that can be safely delivered, said AHIP spokesman David Allen.
In addition to having the same supply chain safety requirements as any other dispensing pharmacy, “specialty pharmacies also must meet additional safety requirements for specialty drugs” to ensure “the safe storage, handling, and dispensing of the drugs,” Mr. Allen explained.
However, oncologists argue that white bagging can be dangerous.
With white bagging, specialty pharmacies send a specified dose to practices, which does not allow practices to source and mix the drug themselves or make essential last-minute dose-related changes — something that happens every day in the clinic, said Debra Patt, MD, PhD, MBA, executive vice president for policy and strategy for Texas Oncology, Dallas.
White bagging also increases the risk for drug contamination, results in drug waste if the medication can’t be used, and can create delays in care.
Essentially, white bagging takes control away from oncologists and makes patient care more unpredictable and complex, explained Dr. Patt, president of the Texas Society of Clinical Oncology, Rockville, Maryland.
Dr. Patt, who does not allow white bagging in her practice, recalled a recent patient with metastatic breast cancer who came to the clinic for trastuzumab deruxtecan. The patient had been experiencing acute abdominal pain. After an exam and CT, Dr. Patt found the breast cancer had grown and moved into the patient’s liver.
“I had to discontinue that plan and change to a different chemotherapy,” she said. “If we had white bagged, that would have been a waste of several thousand dollars. Also, the patient would have to wait for the new medication to be white bagged, a delay that would be at least a week and the patient would have to come back at another time.”
When asked about the safety concerns associated with white bagging, Lemrey “Al” Carter, MS, PharmD, RPh, executive director of the National Association of Boards of Pharmacy (NABP), said the NABP “acknowledges that all these issues exist.
“It is unfortunate if patient care or costs are negatively impacted,” Dr. Carter said, adding that “boards of pharmacy can investigate if they are made aware of safety concerns at the pharmacy level. If a violation of the pharmacy laws or rules is found, boards can take action.”
More Legislation to Prevent Bagging
As white bagging mandates from insurance companies ramp up, more practices and states are banning it.
In the Association of Community Cancer Centers’ 2021 survey, 59% of members said their cancer program or practice does not allow white bagging.
At least 15 states have introduced legislation that restricts and/or prohibits white and brown bagging practices, according to a 2023 report by the Institute for Clinical and Economic Review. Some of the proposed laws would restrict mandates by stipulating that physicians are reimbursed at the contracted amount for clinician-administered drugs, whether obtained from a pharmacy or the manufacturer.
Louisiana, Vermont, and Minnesota were the first to enact anti–white bagging laws. Louisiana’s law, for example, enacted in 2021, bans white bagging and requires insurers to reimburse providers for physician-administered drugs if obtained from out-of-network pharmacies.
When the legislation passed, white bagging was just starting to enter the healthcare market in Louisiana, and the state wanted to act proactively, said Kathy W. Oubre, MS, CEO of the Pontchartrain Cancer Center, Covington, Louisiana, and president of the Coalition of Hematology and Oncology Practices, Mountain View, California.
“We recognized the growing concern around it,” Ms. Oubre said. The state legislature at the time included physicians and pharmacists who “really understood from a practice and patient perspective, the harm that policy could do.”
Ms. Oubre would like to see more legislation in other states and believes Louisiana’s law is a good model.
At the federal level, the American Hospital Association and American Society of Health-System Pharmacists have also urged the US Food and Drug Administration to take appropriate enforcement action to protect patients from white bagging.
Legislation that bars white bagging mandates is the most reasonable way to support timely and appropriate access to cancer care, Dr. Patt said. In the absence of such legislation, she said oncologists can only opt out of insurance contracts that may require the practice.
“That is a difficult position to put oncologists in,” she said.
A version of this article appeared on Medscape.com.
For years, oncologist John DiPersio, MD, PhD, had faced frustrating encounters with insurers that only cover medications through a process called white bagging.
Instead of the traditional buy-and-bill pathway where oncologists purchase specialty drugs, such as infusion medications, directly from the distributor or manufacturer, white bagging requires physicians to receive these drugs from a specialty pharmacy.
On its face, the differences may seem minor. However, as Dr. DiPersio knows well, the consequences for oncologists and patients are not.
That is why Dr. DiPersio’s cancer center does not allow white bagging.
And when insurers refuse to reconsider the white bagging policy, his cancer team is left with few options.
“Sometimes, we have to redirect patients to other places,” said Dr. DiPersio, a bone marrow transplant specialist at Siteman Cancer Center, Washington University, St. Louis.
In emergency instances where patients cannot wait, Dr. DiPersio’s team will administer their own stock of a drug. In such cases, “we accept the fact that by not allowing white bagging, there may be nonpayment. We take the hit as far as cost.”
Increasingly, white bagging mandates are becoming harder for practices to avoid.
In a 2021 survey, 87% of Association of Community Cancer Centers members said white bagging has become an insurer mandate for some of their patients.
A 2023 analysis from Adam J. Fein, PhD, of Drug Channels Institute, Philadelphia, found that white bagging accounted for 17% of infused oncology product sourcing from clinics and 38% from hospital outpatient departments, up from 15% to 28% in 2019. Another practice called brown bagging, where specialty pharmacies send drugs directly to patients, creates many of the same issues but is much less prevalent than white bagging.
This change reflects “the broader battle over oncology margins” and insurers’ “attempts to shift costs to providers, patients, and manufacturers,” Dr. Fein wrote in his 2023 report.
White Bagging: Who Benefits?
At its core, white bagging changes how drugs are covered and reimbursed. Under buy and bill, drugs fall under a patient’s medical benefit. Oncologists purchase drugs directly from the manufacturer or distributor and receive reimbursement from the insurance company for both the cost of the drug as well as for administering it to patients.
Under white bagging, drugs fall under a patient’s pharmacy benefit. In these instances, a specialty pharmacy prepares the infusion ahead of time and ships it directly to the physician’s office or clinic. Because oncologists do not purchase the drug directly, they cannot bill insurers for it; instead, the pharmacy receives reimbursement for the drug and the provider is reimbursed for administering it.
Insurance companies argue that white bagging reduces patients’ out-of-pocket costs “by preventing hospitals and physicians from charging exorbitant fees to buy and store specialty medicines themselves,” according to advocacy group America’s Health Insurance Plans (AHIP).
Data from AHIP suggested that hospitals mark up the price of cancer drugs considerably, charging about twice as much as a specialty pharmacy, and that physician’s offices also charge about 23% more. However, these figures highlight how much insurers are billed, not necessarily how much patients ultimately pay.
Other evidence shows that white bagging raises costs for patients while reducing reimbursement for oncologists and saving insurance companies money.
A recent analysis in JAMA Network Open, which looked at 50 cancer drugs associated with the highest total spending from the 2020 Medicare Part B, found that mean insurance payments to providers were more than $2000 lower for drugs distributed under bagging than traditional buy and bill: $7405 vs $9547 per patient per month. Investigators found the same pattern in median insurance payments: $5746 vs $6681. Patients also paid more out-of-pocket each month with bagging vs buy and bill: $315 vs $145.
For patients with private insurance, “out-of-pocket costs were higher under bagging practice than the traditional buy-and-bill practice,” said lead author Ya-Chen Tina Shih, PhD, a professor in the department of radiation oncology at UCLA Health, Los Angeles.
White bagging is entirely for the profit of health insurers, specialty pharmacies, and pharmacy benefit managers, the middlemen who negotiate drug prices on behalf of payers.
Many people may not realize the underlying money-making strategies behind white bagging, explained Ted Okon, executive director for Community Oncology Alliance, which opposes the practice. Often, an insurer, pharmacy benefit manager, and mail order pharmacy involved in the process are all affiliated with the same corporation. In such cases, an insurer has a financial motive to control the source of medications and steer business to its affiliated pharmacies, Mr. Okon said.
When a single corporation owns numerous parts of the drug supply chain, insurers end up having “sway over what drug to use and then how the patient is going to get it,” Mr. Okon said. If the specialty pharmacy is a 340B contract pharmacy, it likely also receives a sizable discount on the drug and can make more money through white bagging.
Dangerous to Patients?
On the safety front, proponents of white bagging say the process is safe and efficient.
Specialty pharmacies are used only for prescription drugs that can be safely delivered, said AHIP spokesman David Allen.
In addition to having the same supply chain safety requirements as any other dispensing pharmacy, “specialty pharmacies also must meet additional safety requirements for specialty drugs” to ensure “the safe storage, handling, and dispensing of the drugs,” Mr. Allen explained.
However, oncologists argue that white bagging can be dangerous.
With white bagging, specialty pharmacies send a specified dose to practices, which does not allow practices to source and mix the drug themselves or make essential last-minute dose-related changes — something that happens every day in the clinic, said Debra Patt, MD, PhD, MBA, executive vice president for policy and strategy for Texas Oncology, Dallas.
White bagging also increases the risk for drug contamination, results in drug waste if the medication can’t be used, and can create delays in care.
Essentially, white bagging takes control away from oncologists and makes patient care more unpredictable and complex, explained Dr. Patt, president of the Texas Society of Clinical Oncology, Rockville, Maryland.
Dr. Patt, who does not allow white bagging in her practice, recalled a recent patient with metastatic breast cancer who came to the clinic for trastuzumab deruxtecan. The patient had been experiencing acute abdominal pain. After an exam and CT, Dr. Patt found the breast cancer had grown and moved into the patient’s liver.
“I had to discontinue that plan and change to a different chemotherapy,” she said. “If we had white bagged, that would have been a waste of several thousand dollars. Also, the patient would have to wait for the new medication to be white bagged, a delay that would be at least a week and the patient would have to come back at another time.”
When asked about the safety concerns associated with white bagging, Lemrey “Al” Carter, MS, PharmD, RPh, executive director of the National Association of Boards of Pharmacy (NABP), said the NABP “acknowledges that all these issues exist.
“It is unfortunate if patient care or costs are negatively impacted,” Dr. Carter said, adding that “boards of pharmacy can investigate if they are made aware of safety concerns at the pharmacy level. If a violation of the pharmacy laws or rules is found, boards can take action.”
More Legislation to Prevent Bagging
As white bagging mandates from insurance companies ramp up, more practices and states are banning it.
In the Association of Community Cancer Centers’ 2021 survey, 59% of members said their cancer program or practice does not allow white bagging.
At least 15 states have introduced legislation that restricts and/or prohibits white and brown bagging practices, according to a 2023 report by the Institute for Clinical and Economic Review. Some of the proposed laws would restrict mandates by stipulating that physicians are reimbursed at the contracted amount for clinician-administered drugs, whether obtained from a pharmacy or the manufacturer.
Louisiana, Vermont, and Minnesota were the first to enact anti–white bagging laws. Louisiana’s law, for example, enacted in 2021, bans white bagging and requires insurers to reimburse providers for physician-administered drugs if obtained from out-of-network pharmacies.
When the legislation passed, white bagging was just starting to enter the healthcare market in Louisiana, and the state wanted to act proactively, said Kathy W. Oubre, MS, CEO of the Pontchartrain Cancer Center, Covington, Louisiana, and president of the Coalition of Hematology and Oncology Practices, Mountain View, California.
“We recognized the growing concern around it,” Ms. Oubre said. The state legislature at the time included physicians and pharmacists who “really understood from a practice and patient perspective, the harm that policy could do.”
Ms. Oubre would like to see more legislation in other states and believes Louisiana’s law is a good model.
At the federal level, the American Hospital Association and American Society of Health-System Pharmacists have also urged the US Food and Drug Administration to take appropriate enforcement action to protect patients from white bagging.
Legislation that bars white bagging mandates is the most reasonable way to support timely and appropriate access to cancer care, Dr. Patt said. In the absence of such legislation, she said oncologists can only opt out of insurance contracts that may require the practice.
“That is a difficult position to put oncologists in,” she said.
A version of this article appeared on Medscape.com.
New Federal Rule for Prior Authorizations a ‘Major Win’ for Patients, Doctors
Physicians groups on January 17 hailed a new federal rule requiring health insurers to streamline and disclose more information about their prior authorization processes, saying it will improve patient care and reduce doctors’ administrative burden.
Health insurers participating in federal programs, including Medicare Advantage and Medicaid, must now respond to expedited prior authorization requests within 72 hours and other requests within 7 days under the long-awaited final rule, released on January 17 by the Centers for Medicare & Medicaid Services (CMS).
Insurers also must include their reasons for denying a prior authorization request and will be required to publicly release data on denial and approval rates for medical treatment. They’ll also need to give patients more information about their decisions to deny care. Insurers must comply with some of the rule’s provisions by January 2026 and others by January 2027.
The final rule “is an important step forward” toward the Medical Group Management Association’s goal of reducing the overall volume of prior authorization requests, said Anders Gilberg, the group’s senior vice president for government affairs, in a statement.
“Only then will medical groups find meaningful reprieve from these onerous, ill-intentioned administrative requirements that dangerously impede patient care,” Mr. Gilberg said.
Health insurers have long lobbied against increased regulation of prior authorization, arguing that it’s needed to rein in healthcare costs and prevent unnecessary treatment.
“We appreciate CMS’s announcement of enforcement discretion that will permit plans to use one standard, rather than mixing and matching, to reduce costs and speed implementation,” said America’s Health Insurance Plans, an insurers’ lobbying group, in an unsigned statement. “However, we must remember that the CMS rule is only half the picture; the Office of the Coordinator for Health Information Technology (ONC) should swiftly require vendors to build electronic prior authorization capabilities into the electronic health record so that providers can do their part, or plans will build a bridge to nowhere.”
The rule comes as health insurers have increasingly been criticized for onerous and time-consuming prior authorization procedures that physicians say unfairly delay or deny the medical treatment that their patients need. With federal legislation to rein in prior authorization overuse at a standstill, 30 states have introduced their own bills to address the problem. Regulators and lawsuits also have called attention to insurers’ increasing use of artificial intelligence and algorithms to deny claims without human review.
“Family physicians know firsthand how prior authorizations divert valuable time and resources away from direct patient care. We also know that these types of administrative requirements are driving physicians away from the workforce and worsening physician shortages,” said Steven P. Furr, MD, president of the American Academy of Family Physicians, in a statement praising the new rule.
Jesse M. Ehrenfeld, MD, MPH, president of the American Medical Association, called the final rule “ a major win” for patients and physicians, adding that its requirements for health insurers to integrate their prior authorization procedures into physicians’ electronic health records systems will also help make “the current time-consuming, manual workflow” more efficient.
A version of this article first appeared on Medscape.com.
Physicians groups on January 17 hailed a new federal rule requiring health insurers to streamline and disclose more information about their prior authorization processes, saying it will improve patient care and reduce doctors’ administrative burden.
Health insurers participating in federal programs, including Medicare Advantage and Medicaid, must now respond to expedited prior authorization requests within 72 hours and other requests within 7 days under the long-awaited final rule, released on January 17 by the Centers for Medicare & Medicaid Services (CMS).
Insurers also must include their reasons for denying a prior authorization request and will be required to publicly release data on denial and approval rates for medical treatment. They’ll also need to give patients more information about their decisions to deny care. Insurers must comply with some of the rule’s provisions by January 2026 and others by January 2027.
The final rule “is an important step forward” toward the Medical Group Management Association’s goal of reducing the overall volume of prior authorization requests, said Anders Gilberg, the group’s senior vice president for government affairs, in a statement.
“Only then will medical groups find meaningful reprieve from these onerous, ill-intentioned administrative requirements that dangerously impede patient care,” Mr. Gilberg said.
Health insurers have long lobbied against increased regulation of prior authorization, arguing that it’s needed to rein in healthcare costs and prevent unnecessary treatment.
“We appreciate CMS’s announcement of enforcement discretion that will permit plans to use one standard, rather than mixing and matching, to reduce costs and speed implementation,” said America’s Health Insurance Plans, an insurers’ lobbying group, in an unsigned statement. “However, we must remember that the CMS rule is only half the picture; the Office of the Coordinator for Health Information Technology (ONC) should swiftly require vendors to build electronic prior authorization capabilities into the electronic health record so that providers can do their part, or plans will build a bridge to nowhere.”
The rule comes as health insurers have increasingly been criticized for onerous and time-consuming prior authorization procedures that physicians say unfairly delay or deny the medical treatment that their patients need. With federal legislation to rein in prior authorization overuse at a standstill, 30 states have introduced their own bills to address the problem. Regulators and lawsuits also have called attention to insurers’ increasing use of artificial intelligence and algorithms to deny claims without human review.
“Family physicians know firsthand how prior authorizations divert valuable time and resources away from direct patient care. We also know that these types of administrative requirements are driving physicians away from the workforce and worsening physician shortages,” said Steven P. Furr, MD, president of the American Academy of Family Physicians, in a statement praising the new rule.
Jesse M. Ehrenfeld, MD, MPH, president of the American Medical Association, called the final rule “ a major win” for patients and physicians, adding that its requirements for health insurers to integrate their prior authorization procedures into physicians’ electronic health records systems will also help make “the current time-consuming, manual workflow” more efficient.
A version of this article first appeared on Medscape.com.
Physicians groups on January 17 hailed a new federal rule requiring health insurers to streamline and disclose more information about their prior authorization processes, saying it will improve patient care and reduce doctors’ administrative burden.
Health insurers participating in federal programs, including Medicare Advantage and Medicaid, must now respond to expedited prior authorization requests within 72 hours and other requests within 7 days under the long-awaited final rule, released on January 17 by the Centers for Medicare & Medicaid Services (CMS).
Insurers also must include their reasons for denying a prior authorization request and will be required to publicly release data on denial and approval rates for medical treatment. They’ll also need to give patients more information about their decisions to deny care. Insurers must comply with some of the rule’s provisions by January 2026 and others by January 2027.
The final rule “is an important step forward” toward the Medical Group Management Association’s goal of reducing the overall volume of prior authorization requests, said Anders Gilberg, the group’s senior vice president for government affairs, in a statement.
“Only then will medical groups find meaningful reprieve from these onerous, ill-intentioned administrative requirements that dangerously impede patient care,” Mr. Gilberg said.
Health insurers have long lobbied against increased regulation of prior authorization, arguing that it’s needed to rein in healthcare costs and prevent unnecessary treatment.
“We appreciate CMS’s announcement of enforcement discretion that will permit plans to use one standard, rather than mixing and matching, to reduce costs and speed implementation,” said America’s Health Insurance Plans, an insurers’ lobbying group, in an unsigned statement. “However, we must remember that the CMS rule is only half the picture; the Office of the Coordinator for Health Information Technology (ONC) should swiftly require vendors to build electronic prior authorization capabilities into the electronic health record so that providers can do their part, or plans will build a bridge to nowhere.”
The rule comes as health insurers have increasingly been criticized for onerous and time-consuming prior authorization procedures that physicians say unfairly delay or deny the medical treatment that their patients need. With federal legislation to rein in prior authorization overuse at a standstill, 30 states have introduced their own bills to address the problem. Regulators and lawsuits also have called attention to insurers’ increasing use of artificial intelligence and algorithms to deny claims without human review.
“Family physicians know firsthand how prior authorizations divert valuable time and resources away from direct patient care. We also know that these types of administrative requirements are driving physicians away from the workforce and worsening physician shortages,” said Steven P. Furr, MD, president of the American Academy of Family Physicians, in a statement praising the new rule.
Jesse M. Ehrenfeld, MD, MPH, president of the American Medical Association, called the final rule “ a major win” for patients and physicians, adding that its requirements for health insurers to integrate their prior authorization procedures into physicians’ electronic health records systems will also help make “the current time-consuming, manual workflow” more efficient.
A version of this article first appeared on Medscape.com.
Magic Wand Initiative Empowers Dermatologists to Innovate
NEW YORK – .
The program was founded in 2013 by two Harvard Medical School dermatologists, Lilit Garibyan, MD, PhD, the program director, and her mentor R. Rox Anderson MD, director of the Wellman Center for Photomedicine at Massachusetts General Hospital (MGH), Boston. It was based on the idea that clinicians are in a unique position to identify gaps in patient care and should be active in developing medical solutions to address those gaps.
“I truly believe that if we do a better job educating, training, and empowering our clinicians to become innovators, this will benefit patients and hospitals and physicians,” Dr. Garibyan said at the 26th annual Mount Sinai Winter Symposium — Advances in Medical and Surgical Dermatology.
One of the seeds for the project was her own experience with cryolipolysis which involves topical cooling, a noninvasive method of removing subcutaneous fat for body contouring, which relies on conducting heat from subcutaneous fat across the skin and therefore, does not reach fat far from the dermis. With Dr. Anderson’s mentorship, she developed injectable cooling technology (ICT), a procedure where “ice slurry,” composed of normal saline and glycerol, is directly injected into adipose tissue, possibly leading to more efficient and effective cryolipolysis.
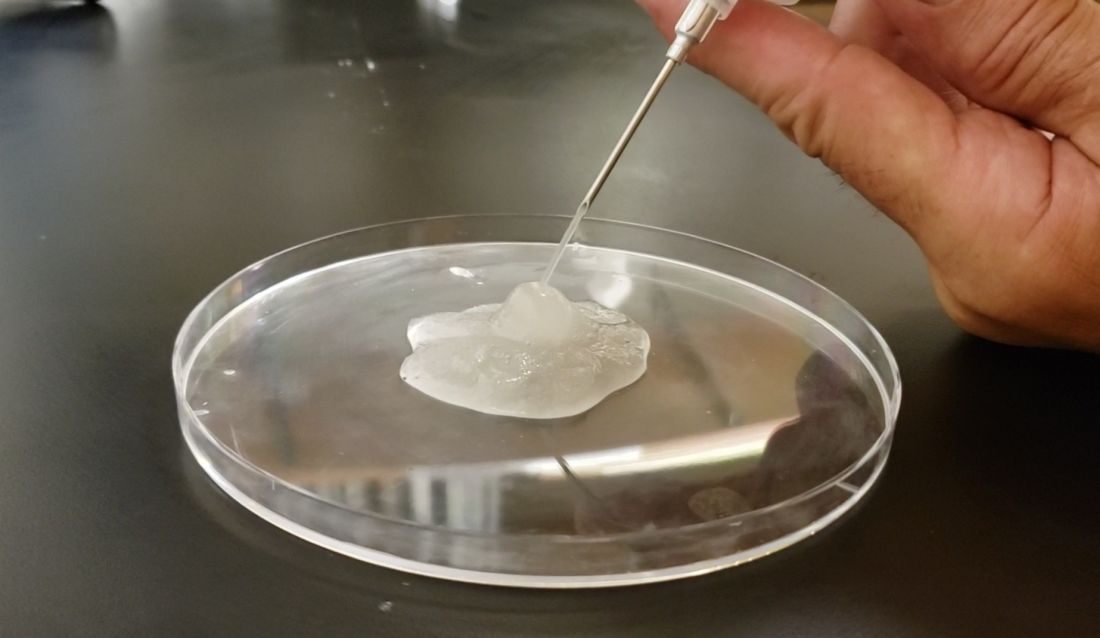
After nearly 10 years of animal studies at MGH, led by Dr. Garibyan as proof of concept trials, ice slurry (Coolio Therapy) recently received FDA breakthrough designation for long-term pain control and early-stage human trials of clinical applications are underway, she noted.
Magic Wand Program
In the Magic Wand program, participating physicians start by recording areas of unmet needs in their day-to-day practices, and in groups, engage in clinician-only brainstorming sessions to screen ideas, define problems, and generate lists of specifications and tools needed to address clinical problems. After working together to define challenges and possible solutions, they take their ideas to a development team, where scientists, engineers, regulatory experts, and industry professionals meet and help clinicians start pilot proof-of-concept projects, develop prototypes, and gain support for studies, followed by pilot feasibility studies.
Part of the project is the Virtual Magic Wand (VMW) Initiative, a 10-month online instructive and interactive course open to clinicians in the United States and Europe, designed to bring together dermatologists “interested in deeply understanding a dermatologic clinical problem worth solving,” according to Dr. Garibyan. Currently, there are more than 86 VMW scholars from 46 institutions, and military and private practice sites in the United States. The VMW was expanded to Europe in 2021 and there are plans to expand to Asia as well, she said.
The success of the program is not only attributed to its clinical methods but the fact that it provides a benefit to doctors at all stages of their careers, patients, and industry. “This is the only program that aims to engage in innovation from resident to full professor. We provide ideas that industry can then support and bring to market. Everyone including patients, doctors, and healthcare companies can benefit from active, engaged, and innovative physicians,” Dr. Garibyan said.
One of the success stories is that of Veradermics, a company founded by Kansas City dermatologist, Reid A. Waldman, MD, the company’s CEO, and Tim Durso, MD, the president, who met while participating in the VMW program in 2020, which eventually led them to start a company addressing an unmet need in dermatology, a kid-friendly treatment of warts.
In an interview with this news organization, Dr. Waldman explained how the program informed his company’s ethos. “Magic Wand Initiative is about identifying problems worth solving,” he said. At the company, “we find problems or unmet needs that are large enough to motivate prescribing changes, so we’ve really taken the philosophy I learned in the program into this company and building our portfolio.”
One of the first needs that Veradermics addressed was the fact that treatment for common warts, cryotherapy with liquid nitrogen, is painful and can frighten children, and, with a response rate of “at best, 50%,” Dr. Waldman said. Veradermics is in the process of creating a nearly painless, child-friendly wart treatment: an “immunostimulatory dissolvable microarray” patch that contains Candida antigen extract, which is currently being evaluated for treating warts in a phase 2 clinical trial started in 2023.
Although the Magic Wand Initiative was initially restricted to dermatologists at MGH, stories like that of Veradermics have made the program so popular that it has branched out to include anesthesiologists and otolaryngologists, as well as general and orthopedic surgeons at MGH, Dr. Garibyan said at the Mount Sinai meeting.
Dr. Garibyan disclosed that she is a cofounder of and has equity in Brixton Biosciences and EyeCool, and is a consultant for and/or investor in Brixton and Clarity Cosmetics. Royalties/inventorship are assigned to MGH.
NEW YORK – .
The program was founded in 2013 by two Harvard Medical School dermatologists, Lilit Garibyan, MD, PhD, the program director, and her mentor R. Rox Anderson MD, director of the Wellman Center for Photomedicine at Massachusetts General Hospital (MGH), Boston. It was based on the idea that clinicians are in a unique position to identify gaps in patient care and should be active in developing medical solutions to address those gaps.
“I truly believe that if we do a better job educating, training, and empowering our clinicians to become innovators, this will benefit patients and hospitals and physicians,” Dr. Garibyan said at the 26th annual Mount Sinai Winter Symposium — Advances in Medical and Surgical Dermatology.
One of the seeds for the project was her own experience with cryolipolysis which involves topical cooling, a noninvasive method of removing subcutaneous fat for body contouring, which relies on conducting heat from subcutaneous fat across the skin and therefore, does not reach fat far from the dermis. With Dr. Anderson’s mentorship, she developed injectable cooling technology (ICT), a procedure where “ice slurry,” composed of normal saline and glycerol, is directly injected into adipose tissue, possibly leading to more efficient and effective cryolipolysis.
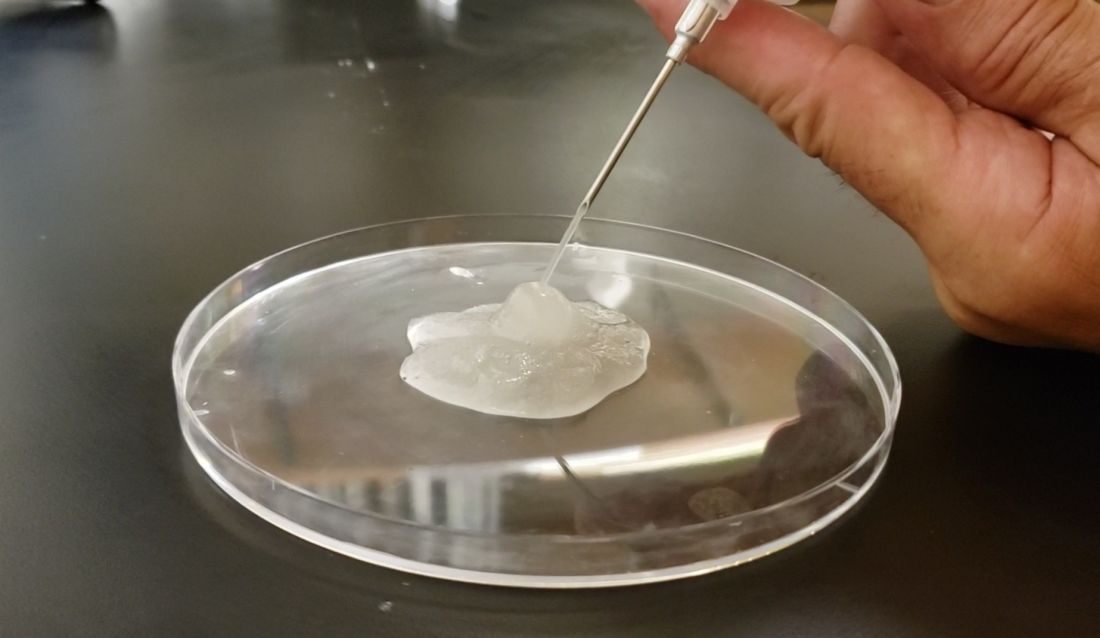
After nearly 10 years of animal studies at MGH, led by Dr. Garibyan as proof of concept trials, ice slurry (Coolio Therapy) recently received FDA breakthrough designation for long-term pain control and early-stage human trials of clinical applications are underway, she noted.
Magic Wand Program
In the Magic Wand program, participating physicians start by recording areas of unmet needs in their day-to-day practices, and in groups, engage in clinician-only brainstorming sessions to screen ideas, define problems, and generate lists of specifications and tools needed to address clinical problems. After working together to define challenges and possible solutions, they take their ideas to a development team, where scientists, engineers, regulatory experts, and industry professionals meet and help clinicians start pilot proof-of-concept projects, develop prototypes, and gain support for studies, followed by pilot feasibility studies.
Part of the project is the Virtual Magic Wand (VMW) Initiative, a 10-month online instructive and interactive course open to clinicians in the United States and Europe, designed to bring together dermatologists “interested in deeply understanding a dermatologic clinical problem worth solving,” according to Dr. Garibyan. Currently, there are more than 86 VMW scholars from 46 institutions, and military and private practice sites in the United States. The VMW was expanded to Europe in 2021 and there are plans to expand to Asia as well, she said.
The success of the program is not only attributed to its clinical methods but the fact that it provides a benefit to doctors at all stages of their careers, patients, and industry. “This is the only program that aims to engage in innovation from resident to full professor. We provide ideas that industry can then support and bring to market. Everyone including patients, doctors, and healthcare companies can benefit from active, engaged, and innovative physicians,” Dr. Garibyan said.
One of the success stories is that of Veradermics, a company founded by Kansas City dermatologist, Reid A. Waldman, MD, the company’s CEO, and Tim Durso, MD, the president, who met while participating in the VMW program in 2020, which eventually led them to start a company addressing an unmet need in dermatology, a kid-friendly treatment of warts.
In an interview with this news organization, Dr. Waldman explained how the program informed his company’s ethos. “Magic Wand Initiative is about identifying problems worth solving,” he said. At the company, “we find problems or unmet needs that are large enough to motivate prescribing changes, so we’ve really taken the philosophy I learned in the program into this company and building our portfolio.”
One of the first needs that Veradermics addressed was the fact that treatment for common warts, cryotherapy with liquid nitrogen, is painful and can frighten children, and, with a response rate of “at best, 50%,” Dr. Waldman said. Veradermics is in the process of creating a nearly painless, child-friendly wart treatment: an “immunostimulatory dissolvable microarray” patch that contains Candida antigen extract, which is currently being evaluated for treating warts in a phase 2 clinical trial started in 2023.
Although the Magic Wand Initiative was initially restricted to dermatologists at MGH, stories like that of Veradermics have made the program so popular that it has branched out to include anesthesiologists and otolaryngologists, as well as general and orthopedic surgeons at MGH, Dr. Garibyan said at the Mount Sinai meeting.
Dr. Garibyan disclosed that she is a cofounder of and has equity in Brixton Biosciences and EyeCool, and is a consultant for and/or investor in Brixton and Clarity Cosmetics. Royalties/inventorship are assigned to MGH.
NEW YORK – .
The program was founded in 2013 by two Harvard Medical School dermatologists, Lilit Garibyan, MD, PhD, the program director, and her mentor R. Rox Anderson MD, director of the Wellman Center for Photomedicine at Massachusetts General Hospital (MGH), Boston. It was based on the idea that clinicians are in a unique position to identify gaps in patient care and should be active in developing medical solutions to address those gaps.
“I truly believe that if we do a better job educating, training, and empowering our clinicians to become innovators, this will benefit patients and hospitals and physicians,” Dr. Garibyan said at the 26th annual Mount Sinai Winter Symposium — Advances in Medical and Surgical Dermatology.
One of the seeds for the project was her own experience with cryolipolysis which involves topical cooling, a noninvasive method of removing subcutaneous fat for body contouring, which relies on conducting heat from subcutaneous fat across the skin and therefore, does not reach fat far from the dermis. With Dr. Anderson’s mentorship, she developed injectable cooling technology (ICT), a procedure where “ice slurry,” composed of normal saline and glycerol, is directly injected into adipose tissue, possibly leading to more efficient and effective cryolipolysis.
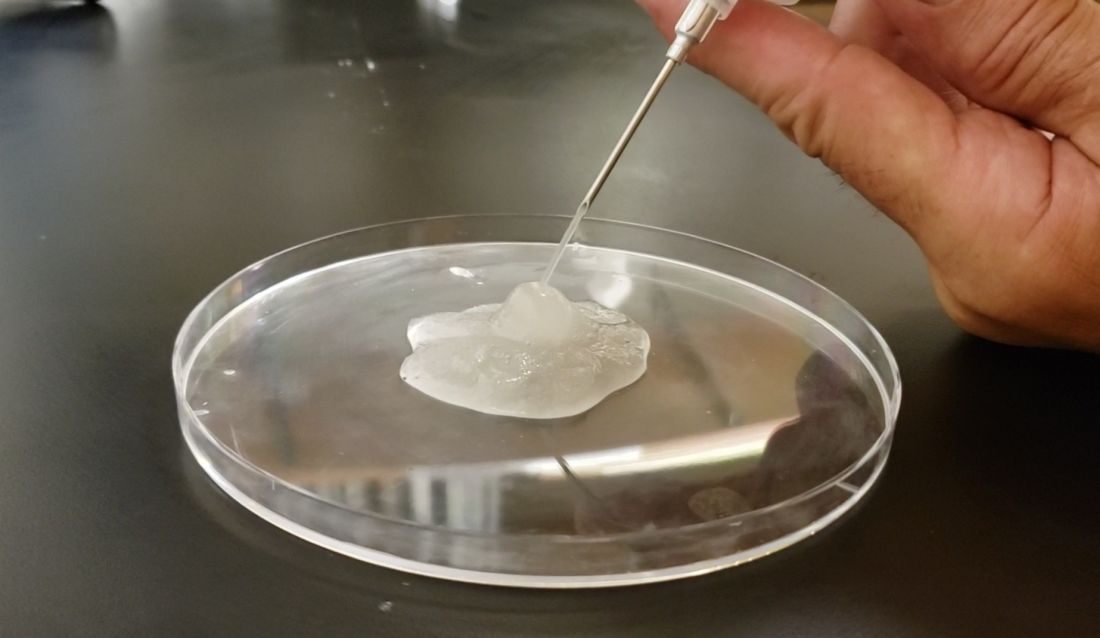
After nearly 10 years of animal studies at MGH, led by Dr. Garibyan as proof of concept trials, ice slurry (Coolio Therapy) recently received FDA breakthrough designation for long-term pain control and early-stage human trials of clinical applications are underway, she noted.
Magic Wand Program
In the Magic Wand program, participating physicians start by recording areas of unmet needs in their day-to-day practices, and in groups, engage in clinician-only brainstorming sessions to screen ideas, define problems, and generate lists of specifications and tools needed to address clinical problems. After working together to define challenges and possible solutions, they take their ideas to a development team, where scientists, engineers, regulatory experts, and industry professionals meet and help clinicians start pilot proof-of-concept projects, develop prototypes, and gain support for studies, followed by pilot feasibility studies.
Part of the project is the Virtual Magic Wand (VMW) Initiative, a 10-month online instructive and interactive course open to clinicians in the United States and Europe, designed to bring together dermatologists “interested in deeply understanding a dermatologic clinical problem worth solving,” according to Dr. Garibyan. Currently, there are more than 86 VMW scholars from 46 institutions, and military and private practice sites in the United States. The VMW was expanded to Europe in 2021 and there are plans to expand to Asia as well, she said.
The success of the program is not only attributed to its clinical methods but the fact that it provides a benefit to doctors at all stages of their careers, patients, and industry. “This is the only program that aims to engage in innovation from resident to full professor. We provide ideas that industry can then support and bring to market. Everyone including patients, doctors, and healthcare companies can benefit from active, engaged, and innovative physicians,” Dr. Garibyan said.
One of the success stories is that of Veradermics, a company founded by Kansas City dermatologist, Reid A. Waldman, MD, the company’s CEO, and Tim Durso, MD, the president, who met while participating in the VMW program in 2020, which eventually led them to start a company addressing an unmet need in dermatology, a kid-friendly treatment of warts.
In an interview with this news organization, Dr. Waldman explained how the program informed his company’s ethos. “Magic Wand Initiative is about identifying problems worth solving,” he said. At the company, “we find problems or unmet needs that are large enough to motivate prescribing changes, so we’ve really taken the philosophy I learned in the program into this company and building our portfolio.”
One of the first needs that Veradermics addressed was the fact that treatment for common warts, cryotherapy with liquid nitrogen, is painful and can frighten children, and, with a response rate of “at best, 50%,” Dr. Waldman said. Veradermics is in the process of creating a nearly painless, child-friendly wart treatment: an “immunostimulatory dissolvable microarray” patch that contains Candida antigen extract, which is currently being evaluated for treating warts in a phase 2 clinical trial started in 2023.
Although the Magic Wand Initiative was initially restricted to dermatologists at MGH, stories like that of Veradermics have made the program so popular that it has branched out to include anesthesiologists and otolaryngologists, as well as general and orthopedic surgeons at MGH, Dr. Garibyan said at the Mount Sinai meeting.
Dr. Garibyan disclosed that she is a cofounder of and has equity in Brixton Biosciences and EyeCool, and is a consultant for and/or investor in Brixton and Clarity Cosmetics. Royalties/inventorship are assigned to MGH.
Biosimilar Business Deals Keep Up ‘Musical Chairs’ Game of Formulary Construction
As the saying goes, “The more things change, the more they stay the same.” That is particularly true when it comes to the affordability of drugs for our patients even after the launch of so many Humira biosimilars. And we still have the “musical chairs” game of formulary construction — when the music stops, who knows whether your patient’s drug found a chair to sit on. There seems to be only a few chairs available for the many adalimumab biosimilars playing the game.
Nothing has changed since my testimony before the FDA Arthritis Advisory Committee in July 2016 during the approval hearing of the first Humira biosimilar. Below is a quote from that meeting where I was speaking predominantly about the pharmacy side of drugs.
“I’d like to highlight the term ‘access’ because none of us are really naive enough to believe that just approving a biosimilar gives a patient true, hands-on access to the medication, because even if the biosimilar is offered at a 30% discount, I don’t have any patients that can afford it. This means that access is ultimately controlled by third-party payers.”
My prediction, that approving and launching biosimilars with lower prices would not ensure patient access to the drug unless it is paid for by insurance, is now our reality. Today, a drug with an 85% discount on the price of Humira is still unattainable for patients without a “payer.”
Competition and Lower Prices
Lawmakers and some in the media cry for more competition to lower prices. This is the main reason that there has been such a push to get biosimilars to the market as quickly as possible. It is abundantly clear that competition to get on the formulary is fierce. Placement of a medication on a formulary can make or break a manufacturer’s ability to get a return on the R&D and make a profit on that medication. For a small biotech manufacturer, it can be the difference between “life and death” of the company.
Does anyone remember when the first interchangeable biosimilar for the reference insulin glargine product Lantus (insulin glargine-yfgn; Semglee) came to market in 2021? Janet Woodcock, MD, then acting FDA commissioner, called it a “momentous day” and further said, “Today’s approval of the first interchangeable biosimilar product furthers FDA’s longstanding commitment to support a competitive marketplace for biological products and ultimately empowers patients by helping to increase access to safe, effective and high-quality medications at potentially lower cost.” There was a high-priced interchangeable biosimilar and an identical unbranded low-priced interchangeable biosimilar, and the only one that could get formulary placement was the high-priced drug.
Patients pay their cost share on the list price of the drug, and because most pharmacy benefit managers’ (PBMs’) formularies cover only the high-priced biosimilar, patients never share in the savings. So much for the “competitive marketplace” creating lower costs for patients. This is just one of hundreds of examples in which lower-priced drugs are excluded from the formulary. It is unfortunate that the bidding process from manufacturers to PBMs to “win” preferred formulary placement is like an art auction, where the highest bidder wins.
Biosimilars and Formulary Construction
For those of us who have been looking into PBMs for many years, it is no surprise that PBMs’ formulary construction has become a profit center for them. Now, with so many adalimumab biosimilars having entered the market, it has become the Wild West where only those with the most money to fork over to the PBMs get preferred placement. Unfortunately, many of the choices that make money for the PBM cost employers and patients more.
How did we get here? In the 1980s and 90s, the price of medications began to increase to the point that many were not affordable without insurance. And who better to construct the list of drugs that would be covered by insurance (formulary) than the PBMs who were already adjudicating the claims for these drugs. The Federal Trade Commission (FTC) realized the power inherent in constructing this list of medications known as the formulary. So when the manufacturer Merck acquired the PBM Medco in the mid-1990s, the FTC stepped in. The FTC surmised that making the drugs and deciding which ones will be paid for created a “conflict of interest” with anticompetitive ramifications.
So, in 1998, William J. Baer, director of the FTC’s Bureau of Competition, said, “Our investigation into the PBM industry has revealed that Merck’s acquisition of Medco has reduced competition in the market for pharmaceutical products … We have found that Medco has given favorable treatment to Merck drugs. As a result, in some cases, consumers have been denied access to the drugs of competing manufacturers. In addition, the merger has made it possible for Medco to share with Merck sensitive pricing information it gets from Merck’s competitors, which could foster collusion among drug manufacturers.” Wow!
These anticompetitive behaviors and conflicts of interest resulting from the Medco acquisition led the FTC to propose a consent agreement.
The agreement would require Merck-Medco to maintain an “open formulary” — one that includes drugs selected and approved by an independent Pharmacy and Therapeutics Committee regardless of the manufacturer. Medco would have to accept rebates and other price concessions and reflect these in the ranking of the drugs on the formulary. Merck would have to make known the availability of the open formulary to any drug maker with an agreement with Medco.
Let’s hope the FTC of 2024 remembers the stance of the FTC in the 1990s regarding anticompetitive behavior involved in formulary construction.
Conflicts of Interest
But today it is apparent that crafting formularies that pay only for the drugs that make the most money for the PBM is not a conflict of interest. In its policy manual, Cigna directly tells employers and employees that they are collecting and keeping rebates and fees on medical pharmaceuticals, and they are not for the benefit of the employer or the plan.
And now, in August 2023, CVS launched Cordavis, a subsidiary wholly owned by CVS. Cordavis/CVS has partnered with Sandoz, which makes Hyrimoz, an adalimumab biosimilar. There is a high-priced version that is discounted 5% from Humira, a lower-cost unbranded version that is discounted 80% off the list price of Humira, and a co-branded CVS/Sandoz version of Hyrimoz that is lower priced as well.
It isn’t a surprise that CVS’ Standard and Advanced Commercial and Chart formularies are offering only Sandoz adalimumab biosimilar products. While these formularies have excluded Humira, CVS has entered into an agreement with AbbVie to allow Humira on a number of their other formularies. It can be very confusing.
As stated earlier, in the 1990s, the FTC frowned upon manufacturers owning PBMs and allowing them to construct their own formularies. Here we have CVS Health, mothership for the PBM CVS Caremark, owning a company that will be co-producing biosimilars with other manufacturers and then determining which biosimilars are on their formularies. The FTC knew back then that the tendency would be to offer only their own drugs for coverage, thus reducing competition. This is exactly what the CVS-Cordavis-Sandoz partnership has done for their Standard and Advanced Commercial and Chart formularies. It is perhaps anti-competitive but certainly profitable.
Perhaps the FTC should require the same consent agreement that was given to Merck in 1998. CVS Caremark would then have to open their formularies to all competitors of their co-branded, co-produced Sandoz biosimilar.
Summary
It is the same old adage, “The more things change, the more they stay the same.” PBMs are still constructing formularies with biosimilars based on their profitability, with huge differences between gross and net cost. Patients still pay their cost share on the list (gross) price. With the CVS-Cordavis-Sandoz partnership, more vertical integration has led to yet another profit river. Self-funded employers are still getting the wool pulled over their eyes by the big three PBMs who threaten to take away rebates if they don’t choose the preferred formularies. The employers don’t realize that sometimes it is less expensive to choose the lower-priced drugs with no rebates, and that holds true for biosimilars as well.
Let’s hope that the FTC investigates the situation of a PBM partnering with a manufacturer and then choosing only that manufacturer’s drugs for many of their formularies.
We need to continue our advocacy for our patients because the medication that has kept them stable for so long may find itself without a chair the next time the music stops.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
As the saying goes, “The more things change, the more they stay the same.” That is particularly true when it comes to the affordability of drugs for our patients even after the launch of so many Humira biosimilars. And we still have the “musical chairs” game of formulary construction — when the music stops, who knows whether your patient’s drug found a chair to sit on. There seems to be only a few chairs available for the many adalimumab biosimilars playing the game.
Nothing has changed since my testimony before the FDA Arthritis Advisory Committee in July 2016 during the approval hearing of the first Humira biosimilar. Below is a quote from that meeting where I was speaking predominantly about the pharmacy side of drugs.
“I’d like to highlight the term ‘access’ because none of us are really naive enough to believe that just approving a biosimilar gives a patient true, hands-on access to the medication, because even if the biosimilar is offered at a 30% discount, I don’t have any patients that can afford it. This means that access is ultimately controlled by third-party payers.”
My prediction, that approving and launching biosimilars with lower prices would not ensure patient access to the drug unless it is paid for by insurance, is now our reality. Today, a drug with an 85% discount on the price of Humira is still unattainable for patients without a “payer.”
Competition and Lower Prices
Lawmakers and some in the media cry for more competition to lower prices. This is the main reason that there has been such a push to get biosimilars to the market as quickly as possible. It is abundantly clear that competition to get on the formulary is fierce. Placement of a medication on a formulary can make or break a manufacturer’s ability to get a return on the R&D and make a profit on that medication. For a small biotech manufacturer, it can be the difference between “life and death” of the company.
Does anyone remember when the first interchangeable biosimilar for the reference insulin glargine product Lantus (insulin glargine-yfgn; Semglee) came to market in 2021? Janet Woodcock, MD, then acting FDA commissioner, called it a “momentous day” and further said, “Today’s approval of the first interchangeable biosimilar product furthers FDA’s longstanding commitment to support a competitive marketplace for biological products and ultimately empowers patients by helping to increase access to safe, effective and high-quality medications at potentially lower cost.” There was a high-priced interchangeable biosimilar and an identical unbranded low-priced interchangeable biosimilar, and the only one that could get formulary placement was the high-priced drug.
Patients pay their cost share on the list price of the drug, and because most pharmacy benefit managers’ (PBMs’) formularies cover only the high-priced biosimilar, patients never share in the savings. So much for the “competitive marketplace” creating lower costs for patients. This is just one of hundreds of examples in which lower-priced drugs are excluded from the formulary. It is unfortunate that the bidding process from manufacturers to PBMs to “win” preferred formulary placement is like an art auction, where the highest bidder wins.
Biosimilars and Formulary Construction
For those of us who have been looking into PBMs for many years, it is no surprise that PBMs’ formulary construction has become a profit center for them. Now, with so many adalimumab biosimilars having entered the market, it has become the Wild West where only those with the most money to fork over to the PBMs get preferred placement. Unfortunately, many of the choices that make money for the PBM cost employers and patients more.
How did we get here? In the 1980s and 90s, the price of medications began to increase to the point that many were not affordable without insurance. And who better to construct the list of drugs that would be covered by insurance (formulary) than the PBMs who were already adjudicating the claims for these drugs. The Federal Trade Commission (FTC) realized the power inherent in constructing this list of medications known as the formulary. So when the manufacturer Merck acquired the PBM Medco in the mid-1990s, the FTC stepped in. The FTC surmised that making the drugs and deciding which ones will be paid for created a “conflict of interest” with anticompetitive ramifications.
So, in 1998, William J. Baer, director of the FTC’s Bureau of Competition, said, “Our investigation into the PBM industry has revealed that Merck’s acquisition of Medco has reduced competition in the market for pharmaceutical products … We have found that Medco has given favorable treatment to Merck drugs. As a result, in some cases, consumers have been denied access to the drugs of competing manufacturers. In addition, the merger has made it possible for Medco to share with Merck sensitive pricing information it gets from Merck’s competitors, which could foster collusion among drug manufacturers.” Wow!
These anticompetitive behaviors and conflicts of interest resulting from the Medco acquisition led the FTC to propose a consent agreement.
The agreement would require Merck-Medco to maintain an “open formulary” — one that includes drugs selected and approved by an independent Pharmacy and Therapeutics Committee regardless of the manufacturer. Medco would have to accept rebates and other price concessions and reflect these in the ranking of the drugs on the formulary. Merck would have to make known the availability of the open formulary to any drug maker with an agreement with Medco.
Let’s hope the FTC of 2024 remembers the stance of the FTC in the 1990s regarding anticompetitive behavior involved in formulary construction.
Conflicts of Interest
But today it is apparent that crafting formularies that pay only for the drugs that make the most money for the PBM is not a conflict of interest. In its policy manual, Cigna directly tells employers and employees that they are collecting and keeping rebates and fees on medical pharmaceuticals, and they are not for the benefit of the employer or the plan.
And now, in August 2023, CVS launched Cordavis, a subsidiary wholly owned by CVS. Cordavis/CVS has partnered with Sandoz, which makes Hyrimoz, an adalimumab biosimilar. There is a high-priced version that is discounted 5% from Humira, a lower-cost unbranded version that is discounted 80% off the list price of Humira, and a co-branded CVS/Sandoz version of Hyrimoz that is lower priced as well.
It isn’t a surprise that CVS’ Standard and Advanced Commercial and Chart formularies are offering only Sandoz adalimumab biosimilar products. While these formularies have excluded Humira, CVS has entered into an agreement with AbbVie to allow Humira on a number of their other formularies. It can be very confusing.
As stated earlier, in the 1990s, the FTC frowned upon manufacturers owning PBMs and allowing them to construct their own formularies. Here we have CVS Health, mothership for the PBM CVS Caremark, owning a company that will be co-producing biosimilars with other manufacturers and then determining which biosimilars are on their formularies. The FTC knew back then that the tendency would be to offer only their own drugs for coverage, thus reducing competition. This is exactly what the CVS-Cordavis-Sandoz partnership has done for their Standard and Advanced Commercial and Chart formularies. It is perhaps anti-competitive but certainly profitable.
Perhaps the FTC should require the same consent agreement that was given to Merck in 1998. CVS Caremark would then have to open their formularies to all competitors of their co-branded, co-produced Sandoz biosimilar.
Summary
It is the same old adage, “The more things change, the more they stay the same.” PBMs are still constructing formularies with biosimilars based on their profitability, with huge differences between gross and net cost. Patients still pay their cost share on the list (gross) price. With the CVS-Cordavis-Sandoz partnership, more vertical integration has led to yet another profit river. Self-funded employers are still getting the wool pulled over their eyes by the big three PBMs who threaten to take away rebates if they don’t choose the preferred formularies. The employers don’t realize that sometimes it is less expensive to choose the lower-priced drugs with no rebates, and that holds true for biosimilars as well.
Let’s hope that the FTC investigates the situation of a PBM partnering with a manufacturer and then choosing only that manufacturer’s drugs for many of their formularies.
We need to continue our advocacy for our patients because the medication that has kept them stable for so long may find itself without a chair the next time the music stops.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
As the saying goes, “The more things change, the more they stay the same.” That is particularly true when it comes to the affordability of drugs for our patients even after the launch of so many Humira biosimilars. And we still have the “musical chairs” game of formulary construction — when the music stops, who knows whether your patient’s drug found a chair to sit on. There seems to be only a few chairs available for the many adalimumab biosimilars playing the game.
Nothing has changed since my testimony before the FDA Arthritis Advisory Committee in July 2016 during the approval hearing of the first Humira biosimilar. Below is a quote from that meeting where I was speaking predominantly about the pharmacy side of drugs.
“I’d like to highlight the term ‘access’ because none of us are really naive enough to believe that just approving a biosimilar gives a patient true, hands-on access to the medication, because even if the biosimilar is offered at a 30% discount, I don’t have any patients that can afford it. This means that access is ultimately controlled by third-party payers.”
My prediction, that approving and launching biosimilars with lower prices would not ensure patient access to the drug unless it is paid for by insurance, is now our reality. Today, a drug with an 85% discount on the price of Humira is still unattainable for patients without a “payer.”
Competition and Lower Prices
Lawmakers and some in the media cry for more competition to lower prices. This is the main reason that there has been such a push to get biosimilars to the market as quickly as possible. It is abundantly clear that competition to get on the formulary is fierce. Placement of a medication on a formulary can make or break a manufacturer’s ability to get a return on the R&D and make a profit on that medication. For a small biotech manufacturer, it can be the difference between “life and death” of the company.
Does anyone remember when the first interchangeable biosimilar for the reference insulin glargine product Lantus (insulin glargine-yfgn; Semglee) came to market in 2021? Janet Woodcock, MD, then acting FDA commissioner, called it a “momentous day” and further said, “Today’s approval of the first interchangeable biosimilar product furthers FDA’s longstanding commitment to support a competitive marketplace for biological products and ultimately empowers patients by helping to increase access to safe, effective and high-quality medications at potentially lower cost.” There was a high-priced interchangeable biosimilar and an identical unbranded low-priced interchangeable biosimilar, and the only one that could get formulary placement was the high-priced drug.
Patients pay their cost share on the list price of the drug, and because most pharmacy benefit managers’ (PBMs’) formularies cover only the high-priced biosimilar, patients never share in the savings. So much for the “competitive marketplace” creating lower costs for patients. This is just one of hundreds of examples in which lower-priced drugs are excluded from the formulary. It is unfortunate that the bidding process from manufacturers to PBMs to “win” preferred formulary placement is like an art auction, where the highest bidder wins.
Biosimilars and Formulary Construction
For those of us who have been looking into PBMs for many years, it is no surprise that PBMs’ formulary construction has become a profit center for them. Now, with so many adalimumab biosimilars having entered the market, it has become the Wild West where only those with the most money to fork over to the PBMs get preferred placement. Unfortunately, many of the choices that make money for the PBM cost employers and patients more.
How did we get here? In the 1980s and 90s, the price of medications began to increase to the point that many were not affordable without insurance. And who better to construct the list of drugs that would be covered by insurance (formulary) than the PBMs who were already adjudicating the claims for these drugs. The Federal Trade Commission (FTC) realized the power inherent in constructing this list of medications known as the formulary. So when the manufacturer Merck acquired the PBM Medco in the mid-1990s, the FTC stepped in. The FTC surmised that making the drugs and deciding which ones will be paid for created a “conflict of interest” with anticompetitive ramifications.
So, in 1998, William J. Baer, director of the FTC’s Bureau of Competition, said, “Our investigation into the PBM industry has revealed that Merck’s acquisition of Medco has reduced competition in the market for pharmaceutical products … We have found that Medco has given favorable treatment to Merck drugs. As a result, in some cases, consumers have been denied access to the drugs of competing manufacturers. In addition, the merger has made it possible for Medco to share with Merck sensitive pricing information it gets from Merck’s competitors, which could foster collusion among drug manufacturers.” Wow!
These anticompetitive behaviors and conflicts of interest resulting from the Medco acquisition led the FTC to propose a consent agreement.
The agreement would require Merck-Medco to maintain an “open formulary” — one that includes drugs selected and approved by an independent Pharmacy and Therapeutics Committee regardless of the manufacturer. Medco would have to accept rebates and other price concessions and reflect these in the ranking of the drugs on the formulary. Merck would have to make known the availability of the open formulary to any drug maker with an agreement with Medco.
Let’s hope the FTC of 2024 remembers the stance of the FTC in the 1990s regarding anticompetitive behavior involved in formulary construction.
Conflicts of Interest
But today it is apparent that crafting formularies that pay only for the drugs that make the most money for the PBM is not a conflict of interest. In its policy manual, Cigna directly tells employers and employees that they are collecting and keeping rebates and fees on medical pharmaceuticals, and they are not for the benefit of the employer or the plan.
And now, in August 2023, CVS launched Cordavis, a subsidiary wholly owned by CVS. Cordavis/CVS has partnered with Sandoz, which makes Hyrimoz, an adalimumab biosimilar. There is a high-priced version that is discounted 5% from Humira, a lower-cost unbranded version that is discounted 80% off the list price of Humira, and a co-branded CVS/Sandoz version of Hyrimoz that is lower priced as well.
It isn’t a surprise that CVS’ Standard and Advanced Commercial and Chart formularies are offering only Sandoz adalimumab biosimilar products. While these formularies have excluded Humira, CVS has entered into an agreement with AbbVie to allow Humira on a number of their other formularies. It can be very confusing.
As stated earlier, in the 1990s, the FTC frowned upon manufacturers owning PBMs and allowing them to construct their own formularies. Here we have CVS Health, mothership for the PBM CVS Caremark, owning a company that will be co-producing biosimilars with other manufacturers and then determining which biosimilars are on their formularies. The FTC knew back then that the tendency would be to offer only their own drugs for coverage, thus reducing competition. This is exactly what the CVS-Cordavis-Sandoz partnership has done for their Standard and Advanced Commercial and Chart formularies. It is perhaps anti-competitive but certainly profitable.
Perhaps the FTC should require the same consent agreement that was given to Merck in 1998. CVS Caremark would then have to open their formularies to all competitors of their co-branded, co-produced Sandoz biosimilar.
Summary
It is the same old adage, “The more things change, the more they stay the same.” PBMs are still constructing formularies with biosimilars based on their profitability, with huge differences between gross and net cost. Patients still pay their cost share on the list (gross) price. With the CVS-Cordavis-Sandoz partnership, more vertical integration has led to yet another profit river. Self-funded employers are still getting the wool pulled over their eyes by the big three PBMs who threaten to take away rebates if they don’t choose the preferred formularies. The employers don’t realize that sometimes it is less expensive to choose the lower-priced drugs with no rebates, and that holds true for biosimilars as well.
Let’s hope that the FTC investigates the situation of a PBM partnering with a manufacturer and then choosing only that manufacturer’s drugs for many of their formularies.
We need to continue our advocacy for our patients because the medication that has kept them stable for so long may find itself without a chair the next time the music stops.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
Coffee, COVID, and the Universal Antimicrobial
A recent article in Cell & Bioscience suggested that regular coffee consumption can reduce the risk of COVID infections.
The study does make some interesting points about the benefits of coffee’s different polyphenols and antioxidants and their effects on different COVID variants. Most of it is based on lab data, although one section, using serum from coffee versus water drinkers, did find that it was more effective at inhibiting the virions. Caffeinated versus decaffeinated didn’t matter.
I’m not saying coffee doesn’t impair the virus. The data are worth looking at. But the majority of adults in North America, Europe, and pretty much the entire planet drink coffee on a regular basis. A large number of them still caught COVID. Would they have had worse cases if they didn’t drink coffee? Maybe, maybe not.
The problem here is that, as always, preliminary data like this get pushed into mass media, making it sound like “COFFEE CURES COVID!!!” Never mind that that’s not what the article said, but it sure gets clicks and retweets and FaceBook “likes.”
Suddenly fringe groups are claiming the coffee cure was there all along, and hidden from them by the evil government-pharma-medical cartel. Others claim the research is flawed because of this or that. The signal gets drowned out by the noise.
Definitely, food can be a medicine. Look at all the benefits proven of the Mediterranean diet. Coffee may help, especially if we can identify and isolate the specific components that reduce COVID risk. But, as they always say at the end, the study is preliminary and further research is needed.
Once or twice a year, an adult with epilepsy comes in, waving a copy of the ketogenic diet around and upset that I never tried it on them — again proof of the evil government-pharma-medical cartel that I’m in league with. I calm them down and explain the diet in detail. Maybe 50% of them decide to go ahead with it. In 25 years of practice, my record for an otherwise normal adult sticking with it is 5 days.
You don’t have to go too far back to remember Linus Pauling, an absolutely brilliant scientist, but not the best of nutritionists. With two Nobel prizes behind him, he took a stab at medicine in the 1970s, arguing that megadoses of vitamin C worked for the common cold. While it may be good for us, and certainly most people like orange juice, but those claims about the common cold never panned out. In fact, we’re no closer to curing it now than we were then.
It might, but this doesn’t mean the “truth” is being maliciously hidden by an evil cartel. It just means we have (as always) more to learn.
I’ll still drink my single cup of coffee every weekday morning. I’m a creature of habit, and heaven knows I need the caffeine. If it also boosts my immune system, so much the better.
Besides, we still have that universal antimicrobial called chicken soup.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A recent article in Cell & Bioscience suggested that regular coffee consumption can reduce the risk of COVID infections.
The study does make some interesting points about the benefits of coffee’s different polyphenols and antioxidants and their effects on different COVID variants. Most of it is based on lab data, although one section, using serum from coffee versus water drinkers, did find that it was more effective at inhibiting the virions. Caffeinated versus decaffeinated didn’t matter.
I’m not saying coffee doesn’t impair the virus. The data are worth looking at. But the majority of adults in North America, Europe, and pretty much the entire planet drink coffee on a regular basis. A large number of them still caught COVID. Would they have had worse cases if they didn’t drink coffee? Maybe, maybe not.
The problem here is that, as always, preliminary data like this get pushed into mass media, making it sound like “COFFEE CURES COVID!!!” Never mind that that’s not what the article said, but it sure gets clicks and retweets and FaceBook “likes.”
Suddenly fringe groups are claiming the coffee cure was there all along, and hidden from them by the evil government-pharma-medical cartel. Others claim the research is flawed because of this or that. The signal gets drowned out by the noise.
Definitely, food can be a medicine. Look at all the benefits proven of the Mediterranean diet. Coffee may help, especially if we can identify and isolate the specific components that reduce COVID risk. But, as they always say at the end, the study is preliminary and further research is needed.
Once or twice a year, an adult with epilepsy comes in, waving a copy of the ketogenic diet around and upset that I never tried it on them — again proof of the evil government-pharma-medical cartel that I’m in league with. I calm them down and explain the diet in detail. Maybe 50% of them decide to go ahead with it. In 25 years of practice, my record for an otherwise normal adult sticking with it is 5 days.
You don’t have to go too far back to remember Linus Pauling, an absolutely brilliant scientist, but not the best of nutritionists. With two Nobel prizes behind him, he took a stab at medicine in the 1970s, arguing that megadoses of vitamin C worked for the common cold. While it may be good for us, and certainly most people like orange juice, but those claims about the common cold never panned out. In fact, we’re no closer to curing it now than we were then.
It might, but this doesn’t mean the “truth” is being maliciously hidden by an evil cartel. It just means we have (as always) more to learn.
I’ll still drink my single cup of coffee every weekday morning. I’m a creature of habit, and heaven knows I need the caffeine. If it also boosts my immune system, so much the better.
Besides, we still have that universal antimicrobial called chicken soup.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A recent article in Cell & Bioscience suggested that regular coffee consumption can reduce the risk of COVID infections.
The study does make some interesting points about the benefits of coffee’s different polyphenols and antioxidants and their effects on different COVID variants. Most of it is based on lab data, although one section, using serum from coffee versus water drinkers, did find that it was more effective at inhibiting the virions. Caffeinated versus decaffeinated didn’t matter.
I’m not saying coffee doesn’t impair the virus. The data are worth looking at. But the majority of adults in North America, Europe, and pretty much the entire planet drink coffee on a regular basis. A large number of them still caught COVID. Would they have had worse cases if they didn’t drink coffee? Maybe, maybe not.
The problem here is that, as always, preliminary data like this get pushed into mass media, making it sound like “COFFEE CURES COVID!!!” Never mind that that’s not what the article said, but it sure gets clicks and retweets and FaceBook “likes.”
Suddenly fringe groups are claiming the coffee cure was there all along, and hidden from them by the evil government-pharma-medical cartel. Others claim the research is flawed because of this or that. The signal gets drowned out by the noise.
Definitely, food can be a medicine. Look at all the benefits proven of the Mediterranean diet. Coffee may help, especially if we can identify and isolate the specific components that reduce COVID risk. But, as they always say at the end, the study is preliminary and further research is needed.
Once or twice a year, an adult with epilepsy comes in, waving a copy of the ketogenic diet around and upset that I never tried it on them — again proof of the evil government-pharma-medical cartel that I’m in league with. I calm them down and explain the diet in detail. Maybe 50% of them decide to go ahead with it. In 25 years of practice, my record for an otherwise normal adult sticking with it is 5 days.
You don’t have to go too far back to remember Linus Pauling, an absolutely brilliant scientist, but not the best of nutritionists. With two Nobel prizes behind him, he took a stab at medicine in the 1970s, arguing that megadoses of vitamin C worked for the common cold. While it may be good for us, and certainly most people like orange juice, but those claims about the common cold never panned out. In fact, we’re no closer to curing it now than we were then.
It might, but this doesn’t mean the “truth” is being maliciously hidden by an evil cartel. It just means we have (as always) more to learn.
I’ll still drink my single cup of coffee every weekday morning. I’m a creature of habit, and heaven knows I need the caffeine. If it also boosts my immune system, so much the better.
Besides, we still have that universal antimicrobial called chicken soup.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Left-Handed Med Students Still ‘Left Out’ in Surgery
of 31 individuals from 15 US institutions.
“Surgical education is designed for the right-handed,” wrote Timothy J. Gilbert, MD, of the University of Michigan, Ann Arbor, and colleagues. Left-handed medical students “contend with instruments designed for right-handed use, perform worse on surgical skills assessments that are biased toward the right-handed, and are assumed to be right-handed by educators,” they said.
Challenges for left-handed medical students are not new. A study published in 2010 in the Journal of Surgical Education identified eight major issues for left-handed surgeons:
- Anxiety about laterality
- Lack of mentoring on lateral preference
- Difficulty handling traditional instruments
- Difficulty with minimally invasive instruments
- Inconvenience while assisting a right-handed person
- Pressure to change lateral preference
- Possible disadvantages with certain procedures
- Possible advantage situs inversus
Previous studies have shown reports of stigmatization and a lack of training and educational resources as barriers to improving the experience and fostering the skills of left-handed students, but the current data on the subjective experiences of left-handed students are limited, the authors said.
“Some of the members of the research team are left-handed, and I think their personal experience/understanding of the topic informed their desire to do projects within this space, since handedness is so thoroughly taken for granted by the right-handed majority,” Dr. Gilbert, who is right-handed, said in an interview. “It was important for our study to have parity between handedness to reduce bias in data interpretation,” he said. “In an era where much has been done to ensure equity between different groups, there’s not as much discussion about handedness within surgery as I believe there should be.”
In a new study published in Academic Medicine, the researchers recruited 31 self-identified left-handed surgical residents and fellows in six surgical specialties (general surgery, urology, plastic surgery, obstetrics and gynecology, otolaryngology, and neurosurgery) and conducted semi-structured interviews between January 31, 2021, and June 20, 2021. The study population included 21 seniors (postgraduate year of 3 or higher), five juniors (postgraduate years 1 or 2), and five surgical fellows.
Overall, three themes surfaced from the participants’ educational experiences:
- Disorienting advice from faculty or residents
- Discouraging right-handed pressures and left-handed stigmatization
- Expression of the educational wishes of left-handed medical students
Conflicting Advice
The interviewees described feeling confused by conflicting advice about how to manage surgical procedures given their left-handedness, the researchers said. Some respondents reported being told to learn to do everything with the right hand; others were told to use their dominant hand (right or left) for fine motor skill elements but use the right hand for sewing.
Persistent Stigma and Switching
Survey respondents reported perceptions that others in the surgical setting were judgmental and inconsiderate; workshops involved demonstrations with a right-handed focus; and surgical technicians prepared needles that were loaded right-handed. “To minimize this negativity, participants often changed to their right hand,” the authors wrote. Some students who changed handedness reported an improved learning experience, in part because their handedness aligned with the instruments they used.
Educational Wish List
Study participants expressed the need for destigmatization of left-handedness in surgical through strategies including tangible mentorship, more granular and meaningful instruction, and normalization of left-handedness.
The study was limited by several factors including the focus only on surgical residents and fellows, with no left-handed medical students who pursued other specialties, the researchers noted. Other limitations included the retrospective design and potential bias from left-handed members of the research team, they said.
Notably, left-handed medical students reported negative experiences during training whether they operated with the right or left hand, the researchers wrote in their discussion. “From a strictly technical perspective, a left-handed medical student who is operatively left-handed will struggle to use hand-discordant tools in their dominant hand, whereas one who is operatively right-handed will struggle to use hand-concordant tools in their nondominant hand,” they said.
The researchers emphasized the need to consider the data in context; a nervous left-handed student who has been shown only right-handed tools and techniques and has not disclosed their left-handedness struggles when asked to close an incision may see themselves as the problem rather than the surgical education.
Takeaways to Improve Training
The current study showed the diversity of needs of left-handed surgical trainees and how more positive encouragement and support could improve their experiences, Dr. Gilbert told this news organization.
The strategies to improve training for left-handed medical students vary according to educational level, said Dr. Gilbert. “If you’re a surgical fellow or chief resident, you probably want more formal training, different tools, access to attendings who have experience performing an operation left-handed. If you’re a medical student, that is likely less important than feeling like you won’t be penalized of looked down upon for your handedness,” he said.
In the survey responses, “I at least was struck by how far a few accepting words could do when said in the right way at the right time,” he said.
“I think the most important takeaway is that educators should consider more what they say and do in the operating room to these junior students/trainees, as our data suggest even a single sentence at such a vulnerable point in time can push them into a choosing their handedness,” Dr. Gilbert said. “That’s not a small decision to make, and educators should be more thoughtful when engaging in the topic.”
Also, educators should offer left-handed resources during clerkship orientations on techniques such as knot-tying, he said. “This normalized handedness and may make students more comfortable with themselves in the operating room.”
Finally, “educators should be able to teach medical students the level-appropriate skills in either hand. If a medical student asks how to tie a knot or throw a stitch in their left hand, the educator should be able to demonstrate this to them effectively,” Dr. Gilbert added.
More research is needed to understand the needs and wants of left-handed medical students, including those who do not pursue surgery and of the skills of the residents and attendings who are tasked with educating these students, Dr. Gilbert told this news organization.
“Eventually, the goal is to implement concrete changes to improve resources for these students, but I think the most effective way to design these resources is to fully grasp the desires and concerns of all involved parties,” he said.
Residency Director Perspective
“We are increasingly sensitive to individual differences, but for some reason, left-handedness is a blind spot, although 10% of the population is left-handed,” said Stephen M. Kavic, MD, professor of surgery at the University of Maryland School of Medicine, in an interview.
“Interestingly, we do not ask handedness on residency applications, suggesting that it may be viewed as a negative trait in the selection process,” said Dr. Kavic, who also serves as program director of residency in surgery at the University of Maryland.
“While not left-handed myself, as Program Director, I have been tasked with training left-handed residents, and I appreciate the challenges,” Dr. Kavic said. “Our department is about 6% left-handed. Most left-handed surgeons are far more comfortable with their nondominant hand than right-handers are with theirs,” he noted. “We do have left-handed instruments available, but the ratio of sets is easily 100:1 right to left.”
With regard to the current study, Dr. Kavic said it was understandable that left-handed medical students feel stigmatized. A message for educators is to not presume right-handedness; instead, ask students about the hand preference on first meeting, and then training will be more inclusive, he said.
“There is a fundamental difference in mirror image training when a righty tries to teach a lefty. How do we do this better and in a standardized fashion? This article clearly shows that we still have a problem; now we must do the work to fix it,” Dr. Kavic said.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Kavic had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
of 31 individuals from 15 US institutions.
“Surgical education is designed for the right-handed,” wrote Timothy J. Gilbert, MD, of the University of Michigan, Ann Arbor, and colleagues. Left-handed medical students “contend with instruments designed for right-handed use, perform worse on surgical skills assessments that are biased toward the right-handed, and are assumed to be right-handed by educators,” they said.
Challenges for left-handed medical students are not new. A study published in 2010 in the Journal of Surgical Education identified eight major issues for left-handed surgeons:
- Anxiety about laterality
- Lack of mentoring on lateral preference
- Difficulty handling traditional instruments
- Difficulty with minimally invasive instruments
- Inconvenience while assisting a right-handed person
- Pressure to change lateral preference
- Possible disadvantages with certain procedures
- Possible advantage situs inversus
Previous studies have shown reports of stigmatization and a lack of training and educational resources as barriers to improving the experience and fostering the skills of left-handed students, but the current data on the subjective experiences of left-handed students are limited, the authors said.
“Some of the members of the research team are left-handed, and I think their personal experience/understanding of the topic informed their desire to do projects within this space, since handedness is so thoroughly taken for granted by the right-handed majority,” Dr. Gilbert, who is right-handed, said in an interview. “It was important for our study to have parity between handedness to reduce bias in data interpretation,” he said. “In an era where much has been done to ensure equity between different groups, there’s not as much discussion about handedness within surgery as I believe there should be.”
In a new study published in Academic Medicine, the researchers recruited 31 self-identified left-handed surgical residents and fellows in six surgical specialties (general surgery, urology, plastic surgery, obstetrics and gynecology, otolaryngology, and neurosurgery) and conducted semi-structured interviews between January 31, 2021, and June 20, 2021. The study population included 21 seniors (postgraduate year of 3 or higher), five juniors (postgraduate years 1 or 2), and five surgical fellows.
Overall, three themes surfaced from the participants’ educational experiences:
- Disorienting advice from faculty or residents
- Discouraging right-handed pressures and left-handed stigmatization
- Expression of the educational wishes of left-handed medical students
Conflicting Advice
The interviewees described feeling confused by conflicting advice about how to manage surgical procedures given their left-handedness, the researchers said. Some respondents reported being told to learn to do everything with the right hand; others were told to use their dominant hand (right or left) for fine motor skill elements but use the right hand for sewing.
Persistent Stigma and Switching
Survey respondents reported perceptions that others in the surgical setting were judgmental and inconsiderate; workshops involved demonstrations with a right-handed focus; and surgical technicians prepared needles that were loaded right-handed. “To minimize this negativity, participants often changed to their right hand,” the authors wrote. Some students who changed handedness reported an improved learning experience, in part because their handedness aligned with the instruments they used.
Educational Wish List
Study participants expressed the need for destigmatization of left-handedness in surgical through strategies including tangible mentorship, more granular and meaningful instruction, and normalization of left-handedness.
The study was limited by several factors including the focus only on surgical residents and fellows, with no left-handed medical students who pursued other specialties, the researchers noted. Other limitations included the retrospective design and potential bias from left-handed members of the research team, they said.
Notably, left-handed medical students reported negative experiences during training whether they operated with the right or left hand, the researchers wrote in their discussion. “From a strictly technical perspective, a left-handed medical student who is operatively left-handed will struggle to use hand-discordant tools in their dominant hand, whereas one who is operatively right-handed will struggle to use hand-concordant tools in their nondominant hand,” they said.
The researchers emphasized the need to consider the data in context; a nervous left-handed student who has been shown only right-handed tools and techniques and has not disclosed their left-handedness struggles when asked to close an incision may see themselves as the problem rather than the surgical education.
Takeaways to Improve Training
The current study showed the diversity of needs of left-handed surgical trainees and how more positive encouragement and support could improve their experiences, Dr. Gilbert told this news organization.
The strategies to improve training for left-handed medical students vary according to educational level, said Dr. Gilbert. “If you’re a surgical fellow or chief resident, you probably want more formal training, different tools, access to attendings who have experience performing an operation left-handed. If you’re a medical student, that is likely less important than feeling like you won’t be penalized of looked down upon for your handedness,” he said.
In the survey responses, “I at least was struck by how far a few accepting words could do when said in the right way at the right time,” he said.
“I think the most important takeaway is that educators should consider more what they say and do in the operating room to these junior students/trainees, as our data suggest even a single sentence at such a vulnerable point in time can push them into a choosing their handedness,” Dr. Gilbert said. “That’s not a small decision to make, and educators should be more thoughtful when engaging in the topic.”
Also, educators should offer left-handed resources during clerkship orientations on techniques such as knot-tying, he said. “This normalized handedness and may make students more comfortable with themselves in the operating room.”
Finally, “educators should be able to teach medical students the level-appropriate skills in either hand. If a medical student asks how to tie a knot or throw a stitch in their left hand, the educator should be able to demonstrate this to them effectively,” Dr. Gilbert added.
More research is needed to understand the needs and wants of left-handed medical students, including those who do not pursue surgery and of the skills of the residents and attendings who are tasked with educating these students, Dr. Gilbert told this news organization.
“Eventually, the goal is to implement concrete changes to improve resources for these students, but I think the most effective way to design these resources is to fully grasp the desires and concerns of all involved parties,” he said.
Residency Director Perspective
“We are increasingly sensitive to individual differences, but for some reason, left-handedness is a blind spot, although 10% of the population is left-handed,” said Stephen M. Kavic, MD, professor of surgery at the University of Maryland School of Medicine, in an interview.
“Interestingly, we do not ask handedness on residency applications, suggesting that it may be viewed as a negative trait in the selection process,” said Dr. Kavic, who also serves as program director of residency in surgery at the University of Maryland.
“While not left-handed myself, as Program Director, I have been tasked with training left-handed residents, and I appreciate the challenges,” Dr. Kavic said. “Our department is about 6% left-handed. Most left-handed surgeons are far more comfortable with their nondominant hand than right-handers are with theirs,” he noted. “We do have left-handed instruments available, but the ratio of sets is easily 100:1 right to left.”
With regard to the current study, Dr. Kavic said it was understandable that left-handed medical students feel stigmatized. A message for educators is to not presume right-handedness; instead, ask students about the hand preference on first meeting, and then training will be more inclusive, he said.
“There is a fundamental difference in mirror image training when a righty tries to teach a lefty. How do we do this better and in a standardized fashion? This article clearly shows that we still have a problem; now we must do the work to fix it,” Dr. Kavic said.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Kavic had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
of 31 individuals from 15 US institutions.
“Surgical education is designed for the right-handed,” wrote Timothy J. Gilbert, MD, of the University of Michigan, Ann Arbor, and colleagues. Left-handed medical students “contend with instruments designed for right-handed use, perform worse on surgical skills assessments that are biased toward the right-handed, and are assumed to be right-handed by educators,” they said.
Challenges for left-handed medical students are not new. A study published in 2010 in the Journal of Surgical Education identified eight major issues for left-handed surgeons:
- Anxiety about laterality
- Lack of mentoring on lateral preference
- Difficulty handling traditional instruments
- Difficulty with minimally invasive instruments
- Inconvenience while assisting a right-handed person
- Pressure to change lateral preference
- Possible disadvantages with certain procedures
- Possible advantage situs inversus
Previous studies have shown reports of stigmatization and a lack of training and educational resources as barriers to improving the experience and fostering the skills of left-handed students, but the current data on the subjective experiences of left-handed students are limited, the authors said.
“Some of the members of the research team are left-handed, and I think their personal experience/understanding of the topic informed their desire to do projects within this space, since handedness is so thoroughly taken for granted by the right-handed majority,” Dr. Gilbert, who is right-handed, said in an interview. “It was important for our study to have parity between handedness to reduce bias in data interpretation,” he said. “In an era where much has been done to ensure equity between different groups, there’s not as much discussion about handedness within surgery as I believe there should be.”
In a new study published in Academic Medicine, the researchers recruited 31 self-identified left-handed surgical residents and fellows in six surgical specialties (general surgery, urology, plastic surgery, obstetrics and gynecology, otolaryngology, and neurosurgery) and conducted semi-structured interviews between January 31, 2021, and June 20, 2021. The study population included 21 seniors (postgraduate year of 3 or higher), five juniors (postgraduate years 1 or 2), and five surgical fellows.
Overall, three themes surfaced from the participants’ educational experiences:
- Disorienting advice from faculty or residents
- Discouraging right-handed pressures and left-handed stigmatization
- Expression of the educational wishes of left-handed medical students
Conflicting Advice
The interviewees described feeling confused by conflicting advice about how to manage surgical procedures given their left-handedness, the researchers said. Some respondents reported being told to learn to do everything with the right hand; others were told to use their dominant hand (right or left) for fine motor skill elements but use the right hand for sewing.
Persistent Stigma and Switching
Survey respondents reported perceptions that others in the surgical setting were judgmental and inconsiderate; workshops involved demonstrations with a right-handed focus; and surgical technicians prepared needles that were loaded right-handed. “To minimize this negativity, participants often changed to their right hand,” the authors wrote. Some students who changed handedness reported an improved learning experience, in part because their handedness aligned with the instruments they used.
Educational Wish List
Study participants expressed the need for destigmatization of left-handedness in surgical through strategies including tangible mentorship, more granular and meaningful instruction, and normalization of left-handedness.
The study was limited by several factors including the focus only on surgical residents and fellows, with no left-handed medical students who pursued other specialties, the researchers noted. Other limitations included the retrospective design and potential bias from left-handed members of the research team, they said.
Notably, left-handed medical students reported negative experiences during training whether they operated with the right or left hand, the researchers wrote in their discussion. “From a strictly technical perspective, a left-handed medical student who is operatively left-handed will struggle to use hand-discordant tools in their dominant hand, whereas one who is operatively right-handed will struggle to use hand-concordant tools in their nondominant hand,” they said.
The researchers emphasized the need to consider the data in context; a nervous left-handed student who has been shown only right-handed tools and techniques and has not disclosed their left-handedness struggles when asked to close an incision may see themselves as the problem rather than the surgical education.
Takeaways to Improve Training
The current study showed the diversity of needs of left-handed surgical trainees and how more positive encouragement and support could improve their experiences, Dr. Gilbert told this news organization.
The strategies to improve training for left-handed medical students vary according to educational level, said Dr. Gilbert. “If you’re a surgical fellow or chief resident, you probably want more formal training, different tools, access to attendings who have experience performing an operation left-handed. If you’re a medical student, that is likely less important than feeling like you won’t be penalized of looked down upon for your handedness,” he said.
In the survey responses, “I at least was struck by how far a few accepting words could do when said in the right way at the right time,” he said.
“I think the most important takeaway is that educators should consider more what they say and do in the operating room to these junior students/trainees, as our data suggest even a single sentence at such a vulnerable point in time can push them into a choosing their handedness,” Dr. Gilbert said. “That’s not a small decision to make, and educators should be more thoughtful when engaging in the topic.”
Also, educators should offer left-handed resources during clerkship orientations on techniques such as knot-tying, he said. “This normalized handedness and may make students more comfortable with themselves in the operating room.”
Finally, “educators should be able to teach medical students the level-appropriate skills in either hand. If a medical student asks how to tie a knot or throw a stitch in their left hand, the educator should be able to demonstrate this to them effectively,” Dr. Gilbert added.
More research is needed to understand the needs and wants of left-handed medical students, including those who do not pursue surgery and of the skills of the residents and attendings who are tasked with educating these students, Dr. Gilbert told this news organization.
“Eventually, the goal is to implement concrete changes to improve resources for these students, but I think the most effective way to design these resources is to fully grasp the desires and concerns of all involved parties,” he said.
Residency Director Perspective
“We are increasingly sensitive to individual differences, but for some reason, left-handedness is a blind spot, although 10% of the population is left-handed,” said Stephen M. Kavic, MD, professor of surgery at the University of Maryland School of Medicine, in an interview.
“Interestingly, we do not ask handedness on residency applications, suggesting that it may be viewed as a negative trait in the selection process,” said Dr. Kavic, who also serves as program director of residency in surgery at the University of Maryland.
“While not left-handed myself, as Program Director, I have been tasked with training left-handed residents, and I appreciate the challenges,” Dr. Kavic said. “Our department is about 6% left-handed. Most left-handed surgeons are far more comfortable with their nondominant hand than right-handers are with theirs,” he noted. “We do have left-handed instruments available, but the ratio of sets is easily 100:1 right to left.”
With regard to the current study, Dr. Kavic said it was understandable that left-handed medical students feel stigmatized. A message for educators is to not presume right-handedness; instead, ask students about the hand preference on first meeting, and then training will be more inclusive, he said.
“There is a fundamental difference in mirror image training when a righty tries to teach a lefty. How do we do this better and in a standardized fashion? This article clearly shows that we still have a problem; now we must do the work to fix it,” Dr. Kavic said.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Kavic had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
FROM ACADEMIC MEDICINE
CMS Okays Payment for Novel AI Prostate Test
The Centers for Medicare & Medicare Services (CMS) on January 1 approved the payment rate for ArteraAI as a clinical diagnostic laboratory test. The test is the first that can both predict therapeutic benefit and prognosticate long-term outcomes in localized prostate cancer.
Daniel Spratt, MD, chair of radiation oncology at UH Seidman Cancer Center in Cleveland, who has been involved in researching ArteraAI, told this news organization that the test improves risk stratification or prognostication over standard clinical and pathologic tools, such as prostate-specific antigen, Gleason score, and T-stage, or risk groupings such as those from the National Comprehensive Cancer Network (NCCN).
“Medicare approval allows this test to reach more patients without the financial burden of covering the test out of pocket. The test is found among other tests in NCCN guidelines as a tool to improve risk stratification and personalization of treatment,” said Dr. Spratt, who serves on the network’s prostate cancer panel.
ArteraAI combines a patient’s standard clinical and pathologic information into an algorithm, alongside a digitized image analysis of the patients’ prostate biopsy. The result is a score that estimates a patient’s risk of developing metastasis or dying from prostate cancer.
Dr. Spratt was the lead author of article last June in NEJM Evidence that validated ArteraAI. He said ArteraAI is 80% accurate as a prognostic test compared with 65% accuracy using NCCN stratification systems.
The AI test spares about two thirds of men with intermediate-risk prostate cancer who are starting radiation therapy from androgen deprivation and its side effects, such as weight gain, breast enlargement, hot flashes, heart disease, and brain problems, Dr. Spratt added.
Andre Esteva, CEO and co-founder of San Francisco-based ArteraAI, said, “After someone is diagnosed with localized prostate cancer, deciding on a treatment can feel very overwhelming as there are so many factors to consider. During this time, knowledge is power, and having detailed, personalized information can increase confidence when making these challenging decisions. The ArteraAI Prostate Test was developed with this in mind and can predict whether a patient will benefit from hormone therapy and estimate long-term outcomes.”
Bruno Barrey is one of Dr. Spratt’s patients. Barrey, a robotics engineer from suburban Detroit who was transitioning from active surveillance with Gleason 3+4 intermediate-risk prostate cancer to radiation therapy, said, “I was concerned about the side effects from androgen-deprivation therapy. I was relieved that the AI test allowed me to avoid hormone therapy.”
Dr. Spratt reported working with NRG Oncology, a clinical trials group funded by the National Cancer Institute, and as an academic collaborator with ArteraAI.
A version of this article appeared on Medscape.com.
The Centers for Medicare & Medicare Services (CMS) on January 1 approved the payment rate for ArteraAI as a clinical diagnostic laboratory test. The test is the first that can both predict therapeutic benefit and prognosticate long-term outcomes in localized prostate cancer.
Daniel Spratt, MD, chair of radiation oncology at UH Seidman Cancer Center in Cleveland, who has been involved in researching ArteraAI, told this news organization that the test improves risk stratification or prognostication over standard clinical and pathologic tools, such as prostate-specific antigen, Gleason score, and T-stage, or risk groupings such as those from the National Comprehensive Cancer Network (NCCN).
“Medicare approval allows this test to reach more patients without the financial burden of covering the test out of pocket. The test is found among other tests in NCCN guidelines as a tool to improve risk stratification and personalization of treatment,” said Dr. Spratt, who serves on the network’s prostate cancer panel.
ArteraAI combines a patient’s standard clinical and pathologic information into an algorithm, alongside a digitized image analysis of the patients’ prostate biopsy. The result is a score that estimates a patient’s risk of developing metastasis or dying from prostate cancer.
Dr. Spratt was the lead author of article last June in NEJM Evidence that validated ArteraAI. He said ArteraAI is 80% accurate as a prognostic test compared with 65% accuracy using NCCN stratification systems.
The AI test spares about two thirds of men with intermediate-risk prostate cancer who are starting radiation therapy from androgen deprivation and its side effects, such as weight gain, breast enlargement, hot flashes, heart disease, and brain problems, Dr. Spratt added.
Andre Esteva, CEO and co-founder of San Francisco-based ArteraAI, said, “After someone is diagnosed with localized prostate cancer, deciding on a treatment can feel very overwhelming as there are so many factors to consider. During this time, knowledge is power, and having detailed, personalized information can increase confidence when making these challenging decisions. The ArteraAI Prostate Test was developed with this in mind and can predict whether a patient will benefit from hormone therapy and estimate long-term outcomes.”
Bruno Barrey is one of Dr. Spratt’s patients. Barrey, a robotics engineer from suburban Detroit who was transitioning from active surveillance with Gleason 3+4 intermediate-risk prostate cancer to radiation therapy, said, “I was concerned about the side effects from androgen-deprivation therapy. I was relieved that the AI test allowed me to avoid hormone therapy.”
Dr. Spratt reported working with NRG Oncology, a clinical trials group funded by the National Cancer Institute, and as an academic collaborator with ArteraAI.
A version of this article appeared on Medscape.com.
The Centers for Medicare & Medicare Services (CMS) on January 1 approved the payment rate for ArteraAI as a clinical diagnostic laboratory test. The test is the first that can both predict therapeutic benefit and prognosticate long-term outcomes in localized prostate cancer.
Daniel Spratt, MD, chair of radiation oncology at UH Seidman Cancer Center in Cleveland, who has been involved in researching ArteraAI, told this news organization that the test improves risk stratification or prognostication over standard clinical and pathologic tools, such as prostate-specific antigen, Gleason score, and T-stage, or risk groupings such as those from the National Comprehensive Cancer Network (NCCN).
“Medicare approval allows this test to reach more patients without the financial burden of covering the test out of pocket. The test is found among other tests in NCCN guidelines as a tool to improve risk stratification and personalization of treatment,” said Dr. Spratt, who serves on the network’s prostate cancer panel.
ArteraAI combines a patient’s standard clinical and pathologic information into an algorithm, alongside a digitized image analysis of the patients’ prostate biopsy. The result is a score that estimates a patient’s risk of developing metastasis or dying from prostate cancer.
Dr. Spratt was the lead author of article last June in NEJM Evidence that validated ArteraAI. He said ArteraAI is 80% accurate as a prognostic test compared with 65% accuracy using NCCN stratification systems.
The AI test spares about two thirds of men with intermediate-risk prostate cancer who are starting radiation therapy from androgen deprivation and its side effects, such as weight gain, breast enlargement, hot flashes, heart disease, and brain problems, Dr. Spratt added.
Andre Esteva, CEO and co-founder of San Francisco-based ArteraAI, said, “After someone is diagnosed with localized prostate cancer, deciding on a treatment can feel very overwhelming as there are so many factors to consider. During this time, knowledge is power, and having detailed, personalized information can increase confidence when making these challenging decisions. The ArteraAI Prostate Test was developed with this in mind and can predict whether a patient will benefit from hormone therapy and estimate long-term outcomes.”
Bruno Barrey is one of Dr. Spratt’s patients. Barrey, a robotics engineer from suburban Detroit who was transitioning from active surveillance with Gleason 3+4 intermediate-risk prostate cancer to radiation therapy, said, “I was concerned about the side effects from androgen-deprivation therapy. I was relieved that the AI test allowed me to avoid hormone therapy.”
Dr. Spratt reported working with NRG Oncology, a clinical trials group funded by the National Cancer Institute, and as an academic collaborator with ArteraAI.
A version of this article appeared on Medscape.com.
Time Off Isn’t Really Off-Time for Most Physicians, Study Finds
About 20% of US physicians took less than 1 week of vacation in the previous year, a new study found. When doctors did go on vacation, 70% reported working on their days off to handle patient-related tasks.
, according to the cross-sectional study, which was published on January 12, 2024, in JAMA Network Open.“It’s important to provide physicians with adequate time to disconnect from work and recharge,” said study coauthor Tait Shanafelt, MD, chief wellness officer at Stanford Medicine, in an interview.
The study’s conclusion that most US physicians work on their days off “is a marker of inadequate staffing, suboptimal teamwork, and poorly designed coverage systems,” he added. “Simply allocating people a number of vacation days is not enough.”
According to Dr. Shanafelt, there’s been little research into vacation’s impact on physician well-being. However, it is clear that work overload and exhaustion are major problems among American physicians. “Inadequate time off may magnify these challenges.”
Research suggests that physicians suffer more burnout than other US workers even after adjusting for confounders, he said. Extensive evidence shows that burnout in physicians contributes to medical errors and erodes quality of care and patient satisfaction, he added.
For the new study, researchers mailed surveys to 3671 members of the American Medical Association from 2020 to 2021, and 1162 (31.7%) responded. Another 6348 (7.1%) responded to an email survey sent to 90,000 physicians. An analysis suggested the respondents were representative of all US practicing physicians.
Among 3024 respondents who responded to a subsurvey about vacations, about 40% took more than 15 days of vacation over the past year, about 40% took 6-15 days, and about 20% took 5 or fewer days.
Fewer than half of physicians said their electronic health record (EHR) inboxes were fully covered by others while they were away. About 70% said they worked while on vacation, with nearly 15% working an hour or more each day.
Emergency physicians were the least likely and anesthesiologists were the most likely to take at least 15 days of vacation per year, according to the study.
Women were more likely than men to work 30 or more minutes a day on vacation. Physicians aged 65 years and older were more likely to take 15 or more days of vacation per year than those under 35 years.
An adjusted analysis linked complete EHR inbox coverage to lower odds of taking time during vacation to work (odds ratio [OR], 0.68; 95% CI, 0.57-0.80).
“For many, difficulty finding clinical coverage, lack of EHR inbox coverage, and returning to an overwhelming backlog of EHR inbox work at were identified as barriers to taking vacation,” Dr. Shanafelt said.
Researchers linked lower rates of burnout to taking more than 3 weeks of vacation per year (OR, 0.59-0.66, depending on time spent; 95% CI, 0.40-0.98) vs none. They also linked less burnout to full EHR inbox coverage while on vacation (OR, 0.74; 95% CI, 0.63-0.88) and more burnout to spending 30 minutes or more on work while on a typical vacation day (OR, 1.58-1.97, depending on time spent; 95% CI, 1.22-2.77).
Study limitations include the low participation rate and lack of insight into causation. It’s not clear how burnout and less vacation time are related and whether one causes the other, Shanafelt said. “It is possible there are a number of interacting factors rather than a simple, linear relationship.”
In an interview, Lazar J. Greenfield, Jr., MD, PhD, professor and chairman of neurology at UConn Health, Farmington, Connecticut, said his department encourages clinicians to plan vacations well ahead of time, and “we make a real strong effort to make sure that people are fully covered and someone has their Epic inbox.”
Dr. Greenfield, who wasn’t involved in the new study, recommended that physicians plan active vacations, so they have less downtime to catch up on work matters. But he acknowledged that stepping away from emails can be difficult, especially when physicians fear pileups of work upon their return or don’t want to annoy patients with tardy responses.
“They have a hard time disengaging from their moral obligations to patients,” he said. “Another issue, particularly in my field of neurology, is that there’s a lot of subspecialties. Finding somebody with the exact subspecialty and expertise to cover a very specific patient population they treat can be really hard.”
The Stanford WellMD Center, Mayo Clinic Department of Medicine Program on Physician Well-being, and American Medical Association funded the study.
Dr. Shanafelt discloses coinventing the Well-Being Index and its derivatives with another study author; Mayo Clinic licensed the Well-Being Index and pays them royalties outside the submitted work. Dr. Shanafelt also reported support for grand rounds, lectures, and advising for healthcare organizations outside the submitted work. Other authors reported personal fees from Marvin Behavioral Health and grants from the National Institute of Nursing Research, National Science Foundation, and Med Ed Solutions.
Dr. Greenfield had no disclosures.
A version of this article appeared on Medscape.com.
About 20% of US physicians took less than 1 week of vacation in the previous year, a new study found. When doctors did go on vacation, 70% reported working on their days off to handle patient-related tasks.
, according to the cross-sectional study, which was published on January 12, 2024, in JAMA Network Open.“It’s important to provide physicians with adequate time to disconnect from work and recharge,” said study coauthor Tait Shanafelt, MD, chief wellness officer at Stanford Medicine, in an interview.
The study’s conclusion that most US physicians work on their days off “is a marker of inadequate staffing, suboptimal teamwork, and poorly designed coverage systems,” he added. “Simply allocating people a number of vacation days is not enough.”
According to Dr. Shanafelt, there’s been little research into vacation’s impact on physician well-being. However, it is clear that work overload and exhaustion are major problems among American physicians. “Inadequate time off may magnify these challenges.”
Research suggests that physicians suffer more burnout than other US workers even after adjusting for confounders, he said. Extensive evidence shows that burnout in physicians contributes to medical errors and erodes quality of care and patient satisfaction, he added.
For the new study, researchers mailed surveys to 3671 members of the American Medical Association from 2020 to 2021, and 1162 (31.7%) responded. Another 6348 (7.1%) responded to an email survey sent to 90,000 physicians. An analysis suggested the respondents were representative of all US practicing physicians.
Among 3024 respondents who responded to a subsurvey about vacations, about 40% took more than 15 days of vacation over the past year, about 40% took 6-15 days, and about 20% took 5 or fewer days.
Fewer than half of physicians said their electronic health record (EHR) inboxes were fully covered by others while they were away. About 70% said they worked while on vacation, with nearly 15% working an hour or more each day.
Emergency physicians were the least likely and anesthesiologists were the most likely to take at least 15 days of vacation per year, according to the study.
Women were more likely than men to work 30 or more minutes a day on vacation. Physicians aged 65 years and older were more likely to take 15 or more days of vacation per year than those under 35 years.
An adjusted analysis linked complete EHR inbox coverage to lower odds of taking time during vacation to work (odds ratio [OR], 0.68; 95% CI, 0.57-0.80).
“For many, difficulty finding clinical coverage, lack of EHR inbox coverage, and returning to an overwhelming backlog of EHR inbox work at were identified as barriers to taking vacation,” Dr. Shanafelt said.
Researchers linked lower rates of burnout to taking more than 3 weeks of vacation per year (OR, 0.59-0.66, depending on time spent; 95% CI, 0.40-0.98) vs none. They also linked less burnout to full EHR inbox coverage while on vacation (OR, 0.74; 95% CI, 0.63-0.88) and more burnout to spending 30 minutes or more on work while on a typical vacation day (OR, 1.58-1.97, depending on time spent; 95% CI, 1.22-2.77).
Study limitations include the low participation rate and lack of insight into causation. It’s not clear how burnout and less vacation time are related and whether one causes the other, Shanafelt said. “It is possible there are a number of interacting factors rather than a simple, linear relationship.”
In an interview, Lazar J. Greenfield, Jr., MD, PhD, professor and chairman of neurology at UConn Health, Farmington, Connecticut, said his department encourages clinicians to plan vacations well ahead of time, and “we make a real strong effort to make sure that people are fully covered and someone has their Epic inbox.”
Dr. Greenfield, who wasn’t involved in the new study, recommended that physicians plan active vacations, so they have less downtime to catch up on work matters. But he acknowledged that stepping away from emails can be difficult, especially when physicians fear pileups of work upon their return or don’t want to annoy patients with tardy responses.
“They have a hard time disengaging from their moral obligations to patients,” he said. “Another issue, particularly in my field of neurology, is that there’s a lot of subspecialties. Finding somebody with the exact subspecialty and expertise to cover a very specific patient population they treat can be really hard.”
The Stanford WellMD Center, Mayo Clinic Department of Medicine Program on Physician Well-being, and American Medical Association funded the study.
Dr. Shanafelt discloses coinventing the Well-Being Index and its derivatives with another study author; Mayo Clinic licensed the Well-Being Index and pays them royalties outside the submitted work. Dr. Shanafelt also reported support for grand rounds, lectures, and advising for healthcare organizations outside the submitted work. Other authors reported personal fees from Marvin Behavioral Health and grants from the National Institute of Nursing Research, National Science Foundation, and Med Ed Solutions.
Dr. Greenfield had no disclosures.
A version of this article appeared on Medscape.com.
About 20% of US physicians took less than 1 week of vacation in the previous year, a new study found. When doctors did go on vacation, 70% reported working on their days off to handle patient-related tasks.
, according to the cross-sectional study, which was published on January 12, 2024, in JAMA Network Open.“It’s important to provide physicians with adequate time to disconnect from work and recharge,” said study coauthor Tait Shanafelt, MD, chief wellness officer at Stanford Medicine, in an interview.
The study’s conclusion that most US physicians work on their days off “is a marker of inadequate staffing, suboptimal teamwork, and poorly designed coverage systems,” he added. “Simply allocating people a number of vacation days is not enough.”
According to Dr. Shanafelt, there’s been little research into vacation’s impact on physician well-being. However, it is clear that work overload and exhaustion are major problems among American physicians. “Inadequate time off may magnify these challenges.”
Research suggests that physicians suffer more burnout than other US workers even after adjusting for confounders, he said. Extensive evidence shows that burnout in physicians contributes to medical errors and erodes quality of care and patient satisfaction, he added.
For the new study, researchers mailed surveys to 3671 members of the American Medical Association from 2020 to 2021, and 1162 (31.7%) responded. Another 6348 (7.1%) responded to an email survey sent to 90,000 physicians. An analysis suggested the respondents were representative of all US practicing physicians.
Among 3024 respondents who responded to a subsurvey about vacations, about 40% took more than 15 days of vacation over the past year, about 40% took 6-15 days, and about 20% took 5 or fewer days.
Fewer than half of physicians said their electronic health record (EHR) inboxes were fully covered by others while they were away. About 70% said they worked while on vacation, with nearly 15% working an hour or more each day.
Emergency physicians were the least likely and anesthesiologists were the most likely to take at least 15 days of vacation per year, according to the study.
Women were more likely than men to work 30 or more minutes a day on vacation. Physicians aged 65 years and older were more likely to take 15 or more days of vacation per year than those under 35 years.
An adjusted analysis linked complete EHR inbox coverage to lower odds of taking time during vacation to work (odds ratio [OR], 0.68; 95% CI, 0.57-0.80).
“For many, difficulty finding clinical coverage, lack of EHR inbox coverage, and returning to an overwhelming backlog of EHR inbox work at were identified as barriers to taking vacation,” Dr. Shanafelt said.
Researchers linked lower rates of burnout to taking more than 3 weeks of vacation per year (OR, 0.59-0.66, depending on time spent; 95% CI, 0.40-0.98) vs none. They also linked less burnout to full EHR inbox coverage while on vacation (OR, 0.74; 95% CI, 0.63-0.88) and more burnout to spending 30 minutes or more on work while on a typical vacation day (OR, 1.58-1.97, depending on time spent; 95% CI, 1.22-2.77).
Study limitations include the low participation rate and lack of insight into causation. It’s not clear how burnout and less vacation time are related and whether one causes the other, Shanafelt said. “It is possible there are a number of interacting factors rather than a simple, linear relationship.”
In an interview, Lazar J. Greenfield, Jr., MD, PhD, professor and chairman of neurology at UConn Health, Farmington, Connecticut, said his department encourages clinicians to plan vacations well ahead of time, and “we make a real strong effort to make sure that people are fully covered and someone has their Epic inbox.”
Dr. Greenfield, who wasn’t involved in the new study, recommended that physicians plan active vacations, so they have less downtime to catch up on work matters. But he acknowledged that stepping away from emails can be difficult, especially when physicians fear pileups of work upon their return or don’t want to annoy patients with tardy responses.
“They have a hard time disengaging from their moral obligations to patients,” he said. “Another issue, particularly in my field of neurology, is that there’s a lot of subspecialties. Finding somebody with the exact subspecialty and expertise to cover a very specific patient population they treat can be really hard.”
The Stanford WellMD Center, Mayo Clinic Department of Medicine Program on Physician Well-being, and American Medical Association funded the study.
Dr. Shanafelt discloses coinventing the Well-Being Index and its derivatives with another study author; Mayo Clinic licensed the Well-Being Index and pays them royalties outside the submitted work. Dr. Shanafelt also reported support for grand rounds, lectures, and advising for healthcare organizations outside the submitted work. Other authors reported personal fees from Marvin Behavioral Health and grants from the National Institute of Nursing Research, National Science Foundation, and Med Ed Solutions.
Dr. Greenfield had no disclosures.
A version of this article appeared on Medscape.com.
FROM JAMA NETWORK OPEN









