User login
The Long, Controversial Search for a ‘Cancer Microbiome’
Last year, the controversy heightened when experts questioned a high-profile study — a 2020 analysis claiming that the tumors of 33 different cancers had their own unique microbiomes — on whether the “signature” of these bacterial compositions could help diagnose cancer.
The incident renewed the spotlight on “tumor microbiomes” because of the bold claims of the original paper and the strongly worded refutations of those claims. The broader field has focused primarily on ways the body’s microbiome interacts with cancers and cancer treatment.
This controversy has highlighted the challenges of making headway in a field where researchers may not even have the tools yet to puzzle-out the wide-ranging implications the microbiome holds for cancer diagnosis and treatment.
But it is also part of a provocative question within that larger field: whether tumors in the body, far from the natural microbiome in the gut, have their own thriving communities of bacteria, viruses, and fungi. And, if they do, how do those tumor microbiomes affect the development and progression of the cancer and the effectiveness of cancer therapies?
Cancer Controversy
The evidence is undeniable that some microbes can directly cause certain cancers and that the human gut microbiome can influence the effectiveness of certain therapies. Beyond that established science, however, the research has raised as many questions as answers about what we do and don’t know about microbiota and cancer.
The only confirmed microbiomes are on the skin and in the gut, mouth, and vagina, which are all areas with an easy direct route for bacteria to enter and grow in or on the body. A series of papers in recent years have suggested that other internal organs, and tumors within them, may have their own microbiomes.
“Whether microbes exist in tumors of internal organs beyond body surfaces exposed to the environment is a different matter,” said Ivan Vujkovic-Cvijin, PhD, an assistant professor of biomedical sciences and gastroenterology at Cedars-Sinai Medical Center in Los Angeles, whose lab studies how human gut microbes affect inflammatory diseases. “We’ve only recently had the tools to study that question on a molecular level, and the reported results have been conflicting.”
For example, research allegedly identified microbiota in the human placenta nearly one decade ago. But subsequent research contradicted those claims and showed that the source of the “placental microbiome” was actually contamination. Subsequent similar studies for other parts of the body faced the same scrutiny and, often, eventual debunking.
“Most likely, our immune system has undergone selective pressure to eliminate everything that crosses the gut barrier because there’s not much benefit to the body to have bacteria run amok in our internal organs,” Dr. Vujkovic-Cvijin said. “That can only disrupt the functioning of our tissues, to have an external organism living inside them.”
The controversy that erupted last summer, surrounding research from the lab of Rob Knight, PhD, at the University of California, San Diego, centered on a slightly different but related question: Could tumors harbor their own microbiomes?
This news organization spoke with two of the authors who published a paper contesting Dr. Knight’s findings: Steven Salzberg, PhD, a professor of biomedical engineering at John Hopkins Medicine, Baltimore, Maryland, and Abraham Gihawi, PhD, a research fellow at Norwich Medical School at the University of East Anglia in the United Kingdom.
Dr. Salzberg described two major problems with Dr. Knight’s study.
“What they found were false positives because of contamination in the database and flaws in their methods,” Dr. Salzberg said. “I can’t prove there’s no cancer microbiome, but I can say the cancer microbiomes that they reported don’t exist because the species they were finding aren’t there.”
Dr. Knight disagrees with Dr. Salzberg’s findings, noting that Dr. Salzberg and his co-authors did not examine the publicly available databases used in his study. In a written response, he said that his team’s examination of the database revealed that less than 1% of the microbial genomes overlapped with human ones and that removing them did not change their findings.
Dr. Knight also noted that his team could still “distinguish cancer types by their microbiome” even after running their analysis without the technique that Dr. Salzberg found fault with.
Dr. Salzberg said that the database linked above is not the one Dr. Knight’s study used, however. “The primary database in their study was never made public (it’s too large, they said), and it has/had about 69,000 genomes,” Dr. Salzberg said by email. “But even if we did, this is irrelevant. He’s trying to distract from the primary errors in their study,” which Dr. Salzberg said Dr. Knight’s team has not addressed.
The critiques Dr. Salzberg raised have been leveled at other studies investigating microbiomes specifically within tumors and independent of the body’s microbiome.
For example, a 2019 study in Nature described a fungal microbiome in pancreatic cancer that a Nature paper 4 years later directly contradicted, citing flaws that invalidated the original findings. A different 2019 study in Cell examined pancreatic tumor microbiota and patient outcomes, but it’s unclear whether the microorganisms moved from the gut to the pancreas or “constitute a durably colonized community that lives inside the tumor,” which remains a matter of debate, Dr. Vujkovic-Cvijin said.
A 2020 study in Science suggested diverse microbial communities in seven tumor types, but those findings were similarly called into question. That study stated that “bacteria were first detected in human tumors more than 100 years ago” and that “bacteria are well-known residents in human tumors,” but Dr. Salzberg considers those statements misleading.
It’s true that bacteria and viruses have been detected in tumors because “there’s very good evidence that an acute infection caused by a very small number of viruses and bacteria can cause a tumor,” Dr. Salzberg said. Human papillomavirus, for example, can cause six different types of cancer. Inflammation and ulcers caused by Helicobacter pylori may progress to stomach cancer, and Fusobacterium nucleatum and Enterococcus faecalis have been shown to contribute to colorectal cancer. Those examples differ from a microbiome; this “a community of bacteria and possibly other microscopic bugs, like fungi, that are happily living in the tumor” the same way microbes reside in our guts, he said.
Dr. Knight said that many bacteria his team identified “have been confirmed independently in subsequent work.” He acknowledged, however, that more research is needed.
Several of the contested studies above were among a lengthy list that Dr. Knight provided, noting that most of the disagreements “have two sides to them, and critiques from one particular group does not immediately invalidate a reported finding.”
Yet, many of the papers Dr. Knight listed are precisely the types that skeptics like Dr. Salzberg believe are too flawed to draw reliable conclusions.
“I think many agree that microbes may exist within tumors that are exposed to the environment, like tumors of the skin, gut, and mouth,” Dr. Vujkovic-Cvijin said. It’s less clear, however, whether tumors further from the body’s microbiome harbor any microbes or where they came from if they do. Microbial signals in organs elsewhere in the body become faint quickly, he said.
Underdeveloped Technology
Though Dr. Salzberg said that the concept of a tumor microbiome is “implausible” because there’s no easy route for bacteria to reach internal organs, it’s unclear whether scientists have the technology yet to adequately answer this question.
For one thing, samples in these types of studies are typically “ultra-low biomass samples, where the signal — the amount of microbes in the sample — is so low that it’s comparable to how much would be expected to be found in reagents and environmental contamination through processing,” Dr. Vujkovic-Cvijin explained. Many polymerases used to amplify a DNA signal, for example, are made in bacteria and may retain trace amounts identified in these studies.
Dr. Knight agreed that low biomass is a challenge in this field but is not an unsurmountable one.
Another challenge is that study samples, as with Dr. Knight’s work, were collected during routine surgeries without the intent to find a microbial signal. Simply using a scalpel to cut through the skin means cutting through a layer of bacteria, and surgery rooms are not designed to eliminate all bacteria. Some work has even shown there is a “hospital microbiome,” so “you can easily have that creep into your signal and mistake it for tumor-resident bacteria,” Dr. Vujkovic-Cvijin said.
Dr. Knight asserted that the samples are taken under sterile conditions, but other researchers do not think the level of sterility necessary for completely clean samples is possible.
“Just because it’s in your sample doesn’t mean it was in your tumor,” Dr. Gihawi said.
Even if scientists can retrieve a reliable sample without contamination, analyzing it requires comparing the genetic material to existing databases of microbial genomes. Yet, contamination and misclassification of genetic sequences can be problems in those reference genomes too, Dr. Gihawi explained.
Machine learning algorithms have a role in interpreting data, but “we need to be careful of what we use them for,” he added.
“These techniques are in their infancy, and we’re starting to chase them down, which is why we need to move microbiome research in a way that can be used clinically,” Dr. Gihawi said.
Influence on Cancer Treatment Outcomes
Again, however, the question of whether microbiomes exist within tumors is only one slice of the much larger field looking at microbiomes and cancer, including its influence on cancer treatment outcomes. Although much remains to be learned, less controversy exists over the thousands of studies in the past two decades that have gradually revealed how the body’s microbiome can affect both the course of a cancer and the effectiveness of different treatments.
The growing research showing the importance of the gut microbiome in cancer treatments is not surprising given its role in immunity more broadly. Because the human immune system must recognize and defend against microbes, the microbiome helps train it, Dr. Vujkovic-Cvijin said.
Some bacteria can escape the gut — a phenomenon called bacterial translocation — and may aid in fighting tumors. To grow large enough to be seen on imaging, tumors need to evolve several abilities, such as growing enough vascularization to receive blood flow and shutting down local immune responses.
“Any added boost, like immunotherapy, has a chance of breaking through that immune forcefield and killing the tumor cells,” Dr. Vujkovic-Cvijin said. Escaped gut bacteria may provide that boost.
“There’s a lot of evidence that depletion of the gut microbiome impairs immunotherapy and chemotherapy. The thinking behind some of those studies is that gut microbes can cross the gut barrier and when they do, they activate the immune system,” he said.
In mice engineered to have sterile guts, for example, the lack of bacteria results in less effective immune systems, Dr. Vujkovic-Cvijin pointed out. A host of research has shown that antibiotic exposure during and even 6 months before immunotherapy dramatically reduces survival rates. “That’s pretty convincing to me that gut microbes are important,” he said.
Dr. Vujkovic-Cvijin cautioned that there continues to be controversy on understanding which bacteria are important for response to immunotherapy. “The field is still in its infancy in terms of understanding which bacteria are most important for these effects,” he said.
Dr. Knight suggested that escaped bacteria may be the genesis of the ones that he and other researchers believe exist in tumors. “Because tumor microbes must come from somewhere, it is to be expected that some of those microbes will be co-opted from body-site specific commensals.”
It’s also possible that metabolites released from gut bacteria escape the gut and could theoretically affect distant tumor growth, Dr. Gihawi said. The most promising avenue of research in this area is metabolites being used as biomarkers, added Dr. Gihawi, whose lab published research on a link between bacteria detected in men’s urine and a more aggressive subset of prostate cancers. But that research is not far enough along to develop lab tests for clinical use, he noted.
No Consensus Yet
Even before the controversy erupted around Dr. Knight’s research, he co-founded the company Micronoma to develop cancer tests based on his microbe findings. The company has raised $17.5 million from private investors as of August 2023 and received the US Food and Drug Administration’s Breakthrough Device designation, allowing the firm to fast-track clinical trials testing the technology. The recent critiques have not changed the company’s plans.
It’s safe to say that scientists will continue to research and debate the possibility of tumor microbiomes until a consensus emerges.
“The field is evolving and studies testing the reproducibility of tumor-resident microbial signals are essential for developing our understanding in this area,” Dr. Vujkovic-Cvijin said.
Even if that path ultimately leads nowhere, as Dr. Salzberg expects, research into microbiomes and cancer has plenty of other directions to go.
“I’m actually quite an optimist,” Dr. Gihawi said. “I think there’s a lot of scope for some really good research here, especially in the sites where we know there is a strong microbiome, such as the gastrointestinal tract.”
A version of this article appeared on Medscape.com.
Last year, the controversy heightened when experts questioned a high-profile study — a 2020 analysis claiming that the tumors of 33 different cancers had their own unique microbiomes — on whether the “signature” of these bacterial compositions could help diagnose cancer.
The incident renewed the spotlight on “tumor microbiomes” because of the bold claims of the original paper and the strongly worded refutations of those claims. The broader field has focused primarily on ways the body’s microbiome interacts with cancers and cancer treatment.
This controversy has highlighted the challenges of making headway in a field where researchers may not even have the tools yet to puzzle-out the wide-ranging implications the microbiome holds for cancer diagnosis and treatment.
But it is also part of a provocative question within that larger field: whether tumors in the body, far from the natural microbiome in the gut, have their own thriving communities of bacteria, viruses, and fungi. And, if they do, how do those tumor microbiomes affect the development and progression of the cancer and the effectiveness of cancer therapies?
Cancer Controversy
The evidence is undeniable that some microbes can directly cause certain cancers and that the human gut microbiome can influence the effectiveness of certain therapies. Beyond that established science, however, the research has raised as many questions as answers about what we do and don’t know about microbiota and cancer.
The only confirmed microbiomes are on the skin and in the gut, mouth, and vagina, which are all areas with an easy direct route for bacteria to enter and grow in or on the body. A series of papers in recent years have suggested that other internal organs, and tumors within them, may have their own microbiomes.
“Whether microbes exist in tumors of internal organs beyond body surfaces exposed to the environment is a different matter,” said Ivan Vujkovic-Cvijin, PhD, an assistant professor of biomedical sciences and gastroenterology at Cedars-Sinai Medical Center in Los Angeles, whose lab studies how human gut microbes affect inflammatory diseases. “We’ve only recently had the tools to study that question on a molecular level, and the reported results have been conflicting.”
For example, research allegedly identified microbiota in the human placenta nearly one decade ago. But subsequent research contradicted those claims and showed that the source of the “placental microbiome” was actually contamination. Subsequent similar studies for other parts of the body faced the same scrutiny and, often, eventual debunking.
“Most likely, our immune system has undergone selective pressure to eliminate everything that crosses the gut barrier because there’s not much benefit to the body to have bacteria run amok in our internal organs,” Dr. Vujkovic-Cvijin said. “That can only disrupt the functioning of our tissues, to have an external organism living inside them.”
The controversy that erupted last summer, surrounding research from the lab of Rob Knight, PhD, at the University of California, San Diego, centered on a slightly different but related question: Could tumors harbor their own microbiomes?
This news organization spoke with two of the authors who published a paper contesting Dr. Knight’s findings: Steven Salzberg, PhD, a professor of biomedical engineering at John Hopkins Medicine, Baltimore, Maryland, and Abraham Gihawi, PhD, a research fellow at Norwich Medical School at the University of East Anglia in the United Kingdom.
Dr. Salzberg described two major problems with Dr. Knight’s study.
“What they found were false positives because of contamination in the database and flaws in their methods,” Dr. Salzberg said. “I can’t prove there’s no cancer microbiome, but I can say the cancer microbiomes that they reported don’t exist because the species they were finding aren’t there.”
Dr. Knight disagrees with Dr. Salzberg’s findings, noting that Dr. Salzberg and his co-authors did not examine the publicly available databases used in his study. In a written response, he said that his team’s examination of the database revealed that less than 1% of the microbial genomes overlapped with human ones and that removing them did not change their findings.
Dr. Knight also noted that his team could still “distinguish cancer types by their microbiome” even after running their analysis without the technique that Dr. Salzberg found fault with.
Dr. Salzberg said that the database linked above is not the one Dr. Knight’s study used, however. “The primary database in their study was never made public (it’s too large, they said), and it has/had about 69,000 genomes,” Dr. Salzberg said by email. “But even if we did, this is irrelevant. He’s trying to distract from the primary errors in their study,” which Dr. Salzberg said Dr. Knight’s team has not addressed.
The critiques Dr. Salzberg raised have been leveled at other studies investigating microbiomes specifically within tumors and independent of the body’s microbiome.
For example, a 2019 study in Nature described a fungal microbiome in pancreatic cancer that a Nature paper 4 years later directly contradicted, citing flaws that invalidated the original findings. A different 2019 study in Cell examined pancreatic tumor microbiota and patient outcomes, but it’s unclear whether the microorganisms moved from the gut to the pancreas or “constitute a durably colonized community that lives inside the tumor,” which remains a matter of debate, Dr. Vujkovic-Cvijin said.
A 2020 study in Science suggested diverse microbial communities in seven tumor types, but those findings were similarly called into question. That study stated that “bacteria were first detected in human tumors more than 100 years ago” and that “bacteria are well-known residents in human tumors,” but Dr. Salzberg considers those statements misleading.
It’s true that bacteria and viruses have been detected in tumors because “there’s very good evidence that an acute infection caused by a very small number of viruses and bacteria can cause a tumor,” Dr. Salzberg said. Human papillomavirus, for example, can cause six different types of cancer. Inflammation and ulcers caused by Helicobacter pylori may progress to stomach cancer, and Fusobacterium nucleatum and Enterococcus faecalis have been shown to contribute to colorectal cancer. Those examples differ from a microbiome; this “a community of bacteria and possibly other microscopic bugs, like fungi, that are happily living in the tumor” the same way microbes reside in our guts, he said.
Dr. Knight said that many bacteria his team identified “have been confirmed independently in subsequent work.” He acknowledged, however, that more research is needed.
Several of the contested studies above were among a lengthy list that Dr. Knight provided, noting that most of the disagreements “have two sides to them, and critiques from one particular group does not immediately invalidate a reported finding.”
Yet, many of the papers Dr. Knight listed are precisely the types that skeptics like Dr. Salzberg believe are too flawed to draw reliable conclusions.
“I think many agree that microbes may exist within tumors that are exposed to the environment, like tumors of the skin, gut, and mouth,” Dr. Vujkovic-Cvijin said. It’s less clear, however, whether tumors further from the body’s microbiome harbor any microbes or where they came from if they do. Microbial signals in organs elsewhere in the body become faint quickly, he said.
Underdeveloped Technology
Though Dr. Salzberg said that the concept of a tumor microbiome is “implausible” because there’s no easy route for bacteria to reach internal organs, it’s unclear whether scientists have the technology yet to adequately answer this question.
For one thing, samples in these types of studies are typically “ultra-low biomass samples, where the signal — the amount of microbes in the sample — is so low that it’s comparable to how much would be expected to be found in reagents and environmental contamination through processing,” Dr. Vujkovic-Cvijin explained. Many polymerases used to amplify a DNA signal, for example, are made in bacteria and may retain trace amounts identified in these studies.
Dr. Knight agreed that low biomass is a challenge in this field but is not an unsurmountable one.
Another challenge is that study samples, as with Dr. Knight’s work, were collected during routine surgeries without the intent to find a microbial signal. Simply using a scalpel to cut through the skin means cutting through a layer of bacteria, and surgery rooms are not designed to eliminate all bacteria. Some work has even shown there is a “hospital microbiome,” so “you can easily have that creep into your signal and mistake it for tumor-resident bacteria,” Dr. Vujkovic-Cvijin said.
Dr. Knight asserted that the samples are taken under sterile conditions, but other researchers do not think the level of sterility necessary for completely clean samples is possible.
“Just because it’s in your sample doesn’t mean it was in your tumor,” Dr. Gihawi said.
Even if scientists can retrieve a reliable sample without contamination, analyzing it requires comparing the genetic material to existing databases of microbial genomes. Yet, contamination and misclassification of genetic sequences can be problems in those reference genomes too, Dr. Gihawi explained.
Machine learning algorithms have a role in interpreting data, but “we need to be careful of what we use them for,” he added.
“These techniques are in their infancy, and we’re starting to chase them down, which is why we need to move microbiome research in a way that can be used clinically,” Dr. Gihawi said.
Influence on Cancer Treatment Outcomes
Again, however, the question of whether microbiomes exist within tumors is only one slice of the much larger field looking at microbiomes and cancer, including its influence on cancer treatment outcomes. Although much remains to be learned, less controversy exists over the thousands of studies in the past two decades that have gradually revealed how the body’s microbiome can affect both the course of a cancer and the effectiveness of different treatments.
The growing research showing the importance of the gut microbiome in cancer treatments is not surprising given its role in immunity more broadly. Because the human immune system must recognize and defend against microbes, the microbiome helps train it, Dr. Vujkovic-Cvijin said.
Some bacteria can escape the gut — a phenomenon called bacterial translocation — and may aid in fighting tumors. To grow large enough to be seen on imaging, tumors need to evolve several abilities, such as growing enough vascularization to receive blood flow and shutting down local immune responses.
“Any added boost, like immunotherapy, has a chance of breaking through that immune forcefield and killing the tumor cells,” Dr. Vujkovic-Cvijin said. Escaped gut bacteria may provide that boost.
“There’s a lot of evidence that depletion of the gut microbiome impairs immunotherapy and chemotherapy. The thinking behind some of those studies is that gut microbes can cross the gut barrier and when they do, they activate the immune system,” he said.
In mice engineered to have sterile guts, for example, the lack of bacteria results in less effective immune systems, Dr. Vujkovic-Cvijin pointed out. A host of research has shown that antibiotic exposure during and even 6 months before immunotherapy dramatically reduces survival rates. “That’s pretty convincing to me that gut microbes are important,” he said.
Dr. Vujkovic-Cvijin cautioned that there continues to be controversy on understanding which bacteria are important for response to immunotherapy. “The field is still in its infancy in terms of understanding which bacteria are most important for these effects,” he said.
Dr. Knight suggested that escaped bacteria may be the genesis of the ones that he and other researchers believe exist in tumors. “Because tumor microbes must come from somewhere, it is to be expected that some of those microbes will be co-opted from body-site specific commensals.”
It’s also possible that metabolites released from gut bacteria escape the gut and could theoretically affect distant tumor growth, Dr. Gihawi said. The most promising avenue of research in this area is metabolites being used as biomarkers, added Dr. Gihawi, whose lab published research on a link between bacteria detected in men’s urine and a more aggressive subset of prostate cancers. But that research is not far enough along to develop lab tests for clinical use, he noted.
No Consensus Yet
Even before the controversy erupted around Dr. Knight’s research, he co-founded the company Micronoma to develop cancer tests based on his microbe findings. The company has raised $17.5 million from private investors as of August 2023 and received the US Food and Drug Administration’s Breakthrough Device designation, allowing the firm to fast-track clinical trials testing the technology. The recent critiques have not changed the company’s plans.
It’s safe to say that scientists will continue to research and debate the possibility of tumor microbiomes until a consensus emerges.
“The field is evolving and studies testing the reproducibility of tumor-resident microbial signals are essential for developing our understanding in this area,” Dr. Vujkovic-Cvijin said.
Even if that path ultimately leads nowhere, as Dr. Salzberg expects, research into microbiomes and cancer has plenty of other directions to go.
“I’m actually quite an optimist,” Dr. Gihawi said. “I think there’s a lot of scope for some really good research here, especially in the sites where we know there is a strong microbiome, such as the gastrointestinal tract.”
A version of this article appeared on Medscape.com.
Last year, the controversy heightened when experts questioned a high-profile study — a 2020 analysis claiming that the tumors of 33 different cancers had their own unique microbiomes — on whether the “signature” of these bacterial compositions could help diagnose cancer.
The incident renewed the spotlight on “tumor microbiomes” because of the bold claims of the original paper and the strongly worded refutations of those claims. The broader field has focused primarily on ways the body’s microbiome interacts with cancers and cancer treatment.
This controversy has highlighted the challenges of making headway in a field where researchers may not even have the tools yet to puzzle-out the wide-ranging implications the microbiome holds for cancer diagnosis and treatment.
But it is also part of a provocative question within that larger field: whether tumors in the body, far from the natural microbiome in the gut, have their own thriving communities of bacteria, viruses, and fungi. And, if they do, how do those tumor microbiomes affect the development and progression of the cancer and the effectiveness of cancer therapies?
Cancer Controversy
The evidence is undeniable that some microbes can directly cause certain cancers and that the human gut microbiome can influence the effectiveness of certain therapies. Beyond that established science, however, the research has raised as many questions as answers about what we do and don’t know about microbiota and cancer.
The only confirmed microbiomes are on the skin and in the gut, mouth, and vagina, which are all areas with an easy direct route for bacteria to enter and grow in or on the body. A series of papers in recent years have suggested that other internal organs, and tumors within them, may have their own microbiomes.
“Whether microbes exist in tumors of internal organs beyond body surfaces exposed to the environment is a different matter,” said Ivan Vujkovic-Cvijin, PhD, an assistant professor of biomedical sciences and gastroenterology at Cedars-Sinai Medical Center in Los Angeles, whose lab studies how human gut microbes affect inflammatory diseases. “We’ve only recently had the tools to study that question on a molecular level, and the reported results have been conflicting.”
For example, research allegedly identified microbiota in the human placenta nearly one decade ago. But subsequent research contradicted those claims and showed that the source of the “placental microbiome” was actually contamination. Subsequent similar studies for other parts of the body faced the same scrutiny and, often, eventual debunking.
“Most likely, our immune system has undergone selective pressure to eliminate everything that crosses the gut barrier because there’s not much benefit to the body to have bacteria run amok in our internal organs,” Dr. Vujkovic-Cvijin said. “That can only disrupt the functioning of our tissues, to have an external organism living inside them.”
The controversy that erupted last summer, surrounding research from the lab of Rob Knight, PhD, at the University of California, San Diego, centered on a slightly different but related question: Could tumors harbor their own microbiomes?
This news organization spoke with two of the authors who published a paper contesting Dr. Knight’s findings: Steven Salzberg, PhD, a professor of biomedical engineering at John Hopkins Medicine, Baltimore, Maryland, and Abraham Gihawi, PhD, a research fellow at Norwich Medical School at the University of East Anglia in the United Kingdom.
Dr. Salzberg described two major problems with Dr. Knight’s study.
“What they found were false positives because of contamination in the database and flaws in their methods,” Dr. Salzberg said. “I can’t prove there’s no cancer microbiome, but I can say the cancer microbiomes that they reported don’t exist because the species they were finding aren’t there.”
Dr. Knight disagrees with Dr. Salzberg’s findings, noting that Dr. Salzberg and his co-authors did not examine the publicly available databases used in his study. In a written response, he said that his team’s examination of the database revealed that less than 1% of the microbial genomes overlapped with human ones and that removing them did not change their findings.
Dr. Knight also noted that his team could still “distinguish cancer types by their microbiome” even after running their analysis without the technique that Dr. Salzberg found fault with.
Dr. Salzberg said that the database linked above is not the one Dr. Knight’s study used, however. “The primary database in their study was never made public (it’s too large, they said), and it has/had about 69,000 genomes,” Dr. Salzberg said by email. “But even if we did, this is irrelevant. He’s trying to distract from the primary errors in their study,” which Dr. Salzberg said Dr. Knight’s team has not addressed.
The critiques Dr. Salzberg raised have been leveled at other studies investigating microbiomes specifically within tumors and independent of the body’s microbiome.
For example, a 2019 study in Nature described a fungal microbiome in pancreatic cancer that a Nature paper 4 years later directly contradicted, citing flaws that invalidated the original findings. A different 2019 study in Cell examined pancreatic tumor microbiota and patient outcomes, but it’s unclear whether the microorganisms moved from the gut to the pancreas or “constitute a durably colonized community that lives inside the tumor,” which remains a matter of debate, Dr. Vujkovic-Cvijin said.
A 2020 study in Science suggested diverse microbial communities in seven tumor types, but those findings were similarly called into question. That study stated that “bacteria were first detected in human tumors more than 100 years ago” and that “bacteria are well-known residents in human tumors,” but Dr. Salzberg considers those statements misleading.
It’s true that bacteria and viruses have been detected in tumors because “there’s very good evidence that an acute infection caused by a very small number of viruses and bacteria can cause a tumor,” Dr. Salzberg said. Human papillomavirus, for example, can cause six different types of cancer. Inflammation and ulcers caused by Helicobacter pylori may progress to stomach cancer, and Fusobacterium nucleatum and Enterococcus faecalis have been shown to contribute to colorectal cancer. Those examples differ from a microbiome; this “a community of bacteria and possibly other microscopic bugs, like fungi, that are happily living in the tumor” the same way microbes reside in our guts, he said.
Dr. Knight said that many bacteria his team identified “have been confirmed independently in subsequent work.” He acknowledged, however, that more research is needed.
Several of the contested studies above were among a lengthy list that Dr. Knight provided, noting that most of the disagreements “have two sides to them, and critiques from one particular group does not immediately invalidate a reported finding.”
Yet, many of the papers Dr. Knight listed are precisely the types that skeptics like Dr. Salzberg believe are too flawed to draw reliable conclusions.
“I think many agree that microbes may exist within tumors that are exposed to the environment, like tumors of the skin, gut, and mouth,” Dr. Vujkovic-Cvijin said. It’s less clear, however, whether tumors further from the body’s microbiome harbor any microbes or where they came from if they do. Microbial signals in organs elsewhere in the body become faint quickly, he said.
Underdeveloped Technology
Though Dr. Salzberg said that the concept of a tumor microbiome is “implausible” because there’s no easy route for bacteria to reach internal organs, it’s unclear whether scientists have the technology yet to adequately answer this question.
For one thing, samples in these types of studies are typically “ultra-low biomass samples, where the signal — the amount of microbes in the sample — is so low that it’s comparable to how much would be expected to be found in reagents and environmental contamination through processing,” Dr. Vujkovic-Cvijin explained. Many polymerases used to amplify a DNA signal, for example, are made in bacteria and may retain trace amounts identified in these studies.
Dr. Knight agreed that low biomass is a challenge in this field but is not an unsurmountable one.
Another challenge is that study samples, as with Dr. Knight’s work, were collected during routine surgeries without the intent to find a microbial signal. Simply using a scalpel to cut through the skin means cutting through a layer of bacteria, and surgery rooms are not designed to eliminate all bacteria. Some work has even shown there is a “hospital microbiome,” so “you can easily have that creep into your signal and mistake it for tumor-resident bacteria,” Dr. Vujkovic-Cvijin said.
Dr. Knight asserted that the samples are taken under sterile conditions, but other researchers do not think the level of sterility necessary for completely clean samples is possible.
“Just because it’s in your sample doesn’t mean it was in your tumor,” Dr. Gihawi said.
Even if scientists can retrieve a reliable sample without contamination, analyzing it requires comparing the genetic material to existing databases of microbial genomes. Yet, contamination and misclassification of genetic sequences can be problems in those reference genomes too, Dr. Gihawi explained.
Machine learning algorithms have a role in interpreting data, but “we need to be careful of what we use them for,” he added.
“These techniques are in their infancy, and we’re starting to chase them down, which is why we need to move microbiome research in a way that can be used clinically,” Dr. Gihawi said.
Influence on Cancer Treatment Outcomes
Again, however, the question of whether microbiomes exist within tumors is only one slice of the much larger field looking at microbiomes and cancer, including its influence on cancer treatment outcomes. Although much remains to be learned, less controversy exists over the thousands of studies in the past two decades that have gradually revealed how the body’s microbiome can affect both the course of a cancer and the effectiveness of different treatments.
The growing research showing the importance of the gut microbiome in cancer treatments is not surprising given its role in immunity more broadly. Because the human immune system must recognize and defend against microbes, the microbiome helps train it, Dr. Vujkovic-Cvijin said.
Some bacteria can escape the gut — a phenomenon called bacterial translocation — and may aid in fighting tumors. To grow large enough to be seen on imaging, tumors need to evolve several abilities, such as growing enough vascularization to receive blood flow and shutting down local immune responses.
“Any added boost, like immunotherapy, has a chance of breaking through that immune forcefield and killing the tumor cells,” Dr. Vujkovic-Cvijin said. Escaped gut bacteria may provide that boost.
“There’s a lot of evidence that depletion of the gut microbiome impairs immunotherapy and chemotherapy. The thinking behind some of those studies is that gut microbes can cross the gut barrier and when they do, they activate the immune system,” he said.
In mice engineered to have sterile guts, for example, the lack of bacteria results in less effective immune systems, Dr. Vujkovic-Cvijin pointed out. A host of research has shown that antibiotic exposure during and even 6 months before immunotherapy dramatically reduces survival rates. “That’s pretty convincing to me that gut microbes are important,” he said.
Dr. Vujkovic-Cvijin cautioned that there continues to be controversy on understanding which bacteria are important for response to immunotherapy. “The field is still in its infancy in terms of understanding which bacteria are most important for these effects,” he said.
Dr. Knight suggested that escaped bacteria may be the genesis of the ones that he and other researchers believe exist in tumors. “Because tumor microbes must come from somewhere, it is to be expected that some of those microbes will be co-opted from body-site specific commensals.”
It’s also possible that metabolites released from gut bacteria escape the gut and could theoretically affect distant tumor growth, Dr. Gihawi said. The most promising avenue of research in this area is metabolites being used as biomarkers, added Dr. Gihawi, whose lab published research on a link between bacteria detected in men’s urine and a more aggressive subset of prostate cancers. But that research is not far enough along to develop lab tests for clinical use, he noted.
No Consensus Yet
Even before the controversy erupted around Dr. Knight’s research, he co-founded the company Micronoma to develop cancer tests based on his microbe findings. The company has raised $17.5 million from private investors as of August 2023 and received the US Food and Drug Administration’s Breakthrough Device designation, allowing the firm to fast-track clinical trials testing the technology. The recent critiques have not changed the company’s plans.
It’s safe to say that scientists will continue to research and debate the possibility of tumor microbiomes until a consensus emerges.
“The field is evolving and studies testing the reproducibility of tumor-resident microbial signals are essential for developing our understanding in this area,” Dr. Vujkovic-Cvijin said.
Even if that path ultimately leads nowhere, as Dr. Salzberg expects, research into microbiomes and cancer has plenty of other directions to go.
“I’m actually quite an optimist,” Dr. Gihawi said. “I think there’s a lot of scope for some really good research here, especially in the sites where we know there is a strong microbiome, such as the gastrointestinal tract.”
A version of this article appeared on Medscape.com.
Late-Stage Incidence Rates Support CRC Screening From Age 45
, a cross-sectional study of stage-stratified CRC found.
It is well known that CRC is becoming more prevalent generally in the under 50-year population, but stage-related analyses have not been done.
Staging analysis in this age group is important, however, as an increasing burden of advance-staged disease would provide further evidence for earlier screening initiation, wrote Eric M. Montminy, MD, a gastroenterologist at John H. Stroger Hospital of County Cook, Chicago, Illinois, and colleagues in JAMA Network Open.
The United States Preventive Services Task Force (USPSTF) has recommended that average-risk screening begin at 45 years of age, as do the American Gastroenterological Association and other GI societies, although the American College of Physicians last year published clinical guidance recommending 50 years as the age to start screening for CRC for patients with average risk.
“Patients aged 46-49 may become confused on which guideline to follow, similar to confusion occurring with prior breast cancer screening changes,” Dr. Montminy said in an interview. “We wanted to demonstrate incidence rates with stage stratification to help clarify the incidence trends in this age group. Stage stratification is a key because it provides insight into the relationship between time and cancer incidence, ie, is screening finding early cancer or not?”
A 2020 study in JAMA Network Open demonstrated a 46.1% increase in CRC incidence rates (IRs) in persons aged 49-50 years. This steep increase is consistent with the presence of a large preexisting and undetected case burden.
“Our results demonstrate that adults aged 46-49 years, who are between now-conflicting guidelines on whether to start screening at age 45 or 50 years, have an increasing burden of more advanced-stage CRC and thus may be at an increased risk if screening is not initiated at age 45 years,” Dr. Montminy’s group wrote.
Using incidence data per 100,000 population from the National Cancer Institute’s Surveillance, Epidemiology, and End Results registry, the investigators observed the following IRs for early-onset CRC in the age group of 46-49 years:
- Distant adenocarcinoma IRs increased faster than other stages: annual percentage change (APC), 2.2 (95% CI, 1.8-2.6).
- Regional IRs also significantly increased: APC, 1.3 (95% CI, 0.8-1.7).
- Absolute regional IRs of CRC in the age bracket of 46-49 years are similar to total pancreatic cancer IRs in all ages and all stages combined (13.2 of 100,000) over similar years. When distant IRs for CRC are included with regional IRs, those for IRs for CRC are double those for pancreatic cancer of all stages combined.
- The only decrease was seen in localized IRs: APC, -0.6 (95% CI, -1 to -0.2).
“My best advice for clinicians is to provide the facts from the data to patients so they can make an informed health decision,” Dr. Montminy said. “This includes taking an appropriate personal and family history and having the patient factor this aspect into their decision on when and how they want to perform colon cancer screening.”
His institution adheres to the USPSTF recommendation of initiation of CRC screening at age 45 years.
Findings From 2000 to 2020
During 2000-2020 period, 26,887 CRCs were diagnosed in adults aged 46-49 years (54.5% in men).
As of 2020, the localized adenocarcinoma IR decreased to 7.7 of 100,000, but regional adenocarcinoma IR increased to 13.4 of 100,000 and distant adenocarcinoma IR increased to 9.0 of 100,000.
Regional adenocarcinoma IR remained the highest of all stages in 2000-2020. From 2014 to 2020, distant IRs became similar to localized IRs, except in 2017 when distant IRs were significantly higher than localized.
Why the CRC Uptick?
“It remains an enigma at this time as to why we’re seeing this shift,” Dr. Montminy said, noting that etiologies from the colonic microbiome to cellphones have been postulated. “To date, no theory has substantially provided causality. But whatever the source is, it is affecting Western countries in unison with data demonstrating a birth cohort effect as well,” he added. “We additionally know, based on the current epidemiologic data, that current screening practices are failing, and a unified discussion must occur in order to prevent young patients from developing advanced colon cancer.”
Offering his perspective on the findings, Joshua Meyer, MD, vice chair of translational research in the Department of Radiation Oncology at Fox Chase Cancer Center in Philadelphia, said the findings reinforce the practice of offering screening to average-risk individuals starting at age 45 years, the threshold at his institution. “There are previously published data demonstrating an increase in advanced stage at the time of screening initiation, and these data support that,” said Dr. Meyer, who was not involved in the present analysis.
More research needs to be done, he continued, not just on optimal age but also on the effect of multiple other factors impacting risk. “These may include family history and genetic risk as well as the role of blood- and stool-based screening assays in an integrated strategy to screen for colorectal cancer.”
There are multiple screening tests, and while colonoscopy, the gold standard, is very safe, it is not completely without risks, Dr. Meyer added. “And the question of the appropriate allocation of limited societal resources continues to be discussed on a broader level and largely explains the difference between the two guidelines.”
This study received no specific funding. Co-author Jordan J. Karlitz, MD, reported personal fees from GRAIL (senior medical director) and an equity position from Gastro Girl/GI On Demand outside f the submitted work. Dr. Meyer disclosed no conflicts of interest relevant to his comments.
, a cross-sectional study of stage-stratified CRC found.
It is well known that CRC is becoming more prevalent generally in the under 50-year population, but stage-related analyses have not been done.
Staging analysis in this age group is important, however, as an increasing burden of advance-staged disease would provide further evidence for earlier screening initiation, wrote Eric M. Montminy, MD, a gastroenterologist at John H. Stroger Hospital of County Cook, Chicago, Illinois, and colleagues in JAMA Network Open.
The United States Preventive Services Task Force (USPSTF) has recommended that average-risk screening begin at 45 years of age, as do the American Gastroenterological Association and other GI societies, although the American College of Physicians last year published clinical guidance recommending 50 years as the age to start screening for CRC for patients with average risk.
“Patients aged 46-49 may become confused on which guideline to follow, similar to confusion occurring with prior breast cancer screening changes,” Dr. Montminy said in an interview. “We wanted to demonstrate incidence rates with stage stratification to help clarify the incidence trends in this age group. Stage stratification is a key because it provides insight into the relationship between time and cancer incidence, ie, is screening finding early cancer or not?”
A 2020 study in JAMA Network Open demonstrated a 46.1% increase in CRC incidence rates (IRs) in persons aged 49-50 years. This steep increase is consistent with the presence of a large preexisting and undetected case burden.
“Our results demonstrate that adults aged 46-49 years, who are between now-conflicting guidelines on whether to start screening at age 45 or 50 years, have an increasing burden of more advanced-stage CRC and thus may be at an increased risk if screening is not initiated at age 45 years,” Dr. Montminy’s group wrote.
Using incidence data per 100,000 population from the National Cancer Institute’s Surveillance, Epidemiology, and End Results registry, the investigators observed the following IRs for early-onset CRC in the age group of 46-49 years:
- Distant adenocarcinoma IRs increased faster than other stages: annual percentage change (APC), 2.2 (95% CI, 1.8-2.6).
- Regional IRs also significantly increased: APC, 1.3 (95% CI, 0.8-1.7).
- Absolute regional IRs of CRC in the age bracket of 46-49 years are similar to total pancreatic cancer IRs in all ages and all stages combined (13.2 of 100,000) over similar years. When distant IRs for CRC are included with regional IRs, those for IRs for CRC are double those for pancreatic cancer of all stages combined.
- The only decrease was seen in localized IRs: APC, -0.6 (95% CI, -1 to -0.2).
“My best advice for clinicians is to provide the facts from the data to patients so they can make an informed health decision,” Dr. Montminy said. “This includes taking an appropriate personal and family history and having the patient factor this aspect into their decision on when and how they want to perform colon cancer screening.”
His institution adheres to the USPSTF recommendation of initiation of CRC screening at age 45 years.
Findings From 2000 to 2020
During 2000-2020 period, 26,887 CRCs were diagnosed in adults aged 46-49 years (54.5% in men).
As of 2020, the localized adenocarcinoma IR decreased to 7.7 of 100,000, but regional adenocarcinoma IR increased to 13.4 of 100,000 and distant adenocarcinoma IR increased to 9.0 of 100,000.
Regional adenocarcinoma IR remained the highest of all stages in 2000-2020. From 2014 to 2020, distant IRs became similar to localized IRs, except in 2017 when distant IRs were significantly higher than localized.
Why the CRC Uptick?
“It remains an enigma at this time as to why we’re seeing this shift,” Dr. Montminy said, noting that etiologies from the colonic microbiome to cellphones have been postulated. “To date, no theory has substantially provided causality. But whatever the source is, it is affecting Western countries in unison with data demonstrating a birth cohort effect as well,” he added. “We additionally know, based on the current epidemiologic data, that current screening practices are failing, and a unified discussion must occur in order to prevent young patients from developing advanced colon cancer.”
Offering his perspective on the findings, Joshua Meyer, MD, vice chair of translational research in the Department of Radiation Oncology at Fox Chase Cancer Center in Philadelphia, said the findings reinforce the practice of offering screening to average-risk individuals starting at age 45 years, the threshold at his institution. “There are previously published data demonstrating an increase in advanced stage at the time of screening initiation, and these data support that,” said Dr. Meyer, who was not involved in the present analysis.
More research needs to be done, he continued, not just on optimal age but also on the effect of multiple other factors impacting risk. “These may include family history and genetic risk as well as the role of blood- and stool-based screening assays in an integrated strategy to screen for colorectal cancer.”
There are multiple screening tests, and while colonoscopy, the gold standard, is very safe, it is not completely without risks, Dr. Meyer added. “And the question of the appropriate allocation of limited societal resources continues to be discussed on a broader level and largely explains the difference between the two guidelines.”
This study received no specific funding. Co-author Jordan J. Karlitz, MD, reported personal fees from GRAIL (senior medical director) and an equity position from Gastro Girl/GI On Demand outside f the submitted work. Dr. Meyer disclosed no conflicts of interest relevant to his comments.
, a cross-sectional study of stage-stratified CRC found.
It is well known that CRC is becoming more prevalent generally in the under 50-year population, but stage-related analyses have not been done.
Staging analysis in this age group is important, however, as an increasing burden of advance-staged disease would provide further evidence for earlier screening initiation, wrote Eric M. Montminy, MD, a gastroenterologist at John H. Stroger Hospital of County Cook, Chicago, Illinois, and colleagues in JAMA Network Open.
The United States Preventive Services Task Force (USPSTF) has recommended that average-risk screening begin at 45 years of age, as do the American Gastroenterological Association and other GI societies, although the American College of Physicians last year published clinical guidance recommending 50 years as the age to start screening for CRC for patients with average risk.
“Patients aged 46-49 may become confused on which guideline to follow, similar to confusion occurring with prior breast cancer screening changes,” Dr. Montminy said in an interview. “We wanted to demonstrate incidence rates with stage stratification to help clarify the incidence trends in this age group. Stage stratification is a key because it provides insight into the relationship between time and cancer incidence, ie, is screening finding early cancer or not?”
A 2020 study in JAMA Network Open demonstrated a 46.1% increase in CRC incidence rates (IRs) in persons aged 49-50 years. This steep increase is consistent with the presence of a large preexisting and undetected case burden.
“Our results demonstrate that adults aged 46-49 years, who are between now-conflicting guidelines on whether to start screening at age 45 or 50 years, have an increasing burden of more advanced-stage CRC and thus may be at an increased risk if screening is not initiated at age 45 years,” Dr. Montminy’s group wrote.
Using incidence data per 100,000 population from the National Cancer Institute’s Surveillance, Epidemiology, and End Results registry, the investigators observed the following IRs for early-onset CRC in the age group of 46-49 years:
- Distant adenocarcinoma IRs increased faster than other stages: annual percentage change (APC), 2.2 (95% CI, 1.8-2.6).
- Regional IRs also significantly increased: APC, 1.3 (95% CI, 0.8-1.7).
- Absolute regional IRs of CRC in the age bracket of 46-49 years are similar to total pancreatic cancer IRs in all ages and all stages combined (13.2 of 100,000) over similar years. When distant IRs for CRC are included with regional IRs, those for IRs for CRC are double those for pancreatic cancer of all stages combined.
- The only decrease was seen in localized IRs: APC, -0.6 (95% CI, -1 to -0.2).
“My best advice for clinicians is to provide the facts from the data to patients so they can make an informed health decision,” Dr. Montminy said. “This includes taking an appropriate personal and family history and having the patient factor this aspect into their decision on when and how they want to perform colon cancer screening.”
His institution adheres to the USPSTF recommendation of initiation of CRC screening at age 45 years.
Findings From 2000 to 2020
During 2000-2020 period, 26,887 CRCs were diagnosed in adults aged 46-49 years (54.5% in men).
As of 2020, the localized adenocarcinoma IR decreased to 7.7 of 100,000, but regional adenocarcinoma IR increased to 13.4 of 100,000 and distant adenocarcinoma IR increased to 9.0 of 100,000.
Regional adenocarcinoma IR remained the highest of all stages in 2000-2020. From 2014 to 2020, distant IRs became similar to localized IRs, except in 2017 when distant IRs were significantly higher than localized.
Why the CRC Uptick?
“It remains an enigma at this time as to why we’re seeing this shift,” Dr. Montminy said, noting that etiologies from the colonic microbiome to cellphones have been postulated. “To date, no theory has substantially provided causality. But whatever the source is, it is affecting Western countries in unison with data demonstrating a birth cohort effect as well,” he added. “We additionally know, based on the current epidemiologic data, that current screening practices are failing, and a unified discussion must occur in order to prevent young patients from developing advanced colon cancer.”
Offering his perspective on the findings, Joshua Meyer, MD, vice chair of translational research in the Department of Radiation Oncology at Fox Chase Cancer Center in Philadelphia, said the findings reinforce the practice of offering screening to average-risk individuals starting at age 45 years, the threshold at his institution. “There are previously published data demonstrating an increase in advanced stage at the time of screening initiation, and these data support that,” said Dr. Meyer, who was not involved in the present analysis.
More research needs to be done, he continued, not just on optimal age but also on the effect of multiple other factors impacting risk. “These may include family history and genetic risk as well as the role of blood- and stool-based screening assays in an integrated strategy to screen for colorectal cancer.”
There are multiple screening tests, and while colonoscopy, the gold standard, is very safe, it is not completely without risks, Dr. Meyer added. “And the question of the appropriate allocation of limited societal resources continues to be discussed on a broader level and largely explains the difference between the two guidelines.”
This study received no specific funding. Co-author Jordan J. Karlitz, MD, reported personal fees from GRAIL (senior medical director) and an equity position from Gastro Girl/GI On Demand outside f the submitted work. Dr. Meyer disclosed no conflicts of interest relevant to his comments.
FROM JAMA NETWORK OPEN
Improving Fecal Immunochemical Test Collection for Colorectal Cancer Screening During the COVID-19 Pandemic
Colorectal cancer (CRC) is the third-most common cancer worldwide and accounts for almost 11% of all cancer diagnoses, with > 1.9 million cases reported globally.1,2 CRC is the second-most deadly cancer, responsible for about 935,000 deaths.1 Over the past several decades, a steady decline in CRC incidence and mortality has been reported in developed countries, including the US.3,4 From 2008 through 2017, an annual reduction of 3% in CRC death rates was reported in individuals aged ≥ 65 years.5 This decline can mainly be attributed to improvements made in health systems and advancements in CRC screening programs.3,5
US Preventive Services Task Force (USPSTF) recommends CRC screening in individuals aged 45 to 75 years. USPSTF recommends direct visualization tests, such as colonoscopy and flexible sigmoidoscopy for CRC screening.6 Although colonoscopy is commonly used for CRC screening, it is an invasive procedure that requires bowel preparation and sedation, and has the potential risk of colonic perforation, bleeding, and infection. Additionally, social determinants—such as health care costs, missed work, and geographic location (eg, rural communities)—may limit colonoscopy utilization.7 As a result, other cost-effective, noninvasive tests such as high-sensitivity guaiac-based fecal occult blood test (gFOBT) and fecal immunochemical test (FIT) are also used for CRC screening. These tests detect occult blood in the stool of individuals who may be at risk for CRC, helping direct them to colonoscopy if they screen positive.8
The gFOBT relies on simple oxidation and requires a stool sample to detect the presence of the heme component of blood.9 If heme is present in the stool sample, it will enable the oxidation of guaiac to form a blue-colored dye when added to hydrogen peroxide. It is important to note that the oxidation component of this test may lead to false-positive results, as it may detect dietary hemoglobin present in red meat. Medications or foods that have peroxidase properties may also result in a false-positive gFOBT result. Additionally, false-negative results may be caused by antioxidants, which may interfere with the oxidation of guaiac.
FIT uses antibodies, which bind to the intact globin component of human hemoglobin.9 The quantity of bound antibody-hemoglobin complex is detected and measured by a variety of automated quantitative techniques. This testing strategy eliminates the need for food or medication restrictions and the subjective visual assessment of change in color, as required for the gFOBT.9 A 2016 meta-analysis found that FIT performed better compared with gFOBT in terms of specificity, positivity rate, number needed to scope, and number needed to screen.8 The FIT screening method has also been found to have greater adherence rates, which is likely due to fewer stool sampling requirements and the lack of medication or dietary restrictions, compared with gFOBT.7,8
The COVID-19 pandemic had a drastic impact on CRC preventive care services. In March 2020, elective colonoscopies were temporarily ceased across the country and the US Department of Veterans Affairs (VA) deferred all elective surgeries and medical procedures, including screening and surveillance colonoscopies. In line with these recommendations, elective colonoscopies were temporarily ceased across the country.10 The National Cancer Institute’s Population-Based Research to Optimize the Screening Process consortium reported that CRC screening rates decreased by 82% across the US in 2020.11 Public health measures are likely the main reason for this decline, but other factors may include a lack of resource availability in outpatient settings and public fear of the pandemic.10
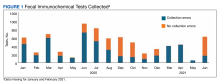
The James A. Haley Veterans Affairs Hospital (JAHVAH) in Tampa, Florida, encouraged the use of FIT in place of colonoscopies to avoid delaying preventive services. The initiative to continue CRC screening methods via FIT was scrutinized when laboratory personnel reported that in fiscal year (FY) 2020, 62% of the FIT kits that patients returned to the laboratory were missing information or had other errors (Figure 1). These improperly returned FIT kits led to delayed processing, canceled orders, increased staff workload, and more costs for FIT repetition.
Research shows many patients often fail to adhere to the instructions for proper FIT sample collection and return. Wang and colleagues reported that of 4916 FIT samples returned to the laboratory, 971 (20%) had collection errors, and 910 (94%) of those samples were missing a sample collection date.12 The sample collection date is important because hemoglobin degradation occurs over time, which may create false-negative FIT results. Although studies have found that sample return times of ≤ 10 days are not associated with a decrease in FIT positive rates, it is recommended to mail completed FITs within 24 hours of sample collection.13
Because remote screening methods like FIT were preferred during the COVID-19 pandemic, we conducted a quality improvement (QI) project to address FIT inefficiency. The aim of this initiative was to determine the root cause behind incorrectly returned FIT kits and to increase correctly collected and testable FIT kits upon initial laboratory arrival by at least 20% by the second quarter of FY 2021.
Quality Improvement Project
This QI project was conducted from July 2020 to June 2021 at the JAHVAH, which provides primary care and specialty health services to veterans in central and south Florida. The QI was designed based on the Plan-Do-Study-Act (PDSA) model of health care improvement. The QI team consisted of physicians, nurses, administrative staff, and laboratory personnel. A SIPOC (Suppliers, Input, Process, Output, Customers) map was initially designed to help clarify the different groups involved in the process of FIT kit distribution and return. This map helped the team decide who should be involved in the solution process.
The QI team performed a root cause analysis using a fishbone diagram and identified the reasons FIT kits were returned to the laboratory with errors that prevented processing. The team brainstormed potential change ideas and created an impact vs effort chart to increase the number of correctly returned and testable FIT kits upon initial arrival at the laboratory by at least 20% by the second quarter of FY 2021. We identified strengths and prioritized change ideas to improve the number of testable and correctly returned FIT kits to the hospital laboratory. These ideas included centralizing FIT kit dispersal to a new administrative group, building redundant patient reminders on kit completion and giving patients more accessible places for kit return.
Patients included in the study were adults aged 50 to 75 years seen at the JAHVAH outpatient clinic who were asked to undergo FIT CRC screening. FIT orders for other facilities were excluded. The primary endpoint of this project was to improve the number of correctly returned FITs. The number of correct and incorrect returned FITs were measured from July 2020 to June 2021. FITs returned with errors were categorized by the type of error, including: no order on file in the electronic health record (EHR), canceled test, expired test, unable to identify test, missing information, and missing collection date.
We attempted to calculate costs of FITs that were returned to the laboratory but could not be analyzed and were discarded. In FY 2020, 1568 FITs were discarded. Each FIT cost about $7.80 to process for an annualized expense of $12,230 for discarded FITs.
Root Cause Analysis
Root causes were obtained by making a fishbone diagram. From this diagram, an impact vs effort chart was created to form and prioritize ideas for our PDSA cycles. Data about correctly and incorrectly returned kits were collected monthly from laboratory personnel, then analyzed by the QI team using run charts to look for change in frequency and patterns.
To improve this process, a swim lane chart for FIT processing was assembled and later used to make a comprehensive fishbone diagram to establish the 6 main root cause errors: missing FIT EHR order, cancelled FIT EHR order, expired stool specimen, partial patient identifiers, no patient identifiers, and no stool collection date. Pareto and run charts were superimposed with the laboratory data. The most common cause of incorrectly returned FITs was no collection date.
PDSA Cycles
Beginning in January 2021, PDSA cycles from the ideas in the impact vs effort chart were used. Organization and implementation of the project occurred from July 2020 to April 2021. The team reassessed the data in April 2021 to evaluate progress after PDSA initiation. The mean rate of missing collection date dropped from 24% in FY 2020 prior to PDSA cycles to 14% in April 2021; however, the number of incorrectly returned kits was similar to the baseline level. When reviewing this discrepancy, the QI team found that although the missing collection date rate had improved, the rate of FITs with not enough information had increased from 5% in FY 2020 to 67% in April 2021 (Figure 2). After discussing with laboratory personnel, it was determined that the EHR order was missing when the process pathway changed. Our PDSA initiative changed the process pathway and different individuals were responsible for FIT dispersal. The error was quickly addressed with the help of clinical and administrative staff; a 30-day follow-up on June 21, 2021, revealed that only 9% of the patients had sent back kits with not enough information.
After troubleshooting, the team achieved a sustainable increase in the number of correctly returned FIT kits from an average of 38% before the project to 72% after 30-day follow-up.
Discussion
Proper collection and return of FIT samples are vital for process efficiency for both physicians and patients. This initiative aimed to improve the rate of correctly returned FIT kits by 20%, but its final numbers showed an improvement of 33.6%. Operational benefits from this project included early detection of CRC, improved laboratory workflow, decreased FIT kit waste, and increased patient satisfaction.
The multipronged PDSA cycle attempted to increase the rate of correctly returned FIT kits. We improved kit comprehension and laboratory accessibility, and instituted redundant return reminders for patients. We also centralized a new process pathway for FIT distribution and educated physicians and support staff. Sampling and FIT return may seem like a simple procedure, but the FIT can be cumbersome for patients and directions can be confusing. Therefore, to maximize screening participation, it is essential to minimize confusion in the collection and return of a FIT sample.14,15
This QI initiative was presented at Grand Rounds at the University of South Florida in June 2021 and has since been shared with other VA hospitals. It was also presented at the American College of Gastroenterology Conference in 2021.
Limitations
This study was a single-center QI project and focused mostly on FIT kit return rates. To fully address CRC screening, it is important to ensure that individuals with a positive screen are appropriately followed up with a colonoscopy. Although follow-up was not in the scope of this project, it is key to CRC screening in general and should be the subject of future research.
Conclusions
FIT is a useful method for CRC screening that can be particularly helpful when in-person visits are limited, as seen during the COVID-19 pandemic. This increase in demand for FITs during the pandemic revealed process deficiencies and gave JAHVAH an opportunity to improve workflow. Through the aid of a multidisciplinary team, the process to complete and return FITs improved and surpassed the goal of 20% improvement. Our goal is to continue to fine-tune the workflow and troubleshoot the system as needed.
1. Sawicki T, Ruszkowska M, Danielewicz A, Niedz′wiedzka E, Arłukowicz T, Przybyłowicz KE. A review of colorectal cancer in terms of epidemiology, risk factors, development, symptoms and diagnosis. Cancers (Basel). 2021;13(9):2025. Published 2021 Apr 22. doi:10.3390/cancers13092025
2. Rawla P, Sunkara T, Barsouk A. Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol. 2019;14(2):89-103. doi:10.5114/pg.2018.81072
3. Yang DX, Gross CP, Soulos PR, Yu JB. Estimating the magnitude of colorectal cancers prevented during the era of screening: 1976 to 2009. Cancer. 2014;120(18):2893-2901. doi:10.1002/cncr.28794
4. Naishadham D, Lansdorp-Vogelaar I, Siegel R, Cokkinides V, Jemal A. State disparities in colorectal cancer mortality patterns in the United States. Cancer Epidemiol Biomarkers Prev. 2011;20(7):1296-1302. doi:10.1158/1055-9965.EPI-11-0250
5. Siegel RL, Miller KD, Goding Sauer A, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145-164. doi:10.3322/caac.21601
6. US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Screening for colorectal cancer: US Preventive
Colorectal cancer (CRC) is the third-most common cancer worldwide and accounts for almost 11% of all cancer diagnoses, with > 1.9 million cases reported globally.1,2 CRC is the second-most deadly cancer, responsible for about 935,000 deaths.1 Over the past several decades, a steady decline in CRC incidence and mortality has been reported in developed countries, including the US.3,4 From 2008 through 2017, an annual reduction of 3% in CRC death rates was reported in individuals aged ≥ 65 years.5 This decline can mainly be attributed to improvements made in health systems and advancements in CRC screening programs.3,5
US Preventive Services Task Force (USPSTF) recommends CRC screening in individuals aged 45 to 75 years. USPSTF recommends direct visualization tests, such as colonoscopy and flexible sigmoidoscopy for CRC screening.6 Although colonoscopy is commonly used for CRC screening, it is an invasive procedure that requires bowel preparation and sedation, and has the potential risk of colonic perforation, bleeding, and infection. Additionally, social determinants—such as health care costs, missed work, and geographic location (eg, rural communities)—may limit colonoscopy utilization.7 As a result, other cost-effective, noninvasive tests such as high-sensitivity guaiac-based fecal occult blood test (gFOBT) and fecal immunochemical test (FIT) are also used for CRC screening. These tests detect occult blood in the stool of individuals who may be at risk for CRC, helping direct them to colonoscopy if they screen positive.8
The gFOBT relies on simple oxidation and requires a stool sample to detect the presence of the heme component of blood.9 If heme is present in the stool sample, it will enable the oxidation of guaiac to form a blue-colored dye when added to hydrogen peroxide. It is important to note that the oxidation component of this test may lead to false-positive results, as it may detect dietary hemoglobin present in red meat. Medications or foods that have peroxidase properties may also result in a false-positive gFOBT result. Additionally, false-negative results may be caused by antioxidants, which may interfere with the oxidation of guaiac.
FIT uses antibodies, which bind to the intact globin component of human hemoglobin.9 The quantity of bound antibody-hemoglobin complex is detected and measured by a variety of automated quantitative techniques. This testing strategy eliminates the need for food or medication restrictions and the subjective visual assessment of change in color, as required for the gFOBT.9 A 2016 meta-analysis found that FIT performed better compared with gFOBT in terms of specificity, positivity rate, number needed to scope, and number needed to screen.8 The FIT screening method has also been found to have greater adherence rates, which is likely due to fewer stool sampling requirements and the lack of medication or dietary restrictions, compared with gFOBT.7,8
The COVID-19 pandemic had a drastic impact on CRC preventive care services. In March 2020, elective colonoscopies were temporarily ceased across the country and the US Department of Veterans Affairs (VA) deferred all elective surgeries and medical procedures, including screening and surveillance colonoscopies. In line with these recommendations, elective colonoscopies were temporarily ceased across the country.10 The National Cancer Institute’s Population-Based Research to Optimize the Screening Process consortium reported that CRC screening rates decreased by 82% across the US in 2020.11 Public health measures are likely the main reason for this decline, but other factors may include a lack of resource availability in outpatient settings and public fear of the pandemic.10
The James A. Haley Veterans Affairs Hospital (JAHVAH) in Tampa, Florida, encouraged the use of FIT in place of colonoscopies to avoid delaying preventive services. The initiative to continue CRC screening methods via FIT was scrutinized when laboratory personnel reported that in fiscal year (FY) 2020, 62% of the FIT kits that patients returned to the laboratory were missing information or had other errors (Figure 1). These improperly returned FIT kits led to delayed processing, canceled orders, increased staff workload, and more costs for FIT repetition.
Research shows many patients often fail to adhere to the instructions for proper FIT sample collection and return. Wang and colleagues reported that of 4916 FIT samples returned to the laboratory, 971 (20%) had collection errors, and 910 (94%) of those samples were missing a sample collection date.12 The sample collection date is important because hemoglobin degradation occurs over time, which may create false-negative FIT results. Although studies have found that sample return times of ≤ 10 days are not associated with a decrease in FIT positive rates, it is recommended to mail completed FITs within 24 hours of sample collection.13
Because remote screening methods like FIT were preferred during the COVID-19 pandemic, we conducted a quality improvement (QI) project to address FIT inefficiency. The aim of this initiative was to determine the root cause behind incorrectly returned FIT kits and to increase correctly collected and testable FIT kits upon initial laboratory arrival by at least 20% by the second quarter of FY 2021.
Quality Improvement Project
This QI project was conducted from July 2020 to June 2021 at the JAHVAH, which provides primary care and specialty health services to veterans in central and south Florida. The QI was designed based on the Plan-Do-Study-Act (PDSA) model of health care improvement. The QI team consisted of physicians, nurses, administrative staff, and laboratory personnel. A SIPOC (Suppliers, Input, Process, Output, Customers) map was initially designed to help clarify the different groups involved in the process of FIT kit distribution and return. This map helped the team decide who should be involved in the solution process.
The QI team performed a root cause analysis using a fishbone diagram and identified the reasons FIT kits were returned to the laboratory with errors that prevented processing. The team brainstormed potential change ideas and created an impact vs effort chart to increase the number of correctly returned and testable FIT kits upon initial arrival at the laboratory by at least 20% by the second quarter of FY 2021. We identified strengths and prioritized change ideas to improve the number of testable and correctly returned FIT kits to the hospital laboratory. These ideas included centralizing FIT kit dispersal to a new administrative group, building redundant patient reminders on kit completion and giving patients more accessible places for kit return.
Patients included in the study were adults aged 50 to 75 years seen at the JAHVAH outpatient clinic who were asked to undergo FIT CRC screening. FIT orders for other facilities were excluded. The primary endpoint of this project was to improve the number of correctly returned FITs. The number of correct and incorrect returned FITs were measured from July 2020 to June 2021. FITs returned with errors were categorized by the type of error, including: no order on file in the electronic health record (EHR), canceled test, expired test, unable to identify test, missing information, and missing collection date.
We attempted to calculate costs of FITs that were returned to the laboratory but could not be analyzed and were discarded. In FY 2020, 1568 FITs were discarded. Each FIT cost about $7.80 to process for an annualized expense of $12,230 for discarded FITs.
Root Cause Analysis
Root causes were obtained by making a fishbone diagram. From this diagram, an impact vs effort chart was created to form and prioritize ideas for our PDSA cycles. Data about correctly and incorrectly returned kits were collected monthly from laboratory personnel, then analyzed by the QI team using run charts to look for change in frequency and patterns.
To improve this process, a swim lane chart for FIT processing was assembled and later used to make a comprehensive fishbone diagram to establish the 6 main root cause errors: missing FIT EHR order, cancelled FIT EHR order, expired stool specimen, partial patient identifiers, no patient identifiers, and no stool collection date. Pareto and run charts were superimposed with the laboratory data. The most common cause of incorrectly returned FITs was no collection date.
PDSA Cycles
Beginning in January 2021, PDSA cycles from the ideas in the impact vs effort chart were used. Organization and implementation of the project occurred from July 2020 to April 2021. The team reassessed the data in April 2021 to evaluate progress after PDSA initiation. The mean rate of missing collection date dropped from 24% in FY 2020 prior to PDSA cycles to 14% in April 2021; however, the number of incorrectly returned kits was similar to the baseline level. When reviewing this discrepancy, the QI team found that although the missing collection date rate had improved, the rate of FITs with not enough information had increased from 5% in FY 2020 to 67% in April 2021 (Figure 2). After discussing with laboratory personnel, it was determined that the EHR order was missing when the process pathway changed. Our PDSA initiative changed the process pathway and different individuals were responsible for FIT dispersal. The error was quickly addressed with the help of clinical and administrative staff; a 30-day follow-up on June 21, 2021, revealed that only 9% of the patients had sent back kits with not enough information.
After troubleshooting, the team achieved a sustainable increase in the number of correctly returned FIT kits from an average of 38% before the project to 72% after 30-day follow-up.
Discussion
Proper collection and return of FIT samples are vital for process efficiency for both physicians and patients. This initiative aimed to improve the rate of correctly returned FIT kits by 20%, but its final numbers showed an improvement of 33.6%. Operational benefits from this project included early detection of CRC, improved laboratory workflow, decreased FIT kit waste, and increased patient satisfaction.
The multipronged PDSA cycle attempted to increase the rate of correctly returned FIT kits. We improved kit comprehension and laboratory accessibility, and instituted redundant return reminders for patients. We also centralized a new process pathway for FIT distribution and educated physicians and support staff. Sampling and FIT return may seem like a simple procedure, but the FIT can be cumbersome for patients and directions can be confusing. Therefore, to maximize screening participation, it is essential to minimize confusion in the collection and return of a FIT sample.14,15
This QI initiative was presented at Grand Rounds at the University of South Florida in June 2021 and has since been shared with other VA hospitals. It was also presented at the American College of Gastroenterology Conference in 2021.
Limitations
This study was a single-center QI project and focused mostly on FIT kit return rates. To fully address CRC screening, it is important to ensure that individuals with a positive screen are appropriately followed up with a colonoscopy. Although follow-up was not in the scope of this project, it is key to CRC screening in general and should be the subject of future research.
Conclusions
FIT is a useful method for CRC screening that can be particularly helpful when in-person visits are limited, as seen during the COVID-19 pandemic. This increase in demand for FITs during the pandemic revealed process deficiencies and gave JAHVAH an opportunity to improve workflow. Through the aid of a multidisciplinary team, the process to complete and return FITs improved and surpassed the goal of 20% improvement. Our goal is to continue to fine-tune the workflow and troubleshoot the system as needed.
Colorectal cancer (CRC) is the third-most common cancer worldwide and accounts for almost 11% of all cancer diagnoses, with > 1.9 million cases reported globally.1,2 CRC is the second-most deadly cancer, responsible for about 935,000 deaths.1 Over the past several decades, a steady decline in CRC incidence and mortality has been reported in developed countries, including the US.3,4 From 2008 through 2017, an annual reduction of 3% in CRC death rates was reported in individuals aged ≥ 65 years.5 This decline can mainly be attributed to improvements made in health systems and advancements in CRC screening programs.3,5
US Preventive Services Task Force (USPSTF) recommends CRC screening in individuals aged 45 to 75 years. USPSTF recommends direct visualization tests, such as colonoscopy and flexible sigmoidoscopy for CRC screening.6 Although colonoscopy is commonly used for CRC screening, it is an invasive procedure that requires bowel preparation and sedation, and has the potential risk of colonic perforation, bleeding, and infection. Additionally, social determinants—such as health care costs, missed work, and geographic location (eg, rural communities)—may limit colonoscopy utilization.7 As a result, other cost-effective, noninvasive tests such as high-sensitivity guaiac-based fecal occult blood test (gFOBT) and fecal immunochemical test (FIT) are also used for CRC screening. These tests detect occult blood in the stool of individuals who may be at risk for CRC, helping direct them to colonoscopy if they screen positive.8
The gFOBT relies on simple oxidation and requires a stool sample to detect the presence of the heme component of blood.9 If heme is present in the stool sample, it will enable the oxidation of guaiac to form a blue-colored dye when added to hydrogen peroxide. It is important to note that the oxidation component of this test may lead to false-positive results, as it may detect dietary hemoglobin present in red meat. Medications or foods that have peroxidase properties may also result in a false-positive gFOBT result. Additionally, false-negative results may be caused by antioxidants, which may interfere with the oxidation of guaiac.
FIT uses antibodies, which bind to the intact globin component of human hemoglobin.9 The quantity of bound antibody-hemoglobin complex is detected and measured by a variety of automated quantitative techniques. This testing strategy eliminates the need for food or medication restrictions and the subjective visual assessment of change in color, as required for the gFOBT.9 A 2016 meta-analysis found that FIT performed better compared with gFOBT in terms of specificity, positivity rate, number needed to scope, and number needed to screen.8 The FIT screening method has also been found to have greater adherence rates, which is likely due to fewer stool sampling requirements and the lack of medication or dietary restrictions, compared with gFOBT.7,8
The COVID-19 pandemic had a drastic impact on CRC preventive care services. In March 2020, elective colonoscopies were temporarily ceased across the country and the US Department of Veterans Affairs (VA) deferred all elective surgeries and medical procedures, including screening and surveillance colonoscopies. In line with these recommendations, elective colonoscopies were temporarily ceased across the country.10 The National Cancer Institute’s Population-Based Research to Optimize the Screening Process consortium reported that CRC screening rates decreased by 82% across the US in 2020.11 Public health measures are likely the main reason for this decline, but other factors may include a lack of resource availability in outpatient settings and public fear of the pandemic.10
The James A. Haley Veterans Affairs Hospital (JAHVAH) in Tampa, Florida, encouraged the use of FIT in place of colonoscopies to avoid delaying preventive services. The initiative to continue CRC screening methods via FIT was scrutinized when laboratory personnel reported that in fiscal year (FY) 2020, 62% of the FIT kits that patients returned to the laboratory were missing information or had other errors (Figure 1). These improperly returned FIT kits led to delayed processing, canceled orders, increased staff workload, and more costs for FIT repetition.
Research shows many patients often fail to adhere to the instructions for proper FIT sample collection and return. Wang and colleagues reported that of 4916 FIT samples returned to the laboratory, 971 (20%) had collection errors, and 910 (94%) of those samples were missing a sample collection date.12 The sample collection date is important because hemoglobin degradation occurs over time, which may create false-negative FIT results. Although studies have found that sample return times of ≤ 10 days are not associated with a decrease in FIT positive rates, it is recommended to mail completed FITs within 24 hours of sample collection.13
Because remote screening methods like FIT were preferred during the COVID-19 pandemic, we conducted a quality improvement (QI) project to address FIT inefficiency. The aim of this initiative was to determine the root cause behind incorrectly returned FIT kits and to increase correctly collected and testable FIT kits upon initial laboratory arrival by at least 20% by the second quarter of FY 2021.
Quality Improvement Project
This QI project was conducted from July 2020 to June 2021 at the JAHVAH, which provides primary care and specialty health services to veterans in central and south Florida. The QI was designed based on the Plan-Do-Study-Act (PDSA) model of health care improvement. The QI team consisted of physicians, nurses, administrative staff, and laboratory personnel. A SIPOC (Suppliers, Input, Process, Output, Customers) map was initially designed to help clarify the different groups involved in the process of FIT kit distribution and return. This map helped the team decide who should be involved in the solution process.
The QI team performed a root cause analysis using a fishbone diagram and identified the reasons FIT kits were returned to the laboratory with errors that prevented processing. The team brainstormed potential change ideas and created an impact vs effort chart to increase the number of correctly returned and testable FIT kits upon initial arrival at the laboratory by at least 20% by the second quarter of FY 2021. We identified strengths and prioritized change ideas to improve the number of testable and correctly returned FIT kits to the hospital laboratory. These ideas included centralizing FIT kit dispersal to a new administrative group, building redundant patient reminders on kit completion and giving patients more accessible places for kit return.
Patients included in the study were adults aged 50 to 75 years seen at the JAHVAH outpatient clinic who were asked to undergo FIT CRC screening. FIT orders for other facilities were excluded. The primary endpoint of this project was to improve the number of correctly returned FITs. The number of correct and incorrect returned FITs were measured from July 2020 to June 2021. FITs returned with errors were categorized by the type of error, including: no order on file in the electronic health record (EHR), canceled test, expired test, unable to identify test, missing information, and missing collection date.
We attempted to calculate costs of FITs that were returned to the laboratory but could not be analyzed and were discarded. In FY 2020, 1568 FITs were discarded. Each FIT cost about $7.80 to process for an annualized expense of $12,230 for discarded FITs.
Root Cause Analysis
Root causes were obtained by making a fishbone diagram. From this diagram, an impact vs effort chart was created to form and prioritize ideas for our PDSA cycles. Data about correctly and incorrectly returned kits were collected monthly from laboratory personnel, then analyzed by the QI team using run charts to look for change in frequency and patterns.
To improve this process, a swim lane chart for FIT processing was assembled and later used to make a comprehensive fishbone diagram to establish the 6 main root cause errors: missing FIT EHR order, cancelled FIT EHR order, expired stool specimen, partial patient identifiers, no patient identifiers, and no stool collection date. Pareto and run charts were superimposed with the laboratory data. The most common cause of incorrectly returned FITs was no collection date.
PDSA Cycles
Beginning in January 2021, PDSA cycles from the ideas in the impact vs effort chart were used. Organization and implementation of the project occurred from July 2020 to April 2021. The team reassessed the data in April 2021 to evaluate progress after PDSA initiation. The mean rate of missing collection date dropped from 24% in FY 2020 prior to PDSA cycles to 14% in April 2021; however, the number of incorrectly returned kits was similar to the baseline level. When reviewing this discrepancy, the QI team found that although the missing collection date rate had improved, the rate of FITs with not enough information had increased from 5% in FY 2020 to 67% in April 2021 (Figure 2). After discussing with laboratory personnel, it was determined that the EHR order was missing when the process pathway changed. Our PDSA initiative changed the process pathway and different individuals were responsible for FIT dispersal. The error was quickly addressed with the help of clinical and administrative staff; a 30-day follow-up on June 21, 2021, revealed that only 9% of the patients had sent back kits with not enough information.
After troubleshooting, the team achieved a sustainable increase in the number of correctly returned FIT kits from an average of 38% before the project to 72% after 30-day follow-up.
Discussion
Proper collection and return of FIT samples are vital for process efficiency for both physicians and patients. This initiative aimed to improve the rate of correctly returned FIT kits by 20%, but its final numbers showed an improvement of 33.6%. Operational benefits from this project included early detection of CRC, improved laboratory workflow, decreased FIT kit waste, and increased patient satisfaction.
The multipronged PDSA cycle attempted to increase the rate of correctly returned FIT kits. We improved kit comprehension and laboratory accessibility, and instituted redundant return reminders for patients. We also centralized a new process pathway for FIT distribution and educated physicians and support staff. Sampling and FIT return may seem like a simple procedure, but the FIT can be cumbersome for patients and directions can be confusing. Therefore, to maximize screening participation, it is essential to minimize confusion in the collection and return of a FIT sample.14,15
This QI initiative was presented at Grand Rounds at the University of South Florida in June 2021 and has since been shared with other VA hospitals. It was also presented at the American College of Gastroenterology Conference in 2021.
Limitations
This study was a single-center QI project and focused mostly on FIT kit return rates. To fully address CRC screening, it is important to ensure that individuals with a positive screen are appropriately followed up with a colonoscopy. Although follow-up was not in the scope of this project, it is key to CRC screening in general and should be the subject of future research.
Conclusions
FIT is a useful method for CRC screening that can be particularly helpful when in-person visits are limited, as seen during the COVID-19 pandemic. This increase in demand for FITs during the pandemic revealed process deficiencies and gave JAHVAH an opportunity to improve workflow. Through the aid of a multidisciplinary team, the process to complete and return FITs improved and surpassed the goal of 20% improvement. Our goal is to continue to fine-tune the workflow and troubleshoot the system as needed.
1. Sawicki T, Ruszkowska M, Danielewicz A, Niedz′wiedzka E, Arłukowicz T, Przybyłowicz KE. A review of colorectal cancer in terms of epidemiology, risk factors, development, symptoms and diagnosis. Cancers (Basel). 2021;13(9):2025. Published 2021 Apr 22. doi:10.3390/cancers13092025
2. Rawla P, Sunkara T, Barsouk A. Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol. 2019;14(2):89-103. doi:10.5114/pg.2018.81072
3. Yang DX, Gross CP, Soulos PR, Yu JB. Estimating the magnitude of colorectal cancers prevented during the era of screening: 1976 to 2009. Cancer. 2014;120(18):2893-2901. doi:10.1002/cncr.28794
4. Naishadham D, Lansdorp-Vogelaar I, Siegel R, Cokkinides V, Jemal A. State disparities in colorectal cancer mortality patterns in the United States. Cancer Epidemiol Biomarkers Prev. 2011;20(7):1296-1302. doi:10.1158/1055-9965.EPI-11-0250
5. Siegel RL, Miller KD, Goding Sauer A, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145-164. doi:10.3322/caac.21601
6. US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Screening for colorectal cancer: US Preventive
1. Sawicki T, Ruszkowska M, Danielewicz A, Niedz′wiedzka E, Arłukowicz T, Przybyłowicz KE. A review of colorectal cancer in terms of epidemiology, risk factors, development, symptoms and diagnosis. Cancers (Basel). 2021;13(9):2025. Published 2021 Apr 22. doi:10.3390/cancers13092025
2. Rawla P, Sunkara T, Barsouk A. Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol. 2019;14(2):89-103. doi:10.5114/pg.2018.81072
3. Yang DX, Gross CP, Soulos PR, Yu JB. Estimating the magnitude of colorectal cancers prevented during the era of screening: 1976 to 2009. Cancer. 2014;120(18):2893-2901. doi:10.1002/cncr.28794
4. Naishadham D, Lansdorp-Vogelaar I, Siegel R, Cokkinides V, Jemal A. State disparities in colorectal cancer mortality patterns in the United States. Cancer Epidemiol Biomarkers Prev. 2011;20(7):1296-1302. doi:10.1158/1055-9965.EPI-11-0250
5. Siegel RL, Miller KD, Goding Sauer A, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145-164. doi:10.3322/caac.21601
6. US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Screening for colorectal cancer: US Preventive
Potential Impact of USPS Mail Delivery Delays on Colorectal Cancer Screening Programs
Colorectal cancer (CRC) is the second leading cause of cancer deaths in the United States.1 In 2022, there were an estimated 151,030 new CRC cases and 52,580 deaths.1 Options for CRC screening of patients at average risk include stool tests (annual fecal immunochemical test [FIT], annual guaiac-based fecal occult blood test, or stool FIT-DNA test every 1 to 3 years), colonoscopies every 10 years, flexible sigmoidoscopies every 5 years (or every 10 years with annual FIT), and computed tomography (CT) colonography every 5 years.2 Many health care systems use annual FIT for patients at average risk. Compared with guaiac-based fecal occult blood testing, FIT does not require dietary or medication modifications and yields greater sensitivity and patient participation.3
The COVID-19 pandemic and staffing issues have caused a scheduling backlog for screening, diagnostic, and surveillance endoscopies at some medical centers. As a result, FIT has become the primary means of CRC screening at these institutions. FIT kits for home use are typically distributed to eligible patients at an office visit or by mail, and patients are then instructed to mail the kits back to the laboratory. For the test to be as sensitive as possible, FIT kit manufacturers advise laboratory analysis within 14 to 15 days of collection, if stored at ambient temperature, and to reject the sample if it does not meet testing criteria for stability. Delayed FIT sample analysis has been associated with higher false-negative rates because of hemoglobin degradation.4 FIT sample exposure to high ambient temperatures also has been linked to decreased sensitivity for detecting CRC.5
US Postal Service (USPS) mail delivery delays have plagued many areas of the country. A variety of factors, including the COVID-19 pandemic, understaffing, changes in USPS policies, closure of post offices, and changes in mail delivery standards, may also be contributory causes. According to the USPS website, delivery standard for first-class mail is 1 to 5 days, but this is not guaranteed.6
The Jesse Brown Veterans Affairs Medical Center (JBVAMC) laboratory in Chicago has reported receiving FIT kit envelopes in batches by the USPS, with some prepaid first-class business reply envelopes delivered up to 60 days after the time of sample collection. Polymedco, a company that assists US Department of Veterans Affairs (VA) medical centers with logistics of FIT programs for CRC screening, reports that USPS batching of FIT kits leading to delayed delivery has been a periodic problem for medical centers around the country. Polymedco staff remind USPS staff about 4 points when they encounter this issue: Mailers are first-class mail; mailers contain a human biologic specimen that has limited viability; the biological sample used for detecting cancer is time sensitive; and delays in delivery by holding/batching kits could impact morbidity and mortality. Reviewing these key points with local USPS staff usually helps, however, batching and delayed delivery of the FIT kits can sometimes recur with USPS staffing turnover.
Tracking and identifying when a patient receives the FIT kit is difficult. Patients are instructed to write the date of collection on the kit, so the receiving laboratory knows whether the sample can be reliably analyzed. When patients are notified about delayed delivery of their sample, a staff member asks if they postponed dropping the kit in the mail. Most patients report mailing the sample within 1 to 2 days of collection. Tracking and dating each step of FIT kit events is not feasible with a mass mailing campaign. In our experience, most patients write the date of collection on the kit. If a collection date is not provided, the laboratory will call the patient to confirm a date. Cheng and colleagues reviewed the causes for FIT specimen rejection in a laboratory analyzing specimens for VA patients and found that 14% of submitted samples were rejected because the specimen was received > 14 days after collection, and 6% because the patient did not record the collection date. With a series of interventions aimed at reminding patients and improving laboratory procedures, rates of rejection for these 2 causes were reduced to < 4%.7 USPS delays were not identified as a factor or tracked in this study.
It is unclear why the USPS sometimes holds FIT kits at their facilities and then delivers large bins of them at the same time. Because FIT kits should be analyzed within 14 to 15 days of sample collection to assure reliable results, mail delivery delays can result in increased sample rejection. Based on the JBVAMC experience, up to 30% of submitted samples might need to be discarded when batched delivery takes place. In these cases, patients need to be contacted, informed of the problem, and asked to submit new kits. Understandably, patients are reluctant to repeat this type of testing, and we are concerned this could lead to reduced rates of CRC screening in affected communities.
As an alternative to discarding delayed samples, laboratories could report the results of delayed FIT kits with an added comment that “negative test results may be less reliable due to delayed processing,” but this approach would raise quality and medicolegal concerns. Clinicians have reached out to local USPS supervisory personnel with mixed results. Sometimes batching and delayed deliveries stop for a few months, only to resume without warning. Dropping off the sample directly at the laboratory is not a realistic option for most patients. Some patients can be convinced to submit another sample, some elect to switch to other CRC screening strategies, while others, unfortunately, decline further screening efforts.
Laboratory staff can be overwhelmed with having to process hundreds of samples in a short time frame, especially because there is no way of knowing when USPS will make a batched delivery. Laboratory capacities can limit staff at some facilities to performing analysis of only 10 tests at a time. The FIT kits should be delivered on a rolling basis and without delay so that the samples can be reliably analyzed with a predictable workload for the laboratory personnel and without unexpected surges.
When health care facilities identify delayed mail delivery of FIT kits via USPS, laboratories should first ensure that the correct postage rates are used on the prepaid envelopes and that their USPS accounts are properly funded, so that insufficient funds are not contributing to delayed deliveries. Stakeholders should then reach out to local USPS supervisory staff and request that the practice of batching the delivery of FIT kits be stopped. Educating USPS supervisory staff about concerns related to decreased test reliability associated with delayed mail delivery can be a persuasive argument. Adding additional language to the preprinted envelopes, such as “time sensitive,” may also be helpful. Unfortunately, the JBVAMC experience has been that the problem initially gets better after contacting the USPS, only to unexpectedly resurface months later. This cycle has been repeated several times in the past 2 years at JBVAMC.
All clinicians involved in CRC screening and treatment at institutions that use FIT kits need to be aware of the impact that local USPS delays can have on the reliability of these results. Health care systems should be prepared to implement mitigation strategies if they encounter significant delays with mail delivery. If delays cannot be reliably resolved by working with the local USPS staff, consider involving national USPS oversight bodies. And if the problems persist despite an attempt to work with the USPS, some institutions might find it feasible to offer drop boxes at their clinics and instruct patients to drop off FIT kits immediately following collection, in lieu of mailing them. Switching to private carriers is not a cost-effective alternative for most health care systems, and some may exclude rural areas. Depending on the local availability and capacity of endoscopists, some clinicians might prioritize referring patients for screening colonoscopies or screening flexible sigmoidoscopies, and might deemphasize FIT kits as a preferred option for CRC screening. CT colonography is an alternative screening method that is not as widely offered, nor as widely accepted at this time.
Conclusions
CRC screening is an essential part of preventive medicine, and the percentage of eligible patients screened is a well-established quality metric in primary care settings. Health care systems, clinicians, and laboratories must be vigilant to ensure that USPS delays in delivering FIT kits do not negatively impact their CRC screening programs. Facilities should actively monitor for delays in the return of FIT kits.
Despite the widespread use of mail-order pharmacies and the use of mail to communicate notifications about test results and follow-up appointments, unreliable or delayed mail delivery traditionally has not been considered a social determinant of health.8 This article highlights the impact delayed mail delivery can have on health outcomes. Disadvantaged communities in inner cities and rural areas have been disproportionately affected by the worsening performance of the USPS over the past few years.9 This represents an underappreciated public health concern in need of a sustainable solution.
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33. doi:10.3322/caac.21708
2. Centers for Disease Control and Prevention. Colorectal cancer screening tests. Updated February 23, 2023. Accessed March 14, 2024. https://www.cdc.gov/cancer/colorectal/basic_info/screening/tests.htm
3. van Rossum LG, van Rijn AF, Laheij RJ, et al. Random comparison of guaiac and immunochemical fecal occult blood tests for colorectal cancer in a screening population. Gastroenterology. 2008;135(1):82-90. doi:10.1053/j.gastro.2008.03.040
4. van Rossum LG, van Rijn AF, van Oijen MG, et al. False negative fecal occult blood tests due to delayed sample return in colorectal cancer screening. Int J Cancer. 2009;125(4):746-750. doi:10.1002/ijc.24458
5. Doubeni CA, Jensen CD, Fedewa SA, et al. Fecal immunochemical test (FIT) for colon cancer screening: variable performance with ambient temperature. J Am Board Fam Med. 2016;29(6):672-681. doi:10.3122/jabfm.2016.06.160060
6. United States Postal Service. Shipping and mailing with USPS. Accessed March 14, 2024. https://www.usps.com/ship
7. Cheng C, Ganz DA, Chang ET, Huynh A, De Peralta S. Reducing rejected fecal immunochemical tests received in the laboratory for colorectal cancer screening. J Healthc Qual. 2019;41(2):75-82.doi:10.1097/JHQ.0000000000000181
8. Hussaini SMQ, Alexander GC. The United States Postal Service: an essential public health agency? J Gen Intern Med. 2020;35(12):3699-3701. doi:10.1007/s11606-020-06275-2
9. Hampton DJ. Colorado mountain towns are plagued by post office delays as residents wait weeks for medication and retirement checks. NBC News. February 25, 2023. Accessed March 14, 2024. https://www.nbcnews.com/news/us-news/colo-mountain-towns-are-plagued-post-office-delays-residents-wait-week-rcna72085
Colorectal cancer (CRC) is the second leading cause of cancer deaths in the United States.1 In 2022, there were an estimated 151,030 new CRC cases and 52,580 deaths.1 Options for CRC screening of patients at average risk include stool tests (annual fecal immunochemical test [FIT], annual guaiac-based fecal occult blood test, or stool FIT-DNA test every 1 to 3 years), colonoscopies every 10 years, flexible sigmoidoscopies every 5 years (or every 10 years with annual FIT), and computed tomography (CT) colonography every 5 years.2 Many health care systems use annual FIT for patients at average risk. Compared with guaiac-based fecal occult blood testing, FIT does not require dietary or medication modifications and yields greater sensitivity and patient participation.3
The COVID-19 pandemic and staffing issues have caused a scheduling backlog for screening, diagnostic, and surveillance endoscopies at some medical centers. As a result, FIT has become the primary means of CRC screening at these institutions. FIT kits for home use are typically distributed to eligible patients at an office visit or by mail, and patients are then instructed to mail the kits back to the laboratory. For the test to be as sensitive as possible, FIT kit manufacturers advise laboratory analysis within 14 to 15 days of collection, if stored at ambient temperature, and to reject the sample if it does not meet testing criteria for stability. Delayed FIT sample analysis has been associated with higher false-negative rates because of hemoglobin degradation.4 FIT sample exposure to high ambient temperatures also has been linked to decreased sensitivity for detecting CRC.5
US Postal Service (USPS) mail delivery delays have plagued many areas of the country. A variety of factors, including the COVID-19 pandemic, understaffing, changes in USPS policies, closure of post offices, and changes in mail delivery standards, may also be contributory causes. According to the USPS website, delivery standard for first-class mail is 1 to 5 days, but this is not guaranteed.6
The Jesse Brown Veterans Affairs Medical Center (JBVAMC) laboratory in Chicago has reported receiving FIT kit envelopes in batches by the USPS, with some prepaid first-class business reply envelopes delivered up to 60 days after the time of sample collection. Polymedco, a company that assists US Department of Veterans Affairs (VA) medical centers with logistics of FIT programs for CRC screening, reports that USPS batching of FIT kits leading to delayed delivery has been a periodic problem for medical centers around the country. Polymedco staff remind USPS staff about 4 points when they encounter this issue: Mailers are first-class mail; mailers contain a human biologic specimen that has limited viability; the biological sample used for detecting cancer is time sensitive; and delays in delivery by holding/batching kits could impact morbidity and mortality. Reviewing these key points with local USPS staff usually helps, however, batching and delayed delivery of the FIT kits can sometimes recur with USPS staffing turnover.
Tracking and identifying when a patient receives the FIT kit is difficult. Patients are instructed to write the date of collection on the kit, so the receiving laboratory knows whether the sample can be reliably analyzed. When patients are notified about delayed delivery of their sample, a staff member asks if they postponed dropping the kit in the mail. Most patients report mailing the sample within 1 to 2 days of collection. Tracking and dating each step of FIT kit events is not feasible with a mass mailing campaign. In our experience, most patients write the date of collection on the kit. If a collection date is not provided, the laboratory will call the patient to confirm a date. Cheng and colleagues reviewed the causes for FIT specimen rejection in a laboratory analyzing specimens for VA patients and found that 14% of submitted samples were rejected because the specimen was received > 14 days after collection, and 6% because the patient did not record the collection date. With a series of interventions aimed at reminding patients and improving laboratory procedures, rates of rejection for these 2 causes were reduced to < 4%.7 USPS delays were not identified as a factor or tracked in this study.
It is unclear why the USPS sometimes holds FIT kits at their facilities and then delivers large bins of them at the same time. Because FIT kits should be analyzed within 14 to 15 days of sample collection to assure reliable results, mail delivery delays can result in increased sample rejection. Based on the JBVAMC experience, up to 30% of submitted samples might need to be discarded when batched delivery takes place. In these cases, patients need to be contacted, informed of the problem, and asked to submit new kits. Understandably, patients are reluctant to repeat this type of testing, and we are concerned this could lead to reduced rates of CRC screening in affected communities.
As an alternative to discarding delayed samples, laboratories could report the results of delayed FIT kits with an added comment that “negative test results may be less reliable due to delayed processing,” but this approach would raise quality and medicolegal concerns. Clinicians have reached out to local USPS supervisory personnel with mixed results. Sometimes batching and delayed deliveries stop for a few months, only to resume without warning. Dropping off the sample directly at the laboratory is not a realistic option for most patients. Some patients can be convinced to submit another sample, some elect to switch to other CRC screening strategies, while others, unfortunately, decline further screening efforts.
Laboratory staff can be overwhelmed with having to process hundreds of samples in a short time frame, especially because there is no way of knowing when USPS will make a batched delivery. Laboratory capacities can limit staff at some facilities to performing analysis of only 10 tests at a time. The FIT kits should be delivered on a rolling basis and without delay so that the samples can be reliably analyzed with a predictable workload for the laboratory personnel and without unexpected surges.
When health care facilities identify delayed mail delivery of FIT kits via USPS, laboratories should first ensure that the correct postage rates are used on the prepaid envelopes and that their USPS accounts are properly funded, so that insufficient funds are not contributing to delayed deliveries. Stakeholders should then reach out to local USPS supervisory staff and request that the practice of batching the delivery of FIT kits be stopped. Educating USPS supervisory staff about concerns related to decreased test reliability associated with delayed mail delivery can be a persuasive argument. Adding additional language to the preprinted envelopes, such as “time sensitive,” may also be helpful. Unfortunately, the JBVAMC experience has been that the problem initially gets better after contacting the USPS, only to unexpectedly resurface months later. This cycle has been repeated several times in the past 2 years at JBVAMC.
All clinicians involved in CRC screening and treatment at institutions that use FIT kits need to be aware of the impact that local USPS delays can have on the reliability of these results. Health care systems should be prepared to implement mitigation strategies if they encounter significant delays with mail delivery. If delays cannot be reliably resolved by working with the local USPS staff, consider involving national USPS oversight bodies. And if the problems persist despite an attempt to work with the USPS, some institutions might find it feasible to offer drop boxes at their clinics and instruct patients to drop off FIT kits immediately following collection, in lieu of mailing them. Switching to private carriers is not a cost-effective alternative for most health care systems, and some may exclude rural areas. Depending on the local availability and capacity of endoscopists, some clinicians might prioritize referring patients for screening colonoscopies or screening flexible sigmoidoscopies, and might deemphasize FIT kits as a preferred option for CRC screening. CT colonography is an alternative screening method that is not as widely offered, nor as widely accepted at this time.
Conclusions
CRC screening is an essential part of preventive medicine, and the percentage of eligible patients screened is a well-established quality metric in primary care settings. Health care systems, clinicians, and laboratories must be vigilant to ensure that USPS delays in delivering FIT kits do not negatively impact their CRC screening programs. Facilities should actively monitor for delays in the return of FIT kits.
Despite the widespread use of mail-order pharmacies and the use of mail to communicate notifications about test results and follow-up appointments, unreliable or delayed mail delivery traditionally has not been considered a social determinant of health.8 This article highlights the impact delayed mail delivery can have on health outcomes. Disadvantaged communities in inner cities and rural areas have been disproportionately affected by the worsening performance of the USPS over the past few years.9 This represents an underappreciated public health concern in need of a sustainable solution.
Colorectal cancer (CRC) is the second leading cause of cancer deaths in the United States.1 In 2022, there were an estimated 151,030 new CRC cases and 52,580 deaths.1 Options for CRC screening of patients at average risk include stool tests (annual fecal immunochemical test [FIT], annual guaiac-based fecal occult blood test, or stool FIT-DNA test every 1 to 3 years), colonoscopies every 10 years, flexible sigmoidoscopies every 5 years (or every 10 years with annual FIT), and computed tomography (CT) colonography every 5 years.2 Many health care systems use annual FIT for patients at average risk. Compared with guaiac-based fecal occult blood testing, FIT does not require dietary or medication modifications and yields greater sensitivity and patient participation.3
The COVID-19 pandemic and staffing issues have caused a scheduling backlog for screening, diagnostic, and surveillance endoscopies at some medical centers. As a result, FIT has become the primary means of CRC screening at these institutions. FIT kits for home use are typically distributed to eligible patients at an office visit or by mail, and patients are then instructed to mail the kits back to the laboratory. For the test to be as sensitive as possible, FIT kit manufacturers advise laboratory analysis within 14 to 15 days of collection, if stored at ambient temperature, and to reject the sample if it does not meet testing criteria for stability. Delayed FIT sample analysis has been associated with higher false-negative rates because of hemoglobin degradation.4 FIT sample exposure to high ambient temperatures also has been linked to decreased sensitivity for detecting CRC.5
US Postal Service (USPS) mail delivery delays have plagued many areas of the country. A variety of factors, including the COVID-19 pandemic, understaffing, changes in USPS policies, closure of post offices, and changes in mail delivery standards, may also be contributory causes. According to the USPS website, delivery standard for first-class mail is 1 to 5 days, but this is not guaranteed.6
The Jesse Brown Veterans Affairs Medical Center (JBVAMC) laboratory in Chicago has reported receiving FIT kit envelopes in batches by the USPS, with some prepaid first-class business reply envelopes delivered up to 60 days after the time of sample collection. Polymedco, a company that assists US Department of Veterans Affairs (VA) medical centers with logistics of FIT programs for CRC screening, reports that USPS batching of FIT kits leading to delayed delivery has been a periodic problem for medical centers around the country. Polymedco staff remind USPS staff about 4 points when they encounter this issue: Mailers are first-class mail; mailers contain a human biologic specimen that has limited viability; the biological sample used for detecting cancer is time sensitive; and delays in delivery by holding/batching kits could impact morbidity and mortality. Reviewing these key points with local USPS staff usually helps, however, batching and delayed delivery of the FIT kits can sometimes recur with USPS staffing turnover.
Tracking and identifying when a patient receives the FIT kit is difficult. Patients are instructed to write the date of collection on the kit, so the receiving laboratory knows whether the sample can be reliably analyzed. When patients are notified about delayed delivery of their sample, a staff member asks if they postponed dropping the kit in the mail. Most patients report mailing the sample within 1 to 2 days of collection. Tracking and dating each step of FIT kit events is not feasible with a mass mailing campaign. In our experience, most patients write the date of collection on the kit. If a collection date is not provided, the laboratory will call the patient to confirm a date. Cheng and colleagues reviewed the causes for FIT specimen rejection in a laboratory analyzing specimens for VA patients and found that 14% of submitted samples were rejected because the specimen was received > 14 days after collection, and 6% because the patient did not record the collection date. With a series of interventions aimed at reminding patients and improving laboratory procedures, rates of rejection for these 2 causes were reduced to < 4%.7 USPS delays were not identified as a factor or tracked in this study.
It is unclear why the USPS sometimes holds FIT kits at their facilities and then delivers large bins of them at the same time. Because FIT kits should be analyzed within 14 to 15 days of sample collection to assure reliable results, mail delivery delays can result in increased sample rejection. Based on the JBVAMC experience, up to 30% of submitted samples might need to be discarded when batched delivery takes place. In these cases, patients need to be contacted, informed of the problem, and asked to submit new kits. Understandably, patients are reluctant to repeat this type of testing, and we are concerned this could lead to reduced rates of CRC screening in affected communities.
As an alternative to discarding delayed samples, laboratories could report the results of delayed FIT kits with an added comment that “negative test results may be less reliable due to delayed processing,” but this approach would raise quality and medicolegal concerns. Clinicians have reached out to local USPS supervisory personnel with mixed results. Sometimes batching and delayed deliveries stop for a few months, only to resume without warning. Dropping off the sample directly at the laboratory is not a realistic option for most patients. Some patients can be convinced to submit another sample, some elect to switch to other CRC screening strategies, while others, unfortunately, decline further screening efforts.
Laboratory staff can be overwhelmed with having to process hundreds of samples in a short time frame, especially because there is no way of knowing when USPS will make a batched delivery. Laboratory capacities can limit staff at some facilities to performing analysis of only 10 tests at a time. The FIT kits should be delivered on a rolling basis and without delay so that the samples can be reliably analyzed with a predictable workload for the laboratory personnel and without unexpected surges.
When health care facilities identify delayed mail delivery of FIT kits via USPS, laboratories should first ensure that the correct postage rates are used on the prepaid envelopes and that their USPS accounts are properly funded, so that insufficient funds are not contributing to delayed deliveries. Stakeholders should then reach out to local USPS supervisory staff and request that the practice of batching the delivery of FIT kits be stopped. Educating USPS supervisory staff about concerns related to decreased test reliability associated with delayed mail delivery can be a persuasive argument. Adding additional language to the preprinted envelopes, such as “time sensitive,” may also be helpful. Unfortunately, the JBVAMC experience has been that the problem initially gets better after contacting the USPS, only to unexpectedly resurface months later. This cycle has been repeated several times in the past 2 years at JBVAMC.
All clinicians involved in CRC screening and treatment at institutions that use FIT kits need to be aware of the impact that local USPS delays can have on the reliability of these results. Health care systems should be prepared to implement mitigation strategies if they encounter significant delays with mail delivery. If delays cannot be reliably resolved by working with the local USPS staff, consider involving national USPS oversight bodies. And if the problems persist despite an attempt to work with the USPS, some institutions might find it feasible to offer drop boxes at their clinics and instruct patients to drop off FIT kits immediately following collection, in lieu of mailing them. Switching to private carriers is not a cost-effective alternative for most health care systems, and some may exclude rural areas. Depending on the local availability and capacity of endoscopists, some clinicians might prioritize referring patients for screening colonoscopies or screening flexible sigmoidoscopies, and might deemphasize FIT kits as a preferred option for CRC screening. CT colonography is an alternative screening method that is not as widely offered, nor as widely accepted at this time.
Conclusions
CRC screening is an essential part of preventive medicine, and the percentage of eligible patients screened is a well-established quality metric in primary care settings. Health care systems, clinicians, and laboratories must be vigilant to ensure that USPS delays in delivering FIT kits do not negatively impact their CRC screening programs. Facilities should actively monitor for delays in the return of FIT kits.
Despite the widespread use of mail-order pharmacies and the use of mail to communicate notifications about test results and follow-up appointments, unreliable or delayed mail delivery traditionally has not been considered a social determinant of health.8 This article highlights the impact delayed mail delivery can have on health outcomes. Disadvantaged communities in inner cities and rural areas have been disproportionately affected by the worsening performance of the USPS over the past few years.9 This represents an underappreciated public health concern in need of a sustainable solution.
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33. doi:10.3322/caac.21708
2. Centers for Disease Control and Prevention. Colorectal cancer screening tests. Updated February 23, 2023. Accessed March 14, 2024. https://www.cdc.gov/cancer/colorectal/basic_info/screening/tests.htm
3. van Rossum LG, van Rijn AF, Laheij RJ, et al. Random comparison of guaiac and immunochemical fecal occult blood tests for colorectal cancer in a screening population. Gastroenterology. 2008;135(1):82-90. doi:10.1053/j.gastro.2008.03.040
4. van Rossum LG, van Rijn AF, van Oijen MG, et al. False negative fecal occult blood tests due to delayed sample return in colorectal cancer screening. Int J Cancer. 2009;125(4):746-750. doi:10.1002/ijc.24458
5. Doubeni CA, Jensen CD, Fedewa SA, et al. Fecal immunochemical test (FIT) for colon cancer screening: variable performance with ambient temperature. J Am Board Fam Med. 2016;29(6):672-681. doi:10.3122/jabfm.2016.06.160060
6. United States Postal Service. Shipping and mailing with USPS. Accessed March 14, 2024. https://www.usps.com/ship
7. Cheng C, Ganz DA, Chang ET, Huynh A, De Peralta S. Reducing rejected fecal immunochemical tests received in the laboratory for colorectal cancer screening. J Healthc Qual. 2019;41(2):75-82.doi:10.1097/JHQ.0000000000000181
8. Hussaini SMQ, Alexander GC. The United States Postal Service: an essential public health agency? J Gen Intern Med. 2020;35(12):3699-3701. doi:10.1007/s11606-020-06275-2
9. Hampton DJ. Colorado mountain towns are plagued by post office delays as residents wait weeks for medication and retirement checks. NBC News. February 25, 2023. Accessed March 14, 2024. https://www.nbcnews.com/news/us-news/colo-mountain-towns-are-plagued-post-office-delays-residents-wait-week-rcna72085
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33. doi:10.3322/caac.21708
2. Centers for Disease Control and Prevention. Colorectal cancer screening tests. Updated February 23, 2023. Accessed March 14, 2024. https://www.cdc.gov/cancer/colorectal/basic_info/screening/tests.htm
3. van Rossum LG, van Rijn AF, Laheij RJ, et al. Random comparison of guaiac and immunochemical fecal occult blood tests for colorectal cancer in a screening population. Gastroenterology. 2008;135(1):82-90. doi:10.1053/j.gastro.2008.03.040
4. van Rossum LG, van Rijn AF, van Oijen MG, et al. False negative fecal occult blood tests due to delayed sample return in colorectal cancer screening. Int J Cancer. 2009;125(4):746-750. doi:10.1002/ijc.24458
5. Doubeni CA, Jensen CD, Fedewa SA, et al. Fecal immunochemical test (FIT) for colon cancer screening: variable performance with ambient temperature. J Am Board Fam Med. 2016;29(6):672-681. doi:10.3122/jabfm.2016.06.160060
6. United States Postal Service. Shipping and mailing with USPS. Accessed March 14, 2024. https://www.usps.com/ship
7. Cheng C, Ganz DA, Chang ET, Huynh A, De Peralta S. Reducing rejected fecal immunochemical tests received in the laboratory for colorectal cancer screening. J Healthc Qual. 2019;41(2):75-82.doi:10.1097/JHQ.0000000000000181
8. Hussaini SMQ, Alexander GC. The United States Postal Service: an essential public health agency? J Gen Intern Med. 2020;35(12):3699-3701. doi:10.1007/s11606-020-06275-2
9. Hampton DJ. Colorado mountain towns are plagued by post office delays as residents wait weeks for medication and retirement checks. NBC News. February 25, 2023. Accessed March 14, 2024. https://www.nbcnews.com/news/us-news/colo-mountain-towns-are-plagued-post-office-delays-residents-wait-week-rcna72085
Few Cancer Survivors Meet ACS Nutrition, Exercise Guidelines
TOPLINE:
METHODOLOGY:
- The ACS has published nutrition and exercise guidelines for cancer survivors, which include recommendations to maintain a healthy weight and diet, cut out alcohol, and participate in regular physical activities. Engaging in these behaviors is associated with longer survival among cancer survivors, but whether survivors follow these nutrition and activity recommendations has not been systematically tracked.
- Researchers evaluated data on 10,020 individuals (mean age, 64.2 years) who had completed cancer treatment. Data came from the Behavioral Risk Factor Surveillance System telephone-based survey administered in 2017, 2019, and 2021, which represents 2.7 million cancer survivors.
- The researchers estimated survivors’ adherence to guidelines across four domains: Weight, physical activity, fruit and vegetable consumption, and alcohol intake. Factors associated with adherence were also evaluated.
- Overall, 9,121 survivors (91%) completed questionnaires for all four domains.
TAKEAWAY:
Only 4% of patients (365 of 9121) followed ACS guidelines in all four categories.
When assessing adherence to each category, the researchers found that 72% of cancer survivors reported engaging in recommended levels of physical activity, 68% maintained a nonobese weight, 50% said they did not consume alcohol, and 12% said they consumed recommended quantities of fruits and vegetables.
Compared with people in the general population, cancer survivors generally engaged in fewer healthy behaviors than those who had never been diagnosed with cancer.
The authors identified certain factors associated with greater guideline adherence, including female sex, older age, Black (vs White) race, and higher education level (college graduate).
IN PRACTICE:
This study highlights a potential “gap between published guidelines regarding behavioral modifications for cancer survivors and uptake of these behaviors,” the authors wrote, adding that “it is essential for oncologists and general internists to improve widespread and systematic counseling on these guidelines to improve uptake of healthy behaviors in this vulnerable patient population.”
SOURCE:
This work, led by Carter Baughman, MD, from the Division of Internal Medicine at Beth Israel Deaconess Medical Center, Boston, Massachusetts, was published online in JAMA Oncology.
LIMITATIONS:
The authors reported several study limitations, most notably that self-reported data may introduce biases.
DISCLOSURES:
The study funding source was not reported. One author received grants from the US Highbush Blueberry Council outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The ACS has published nutrition and exercise guidelines for cancer survivors, which include recommendations to maintain a healthy weight and diet, cut out alcohol, and participate in regular physical activities. Engaging in these behaviors is associated with longer survival among cancer survivors, but whether survivors follow these nutrition and activity recommendations has not been systematically tracked.
- Researchers evaluated data on 10,020 individuals (mean age, 64.2 years) who had completed cancer treatment. Data came from the Behavioral Risk Factor Surveillance System telephone-based survey administered in 2017, 2019, and 2021, which represents 2.7 million cancer survivors.
- The researchers estimated survivors’ adherence to guidelines across four domains: Weight, physical activity, fruit and vegetable consumption, and alcohol intake. Factors associated with adherence were also evaluated.
- Overall, 9,121 survivors (91%) completed questionnaires for all four domains.
TAKEAWAY:
Only 4% of patients (365 of 9121) followed ACS guidelines in all four categories.
When assessing adherence to each category, the researchers found that 72% of cancer survivors reported engaging in recommended levels of physical activity, 68% maintained a nonobese weight, 50% said they did not consume alcohol, and 12% said they consumed recommended quantities of fruits and vegetables.
Compared with people in the general population, cancer survivors generally engaged in fewer healthy behaviors than those who had never been diagnosed with cancer.
The authors identified certain factors associated with greater guideline adherence, including female sex, older age, Black (vs White) race, and higher education level (college graduate).
IN PRACTICE:
This study highlights a potential “gap between published guidelines regarding behavioral modifications for cancer survivors and uptake of these behaviors,” the authors wrote, adding that “it is essential for oncologists and general internists to improve widespread and systematic counseling on these guidelines to improve uptake of healthy behaviors in this vulnerable patient population.”
SOURCE:
This work, led by Carter Baughman, MD, from the Division of Internal Medicine at Beth Israel Deaconess Medical Center, Boston, Massachusetts, was published online in JAMA Oncology.
LIMITATIONS:
The authors reported several study limitations, most notably that self-reported data may introduce biases.
DISCLOSURES:
The study funding source was not reported. One author received grants from the US Highbush Blueberry Council outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The ACS has published nutrition and exercise guidelines for cancer survivors, which include recommendations to maintain a healthy weight and diet, cut out alcohol, and participate in regular physical activities. Engaging in these behaviors is associated with longer survival among cancer survivors, but whether survivors follow these nutrition and activity recommendations has not been systematically tracked.
- Researchers evaluated data on 10,020 individuals (mean age, 64.2 years) who had completed cancer treatment. Data came from the Behavioral Risk Factor Surveillance System telephone-based survey administered in 2017, 2019, and 2021, which represents 2.7 million cancer survivors.
- The researchers estimated survivors’ adherence to guidelines across four domains: Weight, physical activity, fruit and vegetable consumption, and alcohol intake. Factors associated with adherence were also evaluated.
- Overall, 9,121 survivors (91%) completed questionnaires for all four domains.
TAKEAWAY:
Only 4% of patients (365 of 9121) followed ACS guidelines in all four categories.
When assessing adherence to each category, the researchers found that 72% of cancer survivors reported engaging in recommended levels of physical activity, 68% maintained a nonobese weight, 50% said they did not consume alcohol, and 12% said they consumed recommended quantities of fruits and vegetables.
Compared with people in the general population, cancer survivors generally engaged in fewer healthy behaviors than those who had never been diagnosed with cancer.
The authors identified certain factors associated with greater guideline adherence, including female sex, older age, Black (vs White) race, and higher education level (college graduate).
IN PRACTICE:
This study highlights a potential “gap between published guidelines regarding behavioral modifications for cancer survivors and uptake of these behaviors,” the authors wrote, adding that “it is essential for oncologists and general internists to improve widespread and systematic counseling on these guidelines to improve uptake of healthy behaviors in this vulnerable patient population.”
SOURCE:
This work, led by Carter Baughman, MD, from the Division of Internal Medicine at Beth Israel Deaconess Medical Center, Boston, Massachusetts, was published online in JAMA Oncology.
LIMITATIONS:
The authors reported several study limitations, most notably that self-reported data may introduce biases.
DISCLOSURES:
The study funding source was not reported. One author received grants from the US Highbush Blueberry Council outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
Can Rectal Cancer Patients Benefit from Deintensification of Treatment?
New and evolving research in locally advanced rectal cancer suggests that selective use of treatments in some patients can achieve outcomes similar to those of standard regimens, according to the chair of the Department of Radiation Oncology at Duke University School of Medicine, Durham, North Carolina.
Total neoadjuvant therapy (TNT) is the standard treatment that involves systemic chemotherapy and radiation therapy before surgery for patients with locally advanced rectal cancer, Christopher G. Willett, MD, explained, in an interview. However, recent clinical trials support several strategies for “deintensification” of TNT for patients with locally advanced rectal cancer, he said.
Some patients may not require surgery or radiation therapy, or they may not require any treatment modalities including radiation therapy, chemotherapy, and surgery, Dr. Willett continued.
However, “these patients require close surveillance post treatment to identify any recurrence that may require salvage treatment,” he added.
During a presentation at the 2024 National Comprehensive Cancer Network Annual Conference, Dr. Willett primarily discussed the following three strategies for deintensifying overall therapy for locally advanced rectal cancer:
- Selective surgical omission for patients with rectal cancer having a complete clinical response after TNT with close surveillance following treatment.
- Selective omission of radiation therapy for patients with surgery such as sphincter-sparing surgery.
- Selective omission of all treatment modalities (radiation therapy, chemotherapy and surgery).
Does Watch and Wait Work?
Selective surgical omission, also known as a “watch and wait” or nonoperative management (NOM), involves treating patients with chemotherapy or a combination of chemo and radiation therapy but without surgery, Dr. Willett said during his presentation at the meeting.
Data from the OPRA trial published in the Journal of Clinical Oncology showed that 36% of patients who started on NOM developed tumor regrowth, most of which occurred in the first 2-3 years. Five-year disease-free survival rates were similar in patients who had total mesorectal excision (TME) upfront and those who had salvage TME procedures after tumor regrowth (61% and 62%, respectively). An update to the OPRA trial showed that the clinical outcomes persisted, and the results suggest no significant differences in disease-free survival between upfront surgery vs. watch and wait, Dr. Willett said.
Does Selective Omission of Radiotherapy Work?
Selective omission of radiotherapy is another option for reducing the overall treatment burden in patients with locally advanced rectal cancer, Dr. Willett. For these patients, who are at relatively low risk for recurrence, radiation along with surgery may not be needed.
Data from the FOWARC trial, published in the Journal of Clinical Oncology in 2016 and 2019, included 495 patients from 15 centers in China. In the randomized trial, the researchers found no significant difference in the primary outcome of disease-free survival between patients assigned in a 1:1:1 ratio to three arms:
- FOLFOX chemotherapy alone (a combination of chemotherapy drugs including folinic acid, fluorouracil, and oxaliplatin).
- FOLFOX plus chemoradiation.
- FU (fluorouracil)/LV (leucovorin calcium) plus chemoradiation.
Although the data were ultimately inconclusive because of potential staging bias, the findings were “promising for recommending radiation omission in these patients,” Dr. Willett said.
The larger PROSPECT study published in The New England Journal of Medicine in 2023 was similarly encouraging, he said. In this trial, 1194 patients with locally advanced rectal cancer were randomized to FOLFOX or chemoradiation prior to sphincter-sparing surgery. The two groups showed similar 5-year estimated overall survival, complete resection (R0), and pathological complete response.
“These further data support the idea that we don’t need radiotherapy anymore,” Dr. Willett said.
PROSPECT was “a very well-done trial” that also showed important patient reported outcomes, he said. At 12 months after surgery, patients in the chemoradiation group had higher scores on fatigue and neuropathy measures, but less than 15% were severe. Sexual function scores for men and women were worse in the chemoradiation group, although overall health-related quality-of-life scores were not significantly different between the groups, he noted.
Does Dropping Everything But Immunotherapy Work?
Research is very preliminary, but a small study of 12 patients with mismatch repair-deficit (MMRd) locally advanced rectal cancer published in The New England Journal of Medicine “lends optimism” to a personalized treatment approach via a programmed death 1 (PD-1) blockade, Dr. Willett said. The “small, but impressive numbers” showed that all 12 patients treated with dostarlimab only (an anti-PD-1 monoclonal antibody) had durable disease control at a follow-up of 6-24 months.
This option is feasible for patients with MMRd locally advanced rectal cancer, Dr. Willett said in an interview. “Patients treated with only dostarlimab (a PD-1 inhibitor) had excellent outcomes and did not require radiation therapy, chemotherapy, and surgery. This is potentially a new paradigm of treatment for MMRd rectal cancer.”
What are the Clinical Implications and Next Steps?
Patients should be carefully evaluated and selected for treatment approaches by experienced multidisciplinary teams with vigilant posttreatment surveillance, including history and physical exam, endoscopy, computed tomography (CT) of the chest, and abdomen and pelvic magnetic resonance imaging (MRI), Dr. Willett said in the interview.
Data on the treatment of patients with MMRd rectal cancer using dostarlimab and other immune checkpoint inhibitors are preliminary; more patients and further follow-up are required, he said. This treatment is applicable to only 5%-10% of patients with rectal cancer, he continued.
“There is a need for biomarkers such as circulating tumor DNA to further aid in selection and monitoring of patients with rectal cancer,” Dr. Willett said.
Other preliminary research is examining circulating tumor DNA analysis to guide adjuvant treatment for patients with resected stage II colon cancer, he noted in his presentation. Currently, ctDNA-driven therapy is not recommended by the NCCN, but more research is needed to determine whether this strategy might be applied to decision-making in rectal cancer patients, especially with watch and wait/nonoperative strategies, he said.
What Are the Takeaways for Deintensifying Treatment of Rectal Cancer?
The global continuum of rectal cancer clinical trials has provided significant evidence that, for select patients, the deintensification of treatment strategies may result in the avoidance of radiation and even avoidance of surgery, which can profoundly improve long-term quality of life, Al B. Benson III, MD, said in an interview.
“A critical takeaway message for clinicians who are determining which individual patient might benefit from a less intensive regimen to treat locally advanced rectal cancer is to first have a multidisciplinary consensus which should encompass review of a rectal MRI, pathology, chest and abdominal imaging, colonoscopy, as well as the patient’s clinical status including comorbidities,” said Dr. Benson, who served as chair of the NCCN Guidelines Panel for Colon/Rectal/Anal Cancers and Small Intestine Adenocarcinoma.
“The location of the rectal tumor (distal versus proximal) and clinical TNM stage also will inform the discussion as to which of the potential total neoadjuvant therapy regimens would be most optimal to reduce the risk of local recurrence and maintain long-term quality of life for the individual patient,” explained Dr. Benson, professor of medicine at Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago.
The effectiveness of less intense treatment for rectal cancer remains a work in progress, Dr. Benson said in an interview. “There is much we still do not know, such as the optimal selection of patients and the durability of this approach over time.”
Patients who undergo watch and wait require intensive follow-up, including sigmoidoscopy, digital rectal exam, and rectal MRI, to detect any evidence of local recurrence that would warrant further intervention, including possible radiation and surgery, he said. A highly skilled multidisciplinary team is a must for individuals who are potential candidates for a less intense treatment regimen, he emphasized.
The treatment of locally advanced rectal cancer continues to evolve, but there is no question that TNT has transformed patient outcomes, including the ability to deintensify treatment for select patients, Dr. Benson said.
However, many research gaps remain, Dr. Benson said in an interview. “For the MSI/dMMR patient who has achieved a complete response from immunotherapy we will need more long-term data to determine the durability of a complete clinical response and long-term avoidance of other interventions including radiation, chemotherapy and surgery.
“The wait and watch strategy for the much more common MSS patient also will require much longer follow-up to determine which patients are destined to recur and which are not,” he added.
“The introduction of monitoring with ctDNA determination over time offers an opportunity to streamline surveillance of patients who have completed combination therapy and for those undergoing watch and wait; however, much more information is required to determine which of the various ctDNA assays are most optimal, and the frequency and duration of ctDNA determination that will lend this approach as a standard of care,” Dr. Benson said.
Dr. Willett and Dr. Benson had no financial conflicts to disclose.
New and evolving research in locally advanced rectal cancer suggests that selective use of treatments in some patients can achieve outcomes similar to those of standard regimens, according to the chair of the Department of Radiation Oncology at Duke University School of Medicine, Durham, North Carolina.
Total neoadjuvant therapy (TNT) is the standard treatment that involves systemic chemotherapy and radiation therapy before surgery for patients with locally advanced rectal cancer, Christopher G. Willett, MD, explained, in an interview. However, recent clinical trials support several strategies for “deintensification” of TNT for patients with locally advanced rectal cancer, he said.
Some patients may not require surgery or radiation therapy, or they may not require any treatment modalities including radiation therapy, chemotherapy, and surgery, Dr. Willett continued.
However, “these patients require close surveillance post treatment to identify any recurrence that may require salvage treatment,” he added.
During a presentation at the 2024 National Comprehensive Cancer Network Annual Conference, Dr. Willett primarily discussed the following three strategies for deintensifying overall therapy for locally advanced rectal cancer:
- Selective surgical omission for patients with rectal cancer having a complete clinical response after TNT with close surveillance following treatment.
- Selective omission of radiation therapy for patients with surgery such as sphincter-sparing surgery.
- Selective omission of all treatment modalities (radiation therapy, chemotherapy and surgery).
Does Watch and Wait Work?
Selective surgical omission, also known as a “watch and wait” or nonoperative management (NOM), involves treating patients with chemotherapy or a combination of chemo and radiation therapy but without surgery, Dr. Willett said during his presentation at the meeting.
Data from the OPRA trial published in the Journal of Clinical Oncology showed that 36% of patients who started on NOM developed tumor regrowth, most of which occurred in the first 2-3 years. Five-year disease-free survival rates were similar in patients who had total mesorectal excision (TME) upfront and those who had salvage TME procedures after tumor regrowth (61% and 62%, respectively). An update to the OPRA trial showed that the clinical outcomes persisted, and the results suggest no significant differences in disease-free survival between upfront surgery vs. watch and wait, Dr. Willett said.
Does Selective Omission of Radiotherapy Work?
Selective omission of radiotherapy is another option for reducing the overall treatment burden in patients with locally advanced rectal cancer, Dr. Willett. For these patients, who are at relatively low risk for recurrence, radiation along with surgery may not be needed.
Data from the FOWARC trial, published in the Journal of Clinical Oncology in 2016 and 2019, included 495 patients from 15 centers in China. In the randomized trial, the researchers found no significant difference in the primary outcome of disease-free survival between patients assigned in a 1:1:1 ratio to three arms:
- FOLFOX chemotherapy alone (a combination of chemotherapy drugs including folinic acid, fluorouracil, and oxaliplatin).
- FOLFOX plus chemoradiation.
- FU (fluorouracil)/LV (leucovorin calcium) plus chemoradiation.
Although the data were ultimately inconclusive because of potential staging bias, the findings were “promising for recommending radiation omission in these patients,” Dr. Willett said.
The larger PROSPECT study published in The New England Journal of Medicine in 2023 was similarly encouraging, he said. In this trial, 1194 patients with locally advanced rectal cancer were randomized to FOLFOX or chemoradiation prior to sphincter-sparing surgery. The two groups showed similar 5-year estimated overall survival, complete resection (R0), and pathological complete response.
“These further data support the idea that we don’t need radiotherapy anymore,” Dr. Willett said.
PROSPECT was “a very well-done trial” that also showed important patient reported outcomes, he said. At 12 months after surgery, patients in the chemoradiation group had higher scores on fatigue and neuropathy measures, but less than 15% were severe. Sexual function scores for men and women were worse in the chemoradiation group, although overall health-related quality-of-life scores were not significantly different between the groups, he noted.
Does Dropping Everything But Immunotherapy Work?
Research is very preliminary, but a small study of 12 patients with mismatch repair-deficit (MMRd) locally advanced rectal cancer published in The New England Journal of Medicine “lends optimism” to a personalized treatment approach via a programmed death 1 (PD-1) blockade, Dr. Willett said. The “small, but impressive numbers” showed that all 12 patients treated with dostarlimab only (an anti-PD-1 monoclonal antibody) had durable disease control at a follow-up of 6-24 months.
This option is feasible for patients with MMRd locally advanced rectal cancer, Dr. Willett said in an interview. “Patients treated with only dostarlimab (a PD-1 inhibitor) had excellent outcomes and did not require radiation therapy, chemotherapy, and surgery. This is potentially a new paradigm of treatment for MMRd rectal cancer.”
What are the Clinical Implications and Next Steps?
Patients should be carefully evaluated and selected for treatment approaches by experienced multidisciplinary teams with vigilant posttreatment surveillance, including history and physical exam, endoscopy, computed tomography (CT) of the chest, and abdomen and pelvic magnetic resonance imaging (MRI), Dr. Willett said in the interview.
Data on the treatment of patients with MMRd rectal cancer using dostarlimab and other immune checkpoint inhibitors are preliminary; more patients and further follow-up are required, he said. This treatment is applicable to only 5%-10% of patients with rectal cancer, he continued.
“There is a need for biomarkers such as circulating tumor DNA to further aid in selection and monitoring of patients with rectal cancer,” Dr. Willett said.
Other preliminary research is examining circulating tumor DNA analysis to guide adjuvant treatment for patients with resected stage II colon cancer, he noted in his presentation. Currently, ctDNA-driven therapy is not recommended by the NCCN, but more research is needed to determine whether this strategy might be applied to decision-making in rectal cancer patients, especially with watch and wait/nonoperative strategies, he said.
What Are the Takeaways for Deintensifying Treatment of Rectal Cancer?
The global continuum of rectal cancer clinical trials has provided significant evidence that, for select patients, the deintensification of treatment strategies may result in the avoidance of radiation and even avoidance of surgery, which can profoundly improve long-term quality of life, Al B. Benson III, MD, said in an interview.
“A critical takeaway message for clinicians who are determining which individual patient might benefit from a less intensive regimen to treat locally advanced rectal cancer is to first have a multidisciplinary consensus which should encompass review of a rectal MRI, pathology, chest and abdominal imaging, colonoscopy, as well as the patient’s clinical status including comorbidities,” said Dr. Benson, who served as chair of the NCCN Guidelines Panel for Colon/Rectal/Anal Cancers and Small Intestine Adenocarcinoma.
“The location of the rectal tumor (distal versus proximal) and clinical TNM stage also will inform the discussion as to which of the potential total neoadjuvant therapy regimens would be most optimal to reduce the risk of local recurrence and maintain long-term quality of life for the individual patient,” explained Dr. Benson, professor of medicine at Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago.
The effectiveness of less intense treatment for rectal cancer remains a work in progress, Dr. Benson said in an interview. “There is much we still do not know, such as the optimal selection of patients and the durability of this approach over time.”
Patients who undergo watch and wait require intensive follow-up, including sigmoidoscopy, digital rectal exam, and rectal MRI, to detect any evidence of local recurrence that would warrant further intervention, including possible radiation and surgery, he said. A highly skilled multidisciplinary team is a must for individuals who are potential candidates for a less intense treatment regimen, he emphasized.
The treatment of locally advanced rectal cancer continues to evolve, but there is no question that TNT has transformed patient outcomes, including the ability to deintensify treatment for select patients, Dr. Benson said.
However, many research gaps remain, Dr. Benson said in an interview. “For the MSI/dMMR patient who has achieved a complete response from immunotherapy we will need more long-term data to determine the durability of a complete clinical response and long-term avoidance of other interventions including radiation, chemotherapy and surgery.
“The wait and watch strategy for the much more common MSS patient also will require much longer follow-up to determine which patients are destined to recur and which are not,” he added.
“The introduction of monitoring with ctDNA determination over time offers an opportunity to streamline surveillance of patients who have completed combination therapy and for those undergoing watch and wait; however, much more information is required to determine which of the various ctDNA assays are most optimal, and the frequency and duration of ctDNA determination that will lend this approach as a standard of care,” Dr. Benson said.
Dr. Willett and Dr. Benson had no financial conflicts to disclose.
New and evolving research in locally advanced rectal cancer suggests that selective use of treatments in some patients can achieve outcomes similar to those of standard regimens, according to the chair of the Department of Radiation Oncology at Duke University School of Medicine, Durham, North Carolina.
Total neoadjuvant therapy (TNT) is the standard treatment that involves systemic chemotherapy and radiation therapy before surgery for patients with locally advanced rectal cancer, Christopher G. Willett, MD, explained, in an interview. However, recent clinical trials support several strategies for “deintensification” of TNT for patients with locally advanced rectal cancer, he said.
Some patients may not require surgery or radiation therapy, or they may not require any treatment modalities including radiation therapy, chemotherapy, and surgery, Dr. Willett continued.
However, “these patients require close surveillance post treatment to identify any recurrence that may require salvage treatment,” he added.
During a presentation at the 2024 National Comprehensive Cancer Network Annual Conference, Dr. Willett primarily discussed the following three strategies for deintensifying overall therapy for locally advanced rectal cancer:
- Selective surgical omission for patients with rectal cancer having a complete clinical response after TNT with close surveillance following treatment.
- Selective omission of radiation therapy for patients with surgery such as sphincter-sparing surgery.
- Selective omission of all treatment modalities (radiation therapy, chemotherapy and surgery).
Does Watch and Wait Work?
Selective surgical omission, also known as a “watch and wait” or nonoperative management (NOM), involves treating patients with chemotherapy or a combination of chemo and radiation therapy but without surgery, Dr. Willett said during his presentation at the meeting.
Data from the OPRA trial published in the Journal of Clinical Oncology showed that 36% of patients who started on NOM developed tumor regrowth, most of which occurred in the first 2-3 years. Five-year disease-free survival rates were similar in patients who had total mesorectal excision (TME) upfront and those who had salvage TME procedures after tumor regrowth (61% and 62%, respectively). An update to the OPRA trial showed that the clinical outcomes persisted, and the results suggest no significant differences in disease-free survival between upfront surgery vs. watch and wait, Dr. Willett said.
Does Selective Omission of Radiotherapy Work?
Selective omission of radiotherapy is another option for reducing the overall treatment burden in patients with locally advanced rectal cancer, Dr. Willett. For these patients, who are at relatively low risk for recurrence, radiation along with surgery may not be needed.
Data from the FOWARC trial, published in the Journal of Clinical Oncology in 2016 and 2019, included 495 patients from 15 centers in China. In the randomized trial, the researchers found no significant difference in the primary outcome of disease-free survival between patients assigned in a 1:1:1 ratio to three arms:
- FOLFOX chemotherapy alone (a combination of chemotherapy drugs including folinic acid, fluorouracil, and oxaliplatin).
- FOLFOX plus chemoradiation.
- FU (fluorouracil)/LV (leucovorin calcium) plus chemoradiation.
Although the data were ultimately inconclusive because of potential staging bias, the findings were “promising for recommending radiation omission in these patients,” Dr. Willett said.
The larger PROSPECT study published in The New England Journal of Medicine in 2023 was similarly encouraging, he said. In this trial, 1194 patients with locally advanced rectal cancer were randomized to FOLFOX or chemoradiation prior to sphincter-sparing surgery. The two groups showed similar 5-year estimated overall survival, complete resection (R0), and pathological complete response.
“These further data support the idea that we don’t need radiotherapy anymore,” Dr. Willett said.
PROSPECT was “a very well-done trial” that also showed important patient reported outcomes, he said. At 12 months after surgery, patients in the chemoradiation group had higher scores on fatigue and neuropathy measures, but less than 15% were severe. Sexual function scores for men and women were worse in the chemoradiation group, although overall health-related quality-of-life scores were not significantly different between the groups, he noted.
Does Dropping Everything But Immunotherapy Work?
Research is very preliminary, but a small study of 12 patients with mismatch repair-deficit (MMRd) locally advanced rectal cancer published in The New England Journal of Medicine “lends optimism” to a personalized treatment approach via a programmed death 1 (PD-1) blockade, Dr. Willett said. The “small, but impressive numbers” showed that all 12 patients treated with dostarlimab only (an anti-PD-1 monoclonal antibody) had durable disease control at a follow-up of 6-24 months.
This option is feasible for patients with MMRd locally advanced rectal cancer, Dr. Willett said in an interview. “Patients treated with only dostarlimab (a PD-1 inhibitor) had excellent outcomes and did not require radiation therapy, chemotherapy, and surgery. This is potentially a new paradigm of treatment for MMRd rectal cancer.”
What are the Clinical Implications and Next Steps?
Patients should be carefully evaluated and selected for treatment approaches by experienced multidisciplinary teams with vigilant posttreatment surveillance, including history and physical exam, endoscopy, computed tomography (CT) of the chest, and abdomen and pelvic magnetic resonance imaging (MRI), Dr. Willett said in the interview.
Data on the treatment of patients with MMRd rectal cancer using dostarlimab and other immune checkpoint inhibitors are preliminary; more patients and further follow-up are required, he said. This treatment is applicable to only 5%-10% of patients with rectal cancer, he continued.
“There is a need for biomarkers such as circulating tumor DNA to further aid in selection and monitoring of patients with rectal cancer,” Dr. Willett said.
Other preliminary research is examining circulating tumor DNA analysis to guide adjuvant treatment for patients with resected stage II colon cancer, he noted in his presentation. Currently, ctDNA-driven therapy is not recommended by the NCCN, but more research is needed to determine whether this strategy might be applied to decision-making in rectal cancer patients, especially with watch and wait/nonoperative strategies, he said.
What Are the Takeaways for Deintensifying Treatment of Rectal Cancer?
The global continuum of rectal cancer clinical trials has provided significant evidence that, for select patients, the deintensification of treatment strategies may result in the avoidance of radiation and even avoidance of surgery, which can profoundly improve long-term quality of life, Al B. Benson III, MD, said in an interview.
“A critical takeaway message for clinicians who are determining which individual patient might benefit from a less intensive regimen to treat locally advanced rectal cancer is to first have a multidisciplinary consensus which should encompass review of a rectal MRI, pathology, chest and abdominal imaging, colonoscopy, as well as the patient’s clinical status including comorbidities,” said Dr. Benson, who served as chair of the NCCN Guidelines Panel for Colon/Rectal/Anal Cancers and Small Intestine Adenocarcinoma.
“The location of the rectal tumor (distal versus proximal) and clinical TNM stage also will inform the discussion as to which of the potential total neoadjuvant therapy regimens would be most optimal to reduce the risk of local recurrence and maintain long-term quality of life for the individual patient,” explained Dr. Benson, professor of medicine at Robert H. Lurie Comprehensive Cancer Center of Northwestern University in Chicago.
The effectiveness of less intense treatment for rectal cancer remains a work in progress, Dr. Benson said in an interview. “There is much we still do not know, such as the optimal selection of patients and the durability of this approach over time.”
Patients who undergo watch and wait require intensive follow-up, including sigmoidoscopy, digital rectal exam, and rectal MRI, to detect any evidence of local recurrence that would warrant further intervention, including possible radiation and surgery, he said. A highly skilled multidisciplinary team is a must for individuals who are potential candidates for a less intense treatment regimen, he emphasized.
The treatment of locally advanced rectal cancer continues to evolve, but there is no question that TNT has transformed patient outcomes, including the ability to deintensify treatment for select patients, Dr. Benson said.
However, many research gaps remain, Dr. Benson said in an interview. “For the MSI/dMMR patient who has achieved a complete response from immunotherapy we will need more long-term data to determine the durability of a complete clinical response and long-term avoidance of other interventions including radiation, chemotherapy and surgery.
“The wait and watch strategy for the much more common MSS patient also will require much longer follow-up to determine which patients are destined to recur and which are not,” he added.
“The introduction of monitoring with ctDNA determination over time offers an opportunity to streamline surveillance of patients who have completed combination therapy and for those undergoing watch and wait; however, much more information is required to determine which of the various ctDNA assays are most optimal, and the frequency and duration of ctDNA determination that will lend this approach as a standard of care,” Dr. Benson said.
Dr. Willett and Dr. Benson had no financial conflicts to disclose.
FROM NCCN 2024
CRC Screening in Primary Care: The Blood Test Option
Last year, I concluded a commentary for this news organization on colorectal cancer (CRC) screening guidelines by stating that between stool-based tests, flexible sigmoidoscopy, and colonoscopy, “the best screening test is the test that gets done.” But should that maxim apply to the new blood-based screening test, Guardant Health Shield? This proprietary test, which costs $895 and is not generally covered by insurance, identifies alterations in cell-free DNA that are characteristic of CRC.
Shield’s test characteristics were recently evaluated in a prospective study of more than 10,000 adults aged 45-84 at average risk for CRC. The test had an 87.5% sensitivity for stage I, II, or III colorectal cancer but only a 13% sensitivity for advanced precancerous lesions. Test specificity was 89.6%, meaning that about 1 in 10 participants without CRC or advanced precancerous lesions on colonoscopy had a false-positive result.
Although the Shield blood test has a higher rate of false positives than the traditional fecal immunochemical test (FIT) and lower sensitivity and specificity than a multitarget stool DNA (FIT-DNA) test designed to improve on Cologuard, it meets the previously established criteria set forth by the Centers for Medicare & Medicaid Services (CMS) to be covered for Medicare beneficiaries at 3-year intervals, pending FDA approval.
A big concern, however, is that the availability of a blood test may cause patients who would have otherwise been screened with colonoscopy or stool tests to switch to the blood test. A cost-effectiveness analysis found that offering a blood test to patients who decline screening colonoscopy saves additional lives, but at the cost of more than $377,000 per life-year gained. Another study relying on three microsimulation models previously utilized by the US Preventive Services Task Force (USPSTF) found that annual FIT results in more life-years gained at substantially lower cost than blood-based screening every 3 years “even when uptake of blood-based screening was 20 percentage points higher than uptake of FIT.” As a result, a multidisciplinary expert panel concluded that blood-based screening should not substitute for established CRC screening tests, but instead be offered only to patients who decline those tests.
In practice, this will increase the complexity of the CRC screening conversations we have with patients. We will need to be clear that the blood test is not yet endorsed by the USPSTF or any major guideline group and is a second-line test that will miss most precancerous polyps. As with the stool tests, it is essential to emphasize that a positive result must be followed by diagnostic colonoscopy. To addend the cancer screening maxim I mentioned before, the blood test is not the best test for CRC, but it’s probably better than no test at all.
Dr. Lin is a family physician and associate director, Family Medicine Residency Program, Lancaster General Hospital, Lancaster, Pennsylvania. He blogs at Common Sense Family Doctor.
A version of this article appeared on Medscape.com.
Last year, I concluded a commentary for this news organization on colorectal cancer (CRC) screening guidelines by stating that between stool-based tests, flexible sigmoidoscopy, and colonoscopy, “the best screening test is the test that gets done.” But should that maxim apply to the new blood-based screening test, Guardant Health Shield? This proprietary test, which costs $895 and is not generally covered by insurance, identifies alterations in cell-free DNA that are characteristic of CRC.
Shield’s test characteristics were recently evaluated in a prospective study of more than 10,000 adults aged 45-84 at average risk for CRC. The test had an 87.5% sensitivity for stage I, II, or III colorectal cancer but only a 13% sensitivity for advanced precancerous lesions. Test specificity was 89.6%, meaning that about 1 in 10 participants without CRC or advanced precancerous lesions on colonoscopy had a false-positive result.
Although the Shield blood test has a higher rate of false positives than the traditional fecal immunochemical test (FIT) and lower sensitivity and specificity than a multitarget stool DNA (FIT-DNA) test designed to improve on Cologuard, it meets the previously established criteria set forth by the Centers for Medicare & Medicaid Services (CMS) to be covered for Medicare beneficiaries at 3-year intervals, pending FDA approval.
A big concern, however, is that the availability of a blood test may cause patients who would have otherwise been screened with colonoscopy or stool tests to switch to the blood test. A cost-effectiveness analysis found that offering a blood test to patients who decline screening colonoscopy saves additional lives, but at the cost of more than $377,000 per life-year gained. Another study relying on three microsimulation models previously utilized by the US Preventive Services Task Force (USPSTF) found that annual FIT results in more life-years gained at substantially lower cost than blood-based screening every 3 years “even when uptake of blood-based screening was 20 percentage points higher than uptake of FIT.” As a result, a multidisciplinary expert panel concluded that blood-based screening should not substitute for established CRC screening tests, but instead be offered only to patients who decline those tests.
In practice, this will increase the complexity of the CRC screening conversations we have with patients. We will need to be clear that the blood test is not yet endorsed by the USPSTF or any major guideline group and is a second-line test that will miss most precancerous polyps. As with the stool tests, it is essential to emphasize that a positive result must be followed by diagnostic colonoscopy. To addend the cancer screening maxim I mentioned before, the blood test is not the best test for CRC, but it’s probably better than no test at all.
Dr. Lin is a family physician and associate director, Family Medicine Residency Program, Lancaster General Hospital, Lancaster, Pennsylvania. He blogs at Common Sense Family Doctor.
A version of this article appeared on Medscape.com.
Last year, I concluded a commentary for this news organization on colorectal cancer (CRC) screening guidelines by stating that between stool-based tests, flexible sigmoidoscopy, and colonoscopy, “the best screening test is the test that gets done.” But should that maxim apply to the new blood-based screening test, Guardant Health Shield? This proprietary test, which costs $895 and is not generally covered by insurance, identifies alterations in cell-free DNA that are characteristic of CRC.
Shield’s test characteristics were recently evaluated in a prospective study of more than 10,000 adults aged 45-84 at average risk for CRC. The test had an 87.5% sensitivity for stage I, II, or III colorectal cancer but only a 13% sensitivity for advanced precancerous lesions. Test specificity was 89.6%, meaning that about 1 in 10 participants without CRC or advanced precancerous lesions on colonoscopy had a false-positive result.
Although the Shield blood test has a higher rate of false positives than the traditional fecal immunochemical test (FIT) and lower sensitivity and specificity than a multitarget stool DNA (FIT-DNA) test designed to improve on Cologuard, it meets the previously established criteria set forth by the Centers for Medicare & Medicaid Services (CMS) to be covered for Medicare beneficiaries at 3-year intervals, pending FDA approval.
A big concern, however, is that the availability of a blood test may cause patients who would have otherwise been screened with colonoscopy or stool tests to switch to the blood test. A cost-effectiveness analysis found that offering a blood test to patients who decline screening colonoscopy saves additional lives, but at the cost of more than $377,000 per life-year gained. Another study relying on three microsimulation models previously utilized by the US Preventive Services Task Force (USPSTF) found that annual FIT results in more life-years gained at substantially lower cost than blood-based screening every 3 years “even when uptake of blood-based screening was 20 percentage points higher than uptake of FIT.” As a result, a multidisciplinary expert panel concluded that blood-based screening should not substitute for established CRC screening tests, but instead be offered only to patients who decline those tests.
In practice, this will increase the complexity of the CRC screening conversations we have with patients. We will need to be clear that the blood test is not yet endorsed by the USPSTF or any major guideline group and is a second-line test that will miss most precancerous polyps. As with the stool tests, it is essential to emphasize that a positive result must be followed by diagnostic colonoscopy. To addend the cancer screening maxim I mentioned before, the blood test is not the best test for CRC, but it’s probably better than no test at all.
Dr. Lin is a family physician and associate director, Family Medicine Residency Program, Lancaster General Hospital, Lancaster, Pennsylvania. He blogs at Common Sense Family Doctor.
A version of this article appeared on Medscape.com.
Microbial Signature of KRAS-Mutated Colorectal Cancer Identified
Their findings suggest that the gut microbes may serve as noninvasive biomarkers to help identify subtypes of CRC and guide personalized treatment recommendations.
“Our new work contributes to the growing body of evidence highlighting the significance of microbiota-driven mechanisms in cancer pathogenesis,” lead investigator Weizhong Tang, MD, with Guangxi Medical University Cancer Hospital in Nanning, China, said in a statement.
The research was recently published online in Microbiology Spectrum.
The onset and growth of CRC has been linked both to imbalances in the gut microbiome and to mutations in the KRAS gene — about 40% of people with CRC have a KRAS mutation. Yet, the interplay between gut dysbiosis and KRAS mutations in CRC remains unclear.
To investigate further, Dr. Tang and colleagues used 16s rRNA sequencing to analyze stool samples from 94 patients with CRC, including 24 with KRAS-mutated CRC and 70 with KRAS wild-type (nonmutated) CRC.
The researchers identified 26 distinct types of gut microbiota with statistically significant differences in abundance between the KRAS mutant and KRAS wild-type CRC patients.
At the genus level, Fusobacterium, Clostridium, and Shewanella were all abundant in the KRAS mutant group.
Fusobacterium is a Gram-negative microbe found in the gastrointestinal tract and the oral cavity. Recent studies have established a strong link between Fusobacterium and CRC development. Other work found elevated levels of Fusobacterium nucleatum were not only closely associated with KRAS mutation but also correlated with chemoresistance in CRC.
Clostridium produces metabolites in the large intestine, which are known to cause DNA damage and trigger inflammatory responses, thereby increasing the risk of CRC development.
Similarly, Shewanella has been proven to be a contributor to CRC development.
The researchers say it’s “plausible” to consider all three as potential noninvasive biomarkers for identifying KRAS mutation in CRC patients.
In contrast, Bifidobacterium and Akkermansia were abundant in the KRAS wild-type group.
Bifidobacterium is a probiotic with antitumor activity and Akkermansia is a Gram-negative anaerobic bacterium abundant in the gut and currently recognized as a potential probiotic.
The researchers speculated that CRC patients may have a reduced likelihood of developing KRAS mutation in the presence of Bifidobacterium and Akkermansia.
Analyses of biological pathways of gut microbiota associated with KRAS mutation status in CRC revealed a significantly higher abundance of the isoflavonoid biosynthesis pathway in the KRAS wild-type group compared with the KRAS mutant group.
“In comparison to KRAS mutant CRC, it is postulated that KRAS wild-type CRC may be less aggressive due to the upregulation of the isoflavonoid biosynthesis pathway, which may inhibit CRC development and progression,” the authors wrote.
Promising Predictive Model
Dr. Tang and colleagues also developed a machine learning model to predict KRAS mutation status in CRC patients based on the gut microbiota signature in KRAS mutant CRC.
The initial results underscore the model’s predictive efficacy and suggest that it has “considerable potential for clinical application, offering a novel dimension in the prediction of KRAS mutation status among CRC patients in a clinical setting,” the authors wrote.
They caution that the model requires data from a larger cohort to improve its efficacy, and they plan to do larger studies to validate the findings.
The study had no commercial funding. The authors declared no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Their findings suggest that the gut microbes may serve as noninvasive biomarkers to help identify subtypes of CRC and guide personalized treatment recommendations.
“Our new work contributes to the growing body of evidence highlighting the significance of microbiota-driven mechanisms in cancer pathogenesis,” lead investigator Weizhong Tang, MD, with Guangxi Medical University Cancer Hospital in Nanning, China, said in a statement.
The research was recently published online in Microbiology Spectrum.
The onset and growth of CRC has been linked both to imbalances in the gut microbiome and to mutations in the KRAS gene — about 40% of people with CRC have a KRAS mutation. Yet, the interplay between gut dysbiosis and KRAS mutations in CRC remains unclear.
To investigate further, Dr. Tang and colleagues used 16s rRNA sequencing to analyze stool samples from 94 patients with CRC, including 24 with KRAS-mutated CRC and 70 with KRAS wild-type (nonmutated) CRC.
The researchers identified 26 distinct types of gut microbiota with statistically significant differences in abundance between the KRAS mutant and KRAS wild-type CRC patients.
At the genus level, Fusobacterium, Clostridium, and Shewanella were all abundant in the KRAS mutant group.
Fusobacterium is a Gram-negative microbe found in the gastrointestinal tract and the oral cavity. Recent studies have established a strong link between Fusobacterium and CRC development. Other work found elevated levels of Fusobacterium nucleatum were not only closely associated with KRAS mutation but also correlated with chemoresistance in CRC.
Clostridium produces metabolites in the large intestine, which are known to cause DNA damage and trigger inflammatory responses, thereby increasing the risk of CRC development.
Similarly, Shewanella has been proven to be a contributor to CRC development.
The researchers say it’s “plausible” to consider all three as potential noninvasive biomarkers for identifying KRAS mutation in CRC patients.
In contrast, Bifidobacterium and Akkermansia were abundant in the KRAS wild-type group.
Bifidobacterium is a probiotic with antitumor activity and Akkermansia is a Gram-negative anaerobic bacterium abundant in the gut and currently recognized as a potential probiotic.
The researchers speculated that CRC patients may have a reduced likelihood of developing KRAS mutation in the presence of Bifidobacterium and Akkermansia.
Analyses of biological pathways of gut microbiota associated with KRAS mutation status in CRC revealed a significantly higher abundance of the isoflavonoid biosynthesis pathway in the KRAS wild-type group compared with the KRAS mutant group.
“In comparison to KRAS mutant CRC, it is postulated that KRAS wild-type CRC may be less aggressive due to the upregulation of the isoflavonoid biosynthesis pathway, which may inhibit CRC development and progression,” the authors wrote.
Promising Predictive Model
Dr. Tang and colleagues also developed a machine learning model to predict KRAS mutation status in CRC patients based on the gut microbiota signature in KRAS mutant CRC.
The initial results underscore the model’s predictive efficacy and suggest that it has “considerable potential for clinical application, offering a novel dimension in the prediction of KRAS mutation status among CRC patients in a clinical setting,” the authors wrote.
They caution that the model requires data from a larger cohort to improve its efficacy, and they plan to do larger studies to validate the findings.
The study had no commercial funding. The authors declared no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Their findings suggest that the gut microbes may serve as noninvasive biomarkers to help identify subtypes of CRC and guide personalized treatment recommendations.
“Our new work contributes to the growing body of evidence highlighting the significance of microbiota-driven mechanisms in cancer pathogenesis,” lead investigator Weizhong Tang, MD, with Guangxi Medical University Cancer Hospital in Nanning, China, said in a statement.
The research was recently published online in Microbiology Spectrum.
The onset and growth of CRC has been linked both to imbalances in the gut microbiome and to mutations in the KRAS gene — about 40% of people with CRC have a KRAS mutation. Yet, the interplay between gut dysbiosis and KRAS mutations in CRC remains unclear.
To investigate further, Dr. Tang and colleagues used 16s rRNA sequencing to analyze stool samples from 94 patients with CRC, including 24 with KRAS-mutated CRC and 70 with KRAS wild-type (nonmutated) CRC.
The researchers identified 26 distinct types of gut microbiota with statistically significant differences in abundance between the KRAS mutant and KRAS wild-type CRC patients.
At the genus level, Fusobacterium, Clostridium, and Shewanella were all abundant in the KRAS mutant group.
Fusobacterium is a Gram-negative microbe found in the gastrointestinal tract and the oral cavity. Recent studies have established a strong link between Fusobacterium and CRC development. Other work found elevated levels of Fusobacterium nucleatum were not only closely associated with KRAS mutation but also correlated with chemoresistance in CRC.
Clostridium produces metabolites in the large intestine, which are known to cause DNA damage and trigger inflammatory responses, thereby increasing the risk of CRC development.
Similarly, Shewanella has been proven to be a contributor to CRC development.
The researchers say it’s “plausible” to consider all three as potential noninvasive biomarkers for identifying KRAS mutation in CRC patients.
In contrast, Bifidobacterium and Akkermansia were abundant in the KRAS wild-type group.
Bifidobacterium is a probiotic with antitumor activity and Akkermansia is a Gram-negative anaerobic bacterium abundant in the gut and currently recognized as a potential probiotic.
The researchers speculated that CRC patients may have a reduced likelihood of developing KRAS mutation in the presence of Bifidobacterium and Akkermansia.
Analyses of biological pathways of gut microbiota associated with KRAS mutation status in CRC revealed a significantly higher abundance of the isoflavonoid biosynthesis pathway in the KRAS wild-type group compared with the KRAS mutant group.
“In comparison to KRAS mutant CRC, it is postulated that KRAS wild-type CRC may be less aggressive due to the upregulation of the isoflavonoid biosynthesis pathway, which may inhibit CRC development and progression,” the authors wrote.
Promising Predictive Model
Dr. Tang and colleagues also developed a machine learning model to predict KRAS mutation status in CRC patients based on the gut microbiota signature in KRAS mutant CRC.
The initial results underscore the model’s predictive efficacy and suggest that it has “considerable potential for clinical application, offering a novel dimension in the prediction of KRAS mutation status among CRC patients in a clinical setting,” the authors wrote.
They caution that the model requires data from a larger cohort to improve its efficacy, and they plan to do larger studies to validate the findings.
The study had no commercial funding. The authors declared no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Most Targeted Cancer Drugs Lack Substantial Clinical Benefit
TOPLINE:
METHODOLOGY:
- The strength and quality of evidence supporting genome-targeted cancer drug approvals vary. A big reason is the growing number of cancer drug approvals based on surrogate endpoints, such as disease-free and progression-free survival, instead of clinical endpoints, such as overall survival or quality of life. The US Food and Drug Administration (FDA) has also approved genome-targeted cancer drugs based on phase 1 or single-arm trials.
- Given these less rigorous considerations for approval, “the validity and value of the targets and surrogate measures underlying FDA genome-targeted cancer drug approvals are uncertain,” the researchers explained.
- In the current analysis, researchers assessed the validity of the molecular targets as well as the clinical benefits of genome-targeted cancer drugs approved in the United States from 2015 to 2022 based on results from pivotal trials.
- The researchers evaluated the strength of evidence supporting molecular targetability using the European Society for Medical Oncology (ESMO) Scale for Clinical Actionability of Molecular Targets (ESCAT) and the clinical benefit using the ESMO–Magnitude of Clinical Benefit Scale (ESMO-MCBS).
- The authors defined a substantial clinical benefit as an A or B grade for curative intent and a 4 or 5 for noncurative intent. High-benefit genomic-based cancer treatments were defined as those associated with a substantial clinical benefit (ESMO-MCBS) and that qualified as ESCAT category level I-A (a clinical benefit based on prospective randomized data) or I-B (prospective nonrandomized data).
TAKEAWAY:
- The analyses focused on 50 molecular-targeted cancer drugs covering 84 indications. Of which, 45 indications (54%) were approved based on phase 1 or 2 pivotal trials, 45 (54%) were supported by single-arm pivotal trials and the remaining 39 (46%) by randomized trial, and 48 (57%) were approved based on subgroup analyses.
- Among the 84 indications, more than half (55%) of the pivotal trials supporting approval used overall response rate as a primary endpoint, 31% used progression-free survival, and 6% used disease-free survival. Only seven indications (8%) were supported by pivotal trials demonstrating an improvement in overall survival.
- Among the 84 trials, 24 (29%) met the ESMO-MCBS threshold for substantial clinical benefit.
- Overall, when combining all ratings, only 24 of the 84 indications (29%) were considered high-benefit genomic-based cancer treatments.
IN PRACTICE:
“We applied the ESMO-MCBS and ESCAT value frameworks to identify therapies and molecular targets providing high clinical value that should be widely available to patients” and “found that drug indications supported by these characteristics represent a minority of cancer drug approvals in recent years,” the authors said. Using these value frameworks could help payers, governments, and individual patients “prioritize the availability of high-value molecular-targeted therapies.”
SOURCE:
The study, with first author Ariadna Tibau, MD, PhD, Brigham and Women’s Hospital and Harvard Medical School, Boston, was published online in JAMA Oncology.
LIMITATIONS:
The study evaluated only trials that supported regulatory approval and did not include outcomes of postapproval clinical studies, which could lead to changes in ESMO-MCBS grades and ESCAT levels of evidence over time.
DISCLOSURES:
The study was funded by the Kaiser Permanente Institute for Health Policy, Arnold Ventures, and the Commonwealth Fund. The authors had no relevant disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The strength and quality of evidence supporting genome-targeted cancer drug approvals vary. A big reason is the growing number of cancer drug approvals based on surrogate endpoints, such as disease-free and progression-free survival, instead of clinical endpoints, such as overall survival or quality of life. The US Food and Drug Administration (FDA) has also approved genome-targeted cancer drugs based on phase 1 or single-arm trials.
- Given these less rigorous considerations for approval, “the validity and value of the targets and surrogate measures underlying FDA genome-targeted cancer drug approvals are uncertain,” the researchers explained.
- In the current analysis, researchers assessed the validity of the molecular targets as well as the clinical benefits of genome-targeted cancer drugs approved in the United States from 2015 to 2022 based on results from pivotal trials.
- The researchers evaluated the strength of evidence supporting molecular targetability using the European Society for Medical Oncology (ESMO) Scale for Clinical Actionability of Molecular Targets (ESCAT) and the clinical benefit using the ESMO–Magnitude of Clinical Benefit Scale (ESMO-MCBS).
- The authors defined a substantial clinical benefit as an A or B grade for curative intent and a 4 or 5 for noncurative intent. High-benefit genomic-based cancer treatments were defined as those associated with a substantial clinical benefit (ESMO-MCBS) and that qualified as ESCAT category level I-A (a clinical benefit based on prospective randomized data) or I-B (prospective nonrandomized data).
TAKEAWAY:
- The analyses focused on 50 molecular-targeted cancer drugs covering 84 indications. Of which, 45 indications (54%) were approved based on phase 1 or 2 pivotal trials, 45 (54%) were supported by single-arm pivotal trials and the remaining 39 (46%) by randomized trial, and 48 (57%) were approved based on subgroup analyses.
- Among the 84 indications, more than half (55%) of the pivotal trials supporting approval used overall response rate as a primary endpoint, 31% used progression-free survival, and 6% used disease-free survival. Only seven indications (8%) were supported by pivotal trials demonstrating an improvement in overall survival.
- Among the 84 trials, 24 (29%) met the ESMO-MCBS threshold for substantial clinical benefit.
- Overall, when combining all ratings, only 24 of the 84 indications (29%) were considered high-benefit genomic-based cancer treatments.
IN PRACTICE:
“We applied the ESMO-MCBS and ESCAT value frameworks to identify therapies and molecular targets providing high clinical value that should be widely available to patients” and “found that drug indications supported by these characteristics represent a minority of cancer drug approvals in recent years,” the authors said. Using these value frameworks could help payers, governments, and individual patients “prioritize the availability of high-value molecular-targeted therapies.”
SOURCE:
The study, with first author Ariadna Tibau, MD, PhD, Brigham and Women’s Hospital and Harvard Medical School, Boston, was published online in JAMA Oncology.
LIMITATIONS:
The study evaluated only trials that supported regulatory approval and did not include outcomes of postapproval clinical studies, which could lead to changes in ESMO-MCBS grades and ESCAT levels of evidence over time.
DISCLOSURES:
The study was funded by the Kaiser Permanente Institute for Health Policy, Arnold Ventures, and the Commonwealth Fund. The authors had no relevant disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The strength and quality of evidence supporting genome-targeted cancer drug approvals vary. A big reason is the growing number of cancer drug approvals based on surrogate endpoints, such as disease-free and progression-free survival, instead of clinical endpoints, such as overall survival or quality of life. The US Food and Drug Administration (FDA) has also approved genome-targeted cancer drugs based on phase 1 or single-arm trials.
- Given these less rigorous considerations for approval, “the validity and value of the targets and surrogate measures underlying FDA genome-targeted cancer drug approvals are uncertain,” the researchers explained.
- In the current analysis, researchers assessed the validity of the molecular targets as well as the clinical benefits of genome-targeted cancer drugs approved in the United States from 2015 to 2022 based on results from pivotal trials.
- The researchers evaluated the strength of evidence supporting molecular targetability using the European Society for Medical Oncology (ESMO) Scale for Clinical Actionability of Molecular Targets (ESCAT) and the clinical benefit using the ESMO–Magnitude of Clinical Benefit Scale (ESMO-MCBS).
- The authors defined a substantial clinical benefit as an A or B grade for curative intent and a 4 or 5 for noncurative intent. High-benefit genomic-based cancer treatments were defined as those associated with a substantial clinical benefit (ESMO-MCBS) and that qualified as ESCAT category level I-A (a clinical benefit based on prospective randomized data) or I-B (prospective nonrandomized data).
TAKEAWAY:
- The analyses focused on 50 molecular-targeted cancer drugs covering 84 indications. Of which, 45 indications (54%) were approved based on phase 1 or 2 pivotal trials, 45 (54%) were supported by single-arm pivotal trials and the remaining 39 (46%) by randomized trial, and 48 (57%) were approved based on subgroup analyses.
- Among the 84 indications, more than half (55%) of the pivotal trials supporting approval used overall response rate as a primary endpoint, 31% used progression-free survival, and 6% used disease-free survival. Only seven indications (8%) were supported by pivotal trials demonstrating an improvement in overall survival.
- Among the 84 trials, 24 (29%) met the ESMO-MCBS threshold for substantial clinical benefit.
- Overall, when combining all ratings, only 24 of the 84 indications (29%) were considered high-benefit genomic-based cancer treatments.
IN PRACTICE:
“We applied the ESMO-MCBS and ESCAT value frameworks to identify therapies and molecular targets providing high clinical value that should be widely available to patients” and “found that drug indications supported by these characteristics represent a minority of cancer drug approvals in recent years,” the authors said. Using these value frameworks could help payers, governments, and individual patients “prioritize the availability of high-value molecular-targeted therapies.”
SOURCE:
The study, with first author Ariadna Tibau, MD, PhD, Brigham and Women’s Hospital and Harvard Medical School, Boston, was published online in JAMA Oncology.
LIMITATIONS:
The study evaluated only trials that supported regulatory approval and did not include outcomes of postapproval clinical studies, which could lead to changes in ESMO-MCBS grades and ESCAT levels of evidence over time.
DISCLOSURES:
The study was funded by the Kaiser Permanente Institute for Health Policy, Arnold Ventures, and the Commonwealth Fund. The authors had no relevant disclosures.
A version of this article appeared on Medscape.com.
Blood Test Shows Promise for Improving CRC Screening
say the authors of new research.
Rachel B. Issaka, MD, MAS, of the Fred Hutchinson Cancer Center, Seattle, presented the clinical data, which was published in The New England Journal of Medicine, at the American Association for Cancer Research annual meeting.
The authors of the study evaluated the performance of a cfDNA blood-based test in a population eligible for colorectal cancer screening. The researchers found that the test had high sensitivity for the detection of colorectal cancer and high specificity for advanced precancerous lesions.
This novel blood test could improve screening adherence and, ultimately, reduce colorectal cancer-related mortality, Dr. Issaka said during her presentation.
“This test has the potential to help us reach the 80% screening target in colorectal cancer. However, this will depend on many factors, including access, implementation, follow-up colonoscopy, and characteristics of the test,” Dr. Issaka said in an interview.
She added that, when approved for broader use, anyone who wants to use this blood test for colorectal cancer screening should have a frank conversation with their healthcare provider.
“Considering the person’s age, medical history, family history, and any potential symptoms, and how the test performs will dictate if it’s the right test for that person versus another screening strategy,” Dr. Issaka explained.
The Blood Test Detects Colorectal Cancer With High Accuracy
The investigators of the observational ECLIPSE trial evaluated the performance of the cfDNA-based blood test in 7861 individuals who were eligible for colorectal cancer screening. The study population included people from more than 200 rural and urban sites across 34 states, including community hospitals, private practices, gastroenterology clinics, and academic centers. “The study enrolled a diverse cohort that is reflective of the demographics of the intended use population in the US,” Dr. Issaka said during her talk.
The co-primary outcomes of the study were the test’s sensitivity for detecting colorectal cancer and its specificity for identifying advanced neoplasia.
In her presentation, Dr. Issaka highlighted that the test had 83.1% (95% confidence interval [CI], 72.2%-90.3%) sensitivity for the detection of colorectal cancer, meaning that it was able to correctly identify most participants with the disease. The test’s sensitivity was even higher (87.5%; 95% CI, 75.3%-94.1%) for stage I, II, or III colorectal cancer. “These are the stages at which early intervention can have the greatest impact on patient prognosis,” Dr. Issaka said.
Moreover, the blood test showed 89.6% (95% CI, 88.8%-90.3%) specificity for advanced neoplasia, including colorectal cancer and advanced precancerous lesions. The specificity of the test for negative colonoscopy results (no colorectal cancer, advanced precancerous lesions, or nonadvanced precancerous lesions) was 89.9% (95% CI, 89.0%-90.7%).
Dr. Issaka highlighted that this cfDNA assay is the first blood-based test with performance comparable to current guideline-recommended noninvasive options for CRC.
The Blood Test Shows Limited Ability To Detect Advanced Precancerous Lesions
During her presentation, Dr. Issaka acknowledged that the cfDNA-based blood test had a lower sensitivity (13.2%; 95% CI, 11.3%-15.3%) for the detection of advanced precancerous lesions, suggesting that it may be more effective at identifying established cancers than early-stage precancerous changes. Low sensitivity was also observed for high-grade dysplasia (22.6%; 95% CI, 11.4%-39.8%). However, she emphasized that the test could still play a valuable role in a comprehensive screening approach, potentially serving as a first-line tool to identify individuals who would then undergo follow-up colonoscopy.
“Although blood-based tests perform well at finding cancers, they do not do so well at finding precancerous polyps. This is relevant because colorectal cancer is one of the few cancers that we can prevent by finding and removing precancerous polyps,” Folasade P. May, MD, PhD, MPhil, said in an interview.
“Users must also understand that if the test result is abnormal, a colonoscopy is required to look for cancers and polyps that might have caused the abnormal result,” added Dr. May, associate professor at UCLA. She was not involved in the study.
Clinical Implications and Future Steps
According to the study published in the NEJM, colorectal cancer is the third most commonly diagnosed cancer in the United States, and early detection is crucial for effective treatment. However, over a third of eligible individuals are not up to date with recommended screening.
During her talk, Dr. Issaka noted that colonoscopy is the most commonly used screening method for colorectal cancer. What contributes to the low adherence to getting a colonoscopy among the eligible population is that some find it inconvenient, and the test is invasive, she added.
According to Dr. May, the key advantage of cfDNA-based screening is that many people will find it easier to complete a blood test than the currently available screening tests.
“This option may allow us to screen individuals that we have previously struggled to convince to get screened for colorectal cancer,” she said.
In an interview, Dr. Issaka acknowledged that the potential public health impact of any noninvasive screening test depends on how many people with abnormal results complete a follow-up colonoscopy. “This is an important quality metric to track,” she said.
In an interview, Dr. Issaka emphasized that comparing this cfDNA blood test with emerging blood tests and other noninvasive screening strategies will empower patients and clinicians to select the right test at the right time for the right patient.
She added that the study was conducted in an average-risk screening population and that further research is needed to evaluate the test’s performance in higher-risk groups and to assess its real-world impact on screening adherence and colorectal cancer-related outcomes.
Commenting on potential challenges with implementing this cfDNA blood test in clinical practice, Dr. May said, “As we consider incorporating blood-based tests into clinical practice, some challenges include cost, equitable access to tests and follow-up, performance in young adults who are newly eligible for screening, and follow-up after abnormal results.”
She added that, if there is uptake of these tests, it will be important to track how that impacts colorectal cancer screening rates, stage at diagnosis, and whether there is stage migration, incidence, and mortality.
“At this time, I feel that these tests are appropriate for individuals who will not or cannot participate in one of the currently recommended screening tests. These include colonoscopy and stool-based tests, like FIT and FIT-DNA,” Dr. May concluded.
Dr. Issaka reported financial relationships with the National Institutes of Health/National Cancer Institute, American College of Gastroenterology, and Guardant Health Inc. Dr. May reported financial relationships with Takeda, Medtronic, Johnson & Johnson, Saint Supply, Exact Sciences, Freenome, Geneoscopy, Guardant Health, InterVenn, Natura, National Institutes of Health/National Cancer Institute, Veterans Affairs HSR&D, Broad Institute, Stand up to Cancer, and NRG Oncology.
say the authors of new research.
Rachel B. Issaka, MD, MAS, of the Fred Hutchinson Cancer Center, Seattle, presented the clinical data, which was published in The New England Journal of Medicine, at the American Association for Cancer Research annual meeting.
The authors of the study evaluated the performance of a cfDNA blood-based test in a population eligible for colorectal cancer screening. The researchers found that the test had high sensitivity for the detection of colorectal cancer and high specificity for advanced precancerous lesions.
This novel blood test could improve screening adherence and, ultimately, reduce colorectal cancer-related mortality, Dr. Issaka said during her presentation.
“This test has the potential to help us reach the 80% screening target in colorectal cancer. However, this will depend on many factors, including access, implementation, follow-up colonoscopy, and characteristics of the test,” Dr. Issaka said in an interview.
She added that, when approved for broader use, anyone who wants to use this blood test for colorectal cancer screening should have a frank conversation with their healthcare provider.
“Considering the person’s age, medical history, family history, and any potential symptoms, and how the test performs will dictate if it’s the right test for that person versus another screening strategy,” Dr. Issaka explained.
The Blood Test Detects Colorectal Cancer With High Accuracy
The investigators of the observational ECLIPSE trial evaluated the performance of the cfDNA-based blood test in 7861 individuals who were eligible for colorectal cancer screening. The study population included people from more than 200 rural and urban sites across 34 states, including community hospitals, private practices, gastroenterology clinics, and academic centers. “The study enrolled a diverse cohort that is reflective of the demographics of the intended use population in the US,” Dr. Issaka said during her talk.
The co-primary outcomes of the study were the test’s sensitivity for detecting colorectal cancer and its specificity for identifying advanced neoplasia.
In her presentation, Dr. Issaka highlighted that the test had 83.1% (95% confidence interval [CI], 72.2%-90.3%) sensitivity for the detection of colorectal cancer, meaning that it was able to correctly identify most participants with the disease. The test’s sensitivity was even higher (87.5%; 95% CI, 75.3%-94.1%) for stage I, II, or III colorectal cancer. “These are the stages at which early intervention can have the greatest impact on patient prognosis,” Dr. Issaka said.
Moreover, the blood test showed 89.6% (95% CI, 88.8%-90.3%) specificity for advanced neoplasia, including colorectal cancer and advanced precancerous lesions. The specificity of the test for negative colonoscopy results (no colorectal cancer, advanced precancerous lesions, or nonadvanced precancerous lesions) was 89.9% (95% CI, 89.0%-90.7%).
Dr. Issaka highlighted that this cfDNA assay is the first blood-based test with performance comparable to current guideline-recommended noninvasive options for CRC.
The Blood Test Shows Limited Ability To Detect Advanced Precancerous Lesions
During her presentation, Dr. Issaka acknowledged that the cfDNA-based blood test had a lower sensitivity (13.2%; 95% CI, 11.3%-15.3%) for the detection of advanced precancerous lesions, suggesting that it may be more effective at identifying established cancers than early-stage precancerous changes. Low sensitivity was also observed for high-grade dysplasia (22.6%; 95% CI, 11.4%-39.8%). However, she emphasized that the test could still play a valuable role in a comprehensive screening approach, potentially serving as a first-line tool to identify individuals who would then undergo follow-up colonoscopy.
“Although blood-based tests perform well at finding cancers, they do not do so well at finding precancerous polyps. This is relevant because colorectal cancer is one of the few cancers that we can prevent by finding and removing precancerous polyps,” Folasade P. May, MD, PhD, MPhil, said in an interview.
“Users must also understand that if the test result is abnormal, a colonoscopy is required to look for cancers and polyps that might have caused the abnormal result,” added Dr. May, associate professor at UCLA. She was not involved in the study.
Clinical Implications and Future Steps
According to the study published in the NEJM, colorectal cancer is the third most commonly diagnosed cancer in the United States, and early detection is crucial for effective treatment. However, over a third of eligible individuals are not up to date with recommended screening.
During her talk, Dr. Issaka noted that colonoscopy is the most commonly used screening method for colorectal cancer. What contributes to the low adherence to getting a colonoscopy among the eligible population is that some find it inconvenient, and the test is invasive, she added.
According to Dr. May, the key advantage of cfDNA-based screening is that many people will find it easier to complete a blood test than the currently available screening tests.
“This option may allow us to screen individuals that we have previously struggled to convince to get screened for colorectal cancer,” she said.
In an interview, Dr. Issaka acknowledged that the potential public health impact of any noninvasive screening test depends on how many people with abnormal results complete a follow-up colonoscopy. “This is an important quality metric to track,” she said.
In an interview, Dr. Issaka emphasized that comparing this cfDNA blood test with emerging blood tests and other noninvasive screening strategies will empower patients and clinicians to select the right test at the right time for the right patient.
She added that the study was conducted in an average-risk screening population and that further research is needed to evaluate the test’s performance in higher-risk groups and to assess its real-world impact on screening adherence and colorectal cancer-related outcomes.
Commenting on potential challenges with implementing this cfDNA blood test in clinical practice, Dr. May said, “As we consider incorporating blood-based tests into clinical practice, some challenges include cost, equitable access to tests and follow-up, performance in young adults who are newly eligible for screening, and follow-up after abnormal results.”
She added that, if there is uptake of these tests, it will be important to track how that impacts colorectal cancer screening rates, stage at diagnosis, and whether there is stage migration, incidence, and mortality.
“At this time, I feel that these tests are appropriate for individuals who will not or cannot participate in one of the currently recommended screening tests. These include colonoscopy and stool-based tests, like FIT and FIT-DNA,” Dr. May concluded.
Dr. Issaka reported financial relationships with the National Institutes of Health/National Cancer Institute, American College of Gastroenterology, and Guardant Health Inc. Dr. May reported financial relationships with Takeda, Medtronic, Johnson & Johnson, Saint Supply, Exact Sciences, Freenome, Geneoscopy, Guardant Health, InterVenn, Natura, National Institutes of Health/National Cancer Institute, Veterans Affairs HSR&D, Broad Institute, Stand up to Cancer, and NRG Oncology.
say the authors of new research.
Rachel B. Issaka, MD, MAS, of the Fred Hutchinson Cancer Center, Seattle, presented the clinical data, which was published in The New England Journal of Medicine, at the American Association for Cancer Research annual meeting.
The authors of the study evaluated the performance of a cfDNA blood-based test in a population eligible for colorectal cancer screening. The researchers found that the test had high sensitivity for the detection of colorectal cancer and high specificity for advanced precancerous lesions.
This novel blood test could improve screening adherence and, ultimately, reduce colorectal cancer-related mortality, Dr. Issaka said during her presentation.
“This test has the potential to help us reach the 80% screening target in colorectal cancer. However, this will depend on many factors, including access, implementation, follow-up colonoscopy, and characteristics of the test,” Dr. Issaka said in an interview.
She added that, when approved for broader use, anyone who wants to use this blood test for colorectal cancer screening should have a frank conversation with their healthcare provider.
“Considering the person’s age, medical history, family history, and any potential symptoms, and how the test performs will dictate if it’s the right test for that person versus another screening strategy,” Dr. Issaka explained.
The Blood Test Detects Colorectal Cancer With High Accuracy
The investigators of the observational ECLIPSE trial evaluated the performance of the cfDNA-based blood test in 7861 individuals who were eligible for colorectal cancer screening. The study population included people from more than 200 rural and urban sites across 34 states, including community hospitals, private practices, gastroenterology clinics, and academic centers. “The study enrolled a diverse cohort that is reflective of the demographics of the intended use population in the US,” Dr. Issaka said during her talk.
The co-primary outcomes of the study were the test’s sensitivity for detecting colorectal cancer and its specificity for identifying advanced neoplasia.
In her presentation, Dr. Issaka highlighted that the test had 83.1% (95% confidence interval [CI], 72.2%-90.3%) sensitivity for the detection of colorectal cancer, meaning that it was able to correctly identify most participants with the disease. The test’s sensitivity was even higher (87.5%; 95% CI, 75.3%-94.1%) for stage I, II, or III colorectal cancer. “These are the stages at which early intervention can have the greatest impact on patient prognosis,” Dr. Issaka said.
Moreover, the blood test showed 89.6% (95% CI, 88.8%-90.3%) specificity for advanced neoplasia, including colorectal cancer and advanced precancerous lesions. The specificity of the test for negative colonoscopy results (no colorectal cancer, advanced precancerous lesions, or nonadvanced precancerous lesions) was 89.9% (95% CI, 89.0%-90.7%).
Dr. Issaka highlighted that this cfDNA assay is the first blood-based test with performance comparable to current guideline-recommended noninvasive options for CRC.
The Blood Test Shows Limited Ability To Detect Advanced Precancerous Lesions
During her presentation, Dr. Issaka acknowledged that the cfDNA-based blood test had a lower sensitivity (13.2%; 95% CI, 11.3%-15.3%) for the detection of advanced precancerous lesions, suggesting that it may be more effective at identifying established cancers than early-stage precancerous changes. Low sensitivity was also observed for high-grade dysplasia (22.6%; 95% CI, 11.4%-39.8%). However, she emphasized that the test could still play a valuable role in a comprehensive screening approach, potentially serving as a first-line tool to identify individuals who would then undergo follow-up colonoscopy.
“Although blood-based tests perform well at finding cancers, they do not do so well at finding precancerous polyps. This is relevant because colorectal cancer is one of the few cancers that we can prevent by finding and removing precancerous polyps,” Folasade P. May, MD, PhD, MPhil, said in an interview.
“Users must also understand that if the test result is abnormal, a colonoscopy is required to look for cancers and polyps that might have caused the abnormal result,” added Dr. May, associate professor at UCLA. She was not involved in the study.
Clinical Implications and Future Steps
According to the study published in the NEJM, colorectal cancer is the third most commonly diagnosed cancer in the United States, and early detection is crucial for effective treatment. However, over a third of eligible individuals are not up to date with recommended screening.
During her talk, Dr. Issaka noted that colonoscopy is the most commonly used screening method for colorectal cancer. What contributes to the low adherence to getting a colonoscopy among the eligible population is that some find it inconvenient, and the test is invasive, she added.
According to Dr. May, the key advantage of cfDNA-based screening is that many people will find it easier to complete a blood test than the currently available screening tests.
“This option may allow us to screen individuals that we have previously struggled to convince to get screened for colorectal cancer,” she said.
In an interview, Dr. Issaka acknowledged that the potential public health impact of any noninvasive screening test depends on how many people with abnormal results complete a follow-up colonoscopy. “This is an important quality metric to track,” she said.
In an interview, Dr. Issaka emphasized that comparing this cfDNA blood test with emerging blood tests and other noninvasive screening strategies will empower patients and clinicians to select the right test at the right time for the right patient.
She added that the study was conducted in an average-risk screening population and that further research is needed to evaluate the test’s performance in higher-risk groups and to assess its real-world impact on screening adherence and colorectal cancer-related outcomes.
Commenting on potential challenges with implementing this cfDNA blood test in clinical practice, Dr. May said, “As we consider incorporating blood-based tests into clinical practice, some challenges include cost, equitable access to tests and follow-up, performance in young adults who are newly eligible for screening, and follow-up after abnormal results.”
She added that, if there is uptake of these tests, it will be important to track how that impacts colorectal cancer screening rates, stage at diagnosis, and whether there is stage migration, incidence, and mortality.
“At this time, I feel that these tests are appropriate for individuals who will not or cannot participate in one of the currently recommended screening tests. These include colonoscopy and stool-based tests, like FIT and FIT-DNA,” Dr. May concluded.
Dr. Issaka reported financial relationships with the National Institutes of Health/National Cancer Institute, American College of Gastroenterology, and Guardant Health Inc. Dr. May reported financial relationships with Takeda, Medtronic, Johnson & Johnson, Saint Supply, Exact Sciences, Freenome, Geneoscopy, Guardant Health, InterVenn, Natura, National Institutes of Health/National Cancer Institute, Veterans Affairs HSR&D, Broad Institute, Stand up to Cancer, and NRG Oncology.