User login
Youth-led sexual health program improves teen knowledge, autonomy
BALTIMORE – , according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
While the small pilot study focused primarily on assessing feasibility and effectiveness, the results suggest potential for scaling the program up to reach a larger audience and assessing the knowledge disseminated from direct youth participants.
“The good thing about this subject is that not a lot of it has to be context-specific,” Saumya Sao, a clinical researcher in gynecology and obstetrics at the Johns Hopkins University, Baltimore, and the study’s lead author, said in an interview. “A lot of it is just baseline information that everybody needs and doesn’t get.”
Jaime Friedman, MD, a pediatrician and director of marketing at Children’s Primary Care Medical Group in San Diego, was not involved in the study but was impressed with the program’s objectives and results so far.
“While education is massively important, teens don’t always want to hear it from their parents or other adults,” Dr. Friedman said in an interview. “Learning from their peers is one way to overcome this hurdle.”
Given the high rate of sexually transmitted infections and unintended pregnancies in youth, paired with low sexual and reproductive health literacy in this population, the researchers sought to learn whether a program focused on peer-to-peer health education on these topics was feasible. The goal was to increase youth sexual and reproductive health knowledge, self-efficacy, and autonomy using a youth-led intervention.
The researchers hosted nine monthly, interactive, youth-led sessions that lasted 2 hours over Zoom or in person. Incorporated into the meetings were principles from Youth Participatory Action Research (YPAR) and Positive Youth Development (PYD).
The major topics included the following: Use of social media, values and goal-setting, anatomy and menstrual health, risk factors of sexual activities , STI and HIV prevention, contraceptive methods, healthy relationships and consent, practice responding to unhealthy behavior, gender and sexuality, and social media and body image.
The 24 participants were provided with transportation to the study site at the researchers’ institution and received financial compensation for their participation. They were an average 15.8 years old, lived in the greater Baltimore area, and mostly self-identified as female. Eight percent identified as non-binary and half (50%) identified as LGBTQIA+. Just over half the participants (52%) were Black/African American, 28% were Asian/Asian American, 12% were White, and 8% were Hispanic. The participants attended an average 88% of the sessions throughout the full intervention.
For each of the nine sessions, more than 50% of participants reported that they “learned a lot,” and only one participant reported for one session (session 5) that they “didn’t learn” anything. The researchers assessed participants’ knowledge, self-efficacy, and sense of autonomy at baseline and after completion of the intervention. Significant improvements occurred across all areas.
The average score improved by 31% in sexual and reproductive health knowledge (P < .001), 33% in sexual and reproductive health services awareness (P = .002), 46% in advocacy and empowerment (P < .001), 16% in general perceived efficacy (P = .002), and 22% personal sexuality empowerment (P = .006).
Ms. Sao said she was very pleased to see that the improvements were significant in every domain they measured, which she attributed largely to the incorporation of YPAR and PYD into the program.
“We approached it using these two frameworks that really do focus on involving youth in the teaching themselves, so I think that’s what increased their general perceived efficacy and advocacy empowerment without us necessarily having to emphasize, ‘You are advocates,’” Ms. Sao said. “Those frameworks ask the youth for their opinions and then give the youth an opportunity in every single session to be teachers themselves, and I think that lends itself well to all of the domains.”
Ms. Sao was also pleasantly surprised at the high level of retention across the 9 months.
“Every single session was slotted for 2 hours, but they would want to stay for 3 hours. Eventually, we actually started meeting with them twice a month, just adding an extra session,” she said. “As they gained confidence, they were so excited to be peer educators and realized, ‘I can really do this. I can teach my peers. We’re not getting this from anywhere else.’ ”
Ms. Sao and another study author, Maclaine Barré-Quick, an undergraduate research assistant at Johns Hopkins University, said the participants quickly discovered how easy it was to have a non-stigmatizing conversation about many of the topics once a subject was brought up.
“They’re actively looking for that opportunity,” Ms. Barré-Quick said in an interview.
Dr. Friedman agreed that this type of program provides what many adolescents need in a way that they may welcome more than through other methods.
“Adolescents’ bodies are approaching adulthood and function like adults, but their brains are still developing. They don’t have the worldly experience and education of adults, but they think they know everything,” Dr. Friedman said. “They are a population known for their high risk behavior due to their natural impulsivity. This can be a scary combination, especially when it comes to sexual health.”
But if teens don’t want to hear some of the information they need from adults, they may be more open to hearing it from other teens, Dr. Friedman said.
“Using an evidence-based approach ensures the desired outcome of healthier habits, decreased STIs and decreased teen pregnancy,” Dr. Friedman said. “It also adds weight to the argument against abstinence-only education. Teens deserve accurate and evidence-based education about their own bodies.”
Ms. Sao said the next steps will be exploring ways to scale the program up, such as putting the curriculum resources into a bundle available to other educators. They’re also looking at ways to put it into an online platform that’s self-paced, though that requires solving the challenge of having synchronous meetings for youth-led discussion.
“There are certain kinks that we have to work out because there were some activities where I think the students really benefited from having those open discussions with each other, so [we need to determine] how to replicate that in an online format,” Ms. Sao said.
Dr. Friedman agreed that scalability appears to be the biggest challenge, along with funding programs. But if those obstacles can be overcome, such programs would complement and expand on the education she does currently with families.
“I don’t have time for a full sex ed course at each visit,” Dr. Friedman said. “I would like to be able to direct them to a program that I know works and would be easy for them to complete. Even better, this would be an amazing program to ‘sell’ to practices interested in hosting these sessions themselves.”
Ms. Sao said they also hope to assess the impact of the intervention on the participants’ peers to see how well the knowledge and self-efficacy spread through the youths’ teaching.
No external funding was noted. One author reported research support from Hologic and Merck. Dr. Friedman had no disclosures.
BALTIMORE – , according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
While the small pilot study focused primarily on assessing feasibility and effectiveness, the results suggest potential for scaling the program up to reach a larger audience and assessing the knowledge disseminated from direct youth participants.
“The good thing about this subject is that not a lot of it has to be context-specific,” Saumya Sao, a clinical researcher in gynecology and obstetrics at the Johns Hopkins University, Baltimore, and the study’s lead author, said in an interview. “A lot of it is just baseline information that everybody needs and doesn’t get.”
Jaime Friedman, MD, a pediatrician and director of marketing at Children’s Primary Care Medical Group in San Diego, was not involved in the study but was impressed with the program’s objectives and results so far.
“While education is massively important, teens don’t always want to hear it from their parents or other adults,” Dr. Friedman said in an interview. “Learning from their peers is one way to overcome this hurdle.”
Given the high rate of sexually transmitted infections and unintended pregnancies in youth, paired with low sexual and reproductive health literacy in this population, the researchers sought to learn whether a program focused on peer-to-peer health education on these topics was feasible. The goal was to increase youth sexual and reproductive health knowledge, self-efficacy, and autonomy using a youth-led intervention.
The researchers hosted nine monthly, interactive, youth-led sessions that lasted 2 hours over Zoom or in person. Incorporated into the meetings were principles from Youth Participatory Action Research (YPAR) and Positive Youth Development (PYD).
The major topics included the following: Use of social media, values and goal-setting, anatomy and menstrual health, risk factors of sexual activities , STI and HIV prevention, contraceptive methods, healthy relationships and consent, practice responding to unhealthy behavior, gender and sexuality, and social media and body image.
The 24 participants were provided with transportation to the study site at the researchers’ institution and received financial compensation for their participation. They were an average 15.8 years old, lived in the greater Baltimore area, and mostly self-identified as female. Eight percent identified as non-binary and half (50%) identified as LGBTQIA+. Just over half the participants (52%) were Black/African American, 28% were Asian/Asian American, 12% were White, and 8% were Hispanic. The participants attended an average 88% of the sessions throughout the full intervention.
For each of the nine sessions, more than 50% of participants reported that they “learned a lot,” and only one participant reported for one session (session 5) that they “didn’t learn” anything. The researchers assessed participants’ knowledge, self-efficacy, and sense of autonomy at baseline and after completion of the intervention. Significant improvements occurred across all areas.
The average score improved by 31% in sexual and reproductive health knowledge (P < .001), 33% in sexual and reproductive health services awareness (P = .002), 46% in advocacy and empowerment (P < .001), 16% in general perceived efficacy (P = .002), and 22% personal sexuality empowerment (P = .006).
Ms. Sao said she was very pleased to see that the improvements were significant in every domain they measured, which she attributed largely to the incorporation of YPAR and PYD into the program.
“We approached it using these two frameworks that really do focus on involving youth in the teaching themselves, so I think that’s what increased their general perceived efficacy and advocacy empowerment without us necessarily having to emphasize, ‘You are advocates,’” Ms. Sao said. “Those frameworks ask the youth for their opinions and then give the youth an opportunity in every single session to be teachers themselves, and I think that lends itself well to all of the domains.”
Ms. Sao was also pleasantly surprised at the high level of retention across the 9 months.
“Every single session was slotted for 2 hours, but they would want to stay for 3 hours. Eventually, we actually started meeting with them twice a month, just adding an extra session,” she said. “As they gained confidence, they were so excited to be peer educators and realized, ‘I can really do this. I can teach my peers. We’re not getting this from anywhere else.’ ”
Ms. Sao and another study author, Maclaine Barré-Quick, an undergraduate research assistant at Johns Hopkins University, said the participants quickly discovered how easy it was to have a non-stigmatizing conversation about many of the topics once a subject was brought up.
“They’re actively looking for that opportunity,” Ms. Barré-Quick said in an interview.
Dr. Friedman agreed that this type of program provides what many adolescents need in a way that they may welcome more than through other methods.
“Adolescents’ bodies are approaching adulthood and function like adults, but their brains are still developing. They don’t have the worldly experience and education of adults, but they think they know everything,” Dr. Friedman said. “They are a population known for their high risk behavior due to their natural impulsivity. This can be a scary combination, especially when it comes to sexual health.”
But if teens don’t want to hear some of the information they need from adults, they may be more open to hearing it from other teens, Dr. Friedman said.
“Using an evidence-based approach ensures the desired outcome of healthier habits, decreased STIs and decreased teen pregnancy,” Dr. Friedman said. “It also adds weight to the argument against abstinence-only education. Teens deserve accurate and evidence-based education about their own bodies.”
Ms. Sao said the next steps will be exploring ways to scale the program up, such as putting the curriculum resources into a bundle available to other educators. They’re also looking at ways to put it into an online platform that’s self-paced, though that requires solving the challenge of having synchronous meetings for youth-led discussion.
“There are certain kinks that we have to work out because there were some activities where I think the students really benefited from having those open discussions with each other, so [we need to determine] how to replicate that in an online format,” Ms. Sao said.
Dr. Friedman agreed that scalability appears to be the biggest challenge, along with funding programs. But if those obstacles can be overcome, such programs would complement and expand on the education she does currently with families.
“I don’t have time for a full sex ed course at each visit,” Dr. Friedman said. “I would like to be able to direct them to a program that I know works and would be easy for them to complete. Even better, this would be an amazing program to ‘sell’ to practices interested in hosting these sessions themselves.”
Ms. Sao said they also hope to assess the impact of the intervention on the participants’ peers to see how well the knowledge and self-efficacy spread through the youths’ teaching.
No external funding was noted. One author reported research support from Hologic and Merck. Dr. Friedman had no disclosures.
BALTIMORE – , according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
While the small pilot study focused primarily on assessing feasibility and effectiveness, the results suggest potential for scaling the program up to reach a larger audience and assessing the knowledge disseminated from direct youth participants.
“The good thing about this subject is that not a lot of it has to be context-specific,” Saumya Sao, a clinical researcher in gynecology and obstetrics at the Johns Hopkins University, Baltimore, and the study’s lead author, said in an interview. “A lot of it is just baseline information that everybody needs and doesn’t get.”
Jaime Friedman, MD, a pediatrician and director of marketing at Children’s Primary Care Medical Group in San Diego, was not involved in the study but was impressed with the program’s objectives and results so far.
“While education is massively important, teens don’t always want to hear it from their parents or other adults,” Dr. Friedman said in an interview. “Learning from their peers is one way to overcome this hurdle.”
Given the high rate of sexually transmitted infections and unintended pregnancies in youth, paired with low sexual and reproductive health literacy in this population, the researchers sought to learn whether a program focused on peer-to-peer health education on these topics was feasible. The goal was to increase youth sexual and reproductive health knowledge, self-efficacy, and autonomy using a youth-led intervention.
The researchers hosted nine monthly, interactive, youth-led sessions that lasted 2 hours over Zoom or in person. Incorporated into the meetings were principles from Youth Participatory Action Research (YPAR) and Positive Youth Development (PYD).
The major topics included the following: Use of social media, values and goal-setting, anatomy and menstrual health, risk factors of sexual activities , STI and HIV prevention, contraceptive methods, healthy relationships and consent, practice responding to unhealthy behavior, gender and sexuality, and social media and body image.
The 24 participants were provided with transportation to the study site at the researchers’ institution and received financial compensation for their participation. They were an average 15.8 years old, lived in the greater Baltimore area, and mostly self-identified as female. Eight percent identified as non-binary and half (50%) identified as LGBTQIA+. Just over half the participants (52%) were Black/African American, 28% were Asian/Asian American, 12% were White, and 8% were Hispanic. The participants attended an average 88% of the sessions throughout the full intervention.
For each of the nine sessions, more than 50% of participants reported that they “learned a lot,” and only one participant reported for one session (session 5) that they “didn’t learn” anything. The researchers assessed participants’ knowledge, self-efficacy, and sense of autonomy at baseline and after completion of the intervention. Significant improvements occurred across all areas.
The average score improved by 31% in sexual and reproductive health knowledge (P < .001), 33% in sexual and reproductive health services awareness (P = .002), 46% in advocacy and empowerment (P < .001), 16% in general perceived efficacy (P = .002), and 22% personal sexuality empowerment (P = .006).
Ms. Sao said she was very pleased to see that the improvements were significant in every domain they measured, which she attributed largely to the incorporation of YPAR and PYD into the program.
“We approached it using these two frameworks that really do focus on involving youth in the teaching themselves, so I think that’s what increased their general perceived efficacy and advocacy empowerment without us necessarily having to emphasize, ‘You are advocates,’” Ms. Sao said. “Those frameworks ask the youth for their opinions and then give the youth an opportunity in every single session to be teachers themselves, and I think that lends itself well to all of the domains.”
Ms. Sao was also pleasantly surprised at the high level of retention across the 9 months.
“Every single session was slotted for 2 hours, but they would want to stay for 3 hours. Eventually, we actually started meeting with them twice a month, just adding an extra session,” she said. “As they gained confidence, they were so excited to be peer educators and realized, ‘I can really do this. I can teach my peers. We’re not getting this from anywhere else.’ ”
Ms. Sao and another study author, Maclaine Barré-Quick, an undergraduate research assistant at Johns Hopkins University, said the participants quickly discovered how easy it was to have a non-stigmatizing conversation about many of the topics once a subject was brought up.
“They’re actively looking for that opportunity,” Ms. Barré-Quick said in an interview.
Dr. Friedman agreed that this type of program provides what many adolescents need in a way that they may welcome more than through other methods.
“Adolescents’ bodies are approaching adulthood and function like adults, but their brains are still developing. They don’t have the worldly experience and education of adults, but they think they know everything,” Dr. Friedman said. “They are a population known for their high risk behavior due to their natural impulsivity. This can be a scary combination, especially when it comes to sexual health.”
But if teens don’t want to hear some of the information they need from adults, they may be more open to hearing it from other teens, Dr. Friedman said.
“Using an evidence-based approach ensures the desired outcome of healthier habits, decreased STIs and decreased teen pregnancy,” Dr. Friedman said. “It also adds weight to the argument against abstinence-only education. Teens deserve accurate and evidence-based education about their own bodies.”
Ms. Sao said the next steps will be exploring ways to scale the program up, such as putting the curriculum resources into a bundle available to other educators. They’re also looking at ways to put it into an online platform that’s self-paced, though that requires solving the challenge of having synchronous meetings for youth-led discussion.
“There are certain kinks that we have to work out because there were some activities where I think the students really benefited from having those open discussions with each other, so [we need to determine] how to replicate that in an online format,” Ms. Sao said.
Dr. Friedman agreed that scalability appears to be the biggest challenge, along with funding programs. But if those obstacles can be overcome, such programs would complement and expand on the education she does currently with families.
“I don’t have time for a full sex ed course at each visit,” Dr. Friedman said. “I would like to be able to direct them to a program that I know works and would be easy for them to complete. Even better, this would be an amazing program to ‘sell’ to practices interested in hosting these sessions themselves.”
Ms. Sao said they also hope to assess the impact of the intervention on the participants’ peers to see how well the knowledge and self-efficacy spread through the youths’ teaching.
No external funding was noted. One author reported research support from Hologic and Merck. Dr. Friedman had no disclosures.
AT ACOG 2023
Scheduled bleeding may boost tolerability of hormone implants
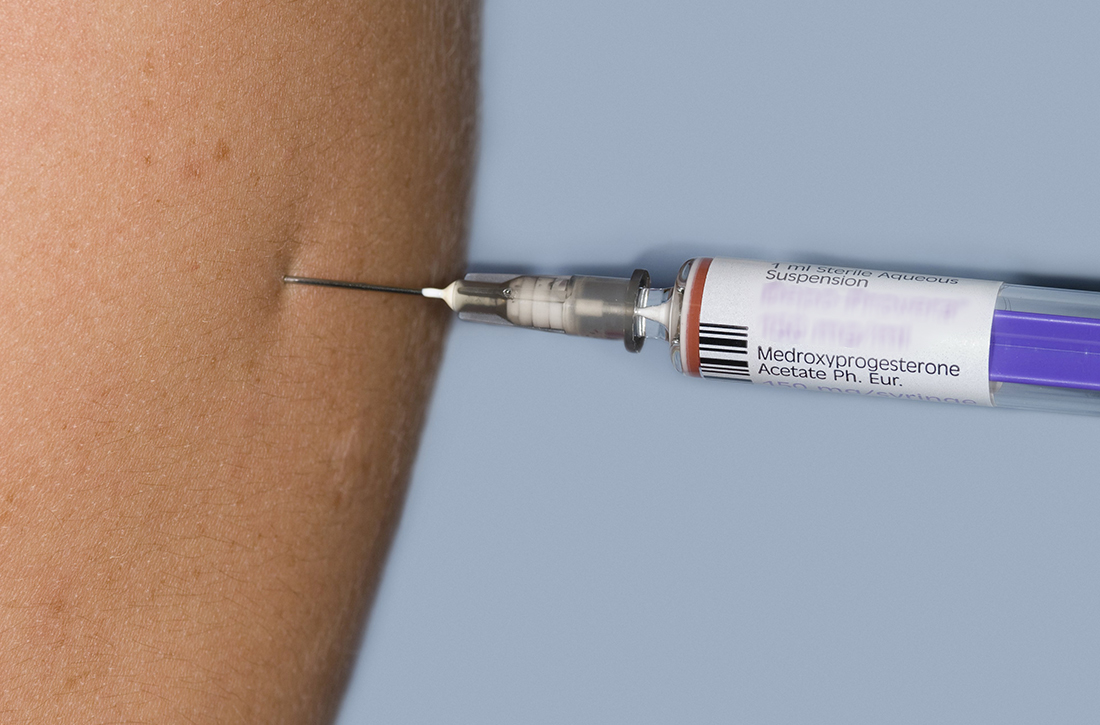
BALTIMORE – The bleeding causes some women to have the device removed, according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
In a randomized, double-blinded, placebo-controlled trial of 51 patients desiring the implants – which suppress ovulation by releasing progestin over a 3-year period – taking norethindrone acetate for 1 week every 4 weeks led to 80% of participants in the treatment group reporting satisfactory bleeding patterns with the etonogestrel implants in place.
Rates of early discontinuation have been variable, according to published literature, ranging from 13% to 21.1%, said Jordan Gray, MD, a fourth-year resident in ob.gyn. at Baylor Scott and White Medical Center, Temple, Tex., who helped conduct the new study. Reasons included bothersome bleeding. Dr. Gray and colleagues found that 24% of women in the placebo group requested removal of the implant, compared with 9% of those in the treatment group. Among these women, none requested removal for bothersome bleeding but rather for reasons such as wanting to get pregnant. One person requested removal because she did not like amenorrhea.
While the results of the study did not achieve statistical significance, owing to its size and noncompliance among some participants, it does indicate that norethindrone acetate may be helpful, Dr. Gray said.
During the study, participants in the treatment group (n = 22) received a monthly treatment regimen of 5 mg of oral norethindrone acetate daily for 7 days each month for the first 6 months after placement of an etonogestrel implant. The placebo group (n = 29) was given inert tablets prescribed in the same regimen. Both groups received products from a mail-order pharmacy.
Participants were women aged 18-48 years who desired an implant or those aged 14 years who had permission from a parent or guardian to receive the contraceptive. The study excluded people with known or suspected pregnancy, those less than 8 weeks’ post partum, those who experienced menarche less than 2 years ago, those with body mass index greater than 40, and those who received depot medroxyprogesterone acetate within the previous 12 weeks. Excessive bleeding was defined as bleeding or spotting on more than 7 consecutive days or a fifth episode of bleeding in 90 days.
Overall, 11 patients (38%) in the placebo group and 10 (45%) in the treatment arm withdrew from the study. Reasons included wanting to get pregnant, mood changes, or noncompliance with study parameters, which included not responding or returning bleeding diaries, Dr. Gray said.
A limitation of the study was that compliance was less than expected. In addition, there were challenges with rates of responses, Dr. Gray said. The study was conducted during the COVID-19 pandemic, when all in-person visits were transitioned to telehealth. Although the investigators offered payment to participants, not all returned text-message surveys. The researchers had intended to enroll 124 participants but curtailed the study early, owing to the limited number of participants.
Given that there is no standard approach to treating prolonged or excessive bleeding with etonogestrel implants, Dr. Gray said, “Our data suggests that this regimen is a simple and acceptable method to treat bothersome bleeding and that predictable bleeding may be more satisfactory than unpredictable bleeding.”
Veronica Maria Pimentel, MD, moderator of the session and a maternal-fetal medicine specialist and director of research for the ob.gyn. residency program at St. Francis Hospital, part of Trinity Health of New England in Hartford, Conn., praised the researchers for a well-designed study.
“However, unfortunately, they were not able to recruit the number of patients that they needed in order to achieve the power to show the difference [between treatment arms], so another study would have to be done to show if there is a difference,” Dr. Pimentel said.
Dr. Pimentel complimented Dr. Gray following her presentation, congratulating her for conducting a randomized, controlled trial: “That’s not easy, as you have shown, but it’s also a good try, so you can actually see how hard it is to obtain quality data from research.”
The study was supported in part by a research grant from the Investigator-Initiated Studies Program of Organon. Dr. Gray is a consultant for Johnson & Johnson. Dr. Pimentel has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BALTIMORE – The bleeding causes some women to have the device removed, according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
In a randomized, double-blinded, placebo-controlled trial of 51 patients desiring the implants – which suppress ovulation by releasing progestin over a 3-year period – taking norethindrone acetate for 1 week every 4 weeks led to 80% of participants in the treatment group reporting satisfactory bleeding patterns with the etonogestrel implants in place.
Rates of early discontinuation have been variable, according to published literature, ranging from 13% to 21.1%, said Jordan Gray, MD, a fourth-year resident in ob.gyn. at Baylor Scott and White Medical Center, Temple, Tex., who helped conduct the new study. Reasons included bothersome bleeding. Dr. Gray and colleagues found that 24% of women in the placebo group requested removal of the implant, compared with 9% of those in the treatment group. Among these women, none requested removal for bothersome bleeding but rather for reasons such as wanting to get pregnant. One person requested removal because she did not like amenorrhea.
While the results of the study did not achieve statistical significance, owing to its size and noncompliance among some participants, it does indicate that norethindrone acetate may be helpful, Dr. Gray said.
During the study, participants in the treatment group (n = 22) received a monthly treatment regimen of 5 mg of oral norethindrone acetate daily for 7 days each month for the first 6 months after placement of an etonogestrel implant. The placebo group (n = 29) was given inert tablets prescribed in the same regimen. Both groups received products from a mail-order pharmacy.
Participants were women aged 18-48 years who desired an implant or those aged 14 years who had permission from a parent or guardian to receive the contraceptive. The study excluded people with known or suspected pregnancy, those less than 8 weeks’ post partum, those who experienced menarche less than 2 years ago, those with body mass index greater than 40, and those who received depot medroxyprogesterone acetate within the previous 12 weeks. Excessive bleeding was defined as bleeding or spotting on more than 7 consecutive days or a fifth episode of bleeding in 90 days.
Overall, 11 patients (38%) in the placebo group and 10 (45%) in the treatment arm withdrew from the study. Reasons included wanting to get pregnant, mood changes, or noncompliance with study parameters, which included not responding or returning bleeding diaries, Dr. Gray said.
A limitation of the study was that compliance was less than expected. In addition, there were challenges with rates of responses, Dr. Gray said. The study was conducted during the COVID-19 pandemic, when all in-person visits were transitioned to telehealth. Although the investigators offered payment to participants, not all returned text-message surveys. The researchers had intended to enroll 124 participants but curtailed the study early, owing to the limited number of participants.
Given that there is no standard approach to treating prolonged or excessive bleeding with etonogestrel implants, Dr. Gray said, “Our data suggests that this regimen is a simple and acceptable method to treat bothersome bleeding and that predictable bleeding may be more satisfactory than unpredictable bleeding.”
Veronica Maria Pimentel, MD, moderator of the session and a maternal-fetal medicine specialist and director of research for the ob.gyn. residency program at St. Francis Hospital, part of Trinity Health of New England in Hartford, Conn., praised the researchers for a well-designed study.
“However, unfortunately, they were not able to recruit the number of patients that they needed in order to achieve the power to show the difference [between treatment arms], so another study would have to be done to show if there is a difference,” Dr. Pimentel said.
Dr. Pimentel complimented Dr. Gray following her presentation, congratulating her for conducting a randomized, controlled trial: “That’s not easy, as you have shown, but it’s also a good try, so you can actually see how hard it is to obtain quality data from research.”
The study was supported in part by a research grant from the Investigator-Initiated Studies Program of Organon. Dr. Gray is a consultant for Johnson & Johnson. Dr. Pimentel has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BALTIMORE – The bleeding causes some women to have the device removed, according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
In a randomized, double-blinded, placebo-controlled trial of 51 patients desiring the implants – which suppress ovulation by releasing progestin over a 3-year period – taking norethindrone acetate for 1 week every 4 weeks led to 80% of participants in the treatment group reporting satisfactory bleeding patterns with the etonogestrel implants in place.
Rates of early discontinuation have been variable, according to published literature, ranging from 13% to 21.1%, said Jordan Gray, MD, a fourth-year resident in ob.gyn. at Baylor Scott and White Medical Center, Temple, Tex., who helped conduct the new study. Reasons included bothersome bleeding. Dr. Gray and colleagues found that 24% of women in the placebo group requested removal of the implant, compared with 9% of those in the treatment group. Among these women, none requested removal for bothersome bleeding but rather for reasons such as wanting to get pregnant. One person requested removal because she did not like amenorrhea.
While the results of the study did not achieve statistical significance, owing to its size and noncompliance among some participants, it does indicate that norethindrone acetate may be helpful, Dr. Gray said.
During the study, participants in the treatment group (n = 22) received a monthly treatment regimen of 5 mg of oral norethindrone acetate daily for 7 days each month for the first 6 months after placement of an etonogestrel implant. The placebo group (n = 29) was given inert tablets prescribed in the same regimen. Both groups received products from a mail-order pharmacy.
Participants were women aged 18-48 years who desired an implant or those aged 14 years who had permission from a parent or guardian to receive the contraceptive. The study excluded people with known or suspected pregnancy, those less than 8 weeks’ post partum, those who experienced menarche less than 2 years ago, those with body mass index greater than 40, and those who received depot medroxyprogesterone acetate within the previous 12 weeks. Excessive bleeding was defined as bleeding or spotting on more than 7 consecutive days or a fifth episode of bleeding in 90 days.
Overall, 11 patients (38%) in the placebo group and 10 (45%) in the treatment arm withdrew from the study. Reasons included wanting to get pregnant, mood changes, or noncompliance with study parameters, which included not responding or returning bleeding diaries, Dr. Gray said.
A limitation of the study was that compliance was less than expected. In addition, there were challenges with rates of responses, Dr. Gray said. The study was conducted during the COVID-19 pandemic, when all in-person visits were transitioned to telehealth. Although the investigators offered payment to participants, not all returned text-message surveys. The researchers had intended to enroll 124 participants but curtailed the study early, owing to the limited number of participants.
Given that there is no standard approach to treating prolonged or excessive bleeding with etonogestrel implants, Dr. Gray said, “Our data suggests that this regimen is a simple and acceptable method to treat bothersome bleeding and that predictable bleeding may be more satisfactory than unpredictable bleeding.”
Veronica Maria Pimentel, MD, moderator of the session and a maternal-fetal medicine specialist and director of research for the ob.gyn. residency program at St. Francis Hospital, part of Trinity Health of New England in Hartford, Conn., praised the researchers for a well-designed study.
“However, unfortunately, they were not able to recruit the number of patients that they needed in order to achieve the power to show the difference [between treatment arms], so another study would have to be done to show if there is a difference,” Dr. Pimentel said.
Dr. Pimentel complimented Dr. Gray following her presentation, congratulating her for conducting a randomized, controlled trial: “That’s not easy, as you have shown, but it’s also a good try, so you can actually see how hard it is to obtain quality data from research.”
The study was supported in part by a research grant from the Investigator-Initiated Studies Program of Organon. Dr. Gray is a consultant for Johnson & Johnson. Dr. Pimentel has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ACOG 2023
Cycle timing may reduce hormonal dosage for contraception
Progesterone and estrogen are often used for contraception by preventing ovulation, but the adverse effects associated with large doses of these hormones remain a concern, wrote Brenda Lyn A. Gavina, a PhD candidate at the University of the Philippines Diliman, Quezon City, and colleagues.
In a study published in PLoS Computational Biology, the researchers examined how the timing of hormone administration during a cycle might impact the amount of hormones needed for contraception. Previous research shown that combining hormones can reduce the dosage needed, but the impact of timing on further dose reduction has not been well studied, they said.
The researchers applied optimal control theory in a mathematical model to show the contraceptive effect of estrogen and/or progesterone at different times in the menstrual cycle. The model was based on a normal menstrual cycle with pituitary and ovarian phases. The model assumed that synthesis of luteinizing hormone and follicle-stimulating hormone occurs in the pituitary, that LH and FSH are held in reserve before release into the bloodstream, and that the follicular/luteal mass goes through nine ovarian stages of development. The model also included the activity of ovarian hormones estradiol (E2), progesterone (P4), and inhibin (Inh), in a normal cycle. In the model, LH, FSH, and E2 peaked in the late follicular phase, and P4 and Inh peaked in the luteal phase.
The pituitary model predicted the synthesis, release, and clearance of LH and FSH, and the response of the pituitary to E2, P4, and Inh. The ovarian model predicted the response of E2, P4, and Inh as functions of LH and FSH.
The researchers simulated a constant dose of exogenous progesterone monotherapy and combined exogenous estrogen/progesterone. They determined that a P4 peak of 4.99 ng/mL was taken as the optimum constant dosage for progesterone monotherapy, and for combination estrogen/progesterone.
The researchers then assessed the impact of time on dosage. They found that estrogen administration starting on the first day of a normal cycle preventing FHS from reaching maximum value, and that the low level of FHS in the follicular phase and additional P4 inhibition slowed follicular growth, and use of combination estrogen/progesterone caused similar inhibition at a later follicular stage.
“The combination therapy suggests that time-varying doses of estrogen and progesterone given simultaneously from the start to the end of the 28-day period, only requires a surge in estrogen dose around the 12th day of the cycle (a delayed administration compared to the estrogen monotherapy),” they noted.
With attention to timing, the maximum progesterone levels throughout a menstrual cycle were 4.43 ng/mL, 4.66 ng/mL, and 4.31 ng/mL for estrogen monotherapy, progesterone monotherapy, and combination therapy, respectively. Total doses of the optimal exogenous hormone were 77.76 pg/mL and 48.84 ng/mL for estrogen and progesterone monotherapy, respectively, and 35.58 pg/mL and 21.67 ng/mL for estrogen and progesterone in combination.
The findings were limited by the use of a standard model that does not account for variations in cycle length, the researchers noted. However, the results reflect other studies of hormonal activity, and the model can be used in future studies of the effect of hormones on cycle length, they said.
Overall, the researchers determined that timing dosage with estrogen monotherapy based on their model could provide effective contraception with about 92% of the minimum total constant dosage, while progesterone monotherapy would be effective with approximately 43% of the total constant dose.
Although more work is needed, the current study results may guide clinicians in experimenting with the optimal treatment regimen for anovulation, the researchers said.
“The results presented here give insights on construction of timed devices that give contraception at certain parts of the menstrual cycle,” they concluded.
Model aims to improve women’s control of contraception
“Aside from wanting to contribute to controlling population growth, we aim to empower women more by giving them more control on when to conceive and start motherhood,” and be in control of contraception in a safer way, said lead author Ms. Gavina, in an interview. In addition, studies are showing the noncontraceptive benefits of suppressing ovulation for managing premenstrual syndromes such as breast tenderness and irritability, and for managing diseases such as endometriosis, she said. “Anovulation also lowers the risk of ACL injuries in female athletes,” she added.
Ms. Gavina said that she was surprised primarily by the optimal control result for estrogen monotherapy. “It was surprising that, theoretically, our mathematical model, with the simplifying assumptions, showed that as low as 10% of the total dose in constant administration could achieve contraception as long as the administration of this dosage is perfectly timed, and the timing was also shown in our optimization result,” she said.
“Our model does not capture all factors in contraception, since the reproductive function in women is a very complex multiscale dynamical system highly dependent on both endogenous and exogenous hormones,” Ms. Gavina told this news organization. However, “with the emergence of more data, it can be refined to address other contraception issues. Further, although the results of this study are not directly translatable to the clinical setting, we hope that these results may aid clinicians in identifying the minimum dose and treatment schedule for contraception,” she said.
Future research directions include examining within and between women’s variabilities and adding a pharmacokinetics model to account for the effects of specific drugs, she said. “We also hope to expand or modify the current model to investigate reproductive health concerns in women, such as [polycystic ovary syndrome] and ovarian cysts,” she added.
Ms. Gavina disclosed support from the University of the Philippines Office of International Linkages, a Continuous Operational and Outcomes-based Partnership for Excellence in Research and Academic Training Enhancement grant, and a Commission on Higher Education Faculty Development Program-II scholarship.
Progesterone and estrogen are often used for contraception by preventing ovulation, but the adverse effects associated with large doses of these hormones remain a concern, wrote Brenda Lyn A. Gavina, a PhD candidate at the University of the Philippines Diliman, Quezon City, and colleagues.
In a study published in PLoS Computational Biology, the researchers examined how the timing of hormone administration during a cycle might impact the amount of hormones needed for contraception. Previous research shown that combining hormones can reduce the dosage needed, but the impact of timing on further dose reduction has not been well studied, they said.
The researchers applied optimal control theory in a mathematical model to show the contraceptive effect of estrogen and/or progesterone at different times in the menstrual cycle. The model was based on a normal menstrual cycle with pituitary and ovarian phases. The model assumed that synthesis of luteinizing hormone and follicle-stimulating hormone occurs in the pituitary, that LH and FSH are held in reserve before release into the bloodstream, and that the follicular/luteal mass goes through nine ovarian stages of development. The model also included the activity of ovarian hormones estradiol (E2), progesterone (P4), and inhibin (Inh), in a normal cycle. In the model, LH, FSH, and E2 peaked in the late follicular phase, and P4 and Inh peaked in the luteal phase.
The pituitary model predicted the synthesis, release, and clearance of LH and FSH, and the response of the pituitary to E2, P4, and Inh. The ovarian model predicted the response of E2, P4, and Inh as functions of LH and FSH.
The researchers simulated a constant dose of exogenous progesterone monotherapy and combined exogenous estrogen/progesterone. They determined that a P4 peak of 4.99 ng/mL was taken as the optimum constant dosage for progesterone monotherapy, and for combination estrogen/progesterone.
The researchers then assessed the impact of time on dosage. They found that estrogen administration starting on the first day of a normal cycle preventing FHS from reaching maximum value, and that the low level of FHS in the follicular phase and additional P4 inhibition slowed follicular growth, and use of combination estrogen/progesterone caused similar inhibition at a later follicular stage.
“The combination therapy suggests that time-varying doses of estrogen and progesterone given simultaneously from the start to the end of the 28-day period, only requires a surge in estrogen dose around the 12th day of the cycle (a delayed administration compared to the estrogen monotherapy),” they noted.
With attention to timing, the maximum progesterone levels throughout a menstrual cycle were 4.43 ng/mL, 4.66 ng/mL, and 4.31 ng/mL for estrogen monotherapy, progesterone monotherapy, and combination therapy, respectively. Total doses of the optimal exogenous hormone were 77.76 pg/mL and 48.84 ng/mL for estrogen and progesterone monotherapy, respectively, and 35.58 pg/mL and 21.67 ng/mL for estrogen and progesterone in combination.
The findings were limited by the use of a standard model that does not account for variations in cycle length, the researchers noted. However, the results reflect other studies of hormonal activity, and the model can be used in future studies of the effect of hormones on cycle length, they said.
Overall, the researchers determined that timing dosage with estrogen monotherapy based on their model could provide effective contraception with about 92% of the minimum total constant dosage, while progesterone monotherapy would be effective with approximately 43% of the total constant dose.
Although more work is needed, the current study results may guide clinicians in experimenting with the optimal treatment regimen for anovulation, the researchers said.
“The results presented here give insights on construction of timed devices that give contraception at certain parts of the menstrual cycle,” they concluded.
Model aims to improve women’s control of contraception
“Aside from wanting to contribute to controlling population growth, we aim to empower women more by giving them more control on when to conceive and start motherhood,” and be in control of contraception in a safer way, said lead author Ms. Gavina, in an interview. In addition, studies are showing the noncontraceptive benefits of suppressing ovulation for managing premenstrual syndromes such as breast tenderness and irritability, and for managing diseases such as endometriosis, she said. “Anovulation also lowers the risk of ACL injuries in female athletes,” she added.
Ms. Gavina said that she was surprised primarily by the optimal control result for estrogen monotherapy. “It was surprising that, theoretically, our mathematical model, with the simplifying assumptions, showed that as low as 10% of the total dose in constant administration could achieve contraception as long as the administration of this dosage is perfectly timed, and the timing was also shown in our optimization result,” she said.
“Our model does not capture all factors in contraception, since the reproductive function in women is a very complex multiscale dynamical system highly dependent on both endogenous and exogenous hormones,” Ms. Gavina told this news organization. However, “with the emergence of more data, it can be refined to address other contraception issues. Further, although the results of this study are not directly translatable to the clinical setting, we hope that these results may aid clinicians in identifying the minimum dose and treatment schedule for contraception,” she said.
Future research directions include examining within and between women’s variabilities and adding a pharmacokinetics model to account for the effects of specific drugs, she said. “We also hope to expand or modify the current model to investigate reproductive health concerns in women, such as [polycystic ovary syndrome] and ovarian cysts,” she added.
Ms. Gavina disclosed support from the University of the Philippines Office of International Linkages, a Continuous Operational and Outcomes-based Partnership for Excellence in Research and Academic Training Enhancement grant, and a Commission on Higher Education Faculty Development Program-II scholarship.
Progesterone and estrogen are often used for contraception by preventing ovulation, but the adverse effects associated with large doses of these hormones remain a concern, wrote Brenda Lyn A. Gavina, a PhD candidate at the University of the Philippines Diliman, Quezon City, and colleagues.
In a study published in PLoS Computational Biology, the researchers examined how the timing of hormone administration during a cycle might impact the amount of hormones needed for contraception. Previous research shown that combining hormones can reduce the dosage needed, but the impact of timing on further dose reduction has not been well studied, they said.
The researchers applied optimal control theory in a mathematical model to show the contraceptive effect of estrogen and/or progesterone at different times in the menstrual cycle. The model was based on a normal menstrual cycle with pituitary and ovarian phases. The model assumed that synthesis of luteinizing hormone and follicle-stimulating hormone occurs in the pituitary, that LH and FSH are held in reserve before release into the bloodstream, and that the follicular/luteal mass goes through nine ovarian stages of development. The model also included the activity of ovarian hormones estradiol (E2), progesterone (P4), and inhibin (Inh), in a normal cycle. In the model, LH, FSH, and E2 peaked in the late follicular phase, and P4 and Inh peaked in the luteal phase.
The pituitary model predicted the synthesis, release, and clearance of LH and FSH, and the response of the pituitary to E2, P4, and Inh. The ovarian model predicted the response of E2, P4, and Inh as functions of LH and FSH.
The researchers simulated a constant dose of exogenous progesterone monotherapy and combined exogenous estrogen/progesterone. They determined that a P4 peak of 4.99 ng/mL was taken as the optimum constant dosage for progesterone monotherapy, and for combination estrogen/progesterone.
The researchers then assessed the impact of time on dosage. They found that estrogen administration starting on the first day of a normal cycle preventing FHS from reaching maximum value, and that the low level of FHS in the follicular phase and additional P4 inhibition slowed follicular growth, and use of combination estrogen/progesterone caused similar inhibition at a later follicular stage.
“The combination therapy suggests that time-varying doses of estrogen and progesterone given simultaneously from the start to the end of the 28-day period, only requires a surge in estrogen dose around the 12th day of the cycle (a delayed administration compared to the estrogen monotherapy),” they noted.
With attention to timing, the maximum progesterone levels throughout a menstrual cycle were 4.43 ng/mL, 4.66 ng/mL, and 4.31 ng/mL for estrogen monotherapy, progesterone monotherapy, and combination therapy, respectively. Total doses of the optimal exogenous hormone were 77.76 pg/mL and 48.84 ng/mL for estrogen and progesterone monotherapy, respectively, and 35.58 pg/mL and 21.67 ng/mL for estrogen and progesterone in combination.
The findings were limited by the use of a standard model that does not account for variations in cycle length, the researchers noted. However, the results reflect other studies of hormonal activity, and the model can be used in future studies of the effect of hormones on cycle length, they said.
Overall, the researchers determined that timing dosage with estrogen monotherapy based on their model could provide effective contraception with about 92% of the minimum total constant dosage, while progesterone monotherapy would be effective with approximately 43% of the total constant dose.
Although more work is needed, the current study results may guide clinicians in experimenting with the optimal treatment regimen for anovulation, the researchers said.
“The results presented here give insights on construction of timed devices that give contraception at certain parts of the menstrual cycle,” they concluded.
Model aims to improve women’s control of contraception
“Aside from wanting to contribute to controlling population growth, we aim to empower women more by giving them more control on when to conceive and start motherhood,” and be in control of contraception in a safer way, said lead author Ms. Gavina, in an interview. In addition, studies are showing the noncontraceptive benefits of suppressing ovulation for managing premenstrual syndromes such as breast tenderness and irritability, and for managing diseases such as endometriosis, she said. “Anovulation also lowers the risk of ACL injuries in female athletes,” she added.
Ms. Gavina said that she was surprised primarily by the optimal control result for estrogen monotherapy. “It was surprising that, theoretically, our mathematical model, with the simplifying assumptions, showed that as low as 10% of the total dose in constant administration could achieve contraception as long as the administration of this dosage is perfectly timed, and the timing was also shown in our optimization result,” she said.
“Our model does not capture all factors in contraception, since the reproductive function in women is a very complex multiscale dynamical system highly dependent on both endogenous and exogenous hormones,” Ms. Gavina told this news organization. However, “with the emergence of more data, it can be refined to address other contraception issues. Further, although the results of this study are not directly translatable to the clinical setting, we hope that these results may aid clinicians in identifying the minimum dose and treatment schedule for contraception,” she said.
Future research directions include examining within and between women’s variabilities and adding a pharmacokinetics model to account for the effects of specific drugs, she said. “We also hope to expand or modify the current model to investigate reproductive health concerns in women, such as [polycystic ovary syndrome] and ovarian cysts,” she added.
Ms. Gavina disclosed support from the University of the Philippines Office of International Linkages, a Continuous Operational and Outcomes-based Partnership for Excellence in Research and Academic Training Enhancement grant, and a Commission on Higher Education Faculty Development Program-II scholarship.
FROM PLOS COMPUTATIONAL BIOLOGY
Neuropsychiatric side effects of hormonal contraceptives: More common than you think!
Since its introduction in 1950, the combined oral contraceptive pill has been used by countless women as a method for birth control (Liao P. Can Fam Physician. 2012 Dec; 58[12]:e757-e760).
Hormonal contraception (HC) provides women with both contraceptive and noncontraceptive benefits, most notably a method for avoiding unintended pregnancy. In addition to being an effective method of contraception, oral contraceptive pills (OCPs) are well established for treating conditions such as hirsutism, pain symptoms associated with endometriosis and adenomyosis, and pelvic inflammatory disease, among others (Schindler A. Int J Endocrinol Metab. 2013 Winter;11[1]:41-7).
Combined hormonal contraceptives are also first-line treatment for women with menstrual disorders, and in women with polycystic ovary syndrome, can offer an effective long-term method to regulate their menstrual cycle, decrease androgens, clear up oily skin and acne, and reduce facial hair while also providing them with effective contraception (de Melo et al. Open Access J Contracept. 2017;8:13-23).
Associations between ‘the pill’ and mood effects remain controversial
More than 100 million women worldwide use hormonal contraceptives today, yet despite this, the data are mixed regarding the prevalence and extent of neuropsychiatric symptoms and mood changes associated with use of “the pill.” Some studies show combined oral contraceptives are associated with a decrease in general well-being, but had no effect on depression, in women compared with placebo (Zethraeus N et al. Fertil Steril. 2017 May;107[5]:1238-45).
However, a large Danish study published in JAMA Psychiatry of more than 1 million women found a significant association between use of hormonal contraception and antidepressant use or first diagnosis of depression, with adolescents having a higher rate of first depression diagnosis and antidepressant use compared with women 20–30 years old (Skovlund C et al. JAMA Psychiatry. 2016 Nov 1;73[11]:1154-62).
Studies have also shown long-term exposure to levonorgestrel is significantly associated with anxiety and sleep problems in women without a history of these issues (Slattery J et al. Drug Saf. 2018 Oct;41[10]:951-8). A recent small nationwide cohort study in France suggests this may also be true of levonorgestrel delivered by intrauterine devices (IUD) and the association may be dose-dependent (Roland N et al. JAMA. 2023;329[3]:257-9).
Of note, a study published in the American Journal of Psychiatry found a nearly twofold risk of suicide attempt and over threefold risk of suicide among women taking hormonal contraception compared with women who had never used hormonal contraceptives (Skovlund et al. Am J Psychiatry. 2017 Nov 17:appiajp201717060616).
Knowledge gaps make drawing conclusions difficult
The latest information on use of antidepressant and antianxiety medications in women of reproductive age (18-44 years) is sparse and, in some cases, outdated. According to data from the National Health and Nutrition Examination Survey, 18.6% of adult women 18 years or older reported using antidepressant medications within the last 30 days in 2017-2018, an increase from 13.8% in 2009-2010. Among women aged 15-44 year with private employer–sponsored insurance surveyed during 2008-2013, the results showed 15.4% of women filled a prescription for an antidepressant. We must look back further to find data on antianxiety medication use among women aged 18-44 years where use of antianxiety drugs (anxiolytics, sedatives, and hypnotics) was 4.3% between 2005 and 2008.
A lack of literature in this area is likely due to significant underreporting, and an inability to select patients who are sensitive to or at risk of developing neuropsychiatric symptoms resulting from hormonal contraception use because the true pathophysiology is unknown. Existing studies tend to use varying methods to assess mood changes, and do not usually specify hormonal contraceptive use type in their analyses (Schaffir J et al. Eur J Contracept Reprod Health Care. 2016 Oct;21[5]:347-55).
Studies of this nature also require large sample sizes, but the percentage of women who develop neuropsychiatric symptoms from hormonal contraceptive use has historically been relatively small. In the late 1990s, Rosenberg and colleagues found 46% of 1,657 women discontinued oral contraceptives due to side effects within 6 months of starting a new prescription; of these women, 5% reported mood changes as their reason for discontinuing oral contraceptives (Rosenberg M et al. Am J Obstet Gynecol. 1998 Sep;179[3 Pt 1]:577-82).
One might expect that, as lower dosage combined hormonal contraceptives were developed in the 1980s, that the rate of reporting psychological side effects would continue to decrease as well. Yet greater awareness of the potential for mood changes while on “the pill” as outlined by the lay press and social media may be leading to increased reporting of neuropsychiatric effects in women. In a recent cross-sectional survey of 188 women in New York, 43.6% said they experienced mood changes while on hormonal contraceptives, and 61.2% of women with histories of psychiatric illness reported mood changes they attributed to hormonal contraceptives (Martell S et al. Contracept Reprod Med. 2023;8:9).
Martell and colleagues found 48.3% of women cited side effects as a reason for discontinuing hormonal contraception, and 43 participants mentioned psychological side effects unprompted, including 2 patients with suicidal thoughts. The authors said this suggests “psychological side effects, at least in part, may have impacted” HC users’ decisions to switch from OCPs to an alternative method of contraception.
It is also not clear what risk factors exist for women who develop neuropsychiatric symptoms from hormonal contraceptive use. First, it is important to note that both progestin-only contraceptives and combined hormonal contraceptives are classified by the Centers for Disease Control and Prevention’s US Medical Eligibility Criteria for Contraceptive Use, 2016 as having no restrictions for use, including among patients with depression. While women in a smaller subgroup have significant neuropsychiatric symptoms related to their hormonal contraceptives, the underlying mechanism is unknown, and is thought to be largely related to the progestogen component of combined hormonal contraceptives or progestogen-only contraceptives (Mu E. Aust Prescr. 2022 Jun; 45[3]:75-9). We know that some women are hormone sensitive, while others are less so, and some not at all. Progestogens could affect mood as a direct action of the progestogen, because progestogens can be neurosteroids, or the progestogen effect could be mediated secondarily through a change in that woman’s own production of or bioavailability of androgens or naturally occurring estrogens (Giatti S. J Mol Endocrinol. 2016 Aug;57[2]:R109-26).
Here, we also find that currently available evidence limits our ability to draw firm conclusions. A study by Berry-Bibee and colleagues found a “low concern for clinically significant interactions” between hormonal contraception and psychotropic drugs, but was limited by quality/quantity of evidence (Berry-Bibee E et al. Contraception. 2016 Dec;94[6]:650-67). Interestingly, a study by Robinson and colleagues from the mid-2000s posited based on low evidence that “psychological response to the practice of contraception” was a potential explanation for the side effect profile of hormonal contraception (Robinson S et al. Med Hypotheses. 2004;63[2]:268-73).
Further, it may be that women with premenstrual dysphoric disorder (PMDD) might be selected for oral contraceptives, and they are predisposed to other neuropsychiatric problems. Estimates have placed the prevalence of comorbid psychiatric disorders such as anxiety, major depression, bipolar disorder, and posttraumatic stress disorder as high as 70% for women with PMDD (Sepede G et al. Neuropsychiatr Dis Treat. 2020;16:415-26). This phenomenon is not new, having been characterized in the lay literature nearly 20 years ago, by endocrinologist Geoffrey P. Redmond, MD (Redmond GP. The Hormonally Vulnerable Woman. New York: HarperCollins; 2005).
While the cause is not exactly idiosyncratic, They tend to have an entire spectrum of responses to the progestogens in combined or progestin-only contraceptives, ranging from just a flattened affect – which could easily be explained by their flattened level of endogenous hormones – to frank depression. Their frank depression, in turn, can be demonstrated to include suicidal ideation and actual suicide.
Compounding this issue is a woman’s perception of her sexuality. Some women with low sexual desire or sexual problems who are younger may have more distress about their problems compared with women of older reproductive age. While the reason for that is not clear, it may be that in the sexual arena, it is more important for some younger women to be a sexual person than in perimenopausal women, or that women who are younger are more likely to be partnered than women of older reproductive age. While the European Society of Sexual Medicine concluded in a 2019 position statement that there is inconclusive evidence whether hormonal contraception may be contributing to changes in sexual desire and sexual dysfunction, it appears that “a minority of women” experience “better or worse sexual functioning” from taking combined oral contraceptives (Both S et al. J Sex Med. 2019 Nov;16[11]:1681-95), suggesting that the majority of women report no significant changes.
Practitioners should discuss mood effects during consultation
An ob.gyn., primary care physicians, or others with prescriptive authority (i.e. nurse practitioners and physician assistants) in clinical practice may encounter a patient who seems to have mood side effects owing to progestogen-containing contraceptives that they prescribe. However, many ob.gyns. are likely unaware of the prevalence, or that some of those same patients can have such significant mood effects that they would become or are suicidal.
I believe questioning patients about mood effects during consultation and particularly during follow-up following the initiation of any hormonal contraceptive is worth a passing comment for every patient, which should include mood effects in broader discussion for anyone currently using an antidepressant, patients with a history of antidepressant use, and patients who have considered suicide. As we do with other drugs, these questions can be posed in the form of a questionnaire followed up by the practitioner in counseling.
Practitioners who encounter a patient with mood changes as a result of hormonal contraceptive use can consider changing to a nonhormonal method of birth control, or recommending the patient use a barrier method during sexual activity, as none of these options have neuropsychiatric side effects.
Ultimately, practitioners of all types need to engage in shared decision-making to identify the key benefits and risks of hormonal contraceptive use for each patient, which may involve trial and error to determine the ideal treatment. It is critical that practitioners of all types strike a balance between alleviating patient concerns about potential mood changes, monitoring patients with an appreciable risk of mood changes, and continuing patients on hormonal contraception for whom the benefits outweigh the risks.
Dr. Simon is a clinical professor at George Washington University and the medical director and founder of IntimMedicine Specialists in Washington, which provides patient-focused care for women across the reproductive life cycle. He is a past president of the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Dr. Simon has been a consultant to, received grant and research support from, and served on the speakers bureau for various pharmaceutical companies that develop combination hormonal contraceptives. Email Dr. Simon at [email protected].
Since its introduction in 1950, the combined oral contraceptive pill has been used by countless women as a method for birth control (Liao P. Can Fam Physician. 2012 Dec; 58[12]:e757-e760).
Hormonal contraception (HC) provides women with both contraceptive and noncontraceptive benefits, most notably a method for avoiding unintended pregnancy. In addition to being an effective method of contraception, oral contraceptive pills (OCPs) are well established for treating conditions such as hirsutism, pain symptoms associated with endometriosis and adenomyosis, and pelvic inflammatory disease, among others (Schindler A. Int J Endocrinol Metab. 2013 Winter;11[1]:41-7).
Combined hormonal contraceptives are also first-line treatment for women with menstrual disorders, and in women with polycystic ovary syndrome, can offer an effective long-term method to regulate their menstrual cycle, decrease androgens, clear up oily skin and acne, and reduce facial hair while also providing them with effective contraception (de Melo et al. Open Access J Contracept. 2017;8:13-23).
Associations between ‘the pill’ and mood effects remain controversial
More than 100 million women worldwide use hormonal contraceptives today, yet despite this, the data are mixed regarding the prevalence and extent of neuropsychiatric symptoms and mood changes associated with use of “the pill.” Some studies show combined oral contraceptives are associated with a decrease in general well-being, but had no effect on depression, in women compared with placebo (Zethraeus N et al. Fertil Steril. 2017 May;107[5]:1238-45).
However, a large Danish study published in JAMA Psychiatry of more than 1 million women found a significant association between use of hormonal contraception and antidepressant use or first diagnosis of depression, with adolescents having a higher rate of first depression diagnosis and antidepressant use compared with women 20–30 years old (Skovlund C et al. JAMA Psychiatry. 2016 Nov 1;73[11]:1154-62).
Studies have also shown long-term exposure to levonorgestrel is significantly associated with anxiety and sleep problems in women without a history of these issues (Slattery J et al. Drug Saf. 2018 Oct;41[10]:951-8). A recent small nationwide cohort study in France suggests this may also be true of levonorgestrel delivered by intrauterine devices (IUD) and the association may be dose-dependent (Roland N et al. JAMA. 2023;329[3]:257-9).
Of note, a study published in the American Journal of Psychiatry found a nearly twofold risk of suicide attempt and over threefold risk of suicide among women taking hormonal contraception compared with women who had never used hormonal contraceptives (Skovlund et al. Am J Psychiatry. 2017 Nov 17:appiajp201717060616).
Knowledge gaps make drawing conclusions difficult
The latest information on use of antidepressant and antianxiety medications in women of reproductive age (18-44 years) is sparse and, in some cases, outdated. According to data from the National Health and Nutrition Examination Survey, 18.6% of adult women 18 years or older reported using antidepressant medications within the last 30 days in 2017-2018, an increase from 13.8% in 2009-2010. Among women aged 15-44 year with private employer–sponsored insurance surveyed during 2008-2013, the results showed 15.4% of women filled a prescription for an antidepressant. We must look back further to find data on antianxiety medication use among women aged 18-44 years where use of antianxiety drugs (anxiolytics, sedatives, and hypnotics) was 4.3% between 2005 and 2008.
A lack of literature in this area is likely due to significant underreporting, and an inability to select patients who are sensitive to or at risk of developing neuropsychiatric symptoms resulting from hormonal contraception use because the true pathophysiology is unknown. Existing studies tend to use varying methods to assess mood changes, and do not usually specify hormonal contraceptive use type in their analyses (Schaffir J et al. Eur J Contracept Reprod Health Care. 2016 Oct;21[5]:347-55).
Studies of this nature also require large sample sizes, but the percentage of women who develop neuropsychiatric symptoms from hormonal contraceptive use has historically been relatively small. In the late 1990s, Rosenberg and colleagues found 46% of 1,657 women discontinued oral contraceptives due to side effects within 6 months of starting a new prescription; of these women, 5% reported mood changes as their reason for discontinuing oral contraceptives (Rosenberg M et al. Am J Obstet Gynecol. 1998 Sep;179[3 Pt 1]:577-82).
One might expect that, as lower dosage combined hormonal contraceptives were developed in the 1980s, that the rate of reporting psychological side effects would continue to decrease as well. Yet greater awareness of the potential for mood changes while on “the pill” as outlined by the lay press and social media may be leading to increased reporting of neuropsychiatric effects in women. In a recent cross-sectional survey of 188 women in New York, 43.6% said they experienced mood changes while on hormonal contraceptives, and 61.2% of women with histories of psychiatric illness reported mood changes they attributed to hormonal contraceptives (Martell S et al. Contracept Reprod Med. 2023;8:9).
Martell and colleagues found 48.3% of women cited side effects as a reason for discontinuing hormonal contraception, and 43 participants mentioned psychological side effects unprompted, including 2 patients with suicidal thoughts. The authors said this suggests “psychological side effects, at least in part, may have impacted” HC users’ decisions to switch from OCPs to an alternative method of contraception.
It is also not clear what risk factors exist for women who develop neuropsychiatric symptoms from hormonal contraceptive use. First, it is important to note that both progestin-only contraceptives and combined hormonal contraceptives are classified by the Centers for Disease Control and Prevention’s US Medical Eligibility Criteria for Contraceptive Use, 2016 as having no restrictions for use, including among patients with depression. While women in a smaller subgroup have significant neuropsychiatric symptoms related to their hormonal contraceptives, the underlying mechanism is unknown, and is thought to be largely related to the progestogen component of combined hormonal contraceptives or progestogen-only contraceptives (Mu E. Aust Prescr. 2022 Jun; 45[3]:75-9). We know that some women are hormone sensitive, while others are less so, and some not at all. Progestogens could affect mood as a direct action of the progestogen, because progestogens can be neurosteroids, or the progestogen effect could be mediated secondarily through a change in that woman’s own production of or bioavailability of androgens or naturally occurring estrogens (Giatti S. J Mol Endocrinol. 2016 Aug;57[2]:R109-26).
Here, we also find that currently available evidence limits our ability to draw firm conclusions. A study by Berry-Bibee and colleagues found a “low concern for clinically significant interactions” between hormonal contraception and psychotropic drugs, but was limited by quality/quantity of evidence (Berry-Bibee E et al. Contraception. 2016 Dec;94[6]:650-67). Interestingly, a study by Robinson and colleagues from the mid-2000s posited based on low evidence that “psychological response to the practice of contraception” was a potential explanation for the side effect profile of hormonal contraception (Robinson S et al. Med Hypotheses. 2004;63[2]:268-73).
Further, it may be that women with premenstrual dysphoric disorder (PMDD) might be selected for oral contraceptives, and they are predisposed to other neuropsychiatric problems. Estimates have placed the prevalence of comorbid psychiatric disorders such as anxiety, major depression, bipolar disorder, and posttraumatic stress disorder as high as 70% for women with PMDD (Sepede G et al. Neuropsychiatr Dis Treat. 2020;16:415-26). This phenomenon is not new, having been characterized in the lay literature nearly 20 years ago, by endocrinologist Geoffrey P. Redmond, MD (Redmond GP. The Hormonally Vulnerable Woman. New York: HarperCollins; 2005).
While the cause is not exactly idiosyncratic, They tend to have an entire spectrum of responses to the progestogens in combined or progestin-only contraceptives, ranging from just a flattened affect – which could easily be explained by their flattened level of endogenous hormones – to frank depression. Their frank depression, in turn, can be demonstrated to include suicidal ideation and actual suicide.
Compounding this issue is a woman’s perception of her sexuality. Some women with low sexual desire or sexual problems who are younger may have more distress about their problems compared with women of older reproductive age. While the reason for that is not clear, it may be that in the sexual arena, it is more important for some younger women to be a sexual person than in perimenopausal women, or that women who are younger are more likely to be partnered than women of older reproductive age. While the European Society of Sexual Medicine concluded in a 2019 position statement that there is inconclusive evidence whether hormonal contraception may be contributing to changes in sexual desire and sexual dysfunction, it appears that “a minority of women” experience “better or worse sexual functioning” from taking combined oral contraceptives (Both S et al. J Sex Med. 2019 Nov;16[11]:1681-95), suggesting that the majority of women report no significant changes.
Practitioners should discuss mood effects during consultation
An ob.gyn., primary care physicians, or others with prescriptive authority (i.e. nurse practitioners and physician assistants) in clinical practice may encounter a patient who seems to have mood side effects owing to progestogen-containing contraceptives that they prescribe. However, many ob.gyns. are likely unaware of the prevalence, or that some of those same patients can have such significant mood effects that they would become or are suicidal.
I believe questioning patients about mood effects during consultation and particularly during follow-up following the initiation of any hormonal contraceptive is worth a passing comment for every patient, which should include mood effects in broader discussion for anyone currently using an antidepressant, patients with a history of antidepressant use, and patients who have considered suicide. As we do with other drugs, these questions can be posed in the form of a questionnaire followed up by the practitioner in counseling.
Practitioners who encounter a patient with mood changes as a result of hormonal contraceptive use can consider changing to a nonhormonal method of birth control, or recommending the patient use a barrier method during sexual activity, as none of these options have neuropsychiatric side effects.
Ultimately, practitioners of all types need to engage in shared decision-making to identify the key benefits and risks of hormonal contraceptive use for each patient, which may involve trial and error to determine the ideal treatment. It is critical that practitioners of all types strike a balance between alleviating patient concerns about potential mood changes, monitoring patients with an appreciable risk of mood changes, and continuing patients on hormonal contraception for whom the benefits outweigh the risks.
Dr. Simon is a clinical professor at George Washington University and the medical director and founder of IntimMedicine Specialists in Washington, which provides patient-focused care for women across the reproductive life cycle. He is a past president of the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Dr. Simon has been a consultant to, received grant and research support from, and served on the speakers bureau for various pharmaceutical companies that develop combination hormonal contraceptives. Email Dr. Simon at [email protected].
Since its introduction in 1950, the combined oral contraceptive pill has been used by countless women as a method for birth control (Liao P. Can Fam Physician. 2012 Dec; 58[12]:e757-e760).
Hormonal contraception (HC) provides women with both contraceptive and noncontraceptive benefits, most notably a method for avoiding unintended pregnancy. In addition to being an effective method of contraception, oral contraceptive pills (OCPs) are well established for treating conditions such as hirsutism, pain symptoms associated with endometriosis and adenomyosis, and pelvic inflammatory disease, among others (Schindler A. Int J Endocrinol Metab. 2013 Winter;11[1]:41-7).
Combined hormonal contraceptives are also first-line treatment for women with menstrual disorders, and in women with polycystic ovary syndrome, can offer an effective long-term method to regulate their menstrual cycle, decrease androgens, clear up oily skin and acne, and reduce facial hair while also providing them with effective contraception (de Melo et al. Open Access J Contracept. 2017;8:13-23).
Associations between ‘the pill’ and mood effects remain controversial
More than 100 million women worldwide use hormonal contraceptives today, yet despite this, the data are mixed regarding the prevalence and extent of neuropsychiatric symptoms and mood changes associated with use of “the pill.” Some studies show combined oral contraceptives are associated with a decrease in general well-being, but had no effect on depression, in women compared with placebo (Zethraeus N et al. Fertil Steril. 2017 May;107[5]:1238-45).
However, a large Danish study published in JAMA Psychiatry of more than 1 million women found a significant association between use of hormonal contraception and antidepressant use or first diagnosis of depression, with adolescents having a higher rate of first depression diagnosis and antidepressant use compared with women 20–30 years old (Skovlund C et al. JAMA Psychiatry. 2016 Nov 1;73[11]:1154-62).
Studies have also shown long-term exposure to levonorgestrel is significantly associated with anxiety and sleep problems in women without a history of these issues (Slattery J et al. Drug Saf. 2018 Oct;41[10]:951-8). A recent small nationwide cohort study in France suggests this may also be true of levonorgestrel delivered by intrauterine devices (IUD) and the association may be dose-dependent (Roland N et al. JAMA. 2023;329[3]:257-9).
Of note, a study published in the American Journal of Psychiatry found a nearly twofold risk of suicide attempt and over threefold risk of suicide among women taking hormonal contraception compared with women who had never used hormonal contraceptives (Skovlund et al. Am J Psychiatry. 2017 Nov 17:appiajp201717060616).
Knowledge gaps make drawing conclusions difficult
The latest information on use of antidepressant and antianxiety medications in women of reproductive age (18-44 years) is sparse and, in some cases, outdated. According to data from the National Health and Nutrition Examination Survey, 18.6% of adult women 18 years or older reported using antidepressant medications within the last 30 days in 2017-2018, an increase from 13.8% in 2009-2010. Among women aged 15-44 year with private employer–sponsored insurance surveyed during 2008-2013, the results showed 15.4% of women filled a prescription for an antidepressant. We must look back further to find data on antianxiety medication use among women aged 18-44 years where use of antianxiety drugs (anxiolytics, sedatives, and hypnotics) was 4.3% between 2005 and 2008.
A lack of literature in this area is likely due to significant underreporting, and an inability to select patients who are sensitive to or at risk of developing neuropsychiatric symptoms resulting from hormonal contraception use because the true pathophysiology is unknown. Existing studies tend to use varying methods to assess mood changes, and do not usually specify hormonal contraceptive use type in their analyses (Schaffir J et al. Eur J Contracept Reprod Health Care. 2016 Oct;21[5]:347-55).
Studies of this nature also require large sample sizes, but the percentage of women who develop neuropsychiatric symptoms from hormonal contraceptive use has historically been relatively small. In the late 1990s, Rosenberg and colleagues found 46% of 1,657 women discontinued oral contraceptives due to side effects within 6 months of starting a new prescription; of these women, 5% reported mood changes as their reason for discontinuing oral contraceptives (Rosenberg M et al. Am J Obstet Gynecol. 1998 Sep;179[3 Pt 1]:577-82).
One might expect that, as lower dosage combined hormonal contraceptives were developed in the 1980s, that the rate of reporting psychological side effects would continue to decrease as well. Yet greater awareness of the potential for mood changes while on “the pill” as outlined by the lay press and social media may be leading to increased reporting of neuropsychiatric effects in women. In a recent cross-sectional survey of 188 women in New York, 43.6% said they experienced mood changes while on hormonal contraceptives, and 61.2% of women with histories of psychiatric illness reported mood changes they attributed to hormonal contraceptives (Martell S et al. Contracept Reprod Med. 2023;8:9).
Martell and colleagues found 48.3% of women cited side effects as a reason for discontinuing hormonal contraception, and 43 participants mentioned psychological side effects unprompted, including 2 patients with suicidal thoughts. The authors said this suggests “psychological side effects, at least in part, may have impacted” HC users’ decisions to switch from OCPs to an alternative method of contraception.
It is also not clear what risk factors exist for women who develop neuropsychiatric symptoms from hormonal contraceptive use. First, it is important to note that both progestin-only contraceptives and combined hormonal contraceptives are classified by the Centers for Disease Control and Prevention’s US Medical Eligibility Criteria for Contraceptive Use, 2016 as having no restrictions for use, including among patients with depression. While women in a smaller subgroup have significant neuropsychiatric symptoms related to their hormonal contraceptives, the underlying mechanism is unknown, and is thought to be largely related to the progestogen component of combined hormonal contraceptives or progestogen-only contraceptives (Mu E. Aust Prescr. 2022 Jun; 45[3]:75-9). We know that some women are hormone sensitive, while others are less so, and some not at all. Progestogens could affect mood as a direct action of the progestogen, because progestogens can be neurosteroids, or the progestogen effect could be mediated secondarily through a change in that woman’s own production of or bioavailability of androgens or naturally occurring estrogens (Giatti S. J Mol Endocrinol. 2016 Aug;57[2]:R109-26).
Here, we also find that currently available evidence limits our ability to draw firm conclusions. A study by Berry-Bibee and colleagues found a “low concern for clinically significant interactions” between hormonal contraception and psychotropic drugs, but was limited by quality/quantity of evidence (Berry-Bibee E et al. Contraception. 2016 Dec;94[6]:650-67). Interestingly, a study by Robinson and colleagues from the mid-2000s posited based on low evidence that “psychological response to the practice of contraception” was a potential explanation for the side effect profile of hormonal contraception (Robinson S et al. Med Hypotheses. 2004;63[2]:268-73).
Further, it may be that women with premenstrual dysphoric disorder (PMDD) might be selected for oral contraceptives, and they are predisposed to other neuropsychiatric problems. Estimates have placed the prevalence of comorbid psychiatric disorders such as anxiety, major depression, bipolar disorder, and posttraumatic stress disorder as high as 70% for women with PMDD (Sepede G et al. Neuropsychiatr Dis Treat. 2020;16:415-26). This phenomenon is not new, having been characterized in the lay literature nearly 20 years ago, by endocrinologist Geoffrey P. Redmond, MD (Redmond GP. The Hormonally Vulnerable Woman. New York: HarperCollins; 2005).
While the cause is not exactly idiosyncratic, They tend to have an entire spectrum of responses to the progestogens in combined or progestin-only contraceptives, ranging from just a flattened affect – which could easily be explained by their flattened level of endogenous hormones – to frank depression. Their frank depression, in turn, can be demonstrated to include suicidal ideation and actual suicide.
Compounding this issue is a woman’s perception of her sexuality. Some women with low sexual desire or sexual problems who are younger may have more distress about their problems compared with women of older reproductive age. While the reason for that is not clear, it may be that in the sexual arena, it is more important for some younger women to be a sexual person than in perimenopausal women, or that women who are younger are more likely to be partnered than women of older reproductive age. While the European Society of Sexual Medicine concluded in a 2019 position statement that there is inconclusive evidence whether hormonal contraception may be contributing to changes in sexual desire and sexual dysfunction, it appears that “a minority of women” experience “better or worse sexual functioning” from taking combined oral contraceptives (Both S et al. J Sex Med. 2019 Nov;16[11]:1681-95), suggesting that the majority of women report no significant changes.
Practitioners should discuss mood effects during consultation
An ob.gyn., primary care physicians, or others with prescriptive authority (i.e. nurse practitioners and physician assistants) in clinical practice may encounter a patient who seems to have mood side effects owing to progestogen-containing contraceptives that they prescribe. However, many ob.gyns. are likely unaware of the prevalence, or that some of those same patients can have such significant mood effects that they would become or are suicidal.
I believe questioning patients about mood effects during consultation and particularly during follow-up following the initiation of any hormonal contraceptive is worth a passing comment for every patient, which should include mood effects in broader discussion for anyone currently using an antidepressant, patients with a history of antidepressant use, and patients who have considered suicide. As we do with other drugs, these questions can be posed in the form of a questionnaire followed up by the practitioner in counseling.
Practitioners who encounter a patient with mood changes as a result of hormonal contraceptive use can consider changing to a nonhormonal method of birth control, or recommending the patient use a barrier method during sexual activity, as none of these options have neuropsychiatric side effects.
Ultimately, practitioners of all types need to engage in shared decision-making to identify the key benefits and risks of hormonal contraceptive use for each patient, which may involve trial and error to determine the ideal treatment. It is critical that practitioners of all types strike a balance between alleviating patient concerns about potential mood changes, monitoring patients with an appreciable risk of mood changes, and continuing patients on hormonal contraception for whom the benefits outweigh the risks.
Dr. Simon is a clinical professor at George Washington University and the medical director and founder of IntimMedicine Specialists in Washington, which provides patient-focused care for women across the reproductive life cycle. He is a past president of the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Dr. Simon has been a consultant to, received grant and research support from, and served on the speakers bureau for various pharmaceutical companies that develop combination hormonal contraceptives. Email Dr. Simon at [email protected].
Adherence to oral contraceptive protocols prevents pregnancy
Combined oral contraceptives (COCs) remain a popular method of pregnancy prevention worldwide, but efficacy and failure rates can be difficult to determine, as real-word use does not always mirror clinical trials, wrote Mitchell D. Creinin, MD, of the University of California, Davis, and colleagues. Clinical trials include perfect use or method-failure rates, but data on pregnancy risk based on reported adherence alone are lacking, they said.
To assess the effects of missed pills on COC efficacy, the researchers reviewed data from a pair of parallel phase 3 trials, focusing only on adherence to the pill dosing regimen. The findings were published in Obstetrics & Gynecology.
The study population included 1,864 individuals from the United States and Canada, and 1,553 from Europe and Russia.
The participants were healthy, sexually active adults aged 16-50 years in monogamous relationships from 2016 through 2018 who agreed to used estetrol 15 mg and drospirenone 3 mg for up to 13 28-day cycles as their only contraceptive method. Condom use was permitted for protection against sexually transmitted infections if needed. The 28-day COCs included 24 hormonal tablets and 4 placebo tablets. Participants received written instructions for what to do it they missed pills.
The primary outcome was the relationship between missed pills and pregnancies.
A total of 31 pregnancies occurred across both studies; none of these occurred during cycles in which other contraception was used. Of 22 pregnancies in participants who reported taking all pills, 21 reported daily pill use during the cycle in which pregnancy occurred. One participant reported not taking one pill and one participant reported not taking two pills; neither correctly followed the instructions for missed pills.
Pregnancies occurred in .09% of cycles in which participants reported taking all pills, and in 0.25%, 0.83%, and 1.6% of cycles in which participants reported missing one pill, two pills, or more than two pills, respectively.
“Pregnancy rates exceeded 1% only in participants who did not correctly follow missed-pill instructions,” the researchers noted.
Pregnancy rates per cycle ranged from 0% to 0.21%, and 48.4% of the pregnancies occurred during the first four cycles of COC use. Approximately one-third (32.3%) of pregnancies occurred within the first week of a new pill pack.
“Fertilization does not appear to be related to the timing of missed pills within the cycle because pregnancy did not occur more frequently earlier in the cycle (after the placebo pills),” the researchers wrote in their discussion. This finding contradicts previous research suggesting that contraceptive failure rates decrease over the first year of use, they said. In addition, the formulation of the pill used may affect pregnancy rates when pills are missed, as some hormones have longer half-lives, they noted.
The study findings were limited by several factors, including the lack of adjustment for outcomes based on reported sexual activity per cycle, and by the reliance on self-reports.
However, the results were strengthened by the use of the clinical outcomes of pregnancy as the primary outcome, rather than characteristics and predictors of participants who missed pills, the researchers said.
The cycle-based methodology used in the current study may provide insight on the relationship between COC adherence and pregnancy risk that can inform future studies, they concluded.
Findings highlight the importance of options
“With increasing restrictions on abortion care, offering more contraceptive options for people is critical,” Lauren Owens, MD, associate professor of obstetrics and gynecology at the University of Washington, Seattle, said in an interview. “That’s not to say that having another pill option makes up for the harm people are experiencing as they navigate abortion bans and legal interference in their health care, but no one pill works for all people, and having more options is helpful,” she said.
Dr. Owens noted that the rates of pregnancy in the current study were lower than she traditionally associates with COCs, “although I usually discuss annual failure rates with patients, not failure rates per cycle, and the latter will clearly be lower.” In the current study, “The authors hypothesize some of this may be due to the longer half-life that estetrol has compared to ethinyl estradiol, the estrogen form more commonly found in oral contraceptive pills,” she said.
From a clinical standpoint, “I appreciated the linkage between number of missed pills and pregnancies occurring,” Dr. Owens said. “This is a good reminder to clinicians to talk to patients ahead of time about what to do when missed pills occur and to provide resources in advance that patients can reference when needed,” she said.
“The authors published other studies on this pill in the last year and it seems to work well and have a reasonable safety profile,” Dr. Owens told this news organization. However, “We still need to broaden the methods available to patients, particularly methods that people producing sperm can use. In the face of ongoing and escalating attacks on access to contraceptive care and abortion care, it’s more important than ever to do what we can to improve options for patients,” she said.
The study was supported by Estetra SRL, an affiliate company of Mithra Pharmaceuticals. Dr. Creinin disclosed relationships with multiple companies including Gedeon Richter, Mayne, and Organon. He disclosed serving on the advisory boards for Evofem, Fuji Pharma, Gedeon Richter, GlaxoSmithKline, Mayne, Merck, OLIC, Organon, and Searchlight, and serving as a consultant for Estetra SRL (including the current study), Libbs, Mayne, and Medicines360; his university department receives contraceptive research funding from Chemo Research SL, Evofem, HRA Pharma, Medicines360, Merck, and Sebela. Dr. Owens had no relevant financial conflicts to disclose.
Combined oral contraceptives (COCs) remain a popular method of pregnancy prevention worldwide, but efficacy and failure rates can be difficult to determine, as real-word use does not always mirror clinical trials, wrote Mitchell D. Creinin, MD, of the University of California, Davis, and colleagues. Clinical trials include perfect use or method-failure rates, but data on pregnancy risk based on reported adherence alone are lacking, they said.
To assess the effects of missed pills on COC efficacy, the researchers reviewed data from a pair of parallel phase 3 trials, focusing only on adherence to the pill dosing regimen. The findings were published in Obstetrics & Gynecology.
The study population included 1,864 individuals from the United States and Canada, and 1,553 from Europe and Russia.
The participants were healthy, sexually active adults aged 16-50 years in monogamous relationships from 2016 through 2018 who agreed to used estetrol 15 mg and drospirenone 3 mg for up to 13 28-day cycles as their only contraceptive method. Condom use was permitted for protection against sexually transmitted infections if needed. The 28-day COCs included 24 hormonal tablets and 4 placebo tablets. Participants received written instructions for what to do it they missed pills.
The primary outcome was the relationship between missed pills and pregnancies.
A total of 31 pregnancies occurred across both studies; none of these occurred during cycles in which other contraception was used. Of 22 pregnancies in participants who reported taking all pills, 21 reported daily pill use during the cycle in which pregnancy occurred. One participant reported not taking one pill and one participant reported not taking two pills; neither correctly followed the instructions for missed pills.
Pregnancies occurred in .09% of cycles in which participants reported taking all pills, and in 0.25%, 0.83%, and 1.6% of cycles in which participants reported missing one pill, two pills, or more than two pills, respectively.
“Pregnancy rates exceeded 1% only in participants who did not correctly follow missed-pill instructions,” the researchers noted.
Pregnancy rates per cycle ranged from 0% to 0.21%, and 48.4% of the pregnancies occurred during the first four cycles of COC use. Approximately one-third (32.3%) of pregnancies occurred within the first week of a new pill pack.
“Fertilization does not appear to be related to the timing of missed pills within the cycle because pregnancy did not occur more frequently earlier in the cycle (after the placebo pills),” the researchers wrote in their discussion. This finding contradicts previous research suggesting that contraceptive failure rates decrease over the first year of use, they said. In addition, the formulation of the pill used may affect pregnancy rates when pills are missed, as some hormones have longer half-lives, they noted.
The study findings were limited by several factors, including the lack of adjustment for outcomes based on reported sexual activity per cycle, and by the reliance on self-reports.
However, the results were strengthened by the use of the clinical outcomes of pregnancy as the primary outcome, rather than characteristics and predictors of participants who missed pills, the researchers said.
The cycle-based methodology used in the current study may provide insight on the relationship between COC adherence and pregnancy risk that can inform future studies, they concluded.
Findings highlight the importance of options
“With increasing restrictions on abortion care, offering more contraceptive options for people is critical,” Lauren Owens, MD, associate professor of obstetrics and gynecology at the University of Washington, Seattle, said in an interview. “That’s not to say that having another pill option makes up for the harm people are experiencing as they navigate abortion bans and legal interference in their health care, but no one pill works for all people, and having more options is helpful,” she said.
Dr. Owens noted that the rates of pregnancy in the current study were lower than she traditionally associates with COCs, “although I usually discuss annual failure rates with patients, not failure rates per cycle, and the latter will clearly be lower.” In the current study, “The authors hypothesize some of this may be due to the longer half-life that estetrol has compared to ethinyl estradiol, the estrogen form more commonly found in oral contraceptive pills,” she said.
From a clinical standpoint, “I appreciated the linkage between number of missed pills and pregnancies occurring,” Dr. Owens said. “This is a good reminder to clinicians to talk to patients ahead of time about what to do when missed pills occur and to provide resources in advance that patients can reference when needed,” she said.
“The authors published other studies on this pill in the last year and it seems to work well and have a reasonable safety profile,” Dr. Owens told this news organization. However, “We still need to broaden the methods available to patients, particularly methods that people producing sperm can use. In the face of ongoing and escalating attacks on access to contraceptive care and abortion care, it’s more important than ever to do what we can to improve options for patients,” she said.
The study was supported by Estetra SRL, an affiliate company of Mithra Pharmaceuticals. Dr. Creinin disclosed relationships with multiple companies including Gedeon Richter, Mayne, and Organon. He disclosed serving on the advisory boards for Evofem, Fuji Pharma, Gedeon Richter, GlaxoSmithKline, Mayne, Merck, OLIC, Organon, and Searchlight, and serving as a consultant for Estetra SRL (including the current study), Libbs, Mayne, and Medicines360; his university department receives contraceptive research funding from Chemo Research SL, Evofem, HRA Pharma, Medicines360, Merck, and Sebela. Dr. Owens had no relevant financial conflicts to disclose.
Combined oral contraceptives (COCs) remain a popular method of pregnancy prevention worldwide, but efficacy and failure rates can be difficult to determine, as real-word use does not always mirror clinical trials, wrote Mitchell D. Creinin, MD, of the University of California, Davis, and colleagues. Clinical trials include perfect use or method-failure rates, but data on pregnancy risk based on reported adherence alone are lacking, they said.
To assess the effects of missed pills on COC efficacy, the researchers reviewed data from a pair of parallel phase 3 trials, focusing only on adherence to the pill dosing regimen. The findings were published in Obstetrics & Gynecology.
The study population included 1,864 individuals from the United States and Canada, and 1,553 from Europe and Russia.
The participants were healthy, sexually active adults aged 16-50 years in monogamous relationships from 2016 through 2018 who agreed to used estetrol 15 mg and drospirenone 3 mg for up to 13 28-day cycles as their only contraceptive method. Condom use was permitted for protection against sexually transmitted infections if needed. The 28-day COCs included 24 hormonal tablets and 4 placebo tablets. Participants received written instructions for what to do it they missed pills.
The primary outcome was the relationship between missed pills and pregnancies.
A total of 31 pregnancies occurred across both studies; none of these occurred during cycles in which other contraception was used. Of 22 pregnancies in participants who reported taking all pills, 21 reported daily pill use during the cycle in which pregnancy occurred. One participant reported not taking one pill and one participant reported not taking two pills; neither correctly followed the instructions for missed pills.
Pregnancies occurred in .09% of cycles in which participants reported taking all pills, and in 0.25%, 0.83%, and 1.6% of cycles in which participants reported missing one pill, two pills, or more than two pills, respectively.
“Pregnancy rates exceeded 1% only in participants who did not correctly follow missed-pill instructions,” the researchers noted.
Pregnancy rates per cycle ranged from 0% to 0.21%, and 48.4% of the pregnancies occurred during the first four cycles of COC use. Approximately one-third (32.3%) of pregnancies occurred within the first week of a new pill pack.
“Fertilization does not appear to be related to the timing of missed pills within the cycle because pregnancy did not occur more frequently earlier in the cycle (after the placebo pills),” the researchers wrote in their discussion. This finding contradicts previous research suggesting that contraceptive failure rates decrease over the first year of use, they said. In addition, the formulation of the pill used may affect pregnancy rates when pills are missed, as some hormones have longer half-lives, they noted.
The study findings were limited by several factors, including the lack of adjustment for outcomes based on reported sexual activity per cycle, and by the reliance on self-reports.
However, the results were strengthened by the use of the clinical outcomes of pregnancy as the primary outcome, rather than characteristics and predictors of participants who missed pills, the researchers said.
The cycle-based methodology used in the current study may provide insight on the relationship between COC adherence and pregnancy risk that can inform future studies, they concluded.
Findings highlight the importance of options
“With increasing restrictions on abortion care, offering more contraceptive options for people is critical,” Lauren Owens, MD, associate professor of obstetrics and gynecology at the University of Washington, Seattle, said in an interview. “That’s not to say that having another pill option makes up for the harm people are experiencing as they navigate abortion bans and legal interference in their health care, but no one pill works for all people, and having more options is helpful,” she said.
Dr. Owens noted that the rates of pregnancy in the current study were lower than she traditionally associates with COCs, “although I usually discuss annual failure rates with patients, not failure rates per cycle, and the latter will clearly be lower.” In the current study, “The authors hypothesize some of this may be due to the longer half-life that estetrol has compared to ethinyl estradiol, the estrogen form more commonly found in oral contraceptive pills,” she said.
From a clinical standpoint, “I appreciated the linkage between number of missed pills and pregnancies occurring,” Dr. Owens said. “This is a good reminder to clinicians to talk to patients ahead of time about what to do when missed pills occur and to provide resources in advance that patients can reference when needed,” she said.
“The authors published other studies on this pill in the last year and it seems to work well and have a reasonable safety profile,” Dr. Owens told this news organization. However, “We still need to broaden the methods available to patients, particularly methods that people producing sperm can use. In the face of ongoing and escalating attacks on access to contraceptive care and abortion care, it’s more important than ever to do what we can to improve options for patients,” she said.
The study was supported by Estetra SRL, an affiliate company of Mithra Pharmaceuticals. Dr. Creinin disclosed relationships with multiple companies including Gedeon Richter, Mayne, and Organon. He disclosed serving on the advisory boards for Evofem, Fuji Pharma, Gedeon Richter, GlaxoSmithKline, Mayne, Merck, OLIC, Organon, and Searchlight, and serving as a consultant for Estetra SRL (including the current study), Libbs, Mayne, and Medicines360; his university department receives contraceptive research funding from Chemo Research SL, Evofem, HRA Pharma, Medicines360, Merck, and Sebela. Dr. Owens had no relevant financial conflicts to disclose.
FROM OBSTETRICS & GYNECOLOGY
Frustration over iPLEDGE evident at FDA meeting
During 2 days of after the chaotic rollout of the new REMS platform at the end of 2021.
On March 29, at the end of the FDA’s joint meeting of two advisory committees that addressed ways to improve the iPLEDGE program, most panelists voted to change the 19-day lockout period for patients who can become pregnant, and the requirement that every month, providers must document counseling of those who cannot get pregnant and are taking the drug for acne.
However, there was no consensus on whether there should be a lockout at all or for how long, and what an appropriate interval for counseling those who cannot get pregnant would be, if not monthly. Those voting on the questions repeatedly cited a lack of data to make well-informed decisions.
The meeting of the two panels, the FDA’s Drug Safety and Risk Management Advisory Committee and the Dermatologic and Ophthalmic Drugs Advisory Committee, was held March 28-29, to discuss proposed changes to iPLEDGE requirements, to minimize the program’s burden on patients, prescribers, and pharmacies – while maintaining safe use of the highly teratogenic drug.
Lockout based on outdated reasoning
John S. Barbieri, MD, a dermatologist and epidemiologist, and director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital in Boston, speaking as deputy chair of the American Academy of Dermatology Association (AADA) iPLEDGE work group, described the burden of getting the drug to patients. He was not on the panel, but spoke during the open public hearing.
“Compared to other acne medications, the time it takes to successfully go from prescribed (isotretinoin) to when the patient actually has it in their hands is 5- to 10-fold higher,” he said.
Among the barriers is the 19-day lockout period for people who can get pregnant and miss the 7-day window for picking up their prescriptions. They must then wait 19 days to get a pregnancy test to clear them for receiving the medication.
Gregory Wedin, PharmD, pharmacovigilance and risk management director of Upsher-Smith Laboratories, who spoke on behalf of the Isotretinoin Products Manufacturer Group (IPMG), which manages iPLEDGE, said, “The rationale for the 19-day wait is to ensure the next confirmatory pregnancy test is completed after the most fertile period of the menstrual cycle is passed.”
Many don’t have a monthly cycle
But Dr. Barbieri said that reasoning is outdated.
“The current program’s focus on the menstrual cycle is really an antiquated approach,” he said. “Many patients do not have a monthly cycle due to medical conditions like polycystic ovarian syndrome, or due to [certain kinds of] contraception.”
He added, “By removing this 19-day lockout and, really, the archaic timing around the menstrual cycle in general in this program, we can simplify the program, improve it, and better align it with the real-world biology of our patients.” He added that patients are often missing the 7-day window for picking up their prescriptions through no fault of their own. Speakers at the hearing also mentioned insurance hassles and ordering delays.
Communication with IPMG
Ilona Frieden, MD, professor of dermatology and pediatrics at the University of California, San Francisco, and outgoing chair of the AADA iPLEDGE work group, cited difficulty in working with IPMG on modifications as another barrier. She also spoke during the open public hearing.
“Despite many, many attempts to work with the IPMG, we are not aware of any organizational structure or key leaders to communicate with. Instead we have been given repeatedly a generic email address for trying to establish a working relationship and we believe this may explain the inaction of the IPMG since our proposals 4 years ago in 2019.”
Among those proposals, she said, were allowing telemedicine visits as part of the iPLEDGE REMS program and reducing counseling attestation to every 6 months instead of monthly for those who cannot become pregnant.
She pointed to the chaotic rollout of modifications to the iPLEDGE program on a new website at the end of 2021.
In 2021, she said, “despite 6 months of notification, no prescriber input was solicited before revamping the website. This lack of transparency and accountability has been a major hurdle in improving iPLEDGE.”
Dr. Barbieri called the rollout “a debacle” that could have been mitigated with communication with IPMG. “We warned about every issue that happened and talked about ways to mitigate it and were largely ignored,” he said.
“By including dermatologists and key stakeholders in these discussions, as we move forward with changes to improve this program, we can make sure that it’s patient-centered.”
IPMG did not address the specific complaints about the working relationship with the AADA workgroup at the meeting.
Monthly attestation for counseling patients who cannot get pregnant
Dr. Barbieri said the monthly requirement to counsel patients who cannot get pregnant and document that counseling unfairly burdens clinicians and patients. “We’re essentially asking patients to come in monthly just to tell them not to share their drugs [or] donate blood,” he said.
Ken Katz, MD, MSc, a dermatologist at Kaiser Permanente in San Francisco, was among the panel members voting not to continue the 19-day lockout.
“I think this places an unduly high burden physically and psychologically on our patients. It seems arbitrary,” he said. “Likely we will miss some pregnancies; we are missing some already. But the burden is not matched by the benefit.”
IPMG representative Dr. Wedin, said, “while we cannot support eliminating or extending the confirmation interval to a year, the [iPLEDGE] sponsors are agreeable [to] a 120-day confirmation interval.”
He said that while an extension to 120 days would reduce burden on prescribers, it comes with the risk in reducing oversight by a certified iPLEDGE prescriber and potentially increasing the risk for drug sharing.
“A patient may be more likely to share their drug with another person the further along with therapy they get as their condition improves,” Dr. Wedin said.
Home pregnancy testing
The advisory groups were also tasked with discussing whether home pregnancy tests, allowed during the COVID-19 public health emergency, should continue to be allowed. Most committee members and those in the public hearing who spoke on the issue agreed that home tests should continue in an effort to increase access and decrease burden.
During the pandemic, iPLEDGE rules have been relaxed from having a pregnancy test done only at a Clinical Laboratory Improvement Amendments–certified laboratory.
Lindsey Crist, PharmD, a risk management analyst at the FDA, who presented the FDA review committee’s analysis, said that the FDA’s review committee recommends ending the allowance of home tests, citing insufficient data on use and the discovery of instances of falsification of pregnancy tests.
“One study at an academic medical center reviewed the medical records of 89 patients who used home pregnancy tests while taking isotretinoin during the public health emergency. It found that 15.7% submitted falsified pregnancy test results,” Dr. Crist said.
Dr. Crist added, however, that the review committee recommends allowing the tests to be done in a provider’s office as an alternative.
Workaround to avoid falsification
Advisory committee member Brian P. Green, DO, associate professor of dermatology at Penn State University, Hershey, Pa., spoke in support of home pregnancy tests.
“What we have people do for telemedicine is take the stick, write their name, write the date on it, and send a picture of that the same day as their visit,” he said. “That way we have the pregnancy test the same day. Allowing this to continue to happen at home is important. Bringing people in is burdensome and costly.”
Emmy Graber, MD, a dermatologist who practices in Boston, and a director of the American Acne and Rosacea Society (AARS), relayed an example of the burden for a patient using isotretinoin who lives 1.5 hours away from the dermatology office. She is able to meet the requirements of iPLEDGE only through telehealth.
“Home pregnancy tests are highly sensitive, equal to the ones done in CLIA-certified labs, and highly accurate when interpreted by a dermatology provider,” said Dr. Graber, who spoke on behalf of the AARS during the open public hearing.
“Notably, CLIA [Clinical Laboratory Improvement Amendments] certification is not required by other REMS programs” for teratogenic drugs, she added.
Dr. Graber said it’s important to note that in the time the pandemic exceptions have been made for isotretinoin patients, “there has been no reported spike in pregnancy in the past three years.
“We do have some data to show that it is not imposing additional harms,” she said.
Suggestions for improvement
At the end of the hearing, advisory committee members were asked to propose improvements to the iPLEDGE REMS program.
Dr. Green advocated for the addition of an iPLEDGE mobile app.
“Most people go to their phones rather than their computers, particularly teenagers and younger people,” he noted.
Advisory committee member Megha M. Tollefson, MD, professor of dermatology and pediatric and adolescent medicine at Mayo Clinic in Rochester, Minn., echoed the need for an iPLEDGE app.
The young patients getting isotretinoin “don’t respond to email, they don’t necessarily go onto web pages. If we’re going to be as effective as possible, it’s going to have to be through an app-based system.”
Dr. Tollefson said she would like to see patient counseling standardized through the app. “I think there’s a lot of variability in what counseling is given when it’s left to the individual prescriber or practice,” she said.
Exceptions for long-acting contraceptives?
Advisory committee member Abbey B. Berenson, MD, PhD, professor of obstetrics and gynecology at University of Texas Medical Branch in Galveston, said that patients taking long-acting reversible contraceptives (LARCs) may need to be considered differently when deciding the intervals for attestation or whether to have a lockout period.
“LARC methods’ rate of failure is extremely low,” she said. “While it is true, as it has been pointed out, that all methods can fail, when they’re over 99% effective, I think that we can treat those methods differently than we treat methods such as birth control pills or abstinence that fail far more often. That is one way we could minimize burden on the providers and the patients.”
She also suggested using members of the health care team other than physicians to complete counseling, such as a nurse or pharmacist.
Prescriptions for emergency contraception
Advisory committee member Sascha Dublin, MD, PhD, senior scientific investigator for Kaiser Permanente Washington Health Research Institute in Seattle, said most patients taking the drug who can get pregnant should get a prescription for emergency contraception at the time of the first isotretinoin prescription.
“They don’t have to buy it, but to make it available at the very beginning sets the expectation that it would be good to have in your medicine cabinet, particularly if the [contraception] choice is abstinence or birth control pills.”
Dr. Dublin also called for better transparency surrounding the role of IPMG.
She said IPMG should be expected to collect data in a way that allows examination of health disparities, including by race and ethnicity and insurance status. Dr. Dublin added that she was concerned about the poor communication between dermatological societies and IPMG.
“The FDA should really require that IPMG hold periodic, regularly scheduled stakeholder forums,” she said. “There has to be a mechanism in place for IPMG to listen to those concerns in real time and respond.”
The advisory committees’ recommendations to the FDA are nonbinding, but the FDA generally follows the recommendations of advisory panels.
During 2 days of after the chaotic rollout of the new REMS platform at the end of 2021.
On March 29, at the end of the FDA’s joint meeting of two advisory committees that addressed ways to improve the iPLEDGE program, most panelists voted to change the 19-day lockout period for patients who can become pregnant, and the requirement that every month, providers must document counseling of those who cannot get pregnant and are taking the drug for acne.
However, there was no consensus on whether there should be a lockout at all or for how long, and what an appropriate interval for counseling those who cannot get pregnant would be, if not monthly. Those voting on the questions repeatedly cited a lack of data to make well-informed decisions.
The meeting of the two panels, the FDA’s Drug Safety and Risk Management Advisory Committee and the Dermatologic and Ophthalmic Drugs Advisory Committee, was held March 28-29, to discuss proposed changes to iPLEDGE requirements, to minimize the program’s burden on patients, prescribers, and pharmacies – while maintaining safe use of the highly teratogenic drug.
Lockout based on outdated reasoning
John S. Barbieri, MD, a dermatologist and epidemiologist, and director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital in Boston, speaking as deputy chair of the American Academy of Dermatology Association (AADA) iPLEDGE work group, described the burden of getting the drug to patients. He was not on the panel, but spoke during the open public hearing.
“Compared to other acne medications, the time it takes to successfully go from prescribed (isotretinoin) to when the patient actually has it in their hands is 5- to 10-fold higher,” he said.
Among the barriers is the 19-day lockout period for people who can get pregnant and miss the 7-day window for picking up their prescriptions. They must then wait 19 days to get a pregnancy test to clear them for receiving the medication.
Gregory Wedin, PharmD, pharmacovigilance and risk management director of Upsher-Smith Laboratories, who spoke on behalf of the Isotretinoin Products Manufacturer Group (IPMG), which manages iPLEDGE, said, “The rationale for the 19-day wait is to ensure the next confirmatory pregnancy test is completed after the most fertile period of the menstrual cycle is passed.”
Many don’t have a monthly cycle
But Dr. Barbieri said that reasoning is outdated.
“The current program’s focus on the menstrual cycle is really an antiquated approach,” he said. “Many patients do not have a monthly cycle due to medical conditions like polycystic ovarian syndrome, or due to [certain kinds of] contraception.”
He added, “By removing this 19-day lockout and, really, the archaic timing around the menstrual cycle in general in this program, we can simplify the program, improve it, and better align it with the real-world biology of our patients.” He added that patients are often missing the 7-day window for picking up their prescriptions through no fault of their own. Speakers at the hearing also mentioned insurance hassles and ordering delays.
Communication with IPMG
Ilona Frieden, MD, professor of dermatology and pediatrics at the University of California, San Francisco, and outgoing chair of the AADA iPLEDGE work group, cited difficulty in working with IPMG on modifications as another barrier. She also spoke during the open public hearing.
“Despite many, many attempts to work with the IPMG, we are not aware of any organizational structure or key leaders to communicate with. Instead we have been given repeatedly a generic email address for trying to establish a working relationship and we believe this may explain the inaction of the IPMG since our proposals 4 years ago in 2019.”
Among those proposals, she said, were allowing telemedicine visits as part of the iPLEDGE REMS program and reducing counseling attestation to every 6 months instead of monthly for those who cannot become pregnant.
She pointed to the chaotic rollout of modifications to the iPLEDGE program on a new website at the end of 2021.
In 2021, she said, “despite 6 months of notification, no prescriber input was solicited before revamping the website. This lack of transparency and accountability has been a major hurdle in improving iPLEDGE.”
Dr. Barbieri called the rollout “a debacle” that could have been mitigated with communication with IPMG. “We warned about every issue that happened and talked about ways to mitigate it and were largely ignored,” he said.
“By including dermatologists and key stakeholders in these discussions, as we move forward with changes to improve this program, we can make sure that it’s patient-centered.”
IPMG did not address the specific complaints about the working relationship with the AADA workgroup at the meeting.
Monthly attestation for counseling patients who cannot get pregnant
Dr. Barbieri said the monthly requirement to counsel patients who cannot get pregnant and document that counseling unfairly burdens clinicians and patients. “We’re essentially asking patients to come in monthly just to tell them not to share their drugs [or] donate blood,” he said.
Ken Katz, MD, MSc, a dermatologist at Kaiser Permanente in San Francisco, was among the panel members voting not to continue the 19-day lockout.
“I think this places an unduly high burden physically and psychologically on our patients. It seems arbitrary,” he said. “Likely we will miss some pregnancies; we are missing some already. But the burden is not matched by the benefit.”
IPMG representative Dr. Wedin, said, “while we cannot support eliminating or extending the confirmation interval to a year, the [iPLEDGE] sponsors are agreeable [to] a 120-day confirmation interval.”
He said that while an extension to 120 days would reduce burden on prescribers, it comes with the risk in reducing oversight by a certified iPLEDGE prescriber and potentially increasing the risk for drug sharing.
“A patient may be more likely to share their drug with another person the further along with therapy they get as their condition improves,” Dr. Wedin said.
Home pregnancy testing
The advisory groups were also tasked with discussing whether home pregnancy tests, allowed during the COVID-19 public health emergency, should continue to be allowed. Most committee members and those in the public hearing who spoke on the issue agreed that home tests should continue in an effort to increase access and decrease burden.
During the pandemic, iPLEDGE rules have been relaxed from having a pregnancy test done only at a Clinical Laboratory Improvement Amendments–certified laboratory.
Lindsey Crist, PharmD, a risk management analyst at the FDA, who presented the FDA review committee’s analysis, said that the FDA’s review committee recommends ending the allowance of home tests, citing insufficient data on use and the discovery of instances of falsification of pregnancy tests.
“One study at an academic medical center reviewed the medical records of 89 patients who used home pregnancy tests while taking isotretinoin during the public health emergency. It found that 15.7% submitted falsified pregnancy test results,” Dr. Crist said.
Dr. Crist added, however, that the review committee recommends allowing the tests to be done in a provider’s office as an alternative.
Workaround to avoid falsification
Advisory committee member Brian P. Green, DO, associate professor of dermatology at Penn State University, Hershey, Pa., spoke in support of home pregnancy tests.
“What we have people do for telemedicine is take the stick, write their name, write the date on it, and send a picture of that the same day as their visit,” he said. “That way we have the pregnancy test the same day. Allowing this to continue to happen at home is important. Bringing people in is burdensome and costly.”
Emmy Graber, MD, a dermatologist who practices in Boston, and a director of the American Acne and Rosacea Society (AARS), relayed an example of the burden for a patient using isotretinoin who lives 1.5 hours away from the dermatology office. She is able to meet the requirements of iPLEDGE only through telehealth.
“Home pregnancy tests are highly sensitive, equal to the ones done in CLIA-certified labs, and highly accurate when interpreted by a dermatology provider,” said Dr. Graber, who spoke on behalf of the AARS during the open public hearing.
“Notably, CLIA [Clinical Laboratory Improvement Amendments] certification is not required by other REMS programs” for teratogenic drugs, she added.
Dr. Graber said it’s important to note that in the time the pandemic exceptions have been made for isotretinoin patients, “there has been no reported spike in pregnancy in the past three years.
“We do have some data to show that it is not imposing additional harms,” she said.
Suggestions for improvement
At the end of the hearing, advisory committee members were asked to propose improvements to the iPLEDGE REMS program.
Dr. Green advocated for the addition of an iPLEDGE mobile app.
“Most people go to their phones rather than their computers, particularly teenagers and younger people,” he noted.
Advisory committee member Megha M. Tollefson, MD, professor of dermatology and pediatric and adolescent medicine at Mayo Clinic in Rochester, Minn., echoed the need for an iPLEDGE app.
The young patients getting isotretinoin “don’t respond to email, they don’t necessarily go onto web pages. If we’re going to be as effective as possible, it’s going to have to be through an app-based system.”
Dr. Tollefson said she would like to see patient counseling standardized through the app. “I think there’s a lot of variability in what counseling is given when it’s left to the individual prescriber or practice,” she said.
Exceptions for long-acting contraceptives?
Advisory committee member Abbey B. Berenson, MD, PhD, professor of obstetrics and gynecology at University of Texas Medical Branch in Galveston, said that patients taking long-acting reversible contraceptives (LARCs) may need to be considered differently when deciding the intervals for attestation or whether to have a lockout period.
“LARC methods’ rate of failure is extremely low,” she said. “While it is true, as it has been pointed out, that all methods can fail, when they’re over 99% effective, I think that we can treat those methods differently than we treat methods such as birth control pills or abstinence that fail far more often. That is one way we could minimize burden on the providers and the patients.”
She also suggested using members of the health care team other than physicians to complete counseling, such as a nurse or pharmacist.
Prescriptions for emergency contraception
Advisory committee member Sascha Dublin, MD, PhD, senior scientific investigator for Kaiser Permanente Washington Health Research Institute in Seattle, said most patients taking the drug who can get pregnant should get a prescription for emergency contraception at the time of the first isotretinoin prescription.
“They don’t have to buy it, but to make it available at the very beginning sets the expectation that it would be good to have in your medicine cabinet, particularly if the [contraception] choice is abstinence or birth control pills.”
Dr. Dublin also called for better transparency surrounding the role of IPMG.
She said IPMG should be expected to collect data in a way that allows examination of health disparities, including by race and ethnicity and insurance status. Dr. Dublin added that she was concerned about the poor communication between dermatological societies and IPMG.
“The FDA should really require that IPMG hold periodic, regularly scheduled stakeholder forums,” she said. “There has to be a mechanism in place for IPMG to listen to those concerns in real time and respond.”
The advisory committees’ recommendations to the FDA are nonbinding, but the FDA generally follows the recommendations of advisory panels.
During 2 days of after the chaotic rollout of the new REMS platform at the end of 2021.
On March 29, at the end of the FDA’s joint meeting of two advisory committees that addressed ways to improve the iPLEDGE program, most panelists voted to change the 19-day lockout period for patients who can become pregnant, and the requirement that every month, providers must document counseling of those who cannot get pregnant and are taking the drug for acne.
However, there was no consensus on whether there should be a lockout at all or for how long, and what an appropriate interval for counseling those who cannot get pregnant would be, if not monthly. Those voting on the questions repeatedly cited a lack of data to make well-informed decisions.
The meeting of the two panels, the FDA’s Drug Safety and Risk Management Advisory Committee and the Dermatologic and Ophthalmic Drugs Advisory Committee, was held March 28-29, to discuss proposed changes to iPLEDGE requirements, to minimize the program’s burden on patients, prescribers, and pharmacies – while maintaining safe use of the highly teratogenic drug.
Lockout based on outdated reasoning
John S. Barbieri, MD, a dermatologist and epidemiologist, and director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital in Boston, speaking as deputy chair of the American Academy of Dermatology Association (AADA) iPLEDGE work group, described the burden of getting the drug to patients. He was not on the panel, but spoke during the open public hearing.
“Compared to other acne medications, the time it takes to successfully go from prescribed (isotretinoin) to when the patient actually has it in their hands is 5- to 10-fold higher,” he said.
Among the barriers is the 19-day lockout period for people who can get pregnant and miss the 7-day window for picking up their prescriptions. They must then wait 19 days to get a pregnancy test to clear them for receiving the medication.
Gregory Wedin, PharmD, pharmacovigilance and risk management director of Upsher-Smith Laboratories, who spoke on behalf of the Isotretinoin Products Manufacturer Group (IPMG), which manages iPLEDGE, said, “The rationale for the 19-day wait is to ensure the next confirmatory pregnancy test is completed after the most fertile period of the menstrual cycle is passed.”
Many don’t have a monthly cycle
But Dr. Barbieri said that reasoning is outdated.
“The current program’s focus on the menstrual cycle is really an antiquated approach,” he said. “Many patients do not have a monthly cycle due to medical conditions like polycystic ovarian syndrome, or due to [certain kinds of] contraception.”
He added, “By removing this 19-day lockout and, really, the archaic timing around the menstrual cycle in general in this program, we can simplify the program, improve it, and better align it with the real-world biology of our patients.” He added that patients are often missing the 7-day window for picking up their prescriptions through no fault of their own. Speakers at the hearing also mentioned insurance hassles and ordering delays.
Communication with IPMG
Ilona Frieden, MD, professor of dermatology and pediatrics at the University of California, San Francisco, and outgoing chair of the AADA iPLEDGE work group, cited difficulty in working with IPMG on modifications as another barrier. She also spoke during the open public hearing.
“Despite many, many attempts to work with the IPMG, we are not aware of any organizational structure or key leaders to communicate with. Instead we have been given repeatedly a generic email address for trying to establish a working relationship and we believe this may explain the inaction of the IPMG since our proposals 4 years ago in 2019.”
Among those proposals, she said, were allowing telemedicine visits as part of the iPLEDGE REMS program and reducing counseling attestation to every 6 months instead of monthly for those who cannot become pregnant.
She pointed to the chaotic rollout of modifications to the iPLEDGE program on a new website at the end of 2021.
In 2021, she said, “despite 6 months of notification, no prescriber input was solicited before revamping the website. This lack of transparency and accountability has been a major hurdle in improving iPLEDGE.”
Dr. Barbieri called the rollout “a debacle” that could have been mitigated with communication with IPMG. “We warned about every issue that happened and talked about ways to mitigate it and were largely ignored,” he said.
“By including dermatologists and key stakeholders in these discussions, as we move forward with changes to improve this program, we can make sure that it’s patient-centered.”
IPMG did not address the specific complaints about the working relationship with the AADA workgroup at the meeting.
Monthly attestation for counseling patients who cannot get pregnant
Dr. Barbieri said the monthly requirement to counsel patients who cannot get pregnant and document that counseling unfairly burdens clinicians and patients. “We’re essentially asking patients to come in monthly just to tell them not to share their drugs [or] donate blood,” he said.
Ken Katz, MD, MSc, a dermatologist at Kaiser Permanente in San Francisco, was among the panel members voting not to continue the 19-day lockout.
“I think this places an unduly high burden physically and psychologically on our patients. It seems arbitrary,” he said. “Likely we will miss some pregnancies; we are missing some already. But the burden is not matched by the benefit.”
IPMG representative Dr. Wedin, said, “while we cannot support eliminating or extending the confirmation interval to a year, the [iPLEDGE] sponsors are agreeable [to] a 120-day confirmation interval.”
He said that while an extension to 120 days would reduce burden on prescribers, it comes with the risk in reducing oversight by a certified iPLEDGE prescriber and potentially increasing the risk for drug sharing.
“A patient may be more likely to share their drug with another person the further along with therapy they get as their condition improves,” Dr. Wedin said.
Home pregnancy testing
The advisory groups were also tasked with discussing whether home pregnancy tests, allowed during the COVID-19 public health emergency, should continue to be allowed. Most committee members and those in the public hearing who spoke on the issue agreed that home tests should continue in an effort to increase access and decrease burden.
During the pandemic, iPLEDGE rules have been relaxed from having a pregnancy test done only at a Clinical Laboratory Improvement Amendments–certified laboratory.
Lindsey Crist, PharmD, a risk management analyst at the FDA, who presented the FDA review committee’s analysis, said that the FDA’s review committee recommends ending the allowance of home tests, citing insufficient data on use and the discovery of instances of falsification of pregnancy tests.
“One study at an academic medical center reviewed the medical records of 89 patients who used home pregnancy tests while taking isotretinoin during the public health emergency. It found that 15.7% submitted falsified pregnancy test results,” Dr. Crist said.
Dr. Crist added, however, that the review committee recommends allowing the tests to be done in a provider’s office as an alternative.
Workaround to avoid falsification
Advisory committee member Brian P. Green, DO, associate professor of dermatology at Penn State University, Hershey, Pa., spoke in support of home pregnancy tests.
“What we have people do for telemedicine is take the stick, write their name, write the date on it, and send a picture of that the same day as their visit,” he said. “That way we have the pregnancy test the same day. Allowing this to continue to happen at home is important. Bringing people in is burdensome and costly.”
Emmy Graber, MD, a dermatologist who practices in Boston, and a director of the American Acne and Rosacea Society (AARS), relayed an example of the burden for a patient using isotretinoin who lives 1.5 hours away from the dermatology office. She is able to meet the requirements of iPLEDGE only through telehealth.
“Home pregnancy tests are highly sensitive, equal to the ones done in CLIA-certified labs, and highly accurate when interpreted by a dermatology provider,” said Dr. Graber, who spoke on behalf of the AARS during the open public hearing.
“Notably, CLIA [Clinical Laboratory Improvement Amendments] certification is not required by other REMS programs” for teratogenic drugs, she added.
Dr. Graber said it’s important to note that in the time the pandemic exceptions have been made for isotretinoin patients, “there has been no reported spike in pregnancy in the past three years.
“We do have some data to show that it is not imposing additional harms,” she said.
Suggestions for improvement
At the end of the hearing, advisory committee members were asked to propose improvements to the iPLEDGE REMS program.
Dr. Green advocated for the addition of an iPLEDGE mobile app.
“Most people go to their phones rather than their computers, particularly teenagers and younger people,” he noted.
Advisory committee member Megha M. Tollefson, MD, professor of dermatology and pediatric and adolescent medicine at Mayo Clinic in Rochester, Minn., echoed the need for an iPLEDGE app.
The young patients getting isotretinoin “don’t respond to email, they don’t necessarily go onto web pages. If we’re going to be as effective as possible, it’s going to have to be through an app-based system.”
Dr. Tollefson said she would like to see patient counseling standardized through the app. “I think there’s a lot of variability in what counseling is given when it’s left to the individual prescriber or practice,” she said.
Exceptions for long-acting contraceptives?
Advisory committee member Abbey B. Berenson, MD, PhD, professor of obstetrics and gynecology at University of Texas Medical Branch in Galveston, said that patients taking long-acting reversible contraceptives (LARCs) may need to be considered differently when deciding the intervals for attestation or whether to have a lockout period.
“LARC methods’ rate of failure is extremely low,” she said. “While it is true, as it has been pointed out, that all methods can fail, when they’re over 99% effective, I think that we can treat those methods differently than we treat methods such as birth control pills or abstinence that fail far more often. That is one way we could minimize burden on the providers and the patients.”
She also suggested using members of the health care team other than physicians to complete counseling, such as a nurse or pharmacist.
Prescriptions for emergency contraception
Advisory committee member Sascha Dublin, MD, PhD, senior scientific investigator for Kaiser Permanente Washington Health Research Institute in Seattle, said most patients taking the drug who can get pregnant should get a prescription for emergency contraception at the time of the first isotretinoin prescription.
“They don’t have to buy it, but to make it available at the very beginning sets the expectation that it would be good to have in your medicine cabinet, particularly if the [contraception] choice is abstinence or birth control pills.”
Dr. Dublin also called for better transparency surrounding the role of IPMG.
She said IPMG should be expected to collect data in a way that allows examination of health disparities, including by race and ethnicity and insurance status. Dr. Dublin added that she was concerned about the poor communication between dermatological societies and IPMG.
“The FDA should really require that IPMG hold periodic, regularly scheduled stakeholder forums,” she said. “There has to be a mechanism in place for IPMG to listen to those concerns in real time and respond.”
The advisory committees’ recommendations to the FDA are nonbinding, but the FDA generally follows the recommendations of advisory panels.
FDA Advisory panels consider easing isotretinoin requirements
for patients, pharmacies, and prescribers.
Isotretinoin, previously called Accutane, is marketed as Absorica, Absorica LD, Claravis, Amnesteem, Myorisan, and Zenatane.
In a joint meeting of the FDA’s Drug Safety and Risk Management Advisory Committee and Dermatologic and Ophthalmic Drugs Advisory Committee, experts addressed ways to improve the modified iPLEDGE Risk Evaluation and Mitigation Strategy (iPLEDGE REMS) for isotretinoin that caused chaos after its rollout at the end of 2021.
In January 2022, problems were multiplying with the program for clinicians, pharmacists, and patients, causing extensive delays and prescription denials. In response, the FDA said it would continue to meet with the Isotretinoin Products Manufacturers Group (IPMG) to resolve problems.
March 28 was the first day of a 2-day meeting addressing what can be done to reduce burden with the iPLEDGE REMS while maintaining safety and preventing fetal exposure to the drug.
Key areas of concern
The meeting focused on several key areas.
The 19-day lockout period
The lockout is a current restriction for patients who can become pregnant and do not pick up their first prescription of isotretinoin within the specified 7-day prescription window. Currently, those who miss the window must wait 19 days from the date of the first pregnancy test to take an additional pregnancy test to be eligible to receive the drug.
Lindsey Crist, PharmD, a risk management analyst for the FDA, who presented the FDA review committee’s analysis, acknowledged that the lockout period causes delays in treatment and adds frustration and costs.
She said it’s important to remember that the lockout applies only to the first prescription. “It’s intended as an additional layer of screening to detect pregnancy,” she said.
“At least 12 pregnancies have been identified during the 19-day lockout from March 2017–September of 2022,” she noted.
The FDA is looking to the advisory committee to provide recommendations on whether the lockout period should be changed.
Home testing
During the pandemic, iPLEDGE rules have been relaxed from having a pregnancy test done only at a Clinical Laboratory Improvement Amendments–certified laboratory and home pregnancy tests have been allowed. The question now is whether home tests should continue to be allowed.
Ms. Crist said that the FDA’s review committee recommends ending the allowance of home tests, citing insufficient data on use and the discovery of instances of falsification of pregnancy tests.
“One study at an academic medical center reviewed the medical records of 89 patients who used home pregnancy tests while taking isotretinoin during the public health emergency. It found that 15.7% submitted falsified pregnancy test results,” she said.
Ms. Crist added, however, that the review committee recommends allowing the tests to be done in a provider’s office as an alternative.
Documenting counseling patients who cannot get pregnant
Currently, this documentation must be done monthly, primarily to counsel patients against drug sharing or giving blood. Proposed changes include extending the intervals for attestation or eliminating it to reduce burden on clinicians.
IPMG representative Gregory Wedin, PharmD, pharmacovigilance and risk management director for Upsher-Smith Laboratories, said, “while we cannot support eliminating or extending the confirmation interval to a year, the [iPLEDGE] sponsors are agreeable [to] a 120-day confirmation interval.”
He said that while extending to 120 days would reduce burden on prescribers, it comes with risk in reducing oversight by a certified iPLEDGE prescriber and potentially increasing the risk for drug sharing.
“A patient may be more likely to share their drug with another person the further along with therapy they get as their condition improves,” Mr. Wedin said.
On March 29, the panel will hear more recommendations for and against modifications to iPLEDGE REMS and will vote on select modifications at the end of the meeting.
A version of this article first appeared on Medscape.com.
for patients, pharmacies, and prescribers.
Isotretinoin, previously called Accutane, is marketed as Absorica, Absorica LD, Claravis, Amnesteem, Myorisan, and Zenatane.
In a joint meeting of the FDA’s Drug Safety and Risk Management Advisory Committee and Dermatologic and Ophthalmic Drugs Advisory Committee, experts addressed ways to improve the modified iPLEDGE Risk Evaluation and Mitigation Strategy (iPLEDGE REMS) for isotretinoin that caused chaos after its rollout at the end of 2021.
In January 2022, problems were multiplying with the program for clinicians, pharmacists, and patients, causing extensive delays and prescription denials. In response, the FDA said it would continue to meet with the Isotretinoin Products Manufacturers Group (IPMG) to resolve problems.
March 28 was the first day of a 2-day meeting addressing what can be done to reduce burden with the iPLEDGE REMS while maintaining safety and preventing fetal exposure to the drug.
Key areas of concern
The meeting focused on several key areas.
The 19-day lockout period
The lockout is a current restriction for patients who can become pregnant and do not pick up their first prescription of isotretinoin within the specified 7-day prescription window. Currently, those who miss the window must wait 19 days from the date of the first pregnancy test to take an additional pregnancy test to be eligible to receive the drug.
Lindsey Crist, PharmD, a risk management analyst for the FDA, who presented the FDA review committee’s analysis, acknowledged that the lockout period causes delays in treatment and adds frustration and costs.
She said it’s important to remember that the lockout applies only to the first prescription. “It’s intended as an additional layer of screening to detect pregnancy,” she said.
“At least 12 pregnancies have been identified during the 19-day lockout from March 2017–September of 2022,” she noted.
The FDA is looking to the advisory committee to provide recommendations on whether the lockout period should be changed.
Home testing
During the pandemic, iPLEDGE rules have been relaxed from having a pregnancy test done only at a Clinical Laboratory Improvement Amendments–certified laboratory and home pregnancy tests have been allowed. The question now is whether home tests should continue to be allowed.
Ms. Crist said that the FDA’s review committee recommends ending the allowance of home tests, citing insufficient data on use and the discovery of instances of falsification of pregnancy tests.
“One study at an academic medical center reviewed the medical records of 89 patients who used home pregnancy tests while taking isotretinoin during the public health emergency. It found that 15.7% submitted falsified pregnancy test results,” she said.
Ms. Crist added, however, that the review committee recommends allowing the tests to be done in a provider’s office as an alternative.
Documenting counseling patients who cannot get pregnant
Currently, this documentation must be done monthly, primarily to counsel patients against drug sharing or giving blood. Proposed changes include extending the intervals for attestation or eliminating it to reduce burden on clinicians.
IPMG representative Gregory Wedin, PharmD, pharmacovigilance and risk management director for Upsher-Smith Laboratories, said, “while we cannot support eliminating or extending the confirmation interval to a year, the [iPLEDGE] sponsors are agreeable [to] a 120-day confirmation interval.”
He said that while extending to 120 days would reduce burden on prescribers, it comes with risk in reducing oversight by a certified iPLEDGE prescriber and potentially increasing the risk for drug sharing.
“A patient may be more likely to share their drug with another person the further along with therapy they get as their condition improves,” Mr. Wedin said.
On March 29, the panel will hear more recommendations for and against modifications to iPLEDGE REMS and will vote on select modifications at the end of the meeting.
A version of this article first appeared on Medscape.com.
for patients, pharmacies, and prescribers.
Isotretinoin, previously called Accutane, is marketed as Absorica, Absorica LD, Claravis, Amnesteem, Myorisan, and Zenatane.
In a joint meeting of the FDA’s Drug Safety and Risk Management Advisory Committee and Dermatologic and Ophthalmic Drugs Advisory Committee, experts addressed ways to improve the modified iPLEDGE Risk Evaluation and Mitigation Strategy (iPLEDGE REMS) for isotretinoin that caused chaos after its rollout at the end of 2021.
In January 2022, problems were multiplying with the program for clinicians, pharmacists, and patients, causing extensive delays and prescription denials. In response, the FDA said it would continue to meet with the Isotretinoin Products Manufacturers Group (IPMG) to resolve problems.
March 28 was the first day of a 2-day meeting addressing what can be done to reduce burden with the iPLEDGE REMS while maintaining safety and preventing fetal exposure to the drug.
Key areas of concern
The meeting focused on several key areas.
The 19-day lockout period
The lockout is a current restriction for patients who can become pregnant and do not pick up their first prescription of isotretinoin within the specified 7-day prescription window. Currently, those who miss the window must wait 19 days from the date of the first pregnancy test to take an additional pregnancy test to be eligible to receive the drug.
Lindsey Crist, PharmD, a risk management analyst for the FDA, who presented the FDA review committee’s analysis, acknowledged that the lockout period causes delays in treatment and adds frustration and costs.
She said it’s important to remember that the lockout applies only to the first prescription. “It’s intended as an additional layer of screening to detect pregnancy,” she said.
“At least 12 pregnancies have been identified during the 19-day lockout from March 2017–September of 2022,” she noted.
The FDA is looking to the advisory committee to provide recommendations on whether the lockout period should be changed.
Home testing
During the pandemic, iPLEDGE rules have been relaxed from having a pregnancy test done only at a Clinical Laboratory Improvement Amendments–certified laboratory and home pregnancy tests have been allowed. The question now is whether home tests should continue to be allowed.
Ms. Crist said that the FDA’s review committee recommends ending the allowance of home tests, citing insufficient data on use and the discovery of instances of falsification of pregnancy tests.
“One study at an academic medical center reviewed the medical records of 89 patients who used home pregnancy tests while taking isotretinoin during the public health emergency. It found that 15.7% submitted falsified pregnancy test results,” she said.
Ms. Crist added, however, that the review committee recommends allowing the tests to be done in a provider’s office as an alternative.
Documenting counseling patients who cannot get pregnant
Currently, this documentation must be done monthly, primarily to counsel patients against drug sharing or giving blood. Proposed changes include extending the intervals for attestation or eliminating it to reduce burden on clinicians.
IPMG representative Gregory Wedin, PharmD, pharmacovigilance and risk management director for Upsher-Smith Laboratories, said, “while we cannot support eliminating or extending the confirmation interval to a year, the [iPLEDGE] sponsors are agreeable [to] a 120-day confirmation interval.”
He said that while extending to 120 days would reduce burden on prescribers, it comes with risk in reducing oversight by a certified iPLEDGE prescriber and potentially increasing the risk for drug sharing.
“A patient may be more likely to share their drug with another person the further along with therapy they get as their condition improves,” Mr. Wedin said.
On March 29, the panel will hear more recommendations for and against modifications to iPLEDGE REMS and will vote on select modifications at the end of the meeting.
A version of this article first appeared on Medscape.com.
Risk of expulsion low after early postpartum IUD placement
Intrauterine device (IUD) placement at 2-4 weeks postpartum was noninferior to placement at 6-8 weeks postpartum for complete expulsion, and carried only a slightly higher risk of partial expulsion. A randomized study of expulsion rates reports the risk of expulsion at these points may help patients and clinicians make informed choices about the timing of IUD insertion, wrote the study authors, led by Sarah H. Averbach, MD, MAS, an obstetrician-gynecologist at the University of California, San Diego. “We found that the risk of complete IUD expulsion was low at 2% after early IUD placement 2-4 weeks after delivery, and was noninferior to interval placement 6-8 weeks after delivery at 0%,” Dr. Averbach said in an interview.
Although the risks of partial expulsion and malposition were modestly greater after early placement, “the possibility of a small increase in the risk of IUD expulsion or malposition with early IUD placement should be weighed against the risk of undesired pregnancy and short-interval pregnancy by delaying placement.”
The timing of IUD placement in the postpartum period should be guided by patients’ goals and preferences, she added. The early postpartum period 2-4 weeks after birth has the advantage of convenience since it coincides with early-postpartum or well-baby visits. The absolute risk differences observed between early and interval placement were small for both complete or partial expulsion at 3.8%, and the rate for complete expulsion after early placement was much lower than historical expulsion rates for immediate postpartum placement within in few days of delivery.
Last year, a large study showed an increase in expulsion risk with IUD insertion within 3 days of delivery. Current guidelines, however, support immediate insertion as a safe practice.
The study
Enrolling 404 participants from diverse settings during the period of 2018 to July 2021, researchers for the noninferiority trial randomly assigned 203 to early IUD placement 14-28 days postpartum and 201 to standard-interval placement at 42-56 days. Patients had a mean age of 29.9 years, 11.4% were Black, 56.4% were White, and 43.3% were Hispanic (some Hispanic participants self-identified as White and some as Black). By 6 months postpartum, 73% of the cohort had received an IUD and completed 6-months of follow-up, while 13% had never received an IUD and 14% were lost to follow-up. Complete expulsion rates were 3 of 149, or 2.0% (95% confidence interval [CI], 0.4-5.8) in the early group and 0 of 145, or 0% (95% CI, 0.0-2.5) in the standard group, for a between-group difference of 2.0 percentage points (95% CI, −0.5 to 5.7, P = .04). Two women chose to replace their IUDs.
Partial expulsion occurred in 14, or 9.4% (95% CI, 5.2-15.3) of patients in the early group and 11, or 7.6% (95% CI, 3.9-13.2) in the standard-interval group, for a between-group difference of 1.8 (95% CI, −4.8 to 8.6) percentage points (P = .22).
The small absolute increase in risk of partial expulsion in the early arm did not meet the prespecified criterion for noninferiority of 6%. Three pelvic infections occurred in the early placement arm.
There were 42 IUD removals: 25 in the early placement group and 17 in the standard interval group. Thirteen participants had their IUDs removed for symptoms such as cramping and bothersome vaginal bleeding.
No perforations were identified in either group at 6 months, suggesting that the rate of uterine perforations is low when IUDs are placed in the early and standard-interval postpartum periods. IUD use at 6 months remained comparable between arms: 69.5% in the early group vs. 67.2% in the standard-interval group.
Commenting on the trial but not involved in it, Maureen K. Baldwin, MD, MPH, associate professor of obstetrics and gynecology at Oregon Health & Science University in Portland, said it provides further data on the prevalence of expulsion and malposition after placements using ultrasonography as needed. While two failures occurred with asymptomatic malposition, she added, “It should be noted that IUD position can change as a result of pregnancy, so it was not determined that malposition occurred prior to contraceptive failure.”
According to Dr. Baldwin, one strategy to reduce concerns is to use transvaginal ultrasonography at a later time or in the presence of unusual symptoms.
Overall, the study establishes that postpartum placement is an option equivalent to standard timing and it should be incorporated into patient preferences, she said. “Pain may be lowest at early placement compared to other timings, particularly for those who had vaginal birth.”
The study was supported by the Society of Family Planning research fund and the National Institutes of Health - National Institute of Child Health and Human Development. Dr. Averbach reported personal fees from Bayer Pharmaceuticals for advice on postpartum IUD placement as well as grants from the NIH outside of the submitted work. Dr. Baldwin disclosed no potential conflicts of interest with regard to her comments.
Intrauterine device (IUD) placement at 2-4 weeks postpartum was noninferior to placement at 6-8 weeks postpartum for complete expulsion, and carried only a slightly higher risk of partial expulsion. A randomized study of expulsion rates reports the risk of expulsion at these points may help patients and clinicians make informed choices about the timing of IUD insertion, wrote the study authors, led by Sarah H. Averbach, MD, MAS, an obstetrician-gynecologist at the University of California, San Diego. “We found that the risk of complete IUD expulsion was low at 2% after early IUD placement 2-4 weeks after delivery, and was noninferior to interval placement 6-8 weeks after delivery at 0%,” Dr. Averbach said in an interview.
Although the risks of partial expulsion and malposition were modestly greater after early placement, “the possibility of a small increase in the risk of IUD expulsion or malposition with early IUD placement should be weighed against the risk of undesired pregnancy and short-interval pregnancy by delaying placement.”
The timing of IUD placement in the postpartum period should be guided by patients’ goals and preferences, she added. The early postpartum period 2-4 weeks after birth has the advantage of convenience since it coincides with early-postpartum or well-baby visits. The absolute risk differences observed between early and interval placement were small for both complete or partial expulsion at 3.8%, and the rate for complete expulsion after early placement was much lower than historical expulsion rates for immediate postpartum placement within in few days of delivery.
Last year, a large study showed an increase in expulsion risk with IUD insertion within 3 days of delivery. Current guidelines, however, support immediate insertion as a safe practice.
The study
Enrolling 404 participants from diverse settings during the period of 2018 to July 2021, researchers for the noninferiority trial randomly assigned 203 to early IUD placement 14-28 days postpartum and 201 to standard-interval placement at 42-56 days. Patients had a mean age of 29.9 years, 11.4% were Black, 56.4% were White, and 43.3% were Hispanic (some Hispanic participants self-identified as White and some as Black). By 6 months postpartum, 73% of the cohort had received an IUD and completed 6-months of follow-up, while 13% had never received an IUD and 14% were lost to follow-up. Complete expulsion rates were 3 of 149, or 2.0% (95% confidence interval [CI], 0.4-5.8) in the early group and 0 of 145, or 0% (95% CI, 0.0-2.5) in the standard group, for a between-group difference of 2.0 percentage points (95% CI, −0.5 to 5.7, P = .04). Two women chose to replace their IUDs.
Partial expulsion occurred in 14, or 9.4% (95% CI, 5.2-15.3) of patients in the early group and 11, or 7.6% (95% CI, 3.9-13.2) in the standard-interval group, for a between-group difference of 1.8 (95% CI, −4.8 to 8.6) percentage points (P = .22).
The small absolute increase in risk of partial expulsion in the early arm did not meet the prespecified criterion for noninferiority of 6%. Three pelvic infections occurred in the early placement arm.
There were 42 IUD removals: 25 in the early placement group and 17 in the standard interval group. Thirteen participants had their IUDs removed for symptoms such as cramping and bothersome vaginal bleeding.
No perforations were identified in either group at 6 months, suggesting that the rate of uterine perforations is low when IUDs are placed in the early and standard-interval postpartum periods. IUD use at 6 months remained comparable between arms: 69.5% in the early group vs. 67.2% in the standard-interval group.
Commenting on the trial but not involved in it, Maureen K. Baldwin, MD, MPH, associate professor of obstetrics and gynecology at Oregon Health & Science University in Portland, said it provides further data on the prevalence of expulsion and malposition after placements using ultrasonography as needed. While two failures occurred with asymptomatic malposition, she added, “It should be noted that IUD position can change as a result of pregnancy, so it was not determined that malposition occurred prior to contraceptive failure.”
According to Dr. Baldwin, one strategy to reduce concerns is to use transvaginal ultrasonography at a later time or in the presence of unusual symptoms.
Overall, the study establishes that postpartum placement is an option equivalent to standard timing and it should be incorporated into patient preferences, she said. “Pain may be lowest at early placement compared to other timings, particularly for those who had vaginal birth.”
The study was supported by the Society of Family Planning research fund and the National Institutes of Health - National Institute of Child Health and Human Development. Dr. Averbach reported personal fees from Bayer Pharmaceuticals for advice on postpartum IUD placement as well as grants from the NIH outside of the submitted work. Dr. Baldwin disclosed no potential conflicts of interest with regard to her comments.
Intrauterine device (IUD) placement at 2-4 weeks postpartum was noninferior to placement at 6-8 weeks postpartum for complete expulsion, and carried only a slightly higher risk of partial expulsion. A randomized study of expulsion rates reports the risk of expulsion at these points may help patients and clinicians make informed choices about the timing of IUD insertion, wrote the study authors, led by Sarah H. Averbach, MD, MAS, an obstetrician-gynecologist at the University of California, San Diego. “We found that the risk of complete IUD expulsion was low at 2% after early IUD placement 2-4 weeks after delivery, and was noninferior to interval placement 6-8 weeks after delivery at 0%,” Dr. Averbach said in an interview.
Although the risks of partial expulsion and malposition were modestly greater after early placement, “the possibility of a small increase in the risk of IUD expulsion or malposition with early IUD placement should be weighed against the risk of undesired pregnancy and short-interval pregnancy by delaying placement.”
The timing of IUD placement in the postpartum period should be guided by patients’ goals and preferences, she added. The early postpartum period 2-4 weeks after birth has the advantage of convenience since it coincides with early-postpartum or well-baby visits. The absolute risk differences observed between early and interval placement were small for both complete or partial expulsion at 3.8%, and the rate for complete expulsion after early placement was much lower than historical expulsion rates for immediate postpartum placement within in few days of delivery.
Last year, a large study showed an increase in expulsion risk with IUD insertion within 3 days of delivery. Current guidelines, however, support immediate insertion as a safe practice.
The study
Enrolling 404 participants from diverse settings during the period of 2018 to July 2021, researchers for the noninferiority trial randomly assigned 203 to early IUD placement 14-28 days postpartum and 201 to standard-interval placement at 42-56 days. Patients had a mean age of 29.9 years, 11.4% were Black, 56.4% were White, and 43.3% were Hispanic (some Hispanic participants self-identified as White and some as Black). By 6 months postpartum, 73% of the cohort had received an IUD and completed 6-months of follow-up, while 13% had never received an IUD and 14% were lost to follow-up. Complete expulsion rates were 3 of 149, or 2.0% (95% confidence interval [CI], 0.4-5.8) in the early group and 0 of 145, or 0% (95% CI, 0.0-2.5) in the standard group, for a between-group difference of 2.0 percentage points (95% CI, −0.5 to 5.7, P = .04). Two women chose to replace their IUDs.
Partial expulsion occurred in 14, or 9.4% (95% CI, 5.2-15.3) of patients in the early group and 11, or 7.6% (95% CI, 3.9-13.2) in the standard-interval group, for a between-group difference of 1.8 (95% CI, −4.8 to 8.6) percentage points (P = .22).
The small absolute increase in risk of partial expulsion in the early arm did not meet the prespecified criterion for noninferiority of 6%. Three pelvic infections occurred in the early placement arm.
There were 42 IUD removals: 25 in the early placement group and 17 in the standard interval group. Thirteen participants had their IUDs removed for symptoms such as cramping and bothersome vaginal bleeding.
No perforations were identified in either group at 6 months, suggesting that the rate of uterine perforations is low when IUDs are placed in the early and standard-interval postpartum periods. IUD use at 6 months remained comparable between arms: 69.5% in the early group vs. 67.2% in the standard-interval group.
Commenting on the trial but not involved in it, Maureen K. Baldwin, MD, MPH, associate professor of obstetrics and gynecology at Oregon Health & Science University in Portland, said it provides further data on the prevalence of expulsion and malposition after placements using ultrasonography as needed. While two failures occurred with asymptomatic malposition, she added, “It should be noted that IUD position can change as a result of pregnancy, so it was not determined that malposition occurred prior to contraceptive failure.”
According to Dr. Baldwin, one strategy to reduce concerns is to use transvaginal ultrasonography at a later time or in the presence of unusual symptoms.
Overall, the study establishes that postpartum placement is an option equivalent to standard timing and it should be incorporated into patient preferences, she said. “Pain may be lowest at early placement compared to other timings, particularly for those who had vaginal birth.”
The study was supported by the Society of Family Planning research fund and the National Institutes of Health - National Institute of Child Health and Human Development. Dr. Averbach reported personal fees from Bayer Pharmaceuticals for advice on postpartum IUD placement as well as grants from the NIH outside of the submitted work. Dr. Baldwin disclosed no potential conflicts of interest with regard to her comments.
FROM JAMA
Ectopic pregnancy risk and levonorgestrel-releasing IUDs
Researchers report that use of any levonorgestrel-releasing intrauterine system was associated with a significantly increased risk of ectopic pregnancy, compared with other hormonal contraceptives, in a study published in JAMA.
A national health database analysis headed by Amani Meaidi, MD, PhD, of the Danish Cancer Society Research Center, Cancer Surveillance and Pharmacoepidemiology, in Copenhagen, compared the 13.5-mg with the 19.5-mg and 52-mg dosages of levonorgestrel-releasing intrauterine systems (IUSs).
The hormone content in levonorgestrel-releasing IUSs must be high enough to maintain optimal contraceptive effect but sufficiently low to minimize progestin-related adverse events, Dr. Meaidi and colleagues noted; they advised using the middle dosage of 19.5 mg. All dosages are recommended for contraception, with the highest dosage also recommended for heavy menstrual bleeding.
“If 10,000 women using the hormonal IUD for 1 year were given the 19.5-mg hormonal IUD instead of the 13.5-mg hormonal IUD, around nine ectopic pregnancies would be avoided,” Dr. Meaidi said in an interview.
“Ectopic pregnancy is an acknowledged adverse event of hormonal IUD use. Although a rare event, it is a serious one, and a difference in ectopic pregnancy safety between the two low-dose hormonal IUDs would impact my recommendations to women.”
The study
Dr. Meaidi’s group followed 963,964 women for 7.8 million person-years. For users of levonorgestrel IUS dosages 52 mg, 19.5 mg, and 13.5 mg, and other hormonal contraceptives, the median ages were 24, 22, 22, and 21 years, respectively.
Eligible women were nulliparous with no previous ectopic pregnancy, abdominal or pelvic surgery, infertility treatment, endometriosis, or use of a levonorgestrel IUS. They were followed from Jan. 1, 2001, or their 15th birthday, until July 1, 2021, age 35, pregnancy, death, emigration, or the occurrence of any exclusion criterion.
During the study period, the cohort registered 2,925 ectopic pregnancies, including 35 at 52 mg, 32 at 19.5 mg, and 80 at 13.5 mg of levonorgestrel. For all other types of hormonal contraception, there were 763 ectopic pregnancies.
In terms of adjusted absolute rates of ectopic pregnancy per 10,000 person-years, compared with other hormonal contraceptives (rate = 2.4), these were 7.7 with 52 mg levonorgestrel IUS, 7.1 with 19.5 mg, and 15.7 with 13.5 mg. They translated to comparative differences of 5.3 (95% confidence interval, 1.9-8.7), 4.8 (95% CI, 1.5-8.0), and 13.4 (95% CI, 8.8-18.1), respectively.
Corresponding adjusted relative rate ratios were 3.4, 4.1, and 7.9. For each levonorgestrel IUS dosage; the ectopic pregnancy rate increased with duration of use.
The adjusted ectopic pregnancy rate difference per 10,000 person-years between the 19.5-mg and 52-mg levonorgestrel dosages was −0.6 , and between the 13.5-mg and 52-mg doses, 8.0, with a rate ratio of 2.3. The rate difference between the 13.5-mg and 19.5-mg levonorgestrel IUS was 8.6, with a rate ratio of 1.9.
An outsider’s perspective
Offering an outsider’s perspective on the study, Eran Bornstein, MD, vice-chair of obstetrics and gynecology at Lenox Hill Hospital in New York, said these data should spark further evaluation of risk of ectopic pregnancy with levonorgestrel-releasing IUDs. “The best advice for clinicians is to individualize the choice of which contraceptive to use, and when levonorgestrel IUD is selected, to individualize the appropriate dose and timing of placement,” he said in an interview.
Several additional factors may determine the best choice, Dr. Bornstein added, including medical conditions that contraindicate other contraceptives and those conditions that justify avoidance of pregnancy, as well as uterine myomas or malformation, the ability of the patient to comply with other options, and informed patient choice. “It is important to remember the potential risk for expulsion and ectopic pregnancy, maintain alertness, and use ultrasound to exclude these potential complications if suspected,” he said.
Dr. Meaidi said the mechanism of ectopic pregnancy with hormonal IUDs is unclear, but in vitro and animal studies have observed that levonorgestrel reduces the ciliary beat frequency in the fallopian tubes. “Thus, it could be hypothesized that if a woman was unfortunate enough to become pregnant using a hormonal IUD, the hormone could inhibit or slow down the movement of the zygote into the uterus for rightful intrauterine implantation and thereby increase the risk of ectopic pregnancy.”
Two coauthors of the study reported financial support from private-sector companies. Dr. Meaidi had no conflicts of interest. Dr. Bornstein disclosed no competing interests.
Researchers report that use of any levonorgestrel-releasing intrauterine system was associated with a significantly increased risk of ectopic pregnancy, compared with other hormonal contraceptives, in a study published in JAMA.
A national health database analysis headed by Amani Meaidi, MD, PhD, of the Danish Cancer Society Research Center, Cancer Surveillance and Pharmacoepidemiology, in Copenhagen, compared the 13.5-mg with the 19.5-mg and 52-mg dosages of levonorgestrel-releasing intrauterine systems (IUSs).
The hormone content in levonorgestrel-releasing IUSs must be high enough to maintain optimal contraceptive effect but sufficiently low to minimize progestin-related adverse events, Dr. Meaidi and colleagues noted; they advised using the middle dosage of 19.5 mg. All dosages are recommended for contraception, with the highest dosage also recommended for heavy menstrual bleeding.
“If 10,000 women using the hormonal IUD for 1 year were given the 19.5-mg hormonal IUD instead of the 13.5-mg hormonal IUD, around nine ectopic pregnancies would be avoided,” Dr. Meaidi said in an interview.
“Ectopic pregnancy is an acknowledged adverse event of hormonal IUD use. Although a rare event, it is a serious one, and a difference in ectopic pregnancy safety between the two low-dose hormonal IUDs would impact my recommendations to women.”
The study
Dr. Meaidi’s group followed 963,964 women for 7.8 million person-years. For users of levonorgestrel IUS dosages 52 mg, 19.5 mg, and 13.5 mg, and other hormonal contraceptives, the median ages were 24, 22, 22, and 21 years, respectively.
Eligible women were nulliparous with no previous ectopic pregnancy, abdominal or pelvic surgery, infertility treatment, endometriosis, or use of a levonorgestrel IUS. They were followed from Jan. 1, 2001, or their 15th birthday, until July 1, 2021, age 35, pregnancy, death, emigration, or the occurrence of any exclusion criterion.
During the study period, the cohort registered 2,925 ectopic pregnancies, including 35 at 52 mg, 32 at 19.5 mg, and 80 at 13.5 mg of levonorgestrel. For all other types of hormonal contraception, there were 763 ectopic pregnancies.
In terms of adjusted absolute rates of ectopic pregnancy per 10,000 person-years, compared with other hormonal contraceptives (rate = 2.4), these were 7.7 with 52 mg levonorgestrel IUS, 7.1 with 19.5 mg, and 15.7 with 13.5 mg. They translated to comparative differences of 5.3 (95% confidence interval, 1.9-8.7), 4.8 (95% CI, 1.5-8.0), and 13.4 (95% CI, 8.8-18.1), respectively.
Corresponding adjusted relative rate ratios were 3.4, 4.1, and 7.9. For each levonorgestrel IUS dosage; the ectopic pregnancy rate increased with duration of use.
The adjusted ectopic pregnancy rate difference per 10,000 person-years between the 19.5-mg and 52-mg levonorgestrel dosages was −0.6 , and between the 13.5-mg and 52-mg doses, 8.0, with a rate ratio of 2.3. The rate difference between the 13.5-mg and 19.5-mg levonorgestrel IUS was 8.6, with a rate ratio of 1.9.
An outsider’s perspective
Offering an outsider’s perspective on the study, Eran Bornstein, MD, vice-chair of obstetrics and gynecology at Lenox Hill Hospital in New York, said these data should spark further evaluation of risk of ectopic pregnancy with levonorgestrel-releasing IUDs. “The best advice for clinicians is to individualize the choice of which contraceptive to use, and when levonorgestrel IUD is selected, to individualize the appropriate dose and timing of placement,” he said in an interview.
Several additional factors may determine the best choice, Dr. Bornstein added, including medical conditions that contraindicate other contraceptives and those conditions that justify avoidance of pregnancy, as well as uterine myomas or malformation, the ability of the patient to comply with other options, and informed patient choice. “It is important to remember the potential risk for expulsion and ectopic pregnancy, maintain alertness, and use ultrasound to exclude these potential complications if suspected,” he said.
Dr. Meaidi said the mechanism of ectopic pregnancy with hormonal IUDs is unclear, but in vitro and animal studies have observed that levonorgestrel reduces the ciliary beat frequency in the fallopian tubes. “Thus, it could be hypothesized that if a woman was unfortunate enough to become pregnant using a hormonal IUD, the hormone could inhibit or slow down the movement of the zygote into the uterus for rightful intrauterine implantation and thereby increase the risk of ectopic pregnancy.”
Two coauthors of the study reported financial support from private-sector companies. Dr. Meaidi had no conflicts of interest. Dr. Bornstein disclosed no competing interests.
Researchers report that use of any levonorgestrel-releasing intrauterine system was associated with a significantly increased risk of ectopic pregnancy, compared with other hormonal contraceptives, in a study published in JAMA.
A national health database analysis headed by Amani Meaidi, MD, PhD, of the Danish Cancer Society Research Center, Cancer Surveillance and Pharmacoepidemiology, in Copenhagen, compared the 13.5-mg with the 19.5-mg and 52-mg dosages of levonorgestrel-releasing intrauterine systems (IUSs).
The hormone content in levonorgestrel-releasing IUSs must be high enough to maintain optimal contraceptive effect but sufficiently low to minimize progestin-related adverse events, Dr. Meaidi and colleagues noted; they advised using the middle dosage of 19.5 mg. All dosages are recommended for contraception, with the highest dosage also recommended for heavy menstrual bleeding.
“If 10,000 women using the hormonal IUD for 1 year were given the 19.5-mg hormonal IUD instead of the 13.5-mg hormonal IUD, around nine ectopic pregnancies would be avoided,” Dr. Meaidi said in an interview.
“Ectopic pregnancy is an acknowledged adverse event of hormonal IUD use. Although a rare event, it is a serious one, and a difference in ectopic pregnancy safety between the two low-dose hormonal IUDs would impact my recommendations to women.”
The study
Dr. Meaidi’s group followed 963,964 women for 7.8 million person-years. For users of levonorgestrel IUS dosages 52 mg, 19.5 mg, and 13.5 mg, and other hormonal contraceptives, the median ages were 24, 22, 22, and 21 years, respectively.
Eligible women were nulliparous with no previous ectopic pregnancy, abdominal or pelvic surgery, infertility treatment, endometriosis, or use of a levonorgestrel IUS. They were followed from Jan. 1, 2001, or their 15th birthday, until July 1, 2021, age 35, pregnancy, death, emigration, or the occurrence of any exclusion criterion.
During the study period, the cohort registered 2,925 ectopic pregnancies, including 35 at 52 mg, 32 at 19.5 mg, and 80 at 13.5 mg of levonorgestrel. For all other types of hormonal contraception, there were 763 ectopic pregnancies.
In terms of adjusted absolute rates of ectopic pregnancy per 10,000 person-years, compared with other hormonal contraceptives (rate = 2.4), these were 7.7 with 52 mg levonorgestrel IUS, 7.1 with 19.5 mg, and 15.7 with 13.5 mg. They translated to comparative differences of 5.3 (95% confidence interval, 1.9-8.7), 4.8 (95% CI, 1.5-8.0), and 13.4 (95% CI, 8.8-18.1), respectively.
Corresponding adjusted relative rate ratios were 3.4, 4.1, and 7.9. For each levonorgestrel IUS dosage; the ectopic pregnancy rate increased with duration of use.
The adjusted ectopic pregnancy rate difference per 10,000 person-years between the 19.5-mg and 52-mg levonorgestrel dosages was −0.6 , and between the 13.5-mg and 52-mg doses, 8.0, with a rate ratio of 2.3. The rate difference between the 13.5-mg and 19.5-mg levonorgestrel IUS was 8.6, with a rate ratio of 1.9.
An outsider’s perspective
Offering an outsider’s perspective on the study, Eran Bornstein, MD, vice-chair of obstetrics and gynecology at Lenox Hill Hospital in New York, said these data should spark further evaluation of risk of ectopic pregnancy with levonorgestrel-releasing IUDs. “The best advice for clinicians is to individualize the choice of which contraceptive to use, and when levonorgestrel IUD is selected, to individualize the appropriate dose and timing of placement,” he said in an interview.
Several additional factors may determine the best choice, Dr. Bornstein added, including medical conditions that contraindicate other contraceptives and those conditions that justify avoidance of pregnancy, as well as uterine myomas or malformation, the ability of the patient to comply with other options, and informed patient choice. “It is important to remember the potential risk for expulsion and ectopic pregnancy, maintain alertness, and use ultrasound to exclude these potential complications if suspected,” he said.
Dr. Meaidi said the mechanism of ectopic pregnancy with hormonal IUDs is unclear, but in vitro and animal studies have observed that levonorgestrel reduces the ciliary beat frequency in the fallopian tubes. “Thus, it could be hypothesized that if a woman was unfortunate enough to become pregnant using a hormonal IUD, the hormone could inhibit or slow down the movement of the zygote into the uterus for rightful intrauterine implantation and thereby increase the risk of ectopic pregnancy.”
Two coauthors of the study reported financial support from private-sector companies. Dr. Meaidi had no conflicts of interest. Dr. Bornstein disclosed no competing interests.
FROM JAMA
Is self-administered DMPA an answer to contraception access in the post-Roe era?
ILLUSTRATIVE CASE
A 32-year-old woman with a history of migraine with aura presents to your office for contraception management. She works full-time, has 2 children, and has transportation barriers. She previously used injectable DMPA (administered every 3 months at a health care facility) and would like to restart it. However, because she had to reschedule her last appointment due to a lack of transportation, she missed her injection window and subsequently became pregnant with her second child. She would still prefer injectable DMPA over the other contraceptive options offered—etonogestrel implant, oral contraceptive, or intrauterine device (IUD)—given her migraine history. However, she’s concerned she may have difficulty coming to the office every 3 months for her injection. What alternative injectable option can you offer?
When not pregnant or seeking to become pregnant, women may spend a significant amount of their lives trying to avoid pregnancy, and almost all women use contraception at some point.2 During the childbearing years of 15 to 49, 65% of women report using contraception.2 Although DMPA is a safe and effective option, only 2% of women report using it for contraception.2
For patients who have migraine with aura, there are fewer contraception options because their risk for ischemic stroke is increased 2- to 4-fold if they use combined hormonal contraceptives in pill, patch, or vaginal ring form.3 Safe options for these patients include the copper IUD, levonorgestrel-releasing intrauterine system, progestin implant, and DMPA injection.3
DMPA is a progestogen-only contraceptive approved by the US Food and Drug Administration to prevent pregnancy. It is available in an intramuscular formulation (DMPA-IM; 150 mg/mL every 13 weeks) and a subcutaneous formulation (DMPA-SC; 104 mg/0.65 mL every 12-14 weeks). DMPA-IM is administered by a health care provider and thus requires patients to present every 3 months for an injection. About 6% of DMPA-IM users have an unintended pregnancy in the first year due to inconsistent or incorrect use or late receipt of injection.4 DMPA-SC is produced as a prefilled needle that can be self-injected by patients.
Barriers to access are a growing concern. During the COVID-19 pandemic, one-third of women surveyed by the Guttmacher Institute (n = 2009) reported delaying or canceling a health care visit or having difficulty obtaining their contraception. Barriers to health care and contraception access were more common among Black and Hispanic women (vs White women), queer women (vs straight women), and low-income women (vs higher-income women).5
Following the overturning of Roe v Wade in June 2022, abortion access is now limited in parts of the United States. Given this significant policy change, physicians have an increasingly important role in providing contraception care and reducing barriers to contraception access. Since the SC forms of injectable contraception can be administered at home rather than in the health care setting, both the World Health Organization and the Centers for Disease Control and Prevention have recommended that self-administered injectable contraception be made widely available to expand access to contraception.6,7
STUDY SUMMARY
Higher contraceptive continuation rates with comparable safety and efficacy
This 2019 systematic review and meta-analysis evaluated the outcomes associated with use of self-administered DMPA-SC vs provider-administered DMPA in 5 countries.1 The authors searched several electronic databases for peer-reviewed studies of women who chose the option to self-administer DMPA-SC vs those who received DMPA injections from a health care provider.
Continue to: Outcomes included pregnancy
Outcomes included pregnancy; adverse effects or events (bleeding, injection site reactions, mental health concerns); initial use of injectable contraception (contraception uptake); and continuation rate of injectable contraception. Two reviewers extracted the data and assessed trials for bias. The authors used random-effects models to calculate pooled relative risk (RR) for studies with the same outcomes.
The analysis included a total of 6 trials (N = 3851): 3 RCTs (n = 1263) and 3 controlled cohort studies (n = 2588), conducted in the United States (2 trials), Malawi, Scotland, Uganda, and Senegal. All studies compared 12-month continuation rates of self-injected DMPA-SC vs provider-administered DMPA-SC or DMPA-IM every 3 months (12-13 weeks, with a window for early and late injections). Participants were at least 15 years of age (mean range, 26 to 29 years). In some studies, reminders (eg, texts, emails, calendar notifications) were provided to either the self-injection cohort only or to both cohorts of the trial. The RCTs were generally graded as having a low risk for bias, except for nonblinding of participants and personnel, given the nature of the interventions. The authors reported no evidence of significant heterogeneity in the studies.
The meta-analysis found higher continuation rates at 12 months with self-administrated DMPA compared with provider administration in the RCTs (RR = 1.27; 95% CI, 1.16-1.39) and in the observational cohort studies (RR = 1.18; 95% CI, 1.10-1.26). Pregnancy outcomes were reported in 4 studies, with the meta-analysis finding no significant difference in pregnancy rates in 2 RCTs (RR = 0.58; 95% CI, 0.15-2.22) or 2 observational cohort studies (RR = 1.1; 95% CI, 0.23-5.26).
Adverse effects or events were reported in 4 studies: 2 cohort studies reported increased injection site reactions with self-administration, and 1 RCT reported increased injection site pain or irritation with self-administration at 3 and 9 months. No other reported adverse effects occurred at higher rates with self-administration vs provider administration.
WHAT’S NEW
Demonstrated effectiveness of self-administered formulation
This systematic review and meta-analysis demonstrated that self-administration of DMPA-SC leads to higher contraception continuation rates at 12 months, without notable increased pregnancy rates or adverse effects, when compared with provider-administered DMPA.
Continue to: CAVEATS
CAVEATS
Outcome data limited to 12 months
Although self-administered DMPA-SC has the theoretical risk for user error and incorrect administration, this study did not find increased rates of pregnancy despite administration outside a health care center. However, the total number of pregnancies in each of the 4 studies measuring this outcome was low (< 5), and thus the authors noted that the effect size estimates may not be accurate.
Currently, there are no data on long-term outcomes beyond 12 months. Additionally, the health care visits for provider-administered DMPA every 3 months may afford other benefits, such as regular discussion of reproductive health concerns or testing for sexually transmitted infections, which must be weighed against the benefit of increased contraception access with self-administration. However, using the DMPA-SC self-administered formulation at home would not inhibit women from making separate health care visits as needed.
CHALLENGES TO IMPLEMENTATION
Limited resources to teach patients how to self-inject
Barriers to implementation include limited experience with prescribing DMPA-SC and changing practice culture to offer it to patients. Additionally, successful implementation of self-administered DMPA-SC is reliant on providing patients with appropriate information and training on self-injection, which requires knowledge, time, and other resources that may be limited in practices. Another potential barrier is product access, as not all insurers cover DMPA-SC and some pharmacies do not carry it.
1. Kennedy CE, Yeh PT, Gaffield ML, et al. Self-administration of injectable contraception: a systematic review and meta-analysis. BMJ Glob Health. 2019;4:e001350. doi: 10.1136/bmjgh-2018-001350
2. Daniels K, Abma J. Current contraceptive status among women aged 15-49: United States, 2017-2019. NCHS Data Brief. 2020;(388):1-8.
3. Paradise SL, Landis CA, Klein DA. Evidence-based contraception: common questions and answers. Am Fam Physician. 2022;106:251-259.
4. Marx M. Evidence‐based guidance for self‐administration of injectable contraception. J Midwifery Womens Health. 2021;66:108-112. doi: 10.1111/jmwh.13190
5. Lindberg LD, VandeVusse A, Mueller J, et al. Early Impacts of the COVID-19 Pandemic: Findings from the 2020 Guttmacher Survey of Reproductive Health Experiences. Guttmacher Institute; 2020. Accessed October 25, 2022. www.guttmacher.org/report/early-impacts-covid-19-pandemic-findings-2020-guttmacher-survey-reproductive-health
6. World Health Organization. WHO consolidated guidance on self-care interventions for health: sexual and reproductive health and rights. Published 2019. Accessed February 14, 2023. https://apps.who.int/iris/bitstream/handle/10665/325480/9789241550550-eng.pdf
7. Curtis KM, Nguyen A, Reeves JA, et al. Update to US selected practice recommendations for contraceptive use: self-administration of subcutaneous depot medroxyprogesterone acetate. MMWR Morb Mortal Wkly Rep. 2021;70:739-743. doi: 10.15585/mmwr.mm7020a2
ILLUSTRATIVE CASE
A 32-year-old woman with a history of migraine with aura presents to your office for contraception management. She works full-time, has 2 children, and has transportation barriers. She previously used injectable DMPA (administered every 3 months at a health care facility) and would like to restart it. However, because she had to reschedule her last appointment due to a lack of transportation, she missed her injection window and subsequently became pregnant with her second child. She would still prefer injectable DMPA over the other contraceptive options offered—etonogestrel implant, oral contraceptive, or intrauterine device (IUD)—given her migraine history. However, she’s concerned she may have difficulty coming to the office every 3 months for her injection. What alternative injectable option can you offer?
When not pregnant or seeking to become pregnant, women may spend a significant amount of their lives trying to avoid pregnancy, and almost all women use contraception at some point.2 During the childbearing years of 15 to 49, 65% of women report using contraception.2 Although DMPA is a safe and effective option, only 2% of women report using it for contraception.2
For patients who have migraine with aura, there are fewer contraception options because their risk for ischemic stroke is increased 2- to 4-fold if they use combined hormonal contraceptives in pill, patch, or vaginal ring form.3 Safe options for these patients include the copper IUD, levonorgestrel-releasing intrauterine system, progestin implant, and DMPA injection.3
DMPA is a progestogen-only contraceptive approved by the US Food and Drug Administration to prevent pregnancy. It is available in an intramuscular formulation (DMPA-IM; 150 mg/mL every 13 weeks) and a subcutaneous formulation (DMPA-SC; 104 mg/0.65 mL every 12-14 weeks). DMPA-IM is administered by a health care provider and thus requires patients to present every 3 months for an injection. About 6% of DMPA-IM users have an unintended pregnancy in the first year due to inconsistent or incorrect use or late receipt of injection.4 DMPA-SC is produced as a prefilled needle that can be self-injected by patients.
Barriers to access are a growing concern. During the COVID-19 pandemic, one-third of women surveyed by the Guttmacher Institute (n = 2009) reported delaying or canceling a health care visit or having difficulty obtaining their contraception. Barriers to health care and contraception access were more common among Black and Hispanic women (vs White women), queer women (vs straight women), and low-income women (vs higher-income women).5
Following the overturning of Roe v Wade in June 2022, abortion access is now limited in parts of the United States. Given this significant policy change, physicians have an increasingly important role in providing contraception care and reducing barriers to contraception access. Since the SC forms of injectable contraception can be administered at home rather than in the health care setting, both the World Health Organization and the Centers for Disease Control and Prevention have recommended that self-administered injectable contraception be made widely available to expand access to contraception.6,7
STUDY SUMMARY
Higher contraceptive continuation rates with comparable safety and efficacy
This 2019 systematic review and meta-analysis evaluated the outcomes associated with use of self-administered DMPA-SC vs provider-administered DMPA in 5 countries.1 The authors searched several electronic databases for peer-reviewed studies of women who chose the option to self-administer DMPA-SC vs those who received DMPA injections from a health care provider.
Continue to: Outcomes included pregnancy
Outcomes included pregnancy; adverse effects or events (bleeding, injection site reactions, mental health concerns); initial use of injectable contraception (contraception uptake); and continuation rate of injectable contraception. Two reviewers extracted the data and assessed trials for bias. The authors used random-effects models to calculate pooled relative risk (RR) for studies with the same outcomes.
The analysis included a total of 6 trials (N = 3851): 3 RCTs (n = 1263) and 3 controlled cohort studies (n = 2588), conducted in the United States (2 trials), Malawi, Scotland, Uganda, and Senegal. All studies compared 12-month continuation rates of self-injected DMPA-SC vs provider-administered DMPA-SC or DMPA-IM every 3 months (12-13 weeks, with a window for early and late injections). Participants were at least 15 years of age (mean range, 26 to 29 years). In some studies, reminders (eg, texts, emails, calendar notifications) were provided to either the self-injection cohort only or to both cohorts of the trial. The RCTs were generally graded as having a low risk for bias, except for nonblinding of participants and personnel, given the nature of the interventions. The authors reported no evidence of significant heterogeneity in the studies.
The meta-analysis found higher continuation rates at 12 months with self-administrated DMPA compared with provider administration in the RCTs (RR = 1.27; 95% CI, 1.16-1.39) and in the observational cohort studies (RR = 1.18; 95% CI, 1.10-1.26). Pregnancy outcomes were reported in 4 studies, with the meta-analysis finding no significant difference in pregnancy rates in 2 RCTs (RR = 0.58; 95% CI, 0.15-2.22) or 2 observational cohort studies (RR = 1.1; 95% CI, 0.23-5.26).
Adverse effects or events were reported in 4 studies: 2 cohort studies reported increased injection site reactions with self-administration, and 1 RCT reported increased injection site pain or irritation with self-administration at 3 and 9 months. No other reported adverse effects occurred at higher rates with self-administration vs provider administration.
WHAT’S NEW
Demonstrated effectiveness of self-administered formulation
This systematic review and meta-analysis demonstrated that self-administration of DMPA-SC leads to higher contraception continuation rates at 12 months, without notable increased pregnancy rates or adverse effects, when compared with provider-administered DMPA.
Continue to: CAVEATS
CAVEATS
Outcome data limited to 12 months
Although self-administered DMPA-SC has the theoretical risk for user error and incorrect administration, this study did not find increased rates of pregnancy despite administration outside a health care center. However, the total number of pregnancies in each of the 4 studies measuring this outcome was low (< 5), and thus the authors noted that the effect size estimates may not be accurate.
Currently, there are no data on long-term outcomes beyond 12 months. Additionally, the health care visits for provider-administered DMPA every 3 months may afford other benefits, such as regular discussion of reproductive health concerns or testing for sexually transmitted infections, which must be weighed against the benefit of increased contraception access with self-administration. However, using the DMPA-SC self-administered formulation at home would not inhibit women from making separate health care visits as needed.
CHALLENGES TO IMPLEMENTATION
Limited resources to teach patients how to self-inject
Barriers to implementation include limited experience with prescribing DMPA-SC and changing practice culture to offer it to patients. Additionally, successful implementation of self-administered DMPA-SC is reliant on providing patients with appropriate information and training on self-injection, which requires knowledge, time, and other resources that may be limited in practices. Another potential barrier is product access, as not all insurers cover DMPA-SC and some pharmacies do not carry it.
ILLUSTRATIVE CASE
A 32-year-old woman with a history of migraine with aura presents to your office for contraception management. She works full-time, has 2 children, and has transportation barriers. She previously used injectable DMPA (administered every 3 months at a health care facility) and would like to restart it. However, because she had to reschedule her last appointment due to a lack of transportation, she missed her injection window and subsequently became pregnant with her second child. She would still prefer injectable DMPA over the other contraceptive options offered—etonogestrel implant, oral contraceptive, or intrauterine device (IUD)—given her migraine history. However, she’s concerned she may have difficulty coming to the office every 3 months for her injection. What alternative injectable option can you offer?
When not pregnant or seeking to become pregnant, women may spend a significant amount of their lives trying to avoid pregnancy, and almost all women use contraception at some point.2 During the childbearing years of 15 to 49, 65% of women report using contraception.2 Although DMPA is a safe and effective option, only 2% of women report using it for contraception.2
For patients who have migraine with aura, there are fewer contraception options because their risk for ischemic stroke is increased 2- to 4-fold if they use combined hormonal contraceptives in pill, patch, or vaginal ring form.3 Safe options for these patients include the copper IUD, levonorgestrel-releasing intrauterine system, progestin implant, and DMPA injection.3
DMPA is a progestogen-only contraceptive approved by the US Food and Drug Administration to prevent pregnancy. It is available in an intramuscular formulation (DMPA-IM; 150 mg/mL every 13 weeks) and a subcutaneous formulation (DMPA-SC; 104 mg/0.65 mL every 12-14 weeks). DMPA-IM is administered by a health care provider and thus requires patients to present every 3 months for an injection. About 6% of DMPA-IM users have an unintended pregnancy in the first year due to inconsistent or incorrect use or late receipt of injection.4 DMPA-SC is produced as a prefilled needle that can be self-injected by patients.
Barriers to access are a growing concern. During the COVID-19 pandemic, one-third of women surveyed by the Guttmacher Institute (n = 2009) reported delaying or canceling a health care visit or having difficulty obtaining their contraception. Barriers to health care and contraception access were more common among Black and Hispanic women (vs White women), queer women (vs straight women), and low-income women (vs higher-income women).5
Following the overturning of Roe v Wade in June 2022, abortion access is now limited in parts of the United States. Given this significant policy change, physicians have an increasingly important role in providing contraception care and reducing barriers to contraception access. Since the SC forms of injectable contraception can be administered at home rather than in the health care setting, both the World Health Organization and the Centers for Disease Control and Prevention have recommended that self-administered injectable contraception be made widely available to expand access to contraception.6,7
STUDY SUMMARY
Higher contraceptive continuation rates with comparable safety and efficacy
This 2019 systematic review and meta-analysis evaluated the outcomes associated with use of self-administered DMPA-SC vs provider-administered DMPA in 5 countries.1 The authors searched several electronic databases for peer-reviewed studies of women who chose the option to self-administer DMPA-SC vs those who received DMPA injections from a health care provider.
Continue to: Outcomes included pregnancy
Outcomes included pregnancy; adverse effects or events (bleeding, injection site reactions, mental health concerns); initial use of injectable contraception (contraception uptake); and continuation rate of injectable contraception. Two reviewers extracted the data and assessed trials for bias. The authors used random-effects models to calculate pooled relative risk (RR) for studies with the same outcomes.
The analysis included a total of 6 trials (N = 3851): 3 RCTs (n = 1263) and 3 controlled cohort studies (n = 2588), conducted in the United States (2 trials), Malawi, Scotland, Uganda, and Senegal. All studies compared 12-month continuation rates of self-injected DMPA-SC vs provider-administered DMPA-SC or DMPA-IM every 3 months (12-13 weeks, with a window for early and late injections). Participants were at least 15 years of age (mean range, 26 to 29 years). In some studies, reminders (eg, texts, emails, calendar notifications) were provided to either the self-injection cohort only or to both cohorts of the trial. The RCTs were generally graded as having a low risk for bias, except for nonblinding of participants and personnel, given the nature of the interventions. The authors reported no evidence of significant heterogeneity in the studies.
The meta-analysis found higher continuation rates at 12 months with self-administrated DMPA compared with provider administration in the RCTs (RR = 1.27; 95% CI, 1.16-1.39) and in the observational cohort studies (RR = 1.18; 95% CI, 1.10-1.26). Pregnancy outcomes were reported in 4 studies, with the meta-analysis finding no significant difference in pregnancy rates in 2 RCTs (RR = 0.58; 95% CI, 0.15-2.22) or 2 observational cohort studies (RR = 1.1; 95% CI, 0.23-5.26).
Adverse effects or events were reported in 4 studies: 2 cohort studies reported increased injection site reactions with self-administration, and 1 RCT reported increased injection site pain or irritation with self-administration at 3 and 9 months. No other reported adverse effects occurred at higher rates with self-administration vs provider administration.
WHAT’S NEW
Demonstrated effectiveness of self-administered formulation
This systematic review and meta-analysis demonstrated that self-administration of DMPA-SC leads to higher contraception continuation rates at 12 months, without notable increased pregnancy rates or adverse effects, when compared with provider-administered DMPA.
Continue to: CAVEATS
CAVEATS
Outcome data limited to 12 months
Although self-administered DMPA-SC has the theoretical risk for user error and incorrect administration, this study did not find increased rates of pregnancy despite administration outside a health care center. However, the total number of pregnancies in each of the 4 studies measuring this outcome was low (< 5), and thus the authors noted that the effect size estimates may not be accurate.
Currently, there are no data on long-term outcomes beyond 12 months. Additionally, the health care visits for provider-administered DMPA every 3 months may afford other benefits, such as regular discussion of reproductive health concerns or testing for sexually transmitted infections, which must be weighed against the benefit of increased contraception access with self-administration. However, using the DMPA-SC self-administered formulation at home would not inhibit women from making separate health care visits as needed.
CHALLENGES TO IMPLEMENTATION
Limited resources to teach patients how to self-inject
Barriers to implementation include limited experience with prescribing DMPA-SC and changing practice culture to offer it to patients. Additionally, successful implementation of self-administered DMPA-SC is reliant on providing patients with appropriate information and training on self-injection, which requires knowledge, time, and other resources that may be limited in practices. Another potential barrier is product access, as not all insurers cover DMPA-SC and some pharmacies do not carry it.
1. Kennedy CE, Yeh PT, Gaffield ML, et al. Self-administration of injectable contraception: a systematic review and meta-analysis. BMJ Glob Health. 2019;4:e001350. doi: 10.1136/bmjgh-2018-001350
2. Daniels K, Abma J. Current contraceptive status among women aged 15-49: United States, 2017-2019. NCHS Data Brief. 2020;(388):1-8.
3. Paradise SL, Landis CA, Klein DA. Evidence-based contraception: common questions and answers. Am Fam Physician. 2022;106:251-259.
4. Marx M. Evidence‐based guidance for self‐administration of injectable contraception. J Midwifery Womens Health. 2021;66:108-112. doi: 10.1111/jmwh.13190
5. Lindberg LD, VandeVusse A, Mueller J, et al. Early Impacts of the COVID-19 Pandemic: Findings from the 2020 Guttmacher Survey of Reproductive Health Experiences. Guttmacher Institute; 2020. Accessed October 25, 2022. www.guttmacher.org/report/early-impacts-covid-19-pandemic-findings-2020-guttmacher-survey-reproductive-health
6. World Health Organization. WHO consolidated guidance on self-care interventions for health: sexual and reproductive health and rights. Published 2019. Accessed February 14, 2023. https://apps.who.int/iris/bitstream/handle/10665/325480/9789241550550-eng.pdf
7. Curtis KM, Nguyen A, Reeves JA, et al. Update to US selected practice recommendations for contraceptive use: self-administration of subcutaneous depot medroxyprogesterone acetate. MMWR Morb Mortal Wkly Rep. 2021;70:739-743. doi: 10.15585/mmwr.mm7020a2
1. Kennedy CE, Yeh PT, Gaffield ML, et al. Self-administration of injectable contraception: a systematic review and meta-analysis. BMJ Glob Health. 2019;4:e001350. doi: 10.1136/bmjgh-2018-001350
2. Daniels K, Abma J. Current contraceptive status among women aged 15-49: United States, 2017-2019. NCHS Data Brief. 2020;(388):1-8.
3. Paradise SL, Landis CA, Klein DA. Evidence-based contraception: common questions and answers. Am Fam Physician. 2022;106:251-259.
4. Marx M. Evidence‐based guidance for self‐administration of injectable contraception. J Midwifery Womens Health. 2021;66:108-112. doi: 10.1111/jmwh.13190
5. Lindberg LD, VandeVusse A, Mueller J, et al. Early Impacts of the COVID-19 Pandemic: Findings from the 2020 Guttmacher Survey of Reproductive Health Experiences. Guttmacher Institute; 2020. Accessed October 25, 2022. www.guttmacher.org/report/early-impacts-covid-19-pandemic-findings-2020-guttmacher-survey-reproductive-health
6. World Health Organization. WHO consolidated guidance on self-care interventions for health: sexual and reproductive health and rights. Published 2019. Accessed February 14, 2023. https://apps.who.int/iris/bitstream/handle/10665/325480/9789241550550-eng.pdf
7. Curtis KM, Nguyen A, Reeves JA, et al. Update to US selected practice recommendations for contraceptive use: self-administration of subcutaneous depot medroxyprogesterone acetate. MMWR Morb Mortal Wkly Rep. 2021;70:739-743. doi: 10.15585/mmwr.mm7020a2
PRACTICE CHANGER
Consider prescribing self-administered subcutaneous depot medroxyprogesterone acetate (DMPA) for contraception instead of provider-administered DMPA. Self-administration improves contraception continuation rates without notable increases in pregnancy or adverse effects.
STRENGTH OF RECOMMENDATION
A: Based on a meta-analysis of randomized controlled trials (RCTs) and cohort studies.1
Kennedy CE, Yeh PT, Gaffield ML, et al. Self-administration of injectable contraception: a systematic review and meta-analysis. BMJ Glob Health. 2019;4:e001350. doi: 10.1136/bmjgh-2018-001350