User login
Should we always offer CPR?
Some details have been changed to protect the patient’s identity.
The first thing I noticed about Mr. Barry as I entered the intensive care unit was his left foot: Half of it was black, shriveled, and gangrenous, jutting out from under the white blanket. The soft rays of the morning sun illuminated his gaunt, unshaven, hollow cheeks. Sedated on propofol, with a green endotracheal tube sticking out of his chapped lips, he looked frail. His nurse, Becky, had just cleaned him after he passed tarry, maroon-colored stool. As she turned him over, I saw that the skin over his tailbone was broken. He had a large decubitus ulcer, the edges of which were now dried and black. The Foley bag, hanging next to his bed, was empty; there had been no urine for several hours now.
No one knew much about Mr. Barry. I don’t mean his current medical status – I mean what he did in life, who he loved, whether he had kids, what he valued. All we knew was that he was 83 years old and lived alone. No prior records in our system. No advanced directives. No information on any family. One of his neighbors called 911 after he was not seen for at least 10 days. Emergency medical services found Mr. Barry in bed, nearly lifeless. In the emergency room, he was noted to be in shock, with a dangerously low blood pressure. He was dry as a bone with markedly elevated sodium levels. His laboratory makers for kidney and liver function were deranged. He was admitted to the medical ICU with a diagnosis of hypovolemic shock and/or septic shock with multiorgan dysfunction. With 48 hours of supportive management with intravenous fluids and antibiotics, he did not improve. Blood cultures were positive for gram-positive cocci. The doses for medications used to maintain the blood pressure increased steadily. He also developed gastrointestinal bleeding.
Futile vs. potentially inappropriate
I was called for a cardiology consult because he had transient ST elevation in inferolateral leads on the monitor. Given his clinical scenario, the likelihood of type 1 myocardial infarction from plaque rupture was low; the ST elevations were probably related to vasospasm from increasing pressor requirement. Diagnostic cardiac catheterization showed clean coronary arteries. Continuous renal replacement therapy was soon started. Given Mr Barry’s multiorgan dysfunction and extremely poor prognosis, I recommended making all efforts to find his family or surrogate decision-maker to discuss goals of care or having a two-physician sign-off to place a DNR order.
Despite all efforts, we could not trace the family. We physicians vary individually on how we define value as related to life. We also vary on the degree of uncertainty about prognostication that we are comfortable with. This is one of the reasons the term “futility” is controversial and there is a push to use “potentially inappropriate” instead. The primary team had a different threshold for placing a DNR order and did not do it. That night, after I left the hospital, Mr Barry had a PEA (pulseless electrical activity) arrest and was resuscitated after 10 minutes of CPR. The next day, I noticed his bruised chest. He was on multiple medications to support his blood pressure.
My patient and a Hemingway protagonist
Whether by coincidence or irony, I started reading Ernest Hemingway’s short story “The Snows of Kilimanjaro” the same day that I met Mr. Barry. He reminded me of the story’s protagonist, Harry, lying on the cot with a gangrenous leg, waiting to die. Harry could sense death approaching. He reminisced about his past. All he wanted was to drink his “whiskey-soda.” “Darling, don’t drink that. We have to do everything we can,” his wife said. “You do it. I am tired,” Harry said, and continued to drink his whiskey-soda.
Mr. Barry looked tired. Tired of life? I can’t say with certainty. However, if I had to guess, the medical team’s heroics meant nothing to him. Unfortunately, he was not awake like Harry and could not do what he wished. I wondered what snippets of his life flashed before him as he lay on his bed at home for days. Did he want to have a whiskey-soda before dying? But we are not letting him die. Not easily anyway. We have to do everything we can: medications, coronary angiogram, dialysis, multiple rounds of CPR. Why?
In this country, we need permission to forgo CPR. If there are no advanced directives or next of kin available to discuss end-of-life care, performing CPR is the default status for all hospitalized patients, irrespective of the underlying severity of the illness. A unilateral DNR order written by a physician in good conscience (in a medically futile situation), but to which the patient has not consented, is generally invalid in most U.S. states. If health directives are not available, CPR will be administered on the presumption that the patient would want us to “do everything we can.” The medicolegal consequences and fear of not administering CPR is more profound than being found wrong and defying a patient’s wishes against CPR.
In patients with outside-hospital cardiac arrest, especially if related to ventricular fibrillation, early bystander CPR improves the survival rate. Hence, it makes sense for first responders and paramedics to administer CPR as the default option, focusing on the technique, rather than thinking about its utility based on the patient’s underlying comorbidities.
In the inpatient setting, however, physicians have enough information to comprehensively evaluate the patient. In a cohort of 5,690 critically ill ICU patients, obtained from a U.S. registry, the rate of survival to discharge after inpatient cardiac arrest is very low at 12.5%. Chronic health conditions, malignancy, end-stage renal disease, multiorgan dysfunction, need for vasopressor support, prior CPR, initial rhythm of asystole, or PEA advanced age were all associated with a less than 10% survival rate after CPR.
Dying is a process. Administering CPR to a dying patient is of little to no value. For Mr. Barry, it resulted in a bruised chest and broken ribs. James R. Jude, MD, one of the pioneers of closed chest compression, or modern-day CPR, wrote in 1965 that “resuscitation of the dying patient with irreparable damage to lungs, heart, kidneys, brain or any other vital system of the body has no medical, ethical, or moral justification. The techniques described in this monograph were designed to resuscitate the victim of acute insult, whether be it from drowning, electrical shock, untoward effect of drugs, anesthetic accident, heart block, acute myocardial infarction, or surgery.”
Yet, doctors continue to provide futile treatments at end of life for a variety of reasons: concerns about medico-legal risks, discomfort or inexperience with death and dying, uncertainty in prognostication, family requests, and organizational barriers such as lack of palliative services that can help lead end-of-life care discussions. Despite knowing that CPR has little benefit in critically ill patients with terminal illness and multiorgan dysfunction, we often ask the patient and their surrogate decision-makers: “If your heart stops, do you want us to restore your heart by pressing on the chest and giving electric shocks?” The very act of asking the question implies that CPR may be beneficial. We often do not go over the risks or offer an opinion on whether CPR should be performed. We take a neutral stance.
Anoxic brain injury, pain from broken ribs, and low likelihood of survival to discharge with acceptable neurologic recovery are rarely discussed in detail. Laypeople may overestimate the chances of survival after CPR and they may not comprehend that it does not reverse the dying process in patients with a terminal illness. When you ask about CPR, most families hear: “Do you want your loved one to live?” and the answer is nearly always “Yes.” We then administer CPR, thinking that we are respecting the patient’s autonomy in the medical decision-making process. However, in end-of-life care, elderly patients or surrogates may not fully understand the complexities involved or the outcomes of CPR. So, are we truly respecting their autonomy?
When to offer CPR?
In 2011, Billings and Krakauer, palliative care specialists from Massachusetts General Hospital, Boston, suggested that we focus on understanding our patient’s values and goals of care, and then decide whether to offer CPR, rather than taking a neutral stance. With this approach, we continue to respect the patient’s autonomy and also affirm our responsibility in providing care consistent with medical reality. We need to have the humility to accept that death is inevitable.
It has been 10 years since a group of physicians from Columbia University Medical Center, Harvard Medical School, MGH, and Boston Children’s Hospital proposed changes to how we determine resuscitation status. Instead of assuming that CPR is always wanted, they suggested three distinct approaches: consider CPR when the benefits versus risks are uncertain, and the patient is not end stage; recommend against CPR when there is a low likelihood of benefit and high likelihood of harm (e.g., patients with anoxic brain injury, advanced incurable cancer, or end-stage multiorgan dysfunction); and do not offer CPR to patients who will die imminently and have no chance of surviving CPR (e.g., patients with multiorgan dysfunction, increasing pressor requirements, and those who are actively dying without a single immediately reversible cause). I agree with their proposal.
Mr. Barry was actively dying. Unfortunately, we had neither his advanced directives nor access to family members or surrogates to discuss values and goals of care. Given the futility of administering CPR again, and based on our humanitarian principles, a moral and ethical responsibility to ensure a peaceful dying process, I and another ICU attending placed the DNR order. He passed away, peacefully, within a few hours.
That evening, as I was sitting on my porch reading the last page of “The Snows of Kilimanjaro,” my phone pinged. It was an email asking me to complete the final attestation for the death certificate. I imagined that Mr. Barry knew where he was going. He probably had his own special place – something beautiful and majestic, great and tall, dazzlingly white in the hot sun, like the snow-capped mountain of Kilimanjaro that Harry saw at the time of his death.
Dr. Mallidi is a general cardiologist at Zuckerberg San Francisco General Hospital, UCSF. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Some details have been changed to protect the patient’s identity.
The first thing I noticed about Mr. Barry as I entered the intensive care unit was his left foot: Half of it was black, shriveled, and gangrenous, jutting out from under the white blanket. The soft rays of the morning sun illuminated his gaunt, unshaven, hollow cheeks. Sedated on propofol, with a green endotracheal tube sticking out of his chapped lips, he looked frail. His nurse, Becky, had just cleaned him after he passed tarry, maroon-colored stool. As she turned him over, I saw that the skin over his tailbone was broken. He had a large decubitus ulcer, the edges of which were now dried and black. The Foley bag, hanging next to his bed, was empty; there had been no urine for several hours now.
No one knew much about Mr. Barry. I don’t mean his current medical status – I mean what he did in life, who he loved, whether he had kids, what he valued. All we knew was that he was 83 years old and lived alone. No prior records in our system. No advanced directives. No information on any family. One of his neighbors called 911 after he was not seen for at least 10 days. Emergency medical services found Mr. Barry in bed, nearly lifeless. In the emergency room, he was noted to be in shock, with a dangerously low blood pressure. He was dry as a bone with markedly elevated sodium levels. His laboratory makers for kidney and liver function were deranged. He was admitted to the medical ICU with a diagnosis of hypovolemic shock and/or septic shock with multiorgan dysfunction. With 48 hours of supportive management with intravenous fluids and antibiotics, he did not improve. Blood cultures were positive for gram-positive cocci. The doses for medications used to maintain the blood pressure increased steadily. He also developed gastrointestinal bleeding.
Futile vs. potentially inappropriate
I was called for a cardiology consult because he had transient ST elevation in inferolateral leads on the monitor. Given his clinical scenario, the likelihood of type 1 myocardial infarction from plaque rupture was low; the ST elevations were probably related to vasospasm from increasing pressor requirement. Diagnostic cardiac catheterization showed clean coronary arteries. Continuous renal replacement therapy was soon started. Given Mr Barry’s multiorgan dysfunction and extremely poor prognosis, I recommended making all efforts to find his family or surrogate decision-maker to discuss goals of care or having a two-physician sign-off to place a DNR order.
Despite all efforts, we could not trace the family. We physicians vary individually on how we define value as related to life. We also vary on the degree of uncertainty about prognostication that we are comfortable with. This is one of the reasons the term “futility” is controversial and there is a push to use “potentially inappropriate” instead. The primary team had a different threshold for placing a DNR order and did not do it. That night, after I left the hospital, Mr Barry had a PEA (pulseless electrical activity) arrest and was resuscitated after 10 minutes of CPR. The next day, I noticed his bruised chest. He was on multiple medications to support his blood pressure.
My patient and a Hemingway protagonist
Whether by coincidence or irony, I started reading Ernest Hemingway’s short story “The Snows of Kilimanjaro” the same day that I met Mr. Barry. He reminded me of the story’s protagonist, Harry, lying on the cot with a gangrenous leg, waiting to die. Harry could sense death approaching. He reminisced about his past. All he wanted was to drink his “whiskey-soda.” “Darling, don’t drink that. We have to do everything we can,” his wife said. “You do it. I am tired,” Harry said, and continued to drink his whiskey-soda.
Mr. Barry looked tired. Tired of life? I can’t say with certainty. However, if I had to guess, the medical team’s heroics meant nothing to him. Unfortunately, he was not awake like Harry and could not do what he wished. I wondered what snippets of his life flashed before him as he lay on his bed at home for days. Did he want to have a whiskey-soda before dying? But we are not letting him die. Not easily anyway. We have to do everything we can: medications, coronary angiogram, dialysis, multiple rounds of CPR. Why?
In this country, we need permission to forgo CPR. If there are no advanced directives or next of kin available to discuss end-of-life care, performing CPR is the default status for all hospitalized patients, irrespective of the underlying severity of the illness. A unilateral DNR order written by a physician in good conscience (in a medically futile situation), but to which the patient has not consented, is generally invalid in most U.S. states. If health directives are not available, CPR will be administered on the presumption that the patient would want us to “do everything we can.” The medicolegal consequences and fear of not administering CPR is more profound than being found wrong and defying a patient’s wishes against CPR.
In patients with outside-hospital cardiac arrest, especially if related to ventricular fibrillation, early bystander CPR improves the survival rate. Hence, it makes sense for first responders and paramedics to administer CPR as the default option, focusing on the technique, rather than thinking about its utility based on the patient’s underlying comorbidities.
In the inpatient setting, however, physicians have enough information to comprehensively evaluate the patient. In a cohort of 5,690 critically ill ICU patients, obtained from a U.S. registry, the rate of survival to discharge after inpatient cardiac arrest is very low at 12.5%. Chronic health conditions, malignancy, end-stage renal disease, multiorgan dysfunction, need for vasopressor support, prior CPR, initial rhythm of asystole, or PEA advanced age were all associated with a less than 10% survival rate after CPR.
Dying is a process. Administering CPR to a dying patient is of little to no value. For Mr. Barry, it resulted in a bruised chest and broken ribs. James R. Jude, MD, one of the pioneers of closed chest compression, or modern-day CPR, wrote in 1965 that “resuscitation of the dying patient with irreparable damage to lungs, heart, kidneys, brain or any other vital system of the body has no medical, ethical, or moral justification. The techniques described in this monograph were designed to resuscitate the victim of acute insult, whether be it from drowning, electrical shock, untoward effect of drugs, anesthetic accident, heart block, acute myocardial infarction, or surgery.”
Yet, doctors continue to provide futile treatments at end of life for a variety of reasons: concerns about medico-legal risks, discomfort or inexperience with death and dying, uncertainty in prognostication, family requests, and organizational barriers such as lack of palliative services that can help lead end-of-life care discussions. Despite knowing that CPR has little benefit in critically ill patients with terminal illness and multiorgan dysfunction, we often ask the patient and their surrogate decision-makers: “If your heart stops, do you want us to restore your heart by pressing on the chest and giving electric shocks?” The very act of asking the question implies that CPR may be beneficial. We often do not go over the risks or offer an opinion on whether CPR should be performed. We take a neutral stance.
Anoxic brain injury, pain from broken ribs, and low likelihood of survival to discharge with acceptable neurologic recovery are rarely discussed in detail. Laypeople may overestimate the chances of survival after CPR and they may not comprehend that it does not reverse the dying process in patients with a terminal illness. When you ask about CPR, most families hear: “Do you want your loved one to live?” and the answer is nearly always “Yes.” We then administer CPR, thinking that we are respecting the patient’s autonomy in the medical decision-making process. However, in end-of-life care, elderly patients or surrogates may not fully understand the complexities involved or the outcomes of CPR. So, are we truly respecting their autonomy?
When to offer CPR?
In 2011, Billings and Krakauer, palliative care specialists from Massachusetts General Hospital, Boston, suggested that we focus on understanding our patient’s values and goals of care, and then decide whether to offer CPR, rather than taking a neutral stance. With this approach, we continue to respect the patient’s autonomy and also affirm our responsibility in providing care consistent with medical reality. We need to have the humility to accept that death is inevitable.
It has been 10 years since a group of physicians from Columbia University Medical Center, Harvard Medical School, MGH, and Boston Children’s Hospital proposed changes to how we determine resuscitation status. Instead of assuming that CPR is always wanted, they suggested three distinct approaches: consider CPR when the benefits versus risks are uncertain, and the patient is not end stage; recommend against CPR when there is a low likelihood of benefit and high likelihood of harm (e.g., patients with anoxic brain injury, advanced incurable cancer, or end-stage multiorgan dysfunction); and do not offer CPR to patients who will die imminently and have no chance of surviving CPR (e.g., patients with multiorgan dysfunction, increasing pressor requirements, and those who are actively dying without a single immediately reversible cause). I agree with their proposal.
Mr. Barry was actively dying. Unfortunately, we had neither his advanced directives nor access to family members or surrogates to discuss values and goals of care. Given the futility of administering CPR again, and based on our humanitarian principles, a moral and ethical responsibility to ensure a peaceful dying process, I and another ICU attending placed the DNR order. He passed away, peacefully, within a few hours.
That evening, as I was sitting on my porch reading the last page of “The Snows of Kilimanjaro,” my phone pinged. It was an email asking me to complete the final attestation for the death certificate. I imagined that Mr. Barry knew where he was going. He probably had his own special place – something beautiful and majestic, great and tall, dazzlingly white in the hot sun, like the snow-capped mountain of Kilimanjaro that Harry saw at the time of his death.
Dr. Mallidi is a general cardiologist at Zuckerberg San Francisco General Hospital, UCSF. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Some details have been changed to protect the patient’s identity.
The first thing I noticed about Mr. Barry as I entered the intensive care unit was his left foot: Half of it was black, shriveled, and gangrenous, jutting out from under the white blanket. The soft rays of the morning sun illuminated his gaunt, unshaven, hollow cheeks. Sedated on propofol, with a green endotracheal tube sticking out of his chapped lips, he looked frail. His nurse, Becky, had just cleaned him after he passed tarry, maroon-colored stool. As she turned him over, I saw that the skin over his tailbone was broken. He had a large decubitus ulcer, the edges of which were now dried and black. The Foley bag, hanging next to his bed, was empty; there had been no urine for several hours now.
No one knew much about Mr. Barry. I don’t mean his current medical status – I mean what he did in life, who he loved, whether he had kids, what he valued. All we knew was that he was 83 years old and lived alone. No prior records in our system. No advanced directives. No information on any family. One of his neighbors called 911 after he was not seen for at least 10 days. Emergency medical services found Mr. Barry in bed, nearly lifeless. In the emergency room, he was noted to be in shock, with a dangerously low blood pressure. He was dry as a bone with markedly elevated sodium levels. His laboratory makers for kidney and liver function were deranged. He was admitted to the medical ICU with a diagnosis of hypovolemic shock and/or septic shock with multiorgan dysfunction. With 48 hours of supportive management with intravenous fluids and antibiotics, he did not improve. Blood cultures were positive for gram-positive cocci. The doses for medications used to maintain the blood pressure increased steadily. He also developed gastrointestinal bleeding.
Futile vs. potentially inappropriate
I was called for a cardiology consult because he had transient ST elevation in inferolateral leads on the monitor. Given his clinical scenario, the likelihood of type 1 myocardial infarction from plaque rupture was low; the ST elevations were probably related to vasospasm from increasing pressor requirement. Diagnostic cardiac catheterization showed clean coronary arteries. Continuous renal replacement therapy was soon started. Given Mr Barry’s multiorgan dysfunction and extremely poor prognosis, I recommended making all efforts to find his family or surrogate decision-maker to discuss goals of care or having a two-physician sign-off to place a DNR order.
Despite all efforts, we could not trace the family. We physicians vary individually on how we define value as related to life. We also vary on the degree of uncertainty about prognostication that we are comfortable with. This is one of the reasons the term “futility” is controversial and there is a push to use “potentially inappropriate” instead. The primary team had a different threshold for placing a DNR order and did not do it. That night, after I left the hospital, Mr Barry had a PEA (pulseless electrical activity) arrest and was resuscitated after 10 minutes of CPR. The next day, I noticed his bruised chest. He was on multiple medications to support his blood pressure.
My patient and a Hemingway protagonist
Whether by coincidence or irony, I started reading Ernest Hemingway’s short story “The Snows of Kilimanjaro” the same day that I met Mr. Barry. He reminded me of the story’s protagonist, Harry, lying on the cot with a gangrenous leg, waiting to die. Harry could sense death approaching. He reminisced about his past. All he wanted was to drink his “whiskey-soda.” “Darling, don’t drink that. We have to do everything we can,” his wife said. “You do it. I am tired,” Harry said, and continued to drink his whiskey-soda.
Mr. Barry looked tired. Tired of life? I can’t say with certainty. However, if I had to guess, the medical team’s heroics meant nothing to him. Unfortunately, he was not awake like Harry and could not do what he wished. I wondered what snippets of his life flashed before him as he lay on his bed at home for days. Did he want to have a whiskey-soda before dying? But we are not letting him die. Not easily anyway. We have to do everything we can: medications, coronary angiogram, dialysis, multiple rounds of CPR. Why?
In this country, we need permission to forgo CPR. If there are no advanced directives or next of kin available to discuss end-of-life care, performing CPR is the default status for all hospitalized patients, irrespective of the underlying severity of the illness. A unilateral DNR order written by a physician in good conscience (in a medically futile situation), but to which the patient has not consented, is generally invalid in most U.S. states. If health directives are not available, CPR will be administered on the presumption that the patient would want us to “do everything we can.” The medicolegal consequences and fear of not administering CPR is more profound than being found wrong and defying a patient’s wishes against CPR.
In patients with outside-hospital cardiac arrest, especially if related to ventricular fibrillation, early bystander CPR improves the survival rate. Hence, it makes sense for first responders and paramedics to administer CPR as the default option, focusing on the technique, rather than thinking about its utility based on the patient’s underlying comorbidities.
In the inpatient setting, however, physicians have enough information to comprehensively evaluate the patient. In a cohort of 5,690 critically ill ICU patients, obtained from a U.S. registry, the rate of survival to discharge after inpatient cardiac arrest is very low at 12.5%. Chronic health conditions, malignancy, end-stage renal disease, multiorgan dysfunction, need for vasopressor support, prior CPR, initial rhythm of asystole, or PEA advanced age were all associated with a less than 10% survival rate after CPR.
Dying is a process. Administering CPR to a dying patient is of little to no value. For Mr. Barry, it resulted in a bruised chest and broken ribs. James R. Jude, MD, one of the pioneers of closed chest compression, or modern-day CPR, wrote in 1965 that “resuscitation of the dying patient with irreparable damage to lungs, heart, kidneys, brain or any other vital system of the body has no medical, ethical, or moral justification. The techniques described in this monograph were designed to resuscitate the victim of acute insult, whether be it from drowning, electrical shock, untoward effect of drugs, anesthetic accident, heart block, acute myocardial infarction, or surgery.”
Yet, doctors continue to provide futile treatments at end of life for a variety of reasons: concerns about medico-legal risks, discomfort or inexperience with death and dying, uncertainty in prognostication, family requests, and organizational barriers such as lack of palliative services that can help lead end-of-life care discussions. Despite knowing that CPR has little benefit in critically ill patients with terminal illness and multiorgan dysfunction, we often ask the patient and their surrogate decision-makers: “If your heart stops, do you want us to restore your heart by pressing on the chest and giving electric shocks?” The very act of asking the question implies that CPR may be beneficial. We often do not go over the risks or offer an opinion on whether CPR should be performed. We take a neutral stance.
Anoxic brain injury, pain from broken ribs, and low likelihood of survival to discharge with acceptable neurologic recovery are rarely discussed in detail. Laypeople may overestimate the chances of survival after CPR and they may not comprehend that it does not reverse the dying process in patients with a terminal illness. When you ask about CPR, most families hear: “Do you want your loved one to live?” and the answer is nearly always “Yes.” We then administer CPR, thinking that we are respecting the patient’s autonomy in the medical decision-making process. However, in end-of-life care, elderly patients or surrogates may not fully understand the complexities involved or the outcomes of CPR. So, are we truly respecting their autonomy?
When to offer CPR?
In 2011, Billings and Krakauer, palliative care specialists from Massachusetts General Hospital, Boston, suggested that we focus on understanding our patient’s values and goals of care, and then decide whether to offer CPR, rather than taking a neutral stance. With this approach, we continue to respect the patient’s autonomy and also affirm our responsibility in providing care consistent with medical reality. We need to have the humility to accept that death is inevitable.
It has been 10 years since a group of physicians from Columbia University Medical Center, Harvard Medical School, MGH, and Boston Children’s Hospital proposed changes to how we determine resuscitation status. Instead of assuming that CPR is always wanted, they suggested three distinct approaches: consider CPR when the benefits versus risks are uncertain, and the patient is not end stage; recommend against CPR when there is a low likelihood of benefit and high likelihood of harm (e.g., patients with anoxic brain injury, advanced incurable cancer, or end-stage multiorgan dysfunction); and do not offer CPR to patients who will die imminently and have no chance of surviving CPR (e.g., patients with multiorgan dysfunction, increasing pressor requirements, and those who are actively dying without a single immediately reversible cause). I agree with their proposal.
Mr. Barry was actively dying. Unfortunately, we had neither his advanced directives nor access to family members or surrogates to discuss values and goals of care. Given the futility of administering CPR again, and based on our humanitarian principles, a moral and ethical responsibility to ensure a peaceful dying process, I and another ICU attending placed the DNR order. He passed away, peacefully, within a few hours.
That evening, as I was sitting on my porch reading the last page of “The Snows of Kilimanjaro,” my phone pinged. It was an email asking me to complete the final attestation for the death certificate. I imagined that Mr. Barry knew where he was going. He probably had his own special place – something beautiful and majestic, great and tall, dazzlingly white in the hot sun, like the snow-capped mountain of Kilimanjaro that Harry saw at the time of his death.
Dr. Mallidi is a general cardiologist at Zuckerberg San Francisco General Hospital, UCSF. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Make America beautiful: Support mask mandates
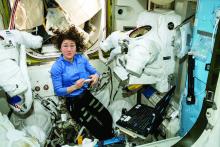
In space, no one can hear your red blood cells scream
There are many reasons why space is the final frontier, not least of which are the major health issues space travel places on the human body. So until a shady billionaire finds an alien protomolecule on a Saturnian moon and starts splicing it with human DNA so we can hang out in space all day without a spacesuit, we’re stuck with things like space anemia, a condition many astronauts develop after extended time in space.
Space anemia has been known for many years, but it was assumed that it developed as a reaction to microgravity and was a short-term phenomenon only – a temporary compensation as fluids and blood volume adjusted themselves. But as new research shows, that assumption seems to be wrong.
For the study, published in Nature Medicine, 13 astronauts who were in space for at least 120 days – long enough for all their red blood cells to have been produced in space – had their blood tested consistently. Before their flights, the astronauts created and destroyed 2 million red blood cells per second, but while they were in space, they destroyed 3 million cells per second. Notably, this process continued for the entire duration of the space flight. So, not a temporary reaction.
Consequently, 5 of the 13 astronauts developed anemia when they returned to Earth. (Interesting space fact: Having fewer blood cells isn’t a problem while you’re in space; the effects of anemia only manifest when the body returns to full gravity.) The anemia disappeared after a few months, but the astronauts were still destroying 30% more red blood cells a year after their spaceflight than they were before leaving Earth.
You may be thinking: Well, if they were destroying 50% more red blood cells while in space, how come they didn’t all develop severe anemia? The researchers theorized that production was boosted as well, which sounds like a good thing. The body is compensating, as it should. Unfortunately, that increased production stresses bone marrow function and the demand for energy spikes. That’s not such a good thing. And of course, many of the astronauts got anemia anyway.
To tackle the issue, the researchers emphasized the importance of feeding astronauts a proper diet, plus potential supplements before spaceflight. So don’t worry, Captain Kirk will be able to arm wrestle Klingons and romance suspiciously human-looking aliens without fear of keeling over from anemia-induced fatigue. Earth will stay safe.
Tell me with your eyes
Communication can be hard, even under the best of circumstances, but for many nonverbal patients in the intensive care unit who can’t move, getting a point across to the health care team can be a huge struggle in itself.
Health care professionals have been making do with eye-blinking or head-nodding, but what if that’s just not enough? New research shows that it’s not, and there’s a more effective way for patients to say what they mean just by looking.
In a study published in the Journal of Trauma and Acute Care Surgery, researchers looked into using eye-tracking systems for nonverbal ICU patients to communicate. Eye-tracking isn’t anything new, but using it as a form of communication among nonverbal patients with critical illness hasn’t been looked at before.
How does it work? The eye-tracking system is set up in the patient’s line of sight and its various algorithms and software collect data to calculate where exactly the patient is looking. Established scores and scales assess the patient’s mood, quality of life, pain, and self-esteem.
The researchers found that participating patients were actually experiencing more negative moods, pain, and feelings of frustration than was once believed. Making this tool even more valuable for treatment adjustment and meeting patients’ needs.
In this case, it means that health care providers are getting an eyeful … of communication.
Make America grave again
Here we go again. Somebody just found something else that the United States is not the best at. To go along with math and science education, infrastructure investment, quality of life …
That’s going to go on for a while, so let’s get to the new stuff. An international group of researchers surveyed end-of-life care in 81 countries and ranked them based on the assessment of 181 experts in those countries. They looked at 13 different factors, including proper management of pain and comfort, having a clean and safe space, being treated kindly, lack of cost barriers to appropriate care, and treatments that address quality of life and don’t just extend life.
… press freedom, industrial production, racial equality, Internet connectivity …
Their report card, published in the Journal of Pain and Symptom Management, gave six countries an A, with Great Britain at the top. The other five were Ireland, Taiwan, Australia, South Korea, and Costa Rica. The lowest grade went to Paraguay in 81st place, with Lebanon, Brazil, Senegal, and Haiti just ahead.
… environmental stewardship, body-mass index, social mobility, COVID safeness …
The United States, getting a firm grasp on mediocrity, ranked 43rd. Here are some countries that did better: North Macedonia (7th), Sri Lanka (16th), Uganda (31st), and Uruguay 33rd). In the United States, “we spend so much money trying to get people to live longer, but we don’t spend enough money in helping people die better,” lead author Eric A. Finkelstein, PhD, said in a written statement.
… economic stability, and soccer; we’re also not the best at dying. Wait, did we already say that?
The face mask that launched a thousand ships
Face masks, clearly, have been a source of social strife during the pandemic. People may not agree on mandates, but a mask can be a pretty-low-maintenance face shield if you don’t feel like putting on make-up or want to cover up some blemishes.
Before the pandemic, people thought that those wearing face masks were less attractive because the masks represented illness or disease, according to Dr. Michael Lewis of Cardiff (Wales) University. Back then, no one really wore masks besides doctors and nurses, so if you saw someone wearing one on the street, you probably wondered what they were trying to hide.
Now, though, the subject of face mask attractiveness has been revisited by Dr. Lewis and his associate, Oliver Hies, who found that face masks now make people more attractive.
“Our study suggests faces are considered most attractive when covered by medical face masks. … At a time when we feel vulnerable, we may find the wearing of medical masks reassuring and so feel more positive towards the wearer,” Dr. Lewis told the Guardian.
He suggested that we’re no longer looking at people wearing a mask as disease riddled, but rather doing their part to protect society. Or maybe we focus more on someone’s eyes when that’s all there is to look at. Or, maybe we wind up making up what the rest of someone’s face looks like to meet our attractiveness criteria.
However you feel about masks, they’re cheaper than plastic surgery. And you can go out wearing a new face every day.
In space, no one can hear your red blood cells scream
There are many reasons why space is the final frontier, not least of which are the major health issues space travel places on the human body. So until a shady billionaire finds an alien protomolecule on a Saturnian moon and starts splicing it with human DNA so we can hang out in space all day without a spacesuit, we’re stuck with things like space anemia, a condition many astronauts develop after extended time in space.
Space anemia has been known for many years, but it was assumed that it developed as a reaction to microgravity and was a short-term phenomenon only – a temporary compensation as fluids and blood volume adjusted themselves. But as new research shows, that assumption seems to be wrong.
For the study, published in Nature Medicine, 13 astronauts who were in space for at least 120 days – long enough for all their red blood cells to have been produced in space – had their blood tested consistently. Before their flights, the astronauts created and destroyed 2 million red blood cells per second, but while they were in space, they destroyed 3 million cells per second. Notably, this process continued for the entire duration of the space flight. So, not a temporary reaction.
Consequently, 5 of the 13 astronauts developed anemia when they returned to Earth. (Interesting space fact: Having fewer blood cells isn’t a problem while you’re in space; the effects of anemia only manifest when the body returns to full gravity.) The anemia disappeared after a few months, but the astronauts were still destroying 30% more red blood cells a year after their spaceflight than they were before leaving Earth.
You may be thinking: Well, if they were destroying 50% more red blood cells while in space, how come they didn’t all develop severe anemia? The researchers theorized that production was boosted as well, which sounds like a good thing. The body is compensating, as it should. Unfortunately, that increased production stresses bone marrow function and the demand for energy spikes. That’s not such a good thing. And of course, many of the astronauts got anemia anyway.
To tackle the issue, the researchers emphasized the importance of feeding astronauts a proper diet, plus potential supplements before spaceflight. So don’t worry, Captain Kirk will be able to arm wrestle Klingons and romance suspiciously human-looking aliens without fear of keeling over from anemia-induced fatigue. Earth will stay safe.
Tell me with your eyes
Communication can be hard, even under the best of circumstances, but for many nonverbal patients in the intensive care unit who can’t move, getting a point across to the health care team can be a huge struggle in itself.
Health care professionals have been making do with eye-blinking or head-nodding, but what if that’s just not enough? New research shows that it’s not, and there’s a more effective way for patients to say what they mean just by looking.
In a study published in the Journal of Trauma and Acute Care Surgery, researchers looked into using eye-tracking systems for nonverbal ICU patients to communicate. Eye-tracking isn’t anything new, but using it as a form of communication among nonverbal patients with critical illness hasn’t been looked at before.
How does it work? The eye-tracking system is set up in the patient’s line of sight and its various algorithms and software collect data to calculate where exactly the patient is looking. Established scores and scales assess the patient’s mood, quality of life, pain, and self-esteem.
The researchers found that participating patients were actually experiencing more negative moods, pain, and feelings of frustration than was once believed. Making this tool even more valuable for treatment adjustment and meeting patients’ needs.
In this case, it means that health care providers are getting an eyeful … of communication.
Make America grave again
Here we go again. Somebody just found something else that the United States is not the best at. To go along with math and science education, infrastructure investment, quality of life …
That’s going to go on for a while, so let’s get to the new stuff. An international group of researchers surveyed end-of-life care in 81 countries and ranked them based on the assessment of 181 experts in those countries. They looked at 13 different factors, including proper management of pain and comfort, having a clean and safe space, being treated kindly, lack of cost barriers to appropriate care, and treatments that address quality of life and don’t just extend life.
… press freedom, industrial production, racial equality, Internet connectivity …
Their report card, published in the Journal of Pain and Symptom Management, gave six countries an A, with Great Britain at the top. The other five were Ireland, Taiwan, Australia, South Korea, and Costa Rica. The lowest grade went to Paraguay in 81st place, with Lebanon, Brazil, Senegal, and Haiti just ahead.
… environmental stewardship, body-mass index, social mobility, COVID safeness …
The United States, getting a firm grasp on mediocrity, ranked 43rd. Here are some countries that did better: North Macedonia (7th), Sri Lanka (16th), Uganda (31st), and Uruguay 33rd). In the United States, “we spend so much money trying to get people to live longer, but we don’t spend enough money in helping people die better,” lead author Eric A. Finkelstein, PhD, said in a written statement.
… economic stability, and soccer; we’re also not the best at dying. Wait, did we already say that?
The face mask that launched a thousand ships
Face masks, clearly, have been a source of social strife during the pandemic. People may not agree on mandates, but a mask can be a pretty-low-maintenance face shield if you don’t feel like putting on make-up or want to cover up some blemishes.
Before the pandemic, people thought that those wearing face masks were less attractive because the masks represented illness or disease, according to Dr. Michael Lewis of Cardiff (Wales) University. Back then, no one really wore masks besides doctors and nurses, so if you saw someone wearing one on the street, you probably wondered what they were trying to hide.
Now, though, the subject of face mask attractiveness has been revisited by Dr. Lewis and his associate, Oliver Hies, who found that face masks now make people more attractive.
“Our study suggests faces are considered most attractive when covered by medical face masks. … At a time when we feel vulnerable, we may find the wearing of medical masks reassuring and so feel more positive towards the wearer,” Dr. Lewis told the Guardian.
He suggested that we’re no longer looking at people wearing a mask as disease riddled, but rather doing their part to protect society. Or maybe we focus more on someone’s eyes when that’s all there is to look at. Or, maybe we wind up making up what the rest of someone’s face looks like to meet our attractiveness criteria.
However you feel about masks, they’re cheaper than plastic surgery. And you can go out wearing a new face every day.
In space, no one can hear your red blood cells scream
There are many reasons why space is the final frontier, not least of which are the major health issues space travel places on the human body. So until a shady billionaire finds an alien protomolecule on a Saturnian moon and starts splicing it with human DNA so we can hang out in space all day without a spacesuit, we’re stuck with things like space anemia, a condition many astronauts develop after extended time in space.
Space anemia has been known for many years, but it was assumed that it developed as a reaction to microgravity and was a short-term phenomenon only – a temporary compensation as fluids and blood volume adjusted themselves. But as new research shows, that assumption seems to be wrong.
For the study, published in Nature Medicine, 13 astronauts who were in space for at least 120 days – long enough for all their red blood cells to have been produced in space – had their blood tested consistently. Before their flights, the astronauts created and destroyed 2 million red blood cells per second, but while they were in space, they destroyed 3 million cells per second. Notably, this process continued for the entire duration of the space flight. So, not a temporary reaction.
Consequently, 5 of the 13 astronauts developed anemia when they returned to Earth. (Interesting space fact: Having fewer blood cells isn’t a problem while you’re in space; the effects of anemia only manifest when the body returns to full gravity.) The anemia disappeared after a few months, but the astronauts were still destroying 30% more red blood cells a year after their spaceflight than they were before leaving Earth.
You may be thinking: Well, if they were destroying 50% more red blood cells while in space, how come they didn’t all develop severe anemia? The researchers theorized that production was boosted as well, which sounds like a good thing. The body is compensating, as it should. Unfortunately, that increased production stresses bone marrow function and the demand for energy spikes. That’s not such a good thing. And of course, many of the astronauts got anemia anyway.
To tackle the issue, the researchers emphasized the importance of feeding astronauts a proper diet, plus potential supplements before spaceflight. So don’t worry, Captain Kirk will be able to arm wrestle Klingons and romance suspiciously human-looking aliens without fear of keeling over from anemia-induced fatigue. Earth will stay safe.
Tell me with your eyes
Communication can be hard, even under the best of circumstances, but for many nonverbal patients in the intensive care unit who can’t move, getting a point across to the health care team can be a huge struggle in itself.
Health care professionals have been making do with eye-blinking or head-nodding, but what if that’s just not enough? New research shows that it’s not, and there’s a more effective way for patients to say what they mean just by looking.
In a study published in the Journal of Trauma and Acute Care Surgery, researchers looked into using eye-tracking systems for nonverbal ICU patients to communicate. Eye-tracking isn’t anything new, but using it as a form of communication among nonverbal patients with critical illness hasn’t been looked at before.
How does it work? The eye-tracking system is set up in the patient’s line of sight and its various algorithms and software collect data to calculate where exactly the patient is looking. Established scores and scales assess the patient’s mood, quality of life, pain, and self-esteem.
The researchers found that participating patients were actually experiencing more negative moods, pain, and feelings of frustration than was once believed. Making this tool even more valuable for treatment adjustment and meeting patients’ needs.
In this case, it means that health care providers are getting an eyeful … of communication.
Make America grave again
Here we go again. Somebody just found something else that the United States is not the best at. To go along with math and science education, infrastructure investment, quality of life …
That’s going to go on for a while, so let’s get to the new stuff. An international group of researchers surveyed end-of-life care in 81 countries and ranked them based on the assessment of 181 experts in those countries. They looked at 13 different factors, including proper management of pain and comfort, having a clean and safe space, being treated kindly, lack of cost barriers to appropriate care, and treatments that address quality of life and don’t just extend life.
… press freedom, industrial production, racial equality, Internet connectivity …
Their report card, published in the Journal of Pain and Symptom Management, gave six countries an A, with Great Britain at the top. The other five were Ireland, Taiwan, Australia, South Korea, and Costa Rica. The lowest grade went to Paraguay in 81st place, with Lebanon, Brazil, Senegal, and Haiti just ahead.
… environmental stewardship, body-mass index, social mobility, COVID safeness …
The United States, getting a firm grasp on mediocrity, ranked 43rd. Here are some countries that did better: North Macedonia (7th), Sri Lanka (16th), Uganda (31st), and Uruguay 33rd). In the United States, “we spend so much money trying to get people to live longer, but we don’t spend enough money in helping people die better,” lead author Eric A. Finkelstein, PhD, said in a written statement.
… economic stability, and soccer; we’re also not the best at dying. Wait, did we already say that?
The face mask that launched a thousand ships
Face masks, clearly, have been a source of social strife during the pandemic. People may not agree on mandates, but a mask can be a pretty-low-maintenance face shield if you don’t feel like putting on make-up or want to cover up some blemishes.
Before the pandemic, people thought that those wearing face masks were less attractive because the masks represented illness or disease, according to Dr. Michael Lewis of Cardiff (Wales) University. Back then, no one really wore masks besides doctors and nurses, so if you saw someone wearing one on the street, you probably wondered what they were trying to hide.
Now, though, the subject of face mask attractiveness has been revisited by Dr. Lewis and his associate, Oliver Hies, who found that face masks now make people more attractive.
“Our study suggests faces are considered most attractive when covered by medical face masks. … At a time when we feel vulnerable, we may find the wearing of medical masks reassuring and so feel more positive towards the wearer,” Dr. Lewis told the Guardian.
He suggested that we’re no longer looking at people wearing a mask as disease riddled, but rather doing their part to protect society. Or maybe we focus more on someone’s eyes when that’s all there is to look at. Or, maybe we wind up making up what the rest of someone’s face looks like to meet our attractiveness criteria.
However you feel about masks, they’re cheaper than plastic surgery. And you can go out wearing a new face every day.
Could the Omicron surge hasten the transition from pandemic to endemic?
The record-setting surge in COVID-19 cases nationwide – including more than one million new infections reported on Jan. 3 – raises questions about whether the higher Omicron variant transmissibility will accelerate a transition from pandemic to endemic disease.
Furthermore,
Infectious disease experts weigh in on these possibilities.
An endemic eventuality?
Whether the current surge will mean the predicted switch to endemic COVID-19 will come sooner “is very hard to predict,” Michael Lin, MD, MPH, told this news organization.
“It’s an open question,” he said, “if another highly transmissible variant will emerge.”
On a positive note, “at this point many more people have received their vaccinations or been infected. And over time, repeated infections have led to milder symptoms,” added Dr. Lin, hospital epidemiologist at Rush Medical College, Chicago.
“It could end up being a seasonal variant,” he said.
COVID-19 going endemic is “a real possibility, but unfortunately ... it doesn’t seem necessarily that we’re going to have the same predictable pattern we have with the flu,” said Eleftherios Mylonakis, MD, PhD, chief of infectious diseases for Lifespan and its affiliates at Rhode Island Hospital and Miriam Hospital in Providence.
“We have a number of other viruses that don’t follow the same annual pattern,” he said.
Unknowns include how long individuals’ immune responses, including T-cell defenses, will last going forward.
A transition from pandemic to endemic is “not a light switch, and there are no metrics associated with what endemic means for COVID-19,” said Syra Madad, DHSc., MSc, MCP, an infectious disease epidemiologist at Harvard’s Belfer Center for Science and International Affairs, Boston.
“Instead, we should continue to focus on decreasing transmission rates and preventing our hospitals from getting overwhelmed,” she said.
A hastening to herd immunity?
“The short answer is yes,” Dr. Lin said when asked if the increased transmissibility and increased cases linked to the Omicron surge could get the U.S. closer to herd immunity.
“The twist in this whole story,” he said, “is the virus mutated enough to escape first-line immune defenses, specifically antibodies. That is why we are seeing breakthrough infections, even in highly vaccinated populations.”
Dr. Mylonakis was more skeptical regarding herd immunity.
“The concept of herd immunity with a rapidly evolving virus is very difficult” to address, he said.
One reason is the number of unknown factors, Dr. Mylonakis said. He predicted a clearer picture will emerge after the Omicrons surge subsides. Also, with so many people infected by the Omicron variant, immune protection should peak.
“People will have boosted immunity. Not everybody, unfortunately, because there are people who cannot really mount [a full immune response] because of age, because of immunosuppression, etc.,” said Dr. Mylonakis, who is also professor of infectious diseases at Brown University.
“But the majority of the population will be exposed and will mount some degree of immunity.”
Dr. Madad agreed. “The omicron variant will add much more immunity into our population by both the preferred pathway – which is through vaccination – as well as through those that are unvaccinated and get infected with omicron,” she said.
“The pathway to gain immunity from vaccination is the safest option, and already over 1 million doses of the COVID-19 vaccine are going into arms per day – this includes first, second, and additional doses like boosters,” added Dr. Madad, who is also senior director of the System-wide Special Pathogens Program at New York City Health and Hospitals.
A shorter, more intense surge?
The United Kingdom’s experience with COVID-19 has often served as a bellwether of what is likely to happen in the U.S. If that is the case with the Omicron surge, the peak should last about 4 weeks, Dr. Mylonakis said.
In other words, the accelerated spread of Omicron could mean this surge passes more quickly than Delta.
Furthermore, some evidence suggests neutralizing antibodies produced by Omicron infection remain effective against the Delta variant – thereby reducing the risk of Delta reinfections over time.
The ability to neutralize the Delta variant increased more than fourfold after a median 14 days, according to data from a preprint study posted Dec. 27 on MedRxiv.
At the same time, neutralization of the Omicron variant increased 14-fold as participants mounted an antibody response. The study was conducted in vaccinated and unvaccinated people infected by Omicron in South Africa shortly after symptoms started. It has yet to be peer reviewed.
Eric Topol, MD, editor-in-chief of Medscape, described the results as “especially good news” in a tweet.
The current surge could also mean enhanced protection in the future.
“As we look at getting to the other side of this Omicron wave, we will end up with more immunity,” Dr. Madad said. “And with more immunity means we’ll be better guarded against the next emerging variant.”
A version of this article first appeared on Medscape.com.
The record-setting surge in COVID-19 cases nationwide – including more than one million new infections reported on Jan. 3 – raises questions about whether the higher Omicron variant transmissibility will accelerate a transition from pandemic to endemic disease.
Furthermore,
Infectious disease experts weigh in on these possibilities.
An endemic eventuality?
Whether the current surge will mean the predicted switch to endemic COVID-19 will come sooner “is very hard to predict,” Michael Lin, MD, MPH, told this news organization.
“It’s an open question,” he said, “if another highly transmissible variant will emerge.”
On a positive note, “at this point many more people have received their vaccinations or been infected. And over time, repeated infections have led to milder symptoms,” added Dr. Lin, hospital epidemiologist at Rush Medical College, Chicago.
“It could end up being a seasonal variant,” he said.
COVID-19 going endemic is “a real possibility, but unfortunately ... it doesn’t seem necessarily that we’re going to have the same predictable pattern we have with the flu,” said Eleftherios Mylonakis, MD, PhD, chief of infectious diseases for Lifespan and its affiliates at Rhode Island Hospital and Miriam Hospital in Providence.
“We have a number of other viruses that don’t follow the same annual pattern,” he said.
Unknowns include how long individuals’ immune responses, including T-cell defenses, will last going forward.
A transition from pandemic to endemic is “not a light switch, and there are no metrics associated with what endemic means for COVID-19,” said Syra Madad, DHSc., MSc, MCP, an infectious disease epidemiologist at Harvard’s Belfer Center for Science and International Affairs, Boston.
“Instead, we should continue to focus on decreasing transmission rates and preventing our hospitals from getting overwhelmed,” she said.
A hastening to herd immunity?
“The short answer is yes,” Dr. Lin said when asked if the increased transmissibility and increased cases linked to the Omicron surge could get the U.S. closer to herd immunity.
“The twist in this whole story,” he said, “is the virus mutated enough to escape first-line immune defenses, specifically antibodies. That is why we are seeing breakthrough infections, even in highly vaccinated populations.”
Dr. Mylonakis was more skeptical regarding herd immunity.
“The concept of herd immunity with a rapidly evolving virus is very difficult” to address, he said.
One reason is the number of unknown factors, Dr. Mylonakis said. He predicted a clearer picture will emerge after the Omicrons surge subsides. Also, with so many people infected by the Omicron variant, immune protection should peak.
“People will have boosted immunity. Not everybody, unfortunately, because there are people who cannot really mount [a full immune response] because of age, because of immunosuppression, etc.,” said Dr. Mylonakis, who is also professor of infectious diseases at Brown University.
“But the majority of the population will be exposed and will mount some degree of immunity.”
Dr. Madad agreed. “The omicron variant will add much more immunity into our population by both the preferred pathway – which is through vaccination – as well as through those that are unvaccinated and get infected with omicron,” she said.
“The pathway to gain immunity from vaccination is the safest option, and already over 1 million doses of the COVID-19 vaccine are going into arms per day – this includes first, second, and additional doses like boosters,” added Dr. Madad, who is also senior director of the System-wide Special Pathogens Program at New York City Health and Hospitals.
A shorter, more intense surge?
The United Kingdom’s experience with COVID-19 has often served as a bellwether of what is likely to happen in the U.S. If that is the case with the Omicron surge, the peak should last about 4 weeks, Dr. Mylonakis said.
In other words, the accelerated spread of Omicron could mean this surge passes more quickly than Delta.
Furthermore, some evidence suggests neutralizing antibodies produced by Omicron infection remain effective against the Delta variant – thereby reducing the risk of Delta reinfections over time.
The ability to neutralize the Delta variant increased more than fourfold after a median 14 days, according to data from a preprint study posted Dec. 27 on MedRxiv.
At the same time, neutralization of the Omicron variant increased 14-fold as participants mounted an antibody response. The study was conducted in vaccinated and unvaccinated people infected by Omicron in South Africa shortly after symptoms started. It has yet to be peer reviewed.
Eric Topol, MD, editor-in-chief of Medscape, described the results as “especially good news” in a tweet.
The current surge could also mean enhanced protection in the future.
“As we look at getting to the other side of this Omicron wave, we will end up with more immunity,” Dr. Madad said. “And with more immunity means we’ll be better guarded against the next emerging variant.”
A version of this article first appeared on Medscape.com.
The record-setting surge in COVID-19 cases nationwide – including more than one million new infections reported on Jan. 3 – raises questions about whether the higher Omicron variant transmissibility will accelerate a transition from pandemic to endemic disease.
Furthermore,
Infectious disease experts weigh in on these possibilities.
An endemic eventuality?
Whether the current surge will mean the predicted switch to endemic COVID-19 will come sooner “is very hard to predict,” Michael Lin, MD, MPH, told this news organization.
“It’s an open question,” he said, “if another highly transmissible variant will emerge.”
On a positive note, “at this point many more people have received their vaccinations or been infected. And over time, repeated infections have led to milder symptoms,” added Dr. Lin, hospital epidemiologist at Rush Medical College, Chicago.
“It could end up being a seasonal variant,” he said.
COVID-19 going endemic is “a real possibility, but unfortunately ... it doesn’t seem necessarily that we’re going to have the same predictable pattern we have with the flu,” said Eleftherios Mylonakis, MD, PhD, chief of infectious diseases for Lifespan and its affiliates at Rhode Island Hospital and Miriam Hospital in Providence.
“We have a number of other viruses that don’t follow the same annual pattern,” he said.
Unknowns include how long individuals’ immune responses, including T-cell defenses, will last going forward.
A transition from pandemic to endemic is “not a light switch, and there are no metrics associated with what endemic means for COVID-19,” said Syra Madad, DHSc., MSc, MCP, an infectious disease epidemiologist at Harvard’s Belfer Center for Science and International Affairs, Boston.
“Instead, we should continue to focus on decreasing transmission rates and preventing our hospitals from getting overwhelmed,” she said.
A hastening to herd immunity?
“The short answer is yes,” Dr. Lin said when asked if the increased transmissibility and increased cases linked to the Omicron surge could get the U.S. closer to herd immunity.
“The twist in this whole story,” he said, “is the virus mutated enough to escape first-line immune defenses, specifically antibodies. That is why we are seeing breakthrough infections, even in highly vaccinated populations.”
Dr. Mylonakis was more skeptical regarding herd immunity.
“The concept of herd immunity with a rapidly evolving virus is very difficult” to address, he said.
One reason is the number of unknown factors, Dr. Mylonakis said. He predicted a clearer picture will emerge after the Omicrons surge subsides. Also, with so many people infected by the Omicron variant, immune protection should peak.
“People will have boosted immunity. Not everybody, unfortunately, because there are people who cannot really mount [a full immune response] because of age, because of immunosuppression, etc.,” said Dr. Mylonakis, who is also professor of infectious diseases at Brown University.
“But the majority of the population will be exposed and will mount some degree of immunity.”
Dr. Madad agreed. “The omicron variant will add much more immunity into our population by both the preferred pathway – which is through vaccination – as well as through those that are unvaccinated and get infected with omicron,” she said.
“The pathway to gain immunity from vaccination is the safest option, and already over 1 million doses of the COVID-19 vaccine are going into arms per day – this includes first, second, and additional doses like boosters,” added Dr. Madad, who is also senior director of the System-wide Special Pathogens Program at New York City Health and Hospitals.
A shorter, more intense surge?
The United Kingdom’s experience with COVID-19 has often served as a bellwether of what is likely to happen in the U.S. If that is the case with the Omicron surge, the peak should last about 4 weeks, Dr. Mylonakis said.
In other words, the accelerated spread of Omicron could mean this surge passes more quickly than Delta.
Furthermore, some evidence suggests neutralizing antibodies produced by Omicron infection remain effective against the Delta variant – thereby reducing the risk of Delta reinfections over time.
The ability to neutralize the Delta variant increased more than fourfold after a median 14 days, according to data from a preprint study posted Dec. 27 on MedRxiv.
At the same time, neutralization of the Omicron variant increased 14-fold as participants mounted an antibody response. The study was conducted in vaccinated and unvaccinated people infected by Omicron in South Africa shortly after symptoms started. It has yet to be peer reviewed.
Eric Topol, MD, editor-in-chief of Medscape, described the results as “especially good news” in a tweet.
The current surge could also mean enhanced protection in the future.
“As we look at getting to the other side of this Omicron wave, we will end up with more immunity,” Dr. Madad said. “And with more immunity means we’ll be better guarded against the next emerging variant.”
A version of this article first appeared on Medscape.com.
As Omicron surges, hospital beds fill, but ICUs less affected
So far, hospitalizations caused by the Omicron variant appear to be milder than in previous waves.
“We are seeing an increase in the number of hospitalizations,” Rahul Sharma, MD, emergency physician-in-chief for New York–Presbyterian/Weill Cornell Medicine, told the New York Times.
“We’re not sending as many patients to the ICU, we’re not intubating as many patients, and actually, most of our patients that are coming to the emergency department that do test positive are actually being discharged,” he said.
Most Omicron patients in ICUs are unvaccinated or have severely compromised immune systems, doctors told the newspaper.
Currently, about 113,000 COVID-19 patients are hospitalized across the country, according to the latest data from the Department of Health & Human Services. About 76% of inpatient beds are in use nationwide, with about 16% of inpatient beds in use for COVID-19.
Early data suggests that the Omicron variant may cause less severe disease. But it’s easier to catch the variant, so more people are getting the virus, including people who have some immunity through prior infection or vaccination, which is driving up hospitalization numbers.
In New York, for instance, COVID-19 hospitalizations have surpassed the peak of last winter’s surge, the newspaper reported. In addition, Maryland Gov. Larry Hogan declared a state of emergency on Jan. 4, noting that the state had more hospitalized COVID-19 patients than at any other time during the pandemic.
“We’re in truly crushed mode,” Gabe Kelen, MD, chair of the department of emergency medicine for the Johns Hopkins University, Baltimore, told the Times.
Earlier in the pandemic, hospitals faced challenges with stockpiling ventilators and personal protective equipment, doctors told the newspaper. Now they’re dealing with limits on hospital beds and staffing as health care workers test positive. The increase in COVID-19 cases has also come along with a rise in hospitalizations for other conditions such as heart attacks and strokes.
In response, some hospitals are considering cutting elective surgeries because of staff shortages and limited bed capacity, the newspaper reported. In the meantime, hospital staff and administrators are watching case numbers to see how high hospitalizations may soar because of the Omicron variant.
“How high will it go? Can’t tell you. Don’t know,” James Musser, MD, chair of pathology and genomic medicine at Houston Methodist, told the Times. “We’re all watching it, obviously, very, very closely.”
A version of this article first appeared on WebMD.com.
So far, hospitalizations caused by the Omicron variant appear to be milder than in previous waves.
“We are seeing an increase in the number of hospitalizations,” Rahul Sharma, MD, emergency physician-in-chief for New York–Presbyterian/Weill Cornell Medicine, told the New York Times.
“We’re not sending as many patients to the ICU, we’re not intubating as many patients, and actually, most of our patients that are coming to the emergency department that do test positive are actually being discharged,” he said.
Most Omicron patients in ICUs are unvaccinated or have severely compromised immune systems, doctors told the newspaper.
Currently, about 113,000 COVID-19 patients are hospitalized across the country, according to the latest data from the Department of Health & Human Services. About 76% of inpatient beds are in use nationwide, with about 16% of inpatient beds in use for COVID-19.
Early data suggests that the Omicron variant may cause less severe disease. But it’s easier to catch the variant, so more people are getting the virus, including people who have some immunity through prior infection or vaccination, which is driving up hospitalization numbers.
In New York, for instance, COVID-19 hospitalizations have surpassed the peak of last winter’s surge, the newspaper reported. In addition, Maryland Gov. Larry Hogan declared a state of emergency on Jan. 4, noting that the state had more hospitalized COVID-19 patients than at any other time during the pandemic.
“We’re in truly crushed mode,” Gabe Kelen, MD, chair of the department of emergency medicine for the Johns Hopkins University, Baltimore, told the Times.
Earlier in the pandemic, hospitals faced challenges with stockpiling ventilators and personal protective equipment, doctors told the newspaper. Now they’re dealing with limits on hospital beds and staffing as health care workers test positive. The increase in COVID-19 cases has also come along with a rise in hospitalizations for other conditions such as heart attacks and strokes.
In response, some hospitals are considering cutting elective surgeries because of staff shortages and limited bed capacity, the newspaper reported. In the meantime, hospital staff and administrators are watching case numbers to see how high hospitalizations may soar because of the Omicron variant.
“How high will it go? Can’t tell you. Don’t know,” James Musser, MD, chair of pathology and genomic medicine at Houston Methodist, told the Times. “We’re all watching it, obviously, very, very closely.”
A version of this article first appeared on WebMD.com.
So far, hospitalizations caused by the Omicron variant appear to be milder than in previous waves.
“We are seeing an increase in the number of hospitalizations,” Rahul Sharma, MD, emergency physician-in-chief for New York–Presbyterian/Weill Cornell Medicine, told the New York Times.
“We’re not sending as many patients to the ICU, we’re not intubating as many patients, and actually, most of our patients that are coming to the emergency department that do test positive are actually being discharged,” he said.
Most Omicron patients in ICUs are unvaccinated or have severely compromised immune systems, doctors told the newspaper.
Currently, about 113,000 COVID-19 patients are hospitalized across the country, according to the latest data from the Department of Health & Human Services. About 76% of inpatient beds are in use nationwide, with about 16% of inpatient beds in use for COVID-19.
Early data suggests that the Omicron variant may cause less severe disease. But it’s easier to catch the variant, so more people are getting the virus, including people who have some immunity through prior infection or vaccination, which is driving up hospitalization numbers.
In New York, for instance, COVID-19 hospitalizations have surpassed the peak of last winter’s surge, the newspaper reported. In addition, Maryland Gov. Larry Hogan declared a state of emergency on Jan. 4, noting that the state had more hospitalized COVID-19 patients than at any other time during the pandemic.
“We’re in truly crushed mode,” Gabe Kelen, MD, chair of the department of emergency medicine for the Johns Hopkins University, Baltimore, told the Times.
Earlier in the pandemic, hospitals faced challenges with stockpiling ventilators and personal protective equipment, doctors told the newspaper. Now they’re dealing with limits on hospital beds and staffing as health care workers test positive. The increase in COVID-19 cases has also come along with a rise in hospitalizations for other conditions such as heart attacks and strokes.
In response, some hospitals are considering cutting elective surgeries because of staff shortages and limited bed capacity, the newspaper reported. In the meantime, hospital staff and administrators are watching case numbers to see how high hospitalizations may soar because of the Omicron variant.
“How high will it go? Can’t tell you. Don’t know,” James Musser, MD, chair of pathology and genomic medicine at Houston Methodist, told the Times. “We’re all watching it, obviously, very, very closely.”
A version of this article first appeared on WebMD.com.
Convalescent plasma cuts COVID-19 hospitalizations in half: Study
A “definitive study” from Johns Hopkins University researchers and others shows that convalescent plasma can cut hospital admissions for COVID-19 by 54% if therapy is administered within 8 days of symptom onset.
In the study of 1,181 adults randomly assigned to high-titer convalescent plasma or placebo, 2.9% of people receiving the therapy were hospitalized, compared with 6.3% who received placebo control plasma.
This translates to a 54% risk reduction for hospitalization with convalescent plasma.
“We have a clear difference,” principal investigator David Sullivan, MD, a professor at Johns Hopkins University, Baltimore, said during a Dec. 21 media briefing.
“This is very good news since we are in the midst of the Omicron surge, which has defeated [some of] our major monocular antibody therapies,” said Arturo Casadevall, MD, chair of the department of molecular microbiology and immunology at Johns Hopkins.
“So we have a new tool to keep people from progressing in their disease and to reduce progression or hospitalization,” Dr. Casadevall said.
The findings were published as a preprint study on Dec. 21, 2021, on medRxiv. The study has not yet been peer reviewed.
Whereas many convalescent plasma studies were done in hospitalized patients, this is one of only a handful performed in outpatients, the researchers noted.
There is a regulatory catch. The Food and Drug Administration restricted emergency use authorization (EUA) for convalescent plasma in February 2021 to include only high-dose titer plasma and to limit the therapy to hospitalized patients with early disease or for immunocompromised people who cannot mount an adequate antibody response.
Dr. Sullivan and colleagues hoped their findings will prompt the FDA to expand the EUA to include outpatients.
“We have shared this data with both the World Health Organization and the FDA,” study coauthor Kelly Gebo, MD, MPH, said during the media briefing.
“We do believe that this could be scaled up quickly,” added Dr. Gebo, professor of medicine at Johns Hopkins University. Convalescent plasma “could be used as a potential treatment as variants continue to evolve, such as we’ve seen with Omicron.”
Pre-Omicron results
The study was conducted at Johns Hopkins University and 23 other sites nationwide between June 2020 and October 2021. This means researchers enrolled symptomatic adults during circulation of the SARS-CoV-2 ancestral strain and the Alpha and Delta variants.
However, Dr. Sullivan said, “we think that ... plasma with high levels of antibodies can adapt faster to Omicron, although it will take us longer to get an Omicron-specific supply.”
Because of the timing of the study, 80% of participants were unvaccinated. Mean age was 44 years and 57% were women. Black and Hispanic participants each accounted for more than 12% of the study population.
On average, participants received a transfusion within 6 days of the start of symptoms.
In the study, 37 people out of 589 control group participants were hospitalized, compared with 17 of the 592 who received the convalescent plasma.
“We know antibodies work against SARS-CoV-2. The vaccines have been spectacular – producing antibodies that reduce hospitalizations and prevent transmission,” Dr. Sullivan said. “Convalescent plasma provides much of the same antibodies instantly.”
Convalescent and controversial
Convalescent plasma has been one of the controversial treatments for people with COVID-19 – with studies going back and forth on the potential benefits and efficacy. A National Institutes of Health–funded study published in August 2021, for example, showed no significant benefit.
“As you know, convalescent plasma has had a rocky ride,” Dr. Casadevall said.
“It was deployed with great excitement in the terrible, early days of the pandemic. Unfortunately, the early excitement and optimism was dampened with some of the randomized control trials appearing to show no benefit in reducing mortality and hospitalized patients,” he added.
In contrast, the current study shows “where convalescent plasma works using the latest, most rigorous clinical investigation tools available: a double-blinded, randomized, placebo-control trial,” Dr. Casadevall said.
Why a preprint, and why now?
The researchers decided to release their data in recognition of the lag time between reporting of COVID-19 cases and hospitalizations, Dr. Sullivan said. “That’s part of the reason we decided to act now with this knowledge – that it does take a couple of weeks – with cases of Omicron going up.”
Furthermore, “we thought this was actionable data for decision-makers,” he added.
A reporter asked why the Johns Hopkins researchers chose to hold a media briefing for a preprint study.
A preprint is “not so unusual given the SARS-CoV-2 pandemic,” said study senior author Daniel Hanley, MD, division director of brain injury outcomes at Johns Hopkins University.
“The data are the data,” Dr. Casadevall added. “This is not going to change from peer review.”
Peer review may change some of the wording of the manuscript, but not the numbers, he added.
“Now with the Omicron crisis and the fact that we have lost some more main monoclonal antibodies, it is essential to get this information out,” Dr. Casadevall said.
Plasma therapy nothing new
Donation and transfusion of convalescent plasma is highly regulated with strict criteria, said Evan Bloch, MBChB, associate director of the transfusion medicine division at Johns Hopkins University.
If the FDA opts to expand the EUA based on this or other evidence, administration of convalescent plasma could be rolled out fairly quickly, the researchers noted.
Plasma transfusion takes place in hospitals and at infusion centers every day. The infrastructure is in place in many countries, even low- and middle-resource nations, around the world to provide convalescent plasma therapy. The major difference between traditional plasma and SARS-CoV-2 convalescent plasma is the indication, Dr. Bloch added.
In addition, convalescent plasma has a polyclonal composition – a benefit compared with monoclonal antibodies, he added. “It’s more durable or adaptive [compared with] some of the targeted therapies, such as monoclonal antibodies, where we’ve witnessed this diminished efficacy with viral evolution.”
A version of this article first appeared on Medscape.com.
A “definitive study” from Johns Hopkins University researchers and others shows that convalescent plasma can cut hospital admissions for COVID-19 by 54% if therapy is administered within 8 days of symptom onset.
In the study of 1,181 adults randomly assigned to high-titer convalescent plasma or placebo, 2.9% of people receiving the therapy were hospitalized, compared with 6.3% who received placebo control plasma.
This translates to a 54% risk reduction for hospitalization with convalescent plasma.
“We have a clear difference,” principal investigator David Sullivan, MD, a professor at Johns Hopkins University, Baltimore, said during a Dec. 21 media briefing.
“This is very good news since we are in the midst of the Omicron surge, which has defeated [some of] our major monocular antibody therapies,” said Arturo Casadevall, MD, chair of the department of molecular microbiology and immunology at Johns Hopkins.
“So we have a new tool to keep people from progressing in their disease and to reduce progression or hospitalization,” Dr. Casadevall said.
The findings were published as a preprint study on Dec. 21, 2021, on medRxiv. The study has not yet been peer reviewed.
Whereas many convalescent plasma studies were done in hospitalized patients, this is one of only a handful performed in outpatients, the researchers noted.
There is a regulatory catch. The Food and Drug Administration restricted emergency use authorization (EUA) for convalescent plasma in February 2021 to include only high-dose titer plasma and to limit the therapy to hospitalized patients with early disease or for immunocompromised people who cannot mount an adequate antibody response.
Dr. Sullivan and colleagues hoped their findings will prompt the FDA to expand the EUA to include outpatients.
“We have shared this data with both the World Health Organization and the FDA,” study coauthor Kelly Gebo, MD, MPH, said during the media briefing.
“We do believe that this could be scaled up quickly,” added Dr. Gebo, professor of medicine at Johns Hopkins University. Convalescent plasma “could be used as a potential treatment as variants continue to evolve, such as we’ve seen with Omicron.”
Pre-Omicron results
The study was conducted at Johns Hopkins University and 23 other sites nationwide between June 2020 and October 2021. This means researchers enrolled symptomatic adults during circulation of the SARS-CoV-2 ancestral strain and the Alpha and Delta variants.
However, Dr. Sullivan said, “we think that ... plasma with high levels of antibodies can adapt faster to Omicron, although it will take us longer to get an Omicron-specific supply.”
Because of the timing of the study, 80% of participants were unvaccinated. Mean age was 44 years and 57% were women. Black and Hispanic participants each accounted for more than 12% of the study population.
On average, participants received a transfusion within 6 days of the start of symptoms.
In the study, 37 people out of 589 control group participants were hospitalized, compared with 17 of the 592 who received the convalescent plasma.
“We know antibodies work against SARS-CoV-2. The vaccines have been spectacular – producing antibodies that reduce hospitalizations and prevent transmission,” Dr. Sullivan said. “Convalescent plasma provides much of the same antibodies instantly.”
Convalescent and controversial
Convalescent plasma has been one of the controversial treatments for people with COVID-19 – with studies going back and forth on the potential benefits and efficacy. A National Institutes of Health–funded study published in August 2021, for example, showed no significant benefit.
“As you know, convalescent plasma has had a rocky ride,” Dr. Casadevall said.
“It was deployed with great excitement in the terrible, early days of the pandemic. Unfortunately, the early excitement and optimism was dampened with some of the randomized control trials appearing to show no benefit in reducing mortality and hospitalized patients,” he added.
In contrast, the current study shows “where convalescent plasma works using the latest, most rigorous clinical investigation tools available: a double-blinded, randomized, placebo-control trial,” Dr. Casadevall said.
Why a preprint, and why now?
The researchers decided to release their data in recognition of the lag time between reporting of COVID-19 cases and hospitalizations, Dr. Sullivan said. “That’s part of the reason we decided to act now with this knowledge – that it does take a couple of weeks – with cases of Omicron going up.”
Furthermore, “we thought this was actionable data for decision-makers,” he added.
A reporter asked why the Johns Hopkins researchers chose to hold a media briefing for a preprint study.
A preprint is “not so unusual given the SARS-CoV-2 pandemic,” said study senior author Daniel Hanley, MD, division director of brain injury outcomes at Johns Hopkins University.
“The data are the data,” Dr. Casadevall added. “This is not going to change from peer review.”
Peer review may change some of the wording of the manuscript, but not the numbers, he added.
“Now with the Omicron crisis and the fact that we have lost some more main monoclonal antibodies, it is essential to get this information out,” Dr. Casadevall said.
Plasma therapy nothing new
Donation and transfusion of convalescent plasma is highly regulated with strict criteria, said Evan Bloch, MBChB, associate director of the transfusion medicine division at Johns Hopkins University.
If the FDA opts to expand the EUA based on this or other evidence, administration of convalescent plasma could be rolled out fairly quickly, the researchers noted.
Plasma transfusion takes place in hospitals and at infusion centers every day. The infrastructure is in place in many countries, even low- and middle-resource nations, around the world to provide convalescent plasma therapy. The major difference between traditional plasma and SARS-CoV-2 convalescent plasma is the indication, Dr. Bloch added.
In addition, convalescent plasma has a polyclonal composition – a benefit compared with monoclonal antibodies, he added. “It’s more durable or adaptive [compared with] some of the targeted therapies, such as monoclonal antibodies, where we’ve witnessed this diminished efficacy with viral evolution.”
A version of this article first appeared on Medscape.com.
A “definitive study” from Johns Hopkins University researchers and others shows that convalescent plasma can cut hospital admissions for COVID-19 by 54% if therapy is administered within 8 days of symptom onset.
In the study of 1,181 adults randomly assigned to high-titer convalescent plasma or placebo, 2.9% of people receiving the therapy were hospitalized, compared with 6.3% who received placebo control plasma.
This translates to a 54% risk reduction for hospitalization with convalescent plasma.
“We have a clear difference,” principal investigator David Sullivan, MD, a professor at Johns Hopkins University, Baltimore, said during a Dec. 21 media briefing.
“This is very good news since we are in the midst of the Omicron surge, which has defeated [some of] our major monocular antibody therapies,” said Arturo Casadevall, MD, chair of the department of molecular microbiology and immunology at Johns Hopkins.
“So we have a new tool to keep people from progressing in their disease and to reduce progression or hospitalization,” Dr. Casadevall said.
The findings were published as a preprint study on Dec. 21, 2021, on medRxiv. The study has not yet been peer reviewed.
Whereas many convalescent plasma studies were done in hospitalized patients, this is one of only a handful performed in outpatients, the researchers noted.
There is a regulatory catch. The Food and Drug Administration restricted emergency use authorization (EUA) for convalescent plasma in February 2021 to include only high-dose titer plasma and to limit the therapy to hospitalized patients with early disease or for immunocompromised people who cannot mount an adequate antibody response.
Dr. Sullivan and colleagues hoped their findings will prompt the FDA to expand the EUA to include outpatients.
“We have shared this data with both the World Health Organization and the FDA,” study coauthor Kelly Gebo, MD, MPH, said during the media briefing.
“We do believe that this could be scaled up quickly,” added Dr. Gebo, professor of medicine at Johns Hopkins University. Convalescent plasma “could be used as a potential treatment as variants continue to evolve, such as we’ve seen with Omicron.”
Pre-Omicron results
The study was conducted at Johns Hopkins University and 23 other sites nationwide between June 2020 and October 2021. This means researchers enrolled symptomatic adults during circulation of the SARS-CoV-2 ancestral strain and the Alpha and Delta variants.
However, Dr. Sullivan said, “we think that ... plasma with high levels of antibodies can adapt faster to Omicron, although it will take us longer to get an Omicron-specific supply.”
Because of the timing of the study, 80% of participants were unvaccinated. Mean age was 44 years and 57% were women. Black and Hispanic participants each accounted for more than 12% of the study population.
On average, participants received a transfusion within 6 days of the start of symptoms.
In the study, 37 people out of 589 control group participants were hospitalized, compared with 17 of the 592 who received the convalescent plasma.
“We know antibodies work against SARS-CoV-2. The vaccines have been spectacular – producing antibodies that reduce hospitalizations and prevent transmission,” Dr. Sullivan said. “Convalescent plasma provides much of the same antibodies instantly.”
Convalescent and controversial
Convalescent plasma has been one of the controversial treatments for people with COVID-19 – with studies going back and forth on the potential benefits and efficacy. A National Institutes of Health–funded study published in August 2021, for example, showed no significant benefit.
“As you know, convalescent plasma has had a rocky ride,” Dr. Casadevall said.
“It was deployed with great excitement in the terrible, early days of the pandemic. Unfortunately, the early excitement and optimism was dampened with some of the randomized control trials appearing to show no benefit in reducing mortality and hospitalized patients,” he added.
In contrast, the current study shows “where convalescent plasma works using the latest, most rigorous clinical investigation tools available: a double-blinded, randomized, placebo-control trial,” Dr. Casadevall said.
Why a preprint, and why now?
The researchers decided to release their data in recognition of the lag time between reporting of COVID-19 cases and hospitalizations, Dr. Sullivan said. “That’s part of the reason we decided to act now with this knowledge – that it does take a couple of weeks – with cases of Omicron going up.”
Furthermore, “we thought this was actionable data for decision-makers,” he added.
A reporter asked why the Johns Hopkins researchers chose to hold a media briefing for a preprint study.
A preprint is “not so unusual given the SARS-CoV-2 pandemic,” said study senior author Daniel Hanley, MD, division director of brain injury outcomes at Johns Hopkins University.
“The data are the data,” Dr. Casadevall added. “This is not going to change from peer review.”
Peer review may change some of the wording of the manuscript, but not the numbers, he added.
“Now with the Omicron crisis and the fact that we have lost some more main monoclonal antibodies, it is essential to get this information out,” Dr. Casadevall said.
Plasma therapy nothing new
Donation and transfusion of convalescent plasma is highly regulated with strict criteria, said Evan Bloch, MBChB, associate director of the transfusion medicine division at Johns Hopkins University.
If the FDA opts to expand the EUA based on this or other evidence, administration of convalescent plasma could be rolled out fairly quickly, the researchers noted.
Plasma transfusion takes place in hospitals and at infusion centers every day. The infrastructure is in place in many countries, even low- and middle-resource nations, around the world to provide convalescent plasma therapy. The major difference between traditional plasma and SARS-CoV-2 convalescent plasma is the indication, Dr. Bloch added.
In addition, convalescent plasma has a polyclonal composition – a benefit compared with monoclonal antibodies, he added. “It’s more durable or adaptive [compared with] some of the targeted therapies, such as monoclonal antibodies, where we’ve witnessed this diminished efficacy with viral evolution.”
A version of this article first appeared on Medscape.com.
FROM MEDRXIV
Bamlanivimab’s effects in COVID-19 depend on antibodies
In the randomized controlled trial, in both the group who received bamlanivimab and the group who received placebo, higher antigen and viral RNA levels were associated with a lower proportion of patients achieving recovery.
Other studies have shown that the use of monoclonal antibodies reduces hospitalization risk in outpatients with early COVID-19, and appears to promote viral load decline in the nasopharynx, wrote Jens D. Lundgren, MD, of the University of Copenhagen and colleagues in their article published in the Annals of Internal Medicine. What had been missing prior to this new research was final results from hospitalized patients, the authors said.
In the new study, the researchers randomized 314 adults hospitalized with COVID-19 but without end-organ failure to receive 7,000 mg bamlanivimab (163 patients) or a placebo (151 patients). All patients received study-supplied remdesivir unless contraindicated. The researchers compared the efficacy of bamlanivimab versus placebo, but considered remdesivir the standard of care in this study.
At baseline, 50% of patients overall had antispike endogenous neutralizing antibodies (nAbs), and 50% had SARS-CoV-2 nucleocapsid plasma antigen levels of at least 1,000 ng/L.
The median time to sustained recovery, 19 days, was not significantly different between the bamlanivimab and placebo groups (subhazard ratio, 0.99).
“As hypothesized, among those who were negative for nAb, the difference between bamlanivimab and placebo was more evident if levels of plasma antigen or nasal-swab viral RNA were above the median entry levels,” with subhazard ratios of 1.48 and 1.89, respectively, the researchers explained.
However, the hazard ratio for death for bamlanivimab vs. placebo was 0.45 for patients negative for nAb vs. 3.53 for those positive for nAb. These differences with respect to nAb status were similar across all 90 elements of a composite safety outcome, the researchers said.
Potential benefits remain unclear
The use of neutralizing monoclonal antibodies has been extensively documented as an effective treatment for COVID-19 among ambulatory patients, corresponding author Dr. Lundgren said in an interview.
“Conversely, among admitted patients with COVID-19 pneumonia, the benefit has been questionable,” he said.
The researchers examined a hypothesis that the null finding in hospitalized patients may stem from differences in underlying mechanisms, “either from uncontrolled viral replication – which would be predicted to occur in particular among those not yet been able to mount an endogenous immune response – or from hyperinflammation among those that have mounted such a response,” Dr. Lundgren said.
The study findings supported the stated hypothesis, said Dr. Lundgren. “However, it was surprising that not only was the neutralizing antibody without any benefit among those that had mounted an endogenous immune response, but it actually may have been harmful,” he said.
Bamlanivimab was effective against the viral strain that circulated at the time of enrollment in the study, but subsequent viral strains have appeared to be unaffected by the neutralizing activity of the antibody, said Dr. Lundgren.
From a practical standpoint, “the findings would suggest that use of neutralizing monoclonal antibodies for patients admitted to a hospital with COVID pneumonia should be restricted to those that have not yet mounted an endogenous immune response, as determined by lack of detectable neutralizing antibodies at the time of admission,” Dr. Lundgren said.
Looking ahead, studies are currently underway to examine how the findings translate to vaccinated patients, he added. Other questions to be addressed include whether the benefits and harms apply to some or all neutralizing antibody products, he said.
In addition, “our research consortium is currently doing field testing of several point-of-care test candidates to examine their reliability and functionality,” for how quickly they might identify an endogenous neutralizing antibody response in an admitted COVID pneumonia patient,” Dr. Lundgren noted.
Findings show bamlanivimab’s limits
“Based on the findings of the current study, no clear subgroup of patients could be identified who would benefit from bamlanivimab when hospitalized with COVID-19,” said Suman Pal, MD, of the University of New Mexico, Albuquerque, in an interview.
“The study findings also show possible harm of using bamlanivimab in hospitalized COVID-19 patients who were seropositive for neutralizing antibodies prior to receiving therapy,” Dr. Pal emphasized. “Moreover, the study did not include participants with COVID-19 from variant strains, such as delta and omicron, which currently account for a large number of cases.” “Therefore, the results of this study do not support the use of bamlanivimab in the clinical setting until further evidence is available to guide the selection of patients who may benefit from therapy,” he explained.
“The possible benefit of bamlanivimab does not outweigh the risks in patients hospitalized with COVID-19,” he concluded.
Dr. Pal emphasized the need for larger prospective studies to establish whether bamlanivimab may have benefits in a subgroup of patients, but “well-validated point-of-care tests to identify such patients need to be readily available before this therapy can be considered by clinicians at the bedside,” he concluded.
Diligent screening required before use
Monoclonal antibody treatment has been administered to individuals with diagnosis of COVID-19 infection as outpatients as well as for hospitalized inpatients, said Noel Deep, MD, an internist in Antigo, Wisc., in an interview. “This study is important because it helps physicians and health care institutions to evaluate whether continued use of the monoclonal antibodies would be beneficial and, if so, in what patient populations,” he said.
The findings present interesting implications for the care of COVID-19 patients, said Dr. Deep. “This study indicates that bamlanivimab does not provide the benefit that was initially envisioned when the monoclonal antibody infusions were initially initiated in the treatment of COVID-19 infections. “Serological screening of the patients would help to identify that subgroup of individuals who could benefit from this monoclonal antibody rather than administering it to every COVID-19–positive individual,” he explained.
However, “it is important to note that the emergency use authorization (EUA) for single-agent bamlanivimab has been revoked,” Dr. Deep said.
“The potential benefits of bamlanivimab can be realized only if adequate attention is paid to identifying the appropriate candidates based on serological screening, and administering bamlanivimab to those who are already producing endogenous antibodies could lead to increased risk to those individuals,” he said. Dr. Deep added that he would favor administration of bamlanivimab “in those appropriately screened and eligible candidates, and it is my opinion that the benefits outweigh the risks in those individuals.”
Although the EUA for single-agent bamlanivimab has been revoked, “alternative monoclonal antibody therapies remain available under EUA, including REGEN-COV (casirivimab and imdevimab, administered together), and bamlanivimab and etesevimab administered together, for the same uses as previously authorized for bamlanivimab alone,” Dr. Deep said. “The FDA believes that these alternative monoclonal antibody therapies remain appropriate to treat patients with COVID-19, and I would like to see some data about the benefits and risks of these agents,” he noted.
Limitations, funding, and disclosures
The main limitation of the study was the small size and the fact that it was a subgroup analysis of a trial that ended early because of futility, the researchers wrote. However, the Therapeutics for Inpatients With COVID-19 (TICO) platform will proceed with clinical evaluation of additional COVID-19 treatments, they said.
The study was supported primarily by the U.S. government Operation Warp Speed and the National Institute of Allergy and Infectious Diseases. Other funding sources included the Division of Clinical Research and Leidos Biomedical Research for the INSIGHT (International Network for Strategic Initiatives in Global HIV Trials) Network, as well as an agreement between the National Heart, Lung, and Blood Institute and the Research Triangle Institute for the PETAL (Prevention & Early Treatment of Acute Lung Injury) Network and CTSN (Cardiothoracic Surgical Trials Network). Other support came from the U.S. Department of Veterans Affairs and the governments of Denmark (National Research Foundation), Australia (National Health and Medical Research Council), and the United Kingdom (Medical Research Council).
The medications used in the study were donated by Gilead Sciences and Eli Lilly.
The researchers had no financial conflicts do disclose. Dr. Deep and Dr. Pal had no relevant financial conflicts to disclose.
In the randomized controlled trial, in both the group who received bamlanivimab and the group who received placebo, higher antigen and viral RNA levels were associated with a lower proportion of patients achieving recovery.
Other studies have shown that the use of monoclonal antibodies reduces hospitalization risk in outpatients with early COVID-19, and appears to promote viral load decline in the nasopharynx, wrote Jens D. Lundgren, MD, of the University of Copenhagen and colleagues in their article published in the Annals of Internal Medicine. What had been missing prior to this new research was final results from hospitalized patients, the authors said.
In the new study, the researchers randomized 314 adults hospitalized with COVID-19 but without end-organ failure to receive 7,000 mg bamlanivimab (163 patients) or a placebo (151 patients). All patients received study-supplied remdesivir unless contraindicated. The researchers compared the efficacy of bamlanivimab versus placebo, but considered remdesivir the standard of care in this study.
At baseline, 50% of patients overall had antispike endogenous neutralizing antibodies (nAbs), and 50% had SARS-CoV-2 nucleocapsid plasma antigen levels of at least 1,000 ng/L.
The median time to sustained recovery, 19 days, was not significantly different between the bamlanivimab and placebo groups (subhazard ratio, 0.99).
“As hypothesized, among those who were negative for nAb, the difference between bamlanivimab and placebo was more evident if levels of plasma antigen or nasal-swab viral RNA were above the median entry levels,” with subhazard ratios of 1.48 and 1.89, respectively, the researchers explained.
However, the hazard ratio for death for bamlanivimab vs. placebo was 0.45 for patients negative for nAb vs. 3.53 for those positive for nAb. These differences with respect to nAb status were similar across all 90 elements of a composite safety outcome, the researchers said.
Potential benefits remain unclear
The use of neutralizing monoclonal antibodies has been extensively documented as an effective treatment for COVID-19 among ambulatory patients, corresponding author Dr. Lundgren said in an interview.
“Conversely, among admitted patients with COVID-19 pneumonia, the benefit has been questionable,” he said.
The researchers examined a hypothesis that the null finding in hospitalized patients may stem from differences in underlying mechanisms, “either from uncontrolled viral replication – which would be predicted to occur in particular among those not yet been able to mount an endogenous immune response – or from hyperinflammation among those that have mounted such a response,” Dr. Lundgren said.
The study findings supported the stated hypothesis, said Dr. Lundgren. “However, it was surprising that not only was the neutralizing antibody without any benefit among those that had mounted an endogenous immune response, but it actually may have been harmful,” he said.
Bamlanivimab was effective against the viral strain that circulated at the time of enrollment in the study, but subsequent viral strains have appeared to be unaffected by the neutralizing activity of the antibody, said Dr. Lundgren.
From a practical standpoint, “the findings would suggest that use of neutralizing monoclonal antibodies for patients admitted to a hospital with COVID pneumonia should be restricted to those that have not yet mounted an endogenous immune response, as determined by lack of detectable neutralizing antibodies at the time of admission,” Dr. Lundgren said.
Looking ahead, studies are currently underway to examine how the findings translate to vaccinated patients, he added. Other questions to be addressed include whether the benefits and harms apply to some or all neutralizing antibody products, he said.
In addition, “our research consortium is currently doing field testing of several point-of-care test candidates to examine their reliability and functionality,” for how quickly they might identify an endogenous neutralizing antibody response in an admitted COVID pneumonia patient,” Dr. Lundgren noted.
Findings show bamlanivimab’s limits
“Based on the findings of the current study, no clear subgroup of patients could be identified who would benefit from bamlanivimab when hospitalized with COVID-19,” said Suman Pal, MD, of the University of New Mexico, Albuquerque, in an interview.
“The study findings also show possible harm of using bamlanivimab in hospitalized COVID-19 patients who were seropositive for neutralizing antibodies prior to receiving therapy,” Dr. Pal emphasized. “Moreover, the study did not include participants with COVID-19 from variant strains, such as delta and omicron, which currently account for a large number of cases.” “Therefore, the results of this study do not support the use of bamlanivimab in the clinical setting until further evidence is available to guide the selection of patients who may benefit from therapy,” he explained.
“The possible benefit of bamlanivimab does not outweigh the risks in patients hospitalized with COVID-19,” he concluded.
Dr. Pal emphasized the need for larger prospective studies to establish whether bamlanivimab may have benefits in a subgroup of patients, but “well-validated point-of-care tests to identify such patients need to be readily available before this therapy can be considered by clinicians at the bedside,” he concluded.
Diligent screening required before use
Monoclonal antibody treatment has been administered to individuals with diagnosis of COVID-19 infection as outpatients as well as for hospitalized inpatients, said Noel Deep, MD, an internist in Antigo, Wisc., in an interview. “This study is important because it helps physicians and health care institutions to evaluate whether continued use of the monoclonal antibodies would be beneficial and, if so, in what patient populations,” he said.
The findings present interesting implications for the care of COVID-19 patients, said Dr. Deep. “This study indicates that bamlanivimab does not provide the benefit that was initially envisioned when the monoclonal antibody infusions were initially initiated in the treatment of COVID-19 infections. “Serological screening of the patients would help to identify that subgroup of individuals who could benefit from this monoclonal antibody rather than administering it to every COVID-19–positive individual,” he explained.
However, “it is important to note that the emergency use authorization (EUA) for single-agent bamlanivimab has been revoked,” Dr. Deep said.
“The potential benefits of bamlanivimab can be realized only if adequate attention is paid to identifying the appropriate candidates based on serological screening, and administering bamlanivimab to those who are already producing endogenous antibodies could lead to increased risk to those individuals,” he said. Dr. Deep added that he would favor administration of bamlanivimab “in those appropriately screened and eligible candidates, and it is my opinion that the benefits outweigh the risks in those individuals.”
Although the EUA for single-agent bamlanivimab has been revoked, “alternative monoclonal antibody therapies remain available under EUA, including REGEN-COV (casirivimab and imdevimab, administered together), and bamlanivimab and etesevimab administered together, for the same uses as previously authorized for bamlanivimab alone,” Dr. Deep said. “The FDA believes that these alternative monoclonal antibody therapies remain appropriate to treat patients with COVID-19, and I would like to see some data about the benefits and risks of these agents,” he noted.
Limitations, funding, and disclosures
The main limitation of the study was the small size and the fact that it was a subgroup analysis of a trial that ended early because of futility, the researchers wrote. However, the Therapeutics for Inpatients With COVID-19 (TICO) platform will proceed with clinical evaluation of additional COVID-19 treatments, they said.
The study was supported primarily by the U.S. government Operation Warp Speed and the National Institute of Allergy and Infectious Diseases. Other funding sources included the Division of Clinical Research and Leidos Biomedical Research for the INSIGHT (International Network for Strategic Initiatives in Global HIV Trials) Network, as well as an agreement between the National Heart, Lung, and Blood Institute and the Research Triangle Institute for the PETAL (Prevention & Early Treatment of Acute Lung Injury) Network and CTSN (Cardiothoracic Surgical Trials Network). Other support came from the U.S. Department of Veterans Affairs and the governments of Denmark (National Research Foundation), Australia (National Health and Medical Research Council), and the United Kingdom (Medical Research Council).
The medications used in the study were donated by Gilead Sciences and Eli Lilly.
The researchers had no financial conflicts do disclose. Dr. Deep and Dr. Pal had no relevant financial conflicts to disclose.
In the randomized controlled trial, in both the group who received bamlanivimab and the group who received placebo, higher antigen and viral RNA levels were associated with a lower proportion of patients achieving recovery.
Other studies have shown that the use of monoclonal antibodies reduces hospitalization risk in outpatients with early COVID-19, and appears to promote viral load decline in the nasopharynx, wrote Jens D. Lundgren, MD, of the University of Copenhagen and colleagues in their article published in the Annals of Internal Medicine. What had been missing prior to this new research was final results from hospitalized patients, the authors said.
In the new study, the researchers randomized 314 adults hospitalized with COVID-19 but without end-organ failure to receive 7,000 mg bamlanivimab (163 patients) or a placebo (151 patients). All patients received study-supplied remdesivir unless contraindicated. The researchers compared the efficacy of bamlanivimab versus placebo, but considered remdesivir the standard of care in this study.
At baseline, 50% of patients overall had antispike endogenous neutralizing antibodies (nAbs), and 50% had SARS-CoV-2 nucleocapsid plasma antigen levels of at least 1,000 ng/L.
The median time to sustained recovery, 19 days, was not significantly different between the bamlanivimab and placebo groups (subhazard ratio, 0.99).
“As hypothesized, among those who were negative for nAb, the difference between bamlanivimab and placebo was more evident if levels of plasma antigen or nasal-swab viral RNA were above the median entry levels,” with subhazard ratios of 1.48 and 1.89, respectively, the researchers explained.
However, the hazard ratio for death for bamlanivimab vs. placebo was 0.45 for patients negative for nAb vs. 3.53 for those positive for nAb. These differences with respect to nAb status were similar across all 90 elements of a composite safety outcome, the researchers said.
Potential benefits remain unclear
The use of neutralizing monoclonal antibodies has been extensively documented as an effective treatment for COVID-19 among ambulatory patients, corresponding author Dr. Lundgren said in an interview.
“Conversely, among admitted patients with COVID-19 pneumonia, the benefit has been questionable,” he said.
The researchers examined a hypothesis that the null finding in hospitalized patients may stem from differences in underlying mechanisms, “either from uncontrolled viral replication – which would be predicted to occur in particular among those not yet been able to mount an endogenous immune response – or from hyperinflammation among those that have mounted such a response,” Dr. Lundgren said.
The study findings supported the stated hypothesis, said Dr. Lundgren. “However, it was surprising that not only was the neutralizing antibody without any benefit among those that had mounted an endogenous immune response, but it actually may have been harmful,” he said.
Bamlanivimab was effective against the viral strain that circulated at the time of enrollment in the study, but subsequent viral strains have appeared to be unaffected by the neutralizing activity of the antibody, said Dr. Lundgren.
From a practical standpoint, “the findings would suggest that use of neutralizing monoclonal antibodies for patients admitted to a hospital with COVID pneumonia should be restricted to those that have not yet mounted an endogenous immune response, as determined by lack of detectable neutralizing antibodies at the time of admission,” Dr. Lundgren said.
Looking ahead, studies are currently underway to examine how the findings translate to vaccinated patients, he added. Other questions to be addressed include whether the benefits and harms apply to some or all neutralizing antibody products, he said.
In addition, “our research consortium is currently doing field testing of several point-of-care test candidates to examine their reliability and functionality,” for how quickly they might identify an endogenous neutralizing antibody response in an admitted COVID pneumonia patient,” Dr. Lundgren noted.
Findings show bamlanivimab’s limits
“Based on the findings of the current study, no clear subgroup of patients could be identified who would benefit from bamlanivimab when hospitalized with COVID-19,” said Suman Pal, MD, of the University of New Mexico, Albuquerque, in an interview.
“The study findings also show possible harm of using bamlanivimab in hospitalized COVID-19 patients who were seropositive for neutralizing antibodies prior to receiving therapy,” Dr. Pal emphasized. “Moreover, the study did not include participants with COVID-19 from variant strains, such as delta and omicron, which currently account for a large number of cases.” “Therefore, the results of this study do not support the use of bamlanivimab in the clinical setting until further evidence is available to guide the selection of patients who may benefit from therapy,” he explained.
“The possible benefit of bamlanivimab does not outweigh the risks in patients hospitalized with COVID-19,” he concluded.
Dr. Pal emphasized the need for larger prospective studies to establish whether bamlanivimab may have benefits in a subgroup of patients, but “well-validated point-of-care tests to identify such patients need to be readily available before this therapy can be considered by clinicians at the bedside,” he concluded.
Diligent screening required before use
Monoclonal antibody treatment has been administered to individuals with diagnosis of COVID-19 infection as outpatients as well as for hospitalized inpatients, said Noel Deep, MD, an internist in Antigo, Wisc., in an interview. “This study is important because it helps physicians and health care institutions to evaluate whether continued use of the monoclonal antibodies would be beneficial and, if so, in what patient populations,” he said.
The findings present interesting implications for the care of COVID-19 patients, said Dr. Deep. “This study indicates that bamlanivimab does not provide the benefit that was initially envisioned when the monoclonal antibody infusions were initially initiated in the treatment of COVID-19 infections. “Serological screening of the patients would help to identify that subgroup of individuals who could benefit from this monoclonal antibody rather than administering it to every COVID-19–positive individual,” he explained.
However, “it is important to note that the emergency use authorization (EUA) for single-agent bamlanivimab has been revoked,” Dr. Deep said.
“The potential benefits of bamlanivimab can be realized only if adequate attention is paid to identifying the appropriate candidates based on serological screening, and administering bamlanivimab to those who are already producing endogenous antibodies could lead to increased risk to those individuals,” he said. Dr. Deep added that he would favor administration of bamlanivimab “in those appropriately screened and eligible candidates, and it is my opinion that the benefits outweigh the risks in those individuals.”
Although the EUA for single-agent bamlanivimab has been revoked, “alternative monoclonal antibody therapies remain available under EUA, including REGEN-COV (casirivimab and imdevimab, administered together), and bamlanivimab and etesevimab administered together, for the same uses as previously authorized for bamlanivimab alone,” Dr. Deep said. “The FDA believes that these alternative monoclonal antibody therapies remain appropriate to treat patients with COVID-19, and I would like to see some data about the benefits and risks of these agents,” he noted.
Limitations, funding, and disclosures
The main limitation of the study was the small size and the fact that it was a subgroup analysis of a trial that ended early because of futility, the researchers wrote. However, the Therapeutics for Inpatients With COVID-19 (TICO) platform will proceed with clinical evaluation of additional COVID-19 treatments, they said.
The study was supported primarily by the U.S. government Operation Warp Speed and the National Institute of Allergy and Infectious Diseases. Other funding sources included the Division of Clinical Research and Leidos Biomedical Research for the INSIGHT (International Network for Strategic Initiatives in Global HIV Trials) Network, as well as an agreement between the National Heart, Lung, and Blood Institute and the Research Triangle Institute for the PETAL (Prevention & Early Treatment of Acute Lung Injury) Network and CTSN (Cardiothoracic Surgical Trials Network). Other support came from the U.S. Department of Veterans Affairs and the governments of Denmark (National Research Foundation), Australia (National Health and Medical Research Council), and the United Kingdom (Medical Research Council).
The medications used in the study were donated by Gilead Sciences and Eli Lilly.
The researchers had no financial conflicts do disclose. Dr. Deep and Dr. Pal had no relevant financial conflicts to disclose.
FROM ANNALS OF INTERNAL MEDICINE
D-dimer thresholds rule out PE in meta-analysis
In a patient suspected to have a PE, “diagnosis is made radiographically, usually with CT pulmonary angiogram, or V/Q scan,” Suman Pal, MD, of the University of New Mexico, Albuquerque, said in an interview.
“Validated clinical decision tools such as Wells’ score or Geneva score may be used to identify patients at low pretest probability of PE who may initially get a D-dimer level check, followed by imaging only if D-dimer level is elevated,” explained Dr. Pal, who was not involved with the new research, which was published in the Annals of Internal Medicine.
According to the authors of the new paper, while current diagnostic strategies in patients with suspected PE include use of a validated clinical decision rule (CDR) and D-dimer testing to rule out PE without imaging tests, the effectiveness of D-dimer tests in older patients, inpatients, cancer patients, and other high-risk groups has not been well-studied.
Lead author of the paper, Milou A.M. Stals, MD, and colleagues said their goal was to evaluate the safety and efficiency of the Wells rule and revised Geneva score in combination with D-dimer tests, and also the YEARS algorithm for D-dimer thresholds, in their paper.
Dr. Stals, of Leiden (the Netherlands) University Medical Center, and the coinvestigators conducted an international systemic review and individual patient data meta-analysis that included 16 studies and 20,553 patients, with all studies having been published between Jan. 1, 1995, and Jan. 1, 2021. Their primary outcomes were the safety and efficiency of each of these three strategies.
In the review, the researchers defined safety as the 3-month incidence of venous thromboembolism after PE was ruled out without imaging at baseline. They defined efficiency as the proportion patients for whom PE was ruled out based on D-dimer thresholds without imaging.
Overall, efficiency was highest in the subset of patients aged younger than 40 years, ranging from 47% to 68% in this group. Efficiency was lowest in patients aged 80 years and older (6.0%-23%), and in patients with cancer (9.6%-26%).
The efficiency was higher when D-dimer thresholds based on pretest probability were used, compared with when fixed or age-adjusted D-dimer thresholds were used.
The key finding was the significant variability in performance of the diagnostic strategies, the researchers said.
“The predicted failure rate was generally highest for strategies incorporating adapted D-dimer thresholds. However, at the same time, predicted overall efficiency was substantially higher with these strategies versus strategies with a fixed D-dimer threshold as well,” they said. Given that the benefits of each of the three diagnostic strategies depends on their correct application, the researchers recommended that an individual hospitalist choose one strategy for their institution.
“Whether clinicians should rely on the Wells rule, the YEARS algorithm, or the revised Geneva score becomes a matter of local preference and experience,” Dr. Stals and colleagues wrote.
The study findings were limited by several factors including between-study differences in scoring predictors and D-dimer assays. Another limitation was that differential verification biases for classifying fatal events and PE may have contributed to overestimation of failure rates of the adapted D-dimer thresholds.
Strengths of the study included its large sample size and original data on pretest probability, and that data support the use of any of the three strategies for ruling out PE in the identified subgroups without the need for imaging tests, the authors wrote.
“Pending the results of ongoing diagnostic randomized trials, physicians and guideline committees should balance the interlink between safety and efficiency of available diagnostic strategies,” they concluded.
Adapted D-dimer benefits some patients
“Clearly, increasing the D-dimer cutoff will lower the number of patients who require radiographic imaging (improved specificity), but this comes with a risk for missing PE (lower sensitivity). Is this risk worth taking?” Daniel J. Brotman, MD, of Johns Hopkins University, Baltimore, asked in an editorial accompanying the new study.
Dr. Brotman was not surprised by the study findings.
“Conditions that predispose to thrombosis through activated hemostasis – such as advanced age, cancer, inflammation, prolonged hospitalization, and trauma – drive D-dimer levels higher independent of the presence or absence of radiographically apparent thrombosis,” he said. However, these patients are unlikely to have normal D-dimer levels regardless of the cutoff used.
Adapted D-dimer cutoffs may benefit some patients, including those with contraindications or limited access to imaging, said Dr. Brotman. D-dimer may be used for risk stratification regardless of PE, since patients with marginally elevated D-dimers have better prognoses than those with higher D-dimer elevations, even if a small PE is missed.
Dr. Brotman wrote that increasing D-dimer cutoffs for high-risk patients in the subgroups analyzed may spare some patients radiographic testing, but doing so carries an increased risk for diagnostic failure. Overall, “the important work by Stals and colleagues offers reassurance that modifying D-dimer thresholds according to age or pretest probability is safe enough for widespread practice, even in high-risk groups.”
Focus on single strategy ‘based on local needs’
“Several validated clinical decision tools, along with age or pretest probability adjusted D-dimer threshold are currently in use as diagnostic strategies for ruling out pulmonary embolism,” Dr. Pal said in an interview.
The current study is important because of limited data on the performance of these strategies in specific subgroups of patients whose risk of PE may differ from the overall patient population, he noted.
“Different diagnostic strategies for PE have a variable performance in patients with differences of age, active cancer, and history of VTE,” said Dr. Pal. “However, in this study, no clear preference for one strategy over others could be established for these subgroups, and clinicians should continue to follow institution-specific guidance.
“A single strategy should be adopted at each institution based on local needs and used as the standard of care until further data are available,” he said.
“The use of D-dimer to rule out PE, either with fixed threshold or age-adjusted thresholds, can be confounded in clinical settings by other comorbid conditions such as sepsis, recent surgery, and more recently, COVID-19,” he said.
“Since the findings of this study do not show a clear benefit of one diagnostic strategy over others in the analyzed subgroups of patients, further prospective head-to-head comparison among the subgroups of interest would be helpful to guide clinical decision making,” Dr. Pal added.
YEARS-specific study supports D-dimer safety and value
A recent paper published in JAMA supported the results of the meta-analysis. In that study, Yonathan Freund, MD, of Sorbonne Université, Paris, and colleagues focused on the YEARS strategy combined with age-adjusted D-dimer thresholds as a way to rule out PE in PERC-positive ED patients.
The authors of this paper randomized 18 EDs to either a protocol of intervention followed by control, or control followed by intervention. The study population included 726 patients in the intervention group and 688 in the control group.
The intervention strategy to rule out PE consisted of assessing the YEARS criteria and D-dimer testing. PE was ruled out in patients with no YEARS criteria and a D-dimer level below 1,000 ng/mL and in patients with one or more YEARS criteria and D-dimers below an age-adjusted threshold (defined as age times 10 ng/mL in patients aged 50 years and older).
The control strategy consisted of D-dimer testing for all patients with the threshold at age-adjusted levels; D-dimers about these levels prompted chest imaging.
Overall, the risk of a missed VTE at 3 months was noninferior between the groups (0.15% in the intervention group and 0.80% in the controls).
“The intervention was associated with a statistically significant reduction in chest imaging use,” the researchers wrote.
This study’s findings were limited by randomization at the center level, rather than the patient level, and the use of imaging on some patients despite negative D-dimer tests, the researchers wrote. However, their findings support those of previous studies and especially support the safety of the intervention, in an emergency medicine setting, as no PEs occurred in patients with a YEARS score of zero who underwent the intervention.
Downsides to applying algorithms to every patient explained
In an editorial accompanying the JAMA study, Marcel Levi, MD, and Nick van Es, MD, of Amsterdam University Medical Center, emphasized the challenges of diagnosing PE given that many patients present with nonspecific clinical manifestations and without typical signs and symptoms. High-resolution CT pulmonary angiography allows for a fast and easy diagnosis in an emergency setting. However, efforts are ongoing to develop alternative strategies that avoid unnecessary scanning for potential PE patients, many of whom have alternative diagnoses such as pulmonary infections, cardiac conditions, pleural disease, or musculoskeletal problems.
On review of the JAMA study using the YEARS rule with adjusted D-dimer thresholds, the editorialists noted that the data were robust and indicated a 10% reduction in chest imaging. They also emphasized the potential to overwhelm busy clinicians with more algorithms.
“Blindly applying algorithms to every patient may be less appropriate or even undesirable in specific situations in which deviation from the rules on clinical grounds is indicated,” but a complex imaging approach may be time consuming and challenging in the acute setting, and a simple algorithm may be safe and efficient in many cases, they wrote. “From a patient perspective, a negative diagnostic algorithm for pulmonary embolism does not diminish the physician’s obligation to consider other diagnoses that explain the symptoms, for which chest CT scans may still be needed and helpful.”
The Annals of Internal Medicine study was supported by the Dutch Research Council. The JAMA study was supported by the French Health Ministry. Dr. Stals, Dr. Freund, Dr. Pal, Dr. Levi, and Dr. van Es had no financial conflicts to disclose.
In a patient suspected to have a PE, “diagnosis is made radiographically, usually with CT pulmonary angiogram, or V/Q scan,” Suman Pal, MD, of the University of New Mexico, Albuquerque, said in an interview.
“Validated clinical decision tools such as Wells’ score or Geneva score may be used to identify patients at low pretest probability of PE who may initially get a D-dimer level check, followed by imaging only if D-dimer level is elevated,” explained Dr. Pal, who was not involved with the new research, which was published in the Annals of Internal Medicine.
According to the authors of the new paper, while current diagnostic strategies in patients with suspected PE include use of a validated clinical decision rule (CDR) and D-dimer testing to rule out PE without imaging tests, the effectiveness of D-dimer tests in older patients, inpatients, cancer patients, and other high-risk groups has not been well-studied.
Lead author of the paper, Milou A.M. Stals, MD, and colleagues said their goal was to evaluate the safety and efficiency of the Wells rule and revised Geneva score in combination with D-dimer tests, and also the YEARS algorithm for D-dimer thresholds, in their paper.
Dr. Stals, of Leiden (the Netherlands) University Medical Center, and the coinvestigators conducted an international systemic review and individual patient data meta-analysis that included 16 studies and 20,553 patients, with all studies having been published between Jan. 1, 1995, and Jan. 1, 2021. Their primary outcomes were the safety and efficiency of each of these three strategies.
In the review, the researchers defined safety as the 3-month incidence of venous thromboembolism after PE was ruled out without imaging at baseline. They defined efficiency as the proportion patients for whom PE was ruled out based on D-dimer thresholds without imaging.
Overall, efficiency was highest in the subset of patients aged younger than 40 years, ranging from 47% to 68% in this group. Efficiency was lowest in patients aged 80 years and older (6.0%-23%), and in patients with cancer (9.6%-26%).
The efficiency was higher when D-dimer thresholds based on pretest probability were used, compared with when fixed or age-adjusted D-dimer thresholds were used.
The key finding was the significant variability in performance of the diagnostic strategies, the researchers said.
“The predicted failure rate was generally highest for strategies incorporating adapted D-dimer thresholds. However, at the same time, predicted overall efficiency was substantially higher with these strategies versus strategies with a fixed D-dimer threshold as well,” they said. Given that the benefits of each of the three diagnostic strategies depends on their correct application, the researchers recommended that an individual hospitalist choose one strategy for their institution.
“Whether clinicians should rely on the Wells rule, the YEARS algorithm, or the revised Geneva score becomes a matter of local preference and experience,” Dr. Stals and colleagues wrote.
The study findings were limited by several factors including between-study differences in scoring predictors and D-dimer assays. Another limitation was that differential verification biases for classifying fatal events and PE may have contributed to overestimation of failure rates of the adapted D-dimer thresholds.
Strengths of the study included its large sample size and original data on pretest probability, and that data support the use of any of the three strategies for ruling out PE in the identified subgroups without the need for imaging tests, the authors wrote.
“Pending the results of ongoing diagnostic randomized trials, physicians and guideline committees should balance the interlink between safety and efficiency of available diagnostic strategies,” they concluded.
Adapted D-dimer benefits some patients
“Clearly, increasing the D-dimer cutoff will lower the number of patients who require radiographic imaging (improved specificity), but this comes with a risk for missing PE (lower sensitivity). Is this risk worth taking?” Daniel J. Brotman, MD, of Johns Hopkins University, Baltimore, asked in an editorial accompanying the new study.
Dr. Brotman was not surprised by the study findings.
“Conditions that predispose to thrombosis through activated hemostasis – such as advanced age, cancer, inflammation, prolonged hospitalization, and trauma – drive D-dimer levels higher independent of the presence or absence of radiographically apparent thrombosis,” he said. However, these patients are unlikely to have normal D-dimer levels regardless of the cutoff used.
Adapted D-dimer cutoffs may benefit some patients, including those with contraindications or limited access to imaging, said Dr. Brotman. D-dimer may be used for risk stratification regardless of PE, since patients with marginally elevated D-dimers have better prognoses than those with higher D-dimer elevations, even if a small PE is missed.
Dr. Brotman wrote that increasing D-dimer cutoffs for high-risk patients in the subgroups analyzed may spare some patients radiographic testing, but doing so carries an increased risk for diagnostic failure. Overall, “the important work by Stals and colleagues offers reassurance that modifying D-dimer thresholds according to age or pretest probability is safe enough for widespread practice, even in high-risk groups.”
Focus on single strategy ‘based on local needs’
“Several validated clinical decision tools, along with age or pretest probability adjusted D-dimer threshold are currently in use as diagnostic strategies for ruling out pulmonary embolism,” Dr. Pal said in an interview.
The current study is important because of limited data on the performance of these strategies in specific subgroups of patients whose risk of PE may differ from the overall patient population, he noted.
“Different diagnostic strategies for PE have a variable performance in patients with differences of age, active cancer, and history of VTE,” said Dr. Pal. “However, in this study, no clear preference for one strategy over others could be established for these subgroups, and clinicians should continue to follow institution-specific guidance.
“A single strategy should be adopted at each institution based on local needs and used as the standard of care until further data are available,” he said.
“The use of D-dimer to rule out PE, either with fixed threshold or age-adjusted thresholds, can be confounded in clinical settings by other comorbid conditions such as sepsis, recent surgery, and more recently, COVID-19,” he said.
“Since the findings of this study do not show a clear benefit of one diagnostic strategy over others in the analyzed subgroups of patients, further prospective head-to-head comparison among the subgroups of interest would be helpful to guide clinical decision making,” Dr. Pal added.
YEARS-specific study supports D-dimer safety and value
A recent paper published in JAMA supported the results of the meta-analysis. In that study, Yonathan Freund, MD, of Sorbonne Université, Paris, and colleagues focused on the YEARS strategy combined with age-adjusted D-dimer thresholds as a way to rule out PE in PERC-positive ED patients.
The authors of this paper randomized 18 EDs to either a protocol of intervention followed by control, or control followed by intervention. The study population included 726 patients in the intervention group and 688 in the control group.
The intervention strategy to rule out PE consisted of assessing the YEARS criteria and D-dimer testing. PE was ruled out in patients with no YEARS criteria and a D-dimer level below 1,000 ng/mL and in patients with one or more YEARS criteria and D-dimers below an age-adjusted threshold (defined as age times 10 ng/mL in patients aged 50 years and older).
The control strategy consisted of D-dimer testing for all patients with the threshold at age-adjusted levels; D-dimers about these levels prompted chest imaging.
Overall, the risk of a missed VTE at 3 months was noninferior between the groups (0.15% in the intervention group and 0.80% in the controls).
“The intervention was associated with a statistically significant reduction in chest imaging use,” the researchers wrote.
This study’s findings were limited by randomization at the center level, rather than the patient level, and the use of imaging on some patients despite negative D-dimer tests, the researchers wrote. However, their findings support those of previous studies and especially support the safety of the intervention, in an emergency medicine setting, as no PEs occurred in patients with a YEARS score of zero who underwent the intervention.
Downsides to applying algorithms to every patient explained
In an editorial accompanying the JAMA study, Marcel Levi, MD, and Nick van Es, MD, of Amsterdam University Medical Center, emphasized the challenges of diagnosing PE given that many patients present with nonspecific clinical manifestations and without typical signs and symptoms. High-resolution CT pulmonary angiography allows for a fast and easy diagnosis in an emergency setting. However, efforts are ongoing to develop alternative strategies that avoid unnecessary scanning for potential PE patients, many of whom have alternative diagnoses such as pulmonary infections, cardiac conditions, pleural disease, or musculoskeletal problems.
On review of the JAMA study using the YEARS rule with adjusted D-dimer thresholds, the editorialists noted that the data were robust and indicated a 10% reduction in chest imaging. They also emphasized the potential to overwhelm busy clinicians with more algorithms.
“Blindly applying algorithms to every patient may be less appropriate or even undesirable in specific situations in which deviation from the rules on clinical grounds is indicated,” but a complex imaging approach may be time consuming and challenging in the acute setting, and a simple algorithm may be safe and efficient in many cases, they wrote. “From a patient perspective, a negative diagnostic algorithm for pulmonary embolism does not diminish the physician’s obligation to consider other diagnoses that explain the symptoms, for which chest CT scans may still be needed and helpful.”
The Annals of Internal Medicine study was supported by the Dutch Research Council. The JAMA study was supported by the French Health Ministry. Dr. Stals, Dr. Freund, Dr. Pal, Dr. Levi, and Dr. van Es had no financial conflicts to disclose.
In a patient suspected to have a PE, “diagnosis is made radiographically, usually with CT pulmonary angiogram, or V/Q scan,” Suman Pal, MD, of the University of New Mexico, Albuquerque, said in an interview.
“Validated clinical decision tools such as Wells’ score or Geneva score may be used to identify patients at low pretest probability of PE who may initially get a D-dimer level check, followed by imaging only if D-dimer level is elevated,” explained Dr. Pal, who was not involved with the new research, which was published in the Annals of Internal Medicine.
According to the authors of the new paper, while current diagnostic strategies in patients with suspected PE include use of a validated clinical decision rule (CDR) and D-dimer testing to rule out PE without imaging tests, the effectiveness of D-dimer tests in older patients, inpatients, cancer patients, and other high-risk groups has not been well-studied.
Lead author of the paper, Milou A.M. Stals, MD, and colleagues said their goal was to evaluate the safety and efficiency of the Wells rule and revised Geneva score in combination with D-dimer tests, and also the YEARS algorithm for D-dimer thresholds, in their paper.
Dr. Stals, of Leiden (the Netherlands) University Medical Center, and the coinvestigators conducted an international systemic review and individual patient data meta-analysis that included 16 studies and 20,553 patients, with all studies having been published between Jan. 1, 1995, and Jan. 1, 2021. Their primary outcomes were the safety and efficiency of each of these three strategies.
In the review, the researchers defined safety as the 3-month incidence of venous thromboembolism after PE was ruled out without imaging at baseline. They defined efficiency as the proportion patients for whom PE was ruled out based on D-dimer thresholds without imaging.
Overall, efficiency was highest in the subset of patients aged younger than 40 years, ranging from 47% to 68% in this group. Efficiency was lowest in patients aged 80 years and older (6.0%-23%), and in patients with cancer (9.6%-26%).
The efficiency was higher when D-dimer thresholds based on pretest probability were used, compared with when fixed or age-adjusted D-dimer thresholds were used.
The key finding was the significant variability in performance of the diagnostic strategies, the researchers said.
“The predicted failure rate was generally highest for strategies incorporating adapted D-dimer thresholds. However, at the same time, predicted overall efficiency was substantially higher with these strategies versus strategies with a fixed D-dimer threshold as well,” they said. Given that the benefits of each of the three diagnostic strategies depends on their correct application, the researchers recommended that an individual hospitalist choose one strategy for their institution.
“Whether clinicians should rely on the Wells rule, the YEARS algorithm, or the revised Geneva score becomes a matter of local preference and experience,” Dr. Stals and colleagues wrote.
The study findings were limited by several factors including between-study differences in scoring predictors and D-dimer assays. Another limitation was that differential verification biases for classifying fatal events and PE may have contributed to overestimation of failure rates of the adapted D-dimer thresholds.
Strengths of the study included its large sample size and original data on pretest probability, and that data support the use of any of the three strategies for ruling out PE in the identified subgroups without the need for imaging tests, the authors wrote.
“Pending the results of ongoing diagnostic randomized trials, physicians and guideline committees should balance the interlink between safety and efficiency of available diagnostic strategies,” they concluded.
Adapted D-dimer benefits some patients
“Clearly, increasing the D-dimer cutoff will lower the number of patients who require radiographic imaging (improved specificity), but this comes with a risk for missing PE (lower sensitivity). Is this risk worth taking?” Daniel J. Brotman, MD, of Johns Hopkins University, Baltimore, asked in an editorial accompanying the new study.
Dr. Brotman was not surprised by the study findings.
“Conditions that predispose to thrombosis through activated hemostasis – such as advanced age, cancer, inflammation, prolonged hospitalization, and trauma – drive D-dimer levels higher independent of the presence or absence of radiographically apparent thrombosis,” he said. However, these patients are unlikely to have normal D-dimer levels regardless of the cutoff used.
Adapted D-dimer cutoffs may benefit some patients, including those with contraindications or limited access to imaging, said Dr. Brotman. D-dimer may be used for risk stratification regardless of PE, since patients with marginally elevated D-dimers have better prognoses than those with higher D-dimer elevations, even if a small PE is missed.
Dr. Brotman wrote that increasing D-dimer cutoffs for high-risk patients in the subgroups analyzed may spare some patients radiographic testing, but doing so carries an increased risk for diagnostic failure. Overall, “the important work by Stals and colleagues offers reassurance that modifying D-dimer thresholds according to age or pretest probability is safe enough for widespread practice, even in high-risk groups.”
Focus on single strategy ‘based on local needs’
“Several validated clinical decision tools, along with age or pretest probability adjusted D-dimer threshold are currently in use as diagnostic strategies for ruling out pulmonary embolism,” Dr. Pal said in an interview.
The current study is important because of limited data on the performance of these strategies in specific subgroups of patients whose risk of PE may differ from the overall patient population, he noted.
“Different diagnostic strategies for PE have a variable performance in patients with differences of age, active cancer, and history of VTE,” said Dr. Pal. “However, in this study, no clear preference for one strategy over others could be established for these subgroups, and clinicians should continue to follow institution-specific guidance.
“A single strategy should be adopted at each institution based on local needs and used as the standard of care until further data are available,” he said.
“The use of D-dimer to rule out PE, either with fixed threshold or age-adjusted thresholds, can be confounded in clinical settings by other comorbid conditions such as sepsis, recent surgery, and more recently, COVID-19,” he said.
“Since the findings of this study do not show a clear benefit of one diagnostic strategy over others in the analyzed subgroups of patients, further prospective head-to-head comparison among the subgroups of interest would be helpful to guide clinical decision making,” Dr. Pal added.
YEARS-specific study supports D-dimer safety and value
A recent paper published in JAMA supported the results of the meta-analysis. In that study, Yonathan Freund, MD, of Sorbonne Université, Paris, and colleagues focused on the YEARS strategy combined with age-adjusted D-dimer thresholds as a way to rule out PE in PERC-positive ED patients.
The authors of this paper randomized 18 EDs to either a protocol of intervention followed by control, or control followed by intervention. The study population included 726 patients in the intervention group and 688 in the control group.
The intervention strategy to rule out PE consisted of assessing the YEARS criteria and D-dimer testing. PE was ruled out in patients with no YEARS criteria and a D-dimer level below 1,000 ng/mL and in patients with one or more YEARS criteria and D-dimers below an age-adjusted threshold (defined as age times 10 ng/mL in patients aged 50 years and older).
The control strategy consisted of D-dimer testing for all patients with the threshold at age-adjusted levels; D-dimers about these levels prompted chest imaging.
Overall, the risk of a missed VTE at 3 months was noninferior between the groups (0.15% in the intervention group and 0.80% in the controls).
“The intervention was associated with a statistically significant reduction in chest imaging use,” the researchers wrote.
This study’s findings were limited by randomization at the center level, rather than the patient level, and the use of imaging on some patients despite negative D-dimer tests, the researchers wrote. However, their findings support those of previous studies and especially support the safety of the intervention, in an emergency medicine setting, as no PEs occurred in patients with a YEARS score of zero who underwent the intervention.
Downsides to applying algorithms to every patient explained
In an editorial accompanying the JAMA study, Marcel Levi, MD, and Nick van Es, MD, of Amsterdam University Medical Center, emphasized the challenges of diagnosing PE given that many patients present with nonspecific clinical manifestations and without typical signs and symptoms. High-resolution CT pulmonary angiography allows for a fast and easy diagnosis in an emergency setting. However, efforts are ongoing to develop alternative strategies that avoid unnecessary scanning for potential PE patients, many of whom have alternative diagnoses such as pulmonary infections, cardiac conditions, pleural disease, or musculoskeletal problems.
On review of the JAMA study using the YEARS rule with adjusted D-dimer thresholds, the editorialists noted that the data were robust and indicated a 10% reduction in chest imaging. They also emphasized the potential to overwhelm busy clinicians with more algorithms.
“Blindly applying algorithms to every patient may be less appropriate or even undesirable in specific situations in which deviation from the rules on clinical grounds is indicated,” but a complex imaging approach may be time consuming and challenging in the acute setting, and a simple algorithm may be safe and efficient in many cases, they wrote. “From a patient perspective, a negative diagnostic algorithm for pulmonary embolism does not diminish the physician’s obligation to consider other diagnoses that explain the symptoms, for which chest CT scans may still be needed and helpful.”
The Annals of Internal Medicine study was supported by the Dutch Research Council. The JAMA study was supported by the French Health Ministry. Dr. Stals, Dr. Freund, Dr. Pal, Dr. Levi, and Dr. van Es had no financial conflicts to disclose.
FROM THE ANNALS OF INTERNAL MEDICINE
For leukemias, COVID-19 death risks tied to poor prognoses, ICU deferrals
, results of an American Society of Hematology (ASH) COVID-19 registry study suggest.
Rates of severe COVID-19 were significantly higher among patients who had active disease or neutropenia at the time of their COVID-19 diagnosis. Mortality related to COVID-19 was linked to neutropenia, primary disease prognosis of less than 6 months, and deferral of recommended ICU care, study results show.
By contrast, mortality was not associated with active primary disease or its treatment, according to researcher Pinkal Desai, MD, MPH.
Taken together, these findings provide preliminary evidence to support the use of aggressive supportive treatment of COVID-19 in patients with acute leukemias and myelodysplastic syndromes, said Dr. Desai, a hematologist-oncologist with Weill Cornell Medicine and NewYork-Presbyterian in New York.
“If desired by patients, aggressive support for hospitalized patients with COVID-19 is appropriate, regardless of remission status, given the results of our study,” Dr. Desai said in a press conference during the annual meeting of the American Society of Hematology.
In non-cancer patient populations, advanced age and cytopenias have been associated with mortality related to COVID-19, Dr. Desai said. Likewise, patients with acute leukemias and myelodysplastic syndrome are generally older and have disease- or treatment-related cytopenias, which might affect the severity of and mortality from COVID-19, she added.
With that concern in mind, Dr. Desai and co-investigators looked at predictors of severe COVID-19 disease and death among patients in the ASH Research Collaborative (ASH RC) COVID-19 Registry for Hematology.
This registry was started in the early days of the pandemic to provide real-time observational COVID-19 data to clinicians, according to an ASH news release.
The analysis by Dr. Desai and co-authors included 257 patients with COVID-19 as determined by their physician, including 135 with a primary diagnosis of acute myeloid leukemia, 82 with acute lymphocytic leukemia, and 40 with myelodysplastic syndromes. Sixty percent of the patients were hospitalized due to COVID-19.
At the time of COVID-19 diagnosis, 46% of patients were in remission, and 44% had active disease, according to the report.
Both neutropenia and active disease status at COVID-19 diagnosis were linked to severe COVID-19, defined as ICU admission due to a COVID-19-related reason, according to results of multivariable analysis. Among patients with severe COVID-19, 67% had active disease, meaning just 33% were in remission, Dr. Desai noted.
In multivariable analysis, two factors were significantly associated with mortality, she added: having an estimated pre-COVID-19 prognosis from the primary disease of less than 6 months, and deferral of ICU care when it was recommended to the patient.
Mortality was 21% overall, higher than would be expected in a non-cancer population, Dr. Desai said. For patients with COVID-19 requiring hospitalization, the mortality rate was 34% and for those patients who did go to the ICU, the mortality rate was 68%.
By contrast, there was no significant association between mortality and active disease as compared to disease in remission, Dr. Desai noted in her presentation. Likewise, mortality was not associated with active treatment at the time of COVID-19 diagnosis as compared to no treatment.
Gwen Nichols, MD, executive vice president and chief medical officer of the Leukemia & Lymphoma Society, New York, said those are reassuring data for patients with acute leukemias and myelodysplastic syndromes and their healthcare providers.
“From our point of view, it helps us say, ‘do not stop your treatment because of worries about COVID-19—it’s more important that you treat your cancer,” Dr. Nichols said in an interview. “We now know we can help people through COVID-19, and I think this is just really important data to back that up,” she added.
Dr. Desai provided disclosures related to Agios, Kura Oncology, and Bristol Myers Squibb (consultancy), and to Janssen R&D and Astex (research funding).
, results of an American Society of Hematology (ASH) COVID-19 registry study suggest.
Rates of severe COVID-19 were significantly higher among patients who had active disease or neutropenia at the time of their COVID-19 diagnosis. Mortality related to COVID-19 was linked to neutropenia, primary disease prognosis of less than 6 months, and deferral of recommended ICU care, study results show.
By contrast, mortality was not associated with active primary disease or its treatment, according to researcher Pinkal Desai, MD, MPH.
Taken together, these findings provide preliminary evidence to support the use of aggressive supportive treatment of COVID-19 in patients with acute leukemias and myelodysplastic syndromes, said Dr. Desai, a hematologist-oncologist with Weill Cornell Medicine and NewYork-Presbyterian in New York.
“If desired by patients, aggressive support for hospitalized patients with COVID-19 is appropriate, regardless of remission status, given the results of our study,” Dr. Desai said in a press conference during the annual meeting of the American Society of Hematology.
In non-cancer patient populations, advanced age and cytopenias have been associated with mortality related to COVID-19, Dr. Desai said. Likewise, patients with acute leukemias and myelodysplastic syndrome are generally older and have disease- or treatment-related cytopenias, which might affect the severity of and mortality from COVID-19, she added.
With that concern in mind, Dr. Desai and co-investigators looked at predictors of severe COVID-19 disease and death among patients in the ASH Research Collaborative (ASH RC) COVID-19 Registry for Hematology.
This registry was started in the early days of the pandemic to provide real-time observational COVID-19 data to clinicians, according to an ASH news release.
The analysis by Dr. Desai and co-authors included 257 patients with COVID-19 as determined by their physician, including 135 with a primary diagnosis of acute myeloid leukemia, 82 with acute lymphocytic leukemia, and 40 with myelodysplastic syndromes. Sixty percent of the patients were hospitalized due to COVID-19.
At the time of COVID-19 diagnosis, 46% of patients were in remission, and 44% had active disease, according to the report.
Both neutropenia and active disease status at COVID-19 diagnosis were linked to severe COVID-19, defined as ICU admission due to a COVID-19-related reason, according to results of multivariable analysis. Among patients with severe COVID-19, 67% had active disease, meaning just 33% were in remission, Dr. Desai noted.
In multivariable analysis, two factors were significantly associated with mortality, she added: having an estimated pre-COVID-19 prognosis from the primary disease of less than 6 months, and deferral of ICU care when it was recommended to the patient.
Mortality was 21% overall, higher than would be expected in a non-cancer population, Dr. Desai said. For patients with COVID-19 requiring hospitalization, the mortality rate was 34% and for those patients who did go to the ICU, the mortality rate was 68%.
By contrast, there was no significant association between mortality and active disease as compared to disease in remission, Dr. Desai noted in her presentation. Likewise, mortality was not associated with active treatment at the time of COVID-19 diagnosis as compared to no treatment.
Gwen Nichols, MD, executive vice president and chief medical officer of the Leukemia & Lymphoma Society, New York, said those are reassuring data for patients with acute leukemias and myelodysplastic syndromes and their healthcare providers.
“From our point of view, it helps us say, ‘do not stop your treatment because of worries about COVID-19—it’s more important that you treat your cancer,” Dr. Nichols said in an interview. “We now know we can help people through COVID-19, and I think this is just really important data to back that up,” she added.
Dr. Desai provided disclosures related to Agios, Kura Oncology, and Bristol Myers Squibb (consultancy), and to Janssen R&D and Astex (research funding).
, results of an American Society of Hematology (ASH) COVID-19 registry study suggest.
Rates of severe COVID-19 were significantly higher among patients who had active disease or neutropenia at the time of their COVID-19 diagnosis. Mortality related to COVID-19 was linked to neutropenia, primary disease prognosis of less than 6 months, and deferral of recommended ICU care, study results show.
By contrast, mortality was not associated with active primary disease or its treatment, according to researcher Pinkal Desai, MD, MPH.
Taken together, these findings provide preliminary evidence to support the use of aggressive supportive treatment of COVID-19 in patients with acute leukemias and myelodysplastic syndromes, said Dr. Desai, a hematologist-oncologist with Weill Cornell Medicine and NewYork-Presbyterian in New York.
“If desired by patients, aggressive support for hospitalized patients with COVID-19 is appropriate, regardless of remission status, given the results of our study,” Dr. Desai said in a press conference during the annual meeting of the American Society of Hematology.
In non-cancer patient populations, advanced age and cytopenias have been associated with mortality related to COVID-19, Dr. Desai said. Likewise, patients with acute leukemias and myelodysplastic syndrome are generally older and have disease- or treatment-related cytopenias, which might affect the severity of and mortality from COVID-19, she added.
With that concern in mind, Dr. Desai and co-investigators looked at predictors of severe COVID-19 disease and death among patients in the ASH Research Collaborative (ASH RC) COVID-19 Registry for Hematology.
This registry was started in the early days of the pandemic to provide real-time observational COVID-19 data to clinicians, according to an ASH news release.
The analysis by Dr. Desai and co-authors included 257 patients with COVID-19 as determined by their physician, including 135 with a primary diagnosis of acute myeloid leukemia, 82 with acute lymphocytic leukemia, and 40 with myelodysplastic syndromes. Sixty percent of the patients were hospitalized due to COVID-19.
At the time of COVID-19 diagnosis, 46% of patients were in remission, and 44% had active disease, according to the report.
Both neutropenia and active disease status at COVID-19 diagnosis were linked to severe COVID-19, defined as ICU admission due to a COVID-19-related reason, according to results of multivariable analysis. Among patients with severe COVID-19, 67% had active disease, meaning just 33% were in remission, Dr. Desai noted.
In multivariable analysis, two factors were significantly associated with mortality, she added: having an estimated pre-COVID-19 prognosis from the primary disease of less than 6 months, and deferral of ICU care when it was recommended to the patient.
Mortality was 21% overall, higher than would be expected in a non-cancer population, Dr. Desai said. For patients with COVID-19 requiring hospitalization, the mortality rate was 34% and for those patients who did go to the ICU, the mortality rate was 68%.
By contrast, there was no significant association between mortality and active disease as compared to disease in remission, Dr. Desai noted in her presentation. Likewise, mortality was not associated with active treatment at the time of COVID-19 diagnosis as compared to no treatment.
Gwen Nichols, MD, executive vice president and chief medical officer of the Leukemia & Lymphoma Society, New York, said those are reassuring data for patients with acute leukemias and myelodysplastic syndromes and their healthcare providers.
“From our point of view, it helps us say, ‘do not stop your treatment because of worries about COVID-19—it’s more important that you treat your cancer,” Dr. Nichols said in an interview. “We now know we can help people through COVID-19, and I think this is just really important data to back that up,” she added.
Dr. Desai provided disclosures related to Agios, Kura Oncology, and Bristol Myers Squibb (consultancy), and to Janssen R&D and Astex (research funding).
FROM ASH 2021
Decreasing the burden of postacute sequelae of SARS-CoV-2 infection: What we know
On March 11, 2020, the World Health Organization (WHO) declared SARS-CoV-2 a pandemic. As of October 2021, there are over 240 million confirmed COVID-19 cases and over 4 million deaths globally, with the United States having the highest incidence of both cases and deaths (https://covid.cdc.gov/covid-data-tracker/#datatracker-home). As many as 87% of COVID-19 survivors experience persistent symptoms that last beyond the acute phase of illness (Carfi A, et al. JAMA. 2020;324[6]:603-5). In February 2021, the National Institutes of Health (NIH) called for a consensus term to describe this protracted form of COVID-19, and defined it as Post-acute Sequelae of SARS-CoV-2 infection (PASC) (https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nih-launches-new-initiative-study-long-covid).
What are the PASC manifestations?
PASC has a heterogeneous presentation with a broad spectrum of manifestations and can vary from single to multiorgan system involvement. Commonly, PASC involves pulmonary abnormalities (shortness of breath, exercise intolerance, abnormal pulmonary functional test [PFT] and chest imaging), neurocognitive impairments (difficulty concentrating and memory loss), mental health disorders (anxiety, depression, and post-traumatic stress disorder), functional mobility impairments, as well as general and constitutional symptoms (fatigue and muscle weakness) (Groff D, et al. JAMA Netw Open. 2021;4[10]). The most prevalent pulmonary physiologic impairment is reduced diffusion capacity that has been shown to be associated with the severity of acute illness, while the most common radiologic abnormalities on chest CT scan are ground glass opacities. Some studies have shown a temporal improvement in pulmonary physiology and exercise capacity; however, persistent physiological and radiographic abnormalities persist in some patients up to 12 months after discharge (Wu X, et al. Lancet Respir Med. 2021;9:747-54). An abnormal or persistent hyper-inflammatory state, viral-induced autoimmune reaction, and ongoing viral activity have been proposed as possible biological mechanisms for PASC; however, the pathophysiology remains mostly unknown.
Who does PASC affect?
PASC affects patients irrespective of premorbid condition and severity of symptoms in the acute phase. It spans from those who had mild disease not requiring hospitalization to those who had critical illness requiring intensive care unit (ICU) management. COVID-19 ICU survivors seem to have an overlap of PASC and post-intensive care syndrome (PICS), defined by new or worsening physical, cognitive, and/or psychiatric impairments after critical illness. (Biehl M, et al. Cleve Clin J Med. 2020 Aug 5).
Who do we evaluate for PASC?
Given the complexity and chronicity of the associated symptoms and their impact on several major organ systems, a comprehensive and multidisciplinary approach is essential to assist with diagnosis and management of PASC. Listening empathically to patients and acknowledging their symptoms are key factors. Access to ambulatory care, establishment of rapport, effective collaboration and coordination of care among different disciplines, management of comorbidities, continuity of care, access to rehabilitation programs, and reduction of disease burden are some of the principles that guided the creation of dedicated COVID-19 clinics throughout the world. The most common services offered are primary care, pulmonology, cardiology, mental health, neurology, speech and language pathology, physical and occupational therapy, pharmacy, and case management. The involvement of specialties varies depending on the specific patient’s needs (Parker A, et al. The Lancet Respir Med. 2021;S2213-2600[21]00385-4).
The development of diagnostic and care pathways by different specialties ensures standardization of clinical assessment and management while allowing for individualized care. The commonly used tools to assess the respiratory system are the 6-minute walk test, PFT, chest imaging including radiographs and high-resolution CT scan, ventilation perfusion scan, and echocardiography. Some patients exhibit persistent cardiopulmonary symptoms with no evidence of organ injury. These patients have persistent exertional and functional limitation with normal PFT, resting echocardiography, and chest imaging. Cardiopulmonary exercise testing (CPET) and, more specifically, invasive CPET can be used to further investigate the decreased exercise capacity. CPET studies have identified an augmented exercise hyperventilation, and the causes of exercise limitation varied from anemia and reduced oxygen extraction by peripheral muscles to deconditioning, obesity, and lower ventilatory efficiency. A study looking at invasive CPET showed reduced peak exercise aerobic capacity in post COVID-19 patients compared with control participants and was associated with impaired systemic oxygen extraction and an exaggerated hyperventilatory response (Singh, et al. Chest. 2021;S0012-3692[21]03635). A subset of COVID-19 survivors presents with symptoms of autonomic dysfunction such as orthostatic intolerance and postural orthostatic tachycardia. These symptoms have been reported after other viral infections and could be secondary to gastrointestinal fluid loss, prolonged bed rest, and deconditioning of the cardiovascular system. More research is needed to characterize the dysautonomia in patients post–COVID-19.
What is the treatment?
Therapies depend on symptoms and organ involvement. The duration of pulmonary symptoms in long-haulers is not yet known, with cough and exercise intolerance/dyspnea ranking among the most common complaints in these patients. Exercise therapy plays an essential part in the rehabilitation of long-haulers and several studies are underway to assess different exercise and rehabilitation programs. For most patients with normal laboratory, physiologic, and imaging tests, post–COVID-19 clinics are offering physical therapy, occupational therapy, and neuropsychological rehabilitation. While steroids have been shown to improve mortality in hospitalized patients with COVID-19 requiring mechanical ventilation or supplemental oxygen, their role in outpatient COVID-19 infections and for post–COVID-19 lung disease/organizing pneumonia remains unclear. In a UK study of patients admitted to the hospital with COVID-19 disease of varying severity, interstitial abnormalities were noted in ~5% of patients at 6 weeks postdischarge and in 10.8% of patients with persistent respiratory symptoms (Myall, et al. Ann Am Thorac Soc. 2021;18[5]:799). The most common radiological findings (in > 50% of cases) were consistent with organizing pneumonia. Patients with persistent physiological abnormalities and interstitial findings improved with steroids. However, since the trajectory of the disease is unknown, further studies are required to understand the natural history of the disease and assess treatment strategies in patients with persistent inflammatory lung changes. Several studies looking at systemic or inhaled steroids in different phases of COVID-19 infection and varying disease severity are ongoing (ClinicalTrials.gov). Antifibrotics used to treat idiopathic pulmonary fibrosis and progressive fibrotic ILD are also being investigated in COVID-19 lung disease. The rationale for their use is to treat and prevent severe COVID-19 lung injury and prevent lung fibrosis.
The role of vaccinations
Whether patients who were infected with COVID-19, and, more specifically, patients with long-term symptoms post-COVID-19, should get vaccinated is actively being investigated. Vaccinations are protective at preventing infections and severe illness. Studies showed that patients who had COVID-19 infection and got vaccinated had a significantly higher antibody response than previously uninfected vaccine recipients. A review showed that the protective effect of prior SARS-CoV-2 infection on reinfection is high and similar to that of vaccination. However, a recent study of hospitalized patients revealed higher rates of COVID-19 among unvaccinated adults with previous infection compared with vaccinated adults (http://dx.doi.org/10.15585/mmwr.mm7044e1). On the other hand, the impact of vaccine on long-hauler symptoms has raised interest. A UK survey (not peer reviewed) on more than 800 long-haulers reported about 57% with overall improvement in their symptoms, 24% no change, and 19% with worsening symptoms after their first dose of vaccine, suggesting that the chances of experiencing an overall worsening of symptoms after vaccination is small, with more than half experiencing improvement (go.nature.com/3yfqem2). While awaiting longitudinal trials, the main argument to guide vaccination in long-haulers is that COVID-19 vaccinations provide protection from reinfection and appear to have the potential to improve symptoms.
The availability of a patient’s support system, peer support, and patient advocacy groups assist in providing equitable care and are critical in sustaining the recovery of COVID-19 survivors. Providing social, financial, and cultural support is imperative in decreasing the burden of COVID-19. The dedicated post–COVID-19 clinics will not only offer care to COVID-19 survivors, but will also help our understanding of the determinants and course of PASC, and will provide opportunities for research. Long-term longitudinal observational studies and clinical trials are critical to identify those at high risk for PASC, clarify the extent of health consequences attributable to COVID-19, and define best practices for COVID-19 survivors.
Dr. Biehl is Staff Physician, Pulmonary & Critical Care Medicine, Director, Post-ICU Recovery Clinic Respiratory Institute, Cleveland Clinic; Dr.Farha is with Respiratory and Lerner Institutes, Cleveland Clinic.
On March 11, 2020, the World Health Organization (WHO) declared SARS-CoV-2 a pandemic. As of October 2021, there are over 240 million confirmed COVID-19 cases and over 4 million deaths globally, with the United States having the highest incidence of both cases and deaths (https://covid.cdc.gov/covid-data-tracker/#datatracker-home). As many as 87% of COVID-19 survivors experience persistent symptoms that last beyond the acute phase of illness (Carfi A, et al. JAMA. 2020;324[6]:603-5). In February 2021, the National Institutes of Health (NIH) called for a consensus term to describe this protracted form of COVID-19, and defined it as Post-acute Sequelae of SARS-CoV-2 infection (PASC) (https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nih-launches-new-initiative-study-long-covid).
What are the PASC manifestations?
PASC has a heterogeneous presentation with a broad spectrum of manifestations and can vary from single to multiorgan system involvement. Commonly, PASC involves pulmonary abnormalities (shortness of breath, exercise intolerance, abnormal pulmonary functional test [PFT] and chest imaging), neurocognitive impairments (difficulty concentrating and memory loss), mental health disorders (anxiety, depression, and post-traumatic stress disorder), functional mobility impairments, as well as general and constitutional symptoms (fatigue and muscle weakness) (Groff D, et al. JAMA Netw Open. 2021;4[10]). The most prevalent pulmonary physiologic impairment is reduced diffusion capacity that has been shown to be associated with the severity of acute illness, while the most common radiologic abnormalities on chest CT scan are ground glass opacities. Some studies have shown a temporal improvement in pulmonary physiology and exercise capacity; however, persistent physiological and radiographic abnormalities persist in some patients up to 12 months after discharge (Wu X, et al. Lancet Respir Med. 2021;9:747-54). An abnormal or persistent hyper-inflammatory state, viral-induced autoimmune reaction, and ongoing viral activity have been proposed as possible biological mechanisms for PASC; however, the pathophysiology remains mostly unknown.
Who does PASC affect?
PASC affects patients irrespective of premorbid condition and severity of symptoms in the acute phase. It spans from those who had mild disease not requiring hospitalization to those who had critical illness requiring intensive care unit (ICU) management. COVID-19 ICU survivors seem to have an overlap of PASC and post-intensive care syndrome (PICS), defined by new or worsening physical, cognitive, and/or psychiatric impairments after critical illness. (Biehl M, et al. Cleve Clin J Med. 2020 Aug 5).
Who do we evaluate for PASC?
Given the complexity and chronicity of the associated symptoms and their impact on several major organ systems, a comprehensive and multidisciplinary approach is essential to assist with diagnosis and management of PASC. Listening empathically to patients and acknowledging their symptoms are key factors. Access to ambulatory care, establishment of rapport, effective collaboration and coordination of care among different disciplines, management of comorbidities, continuity of care, access to rehabilitation programs, and reduction of disease burden are some of the principles that guided the creation of dedicated COVID-19 clinics throughout the world. The most common services offered are primary care, pulmonology, cardiology, mental health, neurology, speech and language pathology, physical and occupational therapy, pharmacy, and case management. The involvement of specialties varies depending on the specific patient’s needs (Parker A, et al. The Lancet Respir Med. 2021;S2213-2600[21]00385-4).
The development of diagnostic and care pathways by different specialties ensures standardization of clinical assessment and management while allowing for individualized care. The commonly used tools to assess the respiratory system are the 6-minute walk test, PFT, chest imaging including radiographs and high-resolution CT scan, ventilation perfusion scan, and echocardiography. Some patients exhibit persistent cardiopulmonary symptoms with no evidence of organ injury. These patients have persistent exertional and functional limitation with normal PFT, resting echocardiography, and chest imaging. Cardiopulmonary exercise testing (CPET) and, more specifically, invasive CPET can be used to further investigate the decreased exercise capacity. CPET studies have identified an augmented exercise hyperventilation, and the causes of exercise limitation varied from anemia and reduced oxygen extraction by peripheral muscles to deconditioning, obesity, and lower ventilatory efficiency. A study looking at invasive CPET showed reduced peak exercise aerobic capacity in post COVID-19 patients compared with control participants and was associated with impaired systemic oxygen extraction and an exaggerated hyperventilatory response (Singh, et al. Chest. 2021;S0012-3692[21]03635). A subset of COVID-19 survivors presents with symptoms of autonomic dysfunction such as orthostatic intolerance and postural orthostatic tachycardia. These symptoms have been reported after other viral infections and could be secondary to gastrointestinal fluid loss, prolonged bed rest, and deconditioning of the cardiovascular system. More research is needed to characterize the dysautonomia in patients post–COVID-19.
What is the treatment?
Therapies depend on symptoms and organ involvement. The duration of pulmonary symptoms in long-haulers is not yet known, with cough and exercise intolerance/dyspnea ranking among the most common complaints in these patients. Exercise therapy plays an essential part in the rehabilitation of long-haulers and several studies are underway to assess different exercise and rehabilitation programs. For most patients with normal laboratory, physiologic, and imaging tests, post–COVID-19 clinics are offering physical therapy, occupational therapy, and neuropsychological rehabilitation. While steroids have been shown to improve mortality in hospitalized patients with COVID-19 requiring mechanical ventilation or supplemental oxygen, their role in outpatient COVID-19 infections and for post–COVID-19 lung disease/organizing pneumonia remains unclear. In a UK study of patients admitted to the hospital with COVID-19 disease of varying severity, interstitial abnormalities were noted in ~5% of patients at 6 weeks postdischarge and in 10.8% of patients with persistent respiratory symptoms (Myall, et al. Ann Am Thorac Soc. 2021;18[5]:799). The most common radiological findings (in > 50% of cases) were consistent with organizing pneumonia. Patients with persistent physiological abnormalities and interstitial findings improved with steroids. However, since the trajectory of the disease is unknown, further studies are required to understand the natural history of the disease and assess treatment strategies in patients with persistent inflammatory lung changes. Several studies looking at systemic or inhaled steroids in different phases of COVID-19 infection and varying disease severity are ongoing (ClinicalTrials.gov). Antifibrotics used to treat idiopathic pulmonary fibrosis and progressive fibrotic ILD are also being investigated in COVID-19 lung disease. The rationale for their use is to treat and prevent severe COVID-19 lung injury and prevent lung fibrosis.
The role of vaccinations
Whether patients who were infected with COVID-19, and, more specifically, patients with long-term symptoms post-COVID-19, should get vaccinated is actively being investigated. Vaccinations are protective at preventing infections and severe illness. Studies showed that patients who had COVID-19 infection and got vaccinated had a significantly higher antibody response than previously uninfected vaccine recipients. A review showed that the protective effect of prior SARS-CoV-2 infection on reinfection is high and similar to that of vaccination. However, a recent study of hospitalized patients revealed higher rates of COVID-19 among unvaccinated adults with previous infection compared with vaccinated adults (http://dx.doi.org/10.15585/mmwr.mm7044e1). On the other hand, the impact of vaccine on long-hauler symptoms has raised interest. A UK survey (not peer reviewed) on more than 800 long-haulers reported about 57% with overall improvement in their symptoms, 24% no change, and 19% with worsening symptoms after their first dose of vaccine, suggesting that the chances of experiencing an overall worsening of symptoms after vaccination is small, with more than half experiencing improvement (go.nature.com/3yfqem2). While awaiting longitudinal trials, the main argument to guide vaccination in long-haulers is that COVID-19 vaccinations provide protection from reinfection and appear to have the potential to improve symptoms.
The availability of a patient’s support system, peer support, and patient advocacy groups assist in providing equitable care and are critical in sustaining the recovery of COVID-19 survivors. Providing social, financial, and cultural support is imperative in decreasing the burden of COVID-19. The dedicated post–COVID-19 clinics will not only offer care to COVID-19 survivors, but will also help our understanding of the determinants and course of PASC, and will provide opportunities for research. Long-term longitudinal observational studies and clinical trials are critical to identify those at high risk for PASC, clarify the extent of health consequences attributable to COVID-19, and define best practices for COVID-19 survivors.
Dr. Biehl is Staff Physician, Pulmonary & Critical Care Medicine, Director, Post-ICU Recovery Clinic Respiratory Institute, Cleveland Clinic; Dr.Farha is with Respiratory and Lerner Institutes, Cleveland Clinic.
On March 11, 2020, the World Health Organization (WHO) declared SARS-CoV-2 a pandemic. As of October 2021, there are over 240 million confirmed COVID-19 cases and over 4 million deaths globally, with the United States having the highest incidence of both cases and deaths (https://covid.cdc.gov/covid-data-tracker/#datatracker-home). As many as 87% of COVID-19 survivors experience persistent symptoms that last beyond the acute phase of illness (Carfi A, et al. JAMA. 2020;324[6]:603-5). In February 2021, the National Institutes of Health (NIH) called for a consensus term to describe this protracted form of COVID-19, and defined it as Post-acute Sequelae of SARS-CoV-2 infection (PASC) (https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nih-launches-new-initiative-study-long-covid).
What are the PASC manifestations?
PASC has a heterogeneous presentation with a broad spectrum of manifestations and can vary from single to multiorgan system involvement. Commonly, PASC involves pulmonary abnormalities (shortness of breath, exercise intolerance, abnormal pulmonary functional test [PFT] and chest imaging), neurocognitive impairments (difficulty concentrating and memory loss), mental health disorders (anxiety, depression, and post-traumatic stress disorder), functional mobility impairments, as well as general and constitutional symptoms (fatigue and muscle weakness) (Groff D, et al. JAMA Netw Open. 2021;4[10]). The most prevalent pulmonary physiologic impairment is reduced diffusion capacity that has been shown to be associated with the severity of acute illness, while the most common radiologic abnormalities on chest CT scan are ground glass opacities. Some studies have shown a temporal improvement in pulmonary physiology and exercise capacity; however, persistent physiological and radiographic abnormalities persist in some patients up to 12 months after discharge (Wu X, et al. Lancet Respir Med. 2021;9:747-54). An abnormal or persistent hyper-inflammatory state, viral-induced autoimmune reaction, and ongoing viral activity have been proposed as possible biological mechanisms for PASC; however, the pathophysiology remains mostly unknown.
Who does PASC affect?
PASC affects patients irrespective of premorbid condition and severity of symptoms in the acute phase. It spans from those who had mild disease not requiring hospitalization to those who had critical illness requiring intensive care unit (ICU) management. COVID-19 ICU survivors seem to have an overlap of PASC and post-intensive care syndrome (PICS), defined by new or worsening physical, cognitive, and/or psychiatric impairments after critical illness. (Biehl M, et al. Cleve Clin J Med. 2020 Aug 5).
Who do we evaluate for PASC?
Given the complexity and chronicity of the associated symptoms and their impact on several major organ systems, a comprehensive and multidisciplinary approach is essential to assist with diagnosis and management of PASC. Listening empathically to patients and acknowledging their symptoms are key factors. Access to ambulatory care, establishment of rapport, effective collaboration and coordination of care among different disciplines, management of comorbidities, continuity of care, access to rehabilitation programs, and reduction of disease burden are some of the principles that guided the creation of dedicated COVID-19 clinics throughout the world. The most common services offered are primary care, pulmonology, cardiology, mental health, neurology, speech and language pathology, physical and occupational therapy, pharmacy, and case management. The involvement of specialties varies depending on the specific patient’s needs (Parker A, et al. The Lancet Respir Med. 2021;S2213-2600[21]00385-4).
The development of diagnostic and care pathways by different specialties ensures standardization of clinical assessment and management while allowing for individualized care. The commonly used tools to assess the respiratory system are the 6-minute walk test, PFT, chest imaging including radiographs and high-resolution CT scan, ventilation perfusion scan, and echocardiography. Some patients exhibit persistent cardiopulmonary symptoms with no evidence of organ injury. These patients have persistent exertional and functional limitation with normal PFT, resting echocardiography, and chest imaging. Cardiopulmonary exercise testing (CPET) and, more specifically, invasive CPET can be used to further investigate the decreased exercise capacity. CPET studies have identified an augmented exercise hyperventilation, and the causes of exercise limitation varied from anemia and reduced oxygen extraction by peripheral muscles to deconditioning, obesity, and lower ventilatory efficiency. A study looking at invasive CPET showed reduced peak exercise aerobic capacity in post COVID-19 patients compared with control participants and was associated with impaired systemic oxygen extraction and an exaggerated hyperventilatory response (Singh, et al. Chest. 2021;S0012-3692[21]03635). A subset of COVID-19 survivors presents with symptoms of autonomic dysfunction such as orthostatic intolerance and postural orthostatic tachycardia. These symptoms have been reported after other viral infections and could be secondary to gastrointestinal fluid loss, prolonged bed rest, and deconditioning of the cardiovascular system. More research is needed to characterize the dysautonomia in patients post–COVID-19.
What is the treatment?
Therapies depend on symptoms and organ involvement. The duration of pulmonary symptoms in long-haulers is not yet known, with cough and exercise intolerance/dyspnea ranking among the most common complaints in these patients. Exercise therapy plays an essential part in the rehabilitation of long-haulers and several studies are underway to assess different exercise and rehabilitation programs. For most patients with normal laboratory, physiologic, and imaging tests, post–COVID-19 clinics are offering physical therapy, occupational therapy, and neuropsychological rehabilitation. While steroids have been shown to improve mortality in hospitalized patients with COVID-19 requiring mechanical ventilation or supplemental oxygen, their role in outpatient COVID-19 infections and for post–COVID-19 lung disease/organizing pneumonia remains unclear. In a UK study of patients admitted to the hospital with COVID-19 disease of varying severity, interstitial abnormalities were noted in ~5% of patients at 6 weeks postdischarge and in 10.8% of patients with persistent respiratory symptoms (Myall, et al. Ann Am Thorac Soc. 2021;18[5]:799). The most common radiological findings (in > 50% of cases) were consistent with organizing pneumonia. Patients with persistent physiological abnormalities and interstitial findings improved with steroids. However, since the trajectory of the disease is unknown, further studies are required to understand the natural history of the disease and assess treatment strategies in patients with persistent inflammatory lung changes. Several studies looking at systemic or inhaled steroids in different phases of COVID-19 infection and varying disease severity are ongoing (ClinicalTrials.gov). Antifibrotics used to treat idiopathic pulmonary fibrosis and progressive fibrotic ILD are also being investigated in COVID-19 lung disease. The rationale for their use is to treat and prevent severe COVID-19 lung injury and prevent lung fibrosis.
The role of vaccinations
Whether patients who were infected with COVID-19, and, more specifically, patients with long-term symptoms post-COVID-19, should get vaccinated is actively being investigated. Vaccinations are protective at preventing infections and severe illness. Studies showed that patients who had COVID-19 infection and got vaccinated had a significantly higher antibody response than previously uninfected vaccine recipients. A review showed that the protective effect of prior SARS-CoV-2 infection on reinfection is high and similar to that of vaccination. However, a recent study of hospitalized patients revealed higher rates of COVID-19 among unvaccinated adults with previous infection compared with vaccinated adults (http://dx.doi.org/10.15585/mmwr.mm7044e1). On the other hand, the impact of vaccine on long-hauler symptoms has raised interest. A UK survey (not peer reviewed) on more than 800 long-haulers reported about 57% with overall improvement in their symptoms, 24% no change, and 19% with worsening symptoms after their first dose of vaccine, suggesting that the chances of experiencing an overall worsening of symptoms after vaccination is small, with more than half experiencing improvement (go.nature.com/3yfqem2). While awaiting longitudinal trials, the main argument to guide vaccination in long-haulers is that COVID-19 vaccinations provide protection from reinfection and appear to have the potential to improve symptoms.
The availability of a patient’s support system, peer support, and patient advocacy groups assist in providing equitable care and are critical in sustaining the recovery of COVID-19 survivors. Providing social, financial, and cultural support is imperative in decreasing the burden of COVID-19. The dedicated post–COVID-19 clinics will not only offer care to COVID-19 survivors, but will also help our understanding of the determinants and course of PASC, and will provide opportunities for research. Long-term longitudinal observational studies and clinical trials are critical to identify those at high risk for PASC, clarify the extent of health consequences attributable to COVID-19, and define best practices for COVID-19 survivors.
Dr. Biehl is Staff Physician, Pulmonary & Critical Care Medicine, Director, Post-ICU Recovery Clinic Respiratory Institute, Cleveland Clinic; Dr.Farha is with Respiratory and Lerner Institutes, Cleveland Clinic.
Timing of initiation of renal-replacement therapy in acute kidney injury
Background: Acute kidney injury (AKI) is a common complication that occurs in seriously ill patients admitted to the ICU, and many of these patients eventually require RRT. When complicated by major metabolic disorders, it is usually clear when therapy should be initiated. However, when these complications are absent, the most appropriate time to initiate RRT is unclear. There are potential advantages to performing early RRT in patients with severe AKI, such as restoring acid-base balance, preventing fluid accumulation, and preventing major electrolyte disturbances.
Study design: Multinational, randomized, controlled trial.
Setting: 168 hospitals in 15 countries.
Synopsis: Eligible patients were adults admitted to an ICU with severe AKI. Patients were randomly assigned to an accelerated strategy of RRT (initiated within 12 hours, 1,465 patients) or a standard strategy of RRT (held until conventional indications developed or AKI lasted more than 72 hours, 1,462 patients). RRT was performed in 1,418 (96.8%) in the accelerated group and 903 (61.8%) in the standard group. At 90 days, 643 deaths (43.9%) occurred in the accelerated group and 639 deaths (43.7%) occurred in the standard group (RR, 1.00; 95% CI, 0.93-1.09; P = .92). Among survivors at 90 days, 85 out of 814 accelerated patients (10.4%) and 49 of 815 standard patients (6.0%) continued to require RRT (RR, 1.75; 95% CI, 1.24-2.43), suggesting the possibility of increased dependence on long-term RRT if introduced early. Limitations include use of clinical equipoise to confirm full eligibility, introducing possible patient heterogeneity into the trial. In addition, broad discretion was given to clinicians on when to start RRT in the standard group resulting in variable initiation times.
Bottom line: In critically ill patients with severe AKI, earlier RRT did not result in lower mortality at 90 days compared with standard therapy and increased the risk of requiring RRT at 90 days.
Citation: Bagshaw SM et al. Timing of initiation of renal-replacement therapy in acute kidney injury. N Engl J Med. 2020;383:240-51. doi: 10.1056/NEJMoa2000741.
Dr. Kim is a hospitalist in the Division of Hospital Medicine, Mount Sinai Health System, New York.
Background: Acute kidney injury (AKI) is a common complication that occurs in seriously ill patients admitted to the ICU, and many of these patients eventually require RRT. When complicated by major metabolic disorders, it is usually clear when therapy should be initiated. However, when these complications are absent, the most appropriate time to initiate RRT is unclear. There are potential advantages to performing early RRT in patients with severe AKI, such as restoring acid-base balance, preventing fluid accumulation, and preventing major electrolyte disturbances.
Study design: Multinational, randomized, controlled trial.
Setting: 168 hospitals in 15 countries.
Synopsis: Eligible patients were adults admitted to an ICU with severe AKI. Patients were randomly assigned to an accelerated strategy of RRT (initiated within 12 hours, 1,465 patients) or a standard strategy of RRT (held until conventional indications developed or AKI lasted more than 72 hours, 1,462 patients). RRT was performed in 1,418 (96.8%) in the accelerated group and 903 (61.8%) in the standard group. At 90 days, 643 deaths (43.9%) occurred in the accelerated group and 639 deaths (43.7%) occurred in the standard group (RR, 1.00; 95% CI, 0.93-1.09; P = .92). Among survivors at 90 days, 85 out of 814 accelerated patients (10.4%) and 49 of 815 standard patients (6.0%) continued to require RRT (RR, 1.75; 95% CI, 1.24-2.43), suggesting the possibility of increased dependence on long-term RRT if introduced early. Limitations include use of clinical equipoise to confirm full eligibility, introducing possible patient heterogeneity into the trial. In addition, broad discretion was given to clinicians on when to start RRT in the standard group resulting in variable initiation times.
Bottom line: In critically ill patients with severe AKI, earlier RRT did not result in lower mortality at 90 days compared with standard therapy and increased the risk of requiring RRT at 90 days.
Citation: Bagshaw SM et al. Timing of initiation of renal-replacement therapy in acute kidney injury. N Engl J Med. 2020;383:240-51. doi: 10.1056/NEJMoa2000741.
Dr. Kim is a hospitalist in the Division of Hospital Medicine, Mount Sinai Health System, New York.
Background: Acute kidney injury (AKI) is a common complication that occurs in seriously ill patients admitted to the ICU, and many of these patients eventually require RRT. When complicated by major metabolic disorders, it is usually clear when therapy should be initiated. However, when these complications are absent, the most appropriate time to initiate RRT is unclear. There are potential advantages to performing early RRT in patients with severe AKI, such as restoring acid-base balance, preventing fluid accumulation, and preventing major electrolyte disturbances.
Study design: Multinational, randomized, controlled trial.
Setting: 168 hospitals in 15 countries.
Synopsis: Eligible patients were adults admitted to an ICU with severe AKI. Patients were randomly assigned to an accelerated strategy of RRT (initiated within 12 hours, 1,465 patients) or a standard strategy of RRT (held until conventional indications developed or AKI lasted more than 72 hours, 1,462 patients). RRT was performed in 1,418 (96.8%) in the accelerated group and 903 (61.8%) in the standard group. At 90 days, 643 deaths (43.9%) occurred in the accelerated group and 639 deaths (43.7%) occurred in the standard group (RR, 1.00; 95% CI, 0.93-1.09; P = .92). Among survivors at 90 days, 85 out of 814 accelerated patients (10.4%) and 49 of 815 standard patients (6.0%) continued to require RRT (RR, 1.75; 95% CI, 1.24-2.43), suggesting the possibility of increased dependence on long-term RRT if introduced early. Limitations include use of clinical equipoise to confirm full eligibility, introducing possible patient heterogeneity into the trial. In addition, broad discretion was given to clinicians on when to start RRT in the standard group resulting in variable initiation times.
Bottom line: In critically ill patients with severe AKI, earlier RRT did not result in lower mortality at 90 days compared with standard therapy and increased the risk of requiring RRT at 90 days.
Citation: Bagshaw SM et al. Timing of initiation of renal-replacement therapy in acute kidney injury. N Engl J Med. 2020;383:240-51. doi: 10.1056/NEJMoa2000741.
Dr. Kim is a hospitalist in the Division of Hospital Medicine, Mount Sinai Health System, New York.