User login
Greater handgrip strength tied to lower risk for depression
, new research suggests.
In a study of more than 115,000 adults, there was a significant association between stronger handgrip, up to 40 kg in men and 27 kg in women, and lower depression risk.
Investigators add that there was a “dose-response” association between physical strength and risk for depression.
“Being physically strong may serve as a preventive factor for depression in older adults, but this is limited to a maximum specific threshold for men and women,” Ruben Lopez-Bueno, PhD, of the department of physical medicine and nursing, University of Zaragoza, Spain, and colleagues write.
The findings were published online in the British Journal of Psychiatry.
Easy, fast, reliable
Depression is a major public health problem, and studies “aimed at examining preventive factors to tackle the increase in depression are required,” the investigators write.
They add that a “growing body of research” is examining the link between depression and muscle strength, with handgrip as an estimator, in healthy middle-aged and older adults.
Handgrip strength is an “easy-to-use, fast and reliable indicator of both sarcopenia (age-related loss of muscle mass) and dynapenia (age-related loss of muscle strength), both of which have been associated with depression,” the researchers note.
It is plausible that there is a “regulatory role of skeletal muscle on brain function affecting this condition,” they add.
They note that exercise seems to play a “key role” because it can improve muscle strength as well as muscle mass, downregulate systemic inflammation, and improve neuroplasticity, neuroendocrine, and oxidative stress responses.
Previous studies have relied either on cross-sectional or prospective cohort models and have focused mostly on a specific country, “not accounting for time-varying changes of both handgrip strength and relevant covariables.”
Moreover, previous evidence has been mixed regarding the “extent to which handgrip strength levels may associate with lower risk of depression, with study results ranging from weak to strong associations,” the investigators write.
So “higher-quality research with representative samples from different countries is required to better clarify the strength of such an association and to confirm directionality,” they add.
SHARE data
To fill this gap, the researchers turned to data from waves 1, 2, 4, 5, 6, and 7 of the Survey of Health, Ageing and Retirement in Europe (SHARE). This encompassed 115,601 individuals aged 50 years and older (mean age, 64.3 years; 54.3% women) residing in European countries and Israel (24 countries total).
Data from wave 3 were not used because handgrip measures were not used in that wave. In the other waves, a handheld dynamometer was used to measure handgrip strength.
The participants were divided into tertiles of handgrip strength, with the “first third” being the lowest tertile of strength and the “final third” representing the highest strength.
All participants were followed for a median of 7.3 years (792,459 person-years), during which 26.1% experienced a risk for depression, as reflected by scores on the EURO-D 12-item scale.
The investigators set the time scale as the months from study entry until either a first depression onset or the end of follow-up.
Covariates that the researchers accounted for included gender, age, education, country, body mass index, physical inactivity, smoking, alcohol consumption, whether living with a partner, wave of inclusion, chronic diseases, consumption of prescribed drugs, and fruit and vegetable consumption.
The researchers used two models: the first adjusted for gender and age at time of the interview, and the second adjusted for all confounders.
In the model that was adjusted only for gender and age, greater handgrip strength was associated with a significantly reduced risk for depression among participants in the second, third, and the final third in comparison with the first third (hazard ratio, 0.65; 95% confidence interval, 0.63-0.68; and HR, 0.50; 95% CI, 0.48-0.53, respectively).
The associations remained consistent in the fully adjusted model, although risk for depression was slightly attenuated in the second and final thirds compared with the first third (HR, 0.76; 95% CI, 0.71-0.81; and HR, 0.64; 95% CI, 0.59-0.69, respectively).
When the researchers conducted analyses using restricted cubic spline modeling, they found a significant association for each kilogram increase of handgrip strength and depression, up to 40 kg in men and 27 kg in women (HR, 1.39; 95% CI, 1.08-1.71; and HR, 1.28; 95% CI, 1.05-1.55, respectively).
There was no greater reduction in depression risk in those with handgrip strength above those values.
Potential depression screen
The investigators suggest several explanations for their findings. For example, handgrip strength has “been used as an overall indicator of health status, including sarcopenia,” they write.
Adults with sarcopenia have been found to be at greater risk for depression because of reduced muscle strength, since neurotrophins are produced by skeletal muscle, among other tissues, and are associated with improvement in mood.
From a psychological point of view, “being physically strong may lead to a sensation of psychological wellbeing,” the researchers write.
Moreover, being physically active “across the lifespan also promotes structural and functional changes in the brain, benefiting cognitive functioning and reducing the risk of neurodegeneration,” they write.
This can be important because aging adults with cognitive impairments can also experience neuromuscular impairments that “presumably will contribute to becoming weaker,” they note.
Overall, the findings “warrant strength training programmes aimed at older adults to reduce depression risk,” the investigators write. Clinicians “may consider using the observed handgrip strength thresholds to screen for potential depression risk in older adults,” they add.
Protective factor?
Commenting for this news organization, Julian Mutz, PhD, postdoctoral research associate at the Social, Genetic and Developmental Psychiatry Centre, King’s College, London, said the study “provides further evidence that physical strength may be a protective factor against depression in older adults.”
This confirms a “plethora of cross-sectional and longitudinal studies,” including one recently conducted by Dr. Mutz’s group.
The design of the current study “allowed the authors to address a number of key limitations of previous studies, for example, by including repeated measurements of grip strength and adjustment for potential confounding factors over time,” said Dr. Mutz, who was not involved with the research.
Additionally, “an important contribution of this study is that the authors show that higher grip strength is only associated with a lower risk of depression up to a specific threshold,” he noted.
“The clinical implication of this finding is that only individuals with grip strength below this threshold are at a higher risk of depression. These individuals especially may benefit from interventions aimed at increasing physical strength,” Dr. Mutz said.
The SHARE data collection has been funded by the European Commission and by DG Employment, Social Affairs and Inclusion. Additional funding was obtained from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, and the U.S. National Institute on Aging. Dr. Lopez-Bueno is supported by the European Union – Next Generation EU. The other investigators and Dr. Mutz have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
In a study of more than 115,000 adults, there was a significant association between stronger handgrip, up to 40 kg in men and 27 kg in women, and lower depression risk.
Investigators add that there was a “dose-response” association between physical strength and risk for depression.
“Being physically strong may serve as a preventive factor for depression in older adults, but this is limited to a maximum specific threshold for men and women,” Ruben Lopez-Bueno, PhD, of the department of physical medicine and nursing, University of Zaragoza, Spain, and colleagues write.
The findings were published online in the British Journal of Psychiatry.
Easy, fast, reliable
Depression is a major public health problem, and studies “aimed at examining preventive factors to tackle the increase in depression are required,” the investigators write.
They add that a “growing body of research” is examining the link between depression and muscle strength, with handgrip as an estimator, in healthy middle-aged and older adults.
Handgrip strength is an “easy-to-use, fast and reliable indicator of both sarcopenia (age-related loss of muscle mass) and dynapenia (age-related loss of muscle strength), both of which have been associated with depression,” the researchers note.
It is plausible that there is a “regulatory role of skeletal muscle on brain function affecting this condition,” they add.
They note that exercise seems to play a “key role” because it can improve muscle strength as well as muscle mass, downregulate systemic inflammation, and improve neuroplasticity, neuroendocrine, and oxidative stress responses.
Previous studies have relied either on cross-sectional or prospective cohort models and have focused mostly on a specific country, “not accounting for time-varying changes of both handgrip strength and relevant covariables.”
Moreover, previous evidence has been mixed regarding the “extent to which handgrip strength levels may associate with lower risk of depression, with study results ranging from weak to strong associations,” the investigators write.
So “higher-quality research with representative samples from different countries is required to better clarify the strength of such an association and to confirm directionality,” they add.
SHARE data
To fill this gap, the researchers turned to data from waves 1, 2, 4, 5, 6, and 7 of the Survey of Health, Ageing and Retirement in Europe (SHARE). This encompassed 115,601 individuals aged 50 years and older (mean age, 64.3 years; 54.3% women) residing in European countries and Israel (24 countries total).
Data from wave 3 were not used because handgrip measures were not used in that wave. In the other waves, a handheld dynamometer was used to measure handgrip strength.
The participants were divided into tertiles of handgrip strength, with the “first third” being the lowest tertile of strength and the “final third” representing the highest strength.
All participants were followed for a median of 7.3 years (792,459 person-years), during which 26.1% experienced a risk for depression, as reflected by scores on the EURO-D 12-item scale.
The investigators set the time scale as the months from study entry until either a first depression onset or the end of follow-up.
Covariates that the researchers accounted for included gender, age, education, country, body mass index, physical inactivity, smoking, alcohol consumption, whether living with a partner, wave of inclusion, chronic diseases, consumption of prescribed drugs, and fruit and vegetable consumption.
The researchers used two models: the first adjusted for gender and age at time of the interview, and the second adjusted for all confounders.
In the model that was adjusted only for gender and age, greater handgrip strength was associated with a significantly reduced risk for depression among participants in the second, third, and the final third in comparison with the first third (hazard ratio, 0.65; 95% confidence interval, 0.63-0.68; and HR, 0.50; 95% CI, 0.48-0.53, respectively).
The associations remained consistent in the fully adjusted model, although risk for depression was slightly attenuated in the second and final thirds compared with the first third (HR, 0.76; 95% CI, 0.71-0.81; and HR, 0.64; 95% CI, 0.59-0.69, respectively).
When the researchers conducted analyses using restricted cubic spline modeling, they found a significant association for each kilogram increase of handgrip strength and depression, up to 40 kg in men and 27 kg in women (HR, 1.39; 95% CI, 1.08-1.71; and HR, 1.28; 95% CI, 1.05-1.55, respectively).
There was no greater reduction in depression risk in those with handgrip strength above those values.
Potential depression screen
The investigators suggest several explanations for their findings. For example, handgrip strength has “been used as an overall indicator of health status, including sarcopenia,” they write.
Adults with sarcopenia have been found to be at greater risk for depression because of reduced muscle strength, since neurotrophins are produced by skeletal muscle, among other tissues, and are associated with improvement in mood.
From a psychological point of view, “being physically strong may lead to a sensation of psychological wellbeing,” the researchers write.
Moreover, being physically active “across the lifespan also promotes structural and functional changes in the brain, benefiting cognitive functioning and reducing the risk of neurodegeneration,” they write.
This can be important because aging adults with cognitive impairments can also experience neuromuscular impairments that “presumably will contribute to becoming weaker,” they note.
Overall, the findings “warrant strength training programmes aimed at older adults to reduce depression risk,” the investigators write. Clinicians “may consider using the observed handgrip strength thresholds to screen for potential depression risk in older adults,” they add.
Protective factor?
Commenting for this news organization, Julian Mutz, PhD, postdoctoral research associate at the Social, Genetic and Developmental Psychiatry Centre, King’s College, London, said the study “provides further evidence that physical strength may be a protective factor against depression in older adults.”
This confirms a “plethora of cross-sectional and longitudinal studies,” including one recently conducted by Dr. Mutz’s group.
The design of the current study “allowed the authors to address a number of key limitations of previous studies, for example, by including repeated measurements of grip strength and adjustment for potential confounding factors over time,” said Dr. Mutz, who was not involved with the research.
Additionally, “an important contribution of this study is that the authors show that higher grip strength is only associated with a lower risk of depression up to a specific threshold,” he noted.
“The clinical implication of this finding is that only individuals with grip strength below this threshold are at a higher risk of depression. These individuals especially may benefit from interventions aimed at increasing physical strength,” Dr. Mutz said.
The SHARE data collection has been funded by the European Commission and by DG Employment, Social Affairs and Inclusion. Additional funding was obtained from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, and the U.S. National Institute on Aging. Dr. Lopez-Bueno is supported by the European Union – Next Generation EU. The other investigators and Dr. Mutz have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
In a study of more than 115,000 adults, there was a significant association between stronger handgrip, up to 40 kg in men and 27 kg in women, and lower depression risk.
Investigators add that there was a “dose-response” association between physical strength and risk for depression.
“Being physically strong may serve as a preventive factor for depression in older adults, but this is limited to a maximum specific threshold for men and women,” Ruben Lopez-Bueno, PhD, of the department of physical medicine and nursing, University of Zaragoza, Spain, and colleagues write.
The findings were published online in the British Journal of Psychiatry.
Easy, fast, reliable
Depression is a major public health problem, and studies “aimed at examining preventive factors to tackle the increase in depression are required,” the investigators write.
They add that a “growing body of research” is examining the link between depression and muscle strength, with handgrip as an estimator, in healthy middle-aged and older adults.
Handgrip strength is an “easy-to-use, fast and reliable indicator of both sarcopenia (age-related loss of muscle mass) and dynapenia (age-related loss of muscle strength), both of which have been associated with depression,” the researchers note.
It is plausible that there is a “regulatory role of skeletal muscle on brain function affecting this condition,” they add.
They note that exercise seems to play a “key role” because it can improve muscle strength as well as muscle mass, downregulate systemic inflammation, and improve neuroplasticity, neuroendocrine, and oxidative stress responses.
Previous studies have relied either on cross-sectional or prospective cohort models and have focused mostly on a specific country, “not accounting for time-varying changes of both handgrip strength and relevant covariables.”
Moreover, previous evidence has been mixed regarding the “extent to which handgrip strength levels may associate with lower risk of depression, with study results ranging from weak to strong associations,” the investigators write.
So “higher-quality research with representative samples from different countries is required to better clarify the strength of such an association and to confirm directionality,” they add.
SHARE data
To fill this gap, the researchers turned to data from waves 1, 2, 4, 5, 6, and 7 of the Survey of Health, Ageing and Retirement in Europe (SHARE). This encompassed 115,601 individuals aged 50 years and older (mean age, 64.3 years; 54.3% women) residing in European countries and Israel (24 countries total).
Data from wave 3 were not used because handgrip measures were not used in that wave. In the other waves, a handheld dynamometer was used to measure handgrip strength.
The participants were divided into tertiles of handgrip strength, with the “first third” being the lowest tertile of strength and the “final third” representing the highest strength.
All participants were followed for a median of 7.3 years (792,459 person-years), during which 26.1% experienced a risk for depression, as reflected by scores on the EURO-D 12-item scale.
The investigators set the time scale as the months from study entry until either a first depression onset or the end of follow-up.
Covariates that the researchers accounted for included gender, age, education, country, body mass index, physical inactivity, smoking, alcohol consumption, whether living with a partner, wave of inclusion, chronic diseases, consumption of prescribed drugs, and fruit and vegetable consumption.
The researchers used two models: the first adjusted for gender and age at time of the interview, and the second adjusted for all confounders.
In the model that was adjusted only for gender and age, greater handgrip strength was associated with a significantly reduced risk for depression among participants in the second, third, and the final third in comparison with the first third (hazard ratio, 0.65; 95% confidence interval, 0.63-0.68; and HR, 0.50; 95% CI, 0.48-0.53, respectively).
The associations remained consistent in the fully adjusted model, although risk for depression was slightly attenuated in the second and final thirds compared with the first third (HR, 0.76; 95% CI, 0.71-0.81; and HR, 0.64; 95% CI, 0.59-0.69, respectively).
When the researchers conducted analyses using restricted cubic spline modeling, they found a significant association for each kilogram increase of handgrip strength and depression, up to 40 kg in men and 27 kg in women (HR, 1.39; 95% CI, 1.08-1.71; and HR, 1.28; 95% CI, 1.05-1.55, respectively).
There was no greater reduction in depression risk in those with handgrip strength above those values.
Potential depression screen
The investigators suggest several explanations for their findings. For example, handgrip strength has “been used as an overall indicator of health status, including sarcopenia,” they write.
Adults with sarcopenia have been found to be at greater risk for depression because of reduced muscle strength, since neurotrophins are produced by skeletal muscle, among other tissues, and are associated with improvement in mood.
From a psychological point of view, “being physically strong may lead to a sensation of psychological wellbeing,” the researchers write.
Moreover, being physically active “across the lifespan also promotes structural and functional changes in the brain, benefiting cognitive functioning and reducing the risk of neurodegeneration,” they write.
This can be important because aging adults with cognitive impairments can also experience neuromuscular impairments that “presumably will contribute to becoming weaker,” they note.
Overall, the findings “warrant strength training programmes aimed at older adults to reduce depression risk,” the investigators write. Clinicians “may consider using the observed handgrip strength thresholds to screen for potential depression risk in older adults,” they add.
Protective factor?
Commenting for this news organization, Julian Mutz, PhD, postdoctoral research associate at the Social, Genetic and Developmental Psychiatry Centre, King’s College, London, said the study “provides further evidence that physical strength may be a protective factor against depression in older adults.”
This confirms a “plethora of cross-sectional and longitudinal studies,” including one recently conducted by Dr. Mutz’s group.
The design of the current study “allowed the authors to address a number of key limitations of previous studies, for example, by including repeated measurements of grip strength and adjustment for potential confounding factors over time,” said Dr. Mutz, who was not involved with the research.
Additionally, “an important contribution of this study is that the authors show that higher grip strength is only associated with a lower risk of depression up to a specific threshold,” he noted.
“The clinical implication of this finding is that only individuals with grip strength below this threshold are at a higher risk of depression. These individuals especially may benefit from interventions aimed at increasing physical strength,” Dr. Mutz said.
The SHARE data collection has been funded by the European Commission and by DG Employment, Social Affairs and Inclusion. Additional funding was obtained from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, and the U.S. National Institute on Aging. Dr. Lopez-Bueno is supported by the European Union – Next Generation EU. The other investigators and Dr. Mutz have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF PSYCHIATRY
Behavioral treatment tied to lower medical, pharmacy costs
Results of a large retrospective study showed that patients newly diagnosed with a BHC who receive OPBHT following diagnosis incur lower medical and pharmacy costs over roughly the next 1 to 2 years, compared with peers who don’t receive OPBHT.
“Our findings suggest that promoting OPBHT as part of a population health strategy is associated with improved overall medical spending, particularly among adults,” the investigators write.
The study was published online in JAMA Network Open.
Common, undertreated
Nearly a quarter of adults in the United States have a BHC, and they incur greater medical costs than those without a BHC. However, diagnosis of a BHC is often delayed, and most affected individuals receive little to no treatment.
In their cost analysis, Johanna Bellon, PhD, and colleagues with Evernorth Health, St. Louis, analyzed commercial insurance claims data for 203,401 U.S. individuals newly diagnosed with one or more BHCs between 2017 and 2018.
About half of participants had depression and/or anxiety, 11% had substance use or alcohol use disorder, and 6% had a higher-acuity diagnosis, such as bipolar disorder, severe depression, eating disorder, psychotic disorder, or autism spectrum disorder.
About 1 in 5 (22%) had at least one chronic medical condition along with their BHC.
The researchers found that having at least one OPBHT visit was associated with lower medical and pharmacy costs during 15- and 27-month follow-up periods.
Over 15 months, the adjusted mean per member per month (PMPM) medical/pharmacy cost was $686 with no OPBHT visit, compared with $571 with one or more OPBHT visits.
Over 27 months, the adjusted mean PMPM was $464 with no OPBHT, versus $391 with one or more OPBHT visits.
Dose-response effect
In addition, there was a “dose-response” relationship between OPBHT and medical/pharmacy costs, such that estimated cost savings were significantly lower in the treated versus the untreated groups at almost every level of treatment.
“Our findings were also largely age independent, especially over 15 months, suggesting that OPBHT has favorable effects among children, young adults, and adults,” the researchers report.
“This is promising given that disease etiology and progression, treatment paradigms, presence of comorbid medical conditions, and overall medical and pharmacy costs differ among the three groups,” they say.
Notably, the dataset largely encompassed in-person OPBHT, because the study period preceded the transition into virtual care that occurred in 2020.
However, overall use of OPBHT was low – older adults, adults with lower income, individuals with comorbid medical conditions, and persons of racial and ethnic minorities were less likely to receive OPBHT, they found.
“These findings support the cost-effectiveness of practitioner- and insurance-based interventions to increase OPBHT utilization, which is a critical resource as new BHC diagnoses continue to increase,” the researchers say.
“Future research should validate these findings in other populations, including government-insured individuals, and explore data by chronic disease category, over longer time horizons, by type and quality of OPBHT, by type of medical spending, within subpopulations with BHCs, and including virtual and digital behavioral health services,” they suggest.
The study had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large retrospective study showed that patients newly diagnosed with a BHC who receive OPBHT following diagnosis incur lower medical and pharmacy costs over roughly the next 1 to 2 years, compared with peers who don’t receive OPBHT.
“Our findings suggest that promoting OPBHT as part of a population health strategy is associated with improved overall medical spending, particularly among adults,” the investigators write.
The study was published online in JAMA Network Open.
Common, undertreated
Nearly a quarter of adults in the United States have a BHC, and they incur greater medical costs than those without a BHC. However, diagnosis of a BHC is often delayed, and most affected individuals receive little to no treatment.
In their cost analysis, Johanna Bellon, PhD, and colleagues with Evernorth Health, St. Louis, analyzed commercial insurance claims data for 203,401 U.S. individuals newly diagnosed with one or more BHCs between 2017 and 2018.
About half of participants had depression and/or anxiety, 11% had substance use or alcohol use disorder, and 6% had a higher-acuity diagnosis, such as bipolar disorder, severe depression, eating disorder, psychotic disorder, or autism spectrum disorder.
About 1 in 5 (22%) had at least one chronic medical condition along with their BHC.
The researchers found that having at least one OPBHT visit was associated with lower medical and pharmacy costs during 15- and 27-month follow-up periods.
Over 15 months, the adjusted mean per member per month (PMPM) medical/pharmacy cost was $686 with no OPBHT visit, compared with $571 with one or more OPBHT visits.
Over 27 months, the adjusted mean PMPM was $464 with no OPBHT, versus $391 with one or more OPBHT visits.
Dose-response effect
In addition, there was a “dose-response” relationship between OPBHT and medical/pharmacy costs, such that estimated cost savings were significantly lower in the treated versus the untreated groups at almost every level of treatment.
“Our findings were also largely age independent, especially over 15 months, suggesting that OPBHT has favorable effects among children, young adults, and adults,” the researchers report.
“This is promising given that disease etiology and progression, treatment paradigms, presence of comorbid medical conditions, and overall medical and pharmacy costs differ among the three groups,” they say.
Notably, the dataset largely encompassed in-person OPBHT, because the study period preceded the transition into virtual care that occurred in 2020.
However, overall use of OPBHT was low – older adults, adults with lower income, individuals with comorbid medical conditions, and persons of racial and ethnic minorities were less likely to receive OPBHT, they found.
“These findings support the cost-effectiveness of practitioner- and insurance-based interventions to increase OPBHT utilization, which is a critical resource as new BHC diagnoses continue to increase,” the researchers say.
“Future research should validate these findings in other populations, including government-insured individuals, and explore data by chronic disease category, over longer time horizons, by type and quality of OPBHT, by type of medical spending, within subpopulations with BHCs, and including virtual and digital behavioral health services,” they suggest.
The study had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large retrospective study showed that patients newly diagnosed with a BHC who receive OPBHT following diagnosis incur lower medical and pharmacy costs over roughly the next 1 to 2 years, compared with peers who don’t receive OPBHT.
“Our findings suggest that promoting OPBHT as part of a population health strategy is associated with improved overall medical spending, particularly among adults,” the investigators write.
The study was published online in JAMA Network Open.
Common, undertreated
Nearly a quarter of adults in the United States have a BHC, and they incur greater medical costs than those without a BHC. However, diagnosis of a BHC is often delayed, and most affected individuals receive little to no treatment.
In their cost analysis, Johanna Bellon, PhD, and colleagues with Evernorth Health, St. Louis, analyzed commercial insurance claims data for 203,401 U.S. individuals newly diagnosed with one or more BHCs between 2017 and 2018.
About half of participants had depression and/or anxiety, 11% had substance use or alcohol use disorder, and 6% had a higher-acuity diagnosis, such as bipolar disorder, severe depression, eating disorder, psychotic disorder, or autism spectrum disorder.
About 1 in 5 (22%) had at least one chronic medical condition along with their BHC.
The researchers found that having at least one OPBHT visit was associated with lower medical and pharmacy costs during 15- and 27-month follow-up periods.
Over 15 months, the adjusted mean per member per month (PMPM) medical/pharmacy cost was $686 with no OPBHT visit, compared with $571 with one or more OPBHT visits.
Over 27 months, the adjusted mean PMPM was $464 with no OPBHT, versus $391 with one or more OPBHT visits.
Dose-response effect
In addition, there was a “dose-response” relationship between OPBHT and medical/pharmacy costs, such that estimated cost savings were significantly lower in the treated versus the untreated groups at almost every level of treatment.
“Our findings were also largely age independent, especially over 15 months, suggesting that OPBHT has favorable effects among children, young adults, and adults,” the researchers report.
“This is promising given that disease etiology and progression, treatment paradigms, presence of comorbid medical conditions, and overall medical and pharmacy costs differ among the three groups,” they say.
Notably, the dataset largely encompassed in-person OPBHT, because the study period preceded the transition into virtual care that occurred in 2020.
However, overall use of OPBHT was low – older adults, adults with lower income, individuals with comorbid medical conditions, and persons of racial and ethnic minorities were less likely to receive OPBHT, they found.
“These findings support the cost-effectiveness of practitioner- and insurance-based interventions to increase OPBHT utilization, which is a critical resource as new BHC diagnoses continue to increase,” the researchers say.
“Future research should validate these findings in other populations, including government-insured individuals, and explore data by chronic disease category, over longer time horizons, by type and quality of OPBHT, by type of medical spending, within subpopulations with BHCs, and including virtual and digital behavioral health services,” they suggest.
The study had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Can a Mediterranean diet ease depression in young men?
This transcript has been edited for clarity.
Drew Ramsey, MD: Welcome back, everyone. I’m Dr. Drew Ramsey. I’m on the editorial board with Medscape Psychiatry and I’m an assistant clinical professor of psychiatry at Columbia University. We have a special guest today.
I’m here with nutritionist Jessica Bayes, who’s at the University of Technology Sydney, and she’s the lead author of the AMMEND trial. [Editor’s note: Since completing her PhD, Bayes is now at Southern Cross University.]
Jessica, welcome to Medscape.
Jessica Bayes, PhD: Thank you for having me.
The AMMEND Trial
Dr. Ramsey: Thank you for coming on board and helping all of us as clinicians understand some of your research and some of what is suggested by your research – that young men can change their diet and it helped their depression. Tell us a little bit about the AMMEND trial.
Dr. Bayes: The AMMEND trial was a 12-week randomized controlled trial in young men, 18-25 years old, who had diagnosed moderate to severe clinical depression. They had a poor baseline diet and we got them to eat a healthy Mediterranean diet, which improved their symptoms of depression.
Dr. Ramsey: It was a remarkable trial. Jessica, if I recall, you helped individuals improve the Mediterranean dietary pattern score by 8 points on a 14-point scale. That led to a 20-point reduction in their Beck Depression Inventory. Tell us what that looked like on the ground.
Dr. Bayes: It’s a huge improvement. Obviously, they were feeling much better in the end in terms of their depressive symptoms, but we also measured their energy, sleep, and quality of life. Many of them at the end were at a score cutoff that suggests no depression or in remission.
Dr. Ramsey: There were 72 people in your total trial, so 36% in your intervention arm went into full remission.
Dr. Bayes: Which is just amazing.
Dr. Ramsey: It also follows up the SMILES trial, which was a little bit of a different trial. You had two nutritional counseling sessions and the SMILES trial had seven, but in the SMILES trial, 32.3% of the patients went into full remission when they adopted a Mediterranean-style diet.
Jessica, what is the secret that you and your team know? I think many clinicians, especially clinicians who are parents and have teens, are kind of shaking their heads in disbelief. They’ve been telling their kids to eat healthy. What do you guys know about how to help young men change their diet?
How to Aid Adherence to Mediterranean Diet
Dr. Bayes: Prior to starting this, when I would say this idea to people, everyone would say, “Great idea. There’s no way you’re going to get depressed young men to change their diet. Not going to happen.” We went to them and we asked them. We said, “We’re going to do this study. What do you want from us? What resources would you need? How many appointments would you like? What’s too little or too many?”
We really got their feedback on board when we designed the study, and that obviously paid off. We had a personalized approach and we met them where they were at. We gave them the skills, resources, recipes, meal ideas – all those things – so we could really set them up to succeed.
Dr. Ramsey: You were telling me earlier about a few of the dietary changes that you felt made a big difference for these young men. What were those?
Dr. Bayes: Increasing the vegetables, olive oil, and legumes are probably the big ones that most of them were really not doing beforehand. They were really able to take that on board and make significant improvements in those areas.
Dr. Ramsey: These are really some of the top food categories in nutritional psychiatry as we think about how we help our efforts to improve mental health by thinking about nutrition, nutritional quality, and nutritional density. Certainly, those food categories – nuts and legumes, plants, and olive oil – are really what help get us there.
You also gave the students a food hamper. If you were going to be in charge of mental health in Australia and America and you got to give every college freshman a little box with a note, what would be in that box?
Dr. Bayes: I’d want to put everything in that box! It would be full of brightly colored fruits and vegetables, different nuts and seeds, and legumes. It would be full of recipes and ideas of how to cook things and how to prepare really delicious things. It would be full of different herbs and spices and all of those things to get people really excited about food.
Dr. Ramsey: Did the young men pick up on your enthusiasm and excitement around food? Did they begin to adopt some of that, shifting their view of how they saw the food and how they saw that it is related to their depression?
Dr. Bayes: Hopefully. I do think energy is infectious. I’m sure that played a role somewhat, but trying to get them excited about food can be really quite daunting, thinking, I’ve got to change my entire diet and I’ve got to learn to cook and go out and buy groceries. I don’t even know what to do with a piece of salmon. Trying to get them curious, interested, and just reminding them that it’s not all-or-nothing. Make small changes, give it a go, and have fun.
Dr. Ramsey: You also have a unique aspect of your research that you’re interested in male mental health, and that’s not something that’s been widely researched. Can you tell us a little bit about what these men were like in terms of coming into your trial as depressed young men?
Dr. Bayes: In the context of the COVID-19 pandemic, mental health was at the forefront of many people’s minds. They joined the study saying, “I’ve never seen anything like this before. I’ve never seen myself represented in research. I wanted to contribute. I want to add to that conversation because I feel like we are overlooked.”
Dr. Ramsey: I love hearing this notion that maybe young men aren’t quite who we think they are. They are wanting to be seen around their mental health. They can learn to use olive oil and to cook, and they can engage in mental health interventions that work. We just need to ask, give them some food, encourage them, and it makes a big difference.
Jessica Bayes, thank you so much for joining us and sharing some of your research. Everyone, it’s the AMMEND trial. We will drop a link to the trial below so you can take a peek and tell us what you think.
Please, in the comments, let us know what you think about this notion of helping young men with depression through nutritional interventions. Take a peek at the great work that Jessica and Professor Sibbritt from the University of Technology Sydney have published and put out into the scientific literature for us all.
Thanks so much, Jessica. I look forward to seeing you soon.
Dr. Bayes: Thank you.
Dr. Ramsey is assistant clinical professor, department of psychiatry, Columbia University, New York. He has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for InterContinental Hotels Group; National Kale Day 501(c)3. Received income in an amount equal to or greater than $250 from: Sharecare. Dr. Bayes is a postdoctoral research fellow; clinical nutritionist, Southern Cross University, National Center for Naturopathic Medicine, Lismore, New South Wales, Australia. She has disclosed the following relevant financial relationships: Received research grant from Endeavour College. A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Drew Ramsey, MD: Welcome back, everyone. I’m Dr. Drew Ramsey. I’m on the editorial board with Medscape Psychiatry and I’m an assistant clinical professor of psychiatry at Columbia University. We have a special guest today.
I’m here with nutritionist Jessica Bayes, who’s at the University of Technology Sydney, and she’s the lead author of the AMMEND trial. [Editor’s note: Since completing her PhD, Bayes is now at Southern Cross University.]
Jessica, welcome to Medscape.
Jessica Bayes, PhD: Thank you for having me.
The AMMEND Trial
Dr. Ramsey: Thank you for coming on board and helping all of us as clinicians understand some of your research and some of what is suggested by your research – that young men can change their diet and it helped their depression. Tell us a little bit about the AMMEND trial.
Dr. Bayes: The AMMEND trial was a 12-week randomized controlled trial in young men, 18-25 years old, who had diagnosed moderate to severe clinical depression. They had a poor baseline diet and we got them to eat a healthy Mediterranean diet, which improved their symptoms of depression.
Dr. Ramsey: It was a remarkable trial. Jessica, if I recall, you helped individuals improve the Mediterranean dietary pattern score by 8 points on a 14-point scale. That led to a 20-point reduction in their Beck Depression Inventory. Tell us what that looked like on the ground.
Dr. Bayes: It’s a huge improvement. Obviously, they were feeling much better in the end in terms of their depressive symptoms, but we also measured their energy, sleep, and quality of life. Many of them at the end were at a score cutoff that suggests no depression or in remission.
Dr. Ramsey: There were 72 people in your total trial, so 36% in your intervention arm went into full remission.
Dr. Bayes: Which is just amazing.
Dr. Ramsey: It also follows up the SMILES trial, which was a little bit of a different trial. You had two nutritional counseling sessions and the SMILES trial had seven, but in the SMILES trial, 32.3% of the patients went into full remission when they adopted a Mediterranean-style diet.
Jessica, what is the secret that you and your team know? I think many clinicians, especially clinicians who are parents and have teens, are kind of shaking their heads in disbelief. They’ve been telling their kids to eat healthy. What do you guys know about how to help young men change their diet?
How to Aid Adherence to Mediterranean Diet
Dr. Bayes: Prior to starting this, when I would say this idea to people, everyone would say, “Great idea. There’s no way you’re going to get depressed young men to change their diet. Not going to happen.” We went to them and we asked them. We said, “We’re going to do this study. What do you want from us? What resources would you need? How many appointments would you like? What’s too little or too many?”
We really got their feedback on board when we designed the study, and that obviously paid off. We had a personalized approach and we met them where they were at. We gave them the skills, resources, recipes, meal ideas – all those things – so we could really set them up to succeed.
Dr. Ramsey: You were telling me earlier about a few of the dietary changes that you felt made a big difference for these young men. What were those?
Dr. Bayes: Increasing the vegetables, olive oil, and legumes are probably the big ones that most of them were really not doing beforehand. They were really able to take that on board and make significant improvements in those areas.
Dr. Ramsey: These are really some of the top food categories in nutritional psychiatry as we think about how we help our efforts to improve mental health by thinking about nutrition, nutritional quality, and nutritional density. Certainly, those food categories – nuts and legumes, plants, and olive oil – are really what help get us there.
You also gave the students a food hamper. If you were going to be in charge of mental health in Australia and America and you got to give every college freshman a little box with a note, what would be in that box?
Dr. Bayes: I’d want to put everything in that box! It would be full of brightly colored fruits and vegetables, different nuts and seeds, and legumes. It would be full of recipes and ideas of how to cook things and how to prepare really delicious things. It would be full of different herbs and spices and all of those things to get people really excited about food.
Dr. Ramsey: Did the young men pick up on your enthusiasm and excitement around food? Did they begin to adopt some of that, shifting their view of how they saw the food and how they saw that it is related to their depression?
Dr. Bayes: Hopefully. I do think energy is infectious. I’m sure that played a role somewhat, but trying to get them excited about food can be really quite daunting, thinking, I’ve got to change my entire diet and I’ve got to learn to cook and go out and buy groceries. I don’t even know what to do with a piece of salmon. Trying to get them curious, interested, and just reminding them that it’s not all-or-nothing. Make small changes, give it a go, and have fun.
Dr. Ramsey: You also have a unique aspect of your research that you’re interested in male mental health, and that’s not something that’s been widely researched. Can you tell us a little bit about what these men were like in terms of coming into your trial as depressed young men?
Dr. Bayes: In the context of the COVID-19 pandemic, mental health was at the forefront of many people’s minds. They joined the study saying, “I’ve never seen anything like this before. I’ve never seen myself represented in research. I wanted to contribute. I want to add to that conversation because I feel like we are overlooked.”
Dr. Ramsey: I love hearing this notion that maybe young men aren’t quite who we think they are. They are wanting to be seen around their mental health. They can learn to use olive oil and to cook, and they can engage in mental health interventions that work. We just need to ask, give them some food, encourage them, and it makes a big difference.
Jessica Bayes, thank you so much for joining us and sharing some of your research. Everyone, it’s the AMMEND trial. We will drop a link to the trial below so you can take a peek and tell us what you think.
Please, in the comments, let us know what you think about this notion of helping young men with depression through nutritional interventions. Take a peek at the great work that Jessica and Professor Sibbritt from the University of Technology Sydney have published and put out into the scientific literature for us all.
Thanks so much, Jessica. I look forward to seeing you soon.
Dr. Bayes: Thank you.
Dr. Ramsey is assistant clinical professor, department of psychiatry, Columbia University, New York. He has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for InterContinental Hotels Group; National Kale Day 501(c)3. Received income in an amount equal to or greater than $250 from: Sharecare. Dr. Bayes is a postdoctoral research fellow; clinical nutritionist, Southern Cross University, National Center for Naturopathic Medicine, Lismore, New South Wales, Australia. She has disclosed the following relevant financial relationships: Received research grant from Endeavour College. A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Drew Ramsey, MD: Welcome back, everyone. I’m Dr. Drew Ramsey. I’m on the editorial board with Medscape Psychiatry and I’m an assistant clinical professor of psychiatry at Columbia University. We have a special guest today.
I’m here with nutritionist Jessica Bayes, who’s at the University of Technology Sydney, and she’s the lead author of the AMMEND trial. [Editor’s note: Since completing her PhD, Bayes is now at Southern Cross University.]
Jessica, welcome to Medscape.
Jessica Bayes, PhD: Thank you for having me.
The AMMEND Trial
Dr. Ramsey: Thank you for coming on board and helping all of us as clinicians understand some of your research and some of what is suggested by your research – that young men can change their diet and it helped their depression. Tell us a little bit about the AMMEND trial.
Dr. Bayes: The AMMEND trial was a 12-week randomized controlled trial in young men, 18-25 years old, who had diagnosed moderate to severe clinical depression. They had a poor baseline diet and we got them to eat a healthy Mediterranean diet, which improved their symptoms of depression.
Dr. Ramsey: It was a remarkable trial. Jessica, if I recall, you helped individuals improve the Mediterranean dietary pattern score by 8 points on a 14-point scale. That led to a 20-point reduction in their Beck Depression Inventory. Tell us what that looked like on the ground.
Dr. Bayes: It’s a huge improvement. Obviously, they were feeling much better in the end in terms of their depressive symptoms, but we also measured their energy, sleep, and quality of life. Many of them at the end were at a score cutoff that suggests no depression or in remission.
Dr. Ramsey: There were 72 people in your total trial, so 36% in your intervention arm went into full remission.
Dr. Bayes: Which is just amazing.
Dr. Ramsey: It also follows up the SMILES trial, which was a little bit of a different trial. You had two nutritional counseling sessions and the SMILES trial had seven, but in the SMILES trial, 32.3% of the patients went into full remission when they adopted a Mediterranean-style diet.
Jessica, what is the secret that you and your team know? I think many clinicians, especially clinicians who are parents and have teens, are kind of shaking their heads in disbelief. They’ve been telling their kids to eat healthy. What do you guys know about how to help young men change their diet?
How to Aid Adherence to Mediterranean Diet
Dr. Bayes: Prior to starting this, when I would say this idea to people, everyone would say, “Great idea. There’s no way you’re going to get depressed young men to change their diet. Not going to happen.” We went to them and we asked them. We said, “We’re going to do this study. What do you want from us? What resources would you need? How many appointments would you like? What’s too little or too many?”
We really got their feedback on board when we designed the study, and that obviously paid off. We had a personalized approach and we met them where they were at. We gave them the skills, resources, recipes, meal ideas – all those things – so we could really set them up to succeed.
Dr. Ramsey: You were telling me earlier about a few of the dietary changes that you felt made a big difference for these young men. What were those?
Dr. Bayes: Increasing the vegetables, olive oil, and legumes are probably the big ones that most of them were really not doing beforehand. They were really able to take that on board and make significant improvements in those areas.
Dr. Ramsey: These are really some of the top food categories in nutritional psychiatry as we think about how we help our efforts to improve mental health by thinking about nutrition, nutritional quality, and nutritional density. Certainly, those food categories – nuts and legumes, plants, and olive oil – are really what help get us there.
You also gave the students a food hamper. If you were going to be in charge of mental health in Australia and America and you got to give every college freshman a little box with a note, what would be in that box?
Dr. Bayes: I’d want to put everything in that box! It would be full of brightly colored fruits and vegetables, different nuts and seeds, and legumes. It would be full of recipes and ideas of how to cook things and how to prepare really delicious things. It would be full of different herbs and spices and all of those things to get people really excited about food.
Dr. Ramsey: Did the young men pick up on your enthusiasm and excitement around food? Did they begin to adopt some of that, shifting their view of how they saw the food and how they saw that it is related to their depression?
Dr. Bayes: Hopefully. I do think energy is infectious. I’m sure that played a role somewhat, but trying to get them excited about food can be really quite daunting, thinking, I’ve got to change my entire diet and I’ve got to learn to cook and go out and buy groceries. I don’t even know what to do with a piece of salmon. Trying to get them curious, interested, and just reminding them that it’s not all-or-nothing. Make small changes, give it a go, and have fun.
Dr. Ramsey: You also have a unique aspect of your research that you’re interested in male mental health, and that’s not something that’s been widely researched. Can you tell us a little bit about what these men were like in terms of coming into your trial as depressed young men?
Dr. Bayes: In the context of the COVID-19 pandemic, mental health was at the forefront of many people’s minds. They joined the study saying, “I’ve never seen anything like this before. I’ve never seen myself represented in research. I wanted to contribute. I want to add to that conversation because I feel like we are overlooked.”
Dr. Ramsey: I love hearing this notion that maybe young men aren’t quite who we think they are. They are wanting to be seen around their mental health. They can learn to use olive oil and to cook, and they can engage in mental health interventions that work. We just need to ask, give them some food, encourage them, and it makes a big difference.
Jessica Bayes, thank you so much for joining us and sharing some of your research. Everyone, it’s the AMMEND trial. We will drop a link to the trial below so you can take a peek and tell us what you think.
Please, in the comments, let us know what you think about this notion of helping young men with depression through nutritional interventions. Take a peek at the great work that Jessica and Professor Sibbritt from the University of Technology Sydney have published and put out into the scientific literature for us all.
Thanks so much, Jessica. I look forward to seeing you soon.
Dr. Bayes: Thank you.
Dr. Ramsey is assistant clinical professor, department of psychiatry, Columbia University, New York. He has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for InterContinental Hotels Group; National Kale Day 501(c)3. Received income in an amount equal to or greater than $250 from: Sharecare. Dr. Bayes is a postdoctoral research fellow; clinical nutritionist, Southern Cross University, National Center for Naturopathic Medicine, Lismore, New South Wales, Australia. She has disclosed the following relevant financial relationships: Received research grant from Endeavour College. A version of this article first appeared on Medscape.com.
The kids may not be alright, but psychiatry can help
When I was growing up, I can remember experiencing “duck and cover” drills at school. If a flash appeared in our peripheral vision, we were told we should not look at it but crawl under our desks. My classmates and I were being taught how to protect ourselves in case of a nuclear attack.
Clearly, had there been such an attack, ducking under our desks would not have saved us. Thankfully, such a conflict never occurred – and hopefully never will. Still, the warning did penetrate our psyches. In those days, families and children in schools were worried, and some were scared.
The situation is quite different today. Our children and grandchildren are being taught to protect themselves not from actions overseas – that never happened – but from what someone living in their community might do that has been occurring in real time. According to my daughter-in-law, her young children are taught during “lockdowns” to hide in their classrooms’ closets. During these drills, some children are directed to line up against a wall that would be out of sight of a shooter, and to stay as still as possible.
Since 2017, the number of intentional shootings in U.S. kindergarten through grade 12 schools increased precipitously (Prev Med. 2022 Dec. doi: 10.1016/j.ypmed.2022.107280). Imagine the psychological impact that the vigilance required to deal with such impending threats must be having on our children, as they learn to fear injury and possible death every day they go to school. I’ve talked with numerous parents about this, including my own adult children, and this is clearly a new dimension of life that is on everyone’s minds. Schools, once bastions of safety, are no longer that safe.
For many years, I’ve written about the need to destigmatize mental illness so that it is treated on a par with physical illness. As we look at the challenges faced by young people, reframing mental illness is more important now than ever. This means finding ways to increase the funding of studies that help us understand young people with mental health issues. It also means encouraging patients to pursue treatment from psychiatrists, psychologists, or mental health counselors who specialize in short-term therapy.
The emphasis here on short-term therapy is not to discourage longer-term care when needed, but clearly short-term care strategies, such as cognitive-behavioral therapies, not only work for problem resolution, they also help in the destigmatization of mental health care – as the circumscribed treatment with a clear beginning, middle, and end is consistent with CBT and consistent with much of medical care for physical disorders.
Furthermore, as we aim to destigmatize mental health care, it’s important to equate it with physical care. For example, taking a day or two from school or work for a sprained ankle, seeing a dentist, or an eye exam, plus a myriad of physical issues is quite acceptable. Why is it not also acceptable for a mental health issue and evaluation, such as for anxiety or PTSD, plus being able to talk about it without stigma? Seeing the “shrink” needs to be removed as a negative but viewed as a very positive move toward care for oneself.
In addition, children and adolescents are battling countless other health challenges that could have implications for mental health professionals, for example:
- During the height of the coronavirus pandemic, pediatric endocrinologists reportedly saw a surge of referrals for girls experiencing early puberty. Puberty should never be medicalized, but early maturation has been linked to numerous psychiatric disorders such as depression, anxiety, and eating disorders (J Pediatr Adolec Gynecol. 2022 Oct. doi: 10.1016/j.jpag.2022.05.005).
- A global epidemiologic study of children estimates that nearly 8 million youth lost a parent or caregiver because of a pandemic-related cause between Jan. 1, 2020, and May 1, 2022. An additional 2.5 million children were affected by the loss of secondary caregivers such as grandparents (JAMA Pediatr. 2022 Sept. doi: 10.1001/jamapediatrics.2022.3157).
- The inpatient and outpatient volume of adolescents and young adults receiving care for eating disorders skyrocketed before and after the pandemic, according to the results of case study series (JAMA Pediatrics. 2022 Nov 7. doi: 10.1001/jamapediatrics.2022.4346).
- Children and adolescents who developed COVID-19 suffered tremendously during the height of the pandemic. A nationwide analysis shows that COVID-19 nearly tripled children’s risks of developing new mental health illnesses, such as attention-deficit/hyperactivity disorder, anxiety, trauma, or stress disorder (Psychiatric Services. 2022 Jun 2. doi: 10.1176/appi.ps.202100646).
In addition to those challenges, young children are facing an increase in respiratory syncytial virus (RSV) infection. We were told the “flu” would be quite bad this year and to beware of monkeypox. However, very little mention is made of the equally distressing “epidemic” of mental health issues, PTSD, anxiety, and depression as we are still in the midst of the COVID pandemic in the United States with almost 400 deaths a day – a very unacceptable number.
Interestingly, we seem to have abandoned the use of masks as protection against COVID and other respiratory diseases, despite their effectiveness. A study in Boston that looked at children in two school districts that did not lift mask mandates demonstrated that mask wearing does indeed lead to significant reductions in the number of pediatric COVID cases. In addition to societal violence and school shootings – which certainly exacerbate anxiety – the fear of dying or the death of a loved one, tied to COVID, may lead to epidemic proportions of PTSD in children. As an article in WebMD noted, “pediatricians are imploring the federal government to declare a national emergency as cases of pediatric respiratory illnesses continue to soar.”
In light of the acknowledged mental health crisis in children, which appears epidemic, I would hope the psychiatric and psychological associations would publicly sound an alarm so that resources could be brought to bear to address this critical issue. I believe doing so would also aid in destigmatizing mental disorders, and increase education and treatment.
Layered on top of those issues are natural disasters, such as the fallout from Tropical Storm Nicole when it recently caused devastation across western Florida. The mental health trauma caused by recent tropical storms seems all but forgotten – except for those who are still suffering. All of this adds up to a society-wide mental health crisis, which seems far more expansive than monkeypox, for example. Yet monkeypox, which did lead to thousands of cases and approximately 29 deaths in the United States, was declared a national public health emergency.
Additionally, RSV killed 100-500 U.S. children under age 5 each year before the pandemic, according to the Centers for Disease Control and Prevention, and currently it appears even worse. Yet despite the seriousness of RSV, it nowhere matches the emotional toll COVID has taken on children globally.
Let’s make it standard practice for children – and of course, adults – to be taught that anxiety is a normal response at times. We should teach that, in some cases, feeling “down” or in despair and even experiencing symptoms of PTSD based on what’s going on personally and within our environment (i.e., COVID, school shootings, etc.) are triggers and responses that can be addressed and often quickly treated by talking with a mental health professional.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
When I was growing up, I can remember experiencing “duck and cover” drills at school. If a flash appeared in our peripheral vision, we were told we should not look at it but crawl under our desks. My classmates and I were being taught how to protect ourselves in case of a nuclear attack.
Clearly, had there been such an attack, ducking under our desks would not have saved us. Thankfully, such a conflict never occurred – and hopefully never will. Still, the warning did penetrate our psyches. In those days, families and children in schools were worried, and some were scared.
The situation is quite different today. Our children and grandchildren are being taught to protect themselves not from actions overseas – that never happened – but from what someone living in their community might do that has been occurring in real time. According to my daughter-in-law, her young children are taught during “lockdowns” to hide in their classrooms’ closets. During these drills, some children are directed to line up against a wall that would be out of sight of a shooter, and to stay as still as possible.
Since 2017, the number of intentional shootings in U.S. kindergarten through grade 12 schools increased precipitously (Prev Med. 2022 Dec. doi: 10.1016/j.ypmed.2022.107280). Imagine the psychological impact that the vigilance required to deal with such impending threats must be having on our children, as they learn to fear injury and possible death every day they go to school. I’ve talked with numerous parents about this, including my own adult children, and this is clearly a new dimension of life that is on everyone’s minds. Schools, once bastions of safety, are no longer that safe.
For many years, I’ve written about the need to destigmatize mental illness so that it is treated on a par with physical illness. As we look at the challenges faced by young people, reframing mental illness is more important now than ever. This means finding ways to increase the funding of studies that help us understand young people with mental health issues. It also means encouraging patients to pursue treatment from psychiatrists, psychologists, or mental health counselors who specialize in short-term therapy.
The emphasis here on short-term therapy is not to discourage longer-term care when needed, but clearly short-term care strategies, such as cognitive-behavioral therapies, not only work for problem resolution, they also help in the destigmatization of mental health care – as the circumscribed treatment with a clear beginning, middle, and end is consistent with CBT and consistent with much of medical care for physical disorders.
Furthermore, as we aim to destigmatize mental health care, it’s important to equate it with physical care. For example, taking a day or two from school or work for a sprained ankle, seeing a dentist, or an eye exam, plus a myriad of physical issues is quite acceptable. Why is it not also acceptable for a mental health issue and evaluation, such as for anxiety or PTSD, plus being able to talk about it without stigma? Seeing the “shrink” needs to be removed as a negative but viewed as a very positive move toward care for oneself.
In addition, children and adolescents are battling countless other health challenges that could have implications for mental health professionals, for example:
- During the height of the coronavirus pandemic, pediatric endocrinologists reportedly saw a surge of referrals for girls experiencing early puberty. Puberty should never be medicalized, but early maturation has been linked to numerous psychiatric disorders such as depression, anxiety, and eating disorders (J Pediatr Adolec Gynecol. 2022 Oct. doi: 10.1016/j.jpag.2022.05.005).
- A global epidemiologic study of children estimates that nearly 8 million youth lost a parent or caregiver because of a pandemic-related cause between Jan. 1, 2020, and May 1, 2022. An additional 2.5 million children were affected by the loss of secondary caregivers such as grandparents (JAMA Pediatr. 2022 Sept. doi: 10.1001/jamapediatrics.2022.3157).
- The inpatient and outpatient volume of adolescents and young adults receiving care for eating disorders skyrocketed before and after the pandemic, according to the results of case study series (JAMA Pediatrics. 2022 Nov 7. doi: 10.1001/jamapediatrics.2022.4346).
- Children and adolescents who developed COVID-19 suffered tremendously during the height of the pandemic. A nationwide analysis shows that COVID-19 nearly tripled children’s risks of developing new mental health illnesses, such as attention-deficit/hyperactivity disorder, anxiety, trauma, or stress disorder (Psychiatric Services. 2022 Jun 2. doi: 10.1176/appi.ps.202100646).
In addition to those challenges, young children are facing an increase in respiratory syncytial virus (RSV) infection. We were told the “flu” would be quite bad this year and to beware of monkeypox. However, very little mention is made of the equally distressing “epidemic” of mental health issues, PTSD, anxiety, and depression as we are still in the midst of the COVID pandemic in the United States with almost 400 deaths a day – a very unacceptable number.
Interestingly, we seem to have abandoned the use of masks as protection against COVID and other respiratory diseases, despite their effectiveness. A study in Boston that looked at children in two school districts that did not lift mask mandates demonstrated that mask wearing does indeed lead to significant reductions in the number of pediatric COVID cases. In addition to societal violence and school shootings – which certainly exacerbate anxiety – the fear of dying or the death of a loved one, tied to COVID, may lead to epidemic proportions of PTSD in children. As an article in WebMD noted, “pediatricians are imploring the federal government to declare a national emergency as cases of pediatric respiratory illnesses continue to soar.”
In light of the acknowledged mental health crisis in children, which appears epidemic, I would hope the psychiatric and psychological associations would publicly sound an alarm so that resources could be brought to bear to address this critical issue. I believe doing so would also aid in destigmatizing mental disorders, and increase education and treatment.
Layered on top of those issues are natural disasters, such as the fallout from Tropical Storm Nicole when it recently caused devastation across western Florida. The mental health trauma caused by recent tropical storms seems all but forgotten – except for those who are still suffering. All of this adds up to a society-wide mental health crisis, which seems far more expansive than monkeypox, for example. Yet monkeypox, which did lead to thousands of cases and approximately 29 deaths in the United States, was declared a national public health emergency.
Additionally, RSV killed 100-500 U.S. children under age 5 each year before the pandemic, according to the Centers for Disease Control and Prevention, and currently it appears even worse. Yet despite the seriousness of RSV, it nowhere matches the emotional toll COVID has taken on children globally.
Let’s make it standard practice for children – and of course, adults – to be taught that anxiety is a normal response at times. We should teach that, in some cases, feeling “down” or in despair and even experiencing symptoms of PTSD based on what’s going on personally and within our environment (i.e., COVID, school shootings, etc.) are triggers and responses that can be addressed and often quickly treated by talking with a mental health professional.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
When I was growing up, I can remember experiencing “duck and cover” drills at school. If a flash appeared in our peripheral vision, we were told we should not look at it but crawl under our desks. My classmates and I were being taught how to protect ourselves in case of a nuclear attack.
Clearly, had there been such an attack, ducking under our desks would not have saved us. Thankfully, such a conflict never occurred – and hopefully never will. Still, the warning did penetrate our psyches. In those days, families and children in schools were worried, and some were scared.
The situation is quite different today. Our children and grandchildren are being taught to protect themselves not from actions overseas – that never happened – but from what someone living in their community might do that has been occurring in real time. According to my daughter-in-law, her young children are taught during “lockdowns” to hide in their classrooms’ closets. During these drills, some children are directed to line up against a wall that would be out of sight of a shooter, and to stay as still as possible.
Since 2017, the number of intentional shootings in U.S. kindergarten through grade 12 schools increased precipitously (Prev Med. 2022 Dec. doi: 10.1016/j.ypmed.2022.107280). Imagine the psychological impact that the vigilance required to deal with such impending threats must be having on our children, as they learn to fear injury and possible death every day they go to school. I’ve talked with numerous parents about this, including my own adult children, and this is clearly a new dimension of life that is on everyone’s minds. Schools, once bastions of safety, are no longer that safe.
For many years, I’ve written about the need to destigmatize mental illness so that it is treated on a par with physical illness. As we look at the challenges faced by young people, reframing mental illness is more important now than ever. This means finding ways to increase the funding of studies that help us understand young people with mental health issues. It also means encouraging patients to pursue treatment from psychiatrists, psychologists, or mental health counselors who specialize in short-term therapy.
The emphasis here on short-term therapy is not to discourage longer-term care when needed, but clearly short-term care strategies, such as cognitive-behavioral therapies, not only work for problem resolution, they also help in the destigmatization of mental health care – as the circumscribed treatment with a clear beginning, middle, and end is consistent with CBT and consistent with much of medical care for physical disorders.
Furthermore, as we aim to destigmatize mental health care, it’s important to equate it with physical care. For example, taking a day or two from school or work for a sprained ankle, seeing a dentist, or an eye exam, plus a myriad of physical issues is quite acceptable. Why is it not also acceptable for a mental health issue and evaluation, such as for anxiety or PTSD, plus being able to talk about it without stigma? Seeing the “shrink” needs to be removed as a negative but viewed as a very positive move toward care for oneself.
In addition, children and adolescents are battling countless other health challenges that could have implications for mental health professionals, for example:
- During the height of the coronavirus pandemic, pediatric endocrinologists reportedly saw a surge of referrals for girls experiencing early puberty. Puberty should never be medicalized, but early maturation has been linked to numerous psychiatric disorders such as depression, anxiety, and eating disorders (J Pediatr Adolec Gynecol. 2022 Oct. doi: 10.1016/j.jpag.2022.05.005).
- A global epidemiologic study of children estimates that nearly 8 million youth lost a parent or caregiver because of a pandemic-related cause between Jan. 1, 2020, and May 1, 2022. An additional 2.5 million children were affected by the loss of secondary caregivers such as grandparents (JAMA Pediatr. 2022 Sept. doi: 10.1001/jamapediatrics.2022.3157).
- The inpatient and outpatient volume of adolescents and young adults receiving care for eating disorders skyrocketed before and after the pandemic, according to the results of case study series (JAMA Pediatrics. 2022 Nov 7. doi: 10.1001/jamapediatrics.2022.4346).
- Children and adolescents who developed COVID-19 suffered tremendously during the height of the pandemic. A nationwide analysis shows that COVID-19 nearly tripled children’s risks of developing new mental health illnesses, such as attention-deficit/hyperactivity disorder, anxiety, trauma, or stress disorder (Psychiatric Services. 2022 Jun 2. doi: 10.1176/appi.ps.202100646).
In addition to those challenges, young children are facing an increase in respiratory syncytial virus (RSV) infection. We were told the “flu” would be quite bad this year and to beware of monkeypox. However, very little mention is made of the equally distressing “epidemic” of mental health issues, PTSD, anxiety, and depression as we are still in the midst of the COVID pandemic in the United States with almost 400 deaths a day – a very unacceptable number.
Interestingly, we seem to have abandoned the use of masks as protection against COVID and other respiratory diseases, despite their effectiveness. A study in Boston that looked at children in two school districts that did not lift mask mandates demonstrated that mask wearing does indeed lead to significant reductions in the number of pediatric COVID cases. In addition to societal violence and school shootings – which certainly exacerbate anxiety – the fear of dying or the death of a loved one, tied to COVID, may lead to epidemic proportions of PTSD in children. As an article in WebMD noted, “pediatricians are imploring the federal government to declare a national emergency as cases of pediatric respiratory illnesses continue to soar.”
In light of the acknowledged mental health crisis in children, which appears epidemic, I would hope the psychiatric and psychological associations would publicly sound an alarm so that resources could be brought to bear to address this critical issue. I believe doing so would also aid in destigmatizing mental disorders, and increase education and treatment.
Layered on top of those issues are natural disasters, such as the fallout from Tropical Storm Nicole when it recently caused devastation across western Florida. The mental health trauma caused by recent tropical storms seems all but forgotten – except for those who are still suffering. All of this adds up to a society-wide mental health crisis, which seems far more expansive than monkeypox, for example. Yet monkeypox, which did lead to thousands of cases and approximately 29 deaths in the United States, was declared a national public health emergency.
Additionally, RSV killed 100-500 U.S. children under age 5 each year before the pandemic, according to the Centers for Disease Control and Prevention, and currently it appears even worse. Yet despite the seriousness of RSV, it nowhere matches the emotional toll COVID has taken on children globally.
Let’s make it standard practice for children – and of course, adults – to be taught that anxiety is a normal response at times. We should teach that, in some cases, feeling “down” or in despair and even experiencing symptoms of PTSD based on what’s going on personally and within our environment (i.e., COVID, school shootings, etc.) are triggers and responses that can be addressed and often quickly treated by talking with a mental health professional.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Immune dysregulation may drive long-term postpartum depression
Postpartum depression, anxiety, and posttraumatic stress disorder that persist 2-3 years after birth are associated with a dysregulated immune system that is characterized by increased inflammatory signaling, according to investigators.
These findings suggest that mental health screening for women who have given birth should continue beyond the first year post partum, reported lead author Jennifer M. Nicoloro-SantaBarbara, PhD, of Brigham and Women’s Hospital, Harvard Medical School, Boston, and colleagues.
“Delayed postpartum depression, also known as late-onset postpartum depression, can affect women up to 18 months after delivery,” the investigators wrote in the American Journal of Reproductive Immunology. “It can appear even later in some women, depending on the hormonal changes that occur after having a baby (for example, timing of weaning). However, the majority of research on maternal mental health focuses on the first year post birth, leaving a gap in research beyond 12 months post partum.”
To address this gap, the investigators enrolled 33 women who were 2-3 years post partum. Participants completed self-guided questionnaires on PTSD, depression, and anxiety, and provided blood samples for gene expression analysis.
Sixteen of the 33 women had clinically significant mood disturbances. and significantly reduced activation of genes associated with viral response.
“The results provide preliminary evidence of a mechanism (e.g., immune dysregulation) that might be contributing to mood disorders and bring us closer to the goal of identifying targetable biomarkers for mood disorders,” Dr. Nicoloro-SantaBarbara said in a written comment. “This work highlights the need for standardized and continual depression and anxiety screening in ob.gyn. and primary care settings that extends beyond the 6-week maternal visit and possibly beyond the first postpartum year.”
Findings draw skepticism
“The authors argue that mothers need to be screened for depression/anxiety longer than the first year post partum, and this is true, but it has nothing to do with their findings,” said Jennifer L. Payne, MD, an expert in reproductive psychiatry at the University of Virginia, Charlottesville.
In a written comment, she explained that the cross-sectional design makes it impossible to know whether the mood disturbances were linked with delivery at all.
“It is unclear if the depression/anxiety symptoms began after delivery or not,” Dr. Payne said. “In addition, it is unclear if the findings are causative or a result of depression/anxiety symptoms (the authors admit this in the limitations section). It is likely that the findings are not specific or even related to having delivered a child, but rather reflect a more general process related to depression/anxiety outside of the postpartum time period.”
Only prospective studies can answer these questions, she said.
Dr. Nicoloro-SantaBarbara agreed that further research is needed.
“Our findings are exciting, but still need to be replicated in larger samples with diverse women in order to make sure they generalize,” she said. “More work is needed to understand why inflammation plays a role in postpartum mental illness for some women and not others.”
The study was supported by a Cedars-Sinai Precision Health Grant, the Cousins Center for Psychoneuroimmunology, University of California, Los Angeles, and the National Institute of Mental Health. The investigators and Dr. Payne disclosed no relevant conflicts of interest.
Postpartum depression, anxiety, and posttraumatic stress disorder that persist 2-3 years after birth are associated with a dysregulated immune system that is characterized by increased inflammatory signaling, according to investigators.
These findings suggest that mental health screening for women who have given birth should continue beyond the first year post partum, reported lead author Jennifer M. Nicoloro-SantaBarbara, PhD, of Brigham and Women’s Hospital, Harvard Medical School, Boston, and colleagues.
“Delayed postpartum depression, also known as late-onset postpartum depression, can affect women up to 18 months after delivery,” the investigators wrote in the American Journal of Reproductive Immunology. “It can appear even later in some women, depending on the hormonal changes that occur after having a baby (for example, timing of weaning). However, the majority of research on maternal mental health focuses on the first year post birth, leaving a gap in research beyond 12 months post partum.”
To address this gap, the investigators enrolled 33 women who were 2-3 years post partum. Participants completed self-guided questionnaires on PTSD, depression, and anxiety, and provided blood samples for gene expression analysis.
Sixteen of the 33 women had clinically significant mood disturbances. and significantly reduced activation of genes associated with viral response.
“The results provide preliminary evidence of a mechanism (e.g., immune dysregulation) that might be contributing to mood disorders and bring us closer to the goal of identifying targetable biomarkers for mood disorders,” Dr. Nicoloro-SantaBarbara said in a written comment. “This work highlights the need for standardized and continual depression and anxiety screening in ob.gyn. and primary care settings that extends beyond the 6-week maternal visit and possibly beyond the first postpartum year.”
Findings draw skepticism
“The authors argue that mothers need to be screened for depression/anxiety longer than the first year post partum, and this is true, but it has nothing to do with their findings,” said Jennifer L. Payne, MD, an expert in reproductive psychiatry at the University of Virginia, Charlottesville.
In a written comment, she explained that the cross-sectional design makes it impossible to know whether the mood disturbances were linked with delivery at all.
“It is unclear if the depression/anxiety symptoms began after delivery or not,” Dr. Payne said. “In addition, it is unclear if the findings are causative or a result of depression/anxiety symptoms (the authors admit this in the limitations section). It is likely that the findings are not specific or even related to having delivered a child, but rather reflect a more general process related to depression/anxiety outside of the postpartum time period.”
Only prospective studies can answer these questions, she said.
Dr. Nicoloro-SantaBarbara agreed that further research is needed.
“Our findings are exciting, but still need to be replicated in larger samples with diverse women in order to make sure they generalize,” she said. “More work is needed to understand why inflammation plays a role in postpartum mental illness for some women and not others.”
The study was supported by a Cedars-Sinai Precision Health Grant, the Cousins Center for Psychoneuroimmunology, University of California, Los Angeles, and the National Institute of Mental Health. The investigators and Dr. Payne disclosed no relevant conflicts of interest.
Postpartum depression, anxiety, and posttraumatic stress disorder that persist 2-3 years after birth are associated with a dysregulated immune system that is characterized by increased inflammatory signaling, according to investigators.
These findings suggest that mental health screening for women who have given birth should continue beyond the first year post partum, reported lead author Jennifer M. Nicoloro-SantaBarbara, PhD, of Brigham and Women’s Hospital, Harvard Medical School, Boston, and colleagues.
“Delayed postpartum depression, also known as late-onset postpartum depression, can affect women up to 18 months after delivery,” the investigators wrote in the American Journal of Reproductive Immunology. “It can appear even later in some women, depending on the hormonal changes that occur after having a baby (for example, timing of weaning). However, the majority of research on maternal mental health focuses on the first year post birth, leaving a gap in research beyond 12 months post partum.”
To address this gap, the investigators enrolled 33 women who were 2-3 years post partum. Participants completed self-guided questionnaires on PTSD, depression, and anxiety, and provided blood samples for gene expression analysis.
Sixteen of the 33 women had clinically significant mood disturbances. and significantly reduced activation of genes associated with viral response.
“The results provide preliminary evidence of a mechanism (e.g., immune dysregulation) that might be contributing to mood disorders and bring us closer to the goal of identifying targetable biomarkers for mood disorders,” Dr. Nicoloro-SantaBarbara said in a written comment. “This work highlights the need for standardized and continual depression and anxiety screening in ob.gyn. and primary care settings that extends beyond the 6-week maternal visit and possibly beyond the first postpartum year.”
Findings draw skepticism
“The authors argue that mothers need to be screened for depression/anxiety longer than the first year post partum, and this is true, but it has nothing to do with their findings,” said Jennifer L. Payne, MD, an expert in reproductive psychiatry at the University of Virginia, Charlottesville.
In a written comment, she explained that the cross-sectional design makes it impossible to know whether the mood disturbances were linked with delivery at all.
“It is unclear if the depression/anxiety symptoms began after delivery or not,” Dr. Payne said. “In addition, it is unclear if the findings are causative or a result of depression/anxiety symptoms (the authors admit this in the limitations section). It is likely that the findings are not specific or even related to having delivered a child, but rather reflect a more general process related to depression/anxiety outside of the postpartum time period.”
Only prospective studies can answer these questions, she said.
Dr. Nicoloro-SantaBarbara agreed that further research is needed.
“Our findings are exciting, but still need to be replicated in larger samples with diverse women in order to make sure they generalize,” she said. “More work is needed to understand why inflammation plays a role in postpartum mental illness for some women and not others.”
The study was supported by a Cedars-Sinai Precision Health Grant, the Cousins Center for Psychoneuroimmunology, University of California, Los Angeles, and the National Institute of Mental Health. The investigators and Dr. Payne disclosed no relevant conflicts of interest.
FROM THE AMERICAN JOURNAL OF REPRODUCTIVE IMMUNOLOGY
‘Striking’ rate of mental health comorbidities in epilepsy
NASHVILLE, TENN. – , new research reveals.
“We hope these results inspire epileptologists and neurologists to both recognize and screen for suicide ideation and behaviors in their adolescent patients,” said study investigator Hadley Greenwood, a third-year medical student at New York University.
The new data should also encourage providers “to become more comfortable” providing support to patients, “be that by increasing their familiarity with prescribing different antidepressants or by being well versed in how to connect patients to resources within their community,” said Mr. Greenwood.
The findings were presented here at the annual meeting of the American Epilepsy Society.
Little research
Previous studies have reported on the prevalence of suicidality as well as depression and anxiety among adults with epilepsy. “We wanted to look at adolescents because there’s much less in the literature out there about psychiatric comorbidity, and specifically suicidality, in this population,” said Mr. Greenwood.
Researchers used data from the Human Epilepsy Project, a study that collected data from 34 sites in the United States, Canada, Europe, and Australia from 2012 to 2017.
From a cohort of more than 400 participants, researchers identified 67 patients aged 11-17 years who were enrolled within 4 months of starting treatment for focal epilepsy.
Participants completed the Columbia–Suicide Severity Rating Scale (C-SSRS) at enrollment and at follow-ups over 36 months. The C-SSRS measures suicidal ideation and severity, said Mr. Greenwood.
“It’s scaled from passive suicide ideation, such as thoughts of ‘I wish I were dead’ without active intent, all the way up to active suicidal ideation with a plan and intent.”
Researchers were able to distinguish individuals with passive suicide ideation from those with more serious intentions, said Mr. Greenwood. They used medical records to evaluate the prevalence of suicidal ideation and behavior.
The investigators found that more than one in five (20.9%) teens endorsed any lifetime suicide ideation. This, said Mr. Greenwood, is “roughly equivalent” to the prevalence reported earlier in the adult cohort of the Human Epilepsy Project (21.6%).
‘Striking’ rate
The fact that one in five adolescents had any lifetime suicide ideation is “definitely a striking number,” said Mr. Greenwood.
Researchers found that 15% of patients experienced active suicide ideation, 7.5% exhibited preparatory or suicidal behaviors, and 3% had made a prior suicide attempt.
All of these percentages increased at 3 years: Thirty-one percent for suicide ideation; 25% for active suicide behavior, 15% for preparatory or suicide behaviors, and 5% for prior suicide attempt.
The fact that nearly one in three adolescents endorsed suicide ideation at 3 years is another “striking” finding, said Mr. Greenwood.
Of the 53 adolescents who had never had suicide ideation at the time of enrollment, 7 endorsed new-onset suicide ideation in the follow-up period. Five of 14 who had had suicide ideation at some point prior to enrollment continued to endorse it.
“The value of the study is identifying the prevalence and identifying the significant number of adolescents with epilepsy who are endorsing either suicide ideation or suicidal behaviors,” said Mr. Greenwood.
The researchers found that among younger teens (aged 11–14 years) rates of suicide ideation were higher than among their older counterparts (aged 15–17 years).
The study does not shed light on the biological connection between epilepsy and suicidality, but Mr. Greenwood noted that prior research has suggested a bidirectional relationship.
“Depression and other psychiatric comorbidities might exist prior to epileptic activity and actually predispose to epileptic activity.”
Mr. Greenwood noted that suicide ideation has “spiked” recently across the general population, and so it’s difficult to compare the prevalence in her study with “today’s prevalence.”
However, other research generally shows that the suicide ideation rate in the general adolescent population is much lower than in teens with epilepsy.
Unique aspects of the current study are that it reports suicide ideation and behaviors at around the time of an epilepsy diagnosis and documents how suicidality progresses or resolves over time, said Mr. Greenwood.
Underdiagnosed, undertreated
Commenting on the research, Elizabeth Donner, MD, director of the comprehensive epilepsy program, Hospital for Sick Children, and associate professor, department of pediatrics, University of Toronto, said a “key point” from the study is that the suicidality rate among teens with epilepsy exceeds that of children not living with epilepsy.
“We are significantly underdiagnosing and undertreating the mental health comorbidities in epilepsy,” said Dr. Donner. “Epilepsy is a brain disease and so are mental health disorders, so it shouldn’t come as any surprise that they coexist in individuals with epilepsy.”
The new results contribute to what is already known about the significant mortality rates among persons with epilepsy, said Dr. Donner. She referred to a 2018 study that showed that people with epilepsy were 3.5 times more likely to die by suicide.
Other research has shown that people with epilepsy are 10 times more likely to die by drowning, mostly in the bathtub, said Dr. Donner.
“You would think that we’re educating these people about risks related to their epilepsy, but either the messages don’t get through, or they don’t know how to keep themselves safe,” she said.
“This needs to be seen in a bigger picture, and the bigger picture is we need to recognize comorbid mental health issues; we need to address them once recognized; and then we need to counsel and support people to live safely with their epilepsy.
The study received funding from the Epilepsy Study Consortium, Finding a Cure for Epilepsy and Seizures (FACES) and other related foundations, UCB, Pfizer, Eisai, Lundbeck, and Sunovion. Mr. Greenwood and Dr. Donner report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NASHVILLE, TENN. – , new research reveals.
“We hope these results inspire epileptologists and neurologists to both recognize and screen for suicide ideation and behaviors in their adolescent patients,” said study investigator Hadley Greenwood, a third-year medical student at New York University.
The new data should also encourage providers “to become more comfortable” providing support to patients, “be that by increasing their familiarity with prescribing different antidepressants or by being well versed in how to connect patients to resources within their community,” said Mr. Greenwood.
The findings were presented here at the annual meeting of the American Epilepsy Society.
Little research
Previous studies have reported on the prevalence of suicidality as well as depression and anxiety among adults with epilepsy. “We wanted to look at adolescents because there’s much less in the literature out there about psychiatric comorbidity, and specifically suicidality, in this population,” said Mr. Greenwood.
Researchers used data from the Human Epilepsy Project, a study that collected data from 34 sites in the United States, Canada, Europe, and Australia from 2012 to 2017.
From a cohort of more than 400 participants, researchers identified 67 patients aged 11-17 years who were enrolled within 4 months of starting treatment for focal epilepsy.
Participants completed the Columbia–Suicide Severity Rating Scale (C-SSRS) at enrollment and at follow-ups over 36 months. The C-SSRS measures suicidal ideation and severity, said Mr. Greenwood.
“It’s scaled from passive suicide ideation, such as thoughts of ‘I wish I were dead’ without active intent, all the way up to active suicidal ideation with a plan and intent.”
Researchers were able to distinguish individuals with passive suicide ideation from those with more serious intentions, said Mr. Greenwood. They used medical records to evaluate the prevalence of suicidal ideation and behavior.
The investigators found that more than one in five (20.9%) teens endorsed any lifetime suicide ideation. This, said Mr. Greenwood, is “roughly equivalent” to the prevalence reported earlier in the adult cohort of the Human Epilepsy Project (21.6%).
‘Striking’ rate
The fact that one in five adolescents had any lifetime suicide ideation is “definitely a striking number,” said Mr. Greenwood.
Researchers found that 15% of patients experienced active suicide ideation, 7.5% exhibited preparatory or suicidal behaviors, and 3% had made a prior suicide attempt.
All of these percentages increased at 3 years: Thirty-one percent for suicide ideation; 25% for active suicide behavior, 15% for preparatory or suicide behaviors, and 5% for prior suicide attempt.
The fact that nearly one in three adolescents endorsed suicide ideation at 3 years is another “striking” finding, said Mr. Greenwood.
Of the 53 adolescents who had never had suicide ideation at the time of enrollment, 7 endorsed new-onset suicide ideation in the follow-up period. Five of 14 who had had suicide ideation at some point prior to enrollment continued to endorse it.
“The value of the study is identifying the prevalence and identifying the significant number of adolescents with epilepsy who are endorsing either suicide ideation or suicidal behaviors,” said Mr. Greenwood.
The researchers found that among younger teens (aged 11–14 years) rates of suicide ideation were higher than among their older counterparts (aged 15–17 years).
The study does not shed light on the biological connection between epilepsy and suicidality, but Mr. Greenwood noted that prior research has suggested a bidirectional relationship.
“Depression and other psychiatric comorbidities might exist prior to epileptic activity and actually predispose to epileptic activity.”
Mr. Greenwood noted that suicide ideation has “spiked” recently across the general population, and so it’s difficult to compare the prevalence in her study with “today’s prevalence.”
However, other research generally shows that the suicide ideation rate in the general adolescent population is much lower than in teens with epilepsy.
Unique aspects of the current study are that it reports suicide ideation and behaviors at around the time of an epilepsy diagnosis and documents how suicidality progresses or resolves over time, said Mr. Greenwood.
Underdiagnosed, undertreated
Commenting on the research, Elizabeth Donner, MD, director of the comprehensive epilepsy program, Hospital for Sick Children, and associate professor, department of pediatrics, University of Toronto, said a “key point” from the study is that the suicidality rate among teens with epilepsy exceeds that of children not living with epilepsy.
“We are significantly underdiagnosing and undertreating the mental health comorbidities in epilepsy,” said Dr. Donner. “Epilepsy is a brain disease and so are mental health disorders, so it shouldn’t come as any surprise that they coexist in individuals with epilepsy.”
The new results contribute to what is already known about the significant mortality rates among persons with epilepsy, said Dr. Donner. She referred to a 2018 study that showed that people with epilepsy were 3.5 times more likely to die by suicide.
Other research has shown that people with epilepsy are 10 times more likely to die by drowning, mostly in the bathtub, said Dr. Donner.
“You would think that we’re educating these people about risks related to their epilepsy, but either the messages don’t get through, or they don’t know how to keep themselves safe,” she said.
“This needs to be seen in a bigger picture, and the bigger picture is we need to recognize comorbid mental health issues; we need to address them once recognized; and then we need to counsel and support people to live safely with their epilepsy.
The study received funding from the Epilepsy Study Consortium, Finding a Cure for Epilepsy and Seizures (FACES) and other related foundations, UCB, Pfizer, Eisai, Lundbeck, and Sunovion. Mr. Greenwood and Dr. Donner report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NASHVILLE, TENN. – , new research reveals.
“We hope these results inspire epileptologists and neurologists to both recognize and screen for suicide ideation and behaviors in their adolescent patients,” said study investigator Hadley Greenwood, a third-year medical student at New York University.
The new data should also encourage providers “to become more comfortable” providing support to patients, “be that by increasing their familiarity with prescribing different antidepressants or by being well versed in how to connect patients to resources within their community,” said Mr. Greenwood.
The findings were presented here at the annual meeting of the American Epilepsy Society.
Little research
Previous studies have reported on the prevalence of suicidality as well as depression and anxiety among adults with epilepsy. “We wanted to look at adolescents because there’s much less in the literature out there about psychiatric comorbidity, and specifically suicidality, in this population,” said Mr. Greenwood.
Researchers used data from the Human Epilepsy Project, a study that collected data from 34 sites in the United States, Canada, Europe, and Australia from 2012 to 2017.
From a cohort of more than 400 participants, researchers identified 67 patients aged 11-17 years who were enrolled within 4 months of starting treatment for focal epilepsy.
Participants completed the Columbia–Suicide Severity Rating Scale (C-SSRS) at enrollment and at follow-ups over 36 months. The C-SSRS measures suicidal ideation and severity, said Mr. Greenwood.
“It’s scaled from passive suicide ideation, such as thoughts of ‘I wish I were dead’ without active intent, all the way up to active suicidal ideation with a plan and intent.”
Researchers were able to distinguish individuals with passive suicide ideation from those with more serious intentions, said Mr. Greenwood. They used medical records to evaluate the prevalence of suicidal ideation and behavior.
The investigators found that more than one in five (20.9%) teens endorsed any lifetime suicide ideation. This, said Mr. Greenwood, is “roughly equivalent” to the prevalence reported earlier in the adult cohort of the Human Epilepsy Project (21.6%).
‘Striking’ rate
The fact that one in five adolescents had any lifetime suicide ideation is “definitely a striking number,” said Mr. Greenwood.
Researchers found that 15% of patients experienced active suicide ideation, 7.5% exhibited preparatory or suicidal behaviors, and 3% had made a prior suicide attempt.
All of these percentages increased at 3 years: Thirty-one percent for suicide ideation; 25% for active suicide behavior, 15% for preparatory or suicide behaviors, and 5% for prior suicide attempt.
The fact that nearly one in three adolescents endorsed suicide ideation at 3 years is another “striking” finding, said Mr. Greenwood.
Of the 53 adolescents who had never had suicide ideation at the time of enrollment, 7 endorsed new-onset suicide ideation in the follow-up period. Five of 14 who had had suicide ideation at some point prior to enrollment continued to endorse it.
“The value of the study is identifying the prevalence and identifying the significant number of adolescents with epilepsy who are endorsing either suicide ideation or suicidal behaviors,” said Mr. Greenwood.
The researchers found that among younger teens (aged 11–14 years) rates of suicide ideation were higher than among their older counterparts (aged 15–17 years).
The study does not shed light on the biological connection between epilepsy and suicidality, but Mr. Greenwood noted that prior research has suggested a bidirectional relationship.
“Depression and other psychiatric comorbidities might exist prior to epileptic activity and actually predispose to epileptic activity.”
Mr. Greenwood noted that suicide ideation has “spiked” recently across the general population, and so it’s difficult to compare the prevalence in her study with “today’s prevalence.”
However, other research generally shows that the suicide ideation rate in the general adolescent population is much lower than in teens with epilepsy.
Unique aspects of the current study are that it reports suicide ideation and behaviors at around the time of an epilepsy diagnosis and documents how suicidality progresses or resolves over time, said Mr. Greenwood.
Underdiagnosed, undertreated
Commenting on the research, Elizabeth Donner, MD, director of the comprehensive epilepsy program, Hospital for Sick Children, and associate professor, department of pediatrics, University of Toronto, said a “key point” from the study is that the suicidality rate among teens with epilepsy exceeds that of children not living with epilepsy.
“We are significantly underdiagnosing and undertreating the mental health comorbidities in epilepsy,” said Dr. Donner. “Epilepsy is a brain disease and so are mental health disorders, so it shouldn’t come as any surprise that they coexist in individuals with epilepsy.”
The new results contribute to what is already known about the significant mortality rates among persons with epilepsy, said Dr. Donner. She referred to a 2018 study that showed that people with epilepsy were 3.5 times more likely to die by suicide.
Other research has shown that people with epilepsy are 10 times more likely to die by drowning, mostly in the bathtub, said Dr. Donner.
“You would think that we’re educating these people about risks related to their epilepsy, but either the messages don’t get through, or they don’t know how to keep themselves safe,” she said.
“This needs to be seen in a bigger picture, and the bigger picture is we need to recognize comorbid mental health issues; we need to address them once recognized; and then we need to counsel and support people to live safely with their epilepsy.
The study received funding from the Epilepsy Study Consortium, Finding a Cure for Epilepsy and Seizures (FACES) and other related foundations, UCB, Pfizer, Eisai, Lundbeck, and Sunovion. Mr. Greenwood and Dr. Donner report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT AES 2022
SSRI tied to improved cognition in comorbid depression, dementia
The results of the 12-week open-label, single-group study are positive, study investigator Michael Cronquist Christensen, MPA, DrPH, a director with the Lundbeck pharmaceutical company, told this news organization before presenting the results in a poster at the 15th Clinical Trials on Alzheimer’s Disease conference.
“The study confirms earlier findings of improvement in both depressive symptoms and cognitive performance with vortioxetine in patients with depression and dementia and adds to this research that these clinical effects also extend to improvement in health-related quality of life and patients’ daily functioning,” Dr. Christensen said.
“It also demonstrates that patients with depression and comorbid dementia can be safely treated with 20 mg vortioxetine – starting dose of 5 mg for the first week and up-titration to 10 mg at day 8,” he added.
However, he reported that Lundbeck doesn’t plan to seek approval from the U.S. Food and Drug Administration for a new indication. Vortioxetine received FDA approval in 2013 to treat MDD, but 3 years later the agency rejected an expansion of its indication to include cognitive dysfunction.
“Vortioxetine is approved for MDD, but the product can be used in patients with MDD who have other diseases, including other mental illnesses,” Dr. Christensen said.
Potential neurotransmission modulator
Vortioxetine is a selective serotonin reuptake inhibitor and serotonin receptor modulator. According to Dr. Christensen, evidence suggests the drug’s receptor targets “have the potential to modulate neurotransmitter systems that are essential for regulation of cognitive function.”
The researchers recruited 83 individuals aged 55-85 with recurrent MDD that had started before the age of 55. All had MDD episodes within the previous 6 months and comorbid dementia for at least 6 months.
Of the participants, 65.9% were female. In addition, 42.7% had Alzheimer’s disease, 26.8% had mixed-type dementia, and the rest had other types of dementia.
The daily oral dose of vortioxetine started at 5 mg for up to week 1 and then was increased to 10 mg. It was then increased to 20 mg or decreased to 5 mg “based on investigator judgment and patient response.” The average daily dose was 12.3 mg.
In regard to the primary outcome, at week 12 (n = 70), scores on the Montgomery-Åsberg Depression Rating Scale (MADRS) fell by a mean of –12.4 (.78, P < .0001), which researchers deemed to be a significant reduction in severe symptoms.
“A significant and clinically meaningful effect was observed from week 1,” the researchers reported.
“As a basis for comparison, we typically see an improvement around 13-14 points during 8 weeks of antidepressant treatment in adults with MDD who do not have dementia,” Dr. Christensen added.
More than a third of patients (35.7%) saw a reduction in MADRS score by more than 50% at week 12, and 17.2% were considered to have reached MDD depression remission, defined as a MADRS score at or under 10.
For secondary outcomes, the total Digit Symbol Substitution test score grew by 0.65 (standardized effect size) by week 12, showing significant improvement (P < .0001). In addition, participants improved on some other cognitive measures, and Dr. Christensen noted that “significant improvement was also observed in the patients’ health-related quality of life and daily functioning.”
A third of patients had drug-related treatment-emergent adverse events.
Vortioxetine is one of the most expensive antidepressants: It has a list price of $444 a month, and no generic version is currently available.
Small trial, open-label design
In a comment, Claire Sexton, DPhil, senior director of scientific programs and outreach at the Alzheimer’s Association, said the study “reflects a valuable aspect of treatment research because of the close connection between depression and dementia. Depression is a known risk factor for dementia, including Alzheimer’s disease, and those who have dementia may experience depression.”
She cautioned, however, that the trial was small and had an open-label design instead of the “gold standard” of a double-blinded trial with a control group.
The study was funded by Lundbeck, where Dr. Christensen is an employee. Another author is a Lundbeck employee, and a third author reported various disclosures. Dr. Sexton reported no disclosures.
A version of this article first appeared on Medscape.com.
The results of the 12-week open-label, single-group study are positive, study investigator Michael Cronquist Christensen, MPA, DrPH, a director with the Lundbeck pharmaceutical company, told this news organization before presenting the results in a poster at the 15th Clinical Trials on Alzheimer’s Disease conference.
“The study confirms earlier findings of improvement in both depressive symptoms and cognitive performance with vortioxetine in patients with depression and dementia and adds to this research that these clinical effects also extend to improvement in health-related quality of life and patients’ daily functioning,” Dr. Christensen said.
“It also demonstrates that patients with depression and comorbid dementia can be safely treated with 20 mg vortioxetine – starting dose of 5 mg for the first week and up-titration to 10 mg at day 8,” he added.
However, he reported that Lundbeck doesn’t plan to seek approval from the U.S. Food and Drug Administration for a new indication. Vortioxetine received FDA approval in 2013 to treat MDD, but 3 years later the agency rejected an expansion of its indication to include cognitive dysfunction.
“Vortioxetine is approved for MDD, but the product can be used in patients with MDD who have other diseases, including other mental illnesses,” Dr. Christensen said.
Potential neurotransmission modulator
Vortioxetine is a selective serotonin reuptake inhibitor and serotonin receptor modulator. According to Dr. Christensen, evidence suggests the drug’s receptor targets “have the potential to modulate neurotransmitter systems that are essential for regulation of cognitive function.”
The researchers recruited 83 individuals aged 55-85 with recurrent MDD that had started before the age of 55. All had MDD episodes within the previous 6 months and comorbid dementia for at least 6 months.
Of the participants, 65.9% were female. In addition, 42.7% had Alzheimer’s disease, 26.8% had mixed-type dementia, and the rest had other types of dementia.
The daily oral dose of vortioxetine started at 5 mg for up to week 1 and then was increased to 10 mg. It was then increased to 20 mg or decreased to 5 mg “based on investigator judgment and patient response.” The average daily dose was 12.3 mg.
In regard to the primary outcome, at week 12 (n = 70), scores on the Montgomery-Åsberg Depression Rating Scale (MADRS) fell by a mean of –12.4 (.78, P < .0001), which researchers deemed to be a significant reduction in severe symptoms.
“A significant and clinically meaningful effect was observed from week 1,” the researchers reported.
“As a basis for comparison, we typically see an improvement around 13-14 points during 8 weeks of antidepressant treatment in adults with MDD who do not have dementia,” Dr. Christensen added.
More than a third of patients (35.7%) saw a reduction in MADRS score by more than 50% at week 12, and 17.2% were considered to have reached MDD depression remission, defined as a MADRS score at or under 10.
For secondary outcomes, the total Digit Symbol Substitution test score grew by 0.65 (standardized effect size) by week 12, showing significant improvement (P < .0001). In addition, participants improved on some other cognitive measures, and Dr. Christensen noted that “significant improvement was also observed in the patients’ health-related quality of life and daily functioning.”
A third of patients had drug-related treatment-emergent adverse events.
Vortioxetine is one of the most expensive antidepressants: It has a list price of $444 a month, and no generic version is currently available.
Small trial, open-label design
In a comment, Claire Sexton, DPhil, senior director of scientific programs and outreach at the Alzheimer’s Association, said the study “reflects a valuable aspect of treatment research because of the close connection between depression and dementia. Depression is a known risk factor for dementia, including Alzheimer’s disease, and those who have dementia may experience depression.”
She cautioned, however, that the trial was small and had an open-label design instead of the “gold standard” of a double-blinded trial with a control group.
The study was funded by Lundbeck, where Dr. Christensen is an employee. Another author is a Lundbeck employee, and a third author reported various disclosures. Dr. Sexton reported no disclosures.
A version of this article first appeared on Medscape.com.
The results of the 12-week open-label, single-group study are positive, study investigator Michael Cronquist Christensen, MPA, DrPH, a director with the Lundbeck pharmaceutical company, told this news organization before presenting the results in a poster at the 15th Clinical Trials on Alzheimer’s Disease conference.
“The study confirms earlier findings of improvement in both depressive symptoms and cognitive performance with vortioxetine in patients with depression and dementia and adds to this research that these clinical effects also extend to improvement in health-related quality of life and patients’ daily functioning,” Dr. Christensen said.
“It also demonstrates that patients with depression and comorbid dementia can be safely treated with 20 mg vortioxetine – starting dose of 5 mg for the first week and up-titration to 10 mg at day 8,” he added.
However, he reported that Lundbeck doesn’t plan to seek approval from the U.S. Food and Drug Administration for a new indication. Vortioxetine received FDA approval in 2013 to treat MDD, but 3 years later the agency rejected an expansion of its indication to include cognitive dysfunction.
“Vortioxetine is approved for MDD, but the product can be used in patients with MDD who have other diseases, including other mental illnesses,” Dr. Christensen said.
Potential neurotransmission modulator
Vortioxetine is a selective serotonin reuptake inhibitor and serotonin receptor modulator. According to Dr. Christensen, evidence suggests the drug’s receptor targets “have the potential to modulate neurotransmitter systems that are essential for regulation of cognitive function.”
The researchers recruited 83 individuals aged 55-85 with recurrent MDD that had started before the age of 55. All had MDD episodes within the previous 6 months and comorbid dementia for at least 6 months.
Of the participants, 65.9% were female. In addition, 42.7% had Alzheimer’s disease, 26.8% had mixed-type dementia, and the rest had other types of dementia.
The daily oral dose of vortioxetine started at 5 mg for up to week 1 and then was increased to 10 mg. It was then increased to 20 mg or decreased to 5 mg “based on investigator judgment and patient response.” The average daily dose was 12.3 mg.
In regard to the primary outcome, at week 12 (n = 70), scores on the Montgomery-Åsberg Depression Rating Scale (MADRS) fell by a mean of –12.4 (.78, P < .0001), which researchers deemed to be a significant reduction in severe symptoms.
“A significant and clinically meaningful effect was observed from week 1,” the researchers reported.
“As a basis for comparison, we typically see an improvement around 13-14 points during 8 weeks of antidepressant treatment in adults with MDD who do not have dementia,” Dr. Christensen added.
More than a third of patients (35.7%) saw a reduction in MADRS score by more than 50% at week 12, and 17.2% were considered to have reached MDD depression remission, defined as a MADRS score at or under 10.
For secondary outcomes, the total Digit Symbol Substitution test score grew by 0.65 (standardized effect size) by week 12, showing significant improvement (P < .0001). In addition, participants improved on some other cognitive measures, and Dr. Christensen noted that “significant improvement was also observed in the patients’ health-related quality of life and daily functioning.”
A third of patients had drug-related treatment-emergent adverse events.
Vortioxetine is one of the most expensive antidepressants: It has a list price of $444 a month, and no generic version is currently available.
Small trial, open-label design
In a comment, Claire Sexton, DPhil, senior director of scientific programs and outreach at the Alzheimer’s Association, said the study “reflects a valuable aspect of treatment research because of the close connection between depression and dementia. Depression is a known risk factor for dementia, including Alzheimer’s disease, and those who have dementia may experience depression.”
She cautioned, however, that the trial was small and had an open-label design instead of the “gold standard” of a double-blinded trial with a control group.
The study was funded by Lundbeck, where Dr. Christensen is an employee. Another author is a Lundbeck employee, and a third author reported various disclosures. Dr. Sexton reported no disclosures.
A version of this article first appeared on Medscape.com.
FROM CTAD 2022
Mood stabilizers, particularly lithium, potential lifesavers in bipolar disorder
Investigators led by Pao-Huan Chen, MD, of the department of psychiatry, Taipei Medical University Hospital, Taiwan, evaluated the association between the use of mood stabilizers and the risks for all-cause mortality, suicide, and natural mortality in more than 25,000 patients with BD and found that those with BD had higher mortality.
However, they also found that patients with BD had a significantly decreased adjusted 5-year risk of dying from any cause, suicide, and natural causes. Lithium was associated with the largest risk reduction compared with the other mood stabilizers.
“The present findings highlight the potential role of mood stabilizers, particularly lithium, in reducing mortality among patients with bipolar disorder,” the authors write.
“The findings of this study could inform future clinical and mechanistic research evaluating the multifaceted effects of mood stabilizers, particularly lithium, on the psychological and physiological statuses of patients with bipolar disorder,” they add.
The study was published online in Acta Psychiatrica Scandinavica.
Research gap
Patients with BD have an elevated risk for multiple comorbidities in addition to mood symptoms and neurocognitive dysfunction, with previous research suggesting a mortality rate due to suicide and natural causes that is at least twice as high as that of the general population, the authors write.
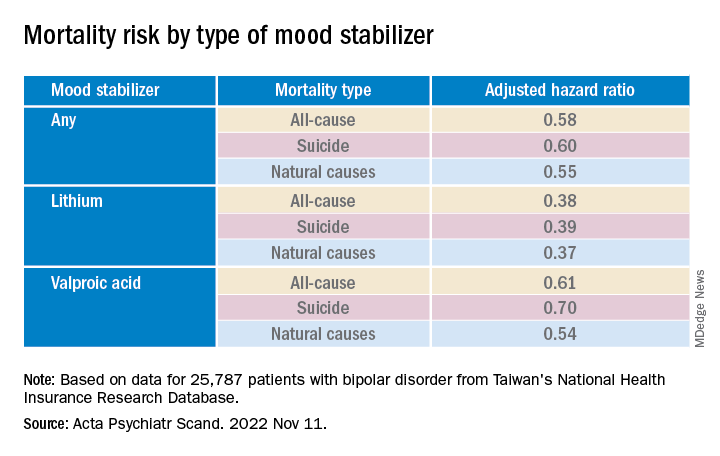
Lithium, in particular, has been associated with decreased risk for all-cause mortality and suicide in patients with BD, but findings regarding anticonvulsant mood stabilizers have been “inconsistent.”
To fill this research gap, the researchers evaluated 16 years of data from Taiwan’s National Health Insurance Research Database, which includes information about more than 23 million residents of Taiwan. The current study, which encompassed 25,787 patients with BD, looked at data from the 5-year period after index hospitalization.
The researchers hypothesized that mood stabilizers “would decrease the risk of mortality” among patients with BD and that “different mood stabilizers would exhibit different associations with mortality, owing to their varying effects on mood symptoms and physiological function.”
Covariates included sex, age, employment status, comorbidities, and concomitant drugs.
Of the patients with BD, 4,000 died within the 5-year period. Suicide and natural causes accounted for 19.0% and 73.7% of these deaths, respectively.
Cardioprotective effects?
The standardized mortality ratios (SMRs) – the ratios of observed mortality in the BD cohort to the number of expected deaths in the general population – were 5.26 for all causes (95% confidence interval, 5.10-5.43), 26.02 for suicide (95% CI, 24.20-27.93), and 4.68 for natural causes (95% CI, 4.51-4.85).
The cumulative mortality rate was higher among men vs. women, a difference that was even larger among patients who had died from any cause or natural causes (crude hazard ratios, .60 and .52, respectively; both Ps < .001).
The suicide risk peaked between ages 45 and 65 years, whereas the risks for all-cause and natural mortality increased with age and were highest in those older than 65 years.
Patients who had died from any cause or from natural causes had a higher risk for physical and psychiatric comorbidities, whereas those who had died by suicide had a higher risk for primarily psychiatric comorbidities.
Mood stabilizers were associated with decreased risks for all-cause mortality and natural mortality, with lithium and valproic acid tied to the lowest risk for all three mortality types (all Ps < .001).
Lamotrigine and carbamazepine were “not significantly associated with any type of mortality,” the authors report.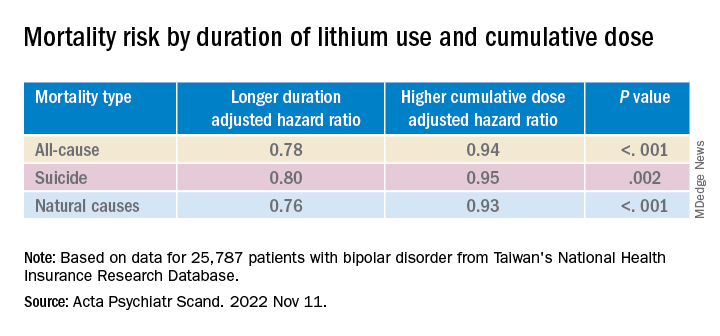
Longer duration of lithium use and a higher cumulative dose of lithium were both associated with lower risks for all three types of mortality (all Ps < .001).
Valproic acid was associated with dose-dependent decreases in all-cause and natural mortality risks.
The findings suggest that mood stabilizers “may improve not only psychosocial outcomes but also the physical health of patients with BD,” the investigators note.
The association between mood stabilizer use and reduced natural mortality risk “may be attributable to the potential benefits of psychiatric care” but may also “have resulted from the direct effects of mood stabilizers on physiological functions,” they add.
Some research suggests lithium treatment may reduce the risk for cardiovascular disease in patients with BD. Mechanistic studies have also pointed to potential cardioprotective effects from valproic acid.
The authors note several study limitations. Focusing on hospitalized patients “may have led to selection bias and overestimated mortality risk.” Moreover, the analyses were “based on the prescription, not the consumption, of mood stabilizers” and information regarding adherence was unavailable.
The absence of a protective mechanism of lamotrigine and carbamazepine may be attributable to “bias toward the relatively poor treatment responses” of these agents, neither of which is used as a first-line medication to treat BD in Taiwan. Patients taking these agents “may not receive medical care at a level equal to those taking lithium, who tend to receive closer surveillance, owing to the narrow therapeutic index.”
First-line treatment
Commenting on the study, Roger S. McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the mood disorders psychopharmacology unit, said that the data “add to a growing confluence of data from observational studies indicating that lithium especially is capable of reducing all-cause mortality, suicide mortality, and natural mortality.”
Dr. McIntyre, chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, who was not involved with the study, agreed with the authors that lamotrigine is “not a very popular drug in Taiwan, therefore we may not have sufficient assay sensitivity to document the effect.”
But lamotrigine “does have recurrence prevention effects in BD, especially bipolar depression, and it would be expected that it would reduce suicide potentially especially in such a large sample.”
The study’s take-home message “is that the extant evidence now indicates that lithium should be a first-line treatment in persons who live with BD who are experiencing suicidal ideation and/or behavior and these data should inform algorithms of treatment selection and sequencing in clinical practice guidelines,” said Dr. McIntyre.
This research was supported by grants from the Ministry of Science and Technology in Taiwan and Taipei City Hospital. The authors declared no relevant financial relationships. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China, and the Milken Institute; and speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe Pharma, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, AbbVie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
Investigators led by Pao-Huan Chen, MD, of the department of psychiatry, Taipei Medical University Hospital, Taiwan, evaluated the association between the use of mood stabilizers and the risks for all-cause mortality, suicide, and natural mortality in more than 25,000 patients with BD and found that those with BD had higher mortality.
However, they also found that patients with BD had a significantly decreased adjusted 5-year risk of dying from any cause, suicide, and natural causes. Lithium was associated with the largest risk reduction compared with the other mood stabilizers.
“The present findings highlight the potential role of mood stabilizers, particularly lithium, in reducing mortality among patients with bipolar disorder,” the authors write.
“The findings of this study could inform future clinical and mechanistic research evaluating the multifaceted effects of mood stabilizers, particularly lithium, on the psychological and physiological statuses of patients with bipolar disorder,” they add.
The study was published online in Acta Psychiatrica Scandinavica.
Research gap
Patients with BD have an elevated risk for multiple comorbidities in addition to mood symptoms and neurocognitive dysfunction, with previous research suggesting a mortality rate due to suicide and natural causes that is at least twice as high as that of the general population, the authors write.
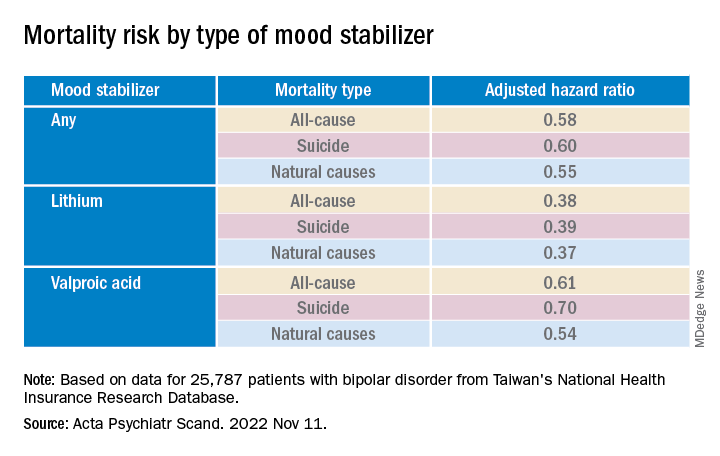
Lithium, in particular, has been associated with decreased risk for all-cause mortality and suicide in patients with BD, but findings regarding anticonvulsant mood stabilizers have been “inconsistent.”
To fill this research gap, the researchers evaluated 16 years of data from Taiwan’s National Health Insurance Research Database, which includes information about more than 23 million residents of Taiwan. The current study, which encompassed 25,787 patients with BD, looked at data from the 5-year period after index hospitalization.
The researchers hypothesized that mood stabilizers “would decrease the risk of mortality” among patients with BD and that “different mood stabilizers would exhibit different associations with mortality, owing to their varying effects on mood symptoms and physiological function.”
Covariates included sex, age, employment status, comorbidities, and concomitant drugs.
Of the patients with BD, 4,000 died within the 5-year period. Suicide and natural causes accounted for 19.0% and 73.7% of these deaths, respectively.
Cardioprotective effects?
The standardized mortality ratios (SMRs) – the ratios of observed mortality in the BD cohort to the number of expected deaths in the general population – were 5.26 for all causes (95% confidence interval, 5.10-5.43), 26.02 for suicide (95% CI, 24.20-27.93), and 4.68 for natural causes (95% CI, 4.51-4.85).
The cumulative mortality rate was higher among men vs. women, a difference that was even larger among patients who had died from any cause or natural causes (crude hazard ratios, .60 and .52, respectively; both Ps < .001).
The suicide risk peaked between ages 45 and 65 years, whereas the risks for all-cause and natural mortality increased with age and were highest in those older than 65 years.
Patients who had died from any cause or from natural causes had a higher risk for physical and psychiatric comorbidities, whereas those who had died by suicide had a higher risk for primarily psychiatric comorbidities.
Mood stabilizers were associated with decreased risks for all-cause mortality and natural mortality, with lithium and valproic acid tied to the lowest risk for all three mortality types (all Ps < .001).
Lamotrigine and carbamazepine were “not significantly associated with any type of mortality,” the authors report.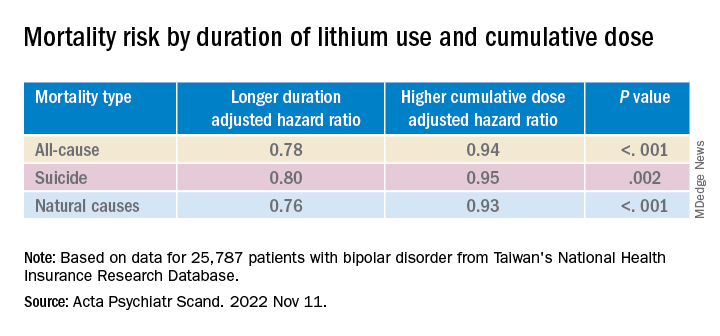
Longer duration of lithium use and a higher cumulative dose of lithium were both associated with lower risks for all three types of mortality (all Ps < .001).
Valproic acid was associated with dose-dependent decreases in all-cause and natural mortality risks.
The findings suggest that mood stabilizers “may improve not only psychosocial outcomes but also the physical health of patients with BD,” the investigators note.
The association between mood stabilizer use and reduced natural mortality risk “may be attributable to the potential benefits of psychiatric care” but may also “have resulted from the direct effects of mood stabilizers on physiological functions,” they add.
Some research suggests lithium treatment may reduce the risk for cardiovascular disease in patients with BD. Mechanistic studies have also pointed to potential cardioprotective effects from valproic acid.
The authors note several study limitations. Focusing on hospitalized patients “may have led to selection bias and overestimated mortality risk.” Moreover, the analyses were “based on the prescription, not the consumption, of mood stabilizers” and information regarding adherence was unavailable.
The absence of a protective mechanism of lamotrigine and carbamazepine may be attributable to “bias toward the relatively poor treatment responses” of these agents, neither of which is used as a first-line medication to treat BD in Taiwan. Patients taking these agents “may not receive medical care at a level equal to those taking lithium, who tend to receive closer surveillance, owing to the narrow therapeutic index.”
First-line treatment
Commenting on the study, Roger S. McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the mood disorders psychopharmacology unit, said that the data “add to a growing confluence of data from observational studies indicating that lithium especially is capable of reducing all-cause mortality, suicide mortality, and natural mortality.”
Dr. McIntyre, chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, who was not involved with the study, agreed with the authors that lamotrigine is “not a very popular drug in Taiwan, therefore we may not have sufficient assay sensitivity to document the effect.”
But lamotrigine “does have recurrence prevention effects in BD, especially bipolar depression, and it would be expected that it would reduce suicide potentially especially in such a large sample.”
The study’s take-home message “is that the extant evidence now indicates that lithium should be a first-line treatment in persons who live with BD who are experiencing suicidal ideation and/or behavior and these data should inform algorithms of treatment selection and sequencing in clinical practice guidelines,” said Dr. McIntyre.
This research was supported by grants from the Ministry of Science and Technology in Taiwan and Taipei City Hospital. The authors declared no relevant financial relationships. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China, and the Milken Institute; and speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe Pharma, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, AbbVie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
Investigators led by Pao-Huan Chen, MD, of the department of psychiatry, Taipei Medical University Hospital, Taiwan, evaluated the association between the use of mood stabilizers and the risks for all-cause mortality, suicide, and natural mortality in more than 25,000 patients with BD and found that those with BD had higher mortality.
However, they also found that patients with BD had a significantly decreased adjusted 5-year risk of dying from any cause, suicide, and natural causes. Lithium was associated with the largest risk reduction compared with the other mood stabilizers.
“The present findings highlight the potential role of mood stabilizers, particularly lithium, in reducing mortality among patients with bipolar disorder,” the authors write.
“The findings of this study could inform future clinical and mechanistic research evaluating the multifaceted effects of mood stabilizers, particularly lithium, on the psychological and physiological statuses of patients with bipolar disorder,” they add.
The study was published online in Acta Psychiatrica Scandinavica.
Research gap
Patients with BD have an elevated risk for multiple comorbidities in addition to mood symptoms and neurocognitive dysfunction, with previous research suggesting a mortality rate due to suicide and natural causes that is at least twice as high as that of the general population, the authors write.
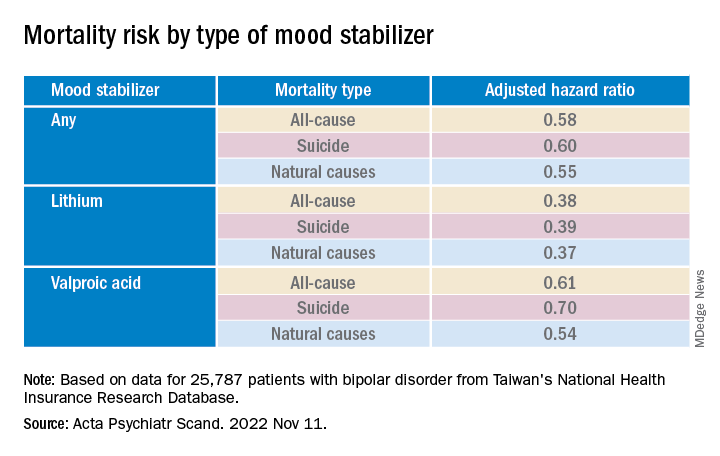
Lithium, in particular, has been associated with decreased risk for all-cause mortality and suicide in patients with BD, but findings regarding anticonvulsant mood stabilizers have been “inconsistent.”
To fill this research gap, the researchers evaluated 16 years of data from Taiwan’s National Health Insurance Research Database, which includes information about more than 23 million residents of Taiwan. The current study, which encompassed 25,787 patients with BD, looked at data from the 5-year period after index hospitalization.
The researchers hypothesized that mood stabilizers “would decrease the risk of mortality” among patients with BD and that “different mood stabilizers would exhibit different associations with mortality, owing to their varying effects on mood symptoms and physiological function.”
Covariates included sex, age, employment status, comorbidities, and concomitant drugs.
Of the patients with BD, 4,000 died within the 5-year period. Suicide and natural causes accounted for 19.0% and 73.7% of these deaths, respectively.
Cardioprotective effects?
The standardized mortality ratios (SMRs) – the ratios of observed mortality in the BD cohort to the number of expected deaths in the general population – were 5.26 for all causes (95% confidence interval, 5.10-5.43), 26.02 for suicide (95% CI, 24.20-27.93), and 4.68 for natural causes (95% CI, 4.51-4.85).
The cumulative mortality rate was higher among men vs. women, a difference that was even larger among patients who had died from any cause or natural causes (crude hazard ratios, .60 and .52, respectively; both Ps < .001).
The suicide risk peaked between ages 45 and 65 years, whereas the risks for all-cause and natural mortality increased with age and were highest in those older than 65 years.
Patients who had died from any cause or from natural causes had a higher risk for physical and psychiatric comorbidities, whereas those who had died by suicide had a higher risk for primarily psychiatric comorbidities.
Mood stabilizers were associated with decreased risks for all-cause mortality and natural mortality, with lithium and valproic acid tied to the lowest risk for all three mortality types (all Ps < .001).
Lamotrigine and carbamazepine were “not significantly associated with any type of mortality,” the authors report.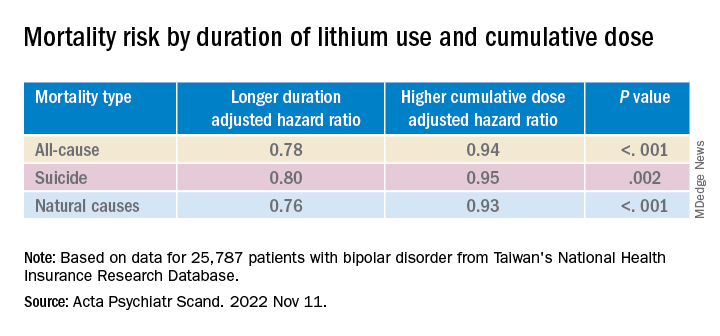
Longer duration of lithium use and a higher cumulative dose of lithium were both associated with lower risks for all three types of mortality (all Ps < .001).
Valproic acid was associated with dose-dependent decreases in all-cause and natural mortality risks.
The findings suggest that mood stabilizers “may improve not only psychosocial outcomes but also the physical health of patients with BD,” the investigators note.
The association between mood stabilizer use and reduced natural mortality risk “may be attributable to the potential benefits of psychiatric care” but may also “have resulted from the direct effects of mood stabilizers on physiological functions,” they add.
Some research suggests lithium treatment may reduce the risk for cardiovascular disease in patients with BD. Mechanistic studies have also pointed to potential cardioprotective effects from valproic acid.
The authors note several study limitations. Focusing on hospitalized patients “may have led to selection bias and overestimated mortality risk.” Moreover, the analyses were “based on the prescription, not the consumption, of mood stabilizers” and information regarding adherence was unavailable.
The absence of a protective mechanism of lamotrigine and carbamazepine may be attributable to “bias toward the relatively poor treatment responses” of these agents, neither of which is used as a first-line medication to treat BD in Taiwan. Patients taking these agents “may not receive medical care at a level equal to those taking lithium, who tend to receive closer surveillance, owing to the narrow therapeutic index.”
First-line treatment
Commenting on the study, Roger S. McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the mood disorders psychopharmacology unit, said that the data “add to a growing confluence of data from observational studies indicating that lithium especially is capable of reducing all-cause mortality, suicide mortality, and natural mortality.”
Dr. McIntyre, chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, who was not involved with the study, agreed with the authors that lamotrigine is “not a very popular drug in Taiwan, therefore we may not have sufficient assay sensitivity to document the effect.”
But lamotrigine “does have recurrence prevention effects in BD, especially bipolar depression, and it would be expected that it would reduce suicide potentially especially in such a large sample.”
The study’s take-home message “is that the extant evidence now indicates that lithium should be a first-line treatment in persons who live with BD who are experiencing suicidal ideation and/or behavior and these data should inform algorithms of treatment selection and sequencing in clinical practice guidelines,” said Dr. McIntyre.
This research was supported by grants from the Ministry of Science and Technology in Taiwan and Taipei City Hospital. The authors declared no relevant financial relationships. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China, and the Milken Institute; and speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe Pharma, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, AbbVie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
FROM ACTA PSYCHIATRICA SCANDINAVICA
Clinical factors drive hospitalization after self-harm
Clinicians who assess suicidal patients in the emergency department setting face the challenge of whether to admit the patient to inpatient or outpatient care, and data on predictors of compulsory admission are limited, wrote Laurent Michaud, MD, of the University of Lausanne, Switzerland, and colleagues.
To better identify predictors of hospitalization after self-harm, the researchers reviewed data from 1,832 patients aged 18 years and older admitted to four emergency departments in Switzerland between December 2016 and November 2019 .
Self-harm (SH) was defined in this study as “all nonfatal intentional acts of self-poisoning or self-injury, irrespective of degree of suicidal intent or other types of motivation,” the researchers noted. The study included 2,142 episodes of self-harm.
The researchers conducted two analyses. They compared episodes followed by any hospitalization and those with outpatient follow-up (1,083 episodes vs. 1,059 episodes) and episodes followed by compulsory hospitalization (357 episodes) with all other episodes followed by either outpatient care or voluntary hospitalization (1,785 episodes).
Overall, women were significantly more likely to be referred to outpatient follow-up compared with men (61.8% vs. 38.1%), and hospitalized patients were significantly older than outpatients (mean age of 41 years vs. 36 years, P < .001 for both).
“Not surprisingly, major psychopathological conditions such as depression, mania, dementia, and schizophrenia were predictive of hospitalization,” the researchers noted.
Other sociodemographic factors associated with hospitalization included living alone, no children, problematic socioeconomic status, and unemployment. Clinical factors associated with hospitalization included physical pain, more lethal suicide attempt method, and clear intent to die.
In a multivariate analysis, independent predictors of any hospitalization included male gender, older age, assessment in the Neuchatel location vs. Lausanne, depression vs. personality disorders, substance use, or anxiety disorder, difficult socioeconomic status, a clear vs. unclear intent to die, and a serious suicide attempt vs. less serious.
Differences in hospitalization based on hospital setting was a striking finding, the researchers wrote in their discussion. These differences may be largely explained by the organization of local mental health services and specific institutional cultures; the workload of staff and availability of beds also may have played a role in decisions to hospitalize, they said.
The findings were limited by several factors including the lack of data on the realization level of a self-harm episode and significant events such as a breakup, the researchers explained. Other limitations included missing data, multiple analyses that could increase the risk of false positives, the reliance on clinical diagnosis rather than formal instruments, and the cross-sectional study design, they said.
However, the results have clinical implications, as the clinical factors identified could be used to target subgroups of suicidal populations and refine treatment strategies, they concluded.
The study was supported by institutional funding and the Swiss Federal Office of Public Health. The researchers had no financial conflicts to disclose.
Clinicians who assess suicidal patients in the emergency department setting face the challenge of whether to admit the patient to inpatient or outpatient care, and data on predictors of compulsory admission are limited, wrote Laurent Michaud, MD, of the University of Lausanne, Switzerland, and colleagues.
To better identify predictors of hospitalization after self-harm, the researchers reviewed data from 1,832 patients aged 18 years and older admitted to four emergency departments in Switzerland between December 2016 and November 2019 .
Self-harm (SH) was defined in this study as “all nonfatal intentional acts of self-poisoning or self-injury, irrespective of degree of suicidal intent or other types of motivation,” the researchers noted. The study included 2,142 episodes of self-harm.
The researchers conducted two analyses. They compared episodes followed by any hospitalization and those with outpatient follow-up (1,083 episodes vs. 1,059 episodes) and episodes followed by compulsory hospitalization (357 episodes) with all other episodes followed by either outpatient care or voluntary hospitalization (1,785 episodes).
Overall, women were significantly more likely to be referred to outpatient follow-up compared with men (61.8% vs. 38.1%), and hospitalized patients were significantly older than outpatients (mean age of 41 years vs. 36 years, P < .001 for both).
“Not surprisingly, major psychopathological conditions such as depression, mania, dementia, and schizophrenia were predictive of hospitalization,” the researchers noted.
Other sociodemographic factors associated with hospitalization included living alone, no children, problematic socioeconomic status, and unemployment. Clinical factors associated with hospitalization included physical pain, more lethal suicide attempt method, and clear intent to die.
In a multivariate analysis, independent predictors of any hospitalization included male gender, older age, assessment in the Neuchatel location vs. Lausanne, depression vs. personality disorders, substance use, or anxiety disorder, difficult socioeconomic status, a clear vs. unclear intent to die, and a serious suicide attempt vs. less serious.
Differences in hospitalization based on hospital setting was a striking finding, the researchers wrote in their discussion. These differences may be largely explained by the organization of local mental health services and specific institutional cultures; the workload of staff and availability of beds also may have played a role in decisions to hospitalize, they said.
The findings were limited by several factors including the lack of data on the realization level of a self-harm episode and significant events such as a breakup, the researchers explained. Other limitations included missing data, multiple analyses that could increase the risk of false positives, the reliance on clinical diagnosis rather than formal instruments, and the cross-sectional study design, they said.
However, the results have clinical implications, as the clinical factors identified could be used to target subgroups of suicidal populations and refine treatment strategies, they concluded.
The study was supported by institutional funding and the Swiss Federal Office of Public Health. The researchers had no financial conflicts to disclose.
Clinicians who assess suicidal patients in the emergency department setting face the challenge of whether to admit the patient to inpatient or outpatient care, and data on predictors of compulsory admission are limited, wrote Laurent Michaud, MD, of the University of Lausanne, Switzerland, and colleagues.
To better identify predictors of hospitalization after self-harm, the researchers reviewed data from 1,832 patients aged 18 years and older admitted to four emergency departments in Switzerland between December 2016 and November 2019 .
Self-harm (SH) was defined in this study as “all nonfatal intentional acts of self-poisoning or self-injury, irrespective of degree of suicidal intent or other types of motivation,” the researchers noted. The study included 2,142 episodes of self-harm.
The researchers conducted two analyses. They compared episodes followed by any hospitalization and those with outpatient follow-up (1,083 episodes vs. 1,059 episodes) and episodes followed by compulsory hospitalization (357 episodes) with all other episodes followed by either outpatient care or voluntary hospitalization (1,785 episodes).
Overall, women were significantly more likely to be referred to outpatient follow-up compared with men (61.8% vs. 38.1%), and hospitalized patients were significantly older than outpatients (mean age of 41 years vs. 36 years, P < .001 for both).
“Not surprisingly, major psychopathological conditions such as depression, mania, dementia, and schizophrenia were predictive of hospitalization,” the researchers noted.
Other sociodemographic factors associated with hospitalization included living alone, no children, problematic socioeconomic status, and unemployment. Clinical factors associated with hospitalization included physical pain, more lethal suicide attempt method, and clear intent to die.
In a multivariate analysis, independent predictors of any hospitalization included male gender, older age, assessment in the Neuchatel location vs. Lausanne, depression vs. personality disorders, substance use, or anxiety disorder, difficult socioeconomic status, a clear vs. unclear intent to die, and a serious suicide attempt vs. less serious.
Differences in hospitalization based on hospital setting was a striking finding, the researchers wrote in their discussion. These differences may be largely explained by the organization of local mental health services and specific institutional cultures; the workload of staff and availability of beds also may have played a role in decisions to hospitalize, they said.
The findings were limited by several factors including the lack of data on the realization level of a self-harm episode and significant events such as a breakup, the researchers explained. Other limitations included missing data, multiple analyses that could increase the risk of false positives, the reliance on clinical diagnosis rather than formal instruments, and the cross-sectional study design, they said.
However, the results have clinical implications, as the clinical factors identified could be used to target subgroups of suicidal populations and refine treatment strategies, they concluded.
The study was supported by institutional funding and the Swiss Federal Office of Public Health. The researchers had no financial conflicts to disclose.
FROM PSYCHIATRIC RESEARCH
Strong two-way link between epilepsy and depression
, with implications for diagnosis and patient care. The findings “strongly support previous observations of a bidirectional association between these two brain disorders,” said Eva Bølling-Ladegaard, MD, a PhD student, department of clinical medicine (Neurology), Aarhus (Denmark) University.
“We add to the existing evidence in temporal range, showing that the increased risks of depression following epilepsy, and vice versa, are sustained over a much more extended time period than previously shown; that is, 20 years on both sides of receiving a diagnosis of the index disorder,” Ms. Bølling-Ladegaard said.
The study was published online in Neurology.
Epilepsy then depression
The researchers examined the magnitude and long-term temporal association between epilepsy and depression. They compared the risk of the two brain disorders following another chronic disorder (asthma) in a nationwide, register-based, matched cohort study.
In a population of more than 8.7 million people, they identified 139,014 persons with epilepsy (54% males; median age at diagnosis, 43 years), 219,990 with depression (37% males; median age at diagnosis, 43 years), and 358,821 with asthma (49% males; median age at diagnosis, 29 years).
The rate of developing depression was increased nearly twofold among people with epilepsy compared with the matched population who did not have epilepsy (adjusted hazard ratio, 1.88; 95% confidence interval, 1.82-1.95).
The rate of depression was highest during the first months and years after epilepsy diagnosis. It declined over time, yet remained significantly elevated throughout the 20+ years of observation.
The cumulative incidence of depression at 5 and 35 years’ follow-up in the epilepsy cohort was 1.37% and 6.05%, respectively, compared with 0.59% and 3.92% in the reference population.
The highest rate of depression after epilepsy was among individuals aged 40-59 years, and the lowest was among those aged 0-19 years at first epilepsy diagnosis.
Depression then epilepsy
The rate of developing epilepsy was increased more than twofold among patients with incident depression compared with the matched population who were without depression (aHR, 2.35; 95% CI, 2.25-2.44).
As in the opposite analysis, the rate of epilepsy was highest during the first months and years after depression diagnosis and declined over time.
The cumulative incidence of epilepsy at 5 and 35 years after depression diagnosis was 1.10% and 4.19%, respectively, compared with 0.32% and 2.06% in the reference population.
The rate of epilepsy was highest among those aged 0-19 years at time of first depression diagnosis and was lowest among those aged 80+ at first depression diagnosis.
For comparison, after asthma diagnosis, rates of depression and epilepsy were increased 1.63-fold (95% CI, 1.59-1.67) and 1.48-fold (95% CI, 1.44-1.53), respectively, compared with matched individuals without asthma.
Using admission with seizures as a proxy for treatment failure, the researchers observed an increased risk of treatment failure among people with epilepsy who were diagnosed with depression.
“Our results support previous findings indicating worse seizure outcomes in people with epilepsy and coexisting depression,” said Ms. Bølling-Ladegaard.
“Increased clinical awareness of the association between epilepsy and depression is therefore needed in order to increase the proportion of patients that receive appropriate treatment and improve outcomes for these patient groups,” she said.
Clinical implications
Reached for comment, Zulfi Haneef, MBBS, MD, associate professor of neurology, Baylor College of Medicine, Houston, noted that the link between epilepsy and depression is “well-known.”
“However, typically one thinks of epilepsy as leading to depression, not vice versa. Here they show the risk of epilepsy following depression to be high (highest of the risks given), which is thought provoking. However, association does not imply causation,” Dr. Haneef said.
“Prima facie, there is no biological rationale for depression to lead to epilepsy,” he said. He noted that some antidepressants can reduce the seizure threshold.
The findings do have implications for care, he said.
“For neurologists, this is another study that exhorts them to screen for depression and treat adequately in all patients with epilepsy,” Dr. Haneef said.
“For psychiatrists, this study may give guidance to watch more carefully for seizures in patients with depression, especially when using antidepressant medications that induce seizures.
“For the general public with either epilepsy or depression, it would help them be aware about this bidirectional association,” Dr. Haneef said.
The study was funded by the Lundbeck Foundation, the Danish Epilepsy Association, and the Novo Nordisk Foundation. Ms. Bølling-Ladegaard and Dr. Haneef have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, with implications for diagnosis and patient care. The findings “strongly support previous observations of a bidirectional association between these two brain disorders,” said Eva Bølling-Ladegaard, MD, a PhD student, department of clinical medicine (Neurology), Aarhus (Denmark) University.
“We add to the existing evidence in temporal range, showing that the increased risks of depression following epilepsy, and vice versa, are sustained over a much more extended time period than previously shown; that is, 20 years on both sides of receiving a diagnosis of the index disorder,” Ms. Bølling-Ladegaard said.
The study was published online in Neurology.
Epilepsy then depression
The researchers examined the magnitude and long-term temporal association between epilepsy and depression. They compared the risk of the two brain disorders following another chronic disorder (asthma) in a nationwide, register-based, matched cohort study.
In a population of more than 8.7 million people, they identified 139,014 persons with epilepsy (54% males; median age at diagnosis, 43 years), 219,990 with depression (37% males; median age at diagnosis, 43 years), and 358,821 with asthma (49% males; median age at diagnosis, 29 years).
The rate of developing depression was increased nearly twofold among people with epilepsy compared with the matched population who did not have epilepsy (adjusted hazard ratio, 1.88; 95% confidence interval, 1.82-1.95).
The rate of depression was highest during the first months and years after epilepsy diagnosis. It declined over time, yet remained significantly elevated throughout the 20+ years of observation.
The cumulative incidence of depression at 5 and 35 years’ follow-up in the epilepsy cohort was 1.37% and 6.05%, respectively, compared with 0.59% and 3.92% in the reference population.
The highest rate of depression after epilepsy was among individuals aged 40-59 years, and the lowest was among those aged 0-19 years at first epilepsy diagnosis.
Depression then epilepsy
The rate of developing epilepsy was increased more than twofold among patients with incident depression compared with the matched population who were without depression (aHR, 2.35; 95% CI, 2.25-2.44).
As in the opposite analysis, the rate of epilepsy was highest during the first months and years after depression diagnosis and declined over time.
The cumulative incidence of epilepsy at 5 and 35 years after depression diagnosis was 1.10% and 4.19%, respectively, compared with 0.32% and 2.06% in the reference population.
The rate of epilepsy was highest among those aged 0-19 years at time of first depression diagnosis and was lowest among those aged 80+ at first depression diagnosis.
For comparison, after asthma diagnosis, rates of depression and epilepsy were increased 1.63-fold (95% CI, 1.59-1.67) and 1.48-fold (95% CI, 1.44-1.53), respectively, compared with matched individuals without asthma.
Using admission with seizures as a proxy for treatment failure, the researchers observed an increased risk of treatment failure among people with epilepsy who were diagnosed with depression.
“Our results support previous findings indicating worse seizure outcomes in people with epilepsy and coexisting depression,” said Ms. Bølling-Ladegaard.
“Increased clinical awareness of the association between epilepsy and depression is therefore needed in order to increase the proportion of patients that receive appropriate treatment and improve outcomes for these patient groups,” she said.
Clinical implications
Reached for comment, Zulfi Haneef, MBBS, MD, associate professor of neurology, Baylor College of Medicine, Houston, noted that the link between epilepsy and depression is “well-known.”
“However, typically one thinks of epilepsy as leading to depression, not vice versa. Here they show the risk of epilepsy following depression to be high (highest of the risks given), which is thought provoking. However, association does not imply causation,” Dr. Haneef said.
“Prima facie, there is no biological rationale for depression to lead to epilepsy,” he said. He noted that some antidepressants can reduce the seizure threshold.
The findings do have implications for care, he said.
“For neurologists, this is another study that exhorts them to screen for depression and treat adequately in all patients with epilepsy,” Dr. Haneef said.
“For psychiatrists, this study may give guidance to watch more carefully for seizures in patients with depression, especially when using antidepressant medications that induce seizures.
“For the general public with either epilepsy or depression, it would help them be aware about this bidirectional association,” Dr. Haneef said.
The study was funded by the Lundbeck Foundation, the Danish Epilepsy Association, and the Novo Nordisk Foundation. Ms. Bølling-Ladegaard and Dr. Haneef have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, with implications for diagnosis and patient care. The findings “strongly support previous observations of a bidirectional association between these two brain disorders,” said Eva Bølling-Ladegaard, MD, a PhD student, department of clinical medicine (Neurology), Aarhus (Denmark) University.
“We add to the existing evidence in temporal range, showing that the increased risks of depression following epilepsy, and vice versa, are sustained over a much more extended time period than previously shown; that is, 20 years on both sides of receiving a diagnosis of the index disorder,” Ms. Bølling-Ladegaard said.
The study was published online in Neurology.
Epilepsy then depression
The researchers examined the magnitude and long-term temporal association between epilepsy and depression. They compared the risk of the two brain disorders following another chronic disorder (asthma) in a nationwide, register-based, matched cohort study.
In a population of more than 8.7 million people, they identified 139,014 persons with epilepsy (54% males; median age at diagnosis, 43 years), 219,990 with depression (37% males; median age at diagnosis, 43 years), and 358,821 with asthma (49% males; median age at diagnosis, 29 years).
The rate of developing depression was increased nearly twofold among people with epilepsy compared with the matched population who did not have epilepsy (adjusted hazard ratio, 1.88; 95% confidence interval, 1.82-1.95).
The rate of depression was highest during the first months and years after epilepsy diagnosis. It declined over time, yet remained significantly elevated throughout the 20+ years of observation.
The cumulative incidence of depression at 5 and 35 years’ follow-up in the epilepsy cohort was 1.37% and 6.05%, respectively, compared with 0.59% and 3.92% in the reference population.
The highest rate of depression after epilepsy was among individuals aged 40-59 years, and the lowest was among those aged 0-19 years at first epilepsy diagnosis.
Depression then epilepsy
The rate of developing epilepsy was increased more than twofold among patients with incident depression compared with the matched population who were without depression (aHR, 2.35; 95% CI, 2.25-2.44).
As in the opposite analysis, the rate of epilepsy was highest during the first months and years after depression diagnosis and declined over time.
The cumulative incidence of epilepsy at 5 and 35 years after depression diagnosis was 1.10% and 4.19%, respectively, compared with 0.32% and 2.06% in the reference population.
The rate of epilepsy was highest among those aged 0-19 years at time of first depression diagnosis and was lowest among those aged 80+ at first depression diagnosis.
For comparison, after asthma diagnosis, rates of depression and epilepsy were increased 1.63-fold (95% CI, 1.59-1.67) and 1.48-fold (95% CI, 1.44-1.53), respectively, compared with matched individuals without asthma.
Using admission with seizures as a proxy for treatment failure, the researchers observed an increased risk of treatment failure among people with epilepsy who were diagnosed with depression.
“Our results support previous findings indicating worse seizure outcomes in people with epilepsy and coexisting depression,” said Ms. Bølling-Ladegaard.
“Increased clinical awareness of the association between epilepsy and depression is therefore needed in order to increase the proportion of patients that receive appropriate treatment and improve outcomes for these patient groups,” she said.
Clinical implications
Reached for comment, Zulfi Haneef, MBBS, MD, associate professor of neurology, Baylor College of Medicine, Houston, noted that the link between epilepsy and depression is “well-known.”
“However, typically one thinks of epilepsy as leading to depression, not vice versa. Here they show the risk of epilepsy following depression to be high (highest of the risks given), which is thought provoking. However, association does not imply causation,” Dr. Haneef said.
“Prima facie, there is no biological rationale for depression to lead to epilepsy,” he said. He noted that some antidepressants can reduce the seizure threshold.
The findings do have implications for care, he said.
“For neurologists, this is another study that exhorts them to screen for depression and treat adequately in all patients with epilepsy,” Dr. Haneef said.
“For psychiatrists, this study may give guidance to watch more carefully for seizures in patients with depression, especially when using antidepressant medications that induce seizures.
“For the general public with either epilepsy or depression, it would help them be aware about this bidirectional association,” Dr. Haneef said.
The study was funded by the Lundbeck Foundation, the Danish Epilepsy Association, and the Novo Nordisk Foundation. Ms. Bølling-Ladegaard and Dr. Haneef have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY






