User login
Treatment-resistant depression ups risk for comorbidities, death
In a population study of more than 145,000 patients, participants with TRD used outpatient resources and missed work at twice the rate as patients with treatment-responsive depression. They also had a threefold higher number of days spent in hospital.
Patients with TRD also had a 23% higher risk of dying during the time they were observed, compared with their matched counterparts with non-TRD depression, and their self-harm rates were twice as high.
In addition, it took an average of 1.5 years for patients with TRD to undergo two unsuccessful treatment attempts and reach their third treatment trial, which is several months longer than is recommended for assessing the efficacy of a treatment for depression.
“It seemed like ineffective treatments were allowed to continue for longer than should be needed and what is recommended in current guidelines,” lead investigator Johan Lundberg, MD, PhD, adjunct professor of psychiatry in the department of clinical neuroscience and head of the mood disorder section at the Northern Stockholm Psychiatry Clinic, told this news organization.
“If this is true, patients would most likely benefit from a more frequent evaluation of treatment effect and, when needed, optimization of ineffective treatments,” Dr. Lundberg said.
The findings were published online in JAMA Psychiatry.
More anxiety, sleep disorders, substance use
Using data from the Region Stockholm’s administrative health care database and the Swedish social insurance agency, the investigators identified nearly 160,000 unipolar major depressive disorder (MDD) episodes in 145,577 patients who sought treatment between January 2012 and December 2017.
Of those episodes, 12,800 fulfilled criteria for TRD, which meant there were three or more treatment trials with antidepressants, add-on medication (aripiprazole, lithium, olanzapine, quetiapine, and/or risperidone), electroshock therapy, or repetitive transcranial magnetic stimulation.
Each new treatment had to be initiated within the MDD episode more than 28 days after previous treatment initiation.
Investigators matched each TRD episode with up to five non-TRD episodes and found that patients with TRD were more likely to have comorbid psychiatric conditions than were their non-TRD counterparts.
This included anxiety (60% vs. 44%, respectively), sleep disorders (28% vs. 19%), substance use (15% vs. 11%) or alcohol use (10% vs. 7%) disorders, and personality disorders (6% vs. 3%). Rates of intentional self-harm were also higher in the TRD group (5% vs. 2%).
Perhaps in part because of the comorbid problems, patients with TRD had a more than 50% higher mean number of outpatient physician visits 1 year before and after the index date, defined as the date of the initiation of the third treatment trial.
The most important predictor of TRD depression was the severity of depression at diagnosis on the self-rated Montgomery Åsberg Depression Rating Scale, the researchers report.
Not generalizable?
Patients with TRD also had three times the number of inpatient bed days as did those with depression that responded to treatment (mean, 3.9 days vs. 1.3 days, respectively) and significantly more lost workdays (132.3 days vs. 58.7 days).
Most notably, patients with TRD episodes had a 23% higher risk of dying during the time they were observed than did their non-TRD counterparts.
“This finding in itself could be a reason to focus on how to avoid putting a patient on the TRD path. This could be done through prospective studies comparing different treatment options and their risk of leading to TRD,” Dr. Lundberg said.
Interestingly, he noted that the study results may not be generalizable to other populations, such as the United States.
“The biggest difference between Stockholm and the U.S. may not be the demographics, but the access to health care,” Dr. Lundberg said.
“In Stockholm, there is a universal access health care system, meaning that these results are what you can expect if you are able to get care. In the U.S., this is not the case, meaning that people outside the health care system may fare worse than what our study suggests,” he added.
Quality over quantity
In a comment, Sidney Zisook, MD, distinguished professor of psychiatry at the University of California, San Diego, said that the findings “highlight the need for our field to develop better-tolerated, more effective, and sustainable treatments for major depressive disorder and for better education of clinicians so they can employ up-to-date, evidence-based treatments and integrate sound clinical guidelines into clinical practice.”
Dr. Zisook has independently researched TRD but was not involved with the current study.
He noted that it was “striking how long patients remained on the same antidepressant, apparently despite suboptimal outcomes, without taking next steps.”
However, Dr. Zisook expressed concern that the diagnosis of TRD in the study was solely on the basis of the number of treatment trials for an episode.
“Somebody might have had three different antidepressant trials because they had had three episodes with interepisode periods of recovery followed by recurrent episodes. That would not be considered treatment-resistant depression,” he said.
Dr. Zisook also noted that patients might be given a new antidepressant for reasons other than treatment resistance. “For example, they lost an initial good response – this used to be called Prozac poop out, were nonadherent, or had troublesome side effects,” he said.
“We usually define treatment-resistant depression not only on the basis of number of trials but also the quality of the trial, taking both dose and duration into account,” Dr. Zisook added.
The study was funded by Region Stockholm. Dr. Zisook reports receiving research funding from COMPASS Pathways.
A version of this article first appeared on Medscape.com.
In a population study of more than 145,000 patients, participants with TRD used outpatient resources and missed work at twice the rate as patients with treatment-responsive depression. They also had a threefold higher number of days spent in hospital.
Patients with TRD also had a 23% higher risk of dying during the time they were observed, compared with their matched counterparts with non-TRD depression, and their self-harm rates were twice as high.
In addition, it took an average of 1.5 years for patients with TRD to undergo two unsuccessful treatment attempts and reach their third treatment trial, which is several months longer than is recommended for assessing the efficacy of a treatment for depression.
“It seemed like ineffective treatments were allowed to continue for longer than should be needed and what is recommended in current guidelines,” lead investigator Johan Lundberg, MD, PhD, adjunct professor of psychiatry in the department of clinical neuroscience and head of the mood disorder section at the Northern Stockholm Psychiatry Clinic, told this news organization.
“If this is true, patients would most likely benefit from a more frequent evaluation of treatment effect and, when needed, optimization of ineffective treatments,” Dr. Lundberg said.
The findings were published online in JAMA Psychiatry.
More anxiety, sleep disorders, substance use
Using data from the Region Stockholm’s administrative health care database and the Swedish social insurance agency, the investigators identified nearly 160,000 unipolar major depressive disorder (MDD) episodes in 145,577 patients who sought treatment between January 2012 and December 2017.
Of those episodes, 12,800 fulfilled criteria for TRD, which meant there were three or more treatment trials with antidepressants, add-on medication (aripiprazole, lithium, olanzapine, quetiapine, and/or risperidone), electroshock therapy, or repetitive transcranial magnetic stimulation.
Each new treatment had to be initiated within the MDD episode more than 28 days after previous treatment initiation.
Investigators matched each TRD episode with up to five non-TRD episodes and found that patients with TRD were more likely to have comorbid psychiatric conditions than were their non-TRD counterparts.
This included anxiety (60% vs. 44%, respectively), sleep disorders (28% vs. 19%), substance use (15% vs. 11%) or alcohol use (10% vs. 7%) disorders, and personality disorders (6% vs. 3%). Rates of intentional self-harm were also higher in the TRD group (5% vs. 2%).
Perhaps in part because of the comorbid problems, patients with TRD had a more than 50% higher mean number of outpatient physician visits 1 year before and after the index date, defined as the date of the initiation of the third treatment trial.
The most important predictor of TRD depression was the severity of depression at diagnosis on the self-rated Montgomery Åsberg Depression Rating Scale, the researchers report.
Not generalizable?
Patients with TRD also had three times the number of inpatient bed days as did those with depression that responded to treatment (mean, 3.9 days vs. 1.3 days, respectively) and significantly more lost workdays (132.3 days vs. 58.7 days).
Most notably, patients with TRD episodes had a 23% higher risk of dying during the time they were observed than did their non-TRD counterparts.
“This finding in itself could be a reason to focus on how to avoid putting a patient on the TRD path. This could be done through prospective studies comparing different treatment options and their risk of leading to TRD,” Dr. Lundberg said.
Interestingly, he noted that the study results may not be generalizable to other populations, such as the United States.
“The biggest difference between Stockholm and the U.S. may not be the demographics, but the access to health care,” Dr. Lundberg said.
“In Stockholm, there is a universal access health care system, meaning that these results are what you can expect if you are able to get care. In the U.S., this is not the case, meaning that people outside the health care system may fare worse than what our study suggests,” he added.
Quality over quantity
In a comment, Sidney Zisook, MD, distinguished professor of psychiatry at the University of California, San Diego, said that the findings “highlight the need for our field to develop better-tolerated, more effective, and sustainable treatments for major depressive disorder and for better education of clinicians so they can employ up-to-date, evidence-based treatments and integrate sound clinical guidelines into clinical practice.”
Dr. Zisook has independently researched TRD but was not involved with the current study.
He noted that it was “striking how long patients remained on the same antidepressant, apparently despite suboptimal outcomes, without taking next steps.”
However, Dr. Zisook expressed concern that the diagnosis of TRD in the study was solely on the basis of the number of treatment trials for an episode.
“Somebody might have had three different antidepressant trials because they had had three episodes with interepisode periods of recovery followed by recurrent episodes. That would not be considered treatment-resistant depression,” he said.
Dr. Zisook also noted that patients might be given a new antidepressant for reasons other than treatment resistance. “For example, they lost an initial good response – this used to be called Prozac poop out, were nonadherent, or had troublesome side effects,” he said.
“We usually define treatment-resistant depression not only on the basis of number of trials but also the quality of the trial, taking both dose and duration into account,” Dr. Zisook added.
The study was funded by Region Stockholm. Dr. Zisook reports receiving research funding from COMPASS Pathways.
A version of this article first appeared on Medscape.com.
In a population study of more than 145,000 patients, participants with TRD used outpatient resources and missed work at twice the rate as patients with treatment-responsive depression. They also had a threefold higher number of days spent in hospital.
Patients with TRD also had a 23% higher risk of dying during the time they were observed, compared with their matched counterparts with non-TRD depression, and their self-harm rates were twice as high.
In addition, it took an average of 1.5 years for patients with TRD to undergo two unsuccessful treatment attempts and reach their third treatment trial, which is several months longer than is recommended for assessing the efficacy of a treatment for depression.
“It seemed like ineffective treatments were allowed to continue for longer than should be needed and what is recommended in current guidelines,” lead investigator Johan Lundberg, MD, PhD, adjunct professor of psychiatry in the department of clinical neuroscience and head of the mood disorder section at the Northern Stockholm Psychiatry Clinic, told this news organization.
“If this is true, patients would most likely benefit from a more frequent evaluation of treatment effect and, when needed, optimization of ineffective treatments,” Dr. Lundberg said.
The findings were published online in JAMA Psychiatry.
More anxiety, sleep disorders, substance use
Using data from the Region Stockholm’s administrative health care database and the Swedish social insurance agency, the investigators identified nearly 160,000 unipolar major depressive disorder (MDD) episodes in 145,577 patients who sought treatment between January 2012 and December 2017.
Of those episodes, 12,800 fulfilled criteria for TRD, which meant there were three or more treatment trials with antidepressants, add-on medication (aripiprazole, lithium, olanzapine, quetiapine, and/or risperidone), electroshock therapy, or repetitive transcranial magnetic stimulation.
Each new treatment had to be initiated within the MDD episode more than 28 days after previous treatment initiation.
Investigators matched each TRD episode with up to five non-TRD episodes and found that patients with TRD were more likely to have comorbid psychiatric conditions than were their non-TRD counterparts.
This included anxiety (60% vs. 44%, respectively), sleep disorders (28% vs. 19%), substance use (15% vs. 11%) or alcohol use (10% vs. 7%) disorders, and personality disorders (6% vs. 3%). Rates of intentional self-harm were also higher in the TRD group (5% vs. 2%).
Perhaps in part because of the comorbid problems, patients with TRD had a more than 50% higher mean number of outpatient physician visits 1 year before and after the index date, defined as the date of the initiation of the third treatment trial.
The most important predictor of TRD depression was the severity of depression at diagnosis on the self-rated Montgomery Åsberg Depression Rating Scale, the researchers report.
Not generalizable?
Patients with TRD also had three times the number of inpatient bed days as did those with depression that responded to treatment (mean, 3.9 days vs. 1.3 days, respectively) and significantly more lost workdays (132.3 days vs. 58.7 days).
Most notably, patients with TRD episodes had a 23% higher risk of dying during the time they were observed than did their non-TRD counterparts.
“This finding in itself could be a reason to focus on how to avoid putting a patient on the TRD path. This could be done through prospective studies comparing different treatment options and their risk of leading to TRD,” Dr. Lundberg said.
Interestingly, he noted that the study results may not be generalizable to other populations, such as the United States.
“The biggest difference between Stockholm and the U.S. may not be the demographics, but the access to health care,” Dr. Lundberg said.
“In Stockholm, there is a universal access health care system, meaning that these results are what you can expect if you are able to get care. In the U.S., this is not the case, meaning that people outside the health care system may fare worse than what our study suggests,” he added.
Quality over quantity
In a comment, Sidney Zisook, MD, distinguished professor of psychiatry at the University of California, San Diego, said that the findings “highlight the need for our field to develop better-tolerated, more effective, and sustainable treatments for major depressive disorder and for better education of clinicians so they can employ up-to-date, evidence-based treatments and integrate sound clinical guidelines into clinical practice.”
Dr. Zisook has independently researched TRD but was not involved with the current study.
He noted that it was “striking how long patients remained on the same antidepressant, apparently despite suboptimal outcomes, without taking next steps.”
However, Dr. Zisook expressed concern that the diagnosis of TRD in the study was solely on the basis of the number of treatment trials for an episode.
“Somebody might have had three different antidepressant trials because they had had three episodes with interepisode periods of recovery followed by recurrent episodes. That would not be considered treatment-resistant depression,” he said.
Dr. Zisook also noted that patients might be given a new antidepressant for reasons other than treatment resistance. “For example, they lost an initial good response – this used to be called Prozac poop out, were nonadherent, or had troublesome side effects,” he said.
“We usually define treatment-resistant depression not only on the basis of number of trials but also the quality of the trial, taking both dose and duration into account,” Dr. Zisook added.
The study was funded by Region Stockholm. Dr. Zisook reports receiving research funding from COMPASS Pathways.
A version of this article first appeared on Medscape.com.
FROM PSYCHIATRY
Physical activity eases depressive symptoms in young people
Intervening with physical activity appears to mitigate depressive symptoms in children and adolescents, a systematic review and meta-analysis of almost 2,500 participants found. Greater reductions were observed for children older than 13 years and those having a diagnosis of mental illness and/or depression versus other conditions, according to Hong Kong researchers reporting in JAMA Pediatrics.
“There is an urgent need to explore novel treatment approaches that can be safely, feasibly, and widely implemented in the daily routine of depressed children and adolescents,” said study coauthor Parco M. Siu, PhD, exercise physiologist and associate professor in the school of public health at the University of Hong Kong, in an interview. “Given the observed association with significant reductions in symptoms, clinical practice guidelines should consider the role of physical activity for improving the mental health of young populations.”
Dr. Siu further noted that while current guidelines suggest psychotherapy and/or pharmacotherapy for children with this common mood disorder, adherence to these can be problematic, and surveys show that nearly 80% do not receive appropriate disorder-specific medical care.
The analysis
Dr. Siu’s team drew on 21 international studies, including 17 randomized controlled trials, published from 1987 to 2021 and comprising 2,444 young participants, mean age 14, 53% girls. Eligible studies compared the effect of exercise on depression versus a control condition.
In 12 studies, participants had a somatic or psychiatric disorder such as obesity, diabetes, depression, and attention-deficit/hyperactivity disorder. The mean duration of the prescribed physical activity program was 22 weeks (6-144 weeks), while the frequency of weekly sessions ranged from 2 to 5 days, with 3 days per week most common and mean duration of 50 minutes (30-120 minutes). Regimens ranged from aerobic exercise on fitness equipment such as treadmills, stationary bikes, and ellipticals, to running, swimming, dancing, sports, and exercise games.
In meta-analysis of postintervention differences, physical activity was associated with a significant reduction in the pooled estimate of depressive symptoms compared with the control condition (Hedges g statistic [effect size] = −0.29; 95% confidence interval, −0.47 to −0.10; P = .004). This was driven by moderate to large effect sizes in adolescents (g = −0.44) and children with diagnosed depression (g = −0.75).The differences, however, were not detectable after a mean follow-up of 21 weeks, possibly owing to the limited number of studies with follow-up outcomes, the authors conceded.
Despite the strong association, the mechanisms underlying the antidepressant properties of physical activity remain uncertain. “Potential pathways include the activation of the endocannabinoid system to stimulate the release of endorphins, an increase in the bioavailability of brain neurotransmitters such as serotonin, dopamine, and noradrenaline, which are reduced in depression, as well as long-term changes in brain plasticity,” Dr. Siu said.
In addition, psychosocial and behavioral hypotheses suggest that physical activity can lead to improvements in self-perception, social interactions, and self-confidence. However, he added, depressive phenomenology is multifaceted and individual, so isolating the effects that physical activity have on specific symptoms may not be possible.
Physical activity appears to enhance the treatment of cognitive and affective symptoms in depression, Dr. Siu continued, and a combination of physical activity and pharmacotherapy may also reduce relapse risk, improve adherence to antidepressants, and promote better management of adverse effects, compared with pharmacotherapy alone. “More research is warranted to explain if and how these mechanisms moderate the effect of physical activity, and whether these changes are also present in younger populations,” he said.
Still unanswered is the question of how vigorous activity has to be in order to have an effect, Dr. Siu said. “Future studies should investigate the influence of parameters such as frequency, duration, and supervision of exercise sessions to determine the optimal dose and mode of delivery of the intervention for depressive symptom management.”
But would group activity likely have broader benefits than solitary exercise? “It is still unclear whether there’s a difference between the effect of solitary activities and team sports,” Dr. Siu said.
In an accompanying editorial on the meta-analysis, Eduardo E. Bustamante, PhD, an exercise psychologist in the department of kinesiology and nutrition at the University of Illinois at Chicago, and colleagues called the meta-analysis “part of a potential watershed moment” in the field of exercise as therapy for psychological disorders. “The work is timely, aligning with the rise of mental health disorders in adolescents, and the methods are rigorous (e.g., random-effects models, risk-of-bias assessment, sensitivity analyses).”
Dr. Bustamante said the literature on physical activity in children has lagged behind that for adults, so this meta-analysis provides a welcome “critical mass” of evidence of benefit in children, in an interview. “Though the benefit is relatively small, it’s exciting to see the results come in positive specifically to depression.” In his view, the effect of exercise is likely to be less pronounced in children than in adults, especially older ones, as they have fewer inflammatory and other systemic health problems that might improve with exercise. “And we tend to see bigger effects in children with a diagnosis like ADHD or clinical depression.”
But the bottom line is clear: “The evidence that physical activity is effective medicine for mental health is robust; now we need to find ways to get people to take it.”
This work was supported by the Health and Medical Research Fund of the Food and Health Bureau, Hong Kong Special Administrative Region Government, and the Seed Fund for Basic Research of the University of Hong Kong. The authors and editorial commentators disclosed no conflicts of interest.
Intervening with physical activity appears to mitigate depressive symptoms in children and adolescents, a systematic review and meta-analysis of almost 2,500 participants found. Greater reductions were observed for children older than 13 years and those having a diagnosis of mental illness and/or depression versus other conditions, according to Hong Kong researchers reporting in JAMA Pediatrics.
“There is an urgent need to explore novel treatment approaches that can be safely, feasibly, and widely implemented in the daily routine of depressed children and adolescents,” said study coauthor Parco M. Siu, PhD, exercise physiologist and associate professor in the school of public health at the University of Hong Kong, in an interview. “Given the observed association with significant reductions in symptoms, clinical practice guidelines should consider the role of physical activity for improving the mental health of young populations.”
Dr. Siu further noted that while current guidelines suggest psychotherapy and/or pharmacotherapy for children with this common mood disorder, adherence to these can be problematic, and surveys show that nearly 80% do not receive appropriate disorder-specific medical care.
The analysis
Dr. Siu’s team drew on 21 international studies, including 17 randomized controlled trials, published from 1987 to 2021 and comprising 2,444 young participants, mean age 14, 53% girls. Eligible studies compared the effect of exercise on depression versus a control condition.
In 12 studies, participants had a somatic or psychiatric disorder such as obesity, diabetes, depression, and attention-deficit/hyperactivity disorder. The mean duration of the prescribed physical activity program was 22 weeks (6-144 weeks), while the frequency of weekly sessions ranged from 2 to 5 days, with 3 days per week most common and mean duration of 50 minutes (30-120 minutes). Regimens ranged from aerobic exercise on fitness equipment such as treadmills, stationary bikes, and ellipticals, to running, swimming, dancing, sports, and exercise games.
In meta-analysis of postintervention differences, physical activity was associated with a significant reduction in the pooled estimate of depressive symptoms compared with the control condition (Hedges g statistic [effect size] = −0.29; 95% confidence interval, −0.47 to −0.10; P = .004). This was driven by moderate to large effect sizes in adolescents (g = −0.44) and children with diagnosed depression (g = −0.75).The differences, however, were not detectable after a mean follow-up of 21 weeks, possibly owing to the limited number of studies with follow-up outcomes, the authors conceded.
Despite the strong association, the mechanisms underlying the antidepressant properties of physical activity remain uncertain. “Potential pathways include the activation of the endocannabinoid system to stimulate the release of endorphins, an increase in the bioavailability of brain neurotransmitters such as serotonin, dopamine, and noradrenaline, which are reduced in depression, as well as long-term changes in brain plasticity,” Dr. Siu said.
In addition, psychosocial and behavioral hypotheses suggest that physical activity can lead to improvements in self-perception, social interactions, and self-confidence. However, he added, depressive phenomenology is multifaceted and individual, so isolating the effects that physical activity have on specific symptoms may not be possible.
Physical activity appears to enhance the treatment of cognitive and affective symptoms in depression, Dr. Siu continued, and a combination of physical activity and pharmacotherapy may also reduce relapse risk, improve adherence to antidepressants, and promote better management of adverse effects, compared with pharmacotherapy alone. “More research is warranted to explain if and how these mechanisms moderate the effect of physical activity, and whether these changes are also present in younger populations,” he said.
Still unanswered is the question of how vigorous activity has to be in order to have an effect, Dr. Siu said. “Future studies should investigate the influence of parameters such as frequency, duration, and supervision of exercise sessions to determine the optimal dose and mode of delivery of the intervention for depressive symptom management.”
But would group activity likely have broader benefits than solitary exercise? “It is still unclear whether there’s a difference between the effect of solitary activities and team sports,” Dr. Siu said.
In an accompanying editorial on the meta-analysis, Eduardo E. Bustamante, PhD, an exercise psychologist in the department of kinesiology and nutrition at the University of Illinois at Chicago, and colleagues called the meta-analysis “part of a potential watershed moment” in the field of exercise as therapy for psychological disorders. “The work is timely, aligning with the rise of mental health disorders in adolescents, and the methods are rigorous (e.g., random-effects models, risk-of-bias assessment, sensitivity analyses).”
Dr. Bustamante said the literature on physical activity in children has lagged behind that for adults, so this meta-analysis provides a welcome “critical mass” of evidence of benefit in children, in an interview. “Though the benefit is relatively small, it’s exciting to see the results come in positive specifically to depression.” In his view, the effect of exercise is likely to be less pronounced in children than in adults, especially older ones, as they have fewer inflammatory and other systemic health problems that might improve with exercise. “And we tend to see bigger effects in children with a diagnosis like ADHD or clinical depression.”
But the bottom line is clear: “The evidence that physical activity is effective medicine for mental health is robust; now we need to find ways to get people to take it.”
This work was supported by the Health and Medical Research Fund of the Food and Health Bureau, Hong Kong Special Administrative Region Government, and the Seed Fund for Basic Research of the University of Hong Kong. The authors and editorial commentators disclosed no conflicts of interest.
Intervening with physical activity appears to mitigate depressive symptoms in children and adolescents, a systematic review and meta-analysis of almost 2,500 participants found. Greater reductions were observed for children older than 13 years and those having a diagnosis of mental illness and/or depression versus other conditions, according to Hong Kong researchers reporting in JAMA Pediatrics.
“There is an urgent need to explore novel treatment approaches that can be safely, feasibly, and widely implemented in the daily routine of depressed children and adolescents,” said study coauthor Parco M. Siu, PhD, exercise physiologist and associate professor in the school of public health at the University of Hong Kong, in an interview. “Given the observed association with significant reductions in symptoms, clinical practice guidelines should consider the role of physical activity for improving the mental health of young populations.”
Dr. Siu further noted that while current guidelines suggest psychotherapy and/or pharmacotherapy for children with this common mood disorder, adherence to these can be problematic, and surveys show that nearly 80% do not receive appropriate disorder-specific medical care.
The analysis
Dr. Siu’s team drew on 21 international studies, including 17 randomized controlled trials, published from 1987 to 2021 and comprising 2,444 young participants, mean age 14, 53% girls. Eligible studies compared the effect of exercise on depression versus a control condition.
In 12 studies, participants had a somatic or psychiatric disorder such as obesity, diabetes, depression, and attention-deficit/hyperactivity disorder. The mean duration of the prescribed physical activity program was 22 weeks (6-144 weeks), while the frequency of weekly sessions ranged from 2 to 5 days, with 3 days per week most common and mean duration of 50 minutes (30-120 minutes). Regimens ranged from aerobic exercise on fitness equipment such as treadmills, stationary bikes, and ellipticals, to running, swimming, dancing, sports, and exercise games.
In meta-analysis of postintervention differences, physical activity was associated with a significant reduction in the pooled estimate of depressive symptoms compared with the control condition (Hedges g statistic [effect size] = −0.29; 95% confidence interval, −0.47 to −0.10; P = .004). This was driven by moderate to large effect sizes in adolescents (g = −0.44) and children with diagnosed depression (g = −0.75).The differences, however, were not detectable after a mean follow-up of 21 weeks, possibly owing to the limited number of studies with follow-up outcomes, the authors conceded.
Despite the strong association, the mechanisms underlying the antidepressant properties of physical activity remain uncertain. “Potential pathways include the activation of the endocannabinoid system to stimulate the release of endorphins, an increase in the bioavailability of brain neurotransmitters such as serotonin, dopamine, and noradrenaline, which are reduced in depression, as well as long-term changes in brain plasticity,” Dr. Siu said.
In addition, psychosocial and behavioral hypotheses suggest that physical activity can lead to improvements in self-perception, social interactions, and self-confidence. However, he added, depressive phenomenology is multifaceted and individual, so isolating the effects that physical activity have on specific symptoms may not be possible.
Physical activity appears to enhance the treatment of cognitive and affective symptoms in depression, Dr. Siu continued, and a combination of physical activity and pharmacotherapy may also reduce relapse risk, improve adherence to antidepressants, and promote better management of adverse effects, compared with pharmacotherapy alone. “More research is warranted to explain if and how these mechanisms moderate the effect of physical activity, and whether these changes are also present in younger populations,” he said.
Still unanswered is the question of how vigorous activity has to be in order to have an effect, Dr. Siu said. “Future studies should investigate the influence of parameters such as frequency, duration, and supervision of exercise sessions to determine the optimal dose and mode of delivery of the intervention for depressive symptom management.”
But would group activity likely have broader benefits than solitary exercise? “It is still unclear whether there’s a difference between the effect of solitary activities and team sports,” Dr. Siu said.
In an accompanying editorial on the meta-analysis, Eduardo E. Bustamante, PhD, an exercise psychologist in the department of kinesiology and nutrition at the University of Illinois at Chicago, and colleagues called the meta-analysis “part of a potential watershed moment” in the field of exercise as therapy for psychological disorders. “The work is timely, aligning with the rise of mental health disorders in adolescents, and the methods are rigorous (e.g., random-effects models, risk-of-bias assessment, sensitivity analyses).”
Dr. Bustamante said the literature on physical activity in children has lagged behind that for adults, so this meta-analysis provides a welcome “critical mass” of evidence of benefit in children, in an interview. “Though the benefit is relatively small, it’s exciting to see the results come in positive specifically to depression.” In his view, the effect of exercise is likely to be less pronounced in children than in adults, especially older ones, as they have fewer inflammatory and other systemic health problems that might improve with exercise. “And we tend to see bigger effects in children with a diagnosis like ADHD or clinical depression.”
But the bottom line is clear: “The evidence that physical activity is effective medicine for mental health is robust; now we need to find ways to get people to take it.”
This work was supported by the Health and Medical Research Fund of the Food and Health Bureau, Hong Kong Special Administrative Region Government, and the Seed Fund for Basic Research of the University of Hong Kong. The authors and editorial commentators disclosed no conflicts of interest.
FROM JAMA PEDIATRICS
The anecdote as antidote: Psychiatric paradigms in Disney films
A common refrain in psychiatry is that the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, (DSM-5-TR), published in 2022, is the best we can do.
Since the DSM-III was released in 1980, the American Psychiatric Association, which publishes the manual, has espoused the position that we should list symptoms, in a manner that is reminiscent of a checklist. For example, having a depressed mood on most days for a 2-week period, or a loss of interest in pleasurable things, as well as 4 additional symptoms – among them changes in appetite, changes in sleep, changes in psychomotor activity, fatigue, worthlessness, poor concentration, or thoughts of death – can lead to a diagnosis of a major depressive episode as part of a major depressive disorder.
Criticisms of this approach can be apparent. Patients subjected to such checklists, including being repeatedly asked to complete the Patient Health Questionnaire 9 (PHQ-9), which closely follows those criteria, can feel lost and even alienated by their providers. After all, one can ask all those questions and make a diagnosis of depression without even knowing about the patient’s stressors, their history, or their social context.
The DSM permits the diagnosis of psychiatric disorders without an understanding of the narrative of the patient. In its defense, the DSM is not a textbook of psychiatry, it is a guide on how to diagnose individuals. The DSM does not demand that psychiatrists only ask about the symptoms on the checklists; it is the providers who can choose to dismiss asking about the important facets of one’s life.
Yet every time we attend a lecture that starts by enumerating the DSM symptoms of the disorder being discussed, we are left with the dissatisfying impression that a specialist of this disorder should have a more nuanced and interesting description of their disorder of study. This feeling of discontent is compounded when we see a movie that encompasses so much of what is missing in today’s psychiatric parlance, and even more so if that movie is ostensibly made for children. Movies, by design, are particularly adept at encapsulating the narrative of someone’s life in a way that psychiatry can learn from.
Other than the embarrassment of not knowing a patient outside the checklist, the importance of narrative cannot be understated. Dr. Erik Erikson rightfully suggested that the point of life is “the acceptance of one’s one and only life cycle”1 or rather to know it was okay to have been oneself without additions or substitutions. Therefore, one must know what it has meant to be themselves to reconcile this question and achieve Ego Integrity rather than disgust and despair. Narrative is the way in which we understand who we are and what it has meant to be ourselves. An understanding of our personal narrative presents a unique opportunity in expressing what is missing in the DSM. Below, we provide two of our favorite examples in Disney films, among many.
‘Ratatouille’ (2007)
One of the missing features of the DSM is its inability to explain to patients the intrapsychic processes that guide us. One of these processes is how our values can lead us to a deep sense of guilt, shame, and the resulting feelings of alienation. It is extremely common for patients to enter our clinical practice feeling shackled by beliefs that they should accomplish more and be more than they are.
The animated film “Ratatouille” does an excellent job at addressing this feeling. The film follows Remy, the protagonist rat, and his adventures as he explores his passion for cooking. Remy teams up with the inept but good-natured human Alfredo Linguini and guides him through cooking while hiding under his chef’s hat. The primary antagonist, Anton Ego, is a particularly harsh food critic. His presence and appearance are somber. He exudes disdain. His trim physique and scarf suggest a man that will break and react to anything, and his skull-shaped typewriter in his coffin-shaped office informs the viewer that he is out to kill with his cruel words. Anton Ego serves as our projected super-ego. He is not an external judge but the judgment deep inside ourselves, goading us to be better with such severity that we are ultimately left feeling condemned.
Remy is the younger of two siblings. He is less physically adept but more intellectual than his older brother, who does not understand why Remy isn’t content eating scraps from the garbage like the rest of their rat clan. Remy is the creative part within us that wants to challenge the status quo and try something new. Remy also represents our shame and guilt for leaving our home. On one hand, we want to dare greatly, in this case at being an extraordinary chef, but on the other we are shy and cook in secret, hiding within the hat of another person. Remy struggles with the deep feeling that we do not deserve our success, that our family will leave us for being who we are, and that we are better off isolating and segregating from our challenges.
The movie concludes that through talent and hard work, our critics will accept us. Furthermore, once accepted for what we do, we can be further accepted for who we are. The movie ends with Remy cooking the eponymous dish ratatouille. He prepares it so remarkably well, the dish transports Anton Ego back to a sublime experience of eating ratatouille as a child, a touching moment which not only underscores food’s evocative link to memory but gives a glimpse at Anton Ego’s own narrative.
Ego is first won over by the dish, and only afterward learns of Remy’s true identity. Remy’s talent is undeniable though, and even the stuffy Ego must accept the film’s theme that “Anyone can cook,” even a rat – the rat that we all sometimes feel we are deep inside, rotten to the core but trying so hard to be accepted by others, and ultimately by ourselves. In the end, we overcome the disgust inherent in the imagery of a rat in a kitchen and instead embrace our hero’s achievement of ego integrity as he combines his identities as a member of a clan of rats, and one of Paris’s finest chefs.
While modern psychiatry can favor looking at people through the lens of biology rather than narrative, “Ratatouille” can serve as a reminder of the powerful unconscious forces that guide our lives. “Ratatouille” is not a successful movie only because of the compelling narrative, but also because the narrative matches the important psychic paradigms that psychiatry once embraced.
‘Inside Out’ (2015)
Another missing feature of the DSM is its inability to explain how symptoms feel and manifest psychologically. One such feeling is that of control – whether one is in control of one’s life, feelings, and action or rather a victim of external forces. It is extremely common for patients to enter our clinical practice feeling traumatized by the life they’ve lived and powerless to produce any change. Part of our role is to guide them through this journey from the object of their lives to the subject of their lives.
In the animated feature “Inside Out,” Riley, a preteen girl, goes through the tribulation of growing up and learning about herself. This seemingly happy child, content playing hockey with her best friend, Meg, on the picturesque frozen lakes of Minnesota, reaches her inevitable conflict. Her parents uproot her life, moving the family to San Francisco. By doing so, they disconnect her from her school, her friends, and her hobbies. While all this is happening, we spend time inside Riley’s psyche with the personified characters of Riley’s emotions as they affect her decisions and daily actions amidst the backdrop of her core memories and islands of personality.
During the move, her parents seemingly change and ultimately destroy every facet of Riley’s sense of self, which is animated as the collapse of her personality islands. Her best friend engages Riley in a video call just to inform her that she has a new friend who plays hockey equally well. Her parents do not hear Riley’s concerns and are portrayed as distracted by their adult problems. Riley feels ridiculed in her new school and unable to share her feelings with her parents, who ask her to still be their “happy girl” and indirectly ask her to fake pleasure to alleviate their own anxiety.
The climax of the movie is when Riley decides to run away from San Francisco and her parents, to return to her perceived true home, Minnesota. The climax is resolved when Riley realizes that her parents’ love, representing the connection we have to others, transcends her need for control. To some degree, we are all powerless in the face of the tremendous forces of life and share the difficult task of accepting the cards we were dealt, thus making the story of Riley so compelling.
Additionally, the climax is further resolved by another argument that psychiatry (and the DSM) should consider embracing. Emotions are not all symptoms and living without negative emotion is not the goal of life. Riley grows from preteen to teenager, and from object to subject of her life, by realizing that her symptoms/feelings are not just nuisances to avoid and hide, but the key to meaning. Our anger drives us to try hard. Our fear protects us from harm. Our sadness attracts the warmth and care of others. Our disgust protects us physically from noxious material (symbolized as a dreaded broccoli floret for preteen Riley) and socially by encouraging us to share societal norms. Similarly, patients and people in general would benefit by being taught that, while symptoms may permit the better assessment of psychiatric conditions using the DSM, life is much more than that.
It is unfair to blame the DSM for things it was not designed to do. The DSM doesn’t advertise itself as a guidebook of all behaviors, at all times. However, for a variety of reasons, it has become the main way psychiatry describes people. While we commend the APA for its effort and do not know that we could make it any better, we are frequently happily reminded that in about 90 minutes, filmmakers are able to display an empathic understanding of personal narratives that biologic psychiatry can miss.
Dr. Pulido is a psychiatry resident at the University of California, San Diego. She is interested in women’s mental health, medical education, and outpatient psychiatry. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Erikson, EH. Childhood and society (New York: WW Norton, 1950).
A common refrain in psychiatry is that the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, (DSM-5-TR), published in 2022, is the best we can do.
Since the DSM-III was released in 1980, the American Psychiatric Association, which publishes the manual, has espoused the position that we should list symptoms, in a manner that is reminiscent of a checklist. For example, having a depressed mood on most days for a 2-week period, or a loss of interest in pleasurable things, as well as 4 additional symptoms – among them changes in appetite, changes in sleep, changes in psychomotor activity, fatigue, worthlessness, poor concentration, or thoughts of death – can lead to a diagnosis of a major depressive episode as part of a major depressive disorder.
Criticisms of this approach can be apparent. Patients subjected to such checklists, including being repeatedly asked to complete the Patient Health Questionnaire 9 (PHQ-9), which closely follows those criteria, can feel lost and even alienated by their providers. After all, one can ask all those questions and make a diagnosis of depression without even knowing about the patient’s stressors, their history, or their social context.
The DSM permits the diagnosis of psychiatric disorders without an understanding of the narrative of the patient. In its defense, the DSM is not a textbook of psychiatry, it is a guide on how to diagnose individuals. The DSM does not demand that psychiatrists only ask about the symptoms on the checklists; it is the providers who can choose to dismiss asking about the important facets of one’s life.
Yet every time we attend a lecture that starts by enumerating the DSM symptoms of the disorder being discussed, we are left with the dissatisfying impression that a specialist of this disorder should have a more nuanced and interesting description of their disorder of study. This feeling of discontent is compounded when we see a movie that encompasses so much of what is missing in today’s psychiatric parlance, and even more so if that movie is ostensibly made for children. Movies, by design, are particularly adept at encapsulating the narrative of someone’s life in a way that psychiatry can learn from.
Other than the embarrassment of not knowing a patient outside the checklist, the importance of narrative cannot be understated. Dr. Erik Erikson rightfully suggested that the point of life is “the acceptance of one’s one and only life cycle”1 or rather to know it was okay to have been oneself without additions or substitutions. Therefore, one must know what it has meant to be themselves to reconcile this question and achieve Ego Integrity rather than disgust and despair. Narrative is the way in which we understand who we are and what it has meant to be ourselves. An understanding of our personal narrative presents a unique opportunity in expressing what is missing in the DSM. Below, we provide two of our favorite examples in Disney films, among many.
‘Ratatouille’ (2007)
One of the missing features of the DSM is its inability to explain to patients the intrapsychic processes that guide us. One of these processes is how our values can lead us to a deep sense of guilt, shame, and the resulting feelings of alienation. It is extremely common for patients to enter our clinical practice feeling shackled by beliefs that they should accomplish more and be more than they are.
The animated film “Ratatouille” does an excellent job at addressing this feeling. The film follows Remy, the protagonist rat, and his adventures as he explores his passion for cooking. Remy teams up with the inept but good-natured human Alfredo Linguini and guides him through cooking while hiding under his chef’s hat. The primary antagonist, Anton Ego, is a particularly harsh food critic. His presence and appearance are somber. He exudes disdain. His trim physique and scarf suggest a man that will break and react to anything, and his skull-shaped typewriter in his coffin-shaped office informs the viewer that he is out to kill with his cruel words. Anton Ego serves as our projected super-ego. He is not an external judge but the judgment deep inside ourselves, goading us to be better with such severity that we are ultimately left feeling condemned.
Remy is the younger of two siblings. He is less physically adept but more intellectual than his older brother, who does not understand why Remy isn’t content eating scraps from the garbage like the rest of their rat clan. Remy is the creative part within us that wants to challenge the status quo and try something new. Remy also represents our shame and guilt for leaving our home. On one hand, we want to dare greatly, in this case at being an extraordinary chef, but on the other we are shy and cook in secret, hiding within the hat of another person. Remy struggles with the deep feeling that we do not deserve our success, that our family will leave us for being who we are, and that we are better off isolating and segregating from our challenges.
The movie concludes that through talent and hard work, our critics will accept us. Furthermore, once accepted for what we do, we can be further accepted for who we are. The movie ends with Remy cooking the eponymous dish ratatouille. He prepares it so remarkably well, the dish transports Anton Ego back to a sublime experience of eating ratatouille as a child, a touching moment which not only underscores food’s evocative link to memory but gives a glimpse at Anton Ego’s own narrative.
Ego is first won over by the dish, and only afterward learns of Remy’s true identity. Remy’s talent is undeniable though, and even the stuffy Ego must accept the film’s theme that “Anyone can cook,” even a rat – the rat that we all sometimes feel we are deep inside, rotten to the core but trying so hard to be accepted by others, and ultimately by ourselves. In the end, we overcome the disgust inherent in the imagery of a rat in a kitchen and instead embrace our hero’s achievement of ego integrity as he combines his identities as a member of a clan of rats, and one of Paris’s finest chefs.
While modern psychiatry can favor looking at people through the lens of biology rather than narrative, “Ratatouille” can serve as a reminder of the powerful unconscious forces that guide our lives. “Ratatouille” is not a successful movie only because of the compelling narrative, but also because the narrative matches the important psychic paradigms that psychiatry once embraced.
‘Inside Out’ (2015)
Another missing feature of the DSM is its inability to explain how symptoms feel and manifest psychologically. One such feeling is that of control – whether one is in control of one’s life, feelings, and action or rather a victim of external forces. It is extremely common for patients to enter our clinical practice feeling traumatized by the life they’ve lived and powerless to produce any change. Part of our role is to guide them through this journey from the object of their lives to the subject of their lives.
In the animated feature “Inside Out,” Riley, a preteen girl, goes through the tribulation of growing up and learning about herself. This seemingly happy child, content playing hockey with her best friend, Meg, on the picturesque frozen lakes of Minnesota, reaches her inevitable conflict. Her parents uproot her life, moving the family to San Francisco. By doing so, they disconnect her from her school, her friends, and her hobbies. While all this is happening, we spend time inside Riley’s psyche with the personified characters of Riley’s emotions as they affect her decisions and daily actions amidst the backdrop of her core memories and islands of personality.
During the move, her parents seemingly change and ultimately destroy every facet of Riley’s sense of self, which is animated as the collapse of her personality islands. Her best friend engages Riley in a video call just to inform her that she has a new friend who plays hockey equally well. Her parents do not hear Riley’s concerns and are portrayed as distracted by their adult problems. Riley feels ridiculed in her new school and unable to share her feelings with her parents, who ask her to still be their “happy girl” and indirectly ask her to fake pleasure to alleviate their own anxiety.
The climax of the movie is when Riley decides to run away from San Francisco and her parents, to return to her perceived true home, Minnesota. The climax is resolved when Riley realizes that her parents’ love, representing the connection we have to others, transcends her need for control. To some degree, we are all powerless in the face of the tremendous forces of life and share the difficult task of accepting the cards we were dealt, thus making the story of Riley so compelling.
Additionally, the climax is further resolved by another argument that psychiatry (and the DSM) should consider embracing. Emotions are not all symptoms and living without negative emotion is not the goal of life. Riley grows from preteen to teenager, and from object to subject of her life, by realizing that her symptoms/feelings are not just nuisances to avoid and hide, but the key to meaning. Our anger drives us to try hard. Our fear protects us from harm. Our sadness attracts the warmth and care of others. Our disgust protects us physically from noxious material (symbolized as a dreaded broccoli floret for preteen Riley) and socially by encouraging us to share societal norms. Similarly, patients and people in general would benefit by being taught that, while symptoms may permit the better assessment of psychiatric conditions using the DSM, life is much more than that.
It is unfair to blame the DSM for things it was not designed to do. The DSM doesn’t advertise itself as a guidebook of all behaviors, at all times. However, for a variety of reasons, it has become the main way psychiatry describes people. While we commend the APA for its effort and do not know that we could make it any better, we are frequently happily reminded that in about 90 minutes, filmmakers are able to display an empathic understanding of personal narratives that biologic psychiatry can miss.
Dr. Pulido is a psychiatry resident at the University of California, San Diego. She is interested in women’s mental health, medical education, and outpatient psychiatry. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Erikson, EH. Childhood and society (New York: WW Norton, 1950).
A common refrain in psychiatry is that the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, (DSM-5-TR), published in 2022, is the best we can do.
Since the DSM-III was released in 1980, the American Psychiatric Association, which publishes the manual, has espoused the position that we should list symptoms, in a manner that is reminiscent of a checklist. For example, having a depressed mood on most days for a 2-week period, or a loss of interest in pleasurable things, as well as 4 additional symptoms – among them changes in appetite, changes in sleep, changes in psychomotor activity, fatigue, worthlessness, poor concentration, or thoughts of death – can lead to a diagnosis of a major depressive episode as part of a major depressive disorder.
Criticisms of this approach can be apparent. Patients subjected to such checklists, including being repeatedly asked to complete the Patient Health Questionnaire 9 (PHQ-9), which closely follows those criteria, can feel lost and even alienated by their providers. After all, one can ask all those questions and make a diagnosis of depression without even knowing about the patient’s stressors, their history, or their social context.
The DSM permits the diagnosis of psychiatric disorders without an understanding of the narrative of the patient. In its defense, the DSM is not a textbook of psychiatry, it is a guide on how to diagnose individuals. The DSM does not demand that psychiatrists only ask about the symptoms on the checklists; it is the providers who can choose to dismiss asking about the important facets of one’s life.
Yet every time we attend a lecture that starts by enumerating the DSM symptoms of the disorder being discussed, we are left with the dissatisfying impression that a specialist of this disorder should have a more nuanced and interesting description of their disorder of study. This feeling of discontent is compounded when we see a movie that encompasses so much of what is missing in today’s psychiatric parlance, and even more so if that movie is ostensibly made for children. Movies, by design, are particularly adept at encapsulating the narrative of someone’s life in a way that psychiatry can learn from.
Other than the embarrassment of not knowing a patient outside the checklist, the importance of narrative cannot be understated. Dr. Erik Erikson rightfully suggested that the point of life is “the acceptance of one’s one and only life cycle”1 or rather to know it was okay to have been oneself without additions or substitutions. Therefore, one must know what it has meant to be themselves to reconcile this question and achieve Ego Integrity rather than disgust and despair. Narrative is the way in which we understand who we are and what it has meant to be ourselves. An understanding of our personal narrative presents a unique opportunity in expressing what is missing in the DSM. Below, we provide two of our favorite examples in Disney films, among many.
‘Ratatouille’ (2007)
One of the missing features of the DSM is its inability to explain to patients the intrapsychic processes that guide us. One of these processes is how our values can lead us to a deep sense of guilt, shame, and the resulting feelings of alienation. It is extremely common for patients to enter our clinical practice feeling shackled by beliefs that they should accomplish more and be more than they are.
The animated film “Ratatouille” does an excellent job at addressing this feeling. The film follows Remy, the protagonist rat, and his adventures as he explores his passion for cooking. Remy teams up with the inept but good-natured human Alfredo Linguini and guides him through cooking while hiding under his chef’s hat. The primary antagonist, Anton Ego, is a particularly harsh food critic. His presence and appearance are somber. He exudes disdain. His trim physique and scarf suggest a man that will break and react to anything, and his skull-shaped typewriter in his coffin-shaped office informs the viewer that he is out to kill with his cruel words. Anton Ego serves as our projected super-ego. He is not an external judge but the judgment deep inside ourselves, goading us to be better with such severity that we are ultimately left feeling condemned.
Remy is the younger of two siblings. He is less physically adept but more intellectual than his older brother, who does not understand why Remy isn’t content eating scraps from the garbage like the rest of their rat clan. Remy is the creative part within us that wants to challenge the status quo and try something new. Remy also represents our shame and guilt for leaving our home. On one hand, we want to dare greatly, in this case at being an extraordinary chef, but on the other we are shy and cook in secret, hiding within the hat of another person. Remy struggles with the deep feeling that we do not deserve our success, that our family will leave us for being who we are, and that we are better off isolating and segregating from our challenges.
The movie concludes that through talent and hard work, our critics will accept us. Furthermore, once accepted for what we do, we can be further accepted for who we are. The movie ends with Remy cooking the eponymous dish ratatouille. He prepares it so remarkably well, the dish transports Anton Ego back to a sublime experience of eating ratatouille as a child, a touching moment which not only underscores food’s evocative link to memory but gives a glimpse at Anton Ego’s own narrative.
Ego is first won over by the dish, and only afterward learns of Remy’s true identity. Remy’s talent is undeniable though, and even the stuffy Ego must accept the film’s theme that “Anyone can cook,” even a rat – the rat that we all sometimes feel we are deep inside, rotten to the core but trying so hard to be accepted by others, and ultimately by ourselves. In the end, we overcome the disgust inherent in the imagery of a rat in a kitchen and instead embrace our hero’s achievement of ego integrity as he combines his identities as a member of a clan of rats, and one of Paris’s finest chefs.
While modern psychiatry can favor looking at people through the lens of biology rather than narrative, “Ratatouille” can serve as a reminder of the powerful unconscious forces that guide our lives. “Ratatouille” is not a successful movie only because of the compelling narrative, but also because the narrative matches the important psychic paradigms that psychiatry once embraced.
‘Inside Out’ (2015)
Another missing feature of the DSM is its inability to explain how symptoms feel and manifest psychologically. One such feeling is that of control – whether one is in control of one’s life, feelings, and action or rather a victim of external forces. It is extremely common for patients to enter our clinical practice feeling traumatized by the life they’ve lived and powerless to produce any change. Part of our role is to guide them through this journey from the object of their lives to the subject of their lives.
In the animated feature “Inside Out,” Riley, a preteen girl, goes through the tribulation of growing up and learning about herself. This seemingly happy child, content playing hockey with her best friend, Meg, on the picturesque frozen lakes of Minnesota, reaches her inevitable conflict. Her parents uproot her life, moving the family to San Francisco. By doing so, they disconnect her from her school, her friends, and her hobbies. While all this is happening, we spend time inside Riley’s psyche with the personified characters of Riley’s emotions as they affect her decisions and daily actions amidst the backdrop of her core memories and islands of personality.
During the move, her parents seemingly change and ultimately destroy every facet of Riley’s sense of self, which is animated as the collapse of her personality islands. Her best friend engages Riley in a video call just to inform her that she has a new friend who plays hockey equally well. Her parents do not hear Riley’s concerns and are portrayed as distracted by their adult problems. Riley feels ridiculed in her new school and unable to share her feelings with her parents, who ask her to still be their “happy girl” and indirectly ask her to fake pleasure to alleviate their own anxiety.
The climax of the movie is when Riley decides to run away from San Francisco and her parents, to return to her perceived true home, Minnesota. The climax is resolved when Riley realizes that her parents’ love, representing the connection we have to others, transcends her need for control. To some degree, we are all powerless in the face of the tremendous forces of life and share the difficult task of accepting the cards we were dealt, thus making the story of Riley so compelling.
Additionally, the climax is further resolved by another argument that psychiatry (and the DSM) should consider embracing. Emotions are not all symptoms and living without negative emotion is not the goal of life. Riley grows from preteen to teenager, and from object to subject of her life, by realizing that her symptoms/feelings are not just nuisances to avoid and hide, but the key to meaning. Our anger drives us to try hard. Our fear protects us from harm. Our sadness attracts the warmth and care of others. Our disgust protects us physically from noxious material (symbolized as a dreaded broccoli floret for preteen Riley) and socially by encouraging us to share societal norms. Similarly, patients and people in general would benefit by being taught that, while symptoms may permit the better assessment of psychiatric conditions using the DSM, life is much more than that.
It is unfair to blame the DSM for things it was not designed to do. The DSM doesn’t advertise itself as a guidebook of all behaviors, at all times. However, for a variety of reasons, it has become the main way psychiatry describes people. While we commend the APA for its effort and do not know that we could make it any better, we are frequently happily reminded that in about 90 minutes, filmmakers are able to display an empathic understanding of personal narratives that biologic psychiatry can miss.
Dr. Pulido is a psychiatry resident at the University of California, San Diego. She is interested in women’s mental health, medical education, and outpatient psychiatry. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest.
References
1. Erikson, EH. Childhood and society (New York: WW Norton, 1950).
Vegetarians suffer more depression than meat eaters
People who follow a vegetarian lifestyle have around twice as many depressive episodes as those who eat meat, according to the Brazilian Longitudinal Study of Adult Health.
What to know
, including the vegetarian social experience; depression itself may increase the likelihood of becoming vegetarian, or both vegetarianism and depression may be associated with guilt through factors involving the meat industry.
Adopting a vegetarian diet might affect one’s relationship with others and involvement in social activities and may sometimes be associated with teasing or other forms of social ostracism.
It is possible that being depressed and dwelling on negative thoughts cause people to be more likely to become vegetarian rather than the other way around.
Videos depicting violence and cruelty in the meat industry may affect depressed people, causing them to dwell on the images, feel guilty for their part in creating the demand for meat, and become vegetarian.
Survey data were collected in Brazil, a country famous for its meat-heavy diet, and while there has been a sharp increase in vegetarianism, vegetarians still account for less than 0.5%.
This is a summary of the article, “Association Between Meatless Diet and Depressive Episodes: A Cross-sectional Analysis of Baseline Data From the Longitudinal Study of Adult Health (ELSA-Brasil),” published in the Journal of Affective Disorders. The full article can be found at sciencedirect.com.
A version of this article first appeared on Medscape.com.
People who follow a vegetarian lifestyle have around twice as many depressive episodes as those who eat meat, according to the Brazilian Longitudinal Study of Adult Health.
What to know
, including the vegetarian social experience; depression itself may increase the likelihood of becoming vegetarian, or both vegetarianism and depression may be associated with guilt through factors involving the meat industry.
Adopting a vegetarian diet might affect one’s relationship with others and involvement in social activities and may sometimes be associated with teasing or other forms of social ostracism.
It is possible that being depressed and dwelling on negative thoughts cause people to be more likely to become vegetarian rather than the other way around.
Videos depicting violence and cruelty in the meat industry may affect depressed people, causing them to dwell on the images, feel guilty for their part in creating the demand for meat, and become vegetarian.
Survey data were collected in Brazil, a country famous for its meat-heavy diet, and while there has been a sharp increase in vegetarianism, vegetarians still account for less than 0.5%.
This is a summary of the article, “Association Between Meatless Diet and Depressive Episodes: A Cross-sectional Analysis of Baseline Data From the Longitudinal Study of Adult Health (ELSA-Brasil),” published in the Journal of Affective Disorders. The full article can be found at sciencedirect.com.
A version of this article first appeared on Medscape.com.
People who follow a vegetarian lifestyle have around twice as many depressive episodes as those who eat meat, according to the Brazilian Longitudinal Study of Adult Health.
What to know
, including the vegetarian social experience; depression itself may increase the likelihood of becoming vegetarian, or both vegetarianism and depression may be associated with guilt through factors involving the meat industry.
Adopting a vegetarian diet might affect one’s relationship with others and involvement in social activities and may sometimes be associated with teasing or other forms of social ostracism.
It is possible that being depressed and dwelling on negative thoughts cause people to be more likely to become vegetarian rather than the other way around.
Videos depicting violence and cruelty in the meat industry may affect depressed people, causing them to dwell on the images, feel guilty for their part in creating the demand for meat, and become vegetarian.
Survey data were collected in Brazil, a country famous for its meat-heavy diet, and while there has been a sharp increase in vegetarianism, vegetarians still account for less than 0.5%.
This is a summary of the article, “Association Between Meatless Diet and Depressive Episodes: A Cross-sectional Analysis of Baseline Data From the Longitudinal Study of Adult Health (ELSA-Brasil),” published in the Journal of Affective Disorders. The full article can be found at sciencedirect.com.
A version of this article first appeared on Medscape.com.
The trauma of sudden death
“It is one of life’s most self-evident truths that everything fades, that we fear the fading, and that we must live, nonetheless, in the face of the fear.” – Irvin D. Yalom, MD, Existential Psychotherapy, 1980
The email was titled simply, “A sorrowful note,” and I knew that someone had died. I held my breath and read as Dr. Jimmy Potash informed our entire department that Dr. Cait McFarland died in a car accident on December 7 while driving to work at West Cecil Health Center, Conowingo, Md., where she was director of psychiatry.
Sadness swelled as I remembered the outspoken resident who was interested in LGBTQ issues. Cait graduated from the Johns Hopkins residency program in 2020, she had recently married a social worker in the department, and the plan was for her to return to Hopkins full-time in July 2023 to be director of a clinic focused on mental health for people who are transgendered.
Sudden deaths are tragic and jarring and they call to the surface our losses from the past. These deaths don’t stand alone – I found myself thinking of my editor at Medscape, Dr. Bret Stetka, who died unexpectedly in August 2022, and then of Dr. Lidia Palcan Wenz, a psychiatrist I trained with, who died in a motor vehicle accident in 2004. Lidia’s husband also died in the accident, while their two young children in the back seat survived – this tragedy haunted me for some time. None of these people was close to me, but I am no stranger to the impact of unexpected death: My parents and brother all died from cardiac events, and any sudden death is a reminder of those losses.
Julia Riddle, MD, trained with Cait McFarland and was her close friend for years. “I don’t have a belief in ‘the afterlife’ but do like to think of the people that I have lost together in my memory – as if they are all suddenly in a new room together. And, with each loss, all the other occupants of that room come freshly to life again,” Dr. Riddle said.
Death is our shared destination in life, but sudden and unexpected deaths carry their own weight. There is no chance to tie up loose ends, to repair riffs, to say goodbye. Nothing is put in order, and the life that was to be lived goes on for some time as bills arrive, social and work events go unattended, vacations are canceled, and there is the awkward moment of running into someone who didn’t know your loved one has died.
Roger Lewin, MD, is a psychiatrist and writer in Towson, Md. He has both personal and professional experience with sudden death. “There is no way to prepare beforehand, so we have to get ready for what has already happened, and that is hard,” he said. “We invent a life for ourselves and others that extends into the future, and that gets interrupted.”
Most people become ill and die on a vaguely predictable schedule. There may be a chance to plan, to know and honor the wishes of the individual, and often there is the opportunity for loved ones to begin the grieving process gradually as death approaches. For those who are elderly, there may be a sense that this is the natural order of things – which may or may not temper the intensity of the grief for those who remain. If the person has suffered, the end may come with relief.
Still, I sometimes find myself surprised at the length and intensity of anguish that some people experience after losing a loved one who has lived a long and full life, who declined and suffered, but whose absence remains a gaping wound that takes years to form a scar.
Sudden death is not rare; accidents, homicide, and suicide are the top killers among young people, and cardiovascular deaths are number one among those who are older. Natural disasters and terrorist attacks can cause catastrophic numbers of sudden deaths and leave survivors to grieve not only the dead, but the loss of all that was familiar to them.
Psychiatry has been a bit lost as to how we approach grief. We often hear patients talk about anxiety surrounding death and illness, be it a fear of death or a longing for it. These fears can seem irrational – I am reminded of a patient who was afraid to eat romaine because of news reports that it was responsible for food poisoning in other states, but not Maryland, where the person lived. I found it odd that he worried about eating lettuce, but not about smoking two packs of cigarettes a day.
But our fears are like that – they move to what the media sensationalizes, or to what may be remote, because otherwise no one would get in a car or clear their walkway of snow. Life is most easily lived with a bit of denial: We shut out the reality that we can be here one moment, overscheduled and overwhelmed, with deadlines, mortgage payments, and summer vacation plans, oblivious to the fact that life may end at any moment. The early months of COVID-19 felt like a global game of Russian roulette, with each venture out a pull of the trigger and everyone’s defenses stripped bare.
While death belongs to us all, we relegate it to the disciplines of religion, philosophy, the arts, and psychology. Religion offers answers – whether a heaven, a hell, or continual reincarnation until the individual attains enlightenment, there is a destination. Perhaps it will be pleasant, perhaps not, and for some there is the hope that one gets to be the driver by having the right beliefs or doing good deeds, while others are comforted by the hope of being reunited with loved ones.
“The suddenness endures and the shock lasts – it’s like a meteor that creates a crater and we revisit it in different ways from different angles,” Dr. Lewin said. “It may leap on us unexpectedly, often many years later.”
Patients talk about death, and when their fears seem unrealistic we may long to reassure them, yet there is no reassurance and psychiatry grasps for how to help. Psychiatry has looked to draw lines for when normal grief crosses to abnormal. Is it an adjustment disorder, complicated grief, “prolonged” grief, pathology in need of medication and medicalization, or something one experiences individually, sometimes for a very long time even with treatment?
One justification for pathologizing “prolonged” reactions includes the fact that insurers will pay for treatment only if there is a diagnosis code, and shouldn’t people in distress be entitled to psychotherapy or medication? Yet there is something offensive about telling someone that they are mentally ill if they don’t grieve along a prescribed timeline, as much as there is about denying them the possible benefits of therapy or medication if they seek it, but are suffering in all the “right” ways. Psychiatry’s approach to death is inelegant at best.
In his poignant podcast series, All There Is, Anderson Cooper is tasked with sorting through his mother’s apartment after her death at age 95. In the course of packing up her belongings, he brings on other guests to talk about their emotional reactions to death. Mr. Cooper’s mother, Gloria Vanderbilt, died at an advanced age, but his father died after a brief cardiac illness when Mr. Cooper was a child, and his brother died by suicide when he was 21. He uses these experiences as a springboard to examine childhood losses, the aftermath of suicide, and the loneliness of grief.
“Loss and grief is this universal experience that we will all go through multiple times in our lives,” Mr. Cooper says, “And yet it leaves us feeling so alone and so separated from other people. At least it does me and has my entire life.”
When we talk about grief and loss, we talk about “getting over it,” or “moving on.” But loss doesn’t work that way – time usually eases the pain, leaving scars that are part of the road map for who we are on the journey that defines us.
Sudden death is hard, and the unexpected death of a young person is tragic. For Cait McFarland, there are the decades she won’t get to experience. For her family and friends, it may be excruciating, and for all the patients who have lost a psychiatrist, may time bring healing and peace.
The Dr. Caitlin McFarland Educational Fund for LGBTQI+ Mental Health is being established, and donations are being accepted at https://www.gofundme.com/f/in-memory-of-cait-mcfarland.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships.
“It is one of life’s most self-evident truths that everything fades, that we fear the fading, and that we must live, nonetheless, in the face of the fear.” – Irvin D. Yalom, MD, Existential Psychotherapy, 1980
The email was titled simply, “A sorrowful note,” and I knew that someone had died. I held my breath and read as Dr. Jimmy Potash informed our entire department that Dr. Cait McFarland died in a car accident on December 7 while driving to work at West Cecil Health Center, Conowingo, Md., where she was director of psychiatry.
Sadness swelled as I remembered the outspoken resident who was interested in LGBTQ issues. Cait graduated from the Johns Hopkins residency program in 2020, she had recently married a social worker in the department, and the plan was for her to return to Hopkins full-time in July 2023 to be director of a clinic focused on mental health for people who are transgendered.
Sudden deaths are tragic and jarring and they call to the surface our losses from the past. These deaths don’t stand alone – I found myself thinking of my editor at Medscape, Dr. Bret Stetka, who died unexpectedly in August 2022, and then of Dr. Lidia Palcan Wenz, a psychiatrist I trained with, who died in a motor vehicle accident in 2004. Lidia’s husband also died in the accident, while their two young children in the back seat survived – this tragedy haunted me for some time. None of these people was close to me, but I am no stranger to the impact of unexpected death: My parents and brother all died from cardiac events, and any sudden death is a reminder of those losses.
Julia Riddle, MD, trained with Cait McFarland and was her close friend for years. “I don’t have a belief in ‘the afterlife’ but do like to think of the people that I have lost together in my memory – as if they are all suddenly in a new room together. And, with each loss, all the other occupants of that room come freshly to life again,” Dr. Riddle said.
Death is our shared destination in life, but sudden and unexpected deaths carry their own weight. There is no chance to tie up loose ends, to repair riffs, to say goodbye. Nothing is put in order, and the life that was to be lived goes on for some time as bills arrive, social and work events go unattended, vacations are canceled, and there is the awkward moment of running into someone who didn’t know your loved one has died.
Roger Lewin, MD, is a psychiatrist and writer in Towson, Md. He has both personal and professional experience with sudden death. “There is no way to prepare beforehand, so we have to get ready for what has already happened, and that is hard,” he said. “We invent a life for ourselves and others that extends into the future, and that gets interrupted.”
Most people become ill and die on a vaguely predictable schedule. There may be a chance to plan, to know and honor the wishes of the individual, and often there is the opportunity for loved ones to begin the grieving process gradually as death approaches. For those who are elderly, there may be a sense that this is the natural order of things – which may or may not temper the intensity of the grief for those who remain. If the person has suffered, the end may come with relief.
Still, I sometimes find myself surprised at the length and intensity of anguish that some people experience after losing a loved one who has lived a long and full life, who declined and suffered, but whose absence remains a gaping wound that takes years to form a scar.
Sudden death is not rare; accidents, homicide, and suicide are the top killers among young people, and cardiovascular deaths are number one among those who are older. Natural disasters and terrorist attacks can cause catastrophic numbers of sudden deaths and leave survivors to grieve not only the dead, but the loss of all that was familiar to them.
Psychiatry has been a bit lost as to how we approach grief. We often hear patients talk about anxiety surrounding death and illness, be it a fear of death or a longing for it. These fears can seem irrational – I am reminded of a patient who was afraid to eat romaine because of news reports that it was responsible for food poisoning in other states, but not Maryland, where the person lived. I found it odd that he worried about eating lettuce, but not about smoking two packs of cigarettes a day.
But our fears are like that – they move to what the media sensationalizes, or to what may be remote, because otherwise no one would get in a car or clear their walkway of snow. Life is most easily lived with a bit of denial: We shut out the reality that we can be here one moment, overscheduled and overwhelmed, with deadlines, mortgage payments, and summer vacation plans, oblivious to the fact that life may end at any moment. The early months of COVID-19 felt like a global game of Russian roulette, with each venture out a pull of the trigger and everyone’s defenses stripped bare.
While death belongs to us all, we relegate it to the disciplines of religion, philosophy, the arts, and psychology. Religion offers answers – whether a heaven, a hell, or continual reincarnation until the individual attains enlightenment, there is a destination. Perhaps it will be pleasant, perhaps not, and for some there is the hope that one gets to be the driver by having the right beliefs or doing good deeds, while others are comforted by the hope of being reunited with loved ones.
“The suddenness endures and the shock lasts – it’s like a meteor that creates a crater and we revisit it in different ways from different angles,” Dr. Lewin said. “It may leap on us unexpectedly, often many years later.”
Patients talk about death, and when their fears seem unrealistic we may long to reassure them, yet there is no reassurance and psychiatry grasps for how to help. Psychiatry has looked to draw lines for when normal grief crosses to abnormal. Is it an adjustment disorder, complicated grief, “prolonged” grief, pathology in need of medication and medicalization, or something one experiences individually, sometimes for a very long time even with treatment?
One justification for pathologizing “prolonged” reactions includes the fact that insurers will pay for treatment only if there is a diagnosis code, and shouldn’t people in distress be entitled to psychotherapy or medication? Yet there is something offensive about telling someone that they are mentally ill if they don’t grieve along a prescribed timeline, as much as there is about denying them the possible benefits of therapy or medication if they seek it, but are suffering in all the “right” ways. Psychiatry’s approach to death is inelegant at best.
In his poignant podcast series, All There Is, Anderson Cooper is tasked with sorting through his mother’s apartment after her death at age 95. In the course of packing up her belongings, he brings on other guests to talk about their emotional reactions to death. Mr. Cooper’s mother, Gloria Vanderbilt, died at an advanced age, but his father died after a brief cardiac illness when Mr. Cooper was a child, and his brother died by suicide when he was 21. He uses these experiences as a springboard to examine childhood losses, the aftermath of suicide, and the loneliness of grief.
“Loss and grief is this universal experience that we will all go through multiple times in our lives,” Mr. Cooper says, “And yet it leaves us feeling so alone and so separated from other people. At least it does me and has my entire life.”
When we talk about grief and loss, we talk about “getting over it,” or “moving on.” But loss doesn’t work that way – time usually eases the pain, leaving scars that are part of the road map for who we are on the journey that defines us.
Sudden death is hard, and the unexpected death of a young person is tragic. For Cait McFarland, there are the decades she won’t get to experience. For her family and friends, it may be excruciating, and for all the patients who have lost a psychiatrist, may time bring healing and peace.
The Dr. Caitlin McFarland Educational Fund for LGBTQI+ Mental Health is being established, and donations are being accepted at https://www.gofundme.com/f/in-memory-of-cait-mcfarland.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships.
“It is one of life’s most self-evident truths that everything fades, that we fear the fading, and that we must live, nonetheless, in the face of the fear.” – Irvin D. Yalom, MD, Existential Psychotherapy, 1980
The email was titled simply, “A sorrowful note,” and I knew that someone had died. I held my breath and read as Dr. Jimmy Potash informed our entire department that Dr. Cait McFarland died in a car accident on December 7 while driving to work at West Cecil Health Center, Conowingo, Md., where she was director of psychiatry.
Sadness swelled as I remembered the outspoken resident who was interested in LGBTQ issues. Cait graduated from the Johns Hopkins residency program in 2020, she had recently married a social worker in the department, and the plan was for her to return to Hopkins full-time in July 2023 to be director of a clinic focused on mental health for people who are transgendered.
Sudden deaths are tragic and jarring and they call to the surface our losses from the past. These deaths don’t stand alone – I found myself thinking of my editor at Medscape, Dr. Bret Stetka, who died unexpectedly in August 2022, and then of Dr. Lidia Palcan Wenz, a psychiatrist I trained with, who died in a motor vehicle accident in 2004. Lidia’s husband also died in the accident, while their two young children in the back seat survived – this tragedy haunted me for some time. None of these people was close to me, but I am no stranger to the impact of unexpected death: My parents and brother all died from cardiac events, and any sudden death is a reminder of those losses.
Julia Riddle, MD, trained with Cait McFarland and was her close friend for years. “I don’t have a belief in ‘the afterlife’ but do like to think of the people that I have lost together in my memory – as if they are all suddenly in a new room together. And, with each loss, all the other occupants of that room come freshly to life again,” Dr. Riddle said.
Death is our shared destination in life, but sudden and unexpected deaths carry their own weight. There is no chance to tie up loose ends, to repair riffs, to say goodbye. Nothing is put in order, and the life that was to be lived goes on for some time as bills arrive, social and work events go unattended, vacations are canceled, and there is the awkward moment of running into someone who didn’t know your loved one has died.
Roger Lewin, MD, is a psychiatrist and writer in Towson, Md. He has both personal and professional experience with sudden death. “There is no way to prepare beforehand, so we have to get ready for what has already happened, and that is hard,” he said. “We invent a life for ourselves and others that extends into the future, and that gets interrupted.”
Most people become ill and die on a vaguely predictable schedule. There may be a chance to plan, to know and honor the wishes of the individual, and often there is the opportunity for loved ones to begin the grieving process gradually as death approaches. For those who are elderly, there may be a sense that this is the natural order of things – which may or may not temper the intensity of the grief for those who remain. If the person has suffered, the end may come with relief.
Still, I sometimes find myself surprised at the length and intensity of anguish that some people experience after losing a loved one who has lived a long and full life, who declined and suffered, but whose absence remains a gaping wound that takes years to form a scar.
Sudden death is not rare; accidents, homicide, and suicide are the top killers among young people, and cardiovascular deaths are number one among those who are older. Natural disasters and terrorist attacks can cause catastrophic numbers of sudden deaths and leave survivors to grieve not only the dead, but the loss of all that was familiar to them.
Psychiatry has been a bit lost as to how we approach grief. We often hear patients talk about anxiety surrounding death and illness, be it a fear of death or a longing for it. These fears can seem irrational – I am reminded of a patient who was afraid to eat romaine because of news reports that it was responsible for food poisoning in other states, but not Maryland, where the person lived. I found it odd that he worried about eating lettuce, but not about smoking two packs of cigarettes a day.
But our fears are like that – they move to what the media sensationalizes, or to what may be remote, because otherwise no one would get in a car or clear their walkway of snow. Life is most easily lived with a bit of denial: We shut out the reality that we can be here one moment, overscheduled and overwhelmed, with deadlines, mortgage payments, and summer vacation plans, oblivious to the fact that life may end at any moment. The early months of COVID-19 felt like a global game of Russian roulette, with each venture out a pull of the trigger and everyone’s defenses stripped bare.
While death belongs to us all, we relegate it to the disciplines of religion, philosophy, the arts, and psychology. Religion offers answers – whether a heaven, a hell, or continual reincarnation until the individual attains enlightenment, there is a destination. Perhaps it will be pleasant, perhaps not, and for some there is the hope that one gets to be the driver by having the right beliefs or doing good deeds, while others are comforted by the hope of being reunited with loved ones.
“The suddenness endures and the shock lasts – it’s like a meteor that creates a crater and we revisit it in different ways from different angles,” Dr. Lewin said. “It may leap on us unexpectedly, often many years later.”
Patients talk about death, and when their fears seem unrealistic we may long to reassure them, yet there is no reassurance and psychiatry grasps for how to help. Psychiatry has looked to draw lines for when normal grief crosses to abnormal. Is it an adjustment disorder, complicated grief, “prolonged” grief, pathology in need of medication and medicalization, or something one experiences individually, sometimes for a very long time even with treatment?
One justification for pathologizing “prolonged” reactions includes the fact that insurers will pay for treatment only if there is a diagnosis code, and shouldn’t people in distress be entitled to psychotherapy or medication? Yet there is something offensive about telling someone that they are mentally ill if they don’t grieve along a prescribed timeline, as much as there is about denying them the possible benefits of therapy or medication if they seek it, but are suffering in all the “right” ways. Psychiatry’s approach to death is inelegant at best.
In his poignant podcast series, All There Is, Anderson Cooper is tasked with sorting through his mother’s apartment after her death at age 95. In the course of packing up her belongings, he brings on other guests to talk about their emotional reactions to death. Mr. Cooper’s mother, Gloria Vanderbilt, died at an advanced age, but his father died after a brief cardiac illness when Mr. Cooper was a child, and his brother died by suicide when he was 21. He uses these experiences as a springboard to examine childhood losses, the aftermath of suicide, and the loneliness of grief.
“Loss and grief is this universal experience that we will all go through multiple times in our lives,” Mr. Cooper says, “And yet it leaves us feeling so alone and so separated from other people. At least it does me and has my entire life.”
When we talk about grief and loss, we talk about “getting over it,” or “moving on.” But loss doesn’t work that way – time usually eases the pain, leaving scars that are part of the road map for who we are on the journey that defines us.
Sudden death is hard, and the unexpected death of a young person is tragic. For Cait McFarland, there are the decades she won’t get to experience. For her family and friends, it may be excruciating, and for all the patients who have lost a psychiatrist, may time bring healing and peace.
The Dr. Caitlin McFarland Educational Fund for LGBTQI+ Mental Health is being established, and donations are being accepted at https://www.gofundme.com/f/in-memory-of-cait-mcfarland.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore. She has disclosed no relevant financial relationships.
Depression: Think outside of the box for diagnosis, treatment
In the treatment of depression, clinicians are commonly dealing with a mix of comorbidities that are more complex than just depression, and as such, effective treatment options may likewise require thinking outside of the box – and beyond the definitions of the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision).
“The DSM-5 isn’t handed to us on tablets from Mount Sinai,” said Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral sciences at the Mulva Clinic for the Neurosciences at the University of Texas at Austin. He spoke at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Our patients don’t fall into these very convenient buckets,” Dr. Nemeroff said. “The problem with depression is patients have very high rates of morbidity and comorbidity.”
The array of potential psychiatric comorbidities that are common in depression is somewhat staggering: As many as 70% of patients also have social anxiety disorder; 67% of patients have obsessive-compulsive disorder (OCD); up to 65% of patients have panic disorder; 48% of patients have posttraumatic stress disorder (PTSD); and 42% have generalized anxiety disorder, Dr. Nemeroff said.
And while the DSM-5 may have all those bases covered, in real world clinical practice, cracking the code of each patient’s unique and often more complicated psychiatric profile – and how to best manage it – can be a challenge. But Dr. Nemeroff said important clues can guide the clinician’s path.
A key starting point is making sure to gauge the severity of the patient’s core depression with one of the validated depression scales – whether it’s the self-reported Beck Depression Inventory, the clinician-rated Hamilton Rating Scale for Depression, the clinician-rated Montgomery Asberg Depression Rating Scale, or the Inventory of Depressive Symptoms, clinicians should pick one and track the score with each visit, Dr. Nemeroff advised.
“It doesn’t matter which tool you prefer – most tend to like the Beck Depression Scale, but the bottom line is that you have to get a measure of severity at every visit,” he said.
Among the most important comorbidities to identify as soon as possible is bipolar disorder, due to the potential worsening of the condition that can occur among those patients if treated with antidepressants, Dr. Nemeroff said.
“The question of whether the patient is bipolar should always be in the back of your mind,” he cautioned. “And if patients have been started on antidepressants, the clues may become evident very quickly.”
The most important indicator that the patient has bipolar disorder “is if they tell you that they were prescribed an antidepressant and it resulted in an increase in what we know to be hypomania – they may describe it as agitation or an inability to sleep,” Dr. Nemeroff said.
Of note, the effect is much more common with SNRIs [serotonin norepinephrine reuptake inhibitors] than SSRIs [selective serotonin reuptake inhibitors], he said.
“The effect is particularly notable with venlafaxine,” he said. “But SNRIs all have the propensity to switch people with depression into hypomania, but only patients who have bipolar disorder.”
“If you give a patient 150 mg of venlafaxine and they switch to developing hypomania, you now have the diagnosis of bipolar disorder, and you can treat them appropriately.”
Other important clues of bipolarity in depressed patients include:
- Family history: Most cases are genetically driven.
- Earlier age of onset (younger than age 25): “If the patient tells you they were depressed prepuberty, you should be thinking about the possibility of bipolar disorder, as it often presents as depression in childhood.”
- Psychotic features: As many as 80% of patients with psychotic depression end up being bipolar, Dr. Nemeroff said.
- Atypical depression: For example, depression with hypersomnia, or having an increased appetite instead of decreased, or a high amount of anxiety.
Remission should be the goal of treatment, and Dr. Nemeroff said that in efforts to accomplish that with the help of medications, psychiatrists may need to think “outside of the box” – or beyond the label.
“Many practitioners become slaves to the PDR [Physicians’ Desk Reference],” he said. “It is only a guide to what the clinical trials show, and not a mandate in terms of dosing.”
“There’s often strong data in the literature that supports going to a higher dose, if necessary, and I have [plenty] of patients, for instance, on 450 or 600 mg of venlafaxine who had not responded to 150 or even 300 mg.”
Treatment resistance
When patients continue to fail to respond, regardless of dosing or medication adjustments, Dr. Nemeroff suggested that clinicians should consider the potential important reasons. For instance, in addition to comorbid psychiatric conditions, practitioners should determine if there are medical conditions that they are not aware of.
“Does the patient have an underlying medical condition, such as thyroid dysfunction, early Parkinson’s disease, or even something like cancer?” he said.
There is also the inevitable question of whether the patient is indeed taking the medication. “We know that 30% of our patients do not follow their prescriptions, so of course that’s an important question to ask,” Dr. Nemeroff said.
Finally, while some pharmacogenomic tests are emerging with the suggestion of identifying which patients may or may not respond to certain drugs, Dr. Nemeroff says he’s seen little convincing evidence of their benefits.
“We have a problem in this field in that we don’t have the kinds of markers that they do in oncology, so we’re left with having to generally play trial and error,” he said.
“But when it comes to these pharmacogenomic tests, there’s just no ‘there there’,” he asserted. “From what I’ve seen so far, it’s frankly neuro-mythology.”
Dr. Nemeroff disclosed that he receives grant/research support from the National Institutes of Health and serves as a consultant for and/or on the advisory boards of multiple pharmaceutical companies.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
In the treatment of depression, clinicians are commonly dealing with a mix of comorbidities that are more complex than just depression, and as such, effective treatment options may likewise require thinking outside of the box – and beyond the definitions of the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision).
“The DSM-5 isn’t handed to us on tablets from Mount Sinai,” said Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral sciences at the Mulva Clinic for the Neurosciences at the University of Texas at Austin. He spoke at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Our patients don’t fall into these very convenient buckets,” Dr. Nemeroff said. “The problem with depression is patients have very high rates of morbidity and comorbidity.”
The array of potential psychiatric comorbidities that are common in depression is somewhat staggering: As many as 70% of patients also have social anxiety disorder; 67% of patients have obsessive-compulsive disorder (OCD); up to 65% of patients have panic disorder; 48% of patients have posttraumatic stress disorder (PTSD); and 42% have generalized anxiety disorder, Dr. Nemeroff said.
And while the DSM-5 may have all those bases covered, in real world clinical practice, cracking the code of each patient’s unique and often more complicated psychiatric profile – and how to best manage it – can be a challenge. But Dr. Nemeroff said important clues can guide the clinician’s path.
A key starting point is making sure to gauge the severity of the patient’s core depression with one of the validated depression scales – whether it’s the self-reported Beck Depression Inventory, the clinician-rated Hamilton Rating Scale for Depression, the clinician-rated Montgomery Asberg Depression Rating Scale, or the Inventory of Depressive Symptoms, clinicians should pick one and track the score with each visit, Dr. Nemeroff advised.
“It doesn’t matter which tool you prefer – most tend to like the Beck Depression Scale, but the bottom line is that you have to get a measure of severity at every visit,” he said.
Among the most important comorbidities to identify as soon as possible is bipolar disorder, due to the potential worsening of the condition that can occur among those patients if treated with antidepressants, Dr. Nemeroff said.
“The question of whether the patient is bipolar should always be in the back of your mind,” he cautioned. “And if patients have been started on antidepressants, the clues may become evident very quickly.”
The most important indicator that the patient has bipolar disorder “is if they tell you that they were prescribed an antidepressant and it resulted in an increase in what we know to be hypomania – they may describe it as agitation or an inability to sleep,” Dr. Nemeroff said.
Of note, the effect is much more common with SNRIs [serotonin norepinephrine reuptake inhibitors] than SSRIs [selective serotonin reuptake inhibitors], he said.
“The effect is particularly notable with venlafaxine,” he said. “But SNRIs all have the propensity to switch people with depression into hypomania, but only patients who have bipolar disorder.”
“If you give a patient 150 mg of venlafaxine and they switch to developing hypomania, you now have the diagnosis of bipolar disorder, and you can treat them appropriately.”
Other important clues of bipolarity in depressed patients include:
- Family history: Most cases are genetically driven.
- Earlier age of onset (younger than age 25): “If the patient tells you they were depressed prepuberty, you should be thinking about the possibility of bipolar disorder, as it often presents as depression in childhood.”
- Psychotic features: As many as 80% of patients with psychotic depression end up being bipolar, Dr. Nemeroff said.
- Atypical depression: For example, depression with hypersomnia, or having an increased appetite instead of decreased, or a high amount of anxiety.
Remission should be the goal of treatment, and Dr. Nemeroff said that in efforts to accomplish that with the help of medications, psychiatrists may need to think “outside of the box” – or beyond the label.
“Many practitioners become slaves to the PDR [Physicians’ Desk Reference],” he said. “It is only a guide to what the clinical trials show, and not a mandate in terms of dosing.”
“There’s often strong data in the literature that supports going to a higher dose, if necessary, and I have [plenty] of patients, for instance, on 450 or 600 mg of venlafaxine who had not responded to 150 or even 300 mg.”
Treatment resistance
When patients continue to fail to respond, regardless of dosing or medication adjustments, Dr. Nemeroff suggested that clinicians should consider the potential important reasons. For instance, in addition to comorbid psychiatric conditions, practitioners should determine if there are medical conditions that they are not aware of.
“Does the patient have an underlying medical condition, such as thyroid dysfunction, early Parkinson’s disease, or even something like cancer?” he said.
There is also the inevitable question of whether the patient is indeed taking the medication. “We know that 30% of our patients do not follow their prescriptions, so of course that’s an important question to ask,” Dr. Nemeroff said.
Finally, while some pharmacogenomic tests are emerging with the suggestion of identifying which patients may or may not respond to certain drugs, Dr. Nemeroff says he’s seen little convincing evidence of their benefits.
“We have a problem in this field in that we don’t have the kinds of markers that they do in oncology, so we’re left with having to generally play trial and error,” he said.
“But when it comes to these pharmacogenomic tests, there’s just no ‘there there’,” he asserted. “From what I’ve seen so far, it’s frankly neuro-mythology.”
Dr. Nemeroff disclosed that he receives grant/research support from the National Institutes of Health and serves as a consultant for and/or on the advisory boards of multiple pharmaceutical companies.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
In the treatment of depression, clinicians are commonly dealing with a mix of comorbidities that are more complex than just depression, and as such, effective treatment options may likewise require thinking outside of the box – and beyond the definitions of the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision).
“The DSM-5 isn’t handed to us on tablets from Mount Sinai,” said Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral sciences at the Mulva Clinic for the Neurosciences at the University of Texas at Austin. He spoke at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Our patients don’t fall into these very convenient buckets,” Dr. Nemeroff said. “The problem with depression is patients have very high rates of morbidity and comorbidity.”
The array of potential psychiatric comorbidities that are common in depression is somewhat staggering: As many as 70% of patients also have social anxiety disorder; 67% of patients have obsessive-compulsive disorder (OCD); up to 65% of patients have panic disorder; 48% of patients have posttraumatic stress disorder (PTSD); and 42% have generalized anxiety disorder, Dr. Nemeroff said.
And while the DSM-5 may have all those bases covered, in real world clinical practice, cracking the code of each patient’s unique and often more complicated psychiatric profile – and how to best manage it – can be a challenge. But Dr. Nemeroff said important clues can guide the clinician’s path.
A key starting point is making sure to gauge the severity of the patient’s core depression with one of the validated depression scales – whether it’s the self-reported Beck Depression Inventory, the clinician-rated Hamilton Rating Scale for Depression, the clinician-rated Montgomery Asberg Depression Rating Scale, or the Inventory of Depressive Symptoms, clinicians should pick one and track the score with each visit, Dr. Nemeroff advised.
“It doesn’t matter which tool you prefer – most tend to like the Beck Depression Scale, but the bottom line is that you have to get a measure of severity at every visit,” he said.
Among the most important comorbidities to identify as soon as possible is bipolar disorder, due to the potential worsening of the condition that can occur among those patients if treated with antidepressants, Dr. Nemeroff said.
“The question of whether the patient is bipolar should always be in the back of your mind,” he cautioned. “And if patients have been started on antidepressants, the clues may become evident very quickly.”
The most important indicator that the patient has bipolar disorder “is if they tell you that they were prescribed an antidepressant and it resulted in an increase in what we know to be hypomania – they may describe it as agitation or an inability to sleep,” Dr. Nemeroff said.
Of note, the effect is much more common with SNRIs [serotonin norepinephrine reuptake inhibitors] than SSRIs [selective serotonin reuptake inhibitors], he said.
“The effect is particularly notable with venlafaxine,” he said. “But SNRIs all have the propensity to switch people with depression into hypomania, but only patients who have bipolar disorder.”
“If you give a patient 150 mg of venlafaxine and they switch to developing hypomania, you now have the diagnosis of bipolar disorder, and you can treat them appropriately.”
Other important clues of bipolarity in depressed patients include:
- Family history: Most cases are genetically driven.
- Earlier age of onset (younger than age 25): “If the patient tells you they were depressed prepuberty, you should be thinking about the possibility of bipolar disorder, as it often presents as depression in childhood.”
- Psychotic features: As many as 80% of patients with psychotic depression end up being bipolar, Dr. Nemeroff said.
- Atypical depression: For example, depression with hypersomnia, or having an increased appetite instead of decreased, or a high amount of anxiety.
Remission should be the goal of treatment, and Dr. Nemeroff said that in efforts to accomplish that with the help of medications, psychiatrists may need to think “outside of the box” – or beyond the label.
“Many practitioners become slaves to the PDR [Physicians’ Desk Reference],” he said. “It is only a guide to what the clinical trials show, and not a mandate in terms of dosing.”
“There’s often strong data in the literature that supports going to a higher dose, if necessary, and I have [plenty] of patients, for instance, on 450 or 600 mg of venlafaxine who had not responded to 150 or even 300 mg.”
Treatment resistance
When patients continue to fail to respond, regardless of dosing or medication adjustments, Dr. Nemeroff suggested that clinicians should consider the potential important reasons. For instance, in addition to comorbid psychiatric conditions, practitioners should determine if there are medical conditions that they are not aware of.
“Does the patient have an underlying medical condition, such as thyroid dysfunction, early Parkinson’s disease, or even something like cancer?” he said.
There is also the inevitable question of whether the patient is indeed taking the medication. “We know that 30% of our patients do not follow their prescriptions, so of course that’s an important question to ask,” Dr. Nemeroff said.
Finally, while some pharmacogenomic tests are emerging with the suggestion of identifying which patients may or may not respond to certain drugs, Dr. Nemeroff says he’s seen little convincing evidence of their benefits.
“We have a problem in this field in that we don’t have the kinds of markers that they do in oncology, so we’re left with having to generally play trial and error,” he said.
“But when it comes to these pharmacogenomic tests, there’s just no ‘there there’,” he asserted. “From what I’ve seen so far, it’s frankly neuro-mythology.”
Dr. Nemeroff disclosed that he receives grant/research support from the National Institutes of Health and serves as a consultant for and/or on the advisory boards of multiple pharmaceutical companies.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
FROM PSYCHOPHARMACOLOGY UPDATE
Suicidality in an older patient with chronic kidney disease
CASE Depressed, anxious, and suicidal
Mr. J, age 72, is brought to the emergency department by law enforcement at his wife’s request due to worsening suicidal thoughts and anxiety. He has a history of major depressive disorder (MDD) and chronic kidney disease (CKD). Mr. J has been compliant with his medications, but they seem to no longer be effective. He is admitted to the geriatric psychiatry unit.
HISTORY Increased debilitation
Over the past several years, Mr. J has experienced increasing debilitation at home, including difficulty walking and an inability to perform activities of daily life. Recently, he has begun to ask for multiple pills in an attempt to take his own life.
Mr. J has been previously treated in a psychiatric clinic with duloxetine 60 mg/d, mirtazapine 30 mg/d at bedtime, buspirone 15 mg 3 times a day, and trazodone 50 mg/d at bedtime. He is also taking amlodipine 5 mg twice daily for hypertension, lisinopril 2.5 mg/d for hypertension, furosemide 20 mg/d orally for CKD, and potassium chloride 10 mEq/d for hypokalemia secondary to CKD and furosemide use. Over the past year, his psychiatric medications have been steadily increased to target his MDD and anxiety.
EVALUATION Disorientation and Stage 3A CKD
In the psychiatric unit, Mr. J describes panic, feelings of impending doom, and profound anxiety. He states he has increasing anxiety related to “being a burden” on his family and wife. Additionally, he describes decreased appetite, difficulty sleeping, low energy, difficulty concentrating, no interest in outside activities, and feelings of hopelessness.
Mr. J’s temperature is 39.2o C; heart rate is 109 beats per minute; respiratory rate is 18 breaths per minute; blood pressure is 157/83 mm Hg; and pulse oximetry is 97%. Laboratory screening indicates a red blood cell count of 3.57, hemoglobin 11.2, hematocrit 33.8, red blood cell distribution width 17.5, blood urea nitrogen 45, creatinine 1.5 with no known baseline, and an estimated glomerular filtration rate (GFR) of 46 mL/min, indicating Stage 3A CKD (Table 11). Additional testing rules out other potential causes of delirium and psychosis.
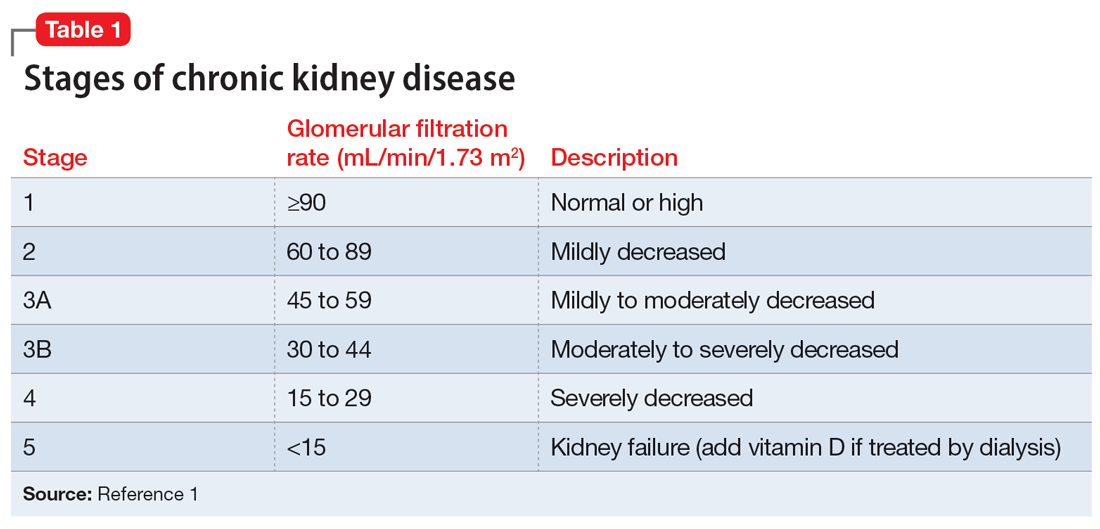
A physical exam reveals Mr. J has a fine tremor, myoclonus, muscle rigidity, and hyperreflexia. He is oriented to name, but not to date, place, or situation, and is easily confused. Mr. J uses a walker but has significant tremors while walking and immediately asks for assistance due to profound anxiety related to a fear of falling. Mr. J’s mood and affect are labile with tearful and anxious episodes. His anxiety focuses on overvalued thoughts of minor or irrelevant concerns. Additionally, he has poor insight and judgment. When asked about the cause of his anxiety, Mr. J says, “I don’t know why I’m anxious; I’m just a worrywart.” His memory is impaired, and he does not know why he is in the hospital. Mr. J scores 24 on the Montreal Cognitive Assessment, which indicates mild impairment.
Mr. J continues to endorse suicidal ideation but denies homicidal thoughts. Based on these symptoms, the differential diagnosis includes serotonin syndrome, MDD with suicidal ideation, generalized anxiety disorder, and panic disorder.
Continue to: The authors' observations
[polldaddy:11273789]
The authors’ observations
GFR is used to determine the level of renal impairment. Mr. J’s GFR of 46 mL/min indicates Stage 3A CKD (Table 11 ). Additionally, he displayed anemia and increased creatinine due to CKD. Twenty percent of patients with CKD also experience MDD.2 In a prospective observational cohort study, Hedayati et al3 found that Stage 2 to Stage 5 CKD with MDD leads to an increased risk of death, hospitalization, or progression to dialysis. It is important to properly manage Mr. J’s MDD and CKD to prevent future comorbidities. Renal impairment is common in people age >65.4 Even when GFR is normal, it is recommended to decrease dosing of medications in older adults due to age-related decreased renal excretion. As kidneys decrease in function, their ability to excrete normal amounts of medications also decreases, leading to increased serum levels and potential toxicity.
A combination of 4 serotonergic psychotropic medications may not be unusual to address treatment-resistant depression in a healthy, nongeriatric adult. However, Mr. J displayed signs of serotonin toxicity, such as hyperthermia, tachycardia, increased blood pressure, increased tremors, myoclonus, hyperreflexia, and muscle rigidity. These are classic signs of serotonin toxicity. For Mr. J, serotonin toxicity can be treated with the removal of serotonergic medications and lorazepam for symptom relief. If symptoms persist, cyproheptadine, a serotonin antagonist, can be used. Mr. J’s psychotropic medications were increased in an outpatient setting and he was unable to renally excrete higher doses of these serotonergic agents, which lead to chronic serotonin toxicity.
It is important to rule out other causes of psychosis or delirium in geriatric patients. A study by Marcantonio et al5 found that >40% of patients referred to a consulting psychiatrist for depression ultimately had delirium, and this was more likely in geriatric patients.
TREATMENT Adjustments to the medication regimen
The treatment team decides to taper and discontinue duloxetine, buspirone, and trazodone and reduce mirtazapine to 15 mg/d at bedtime. Additionally, oral lorazepam 1 mg as needed is prescribed to alleviate agitation and correct vital signs. Mr. J’s vital signs improve, with decreased temperature and normal cardiac and respiratory rhythms.
Mr. J’s Stage 3A CKD is treated with oral fluids, and his hypertension is managed with an increase of lisinopril from 2.5 mg/d to 10 mg/d. After 10 days on the psychiatric unit, he shows improvement, decreased anxiety, and remission of suicidal ideation.
Continue to: The authors' observations
[polldaddy:11273790]
The authors’ observations
In 2019, the American Geriatric Society (AGS) updated the Beers Criteria for potentially inappropriate medication use in older adults.4 The Beers Criteria were created to educate clinicians about the use of potentially inappropriate medications that have an unfavorable balance of benefits and risks compared to alternative treatments. The AGS lists medications that should be avoided or have their dosage reduced with varying levels of kidney function in older adults. Duloxetine is one of the medications listed with the recommendation to avoid for patients with a creatinine clearance <30 mL/min. Creatinine clearance is an estimation of GFR.
Although duloxetine is mentioned in the Beers Criteria, many other antidepressants have metabolites excreted by the kidneys.6 Potential adverse effects include increased bleeding, nausea, vomiting, and serotonin toxicity symptoms.7 Mr. J has Stage 3A CKD and takes 4 psychotropics, which will additively increase the serum concentration of serotonergic medications. In terms of treatment for serotonin toxicity, it is important to remove the causative medications. After discontinuing serotonergic medications, lorazepam can be administered as needed. If a patient continues to have symptoms, cyproheptadine is an option.
For patients with impaired renal function, adding nonpharmacologic options should be considered, such as cognitive-behavioral therapy, electroconvulsive therapy, and transcranial magnetic stimulation. Table 24,8-18 lists the minimum effective doses for well-known medications for treating MDD.
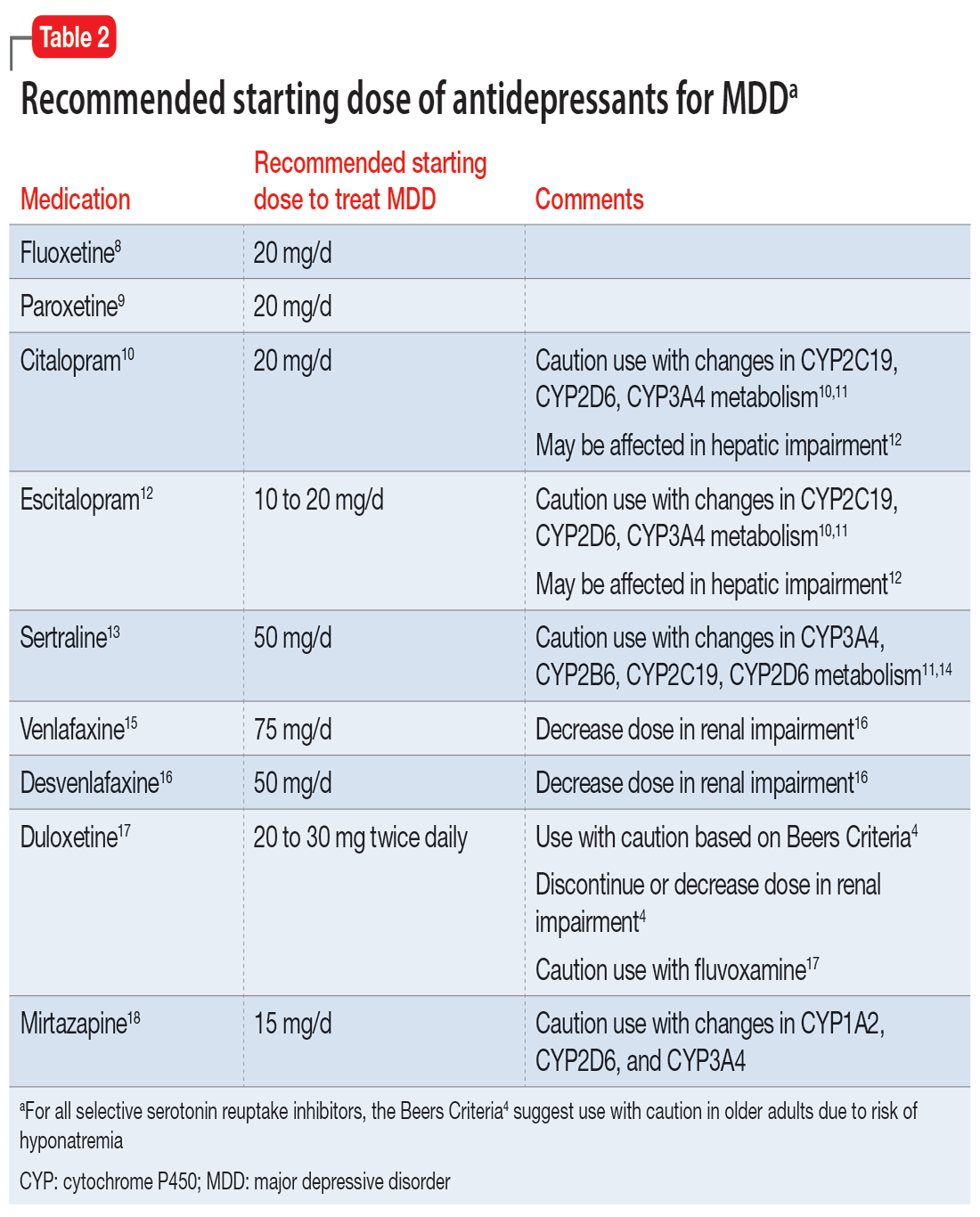
OUTCOME Improvement and discharge
Mr. J’s confusion improves, his heart rate decreases, and his feelings of panic and doom improve. He continues to have depressive symptoms, but his suicidal ideation stops. At discharge, Mr. J is receiving mirtazapine 15 mg/d, potassium chloride 10 mEq/d orally, lisinopril 20 mg/d orally at bedtime, furosemide 20 mg/d orally, and amlodipine 5 mg orally twice a day. Additionally, the treatment team recommends psychotherapy to Mr. J to address his anxiety and depression.
Bottom Line
Older patients are more sensitive to psychotropic medications, regardless of any comorbidities. It is important to review each patient’s glomerular filtration rate to better understand their renal function and adjust medications accordingly.
Related Resources
- Whittaker P, Vordenberg SE, Coe AB. Deprescribing in older adults: an overview. Current Psychiatry. 2022;21(5):40-43. doi:10.12788/cp.0246
- Gibson G, Kennedy LH, Barlow G. Polypharmacy in older adults. Current Psychiatry. 2020;19(4):40-46.
- Barr R, Miskle B, Thomas C. Management of major depressive disorder with psychotic features. Current Psychiatry. 2021;20(2):30-33. doi:10.12788/cp.0092
Drug Brand Names
Amlodipine • Norvasc
Buspirone • BuSpar
Citalopram • Celexa
Cyproheptadine • Periactin
Desvenlafaxine • Pristiq
Duloxetine • Cymbalta
Escitalopram • Lexapro
Fluoxetine • Prozac
Furosemide • Lasix
Lisinopril • Zestril
Lorazepam • Ativan
Mirtazapine • Remeron
Paroxetine • Paxil
Sertraline • Zoloft
Trazodone • Desyrel
Venlafaxine • Effexor
1. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1-S266.
2. Shirazian S, Grant CD, Aina O, et al. Depression in chronic kidney disease and end-stage renal disease: similarities and differences in diagnosis, epidemiology, and management. Kidney Int Rep. 2017;2(1):94-107.
3. Hedayati SS, Minhajuddin AT, Afshar M, et al. Association between major depressive episodes in patients with chronic kidney disease and initiation of dialysis, hospitalization, or death. JAMA. 2010;303(19):1946-1953.
4. 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-694.
5. Marcantonio E, Ta T, Duthie E, et al. Delirium severity and psychomotor types: their relationship with outcomes after hip fracture repair. J Am Geriatr Soc. 2002;50(5):850-857.
6. Cukor D, Cohen, SD, Peterson RA, et al. Psychosocial aspects of chronic disease: ESRD as a paradigmatic illness. J Am Soc Nephrol. 2007;18(12):3042-3055.
7. Cohen SD, Norris L, Acquaviva K, et al. Screening, diagnosis, and treatment of depression in patients with end-stage renal disease. Clin J Am Soc Nephrol. 2007;2(6):1332-1342.
8. Sommi RW, Crismon ML, Bowden CL. Fluoxetine: a serotonin-specific, second-generation antidepressant. Pharmacotherapy. 1987;7(1):1-15.
9. Jenner PN. Paroxetine: an overview of dosage, tolerability, and safety. Int Clin Psychopharmacol. 1992;6(Suppl 4):69-80.
10. Montgomery SA. Selecting the optimum therapeutic dose of serotonin reuptake inhibitors: studies with citalopram. Int Clin Psychopharmacol. 1995;10(Suppl 1):23-27.
11. Milosavljevic F, Bukvic N, Pavlovic Z, et al. Association of CYP2C19 and CYP2D6 poor and intermediate metabolizer status with antidepressant and antipsychotic exposure: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78(3):270-280.
12. Rao N. The clinical pharmacokinetics of escitalopram. Clin Pharmacokinet. 2007;46(4):281-290.
13. Preskorn SH, Lane RM. Sertraline 50 mg daily: the optimal dose in the treatment of depression. Int Clin Psychopharmacol. 1995;10(3):129-141.
14. Huddart R, Hicks JK, Ramsey LB, et al. PharmGKB summary: sertraline pathway, pharmacokinetics. Pharmacogenet Genomics. 2020;30(2):26-33.
15. Furukawa TA, Cipriani A, Cowen PJ, et al. Optimal dose of selective serotonin reuptake inhibitors, venlafaxine, and mirtazapine in major depression: a systematic review and dose-response meta-analysis. Lancet Psychiatry. 2019;6(7):601-609.
16. Norman TR, Olver JS. Desvenlafaxine in the treatment of major depression: an updated overview. Expert Opin Pharmacother. 2021;22(9):1087-1097.
17. Knadler MP, Lobo E, Chappell J, et al. Duloxetine: clinical pharmacokinetics and drug interactions. Clin Pharmacokinet. 2011;50(5):281-294.
18. Anttila SA, Leinonen EV. A review of the pharmacological and clinical profile of mirtazapine. CNS Drug Rev. 2001;7(3):249-264.
CASE Depressed, anxious, and suicidal
Mr. J, age 72, is brought to the emergency department by law enforcement at his wife’s request due to worsening suicidal thoughts and anxiety. He has a history of major depressive disorder (MDD) and chronic kidney disease (CKD). Mr. J has been compliant with his medications, but they seem to no longer be effective. He is admitted to the geriatric psychiatry unit.
HISTORY Increased debilitation
Over the past several years, Mr. J has experienced increasing debilitation at home, including difficulty walking and an inability to perform activities of daily life. Recently, he has begun to ask for multiple pills in an attempt to take his own life.
Mr. J has been previously treated in a psychiatric clinic with duloxetine 60 mg/d, mirtazapine 30 mg/d at bedtime, buspirone 15 mg 3 times a day, and trazodone 50 mg/d at bedtime. He is also taking amlodipine 5 mg twice daily for hypertension, lisinopril 2.5 mg/d for hypertension, furosemide 20 mg/d orally for CKD, and potassium chloride 10 mEq/d for hypokalemia secondary to CKD and furosemide use. Over the past year, his psychiatric medications have been steadily increased to target his MDD and anxiety.
EVALUATION Disorientation and Stage 3A CKD
In the psychiatric unit, Mr. J describes panic, feelings of impending doom, and profound anxiety. He states he has increasing anxiety related to “being a burden” on his family and wife. Additionally, he describes decreased appetite, difficulty sleeping, low energy, difficulty concentrating, no interest in outside activities, and feelings of hopelessness.
Mr. J’s temperature is 39.2o C; heart rate is 109 beats per minute; respiratory rate is 18 breaths per minute; blood pressure is 157/83 mm Hg; and pulse oximetry is 97%. Laboratory screening indicates a red blood cell count of 3.57, hemoglobin 11.2, hematocrit 33.8, red blood cell distribution width 17.5, blood urea nitrogen 45, creatinine 1.5 with no known baseline, and an estimated glomerular filtration rate (GFR) of 46 mL/min, indicating Stage 3A CKD (Table 11). Additional testing rules out other potential causes of delirium and psychosis.
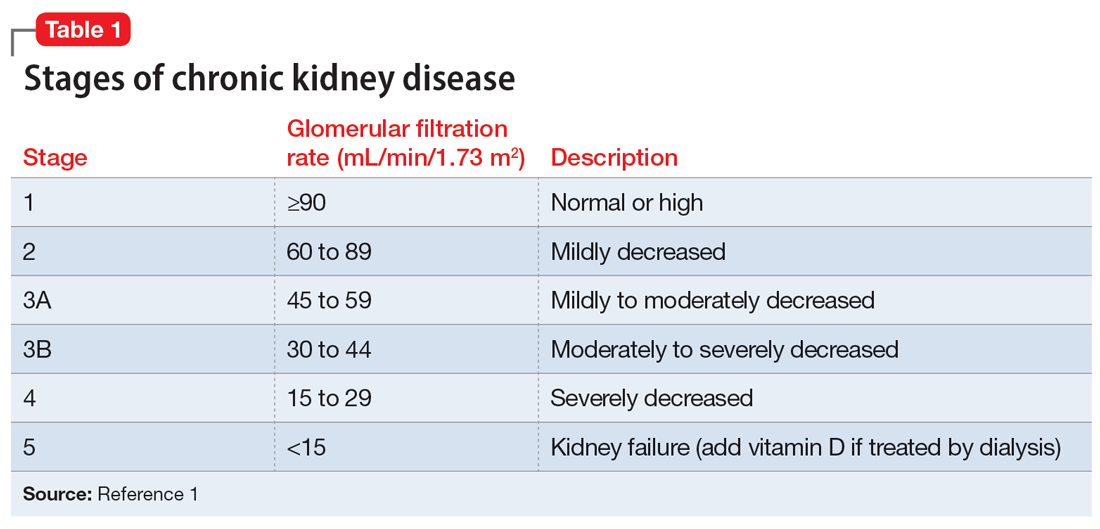
A physical exam reveals Mr. J has a fine tremor, myoclonus, muscle rigidity, and hyperreflexia. He is oriented to name, but not to date, place, or situation, and is easily confused. Mr. J uses a walker but has significant tremors while walking and immediately asks for assistance due to profound anxiety related to a fear of falling. Mr. J’s mood and affect are labile with tearful and anxious episodes. His anxiety focuses on overvalued thoughts of minor or irrelevant concerns. Additionally, he has poor insight and judgment. When asked about the cause of his anxiety, Mr. J says, “I don’t know why I’m anxious; I’m just a worrywart.” His memory is impaired, and he does not know why he is in the hospital. Mr. J scores 24 on the Montreal Cognitive Assessment, which indicates mild impairment.
Mr. J continues to endorse suicidal ideation but denies homicidal thoughts. Based on these symptoms, the differential diagnosis includes serotonin syndrome, MDD with suicidal ideation, generalized anxiety disorder, and panic disorder.
Continue to: The authors' observations
[polldaddy:11273789]
The authors’ observations
GFR is used to determine the level of renal impairment. Mr. J’s GFR of 46 mL/min indicates Stage 3A CKD (Table 11 ). Additionally, he displayed anemia and increased creatinine due to CKD. Twenty percent of patients with CKD also experience MDD.2 In a prospective observational cohort study, Hedayati et al3 found that Stage 2 to Stage 5 CKD with MDD leads to an increased risk of death, hospitalization, or progression to dialysis. It is important to properly manage Mr. J’s MDD and CKD to prevent future comorbidities. Renal impairment is common in people age >65.4 Even when GFR is normal, it is recommended to decrease dosing of medications in older adults due to age-related decreased renal excretion. As kidneys decrease in function, their ability to excrete normal amounts of medications also decreases, leading to increased serum levels and potential toxicity.
A combination of 4 serotonergic psychotropic medications may not be unusual to address treatment-resistant depression in a healthy, nongeriatric adult. However, Mr. J displayed signs of serotonin toxicity, such as hyperthermia, tachycardia, increased blood pressure, increased tremors, myoclonus, hyperreflexia, and muscle rigidity. These are classic signs of serotonin toxicity. For Mr. J, serotonin toxicity can be treated with the removal of serotonergic medications and lorazepam for symptom relief. If symptoms persist, cyproheptadine, a serotonin antagonist, can be used. Mr. J’s psychotropic medications were increased in an outpatient setting and he was unable to renally excrete higher doses of these serotonergic agents, which lead to chronic serotonin toxicity.
It is important to rule out other causes of psychosis or delirium in geriatric patients. A study by Marcantonio et al5 found that >40% of patients referred to a consulting psychiatrist for depression ultimately had delirium, and this was more likely in geriatric patients.
TREATMENT Adjustments to the medication regimen
The treatment team decides to taper and discontinue duloxetine, buspirone, and trazodone and reduce mirtazapine to 15 mg/d at bedtime. Additionally, oral lorazepam 1 mg as needed is prescribed to alleviate agitation and correct vital signs. Mr. J’s vital signs improve, with decreased temperature and normal cardiac and respiratory rhythms.
Mr. J’s Stage 3A CKD is treated with oral fluids, and his hypertension is managed with an increase of lisinopril from 2.5 mg/d to 10 mg/d. After 10 days on the psychiatric unit, he shows improvement, decreased anxiety, and remission of suicidal ideation.
Continue to: The authors' observations
[polldaddy:11273790]
The authors’ observations
In 2019, the American Geriatric Society (AGS) updated the Beers Criteria for potentially inappropriate medication use in older adults.4 The Beers Criteria were created to educate clinicians about the use of potentially inappropriate medications that have an unfavorable balance of benefits and risks compared to alternative treatments. The AGS lists medications that should be avoided or have their dosage reduced with varying levels of kidney function in older adults. Duloxetine is one of the medications listed with the recommendation to avoid for patients with a creatinine clearance <30 mL/min. Creatinine clearance is an estimation of GFR.
Although duloxetine is mentioned in the Beers Criteria, many other antidepressants have metabolites excreted by the kidneys.6 Potential adverse effects include increased bleeding, nausea, vomiting, and serotonin toxicity symptoms.7 Mr. J has Stage 3A CKD and takes 4 psychotropics, which will additively increase the serum concentration of serotonergic medications. In terms of treatment for serotonin toxicity, it is important to remove the causative medications. After discontinuing serotonergic medications, lorazepam can be administered as needed. If a patient continues to have symptoms, cyproheptadine is an option.
For patients with impaired renal function, adding nonpharmacologic options should be considered, such as cognitive-behavioral therapy, electroconvulsive therapy, and transcranial magnetic stimulation. Table 24,8-18 lists the minimum effective doses for well-known medications for treating MDD.
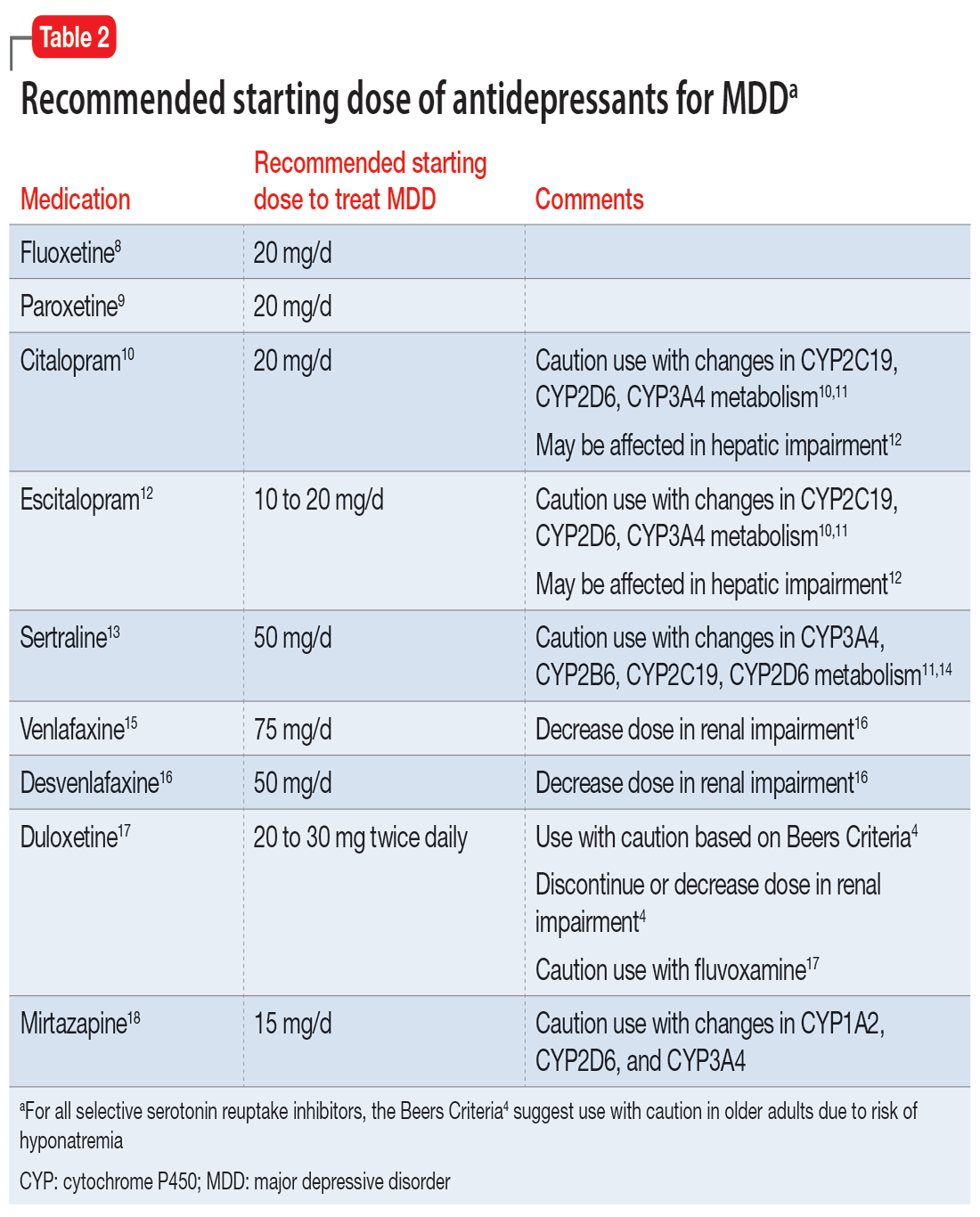
OUTCOME Improvement and discharge
Mr. J’s confusion improves, his heart rate decreases, and his feelings of panic and doom improve. He continues to have depressive symptoms, but his suicidal ideation stops. At discharge, Mr. J is receiving mirtazapine 15 mg/d, potassium chloride 10 mEq/d orally, lisinopril 20 mg/d orally at bedtime, furosemide 20 mg/d orally, and amlodipine 5 mg orally twice a day. Additionally, the treatment team recommends psychotherapy to Mr. J to address his anxiety and depression.
Bottom Line
Older patients are more sensitive to psychotropic medications, regardless of any comorbidities. It is important to review each patient’s glomerular filtration rate to better understand their renal function and adjust medications accordingly.
Related Resources
- Whittaker P, Vordenberg SE, Coe AB. Deprescribing in older adults: an overview. Current Psychiatry. 2022;21(5):40-43. doi:10.12788/cp.0246
- Gibson G, Kennedy LH, Barlow G. Polypharmacy in older adults. Current Psychiatry. 2020;19(4):40-46.
- Barr R, Miskle B, Thomas C. Management of major depressive disorder with psychotic features. Current Psychiatry. 2021;20(2):30-33. doi:10.12788/cp.0092
Drug Brand Names
Amlodipine • Norvasc
Buspirone • BuSpar
Citalopram • Celexa
Cyproheptadine • Periactin
Desvenlafaxine • Pristiq
Duloxetine • Cymbalta
Escitalopram • Lexapro
Fluoxetine • Prozac
Furosemide • Lasix
Lisinopril • Zestril
Lorazepam • Ativan
Mirtazapine • Remeron
Paroxetine • Paxil
Sertraline • Zoloft
Trazodone • Desyrel
Venlafaxine • Effexor
CASE Depressed, anxious, and suicidal
Mr. J, age 72, is brought to the emergency department by law enforcement at his wife’s request due to worsening suicidal thoughts and anxiety. He has a history of major depressive disorder (MDD) and chronic kidney disease (CKD). Mr. J has been compliant with his medications, but they seem to no longer be effective. He is admitted to the geriatric psychiatry unit.
HISTORY Increased debilitation
Over the past several years, Mr. J has experienced increasing debilitation at home, including difficulty walking and an inability to perform activities of daily life. Recently, he has begun to ask for multiple pills in an attempt to take his own life.
Mr. J has been previously treated in a psychiatric clinic with duloxetine 60 mg/d, mirtazapine 30 mg/d at bedtime, buspirone 15 mg 3 times a day, and trazodone 50 mg/d at bedtime. He is also taking amlodipine 5 mg twice daily for hypertension, lisinopril 2.5 mg/d for hypertension, furosemide 20 mg/d orally for CKD, and potassium chloride 10 mEq/d for hypokalemia secondary to CKD and furosemide use. Over the past year, his psychiatric medications have been steadily increased to target his MDD and anxiety.
EVALUATION Disorientation and Stage 3A CKD
In the psychiatric unit, Mr. J describes panic, feelings of impending doom, and profound anxiety. He states he has increasing anxiety related to “being a burden” on his family and wife. Additionally, he describes decreased appetite, difficulty sleeping, low energy, difficulty concentrating, no interest in outside activities, and feelings of hopelessness.
Mr. J’s temperature is 39.2o C; heart rate is 109 beats per minute; respiratory rate is 18 breaths per minute; blood pressure is 157/83 mm Hg; and pulse oximetry is 97%. Laboratory screening indicates a red blood cell count of 3.57, hemoglobin 11.2, hematocrit 33.8, red blood cell distribution width 17.5, blood urea nitrogen 45, creatinine 1.5 with no known baseline, and an estimated glomerular filtration rate (GFR) of 46 mL/min, indicating Stage 3A CKD (Table 11). Additional testing rules out other potential causes of delirium and psychosis.
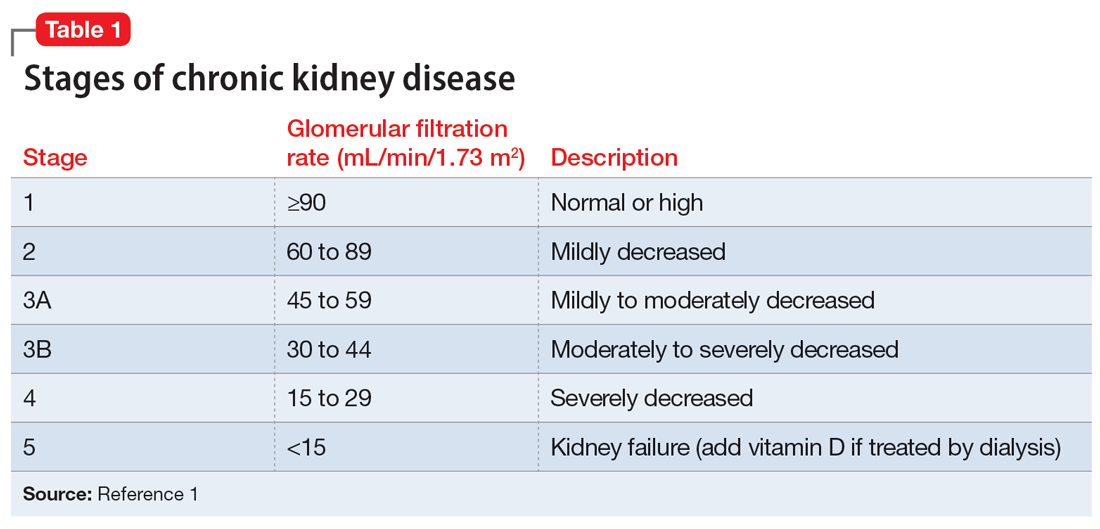
A physical exam reveals Mr. J has a fine tremor, myoclonus, muscle rigidity, and hyperreflexia. He is oriented to name, but not to date, place, or situation, and is easily confused. Mr. J uses a walker but has significant tremors while walking and immediately asks for assistance due to profound anxiety related to a fear of falling. Mr. J’s mood and affect are labile with tearful and anxious episodes. His anxiety focuses on overvalued thoughts of minor or irrelevant concerns. Additionally, he has poor insight and judgment. When asked about the cause of his anxiety, Mr. J says, “I don’t know why I’m anxious; I’m just a worrywart.” His memory is impaired, and he does not know why he is in the hospital. Mr. J scores 24 on the Montreal Cognitive Assessment, which indicates mild impairment.
Mr. J continues to endorse suicidal ideation but denies homicidal thoughts. Based on these symptoms, the differential diagnosis includes serotonin syndrome, MDD with suicidal ideation, generalized anxiety disorder, and panic disorder.
Continue to: The authors' observations
[polldaddy:11273789]
The authors’ observations
GFR is used to determine the level of renal impairment. Mr. J’s GFR of 46 mL/min indicates Stage 3A CKD (Table 11 ). Additionally, he displayed anemia and increased creatinine due to CKD. Twenty percent of patients with CKD also experience MDD.2 In a prospective observational cohort study, Hedayati et al3 found that Stage 2 to Stage 5 CKD with MDD leads to an increased risk of death, hospitalization, or progression to dialysis. It is important to properly manage Mr. J’s MDD and CKD to prevent future comorbidities. Renal impairment is common in people age >65.4 Even when GFR is normal, it is recommended to decrease dosing of medications in older adults due to age-related decreased renal excretion. As kidneys decrease in function, their ability to excrete normal amounts of medications also decreases, leading to increased serum levels and potential toxicity.
A combination of 4 serotonergic psychotropic medications may not be unusual to address treatment-resistant depression in a healthy, nongeriatric adult. However, Mr. J displayed signs of serotonin toxicity, such as hyperthermia, tachycardia, increased blood pressure, increased tremors, myoclonus, hyperreflexia, and muscle rigidity. These are classic signs of serotonin toxicity. For Mr. J, serotonin toxicity can be treated with the removal of serotonergic medications and lorazepam for symptom relief. If symptoms persist, cyproheptadine, a serotonin antagonist, can be used. Mr. J’s psychotropic medications were increased in an outpatient setting and he was unable to renally excrete higher doses of these serotonergic agents, which lead to chronic serotonin toxicity.
It is important to rule out other causes of psychosis or delirium in geriatric patients. A study by Marcantonio et al5 found that >40% of patients referred to a consulting psychiatrist for depression ultimately had delirium, and this was more likely in geriatric patients.
TREATMENT Adjustments to the medication regimen
The treatment team decides to taper and discontinue duloxetine, buspirone, and trazodone and reduce mirtazapine to 15 mg/d at bedtime. Additionally, oral lorazepam 1 mg as needed is prescribed to alleviate agitation and correct vital signs. Mr. J’s vital signs improve, with decreased temperature and normal cardiac and respiratory rhythms.
Mr. J’s Stage 3A CKD is treated with oral fluids, and his hypertension is managed with an increase of lisinopril from 2.5 mg/d to 10 mg/d. After 10 days on the psychiatric unit, he shows improvement, decreased anxiety, and remission of suicidal ideation.
Continue to: The authors' observations
[polldaddy:11273790]
The authors’ observations
In 2019, the American Geriatric Society (AGS) updated the Beers Criteria for potentially inappropriate medication use in older adults.4 The Beers Criteria were created to educate clinicians about the use of potentially inappropriate medications that have an unfavorable balance of benefits and risks compared to alternative treatments. The AGS lists medications that should be avoided or have their dosage reduced with varying levels of kidney function in older adults. Duloxetine is one of the medications listed with the recommendation to avoid for patients with a creatinine clearance <30 mL/min. Creatinine clearance is an estimation of GFR.
Although duloxetine is mentioned in the Beers Criteria, many other antidepressants have metabolites excreted by the kidneys.6 Potential adverse effects include increased bleeding, nausea, vomiting, and serotonin toxicity symptoms.7 Mr. J has Stage 3A CKD and takes 4 psychotropics, which will additively increase the serum concentration of serotonergic medications. In terms of treatment for serotonin toxicity, it is important to remove the causative medications. After discontinuing serotonergic medications, lorazepam can be administered as needed. If a patient continues to have symptoms, cyproheptadine is an option.
For patients with impaired renal function, adding nonpharmacologic options should be considered, such as cognitive-behavioral therapy, electroconvulsive therapy, and transcranial magnetic stimulation. Table 24,8-18 lists the minimum effective doses for well-known medications for treating MDD.
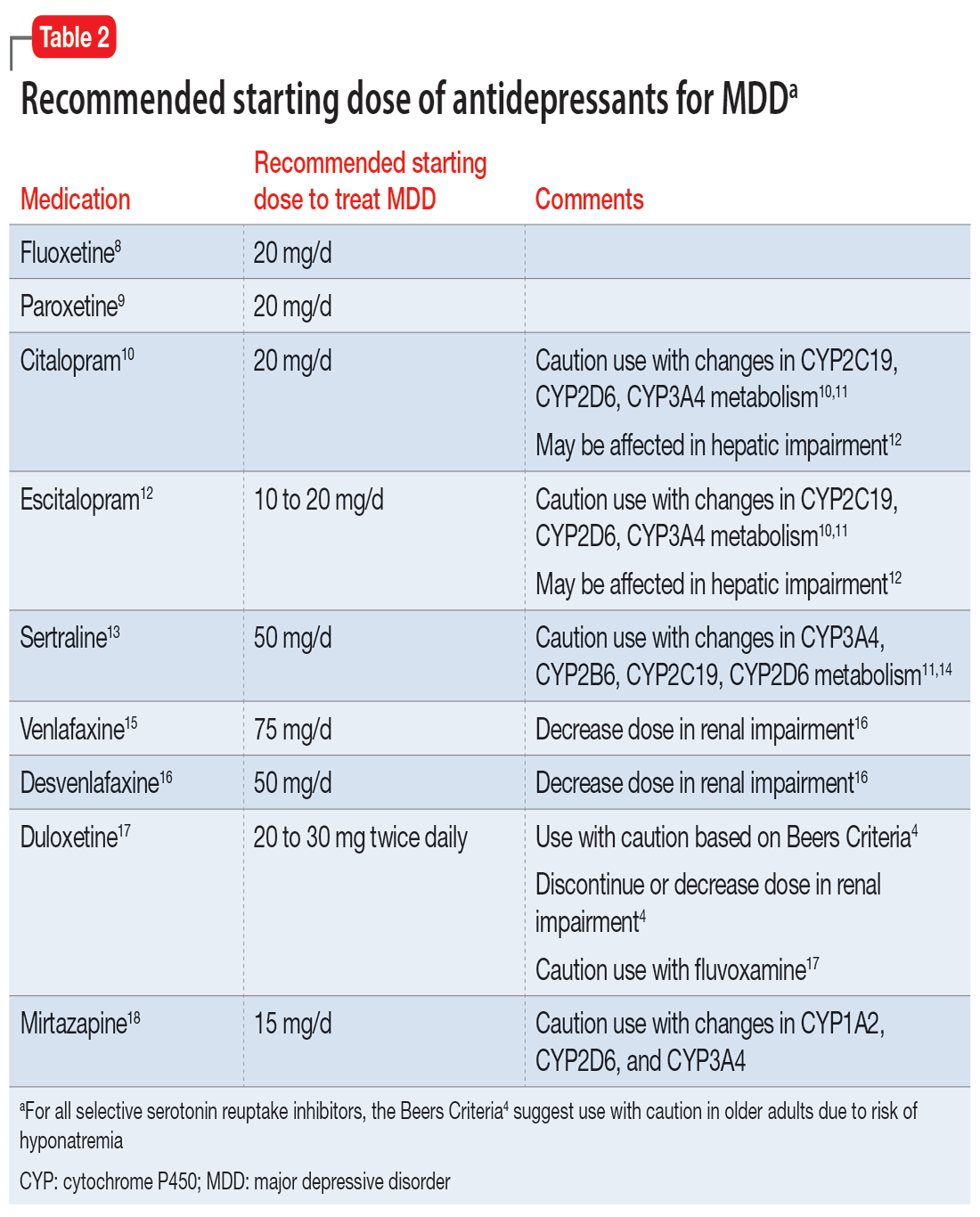
OUTCOME Improvement and discharge
Mr. J’s confusion improves, his heart rate decreases, and his feelings of panic and doom improve. He continues to have depressive symptoms, but his suicidal ideation stops. At discharge, Mr. J is receiving mirtazapine 15 mg/d, potassium chloride 10 mEq/d orally, lisinopril 20 mg/d orally at bedtime, furosemide 20 mg/d orally, and amlodipine 5 mg orally twice a day. Additionally, the treatment team recommends psychotherapy to Mr. J to address his anxiety and depression.
Bottom Line
Older patients are more sensitive to psychotropic medications, regardless of any comorbidities. It is important to review each patient’s glomerular filtration rate to better understand their renal function and adjust medications accordingly.
Related Resources
- Whittaker P, Vordenberg SE, Coe AB. Deprescribing in older adults: an overview. Current Psychiatry. 2022;21(5):40-43. doi:10.12788/cp.0246
- Gibson G, Kennedy LH, Barlow G. Polypharmacy in older adults. Current Psychiatry. 2020;19(4):40-46.
- Barr R, Miskle B, Thomas C. Management of major depressive disorder with psychotic features. Current Psychiatry. 2021;20(2):30-33. doi:10.12788/cp.0092
Drug Brand Names
Amlodipine • Norvasc
Buspirone • BuSpar
Citalopram • Celexa
Cyproheptadine • Periactin
Desvenlafaxine • Pristiq
Duloxetine • Cymbalta
Escitalopram • Lexapro
Fluoxetine • Prozac
Furosemide • Lasix
Lisinopril • Zestril
Lorazepam • Ativan
Mirtazapine • Remeron
Paroxetine • Paxil
Sertraline • Zoloft
Trazodone • Desyrel
Venlafaxine • Effexor
1. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1-S266.
2. Shirazian S, Grant CD, Aina O, et al. Depression in chronic kidney disease and end-stage renal disease: similarities and differences in diagnosis, epidemiology, and management. Kidney Int Rep. 2017;2(1):94-107.
3. Hedayati SS, Minhajuddin AT, Afshar M, et al. Association between major depressive episodes in patients with chronic kidney disease and initiation of dialysis, hospitalization, or death. JAMA. 2010;303(19):1946-1953.
4. 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-694.
5. Marcantonio E, Ta T, Duthie E, et al. Delirium severity and psychomotor types: their relationship with outcomes after hip fracture repair. J Am Geriatr Soc. 2002;50(5):850-857.
6. Cukor D, Cohen, SD, Peterson RA, et al. Psychosocial aspects of chronic disease: ESRD as a paradigmatic illness. J Am Soc Nephrol. 2007;18(12):3042-3055.
7. Cohen SD, Norris L, Acquaviva K, et al. Screening, diagnosis, and treatment of depression in patients with end-stage renal disease. Clin J Am Soc Nephrol. 2007;2(6):1332-1342.
8. Sommi RW, Crismon ML, Bowden CL. Fluoxetine: a serotonin-specific, second-generation antidepressant. Pharmacotherapy. 1987;7(1):1-15.
9. Jenner PN. Paroxetine: an overview of dosage, tolerability, and safety. Int Clin Psychopharmacol. 1992;6(Suppl 4):69-80.
10. Montgomery SA. Selecting the optimum therapeutic dose of serotonin reuptake inhibitors: studies with citalopram. Int Clin Psychopharmacol. 1995;10(Suppl 1):23-27.
11. Milosavljevic F, Bukvic N, Pavlovic Z, et al. Association of CYP2C19 and CYP2D6 poor and intermediate metabolizer status with antidepressant and antipsychotic exposure: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78(3):270-280.
12. Rao N. The clinical pharmacokinetics of escitalopram. Clin Pharmacokinet. 2007;46(4):281-290.
13. Preskorn SH, Lane RM. Sertraline 50 mg daily: the optimal dose in the treatment of depression. Int Clin Psychopharmacol. 1995;10(3):129-141.
14. Huddart R, Hicks JK, Ramsey LB, et al. PharmGKB summary: sertraline pathway, pharmacokinetics. Pharmacogenet Genomics. 2020;30(2):26-33.
15. Furukawa TA, Cipriani A, Cowen PJ, et al. Optimal dose of selective serotonin reuptake inhibitors, venlafaxine, and mirtazapine in major depression: a systematic review and dose-response meta-analysis. Lancet Psychiatry. 2019;6(7):601-609.
16. Norman TR, Olver JS. Desvenlafaxine in the treatment of major depression: an updated overview. Expert Opin Pharmacother. 2021;22(9):1087-1097.
17. Knadler MP, Lobo E, Chappell J, et al. Duloxetine: clinical pharmacokinetics and drug interactions. Clin Pharmacokinet. 2011;50(5):281-294.
18. Anttila SA, Leinonen EV. A review of the pharmacological and clinical profile of mirtazapine. CNS Drug Rev. 2001;7(3):249-264.
1. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1-S266.
2. Shirazian S, Grant CD, Aina O, et al. Depression in chronic kidney disease and end-stage renal disease: similarities and differences in diagnosis, epidemiology, and management. Kidney Int Rep. 2017;2(1):94-107.
3. Hedayati SS, Minhajuddin AT, Afshar M, et al. Association between major depressive episodes in patients with chronic kidney disease and initiation of dialysis, hospitalization, or death. JAMA. 2010;303(19):1946-1953.
4. 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-694.
5. Marcantonio E, Ta T, Duthie E, et al. Delirium severity and psychomotor types: their relationship with outcomes after hip fracture repair. J Am Geriatr Soc. 2002;50(5):850-857.
6. Cukor D, Cohen, SD, Peterson RA, et al. Psychosocial aspects of chronic disease: ESRD as a paradigmatic illness. J Am Soc Nephrol. 2007;18(12):3042-3055.
7. Cohen SD, Norris L, Acquaviva K, et al. Screening, diagnosis, and treatment of depression in patients with end-stage renal disease. Clin J Am Soc Nephrol. 2007;2(6):1332-1342.
8. Sommi RW, Crismon ML, Bowden CL. Fluoxetine: a serotonin-specific, second-generation antidepressant. Pharmacotherapy. 1987;7(1):1-15.
9. Jenner PN. Paroxetine: an overview of dosage, tolerability, and safety. Int Clin Psychopharmacol. 1992;6(Suppl 4):69-80.
10. Montgomery SA. Selecting the optimum therapeutic dose of serotonin reuptake inhibitors: studies with citalopram. Int Clin Psychopharmacol. 1995;10(Suppl 1):23-27.
11. Milosavljevic F, Bukvic N, Pavlovic Z, et al. Association of CYP2C19 and CYP2D6 poor and intermediate metabolizer status with antidepressant and antipsychotic exposure: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78(3):270-280.
12. Rao N. The clinical pharmacokinetics of escitalopram. Clin Pharmacokinet. 2007;46(4):281-290.
13. Preskorn SH, Lane RM. Sertraline 50 mg daily: the optimal dose in the treatment of depression. Int Clin Psychopharmacol. 1995;10(3):129-141.
14. Huddart R, Hicks JK, Ramsey LB, et al. PharmGKB summary: sertraline pathway, pharmacokinetics. Pharmacogenet Genomics. 2020;30(2):26-33.
15. Furukawa TA, Cipriani A, Cowen PJ, et al. Optimal dose of selective serotonin reuptake inhibitors, venlafaxine, and mirtazapine in major depression: a systematic review and dose-response meta-analysis. Lancet Psychiatry. 2019;6(7):601-609.
16. Norman TR, Olver JS. Desvenlafaxine in the treatment of major depression: an updated overview. Expert Opin Pharmacother. 2021;22(9):1087-1097.
17. Knadler MP, Lobo E, Chappell J, et al. Duloxetine: clinical pharmacokinetics and drug interactions. Clin Pharmacokinet. 2011;50(5):281-294.
18. Anttila SA, Leinonen EV. A review of the pharmacological and clinical profile of mirtazapine. CNS Drug Rev. 2001;7(3):249-264.
Contemporary psychiatry: A SWOT analysis
Editor’s note: This article was adapted with permission from a version originally published in the Ohio Psychiatric Physician Association’s newsletter, Insight Matters, Fall 2022.
Acknowledging and analyzing strengths, weaknesses, opportunities, and threats (SWOT) is an important tactic many organizations use to develop a strategic plan to grow, move forward, and thrive. A SWOT analysis can provide a “big picture” view of the status and the desired future directions not only for companies but for medical disciplines such as psychiatry. So here are my perspectives on psychiatry’s strengths, weaknesses, opportunities, and threats. It is a work in progress, and I welcome (and encourage) you to send additional items or comments to me at [email protected].
Strengths
- The American Psychiatric Association (APA) is the oldest medical professional organization, established in 1844 (3 years before the American Medical Association)1
- Strong organizational structure and governance, and a “big tent” with several tiers of membership
- Effective, member-driven District Branches
- The medical identity at the core of psychiatry—we are psychiatric physicians2
- Escalating number of senior medical students choosing psychiatry as a career, far more than a decade ago
- High demand for psychiatrists in all settings around the country
- Increased compensation for psychiatrists (market forces of supply and demand)
- Psychiatry is continuously evolving and reinventing itself: seismic shifts in etiopathogenesis, disease conceptualization, terminology, and therapies (4 major shifts over the past century)3
- An abundant body of evidence supporting that all psychiatric disorders are brain disorders and transdiagnostic in nature4
- Many vibrant subspecialty societies
- Substantial number of Tier 1, evidence-based treatments
- Novel mechanisms of action and treatment strategies are being introduced on a regular basis for psychotic and mood disorders5,6
- Advances in neuromodulation techniques to treat a wide spectrum of psychiatric disorders, including electroconvulsive therapy, transcranial magnetic stimulation, vagus nerve stimulation, transcranial direct current stimulation, deep brain stimulation, cranial electric stimulation, epidural cortical stimulation, focused ultrasound, low field magnetic stimulation, magnetic seizure therapy, and near infrared light therapy, with mechanisms that are electric, ultrasound, magnetic, or optical7,8
- Psychiatric physicians develop wisdom by practicing psychiatry (ie, they become more empathic, tolerant of ambiguity, prosocial, introspective, aware of one’s strengths and limitations). Neuroplasticity in the frontal cortex is triggered by conducting psychotherapy9
Weaknesses
- Shrinking workforce due to a static number of residency training slots for 40 years10
- High rate of retirement by aging psychiatrists
- Persistent stigma around mental disorders despite massive scientific and medical advances11
- Still no real parity! We need succinct laws with “teeth”12
- Demedicalization in the public sector, referring to psychiatric physicians as “providers” and labeling patients as “clients”2
- Not enough graduating residents choosing to do subspecialty fellowships (especially geriatric, addiction, psychosomatic psychiatry) to meet escalating societal needs
- Very low presence in rural areas (both psychiatrists and psychiatric hospitals)
- Persistent APA member apathy: only 10% to 15% vote in the APA national elections or volunteer to serve on committees
- Widespread member dissatisfaction with maintenance of certification
- Neuroscience advances are not being translated fast enough for practical clinical applications
- Many in the public at large do not realize psychiatric symptoms are generated from anomalous brain circuits or that psychiatric disorders are highly genetic but also have environmental and epigenetic etiologies
- The DSM diagnostic system needs a paradigm shift: it is still based on a menu of clinical signs and symptoms and is devoid of objective diagnostic measures such as biomarkers4
- Neuroscience literacy among busy psychiatric practitioners is insufficient at a time of explosive growth in basic and clinical neuroscience13
- No effective treatment for alcohol or substance use disorders despite their very high morbidity and mortality
- Major psychiatric disorders are still associated with significant disability (schizophrenia, bipolar disorder, major depressive disorder, anxiety disorders, eating disorders, substance use disorders)
- Suicide rate (other than opioid deaths) has continued to rise in the past 3 decades14
Opportunities
- Potentially momentous clinical applications of the neuroscience breakthroughs
- Collaborative care with primary care physicians and increasing colocalization
- Dramatic increase in public awareness about the importance of mental health due to the COVID-19 pandemic15
- Powerful new data management tools, including machine learning, artificial intelligence, super computers, big data, deep learning, nanotechnology, and metabolomics, all of which are expediting neurobiological discoveries16
- The potential of reclassifying psychiatric disorders as neurological disorders, which will improve reimbursement for patient health care and reduce stigma17
- Emergence of new mechanisms of action of disease etiology, such as microbiota, mitochondrial dysfunction, permeable blood-brain barrier, and neuroimmune dysregulation18,19
- The advent and growth of “precision psychiatry”20
- The tremendous potential of molecular genetics and gene therapy for psychiatric disorders, most of which are genetic in etiology
- Expanding applications of neuroimaging techniques, including morphological, spectroscopic, functional, diffusion tensor imaging, and receptor imaging21
- Epigenetic advances in neuropsychiatric disorders
- Remarkably powerful research methods, such as pluripotent cells (producing neurons from skin cells), optogenetics (activating genes with light), gene-wide association studies, CRISPR (clustered regularly interspaced short palindromic repeats, which serve as genetic scissors to remove and replace abnormal genes), and brain connectomics22
- Psychiatry should develop and promote an “annual mental health checkup” for all age groups, similar to an annual physical exam23
- Focus on the social determinants of health
- Address the unmet mental health needs of individuals who are members of minority groups
- Lobby ferociously for a much larger budget for the National Institute of Mental Health to advance funding for research of serious psychiatric brain disorders
- Remind Congress continuously that the cost of mental illness is $700 billion annually and costs can only be reduced by funding neurobiological research1
- Partner with the pharmaceutical industry instead of demonizing them. They are the only entity that develops medication for psychiatry, where 80% of disorders have no FDA-approved drugs.24 Without the pharmaceutical industry and the help of medications, many psychiatric patients would still be institutionalized and unable to lead a normal life. We must recognize the contributions of pharmaceutical companies to the health of our patients, similar to the warp speed development of vaccines for the deadly coronavirus
- Psychiatric clinicians must refer patients to clinical trials because without patients enrolling in FDA studies, no drug developments can take place
- Many “out-of-the-box” therapies are being developed, such as antiapoptotic therapy, microglia inhibition, mitochondrial repair, white matter fiber remyelination, neuroprotection, and reversing N-methyl-
d -aspartate receptor hypofunction25 - The emerging evidence that psychotherapy is in fact a biological treatment that induces brain changes (neuroplasticity) and can modulate the immune system26
- Druggable genes, providing innovative new medications27
- Reposition psychedelics as revolutionary new treatments28
- Emphasize measurement-based care (rating scales), which can upgrade patient care29
- Because psychosis is associated with brain tissue loss, just like heart attacks are associated with myocardium destruction, psychiatrists must act like cardiologists30 and treat psychotic episodes urgently, like a stroke,31 to reduce the duration of untreated psychosis and improve patient outcomes
Threats
- Antipsychiatry cults continue to disparage and attack psychiatry32
- Health delivery systems are replacing psychiatric physicians with nurse practitioners to lower costs, regardless of quality and experience, and they inappropriately lump them together as “providers”2
- Psychologists continue to seek prescribing privileges with absurdly sketchy, predominantly online training supervised by other psychologists33
- Many legislators and policymakers, as well as the public, still don’t understand the difference between psychiatrists and psychologists, and the extensively disparate medical training in quality and quantity
- A dearth of psychiatric physician-scientists because very few residents are pursuing research fellowships after training34
- Disproportionate emphasis on clinical care and generating clinical revenue (relative value units) in academic institutions, with fewer tenure-track faculty members having protected time to write grants for federal or foundation grants to support their salaries and research operations35
- Meager financial support for teaching in psychiatry departments
- Many seriously psychiatrically ill persons do not have access to psychiatric medical care (and often to primary care as well)
- Many in the public falsely believe psychiatric disorders are hopeless and untreatable, which perpetuates stigma
- Long-acting injectable antipsychotic formulations are not used early enough in patients with psychosis, who are known to have a high nonadherence rate with oral medications following discharge from their first hospitalization. This leads to many recurrences with multiple devastating consequences, including progressive brain tissue loss, treatment resistance, disability, incarceration, and suicide36
- Many clinicians do not have full-text access to all studies indexed in PubMed, which is vital for lifelong learning in a rapidly growing medical discipline such as psychiatry
- Psychiatrists are often unable to prescribe medications shortly after they are approved by the FDA due to the insurance companies’ outrageous preauthorization racket that enforces a fail-first policy with cheaper generics, even if generic medications are associated with safety and tolerability problems37
- The continued use of decades-old first-generation antipsychotic medications despite 32 published studies reporting their neurotoxicity and the death of brain cells38
Using this analysis to benefit our patients
Despite its strengths, psychiatry must overcome its weaknesses, fend off its threats, and exploit its many opportunities. The only way to do that is for psychiatrists to unify and for the APA to provide inspired leadership to achieve the aspirational goals of our field. However, we must adopt “moonshot thinking”39 to magnify the Ss, diminish the Ws, exploit the Os, and stave off the Ts of our SWOT, thereby attaining all our cherished and lofty goals. Ultimately, the greatest beneficiaries will be our patients.
1. Nasrallah HA. 20 reasons to celebrate our APA membership. Current Psychiatry. 2020;19(1):6-9.
2. Nasrallah HA. We are physicians, not providers, and we treat patients, not clients! Current Psychiatry. 2020;19(2):5-8.
3. Nasrallah HA. From bedlam to biomarkers: the transformation of psychiatry’s terminology reflects its 4 conceptual earthquakes. Current Psychiatry. 2015;14(1):5-7.
4. Nasrallah HA. Re-inventing the DSM as a transdiagnostic model: psychiatric disorders are extensively interconnected. Ann Clin Psychiatry. 2021;33(3):148-150.
5. Nasrallah HA. Psychopharmacology 3.0. Current Psychiatry. 2081;17(11):4-7.
6. Nasrallah HA. Reversing depression: a plethora of therapeutic strategies and mechanisms. Current Psychiatry. 2022;21(8):4-6.
7. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Psychopharmacology. 2012;37(1):102-116.
8. Nasrallah HA. Optimal psychiatric treatment: target the brain and avoid the body. Current Psychiatry. 2022;21(12):3-6.
9. Nasrallah HA. Does psychiatry practice make us wise? Current Psychiatry. 2009;8(10):12-14.
10. Buckley PF, Nasrallah HA. The psychiatry workforce pool is shrinking. What are we doing about it? Current Psychiatry. 2016;15(9):23-24,95.
11. Nasrallah HA. A psychiatric manifesto: stigma is hate speech and a hate crime. Current Psychiatry. 2022;21(6):6-8.
12. Nasrallah HA. The travesty of disparity and non-parity. Current Psychiatry. 2014;13(1):8,19.
13. Nasrallah HA. Advancing clinical neuroscience literacy among psychiatric practitioners. Current Psychiatry. 2017;16(9):17-18.
14. Nasrallah HA. The scourge of societal anosognosia about the mentally ill. Current Psychiatry. 2016;15(6):19-24.
15. Nasrallah HA. 10 silver linings of the COVID-19 pandemic. Insight Matters. 2021;45:3-4.
16. Kalenderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019:18(8):33-38.
17. Nasrallah HA. Let’s tear down the silos and re-unify psychiatry and neurology! Current Psychiatry. 2013;12(8):8-9.
18. Nasrallah HA. It takes guts to be mentally ill: microbiota and psychopathology. Current Psychiatry. 2018;17(9):4-6.
19. Schrenk DA, Nasrallah HA. Faulty fences: blood-brain barrier dysfunction in schizophrenia. Current Psychiatry. 2022;21(10):28-32.
20. Nasrallah HA. The dawn of precision psychiatry. Current Psychiatry. 2017;16(12):7-8,11.
21. Nasrallah HA. Today’s psychiatric neuroscience advances were science fiction during my residency. Current Psychiatry 2021;20(4):5-7,12,24.
22. Nasrallah HA. Transformative advances are unfolding in psychiatry. Current Psychiatry. 2019;18(9):10-12.
23. Nasrallah HA. I have a dream…for psychiatry. Current Psychiatry. 2021;20(11):12-14.
24. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian J Psychiatry. 2009;2(1):29-36.
25. Nasrallah HA. Transformative advances are unfolding in psychiatry. Current Psychiatry. 2019;18(9):10-12.
26. Nasrallah HA. Repositioning psychotherapy as a neurobiological intervention. Current Psychiatry. 2013;12(12):18-19.
27. Nasrallah HA. Druggable genes, promiscuous drugs, repurposed medications. Current Psychiatry. 2016;15(5):23,27.
28. Nasrallah HA. Long overdue: measurement-based psychiatric practice. Current Psychiatry. 2009;8(4):14-16.
29. Nasrallah HA. Maddening therapies: how hallucinogens morphed into novel treatments. Current Psychiatry. 2017:16(1):19-21.
30. Nasrallah HA. For first episode psychosis, psychiatrists should behave like cardiologists. Current Psychiatry. 2017;16(8):4-7.
31. Nasrallah HA, Roque A. FAST and RAPID: acronyms to prevent brain damage in stroke and psychosis. Current Psychiatry. 2018;17(8):6-8.
32. Nasrallah HA. The antipsychiatry movement: who and why. Current Psychiatry. 2011;10(12):4,6,53.
33. Nasrallah HA. Prescribing is the culmination of extensive medical training and psychologists do not qualify. Current Psychiatry. 2017;16(6):11-12,14-16.
34. Fenton W, James R, Insel T. Psychiatry residency training, the physician-scientist, and the future of psychiatry. Acad Psychiatry. 2004;28(4):263-266.
35. Balon R, Morreale MK. The precipitous decline of academic medicine in the United States. Ann Clin Psychiatry. 2020;32(4):225-227.
36. Nasrallah HA. 10 devastating consequences of psychotic relapses. Current Psychiatry. 2021;20(5):9-12.
37. Nasrallah HA. Pre-authorization is illegal, unethical, and adversely disrupts patient care. Current Psychiatry. 2020;19(4):5-11.
38. Nasrallah HA, Chen AT. Multiple neurotoxic effects of haloperidol resulting in neuronal death. Ann Clin Psychiatry. 2017;29(3):195-202.
39. Nasrallah HA. It’s time for moonshot thinking in psychiatry. Current Psychiatry. 2022;21(2):8-10.
Editor’s note: This article was adapted with permission from a version originally published in the Ohio Psychiatric Physician Association’s newsletter, Insight Matters, Fall 2022.
Acknowledging and analyzing strengths, weaknesses, opportunities, and threats (SWOT) is an important tactic many organizations use to develop a strategic plan to grow, move forward, and thrive. A SWOT analysis can provide a “big picture” view of the status and the desired future directions not only for companies but for medical disciplines such as psychiatry. So here are my perspectives on psychiatry’s strengths, weaknesses, opportunities, and threats. It is a work in progress, and I welcome (and encourage) you to send additional items or comments to me at [email protected].
Strengths
- The American Psychiatric Association (APA) is the oldest medical professional organization, established in 1844 (3 years before the American Medical Association)1
- Strong organizational structure and governance, and a “big tent” with several tiers of membership
- Effective, member-driven District Branches
- The medical identity at the core of psychiatry—we are psychiatric physicians2
- Escalating number of senior medical students choosing psychiatry as a career, far more than a decade ago
- High demand for psychiatrists in all settings around the country
- Increased compensation for psychiatrists (market forces of supply and demand)
- Psychiatry is continuously evolving and reinventing itself: seismic shifts in etiopathogenesis, disease conceptualization, terminology, and therapies (4 major shifts over the past century)3
- An abundant body of evidence supporting that all psychiatric disorders are brain disorders and transdiagnostic in nature4
- Many vibrant subspecialty societies
- Substantial number of Tier 1, evidence-based treatments
- Novel mechanisms of action and treatment strategies are being introduced on a regular basis for psychotic and mood disorders5,6
- Advances in neuromodulation techniques to treat a wide spectrum of psychiatric disorders, including electroconvulsive therapy, transcranial magnetic stimulation, vagus nerve stimulation, transcranial direct current stimulation, deep brain stimulation, cranial electric stimulation, epidural cortical stimulation, focused ultrasound, low field magnetic stimulation, magnetic seizure therapy, and near infrared light therapy, with mechanisms that are electric, ultrasound, magnetic, or optical7,8
- Psychiatric physicians develop wisdom by practicing psychiatry (ie, they become more empathic, tolerant of ambiguity, prosocial, introspective, aware of one’s strengths and limitations). Neuroplasticity in the frontal cortex is triggered by conducting psychotherapy9
Weaknesses
- Shrinking workforce due to a static number of residency training slots for 40 years10
- High rate of retirement by aging psychiatrists
- Persistent stigma around mental disorders despite massive scientific and medical advances11
- Still no real parity! We need succinct laws with “teeth”12
- Demedicalization in the public sector, referring to psychiatric physicians as “providers” and labeling patients as “clients”2
- Not enough graduating residents choosing to do subspecialty fellowships (especially geriatric, addiction, psychosomatic psychiatry) to meet escalating societal needs
- Very low presence in rural areas (both psychiatrists and psychiatric hospitals)
- Persistent APA member apathy: only 10% to 15% vote in the APA national elections or volunteer to serve on committees
- Widespread member dissatisfaction with maintenance of certification
- Neuroscience advances are not being translated fast enough for practical clinical applications
- Many in the public at large do not realize psychiatric symptoms are generated from anomalous brain circuits or that psychiatric disorders are highly genetic but also have environmental and epigenetic etiologies
- The DSM diagnostic system needs a paradigm shift: it is still based on a menu of clinical signs and symptoms and is devoid of objective diagnostic measures such as biomarkers4
- Neuroscience literacy among busy psychiatric practitioners is insufficient at a time of explosive growth in basic and clinical neuroscience13
- No effective treatment for alcohol or substance use disorders despite their very high morbidity and mortality
- Major psychiatric disorders are still associated with significant disability (schizophrenia, bipolar disorder, major depressive disorder, anxiety disorders, eating disorders, substance use disorders)
- Suicide rate (other than opioid deaths) has continued to rise in the past 3 decades14
Opportunities
- Potentially momentous clinical applications of the neuroscience breakthroughs
- Collaborative care with primary care physicians and increasing colocalization
- Dramatic increase in public awareness about the importance of mental health due to the COVID-19 pandemic15
- Powerful new data management tools, including machine learning, artificial intelligence, super computers, big data, deep learning, nanotechnology, and metabolomics, all of which are expediting neurobiological discoveries16
- The potential of reclassifying psychiatric disorders as neurological disorders, which will improve reimbursement for patient health care and reduce stigma17
- Emergence of new mechanisms of action of disease etiology, such as microbiota, mitochondrial dysfunction, permeable blood-brain barrier, and neuroimmune dysregulation18,19
- The advent and growth of “precision psychiatry”20
- The tremendous potential of molecular genetics and gene therapy for psychiatric disorders, most of which are genetic in etiology
- Expanding applications of neuroimaging techniques, including morphological, spectroscopic, functional, diffusion tensor imaging, and receptor imaging21
- Epigenetic advances in neuropsychiatric disorders
- Remarkably powerful research methods, such as pluripotent cells (producing neurons from skin cells), optogenetics (activating genes with light), gene-wide association studies, CRISPR (clustered regularly interspaced short palindromic repeats, which serve as genetic scissors to remove and replace abnormal genes), and brain connectomics22
- Psychiatry should develop and promote an “annual mental health checkup” for all age groups, similar to an annual physical exam23
- Focus on the social determinants of health
- Address the unmet mental health needs of individuals who are members of minority groups
- Lobby ferociously for a much larger budget for the National Institute of Mental Health to advance funding for research of serious psychiatric brain disorders
- Remind Congress continuously that the cost of mental illness is $700 billion annually and costs can only be reduced by funding neurobiological research1
- Partner with the pharmaceutical industry instead of demonizing them. They are the only entity that develops medication for psychiatry, where 80% of disorders have no FDA-approved drugs.24 Without the pharmaceutical industry and the help of medications, many psychiatric patients would still be institutionalized and unable to lead a normal life. We must recognize the contributions of pharmaceutical companies to the health of our patients, similar to the warp speed development of vaccines for the deadly coronavirus
- Psychiatric clinicians must refer patients to clinical trials because without patients enrolling in FDA studies, no drug developments can take place
- Many “out-of-the-box” therapies are being developed, such as antiapoptotic therapy, microglia inhibition, mitochondrial repair, white matter fiber remyelination, neuroprotection, and reversing N-methyl-
d -aspartate receptor hypofunction25 - The emerging evidence that psychotherapy is in fact a biological treatment that induces brain changes (neuroplasticity) and can modulate the immune system26
- Druggable genes, providing innovative new medications27
- Reposition psychedelics as revolutionary new treatments28
- Emphasize measurement-based care (rating scales), which can upgrade patient care29
- Because psychosis is associated with brain tissue loss, just like heart attacks are associated with myocardium destruction, psychiatrists must act like cardiologists30 and treat psychotic episodes urgently, like a stroke,31 to reduce the duration of untreated psychosis and improve patient outcomes
Threats
- Antipsychiatry cults continue to disparage and attack psychiatry32
- Health delivery systems are replacing psychiatric physicians with nurse practitioners to lower costs, regardless of quality and experience, and they inappropriately lump them together as “providers”2
- Psychologists continue to seek prescribing privileges with absurdly sketchy, predominantly online training supervised by other psychologists33
- Many legislators and policymakers, as well as the public, still don’t understand the difference between psychiatrists and psychologists, and the extensively disparate medical training in quality and quantity
- A dearth of psychiatric physician-scientists because very few residents are pursuing research fellowships after training34
- Disproportionate emphasis on clinical care and generating clinical revenue (relative value units) in academic institutions, with fewer tenure-track faculty members having protected time to write grants for federal or foundation grants to support their salaries and research operations35
- Meager financial support for teaching in psychiatry departments
- Many seriously psychiatrically ill persons do not have access to psychiatric medical care (and often to primary care as well)
- Many in the public falsely believe psychiatric disorders are hopeless and untreatable, which perpetuates stigma
- Long-acting injectable antipsychotic formulations are not used early enough in patients with psychosis, who are known to have a high nonadherence rate with oral medications following discharge from their first hospitalization. This leads to many recurrences with multiple devastating consequences, including progressive brain tissue loss, treatment resistance, disability, incarceration, and suicide36
- Many clinicians do not have full-text access to all studies indexed in PubMed, which is vital for lifelong learning in a rapidly growing medical discipline such as psychiatry
- Psychiatrists are often unable to prescribe medications shortly after they are approved by the FDA due to the insurance companies’ outrageous preauthorization racket that enforces a fail-first policy with cheaper generics, even if generic medications are associated with safety and tolerability problems37
- The continued use of decades-old first-generation antipsychotic medications despite 32 published studies reporting their neurotoxicity and the death of brain cells38
Using this analysis to benefit our patients
Despite its strengths, psychiatry must overcome its weaknesses, fend off its threats, and exploit its many opportunities. The only way to do that is for psychiatrists to unify and for the APA to provide inspired leadership to achieve the aspirational goals of our field. However, we must adopt “moonshot thinking”39 to magnify the Ss, diminish the Ws, exploit the Os, and stave off the Ts of our SWOT, thereby attaining all our cherished and lofty goals. Ultimately, the greatest beneficiaries will be our patients.
Editor’s note: This article was adapted with permission from a version originally published in the Ohio Psychiatric Physician Association’s newsletter, Insight Matters, Fall 2022.
Acknowledging and analyzing strengths, weaknesses, opportunities, and threats (SWOT) is an important tactic many organizations use to develop a strategic plan to grow, move forward, and thrive. A SWOT analysis can provide a “big picture” view of the status and the desired future directions not only for companies but for medical disciplines such as psychiatry. So here are my perspectives on psychiatry’s strengths, weaknesses, opportunities, and threats. It is a work in progress, and I welcome (and encourage) you to send additional items or comments to me at [email protected].
Strengths
- The American Psychiatric Association (APA) is the oldest medical professional organization, established in 1844 (3 years before the American Medical Association)1
- Strong organizational structure and governance, and a “big tent” with several tiers of membership
- Effective, member-driven District Branches
- The medical identity at the core of psychiatry—we are psychiatric physicians2
- Escalating number of senior medical students choosing psychiatry as a career, far more than a decade ago
- High demand for psychiatrists in all settings around the country
- Increased compensation for psychiatrists (market forces of supply and demand)
- Psychiatry is continuously evolving and reinventing itself: seismic shifts in etiopathogenesis, disease conceptualization, terminology, and therapies (4 major shifts over the past century)3
- An abundant body of evidence supporting that all psychiatric disorders are brain disorders and transdiagnostic in nature4
- Many vibrant subspecialty societies
- Substantial number of Tier 1, evidence-based treatments
- Novel mechanisms of action and treatment strategies are being introduced on a regular basis for psychotic and mood disorders5,6
- Advances in neuromodulation techniques to treat a wide spectrum of psychiatric disorders, including electroconvulsive therapy, transcranial magnetic stimulation, vagus nerve stimulation, transcranial direct current stimulation, deep brain stimulation, cranial electric stimulation, epidural cortical stimulation, focused ultrasound, low field magnetic stimulation, magnetic seizure therapy, and near infrared light therapy, with mechanisms that are electric, ultrasound, magnetic, or optical7,8
- Psychiatric physicians develop wisdom by practicing psychiatry (ie, they become more empathic, tolerant of ambiguity, prosocial, introspective, aware of one’s strengths and limitations). Neuroplasticity in the frontal cortex is triggered by conducting psychotherapy9
Weaknesses
- Shrinking workforce due to a static number of residency training slots for 40 years10
- High rate of retirement by aging psychiatrists
- Persistent stigma around mental disorders despite massive scientific and medical advances11
- Still no real parity! We need succinct laws with “teeth”12
- Demedicalization in the public sector, referring to psychiatric physicians as “providers” and labeling patients as “clients”2
- Not enough graduating residents choosing to do subspecialty fellowships (especially geriatric, addiction, psychosomatic psychiatry) to meet escalating societal needs
- Very low presence in rural areas (both psychiatrists and psychiatric hospitals)
- Persistent APA member apathy: only 10% to 15% vote in the APA national elections or volunteer to serve on committees
- Widespread member dissatisfaction with maintenance of certification
- Neuroscience advances are not being translated fast enough for practical clinical applications
- Many in the public at large do not realize psychiatric symptoms are generated from anomalous brain circuits or that psychiatric disorders are highly genetic but also have environmental and epigenetic etiologies
- The DSM diagnostic system needs a paradigm shift: it is still based on a menu of clinical signs and symptoms and is devoid of objective diagnostic measures such as biomarkers4
- Neuroscience literacy among busy psychiatric practitioners is insufficient at a time of explosive growth in basic and clinical neuroscience13
- No effective treatment for alcohol or substance use disorders despite their very high morbidity and mortality
- Major psychiatric disorders are still associated with significant disability (schizophrenia, bipolar disorder, major depressive disorder, anxiety disorders, eating disorders, substance use disorders)
- Suicide rate (other than opioid deaths) has continued to rise in the past 3 decades14
Opportunities
- Potentially momentous clinical applications of the neuroscience breakthroughs
- Collaborative care with primary care physicians and increasing colocalization
- Dramatic increase in public awareness about the importance of mental health due to the COVID-19 pandemic15
- Powerful new data management tools, including machine learning, artificial intelligence, super computers, big data, deep learning, nanotechnology, and metabolomics, all of which are expediting neurobiological discoveries16
- The potential of reclassifying psychiatric disorders as neurological disorders, which will improve reimbursement for patient health care and reduce stigma17
- Emergence of new mechanisms of action of disease etiology, such as microbiota, mitochondrial dysfunction, permeable blood-brain barrier, and neuroimmune dysregulation18,19
- The advent and growth of “precision psychiatry”20
- The tremendous potential of molecular genetics and gene therapy for psychiatric disorders, most of which are genetic in etiology
- Expanding applications of neuroimaging techniques, including morphological, spectroscopic, functional, diffusion tensor imaging, and receptor imaging21
- Epigenetic advances in neuropsychiatric disorders
- Remarkably powerful research methods, such as pluripotent cells (producing neurons from skin cells), optogenetics (activating genes with light), gene-wide association studies, CRISPR (clustered regularly interspaced short palindromic repeats, which serve as genetic scissors to remove and replace abnormal genes), and brain connectomics22
- Psychiatry should develop and promote an “annual mental health checkup” for all age groups, similar to an annual physical exam23
- Focus on the social determinants of health
- Address the unmet mental health needs of individuals who are members of minority groups
- Lobby ferociously for a much larger budget for the National Institute of Mental Health to advance funding for research of serious psychiatric brain disorders
- Remind Congress continuously that the cost of mental illness is $700 billion annually and costs can only be reduced by funding neurobiological research1
- Partner with the pharmaceutical industry instead of demonizing them. They are the only entity that develops medication for psychiatry, where 80% of disorders have no FDA-approved drugs.24 Without the pharmaceutical industry and the help of medications, many psychiatric patients would still be institutionalized and unable to lead a normal life. We must recognize the contributions of pharmaceutical companies to the health of our patients, similar to the warp speed development of vaccines for the deadly coronavirus
- Psychiatric clinicians must refer patients to clinical trials because without patients enrolling in FDA studies, no drug developments can take place
- Many “out-of-the-box” therapies are being developed, such as antiapoptotic therapy, microglia inhibition, mitochondrial repair, white matter fiber remyelination, neuroprotection, and reversing N-methyl-
d -aspartate receptor hypofunction25 - The emerging evidence that psychotherapy is in fact a biological treatment that induces brain changes (neuroplasticity) and can modulate the immune system26
- Druggable genes, providing innovative new medications27
- Reposition psychedelics as revolutionary new treatments28
- Emphasize measurement-based care (rating scales), which can upgrade patient care29
- Because psychosis is associated with brain tissue loss, just like heart attacks are associated with myocardium destruction, psychiatrists must act like cardiologists30 and treat psychotic episodes urgently, like a stroke,31 to reduce the duration of untreated psychosis and improve patient outcomes
Threats
- Antipsychiatry cults continue to disparage and attack psychiatry32
- Health delivery systems are replacing psychiatric physicians with nurse practitioners to lower costs, regardless of quality and experience, and they inappropriately lump them together as “providers”2
- Psychologists continue to seek prescribing privileges with absurdly sketchy, predominantly online training supervised by other psychologists33
- Many legislators and policymakers, as well as the public, still don’t understand the difference between psychiatrists and psychologists, and the extensively disparate medical training in quality and quantity
- A dearth of psychiatric physician-scientists because very few residents are pursuing research fellowships after training34
- Disproportionate emphasis on clinical care and generating clinical revenue (relative value units) in academic institutions, with fewer tenure-track faculty members having protected time to write grants for federal or foundation grants to support their salaries and research operations35
- Meager financial support for teaching in psychiatry departments
- Many seriously psychiatrically ill persons do not have access to psychiatric medical care (and often to primary care as well)
- Many in the public falsely believe psychiatric disorders are hopeless and untreatable, which perpetuates stigma
- Long-acting injectable antipsychotic formulations are not used early enough in patients with psychosis, who are known to have a high nonadherence rate with oral medications following discharge from their first hospitalization. This leads to many recurrences with multiple devastating consequences, including progressive brain tissue loss, treatment resistance, disability, incarceration, and suicide36
- Many clinicians do not have full-text access to all studies indexed in PubMed, which is vital for lifelong learning in a rapidly growing medical discipline such as psychiatry
- Psychiatrists are often unable to prescribe medications shortly after they are approved by the FDA due to the insurance companies’ outrageous preauthorization racket that enforces a fail-first policy with cheaper generics, even if generic medications are associated with safety and tolerability problems37
- The continued use of decades-old first-generation antipsychotic medications despite 32 published studies reporting their neurotoxicity and the death of brain cells38
Using this analysis to benefit our patients
Despite its strengths, psychiatry must overcome its weaknesses, fend off its threats, and exploit its many opportunities. The only way to do that is for psychiatrists to unify and for the APA to provide inspired leadership to achieve the aspirational goals of our field. However, we must adopt “moonshot thinking”39 to magnify the Ss, diminish the Ws, exploit the Os, and stave off the Ts of our SWOT, thereby attaining all our cherished and lofty goals. Ultimately, the greatest beneficiaries will be our patients.
1. Nasrallah HA. 20 reasons to celebrate our APA membership. Current Psychiatry. 2020;19(1):6-9.
2. Nasrallah HA. We are physicians, not providers, and we treat patients, not clients! Current Psychiatry. 2020;19(2):5-8.
3. Nasrallah HA. From bedlam to biomarkers: the transformation of psychiatry’s terminology reflects its 4 conceptual earthquakes. Current Psychiatry. 2015;14(1):5-7.
4. Nasrallah HA. Re-inventing the DSM as a transdiagnostic model: psychiatric disorders are extensively interconnected. Ann Clin Psychiatry. 2021;33(3):148-150.
5. Nasrallah HA. Psychopharmacology 3.0. Current Psychiatry. 2081;17(11):4-7.
6. Nasrallah HA. Reversing depression: a plethora of therapeutic strategies and mechanisms. Current Psychiatry. 2022;21(8):4-6.
7. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Psychopharmacology. 2012;37(1):102-116.
8. Nasrallah HA. Optimal psychiatric treatment: target the brain and avoid the body. Current Psychiatry. 2022;21(12):3-6.
9. Nasrallah HA. Does psychiatry practice make us wise? Current Psychiatry. 2009;8(10):12-14.
10. Buckley PF, Nasrallah HA. The psychiatry workforce pool is shrinking. What are we doing about it? Current Psychiatry. 2016;15(9):23-24,95.
11. Nasrallah HA. A psychiatric manifesto: stigma is hate speech and a hate crime. Current Psychiatry. 2022;21(6):6-8.
12. Nasrallah HA. The travesty of disparity and non-parity. Current Psychiatry. 2014;13(1):8,19.
13. Nasrallah HA. Advancing clinical neuroscience literacy among psychiatric practitioners. Current Psychiatry. 2017;16(9):17-18.
14. Nasrallah HA. The scourge of societal anosognosia about the mentally ill. Current Psychiatry. 2016;15(6):19-24.
15. Nasrallah HA. 10 silver linings of the COVID-19 pandemic. Insight Matters. 2021;45:3-4.
16. Kalenderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019:18(8):33-38.
17. Nasrallah HA. Let’s tear down the silos and re-unify psychiatry and neurology! Current Psychiatry. 2013;12(8):8-9.
18. Nasrallah HA. It takes guts to be mentally ill: microbiota and psychopathology. Current Psychiatry. 2018;17(9):4-6.
19. Schrenk DA, Nasrallah HA. Faulty fences: blood-brain barrier dysfunction in schizophrenia. Current Psychiatry. 2022;21(10):28-32.
20. Nasrallah HA. The dawn of precision psychiatry. Current Psychiatry. 2017;16(12):7-8,11.
21. Nasrallah HA. Today’s psychiatric neuroscience advances were science fiction during my residency. Current Psychiatry 2021;20(4):5-7,12,24.
22. Nasrallah HA. Transformative advances are unfolding in psychiatry. Current Psychiatry. 2019;18(9):10-12.
23. Nasrallah HA. I have a dream…for psychiatry. Current Psychiatry. 2021;20(11):12-14.
24. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian J Psychiatry. 2009;2(1):29-36.
25. Nasrallah HA. Transformative advances are unfolding in psychiatry. Current Psychiatry. 2019;18(9):10-12.
26. Nasrallah HA. Repositioning psychotherapy as a neurobiological intervention. Current Psychiatry. 2013;12(12):18-19.
27. Nasrallah HA. Druggable genes, promiscuous drugs, repurposed medications. Current Psychiatry. 2016;15(5):23,27.
28. Nasrallah HA. Long overdue: measurement-based psychiatric practice. Current Psychiatry. 2009;8(4):14-16.
29. Nasrallah HA. Maddening therapies: how hallucinogens morphed into novel treatments. Current Psychiatry. 2017:16(1):19-21.
30. Nasrallah HA. For first episode psychosis, psychiatrists should behave like cardiologists. Current Psychiatry. 2017;16(8):4-7.
31. Nasrallah HA, Roque A. FAST and RAPID: acronyms to prevent brain damage in stroke and psychosis. Current Psychiatry. 2018;17(8):6-8.
32. Nasrallah HA. The antipsychiatry movement: who and why. Current Psychiatry. 2011;10(12):4,6,53.
33. Nasrallah HA. Prescribing is the culmination of extensive medical training and psychologists do not qualify. Current Psychiatry. 2017;16(6):11-12,14-16.
34. Fenton W, James R, Insel T. Psychiatry residency training, the physician-scientist, and the future of psychiatry. Acad Psychiatry. 2004;28(4):263-266.
35. Balon R, Morreale MK. The precipitous decline of academic medicine in the United States. Ann Clin Psychiatry. 2020;32(4):225-227.
36. Nasrallah HA. 10 devastating consequences of psychotic relapses. Current Psychiatry. 2021;20(5):9-12.
37. Nasrallah HA. Pre-authorization is illegal, unethical, and adversely disrupts patient care. Current Psychiatry. 2020;19(4):5-11.
38. Nasrallah HA, Chen AT. Multiple neurotoxic effects of haloperidol resulting in neuronal death. Ann Clin Psychiatry. 2017;29(3):195-202.
39. Nasrallah HA. It’s time for moonshot thinking in psychiatry. Current Psychiatry. 2022;21(2):8-10.
1. Nasrallah HA. 20 reasons to celebrate our APA membership. Current Psychiatry. 2020;19(1):6-9.
2. Nasrallah HA. We are physicians, not providers, and we treat patients, not clients! Current Psychiatry. 2020;19(2):5-8.
3. Nasrallah HA. From bedlam to biomarkers: the transformation of psychiatry’s terminology reflects its 4 conceptual earthquakes. Current Psychiatry. 2015;14(1):5-7.
4. Nasrallah HA. Re-inventing the DSM as a transdiagnostic model: psychiatric disorders are extensively interconnected. Ann Clin Psychiatry. 2021;33(3):148-150.
5. Nasrallah HA. Psychopharmacology 3.0. Current Psychiatry. 2081;17(11):4-7.
6. Nasrallah HA. Reversing depression: a plethora of therapeutic strategies and mechanisms. Current Psychiatry. 2022;21(8):4-6.
7. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Psychopharmacology. 2012;37(1):102-116.
8. Nasrallah HA. Optimal psychiatric treatment: target the brain and avoid the body. Current Psychiatry. 2022;21(12):3-6.
9. Nasrallah HA. Does psychiatry practice make us wise? Current Psychiatry. 2009;8(10):12-14.
10. Buckley PF, Nasrallah HA. The psychiatry workforce pool is shrinking. What are we doing about it? Current Psychiatry. 2016;15(9):23-24,95.
11. Nasrallah HA. A psychiatric manifesto: stigma is hate speech and a hate crime. Current Psychiatry. 2022;21(6):6-8.
12. Nasrallah HA. The travesty of disparity and non-parity. Current Psychiatry. 2014;13(1):8,19.
13. Nasrallah HA. Advancing clinical neuroscience literacy among psychiatric practitioners. Current Psychiatry. 2017;16(9):17-18.
14. Nasrallah HA. The scourge of societal anosognosia about the mentally ill. Current Psychiatry. 2016;15(6):19-24.
15. Nasrallah HA. 10 silver linings of the COVID-19 pandemic. Insight Matters. 2021;45:3-4.
16. Kalenderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019:18(8):33-38.
17. Nasrallah HA. Let’s tear down the silos and re-unify psychiatry and neurology! Current Psychiatry. 2013;12(8):8-9.
18. Nasrallah HA. It takes guts to be mentally ill: microbiota and psychopathology. Current Psychiatry. 2018;17(9):4-6.
19. Schrenk DA, Nasrallah HA. Faulty fences: blood-brain barrier dysfunction in schizophrenia. Current Psychiatry. 2022;21(10):28-32.
20. Nasrallah HA. The dawn of precision psychiatry. Current Psychiatry. 2017;16(12):7-8,11.
21. Nasrallah HA. Today’s psychiatric neuroscience advances were science fiction during my residency. Current Psychiatry 2021;20(4):5-7,12,24.
22. Nasrallah HA. Transformative advances are unfolding in psychiatry. Current Psychiatry. 2019;18(9):10-12.
23. Nasrallah HA. I have a dream…for psychiatry. Current Psychiatry. 2021;20(11):12-14.
24. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian J Psychiatry. 2009;2(1):29-36.
25. Nasrallah HA. Transformative advances are unfolding in psychiatry. Current Psychiatry. 2019;18(9):10-12.
26. Nasrallah HA. Repositioning psychotherapy as a neurobiological intervention. Current Psychiatry. 2013;12(12):18-19.
27. Nasrallah HA. Druggable genes, promiscuous drugs, repurposed medications. Current Psychiatry. 2016;15(5):23,27.
28. Nasrallah HA. Long overdue: measurement-based psychiatric practice. Current Psychiatry. 2009;8(4):14-16.
29. Nasrallah HA. Maddening therapies: how hallucinogens morphed into novel treatments. Current Psychiatry. 2017:16(1):19-21.
30. Nasrallah HA. For first episode psychosis, psychiatrists should behave like cardiologists. Current Psychiatry. 2017;16(8):4-7.
31. Nasrallah HA, Roque A. FAST and RAPID: acronyms to prevent brain damage in stroke and psychosis. Current Psychiatry. 2018;17(8):6-8.
32. Nasrallah HA. The antipsychiatry movement: who and why. Current Psychiatry. 2011;10(12):4,6,53.
33. Nasrallah HA. Prescribing is the culmination of extensive medical training and psychologists do not qualify. Current Psychiatry. 2017;16(6):11-12,14-16.
34. Fenton W, James R, Insel T. Psychiatry residency training, the physician-scientist, and the future of psychiatry. Acad Psychiatry. 2004;28(4):263-266.
35. Balon R, Morreale MK. The precipitous decline of academic medicine in the United States. Ann Clin Psychiatry. 2020;32(4):225-227.
36. Nasrallah HA. 10 devastating consequences of psychotic relapses. Current Psychiatry. 2021;20(5):9-12.
37. Nasrallah HA. Pre-authorization is illegal, unethical, and adversely disrupts patient care. Current Psychiatry. 2020;19(4):5-11.
38. Nasrallah HA, Chen AT. Multiple neurotoxic effects of haloperidol resulting in neuronal death. Ann Clin Psychiatry. 2017;29(3):195-202.
39. Nasrallah HA. It’s time for moonshot thinking in psychiatry. Current Psychiatry. 2022;21(2):8-10.
From debate to stalemate and hate: An epidemic of intellectual constipation
Groupthink is hazardous, especially when perfused with religious fervor. It can lead to adopting irrational thinking1 and aversion to new ideas or facts. Tenaciously clinging to 1 ideology as “the absolute truth” precludes an open-minded, constructive debate with any other point of view.
Three historical examples come to mind:
- The discovery of chlorpromazine in 1952 was a scientifically and clinically seismic and transformational event for the treatment of psychosis, which for centuries had been dogmatically deemed irreversible. Jean Delay, MD, the French psychiatrist and co-discoverer of chlorpromazine, was the first physician to witness the magical and dazzling dissolution of delusions and hallucinations in chronically institutionalized patients with psychosis.2 He published his landmark clinical observations and then traveled to the United States to share the great news and present his findings at a large psychiatric conference, hoping to enthrall American psychiatrists with the historic breakthrough in treating psychosis. This was an era in which psychoanalysis dominated American psychiatry (despite its dearth of empirical evidence). Dr. Delay was shocked when the audience of psychoanalysts booed him for saying that psychosis can be treated with a medication instead of with psychoanalysis (which, in the most intense groupthink in the history of psychiatry, they all believed was the only therapy for psychosis). Deeply disheartened, Dr. Delay returned to France and never returned to the United States. This groupthink was a prime example of intellectual constipation. Since then, not surprisingly, psychopharmacology grew meteorically while psychoanalysis declined precipitously.
- The monoamine hypothesis of depression, first propagated 60 years ago, became a groupthink dogma among psychiatric researchers for the next several decades, stultifying broader antidepressant medication development by focusing only on monoamines (eg, serotonin, norepinephrine, and dopamine). More recently, researchers have become more open-minded, and the monoamine hypothesis has taken a backseat to innovative new models of antidepressant therapy based on advances in the pathophysiology of depression, such as glutamatergic, opioid, and sigma pathways as well as neuroplasticity models.3 The consequence of groupthink in antidepressant research was a half-century delay in the development of effective alternative treatments that could have helped millions of patients recover from a life-threatening brain disorder such as major depressive disorder.
- Peptic ulcer and its serious gastritis were long believed to be due to stress and increased stomach acidity. So the groupthink gastroenterologists mocked 2 Australian researchers, Barry Marshall and Robin Warren, when they proposed that peptic ulcer may be due to an infection with a bacterium called Helicobacter pylori, and published their data demonstrating it.4 Marshall and Warren had the last laugh when they were awarded the 2005 Nobel Prize in Medicine and Physiology. It is ironic that even gastroenterologists are not immune to the affliction of intellectual constipation!
Intellectual constipation’s effects on youth
The principle of a civilized debate of contrarian ideas must be inculcated early, especially during college years. Youth should be mentored about not cowering into an ideological cocoon and shun listening to different or opposing points of view.5 Institutions of higher learning are incubators of future leaders. They must provide their young students with a wide diversity of ideas and philosophies and encourage them to critique those ideas, not “shelter” or isolate them from any ideas. Youth need to recognize that the complex societies in which we all live and work are not placid or unidimensional but a hotbed of clashing ideas and perspectives. An open-minded approach to education will inoculate young minds from developing intellectual constipation in adulthood.
Avoiding or insulating oneself from the ideas of others—no matter how disagreeable—leads to cognitive cowardice and behavioral intolerance. Healthy and vibrant debate is necessary as an inoculation against extremism, hate, paranoia, and, ultimately, violence. Psychiatrists help patients to self-reflect, gain insight, and consider changing their view of themselves and the world to help them grow into mature and resilient individuals. But for the millions of people with intellectual constipation, a potent cerebral enema comprised of a salubrious concoction of insight, common sense, and compromise may be the prescription to forestall lethal intellectual ileus.
1. Nasrallah HA. Irrational beliefs: a ubiquitous human trait. Current Psychiatry. 2007;6(2):15-16.
2. Ban TA. Fifty years chlorpromazine: a historical perspective. Neuropsychiatr Dis Treat. 2007;3(4):495-500.
3. Boku S, Nakagawa S, Toda H, et al. Neural basis of major depressive disorder: beyond monoamine hypothesis. Psychiatry Clin Neurosci. 2018;72(1):3-12.
4. Warren JR, Marshall B. Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet. 1983;1(8336):1273-1275.
5. Lukianoff G, Haidt J. The Coddling of the American Mind: How Good Intentions and Bad Ideas Are Setting Up a Generation for Failure. Penguin Books; 2018.
Groupthink is hazardous, especially when perfused with religious fervor. It can lead to adopting irrational thinking1 and aversion to new ideas or facts. Tenaciously clinging to 1 ideology as “the absolute truth” precludes an open-minded, constructive debate with any other point of view.
Three historical examples come to mind:
- The discovery of chlorpromazine in 1952 was a scientifically and clinically seismic and transformational event for the treatment of psychosis, which for centuries had been dogmatically deemed irreversible. Jean Delay, MD, the French psychiatrist and co-discoverer of chlorpromazine, was the first physician to witness the magical and dazzling dissolution of delusions and hallucinations in chronically institutionalized patients with psychosis.2 He published his landmark clinical observations and then traveled to the United States to share the great news and present his findings at a large psychiatric conference, hoping to enthrall American psychiatrists with the historic breakthrough in treating psychosis. This was an era in which psychoanalysis dominated American psychiatry (despite its dearth of empirical evidence). Dr. Delay was shocked when the audience of psychoanalysts booed him for saying that psychosis can be treated with a medication instead of with psychoanalysis (which, in the most intense groupthink in the history of psychiatry, they all believed was the only therapy for psychosis). Deeply disheartened, Dr. Delay returned to France and never returned to the United States. This groupthink was a prime example of intellectual constipation. Since then, not surprisingly, psychopharmacology grew meteorically while psychoanalysis declined precipitously.
- The monoamine hypothesis of depression, first propagated 60 years ago, became a groupthink dogma among psychiatric researchers for the next several decades, stultifying broader antidepressant medication development by focusing only on monoamines (eg, serotonin, norepinephrine, and dopamine). More recently, researchers have become more open-minded, and the monoamine hypothesis has taken a backseat to innovative new models of antidepressant therapy based on advances in the pathophysiology of depression, such as glutamatergic, opioid, and sigma pathways as well as neuroplasticity models.3 The consequence of groupthink in antidepressant research was a half-century delay in the development of effective alternative treatments that could have helped millions of patients recover from a life-threatening brain disorder such as major depressive disorder.
- Peptic ulcer and its serious gastritis were long believed to be due to stress and increased stomach acidity. So the groupthink gastroenterologists mocked 2 Australian researchers, Barry Marshall and Robin Warren, when they proposed that peptic ulcer may be due to an infection with a bacterium called Helicobacter pylori, and published their data demonstrating it.4 Marshall and Warren had the last laugh when they were awarded the 2005 Nobel Prize in Medicine and Physiology. It is ironic that even gastroenterologists are not immune to the affliction of intellectual constipation!
Intellectual constipation’s effects on youth
The principle of a civilized debate of contrarian ideas must be inculcated early, especially during college years. Youth should be mentored about not cowering into an ideological cocoon and shun listening to different or opposing points of view.5 Institutions of higher learning are incubators of future leaders. They must provide their young students with a wide diversity of ideas and philosophies and encourage them to critique those ideas, not “shelter” or isolate them from any ideas. Youth need to recognize that the complex societies in which we all live and work are not placid or unidimensional but a hotbed of clashing ideas and perspectives. An open-minded approach to education will inoculate young minds from developing intellectual constipation in adulthood.
Avoiding or insulating oneself from the ideas of others—no matter how disagreeable—leads to cognitive cowardice and behavioral intolerance. Healthy and vibrant debate is necessary as an inoculation against extremism, hate, paranoia, and, ultimately, violence. Psychiatrists help patients to self-reflect, gain insight, and consider changing their view of themselves and the world to help them grow into mature and resilient individuals. But for the millions of people with intellectual constipation, a potent cerebral enema comprised of a salubrious concoction of insight, common sense, and compromise may be the prescription to forestall lethal intellectual ileus.
Groupthink is hazardous, especially when perfused with religious fervor. It can lead to adopting irrational thinking1 and aversion to new ideas or facts. Tenaciously clinging to 1 ideology as “the absolute truth” precludes an open-minded, constructive debate with any other point of view.
Three historical examples come to mind:
- The discovery of chlorpromazine in 1952 was a scientifically and clinically seismic and transformational event for the treatment of psychosis, which for centuries had been dogmatically deemed irreversible. Jean Delay, MD, the French psychiatrist and co-discoverer of chlorpromazine, was the first physician to witness the magical and dazzling dissolution of delusions and hallucinations in chronically institutionalized patients with psychosis.2 He published his landmark clinical observations and then traveled to the United States to share the great news and present his findings at a large psychiatric conference, hoping to enthrall American psychiatrists with the historic breakthrough in treating psychosis. This was an era in which psychoanalysis dominated American psychiatry (despite its dearth of empirical evidence). Dr. Delay was shocked when the audience of psychoanalysts booed him for saying that psychosis can be treated with a medication instead of with psychoanalysis (which, in the most intense groupthink in the history of psychiatry, they all believed was the only therapy for psychosis). Deeply disheartened, Dr. Delay returned to France and never returned to the United States. This groupthink was a prime example of intellectual constipation. Since then, not surprisingly, psychopharmacology grew meteorically while psychoanalysis declined precipitously.
- The monoamine hypothesis of depression, first propagated 60 years ago, became a groupthink dogma among psychiatric researchers for the next several decades, stultifying broader antidepressant medication development by focusing only on monoamines (eg, serotonin, norepinephrine, and dopamine). More recently, researchers have become more open-minded, and the monoamine hypothesis has taken a backseat to innovative new models of antidepressant therapy based on advances in the pathophysiology of depression, such as glutamatergic, opioid, and sigma pathways as well as neuroplasticity models.3 The consequence of groupthink in antidepressant research was a half-century delay in the development of effective alternative treatments that could have helped millions of patients recover from a life-threatening brain disorder such as major depressive disorder.
- Peptic ulcer and its serious gastritis were long believed to be due to stress and increased stomach acidity. So the groupthink gastroenterologists mocked 2 Australian researchers, Barry Marshall and Robin Warren, when they proposed that peptic ulcer may be due to an infection with a bacterium called Helicobacter pylori, and published their data demonstrating it.4 Marshall and Warren had the last laugh when they were awarded the 2005 Nobel Prize in Medicine and Physiology. It is ironic that even gastroenterologists are not immune to the affliction of intellectual constipation!
Intellectual constipation’s effects on youth
The principle of a civilized debate of contrarian ideas must be inculcated early, especially during college years. Youth should be mentored about not cowering into an ideological cocoon and shun listening to different or opposing points of view.5 Institutions of higher learning are incubators of future leaders. They must provide their young students with a wide diversity of ideas and philosophies and encourage them to critique those ideas, not “shelter” or isolate them from any ideas. Youth need to recognize that the complex societies in which we all live and work are not placid or unidimensional but a hotbed of clashing ideas and perspectives. An open-minded approach to education will inoculate young minds from developing intellectual constipation in adulthood.
Avoiding or insulating oneself from the ideas of others—no matter how disagreeable—leads to cognitive cowardice and behavioral intolerance. Healthy and vibrant debate is necessary as an inoculation against extremism, hate, paranoia, and, ultimately, violence. Psychiatrists help patients to self-reflect, gain insight, and consider changing their view of themselves and the world to help them grow into mature and resilient individuals. But for the millions of people with intellectual constipation, a potent cerebral enema comprised of a salubrious concoction of insight, common sense, and compromise may be the prescription to forestall lethal intellectual ileus.
1. Nasrallah HA. Irrational beliefs: a ubiquitous human trait. Current Psychiatry. 2007;6(2):15-16.
2. Ban TA. Fifty years chlorpromazine: a historical perspective. Neuropsychiatr Dis Treat. 2007;3(4):495-500.
3. Boku S, Nakagawa S, Toda H, et al. Neural basis of major depressive disorder: beyond monoamine hypothesis. Psychiatry Clin Neurosci. 2018;72(1):3-12.
4. Warren JR, Marshall B. Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet. 1983;1(8336):1273-1275.
5. Lukianoff G, Haidt J. The Coddling of the American Mind: How Good Intentions and Bad Ideas Are Setting Up a Generation for Failure. Penguin Books; 2018.
1. Nasrallah HA. Irrational beliefs: a ubiquitous human trait. Current Psychiatry. 2007;6(2):15-16.
2. Ban TA. Fifty years chlorpromazine: a historical perspective. Neuropsychiatr Dis Treat. 2007;3(4):495-500.
3. Boku S, Nakagawa S, Toda H, et al. Neural basis of major depressive disorder: beyond monoamine hypothesis. Psychiatry Clin Neurosci. 2018;72(1):3-12.
4. Warren JR, Marshall B. Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet. 1983;1(8336):1273-1275.
5. Lukianoff G, Haidt J. The Coddling of the American Mind: How Good Intentions and Bad Ideas Are Setting Up a Generation for Failure. Penguin Books; 2018.
Positive psychotherapy: Core principles
In a time of great national and global upheaval, increasing social problems, migration, climate crisis, globalization, and increasingly multicultural societies, our patients and their needs are unique, diverse, and changing. We need a new understanding of mental health to be able to adequately meet the demands of an ever-changing world. Treatment exclusively with psychotropic medications or years of psychoanalysis will not meet these needs.
Psychiatrists and psychotherapists feel (and actually have) a social responsibility, particularly in a multifaceted global society. Psychotherapeutic interventions may contribute to a more peaceful society1 by reducing individuals’ inner stress, solving (unconscious) conflicts, and conveying a humanistic worldview. As an integrative and transcultural method, positive psychotherapy has been applied for more than 45 years in more than 60 countries and is an active force within a “positive mental health movement.”2
The term “positive psychotherapy” describes 2 different approaches3: positive psychotherapy (1977) by Nossrat Peseschkian,4 which is a humanistic psychodynamic approach, and positive psychotherapy (2006) by Martin E.P. Seligman, Tayyab Rashid, and Acacia C. Parks,5 which is a more cognitive-behavioral therapy (CBT)–based approach. This article focuses on the first approach.
Why ‘positive’ psychotherapy?
The term “positive” implies that positive psychotherapy focuses on the patient’s possibilities and capacities. Symptoms and disorders are seen as capacities to react to a conflict. The Latin term “positum” or “positivus” is applied in its original meaning—the factual, the given, the actual. Factual and given are not only the disorder, the symptoms, and the problems but also the capacity to become healthy and/or cope with this situation. This positive meaning confronts the patient (and the therapist) with a lesser-known aspect of the illness, but one that is just as important for the understanding and clinical treatment of the affliction: its function, its meaning, and, consequently, its positive aspects.6
Positive psychotherapy is a humanistic psychodynamic psychotherapy approach developed by Nossrat Peseschkian (1933-2010).4,7 Positive psychotherapy has been developed since the 1970s in the clinical setting with neurotic and psychosomatic patients. It integrates approaches of the 4 main modalities of psychotherapy:
- a humanistic view of human beings
- a systemic approach toward culture, work, and environment
- a psychodynamic understanding of disorders
- a practical, goal-oriented approach with some cognitive-behavioral techniques.
The concept of balance
Based on a humanistic view of human beings and the resources every patient possesses, a key concept of positive psychotherapy is the importance of balance in one’s life. The balance model (Figure) is the core of positive psychotherapy and is applied in clinical and nonclinical settings. This model is based on the concept that there are 4 main areas of life in which a human being lives and functions. These areas influence one’s satisfaction in life, one’s feelings of self-worth, and the way one deals with conflicts and challenges. Although all 4 capacities are latent in every human being, depending on one`s education, environment, and zeitgeist, some will be more developed than others. Our life energies, activities, and reactions belong to these 4 areas of life:
- physical: eating, tenderness, sexuality, sleep, relaxation, sports, appearance, clothing
- achievement: work, job, career, money
- relationships: partner, family, friends, acquaintances and strangers, community life
- meaning and future: existential questions, spirituality, religious practices, future plans, fantasy.
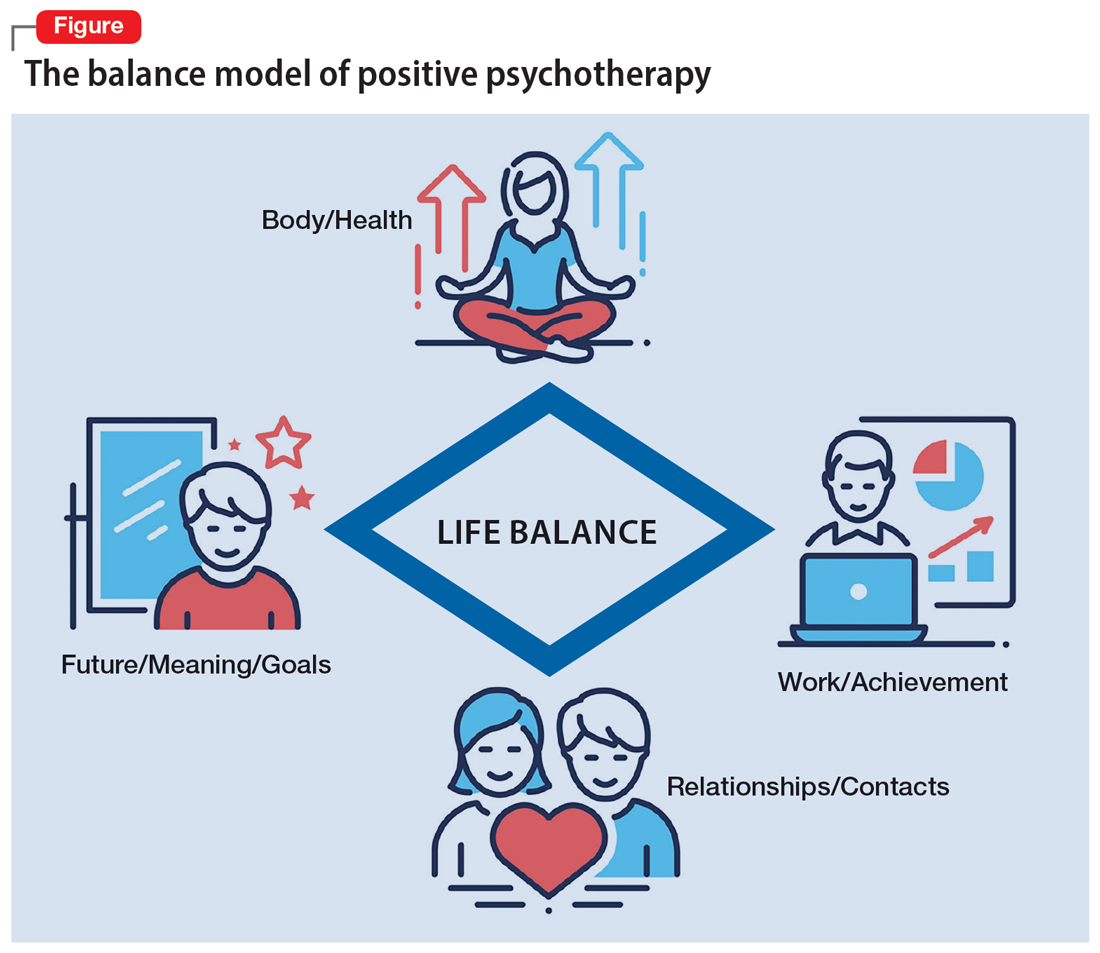
A goal of treatment is to help the patient recognize their own resources and mobilize them with the goal of bringing them into a dynamic equilibrium. This goal places value on a balanced distribution of energy (25% to each area), not of time. According to positive psychotherapy, a person does not become ill because one sphere of life is overemphasized but because of the areas that have been neglected. In the case vignette described in the Box, the problem is not the patient’s work but that his physical health, family and friends, and existential questions are being neglected. That the therapist is not critical from the start of treatment is a constructive experience for the patient and is important and fruitful for building the relationship between the therapist and the patient. Instead of emphasizing the deficits or the disorders, the patient and his family hear that he has neglected other areas of life and not developed them yet.
Box
Mr. M, a 52-year-old manager, is “sent” by his wife to see a psychotherapist. “My wife says I am married to my job, and I should spend more time with her and the children. I understand this, but I love my job. It is no stress for me, but a few minutes at home, and I feel totally stressed out,” he says. During the first interview, the therapist asks Mr. M to draw his energy distribution in the balance model (Figure), and it becomes clear he spends more than 80% of his time and energy on his job.
That is not such a surprise for him. But after some explanation, the therapist tells him that he should continue to do so and that it is an ability to be able to spend so much time every day for his job. Mr. M says, “You are the first person to tell me that it is good that I am working so much. I expected you, like all the others, to tell me I must reduce my working hours immediately, go on vacation, etc.”
Continue to: The balance model...
The balance model also embodies the 4 potential sources of self-esteem. Usually, only 1 or 2 areas provide self-esteem, but in the therapeutic process a patient can learn to uncover the neglected areas so that their self-esteem will have additional pillars of support. By emphasizing how therapy can help to develop one’s self-esteem, many patients can be motivated for the therapeutic process. The balance model, with its concept of devoting 25% of one’s energy to each sphere of life, gives the patient a clear vision about their life and how they can be healthy over the long run by avoiding one-sidedness.8
The transcultural approach
In positive psychotherapy, the term “transcultural” (or cross-cultural) means not only consideration of cultural factors when the therapist and patient come from diverse cultural backgrounds (intercultural psychotherapy or “migrant psychotherapy”) but specifically the consideration of cultural factors in every therapeutic relationship, as a therapeutic attitude and consequently as a sociopolitical dimension of our thinking and behavior. This consideration of the uniqueness of each person, of the relativity of human behavior, and of “unity in diversity” is an essential reason positive psychotherapy is not a “Western” method in the sense of “psychological colonization.”9 Rather, this approach is a culture-sensitive method that can be modified to adapt to particular cultures and life situations.
Transcultural positive psychotherapy begins with answering 2 questions: “How are people different?” and “What do all people have in common?”4 During the therapeutic process, the therapist gives examples from other cultures to the patient to help them relativize their own perspective and broaden their repertoire of behavior.
The use of stories, tales, proverbs, and anecdotes
A special technique of positive psychotherapy is the therapeutic use of stories, tales, proverbs, and anecdotes.10 Often stories from other cultures are used because they offer another perspective when the patient sees none. This has been shown to be highly effective in psychiatric settings, especially in group settings. Psychiatric patients can often easily relate to the images created by stories. In psychiatry and psychotherapy, stories can be a means of changing a patient’s point of view. Such narratives can free up the listener’s feelings and thoughts and often lead to “Aha!” moments. The mirror function of storytelling leads to identification. In the narratives, the reader or listener recognizes themself as well as their needs and situation. They can reflect on the stories without personally becoming the focus of these reflections and remember their own experiences. Stories present solutions that can be models against which one’s own approach can be compared but that also leave room for broader interpretation. Storytelling is particularly useful in bringing about change in patients who are holding fast to old and outworn ideas.
The positive interpretation of disorders
Positive psychotherapy is based on a humanistic view that every human being is good by nature and endowed with unique capacities.11 This positive perspective leads not only to a new quality of relationship between the therapist and patient but also to a new perspective on disorders (Table). Thus, disorders can be “interpreted” in a positive way6: What does the patient unconsciously want to express with their symptoms? What is the function of their disorder? The positive process brings with it a change in perspective to all those concerned: the patient, their family, and the therapist/physician. In this way, one moves from the symptom (which is the disorder and often already has been very thoroughly examined) to the conflict (and the function of the disorder). The positive interpretations are only offered to the patient (“What do you say to this explanation?” “Can you apply this to your own situation?”).
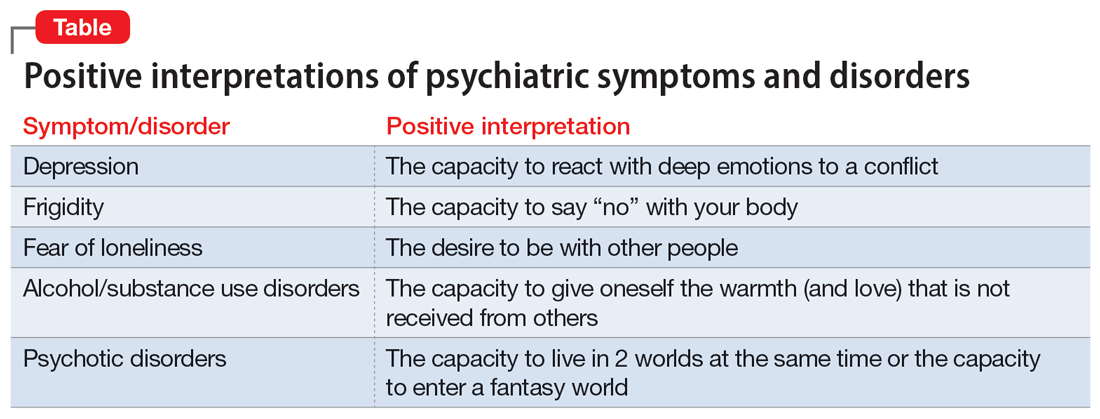
Continue to: This process also helps us...
This process also helps us focus on the “true” patient, who often is not our patient. The patient who comes to us functions as a symptom carrier and can be seen as the “weakest link” in the family chain. The “real patient” is often sitting at home. The positive interpretation of illnesses confronts the patient with the possible function and psychodynamic meaning of their illness for themself and their social milieu, encouraging the patient (and their family) to see their abilities and not merely the pathological aspects.12
Fields of application of positive psychotherapy
As a method positioned between manualized CBT and process-oriented analytical psychotherapy, positive psychotherapy pursues a semi-structured approach in diagnostics (first interview), treatment, posttherapeutic self-help, and training. Positive psychotherapy is applied for the treatment of mood (affective), neurotic, stress-related, and somatoform disorders; behavioral syndromes; and, to some extent, personality disorders. Positive psychotherapy has been employed successfully side-by-side with classical individual therapy as well as in the settings of couple, family, and group therapy.13
What makes positive psychotherapy attractive for mental health professionals?
- As a method that integrates the 4 main modalities of psychotherapy, it does not engage in the conflicts between different schools but combines effective elements into a single approach.
- As an integrative approach, it adjusts to the patient and not vice versa. It gives the therapist the possibility of focusing more on either the actual problems (supportive approach) or the basic conflict (psychodynamic approach).
- It uses vocabulary and terms that can be understood by patients from all strata of society.
- As a culturally sensitive method, it can be applied to patients from different cultures and does not require cultural adaptation.
- As a psychodynamic method, it does not stop after early life conflicts have become more conscious but helps the patient to apply the gained insights using practical techniques.
- It starts with positive affirmations and encouragement but does not later “forget” the unconscious conflicts that have led to disorders. It is not perceived as superficial.
- As a method originally coming from psychiatry and medical practice, it builds a bridge between a scientific basis and psychotherapeutic insights. It favors the biopsychosocial approach.
Bottom Line
Positive psychotherapy combines humanistic, systemic, psychodynamic, and cognitive-behavioral aspects. It is based on a resource-oriented view of human beings in which disorders are interpreted as capacities to react in a specific and unique way to life events and circumstances. Positive psychotherapy can be applied in psychiatry and psychotherapy. This short-term method is easily understood by patients from diverse cultures and social backgrounds.
Related Resources
- Peseschkian H, Remmers A. Positive psychotherapy: an introduction. In: Messias E, Peseschkian H, Cagande C, eds. Positive Psychiatry, Psychotherapy and Psychology. Springer; 2020:11-32. https://doi.org/10.1007/978-3-030-33264-8_2
- Tritt K, Loew T, Meyer M, et al. Positive psychotherapy: effectiveness of an interdisciplinary approach. Eur J Psychiatry. 1999;13(4):231-241.
- World Association for Positive and Transcultural Psychotherapy. http://www.positum.org
1. Mackenthun G. Passt Psychotherapie an ‚die Gesellschaft’ an? Dynamische Psychiatrie. 1991;24(5-6):326-333.
2. Jeste DV. Foreword: positive mental health. In: Messias E, Peseschkian H, Cagande C, eds. Positive Psychiatry, Psychotherapy and Psychology. Springer; 2020:vii-xiii.
3. Dobiała E, Winkler P. ‘Positive psychotherapy’ according to Seligman and ‘positive psychotherapy’ according to Peseschkian: a comparison. Int J Psychother. 2016;20(3):5-17.
4. Peseschkian N. Positive Psychotherapy: Theory and Practice of a New Method. Springer; 1987.
5. Seligman MEP, Rashid T, Parks AC. Positive psychotherapy. Am Psychol. 2006;61(8):774-788.
6. Peseschkian N. Positive Psychosomatics: Clinical Manual of Positive Psychotherapy. AuthorHouse; 2016.
7. Peseschkian N. Positive psychotherapy. In: Pritz A, ed. Globalized Psychotherapy. Facultas Universitätsverlag; 2002.
8. Peseschkian H, Remmers A. Positive psychotherapy: an introduction. In: Messias E, Peseschkian H, Cagande C, eds. Positive Psychiatry, Psychotherapy and Psychology. Springer; 2020:11-32.
9. Moghaddam FM, Harre R. But is it science? Traditional and alternative approaches to the study of social behavior. World Psychol. 1995;1(4):47-78.
10. Peseschkian N. Oriental Stories as Techniques in Positive Psychotherapy. AuthorHouse; 2016.
11. Cope TA. Positive psychotherapy’s theory of the capacity to know as explication of unconscious contents. J Relig Health. 2009;48(1):79-89.
12. Huebner G. Health-illness from the perspective of positive psychotherapy. Global Psychother. 2021;1(1):57-61.
13. Sinici E. A ‘balance model’ for patients with post-traumatic stress disorder. Int J Psychother. 2015;19(3):13-19.
In a time of great national and global upheaval, increasing social problems, migration, climate crisis, globalization, and increasingly multicultural societies, our patients and their needs are unique, diverse, and changing. We need a new understanding of mental health to be able to adequately meet the demands of an ever-changing world. Treatment exclusively with psychotropic medications or years of psychoanalysis will not meet these needs.
Psychiatrists and psychotherapists feel (and actually have) a social responsibility, particularly in a multifaceted global society. Psychotherapeutic interventions may contribute to a more peaceful society1 by reducing individuals’ inner stress, solving (unconscious) conflicts, and conveying a humanistic worldview. As an integrative and transcultural method, positive psychotherapy has been applied for more than 45 years in more than 60 countries and is an active force within a “positive mental health movement.”2
The term “positive psychotherapy” describes 2 different approaches3: positive psychotherapy (1977) by Nossrat Peseschkian,4 which is a humanistic psychodynamic approach, and positive psychotherapy (2006) by Martin E.P. Seligman, Tayyab Rashid, and Acacia C. Parks,5 which is a more cognitive-behavioral therapy (CBT)–based approach. This article focuses on the first approach.
Why ‘positive’ psychotherapy?
The term “positive” implies that positive psychotherapy focuses on the patient’s possibilities and capacities. Symptoms and disorders are seen as capacities to react to a conflict. The Latin term “positum” or “positivus” is applied in its original meaning—the factual, the given, the actual. Factual and given are not only the disorder, the symptoms, and the problems but also the capacity to become healthy and/or cope with this situation. This positive meaning confronts the patient (and the therapist) with a lesser-known aspect of the illness, but one that is just as important for the understanding and clinical treatment of the affliction: its function, its meaning, and, consequently, its positive aspects.6
Positive psychotherapy is a humanistic psychodynamic psychotherapy approach developed by Nossrat Peseschkian (1933-2010).4,7 Positive psychotherapy has been developed since the 1970s in the clinical setting with neurotic and psychosomatic patients. It integrates approaches of the 4 main modalities of psychotherapy:
- a humanistic view of human beings
- a systemic approach toward culture, work, and environment
- a psychodynamic understanding of disorders
- a practical, goal-oriented approach with some cognitive-behavioral techniques.
The concept of balance
Based on a humanistic view of human beings and the resources every patient possesses, a key concept of positive psychotherapy is the importance of balance in one’s life. The balance model (Figure) is the core of positive psychotherapy and is applied in clinical and nonclinical settings. This model is based on the concept that there are 4 main areas of life in which a human being lives and functions. These areas influence one’s satisfaction in life, one’s feelings of self-worth, and the way one deals with conflicts and challenges. Although all 4 capacities are latent in every human being, depending on one`s education, environment, and zeitgeist, some will be more developed than others. Our life energies, activities, and reactions belong to these 4 areas of life:
- physical: eating, tenderness, sexuality, sleep, relaxation, sports, appearance, clothing
- achievement: work, job, career, money
- relationships: partner, family, friends, acquaintances and strangers, community life
- meaning and future: existential questions, spirituality, religious practices, future plans, fantasy.
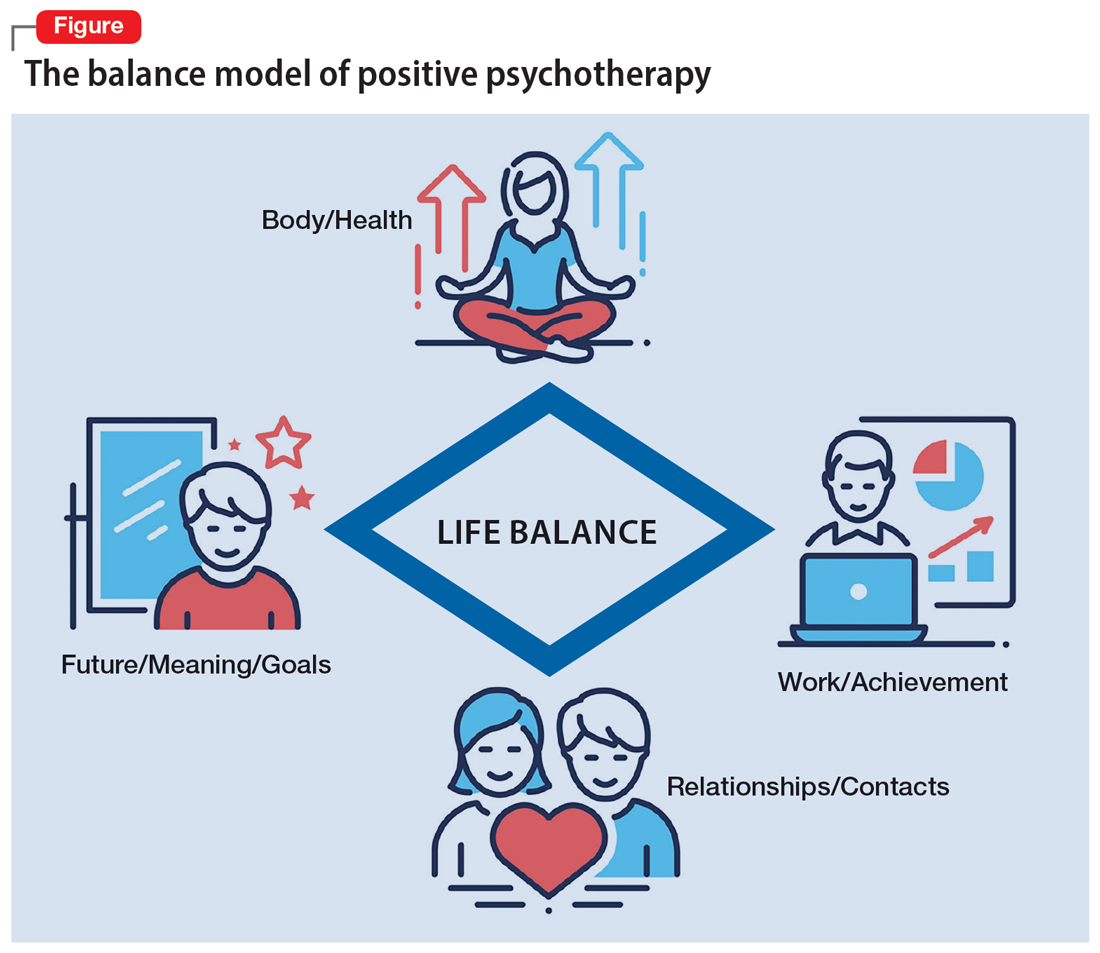
A goal of treatment is to help the patient recognize their own resources and mobilize them with the goal of bringing them into a dynamic equilibrium. This goal places value on a balanced distribution of energy (25% to each area), not of time. According to positive psychotherapy, a person does not become ill because one sphere of life is overemphasized but because of the areas that have been neglected. In the case vignette described in the Box, the problem is not the patient’s work but that his physical health, family and friends, and existential questions are being neglected. That the therapist is not critical from the start of treatment is a constructive experience for the patient and is important and fruitful for building the relationship between the therapist and the patient. Instead of emphasizing the deficits or the disorders, the patient and his family hear that he has neglected other areas of life and not developed them yet.
Box
Mr. M, a 52-year-old manager, is “sent” by his wife to see a psychotherapist. “My wife says I am married to my job, and I should spend more time with her and the children. I understand this, but I love my job. It is no stress for me, but a few minutes at home, and I feel totally stressed out,” he says. During the first interview, the therapist asks Mr. M to draw his energy distribution in the balance model (Figure), and it becomes clear he spends more than 80% of his time and energy on his job.
That is not such a surprise for him. But after some explanation, the therapist tells him that he should continue to do so and that it is an ability to be able to spend so much time every day for his job. Mr. M says, “You are the first person to tell me that it is good that I am working so much. I expected you, like all the others, to tell me I must reduce my working hours immediately, go on vacation, etc.”
Continue to: The balance model...
The balance model also embodies the 4 potential sources of self-esteem. Usually, only 1 or 2 areas provide self-esteem, but in the therapeutic process a patient can learn to uncover the neglected areas so that their self-esteem will have additional pillars of support. By emphasizing how therapy can help to develop one’s self-esteem, many patients can be motivated for the therapeutic process. The balance model, with its concept of devoting 25% of one’s energy to each sphere of life, gives the patient a clear vision about their life and how they can be healthy over the long run by avoiding one-sidedness.8
The transcultural approach
In positive psychotherapy, the term “transcultural” (or cross-cultural) means not only consideration of cultural factors when the therapist and patient come from diverse cultural backgrounds (intercultural psychotherapy or “migrant psychotherapy”) but specifically the consideration of cultural factors in every therapeutic relationship, as a therapeutic attitude and consequently as a sociopolitical dimension of our thinking and behavior. This consideration of the uniqueness of each person, of the relativity of human behavior, and of “unity in diversity” is an essential reason positive psychotherapy is not a “Western” method in the sense of “psychological colonization.”9 Rather, this approach is a culture-sensitive method that can be modified to adapt to particular cultures and life situations.
Transcultural positive psychotherapy begins with answering 2 questions: “How are people different?” and “What do all people have in common?”4 During the therapeutic process, the therapist gives examples from other cultures to the patient to help them relativize their own perspective and broaden their repertoire of behavior.
The use of stories, tales, proverbs, and anecdotes
A special technique of positive psychotherapy is the therapeutic use of stories, tales, proverbs, and anecdotes.10 Often stories from other cultures are used because they offer another perspective when the patient sees none. This has been shown to be highly effective in psychiatric settings, especially in group settings. Psychiatric patients can often easily relate to the images created by stories. In psychiatry and psychotherapy, stories can be a means of changing a patient’s point of view. Such narratives can free up the listener’s feelings and thoughts and often lead to “Aha!” moments. The mirror function of storytelling leads to identification. In the narratives, the reader or listener recognizes themself as well as their needs and situation. They can reflect on the stories without personally becoming the focus of these reflections and remember their own experiences. Stories present solutions that can be models against which one’s own approach can be compared but that also leave room for broader interpretation. Storytelling is particularly useful in bringing about change in patients who are holding fast to old and outworn ideas.
The positive interpretation of disorders
Positive psychotherapy is based on a humanistic view that every human being is good by nature and endowed with unique capacities.11 This positive perspective leads not only to a new quality of relationship between the therapist and patient but also to a new perspective on disorders (Table). Thus, disorders can be “interpreted” in a positive way6: What does the patient unconsciously want to express with their symptoms? What is the function of their disorder? The positive process brings with it a change in perspective to all those concerned: the patient, their family, and the therapist/physician. In this way, one moves from the symptom (which is the disorder and often already has been very thoroughly examined) to the conflict (and the function of the disorder). The positive interpretations are only offered to the patient (“What do you say to this explanation?” “Can you apply this to your own situation?”).
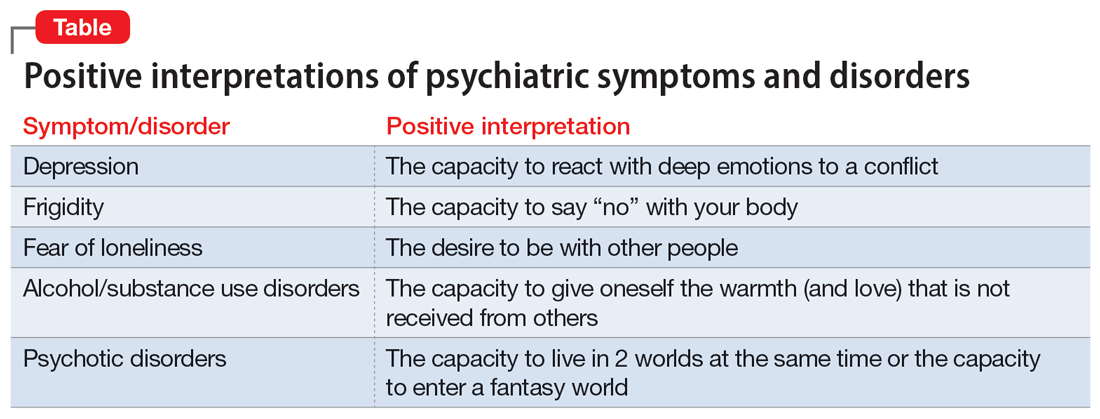
Continue to: This process also helps us...
This process also helps us focus on the “true” patient, who often is not our patient. The patient who comes to us functions as a symptom carrier and can be seen as the “weakest link” in the family chain. The “real patient” is often sitting at home. The positive interpretation of illnesses confronts the patient with the possible function and psychodynamic meaning of their illness for themself and their social milieu, encouraging the patient (and their family) to see their abilities and not merely the pathological aspects.12
Fields of application of positive psychotherapy
As a method positioned between manualized CBT and process-oriented analytical psychotherapy, positive psychotherapy pursues a semi-structured approach in diagnostics (first interview), treatment, posttherapeutic self-help, and training. Positive psychotherapy is applied for the treatment of mood (affective), neurotic, stress-related, and somatoform disorders; behavioral syndromes; and, to some extent, personality disorders. Positive psychotherapy has been employed successfully side-by-side with classical individual therapy as well as in the settings of couple, family, and group therapy.13
What makes positive psychotherapy attractive for mental health professionals?
- As a method that integrates the 4 main modalities of psychotherapy, it does not engage in the conflicts between different schools but combines effective elements into a single approach.
- As an integrative approach, it adjusts to the patient and not vice versa. It gives the therapist the possibility of focusing more on either the actual problems (supportive approach) or the basic conflict (psychodynamic approach).
- It uses vocabulary and terms that can be understood by patients from all strata of society.
- As a culturally sensitive method, it can be applied to patients from different cultures and does not require cultural adaptation.
- As a psychodynamic method, it does not stop after early life conflicts have become more conscious but helps the patient to apply the gained insights using practical techniques.
- It starts with positive affirmations and encouragement but does not later “forget” the unconscious conflicts that have led to disorders. It is not perceived as superficial.
- As a method originally coming from psychiatry and medical practice, it builds a bridge between a scientific basis and psychotherapeutic insights. It favors the biopsychosocial approach.
Bottom Line
Positive psychotherapy combines humanistic, systemic, psychodynamic, and cognitive-behavioral aspects. It is based on a resource-oriented view of human beings in which disorders are interpreted as capacities to react in a specific and unique way to life events and circumstances. Positive psychotherapy can be applied in psychiatry and psychotherapy. This short-term method is easily understood by patients from diverse cultures and social backgrounds.
Related Resources
- Peseschkian H, Remmers A. Positive psychotherapy: an introduction. In: Messias E, Peseschkian H, Cagande C, eds. Positive Psychiatry, Psychotherapy and Psychology. Springer; 2020:11-32. https://doi.org/10.1007/978-3-030-33264-8_2
- Tritt K, Loew T, Meyer M, et al. Positive psychotherapy: effectiveness of an interdisciplinary approach. Eur J Psychiatry. 1999;13(4):231-241.
- World Association for Positive and Transcultural Psychotherapy. http://www.positum.org
In a time of great national and global upheaval, increasing social problems, migration, climate crisis, globalization, and increasingly multicultural societies, our patients and their needs are unique, diverse, and changing. We need a new understanding of mental health to be able to adequately meet the demands of an ever-changing world. Treatment exclusively with psychotropic medications or years of psychoanalysis will not meet these needs.
Psychiatrists and psychotherapists feel (and actually have) a social responsibility, particularly in a multifaceted global society. Psychotherapeutic interventions may contribute to a more peaceful society1 by reducing individuals’ inner stress, solving (unconscious) conflicts, and conveying a humanistic worldview. As an integrative and transcultural method, positive psychotherapy has been applied for more than 45 years in more than 60 countries and is an active force within a “positive mental health movement.”2
The term “positive psychotherapy” describes 2 different approaches3: positive psychotherapy (1977) by Nossrat Peseschkian,4 which is a humanistic psychodynamic approach, and positive psychotherapy (2006) by Martin E.P. Seligman, Tayyab Rashid, and Acacia C. Parks,5 which is a more cognitive-behavioral therapy (CBT)–based approach. This article focuses on the first approach.
Why ‘positive’ psychotherapy?
The term “positive” implies that positive psychotherapy focuses on the patient’s possibilities and capacities. Symptoms and disorders are seen as capacities to react to a conflict. The Latin term “positum” or “positivus” is applied in its original meaning—the factual, the given, the actual. Factual and given are not only the disorder, the symptoms, and the problems but also the capacity to become healthy and/or cope with this situation. This positive meaning confronts the patient (and the therapist) with a lesser-known aspect of the illness, but one that is just as important for the understanding and clinical treatment of the affliction: its function, its meaning, and, consequently, its positive aspects.6
Positive psychotherapy is a humanistic psychodynamic psychotherapy approach developed by Nossrat Peseschkian (1933-2010).4,7 Positive psychotherapy has been developed since the 1970s in the clinical setting with neurotic and psychosomatic patients. It integrates approaches of the 4 main modalities of psychotherapy:
- a humanistic view of human beings
- a systemic approach toward culture, work, and environment
- a psychodynamic understanding of disorders
- a practical, goal-oriented approach with some cognitive-behavioral techniques.
The concept of balance
Based on a humanistic view of human beings and the resources every patient possesses, a key concept of positive psychotherapy is the importance of balance in one’s life. The balance model (Figure) is the core of positive psychotherapy and is applied in clinical and nonclinical settings. This model is based on the concept that there are 4 main areas of life in which a human being lives and functions. These areas influence one’s satisfaction in life, one’s feelings of self-worth, and the way one deals with conflicts and challenges. Although all 4 capacities are latent in every human being, depending on one`s education, environment, and zeitgeist, some will be more developed than others. Our life energies, activities, and reactions belong to these 4 areas of life:
- physical: eating, tenderness, sexuality, sleep, relaxation, sports, appearance, clothing
- achievement: work, job, career, money
- relationships: partner, family, friends, acquaintances and strangers, community life
- meaning and future: existential questions, spirituality, religious practices, future plans, fantasy.
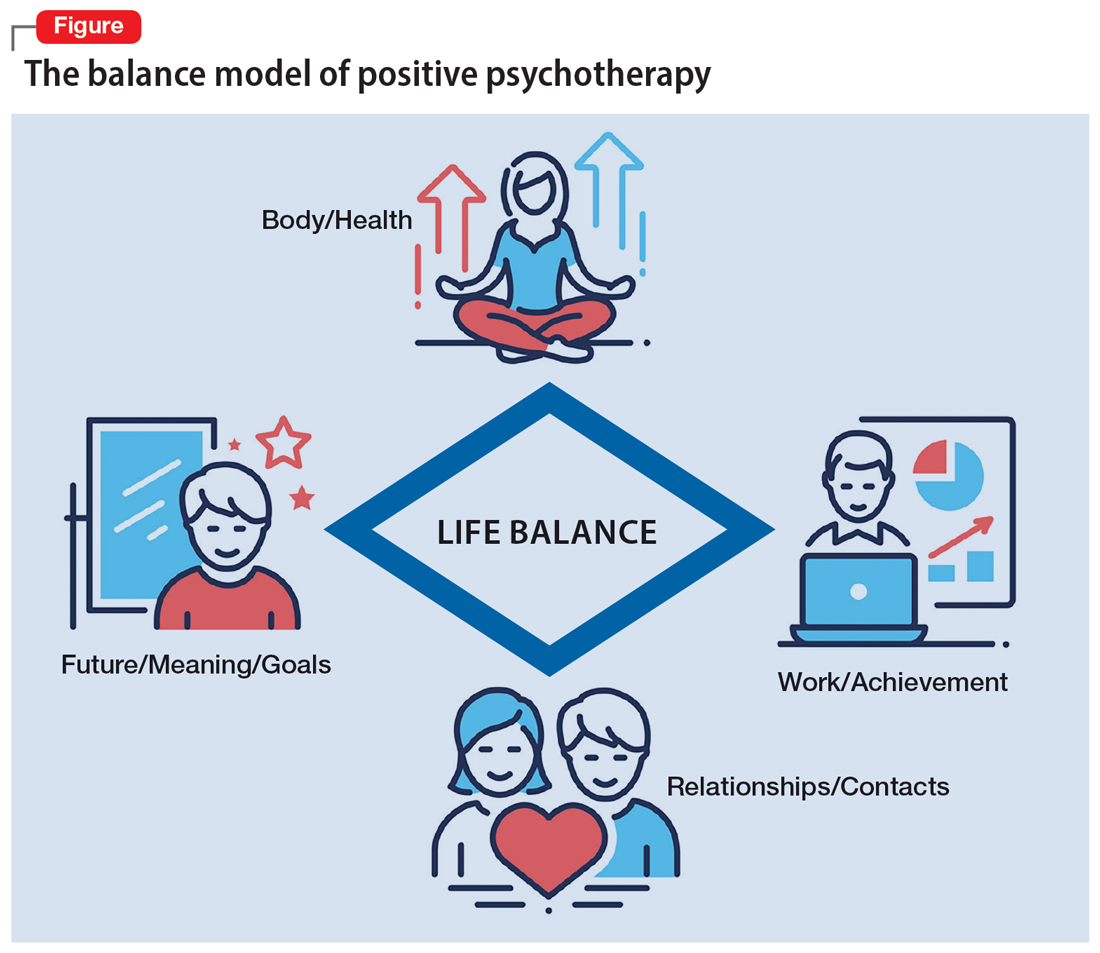
A goal of treatment is to help the patient recognize their own resources and mobilize them with the goal of bringing them into a dynamic equilibrium. This goal places value on a balanced distribution of energy (25% to each area), not of time. According to positive psychotherapy, a person does not become ill because one sphere of life is overemphasized but because of the areas that have been neglected. In the case vignette described in the Box, the problem is not the patient’s work but that his physical health, family and friends, and existential questions are being neglected. That the therapist is not critical from the start of treatment is a constructive experience for the patient and is important and fruitful for building the relationship between the therapist and the patient. Instead of emphasizing the deficits or the disorders, the patient and his family hear that he has neglected other areas of life and not developed them yet.
Box
Mr. M, a 52-year-old manager, is “sent” by his wife to see a psychotherapist. “My wife says I am married to my job, and I should spend more time with her and the children. I understand this, but I love my job. It is no stress for me, but a few minutes at home, and I feel totally stressed out,” he says. During the first interview, the therapist asks Mr. M to draw his energy distribution in the balance model (Figure), and it becomes clear he spends more than 80% of his time and energy on his job.
That is not such a surprise for him. But after some explanation, the therapist tells him that he should continue to do so and that it is an ability to be able to spend so much time every day for his job. Mr. M says, “You are the first person to tell me that it is good that I am working so much. I expected you, like all the others, to tell me I must reduce my working hours immediately, go on vacation, etc.”
Continue to: The balance model...
The balance model also embodies the 4 potential sources of self-esteem. Usually, only 1 or 2 areas provide self-esteem, but in the therapeutic process a patient can learn to uncover the neglected areas so that their self-esteem will have additional pillars of support. By emphasizing how therapy can help to develop one’s self-esteem, many patients can be motivated for the therapeutic process. The balance model, with its concept of devoting 25% of one’s energy to each sphere of life, gives the patient a clear vision about their life and how they can be healthy over the long run by avoiding one-sidedness.8
The transcultural approach
In positive psychotherapy, the term “transcultural” (or cross-cultural) means not only consideration of cultural factors when the therapist and patient come from diverse cultural backgrounds (intercultural psychotherapy or “migrant psychotherapy”) but specifically the consideration of cultural factors in every therapeutic relationship, as a therapeutic attitude and consequently as a sociopolitical dimension of our thinking and behavior. This consideration of the uniqueness of each person, of the relativity of human behavior, and of “unity in diversity” is an essential reason positive psychotherapy is not a “Western” method in the sense of “psychological colonization.”9 Rather, this approach is a culture-sensitive method that can be modified to adapt to particular cultures and life situations.
Transcultural positive psychotherapy begins with answering 2 questions: “How are people different?” and “What do all people have in common?”4 During the therapeutic process, the therapist gives examples from other cultures to the patient to help them relativize their own perspective and broaden their repertoire of behavior.
The use of stories, tales, proverbs, and anecdotes
A special technique of positive psychotherapy is the therapeutic use of stories, tales, proverbs, and anecdotes.10 Often stories from other cultures are used because they offer another perspective when the patient sees none. This has been shown to be highly effective in psychiatric settings, especially in group settings. Psychiatric patients can often easily relate to the images created by stories. In psychiatry and psychotherapy, stories can be a means of changing a patient’s point of view. Such narratives can free up the listener’s feelings and thoughts and often lead to “Aha!” moments. The mirror function of storytelling leads to identification. In the narratives, the reader or listener recognizes themself as well as their needs and situation. They can reflect on the stories without personally becoming the focus of these reflections and remember their own experiences. Stories present solutions that can be models against which one’s own approach can be compared but that also leave room for broader interpretation. Storytelling is particularly useful in bringing about change in patients who are holding fast to old and outworn ideas.
The positive interpretation of disorders
Positive psychotherapy is based on a humanistic view that every human being is good by nature and endowed with unique capacities.11 This positive perspective leads not only to a new quality of relationship between the therapist and patient but also to a new perspective on disorders (Table). Thus, disorders can be “interpreted” in a positive way6: What does the patient unconsciously want to express with their symptoms? What is the function of their disorder? The positive process brings with it a change in perspective to all those concerned: the patient, their family, and the therapist/physician. In this way, one moves from the symptom (which is the disorder and often already has been very thoroughly examined) to the conflict (and the function of the disorder). The positive interpretations are only offered to the patient (“What do you say to this explanation?” “Can you apply this to your own situation?”).
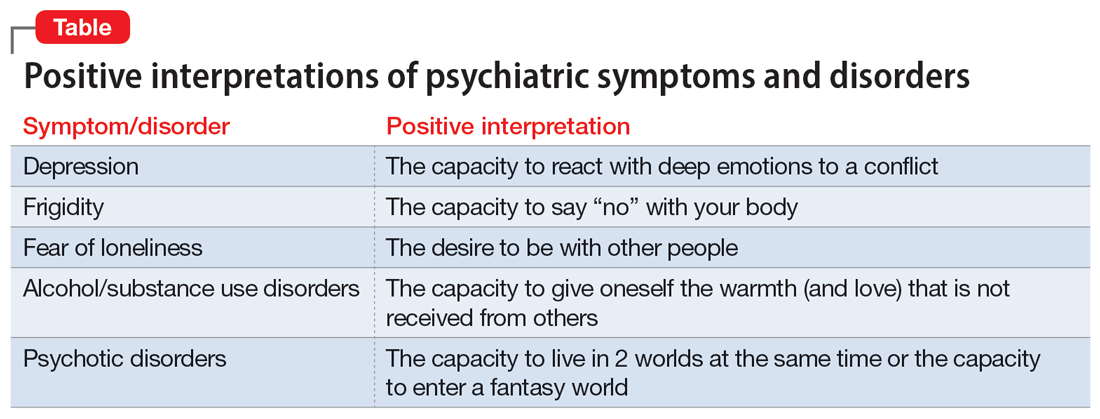
Continue to: This process also helps us...
This process also helps us focus on the “true” patient, who often is not our patient. The patient who comes to us functions as a symptom carrier and can be seen as the “weakest link” in the family chain. The “real patient” is often sitting at home. The positive interpretation of illnesses confronts the patient with the possible function and psychodynamic meaning of their illness for themself and their social milieu, encouraging the patient (and their family) to see their abilities and not merely the pathological aspects.12
Fields of application of positive psychotherapy
As a method positioned between manualized CBT and process-oriented analytical psychotherapy, positive psychotherapy pursues a semi-structured approach in diagnostics (first interview), treatment, posttherapeutic self-help, and training. Positive psychotherapy is applied for the treatment of mood (affective), neurotic, stress-related, and somatoform disorders; behavioral syndromes; and, to some extent, personality disorders. Positive psychotherapy has been employed successfully side-by-side with classical individual therapy as well as in the settings of couple, family, and group therapy.13
What makes positive psychotherapy attractive for mental health professionals?
- As a method that integrates the 4 main modalities of psychotherapy, it does not engage in the conflicts between different schools but combines effective elements into a single approach.
- As an integrative approach, it adjusts to the patient and not vice versa. It gives the therapist the possibility of focusing more on either the actual problems (supportive approach) or the basic conflict (psychodynamic approach).
- It uses vocabulary and terms that can be understood by patients from all strata of society.
- As a culturally sensitive method, it can be applied to patients from different cultures and does not require cultural adaptation.
- As a psychodynamic method, it does not stop after early life conflicts have become more conscious but helps the patient to apply the gained insights using practical techniques.
- It starts with positive affirmations and encouragement but does not later “forget” the unconscious conflicts that have led to disorders. It is not perceived as superficial.
- As a method originally coming from psychiatry and medical practice, it builds a bridge between a scientific basis and psychotherapeutic insights. It favors the biopsychosocial approach.
Bottom Line
Positive psychotherapy combines humanistic, systemic, psychodynamic, and cognitive-behavioral aspects. It is based on a resource-oriented view of human beings in which disorders are interpreted as capacities to react in a specific and unique way to life events and circumstances. Positive psychotherapy can be applied in psychiatry and psychotherapy. This short-term method is easily understood by patients from diverse cultures and social backgrounds.
Related Resources
- Peseschkian H, Remmers A. Positive psychotherapy: an introduction. In: Messias E, Peseschkian H, Cagande C, eds. Positive Psychiatry, Psychotherapy and Psychology. Springer; 2020:11-32. https://doi.org/10.1007/978-3-030-33264-8_2
- Tritt K, Loew T, Meyer M, et al. Positive psychotherapy: effectiveness of an interdisciplinary approach. Eur J Psychiatry. 1999;13(4):231-241.
- World Association for Positive and Transcultural Psychotherapy. http://www.positum.org
1. Mackenthun G. Passt Psychotherapie an ‚die Gesellschaft’ an? Dynamische Psychiatrie. 1991;24(5-6):326-333.
2. Jeste DV. Foreword: positive mental health. In: Messias E, Peseschkian H, Cagande C, eds. Positive Psychiatry, Psychotherapy and Psychology. Springer; 2020:vii-xiii.
3. Dobiała E, Winkler P. ‘Positive psychotherapy’ according to Seligman and ‘positive psychotherapy’ according to Peseschkian: a comparison. Int J Psychother. 2016;20(3):5-17.
4. Peseschkian N. Positive Psychotherapy: Theory and Practice of a New Method. Springer; 1987.
5. Seligman MEP, Rashid T, Parks AC. Positive psychotherapy. Am Psychol. 2006;61(8):774-788.
6. Peseschkian N. Positive Psychosomatics: Clinical Manual of Positive Psychotherapy. AuthorHouse; 2016.
7. Peseschkian N. Positive psychotherapy. In: Pritz A, ed. Globalized Psychotherapy. Facultas Universitätsverlag; 2002.
8. Peseschkian H, Remmers A. Positive psychotherapy: an introduction. In: Messias E, Peseschkian H, Cagande C, eds. Positive Psychiatry, Psychotherapy and Psychology. Springer; 2020:11-32.
9. Moghaddam FM, Harre R. But is it science? Traditional and alternative approaches to the study of social behavior. World Psychol. 1995;1(4):47-78.
10. Peseschkian N. Oriental Stories as Techniques in Positive Psychotherapy. AuthorHouse; 2016.
11. Cope TA. Positive psychotherapy’s theory of the capacity to know as explication of unconscious contents. J Relig Health. 2009;48(1):79-89.
12. Huebner G. Health-illness from the perspective of positive psychotherapy. Global Psychother. 2021;1(1):57-61.
13. Sinici E. A ‘balance model’ for patients with post-traumatic stress disorder. Int J Psychother. 2015;19(3):13-19.
1. Mackenthun G. Passt Psychotherapie an ‚die Gesellschaft’ an? Dynamische Psychiatrie. 1991;24(5-6):326-333.
2. Jeste DV. Foreword: positive mental health. In: Messias E, Peseschkian H, Cagande C, eds. Positive Psychiatry, Psychotherapy and Psychology. Springer; 2020:vii-xiii.
3. Dobiała E, Winkler P. ‘Positive psychotherapy’ according to Seligman and ‘positive psychotherapy’ according to Peseschkian: a comparison. Int J Psychother. 2016;20(3):5-17.
4. Peseschkian N. Positive Psychotherapy: Theory and Practice of a New Method. Springer; 1987.
5. Seligman MEP, Rashid T, Parks AC. Positive psychotherapy. Am Psychol. 2006;61(8):774-788.
6. Peseschkian N. Positive Psychosomatics: Clinical Manual of Positive Psychotherapy. AuthorHouse; 2016.
7. Peseschkian N. Positive psychotherapy. In: Pritz A, ed. Globalized Psychotherapy. Facultas Universitätsverlag; 2002.
8. Peseschkian H, Remmers A. Positive psychotherapy: an introduction. In: Messias E, Peseschkian H, Cagande C, eds. Positive Psychiatry, Psychotherapy and Psychology. Springer; 2020:11-32.
9. Moghaddam FM, Harre R. But is it science? Traditional and alternative approaches to the study of social behavior. World Psychol. 1995;1(4):47-78.
10. Peseschkian N. Oriental Stories as Techniques in Positive Psychotherapy. AuthorHouse; 2016.
11. Cope TA. Positive psychotherapy’s theory of the capacity to know as explication of unconscious contents. J Relig Health. 2009;48(1):79-89.
12. Huebner G. Health-illness from the perspective of positive psychotherapy. Global Psychother. 2021;1(1):57-61.
13. Sinici E. A ‘balance model’ for patients with post-traumatic stress disorder. Int J Psychother. 2015;19(3):13-19.