User login
Long-term erratic sleep may foretell cognitive problems
CHARLOTTE, N.C. – Erratic sleep patterns over years or even decades, along with a patient’s age and history of depression, may be harbingers of cognitive impairment later in life, an analysis of decades of data from a large sleep study has found.
“What we were a little surprised to find in this model was that sleep duration, whether short, long or average, was not significant, but the sleep variability – the change in sleep across those time measurements—was significantly impacting the incidence of cognitive impairment,” Samantha Keil, PhD, a postdoctoral fellow at the University of Washington, Seattle, reported at the at the annual meeting of the Associated Professional Sleep Societies.
The researchers analyzed sleep and cognition data collected over decades on 1,104 adults who participated in the Seattle Longitudinal Study. Study participants ranged from age 55 to over 100, with almost 80% of the study cohort aged 65 and older.
The Seattle Longitudinal Study first started gathering data in the 1950s. Participants in the study cohort underwent an extensive cognitive battery, which was added to the study in 1984 and gathered every 5-7 years, and completed a health behavioral questionnaire (HBQ), which was added in 1993 and administered every 3-5 years, Dr. Keil said. The HBQ included a question on average nightly sleep duration.
The study used a multivariable Cox proportional hazard regression model to evaluate the overall effect of average sleep duration and changes in sleep duration over time on cognitive impairment. Covariates used in the model included apolipoprotein E4 (APOE4) genotype, gender, years of education, ethnicity, and depression.
Dr. Keil said the model found, as expected, that the demographic variables of education, APOE status, and depression were significantly associated with cognitive impairment (hazard ratios of 1.11; 95% confidence interval [CI], 1.02-1.21; P = .01; and 2.08; 95% CI, 1.31-3.31; P < .005; and 1.08; 95% CI, 1.04-1.13; P < .005, respectively). Importantly, when evaluating the duration, change and variability of sleep, the researchers found that increased sleep variability was significantly associated with cognitive impairment (HR, 3.15; 95% CI, 1.69-5.87; P < .005).
Under this analysis, “sleep variability over time and not median sleep duration was associated with cognitive impairment,” she said. When sleep variability was added into the model, it improved the concordance score – a value that reflects the ability of a model to predict an outcome better than random chance – from .63 to .73 (a value of .5 indicates the model is no better at predicting an outcome than a random chance model; a value of .7 or greater indicates a good model).
Identification of sleep variability as a sleep pattern of interest in longitudinal studies is important, Dr. Keil said, because simply evaluating mean or median sleep duration across time might not account for a subject’s variable sleep phenotype. Most importantly, further evaluation of sleep variability with a linear regression prediction analysis (F statistic 8.796, P < .0001, adjusted R-squared .235) found that increased age, depression, and sleep variability significantly predicted cognitive impairment 10 years downstream. “Longitudinal sleep variability is perhaps for the first time being reported as significantly associated with the development of downstream cognitive impairment,” Dr. Keil said.
What makes this study unique, Dr. Keil said in an interview, is that it used self-reported longitudinal data gathered at 3- to 5-year intervals for up to 25 years, allowing for the assessment of variation of sleep duration across this entire time frame. “If you could use that shift in sleep duration as a point of therapeutic intervention, that would be really exciting,” she said.
Future research will evaluate how sleep variability and cognitive function are impacted by other variables gathered in the Seattle Longitudinal Study over the years, including factors such as diabetes and hypertension status, diet, alcohol and tobacco use, and marital and family status. Follow-up studies will be investigating the impact of sleep variability on neuropathologic disease progression and lymphatic system impairment, Dr. Keil said.
A newer approach
By linking sleep variability and daytime functioning, the study employs a “newer approach,” said Joseph M. Dzierzewski, PhD, director of behavioral medicine concentration in the department of psychology at Virginia Commonwealth University in Richmond. “While some previous work has examined night-to-night fluctuation in various sleep characteristics and cognitive functioning, what differentiates the present study from these previous works is the duration of the investigation,” he said. The “richness of data” in the Seattle Longitudinal Study and how it tracks sleep and cognition over years make it “quite unique and novel.”
Future studies, he said, should be deliberate in how they evaluate sleep and neurocognitive function across years. “Disentangling short-term moment-to-moment and day-to-day fluctuation, which may be more reversible in nature, from long-term, enduring month-to-month or year-to-year fluctuation, which may be more permanent, will be important for continuing to advance our understanding of these complex phenomena,” Dr. Dzierzewski said. “An additional important area of future investigation would be to continue the hunt for a common biological factor underpinning both sleep variability and Alzheimer’s disease.” That, he said, may help identify potential intervention targets.
Dr. Keil and Dr. Dzierzewski have no relevant disclosures.
CHARLOTTE, N.C. – Erratic sleep patterns over years or even decades, along with a patient’s age and history of depression, may be harbingers of cognitive impairment later in life, an analysis of decades of data from a large sleep study has found.
“What we were a little surprised to find in this model was that sleep duration, whether short, long or average, was not significant, but the sleep variability – the change in sleep across those time measurements—was significantly impacting the incidence of cognitive impairment,” Samantha Keil, PhD, a postdoctoral fellow at the University of Washington, Seattle, reported at the at the annual meeting of the Associated Professional Sleep Societies.
The researchers analyzed sleep and cognition data collected over decades on 1,104 adults who participated in the Seattle Longitudinal Study. Study participants ranged from age 55 to over 100, with almost 80% of the study cohort aged 65 and older.
The Seattle Longitudinal Study first started gathering data in the 1950s. Participants in the study cohort underwent an extensive cognitive battery, which was added to the study in 1984 and gathered every 5-7 years, and completed a health behavioral questionnaire (HBQ), which was added in 1993 and administered every 3-5 years, Dr. Keil said. The HBQ included a question on average nightly sleep duration.
The study used a multivariable Cox proportional hazard regression model to evaluate the overall effect of average sleep duration and changes in sleep duration over time on cognitive impairment. Covariates used in the model included apolipoprotein E4 (APOE4) genotype, gender, years of education, ethnicity, and depression.
Dr. Keil said the model found, as expected, that the demographic variables of education, APOE status, and depression were significantly associated with cognitive impairment (hazard ratios of 1.11; 95% confidence interval [CI], 1.02-1.21; P = .01; and 2.08; 95% CI, 1.31-3.31; P < .005; and 1.08; 95% CI, 1.04-1.13; P < .005, respectively). Importantly, when evaluating the duration, change and variability of sleep, the researchers found that increased sleep variability was significantly associated with cognitive impairment (HR, 3.15; 95% CI, 1.69-5.87; P < .005).
Under this analysis, “sleep variability over time and not median sleep duration was associated with cognitive impairment,” she said. When sleep variability was added into the model, it improved the concordance score – a value that reflects the ability of a model to predict an outcome better than random chance – from .63 to .73 (a value of .5 indicates the model is no better at predicting an outcome than a random chance model; a value of .7 or greater indicates a good model).
Identification of sleep variability as a sleep pattern of interest in longitudinal studies is important, Dr. Keil said, because simply evaluating mean or median sleep duration across time might not account for a subject’s variable sleep phenotype. Most importantly, further evaluation of sleep variability with a linear regression prediction analysis (F statistic 8.796, P < .0001, adjusted R-squared .235) found that increased age, depression, and sleep variability significantly predicted cognitive impairment 10 years downstream. “Longitudinal sleep variability is perhaps for the first time being reported as significantly associated with the development of downstream cognitive impairment,” Dr. Keil said.
What makes this study unique, Dr. Keil said in an interview, is that it used self-reported longitudinal data gathered at 3- to 5-year intervals for up to 25 years, allowing for the assessment of variation of sleep duration across this entire time frame. “If you could use that shift in sleep duration as a point of therapeutic intervention, that would be really exciting,” she said.
Future research will evaluate how sleep variability and cognitive function are impacted by other variables gathered in the Seattle Longitudinal Study over the years, including factors such as diabetes and hypertension status, diet, alcohol and tobacco use, and marital and family status. Follow-up studies will be investigating the impact of sleep variability on neuropathologic disease progression and lymphatic system impairment, Dr. Keil said.
A newer approach
By linking sleep variability and daytime functioning, the study employs a “newer approach,” said Joseph M. Dzierzewski, PhD, director of behavioral medicine concentration in the department of psychology at Virginia Commonwealth University in Richmond. “While some previous work has examined night-to-night fluctuation in various sleep characteristics and cognitive functioning, what differentiates the present study from these previous works is the duration of the investigation,” he said. The “richness of data” in the Seattle Longitudinal Study and how it tracks sleep and cognition over years make it “quite unique and novel.”
Future studies, he said, should be deliberate in how they evaluate sleep and neurocognitive function across years. “Disentangling short-term moment-to-moment and day-to-day fluctuation, which may be more reversible in nature, from long-term, enduring month-to-month or year-to-year fluctuation, which may be more permanent, will be important for continuing to advance our understanding of these complex phenomena,” Dr. Dzierzewski said. “An additional important area of future investigation would be to continue the hunt for a common biological factor underpinning both sleep variability and Alzheimer’s disease.” That, he said, may help identify potential intervention targets.
Dr. Keil and Dr. Dzierzewski have no relevant disclosures.
CHARLOTTE, N.C. – Erratic sleep patterns over years or even decades, along with a patient’s age and history of depression, may be harbingers of cognitive impairment later in life, an analysis of decades of data from a large sleep study has found.
“What we were a little surprised to find in this model was that sleep duration, whether short, long or average, was not significant, but the sleep variability – the change in sleep across those time measurements—was significantly impacting the incidence of cognitive impairment,” Samantha Keil, PhD, a postdoctoral fellow at the University of Washington, Seattle, reported at the at the annual meeting of the Associated Professional Sleep Societies.
The researchers analyzed sleep and cognition data collected over decades on 1,104 adults who participated in the Seattle Longitudinal Study. Study participants ranged from age 55 to over 100, with almost 80% of the study cohort aged 65 and older.
The Seattle Longitudinal Study first started gathering data in the 1950s. Participants in the study cohort underwent an extensive cognitive battery, which was added to the study in 1984 and gathered every 5-7 years, and completed a health behavioral questionnaire (HBQ), which was added in 1993 and administered every 3-5 years, Dr. Keil said. The HBQ included a question on average nightly sleep duration.
The study used a multivariable Cox proportional hazard regression model to evaluate the overall effect of average sleep duration and changes in sleep duration over time on cognitive impairment. Covariates used in the model included apolipoprotein E4 (APOE4) genotype, gender, years of education, ethnicity, and depression.
Dr. Keil said the model found, as expected, that the demographic variables of education, APOE status, and depression were significantly associated with cognitive impairment (hazard ratios of 1.11; 95% confidence interval [CI], 1.02-1.21; P = .01; and 2.08; 95% CI, 1.31-3.31; P < .005; and 1.08; 95% CI, 1.04-1.13; P < .005, respectively). Importantly, when evaluating the duration, change and variability of sleep, the researchers found that increased sleep variability was significantly associated with cognitive impairment (HR, 3.15; 95% CI, 1.69-5.87; P < .005).
Under this analysis, “sleep variability over time and not median sleep duration was associated with cognitive impairment,” she said. When sleep variability was added into the model, it improved the concordance score – a value that reflects the ability of a model to predict an outcome better than random chance – from .63 to .73 (a value of .5 indicates the model is no better at predicting an outcome than a random chance model; a value of .7 or greater indicates a good model).
Identification of sleep variability as a sleep pattern of interest in longitudinal studies is important, Dr. Keil said, because simply evaluating mean or median sleep duration across time might not account for a subject’s variable sleep phenotype. Most importantly, further evaluation of sleep variability with a linear regression prediction analysis (F statistic 8.796, P < .0001, adjusted R-squared .235) found that increased age, depression, and sleep variability significantly predicted cognitive impairment 10 years downstream. “Longitudinal sleep variability is perhaps for the first time being reported as significantly associated with the development of downstream cognitive impairment,” Dr. Keil said.
What makes this study unique, Dr. Keil said in an interview, is that it used self-reported longitudinal data gathered at 3- to 5-year intervals for up to 25 years, allowing for the assessment of variation of sleep duration across this entire time frame. “If you could use that shift in sleep duration as a point of therapeutic intervention, that would be really exciting,” she said.
Future research will evaluate how sleep variability and cognitive function are impacted by other variables gathered in the Seattle Longitudinal Study over the years, including factors such as diabetes and hypertension status, diet, alcohol and tobacco use, and marital and family status. Follow-up studies will be investigating the impact of sleep variability on neuropathologic disease progression and lymphatic system impairment, Dr. Keil said.
A newer approach
By linking sleep variability and daytime functioning, the study employs a “newer approach,” said Joseph M. Dzierzewski, PhD, director of behavioral medicine concentration in the department of psychology at Virginia Commonwealth University in Richmond. “While some previous work has examined night-to-night fluctuation in various sleep characteristics and cognitive functioning, what differentiates the present study from these previous works is the duration of the investigation,” he said. The “richness of data” in the Seattle Longitudinal Study and how it tracks sleep and cognition over years make it “quite unique and novel.”
Future studies, he said, should be deliberate in how they evaluate sleep and neurocognitive function across years. “Disentangling short-term moment-to-moment and day-to-day fluctuation, which may be more reversible in nature, from long-term, enduring month-to-month or year-to-year fluctuation, which may be more permanent, will be important for continuing to advance our understanding of these complex phenomena,” Dr. Dzierzewski said. “An additional important area of future investigation would be to continue the hunt for a common biological factor underpinning both sleep variability and Alzheimer’s disease.” That, he said, may help identify potential intervention targets.
Dr. Keil and Dr. Dzierzewski have no relevant disclosures.
AT SLEEP 2022
New onset-depression after RA diagnosis raises mortality risk ‘more than sixfold’
The development of depression after a rheumatoid arthritis diagnosis increased the risk for death “more than sixfold” when compared with having no depression at diagnosis, according to Danish researchers.
Cumulative mortality at 10 years was approximately 37% in patients with comorbid RA and depression versus around 13.5% of RA patients with no depression, Jens Kristian Pedersen, MD, PhD, of Odense (Denmark) University Hospital–Svendborg Hospital and the department of clinical research at the University of Southern Denmark, also in Odense, reported at the annual European Congress of Rheumatology.
“According to [antidepressant] exposure status, the cumulative mortality followed two clearly different paths,” Dr. Pedersen said. “The mortality curves separated early and already within the first and second year of follow-up.”
RA, depression, and mortality
Rates of depression in patients with RA are high, Dr. Pedersen said, and while it’s previously been reported that their coexistence can increase mortality, this is the first time that the link has been investigated in a population newly diagnosed with RA.
In this study, Dr. Pedersen and collaborators wanted to look at the association in incident RA and defined depression as the first filling of an antidepressant prescription.
“Although antidepressants are used for different indications, we have recently described that in RA the most frequent indication for filling antidepressants is depression,” he explained. Moreover, that research found that “the frequency of filling coincides with the occurrence of depressive disorder previously reported in the scientific literature.”
Data sourced from multiple Danish registers
To examine the mortality risk associated with newly diagnosed RA and new-onset depression, Dr. Pedersen described how five different Danish registers were used.
First, data from the DANBIO register were used to identify patients with incident RA living in Denmark over a 10-year period ending in December 2018. Although perhaps widely known as a biologics register, DANBIO is required by the Danish National Board of Health to collect information on all patients with RA, regardless of their treatment.
Next, the Danish National Prescription Register and Danish National Patient Register were consulted to obtain data on patients who had a first prescription for antidepressant treatment and information on those who developed a diagnosis of depression. Demographic, vital status, and socioeconomic data were collated from the Danish Civil Registration System and Statistics Denmark databases.
To be sure they were looking at incident cases of RA and new cases of depression, the researchers excluded anyone with an existing prescription of antidepressants or methotrexate, or who had a confirmed diagnosis of either disorder 3 years prior to the index date of Jan. 1, 2008.
This meant that, from a total population of 18,000 patients in the DANBIO database, there were just over 11,000 who could be included in the analyses.
Overall, the median age at RA diagnosis was 61 years, two-thirds were female, and two-thirds had seropositive disease.
New-onset depression in incident RA
“During follow-up, about 10% filled a prescription of antidepressants,” said Dr. Pedersen, adding that there were 671 deaths, representing around 57,000 person-years at risk.
“The majority died from natural causes,” he said, although the cause of death was unknown in 30% of cases.
Comparing those who did and did not have a prescription for antidepressants, there were some differences in the age at which death occurred, the percentage of females to males, the presence of other comorbidities, and levels of higher education and income. These were all adjusted for in the analyses.
Adjusted hazard rate ratios were calculated to look at the mortality risk in patients who had antidepressant exposure. The highest HRR for mortality with antidepressant use was seen in patients aged 55 years or younger at 6.66, with the next highest HRRs being for male gender (3.70) and seropositive RA (3.45).
But HRRs for seronegative RA, female gender, and age 55-70 years or older than 75 years were all still around 3.0.
Depression definition questioned
“My only concern is about the definition of depression in your analysis,” said a member of the audience at the congress.
“You used antidepressant use as a proxy of depression diagnosis, but it might be that most or many patients have taken [medication] like duloxetine for pain control, and you are just seeing higher disease activity and more aggressive RA.”
Dr. Pedersen responded: “After the EULAR 2022 submission deadline, we reanalyzed our data using two other measures of depression.
“First, we use treatment with antidepressants with a positive indication of depression, according to the prescribing physician, and secondly, we used first diagnosis with depression according to ICD-10 Code F32 – ‘depressive episode after discharge from hospital as an outpatient,’ ” he said.
“All definitions end up with a hazard rate ratio of about three. So, in my opinion, it doesn’t matter whether you focus on one measure of depression or the other.”
David Isenberg, MD, FRCP, professor of rheumatology at University College London, wanted to know more about the antecedent history of depression and whether people who had been depressed maybe a decade or 2 decades before, were more likely to get RA.
That calculation has not been done, Dr. Pedersen said, adding that the study also can’t account for people who may have had recurrent depression. Depression treatment guidelines often recommend nonpharmacologic intervention in the first instance, “so we do not necessarily get the right picture of recurrent depression if we look further back.”
Pointing out that the sixfold increase in mortality was impressive, another delegate asked about whether it was because of a higher disease activity or joint damage and if the mortality risk might be lower in patients who are in remission.
“We don’t know that yet,” Dr. Pedersen answered. “We haven’t done the calculations, but there is the issue of residual confounding if we don’t take all relevant covariates into account. So, we need to do that calculation as well.”
The study was supported by the Danish Rheumatism Association. Dr. Pedersen had no conflicts of interest to disclose.
The development of depression after a rheumatoid arthritis diagnosis increased the risk for death “more than sixfold” when compared with having no depression at diagnosis, according to Danish researchers.
Cumulative mortality at 10 years was approximately 37% in patients with comorbid RA and depression versus around 13.5% of RA patients with no depression, Jens Kristian Pedersen, MD, PhD, of Odense (Denmark) University Hospital–Svendborg Hospital and the department of clinical research at the University of Southern Denmark, also in Odense, reported at the annual European Congress of Rheumatology.
“According to [antidepressant] exposure status, the cumulative mortality followed two clearly different paths,” Dr. Pedersen said. “The mortality curves separated early and already within the first and second year of follow-up.”
RA, depression, and mortality
Rates of depression in patients with RA are high, Dr. Pedersen said, and while it’s previously been reported that their coexistence can increase mortality, this is the first time that the link has been investigated in a population newly diagnosed with RA.
In this study, Dr. Pedersen and collaborators wanted to look at the association in incident RA and defined depression as the first filling of an antidepressant prescription.
“Although antidepressants are used for different indications, we have recently described that in RA the most frequent indication for filling antidepressants is depression,” he explained. Moreover, that research found that “the frequency of filling coincides with the occurrence of depressive disorder previously reported in the scientific literature.”
Data sourced from multiple Danish registers
To examine the mortality risk associated with newly diagnosed RA and new-onset depression, Dr. Pedersen described how five different Danish registers were used.
First, data from the DANBIO register were used to identify patients with incident RA living in Denmark over a 10-year period ending in December 2018. Although perhaps widely known as a biologics register, DANBIO is required by the Danish National Board of Health to collect information on all patients with RA, regardless of their treatment.
Next, the Danish National Prescription Register and Danish National Patient Register were consulted to obtain data on patients who had a first prescription for antidepressant treatment and information on those who developed a diagnosis of depression. Demographic, vital status, and socioeconomic data were collated from the Danish Civil Registration System and Statistics Denmark databases.
To be sure they were looking at incident cases of RA and new cases of depression, the researchers excluded anyone with an existing prescription of antidepressants or methotrexate, or who had a confirmed diagnosis of either disorder 3 years prior to the index date of Jan. 1, 2008.
This meant that, from a total population of 18,000 patients in the DANBIO database, there were just over 11,000 who could be included in the analyses.
Overall, the median age at RA diagnosis was 61 years, two-thirds were female, and two-thirds had seropositive disease.
New-onset depression in incident RA
“During follow-up, about 10% filled a prescription of antidepressants,” said Dr. Pedersen, adding that there were 671 deaths, representing around 57,000 person-years at risk.
“The majority died from natural causes,” he said, although the cause of death was unknown in 30% of cases.
Comparing those who did and did not have a prescription for antidepressants, there were some differences in the age at which death occurred, the percentage of females to males, the presence of other comorbidities, and levels of higher education and income. These were all adjusted for in the analyses.
Adjusted hazard rate ratios were calculated to look at the mortality risk in patients who had antidepressant exposure. The highest HRR for mortality with antidepressant use was seen in patients aged 55 years or younger at 6.66, with the next highest HRRs being for male gender (3.70) and seropositive RA (3.45).
But HRRs for seronegative RA, female gender, and age 55-70 years or older than 75 years were all still around 3.0.
Depression definition questioned
“My only concern is about the definition of depression in your analysis,” said a member of the audience at the congress.
“You used antidepressant use as a proxy of depression diagnosis, but it might be that most or many patients have taken [medication] like duloxetine for pain control, and you are just seeing higher disease activity and more aggressive RA.”
Dr. Pedersen responded: “After the EULAR 2022 submission deadline, we reanalyzed our data using two other measures of depression.
“First, we use treatment with antidepressants with a positive indication of depression, according to the prescribing physician, and secondly, we used first diagnosis with depression according to ICD-10 Code F32 – ‘depressive episode after discharge from hospital as an outpatient,’ ” he said.
“All definitions end up with a hazard rate ratio of about three. So, in my opinion, it doesn’t matter whether you focus on one measure of depression or the other.”
David Isenberg, MD, FRCP, professor of rheumatology at University College London, wanted to know more about the antecedent history of depression and whether people who had been depressed maybe a decade or 2 decades before, were more likely to get RA.
That calculation has not been done, Dr. Pedersen said, adding that the study also can’t account for people who may have had recurrent depression. Depression treatment guidelines often recommend nonpharmacologic intervention in the first instance, “so we do not necessarily get the right picture of recurrent depression if we look further back.”
Pointing out that the sixfold increase in mortality was impressive, another delegate asked about whether it was because of a higher disease activity or joint damage and if the mortality risk might be lower in patients who are in remission.
“We don’t know that yet,” Dr. Pedersen answered. “We haven’t done the calculations, but there is the issue of residual confounding if we don’t take all relevant covariates into account. So, we need to do that calculation as well.”
The study was supported by the Danish Rheumatism Association. Dr. Pedersen had no conflicts of interest to disclose.
The development of depression after a rheumatoid arthritis diagnosis increased the risk for death “more than sixfold” when compared with having no depression at diagnosis, according to Danish researchers.
Cumulative mortality at 10 years was approximately 37% in patients with comorbid RA and depression versus around 13.5% of RA patients with no depression, Jens Kristian Pedersen, MD, PhD, of Odense (Denmark) University Hospital–Svendborg Hospital and the department of clinical research at the University of Southern Denmark, also in Odense, reported at the annual European Congress of Rheumatology.
“According to [antidepressant] exposure status, the cumulative mortality followed two clearly different paths,” Dr. Pedersen said. “The mortality curves separated early and already within the first and second year of follow-up.”
RA, depression, and mortality
Rates of depression in patients with RA are high, Dr. Pedersen said, and while it’s previously been reported that their coexistence can increase mortality, this is the first time that the link has been investigated in a population newly diagnosed with RA.
In this study, Dr. Pedersen and collaborators wanted to look at the association in incident RA and defined depression as the first filling of an antidepressant prescription.
“Although antidepressants are used for different indications, we have recently described that in RA the most frequent indication for filling antidepressants is depression,” he explained. Moreover, that research found that “the frequency of filling coincides with the occurrence of depressive disorder previously reported in the scientific literature.”
Data sourced from multiple Danish registers
To examine the mortality risk associated with newly diagnosed RA and new-onset depression, Dr. Pedersen described how five different Danish registers were used.
First, data from the DANBIO register were used to identify patients with incident RA living in Denmark over a 10-year period ending in December 2018. Although perhaps widely known as a biologics register, DANBIO is required by the Danish National Board of Health to collect information on all patients with RA, regardless of their treatment.
Next, the Danish National Prescription Register and Danish National Patient Register were consulted to obtain data on patients who had a first prescription for antidepressant treatment and information on those who developed a diagnosis of depression. Demographic, vital status, and socioeconomic data were collated from the Danish Civil Registration System and Statistics Denmark databases.
To be sure they were looking at incident cases of RA and new cases of depression, the researchers excluded anyone with an existing prescription of antidepressants or methotrexate, or who had a confirmed diagnosis of either disorder 3 years prior to the index date of Jan. 1, 2008.
This meant that, from a total population of 18,000 patients in the DANBIO database, there were just over 11,000 who could be included in the analyses.
Overall, the median age at RA diagnosis was 61 years, two-thirds were female, and two-thirds had seropositive disease.
New-onset depression in incident RA
“During follow-up, about 10% filled a prescription of antidepressants,” said Dr. Pedersen, adding that there were 671 deaths, representing around 57,000 person-years at risk.
“The majority died from natural causes,” he said, although the cause of death was unknown in 30% of cases.
Comparing those who did and did not have a prescription for antidepressants, there were some differences in the age at which death occurred, the percentage of females to males, the presence of other comorbidities, and levels of higher education and income. These were all adjusted for in the analyses.
Adjusted hazard rate ratios were calculated to look at the mortality risk in patients who had antidepressant exposure. The highest HRR for mortality with antidepressant use was seen in patients aged 55 years or younger at 6.66, with the next highest HRRs being for male gender (3.70) and seropositive RA (3.45).
But HRRs for seronegative RA, female gender, and age 55-70 years or older than 75 years were all still around 3.0.
Depression definition questioned
“My only concern is about the definition of depression in your analysis,” said a member of the audience at the congress.
“You used antidepressant use as a proxy of depression diagnosis, but it might be that most or many patients have taken [medication] like duloxetine for pain control, and you are just seeing higher disease activity and more aggressive RA.”
Dr. Pedersen responded: “After the EULAR 2022 submission deadline, we reanalyzed our data using two other measures of depression.
“First, we use treatment with antidepressants with a positive indication of depression, according to the prescribing physician, and secondly, we used first diagnosis with depression according to ICD-10 Code F32 – ‘depressive episode after discharge from hospital as an outpatient,’ ” he said.
“All definitions end up with a hazard rate ratio of about three. So, in my opinion, it doesn’t matter whether you focus on one measure of depression or the other.”
David Isenberg, MD, FRCP, professor of rheumatology at University College London, wanted to know more about the antecedent history of depression and whether people who had been depressed maybe a decade or 2 decades before, were more likely to get RA.
That calculation has not been done, Dr. Pedersen said, adding that the study also can’t account for people who may have had recurrent depression. Depression treatment guidelines often recommend nonpharmacologic intervention in the first instance, “so we do not necessarily get the right picture of recurrent depression if we look further back.”
Pointing out that the sixfold increase in mortality was impressive, another delegate asked about whether it was because of a higher disease activity or joint damage and if the mortality risk might be lower in patients who are in remission.
“We don’t know that yet,” Dr. Pedersen answered. “We haven’t done the calculations, but there is the issue of residual confounding if we don’t take all relevant covariates into account. So, we need to do that calculation as well.”
The study was supported by the Danish Rheumatism Association. Dr. Pedersen had no conflicts of interest to disclose.
FROM THE EULAR 2022 CONGRESS
Adjunctive psychotherapy may offer no benefit in severe depression
Results of a cross-sectional, naturalistic, multicenter European study showed there were no significant differences in response rates between patients with major depressive disorder (MDD) who received combination treatment with psychotherapy and antidepressant medication in comparison with those who received antidepressant monotherapy, even when comparing different types of psychotherapy.
This “might emphasize the fundamental role of the underlying complex biological interrelationships in MDD and its treatment,” said study investigator Lucie Bartova, MD, PhD, Clinical Division of General Psychiatry, Medical University of Vienna.
However, she noted that patients who received psychotherapy in combination with antidepressants also had “beneficial sociodemographic and clinical characteristics,” which might reflect poorer access to “psychotherapeutic techniques for patients who are more severely ill and have less socioeconomic privilege.”
The resulting selection bias may cause patients with more severe illness to “fall by the wayside,” Dr. Bartova said.
Lead researcher Siegfried Kasper, MD, also from the Medical University of Vienna, agreed, saying in a press release that, by implication, “additional psychotherapy tends to be given to more highly educated and healthier patients, which may reflect the greater availability of psychotherapy to more socially and economically advantaged patients.”
The findings, some of which were previously published in the Journal of Psychiatry Research, were presented at the virtual European Psychiatric Association 2022 Congress.
Inconsistent guidelines
During her presentation, Dr. Bartova said that while “numerous effective antidepressant strategies are available for the treatment of MDD, many patients do not achieve a satisfactory treatment response,” which often leads to further management refinement and the use of off-label treatments.
She continued, saying that the “most obvious” approach in these situations is to try the available treatment options in a “systematic and individualized” manner, ideally by following recommended treatment algorithms.
Meta-analyses have suggested that standardized psychotherapy with fixed, regular sessions that follows an established rationale and is based on a defined school of thought is effective in MDD, “with at least moderate effects.”
Among the psychotherapy approaches, cognitive-behavioral therapy (CBT) is the “best and most investigated,” Dr. Bartova said, but international clinical practice guidelines “lack consistency” regarding recommendations for psychotherapy.
To examine the use and impact of psychotherapy for MDD patients, the researchers studied 1,410 adult inpatients and outpatients from 10 centers in eight countries who were surveyed between 2011 and 2016 by the European Group for the Study of Resistant Depression.
Participants were assessed via the Mini–International Neuropsychiatric Interview, the Montgomery-Åsberg Depression Rating Scale, and the Hamilton Depression Rating Scale.
Results showed that among 1,279 MDD patients who were included in the final analysis, 880 (68.8%) received only antidepressants, while 399 (31.2%) received some form of structured psychotherapy as part of their treatment.
These patients included 22.8% who received CBT, 3.4% who underwent psychoanalytic psychotherapy, and 1.3% who received systemic psychotherapy. The additional psychotherapy was not specified for 3.8%.
Dr. Bartova explained that the use of psychotherapy in combination pharmacologic treatment was significantly associated with younger age, higher educational attainment, and ongoing employment in comparison with antidepressant use alone (P < .001 for all).
In addition, combination therapy was associated with an earlier average age of MDD onset, lower severity of current depressive symptoms, a lower risk of suicidality, higher rates of additional melancholic features in the patients’ symptomatology, and higher rates of comorbid asthma and migraine (P < .001 for all).
There was also a significant association between the use of psychotherapy plus pharmacologic treatment and lower average daily doses of first-line antidepressant medication (P < .001), as well as more frequent administration of agomelatine (P < .001) and a trend toward greater use of vortioxetine (P = .006).
In contrast, among patients who received antidepressants alone, there was a trend toward higher rates of additional psychotic features (P = .054), and the patients were more likely to have received selective serotonin reuptake inhibitors as their first-line antidepressant medication (P < .001).
The researchers found there was no significant difference in rates of response, nonresponse, and treatment-resistant depression (TRD) between patients who received combination psychotherapy and pharmacotherapy and those who received antidepressants alone (P = .369).
Dr. Bartova showed that 25.8% of MDD patients who received combination therapy were classified as responders, compared with 23.5% of those given only antidepressants. Nonresponse was identified in 35.6% and 33.8% of patients, respectively, while 38.6% versus 42.7% had TRD.
Dr. Bartova and colleagues performed an additional analysis to determine whether there was any difference in response depending on the type of psychotherapy.
They divided patients who received combination therapy into those who had received CBT and those who had been given another form of psychotherapy.
Again, there were no significant differences in response, nonresponse, and TRD (P = .256). The response rate was 27.1% among patients given combination CBT, versus 22.4% among those who received another psychotherapy.
“Despite clinical guidelines and studies which advocate for psychotherapy and combining psychotherapy with antidepressants, this study shows that in real life, no added value can be demonstrated for psychotherapy in those already treated with antidepressants for severe depression,” Livia De Picker, MD, PhD, Collaborative Antwerp Psychiatric Research Institute, University of Antwerp, Belgium, said in the press release.
“This doesn’t necessarily mean that psychotherapy is not useful, but it is a clear sign that the way we are currently managing these depressed patients with psychotherapy is not effective and needs critical evaluation,” added Dr. De Picker, who was not involved in the research.
However, Michael E. Thase, MD, professor of psychiatry, University of Pennsylvania, Philadelphia, told this news organization that the current study “is a secondary analysis of a naturalistic study.”
Consequently, it is not possible to account for the “dose and duration, and quality, of the psychotherapy provided.”
Therefore, the findings simply suggest that “the kinds of psychotherapy provided to these patients was not so powerful that people who received it consistently did better than those who did not,” Dr. Thase said.
The European Group for the Study of Resistant Depression obtained an unrestricted grant sponsored by Lundbeck A/S. Dr. Bartova has relationships with AOP Orphan, Medizin Medien Austria, Universimed, Vertretungsnetz, Dialectica, Diagnosia, Schwabe, Janssen, Lundbeck, and Angelini. No other relevant financial relationships have been disclosed.
A version of this article first appeared on Medscape.com.
Results of a cross-sectional, naturalistic, multicenter European study showed there were no significant differences in response rates between patients with major depressive disorder (MDD) who received combination treatment with psychotherapy and antidepressant medication in comparison with those who received antidepressant monotherapy, even when comparing different types of psychotherapy.
This “might emphasize the fundamental role of the underlying complex biological interrelationships in MDD and its treatment,” said study investigator Lucie Bartova, MD, PhD, Clinical Division of General Psychiatry, Medical University of Vienna.
However, she noted that patients who received psychotherapy in combination with antidepressants also had “beneficial sociodemographic and clinical characteristics,” which might reflect poorer access to “psychotherapeutic techniques for patients who are more severely ill and have less socioeconomic privilege.”
The resulting selection bias may cause patients with more severe illness to “fall by the wayside,” Dr. Bartova said.
Lead researcher Siegfried Kasper, MD, also from the Medical University of Vienna, agreed, saying in a press release that, by implication, “additional psychotherapy tends to be given to more highly educated and healthier patients, which may reflect the greater availability of psychotherapy to more socially and economically advantaged patients.”
The findings, some of which were previously published in the Journal of Psychiatry Research, were presented at the virtual European Psychiatric Association 2022 Congress.
Inconsistent guidelines
During her presentation, Dr. Bartova said that while “numerous effective antidepressant strategies are available for the treatment of MDD, many patients do not achieve a satisfactory treatment response,” which often leads to further management refinement and the use of off-label treatments.
She continued, saying that the “most obvious” approach in these situations is to try the available treatment options in a “systematic and individualized” manner, ideally by following recommended treatment algorithms.
Meta-analyses have suggested that standardized psychotherapy with fixed, regular sessions that follows an established rationale and is based on a defined school of thought is effective in MDD, “with at least moderate effects.”
Among the psychotherapy approaches, cognitive-behavioral therapy (CBT) is the “best and most investigated,” Dr. Bartova said, but international clinical practice guidelines “lack consistency” regarding recommendations for psychotherapy.
To examine the use and impact of psychotherapy for MDD patients, the researchers studied 1,410 adult inpatients and outpatients from 10 centers in eight countries who were surveyed between 2011 and 2016 by the European Group for the Study of Resistant Depression.
Participants were assessed via the Mini–International Neuropsychiatric Interview, the Montgomery-Åsberg Depression Rating Scale, and the Hamilton Depression Rating Scale.
Results showed that among 1,279 MDD patients who were included in the final analysis, 880 (68.8%) received only antidepressants, while 399 (31.2%) received some form of structured psychotherapy as part of their treatment.
These patients included 22.8% who received CBT, 3.4% who underwent psychoanalytic psychotherapy, and 1.3% who received systemic psychotherapy. The additional psychotherapy was not specified for 3.8%.
Dr. Bartova explained that the use of psychotherapy in combination pharmacologic treatment was significantly associated with younger age, higher educational attainment, and ongoing employment in comparison with antidepressant use alone (P < .001 for all).
In addition, combination therapy was associated with an earlier average age of MDD onset, lower severity of current depressive symptoms, a lower risk of suicidality, higher rates of additional melancholic features in the patients’ symptomatology, and higher rates of comorbid asthma and migraine (P < .001 for all).
There was also a significant association between the use of psychotherapy plus pharmacologic treatment and lower average daily doses of first-line antidepressant medication (P < .001), as well as more frequent administration of agomelatine (P < .001) and a trend toward greater use of vortioxetine (P = .006).
In contrast, among patients who received antidepressants alone, there was a trend toward higher rates of additional psychotic features (P = .054), and the patients were more likely to have received selective serotonin reuptake inhibitors as their first-line antidepressant medication (P < .001).
The researchers found there was no significant difference in rates of response, nonresponse, and treatment-resistant depression (TRD) between patients who received combination psychotherapy and pharmacotherapy and those who received antidepressants alone (P = .369).
Dr. Bartova showed that 25.8% of MDD patients who received combination therapy were classified as responders, compared with 23.5% of those given only antidepressants. Nonresponse was identified in 35.6% and 33.8% of patients, respectively, while 38.6% versus 42.7% had TRD.
Dr. Bartova and colleagues performed an additional analysis to determine whether there was any difference in response depending on the type of psychotherapy.
They divided patients who received combination therapy into those who had received CBT and those who had been given another form of psychotherapy.
Again, there were no significant differences in response, nonresponse, and TRD (P = .256). The response rate was 27.1% among patients given combination CBT, versus 22.4% among those who received another psychotherapy.
“Despite clinical guidelines and studies which advocate for psychotherapy and combining psychotherapy with antidepressants, this study shows that in real life, no added value can be demonstrated for psychotherapy in those already treated with antidepressants for severe depression,” Livia De Picker, MD, PhD, Collaborative Antwerp Psychiatric Research Institute, University of Antwerp, Belgium, said in the press release.
“This doesn’t necessarily mean that psychotherapy is not useful, but it is a clear sign that the way we are currently managing these depressed patients with psychotherapy is not effective and needs critical evaluation,” added Dr. De Picker, who was not involved in the research.
However, Michael E. Thase, MD, professor of psychiatry, University of Pennsylvania, Philadelphia, told this news organization that the current study “is a secondary analysis of a naturalistic study.”
Consequently, it is not possible to account for the “dose and duration, and quality, of the psychotherapy provided.”
Therefore, the findings simply suggest that “the kinds of psychotherapy provided to these patients was not so powerful that people who received it consistently did better than those who did not,” Dr. Thase said.
The European Group for the Study of Resistant Depression obtained an unrestricted grant sponsored by Lundbeck A/S. Dr. Bartova has relationships with AOP Orphan, Medizin Medien Austria, Universimed, Vertretungsnetz, Dialectica, Diagnosia, Schwabe, Janssen, Lundbeck, and Angelini. No other relevant financial relationships have been disclosed.
A version of this article first appeared on Medscape.com.
Results of a cross-sectional, naturalistic, multicenter European study showed there were no significant differences in response rates between patients with major depressive disorder (MDD) who received combination treatment with psychotherapy and antidepressant medication in comparison with those who received antidepressant monotherapy, even when comparing different types of psychotherapy.
This “might emphasize the fundamental role of the underlying complex biological interrelationships in MDD and its treatment,” said study investigator Lucie Bartova, MD, PhD, Clinical Division of General Psychiatry, Medical University of Vienna.
However, she noted that patients who received psychotherapy in combination with antidepressants also had “beneficial sociodemographic and clinical characteristics,” which might reflect poorer access to “psychotherapeutic techniques for patients who are more severely ill and have less socioeconomic privilege.”
The resulting selection bias may cause patients with more severe illness to “fall by the wayside,” Dr. Bartova said.
Lead researcher Siegfried Kasper, MD, also from the Medical University of Vienna, agreed, saying in a press release that, by implication, “additional psychotherapy tends to be given to more highly educated and healthier patients, which may reflect the greater availability of psychotherapy to more socially and economically advantaged patients.”
The findings, some of which were previously published in the Journal of Psychiatry Research, were presented at the virtual European Psychiatric Association 2022 Congress.
Inconsistent guidelines
During her presentation, Dr. Bartova said that while “numerous effective antidepressant strategies are available for the treatment of MDD, many patients do not achieve a satisfactory treatment response,” which often leads to further management refinement and the use of off-label treatments.
She continued, saying that the “most obvious” approach in these situations is to try the available treatment options in a “systematic and individualized” manner, ideally by following recommended treatment algorithms.
Meta-analyses have suggested that standardized psychotherapy with fixed, regular sessions that follows an established rationale and is based on a defined school of thought is effective in MDD, “with at least moderate effects.”
Among the psychotherapy approaches, cognitive-behavioral therapy (CBT) is the “best and most investigated,” Dr. Bartova said, but international clinical practice guidelines “lack consistency” regarding recommendations for psychotherapy.
To examine the use and impact of psychotherapy for MDD patients, the researchers studied 1,410 adult inpatients and outpatients from 10 centers in eight countries who were surveyed between 2011 and 2016 by the European Group for the Study of Resistant Depression.
Participants were assessed via the Mini–International Neuropsychiatric Interview, the Montgomery-Åsberg Depression Rating Scale, and the Hamilton Depression Rating Scale.
Results showed that among 1,279 MDD patients who were included in the final analysis, 880 (68.8%) received only antidepressants, while 399 (31.2%) received some form of structured psychotherapy as part of their treatment.
These patients included 22.8% who received CBT, 3.4% who underwent psychoanalytic psychotherapy, and 1.3% who received systemic psychotherapy. The additional psychotherapy was not specified for 3.8%.
Dr. Bartova explained that the use of psychotherapy in combination pharmacologic treatment was significantly associated with younger age, higher educational attainment, and ongoing employment in comparison with antidepressant use alone (P < .001 for all).
In addition, combination therapy was associated with an earlier average age of MDD onset, lower severity of current depressive symptoms, a lower risk of suicidality, higher rates of additional melancholic features in the patients’ symptomatology, and higher rates of comorbid asthma and migraine (P < .001 for all).
There was also a significant association between the use of psychotherapy plus pharmacologic treatment and lower average daily doses of first-line antidepressant medication (P < .001), as well as more frequent administration of agomelatine (P < .001) and a trend toward greater use of vortioxetine (P = .006).
In contrast, among patients who received antidepressants alone, there was a trend toward higher rates of additional psychotic features (P = .054), and the patients were more likely to have received selective serotonin reuptake inhibitors as their first-line antidepressant medication (P < .001).
The researchers found there was no significant difference in rates of response, nonresponse, and treatment-resistant depression (TRD) between patients who received combination psychotherapy and pharmacotherapy and those who received antidepressants alone (P = .369).
Dr. Bartova showed that 25.8% of MDD patients who received combination therapy were classified as responders, compared with 23.5% of those given only antidepressants. Nonresponse was identified in 35.6% and 33.8% of patients, respectively, while 38.6% versus 42.7% had TRD.
Dr. Bartova and colleagues performed an additional analysis to determine whether there was any difference in response depending on the type of psychotherapy.
They divided patients who received combination therapy into those who had received CBT and those who had been given another form of psychotherapy.
Again, there were no significant differences in response, nonresponse, and TRD (P = .256). The response rate was 27.1% among patients given combination CBT, versus 22.4% among those who received another psychotherapy.
“Despite clinical guidelines and studies which advocate for psychotherapy and combining psychotherapy with antidepressants, this study shows that in real life, no added value can be demonstrated for psychotherapy in those already treated with antidepressants for severe depression,” Livia De Picker, MD, PhD, Collaborative Antwerp Psychiatric Research Institute, University of Antwerp, Belgium, said in the press release.
“This doesn’t necessarily mean that psychotherapy is not useful, but it is a clear sign that the way we are currently managing these depressed patients with psychotherapy is not effective and needs critical evaluation,” added Dr. De Picker, who was not involved in the research.
However, Michael E. Thase, MD, professor of psychiatry, University of Pennsylvania, Philadelphia, told this news organization that the current study “is a secondary analysis of a naturalistic study.”
Consequently, it is not possible to account for the “dose and duration, and quality, of the psychotherapy provided.”
Therefore, the findings simply suggest that “the kinds of psychotherapy provided to these patients was not so powerful that people who received it consistently did better than those who did not,” Dr. Thase said.
The European Group for the Study of Resistant Depression obtained an unrestricted grant sponsored by Lundbeck A/S. Dr. Bartova has relationships with AOP Orphan, Medizin Medien Austria, Universimed, Vertretungsnetz, Dialectica, Diagnosia, Schwabe, Janssen, Lundbeck, and Angelini. No other relevant financial relationships have been disclosed.
A version of this article first appeared on Medscape.com.
FROM EPA 2022
A ‘crisis’ of suicidal thoughts, attempts in transgender youth
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
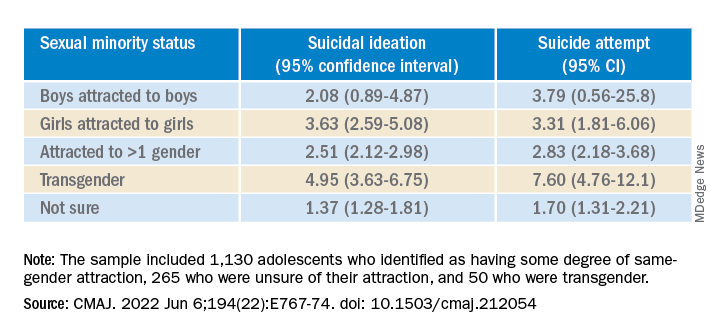
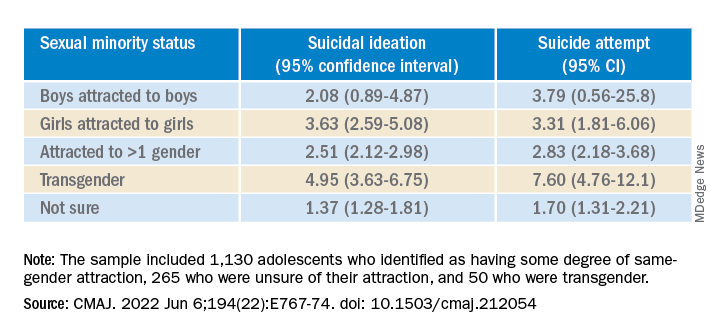
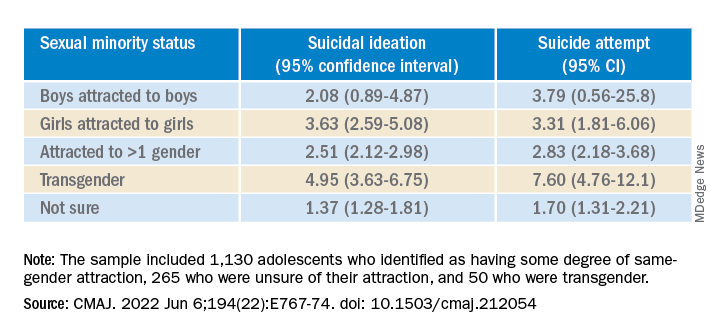
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE CANADIAN MEDICAL ASSOCIATION JOURNAL
Hormonal contraceptives protective against suicide?
Contrary to previous analyses, new research suggests.
In a study of more than 800 women younger than age 50 who attempted suicide and more than 3,000 age-matched peers, results showed those who took hormonal contraceptives had a 27% reduced risk for attempted suicide.
Further analysis showed this was confined to women without a history of psychiatric illness and the reduction in risk rose to 43% among those who took combined hormonal contraceptives rather than progestin-only versions.
The protective effect against attempted suicide increased further to 46% if ethinyl estradiol (EE)–containing preparations were used. Moreover, the beneficial effect of contraceptive use increased over time.
The main message is the “current use of hormonal contraceptives is not associated with an increased risk of attempted suicide in our population,” study presenter Elena Toffol, MD, PhD, department of public health, University of Helsinki, told meeting attendees at the European Psychiatric Association 2022 Congress.
Age range differences
Dr. Toffol said there could be “several reasons” why the results are different from those in previous studies, including that the researchers included a “larger age range.” She noted it is known that “older women have a lower rate of attempted suicide and use different types of contraceptives.”
Dr. Toffol said in an interview that, although it’s “hard to estimate any causality” because this is an observational study, it is “tempting to speculate, and it is plausible, that hormones partly play a role with some, but not all, women being more sensitive to hormonal influences.”
However, the results “may also reflect life choices or a protective life status; for example, more stable relationships or more conscious and health-focused behaviors,” she said.
“It may also be that the underlying characteristics of women who are prescribed or opt for certain types of contraceptives are somehow related to their suicidal risk,” she added.
In 2019, the global age-standardized suicide rate was 9.0 per 100,000, which translates into more than 700,000 deaths every year, Dr. Toffol noted.
However, she emphasized the World Health Organization has calculated that, for every adult who dies by suicide, more than 20 people attempt suicide. In addition, data from the U.S. Centers for Disease Control and Prevention indicate that attempted suicides are three times more common among young women than in men.
“What are the reasons for this gender gap?” Dr. Toffol asked during her presentation.
“It is known that the major risk factor for suicidal behavior is a psychiatric disorder, and in particular depression and mood disorders. And depression and mood disorders are more common in women than in men,” she said.
However, there is also “growing interest into the role of biological factors” in the risk for suicide, including hormones and hormonal contraception. Some studies have also suggested that there is an increased risk for depression and “both completed and attempted suicide” after starting hormonal contraception.
Dr. Toffol added that about 70% of European women use some form of contraception and, among Finnish women, 40% choose a hormonal contraceptive.
Nested analysis
The researchers conducted a nested case-control analysis combining 2017 national prescription data on 587,823 women aged 15-49 years with information from general and primary healthcare registers for the years 2018 to 2019.
They were able to identify 818 cases of attempted suicide among the women. These were matched 4:1 with 3,272 age-matched healthy women who acted as the control group. Use of hormonal contraceptives in the previous 180 days was determined for the whole cohort.
Among users of hormonal contraceptives, there were 344 attempted suicides in 2017, at an incidence rate of 0.59 per 1,000 person-years. This compared with 474 attempted suicides among nonusers, at an incidence rate of 0.81 per 1000 person-years.
Kaplan-Meier analysis showed there was a significant difference in rates for attempted suicide among hormonal contraceptive users versus nonusers, at an incidence rate ratio of 0.73 (P < .0001) – and the difference increased over time.
In addition, the incidence of attempted suicide decreased with increasing age, with the highest incidence rate in women aged 15-19 years (1.62 per 1,000 person-years).
Conditional logistic regression analysis that controlled for education, marital status, chronic disease, recent psychiatric hospitalization, and current use of psychotropic medication showed hormonal contraceptive use was not linked to an increased risk of attempted suicide overall, at an odds ratio of 0.79 (95% confidence interval, 0.56-1.11).
However, when they looked specifically at women without a history of psychiatric illness, the association became significant, at an OR of 0.73 for attempted suicide among hormonal contraceptive users (95% CI, 0.58-0.91), while the relationship remained nonsignificant in women with a history of psychiatric disorders.
Further analysis suggested the significant association was confined to women taking combined hormonal contraceptives, at an OR of 0.57 for suicide attempt versus nonusers (95% CI, 0.44-0.75), and those use EE-containing preparations (OR, 0.54; 95% CI, 0.40-0.73).
There was a suggestion in the data that hormonal contraceptives containing desogestrel or drospirenone alongside EE may offer the greatest reduction in attempted suicide risk, but that did not survive multivariate analysis.
Dr. Toffol also noted that they were not able to capture data on use of intrauterine devices in their analysis.
“There is a growing number of municipalities in Finland that are providing free-of-charge contraception to young women” that is often an intrauterine device, she said. The researchers hope to include these women in a future analysis.
‘Age matters’
Commenting on the findings, Alexis C. Edwards, PhD, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said the current study’s findings “made a lot of sense.” Dr. Edwards wasn’t involved with this study but conducted a previous study of 216,702 Swedish women aged 15-22 years that showed use of combination or progestin-only oral contraceptives was associated with an increased risk for suicidal behavior.
She agreed with Dr. Toffol that the “much larger age range” in the new study may have played a role in showing the opposite result.
“The trajectory that we saw if we had been able to continue following the women for longer – which we couldn’t, due to limitations of the registries – [was that] using hormonal contraceptives was going to end up being protective, so I do think that it matters what age you’re looking at,” she said.
Dr. Edwards noted the takeaway from both studies “is that, even if there is a slight increase in risk from using hormonal contraceptives, it’s short lived and it’s probably specific to young women, which is important.”
She suggested the hormonal benefit from extended contraceptive use could come from the regulation of mood, as it offers a “more stable hormonal course than what their body might be putting them through in the absence of using the pill.”
Overall, it is “really lovely to see very well-executed studies on this, providing more empirical evidence on this question, because it is something that’s relevant to anyone who’s potentially going to be using hormonal contraception,” Dr. Edwards said.
Clinical implications?
Andrea Fiorillo, MD, PhD, department of psychiatry, University of Campania “Luigi Vanvitelli,” Naples, Italy, said in a press release that the “striking” findings of the current study need “careful evaluation.”
They also need to be replicated in “different cohorts of women and controlled for the impact of several psychosocial stressors, such as economic upheavals, social insecurity, and uncertainty due to the COVID pandemic,” said Dr. Fiorillo, who was not involved with the research.
Nevertheless, she believes the “clinical implications of the study are obvious and may help to destigmatize the use of hormonal contraceptives.”
The study was funded by the Jane and Aatos Erkko Foundation, the Avohoidon Tsukimis äätiö (Foundation for Primary Care Research), the Yrj ö Jahnsson Foundation, and the Finnish Cultural Foundation. No relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
Contrary to previous analyses, new research suggests.
In a study of more than 800 women younger than age 50 who attempted suicide and more than 3,000 age-matched peers, results showed those who took hormonal contraceptives had a 27% reduced risk for attempted suicide.
Further analysis showed this was confined to women without a history of psychiatric illness and the reduction in risk rose to 43% among those who took combined hormonal contraceptives rather than progestin-only versions.
The protective effect against attempted suicide increased further to 46% if ethinyl estradiol (EE)–containing preparations were used. Moreover, the beneficial effect of contraceptive use increased over time.
The main message is the “current use of hormonal contraceptives is not associated with an increased risk of attempted suicide in our population,” study presenter Elena Toffol, MD, PhD, department of public health, University of Helsinki, told meeting attendees at the European Psychiatric Association 2022 Congress.
Age range differences
Dr. Toffol said there could be “several reasons” why the results are different from those in previous studies, including that the researchers included a “larger age range.” She noted it is known that “older women have a lower rate of attempted suicide and use different types of contraceptives.”
Dr. Toffol said in an interview that, although it’s “hard to estimate any causality” because this is an observational study, it is “tempting to speculate, and it is plausible, that hormones partly play a role with some, but not all, women being more sensitive to hormonal influences.”
However, the results “may also reflect life choices or a protective life status; for example, more stable relationships or more conscious and health-focused behaviors,” she said.
“It may also be that the underlying characteristics of women who are prescribed or opt for certain types of contraceptives are somehow related to their suicidal risk,” she added.
In 2019, the global age-standardized suicide rate was 9.0 per 100,000, which translates into more than 700,000 deaths every year, Dr. Toffol noted.
However, she emphasized the World Health Organization has calculated that, for every adult who dies by suicide, more than 20 people attempt suicide. In addition, data from the U.S. Centers for Disease Control and Prevention indicate that attempted suicides are three times more common among young women than in men.
“What are the reasons for this gender gap?” Dr. Toffol asked during her presentation.
“It is known that the major risk factor for suicidal behavior is a psychiatric disorder, and in particular depression and mood disorders. And depression and mood disorders are more common in women than in men,” she said.
However, there is also “growing interest into the role of biological factors” in the risk for suicide, including hormones and hormonal contraception. Some studies have also suggested that there is an increased risk for depression and “both completed and attempted suicide” after starting hormonal contraception.
Dr. Toffol added that about 70% of European women use some form of contraception and, among Finnish women, 40% choose a hormonal contraceptive.
Nested analysis
The researchers conducted a nested case-control analysis combining 2017 national prescription data on 587,823 women aged 15-49 years with information from general and primary healthcare registers for the years 2018 to 2019.
They were able to identify 818 cases of attempted suicide among the women. These were matched 4:1 with 3,272 age-matched healthy women who acted as the control group. Use of hormonal contraceptives in the previous 180 days was determined for the whole cohort.
Among users of hormonal contraceptives, there were 344 attempted suicides in 2017, at an incidence rate of 0.59 per 1,000 person-years. This compared with 474 attempted suicides among nonusers, at an incidence rate of 0.81 per 1000 person-years.
Kaplan-Meier analysis showed there was a significant difference in rates for attempted suicide among hormonal contraceptive users versus nonusers, at an incidence rate ratio of 0.73 (P < .0001) – and the difference increased over time.
In addition, the incidence of attempted suicide decreased with increasing age, with the highest incidence rate in women aged 15-19 years (1.62 per 1,000 person-years).
Conditional logistic regression analysis that controlled for education, marital status, chronic disease, recent psychiatric hospitalization, and current use of psychotropic medication showed hormonal contraceptive use was not linked to an increased risk of attempted suicide overall, at an odds ratio of 0.79 (95% confidence interval, 0.56-1.11).
However, when they looked specifically at women without a history of psychiatric illness, the association became significant, at an OR of 0.73 for attempted suicide among hormonal contraceptive users (95% CI, 0.58-0.91), while the relationship remained nonsignificant in women with a history of psychiatric disorders.
Further analysis suggested the significant association was confined to women taking combined hormonal contraceptives, at an OR of 0.57 for suicide attempt versus nonusers (95% CI, 0.44-0.75), and those use EE-containing preparations (OR, 0.54; 95% CI, 0.40-0.73).
There was a suggestion in the data that hormonal contraceptives containing desogestrel or drospirenone alongside EE may offer the greatest reduction in attempted suicide risk, but that did not survive multivariate analysis.
Dr. Toffol also noted that they were not able to capture data on use of intrauterine devices in their analysis.
“There is a growing number of municipalities in Finland that are providing free-of-charge contraception to young women” that is often an intrauterine device, she said. The researchers hope to include these women in a future analysis.
‘Age matters’
Commenting on the findings, Alexis C. Edwards, PhD, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said the current study’s findings “made a lot of sense.” Dr. Edwards wasn’t involved with this study but conducted a previous study of 216,702 Swedish women aged 15-22 years that showed use of combination or progestin-only oral contraceptives was associated with an increased risk for suicidal behavior.
She agreed with Dr. Toffol that the “much larger age range” in the new study may have played a role in showing the opposite result.
“The trajectory that we saw if we had been able to continue following the women for longer – which we couldn’t, due to limitations of the registries – [was that] using hormonal contraceptives was going to end up being protective, so I do think that it matters what age you’re looking at,” she said.
Dr. Edwards noted the takeaway from both studies “is that, even if there is a slight increase in risk from using hormonal contraceptives, it’s short lived and it’s probably specific to young women, which is important.”
She suggested the hormonal benefit from extended contraceptive use could come from the regulation of mood, as it offers a “more stable hormonal course than what their body might be putting them through in the absence of using the pill.”
Overall, it is “really lovely to see very well-executed studies on this, providing more empirical evidence on this question, because it is something that’s relevant to anyone who’s potentially going to be using hormonal contraception,” Dr. Edwards said.
Clinical implications?
Andrea Fiorillo, MD, PhD, department of psychiatry, University of Campania “Luigi Vanvitelli,” Naples, Italy, said in a press release that the “striking” findings of the current study need “careful evaluation.”
They also need to be replicated in “different cohorts of women and controlled for the impact of several psychosocial stressors, such as economic upheavals, social insecurity, and uncertainty due to the COVID pandemic,” said Dr. Fiorillo, who was not involved with the research.
Nevertheless, she believes the “clinical implications of the study are obvious and may help to destigmatize the use of hormonal contraceptives.”
The study was funded by the Jane and Aatos Erkko Foundation, the Avohoidon Tsukimis äätiö (Foundation for Primary Care Research), the Yrj ö Jahnsson Foundation, and the Finnish Cultural Foundation. No relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
Contrary to previous analyses, new research suggests.
In a study of more than 800 women younger than age 50 who attempted suicide and more than 3,000 age-matched peers, results showed those who took hormonal contraceptives had a 27% reduced risk for attempted suicide.
Further analysis showed this was confined to women without a history of psychiatric illness and the reduction in risk rose to 43% among those who took combined hormonal contraceptives rather than progestin-only versions.
The protective effect against attempted suicide increased further to 46% if ethinyl estradiol (EE)–containing preparations were used. Moreover, the beneficial effect of contraceptive use increased over time.
The main message is the “current use of hormonal contraceptives is not associated with an increased risk of attempted suicide in our population,” study presenter Elena Toffol, MD, PhD, department of public health, University of Helsinki, told meeting attendees at the European Psychiatric Association 2022 Congress.
Age range differences
Dr. Toffol said there could be “several reasons” why the results are different from those in previous studies, including that the researchers included a “larger age range.” She noted it is known that “older women have a lower rate of attempted suicide and use different types of contraceptives.”
Dr. Toffol said in an interview that, although it’s “hard to estimate any causality” because this is an observational study, it is “tempting to speculate, and it is plausible, that hormones partly play a role with some, but not all, women being more sensitive to hormonal influences.”
However, the results “may also reflect life choices or a protective life status; for example, more stable relationships or more conscious and health-focused behaviors,” she said.
“It may also be that the underlying characteristics of women who are prescribed or opt for certain types of contraceptives are somehow related to their suicidal risk,” she added.
In 2019, the global age-standardized suicide rate was 9.0 per 100,000, which translates into more than 700,000 deaths every year, Dr. Toffol noted.
However, she emphasized the World Health Organization has calculated that, for every adult who dies by suicide, more than 20 people attempt suicide. In addition, data from the U.S. Centers for Disease Control and Prevention indicate that attempted suicides are three times more common among young women than in men.
“What are the reasons for this gender gap?” Dr. Toffol asked during her presentation.
“It is known that the major risk factor for suicidal behavior is a psychiatric disorder, and in particular depression and mood disorders. And depression and mood disorders are more common in women than in men,” she said.
However, there is also “growing interest into the role of biological factors” in the risk for suicide, including hormones and hormonal contraception. Some studies have also suggested that there is an increased risk for depression and “both completed and attempted suicide” after starting hormonal contraception.
Dr. Toffol added that about 70% of European women use some form of contraception and, among Finnish women, 40% choose a hormonal contraceptive.
Nested analysis
The researchers conducted a nested case-control analysis combining 2017 national prescription data on 587,823 women aged 15-49 years with information from general and primary healthcare registers for the years 2018 to 2019.
They were able to identify 818 cases of attempted suicide among the women. These were matched 4:1 with 3,272 age-matched healthy women who acted as the control group. Use of hormonal contraceptives in the previous 180 days was determined for the whole cohort.
Among users of hormonal contraceptives, there were 344 attempted suicides in 2017, at an incidence rate of 0.59 per 1,000 person-years. This compared with 474 attempted suicides among nonusers, at an incidence rate of 0.81 per 1000 person-years.
Kaplan-Meier analysis showed there was a significant difference in rates for attempted suicide among hormonal contraceptive users versus nonusers, at an incidence rate ratio of 0.73 (P < .0001) – and the difference increased over time.
In addition, the incidence of attempted suicide decreased with increasing age, with the highest incidence rate in women aged 15-19 years (1.62 per 1,000 person-years).
Conditional logistic regression analysis that controlled for education, marital status, chronic disease, recent psychiatric hospitalization, and current use of psychotropic medication showed hormonal contraceptive use was not linked to an increased risk of attempted suicide overall, at an odds ratio of 0.79 (95% confidence interval, 0.56-1.11).
However, when they looked specifically at women without a history of psychiatric illness, the association became significant, at an OR of 0.73 for attempted suicide among hormonal contraceptive users (95% CI, 0.58-0.91), while the relationship remained nonsignificant in women with a history of psychiatric disorders.
Further analysis suggested the significant association was confined to women taking combined hormonal contraceptives, at an OR of 0.57 for suicide attempt versus nonusers (95% CI, 0.44-0.75), and those use EE-containing preparations (OR, 0.54; 95% CI, 0.40-0.73).
There was a suggestion in the data that hormonal contraceptives containing desogestrel or drospirenone alongside EE may offer the greatest reduction in attempted suicide risk, but that did not survive multivariate analysis.
Dr. Toffol also noted that they were not able to capture data on use of intrauterine devices in their analysis.
“There is a growing number of municipalities in Finland that are providing free-of-charge contraception to young women” that is often an intrauterine device, she said. The researchers hope to include these women in a future analysis.
‘Age matters’
Commenting on the findings, Alexis C. Edwards, PhD, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said the current study’s findings “made a lot of sense.” Dr. Edwards wasn’t involved with this study but conducted a previous study of 216,702 Swedish women aged 15-22 years that showed use of combination or progestin-only oral contraceptives was associated with an increased risk for suicidal behavior.
She agreed with Dr. Toffol that the “much larger age range” in the new study may have played a role in showing the opposite result.
“The trajectory that we saw if we had been able to continue following the women for longer – which we couldn’t, due to limitations of the registries – [was that] using hormonal contraceptives was going to end up being protective, so I do think that it matters what age you’re looking at,” she said.
Dr. Edwards noted the takeaway from both studies “is that, even if there is a slight increase in risk from using hormonal contraceptives, it’s short lived and it’s probably specific to young women, which is important.”
She suggested the hormonal benefit from extended contraceptive use could come from the regulation of mood, as it offers a “more stable hormonal course than what their body might be putting them through in the absence of using the pill.”
Overall, it is “really lovely to see very well-executed studies on this, providing more empirical evidence on this question, because it is something that’s relevant to anyone who’s potentially going to be using hormonal contraception,” Dr. Edwards said.
Clinical implications?
Andrea Fiorillo, MD, PhD, department of psychiatry, University of Campania “Luigi Vanvitelli,” Naples, Italy, said in a press release that the “striking” findings of the current study need “careful evaluation.”
They also need to be replicated in “different cohorts of women and controlled for the impact of several psychosocial stressors, such as economic upheavals, social insecurity, and uncertainty due to the COVID pandemic,” said Dr. Fiorillo, who was not involved with the research.
Nevertheless, she believes the “clinical implications of the study are obvious and may help to destigmatize the use of hormonal contraceptives.”
The study was funded by the Jane and Aatos Erkko Foundation, the Avohoidon Tsukimis äätiö (Foundation for Primary Care Research), the Yrj ö Jahnsson Foundation, and the Finnish Cultural Foundation. No relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
FROM EPA 2022
When suffering defies diagnosis
I still remember the woman who came to my office that day, years ago. She was struggling and uncomfortable, and she wanted “something” for stress. She described her life, and to me, it sounded stressful. She lived in a blended family and she described the chaos that one might expect to find in a household with four teens, their friends, their activities, and all it took to keep the household going. I spent 2 hours evaluating the patient, and I could not find a diagnosis that fit this problem nor – I believed – a pill that would fix it. She didn’t “meet criteria” for a psychiatric disorder, but she insisted she was uncomfortable and she wanted to try medication. I admit, I relented and I gave her a prescription for fluoxetine.
When she returned a few weeks later, my patient said she felt better, and what I remember decades later was her statement: “Now I can see dishes in the sink and be okay with it.” Perhaps she had downplayed her anxiety during our first meeting, but what I took from this was that some people are uncomfortable in ways that our lexicon does not capture, and sometimes medication helps with this discomfort.
The APA’s Diagnostic and Statistical Manual of Mental Disorders attempts to capture the problems of emotional and behavioral distress and classify them into discrete syndromes that can be validated and reliably diagnosed by different evaluators. Our disorders are syndromic; they are defined by clusters of symptoms that occur together, and not by a single symptom, lab value, or radiologic finding. The DSM is rewritten periodically so that what is or is not a disorder can bend with new discoveries and with a changing culture. And for better or for worse, when there is an available medication that can alleviate a problem, this may influence what once was a variant of normal into becoming a disorder.
Our illnesses often lie along a spectrum, so there is no precise point where someone who is easily distracted is a person with attention deficit disorder as opposed to being a mentally healthy person who is easily distracted, or a shy person is someone with social anxiety disorder. whether they want to address this with medications, and whether their distress warrants taking a chance that they might have side effects or an adverse reaction to a medication.
When we look at our criteria, sometimes we fall short. One needs to have at least five symptoms out of nine options, to be present for 2 weeks to be diagnosed with major depression, yet I don’t know a single psychiatrist who would not offer medication to a patient who ascribed to feeling profoundly sad with thoughts of suicide in the absence of other symptoms of depression. These issues have come to the forefront with the recent inclusion of prolonged grief in the DSM, as a disorder that is distinct from both normal grieving and from major depression.
In recent weeks, mass murder has been on everyone’s mind as we mourn those lost in Uvalde, Buffalo, and unfortunately, in so many other places. Absolutely no one thinks that someone who shoots strangers is “normal” or emotionally well. Yet psychiatry is often tasked with figuring out if someone is mad (mentally ill), bad (evil), or both. We don’t have a clear path for how to treat and manage people who commit horrendous acts of violence unless they meet criteria for another illness. Yet no one would argue that a person who informs others that he is thinking of killing strangers is in need of some type of intervention, regardless of his motive. We struggle too, with how to manage people who have more regular angry outbursts or emotional dysregulation. Perhaps we diagnose intermittent explosive disorder, or irritability caused by a mood disorder, but we don’t always know how to help people to control their tempers and modulate their emotions. And our semantics to describe psychic pain and anguish are surprisingly limited – sometimes we can only assume that someone who lashes out must be in turmoil.
Psychiatry continues to struggle with our relationship with human suffering. Suffering is part of life, not necessarily a sign of illness, and in his iconic memoir, “Man’s Search for Meaning,” psychiatrist Viktor Frankl, MD, wrote of the atrocities he endured in a Nazi concentration camp. It was through his suffering that Dr. Frankl found meaning and he used these harrowing experiences to fuel positive emotions later in life. Dr. Frankl wrote: “If there is a meaning in life at all, then there must be a meaning in suffering. Suffering is an ineradicable part of life, even as fate and death. Without suffering and death, human life cannot be complete.”
Suffering may be the kindling for acts of violence, or for profound creativity. Would we have music, art, cinema, poetry, or fiction if no one ever suffered? Yet suffering and emotional torment are often what leads people to seek treatment, and what leads us, as healers, to offer any range of therapies. For years, suicide rates have been rising, as have overdose death. And now, in addition to these “deaths of despair,” we are hearing about skyrocketing rates of depression and anxiety in our world that is so full of reasons to be sad and anxious. Access to treatment is limited by so many things, and it is not always clear when one needs psychiatric interventions or when problems will heal on their own, leaving scars or not.
I wrote this article in response to the hundreds of comments that were placed on an article I wrote after the horrors at Uvalde and Buffalo: “Don’t Equate Mass Shootings with Mental Illness.” Many of the commenters suggested I believe the shooter was perfectly sane, and that I am naive (or worse). Many wrote in with their own thoughts about what causes people to become mass murderers. One commenter wrote: “To suggest that random killers do not have mental health issues and their behavior is normal is ridiculous.” I don’t believe that I ever suggested that such behavior was normal, but – for many of these crimes – we as a society have decided to treat the behavior as criminal and not as the product of our current concept of mental disorders. Obviously, people who are well, who are emotionally at peace and comfortable in their own skin, don’t kill strangers.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore.
I still remember the woman who came to my office that day, years ago. She was struggling and uncomfortable, and she wanted “something” for stress. She described her life, and to me, it sounded stressful. She lived in a blended family and she described the chaos that one might expect to find in a household with four teens, their friends, their activities, and all it took to keep the household going. I spent 2 hours evaluating the patient, and I could not find a diagnosis that fit this problem nor – I believed – a pill that would fix it. She didn’t “meet criteria” for a psychiatric disorder, but she insisted she was uncomfortable and she wanted to try medication. I admit, I relented and I gave her a prescription for fluoxetine.
When she returned a few weeks later, my patient said she felt better, and what I remember decades later was her statement: “Now I can see dishes in the sink and be okay with it.” Perhaps she had downplayed her anxiety during our first meeting, but what I took from this was that some people are uncomfortable in ways that our lexicon does not capture, and sometimes medication helps with this discomfort.
The APA’s Diagnostic and Statistical Manual of Mental Disorders attempts to capture the problems of emotional and behavioral distress and classify them into discrete syndromes that can be validated and reliably diagnosed by different evaluators. Our disorders are syndromic; they are defined by clusters of symptoms that occur together, and not by a single symptom, lab value, or radiologic finding. The DSM is rewritten periodically so that what is or is not a disorder can bend with new discoveries and with a changing culture. And for better or for worse, when there is an available medication that can alleviate a problem, this may influence what once was a variant of normal into becoming a disorder.
Our illnesses often lie along a spectrum, so there is no precise point where someone who is easily distracted is a person with attention deficit disorder as opposed to being a mentally healthy person who is easily distracted, or a shy person is someone with social anxiety disorder. whether they want to address this with medications, and whether their distress warrants taking a chance that they might have side effects or an adverse reaction to a medication.
When we look at our criteria, sometimes we fall short. One needs to have at least five symptoms out of nine options, to be present for 2 weeks to be diagnosed with major depression, yet I don’t know a single psychiatrist who would not offer medication to a patient who ascribed to feeling profoundly sad with thoughts of suicide in the absence of other symptoms of depression. These issues have come to the forefront with the recent inclusion of prolonged grief in the DSM, as a disorder that is distinct from both normal grieving and from major depression.
In recent weeks, mass murder has been on everyone’s mind as we mourn those lost in Uvalde, Buffalo, and unfortunately, in so many other places. Absolutely no one thinks that someone who shoots strangers is “normal” or emotionally well. Yet psychiatry is often tasked with figuring out if someone is mad (mentally ill), bad (evil), or both. We don’t have a clear path for how to treat and manage people who commit horrendous acts of violence unless they meet criteria for another illness. Yet no one would argue that a person who informs others that he is thinking of killing strangers is in need of some type of intervention, regardless of his motive. We struggle too, with how to manage people who have more regular angry outbursts or emotional dysregulation. Perhaps we diagnose intermittent explosive disorder, or irritability caused by a mood disorder, but we don’t always know how to help people to control their tempers and modulate their emotions. And our semantics to describe psychic pain and anguish are surprisingly limited – sometimes we can only assume that someone who lashes out must be in turmoil.
Psychiatry continues to struggle with our relationship with human suffering. Suffering is part of life, not necessarily a sign of illness, and in his iconic memoir, “Man’s Search for Meaning,” psychiatrist Viktor Frankl, MD, wrote of the atrocities he endured in a Nazi concentration camp. It was through his suffering that Dr. Frankl found meaning and he used these harrowing experiences to fuel positive emotions later in life. Dr. Frankl wrote: “If there is a meaning in life at all, then there must be a meaning in suffering. Suffering is an ineradicable part of life, even as fate and death. Without suffering and death, human life cannot be complete.”
Suffering may be the kindling for acts of violence, or for profound creativity. Would we have music, art, cinema, poetry, or fiction if no one ever suffered? Yet suffering and emotional torment are often what leads people to seek treatment, and what leads us, as healers, to offer any range of therapies. For years, suicide rates have been rising, as have overdose death. And now, in addition to these “deaths of despair,” we are hearing about skyrocketing rates of depression and anxiety in our world that is so full of reasons to be sad and anxious. Access to treatment is limited by so many things, and it is not always clear when one needs psychiatric interventions or when problems will heal on their own, leaving scars or not.
I wrote this article in response to the hundreds of comments that were placed on an article I wrote after the horrors at Uvalde and Buffalo: “Don’t Equate Mass Shootings with Mental Illness.” Many of the commenters suggested I believe the shooter was perfectly sane, and that I am naive (or worse). Many wrote in with their own thoughts about what causes people to become mass murderers. One commenter wrote: “To suggest that random killers do not have mental health issues and their behavior is normal is ridiculous.” I don’t believe that I ever suggested that such behavior was normal, but – for many of these crimes – we as a society have decided to treat the behavior as criminal and not as the product of our current concept of mental disorders. Obviously, people who are well, who are emotionally at peace and comfortable in their own skin, don’t kill strangers.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore.
I still remember the woman who came to my office that day, years ago. She was struggling and uncomfortable, and she wanted “something” for stress. She described her life, and to me, it sounded stressful. She lived in a blended family and she described the chaos that one might expect to find in a household with four teens, their friends, their activities, and all it took to keep the household going. I spent 2 hours evaluating the patient, and I could not find a diagnosis that fit this problem nor – I believed – a pill that would fix it. She didn’t “meet criteria” for a psychiatric disorder, but she insisted she was uncomfortable and she wanted to try medication. I admit, I relented and I gave her a prescription for fluoxetine.
When she returned a few weeks later, my patient said she felt better, and what I remember decades later was her statement: “Now I can see dishes in the sink and be okay with it.” Perhaps she had downplayed her anxiety during our first meeting, but what I took from this was that some people are uncomfortable in ways that our lexicon does not capture, and sometimes medication helps with this discomfort.
The APA’s Diagnostic and Statistical Manual of Mental Disorders attempts to capture the problems of emotional and behavioral distress and classify them into discrete syndromes that can be validated and reliably diagnosed by different evaluators. Our disorders are syndromic; they are defined by clusters of symptoms that occur together, and not by a single symptom, lab value, or radiologic finding. The DSM is rewritten periodically so that what is or is not a disorder can bend with new discoveries and with a changing culture. And for better or for worse, when there is an available medication that can alleviate a problem, this may influence what once was a variant of normal into becoming a disorder.
Our illnesses often lie along a spectrum, so there is no precise point where someone who is easily distracted is a person with attention deficit disorder as opposed to being a mentally healthy person who is easily distracted, or a shy person is someone with social anxiety disorder. whether they want to address this with medications, and whether their distress warrants taking a chance that they might have side effects or an adverse reaction to a medication.
When we look at our criteria, sometimes we fall short. One needs to have at least five symptoms out of nine options, to be present for 2 weeks to be diagnosed with major depression, yet I don’t know a single psychiatrist who would not offer medication to a patient who ascribed to feeling profoundly sad with thoughts of suicide in the absence of other symptoms of depression. These issues have come to the forefront with the recent inclusion of prolonged grief in the DSM, as a disorder that is distinct from both normal grieving and from major depression.
In recent weeks, mass murder has been on everyone’s mind as we mourn those lost in Uvalde, Buffalo, and unfortunately, in so many other places. Absolutely no one thinks that someone who shoots strangers is “normal” or emotionally well. Yet psychiatry is often tasked with figuring out if someone is mad (mentally ill), bad (evil), or both. We don’t have a clear path for how to treat and manage people who commit horrendous acts of violence unless they meet criteria for another illness. Yet no one would argue that a person who informs others that he is thinking of killing strangers is in need of some type of intervention, regardless of his motive. We struggle too, with how to manage people who have more regular angry outbursts or emotional dysregulation. Perhaps we diagnose intermittent explosive disorder, or irritability caused by a mood disorder, but we don’t always know how to help people to control their tempers and modulate their emotions. And our semantics to describe psychic pain and anguish are surprisingly limited – sometimes we can only assume that someone who lashes out must be in turmoil.
Psychiatry continues to struggle with our relationship with human suffering. Suffering is part of life, not necessarily a sign of illness, and in his iconic memoir, “Man’s Search for Meaning,” psychiatrist Viktor Frankl, MD, wrote of the atrocities he endured in a Nazi concentration camp. It was through his suffering that Dr. Frankl found meaning and he used these harrowing experiences to fuel positive emotions later in life. Dr. Frankl wrote: “If there is a meaning in life at all, then there must be a meaning in suffering. Suffering is an ineradicable part of life, even as fate and death. Without suffering and death, human life cannot be complete.”
Suffering may be the kindling for acts of violence, or for profound creativity. Would we have music, art, cinema, poetry, or fiction if no one ever suffered? Yet suffering and emotional torment are often what leads people to seek treatment, and what leads us, as healers, to offer any range of therapies. For years, suicide rates have been rising, as have overdose death. And now, in addition to these “deaths of despair,” we are hearing about skyrocketing rates of depression and anxiety in our world that is so full of reasons to be sad and anxious. Access to treatment is limited by so many things, and it is not always clear when one needs psychiatric interventions or when problems will heal on their own, leaving scars or not.
I wrote this article in response to the hundreds of comments that were placed on an article I wrote after the horrors at Uvalde and Buffalo: “Don’t Equate Mass Shootings with Mental Illness.” Many of the commenters suggested I believe the shooter was perfectly sane, and that I am naive (or worse). Many wrote in with their own thoughts about what causes people to become mass murderers. One commenter wrote: “To suggest that random killers do not have mental health issues and their behavior is normal is ridiculous.” I don’t believe that I ever suggested that such behavior was normal, but – for many of these crimes – we as a society have decided to treat the behavior as criminal and not as the product of our current concept of mental disorders. Obviously, people who are well, who are emotionally at peace and comfortable in their own skin, don’t kill strangers.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore.
A prescription for de-diagnosing
In 2016, Gupta and Cahill challenged the field of psychiatry to reexamine prescribing patterns.1 They warned against the use of polypharmacy when not attached to improved patient functioning. They were concerned with the limited evidence for polypharmacy as well as DSM diagnostic criteria. In their inspiring article, they described a process of deprescribing.
In an effort to study and practice their recommendations, we have noticed a lack of literature examining the elimination of diagnostic labels. While there have been some studies looking at comorbidity, especially with substance use disorders,2 there is a paucity of scientific evidence on patients with numerous diagnoses. Yet our practices are filled with patients who have been labeled with multiple conflicting or redundant diagnoses throughout their lives depending on the setting or the orientation of the practitioner.
The DSM-5 warns against diagnosing disorders when “the occurrence … is not better explained by” another disorder.3 A mix of diagnoses creates confusion for patients as well as clinicians trying to sort through their reported psychiatric histories.
A routine example would include a patient presenting for an initial evaluation and stating “I’ve been diagnosed as manic-depressive, high anxiety, split personality, posttraumatic stress, insomnia, ADD, and depression.” A review of the medical record will reveal a list of diagnoses, including bipolar II, generalized anxiety disorder, borderline personality disorder, posttraumatic stress disorder, unspecified insomnia, attention-deficit/hyperactivity disorder, and major depressive disorder. The medication list includes lamotrigine, valproic acid, citalopram, bupropion, buspirone, prazosin, methylphenidate, clonazepam, hydroxyzine, and low-dose quetiapine at night as needed.
This is an example of polypharmacy treating multiple, and at times conflicting, diagnoses. While an extreme case, in our experience, cases like this are not uncommon. It was actually in our efforts to examine deprescribing that we noticed this quandary. When inquiring about patients on many psychotropic medications, we often receive this retort: the patient is only prescribed one medication per disorder. Some providers have the belief that multiple disorders justify multiple medications, and that this tautological thinking legitimizes polypharmacy.
A patient who has varying moods, some fears, a fluctuating temperament, past traumas, occasional difficulty sleeping, intermittent inattention, and some sadness may be given all the diagnoses listed above and the resulting medication list. The multiplication of diagnoses, “polydiagnosing,” is a convenient justification for future polypharmacy. A lack of careful assessment and thinking in the application of new diagnoses permits the use of increasing numbers of pharmacological agents. A constellation of symptoms of anxiety, concentration deficits, affective dysregulation, and psychosis may justify the combination of benzodiazepines, stimulants, mood stabilizers, and antipsychotics, while a patient with “just” schizophrenia who is sometimes sad, scared, or distracted is more likely to be kept on just one medication, likely an antipsychotic.
Contrary to most medical disorders (for example, tuberculosis) but similar to others (for example, chronic pain), psychiatric disorders are based on the opinion of a “modest number of ‘expert’ classifications.”4 While the broad categories of disorders are justifiable, individual diagnoses are burdened with high rates of comorbidity; lack of treatment specificity; and evidence that distinct syndromes share a genetic basis. Those concerns were exemplified in the study examining the inter-rater reliability of DSM-5 diagnoses, where many disorders were found to have questionable validity.5
A psychiatric diagnosis should be based on biological, psychological, and social factors, which align with our understanding of the natural course of an illness. A patient presenting with transient symptoms of sadness in the context of significant social factors like homelessness and/or significant biological factors associated with schizophrenia should not reflexively receive an additional diagnosis of a depressive disorder. A patient reporting poor concentration in the context of a manic episode should not receive an additional diagnosis of attention-deficit disorder. An older patient with depression on multiple antipsychotics for adjunctive treatment should not necessarily receive a diagnosis of cognitive disorder at the first sign of memory problems.
The cavalier and inconsistent use of diagnoses renders the patients with no clear narrative of who they are. They end up integrating the varying providers’ opinions as a cacophony of labels of unclear significance. Many patients have contradictory diagnoses like major depressive disorder and bipolar disorder, or schizophrenia and schizoaffective disorder. Those inaccurate diagnoses could not only lead to treatment mistakes, but also psychological harm.6
A clearer diagnostic picture is not only more scientifically sound but also more coherent to the patient. This in turn can lead to an improved treatment alliance and buy-in from the patient.
How should a provider practice de-diagnosing? Based on the work of Reeve, et al.,7 on the principles crucial to deprescribing, and subsequent research by Gupta and Cahill,8 we compiled a list of considerations for practitioners wishing to engage in this type of work with their patients.
Choose the right time. While insurance companies require diagnostic findings from the first visit, abrupt de-diagnosing for the sake of simplifying the record from that first visit could be detrimental. Patients can become attached to and find meaning in their diagnostic labels. This was exemplified with the removal of Asperger’s syndrome from the DSM-5.9 Acute symptomatology may be an opportune time to revisit the core pathology of a patient, or a poor time for a patient to have this discussion.
Compile a list of all the patient’s diagnoses. Our initial visits are often illuminated when patients enumerate the vast number of diagnoses they have been given by different providers. Patients will often list half a dozen diagnoses. The patterns often follow life courses with ADHD, conduct disorder, and learning disability in childhood; with anxiety, depression, and/or bipolar disorder in early adulthood; to complicated grief, depression with pseudodementia, and neurocognitive disorders in older adults. Yet patients rarely appreciate the temporary or episodic nature of mental disorders and instead accumulate diagnoses at each change of provider.
Initiate discussion with the patient. It is meaningful to see if patients resonate with the question, “Do you ever feel like every psychiatrist you have seen has given you a different diagnosis?” In our experience, patients’ reactions to this question usually exemplify the problematic nature of the vast array of diagnoses our patients are given. The majority of them are unable to confidently explain the meaning of those diagnoses, the context in which they were given, or their significance. This simple exercise has a powerful effect on raising awareness to patients of the problematic nature of polydiagnosing.
Introduce de-diagnosing. The engagement of patients in the diagnostic process has a significant effect. Reviewing not only diagnostic criteria but also nosology and debates in our understanding of diagnoses can provide patients with further engagement in their care. A simple review of the debate of the bereavement exclusion may permit a patient to not only understand the complexity, but also the changing nature of diagnoses. Suddenly, they are no longer bystanders, but informed participants in their care.
Identify diagnoses most appropriate for removal. Contradictory diagnoses are common in the clinical settings we work in. We routinely see patients carrying multiple mood diagnoses, despite our diagnostic systems not permitting one to have both unipolar and bipolar depression. Superfluous diagnoses are also frequent, with patients receiving depressive, or anxious labels when in an acute state of psychosis or mania. This is exemplified by patients suffering from thought blocking and receiving cognitive or attention-related diagnoses. Concurrent yet different diagnoses are also common in patients with a different list of diagnoses by their primary care provider, their therapist, and their psychiatrist. This is particularly problematic as it forces the patient to alternate their thinking or choose between their providers.
Create a new narrative for the patient. Once diagnoses are explained, clarified, and understood, patients with the help of their providers can reexamine their life story under a new and simplified construct. This process often leads to a less confusing sense of self, an increased dedication to the treatment process, whether behavioral, social, psychological, or pharmacologic.
Consider deprescribing. With a more straightforward and more grounded list of diagnoses (or simply one diagnosis), we find the process of deprescribing to be simpler and more engaging for patients. For example, patients can clearly understand the lack of necessity of an antipsychotic prescription for a resolved substance-induced psychosis. Patients are more engaged in their care, leading to improved medication compliance and less attachment to discontinued medications.
Monitor and adapt. One should of course reevaluate diagnoses as the course of illness provides us with additional information. However, we suggest waiting for a manic episode to emerge prior to diagnosing bipolar rather than suggesting the diagnosis because a patient was wearing red shoes, spoke multiple languages, had multiple degrees and was creative.10 The contextual basis and progression of the symptoms should lead to continual reassessment of diagnoses.
Physicians are aware of the balance between Occam’s razor, which promotes the simplest single explanation for a problem, versus Hickam’s dictum that reminds us that patients can have as many diseases as they please. However, similarly to polypharmacy, “polydiagnosing” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to diagnose their patients with the growing number of diagnoses, patients still need and benefit from a coherent and clear medical narrative. Psychiatry would be wise to recognize this concerning trend, in its attempt at rectifying polypharmacy.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest. Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest.
References
1. Gupta S & Cahill JD. A prescription for “deprescribing” in psychiatry. Psychiatr Serv. 2016 Aug 1;67(8):904-7. doi: 10.1176/appi.ps.201500359.
2. Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. 2006 Sep;101 Suppl 1:76-88. doi: 10.1111/j.1360-0443.2006.01592.x.
3. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). American Psychiatric Association, 2022. https://psychiatry.org/psychiatrists/practice/dsm.
4. Kendler KS. An historical framework for psychiatric nosology. Psychol Med. 2009 Dec;39(12):1935-41. doi: 10.1017/S0033291709005753.
5. Regier DA et al. DSM-5 field trials in the United States and Canada. Am J Psychiatry. 2013 Jan;170(1):59-70. doi: 10.1176/appi.ajp.2012.12070999.
6. Bhattacharya R et al. When good news is bad news: psychological impact of false-positive diagnosis of HIV. AIDS Care. 2008 May;20(5):560-4. doi: 10.1080/09540120701867206.
7. Reeve E et al. Review of deprescribing processes and development of an evidence‐based, patient‐centred deprescribing process. Br J Clin Pharmacol. 2014 Oct;78(4):738-47. doi: 10.1111/bcp.12386.
8. Gupta S and Cahill JD. A prescription for “deprescribing” in psychiatry.
9. Solomon M. “On the appearance and disappearance of Asperger’s syndrome” in Kendler and Parnas (eds.) Philosophical Issues in Psychiatry IV: Classification of Psychiatric Illness. Oxford University Press, 2017. doi: 10.1093/med/9780198796022.003.0023.
10. Akiskal HS. Searching for behavioral indicators of bipolar II in patients presenting with major depressive episodes: The “red sign,” the “rule of three,” and other biographic signs of temperamental extravagance, activation, and hypomania. J Affect Disord. 2005 Feb;84(2-3):279-90. doi: 10.1016/j.jad.2004.06.002.
In 2016, Gupta and Cahill challenged the field of psychiatry to reexamine prescribing patterns.1 They warned against the use of polypharmacy when not attached to improved patient functioning. They were concerned with the limited evidence for polypharmacy as well as DSM diagnostic criteria. In their inspiring article, they described a process of deprescribing.
In an effort to study and practice their recommendations, we have noticed a lack of literature examining the elimination of diagnostic labels. While there have been some studies looking at comorbidity, especially with substance use disorders,2 there is a paucity of scientific evidence on patients with numerous diagnoses. Yet our practices are filled with patients who have been labeled with multiple conflicting or redundant diagnoses throughout their lives depending on the setting or the orientation of the practitioner.
The DSM-5 warns against diagnosing disorders when “the occurrence … is not better explained by” another disorder.3 A mix of diagnoses creates confusion for patients as well as clinicians trying to sort through their reported psychiatric histories.
A routine example would include a patient presenting for an initial evaluation and stating “I’ve been diagnosed as manic-depressive, high anxiety, split personality, posttraumatic stress, insomnia, ADD, and depression.” A review of the medical record will reveal a list of diagnoses, including bipolar II, generalized anxiety disorder, borderline personality disorder, posttraumatic stress disorder, unspecified insomnia, attention-deficit/hyperactivity disorder, and major depressive disorder. The medication list includes lamotrigine, valproic acid, citalopram, bupropion, buspirone, prazosin, methylphenidate, clonazepam, hydroxyzine, and low-dose quetiapine at night as needed.
This is an example of polypharmacy treating multiple, and at times conflicting, diagnoses. While an extreme case, in our experience, cases like this are not uncommon. It was actually in our efforts to examine deprescribing that we noticed this quandary. When inquiring about patients on many psychotropic medications, we often receive this retort: the patient is only prescribed one medication per disorder. Some providers have the belief that multiple disorders justify multiple medications, and that this tautological thinking legitimizes polypharmacy.
A patient who has varying moods, some fears, a fluctuating temperament, past traumas, occasional difficulty sleeping, intermittent inattention, and some sadness may be given all the diagnoses listed above and the resulting medication list. The multiplication of diagnoses, “polydiagnosing,” is a convenient justification for future polypharmacy. A lack of careful assessment and thinking in the application of new diagnoses permits the use of increasing numbers of pharmacological agents. A constellation of symptoms of anxiety, concentration deficits, affective dysregulation, and psychosis may justify the combination of benzodiazepines, stimulants, mood stabilizers, and antipsychotics, while a patient with “just” schizophrenia who is sometimes sad, scared, or distracted is more likely to be kept on just one medication, likely an antipsychotic.
Contrary to most medical disorders (for example, tuberculosis) but similar to others (for example, chronic pain), psychiatric disorders are based on the opinion of a “modest number of ‘expert’ classifications.”4 While the broad categories of disorders are justifiable, individual diagnoses are burdened with high rates of comorbidity; lack of treatment specificity; and evidence that distinct syndromes share a genetic basis. Those concerns were exemplified in the study examining the inter-rater reliability of DSM-5 diagnoses, where many disorders were found to have questionable validity.5
A psychiatric diagnosis should be based on biological, psychological, and social factors, which align with our understanding of the natural course of an illness. A patient presenting with transient symptoms of sadness in the context of significant social factors like homelessness and/or significant biological factors associated with schizophrenia should not reflexively receive an additional diagnosis of a depressive disorder. A patient reporting poor concentration in the context of a manic episode should not receive an additional diagnosis of attention-deficit disorder. An older patient with depression on multiple antipsychotics for adjunctive treatment should not necessarily receive a diagnosis of cognitive disorder at the first sign of memory problems.
The cavalier and inconsistent use of diagnoses renders the patients with no clear narrative of who they are. They end up integrating the varying providers’ opinions as a cacophony of labels of unclear significance. Many patients have contradictory diagnoses like major depressive disorder and bipolar disorder, or schizophrenia and schizoaffective disorder. Those inaccurate diagnoses could not only lead to treatment mistakes, but also psychological harm.6
A clearer diagnostic picture is not only more scientifically sound but also more coherent to the patient. This in turn can lead to an improved treatment alliance and buy-in from the patient.
How should a provider practice de-diagnosing? Based on the work of Reeve, et al.,7 on the principles crucial to deprescribing, and subsequent research by Gupta and Cahill,8 we compiled a list of considerations for practitioners wishing to engage in this type of work with their patients.
Choose the right time. While insurance companies require diagnostic findings from the first visit, abrupt de-diagnosing for the sake of simplifying the record from that first visit could be detrimental. Patients can become attached to and find meaning in their diagnostic labels. This was exemplified with the removal of Asperger’s syndrome from the DSM-5.9 Acute symptomatology may be an opportune time to revisit the core pathology of a patient, or a poor time for a patient to have this discussion.
Compile a list of all the patient’s diagnoses. Our initial visits are often illuminated when patients enumerate the vast number of diagnoses they have been given by different providers. Patients will often list half a dozen diagnoses. The patterns often follow life courses with ADHD, conduct disorder, and learning disability in childhood; with anxiety, depression, and/or bipolar disorder in early adulthood; to complicated grief, depression with pseudodementia, and neurocognitive disorders in older adults. Yet patients rarely appreciate the temporary or episodic nature of mental disorders and instead accumulate diagnoses at each change of provider.
Initiate discussion with the patient. It is meaningful to see if patients resonate with the question, “Do you ever feel like every psychiatrist you have seen has given you a different diagnosis?” In our experience, patients’ reactions to this question usually exemplify the problematic nature of the vast array of diagnoses our patients are given. The majority of them are unable to confidently explain the meaning of those diagnoses, the context in which they were given, or their significance. This simple exercise has a powerful effect on raising awareness to patients of the problematic nature of polydiagnosing.
Introduce de-diagnosing. The engagement of patients in the diagnostic process has a significant effect. Reviewing not only diagnostic criteria but also nosology and debates in our understanding of diagnoses can provide patients with further engagement in their care. A simple review of the debate of the bereavement exclusion may permit a patient to not only understand the complexity, but also the changing nature of diagnoses. Suddenly, they are no longer bystanders, but informed participants in their care.
Identify diagnoses most appropriate for removal. Contradictory diagnoses are common in the clinical settings we work in. We routinely see patients carrying multiple mood diagnoses, despite our diagnostic systems not permitting one to have both unipolar and bipolar depression. Superfluous diagnoses are also frequent, with patients receiving depressive, or anxious labels when in an acute state of psychosis or mania. This is exemplified by patients suffering from thought blocking and receiving cognitive or attention-related diagnoses. Concurrent yet different diagnoses are also common in patients with a different list of diagnoses by their primary care provider, their therapist, and their psychiatrist. This is particularly problematic as it forces the patient to alternate their thinking or choose between their providers.
Create a new narrative for the patient. Once diagnoses are explained, clarified, and understood, patients with the help of their providers can reexamine their life story under a new and simplified construct. This process often leads to a less confusing sense of self, an increased dedication to the treatment process, whether behavioral, social, psychological, or pharmacologic.
Consider deprescribing. With a more straightforward and more grounded list of diagnoses (or simply one diagnosis), we find the process of deprescribing to be simpler and more engaging for patients. For example, patients can clearly understand the lack of necessity of an antipsychotic prescription for a resolved substance-induced psychosis. Patients are more engaged in their care, leading to improved medication compliance and less attachment to discontinued medications.
Monitor and adapt. One should of course reevaluate diagnoses as the course of illness provides us with additional information. However, we suggest waiting for a manic episode to emerge prior to diagnosing bipolar rather than suggesting the diagnosis because a patient was wearing red shoes, spoke multiple languages, had multiple degrees and was creative.10 The contextual basis and progression of the symptoms should lead to continual reassessment of diagnoses.
Physicians are aware of the balance between Occam’s razor, which promotes the simplest single explanation for a problem, versus Hickam’s dictum that reminds us that patients can have as many diseases as they please. However, similarly to polypharmacy, “polydiagnosing” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to diagnose their patients with the growing number of diagnoses, patients still need and benefit from a coherent and clear medical narrative. Psychiatry would be wise to recognize this concerning trend, in its attempt at rectifying polypharmacy.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest. Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest.
References
1. Gupta S & Cahill JD. A prescription for “deprescribing” in psychiatry. Psychiatr Serv. 2016 Aug 1;67(8):904-7. doi: 10.1176/appi.ps.201500359.
2. Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. 2006 Sep;101 Suppl 1:76-88. doi: 10.1111/j.1360-0443.2006.01592.x.
3. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). American Psychiatric Association, 2022. https://psychiatry.org/psychiatrists/practice/dsm.
4. Kendler KS. An historical framework for psychiatric nosology. Psychol Med. 2009 Dec;39(12):1935-41. doi: 10.1017/S0033291709005753.
5. Regier DA et al. DSM-5 field trials in the United States and Canada. Am J Psychiatry. 2013 Jan;170(1):59-70. doi: 10.1176/appi.ajp.2012.12070999.
6. Bhattacharya R et al. When good news is bad news: psychological impact of false-positive diagnosis of HIV. AIDS Care. 2008 May;20(5):560-4. doi: 10.1080/09540120701867206.
7. Reeve E et al. Review of deprescribing processes and development of an evidence‐based, patient‐centred deprescribing process. Br J Clin Pharmacol. 2014 Oct;78(4):738-47. doi: 10.1111/bcp.12386.
8. Gupta S and Cahill JD. A prescription for “deprescribing” in psychiatry.
9. Solomon M. “On the appearance and disappearance of Asperger’s syndrome” in Kendler and Parnas (eds.) Philosophical Issues in Psychiatry IV: Classification of Psychiatric Illness. Oxford University Press, 2017. doi: 10.1093/med/9780198796022.003.0023.
10. Akiskal HS. Searching for behavioral indicators of bipolar II in patients presenting with major depressive episodes: The “red sign,” the “rule of three,” and other biographic signs of temperamental extravagance, activation, and hypomania. J Affect Disord. 2005 Feb;84(2-3):279-90. doi: 10.1016/j.jad.2004.06.002.
In 2016, Gupta and Cahill challenged the field of psychiatry to reexamine prescribing patterns.1 They warned against the use of polypharmacy when not attached to improved patient functioning. They were concerned with the limited evidence for polypharmacy as well as DSM diagnostic criteria. In their inspiring article, they described a process of deprescribing.
In an effort to study and practice their recommendations, we have noticed a lack of literature examining the elimination of diagnostic labels. While there have been some studies looking at comorbidity, especially with substance use disorders,2 there is a paucity of scientific evidence on patients with numerous diagnoses. Yet our practices are filled with patients who have been labeled with multiple conflicting or redundant diagnoses throughout their lives depending on the setting or the orientation of the practitioner.
The DSM-5 warns against diagnosing disorders when “the occurrence … is not better explained by” another disorder.3 A mix of diagnoses creates confusion for patients as well as clinicians trying to sort through their reported psychiatric histories.
A routine example would include a patient presenting for an initial evaluation and stating “I’ve been diagnosed as manic-depressive, high anxiety, split personality, posttraumatic stress, insomnia, ADD, and depression.” A review of the medical record will reveal a list of diagnoses, including bipolar II, generalized anxiety disorder, borderline personality disorder, posttraumatic stress disorder, unspecified insomnia, attention-deficit/hyperactivity disorder, and major depressive disorder. The medication list includes lamotrigine, valproic acid, citalopram, bupropion, buspirone, prazosin, methylphenidate, clonazepam, hydroxyzine, and low-dose quetiapine at night as needed.
This is an example of polypharmacy treating multiple, and at times conflicting, diagnoses. While an extreme case, in our experience, cases like this are not uncommon. It was actually in our efforts to examine deprescribing that we noticed this quandary. When inquiring about patients on many psychotropic medications, we often receive this retort: the patient is only prescribed one medication per disorder. Some providers have the belief that multiple disorders justify multiple medications, and that this tautological thinking legitimizes polypharmacy.
A patient who has varying moods, some fears, a fluctuating temperament, past traumas, occasional difficulty sleeping, intermittent inattention, and some sadness may be given all the diagnoses listed above and the resulting medication list. The multiplication of diagnoses, “polydiagnosing,” is a convenient justification for future polypharmacy. A lack of careful assessment and thinking in the application of new diagnoses permits the use of increasing numbers of pharmacological agents. A constellation of symptoms of anxiety, concentration deficits, affective dysregulation, and psychosis may justify the combination of benzodiazepines, stimulants, mood stabilizers, and antipsychotics, while a patient with “just” schizophrenia who is sometimes sad, scared, or distracted is more likely to be kept on just one medication, likely an antipsychotic.
Contrary to most medical disorders (for example, tuberculosis) but similar to others (for example, chronic pain), psychiatric disorders are based on the opinion of a “modest number of ‘expert’ classifications.”4 While the broad categories of disorders are justifiable, individual diagnoses are burdened with high rates of comorbidity; lack of treatment specificity; and evidence that distinct syndromes share a genetic basis. Those concerns were exemplified in the study examining the inter-rater reliability of DSM-5 diagnoses, where many disorders were found to have questionable validity.5
A psychiatric diagnosis should be based on biological, psychological, and social factors, which align with our understanding of the natural course of an illness. A patient presenting with transient symptoms of sadness in the context of significant social factors like homelessness and/or significant biological factors associated with schizophrenia should not reflexively receive an additional diagnosis of a depressive disorder. A patient reporting poor concentration in the context of a manic episode should not receive an additional diagnosis of attention-deficit disorder. An older patient with depression on multiple antipsychotics for adjunctive treatment should not necessarily receive a diagnosis of cognitive disorder at the first sign of memory problems.
The cavalier and inconsistent use of diagnoses renders the patients with no clear narrative of who they are. They end up integrating the varying providers’ opinions as a cacophony of labels of unclear significance. Many patients have contradictory diagnoses like major depressive disorder and bipolar disorder, or schizophrenia and schizoaffective disorder. Those inaccurate diagnoses could not only lead to treatment mistakes, but also psychological harm.6
A clearer diagnostic picture is not only more scientifically sound but also more coherent to the patient. This in turn can lead to an improved treatment alliance and buy-in from the patient.
How should a provider practice de-diagnosing? Based on the work of Reeve, et al.,7 on the principles crucial to deprescribing, and subsequent research by Gupta and Cahill,8 we compiled a list of considerations for practitioners wishing to engage in this type of work with their patients.
Choose the right time. While insurance companies require diagnostic findings from the first visit, abrupt de-diagnosing for the sake of simplifying the record from that first visit could be detrimental. Patients can become attached to and find meaning in their diagnostic labels. This was exemplified with the removal of Asperger’s syndrome from the DSM-5.9 Acute symptomatology may be an opportune time to revisit the core pathology of a patient, or a poor time for a patient to have this discussion.
Compile a list of all the patient’s diagnoses. Our initial visits are often illuminated when patients enumerate the vast number of diagnoses they have been given by different providers. Patients will often list half a dozen diagnoses. The patterns often follow life courses with ADHD, conduct disorder, and learning disability in childhood; with anxiety, depression, and/or bipolar disorder in early adulthood; to complicated grief, depression with pseudodementia, and neurocognitive disorders in older adults. Yet patients rarely appreciate the temporary or episodic nature of mental disorders and instead accumulate diagnoses at each change of provider.
Initiate discussion with the patient. It is meaningful to see if patients resonate with the question, “Do you ever feel like every psychiatrist you have seen has given you a different diagnosis?” In our experience, patients’ reactions to this question usually exemplify the problematic nature of the vast array of diagnoses our patients are given. The majority of them are unable to confidently explain the meaning of those diagnoses, the context in which they were given, or their significance. This simple exercise has a powerful effect on raising awareness to patients of the problematic nature of polydiagnosing.
Introduce de-diagnosing. The engagement of patients in the diagnostic process has a significant effect. Reviewing not only diagnostic criteria but also nosology and debates in our understanding of diagnoses can provide patients with further engagement in their care. A simple review of the debate of the bereavement exclusion may permit a patient to not only understand the complexity, but also the changing nature of diagnoses. Suddenly, they are no longer bystanders, but informed participants in their care.
Identify diagnoses most appropriate for removal. Contradictory diagnoses are common in the clinical settings we work in. We routinely see patients carrying multiple mood diagnoses, despite our diagnostic systems not permitting one to have both unipolar and bipolar depression. Superfluous diagnoses are also frequent, with patients receiving depressive, or anxious labels when in an acute state of psychosis or mania. This is exemplified by patients suffering from thought blocking and receiving cognitive or attention-related diagnoses. Concurrent yet different diagnoses are also common in patients with a different list of diagnoses by their primary care provider, their therapist, and their psychiatrist. This is particularly problematic as it forces the patient to alternate their thinking or choose between their providers.
Create a new narrative for the patient. Once diagnoses are explained, clarified, and understood, patients with the help of their providers can reexamine their life story under a new and simplified construct. This process often leads to a less confusing sense of self, an increased dedication to the treatment process, whether behavioral, social, psychological, or pharmacologic.
Consider deprescribing. With a more straightforward and more grounded list of diagnoses (or simply one diagnosis), we find the process of deprescribing to be simpler and more engaging for patients. For example, patients can clearly understand the lack of necessity of an antipsychotic prescription for a resolved substance-induced psychosis. Patients are more engaged in their care, leading to improved medication compliance and less attachment to discontinued medications.
Monitor and adapt. One should of course reevaluate diagnoses as the course of illness provides us with additional information. However, we suggest waiting for a manic episode to emerge prior to diagnosing bipolar rather than suggesting the diagnosis because a patient was wearing red shoes, spoke multiple languages, had multiple degrees and was creative.10 The contextual basis and progression of the symptoms should lead to continual reassessment of diagnoses.
Physicians are aware of the balance between Occam’s razor, which promotes the simplest single explanation for a problem, versus Hickam’s dictum that reminds us that patients can have as many diseases as they please. However, similarly to polypharmacy, “polydiagnosing” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to diagnose their patients with the growing number of diagnoses, patients still need and benefit from a coherent and clear medical narrative. Psychiatry would be wise to recognize this concerning trend, in its attempt at rectifying polypharmacy.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest. Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest.
References
1. Gupta S & Cahill JD. A prescription for “deprescribing” in psychiatry. Psychiatr Serv. 2016 Aug 1;67(8):904-7. doi: 10.1176/appi.ps.201500359.
2. Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. 2006 Sep;101 Suppl 1:76-88. doi: 10.1111/j.1360-0443.2006.01592.x.
3. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). American Psychiatric Association, 2022. https://psychiatry.org/psychiatrists/practice/dsm.
4. Kendler KS. An historical framework for psychiatric nosology. Psychol Med. 2009 Dec;39(12):1935-41. doi: 10.1017/S0033291709005753.
5. Regier DA et al. DSM-5 field trials in the United States and Canada. Am J Psychiatry. 2013 Jan;170(1):59-70. doi: 10.1176/appi.ajp.2012.12070999.
6. Bhattacharya R et al. When good news is bad news: psychological impact of false-positive diagnosis of HIV. AIDS Care. 2008 May;20(5):560-4. doi: 10.1080/09540120701867206.
7. Reeve E et al. Review of deprescribing processes and development of an evidence‐based, patient‐centred deprescribing process. Br J Clin Pharmacol. 2014 Oct;78(4):738-47. doi: 10.1111/bcp.12386.
8. Gupta S and Cahill JD. A prescription for “deprescribing” in psychiatry.
9. Solomon M. “On the appearance and disappearance of Asperger’s syndrome” in Kendler and Parnas (eds.) Philosophical Issues in Psychiatry IV: Classification of Psychiatric Illness. Oxford University Press, 2017. doi: 10.1093/med/9780198796022.003.0023.
10. Akiskal HS. Searching for behavioral indicators of bipolar II in patients presenting with major depressive episodes: The “red sign,” the “rule of three,” and other biographic signs of temperamental extravagance, activation, and hypomania. J Affect Disord. 2005 Feb;84(2-3):279-90. doi: 10.1016/j.jad.2004.06.002.
ECT may reduce all-cause mortality in major depression
In an analysis of data from a large database of inpatients across the United States, use of ECT for those with resistant MDD was associated with significantly lower in-hospital mortality compared with those who did not receive ECT.
This held true even after the researchers controlled for demographics and loss of function due to comorbid medical conditions.
“I think the risks of ECT are far less than the benefits in this population,” coinvestigator Nagy A. Youssef, MD, PhD, professor of psychiatry and director of clinical research, The Ohio State University, Columbus, told this news organization.
“My hope is that providers will not be afraid to refer appropriate cases for ECT. If meds and other therapeutics are not working, you should start discussing ECT as a second or third line,” he said.
The findings were presented at the American Society of Clinical Psychopharmacology annual meeting.
Lower mortality
Dr. Youssef, a brain stimulation researcher who uses ECT in his clinical practice, said that in his experience, it is a highly effective therapy for resistant depression.
“I see great responses in patients who have tried everything else. Most of the time, it works very well, and results are very rewarding.”
For the study, the investigators used a large, national insurance claims database that included 949,394 adult inpatients with MDD across the United States from 2012 to 2014. The cohort represented over 4,000 hospitals across the country.
The investigators used logistic regression to determine the odds ratio for in-hospital all-cause mortality for the 25,535 MDD patients who were treated with ECT in comparison with 923,859 patients with MDD who were not treated with ECT.
Results showed that ECT use was significantly higher among older patients (mean age, 56.9 years), women (64%), and White patients (86.9%). In addition, patients in the ECT group were physically sicker than were their peers in the non-ECT group.
A higher proportion of patients in the ECT group in comparison with the non-ECT group had experienced major loss of physical function (37% vs. 5%, respectively) and extreme loss of physical function (63% vs. 0.2%).
“By loss of function, I mean the degree of impairment caused by medical disease,” said Dr. Youssef.
He added that patients with MDD are more likely to care less for their health and do things that are not good for their well-being, such as drinking alcohol or using drugs, and are less likely to adhere to prescribed medication regimens or seek medical attention for physical illness.
“Also, there is probably a biological component where depression, by dysregulation of the hypothalamus and pituitary regions of the brain, can increase the likelihood of physical illness or disease,” Dr. Youssef said.
After adjusting for demographics and extreme loss of function because of medical conditions, the investigators found that in-hospital mortality was significantly lower in the ECT group (odds ratio [OR], 0.05; 95% confidence interval [CI], 0.02-0.11; P < .001).
In-hospital mortality was numerically but not statistically significantly lower in the ECT group (OR, 0.7; 95% CI, 0.41-1.50; P < .47) when adjusted for demographics and major loss of function.
“While this was not statistically significant with marked loss of function, it is clinically important and meaningful. With extreme loss of function, the decrease in mortality was statistically significant,” Dr. Youssef noted.
Designations of extreme and major loss of function were derived from ICD codes.
“This is a complex grading system that takes into account how sick the patient is and includes medical disease severity and comorbidities assessed by the clinician,” he said.
A lifesaving treatment
Commenting on the study, Jair C. Soares, MD, PhD, professor and chair, Pat Rutherford Chair in Psychiatry, UT Houston Medical School, Texas, said, “These are interesting results in a very large national sample suggesting some potential benefits of ECT.
“For the most severely ill patients with major depression who do not respond to currently available medications, ECT is still the most efficacious treatment and indeed a lifesaving treatment modality for many patients,” said Dr. Soares, who was not part of the study.
He noted that ECT is not right for everyone, but “as administered these days, with careful patient selection, it is indeed a safe treatment that can save many lives,” Dr. Soares said.
Dr. Youssef reports a financial relationship with Mecta. Dr. Soares reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In an analysis of data from a large database of inpatients across the United States, use of ECT for those with resistant MDD was associated with significantly lower in-hospital mortality compared with those who did not receive ECT.
This held true even after the researchers controlled for demographics and loss of function due to comorbid medical conditions.
“I think the risks of ECT are far less than the benefits in this population,” coinvestigator Nagy A. Youssef, MD, PhD, professor of psychiatry and director of clinical research, The Ohio State University, Columbus, told this news organization.
“My hope is that providers will not be afraid to refer appropriate cases for ECT. If meds and other therapeutics are not working, you should start discussing ECT as a second or third line,” he said.
The findings were presented at the American Society of Clinical Psychopharmacology annual meeting.
Lower mortality
Dr. Youssef, a brain stimulation researcher who uses ECT in his clinical practice, said that in his experience, it is a highly effective therapy for resistant depression.
“I see great responses in patients who have tried everything else. Most of the time, it works very well, and results are very rewarding.”
For the study, the investigators used a large, national insurance claims database that included 949,394 adult inpatients with MDD across the United States from 2012 to 2014. The cohort represented over 4,000 hospitals across the country.
The investigators used logistic regression to determine the odds ratio for in-hospital all-cause mortality for the 25,535 MDD patients who were treated with ECT in comparison with 923,859 patients with MDD who were not treated with ECT.
Results showed that ECT use was significantly higher among older patients (mean age, 56.9 years), women (64%), and White patients (86.9%). In addition, patients in the ECT group were physically sicker than were their peers in the non-ECT group.
A higher proportion of patients in the ECT group in comparison with the non-ECT group had experienced major loss of physical function (37% vs. 5%, respectively) and extreme loss of physical function (63% vs. 0.2%).
“By loss of function, I mean the degree of impairment caused by medical disease,” said Dr. Youssef.
He added that patients with MDD are more likely to care less for their health and do things that are not good for their well-being, such as drinking alcohol or using drugs, and are less likely to adhere to prescribed medication regimens or seek medical attention for physical illness.
“Also, there is probably a biological component where depression, by dysregulation of the hypothalamus and pituitary regions of the brain, can increase the likelihood of physical illness or disease,” Dr. Youssef said.
After adjusting for demographics and extreme loss of function because of medical conditions, the investigators found that in-hospital mortality was significantly lower in the ECT group (odds ratio [OR], 0.05; 95% confidence interval [CI], 0.02-0.11; P < .001).
In-hospital mortality was numerically but not statistically significantly lower in the ECT group (OR, 0.7; 95% CI, 0.41-1.50; P < .47) when adjusted for demographics and major loss of function.
“While this was not statistically significant with marked loss of function, it is clinically important and meaningful. With extreme loss of function, the decrease in mortality was statistically significant,” Dr. Youssef noted.
Designations of extreme and major loss of function were derived from ICD codes.
“This is a complex grading system that takes into account how sick the patient is and includes medical disease severity and comorbidities assessed by the clinician,” he said.
A lifesaving treatment
Commenting on the study, Jair C. Soares, MD, PhD, professor and chair, Pat Rutherford Chair in Psychiatry, UT Houston Medical School, Texas, said, “These are interesting results in a very large national sample suggesting some potential benefits of ECT.
“For the most severely ill patients with major depression who do not respond to currently available medications, ECT is still the most efficacious treatment and indeed a lifesaving treatment modality for many patients,” said Dr. Soares, who was not part of the study.
He noted that ECT is not right for everyone, but “as administered these days, with careful patient selection, it is indeed a safe treatment that can save many lives,” Dr. Soares said.
Dr. Youssef reports a financial relationship with Mecta. Dr. Soares reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In an analysis of data from a large database of inpatients across the United States, use of ECT for those with resistant MDD was associated with significantly lower in-hospital mortality compared with those who did not receive ECT.
This held true even after the researchers controlled for demographics and loss of function due to comorbid medical conditions.
“I think the risks of ECT are far less than the benefits in this population,” coinvestigator Nagy A. Youssef, MD, PhD, professor of psychiatry and director of clinical research, The Ohio State University, Columbus, told this news organization.
“My hope is that providers will not be afraid to refer appropriate cases for ECT. If meds and other therapeutics are not working, you should start discussing ECT as a second or third line,” he said.
The findings were presented at the American Society of Clinical Psychopharmacology annual meeting.
Lower mortality
Dr. Youssef, a brain stimulation researcher who uses ECT in his clinical practice, said that in his experience, it is a highly effective therapy for resistant depression.
“I see great responses in patients who have tried everything else. Most of the time, it works very well, and results are very rewarding.”
For the study, the investigators used a large, national insurance claims database that included 949,394 adult inpatients with MDD across the United States from 2012 to 2014. The cohort represented over 4,000 hospitals across the country.
The investigators used logistic regression to determine the odds ratio for in-hospital all-cause mortality for the 25,535 MDD patients who were treated with ECT in comparison with 923,859 patients with MDD who were not treated with ECT.
Results showed that ECT use was significantly higher among older patients (mean age, 56.9 years), women (64%), and White patients (86.9%). In addition, patients in the ECT group were physically sicker than were their peers in the non-ECT group.
A higher proportion of patients in the ECT group in comparison with the non-ECT group had experienced major loss of physical function (37% vs. 5%, respectively) and extreme loss of physical function (63% vs. 0.2%).
“By loss of function, I mean the degree of impairment caused by medical disease,” said Dr. Youssef.
He added that patients with MDD are more likely to care less for their health and do things that are not good for their well-being, such as drinking alcohol or using drugs, and are less likely to adhere to prescribed medication regimens or seek medical attention for physical illness.
“Also, there is probably a biological component where depression, by dysregulation of the hypothalamus and pituitary regions of the brain, can increase the likelihood of physical illness or disease,” Dr. Youssef said.
After adjusting for demographics and extreme loss of function because of medical conditions, the investigators found that in-hospital mortality was significantly lower in the ECT group (odds ratio [OR], 0.05; 95% confidence interval [CI], 0.02-0.11; P < .001).
In-hospital mortality was numerically but not statistically significantly lower in the ECT group (OR, 0.7; 95% CI, 0.41-1.50; P < .47) when adjusted for demographics and major loss of function.
“While this was not statistically significant with marked loss of function, it is clinically important and meaningful. With extreme loss of function, the decrease in mortality was statistically significant,” Dr. Youssef noted.
Designations of extreme and major loss of function were derived from ICD codes.
“This is a complex grading system that takes into account how sick the patient is and includes medical disease severity and comorbidities assessed by the clinician,” he said.
A lifesaving treatment
Commenting on the study, Jair C. Soares, MD, PhD, professor and chair, Pat Rutherford Chair in Psychiatry, UT Houston Medical School, Texas, said, “These are interesting results in a very large national sample suggesting some potential benefits of ECT.
“For the most severely ill patients with major depression who do not respond to currently available medications, ECT is still the most efficacious treatment and indeed a lifesaving treatment modality for many patients,” said Dr. Soares, who was not part of the study.
He noted that ECT is not right for everyone, but “as administered these days, with careful patient selection, it is indeed a safe treatment that can save many lives,” Dr. Soares said.
Dr. Youssef reports a financial relationship with Mecta. Dr. Soares reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ASCP 2022
Asian American teens have highest rate of suicidal ideation
NEW ORLEANS – In an unexpected finding, researchers discovered that According to a weighted analysis, 24% of Asian Americans reported thinking about or planning suicide vs. 22% of Whites and Blacks and 20% of Hispanics (P < .01).
“We were shocked,” said study lead author Esha Hansoti, MD, who conducted the research at UT Southwestern Medical Center, Dallas, and is now a psychiatry resident at Zucker Hillside Hospital Northwell/Hofstra in Glen Oaks, NY. The findings were released at the annual meeting of the American Psychiatric Association.
Dr. Hansoti and colleagues launched the analysis in light of sparse research into Asian American mental health, she said. Even within this population, she said, mental illness “tends to be overlooked” and discussion of the topic may be considered taboo.
For the new study, researchers analyzed the 2019 Youth Risk Behavior Survey, conducted biennially by the Centers for Disease Control and Prevention, which had more than 13,000 participants in grades 9-12.
A weighted bivariate analysis of 618 Asian American adolescents – adjusted for age, sex, and depressive symptoms – found no statistically significant impact on suicidal ideation by gender, age, substance use, sexual/physical dating violence, or fluency in English.
However, several groups had a statistically significant higher risk, including victims of forced sexual intercourse and those who were threatened or bullied at school.
Those who didn’t get mostly A grades were also at high risk: Adolescents with mostly Ds and Fs were more likely to have acknowledged suicidal ideation than those with mostly As (adjusted odds ratio [AOR] = 3.2).
Gays and lesbians (AOR = 7.9 vs. heterosexuals), and bisexuals (AOR = 5.2 vs. heterosexuals) also showed sharply higher rates of suicidal ideation.
It’s not clear why Asian American adolescents may be at higher risk of suicidal ideation. The survey was completed prior to the COVID-19 pandemic, which spawned bigotry against people of Asian descent and an ongoing outbreak of high-profile violence against Asian Americans across the country.
Dr. Hansoti noted that Asian Americans face the pressures to live up to the standards of being a “model minority.” In addition, “very few Asian American adolescents are taken to a therapist, and few mental health providers are Asian Americans.”
She urged fellow psychiatrists “to remember that our perceptions of Asian Americans might hinder some of the diagnoses we could be making. Be thoughtful about how their ethnicity and race affects their presentation and their own perception of their illness.”
She added that Asian Americans may experience mental illness and anxiety “more somatically and physically than emotionally.”
In an interview, Anne Saw, PhD, associate professor of clinical-community psychology at DePaul University, Chicago, said the findings are “helpful for corroborating other studies identifying risk factors of suicidal ideation among Asian American adolescents. Since this research utilizes the Youth Risk Behavior Survey, these findings can be compared with risk factors of suicidal ideation among adolescents from other racial/ethnic backgrounds to pinpoint general as well as specific risk factors, thus informing how we can tailor interventions for specific groups.”
According to Dr. Saw, while it’s clear that suicide is a leading cause of death among Asian American adolescents, it’s still unknown which specific subgroups other than girls and LGBTIA+ individuals are especially vulnerable and which culturally tailored interventions are most effective for decreasing suicide risk.
“Psychiatrists should understand that risk and protective factors for suicidal behavior in Asian American adolescents are multifaceted and require careful attention and intervention across different environments,” she said.
No funding and no disclosures were reported.
NEW ORLEANS – In an unexpected finding, researchers discovered that According to a weighted analysis, 24% of Asian Americans reported thinking about or planning suicide vs. 22% of Whites and Blacks and 20% of Hispanics (P < .01).
“We were shocked,” said study lead author Esha Hansoti, MD, who conducted the research at UT Southwestern Medical Center, Dallas, and is now a psychiatry resident at Zucker Hillside Hospital Northwell/Hofstra in Glen Oaks, NY. The findings were released at the annual meeting of the American Psychiatric Association.
Dr. Hansoti and colleagues launched the analysis in light of sparse research into Asian American mental health, she said. Even within this population, she said, mental illness “tends to be overlooked” and discussion of the topic may be considered taboo.
For the new study, researchers analyzed the 2019 Youth Risk Behavior Survey, conducted biennially by the Centers for Disease Control and Prevention, which had more than 13,000 participants in grades 9-12.
A weighted bivariate analysis of 618 Asian American adolescents – adjusted for age, sex, and depressive symptoms – found no statistically significant impact on suicidal ideation by gender, age, substance use, sexual/physical dating violence, or fluency in English.
However, several groups had a statistically significant higher risk, including victims of forced sexual intercourse and those who were threatened or bullied at school.
Those who didn’t get mostly A grades were also at high risk: Adolescents with mostly Ds and Fs were more likely to have acknowledged suicidal ideation than those with mostly As (adjusted odds ratio [AOR] = 3.2).
Gays and lesbians (AOR = 7.9 vs. heterosexuals), and bisexuals (AOR = 5.2 vs. heterosexuals) also showed sharply higher rates of suicidal ideation.
It’s not clear why Asian American adolescents may be at higher risk of suicidal ideation. The survey was completed prior to the COVID-19 pandemic, which spawned bigotry against people of Asian descent and an ongoing outbreak of high-profile violence against Asian Americans across the country.
Dr. Hansoti noted that Asian Americans face the pressures to live up to the standards of being a “model minority.” In addition, “very few Asian American adolescents are taken to a therapist, and few mental health providers are Asian Americans.”
She urged fellow psychiatrists “to remember that our perceptions of Asian Americans might hinder some of the diagnoses we could be making. Be thoughtful about how their ethnicity and race affects their presentation and their own perception of their illness.”
She added that Asian Americans may experience mental illness and anxiety “more somatically and physically than emotionally.”
In an interview, Anne Saw, PhD, associate professor of clinical-community psychology at DePaul University, Chicago, said the findings are “helpful for corroborating other studies identifying risk factors of suicidal ideation among Asian American adolescents. Since this research utilizes the Youth Risk Behavior Survey, these findings can be compared with risk factors of suicidal ideation among adolescents from other racial/ethnic backgrounds to pinpoint general as well as specific risk factors, thus informing how we can tailor interventions for specific groups.”
According to Dr. Saw, while it’s clear that suicide is a leading cause of death among Asian American adolescents, it’s still unknown which specific subgroups other than girls and LGBTIA+ individuals are especially vulnerable and which culturally tailored interventions are most effective for decreasing suicide risk.
“Psychiatrists should understand that risk and protective factors for suicidal behavior in Asian American adolescents are multifaceted and require careful attention and intervention across different environments,” she said.
No funding and no disclosures were reported.
NEW ORLEANS – In an unexpected finding, researchers discovered that According to a weighted analysis, 24% of Asian Americans reported thinking about or planning suicide vs. 22% of Whites and Blacks and 20% of Hispanics (P < .01).
“We were shocked,” said study lead author Esha Hansoti, MD, who conducted the research at UT Southwestern Medical Center, Dallas, and is now a psychiatry resident at Zucker Hillside Hospital Northwell/Hofstra in Glen Oaks, NY. The findings were released at the annual meeting of the American Psychiatric Association.
Dr. Hansoti and colleagues launched the analysis in light of sparse research into Asian American mental health, she said. Even within this population, she said, mental illness “tends to be overlooked” and discussion of the topic may be considered taboo.
For the new study, researchers analyzed the 2019 Youth Risk Behavior Survey, conducted biennially by the Centers for Disease Control and Prevention, which had more than 13,000 participants in grades 9-12.
A weighted bivariate analysis of 618 Asian American adolescents – adjusted for age, sex, and depressive symptoms – found no statistically significant impact on suicidal ideation by gender, age, substance use, sexual/physical dating violence, or fluency in English.
However, several groups had a statistically significant higher risk, including victims of forced sexual intercourse and those who were threatened or bullied at school.
Those who didn’t get mostly A grades were also at high risk: Adolescents with mostly Ds and Fs were more likely to have acknowledged suicidal ideation than those with mostly As (adjusted odds ratio [AOR] = 3.2).
Gays and lesbians (AOR = 7.9 vs. heterosexuals), and bisexuals (AOR = 5.2 vs. heterosexuals) also showed sharply higher rates of suicidal ideation.
It’s not clear why Asian American adolescents may be at higher risk of suicidal ideation. The survey was completed prior to the COVID-19 pandemic, which spawned bigotry against people of Asian descent and an ongoing outbreak of high-profile violence against Asian Americans across the country.
Dr. Hansoti noted that Asian Americans face the pressures to live up to the standards of being a “model minority.” In addition, “very few Asian American adolescents are taken to a therapist, and few mental health providers are Asian Americans.”
She urged fellow psychiatrists “to remember that our perceptions of Asian Americans might hinder some of the diagnoses we could be making. Be thoughtful about how their ethnicity and race affects their presentation and their own perception of their illness.”
She added that Asian Americans may experience mental illness and anxiety “more somatically and physically than emotionally.”
In an interview, Anne Saw, PhD, associate professor of clinical-community psychology at DePaul University, Chicago, said the findings are “helpful for corroborating other studies identifying risk factors of suicidal ideation among Asian American adolescents. Since this research utilizes the Youth Risk Behavior Survey, these findings can be compared with risk factors of suicidal ideation among adolescents from other racial/ethnic backgrounds to pinpoint general as well as specific risk factors, thus informing how we can tailor interventions for specific groups.”
According to Dr. Saw, while it’s clear that suicide is a leading cause of death among Asian American adolescents, it’s still unknown which specific subgroups other than girls and LGBTIA+ individuals are especially vulnerable and which culturally tailored interventions are most effective for decreasing suicide risk.
“Psychiatrists should understand that risk and protective factors for suicidal behavior in Asian American adolescents are multifaceted and require careful attention and intervention across different environments,” she said.
No funding and no disclosures were reported.
AT APA 2022
Genetic testing for best antidepressant accurate, cost effective
new research suggests.
CYP2D6 and CYP2C19, from the cytochrome P450 family, are involved in the metabolism and elimination of various molecules, including medications. Variants in the genes encoding these enzymes affect the speed at which drugs are metabolized, altering their pharmacokinetic profiles.
The researchers studied 125 patients with MDD and used CYP2D6 and CYP2C19 genotyping to determine the presence of actionable phenotypes in line with Food and Drug Administration labeling.
They found that, in many cases, pharmacogenetic testing could have predicted poor response to the initial treatment selection and could have helped guide subsequent choices to improve outcomes.
In addition, a pharmacoeconomic evaluation that combined direct and indirect costs resulting from MDD with the prevalence of CYP2D6 and CYP2C19 phenotypes showed that testing for functional variants in both genes would be cost effective at a national level.
Had psychiatrists who treated patients in the study known about their metabolizing profiles, it “might have contributed to switches in medication” and could have reduced “delays in response,” said lead researcher Alessio Squassina, PhD, associate professor of pharmacology at the University of Cagliari (Italy).
The findings were presented at the European Psychiatric Association 2022 Congress.
Highly variable response rates
Dr. Squassina noted that the response to antidepressants is a “highly variable trait,” and while it is known that genetics play a role, their contribution is “still not completely understood.”
He explained that the use of pharmacogenetics, which leverages genetic information to guide treatment decision-making, has increased significantly.
While regulatory bodies, including the FDA, have been “very active” in defining strict criteria for interpreting the information from pharmacogenetic tests, there remains some “discrepancy” in their clinical utility.
Dr. Squassina said the FDA provides guidance on use of genetic testing on the labels of 34 psychiatric medications. Of these, 79% relate to CYP2D6, 12% relate to CYP2C19, and 9% relate to other genes.
These labels provide guidance on when genetic testing is recommended or required, as well as potentially clinically actionable gene-drug associations in patients with certain functional alleles.
However, Dr. Squassina noted that the distribution of such alleles is not the same across Europe, so it’s possible that a psychiatrist in Italy may be less likely to treat a patient with a phenotype affecting response to treatment or risk of adverse events than one in Norway or Sweden.
For the study, the investigators examined the frequency of CYP2D6 and CYP2C19 phenotypes in psychiatric patients in Sardinia and their relationship with pharmacologic treatment and cost-effectiveness.
They set out to recruit 200 patients with MDD who had a documented 5-year medical and treatment history, including alterations in treatment, adverse events, hospitalizations, suicide, and symptom scores, as well as sociodemographic variables.
An interim analysis of the first 125 patients recruited to the study showed that the most common CYP2D6 phenotype was normal metabolizers (NM), at 60.5%, followed by intermediate metabolizers (IM), at 28.2%, ultrarapid metabolizers (UR), at 8.9%, and poor metabolizers (PM), at 2.4%.
For CYP2C19, the most common phenotype was NM (49%), followed by IM (29.0%), UR (25.0%), and PM (4.0%). While there were differences in the overall European averages, they were not significant.
To highlight the potential impact that pharmacogenetic testing could have had on patient care and outcome, Dr. Squassina highlighted two cases.
The first concerned a patient with a CYP2D6 IM and CYP2C19 UR phenotype, who did not respond to escitalopram. The FDA drug label indicates this phenotype is actionable and recommends an alternative drug.
The patient was subsequently switched to venlafaxine. The FDA drug label on venlafaxine notes that patients with this phenotype are likely to have a suboptimal response to this drug, and again, this patient did not respond to treatment.
Another patient with a CYP2D6 NM and CYP2C19 IM phenotype was also prescribed escitalopram. The FDA label on this drug notes that patients with this phenotype can try venlafaxine but may not respond. Indeed, this patient did not respond and was switched to venlafaxine and started responding.
“The psychiatrists [in these cases] may made have made different [drug] choices if they had known the genotypes in advance,” Dr. Squassina said.
Cost effective?
To determine the cost-effectiveness of screening for CYP2D6 and CYP2C19 phenotypes in patients with MDD, the researchers used real-world data to develop a Markov model with a hypothetical cohort of 2000 MDD patients, half of whom underwent pharmacogenetic testing, to determine the potential impact on outcomes over an 18-week period.
The model included the cost of medications and hospitalization, psychiatric counseling, loss of productivity, and the estimated probability of response and adverse events, adjusted for the patient’s likelihood of having a particular metabolizing phenotype.
Results showed that, for CYP2C19, compared to no testing, pharmacogenetic testing would be cost-effective at an incremental cost-effective ratio (ICER) of €60,000 ($64,000 USD) per quality-adjusted life-year (QALY).
This, Squassina said, is “below the willingness to pay threshold” for health authorities in developed countries.
For CYP2D6, pharmacogenetic testing would become cost-effective at an ICER of approximately €47,000 ($40,000 USD) per QALY.
The team plans to complete recruitment and perform a “detailed evaluation of all the variables, especially those relating to the medication history and changes in dosage, and adverse drug reactions.” The researchers would also like to study genetic phenotypes for other metabolizing enzymes and repeat the pharmacoeconomic analysis with the complete dataset.
A glimpse into the future
Approached for comment, Alessandro Serretti, MD, PhD, department of biomedical and neuromotor sciences, University of Bologna (Italy), who was not involved in the study, said the findings show there is a “small but evident benefit” from CYP profiling, “which makes sense.”
He added that in the Netherlands and other European countries, efforts are already underway to record the CYP status of patients at a national level. “Sooner or later, all Western countries will implement it as a routine,” he said in an interview.
He explained that, when such testing is widely available, electronic health record data will allow physicians to immediately select the optimal antidepressant for an individual patient. This will end the current trial-and-error process that leads to delayed treatment and will help avoid serious consequences, such as suicide.
While reducing a single patient’s treatment by a few weeks with the most appropriate antidepressant choice does not make a large difference in the cost per episode, at a population level, it has the potential to make a significant difference.
Dr. Serretti does not envisage genotyping all 333 million Europeans for the CYP phenotype at this point but imagines that in the future, individuals will undergo whole-genome sequencing to determine risks for cancer, dementia, and heart disease, at which point they will also undergo CYP functional allele profiling, and all these data will be recorded on individuals’ EHR.
“So, every doctor, a psychiatrist or cardiologist, can see everything, whenever they need it,” he said.
The study was funded by Fondazione di Sardegna and Regione Autonoma della Sardegna. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
CYP2D6 and CYP2C19, from the cytochrome P450 family, are involved in the metabolism and elimination of various molecules, including medications. Variants in the genes encoding these enzymes affect the speed at which drugs are metabolized, altering their pharmacokinetic profiles.
The researchers studied 125 patients with MDD and used CYP2D6 and CYP2C19 genotyping to determine the presence of actionable phenotypes in line with Food and Drug Administration labeling.
They found that, in many cases, pharmacogenetic testing could have predicted poor response to the initial treatment selection and could have helped guide subsequent choices to improve outcomes.
In addition, a pharmacoeconomic evaluation that combined direct and indirect costs resulting from MDD with the prevalence of CYP2D6 and CYP2C19 phenotypes showed that testing for functional variants in both genes would be cost effective at a national level.
Had psychiatrists who treated patients in the study known about their metabolizing profiles, it “might have contributed to switches in medication” and could have reduced “delays in response,” said lead researcher Alessio Squassina, PhD, associate professor of pharmacology at the University of Cagliari (Italy).
The findings were presented at the European Psychiatric Association 2022 Congress.
Highly variable response rates
Dr. Squassina noted that the response to antidepressants is a “highly variable trait,” and while it is known that genetics play a role, their contribution is “still not completely understood.”
He explained that the use of pharmacogenetics, which leverages genetic information to guide treatment decision-making, has increased significantly.
While regulatory bodies, including the FDA, have been “very active” in defining strict criteria for interpreting the information from pharmacogenetic tests, there remains some “discrepancy” in their clinical utility.
Dr. Squassina said the FDA provides guidance on use of genetic testing on the labels of 34 psychiatric medications. Of these, 79% relate to CYP2D6, 12% relate to CYP2C19, and 9% relate to other genes.
These labels provide guidance on when genetic testing is recommended or required, as well as potentially clinically actionable gene-drug associations in patients with certain functional alleles.
However, Dr. Squassina noted that the distribution of such alleles is not the same across Europe, so it’s possible that a psychiatrist in Italy may be less likely to treat a patient with a phenotype affecting response to treatment or risk of adverse events than one in Norway or Sweden.
For the study, the investigators examined the frequency of CYP2D6 and CYP2C19 phenotypes in psychiatric patients in Sardinia and their relationship with pharmacologic treatment and cost-effectiveness.
They set out to recruit 200 patients with MDD who had a documented 5-year medical and treatment history, including alterations in treatment, adverse events, hospitalizations, suicide, and symptom scores, as well as sociodemographic variables.
An interim analysis of the first 125 patients recruited to the study showed that the most common CYP2D6 phenotype was normal metabolizers (NM), at 60.5%, followed by intermediate metabolizers (IM), at 28.2%, ultrarapid metabolizers (UR), at 8.9%, and poor metabolizers (PM), at 2.4%.
For CYP2C19, the most common phenotype was NM (49%), followed by IM (29.0%), UR (25.0%), and PM (4.0%). While there were differences in the overall European averages, they were not significant.
To highlight the potential impact that pharmacogenetic testing could have had on patient care and outcome, Dr. Squassina highlighted two cases.
The first concerned a patient with a CYP2D6 IM and CYP2C19 UR phenotype, who did not respond to escitalopram. The FDA drug label indicates this phenotype is actionable and recommends an alternative drug.
The patient was subsequently switched to venlafaxine. The FDA drug label on venlafaxine notes that patients with this phenotype are likely to have a suboptimal response to this drug, and again, this patient did not respond to treatment.
Another patient with a CYP2D6 NM and CYP2C19 IM phenotype was also prescribed escitalopram. The FDA label on this drug notes that patients with this phenotype can try venlafaxine but may not respond. Indeed, this patient did not respond and was switched to venlafaxine and started responding.
“The psychiatrists [in these cases] may made have made different [drug] choices if they had known the genotypes in advance,” Dr. Squassina said.
Cost effective?
To determine the cost-effectiveness of screening for CYP2D6 and CYP2C19 phenotypes in patients with MDD, the researchers used real-world data to develop a Markov model with a hypothetical cohort of 2000 MDD patients, half of whom underwent pharmacogenetic testing, to determine the potential impact on outcomes over an 18-week period.
The model included the cost of medications and hospitalization, psychiatric counseling, loss of productivity, and the estimated probability of response and adverse events, adjusted for the patient’s likelihood of having a particular metabolizing phenotype.
Results showed that, for CYP2C19, compared to no testing, pharmacogenetic testing would be cost-effective at an incremental cost-effective ratio (ICER) of €60,000 ($64,000 USD) per quality-adjusted life-year (QALY).
This, Squassina said, is “below the willingness to pay threshold” for health authorities in developed countries.
For CYP2D6, pharmacogenetic testing would become cost-effective at an ICER of approximately €47,000 ($40,000 USD) per QALY.
The team plans to complete recruitment and perform a “detailed evaluation of all the variables, especially those relating to the medication history and changes in dosage, and adverse drug reactions.” The researchers would also like to study genetic phenotypes for other metabolizing enzymes and repeat the pharmacoeconomic analysis with the complete dataset.
A glimpse into the future
Approached for comment, Alessandro Serretti, MD, PhD, department of biomedical and neuromotor sciences, University of Bologna (Italy), who was not involved in the study, said the findings show there is a “small but evident benefit” from CYP profiling, “which makes sense.”
He added that in the Netherlands and other European countries, efforts are already underway to record the CYP status of patients at a national level. “Sooner or later, all Western countries will implement it as a routine,” he said in an interview.
He explained that, when such testing is widely available, electronic health record data will allow physicians to immediately select the optimal antidepressant for an individual patient. This will end the current trial-and-error process that leads to delayed treatment and will help avoid serious consequences, such as suicide.
While reducing a single patient’s treatment by a few weeks with the most appropriate antidepressant choice does not make a large difference in the cost per episode, at a population level, it has the potential to make a significant difference.
Dr. Serretti does not envisage genotyping all 333 million Europeans for the CYP phenotype at this point but imagines that in the future, individuals will undergo whole-genome sequencing to determine risks for cancer, dementia, and heart disease, at which point they will also undergo CYP functional allele profiling, and all these data will be recorded on individuals’ EHR.
“So, every doctor, a psychiatrist or cardiologist, can see everything, whenever they need it,” he said.
The study was funded by Fondazione di Sardegna and Regione Autonoma della Sardegna. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
CYP2D6 and CYP2C19, from the cytochrome P450 family, are involved in the metabolism and elimination of various molecules, including medications. Variants in the genes encoding these enzymes affect the speed at which drugs are metabolized, altering their pharmacokinetic profiles.
The researchers studied 125 patients with MDD and used CYP2D6 and CYP2C19 genotyping to determine the presence of actionable phenotypes in line with Food and Drug Administration labeling.
They found that, in many cases, pharmacogenetic testing could have predicted poor response to the initial treatment selection and could have helped guide subsequent choices to improve outcomes.
In addition, a pharmacoeconomic evaluation that combined direct and indirect costs resulting from MDD with the prevalence of CYP2D6 and CYP2C19 phenotypes showed that testing for functional variants in both genes would be cost effective at a national level.
Had psychiatrists who treated patients in the study known about their metabolizing profiles, it “might have contributed to switches in medication” and could have reduced “delays in response,” said lead researcher Alessio Squassina, PhD, associate professor of pharmacology at the University of Cagliari (Italy).
The findings were presented at the European Psychiatric Association 2022 Congress.
Highly variable response rates
Dr. Squassina noted that the response to antidepressants is a “highly variable trait,” and while it is known that genetics play a role, their contribution is “still not completely understood.”
He explained that the use of pharmacogenetics, which leverages genetic information to guide treatment decision-making, has increased significantly.
While regulatory bodies, including the FDA, have been “very active” in defining strict criteria for interpreting the information from pharmacogenetic tests, there remains some “discrepancy” in their clinical utility.
Dr. Squassina said the FDA provides guidance on use of genetic testing on the labels of 34 psychiatric medications. Of these, 79% relate to CYP2D6, 12% relate to CYP2C19, and 9% relate to other genes.
These labels provide guidance on when genetic testing is recommended or required, as well as potentially clinically actionable gene-drug associations in patients with certain functional alleles.
However, Dr. Squassina noted that the distribution of such alleles is not the same across Europe, so it’s possible that a psychiatrist in Italy may be less likely to treat a patient with a phenotype affecting response to treatment or risk of adverse events than one in Norway or Sweden.
For the study, the investigators examined the frequency of CYP2D6 and CYP2C19 phenotypes in psychiatric patients in Sardinia and their relationship with pharmacologic treatment and cost-effectiveness.
They set out to recruit 200 patients with MDD who had a documented 5-year medical and treatment history, including alterations in treatment, adverse events, hospitalizations, suicide, and symptom scores, as well as sociodemographic variables.
An interim analysis of the first 125 patients recruited to the study showed that the most common CYP2D6 phenotype was normal metabolizers (NM), at 60.5%, followed by intermediate metabolizers (IM), at 28.2%, ultrarapid metabolizers (UR), at 8.9%, and poor metabolizers (PM), at 2.4%.
For CYP2C19, the most common phenotype was NM (49%), followed by IM (29.0%), UR (25.0%), and PM (4.0%). While there were differences in the overall European averages, they were not significant.
To highlight the potential impact that pharmacogenetic testing could have had on patient care and outcome, Dr. Squassina highlighted two cases.
The first concerned a patient with a CYP2D6 IM and CYP2C19 UR phenotype, who did not respond to escitalopram. The FDA drug label indicates this phenotype is actionable and recommends an alternative drug.
The patient was subsequently switched to venlafaxine. The FDA drug label on venlafaxine notes that patients with this phenotype are likely to have a suboptimal response to this drug, and again, this patient did not respond to treatment.
Another patient with a CYP2D6 NM and CYP2C19 IM phenotype was also prescribed escitalopram. The FDA label on this drug notes that patients with this phenotype can try venlafaxine but may not respond. Indeed, this patient did not respond and was switched to venlafaxine and started responding.
“The psychiatrists [in these cases] may made have made different [drug] choices if they had known the genotypes in advance,” Dr. Squassina said.
Cost effective?
To determine the cost-effectiveness of screening for CYP2D6 and CYP2C19 phenotypes in patients with MDD, the researchers used real-world data to develop a Markov model with a hypothetical cohort of 2000 MDD patients, half of whom underwent pharmacogenetic testing, to determine the potential impact on outcomes over an 18-week period.
The model included the cost of medications and hospitalization, psychiatric counseling, loss of productivity, and the estimated probability of response and adverse events, adjusted for the patient’s likelihood of having a particular metabolizing phenotype.
Results showed that, for CYP2C19, compared to no testing, pharmacogenetic testing would be cost-effective at an incremental cost-effective ratio (ICER) of €60,000 ($64,000 USD) per quality-adjusted life-year (QALY).
This, Squassina said, is “below the willingness to pay threshold” for health authorities in developed countries.
For CYP2D6, pharmacogenetic testing would become cost-effective at an ICER of approximately €47,000 ($40,000 USD) per QALY.
The team plans to complete recruitment and perform a “detailed evaluation of all the variables, especially those relating to the medication history and changes in dosage, and adverse drug reactions.” The researchers would also like to study genetic phenotypes for other metabolizing enzymes and repeat the pharmacoeconomic analysis with the complete dataset.
A glimpse into the future
Approached for comment, Alessandro Serretti, MD, PhD, department of biomedical and neuromotor sciences, University of Bologna (Italy), who was not involved in the study, said the findings show there is a “small but evident benefit” from CYP profiling, “which makes sense.”
He added that in the Netherlands and other European countries, efforts are already underway to record the CYP status of patients at a national level. “Sooner or later, all Western countries will implement it as a routine,” he said in an interview.
He explained that, when such testing is widely available, electronic health record data will allow physicians to immediately select the optimal antidepressant for an individual patient. This will end the current trial-and-error process that leads to delayed treatment and will help avoid serious consequences, such as suicide.
While reducing a single patient’s treatment by a few weeks with the most appropriate antidepressant choice does not make a large difference in the cost per episode, at a population level, it has the potential to make a significant difference.
Dr. Serretti does not envisage genotyping all 333 million Europeans for the CYP phenotype at this point but imagines that in the future, individuals will undergo whole-genome sequencing to determine risks for cancer, dementia, and heart disease, at which point they will also undergo CYP functional allele profiling, and all these data will be recorded on individuals’ EHR.
“So, every doctor, a psychiatrist or cardiologist, can see everything, whenever they need it,” he said.
The study was funded by Fondazione di Sardegna and Regione Autonoma della Sardegna. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EPA 2022



















