User login
Debate heats up on how best to treat gender-questioning kids
The past week has seen heated debate about the complex issue of how to best treat children with gender dysphoria, with further developments in a number of U.S. states and in Sweden.
In the U.S., more states have moved to prevent the use of any medical treatment, such as puberty blockers or cross-sex hormones, in kids younger than the age of 18, most recently in a state Senate vote in Alabama last week, and in Texas, where Governor Greg Abbott is said to have ordered state agencies to investigate reports of gender-transition procedures on children as “child abuse.”
At least one parent has, because of this, established a crowdfunding page to try to raise money to move away from Texas, fearful of being accused of child abuse if their child with gender dysphoria receives hormone therapy. And a countersuit has been filed there by the ACLU of Texas and Lambda Legal, a civil rights organization, on behalf of one parent said to be under investigation.
But on the flip side, parents living in more liberal states – where children under the age of 18 can often get hormones to transition without parental consent – are considering moving out of them to protect their children. These parents are concerned that their kids do not know enough about the side effects of puberty blockers, or lifetime use of cross-sex hormones and its implications, to be able to make properly informed decisions at such a young age.
Meanwhile, Sweden has further tightened its restrictions on medical therapy to treat gender-questioning kids, with a recent announcement from its National Board of Health and Welfare (NBHW), on Feb. 22, urging restraint in hormone treatment of minors with gender dysphoria following a review by the agency there that assesses health technologies, the SBU.
Based on the review results, the NBHW’s overall conclusion is that the risks of puberty blocking and cross-sex hormone treatment for those under 18 currently outweigh the possible benefits for the group as a whole. The agency now says hormone treatment should only be offered in exceptional cases outside the framework of research, and principally, only in adolescents with childhood-onset gender dysphoria, as opposed to those who develop it during puberty, or in their teens, as is the case with most teenagers currently presenting.
At the same time, gender-affirming hormone treatment for adolescents who identify as transgender or nonbinary is associated with changes in depression and suicidality, according to a new U.S. survey published Feb. 25 in JAMA Network Health.
However, experts who spoke to this news organization were critical of the study, noting it was small, conducted in just 104 youth who were an average age of 15.8 years and of whom only 63% completed the survey at the final timepoint, just 1 year after starting therapy. In addition, there was no control group, among other limitations.
“The most worrying thing is that they haven’t described the pros and cons of the treatment that they are researching. We know that there are risks inherent in using gender-affirming medicine, as with all medications,” Anna Hutchinson, DClinPsych, of the Integrated Psychology Clinic, London, told this news organization.
“For example, when people with gender dysphoria use cross-sex hormones, there is a burden of treatment that can last a lifetime, both for those who benefit from the treatment and those who detransition or regret later on,” said Dr. Hutchinson, who has extensive experience of working with young people with issues related to sexuality or gender.
“This isn’t mentioned at all, which makes the paper appear quite biased towards using one approach for managing gender dysphoria and related distress, whilst not acknowledging any risks of doing so or considering alternatives,” she noted.
Why were some treated with hormones while others weren’t?
The newly published survey is by PhD student Diana M. Tordoff, MPH, of the Department of Epidemiology, University of Washington, Seattle, and colleagues. Published alongside was an invited commentary by Brett Dolotina, BS, of Massachusetts General Hospital, Boston, and Jack L. Turban, MD, MHS, of Stanford (Calif.) University.
The study was conducted at an urban multidisciplinary gender clinic in Seattle among transgender and nonbinary adolescents and young adults seeking gender-affirming care from August 2017 to June 2018. Data were analyzed from August 2020 to November 2021.
Participating in the study were 104 youths aged 13-20 years (mean age, 15.8 years), 63 transmasculine (born female) individuals (60.6%), 27 transfeminine (born male) individuals (26.0%), 10 nonbinary or gender-fluid individuals (9.6%), and four youths who responded, “I don’t know,” or did not respond to the gender-identity question (3.8%).
At baseline, 59 individuals (56.7%) had moderate-to-severe depression, 52 individuals (50.0%) had moderate-to-severe anxiety, and 45 individuals (43.3%) reported self-harm or suicidal thoughts.
By the end of the study, 69 youths (66.3%) had received puberty blockers, cross-sex hormones (testosterone for girls transitioning to male and estrogen for boys transitioning to female), or both interventions, while 35 youths had not received either intervention (33.7%).
After adjustment for temporal trends and potential confounders, there were a 60% lower odds of depression (adjusted odds ratio, 0.40; 95% confidence interval, 0.17-0.95) and 73% lower odds of suicidality (aOR, 0.27; 95% CI, 0.11-0.65) among youths who had initiated puberty blockers or cross-sex hormones.
There was no association between these treatments and anxiety, however (aOR, 1.01; 95% CI, 0.41-2.51).
Dr. Hutchinson points out that nonbinary and gender fluid “are not diagnostic or clinical terms,” adding, “there is no information about how the groups were chosen or if any of them met the criteria for gender dysphoria. It seems strange to not have measured gender dysphoria, both before and after interventions, in a group of children presenting with gender dysphoria.”
She adds: “I am questioning why ‘gender-affirming’ medicine appears to be being used here as a specific intervention for depression and suicidality? [That] wouldn’t usually be the first reason to commence these particular treatments. Why didn’t they provide therapy or antidepressant medication to this group of young people, as is routine for managing mood and/or suicidality in all other patient cohorts?”
In their commentary, Mr. Dolotina and Dr. Turban observe: “The rate of suicidality among the Tordoff et al. sample after receiving gender-affirming care was still much higher than national rates of suicidality among youth in the U.S., denoting that ... other mental health determinants must be addressed ... including gender minority stress.”
Small study, no control group, large loss to follow-up
Dr. Hutchinson also criticizes the small sample size of just 104 youth and “large loss to follow-up, whereby only 65 of those 104 [youth] completed the final survey in a short time [1 year].” This could indicate “that only the most satisfied kids stayed the course,” she suggests.
And importantly, the findings on depression and suicidality rely on the experience of only five people in the no-treatment group at 12 months, she points out.
Also, as the authors themselves acknowledge, they didn’t control for other psychiatric medicines that the participants might have been taking at baseline.
“It’s important to know more about all of this in order to draw accurate conclusions about what works, or does not, for whom,” noted Dr. Hutchinson.
Most patients, too, she notes, were females-to-males taking testosterone. Therefore, the finding that they experienced a reduction in depression might simply reflect the widely reported antidepressant effects of testosterone.
Also expressing concern about the small sample size and “lack of a control group” is Michelle Mackness, MC, a Canadian counselor in private practice who has experience working with gender-questioning individuals, detransitioners, and those experiencing complications related to their transition.
“Tordoff et al.’s assertion that there is a ‘robust evidence base’ supporting pediatric transition seems out-of-step with recent global developments in care policies and protocols for gender-questioning youth,” she points out.
“Neither the study authors or commentators acknowledge, let alone address, the fact that Finland, the U.K., and Sweden have recently determined that the evidence allegedly supporting medical interventions for pediatric transition is ‘inconclusive’,” she adds.
Asked to respond, Ms. Tordoff did not directly address this question. Rather, she reiterated to this news organization: “We found that receipt of puberty blockers and gender-affirming hormones was associated with a 60% lower odds of depression and a 73% lower odds of suicidal thoughts by the end of our study follow-up. We conducted extensive sensitivity analyses, which support the robustness of our study findings.”
She added: “These results are consistent with other recently published prospective cohort studies (please see citations provided within the manuscript).”
Parents may move states
It is this concern about the lifetime burden of treatment involved with transitioning that gives some parents of children with gender dysphoria pause for thought, especially those who live in more liberal U.S. states.
Indeed, two of America’s leading psychologists who work in this field, including one who is transgender herself, told this news organization in November they are now concerned about a lack of adequate psychological evaluations of youth with gender dysphoria before any medical treatment is considered.
So while one parent, Violet A., last week established a GoFundMe page for her child, entitled, “Help Us Move Isa to Safety,” stating she needed to move from Texas due to Governor Abbott’s pronouncements there “to a state that won’t consider me an abuser when I seek medical care for my trans child and potentially remove her from my custody,” some parents feel the need instead to move from more liberal states.
Some tell their stories anonymously, as they don’t want to risk causing their gender-questioning children further distress, as detailed on the Genspect website.
A version of this article first appeared on Medscape.com.
The past week has seen heated debate about the complex issue of how to best treat children with gender dysphoria, with further developments in a number of U.S. states and in Sweden.
In the U.S., more states have moved to prevent the use of any medical treatment, such as puberty blockers or cross-sex hormones, in kids younger than the age of 18, most recently in a state Senate vote in Alabama last week, and in Texas, where Governor Greg Abbott is said to have ordered state agencies to investigate reports of gender-transition procedures on children as “child abuse.”
At least one parent has, because of this, established a crowdfunding page to try to raise money to move away from Texas, fearful of being accused of child abuse if their child with gender dysphoria receives hormone therapy. And a countersuit has been filed there by the ACLU of Texas and Lambda Legal, a civil rights organization, on behalf of one parent said to be under investigation.
But on the flip side, parents living in more liberal states – where children under the age of 18 can often get hormones to transition without parental consent – are considering moving out of them to protect their children. These parents are concerned that their kids do not know enough about the side effects of puberty blockers, or lifetime use of cross-sex hormones and its implications, to be able to make properly informed decisions at such a young age.
Meanwhile, Sweden has further tightened its restrictions on medical therapy to treat gender-questioning kids, with a recent announcement from its National Board of Health and Welfare (NBHW), on Feb. 22, urging restraint in hormone treatment of minors with gender dysphoria following a review by the agency there that assesses health technologies, the SBU.
Based on the review results, the NBHW’s overall conclusion is that the risks of puberty blocking and cross-sex hormone treatment for those under 18 currently outweigh the possible benefits for the group as a whole. The agency now says hormone treatment should only be offered in exceptional cases outside the framework of research, and principally, only in adolescents with childhood-onset gender dysphoria, as opposed to those who develop it during puberty, or in their teens, as is the case with most teenagers currently presenting.
At the same time, gender-affirming hormone treatment for adolescents who identify as transgender or nonbinary is associated with changes in depression and suicidality, according to a new U.S. survey published Feb. 25 in JAMA Network Health.
However, experts who spoke to this news organization were critical of the study, noting it was small, conducted in just 104 youth who were an average age of 15.8 years and of whom only 63% completed the survey at the final timepoint, just 1 year after starting therapy. In addition, there was no control group, among other limitations.
“The most worrying thing is that they haven’t described the pros and cons of the treatment that they are researching. We know that there are risks inherent in using gender-affirming medicine, as with all medications,” Anna Hutchinson, DClinPsych, of the Integrated Psychology Clinic, London, told this news organization.
“For example, when people with gender dysphoria use cross-sex hormones, there is a burden of treatment that can last a lifetime, both for those who benefit from the treatment and those who detransition or regret later on,” said Dr. Hutchinson, who has extensive experience of working with young people with issues related to sexuality or gender.
“This isn’t mentioned at all, which makes the paper appear quite biased towards using one approach for managing gender dysphoria and related distress, whilst not acknowledging any risks of doing so or considering alternatives,” she noted.
Why were some treated with hormones while others weren’t?
The newly published survey is by PhD student Diana M. Tordoff, MPH, of the Department of Epidemiology, University of Washington, Seattle, and colleagues. Published alongside was an invited commentary by Brett Dolotina, BS, of Massachusetts General Hospital, Boston, and Jack L. Turban, MD, MHS, of Stanford (Calif.) University.
The study was conducted at an urban multidisciplinary gender clinic in Seattle among transgender and nonbinary adolescents and young adults seeking gender-affirming care from August 2017 to June 2018. Data were analyzed from August 2020 to November 2021.
Participating in the study were 104 youths aged 13-20 years (mean age, 15.8 years), 63 transmasculine (born female) individuals (60.6%), 27 transfeminine (born male) individuals (26.0%), 10 nonbinary or gender-fluid individuals (9.6%), and four youths who responded, “I don’t know,” or did not respond to the gender-identity question (3.8%).
At baseline, 59 individuals (56.7%) had moderate-to-severe depression, 52 individuals (50.0%) had moderate-to-severe anxiety, and 45 individuals (43.3%) reported self-harm or suicidal thoughts.
By the end of the study, 69 youths (66.3%) had received puberty blockers, cross-sex hormones (testosterone for girls transitioning to male and estrogen for boys transitioning to female), or both interventions, while 35 youths had not received either intervention (33.7%).
After adjustment for temporal trends and potential confounders, there were a 60% lower odds of depression (adjusted odds ratio, 0.40; 95% confidence interval, 0.17-0.95) and 73% lower odds of suicidality (aOR, 0.27; 95% CI, 0.11-0.65) among youths who had initiated puberty blockers or cross-sex hormones.
There was no association between these treatments and anxiety, however (aOR, 1.01; 95% CI, 0.41-2.51).
Dr. Hutchinson points out that nonbinary and gender fluid “are not diagnostic or clinical terms,” adding, “there is no information about how the groups were chosen or if any of them met the criteria for gender dysphoria. It seems strange to not have measured gender dysphoria, both before and after interventions, in a group of children presenting with gender dysphoria.”
She adds: “I am questioning why ‘gender-affirming’ medicine appears to be being used here as a specific intervention for depression and suicidality? [That] wouldn’t usually be the first reason to commence these particular treatments. Why didn’t they provide therapy or antidepressant medication to this group of young people, as is routine for managing mood and/or suicidality in all other patient cohorts?”
In their commentary, Mr. Dolotina and Dr. Turban observe: “The rate of suicidality among the Tordoff et al. sample after receiving gender-affirming care was still much higher than national rates of suicidality among youth in the U.S., denoting that ... other mental health determinants must be addressed ... including gender minority stress.”
Small study, no control group, large loss to follow-up
Dr. Hutchinson also criticizes the small sample size of just 104 youth and “large loss to follow-up, whereby only 65 of those 104 [youth] completed the final survey in a short time [1 year].” This could indicate “that only the most satisfied kids stayed the course,” she suggests.
And importantly, the findings on depression and suicidality rely on the experience of only five people in the no-treatment group at 12 months, she points out.
Also, as the authors themselves acknowledge, they didn’t control for other psychiatric medicines that the participants might have been taking at baseline.
“It’s important to know more about all of this in order to draw accurate conclusions about what works, or does not, for whom,” noted Dr. Hutchinson.
Most patients, too, she notes, were females-to-males taking testosterone. Therefore, the finding that they experienced a reduction in depression might simply reflect the widely reported antidepressant effects of testosterone.
Also expressing concern about the small sample size and “lack of a control group” is Michelle Mackness, MC, a Canadian counselor in private practice who has experience working with gender-questioning individuals, detransitioners, and those experiencing complications related to their transition.
“Tordoff et al.’s assertion that there is a ‘robust evidence base’ supporting pediatric transition seems out-of-step with recent global developments in care policies and protocols for gender-questioning youth,” she points out.
“Neither the study authors or commentators acknowledge, let alone address, the fact that Finland, the U.K., and Sweden have recently determined that the evidence allegedly supporting medical interventions for pediatric transition is ‘inconclusive’,” she adds.
Asked to respond, Ms. Tordoff did not directly address this question. Rather, she reiterated to this news organization: “We found that receipt of puberty blockers and gender-affirming hormones was associated with a 60% lower odds of depression and a 73% lower odds of suicidal thoughts by the end of our study follow-up. We conducted extensive sensitivity analyses, which support the robustness of our study findings.”
She added: “These results are consistent with other recently published prospective cohort studies (please see citations provided within the manuscript).”
Parents may move states
It is this concern about the lifetime burden of treatment involved with transitioning that gives some parents of children with gender dysphoria pause for thought, especially those who live in more liberal U.S. states.
Indeed, two of America’s leading psychologists who work in this field, including one who is transgender herself, told this news organization in November they are now concerned about a lack of adequate psychological evaluations of youth with gender dysphoria before any medical treatment is considered.
So while one parent, Violet A., last week established a GoFundMe page for her child, entitled, “Help Us Move Isa to Safety,” stating she needed to move from Texas due to Governor Abbott’s pronouncements there “to a state that won’t consider me an abuser when I seek medical care for my trans child and potentially remove her from my custody,” some parents feel the need instead to move from more liberal states.
Some tell their stories anonymously, as they don’t want to risk causing their gender-questioning children further distress, as detailed on the Genspect website.
A version of this article first appeared on Medscape.com.
The past week has seen heated debate about the complex issue of how to best treat children with gender dysphoria, with further developments in a number of U.S. states and in Sweden.
In the U.S., more states have moved to prevent the use of any medical treatment, such as puberty blockers or cross-sex hormones, in kids younger than the age of 18, most recently in a state Senate vote in Alabama last week, and in Texas, where Governor Greg Abbott is said to have ordered state agencies to investigate reports of gender-transition procedures on children as “child abuse.”
At least one parent has, because of this, established a crowdfunding page to try to raise money to move away from Texas, fearful of being accused of child abuse if their child with gender dysphoria receives hormone therapy. And a countersuit has been filed there by the ACLU of Texas and Lambda Legal, a civil rights organization, on behalf of one parent said to be under investigation.
But on the flip side, parents living in more liberal states – where children under the age of 18 can often get hormones to transition without parental consent – are considering moving out of them to protect their children. These parents are concerned that their kids do not know enough about the side effects of puberty blockers, or lifetime use of cross-sex hormones and its implications, to be able to make properly informed decisions at such a young age.
Meanwhile, Sweden has further tightened its restrictions on medical therapy to treat gender-questioning kids, with a recent announcement from its National Board of Health and Welfare (NBHW), on Feb. 22, urging restraint in hormone treatment of minors with gender dysphoria following a review by the agency there that assesses health technologies, the SBU.
Based on the review results, the NBHW’s overall conclusion is that the risks of puberty blocking and cross-sex hormone treatment for those under 18 currently outweigh the possible benefits for the group as a whole. The agency now says hormone treatment should only be offered in exceptional cases outside the framework of research, and principally, only in adolescents with childhood-onset gender dysphoria, as opposed to those who develop it during puberty, or in their teens, as is the case with most teenagers currently presenting.
At the same time, gender-affirming hormone treatment for adolescents who identify as transgender or nonbinary is associated with changes in depression and suicidality, according to a new U.S. survey published Feb. 25 in JAMA Network Health.
However, experts who spoke to this news organization were critical of the study, noting it was small, conducted in just 104 youth who were an average age of 15.8 years and of whom only 63% completed the survey at the final timepoint, just 1 year after starting therapy. In addition, there was no control group, among other limitations.
“The most worrying thing is that they haven’t described the pros and cons of the treatment that they are researching. We know that there are risks inherent in using gender-affirming medicine, as with all medications,” Anna Hutchinson, DClinPsych, of the Integrated Psychology Clinic, London, told this news organization.
“For example, when people with gender dysphoria use cross-sex hormones, there is a burden of treatment that can last a lifetime, both for those who benefit from the treatment and those who detransition or regret later on,” said Dr. Hutchinson, who has extensive experience of working with young people with issues related to sexuality or gender.
“This isn’t mentioned at all, which makes the paper appear quite biased towards using one approach for managing gender dysphoria and related distress, whilst not acknowledging any risks of doing so or considering alternatives,” she noted.
Why were some treated with hormones while others weren’t?
The newly published survey is by PhD student Diana M. Tordoff, MPH, of the Department of Epidemiology, University of Washington, Seattle, and colleagues. Published alongside was an invited commentary by Brett Dolotina, BS, of Massachusetts General Hospital, Boston, and Jack L. Turban, MD, MHS, of Stanford (Calif.) University.
The study was conducted at an urban multidisciplinary gender clinic in Seattle among transgender and nonbinary adolescents and young adults seeking gender-affirming care from August 2017 to June 2018. Data were analyzed from August 2020 to November 2021.
Participating in the study were 104 youths aged 13-20 years (mean age, 15.8 years), 63 transmasculine (born female) individuals (60.6%), 27 transfeminine (born male) individuals (26.0%), 10 nonbinary or gender-fluid individuals (9.6%), and four youths who responded, “I don’t know,” or did not respond to the gender-identity question (3.8%).
At baseline, 59 individuals (56.7%) had moderate-to-severe depression, 52 individuals (50.0%) had moderate-to-severe anxiety, and 45 individuals (43.3%) reported self-harm or suicidal thoughts.
By the end of the study, 69 youths (66.3%) had received puberty blockers, cross-sex hormones (testosterone for girls transitioning to male and estrogen for boys transitioning to female), or both interventions, while 35 youths had not received either intervention (33.7%).
After adjustment for temporal trends and potential confounders, there were a 60% lower odds of depression (adjusted odds ratio, 0.40; 95% confidence interval, 0.17-0.95) and 73% lower odds of suicidality (aOR, 0.27; 95% CI, 0.11-0.65) among youths who had initiated puberty blockers or cross-sex hormones.
There was no association between these treatments and anxiety, however (aOR, 1.01; 95% CI, 0.41-2.51).
Dr. Hutchinson points out that nonbinary and gender fluid “are not diagnostic or clinical terms,” adding, “there is no information about how the groups were chosen or if any of them met the criteria for gender dysphoria. It seems strange to not have measured gender dysphoria, both before and after interventions, in a group of children presenting with gender dysphoria.”
She adds: “I am questioning why ‘gender-affirming’ medicine appears to be being used here as a specific intervention for depression and suicidality? [That] wouldn’t usually be the first reason to commence these particular treatments. Why didn’t they provide therapy or antidepressant medication to this group of young people, as is routine for managing mood and/or suicidality in all other patient cohorts?”
In their commentary, Mr. Dolotina and Dr. Turban observe: “The rate of suicidality among the Tordoff et al. sample after receiving gender-affirming care was still much higher than national rates of suicidality among youth in the U.S., denoting that ... other mental health determinants must be addressed ... including gender minority stress.”
Small study, no control group, large loss to follow-up
Dr. Hutchinson also criticizes the small sample size of just 104 youth and “large loss to follow-up, whereby only 65 of those 104 [youth] completed the final survey in a short time [1 year].” This could indicate “that only the most satisfied kids stayed the course,” she suggests.
And importantly, the findings on depression and suicidality rely on the experience of only five people in the no-treatment group at 12 months, she points out.
Also, as the authors themselves acknowledge, they didn’t control for other psychiatric medicines that the participants might have been taking at baseline.
“It’s important to know more about all of this in order to draw accurate conclusions about what works, or does not, for whom,” noted Dr. Hutchinson.
Most patients, too, she notes, were females-to-males taking testosterone. Therefore, the finding that they experienced a reduction in depression might simply reflect the widely reported antidepressant effects of testosterone.
Also expressing concern about the small sample size and “lack of a control group” is Michelle Mackness, MC, a Canadian counselor in private practice who has experience working with gender-questioning individuals, detransitioners, and those experiencing complications related to their transition.
“Tordoff et al.’s assertion that there is a ‘robust evidence base’ supporting pediatric transition seems out-of-step with recent global developments in care policies and protocols for gender-questioning youth,” she points out.
“Neither the study authors or commentators acknowledge, let alone address, the fact that Finland, the U.K., and Sweden have recently determined that the evidence allegedly supporting medical interventions for pediatric transition is ‘inconclusive’,” she adds.
Asked to respond, Ms. Tordoff did not directly address this question. Rather, she reiterated to this news organization: “We found that receipt of puberty blockers and gender-affirming hormones was associated with a 60% lower odds of depression and a 73% lower odds of suicidal thoughts by the end of our study follow-up. We conducted extensive sensitivity analyses, which support the robustness of our study findings.”
She added: “These results are consistent with other recently published prospective cohort studies (please see citations provided within the manuscript).”
Parents may move states
It is this concern about the lifetime burden of treatment involved with transitioning that gives some parents of children with gender dysphoria pause for thought, especially those who live in more liberal U.S. states.
Indeed, two of America’s leading psychologists who work in this field, including one who is transgender herself, told this news organization in November they are now concerned about a lack of adequate psychological evaluations of youth with gender dysphoria before any medical treatment is considered.
So while one parent, Violet A., last week established a GoFundMe page for her child, entitled, “Help Us Move Isa to Safety,” stating she needed to move from Texas due to Governor Abbott’s pronouncements there “to a state that won’t consider me an abuser when I seek medical care for my trans child and potentially remove her from my custody,” some parents feel the need instead to move from more liberal states.
Some tell their stories anonymously, as they don’t want to risk causing their gender-questioning children further distress, as detailed on the Genspect website.
A version of this article first appeared on Medscape.com.
Irregular and long periods linked to NAFLD
Long or irregular menstrual cycles in relatively young women are linked an increased risk of both prevalent and incident nonalcoholic fatty liver disease (NAFLD), according to a cross-sectional study that included data on more than 70,000 women.
“Our results indicate that menstrual irregularity, which is easier to diagnose and usually presented earlier than PCOS [polycystic ovary syndrome] highlights the possibility of identifying premenopausal women at risk of developing NAFLD,” reported a team of authors primarily from Sungkyunkwan University, Seoul, South Korea.
The study evaluated women aged younger than 40 years who were participating in the Kangbuk Samsung Health Study, which involves a comprehensive biennial health examination at health centers in South Korea. Of the 135,090 women enrolled over a 6-year period who had at least one follow-up examination, 72,092 were available for analysis after excluding for a sizable list of confounding factors such as liver disease and infections; exposure to steatogenic medications, such as corticosteroids; hysterectomy; and pregnancy.
NAFLD prevalence climbs with longer menses
Of these women, 36.378 (27.7%) had menstrual cycles of 26-30 days and were identified as the index group. The prevalence of NAFLD in this group was 5.8%. For those with a menstrual cycle of 31-39 days, the prevalence rate climbed to 7.2%. For those with a menstrual cycle of at least 40 days or too irregular to estimate, the prevalence was 9.7%. The prevalence was 7.1% for those with a menstrual cycle less than 21 days.
The results of this study were published in the Journal of Clinical Endocrinology & Metabolism.
In those without NAFLD at baseline who were then followed for a mean of 4.4 years, there were 4,524 incident cases of NAFLD. Incidence density was calculated per 103 patient-years. In the index group, the rate was 18.4. It climbed to 20.2 for those with a menstrual cycle of 31-39 days and then to 22.9 for those with a menstrual cycle of at least 40 days. For those with a cycle of fewer than 21 days, the rate was 26.8.
After adjusting for age, body mass index, insulin resistance, and other confounders, the hazard ratio for incident NAFLD for those with long or irregular menstrual cycles compared with the incident group corresponded with a 22% increased risk (HR, 1.22; 95% confidence interval, 1.14-1.31). When calculated in a time-dependent analysis, the risk of NAFLD was increased by almost 50% (HR, 1.49; 95% CI, 1.38-1.60).
Risk persists with PCOS exclusion
PCOS has previously been associated with increased risk of NAFLD, but the association between long or irregular menstrual cycles and NAFLD persisted after women with PCOS were excluded.
The mechanism that links menstrual irregularity with NAFLD is unclear, but the investigators said that estrogen exposure is implicated. In addition to a previously reported associated between low estradiol levels and antiestrogens such as tamoxifen with increased risk of NAFLD, they cited studies associating estrogen replacement therapy with a reduced risk of NAFLD. The role of estrogen in suppressing inflammation, oxidative stress, and insulin resistance are all activities that might link more regular menses with a reduced risk of NAFLD, the authors contended.
Women older than 40 years were excluded from this analysis to reduce the possibility of perimenopausal changes as a confounding factor.
Of study limitations acknowledged by the investigators, the presence of NAFLD was diagnosed on ultrasonography rather than histology. Information on sex hormone or prolactin levels was not captured in relation to NAFLD incidence, and the lack of exposure to estrogen replacement therapy and oral contraceptives was based on self-reports from the participants.
Still, the large study size and the consistency of results after adjustment for multiple risk factors argue that long and irregular menstrual cycles do identify women at risk for NAFLD. One implication is that irregular menses can be a marker for NAFLD risk.
“Our findings do not prove a causal relationship, but they show that long or irregular menstrual cycles were significantly associated with an increased risk of developing NAFLD,” said Seungho Ryu, MD, PhD, a professor at the Sungkyunkwan University. Senior author of this study, Dr. Ryu emphasized in an interview that the association “was not explained by obesity or any other risk factor for NAFLD.”
Lifestyle changes may lower risk
The message is that “young women with long or irregular menstrual cycles may benefit from lifestyle changes to reduce the risk of NAFLD,” Dr. Ryu stated.
The Study of Women’s Health Across the Nation, which was started in 1994, has not evaluated NAFLD, but it did show a relationship between longer menstrual cycles and more cardiometabolic risk factors, according to Nanette Santoro MD, professor and chair, department of obstetrics & gynecology, University of Colorado at Denver, Aurora.
This suggests that others are “thinking along the same lines,” but in discussing this study with this news organization, she characterized some of the design elements as well as some of the findings in this study as “peculiar.”
In addition to a “very, very narrow definition of regular cycles,” she questioned the consistent hazard ratio for NAFLD for those with long cycles relative to other types of irregular menses. Presuming that the group with longer cycles would have included at least some patients with undiagnosed PCOS, she was would have expected that the risk would have been highest in this group. While conceding that differences in body composition of Korean women is a potential explanation for this apparent discrepancy, “I would like to see confirmed in other samples of women with more detailed metabolic assessments to understand who is at risk,” she said.
Not least problematic for the strength of the conclusions, the hazard ratio for NAFLD among women with long or irregular menstrual cycles was “pretty low.” She described this as a level at which the risk “is very susceptible to confounding and unlikely to influence clinical practice.”
Anuja Dokras, MD, PHD, a professor of obstetrics and gynecology and director of the PCOS Center at the University of Pennsylvania, Philadelphia, also questioned whether undiagnosed PCOS might have skewed the data.
“There is increasing data on the association between PCOS and NAFLD. Irregular menses is a key criterion for PCOS, and PCOS is the commonest reason for anovulation,” she said. Dr. Dokras therefore considered it possible that patients with unrecognized PCOS were included in the study, weakening the claim that risk of NAFLD and long menstrual cycles remains significant after controlling for PCOS.
Dr. Ryu and coinvestigators, Dr. Santoro, and Dr. Dokras reported no potential conflicts of interest.
Long or irregular menstrual cycles in relatively young women are linked an increased risk of both prevalent and incident nonalcoholic fatty liver disease (NAFLD), according to a cross-sectional study that included data on more than 70,000 women.
“Our results indicate that menstrual irregularity, which is easier to diagnose and usually presented earlier than PCOS [polycystic ovary syndrome] highlights the possibility of identifying premenopausal women at risk of developing NAFLD,” reported a team of authors primarily from Sungkyunkwan University, Seoul, South Korea.
The study evaluated women aged younger than 40 years who were participating in the Kangbuk Samsung Health Study, which involves a comprehensive biennial health examination at health centers in South Korea. Of the 135,090 women enrolled over a 6-year period who had at least one follow-up examination, 72,092 were available for analysis after excluding for a sizable list of confounding factors such as liver disease and infections; exposure to steatogenic medications, such as corticosteroids; hysterectomy; and pregnancy.
NAFLD prevalence climbs with longer menses
Of these women, 36.378 (27.7%) had menstrual cycles of 26-30 days and were identified as the index group. The prevalence of NAFLD in this group was 5.8%. For those with a menstrual cycle of 31-39 days, the prevalence rate climbed to 7.2%. For those with a menstrual cycle of at least 40 days or too irregular to estimate, the prevalence was 9.7%. The prevalence was 7.1% for those with a menstrual cycle less than 21 days.
The results of this study were published in the Journal of Clinical Endocrinology & Metabolism.
In those without NAFLD at baseline who were then followed for a mean of 4.4 years, there were 4,524 incident cases of NAFLD. Incidence density was calculated per 103 patient-years. In the index group, the rate was 18.4. It climbed to 20.2 for those with a menstrual cycle of 31-39 days and then to 22.9 for those with a menstrual cycle of at least 40 days. For those with a cycle of fewer than 21 days, the rate was 26.8.
After adjusting for age, body mass index, insulin resistance, and other confounders, the hazard ratio for incident NAFLD for those with long or irregular menstrual cycles compared with the incident group corresponded with a 22% increased risk (HR, 1.22; 95% confidence interval, 1.14-1.31). When calculated in a time-dependent analysis, the risk of NAFLD was increased by almost 50% (HR, 1.49; 95% CI, 1.38-1.60).
Risk persists with PCOS exclusion
PCOS has previously been associated with increased risk of NAFLD, but the association between long or irregular menstrual cycles and NAFLD persisted after women with PCOS were excluded.
The mechanism that links menstrual irregularity with NAFLD is unclear, but the investigators said that estrogen exposure is implicated. In addition to a previously reported associated between low estradiol levels and antiestrogens such as tamoxifen with increased risk of NAFLD, they cited studies associating estrogen replacement therapy with a reduced risk of NAFLD. The role of estrogen in suppressing inflammation, oxidative stress, and insulin resistance are all activities that might link more regular menses with a reduced risk of NAFLD, the authors contended.
Women older than 40 years were excluded from this analysis to reduce the possibility of perimenopausal changes as a confounding factor.
Of study limitations acknowledged by the investigators, the presence of NAFLD was diagnosed on ultrasonography rather than histology. Information on sex hormone or prolactin levels was not captured in relation to NAFLD incidence, and the lack of exposure to estrogen replacement therapy and oral contraceptives was based on self-reports from the participants.
Still, the large study size and the consistency of results after adjustment for multiple risk factors argue that long and irregular menstrual cycles do identify women at risk for NAFLD. One implication is that irregular menses can be a marker for NAFLD risk.
“Our findings do not prove a causal relationship, but they show that long or irregular menstrual cycles were significantly associated with an increased risk of developing NAFLD,” said Seungho Ryu, MD, PhD, a professor at the Sungkyunkwan University. Senior author of this study, Dr. Ryu emphasized in an interview that the association “was not explained by obesity or any other risk factor for NAFLD.”
Lifestyle changes may lower risk
The message is that “young women with long or irregular menstrual cycles may benefit from lifestyle changes to reduce the risk of NAFLD,” Dr. Ryu stated.
The Study of Women’s Health Across the Nation, which was started in 1994, has not evaluated NAFLD, but it did show a relationship between longer menstrual cycles and more cardiometabolic risk factors, according to Nanette Santoro MD, professor and chair, department of obstetrics & gynecology, University of Colorado at Denver, Aurora.
This suggests that others are “thinking along the same lines,” but in discussing this study with this news organization, she characterized some of the design elements as well as some of the findings in this study as “peculiar.”
In addition to a “very, very narrow definition of regular cycles,” she questioned the consistent hazard ratio for NAFLD for those with long cycles relative to other types of irregular menses. Presuming that the group with longer cycles would have included at least some patients with undiagnosed PCOS, she was would have expected that the risk would have been highest in this group. While conceding that differences in body composition of Korean women is a potential explanation for this apparent discrepancy, “I would like to see confirmed in other samples of women with more detailed metabolic assessments to understand who is at risk,” she said.
Not least problematic for the strength of the conclusions, the hazard ratio for NAFLD among women with long or irregular menstrual cycles was “pretty low.” She described this as a level at which the risk “is very susceptible to confounding and unlikely to influence clinical practice.”
Anuja Dokras, MD, PHD, a professor of obstetrics and gynecology and director of the PCOS Center at the University of Pennsylvania, Philadelphia, also questioned whether undiagnosed PCOS might have skewed the data.
“There is increasing data on the association between PCOS and NAFLD. Irregular menses is a key criterion for PCOS, and PCOS is the commonest reason for anovulation,” she said. Dr. Dokras therefore considered it possible that patients with unrecognized PCOS were included in the study, weakening the claim that risk of NAFLD and long menstrual cycles remains significant after controlling for PCOS.
Dr. Ryu and coinvestigators, Dr. Santoro, and Dr. Dokras reported no potential conflicts of interest.
Long or irregular menstrual cycles in relatively young women are linked an increased risk of both prevalent and incident nonalcoholic fatty liver disease (NAFLD), according to a cross-sectional study that included data on more than 70,000 women.
“Our results indicate that menstrual irregularity, which is easier to diagnose and usually presented earlier than PCOS [polycystic ovary syndrome] highlights the possibility of identifying premenopausal women at risk of developing NAFLD,” reported a team of authors primarily from Sungkyunkwan University, Seoul, South Korea.
The study evaluated women aged younger than 40 years who were participating in the Kangbuk Samsung Health Study, which involves a comprehensive biennial health examination at health centers in South Korea. Of the 135,090 women enrolled over a 6-year period who had at least one follow-up examination, 72,092 were available for analysis after excluding for a sizable list of confounding factors such as liver disease and infections; exposure to steatogenic medications, such as corticosteroids; hysterectomy; and pregnancy.
NAFLD prevalence climbs with longer menses
Of these women, 36.378 (27.7%) had menstrual cycles of 26-30 days and were identified as the index group. The prevalence of NAFLD in this group was 5.8%. For those with a menstrual cycle of 31-39 days, the prevalence rate climbed to 7.2%. For those with a menstrual cycle of at least 40 days or too irregular to estimate, the prevalence was 9.7%. The prevalence was 7.1% for those with a menstrual cycle less than 21 days.
The results of this study were published in the Journal of Clinical Endocrinology & Metabolism.
In those without NAFLD at baseline who were then followed for a mean of 4.4 years, there were 4,524 incident cases of NAFLD. Incidence density was calculated per 103 patient-years. In the index group, the rate was 18.4. It climbed to 20.2 for those with a menstrual cycle of 31-39 days and then to 22.9 for those with a menstrual cycle of at least 40 days. For those with a cycle of fewer than 21 days, the rate was 26.8.
After adjusting for age, body mass index, insulin resistance, and other confounders, the hazard ratio for incident NAFLD for those with long or irregular menstrual cycles compared with the incident group corresponded with a 22% increased risk (HR, 1.22; 95% confidence interval, 1.14-1.31). When calculated in a time-dependent analysis, the risk of NAFLD was increased by almost 50% (HR, 1.49; 95% CI, 1.38-1.60).
Risk persists with PCOS exclusion
PCOS has previously been associated with increased risk of NAFLD, but the association between long or irregular menstrual cycles and NAFLD persisted after women with PCOS were excluded.
The mechanism that links menstrual irregularity with NAFLD is unclear, but the investigators said that estrogen exposure is implicated. In addition to a previously reported associated between low estradiol levels and antiestrogens such as tamoxifen with increased risk of NAFLD, they cited studies associating estrogen replacement therapy with a reduced risk of NAFLD. The role of estrogen in suppressing inflammation, oxidative stress, and insulin resistance are all activities that might link more regular menses with a reduced risk of NAFLD, the authors contended.
Women older than 40 years were excluded from this analysis to reduce the possibility of perimenopausal changes as a confounding factor.
Of study limitations acknowledged by the investigators, the presence of NAFLD was diagnosed on ultrasonography rather than histology. Information on sex hormone or prolactin levels was not captured in relation to NAFLD incidence, and the lack of exposure to estrogen replacement therapy and oral contraceptives was based on self-reports from the participants.
Still, the large study size and the consistency of results after adjustment for multiple risk factors argue that long and irregular menstrual cycles do identify women at risk for NAFLD. One implication is that irregular menses can be a marker for NAFLD risk.
“Our findings do not prove a causal relationship, but they show that long or irregular menstrual cycles were significantly associated with an increased risk of developing NAFLD,” said Seungho Ryu, MD, PhD, a professor at the Sungkyunkwan University. Senior author of this study, Dr. Ryu emphasized in an interview that the association “was not explained by obesity or any other risk factor for NAFLD.”
Lifestyle changes may lower risk
The message is that “young women with long or irregular menstrual cycles may benefit from lifestyle changes to reduce the risk of NAFLD,” Dr. Ryu stated.
The Study of Women’s Health Across the Nation, which was started in 1994, has not evaluated NAFLD, but it did show a relationship between longer menstrual cycles and more cardiometabolic risk factors, according to Nanette Santoro MD, professor and chair, department of obstetrics & gynecology, University of Colorado at Denver, Aurora.
This suggests that others are “thinking along the same lines,” but in discussing this study with this news organization, she characterized some of the design elements as well as some of the findings in this study as “peculiar.”
In addition to a “very, very narrow definition of regular cycles,” she questioned the consistent hazard ratio for NAFLD for those with long cycles relative to other types of irregular menses. Presuming that the group with longer cycles would have included at least some patients with undiagnosed PCOS, she was would have expected that the risk would have been highest in this group. While conceding that differences in body composition of Korean women is a potential explanation for this apparent discrepancy, “I would like to see confirmed in other samples of women with more detailed metabolic assessments to understand who is at risk,” she said.
Not least problematic for the strength of the conclusions, the hazard ratio for NAFLD among women with long or irregular menstrual cycles was “pretty low.” She described this as a level at which the risk “is very susceptible to confounding and unlikely to influence clinical practice.”
Anuja Dokras, MD, PHD, a professor of obstetrics and gynecology and director of the PCOS Center at the University of Pennsylvania, Philadelphia, also questioned whether undiagnosed PCOS might have skewed the data.
“There is increasing data on the association between PCOS and NAFLD. Irregular menses is a key criterion for PCOS, and PCOS is the commonest reason for anovulation,” she said. Dr. Dokras therefore considered it possible that patients with unrecognized PCOS were included in the study, weakening the claim that risk of NAFLD and long menstrual cycles remains significant after controlling for PCOS.
Dr. Ryu and coinvestigators, Dr. Santoro, and Dr. Dokras reported no potential conflicts of interest.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
How Lp(a) can help improve ASCVD risk assessment
A look back at a pair of large cohort studies suggests a telling relation between two distinct predictors of atherosclerotic cardiovascular disease (ASCVD) risk and may offer guidance on how to interpret them together.
Elevated levels of lipoprotein(a), or Lp(a), and high coronary artery calcium (CAC) scores were both predictive of ASCVD risk over 10 years, but independent of each other and a host of more traditional cardiovascular risk factors, for example, in the analysis of data from the MESA (Multi-Ethnic Study of Atherosclerosis) and DHS (Dallas Heart Study) longitudinal cohorts.
Notably, the risk when both Lp(a) and CAC scores were high far exceeded that associated with either marker alone. But when CAC scores were less than 100 Agatston units, predicted ASCVD risk wasn’t influenced by levels of Lp(a). Indeed, a CAC score of 0 predicted the lowest levels of ASCVD risk, even with elevated Lp(a).
That is, the findings suggest, the addition of Lp(a) makes a difference to the risk assessment only when CAC scores are high, at least 100 units, and elevated Lp(a) doesn’t mean increased ASCVD risk in the absence of coronary calcium.
“Our novel findings indicate that elevated Lp(a) drives ASCVD risk independent of the subclinical coronary atherosclerosis burden captured by CAC score,” concluded a report on the analysis, published in the Journal of the American College of Cardiology, with lead author Anurag Mehta, MD, Emory University, Atlanta.
There are no formal recommendations on how to interpret Lp(a) and CAC scores together, but the current findings “provide impetus for measuring Lp(a) in more individuals as part of the shared decision-making process,” the authors contended.
“Really, the calcium score carries the majority of the information in terms of risk, except in the highest CAC score group. That is, if you have a high Lp(a) and a high burden of calcium, your risk is significantly higher than if you just have the high calcium score and the normal Lp(a),” senior author Parag H. Joshi, MD, MHS, said in an interview.
“We thought we would see that the group with higher Lp(a) would have more events over 10 years, even among those who didn’t have coronary calcium,” said Dr. Joshi, of the University of Texas Southwestern Medical Center, Dallas. “But we really don’t see that, at least in a statistically significant way.”
A CAC score of 0 would at least support a more conservative approach in a patient with elevated Lp(a) “who is hesitant to be on a statin or to be more aggressive managing their risk,” Dr. Joshi said.
“This study should be very reassuring for a patient like that,” Ron Blankstein, MD, director of cardiac computed tomography at Brigham and Women’s Hospital, Boston, said in an interview.
“If you have a high Lp(a) and you’re concerned, I think this study really supports the role of calcium scoring for further risk assessment,” said Dr. Blankstein, who is not associated with the new report. “We often check Lp(a) in individuals who perhaps have a family history or who come to see us in a preventive cardiology clinic. If it is high and there is concern, a calcium score can be very helpful. If it’s zero, that really means a very low risk of events. And if it’s elevated, I think we’re going to be more concerned about that patient.”
The current analysis suggests “that, when a patient without clinical cardiovascular disease is identified with either CAC ≥100 or Lp(a) >50 mg/dL, the next step in the risk evaluation should be to measure either Lp(a) or CAC, respectively – if not already performed – to identify the patients at highest risk,” Sotirios Tsimikas, MD, director of vascular medicine at University of California, San Diego, wrote in an accompanying editorial.
“Both Lp(a) and CAC should be more broadly applied in clinical care settings in patients without prior ASCVD to identify those that most likely will benefit from more aggressive therapy and, in the future, from Lp(a)-lowering therapies,” he wrote.
The analyses were conducted separately on data from 4,512 initially asymptomatic patients in MESA and 2,078 from the DHS cohort, who were followed for ASCVD events an average of 13 years and 11 years, respectively. Such events included coronary heart disease–related death, nonfatal MI, and fatal or nonfatal stroke.
In the MESA cohort – 52% women, 36.8% White, 29.3% Black, 22.2% Hispanic, and 11.7% Chinese – elevated Lp(a) (quintile 5 vs. quintiles 1-4) and CAC scores of 1-99 and above 100 (both compared with 0) were each independently associated with increased risk for ASCVD events. The hazard ratio was 1.29 (P = .02) for elevated Lp(a), 1.68 (P < .01) for a CAC score of 1-99, and 2.66 (P < .01) for a CAC score of at least 100.
The corresponding HRs in the DHS cohort were 1.54 (P = .07) for Lp(a), 3.32 (P < .01) for a CAC score of 1-99, and 5.21 (P < .01) for a CAC score of at least 100.
Of note, the authors wrote, ASCVD risk among MESA participants with a CAC score of 0 was not significantly different in those with normal and elevated Lp(a).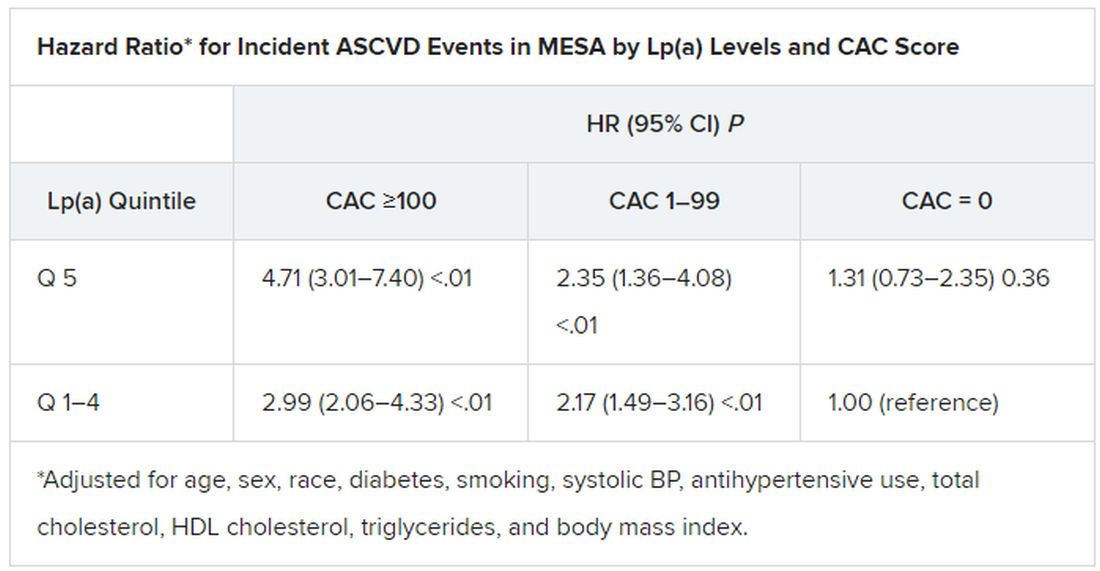
The findings were similar in the corresponding DHS analysis, the authors noted.
When both Lp(a) and CAC scores are considered as dichotomous variables, the highest 10-year ASCVD incidence in MESA was in participants with both elevated Lp(a) (≥50 mg/dL) and a high CAC score (≥100). The lowest risk was seen when Lp(a) was normal (<50 mg/dL) and the CAC score was no more than moderately high (<100).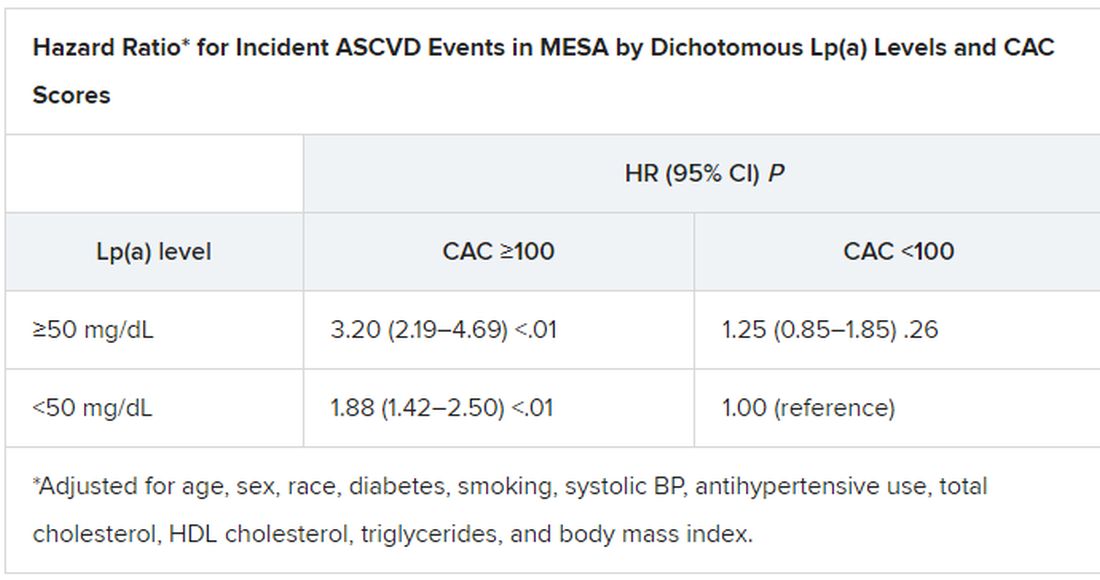
The results in the corresponding DHS analysis, according to the report, again mirrored those from MESA.
“This study has important implications for our patients and also potentially for future clinical trial design,” Dr. Blankstein noted. “A big part of developing a trial in this space is identifying the patients who are at higher risk,” and the current analysis supports CAC scores for identifying the highest-risk patient among those with elevated Lp(a).
Current wisdom is that, for the most part, Lp(a) levels are genetically mediated and are mostly unaffected by interventions such as diet management or exercise. It’s unknown whether reducing elevated Lp(a) levels pharmacologically will cut ASCVD risk, but there are a number of clinical trial programs currently aimed at learning just that. They include the Novartis-sponsored phase 3 HORIZON trial of the antisense agent pelacarsen (TQJ230), with an estimated enrollment of almost 7,700; a randomized, controlled dose-finding study of the small interfering RNA agent olpasiran (AMG890), with 290 patients and funded by Amgen; and an 88-patient phase 1 study of another siRNA agent, SLN360, supported by Silence Therapeutics.
Dr. Mehta reported no relevant relationships. Dr. Joshi has received grant support from Novo Nordisk and consulting income from Bayer and Regeneron; holds equity in G3 Therapeutics; and has served as site investigator for GlaxoSmithKline, Sanofi, AstraZeneca, and Novartis. Dr. Blankstein reported serving as a consultant to Amgen, Novartis, and Silence Therapeutics.
A version of this article first appeared on Medscape.com.
A look back at a pair of large cohort studies suggests a telling relation between two distinct predictors of atherosclerotic cardiovascular disease (ASCVD) risk and may offer guidance on how to interpret them together.
Elevated levels of lipoprotein(a), or Lp(a), and high coronary artery calcium (CAC) scores were both predictive of ASCVD risk over 10 years, but independent of each other and a host of more traditional cardiovascular risk factors, for example, in the analysis of data from the MESA (Multi-Ethnic Study of Atherosclerosis) and DHS (Dallas Heart Study) longitudinal cohorts.
Notably, the risk when both Lp(a) and CAC scores were high far exceeded that associated with either marker alone. But when CAC scores were less than 100 Agatston units, predicted ASCVD risk wasn’t influenced by levels of Lp(a). Indeed, a CAC score of 0 predicted the lowest levels of ASCVD risk, even with elevated Lp(a).
That is, the findings suggest, the addition of Lp(a) makes a difference to the risk assessment only when CAC scores are high, at least 100 units, and elevated Lp(a) doesn’t mean increased ASCVD risk in the absence of coronary calcium.
“Our novel findings indicate that elevated Lp(a) drives ASCVD risk independent of the subclinical coronary atherosclerosis burden captured by CAC score,” concluded a report on the analysis, published in the Journal of the American College of Cardiology, with lead author Anurag Mehta, MD, Emory University, Atlanta.
There are no formal recommendations on how to interpret Lp(a) and CAC scores together, but the current findings “provide impetus for measuring Lp(a) in more individuals as part of the shared decision-making process,” the authors contended.
“Really, the calcium score carries the majority of the information in terms of risk, except in the highest CAC score group. That is, if you have a high Lp(a) and a high burden of calcium, your risk is significantly higher than if you just have the high calcium score and the normal Lp(a),” senior author Parag H. Joshi, MD, MHS, said in an interview.
“We thought we would see that the group with higher Lp(a) would have more events over 10 years, even among those who didn’t have coronary calcium,” said Dr. Joshi, of the University of Texas Southwestern Medical Center, Dallas. “But we really don’t see that, at least in a statistically significant way.”
A CAC score of 0 would at least support a more conservative approach in a patient with elevated Lp(a) “who is hesitant to be on a statin or to be more aggressive managing their risk,” Dr. Joshi said.
“This study should be very reassuring for a patient like that,” Ron Blankstein, MD, director of cardiac computed tomography at Brigham and Women’s Hospital, Boston, said in an interview.
“If you have a high Lp(a) and you’re concerned, I think this study really supports the role of calcium scoring for further risk assessment,” said Dr. Blankstein, who is not associated with the new report. “We often check Lp(a) in individuals who perhaps have a family history or who come to see us in a preventive cardiology clinic. If it is high and there is concern, a calcium score can be very helpful. If it’s zero, that really means a very low risk of events. And if it’s elevated, I think we’re going to be more concerned about that patient.”
The current analysis suggests “that, when a patient without clinical cardiovascular disease is identified with either CAC ≥100 or Lp(a) >50 mg/dL, the next step in the risk evaluation should be to measure either Lp(a) or CAC, respectively – if not already performed – to identify the patients at highest risk,” Sotirios Tsimikas, MD, director of vascular medicine at University of California, San Diego, wrote in an accompanying editorial.
“Both Lp(a) and CAC should be more broadly applied in clinical care settings in patients without prior ASCVD to identify those that most likely will benefit from more aggressive therapy and, in the future, from Lp(a)-lowering therapies,” he wrote.
The analyses were conducted separately on data from 4,512 initially asymptomatic patients in MESA and 2,078 from the DHS cohort, who were followed for ASCVD events an average of 13 years and 11 years, respectively. Such events included coronary heart disease–related death, nonfatal MI, and fatal or nonfatal stroke.
In the MESA cohort – 52% women, 36.8% White, 29.3% Black, 22.2% Hispanic, and 11.7% Chinese – elevated Lp(a) (quintile 5 vs. quintiles 1-4) and CAC scores of 1-99 and above 100 (both compared with 0) were each independently associated with increased risk for ASCVD events. The hazard ratio was 1.29 (P = .02) for elevated Lp(a), 1.68 (P < .01) for a CAC score of 1-99, and 2.66 (P < .01) for a CAC score of at least 100.
The corresponding HRs in the DHS cohort were 1.54 (P = .07) for Lp(a), 3.32 (P < .01) for a CAC score of 1-99, and 5.21 (P < .01) for a CAC score of at least 100.
Of note, the authors wrote, ASCVD risk among MESA participants with a CAC score of 0 was not significantly different in those with normal and elevated Lp(a).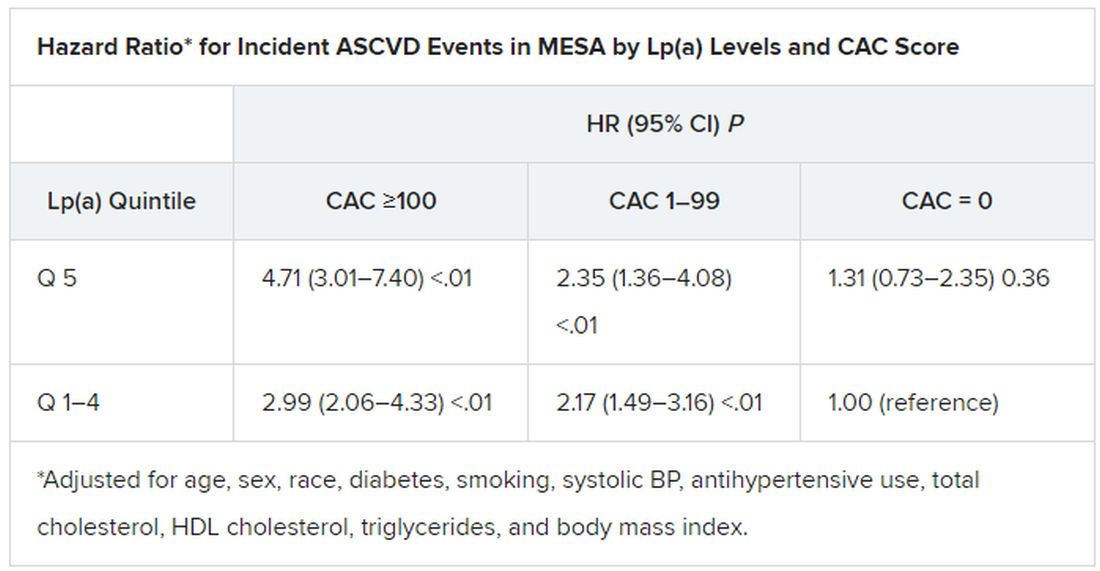
The findings were similar in the corresponding DHS analysis, the authors noted.
When both Lp(a) and CAC scores are considered as dichotomous variables, the highest 10-year ASCVD incidence in MESA was in participants with both elevated Lp(a) (≥50 mg/dL) and a high CAC score (≥100). The lowest risk was seen when Lp(a) was normal (<50 mg/dL) and the CAC score was no more than moderately high (<100).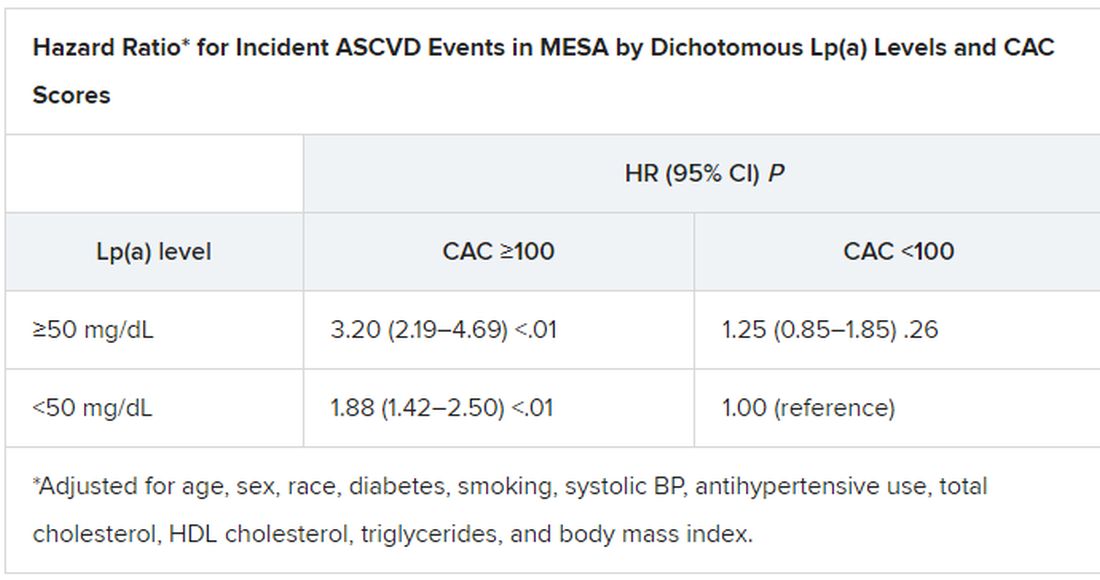
The results in the corresponding DHS analysis, according to the report, again mirrored those from MESA.
“This study has important implications for our patients and also potentially for future clinical trial design,” Dr. Blankstein noted. “A big part of developing a trial in this space is identifying the patients who are at higher risk,” and the current analysis supports CAC scores for identifying the highest-risk patient among those with elevated Lp(a).
Current wisdom is that, for the most part, Lp(a) levels are genetically mediated and are mostly unaffected by interventions such as diet management or exercise. It’s unknown whether reducing elevated Lp(a) levels pharmacologically will cut ASCVD risk, but there are a number of clinical trial programs currently aimed at learning just that. They include the Novartis-sponsored phase 3 HORIZON trial of the antisense agent pelacarsen (TQJ230), with an estimated enrollment of almost 7,700; a randomized, controlled dose-finding study of the small interfering RNA agent olpasiran (AMG890), with 290 patients and funded by Amgen; and an 88-patient phase 1 study of another siRNA agent, SLN360, supported by Silence Therapeutics.
Dr. Mehta reported no relevant relationships. Dr. Joshi has received grant support from Novo Nordisk and consulting income from Bayer and Regeneron; holds equity in G3 Therapeutics; and has served as site investigator for GlaxoSmithKline, Sanofi, AstraZeneca, and Novartis. Dr. Blankstein reported serving as a consultant to Amgen, Novartis, and Silence Therapeutics.
A version of this article first appeared on Medscape.com.
A look back at a pair of large cohort studies suggests a telling relation between two distinct predictors of atherosclerotic cardiovascular disease (ASCVD) risk and may offer guidance on how to interpret them together.
Elevated levels of lipoprotein(a), or Lp(a), and high coronary artery calcium (CAC) scores were both predictive of ASCVD risk over 10 years, but independent of each other and a host of more traditional cardiovascular risk factors, for example, in the analysis of data from the MESA (Multi-Ethnic Study of Atherosclerosis) and DHS (Dallas Heart Study) longitudinal cohorts.
Notably, the risk when both Lp(a) and CAC scores were high far exceeded that associated with either marker alone. But when CAC scores were less than 100 Agatston units, predicted ASCVD risk wasn’t influenced by levels of Lp(a). Indeed, a CAC score of 0 predicted the lowest levels of ASCVD risk, even with elevated Lp(a).
That is, the findings suggest, the addition of Lp(a) makes a difference to the risk assessment only when CAC scores are high, at least 100 units, and elevated Lp(a) doesn’t mean increased ASCVD risk in the absence of coronary calcium.
“Our novel findings indicate that elevated Lp(a) drives ASCVD risk independent of the subclinical coronary atherosclerosis burden captured by CAC score,” concluded a report on the analysis, published in the Journal of the American College of Cardiology, with lead author Anurag Mehta, MD, Emory University, Atlanta.
There are no formal recommendations on how to interpret Lp(a) and CAC scores together, but the current findings “provide impetus for measuring Lp(a) in more individuals as part of the shared decision-making process,” the authors contended.
“Really, the calcium score carries the majority of the information in terms of risk, except in the highest CAC score group. That is, if you have a high Lp(a) and a high burden of calcium, your risk is significantly higher than if you just have the high calcium score and the normal Lp(a),” senior author Parag H. Joshi, MD, MHS, said in an interview.
“We thought we would see that the group with higher Lp(a) would have more events over 10 years, even among those who didn’t have coronary calcium,” said Dr. Joshi, of the University of Texas Southwestern Medical Center, Dallas. “But we really don’t see that, at least in a statistically significant way.”
A CAC score of 0 would at least support a more conservative approach in a patient with elevated Lp(a) “who is hesitant to be on a statin or to be more aggressive managing their risk,” Dr. Joshi said.
“This study should be very reassuring for a patient like that,” Ron Blankstein, MD, director of cardiac computed tomography at Brigham and Women’s Hospital, Boston, said in an interview.
“If you have a high Lp(a) and you’re concerned, I think this study really supports the role of calcium scoring for further risk assessment,” said Dr. Blankstein, who is not associated with the new report. “We often check Lp(a) in individuals who perhaps have a family history or who come to see us in a preventive cardiology clinic. If it is high and there is concern, a calcium score can be very helpful. If it’s zero, that really means a very low risk of events. And if it’s elevated, I think we’re going to be more concerned about that patient.”
The current analysis suggests “that, when a patient without clinical cardiovascular disease is identified with either CAC ≥100 or Lp(a) >50 mg/dL, the next step in the risk evaluation should be to measure either Lp(a) or CAC, respectively – if not already performed – to identify the patients at highest risk,” Sotirios Tsimikas, MD, director of vascular medicine at University of California, San Diego, wrote in an accompanying editorial.
“Both Lp(a) and CAC should be more broadly applied in clinical care settings in patients without prior ASCVD to identify those that most likely will benefit from more aggressive therapy and, in the future, from Lp(a)-lowering therapies,” he wrote.
The analyses were conducted separately on data from 4,512 initially asymptomatic patients in MESA and 2,078 from the DHS cohort, who were followed for ASCVD events an average of 13 years and 11 years, respectively. Such events included coronary heart disease–related death, nonfatal MI, and fatal or nonfatal stroke.
In the MESA cohort – 52% women, 36.8% White, 29.3% Black, 22.2% Hispanic, and 11.7% Chinese – elevated Lp(a) (quintile 5 vs. quintiles 1-4) and CAC scores of 1-99 and above 100 (both compared with 0) were each independently associated with increased risk for ASCVD events. The hazard ratio was 1.29 (P = .02) for elevated Lp(a), 1.68 (P < .01) for a CAC score of 1-99, and 2.66 (P < .01) for a CAC score of at least 100.
The corresponding HRs in the DHS cohort were 1.54 (P = .07) for Lp(a), 3.32 (P < .01) for a CAC score of 1-99, and 5.21 (P < .01) for a CAC score of at least 100.
Of note, the authors wrote, ASCVD risk among MESA participants with a CAC score of 0 was not significantly different in those with normal and elevated Lp(a).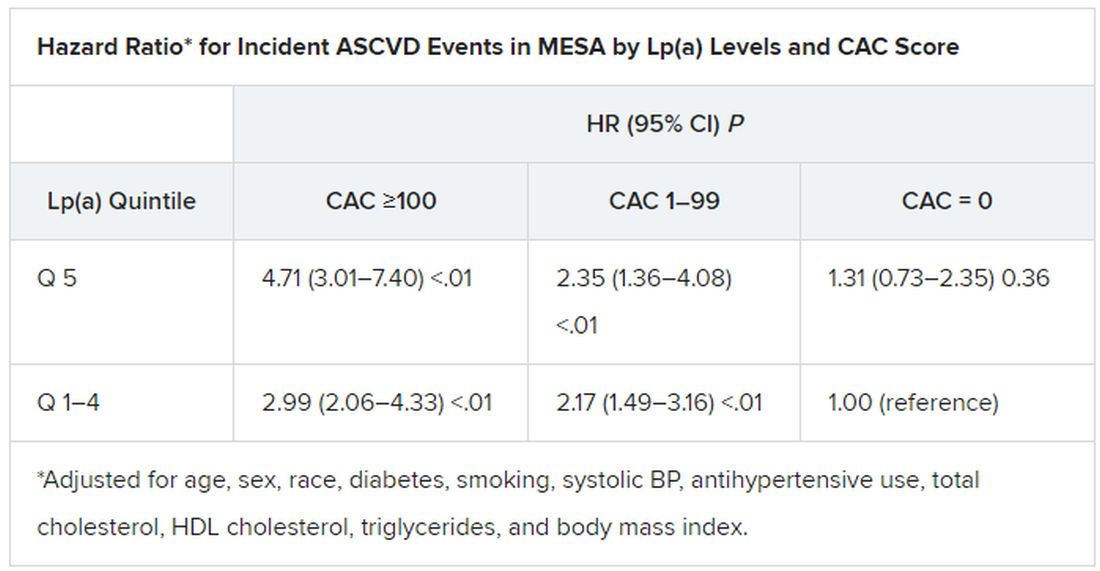
The findings were similar in the corresponding DHS analysis, the authors noted.
When both Lp(a) and CAC scores are considered as dichotomous variables, the highest 10-year ASCVD incidence in MESA was in participants with both elevated Lp(a) (≥50 mg/dL) and a high CAC score (≥100). The lowest risk was seen when Lp(a) was normal (<50 mg/dL) and the CAC score was no more than moderately high (<100).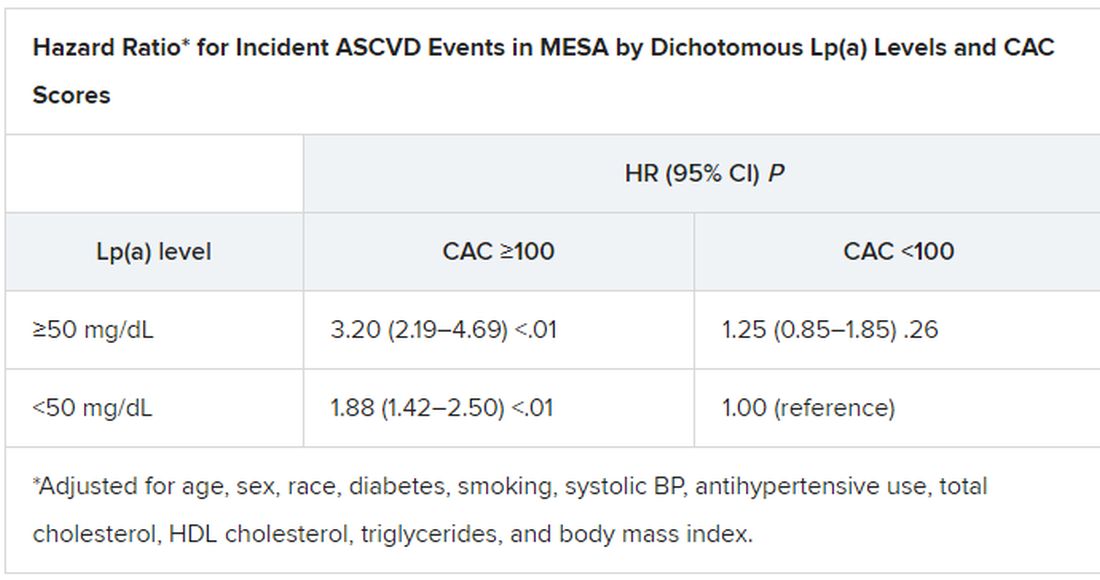
The results in the corresponding DHS analysis, according to the report, again mirrored those from MESA.
“This study has important implications for our patients and also potentially for future clinical trial design,” Dr. Blankstein noted. “A big part of developing a trial in this space is identifying the patients who are at higher risk,” and the current analysis supports CAC scores for identifying the highest-risk patient among those with elevated Lp(a).
Current wisdom is that, for the most part, Lp(a) levels are genetically mediated and are mostly unaffected by interventions such as diet management or exercise. It’s unknown whether reducing elevated Lp(a) levels pharmacologically will cut ASCVD risk, but there are a number of clinical trial programs currently aimed at learning just that. They include the Novartis-sponsored phase 3 HORIZON trial of the antisense agent pelacarsen (TQJ230), with an estimated enrollment of almost 7,700; a randomized, controlled dose-finding study of the small interfering RNA agent olpasiran (AMG890), with 290 patients and funded by Amgen; and an 88-patient phase 1 study of another siRNA agent, SLN360, supported by Silence Therapeutics.
Dr. Mehta reported no relevant relationships. Dr. Joshi has received grant support from Novo Nordisk and consulting income from Bayer and Regeneron; holds equity in G3 Therapeutics; and has served as site investigator for GlaxoSmithKline, Sanofi, AstraZeneca, and Novartis. Dr. Blankstein reported serving as a consultant to Amgen, Novartis, and Silence Therapeutics.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Phthalate exposure via maternal and cord blood affects infant outcomes
Exposure to phthalates through maternal blood and cord blood affected outcomes including head circumference and anogenital index for male and female infants, according to data from 65 mother-infant pairs.
Phthalates are recognized endocrine disruptors that have been associated with adverse birth outcomes, but the specific relationship between maternal phthalate exposure and birth outcomes has not been well studied, wrote Hsiao-Lin Hwa, MD, of National Taiwan University, Taipei, and colleagues.
Previous research suggests that trace exposure to hazardous chemicals during the fetal period “may cause fetal metabolic dysfunction and adversely change the morphology of body systems,” they said. In 2011, “the Taiwan Food and Drug Administration found that di‐2‐ethylhexyl phthalate (DEHP) and DiNP [di‐isononyl phthalate] had been illegally added as emulsifiers to replace palm oil in beverages and food,” they added. The researchers sought to examine the association between infant birth outcomes and phthalate exposure levels in the Taiwanese population after 2011. In a study published in Environmental Toxicology and Chemistry, the researchers recruited 65 pregnant women in Taiwan between 2016 and 2017. Birth length, birth weight, head circumference, anogenital distance (AGD), anoscrotal distance (ASD), and anofourchette distance (AFD) were measured for each newborn at the time of delivery. The average age of the women was 33.6 years, and the rate of low birth weight was 13.7%. The mean measures of birth length, birth weight, head circumference, and chest circumference were 47.6 cm, 3022 g, 32.9 cm, and 30.8 mm, respectively. The mean AFD and ASD were 14.2 mm and 22.3 mm, respectively.
The researchers tested for 12 phthalates in maternal blood and cord blood samples. Of these, the six most frequently detected phthalate metabolites were mono‐ethyl phthalate (MEP), mono‐isobutyl phthalate (MiBP), mono‐n‐butyl phthalate (MnBP), mono‐(2‐ethyl‐5‐oxohexyl)‐phthalate (MEOHP), mono‐(2‐ethyl‐5‐hydroxyhexyl) phthalate (MEHHP), and mono‐n‐octyl phthalate (MOP); these six were present in 80%–100% of the maternal blood samples.
Overall, the mean levels of MEP, MiBP, MnBP, and MEHP were relatively higher in both maternal and infant blood than other phthalates, the researchers noted. The mean concentrations of metabolites in maternal blood and infant cord blood were 0.03-2.27 ng/mL and 0.01-3.74 ng/mL, respectively.
Among male infants, levels of MMP, MiBP, and MEHP in maternal blood were inversely related to anogenital index (AGI), with P values for regression coefficients ranging from .011 to .033. In addition, the total concentration of MEHP, MEOHP, and MEHHP (designated as Σdi‐2‐ethylhexyl phthalate, ΣDEHP) was inversely related to AGI in males.
Among female infants, however, phthalates in cord blood, rather than maternal blood, were positively related to AGI, including MMP, MibP, MnBP, and MOP, with P values for regression coefficients ranging from .001 to .034.
Cord blood levels of MnBP, MEOHP, MEHP, and ΣDEHP were inversely associated with gestational age-adjusted head circumference in all infants, with beta coefficients of –0.15, –0.12, –0.01, and –0.01, respectively (P < .05 for all).
“The detection rates of MEHHP, MEOHP, and MEHP in the cord blood were lower than those in the maternal blood, particularly those of MEHHP and MEOHP, which were approximately 25% lower,” which may be caused by slow placental transfer, the researchers wrote in their discussion section. “The high detection rate of phthalate metabolites indicated that our subjects may continue to be exposed to these phthalates even after the 2011 Taiwan DEHP incident,” they noted.
The study findings were limited by several factors including the possibility for contamination of samples and other environmental confounders, the researchers noted. However, the results support the role of phthalates as endocrine disruptors, and the distinction in effects between males and females “may suggest that phthalate monoesters are potentially estrogenic and antiandrogenic chemicals,” they added.
“Further investigations involving multiple phthalate analyses during pregnancy and measurements throughout childhood are necessary to confirm our findings,” they concluded.
Direct clinical implications remain uncertain
“Phthalates are a group of chemicals that are used to make plastic more durable; they are found in multiple everyday materials, food products, and common household products,” Marissa Platner, MD, of Emory University, Atlanta, said in an interview. “It is known that we are exposed to phthalates on a routine basis but the long-term effects of this exposure are unclear,” she said.
The current study findings “were not entirely surprising given data from prior animal studies because they do imply that there is some placental transfer of the phthalate metabolites that can cause adverse effects on the developing fetus,” said Dr. Platner. “However, they also demonstrate that the placenta acts as a filter for certain larger molecules to protect the fetus,” she said.
“This study was based on a small sample size, therefore the clinical implications are not clear,” Dr. Platner noted. “However it may be worthwhile after further research to encourage our pregnant patients to try to decrease their exposure to phthalates,” she said.
Dr. Platner identified two areas for additional research to explore the role of phthalate exposure.
“The first would be to assess the level of maternal phthalate exposure throughout the pregnancy instead of just at one point in time, and the second would be to assess how the reproductive system differences at birth translate to long-term outcomes in children, such as early puberty in females or decreased fertility in males,” she said.
The study was funded by the Ministry of Science and Technology of Taiwan and the Far Eastern Memorial Hospital‐National Taiwan University Hospital. The researchers and Dr. Platner had no financial conflicts to disclose.
Exposure to phthalates through maternal blood and cord blood affected outcomes including head circumference and anogenital index for male and female infants, according to data from 65 mother-infant pairs.
Phthalates are recognized endocrine disruptors that have been associated with adverse birth outcomes, but the specific relationship between maternal phthalate exposure and birth outcomes has not been well studied, wrote Hsiao-Lin Hwa, MD, of National Taiwan University, Taipei, and colleagues.
Previous research suggests that trace exposure to hazardous chemicals during the fetal period “may cause fetal metabolic dysfunction and adversely change the morphology of body systems,” they said. In 2011, “the Taiwan Food and Drug Administration found that di‐2‐ethylhexyl phthalate (DEHP) and DiNP [di‐isononyl phthalate] had been illegally added as emulsifiers to replace palm oil in beverages and food,” they added. The researchers sought to examine the association between infant birth outcomes and phthalate exposure levels in the Taiwanese population after 2011. In a study published in Environmental Toxicology and Chemistry, the researchers recruited 65 pregnant women in Taiwan between 2016 and 2017. Birth length, birth weight, head circumference, anogenital distance (AGD), anoscrotal distance (ASD), and anofourchette distance (AFD) were measured for each newborn at the time of delivery. The average age of the women was 33.6 years, and the rate of low birth weight was 13.7%. The mean measures of birth length, birth weight, head circumference, and chest circumference were 47.6 cm, 3022 g, 32.9 cm, and 30.8 mm, respectively. The mean AFD and ASD were 14.2 mm and 22.3 mm, respectively.
The researchers tested for 12 phthalates in maternal blood and cord blood samples. Of these, the six most frequently detected phthalate metabolites were mono‐ethyl phthalate (MEP), mono‐isobutyl phthalate (MiBP), mono‐n‐butyl phthalate (MnBP), mono‐(2‐ethyl‐5‐oxohexyl)‐phthalate (MEOHP), mono‐(2‐ethyl‐5‐hydroxyhexyl) phthalate (MEHHP), and mono‐n‐octyl phthalate (MOP); these six were present in 80%–100% of the maternal blood samples.
Overall, the mean levels of MEP, MiBP, MnBP, and MEHP were relatively higher in both maternal and infant blood than other phthalates, the researchers noted. The mean concentrations of metabolites in maternal blood and infant cord blood were 0.03-2.27 ng/mL and 0.01-3.74 ng/mL, respectively.
Among male infants, levels of MMP, MiBP, and MEHP in maternal blood were inversely related to anogenital index (AGI), with P values for regression coefficients ranging from .011 to .033. In addition, the total concentration of MEHP, MEOHP, and MEHHP (designated as Σdi‐2‐ethylhexyl phthalate, ΣDEHP) was inversely related to AGI in males.
Among female infants, however, phthalates in cord blood, rather than maternal blood, were positively related to AGI, including MMP, MibP, MnBP, and MOP, with P values for regression coefficients ranging from .001 to .034.
Cord blood levels of MnBP, MEOHP, MEHP, and ΣDEHP were inversely associated with gestational age-adjusted head circumference in all infants, with beta coefficients of –0.15, –0.12, –0.01, and –0.01, respectively (P < .05 for all).
“The detection rates of MEHHP, MEOHP, and MEHP in the cord blood were lower than those in the maternal blood, particularly those of MEHHP and MEOHP, which were approximately 25% lower,” which may be caused by slow placental transfer, the researchers wrote in their discussion section. “The high detection rate of phthalate metabolites indicated that our subjects may continue to be exposed to these phthalates even after the 2011 Taiwan DEHP incident,” they noted.
The study findings were limited by several factors including the possibility for contamination of samples and other environmental confounders, the researchers noted. However, the results support the role of phthalates as endocrine disruptors, and the distinction in effects between males and females “may suggest that phthalate monoesters are potentially estrogenic and antiandrogenic chemicals,” they added.
“Further investigations involving multiple phthalate analyses during pregnancy and measurements throughout childhood are necessary to confirm our findings,” they concluded.
Direct clinical implications remain uncertain
“Phthalates are a group of chemicals that are used to make plastic more durable; they are found in multiple everyday materials, food products, and common household products,” Marissa Platner, MD, of Emory University, Atlanta, said in an interview. “It is known that we are exposed to phthalates on a routine basis but the long-term effects of this exposure are unclear,” she said.
The current study findings “were not entirely surprising given data from prior animal studies because they do imply that there is some placental transfer of the phthalate metabolites that can cause adverse effects on the developing fetus,” said Dr. Platner. “However, they also demonstrate that the placenta acts as a filter for certain larger molecules to protect the fetus,” she said.
“This study was based on a small sample size, therefore the clinical implications are not clear,” Dr. Platner noted. “However it may be worthwhile after further research to encourage our pregnant patients to try to decrease their exposure to phthalates,” she said.
Dr. Platner identified two areas for additional research to explore the role of phthalate exposure.
“The first would be to assess the level of maternal phthalate exposure throughout the pregnancy instead of just at one point in time, and the second would be to assess how the reproductive system differences at birth translate to long-term outcomes in children, such as early puberty in females or decreased fertility in males,” she said.
The study was funded by the Ministry of Science and Technology of Taiwan and the Far Eastern Memorial Hospital‐National Taiwan University Hospital. The researchers and Dr. Platner had no financial conflicts to disclose.
Exposure to phthalates through maternal blood and cord blood affected outcomes including head circumference and anogenital index for male and female infants, according to data from 65 mother-infant pairs.
Phthalates are recognized endocrine disruptors that have been associated with adverse birth outcomes, but the specific relationship between maternal phthalate exposure and birth outcomes has not been well studied, wrote Hsiao-Lin Hwa, MD, of National Taiwan University, Taipei, and colleagues.
Previous research suggests that trace exposure to hazardous chemicals during the fetal period “may cause fetal metabolic dysfunction and adversely change the morphology of body systems,” they said. In 2011, “the Taiwan Food and Drug Administration found that di‐2‐ethylhexyl phthalate (DEHP) and DiNP [di‐isononyl phthalate] had been illegally added as emulsifiers to replace palm oil in beverages and food,” they added. The researchers sought to examine the association between infant birth outcomes and phthalate exposure levels in the Taiwanese population after 2011. In a study published in Environmental Toxicology and Chemistry, the researchers recruited 65 pregnant women in Taiwan between 2016 and 2017. Birth length, birth weight, head circumference, anogenital distance (AGD), anoscrotal distance (ASD), and anofourchette distance (AFD) were measured for each newborn at the time of delivery. The average age of the women was 33.6 years, and the rate of low birth weight was 13.7%. The mean measures of birth length, birth weight, head circumference, and chest circumference were 47.6 cm, 3022 g, 32.9 cm, and 30.8 mm, respectively. The mean AFD and ASD were 14.2 mm and 22.3 mm, respectively.
The researchers tested for 12 phthalates in maternal blood and cord blood samples. Of these, the six most frequently detected phthalate metabolites were mono‐ethyl phthalate (MEP), mono‐isobutyl phthalate (MiBP), mono‐n‐butyl phthalate (MnBP), mono‐(2‐ethyl‐5‐oxohexyl)‐phthalate (MEOHP), mono‐(2‐ethyl‐5‐hydroxyhexyl) phthalate (MEHHP), and mono‐n‐octyl phthalate (MOP); these six were present in 80%–100% of the maternal blood samples.
Overall, the mean levels of MEP, MiBP, MnBP, and MEHP were relatively higher in both maternal and infant blood than other phthalates, the researchers noted. The mean concentrations of metabolites in maternal blood and infant cord blood were 0.03-2.27 ng/mL and 0.01-3.74 ng/mL, respectively.
Among male infants, levels of MMP, MiBP, and MEHP in maternal blood were inversely related to anogenital index (AGI), with P values for regression coefficients ranging from .011 to .033. In addition, the total concentration of MEHP, MEOHP, and MEHHP (designated as Σdi‐2‐ethylhexyl phthalate, ΣDEHP) was inversely related to AGI in males.
Among female infants, however, phthalates in cord blood, rather than maternal blood, were positively related to AGI, including MMP, MibP, MnBP, and MOP, with P values for regression coefficients ranging from .001 to .034.
Cord blood levels of MnBP, MEOHP, MEHP, and ΣDEHP were inversely associated with gestational age-adjusted head circumference in all infants, with beta coefficients of –0.15, –0.12, –0.01, and –0.01, respectively (P < .05 for all).
“The detection rates of MEHHP, MEOHP, and MEHP in the cord blood were lower than those in the maternal blood, particularly those of MEHHP and MEOHP, which were approximately 25% lower,” which may be caused by slow placental transfer, the researchers wrote in their discussion section. “The high detection rate of phthalate metabolites indicated that our subjects may continue to be exposed to these phthalates even after the 2011 Taiwan DEHP incident,” they noted.
The study findings were limited by several factors including the possibility for contamination of samples and other environmental confounders, the researchers noted. However, the results support the role of phthalates as endocrine disruptors, and the distinction in effects between males and females “may suggest that phthalate monoesters are potentially estrogenic and antiandrogenic chemicals,” they added.
“Further investigations involving multiple phthalate analyses during pregnancy and measurements throughout childhood are necessary to confirm our findings,” they concluded.
Direct clinical implications remain uncertain
“Phthalates are a group of chemicals that are used to make plastic more durable; they are found in multiple everyday materials, food products, and common household products,” Marissa Platner, MD, of Emory University, Atlanta, said in an interview. “It is known that we are exposed to phthalates on a routine basis but the long-term effects of this exposure are unclear,” she said.
The current study findings “were not entirely surprising given data from prior animal studies because they do imply that there is some placental transfer of the phthalate metabolites that can cause adverse effects on the developing fetus,” said Dr. Platner. “However, they also demonstrate that the placenta acts as a filter for certain larger molecules to protect the fetus,” she said.
“This study was based on a small sample size, therefore the clinical implications are not clear,” Dr. Platner noted. “However it may be worthwhile after further research to encourage our pregnant patients to try to decrease their exposure to phthalates,” she said.
Dr. Platner identified two areas for additional research to explore the role of phthalate exposure.
“The first would be to assess the level of maternal phthalate exposure throughout the pregnancy instead of just at one point in time, and the second would be to assess how the reproductive system differences at birth translate to long-term outcomes in children, such as early puberty in females or decreased fertility in males,” she said.
The study was funded by the Ministry of Science and Technology of Taiwan and the Far Eastern Memorial Hospital‐National Taiwan University Hospital. The researchers and Dr. Platner had no financial conflicts to disclose.
FROM ENVIRONMENTAL TOXICOLOGY AND CHEMISTRY
Full-press therapy rare in diabetes with ASCVD
A high percentage of people with type 2 diabetes also have atherosclerotic cardiovascular disease (ASCVD), but fewer than 1 in 20 get the triumvirate of evidence-based medications – drugs to lower cholesterol, blood pressure, and glucose levels – that can mitigate the dominant health risks they face, a large multicenter cohort study reported.
The cohort consisted of 324,706 patients with diabetes and ASCVD in the National Patient-Centered Clinical Research Network in 2018.
Senior study author Christopher B. Granger, MD, said in an interview that the findings represent “a shocking underuse of treatments proven to improve outcomes in this high-risk population.” For example, he noted that high-intensity statins are “inexpensive, well tolerated, and highly effective, but the fact that they’re only used in 26.8% of this population is really an indictment and embarrassment for our health-care system.”
The study analyzed prescriptions of high-intensity statins to lower cholesterol, ACE inhibitors or angiotensin-receptor blockers (ARBs) for blood pressure, and SGLT2 inhibitors or GLP-1 receptor agonists for hyperglycemia in a population with both diabetes and ASCVD.
This study amplifies the perceived treatment gap in cardiovascular risk reduction in persons with diabetes,” Paul S. Jellinger, MD, of the Center for Diabetes and Endocrine Care in Hollywood, Fla., said in an interview. “The unfortunate treatment deficiency documented among 325,000 patients in 12 health systems is carefully quantitated and the message is loud, clear, and simple: There is gross underutilization of agents – ACE inhibitors and ARBs, SGLT-2 inhibitors, GLP-1 receptor agonists, and high-intensity statins – with definitively proven ASCVD benefit.”
In the cohort population, 44% were women and 56% were men; 18.2% were black and 12.8% were Latinx. In terms of care patterns for the 205,885 patients who had specialized visit data from the year before the study, the most (74.8%) saw a primary care physician, while only 8.7% visited an endocrinologist and 26.4% saw a cardiologist.
In terms of the prescriptions they received, 58.6% were on a statin, with less than half on a high-intensity statin; 45.5% were on either an ACE inhibitor or ARB, 3.9% received a GLP-1 receptor agonist, and 2.8% were taking a SGLT2 inhibitor.
The investigators pointed out that figure of 58.6% for patients who got a statin was significantly lower than the 74.6% reported in a study of a database of commercially insured patients, but was more in line with findings a 2018 study of patients with diabetes and ASCVD.
Only 4.8% of patients got all three types of therapies, and a high percentage (42.6%) didn’t get any prescription for the three major risk factors.
Overcoming barriers to prescriptions
The study noted that more work needs to be done to overcome the barriers to more widespread use of these therapies in patients with both diabetes and ASCVD.
Specifically with SGLT2 inhibitors and GLP-1 receptor agonists, cost was more likely to be a barrier than with the other drug groups, but that didn’t explain the low levels of high-intensity statin prescriptions, said Dr. Granger of Duke University, Durham, N.C.
The first barrier he mentioned is what he called “clinical inertia.” He said: “I’m a cardiologist who cares for these patients in my clinic each week, and there are so many different things that we need to be trying to achieve with the brief time we have with each patient in our clinic setting that people tend to miss the opportunity.”
The cost barrier, especially with the glucose-lowering therapies, can be overcome with clinic and health care system programs that aid patients in getting discounted drugs, he noted.
Other barriers Dr. Granger pointed out are lack of education – “So many people think that people with previous muscle aches can’t take a high-intensity statin, and we know that’s not true” – and misinformation, which he called “the more nefarious issue.”
He said, “Part of the problem is that misinformation travels much faster than accurate information. There’s so much out there about statins being toxic, which is just not true.”
Fragmentation of the U.S. health care system and the lack of feedback on quality measures, and physicians deferring decisions on glucose-lowering therapy to endocrinologists also pose barriers to more widespread use of evidence-based therapies in patients with diabetes and ASCVD, Dr. Granger said.
“This is a call to action,” Dr. Granger said. “By clearly describing these gaps, we hope that people will see this as an important opportunity to improve care not only at the level of individual providers, but even more importantly at the level of health systems.”
Dr. Jellinger said the “dismal results” of the study serve as a “wake-up call,” adding that “my own perception among my colleagues, along with the data referred to in this article, point to definitely higher usage among commercially insured patients. However, even in more enriched populations the message is not having its full impact. We have remarkable agents for our patients with diabetes that can make a real impact in diabetes-related morbidity and mortality. Our twofold goal should be to aggressively educate a broad slate of health care professionals and, of course, make patient access easy and affordable without ‘prior authorization.’ ”
The study noted the need to bring the prescribing patterns for patients with both diabetes and ASCVD more in line with evidence-based guidelines. To that end, said Dr. Granger, the researchers are moving ahead on a randomized study of a quality improvement project involving about 45 U.S. cardiology clinics using a feedback loop to apply more consistent prescribing patterns for the three therapy groups. “Hopefully a year from now we’ll have a lot more information about this problem,” Dr. Granger added.
Boehringer Ingelheim and Lilly funded the study. Dr. Granger reported financial relationships with Boehringer Ingelheim, Bristol-Myers Squibb, Janssen, Pfizer, Medtronic, Akros Pharma, Apple, AstraZeneca, Daichi-Sankyo, Novartis, AbbVie, Bayer, Boston Scientific, CeleCor, Correvio, Espero, Merck, Novo Nordisk, Rhoshan Pharmaceuticals, and Roche Diagnostics. Dr. Jellinger is on speaker’s bureaus for Esperion and Amgen.
A high percentage of people with type 2 diabetes also have atherosclerotic cardiovascular disease (ASCVD), but fewer than 1 in 20 get the triumvirate of evidence-based medications – drugs to lower cholesterol, blood pressure, and glucose levels – that can mitigate the dominant health risks they face, a large multicenter cohort study reported.
The cohort consisted of 324,706 patients with diabetes and ASCVD in the National Patient-Centered Clinical Research Network in 2018.
Senior study author Christopher B. Granger, MD, said in an interview that the findings represent “a shocking underuse of treatments proven to improve outcomes in this high-risk population.” For example, he noted that high-intensity statins are “inexpensive, well tolerated, and highly effective, but the fact that they’re only used in 26.8% of this population is really an indictment and embarrassment for our health-care system.”
The study analyzed prescriptions of high-intensity statins to lower cholesterol, ACE inhibitors or angiotensin-receptor blockers (ARBs) for blood pressure, and SGLT2 inhibitors or GLP-1 receptor agonists for hyperglycemia in a population with both diabetes and ASCVD.
This study amplifies the perceived treatment gap in cardiovascular risk reduction in persons with diabetes,” Paul S. Jellinger, MD, of the Center for Diabetes and Endocrine Care in Hollywood, Fla., said in an interview. “The unfortunate treatment deficiency documented among 325,000 patients in 12 health systems is carefully quantitated and the message is loud, clear, and simple: There is gross underutilization of agents – ACE inhibitors and ARBs, SGLT-2 inhibitors, GLP-1 receptor agonists, and high-intensity statins – with definitively proven ASCVD benefit.”
In the cohort population, 44% were women and 56% were men; 18.2% were black and 12.8% were Latinx. In terms of care patterns for the 205,885 patients who had specialized visit data from the year before the study, the most (74.8%) saw a primary care physician, while only 8.7% visited an endocrinologist and 26.4% saw a cardiologist.
In terms of the prescriptions they received, 58.6% were on a statin, with less than half on a high-intensity statin; 45.5% were on either an ACE inhibitor or ARB, 3.9% received a GLP-1 receptor agonist, and 2.8% were taking a SGLT2 inhibitor.
The investigators pointed out that figure of 58.6% for patients who got a statin was significantly lower than the 74.6% reported in a study of a database of commercially insured patients, but was more in line with findings a 2018 study of patients with diabetes and ASCVD.
Only 4.8% of patients got all three types of therapies, and a high percentage (42.6%) didn’t get any prescription for the three major risk factors.
Overcoming barriers to prescriptions
The study noted that more work needs to be done to overcome the barriers to more widespread use of these therapies in patients with both diabetes and ASCVD.
Specifically with SGLT2 inhibitors and GLP-1 receptor agonists, cost was more likely to be a barrier than with the other drug groups, but that didn’t explain the low levels of high-intensity statin prescriptions, said Dr. Granger of Duke University, Durham, N.C.
The first barrier he mentioned is what he called “clinical inertia.” He said: “I’m a cardiologist who cares for these patients in my clinic each week, and there are so many different things that we need to be trying to achieve with the brief time we have with each patient in our clinic setting that people tend to miss the opportunity.”
The cost barrier, especially with the glucose-lowering therapies, can be overcome with clinic and health care system programs that aid patients in getting discounted drugs, he noted.
Other barriers Dr. Granger pointed out are lack of education – “So many people think that people with previous muscle aches can’t take a high-intensity statin, and we know that’s not true” – and misinformation, which he called “the more nefarious issue.”
He said, “Part of the problem is that misinformation travels much faster than accurate information. There’s so much out there about statins being toxic, which is just not true.”
Fragmentation of the U.S. health care system and the lack of feedback on quality measures, and physicians deferring decisions on glucose-lowering therapy to endocrinologists also pose barriers to more widespread use of evidence-based therapies in patients with diabetes and ASCVD, Dr. Granger said.
“This is a call to action,” Dr. Granger said. “By clearly describing these gaps, we hope that people will see this as an important opportunity to improve care not only at the level of individual providers, but even more importantly at the level of health systems.”
Dr. Jellinger said the “dismal results” of the study serve as a “wake-up call,” adding that “my own perception among my colleagues, along with the data referred to in this article, point to definitely higher usage among commercially insured patients. However, even in more enriched populations the message is not having its full impact. We have remarkable agents for our patients with diabetes that can make a real impact in diabetes-related morbidity and mortality. Our twofold goal should be to aggressively educate a broad slate of health care professionals and, of course, make patient access easy and affordable without ‘prior authorization.’ ”
The study noted the need to bring the prescribing patterns for patients with both diabetes and ASCVD more in line with evidence-based guidelines. To that end, said Dr. Granger, the researchers are moving ahead on a randomized study of a quality improvement project involving about 45 U.S. cardiology clinics using a feedback loop to apply more consistent prescribing patterns for the three therapy groups. “Hopefully a year from now we’ll have a lot more information about this problem,” Dr. Granger added.
Boehringer Ingelheim and Lilly funded the study. Dr. Granger reported financial relationships with Boehringer Ingelheim, Bristol-Myers Squibb, Janssen, Pfizer, Medtronic, Akros Pharma, Apple, AstraZeneca, Daichi-Sankyo, Novartis, AbbVie, Bayer, Boston Scientific, CeleCor, Correvio, Espero, Merck, Novo Nordisk, Rhoshan Pharmaceuticals, and Roche Diagnostics. Dr. Jellinger is on speaker’s bureaus for Esperion and Amgen.
A high percentage of people with type 2 diabetes also have atherosclerotic cardiovascular disease (ASCVD), but fewer than 1 in 20 get the triumvirate of evidence-based medications – drugs to lower cholesterol, blood pressure, and glucose levels – that can mitigate the dominant health risks they face, a large multicenter cohort study reported.
The cohort consisted of 324,706 patients with diabetes and ASCVD in the National Patient-Centered Clinical Research Network in 2018.
Senior study author Christopher B. Granger, MD, said in an interview that the findings represent “a shocking underuse of treatments proven to improve outcomes in this high-risk population.” For example, he noted that high-intensity statins are “inexpensive, well tolerated, and highly effective, but the fact that they’re only used in 26.8% of this population is really an indictment and embarrassment for our health-care system.”
The study analyzed prescriptions of high-intensity statins to lower cholesterol, ACE inhibitors or angiotensin-receptor blockers (ARBs) for blood pressure, and SGLT2 inhibitors or GLP-1 receptor agonists for hyperglycemia in a population with both diabetes and ASCVD.
This study amplifies the perceived treatment gap in cardiovascular risk reduction in persons with diabetes,” Paul S. Jellinger, MD, of the Center for Diabetes and Endocrine Care in Hollywood, Fla., said in an interview. “The unfortunate treatment deficiency documented among 325,000 patients in 12 health systems is carefully quantitated and the message is loud, clear, and simple: There is gross underutilization of agents – ACE inhibitors and ARBs, SGLT-2 inhibitors, GLP-1 receptor agonists, and high-intensity statins – with definitively proven ASCVD benefit.”
In the cohort population, 44% were women and 56% were men; 18.2% were black and 12.8% were Latinx. In terms of care patterns for the 205,885 patients who had specialized visit data from the year before the study, the most (74.8%) saw a primary care physician, while only 8.7% visited an endocrinologist and 26.4% saw a cardiologist.
In terms of the prescriptions they received, 58.6% were on a statin, with less than half on a high-intensity statin; 45.5% were on either an ACE inhibitor or ARB, 3.9% received a GLP-1 receptor agonist, and 2.8% were taking a SGLT2 inhibitor.
The investigators pointed out that figure of 58.6% for patients who got a statin was significantly lower than the 74.6% reported in a study of a database of commercially insured patients, but was more in line with findings a 2018 study of patients with diabetes and ASCVD.
Only 4.8% of patients got all three types of therapies, and a high percentage (42.6%) didn’t get any prescription for the three major risk factors.
Overcoming barriers to prescriptions
The study noted that more work needs to be done to overcome the barriers to more widespread use of these therapies in patients with both diabetes and ASCVD.
Specifically with SGLT2 inhibitors and GLP-1 receptor agonists, cost was more likely to be a barrier than with the other drug groups, but that didn’t explain the low levels of high-intensity statin prescriptions, said Dr. Granger of Duke University, Durham, N.C.
The first barrier he mentioned is what he called “clinical inertia.” He said: “I’m a cardiologist who cares for these patients in my clinic each week, and there are so many different things that we need to be trying to achieve with the brief time we have with each patient in our clinic setting that people tend to miss the opportunity.”
The cost barrier, especially with the glucose-lowering therapies, can be overcome with clinic and health care system programs that aid patients in getting discounted drugs, he noted.
Other barriers Dr. Granger pointed out are lack of education – “So many people think that people with previous muscle aches can’t take a high-intensity statin, and we know that’s not true” – and misinformation, which he called “the more nefarious issue.”
He said, “Part of the problem is that misinformation travels much faster than accurate information. There’s so much out there about statins being toxic, which is just not true.”
Fragmentation of the U.S. health care system and the lack of feedback on quality measures, and physicians deferring decisions on glucose-lowering therapy to endocrinologists also pose barriers to more widespread use of evidence-based therapies in patients with diabetes and ASCVD, Dr. Granger said.
“This is a call to action,” Dr. Granger said. “By clearly describing these gaps, we hope that people will see this as an important opportunity to improve care not only at the level of individual providers, but even more importantly at the level of health systems.”
Dr. Jellinger said the “dismal results” of the study serve as a “wake-up call,” adding that “my own perception among my colleagues, along with the data referred to in this article, point to definitely higher usage among commercially insured patients. However, even in more enriched populations the message is not having its full impact. We have remarkable agents for our patients with diabetes that can make a real impact in diabetes-related morbidity and mortality. Our twofold goal should be to aggressively educate a broad slate of health care professionals and, of course, make patient access easy and affordable without ‘prior authorization.’ ”
The study noted the need to bring the prescribing patterns for patients with both diabetes and ASCVD more in line with evidence-based guidelines. To that end, said Dr. Granger, the researchers are moving ahead on a randomized study of a quality improvement project involving about 45 U.S. cardiology clinics using a feedback loop to apply more consistent prescribing patterns for the three therapy groups. “Hopefully a year from now we’ll have a lot more information about this problem,” Dr. Granger added.
Boehringer Ingelheim and Lilly funded the study. Dr. Granger reported financial relationships with Boehringer Ingelheim, Bristol-Myers Squibb, Janssen, Pfizer, Medtronic, Akros Pharma, Apple, AstraZeneca, Daichi-Sankyo, Novartis, AbbVie, Bayer, Boston Scientific, CeleCor, Correvio, Espero, Merck, Novo Nordisk, Rhoshan Pharmaceuticals, and Roche Diagnostics. Dr. Jellinger is on speaker’s bureaus for Esperion and Amgen.
FROM JAMA OPEN NETWORK
Statin intolerance ‘overestimated and overdiagnosed’
Statin intolerance is far less common than previously reported, according to a new meta-analysis, with data on more than 4 million adults from around the world, looking at reported statin adverse effects.
The study puts the prevalence of statin intolerance at 6% to 10%, meaning that statin intolerance is “overestimated and overdiagnosed” in most cases, Maciej Banach, MD, PhD, from the Medical University of Lodz and the University of Zielona Góra, Poland, said in a news release.
It also means that “around 93% of patients on statin therapy can be treated effectively, with very good tolerability and without any safety issues,” Dr. Banach added.
The study, conducted on behalf of the Lipid and Blood Pressure Meta-Analysis Collaboration and the International Lipid Expert Panel, was published online Feb. 16 in the European Heart Journal.
Reassuring data
In a statement from the British nonprofit Science Media Center, Sir Nilesh J. Samani, MBChB, MD, medical director of the British Heart Foundation, said: “Decades of evidence have proven that statins save lives. This latest analysis, showing that the risk of side effects from statins are less than previously thought, should provide reassurance to those who are recommended this medicine to reduce their risk of a heart attack or stroke.”
The reported prevalence of statin intolerance varies widely, from 2% to 3% to as high as 50%, chiefly because “there is still a lack of a clear and easy way to apply the definition of statin intolerance,” Dr. Banach told this news organization.
“The ones we use in lipid clinics – by National Lipid Association (NLA), European Atherosclerosis Society (EAS), and International Lipid Expert Panel (ILEP) – are not used or are rarely used in everyday clinical practice by GPs and other specialists,” Dr. Banach explained.
He also blames “physician inertia: When they listen to a patient complain of muscle pain, or see elevated alanine aminotransferase (ALT), in most of the cases, they will immediately discontinue statins, without any further investigations. One should remember that there are many secondary causes of statin intolerance,” Dr. Banach said.
To get a better handle on the true prevalence of statin intolerance, the study team did a meta-analysis of 4,143,517 patients worldwide from 176 studies: 112 randomized controlled trials and 64 cohort studies.
The overall prevalence of statin intolerance was 9.1% (95% confidence interval, 8.0%-10.0%).
The prevalence of statin intolerance was even lower when assessed with diagnostic criteria from the NLA (7.0%; 95% CI, 6.0%-8.0%), the ILEP (6.7%; 95% CI, 5.0%-8.0%), and the EAS (5.9%; 95% CI, 4.0%-7.0%).
The main factors associated with an increased risk for statin intolerance are female gender, hypothyroidism, high statin dose, advanced age, concomitant use of anti-arrhythmic drugs, and obesity. Other factors include race (being Asian or African American), type 2 diabetes, alcohol use, and chronic liver and renal diseases.
“Our findings mean that we should evaluate patients’ symptoms very carefully, firstly to see whether symptoms are indeed caused by statins, and secondly to evaluate whether it might be patients’ perceptions that statins are harmful – so called nocebo or drucebo effect – which could be responsible for more than 50% of all symptoms, rather than the drug itself,” Dr. Banach said.
He encourages use of the Statin-Associated Muscle Symptom Clinical Index (SAMS-CI) to assess the likelihood that a patient’s muscle symptoms are caused or worsened by statin use.
Substantial analysis, valid results
“This is a substantial analysis [and], based on what we know about statin side effects to date, the results are likely to be broadly valid and indicate that we should not overestimate statin side effects or be too quick to stop statins without due consideration,” Riyaz Patel, MBBS, professor of cardiology, University College London, told the Science Media Center.
“Some patients do experience real side effects, and we do our best to help them with alternative therapies, as with any other medicine. However, for the vast majority of people experiencing statin side effects, we can usually work with the patient to understand the symptoms, use proven strategies to manage these, and ensure they do not miss out on the well-established benefits of statins,” Mr. Patel said.
“This is especially important for people who have already had a heart attack or stroke, where statin therapy is really important in preventing further events,” Mr. Patel added.
Also weighing in on the results, Peter Sever, MB BChir, professor of clinical pharmacology and therapeutics, Imperial College London, said: “The importance for clinicians and patients is to realize that commonly reported symptoms, such as muscle aches and pains and lethargy, are not due to the chemistry of the drug.”
“These ‘nocebo’ symptoms may be psychological in origin, but they are no less real than pharmacological symptoms in how they affect quality of life,” Mr. Sever told the Science Media Center.
“However, it’s important to note that as they are not directly caused by the drug, they should not override the decision to prescribe and take statins on account of their proven benefit in reducing death and disability from heart attacks, strokes, and other cardiovascular conditions,” he added.
This meta-analysis was conducted independently; no company or institution supported it financially. Dr. Banach is on the speakers bureau for Amgen, Herbapol, Kogen, KRKA, Polpharma, Mylan/Viatris, Novartis, Novo Nordisk, Sanofi-Aventis, Teva, and Zentiva; is a consultant to Abbott Vascular, Amgen, Daichii Sankyo, Esperion, FreiaPharmaceuticals, Novartis, Polfarmex, and Sanofi-Aventis; has received grants from Amgen, Mylan/Viatris, Sanofi, and Valeant; and serves as CMO for Nomi Biotech Corporation. Dr. Samani has no relevant disclosures. Mr. Patel has received past honoraria and consulting fees from drug companies manufacturing new cholesterol-lowering drugs and currently works with NICE as a topic advisor for CVD prevention. Mr. Sever has received research grants and consultancy from Pfizer and Amgen.
A version of this article first appeared on Medscape.com.
Statin intolerance is far less common than previously reported, according to a new meta-analysis, with data on more than 4 million adults from around the world, looking at reported statin adverse effects.
The study puts the prevalence of statin intolerance at 6% to 10%, meaning that statin intolerance is “overestimated and overdiagnosed” in most cases, Maciej Banach, MD, PhD, from the Medical University of Lodz and the University of Zielona Góra, Poland, said in a news release.
It also means that “around 93% of patients on statin therapy can be treated effectively, with very good tolerability and without any safety issues,” Dr. Banach added.
The study, conducted on behalf of the Lipid and Blood Pressure Meta-Analysis Collaboration and the International Lipid Expert Panel, was published online Feb. 16 in the European Heart Journal.
Reassuring data
In a statement from the British nonprofit Science Media Center, Sir Nilesh J. Samani, MBChB, MD, medical director of the British Heart Foundation, said: “Decades of evidence have proven that statins save lives. This latest analysis, showing that the risk of side effects from statins are less than previously thought, should provide reassurance to those who are recommended this medicine to reduce their risk of a heart attack or stroke.”
The reported prevalence of statin intolerance varies widely, from 2% to 3% to as high as 50%, chiefly because “there is still a lack of a clear and easy way to apply the definition of statin intolerance,” Dr. Banach told this news organization.
“The ones we use in lipid clinics – by National Lipid Association (NLA), European Atherosclerosis Society (EAS), and International Lipid Expert Panel (ILEP) – are not used or are rarely used in everyday clinical practice by GPs and other specialists,” Dr. Banach explained.
He also blames “physician inertia: When they listen to a patient complain of muscle pain, or see elevated alanine aminotransferase (ALT), in most of the cases, they will immediately discontinue statins, without any further investigations. One should remember that there are many secondary causes of statin intolerance,” Dr. Banach said.
To get a better handle on the true prevalence of statin intolerance, the study team did a meta-analysis of 4,143,517 patients worldwide from 176 studies: 112 randomized controlled trials and 64 cohort studies.
The overall prevalence of statin intolerance was 9.1% (95% confidence interval, 8.0%-10.0%).
The prevalence of statin intolerance was even lower when assessed with diagnostic criteria from the NLA (7.0%; 95% CI, 6.0%-8.0%), the ILEP (6.7%; 95% CI, 5.0%-8.0%), and the EAS (5.9%; 95% CI, 4.0%-7.0%).
The main factors associated with an increased risk for statin intolerance are female gender, hypothyroidism, high statin dose, advanced age, concomitant use of anti-arrhythmic drugs, and obesity. Other factors include race (being Asian or African American), type 2 diabetes, alcohol use, and chronic liver and renal diseases.
“Our findings mean that we should evaluate patients’ symptoms very carefully, firstly to see whether symptoms are indeed caused by statins, and secondly to evaluate whether it might be patients’ perceptions that statins are harmful – so called nocebo or drucebo effect – which could be responsible for more than 50% of all symptoms, rather than the drug itself,” Dr. Banach said.
He encourages use of the Statin-Associated Muscle Symptom Clinical Index (SAMS-CI) to assess the likelihood that a patient’s muscle symptoms are caused or worsened by statin use.
Substantial analysis, valid results
“This is a substantial analysis [and], based on what we know about statin side effects to date, the results are likely to be broadly valid and indicate that we should not overestimate statin side effects or be too quick to stop statins without due consideration,” Riyaz Patel, MBBS, professor of cardiology, University College London, told the Science Media Center.
“Some patients do experience real side effects, and we do our best to help them with alternative therapies, as with any other medicine. However, for the vast majority of people experiencing statin side effects, we can usually work with the patient to understand the symptoms, use proven strategies to manage these, and ensure they do not miss out on the well-established benefits of statins,” Mr. Patel said.
“This is especially important for people who have already had a heart attack or stroke, where statin therapy is really important in preventing further events,” Mr. Patel added.
Also weighing in on the results, Peter Sever, MB BChir, professor of clinical pharmacology and therapeutics, Imperial College London, said: “The importance for clinicians and patients is to realize that commonly reported symptoms, such as muscle aches and pains and lethargy, are not due to the chemistry of the drug.”
“These ‘nocebo’ symptoms may be psychological in origin, but they are no less real than pharmacological symptoms in how they affect quality of life,” Mr. Sever told the Science Media Center.
“However, it’s important to note that as they are not directly caused by the drug, they should not override the decision to prescribe and take statins on account of their proven benefit in reducing death and disability from heart attacks, strokes, and other cardiovascular conditions,” he added.
This meta-analysis was conducted independently; no company or institution supported it financially. Dr. Banach is on the speakers bureau for Amgen, Herbapol, Kogen, KRKA, Polpharma, Mylan/Viatris, Novartis, Novo Nordisk, Sanofi-Aventis, Teva, and Zentiva; is a consultant to Abbott Vascular, Amgen, Daichii Sankyo, Esperion, FreiaPharmaceuticals, Novartis, Polfarmex, and Sanofi-Aventis; has received grants from Amgen, Mylan/Viatris, Sanofi, and Valeant; and serves as CMO for Nomi Biotech Corporation. Dr. Samani has no relevant disclosures. Mr. Patel has received past honoraria and consulting fees from drug companies manufacturing new cholesterol-lowering drugs and currently works with NICE as a topic advisor for CVD prevention. Mr. Sever has received research grants and consultancy from Pfizer and Amgen.
A version of this article first appeared on Medscape.com.
Statin intolerance is far less common than previously reported, according to a new meta-analysis, with data on more than 4 million adults from around the world, looking at reported statin adverse effects.
The study puts the prevalence of statin intolerance at 6% to 10%, meaning that statin intolerance is “overestimated and overdiagnosed” in most cases, Maciej Banach, MD, PhD, from the Medical University of Lodz and the University of Zielona Góra, Poland, said in a news release.
It also means that “around 93% of patients on statin therapy can be treated effectively, with very good tolerability and without any safety issues,” Dr. Banach added.
The study, conducted on behalf of the Lipid and Blood Pressure Meta-Analysis Collaboration and the International Lipid Expert Panel, was published online Feb. 16 in the European Heart Journal.
Reassuring data
In a statement from the British nonprofit Science Media Center, Sir Nilesh J. Samani, MBChB, MD, medical director of the British Heart Foundation, said: “Decades of evidence have proven that statins save lives. This latest analysis, showing that the risk of side effects from statins are less than previously thought, should provide reassurance to those who are recommended this medicine to reduce their risk of a heart attack or stroke.”
The reported prevalence of statin intolerance varies widely, from 2% to 3% to as high as 50%, chiefly because “there is still a lack of a clear and easy way to apply the definition of statin intolerance,” Dr. Banach told this news organization.
“The ones we use in lipid clinics – by National Lipid Association (NLA), European Atherosclerosis Society (EAS), and International Lipid Expert Panel (ILEP) – are not used or are rarely used in everyday clinical practice by GPs and other specialists,” Dr. Banach explained.
He also blames “physician inertia: When they listen to a patient complain of muscle pain, or see elevated alanine aminotransferase (ALT), in most of the cases, they will immediately discontinue statins, without any further investigations. One should remember that there are many secondary causes of statin intolerance,” Dr. Banach said.
To get a better handle on the true prevalence of statin intolerance, the study team did a meta-analysis of 4,143,517 patients worldwide from 176 studies: 112 randomized controlled trials and 64 cohort studies.
The overall prevalence of statin intolerance was 9.1% (95% confidence interval, 8.0%-10.0%).
The prevalence of statin intolerance was even lower when assessed with diagnostic criteria from the NLA (7.0%; 95% CI, 6.0%-8.0%), the ILEP (6.7%; 95% CI, 5.0%-8.0%), and the EAS (5.9%; 95% CI, 4.0%-7.0%).
The main factors associated with an increased risk for statin intolerance are female gender, hypothyroidism, high statin dose, advanced age, concomitant use of anti-arrhythmic drugs, and obesity. Other factors include race (being Asian or African American), type 2 diabetes, alcohol use, and chronic liver and renal diseases.
“Our findings mean that we should evaluate patients’ symptoms very carefully, firstly to see whether symptoms are indeed caused by statins, and secondly to evaluate whether it might be patients’ perceptions that statins are harmful – so called nocebo or drucebo effect – which could be responsible for more than 50% of all symptoms, rather than the drug itself,” Dr. Banach said.
He encourages use of the Statin-Associated Muscle Symptom Clinical Index (SAMS-CI) to assess the likelihood that a patient’s muscle symptoms are caused or worsened by statin use.
Substantial analysis, valid results
“This is a substantial analysis [and], based on what we know about statin side effects to date, the results are likely to be broadly valid and indicate that we should not overestimate statin side effects or be too quick to stop statins without due consideration,” Riyaz Patel, MBBS, professor of cardiology, University College London, told the Science Media Center.
“Some patients do experience real side effects, and we do our best to help them with alternative therapies, as with any other medicine. However, for the vast majority of people experiencing statin side effects, we can usually work with the patient to understand the symptoms, use proven strategies to manage these, and ensure they do not miss out on the well-established benefits of statins,” Mr. Patel said.
“This is especially important for people who have already had a heart attack or stroke, where statin therapy is really important in preventing further events,” Mr. Patel added.
Also weighing in on the results, Peter Sever, MB BChir, professor of clinical pharmacology and therapeutics, Imperial College London, said: “The importance for clinicians and patients is to realize that commonly reported symptoms, such as muscle aches and pains and lethargy, are not due to the chemistry of the drug.”
“These ‘nocebo’ symptoms may be psychological in origin, but they are no less real than pharmacological symptoms in how they affect quality of life,” Mr. Sever told the Science Media Center.
“However, it’s important to note that as they are not directly caused by the drug, they should not override the decision to prescribe and take statins on account of their proven benefit in reducing death and disability from heart attacks, strokes, and other cardiovascular conditions,” he added.
This meta-analysis was conducted independently; no company or institution supported it financially. Dr. Banach is on the speakers bureau for Amgen, Herbapol, Kogen, KRKA, Polpharma, Mylan/Viatris, Novartis, Novo Nordisk, Sanofi-Aventis, Teva, and Zentiva; is a consultant to Abbott Vascular, Amgen, Daichii Sankyo, Esperion, FreiaPharmaceuticals, Novartis, Polfarmex, and Sanofi-Aventis; has received grants from Amgen, Mylan/Viatris, Sanofi, and Valeant; and serves as CMO for Nomi Biotech Corporation. Dr. Samani has no relevant disclosures. Mr. Patel has received past honoraria and consulting fees from drug companies manufacturing new cholesterol-lowering drugs and currently works with NICE as a topic advisor for CVD prevention. Mr. Sever has received research grants and consultancy from Pfizer and Amgen.
A version of this article first appeared on Medscape.com.
Growth hormone therapy for certain children may help them reach their potential
“Dr. Lilley, you’ll always be my favorite doctor; you helped me grow.”
These were the parting words from the last patient that I treated during my endocrinology fellowship. I had watched this young man grow from a prepubertal 17-year-old to a young man who had reached his predicted family height as I treated his delayed puberty caused by Kallmann syndrome, a problem that had been missed for years. It was the appropriate bookend for my chosen specialty.
Watching children grow and develop into who they were meant to be is one of my favorite things about endocrinology, as well as forming meaningful relationships with families. Treating detectable deficiencies in logical and measurable ways is also extremely satisfying.
Too little testosterone? That’s a problem I can solve. Too much thyroid hormone? There’s a blocker for that! Endocrinology can be a straightforward field, and when all goes well, everyone leaves happy.
Except when they don’t.
Gatekeepers for treatment for children’s growth
“Nice to meet you. We’re here to get growth hormone.”
“We’re here because his pediatrician made us come. We’ve already decided we’re not going to put hormones into his body.”
These are common statements I hear when I first meet new patients whose parents are concerned about their children’s growth. Pediatric endocrinologists, after all, are the usual gatekeepers for this treatment.
Growth hormone (GH) often makes the news for controversial reasons – most commonly for its abuse by elite athletes hoping to exploit its anabolic effects – causing parents to have varied opinions about its possible use in their children.
Some refuse endocrinology referrals at all owing to concerns that we will push daily injections on their children. Others demand referrals for their children of average height, hoping for every perceived advantage.
GH deficiency (GHD) – a condition where the pituitary gland fails to produce enough GH – can occur because of congenital pituitary malformations; anatomic, surgical, or traumatic interruptions to the gland; or enzyme deficiencies leading to faulty production.
GHD is just one reason for poor growth, however.
Growth is one of the most important indicators of health in children. A waning growth rate may be an early symptom of serious problems. In my clinic, I’ve diagnosed severe hypothyroidism in a marathon runner, a brain tumor, celiac disease in a teenager with no gastrointestinal complaints, autoimmune hepatitis, and several other diseases needing treatment in children who show no symptoms other than poor growth.
Barriers to normal growth
Sometimes, the die is cast for children to have barriers to normal growth. Several genetic conditions can lead to poor GH production or response, and GH treatment is often necessary to approximate normal height.
These may include:
- Turner syndrome (in females who are missing an X chromosome in whole or part) should be considered in every girl with abnormally short stature; mosaic forms of the condition may be subtle and lack classic features.
- Noonan syndrome is important to detect owing to the possibility of cardiac or renal malformations that may also occur in this condition, caused by a mutation in one of the genes in the RAS-MAPK pathway.
- Russell-Silver syndrome can cause intrauterine GH restriction and has been traced to uniparental disomy of chromosome 7 or duplications, mutations, or methylation defects in chromosome 11.
- Individuals with Prader-Willi syndrome, which is characterized by low muscle tone, hyperphagia, and hypogonadism, have demonstrated dramatic benefits from GH therapy, primarily in maintaining a normal body mass index.
Children who are small for their gestational age may be GH resistant, and those who do not catch up to their growth curve by the age of 2 years may require GH treatment to reach their height potential.
GH therapy isn’t entirely benign. Rare adverse effects of overtreatment can include slipped capital femoral epiphysis (a fracture to the growth plate) and pseudotumor cerebri (idiopathic intracranial hypertension).
Overtreatment can cause acromegaly, which results in coarsened features and large hands and feet.
When is GH therapy warranted?
“Growth hormone therapy has been denied by her insurer. They want you to fill out an appeal.”
Insurance approval in the United States can be a herculean effort because GH is expensive: Out-of-pocket costs are prohibitive for most people without insurance assistance, ranging from $7,000 to $30,000 annually.
Pediatric endocrinologists aren’t in the business of cosmetic endocrinology. Treatment of idiopathic short stature has been controversial since this became an indication for GH treatment.
GH isn’t always necessary. Diagnosing the underlying cause for poor growth is the most important step.
Often, we find constitutional delay of growth and puberty, or “late bloomers.” This condition is characterized by a delayed bone age (growth plates more open than expected for age) and delayed pubertal onset. These children will often reach a normal height despite starting as some of the smallest of their peers.
However, GH plays other roles in the body than simply propelling height. Children with congenital GHD will require GH treatment to prevent hypoglycemia, especially in infancy.
GH is needed even in adults with fused growth plates for normal lipid metabolism, bone accrual, and maintaining normal muscle mass.
I have noticed marked improvements in muscle tone in many children with developmental delays who are treated with GH, and research supports cognitive benefits for certain populations.
The most common regimens for GH focus on treatment via subcutaneous injection nightly, when GH is naturally produced; sometimes, injections are given six nights out of seven to provide a break or for splitting time between households.
Newer once-weekly formulations have recently received approval, as reported by this news organization, and are coming into use.
Pediatric endocrinologists measure height and follow growth factors closely with visits every 3-6 months. GH levels are not useful outside of provocative diagnostic (stimulation) testing.
Insulinlike growth factor 1 or insulinlike growth factor binding protein levels are analyzed per Tanner stage of puberty to assess appropriate response and to make dose adjustments.
Annual standardized films of the left hand help predict progress and anticipated adult height. Treatment usually persists through puberty until growth plates are closed; if true GHD is noticed, much smaller doses are continued through adulthood.
Regardless, conversations about GH happen with your friendly local pediatric endocrinologist.
We are thrilled to help shepherd patients through their growing age to meet their potential. For more information about GH treatment for children, the MAGIC Foundation is the perfect place to start.
Dr. Lilley is director of the pediatric diabetes and lipid program, Mississippi Center for Advanced Medicine, Madison. She disclosed no relevant conflicts of interest. A version of this article first appeared on Medscape.com.
“Dr. Lilley, you’ll always be my favorite doctor; you helped me grow.”
These were the parting words from the last patient that I treated during my endocrinology fellowship. I had watched this young man grow from a prepubertal 17-year-old to a young man who had reached his predicted family height as I treated his delayed puberty caused by Kallmann syndrome, a problem that had been missed for years. It was the appropriate bookend for my chosen specialty.
Watching children grow and develop into who they were meant to be is one of my favorite things about endocrinology, as well as forming meaningful relationships with families. Treating detectable deficiencies in logical and measurable ways is also extremely satisfying.
Too little testosterone? That’s a problem I can solve. Too much thyroid hormone? There’s a blocker for that! Endocrinology can be a straightforward field, and when all goes well, everyone leaves happy.
Except when they don’t.
Gatekeepers for treatment for children’s growth
“Nice to meet you. We’re here to get growth hormone.”
“We’re here because his pediatrician made us come. We’ve already decided we’re not going to put hormones into his body.”
These are common statements I hear when I first meet new patients whose parents are concerned about their children’s growth. Pediatric endocrinologists, after all, are the usual gatekeepers for this treatment.
Growth hormone (GH) often makes the news for controversial reasons – most commonly for its abuse by elite athletes hoping to exploit its anabolic effects – causing parents to have varied opinions about its possible use in their children.
Some refuse endocrinology referrals at all owing to concerns that we will push daily injections on their children. Others demand referrals for their children of average height, hoping for every perceived advantage.
GH deficiency (GHD) – a condition where the pituitary gland fails to produce enough GH – can occur because of congenital pituitary malformations; anatomic, surgical, or traumatic interruptions to the gland; or enzyme deficiencies leading to faulty production.
GHD is just one reason for poor growth, however.
Growth is one of the most important indicators of health in children. A waning growth rate may be an early symptom of serious problems. In my clinic, I’ve diagnosed severe hypothyroidism in a marathon runner, a brain tumor, celiac disease in a teenager with no gastrointestinal complaints, autoimmune hepatitis, and several other diseases needing treatment in children who show no symptoms other than poor growth.
Barriers to normal growth
Sometimes, the die is cast for children to have barriers to normal growth. Several genetic conditions can lead to poor GH production or response, and GH treatment is often necessary to approximate normal height.
These may include:
- Turner syndrome (in females who are missing an X chromosome in whole or part) should be considered in every girl with abnormally short stature; mosaic forms of the condition may be subtle and lack classic features.
- Noonan syndrome is important to detect owing to the possibility of cardiac or renal malformations that may also occur in this condition, caused by a mutation in one of the genes in the RAS-MAPK pathway.
- Russell-Silver syndrome can cause intrauterine GH restriction and has been traced to uniparental disomy of chromosome 7 or duplications, mutations, or methylation defects in chromosome 11.
- Individuals with Prader-Willi syndrome, which is characterized by low muscle tone, hyperphagia, and hypogonadism, have demonstrated dramatic benefits from GH therapy, primarily in maintaining a normal body mass index.
Children who are small for their gestational age may be GH resistant, and those who do not catch up to their growth curve by the age of 2 years may require GH treatment to reach their height potential.
GH therapy isn’t entirely benign. Rare adverse effects of overtreatment can include slipped capital femoral epiphysis (a fracture to the growth plate) and pseudotumor cerebri (idiopathic intracranial hypertension).
Overtreatment can cause acromegaly, which results in coarsened features and large hands and feet.
When is GH therapy warranted?
“Growth hormone therapy has been denied by her insurer. They want you to fill out an appeal.”
Insurance approval in the United States can be a herculean effort because GH is expensive: Out-of-pocket costs are prohibitive for most people without insurance assistance, ranging from $7,000 to $30,000 annually.
Pediatric endocrinologists aren’t in the business of cosmetic endocrinology. Treatment of idiopathic short stature has been controversial since this became an indication for GH treatment.
GH isn’t always necessary. Diagnosing the underlying cause for poor growth is the most important step.
Often, we find constitutional delay of growth and puberty, or “late bloomers.” This condition is characterized by a delayed bone age (growth plates more open than expected for age) and delayed pubertal onset. These children will often reach a normal height despite starting as some of the smallest of their peers.
However, GH plays other roles in the body than simply propelling height. Children with congenital GHD will require GH treatment to prevent hypoglycemia, especially in infancy.
GH is needed even in adults with fused growth plates for normal lipid metabolism, bone accrual, and maintaining normal muscle mass.
I have noticed marked improvements in muscle tone in many children with developmental delays who are treated with GH, and research supports cognitive benefits for certain populations.
The most common regimens for GH focus on treatment via subcutaneous injection nightly, when GH is naturally produced; sometimes, injections are given six nights out of seven to provide a break or for splitting time between households.
Newer once-weekly formulations have recently received approval, as reported by this news organization, and are coming into use.
Pediatric endocrinologists measure height and follow growth factors closely with visits every 3-6 months. GH levels are not useful outside of provocative diagnostic (stimulation) testing.
Insulinlike growth factor 1 or insulinlike growth factor binding protein levels are analyzed per Tanner stage of puberty to assess appropriate response and to make dose adjustments.
Annual standardized films of the left hand help predict progress and anticipated adult height. Treatment usually persists through puberty until growth plates are closed; if true GHD is noticed, much smaller doses are continued through adulthood.
Regardless, conversations about GH happen with your friendly local pediatric endocrinologist.
We are thrilled to help shepherd patients through their growing age to meet their potential. For more information about GH treatment for children, the MAGIC Foundation is the perfect place to start.
Dr. Lilley is director of the pediatric diabetes and lipid program, Mississippi Center for Advanced Medicine, Madison. She disclosed no relevant conflicts of interest. A version of this article first appeared on Medscape.com.
“Dr. Lilley, you’ll always be my favorite doctor; you helped me grow.”
These were the parting words from the last patient that I treated during my endocrinology fellowship. I had watched this young man grow from a prepubertal 17-year-old to a young man who had reached his predicted family height as I treated his delayed puberty caused by Kallmann syndrome, a problem that had been missed for years. It was the appropriate bookend for my chosen specialty.
Watching children grow and develop into who they were meant to be is one of my favorite things about endocrinology, as well as forming meaningful relationships with families. Treating detectable deficiencies in logical and measurable ways is also extremely satisfying.
Too little testosterone? That’s a problem I can solve. Too much thyroid hormone? There’s a blocker for that! Endocrinology can be a straightforward field, and when all goes well, everyone leaves happy.
Except when they don’t.
Gatekeepers for treatment for children’s growth
“Nice to meet you. We’re here to get growth hormone.”
“We’re here because his pediatrician made us come. We’ve already decided we’re not going to put hormones into his body.”
These are common statements I hear when I first meet new patients whose parents are concerned about their children’s growth. Pediatric endocrinologists, after all, are the usual gatekeepers for this treatment.
Growth hormone (GH) often makes the news for controversial reasons – most commonly for its abuse by elite athletes hoping to exploit its anabolic effects – causing parents to have varied opinions about its possible use in their children.
Some refuse endocrinology referrals at all owing to concerns that we will push daily injections on their children. Others demand referrals for their children of average height, hoping for every perceived advantage.
GH deficiency (GHD) – a condition where the pituitary gland fails to produce enough GH – can occur because of congenital pituitary malformations; anatomic, surgical, or traumatic interruptions to the gland; or enzyme deficiencies leading to faulty production.
GHD is just one reason for poor growth, however.
Growth is one of the most important indicators of health in children. A waning growth rate may be an early symptom of serious problems. In my clinic, I’ve diagnosed severe hypothyroidism in a marathon runner, a brain tumor, celiac disease in a teenager with no gastrointestinal complaints, autoimmune hepatitis, and several other diseases needing treatment in children who show no symptoms other than poor growth.
Barriers to normal growth
Sometimes, the die is cast for children to have barriers to normal growth. Several genetic conditions can lead to poor GH production or response, and GH treatment is often necessary to approximate normal height.
These may include:
- Turner syndrome (in females who are missing an X chromosome in whole or part) should be considered in every girl with abnormally short stature; mosaic forms of the condition may be subtle and lack classic features.
- Noonan syndrome is important to detect owing to the possibility of cardiac or renal malformations that may also occur in this condition, caused by a mutation in one of the genes in the RAS-MAPK pathway.
- Russell-Silver syndrome can cause intrauterine GH restriction and has been traced to uniparental disomy of chromosome 7 or duplications, mutations, or methylation defects in chromosome 11.
- Individuals with Prader-Willi syndrome, which is characterized by low muscle tone, hyperphagia, and hypogonadism, have demonstrated dramatic benefits from GH therapy, primarily in maintaining a normal body mass index.
Children who are small for their gestational age may be GH resistant, and those who do not catch up to their growth curve by the age of 2 years may require GH treatment to reach their height potential.
GH therapy isn’t entirely benign. Rare adverse effects of overtreatment can include slipped capital femoral epiphysis (a fracture to the growth plate) and pseudotumor cerebri (idiopathic intracranial hypertension).
Overtreatment can cause acromegaly, which results in coarsened features and large hands and feet.
When is GH therapy warranted?
“Growth hormone therapy has been denied by her insurer. They want you to fill out an appeal.”
Insurance approval in the United States can be a herculean effort because GH is expensive: Out-of-pocket costs are prohibitive for most people without insurance assistance, ranging from $7,000 to $30,000 annually.
Pediatric endocrinologists aren’t in the business of cosmetic endocrinology. Treatment of idiopathic short stature has been controversial since this became an indication for GH treatment.
GH isn’t always necessary. Diagnosing the underlying cause for poor growth is the most important step.
Often, we find constitutional delay of growth and puberty, or “late bloomers.” This condition is characterized by a delayed bone age (growth plates more open than expected for age) and delayed pubertal onset. These children will often reach a normal height despite starting as some of the smallest of their peers.
However, GH plays other roles in the body than simply propelling height. Children with congenital GHD will require GH treatment to prevent hypoglycemia, especially in infancy.
GH is needed even in adults with fused growth plates for normal lipid metabolism, bone accrual, and maintaining normal muscle mass.
I have noticed marked improvements in muscle tone in many children with developmental delays who are treated with GH, and research supports cognitive benefits for certain populations.
The most common regimens for GH focus on treatment via subcutaneous injection nightly, when GH is naturally produced; sometimes, injections are given six nights out of seven to provide a break or for splitting time between households.
Newer once-weekly formulations have recently received approval, as reported by this news organization, and are coming into use.
Pediatric endocrinologists measure height and follow growth factors closely with visits every 3-6 months. GH levels are not useful outside of provocative diagnostic (stimulation) testing.
Insulinlike growth factor 1 or insulinlike growth factor binding protein levels are analyzed per Tanner stage of puberty to assess appropriate response and to make dose adjustments.
Annual standardized films of the left hand help predict progress and anticipated adult height. Treatment usually persists through puberty until growth plates are closed; if true GHD is noticed, much smaller doses are continued through adulthood.
Regardless, conversations about GH happen with your friendly local pediatric endocrinologist.
We are thrilled to help shepherd patients through their growing age to meet their potential. For more information about GH treatment for children, the MAGIC Foundation is the perfect place to start.
Dr. Lilley is director of the pediatric diabetes and lipid program, Mississippi Center for Advanced Medicine, Madison. She disclosed no relevant conflicts of interest. A version of this article first appeared on Medscape.com.
Fewer diabetes complications with NOACs in patients with AFib
The new research, which was published in Annals of Internal Medicine, found that taking non–vitamin K oral anticoagulants was associated with reduced diabetes complications and lower mortality vs. taking warfarin in the group examined.
In their paper, the researchers present the outcomes of a retrospective cohort study involving 30,209 patients with atrial fibrillation and diabetes. Of these, 19,909 were treated with non–vitamin K oral anticoagulants (NOACs) – dabigatran, rivaroxaban, apixaban, or edoxaban – and 10,300 were treated with warfarin.
Dr. Huei-Kai Huang from the Hualien (Taiwan) Tzu Chi Hospital and coauthors wrote that, while diabetes mellitus is an important risk factor for stroke, there’s not yet a good understanding of the effect of different oral anticoagulants on the risk for diabetes-related complications in patients with atrial fibrillation and diabetes.
“Recent evidence has suggested that NOAC and warfarin may have different effects on glycemic control through the vitamin K–related mechanisms,” coauthor Yu-Kang Tu, PhD, from the College of Public Health at the National Taiwan University in Taipei said in an interview. “It was therefore natural to further evaluate whether NOAC could help decrease various diabetes-related complications, compared with warfarin.”
Hazards with NOACS vs. warfarin
The researchers found that patients treated with NOACs had a 16% lower hazard of macrovascular complications – a composite of coronary artery disease, stroke, and peripheral vascular disease (95% confidence interval, 0.78-0.91; P < .001) – and a 21% lower hazard of microvascular complications including dialysis and lower-extremity amputations (95% CI, 0.73-0.85; P < .001).
NOAC therapy was also associated a 22% lower hazard of death (95% CI, 0.75-0.82; P < .001) and a 9% lower hazard for glycemic emergency (95% CI, 0.83-0.99; P = .043), which the authors defined as a composite of diabetic ketoacidosis, hyperosmolar hyperglycemic state, and hypoglycemia.
In particular, patients treated with NOACs showed significantly lower hazards for coronary artery disease, stroke, dialysis, amputation of lower extremities, and death from cardiovascular and noncardiovascular causes, compared with warfarin users.
The study also found that patients on higher volumes of NOAC medication had greater reductions in mortality and diabetes complications.
“Although our main findings can be explained by the potential differences in underlying mechanisms of action between NOAC and warfarin, we were still surprised with the significantly lower risks of retinopathy, neuropathy, and hypoglycemia in patients taking NOAC with high medication possession ratio,” Dr. Tu said.
Study provides more diabetes-specific outcomes data
Commenting on the findings, Dr. Peter Rossing, head of complications research at the Steno Diabetes Center in Copenhagen said there has long been discussion about whether the newer and more expensive NOACs offer greater benefits to patient with diabetes – beyond stroke prevention – compared with the older and cheaper warfarin. As such, this study was important in providing more diabetes-specific outcomes data and in a large population.
“The effect size they find is certainly meaningful and relevant and should support decision-making,” Dr. Rossing noted in an interview. The finding of reduced risk of amputation and mortality “fits in line with theory that maybe if you block vitamin K, you get calcification, you get vascular damage that leads to failure of the kidney and leads to limb amputations, and that is potentially prevented or not developed when you give the NOACs.”
Dr. John Camm, professor of clinical cardiology at St George’s University of London, said the findings of the benefits of NOACs in this patient group ,were confirmation of earlier, smaller studies, and were important not just for patients with atrial fibrillation and diabetes, but also those prone to diabetes.
“We know from previous studies from the same database, and also from Korea, [for example], that patients who are treated with NOACs as opposed to warfarin develop less diabetes,” he explained.
Dr. Camm said many guidelines around the world now suggest NOACs, and, in some cases, even advise against using vitamin K antagonists as a first option, except in certain situations, such as when patients have rheumatic heart disease, mild to moderate mitral stenosis in rheumatic disease, or prosthetic heart valves.
The researchers applied two methods to account for covariates that may have influenced whether patients received one class of treatment or the other. These achieved ‘appropriate balance’ of baseline characteristics such as comorbidities and baseline medication use for diabetes and other conditions, Dr. Tu and colleagues wrote.
The benefits of NOACs were less evident in younger patients, and the reductions in mortality and diabetes complications associated with NOACs did not reach statistical significance in those aged under 65 years. Regarding this, Dr. Camm noted that there was a debate as to whether patients under 65 years with atrial fibrillation and diabetes should be put on an anticoagulant.
The study was funded by Hualien Tzu Chi Hospital. No conflicts of interest were declared.
The new research, which was published in Annals of Internal Medicine, found that taking non–vitamin K oral anticoagulants was associated with reduced diabetes complications and lower mortality vs. taking warfarin in the group examined.
In their paper, the researchers present the outcomes of a retrospective cohort study involving 30,209 patients with atrial fibrillation and diabetes. Of these, 19,909 were treated with non–vitamin K oral anticoagulants (NOACs) – dabigatran, rivaroxaban, apixaban, or edoxaban – and 10,300 were treated with warfarin.
Dr. Huei-Kai Huang from the Hualien (Taiwan) Tzu Chi Hospital and coauthors wrote that, while diabetes mellitus is an important risk factor for stroke, there’s not yet a good understanding of the effect of different oral anticoagulants on the risk for diabetes-related complications in patients with atrial fibrillation and diabetes.
“Recent evidence has suggested that NOAC and warfarin may have different effects on glycemic control through the vitamin K–related mechanisms,” coauthor Yu-Kang Tu, PhD, from the College of Public Health at the National Taiwan University in Taipei said in an interview. “It was therefore natural to further evaluate whether NOAC could help decrease various diabetes-related complications, compared with warfarin.”
Hazards with NOACS vs. warfarin
The researchers found that patients treated with NOACs had a 16% lower hazard of macrovascular complications – a composite of coronary artery disease, stroke, and peripheral vascular disease (95% confidence interval, 0.78-0.91; P < .001) – and a 21% lower hazard of microvascular complications including dialysis and lower-extremity amputations (95% CI, 0.73-0.85; P < .001).
NOAC therapy was also associated a 22% lower hazard of death (95% CI, 0.75-0.82; P < .001) and a 9% lower hazard for glycemic emergency (95% CI, 0.83-0.99; P = .043), which the authors defined as a composite of diabetic ketoacidosis, hyperosmolar hyperglycemic state, and hypoglycemia.
In particular, patients treated with NOACs showed significantly lower hazards for coronary artery disease, stroke, dialysis, amputation of lower extremities, and death from cardiovascular and noncardiovascular causes, compared with warfarin users.
The study also found that patients on higher volumes of NOAC medication had greater reductions in mortality and diabetes complications.
“Although our main findings can be explained by the potential differences in underlying mechanisms of action between NOAC and warfarin, we were still surprised with the significantly lower risks of retinopathy, neuropathy, and hypoglycemia in patients taking NOAC with high medication possession ratio,” Dr. Tu said.
Study provides more diabetes-specific outcomes data
Commenting on the findings, Dr. Peter Rossing, head of complications research at the Steno Diabetes Center in Copenhagen said there has long been discussion about whether the newer and more expensive NOACs offer greater benefits to patient with diabetes – beyond stroke prevention – compared with the older and cheaper warfarin. As such, this study was important in providing more diabetes-specific outcomes data and in a large population.
“The effect size they find is certainly meaningful and relevant and should support decision-making,” Dr. Rossing noted in an interview. The finding of reduced risk of amputation and mortality “fits in line with theory that maybe if you block vitamin K, you get calcification, you get vascular damage that leads to failure of the kidney and leads to limb amputations, and that is potentially prevented or not developed when you give the NOACs.”
Dr. John Camm, professor of clinical cardiology at St George’s University of London, said the findings of the benefits of NOACs in this patient group ,were confirmation of earlier, smaller studies, and were important not just for patients with atrial fibrillation and diabetes, but also those prone to diabetes.
“We know from previous studies from the same database, and also from Korea, [for example], that patients who are treated with NOACs as opposed to warfarin develop less diabetes,” he explained.
Dr. Camm said many guidelines around the world now suggest NOACs, and, in some cases, even advise against using vitamin K antagonists as a first option, except in certain situations, such as when patients have rheumatic heart disease, mild to moderate mitral stenosis in rheumatic disease, or prosthetic heart valves.
The researchers applied two methods to account for covariates that may have influenced whether patients received one class of treatment or the other. These achieved ‘appropriate balance’ of baseline characteristics such as comorbidities and baseline medication use for diabetes and other conditions, Dr. Tu and colleagues wrote.
The benefits of NOACs were less evident in younger patients, and the reductions in mortality and diabetes complications associated with NOACs did not reach statistical significance in those aged under 65 years. Regarding this, Dr. Camm noted that there was a debate as to whether patients under 65 years with atrial fibrillation and diabetes should be put on an anticoagulant.
The study was funded by Hualien Tzu Chi Hospital. No conflicts of interest were declared.
The new research, which was published in Annals of Internal Medicine, found that taking non–vitamin K oral anticoagulants was associated with reduced diabetes complications and lower mortality vs. taking warfarin in the group examined.
In their paper, the researchers present the outcomes of a retrospective cohort study involving 30,209 patients with atrial fibrillation and diabetes. Of these, 19,909 were treated with non–vitamin K oral anticoagulants (NOACs) – dabigatran, rivaroxaban, apixaban, or edoxaban – and 10,300 were treated with warfarin.
Dr. Huei-Kai Huang from the Hualien (Taiwan) Tzu Chi Hospital and coauthors wrote that, while diabetes mellitus is an important risk factor for stroke, there’s not yet a good understanding of the effect of different oral anticoagulants on the risk for diabetes-related complications in patients with atrial fibrillation and diabetes.
“Recent evidence has suggested that NOAC and warfarin may have different effects on glycemic control through the vitamin K–related mechanisms,” coauthor Yu-Kang Tu, PhD, from the College of Public Health at the National Taiwan University in Taipei said in an interview. “It was therefore natural to further evaluate whether NOAC could help decrease various diabetes-related complications, compared with warfarin.”
Hazards with NOACS vs. warfarin
The researchers found that patients treated with NOACs had a 16% lower hazard of macrovascular complications – a composite of coronary artery disease, stroke, and peripheral vascular disease (95% confidence interval, 0.78-0.91; P < .001) – and a 21% lower hazard of microvascular complications including dialysis and lower-extremity amputations (95% CI, 0.73-0.85; P < .001).
NOAC therapy was also associated a 22% lower hazard of death (95% CI, 0.75-0.82; P < .001) and a 9% lower hazard for glycemic emergency (95% CI, 0.83-0.99; P = .043), which the authors defined as a composite of diabetic ketoacidosis, hyperosmolar hyperglycemic state, and hypoglycemia.
In particular, patients treated with NOACs showed significantly lower hazards for coronary artery disease, stroke, dialysis, amputation of lower extremities, and death from cardiovascular and noncardiovascular causes, compared with warfarin users.
The study also found that patients on higher volumes of NOAC medication had greater reductions in mortality and diabetes complications.
“Although our main findings can be explained by the potential differences in underlying mechanisms of action between NOAC and warfarin, we were still surprised with the significantly lower risks of retinopathy, neuropathy, and hypoglycemia in patients taking NOAC with high medication possession ratio,” Dr. Tu said.
Study provides more diabetes-specific outcomes data
Commenting on the findings, Dr. Peter Rossing, head of complications research at the Steno Diabetes Center in Copenhagen said there has long been discussion about whether the newer and more expensive NOACs offer greater benefits to patient with diabetes – beyond stroke prevention – compared with the older and cheaper warfarin. As such, this study was important in providing more diabetes-specific outcomes data and in a large population.
“The effect size they find is certainly meaningful and relevant and should support decision-making,” Dr. Rossing noted in an interview. The finding of reduced risk of amputation and mortality “fits in line with theory that maybe if you block vitamin K, you get calcification, you get vascular damage that leads to failure of the kidney and leads to limb amputations, and that is potentially prevented or not developed when you give the NOACs.”
Dr. John Camm, professor of clinical cardiology at St George’s University of London, said the findings of the benefits of NOACs in this patient group ,were confirmation of earlier, smaller studies, and were important not just for patients with atrial fibrillation and diabetes, but also those prone to diabetes.
“We know from previous studies from the same database, and also from Korea, [for example], that patients who are treated with NOACs as opposed to warfarin develop less diabetes,” he explained.
Dr. Camm said many guidelines around the world now suggest NOACs, and, in some cases, even advise against using vitamin K antagonists as a first option, except in certain situations, such as when patients have rheumatic heart disease, mild to moderate mitral stenosis in rheumatic disease, or prosthetic heart valves.
The researchers applied two methods to account for covariates that may have influenced whether patients received one class of treatment or the other. These achieved ‘appropriate balance’ of baseline characteristics such as comorbidities and baseline medication use for diabetes and other conditions, Dr. Tu and colleagues wrote.
The benefits of NOACs were less evident in younger patients, and the reductions in mortality and diabetes complications associated with NOACs did not reach statistical significance in those aged under 65 years. Regarding this, Dr. Camm noted that there was a debate as to whether patients under 65 years with atrial fibrillation and diabetes should be put on an anticoagulant.
The study was funded by Hualien Tzu Chi Hospital. No conflicts of interest were declared.
FROM ANNALS OF INTERNAL MEDICINE
Sports experts on T2D: Boost activity, cut sedentary time
The American College of Sports Medicine (ACSM) has issued new recommendations for exercise/physical activity in people with type 2 diabetes, which update a 2010 joint ACSM/American Diabetes Association position statement.
The guidance has been published in the February issue of Medicine & Science in Sports & Exercise.
“This consensus statement provides a brief summary of the current evidence and extends and updates the prior recommendations,” the authors explain.
In the past decade, there has been a “considerable amount” of research about exercise in people with type 2 diabetes, they add, while the prevalence of diabetes has steadily increased.
The updated recommendations have been “expanded to include physical activity – a broader, more comprehensive definition of human movement than planned exercise – and reducing sedentary time,” the authors note.
“The latest guidelines are applicable to most individuals with diabetes, including youth, with a few exceptions and modifications,” lead author Jill A. Kanaley, PhD, said in a press release from the ACSM.
The key takeaway is that “all individuals [with type 2 diabetes] should engage in regular physical activity, reduce sedentary time, and break up sitting time with frequent activity breaks,” said Dr. Kanaley, a professor in the department of nutrition and exercise physiology, University of Missouri, Columbia.
“Exercise can play an important role in managing type 2 diabetes, and workouts can be modified to fit the abilities of most people,” she stressed.
And those with type 2 diabetes who want to lose weight “should consider workouts of moderately high volume for 4 to 5 days per week,” she added.
Six key tips for physical activity in adults with type 2 diabetes
The consensus statement gives six key tips for physical activity in adults with type 2 diabetes, as follows.
- Regular aerobic exercise improves glycemic management; meta-analyses have reported fewer daily hyperglycemic episodes and reductions in A1c of 0.5%-0.7%.
- High-intensity resistance exercise, when performed safely, is better than low-to-moderate intensity resistance exercise for glucose management and attenuation of insulin levels. Resistance exercise typically results in improvements of 10% to 15% in strength, bone mineral density, blood pressure, lipid profile, skeletal muscle mass, and insulin sensitivity.
- Exercise after meals, such as taking a walk after dinner at one’s own pace, takes advantage of the blood glucose-stabilizing effects of exercise.
- Reduce sedentary time by taking regular breaks for small “doses” of physical activity, which can modestly attenuate postprandial glucose and insulin levels, particularly in individuals with insulin resistance and a higher body mass index.
- To prevent hypoglycemia during or after exercise, people taking insulin or insulin secretagogues should increase carbohydrate intake, or if possible, reduce insulin.
- People who are taking beta blockers should not rely on a heart monitor to measure workout intensity. They could ask a certified exercise professional about using ratings of perceived exertion to track how a workout feels.
Other recommendations
The consensus statement also summarizes precautions that people with complications of type 2 diabetes (such as neuropathy, retinopathy, kidney disease, and hypertension) should take.
Low impact exercises for flexibility can help introduce sedentary people to physical activity, the consensus group writes. Balance exercises can be helpful for older adults.
Weight loss greater than 5% can benefit A1c, blood lipid, and blood pressure levels. Moderate exercise 4 to 5 days a week can reduce visceral fat.
In studies of youth with type 2 diabetes, intensive lifestyle interventions plus metformin were not superior to metformin alone for managing glycemia. Physical activity goals are the same for youth with or without diabetes.
Pregnant women with diabetes should participate in at least 20 to 30 minutes of moderate-intensity exercise most days of the week.
Participating in an exercise program before and after bariatric surgery may enhance surgical outcomes.
Dr. Kanaley has reported receiving a grant from the National Institutes of Health. Disclosures for the other authors are listed in the article.
A version of this article first appeared on Medscape.com.
The American College of Sports Medicine (ACSM) has issued new recommendations for exercise/physical activity in people with type 2 diabetes, which update a 2010 joint ACSM/American Diabetes Association position statement.
The guidance has been published in the February issue of Medicine & Science in Sports & Exercise.
“This consensus statement provides a brief summary of the current evidence and extends and updates the prior recommendations,” the authors explain.
In the past decade, there has been a “considerable amount” of research about exercise in people with type 2 diabetes, they add, while the prevalence of diabetes has steadily increased.
The updated recommendations have been “expanded to include physical activity – a broader, more comprehensive definition of human movement than planned exercise – and reducing sedentary time,” the authors note.
“The latest guidelines are applicable to most individuals with diabetes, including youth, with a few exceptions and modifications,” lead author Jill A. Kanaley, PhD, said in a press release from the ACSM.
The key takeaway is that “all individuals [with type 2 diabetes] should engage in regular physical activity, reduce sedentary time, and break up sitting time with frequent activity breaks,” said Dr. Kanaley, a professor in the department of nutrition and exercise physiology, University of Missouri, Columbia.
“Exercise can play an important role in managing type 2 diabetes, and workouts can be modified to fit the abilities of most people,” she stressed.
And those with type 2 diabetes who want to lose weight “should consider workouts of moderately high volume for 4 to 5 days per week,” she added.
Six key tips for physical activity in adults with type 2 diabetes
The consensus statement gives six key tips for physical activity in adults with type 2 diabetes, as follows.
- Regular aerobic exercise improves glycemic management; meta-analyses have reported fewer daily hyperglycemic episodes and reductions in A1c of 0.5%-0.7%.
- High-intensity resistance exercise, when performed safely, is better than low-to-moderate intensity resistance exercise for glucose management and attenuation of insulin levels. Resistance exercise typically results in improvements of 10% to 15% in strength, bone mineral density, blood pressure, lipid profile, skeletal muscle mass, and insulin sensitivity.
- Exercise after meals, such as taking a walk after dinner at one’s own pace, takes advantage of the blood glucose-stabilizing effects of exercise.
- Reduce sedentary time by taking regular breaks for small “doses” of physical activity, which can modestly attenuate postprandial glucose and insulin levels, particularly in individuals with insulin resistance and a higher body mass index.
- To prevent hypoglycemia during or after exercise, people taking insulin or insulin secretagogues should increase carbohydrate intake, or if possible, reduce insulin.
- People who are taking beta blockers should not rely on a heart monitor to measure workout intensity. They could ask a certified exercise professional about using ratings of perceived exertion to track how a workout feels.
Other recommendations
The consensus statement also summarizes precautions that people with complications of type 2 diabetes (such as neuropathy, retinopathy, kidney disease, and hypertension) should take.
Low impact exercises for flexibility can help introduce sedentary people to physical activity, the consensus group writes. Balance exercises can be helpful for older adults.
Weight loss greater than 5% can benefit A1c, blood lipid, and blood pressure levels. Moderate exercise 4 to 5 days a week can reduce visceral fat.
In studies of youth with type 2 diabetes, intensive lifestyle interventions plus metformin were not superior to metformin alone for managing glycemia. Physical activity goals are the same for youth with or without diabetes.
Pregnant women with diabetes should participate in at least 20 to 30 minutes of moderate-intensity exercise most days of the week.
Participating in an exercise program before and after bariatric surgery may enhance surgical outcomes.
Dr. Kanaley has reported receiving a grant from the National Institutes of Health. Disclosures for the other authors are listed in the article.
A version of this article first appeared on Medscape.com.
The American College of Sports Medicine (ACSM) has issued new recommendations for exercise/physical activity in people with type 2 diabetes, which update a 2010 joint ACSM/American Diabetes Association position statement.
The guidance has been published in the February issue of Medicine & Science in Sports & Exercise.
“This consensus statement provides a brief summary of the current evidence and extends and updates the prior recommendations,” the authors explain.
In the past decade, there has been a “considerable amount” of research about exercise in people with type 2 diabetes, they add, while the prevalence of diabetes has steadily increased.
The updated recommendations have been “expanded to include physical activity – a broader, more comprehensive definition of human movement than planned exercise – and reducing sedentary time,” the authors note.
“The latest guidelines are applicable to most individuals with diabetes, including youth, with a few exceptions and modifications,” lead author Jill A. Kanaley, PhD, said in a press release from the ACSM.
The key takeaway is that “all individuals [with type 2 diabetes] should engage in regular physical activity, reduce sedentary time, and break up sitting time with frequent activity breaks,” said Dr. Kanaley, a professor in the department of nutrition and exercise physiology, University of Missouri, Columbia.
“Exercise can play an important role in managing type 2 diabetes, and workouts can be modified to fit the abilities of most people,” she stressed.
And those with type 2 diabetes who want to lose weight “should consider workouts of moderately high volume for 4 to 5 days per week,” she added.
Six key tips for physical activity in adults with type 2 diabetes
The consensus statement gives six key tips for physical activity in adults with type 2 diabetes, as follows.
- Regular aerobic exercise improves glycemic management; meta-analyses have reported fewer daily hyperglycemic episodes and reductions in A1c of 0.5%-0.7%.
- High-intensity resistance exercise, when performed safely, is better than low-to-moderate intensity resistance exercise for glucose management and attenuation of insulin levels. Resistance exercise typically results in improvements of 10% to 15% in strength, bone mineral density, blood pressure, lipid profile, skeletal muscle mass, and insulin sensitivity.
- Exercise after meals, such as taking a walk after dinner at one’s own pace, takes advantage of the blood glucose-stabilizing effects of exercise.
- Reduce sedentary time by taking regular breaks for small “doses” of physical activity, which can modestly attenuate postprandial glucose and insulin levels, particularly in individuals with insulin resistance and a higher body mass index.
- To prevent hypoglycemia during or after exercise, people taking insulin or insulin secretagogues should increase carbohydrate intake, or if possible, reduce insulin.
- People who are taking beta blockers should not rely on a heart monitor to measure workout intensity. They could ask a certified exercise professional about using ratings of perceived exertion to track how a workout feels.
Other recommendations
The consensus statement also summarizes precautions that people with complications of type 2 diabetes (such as neuropathy, retinopathy, kidney disease, and hypertension) should take.
Low impact exercises for flexibility can help introduce sedentary people to physical activity, the consensus group writes. Balance exercises can be helpful for older adults.
Weight loss greater than 5% can benefit A1c, blood lipid, and blood pressure levels. Moderate exercise 4 to 5 days a week can reduce visceral fat.
In studies of youth with type 2 diabetes, intensive lifestyle interventions plus metformin were not superior to metformin alone for managing glycemia. Physical activity goals are the same for youth with or without diabetes.
Pregnant women with diabetes should participate in at least 20 to 30 minutes of moderate-intensity exercise most days of the week.
Participating in an exercise program before and after bariatric surgery may enhance surgical outcomes.
Dr. Kanaley has reported receiving a grant from the National Institutes of Health. Disclosures for the other authors are listed in the article.
A version of this article first appeared on Medscape.com.
Body fat linked to lower bone density, particularly in men
an analysis of data from a large, nationally representative sample has found.
Much previous research has suggested that obesity protects against fractures and loss of BMD for a variety of reasons, including the beneficial effects of weight-bearing on the skeleton and hormonal factors linked to body fat. But the new findings should prompt a reconsideration of the relationship between obesity and fracture risk, according to the investigators, whose study appears in the Journal of Clinical Endocrinology & Metabolism.
“While higher BMI [body mass index] is generally associated with higher bone density, our study demonstrates that lean and fat mass affect bone density differently and that obesity is not a guarantee against osteoporosis,” Rajesh K. Jain, MD, of the University of Chicago said in an interview.
Dr. Jain and a colleague, Tamara Vokes, MD, used multivariant modeling to examine the relationship between BMD and body composition of 10,814 men and women aged 20-59 years from the National Health and Nutrition Examination Survey (NHANES) 2011-2018. All underwent total body dual-energy x-ray absorptiometry scans.
Participants were stratified into sex-specific quartiles based on lean mass index (LMI; lean mass divided by height squared) and fat mass index (FMI; fat mass divided by height squared). Lean mass had a strong positive association with bone density, whereas fat mass had a moderate negative effect, the researchers found.
An additional kg/m2 of FMI was associated with a 0.10 lower T score, the number of standard deviations from the expected bone density of a young adult (P < .001). The negative effect was greater in men, who had a 0.13 lower T score per additional 1 kg/m2 of FMI, compared with 0.08 lower in women (P < .001). The effect was most pronounced in people in the highest FMI quartile.
Body composition is not a routine clinical measurement, Dr. Jain and Dr. Vokes noted. Prior studies of the effect of body composition on bone density have been limited by small patient numbers, referral bias, lack of racial or ethnic diversity, and the use of estimates rather than true measures of fat and lean tissue. NHANES is designed to mirror the U.S. population.
The researchers say when it comes to patients with obesity, the findings “should not dissuade clinicians from assessing bone density, particularly if other risk factors are present.”
Useful clinical proxies for body composition
Clinicians have no routine way to measure body composition in an office setting. As a result, Dr. Jain advised clinicians to look at factors that correlate with high body fat, such as the presence of diabetes, or with low lean mass, such as poor performance on physical activity measures like grip strength, when deciding whether to consider osteoporosis screening. Patients with obesity should undergo recommended bone density screening, especially if they have other risk factors such as older age, previous fracture, steroid use, or a family history of fracture.
Although some extra weight may have a beneficial loading effect, too much extra weight can lead to metabolic problems and restrict movement, according to Rodrigo J. Valderrábano, MD, medical director of clinical research for the Research Program in Men’s Health: Aging and Metabolism, Brigham and Women’s Hospital in Boston. “There’s a general sense that the extra weight is only good for your bones if you can carry it around,” said Dr. Valderrábano, who was not involved in the study.
More research is needed to understand why fat affects men and women differently, Dr. Jain noted. The researchers found that testosterone and estradiol values did not fully explain the variation.
Adipokines released by fat cells may be important in driving bone loss but were not measured in the study, Peter R. Ebeling, MD, president of the American Society of Bone and Mineral Research, said in an interview. Distribution of fractures in obesity suggests that a high FMI may preferentially affect cortical bone instead of trabecular bone, but further studies using high-resolution peripheral quantitative CT are required to confirm the difference.
Dr. Ebeling, who was not involved in the new study, agreed that the positive relationship between BMI and BMD has led to false reassurance that people with obesity may be protected from fragility fractures. “The take-home message for clinicians is that we should not neglect bone health in our patients with obesity, both male and female.”
Dr. Jain has reported receiving grant support from the Amgen Foundation and being a consultant for Radius Health. Dr. Vokes has reported being an investigator, consultant, and speaker for Radius Health, investigator and consultant for Takeda Pharmaceutical, and investigator for Ascendis Pharma. Dr. Valderrábano and Dr. Ebeling reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
an analysis of data from a large, nationally representative sample has found.
Much previous research has suggested that obesity protects against fractures and loss of BMD for a variety of reasons, including the beneficial effects of weight-bearing on the skeleton and hormonal factors linked to body fat. But the new findings should prompt a reconsideration of the relationship between obesity and fracture risk, according to the investigators, whose study appears in the Journal of Clinical Endocrinology & Metabolism.
“While higher BMI [body mass index] is generally associated with higher bone density, our study demonstrates that lean and fat mass affect bone density differently and that obesity is not a guarantee against osteoporosis,” Rajesh K. Jain, MD, of the University of Chicago said in an interview.
Dr. Jain and a colleague, Tamara Vokes, MD, used multivariant modeling to examine the relationship between BMD and body composition of 10,814 men and women aged 20-59 years from the National Health and Nutrition Examination Survey (NHANES) 2011-2018. All underwent total body dual-energy x-ray absorptiometry scans.
Participants were stratified into sex-specific quartiles based on lean mass index (LMI; lean mass divided by height squared) and fat mass index (FMI; fat mass divided by height squared). Lean mass had a strong positive association with bone density, whereas fat mass had a moderate negative effect, the researchers found.
An additional kg/m2 of FMI was associated with a 0.10 lower T score, the number of standard deviations from the expected bone density of a young adult (P < .001). The negative effect was greater in men, who had a 0.13 lower T score per additional 1 kg/m2 of FMI, compared with 0.08 lower in women (P < .001). The effect was most pronounced in people in the highest FMI quartile.
Body composition is not a routine clinical measurement, Dr. Jain and Dr. Vokes noted. Prior studies of the effect of body composition on bone density have been limited by small patient numbers, referral bias, lack of racial or ethnic diversity, and the use of estimates rather than true measures of fat and lean tissue. NHANES is designed to mirror the U.S. population.
The researchers say when it comes to patients with obesity, the findings “should not dissuade clinicians from assessing bone density, particularly if other risk factors are present.”
Useful clinical proxies for body composition
Clinicians have no routine way to measure body composition in an office setting. As a result, Dr. Jain advised clinicians to look at factors that correlate with high body fat, such as the presence of diabetes, or with low lean mass, such as poor performance on physical activity measures like grip strength, when deciding whether to consider osteoporosis screening. Patients with obesity should undergo recommended bone density screening, especially if they have other risk factors such as older age, previous fracture, steroid use, or a family history of fracture.
Although some extra weight may have a beneficial loading effect, too much extra weight can lead to metabolic problems and restrict movement, according to Rodrigo J. Valderrábano, MD, medical director of clinical research for the Research Program in Men’s Health: Aging and Metabolism, Brigham and Women’s Hospital in Boston. “There’s a general sense that the extra weight is only good for your bones if you can carry it around,” said Dr. Valderrábano, who was not involved in the study.
More research is needed to understand why fat affects men and women differently, Dr. Jain noted. The researchers found that testosterone and estradiol values did not fully explain the variation.
Adipokines released by fat cells may be important in driving bone loss but were not measured in the study, Peter R. Ebeling, MD, president of the American Society of Bone and Mineral Research, said in an interview. Distribution of fractures in obesity suggests that a high FMI may preferentially affect cortical bone instead of trabecular bone, but further studies using high-resolution peripheral quantitative CT are required to confirm the difference.
Dr. Ebeling, who was not involved in the new study, agreed that the positive relationship between BMI and BMD has led to false reassurance that people with obesity may be protected from fragility fractures. “The take-home message for clinicians is that we should not neglect bone health in our patients with obesity, both male and female.”
Dr. Jain has reported receiving grant support from the Amgen Foundation and being a consultant for Radius Health. Dr. Vokes has reported being an investigator, consultant, and speaker for Radius Health, investigator and consultant for Takeda Pharmaceutical, and investigator for Ascendis Pharma. Dr. Valderrábano and Dr. Ebeling reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
an analysis of data from a large, nationally representative sample has found.
Much previous research has suggested that obesity protects against fractures and loss of BMD for a variety of reasons, including the beneficial effects of weight-bearing on the skeleton and hormonal factors linked to body fat. But the new findings should prompt a reconsideration of the relationship between obesity and fracture risk, according to the investigators, whose study appears in the Journal of Clinical Endocrinology & Metabolism.
“While higher BMI [body mass index] is generally associated with higher bone density, our study demonstrates that lean and fat mass affect bone density differently and that obesity is not a guarantee against osteoporosis,” Rajesh K. Jain, MD, of the University of Chicago said in an interview.
Dr. Jain and a colleague, Tamara Vokes, MD, used multivariant modeling to examine the relationship between BMD and body composition of 10,814 men and women aged 20-59 years from the National Health and Nutrition Examination Survey (NHANES) 2011-2018. All underwent total body dual-energy x-ray absorptiometry scans.
Participants were stratified into sex-specific quartiles based on lean mass index (LMI; lean mass divided by height squared) and fat mass index (FMI; fat mass divided by height squared). Lean mass had a strong positive association with bone density, whereas fat mass had a moderate negative effect, the researchers found.
An additional kg/m2 of FMI was associated with a 0.10 lower T score, the number of standard deviations from the expected bone density of a young adult (P < .001). The negative effect was greater in men, who had a 0.13 lower T score per additional 1 kg/m2 of FMI, compared with 0.08 lower in women (P < .001). The effect was most pronounced in people in the highest FMI quartile.
Body composition is not a routine clinical measurement, Dr. Jain and Dr. Vokes noted. Prior studies of the effect of body composition on bone density have been limited by small patient numbers, referral bias, lack of racial or ethnic diversity, and the use of estimates rather than true measures of fat and lean tissue. NHANES is designed to mirror the U.S. population.
The researchers say when it comes to patients with obesity, the findings “should not dissuade clinicians from assessing bone density, particularly if other risk factors are present.”
Useful clinical proxies for body composition
Clinicians have no routine way to measure body composition in an office setting. As a result, Dr. Jain advised clinicians to look at factors that correlate with high body fat, such as the presence of diabetes, or with low lean mass, such as poor performance on physical activity measures like grip strength, when deciding whether to consider osteoporosis screening. Patients with obesity should undergo recommended bone density screening, especially if they have other risk factors such as older age, previous fracture, steroid use, or a family history of fracture.
Although some extra weight may have a beneficial loading effect, too much extra weight can lead to metabolic problems and restrict movement, according to Rodrigo J. Valderrábano, MD, medical director of clinical research for the Research Program in Men’s Health: Aging and Metabolism, Brigham and Women’s Hospital in Boston. “There’s a general sense that the extra weight is only good for your bones if you can carry it around,” said Dr. Valderrábano, who was not involved in the study.
More research is needed to understand why fat affects men and women differently, Dr. Jain noted. The researchers found that testosterone and estradiol values did not fully explain the variation.
Adipokines released by fat cells may be important in driving bone loss but were not measured in the study, Peter R. Ebeling, MD, president of the American Society of Bone and Mineral Research, said in an interview. Distribution of fractures in obesity suggests that a high FMI may preferentially affect cortical bone instead of trabecular bone, but further studies using high-resolution peripheral quantitative CT are required to confirm the difference.
Dr. Ebeling, who was not involved in the new study, agreed that the positive relationship between BMI and BMD has led to false reassurance that people with obesity may be protected from fragility fractures. “The take-home message for clinicians is that we should not neglect bone health in our patients with obesity, both male and female.”
Dr. Jain has reported receiving grant support from the Amgen Foundation and being a consultant for Radius Health. Dr. Vokes has reported being an investigator, consultant, and speaker for Radius Health, investigator and consultant for Takeda Pharmaceutical, and investigator for Ascendis Pharma. Dr. Valderrábano and Dr. Ebeling reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM