User login
In epilepsy, brain-responsive stimulation passes long-term tests
Two new long-term studies, one an extension trial and the other an analysis of real-world experience, show that Both studies showed that the benefit from the devices increased over time.
That accruing benefit may be because of improved protocols as clinicians gain experience with the device or because of network remodeling that occurs over time as seizures are controlled. “I think it’s both,” said Martha Morrell, MD, a clinical professor of neurology at Stanford (Calif.) University and chief medical officer at NeuroPace, the company that has marketed the device since it gained FDA approval in 2013.
In both studies, the slope of improvement over time was similar, but the real-world study showed greater improvement at the beginning of treatment. “I think the slopes represent physiological changes, but the fact that [the real-world study] starts with better outcomes is, I think, directly attributable to learning. When the long-term study was started in 2004, this had never been done before, and we had to make a highly educated guess about what we should do, and the initial stimulatory parameters were programmed in a way that’s very similar to what was used for movement disorders,” Dr. Morrell said in an interview.
The long-term treatment study appeared online July 20 in the journal Neurology, while the real-world analysis was published July 13 in Epilepsia.
An alternative option
Medications can effectively treat some seizures, but 30%-40% of patients must turn to other options for control. Surgery can sometimes be curative, but is not suitable for some patients. Other stimulation devices include vagus nerve stimulation (VNS), which sends pulses from a chest implant to the vagus nerve, reducing epileptic attacks through an unknown mechanism. Deep brain stimulation (DBS) places electrodes that deliver stimulation to the anterior nucleus of the thalamus, which can spread initially localized seizures.
The RNS device consists of a neurostimulator implanted cranially and connected to leads that are placed based on the individual patient’s seizure focus or foci. It also continuously monitors brain activity and delivers stimulation only when its signal suggests the beginning of a seizure.
That capacity for recording is a key benefit because the information can be stored and analyzed, according to Vikram Rao, MD, PhD, a coinvestigator in the real-world trial and an associate professor and the epilepsy division chief at the University of California, San Francisco, which was one of the trial centers. “You know more precisely than we previously did how many seizures a patient is having. Many of our patients are not able to quantify their seizures with perfect accuracy, so we’re better quantifying their seizure burden,” Dr. Rao said in an interview.
The ability to monitor patients can also improve clinical management. Dr. Morrell recounted an elderly patient who for many years has driven 5 hours for appointments. Recently she was able to review his data from the RNS System remotely. She determined that he was doing fine and, after a telephone consultation, told him he didn’t need to come in for a scheduled visit.
Real-world analysis
In the real-world analysis, researchers led by Babak Razavi, PhD, and Casey Halpern, MD, at Stanford University conducted a chart review of 150 patients at eight centers who underwent treatment with the RNS system between 2013 and 2018. All patients were followed at least 1 year, with a mean of 2.3 years. Patients had a median of 7.7 disabling seizures per month. The mean value was 52 and the numbers ranged from 0.1 to 3,000. A total of 60% had abnormal brain MRI findings.
At 1 year, subjects achieved a mean 67% decrease in seizure frequency (interquartile range, 50%-94%). At 2 years, that grew to 77%; at 3 or more years, 84%. There was no significant difference in seizure reduction at 1 year according to age, age at epilepsy onset, duration of epilepsy, location of seizure foci, presence of brain MRI abnormalities, prior intracranial monitoring, prior epilepsy surgery, or prior VNS treatment. When patients who underwent a resection at the time of RNS placement were excluded, the results were similar. There were no significant differences in outcome by center.
A total of 11.3% of patients experienced a device-related serious adverse event, and 4% developed infections. The rate of infection was not significantly different between patients who had the neurostimulator and leads implanted alone (3.0%) and patients who had intracranial EEG diagnostic monitoring (ICM) electrodes removed at the same time (6.1%; P = .38).
Although about one-third of the patients who started the long-term study dropped out before completion, most were because the participants moved away from treatment centers, according to Dr. Morrell, and other evidence points squarely to patient satisfaction. “At the end of the battery’s longevity, the neurostimulator needs to be replaced. It’s an outpatient, 45-minute procedure. Over 90% of patients chose to have it replaced. It’s not the answer for everybody, but the substantial majority of patients choose to continue,” she said.
Extension trial
The open-label extension trial, led by Dileep Nair, MD, of the Cleveland Clinic Foundation and Dr. Morrell, followed 230 of the 256 patients who participated in 2-year phase 3 study or feasibility studies, extending device usage to 9 years. A total of 162 completed follow-up (mean, 7.5 years). The median reduction of seizure frequency was 58% at the end of year 3, and 75% by year 9 (P < .0001; Wilcoxon signed rank). Although patient population enrichment could have explained this observation, other analyses confirmed that the improvement was real.
Nearly 75% had at least a 50% reduction in seizure frequency; 35% had a 90% or greater reduction in seizure frequency. Some patients (18.4%) had at least a full year with no seizures, and 62% who had a 1-year seizure-free period experienced no seizures at the latest follow-up. Overall, 21% had no seizures in the last 6 months of follow-up.
For those with a seizure-free period of more than 1 year, the average duration was 3.2 years (range, 1.04-9.6 years). There was no difference in response among patients based on previous antiseizure medication use or previous epilepsy surgery, VNS treatment, or intracranial monitoring, and there were no differences by patient age at enrollment, age of seizure onset, brain imaging abnormality, seizure onset locality, or number of foci.
The researchers noted improvement in overall Quality of Life in Epilepsy Inventory–89 scores at 1 year (mean, +3.2; P < .0001), which continued through year 9 (mean, +1.9; P < .05). Improvements were also seen in epilepsy targeted (mean, +4.5; P < .001) and cognitive domains (mean, +2.5; P = .005). Risk of infection was 4.1% per procedure, and 12.1% of subjects overall experienced a serious device-related implant infection. Of 35 infections, 16 led to device removal.
The extension study was funded by NeuroPace. NeuroPace supported data entry and institutional review board submission for the real-world trial. Dr. Morrell owns stock and is an employee of NeuroPace. Dr Rao has received support from and/or consulted for NeuroPace.
SOURCE: Nair DR et al. Neurology. 2020 Jul 20. doi: 10.1212/WNL.0000000000010154. Razavi B et al. Epilepsia. 2020 Jul 13. doi: 10.1111/epi.16593.
Two new long-term studies, one an extension trial and the other an analysis of real-world experience, show that Both studies showed that the benefit from the devices increased over time.
That accruing benefit may be because of improved protocols as clinicians gain experience with the device or because of network remodeling that occurs over time as seizures are controlled. “I think it’s both,” said Martha Morrell, MD, a clinical professor of neurology at Stanford (Calif.) University and chief medical officer at NeuroPace, the company that has marketed the device since it gained FDA approval in 2013.
In both studies, the slope of improvement over time was similar, but the real-world study showed greater improvement at the beginning of treatment. “I think the slopes represent physiological changes, but the fact that [the real-world study] starts with better outcomes is, I think, directly attributable to learning. When the long-term study was started in 2004, this had never been done before, and we had to make a highly educated guess about what we should do, and the initial stimulatory parameters were programmed in a way that’s very similar to what was used for movement disorders,” Dr. Morrell said in an interview.
The long-term treatment study appeared online July 20 in the journal Neurology, while the real-world analysis was published July 13 in Epilepsia.
An alternative option
Medications can effectively treat some seizures, but 30%-40% of patients must turn to other options for control. Surgery can sometimes be curative, but is not suitable for some patients. Other stimulation devices include vagus nerve stimulation (VNS), which sends pulses from a chest implant to the vagus nerve, reducing epileptic attacks through an unknown mechanism. Deep brain stimulation (DBS) places electrodes that deliver stimulation to the anterior nucleus of the thalamus, which can spread initially localized seizures.
The RNS device consists of a neurostimulator implanted cranially and connected to leads that are placed based on the individual patient’s seizure focus or foci. It also continuously monitors brain activity and delivers stimulation only when its signal suggests the beginning of a seizure.
That capacity for recording is a key benefit because the information can be stored and analyzed, according to Vikram Rao, MD, PhD, a coinvestigator in the real-world trial and an associate professor and the epilepsy division chief at the University of California, San Francisco, which was one of the trial centers. “You know more precisely than we previously did how many seizures a patient is having. Many of our patients are not able to quantify their seizures with perfect accuracy, so we’re better quantifying their seizure burden,” Dr. Rao said in an interview.
The ability to monitor patients can also improve clinical management. Dr. Morrell recounted an elderly patient who for many years has driven 5 hours for appointments. Recently she was able to review his data from the RNS System remotely. She determined that he was doing fine and, after a telephone consultation, told him he didn’t need to come in for a scheduled visit.
Real-world analysis
In the real-world analysis, researchers led by Babak Razavi, PhD, and Casey Halpern, MD, at Stanford University conducted a chart review of 150 patients at eight centers who underwent treatment with the RNS system between 2013 and 2018. All patients were followed at least 1 year, with a mean of 2.3 years. Patients had a median of 7.7 disabling seizures per month. The mean value was 52 and the numbers ranged from 0.1 to 3,000. A total of 60% had abnormal brain MRI findings.
At 1 year, subjects achieved a mean 67% decrease in seizure frequency (interquartile range, 50%-94%). At 2 years, that grew to 77%; at 3 or more years, 84%. There was no significant difference in seizure reduction at 1 year according to age, age at epilepsy onset, duration of epilepsy, location of seizure foci, presence of brain MRI abnormalities, prior intracranial monitoring, prior epilepsy surgery, or prior VNS treatment. When patients who underwent a resection at the time of RNS placement were excluded, the results were similar. There were no significant differences in outcome by center.
A total of 11.3% of patients experienced a device-related serious adverse event, and 4% developed infections. The rate of infection was not significantly different between patients who had the neurostimulator and leads implanted alone (3.0%) and patients who had intracranial EEG diagnostic monitoring (ICM) electrodes removed at the same time (6.1%; P = .38).
Although about one-third of the patients who started the long-term study dropped out before completion, most were because the participants moved away from treatment centers, according to Dr. Morrell, and other evidence points squarely to patient satisfaction. “At the end of the battery’s longevity, the neurostimulator needs to be replaced. It’s an outpatient, 45-minute procedure. Over 90% of patients chose to have it replaced. It’s not the answer for everybody, but the substantial majority of patients choose to continue,” she said.
Extension trial
The open-label extension trial, led by Dileep Nair, MD, of the Cleveland Clinic Foundation and Dr. Morrell, followed 230 of the 256 patients who participated in 2-year phase 3 study or feasibility studies, extending device usage to 9 years. A total of 162 completed follow-up (mean, 7.5 years). The median reduction of seizure frequency was 58% at the end of year 3, and 75% by year 9 (P < .0001; Wilcoxon signed rank). Although patient population enrichment could have explained this observation, other analyses confirmed that the improvement was real.
Nearly 75% had at least a 50% reduction in seizure frequency; 35% had a 90% or greater reduction in seizure frequency. Some patients (18.4%) had at least a full year with no seizures, and 62% who had a 1-year seizure-free period experienced no seizures at the latest follow-up. Overall, 21% had no seizures in the last 6 months of follow-up.
For those with a seizure-free period of more than 1 year, the average duration was 3.2 years (range, 1.04-9.6 years). There was no difference in response among patients based on previous antiseizure medication use or previous epilepsy surgery, VNS treatment, or intracranial monitoring, and there were no differences by patient age at enrollment, age of seizure onset, brain imaging abnormality, seizure onset locality, or number of foci.
The researchers noted improvement in overall Quality of Life in Epilepsy Inventory–89 scores at 1 year (mean, +3.2; P < .0001), which continued through year 9 (mean, +1.9; P < .05). Improvements were also seen in epilepsy targeted (mean, +4.5; P < .001) and cognitive domains (mean, +2.5; P = .005). Risk of infection was 4.1% per procedure, and 12.1% of subjects overall experienced a serious device-related implant infection. Of 35 infections, 16 led to device removal.
The extension study was funded by NeuroPace. NeuroPace supported data entry and institutional review board submission for the real-world trial. Dr. Morrell owns stock and is an employee of NeuroPace. Dr Rao has received support from and/or consulted for NeuroPace.
SOURCE: Nair DR et al. Neurology. 2020 Jul 20. doi: 10.1212/WNL.0000000000010154. Razavi B et al. Epilepsia. 2020 Jul 13. doi: 10.1111/epi.16593.
Two new long-term studies, one an extension trial and the other an analysis of real-world experience, show that Both studies showed that the benefit from the devices increased over time.
That accruing benefit may be because of improved protocols as clinicians gain experience with the device or because of network remodeling that occurs over time as seizures are controlled. “I think it’s both,” said Martha Morrell, MD, a clinical professor of neurology at Stanford (Calif.) University and chief medical officer at NeuroPace, the company that has marketed the device since it gained FDA approval in 2013.
In both studies, the slope of improvement over time was similar, but the real-world study showed greater improvement at the beginning of treatment. “I think the slopes represent physiological changes, but the fact that [the real-world study] starts with better outcomes is, I think, directly attributable to learning. When the long-term study was started in 2004, this had never been done before, and we had to make a highly educated guess about what we should do, and the initial stimulatory parameters were programmed in a way that’s very similar to what was used for movement disorders,” Dr. Morrell said in an interview.
The long-term treatment study appeared online July 20 in the journal Neurology, while the real-world analysis was published July 13 in Epilepsia.
An alternative option
Medications can effectively treat some seizures, but 30%-40% of patients must turn to other options for control. Surgery can sometimes be curative, but is not suitable for some patients. Other stimulation devices include vagus nerve stimulation (VNS), which sends pulses from a chest implant to the vagus nerve, reducing epileptic attacks through an unknown mechanism. Deep brain stimulation (DBS) places electrodes that deliver stimulation to the anterior nucleus of the thalamus, which can spread initially localized seizures.
The RNS device consists of a neurostimulator implanted cranially and connected to leads that are placed based on the individual patient’s seizure focus or foci. It also continuously monitors brain activity and delivers stimulation only when its signal suggests the beginning of a seizure.
That capacity for recording is a key benefit because the information can be stored and analyzed, according to Vikram Rao, MD, PhD, a coinvestigator in the real-world trial and an associate professor and the epilepsy division chief at the University of California, San Francisco, which was one of the trial centers. “You know more precisely than we previously did how many seizures a patient is having. Many of our patients are not able to quantify their seizures with perfect accuracy, so we’re better quantifying their seizure burden,” Dr. Rao said in an interview.
The ability to monitor patients can also improve clinical management. Dr. Morrell recounted an elderly patient who for many years has driven 5 hours for appointments. Recently she was able to review his data from the RNS System remotely. She determined that he was doing fine and, after a telephone consultation, told him he didn’t need to come in for a scheduled visit.
Real-world analysis
In the real-world analysis, researchers led by Babak Razavi, PhD, and Casey Halpern, MD, at Stanford University conducted a chart review of 150 patients at eight centers who underwent treatment with the RNS system between 2013 and 2018. All patients were followed at least 1 year, with a mean of 2.3 years. Patients had a median of 7.7 disabling seizures per month. The mean value was 52 and the numbers ranged from 0.1 to 3,000. A total of 60% had abnormal brain MRI findings.
At 1 year, subjects achieved a mean 67% decrease in seizure frequency (interquartile range, 50%-94%). At 2 years, that grew to 77%; at 3 or more years, 84%. There was no significant difference in seizure reduction at 1 year according to age, age at epilepsy onset, duration of epilepsy, location of seizure foci, presence of brain MRI abnormalities, prior intracranial monitoring, prior epilepsy surgery, or prior VNS treatment. When patients who underwent a resection at the time of RNS placement were excluded, the results were similar. There were no significant differences in outcome by center.
A total of 11.3% of patients experienced a device-related serious adverse event, and 4% developed infections. The rate of infection was not significantly different between patients who had the neurostimulator and leads implanted alone (3.0%) and patients who had intracranial EEG diagnostic monitoring (ICM) electrodes removed at the same time (6.1%; P = .38).
Although about one-third of the patients who started the long-term study dropped out before completion, most were because the participants moved away from treatment centers, according to Dr. Morrell, and other evidence points squarely to patient satisfaction. “At the end of the battery’s longevity, the neurostimulator needs to be replaced. It’s an outpatient, 45-minute procedure. Over 90% of patients chose to have it replaced. It’s not the answer for everybody, but the substantial majority of patients choose to continue,” she said.
Extension trial
The open-label extension trial, led by Dileep Nair, MD, of the Cleveland Clinic Foundation and Dr. Morrell, followed 230 of the 256 patients who participated in 2-year phase 3 study or feasibility studies, extending device usage to 9 years. A total of 162 completed follow-up (mean, 7.5 years). The median reduction of seizure frequency was 58% at the end of year 3, and 75% by year 9 (P < .0001; Wilcoxon signed rank). Although patient population enrichment could have explained this observation, other analyses confirmed that the improvement was real.
Nearly 75% had at least a 50% reduction in seizure frequency; 35% had a 90% or greater reduction in seizure frequency. Some patients (18.4%) had at least a full year with no seizures, and 62% who had a 1-year seizure-free period experienced no seizures at the latest follow-up. Overall, 21% had no seizures in the last 6 months of follow-up.
For those with a seizure-free period of more than 1 year, the average duration was 3.2 years (range, 1.04-9.6 years). There was no difference in response among patients based on previous antiseizure medication use or previous epilepsy surgery, VNS treatment, or intracranial monitoring, and there were no differences by patient age at enrollment, age of seizure onset, brain imaging abnormality, seizure onset locality, or number of foci.
The researchers noted improvement in overall Quality of Life in Epilepsy Inventory–89 scores at 1 year (mean, +3.2; P < .0001), which continued through year 9 (mean, +1.9; P < .05). Improvements were also seen in epilepsy targeted (mean, +4.5; P < .001) and cognitive domains (mean, +2.5; P = .005). Risk of infection was 4.1% per procedure, and 12.1% of subjects overall experienced a serious device-related implant infection. Of 35 infections, 16 led to device removal.
The extension study was funded by NeuroPace. NeuroPace supported data entry and institutional review board submission for the real-world trial. Dr. Morrell owns stock and is an employee of NeuroPace. Dr Rao has received support from and/or consulted for NeuroPace.
SOURCE: Nair DR et al. Neurology. 2020 Jul 20. doi: 10.1212/WNL.0000000000010154. Razavi B et al. Epilepsia. 2020 Jul 13. doi: 10.1111/epi.16593.
FROM EPILEPSIA AND FROM NEUROLOGY
Psychiatrists report rare case of woman who thinks she’s a chicken
LEUVEN, Belgium — A 54-year-old woman has suffered the delusion of thinking she is a chicken for 24 hours. This very rare condition, known as zoanthropy, in which people think they are an animal is often not recognised, say researchers from the University of Leuven.
Zoanthropy can include people believing they are, or behaving like, any kind of animal: from a dog, to a lion or tiger, crocodile, snake, or bee.
It’s important to recognise this as a potential symptom of something serious, say the researchers in the July issue of the Belgian Journal of Psychiatry, Tijdschrift voor Psychiatrie.
“Additional investigations with brain imaging and electroencephalogram are therefore advised,” say the authors.
Psychiatrists Need to Be Aware That Clinical Zoanthropy Exists
In their paper, they describe the case of the woman who briefly thought she was a chicken, which was followed by her having a generalized epileptic seizure.
“Clinically, we saw a lady who perspired profusely, trembled, blew up her cheeks, and ... seemed to imitate a chicken, [making noises] like clucking, cackling, and crowing like a rooster,” they say.
“After about 10 minutes she seemed to tighten her muscles for a few seconds, her face turned red and for a short time she didn’t react. These symptoms repeated themselves at intervals of a few minutes [and her] consciousness was fluctuating,” with the patient “disoriented in time and space.”
Lead author Dr Athena Beckers of University Psychiatric Centre, KU Leuven, Belgium, said in an interview with MediQuality: “With only 56 case descriptions in the medical literature from 1850 to the present day, the condition is rare. It amounts to about one description every 3 years.
“We suspect, however, that the delusion is not always noticed: the patient shows bizarre behaviour or makes animal sounds, it is probably often catalogued under the general term ‘psychosis’.”
Dr Beckers adds that it is important that the symptoms are recognised, because of the possible underlying causes which can include epilepsy. So this might require a different or complementary treatment “with, for example, antiepileptic drugs”.
“I myself have only seen this type of delusion once, but I ... heard anecdotal stories from other patients whose family member, for example with schizophrenia, sometimes thought he was a cow [during] ... a psychosis.
“After the publication of my article I was also contacted by someone who told me they had experienced the same thing 30 years ago – he thought he was a chicken.
“I think it’s a good thing that we psychiatrists are aware of the fact that clinical zoanthropy exists and may require additional research,” she observed.
Fortunately, this woman’s experience ended well. After about one year of disability, the patient was able to return to work progressively. Her mood remained stable and there were no more psychotic symptoms or any indication of epileptic episodes.
Such Delusions Are Rare
Dr Georges Otte, a recently retired neuropsychiatrist who formerly worked at Ghent University, Belgium, gave his thoughts to Mediquality: “The interface between neurology and psychiatry ... is a fertile meadow on which many crops thrive. But it is in the darkest corners of psychosis that one finds the most bizarre and also rarest excesses.”
There are a number of delusions of identity, said Dr Otte.
These include Cotard’s syndrome, a rare condition marked by the false belief that the person or their body parts are dead, dying, or don’t exist, or Capgras delusion, where the affected person believes that a spouse or close family member has been replaced with an imposter. Delusions can also occur as a result of substance abuse, for example after using psilocybin (magic mushrooms), he added.
“Delusions in which patients are convinced of ‘shape shifting’ (man to animal) are quite rare,” Dr Otte observed.
“In the literature we know that lycanthropy [a person thinks he or she is turning into a werewolf],” has been reported, and has “apparently inspired many authors of horror stories,” he added.
“But it’s not every day that as a psychiatrist, you will encounter such an extreme psychotic depersonalization as someone turning into a chicken.”
This article first appeared on Medscape.com.
LEUVEN, Belgium — A 54-year-old woman has suffered the delusion of thinking she is a chicken for 24 hours. This very rare condition, known as zoanthropy, in which people think they are an animal is often not recognised, say researchers from the University of Leuven.
Zoanthropy can include people believing they are, or behaving like, any kind of animal: from a dog, to a lion or tiger, crocodile, snake, or bee.
It’s important to recognise this as a potential symptom of something serious, say the researchers in the July issue of the Belgian Journal of Psychiatry, Tijdschrift voor Psychiatrie.
“Additional investigations with brain imaging and electroencephalogram are therefore advised,” say the authors.
Psychiatrists Need to Be Aware That Clinical Zoanthropy Exists
In their paper, they describe the case of the woman who briefly thought she was a chicken, which was followed by her having a generalized epileptic seizure.
“Clinically, we saw a lady who perspired profusely, trembled, blew up her cheeks, and ... seemed to imitate a chicken, [making noises] like clucking, cackling, and crowing like a rooster,” they say.
“After about 10 minutes she seemed to tighten her muscles for a few seconds, her face turned red and for a short time she didn’t react. These symptoms repeated themselves at intervals of a few minutes [and her] consciousness was fluctuating,” with the patient “disoriented in time and space.”
Lead author Dr Athena Beckers of University Psychiatric Centre, KU Leuven, Belgium, said in an interview with MediQuality: “With only 56 case descriptions in the medical literature from 1850 to the present day, the condition is rare. It amounts to about one description every 3 years.
“We suspect, however, that the delusion is not always noticed: the patient shows bizarre behaviour or makes animal sounds, it is probably often catalogued under the general term ‘psychosis’.”
Dr Beckers adds that it is important that the symptoms are recognised, because of the possible underlying causes which can include epilepsy. So this might require a different or complementary treatment “with, for example, antiepileptic drugs”.
“I myself have only seen this type of delusion once, but I ... heard anecdotal stories from other patients whose family member, for example with schizophrenia, sometimes thought he was a cow [during] ... a psychosis.
“After the publication of my article I was also contacted by someone who told me they had experienced the same thing 30 years ago – he thought he was a chicken.
“I think it’s a good thing that we psychiatrists are aware of the fact that clinical zoanthropy exists and may require additional research,” she observed.
Fortunately, this woman’s experience ended well. After about one year of disability, the patient was able to return to work progressively. Her mood remained stable and there were no more psychotic symptoms or any indication of epileptic episodes.
Such Delusions Are Rare
Dr Georges Otte, a recently retired neuropsychiatrist who formerly worked at Ghent University, Belgium, gave his thoughts to Mediquality: “The interface between neurology and psychiatry ... is a fertile meadow on which many crops thrive. But it is in the darkest corners of psychosis that one finds the most bizarre and also rarest excesses.”
There are a number of delusions of identity, said Dr Otte.
These include Cotard’s syndrome, a rare condition marked by the false belief that the person or their body parts are dead, dying, or don’t exist, or Capgras delusion, where the affected person believes that a spouse or close family member has been replaced with an imposter. Delusions can also occur as a result of substance abuse, for example after using psilocybin (magic mushrooms), he added.
“Delusions in which patients are convinced of ‘shape shifting’ (man to animal) are quite rare,” Dr Otte observed.
“In the literature we know that lycanthropy [a person thinks he or she is turning into a werewolf],” has been reported, and has “apparently inspired many authors of horror stories,” he added.
“But it’s not every day that as a psychiatrist, you will encounter such an extreme psychotic depersonalization as someone turning into a chicken.”
This article first appeared on Medscape.com.
LEUVEN, Belgium — A 54-year-old woman has suffered the delusion of thinking she is a chicken for 24 hours. This very rare condition, known as zoanthropy, in which people think they are an animal is often not recognised, say researchers from the University of Leuven.
Zoanthropy can include people believing they are, or behaving like, any kind of animal: from a dog, to a lion or tiger, crocodile, snake, or bee.
It’s important to recognise this as a potential symptom of something serious, say the researchers in the July issue of the Belgian Journal of Psychiatry, Tijdschrift voor Psychiatrie.
“Additional investigations with brain imaging and electroencephalogram are therefore advised,” say the authors.
Psychiatrists Need to Be Aware That Clinical Zoanthropy Exists
In their paper, they describe the case of the woman who briefly thought she was a chicken, which was followed by her having a generalized epileptic seizure.
“Clinically, we saw a lady who perspired profusely, trembled, blew up her cheeks, and ... seemed to imitate a chicken, [making noises] like clucking, cackling, and crowing like a rooster,” they say.
“After about 10 minutes she seemed to tighten her muscles for a few seconds, her face turned red and for a short time she didn’t react. These symptoms repeated themselves at intervals of a few minutes [and her] consciousness was fluctuating,” with the patient “disoriented in time and space.”
Lead author Dr Athena Beckers of University Psychiatric Centre, KU Leuven, Belgium, said in an interview with MediQuality: “With only 56 case descriptions in the medical literature from 1850 to the present day, the condition is rare. It amounts to about one description every 3 years.
“We suspect, however, that the delusion is not always noticed: the patient shows bizarre behaviour or makes animal sounds, it is probably often catalogued under the general term ‘psychosis’.”
Dr Beckers adds that it is important that the symptoms are recognised, because of the possible underlying causes which can include epilepsy. So this might require a different or complementary treatment “with, for example, antiepileptic drugs”.
“I myself have only seen this type of delusion once, but I ... heard anecdotal stories from other patients whose family member, for example with schizophrenia, sometimes thought he was a cow [during] ... a psychosis.
“After the publication of my article I was also contacted by someone who told me they had experienced the same thing 30 years ago – he thought he was a chicken.
“I think it’s a good thing that we psychiatrists are aware of the fact that clinical zoanthropy exists and may require additional research,” she observed.
Fortunately, this woman’s experience ended well. After about one year of disability, the patient was able to return to work progressively. Her mood remained stable and there were no more psychotic symptoms or any indication of epileptic episodes.
Such Delusions Are Rare
Dr Georges Otte, a recently retired neuropsychiatrist who formerly worked at Ghent University, Belgium, gave his thoughts to Mediquality: “The interface between neurology and psychiatry ... is a fertile meadow on which many crops thrive. But it is in the darkest corners of psychosis that one finds the most bizarre and also rarest excesses.”
There are a number of delusions of identity, said Dr Otte.
These include Cotard’s syndrome, a rare condition marked by the false belief that the person or their body parts are dead, dying, or don’t exist, or Capgras delusion, where the affected person believes that a spouse or close family member has been replaced with an imposter. Delusions can also occur as a result of substance abuse, for example after using psilocybin (magic mushrooms), he added.
“Delusions in which patients are convinced of ‘shape shifting’ (man to animal) are quite rare,” Dr Otte observed.
“In the literature we know that lycanthropy [a person thinks he or she is turning into a werewolf],” has been reported, and has “apparently inspired many authors of horror stories,” he added.
“But it’s not every day that as a psychiatrist, you will encounter such an extreme psychotic depersonalization as someone turning into a chicken.”
This article first appeared on Medscape.com.
Move over supplements, here come medical foods
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
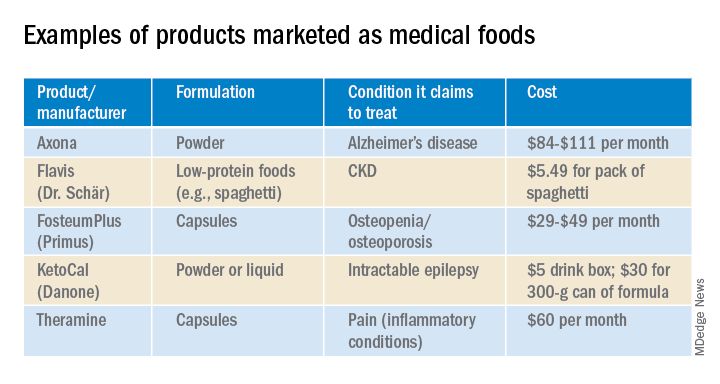
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.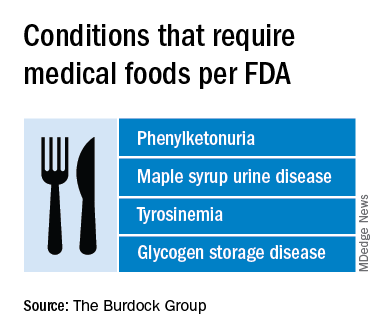
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.
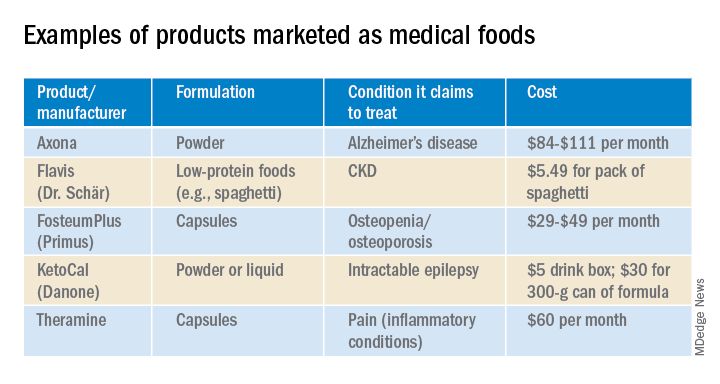
In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.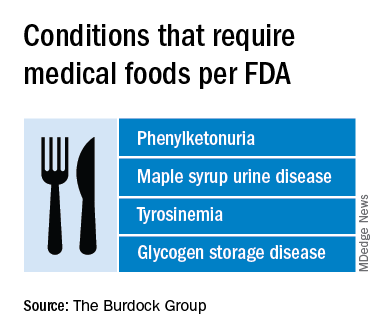
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.
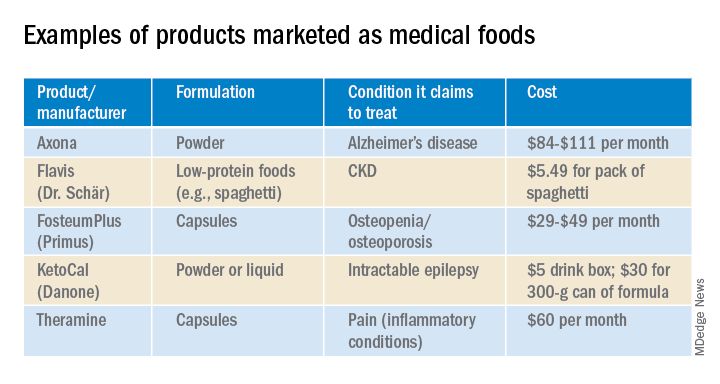
In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
As the Food and Drug Administration focuses on other issues, companies, both big and small, are looking to boost physician and consumer interest in their “medical foods” – products that fall somewhere between drugs and supplements and promise to mitigate symptoms, or even address underlying pathologies, of a range of diseases.
Manufacturers now market an array of medical foods, ranging from powders and capsules for Alzheimer disease to low-protein spaghetti for chronic kidney disease (CKD). The FDA has not been completely absent; it takes a narrow view of what medical conditions qualify for treatment with food products and has warned some manufacturers that their misbranded products are acting more like unapproved drugs.
By the FDA’s definition, medical food is limited to products that provide crucial therapy for patients with inborn errors of metabolism (IEM). An example is specialized baby formula for infants with phenylketonuria. Unlike supplements, medical foods are supposed to be used under the supervision of a physician. This has prompted some sales reps to turn up in the clinic, and most manufacturers have online approval forms for doctors to sign. Manufacturers, advisers, and regulators were interviewed for a closer look at this burgeoning industry.
The market
The global market for medical foods – about $18 billion in 2019 – is expected to grow steadily in the near future. It is drawing more interest, especially in Europe, where medical foods are more accepted by physicians and consumers, Meghan Donnelly, MS, RDN, said in an interview. She is a registered dietitian who conducts physician outreach in the United States for Flavis, a division of Dr. Schär. That company, based in northern Italy, started out targeting IEMs but now also sells gluten-free foods for celiac disease and low-protein foods for CKD.
It is still a niche market in the United States – and isn’t likely to ever approach the size of the supplement market, according to Marcus Charuvastra, the managing director of Targeted Medical Pharma, which markets Theramine capsules for pain management, among many other products. But it could still be a big win for a manufacturer if they get a small slice of a big market, such as for Alzheimer disease.
Defining medical food
According to an update of the Orphan Drug Act in 1988, a medical food is “a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation.” The FDA issued regulations to accompany that law in 1993 but has since only issued a guidance document that is not legally binding.
Medical foods are not drugs and they are not supplements (the latter are intended only for healthy people). The FDA doesn’t require formal approval of a medical food, but, by law, the ingredients must be generally recognized as safe, and manufacturers must follow good manufacturing practices. However, the agency has taken a narrow view of what conditions require medical foods.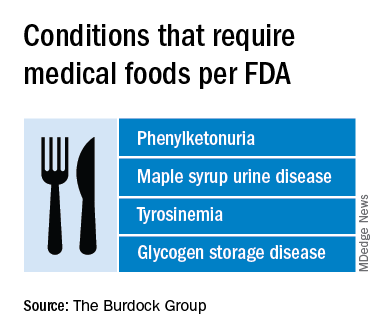
Policing medical foods hasn’t been a priority for the FDA, which is why there has been a proliferation of products that don’t meet the FDA’s view of the statutory definition of medical foods, according to Miriam Guggenheim, a food and drug law attorney in Washington, D.C. The FDA usually takes enforcement action when it sees a risk to the public’s health.
The agency’s stance has led to confusion – among manufacturers, physicians, consumers, and even regulators – making the market a kind of Wild West, according to Paul Hyman, a Washington, D.C.–based attorney who has represented medical food companies.
George A. Burdock, PhD, an Orlando-based regulatory consultant who has worked with medical food makers, believes the FDA will be forced to expand their narrow definition. He foresees a reconsideration of many medical food products in light of an October 2019 White House executive order prohibiting federal agencies from issuing guidance in lieu of rules.
Manufacturers and the FDA differ
One example of a product about which regulators and manufacturers differ is Theramine, which is described as “specially designed to supply the nervous system with the fuel it needs to meet the altered metabolic requirements of chronic pain and inflammatory disorders.”
It is not considered a medical food by the FDA, and the company has had numerous discussions with the agency about their diverging views, according to Mr. Charuvastra. “We’ve had our warning letters and we’ve had our sit downs, and we just had an inspection.”
Targeted Medical Pharma continues to market its products as medical foods but steers away from making any claims that they are like drugs, he said.
Confusion about medical foods has been exposed in the California Workers’ Compensation System by Leslie Wilson, PhD, and colleagues at the University of California, San Francisco. They found that physicians regularly wrote medical food prescriptions for non–FDA-approved uses and that the system reimbursed the majority of the products at a cost of $15.5 million from 2011 to 2013. More than half of these prescriptions were for Theramine.
Dr. Wilson reported that, for most products, no evidence supported effectiveness, and they were frequently mislabeled – for all 36 that were studied, submissions for reimbursement were made using a National Drug Code, an impossibility because medical foods are not drugs, and 14 were labeled “Rx only.”
Big-name companies joining in
The FDA does not keep a list of approved medical foods or manufacturers. Both small businesses and big food companies like Danone, Nestlé, and Abbott are players. Most products are sold online.
In the United States, Danone’s Nutricia division sells formulas and low-protein foods for IEMs. They also sell Ketocal, a powder or ready-to-drink liquid that is pitched as a balanced medical food to simplify and optimize the ketogenic diet for children with intractable epilepsy. Yet the FDA does not include epilepsy among the conditions that medical foods can treat.
Nestlé sells traditional medical foods for IEMs and also markets a range of what it calls nutritional therapies for such conditions as irritable bowel syndrome and dysphagia.
Nestlé is a minority shareholder in Axona, a product originally developed by Accera (Cerecin as of 2018). Jacquelyn Campo, senior director of global communications at Nestlé Health Sciences, said that the company is not actively involved in the operations management of Cerecin. However, on its website, Nestlé touts Axona, which is only available in the United States, as a “medical food” that “is intended for the clinical dietary management of mild to moderate Alzheimer disease.” The Axona site claims that the main ingredient, caprylic triglyceride, is broken down into ketones that provide fuel to treat cerebral hypometabolism, a precursor to Alzheimer disease. In a 2009 study, daily dosing of a preliminary formulation was associated with improved cognitive performance compared with placebo in patients with mild to moderate Alzheimer disease.
In 2013, the FDA warned Accera that it was misbranding Axona as a medical food and that the therapeutic claims the company was making would make the product an unapproved drug. Ms. Campo said Nestlé is aware of the agency’s warning, but added, “to our knowledge, Cerecin provided answers to the issues raised by the FDA.”
With the goal of getting drug approval, Accera went on to test a tweaked formulation in a 400-patient randomized, placebo-controlled trial called NOURISH AD that ultimately failed. Nevertheless, Axona is still marketed as a medical food. It costs about $100 for a month’s supply.
Repeated requests for comment from Cerecin were not answered. Danielle Schor, an FDA spokesperson, said the agency will not discuss the status of individual products.
More disputes and insurance coverage
Mary Ann DeMarco, executive director of sales and marketing for the Scottsdale, Ariz.–based medical food maker Primus Pharmaceuticals, said the company believes its products fit within the FDA’s medical foods rubric.
These include Fosteum Plus capsules, which it markets “for the clinical dietary management of the metabolic processes of osteopenia and osteoporosis.” The capsules contain a combination of genistein, zinc, calcium, phosphate, vitamin K2, and vitamin D. As proof of effectiveness, the company cites clinical data on some of the ingredients – not the product itself.
Primus has run afoul of the FDA before when it similarly positioned another product, called Limbrel, as a medical food for osteoarthritis. From 2007 to 2017, the FDA received 194 adverse event reports associated with Limbrel, including reports of drug-induced liver injury, pancreatitis, and hypersensitivity pneumonitis. In December 2017, the agency urged Primus to recall Limbrel, a move that it said was “necessary to protect the public health and welfare.” Primus withdrew the product but laid out a defense of Limbrel on a devoted website.
The FDA would not comment any further, said Ms. Schor. Ms. DeMarco said that Primus is working with the FDA to bring Limbrel back to market.
A lack of insurance coverage – even for approved medical foods for IEMs – has frustrated advocates, parents, and manufacturers. They are putting their weight behind the Medical Nutrition Equity Act, which would mandate public and private payer coverage of medical foods for IEMs and digestive conditions such as Crohn disease. That 2019 House bill has 56 cosponsors; there is no Senate companion bill.
“If you can get reimbursement, it really makes the market,” for Primus and the other manufacturers, Mr. Hyman said.
Primus Pharmaceuticals has launched its own campaign, Cover My Medical Foods, to enlist consumers and others to the cause.
Partnering with advocates
Although its low-protein breads, pastas, and baking products are not considered medical foods by the FDA, Dr. Schär is marketing them as such in the United States. They are trying to make a mark in CKD, according to Ms. Donnelly. She added that Dr. Schär has been successful in Europe, where nutrition therapy is more integrated in the health care system.
In 2019, Flavis and the National Kidney Foundation joined forces to raise awareness of nutritional interventions and to build enthusiasm for the Flavis products. The partnership has now ended, mostly because Flavis could no longer afford it, according to Ms. Donnelly.
“Information on diet and nutrition is the most requested subject matter from the NKF,” said Anthony Gucciardo, senior vice president of strategic partnerships at the foundation. The partnership “has never been necessarily about promoting their products per se; it’s promoting a healthy diet and really a diet specific for CKD.”
The NKF developed cobranded materials on low-protein foods for physicians and a teaching tool they could use with patients. Consumers could access nutrition information and a discount on Flavis products on a dedicated webpage. The foundation didn’t describe the low-protein products as medical foods, said Mr. Gucciardo, even if Flavis promoted them as such.
In patients with CKD, dietary management can help prevent the progression to end-stage renal disease. Although Medicare covers medical nutrition therapy – in which patients receive personalized assessments and dietary advice – uptake is abysmally low, according to a 2018 study.
Dr. Burdock thinks low-protein foods for CKD do meet the FDA’s criteria for a medical food but that the agency might not necessarily agree with him. The FDA would not comment.
Physician beware
When it comes to medical foods, the FDA has often looked the other way because the ingredients may already have been proven safe and the danger to an individual or to the public’s health is relatively low, according to Dr. Burdock and Mr. Hyman.
However, if the agency “feels that a medical food will prevent people from seeking medical care or there is potential to defraud the public, it is justified in taking action against the company,” said Dr. Burdock.
According to Dr. Wilson, the pharmacist who reported on the inappropriate medical food prescriptions in the California system, the FDA could help by creating a list of approved medical foods. Physicians should take time to learn about the difference between medical foods and supplements, she said, adding that they should also not hesitate to “question the veracity of the claims for them.”
Ms. Guggenheim believed doctors need to know that, for the most part, these are not FDA-approved products. She emphasized the importance of evaluating the products and looking at the data of their impact on a disease or condition.
“Many of these companies strongly believe that the products work and help people, so clinicians need to be very data driven,” she said.
A version of this article originally appeared on Medscape.com.
Epilepsy after TBI linked to worse 12-month outcomes
findings from an analysis of a large, prospective database suggest. “We found that patients essentially have a 10-times greater risk of developing posttraumatic epilepsy and seizures at 12 months [post injury] if the presenting Glasgow Coma Scale GCS) is less than 8,” said lead author John F. Burke, MD, PhD, University of California, San Francisco, in presenting the findings as part of the virtual annual meeting of the American Association of Neurological Surgeons.
Assessing risk factors
While posttraumatic epilepsy represents an estimated 20% of all cases of symptomatic epilepsy, many questions remain on those most at risk and on the long-term effects of posttraumatic epilepsy on TBI outcomes. To probe those issues, Dr. Burke and colleagues turned to the multicenter TRACK-TBI database, which has prospective, longitudinal data on more than 2,700 patients with traumatic brain injuries and is considered the largest source of prospective data on posttraumatic epilepsy.
Using the criteria of no previous epilepsy and having 12 months of follow-up, the team identified 1,493 patients with TBI. In addition, investigators identified 182 orthopedic controls (included and prospectively followed because they have injuries but not specifically head trauma) and 210 controls who are friends of the patients and who do not have injuries but allow researchers to control for socioeconomic and environmental factors.
Of the 1,493 patients with TBI, 41 (2.7%) were determined to have posttraumatic epilepsy, assessed according to a National Institute of Neurological Disorders and Stroke epilepsy screening questionnaire, which is designed to identify patients with posttraumatic epilepsy symptoms. There were no reports of epilepsy symptoms using the screening tool among the controls. Dr. Burke noted that the 2.7% was in agreement with historical reports.
In comparing patients with TBI who did and did not have posttraumatic epilepsy, no differences were observed in the groups in terms of gender, although there was a trend toward younger age among those with PTE (mean age, 35.4 years with posttraumatic injury vs. 41.5 without; P = .05).
A major risk factor for the development of posttraumatic epilepsy was presenting GCS scores. Among those with scores of less than 8, indicative of severe injury, the rate of posttraumatic epilepsy was 6% at 6 months and 12.5% at 12 months. In contrast, those with TBI presenting with GCS scores between 13 and 15, indicative of minor injury, had an incidence of posttraumatic epilepsy of 0.9% at 6 months and 1.4% at 12 months.
Imaging findings in the two groups showed that hemorrhage detected on CT imaging was associated with a significantly higher risk for posttraumatic epilepsy (P < .001).
“The main takeaway is that any hemorrhage in the brain is a major risk factor for developing seizures,” Dr. Burke said. “Whether it is subdural, epidural blood, subarachnoid or contusion, any blood confers a very [high] risk for developing seizures.”
Posttraumatic epilepsy was linked to poorer longer-term outcomes even for patients with lesser injury: Among those with TBI and GCS of 13-15, the mean Glasgow Outcome Scale Extended (GOSE) score at 12 months among those without posttraumatic epilepsy was 7, indicative of a good recovery with minor defects, whereas the mean GOSE score for those with PTE was 4.6, indicative of moderate to severe disability (P < .001).
“It was surprising to us that PTE-positive patients had a very significant decrease in GOSE, compared to PTE-negative patients,” Dr. Burke said. “There was a nearly 2-point drop in the GOSE and that was extremely significant.”
A multivariate analysis showed there was still a significant independent risk for a poor GOSE score with posttraumatic epilepsy after controlling for GCS score, head CT findings, and age (P < .001).
The authors also looked at mood outcomes using the Brief Symptom Inventory–18, which showed significant worse effect in those with posttraumatic epilepsy after multivariate adjustment (P = .01). Additionally, a highly significant worse effect in cognitive outcomes on the Rivermead cognitive metric was observed with posttraumatic epilepsy (P = .001).
“On all metrics tested, posttraumatic epilepsy worsened outcomes,” Dr. Burke said.
He noted that the study has some key limitations, including the 12-month follow-up. A previous study showed a linear increase in posttraumatic follow-up up to 30 years. “The fact that we found 41 patients at 12 months indicates there are probably more that are out there who are going to develop seizures, but because we don’t have the follow-up we can’t look at that.”
Although the screening questionnaires are effective, “the issue is these people are not being seen by an epileptologist or having scalp EEG done, and we need a more accurate way to do this,” he said. A new study, TRACK-TBI EPI, will address those limitations and a host of other issues with a 5-year follow-up.
Capturing the nuances of brain injury
Commenting on the study as a discussant, neurosurgeon Uzma Samadani, MD, PhD, of the Minneapolis Veterans Affairs Medical Center and CentraCare in Minneapolis, suggested that the future work should focus on issues including the wide-ranging mechanisms that could explain the seizure activity.
“For example, it’s known that posttraumatic epilepsy or seizures can be triggered by abnormal conductivity due to multiple different mechanisms associated with brain injury, such as endocrine dysfunction, cortical-spreading depression, and many others,” said Dr. Samadani, who has been a researcher on the TRACK-TBI study.
Factors ranging from genetic differences to comorbid conditions such as alcoholism can play a role in brain injury susceptibility, Dr. Samadani added. Furthermore, outcome measures currently available simply may not capture the unknown nuances of brain injury.
“We have to ask, are these an all-or-none phenomena, or is aberrant electrical activity after brain injury a continuum of dysfunction?” Dr. Samadani speculated.
“I would caution that we are likely underestimating the non–easily measurable consequences of brain injury,” she said. “And the better we can quantitate susceptibility, classify the nature of injury and target acute management, the less posttraumatic epilepsy/aberrant electrical activity our patients will have.”
Dr. Burke and Dr. Samadani disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
findings from an analysis of a large, prospective database suggest. “We found that patients essentially have a 10-times greater risk of developing posttraumatic epilepsy and seizures at 12 months [post injury] if the presenting Glasgow Coma Scale GCS) is less than 8,” said lead author John F. Burke, MD, PhD, University of California, San Francisco, in presenting the findings as part of the virtual annual meeting of the American Association of Neurological Surgeons.
Assessing risk factors
While posttraumatic epilepsy represents an estimated 20% of all cases of symptomatic epilepsy, many questions remain on those most at risk and on the long-term effects of posttraumatic epilepsy on TBI outcomes. To probe those issues, Dr. Burke and colleagues turned to the multicenter TRACK-TBI database, which has prospective, longitudinal data on more than 2,700 patients with traumatic brain injuries and is considered the largest source of prospective data on posttraumatic epilepsy.
Using the criteria of no previous epilepsy and having 12 months of follow-up, the team identified 1,493 patients with TBI. In addition, investigators identified 182 orthopedic controls (included and prospectively followed because they have injuries but not specifically head trauma) and 210 controls who are friends of the patients and who do not have injuries but allow researchers to control for socioeconomic and environmental factors.
Of the 1,493 patients with TBI, 41 (2.7%) were determined to have posttraumatic epilepsy, assessed according to a National Institute of Neurological Disorders and Stroke epilepsy screening questionnaire, which is designed to identify patients with posttraumatic epilepsy symptoms. There were no reports of epilepsy symptoms using the screening tool among the controls. Dr. Burke noted that the 2.7% was in agreement with historical reports.
In comparing patients with TBI who did and did not have posttraumatic epilepsy, no differences were observed in the groups in terms of gender, although there was a trend toward younger age among those with PTE (mean age, 35.4 years with posttraumatic injury vs. 41.5 without; P = .05).
A major risk factor for the development of posttraumatic epilepsy was presenting GCS scores. Among those with scores of less than 8, indicative of severe injury, the rate of posttraumatic epilepsy was 6% at 6 months and 12.5% at 12 months. In contrast, those with TBI presenting with GCS scores between 13 and 15, indicative of minor injury, had an incidence of posttraumatic epilepsy of 0.9% at 6 months and 1.4% at 12 months.
Imaging findings in the two groups showed that hemorrhage detected on CT imaging was associated with a significantly higher risk for posttraumatic epilepsy (P < .001).
“The main takeaway is that any hemorrhage in the brain is a major risk factor for developing seizures,” Dr. Burke said. “Whether it is subdural, epidural blood, subarachnoid or contusion, any blood confers a very [high] risk for developing seizures.”
Posttraumatic epilepsy was linked to poorer longer-term outcomes even for patients with lesser injury: Among those with TBI and GCS of 13-15, the mean Glasgow Outcome Scale Extended (GOSE) score at 12 months among those without posttraumatic epilepsy was 7, indicative of a good recovery with minor defects, whereas the mean GOSE score for those with PTE was 4.6, indicative of moderate to severe disability (P < .001).
“It was surprising to us that PTE-positive patients had a very significant decrease in GOSE, compared to PTE-negative patients,” Dr. Burke said. “There was a nearly 2-point drop in the GOSE and that was extremely significant.”
A multivariate analysis showed there was still a significant independent risk for a poor GOSE score with posttraumatic epilepsy after controlling for GCS score, head CT findings, and age (P < .001).
The authors also looked at mood outcomes using the Brief Symptom Inventory–18, which showed significant worse effect in those with posttraumatic epilepsy after multivariate adjustment (P = .01). Additionally, a highly significant worse effect in cognitive outcomes on the Rivermead cognitive metric was observed with posttraumatic epilepsy (P = .001).
“On all metrics tested, posttraumatic epilepsy worsened outcomes,” Dr. Burke said.
He noted that the study has some key limitations, including the 12-month follow-up. A previous study showed a linear increase in posttraumatic follow-up up to 30 years. “The fact that we found 41 patients at 12 months indicates there are probably more that are out there who are going to develop seizures, but because we don’t have the follow-up we can’t look at that.”
Although the screening questionnaires are effective, “the issue is these people are not being seen by an epileptologist or having scalp EEG done, and we need a more accurate way to do this,” he said. A new study, TRACK-TBI EPI, will address those limitations and a host of other issues with a 5-year follow-up.
Capturing the nuances of brain injury
Commenting on the study as a discussant, neurosurgeon Uzma Samadani, MD, PhD, of the Minneapolis Veterans Affairs Medical Center and CentraCare in Minneapolis, suggested that the future work should focus on issues including the wide-ranging mechanisms that could explain the seizure activity.
“For example, it’s known that posttraumatic epilepsy or seizures can be triggered by abnormal conductivity due to multiple different mechanisms associated with brain injury, such as endocrine dysfunction, cortical-spreading depression, and many others,” said Dr. Samadani, who has been a researcher on the TRACK-TBI study.
Factors ranging from genetic differences to comorbid conditions such as alcoholism can play a role in brain injury susceptibility, Dr. Samadani added. Furthermore, outcome measures currently available simply may not capture the unknown nuances of brain injury.
“We have to ask, are these an all-or-none phenomena, or is aberrant electrical activity after brain injury a continuum of dysfunction?” Dr. Samadani speculated.
“I would caution that we are likely underestimating the non–easily measurable consequences of brain injury,” she said. “And the better we can quantitate susceptibility, classify the nature of injury and target acute management, the less posttraumatic epilepsy/aberrant electrical activity our patients will have.”
Dr. Burke and Dr. Samadani disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
findings from an analysis of a large, prospective database suggest. “We found that patients essentially have a 10-times greater risk of developing posttraumatic epilepsy and seizures at 12 months [post injury] if the presenting Glasgow Coma Scale GCS) is less than 8,” said lead author John F. Burke, MD, PhD, University of California, San Francisco, in presenting the findings as part of the virtual annual meeting of the American Association of Neurological Surgeons.
Assessing risk factors
While posttraumatic epilepsy represents an estimated 20% of all cases of symptomatic epilepsy, many questions remain on those most at risk and on the long-term effects of posttraumatic epilepsy on TBI outcomes. To probe those issues, Dr. Burke and colleagues turned to the multicenter TRACK-TBI database, which has prospective, longitudinal data on more than 2,700 patients with traumatic brain injuries and is considered the largest source of prospective data on posttraumatic epilepsy.
Using the criteria of no previous epilepsy and having 12 months of follow-up, the team identified 1,493 patients with TBI. In addition, investigators identified 182 orthopedic controls (included and prospectively followed because they have injuries but not specifically head trauma) and 210 controls who are friends of the patients and who do not have injuries but allow researchers to control for socioeconomic and environmental factors.
Of the 1,493 patients with TBI, 41 (2.7%) were determined to have posttraumatic epilepsy, assessed according to a National Institute of Neurological Disorders and Stroke epilepsy screening questionnaire, which is designed to identify patients with posttraumatic epilepsy symptoms. There were no reports of epilepsy symptoms using the screening tool among the controls. Dr. Burke noted that the 2.7% was in agreement with historical reports.
In comparing patients with TBI who did and did not have posttraumatic epilepsy, no differences were observed in the groups in terms of gender, although there was a trend toward younger age among those with PTE (mean age, 35.4 years with posttraumatic injury vs. 41.5 without; P = .05).
A major risk factor for the development of posttraumatic epilepsy was presenting GCS scores. Among those with scores of less than 8, indicative of severe injury, the rate of posttraumatic epilepsy was 6% at 6 months and 12.5% at 12 months. In contrast, those with TBI presenting with GCS scores between 13 and 15, indicative of minor injury, had an incidence of posttraumatic epilepsy of 0.9% at 6 months and 1.4% at 12 months.
Imaging findings in the two groups showed that hemorrhage detected on CT imaging was associated with a significantly higher risk for posttraumatic epilepsy (P < .001).
“The main takeaway is that any hemorrhage in the brain is a major risk factor for developing seizures,” Dr. Burke said. “Whether it is subdural, epidural blood, subarachnoid or contusion, any blood confers a very [high] risk for developing seizures.”
Posttraumatic epilepsy was linked to poorer longer-term outcomes even for patients with lesser injury: Among those with TBI and GCS of 13-15, the mean Glasgow Outcome Scale Extended (GOSE) score at 12 months among those without posttraumatic epilepsy was 7, indicative of a good recovery with minor defects, whereas the mean GOSE score for those with PTE was 4.6, indicative of moderate to severe disability (P < .001).
“It was surprising to us that PTE-positive patients had a very significant decrease in GOSE, compared to PTE-negative patients,” Dr. Burke said. “There was a nearly 2-point drop in the GOSE and that was extremely significant.”
A multivariate analysis showed there was still a significant independent risk for a poor GOSE score with posttraumatic epilepsy after controlling for GCS score, head CT findings, and age (P < .001).
The authors also looked at mood outcomes using the Brief Symptom Inventory–18, which showed significant worse effect in those with posttraumatic epilepsy after multivariate adjustment (P = .01). Additionally, a highly significant worse effect in cognitive outcomes on the Rivermead cognitive metric was observed with posttraumatic epilepsy (P = .001).
“On all metrics tested, posttraumatic epilepsy worsened outcomes,” Dr. Burke said.
He noted that the study has some key limitations, including the 12-month follow-up. A previous study showed a linear increase in posttraumatic follow-up up to 30 years. “The fact that we found 41 patients at 12 months indicates there are probably more that are out there who are going to develop seizures, but because we don’t have the follow-up we can’t look at that.”
Although the screening questionnaires are effective, “the issue is these people are not being seen by an epileptologist or having scalp EEG done, and we need a more accurate way to do this,” he said. A new study, TRACK-TBI EPI, will address those limitations and a host of other issues with a 5-year follow-up.
Capturing the nuances of brain injury
Commenting on the study as a discussant, neurosurgeon Uzma Samadani, MD, PhD, of the Minneapolis Veterans Affairs Medical Center and CentraCare in Minneapolis, suggested that the future work should focus on issues including the wide-ranging mechanisms that could explain the seizure activity.
“For example, it’s known that posttraumatic epilepsy or seizures can be triggered by abnormal conductivity due to multiple different mechanisms associated with brain injury, such as endocrine dysfunction, cortical-spreading depression, and many others,” said Dr. Samadani, who has been a researcher on the TRACK-TBI study.
Factors ranging from genetic differences to comorbid conditions such as alcoholism can play a role in brain injury susceptibility, Dr. Samadani added. Furthermore, outcome measures currently available simply may not capture the unknown nuances of brain injury.
“We have to ask, are these an all-or-none phenomena, or is aberrant electrical activity after brain injury a continuum of dysfunction?” Dr. Samadani speculated.
“I would caution that we are likely underestimating the non–easily measurable consequences of brain injury,” she said. “And the better we can quantitate susceptibility, classify the nature of injury and target acute management, the less posttraumatic epilepsy/aberrant electrical activity our patients will have.”
Dr. Burke and Dr. Samadani disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM AANS 2020
New data back use of medical cannabis for epilepsy, pain, anxiety
Two new studies offer positive news about medical cannabis, suggesting that marijuana products improve physical and cognitive symptoms, boost quality of life, and rarely produce signs of problematic use.
In one study, patients with epilepsy who used medical cannabis were nearly half as likely to have needed an emergency department visit within the last 30 days as was a control group. In the other study, 3 of 54 subjects who used medical cannabis showed signs of possible cannabis use disorder (CUD) over 12 months.
The findings show that “there is improvement in a range of outcome variables, and the adverse effects seem to be minimal, compared to what we might have hypothesized based on the bulk of the literature on the negative effects of cannabis on health outcomes,” cannabis researcher Ziva Cooper, PhD, of the University of California at Los Angeles, said in an interview. Dr. Cooper moderated a session about the studies at the virtual annual meeting of the College on Problems of Drug Dependence.
In one study, cannabis researcher Ryan Vandrey, PhD, of Johns Hopkins University, Baltimore, and colleagues compared medical cannabis users (number, 808; mean age, 38; percentage female, 63%) to a control group of people who were interested in medical cannabis (n, 468; mean age, 35; percentage female, 62%).
In both groups, 79% were White. The groups had similar levels of primary medical conditions, such as neurologic (38% and 36%, respectively, for the medical cannabis group and control group) and chronic pain (25% and 23%, respectively.)
The wide majority of those in the medical cannabis group – 58% – were cannabidiol (CBD) users, relying on a component of cannabis (marijuana) that does not make people high. Fewer than 20% used tetrahydrocannabinol (THC), which does make people high, or a combination of both CBD and THC.
Most of those in the medical cannabis group used the drug as an adjunct (39%) to other treatments or last-resort (29%) treatment instead of first line (11%) or second line (18%).
In patients with epilepsy, about 45% of controls reported a past-month ED visit, compared with about 25% of medical cannabis users. The gap in past-month hospital admissions was even wider, at about 35% for the controls and about 15% for the medical cannabis.
After an initial survey, the researchers followed subjects prospectively; some either started or stopped using medical cannabis. From baseline to follow-up, those in the medical cannabis group improved more, compared with those in the control group on a variety of measures of quality of life, anxiety, and depression.
“Folks who were in the control condition at baseline and then initiated cannabis use started to look more like the baseline cannabis users,” Dr. Vandrey said. “The folks who were cannabis users at baseline and then stopped for whatever reason started to look like the controls. And the controls [who never started using medical cannabis] stayed the same.”
As for adverse effects, two-thirds of medical cannabis users reported no problems; the highest number, 14%, reported high cost.
As for limitations, Dr. Vandrey reported missing data, a reliance on self-reports, and poor follow-up with about a third of participants agreeing to complete follow-up assessments. “We are continuing to collect data on this,” he said, “and we’re hoping we’ll be able to drill down more as we get bigger.”
The study was funded by the Realm of Caring Foundation.
In the other study, led by cannabis researcher Staci Gruber, PhD, of McLean Hospital in Belmont, Mass., and Harvard Medical School in Boston, researchers tracked 54 subjects (mean age, 49; 20 male and 34 female; 48 white) for up to 2 years after they began medical cannabis use. Most had pain (36) or anxiety/PTSD (31), and all had to have abstained from recreational cannabis use for at least 1 year.
At follow-ups, the users reported improved mood and anxiety via various measures, and they saw some improvement in quality of life. “We did not see worsening cognitive performance,” Dr. Gruber said. “In fact,
Research has suggested that as many as 30% of recreational cannabis users develop cannabis use disorder (CUD), Dr. Gruber said. But only 3 of the 54 patients showed signs of possible CUD at 12 months, she said, even though frequency of use jumped substantially vs. baseline.
Information about study funding was not available.
Dr. Cooper disclosed relationships with FSD Pharma, Beckley Canopy Therapeutics, and Insys Therapeutics. Dr. Vandrey disclosed work with Zynerba Pharmaceuticals, Canopy Health Innovations, and FSD Pharma. Dr. Gruber reported no disclosures.
Two new studies offer positive news about medical cannabis, suggesting that marijuana products improve physical and cognitive symptoms, boost quality of life, and rarely produce signs of problematic use.
In one study, patients with epilepsy who used medical cannabis were nearly half as likely to have needed an emergency department visit within the last 30 days as was a control group. In the other study, 3 of 54 subjects who used medical cannabis showed signs of possible cannabis use disorder (CUD) over 12 months.
The findings show that “there is improvement in a range of outcome variables, and the adverse effects seem to be minimal, compared to what we might have hypothesized based on the bulk of the literature on the negative effects of cannabis on health outcomes,” cannabis researcher Ziva Cooper, PhD, of the University of California at Los Angeles, said in an interview. Dr. Cooper moderated a session about the studies at the virtual annual meeting of the College on Problems of Drug Dependence.
In one study, cannabis researcher Ryan Vandrey, PhD, of Johns Hopkins University, Baltimore, and colleagues compared medical cannabis users (number, 808; mean age, 38; percentage female, 63%) to a control group of people who were interested in medical cannabis (n, 468; mean age, 35; percentage female, 62%).
In both groups, 79% were White. The groups had similar levels of primary medical conditions, such as neurologic (38% and 36%, respectively, for the medical cannabis group and control group) and chronic pain (25% and 23%, respectively.)
The wide majority of those in the medical cannabis group – 58% – were cannabidiol (CBD) users, relying on a component of cannabis (marijuana) that does not make people high. Fewer than 20% used tetrahydrocannabinol (THC), which does make people high, or a combination of both CBD and THC.
Most of those in the medical cannabis group used the drug as an adjunct (39%) to other treatments or last-resort (29%) treatment instead of first line (11%) or second line (18%).
In patients with epilepsy, about 45% of controls reported a past-month ED visit, compared with about 25% of medical cannabis users. The gap in past-month hospital admissions was even wider, at about 35% for the controls and about 15% for the medical cannabis.
After an initial survey, the researchers followed subjects prospectively; some either started or stopped using medical cannabis. From baseline to follow-up, those in the medical cannabis group improved more, compared with those in the control group on a variety of measures of quality of life, anxiety, and depression.
“Folks who were in the control condition at baseline and then initiated cannabis use started to look more like the baseline cannabis users,” Dr. Vandrey said. “The folks who were cannabis users at baseline and then stopped for whatever reason started to look like the controls. And the controls [who never started using medical cannabis] stayed the same.”
As for adverse effects, two-thirds of medical cannabis users reported no problems; the highest number, 14%, reported high cost.
As for limitations, Dr. Vandrey reported missing data, a reliance on self-reports, and poor follow-up with about a third of participants agreeing to complete follow-up assessments. “We are continuing to collect data on this,” he said, “and we’re hoping we’ll be able to drill down more as we get bigger.”
The study was funded by the Realm of Caring Foundation.
In the other study, led by cannabis researcher Staci Gruber, PhD, of McLean Hospital in Belmont, Mass., and Harvard Medical School in Boston, researchers tracked 54 subjects (mean age, 49; 20 male and 34 female; 48 white) for up to 2 years after they began medical cannabis use. Most had pain (36) or anxiety/PTSD (31), and all had to have abstained from recreational cannabis use for at least 1 year.
At follow-ups, the users reported improved mood and anxiety via various measures, and they saw some improvement in quality of life. “We did not see worsening cognitive performance,” Dr. Gruber said. “In fact,
Research has suggested that as many as 30% of recreational cannabis users develop cannabis use disorder (CUD), Dr. Gruber said. But only 3 of the 54 patients showed signs of possible CUD at 12 months, she said, even though frequency of use jumped substantially vs. baseline.
Information about study funding was not available.
Dr. Cooper disclosed relationships with FSD Pharma, Beckley Canopy Therapeutics, and Insys Therapeutics. Dr. Vandrey disclosed work with Zynerba Pharmaceuticals, Canopy Health Innovations, and FSD Pharma. Dr. Gruber reported no disclosures.
Two new studies offer positive news about medical cannabis, suggesting that marijuana products improve physical and cognitive symptoms, boost quality of life, and rarely produce signs of problematic use.
In one study, patients with epilepsy who used medical cannabis were nearly half as likely to have needed an emergency department visit within the last 30 days as was a control group. In the other study, 3 of 54 subjects who used medical cannabis showed signs of possible cannabis use disorder (CUD) over 12 months.
The findings show that “there is improvement in a range of outcome variables, and the adverse effects seem to be minimal, compared to what we might have hypothesized based on the bulk of the literature on the negative effects of cannabis on health outcomes,” cannabis researcher Ziva Cooper, PhD, of the University of California at Los Angeles, said in an interview. Dr. Cooper moderated a session about the studies at the virtual annual meeting of the College on Problems of Drug Dependence.
In one study, cannabis researcher Ryan Vandrey, PhD, of Johns Hopkins University, Baltimore, and colleagues compared medical cannabis users (number, 808; mean age, 38; percentage female, 63%) to a control group of people who were interested in medical cannabis (n, 468; mean age, 35; percentage female, 62%).
In both groups, 79% were White. The groups had similar levels of primary medical conditions, such as neurologic (38% and 36%, respectively, for the medical cannabis group and control group) and chronic pain (25% and 23%, respectively.)
The wide majority of those in the medical cannabis group – 58% – were cannabidiol (CBD) users, relying on a component of cannabis (marijuana) that does not make people high. Fewer than 20% used tetrahydrocannabinol (THC), which does make people high, or a combination of both CBD and THC.
Most of those in the medical cannabis group used the drug as an adjunct (39%) to other treatments or last-resort (29%) treatment instead of first line (11%) or second line (18%).
In patients with epilepsy, about 45% of controls reported a past-month ED visit, compared with about 25% of medical cannabis users. The gap in past-month hospital admissions was even wider, at about 35% for the controls and about 15% for the medical cannabis.
After an initial survey, the researchers followed subjects prospectively; some either started or stopped using medical cannabis. From baseline to follow-up, those in the medical cannabis group improved more, compared with those in the control group on a variety of measures of quality of life, anxiety, and depression.
“Folks who were in the control condition at baseline and then initiated cannabis use started to look more like the baseline cannabis users,” Dr. Vandrey said. “The folks who were cannabis users at baseline and then stopped for whatever reason started to look like the controls. And the controls [who never started using medical cannabis] stayed the same.”
As for adverse effects, two-thirds of medical cannabis users reported no problems; the highest number, 14%, reported high cost.
As for limitations, Dr. Vandrey reported missing data, a reliance on self-reports, and poor follow-up with about a third of participants agreeing to complete follow-up assessments. “We are continuing to collect data on this,” he said, “and we’re hoping we’ll be able to drill down more as we get bigger.”
The study was funded by the Realm of Caring Foundation.
In the other study, led by cannabis researcher Staci Gruber, PhD, of McLean Hospital in Belmont, Mass., and Harvard Medical School in Boston, researchers tracked 54 subjects (mean age, 49; 20 male and 34 female; 48 white) for up to 2 years after they began medical cannabis use. Most had pain (36) or anxiety/PTSD (31), and all had to have abstained from recreational cannabis use for at least 1 year.
At follow-ups, the users reported improved mood and anxiety via various measures, and they saw some improvement in quality of life. “We did not see worsening cognitive performance,” Dr. Gruber said. “In fact,
Research has suggested that as many as 30% of recreational cannabis users develop cannabis use disorder (CUD), Dr. Gruber said. But only 3 of the 54 patients showed signs of possible CUD at 12 months, she said, even though frequency of use jumped substantially vs. baseline.
Information about study funding was not available.
Dr. Cooper disclosed relationships with FSD Pharma, Beckley Canopy Therapeutics, and Insys Therapeutics. Dr. Vandrey disclosed work with Zynerba Pharmaceuticals, Canopy Health Innovations, and FSD Pharma. Dr. Gruber reported no disclosures.
FROM CPDD 2020
FDA approves new treatment for Dravet syndrome
Dravet syndrome is a rare childhood-onset epilepsy characterized by frequent, drug-resistant convulsive seizures that may contribute to intellectual disability and impairments in motor control, behavior, and cognition, as well as an increased risk of sudden unexpected death in epilepsy (SUDEP).
Dravet syndrome takes a “tremendous toll on both patients and their families. Fintepla offers an additional effective treatment option for the treatment of seizures associated with Dravet syndrome,” Billy Dunn, MD, director, Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, said in a news release.
The FDA approved fenfluramine for Dravet syndrome based on the results of two randomized, double-blind, placebo-controlled phase 3 trials involving children ages 2 to 18 years with Dravet syndrome.
In both studies, children treated with fenfluramine experienced significantly greater reductions in the frequency of convulsive seizures than did their peers who received placebo. These reductions occurred within 3 to 4 weeks, and remained generally consistent over the 14- to 15-week treatment periods, the FDA said.
“There remains a huge unmet need for the many Dravet syndrome patients who continue to experience frequent severe seizures even while taking one or more of the currently available antiseizure medications,” Joseph Sullivan, MD, who worked on the fenfluramine for Dravet syndrome studies, said in a news release.
Given the “profound reductions” in convulsive seizure frequency seen in the clinical trials, combined with the “ongoing, robust safety monitoring,” fenfluramine offers “an extremely important treatment option for Dravet syndrome patients,” said Dr. Sullivan, director of the Pediatric Epilepsy Center of Excellence at the University of California San Francisco (UCSF) Benioff Children’s Hospital.
Fenfluramine is an anorectic agent that was used to treat obesity until it was removed from the market in 1997 over reports of increased risk of valvular heart disease when prescribed in higher doses and most often when prescribed with phentermine. The combination of the two drugs was known as fen-phen.
In the clinical trials of Dravet syndrome, the most common adverse reactions were decreased appetite; somnolence, sedation, lethargy; diarrhea; constipation; abnormal echocardiogram; fatigue, malaise, asthenia; ataxia, balance disorder, gait disturbance; increased blood pressure; drooling, salivary hypersecretion; pyrexia; upper respiratory tract infection; vomiting; decreased weight; fall; and status epilepticus.
The Fintepla label has a boxed warning stating that the drug is associated with valvular heart disease (VHD) and pulmonary arterial hypertension (PAH). Due to these risks, patients must undergo echocardiography before treatment, every 6 months during treatment, and once 3 to 6 months after treatment is stopped.
If signs of VHD, PAH, or other cardiac abnormalities are present, clinicians should weigh the benefits and risks of continuing treatment with Fintepla, the FDA said.
Fintepla is available only through a risk evaluation and mitigation strategy (REMS) program, which requires physicians who prescribe the drug and pharmacies that dispense it to be certified in the Fintepla REMS and that patients be enrolled in the program.
As part of the REMS requirements, prescribers and patients must adhere to the required cardiac monitoring to receive the drug.
Fintepla will be available to certified prescribers in the United States in July. Zogenix is launching Zogenix Central, a comprehensive support service that will provide ongoing product assistance to patients, caregivers, and their medical teams. Further information is available online.
This article first appeared on Medscape.com.
Dravet syndrome is a rare childhood-onset epilepsy characterized by frequent, drug-resistant convulsive seizures that may contribute to intellectual disability and impairments in motor control, behavior, and cognition, as well as an increased risk of sudden unexpected death in epilepsy (SUDEP).
Dravet syndrome takes a “tremendous toll on both patients and their families. Fintepla offers an additional effective treatment option for the treatment of seizures associated with Dravet syndrome,” Billy Dunn, MD, director, Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, said in a news release.
The FDA approved fenfluramine for Dravet syndrome based on the results of two randomized, double-blind, placebo-controlled phase 3 trials involving children ages 2 to 18 years with Dravet syndrome.
In both studies, children treated with fenfluramine experienced significantly greater reductions in the frequency of convulsive seizures than did their peers who received placebo. These reductions occurred within 3 to 4 weeks, and remained generally consistent over the 14- to 15-week treatment periods, the FDA said.
“There remains a huge unmet need for the many Dravet syndrome patients who continue to experience frequent severe seizures even while taking one or more of the currently available antiseizure medications,” Joseph Sullivan, MD, who worked on the fenfluramine for Dravet syndrome studies, said in a news release.
Given the “profound reductions” in convulsive seizure frequency seen in the clinical trials, combined with the “ongoing, robust safety monitoring,” fenfluramine offers “an extremely important treatment option for Dravet syndrome patients,” said Dr. Sullivan, director of the Pediatric Epilepsy Center of Excellence at the University of California San Francisco (UCSF) Benioff Children’s Hospital.
Fenfluramine is an anorectic agent that was used to treat obesity until it was removed from the market in 1997 over reports of increased risk of valvular heart disease when prescribed in higher doses and most often when prescribed with phentermine. The combination of the two drugs was known as fen-phen.
In the clinical trials of Dravet syndrome, the most common adverse reactions were decreased appetite; somnolence, sedation, lethargy; diarrhea; constipation; abnormal echocardiogram; fatigue, malaise, asthenia; ataxia, balance disorder, gait disturbance; increased blood pressure; drooling, salivary hypersecretion; pyrexia; upper respiratory tract infection; vomiting; decreased weight; fall; and status epilepticus.
The Fintepla label has a boxed warning stating that the drug is associated with valvular heart disease (VHD) and pulmonary arterial hypertension (PAH). Due to these risks, patients must undergo echocardiography before treatment, every 6 months during treatment, and once 3 to 6 months after treatment is stopped.
If signs of VHD, PAH, or other cardiac abnormalities are present, clinicians should weigh the benefits and risks of continuing treatment with Fintepla, the FDA said.
Fintepla is available only through a risk evaluation and mitigation strategy (REMS) program, which requires physicians who prescribe the drug and pharmacies that dispense it to be certified in the Fintepla REMS and that patients be enrolled in the program.
As part of the REMS requirements, prescribers and patients must adhere to the required cardiac monitoring to receive the drug.
Fintepla will be available to certified prescribers in the United States in July. Zogenix is launching Zogenix Central, a comprehensive support service that will provide ongoing product assistance to patients, caregivers, and their medical teams. Further information is available online.
This article first appeared on Medscape.com.
Dravet syndrome is a rare childhood-onset epilepsy characterized by frequent, drug-resistant convulsive seizures that may contribute to intellectual disability and impairments in motor control, behavior, and cognition, as well as an increased risk of sudden unexpected death in epilepsy (SUDEP).
Dravet syndrome takes a “tremendous toll on both patients and their families. Fintepla offers an additional effective treatment option for the treatment of seizures associated with Dravet syndrome,” Billy Dunn, MD, director, Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, said in a news release.
The FDA approved fenfluramine for Dravet syndrome based on the results of two randomized, double-blind, placebo-controlled phase 3 trials involving children ages 2 to 18 years with Dravet syndrome.
In both studies, children treated with fenfluramine experienced significantly greater reductions in the frequency of convulsive seizures than did their peers who received placebo. These reductions occurred within 3 to 4 weeks, and remained generally consistent over the 14- to 15-week treatment periods, the FDA said.
“There remains a huge unmet need for the many Dravet syndrome patients who continue to experience frequent severe seizures even while taking one or more of the currently available antiseizure medications,” Joseph Sullivan, MD, who worked on the fenfluramine for Dravet syndrome studies, said in a news release.
Given the “profound reductions” in convulsive seizure frequency seen in the clinical trials, combined with the “ongoing, robust safety monitoring,” fenfluramine offers “an extremely important treatment option for Dravet syndrome patients,” said Dr. Sullivan, director of the Pediatric Epilepsy Center of Excellence at the University of California San Francisco (UCSF) Benioff Children’s Hospital.
Fenfluramine is an anorectic agent that was used to treat obesity until it was removed from the market in 1997 over reports of increased risk of valvular heart disease when prescribed in higher doses and most often when prescribed with phentermine. The combination of the two drugs was known as fen-phen.
In the clinical trials of Dravet syndrome, the most common adverse reactions were decreased appetite; somnolence, sedation, lethargy; diarrhea; constipation; abnormal echocardiogram; fatigue, malaise, asthenia; ataxia, balance disorder, gait disturbance; increased blood pressure; drooling, salivary hypersecretion; pyrexia; upper respiratory tract infection; vomiting; decreased weight; fall; and status epilepticus.
The Fintepla label has a boxed warning stating that the drug is associated with valvular heart disease (VHD) and pulmonary arterial hypertension (PAH). Due to these risks, patients must undergo echocardiography before treatment, every 6 months during treatment, and once 3 to 6 months after treatment is stopped.
If signs of VHD, PAH, or other cardiac abnormalities are present, clinicians should weigh the benefits and risks of continuing treatment with Fintepla, the FDA said.
Fintepla is available only through a risk evaluation and mitigation strategy (REMS) program, which requires physicians who prescribe the drug and pharmacies that dispense it to be certified in the Fintepla REMS and that patients be enrolled in the program.
As part of the REMS requirements, prescribers and patients must adhere to the required cardiac monitoring to receive the drug.
Fintepla will be available to certified prescribers in the United States in July. Zogenix is launching Zogenix Central, a comprehensive support service that will provide ongoing product assistance to patients, caregivers, and their medical teams. Further information is available online.
This article first appeared on Medscape.com.
Most adult epilepsy-related deaths could be avoided
The research shows that such avoidable deaths “remain common and have not declined over time, despite advances in treatment,” Gashirai Mbizvo, MBChB, PhD, clinical research fellow, Muir Maxwell Epilepsy Center, the University of Edinburgh, Scotland, told a press briefing.
The findings were presented at the Congress of the European Academy of Neurology (EAN) 2020, which is being conducted as a virtual/online meeting because of the COVID-19 pandemic.
As his PhD dissertation, Dr. Mbizvo is investigating the rates, causes, and risk factors for epilepsy-related deaths and the percentage of these that are potentially avoidable.
The National Health Service of Scotland contains various linked administrative data sets. Each resident of Scotland has a unique identifier that facilitates investigations across the health system.
Dr. Mbizvo investigated adults and adolescents aged 16 years and older who died because of epilepsy during 2009-2016. He compared this group to patients of similar age who were living with epilepsy to identify risk factors that might help focus resources. During the study period, 2,149 epilepsy-related deaths occurred. Nearly 60% involved at least one seizure-related hospital admission.
Heavy burden
Of the patients who died because of epilepsy, 24% were seen in an outpatient neurologic clinic. “So there’s this heavy burden of admissions not translating to neurology follow-up,” said Dr. Mbizvo.
During the study period, there was no reduction in mortality “despite advances in medical care,” said Dr. Mbizvo.
Younger people with epilepsy were found to be more likely to die. The standardized mortality rate was 6/100,000 (95% confidence interval, 2.3-9.7) among those aged 16-24 years. By contrast, among those aged 45-54 years, the rate was 2/100,000 (95% CI, 1.1-2.1); it was lower in older age groups.
“The overall mortality is not reducing; people are dying young, and neurologists are really not getting involved,” Dr. Mbizvo said.
Among the almost 600 deaths of those aged 16-54 years, 58% were from Scotland’s “most deprived areas,” he noted.
From medical records and antiepileptic drug (AED) use, Dr. Mbizvo looked for risk factors that may have contributed to these epilepsy-related deaths. The most common cause of death in the group aged 16- 54 years was sudden unexpected death in epilepsy (SUDEP), followed by respiratory disorders, such as aspiration pneumonia.
“We think this should be avoidable, in the sense that these are people that could perhaps be targeted early with, for example, antibiotics,” said Dr. Mbizvo.
The next most common cause of death was circulatory disease, largely cardiac arrest.
“The idea is that electroexcitation – an abnormality in the brain – and the heart are related, and maybe that’s translating to a risk of death,” said Dr. Mbizvo.
Worrisome group
Mental and behavioral disorders, largely alcohol related, were the next most common cause of death.
“This is a group I worry about,” said Dr. Mbizvo. “I think they’re seen in the acute services and discharged as alcohol-withdrawal seizures. It’s possible that some have epilepsy and are never referred to a neurologist, and this may translate into increased mortality.”
Dr. Mbizvo is analyzing how these results differ from what is seen in the general population of Scotland among those younger than 75 years.
The top cause of death in the general population is neoplasm of the lungs. Aspiration of the lung is near the top for those who died from epilepsy, but the mechanisms leading to lung-related deaths in these populations may differ, said Dr. Mbizvo.
By applying coding methodology from fields unrelated to epilepsy where this approach has been tried, he determined that 78% of epilepsy-related deaths among those younger than 55 years were potentially avoidable.
“As a method, this is still in its infancy and will require validation, but we see this as a start,” Dr. Mbizvo said.
He provided examples from medical records that illustrate avoidable factors that could contribute to death. These included cases in which patients were discharged with the wrong dose of AED and in which patients drowned in a bath after having not been appropriately educated about seizure safety.
Can’t plug in
Patients with a first seizure are typically referred quickly to an appropriate service, but Dr. Mbizvo is concerned about those with chronic, stable epilepsy. “These people may at some point decompensate, and there’s no channel to plug them back into neurology services to make it easy for them to access a neurologist,” he said.
Currently, experts tell discharged patients to call if a problem occurs, but the system “is rather ad hoc,” said Dr. Mbizvo.
Because of the COVID-19 crisis, the use of telemedicine is increasing. This is helping to improve the system. “We may be able to build a virtual community for people who are on antiepileptic drugs and who suddenly begin to experience seizures again, to enable them to quickly get help, alongside a defined pathway to an epilepsy specialist,” said Dr. Mbizvo.
He hopes to develop a risk index for epilepsy patients similar to one used in cardiology that assesses risks such as smoking, high cholesterol level, and obesity. Although such a risk score might be similar to the SUDEP risk indices being developed, it will take into account death from any epilepsy-related cause, said Dr. Mbizvo. “Having not yet completed the analysis, I’m not sure which aspects will confer the greatest risk,” he said.
He added that, anecdotally, he has noticed a slight trend toward high mortality among patients with epilepsy who present multiple times at emergency departments in a year.
If this trend is statistically valid, “it could help create a traffic light flagging system on A&Es [accident and emergency departments] in which individuals with epilepsy who, for example, have two or more attendances to A&E in a year become flagged as high risk of death and are plugged into a rapid access epilepsy specialist clinic,” he said.
For their part, neurologists should recognize drug-resistant epilepsy early and refer such patients for assessment for resective surgery. If successful, such surgery reduces the risk for premature mortality, said Dr. Mbizvo.
Patients should not become discouraged by drug resistance, either. Research shows that, with careful reassessment of epilepsy type and drug changes, some patients whose condition is thought to be intractable could experience significant improvement in seizure frequency or seizures could be stopped.
“We need to talk to our patients more about the importance of adherence and encourage them to be honest with us if they don’t like the drugs we’re giving them and, as a result, are not taking them as recommended,” Dr. Mbizvo said.
Physicians also need to screen for mood disorders, especially suicidal ideation. Increasingly, specialists are recognizing mental health as an important area of epilepsy care.
They should also conduct a “safety briefing” perhaps twice a year in which they discuss, for example, SUDEP risk, driving concerns, showering instead of bathing, ensuring that a life guard is present at a swimming pool, and other measures.
Commenting on the study, Josemir W. (Ley) Sander, MD, PhD, professor of neurology and clinical epilepsy at University College London, said he welcomes any effort that highlights the problem of premature death among people with epilepsy and that offers possible ways to mitigate it.
Although the study “shows that premature death among people with epilepsy is a major issue,” many health care providers are not fully aware of the extent of this problem, said Dr. Sander. “For many, epilepsy is just a benign condition in which people have seizures,” he said. A risk score that could identify those at high risk for death and establishing preventive measures “would go a long way to decrease the burden of epilepsy,” he noted.
The study was supported by Epilepsy Research UK and the Juliet Bergqvist Memorial Fund. Dr. Mbizvo and Dr. Sander have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The research shows that such avoidable deaths “remain common and have not declined over time, despite advances in treatment,” Gashirai Mbizvo, MBChB, PhD, clinical research fellow, Muir Maxwell Epilepsy Center, the University of Edinburgh, Scotland, told a press briefing.
The findings were presented at the Congress of the European Academy of Neurology (EAN) 2020, which is being conducted as a virtual/online meeting because of the COVID-19 pandemic.
As his PhD dissertation, Dr. Mbizvo is investigating the rates, causes, and risk factors for epilepsy-related deaths and the percentage of these that are potentially avoidable.
The National Health Service of Scotland contains various linked administrative data sets. Each resident of Scotland has a unique identifier that facilitates investigations across the health system.
Dr. Mbizvo investigated adults and adolescents aged 16 years and older who died because of epilepsy during 2009-2016. He compared this group to patients of similar age who were living with epilepsy to identify risk factors that might help focus resources. During the study period, 2,149 epilepsy-related deaths occurred. Nearly 60% involved at least one seizure-related hospital admission.
Heavy burden
Of the patients who died because of epilepsy, 24% were seen in an outpatient neurologic clinic. “So there’s this heavy burden of admissions not translating to neurology follow-up,” said Dr. Mbizvo.
During the study period, there was no reduction in mortality “despite advances in medical care,” said Dr. Mbizvo.
Younger people with epilepsy were found to be more likely to die. The standardized mortality rate was 6/100,000 (95% confidence interval, 2.3-9.7) among those aged 16-24 years. By contrast, among those aged 45-54 years, the rate was 2/100,000 (95% CI, 1.1-2.1); it was lower in older age groups.
“The overall mortality is not reducing; people are dying young, and neurologists are really not getting involved,” Dr. Mbizvo said.
Among the almost 600 deaths of those aged 16-54 years, 58% were from Scotland’s “most deprived areas,” he noted.
From medical records and antiepileptic drug (AED) use, Dr. Mbizvo looked for risk factors that may have contributed to these epilepsy-related deaths. The most common cause of death in the group aged 16- 54 years was sudden unexpected death in epilepsy (SUDEP), followed by respiratory disorders, such as aspiration pneumonia.
“We think this should be avoidable, in the sense that these are people that could perhaps be targeted early with, for example, antibiotics,” said Dr. Mbizvo.
The next most common cause of death was circulatory disease, largely cardiac arrest.
“The idea is that electroexcitation – an abnormality in the brain – and the heart are related, and maybe that’s translating to a risk of death,” said Dr. Mbizvo.
Worrisome group
Mental and behavioral disorders, largely alcohol related, were the next most common cause of death.
“This is a group I worry about,” said Dr. Mbizvo. “I think they’re seen in the acute services and discharged as alcohol-withdrawal seizures. It’s possible that some have epilepsy and are never referred to a neurologist, and this may translate into increased mortality.”
Dr. Mbizvo is analyzing how these results differ from what is seen in the general population of Scotland among those younger than 75 years.
The top cause of death in the general population is neoplasm of the lungs. Aspiration of the lung is near the top for those who died from epilepsy, but the mechanisms leading to lung-related deaths in these populations may differ, said Dr. Mbizvo.
By applying coding methodology from fields unrelated to epilepsy where this approach has been tried, he determined that 78% of epilepsy-related deaths among those younger than 55 years were potentially avoidable.
“As a method, this is still in its infancy and will require validation, but we see this as a start,” Dr. Mbizvo said.
He provided examples from medical records that illustrate avoidable factors that could contribute to death. These included cases in which patients were discharged with the wrong dose of AED and in which patients drowned in a bath after having not been appropriately educated about seizure safety.
Can’t plug in
Patients with a first seizure are typically referred quickly to an appropriate service, but Dr. Mbizvo is concerned about those with chronic, stable epilepsy. “These people may at some point decompensate, and there’s no channel to plug them back into neurology services to make it easy for them to access a neurologist,” he said.
Currently, experts tell discharged patients to call if a problem occurs, but the system “is rather ad hoc,” said Dr. Mbizvo.
Because of the COVID-19 crisis, the use of telemedicine is increasing. This is helping to improve the system. “We may be able to build a virtual community for people who are on antiepileptic drugs and who suddenly begin to experience seizures again, to enable them to quickly get help, alongside a defined pathway to an epilepsy specialist,” said Dr. Mbizvo.
He hopes to develop a risk index for epilepsy patients similar to one used in cardiology that assesses risks such as smoking, high cholesterol level, and obesity. Although such a risk score might be similar to the SUDEP risk indices being developed, it will take into account death from any epilepsy-related cause, said Dr. Mbizvo. “Having not yet completed the analysis, I’m not sure which aspects will confer the greatest risk,” he said.
He added that, anecdotally, he has noticed a slight trend toward high mortality among patients with epilepsy who present multiple times at emergency departments in a year.
If this trend is statistically valid, “it could help create a traffic light flagging system on A&Es [accident and emergency departments] in which individuals with epilepsy who, for example, have two or more attendances to A&E in a year become flagged as high risk of death and are plugged into a rapid access epilepsy specialist clinic,” he said.
For their part, neurologists should recognize drug-resistant epilepsy early and refer such patients for assessment for resective surgery. If successful, such surgery reduces the risk for premature mortality, said Dr. Mbizvo.
Patients should not become discouraged by drug resistance, either. Research shows that, with careful reassessment of epilepsy type and drug changes, some patients whose condition is thought to be intractable could experience significant improvement in seizure frequency or seizures could be stopped.
“We need to talk to our patients more about the importance of adherence and encourage them to be honest with us if they don’t like the drugs we’re giving them and, as a result, are not taking them as recommended,” Dr. Mbizvo said.
Physicians also need to screen for mood disorders, especially suicidal ideation. Increasingly, specialists are recognizing mental health as an important area of epilepsy care.
They should also conduct a “safety briefing” perhaps twice a year in which they discuss, for example, SUDEP risk, driving concerns, showering instead of bathing, ensuring that a life guard is present at a swimming pool, and other measures.
Commenting on the study, Josemir W. (Ley) Sander, MD, PhD, professor of neurology and clinical epilepsy at University College London, said he welcomes any effort that highlights the problem of premature death among people with epilepsy and that offers possible ways to mitigate it.
Although the study “shows that premature death among people with epilepsy is a major issue,” many health care providers are not fully aware of the extent of this problem, said Dr. Sander. “For many, epilepsy is just a benign condition in which people have seizures,” he said. A risk score that could identify those at high risk for death and establishing preventive measures “would go a long way to decrease the burden of epilepsy,” he noted.
The study was supported by Epilepsy Research UK and the Juliet Bergqvist Memorial Fund. Dr. Mbizvo and Dr. Sander have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The research shows that such avoidable deaths “remain common and have not declined over time, despite advances in treatment,” Gashirai Mbizvo, MBChB, PhD, clinical research fellow, Muir Maxwell Epilepsy Center, the University of Edinburgh, Scotland, told a press briefing.
The findings were presented at the Congress of the European Academy of Neurology (EAN) 2020, which is being conducted as a virtual/online meeting because of the COVID-19 pandemic.
As his PhD dissertation, Dr. Mbizvo is investigating the rates, causes, and risk factors for epilepsy-related deaths and the percentage of these that are potentially avoidable.
The National Health Service of Scotland contains various linked administrative data sets. Each resident of Scotland has a unique identifier that facilitates investigations across the health system.
Dr. Mbizvo investigated adults and adolescents aged 16 years and older who died because of epilepsy during 2009-2016. He compared this group to patients of similar age who were living with epilepsy to identify risk factors that might help focus resources. During the study period, 2,149 epilepsy-related deaths occurred. Nearly 60% involved at least one seizure-related hospital admission.
Heavy burden
Of the patients who died because of epilepsy, 24% were seen in an outpatient neurologic clinic. “So there’s this heavy burden of admissions not translating to neurology follow-up,” said Dr. Mbizvo.
During the study period, there was no reduction in mortality “despite advances in medical care,” said Dr. Mbizvo.
Younger people with epilepsy were found to be more likely to die. The standardized mortality rate was 6/100,000 (95% confidence interval, 2.3-9.7) among those aged 16-24 years. By contrast, among those aged 45-54 years, the rate was 2/100,000 (95% CI, 1.1-2.1); it was lower in older age groups.
“The overall mortality is not reducing; people are dying young, and neurologists are really not getting involved,” Dr. Mbizvo said.
Among the almost 600 deaths of those aged 16-54 years, 58% were from Scotland’s “most deprived areas,” he noted.
From medical records and antiepileptic drug (AED) use, Dr. Mbizvo looked for risk factors that may have contributed to these epilepsy-related deaths. The most common cause of death in the group aged 16- 54 years was sudden unexpected death in epilepsy (SUDEP), followed by respiratory disorders, such as aspiration pneumonia.
“We think this should be avoidable, in the sense that these are people that could perhaps be targeted early with, for example, antibiotics,” said Dr. Mbizvo.
The next most common cause of death was circulatory disease, largely cardiac arrest.
“The idea is that electroexcitation – an abnormality in the brain – and the heart are related, and maybe that’s translating to a risk of death,” said Dr. Mbizvo.
Worrisome group
Mental and behavioral disorders, largely alcohol related, were the next most common cause of death.
“This is a group I worry about,” said Dr. Mbizvo. “I think they’re seen in the acute services and discharged as alcohol-withdrawal seizures. It’s possible that some have epilepsy and are never referred to a neurologist, and this may translate into increased mortality.”
Dr. Mbizvo is analyzing how these results differ from what is seen in the general population of Scotland among those younger than 75 years.
The top cause of death in the general population is neoplasm of the lungs. Aspiration of the lung is near the top for those who died from epilepsy, but the mechanisms leading to lung-related deaths in these populations may differ, said Dr. Mbizvo.
By applying coding methodology from fields unrelated to epilepsy where this approach has been tried, he determined that 78% of epilepsy-related deaths among those younger than 55 years were potentially avoidable.
“As a method, this is still in its infancy and will require validation, but we see this as a start,” Dr. Mbizvo said.
He provided examples from medical records that illustrate avoidable factors that could contribute to death. These included cases in which patients were discharged with the wrong dose of AED and in which patients drowned in a bath after having not been appropriately educated about seizure safety.
Can’t plug in
Patients with a first seizure are typically referred quickly to an appropriate service, but Dr. Mbizvo is concerned about those with chronic, stable epilepsy. “These people may at some point decompensate, and there’s no channel to plug them back into neurology services to make it easy for them to access a neurologist,” he said.
Currently, experts tell discharged patients to call if a problem occurs, but the system “is rather ad hoc,” said Dr. Mbizvo.
Because of the COVID-19 crisis, the use of telemedicine is increasing. This is helping to improve the system. “We may be able to build a virtual community for people who are on antiepileptic drugs and who suddenly begin to experience seizures again, to enable them to quickly get help, alongside a defined pathway to an epilepsy specialist,” said Dr. Mbizvo.
He hopes to develop a risk index for epilepsy patients similar to one used in cardiology that assesses risks such as smoking, high cholesterol level, and obesity. Although such a risk score might be similar to the SUDEP risk indices being developed, it will take into account death from any epilepsy-related cause, said Dr. Mbizvo. “Having not yet completed the analysis, I’m not sure which aspects will confer the greatest risk,” he said.
He added that, anecdotally, he has noticed a slight trend toward high mortality among patients with epilepsy who present multiple times at emergency departments in a year.
If this trend is statistically valid, “it could help create a traffic light flagging system on A&Es [accident and emergency departments] in which individuals with epilepsy who, for example, have two or more attendances to A&E in a year become flagged as high risk of death and are plugged into a rapid access epilepsy specialist clinic,” he said.
For their part, neurologists should recognize drug-resistant epilepsy early and refer such patients for assessment for resective surgery. If successful, such surgery reduces the risk for premature mortality, said Dr. Mbizvo.
Patients should not become discouraged by drug resistance, either. Research shows that, with careful reassessment of epilepsy type and drug changes, some patients whose condition is thought to be intractable could experience significant improvement in seizure frequency or seizures could be stopped.
“We need to talk to our patients more about the importance of adherence and encourage them to be honest with us if they don’t like the drugs we’re giving them and, as a result, are not taking them as recommended,” Dr. Mbizvo said.
Physicians also need to screen for mood disorders, especially suicidal ideation. Increasingly, specialists are recognizing mental health as an important area of epilepsy care.
They should also conduct a “safety briefing” perhaps twice a year in which they discuss, for example, SUDEP risk, driving concerns, showering instead of bathing, ensuring that a life guard is present at a swimming pool, and other measures.
Commenting on the study, Josemir W. (Ley) Sander, MD, PhD, professor of neurology and clinical epilepsy at University College London, said he welcomes any effort that highlights the problem of premature death among people with epilepsy and that offers possible ways to mitigate it.
Although the study “shows that premature death among people with epilepsy is a major issue,” many health care providers are not fully aware of the extent of this problem, said Dr. Sander. “For many, epilepsy is just a benign condition in which people have seizures,” he said. A risk score that could identify those at high risk for death and establishing preventive measures “would go a long way to decrease the burden of epilepsy,” he noted.
The study was supported by Epilepsy Research UK and the Juliet Bergqvist Memorial Fund. Dr. Mbizvo and Dr. Sander have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM EAN 2020
Today’s top news highlights: Protests and COVID-19 risk, avoidable epilepsy deaths, and more
Here are the stories our MDedge editors across specialties think you need to know about today:
Mass protests could cause COVID-19 outbreaks
As mass protests continue throughout the country, officials expressed concern about a potential spike in coronavirus cases in the coming days.
“There’s going to be a lot of issues coming out of what’s happened in the last week, but one of them is going to be that chains of transmission will have become lit from these gatherings,” Scott Gottlieb, former FDA commissioner, said on the CBS News show “Face the Nation.”
The protests generally have started peacefully with some demonstrators following physical distancing rules. But they have evolved into sometimes violent gatherings of hundreds or thousands of people where standing six feet apart is impossible. Chanting, singing, and shouting may spread the virus through respiratory droplets.
“If you were out protesting last night, you probably need to go get a COVID test this week,” Atlanta Mayor Keisha Lance Bottoms said Saturday, according to The Associated Press. Read More.
Diabetes: 1 in 10 hospitalized for COVID-19 die within a week
More than 10% of people with diabetes who are hospitalized for COVID-19 die within a week, while nearly a third require mechanical ventilation, new research shows.
Data from the CORONADO study also revealed that body mass index was independently associated with death or intubation at 7 days, while A1c and use of renin-angiotensin-aldosterone system blockers and dipeptidyl peptidase–4 inhibitors were not.
The presence of diabetes-related complications and older age also increased the risk of death.
The findings were published online in Diabetologia.
Previous studies have linked diabetes to worse outcomes in COVID-19, but this is the first to examine specific characteristics before and at the time of hospital admission that predict worse outcomes among people with diabetes, study coauthor Samy Hadjadj, MD, PhD, said in an interview. Read more.
Most adult epilepsy-related deaths could be avoided
Almost 80% of epilepsy deaths among adults are potentially avoidable, results of a new study suggest.
The research shows that such avoidable deaths “remain common and have not declined over time, despite advances in treatment,” Gashirai Mbizvo, MBChB, PhD, of the University of Edinburgh, United Kingdom, said during a press briefing. The findings were presented at the virtual/online Congress of the European Academy of Neurology (EAN) 2020.
Dr. Mbizvo investigated adolescents and adults aged 16 years and older who died because of epilepsy from 2009 to 2016. He compared this group to patients of similar age who were living with epilepsy. A total of 2149 epilepsy-related deaths occurred.
The most common cause of death in the 16- to 54-year age group was sudden unexpected death in epilepsy, followed by respiratory disorders, such as aspiration pneumonia. “We think this should be avoidable, in the sense that these are people that could perhaps be targeted early with, for example, antibiotics,” Dr. Mbizvo said.
The next most common cause of death was circulatory disease, largely cardiac arrest.
“The idea is that electroexcitation – an abnormality in the brain – and the heart are related, and maybe that’s translating to a risk of death,” Dr. Mbizvo said. Read More.
FDA approves combo treatment for hepatocellular cancer
The Food and Drug Administration has approved atezolizumab (Tecentriq) in combination with bevacizumab (Avastin) to treat patients with unresectable or metastatic hepatocellular carcinoma who have not received prior systemic therapy.
The approval was supported by results from the IMbrave150 trial (N Engl J Med 2020; 382:1894-1905). This phase 3 trial enrolled 501 patients with hepatocellular carcinoma who were randomized to receive either sorafenib or atezolizumab plus bevacizumab.
The median overall survival was not reached in patients who received atezolizumab plus bevacizumab, but it was 13.2 months in patients who received sorafenib.
The median progression-free survival was 6.8 months in patients who received atezolizumab plus bevacizumab and 4.3 months for those who received sorafenib. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Mass protests could cause COVID-19 outbreaks
As mass protests continue throughout the country, officials expressed concern about a potential spike in coronavirus cases in the coming days.
“There’s going to be a lot of issues coming out of what’s happened in the last week, but one of them is going to be that chains of transmission will have become lit from these gatherings,” Scott Gottlieb, former FDA commissioner, said on the CBS News show “Face the Nation.”
The protests generally have started peacefully with some demonstrators following physical distancing rules. But they have evolved into sometimes violent gatherings of hundreds or thousands of people where standing six feet apart is impossible. Chanting, singing, and shouting may spread the virus through respiratory droplets.
“If you were out protesting last night, you probably need to go get a COVID test this week,” Atlanta Mayor Keisha Lance Bottoms said Saturday, according to The Associated Press. Read More.
Diabetes: 1 in 10 hospitalized for COVID-19 die within a week
More than 10% of people with diabetes who are hospitalized for COVID-19 die within a week, while nearly a third require mechanical ventilation, new research shows.
Data from the CORONADO study also revealed that body mass index was independently associated with death or intubation at 7 days, while A1c and use of renin-angiotensin-aldosterone system blockers and dipeptidyl peptidase–4 inhibitors were not.
The presence of diabetes-related complications and older age also increased the risk of death.
The findings were published online in Diabetologia.
Previous studies have linked diabetes to worse outcomes in COVID-19, but this is the first to examine specific characteristics before and at the time of hospital admission that predict worse outcomes among people with diabetes, study coauthor Samy Hadjadj, MD, PhD, said in an interview. Read more.
Most adult epilepsy-related deaths could be avoided
Almost 80% of epilepsy deaths among adults are potentially avoidable, results of a new study suggest.
The research shows that such avoidable deaths “remain common and have not declined over time, despite advances in treatment,” Gashirai Mbizvo, MBChB, PhD, of the University of Edinburgh, United Kingdom, said during a press briefing. The findings were presented at the virtual/online Congress of the European Academy of Neurology (EAN) 2020.
Dr. Mbizvo investigated adolescents and adults aged 16 years and older who died because of epilepsy from 2009 to 2016. He compared this group to patients of similar age who were living with epilepsy. A total of 2149 epilepsy-related deaths occurred.
The most common cause of death in the 16- to 54-year age group was sudden unexpected death in epilepsy, followed by respiratory disorders, such as aspiration pneumonia. “We think this should be avoidable, in the sense that these are people that could perhaps be targeted early with, for example, antibiotics,” Dr. Mbizvo said.
The next most common cause of death was circulatory disease, largely cardiac arrest.
“The idea is that electroexcitation – an abnormality in the brain – and the heart are related, and maybe that’s translating to a risk of death,” Dr. Mbizvo said. Read More.
FDA approves combo treatment for hepatocellular cancer
The Food and Drug Administration has approved atezolizumab (Tecentriq) in combination with bevacizumab (Avastin) to treat patients with unresectable or metastatic hepatocellular carcinoma who have not received prior systemic therapy.
The approval was supported by results from the IMbrave150 trial (N Engl J Med 2020; 382:1894-1905). This phase 3 trial enrolled 501 patients with hepatocellular carcinoma who were randomized to receive either sorafenib or atezolizumab plus bevacizumab.
The median overall survival was not reached in patients who received atezolizumab plus bevacizumab, but it was 13.2 months in patients who received sorafenib.
The median progression-free survival was 6.8 months in patients who received atezolizumab plus bevacizumab and 4.3 months for those who received sorafenib. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Mass protests could cause COVID-19 outbreaks
As mass protests continue throughout the country, officials expressed concern about a potential spike in coronavirus cases in the coming days.
“There’s going to be a lot of issues coming out of what’s happened in the last week, but one of them is going to be that chains of transmission will have become lit from these gatherings,” Scott Gottlieb, former FDA commissioner, said on the CBS News show “Face the Nation.”
The protests generally have started peacefully with some demonstrators following physical distancing rules. But they have evolved into sometimes violent gatherings of hundreds or thousands of people where standing six feet apart is impossible. Chanting, singing, and shouting may spread the virus through respiratory droplets.
“If you were out protesting last night, you probably need to go get a COVID test this week,” Atlanta Mayor Keisha Lance Bottoms said Saturday, according to The Associated Press. Read More.
Diabetes: 1 in 10 hospitalized for COVID-19 die within a week
More than 10% of people with diabetes who are hospitalized for COVID-19 die within a week, while nearly a third require mechanical ventilation, new research shows.
Data from the CORONADO study also revealed that body mass index was independently associated with death or intubation at 7 days, while A1c and use of renin-angiotensin-aldosterone system blockers and dipeptidyl peptidase–4 inhibitors were not.
The presence of diabetes-related complications and older age also increased the risk of death.
The findings were published online in Diabetologia.
Previous studies have linked diabetes to worse outcomes in COVID-19, but this is the first to examine specific characteristics before and at the time of hospital admission that predict worse outcomes among people with diabetes, study coauthor Samy Hadjadj, MD, PhD, said in an interview. Read more.
Most adult epilepsy-related deaths could be avoided
Almost 80% of epilepsy deaths among adults are potentially avoidable, results of a new study suggest.
The research shows that such avoidable deaths “remain common and have not declined over time, despite advances in treatment,” Gashirai Mbizvo, MBChB, PhD, of the University of Edinburgh, United Kingdom, said during a press briefing. The findings were presented at the virtual/online Congress of the European Academy of Neurology (EAN) 2020.
Dr. Mbizvo investigated adolescents and adults aged 16 years and older who died because of epilepsy from 2009 to 2016. He compared this group to patients of similar age who were living with epilepsy. A total of 2149 epilepsy-related deaths occurred.
The most common cause of death in the 16- to 54-year age group was sudden unexpected death in epilepsy, followed by respiratory disorders, such as aspiration pneumonia. “We think this should be avoidable, in the sense that these are people that could perhaps be targeted early with, for example, antibiotics,” Dr. Mbizvo said.
The next most common cause of death was circulatory disease, largely cardiac arrest.
“The idea is that electroexcitation – an abnormality in the brain – and the heart are related, and maybe that’s translating to a risk of death,” Dr. Mbizvo said. Read More.
FDA approves combo treatment for hepatocellular cancer
The Food and Drug Administration has approved atezolizumab (Tecentriq) in combination with bevacizumab (Avastin) to treat patients with unresectable or metastatic hepatocellular carcinoma who have not received prior systemic therapy.
The approval was supported by results from the IMbrave150 trial (N Engl J Med 2020; 382:1894-1905). This phase 3 trial enrolled 501 patients with hepatocellular carcinoma who were randomized to receive either sorafenib or atezolizumab plus bevacizumab.
The median overall survival was not reached in patients who received atezolizumab plus bevacizumab, but it was 13.2 months in patients who received sorafenib.
The median progression-free survival was 6.8 months in patients who received atezolizumab plus bevacizumab and 4.3 months for those who received sorafenib. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Neurologists’ pay gets a boost, most happy with career choice
findings from the newly released Medscape Neurologist Compensation Report 2020 show.
Neurologists’ average annual income this year rose to $280,000, up from $267,000 last year. More than half of neurologists (53%) feel fairly compensated, similar to last year’s percentage.
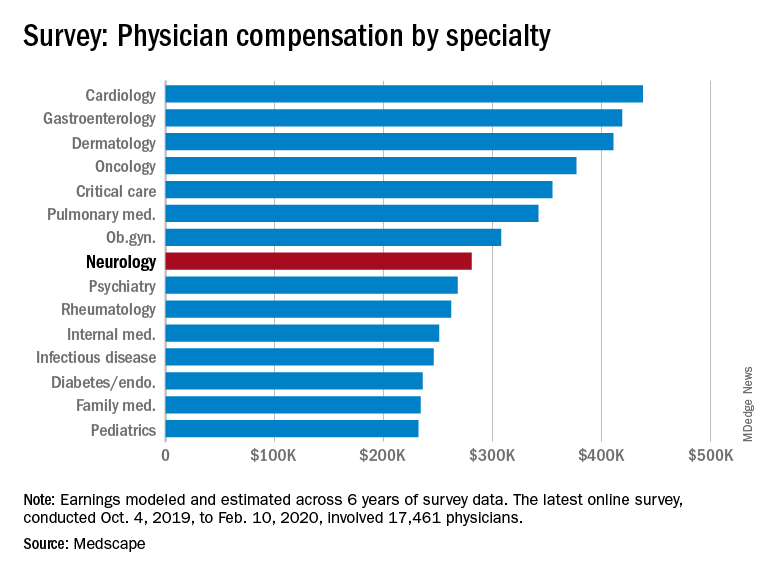
Neurologists are below the middle earners of all physician specialties. At $280,000 in annual compensation for patient care, neurologists rank ninth from the bottom, just below allergists/immunologists ($301,000) but ahead of psychiatrists ($268,000), rheumatologists ($262,000), and internists ($251,000).
Orthopedists are the top earners ($511,000 annual pay), followed by plastic surgeons ($479,000), otolaryngologists ($455,000), and cardiologists ($438,000), according the overall Medscape Physician Compensation Report 2020, which covers U.S. physicians as a whole. The survey included more than 17,000 physicians in over 30 specialties.
COVID-19 impact
An important caveat is that the data for this year’s report were collected prior to Feb. 10, 2020, and therefore reflect physician salary and income prior to the COVID-19 crisis, which has had a huge impact on physicians.
For example, data show that since the start of the crisis, physician practices have seen a 55% dip in revenue and a 60% dip in patient volume on average. Hospitals and physician groups nationwide have implemented layoffs, furloughs, and pay cuts.
In March, 43,000 health care workers were laid off; 9% of independent medical practices reported that they had closed their practices, at least temporarily.
There continues to be a gender pay gap in neurology, with male neurologists earning about 26% more than their female peers ($299,000 vs. $237,000). Among all specialists, men earn 31% more than women, similar to last year’s figure of 33%. There continues to be a 25% gender pay gap among primary care physicians.
More than half of all physicians (56%) say they receive an incentive bonus. Neurologists report that they are eligible for an annual incentive bonus of $35,000. Average annual incentive bonuses are highest among orthopedists ($96,000) and lowest among family medicine physicians ($24,000).
Close to one third of physicians overall who receive incentive bonuses say the prospect of receiving the bonus has encouraged them to work longer hours. A higher percentage of neurologists (41%) say their potential bonus influenced them to increase their work hours.
Fifty-eight percent of neurologists achieve more than three quarters of their potential annual incentive bonus. On average, neurologists achieve about two thirds of their potential bonus, the same proportion as for physicians overall.
However, COVID-19 may change that. Experts who were interviewed recently by Medscape noted that productivity benchmarks for physicians are likely to be lowered in light of plunging patient numbers from COVID-19, and bonuses are expected to take a hit.
Happy at work
On average, male neurologists spend 37.7 hours per week seeing patients, somewhat more hours per week than female neurologists (36.1 hours); the average for all physicians is 37.9 hours per week.
Bureaucratic tasks continue to be a burden for physicians in all specialties. On average, neurologists spend 16.9 hours per week on paperwork and administration, about the same as physicians overall (15.6 hours).
Intensivists top the list regarding such tasks (19.1 hours), followed by internists (18.5), infectious disease physicians (18.5), and psychiatrists (18.3). Anesthesiologists and ophthalmologists spend the least amount of time on paperwork/administration (10.0 and 9.8 hours per week, respectively).
What is most rewarding about being a neurologist? Being good at what they do/finding answers, diagnoses tops the list (33%), followed by making the world a better place/helping others (26%), relationships with and gratitude from patients (18%), and making good money at a job they like (11%). A few cited teaching (5%) and pride in their profession (4%).
The most challenging part of practicing neurology is having to follow so many rules and regulations (26%). Other challenges include having to work long hours (18%), dealing with difficult patients (17%), trouble getting fair reimbursement (13%), and working with electronic health records (10%).
Despite the challenges, if they had to do it all over again, 73% of neurologists would still choose medicine as a career, and 86% would again choose neurology.
Other key findings in the latest report regarding neurologists include the following:
- At 18%, neurologists rank near the middle among physicians with regard to losing money on denied or resubmitted claims. Plastic surgery and emergency medicine have the highest percentage of claims denied or resubmitted (28% and 22%, respectively). One study found that, on average, 63% of denied claims are recoverable, but healthcare professionals spend about $118 per claim on appeals.
- 29% of neurologists say they use physician assistants (PAs) to treat patients in their practices, and 53% use nurse practitioners (NPs); 38% use neither for patient care. Of neurologists who work with PAs and NPs in their offices, 49% say these employees have helped boost profitability.
- Two-thirds of neurologists say they will continue taking new and current Medicare/Medicaid patients; none say they will not take new Medicare patients; and 26% are undecided.
- Neurologists participate in various payment methods; 78% are reimbursed via insurance, 35% have fee-for-service arrangements, and 28% are in accountable care organizations.
- Nearly 40% of neurologists expect to participate in the merit-based incentive payment system option, and 10% expect to participate in alternative payment models.
This article first appeared on Medscape.com.
findings from the newly released Medscape Neurologist Compensation Report 2020 show.
Neurologists’ average annual income this year rose to $280,000, up from $267,000 last year. More than half of neurologists (53%) feel fairly compensated, similar to last year’s percentage.
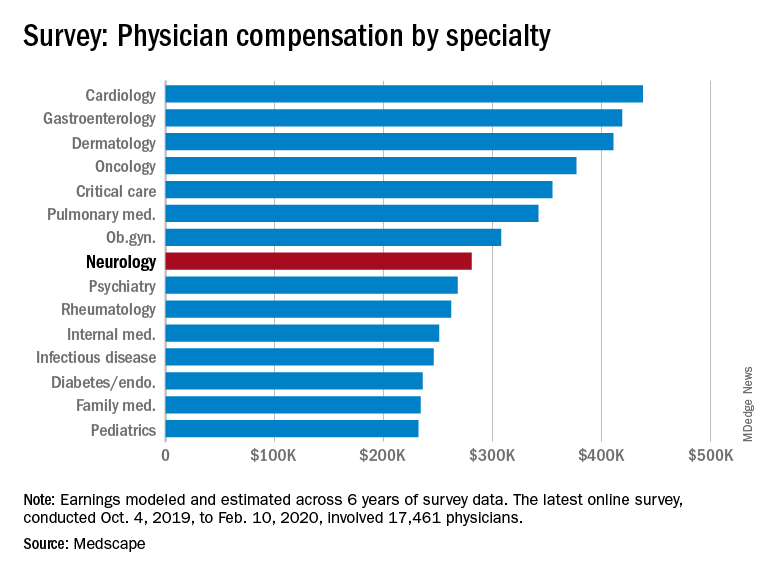
Neurologists are below the middle earners of all physician specialties. At $280,000 in annual compensation for patient care, neurologists rank ninth from the bottom, just below allergists/immunologists ($301,000) but ahead of psychiatrists ($268,000), rheumatologists ($262,000), and internists ($251,000).
Orthopedists are the top earners ($511,000 annual pay), followed by plastic surgeons ($479,000), otolaryngologists ($455,000), and cardiologists ($438,000), according the overall Medscape Physician Compensation Report 2020, which covers U.S. physicians as a whole. The survey included more than 17,000 physicians in over 30 specialties.
COVID-19 impact
An important caveat is that the data for this year’s report were collected prior to Feb. 10, 2020, and therefore reflect physician salary and income prior to the COVID-19 crisis, which has had a huge impact on physicians.
For example, data show that since the start of the crisis, physician practices have seen a 55% dip in revenue and a 60% dip in patient volume on average. Hospitals and physician groups nationwide have implemented layoffs, furloughs, and pay cuts.
In March, 43,000 health care workers were laid off; 9% of independent medical practices reported that they had closed their practices, at least temporarily.
There continues to be a gender pay gap in neurology, with male neurologists earning about 26% more than their female peers ($299,000 vs. $237,000). Among all specialists, men earn 31% more than women, similar to last year’s figure of 33%. There continues to be a 25% gender pay gap among primary care physicians.
More than half of all physicians (56%) say they receive an incentive bonus. Neurologists report that they are eligible for an annual incentive bonus of $35,000. Average annual incentive bonuses are highest among orthopedists ($96,000) and lowest among family medicine physicians ($24,000).
Close to one third of physicians overall who receive incentive bonuses say the prospect of receiving the bonus has encouraged them to work longer hours. A higher percentage of neurologists (41%) say their potential bonus influenced them to increase their work hours.
Fifty-eight percent of neurologists achieve more than three quarters of their potential annual incentive bonus. On average, neurologists achieve about two thirds of their potential bonus, the same proportion as for physicians overall.
However, COVID-19 may change that. Experts who were interviewed recently by Medscape noted that productivity benchmarks for physicians are likely to be lowered in light of plunging patient numbers from COVID-19, and bonuses are expected to take a hit.
Happy at work
On average, male neurologists spend 37.7 hours per week seeing patients, somewhat more hours per week than female neurologists (36.1 hours); the average for all physicians is 37.9 hours per week.
Bureaucratic tasks continue to be a burden for physicians in all specialties. On average, neurologists spend 16.9 hours per week on paperwork and administration, about the same as physicians overall (15.6 hours).
Intensivists top the list regarding such tasks (19.1 hours), followed by internists (18.5), infectious disease physicians (18.5), and psychiatrists (18.3). Anesthesiologists and ophthalmologists spend the least amount of time on paperwork/administration (10.0 and 9.8 hours per week, respectively).
What is most rewarding about being a neurologist? Being good at what they do/finding answers, diagnoses tops the list (33%), followed by making the world a better place/helping others (26%), relationships with and gratitude from patients (18%), and making good money at a job they like (11%). A few cited teaching (5%) and pride in their profession (4%).
The most challenging part of practicing neurology is having to follow so many rules and regulations (26%). Other challenges include having to work long hours (18%), dealing with difficult patients (17%), trouble getting fair reimbursement (13%), and working with electronic health records (10%).
Despite the challenges, if they had to do it all over again, 73% of neurologists would still choose medicine as a career, and 86% would again choose neurology.
Other key findings in the latest report regarding neurologists include the following:
- At 18%, neurologists rank near the middle among physicians with regard to losing money on denied or resubmitted claims. Plastic surgery and emergency medicine have the highest percentage of claims denied or resubmitted (28% and 22%, respectively). One study found that, on average, 63% of denied claims are recoverable, but healthcare professionals spend about $118 per claim on appeals.
- 29% of neurologists say they use physician assistants (PAs) to treat patients in their practices, and 53% use nurse practitioners (NPs); 38% use neither for patient care. Of neurologists who work with PAs and NPs in their offices, 49% say these employees have helped boost profitability.
- Two-thirds of neurologists say they will continue taking new and current Medicare/Medicaid patients; none say they will not take new Medicare patients; and 26% are undecided.
- Neurologists participate in various payment methods; 78% are reimbursed via insurance, 35% have fee-for-service arrangements, and 28% are in accountable care organizations.
- Nearly 40% of neurologists expect to participate in the merit-based incentive payment system option, and 10% expect to participate in alternative payment models.
This article first appeared on Medscape.com.
findings from the newly released Medscape Neurologist Compensation Report 2020 show.
Neurologists’ average annual income this year rose to $280,000, up from $267,000 last year. More than half of neurologists (53%) feel fairly compensated, similar to last year’s percentage.
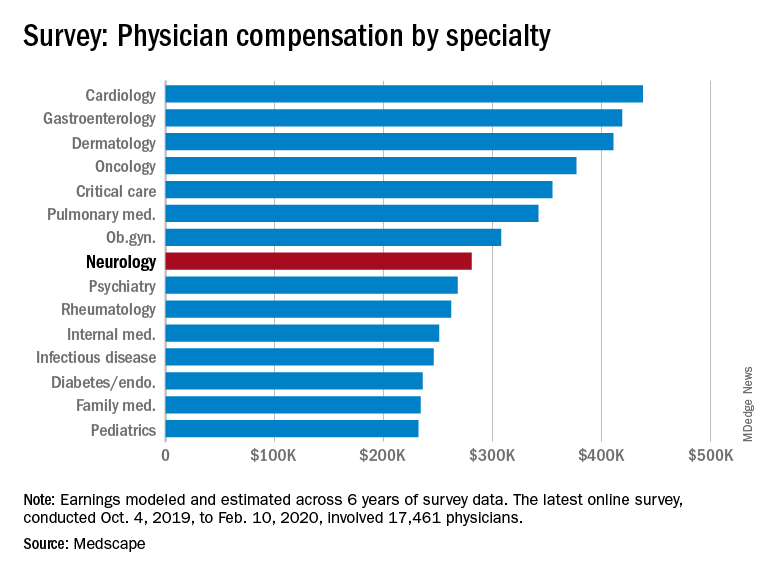
Neurologists are below the middle earners of all physician specialties. At $280,000 in annual compensation for patient care, neurologists rank ninth from the bottom, just below allergists/immunologists ($301,000) but ahead of psychiatrists ($268,000), rheumatologists ($262,000), and internists ($251,000).
Orthopedists are the top earners ($511,000 annual pay), followed by plastic surgeons ($479,000), otolaryngologists ($455,000), and cardiologists ($438,000), according the overall Medscape Physician Compensation Report 2020, which covers U.S. physicians as a whole. The survey included more than 17,000 physicians in over 30 specialties.
COVID-19 impact
An important caveat is that the data for this year’s report were collected prior to Feb. 10, 2020, and therefore reflect physician salary and income prior to the COVID-19 crisis, which has had a huge impact on physicians.
For example, data show that since the start of the crisis, physician practices have seen a 55% dip in revenue and a 60% dip in patient volume on average. Hospitals and physician groups nationwide have implemented layoffs, furloughs, and pay cuts.
In March, 43,000 health care workers were laid off; 9% of independent medical practices reported that they had closed their practices, at least temporarily.
There continues to be a gender pay gap in neurology, with male neurologists earning about 26% more than their female peers ($299,000 vs. $237,000). Among all specialists, men earn 31% more than women, similar to last year’s figure of 33%. There continues to be a 25% gender pay gap among primary care physicians.
More than half of all physicians (56%) say they receive an incentive bonus. Neurologists report that they are eligible for an annual incentive bonus of $35,000. Average annual incentive bonuses are highest among orthopedists ($96,000) and lowest among family medicine physicians ($24,000).
Close to one third of physicians overall who receive incentive bonuses say the prospect of receiving the bonus has encouraged them to work longer hours. A higher percentage of neurologists (41%) say their potential bonus influenced them to increase their work hours.
Fifty-eight percent of neurologists achieve more than three quarters of their potential annual incentive bonus. On average, neurologists achieve about two thirds of their potential bonus, the same proportion as for physicians overall.
However, COVID-19 may change that. Experts who were interviewed recently by Medscape noted that productivity benchmarks for physicians are likely to be lowered in light of plunging patient numbers from COVID-19, and bonuses are expected to take a hit.
Happy at work
On average, male neurologists spend 37.7 hours per week seeing patients, somewhat more hours per week than female neurologists (36.1 hours); the average for all physicians is 37.9 hours per week.
Bureaucratic tasks continue to be a burden for physicians in all specialties. On average, neurologists spend 16.9 hours per week on paperwork and administration, about the same as physicians overall (15.6 hours).
Intensivists top the list regarding such tasks (19.1 hours), followed by internists (18.5), infectious disease physicians (18.5), and psychiatrists (18.3). Anesthesiologists and ophthalmologists spend the least amount of time on paperwork/administration (10.0 and 9.8 hours per week, respectively).
What is most rewarding about being a neurologist? Being good at what they do/finding answers, diagnoses tops the list (33%), followed by making the world a better place/helping others (26%), relationships with and gratitude from patients (18%), and making good money at a job they like (11%). A few cited teaching (5%) and pride in their profession (4%).
The most challenging part of practicing neurology is having to follow so many rules and regulations (26%). Other challenges include having to work long hours (18%), dealing with difficult patients (17%), trouble getting fair reimbursement (13%), and working with electronic health records (10%).
Despite the challenges, if they had to do it all over again, 73% of neurologists would still choose medicine as a career, and 86% would again choose neurology.
Other key findings in the latest report regarding neurologists include the following:
- At 18%, neurologists rank near the middle among physicians with regard to losing money on denied or resubmitted claims. Plastic surgery and emergency medicine have the highest percentage of claims denied or resubmitted (28% and 22%, respectively). One study found that, on average, 63% of denied claims are recoverable, but healthcare professionals spend about $118 per claim on appeals.
- 29% of neurologists say they use physician assistants (PAs) to treat patients in their practices, and 53% use nurse practitioners (NPs); 38% use neither for patient care. Of neurologists who work with PAs and NPs in their offices, 49% say these employees have helped boost profitability.
- Two-thirds of neurologists say they will continue taking new and current Medicare/Medicaid patients; none say they will not take new Medicare patients; and 26% are undecided.
- Neurologists participate in various payment methods; 78% are reimbursed via insurance, 35% have fee-for-service arrangements, and 28% are in accountable care organizations.
- Nearly 40% of neurologists expect to participate in the merit-based incentive payment system option, and 10% expect to participate in alternative payment models.
This article first appeared on Medscape.com.
Frontal lobe glucose abnormalities may indicate increased SUDEP risk
, new research suggests.
“The data provide initial evidence that hypometabolism in certain parts of the frontal cortex may be associated with higher SUDEP risk,” said lead author Maysaa M. Basha, MD, associate professor of neurology and director of the Adult Comprehensive Epilepsy Program, Wayne State University/Detroit Medical Center, in Michigan.
If this research is validated, “it potentially can be used to screen patients for higher SUDEP risk,” she said. The idea is to identify those at high risk and then reduce that risk with more aggressive management of seizures or closer monitoring in certain cases, she added.
The research is being presented online as part of the 2020 American Academy of Neurology (AAN) Science Highlights.
Hypometabolism
Dr. Basha and colleagues were encouraged to pursue this new line of research after a pilot [18F]fluorodeoxyglucose positron-emission tomography (FDG-PET) study revealed frontal lobe hypometabolism among patients who subsequently died.
“We wanted to determine if such a metabolic abnormality is associated with SUDEP risk,” said Dr. Basha. She noted that no PET studies have addressed this question, only MRI studies.
In this new study, researchers aimed to identify specific patterns of objectively detected brain glucose metabolic abnormalities in patients with refractory focal epilepsy who were at risk for SUDEP.
The study included 80 patients (45 female patients) aged 16 to 61 years (mean age, 37 years) who underwent FDG-PET as part of their presurgical evaluation for epilepsy surgery. Patients with large brain lesions, such as an infarct or a large tumor, were excluded from the study; such lesions can affect the accuracy of an objective PET analysis, explained Dr. Basha.
The researchers assessed risk for SUDEP using the seven-item SUDEP inventory (SUDEP-7), which was developed as a marker of clinical SUDEP risk. The 0- to 10-point scale is used to evaluate the frequency of tonic-clonic and other seizures, the duration of epilepsy, the use of antiepileptic drugs, and intellectual disability.
The researchers calculated SUDEP-7 inventory scores as closely as possible to FDG-PET assessments. The mean score in the patient population was 3.6.
The investigators divided participants into two subgroups: 22 patients had a SUDEP score of 5 or greater; and 58 had a score of less than 5 (higher scores indicate higher risk for SUDEP).
The researchers compared PET scans of each of these subgroups to PET scans from healthy adults to determine whether they showed common areas of metabolic abnormality. For this, they used an image analytic software program called Statistical Parametric Mapping, which compares group values of metabolic activity measured in small units of the brain (voxels) with statistical methods.
The analysis showed that the higher-risk group displayed a common pattern of hypometabolism in certain brain areas.
“The epilepsy patient subgroup with high SUDEP risk showed areas of decreased metabolism, as compared to the control group, in portions of the frontal cortex,” said Dr. Basha. “The statistically most significant decreases were in the right frontal lobe area—both lateral convexity and medial cortex.”
Dr. Basha added that these group abnormalities were “remarkably similar” to the individual metabolic abnormalities found in the four SUDEP patients in the previous pilot study who underwent PET scanning and who subsequently died.
A similar group analysis showed that the group at low SUDEP risk displayed no common metabolic abnormalities.
MRI findings were normal for 40 patients.
Dr. Basha and colleagues believe that “this is the first PET study assessing the metabolic correlates of SUDEP risk on the group level.”
Common feature
Interictal glucose hypometabolism is “common in and around epileptic foci,” noted Dr. Basha. However, this could extend into nonepileptic regions—for example, to remote connected regions where seizures can spread from the primary focus and into subcortical gray matter structures, such the thalamus.
Some of these metabolic abnormalities may indicate subtle, microscopic, structural abnormalities in the affected brain, said Dr. Basha.
Abnormalities that are induced by epilepsy and that result from purely metabolic changes could be partly or fully reversed if seizures are controlled on a long-term basis, she said. “Some metabolic abnormalities can be reversed after better seizure control with antiepileptic drugs, epileptic surgery, or other antiepileptic treatment,” she said.
It’s “quite possible” that the same brain pattern would be evident in children with epilepsy, although her team has not performed the same analysis in a younger pediatric group, said Dr. Basha. She noted that it would be unethical to administer PET scans, which involve radiation, to young, healthy control persons.
It’s too early to recommend that all epilepsy patients undergo FDG-PET scanning to see whether this pattern of brain glucose hypometabolism is present, said Dr. Basha. “But if this is proven to be a good biomarker, the next step would be a prospective study” to see whether this brain marker is a true signal of SUDEP risk.
“I don’t think our single study would do that, but ultimately, that would be the goal,” she added.
One more piece of the SUDEP puzzle
Commenting on the study, William Davis Gaillard, MD, president of the American Epilepsy Society and chief of neurology, Children’s National Medical Center, Chevy Chase, Maryland, said this new information provides one more piece of the SUDEP puzzle but doesn’t complete the picture.
The study authors assessed PET scans of a group of patients and found common abnormalities that implicate the right medial frontal cortex. “That’s a pretty reasonable method” of investigation, said Dr. Gaillard.
“The challenge is that they’re looking at people they believe have a risk of SUDEP as opposed to people who died,” said Dr. Gaillard.
But he agreed that the results might signal “a biomarker” that “allows you to identify who’s at high risk, and then you may be able to intervene to save them.”
It’s not clear that people with frontal lobe epilepsy are at greater risk for SUDEP than those with temporal lobe epilepsy, he said.
“What you don’t know is whether this represents people with a seizure focus in that area or this represents a common network implicated in people with diverse forms of focal epilepsy; so you need to do some more work,” he said.
Dr. Gaillard pointed out that other research has implicated regions other than the mesial frontal cortex in SUDEP risk. These regions include the insula, the amygdala, the hippocampus, and the brain stem.
He also noted that the SUDEP-7, which has not been thoroughly validated, is designed for use only in adults.
In his own practice, he asks patients about the frequency of tonic-clonic seizures and whether they occur at night. The number of antiepileptic medications a patient takes reflects the difficulty of controlling seizures and may not be “an independent variable for risk,” said Dr. Gaillard.
“It’s clear one needs a better assessment and better idea of who is at risk,” he said.
The researchers have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
SOURCE: Basha A et al. AAN 2020. Abstract P5.001.
, new research suggests.
“The data provide initial evidence that hypometabolism in certain parts of the frontal cortex may be associated with higher SUDEP risk,” said lead author Maysaa M. Basha, MD, associate professor of neurology and director of the Adult Comprehensive Epilepsy Program, Wayne State University/Detroit Medical Center, in Michigan.
If this research is validated, “it potentially can be used to screen patients for higher SUDEP risk,” she said. The idea is to identify those at high risk and then reduce that risk with more aggressive management of seizures or closer monitoring in certain cases, she added.
The research is being presented online as part of the 2020 American Academy of Neurology (AAN) Science Highlights.
Hypometabolism
Dr. Basha and colleagues were encouraged to pursue this new line of research after a pilot [18F]fluorodeoxyglucose positron-emission tomography (FDG-PET) study revealed frontal lobe hypometabolism among patients who subsequently died.
“We wanted to determine if such a metabolic abnormality is associated with SUDEP risk,” said Dr. Basha. She noted that no PET studies have addressed this question, only MRI studies.
In this new study, researchers aimed to identify specific patterns of objectively detected brain glucose metabolic abnormalities in patients with refractory focal epilepsy who were at risk for SUDEP.
The study included 80 patients (45 female patients) aged 16 to 61 years (mean age, 37 years) who underwent FDG-PET as part of their presurgical evaluation for epilepsy surgery. Patients with large brain lesions, such as an infarct or a large tumor, were excluded from the study; such lesions can affect the accuracy of an objective PET analysis, explained Dr. Basha.
The researchers assessed risk for SUDEP using the seven-item SUDEP inventory (SUDEP-7), which was developed as a marker of clinical SUDEP risk. The 0- to 10-point scale is used to evaluate the frequency of tonic-clonic and other seizures, the duration of epilepsy, the use of antiepileptic drugs, and intellectual disability.
The researchers calculated SUDEP-7 inventory scores as closely as possible to FDG-PET assessments. The mean score in the patient population was 3.6.
The investigators divided participants into two subgroups: 22 patients had a SUDEP score of 5 or greater; and 58 had a score of less than 5 (higher scores indicate higher risk for SUDEP).
The researchers compared PET scans of each of these subgroups to PET scans from healthy adults to determine whether they showed common areas of metabolic abnormality. For this, they used an image analytic software program called Statistical Parametric Mapping, which compares group values of metabolic activity measured in small units of the brain (voxels) with statistical methods.
The analysis showed that the higher-risk group displayed a common pattern of hypometabolism in certain brain areas.
“The epilepsy patient subgroup with high SUDEP risk showed areas of decreased metabolism, as compared to the control group, in portions of the frontal cortex,” said Dr. Basha. “The statistically most significant decreases were in the right frontal lobe area—both lateral convexity and medial cortex.”
Dr. Basha added that these group abnormalities were “remarkably similar” to the individual metabolic abnormalities found in the four SUDEP patients in the previous pilot study who underwent PET scanning and who subsequently died.
A similar group analysis showed that the group at low SUDEP risk displayed no common metabolic abnormalities.
MRI findings were normal for 40 patients.
Dr. Basha and colleagues believe that “this is the first PET study assessing the metabolic correlates of SUDEP risk on the group level.”
Common feature
Interictal glucose hypometabolism is “common in and around epileptic foci,” noted Dr. Basha. However, this could extend into nonepileptic regions—for example, to remote connected regions where seizures can spread from the primary focus and into subcortical gray matter structures, such the thalamus.
Some of these metabolic abnormalities may indicate subtle, microscopic, structural abnormalities in the affected brain, said Dr. Basha.
Abnormalities that are induced by epilepsy and that result from purely metabolic changes could be partly or fully reversed if seizures are controlled on a long-term basis, she said. “Some metabolic abnormalities can be reversed after better seizure control with antiepileptic drugs, epileptic surgery, or other antiepileptic treatment,” she said.
It’s “quite possible” that the same brain pattern would be evident in children with epilepsy, although her team has not performed the same analysis in a younger pediatric group, said Dr. Basha. She noted that it would be unethical to administer PET scans, which involve radiation, to young, healthy control persons.
It’s too early to recommend that all epilepsy patients undergo FDG-PET scanning to see whether this pattern of brain glucose hypometabolism is present, said Dr. Basha. “But if this is proven to be a good biomarker, the next step would be a prospective study” to see whether this brain marker is a true signal of SUDEP risk.
“I don’t think our single study would do that, but ultimately, that would be the goal,” she added.
One more piece of the SUDEP puzzle
Commenting on the study, William Davis Gaillard, MD, president of the American Epilepsy Society and chief of neurology, Children’s National Medical Center, Chevy Chase, Maryland, said this new information provides one more piece of the SUDEP puzzle but doesn’t complete the picture.
The study authors assessed PET scans of a group of patients and found common abnormalities that implicate the right medial frontal cortex. “That’s a pretty reasonable method” of investigation, said Dr. Gaillard.
“The challenge is that they’re looking at people they believe have a risk of SUDEP as opposed to people who died,” said Dr. Gaillard.
But he agreed that the results might signal “a biomarker” that “allows you to identify who’s at high risk, and then you may be able to intervene to save them.”
It’s not clear that people with frontal lobe epilepsy are at greater risk for SUDEP than those with temporal lobe epilepsy, he said.
“What you don’t know is whether this represents people with a seizure focus in that area or this represents a common network implicated in people with diverse forms of focal epilepsy; so you need to do some more work,” he said.
Dr. Gaillard pointed out that other research has implicated regions other than the mesial frontal cortex in SUDEP risk. These regions include the insula, the amygdala, the hippocampus, and the brain stem.
He also noted that the SUDEP-7, which has not been thoroughly validated, is designed for use only in adults.
In his own practice, he asks patients about the frequency of tonic-clonic seizures and whether they occur at night. The number of antiepileptic medications a patient takes reflects the difficulty of controlling seizures and may not be “an independent variable for risk,” said Dr. Gaillard.
“It’s clear one needs a better assessment and better idea of who is at risk,” he said.
The researchers have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
SOURCE: Basha A et al. AAN 2020. Abstract P5.001.
, new research suggests.
“The data provide initial evidence that hypometabolism in certain parts of the frontal cortex may be associated with higher SUDEP risk,” said lead author Maysaa M. Basha, MD, associate professor of neurology and director of the Adult Comprehensive Epilepsy Program, Wayne State University/Detroit Medical Center, in Michigan.
If this research is validated, “it potentially can be used to screen patients for higher SUDEP risk,” she said. The idea is to identify those at high risk and then reduce that risk with more aggressive management of seizures or closer monitoring in certain cases, she added.
The research is being presented online as part of the 2020 American Academy of Neurology (AAN) Science Highlights.
Hypometabolism
Dr. Basha and colleagues were encouraged to pursue this new line of research after a pilot [18F]fluorodeoxyglucose positron-emission tomography (FDG-PET) study revealed frontal lobe hypometabolism among patients who subsequently died.
“We wanted to determine if such a metabolic abnormality is associated with SUDEP risk,” said Dr. Basha. She noted that no PET studies have addressed this question, only MRI studies.
In this new study, researchers aimed to identify specific patterns of objectively detected brain glucose metabolic abnormalities in patients with refractory focal epilepsy who were at risk for SUDEP.
The study included 80 patients (45 female patients) aged 16 to 61 years (mean age, 37 years) who underwent FDG-PET as part of their presurgical evaluation for epilepsy surgery. Patients with large brain lesions, such as an infarct or a large tumor, were excluded from the study; such lesions can affect the accuracy of an objective PET analysis, explained Dr. Basha.
The researchers assessed risk for SUDEP using the seven-item SUDEP inventory (SUDEP-7), which was developed as a marker of clinical SUDEP risk. The 0- to 10-point scale is used to evaluate the frequency of tonic-clonic and other seizures, the duration of epilepsy, the use of antiepileptic drugs, and intellectual disability.
The researchers calculated SUDEP-7 inventory scores as closely as possible to FDG-PET assessments. The mean score in the patient population was 3.6.
The investigators divided participants into two subgroups: 22 patients had a SUDEP score of 5 or greater; and 58 had a score of less than 5 (higher scores indicate higher risk for SUDEP).
The researchers compared PET scans of each of these subgroups to PET scans from healthy adults to determine whether they showed common areas of metabolic abnormality. For this, they used an image analytic software program called Statistical Parametric Mapping, which compares group values of metabolic activity measured in small units of the brain (voxels) with statistical methods.
The analysis showed that the higher-risk group displayed a common pattern of hypometabolism in certain brain areas.
“The epilepsy patient subgroup with high SUDEP risk showed areas of decreased metabolism, as compared to the control group, in portions of the frontal cortex,” said Dr. Basha. “The statistically most significant decreases were in the right frontal lobe area—both lateral convexity and medial cortex.”
Dr. Basha added that these group abnormalities were “remarkably similar” to the individual metabolic abnormalities found in the four SUDEP patients in the previous pilot study who underwent PET scanning and who subsequently died.
A similar group analysis showed that the group at low SUDEP risk displayed no common metabolic abnormalities.
MRI findings were normal for 40 patients.
Dr. Basha and colleagues believe that “this is the first PET study assessing the metabolic correlates of SUDEP risk on the group level.”
Common feature
Interictal glucose hypometabolism is “common in and around epileptic foci,” noted Dr. Basha. However, this could extend into nonepileptic regions—for example, to remote connected regions where seizures can spread from the primary focus and into subcortical gray matter structures, such the thalamus.
Some of these metabolic abnormalities may indicate subtle, microscopic, structural abnormalities in the affected brain, said Dr. Basha.
Abnormalities that are induced by epilepsy and that result from purely metabolic changes could be partly or fully reversed if seizures are controlled on a long-term basis, she said. “Some metabolic abnormalities can be reversed after better seizure control with antiepileptic drugs, epileptic surgery, or other antiepileptic treatment,” she said.
It’s “quite possible” that the same brain pattern would be evident in children with epilepsy, although her team has not performed the same analysis in a younger pediatric group, said Dr. Basha. She noted that it would be unethical to administer PET scans, which involve radiation, to young, healthy control persons.
It’s too early to recommend that all epilepsy patients undergo FDG-PET scanning to see whether this pattern of brain glucose hypometabolism is present, said Dr. Basha. “But if this is proven to be a good biomarker, the next step would be a prospective study” to see whether this brain marker is a true signal of SUDEP risk.
“I don’t think our single study would do that, but ultimately, that would be the goal,” she added.
One more piece of the SUDEP puzzle
Commenting on the study, William Davis Gaillard, MD, president of the American Epilepsy Society and chief of neurology, Children’s National Medical Center, Chevy Chase, Maryland, said this new information provides one more piece of the SUDEP puzzle but doesn’t complete the picture.
The study authors assessed PET scans of a group of patients and found common abnormalities that implicate the right medial frontal cortex. “That’s a pretty reasonable method” of investigation, said Dr. Gaillard.
“The challenge is that they’re looking at people they believe have a risk of SUDEP as opposed to people who died,” said Dr. Gaillard.
But he agreed that the results might signal “a biomarker” that “allows you to identify who’s at high risk, and then you may be able to intervene to save them.”
It’s not clear that people with frontal lobe epilepsy are at greater risk for SUDEP than those with temporal lobe epilepsy, he said.
“What you don’t know is whether this represents people with a seizure focus in that area or this represents a common network implicated in people with diverse forms of focal epilepsy; so you need to do some more work,” he said.
Dr. Gaillard pointed out that other research has implicated regions other than the mesial frontal cortex in SUDEP risk. These regions include the insula, the amygdala, the hippocampus, and the brain stem.
He also noted that the SUDEP-7, which has not been thoroughly validated, is designed for use only in adults.
In his own practice, he asks patients about the frequency of tonic-clonic seizures and whether they occur at night. The number of antiepileptic medications a patient takes reflects the difficulty of controlling seizures and may not be “an independent variable for risk,” said Dr. Gaillard.
“It’s clear one needs a better assessment and better idea of who is at risk,” he said.
The researchers have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
SOURCE: Basha A et al. AAN 2020. Abstract P5.001.

