User login
Reoperation risk doubled in Roux-en-Y over sleeve gastrectomy
CHICAGO – Patients undergoing Roux-en-Y gastric bypass are twice as likely to need a reoperation as those having sleeve gastrectomy, according to ACS NSQIP data.
Reoperation among Roux-en-Y patients was associated with a 10-fold increase in mortality over sleeve gastrectomy (1.2% vs. 0.1%; P less than .01) and a 3-fold increase in length of stay (6 days vs. 2 days; P less than .01), Dr. Matthew Whealon reported at the American College of Surgeons Clinical Congress
The results are consistent with prior contemporary analyses using ACS National Surgical Quality Improvement Program (NSQIP) data reporting reoperation rates of 2.5%-5.1% for Roux-en-Y gastric bypass (RYGB) and 1.6%-3% for sleeve gastrectomy. Those analyses, however, did not include the reasons for reoperation, as these data were not available until the 2012 database release, he said.
With these data now in hand, lead author Dr. Mark Hanna and his fellow investigators at the University of California, Irvine, identified 36,757 adults in the 2012-2013 database who underwent RYGB (n = 19,597) or sleeve gastrectomy (n = 17,160) for morbid obesity and performed multivariate regression analyses to identify risk factors associated with reoperation.
In all, 518 RYGB patients and 231 sleeve gastrectomy patients required an unplanned return to the operating room (2.6% vs. 1.3%), Dr. Whealon said. The mean time from the index procedure to reoperation was 7.6 days and 7.1 days, respectively.
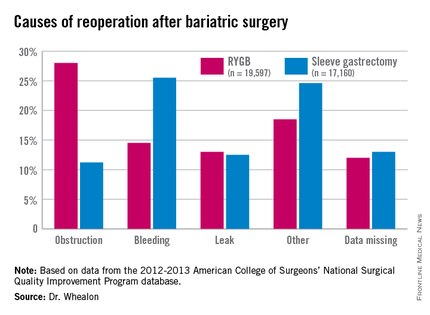
Obstruction was the biggest driver of reoperation following RYGB, accounting for 28% of reoperations. Other causes were bleeding (14.5%), leak (13%), and other unspecified reasons (18.5%), with data missing in 12%.
Bleeding was the most common indication for reoperation after sleeve gastrectomy (25.5%), followed by other unspecified reasons(24.6%), missing data (13%), leak (12.55%), and obstruction (11.2%), he said.
In adjusted multivariate analyses, factors that significantly increased the risk for reoperation were heart failure (adjusted odds ratio, 2.3), dependent functional status (aOR, 2.1), RYGB (aOR, 1.94), chronic obstructive pulmonary disease (aOR, 1.7), open operation (aOR, 1.6), and male sex (aOR, 1.1). The P values were less than .05 for all comparisons.
Factors not significant for reoperation included body mass index, age, smoking status, bleeding disorder, steroid use, dialysis, hypertension, diabetes, preoperative sepsis, emergent admission, elective operation, and preoperative weight loss.
While bariatric surgery remains a safe operation with low mortality and reoperation rates, additional studies are needed, because of the increased mortality associated with reoperation, to identify ways to mitigate these complications, Dr. Whealon said.
Limitations of the study were that ICD-9 codes for postoperative hemorrhage could not differentiate between intra-abdominal and gastrointestinal bleeding, the database is subject to coding errors, and missing data may have introduced bias into the study, he noted.
Discussant Dr. Matthew Goldblatt of the Medical College of Wisconsin in Milwaukee commented that use of the ACS MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) database would have avoided some of the coding errors for reoperation.
He also questioned whether the average 7-day return to surgery interval reflects the use of endoscopy, as few surgeons would wait that long if, as the analysis suggests, a primary reason for reoperation was postoperative bleeding.
Endoscopy was included in the reoperations, Dr. Whealon said, but he could not speak to the exact percentage it comprised.
Finally, Dr. Goldblatt said, “the patients that you identified as being the highest risk for complication, as is often the case in these reviews, are really the ones most likely to gain the most from the procedure. … So how can people avoid operating on these patients when they are the ones that can get the most out of it?”
Dr. Whealon agreed that high-risk patients have the most to gain and suggested that “optimizing their comorbid conditions before operation will help reduce their risk.”
The authors reported having no conflicts of interest.
CHICAGO – Patients undergoing Roux-en-Y gastric bypass are twice as likely to need a reoperation as those having sleeve gastrectomy, according to ACS NSQIP data.
Reoperation among Roux-en-Y patients was associated with a 10-fold increase in mortality over sleeve gastrectomy (1.2% vs. 0.1%; P less than .01) and a 3-fold increase in length of stay (6 days vs. 2 days; P less than .01), Dr. Matthew Whealon reported at the American College of Surgeons Clinical Congress
The results are consistent with prior contemporary analyses using ACS National Surgical Quality Improvement Program (NSQIP) data reporting reoperation rates of 2.5%-5.1% for Roux-en-Y gastric bypass (RYGB) and 1.6%-3% for sleeve gastrectomy. Those analyses, however, did not include the reasons for reoperation, as these data were not available until the 2012 database release, he said.
With these data now in hand, lead author Dr. Mark Hanna and his fellow investigators at the University of California, Irvine, identified 36,757 adults in the 2012-2013 database who underwent RYGB (n = 19,597) or sleeve gastrectomy (n = 17,160) for morbid obesity and performed multivariate regression analyses to identify risk factors associated with reoperation.
In all, 518 RYGB patients and 231 sleeve gastrectomy patients required an unplanned return to the operating room (2.6% vs. 1.3%), Dr. Whealon said. The mean time from the index procedure to reoperation was 7.6 days and 7.1 days, respectively.
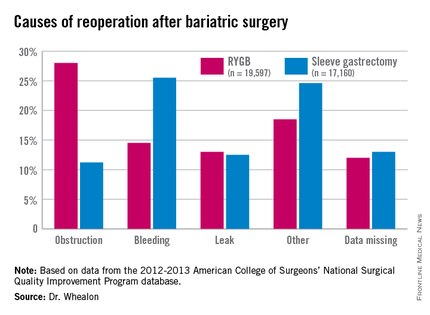
Obstruction was the biggest driver of reoperation following RYGB, accounting for 28% of reoperations. Other causes were bleeding (14.5%), leak (13%), and other unspecified reasons (18.5%), with data missing in 12%.
Bleeding was the most common indication for reoperation after sleeve gastrectomy (25.5%), followed by other unspecified reasons(24.6%), missing data (13%), leak (12.55%), and obstruction (11.2%), he said.
In adjusted multivariate analyses, factors that significantly increased the risk for reoperation were heart failure (adjusted odds ratio, 2.3), dependent functional status (aOR, 2.1), RYGB (aOR, 1.94), chronic obstructive pulmonary disease (aOR, 1.7), open operation (aOR, 1.6), and male sex (aOR, 1.1). The P values were less than .05 for all comparisons.
Factors not significant for reoperation included body mass index, age, smoking status, bleeding disorder, steroid use, dialysis, hypertension, diabetes, preoperative sepsis, emergent admission, elective operation, and preoperative weight loss.
While bariatric surgery remains a safe operation with low mortality and reoperation rates, additional studies are needed, because of the increased mortality associated with reoperation, to identify ways to mitigate these complications, Dr. Whealon said.
Limitations of the study were that ICD-9 codes for postoperative hemorrhage could not differentiate between intra-abdominal and gastrointestinal bleeding, the database is subject to coding errors, and missing data may have introduced bias into the study, he noted.
Discussant Dr. Matthew Goldblatt of the Medical College of Wisconsin in Milwaukee commented that use of the ACS MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) database would have avoided some of the coding errors for reoperation.
He also questioned whether the average 7-day return to surgery interval reflects the use of endoscopy, as few surgeons would wait that long if, as the analysis suggests, a primary reason for reoperation was postoperative bleeding.
Endoscopy was included in the reoperations, Dr. Whealon said, but he could not speak to the exact percentage it comprised.
Finally, Dr. Goldblatt said, “the patients that you identified as being the highest risk for complication, as is often the case in these reviews, are really the ones most likely to gain the most from the procedure. … So how can people avoid operating on these patients when they are the ones that can get the most out of it?”
Dr. Whealon agreed that high-risk patients have the most to gain and suggested that “optimizing their comorbid conditions before operation will help reduce their risk.”
The authors reported having no conflicts of interest.
CHICAGO – Patients undergoing Roux-en-Y gastric bypass are twice as likely to need a reoperation as those having sleeve gastrectomy, according to ACS NSQIP data.
Reoperation among Roux-en-Y patients was associated with a 10-fold increase in mortality over sleeve gastrectomy (1.2% vs. 0.1%; P less than .01) and a 3-fold increase in length of stay (6 days vs. 2 days; P less than .01), Dr. Matthew Whealon reported at the American College of Surgeons Clinical Congress
The results are consistent with prior contemporary analyses using ACS National Surgical Quality Improvement Program (NSQIP) data reporting reoperation rates of 2.5%-5.1% for Roux-en-Y gastric bypass (RYGB) and 1.6%-3% for sleeve gastrectomy. Those analyses, however, did not include the reasons for reoperation, as these data were not available until the 2012 database release, he said.
With these data now in hand, lead author Dr. Mark Hanna and his fellow investigators at the University of California, Irvine, identified 36,757 adults in the 2012-2013 database who underwent RYGB (n = 19,597) or sleeve gastrectomy (n = 17,160) for morbid obesity and performed multivariate regression analyses to identify risk factors associated with reoperation.
In all, 518 RYGB patients and 231 sleeve gastrectomy patients required an unplanned return to the operating room (2.6% vs. 1.3%), Dr. Whealon said. The mean time from the index procedure to reoperation was 7.6 days and 7.1 days, respectively.
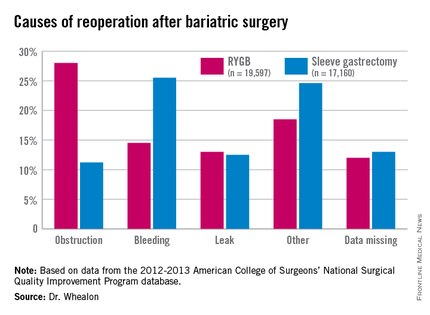
Obstruction was the biggest driver of reoperation following RYGB, accounting for 28% of reoperations. Other causes were bleeding (14.5%), leak (13%), and other unspecified reasons (18.5%), with data missing in 12%.
Bleeding was the most common indication for reoperation after sleeve gastrectomy (25.5%), followed by other unspecified reasons(24.6%), missing data (13%), leak (12.55%), and obstruction (11.2%), he said.
In adjusted multivariate analyses, factors that significantly increased the risk for reoperation were heart failure (adjusted odds ratio, 2.3), dependent functional status (aOR, 2.1), RYGB (aOR, 1.94), chronic obstructive pulmonary disease (aOR, 1.7), open operation (aOR, 1.6), and male sex (aOR, 1.1). The P values were less than .05 for all comparisons.
Factors not significant for reoperation included body mass index, age, smoking status, bleeding disorder, steroid use, dialysis, hypertension, diabetes, preoperative sepsis, emergent admission, elective operation, and preoperative weight loss.
While bariatric surgery remains a safe operation with low mortality and reoperation rates, additional studies are needed, because of the increased mortality associated with reoperation, to identify ways to mitigate these complications, Dr. Whealon said.
Limitations of the study were that ICD-9 codes for postoperative hemorrhage could not differentiate between intra-abdominal and gastrointestinal bleeding, the database is subject to coding errors, and missing data may have introduced bias into the study, he noted.
Discussant Dr. Matthew Goldblatt of the Medical College of Wisconsin in Milwaukee commented that use of the ACS MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) database would have avoided some of the coding errors for reoperation.
He also questioned whether the average 7-day return to surgery interval reflects the use of endoscopy, as few surgeons would wait that long if, as the analysis suggests, a primary reason for reoperation was postoperative bleeding.
Endoscopy was included in the reoperations, Dr. Whealon said, but he could not speak to the exact percentage it comprised.
Finally, Dr. Goldblatt said, “the patients that you identified as being the highest risk for complication, as is often the case in these reviews, are really the ones most likely to gain the most from the procedure. … So how can people avoid operating on these patients when they are the ones that can get the most out of it?”
Dr. Whealon agreed that high-risk patients have the most to gain and suggested that “optimizing their comorbid conditions before operation will help reduce their risk.”
The authors reported having no conflicts of interest.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Patients undergoing Roux-en-Y gastric bypass were twice as likely to need a reoperation as with sleeve gastrectomy, and reoperation increased morbidity 10-fold.
Major finding: The reoperation rate for Roux-en-Y gastric bypass was 2.6% vs. 1.3% for sleeve gastrectomy.
Data source: An ACS NSQIP database analysis of 36,757 patients undergoing bariatric surgery.
Disclosures: The authors reported having no conflicts of interest.
Myth of the Month: Does Colace work?
Myth: Docusate is a stool softener and helps with constipation.
A 60-year-old man is injured in a fall and breaks four ribs. He is in severe pain and is prescribed oxycodone and naproxen for pain. What treatment would you prescribe to help decrease problems with constipation?
A. Docusate.
B. Docusate and polyethylene glycol.
C. Psyllium.
D. Polyethylene glycol.
Constipation is extremely common, occurring in up to 20%-25% of the elderly population and 90% of patients treated with opioids. The formal definition of constipation is fewer than three bowel movements per week. Patients are concerned with other symptoms as well, including hard stool consistency and the feeling of incomplete evacuation.
An extremely commonly prescribed medication for patients with symptoms of constipation/hard stool passage is docusate (Colace). This medication is often a part of bowel programs for institutionalized/hospitalized patients, as well as being frequently prescribed when patients are treated with opiates.
Does it work?
Docusate is frequently prescribed as a “stool softener,” but does it increase water content in stool? In a randomized, controlled trial of docusate vs. psyllium, 170 adult patients with chronic constipation received either 5.1 g twice a day of psyllium or 100 mg twice a day of docusate (Aliment Pharmacol Ther. 1998 May;12[5]:491-7).
Psyllium was superior in its effect on stool frequency, stool water content, total stool output, and the combination of several objective measures of constipation. Compared with baseline, psyllium increased stool water content by 2.33%, vs .01% for docusate (P =. 007), and stool weight was increased in the group treated with psyllium, compared with docusate-treated patients (359.9 g/week vs. 271.9 g/week, respectively; P = .005). Docusate does not appear to have any effect on stool water content or amount of stool.
In a study of constipation treatment in patients receiving opioids, Dr. Yoko Tarumi and her colleagues studied 74 patients admitted to hospice units (J Pain Symptom Manage. 2013 Jan;45[1]:2-13). A total of 74 patients were randomized to receive docusate 100 mg twice a day plus senna, or placebo plus senna. Once the study was started, inclusion criteria were broadened to include hospice patients with nonmalignant disease and patients who were not on opioids.
Almost all patients in the study did receive opioids (94% of the docusate patients and 100% of placebo-treated patients). There were no significant between the groups in stool volume, frequency, consistency, or in perceived completeness of evacuation.
In a randomized, controlled study of elderly patients on a medicine ward, 34 patients were randomized to docusate or control (no laxatives)(J Chronic Dis. 1976 Jan;29[1]:59-63). There was no difference in frequency or quality of stools between groups.
A systematic review of the usefulness of docusate in chronically ill patients concluded that the widespread use of docusate for the treatment of constipation in palliative-care patients is based on inadequate experimental evidence (J Pain Symptom Manage. 2000 Feb;19[2]:130-6).
The Canadian Agency for Drugs and Technologies in Health concluded “the available evidence suggests that docusate is no more effective than placebo in the prevention or management of constipation” (Dioctyl sulfosuccinate or docusate [calcium or sodium] for the prevention or management of constipation: a review of the clinical effectiveness. Canadian Agency for Drugs and Technologies in Health; 2014 Jun 26).
Dr. Davendra Ramkumar and his colleagues published a systematic review of drug trials for the treatment of constipation in 2005 (Am J Gastroenterol. 2005 Apr;100[4]:936-71). Only polyethylene glycol and tegaserod received grade A evidence for published trials. Psyllium and lactulose received grade B evidence. Docusate received a level 3, grade C for evidence (poor quality evidence, poor evidence to support a recommendation for or against the use of the modality).
I have been surprised at how docusate has been the most commonly prescribed laxative agent. Polyethylene glycol or psyllium are better evidence-based options. Docusate is often prescribed as a stool softener, and it has even less evidence that it softens stool than its poor evidence as a laxative.
Acknowledgments
My thanks to the late Dr. David Saunders for teaching me 30 years ago that docusate was not a helpful option for the management of constipation, and to Sarah Steinkruger for doing much of the research that was used in this column.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Myth: Docusate is a stool softener and helps with constipation.
A 60-year-old man is injured in a fall and breaks four ribs. He is in severe pain and is prescribed oxycodone and naproxen for pain. What treatment would you prescribe to help decrease problems with constipation?
A. Docusate.
B. Docusate and polyethylene glycol.
C. Psyllium.
D. Polyethylene glycol.
Constipation is extremely common, occurring in up to 20%-25% of the elderly population and 90% of patients treated with opioids. The formal definition of constipation is fewer than three bowel movements per week. Patients are concerned with other symptoms as well, including hard stool consistency and the feeling of incomplete evacuation.
An extremely commonly prescribed medication for patients with symptoms of constipation/hard stool passage is docusate (Colace). This medication is often a part of bowel programs for institutionalized/hospitalized patients, as well as being frequently prescribed when patients are treated with opiates.
Does it work?
Docusate is frequently prescribed as a “stool softener,” but does it increase water content in stool? In a randomized, controlled trial of docusate vs. psyllium, 170 adult patients with chronic constipation received either 5.1 g twice a day of psyllium or 100 mg twice a day of docusate (Aliment Pharmacol Ther. 1998 May;12[5]:491-7).
Psyllium was superior in its effect on stool frequency, stool water content, total stool output, and the combination of several objective measures of constipation. Compared with baseline, psyllium increased stool water content by 2.33%, vs .01% for docusate (P =. 007), and stool weight was increased in the group treated with psyllium, compared with docusate-treated patients (359.9 g/week vs. 271.9 g/week, respectively; P = .005). Docusate does not appear to have any effect on stool water content or amount of stool.
In a study of constipation treatment in patients receiving opioids, Dr. Yoko Tarumi and her colleagues studied 74 patients admitted to hospice units (J Pain Symptom Manage. 2013 Jan;45[1]:2-13). A total of 74 patients were randomized to receive docusate 100 mg twice a day plus senna, or placebo plus senna. Once the study was started, inclusion criteria were broadened to include hospice patients with nonmalignant disease and patients who were not on opioids.
Almost all patients in the study did receive opioids (94% of the docusate patients and 100% of placebo-treated patients). There were no significant between the groups in stool volume, frequency, consistency, or in perceived completeness of evacuation.
In a randomized, controlled study of elderly patients on a medicine ward, 34 patients were randomized to docusate or control (no laxatives)(J Chronic Dis. 1976 Jan;29[1]:59-63). There was no difference in frequency or quality of stools between groups.
A systematic review of the usefulness of docusate in chronically ill patients concluded that the widespread use of docusate for the treatment of constipation in palliative-care patients is based on inadequate experimental evidence (J Pain Symptom Manage. 2000 Feb;19[2]:130-6).
The Canadian Agency for Drugs and Technologies in Health concluded “the available evidence suggests that docusate is no more effective than placebo in the prevention or management of constipation” (Dioctyl sulfosuccinate or docusate [calcium or sodium] for the prevention or management of constipation: a review of the clinical effectiveness. Canadian Agency for Drugs and Technologies in Health; 2014 Jun 26).
Dr. Davendra Ramkumar and his colleagues published a systematic review of drug trials for the treatment of constipation in 2005 (Am J Gastroenterol. 2005 Apr;100[4]:936-71). Only polyethylene glycol and tegaserod received grade A evidence for published trials. Psyllium and lactulose received grade B evidence. Docusate received a level 3, grade C for evidence (poor quality evidence, poor evidence to support a recommendation for or against the use of the modality).
I have been surprised at how docusate has been the most commonly prescribed laxative agent. Polyethylene glycol or psyllium are better evidence-based options. Docusate is often prescribed as a stool softener, and it has even less evidence that it softens stool than its poor evidence as a laxative.
Acknowledgments
My thanks to the late Dr. David Saunders for teaching me 30 years ago that docusate was not a helpful option for the management of constipation, and to Sarah Steinkruger for doing much of the research that was used in this column.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Myth: Docusate is a stool softener and helps with constipation.
A 60-year-old man is injured in a fall and breaks four ribs. He is in severe pain and is prescribed oxycodone and naproxen for pain. What treatment would you prescribe to help decrease problems with constipation?
A. Docusate.
B. Docusate and polyethylene glycol.
C. Psyllium.
D. Polyethylene glycol.
Constipation is extremely common, occurring in up to 20%-25% of the elderly population and 90% of patients treated with opioids. The formal definition of constipation is fewer than three bowel movements per week. Patients are concerned with other symptoms as well, including hard stool consistency and the feeling of incomplete evacuation.
An extremely commonly prescribed medication for patients with symptoms of constipation/hard stool passage is docusate (Colace). This medication is often a part of bowel programs for institutionalized/hospitalized patients, as well as being frequently prescribed when patients are treated with opiates.
Does it work?
Docusate is frequently prescribed as a “stool softener,” but does it increase water content in stool? In a randomized, controlled trial of docusate vs. psyllium, 170 adult patients with chronic constipation received either 5.1 g twice a day of psyllium or 100 mg twice a day of docusate (Aliment Pharmacol Ther. 1998 May;12[5]:491-7).
Psyllium was superior in its effect on stool frequency, stool water content, total stool output, and the combination of several objective measures of constipation. Compared with baseline, psyllium increased stool water content by 2.33%, vs .01% for docusate (P =. 007), and stool weight was increased in the group treated with psyllium, compared with docusate-treated patients (359.9 g/week vs. 271.9 g/week, respectively; P = .005). Docusate does not appear to have any effect on stool water content or amount of stool.
In a study of constipation treatment in patients receiving opioids, Dr. Yoko Tarumi and her colleagues studied 74 patients admitted to hospice units (J Pain Symptom Manage. 2013 Jan;45[1]:2-13). A total of 74 patients were randomized to receive docusate 100 mg twice a day plus senna, or placebo plus senna. Once the study was started, inclusion criteria were broadened to include hospice patients with nonmalignant disease and patients who were not on opioids.
Almost all patients in the study did receive opioids (94% of the docusate patients and 100% of placebo-treated patients). There were no significant between the groups in stool volume, frequency, consistency, or in perceived completeness of evacuation.
In a randomized, controlled study of elderly patients on a medicine ward, 34 patients were randomized to docusate or control (no laxatives)(J Chronic Dis. 1976 Jan;29[1]:59-63). There was no difference in frequency or quality of stools between groups.
A systematic review of the usefulness of docusate in chronically ill patients concluded that the widespread use of docusate for the treatment of constipation in palliative-care patients is based on inadequate experimental evidence (J Pain Symptom Manage. 2000 Feb;19[2]:130-6).
The Canadian Agency for Drugs and Technologies in Health concluded “the available evidence suggests that docusate is no more effective than placebo in the prevention or management of constipation” (Dioctyl sulfosuccinate or docusate [calcium or sodium] for the prevention or management of constipation: a review of the clinical effectiveness. Canadian Agency for Drugs and Technologies in Health; 2014 Jun 26).
Dr. Davendra Ramkumar and his colleagues published a systematic review of drug trials for the treatment of constipation in 2005 (Am J Gastroenterol. 2005 Apr;100[4]:936-71). Only polyethylene glycol and tegaserod received grade A evidence for published trials. Psyllium and lactulose received grade B evidence. Docusate received a level 3, grade C for evidence (poor quality evidence, poor evidence to support a recommendation for or against the use of the modality).
I have been surprised at how docusate has been the most commonly prescribed laxative agent. Polyethylene glycol or psyllium are better evidence-based options. Docusate is often prescribed as a stool softener, and it has even less evidence that it softens stool than its poor evidence as a laxative.
Acknowledgments
My thanks to the late Dr. David Saunders for teaching me 30 years ago that docusate was not a helpful option for the management of constipation, and to Sarah Steinkruger for doing much of the research that was used in this column.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Complications climb with revisional surgery after adjustable gastric banding
LOS ANGELES – Revisional surgery after failed adjustable gastric banding (AGB) is associated with an increased risk of adverse events and resource utilization, according to Dr. Steven Poplawski, medical director for Barix Clinics in Ypsilanti, Mich.
His conclusion is based on safety outcomes at 30 days for 55,237 patients who underwent primary bariatric surgery and 1,417 patients who underwent AGB revision between June 2006 and July 2015 in the Michigan Bariatric Surgery Collaborative. Patients were excluded from the retrospective evaluation if they had urgent/emergent procedures or more than one previous bariatric operation.
The primary bariatric surgery was Roux-en-Y gastric bypass (RYGB) in 43%, sleeve gastrectomy in 37%, AGB in 19%, and biliopancreatic diversion with duodenal switch (BPD/DS) in 1%.
The patients turned to AGB revision for the same reasons that have prompted its dramatic decline in utilization: weight loss failure (38%), band complications (33%), or both (29%). AGB revisional procedures were sleeve gastrectomy in 54%, RYGB in 35%, AGB in 9%, and BPD/DS in 2%.
Patients undergoing band-to-RYGB conversions had significantly more serious complications, compared with primary RYGB procedures (10.2% vs. 4.4%; P less than .0001), reoperations (5.1% vs. 2.3%; P = .0001), and hospital readmissions (10% vs. 7.3%; P = .0064), and a nonsignificant trend toward more leaks (1.3% vs. 0.7%; P = .13), Dr. Poplawski reported.
Patients undergoing band-to-sleeve conversions had significantly more serious complications when compared with primary sleeve gastrectomy (5% vs. 1.8%; P less than .0001), reoperations (3.3% vs. 1%; P less than .0001), and leaks (1.5% vs. 0.5%; P = .0001), and a nonsignificant trend toward more readmissions (7.7% vs. 4.6%; P = .0685).
Outcomes were not reported for the smaller number of patients undergoing AGB-to-AGB or AGB-to-BPD/DS conversions.
A secondary analysis was performed examining a one-stage versus a two-stage procedure in 525 patients undergoing revisional surgery for weight loss failure only. The only safety outcome to show a significant difference at 30 days was hospital readmissions in the RYGB-conversion group, favoring the one-stage over the two-stage procedure (7.1% vs. 11.5%; P = .0164).
“Clearly, the benefit of a one-stage procedure versus a two-stage procedure is unclear in the way it was studied here,” Dr. Poplawski said at Obesity Week 2015, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
“You can read in some reports that [surgeons] do all [of these procedures as] two-stage because they think it’s safer, but I don’t know that there’s much support for that here. I think it’s reasonable to get most of them done in one stage because there’s also two hospitalizations, two periods of convalescence, and when we talk about the complications of the two-stage operation we aren’t even including the costs to remove the initial band, which are not insignificant,” he noted.
Dr. Raul Rosenthal of the Cleveland Clinic in Weston, Fla., who comoderated the session, said the takeaway message is that “reoperative surgery pays a price. No matter how you look at it, one stage, two stages, with bands or sleeve, you’re going to get in trouble.”
LOS ANGELES – Revisional surgery after failed adjustable gastric banding (AGB) is associated with an increased risk of adverse events and resource utilization, according to Dr. Steven Poplawski, medical director for Barix Clinics in Ypsilanti, Mich.
His conclusion is based on safety outcomes at 30 days for 55,237 patients who underwent primary bariatric surgery and 1,417 patients who underwent AGB revision between June 2006 and July 2015 in the Michigan Bariatric Surgery Collaborative. Patients were excluded from the retrospective evaluation if they had urgent/emergent procedures or more than one previous bariatric operation.
The primary bariatric surgery was Roux-en-Y gastric bypass (RYGB) in 43%, sleeve gastrectomy in 37%, AGB in 19%, and biliopancreatic diversion with duodenal switch (BPD/DS) in 1%.
The patients turned to AGB revision for the same reasons that have prompted its dramatic decline in utilization: weight loss failure (38%), band complications (33%), or both (29%). AGB revisional procedures were sleeve gastrectomy in 54%, RYGB in 35%, AGB in 9%, and BPD/DS in 2%.
Patients undergoing band-to-RYGB conversions had significantly more serious complications, compared with primary RYGB procedures (10.2% vs. 4.4%; P less than .0001), reoperations (5.1% vs. 2.3%; P = .0001), and hospital readmissions (10% vs. 7.3%; P = .0064), and a nonsignificant trend toward more leaks (1.3% vs. 0.7%; P = .13), Dr. Poplawski reported.
Patients undergoing band-to-sleeve conversions had significantly more serious complications when compared with primary sleeve gastrectomy (5% vs. 1.8%; P less than .0001), reoperations (3.3% vs. 1%; P less than .0001), and leaks (1.5% vs. 0.5%; P = .0001), and a nonsignificant trend toward more readmissions (7.7% vs. 4.6%; P = .0685).
Outcomes were not reported for the smaller number of patients undergoing AGB-to-AGB or AGB-to-BPD/DS conversions.
A secondary analysis was performed examining a one-stage versus a two-stage procedure in 525 patients undergoing revisional surgery for weight loss failure only. The only safety outcome to show a significant difference at 30 days was hospital readmissions in the RYGB-conversion group, favoring the one-stage over the two-stage procedure (7.1% vs. 11.5%; P = .0164).
“Clearly, the benefit of a one-stage procedure versus a two-stage procedure is unclear in the way it was studied here,” Dr. Poplawski said at Obesity Week 2015, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
“You can read in some reports that [surgeons] do all [of these procedures as] two-stage because they think it’s safer, but I don’t know that there’s much support for that here. I think it’s reasonable to get most of them done in one stage because there’s also two hospitalizations, two periods of convalescence, and when we talk about the complications of the two-stage operation we aren’t even including the costs to remove the initial band, which are not insignificant,” he noted.
Dr. Raul Rosenthal of the Cleveland Clinic in Weston, Fla., who comoderated the session, said the takeaway message is that “reoperative surgery pays a price. No matter how you look at it, one stage, two stages, with bands or sleeve, you’re going to get in trouble.”
LOS ANGELES – Revisional surgery after failed adjustable gastric banding (AGB) is associated with an increased risk of adverse events and resource utilization, according to Dr. Steven Poplawski, medical director for Barix Clinics in Ypsilanti, Mich.
His conclusion is based on safety outcomes at 30 days for 55,237 patients who underwent primary bariatric surgery and 1,417 patients who underwent AGB revision between June 2006 and July 2015 in the Michigan Bariatric Surgery Collaborative. Patients were excluded from the retrospective evaluation if they had urgent/emergent procedures or more than one previous bariatric operation.
The primary bariatric surgery was Roux-en-Y gastric bypass (RYGB) in 43%, sleeve gastrectomy in 37%, AGB in 19%, and biliopancreatic diversion with duodenal switch (BPD/DS) in 1%.
The patients turned to AGB revision for the same reasons that have prompted its dramatic decline in utilization: weight loss failure (38%), band complications (33%), or both (29%). AGB revisional procedures were sleeve gastrectomy in 54%, RYGB in 35%, AGB in 9%, and BPD/DS in 2%.
Patients undergoing band-to-RYGB conversions had significantly more serious complications, compared with primary RYGB procedures (10.2% vs. 4.4%; P less than .0001), reoperations (5.1% vs. 2.3%; P = .0001), and hospital readmissions (10% vs. 7.3%; P = .0064), and a nonsignificant trend toward more leaks (1.3% vs. 0.7%; P = .13), Dr. Poplawski reported.
Patients undergoing band-to-sleeve conversions had significantly more serious complications when compared with primary sleeve gastrectomy (5% vs. 1.8%; P less than .0001), reoperations (3.3% vs. 1%; P less than .0001), and leaks (1.5% vs. 0.5%; P = .0001), and a nonsignificant trend toward more readmissions (7.7% vs. 4.6%; P = .0685).
Outcomes were not reported for the smaller number of patients undergoing AGB-to-AGB or AGB-to-BPD/DS conversions.
A secondary analysis was performed examining a one-stage versus a two-stage procedure in 525 patients undergoing revisional surgery for weight loss failure only. The only safety outcome to show a significant difference at 30 days was hospital readmissions in the RYGB-conversion group, favoring the one-stage over the two-stage procedure (7.1% vs. 11.5%; P = .0164).
“Clearly, the benefit of a one-stage procedure versus a two-stage procedure is unclear in the way it was studied here,” Dr. Poplawski said at Obesity Week 2015, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
“You can read in some reports that [surgeons] do all [of these procedures as] two-stage because they think it’s safer, but I don’t know that there’s much support for that here. I think it’s reasonable to get most of them done in one stage because there’s also two hospitalizations, two periods of convalescence, and when we talk about the complications of the two-stage operation we aren’t even including the costs to remove the initial band, which are not insignificant,” he noted.
Dr. Raul Rosenthal of the Cleveland Clinic in Weston, Fla., who comoderated the session, said the takeaway message is that “reoperative surgery pays a price. No matter how you look at it, one stage, two stages, with bands or sleeve, you’re going to get in trouble.”
AT OBESITY WEEK 2015
Key clinical point: Conversions of adjustable gastric bands are associated with more 30-day adverse events.
Major finding: Serious complications were higher in AGB–to–Roux-en-Y gastric bypass conversions than in primary RYGB (10.2% vs. 4.4%; P less than .0001) and in AGB-to-sleeve gastrectomy conversions, compared with primary sleeves (5% vs. 1.8%; P less than .0001).
Data source: Retrospective study of 55,237 patients who underwent primary bariatric surgery and 1,417 patients who underwent adjustable gastric band revision.
Disclosures: Dr. Poplawski reported having no disclosures.
ACS: Infected hernia salvage success most likely with lightweight polypropylene
CHICAGO – Infected ventral hernia mesh is most likely to be salvaged if it’s made from lightweight polypropylene, according to data from a series of 161 mesh infection cases at Carolinas Medical Center in Charlotte, N.C.
Investigators there were able to salvage 33% of lightweight polypropylene and 8% of polytetrafluoroethylene mesh patients, but salvage failed in patients with composite, polyester, or heavyweight polypropylene meshes. The overall salvage rate was less than 10%.
“We sometimes think that we’ve salvaged the mesh, but if we follow these patients long enough” – follow-up was an average of 37 months in the series – “the majority of them will need to be excised,” said investigator Dr. Vedra Augenstein of the department of surgery at the medical center.
Wound complications are common in ventral hernia repairs, and mesh infections, said Dr. Augenstein, are among “the most dreaded.” The North Carolina findings help define the small pool of patients in whom salvage might work.
The average body mass index in the series was 36 kg/m2, and patients had an average of 2.6 previous ventral hernia repairs. The majority had a polypropylene mesh. Most of the cases were referred to the medical center from elsewhere, so mesh excision came an average of 10 months after the diagnosis of infection.
Almost a third of patients had their infections diagnosed a year or more after mesh implant, which goes against the common notion that mesh patients are out of the woods after a year. “It took a very long time for some of these infections to present. This was a big surprise for us,” Dr. Augenstein said.
The team tried to salvage all of their patients, using antibiotics in 90%, vacuum-assisted closure and/or debridement in 57%, and percutaneous drainage in 17%.
No patient presented with an obvious fistula, but the investigators found fistulas during surgery in about 16% of patients. Meanwhile, salvage failed in every patient who continued to smoke despite being diagnosed with a mesh infection.
The team assembled their findings into an informal algorithm for considering mesh salvage.
“Think about what you need to ask yourself. First, does the patient have a fistula or do you suspect one” from, for instance, gut bacteria in the wound or oral contrast above the mesh on CT? If so, “they are going to need an operation,” Dr. Augenstein said.
Smoking is the next stop point; salvage is likely to fail in smokers.
Mesh type is the third consideration; lightweight polypropylene is a good sign. “If they have heavyweight polypropylene, composite, or polyester mesh, they were not salvageable in our series,” she said.
For patients still in the running, Methicillin-resistant Staphylococcus aureus (MRSA) is the next concern. If it’s in the wound, mesh is going to be harder to salvage, said Dr. Augenstein. Most of the infections in the series were caused by Staphylococcus, with MRSA present in 45% of patients.
Infection recurrence is common even when salvage seems to work, so “we need to follow these patients for a very, very long time,” Dr. Augenstein said.
Along with clinical exams, the North Carolina team follows C-reactive protein and erythrocyte sedimentation rate. “If the abdomen gets red or if, for example, the C-reactive protein goes up, we’ll do a CT scan or ultrasound to make sure they are not brewing an infection,” she said.
Dr. Augenstein has received research and educational grants from Gore, Ethicon, Novadaq, Bard, and LifeCell.
CHICAGO – Infected ventral hernia mesh is most likely to be salvaged if it’s made from lightweight polypropylene, according to data from a series of 161 mesh infection cases at Carolinas Medical Center in Charlotte, N.C.
Investigators there were able to salvage 33% of lightweight polypropylene and 8% of polytetrafluoroethylene mesh patients, but salvage failed in patients with composite, polyester, or heavyweight polypropylene meshes. The overall salvage rate was less than 10%.
“We sometimes think that we’ve salvaged the mesh, but if we follow these patients long enough” – follow-up was an average of 37 months in the series – “the majority of them will need to be excised,” said investigator Dr. Vedra Augenstein of the department of surgery at the medical center.
Wound complications are common in ventral hernia repairs, and mesh infections, said Dr. Augenstein, are among “the most dreaded.” The North Carolina findings help define the small pool of patients in whom salvage might work.
The average body mass index in the series was 36 kg/m2, and patients had an average of 2.6 previous ventral hernia repairs. The majority had a polypropylene mesh. Most of the cases were referred to the medical center from elsewhere, so mesh excision came an average of 10 months after the diagnosis of infection.
Almost a third of patients had their infections diagnosed a year or more after mesh implant, which goes against the common notion that mesh patients are out of the woods after a year. “It took a very long time for some of these infections to present. This was a big surprise for us,” Dr. Augenstein said.
The team tried to salvage all of their patients, using antibiotics in 90%, vacuum-assisted closure and/or debridement in 57%, and percutaneous drainage in 17%.
No patient presented with an obvious fistula, but the investigators found fistulas during surgery in about 16% of patients. Meanwhile, salvage failed in every patient who continued to smoke despite being diagnosed with a mesh infection.
The team assembled their findings into an informal algorithm for considering mesh salvage.
“Think about what you need to ask yourself. First, does the patient have a fistula or do you suspect one” from, for instance, gut bacteria in the wound or oral contrast above the mesh on CT? If so, “they are going to need an operation,” Dr. Augenstein said.
Smoking is the next stop point; salvage is likely to fail in smokers.
Mesh type is the third consideration; lightweight polypropylene is a good sign. “If they have heavyweight polypropylene, composite, or polyester mesh, they were not salvageable in our series,” she said.
For patients still in the running, Methicillin-resistant Staphylococcus aureus (MRSA) is the next concern. If it’s in the wound, mesh is going to be harder to salvage, said Dr. Augenstein. Most of the infections in the series were caused by Staphylococcus, with MRSA present in 45% of patients.
Infection recurrence is common even when salvage seems to work, so “we need to follow these patients for a very, very long time,” Dr. Augenstein said.
Along with clinical exams, the North Carolina team follows C-reactive protein and erythrocyte sedimentation rate. “If the abdomen gets red or if, for example, the C-reactive protein goes up, we’ll do a CT scan or ultrasound to make sure they are not brewing an infection,” she said.
Dr. Augenstein has received research and educational grants from Gore, Ethicon, Novadaq, Bard, and LifeCell.
CHICAGO – Infected ventral hernia mesh is most likely to be salvaged if it’s made from lightweight polypropylene, according to data from a series of 161 mesh infection cases at Carolinas Medical Center in Charlotte, N.C.
Investigators there were able to salvage 33% of lightweight polypropylene and 8% of polytetrafluoroethylene mesh patients, but salvage failed in patients with composite, polyester, or heavyweight polypropylene meshes. The overall salvage rate was less than 10%.
“We sometimes think that we’ve salvaged the mesh, but if we follow these patients long enough” – follow-up was an average of 37 months in the series – “the majority of them will need to be excised,” said investigator Dr. Vedra Augenstein of the department of surgery at the medical center.
Wound complications are common in ventral hernia repairs, and mesh infections, said Dr. Augenstein, are among “the most dreaded.” The North Carolina findings help define the small pool of patients in whom salvage might work.
The average body mass index in the series was 36 kg/m2, and patients had an average of 2.6 previous ventral hernia repairs. The majority had a polypropylene mesh. Most of the cases were referred to the medical center from elsewhere, so mesh excision came an average of 10 months after the diagnosis of infection.
Almost a third of patients had their infections diagnosed a year or more after mesh implant, which goes against the common notion that mesh patients are out of the woods after a year. “It took a very long time for some of these infections to present. This was a big surprise for us,” Dr. Augenstein said.
The team tried to salvage all of their patients, using antibiotics in 90%, vacuum-assisted closure and/or debridement in 57%, and percutaneous drainage in 17%.
No patient presented with an obvious fistula, but the investigators found fistulas during surgery in about 16% of patients. Meanwhile, salvage failed in every patient who continued to smoke despite being diagnosed with a mesh infection.
The team assembled their findings into an informal algorithm for considering mesh salvage.
“Think about what you need to ask yourself. First, does the patient have a fistula or do you suspect one” from, for instance, gut bacteria in the wound or oral contrast above the mesh on CT? If so, “they are going to need an operation,” Dr. Augenstein said.
Smoking is the next stop point; salvage is likely to fail in smokers.
Mesh type is the third consideration; lightweight polypropylene is a good sign. “If they have heavyweight polypropylene, composite, or polyester mesh, they were not salvageable in our series,” she said.
For patients still in the running, Methicillin-resistant Staphylococcus aureus (MRSA) is the next concern. If it’s in the wound, mesh is going to be harder to salvage, said Dr. Augenstein. Most of the infections in the series were caused by Staphylococcus, with MRSA present in 45% of patients.
Infection recurrence is common even when salvage seems to work, so “we need to follow these patients for a very, very long time,” Dr. Augenstein said.
Along with clinical exams, the North Carolina team follows C-reactive protein and erythrocyte sedimentation rate. “If the abdomen gets red or if, for example, the C-reactive protein goes up, we’ll do a CT scan or ultrasound to make sure they are not brewing an infection,” she said.
Dr. Augenstein has received research and educational grants from Gore, Ethicon, Novadaq, Bard, and LifeCell.
AT THE ACS CLINICAL CONGRESS
Key clinical point: The ideal infected mesh salvage candidate is a MRSA-free nonsmoker with a lightweight polypropylene implant and no fistulas.
Major finding: Mesh salvage worked in about a third of lightweight polypropylene patients and 8% of polytetrafluoroethylene mesh patients but failed in patients with composite, polyester, or heavyweight polypropylene meshes.
Data source: Series of 161 infected ventral hernia mesh patients.
Disclosures: The presenting investigator has received research and educational grants from Gore, Ethicon, Novadaq, Bard, and LifeCell.
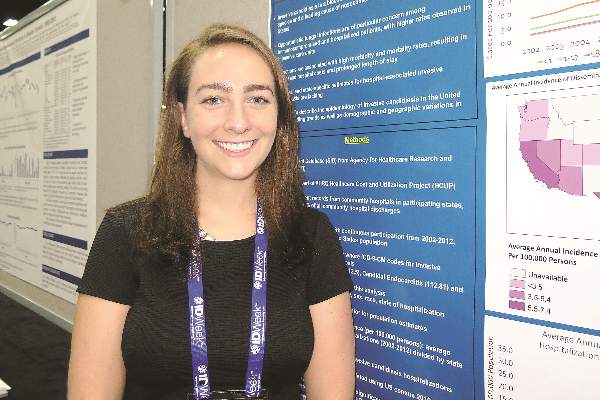
Invasive candidiasis hospitalizations down overall
SAN DIEGO – The incidence of hospitalizations associated with invasive candidiasis decreased between 2007 and 2012, but both elderly and black patients remain at greatest risk for the infection, according to an analysis of national data.
“It’s been noted previously that the incidence of neonatal candidiasis seems to be going down, but we wanted to focus on older populations,” Sara Strollo, M.P.H., a trainee in the division of intramural research at the National Institute of Allergy and Infectious Diseases, Rockville., Md., said in an interview at an annual scientific meeting on infectious diseases.
For the study, which is the first of its kind, Ms. Strollo and her associates analyzed data from the State Inpatient Database from the Agency for Healthcare Research and Quality, which represents 97% of all community hospital discharges. They excluded neonatal cases.
The age-adjusted annual incidence of hospitalizations associated with invasive candidiasis ranged from 4.3 to 6.0 per 100,000 persons between 2002 and 2012. The incidence increased from 2002-2005, was stable through 2007, and decreased significantly between 2007 and 2012 -- by 6.7% among men and by 7.4% among women.
The highest incidence of hospitalization for invasive candidiasis occurred among the oldest age groups and among men. For example, compared with persons aged 50-64, the average annual incidence among those over age 80 years old was 2.6-fold higher among women (7.6 vs. 19.7 per 100,000 persons) and 3.9-fold higher among men (7.6 vs. 30 per 100,000 persons).
The researchers also found that among persons older than 50 years of age, black men and women had more than a two-fold higher incidence, compared with white men and women (23.7 vs. 11.7 per 100,000 persons and 22 vs. 10.4 per 100,000 persons, respectively).
During the overall study period, Ms. Strollo and her associates observed a nearly three-fold variation in the average annual incidence of hospital discharges for candidiasis per 100,000 persons, from 2.7 in Oregon to 7.2 in Florida. States with the highest incidence were Florida, Maryland, Missouri, Michigan, California, and Texas, but temporal trends were similar across states and no clear regional patterns among states were observed.
The investigators limited their analysis to 24 states with continuous reporting from 2002 through 2012, which represents 65% of the United States population. The researchers extracted records for discharges where ICD-9 codes for invasive candidiasis were listed in the primary or secondary discharge fields, including disseminated candidiasis (112.5), candidal endocarditis (112.81), and candidal meningitis (112.83). Age, gender, hospitalization year, and state data were extracted, and U.S. Census Bureau data were used as the denominator for state hospitalization incidence and trends. Poisson regression was used to assess significance of trends.
IDWeek marks the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The study was supported by a training grant from the National Institute of Child Health and Human Development. The researchers reported having no financial disclosures.
SAN DIEGO – The incidence of hospitalizations associated with invasive candidiasis decreased between 2007 and 2012, but both elderly and black patients remain at greatest risk for the infection, according to an analysis of national data.
“It’s been noted previously that the incidence of neonatal candidiasis seems to be going down, but we wanted to focus on older populations,” Sara Strollo, M.P.H., a trainee in the division of intramural research at the National Institute of Allergy and Infectious Diseases, Rockville., Md., said in an interview at an annual scientific meeting on infectious diseases.
For the study, which is the first of its kind, Ms. Strollo and her associates analyzed data from the State Inpatient Database from the Agency for Healthcare Research and Quality, which represents 97% of all community hospital discharges. They excluded neonatal cases.
The age-adjusted annual incidence of hospitalizations associated with invasive candidiasis ranged from 4.3 to 6.0 per 100,000 persons between 2002 and 2012. The incidence increased from 2002-2005, was stable through 2007, and decreased significantly between 2007 and 2012 -- by 6.7% among men and by 7.4% among women.
The highest incidence of hospitalization for invasive candidiasis occurred among the oldest age groups and among men. For example, compared with persons aged 50-64, the average annual incidence among those over age 80 years old was 2.6-fold higher among women (7.6 vs. 19.7 per 100,000 persons) and 3.9-fold higher among men (7.6 vs. 30 per 100,000 persons).
The researchers also found that among persons older than 50 years of age, black men and women had more than a two-fold higher incidence, compared with white men and women (23.7 vs. 11.7 per 100,000 persons and 22 vs. 10.4 per 100,000 persons, respectively).
During the overall study period, Ms. Strollo and her associates observed a nearly three-fold variation in the average annual incidence of hospital discharges for candidiasis per 100,000 persons, from 2.7 in Oregon to 7.2 in Florida. States with the highest incidence were Florida, Maryland, Missouri, Michigan, California, and Texas, but temporal trends were similar across states and no clear regional patterns among states were observed.
The investigators limited their analysis to 24 states with continuous reporting from 2002 through 2012, which represents 65% of the United States population. The researchers extracted records for discharges where ICD-9 codes for invasive candidiasis were listed in the primary or secondary discharge fields, including disseminated candidiasis (112.5), candidal endocarditis (112.81), and candidal meningitis (112.83). Age, gender, hospitalization year, and state data were extracted, and U.S. Census Bureau data were used as the denominator for state hospitalization incidence and trends. Poisson regression was used to assess significance of trends.
IDWeek marks the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The study was supported by a training grant from the National Institute of Child Health and Human Development. The researchers reported having no financial disclosures.
SAN DIEGO – The incidence of hospitalizations associated with invasive candidiasis decreased between 2007 and 2012, but both elderly and black patients remain at greatest risk for the infection, according to an analysis of national data.
“It’s been noted previously that the incidence of neonatal candidiasis seems to be going down, but we wanted to focus on older populations,” Sara Strollo, M.P.H., a trainee in the division of intramural research at the National Institute of Allergy and Infectious Diseases, Rockville., Md., said in an interview at an annual scientific meeting on infectious diseases.
For the study, which is the first of its kind, Ms. Strollo and her associates analyzed data from the State Inpatient Database from the Agency for Healthcare Research and Quality, which represents 97% of all community hospital discharges. They excluded neonatal cases.
The age-adjusted annual incidence of hospitalizations associated with invasive candidiasis ranged from 4.3 to 6.0 per 100,000 persons between 2002 and 2012. The incidence increased from 2002-2005, was stable through 2007, and decreased significantly between 2007 and 2012 -- by 6.7% among men and by 7.4% among women.
The highest incidence of hospitalization for invasive candidiasis occurred among the oldest age groups and among men. For example, compared with persons aged 50-64, the average annual incidence among those over age 80 years old was 2.6-fold higher among women (7.6 vs. 19.7 per 100,000 persons) and 3.9-fold higher among men (7.6 vs. 30 per 100,000 persons).
The researchers also found that among persons older than 50 years of age, black men and women had more than a two-fold higher incidence, compared with white men and women (23.7 vs. 11.7 per 100,000 persons and 22 vs. 10.4 per 100,000 persons, respectively).
During the overall study period, Ms. Strollo and her associates observed a nearly three-fold variation in the average annual incidence of hospital discharges for candidiasis per 100,000 persons, from 2.7 in Oregon to 7.2 in Florida. States with the highest incidence were Florida, Maryland, Missouri, Michigan, California, and Texas, but temporal trends were similar across states and no clear regional patterns among states were observed.
The investigators limited their analysis to 24 states with continuous reporting from 2002 through 2012, which represents 65% of the United States population. The researchers extracted records for discharges where ICD-9 codes for invasive candidiasis were listed in the primary or secondary discharge fields, including disseminated candidiasis (112.5), candidal endocarditis (112.81), and candidal meningitis (112.83). Age, gender, hospitalization year, and state data were extracted, and U.S. Census Bureau data were used as the denominator for state hospitalization incidence and trends. Poisson regression was used to assess significance of trends.
IDWeek marks the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The study was supported by a training grant from the National Institute of Child Health and Human Development. The researchers reported having no financial disclosures.
AT IDWEEK 2015
Key clinical point: As of 2007, the incidence of hospital-associated invasive candidiasis appears to be decreasing.
Major finding: Between 2007 and 2012, the age-adjusted annual incidence of hospitalizations associated with invasive candidiasis in the United States decreased by 6.7% among men and by 7.4% among women.
Data source: A long-term analysis of data from the State Inpatient Database from the Agency for Healthcare Research and Quality.
Disclosures: The researchers reported having no financial disclosures.
Short-term adverse events modest after bariatric surgery in slimmer diabetics
LOS ANGELES – A nationwide analysis shows modest early morbidity and low mortality following bariatric surgery in patients with type 2 diabetes who are not morbidly obese.
At 30 days’ follow-up among 1,003 patients, the composite complication rate, defined as the presence of any of 16 adverse events, was 4.2%; the reoperation rate was 1.6%; and two patients (0.2%) died.
“A 2-hour surgical procedure requiring a 2-day hospital stay that is associated with low morbidity and mortality can lead to remission of a chronic, progressive, and disabling disease,” lead author Dr. Ali Aminian of the Cleveland Clinic said at Obesity Week 2015.
“Based on these findings, bariatric surgery can be considered a relatively safe option for managing type 2 diabetes in patients with mild obesity.”
The analysis included adults with a body mass index of at least 25 kg/m2, but less than 35 kg/m2 (mean, 33 kg/m2).
These data are important because most patients with type 2 diabetes fall into this BMI category, he said.
Most of the patients were women (74.3%), 40% were using insulin, 78% had hypertension, and 9% had cardiac disease, according to the analysis, drawn from the American College of Surgery National Surgical Quality Improvement Program 2005-2013 database.
Roux-en-Y bypass was performed in 574 patients, adjustable gastric banding in 227, sleeve gastrectomy in 189, and duodenal switch in 13.
The most common adverse events overall were blood transfusion and reoperation (both 1.6%), a hospital stay longer than 7 days (0.6%), and organ space surgical-site infection (0.5%).
Composite morbidity and mortality was highest in the Roux-en-Y bypass group, compared with the adjustable banding and sleeve groups (5% vs. 3.1% vs. 3.2%, respectively), Dr. Aminian said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Only 3 of 46 patients with a BMI of less than 30 kg/m2 had an adverse event.
Available randomized controlled trials can’t clearly resolve the safety concerns of bariatric surgery in the subgroup of patients with type 2 diabetes who are overweight and mildly obese because such small trials are unlikely to reveal uncommon but clinically serious complications, Dr. Aminian said. In addition, many of the trials have screened out low-BMI and high-risk patients.
Those in attendance at the presentation, however, weren’t entirely convinced the current analysis could allay all safety concerns.
Session comoderator Dr. Daniel Cottam, a bariatric surgeon in group practice in Salt Lake City, said, “I like the summary; however, the use of the word ‘safe’ can be taken to mean a lot of things. It’s one of those squishy words.”
Though the authors have shown that bariatric surgery can be performed in diabetics with a low BMI, in order to say it is safe, the comparison needs to be drawn to the all-cause mortality for these patients in the general population and with other surgical procedures.
“That would be useful in the manuscript because as we approach our patients, we want to be able to say, ‘Listen, if you live with diabetes and a BMI of 25-35 for 5 years, this is your all-cause mortality, and surgery is going to save your life, not hurt it,’ ” Dr. Cottam said.
Along the same lines, Dr. Harvey Sugerman emeritus professor of surgery at Virginia Commonwealth University in Richmond, commented, “Like the old days of routinely operating on any patient with diabetes and gallstones, the data were that just having one death in a young person and the quality-of-life-years lost, it would take you thousands of gallbladders to make up for that one death.”
Dr. Sugarmen also asked for details on the deaths including where they occurred, in whom, and whether the centers were inexperienced.
Dr. Aminian could not recall at the time, but in an interview with this news organization said one death was in a 61-year-old with a history of cardiac disease and chronic kidney failure secondary to insulin-dependent diabetes who developed postop bleeding after gastric bypass. The second was in a 59-year-old patient, again on insulin, who was discharged without problems after gastric bypass, but died within 30 days after surgery.
Although most serious complications occur in this period, the main limitation of the study is that the dataset does not capture adverse events beyond 30 days after surgery, which can lead to underestimation of real risk, Dr. Aminian told the crowd.
“Further large clinical studies on long-term safety and efficacy outcomes of bariatric surgery in patients with type 2 diabetes and low BMI are warranted,” he said.
LOS ANGELES – A nationwide analysis shows modest early morbidity and low mortality following bariatric surgery in patients with type 2 diabetes who are not morbidly obese.
At 30 days’ follow-up among 1,003 patients, the composite complication rate, defined as the presence of any of 16 adverse events, was 4.2%; the reoperation rate was 1.6%; and two patients (0.2%) died.
“A 2-hour surgical procedure requiring a 2-day hospital stay that is associated with low morbidity and mortality can lead to remission of a chronic, progressive, and disabling disease,” lead author Dr. Ali Aminian of the Cleveland Clinic said at Obesity Week 2015.
“Based on these findings, bariatric surgery can be considered a relatively safe option for managing type 2 diabetes in patients with mild obesity.”
The analysis included adults with a body mass index of at least 25 kg/m2, but less than 35 kg/m2 (mean, 33 kg/m2).
These data are important because most patients with type 2 diabetes fall into this BMI category, he said.
Most of the patients were women (74.3%), 40% were using insulin, 78% had hypertension, and 9% had cardiac disease, according to the analysis, drawn from the American College of Surgery National Surgical Quality Improvement Program 2005-2013 database.
Roux-en-Y bypass was performed in 574 patients, adjustable gastric banding in 227, sleeve gastrectomy in 189, and duodenal switch in 13.
The most common adverse events overall were blood transfusion and reoperation (both 1.6%), a hospital stay longer than 7 days (0.6%), and organ space surgical-site infection (0.5%).
Composite morbidity and mortality was highest in the Roux-en-Y bypass group, compared with the adjustable banding and sleeve groups (5% vs. 3.1% vs. 3.2%, respectively), Dr. Aminian said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Only 3 of 46 patients with a BMI of less than 30 kg/m2 had an adverse event.
Available randomized controlled trials can’t clearly resolve the safety concerns of bariatric surgery in the subgroup of patients with type 2 diabetes who are overweight and mildly obese because such small trials are unlikely to reveal uncommon but clinically serious complications, Dr. Aminian said. In addition, many of the trials have screened out low-BMI and high-risk patients.
Those in attendance at the presentation, however, weren’t entirely convinced the current analysis could allay all safety concerns.
Session comoderator Dr. Daniel Cottam, a bariatric surgeon in group practice in Salt Lake City, said, “I like the summary; however, the use of the word ‘safe’ can be taken to mean a lot of things. It’s one of those squishy words.”
Though the authors have shown that bariatric surgery can be performed in diabetics with a low BMI, in order to say it is safe, the comparison needs to be drawn to the all-cause mortality for these patients in the general population and with other surgical procedures.
“That would be useful in the manuscript because as we approach our patients, we want to be able to say, ‘Listen, if you live with diabetes and a BMI of 25-35 for 5 years, this is your all-cause mortality, and surgery is going to save your life, not hurt it,’ ” Dr. Cottam said.
Along the same lines, Dr. Harvey Sugerman emeritus professor of surgery at Virginia Commonwealth University in Richmond, commented, “Like the old days of routinely operating on any patient with diabetes and gallstones, the data were that just having one death in a young person and the quality-of-life-years lost, it would take you thousands of gallbladders to make up for that one death.”
Dr. Sugarmen also asked for details on the deaths including where they occurred, in whom, and whether the centers were inexperienced.
Dr. Aminian could not recall at the time, but in an interview with this news organization said one death was in a 61-year-old with a history of cardiac disease and chronic kidney failure secondary to insulin-dependent diabetes who developed postop bleeding after gastric bypass. The second was in a 59-year-old patient, again on insulin, who was discharged without problems after gastric bypass, but died within 30 days after surgery.
Although most serious complications occur in this period, the main limitation of the study is that the dataset does not capture adverse events beyond 30 days after surgery, which can lead to underestimation of real risk, Dr. Aminian told the crowd.
“Further large clinical studies on long-term safety and efficacy outcomes of bariatric surgery in patients with type 2 diabetes and low BMI are warranted,” he said.
LOS ANGELES – A nationwide analysis shows modest early morbidity and low mortality following bariatric surgery in patients with type 2 diabetes who are not morbidly obese.
At 30 days’ follow-up among 1,003 patients, the composite complication rate, defined as the presence of any of 16 adverse events, was 4.2%; the reoperation rate was 1.6%; and two patients (0.2%) died.
“A 2-hour surgical procedure requiring a 2-day hospital stay that is associated with low morbidity and mortality can lead to remission of a chronic, progressive, and disabling disease,” lead author Dr. Ali Aminian of the Cleveland Clinic said at Obesity Week 2015.
“Based on these findings, bariatric surgery can be considered a relatively safe option for managing type 2 diabetes in patients with mild obesity.”
The analysis included adults with a body mass index of at least 25 kg/m2, but less than 35 kg/m2 (mean, 33 kg/m2).
These data are important because most patients with type 2 diabetes fall into this BMI category, he said.
Most of the patients were women (74.3%), 40% were using insulin, 78% had hypertension, and 9% had cardiac disease, according to the analysis, drawn from the American College of Surgery National Surgical Quality Improvement Program 2005-2013 database.
Roux-en-Y bypass was performed in 574 patients, adjustable gastric banding in 227, sleeve gastrectomy in 189, and duodenal switch in 13.
The most common adverse events overall were blood transfusion and reoperation (both 1.6%), a hospital stay longer than 7 days (0.6%), and organ space surgical-site infection (0.5%).
Composite morbidity and mortality was highest in the Roux-en-Y bypass group, compared with the adjustable banding and sleeve groups (5% vs. 3.1% vs. 3.2%, respectively), Dr. Aminian said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Only 3 of 46 patients with a BMI of less than 30 kg/m2 had an adverse event.
Available randomized controlled trials can’t clearly resolve the safety concerns of bariatric surgery in the subgroup of patients with type 2 diabetes who are overweight and mildly obese because such small trials are unlikely to reveal uncommon but clinically serious complications, Dr. Aminian said. In addition, many of the trials have screened out low-BMI and high-risk patients.
Those in attendance at the presentation, however, weren’t entirely convinced the current analysis could allay all safety concerns.
Session comoderator Dr. Daniel Cottam, a bariatric surgeon in group practice in Salt Lake City, said, “I like the summary; however, the use of the word ‘safe’ can be taken to mean a lot of things. It’s one of those squishy words.”
Though the authors have shown that bariatric surgery can be performed in diabetics with a low BMI, in order to say it is safe, the comparison needs to be drawn to the all-cause mortality for these patients in the general population and with other surgical procedures.
“That would be useful in the manuscript because as we approach our patients, we want to be able to say, ‘Listen, if you live with diabetes and a BMI of 25-35 for 5 years, this is your all-cause mortality, and surgery is going to save your life, not hurt it,’ ” Dr. Cottam said.
Along the same lines, Dr. Harvey Sugerman emeritus professor of surgery at Virginia Commonwealth University in Richmond, commented, “Like the old days of routinely operating on any patient with diabetes and gallstones, the data were that just having one death in a young person and the quality-of-life-years lost, it would take you thousands of gallbladders to make up for that one death.”
Dr. Sugarmen also asked for details on the deaths including where they occurred, in whom, and whether the centers were inexperienced.
Dr. Aminian could not recall at the time, but in an interview with this news organization said one death was in a 61-year-old with a history of cardiac disease and chronic kidney failure secondary to insulin-dependent diabetes who developed postop bleeding after gastric bypass. The second was in a 59-year-old patient, again on insulin, who was discharged without problems after gastric bypass, but died within 30 days after surgery.
Although most serious complications occur in this period, the main limitation of the study is that the dataset does not capture adverse events beyond 30 days after surgery, which can lead to underestimation of real risk, Dr. Aminian told the crowd.
“Further large clinical studies on long-term safety and efficacy outcomes of bariatric surgery in patients with type 2 diabetes and low BMI are warranted,” he said.
AT OBESITY WEEK 2015
Key clinical point: Short-term outcomes suggest that bariatric surgery may be safe in patients with type 2 diabetes who are not morbidly obese.
Major finding: The composite complication rate was 4.2%, 1.6% required reoperation, and two patients (0.2%) died.
Data source: An ACS-NSQIP safety analysis of 1,003 diabetics undergoing bariatric surgery.
Disclosures: The authors reported having no relevant financial conflicts.
VIDEO: Psoriasis, psoriatic arthritis improve with bariatric surgery
SAN FRANCISCO – It might be time to add psoriasis to the list of comorbidities bariatric surgery is likely to help.
New York University investigators have found a marked improvement in psoriasis and psoriatic arthritis following bariatric surgery, especially with severe disease. The more weight people lose, the better they do.
In an interview at the annual meeting of the American College of Rheumatology, investigator Dr. Soumya Reddy, codirector of NYU’s Psoriatic Arthritis Center in Manhattan, explained how the findings can be used in the clinic and their potential impact on bariatric surgery authorization.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – It might be time to add psoriasis to the list of comorbidities bariatric surgery is likely to help.
New York University investigators have found a marked improvement in psoriasis and psoriatic arthritis following bariatric surgery, especially with severe disease. The more weight people lose, the better they do.
In an interview at the annual meeting of the American College of Rheumatology, investigator Dr. Soumya Reddy, codirector of NYU’s Psoriatic Arthritis Center in Manhattan, explained how the findings can be used in the clinic and their potential impact on bariatric surgery authorization.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – It might be time to add psoriasis to the list of comorbidities bariatric surgery is likely to help.
New York University investigators have found a marked improvement in psoriasis and psoriatic arthritis following bariatric surgery, especially with severe disease. The more weight people lose, the better they do.
In an interview at the annual meeting of the American College of Rheumatology, investigator Dr. Soumya Reddy, codirector of NYU’s Psoriatic Arthritis Center in Manhattan, explained how the findings can be used in the clinic and their potential impact on bariatric surgery authorization.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACR ANNUAL MEETING
ACS: Health, weight benefits of gastric bypass durable at 10 years
CHICAGO – Weight loss and comorbidity reduction from Roux-en-Y gastric bypass remain durable at 10 years, according to a reviewof 651 patients at the University of Virginia in Charlottesville.
Investigators checked up on their patients after a decade because “the long-term durability of this operation remains ill-defined in the American population.” Their study, likely the largest American series with 10-year follow-up, helps “to more clearly define long-term outcomes that may be achieved following performance of Roux-en-Y gastric bypass and establish a benchmark for future clinical investigation,” they said.
The study included 335 open and 316 laparoscopic Roux-en-Y gastric bypass (RYGB) patients. Although gastric bypass is preformed laparoscopically at the university now, the team felt comfortable including open cases in the analysis because patients and outcomes were similar in both groups. The mean preoperative body mass index, for instance, was about 53 kg/m2 and the mean operative time about 230 minutes. Postoperative incisional hernia and anastomotic stenosis were more likely with open surgery.
As in other studies, weight loss peaked at 24 months, with patients shedding a mean of 74% of their excess weight. Although that had fallen to a mean of 52% at 10 years, “they still kept off half of their excess weight, which is outstanding,” investigator and general surgery resident Dr. Hunter Mehaffey said at the annual clinical congress of the American College of Surgeons.
Surgery also led to persistent reductions in obesity-related comorbidities. Before RYGB, for instance, 38% of patients had gastroesophageal reflux disease, versus 29% after 10 years. Similarly, the prevalence of degenerative joint disease fell from 61% to 32%, diabetes from 41% to 18%, obstructive sleep apnea from 36% to 16%, hypertension from 59% to 47%, pulmonary problems from 28% to 13%, and psychiatric issues from 39% to 29%. About a quarter of patients had cardiac comorbidities before RYGB, versus 16% at 10 years after surgery. The data came from chart reviews and patient interviews, and the findings were statistically significant.
Overall, patients seemed glad to have had the operation, reporting an average satisfaction score of 8.7 out of 10 points, he said, adding, “I would expect these findings to be generalizable to other institutions. This is a good, durable operation.”
Given the scope of the comorbidity reductions, “the savings in health care costs” from RYGB “are likely underestimated,” Dr. Mehaffey said.
There was another lesson from the study, as well. It took a while to track down patients for 10-year follow-up because they were no longer seeing their surgeons. “If we are not going to see these patients much after 2 years, we really have to make sure that their primary care physician knows” how to recognize and manage possible complications, such as nutritional deficiency or hypoglycemia, he said.
Dr. Mehaffey had no disclosures, and there was no outside funding for the work.
CHICAGO – Weight loss and comorbidity reduction from Roux-en-Y gastric bypass remain durable at 10 years, according to a reviewof 651 patients at the University of Virginia in Charlottesville.
Investigators checked up on their patients after a decade because “the long-term durability of this operation remains ill-defined in the American population.” Their study, likely the largest American series with 10-year follow-up, helps “to more clearly define long-term outcomes that may be achieved following performance of Roux-en-Y gastric bypass and establish a benchmark for future clinical investigation,” they said.
The study included 335 open and 316 laparoscopic Roux-en-Y gastric bypass (RYGB) patients. Although gastric bypass is preformed laparoscopically at the university now, the team felt comfortable including open cases in the analysis because patients and outcomes were similar in both groups. The mean preoperative body mass index, for instance, was about 53 kg/m2 and the mean operative time about 230 minutes. Postoperative incisional hernia and anastomotic stenosis were more likely with open surgery.
As in other studies, weight loss peaked at 24 months, with patients shedding a mean of 74% of their excess weight. Although that had fallen to a mean of 52% at 10 years, “they still kept off half of their excess weight, which is outstanding,” investigator and general surgery resident Dr. Hunter Mehaffey said at the annual clinical congress of the American College of Surgeons.
Surgery also led to persistent reductions in obesity-related comorbidities. Before RYGB, for instance, 38% of patients had gastroesophageal reflux disease, versus 29% after 10 years. Similarly, the prevalence of degenerative joint disease fell from 61% to 32%, diabetes from 41% to 18%, obstructive sleep apnea from 36% to 16%, hypertension from 59% to 47%, pulmonary problems from 28% to 13%, and psychiatric issues from 39% to 29%. About a quarter of patients had cardiac comorbidities before RYGB, versus 16% at 10 years after surgery. The data came from chart reviews and patient interviews, and the findings were statistically significant.
Overall, patients seemed glad to have had the operation, reporting an average satisfaction score of 8.7 out of 10 points, he said, adding, “I would expect these findings to be generalizable to other institutions. This is a good, durable operation.”
Given the scope of the comorbidity reductions, “the savings in health care costs” from RYGB “are likely underestimated,” Dr. Mehaffey said.
There was another lesson from the study, as well. It took a while to track down patients for 10-year follow-up because they were no longer seeing their surgeons. “If we are not going to see these patients much after 2 years, we really have to make sure that their primary care physician knows” how to recognize and manage possible complications, such as nutritional deficiency or hypoglycemia, he said.
Dr. Mehaffey had no disclosures, and there was no outside funding for the work.
CHICAGO – Weight loss and comorbidity reduction from Roux-en-Y gastric bypass remain durable at 10 years, according to a reviewof 651 patients at the University of Virginia in Charlottesville.
Investigators checked up on their patients after a decade because “the long-term durability of this operation remains ill-defined in the American population.” Their study, likely the largest American series with 10-year follow-up, helps “to more clearly define long-term outcomes that may be achieved following performance of Roux-en-Y gastric bypass and establish a benchmark for future clinical investigation,” they said.
The study included 335 open and 316 laparoscopic Roux-en-Y gastric bypass (RYGB) patients. Although gastric bypass is preformed laparoscopically at the university now, the team felt comfortable including open cases in the analysis because patients and outcomes were similar in both groups. The mean preoperative body mass index, for instance, was about 53 kg/m2 and the mean operative time about 230 minutes. Postoperative incisional hernia and anastomotic stenosis were more likely with open surgery.
As in other studies, weight loss peaked at 24 months, with patients shedding a mean of 74% of their excess weight. Although that had fallen to a mean of 52% at 10 years, “they still kept off half of their excess weight, which is outstanding,” investigator and general surgery resident Dr. Hunter Mehaffey said at the annual clinical congress of the American College of Surgeons.
Surgery also led to persistent reductions in obesity-related comorbidities. Before RYGB, for instance, 38% of patients had gastroesophageal reflux disease, versus 29% after 10 years. Similarly, the prevalence of degenerative joint disease fell from 61% to 32%, diabetes from 41% to 18%, obstructive sleep apnea from 36% to 16%, hypertension from 59% to 47%, pulmonary problems from 28% to 13%, and psychiatric issues from 39% to 29%. About a quarter of patients had cardiac comorbidities before RYGB, versus 16% at 10 years after surgery. The data came from chart reviews and patient interviews, and the findings were statistically significant.
Overall, patients seemed glad to have had the operation, reporting an average satisfaction score of 8.7 out of 10 points, he said, adding, “I would expect these findings to be generalizable to other institutions. This is a good, durable operation.”
Given the scope of the comorbidity reductions, “the savings in health care costs” from RYGB “are likely underestimated,” Dr. Mehaffey said.
There was another lesson from the study, as well. It took a while to track down patients for 10-year follow-up because they were no longer seeing their surgeons. “If we are not going to see these patients much after 2 years, we really have to make sure that their primary care physician knows” how to recognize and manage possible complications, such as nutritional deficiency or hypoglycemia, he said.
Dr. Mehaffey had no disclosures, and there was no outside funding for the work.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Patients considering bariatric surgery can be reassured that many of the benefits are long lasting.
Major finding: At 10 years, patients had kept off a mean of 52% of their excess preoperative weight.
Data source: Follow-up of 651 Roux-en-Y gastric bypass patients 10 years after their surgery.
Disclosures: The lead investigator had no disclosures, and there was no outside funding.
Pain a common cause of revisits after same-day surgery
SAN DIEGO – Nearly one-third of pain-related emergency room visits or hospital readmissions following same-day surgery were attributable to inadequate pain management in the peridischarge period, a large single-center analysis demonstrated.
“Pain management in the perioperative period is largely an anesthesiologist responsibility, but maybe it would be helpful if it was a little bit more multispecialty, if we had more communication,” study author Dr. Martha O. Herbst said in an interview at the annual meeting of the American Society of Anesthesiologists.
“There were some patients who came back for pain because they didn’t even receive prescriptions from their surgeon. Maybe a little better communication between the anesthesiologist and the surgeon on how to optimize specific patients and prevent those readmissions for pain would help,” she said.
Inspired by a similar study published in 2002 (J Clin Anesth. 2002;14[5]:349-53), Dr. Herbst, a fourth-year anesthesiology resident at Beaumont Hospital in Royal Oak, Mich., and her associates retrospectively evaluated the number of readmissions or revisits that occurred among 28,647 patients who underwent same-day surgery in the Beaumont Health system in 2012. A total of 1,559 revisits occurred during the study period. Of these, 621 (39.8%) were revisits related to the surgical procedure and 145 (9.3% overall and 23.3% of readmissions) were due to pain.
The researchers then stratified patients into one of six categories for readmission. These included all-cause pain (16%); surgical-related issues such as wound opening or reinfection (21%); medical issues such as exacerbation of chronic obstructive pulmonary disease (43%); bleeding complications such as hematuria, hemodialysis, and surgical site bleeding (6%); adverse medical reactions (2%); and other (12%).
Of the 145 patients who were readmitted for pain from the same-day surgery, 71% were deemed to have no pre-existing risk for readmission while 29% had at least one risk factor for readmission. These included opioid monotherapy during the procedure (11%), history of chronic pain (9%), no pain medication given during the procedure (4%), inadequate doses of analgesics used (3%), and discharge without a prescription for an analgesic (2%).
“There were people who got tiny doses of pain medications after a huge, painful procedure, so that was surprising,” Dr. Herbst said. “Maybe they weren’t optimally managed at the time of surgery.”
The findings, she concluded, underscore the need for a team-based approach to pain management in the same-day surgery population, with discharge planning focused on patient education, expectation management, multimodal analgesia optimization, and pain risk assessment.
The researchers reported having no financial disclosures.
SAN DIEGO – Nearly one-third of pain-related emergency room visits or hospital readmissions following same-day surgery were attributable to inadequate pain management in the peridischarge period, a large single-center analysis demonstrated.
“Pain management in the perioperative period is largely an anesthesiologist responsibility, but maybe it would be helpful if it was a little bit more multispecialty, if we had more communication,” study author Dr. Martha O. Herbst said in an interview at the annual meeting of the American Society of Anesthesiologists.
“There were some patients who came back for pain because they didn’t even receive prescriptions from their surgeon. Maybe a little better communication between the anesthesiologist and the surgeon on how to optimize specific patients and prevent those readmissions for pain would help,” she said.
Inspired by a similar study published in 2002 (J Clin Anesth. 2002;14[5]:349-53), Dr. Herbst, a fourth-year anesthesiology resident at Beaumont Hospital in Royal Oak, Mich., and her associates retrospectively evaluated the number of readmissions or revisits that occurred among 28,647 patients who underwent same-day surgery in the Beaumont Health system in 2012. A total of 1,559 revisits occurred during the study period. Of these, 621 (39.8%) were revisits related to the surgical procedure and 145 (9.3% overall and 23.3% of readmissions) were due to pain.
The researchers then stratified patients into one of six categories for readmission. These included all-cause pain (16%); surgical-related issues such as wound opening or reinfection (21%); medical issues such as exacerbation of chronic obstructive pulmonary disease (43%); bleeding complications such as hematuria, hemodialysis, and surgical site bleeding (6%); adverse medical reactions (2%); and other (12%).
Of the 145 patients who were readmitted for pain from the same-day surgery, 71% were deemed to have no pre-existing risk for readmission while 29% had at least one risk factor for readmission. These included opioid monotherapy during the procedure (11%), history of chronic pain (9%), no pain medication given during the procedure (4%), inadequate doses of analgesics used (3%), and discharge without a prescription for an analgesic (2%).
“There were people who got tiny doses of pain medications after a huge, painful procedure, so that was surprising,” Dr. Herbst said. “Maybe they weren’t optimally managed at the time of surgery.”
The findings, she concluded, underscore the need for a team-based approach to pain management in the same-day surgery population, with discharge planning focused on patient education, expectation management, multimodal analgesia optimization, and pain risk assessment.
The researchers reported having no financial disclosures.
SAN DIEGO – Nearly one-third of pain-related emergency room visits or hospital readmissions following same-day surgery were attributable to inadequate pain management in the peridischarge period, a large single-center analysis demonstrated.
“Pain management in the perioperative period is largely an anesthesiologist responsibility, but maybe it would be helpful if it was a little bit more multispecialty, if we had more communication,” study author Dr. Martha O. Herbst said in an interview at the annual meeting of the American Society of Anesthesiologists.
“There were some patients who came back for pain because they didn’t even receive prescriptions from their surgeon. Maybe a little better communication between the anesthesiologist and the surgeon on how to optimize specific patients and prevent those readmissions for pain would help,” she said.
Inspired by a similar study published in 2002 (J Clin Anesth. 2002;14[5]:349-53), Dr. Herbst, a fourth-year anesthesiology resident at Beaumont Hospital in Royal Oak, Mich., and her associates retrospectively evaluated the number of readmissions or revisits that occurred among 28,647 patients who underwent same-day surgery in the Beaumont Health system in 2012. A total of 1,559 revisits occurred during the study period. Of these, 621 (39.8%) were revisits related to the surgical procedure and 145 (9.3% overall and 23.3% of readmissions) were due to pain.
The researchers then stratified patients into one of six categories for readmission. These included all-cause pain (16%); surgical-related issues such as wound opening or reinfection (21%); medical issues such as exacerbation of chronic obstructive pulmonary disease (43%); bleeding complications such as hematuria, hemodialysis, and surgical site bleeding (6%); adverse medical reactions (2%); and other (12%).
Of the 145 patients who were readmitted for pain from the same-day surgery, 71% were deemed to have no pre-existing risk for readmission while 29% had at least one risk factor for readmission. These included opioid monotherapy during the procedure (11%), history of chronic pain (9%), no pain medication given during the procedure (4%), inadequate doses of analgesics used (3%), and discharge without a prescription for an analgesic (2%).
“There were people who got tiny doses of pain medications after a huge, painful procedure, so that was surprising,” Dr. Herbst said. “Maybe they weren’t optimally managed at the time of surgery.”
The findings, she concluded, underscore the need for a team-based approach to pain management in the same-day surgery population, with discharge planning focused on patient education, expectation management, multimodal analgesia optimization, and pain risk assessment.
The researchers reported having no financial disclosures.
AT THE ASA ANNUAL MEETING
Key clinical point: Among patients who underwent same-day surgery, pain was a significant cause of readmissions or revisits.
Major finding: Of 145 patients who were readmitted for pain following same-day surgery, 71% were deemed to have no pre-existing risk for readmission, while 29% had at least one risk factor for readmission.
Data source: A retrospective evaluation of the number of readmissions or revisits that occurred among 28,647 patients who underwent same-day surgery at a single health system in 2012.
Disclosures: The researchers reported having no financial disclosures.
After bariatric surgery, pain and disability decline
LOS ANGELES – In the 3 years following bariatric surgery, 50%-70% of adults will experience clinically meaningful easing of bodily pain and improved physical function, a collaborative study shows.
Further, 75% of patients with severe knee and hip pain or disability had lessening of symptoms indicative of osteoarthritis, Wendy C. King, Ph.D., of the University of Pittsburgh Graduate School of Public Health, reported at Obesity Week 2015.
The study also sheds new light on several factors associated with easing of the debilitating joint pain and physical limitations that are common among patients undergoing bariatric surgery.
Previous studies have reported lessening of symptoms after surgery but had small sample sizes, short-term follow-up of 1 year or less, or used obsolete surgical procedures, she said.
The investigators followed 2,221 patients participating in the prospective, observational Longitudinal Assessment of Bariatric Surgery-2 (LABS-2) study who underwent weight-loss surgery at any of ten U.S. hospitals. Most (70%) had Roux-en-Y bypass, 25% laparoscopic adjustable gastric banding, and 5% other procedures. Their median age was 47 years, median body mass index 46 kg/m2, and 79% were female. Follow-up assessment with several validated measures was available in 1,724 (72%) of patients at 3 years.
Short Form Health Survey (SF-36) scores at years 1, 2, and 3 of follow-up were 57.6, 53.5, and 48.6 for bodily pain and 76.5, 74.2, and 70.2 for physical function, Dr. King said.
Knee pain scores on the Western Ontario and McMaster Universities Arthritis Index (WOMAC) were 75.1 at 1 year, 71.6 at year 2, and 71.3 at year 3.
In Poisson mixed models, younger age, higher household income, and fewer depressive symptoms before surgery were among the factors independently related to a higher likelihood of easing of pain and improvements in function, she said. In addition, greater weight loss and lessening of depressive symptoms after surgery predicted easing of pain and improved physical function.
Opioid use and mobility deficits after bariatric surgery, however, proved more thorny outcomes to alter, Dr. King acknowledged.
Less than half of the 353 patients who reported opioid pain medication use at baseline discontinued opioids at years 1, 2, and 3 of follow-up (42.2%, 40.2%, 45.7%).
Only younger age and higher household income at baseline predicted discontinuation, she said. When the SF-36 pain score was added to the model to account for perceived pain, only having less presurgical pain and a more significant postsurgical lessening of pain were related to postsurgical cessation of opioid use.
“It’s possible that the improvement in depressive symptoms and improvement in pain and function are bidirectional,” Dr. King said. “So if you have improvement in pain and function, you may have improvement in depressive symptoms. But I think it’s noteworthy that presurgery depressive symptoms predicted lower likelihood of improvement in pain, suggesting that depressive symptoms may contribute to pain perception in this population.”
Mobility deficits, defined as the inability to complete a timed 400-m walk in 7 minutes, were present in 836 patients (44%) at entry, with deficit remission rates holding steady at each year of follow-up (55.6%, 55.8%, 56.5%).
After controlling for factors related to pain and function (age, income, depressive symptoms, weight loss), baseline pain and easing of pain were related to improvement in function. Thus, effective pain management may also improve physical function in this population, Dr. King suggested.
“These findings may help clinicians identify patients likely to require additional intervention to address pain and physical limitations that may otherwise limit or reduce their quality of life and pose significant barriers to their ability to adopt an active lifestyle,” she said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. “There was some decline in the original improvement between year 1 and year 3, so I think it will be really important for us to get the 7-year data out there to see if that trend continues.”
This is a very-well-done study, but information is needed on how long participants were suffering presurgery, as this could be a confounding factor. While patients clearly had improvements in symptoms, this did not remain constant over follow-up and appeared to decline in year 3. For most measures, there wasn’t a significant difference between years 1 and 3, although SF-36 scores did drop off in a small percentage of patients, possibly because of aging or weight regain.
Dr. Richard M. Peterson is the director of the University of Texas Center for Bariatric and Metabolic Surgery in San Antonio. He was the discussant for the presentation at the meeting.
This is a very-well-done study, but information is needed on how long participants were suffering presurgery, as this could be a confounding factor. While patients clearly had improvements in symptoms, this did not remain constant over follow-up and appeared to decline in year 3. For most measures, there wasn’t a significant difference between years 1 and 3, although SF-36 scores did drop off in a small percentage of patients, possibly because of aging or weight regain.
Dr. Richard M. Peterson is the director of the University of Texas Center for Bariatric and Metabolic Surgery in San Antonio. He was the discussant for the presentation at the meeting.
This is a very-well-done study, but information is needed on how long participants were suffering presurgery, as this could be a confounding factor. While patients clearly had improvements in symptoms, this did not remain constant over follow-up and appeared to decline in year 3. For most measures, there wasn’t a significant difference between years 1 and 3, although SF-36 scores did drop off in a small percentage of patients, possibly because of aging or weight regain.
Dr. Richard M. Peterson is the director of the University of Texas Center for Bariatric and Metabolic Surgery in San Antonio. He was the discussant for the presentation at the meeting.
LOS ANGELES – In the 3 years following bariatric surgery, 50%-70% of adults will experience clinically meaningful easing of bodily pain and improved physical function, a collaborative study shows.
Further, 75% of patients with severe knee and hip pain or disability had lessening of symptoms indicative of osteoarthritis, Wendy C. King, Ph.D., of the University of Pittsburgh Graduate School of Public Health, reported at Obesity Week 2015.
The study also sheds new light on several factors associated with easing of the debilitating joint pain and physical limitations that are common among patients undergoing bariatric surgery.
Previous studies have reported lessening of symptoms after surgery but had small sample sizes, short-term follow-up of 1 year or less, or used obsolete surgical procedures, she said.
The investigators followed 2,221 patients participating in the prospective, observational Longitudinal Assessment of Bariatric Surgery-2 (LABS-2) study who underwent weight-loss surgery at any of ten U.S. hospitals. Most (70%) had Roux-en-Y bypass, 25% laparoscopic adjustable gastric banding, and 5% other procedures. Their median age was 47 years, median body mass index 46 kg/m2, and 79% were female. Follow-up assessment with several validated measures was available in 1,724 (72%) of patients at 3 years.
Short Form Health Survey (SF-36) scores at years 1, 2, and 3 of follow-up were 57.6, 53.5, and 48.6 for bodily pain and 76.5, 74.2, and 70.2 for physical function, Dr. King said.
Knee pain scores on the Western Ontario and McMaster Universities Arthritis Index (WOMAC) were 75.1 at 1 year, 71.6 at year 2, and 71.3 at year 3.
In Poisson mixed models, younger age, higher household income, and fewer depressive symptoms before surgery were among the factors independently related to a higher likelihood of easing of pain and improvements in function, she said. In addition, greater weight loss and lessening of depressive symptoms after surgery predicted easing of pain and improved physical function.
Opioid use and mobility deficits after bariatric surgery, however, proved more thorny outcomes to alter, Dr. King acknowledged.
Less than half of the 353 patients who reported opioid pain medication use at baseline discontinued opioids at years 1, 2, and 3 of follow-up (42.2%, 40.2%, 45.7%).
Only younger age and higher household income at baseline predicted discontinuation, she said. When the SF-36 pain score was added to the model to account for perceived pain, only having less presurgical pain and a more significant postsurgical lessening of pain were related to postsurgical cessation of opioid use.
“It’s possible that the improvement in depressive symptoms and improvement in pain and function are bidirectional,” Dr. King said. “So if you have improvement in pain and function, you may have improvement in depressive symptoms. But I think it’s noteworthy that presurgery depressive symptoms predicted lower likelihood of improvement in pain, suggesting that depressive symptoms may contribute to pain perception in this population.”
Mobility deficits, defined as the inability to complete a timed 400-m walk in 7 minutes, were present in 836 patients (44%) at entry, with deficit remission rates holding steady at each year of follow-up (55.6%, 55.8%, 56.5%).
After controlling for factors related to pain and function (age, income, depressive symptoms, weight loss), baseline pain and easing of pain were related to improvement in function. Thus, effective pain management may also improve physical function in this population, Dr. King suggested.
“These findings may help clinicians identify patients likely to require additional intervention to address pain and physical limitations that may otherwise limit or reduce their quality of life and pose significant barriers to their ability to adopt an active lifestyle,” she said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. “There was some decline in the original improvement between year 1 and year 3, so I think it will be really important for us to get the 7-year data out there to see if that trend continues.”
LOS ANGELES – In the 3 years following bariatric surgery, 50%-70% of adults will experience clinically meaningful easing of bodily pain and improved physical function, a collaborative study shows.
Further, 75% of patients with severe knee and hip pain or disability had lessening of symptoms indicative of osteoarthritis, Wendy C. King, Ph.D., of the University of Pittsburgh Graduate School of Public Health, reported at Obesity Week 2015.
The study also sheds new light on several factors associated with easing of the debilitating joint pain and physical limitations that are common among patients undergoing bariatric surgery.
Previous studies have reported lessening of symptoms after surgery but had small sample sizes, short-term follow-up of 1 year or less, or used obsolete surgical procedures, she said.
The investigators followed 2,221 patients participating in the prospective, observational Longitudinal Assessment of Bariatric Surgery-2 (LABS-2) study who underwent weight-loss surgery at any of ten U.S. hospitals. Most (70%) had Roux-en-Y bypass, 25% laparoscopic adjustable gastric banding, and 5% other procedures. Their median age was 47 years, median body mass index 46 kg/m2, and 79% were female. Follow-up assessment with several validated measures was available in 1,724 (72%) of patients at 3 years.
Short Form Health Survey (SF-36) scores at years 1, 2, and 3 of follow-up were 57.6, 53.5, and 48.6 for bodily pain and 76.5, 74.2, and 70.2 for physical function, Dr. King said.
Knee pain scores on the Western Ontario and McMaster Universities Arthritis Index (WOMAC) were 75.1 at 1 year, 71.6 at year 2, and 71.3 at year 3.
In Poisson mixed models, younger age, higher household income, and fewer depressive symptoms before surgery were among the factors independently related to a higher likelihood of easing of pain and improvements in function, she said. In addition, greater weight loss and lessening of depressive symptoms after surgery predicted easing of pain and improved physical function.
Opioid use and mobility deficits after bariatric surgery, however, proved more thorny outcomes to alter, Dr. King acknowledged.
Less than half of the 353 patients who reported opioid pain medication use at baseline discontinued opioids at years 1, 2, and 3 of follow-up (42.2%, 40.2%, 45.7%).
Only younger age and higher household income at baseline predicted discontinuation, she said. When the SF-36 pain score was added to the model to account for perceived pain, only having less presurgical pain and a more significant postsurgical lessening of pain were related to postsurgical cessation of opioid use.
“It’s possible that the improvement in depressive symptoms and improvement in pain and function are bidirectional,” Dr. King said. “So if you have improvement in pain and function, you may have improvement in depressive symptoms. But I think it’s noteworthy that presurgery depressive symptoms predicted lower likelihood of improvement in pain, suggesting that depressive symptoms may contribute to pain perception in this population.”
Mobility deficits, defined as the inability to complete a timed 400-m walk in 7 minutes, were present in 836 patients (44%) at entry, with deficit remission rates holding steady at each year of follow-up (55.6%, 55.8%, 56.5%).
After controlling for factors related to pain and function (age, income, depressive symptoms, weight loss), baseline pain and easing of pain were related to improvement in function. Thus, effective pain management may also improve physical function in this population, Dr. King suggested.
“These findings may help clinicians identify patients likely to require additional intervention to address pain and physical limitations that may otherwise limit or reduce their quality of life and pose significant barriers to their ability to adopt an active lifestyle,” she said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. “There was some decline in the original improvement between year 1 and year 3, so I think it will be really important for us to get the 7-year data out there to see if that trend continues.”
AT OBESITY WEEK 2015
Key clinical point: In the 3 years following bariatric surgery, most patients will have less pain and improved physical function.
Major finding: SF-36 scores for bodily pain at years 1, 2, and 3 were 57.6, 53.5, and 48.6.
Data source: Analysis of 2,221 severely obese adults.
Disclosures: The study was funded by the National Institute of Diabetes and Digestive and Kidney diseases. Dr. King reported having no disclosures.