User login
U.S. cancer death rates drop for second year in a row
The study was published online Jan. 12 in CA: A Cancer Journal for Clinicians.
“Mortality rates are a better indicator of progress against cancer than incidence or survival because they are less affected by biases resulting from changes in detection practices,” wrote the authors, led by Rebecca Siegel, MPH, American Cancer Society, Atlanta.
“The overall drop of 31% as of 2018 [since the early 1990s] translates to an estimated 3,188,500 fewer cancer deaths (2,170,700 in men and 1,017,800 in women) than what would have occurred if mortality rates had remained at their peak,” the researchers added.
Lung cancer accounted for 46% of the total decline in cancer mortality in the past 5 years, with a record, single-year drop of 2.4% between 2017 and 2018.
The recent and rapid reductions in lung cancer mortality reflect better treatments for NSCLC, the authors suggested. For example, survival rates at 2 years have increased from 34% for patients diagnosed with NSCLC between 2009 and 2010 to 42% for those diagnosed during 2015 and 2016 – an absolute gain of 5%-6% in survival odds for every stage of diagnosis.
On a more somber note, the authors warned that COVID-19 is predicted to have a negative impact on both the diagnosis and outcomes of patients with cancer in the near future.
“We anticipate that disruptions in access to cancer care in 2020 will lead to downstream increases in advanced stage diagnoses that may impede progress in reducing cancer mortality rates in the years to come,” Ms. Siegel said in a statement.
New cancer cases
The report provides an estimated number of new cancer cases and deaths in 2021 in the United States (nationally and state-by-state) based on the most current population-based data for cancer incidence through 2017 and for mortality through 2018. “An estimated 608,570 Americans will die from cancer in 2021, corresponding to more than 1600 deaths per day,” Ms. Siegel and colleagues reported.
The greatest number of deaths are predicted to be from the most common cancers: Lung, prostate, and colorectal cancer in men and lung, breast, and colorectal cancer in women, they added. However, the mortality rates for all four cancers are continuing to fall.
As of 2018, the death rate from lung cancer had dropped by 54% among males and by 30% among females over the past few decades, the investigators noted.
Mortality from female breast cancer has dropped by 41% since 1989; by 52% for prostate cancer since 1993; and by 53% and 59% for colorectal cancer for men (since 1980) and women (since 1969), respectively.
“However, in recent years, mortality declines have slowed for breast cancer and [colorectal cancer] and have halted for prostate cancer,” the researchers noted.
In contrast, the pace of the annual decline in lung cancer mortality doubled among men from 3.1% between 2009 and 2013 to 5.5% between 2014 and 2018, and from 1.8% to 4.4% among women during the same time intervals.
Increase in incidence at common sites
Despite the steady progress in mortality for most cancers, “rates continue to increase for some common sites,” Ms. Siegel and colleagues reported.
For example, death rates from uterine corpus cancer have accelerated from the late 1990s at twice the pace of the increase in its incidence. Death rates also have increased for cancers of the oral cavity and pharynx – although in this cancer, increases in mortality parallel an increase in its incidence.
“Pancreatic cancer death rates [in turn] continued to increase slowly in men ... but remained stable in women, despite incidence [rates] rising by about 1% per year in both sexes,” the authors observed.
Meanwhile, the incidence of cervical cancer, although declining for decades overall, is increasing for patients who present with more distant-stage disease as well as cervical adenocarcinoma, both of which are often undetected by cytology.
“These findings underscore the need for more targeted efforts to increase both HPV [human papillomavirus] vaccination among all individuals aged [26 and younger] and primary HPV testing or HPV/cytology co-testing every 5 years among women beginning at age 25,” the authors emphasized.
On a more positive note, the long-term increase in mortality from liver cancer has recently slowed among women and has stabilized among men, they added.
Once again, disparities in both cancer occurrence and outcomes varied considerably between racial and ethnic groups. For example, cancer is the leading cause of death in people who are Hispanic, Asian American, and Alaska Native. Survival rates at 5 years for almost all cancers are still higher for White patients than for Black patients, although the disparity in cancer mortality between Black persons and White persons has declined to 13% from a peak of 33% in 1993.
Geographic disparities in cancer mortality rates still prevail; the rates are largest for preventable cancers such as lung and cervical cancer, for which mortality varies by as much as fivefold across states.
And although cancer remains the second most common cause of death among children, death rates from cancer have continuously declined over time among both children and adolescents, largely the result of dramatic declines in death rates from leukemia in both age groups.
The study authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The study was published online Jan. 12 in CA: A Cancer Journal for Clinicians.
“Mortality rates are a better indicator of progress against cancer than incidence or survival because they are less affected by biases resulting from changes in detection practices,” wrote the authors, led by Rebecca Siegel, MPH, American Cancer Society, Atlanta.
“The overall drop of 31% as of 2018 [since the early 1990s] translates to an estimated 3,188,500 fewer cancer deaths (2,170,700 in men and 1,017,800 in women) than what would have occurred if mortality rates had remained at their peak,” the researchers added.
Lung cancer accounted for 46% of the total decline in cancer mortality in the past 5 years, with a record, single-year drop of 2.4% between 2017 and 2018.
The recent and rapid reductions in lung cancer mortality reflect better treatments for NSCLC, the authors suggested. For example, survival rates at 2 years have increased from 34% for patients diagnosed with NSCLC between 2009 and 2010 to 42% for those diagnosed during 2015 and 2016 – an absolute gain of 5%-6% in survival odds for every stage of diagnosis.
On a more somber note, the authors warned that COVID-19 is predicted to have a negative impact on both the diagnosis and outcomes of patients with cancer in the near future.
“We anticipate that disruptions in access to cancer care in 2020 will lead to downstream increases in advanced stage diagnoses that may impede progress in reducing cancer mortality rates in the years to come,” Ms. Siegel said in a statement.
New cancer cases
The report provides an estimated number of new cancer cases and deaths in 2021 in the United States (nationally and state-by-state) based on the most current population-based data for cancer incidence through 2017 and for mortality through 2018. “An estimated 608,570 Americans will die from cancer in 2021, corresponding to more than 1600 deaths per day,” Ms. Siegel and colleagues reported.
The greatest number of deaths are predicted to be from the most common cancers: Lung, prostate, and colorectal cancer in men and lung, breast, and colorectal cancer in women, they added. However, the mortality rates for all four cancers are continuing to fall.
As of 2018, the death rate from lung cancer had dropped by 54% among males and by 30% among females over the past few decades, the investigators noted.
Mortality from female breast cancer has dropped by 41% since 1989; by 52% for prostate cancer since 1993; and by 53% and 59% for colorectal cancer for men (since 1980) and women (since 1969), respectively.
“However, in recent years, mortality declines have slowed for breast cancer and [colorectal cancer] and have halted for prostate cancer,” the researchers noted.
In contrast, the pace of the annual decline in lung cancer mortality doubled among men from 3.1% between 2009 and 2013 to 5.5% between 2014 and 2018, and from 1.8% to 4.4% among women during the same time intervals.
Increase in incidence at common sites
Despite the steady progress in mortality for most cancers, “rates continue to increase for some common sites,” Ms. Siegel and colleagues reported.
For example, death rates from uterine corpus cancer have accelerated from the late 1990s at twice the pace of the increase in its incidence. Death rates also have increased for cancers of the oral cavity and pharynx – although in this cancer, increases in mortality parallel an increase in its incidence.
“Pancreatic cancer death rates [in turn] continued to increase slowly in men ... but remained stable in women, despite incidence [rates] rising by about 1% per year in both sexes,” the authors observed.
Meanwhile, the incidence of cervical cancer, although declining for decades overall, is increasing for patients who present with more distant-stage disease as well as cervical adenocarcinoma, both of which are often undetected by cytology.
“These findings underscore the need for more targeted efforts to increase both HPV [human papillomavirus] vaccination among all individuals aged [26 and younger] and primary HPV testing or HPV/cytology co-testing every 5 years among women beginning at age 25,” the authors emphasized.
On a more positive note, the long-term increase in mortality from liver cancer has recently slowed among women and has stabilized among men, they added.
Once again, disparities in both cancer occurrence and outcomes varied considerably between racial and ethnic groups. For example, cancer is the leading cause of death in people who are Hispanic, Asian American, and Alaska Native. Survival rates at 5 years for almost all cancers are still higher for White patients than for Black patients, although the disparity in cancer mortality between Black persons and White persons has declined to 13% from a peak of 33% in 1993.
Geographic disparities in cancer mortality rates still prevail; the rates are largest for preventable cancers such as lung and cervical cancer, for which mortality varies by as much as fivefold across states.
And although cancer remains the second most common cause of death among children, death rates from cancer have continuously declined over time among both children and adolescents, largely the result of dramatic declines in death rates from leukemia in both age groups.
The study authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The study was published online Jan. 12 in CA: A Cancer Journal for Clinicians.
“Mortality rates are a better indicator of progress against cancer than incidence or survival because they are less affected by biases resulting from changes in detection practices,” wrote the authors, led by Rebecca Siegel, MPH, American Cancer Society, Atlanta.
“The overall drop of 31% as of 2018 [since the early 1990s] translates to an estimated 3,188,500 fewer cancer deaths (2,170,700 in men and 1,017,800 in women) than what would have occurred if mortality rates had remained at their peak,” the researchers added.
Lung cancer accounted for 46% of the total decline in cancer mortality in the past 5 years, with a record, single-year drop of 2.4% between 2017 and 2018.
The recent and rapid reductions in lung cancer mortality reflect better treatments for NSCLC, the authors suggested. For example, survival rates at 2 years have increased from 34% for patients diagnosed with NSCLC between 2009 and 2010 to 42% for those diagnosed during 2015 and 2016 – an absolute gain of 5%-6% in survival odds for every stage of diagnosis.
On a more somber note, the authors warned that COVID-19 is predicted to have a negative impact on both the diagnosis and outcomes of patients with cancer in the near future.
“We anticipate that disruptions in access to cancer care in 2020 will lead to downstream increases in advanced stage diagnoses that may impede progress in reducing cancer mortality rates in the years to come,” Ms. Siegel said in a statement.
New cancer cases
The report provides an estimated number of new cancer cases and deaths in 2021 in the United States (nationally and state-by-state) based on the most current population-based data for cancer incidence through 2017 and for mortality through 2018. “An estimated 608,570 Americans will die from cancer in 2021, corresponding to more than 1600 deaths per day,” Ms. Siegel and colleagues reported.
The greatest number of deaths are predicted to be from the most common cancers: Lung, prostate, and colorectal cancer in men and lung, breast, and colorectal cancer in women, they added. However, the mortality rates for all four cancers are continuing to fall.
As of 2018, the death rate from lung cancer had dropped by 54% among males and by 30% among females over the past few decades, the investigators noted.
Mortality from female breast cancer has dropped by 41% since 1989; by 52% for prostate cancer since 1993; and by 53% and 59% for colorectal cancer for men (since 1980) and women (since 1969), respectively.
“However, in recent years, mortality declines have slowed for breast cancer and [colorectal cancer] and have halted for prostate cancer,” the researchers noted.
In contrast, the pace of the annual decline in lung cancer mortality doubled among men from 3.1% between 2009 and 2013 to 5.5% between 2014 and 2018, and from 1.8% to 4.4% among women during the same time intervals.
Increase in incidence at common sites
Despite the steady progress in mortality for most cancers, “rates continue to increase for some common sites,” Ms. Siegel and colleagues reported.
For example, death rates from uterine corpus cancer have accelerated from the late 1990s at twice the pace of the increase in its incidence. Death rates also have increased for cancers of the oral cavity and pharynx – although in this cancer, increases in mortality parallel an increase in its incidence.
“Pancreatic cancer death rates [in turn] continued to increase slowly in men ... but remained stable in women, despite incidence [rates] rising by about 1% per year in both sexes,” the authors observed.
Meanwhile, the incidence of cervical cancer, although declining for decades overall, is increasing for patients who present with more distant-stage disease as well as cervical adenocarcinoma, both of which are often undetected by cytology.
“These findings underscore the need for more targeted efforts to increase both HPV [human papillomavirus] vaccination among all individuals aged [26 and younger] and primary HPV testing or HPV/cytology co-testing every 5 years among women beginning at age 25,” the authors emphasized.
On a more positive note, the long-term increase in mortality from liver cancer has recently slowed among women and has stabilized among men, they added.
Once again, disparities in both cancer occurrence and outcomes varied considerably between racial and ethnic groups. For example, cancer is the leading cause of death in people who are Hispanic, Asian American, and Alaska Native. Survival rates at 5 years for almost all cancers are still higher for White patients than for Black patients, although the disparity in cancer mortality between Black persons and White persons has declined to 13% from a peak of 33% in 1993.
Geographic disparities in cancer mortality rates still prevail; the rates are largest for preventable cancers such as lung and cervical cancer, for which mortality varies by as much as fivefold across states.
And although cancer remains the second most common cause of death among children, death rates from cancer have continuously declined over time among both children and adolescents, largely the result of dramatic declines in death rates from leukemia in both age groups.
The study authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sentinel node biopsy cuts surgery time over lymphadenectomy
Sentinel node biopsy shortens operative time by 13% and may play a role in reducing recovery time and length of hospital stay, reported David L. Tait, MD, of the Levine Cancer Institute, Charlotte, N.C., and colleagues.
In an effort to compare the immediate perioperative outcomes for narcotic usage and use of hospital resources for patients having sentinel node dissection, Dr. Tait and his colleagues conducted a retrospective study of 241 consecutive cases of minimally invasive surgery performed between Jan. 1, 2018, and Aug. 31, 2019, on endometrial cancer patients.
A total of 156 (65%) patients received nodal dissection, including 93 (60%) who received sentinel node biopsy and 63 (40%) who underwent a full lymphadenectomy in accordance with pathological criteria established at the time of surgery. The authors noted no differences between the sentinel group and the lymphadenectomy group in terms of age, body mass index, estimated blood loss, use of a preoperative enhanced recovery after surgery (ERAS) program, tobacco use, or ethanol use. They also found no difference in primary outcome of intravenous narcotics dispensed in surgery, recovery, or total dose.
Sentinel node biopsy offers several advantages
Dr. Tate and colleagues noted that a significantly shorter surgery time, by 27 minutes, on average, was not unexpected with the sentinel node biopsy technique. With lymphadenectomy, surgical procedure and recovery times were longer (214.2 minutes vs. 185.2 minutes and 157.6 minutes vs. 125.2 minutes, respectively) than sentinel biopsy, a difference the researchers could not explain given the similar use of narcotics between the two procedures. Lymphadenectomy also resulted in longer hospital stay than sentinel biopsy (23.5 hours vs. 15.5 hours), with same-day discharge significantly less frequent (16% vs. 50%).
The differences in operative time, recovery time, and hospital stay “are important with respect to improving the efficiency of the operating room, which has become even more important in the era of the COVID-19 pandemic,” the authors noted. They also found noteworthy that recovery and hospital stay are longer after full lymphadenectomy even though there was no difference in overall narcotic administration. Although this suggests surgeon and staff bias, other factors that were not accounted for in the study include distance from hospital, social situation, and functional status.
Change in practice patterns over time and the introduction of a universal ERAS program during the study period were noted as possible limitations. It was also noted that the study did not collect data on functional status or long-term outcome of patients.
The authors did note that using the sentinel node technique was advantageous because it was performed on all patients regardless of risk factors for extra uterine spread since the injection must be performed before hysterectomy. What makes this so beneficial is the potential it offers for detecting nodal metastasis in low-risk patients who may not have otherwise qualified for dissection, said Dr. Tait and colleagues.
In a separate interview, Justin Chura, MD, director of gynecologic oncology and robotic surgery at the Cancer Treatment Centers of America in Philadelphia, observed that “sentinel lymph node [SLN] mapping has been around since the late 1970s. It is most validated in melanoma and breast cancers but has also seen application for gynecological cancers including vulva, cervix, and endometrium. More than 5 years ago, the Society of Gynecologic Oncology issued a clinical practice statement regarding the role of sentinel lymph node mapping for endometrial cancer. An SLN algorithm has been part of [National Comprehensive Cancer Network] guidelines for a similar time frame. The technique faced a lot of skepticism and criticism in the breast cancer literature until randomized studies demonstrated that full axillary adenopathy did not confer a survival benefit. For endometrial cancer, it is unlikely that we will have as robust data, so we often look to retrospective studies such as the one presented by Tait et al.
“The study utilized a data set that was originally collected to assess the impact of an ERAS protocol. So, it is important to note that the data set was not collected with the intent of evaluating SLN mapping versus full lymphadenectomy. This explains why pathological data regarding lymph node yield and final surgicopathologic staging are absent,” he said.
Adoption of sentinel node biopsy is gaining popularity
“Overall, SLN mapping is safe (from a surgical standpoint) and may decrease perioperative morbidity,” Dr. Chura said. “The adoption of SLN mapping also appears to be increasing. Some gyn oncologists (including myself) are even performing SLN mapping on patients with endometrial intraepithelial neoplasia given the risk of malignancy being identified on final pathology.
“The current study provides more of a glimpse into the practice patterns of the authors’ institution where ‘full lymphadenectomy was very dependent upon the surgeon (P < .001)’ than it demonstrates one technique is better than the other. The ultimate question is how we define ‘better?’ Survival? Less morbidity? Improved accuracy of nodal metastasis? Shorter length of stay?” Dr. Chura said.Dr. Tait and colleagues as well as Dr. Chura had no conflicts of interest and no relevant financial disclosures.
SOURCE: Tate DL et al. J Minim Invasive Gynecol. 2020 Dec 19. doi: 10.1016/jmig.2020.12.019.
Sentinel node biopsy shortens operative time by 13% and may play a role in reducing recovery time and length of hospital stay, reported David L. Tait, MD, of the Levine Cancer Institute, Charlotte, N.C., and colleagues.
In an effort to compare the immediate perioperative outcomes for narcotic usage and use of hospital resources for patients having sentinel node dissection, Dr. Tait and his colleagues conducted a retrospective study of 241 consecutive cases of minimally invasive surgery performed between Jan. 1, 2018, and Aug. 31, 2019, on endometrial cancer patients.
A total of 156 (65%) patients received nodal dissection, including 93 (60%) who received sentinel node biopsy and 63 (40%) who underwent a full lymphadenectomy in accordance with pathological criteria established at the time of surgery. The authors noted no differences between the sentinel group and the lymphadenectomy group in terms of age, body mass index, estimated blood loss, use of a preoperative enhanced recovery after surgery (ERAS) program, tobacco use, or ethanol use. They also found no difference in primary outcome of intravenous narcotics dispensed in surgery, recovery, or total dose.
Sentinel node biopsy offers several advantages
Dr. Tate and colleagues noted that a significantly shorter surgery time, by 27 minutes, on average, was not unexpected with the sentinel node biopsy technique. With lymphadenectomy, surgical procedure and recovery times were longer (214.2 minutes vs. 185.2 minutes and 157.6 minutes vs. 125.2 minutes, respectively) than sentinel biopsy, a difference the researchers could not explain given the similar use of narcotics between the two procedures. Lymphadenectomy also resulted in longer hospital stay than sentinel biopsy (23.5 hours vs. 15.5 hours), with same-day discharge significantly less frequent (16% vs. 50%).
The differences in operative time, recovery time, and hospital stay “are important with respect to improving the efficiency of the operating room, which has become even more important in the era of the COVID-19 pandemic,” the authors noted. They also found noteworthy that recovery and hospital stay are longer after full lymphadenectomy even though there was no difference in overall narcotic administration. Although this suggests surgeon and staff bias, other factors that were not accounted for in the study include distance from hospital, social situation, and functional status.
Change in practice patterns over time and the introduction of a universal ERAS program during the study period were noted as possible limitations. It was also noted that the study did not collect data on functional status or long-term outcome of patients.
The authors did note that using the sentinel node technique was advantageous because it was performed on all patients regardless of risk factors for extra uterine spread since the injection must be performed before hysterectomy. What makes this so beneficial is the potential it offers for detecting nodal metastasis in low-risk patients who may not have otherwise qualified for dissection, said Dr. Tait and colleagues.
In a separate interview, Justin Chura, MD, director of gynecologic oncology and robotic surgery at the Cancer Treatment Centers of America in Philadelphia, observed that “sentinel lymph node [SLN] mapping has been around since the late 1970s. It is most validated in melanoma and breast cancers but has also seen application for gynecological cancers including vulva, cervix, and endometrium. More than 5 years ago, the Society of Gynecologic Oncology issued a clinical practice statement regarding the role of sentinel lymph node mapping for endometrial cancer. An SLN algorithm has been part of [National Comprehensive Cancer Network] guidelines for a similar time frame. The technique faced a lot of skepticism and criticism in the breast cancer literature until randomized studies demonstrated that full axillary adenopathy did not confer a survival benefit. For endometrial cancer, it is unlikely that we will have as robust data, so we often look to retrospective studies such as the one presented by Tait et al.
“The study utilized a data set that was originally collected to assess the impact of an ERAS protocol. So, it is important to note that the data set was not collected with the intent of evaluating SLN mapping versus full lymphadenectomy. This explains why pathological data regarding lymph node yield and final surgicopathologic staging are absent,” he said.
Adoption of sentinel node biopsy is gaining popularity
“Overall, SLN mapping is safe (from a surgical standpoint) and may decrease perioperative morbidity,” Dr. Chura said. “The adoption of SLN mapping also appears to be increasing. Some gyn oncologists (including myself) are even performing SLN mapping on patients with endometrial intraepithelial neoplasia given the risk of malignancy being identified on final pathology.
“The current study provides more of a glimpse into the practice patterns of the authors’ institution where ‘full lymphadenectomy was very dependent upon the surgeon (P < .001)’ than it demonstrates one technique is better than the other. The ultimate question is how we define ‘better?’ Survival? Less morbidity? Improved accuracy of nodal metastasis? Shorter length of stay?” Dr. Chura said.Dr. Tait and colleagues as well as Dr. Chura had no conflicts of interest and no relevant financial disclosures.
SOURCE: Tate DL et al. J Minim Invasive Gynecol. 2020 Dec 19. doi: 10.1016/jmig.2020.12.019.
Sentinel node biopsy shortens operative time by 13% and may play a role in reducing recovery time and length of hospital stay, reported David L. Tait, MD, of the Levine Cancer Institute, Charlotte, N.C., and colleagues.
In an effort to compare the immediate perioperative outcomes for narcotic usage and use of hospital resources for patients having sentinel node dissection, Dr. Tait and his colleagues conducted a retrospective study of 241 consecutive cases of minimally invasive surgery performed between Jan. 1, 2018, and Aug. 31, 2019, on endometrial cancer patients.
A total of 156 (65%) patients received nodal dissection, including 93 (60%) who received sentinel node biopsy and 63 (40%) who underwent a full lymphadenectomy in accordance with pathological criteria established at the time of surgery. The authors noted no differences between the sentinel group and the lymphadenectomy group in terms of age, body mass index, estimated blood loss, use of a preoperative enhanced recovery after surgery (ERAS) program, tobacco use, or ethanol use. They also found no difference in primary outcome of intravenous narcotics dispensed in surgery, recovery, or total dose.
Sentinel node biopsy offers several advantages
Dr. Tate and colleagues noted that a significantly shorter surgery time, by 27 minutes, on average, was not unexpected with the sentinel node biopsy technique. With lymphadenectomy, surgical procedure and recovery times were longer (214.2 minutes vs. 185.2 minutes and 157.6 minutes vs. 125.2 minutes, respectively) than sentinel biopsy, a difference the researchers could not explain given the similar use of narcotics between the two procedures. Lymphadenectomy also resulted in longer hospital stay than sentinel biopsy (23.5 hours vs. 15.5 hours), with same-day discharge significantly less frequent (16% vs. 50%).
The differences in operative time, recovery time, and hospital stay “are important with respect to improving the efficiency of the operating room, which has become even more important in the era of the COVID-19 pandemic,” the authors noted. They also found noteworthy that recovery and hospital stay are longer after full lymphadenectomy even though there was no difference in overall narcotic administration. Although this suggests surgeon and staff bias, other factors that were not accounted for in the study include distance from hospital, social situation, and functional status.
Change in practice patterns over time and the introduction of a universal ERAS program during the study period were noted as possible limitations. It was also noted that the study did not collect data on functional status or long-term outcome of patients.
The authors did note that using the sentinel node technique was advantageous because it was performed on all patients regardless of risk factors for extra uterine spread since the injection must be performed before hysterectomy. What makes this so beneficial is the potential it offers for detecting nodal metastasis in low-risk patients who may not have otherwise qualified for dissection, said Dr. Tait and colleagues.
In a separate interview, Justin Chura, MD, director of gynecologic oncology and robotic surgery at the Cancer Treatment Centers of America in Philadelphia, observed that “sentinel lymph node [SLN] mapping has been around since the late 1970s. It is most validated in melanoma and breast cancers but has also seen application for gynecological cancers including vulva, cervix, and endometrium. More than 5 years ago, the Society of Gynecologic Oncology issued a clinical practice statement regarding the role of sentinel lymph node mapping for endometrial cancer. An SLN algorithm has been part of [National Comprehensive Cancer Network] guidelines for a similar time frame. The technique faced a lot of skepticism and criticism in the breast cancer literature until randomized studies demonstrated that full axillary adenopathy did not confer a survival benefit. For endometrial cancer, it is unlikely that we will have as robust data, so we often look to retrospective studies such as the one presented by Tait et al.
“The study utilized a data set that was originally collected to assess the impact of an ERAS protocol. So, it is important to note that the data set was not collected with the intent of evaluating SLN mapping versus full lymphadenectomy. This explains why pathological data regarding lymph node yield and final surgicopathologic staging are absent,” he said.
Adoption of sentinel node biopsy is gaining popularity
“Overall, SLN mapping is safe (from a surgical standpoint) and may decrease perioperative morbidity,” Dr. Chura said. “The adoption of SLN mapping also appears to be increasing. Some gyn oncologists (including myself) are even performing SLN mapping on patients with endometrial intraepithelial neoplasia given the risk of malignancy being identified on final pathology.
“The current study provides more of a glimpse into the practice patterns of the authors’ institution where ‘full lymphadenectomy was very dependent upon the surgeon (P < .001)’ than it demonstrates one technique is better than the other. The ultimate question is how we define ‘better?’ Survival? Less morbidity? Improved accuracy of nodal metastasis? Shorter length of stay?” Dr. Chura said.Dr. Tait and colleagues as well as Dr. Chura had no conflicts of interest and no relevant financial disclosures.
SOURCE: Tate DL et al. J Minim Invasive Gynecol. 2020 Dec 19. doi: 10.1016/jmig.2020.12.019.
FROM THE JOURNAL OF MINIMALLY INVASIVE GYNECOLOGY
‘Impressive’ local control with MRI-guided brachytherapy in cervical cancer
At 5 years, the rate of local control was 92%, and overall survival was 74%. However, nodal and systemic control rates were inferior for node-positive and high-risk patients, and nearly 15% of patients experienced grade 3-5 treatment-related morbidity.
These results were reported at the European Society for Radiology and Oncology 2020 Online Congress.
Historically, brachytherapy dose has been fairly rigidly prescribed, based on dose points defined in two dimensions. By performing imaging before each brachytherapy implant, treatment parameters can be adapted to a patient’s anatomy, taking into account the positions of organs at risk and any tumor regression from prior treatment.
Richard Pötter, MD, emeritus professor at Medical University of Vienna, and colleagues tested MRI-guided adaptive brachytherapy in a multicenter cohort study.
The study’s disease outcome analysis included 1,341 women with cervical cancer of International Federation of Gynecology and Obstetrics stage IB–IVB (52% node positive) being treated with curative intent.
The women underwent definitive external beam radiotherapy (45-50 Gy, using either three-dimensional–conformal radiotherapy or intensity-modulated radiotherapy) with concurrent cisplatin chemotherapy, followed by MRI-guided adaptive brachytherapy based on MRI with the applicator in situ.
“There was no fixed dose prescription for brachytherapy, and there were no constraints for organs at risk,” Dr. Pötter explained. “But there was systematic joint reporting and contouring for the target and organs at risk, and also for doses and volumes.”
Nearly all patients were treated with adaptive MRI-based target and dose-volume and point parameters (99.1%), as well as with individualized multiparametric dose optimization (98.2%). The application technique was adapted, with intracavitary application alone used in 57% of patients, and both intracavitary and interstitial application in 43%.
Efficacy and toxicity
At a median follow-up of 51 months, 7.3% of patients had experienced a local failure, with 3.8% having an isolated local failure and 3.5% having synchronous nodal or systemic failure, Dr. Pötter reported.
The local failure rate was similar going from disease stage IB2 to IVA (8%-9%), even though the target volume more than doubled.
“This favorable result was due to an adaptation of dose, which was quite similar for the different stages and volumes. This is a major message of EMBRACE I,” Dr. Pötter commented.
The Kaplan-Meier–estimated 5-year rate of local control was 92% for the whole cohort. It was 98% in patients with stage IB1 disease and 91%-92% in patients with stage IB2–IVA disease.
The 5-year rate of overall survival was 74% for the entire cohort. It fell with stage, from 83% in patients with stage IB1 disease to 52% in patients with stage IVA disease.
For the entire population, the 5-year pelvic control rate was 87%, the 5-year cancer-specific survival was 79%, and the 5-year disease-free survival was 68%.
Overall, 14.6% of patients experienced grade 3-5 treatment-related morbidity at 5 years: 2.7% developed fistulas, 6.1% had vaginal toxicity, 6.5% had genitourinary toxicity, and 7.6% had gastrointestinal toxicity.
Room for improvement
“MRI-guided adaptive brachytherapy in locally advanced cervical cancer works in multicenter clinical practice, within such a study, with adaptation of the target and application technique, and multiparametric treatment planning and dose prescription,” Dr. Pötter summarized.
However, “the mature clinical outcomes appear challenging,” he added. Specifically, although the rate of local control was high, the rate of nodal control left room for improvement in node-positive patients, and the rates of systemic control and overall survival left room for improvement in high-risk patients.
In addition, “the grade 3-5 morbidity was limited per organ and per endpoint, but was considerable overall, and this asks for a reduction,” Dr. Pötter said.
Two of the areas needing improvement are being addressed in ongoing and planned research, according to Dr. Pötter. “The nodal part is already being addressed in EMBRACE II, intensifying treatment for node-positive patients through a simultaneous integrated boost and a very sophisticated probability planning concept, and also including more patients for paraaortic radiotherapy,” he elaborated. “For the systemic part, we have thought about [a study testing an] additional drug ... and there are thoughts for EMBRACE III to investigate such effect.”
A benchmark for brachytherapy
“This is the largest prospective cohort of patients treated with image-guided brachytherapy. The high rates of local control with long-term follow-up are impressive and speak to the clear value of high-quality brachytherapy,” commented Ann H. Klopp, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston, who was not involved in this study.
With its consistent reporting of detailed dose and toxicity data, the study establishes a benchmark for brachytherapy worldwide, Dr. Klopp said. It also better informs treatment decision-making in cases where replacing brachytherapy with external beam techniques is being considered.
Although MRI guidance is increasingly being used in brachytherapy, the latest studies on patterns of care suggest that overall use is still low, according to Dr. Klopp.
“The challenges are primarily logistical,” she elaborated. “MRI-compatible applicators must be placed, and patients need to wait for the scans to be performed, which can take an hour or more. In addition, the times that patients get scanned can be unpredictable based on procedure times, which can create practical challenges for scheduling. In some cases, cost may also be a deterrent.
“The bar is high for brachytherapy. It’s an excellent treatment modality that provides very high rates of local control with very low toxicity when done optimally,” Dr. Klopp concluded. “I do think that this experience provides very convincing evidence that the best brachytherapy is image-guided and requires care to monitor normal tissue doses in order to reduce the risk of long-term toxicity.”
The study was supported by unrestricted grants from Elekta and Varian. Dr. Pötter and Dr. Klopp disclosed no conflicts of interest.
SOURCE: Pötter R et al. ESTRO 2020, Abstract OC-0437.
At 5 years, the rate of local control was 92%, and overall survival was 74%. However, nodal and systemic control rates were inferior for node-positive and high-risk patients, and nearly 15% of patients experienced grade 3-5 treatment-related morbidity.
These results were reported at the European Society for Radiology and Oncology 2020 Online Congress.
Historically, brachytherapy dose has been fairly rigidly prescribed, based on dose points defined in two dimensions. By performing imaging before each brachytherapy implant, treatment parameters can be adapted to a patient’s anatomy, taking into account the positions of organs at risk and any tumor regression from prior treatment.
Richard Pötter, MD, emeritus professor at Medical University of Vienna, and colleagues tested MRI-guided adaptive brachytherapy in a multicenter cohort study.
The study’s disease outcome analysis included 1,341 women with cervical cancer of International Federation of Gynecology and Obstetrics stage IB–IVB (52% node positive) being treated with curative intent.
The women underwent definitive external beam radiotherapy (45-50 Gy, using either three-dimensional–conformal radiotherapy or intensity-modulated radiotherapy) with concurrent cisplatin chemotherapy, followed by MRI-guided adaptive brachytherapy based on MRI with the applicator in situ.
“There was no fixed dose prescription for brachytherapy, and there were no constraints for organs at risk,” Dr. Pötter explained. “But there was systematic joint reporting and contouring for the target and organs at risk, and also for doses and volumes.”
Nearly all patients were treated with adaptive MRI-based target and dose-volume and point parameters (99.1%), as well as with individualized multiparametric dose optimization (98.2%). The application technique was adapted, with intracavitary application alone used in 57% of patients, and both intracavitary and interstitial application in 43%.
Efficacy and toxicity
At a median follow-up of 51 months, 7.3% of patients had experienced a local failure, with 3.8% having an isolated local failure and 3.5% having synchronous nodal or systemic failure, Dr. Pötter reported.
The local failure rate was similar going from disease stage IB2 to IVA (8%-9%), even though the target volume more than doubled.
“This favorable result was due to an adaptation of dose, which was quite similar for the different stages and volumes. This is a major message of EMBRACE I,” Dr. Pötter commented.
The Kaplan-Meier–estimated 5-year rate of local control was 92% for the whole cohort. It was 98% in patients with stage IB1 disease and 91%-92% in patients with stage IB2–IVA disease.
The 5-year rate of overall survival was 74% for the entire cohort. It fell with stage, from 83% in patients with stage IB1 disease to 52% in patients with stage IVA disease.
For the entire population, the 5-year pelvic control rate was 87%, the 5-year cancer-specific survival was 79%, and the 5-year disease-free survival was 68%.
Overall, 14.6% of patients experienced grade 3-5 treatment-related morbidity at 5 years: 2.7% developed fistulas, 6.1% had vaginal toxicity, 6.5% had genitourinary toxicity, and 7.6% had gastrointestinal toxicity.
Room for improvement
“MRI-guided adaptive brachytherapy in locally advanced cervical cancer works in multicenter clinical practice, within such a study, with adaptation of the target and application technique, and multiparametric treatment planning and dose prescription,” Dr. Pötter summarized.
However, “the mature clinical outcomes appear challenging,” he added. Specifically, although the rate of local control was high, the rate of nodal control left room for improvement in node-positive patients, and the rates of systemic control and overall survival left room for improvement in high-risk patients.
In addition, “the grade 3-5 morbidity was limited per organ and per endpoint, but was considerable overall, and this asks for a reduction,” Dr. Pötter said.
Two of the areas needing improvement are being addressed in ongoing and planned research, according to Dr. Pötter. “The nodal part is already being addressed in EMBRACE II, intensifying treatment for node-positive patients through a simultaneous integrated boost and a very sophisticated probability planning concept, and also including more patients for paraaortic radiotherapy,” he elaborated. “For the systemic part, we have thought about [a study testing an] additional drug ... and there are thoughts for EMBRACE III to investigate such effect.”
A benchmark for brachytherapy
“This is the largest prospective cohort of patients treated with image-guided brachytherapy. The high rates of local control with long-term follow-up are impressive and speak to the clear value of high-quality brachytherapy,” commented Ann H. Klopp, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston, who was not involved in this study.
With its consistent reporting of detailed dose and toxicity data, the study establishes a benchmark for brachytherapy worldwide, Dr. Klopp said. It also better informs treatment decision-making in cases where replacing brachytherapy with external beam techniques is being considered.
Although MRI guidance is increasingly being used in brachytherapy, the latest studies on patterns of care suggest that overall use is still low, according to Dr. Klopp.
“The challenges are primarily logistical,” she elaborated. “MRI-compatible applicators must be placed, and patients need to wait for the scans to be performed, which can take an hour or more. In addition, the times that patients get scanned can be unpredictable based on procedure times, which can create practical challenges for scheduling. In some cases, cost may also be a deterrent.
“The bar is high for brachytherapy. It’s an excellent treatment modality that provides very high rates of local control with very low toxicity when done optimally,” Dr. Klopp concluded. “I do think that this experience provides very convincing evidence that the best brachytherapy is image-guided and requires care to monitor normal tissue doses in order to reduce the risk of long-term toxicity.”
The study was supported by unrestricted grants from Elekta and Varian. Dr. Pötter and Dr. Klopp disclosed no conflicts of interest.
SOURCE: Pötter R et al. ESTRO 2020, Abstract OC-0437.
At 5 years, the rate of local control was 92%, and overall survival was 74%. However, nodal and systemic control rates were inferior for node-positive and high-risk patients, and nearly 15% of patients experienced grade 3-5 treatment-related morbidity.
These results were reported at the European Society for Radiology and Oncology 2020 Online Congress.
Historically, brachytherapy dose has been fairly rigidly prescribed, based on dose points defined in two dimensions. By performing imaging before each brachytherapy implant, treatment parameters can be adapted to a patient’s anatomy, taking into account the positions of organs at risk and any tumor regression from prior treatment.
Richard Pötter, MD, emeritus professor at Medical University of Vienna, and colleagues tested MRI-guided adaptive brachytherapy in a multicenter cohort study.
The study’s disease outcome analysis included 1,341 women with cervical cancer of International Federation of Gynecology and Obstetrics stage IB–IVB (52% node positive) being treated with curative intent.
The women underwent definitive external beam radiotherapy (45-50 Gy, using either three-dimensional–conformal radiotherapy or intensity-modulated radiotherapy) with concurrent cisplatin chemotherapy, followed by MRI-guided adaptive brachytherapy based on MRI with the applicator in situ.
“There was no fixed dose prescription for brachytherapy, and there were no constraints for organs at risk,” Dr. Pötter explained. “But there was systematic joint reporting and contouring for the target and organs at risk, and also for doses and volumes.”
Nearly all patients were treated with adaptive MRI-based target and dose-volume and point parameters (99.1%), as well as with individualized multiparametric dose optimization (98.2%). The application technique was adapted, with intracavitary application alone used in 57% of patients, and both intracavitary and interstitial application in 43%.
Efficacy and toxicity
At a median follow-up of 51 months, 7.3% of patients had experienced a local failure, with 3.8% having an isolated local failure and 3.5% having synchronous nodal or systemic failure, Dr. Pötter reported.
The local failure rate was similar going from disease stage IB2 to IVA (8%-9%), even though the target volume more than doubled.
“This favorable result was due to an adaptation of dose, which was quite similar for the different stages and volumes. This is a major message of EMBRACE I,” Dr. Pötter commented.
The Kaplan-Meier–estimated 5-year rate of local control was 92% for the whole cohort. It was 98% in patients with stage IB1 disease and 91%-92% in patients with stage IB2–IVA disease.
The 5-year rate of overall survival was 74% for the entire cohort. It fell with stage, from 83% in patients with stage IB1 disease to 52% in patients with stage IVA disease.
For the entire population, the 5-year pelvic control rate was 87%, the 5-year cancer-specific survival was 79%, and the 5-year disease-free survival was 68%.
Overall, 14.6% of patients experienced grade 3-5 treatment-related morbidity at 5 years: 2.7% developed fistulas, 6.1% had vaginal toxicity, 6.5% had genitourinary toxicity, and 7.6% had gastrointestinal toxicity.
Room for improvement
“MRI-guided adaptive brachytherapy in locally advanced cervical cancer works in multicenter clinical practice, within such a study, with adaptation of the target and application technique, and multiparametric treatment planning and dose prescription,” Dr. Pötter summarized.
However, “the mature clinical outcomes appear challenging,” he added. Specifically, although the rate of local control was high, the rate of nodal control left room for improvement in node-positive patients, and the rates of systemic control and overall survival left room for improvement in high-risk patients.
In addition, “the grade 3-5 morbidity was limited per organ and per endpoint, but was considerable overall, and this asks for a reduction,” Dr. Pötter said.
Two of the areas needing improvement are being addressed in ongoing and planned research, according to Dr. Pötter. “The nodal part is already being addressed in EMBRACE II, intensifying treatment for node-positive patients through a simultaneous integrated boost and a very sophisticated probability planning concept, and also including more patients for paraaortic radiotherapy,” he elaborated. “For the systemic part, we have thought about [a study testing an] additional drug ... and there are thoughts for EMBRACE III to investigate such effect.”
A benchmark for brachytherapy
“This is the largest prospective cohort of patients treated with image-guided brachytherapy. The high rates of local control with long-term follow-up are impressive and speak to the clear value of high-quality brachytherapy,” commented Ann H. Klopp, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston, who was not involved in this study.
With its consistent reporting of detailed dose and toxicity data, the study establishes a benchmark for brachytherapy worldwide, Dr. Klopp said. It also better informs treatment decision-making in cases where replacing brachytherapy with external beam techniques is being considered.
Although MRI guidance is increasingly being used in brachytherapy, the latest studies on patterns of care suggest that overall use is still low, according to Dr. Klopp.
“The challenges are primarily logistical,” she elaborated. “MRI-compatible applicators must be placed, and patients need to wait for the scans to be performed, which can take an hour or more. In addition, the times that patients get scanned can be unpredictable based on procedure times, which can create practical challenges for scheduling. In some cases, cost may also be a deterrent.
“The bar is high for brachytherapy. It’s an excellent treatment modality that provides very high rates of local control with very low toxicity when done optimally,” Dr. Klopp concluded. “I do think that this experience provides very convincing evidence that the best brachytherapy is image-guided and requires care to monitor normal tissue doses in order to reduce the risk of long-term toxicity.”
The study was supported by unrestricted grants from Elekta and Varian. Dr. Pötter and Dr. Klopp disclosed no conflicts of interest.
SOURCE: Pötter R et al. ESTRO 2020, Abstract OC-0437.
FROM ESTRO 2020
Is diagnostic hysteroscopy safe in patients with type 2 endometrial cancer?
Among women with type 2 endometrial cancer, diagnostic hysteroscopy may not be associated with increased odds of positive peritoneal cytology at the time of surgical staging or with decreased survival, according to a retrospective study of 127 patients.
a researcher said at the meeting sponsored by AAGL, held virtually this year.
Possible associations between cytology and procedures
Prior research has found that positive peritoneal cytology may correlate with greater likelihood of death among patients with endometrial cancer, and researchers have wondered whether pressure on the uterine cavity during hysteroscopy increases the presence of positive peritoneal cytology. “According to some systematic reviews ... it seems that it does,” said study author Luiz Brito, MD, PhD, associate professor of obstetrics and gynecology at the University of Campinas in Brazil.
Nevertheless, research suggests that “most of the time hysteroscopy does not have a powerful impact on the prognosis of these patients,” he said.
Studies have tended to focus on patients with type 1 endometrial cancer, however. Type 2 endometrial cancer, which is more aggressive, “is scarcely studied,” Dr. Brito said. One retrospective study that focused on type 2 endometrial cancer included 140 patients. Among patients who underwent hysteroscopy, 30% had positive cytology. In comparison, 12% of patients in the curettage group had positive cytology. But the difference in disease-specific survival between groups was not statistically significant, and about 33% of the patients in each group developed a recurrence.
To examine associations between diagnostic methods and outcomes in another group of patients with type 2 endometrial cancer, Dr. Brito and colleagues analyzed data from a hospital registry in Brazil.
The database included 1,183 patients with endometrial cancer between 2002 and 2017, including 235 patients with type 2 endometrial cancer. After excluding patients with synchronous tumor and those who did not undergo surgery or did not have peritoneal cytology performed, 127 patients remained for the analysis. The study included follow-up to December 2019.
The researchers compared the prevalence of positive peritoneal cytology among 43 patients who underwent hysteroscopy with that among 84 patients who underwent curettage. The groups had similar baseline characteristics.
Positive peritoneal cytology was more common in the curettage group than in the hysteroscopy group (10.7% vs. 4.6%), although the difference was not statistically significant. Lymphovascular invasion and advanced surgical staging were more common in the curettage group.
In a multivariate analysis, older age and advanced cancer staging were the only factors associated with decreased disease-free survival. Age, advanced cancer staging, and vascular invasion were associated with decreased disease-specific survival.
The researchers also had considered factors such as peritoneal cytology, diagnostic method, age of menarche, menopause time, parity, comorbidities, smoking status, body mass index, abnormal uterine bleeding, histological type, and adjuvant treatment.
A limitation of the study is that it relied on data from a public health system that often has long wait times for diagnosis and treatment, Dr. Brito noted.
Some doctors may forgo cytology
The available research raises questions about the role and relevance of peritoneal cytology in caring for patients with endometrial cancer, René Pareja, MD, a gynecologic oncologist at Instituto Nacional de Cancerología, Bogotá, Colombia, said in a discussion following the presentation.
Peritoneal cytology has not been part of endometrial cancer staging since 2009, Dr. Pareja said. Still, guidelines recommend that surgeons collect cytology during surgical staging, with the idea that the results could inform adjuvant treatment decisions.
“Peritoneal cytology is recommended in the guidelines, but there are no recommendations on how to proceed if it is positive,” Dr. Pareja said. “While some gynecologic oncologists continue to take cytology during endometrial cancer staging, some have stopped doing so. And in Colombia, most of us are not performing pelvic cytology.”
Although some studies indicate that hysteroscopy may increase the rate of positive cytology, positive cytology may not be associated with worse oncological outcomes independent of other risk factors for recurrence, said Dr. Pareja.
So far, studies have been retrospective. Furthermore, the sensitivity and specificity of pelvic cytology tests are not 100%. “Should we continue performing pelvic cytology given the results of this and other studies?” Dr. Pareja asked.
Despite limited knowledge about this variable, physicians may want to be aware if a patient has positive cytology, Dr. Brito suggested. “At least it will give us some red flags so we can be attentive to these patients.”
If researchers were to design a prospective study that incorporates hysteroscopic variables, it could provide more complete answers about the relationship between hysteroscopy and peritoneal cytology and clarify the importance of positive cytology, Dr. Brito said.
Dr. Brito had no relevant disclosures. Dr. Pareja disclosed consulting for Johnson & Johnson.
SOURCE: Oliveira Brito LG et al. J Minim Invasive Gynecol. 2020 Nov. doi: 10.1016/j.jmig.2020.08.356.
Among women with type 2 endometrial cancer, diagnostic hysteroscopy may not be associated with increased odds of positive peritoneal cytology at the time of surgical staging or with decreased survival, according to a retrospective study of 127 patients.
a researcher said at the meeting sponsored by AAGL, held virtually this year.
Possible associations between cytology and procedures
Prior research has found that positive peritoneal cytology may correlate with greater likelihood of death among patients with endometrial cancer, and researchers have wondered whether pressure on the uterine cavity during hysteroscopy increases the presence of positive peritoneal cytology. “According to some systematic reviews ... it seems that it does,” said study author Luiz Brito, MD, PhD, associate professor of obstetrics and gynecology at the University of Campinas in Brazil.
Nevertheless, research suggests that “most of the time hysteroscopy does not have a powerful impact on the prognosis of these patients,” he said.
Studies have tended to focus on patients with type 1 endometrial cancer, however. Type 2 endometrial cancer, which is more aggressive, “is scarcely studied,” Dr. Brito said. One retrospective study that focused on type 2 endometrial cancer included 140 patients. Among patients who underwent hysteroscopy, 30% had positive cytology. In comparison, 12% of patients in the curettage group had positive cytology. But the difference in disease-specific survival between groups was not statistically significant, and about 33% of the patients in each group developed a recurrence.
To examine associations between diagnostic methods and outcomes in another group of patients with type 2 endometrial cancer, Dr. Brito and colleagues analyzed data from a hospital registry in Brazil.
The database included 1,183 patients with endometrial cancer between 2002 and 2017, including 235 patients with type 2 endometrial cancer. After excluding patients with synchronous tumor and those who did not undergo surgery or did not have peritoneal cytology performed, 127 patients remained for the analysis. The study included follow-up to December 2019.
The researchers compared the prevalence of positive peritoneal cytology among 43 patients who underwent hysteroscopy with that among 84 patients who underwent curettage. The groups had similar baseline characteristics.
Positive peritoneal cytology was more common in the curettage group than in the hysteroscopy group (10.7% vs. 4.6%), although the difference was not statistically significant. Lymphovascular invasion and advanced surgical staging were more common in the curettage group.
In a multivariate analysis, older age and advanced cancer staging were the only factors associated with decreased disease-free survival. Age, advanced cancer staging, and vascular invasion were associated with decreased disease-specific survival.
The researchers also had considered factors such as peritoneal cytology, diagnostic method, age of menarche, menopause time, parity, comorbidities, smoking status, body mass index, abnormal uterine bleeding, histological type, and adjuvant treatment.
A limitation of the study is that it relied on data from a public health system that often has long wait times for diagnosis and treatment, Dr. Brito noted.
Some doctors may forgo cytology
The available research raises questions about the role and relevance of peritoneal cytology in caring for patients with endometrial cancer, René Pareja, MD, a gynecologic oncologist at Instituto Nacional de Cancerología, Bogotá, Colombia, said in a discussion following the presentation.
Peritoneal cytology has not been part of endometrial cancer staging since 2009, Dr. Pareja said. Still, guidelines recommend that surgeons collect cytology during surgical staging, with the idea that the results could inform adjuvant treatment decisions.
“Peritoneal cytology is recommended in the guidelines, but there are no recommendations on how to proceed if it is positive,” Dr. Pareja said. “While some gynecologic oncologists continue to take cytology during endometrial cancer staging, some have stopped doing so. And in Colombia, most of us are not performing pelvic cytology.”
Although some studies indicate that hysteroscopy may increase the rate of positive cytology, positive cytology may not be associated with worse oncological outcomes independent of other risk factors for recurrence, said Dr. Pareja.
So far, studies have been retrospective. Furthermore, the sensitivity and specificity of pelvic cytology tests are not 100%. “Should we continue performing pelvic cytology given the results of this and other studies?” Dr. Pareja asked.
Despite limited knowledge about this variable, physicians may want to be aware if a patient has positive cytology, Dr. Brito suggested. “At least it will give us some red flags so we can be attentive to these patients.”
If researchers were to design a prospective study that incorporates hysteroscopic variables, it could provide more complete answers about the relationship between hysteroscopy and peritoneal cytology and clarify the importance of positive cytology, Dr. Brito said.
Dr. Brito had no relevant disclosures. Dr. Pareja disclosed consulting for Johnson & Johnson.
SOURCE: Oliveira Brito LG et al. J Minim Invasive Gynecol. 2020 Nov. doi: 10.1016/j.jmig.2020.08.356.
Among women with type 2 endometrial cancer, diagnostic hysteroscopy may not be associated with increased odds of positive peritoneal cytology at the time of surgical staging or with decreased survival, according to a retrospective study of 127 patients.
a researcher said at the meeting sponsored by AAGL, held virtually this year.
Possible associations between cytology and procedures
Prior research has found that positive peritoneal cytology may correlate with greater likelihood of death among patients with endometrial cancer, and researchers have wondered whether pressure on the uterine cavity during hysteroscopy increases the presence of positive peritoneal cytology. “According to some systematic reviews ... it seems that it does,” said study author Luiz Brito, MD, PhD, associate professor of obstetrics and gynecology at the University of Campinas in Brazil.
Nevertheless, research suggests that “most of the time hysteroscopy does not have a powerful impact on the prognosis of these patients,” he said.
Studies have tended to focus on patients with type 1 endometrial cancer, however. Type 2 endometrial cancer, which is more aggressive, “is scarcely studied,” Dr. Brito said. One retrospective study that focused on type 2 endometrial cancer included 140 patients. Among patients who underwent hysteroscopy, 30% had positive cytology. In comparison, 12% of patients in the curettage group had positive cytology. But the difference in disease-specific survival between groups was not statistically significant, and about 33% of the patients in each group developed a recurrence.
To examine associations between diagnostic methods and outcomes in another group of patients with type 2 endometrial cancer, Dr. Brito and colleagues analyzed data from a hospital registry in Brazil.
The database included 1,183 patients with endometrial cancer between 2002 and 2017, including 235 patients with type 2 endometrial cancer. After excluding patients with synchronous tumor and those who did not undergo surgery or did not have peritoneal cytology performed, 127 patients remained for the analysis. The study included follow-up to December 2019.
The researchers compared the prevalence of positive peritoneal cytology among 43 patients who underwent hysteroscopy with that among 84 patients who underwent curettage. The groups had similar baseline characteristics.
Positive peritoneal cytology was more common in the curettage group than in the hysteroscopy group (10.7% vs. 4.6%), although the difference was not statistically significant. Lymphovascular invasion and advanced surgical staging were more common in the curettage group.
In a multivariate analysis, older age and advanced cancer staging were the only factors associated with decreased disease-free survival. Age, advanced cancer staging, and vascular invasion were associated with decreased disease-specific survival.
The researchers also had considered factors such as peritoneal cytology, diagnostic method, age of menarche, menopause time, parity, comorbidities, smoking status, body mass index, abnormal uterine bleeding, histological type, and adjuvant treatment.
A limitation of the study is that it relied on data from a public health system that often has long wait times for diagnosis and treatment, Dr. Brito noted.
Some doctors may forgo cytology
The available research raises questions about the role and relevance of peritoneal cytology in caring for patients with endometrial cancer, René Pareja, MD, a gynecologic oncologist at Instituto Nacional de Cancerología, Bogotá, Colombia, said in a discussion following the presentation.
Peritoneal cytology has not been part of endometrial cancer staging since 2009, Dr. Pareja said. Still, guidelines recommend that surgeons collect cytology during surgical staging, with the idea that the results could inform adjuvant treatment decisions.
“Peritoneal cytology is recommended in the guidelines, but there are no recommendations on how to proceed if it is positive,” Dr. Pareja said. “While some gynecologic oncologists continue to take cytology during endometrial cancer staging, some have stopped doing so. And in Colombia, most of us are not performing pelvic cytology.”
Although some studies indicate that hysteroscopy may increase the rate of positive cytology, positive cytology may not be associated with worse oncological outcomes independent of other risk factors for recurrence, said Dr. Pareja.
So far, studies have been retrospective. Furthermore, the sensitivity and specificity of pelvic cytology tests are not 100%. “Should we continue performing pelvic cytology given the results of this and other studies?” Dr. Pareja asked.
Despite limited knowledge about this variable, physicians may want to be aware if a patient has positive cytology, Dr. Brito suggested. “At least it will give us some red flags so we can be attentive to these patients.”
If researchers were to design a prospective study that incorporates hysteroscopic variables, it could provide more complete answers about the relationship between hysteroscopy and peritoneal cytology and clarify the importance of positive cytology, Dr. Brito said.
Dr. Brito had no relevant disclosures. Dr. Pareja disclosed consulting for Johnson & Johnson.
SOURCE: Oliveira Brito LG et al. J Minim Invasive Gynecol. 2020 Nov. doi: 10.1016/j.jmig.2020.08.356.
FROM AAGL GLOBAL CONGRESS
COVID-19 vaccines and cancer patients: 4 things to know
Earlier this week, Medscape spoke with Nora Disis, MD, about vaccinating cancer patients. Disis is a medical oncologist and director of both the Institute of Translational Health Sciences and the Cancer Vaccine Institute, the University of Washington, Seattle, Washington. As editor-in-chief of JAMA Oncology, she has watched COVID-19 developments in the oncology community over the past year.
Here are a few themes that Disis said oncologists should be aware of as vaccines eventually begin reaching cancer patients.
We should expect cancer patients to respond to vaccines. Historically, some believed that cancer patients would be unable to mount an immune response to vaccines. Data on other viral vaccines have shown otherwise. For example, there has been a long history of studies of flu vaccination in cancer patients, and in general, those vaccines confer protection. Likewise for pneumococcal vaccine, which, generally speaking, cancer patients should receive.
Special cases may include hematologic malignancies in which the immune system has been destroyed and profound immunosuppression occurs. Data on immunization during this immunosuppressed period are scarce, but what data are available suggest that once cancer patients are through this immunosuppressed period, they can be vaccinated successfully.
The type of vaccine will probably be important for cancer patients. Currently, there are 61 coronavirus vaccines in human clinical trials, and 17 have reached the final stages of testing. At least 85 preclinical vaccines are under active investigation in animals.
Both the Pfizer-BioNTech and Moderna COVID vaccines are mRNA type. There are many other types, including protein-based vaccines, viral vector vaccines based on adenoviruses, and inactivated or attenuated coronavirus vaccines.
The latter vaccines, particularly attenuated live virus vaccines, may not be a good choice for cancer patients. Especially in those with rapidly progressing disease or on chemotherapy, attenuated live viruses may cause a low-grade infection.
Incidentally, the technology used in the genetic, or mRNA, vaccines developed by both Pfizer-BioNTech and Moderna was initially developed for fighting cancer, and studies have shown that patients can generate immune responses to cancer-associated proteins with this type of vaccine.
These genetic vaccines could turn out to be the most effective for cancer patients, especially those with solid tumors.
Our understanding is very limited right now. Neither the Pfizer-BioNTech nor the Moderna early data discuss cancer patients. Two of the most important questions for cancer patients are dosing and booster scheduling. Potential defects in lymphocyte function among cancer patients may require unique initial dosing and booster schedules. In terms of timing, it is unclear how active therapy might affect a patient’s immune response to vaccination and whether vaccines should be timed with therapy cycles.
Vaccine access may depend on whether cancer patients are viewed as a vulnerable population. Those at higher risk for severe COVID-19 clearly have a greater need for vaccination. While there are data suggesting that cancer patients are at higher risk, they are a bit murky, in part because cancer patients are a heterogeneous group. For example, there are data suggesting that lung and blood cancer patients fare worse. There is also a suggestion that, like in the general population, COVID risk in cancer patients remains driven by comorbidities.
It is likely, then, that personalized risk factors such as type of cancer therapy, site of disease, and comorbidities will shape individual choices about vaccination among cancer patients.
A version of this article first appeared on Medscape.com.
Earlier this week, Medscape spoke with Nora Disis, MD, about vaccinating cancer patients. Disis is a medical oncologist and director of both the Institute of Translational Health Sciences and the Cancer Vaccine Institute, the University of Washington, Seattle, Washington. As editor-in-chief of JAMA Oncology, she has watched COVID-19 developments in the oncology community over the past year.
Here are a few themes that Disis said oncologists should be aware of as vaccines eventually begin reaching cancer patients.
We should expect cancer patients to respond to vaccines. Historically, some believed that cancer patients would be unable to mount an immune response to vaccines. Data on other viral vaccines have shown otherwise. For example, there has been a long history of studies of flu vaccination in cancer patients, and in general, those vaccines confer protection. Likewise for pneumococcal vaccine, which, generally speaking, cancer patients should receive.
Special cases may include hematologic malignancies in which the immune system has been destroyed and profound immunosuppression occurs. Data on immunization during this immunosuppressed period are scarce, but what data are available suggest that once cancer patients are through this immunosuppressed period, they can be vaccinated successfully.
The type of vaccine will probably be important for cancer patients. Currently, there are 61 coronavirus vaccines in human clinical trials, and 17 have reached the final stages of testing. At least 85 preclinical vaccines are under active investigation in animals.
Both the Pfizer-BioNTech and Moderna COVID vaccines are mRNA type. There are many other types, including protein-based vaccines, viral vector vaccines based on adenoviruses, and inactivated or attenuated coronavirus vaccines.
The latter vaccines, particularly attenuated live virus vaccines, may not be a good choice for cancer patients. Especially in those with rapidly progressing disease or on chemotherapy, attenuated live viruses may cause a low-grade infection.
Incidentally, the technology used in the genetic, or mRNA, vaccines developed by both Pfizer-BioNTech and Moderna was initially developed for fighting cancer, and studies have shown that patients can generate immune responses to cancer-associated proteins with this type of vaccine.
These genetic vaccines could turn out to be the most effective for cancer patients, especially those with solid tumors.
Our understanding is very limited right now. Neither the Pfizer-BioNTech nor the Moderna early data discuss cancer patients. Two of the most important questions for cancer patients are dosing and booster scheduling. Potential defects in lymphocyte function among cancer patients may require unique initial dosing and booster schedules. In terms of timing, it is unclear how active therapy might affect a patient’s immune response to vaccination and whether vaccines should be timed with therapy cycles.
Vaccine access may depend on whether cancer patients are viewed as a vulnerable population. Those at higher risk for severe COVID-19 clearly have a greater need for vaccination. While there are data suggesting that cancer patients are at higher risk, they are a bit murky, in part because cancer patients are a heterogeneous group. For example, there are data suggesting that lung and blood cancer patients fare worse. There is also a suggestion that, like in the general population, COVID risk in cancer patients remains driven by comorbidities.
It is likely, then, that personalized risk factors such as type of cancer therapy, site of disease, and comorbidities will shape individual choices about vaccination among cancer patients.
A version of this article first appeared on Medscape.com.
Earlier this week, Medscape spoke with Nora Disis, MD, about vaccinating cancer patients. Disis is a medical oncologist and director of both the Institute of Translational Health Sciences and the Cancer Vaccine Institute, the University of Washington, Seattle, Washington. As editor-in-chief of JAMA Oncology, she has watched COVID-19 developments in the oncology community over the past year.
Here are a few themes that Disis said oncologists should be aware of as vaccines eventually begin reaching cancer patients.
We should expect cancer patients to respond to vaccines. Historically, some believed that cancer patients would be unable to mount an immune response to vaccines. Data on other viral vaccines have shown otherwise. For example, there has been a long history of studies of flu vaccination in cancer patients, and in general, those vaccines confer protection. Likewise for pneumococcal vaccine, which, generally speaking, cancer patients should receive.
Special cases may include hematologic malignancies in which the immune system has been destroyed and profound immunosuppression occurs. Data on immunization during this immunosuppressed period are scarce, but what data are available suggest that once cancer patients are through this immunosuppressed period, they can be vaccinated successfully.
The type of vaccine will probably be important for cancer patients. Currently, there are 61 coronavirus vaccines in human clinical trials, and 17 have reached the final stages of testing. At least 85 preclinical vaccines are under active investigation in animals.
Both the Pfizer-BioNTech and Moderna COVID vaccines are mRNA type. There are many other types, including protein-based vaccines, viral vector vaccines based on adenoviruses, and inactivated or attenuated coronavirus vaccines.
The latter vaccines, particularly attenuated live virus vaccines, may not be a good choice for cancer patients. Especially in those with rapidly progressing disease or on chemotherapy, attenuated live viruses may cause a low-grade infection.
Incidentally, the technology used in the genetic, or mRNA, vaccines developed by both Pfizer-BioNTech and Moderna was initially developed for fighting cancer, and studies have shown that patients can generate immune responses to cancer-associated proteins with this type of vaccine.
These genetic vaccines could turn out to be the most effective for cancer patients, especially those with solid tumors.
Our understanding is very limited right now. Neither the Pfizer-BioNTech nor the Moderna early data discuss cancer patients. Two of the most important questions for cancer patients are dosing and booster scheduling. Potential defects in lymphocyte function among cancer patients may require unique initial dosing and booster schedules. In terms of timing, it is unclear how active therapy might affect a patient’s immune response to vaccination and whether vaccines should be timed with therapy cycles.
Vaccine access may depend on whether cancer patients are viewed as a vulnerable population. Those at higher risk for severe COVID-19 clearly have a greater need for vaccination. While there are data suggesting that cancer patients are at higher risk, they are a bit murky, in part because cancer patients are a heterogeneous group. For example, there are data suggesting that lung and blood cancer patients fare worse. There is also a suggestion that, like in the general population, COVID risk in cancer patients remains driven by comorbidities.
It is likely, then, that personalized risk factors such as type of cancer therapy, site of disease, and comorbidities will shape individual choices about vaccination among cancer patients.
A version of this article first appeared on Medscape.com.
NHS England starts pilot trial of blood test for many cancers
“Early detection, particularly for hard-to-treat conditions like ovarian and pancreatic cancer, has the potential to save many lives,” said NHS Chief Executive Sir Simon Stevens in a statement.
The pilot trial will use the Galleri blood test, developed by Grail. Sir Stevens described the blood test as “promising” and said it could “be a game changer in cancer care, helping thousands more people to get successful treatment.”
However, some clinicians have expressed concerns over the potential for false-positive results with the test.
Results of a study of the Galleri blood test, published earlier this year, showed that the test detected 50 types of cancer with a specificity of 99.3% and a false positive rate of 0.7%.
It also correctly identified the originating tissue in 90% of cases. However, the sensitivity was lower, at 67%, for the 12 most common cancers, as reported at the time.
The senior author of that study, Michael Seiden, MD, PhD, president of the U.S. Oncology Network, The Woodlands, Tex., noted that it was not a screening study: the test had been used in patients with cancer and in healthy volunteers. He said the test “is intended to be complementary to, and not replace, existing guideline-recommended screening tests and might provide new avenues of investigation for cancers that don’t currently have screening tests.”
The Galleri test uses next-generation sequencing to analyze the arrangement of methyl groups on circulating cell-free DNA in a blood sample.
Several other blood tests for cancer are under development, including the CancerSEEK test, which has been reported to be able to identify eight common cancers. It measures circulating tumor DNA from 16 genes and eight protein biomarkers and then uses machine learning to analyze the data.
Improving early detection rates
The pilot trial of the blood test is due to start in mid-2021 and will involve 165,000 people.
The trial will include 140,000 individuals aged 50-79 years who were identified through their health records and who have no cancer symptoms. They will undergo blood tests annually for 3 years and will be referred for investigation if a test result is positive.
A second group will include 25,000 people with potential cancer symptoms. These patients will be offered the blood test to speed up their diagnosis after referral to a hospital via the normal channels.
The results of the pilot are expected in 2023. If successful, the test will be rolled out to 1 million individuals from 2024 to 2025.
The pilot trial is part of the NHS Long Term Plan, which aims to increase early detection of cancer. At present, around half of cancers in England are diagnosed in stage I or II; the NHS aims to increase this to 75% by 2028.
“The NHS has set itself an ambitious target,” commented Peter Johnson, MD, PhD, national clinical director for cancer at NHS England and Improvement.
“Tests like this may help us get there far faster, and I am excited to see how this cutting-edge technology will work out as we test it in clinics across the NHS,” he added.
Lord David Prior, chair of NHS England, noted that almost 200,000 people die from cancer in the United Kingdom every year and that “many of these people are diagnosed too late for treatment to be effective.
“This collaboration between the NHS and Grail offers the chance for a wide range of cancers to be diagnosed much earlier and could fundamentally change the outlook for people with cancer,” he said.
However, some clinicians raised potential concerns.
Stephen Duffy, PhD, Center for Cancer Prevention, Queen Mary University of London, described the pilot as “very exciting,” but cautioned: “We will need to find out just how early the test detects cancers and whether it can it be used in a way which minimizes anxiety from false positives.”
Yong-Jie Lu, MD, PhD, also at Queen Mary University of London, said: “It is not clear how early it aims to catch cancer. For a cancer screen test, it needs very high specificity (>99%), otherwise it may end up in a similar situation as the PSA [prostate-specific antigen] test for prostate cancer, or even worse.”
Mangesh Thorat, MD, Cancer Prevention Trials Unit, King’s College London, warned: “It is likely that for every testing round ... there will be about 1,000 false-positive results, and the test may not be able to pinpoint the location of cancer in 3%-4% of those with a true positive result, necessitating a range of imaging and other investigations in these participants.”
No funding for the study has been declared. The investigators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
“Early detection, particularly for hard-to-treat conditions like ovarian and pancreatic cancer, has the potential to save many lives,” said NHS Chief Executive Sir Simon Stevens in a statement.
The pilot trial will use the Galleri blood test, developed by Grail. Sir Stevens described the blood test as “promising” and said it could “be a game changer in cancer care, helping thousands more people to get successful treatment.”
However, some clinicians have expressed concerns over the potential for false-positive results with the test.
Results of a study of the Galleri blood test, published earlier this year, showed that the test detected 50 types of cancer with a specificity of 99.3% and a false positive rate of 0.7%.
It also correctly identified the originating tissue in 90% of cases. However, the sensitivity was lower, at 67%, for the 12 most common cancers, as reported at the time.
The senior author of that study, Michael Seiden, MD, PhD, president of the U.S. Oncology Network, The Woodlands, Tex., noted that it was not a screening study: the test had been used in patients with cancer and in healthy volunteers. He said the test “is intended to be complementary to, and not replace, existing guideline-recommended screening tests and might provide new avenues of investigation for cancers that don’t currently have screening tests.”
The Galleri test uses next-generation sequencing to analyze the arrangement of methyl groups on circulating cell-free DNA in a blood sample.
Several other blood tests for cancer are under development, including the CancerSEEK test, which has been reported to be able to identify eight common cancers. It measures circulating tumor DNA from 16 genes and eight protein biomarkers and then uses machine learning to analyze the data.
Improving early detection rates
The pilot trial of the blood test is due to start in mid-2021 and will involve 165,000 people.
The trial will include 140,000 individuals aged 50-79 years who were identified through their health records and who have no cancer symptoms. They will undergo blood tests annually for 3 years and will be referred for investigation if a test result is positive.
A second group will include 25,000 people with potential cancer symptoms. These patients will be offered the blood test to speed up their diagnosis after referral to a hospital via the normal channels.
The results of the pilot are expected in 2023. If successful, the test will be rolled out to 1 million individuals from 2024 to 2025.
The pilot trial is part of the NHS Long Term Plan, which aims to increase early detection of cancer. At present, around half of cancers in England are diagnosed in stage I or II; the NHS aims to increase this to 75% by 2028.
“The NHS has set itself an ambitious target,” commented Peter Johnson, MD, PhD, national clinical director for cancer at NHS England and Improvement.
“Tests like this may help us get there far faster, and I am excited to see how this cutting-edge technology will work out as we test it in clinics across the NHS,” he added.
Lord David Prior, chair of NHS England, noted that almost 200,000 people die from cancer in the United Kingdom every year and that “many of these people are diagnosed too late for treatment to be effective.
“This collaboration between the NHS and Grail offers the chance for a wide range of cancers to be diagnosed much earlier and could fundamentally change the outlook for people with cancer,” he said.
However, some clinicians raised potential concerns.
Stephen Duffy, PhD, Center for Cancer Prevention, Queen Mary University of London, described the pilot as “very exciting,” but cautioned: “We will need to find out just how early the test detects cancers and whether it can it be used in a way which minimizes anxiety from false positives.”
Yong-Jie Lu, MD, PhD, also at Queen Mary University of London, said: “It is not clear how early it aims to catch cancer. For a cancer screen test, it needs very high specificity (>99%), otherwise it may end up in a similar situation as the PSA [prostate-specific antigen] test for prostate cancer, or even worse.”
Mangesh Thorat, MD, Cancer Prevention Trials Unit, King’s College London, warned: “It is likely that for every testing round ... there will be about 1,000 false-positive results, and the test may not be able to pinpoint the location of cancer in 3%-4% of those with a true positive result, necessitating a range of imaging and other investigations in these participants.”
No funding for the study has been declared. The investigators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
“Early detection, particularly for hard-to-treat conditions like ovarian and pancreatic cancer, has the potential to save many lives,” said NHS Chief Executive Sir Simon Stevens in a statement.
The pilot trial will use the Galleri blood test, developed by Grail. Sir Stevens described the blood test as “promising” and said it could “be a game changer in cancer care, helping thousands more people to get successful treatment.”
However, some clinicians have expressed concerns over the potential for false-positive results with the test.
Results of a study of the Galleri blood test, published earlier this year, showed that the test detected 50 types of cancer with a specificity of 99.3% and a false positive rate of 0.7%.
It also correctly identified the originating tissue in 90% of cases. However, the sensitivity was lower, at 67%, for the 12 most common cancers, as reported at the time.
The senior author of that study, Michael Seiden, MD, PhD, president of the U.S. Oncology Network, The Woodlands, Tex., noted that it was not a screening study: the test had been used in patients with cancer and in healthy volunteers. He said the test “is intended to be complementary to, and not replace, existing guideline-recommended screening tests and might provide new avenues of investigation for cancers that don’t currently have screening tests.”
The Galleri test uses next-generation sequencing to analyze the arrangement of methyl groups on circulating cell-free DNA in a blood sample.
Several other blood tests for cancer are under development, including the CancerSEEK test, which has been reported to be able to identify eight common cancers. It measures circulating tumor DNA from 16 genes and eight protein biomarkers and then uses machine learning to analyze the data.
Improving early detection rates
The pilot trial of the blood test is due to start in mid-2021 and will involve 165,000 people.
The trial will include 140,000 individuals aged 50-79 years who were identified through their health records and who have no cancer symptoms. They will undergo blood tests annually for 3 years and will be referred for investigation if a test result is positive.
A second group will include 25,000 people with potential cancer symptoms. These patients will be offered the blood test to speed up their diagnosis after referral to a hospital via the normal channels.
The results of the pilot are expected in 2023. If successful, the test will be rolled out to 1 million individuals from 2024 to 2025.
The pilot trial is part of the NHS Long Term Plan, which aims to increase early detection of cancer. At present, around half of cancers in England are diagnosed in stage I or II; the NHS aims to increase this to 75% by 2028.
“The NHS has set itself an ambitious target,” commented Peter Johnson, MD, PhD, national clinical director for cancer at NHS England and Improvement.
“Tests like this may help us get there far faster, and I am excited to see how this cutting-edge technology will work out as we test it in clinics across the NHS,” he added.
Lord David Prior, chair of NHS England, noted that almost 200,000 people die from cancer in the United Kingdom every year and that “many of these people are diagnosed too late for treatment to be effective.
“This collaboration between the NHS and Grail offers the chance for a wide range of cancers to be diagnosed much earlier and could fundamentally change the outlook for people with cancer,” he said.
However, some clinicians raised potential concerns.
Stephen Duffy, PhD, Center for Cancer Prevention, Queen Mary University of London, described the pilot as “very exciting,” but cautioned: “We will need to find out just how early the test detects cancers and whether it can it be used in a way which minimizes anxiety from false positives.”
Yong-Jie Lu, MD, PhD, also at Queen Mary University of London, said: “It is not clear how early it aims to catch cancer. For a cancer screen test, it needs very high specificity (>99%), otherwise it may end up in a similar situation as the PSA [prostate-specific antigen] test for prostate cancer, or even worse.”
Mangesh Thorat, MD, Cancer Prevention Trials Unit, King’s College London, warned: “It is likely that for every testing round ... there will be about 1,000 false-positive results, and the test may not be able to pinpoint the location of cancer in 3%-4% of those with a true positive result, necessitating a range of imaging and other investigations in these participants.”
No funding for the study has been declared. The investigators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Cancer rates on the rise in adolescents and young adults
Rates of cancer increased by 30% from 1973 to 2015 in adolescents and young adults (AYAs) aged 15–39 years in the United States, according to a review of almost a half million cases in the National Institutes of Health’s Surveillance, Epidemiology, and End Results database.
There was an annual increase of 0.537 new cases per 100,000 people, from 57.2 cases per 100,000 in 1973 to 74.2 in 2015.
Kidney carcinoma led with the highest rate increase. There were also marked increases in thyroid and colorectal carcinoma, germ cell and trophoblastic neoplasms, and melanoma, among others.
The report was published online December 1 in JAMA Network Open.
“Clinicians should be on the lookout for these cancers in their adolescent and young adult patients,” said senior investigator Nicholas Zaorsky, MD, an assistant professor of radiation oncology and public health sciences at the Penn State Cancer Institute, Hershey, Pennsylvania.
“Now that there is a better understanding of the types of cancer that are prevalent and rising in this age group, prevention, screening, diagnosis and treatment protocols specifically targeted to this population should be developed,” he said in a press release.
The reasons for the increases are unclear, but environmental and dietary factors, increasing obesity, and changing screening practices are likely in play, the authors comment. In addition, “cancer screening and overdiagnosis are thought to account for much of the increasing rates of thyroid and kidney carcinoma, among others,” they add.
The American Cancer Society (ACS) recently found similar increases in thyroid, kidney, and colorectal cancer among AYAs, as well as an increase in uterine cancer.
It’s important to note, however, that “this phenomenon is largely driven by trends for thyroid cancer, which is thought to be a result of overdiagnosis,” said ACS surveillance researcher Kimberly Miller, MPH, when asked to comment on the new study.
“As such, it is extremely important to also consider trends in cancer mortality rates among this age group, which are declining overall but are increasing for colorectal and uterine cancers. The fact that both incidence and mortality rates are increasing for these two cancers suggests a true increase in disease burden and certainly requires further attention and research,” she said.
Historically, management of cancer in AYAs has fallen somewhere between pediatric and adult oncology, neither of which capture the distinct biological, social, and economic needs of AYAs. Research has also focused on childhood and adult cancers, leaving cancer in AYAs inadequately studied.
The new findings are “valuable to guide more targeted research and interventions specifically to AYAs,” Zaorsky and colleagues say in their report.
Among female patients ― 59.1% of the study population ― incidence increased for 15 cancers, including kidney carcinoma (annual percent change [APC], 3.632), thyroid carcinoma (APC, 3.456), and myeloma, mast cell, and miscellaneous lymphoreticular neoplasms not otherwise specified (APC, 2.805). Rates of five cancers declined, led by astrocytoma not otherwise specified (APC, –3.369) and carcinoma of the gonads (APC, –1.743).
Among male patients, incidence increased for 14 cancers, including kidney carcinoma (APC, 3.572), unspecified soft tissue sarcoma (APC 2.543), and thyroid carcinoma (APC, 2.273). Incidence fell for seven, led by astrocytoma not otherwise specified (APC, –3.759) and carcinoma of the trachea, bronchus, and lung (APC, –2.635).
Increased testicular cancer rates (APC, 1.246) could be related to greater prenatal exposure to estrogen and progesterone or through dairy consumption; increasing survival of premature infants; and greater exposure to cannabis, among other possibilities, the investigators say.
Increases in colorectal cancer might be related to fewer vegetables and more fat and processed meat in the diet; lack of exercise; and increasing obesity. Human papillomavirus infection has also been implicated.
Higher rates of melanoma could be related to tanning bed use.
Declines in some cancers could be related to greater use of oral contraceptives; laws reducing exposure to benzene and other chemicals; and fewer people smoking.
Although kidney carcinoma has increased at the greatest rate, it’s uncommon. Colorectal and thyroid carcinoma, melanoma, non-Hodgkin lymphoma, and germ cell and trophoblastic neoplasms of the gonads contribute more to the overall increase in cancers among AYAs, the investigators note.
Almost 80% of the patients were White; 10.3% were Black.
The study was funded by the National Center for Advancing Translational Sciences. The investigators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Rates of cancer increased by 30% from 1973 to 2015 in adolescents and young adults (AYAs) aged 15–39 years in the United States, according to a review of almost a half million cases in the National Institutes of Health’s Surveillance, Epidemiology, and End Results database.
There was an annual increase of 0.537 new cases per 100,000 people, from 57.2 cases per 100,000 in 1973 to 74.2 in 2015.
Kidney carcinoma led with the highest rate increase. There were also marked increases in thyroid and colorectal carcinoma, germ cell and trophoblastic neoplasms, and melanoma, among others.
The report was published online December 1 in JAMA Network Open.
“Clinicians should be on the lookout for these cancers in their adolescent and young adult patients,” said senior investigator Nicholas Zaorsky, MD, an assistant professor of radiation oncology and public health sciences at the Penn State Cancer Institute, Hershey, Pennsylvania.
“Now that there is a better understanding of the types of cancer that are prevalent and rising in this age group, prevention, screening, diagnosis and treatment protocols specifically targeted to this population should be developed,” he said in a press release.
The reasons for the increases are unclear, but environmental and dietary factors, increasing obesity, and changing screening practices are likely in play, the authors comment. In addition, “cancer screening and overdiagnosis are thought to account for much of the increasing rates of thyroid and kidney carcinoma, among others,” they add.
The American Cancer Society (ACS) recently found similar increases in thyroid, kidney, and colorectal cancer among AYAs, as well as an increase in uterine cancer.
It’s important to note, however, that “this phenomenon is largely driven by trends for thyroid cancer, which is thought to be a result of overdiagnosis,” said ACS surveillance researcher Kimberly Miller, MPH, when asked to comment on the new study.
“As such, it is extremely important to also consider trends in cancer mortality rates among this age group, which are declining overall but are increasing for colorectal and uterine cancers. The fact that both incidence and mortality rates are increasing for these two cancers suggests a true increase in disease burden and certainly requires further attention and research,” she said.
Historically, management of cancer in AYAs has fallen somewhere between pediatric and adult oncology, neither of which capture the distinct biological, social, and economic needs of AYAs. Research has also focused on childhood and adult cancers, leaving cancer in AYAs inadequately studied.
The new findings are “valuable to guide more targeted research and interventions specifically to AYAs,” Zaorsky and colleagues say in their report.
Among female patients ― 59.1% of the study population ― incidence increased for 15 cancers, including kidney carcinoma (annual percent change [APC], 3.632), thyroid carcinoma (APC, 3.456), and myeloma, mast cell, and miscellaneous lymphoreticular neoplasms not otherwise specified (APC, 2.805). Rates of five cancers declined, led by astrocytoma not otherwise specified (APC, –3.369) and carcinoma of the gonads (APC, –1.743).
Among male patients, incidence increased for 14 cancers, including kidney carcinoma (APC, 3.572), unspecified soft tissue sarcoma (APC 2.543), and thyroid carcinoma (APC, 2.273). Incidence fell for seven, led by astrocytoma not otherwise specified (APC, –3.759) and carcinoma of the trachea, bronchus, and lung (APC, –2.635).
Increased testicular cancer rates (APC, 1.246) could be related to greater prenatal exposure to estrogen and progesterone or through dairy consumption; increasing survival of premature infants; and greater exposure to cannabis, among other possibilities, the investigators say.
Increases in colorectal cancer might be related to fewer vegetables and more fat and processed meat in the diet; lack of exercise; and increasing obesity. Human papillomavirus infection has also been implicated.
Higher rates of melanoma could be related to tanning bed use.
Declines in some cancers could be related to greater use of oral contraceptives; laws reducing exposure to benzene and other chemicals; and fewer people smoking.
Although kidney carcinoma has increased at the greatest rate, it’s uncommon. Colorectal and thyroid carcinoma, melanoma, non-Hodgkin lymphoma, and germ cell and trophoblastic neoplasms of the gonads contribute more to the overall increase in cancers among AYAs, the investigators note.
Almost 80% of the patients were White; 10.3% were Black.
The study was funded by the National Center for Advancing Translational Sciences. The investigators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Rates of cancer increased by 30% from 1973 to 2015 in adolescents and young adults (AYAs) aged 15–39 years in the United States, according to a review of almost a half million cases in the National Institutes of Health’s Surveillance, Epidemiology, and End Results database.
There was an annual increase of 0.537 new cases per 100,000 people, from 57.2 cases per 100,000 in 1973 to 74.2 in 2015.
Kidney carcinoma led with the highest rate increase. There were also marked increases in thyroid and colorectal carcinoma, germ cell and trophoblastic neoplasms, and melanoma, among others.
The report was published online December 1 in JAMA Network Open.
“Clinicians should be on the lookout for these cancers in their adolescent and young adult patients,” said senior investigator Nicholas Zaorsky, MD, an assistant professor of radiation oncology and public health sciences at the Penn State Cancer Institute, Hershey, Pennsylvania.
“Now that there is a better understanding of the types of cancer that are prevalent and rising in this age group, prevention, screening, diagnosis and treatment protocols specifically targeted to this population should be developed,” he said in a press release.
The reasons for the increases are unclear, but environmental and dietary factors, increasing obesity, and changing screening practices are likely in play, the authors comment. In addition, “cancer screening and overdiagnosis are thought to account for much of the increasing rates of thyroid and kidney carcinoma, among others,” they add.
The American Cancer Society (ACS) recently found similar increases in thyroid, kidney, and colorectal cancer among AYAs, as well as an increase in uterine cancer.
It’s important to note, however, that “this phenomenon is largely driven by trends for thyroid cancer, which is thought to be a result of overdiagnosis,” said ACS surveillance researcher Kimberly Miller, MPH, when asked to comment on the new study.
“As such, it is extremely important to also consider trends in cancer mortality rates among this age group, which are declining overall but are increasing for colorectal and uterine cancers. The fact that both incidence and mortality rates are increasing for these two cancers suggests a true increase in disease burden and certainly requires further attention and research,” she said.
Historically, management of cancer in AYAs has fallen somewhere between pediatric and adult oncology, neither of which capture the distinct biological, social, and economic needs of AYAs. Research has also focused on childhood and adult cancers, leaving cancer in AYAs inadequately studied.
The new findings are “valuable to guide more targeted research and interventions specifically to AYAs,” Zaorsky and colleagues say in their report.
Among female patients ― 59.1% of the study population ― incidence increased for 15 cancers, including kidney carcinoma (annual percent change [APC], 3.632), thyroid carcinoma (APC, 3.456), and myeloma, mast cell, and miscellaneous lymphoreticular neoplasms not otherwise specified (APC, 2.805). Rates of five cancers declined, led by astrocytoma not otherwise specified (APC, –3.369) and carcinoma of the gonads (APC, –1.743).
Among male patients, incidence increased for 14 cancers, including kidney carcinoma (APC, 3.572), unspecified soft tissue sarcoma (APC 2.543), and thyroid carcinoma (APC, 2.273). Incidence fell for seven, led by astrocytoma not otherwise specified (APC, –3.759) and carcinoma of the trachea, bronchus, and lung (APC, –2.635).
Increased testicular cancer rates (APC, 1.246) could be related to greater prenatal exposure to estrogen and progesterone or through dairy consumption; increasing survival of premature infants; and greater exposure to cannabis, among other possibilities, the investigators say.
Increases in colorectal cancer might be related to fewer vegetables and more fat and processed meat in the diet; lack of exercise; and increasing obesity. Human papillomavirus infection has also been implicated.
Higher rates of melanoma could be related to tanning bed use.
Declines in some cancers could be related to greater use of oral contraceptives; laws reducing exposure to benzene and other chemicals; and fewer people smoking.
Although kidney carcinoma has increased at the greatest rate, it’s uncommon. Colorectal and thyroid carcinoma, melanoma, non-Hodgkin lymphoma, and germ cell and trophoblastic neoplasms of the gonads contribute more to the overall increase in cancers among AYAs, the investigators note.
Almost 80% of the patients were White; 10.3% were Black.
The study was funded by the National Center for Advancing Translational Sciences. The investigators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The pill toolbox: How to choose a combined oral contraceptive
In the era of long-acting reversible contraceptives (LARCs), the pill can seem obsolete. However, it is still the second most commonly used birth control method in the United States, chosen by 19% of female contraceptive users as of 2015–2017.1 It also has noncontraceptive benefits, so it is important that obstetrician-gynecologists are well-versed in its uses. In this article, I will focus on combined oral contraceptives (COCs; TABLE 1), reviewing the major risks, benefits, and adverse effects of COCs before focusing on recommendations for particular formulations of COCs for various patient populations.
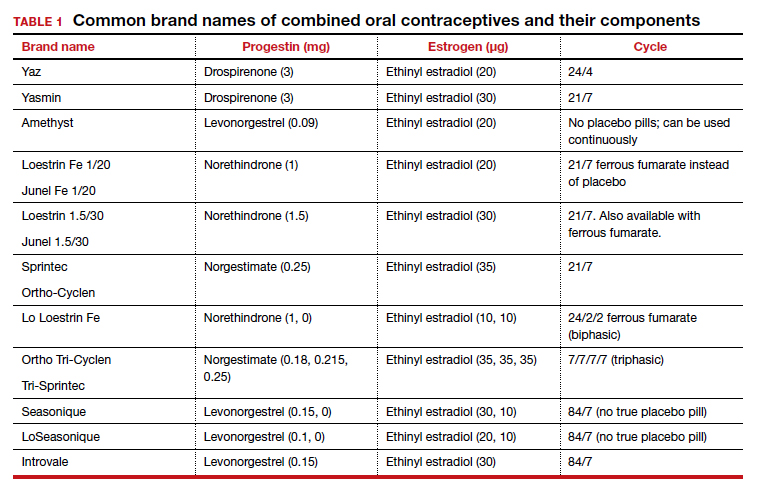
Benefits and risks
There are numerous noncontraceptive benefits of COCs, including menstrual cycle regulation; reduced risk of ovarian, endometrial, and colorectal cancer; and treatment of menorrhagia, dysmenorrhea, acne, menstrual migraine, premenstrual syndrome and premenstrual dysphoric disorder, pelvic pain due to endometriosis, and hirsutism.
Common patient concerns
In terms of adverse effects, there are more potential unwanted effects of concern to women than there are ones validated in the literature. Accepted adverse effects include nausea, breast tenderness, and decreased libido. However, one of the most common concerns voiced during contraceptive counseling is that COCs will cause weight gain. A 2014 Cochrane review identified 49 trials studying the weight gain question.2 Of those, only 4 had a placebo or nonintervention group. Of these 4, there was no significant difference in weight change between the COC-receiving group and the control group. When patients bring up their concerns, it may help to remind them that women tend to gain weight over time whether or not they are taking a COC.
Another common concern is that COCs cause mood changes. A 2016 review by Schaffir and colleagues sheds some light on this topic,3 albeit limited by the paucity of prospective studies. This review identified only 1 randomized controlled trial comparing depression incidence among women initiating a COC versus a placebo. There was no difference in the incidence of depression among the groups at 3 months. Among 4 large retrospective studies of women using COCs, the agents either had no or a beneficial effect on mood. Schaffir’s review reports that there may be greater mood adverse effects with COCs among women with underlying mood disorders.
Patients may worry that COC use will permanently impair their fertility or delay return to fertility after discontinuation. Research does indicate that return of fertility after stopping COCs often takes several months (compared with immediate fertility after discontinuing a barrier method). However, there still seem to be comparable conception rates within 12 months after discontinuing COCs as there are after discontinuing other common nonhormonal or hormonal contraceptive methods. Fertility is not impacted by the duration of COC use. In addition, return to fertility seems to be comparable after discontinuation of extended cycle or continuous COCs compared with traditional-cycle COCs.4
COC safety
Known major risks of COCs include venous thromboembolism (VTE). The risk of VTE is about double among COC users than among nonpregnant nonusers: 3–9 per 10,000 woman-years compared with 1–5.5 In a study by the US Food and Drug Administration, drospirenone-containing COCs had double the risk of VTE than other COCs. However, the position of the American College of Obstetricians and Gynecologists on this increased risk of VTE with drospirenone-containing pills is that it is “possible” and “minimal.”5 It is important to remember that an alternative to COC use is pregnancy, in which the VTE risk is about double that among COC users, at 5–20 per 10,000 woman-years. This risk increases further in the postpartum period, to 40–65 per 10,000 woman-years.5
Another known major risk of COCs is arterial embolic disease, including cerebrovascular accidents and myocardial infarctions. Women at increased risk for these complications include those with hypertension, diabetes, and/or obesity and women who are aged 35 or older and smoke. Interestingly, women with migraines with aura are at increased risk for stroke but not for myocardial infarction. These women increase their risk of stroke 2- to 4-fold if they use COCs.
Continue to: Different pills for different problems...
Different pills for different problems
With so many pills on the market, it is important for clinicians to know how to choose a particular pill for a particular patient. The following discussion assumes that the patient in question desires a COC for contraception, then offers guidance on how to choose a pill with patient-specific noncontraceptive benefits (TABLE 2).
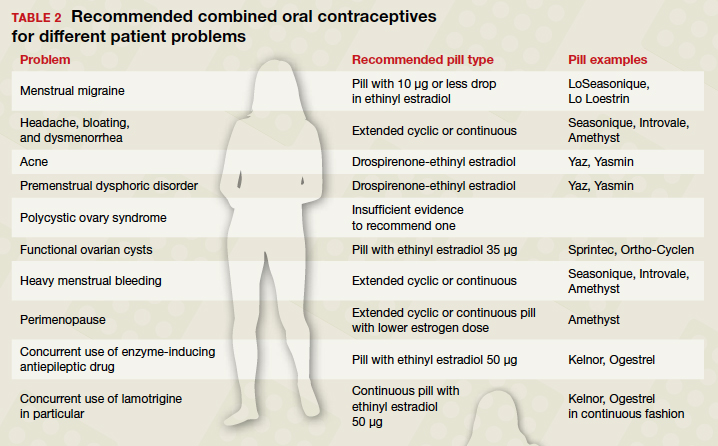
When HMB is a concern. Patients with heavy menstrual bleeding may experience fewer bleeding and/or spotting days with extended cyclic or continuous use of a COC rather than with traditional cyclic use.6 Examples of such COC options include:
- Introvale and Seasonique, both extended-cycle formulations
- Amethyst, which is formulated without placebo pills so that it can be used continuously
- any other COC prescribed with instructions for the patient to skip placebo pills.
An extrapolated benefit to extended-cycle or continuous COCs use for heavy menstrual bleeding is addressing anemia.
For premenstrual dysphoric disorder, the only randomized controlled trials showing improvement involve drospirenone-ethinyl estradiol pills (Yaz and Yasmin).7 There is also evidence that extended cyclic or continuous use of these formulations is more impactful for premenstrual dysphoric disorder than a traditional cycle.8
Keeping migraine avoidance and prevention in mind. Various studies have looked at the impact of different COC formulations on menstrual-related symptoms. There is evidence of greater improvement in headache, bloating, and dysmenorrhea with extended cyclic or continuous use compared with traditional cyclic use.6
In terms of headache, let us delve into menstrual migraine in particular. Menstrual migraines occur sometime between 2 days prior to 2 days after the first day of menses and are linked to a sharp drop in estrogen levels. COCs are contraindicated in women with menstrual migraines with aura because of the increased stroke risk. For women with menstrual migraines without aura, COCs can prevent migraines. Prevention depends on minimizing fluctuations in estrogen levels; any change in estrogen level greater than 10 µg of ethinyl estradiol may trigger an estrogen-related migraine. All currently available regimens of COCs that comprise 21 days of active pills and 7 days of placebo involve a drop of more than 10 µg. Options that involve a drop of 10 µg or less include any continuous formulation, the extended formulation LoSeasonique (levonorgestrel 0.1 mg and ethinyl estradiol 20 µg for 84 days, then ethinyl estradiol 10 µg for 7 days), and Lo Loestrin (ethinyl estradiol 10 µg and norethindrone 1 mg for 24 days, then ethinyl estradiol 10 µg for 2 days, then placebo for 2 days).9
What’s best for acne-prone patients? All COCs should improve acne by increasing levels of sex hormone binding globulin. However, some comparative studies have shown drospirenone-containing COCs to be the most effective for acne. This finding makes sense in light of studies demonstrating antiandrogenic effects of drospirenone.10
Managing PCOS symptoms. It seems logical, by extension, that drospirenone-containing COCs would be particularly beneficial for treating hirsutism associated with polycystic ovary syndrome (PCOS). Other low‒androgenic-potential progestins, such as a third-generation progestin (norgestimate or desogestrel), might similarly be hypothesized to be advantageous. However, there is currently insufficient evidence to recommend any one COC formulation over another for the indication of PCOS.11
Ovarian cysts: Can COCs be helpful? COCs are commonly prescribed by gynecologists for patients with functional ovarian cysts. It is important to note that COCs have not been found to hasten the resolution of existing cysts, so they should not be used for this purpose.12 Studies of early COCs, which had high doses of estrogen (on the order of 50 µg), showed lower rates of cysts among users. This effect seems to be attenuated with the lower-estrogen-dose pills that are currently available, but there still appears to be benefit. Therefore, for a patient prone to cysts who desires an oral contraceptive, a COC containing estrogen 35 µg is likely to be the most beneficial of COCs currently on the market.13,14
Lower-dosage COCs in perimenopause may be beneficial. COCs can ameliorate perimenopausal symptoms including abnormal uterine bleeding and vasomotor symptoms. Clinicians are often hesitant to prescribe COCs for perimenopausal women because of increased risk of VTE, stroke, myocardial infarction, and breast cancer with increasing age. However, age alone is not a contraindication to any contraceptive method. An extended cyclic or continuous regimen COC may be the best choice for a perimenopausal woman in order to avoid vasomotor symptoms that occur during hormone-free intervals. In addition, given the increasing risk of adverse effects like VTE with estrogen dose, a lower estrogen formulation is advisable.15
Patients with epilepsy who are taking antiepileptic drugs (AEDs) are a special population when it comes to COCs. Certain AEDs induce hepatic enzymes involved in the metabolism and protein binding of COCs, which can result in contraceptive failure. Strong inducers are carbamazepine, oxcarbazepine, perampanel, phenobarbital, phenytoin, and primidone. Weak inducers are clobazam, eslicarbazepine, felbamate, lamotrigine, rufinamide, and topiramate. Women taking any of the above AEDs are recommended to choose a different form of contraception than a COC. However, if they are limited to COCs for some reason, a preparation containing estrogen 50 µg is recommended. It is speculated that the efficacy and adverse effects of COCs with increased hormone doses, used in combination with enzyme-inducing AEDs, should be comparable to those with standard doses when not combined with AEDs; however, this speculation is unproven.16 There are few COCs on the market with estrogen doses of 50 µg, but a couple of examples are Kelnor and Ogestrel.
Additional factors have to be considered with concurrent COC use with the AED lamotrigine since COCs increase clearance of this agent. Therefore, patients taking lamotrigine who start COCs will need an increase in lamotrigine dose. To avoid fluctuations in lamotrigine serum levels, use of a continuous COC is recommended.17
Continue to: Pill types to minimize adverse effects or risks...
Pill types to minimize adverse effects or risks
For women who desire to use a COC for contraception but who are at risk for a particular complication or are bothered by a particular adverse effect, ObGyns can optimize the choice of pill (TABLE 3). For example, women who have adverse effects of nausea and/or breast tenderness may benefit from reducing the estrogen dose to 20 µg or lower.18
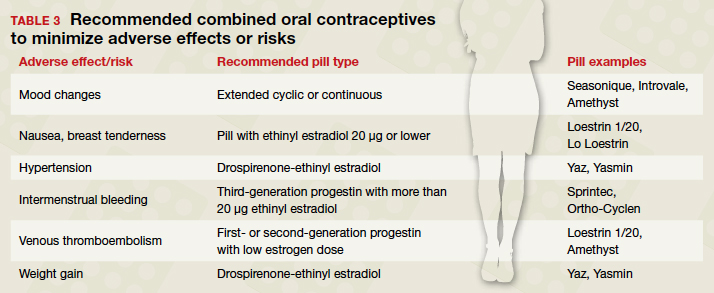
Considering VTE
As discussed previously, VTE is a risk with all COCs, but some pills confer greater risk than others. For one, VTE risk increases with estrogen dose. In addition, VTE risk depends on the type of progestin. Drospirenone and third-generation progestins (norgestimate, gestodene, and desogestrel) confer a higher risk of VTE than first- or second-generation progestins. For example, a pill with estradiol 30 µg and either a third-generation progestin or drospirenone has a 50% to 80% higher risk of VTE compared with a pill with estradiol 30 µg and levonorgestrel.
For patients at particularly high risk for VTE, COCs are contraindicated. For patients for whom COCs are considered medically appropriate but who are at higher risk (eg, obese women), it is wise to use a pill containing a first-generation (norethindrone) or second-generation progestin (levonorgestrel) combined with the lowest dose of estrogen that has tolerable adverse effects.19
What about hypertension concerns?
Let us turn our attention briefly to hypertension and its relation to COC use. While the American College of Cardiology and the American Heart Association redefined hypertension in 2017 using a threshold of 130/80 mm Hg, the American College of Obstetricians and Gynecologists (ACOG) considers hypertension to be 140/90 mm Hg in terms of safety of using COCs. ACOG states, “women with blood pressure below 140/90 mm Hg may use any hormonal contraceptive method.”20 In women with hypertension in the range of 140‒159 mm Hg systolic or 90‒99 mm Hg diastolic, COCs are category 3 according to the US Medical Eligibility Criteria for Contraceptive Use, meaning that the risks usually outweigh the benefits. For women with blood pressures of 160/110 mm Hg or greater, COCs are category 4 (contraindicated). If a woman with mild hypertension is started on a COC, a drospirenone-containing pill may be the best choice because of its diuretic effects. While other contemporary COCs have been associated with a mild increase in blood pressure, drospirenone-containing pills have not shown this association.21
Continue to: At issue: Break-through bleeding, mood, and weight gain...
At issue: Break-through bleeding, mood, and weight gain
For women bothered by intermenstrual bleeding, use of a COC with a third-generation progestin may be preferable to use of one with a first- or second-generation. It may be because of decreased abnormal bleeding that COCs with third-generation progestins have lower discontinuation rates.22 In addition, COCs containing estrogen 20 µg or less are associated with more intermenstrual bleeding than those with more than 20 µg estrogen.23 Keep in mind that it is common with any COC to have intermenstrual bleeding for the first several months.
For women with pre-existing mood disorders or who report mood changes with COCs, it appears that fluctuations in hormone levels are problematic. Consistently, there is evidence that monophasic pills are preferable to multiphasic and that extended cyclic or continuous use is preferable to traditional cyclic use for mitigating mood adverse effects. There is mixed evidence on whether a low dose of ethinyl estradiol is better for mood.3
Although it is discussed above that randomized controlled trials have not shown an association between COC use and weight gain, many women remain concerned. For these women, a drospirenone-containing COC may be the best choice. Drospirenone has antimineralocorticoid activity, so it may help prevent water retention.
A brief word about multiphasic COCs. While these pills were designed to mimic physiologic hormone fluctuations and minimize hormonal adverse effects, there is insufficient evidence to compare their effects to those of monophasic pills.24 Without such evidence, there is little reason to recommend a multiphasic pill to a patient over the more straightforward monophasic formulation.
Conclusion
There are more nuances to prescribing an optimal COC for a patient than may initially come to mind. It is useful to remember that any formulation of pill may be prescribed in an extended or continuous fashion, and there are benefits for such use for premenstrual dysphoric disorder, heavy menstrual bleeding, perimenopause, and menstrual symptoms. Although there are numerous brands of COCs available, a small cadre will suffice for almost all purposes. Such a “toolbox” of pills could include a pill formatted for continuous use (Seasonique), a low estrogen pill (Loestrin), a drospirenone-containing pill (Yaz), and a pill containing a third-generation progestin and a higher dose of estrogen (Sprintec). ●
- Daniels K, Abma JC. Current contraceptive status among women aged 15-49: United States, 2015-2017. NCHS Data Brief, no 327. Hyattsville, MD; 2018.
- Gallo MF, Lopez LM, Grimes DA, et al. Combination contraceptives: effects on weight. Cochrane Database Syst Rev. 2014:CD003987.
- Schaffir J, Worly BL, Gur TL. Combined hormonal contraception and its effects on mood: a critical review. Eur J Contracept Reprod Health Care. 2016;21:347-355.
- Barnhart KT, Schreiber CA. Return to fertility following discontinuation of oral contraceptives. Fertil Steril. 2009;91:659-663.
- American College of Obstetricians and Gynecologists. Committee Opinion #540: Risk of Venous Thromboembolism Among Users of Drospirenone-Containing Oral Contraceptive Pills. Obstet Gynecol. 2012;120:1239-1242.
- Edelman A, Micks E, Gallo MF, et al. Continuous or extended cycle vs. cyclic use of combined hormonal contraceptives for contraception. Cochrane Database Syst Rev. 2014:CD004695.
- American College of Obstetricians and Gynecologists. Practice Bulletin #110: Noncontraceptive Uses of Hormonal Contraceptives. Obstet Gynecol. 2010:206-218.
- Coffee AL, Kuehl TJ, Willis S, et al. Oral contraceptives and premenstrual symptoms: comparison of a 21/7 and extended regimen. Am J Obstet Gynecol. 2006;195:1311-1319.
- Calhoun AH, Batur P. Combined hormonal contraceptives and migraine: an update on the evidence. Cleve Clin J Med. 2017;84:631-638.
- Arowojolu AO, Gallo MF, Lopez LM, et al. Combined oral contraceptive pills for treatment of acne. Cochrane Database Syst Rev. 2012:CD004425.
- McCartney CR, Marshall JC. CLINICAL PRACTICE. Polycystic Ovary Syndrome. N Engl J Med. 2016;375:54-64.
- Grimes DA, Jones LB, Lopez LM, et al. Oral contraceptives for functional ovarian cysts. Cochrane Database Syst Rev. 2014:CD006134.
- Grimes DA, Godwin AJ, Rubin A, et al. Ovulation and follicular development associated with three low-dose oral contraceptives: a randomized controlled trial. Obstet Gynecol. 1994;83:29-34.
- Christensen JT, Boldsen JL, Westergaard JG. Functional ovarian cysts in premenopausal and gynecologically healthy women. Contraception. 2002;66:153-157.
- Hardman SM, Gebbie AE. Hormonal contraceptive regimens in the perimenopause. Maturitas. 2009;63:204-212.
- Zupanc ML. Antiepileptic drugs and hormonal contraceptives in adolescent women with epilepsy. Neurology. 2006;66 (6 suppl 3):S37-S45.
- Wegner I, Edelbroek PM, Bulk S, et al. Lamotrigine kinetics within the menstrual cycle, after menopause, and with oral contraceptives. Neurology. 2009;73:1388-1393.
- Stewart M, Black K. Choosing a combined oral contraceptive pill. Australian Prescriber. 2015;38:6-11.
- de Bastos M, Stegeman BH, Rosendaal FR, et al. Combined oral contraceptives: venous thrombosis. Cochrane Database Syst Rev. 2014:CD010813.
- American College of Obstetricians and Gynecologists. Practice Bulletin #206: use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2019;133:e128-e150.
- de Morais TL, Giribela C, Nisenbaum MG, et al. Effects of a contraceptive containing drospirenone and ethinylestradiol on blood pressure, metabolic profile and neurohumoral axis in hypertensive women at reproductive age. Eur J Obstet Gynecol Reprod Biol. 2014;182:113-117.
- Lawrie TA, Helmerhorst FM, Maitra NK, et al. Types of progestogens in combined oral contraception: effectiveness and side-effects. Cochrane Database Syst Rev. 2011:CD004861.
- Gallo MF, Nanda K, Grimes DA, et al. 20 µg versus >20 µg estrogen combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2013:CD003989.
- van Vliet HA, Grimes DA, Lopez LM, et al. Triphasic versus monophasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2006:CD003553
In the era of long-acting reversible contraceptives (LARCs), the pill can seem obsolete. However, it is still the second most commonly used birth control method in the United States, chosen by 19% of female contraceptive users as of 2015–2017.1 It also has noncontraceptive benefits, so it is important that obstetrician-gynecologists are well-versed in its uses. In this article, I will focus on combined oral contraceptives (COCs; TABLE 1), reviewing the major risks, benefits, and adverse effects of COCs before focusing on recommendations for particular formulations of COCs for various patient populations.
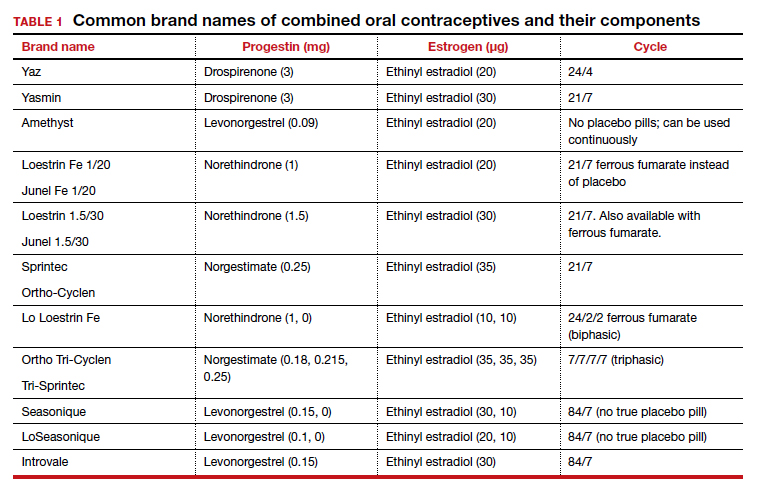
Benefits and risks
There are numerous noncontraceptive benefits of COCs, including menstrual cycle regulation; reduced risk of ovarian, endometrial, and colorectal cancer; and treatment of menorrhagia, dysmenorrhea, acne, menstrual migraine, premenstrual syndrome and premenstrual dysphoric disorder, pelvic pain due to endometriosis, and hirsutism.
Common patient concerns
In terms of adverse effects, there are more potential unwanted effects of concern to women than there are ones validated in the literature. Accepted adverse effects include nausea, breast tenderness, and decreased libido. However, one of the most common concerns voiced during contraceptive counseling is that COCs will cause weight gain. A 2014 Cochrane review identified 49 trials studying the weight gain question.2 Of those, only 4 had a placebo or nonintervention group. Of these 4, there was no significant difference in weight change between the COC-receiving group and the control group. When patients bring up their concerns, it may help to remind them that women tend to gain weight over time whether or not they are taking a COC.
Another common concern is that COCs cause mood changes. A 2016 review by Schaffir and colleagues sheds some light on this topic,3 albeit limited by the paucity of prospective studies. This review identified only 1 randomized controlled trial comparing depression incidence among women initiating a COC versus a placebo. There was no difference in the incidence of depression among the groups at 3 months. Among 4 large retrospective studies of women using COCs, the agents either had no or a beneficial effect on mood. Schaffir’s review reports that there may be greater mood adverse effects with COCs among women with underlying mood disorders.
Patients may worry that COC use will permanently impair their fertility or delay return to fertility after discontinuation. Research does indicate that return of fertility after stopping COCs often takes several months (compared with immediate fertility after discontinuing a barrier method). However, there still seem to be comparable conception rates within 12 months after discontinuing COCs as there are after discontinuing other common nonhormonal or hormonal contraceptive methods. Fertility is not impacted by the duration of COC use. In addition, return to fertility seems to be comparable after discontinuation of extended cycle or continuous COCs compared with traditional-cycle COCs.4
COC safety
Known major risks of COCs include venous thromboembolism (VTE). The risk of VTE is about double among COC users than among nonpregnant nonusers: 3–9 per 10,000 woman-years compared with 1–5.5 In a study by the US Food and Drug Administration, drospirenone-containing COCs had double the risk of VTE than other COCs. However, the position of the American College of Obstetricians and Gynecologists on this increased risk of VTE with drospirenone-containing pills is that it is “possible” and “minimal.”5 It is important to remember that an alternative to COC use is pregnancy, in which the VTE risk is about double that among COC users, at 5–20 per 10,000 woman-years. This risk increases further in the postpartum period, to 40–65 per 10,000 woman-years.5
Another known major risk of COCs is arterial embolic disease, including cerebrovascular accidents and myocardial infarctions. Women at increased risk for these complications include those with hypertension, diabetes, and/or obesity and women who are aged 35 or older and smoke. Interestingly, women with migraines with aura are at increased risk for stroke but not for myocardial infarction. These women increase their risk of stroke 2- to 4-fold if they use COCs.
Continue to: Different pills for different problems...
Different pills for different problems
With so many pills on the market, it is important for clinicians to know how to choose a particular pill for a particular patient. The following discussion assumes that the patient in question desires a COC for contraception, then offers guidance on how to choose a pill with patient-specific noncontraceptive benefits (TABLE 2).
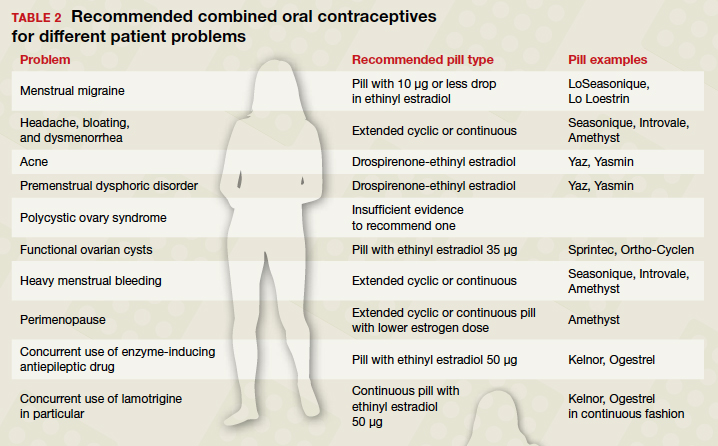
When HMB is a concern. Patients with heavy menstrual bleeding may experience fewer bleeding and/or spotting days with extended cyclic or continuous use of a COC rather than with traditional cyclic use.6 Examples of such COC options include:
- Introvale and Seasonique, both extended-cycle formulations
- Amethyst, which is formulated without placebo pills so that it can be used continuously
- any other COC prescribed with instructions for the patient to skip placebo pills.
An extrapolated benefit to extended-cycle or continuous COCs use for heavy menstrual bleeding is addressing anemia.
For premenstrual dysphoric disorder, the only randomized controlled trials showing improvement involve drospirenone-ethinyl estradiol pills (Yaz and Yasmin).7 There is also evidence that extended cyclic or continuous use of these formulations is more impactful for premenstrual dysphoric disorder than a traditional cycle.8
Keeping migraine avoidance and prevention in mind. Various studies have looked at the impact of different COC formulations on menstrual-related symptoms. There is evidence of greater improvement in headache, bloating, and dysmenorrhea with extended cyclic or continuous use compared with traditional cyclic use.6
In terms of headache, let us delve into menstrual migraine in particular. Menstrual migraines occur sometime between 2 days prior to 2 days after the first day of menses and are linked to a sharp drop in estrogen levels. COCs are contraindicated in women with menstrual migraines with aura because of the increased stroke risk. For women with menstrual migraines without aura, COCs can prevent migraines. Prevention depends on minimizing fluctuations in estrogen levels; any change in estrogen level greater than 10 µg of ethinyl estradiol may trigger an estrogen-related migraine. All currently available regimens of COCs that comprise 21 days of active pills and 7 days of placebo involve a drop of more than 10 µg. Options that involve a drop of 10 µg or less include any continuous formulation, the extended formulation LoSeasonique (levonorgestrel 0.1 mg and ethinyl estradiol 20 µg for 84 days, then ethinyl estradiol 10 µg for 7 days), and Lo Loestrin (ethinyl estradiol 10 µg and norethindrone 1 mg for 24 days, then ethinyl estradiol 10 µg for 2 days, then placebo for 2 days).9
What’s best for acne-prone patients? All COCs should improve acne by increasing levels of sex hormone binding globulin. However, some comparative studies have shown drospirenone-containing COCs to be the most effective for acne. This finding makes sense in light of studies demonstrating antiandrogenic effects of drospirenone.10
Managing PCOS symptoms. It seems logical, by extension, that drospirenone-containing COCs would be particularly beneficial for treating hirsutism associated with polycystic ovary syndrome (PCOS). Other low‒androgenic-potential progestins, such as a third-generation progestin (norgestimate or desogestrel), might similarly be hypothesized to be advantageous. However, there is currently insufficient evidence to recommend any one COC formulation over another for the indication of PCOS.11
Ovarian cysts: Can COCs be helpful? COCs are commonly prescribed by gynecologists for patients with functional ovarian cysts. It is important to note that COCs have not been found to hasten the resolution of existing cysts, so they should not be used for this purpose.12 Studies of early COCs, which had high doses of estrogen (on the order of 50 µg), showed lower rates of cysts among users. This effect seems to be attenuated with the lower-estrogen-dose pills that are currently available, but there still appears to be benefit. Therefore, for a patient prone to cysts who desires an oral contraceptive, a COC containing estrogen 35 µg is likely to be the most beneficial of COCs currently on the market.13,14
Lower-dosage COCs in perimenopause may be beneficial. COCs can ameliorate perimenopausal symptoms including abnormal uterine bleeding and vasomotor symptoms. Clinicians are often hesitant to prescribe COCs for perimenopausal women because of increased risk of VTE, stroke, myocardial infarction, and breast cancer with increasing age. However, age alone is not a contraindication to any contraceptive method. An extended cyclic or continuous regimen COC may be the best choice for a perimenopausal woman in order to avoid vasomotor symptoms that occur during hormone-free intervals. In addition, given the increasing risk of adverse effects like VTE with estrogen dose, a lower estrogen formulation is advisable.15
Patients with epilepsy who are taking antiepileptic drugs (AEDs) are a special population when it comes to COCs. Certain AEDs induce hepatic enzymes involved in the metabolism and protein binding of COCs, which can result in contraceptive failure. Strong inducers are carbamazepine, oxcarbazepine, perampanel, phenobarbital, phenytoin, and primidone. Weak inducers are clobazam, eslicarbazepine, felbamate, lamotrigine, rufinamide, and topiramate. Women taking any of the above AEDs are recommended to choose a different form of contraception than a COC. However, if they are limited to COCs for some reason, a preparation containing estrogen 50 µg is recommended. It is speculated that the efficacy and adverse effects of COCs with increased hormone doses, used in combination with enzyme-inducing AEDs, should be comparable to those with standard doses when not combined with AEDs; however, this speculation is unproven.16 There are few COCs on the market with estrogen doses of 50 µg, but a couple of examples are Kelnor and Ogestrel.
Additional factors have to be considered with concurrent COC use with the AED lamotrigine since COCs increase clearance of this agent. Therefore, patients taking lamotrigine who start COCs will need an increase in lamotrigine dose. To avoid fluctuations in lamotrigine serum levels, use of a continuous COC is recommended.17
Continue to: Pill types to minimize adverse effects or risks...
Pill types to minimize adverse effects or risks
For women who desire to use a COC for contraception but who are at risk for a particular complication or are bothered by a particular adverse effect, ObGyns can optimize the choice of pill (TABLE 3). For example, women who have adverse effects of nausea and/or breast tenderness may benefit from reducing the estrogen dose to 20 µg or lower.18
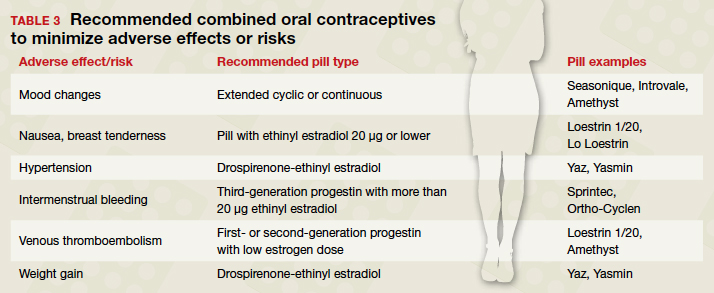
Considering VTE
As discussed previously, VTE is a risk with all COCs, but some pills confer greater risk than others. For one, VTE risk increases with estrogen dose. In addition, VTE risk depends on the type of progestin. Drospirenone and third-generation progestins (norgestimate, gestodene, and desogestrel) confer a higher risk of VTE than first- or second-generation progestins. For example, a pill with estradiol 30 µg and either a third-generation progestin or drospirenone has a 50% to 80% higher risk of VTE compared with a pill with estradiol 30 µg and levonorgestrel.
For patients at particularly high risk for VTE, COCs are contraindicated. For patients for whom COCs are considered medically appropriate but who are at higher risk (eg, obese women), it is wise to use a pill containing a first-generation (norethindrone) or second-generation progestin (levonorgestrel) combined with the lowest dose of estrogen that has tolerable adverse effects.19
What about hypertension concerns?
Let us turn our attention briefly to hypertension and its relation to COC use. While the American College of Cardiology and the American Heart Association redefined hypertension in 2017 using a threshold of 130/80 mm Hg, the American College of Obstetricians and Gynecologists (ACOG) considers hypertension to be 140/90 mm Hg in terms of safety of using COCs. ACOG states, “women with blood pressure below 140/90 mm Hg may use any hormonal contraceptive method.”20 In women with hypertension in the range of 140‒159 mm Hg systolic or 90‒99 mm Hg diastolic, COCs are category 3 according to the US Medical Eligibility Criteria for Contraceptive Use, meaning that the risks usually outweigh the benefits. For women with blood pressures of 160/110 mm Hg or greater, COCs are category 4 (contraindicated). If a woman with mild hypertension is started on a COC, a drospirenone-containing pill may be the best choice because of its diuretic effects. While other contemporary COCs have been associated with a mild increase in blood pressure, drospirenone-containing pills have not shown this association.21
Continue to: At issue: Break-through bleeding, mood, and weight gain...
At issue: Break-through bleeding, mood, and weight gain
For women bothered by intermenstrual bleeding, use of a COC with a third-generation progestin may be preferable to use of one with a first- or second-generation. It may be because of decreased abnormal bleeding that COCs with third-generation progestins have lower discontinuation rates.22 In addition, COCs containing estrogen 20 µg or less are associated with more intermenstrual bleeding than those with more than 20 µg estrogen.23 Keep in mind that it is common with any COC to have intermenstrual bleeding for the first several months.
For women with pre-existing mood disorders or who report mood changes with COCs, it appears that fluctuations in hormone levels are problematic. Consistently, there is evidence that monophasic pills are preferable to multiphasic and that extended cyclic or continuous use is preferable to traditional cyclic use for mitigating mood adverse effects. There is mixed evidence on whether a low dose of ethinyl estradiol is better for mood.3
Although it is discussed above that randomized controlled trials have not shown an association between COC use and weight gain, many women remain concerned. For these women, a drospirenone-containing COC may be the best choice. Drospirenone has antimineralocorticoid activity, so it may help prevent water retention.
A brief word about multiphasic COCs. While these pills were designed to mimic physiologic hormone fluctuations and minimize hormonal adverse effects, there is insufficient evidence to compare their effects to those of monophasic pills.24 Without such evidence, there is little reason to recommend a multiphasic pill to a patient over the more straightforward monophasic formulation.
Conclusion
There are more nuances to prescribing an optimal COC for a patient than may initially come to mind. It is useful to remember that any formulation of pill may be prescribed in an extended or continuous fashion, and there are benefits for such use for premenstrual dysphoric disorder, heavy menstrual bleeding, perimenopause, and menstrual symptoms. Although there are numerous brands of COCs available, a small cadre will suffice for almost all purposes. Such a “toolbox” of pills could include a pill formatted for continuous use (Seasonique), a low estrogen pill (Loestrin), a drospirenone-containing pill (Yaz), and a pill containing a third-generation progestin and a higher dose of estrogen (Sprintec). ●
In the era of long-acting reversible contraceptives (LARCs), the pill can seem obsolete. However, it is still the second most commonly used birth control method in the United States, chosen by 19% of female contraceptive users as of 2015–2017.1 It also has noncontraceptive benefits, so it is important that obstetrician-gynecologists are well-versed in its uses. In this article, I will focus on combined oral contraceptives (COCs; TABLE 1), reviewing the major risks, benefits, and adverse effects of COCs before focusing on recommendations for particular formulations of COCs for various patient populations.
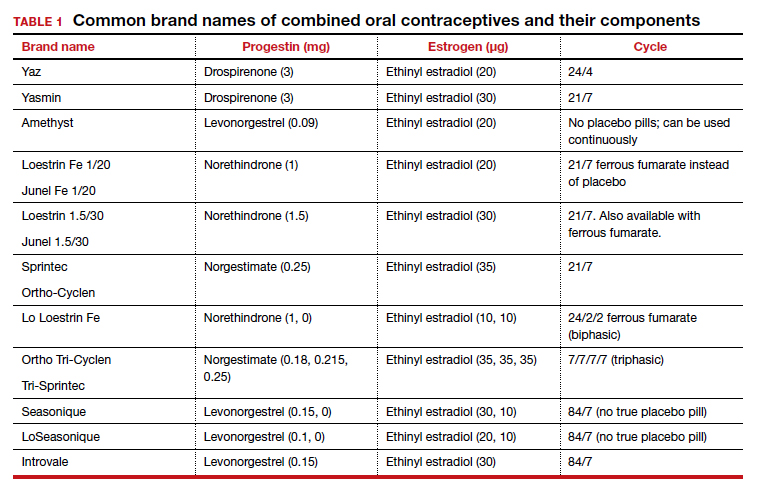
Benefits and risks
There are numerous noncontraceptive benefits of COCs, including menstrual cycle regulation; reduced risk of ovarian, endometrial, and colorectal cancer; and treatment of menorrhagia, dysmenorrhea, acne, menstrual migraine, premenstrual syndrome and premenstrual dysphoric disorder, pelvic pain due to endometriosis, and hirsutism.
Common patient concerns
In terms of adverse effects, there are more potential unwanted effects of concern to women than there are ones validated in the literature. Accepted adverse effects include nausea, breast tenderness, and decreased libido. However, one of the most common concerns voiced during contraceptive counseling is that COCs will cause weight gain. A 2014 Cochrane review identified 49 trials studying the weight gain question.2 Of those, only 4 had a placebo or nonintervention group. Of these 4, there was no significant difference in weight change between the COC-receiving group and the control group. When patients bring up their concerns, it may help to remind them that women tend to gain weight over time whether or not they are taking a COC.
Another common concern is that COCs cause mood changes. A 2016 review by Schaffir and colleagues sheds some light on this topic,3 albeit limited by the paucity of prospective studies. This review identified only 1 randomized controlled trial comparing depression incidence among women initiating a COC versus a placebo. There was no difference in the incidence of depression among the groups at 3 months. Among 4 large retrospective studies of women using COCs, the agents either had no or a beneficial effect on mood. Schaffir’s review reports that there may be greater mood adverse effects with COCs among women with underlying mood disorders.
Patients may worry that COC use will permanently impair their fertility or delay return to fertility after discontinuation. Research does indicate that return of fertility after stopping COCs often takes several months (compared with immediate fertility after discontinuing a barrier method). However, there still seem to be comparable conception rates within 12 months after discontinuing COCs as there are after discontinuing other common nonhormonal or hormonal contraceptive methods. Fertility is not impacted by the duration of COC use. In addition, return to fertility seems to be comparable after discontinuation of extended cycle or continuous COCs compared with traditional-cycle COCs.4
COC safety
Known major risks of COCs include venous thromboembolism (VTE). The risk of VTE is about double among COC users than among nonpregnant nonusers: 3–9 per 10,000 woman-years compared with 1–5.5 In a study by the US Food and Drug Administration, drospirenone-containing COCs had double the risk of VTE than other COCs. However, the position of the American College of Obstetricians and Gynecologists on this increased risk of VTE with drospirenone-containing pills is that it is “possible” and “minimal.”5 It is important to remember that an alternative to COC use is pregnancy, in which the VTE risk is about double that among COC users, at 5–20 per 10,000 woman-years. This risk increases further in the postpartum period, to 40–65 per 10,000 woman-years.5
Another known major risk of COCs is arterial embolic disease, including cerebrovascular accidents and myocardial infarctions. Women at increased risk for these complications include those with hypertension, diabetes, and/or obesity and women who are aged 35 or older and smoke. Interestingly, women with migraines with aura are at increased risk for stroke but not for myocardial infarction. These women increase their risk of stroke 2- to 4-fold if they use COCs.
Continue to: Different pills for different problems...
Different pills for different problems
With so many pills on the market, it is important for clinicians to know how to choose a particular pill for a particular patient. The following discussion assumes that the patient in question desires a COC for contraception, then offers guidance on how to choose a pill with patient-specific noncontraceptive benefits (TABLE 2).
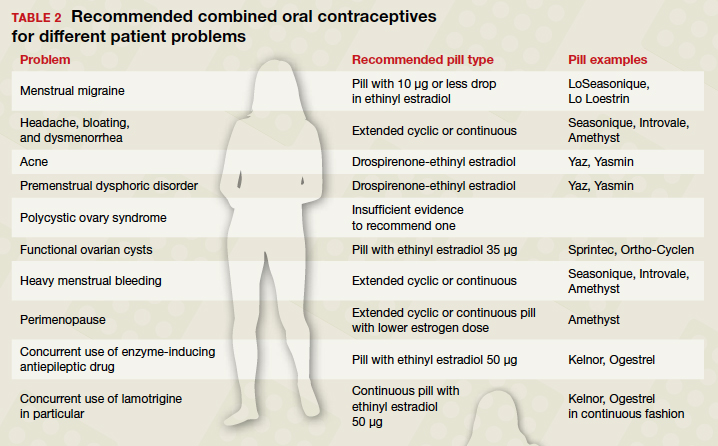
When HMB is a concern. Patients with heavy menstrual bleeding may experience fewer bleeding and/or spotting days with extended cyclic or continuous use of a COC rather than with traditional cyclic use.6 Examples of such COC options include:
- Introvale and Seasonique, both extended-cycle formulations
- Amethyst, which is formulated without placebo pills so that it can be used continuously
- any other COC prescribed with instructions for the patient to skip placebo pills.
An extrapolated benefit to extended-cycle or continuous COCs use for heavy menstrual bleeding is addressing anemia.
For premenstrual dysphoric disorder, the only randomized controlled trials showing improvement involve drospirenone-ethinyl estradiol pills (Yaz and Yasmin).7 There is also evidence that extended cyclic or continuous use of these formulations is more impactful for premenstrual dysphoric disorder than a traditional cycle.8
Keeping migraine avoidance and prevention in mind. Various studies have looked at the impact of different COC formulations on menstrual-related symptoms. There is evidence of greater improvement in headache, bloating, and dysmenorrhea with extended cyclic or continuous use compared with traditional cyclic use.6
In terms of headache, let us delve into menstrual migraine in particular. Menstrual migraines occur sometime between 2 days prior to 2 days after the first day of menses and are linked to a sharp drop in estrogen levels. COCs are contraindicated in women with menstrual migraines with aura because of the increased stroke risk. For women with menstrual migraines without aura, COCs can prevent migraines. Prevention depends on minimizing fluctuations in estrogen levels; any change in estrogen level greater than 10 µg of ethinyl estradiol may trigger an estrogen-related migraine. All currently available regimens of COCs that comprise 21 days of active pills and 7 days of placebo involve a drop of more than 10 µg. Options that involve a drop of 10 µg or less include any continuous formulation, the extended formulation LoSeasonique (levonorgestrel 0.1 mg and ethinyl estradiol 20 µg for 84 days, then ethinyl estradiol 10 µg for 7 days), and Lo Loestrin (ethinyl estradiol 10 µg and norethindrone 1 mg for 24 days, then ethinyl estradiol 10 µg for 2 days, then placebo for 2 days).9
What’s best for acne-prone patients? All COCs should improve acne by increasing levels of sex hormone binding globulin. However, some comparative studies have shown drospirenone-containing COCs to be the most effective for acne. This finding makes sense in light of studies demonstrating antiandrogenic effects of drospirenone.10
Managing PCOS symptoms. It seems logical, by extension, that drospirenone-containing COCs would be particularly beneficial for treating hirsutism associated with polycystic ovary syndrome (PCOS). Other low‒androgenic-potential progestins, such as a third-generation progestin (norgestimate or desogestrel), might similarly be hypothesized to be advantageous. However, there is currently insufficient evidence to recommend any one COC formulation over another for the indication of PCOS.11
Ovarian cysts: Can COCs be helpful? COCs are commonly prescribed by gynecologists for patients with functional ovarian cysts. It is important to note that COCs have not been found to hasten the resolution of existing cysts, so they should not be used for this purpose.12 Studies of early COCs, which had high doses of estrogen (on the order of 50 µg), showed lower rates of cysts among users. This effect seems to be attenuated with the lower-estrogen-dose pills that are currently available, but there still appears to be benefit. Therefore, for a patient prone to cysts who desires an oral contraceptive, a COC containing estrogen 35 µg is likely to be the most beneficial of COCs currently on the market.13,14
Lower-dosage COCs in perimenopause may be beneficial. COCs can ameliorate perimenopausal symptoms including abnormal uterine bleeding and vasomotor symptoms. Clinicians are often hesitant to prescribe COCs for perimenopausal women because of increased risk of VTE, stroke, myocardial infarction, and breast cancer with increasing age. However, age alone is not a contraindication to any contraceptive method. An extended cyclic or continuous regimen COC may be the best choice for a perimenopausal woman in order to avoid vasomotor symptoms that occur during hormone-free intervals. In addition, given the increasing risk of adverse effects like VTE with estrogen dose, a lower estrogen formulation is advisable.15
Patients with epilepsy who are taking antiepileptic drugs (AEDs) are a special population when it comes to COCs. Certain AEDs induce hepatic enzymes involved in the metabolism and protein binding of COCs, which can result in contraceptive failure. Strong inducers are carbamazepine, oxcarbazepine, perampanel, phenobarbital, phenytoin, and primidone. Weak inducers are clobazam, eslicarbazepine, felbamate, lamotrigine, rufinamide, and topiramate. Women taking any of the above AEDs are recommended to choose a different form of contraception than a COC. However, if they are limited to COCs for some reason, a preparation containing estrogen 50 µg is recommended. It is speculated that the efficacy and adverse effects of COCs with increased hormone doses, used in combination with enzyme-inducing AEDs, should be comparable to those with standard doses when not combined with AEDs; however, this speculation is unproven.16 There are few COCs on the market with estrogen doses of 50 µg, but a couple of examples are Kelnor and Ogestrel.
Additional factors have to be considered with concurrent COC use with the AED lamotrigine since COCs increase clearance of this agent. Therefore, patients taking lamotrigine who start COCs will need an increase in lamotrigine dose. To avoid fluctuations in lamotrigine serum levels, use of a continuous COC is recommended.17
Continue to: Pill types to minimize adverse effects or risks...
Pill types to minimize adverse effects or risks
For women who desire to use a COC for contraception but who are at risk for a particular complication or are bothered by a particular adverse effect, ObGyns can optimize the choice of pill (TABLE 3). For example, women who have adverse effects of nausea and/or breast tenderness may benefit from reducing the estrogen dose to 20 µg or lower.18
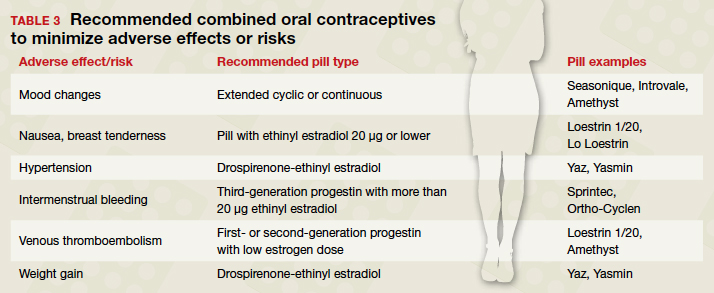
Considering VTE
As discussed previously, VTE is a risk with all COCs, but some pills confer greater risk than others. For one, VTE risk increases with estrogen dose. In addition, VTE risk depends on the type of progestin. Drospirenone and third-generation progestins (norgestimate, gestodene, and desogestrel) confer a higher risk of VTE than first- or second-generation progestins. For example, a pill with estradiol 30 µg and either a third-generation progestin or drospirenone has a 50% to 80% higher risk of VTE compared with a pill with estradiol 30 µg and levonorgestrel.
For patients at particularly high risk for VTE, COCs are contraindicated. For patients for whom COCs are considered medically appropriate but who are at higher risk (eg, obese women), it is wise to use a pill containing a first-generation (norethindrone) or second-generation progestin (levonorgestrel) combined with the lowest dose of estrogen that has tolerable adverse effects.19
What about hypertension concerns?
Let us turn our attention briefly to hypertension and its relation to COC use. While the American College of Cardiology and the American Heart Association redefined hypertension in 2017 using a threshold of 130/80 mm Hg, the American College of Obstetricians and Gynecologists (ACOG) considers hypertension to be 140/90 mm Hg in terms of safety of using COCs. ACOG states, “women with blood pressure below 140/90 mm Hg may use any hormonal contraceptive method.”20 In women with hypertension in the range of 140‒159 mm Hg systolic or 90‒99 mm Hg diastolic, COCs are category 3 according to the US Medical Eligibility Criteria for Contraceptive Use, meaning that the risks usually outweigh the benefits. For women with blood pressures of 160/110 mm Hg or greater, COCs are category 4 (contraindicated). If a woman with mild hypertension is started on a COC, a drospirenone-containing pill may be the best choice because of its diuretic effects. While other contemporary COCs have been associated with a mild increase in blood pressure, drospirenone-containing pills have not shown this association.21
Continue to: At issue: Break-through bleeding, mood, and weight gain...
At issue: Break-through bleeding, mood, and weight gain
For women bothered by intermenstrual bleeding, use of a COC with a third-generation progestin may be preferable to use of one with a first- or second-generation. It may be because of decreased abnormal bleeding that COCs with third-generation progestins have lower discontinuation rates.22 In addition, COCs containing estrogen 20 µg or less are associated with more intermenstrual bleeding than those with more than 20 µg estrogen.23 Keep in mind that it is common with any COC to have intermenstrual bleeding for the first several months.
For women with pre-existing mood disorders or who report mood changes with COCs, it appears that fluctuations in hormone levels are problematic. Consistently, there is evidence that monophasic pills are preferable to multiphasic and that extended cyclic or continuous use is preferable to traditional cyclic use for mitigating mood adverse effects. There is mixed evidence on whether a low dose of ethinyl estradiol is better for mood.3
Although it is discussed above that randomized controlled trials have not shown an association between COC use and weight gain, many women remain concerned. For these women, a drospirenone-containing COC may be the best choice. Drospirenone has antimineralocorticoid activity, so it may help prevent water retention.
A brief word about multiphasic COCs. While these pills were designed to mimic physiologic hormone fluctuations and minimize hormonal adverse effects, there is insufficient evidence to compare their effects to those of monophasic pills.24 Without such evidence, there is little reason to recommend a multiphasic pill to a patient over the more straightforward monophasic formulation.
Conclusion
There are more nuances to prescribing an optimal COC for a patient than may initially come to mind. It is useful to remember that any formulation of pill may be prescribed in an extended or continuous fashion, and there are benefits for such use for premenstrual dysphoric disorder, heavy menstrual bleeding, perimenopause, and menstrual symptoms. Although there are numerous brands of COCs available, a small cadre will suffice for almost all purposes. Such a “toolbox” of pills could include a pill formatted for continuous use (Seasonique), a low estrogen pill (Loestrin), a drospirenone-containing pill (Yaz), and a pill containing a third-generation progestin and a higher dose of estrogen (Sprintec). ●
- Daniels K, Abma JC. Current contraceptive status among women aged 15-49: United States, 2015-2017. NCHS Data Brief, no 327. Hyattsville, MD; 2018.
- Gallo MF, Lopez LM, Grimes DA, et al. Combination contraceptives: effects on weight. Cochrane Database Syst Rev. 2014:CD003987.
- Schaffir J, Worly BL, Gur TL. Combined hormonal contraception and its effects on mood: a critical review. Eur J Contracept Reprod Health Care. 2016;21:347-355.
- Barnhart KT, Schreiber CA. Return to fertility following discontinuation of oral contraceptives. Fertil Steril. 2009;91:659-663.
- American College of Obstetricians and Gynecologists. Committee Opinion #540: Risk of Venous Thromboembolism Among Users of Drospirenone-Containing Oral Contraceptive Pills. Obstet Gynecol. 2012;120:1239-1242.
- Edelman A, Micks E, Gallo MF, et al. Continuous or extended cycle vs. cyclic use of combined hormonal contraceptives for contraception. Cochrane Database Syst Rev. 2014:CD004695.
- American College of Obstetricians and Gynecologists. Practice Bulletin #110: Noncontraceptive Uses of Hormonal Contraceptives. Obstet Gynecol. 2010:206-218.
- Coffee AL, Kuehl TJ, Willis S, et al. Oral contraceptives and premenstrual symptoms: comparison of a 21/7 and extended regimen. Am J Obstet Gynecol. 2006;195:1311-1319.
- Calhoun AH, Batur P. Combined hormonal contraceptives and migraine: an update on the evidence. Cleve Clin J Med. 2017;84:631-638.
- Arowojolu AO, Gallo MF, Lopez LM, et al. Combined oral contraceptive pills for treatment of acne. Cochrane Database Syst Rev. 2012:CD004425.
- McCartney CR, Marshall JC. CLINICAL PRACTICE. Polycystic Ovary Syndrome. N Engl J Med. 2016;375:54-64.
- Grimes DA, Jones LB, Lopez LM, et al. Oral contraceptives for functional ovarian cysts. Cochrane Database Syst Rev. 2014:CD006134.
- Grimes DA, Godwin AJ, Rubin A, et al. Ovulation and follicular development associated with three low-dose oral contraceptives: a randomized controlled trial. Obstet Gynecol. 1994;83:29-34.
- Christensen JT, Boldsen JL, Westergaard JG. Functional ovarian cysts in premenopausal and gynecologically healthy women. Contraception. 2002;66:153-157.
- Hardman SM, Gebbie AE. Hormonal contraceptive regimens in the perimenopause. Maturitas. 2009;63:204-212.
- Zupanc ML. Antiepileptic drugs and hormonal contraceptives in adolescent women with epilepsy. Neurology. 2006;66 (6 suppl 3):S37-S45.
- Wegner I, Edelbroek PM, Bulk S, et al. Lamotrigine kinetics within the menstrual cycle, after menopause, and with oral contraceptives. Neurology. 2009;73:1388-1393.
- Stewart M, Black K. Choosing a combined oral contraceptive pill. Australian Prescriber. 2015;38:6-11.
- de Bastos M, Stegeman BH, Rosendaal FR, et al. Combined oral contraceptives: venous thrombosis. Cochrane Database Syst Rev. 2014:CD010813.
- American College of Obstetricians and Gynecologists. Practice Bulletin #206: use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2019;133:e128-e150.
- de Morais TL, Giribela C, Nisenbaum MG, et al. Effects of a contraceptive containing drospirenone and ethinylestradiol on blood pressure, metabolic profile and neurohumoral axis in hypertensive women at reproductive age. Eur J Obstet Gynecol Reprod Biol. 2014;182:113-117.
- Lawrie TA, Helmerhorst FM, Maitra NK, et al. Types of progestogens in combined oral contraception: effectiveness and side-effects. Cochrane Database Syst Rev. 2011:CD004861.
- Gallo MF, Nanda K, Grimes DA, et al. 20 µg versus >20 µg estrogen combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2013:CD003989.
- van Vliet HA, Grimes DA, Lopez LM, et al. Triphasic versus monophasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2006:CD003553
- Daniels K, Abma JC. Current contraceptive status among women aged 15-49: United States, 2015-2017. NCHS Data Brief, no 327. Hyattsville, MD; 2018.
- Gallo MF, Lopez LM, Grimes DA, et al. Combination contraceptives: effects on weight. Cochrane Database Syst Rev. 2014:CD003987.
- Schaffir J, Worly BL, Gur TL. Combined hormonal contraception and its effects on mood: a critical review. Eur J Contracept Reprod Health Care. 2016;21:347-355.
- Barnhart KT, Schreiber CA. Return to fertility following discontinuation of oral contraceptives. Fertil Steril. 2009;91:659-663.
- American College of Obstetricians and Gynecologists. Committee Opinion #540: Risk of Venous Thromboembolism Among Users of Drospirenone-Containing Oral Contraceptive Pills. Obstet Gynecol. 2012;120:1239-1242.
- Edelman A, Micks E, Gallo MF, et al. Continuous or extended cycle vs. cyclic use of combined hormonal contraceptives for contraception. Cochrane Database Syst Rev. 2014:CD004695.
- American College of Obstetricians and Gynecologists. Practice Bulletin #110: Noncontraceptive Uses of Hormonal Contraceptives. Obstet Gynecol. 2010:206-218.
- Coffee AL, Kuehl TJ, Willis S, et al. Oral contraceptives and premenstrual symptoms: comparison of a 21/7 and extended regimen. Am J Obstet Gynecol. 2006;195:1311-1319.
- Calhoun AH, Batur P. Combined hormonal contraceptives and migraine: an update on the evidence. Cleve Clin J Med. 2017;84:631-638.
- Arowojolu AO, Gallo MF, Lopez LM, et al. Combined oral contraceptive pills for treatment of acne. Cochrane Database Syst Rev. 2012:CD004425.
- McCartney CR, Marshall JC. CLINICAL PRACTICE. Polycystic Ovary Syndrome. N Engl J Med. 2016;375:54-64.
- Grimes DA, Jones LB, Lopez LM, et al. Oral contraceptives for functional ovarian cysts. Cochrane Database Syst Rev. 2014:CD006134.
- Grimes DA, Godwin AJ, Rubin A, et al. Ovulation and follicular development associated with three low-dose oral contraceptives: a randomized controlled trial. Obstet Gynecol. 1994;83:29-34.
- Christensen JT, Boldsen JL, Westergaard JG. Functional ovarian cysts in premenopausal and gynecologically healthy women. Contraception. 2002;66:153-157.
- Hardman SM, Gebbie AE. Hormonal contraceptive regimens in the perimenopause. Maturitas. 2009;63:204-212.
- Zupanc ML. Antiepileptic drugs and hormonal contraceptives in adolescent women with epilepsy. Neurology. 2006;66 (6 suppl 3):S37-S45.
- Wegner I, Edelbroek PM, Bulk S, et al. Lamotrigine kinetics within the menstrual cycle, after menopause, and with oral contraceptives. Neurology. 2009;73:1388-1393.
- Stewart M, Black K. Choosing a combined oral contraceptive pill. Australian Prescriber. 2015;38:6-11.
- de Bastos M, Stegeman BH, Rosendaal FR, et al. Combined oral contraceptives: venous thrombosis. Cochrane Database Syst Rev. 2014:CD010813.
- American College of Obstetricians and Gynecologists. Practice Bulletin #206: use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2019;133:e128-e150.
- de Morais TL, Giribela C, Nisenbaum MG, et al. Effects of a contraceptive containing drospirenone and ethinylestradiol on blood pressure, metabolic profile and neurohumoral axis in hypertensive women at reproductive age. Eur J Obstet Gynecol Reprod Biol. 2014;182:113-117.
- Lawrie TA, Helmerhorst FM, Maitra NK, et al. Types of progestogens in combined oral contraception: effectiveness and side-effects. Cochrane Database Syst Rev. 2011:CD004861.
- Gallo MF, Nanda K, Grimes DA, et al. 20 µg versus >20 µg estrogen combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2013:CD003989.
- van Vliet HA, Grimes DA, Lopez LM, et al. Triphasic versus monophasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2006:CD003553
For obese postmenopausal women, what options may decrease endometrial cancer risk?
Endometrial cancer is the most common gynecologic malignancy, with approximately 59,000 cases diagnosed annually,1 and a lifetime risk of approximately 3.1% in the United States.2 Type I endometrial cancer includes tumors with endometrioid histology that are grade 1 or 2. Type II endometrial cancer includes tumors that have grade 3 endometrioid or nonendometrioid histology, including serous, clear cell, mucinous, squamous transitional cell, mesonephric, and undifferentiated tumors.3 Type I endometrial cancer is hormone sensitive, generally stimulated by estrogen and suppressed by progestins.
Endometrial cancer is diagnosed at a mean age of 63 years,4 and only 15% of cases occur before age 50.5 Women with an elevated body mass index (BMI) have a markedly increased risk of both Types I and II endometrial cancer (TABLE).6 Hence, endometrial cancer is highly prevalent in obese postmenopausal women. For these women health interventions that may reduce the risk of developing endometrial cancer include dieting, physical activity, bariatric surgery, and progestin therapy.

Educating patients is a priority
Many women do not know that postmenopausal bleeding is a sign of endometrial cancer. All postmenopausal women should be advised that if they develop vaginal bleeding they need to be evaluated by a clinician.7 Women who are knowledgeable about the link between postmenopausal vaginal bleeding and endometrial cancer can be encouraged to share this information with their postmenopausal friends in order to reach more people with this important information. All obese postmenopausal women should be advised that weight loss and increased physical activity can reduce the risk of developing endometrial cancer.
How weight loss and physical activity affect risk
Intentional weight loss has been reported to reduce the risk of endometrial cancer in postmenopausal women. As part of the Women’s Health Initiative observational study, 36,794 postmenopausal women aged 50 to 79 years with a uterus had their body weight and height measured at entry into the study and after 3 years of follow-up.8 During the 11 years following study entry, there were 566 incident cases of endometrial cancer. Compared with women who had a stable weight, intentional weight loss of ≥5% was associated with a 40% reduction in the risk of endometrial cancer (hazard ratio [HR], 0.60; 95% confidence interval [CI], 0.42–0.86). Compared with women who had a stable weight, women who had weight gain ≥10% had an increased risk of endometrial cancer (HR, 1.26; 95% CI, 1.00–1.57).
High levels of physical activity may be associated with a decreased risk of endometrial cancer. In one study, compared with a sedentary lifestyle, higher levels of physical activity were reported to be associated with a decreased risk of endometrial cancer.9
Continue to: How bariatric surgery affects risk...
How bariatric surgery affects risk
Many cancers are associated with obesity, including endometrial, breast, colon, pancreas, gallbladder, and renal. Obesity is associated with increased conversion of androgens to estrogens in fat tissue, stimulating excessive endometrial proliferation and increasing the risk of endometrial hyperplasia and cancer. Bariatric surgery reliably causes sustained weight reduction. Multiple studies have reported that bariatric surgery reduces the risk of endometrial cancer.
Schauer and colleagues used data from the Kaiser Permanente health system to identify 22,198 obese people who had undergone bariatric surgery and 66,427 matched controls who were obese but did not have surgery.10 The study population was 81% female, with a mean age of 45 years and a mean BMI of 45 kg/m2. After an average 3.5 years of follow-up there were 2,542 incident cases of cancer, including 322 cases of endometrial cancer. Compared with conventional weight loss treatment, bariatric surgery reduced the risk of endometrial cancer by 50% (HR, 0.50; 95% CI, 0.37–0.67; P<.001).10 In addition, bariatric surgery reduced the risk of colon and pancreatic cancer by 41% and 54%, respectively.10
In the Swedish Obese Subjects (SOS) study, 1,420 women who underwent bariatric surgery and 1,447 matched controls who received conventional obesity treatment were followed for 18 years.11 At study entry, the mean age of the women was approximately 48 years, and the mean BMI was approximately 42 kg/m2. In follow-up there were 76 incident cases of endometrial cancer. Compared with women receiving conventional obesity treatment, women who had bariatric surgery had a non–statistically significant 49% decrease in the risk of developing endometrial cancer (HR, 0.51; 95% CI, 0.24–1.10)
In a systematic review of 5 additional studies (not including publications 10 or 11) of the impact of bariatric surgery on the risk of developing endometrial cancer, the surgery was associated with a 68% risk reduction (odds ratio [OR], 0.32; 95% CI, 0.16–0.63) compared with matched obese women that did not have surgery.12
Although there are no randomized prospective studies showing that bariatric surgery reduces the risk of endometrial cancer, the weight of the observation evidence is strong. In addition, bariatric surgery was reported to reduce all-cause mortality in the SOS study.13 Hence, for obese postmenopausal women, if lifestyle changes do not result in sustained weight loss, bariatric surgery may be an optimal approach to improving health outcomes.
Continue to: Progestin treatment and endometrial cancer risk...
Progestin treatment and endometrial cancer risk
Estrogen stimulates endometrial cell proliferation. Hence, unopposed chronic exposure to estrogen is a major risk factor for developing endometrial hyperplasia and cancer. Progestins block the proliferative effect of estrogen and cause cell differentiation, resulting in stromal decidualization. Progestins also reduce the concentration of estrogen and progesterone receptors and increase the activity of enzymes that convert estradiol to estrone, blocking estrogen-induced endometrial proliferation.14
In women with endometrial hyperplasia, progestins have been shown to be effective in resolving the hyperplasia in approximately 80% of cases. Both oral progestins and the 52-mg levonorgestrel-containing intrauterine device (LNG-IUD) have been reported to be effective in the treatment of endometrial hyperplasia. In a Cochrane systematic review and meta-analysis, the 52-mg LNG-IUD was reported to be somewhat more effective in resolving endometrial hyperplasia than cyclic oral progestins (89% vs 72%, respectively).15
Other studies have also reported that the 52 mg LNG-IUD was more effective than oral progestin therapy for women with complex atypical endometrial hyperplasia.16 There are no large randomized clinical trials of progestin therapy on prevention for future development of endometrial cancer in obese postmenopausal women who have a normal endometrial histology. However, for an obese perimenopausal woman, insertion of a 52-mg LNG-IUD may help to minimize excessive uterine bleeding during the menopause transition and reduce the risk of developing endometrial hyperplasia during the early postmenopause.
We can help our patients reduce their risk of endometrial cancer
Obese postmenopausal women are at increased risk for developing endometrial cancer. Gynecologists play an important role in the prevention and early detection of endometrial cancer. We can make a difference and improve the health of our obese peri- and postmenopausal women by recommending interventions that reduce the risk of endometrial cancer, thereby improving the health of our patients. ●
- American Society of Clinical Oncology. Uterine cancer statistics. https://www.cancer.net/cancer-types/uterine-cancer/statistics#:~:text=This%20year%2C%20an%20
estimated%2065%2C620,cancers%20occur%20in%20the%20endometrium. Accessed November 23, 2020. - Howlader N, Noone AM, Krapcho M, et al (eds). SEER Cancer Statistics Review, 1975-2017. National Cancer Institute: Bethesda, MD. April 15, 2020. https://seer.cancer.gov/csr/1975_2017/. Accessed November 23, 2020.
- Noer MC, Antonsen SL, Ottesen B, et al. Type I versus Type II endometrial cancer: differential impact of comorbidity. Int J Gynecol Cancer. 2018;28:586-593.
- Sorosky JI. Endometrial cancer. Obstet Gynecol. 2008;111:436-437.
- Gallup DG, Stock RJ. Adenocarcinoma of the endometrium in women 40 years of age or younger. Obstet Gynecol. 1984;64:417-420.
- Setiawan VW, Yang HP, Pike MC, et al. Type I and II endometrial cancers: have they different risk factors. J Clin Oncol. 2013;31:2607-2618.
- Saccardi C, Vitagliano A, Marchetti M, et al. Endometrial cancer risk prediction according to indication of diagnostic hysteroscopy in postmenopausal women. Diagnostics (Basel). 2020;10:257.e1-e11.
- Luo J, Chlebowski RT, Hendryx M, et al. Intentional weight loss and endometrial cancer risk. J Clin Oncology. 2017;35:1189-1193.
- Friedenreich CM, Ryder-Burbidge C, McNeil J. Physical activity, obesity and sedentary behavior in cancer etiology: epidemiologic evidence and biological mechanisms. Mol Oncol. August 2, 2020. doi: 10.1001/1878-0261.12772.
- Schauer DP, Feigelson HS, Koebnick C, et al. Bariatric surgery and the risk of cancer in a large multisite cohort. Ann Surg. 2019;269:95-101.
- Anvenden A, Taube M, Peltonen M, et al. Long-term incidence of female-specific cancer after bariatric surgery or usual care in the Swedish Obese Subjects Study. Gynecol Oncol. 2017;145:224-229.
- Winder AA, Kularatna M, MacCormick AD. Does bariatric surgery affect the incidence of endometrial cancer development? A systematic review. Obes Surg. 2018;28:1433-1440.
- Carlsson LM, Sjoholm K, Jacobson P, et al. Life expectancy after bariatric surgery in the Swedish Obese Subjects Study. N Engl J Med. 2020;383:1535-1543.
- Lessey BA, Young SL. In: Strauss JF, Barbieri RL (eds.) Yen and Jaffe’s Reproductive Endocrinology: Physiology, Pathophysiology and Clinical Management. 8th ed. Elsevier Saunders: Philadelphia, PA; 2018:208-212.
- Mittermeier T, Farrant C, Wise MR. Levonorgestrel-releasing intrauterine system for endometrial hyperplasia. Cochrane Database Syst Rev. 2020;CD012658.
- Mandelbaum RS, Ciccone MA, Nusbaum DJ, et al. Progestin therapy for obese women with complex atypical hyperplasia: levonorgestrel-releasing intrauterine device vs systemic therapy. Am J Obstet Gynecol. 2020;223:103.e1-e13.
Endometrial cancer is the most common gynecologic malignancy, with approximately 59,000 cases diagnosed annually,1 and a lifetime risk of approximately 3.1% in the United States.2 Type I endometrial cancer includes tumors with endometrioid histology that are grade 1 or 2. Type II endometrial cancer includes tumors that have grade 3 endometrioid or nonendometrioid histology, including serous, clear cell, mucinous, squamous transitional cell, mesonephric, and undifferentiated tumors.3 Type I endometrial cancer is hormone sensitive, generally stimulated by estrogen and suppressed by progestins.
Endometrial cancer is diagnosed at a mean age of 63 years,4 and only 15% of cases occur before age 50.5 Women with an elevated body mass index (BMI) have a markedly increased risk of both Types I and II endometrial cancer (TABLE).6 Hence, endometrial cancer is highly prevalent in obese postmenopausal women. For these women health interventions that may reduce the risk of developing endometrial cancer include dieting, physical activity, bariatric surgery, and progestin therapy.

Educating patients is a priority
Many women do not know that postmenopausal bleeding is a sign of endometrial cancer. All postmenopausal women should be advised that if they develop vaginal bleeding they need to be evaluated by a clinician.7 Women who are knowledgeable about the link between postmenopausal vaginal bleeding and endometrial cancer can be encouraged to share this information with their postmenopausal friends in order to reach more people with this important information. All obese postmenopausal women should be advised that weight loss and increased physical activity can reduce the risk of developing endometrial cancer.
How weight loss and physical activity affect risk
Intentional weight loss has been reported to reduce the risk of endometrial cancer in postmenopausal women. As part of the Women’s Health Initiative observational study, 36,794 postmenopausal women aged 50 to 79 years with a uterus had their body weight and height measured at entry into the study and after 3 years of follow-up.8 During the 11 years following study entry, there were 566 incident cases of endometrial cancer. Compared with women who had a stable weight, intentional weight loss of ≥5% was associated with a 40% reduction in the risk of endometrial cancer (hazard ratio [HR], 0.60; 95% confidence interval [CI], 0.42–0.86). Compared with women who had a stable weight, women who had weight gain ≥10% had an increased risk of endometrial cancer (HR, 1.26; 95% CI, 1.00–1.57).
High levels of physical activity may be associated with a decreased risk of endometrial cancer. In one study, compared with a sedentary lifestyle, higher levels of physical activity were reported to be associated with a decreased risk of endometrial cancer.9
Continue to: How bariatric surgery affects risk...
How bariatric surgery affects risk
Many cancers are associated with obesity, including endometrial, breast, colon, pancreas, gallbladder, and renal. Obesity is associated with increased conversion of androgens to estrogens in fat tissue, stimulating excessive endometrial proliferation and increasing the risk of endometrial hyperplasia and cancer. Bariatric surgery reliably causes sustained weight reduction. Multiple studies have reported that bariatric surgery reduces the risk of endometrial cancer.
Schauer and colleagues used data from the Kaiser Permanente health system to identify 22,198 obese people who had undergone bariatric surgery and 66,427 matched controls who were obese but did not have surgery.10 The study population was 81% female, with a mean age of 45 years and a mean BMI of 45 kg/m2. After an average 3.5 years of follow-up there were 2,542 incident cases of cancer, including 322 cases of endometrial cancer. Compared with conventional weight loss treatment, bariatric surgery reduced the risk of endometrial cancer by 50% (HR, 0.50; 95% CI, 0.37–0.67; P<.001).10 In addition, bariatric surgery reduced the risk of colon and pancreatic cancer by 41% and 54%, respectively.10
In the Swedish Obese Subjects (SOS) study, 1,420 women who underwent bariatric surgery and 1,447 matched controls who received conventional obesity treatment were followed for 18 years.11 At study entry, the mean age of the women was approximately 48 years, and the mean BMI was approximately 42 kg/m2. In follow-up there were 76 incident cases of endometrial cancer. Compared with women receiving conventional obesity treatment, women who had bariatric surgery had a non–statistically significant 49% decrease in the risk of developing endometrial cancer (HR, 0.51; 95% CI, 0.24–1.10)
In a systematic review of 5 additional studies (not including publications 10 or 11) of the impact of bariatric surgery on the risk of developing endometrial cancer, the surgery was associated with a 68% risk reduction (odds ratio [OR], 0.32; 95% CI, 0.16–0.63) compared with matched obese women that did not have surgery.12
Although there are no randomized prospective studies showing that bariatric surgery reduces the risk of endometrial cancer, the weight of the observation evidence is strong. In addition, bariatric surgery was reported to reduce all-cause mortality in the SOS study.13 Hence, for obese postmenopausal women, if lifestyle changes do not result in sustained weight loss, bariatric surgery may be an optimal approach to improving health outcomes.
Continue to: Progestin treatment and endometrial cancer risk...
Progestin treatment and endometrial cancer risk
Estrogen stimulates endometrial cell proliferation. Hence, unopposed chronic exposure to estrogen is a major risk factor for developing endometrial hyperplasia and cancer. Progestins block the proliferative effect of estrogen and cause cell differentiation, resulting in stromal decidualization. Progestins also reduce the concentration of estrogen and progesterone receptors and increase the activity of enzymes that convert estradiol to estrone, blocking estrogen-induced endometrial proliferation.14
In women with endometrial hyperplasia, progestins have been shown to be effective in resolving the hyperplasia in approximately 80% of cases. Both oral progestins and the 52-mg levonorgestrel-containing intrauterine device (LNG-IUD) have been reported to be effective in the treatment of endometrial hyperplasia. In a Cochrane systematic review and meta-analysis, the 52-mg LNG-IUD was reported to be somewhat more effective in resolving endometrial hyperplasia than cyclic oral progestins (89% vs 72%, respectively).15
Other studies have also reported that the 52 mg LNG-IUD was more effective than oral progestin therapy for women with complex atypical endometrial hyperplasia.16 There are no large randomized clinical trials of progestin therapy on prevention for future development of endometrial cancer in obese postmenopausal women who have a normal endometrial histology. However, for an obese perimenopausal woman, insertion of a 52-mg LNG-IUD may help to minimize excessive uterine bleeding during the menopause transition and reduce the risk of developing endometrial hyperplasia during the early postmenopause.
We can help our patients reduce their risk of endometrial cancer
Obese postmenopausal women are at increased risk for developing endometrial cancer. Gynecologists play an important role in the prevention and early detection of endometrial cancer. We can make a difference and improve the health of our obese peri- and postmenopausal women by recommending interventions that reduce the risk of endometrial cancer, thereby improving the health of our patients. ●
Endometrial cancer is the most common gynecologic malignancy, with approximately 59,000 cases diagnosed annually,1 and a lifetime risk of approximately 3.1% in the United States.2 Type I endometrial cancer includes tumors with endometrioid histology that are grade 1 or 2. Type II endometrial cancer includes tumors that have grade 3 endometrioid or nonendometrioid histology, including serous, clear cell, mucinous, squamous transitional cell, mesonephric, and undifferentiated tumors.3 Type I endometrial cancer is hormone sensitive, generally stimulated by estrogen and suppressed by progestins.
Endometrial cancer is diagnosed at a mean age of 63 years,4 and only 15% of cases occur before age 50.5 Women with an elevated body mass index (BMI) have a markedly increased risk of both Types I and II endometrial cancer (TABLE).6 Hence, endometrial cancer is highly prevalent in obese postmenopausal women. For these women health interventions that may reduce the risk of developing endometrial cancer include dieting, physical activity, bariatric surgery, and progestin therapy.

Educating patients is a priority
Many women do not know that postmenopausal bleeding is a sign of endometrial cancer. All postmenopausal women should be advised that if they develop vaginal bleeding they need to be evaluated by a clinician.7 Women who are knowledgeable about the link between postmenopausal vaginal bleeding and endometrial cancer can be encouraged to share this information with their postmenopausal friends in order to reach more people with this important information. All obese postmenopausal women should be advised that weight loss and increased physical activity can reduce the risk of developing endometrial cancer.
How weight loss and physical activity affect risk
Intentional weight loss has been reported to reduce the risk of endometrial cancer in postmenopausal women. As part of the Women’s Health Initiative observational study, 36,794 postmenopausal women aged 50 to 79 years with a uterus had their body weight and height measured at entry into the study and after 3 years of follow-up.8 During the 11 years following study entry, there were 566 incident cases of endometrial cancer. Compared with women who had a stable weight, intentional weight loss of ≥5% was associated with a 40% reduction in the risk of endometrial cancer (hazard ratio [HR], 0.60; 95% confidence interval [CI], 0.42–0.86). Compared with women who had a stable weight, women who had weight gain ≥10% had an increased risk of endometrial cancer (HR, 1.26; 95% CI, 1.00–1.57).
High levels of physical activity may be associated with a decreased risk of endometrial cancer. In one study, compared with a sedentary lifestyle, higher levels of physical activity were reported to be associated with a decreased risk of endometrial cancer.9
Continue to: How bariatric surgery affects risk...
How bariatric surgery affects risk
Many cancers are associated with obesity, including endometrial, breast, colon, pancreas, gallbladder, and renal. Obesity is associated with increased conversion of androgens to estrogens in fat tissue, stimulating excessive endometrial proliferation and increasing the risk of endometrial hyperplasia and cancer. Bariatric surgery reliably causes sustained weight reduction. Multiple studies have reported that bariatric surgery reduces the risk of endometrial cancer.
Schauer and colleagues used data from the Kaiser Permanente health system to identify 22,198 obese people who had undergone bariatric surgery and 66,427 matched controls who were obese but did not have surgery.10 The study population was 81% female, with a mean age of 45 years and a mean BMI of 45 kg/m2. After an average 3.5 years of follow-up there were 2,542 incident cases of cancer, including 322 cases of endometrial cancer. Compared with conventional weight loss treatment, bariatric surgery reduced the risk of endometrial cancer by 50% (HR, 0.50; 95% CI, 0.37–0.67; P<.001).10 In addition, bariatric surgery reduced the risk of colon and pancreatic cancer by 41% and 54%, respectively.10
In the Swedish Obese Subjects (SOS) study, 1,420 women who underwent bariatric surgery and 1,447 matched controls who received conventional obesity treatment were followed for 18 years.11 At study entry, the mean age of the women was approximately 48 years, and the mean BMI was approximately 42 kg/m2. In follow-up there were 76 incident cases of endometrial cancer. Compared with women receiving conventional obesity treatment, women who had bariatric surgery had a non–statistically significant 49% decrease in the risk of developing endometrial cancer (HR, 0.51; 95% CI, 0.24–1.10)
In a systematic review of 5 additional studies (not including publications 10 or 11) of the impact of bariatric surgery on the risk of developing endometrial cancer, the surgery was associated with a 68% risk reduction (odds ratio [OR], 0.32; 95% CI, 0.16–0.63) compared with matched obese women that did not have surgery.12
Although there are no randomized prospective studies showing that bariatric surgery reduces the risk of endometrial cancer, the weight of the observation evidence is strong. In addition, bariatric surgery was reported to reduce all-cause mortality in the SOS study.13 Hence, for obese postmenopausal women, if lifestyle changes do not result in sustained weight loss, bariatric surgery may be an optimal approach to improving health outcomes.
Continue to: Progestin treatment and endometrial cancer risk...
Progestin treatment and endometrial cancer risk
Estrogen stimulates endometrial cell proliferation. Hence, unopposed chronic exposure to estrogen is a major risk factor for developing endometrial hyperplasia and cancer. Progestins block the proliferative effect of estrogen and cause cell differentiation, resulting in stromal decidualization. Progestins also reduce the concentration of estrogen and progesterone receptors and increase the activity of enzymes that convert estradiol to estrone, blocking estrogen-induced endometrial proliferation.14
In women with endometrial hyperplasia, progestins have been shown to be effective in resolving the hyperplasia in approximately 80% of cases. Both oral progestins and the 52-mg levonorgestrel-containing intrauterine device (LNG-IUD) have been reported to be effective in the treatment of endometrial hyperplasia. In a Cochrane systematic review and meta-analysis, the 52-mg LNG-IUD was reported to be somewhat more effective in resolving endometrial hyperplasia than cyclic oral progestins (89% vs 72%, respectively).15
Other studies have also reported that the 52 mg LNG-IUD was more effective than oral progestin therapy for women with complex atypical endometrial hyperplasia.16 There are no large randomized clinical trials of progestin therapy on prevention for future development of endometrial cancer in obese postmenopausal women who have a normal endometrial histology. However, for an obese perimenopausal woman, insertion of a 52-mg LNG-IUD may help to minimize excessive uterine bleeding during the menopause transition and reduce the risk of developing endometrial hyperplasia during the early postmenopause.
We can help our patients reduce their risk of endometrial cancer
Obese postmenopausal women are at increased risk for developing endometrial cancer. Gynecologists play an important role in the prevention and early detection of endometrial cancer. We can make a difference and improve the health of our obese peri- and postmenopausal women by recommending interventions that reduce the risk of endometrial cancer, thereby improving the health of our patients. ●
- American Society of Clinical Oncology. Uterine cancer statistics. https://www.cancer.net/cancer-types/uterine-cancer/statistics#:~:text=This%20year%2C%20an%20
estimated%2065%2C620,cancers%20occur%20in%20the%20endometrium. Accessed November 23, 2020. - Howlader N, Noone AM, Krapcho M, et al (eds). SEER Cancer Statistics Review, 1975-2017. National Cancer Institute: Bethesda, MD. April 15, 2020. https://seer.cancer.gov/csr/1975_2017/. Accessed November 23, 2020.
- Noer MC, Antonsen SL, Ottesen B, et al. Type I versus Type II endometrial cancer: differential impact of comorbidity. Int J Gynecol Cancer. 2018;28:586-593.
- Sorosky JI. Endometrial cancer. Obstet Gynecol. 2008;111:436-437.
- Gallup DG, Stock RJ. Adenocarcinoma of the endometrium in women 40 years of age or younger. Obstet Gynecol. 1984;64:417-420.
- Setiawan VW, Yang HP, Pike MC, et al. Type I and II endometrial cancers: have they different risk factors. J Clin Oncol. 2013;31:2607-2618.
- Saccardi C, Vitagliano A, Marchetti M, et al. Endometrial cancer risk prediction according to indication of diagnostic hysteroscopy in postmenopausal women. Diagnostics (Basel). 2020;10:257.e1-e11.
- Luo J, Chlebowski RT, Hendryx M, et al. Intentional weight loss and endometrial cancer risk. J Clin Oncology. 2017;35:1189-1193.
- Friedenreich CM, Ryder-Burbidge C, McNeil J. Physical activity, obesity and sedentary behavior in cancer etiology: epidemiologic evidence and biological mechanisms. Mol Oncol. August 2, 2020. doi: 10.1001/1878-0261.12772.
- Schauer DP, Feigelson HS, Koebnick C, et al. Bariatric surgery and the risk of cancer in a large multisite cohort. Ann Surg. 2019;269:95-101.
- Anvenden A, Taube M, Peltonen M, et al. Long-term incidence of female-specific cancer after bariatric surgery or usual care in the Swedish Obese Subjects Study. Gynecol Oncol. 2017;145:224-229.
- Winder AA, Kularatna M, MacCormick AD. Does bariatric surgery affect the incidence of endometrial cancer development? A systematic review. Obes Surg. 2018;28:1433-1440.
- Carlsson LM, Sjoholm K, Jacobson P, et al. Life expectancy after bariatric surgery in the Swedish Obese Subjects Study. N Engl J Med. 2020;383:1535-1543.
- Lessey BA, Young SL. In: Strauss JF, Barbieri RL (eds.) Yen and Jaffe’s Reproductive Endocrinology: Physiology, Pathophysiology and Clinical Management. 8th ed. Elsevier Saunders: Philadelphia, PA; 2018:208-212.
- Mittermeier T, Farrant C, Wise MR. Levonorgestrel-releasing intrauterine system for endometrial hyperplasia. Cochrane Database Syst Rev. 2020;CD012658.
- Mandelbaum RS, Ciccone MA, Nusbaum DJ, et al. Progestin therapy for obese women with complex atypical hyperplasia: levonorgestrel-releasing intrauterine device vs systemic therapy. Am J Obstet Gynecol. 2020;223:103.e1-e13.
- American Society of Clinical Oncology. Uterine cancer statistics. https://www.cancer.net/cancer-types/uterine-cancer/statistics#:~:text=This%20year%2C%20an%20
estimated%2065%2C620,cancers%20occur%20in%20the%20endometrium. Accessed November 23, 2020. - Howlader N, Noone AM, Krapcho M, et al (eds). SEER Cancer Statistics Review, 1975-2017. National Cancer Institute: Bethesda, MD. April 15, 2020. https://seer.cancer.gov/csr/1975_2017/. Accessed November 23, 2020.
- Noer MC, Antonsen SL, Ottesen B, et al. Type I versus Type II endometrial cancer: differential impact of comorbidity. Int J Gynecol Cancer. 2018;28:586-593.
- Sorosky JI. Endometrial cancer. Obstet Gynecol. 2008;111:436-437.
- Gallup DG, Stock RJ. Adenocarcinoma of the endometrium in women 40 years of age or younger. Obstet Gynecol. 1984;64:417-420.
- Setiawan VW, Yang HP, Pike MC, et al. Type I and II endometrial cancers: have they different risk factors. J Clin Oncol. 2013;31:2607-2618.
- Saccardi C, Vitagliano A, Marchetti M, et al. Endometrial cancer risk prediction according to indication of diagnostic hysteroscopy in postmenopausal women. Diagnostics (Basel). 2020;10:257.e1-e11.
- Luo J, Chlebowski RT, Hendryx M, et al. Intentional weight loss and endometrial cancer risk. J Clin Oncology. 2017;35:1189-1193.
- Friedenreich CM, Ryder-Burbidge C, McNeil J. Physical activity, obesity and sedentary behavior in cancer etiology: epidemiologic evidence and biological mechanisms. Mol Oncol. August 2, 2020. doi: 10.1001/1878-0261.12772.
- Schauer DP, Feigelson HS, Koebnick C, et al. Bariatric surgery and the risk of cancer in a large multisite cohort. Ann Surg. 2019;269:95-101.
- Anvenden A, Taube M, Peltonen M, et al. Long-term incidence of female-specific cancer after bariatric surgery or usual care in the Swedish Obese Subjects Study. Gynecol Oncol. 2017;145:224-229.
- Winder AA, Kularatna M, MacCormick AD. Does bariatric surgery affect the incidence of endometrial cancer development? A systematic review. Obes Surg. 2018;28:1433-1440.
- Carlsson LM, Sjoholm K, Jacobson P, et al. Life expectancy after bariatric surgery in the Swedish Obese Subjects Study. N Engl J Med. 2020;383:1535-1543.
- Lessey BA, Young SL. In: Strauss JF, Barbieri RL (eds.) Yen and Jaffe’s Reproductive Endocrinology: Physiology, Pathophysiology and Clinical Management. 8th ed. Elsevier Saunders: Philadelphia, PA; 2018:208-212.
- Mittermeier T, Farrant C, Wise MR. Levonorgestrel-releasing intrauterine system for endometrial hyperplasia. Cochrane Database Syst Rev. 2020;CD012658.
- Mandelbaum RS, Ciccone MA, Nusbaum DJ, et al. Progestin therapy for obese women with complex atypical hyperplasia: levonorgestrel-releasing intrauterine device vs systemic therapy. Am J Obstet Gynecol. 2020;223:103.e1-e13.
Cervical cancer recurrence patterns differ after laparoscopic and open hysterectomy
When cervical cancer recurs after radical hysterectomy, the likelihood of recurrence at certain sites and the timing of recurrence may be associated with the surgical approach, according to a retrospective study.
according to a propensity-matched analysis of data from 105 patients with recurrence.
And recurrence in the pelvic cavity and peritoneal carcinomatosis were more common after laparoscopic hysterectomy than after open surgery. Overall survival was similar between the groups, however.
The different patterns of recurrence may relate to dissemination of the disease during colpotomy, but the reasons are unknown, study author Giorgio Bogani, MD, PhD, said at the meeting sponsored by AAGL.
To examine patterns of recurrence after laparoscopic and open abdominal radical hysterectomy for cervical cancer, Dr. Bogani of the department of gynecologic surgery at the National Cancer Institute in Milan and colleagues analyzed data from patients with cervical cancer who developed recurrence after surgery at two oncologic referral centers between 1990 and 2018 (Int J Gynecol Cancer. 2020 Jul. doi: 10.1136/ijgc-2020-001381).
The investigators applied a propensity-matching algorithm to reduce possible confounding factors. They matched 35 patients who had recurrence after laparoscopic hysterectomy to 70 patients who had recurrence after open surgery. The groups had similar baseline characteristics.
As in the Laparoscopic Approach to Cervical Cancer (LACC) trial, patients who had minimally invasive surgery were more likely to have a worse disease-free survival, compared with patients who had open surgery, Dr. Bogani said. Patients who underwent laparoscopic radical hysterectomy had a median progression-free survival of 8 months, whereas patients who underwent open abdominal procedures had a median progression-free survival of 15.8 months.
Although vaginal, lymphatic, and distant recurrences were similar between the groups, a greater percentage of patients in the laparoscopic hysterectomy group had recurrence in the pelvic cavity (74% vs. 34%) and peritoneal carcinomatosis (17% vs. 1.5%).
The LACC trial, which found significantly lower disease-free and overall survival with laparoscopic hysterectomy, sent a “shockwave through the gynecologic oncology community” when it was published in 2018, said Masoud Azodi, MD, in a discussion following Dr. Bogani’s presentation.
Researchers have raised questions about that trial’s design and validity, noted Dr. Azodi, director of minimally invasive and robotic surgery at Yale University in New Haven, Conn.
It could be that local recurrences are attributable to surgical technique, rather than to the minimally invasive approach in itself, Dr. Azodi said. Prior studies of laparoscopic hysterectomy for cervical cancer had indicated better surgical outcomes and equivalent oncologic results, relative to open surgery.
Before the LACC trial, Dr. Bogani used the minimally invasive approach for almost all surgeries. Since then, he has performed open surgeries. If he were to use a minimally invasive approach now, it would be in the context of a clinical trial, Dr. Bogani said.
Dr. Bogani and Dr. Azodi had no relevant financial disclosures.
SOURCE: Bogani G et al. J Minim Invasive Gynecol. 2020 Nov. doi: 10.1016/j.jmig.2020.08.069.
When cervical cancer recurs after radical hysterectomy, the likelihood of recurrence at certain sites and the timing of recurrence may be associated with the surgical approach, according to a retrospective study.
according to a propensity-matched analysis of data from 105 patients with recurrence.
And recurrence in the pelvic cavity and peritoneal carcinomatosis were more common after laparoscopic hysterectomy than after open surgery. Overall survival was similar between the groups, however.
The different patterns of recurrence may relate to dissemination of the disease during colpotomy, but the reasons are unknown, study author Giorgio Bogani, MD, PhD, said at the meeting sponsored by AAGL.
To examine patterns of recurrence after laparoscopic and open abdominal radical hysterectomy for cervical cancer, Dr. Bogani of the department of gynecologic surgery at the National Cancer Institute in Milan and colleagues analyzed data from patients with cervical cancer who developed recurrence after surgery at two oncologic referral centers between 1990 and 2018 (Int J Gynecol Cancer. 2020 Jul. doi: 10.1136/ijgc-2020-001381).
The investigators applied a propensity-matching algorithm to reduce possible confounding factors. They matched 35 patients who had recurrence after laparoscopic hysterectomy to 70 patients who had recurrence after open surgery. The groups had similar baseline characteristics.
As in the Laparoscopic Approach to Cervical Cancer (LACC) trial, patients who had minimally invasive surgery were more likely to have a worse disease-free survival, compared with patients who had open surgery, Dr. Bogani said. Patients who underwent laparoscopic radical hysterectomy had a median progression-free survival of 8 months, whereas patients who underwent open abdominal procedures had a median progression-free survival of 15.8 months.
Although vaginal, lymphatic, and distant recurrences were similar between the groups, a greater percentage of patients in the laparoscopic hysterectomy group had recurrence in the pelvic cavity (74% vs. 34%) and peritoneal carcinomatosis (17% vs. 1.5%).
The LACC trial, which found significantly lower disease-free and overall survival with laparoscopic hysterectomy, sent a “shockwave through the gynecologic oncology community” when it was published in 2018, said Masoud Azodi, MD, in a discussion following Dr. Bogani’s presentation.
Researchers have raised questions about that trial’s design and validity, noted Dr. Azodi, director of minimally invasive and robotic surgery at Yale University in New Haven, Conn.
It could be that local recurrences are attributable to surgical technique, rather than to the minimally invasive approach in itself, Dr. Azodi said. Prior studies of laparoscopic hysterectomy for cervical cancer had indicated better surgical outcomes and equivalent oncologic results, relative to open surgery.
Before the LACC trial, Dr. Bogani used the minimally invasive approach for almost all surgeries. Since then, he has performed open surgeries. If he were to use a minimally invasive approach now, it would be in the context of a clinical trial, Dr. Bogani said.
Dr. Bogani and Dr. Azodi had no relevant financial disclosures.
SOURCE: Bogani G et al. J Minim Invasive Gynecol. 2020 Nov. doi: 10.1016/j.jmig.2020.08.069.
When cervical cancer recurs after radical hysterectomy, the likelihood of recurrence at certain sites and the timing of recurrence may be associated with the surgical approach, according to a retrospective study.
according to a propensity-matched analysis of data from 105 patients with recurrence.
And recurrence in the pelvic cavity and peritoneal carcinomatosis were more common after laparoscopic hysterectomy than after open surgery. Overall survival was similar between the groups, however.
The different patterns of recurrence may relate to dissemination of the disease during colpotomy, but the reasons are unknown, study author Giorgio Bogani, MD, PhD, said at the meeting sponsored by AAGL.
To examine patterns of recurrence after laparoscopic and open abdominal radical hysterectomy for cervical cancer, Dr. Bogani of the department of gynecologic surgery at the National Cancer Institute in Milan and colleagues analyzed data from patients with cervical cancer who developed recurrence after surgery at two oncologic referral centers between 1990 and 2018 (Int J Gynecol Cancer. 2020 Jul. doi: 10.1136/ijgc-2020-001381).
The investigators applied a propensity-matching algorithm to reduce possible confounding factors. They matched 35 patients who had recurrence after laparoscopic hysterectomy to 70 patients who had recurrence after open surgery. The groups had similar baseline characteristics.
As in the Laparoscopic Approach to Cervical Cancer (LACC) trial, patients who had minimally invasive surgery were more likely to have a worse disease-free survival, compared with patients who had open surgery, Dr. Bogani said. Patients who underwent laparoscopic radical hysterectomy had a median progression-free survival of 8 months, whereas patients who underwent open abdominal procedures had a median progression-free survival of 15.8 months.
Although vaginal, lymphatic, and distant recurrences were similar between the groups, a greater percentage of patients in the laparoscopic hysterectomy group had recurrence in the pelvic cavity (74% vs. 34%) and peritoneal carcinomatosis (17% vs. 1.5%).
The LACC trial, which found significantly lower disease-free and overall survival with laparoscopic hysterectomy, sent a “shockwave through the gynecologic oncology community” when it was published in 2018, said Masoud Azodi, MD, in a discussion following Dr. Bogani’s presentation.
Researchers have raised questions about that trial’s design and validity, noted Dr. Azodi, director of minimally invasive and robotic surgery at Yale University in New Haven, Conn.
It could be that local recurrences are attributable to surgical technique, rather than to the minimally invasive approach in itself, Dr. Azodi said. Prior studies of laparoscopic hysterectomy for cervical cancer had indicated better surgical outcomes and equivalent oncologic results, relative to open surgery.
Before the LACC trial, Dr. Bogani used the minimally invasive approach for almost all surgeries. Since then, he has performed open surgeries. If he were to use a minimally invasive approach now, it would be in the context of a clinical trial, Dr. Bogani said.
Dr. Bogani and Dr. Azodi had no relevant financial disclosures.
SOURCE: Bogani G et al. J Minim Invasive Gynecol. 2020 Nov. doi: 10.1016/j.jmig.2020.08.069.
FROM AAGL GLOBAL CONGRESS