User login
How does long-term OC use affect breast, ovarian, and endometrial cancer risk?
Karlsson T, Johansson T, Hoguland J, et al. Time-dependent effects of oral contraceptive use on breast, ovarian and endometrial cancers. Cancer Research. 2020;canres.2476.2020. doi:10.1158/0008-5472.CAN-20-2476.
EXPERT COMMENTARY
The long-term effects of OC use on gynecologic and breast cancers has been uncertain, with different reports yielding conflicting findings. To assess the time-dependent and long-term associations between OC use and the risk of breast, ovarian, and endometrial cancer in women born between 1939 and 1970, Karlsson and colleagues used data from the UK Biobank (which includes a large cross-sectional cohort of individuals recruited between 2006 and 2010) and national databases.
Details of the study
A total of 256,661 women were included in this study. Of these, 82% (210,443) had used or were currently using OC (ever-users) and 18% (46,218) had never used OC (never-users). There were 17,739; 1,966; and 2,462 cases of breast, ovarian, and endometrial cancer, respectively, identified.
In analyses adjusted for 10 parameters, the ORs for ovarian (OR, 0.72) and endometrial cancer (OR, 0.68) were lower among ever-users of OC compared with never-users (P<.05). However, the OR for breast cancer (OR, 1.02) was similar among ever-users and never-users of OC (P>.05).
Among women followed to age 55, results were similar for the 2 gynecologic cancers but were significantly higher for breast cancer (OR, 1.10; P<.05). With 20 or more years of OC use, greater prevention of ovarian (OR, 0.60) and, particularly, endometrial cancer (OR, 0.36) was observed (P<.05). However, the risk of breast cancer was similar in never-users and long-term users of OC.
Study strengths and limitations
A strength of this study is that, compared with most previous studies, it had a much longer follow-up period.
The authors noted, however, that among the potential limitations in the study design was the fact that only 6% of participants invited to the UK Biobank volunteered to participate in the study. This may have resulted in participation bias within the cohort, reflecting a healthier cohort that is not representative of the overall population. ●
These study findings from a large cross-sectional cohort by Karlsson and colleagues suggest that controversy regarding the association of breast cancer with OC use may reflect different study methodologies with respect to timing. The authors note that while the lifetime risk of breast cancer may not differ between OC ever-users and never-users, there appears to be a transient elevated risk associated with OC use. By contrast, OC use, particularly when used long-term, appears to “dramatically” reduce the risk of ovarian and endometrial cancer, according to the study authors.
ANDREW M. KAUNITZ, MD
Karlsson T, Johansson T, Hoguland J, et al. Time-dependent effects of oral contraceptive use on breast, ovarian and endometrial cancers. Cancer Research. 2020;canres.2476.2020. doi:10.1158/0008-5472.CAN-20-2476.
EXPERT COMMENTARY
The long-term effects of OC use on gynecologic and breast cancers has been uncertain, with different reports yielding conflicting findings. To assess the time-dependent and long-term associations between OC use and the risk of breast, ovarian, and endometrial cancer in women born between 1939 and 1970, Karlsson and colleagues used data from the UK Biobank (which includes a large cross-sectional cohort of individuals recruited between 2006 and 2010) and national databases.
Details of the study
A total of 256,661 women were included in this study. Of these, 82% (210,443) had used or were currently using OC (ever-users) and 18% (46,218) had never used OC (never-users). There were 17,739; 1,966; and 2,462 cases of breast, ovarian, and endometrial cancer, respectively, identified.
In analyses adjusted for 10 parameters, the ORs for ovarian (OR, 0.72) and endometrial cancer (OR, 0.68) were lower among ever-users of OC compared with never-users (P<.05). However, the OR for breast cancer (OR, 1.02) was similar among ever-users and never-users of OC (P>.05).
Among women followed to age 55, results were similar for the 2 gynecologic cancers but were significantly higher for breast cancer (OR, 1.10; P<.05). With 20 or more years of OC use, greater prevention of ovarian (OR, 0.60) and, particularly, endometrial cancer (OR, 0.36) was observed (P<.05). However, the risk of breast cancer was similar in never-users and long-term users of OC.
Study strengths and limitations
A strength of this study is that, compared with most previous studies, it had a much longer follow-up period.
The authors noted, however, that among the potential limitations in the study design was the fact that only 6% of participants invited to the UK Biobank volunteered to participate in the study. This may have resulted in participation bias within the cohort, reflecting a healthier cohort that is not representative of the overall population. ●
These study findings from a large cross-sectional cohort by Karlsson and colleagues suggest that controversy regarding the association of breast cancer with OC use may reflect different study methodologies with respect to timing. The authors note that while the lifetime risk of breast cancer may not differ between OC ever-users and never-users, there appears to be a transient elevated risk associated with OC use. By contrast, OC use, particularly when used long-term, appears to “dramatically” reduce the risk of ovarian and endometrial cancer, according to the study authors.
ANDREW M. KAUNITZ, MD
Karlsson T, Johansson T, Hoguland J, et al. Time-dependent effects of oral contraceptive use on breast, ovarian and endometrial cancers. Cancer Research. 2020;canres.2476.2020. doi:10.1158/0008-5472.CAN-20-2476.
EXPERT COMMENTARY
The long-term effects of OC use on gynecologic and breast cancers has been uncertain, with different reports yielding conflicting findings. To assess the time-dependent and long-term associations between OC use and the risk of breast, ovarian, and endometrial cancer in women born between 1939 and 1970, Karlsson and colleagues used data from the UK Biobank (which includes a large cross-sectional cohort of individuals recruited between 2006 and 2010) and national databases.
Details of the study
A total of 256,661 women were included in this study. Of these, 82% (210,443) had used or were currently using OC (ever-users) and 18% (46,218) had never used OC (never-users). There were 17,739; 1,966; and 2,462 cases of breast, ovarian, and endometrial cancer, respectively, identified.
In analyses adjusted for 10 parameters, the ORs for ovarian (OR, 0.72) and endometrial cancer (OR, 0.68) were lower among ever-users of OC compared with never-users (P<.05). However, the OR for breast cancer (OR, 1.02) was similar among ever-users and never-users of OC (P>.05).
Among women followed to age 55, results were similar for the 2 gynecologic cancers but were significantly higher for breast cancer (OR, 1.10; P<.05). With 20 or more years of OC use, greater prevention of ovarian (OR, 0.60) and, particularly, endometrial cancer (OR, 0.36) was observed (P<.05). However, the risk of breast cancer was similar in never-users and long-term users of OC.
Study strengths and limitations
A strength of this study is that, compared with most previous studies, it had a much longer follow-up period.
The authors noted, however, that among the potential limitations in the study design was the fact that only 6% of participants invited to the UK Biobank volunteered to participate in the study. This may have resulted in participation bias within the cohort, reflecting a healthier cohort that is not representative of the overall population. ●
These study findings from a large cross-sectional cohort by Karlsson and colleagues suggest that controversy regarding the association of breast cancer with OC use may reflect different study methodologies with respect to timing. The authors note that while the lifetime risk of breast cancer may not differ between OC ever-users and never-users, there appears to be a transient elevated risk associated with OC use. By contrast, OC use, particularly when used long-term, appears to “dramatically” reduce the risk of ovarian and endometrial cancer, according to the study authors.
ANDREW M. KAUNITZ, MD
Product update: Breast biopsy system, tamponade mini-sponge, ovulation prediction device and app
Updated option for breast biopsy
Hologic announces updates to its Brevera® Breast Biopsy System with CorLumina® Imaging Technology. The Brevera system is designed for use with the manufacturer’s Affirm® Prone biopsy guidance system.
For more information, visit https://www.hologic.com.
“Mini-sponge” device shows potential to treat PPH
During a pilot study, reports Obstetrx, 9 patients, treated at the University Teaching Hospital in Lusaka, Zambia, did not respond to conventional PPH management options after vaginal birth but did respond, with bleeding resolved in 60 seconds and no adverse events, to the XSTAT device. The device was left in place for a mean time of 1 hour, and none of the patients required further surgical procedures or blood transfusions. The initial placement time of XSTAT (mean time to placement, 62 seconds) was faster than times reported for balloon uterine tamponade devices. The pilot study results were published in Obstetrics & Gynecology.
XSTAT is US Food and Drug Administration–approved to treat high-flow arterial bleeding in prehospital trauma settings, and Obstetrx is planning to submit for 510k clearance in 2022, after the conclusion of a follow-up PPH trial in 2021.
For more information, visit: https://www.obstetrx.com/.
Continue to: AI and ovulation prediction...
AI and ovulation prediction
A woman’s fertility window is typically the 5 days leading up to ovulation, with peak fertility in the 2 to 3 days before ovulation. There are other options for measuring that fertile window, including luteinizing hormone (LH) tests; however, Prima-Temp reports that Priya predicts the fertile window an average of 2.6 days before tests for LH. Utilizing continuous core body temperature measurement, Priya detects subtle changes in temperature patterns that occur prior to ovulation. The app portion of the technology stores and analyzes the temperature measurements, for a high-tech fertility alert system that also offers clinical diagnostic support. Potential users of the Priya system are able to sign up to receive it through the product’s website.
For more information, visit: https://www.priyafertility.com.
Updated option for breast biopsy
Hologic announces updates to its Brevera® Breast Biopsy System with CorLumina® Imaging Technology. The Brevera system is designed for use with the manufacturer’s Affirm® Prone biopsy guidance system.
For more information, visit https://www.hologic.com.
“Mini-sponge” device shows potential to treat PPH
During a pilot study, reports Obstetrx, 9 patients, treated at the University Teaching Hospital in Lusaka, Zambia, did not respond to conventional PPH management options after vaginal birth but did respond, with bleeding resolved in 60 seconds and no adverse events, to the XSTAT device. The device was left in place for a mean time of 1 hour, and none of the patients required further surgical procedures or blood transfusions. The initial placement time of XSTAT (mean time to placement, 62 seconds) was faster than times reported for balloon uterine tamponade devices. The pilot study results were published in Obstetrics & Gynecology.
XSTAT is US Food and Drug Administration–approved to treat high-flow arterial bleeding in prehospital trauma settings, and Obstetrx is planning to submit for 510k clearance in 2022, after the conclusion of a follow-up PPH trial in 2021.
For more information, visit: https://www.obstetrx.com/.
Continue to: AI and ovulation prediction...
AI and ovulation prediction
A woman’s fertility window is typically the 5 days leading up to ovulation, with peak fertility in the 2 to 3 days before ovulation. There are other options for measuring that fertile window, including luteinizing hormone (LH) tests; however, Prima-Temp reports that Priya predicts the fertile window an average of 2.6 days before tests for LH. Utilizing continuous core body temperature measurement, Priya detects subtle changes in temperature patterns that occur prior to ovulation. The app portion of the technology stores and analyzes the temperature measurements, for a high-tech fertility alert system that also offers clinical diagnostic support. Potential users of the Priya system are able to sign up to receive it through the product’s website.
For more information, visit: https://www.priyafertility.com.
Updated option for breast biopsy
Hologic announces updates to its Brevera® Breast Biopsy System with CorLumina® Imaging Technology. The Brevera system is designed for use with the manufacturer’s Affirm® Prone biopsy guidance system.
For more information, visit https://www.hologic.com.
“Mini-sponge” device shows potential to treat PPH
During a pilot study, reports Obstetrx, 9 patients, treated at the University Teaching Hospital in Lusaka, Zambia, did not respond to conventional PPH management options after vaginal birth but did respond, with bleeding resolved in 60 seconds and no adverse events, to the XSTAT device. The device was left in place for a mean time of 1 hour, and none of the patients required further surgical procedures or blood transfusions. The initial placement time of XSTAT (mean time to placement, 62 seconds) was faster than times reported for balloon uterine tamponade devices. The pilot study results were published in Obstetrics & Gynecology.
XSTAT is US Food and Drug Administration–approved to treat high-flow arterial bleeding in prehospital trauma settings, and Obstetrx is planning to submit for 510k clearance in 2022, after the conclusion of a follow-up PPH trial in 2021.
For more information, visit: https://www.obstetrx.com/.
Continue to: AI and ovulation prediction...
AI and ovulation prediction
A woman’s fertility window is typically the 5 days leading up to ovulation, with peak fertility in the 2 to 3 days before ovulation. There are other options for measuring that fertile window, including luteinizing hormone (LH) tests; however, Prima-Temp reports that Priya predicts the fertile window an average of 2.6 days before tests for LH. Utilizing continuous core body temperature measurement, Priya detects subtle changes in temperature patterns that occur prior to ovulation. The app portion of the technology stores and analyzes the temperature measurements, for a high-tech fertility alert system that also offers clinical diagnostic support. Potential users of the Priya system are able to sign up to receive it through the product’s website.
For more information, visit: https://www.priyafertility.com.
Oral contraceptives may reduce ovarian and endometrial cancer risk 35 years after discontinuation
At the same time, oral contraceptive use is associated with a short-term increased risk of breast cancer after discontinuation, although the lifetime risk of breast cancer is not significantly different, the researchers found.
The absolute risk of breast cancer after discontinuation is “extremely small” and should be a limited factor when deciding whether to start oral contraceptive pills (OCPs), a doctor said.
The study was conducted by Torgny Karlsson, PhD, a researcher in the department of immunology, genetics, and pathology at Uppsala (Sweden) University, and colleagues and published online in Cancer Research.
Reinforcing and extending knowledge
“These findings are generally consistent with what is known, but extend that knowledge, most notably by the longer-term follow-up for the cohort,” commented Nancy L. Keating, MD, MPH, professor of health care policy and medicine at Harvard Medical School and a physician at Brigham and Women’s Hospital, both in Boston. “Other studies have also shown that OCPs lower risk of ovarian and endometrial cancer. This study suggests that this protective benefit extends up to 30-35 years after discontinuing OCPs.”
The results “reinforce the message to patients of the protective effect of OCPs on risk of ovarian and endometrial cancer,” Dr. Keating said. “Women concerned about these cancers can be reassured that this protective effect appears to persist for decades after discontinuing use.”
Prior studies have indicated that oral contraceptives may be associated with an increased risk of breast cancer.
In terms of breast cancer risk, the study “again extends follow-up and shows that risk of breast cancer was higher for current and ever users through age 50,” although the lifetime risk was not elevated, Dr. Keating said.
“The counseling regarding the effect on breast cancer is more complex,” she said. “I tell women about the very small increased risk of breast cancer during and immediately after use. Because cancer is very rare among women at the ages when OCPs are typically prescribed, the absolute risk increase is extremely small. This paper adds reassurance that this small increase in risk does not persist.”
For certain patients, the association may be more relevant.
“For most women, this risk is so small that it should be a limited factor in their decision to start OCPs,” Dr. Keating said. “However, for women with a substantially higher risk of breast cancer, or a family history of breast cancer at a young age, the small increased risk of breast cancer during and immediately after OCP use is more relevant, and counseling should include carefully weighing the benefits and harms of OCPs with other forms of contraception (and no contraception).”
Although the protective effects of oral contraceptives on ovarian and endometrial cancer were well known, the study describes long-term outcomes that can further inform patient counseling, said Samuel S. Badalian, MD, PhD, chief of the department of obstetrics and gynecology at Bassett Medical Center in Cooperstown, N.Y., and clinical professor of obstetrics and gynecology at the State University of New York, Syracuse.
“Women with individual or family risk factors of ovarian or endometrial cancers will need to know about the protective effects of oral contraceptives and long-term benefits related with their use (30-35 years after discontinuation),” Dr. Badalian said. “Women with family history of breast cancer need to know that lifetime risk of breast cancer might not differ between ever and never users, even if there is an increased short-term risk.”
Data from the U.K. Biobank
To examine the time-dependent effects between long-term oral contraceptive use and cancer risk, the researchers examined data from 256,661 women from the U.K. Biobank who were born between 1939 and 1970. The researchers identified cancer diagnoses using information from national registers and self-reported data until March 2019.
Of the women included in the study, 82% had used or still were using oral contraceptives, whereas 18% had never used oral contraceptives. Overall, ever users were younger, more frequently smokers, and had a lower body mass index, compared with never users. Most women started using oral contraceptives between 1969 and 1978. Last use of oral contraceptives occurred on average 10.7 years after starting.
The researchers adjusted for covariates and used logistic regression analyses to measure the cumulative risk of cancer. They used Cox regression analysis to examine instantaneous risk, measured using hazard ratios.
In all, there were 17,739 cases of breast cancer (6.9%), 1,966 cases of ovarian cancer (0.76%), and 2,462 cases of endometrial cancer (0.96%).
Among ever users, the likelihood of ovarian cancer (OR, 0.72) and endometrial cancer (OR, 0.68) was lower, compared with never users. “However, we did not see a significant association between oral contraceptive use and breast cancer” for the study period as a whole, the researchers reported. When the researchers limited follow-up to age 50 years, however, the odds ratio for breast cancer was increased (OR, 1.09).
“Surprisingly, we only found a small increased risk of breast cancer among oral contraceptive users, and the increased risk disappeared within a few years after discontinuation,” Åsa Johansson, PhD, a researcher in the department of immunology, genetics, and pathology at Uppsala University and one of the study authors, said in a news release. “Our results suggest that the lifetime risk of breast cancer might not differ between ever and never users, even if there is an increased short-term risk.”
Oral contraceptives today typically use lower doses of estrogen and other types of progesterone, compared with formulas commonly used when participants in the study started taking them, so the results may not directly apply to patients currently taking oral contraceptives, the researchers noted.
The study was supported by the Swedish Research Council, the Swedish Cancer Society, and the Kjell and Märta Beijers, the Marcus Borgström, the Åke Wiberg, and the A and M Rudbergs foundations. The authors, Dr. Keating, and Dr. Badalian had no conflicts of interest.
At the same time, oral contraceptive use is associated with a short-term increased risk of breast cancer after discontinuation, although the lifetime risk of breast cancer is not significantly different, the researchers found.
The absolute risk of breast cancer after discontinuation is “extremely small” and should be a limited factor when deciding whether to start oral contraceptive pills (OCPs), a doctor said.
The study was conducted by Torgny Karlsson, PhD, a researcher in the department of immunology, genetics, and pathology at Uppsala (Sweden) University, and colleagues and published online in Cancer Research.
Reinforcing and extending knowledge
“These findings are generally consistent with what is known, but extend that knowledge, most notably by the longer-term follow-up for the cohort,” commented Nancy L. Keating, MD, MPH, professor of health care policy and medicine at Harvard Medical School and a physician at Brigham and Women’s Hospital, both in Boston. “Other studies have also shown that OCPs lower risk of ovarian and endometrial cancer. This study suggests that this protective benefit extends up to 30-35 years after discontinuing OCPs.”
The results “reinforce the message to patients of the protective effect of OCPs on risk of ovarian and endometrial cancer,” Dr. Keating said. “Women concerned about these cancers can be reassured that this protective effect appears to persist for decades after discontinuing use.”
Prior studies have indicated that oral contraceptives may be associated with an increased risk of breast cancer.
In terms of breast cancer risk, the study “again extends follow-up and shows that risk of breast cancer was higher for current and ever users through age 50,” although the lifetime risk was not elevated, Dr. Keating said.
“The counseling regarding the effect on breast cancer is more complex,” she said. “I tell women about the very small increased risk of breast cancer during and immediately after use. Because cancer is very rare among women at the ages when OCPs are typically prescribed, the absolute risk increase is extremely small. This paper adds reassurance that this small increase in risk does not persist.”
For certain patients, the association may be more relevant.
“For most women, this risk is so small that it should be a limited factor in their decision to start OCPs,” Dr. Keating said. “However, for women with a substantially higher risk of breast cancer, or a family history of breast cancer at a young age, the small increased risk of breast cancer during and immediately after OCP use is more relevant, and counseling should include carefully weighing the benefits and harms of OCPs with other forms of contraception (and no contraception).”
Although the protective effects of oral contraceptives on ovarian and endometrial cancer were well known, the study describes long-term outcomes that can further inform patient counseling, said Samuel S. Badalian, MD, PhD, chief of the department of obstetrics and gynecology at Bassett Medical Center in Cooperstown, N.Y., and clinical professor of obstetrics and gynecology at the State University of New York, Syracuse.
“Women with individual or family risk factors of ovarian or endometrial cancers will need to know about the protective effects of oral contraceptives and long-term benefits related with their use (30-35 years after discontinuation),” Dr. Badalian said. “Women with family history of breast cancer need to know that lifetime risk of breast cancer might not differ between ever and never users, even if there is an increased short-term risk.”
Data from the U.K. Biobank
To examine the time-dependent effects between long-term oral contraceptive use and cancer risk, the researchers examined data from 256,661 women from the U.K. Biobank who were born between 1939 and 1970. The researchers identified cancer diagnoses using information from national registers and self-reported data until March 2019.
Of the women included in the study, 82% had used or still were using oral contraceptives, whereas 18% had never used oral contraceptives. Overall, ever users were younger, more frequently smokers, and had a lower body mass index, compared with never users. Most women started using oral contraceptives between 1969 and 1978. Last use of oral contraceptives occurred on average 10.7 years after starting.
The researchers adjusted for covariates and used logistic regression analyses to measure the cumulative risk of cancer. They used Cox regression analysis to examine instantaneous risk, measured using hazard ratios.
In all, there were 17,739 cases of breast cancer (6.9%), 1,966 cases of ovarian cancer (0.76%), and 2,462 cases of endometrial cancer (0.96%).
Among ever users, the likelihood of ovarian cancer (OR, 0.72) and endometrial cancer (OR, 0.68) was lower, compared with never users. “However, we did not see a significant association between oral contraceptive use and breast cancer” for the study period as a whole, the researchers reported. When the researchers limited follow-up to age 50 years, however, the odds ratio for breast cancer was increased (OR, 1.09).
“Surprisingly, we only found a small increased risk of breast cancer among oral contraceptive users, and the increased risk disappeared within a few years after discontinuation,” Åsa Johansson, PhD, a researcher in the department of immunology, genetics, and pathology at Uppsala University and one of the study authors, said in a news release. “Our results suggest that the lifetime risk of breast cancer might not differ between ever and never users, even if there is an increased short-term risk.”
Oral contraceptives today typically use lower doses of estrogen and other types of progesterone, compared with formulas commonly used when participants in the study started taking them, so the results may not directly apply to patients currently taking oral contraceptives, the researchers noted.
The study was supported by the Swedish Research Council, the Swedish Cancer Society, and the Kjell and Märta Beijers, the Marcus Borgström, the Åke Wiberg, and the A and M Rudbergs foundations. The authors, Dr. Keating, and Dr. Badalian had no conflicts of interest.
At the same time, oral contraceptive use is associated with a short-term increased risk of breast cancer after discontinuation, although the lifetime risk of breast cancer is not significantly different, the researchers found.
The absolute risk of breast cancer after discontinuation is “extremely small” and should be a limited factor when deciding whether to start oral contraceptive pills (OCPs), a doctor said.
The study was conducted by Torgny Karlsson, PhD, a researcher in the department of immunology, genetics, and pathology at Uppsala (Sweden) University, and colleagues and published online in Cancer Research.
Reinforcing and extending knowledge
“These findings are generally consistent with what is known, but extend that knowledge, most notably by the longer-term follow-up for the cohort,” commented Nancy L. Keating, MD, MPH, professor of health care policy and medicine at Harvard Medical School and a physician at Brigham and Women’s Hospital, both in Boston. “Other studies have also shown that OCPs lower risk of ovarian and endometrial cancer. This study suggests that this protective benefit extends up to 30-35 years after discontinuing OCPs.”
The results “reinforce the message to patients of the protective effect of OCPs on risk of ovarian and endometrial cancer,” Dr. Keating said. “Women concerned about these cancers can be reassured that this protective effect appears to persist for decades after discontinuing use.”
Prior studies have indicated that oral contraceptives may be associated with an increased risk of breast cancer.
In terms of breast cancer risk, the study “again extends follow-up and shows that risk of breast cancer was higher for current and ever users through age 50,” although the lifetime risk was not elevated, Dr. Keating said.
“The counseling regarding the effect on breast cancer is more complex,” she said. “I tell women about the very small increased risk of breast cancer during and immediately after use. Because cancer is very rare among women at the ages when OCPs are typically prescribed, the absolute risk increase is extremely small. This paper adds reassurance that this small increase in risk does not persist.”
For certain patients, the association may be more relevant.
“For most women, this risk is so small that it should be a limited factor in their decision to start OCPs,” Dr. Keating said. “However, for women with a substantially higher risk of breast cancer, or a family history of breast cancer at a young age, the small increased risk of breast cancer during and immediately after OCP use is more relevant, and counseling should include carefully weighing the benefits and harms of OCPs with other forms of contraception (and no contraception).”
Although the protective effects of oral contraceptives on ovarian and endometrial cancer were well known, the study describes long-term outcomes that can further inform patient counseling, said Samuel S. Badalian, MD, PhD, chief of the department of obstetrics and gynecology at Bassett Medical Center in Cooperstown, N.Y., and clinical professor of obstetrics and gynecology at the State University of New York, Syracuse.
“Women with individual or family risk factors of ovarian or endometrial cancers will need to know about the protective effects of oral contraceptives and long-term benefits related with their use (30-35 years after discontinuation),” Dr. Badalian said. “Women with family history of breast cancer need to know that lifetime risk of breast cancer might not differ between ever and never users, even if there is an increased short-term risk.”
Data from the U.K. Biobank
To examine the time-dependent effects between long-term oral contraceptive use and cancer risk, the researchers examined data from 256,661 women from the U.K. Biobank who were born between 1939 and 1970. The researchers identified cancer diagnoses using information from national registers and self-reported data until March 2019.
Of the women included in the study, 82% had used or still were using oral contraceptives, whereas 18% had never used oral contraceptives. Overall, ever users were younger, more frequently smokers, and had a lower body mass index, compared with never users. Most women started using oral contraceptives between 1969 and 1978. Last use of oral contraceptives occurred on average 10.7 years after starting.
The researchers adjusted for covariates and used logistic regression analyses to measure the cumulative risk of cancer. They used Cox regression analysis to examine instantaneous risk, measured using hazard ratios.
In all, there were 17,739 cases of breast cancer (6.9%), 1,966 cases of ovarian cancer (0.76%), and 2,462 cases of endometrial cancer (0.96%).
Among ever users, the likelihood of ovarian cancer (OR, 0.72) and endometrial cancer (OR, 0.68) was lower, compared with never users. “However, we did not see a significant association between oral contraceptive use and breast cancer” for the study period as a whole, the researchers reported. When the researchers limited follow-up to age 50 years, however, the odds ratio for breast cancer was increased (OR, 1.09).
“Surprisingly, we only found a small increased risk of breast cancer among oral contraceptive users, and the increased risk disappeared within a few years after discontinuation,” Åsa Johansson, PhD, a researcher in the department of immunology, genetics, and pathology at Uppsala University and one of the study authors, said in a news release. “Our results suggest that the lifetime risk of breast cancer might not differ between ever and never users, even if there is an increased short-term risk.”
Oral contraceptives today typically use lower doses of estrogen and other types of progesterone, compared with formulas commonly used when participants in the study started taking them, so the results may not directly apply to patients currently taking oral contraceptives, the researchers noted.
The study was supported by the Swedish Research Council, the Swedish Cancer Society, and the Kjell and Märta Beijers, the Marcus Borgström, the Åke Wiberg, and the A and M Rudbergs foundations. The authors, Dr. Keating, and Dr. Badalian had no conflicts of interest.
FROM CANCER RESEARCH
COVID-19 vaccination in cancer patients: NCCN outlines priorities
Vaccination timing considerations vary based on factors such as cancer and treatment type, and reasons for delaying vaccination in the general public also apply to cancer patients (recent COVID-19 exposure, for example).
In general, however, patients with cancer should be assigned to Centers for Disease Control and Prevention priority group 1 b/c and immunized when vaccination is available to them, the guidelines state. Exceptions to this recommendation include:
- Patients undergoing hematopoietic stem cell transplant or receiving engineered cellular therapy such as chimeric antigen receptor T-cell therapy. Vaccination should be delayed for at least 3 months in these patients to maximize vaccine efficacy. Caregivers of these patients, however, should be immunized when possible.
- Patients with hematologic malignancies who are receiving intensive cytotoxic chemotherapy, such as cytarabine- or anthracycline-based regimens for acute myeloid leukemia. Vaccination in these patients should be delayed until absolute neutrophil count recovery.
- Patients undergoing major surgery. Vaccination should occur at least a few days before or after surgery.
- Patients who have experienced a severe or immediate adverse reaction to any of the ingredients in the mRNA COVID-19 vaccines.
Conversely, vaccination should occur when available in patients with hematologic malignancies and marrow failure who are expected to have limited or no recovery, patients with hematologic malignancies who are on long-term maintenance therapy, and patients with solid tumors who are receiving cytotoxic chemotherapy, targeted therapy, checkpoint inhibitors and other immunotherapy, or radiotherapy.
Caregivers, household contacts, and other close contacts who are 16 years of age and older should be vaccinated whenever they are eligible.
Unique concerns in patients with cancer
The NCCN recommendations were developed to address the unique issues and concerns with respect to patients with cancer, who have an increased risk of severe illness from SARS-CoV-2 infection. But the guidelines come with a caveat: “[t]here are limited safety and efficacy data in these patients,” the NCCN emphasized in a press statement.
“Right now, there is urgent need and limited data,” Steven Pergam, MD, co-leader of the NCCN COVID-19 Vaccination Committee, said in the statement.
“Our number one goal is helping to get the vaccine to as many people as we can,” Dr. Pergam said. “That means following existing national and regional directions for prioritizing people who are more likely to face death or severe illness from COVID-19.”
Dr. Pergam, associate professor at Fred Hutchinson Cancer Research Center in Seattle, further explained that “people receiving active cancer treatment are at greater risk for worse outcomes from COVID-19, particularly if they are older and have additional comorbidities, like immunosuppression.”
NCCN’s recommendations couldn’t have come at a better time for patients with cancer, according to Nora Disis, MD, a professor at the University of Washington in Seattle.
“The NCCN’s recommendations to prioritize COVID vaccinations for cancer patients on active treatment is an important step forward in protecting our patients from the infection,” Dr. Disis said in an interview.
“Cancer patients may be at higher risk for the complications seen with infection. In addition, cancer is a disease of older people, and a good number of our patients have the comorbidities that would predict a poorer outcome if they should become sick,” Dr. Disis added. “With the correct treatment, many patients with cancer will be long-term survivors. It is important that they be protected from infection with COVID to realize their best outcome.”
Additional vaccine considerations
The NCCN recommendations also address several other issues of importance for cancer patients, including:
- Deprioritizing other vaccines. COVID-19 vaccines should take precedence over other vaccines because data on dual vaccination are lacking. The NCCN recommends waiting 14 days after COVID-19 vaccination to deliver other vaccines.
- Vaccinating clinical trial participants. Trial leads should be consulted to prevent protocol violations or exclusions.
- Decision-making in the setting of limited vaccine availability. The NCCN noted that decisions on allocation must be made in accordance with state and local vaccine guidance but suggests prioritizing appropriate patients on active treatment, those planning to start treatment, and those who have just completed treatment. Additional risk factors for these patients, as well as other factors associated with risk for adverse COVID-19 outcomes, should also be considered. These include advanced age, comorbidities, and adverse social and demographic factors such as poverty and limited health care access.
- The need for ongoing prevention measures. Vaccines have been shown to decrease the incidence of COVID-19 and related complications, but it remains unclear whether vaccines prevent infection and subsequent transmission. This means everyone should continue following prevention recommendations, such as wearing masks and avoiding crowds.
The NCCN stressed that these recommendations are “intended to be a living document that is constantly evolving – it will be updated rapidly whenever new data comes out, as well as any potential new vaccines that may get approved in the future.” The NCCN also noted that the advisory committee will meet regularly to refine the recommendations as needed.
Dr. Pergam disclosed relationships with Chimerix Inc., Merck & Co., Global Life Technologies Inc., and Sanofi-Aventis. Dr. Disis disclosed grants from Pfizer, Bavarian Nordisk, Janssen, and Precigen. She is the founder of EpiThany and editor-in-chief of JAMA Oncology.
Vaccination timing considerations vary based on factors such as cancer and treatment type, and reasons for delaying vaccination in the general public also apply to cancer patients (recent COVID-19 exposure, for example).
In general, however, patients with cancer should be assigned to Centers for Disease Control and Prevention priority group 1 b/c and immunized when vaccination is available to them, the guidelines state. Exceptions to this recommendation include:
- Patients undergoing hematopoietic stem cell transplant or receiving engineered cellular therapy such as chimeric antigen receptor T-cell therapy. Vaccination should be delayed for at least 3 months in these patients to maximize vaccine efficacy. Caregivers of these patients, however, should be immunized when possible.
- Patients with hematologic malignancies who are receiving intensive cytotoxic chemotherapy, such as cytarabine- or anthracycline-based regimens for acute myeloid leukemia. Vaccination in these patients should be delayed until absolute neutrophil count recovery.
- Patients undergoing major surgery. Vaccination should occur at least a few days before or after surgery.
- Patients who have experienced a severe or immediate adverse reaction to any of the ingredients in the mRNA COVID-19 vaccines.
Conversely, vaccination should occur when available in patients with hematologic malignancies and marrow failure who are expected to have limited or no recovery, patients with hematologic malignancies who are on long-term maintenance therapy, and patients with solid tumors who are receiving cytotoxic chemotherapy, targeted therapy, checkpoint inhibitors and other immunotherapy, or radiotherapy.
Caregivers, household contacts, and other close contacts who are 16 years of age and older should be vaccinated whenever they are eligible.
Unique concerns in patients with cancer
The NCCN recommendations were developed to address the unique issues and concerns with respect to patients with cancer, who have an increased risk of severe illness from SARS-CoV-2 infection. But the guidelines come with a caveat: “[t]here are limited safety and efficacy data in these patients,” the NCCN emphasized in a press statement.
“Right now, there is urgent need and limited data,” Steven Pergam, MD, co-leader of the NCCN COVID-19 Vaccination Committee, said in the statement.
“Our number one goal is helping to get the vaccine to as many people as we can,” Dr. Pergam said. “That means following existing national and regional directions for prioritizing people who are more likely to face death or severe illness from COVID-19.”
Dr. Pergam, associate professor at Fred Hutchinson Cancer Research Center in Seattle, further explained that “people receiving active cancer treatment are at greater risk for worse outcomes from COVID-19, particularly if they are older and have additional comorbidities, like immunosuppression.”
NCCN’s recommendations couldn’t have come at a better time for patients with cancer, according to Nora Disis, MD, a professor at the University of Washington in Seattle.
“The NCCN’s recommendations to prioritize COVID vaccinations for cancer patients on active treatment is an important step forward in protecting our patients from the infection,” Dr. Disis said in an interview.
“Cancer patients may be at higher risk for the complications seen with infection. In addition, cancer is a disease of older people, and a good number of our patients have the comorbidities that would predict a poorer outcome if they should become sick,” Dr. Disis added. “With the correct treatment, many patients with cancer will be long-term survivors. It is important that they be protected from infection with COVID to realize their best outcome.”
Additional vaccine considerations
The NCCN recommendations also address several other issues of importance for cancer patients, including:
- Deprioritizing other vaccines. COVID-19 vaccines should take precedence over other vaccines because data on dual vaccination are lacking. The NCCN recommends waiting 14 days after COVID-19 vaccination to deliver other vaccines.
- Vaccinating clinical trial participants. Trial leads should be consulted to prevent protocol violations or exclusions.
- Decision-making in the setting of limited vaccine availability. The NCCN noted that decisions on allocation must be made in accordance with state and local vaccine guidance but suggests prioritizing appropriate patients on active treatment, those planning to start treatment, and those who have just completed treatment. Additional risk factors for these patients, as well as other factors associated with risk for adverse COVID-19 outcomes, should also be considered. These include advanced age, comorbidities, and adverse social and demographic factors such as poverty and limited health care access.
- The need for ongoing prevention measures. Vaccines have been shown to decrease the incidence of COVID-19 and related complications, but it remains unclear whether vaccines prevent infection and subsequent transmission. This means everyone should continue following prevention recommendations, such as wearing masks and avoiding crowds.
The NCCN stressed that these recommendations are “intended to be a living document that is constantly evolving – it will be updated rapidly whenever new data comes out, as well as any potential new vaccines that may get approved in the future.” The NCCN also noted that the advisory committee will meet regularly to refine the recommendations as needed.
Dr. Pergam disclosed relationships with Chimerix Inc., Merck & Co., Global Life Technologies Inc., and Sanofi-Aventis. Dr. Disis disclosed grants from Pfizer, Bavarian Nordisk, Janssen, and Precigen. She is the founder of EpiThany and editor-in-chief of JAMA Oncology.
Vaccination timing considerations vary based on factors such as cancer and treatment type, and reasons for delaying vaccination in the general public also apply to cancer patients (recent COVID-19 exposure, for example).
In general, however, patients with cancer should be assigned to Centers for Disease Control and Prevention priority group 1 b/c and immunized when vaccination is available to them, the guidelines state. Exceptions to this recommendation include:
- Patients undergoing hematopoietic stem cell transplant or receiving engineered cellular therapy such as chimeric antigen receptor T-cell therapy. Vaccination should be delayed for at least 3 months in these patients to maximize vaccine efficacy. Caregivers of these patients, however, should be immunized when possible.
- Patients with hematologic malignancies who are receiving intensive cytotoxic chemotherapy, such as cytarabine- or anthracycline-based regimens for acute myeloid leukemia. Vaccination in these patients should be delayed until absolute neutrophil count recovery.
- Patients undergoing major surgery. Vaccination should occur at least a few days before or after surgery.
- Patients who have experienced a severe or immediate adverse reaction to any of the ingredients in the mRNA COVID-19 vaccines.
Conversely, vaccination should occur when available in patients with hematologic malignancies and marrow failure who are expected to have limited or no recovery, patients with hematologic malignancies who are on long-term maintenance therapy, and patients with solid tumors who are receiving cytotoxic chemotherapy, targeted therapy, checkpoint inhibitors and other immunotherapy, or radiotherapy.
Caregivers, household contacts, and other close contacts who are 16 years of age and older should be vaccinated whenever they are eligible.
Unique concerns in patients with cancer
The NCCN recommendations were developed to address the unique issues and concerns with respect to patients with cancer, who have an increased risk of severe illness from SARS-CoV-2 infection. But the guidelines come with a caveat: “[t]here are limited safety and efficacy data in these patients,” the NCCN emphasized in a press statement.
“Right now, there is urgent need and limited data,” Steven Pergam, MD, co-leader of the NCCN COVID-19 Vaccination Committee, said in the statement.
“Our number one goal is helping to get the vaccine to as many people as we can,” Dr. Pergam said. “That means following existing national and regional directions for prioritizing people who are more likely to face death or severe illness from COVID-19.”
Dr. Pergam, associate professor at Fred Hutchinson Cancer Research Center in Seattle, further explained that “people receiving active cancer treatment are at greater risk for worse outcomes from COVID-19, particularly if they are older and have additional comorbidities, like immunosuppression.”
NCCN’s recommendations couldn’t have come at a better time for patients with cancer, according to Nora Disis, MD, a professor at the University of Washington in Seattle.
“The NCCN’s recommendations to prioritize COVID vaccinations for cancer patients on active treatment is an important step forward in protecting our patients from the infection,” Dr. Disis said in an interview.
“Cancer patients may be at higher risk for the complications seen with infection. In addition, cancer is a disease of older people, and a good number of our patients have the comorbidities that would predict a poorer outcome if they should become sick,” Dr. Disis added. “With the correct treatment, many patients with cancer will be long-term survivors. It is important that they be protected from infection with COVID to realize their best outcome.”
Additional vaccine considerations
The NCCN recommendations also address several other issues of importance for cancer patients, including:
- Deprioritizing other vaccines. COVID-19 vaccines should take precedence over other vaccines because data on dual vaccination are lacking. The NCCN recommends waiting 14 days after COVID-19 vaccination to deliver other vaccines.
- Vaccinating clinical trial participants. Trial leads should be consulted to prevent protocol violations or exclusions.
- Decision-making in the setting of limited vaccine availability. The NCCN noted that decisions on allocation must be made in accordance with state and local vaccine guidance but suggests prioritizing appropriate patients on active treatment, those planning to start treatment, and those who have just completed treatment. Additional risk factors for these patients, as well as other factors associated with risk for adverse COVID-19 outcomes, should also be considered. These include advanced age, comorbidities, and adverse social and demographic factors such as poverty and limited health care access.
- The need for ongoing prevention measures. Vaccines have been shown to decrease the incidence of COVID-19 and related complications, but it remains unclear whether vaccines prevent infection and subsequent transmission. This means everyone should continue following prevention recommendations, such as wearing masks and avoiding crowds.
The NCCN stressed that these recommendations are “intended to be a living document that is constantly evolving – it will be updated rapidly whenever new data comes out, as well as any potential new vaccines that may get approved in the future.” The NCCN also noted that the advisory committee will meet regularly to refine the recommendations as needed.
Dr. Pergam disclosed relationships with Chimerix Inc., Merck & Co., Global Life Technologies Inc., and Sanofi-Aventis. Dr. Disis disclosed grants from Pfizer, Bavarian Nordisk, Janssen, and Precigen. She is the founder of EpiThany and editor-in-chief of JAMA Oncology.
Model predicts acute kidney injury in cancer patients a month in advance
A model that crunches data from routine blood tests can accurately identify cancer patients who will develop acute kidney injury (AKI) up to a month before it happens, according to a cohort study.
The algorithm spotted nearly 74% of the patients who went on to develop AKI within 30 days, providing a window for intervention and possibly prevention, according to investigators.
These results were reported at the AACR Virtual Special Conference: Artificial Intelligence, Diagnosis, and Imaging (abstract PR-11).
“Cancer patients are a high-risk population for AKI due to the nature of their treatment and illness,” said presenter Lauren A. Scanlon, PhD, a data scientist at The Christie NHS Foundation Trust in Huddersfield, England. “AKI causes a huge disruption in treatment and distress for the patient, so it would be amazing if we could, say, predict the AKI before it occurs and prevent it from even happening.”
U.K. health care providers are already using an algorithm to monitor patients’ creatinine levels, comparing new values against historic ones, Dr. Scanlon explained. When that algorithm detects AKI, it issues an alert that triggers implementation of an AKI care bundle, including measures such as fluid monitoring and medication review, within 24 hours.
Taking this concept further, Dr. Scanlon and colleagues developed a random forest model, a type of machine learning algorithm, that incorporates other markers from blood tests routinely obtained for all patients, with the aim of predicting AKI up to 30 days in advance.
“Using routinely collected blood test results will ensure that the model is applicable to all our patients and can be implemented in an automated manner,” Dr. Scanlon noted.
The investigators developed and trained the model using 597,403 blood test results from 48,865 patients undergoing cancer treatment between January 2017 and May 2020.
The model assigns patients to five categories of risk for AKI in the next 30 days: very low, low, medium, high, and very high.
“We wanted the model to output in this way so that it could be used by clinicians alongside their own insight and knowledge on a case-by-case basis,” Dr. Scanlon explained.
The investigators then prospectively validated the model and its risk categories in another 9,913 patients who underwent cancer treatment between June and August 2020.
Using a model threshold of medium risk or higher, the model correctly predicted AKI in 330 (73.8%) of the 447 patients in the validation cohort who ultimately developed AKI.
“This is pretty amazing and shows that this model really is working and can correctly detect these AKIs up to 30 days before they occur, giving a huge window to put in place preventive strategies,” Dr. Scanlon said.
Among the 154 patients in whom the model incorrectly predicted AKI, 9 patients had only a single follow-up blood test and 17 patients did not have any, leaving their actual outcomes unclear.
“Given that AKI detection uses blood tests, an AKI in these patients was never confirmed,” Dr. Scanlon noted. “So this could give a potential benefit of the model that we never intended: It could reduce undiagnosed AKI by flagging those who are at risk.”
“Our next steps are to test the model through a technology clinical trial to see if putting intervention strategies in place does prevent these AKIs from taking place,” Dr. Scanlon concluded. “We are also going to move to ongoing monitoring of the model performance.”
Dr. Scanlon disclosed no conflicts of interest. The study did not receive specific funding.
A model that crunches data from routine blood tests can accurately identify cancer patients who will develop acute kidney injury (AKI) up to a month before it happens, according to a cohort study.
The algorithm spotted nearly 74% of the patients who went on to develop AKI within 30 days, providing a window for intervention and possibly prevention, according to investigators.
These results were reported at the AACR Virtual Special Conference: Artificial Intelligence, Diagnosis, and Imaging (abstract PR-11).
“Cancer patients are a high-risk population for AKI due to the nature of their treatment and illness,” said presenter Lauren A. Scanlon, PhD, a data scientist at The Christie NHS Foundation Trust in Huddersfield, England. “AKI causes a huge disruption in treatment and distress for the patient, so it would be amazing if we could, say, predict the AKI before it occurs and prevent it from even happening.”
U.K. health care providers are already using an algorithm to monitor patients’ creatinine levels, comparing new values against historic ones, Dr. Scanlon explained. When that algorithm detects AKI, it issues an alert that triggers implementation of an AKI care bundle, including measures such as fluid monitoring and medication review, within 24 hours.
Taking this concept further, Dr. Scanlon and colleagues developed a random forest model, a type of machine learning algorithm, that incorporates other markers from blood tests routinely obtained for all patients, with the aim of predicting AKI up to 30 days in advance.
“Using routinely collected blood test results will ensure that the model is applicable to all our patients and can be implemented in an automated manner,” Dr. Scanlon noted.
The investigators developed and trained the model using 597,403 blood test results from 48,865 patients undergoing cancer treatment between January 2017 and May 2020.
The model assigns patients to five categories of risk for AKI in the next 30 days: very low, low, medium, high, and very high.
“We wanted the model to output in this way so that it could be used by clinicians alongside their own insight and knowledge on a case-by-case basis,” Dr. Scanlon explained.
The investigators then prospectively validated the model and its risk categories in another 9,913 patients who underwent cancer treatment between June and August 2020.
Using a model threshold of medium risk or higher, the model correctly predicted AKI in 330 (73.8%) of the 447 patients in the validation cohort who ultimately developed AKI.
“This is pretty amazing and shows that this model really is working and can correctly detect these AKIs up to 30 days before they occur, giving a huge window to put in place preventive strategies,” Dr. Scanlon said.
Among the 154 patients in whom the model incorrectly predicted AKI, 9 patients had only a single follow-up blood test and 17 patients did not have any, leaving their actual outcomes unclear.
“Given that AKI detection uses blood tests, an AKI in these patients was never confirmed,” Dr. Scanlon noted. “So this could give a potential benefit of the model that we never intended: It could reduce undiagnosed AKI by flagging those who are at risk.”
“Our next steps are to test the model through a technology clinical trial to see if putting intervention strategies in place does prevent these AKIs from taking place,” Dr. Scanlon concluded. “We are also going to move to ongoing monitoring of the model performance.”
Dr. Scanlon disclosed no conflicts of interest. The study did not receive specific funding.
A model that crunches data from routine blood tests can accurately identify cancer patients who will develop acute kidney injury (AKI) up to a month before it happens, according to a cohort study.
The algorithm spotted nearly 74% of the patients who went on to develop AKI within 30 days, providing a window for intervention and possibly prevention, according to investigators.
These results were reported at the AACR Virtual Special Conference: Artificial Intelligence, Diagnosis, and Imaging (abstract PR-11).
“Cancer patients are a high-risk population for AKI due to the nature of their treatment and illness,” said presenter Lauren A. Scanlon, PhD, a data scientist at The Christie NHS Foundation Trust in Huddersfield, England. “AKI causes a huge disruption in treatment and distress for the patient, so it would be amazing if we could, say, predict the AKI before it occurs and prevent it from even happening.”
U.K. health care providers are already using an algorithm to monitor patients’ creatinine levels, comparing new values against historic ones, Dr. Scanlon explained. When that algorithm detects AKI, it issues an alert that triggers implementation of an AKI care bundle, including measures such as fluid monitoring and medication review, within 24 hours.
Taking this concept further, Dr. Scanlon and colleagues developed a random forest model, a type of machine learning algorithm, that incorporates other markers from blood tests routinely obtained for all patients, with the aim of predicting AKI up to 30 days in advance.
“Using routinely collected blood test results will ensure that the model is applicable to all our patients and can be implemented in an automated manner,” Dr. Scanlon noted.
The investigators developed and trained the model using 597,403 blood test results from 48,865 patients undergoing cancer treatment between January 2017 and May 2020.
The model assigns patients to five categories of risk for AKI in the next 30 days: very low, low, medium, high, and very high.
“We wanted the model to output in this way so that it could be used by clinicians alongside their own insight and knowledge on a case-by-case basis,” Dr. Scanlon explained.
The investigators then prospectively validated the model and its risk categories in another 9,913 patients who underwent cancer treatment between June and August 2020.
Using a model threshold of medium risk or higher, the model correctly predicted AKI in 330 (73.8%) of the 447 patients in the validation cohort who ultimately developed AKI.
“This is pretty amazing and shows that this model really is working and can correctly detect these AKIs up to 30 days before they occur, giving a huge window to put in place preventive strategies,” Dr. Scanlon said.
Among the 154 patients in whom the model incorrectly predicted AKI, 9 patients had only a single follow-up blood test and 17 patients did not have any, leaving their actual outcomes unclear.
“Given that AKI detection uses blood tests, an AKI in these patients was never confirmed,” Dr. Scanlon noted. “So this could give a potential benefit of the model that we never intended: It could reduce undiagnosed AKI by flagging those who are at risk.”
“Our next steps are to test the model through a technology clinical trial to see if putting intervention strategies in place does prevent these AKIs from taking place,” Dr. Scanlon concluded. “We are also going to move to ongoing monitoring of the model performance.”
Dr. Scanlon disclosed no conflicts of interest. The study did not receive specific funding.
FROM AACR: AI, DIAGNOSIS, AND IMAGING 2021
Intraoperative rupture of ovarian cancer: Does it worsen outcomes?
Intact removal of an ovarian cyst is a well-established gynecologic surgical principle because ovarian cancer is definitively diagnosed only in retrospect (after ovarian extraction) and intraoperative cyst rupture upstages an otherwise nonmetastatic cancer to stage IC. This lumps cancers that are ruptured during surgical extraction together with those that have spontaneously ruptured or have surface excrescences. The theoretical rationale for this “lumping” is that contact between malignant cells from the ruptured cyst may take hold on peritoneal surfaces resulting in development of metastases. To offset this theoretical risk, it has been recommended that all stage IC ovarian cancer is treated with chemotherapy, whereas low-grade stage IA and IB cancers generally are not. No conscientious surgeon wants their surgical intervention to be the cause of a patient needing toxic chemotherapy. But is the contact between malignant cyst fluid and the peritoneum truly as bad as a spontaneous breach of the surface of the tumor? Or is cyst rupture a confounder for other adverse prognostic features, such as histologic cell type and dense pelvic attachments? If ovarian cyst rupture is an independent risk factor for patients with stage I ovarian cancer, strategies should be employed to avoid this occurrence, and we should understand how to counsel and treat patients in whom this has occurred.
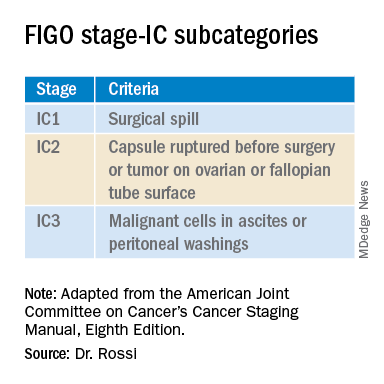
In 2017 the International Federation of Gynecology and Obstetrics (FIGO) staging of epithelial ovarian cancer subcategorized stage IC. This group encompasses women with contact between malignant cells and the peritoneum in the absence of other extraovarian disease. The table includes these distinct groupings. Stage IC1 includes patients in whom intraoperative spill occurred. Stage IC2 includes women with preoperative cyst rupture, and or microscopic or macroscopic surface involvement because the data support that these cases carry a poorer prognosis, compared with those with intraoperative rupture (IC1).1 The final subcategory, IC3, includes women who have washings (obtained at the onset of surgery, prior to manipulation of the tumor) that were positive for malignant cells, denoting preexisting contact between the tumor and peritoneum and a phenotypically more aggressive tumor.
The clinical significance of ovarian cancer capsule rupture has been evaluated in multiple studies with some mixed results.1 Consistently, it is reported that preoperative rupture, surface or capsular involvement, and preexisting peritoneal circulation of metastatic cells all portend a poorer prognosis; however, it is less clear that iatrogenic surgical rupture has the same deleterious association. In a large retrospective series from Japan, the authors evaluated 15,163 cases of stage I ovarian cancer and identified 7,227 cases of iatrogenic (intraoperative) cyst rupture.2 These cases were significantly more likely to occur among clear cell cancers, and were more likely to occur in younger patients. Worse prognosis was associated with cell type (clear cell cancers), but non–clear cell cancers (such as serous, mucinous, and endometrioid) did not have a higher hazard ratio for death when intraoperative rupture occurred. But why would intraoperative cyst rupture result in worse prognosis for only one histologic cell type? The authors hypothesized that perhaps rupture was more likely to occur during extraction of these clear cell tumors because they were associated with dense adhesions from associated endometriosis, and perhaps an adverse biologic phenomenon associated with infiltrative endometriosis is driving the behavior of this cancer.
The Japanese study also looked at the effect of chemotherapy on these same patients’ outcomes. Interestingly, the addition of chemotherapy did not improve survival for the patients with stage IC1 cancers, which was in contrast to the improved survival seen when chemotherapy was given to those with spontaneous rupture or ovarian surface involvement (IC2, IC3). These data support differentiating the subgroups of stage IC cancer in treatment decision-making, and suggest that adjuvant chemotherapy might be avoided for patients with nonclear cell stage IC1 ovarian cancer. While the outcomes are worse for patients with ruptured clear cell cancers, current therapeutic options for clear cell cancers are limited because of their known resistance to traditional agents, and outcomes for women with clear cell cancer can be worse across all stages.
While cyst rupture may not always negatively affect prognosis, the goal of surgery remains an intact removal, which influences decisions regarding surgical approach. Most adnexal masses are removed via minimally invasive surgery (MIS). MIS is associated with benefits of morbidity and cost, and therefore should be considered wherever feasible. However, MIS is associated with an increased risk of ovarian cyst rupture, likely because of the rigid instrumentation used when approaching a curved structure, in addition to the disparity in size of the pathology, compared with the extraction site incision.3 When weighing the benefits and risks of different surgical approaches, it is important to gauge the probability of malignancy. Not all complex ovarian masses associated with elevations in tumor markers are malignant, and certainly most that are associated with normal tumor markers are not. If the preoperative clinical data suggest that the mass is more likely to be malignant (e.g., mostly solid, vascular tumors with very elevated tumor markers), consideration might be made to abandoning a purely minimally invasive approach to a hand-assisted MIS or laparotomy approach. However, it would seem that abandoning an MIS approach to remove every ovarian cyst is unwise given that there is clear patient benefit with MIS and, as discussed above, most cases of iatrogenic malignant cyst rupture are unavoidable even with laparotomy, and do not necessarily independently portend poorer survival or mandate chemotherapy.
Surgeons should be both nuanced and flexible and apply some basic rules of thumb when approaching the diagnostically uncertain adnexal mass. Peritoneal washings should be obtained at the commencement of the case to discriminate those cases of true stage IC3. The peritoneum parallel to the ovarian vessel should be extensively opened to a level above the pelvic brim. In order to do this, the physiological attachments between the sigmoid colon or cecum and the suspensory ligament of the ovary may need to be carefully mobilized. This allows for retroperitoneal identification of the ureter and skeletonization of the ovarian vessels at least 2 cm proximal to their insertion into the ovary and avoidance of contact with the ovary itself (which may have a fragile capsule) or incomplete ovarian resection. If the ovary remains invested close to the sidewall or colonic structures and the appropriate peritoneal and retroperitoneal mobilization has not occurred, the surgeon may unavoidably rupture the ovarian cyst as they try to “hug” the ovary with their bites of tissue in an attempt to avoid visceral injury. There is little role for an ovarian cystectomy in a postmenopausal woman undergoing surgery for a complex adnexal mass, particularly if she has elevated tumor markers, because the process of performing ovarian cystectomy commonly invokes cyst rupture or fragmentation. Ovarian cystectomy should be reserved for premenopausal women with adnexal masses at low suspicion for malignancy. If the adnexa appears densely adherent to adjacent structures – for example, associated with infiltrative endometriosis – consideration for laparotomy or a hand-assisted approach may be necessary; in such cases, even open surgery can result in cyst rupture, and the morbidity of conversion to laparotomy should be weighed for individual cases.
Finally, retrieval of the ovarian specimen should occur intact without morcellation. There should be no uncontained morcellation of adnexal structures during retrieval of even normal-appearing ovaries. The preferred retrieval method is to place the adnexa in an appropriately sized retrieval bag, after which contained morcellation or drainage can occur to facilitate removal through a laparoscopic incision. Contained morcellation is very difficult for large solid masses through a laparoscopic port site; in these cases, extension of the incision may be necessary.
While operative spill of an ovarian cancer does upstage nonmetastatic ovarian cancer, it is unclear that, in most cases, this is independently associated with worse prognosis, and chemotherapy may not always be of added value. However, best surgical practice should always include strategies to minimize the chance of rupture when approaching adnexal masses, particularly those at highest likelihood of malignancy.
References
1. Kim HS et al. Eur J Surg Oncol. 2013 Mar 39(3):279-89.
2. Matsuo K et al. Obstet Gynecol. 2019 Nov;134(5):1017-26.
3. Matsuo K et al. JAMA Oncol. 2020 Jul 1;6(7):1110-3.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
Intact removal of an ovarian cyst is a well-established gynecologic surgical principle because ovarian cancer is definitively diagnosed only in retrospect (after ovarian extraction) and intraoperative cyst rupture upstages an otherwise nonmetastatic cancer to stage IC. This lumps cancers that are ruptured during surgical extraction together with those that have spontaneously ruptured or have surface excrescences. The theoretical rationale for this “lumping” is that contact between malignant cells from the ruptured cyst may take hold on peritoneal surfaces resulting in development of metastases. To offset this theoretical risk, it has been recommended that all stage IC ovarian cancer is treated with chemotherapy, whereas low-grade stage IA and IB cancers generally are not. No conscientious surgeon wants their surgical intervention to be the cause of a patient needing toxic chemotherapy. But is the contact between malignant cyst fluid and the peritoneum truly as bad as a spontaneous breach of the surface of the tumor? Or is cyst rupture a confounder for other adverse prognostic features, such as histologic cell type and dense pelvic attachments? If ovarian cyst rupture is an independent risk factor for patients with stage I ovarian cancer, strategies should be employed to avoid this occurrence, and we should understand how to counsel and treat patients in whom this has occurred.
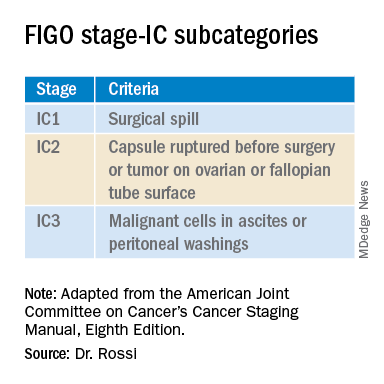
In 2017 the International Federation of Gynecology and Obstetrics (FIGO) staging of epithelial ovarian cancer subcategorized stage IC. This group encompasses women with contact between malignant cells and the peritoneum in the absence of other extraovarian disease. The table includes these distinct groupings. Stage IC1 includes patients in whom intraoperative spill occurred. Stage IC2 includes women with preoperative cyst rupture, and or microscopic or macroscopic surface involvement because the data support that these cases carry a poorer prognosis, compared with those with intraoperative rupture (IC1).1 The final subcategory, IC3, includes women who have washings (obtained at the onset of surgery, prior to manipulation of the tumor) that were positive for malignant cells, denoting preexisting contact between the tumor and peritoneum and a phenotypically more aggressive tumor.
The clinical significance of ovarian cancer capsule rupture has been evaluated in multiple studies with some mixed results.1 Consistently, it is reported that preoperative rupture, surface or capsular involvement, and preexisting peritoneal circulation of metastatic cells all portend a poorer prognosis; however, it is less clear that iatrogenic surgical rupture has the same deleterious association. In a large retrospective series from Japan, the authors evaluated 15,163 cases of stage I ovarian cancer and identified 7,227 cases of iatrogenic (intraoperative) cyst rupture.2 These cases were significantly more likely to occur among clear cell cancers, and were more likely to occur in younger patients. Worse prognosis was associated with cell type (clear cell cancers), but non–clear cell cancers (such as serous, mucinous, and endometrioid) did not have a higher hazard ratio for death when intraoperative rupture occurred. But why would intraoperative cyst rupture result in worse prognosis for only one histologic cell type? The authors hypothesized that perhaps rupture was more likely to occur during extraction of these clear cell tumors because they were associated with dense adhesions from associated endometriosis, and perhaps an adverse biologic phenomenon associated with infiltrative endometriosis is driving the behavior of this cancer.
The Japanese study also looked at the effect of chemotherapy on these same patients’ outcomes. Interestingly, the addition of chemotherapy did not improve survival for the patients with stage IC1 cancers, which was in contrast to the improved survival seen when chemotherapy was given to those with spontaneous rupture or ovarian surface involvement (IC2, IC3). These data support differentiating the subgroups of stage IC cancer in treatment decision-making, and suggest that adjuvant chemotherapy might be avoided for patients with nonclear cell stage IC1 ovarian cancer. While the outcomes are worse for patients with ruptured clear cell cancers, current therapeutic options for clear cell cancers are limited because of their known resistance to traditional agents, and outcomes for women with clear cell cancer can be worse across all stages.
While cyst rupture may not always negatively affect prognosis, the goal of surgery remains an intact removal, which influences decisions regarding surgical approach. Most adnexal masses are removed via minimally invasive surgery (MIS). MIS is associated with benefits of morbidity and cost, and therefore should be considered wherever feasible. However, MIS is associated with an increased risk of ovarian cyst rupture, likely because of the rigid instrumentation used when approaching a curved structure, in addition to the disparity in size of the pathology, compared with the extraction site incision.3 When weighing the benefits and risks of different surgical approaches, it is important to gauge the probability of malignancy. Not all complex ovarian masses associated with elevations in tumor markers are malignant, and certainly most that are associated with normal tumor markers are not. If the preoperative clinical data suggest that the mass is more likely to be malignant (e.g., mostly solid, vascular tumors with very elevated tumor markers), consideration might be made to abandoning a purely minimally invasive approach to a hand-assisted MIS or laparotomy approach. However, it would seem that abandoning an MIS approach to remove every ovarian cyst is unwise given that there is clear patient benefit with MIS and, as discussed above, most cases of iatrogenic malignant cyst rupture are unavoidable even with laparotomy, and do not necessarily independently portend poorer survival or mandate chemotherapy.
Surgeons should be both nuanced and flexible and apply some basic rules of thumb when approaching the diagnostically uncertain adnexal mass. Peritoneal washings should be obtained at the commencement of the case to discriminate those cases of true stage IC3. The peritoneum parallel to the ovarian vessel should be extensively opened to a level above the pelvic brim. In order to do this, the physiological attachments between the sigmoid colon or cecum and the suspensory ligament of the ovary may need to be carefully mobilized. This allows for retroperitoneal identification of the ureter and skeletonization of the ovarian vessels at least 2 cm proximal to their insertion into the ovary and avoidance of contact with the ovary itself (which may have a fragile capsule) or incomplete ovarian resection. If the ovary remains invested close to the sidewall or colonic structures and the appropriate peritoneal and retroperitoneal mobilization has not occurred, the surgeon may unavoidably rupture the ovarian cyst as they try to “hug” the ovary with their bites of tissue in an attempt to avoid visceral injury. There is little role for an ovarian cystectomy in a postmenopausal woman undergoing surgery for a complex adnexal mass, particularly if she has elevated tumor markers, because the process of performing ovarian cystectomy commonly invokes cyst rupture or fragmentation. Ovarian cystectomy should be reserved for premenopausal women with adnexal masses at low suspicion for malignancy. If the adnexa appears densely adherent to adjacent structures – for example, associated with infiltrative endometriosis – consideration for laparotomy or a hand-assisted approach may be necessary; in such cases, even open surgery can result in cyst rupture, and the morbidity of conversion to laparotomy should be weighed for individual cases.
Finally, retrieval of the ovarian specimen should occur intact without morcellation. There should be no uncontained morcellation of adnexal structures during retrieval of even normal-appearing ovaries. The preferred retrieval method is to place the adnexa in an appropriately sized retrieval bag, after which contained morcellation or drainage can occur to facilitate removal through a laparoscopic incision. Contained morcellation is very difficult for large solid masses through a laparoscopic port site; in these cases, extension of the incision may be necessary.
While operative spill of an ovarian cancer does upstage nonmetastatic ovarian cancer, it is unclear that, in most cases, this is independently associated with worse prognosis, and chemotherapy may not always be of added value. However, best surgical practice should always include strategies to minimize the chance of rupture when approaching adnexal masses, particularly those at highest likelihood of malignancy.
References
1. Kim HS et al. Eur J Surg Oncol. 2013 Mar 39(3):279-89.
2. Matsuo K et al. Obstet Gynecol. 2019 Nov;134(5):1017-26.
3. Matsuo K et al. JAMA Oncol. 2020 Jul 1;6(7):1110-3.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
Intact removal of an ovarian cyst is a well-established gynecologic surgical principle because ovarian cancer is definitively diagnosed only in retrospect (after ovarian extraction) and intraoperative cyst rupture upstages an otherwise nonmetastatic cancer to stage IC. This lumps cancers that are ruptured during surgical extraction together with those that have spontaneously ruptured or have surface excrescences. The theoretical rationale for this “lumping” is that contact between malignant cells from the ruptured cyst may take hold on peritoneal surfaces resulting in development of metastases. To offset this theoretical risk, it has been recommended that all stage IC ovarian cancer is treated with chemotherapy, whereas low-grade stage IA and IB cancers generally are not. No conscientious surgeon wants their surgical intervention to be the cause of a patient needing toxic chemotherapy. But is the contact between malignant cyst fluid and the peritoneum truly as bad as a spontaneous breach of the surface of the tumor? Or is cyst rupture a confounder for other adverse prognostic features, such as histologic cell type and dense pelvic attachments? If ovarian cyst rupture is an independent risk factor for patients with stage I ovarian cancer, strategies should be employed to avoid this occurrence, and we should understand how to counsel and treat patients in whom this has occurred.
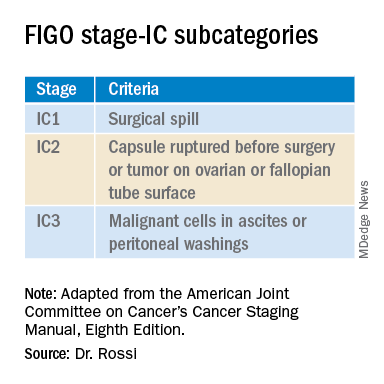
In 2017 the International Federation of Gynecology and Obstetrics (FIGO) staging of epithelial ovarian cancer subcategorized stage IC. This group encompasses women with contact between malignant cells and the peritoneum in the absence of other extraovarian disease. The table includes these distinct groupings. Stage IC1 includes patients in whom intraoperative spill occurred. Stage IC2 includes women with preoperative cyst rupture, and or microscopic or macroscopic surface involvement because the data support that these cases carry a poorer prognosis, compared with those with intraoperative rupture (IC1).1 The final subcategory, IC3, includes women who have washings (obtained at the onset of surgery, prior to manipulation of the tumor) that were positive for malignant cells, denoting preexisting contact between the tumor and peritoneum and a phenotypically more aggressive tumor.
The clinical significance of ovarian cancer capsule rupture has been evaluated in multiple studies with some mixed results.1 Consistently, it is reported that preoperative rupture, surface or capsular involvement, and preexisting peritoneal circulation of metastatic cells all portend a poorer prognosis; however, it is less clear that iatrogenic surgical rupture has the same deleterious association. In a large retrospective series from Japan, the authors evaluated 15,163 cases of stage I ovarian cancer and identified 7,227 cases of iatrogenic (intraoperative) cyst rupture.2 These cases were significantly more likely to occur among clear cell cancers, and were more likely to occur in younger patients. Worse prognosis was associated with cell type (clear cell cancers), but non–clear cell cancers (such as serous, mucinous, and endometrioid) did not have a higher hazard ratio for death when intraoperative rupture occurred. But why would intraoperative cyst rupture result in worse prognosis for only one histologic cell type? The authors hypothesized that perhaps rupture was more likely to occur during extraction of these clear cell tumors because they were associated with dense adhesions from associated endometriosis, and perhaps an adverse biologic phenomenon associated with infiltrative endometriosis is driving the behavior of this cancer.
The Japanese study also looked at the effect of chemotherapy on these same patients’ outcomes. Interestingly, the addition of chemotherapy did not improve survival for the patients with stage IC1 cancers, which was in contrast to the improved survival seen when chemotherapy was given to those with spontaneous rupture or ovarian surface involvement (IC2, IC3). These data support differentiating the subgroups of stage IC cancer in treatment decision-making, and suggest that adjuvant chemotherapy might be avoided for patients with nonclear cell stage IC1 ovarian cancer. While the outcomes are worse for patients with ruptured clear cell cancers, current therapeutic options for clear cell cancers are limited because of their known resistance to traditional agents, and outcomes for women with clear cell cancer can be worse across all stages.
While cyst rupture may not always negatively affect prognosis, the goal of surgery remains an intact removal, which influences decisions regarding surgical approach. Most adnexal masses are removed via minimally invasive surgery (MIS). MIS is associated with benefits of morbidity and cost, and therefore should be considered wherever feasible. However, MIS is associated with an increased risk of ovarian cyst rupture, likely because of the rigid instrumentation used when approaching a curved structure, in addition to the disparity in size of the pathology, compared with the extraction site incision.3 When weighing the benefits and risks of different surgical approaches, it is important to gauge the probability of malignancy. Not all complex ovarian masses associated with elevations in tumor markers are malignant, and certainly most that are associated with normal tumor markers are not. If the preoperative clinical data suggest that the mass is more likely to be malignant (e.g., mostly solid, vascular tumors with very elevated tumor markers), consideration might be made to abandoning a purely minimally invasive approach to a hand-assisted MIS or laparotomy approach. However, it would seem that abandoning an MIS approach to remove every ovarian cyst is unwise given that there is clear patient benefit with MIS and, as discussed above, most cases of iatrogenic malignant cyst rupture are unavoidable even with laparotomy, and do not necessarily independently portend poorer survival or mandate chemotherapy.
Surgeons should be both nuanced and flexible and apply some basic rules of thumb when approaching the diagnostically uncertain adnexal mass. Peritoneal washings should be obtained at the commencement of the case to discriminate those cases of true stage IC3. The peritoneum parallel to the ovarian vessel should be extensively opened to a level above the pelvic brim. In order to do this, the physiological attachments between the sigmoid colon or cecum and the suspensory ligament of the ovary may need to be carefully mobilized. This allows for retroperitoneal identification of the ureter and skeletonization of the ovarian vessels at least 2 cm proximal to their insertion into the ovary and avoidance of contact with the ovary itself (which may have a fragile capsule) or incomplete ovarian resection. If the ovary remains invested close to the sidewall or colonic structures and the appropriate peritoneal and retroperitoneal mobilization has not occurred, the surgeon may unavoidably rupture the ovarian cyst as they try to “hug” the ovary with their bites of tissue in an attempt to avoid visceral injury. There is little role for an ovarian cystectomy in a postmenopausal woman undergoing surgery for a complex adnexal mass, particularly if she has elevated tumor markers, because the process of performing ovarian cystectomy commonly invokes cyst rupture or fragmentation. Ovarian cystectomy should be reserved for premenopausal women with adnexal masses at low suspicion for malignancy. If the adnexa appears densely adherent to adjacent structures – for example, associated with infiltrative endometriosis – consideration for laparotomy or a hand-assisted approach may be necessary; in such cases, even open surgery can result in cyst rupture, and the morbidity of conversion to laparotomy should be weighed for individual cases.
Finally, retrieval of the ovarian specimen should occur intact without morcellation. There should be no uncontained morcellation of adnexal structures during retrieval of even normal-appearing ovaries. The preferred retrieval method is to place the adnexa in an appropriately sized retrieval bag, after which contained morcellation or drainage can occur to facilitate removal through a laparoscopic incision. Contained morcellation is very difficult for large solid masses through a laparoscopic port site; in these cases, extension of the incision may be necessary.
While operative spill of an ovarian cancer does upstage nonmetastatic ovarian cancer, it is unclear that, in most cases, this is independently associated with worse prognosis, and chemotherapy may not always be of added value. However, best surgical practice should always include strategies to minimize the chance of rupture when approaching adnexal masses, particularly those at highest likelihood of malignancy.
References
1. Kim HS et al. Eur J Surg Oncol. 2013 Mar 39(3):279-89.
2. Matsuo K et al. Obstet Gynecol. 2019 Nov;134(5):1017-26.
3. Matsuo K et al. JAMA Oncol. 2020 Jul 1;6(7):1110-3.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill.
Von Willebrand disease guidelines address women’s bleeding concerns
New guidelines issued jointly by four major international hematology groups focus on the management of patients with von Willebrand disease (VWD), the most common bleeding disorder in the world.
The evidence-based guidelines, published in Blood Advances, were developed in collaboration by the American Society of Hematology (ASH), the International Society on Thrombosis and Haemostasis, the National Hemophilia Foundation, and the World Federation of Hemophilia. They outline key recommendations spanning the care of patients with a broad range of therapeutic needs.
“We addressed some of the questions that were most important to the community, but certainly there are a lot of areas that we couldn’t cover” said coauthor Veronica H. Flood, MD, of the Medical College of Wisconsin in Milwaukee.
The guidelines process began with a survey sent to the von Willebrand disease community, including patients, caregivers, nurses, physicians, and scientists. The respondents were asked to prioritize issues that they felt should be addressed in the guidelines.
“Interestingly, some of the issues were the same between patients and caregivers and physicians, and some were different, but there were obviously some areas that we just couldn’t cover,” she said in an interview.
One of the areas of greatest concern for respondents was bleeding in women, and many of the recommendations include specific considerations for management of gynecologic and obstetric patients, Dr. Flood said.
“We also tried to make the questions applicable to as many patients with von Willebrand disease as possible,” she added.
Some of the questions, such as recommendation 1, regarding prophylaxis, are geared toward management of patients with severe disease, while others, such as recommendations for treatment of menstrual bleeding, are more suited for patients with milder VWD.
All of the recommendations in the guidelines are “conditional” (suggested), due to very low certainty in the evidence of effects, the authors noted.
Prophylaxis
The guidelines suggest long-term prophylaxis for patients with a history of severe and frequent bleeds, with periodic assessment of the need for prophylaxis.
Desmopressin
For those patients who may benefit from the use of desmopressin, primarily those with type 1 VWD, and who have a baseline von Willebrand factor (VWF) level below 0.30 IU/mL, the panel issued a conditional recommendation for a desmopressin trial with treatment based on the patient’s results compared with not performing a trial and treating with tranexamic acid or factor concentrate. The guidelines also advise against treating with desmopressin in the absence of a trial. In a section of “good practice statements,” the guidelines indicate that using desmopressin in patients with type 2B VWD is generally contraindicated, because of the risk of thrombocytopenia as a result of increased platelet binding. In addition, desmopressin is generally contraindicated in patients with active cardiovascular disease, patients with seizure disorders, patients less than 2 years old, and patients with type 1C VWD in the setting of surgery.
Antithrombotic therapy
The guideline panelists conditionally recommend antithrombotic therapy with either antiplatelet agents or anticoagulants, with an emphasis on reassessing bleeding risk throughout the course of treatment.
An accompanying good practice statement calls for individualized assessments of risks and benefits of specific antithrombotic therapies by a multidisciplinary team including hematologists, cardiovascular specialists, and the patient.
Major surgery
This section includes a recommendation for targeting both factor VIII and VWF activity levels to a minimum of 50 IU/mL for at least 3 days after surgery, and a suggestion against using factor VIII target levels alone.
Minor surgery/invasive procedures
The panelists suggest increasing VWF activity levels to a minimum of 0.50 IU/mL with desmopressin or factor concentrate with the addition of tranexamic acid over raising VWF levels to at least 0.50 IU/mL with desmopressin or factor concentrate alone.
In addition, the panelists suggest “giving tranexamic acid alone over increasing VWF activity levels to a minimum threshold of 0.50 IU/mL with any intervention in patients with type 1 VWD with baseline VWF activity levels of 0.30 IU/mL and a mild bleeding phenotype undergoing minor mucosal procedures.”
Heavy menstrual bleeding
In women with heavy menstrual bleeding who do not plan to conceive, the panel suggests either combined hormonal therapy or levonorgestrel-releasing intrauterine system, or tranexamic acid over desmopressin.
In women who wish to conceive, the panel suggests using tranexamic acid over desmopressin.
Neuraxial anesthesia during labor
For women in labor for whom neuraxial anesthesia is considered, the guidelines suggest targeting a VWF activity level from 0.50 to 1.50 IU/mL over targeting a level above 1.50 IU/mL.
Postpartum management
“The guideline panel suggests the use of tranexamic acid over not using it in women with type 1 VWD or low VWF levels (and this may also apply to types 2 and 3 VWD) during the postpartum period,” the guidelines say.
An accompanying good practice statement says that tranexamic acid can be provided orally or intravenously. The oral dose is 25 mg/kg three times daily for 10-14 days, or longer if blood loss remains heavy.
Dr. Flood said that the guidelines were developed under the assumption that they would apply to care of patients in regions with a high or moderately high degree of clinical resources.
“We recognize that this eliminates a great deal of the globe, and our hope is that ASH and the other sponsoring organizations are going to let us revise this and do a version for lower-resourced settings,” she said.
New guidelines issued jointly by four major international hematology groups focus on the management of patients with von Willebrand disease (VWD), the most common bleeding disorder in the world.
The evidence-based guidelines, published in Blood Advances, were developed in collaboration by the American Society of Hematology (ASH), the International Society on Thrombosis and Haemostasis, the National Hemophilia Foundation, and the World Federation of Hemophilia. They outline key recommendations spanning the care of patients with a broad range of therapeutic needs.
“We addressed some of the questions that were most important to the community, but certainly there are a lot of areas that we couldn’t cover” said coauthor Veronica H. Flood, MD, of the Medical College of Wisconsin in Milwaukee.
The guidelines process began with a survey sent to the von Willebrand disease community, including patients, caregivers, nurses, physicians, and scientists. The respondents were asked to prioritize issues that they felt should be addressed in the guidelines.
“Interestingly, some of the issues were the same between patients and caregivers and physicians, and some were different, but there were obviously some areas that we just couldn’t cover,” she said in an interview.
One of the areas of greatest concern for respondents was bleeding in women, and many of the recommendations include specific considerations for management of gynecologic and obstetric patients, Dr. Flood said.
“We also tried to make the questions applicable to as many patients with von Willebrand disease as possible,” she added.
Some of the questions, such as recommendation 1, regarding prophylaxis, are geared toward management of patients with severe disease, while others, such as recommendations for treatment of menstrual bleeding, are more suited for patients with milder VWD.
All of the recommendations in the guidelines are “conditional” (suggested), due to very low certainty in the evidence of effects, the authors noted.
Prophylaxis
The guidelines suggest long-term prophylaxis for patients with a history of severe and frequent bleeds, with periodic assessment of the need for prophylaxis.
Desmopressin
For those patients who may benefit from the use of desmopressin, primarily those with type 1 VWD, and who have a baseline von Willebrand factor (VWF) level below 0.30 IU/mL, the panel issued a conditional recommendation for a desmopressin trial with treatment based on the patient’s results compared with not performing a trial and treating with tranexamic acid or factor concentrate. The guidelines also advise against treating with desmopressin in the absence of a trial. In a section of “good practice statements,” the guidelines indicate that using desmopressin in patients with type 2B VWD is generally contraindicated, because of the risk of thrombocytopenia as a result of increased platelet binding. In addition, desmopressin is generally contraindicated in patients with active cardiovascular disease, patients with seizure disorders, patients less than 2 years old, and patients with type 1C VWD in the setting of surgery.
Antithrombotic therapy
The guideline panelists conditionally recommend antithrombotic therapy with either antiplatelet agents or anticoagulants, with an emphasis on reassessing bleeding risk throughout the course of treatment.
An accompanying good practice statement calls for individualized assessments of risks and benefits of specific antithrombotic therapies by a multidisciplinary team including hematologists, cardiovascular specialists, and the patient.
Major surgery
This section includes a recommendation for targeting both factor VIII and VWF activity levels to a minimum of 50 IU/mL for at least 3 days after surgery, and a suggestion against using factor VIII target levels alone.
Minor surgery/invasive procedures
The panelists suggest increasing VWF activity levels to a minimum of 0.50 IU/mL with desmopressin or factor concentrate with the addition of tranexamic acid over raising VWF levels to at least 0.50 IU/mL with desmopressin or factor concentrate alone.
In addition, the panelists suggest “giving tranexamic acid alone over increasing VWF activity levels to a minimum threshold of 0.50 IU/mL with any intervention in patients with type 1 VWD with baseline VWF activity levels of 0.30 IU/mL and a mild bleeding phenotype undergoing minor mucosal procedures.”
Heavy menstrual bleeding
In women with heavy menstrual bleeding who do not plan to conceive, the panel suggests either combined hormonal therapy or levonorgestrel-releasing intrauterine system, or tranexamic acid over desmopressin.
In women who wish to conceive, the panel suggests using tranexamic acid over desmopressin.
Neuraxial anesthesia during labor
For women in labor for whom neuraxial anesthesia is considered, the guidelines suggest targeting a VWF activity level from 0.50 to 1.50 IU/mL over targeting a level above 1.50 IU/mL.
Postpartum management
“The guideline panel suggests the use of tranexamic acid over not using it in women with type 1 VWD or low VWF levels (and this may also apply to types 2 and 3 VWD) during the postpartum period,” the guidelines say.
An accompanying good practice statement says that tranexamic acid can be provided orally or intravenously. The oral dose is 25 mg/kg three times daily for 10-14 days, or longer if blood loss remains heavy.
Dr. Flood said that the guidelines were developed under the assumption that they would apply to care of patients in regions with a high or moderately high degree of clinical resources.
“We recognize that this eliminates a great deal of the globe, and our hope is that ASH and the other sponsoring organizations are going to let us revise this and do a version for lower-resourced settings,” she said.
New guidelines issued jointly by four major international hematology groups focus on the management of patients with von Willebrand disease (VWD), the most common bleeding disorder in the world.
The evidence-based guidelines, published in Blood Advances, were developed in collaboration by the American Society of Hematology (ASH), the International Society on Thrombosis and Haemostasis, the National Hemophilia Foundation, and the World Federation of Hemophilia. They outline key recommendations spanning the care of patients with a broad range of therapeutic needs.
“We addressed some of the questions that were most important to the community, but certainly there are a lot of areas that we couldn’t cover” said coauthor Veronica H. Flood, MD, of the Medical College of Wisconsin in Milwaukee.
The guidelines process began with a survey sent to the von Willebrand disease community, including patients, caregivers, nurses, physicians, and scientists. The respondents were asked to prioritize issues that they felt should be addressed in the guidelines.
“Interestingly, some of the issues were the same between patients and caregivers and physicians, and some were different, but there were obviously some areas that we just couldn’t cover,” she said in an interview.
One of the areas of greatest concern for respondents was bleeding in women, and many of the recommendations include specific considerations for management of gynecologic and obstetric patients, Dr. Flood said.
“We also tried to make the questions applicable to as many patients with von Willebrand disease as possible,” she added.
Some of the questions, such as recommendation 1, regarding prophylaxis, are geared toward management of patients with severe disease, while others, such as recommendations for treatment of menstrual bleeding, are more suited for patients with milder VWD.
All of the recommendations in the guidelines are “conditional” (suggested), due to very low certainty in the evidence of effects, the authors noted.
Prophylaxis
The guidelines suggest long-term prophylaxis for patients with a history of severe and frequent bleeds, with periodic assessment of the need for prophylaxis.
Desmopressin
For those patients who may benefit from the use of desmopressin, primarily those with type 1 VWD, and who have a baseline von Willebrand factor (VWF) level below 0.30 IU/mL, the panel issued a conditional recommendation for a desmopressin trial with treatment based on the patient’s results compared with not performing a trial and treating with tranexamic acid or factor concentrate. The guidelines also advise against treating with desmopressin in the absence of a trial. In a section of “good practice statements,” the guidelines indicate that using desmopressin in patients with type 2B VWD is generally contraindicated, because of the risk of thrombocytopenia as a result of increased platelet binding. In addition, desmopressin is generally contraindicated in patients with active cardiovascular disease, patients with seizure disorders, patients less than 2 years old, and patients with type 1C VWD in the setting of surgery.
Antithrombotic therapy
The guideline panelists conditionally recommend antithrombotic therapy with either antiplatelet agents or anticoagulants, with an emphasis on reassessing bleeding risk throughout the course of treatment.
An accompanying good practice statement calls for individualized assessments of risks and benefits of specific antithrombotic therapies by a multidisciplinary team including hematologists, cardiovascular specialists, and the patient.
Major surgery
This section includes a recommendation for targeting both factor VIII and VWF activity levels to a minimum of 50 IU/mL for at least 3 days after surgery, and a suggestion against using factor VIII target levels alone.
Minor surgery/invasive procedures
The panelists suggest increasing VWF activity levels to a minimum of 0.50 IU/mL with desmopressin or factor concentrate with the addition of tranexamic acid over raising VWF levels to at least 0.50 IU/mL with desmopressin or factor concentrate alone.
In addition, the panelists suggest “giving tranexamic acid alone over increasing VWF activity levels to a minimum threshold of 0.50 IU/mL with any intervention in patients with type 1 VWD with baseline VWF activity levels of 0.30 IU/mL and a mild bleeding phenotype undergoing minor mucosal procedures.”
Heavy menstrual bleeding
In women with heavy menstrual bleeding who do not plan to conceive, the panel suggests either combined hormonal therapy or levonorgestrel-releasing intrauterine system, or tranexamic acid over desmopressin.
In women who wish to conceive, the panel suggests using tranexamic acid over desmopressin.
Neuraxial anesthesia during labor
For women in labor for whom neuraxial anesthesia is considered, the guidelines suggest targeting a VWF activity level from 0.50 to 1.50 IU/mL over targeting a level above 1.50 IU/mL.
Postpartum management
“The guideline panel suggests the use of tranexamic acid over not using it in women with type 1 VWD or low VWF levels (and this may also apply to types 2 and 3 VWD) during the postpartum period,” the guidelines say.
An accompanying good practice statement says that tranexamic acid can be provided orally or intravenously. The oral dose is 25 mg/kg three times daily for 10-14 days, or longer if blood loss remains heavy.
Dr. Flood said that the guidelines were developed under the assumption that they would apply to care of patients in regions with a high or moderately high degree of clinical resources.
“We recognize that this eliminates a great deal of the globe, and our hope is that ASH and the other sponsoring organizations are going to let us revise this and do a version for lower-resourced settings,” she said.
FROM BLOOD ADVANCES
Nulliparity, not ART, likely raises risk of ovarian cancer
Women who receive ovarian stimulation for assisted reproductive technology (ART) procedures don’t have an increased risk of developing ovarian cancer when compared to subfertile women who don’t undergo ART, according to a new study.
The results suggest that nulliparity is likely responsible for the increased risk of ovarian cancer observed in patients treated with ART, the researchers said.
Earlier, shorter studies had only compared ART-treated women with women from the general population.
“Subfertile women differ from women in the general population according to several ovarian cancer risk factors. Therefore, to estimate the risk of ovarian cancer associated with ART, it was important to include a comparison group of women who were subfertile and not treated with ART,” said senior study author Flora E. van Leeuwen, PhD, of Netherlands Cancer Institute in Amsterdam.
She and her colleagues conducted a nationwide cohort study of 30,625 women who received ovarian stimulation for ART during 1983-2000 and 9,988 women who received fertility treatments other than ART.
Incident invasive and borderline ovarian tumors were ascertained through linkage with the Netherlands Cancer Registry and the Dutch Pathology Registry. Ovarian tumor risk in ART-treated women was compared with risks in the general population and the subfertile non-ART group.
The researchers reported the results in the Journal of the National Cancer Institute.
Risk of ovarian cancer
Women treated with ART were no more likely to develop ovarian cancer than subfertile women not treated with ART (adjusted hazard ratio, 1.02), but the ART group did have an increased risk of ovarian cancer when compared to the general population (standardized incidence ratio, 1.43).
“This, however, turned out to be due to the fact that the women who had received ART were less likely to have children. Not having children is a known risk factor for ovarian cancer,” Dr. van Leeuwen said.
Women with more ART procedures that resulted in the birth of a child were at lower risk of developing ovarian cancer, compared with women without any successful cycle (Ptrend = .001). However, women who had only cycles not resulting in a birth were not at higher risk of ovarian cancer when they had a greater number of cycles.
“These results indicate that parity decreases the risk of ovarian cancer, also in ART-treated women. But more unsuccessful ART cycles do not increase the risk of ovarian cancer,” Dr. van Leeuwen said.
Risk of borderline ovarian tumors
The risk of developing borderline ovarian tumors was roughly twice as high in women who had received ART, both compared with women who had received other fertility treatments (hazard ratio, 1.84) and women from the general population (standardized incidence ratio, 2.20).
However, the risk of developing borderline ovarian tumors did not increase in women who had received multiple ART procedures.
“If there was a causal association between ART and increased risk of borderline ovarian tumors, we would expect to see this risk increase with a greater number of ART procedures from more hormones and more stimulation of the ovaries. This makes the direct link between ART and increased risk of borderline tumors a bit uncertain. It might be caused by other factors, such as the severity of infertility,” Dr. van Leeuwen said.
Borderline ovarian tumors are rare in the general population in the Netherlands, and women who develop these tumors generally have a good prognosis, she said.
The risk of developing a borderline tumor before the age of 55 for women in the Netherlands is approximately 0.2%. After ART, the study found a risk of approximately 0.3%.
Causal associations with ART 'unlikely'
“Women who develop cancer and have undergone ART procedures in the past may wonder whether their cancer may be caused by ART. Based on the results from our study, that seems unlikely, and that is a very reassuring message from practicing oncologists to women diagnosed with ovarian cancer. Another important message is that, in ART-treated women, increasing parity reduces the risk of ovarian cancer,” Dr. van Leeuwen said.
She added that the risk of borderline ovarian tumors did not increase in women who received multiple ART procedures, “which makes it somewhat less likely that ART would have caused their borderline ovarian tumor.”
The study does not exclude the possibility that ART might increase the risk of ovarian tumors after age 60.
“Despite our long follow-up, the age of the women at the end of our study was still relatively young [average 56 years]. Because the incidence of ovarian cancer increases with older age, it is vital to continue to follow these women. Only then can we be sure that ART does not increase the risk of ovarian tumors in the very long run,” Dr. van Leeuwen said.
“This study offers confirmation of several previous studies and provides reassurance about the risk of ovarian cancer after ART procedures,” said Daniel Kenigsberg, MD, of RMA Long Island IVF in New York. Dr. Kenigsberg was not involved in this study but has performed more than 30,000 ART procedures over the past 32 years.
“Researchers have looked at whether fertility drugs cause ovarian cancer in different ways and in different countries, and there is no cause-and-effect relationship. There was no dose-response relationship between ART and ovarian tumors in this study. It’s more likely there is something wrong with the women’s ovaries that lead to borderline tumors and infertility more than any treatment,” Dr. Kenigsberg added.
“Perhaps both fertility and cancer relate to an underlying ovarian issue, but this would not explain the increased cancer incidence in those who never attempted pregnancy, that is, women who are voluntarily childless. Pregnancy is statistically protective: more pregnancies lead to less ovarian cancer, but this is far from absolute,” he explained.
Dr. Kenigsberg suggested that oncologists should be aware of a patient’s obstetrical history and fertility history as well as any related medical interventions.
“Borderline tumors look like cancer and have histologic features of cancer but do not meet the criteria for a cancer diagnosis,” he said. “They require close surveillance because their relationship to the development of full-fledged cancer is uncertain.”
This research was supported by grants from the Dutch Cancer Society. The authors and Dr. Kenigsberg have no conflicts of interest.
Women who receive ovarian stimulation for assisted reproductive technology (ART) procedures don’t have an increased risk of developing ovarian cancer when compared to subfertile women who don’t undergo ART, according to a new study.
The results suggest that nulliparity is likely responsible for the increased risk of ovarian cancer observed in patients treated with ART, the researchers said.
Earlier, shorter studies had only compared ART-treated women with women from the general population.
“Subfertile women differ from women in the general population according to several ovarian cancer risk factors. Therefore, to estimate the risk of ovarian cancer associated with ART, it was important to include a comparison group of women who were subfertile and not treated with ART,” said senior study author Flora E. van Leeuwen, PhD, of Netherlands Cancer Institute in Amsterdam.
She and her colleagues conducted a nationwide cohort study of 30,625 women who received ovarian stimulation for ART during 1983-2000 and 9,988 women who received fertility treatments other than ART.
Incident invasive and borderline ovarian tumors were ascertained through linkage with the Netherlands Cancer Registry and the Dutch Pathology Registry. Ovarian tumor risk in ART-treated women was compared with risks in the general population and the subfertile non-ART group.
The researchers reported the results in the Journal of the National Cancer Institute.
Risk of ovarian cancer
Women treated with ART were no more likely to develop ovarian cancer than subfertile women not treated with ART (adjusted hazard ratio, 1.02), but the ART group did have an increased risk of ovarian cancer when compared to the general population (standardized incidence ratio, 1.43).
“This, however, turned out to be due to the fact that the women who had received ART were less likely to have children. Not having children is a known risk factor for ovarian cancer,” Dr. van Leeuwen said.
Women with more ART procedures that resulted in the birth of a child were at lower risk of developing ovarian cancer, compared with women without any successful cycle (Ptrend = .001). However, women who had only cycles not resulting in a birth were not at higher risk of ovarian cancer when they had a greater number of cycles.
“These results indicate that parity decreases the risk of ovarian cancer, also in ART-treated women. But more unsuccessful ART cycles do not increase the risk of ovarian cancer,” Dr. van Leeuwen said.
Risk of borderline ovarian tumors
The risk of developing borderline ovarian tumors was roughly twice as high in women who had received ART, both compared with women who had received other fertility treatments (hazard ratio, 1.84) and women from the general population (standardized incidence ratio, 2.20).
However, the risk of developing borderline ovarian tumors did not increase in women who had received multiple ART procedures.
“If there was a causal association between ART and increased risk of borderline ovarian tumors, we would expect to see this risk increase with a greater number of ART procedures from more hormones and more stimulation of the ovaries. This makes the direct link between ART and increased risk of borderline tumors a bit uncertain. It might be caused by other factors, such as the severity of infertility,” Dr. van Leeuwen said.
Borderline ovarian tumors are rare in the general population in the Netherlands, and women who develop these tumors generally have a good prognosis, she said.
The risk of developing a borderline tumor before the age of 55 for women in the Netherlands is approximately 0.2%. After ART, the study found a risk of approximately 0.3%.
Causal associations with ART 'unlikely'
“Women who develop cancer and have undergone ART procedures in the past may wonder whether their cancer may be caused by ART. Based on the results from our study, that seems unlikely, and that is a very reassuring message from practicing oncologists to women diagnosed with ovarian cancer. Another important message is that, in ART-treated women, increasing parity reduces the risk of ovarian cancer,” Dr. van Leeuwen said.
She added that the risk of borderline ovarian tumors did not increase in women who received multiple ART procedures, “which makes it somewhat less likely that ART would have caused their borderline ovarian tumor.”
The study does not exclude the possibility that ART might increase the risk of ovarian tumors after age 60.
“Despite our long follow-up, the age of the women at the end of our study was still relatively young [average 56 years]. Because the incidence of ovarian cancer increases with older age, it is vital to continue to follow these women. Only then can we be sure that ART does not increase the risk of ovarian tumors in the very long run,” Dr. van Leeuwen said.
“This study offers confirmation of several previous studies and provides reassurance about the risk of ovarian cancer after ART procedures,” said Daniel Kenigsberg, MD, of RMA Long Island IVF in New York. Dr. Kenigsberg was not involved in this study but has performed more than 30,000 ART procedures over the past 32 years.
“Researchers have looked at whether fertility drugs cause ovarian cancer in different ways and in different countries, and there is no cause-and-effect relationship. There was no dose-response relationship between ART and ovarian tumors in this study. It’s more likely there is something wrong with the women’s ovaries that lead to borderline tumors and infertility more than any treatment,” Dr. Kenigsberg added.
“Perhaps both fertility and cancer relate to an underlying ovarian issue, but this would not explain the increased cancer incidence in those who never attempted pregnancy, that is, women who are voluntarily childless. Pregnancy is statistically protective: more pregnancies lead to less ovarian cancer, but this is far from absolute,” he explained.
Dr. Kenigsberg suggested that oncologists should be aware of a patient’s obstetrical history and fertility history as well as any related medical interventions.
“Borderline tumors look like cancer and have histologic features of cancer but do not meet the criteria for a cancer diagnosis,” he said. “They require close surveillance because their relationship to the development of full-fledged cancer is uncertain.”
This research was supported by grants from the Dutch Cancer Society. The authors and Dr. Kenigsberg have no conflicts of interest.
Women who receive ovarian stimulation for assisted reproductive technology (ART) procedures don’t have an increased risk of developing ovarian cancer when compared to subfertile women who don’t undergo ART, according to a new study.
The results suggest that nulliparity is likely responsible for the increased risk of ovarian cancer observed in patients treated with ART, the researchers said.
Earlier, shorter studies had only compared ART-treated women with women from the general population.
“Subfertile women differ from women in the general population according to several ovarian cancer risk factors. Therefore, to estimate the risk of ovarian cancer associated with ART, it was important to include a comparison group of women who were subfertile and not treated with ART,” said senior study author Flora E. van Leeuwen, PhD, of Netherlands Cancer Institute in Amsterdam.
She and her colleagues conducted a nationwide cohort study of 30,625 women who received ovarian stimulation for ART during 1983-2000 and 9,988 women who received fertility treatments other than ART.
Incident invasive and borderline ovarian tumors were ascertained through linkage with the Netherlands Cancer Registry and the Dutch Pathology Registry. Ovarian tumor risk in ART-treated women was compared with risks in the general population and the subfertile non-ART group.
The researchers reported the results in the Journal of the National Cancer Institute.
Risk of ovarian cancer
Women treated with ART were no more likely to develop ovarian cancer than subfertile women not treated with ART (adjusted hazard ratio, 1.02), but the ART group did have an increased risk of ovarian cancer when compared to the general population (standardized incidence ratio, 1.43).
“This, however, turned out to be due to the fact that the women who had received ART were less likely to have children. Not having children is a known risk factor for ovarian cancer,” Dr. van Leeuwen said.
Women with more ART procedures that resulted in the birth of a child were at lower risk of developing ovarian cancer, compared with women without any successful cycle (Ptrend = .001). However, women who had only cycles not resulting in a birth were not at higher risk of ovarian cancer when they had a greater number of cycles.
“These results indicate that parity decreases the risk of ovarian cancer, also in ART-treated women. But more unsuccessful ART cycles do not increase the risk of ovarian cancer,” Dr. van Leeuwen said.
Risk of borderline ovarian tumors
The risk of developing borderline ovarian tumors was roughly twice as high in women who had received ART, both compared with women who had received other fertility treatments (hazard ratio, 1.84) and women from the general population (standardized incidence ratio, 2.20).
However, the risk of developing borderline ovarian tumors did not increase in women who had received multiple ART procedures.
“If there was a causal association between ART and increased risk of borderline ovarian tumors, we would expect to see this risk increase with a greater number of ART procedures from more hormones and more stimulation of the ovaries. This makes the direct link between ART and increased risk of borderline tumors a bit uncertain. It might be caused by other factors, such as the severity of infertility,” Dr. van Leeuwen said.
Borderline ovarian tumors are rare in the general population in the Netherlands, and women who develop these tumors generally have a good prognosis, she said.
The risk of developing a borderline tumor before the age of 55 for women in the Netherlands is approximately 0.2%. After ART, the study found a risk of approximately 0.3%.
Causal associations with ART 'unlikely'
“Women who develop cancer and have undergone ART procedures in the past may wonder whether their cancer may be caused by ART. Based on the results from our study, that seems unlikely, and that is a very reassuring message from practicing oncologists to women diagnosed with ovarian cancer. Another important message is that, in ART-treated women, increasing parity reduces the risk of ovarian cancer,” Dr. van Leeuwen said.
She added that the risk of borderline ovarian tumors did not increase in women who received multiple ART procedures, “which makes it somewhat less likely that ART would have caused their borderline ovarian tumor.”
The study does not exclude the possibility that ART might increase the risk of ovarian tumors after age 60.
“Despite our long follow-up, the age of the women at the end of our study was still relatively young [average 56 years]. Because the incidence of ovarian cancer increases with older age, it is vital to continue to follow these women. Only then can we be sure that ART does not increase the risk of ovarian tumors in the very long run,” Dr. van Leeuwen said.
“This study offers confirmation of several previous studies and provides reassurance about the risk of ovarian cancer after ART procedures,” said Daniel Kenigsberg, MD, of RMA Long Island IVF in New York. Dr. Kenigsberg was not involved in this study but has performed more than 30,000 ART procedures over the past 32 years.
“Researchers have looked at whether fertility drugs cause ovarian cancer in different ways and in different countries, and there is no cause-and-effect relationship. There was no dose-response relationship between ART and ovarian tumors in this study. It’s more likely there is something wrong with the women’s ovaries that lead to borderline tumors and infertility more than any treatment,” Dr. Kenigsberg added.
“Perhaps both fertility and cancer relate to an underlying ovarian issue, but this would not explain the increased cancer incidence in those who never attempted pregnancy, that is, women who are voluntarily childless. Pregnancy is statistically protective: more pregnancies lead to less ovarian cancer, but this is far from absolute,” he explained.
Dr. Kenigsberg suggested that oncologists should be aware of a patient’s obstetrical history and fertility history as well as any related medical interventions.
“Borderline tumors look like cancer and have histologic features of cancer but do not meet the criteria for a cancer diagnosis,” he said. “They require close surveillance because their relationship to the development of full-fledged cancer is uncertain.”
This research was supported by grants from the Dutch Cancer Society. The authors and Dr. Kenigsberg have no conflicts of interest.
FROM JOURNAL OF THE NATIONAL CANCER INSTITUTE
Case study: Maternal cervical cancer linked to neonate lung cancer
That’s the conclusion of two ground-breaking cases from Japan in which investigators describe lung cancer in two boys that “probably developed” from their respective mothers via vaginal transmission during birth.
“Transmission of maternal cancer to offspring is extremely rare and is estimated to occur in approximately 1 infant per every 500,000 mothers with cancer,” wrote Ayumu Arakawa, MD, of the National Cancer Center Hospital in Japan, and colleagues, in a paper published Jan. 7 in The New England Journal of Medicine.
Previous cases, of which only 18 have been recorded, have been presumed to occur via transplacental transmission, they said.
In the two new cases, genetic analyses and other evidence suggest that both boys’ lung cancers developed after aspirating uterine cervical cancer tumor cells into their lungs during passage through the birth canal.
Tragically, both mothers, each of whom was diagnosed with cervical cancer after the births, died while their boys were still infants.
“Most of the maternal-to-infant cases reported have been leukemia or melanoma,” said Mel Greaves, PhD, of the Institute of Cancer Research, London, who was asked for comment. In 2009, Dr. Greaves and colleagues published a case study of maternal-to-infant cancer transmission (presumably via the placenta). “It attracted an enormous amount of publicity and no doubt some alarm,” he said in an interview. He emphasized that the phenomenon is “incredibly rare.”
Dr. Greaves explains why such transmission is so rare. “We suspect that cancer cells do transit from mum to unborn child more often, but the foreign (aka paternal) antigens (HLA) on the tumor cells prompt immunological rejection. The extremely rare cases of successful transmission probably do depend on the fortuitous loss of paternal HLA.”
Advances in genetic technology may allow such cases, which have been recorded since 1950, to be rapidly identified now, he said.
“Where there is an adult-type cancer in an infant or child whose mother carried cancer when pregnant, then whole-genome sequencing should quickly tell if the infant’s tumor was of maternal origin,” Dr. Greaves explained.
“I think we will be seeing more reports like this in the future, now that this phenomenon has been described and next-generation sequencing is more readily available,” added Mae Zakhour, MD, of the University of California, Los Angeles, Jonsson Comprehensive Cancer Center, when asked for comment.
In the case of the Japanese boys, both cases were discovered incidentally during an analysis of the results of routine next-generation sequencing testing in a prospective gene-profiling trial in cancer patients, known as TOP-GEAR.
How do the investigators know that the spread happened vaginally and not via the placenta?
They explained that, in other cases of mother-to-fetus transmission, the offspring presented with multiple metastases in the brain, bones, liver, lungs, and soft tissues, which were “consistent with presumed hematogenous spread from the placenta.” However, in the two boys, tumors were observed only in the lungs and were localized along the bronchi.
That peribronchial pattern of tumor growth “suggested that the tumors arose from mother-to-infant vaginal transmission through aspiration of tumor-contaminated vaginal fluids during birth.”
In addition, the tumors in both boys lacked the Y chromosome and shared multiple somatic mutations, an HPV genome, and SNP alleles with tumors from the mothers.
“The identical molecular profiles of maternal and pediatric tumors demonstrated by next-generation sequencing, as well as the location of the tumors in the children, provides strong evidence for cancer transmission during delivery,” Dr. Zakhour summarized.
C-section question
The first of the cases reported by the Japanese team was a toddler (23 months) who presented to a local hospital with a 2-week history of a productive cough. Computed tomography revealed multiple masses scattered along the bronchi in both lungs, and a biopsy revealed neuroendocrine carcinoma of the lung.
Notably, the mother’s cervical cancer was not diagnosed during her pregnancy. A cervical cytologic test performed in the mother 7 months before the birth was negative. The infant was delivered transvaginally at 39 weeks of gestation.
It was only 3 months after the birth that the 35-year-old mother received a diagnosis of squamous cell carcinoma of the cervix. She then underwent radical hysterectomy with pelvic lymphadenectomy, followed by chemotherapy.
Had it been known that she had cervical cancer, she may have been advised to have a cesarean section.
The study authors propose, on the basis of their paper, that all women with cervical cancer should have a cesarean section.
But a U.S. expert questioned this, and said the situation is “a bit nuanced.”
William Grobman, MD, of Northwestern University in Chicago, said the current standard recommendation for many pregnant women known to have cervical cancer is to have a cesarean section and that “the strength of the recommendation is dependent on factors such as stage and size.”
However, in an interview, he added that “it may be premature to make a blanket recommendation for all people based on two reports without any idea of the frequency of this event, and with such uncertainty, it seems that disclosure of all information and shared decision-making would be a key approach.”
In this case report, the authors also noted that the cancer found in the toddler looked similar to the cancer in the mother.
“Histologic similarities between the tumor samples from the mother and child prompted us to compare the results of their next-generation sequencing tests,” they said.
The result? “The comparison of the gene profiles in the samples of tumor and normal tissue confirmed that transmission of maternal tumor to the child had occurred.”
The lung cancer in the toddler progressed despite two chemotherapy regimens, so he was enrolled in a clinical trial of nivolumab therapy. He had a response that continued for 7 months, with no appearance of new lesions. Lobectomy was performed to resect a single remaining nodule. The boy had no evidence of disease recurrence at 12 months after lobectomy.
His mother was also enrolled in a nivolumab trial, but her cervical cancer had spread, and she died 5 months after disease progression.
Second case
In the second reported case, a 6-year-old boy presented to a local hospital with chest pain on the left side. Computed tomography revealed a mass in the left lung, and mucinous adenocarcinoma was eventually diagnosed.
In this case, the mother had a cervical polypoid tumor detected during pregnancy. But, as in the other case, cervical cytologic analysis was negative. Because the tumor was stable without any intervention, the mother delivered the boy vaginally at 38 weeks of gestation.
However, after the delivery, biopsy of the cervical lesion revealed adenocarcinoma. The mother underwent radical hysterectomy and bilateral salpingo-oophorectomy 3 months after delivery. She died of the disease 2 years after the surgery.
The boy received chemotherapy and had a partial response, with a reduction in levels of the tumor marker CA19-9 to normal levels. But 3 months later, the disease recurred in the left lung. After more chemotherapy, he underwent total left pneumonectomy and was subsequently free of disease.
The study authors said that they did not suspect maternal transmission of the cancer when her child received a diagnosis at 6 years of age. They explained that metastatic cervical cancer is typically a fast-growing tumor and the slow growth in the child seemed inconsistent with the idea that the cancer had been transmitted to him.
However, the pathology exam showed that the boy had mucinous adenocarcinoma, “which is an unusual morphologic finding for a primary lung tumor, but it was similar to the uterine cervical tumor in the mother,” the authors reported.
Samples of the cervical tumor from the mother and from the lung tumor of the child were submitted for next-generation sequencing tests and, said the authors, indicated mother-to-infant transmission.
The study was supported by grants from the Japan Agency for Medical Research and Development; the National Cancer Center Research and Development Fund; and the Ministry of Education, Culture, Sports, Science and Technology; and funding from Ono Pharmaceutical.
A version of this article first appeared on Medscape.com.
That’s the conclusion of two ground-breaking cases from Japan in which investigators describe lung cancer in two boys that “probably developed” from their respective mothers via vaginal transmission during birth.
“Transmission of maternal cancer to offspring is extremely rare and is estimated to occur in approximately 1 infant per every 500,000 mothers with cancer,” wrote Ayumu Arakawa, MD, of the National Cancer Center Hospital in Japan, and colleagues, in a paper published Jan. 7 in The New England Journal of Medicine.
Previous cases, of which only 18 have been recorded, have been presumed to occur via transplacental transmission, they said.
In the two new cases, genetic analyses and other evidence suggest that both boys’ lung cancers developed after aspirating uterine cervical cancer tumor cells into their lungs during passage through the birth canal.
Tragically, both mothers, each of whom was diagnosed with cervical cancer after the births, died while their boys were still infants.
“Most of the maternal-to-infant cases reported have been leukemia or melanoma,” said Mel Greaves, PhD, of the Institute of Cancer Research, London, who was asked for comment. In 2009, Dr. Greaves and colleagues published a case study of maternal-to-infant cancer transmission (presumably via the placenta). “It attracted an enormous amount of publicity and no doubt some alarm,” he said in an interview. He emphasized that the phenomenon is “incredibly rare.”
Dr. Greaves explains why such transmission is so rare. “We suspect that cancer cells do transit from mum to unborn child more often, but the foreign (aka paternal) antigens (HLA) on the tumor cells prompt immunological rejection. The extremely rare cases of successful transmission probably do depend on the fortuitous loss of paternal HLA.”
Advances in genetic technology may allow such cases, which have been recorded since 1950, to be rapidly identified now, he said.
“Where there is an adult-type cancer in an infant or child whose mother carried cancer when pregnant, then whole-genome sequencing should quickly tell if the infant’s tumor was of maternal origin,” Dr. Greaves explained.
“I think we will be seeing more reports like this in the future, now that this phenomenon has been described and next-generation sequencing is more readily available,” added Mae Zakhour, MD, of the University of California, Los Angeles, Jonsson Comprehensive Cancer Center, when asked for comment.
In the case of the Japanese boys, both cases were discovered incidentally during an analysis of the results of routine next-generation sequencing testing in a prospective gene-profiling trial in cancer patients, known as TOP-GEAR.
How do the investigators know that the spread happened vaginally and not via the placenta?
They explained that, in other cases of mother-to-fetus transmission, the offspring presented with multiple metastases in the brain, bones, liver, lungs, and soft tissues, which were “consistent with presumed hematogenous spread from the placenta.” However, in the two boys, tumors were observed only in the lungs and were localized along the bronchi.
That peribronchial pattern of tumor growth “suggested that the tumors arose from mother-to-infant vaginal transmission through aspiration of tumor-contaminated vaginal fluids during birth.”
In addition, the tumors in both boys lacked the Y chromosome and shared multiple somatic mutations, an HPV genome, and SNP alleles with tumors from the mothers.
“The identical molecular profiles of maternal and pediatric tumors demonstrated by next-generation sequencing, as well as the location of the tumors in the children, provides strong evidence for cancer transmission during delivery,” Dr. Zakhour summarized.
C-section question
The first of the cases reported by the Japanese team was a toddler (23 months) who presented to a local hospital with a 2-week history of a productive cough. Computed tomography revealed multiple masses scattered along the bronchi in both lungs, and a biopsy revealed neuroendocrine carcinoma of the lung.
Notably, the mother’s cervical cancer was not diagnosed during her pregnancy. A cervical cytologic test performed in the mother 7 months before the birth was negative. The infant was delivered transvaginally at 39 weeks of gestation.
It was only 3 months after the birth that the 35-year-old mother received a diagnosis of squamous cell carcinoma of the cervix. She then underwent radical hysterectomy with pelvic lymphadenectomy, followed by chemotherapy.
Had it been known that she had cervical cancer, she may have been advised to have a cesarean section.
The study authors propose, on the basis of their paper, that all women with cervical cancer should have a cesarean section.
But a U.S. expert questioned this, and said the situation is “a bit nuanced.”
William Grobman, MD, of Northwestern University in Chicago, said the current standard recommendation for many pregnant women known to have cervical cancer is to have a cesarean section and that “the strength of the recommendation is dependent on factors such as stage and size.”
However, in an interview, he added that “it may be premature to make a blanket recommendation for all people based on two reports without any idea of the frequency of this event, and with such uncertainty, it seems that disclosure of all information and shared decision-making would be a key approach.”
In this case report, the authors also noted that the cancer found in the toddler looked similar to the cancer in the mother.
“Histologic similarities between the tumor samples from the mother and child prompted us to compare the results of their next-generation sequencing tests,” they said.
The result? “The comparison of the gene profiles in the samples of tumor and normal tissue confirmed that transmission of maternal tumor to the child had occurred.”
The lung cancer in the toddler progressed despite two chemotherapy regimens, so he was enrolled in a clinical trial of nivolumab therapy. He had a response that continued for 7 months, with no appearance of new lesions. Lobectomy was performed to resect a single remaining nodule. The boy had no evidence of disease recurrence at 12 months after lobectomy.
His mother was also enrolled in a nivolumab trial, but her cervical cancer had spread, and she died 5 months after disease progression.
Second case
In the second reported case, a 6-year-old boy presented to a local hospital with chest pain on the left side. Computed tomography revealed a mass in the left lung, and mucinous adenocarcinoma was eventually diagnosed.
In this case, the mother had a cervical polypoid tumor detected during pregnancy. But, as in the other case, cervical cytologic analysis was negative. Because the tumor was stable without any intervention, the mother delivered the boy vaginally at 38 weeks of gestation.
However, after the delivery, biopsy of the cervical lesion revealed adenocarcinoma. The mother underwent radical hysterectomy and bilateral salpingo-oophorectomy 3 months after delivery. She died of the disease 2 years after the surgery.
The boy received chemotherapy and had a partial response, with a reduction in levels of the tumor marker CA19-9 to normal levels. But 3 months later, the disease recurred in the left lung. After more chemotherapy, he underwent total left pneumonectomy and was subsequently free of disease.
The study authors said that they did not suspect maternal transmission of the cancer when her child received a diagnosis at 6 years of age. They explained that metastatic cervical cancer is typically a fast-growing tumor and the slow growth in the child seemed inconsistent with the idea that the cancer had been transmitted to him.
However, the pathology exam showed that the boy had mucinous adenocarcinoma, “which is an unusual morphologic finding for a primary lung tumor, but it was similar to the uterine cervical tumor in the mother,” the authors reported.
Samples of the cervical tumor from the mother and from the lung tumor of the child were submitted for next-generation sequencing tests and, said the authors, indicated mother-to-infant transmission.
The study was supported by grants from the Japan Agency for Medical Research and Development; the National Cancer Center Research and Development Fund; and the Ministry of Education, Culture, Sports, Science and Technology; and funding from Ono Pharmaceutical.
A version of this article first appeared on Medscape.com.
That’s the conclusion of two ground-breaking cases from Japan in which investigators describe lung cancer in two boys that “probably developed” from their respective mothers via vaginal transmission during birth.
“Transmission of maternal cancer to offspring is extremely rare and is estimated to occur in approximately 1 infant per every 500,000 mothers with cancer,” wrote Ayumu Arakawa, MD, of the National Cancer Center Hospital in Japan, and colleagues, in a paper published Jan. 7 in The New England Journal of Medicine.
Previous cases, of which only 18 have been recorded, have been presumed to occur via transplacental transmission, they said.
In the two new cases, genetic analyses and other evidence suggest that both boys’ lung cancers developed after aspirating uterine cervical cancer tumor cells into their lungs during passage through the birth canal.
Tragically, both mothers, each of whom was diagnosed with cervical cancer after the births, died while their boys were still infants.
“Most of the maternal-to-infant cases reported have been leukemia or melanoma,” said Mel Greaves, PhD, of the Institute of Cancer Research, London, who was asked for comment. In 2009, Dr. Greaves and colleagues published a case study of maternal-to-infant cancer transmission (presumably via the placenta). “It attracted an enormous amount of publicity and no doubt some alarm,” he said in an interview. He emphasized that the phenomenon is “incredibly rare.”
Dr. Greaves explains why such transmission is so rare. “We suspect that cancer cells do transit from mum to unborn child more often, but the foreign (aka paternal) antigens (HLA) on the tumor cells prompt immunological rejection. The extremely rare cases of successful transmission probably do depend on the fortuitous loss of paternal HLA.”
Advances in genetic technology may allow such cases, which have been recorded since 1950, to be rapidly identified now, he said.
“Where there is an adult-type cancer in an infant or child whose mother carried cancer when pregnant, then whole-genome sequencing should quickly tell if the infant’s tumor was of maternal origin,” Dr. Greaves explained.
“I think we will be seeing more reports like this in the future, now that this phenomenon has been described and next-generation sequencing is more readily available,” added Mae Zakhour, MD, of the University of California, Los Angeles, Jonsson Comprehensive Cancer Center, when asked for comment.
In the case of the Japanese boys, both cases were discovered incidentally during an analysis of the results of routine next-generation sequencing testing in a prospective gene-profiling trial in cancer patients, known as TOP-GEAR.
How do the investigators know that the spread happened vaginally and not via the placenta?
They explained that, in other cases of mother-to-fetus transmission, the offspring presented with multiple metastases in the brain, bones, liver, lungs, and soft tissues, which were “consistent with presumed hematogenous spread from the placenta.” However, in the two boys, tumors were observed only in the lungs and were localized along the bronchi.
That peribronchial pattern of tumor growth “suggested that the tumors arose from mother-to-infant vaginal transmission through aspiration of tumor-contaminated vaginal fluids during birth.”
In addition, the tumors in both boys lacked the Y chromosome and shared multiple somatic mutations, an HPV genome, and SNP alleles with tumors from the mothers.
“The identical molecular profiles of maternal and pediatric tumors demonstrated by next-generation sequencing, as well as the location of the tumors in the children, provides strong evidence for cancer transmission during delivery,” Dr. Zakhour summarized.
C-section question
The first of the cases reported by the Japanese team was a toddler (23 months) who presented to a local hospital with a 2-week history of a productive cough. Computed tomography revealed multiple masses scattered along the bronchi in both lungs, and a biopsy revealed neuroendocrine carcinoma of the lung.
Notably, the mother’s cervical cancer was not diagnosed during her pregnancy. A cervical cytologic test performed in the mother 7 months before the birth was negative. The infant was delivered transvaginally at 39 weeks of gestation.
It was only 3 months after the birth that the 35-year-old mother received a diagnosis of squamous cell carcinoma of the cervix. She then underwent radical hysterectomy with pelvic lymphadenectomy, followed by chemotherapy.
Had it been known that she had cervical cancer, she may have been advised to have a cesarean section.
The study authors propose, on the basis of their paper, that all women with cervical cancer should have a cesarean section.
But a U.S. expert questioned this, and said the situation is “a bit nuanced.”
William Grobman, MD, of Northwestern University in Chicago, said the current standard recommendation for many pregnant women known to have cervical cancer is to have a cesarean section and that “the strength of the recommendation is dependent on factors such as stage and size.”
However, in an interview, he added that “it may be premature to make a blanket recommendation for all people based on two reports without any idea of the frequency of this event, and with such uncertainty, it seems that disclosure of all information and shared decision-making would be a key approach.”
In this case report, the authors also noted that the cancer found in the toddler looked similar to the cancer in the mother.
“Histologic similarities between the tumor samples from the mother and child prompted us to compare the results of their next-generation sequencing tests,” they said.
The result? “The comparison of the gene profiles in the samples of tumor and normal tissue confirmed that transmission of maternal tumor to the child had occurred.”
The lung cancer in the toddler progressed despite two chemotherapy regimens, so he was enrolled in a clinical trial of nivolumab therapy. He had a response that continued for 7 months, with no appearance of new lesions. Lobectomy was performed to resect a single remaining nodule. The boy had no evidence of disease recurrence at 12 months after lobectomy.
His mother was also enrolled in a nivolumab trial, but her cervical cancer had spread, and she died 5 months after disease progression.
Second case
In the second reported case, a 6-year-old boy presented to a local hospital with chest pain on the left side. Computed tomography revealed a mass in the left lung, and mucinous adenocarcinoma was eventually diagnosed.
In this case, the mother had a cervical polypoid tumor detected during pregnancy. But, as in the other case, cervical cytologic analysis was negative. Because the tumor was stable without any intervention, the mother delivered the boy vaginally at 38 weeks of gestation.
However, after the delivery, biopsy of the cervical lesion revealed adenocarcinoma. The mother underwent radical hysterectomy and bilateral salpingo-oophorectomy 3 months after delivery. She died of the disease 2 years after the surgery.
The boy received chemotherapy and had a partial response, with a reduction in levels of the tumor marker CA19-9 to normal levels. But 3 months later, the disease recurred in the left lung. After more chemotherapy, he underwent total left pneumonectomy and was subsequently free of disease.
The study authors said that they did not suspect maternal transmission of the cancer when her child received a diagnosis at 6 years of age. They explained that metastatic cervical cancer is typically a fast-growing tumor and the slow growth in the child seemed inconsistent with the idea that the cancer had been transmitted to him.
However, the pathology exam showed that the boy had mucinous adenocarcinoma, “which is an unusual morphologic finding for a primary lung tumor, but it was similar to the uterine cervical tumor in the mother,” the authors reported.
Samples of the cervical tumor from the mother and from the lung tumor of the child were submitted for next-generation sequencing tests and, said the authors, indicated mother-to-infant transmission.
The study was supported by grants from the Japan Agency for Medical Research and Development; the National Cancer Center Research and Development Fund; and the Ministry of Education, Culture, Sports, Science and Technology; and funding from Ono Pharmaceutical.
A version of this article first appeared on Medscape.com.
Family physicians can help achieve national goals on STIs
Among these are the U.S. Department of Health and Human Services’ first “Sexually Transmitted Infections (STIs) National Strategic Plan for the United States,” which has a strong encompassing vision.
“The United States will be a place where sexually transmitted infections are prevented and where every person has high-quality STI prevention care, and treatment while living free from stigma and discrimination. The vision includes all people, regardless of age, sex, gender identity, sexual orientation, race, ethnicity, religion, disability, geographic location, or socioeconomic circumstance,” the new HHS plan states.1
Family physicians can and should play important roles in helping our country meet this plan’s goals particularly by following two important updated clinical guidelines, one from the U.S. Preventive Services Task Force (USPSTF) and another from the Centers for Disease Control and Prevention (CDC).
This strategic plan includes the following five overarching goals with associated objectives:
- Prevent New STIs.
- Improve the health of people by reducing adverse outcomes of STIs.
- Accelerate progress in STI research, technology, and innovation.
- Reduce STI-related health disparities and health inequities.
- Achieve integrated, coordinated efforts that address the STI epidemic.1
In my opinion, family physicians have important roles to play in order for each of these goals to be achieved.Unfortunately, there are approximately 20 million new cases of STIs each year, and the U.S. has seen increases in the rates of STIs in the past decade.
“Sexually transmitted infections are frequently asymptomatic, which may delay diagnosis and treatment and lead persons to unknowingly transmit STIs to others,” according to a new recommendation statement from the USPSTF.2 STIs may lead to serious health consequences for patients, cause harms to a mother and infant during pregnancy, and lead to cases of cancer among other concerning outcomes. As such, following the HHS new national strategic plan is critical for us to address the needs of our communities.
Preventing new STIs
Family physicians can be vital in achieving the first goal of the plan by helping to prevent new STIs. In August 2020, the USPSTF updated its guideline on behavioral counseling interventions to prevent STIs. In my opinion, the USPSTF offers some practical improvements from the earlier version of this guideline.
The task force provides a grade B recommendation that all sexually active adolescents and adults at increased risk for STIs be provided with behavioral counseling to prevent STIs. The guideline indicates that behavioral counseling interventions reduce the likelihood of those at increased risk for acquiring STIs.2
The 2014 guideline had recommended intensive interventions with a minimum of 30 minutes of counseling. Many family physicians may have found this previous recommendation impractical to implement. These updated recommendations now include a variety of interventions, such as those that take less than 30 minutes.
Although interventions with more than 120 minutes of contact time had the most effect, those with less than 30 minutes still demonstrated statistically significant fewer acquisitions of STIs during follow-up. These options include in-person counseling, and providing written materials, websites, videos, and telephone and text support to patients. These interventions can be delivered directly by the family physician, or patients may be referred to other settings or the media interventions.
The task force’s updated recommendation statement refers to a variety of resources that can be used to identify these interventions. Many of the studies reviewed for this guideline were conducted in STI clinics, and the guideline authors recommended further studies in primary care as opportunities for more generalizability.
In addition to behavioral counseling for STI prevention, family physicians can help prevent STIs in their patients through HPV vaccination and HIV pre-exposure prophylaxis (PrEP provision) within their practices. As the first contact for health care for many patients, we have an opportunity to significantly impact this first goal of prevention.
Treating STIs
Within the second goal of the national strategic plan is treatment of STIs, which family physicians should include in their practices as well as the diagnosis of STIs.
In December 2020, an update to the CDC’s treatment guideline for gonococcal infection was released. Prior to the publishing of this updated recommendation, the CDC recommended combination therapy of 250 mg intramuscular (IM) dose of ceftriaxone and either doxycycline or azithromycin. This recommendation has been changed to a single 500-mg IM dose of ceftriaxone for uncomplicated urogenital, anorectal, and pharyngeal gonorrhea. If chlamydia cannot be excluded, then the addition of oral doxycycline 100 mg twice daily for 7 days is recommended for nonpregnant persons, and 1 g oral azithromycin for pregnant persons. The previous treatment was recommended based on a concern for gonococcal resistance.
This updated guideline reflects increasing concerns for antimicrobial stewardship and emerging azithromycin resistance. It does not recommend a test-of-cure for urogenital or rectal gonorrhea, though did recommend a test-of-cure 7-14 days after treatment of pharyngeal gonorrhea. The guideline also recommends testing for reinfection 3-12 months after treatment as the rate of reinfection ranges from 7% to 12% among those previously treated.3
For some offices, the provision of the IM injection may be challenging, though having this medication in stock with the possibility of provision can greatly improve access and ease of treatment for patients. Family physicians can incorporate these updated recommendations along with those for other STIs such as chlamydia and syphilis with standing orders for treatment and testing within their offices.
Accelerating progress in STI research
Family physicians can also support the national strategic plan by participating in studies looking at the impact of behavioral counseling in the primary care office as opposed to in STI clinics. In addition, by following the STI treatment and screening guidelines, family physicians will contribute to the body of knowledge of prevalence, treatment failure, and reinfection rates of STIs. We can also help advance the research by providing feedback on interventions that have success within our practices.
Reducing STI-related health disparities and inequities
Family physicians are also in important places to support the strategic plan’s fourth goal of reducing health disparities and health inequities.
If we continue to ask the questions to identify those at high risk and ensure that we are offering appropriate STI prevention, care, and treatment services within our clinics, we can expand access to all who need services and improve equity. By offering these services within the primary care office, we may be able to decrease the stigma some may feel going to an STI clinic for services.
By incorporating additional screening and counseling in our practices we may identify some patients who were not aware that they were at risk for an STI and offer them preventive services.
Achieving integrated and coordinated efforts
Finally, as many family physicians have integrated practices, we are uniquely poised to support the fifth goal of the strategic plan of achieving integrated and coordinated efforts addressing the STI epidemic. In our practices we can participate in, lead, and refer to programs for substance use disorders, viral hepatitis, STIs, and HIV as part of full scope primary care.
Family physicians and other primary care providers should work to support the entire strategic plan to ensure that we are fully caring for our patients and communities and stopping the past decade’s increase in STIs. We have an opportunity to use this strategy and make a large impact in our communities.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at [email protected].
References
1. U.S. Department of Health and Human Services. 2020. Sexually Transmitted Infections National Strategic Plan for the United States: 2021-2025. Washington.
2. U.S. Preventive Services Task Force. Behavioral counseling interventions to prevent sexually transmitted infections: U.S. Preventive Services Task Force Recommendation Statement. JAMA. 2020;324(7):674-81. doi: 10.1001/jama.2020.13095.
3. St. Cyr S et al. Update to CDC’s Treatment Guideline for Gonococcal Infection, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1911-6. doi: 10.15585/mmwr.mm6950a6external_icon.
Among these are the U.S. Department of Health and Human Services’ first “Sexually Transmitted Infections (STIs) National Strategic Plan for the United States,” which has a strong encompassing vision.
“The United States will be a place where sexually transmitted infections are prevented and where every person has high-quality STI prevention care, and treatment while living free from stigma and discrimination. The vision includes all people, regardless of age, sex, gender identity, sexual orientation, race, ethnicity, religion, disability, geographic location, or socioeconomic circumstance,” the new HHS plan states.1
Family physicians can and should play important roles in helping our country meet this plan’s goals particularly by following two important updated clinical guidelines, one from the U.S. Preventive Services Task Force (USPSTF) and another from the Centers for Disease Control and Prevention (CDC).
This strategic plan includes the following five overarching goals with associated objectives:
- Prevent New STIs.
- Improve the health of people by reducing adverse outcomes of STIs.
- Accelerate progress in STI research, technology, and innovation.
- Reduce STI-related health disparities and health inequities.
- Achieve integrated, coordinated efforts that address the STI epidemic.1
In my opinion, family physicians have important roles to play in order for each of these goals to be achieved.Unfortunately, there are approximately 20 million new cases of STIs each year, and the U.S. has seen increases in the rates of STIs in the past decade.
“Sexually transmitted infections are frequently asymptomatic, which may delay diagnosis and treatment and lead persons to unknowingly transmit STIs to others,” according to a new recommendation statement from the USPSTF.2 STIs may lead to serious health consequences for patients, cause harms to a mother and infant during pregnancy, and lead to cases of cancer among other concerning outcomes. As such, following the HHS new national strategic plan is critical for us to address the needs of our communities.
Preventing new STIs
Family physicians can be vital in achieving the first goal of the plan by helping to prevent new STIs. In August 2020, the USPSTF updated its guideline on behavioral counseling interventions to prevent STIs. In my opinion, the USPSTF offers some practical improvements from the earlier version of this guideline.
The task force provides a grade B recommendation that all sexually active adolescents and adults at increased risk for STIs be provided with behavioral counseling to prevent STIs. The guideline indicates that behavioral counseling interventions reduce the likelihood of those at increased risk for acquiring STIs.2
The 2014 guideline had recommended intensive interventions with a minimum of 30 minutes of counseling. Many family physicians may have found this previous recommendation impractical to implement. These updated recommendations now include a variety of interventions, such as those that take less than 30 minutes.
Although interventions with more than 120 minutes of contact time had the most effect, those with less than 30 minutes still demonstrated statistically significant fewer acquisitions of STIs during follow-up. These options include in-person counseling, and providing written materials, websites, videos, and telephone and text support to patients. These interventions can be delivered directly by the family physician, or patients may be referred to other settings or the media interventions.
The task force’s updated recommendation statement refers to a variety of resources that can be used to identify these interventions. Many of the studies reviewed for this guideline were conducted in STI clinics, and the guideline authors recommended further studies in primary care as opportunities for more generalizability.
In addition to behavioral counseling for STI prevention, family physicians can help prevent STIs in their patients through HPV vaccination and HIV pre-exposure prophylaxis (PrEP provision) within their practices. As the first contact for health care for many patients, we have an opportunity to significantly impact this first goal of prevention.
Treating STIs
Within the second goal of the national strategic plan is treatment of STIs, which family physicians should include in their practices as well as the diagnosis of STIs.
In December 2020, an update to the CDC’s treatment guideline for gonococcal infection was released. Prior to the publishing of this updated recommendation, the CDC recommended combination therapy of 250 mg intramuscular (IM) dose of ceftriaxone and either doxycycline or azithromycin. This recommendation has been changed to a single 500-mg IM dose of ceftriaxone for uncomplicated urogenital, anorectal, and pharyngeal gonorrhea. If chlamydia cannot be excluded, then the addition of oral doxycycline 100 mg twice daily for 7 days is recommended for nonpregnant persons, and 1 g oral azithromycin for pregnant persons. The previous treatment was recommended based on a concern for gonococcal resistance.
This updated guideline reflects increasing concerns for antimicrobial stewardship and emerging azithromycin resistance. It does not recommend a test-of-cure for urogenital or rectal gonorrhea, though did recommend a test-of-cure 7-14 days after treatment of pharyngeal gonorrhea. The guideline also recommends testing for reinfection 3-12 months after treatment as the rate of reinfection ranges from 7% to 12% among those previously treated.3
For some offices, the provision of the IM injection may be challenging, though having this medication in stock with the possibility of provision can greatly improve access and ease of treatment for patients. Family physicians can incorporate these updated recommendations along with those for other STIs such as chlamydia and syphilis with standing orders for treatment and testing within their offices.
Accelerating progress in STI research
Family physicians can also support the national strategic plan by participating in studies looking at the impact of behavioral counseling in the primary care office as opposed to in STI clinics. In addition, by following the STI treatment and screening guidelines, family physicians will contribute to the body of knowledge of prevalence, treatment failure, and reinfection rates of STIs. We can also help advance the research by providing feedback on interventions that have success within our practices.
Reducing STI-related health disparities and inequities
Family physicians are also in important places to support the strategic plan’s fourth goal of reducing health disparities and health inequities.
If we continue to ask the questions to identify those at high risk and ensure that we are offering appropriate STI prevention, care, and treatment services within our clinics, we can expand access to all who need services and improve equity. By offering these services within the primary care office, we may be able to decrease the stigma some may feel going to an STI clinic for services.
By incorporating additional screening and counseling in our practices we may identify some patients who were not aware that they were at risk for an STI and offer them preventive services.
Achieving integrated and coordinated efforts
Finally, as many family physicians have integrated practices, we are uniquely poised to support the fifth goal of the strategic plan of achieving integrated and coordinated efforts addressing the STI epidemic. In our practices we can participate in, lead, and refer to programs for substance use disorders, viral hepatitis, STIs, and HIV as part of full scope primary care.
Family physicians and other primary care providers should work to support the entire strategic plan to ensure that we are fully caring for our patients and communities and stopping the past decade’s increase in STIs. We have an opportunity to use this strategy and make a large impact in our communities.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at [email protected].
References
1. U.S. Department of Health and Human Services. 2020. Sexually Transmitted Infections National Strategic Plan for the United States: 2021-2025. Washington.
2. U.S. Preventive Services Task Force. Behavioral counseling interventions to prevent sexually transmitted infections: U.S. Preventive Services Task Force Recommendation Statement. JAMA. 2020;324(7):674-81. doi: 10.1001/jama.2020.13095.
3. St. Cyr S et al. Update to CDC’s Treatment Guideline for Gonococcal Infection, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1911-6. doi: 10.15585/mmwr.mm6950a6external_icon.
Among these are the U.S. Department of Health and Human Services’ first “Sexually Transmitted Infections (STIs) National Strategic Plan for the United States,” which has a strong encompassing vision.
“The United States will be a place where sexually transmitted infections are prevented and where every person has high-quality STI prevention care, and treatment while living free from stigma and discrimination. The vision includes all people, regardless of age, sex, gender identity, sexual orientation, race, ethnicity, religion, disability, geographic location, or socioeconomic circumstance,” the new HHS plan states.1
Family physicians can and should play important roles in helping our country meet this plan’s goals particularly by following two important updated clinical guidelines, one from the U.S. Preventive Services Task Force (USPSTF) and another from the Centers for Disease Control and Prevention (CDC).
This strategic plan includes the following five overarching goals with associated objectives:
- Prevent New STIs.
- Improve the health of people by reducing adverse outcomes of STIs.
- Accelerate progress in STI research, technology, and innovation.
- Reduce STI-related health disparities and health inequities.
- Achieve integrated, coordinated efforts that address the STI epidemic.1
In my opinion, family physicians have important roles to play in order for each of these goals to be achieved.Unfortunately, there are approximately 20 million new cases of STIs each year, and the U.S. has seen increases in the rates of STIs in the past decade.
“Sexually transmitted infections are frequently asymptomatic, which may delay diagnosis and treatment and lead persons to unknowingly transmit STIs to others,” according to a new recommendation statement from the USPSTF.2 STIs may lead to serious health consequences for patients, cause harms to a mother and infant during pregnancy, and lead to cases of cancer among other concerning outcomes. As such, following the HHS new national strategic plan is critical for us to address the needs of our communities.
Preventing new STIs
Family physicians can be vital in achieving the first goal of the plan by helping to prevent new STIs. In August 2020, the USPSTF updated its guideline on behavioral counseling interventions to prevent STIs. In my opinion, the USPSTF offers some practical improvements from the earlier version of this guideline.
The task force provides a grade B recommendation that all sexually active adolescents and adults at increased risk for STIs be provided with behavioral counseling to prevent STIs. The guideline indicates that behavioral counseling interventions reduce the likelihood of those at increased risk for acquiring STIs.2
The 2014 guideline had recommended intensive interventions with a minimum of 30 minutes of counseling. Many family physicians may have found this previous recommendation impractical to implement. These updated recommendations now include a variety of interventions, such as those that take less than 30 minutes.
Although interventions with more than 120 minutes of contact time had the most effect, those with less than 30 minutes still demonstrated statistically significant fewer acquisitions of STIs during follow-up. These options include in-person counseling, and providing written materials, websites, videos, and telephone and text support to patients. These interventions can be delivered directly by the family physician, or patients may be referred to other settings or the media interventions.
The task force’s updated recommendation statement refers to a variety of resources that can be used to identify these interventions. Many of the studies reviewed for this guideline were conducted in STI clinics, and the guideline authors recommended further studies in primary care as opportunities for more generalizability.
In addition to behavioral counseling for STI prevention, family physicians can help prevent STIs in their patients through HPV vaccination and HIV pre-exposure prophylaxis (PrEP provision) within their practices. As the first contact for health care for many patients, we have an opportunity to significantly impact this first goal of prevention.
Treating STIs
Within the second goal of the national strategic plan is treatment of STIs, which family physicians should include in their practices as well as the diagnosis of STIs.
In December 2020, an update to the CDC’s treatment guideline for gonococcal infection was released. Prior to the publishing of this updated recommendation, the CDC recommended combination therapy of 250 mg intramuscular (IM) dose of ceftriaxone and either doxycycline or azithromycin. This recommendation has been changed to a single 500-mg IM dose of ceftriaxone for uncomplicated urogenital, anorectal, and pharyngeal gonorrhea. If chlamydia cannot be excluded, then the addition of oral doxycycline 100 mg twice daily for 7 days is recommended for nonpregnant persons, and 1 g oral azithromycin for pregnant persons. The previous treatment was recommended based on a concern for gonococcal resistance.
This updated guideline reflects increasing concerns for antimicrobial stewardship and emerging azithromycin resistance. It does not recommend a test-of-cure for urogenital or rectal gonorrhea, though did recommend a test-of-cure 7-14 days after treatment of pharyngeal gonorrhea. The guideline also recommends testing for reinfection 3-12 months after treatment as the rate of reinfection ranges from 7% to 12% among those previously treated.3
For some offices, the provision of the IM injection may be challenging, though having this medication in stock with the possibility of provision can greatly improve access and ease of treatment for patients. Family physicians can incorporate these updated recommendations along with those for other STIs such as chlamydia and syphilis with standing orders for treatment and testing within their offices.
Accelerating progress in STI research
Family physicians can also support the national strategic plan by participating in studies looking at the impact of behavioral counseling in the primary care office as opposed to in STI clinics. In addition, by following the STI treatment and screening guidelines, family physicians will contribute to the body of knowledge of prevalence, treatment failure, and reinfection rates of STIs. We can also help advance the research by providing feedback on interventions that have success within our practices.
Reducing STI-related health disparities and inequities
Family physicians are also in important places to support the strategic plan’s fourth goal of reducing health disparities and health inequities.
If we continue to ask the questions to identify those at high risk and ensure that we are offering appropriate STI prevention, care, and treatment services within our clinics, we can expand access to all who need services and improve equity. By offering these services within the primary care office, we may be able to decrease the stigma some may feel going to an STI clinic for services.
By incorporating additional screening and counseling in our practices we may identify some patients who were not aware that they were at risk for an STI and offer them preventive services.
Achieving integrated and coordinated efforts
Finally, as many family physicians have integrated practices, we are uniquely poised to support the fifth goal of the strategic plan of achieving integrated and coordinated efforts addressing the STI epidemic. In our practices we can participate in, lead, and refer to programs for substance use disorders, viral hepatitis, STIs, and HIV as part of full scope primary care.
Family physicians and other primary care providers should work to support the entire strategic plan to ensure that we are fully caring for our patients and communities and stopping the past decade’s increase in STIs. We have an opportunity to use this strategy and make a large impact in our communities.
Dr. Wheat is a family physician at Erie Family Health Center in Chicago. She is program director of Northwestern’s McGaw Family Medicine residency program at Humboldt Park, Chicago. Dr. Wheat serves on the editorial advisory board of Family Practice News. You can contact her at [email protected].
References
1. U.S. Department of Health and Human Services. 2020. Sexually Transmitted Infections National Strategic Plan for the United States: 2021-2025. Washington.
2. U.S. Preventive Services Task Force. Behavioral counseling interventions to prevent sexually transmitted infections: U.S. Preventive Services Task Force Recommendation Statement. JAMA. 2020;324(7):674-81. doi: 10.1001/jama.2020.13095.
3. St. Cyr S et al. Update to CDC’s Treatment Guideline for Gonococcal Infection, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1911-6. doi: 10.15585/mmwr.mm6950a6external_icon.












