User login
Opioids: Overprescribing, alternatives, and clinical guidance
Optimal management of pregnant women with opioid misuse
Optimal management of postpartum and postoperative pain
Long-term trend: Women receiving fewer pelvic exams
according to the National Center for Health Statistics.
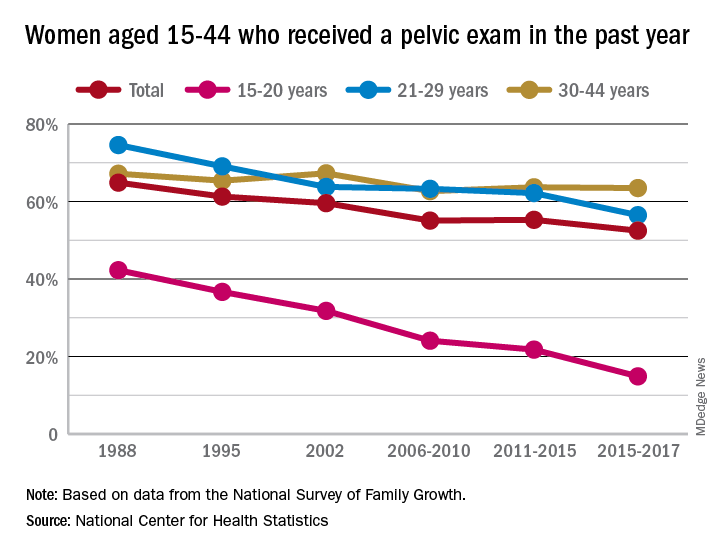
Sixty-five percent of women aged 15-44 years had received a pelvic examination in the past year when asked in 1988 as part of the National Survey of Family Growth, but the 3-year average for the 2015-2017 surveys was 53%, a significant decline, the NCHS said in a recent report.
The decrease was seen in all three of the age subgroups – 15-20 years, 21-29 years, and 30-44 years – over the length of the study period, with the trend in only the oldest women not reaching significance. The 30-44 group also was the only one of the three in which the rate ever increased at any point, the survey data show.
Data for other subgroups focused on the last 3-year period. From 2015 to 2017, non-Hispanic black women were more likely to have received a pelvic examination in the past year (60%) than were non-Hispanic white (54%) or Hispanic women (45%). An association with education level also was seen: Women with a bachelor’s degree or higher were most likely to get an exam (69%), and those with less than a high-school degree were least likely (52%), the researchers reported.
In 2018, the American College of Obstetricians and Gynecologists altered its recommendation that annual pelvic examinations be part of the well-woman visit for those aged 21 years and over, advising instead “that pelvic examinations be performed when indicated by medical history or symptoms,” the NCHS authors explained. They also suggested that their data “could provide a benchmark for estimates of the prevalence of pelvic examinations before the 2018 ACOG-updated guidelines.”
according to the National Center for Health Statistics.
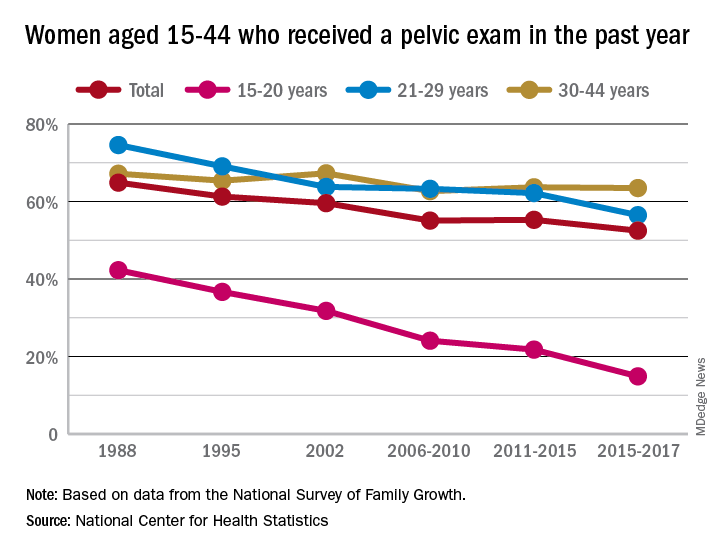
Sixty-five percent of women aged 15-44 years had received a pelvic examination in the past year when asked in 1988 as part of the National Survey of Family Growth, but the 3-year average for the 2015-2017 surveys was 53%, a significant decline, the NCHS said in a recent report.
The decrease was seen in all three of the age subgroups – 15-20 years, 21-29 years, and 30-44 years – over the length of the study period, with the trend in only the oldest women not reaching significance. The 30-44 group also was the only one of the three in which the rate ever increased at any point, the survey data show.
Data for other subgroups focused on the last 3-year period. From 2015 to 2017, non-Hispanic black women were more likely to have received a pelvic examination in the past year (60%) than were non-Hispanic white (54%) or Hispanic women (45%). An association with education level also was seen: Women with a bachelor’s degree or higher were most likely to get an exam (69%), and those with less than a high-school degree were least likely (52%), the researchers reported.
In 2018, the American College of Obstetricians and Gynecologists altered its recommendation that annual pelvic examinations be part of the well-woman visit for those aged 21 years and over, advising instead “that pelvic examinations be performed when indicated by medical history or symptoms,” the NCHS authors explained. They also suggested that their data “could provide a benchmark for estimates of the prevalence of pelvic examinations before the 2018 ACOG-updated guidelines.”
according to the National Center for Health Statistics.
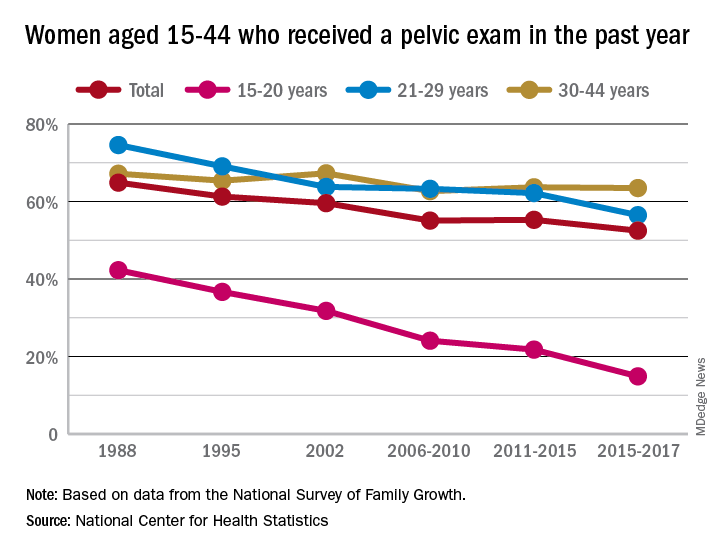
Sixty-five percent of women aged 15-44 years had received a pelvic examination in the past year when asked in 1988 as part of the National Survey of Family Growth, but the 3-year average for the 2015-2017 surveys was 53%, a significant decline, the NCHS said in a recent report.
The decrease was seen in all three of the age subgroups – 15-20 years, 21-29 years, and 30-44 years – over the length of the study period, with the trend in only the oldest women not reaching significance. The 30-44 group also was the only one of the three in which the rate ever increased at any point, the survey data show.
Data for other subgroups focused on the last 3-year period. From 2015 to 2017, non-Hispanic black women were more likely to have received a pelvic examination in the past year (60%) than were non-Hispanic white (54%) or Hispanic women (45%). An association with education level also was seen: Women with a bachelor’s degree or higher were most likely to get an exam (69%), and those with less than a high-school degree were least likely (52%), the researchers reported.
In 2018, the American College of Obstetricians and Gynecologists altered its recommendation that annual pelvic examinations be part of the well-woman visit for those aged 21 years and over, advising instead “that pelvic examinations be performed when indicated by medical history or symptoms,” the NCHS authors explained. They also suggested that their data “could provide a benchmark for estimates of the prevalence of pelvic examinations before the 2018 ACOG-updated guidelines.”
Survey: Patient-provider communication regarding dyspareunia disappoints
NASHVILLE, TENN. – Many women with endometriosis experience dyspareunia, but they are largely unsatisfied when it comes to discussions with health care providers about their symptoms, the results of an online survey suggest.
Of 638 women with self-reported endometriosis who responded to the survey, 81% said they always or usually experience pain during intercourse, 51% described their pain as severe, and 49% said they experience pain lasting more than 24 hours, Roberta Renzelli-Cain, DO, reported during a poster session at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
“The results of our survey suggest that said Dr. Renzelli-Cain, director of the West Virginia National Center of Excellence in Women’s Health and an ob.gyn. at West Virginia University, Morgantown.
In fact, survey responses suggested that dyspareunia has a marked impact on quality of life; 69% of respondents said they find sexual intercourse unpleasant, 31% said they always or usually avoid intercourse, 44% strongly agreed that dyspareunia has affected their relationship with their spouse or partner, 63% said they worry that their spouse or partner will leave, and 63% said they feel depressed because of their dyspareunia, she and her colleagues found.
Most respondents (88%) discussed their symptoms with health care providers (HCPs), and 85% did so with their ob.gyn. Among the other HCPs who respondents spoke with about their dyspareunia were primary care physicians, nurse practitioners, emergency department doctors, fertility specialists, and pain specialists.
Among the reasons given for avoiding discussions with HCPs about painful intercourse were embarrassment (34% of respondents), thinking nothing would help (26%), the physician was a man (5%), and a feeling that the provider was not understanding (3%).
Overall, 18% of respondents said they received no advice from their HCPs regarding how to deal with their dyspareunia, and 39% found nothing that their HCPs suggested to be effective.
Advice given by HCPs included surgery, lubricant use, over-the-counter pain medication, and trying different sexual positions. The percentages of respondents receiving this advice, and the percentages who considered the advice effective, respectively, were 46%, 25% for surgery; 32%, 21% for lubricant use; 36%, 18% for OTC medication; and 21%, 14% for trying different sexual positions, the investigators said.
Importantly, 42% of respondent said they felt it would be easier to discuss dyspareunia if their HCP initiated the subject.
The findings are notable given that 6%-10% of women of childbearing age are affected by endometriosis, and about 30% of those women have related dyspareunia – a “challenging symptom associated with lower sexual functioning, as well as lower self-esteem, and body image,” the investigators wrote.
The 24-question English-language survey was conducted online among women aged 19 years or older who reported having endometriosis and dyspareunia. Participants were recruited via a social network for women with endometriosis (MyEndometriosisTeam.com) and invited by e-mail to participate.
Of the 32,865 invited participants, 361 U.S.-based women and 277 women from outside the United States completed the survey. Most (83%) were aged 19-29 years.
In this online survey, the majority of women reported suboptimal communication with HCPs when seeking help for dyspareunia, the investigators said, concluding that “these results were similar between the U.S.- and non-U.S.–based women, highlighting the need for better medical communication between patients and HCPs, and better advice for patients regarding dyspareunia.”
Dr. Renzelli-Cain reported having no relevant financial disclosures.
NASHVILLE, TENN. – Many women with endometriosis experience dyspareunia, but they are largely unsatisfied when it comes to discussions with health care providers about their symptoms, the results of an online survey suggest.
Of 638 women with self-reported endometriosis who responded to the survey, 81% said they always or usually experience pain during intercourse, 51% described their pain as severe, and 49% said they experience pain lasting more than 24 hours, Roberta Renzelli-Cain, DO, reported during a poster session at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
“The results of our survey suggest that said Dr. Renzelli-Cain, director of the West Virginia National Center of Excellence in Women’s Health and an ob.gyn. at West Virginia University, Morgantown.
In fact, survey responses suggested that dyspareunia has a marked impact on quality of life; 69% of respondents said they find sexual intercourse unpleasant, 31% said they always or usually avoid intercourse, 44% strongly agreed that dyspareunia has affected their relationship with their spouse or partner, 63% said they worry that their spouse or partner will leave, and 63% said they feel depressed because of their dyspareunia, she and her colleagues found.
Most respondents (88%) discussed their symptoms with health care providers (HCPs), and 85% did so with their ob.gyn. Among the other HCPs who respondents spoke with about their dyspareunia were primary care physicians, nurse practitioners, emergency department doctors, fertility specialists, and pain specialists.
Among the reasons given for avoiding discussions with HCPs about painful intercourse were embarrassment (34% of respondents), thinking nothing would help (26%), the physician was a man (5%), and a feeling that the provider was not understanding (3%).
Overall, 18% of respondents said they received no advice from their HCPs regarding how to deal with their dyspareunia, and 39% found nothing that their HCPs suggested to be effective.
Advice given by HCPs included surgery, lubricant use, over-the-counter pain medication, and trying different sexual positions. The percentages of respondents receiving this advice, and the percentages who considered the advice effective, respectively, were 46%, 25% for surgery; 32%, 21% for lubricant use; 36%, 18% for OTC medication; and 21%, 14% for trying different sexual positions, the investigators said.
Importantly, 42% of respondent said they felt it would be easier to discuss dyspareunia if their HCP initiated the subject.
The findings are notable given that 6%-10% of women of childbearing age are affected by endometriosis, and about 30% of those women have related dyspareunia – a “challenging symptom associated with lower sexual functioning, as well as lower self-esteem, and body image,” the investigators wrote.
The 24-question English-language survey was conducted online among women aged 19 years or older who reported having endometriosis and dyspareunia. Participants were recruited via a social network for women with endometriosis (MyEndometriosisTeam.com) and invited by e-mail to participate.
Of the 32,865 invited participants, 361 U.S.-based women and 277 women from outside the United States completed the survey. Most (83%) were aged 19-29 years.
In this online survey, the majority of women reported suboptimal communication with HCPs when seeking help for dyspareunia, the investigators said, concluding that “these results were similar between the U.S.- and non-U.S.–based women, highlighting the need for better medical communication between patients and HCPs, and better advice for patients regarding dyspareunia.”
Dr. Renzelli-Cain reported having no relevant financial disclosures.
NASHVILLE, TENN. – Many women with endometriosis experience dyspareunia, but they are largely unsatisfied when it comes to discussions with health care providers about their symptoms, the results of an online survey suggest.
Of 638 women with self-reported endometriosis who responded to the survey, 81% said they always or usually experience pain during intercourse, 51% described their pain as severe, and 49% said they experience pain lasting more than 24 hours, Roberta Renzelli-Cain, DO, reported during a poster session at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
“The results of our survey suggest that said Dr. Renzelli-Cain, director of the West Virginia National Center of Excellence in Women’s Health and an ob.gyn. at West Virginia University, Morgantown.
In fact, survey responses suggested that dyspareunia has a marked impact on quality of life; 69% of respondents said they find sexual intercourse unpleasant, 31% said they always or usually avoid intercourse, 44% strongly agreed that dyspareunia has affected their relationship with their spouse or partner, 63% said they worry that their spouse or partner will leave, and 63% said they feel depressed because of their dyspareunia, she and her colleagues found.
Most respondents (88%) discussed their symptoms with health care providers (HCPs), and 85% did so with their ob.gyn. Among the other HCPs who respondents spoke with about their dyspareunia were primary care physicians, nurse practitioners, emergency department doctors, fertility specialists, and pain specialists.
Among the reasons given for avoiding discussions with HCPs about painful intercourse were embarrassment (34% of respondents), thinking nothing would help (26%), the physician was a man (5%), and a feeling that the provider was not understanding (3%).
Overall, 18% of respondents said they received no advice from their HCPs regarding how to deal with their dyspareunia, and 39% found nothing that their HCPs suggested to be effective.
Advice given by HCPs included surgery, lubricant use, over-the-counter pain medication, and trying different sexual positions. The percentages of respondents receiving this advice, and the percentages who considered the advice effective, respectively, were 46%, 25% for surgery; 32%, 21% for lubricant use; 36%, 18% for OTC medication; and 21%, 14% for trying different sexual positions, the investigators said.
Importantly, 42% of respondent said they felt it would be easier to discuss dyspareunia if their HCP initiated the subject.
The findings are notable given that 6%-10% of women of childbearing age are affected by endometriosis, and about 30% of those women have related dyspareunia – a “challenging symptom associated with lower sexual functioning, as well as lower self-esteem, and body image,” the investigators wrote.
The 24-question English-language survey was conducted online among women aged 19 years or older who reported having endometriosis and dyspareunia. Participants were recruited via a social network for women with endometriosis (MyEndometriosisTeam.com) and invited by e-mail to participate.
Of the 32,865 invited participants, 361 U.S.-based women and 277 women from outside the United States completed the survey. Most (83%) were aged 19-29 years.
In this online survey, the majority of women reported suboptimal communication with HCPs when seeking help for dyspareunia, the investigators said, concluding that “these results were similar between the U.S.- and non-U.S.–based women, highlighting the need for better medical communication between patients and HCPs, and better advice for patients regarding dyspareunia.”
Dr. Renzelli-Cain reported having no relevant financial disclosures.
REPORTING FROM ACOG 2019
ACIP extends HPV vaccine coverage
according to a unanimous vote at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
This change affects males aged 22 through 26 years; the HPV vaccine is currently recommended for males and females aged 11 or 12 years, with catch-up vaccination through age 21 for males and age 26 for females.
The change was supported in part by increased interest in simplifying and harmonizing the vaccine schedule, said Lauri Markowitz, MD, of the CDC’s National Center for Immunization and Respiratory Diseases (NCIRD), who presented the HPV work group’s considerations.
In addition, the committee voted 10-4 in favor of catch-up HPV vaccination, based on shared clinical decision making, for all adults aged 27 through 45 years.
Although the current program of HPV vaccination for youth has demonstrated effectiveness, data from multiple models suggest that widespread HPV vaccination for adults older than 26 years is much less cost effective, and would yield relatively small additional health benefits, Dr. Markowitz said.
The HPV work group reviewed data from a range of clinical trials, epidemiology, and natural history, as well as results from five different health economic models. They concluded that an assessment of benefits and harms favors expanding the catch-up vaccination to all individuals through 26 years, said Elissa Meites, MD, of the CDC, who presented the official work group opinion. The group’s opinion on the second question was that the additional population level benefit of expanding HPV vaccination to all adults would be minimal and not a reasonable and effective allocation of resources, but that shared clinical decision making would allow flexibility.
The committee expressed strong opinions about the potential for shared clinical decision making as a policy for vaccination for adults older than 26 years. Some felt that this option was a way to include adults at risk for HPV, such as divorced women with new partners, or women getting married for the first time later in life who might not have been exposed to HPV through other relationships. In addition, supporters noted that the shared clinical decision-making option would allow for potential insurance coverage, and would involve discussion between doctors and patients to assess risk.
However, other committee members felt that any recommendation for older adult vaccination would distract clinicians from the importance and value of HPV vaccination for the target age group of 11- and 12-year-olds, and might divert resources from the younger age group in whom it has shown the most benefit.
Resource allocation was a concern voiced by many committee members. Kelly Moore, MD, MPH, of Vanderbilt University, Nashville, Tenn., said she voted no on expanding vaccination to older adults because “we didn’t have details on shared clinical decision making, in the absence of information on what that meant, and in the presence of supply questions, I didn’t feel comfortable expanding vaccination to a huge population,” she said.
Paul Hunter, MD, of the City of Milwaukee Health Department, also voted no, and expressed concern that expanding the HPV vaccination recommendations to older adults would send the message that vaccination for children and teens is not effective or important.
The text of the new recommendations for routine and catch-up vaccination states that the recommendations “also apply to MSM [men who have sex with men], transgender people, and people with immunocompromising conditions.”
The ACIP members had no financial conflicts to disclose.
according to a unanimous vote at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
This change affects males aged 22 through 26 years; the HPV vaccine is currently recommended for males and females aged 11 or 12 years, with catch-up vaccination through age 21 for males and age 26 for females.
The change was supported in part by increased interest in simplifying and harmonizing the vaccine schedule, said Lauri Markowitz, MD, of the CDC’s National Center for Immunization and Respiratory Diseases (NCIRD), who presented the HPV work group’s considerations.
In addition, the committee voted 10-4 in favor of catch-up HPV vaccination, based on shared clinical decision making, for all adults aged 27 through 45 years.
Although the current program of HPV vaccination for youth has demonstrated effectiveness, data from multiple models suggest that widespread HPV vaccination for adults older than 26 years is much less cost effective, and would yield relatively small additional health benefits, Dr. Markowitz said.
The HPV work group reviewed data from a range of clinical trials, epidemiology, and natural history, as well as results from five different health economic models. They concluded that an assessment of benefits and harms favors expanding the catch-up vaccination to all individuals through 26 years, said Elissa Meites, MD, of the CDC, who presented the official work group opinion. The group’s opinion on the second question was that the additional population level benefit of expanding HPV vaccination to all adults would be minimal and not a reasonable and effective allocation of resources, but that shared clinical decision making would allow flexibility.
The committee expressed strong opinions about the potential for shared clinical decision making as a policy for vaccination for adults older than 26 years. Some felt that this option was a way to include adults at risk for HPV, such as divorced women with new partners, or women getting married for the first time later in life who might not have been exposed to HPV through other relationships. In addition, supporters noted that the shared clinical decision-making option would allow for potential insurance coverage, and would involve discussion between doctors and patients to assess risk.
However, other committee members felt that any recommendation for older adult vaccination would distract clinicians from the importance and value of HPV vaccination for the target age group of 11- and 12-year-olds, and might divert resources from the younger age group in whom it has shown the most benefit.
Resource allocation was a concern voiced by many committee members. Kelly Moore, MD, MPH, of Vanderbilt University, Nashville, Tenn., said she voted no on expanding vaccination to older adults because “we didn’t have details on shared clinical decision making, in the absence of information on what that meant, and in the presence of supply questions, I didn’t feel comfortable expanding vaccination to a huge population,” she said.
Paul Hunter, MD, of the City of Milwaukee Health Department, also voted no, and expressed concern that expanding the HPV vaccination recommendations to older adults would send the message that vaccination for children and teens is not effective or important.
The text of the new recommendations for routine and catch-up vaccination states that the recommendations “also apply to MSM [men who have sex with men], transgender people, and people with immunocompromising conditions.”
The ACIP members had no financial conflicts to disclose.
according to a unanimous vote at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
This change affects males aged 22 through 26 years; the HPV vaccine is currently recommended for males and females aged 11 or 12 years, with catch-up vaccination through age 21 for males and age 26 for females.
The change was supported in part by increased interest in simplifying and harmonizing the vaccine schedule, said Lauri Markowitz, MD, of the CDC’s National Center for Immunization and Respiratory Diseases (NCIRD), who presented the HPV work group’s considerations.
In addition, the committee voted 10-4 in favor of catch-up HPV vaccination, based on shared clinical decision making, for all adults aged 27 through 45 years.
Although the current program of HPV vaccination for youth has demonstrated effectiveness, data from multiple models suggest that widespread HPV vaccination for adults older than 26 years is much less cost effective, and would yield relatively small additional health benefits, Dr. Markowitz said.
The HPV work group reviewed data from a range of clinical trials, epidemiology, and natural history, as well as results from five different health economic models. They concluded that an assessment of benefits and harms favors expanding the catch-up vaccination to all individuals through 26 years, said Elissa Meites, MD, of the CDC, who presented the official work group opinion. The group’s opinion on the second question was that the additional population level benefit of expanding HPV vaccination to all adults would be minimal and not a reasonable and effective allocation of resources, but that shared clinical decision making would allow flexibility.
The committee expressed strong opinions about the potential for shared clinical decision making as a policy for vaccination for adults older than 26 years. Some felt that this option was a way to include adults at risk for HPV, such as divorced women with new partners, or women getting married for the first time later in life who might not have been exposed to HPV through other relationships. In addition, supporters noted that the shared clinical decision-making option would allow for potential insurance coverage, and would involve discussion between doctors and patients to assess risk.
However, other committee members felt that any recommendation for older adult vaccination would distract clinicians from the importance and value of HPV vaccination for the target age group of 11- and 12-year-olds, and might divert resources from the younger age group in whom it has shown the most benefit.
Resource allocation was a concern voiced by many committee members. Kelly Moore, MD, MPH, of Vanderbilt University, Nashville, Tenn., said she voted no on expanding vaccination to older adults because “we didn’t have details on shared clinical decision making, in the absence of information on what that meant, and in the presence of supply questions, I didn’t feel comfortable expanding vaccination to a huge population,” she said.
Paul Hunter, MD, of the City of Milwaukee Health Department, also voted no, and expressed concern that expanding the HPV vaccination recommendations to older adults would send the message that vaccination for children and teens is not effective or important.
The text of the new recommendations for routine and catch-up vaccination states that the recommendations “also apply to MSM [men who have sex with men], transgender people, and people with immunocompromising conditions.”
The ACIP members had no financial conflicts to disclose.
REPORTING FROM AN ACIP MEETING
Substantial reductions in HPV infections, CIN2+ after vaccination
The introduction of the human papillomavirus according to a meta-analysis of data from more than 60 million individuals worldwide.
Mélanie Drolet, PhD, from the Centre de recherche du CHU de Québec–Université Laval, and coauthors of the HPV Vaccination Impact Study Group reported the results of a systematic review and meta-analysis of 65 studies showing pre- and postvaccination frequency of at least one HPV-related endpoint published in the Lancet. The studies were conducted in 14 high-income countries, 12 of which were vaccinating only women and girls, with the results at 5-8 years published in the Lancet.
At 5-8 years after a vaccination program was implemented, there was a significant 83% reduction in the prevalence of HPV 16 and 18, both of which are targeted by the vaccine, among girls aged 13-19 years; a 66% reduction among women aged 20-24 years; and a 37% reduction in women aged 25-29 years, even though most of these women were unvaccinated.
There also were significant decreases at 5-8 years in the prevalence of HPV subtypes 31, 33, and 45, which are not included in the vaccine but against which the vaccine appears to offer cross-protection. Among girls aged 13-19 years, there was a significant 54% reduction in the prevalence of these subtypes, among women aged 20-24 years there was a nonsignificant 28% decrease, but among women aged 25-29 years, there was no significant decrease.
The analysis also found significant declines in the prevalence of cervical intraepithelial neoplasias (CINs) of grade 2 or above. At 5-9 years after vaccination was introduced, CIN2+ decreased by 51% among girls aged 15-19 years who also were screened for cervical cancer, and by 31% among women aged 20-24 years.
However, over the same time period, the rates of CIN2+ increased by a significant 19% among mostly unvaccinated women aged 25-29 years and 23% among mostly unvaccinated women aged 30-39 years, despite both groups being screened for cervical abnormalities.
While most of the countries in the study vaccinated only girls and women, two studies did find nonsignificant decreases in the prevalence of HPV 16, 18, 31, 33, and 45 among boys aged 16-19 years, but not among men aged 20-24 years.
HPV vaccination also was associated with significant declines in the incidence of anogenital warts among both males and females. In the first 4 years alone, vaccination was associated with significant reductions in anogenital wart diagnoses among females aged 15-29 years, as well as nonsignificant but “substantial” reductions in unvaccinated boys aged 15-19 years.
After 5-8 years, anogenital wart diagnoses decreased by 67% among girls aged 15-19 years, significantly by 54% among women aged 20-24 years, and 31% among women aged 25-29 years – all significant changes. Among boys aged 15-19 years, anogenital wart diagnoses decreased by a significant 48%, and among men aged 20-24 years they decreased by a significant 32%.
The decreases in anogenital wart diagnoses were even greater in countries that implemented vaccination among multiple cohorts simultaneously and achieved high vaccination coverage, compared with countries that vaccinated only one cohort at a time or had low routine vaccination coverage.
“Our study is the first to show the real-world additional benefit of multicohort HPV vaccination and high routine vaccination coverage, and the fast and substantial herd effects of vaccination in countries which implement these measures,” wrote Dr. Drolet and coauthors. “The greater impact of multicohort vaccination was similar when restricting the analyses to countries with high routine vaccination coverage.”
They pointed to the World Health Organization’s recently revised position on HPV vaccination, which now recommends vaccination of multiple cohorts of girls aged 9-14 years, although they raised the question of what might be the optimal number of age cohorts. “Number needed to vaccinate and cost-effectiveness analyses in high-income countries suggest that vaccinating multiple cohorts of individuals up to 18 years of age is highly efficient and cost effective.”
This analysis by Drolet et al. “provides compelling evidence for HPV vaccine efficacy on all outcomes explored and for almost all age strata,” Dr. Silvia de Sanjose, of PATH in Seattle, and Dr. Sinead Delany-Moretlwe of the Wits Reproductive Health and HIV Institute at the University of Witwatersrand in Johannesburg, said in an accompanying editorial (Lancet. 2019 Jun 26. doi: 10.1016/ S0140-6736[19]30549-5). This study shows just how effective HPV vaccination can be across a range of outcomes and ages, and also demonstrates the herd immunity benefits, particularly when multiple cohorts are vaccinated and there is high vaccination coverage.
One key limitation of this analysis is the lack of data from low- and middle-income countries. The data by Drolet et al. “emphasise the importance of redoubling our efforts to tackle the fiscal, supply, and programmatic barriers that currently limit HPV vaccine programmes; with these efforts, HPV vaccination could become a hallmark investment of cancer prevention in the 21st century,” Dr. de Sanjose and Dr. Delany-Moretlwe concluded.
The study was funded by WHO, Canadian Institutes of Health Research, and Fonds de recherche du Québec–Santé. No conflicts of interest were declared.
Dr. de Sanjose declared previous institutional support from Merck.
SOURCE: Drolet M et al. Lancet 2019 Jun 26. doi: 10.1016/ S0140-6736(19)30298-3.
The introduction of the human papillomavirus according to a meta-analysis of data from more than 60 million individuals worldwide.
Mélanie Drolet, PhD, from the Centre de recherche du CHU de Québec–Université Laval, and coauthors of the HPV Vaccination Impact Study Group reported the results of a systematic review and meta-analysis of 65 studies showing pre- and postvaccination frequency of at least one HPV-related endpoint published in the Lancet. The studies were conducted in 14 high-income countries, 12 of which were vaccinating only women and girls, with the results at 5-8 years published in the Lancet.
At 5-8 years after a vaccination program was implemented, there was a significant 83% reduction in the prevalence of HPV 16 and 18, both of which are targeted by the vaccine, among girls aged 13-19 years; a 66% reduction among women aged 20-24 years; and a 37% reduction in women aged 25-29 years, even though most of these women were unvaccinated.
There also were significant decreases at 5-8 years in the prevalence of HPV subtypes 31, 33, and 45, which are not included in the vaccine but against which the vaccine appears to offer cross-protection. Among girls aged 13-19 years, there was a significant 54% reduction in the prevalence of these subtypes, among women aged 20-24 years there was a nonsignificant 28% decrease, but among women aged 25-29 years, there was no significant decrease.
The analysis also found significant declines in the prevalence of cervical intraepithelial neoplasias (CINs) of grade 2 or above. At 5-9 years after vaccination was introduced, CIN2+ decreased by 51% among girls aged 15-19 years who also were screened for cervical cancer, and by 31% among women aged 20-24 years.
However, over the same time period, the rates of CIN2+ increased by a significant 19% among mostly unvaccinated women aged 25-29 years and 23% among mostly unvaccinated women aged 30-39 years, despite both groups being screened for cervical abnormalities.
While most of the countries in the study vaccinated only girls and women, two studies did find nonsignificant decreases in the prevalence of HPV 16, 18, 31, 33, and 45 among boys aged 16-19 years, but not among men aged 20-24 years.
HPV vaccination also was associated with significant declines in the incidence of anogenital warts among both males and females. In the first 4 years alone, vaccination was associated with significant reductions in anogenital wart diagnoses among females aged 15-29 years, as well as nonsignificant but “substantial” reductions in unvaccinated boys aged 15-19 years.
After 5-8 years, anogenital wart diagnoses decreased by 67% among girls aged 15-19 years, significantly by 54% among women aged 20-24 years, and 31% among women aged 25-29 years – all significant changes. Among boys aged 15-19 years, anogenital wart diagnoses decreased by a significant 48%, and among men aged 20-24 years they decreased by a significant 32%.
The decreases in anogenital wart diagnoses were even greater in countries that implemented vaccination among multiple cohorts simultaneously and achieved high vaccination coverage, compared with countries that vaccinated only one cohort at a time or had low routine vaccination coverage.
“Our study is the first to show the real-world additional benefit of multicohort HPV vaccination and high routine vaccination coverage, and the fast and substantial herd effects of vaccination in countries which implement these measures,” wrote Dr. Drolet and coauthors. “The greater impact of multicohort vaccination was similar when restricting the analyses to countries with high routine vaccination coverage.”
They pointed to the World Health Organization’s recently revised position on HPV vaccination, which now recommends vaccination of multiple cohorts of girls aged 9-14 years, although they raised the question of what might be the optimal number of age cohorts. “Number needed to vaccinate and cost-effectiveness analyses in high-income countries suggest that vaccinating multiple cohorts of individuals up to 18 years of age is highly efficient and cost effective.”
This analysis by Drolet et al. “provides compelling evidence for HPV vaccine efficacy on all outcomes explored and for almost all age strata,” Dr. Silvia de Sanjose, of PATH in Seattle, and Dr. Sinead Delany-Moretlwe of the Wits Reproductive Health and HIV Institute at the University of Witwatersrand in Johannesburg, said in an accompanying editorial (Lancet. 2019 Jun 26. doi: 10.1016/ S0140-6736[19]30549-5). This study shows just how effective HPV vaccination can be across a range of outcomes and ages, and also demonstrates the herd immunity benefits, particularly when multiple cohorts are vaccinated and there is high vaccination coverage.
One key limitation of this analysis is the lack of data from low- and middle-income countries. The data by Drolet et al. “emphasise the importance of redoubling our efforts to tackle the fiscal, supply, and programmatic barriers that currently limit HPV vaccine programmes; with these efforts, HPV vaccination could become a hallmark investment of cancer prevention in the 21st century,” Dr. de Sanjose and Dr. Delany-Moretlwe concluded.
The study was funded by WHO, Canadian Institutes of Health Research, and Fonds de recherche du Québec–Santé. No conflicts of interest were declared.
Dr. de Sanjose declared previous institutional support from Merck.
SOURCE: Drolet M et al. Lancet 2019 Jun 26. doi: 10.1016/ S0140-6736(19)30298-3.
The introduction of the human papillomavirus according to a meta-analysis of data from more than 60 million individuals worldwide.
Mélanie Drolet, PhD, from the Centre de recherche du CHU de Québec–Université Laval, and coauthors of the HPV Vaccination Impact Study Group reported the results of a systematic review and meta-analysis of 65 studies showing pre- and postvaccination frequency of at least one HPV-related endpoint published in the Lancet. The studies were conducted in 14 high-income countries, 12 of which were vaccinating only women and girls, with the results at 5-8 years published in the Lancet.
At 5-8 years after a vaccination program was implemented, there was a significant 83% reduction in the prevalence of HPV 16 and 18, both of which are targeted by the vaccine, among girls aged 13-19 years; a 66% reduction among women aged 20-24 years; and a 37% reduction in women aged 25-29 years, even though most of these women were unvaccinated.
There also were significant decreases at 5-8 years in the prevalence of HPV subtypes 31, 33, and 45, which are not included in the vaccine but against which the vaccine appears to offer cross-protection. Among girls aged 13-19 years, there was a significant 54% reduction in the prevalence of these subtypes, among women aged 20-24 years there was a nonsignificant 28% decrease, but among women aged 25-29 years, there was no significant decrease.
The analysis also found significant declines in the prevalence of cervical intraepithelial neoplasias (CINs) of grade 2 or above. At 5-9 years after vaccination was introduced, CIN2+ decreased by 51% among girls aged 15-19 years who also were screened for cervical cancer, and by 31% among women aged 20-24 years.
However, over the same time period, the rates of CIN2+ increased by a significant 19% among mostly unvaccinated women aged 25-29 years and 23% among mostly unvaccinated women aged 30-39 years, despite both groups being screened for cervical abnormalities.
While most of the countries in the study vaccinated only girls and women, two studies did find nonsignificant decreases in the prevalence of HPV 16, 18, 31, 33, and 45 among boys aged 16-19 years, but not among men aged 20-24 years.
HPV vaccination also was associated with significant declines in the incidence of anogenital warts among both males and females. In the first 4 years alone, vaccination was associated with significant reductions in anogenital wart diagnoses among females aged 15-29 years, as well as nonsignificant but “substantial” reductions in unvaccinated boys aged 15-19 years.
After 5-8 years, anogenital wart diagnoses decreased by 67% among girls aged 15-19 years, significantly by 54% among women aged 20-24 years, and 31% among women aged 25-29 years – all significant changes. Among boys aged 15-19 years, anogenital wart diagnoses decreased by a significant 48%, and among men aged 20-24 years they decreased by a significant 32%.
The decreases in anogenital wart diagnoses were even greater in countries that implemented vaccination among multiple cohorts simultaneously and achieved high vaccination coverage, compared with countries that vaccinated only one cohort at a time or had low routine vaccination coverage.
“Our study is the first to show the real-world additional benefit of multicohort HPV vaccination and high routine vaccination coverage, and the fast and substantial herd effects of vaccination in countries which implement these measures,” wrote Dr. Drolet and coauthors. “The greater impact of multicohort vaccination was similar when restricting the analyses to countries with high routine vaccination coverage.”
They pointed to the World Health Organization’s recently revised position on HPV vaccination, which now recommends vaccination of multiple cohorts of girls aged 9-14 years, although they raised the question of what might be the optimal number of age cohorts. “Number needed to vaccinate and cost-effectiveness analyses in high-income countries suggest that vaccinating multiple cohorts of individuals up to 18 years of age is highly efficient and cost effective.”
This analysis by Drolet et al. “provides compelling evidence for HPV vaccine efficacy on all outcomes explored and for almost all age strata,” Dr. Silvia de Sanjose, of PATH in Seattle, and Dr. Sinead Delany-Moretlwe of the Wits Reproductive Health and HIV Institute at the University of Witwatersrand in Johannesburg, said in an accompanying editorial (Lancet. 2019 Jun 26. doi: 10.1016/ S0140-6736[19]30549-5). This study shows just how effective HPV vaccination can be across a range of outcomes and ages, and also demonstrates the herd immunity benefits, particularly when multiple cohorts are vaccinated and there is high vaccination coverage.
One key limitation of this analysis is the lack of data from low- and middle-income countries. The data by Drolet et al. “emphasise the importance of redoubling our efforts to tackle the fiscal, supply, and programmatic barriers that currently limit HPV vaccine programmes; with these efforts, HPV vaccination could become a hallmark investment of cancer prevention in the 21st century,” Dr. de Sanjose and Dr. Delany-Moretlwe concluded.
The study was funded by WHO, Canadian Institutes of Health Research, and Fonds de recherche du Québec–Santé. No conflicts of interest were declared.
Dr. de Sanjose declared previous institutional support from Merck.
SOURCE: Drolet M et al. Lancet 2019 Jun 26. doi: 10.1016/ S0140-6736(19)30298-3.
FROM THE LANCET
Key clinical point: Significant declines in HPV infections, CIN2+, and anogenital warts have occurred after the introduction of HPV vaccine programs, some because of herd effects.
Major finding: The HPV vaccination program is associated with a significant 83% reduction in the prevalence of HPV 16 and 18 among girls aged 13-19 years in 14 high-income countries.
Study details: Systematic review and meta-analysis of 65 studies involving more than 60 million individuals in 14 countries.
Disclosures: The study was funded by World Health Organization, Canadian Institutes of Health Research, and Fonds de recherche du Québec – Santé. No conflicts of interest were declared.
Source: Drolet M et al. Lancet 2019 Jun 26. doi: 10.1016/ S0140-6736(19)30298-3.
Sexual assault in military linked to sexual pain
according to an observational study involving interviews with more than 1,000 military women.
Female veterans with histories of both childhood sexual abuse and sexual assault in the military were 4.33 times more likely to report sexual pain than female veterans with no history of sexual assault; women whose history of sexual assault occurred in the military only were 2.37 times more likely to report sexual pain. Those with histories of childhood sexual abuse but no military assaults were 1.75 times more likely to report sexual pain than those who had no history of sexual assault.
The findings suggest that sexual assault in the military is more detrimental to sexual function than childhood sexual abuse alone, which “is distinct from the pattern long observed in civilian women that childhood sexual abuse confers a greater risk for sexual pain than adulthood sexual assault,” Carey S. Pulverman, PhD, then of the Department of Veterans Affairs Center of Excellence for Research on Returning War Veterans in Waco, Tex., and coinvestigators wrote in Obstetrics & Gynecology.
The findings come from a secondary analysis of data collected for a larger project titled Sexual Violence and Women Veterans’ Gynecologic Health . The research team conducted telephone interviews with 1,004 female veterans younger than 52 years of age (mean, 38 years) who were enrolled at two large Midwestern VA medical centers and associated clinics. Sexual pain was assessed by one question: “Does it hurt you to have sexual intercourse or penetration?”
The study also identified high comorbidity between sexual pain and mental health concerns. As with sexual pain, rates of depression and PTSD were highest among female veterans with histories of both sexual abuse in childhood and sexual assault in the military, followed by women with histories of sexual assaults in the military alone, and then women with histories of childhood sexual abuse alone. Women with both histories were 6.35 times more likely to report PTSD, and 3.91 times more likely to report depression, compared with female veterans with no history of sexual assault.
Women who experienced sexual assault during their childhood and/or while serving in the military also may have been exposed to sexual assault during their pre- or postmilitary adulthood as well, but this was a small number and its effects were not evaluated, the authors noted.
Especially given the “growing numbers of women serving in the military and prevalence of sexual assault in this population,” there’s a need for more research on the sexual function of female veterans and development of “targeted treatments,” the investigators wrote.
For now, providers should be “more comprehensive in their assessment of sexual assault history” and should consider developing relationships with community providers who specialize in sexual health, they added.
The study was funded by the VA. The authors did not report any relevant financial disclosures.
SOURCE: Pulverman CS et al. Obstet Gynecol. 2019;134:63-71.
according to an observational study involving interviews with more than 1,000 military women.
Female veterans with histories of both childhood sexual abuse and sexual assault in the military were 4.33 times more likely to report sexual pain than female veterans with no history of sexual assault; women whose history of sexual assault occurred in the military only were 2.37 times more likely to report sexual pain. Those with histories of childhood sexual abuse but no military assaults were 1.75 times more likely to report sexual pain than those who had no history of sexual assault.
The findings suggest that sexual assault in the military is more detrimental to sexual function than childhood sexual abuse alone, which “is distinct from the pattern long observed in civilian women that childhood sexual abuse confers a greater risk for sexual pain than adulthood sexual assault,” Carey S. Pulverman, PhD, then of the Department of Veterans Affairs Center of Excellence for Research on Returning War Veterans in Waco, Tex., and coinvestigators wrote in Obstetrics & Gynecology.
The findings come from a secondary analysis of data collected for a larger project titled Sexual Violence and Women Veterans’ Gynecologic Health . The research team conducted telephone interviews with 1,004 female veterans younger than 52 years of age (mean, 38 years) who were enrolled at two large Midwestern VA medical centers and associated clinics. Sexual pain was assessed by one question: “Does it hurt you to have sexual intercourse or penetration?”
The study also identified high comorbidity between sexual pain and mental health concerns. As with sexual pain, rates of depression and PTSD were highest among female veterans with histories of both sexual abuse in childhood and sexual assault in the military, followed by women with histories of sexual assaults in the military alone, and then women with histories of childhood sexual abuse alone. Women with both histories were 6.35 times more likely to report PTSD, and 3.91 times more likely to report depression, compared with female veterans with no history of sexual assault.
Women who experienced sexual assault during their childhood and/or while serving in the military also may have been exposed to sexual assault during their pre- or postmilitary adulthood as well, but this was a small number and its effects were not evaluated, the authors noted.
Especially given the “growing numbers of women serving in the military and prevalence of sexual assault in this population,” there’s a need for more research on the sexual function of female veterans and development of “targeted treatments,” the investigators wrote.
For now, providers should be “more comprehensive in their assessment of sexual assault history” and should consider developing relationships with community providers who specialize in sexual health, they added.
The study was funded by the VA. The authors did not report any relevant financial disclosures.
SOURCE: Pulverman CS et al. Obstet Gynecol. 2019;134:63-71.
according to an observational study involving interviews with more than 1,000 military women.
Female veterans with histories of both childhood sexual abuse and sexual assault in the military were 4.33 times more likely to report sexual pain than female veterans with no history of sexual assault; women whose history of sexual assault occurred in the military only were 2.37 times more likely to report sexual pain. Those with histories of childhood sexual abuse but no military assaults were 1.75 times more likely to report sexual pain than those who had no history of sexual assault.
The findings suggest that sexual assault in the military is more detrimental to sexual function than childhood sexual abuse alone, which “is distinct from the pattern long observed in civilian women that childhood sexual abuse confers a greater risk for sexual pain than adulthood sexual assault,” Carey S. Pulverman, PhD, then of the Department of Veterans Affairs Center of Excellence for Research on Returning War Veterans in Waco, Tex., and coinvestigators wrote in Obstetrics & Gynecology.
The findings come from a secondary analysis of data collected for a larger project titled Sexual Violence and Women Veterans’ Gynecologic Health . The research team conducted telephone interviews with 1,004 female veterans younger than 52 years of age (mean, 38 years) who were enrolled at two large Midwestern VA medical centers and associated clinics. Sexual pain was assessed by one question: “Does it hurt you to have sexual intercourse or penetration?”
The study also identified high comorbidity between sexual pain and mental health concerns. As with sexual pain, rates of depression and PTSD were highest among female veterans with histories of both sexual abuse in childhood and sexual assault in the military, followed by women with histories of sexual assaults in the military alone, and then women with histories of childhood sexual abuse alone. Women with both histories were 6.35 times more likely to report PTSD, and 3.91 times more likely to report depression, compared with female veterans with no history of sexual assault.
Women who experienced sexual assault during their childhood and/or while serving in the military also may have been exposed to sexual assault during their pre- or postmilitary adulthood as well, but this was a small number and its effects were not evaluated, the authors noted.
Especially given the “growing numbers of women serving in the military and prevalence of sexual assault in this population,” there’s a need for more research on the sexual function of female veterans and development of “targeted treatments,” the investigators wrote.
For now, providers should be “more comprehensive in their assessment of sexual assault history” and should consider developing relationships with community providers who specialize in sexual health, they added.
The study was funded by the VA. The authors did not report any relevant financial disclosures.
SOURCE: Pulverman CS et al. Obstet Gynecol. 2019;134:63-71.
FROM OBSTETRICS & GYNECOLOGY
In MS, the challenges for women are unique
SEATTLE – Mitzi Joi Williams, MD.
About three in four people with MS are female – about 750,000 in the United States. And the risk and incidence may be highest in African American women.
In a presentation about the unique needs of women with MS, Dr. Williams, an assistant professor of internal medicine at the Morehouse School of Medicine in Atlanta, offered these tips at the annual meeting of the Consortium of Multiple Sclerosis Centers.
Pay attention to sexual dysfunction
Patients with MS often are ashamed to talk about sexual dysfunction, Dr. Williams said, but it is on many minds. “If I have a program on intimacy in MS, people are out the door.”
She urged colleagues to understand that MS can affect sexuality through three routes: primary, secondary, and tertiary dysfunction.
In primary sexual dysfunction, brain and spinal lesions directly related to MS can cause problems such as lack of sensation or abnormal sensations, decreased libido, vaginal dryness, and difficult orgasm.
Secondary sexual dysfunction refers to problems caused by symptoms of MS such as fatigue, which can worsen as the day progresses and affect nighttime intimacy, she said. Bladder dysfunction is another sensitive area in sexuality, with patients – especially women – “concerned that they will lose control of their bladder or they have already lost control.”
Cognitive dysfunction also can disrupt sexual function. “It is important to focus, and certain things cannot happen if you do not. If you are not able to focus and concentrate, it can affect interest,” Dr. Williams said.
Additionally, medications can improve some symptoms while making others worse. For example, a drug may relieve spasticity but boost fatigue. “We have to walk this tightrope,” she said. “But if we are not asking our patients, they may not volunteer this information.”
Finally, she said, MS can spark tertiary sexual dysfunction – poor body image, depression, anxiety, and disruptive changes in familial roles. For example, one partner may become a caregiver, and “it is hard to go from caregiving to sexy time.”
“It is something we have to acknowledge and find ways to deal with,” Dr. Williams said.
To address these issues, she pointed to strategies for symptomatic relief and disease-modifying therapy (DMT) and pinpointed several treatment options.
- Fatigue – stimulants, diet, exercise.
- Spasticity – muscle relaxants, exercise.
- Bladder dysfunction – fluid restriction, medication.
- Paresthesia – antidepressants, anticonvulsants.
- Numbness – vibrators, devices to increase stimulation.
Sexual therapy, couples therapy, and pelvic floor physical therapy also can be helpful.
Be aware of special needs during prepregnancy and pregnancy
“MS itself does not have a lot of effects on fertility, pregnancy, or pregnancy outcomes,” Dr. Williams said. However, “medications cause concern about how we manage pregnancy and fertility.”
In vitro fertilization may increase the risk of relapse, she added, and patients on dimethyl fumarate who experience vomiting or diarrhea may not be able to properly absorb oral contraceptives.
Women with MS may not need to go off DMT when they are trying to conceive, she said. “If patients have very aggressive disease, they may need to be on DMT through conception, through the first trimester, and even the entire pregnancy to prevent long-term disability.”
What about pregnancy itself? “An MS diagnosis alone does not mean that a pregnancy is high risk,” she said. “There are not necessarily additional tests and ultrasounds that are recommended for our patients based on MS diagnosis alone.”
Treatment discontinuation may be warranted during pregnancy, when MS generally improves. However, some MS symptoms – fatigue, bladder dysfunction, and balance – may increase. Corticosteroids can be appropriate if relapses occur during pregnancy.
Menopause and MS symptoms may overlap
Symptoms such as hot flashes, mood changes, sleep disturbance, bladder dysfunction, and decreased energy may be signs of MS, or they could indicate menopause, Dr. Williams said. “Sometimes patients come in and they are getting worse, and we look into it and discover they are premenopausal.”
A decline in estrogen during menopause may worsen MS symptoms, she added, and hormone therapy may be appropriate. A phase 2 study found a benefit in menopausal patients with MS for estriol in conjunction with a DMT, but more studies are needed.
Dr. Williams reported no relevant financial disclosures.
SEATTLE – Mitzi Joi Williams, MD.
About three in four people with MS are female – about 750,000 in the United States. And the risk and incidence may be highest in African American women.
In a presentation about the unique needs of women with MS, Dr. Williams, an assistant professor of internal medicine at the Morehouse School of Medicine in Atlanta, offered these tips at the annual meeting of the Consortium of Multiple Sclerosis Centers.
Pay attention to sexual dysfunction
Patients with MS often are ashamed to talk about sexual dysfunction, Dr. Williams said, but it is on many minds. “If I have a program on intimacy in MS, people are out the door.”
She urged colleagues to understand that MS can affect sexuality through three routes: primary, secondary, and tertiary dysfunction.
In primary sexual dysfunction, brain and spinal lesions directly related to MS can cause problems such as lack of sensation or abnormal sensations, decreased libido, vaginal dryness, and difficult orgasm.
Secondary sexual dysfunction refers to problems caused by symptoms of MS such as fatigue, which can worsen as the day progresses and affect nighttime intimacy, she said. Bladder dysfunction is another sensitive area in sexuality, with patients – especially women – “concerned that they will lose control of their bladder or they have already lost control.”
Cognitive dysfunction also can disrupt sexual function. “It is important to focus, and certain things cannot happen if you do not. If you are not able to focus and concentrate, it can affect interest,” Dr. Williams said.
Additionally, medications can improve some symptoms while making others worse. For example, a drug may relieve spasticity but boost fatigue. “We have to walk this tightrope,” she said. “But if we are not asking our patients, they may not volunteer this information.”
Finally, she said, MS can spark tertiary sexual dysfunction – poor body image, depression, anxiety, and disruptive changes in familial roles. For example, one partner may become a caregiver, and “it is hard to go from caregiving to sexy time.”
“It is something we have to acknowledge and find ways to deal with,” Dr. Williams said.
To address these issues, she pointed to strategies for symptomatic relief and disease-modifying therapy (DMT) and pinpointed several treatment options.
- Fatigue – stimulants, diet, exercise.
- Spasticity – muscle relaxants, exercise.
- Bladder dysfunction – fluid restriction, medication.
- Paresthesia – antidepressants, anticonvulsants.
- Numbness – vibrators, devices to increase stimulation.
Sexual therapy, couples therapy, and pelvic floor physical therapy also can be helpful.
Be aware of special needs during prepregnancy and pregnancy
“MS itself does not have a lot of effects on fertility, pregnancy, or pregnancy outcomes,” Dr. Williams said. However, “medications cause concern about how we manage pregnancy and fertility.”
In vitro fertilization may increase the risk of relapse, she added, and patients on dimethyl fumarate who experience vomiting or diarrhea may not be able to properly absorb oral contraceptives.
Women with MS may not need to go off DMT when they are trying to conceive, she said. “If patients have very aggressive disease, they may need to be on DMT through conception, through the first trimester, and even the entire pregnancy to prevent long-term disability.”
What about pregnancy itself? “An MS diagnosis alone does not mean that a pregnancy is high risk,” she said. “There are not necessarily additional tests and ultrasounds that are recommended for our patients based on MS diagnosis alone.”
Treatment discontinuation may be warranted during pregnancy, when MS generally improves. However, some MS symptoms – fatigue, bladder dysfunction, and balance – may increase. Corticosteroids can be appropriate if relapses occur during pregnancy.
Menopause and MS symptoms may overlap
Symptoms such as hot flashes, mood changes, sleep disturbance, bladder dysfunction, and decreased energy may be signs of MS, or they could indicate menopause, Dr. Williams said. “Sometimes patients come in and they are getting worse, and we look into it and discover they are premenopausal.”
A decline in estrogen during menopause may worsen MS symptoms, she added, and hormone therapy may be appropriate. A phase 2 study found a benefit in menopausal patients with MS for estriol in conjunction with a DMT, but more studies are needed.
Dr. Williams reported no relevant financial disclosures.
SEATTLE – Mitzi Joi Williams, MD.
About three in four people with MS are female – about 750,000 in the United States. And the risk and incidence may be highest in African American women.
In a presentation about the unique needs of women with MS, Dr. Williams, an assistant professor of internal medicine at the Morehouse School of Medicine in Atlanta, offered these tips at the annual meeting of the Consortium of Multiple Sclerosis Centers.
Pay attention to sexual dysfunction
Patients with MS often are ashamed to talk about sexual dysfunction, Dr. Williams said, but it is on many minds. “If I have a program on intimacy in MS, people are out the door.”
She urged colleagues to understand that MS can affect sexuality through three routes: primary, secondary, and tertiary dysfunction.
In primary sexual dysfunction, brain and spinal lesions directly related to MS can cause problems such as lack of sensation or abnormal sensations, decreased libido, vaginal dryness, and difficult orgasm.
Secondary sexual dysfunction refers to problems caused by symptoms of MS such as fatigue, which can worsen as the day progresses and affect nighttime intimacy, she said. Bladder dysfunction is another sensitive area in sexuality, with patients – especially women – “concerned that they will lose control of their bladder or they have already lost control.”
Cognitive dysfunction also can disrupt sexual function. “It is important to focus, and certain things cannot happen if you do not. If you are not able to focus and concentrate, it can affect interest,” Dr. Williams said.
Additionally, medications can improve some symptoms while making others worse. For example, a drug may relieve spasticity but boost fatigue. “We have to walk this tightrope,” she said. “But if we are not asking our patients, they may not volunteer this information.”
Finally, she said, MS can spark tertiary sexual dysfunction – poor body image, depression, anxiety, and disruptive changes in familial roles. For example, one partner may become a caregiver, and “it is hard to go from caregiving to sexy time.”
“It is something we have to acknowledge and find ways to deal with,” Dr. Williams said.
To address these issues, she pointed to strategies for symptomatic relief and disease-modifying therapy (DMT) and pinpointed several treatment options.
- Fatigue – stimulants, diet, exercise.
- Spasticity – muscle relaxants, exercise.
- Bladder dysfunction – fluid restriction, medication.
- Paresthesia – antidepressants, anticonvulsants.
- Numbness – vibrators, devices to increase stimulation.
Sexual therapy, couples therapy, and pelvic floor physical therapy also can be helpful.
Be aware of special needs during prepregnancy and pregnancy
“MS itself does not have a lot of effects on fertility, pregnancy, or pregnancy outcomes,” Dr. Williams said. However, “medications cause concern about how we manage pregnancy and fertility.”
In vitro fertilization may increase the risk of relapse, she added, and patients on dimethyl fumarate who experience vomiting or diarrhea may not be able to properly absorb oral contraceptives.
Women with MS may not need to go off DMT when they are trying to conceive, she said. “If patients have very aggressive disease, they may need to be on DMT through conception, through the first trimester, and even the entire pregnancy to prevent long-term disability.”
What about pregnancy itself? “An MS diagnosis alone does not mean that a pregnancy is high risk,” she said. “There are not necessarily additional tests and ultrasounds that are recommended for our patients based on MS diagnosis alone.”
Treatment discontinuation may be warranted during pregnancy, when MS generally improves. However, some MS symptoms – fatigue, bladder dysfunction, and balance – may increase. Corticosteroids can be appropriate if relapses occur during pregnancy.
Menopause and MS symptoms may overlap
Symptoms such as hot flashes, mood changes, sleep disturbance, bladder dysfunction, and decreased energy may be signs of MS, or they could indicate menopause, Dr. Williams said. “Sometimes patients come in and they are getting worse, and we look into it and discover they are premenopausal.”
A decline in estrogen during menopause may worsen MS symptoms, she added, and hormone therapy may be appropriate. A phase 2 study found a benefit in menopausal patients with MS for estriol in conjunction with a DMT, but more studies are needed.
Dr. Williams reported no relevant financial disclosures.
EXPERT ANALYSIS FROM CMSC 2019
Nearly two-thirds of gynecologic oncology respondents experienced sexual harassment
CHICAGO – Nearly two-thirds of more than 400 U.S.-based physician members of the Society of Gynecologic Oncology who participated in a recent survey reported experiencing sexual harassment in training or practice.
Notably, of the 255 women and 147 men who responded, 71% and 51%, respectively, reported such sexual harassment – and only 15% overall reported it to officials, Marina Stasenko, MD, reported at the annual meeting of the American Society of Clinical Oncology.
The survey also addressed gender-based discrimination and disparities, including respondents’ views on pay disparities. In this video interview, Dr. Stasenko, a gynecologic oncology fellow at Memorial Sloan Kettering Cancer Center, New York, discusses the findings, their implications and context in this age of #MeToo and #TimesUp, and potential approaches to addressing the ongoing problem and the concerns victims have about reporting harassment.
“We need to start by setting an example, saying these things are not tolerated [and] put that into policy – really show folks how it can be reported and what is being done once that report is filed,” she said.
Dr. Stasenko reported having no disclosures.
SOURCE: Stasenko M et al. ASCO 2019, Abstract LBA10502.
CHICAGO – Nearly two-thirds of more than 400 U.S.-based physician members of the Society of Gynecologic Oncology who participated in a recent survey reported experiencing sexual harassment in training or practice.
Notably, of the 255 women and 147 men who responded, 71% and 51%, respectively, reported such sexual harassment – and only 15% overall reported it to officials, Marina Stasenko, MD, reported at the annual meeting of the American Society of Clinical Oncology.
The survey also addressed gender-based discrimination and disparities, including respondents’ views on pay disparities. In this video interview, Dr. Stasenko, a gynecologic oncology fellow at Memorial Sloan Kettering Cancer Center, New York, discusses the findings, their implications and context in this age of #MeToo and #TimesUp, and potential approaches to addressing the ongoing problem and the concerns victims have about reporting harassment.
“We need to start by setting an example, saying these things are not tolerated [and] put that into policy – really show folks how it can be reported and what is being done once that report is filed,” she said.
Dr. Stasenko reported having no disclosures.
SOURCE: Stasenko M et al. ASCO 2019, Abstract LBA10502.
CHICAGO – Nearly two-thirds of more than 400 U.S.-based physician members of the Society of Gynecologic Oncology who participated in a recent survey reported experiencing sexual harassment in training or practice.
Notably, of the 255 women and 147 men who responded, 71% and 51%, respectively, reported such sexual harassment – and only 15% overall reported it to officials, Marina Stasenko, MD, reported at the annual meeting of the American Society of Clinical Oncology.
The survey also addressed gender-based discrimination and disparities, including respondents’ views on pay disparities. In this video interview, Dr. Stasenko, a gynecologic oncology fellow at Memorial Sloan Kettering Cancer Center, New York, discusses the findings, their implications and context in this age of #MeToo and #TimesUp, and potential approaches to addressing the ongoing problem and the concerns victims have about reporting harassment.
“We need to start by setting an example, saying these things are not tolerated [and] put that into policy – really show folks how it can be reported and what is being done once that report is filed,” she said.
Dr. Stasenko reported having no disclosures.
SOURCE: Stasenko M et al. ASCO 2019, Abstract LBA10502.
REPORTING FROM ASCO 2019











