User login
Mandatory reporting laws
Question: You are moonlighting in the emergency department and have just finished treating a 5-year-old boy with an apparent Colles’ fracture, who was accompanied by his mother with bruises on her face. Her exam revealed additional bruises over her abdominal wall. The mother said they accidentally tripped and fell down the stairs, and spontaneously denied any acts of violence in the family.
Given this scenario, which of the following is best?
A. You suspect both child and spousal abuse, but lack sufficient evidence to report the incident.
B. Failure to report based on reasonable suspicion alone may amount to a criminal offense punishable by possible imprisonment.
C. You may face a potential malpractice lawsuit if subsequent injuries caused by abuse could have been prevented had you reported.
D. Mandatory reporting laws apply not only to abuse of children and spouses, but also of the elderly and other vulnerable adults.
E. All are correct except A.
Answer: E. All doctors, especially those working in emergency departments, treat injuries on a regular basis. Accidents probably account for the majority of these injuries, but the most pernicious are those caused by willful abuse or neglect. Such conduct, believed to be widespread and underrecognized, victimizes children, women, the elderly, and other vulnerable groups.
Mandatory reporting laws arose from the need to identify and prevent these activities that cause serious harm and loss of lives. Physicians and other health care workers are in a prime position to diagnose or raise the suspicion of abuse and neglect. This article focuses on laws that mandate physician reporting of such behavior. Not addressed are other reportable situations such as certain infectious diseases, gunshot wounds, threats to third parties, and so on.
Child abuse
The best-known example of a mandatory reporting law relates to child abuse, which is broadly defined as when a parent or caretaker emotionally, physically, or sexually abuses, neglects, or abandons a child. Child abuse laws are intended to protect children from serious harm without abridging parental discipline of their children.
Cases of child abuse are pervasive; four or five children are tragically killed by abuse or neglect every day, and each year, some 6 million children are reported as victims of child abuse. Henry Kempe’s studies on the “battered child syndrome” in 1962 served to underscore the physician’s role in exposing child maltreatment, and 1973 saw the enactment of the Child Abuse Prevention and Treatment Act, which set standards for mandatory reporting as a condition for federal funding.
All U.S. states have statutes identifying persons who are required to report suspected child maltreatment to an appropriate agency, such as child protective services. Reasonable suspicion, without need for proof, is sufficient to trigger the mandatory reporting duty. A summary of the general reporting requirements, as well as each state’s key statutory features, are available at Child Welfare Information Gateway.1
Bruises, fractures, and burns are recurring examples of injuries resulting from child abuse, but there are many others, including severe emotional harm, which is an important consequence. Clues to abuse include a child’s fearful and anxious demeanor, wearing clothes to hide injuries, and inappropriate sexual conduct.2 The perpetrators and/or complicit parties typically blame an innocent home accident for the victim’s injuries to mislead the health care provider.
Elder abuse
Elder abuse is broadly construed to include physical, sexual, and psychological abuse, as well as financial exploitation and caregiver neglect.3 It is a serious problem in the United States, estimated in 2008 to affect 1 in 10 elders. The figure is likely an underestimate, because many elderly victims are afraid or unwilling to lodge a complaint against the abuser whom they love and may depend upon.4
The law, which protects the “elderly” (e.g., those aged 62 years or older in Hawaii), may also be extended to other younger vulnerable adults, who because of an impairment, are unable to 1) communicate or make responsible decisions to manage one’s own care or resources, 2) carry out or arrange for essential activities of daily living, or 3) protect one’s self from abuse.5
The law mandates reporting where there is reason to believe abuse has occurred or the vulnerable adult is in danger of abuse if immediate action is not taken. Reporting statutes for elder abuse vary somewhat on the identity of mandated reporters (health care providers are always included), the victim’s mental capacity, dwelling place (home or in an assisted-living facility), and type of purported activity that warrants reporting.
Domestic violence
As defined by the National Coalition Against Domestic Violence, “Domestic violence is the willful intimidation, physical assault, battery, sexual assault, and/or other abusive behavior as part of a systematic pattern of power and control perpetrated by one intimate partner against another. ... The frequency and severity of domestic violence can vary dramatically; however, the one constant component of domestic violence is one partner’s consistent efforts to maintain power and control over the other.”6 Domestic violence is said to have reached epidemic proportions, with one in four women experiencing it at some point in her life.
Virtually all states mandate the reporting of domestic violence by health care providers if there is a reasonable suspicion that observed patient injuries are the result of physical abuse.7 California, for example, requires the provider to call local law enforcement as soon as possible or to send in a written report within 48 hours.
There may be exceptions to required reporting, as when an adult victim withholds consent but accepts victim referral services. State laws encourage but do not always require that the health care provider inform the patient about the report, but federal law dictates otherwise unless this puts the patient at risk. Hawaii’s domestic violence laws were originally enacted to deter spousal abuse, but they now also protect other household members.8
Any individual who assumes a duty or responsibility pursuant to all of these reporting laws is immunized from criminal or civil liability. On the other hand, a mandated reporter who knowingly fails to report an incident or who willfully prevents another person from reporting such an incident commits a criminal offence.
In the case of a physician, there is the added risk of a malpractice lawsuit based on “violation of statute” (breach of a legal duty), should another injury occur down the road that was arguably preventable by his or her failure to report.
Experts generally believe that mandatory reporting laws are important in identifying child maltreatment. However, it has been asserted that despite a 5-decade history of mandatory reporting, no clear endpoints attest to the efficacy of this approach, and it is argued that no data exist to demonstrate that incremental increases in reporting have contributed to child safety.
Particularly challenging are attempts at impact comparisons between states with different policies. A number of countries, including the United Kingdom, do not have mandatory reporting laws and regulate reporting by professional societies.9
In addition, some critics of mandatory reporting raise concerns surrounding law enforcement showing up at the victim’s house to question the family about abuse, or to make an arrest or issue warnings. They posit that when the behavior of an abuser is under scrutiny, this can paradoxically create a potentially more dangerous environment for the patient-victim, whom the perpetrator now considers to have betrayed his or her trust. Others bemoan that revealing patient confidences violates the physician’s ethical code.
However, the intolerable incidence of violence against the vulnerable has properly made mandatory reporting the law of the land. Although the criminal penalty is currently light for failure to report, there is a move toward increasing its severity. Hawaii, for example, recently introduced Senate Bill 2477 that makes nonreporting by those required to do so a Class C felony punishable by up to 5 years in prison. The offense currently is a petty misdemeanor punishable by up to 30 days in jail.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Child Welfare Information Gateway (2016). Mandatory reporters of child abuse and neglect. Washington, D.C.: U.S. Department of Health and Human Services, Children’s Bureau. Available at www.childwelfare.gov; email: [email protected]; phone: 800-394-3366.
2. Available at www.childwelfare.gov/topics/can.
3. Available at www.justice.gov/elderjustice/elder-justice-statutes-0.
4. Available at www.cdc.gov/violenceprevention/elderabuse/index.html.
5. Hawaii Revised Statutes, Sec. 346-222, 346-224, 346-250, 412:3-114.5.
6. Available at ncadv.org.
7. Ann Emerg Med. 2002 Jan;39(1):56-60.
8. Hawaii Revised Statutes, Sec. 709-906.
9. Pediatrics. 2017 Apr;139(4). pii: e20163511.
Question: You are moonlighting in the emergency department and have just finished treating a 5-year-old boy with an apparent Colles’ fracture, who was accompanied by his mother with bruises on her face. Her exam revealed additional bruises over her abdominal wall. The mother said they accidentally tripped and fell down the stairs, and spontaneously denied any acts of violence in the family.
Given this scenario, which of the following is best?
A. You suspect both child and spousal abuse, but lack sufficient evidence to report the incident.
B. Failure to report based on reasonable suspicion alone may amount to a criminal offense punishable by possible imprisonment.
C. You may face a potential malpractice lawsuit if subsequent injuries caused by abuse could have been prevented had you reported.
D. Mandatory reporting laws apply not only to abuse of children and spouses, but also of the elderly and other vulnerable adults.
E. All are correct except A.
Answer: E. All doctors, especially those working in emergency departments, treat injuries on a regular basis. Accidents probably account for the majority of these injuries, but the most pernicious are those caused by willful abuse or neglect. Such conduct, believed to be widespread and underrecognized, victimizes children, women, the elderly, and other vulnerable groups.
Mandatory reporting laws arose from the need to identify and prevent these activities that cause serious harm and loss of lives. Physicians and other health care workers are in a prime position to diagnose or raise the suspicion of abuse and neglect. This article focuses on laws that mandate physician reporting of such behavior. Not addressed are other reportable situations such as certain infectious diseases, gunshot wounds, threats to third parties, and so on.
Child abuse
The best-known example of a mandatory reporting law relates to child abuse, which is broadly defined as when a parent or caretaker emotionally, physically, or sexually abuses, neglects, or abandons a child. Child abuse laws are intended to protect children from serious harm without abridging parental discipline of their children.
Cases of child abuse are pervasive; four or five children are tragically killed by abuse or neglect every day, and each year, some 6 million children are reported as victims of child abuse. Henry Kempe’s studies on the “battered child syndrome” in 1962 served to underscore the physician’s role in exposing child maltreatment, and 1973 saw the enactment of the Child Abuse Prevention and Treatment Act, which set standards for mandatory reporting as a condition for federal funding.
All U.S. states have statutes identifying persons who are required to report suspected child maltreatment to an appropriate agency, such as child protective services. Reasonable suspicion, without need for proof, is sufficient to trigger the mandatory reporting duty. A summary of the general reporting requirements, as well as each state’s key statutory features, are available at Child Welfare Information Gateway.1
Bruises, fractures, and burns are recurring examples of injuries resulting from child abuse, but there are many others, including severe emotional harm, which is an important consequence. Clues to abuse include a child’s fearful and anxious demeanor, wearing clothes to hide injuries, and inappropriate sexual conduct.2 The perpetrators and/or complicit parties typically blame an innocent home accident for the victim’s injuries to mislead the health care provider.
Elder abuse
Elder abuse is broadly construed to include physical, sexual, and psychological abuse, as well as financial exploitation and caregiver neglect.3 It is a serious problem in the United States, estimated in 2008 to affect 1 in 10 elders. The figure is likely an underestimate, because many elderly victims are afraid or unwilling to lodge a complaint against the abuser whom they love and may depend upon.4
The law, which protects the “elderly” (e.g., those aged 62 years or older in Hawaii), may also be extended to other younger vulnerable adults, who because of an impairment, are unable to 1) communicate or make responsible decisions to manage one’s own care or resources, 2) carry out or arrange for essential activities of daily living, or 3) protect one’s self from abuse.5
The law mandates reporting where there is reason to believe abuse has occurred or the vulnerable adult is in danger of abuse if immediate action is not taken. Reporting statutes for elder abuse vary somewhat on the identity of mandated reporters (health care providers are always included), the victim’s mental capacity, dwelling place (home or in an assisted-living facility), and type of purported activity that warrants reporting.
Domestic violence
As defined by the National Coalition Against Domestic Violence, “Domestic violence is the willful intimidation, physical assault, battery, sexual assault, and/or other abusive behavior as part of a systematic pattern of power and control perpetrated by one intimate partner against another. ... The frequency and severity of domestic violence can vary dramatically; however, the one constant component of domestic violence is one partner’s consistent efforts to maintain power and control over the other.”6 Domestic violence is said to have reached epidemic proportions, with one in four women experiencing it at some point in her life.
Virtually all states mandate the reporting of domestic violence by health care providers if there is a reasonable suspicion that observed patient injuries are the result of physical abuse.7 California, for example, requires the provider to call local law enforcement as soon as possible or to send in a written report within 48 hours.
There may be exceptions to required reporting, as when an adult victim withholds consent but accepts victim referral services. State laws encourage but do not always require that the health care provider inform the patient about the report, but federal law dictates otherwise unless this puts the patient at risk. Hawaii’s domestic violence laws were originally enacted to deter spousal abuse, but they now also protect other household members.8
Any individual who assumes a duty or responsibility pursuant to all of these reporting laws is immunized from criminal or civil liability. On the other hand, a mandated reporter who knowingly fails to report an incident or who willfully prevents another person from reporting such an incident commits a criminal offence.
In the case of a physician, there is the added risk of a malpractice lawsuit based on “violation of statute” (breach of a legal duty), should another injury occur down the road that was arguably preventable by his or her failure to report.
Experts generally believe that mandatory reporting laws are important in identifying child maltreatment. However, it has been asserted that despite a 5-decade history of mandatory reporting, no clear endpoints attest to the efficacy of this approach, and it is argued that no data exist to demonstrate that incremental increases in reporting have contributed to child safety.
Particularly challenging are attempts at impact comparisons between states with different policies. A number of countries, including the United Kingdom, do not have mandatory reporting laws and regulate reporting by professional societies.9
In addition, some critics of mandatory reporting raise concerns surrounding law enforcement showing up at the victim’s house to question the family about abuse, or to make an arrest or issue warnings. They posit that when the behavior of an abuser is under scrutiny, this can paradoxically create a potentially more dangerous environment for the patient-victim, whom the perpetrator now considers to have betrayed his or her trust. Others bemoan that revealing patient confidences violates the physician’s ethical code.
However, the intolerable incidence of violence against the vulnerable has properly made mandatory reporting the law of the land. Although the criminal penalty is currently light for failure to report, there is a move toward increasing its severity. Hawaii, for example, recently introduced Senate Bill 2477 that makes nonreporting by those required to do so a Class C felony punishable by up to 5 years in prison. The offense currently is a petty misdemeanor punishable by up to 30 days in jail.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Child Welfare Information Gateway (2016). Mandatory reporters of child abuse and neglect. Washington, D.C.: U.S. Department of Health and Human Services, Children’s Bureau. Available at www.childwelfare.gov; email: [email protected]; phone: 800-394-3366.
2. Available at www.childwelfare.gov/topics/can.
3. Available at www.justice.gov/elderjustice/elder-justice-statutes-0.
4. Available at www.cdc.gov/violenceprevention/elderabuse/index.html.
5. Hawaii Revised Statutes, Sec. 346-222, 346-224, 346-250, 412:3-114.5.
6. Available at ncadv.org.
7. Ann Emerg Med. 2002 Jan;39(1):56-60.
8. Hawaii Revised Statutes, Sec. 709-906.
9. Pediatrics. 2017 Apr;139(4). pii: e20163511.
Question: You are moonlighting in the emergency department and have just finished treating a 5-year-old boy with an apparent Colles’ fracture, who was accompanied by his mother with bruises on her face. Her exam revealed additional bruises over her abdominal wall. The mother said they accidentally tripped and fell down the stairs, and spontaneously denied any acts of violence in the family.
Given this scenario, which of the following is best?
A. You suspect both child and spousal abuse, but lack sufficient evidence to report the incident.
B. Failure to report based on reasonable suspicion alone may amount to a criminal offense punishable by possible imprisonment.
C. You may face a potential malpractice lawsuit if subsequent injuries caused by abuse could have been prevented had you reported.
D. Mandatory reporting laws apply not only to abuse of children and spouses, but also of the elderly and other vulnerable adults.
E. All are correct except A.
Answer: E. All doctors, especially those working in emergency departments, treat injuries on a regular basis. Accidents probably account for the majority of these injuries, but the most pernicious are those caused by willful abuse or neglect. Such conduct, believed to be widespread and underrecognized, victimizes children, women, the elderly, and other vulnerable groups.
Mandatory reporting laws arose from the need to identify and prevent these activities that cause serious harm and loss of lives. Physicians and other health care workers are in a prime position to diagnose or raise the suspicion of abuse and neglect. This article focuses on laws that mandate physician reporting of such behavior. Not addressed are other reportable situations such as certain infectious diseases, gunshot wounds, threats to third parties, and so on.
Child abuse
The best-known example of a mandatory reporting law relates to child abuse, which is broadly defined as when a parent or caretaker emotionally, physically, or sexually abuses, neglects, or abandons a child. Child abuse laws are intended to protect children from serious harm without abridging parental discipline of their children.
Cases of child abuse are pervasive; four or five children are tragically killed by abuse or neglect every day, and each year, some 6 million children are reported as victims of child abuse. Henry Kempe’s studies on the “battered child syndrome” in 1962 served to underscore the physician’s role in exposing child maltreatment, and 1973 saw the enactment of the Child Abuse Prevention and Treatment Act, which set standards for mandatory reporting as a condition for federal funding.
All U.S. states have statutes identifying persons who are required to report suspected child maltreatment to an appropriate agency, such as child protective services. Reasonable suspicion, without need for proof, is sufficient to trigger the mandatory reporting duty. A summary of the general reporting requirements, as well as each state’s key statutory features, are available at Child Welfare Information Gateway.1
Bruises, fractures, and burns are recurring examples of injuries resulting from child abuse, but there are many others, including severe emotional harm, which is an important consequence. Clues to abuse include a child’s fearful and anxious demeanor, wearing clothes to hide injuries, and inappropriate sexual conduct.2 The perpetrators and/or complicit parties typically blame an innocent home accident for the victim’s injuries to mislead the health care provider.
Elder abuse
Elder abuse is broadly construed to include physical, sexual, and psychological abuse, as well as financial exploitation and caregiver neglect.3 It is a serious problem in the United States, estimated in 2008 to affect 1 in 10 elders. The figure is likely an underestimate, because many elderly victims are afraid or unwilling to lodge a complaint against the abuser whom they love and may depend upon.4
The law, which protects the “elderly” (e.g., those aged 62 years or older in Hawaii), may also be extended to other younger vulnerable adults, who because of an impairment, are unable to 1) communicate or make responsible decisions to manage one’s own care or resources, 2) carry out or arrange for essential activities of daily living, or 3) protect one’s self from abuse.5
The law mandates reporting where there is reason to believe abuse has occurred or the vulnerable adult is in danger of abuse if immediate action is not taken. Reporting statutes for elder abuse vary somewhat on the identity of mandated reporters (health care providers are always included), the victim’s mental capacity, dwelling place (home or in an assisted-living facility), and type of purported activity that warrants reporting.
Domestic violence
As defined by the National Coalition Against Domestic Violence, “Domestic violence is the willful intimidation, physical assault, battery, sexual assault, and/or other abusive behavior as part of a systematic pattern of power and control perpetrated by one intimate partner against another. ... The frequency and severity of domestic violence can vary dramatically; however, the one constant component of domestic violence is one partner’s consistent efforts to maintain power and control over the other.”6 Domestic violence is said to have reached epidemic proportions, with one in four women experiencing it at some point in her life.
Virtually all states mandate the reporting of domestic violence by health care providers if there is a reasonable suspicion that observed patient injuries are the result of physical abuse.7 California, for example, requires the provider to call local law enforcement as soon as possible or to send in a written report within 48 hours.
There may be exceptions to required reporting, as when an adult victim withholds consent but accepts victim referral services. State laws encourage but do not always require that the health care provider inform the patient about the report, but federal law dictates otherwise unless this puts the patient at risk. Hawaii’s domestic violence laws were originally enacted to deter spousal abuse, but they now also protect other household members.8
Any individual who assumes a duty or responsibility pursuant to all of these reporting laws is immunized from criminal or civil liability. On the other hand, a mandated reporter who knowingly fails to report an incident or who willfully prevents another person from reporting such an incident commits a criminal offence.
In the case of a physician, there is the added risk of a malpractice lawsuit based on “violation of statute” (breach of a legal duty), should another injury occur down the road that was arguably preventable by his or her failure to report.
Experts generally believe that mandatory reporting laws are important in identifying child maltreatment. However, it has been asserted that despite a 5-decade history of mandatory reporting, no clear endpoints attest to the efficacy of this approach, and it is argued that no data exist to demonstrate that incremental increases in reporting have contributed to child safety.
Particularly challenging are attempts at impact comparisons between states with different policies. A number of countries, including the United Kingdom, do not have mandatory reporting laws and regulate reporting by professional societies.9
In addition, some critics of mandatory reporting raise concerns surrounding law enforcement showing up at the victim’s house to question the family about abuse, or to make an arrest or issue warnings. They posit that when the behavior of an abuser is under scrutiny, this can paradoxically create a potentially more dangerous environment for the patient-victim, whom the perpetrator now considers to have betrayed his or her trust. Others bemoan that revealing patient confidences violates the physician’s ethical code.
However, the intolerable incidence of violence against the vulnerable has properly made mandatory reporting the law of the land. Although the criminal penalty is currently light for failure to report, there is a move toward increasing its severity. Hawaii, for example, recently introduced Senate Bill 2477 that makes nonreporting by those required to do so a Class C felony punishable by up to 5 years in prison. The offense currently is a petty misdemeanor punishable by up to 30 days in jail.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Child Welfare Information Gateway (2016). Mandatory reporters of child abuse and neglect. Washington, D.C.: U.S. Department of Health and Human Services, Children’s Bureau. Available at www.childwelfare.gov; email: [email protected]; phone: 800-394-3366.
2. Available at www.childwelfare.gov/topics/can.
3. Available at www.justice.gov/elderjustice/elder-justice-statutes-0.
4. Available at www.cdc.gov/violenceprevention/elderabuse/index.html.
5. Hawaii Revised Statutes, Sec. 346-222, 346-224, 346-250, 412:3-114.5.
6. Available at ncadv.org.
7. Ann Emerg Med. 2002 Jan;39(1):56-60.
8. Hawaii Revised Statutes, Sec. 709-906.
9. Pediatrics. 2017 Apr;139(4). pii: e20163511.
Rural suicidality and resilience
Overall U.S. life expectancy decreased from 78.7 years to 78.6 years from 2016 to 2017. Researchers from the Centers for Disease Control and Prevention noted that, along with drug overdose deaths, suicide also drove the decrease in average lifespan over that time period. Addressing suicide in rural communities presents unique challenges.
Dr. Bonham is vice chair of community behavioral health in the department of psychiatry and behavioral sciences at the University of New Mexico, Albuquerque. Dr. Kriechman is a child, adolescent and family psychiatrist at the university, where he serves as principal investigator on ASPYR – Alliance-building for Suicide Prevention & Youth Resilience.
You can hear more on resilience and suicide from the MDedge Psychcast in these past episodes:
- Find the MDedge Psychcast where ever you listen:
Overall U.S. life expectancy decreased from 78.7 years to 78.6 years from 2016 to 2017. Researchers from the Centers for Disease Control and Prevention noted that, along with drug overdose deaths, suicide also drove the decrease in average lifespan over that time period. Addressing suicide in rural communities presents unique challenges.
Dr. Bonham is vice chair of community behavioral health in the department of psychiatry and behavioral sciences at the University of New Mexico, Albuquerque. Dr. Kriechman is a child, adolescent and family psychiatrist at the university, where he serves as principal investigator on ASPYR – Alliance-building for Suicide Prevention & Youth Resilience.
You can hear more on resilience and suicide from the MDedge Psychcast in these past episodes:
- Find the MDedge Psychcast where ever you listen:
Overall U.S. life expectancy decreased from 78.7 years to 78.6 years from 2016 to 2017. Researchers from the Centers for Disease Control and Prevention noted that, along with drug overdose deaths, suicide also drove the decrease in average lifespan over that time period. Addressing suicide in rural communities presents unique challenges.
Dr. Bonham is vice chair of community behavioral health in the department of psychiatry and behavioral sciences at the University of New Mexico, Albuquerque. Dr. Kriechman is a child, adolescent and family psychiatrist at the university, where he serves as principal investigator on ASPYR – Alliance-building for Suicide Prevention & Youth Resilience.
You can hear more on resilience and suicide from the MDedge Psychcast in these past episodes:
- Find the MDedge Psychcast where ever you listen:
Courts block Trump from eroding contraceptive mandate
Federal judges have blocked the Trump administration from weakening the Affordable Care Act’s contraceptive mandate in two separate orders that bar the President from letting more entities claim exemptions.
On Jan. 14, U.S. District Court Judge Wendy Beetlestone for the Eastern District of Pennsylvania issued a temporary nationwide ban on two rules that would have allowed an expanded group of employers and insurers to object to providing contraception coverage on either religious or moral grounds. The regulations, announced Nov. 7, 2018, were scheduled to take effect Jan. 14. The day before, U.S. District Judge Haywood Gilliam for the Northern District of California issued a similar temporary ban, but his order applied only to the 13 plaintiff states in the case, plus the District of Columbia.
While Pennsylvania and New Jersey are the only plaintiffs in the Judge Beetlestone case, she wrote that a nationwide injunction is required to protect numerous citizens from losing contraceptive coverage and resulting in “significant, direct, and proprietary harm” to states in the form of increased state-funded contraceptive services and increased costs associated with unintended pregnancies. Judge Gilliam provided similar reasoning in his Jan. 13 order, writing that the 13 plaintiff states have proven that rules promulgated by the U.S. Department of Health and Human Services would cause women to lose employer-sponsored contraceptive coverage, resulting in economic harm to the states.
California Attorney General Xavier Becerra, a plaintiff in the second case, said Judge Gilliam’s ruling will stop the Trump administration from denying millions of women and families access to co-pay birth control guaranteed by the Affordable Care Act.
“The law couldn’t be clearer – employers have no business interfering in women’s health care decisions,” Mr. Becerra said in the statement. “[The] court ruling stops another attempt by the Trump administration to trample on women’s access to basic reproductive care.”
At press time, the Trump administration officials had responded publicly to the court orders. The administration previously said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” HHS estimated that the rules would affect no more than 200 employers.
Mark Rienzi, president of the Becket Fund for Religious Liberty, a legal institute that defends religious freedoms, expressed disappointment at the court orders. Becket represents the Little Sisters of the Poor, an organization that has been fighting for several years for an exemption to the contraceptive mandate.
“Government bureaucrats should not be allowed to threaten the rights of the Little Sisters of the Poor to serve according to their Catholic beliefs,” Mr. Rienzi said in a statement. “Now the nuns are forced to keep fighting this unnecessary lawsuit to protect their ability to focus on caring for the poor. We are confident these decisions will be overturned.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
The Trump administration then announced new rules aimed at broadening exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. A second rule would protect nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions would apply to institutions of education, issuers, and individuals, but not to governmental entities.
Thirteen states and the District of Columbia then sued the Trump administration over the rules as well as Pennsylvania and New Jersey in a separate case.
The nationwide ban against the rules will remain in effect while the cases continue through the court system.
Federal judges have blocked the Trump administration from weakening the Affordable Care Act’s contraceptive mandate in two separate orders that bar the President from letting more entities claim exemptions.
On Jan. 14, U.S. District Court Judge Wendy Beetlestone for the Eastern District of Pennsylvania issued a temporary nationwide ban on two rules that would have allowed an expanded group of employers and insurers to object to providing contraception coverage on either religious or moral grounds. The regulations, announced Nov. 7, 2018, were scheduled to take effect Jan. 14. The day before, U.S. District Judge Haywood Gilliam for the Northern District of California issued a similar temporary ban, but his order applied only to the 13 plaintiff states in the case, plus the District of Columbia.
While Pennsylvania and New Jersey are the only plaintiffs in the Judge Beetlestone case, she wrote that a nationwide injunction is required to protect numerous citizens from losing contraceptive coverage and resulting in “significant, direct, and proprietary harm” to states in the form of increased state-funded contraceptive services and increased costs associated with unintended pregnancies. Judge Gilliam provided similar reasoning in his Jan. 13 order, writing that the 13 plaintiff states have proven that rules promulgated by the U.S. Department of Health and Human Services would cause women to lose employer-sponsored contraceptive coverage, resulting in economic harm to the states.
California Attorney General Xavier Becerra, a plaintiff in the second case, said Judge Gilliam’s ruling will stop the Trump administration from denying millions of women and families access to co-pay birth control guaranteed by the Affordable Care Act.
“The law couldn’t be clearer – employers have no business interfering in women’s health care decisions,” Mr. Becerra said in the statement. “[The] court ruling stops another attempt by the Trump administration to trample on women’s access to basic reproductive care.”
At press time, the Trump administration officials had responded publicly to the court orders. The administration previously said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” HHS estimated that the rules would affect no more than 200 employers.
Mark Rienzi, president of the Becket Fund for Religious Liberty, a legal institute that defends religious freedoms, expressed disappointment at the court orders. Becket represents the Little Sisters of the Poor, an organization that has been fighting for several years for an exemption to the contraceptive mandate.
“Government bureaucrats should not be allowed to threaten the rights of the Little Sisters of the Poor to serve according to their Catholic beliefs,” Mr. Rienzi said in a statement. “Now the nuns are forced to keep fighting this unnecessary lawsuit to protect their ability to focus on caring for the poor. We are confident these decisions will be overturned.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
The Trump administration then announced new rules aimed at broadening exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. A second rule would protect nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions would apply to institutions of education, issuers, and individuals, but not to governmental entities.
Thirteen states and the District of Columbia then sued the Trump administration over the rules as well as Pennsylvania and New Jersey in a separate case.
The nationwide ban against the rules will remain in effect while the cases continue through the court system.
Federal judges have blocked the Trump administration from weakening the Affordable Care Act’s contraceptive mandate in two separate orders that bar the President from letting more entities claim exemptions.
On Jan. 14, U.S. District Court Judge Wendy Beetlestone for the Eastern District of Pennsylvania issued a temporary nationwide ban on two rules that would have allowed an expanded group of employers and insurers to object to providing contraception coverage on either religious or moral grounds. The regulations, announced Nov. 7, 2018, were scheduled to take effect Jan. 14. The day before, U.S. District Judge Haywood Gilliam for the Northern District of California issued a similar temporary ban, but his order applied only to the 13 plaintiff states in the case, plus the District of Columbia.
While Pennsylvania and New Jersey are the only plaintiffs in the Judge Beetlestone case, she wrote that a nationwide injunction is required to protect numerous citizens from losing contraceptive coverage and resulting in “significant, direct, and proprietary harm” to states in the form of increased state-funded contraceptive services and increased costs associated with unintended pregnancies. Judge Gilliam provided similar reasoning in his Jan. 13 order, writing that the 13 plaintiff states have proven that rules promulgated by the U.S. Department of Health and Human Services would cause women to lose employer-sponsored contraceptive coverage, resulting in economic harm to the states.
California Attorney General Xavier Becerra, a plaintiff in the second case, said Judge Gilliam’s ruling will stop the Trump administration from denying millions of women and families access to co-pay birth control guaranteed by the Affordable Care Act.
“The law couldn’t be clearer – employers have no business interfering in women’s health care decisions,” Mr. Becerra said in the statement. “[The] court ruling stops another attempt by the Trump administration to trample on women’s access to basic reproductive care.”
At press time, the Trump administration officials had responded publicly to the court orders. The administration previously said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” HHS estimated that the rules would affect no more than 200 employers.
Mark Rienzi, president of the Becket Fund for Religious Liberty, a legal institute that defends religious freedoms, expressed disappointment at the court orders. Becket represents the Little Sisters of the Poor, an organization that has been fighting for several years for an exemption to the contraceptive mandate.
“Government bureaucrats should not be allowed to threaten the rights of the Little Sisters of the Poor to serve according to their Catholic beliefs,” Mr. Rienzi said in a statement. “Now the nuns are forced to keep fighting this unnecessary lawsuit to protect their ability to focus on caring for the poor. We are confident these decisions will be overturned.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
The Trump administration then announced new rules aimed at broadening exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. A second rule would protect nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions would apply to institutions of education, issuers, and individuals, but not to governmental entities.
Thirteen states and the District of Columbia then sued the Trump administration over the rules as well as Pennsylvania and New Jersey in a separate case.
The nationwide ban against the rules will remain in effect while the cases continue through the court system.
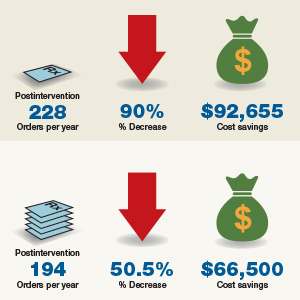
New or existing drugs? Both fuel price inflation
Inflation in existing drugs’ prices and the debut of new drugs are both contributing to the overall rising costs of pharmaceuticals.
.
For oral and injectable specialty drugs, costs increased 20.6% and 12.5%, respectively, with 71.1% and 52.4% attributable to new drugs. Costs of oral and injectable generic drugs grew by 4.4% and 7.3%, also driven by entrants into the market.
Researchers looked at monthly wholesale acquisition costs of 24,877 National Drug Codes for oral drugs and 3,049 injectable drugs from 2005 to 2016. They compared them with pharmacy claims from the UPMC Health Plan, which offers insurance products to more than 3.2 million members across the spectrum of private and public arenas.
“Our analyses yielded three main findings,” explained Inmaculada Hernandez, PharmD, PhD, University of Pittsburgh, and her colleagues in a report published in the January 2019 issue of Health Affairs.
“First, costs increased considerably faster than inflation across all drug classes, and increases were highest for oral specialty drugs and lowest for oral generics,” Dr. Hernandez and her colleagues wrote.
“Second, rising costs of brand-name drugs were driven by inflation in the prices of widely used existing drugs,” they added. A combination of new products and price inflation in existing drugs drove the rising costs of specialty drugs, with new drugs accounting for a larger share of the price increases.
Third, “existing generics tended to decrease the average cost of generic drugs,” Dr. Hernandez noted. However, new generic products cost more than those already on the market, which fueled the annual increases in average costs.
The authors noted that their estimates demonstrate the role of inflation on pharmaceutical cost increases and support policy efforts to control that inflation.
“In the current value-based landscape, increasing drug costs attributable to new products can sometimes be justified on the basis of improved outcomes,” Dr. Hernandez and colleagues stated. “However, rising costs due to inflation do not reflect improved value for patients.”
The researchers noted that the data are limited by the lack of rebate information, which is generally proprietary. Thus, “the contribution of existing drugs may have been lower than we estimated,” they noted. In addition, “because the magnitude of rebates has increased in the past decade, our findings likely overestimated cost increases for brand-name drugs.” The researchers also didn’t examine the effect of drugs transitioning from brand to generic offerings.
The authors provided no disclosures.
SOURCE: Hernandez I et al. Health Aff (Millwood). 2019 Jan 2019. doi: 10.1377/hlthaff.2018.05147.
Inflation in existing drugs’ prices and the debut of new drugs are both contributing to the overall rising costs of pharmaceuticals.
.
For oral and injectable specialty drugs, costs increased 20.6% and 12.5%, respectively, with 71.1% and 52.4% attributable to new drugs. Costs of oral and injectable generic drugs grew by 4.4% and 7.3%, also driven by entrants into the market.
Researchers looked at monthly wholesale acquisition costs of 24,877 National Drug Codes for oral drugs and 3,049 injectable drugs from 2005 to 2016. They compared them with pharmacy claims from the UPMC Health Plan, which offers insurance products to more than 3.2 million members across the spectrum of private and public arenas.
“Our analyses yielded three main findings,” explained Inmaculada Hernandez, PharmD, PhD, University of Pittsburgh, and her colleagues in a report published in the January 2019 issue of Health Affairs.
“First, costs increased considerably faster than inflation across all drug classes, and increases were highest for oral specialty drugs and lowest for oral generics,” Dr. Hernandez and her colleagues wrote.
“Second, rising costs of brand-name drugs were driven by inflation in the prices of widely used existing drugs,” they added. A combination of new products and price inflation in existing drugs drove the rising costs of specialty drugs, with new drugs accounting for a larger share of the price increases.
Third, “existing generics tended to decrease the average cost of generic drugs,” Dr. Hernandez noted. However, new generic products cost more than those already on the market, which fueled the annual increases in average costs.
The authors noted that their estimates demonstrate the role of inflation on pharmaceutical cost increases and support policy efforts to control that inflation.
“In the current value-based landscape, increasing drug costs attributable to new products can sometimes be justified on the basis of improved outcomes,” Dr. Hernandez and colleagues stated. “However, rising costs due to inflation do not reflect improved value for patients.”
The researchers noted that the data are limited by the lack of rebate information, which is generally proprietary. Thus, “the contribution of existing drugs may have been lower than we estimated,” they noted. In addition, “because the magnitude of rebates has increased in the past decade, our findings likely overestimated cost increases for brand-name drugs.” The researchers also didn’t examine the effect of drugs transitioning from brand to generic offerings.
The authors provided no disclosures.
SOURCE: Hernandez I et al. Health Aff (Millwood). 2019 Jan 2019. doi: 10.1377/hlthaff.2018.05147.
Inflation in existing drugs’ prices and the debut of new drugs are both contributing to the overall rising costs of pharmaceuticals.
.
For oral and injectable specialty drugs, costs increased 20.6% and 12.5%, respectively, with 71.1% and 52.4% attributable to new drugs. Costs of oral and injectable generic drugs grew by 4.4% and 7.3%, also driven by entrants into the market.
Researchers looked at monthly wholesale acquisition costs of 24,877 National Drug Codes for oral drugs and 3,049 injectable drugs from 2005 to 2016. They compared them with pharmacy claims from the UPMC Health Plan, which offers insurance products to more than 3.2 million members across the spectrum of private and public arenas.
“Our analyses yielded three main findings,” explained Inmaculada Hernandez, PharmD, PhD, University of Pittsburgh, and her colleagues in a report published in the January 2019 issue of Health Affairs.
“First, costs increased considerably faster than inflation across all drug classes, and increases were highest for oral specialty drugs and lowest for oral generics,” Dr. Hernandez and her colleagues wrote.
“Second, rising costs of brand-name drugs were driven by inflation in the prices of widely used existing drugs,” they added. A combination of new products and price inflation in existing drugs drove the rising costs of specialty drugs, with new drugs accounting for a larger share of the price increases.
Third, “existing generics tended to decrease the average cost of generic drugs,” Dr. Hernandez noted. However, new generic products cost more than those already on the market, which fueled the annual increases in average costs.
The authors noted that their estimates demonstrate the role of inflation on pharmaceutical cost increases and support policy efforts to control that inflation.
“In the current value-based landscape, increasing drug costs attributable to new products can sometimes be justified on the basis of improved outcomes,” Dr. Hernandez and colleagues stated. “However, rising costs due to inflation do not reflect improved value for patients.”
The researchers noted that the data are limited by the lack of rebate information, which is generally proprietary. Thus, “the contribution of existing drugs may have been lower than we estimated,” they noted. In addition, “because the magnitude of rebates has increased in the past decade, our findings likely overestimated cost increases for brand-name drugs.” The researchers also didn’t examine the effect of drugs transitioning from brand to generic offerings.
The authors provided no disclosures.
SOURCE: Hernandez I et al. Health Aff (Millwood). 2019 Jan 2019. doi: 10.1377/hlthaff.2018.05147.
FROM HEALTH AFFAIRS
Key clinical point: Price inflation in existing drugs and new product introductions are driving increases in pharmaceutical costs.
Major finding: 71% of oral specialty drug price increases during 2005-2019 are attributable to new products.
Study details: Researchers analyzed the wholesale acquisition prices of 24,877 oral drugs and 3,049 injectable drugs and compared them with pharmacy claims across all public and private insurance products offered by the UPMC Health Plan.
Disclosures: The authors provided no disclosures.
Source: Hernandez I et al. Health Aff (Millwood). 2019 Jan. doi: 10.1377/hlthaff.2018.05147.
Deep sleep decreases, Alzheimer’s increases
Also today, physician groups are pushing back on Part B of the drug reimbursement proposal, dabigatran matches aspirin for second stroke prevention, and reassurance for pregnancy in atopic dermatitis.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, physician groups are pushing back on Part B of the drug reimbursement proposal, dabigatran matches aspirin for second stroke prevention, and reassurance for pregnancy in atopic dermatitis.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, physician groups are pushing back on Part B of the drug reimbursement proposal, dabigatran matches aspirin for second stroke prevention, and reassurance for pregnancy in atopic dermatitis.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Meeting 21st Century Public Health Needs: Public Health Partnerships at the Uniformed Services University
The Uniformed Services University of the Health Sciences (USU) was established by Congress in 1972 under the Uniformed Services Health Professions Revitalization Act. The only medical school administered by the federal government, “America’s Medical School” as it is affectionately known, has a mission to educate, train, and comprehensively prepare uniformed services health professionals to support the US military and public health system.
The USU School of Medicine (SOM) matriculates about 170 students each year. Although the majority of the medical students receive commissions in the US Army, Navy, or Air Force and serve as military physicians in the Department of Defense (DoD), a small number of students each year are commissioned as officers in the US Public Health Service Commissioned Corps (PHS). The PHS is a uniformed service within the US Department of Health and Human Services (HHS) whose officers serve nationwide in more than 30 government agencies. However, unlike its sister DoD services, the PHS does not participate in the Health Professions Scholarship Program, so admission to USU represents the only direct accession to the PHS Commissioned Corps for prospective physicians.
Beginning with the first graduating class, more than 160 PHS physician officers have now been trained under agreements with PHS agencies and SOM, and numerous others have received training and experience from the other academic programs and research centers within USU. Ten of those graduates achieved the rank of Rear Admiral, the general officer or “flag” position of the PHS.
The benefits of the partnerships between USU, PHS, and the agencies served by PHS to public health outcomes are many. Specifically, investment in PHS students at the SOM has served to ease disparities experienced by American Indians and Alaskan Natives (AI/AN), combat the shortage of primary care physicians (PCPs), generate exceptional clinical researchers, and train health care professionals to be prepared and ready to respond to emerging threats to public health.
Addressing Health Care Disparities Experienced by AI/AN
Through numerous treaties, laws, court cases, and Executive Orders—and most recently reaffirmed by the reauthorization of the Indian Health Care Improvement Act as part of the Patient Protection and Affordable Care Act (2010)–the US federal government holds responsibility for the provision of medical services to AI/AN. The Indian Health Service (IHS) is the principal federal provider of health care services for the AI/AN population. The mission of the IHS is to raise the physical, mental, social, and spiritual health of the AI/AN population to the highest level. It seeks to accomplish this mission by assuring that comprehensive, culturally acceptable personal and public health services are available and accessible to all AI/AN people.
Agency partnerships at USU, like the one between the school and IHS, sponsor medical students to become PHS physicians who can combat health disparities, especially those experienced by AI/AN. AI/AN continue to be subjected to disparities in health status across a wide array of chronic conditions, with significantly higher mortality rates than those of white populations.1 These trends are driven by multifactorial etiologies, including social determinants of health,2 obesity and the metabolic syndrome,3 high rates of tobacco and alcohol use,4 and limited access to medical care.5
Recruitment and retention of health care providers (HCPs) has long been a challenge for the IHS.6 Despite many attractive factors, providing care in a setting of otherwise limited resources and the relative remoteness of most facilities may prove to be deterring factors to prospective applicants. Furthermore, promotion of quality providers to administrative roles and high turnover rates of contractors or temporary staff contribute to poor continuity of care in certain locations. Consequently, efforts are under way to increase provider retention and continuity of care for patients.
This effort is augmented by training officers for a career of service to the IHS within the PHS. After completion of medical school and a residency in primary care, IHS-sponsored graduates from USU serve as officers in the PHS, stationed at an IHS-designated high-priority site for 10 years.7 However, many stay with the IHS for much longer, like IHS Chief Medical Officer, RADM Michael Toedt (USU 1995). In fact, nearly all the officers commissioned in the past 20 years are still on active duty. Within the IHS, physicians focus on community-oriented practice and improving the health of small-town and rural residents at tribal or federally operated clinics and community hospitals. In addition to performing clinical duties, graduates frequently become leaders within the IHS, advocating for systemwide improvements, performing practice-based research, and improving the overall well-being of AI/AN communities.
Combating the PCP Shortage
It has been well documented that primary care is essential for the prevention and control of chronic disease.8 However, fewer US medical school graduates are choosing to practice in primary care specialties, and the number of PCPs is forecasted to be insufficient for the needs of the American population in the coming years.9,10 This deficit is predicted to be especially pronounced in rural and underserved communities.11
Training PHS officers at the USU can fill this growing need by cultivating PCPs committed to a career of service in areas of high need. PHS medical students who are sponsored to attend USU by the IHS select from 1 of 7 approved primary care residencies: emergency medicine, family medicine, general pediatrics, general internal medicine, general psychiatry, obstetrics/gynecology, and general surgery.7 PHS students are permitted to train at military or civilian graduate medical education programs; permission to pursue combination programs is granted on a case-by-case basis, with consideration for the needs of the agency. Previously, such authorizations have included internal medicine/pediatrics, internal medicine/psychiatry, and family medicine/preventive medicine. This requirement, understood at the time of matriculation, selects for students who are passionate about primary care and are willing to live and practice in rural, underserved areas during their 10-year service commitment to the agency.
During medical school, USU students participate in numerous training activities that prepare doctors for practice in isolated or resource-poor settings, including point-of-care ultrasonography and field exercises in stabilization and transport of critically ill patients. The motto of the SOM, “Learning to Care for Those in Harm’s Way,” thereby applies not only to battlefield medicine, but to those who practice medicine in austere environments of all kinds.
Generating Clinical Researchers
Although IHS currently funds most PHS students, sponsorship also is available through the National Institute of Allergy and Infectious Diseases (NIAID), one of the institutes of the National Institutes of Health (NIH) in Bethesda, Maryland. Students selected for this competitive program complete a residency in either internal medicine or pediatrics, then complete an NIH-sponsored fellowship in either infectious diseases or allergy and immunology. Similar to their IHS counterparts, they incur a debt of service—10 years in the PHS Commissioned Corps; however, their service obligation is served at NIH. This track supports the creation of the next generation of clinical researchers and physician-scientists, critical in this time of ever-increasing threats to public health and national security, like emerging infectious diseases and bioterrorism.
Emergency Response Preparations
Combined training with experts from DoD and HHS prepares junior medical officers to serve as leaders in responding to large-scale emergencies and disasters. According to a memorandum of December 11, 1981, then Surgeon General C. Everett Koop described the importance of this skill set, saying that USU students are “ready for instant mobilization to meet military [needs] and [respond to] national disasters.” He continued, “Students are taught the necessary leadership and management skills to command medical units and organizations in the delivery of health services...They are exposed to the problems of dealing with national medical emergencies such as floods, earthquakes, and mass immigrations to this country.”12 Fittingly, physician graduates of USU have recently led disaster response efforts for Hurricanes Harvey, Irma, and Maria and Typhoon Yutu.
Traditional medical school didactic coursework is supplemented by lectures on disaster response, emergency preparedness, and global health engagement. As training progresses, students translate their knowledge into action with practical fieldwork exercises in mass casualty triage, erection of field hospitals using preventive medicine principles, and containment of infectious disease outbreaks among displaced persons—under the close observation and guidance of military and public health subject matter experts from across the country. Medical students complete their clinical training at military treatment facilities around the country and have elective clerkship opportunities in operational medicine nationally and internationally. PHS graduates of USU are well prepared to interface with their military colleagues, building effective joint mission capacity.
Additional Training Opportunities
In addition to the 4-year, tuition-free MD program, the university offers 7 graduate degree programs in public health and residency programs in preventive medicine specialty areas. Continuing education opportunities and graduate certificates are available in global health, tropical medicine and hygiene, travelers’ health, international and domestic disaster response, and other fields of interest to any public health professional, military or civilian. Many programs are available to federal or uniformed service members at no cost, some incur a degree of service commitment. Furthermore, the university is home to multiple research centers, including the National Center for Disaster Medicine and Public Health, which strive to improve public health through research efforts and education.
Conclusion
Though the emerging public health needs of the nation are both varied and daunting, the USU/PHS partnership trains providers that will heed the call and face the modern public health needs head-on. USU remains an important source for commissioning PHS physicians and producing career officers. The unique training provided at USU educates and enables PHS physicians to ease disparities experienced by AI/AN, combat the shortage of PCPs, generate exceptional clinical researchers, and be prepared and ready to respond to emerging threats to public health.
1. Espey DK, Jim MA, Cobb N, et al. Leading causes of death and all-cause mortality in American Indians and Alaska natives. Am J Public Health . 2014;104(S3):S303-S311.
2. Kunitz SJ, Veazie M, Henderson JA. Historical trends and regional differences in all-cause and amenable mortality among American Indians and Alaska Natives since 1950. Am J Public Health. 2014;104(6)(suppl 3):S268-S277.
3. Sinclair KA, Bogart A, Buchwald D, Henderson JA. The prevalence of metabolic syndrome and associated risk factors in Northern Plains and Southwest American Indians. Diabetes Care. 2011;34(1):118-120.
4. Cobb N, Espey D, King J. Health behaviors and risk factors among American Indians and Alaska Natives, 2000–2010. Am J Public Health. 2014;104(6)(suppl 3):S481-S489.
5. Warne D, Frizzell LB. American Indian health policy: historical trends and contemporary issues. Am J Public Health. 2014;104(6)(suppl 3):S263-S267.
6. Noren J, Kindig D, Sprenger A. Challenges to Native American health care. Public Health Rep. 1998;113(1):22-23.
7. Indian Health Services. Follow Your Path: The Uniformed Services University of the Health Sciences Participant Program Guide. https://www.ihs.gov/careeropps/includes/themes/responsive2017/display_objects/documents/USUHS-IHS-Participant-Program-Guide.pdf. Published October 2015. Accessed August 16, 2018.
8. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q . 2005;83(3):457-502.
9. Health Resources and Services Administration. Projecting the supply and demand for primary care practitioners through 2020. https://bhw.hrsa.gov/health-workforce-analysis/primary-care-2020. Accessed December 14, 2018.
10. Dill MJ, Salsberg ES. The complexities of physician supply and demand: projections through 2025. https://members.aamc.org/eweb/upload/The%20Complexities%20of%20Physician%20Supply.pdf. Published November 2008. Accessed December 14, 2018.
11. Wilson N, Couper I, De Vries E, Reid S, Fish T, Marais B. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural Remote Health . 2009;9(2):1060.
12. Department of Health and Human Services. Memorandum. Continued PHS Participation at USUHS. https://profiles.nlm.nih.gov/ps/access/QQBBZV.pdf. Published December 11, 1981. Accessed December 14, 2018.
The Uniformed Services University of the Health Sciences (USU) was established by Congress in 1972 under the Uniformed Services Health Professions Revitalization Act. The only medical school administered by the federal government, “America’s Medical School” as it is affectionately known, has a mission to educate, train, and comprehensively prepare uniformed services health professionals to support the US military and public health system.
The USU School of Medicine (SOM) matriculates about 170 students each year. Although the majority of the medical students receive commissions in the US Army, Navy, or Air Force and serve as military physicians in the Department of Defense (DoD), a small number of students each year are commissioned as officers in the US Public Health Service Commissioned Corps (PHS). The PHS is a uniformed service within the US Department of Health and Human Services (HHS) whose officers serve nationwide in more than 30 government agencies. However, unlike its sister DoD services, the PHS does not participate in the Health Professions Scholarship Program, so admission to USU represents the only direct accession to the PHS Commissioned Corps for prospective physicians.
Beginning with the first graduating class, more than 160 PHS physician officers have now been trained under agreements with PHS agencies and SOM, and numerous others have received training and experience from the other academic programs and research centers within USU. Ten of those graduates achieved the rank of Rear Admiral, the general officer or “flag” position of the PHS.
The benefits of the partnerships between USU, PHS, and the agencies served by PHS to public health outcomes are many. Specifically, investment in PHS students at the SOM has served to ease disparities experienced by American Indians and Alaskan Natives (AI/AN), combat the shortage of primary care physicians (PCPs), generate exceptional clinical researchers, and train health care professionals to be prepared and ready to respond to emerging threats to public health.
Addressing Health Care Disparities Experienced by AI/AN
Through numerous treaties, laws, court cases, and Executive Orders—and most recently reaffirmed by the reauthorization of the Indian Health Care Improvement Act as part of the Patient Protection and Affordable Care Act (2010)–the US federal government holds responsibility for the provision of medical services to AI/AN. The Indian Health Service (IHS) is the principal federal provider of health care services for the AI/AN population. The mission of the IHS is to raise the physical, mental, social, and spiritual health of the AI/AN population to the highest level. It seeks to accomplish this mission by assuring that comprehensive, culturally acceptable personal and public health services are available and accessible to all AI/AN people.
Agency partnerships at USU, like the one between the school and IHS, sponsor medical students to become PHS physicians who can combat health disparities, especially those experienced by AI/AN. AI/AN continue to be subjected to disparities in health status across a wide array of chronic conditions, with significantly higher mortality rates than those of white populations.1 These trends are driven by multifactorial etiologies, including social determinants of health,2 obesity and the metabolic syndrome,3 high rates of tobacco and alcohol use,4 and limited access to medical care.5
Recruitment and retention of health care providers (HCPs) has long been a challenge for the IHS.6 Despite many attractive factors, providing care in a setting of otherwise limited resources and the relative remoteness of most facilities may prove to be deterring factors to prospective applicants. Furthermore, promotion of quality providers to administrative roles and high turnover rates of contractors or temporary staff contribute to poor continuity of care in certain locations. Consequently, efforts are under way to increase provider retention and continuity of care for patients.
This effort is augmented by training officers for a career of service to the IHS within the PHS. After completion of medical school and a residency in primary care, IHS-sponsored graduates from USU serve as officers in the PHS, stationed at an IHS-designated high-priority site for 10 years.7 However, many stay with the IHS for much longer, like IHS Chief Medical Officer, RADM Michael Toedt (USU 1995). In fact, nearly all the officers commissioned in the past 20 years are still on active duty. Within the IHS, physicians focus on community-oriented practice and improving the health of small-town and rural residents at tribal or federally operated clinics and community hospitals. In addition to performing clinical duties, graduates frequently become leaders within the IHS, advocating for systemwide improvements, performing practice-based research, and improving the overall well-being of AI/AN communities.
Combating the PCP Shortage
It has been well documented that primary care is essential for the prevention and control of chronic disease.8 However, fewer US medical school graduates are choosing to practice in primary care specialties, and the number of PCPs is forecasted to be insufficient for the needs of the American population in the coming years.9,10 This deficit is predicted to be especially pronounced in rural and underserved communities.11
Training PHS officers at the USU can fill this growing need by cultivating PCPs committed to a career of service in areas of high need. PHS medical students who are sponsored to attend USU by the IHS select from 1 of 7 approved primary care residencies: emergency medicine, family medicine, general pediatrics, general internal medicine, general psychiatry, obstetrics/gynecology, and general surgery.7 PHS students are permitted to train at military or civilian graduate medical education programs; permission to pursue combination programs is granted on a case-by-case basis, with consideration for the needs of the agency. Previously, such authorizations have included internal medicine/pediatrics, internal medicine/psychiatry, and family medicine/preventive medicine. This requirement, understood at the time of matriculation, selects for students who are passionate about primary care and are willing to live and practice in rural, underserved areas during their 10-year service commitment to the agency.
During medical school, USU students participate in numerous training activities that prepare doctors for practice in isolated or resource-poor settings, including point-of-care ultrasonography and field exercises in stabilization and transport of critically ill patients. The motto of the SOM, “Learning to Care for Those in Harm’s Way,” thereby applies not only to battlefield medicine, but to those who practice medicine in austere environments of all kinds.
Generating Clinical Researchers
Although IHS currently funds most PHS students, sponsorship also is available through the National Institute of Allergy and Infectious Diseases (NIAID), one of the institutes of the National Institutes of Health (NIH) in Bethesda, Maryland. Students selected for this competitive program complete a residency in either internal medicine or pediatrics, then complete an NIH-sponsored fellowship in either infectious diseases or allergy and immunology. Similar to their IHS counterparts, they incur a debt of service—10 years in the PHS Commissioned Corps; however, their service obligation is served at NIH. This track supports the creation of the next generation of clinical researchers and physician-scientists, critical in this time of ever-increasing threats to public health and national security, like emerging infectious diseases and bioterrorism.
Emergency Response Preparations
Combined training with experts from DoD and HHS prepares junior medical officers to serve as leaders in responding to large-scale emergencies and disasters. According to a memorandum of December 11, 1981, then Surgeon General C. Everett Koop described the importance of this skill set, saying that USU students are “ready for instant mobilization to meet military [needs] and [respond to] national disasters.” He continued, “Students are taught the necessary leadership and management skills to command medical units and organizations in the delivery of health services...They are exposed to the problems of dealing with national medical emergencies such as floods, earthquakes, and mass immigrations to this country.”12 Fittingly, physician graduates of USU have recently led disaster response efforts for Hurricanes Harvey, Irma, and Maria and Typhoon Yutu.
Traditional medical school didactic coursework is supplemented by lectures on disaster response, emergency preparedness, and global health engagement. As training progresses, students translate their knowledge into action with practical fieldwork exercises in mass casualty triage, erection of field hospitals using preventive medicine principles, and containment of infectious disease outbreaks among displaced persons—under the close observation and guidance of military and public health subject matter experts from across the country. Medical students complete their clinical training at military treatment facilities around the country and have elective clerkship opportunities in operational medicine nationally and internationally. PHS graduates of USU are well prepared to interface with their military colleagues, building effective joint mission capacity.
Additional Training Opportunities
In addition to the 4-year, tuition-free MD program, the university offers 7 graduate degree programs in public health and residency programs in preventive medicine specialty areas. Continuing education opportunities and graduate certificates are available in global health, tropical medicine and hygiene, travelers’ health, international and domestic disaster response, and other fields of interest to any public health professional, military or civilian. Many programs are available to federal or uniformed service members at no cost, some incur a degree of service commitment. Furthermore, the university is home to multiple research centers, including the National Center for Disaster Medicine and Public Health, which strive to improve public health through research efforts and education.
Conclusion
Though the emerging public health needs of the nation are both varied and daunting, the USU/PHS partnership trains providers that will heed the call and face the modern public health needs head-on. USU remains an important source for commissioning PHS physicians and producing career officers. The unique training provided at USU educates and enables PHS physicians to ease disparities experienced by AI/AN, combat the shortage of PCPs, generate exceptional clinical researchers, and be prepared and ready to respond to emerging threats to public health.
The Uniformed Services University of the Health Sciences (USU) was established by Congress in 1972 under the Uniformed Services Health Professions Revitalization Act. The only medical school administered by the federal government, “America’s Medical School” as it is affectionately known, has a mission to educate, train, and comprehensively prepare uniformed services health professionals to support the US military and public health system.
The USU School of Medicine (SOM) matriculates about 170 students each year. Although the majority of the medical students receive commissions in the US Army, Navy, or Air Force and serve as military physicians in the Department of Defense (DoD), a small number of students each year are commissioned as officers in the US Public Health Service Commissioned Corps (PHS). The PHS is a uniformed service within the US Department of Health and Human Services (HHS) whose officers serve nationwide in more than 30 government agencies. However, unlike its sister DoD services, the PHS does not participate in the Health Professions Scholarship Program, so admission to USU represents the only direct accession to the PHS Commissioned Corps for prospective physicians.
Beginning with the first graduating class, more than 160 PHS physician officers have now been trained under agreements with PHS agencies and SOM, and numerous others have received training and experience from the other academic programs and research centers within USU. Ten of those graduates achieved the rank of Rear Admiral, the general officer or “flag” position of the PHS.
The benefits of the partnerships between USU, PHS, and the agencies served by PHS to public health outcomes are many. Specifically, investment in PHS students at the SOM has served to ease disparities experienced by American Indians and Alaskan Natives (AI/AN), combat the shortage of primary care physicians (PCPs), generate exceptional clinical researchers, and train health care professionals to be prepared and ready to respond to emerging threats to public health.
Addressing Health Care Disparities Experienced by AI/AN
Through numerous treaties, laws, court cases, and Executive Orders—and most recently reaffirmed by the reauthorization of the Indian Health Care Improvement Act as part of the Patient Protection and Affordable Care Act (2010)–the US federal government holds responsibility for the provision of medical services to AI/AN. The Indian Health Service (IHS) is the principal federal provider of health care services for the AI/AN population. The mission of the IHS is to raise the physical, mental, social, and spiritual health of the AI/AN population to the highest level. It seeks to accomplish this mission by assuring that comprehensive, culturally acceptable personal and public health services are available and accessible to all AI/AN people.
Agency partnerships at USU, like the one between the school and IHS, sponsor medical students to become PHS physicians who can combat health disparities, especially those experienced by AI/AN. AI/AN continue to be subjected to disparities in health status across a wide array of chronic conditions, with significantly higher mortality rates than those of white populations.1 These trends are driven by multifactorial etiologies, including social determinants of health,2 obesity and the metabolic syndrome,3 high rates of tobacco and alcohol use,4 and limited access to medical care.5
Recruitment and retention of health care providers (HCPs) has long been a challenge for the IHS.6 Despite many attractive factors, providing care in a setting of otherwise limited resources and the relative remoteness of most facilities may prove to be deterring factors to prospective applicants. Furthermore, promotion of quality providers to administrative roles and high turnover rates of contractors or temporary staff contribute to poor continuity of care in certain locations. Consequently, efforts are under way to increase provider retention and continuity of care for patients.
This effort is augmented by training officers for a career of service to the IHS within the PHS. After completion of medical school and a residency in primary care, IHS-sponsored graduates from USU serve as officers in the PHS, stationed at an IHS-designated high-priority site for 10 years.7 However, many stay with the IHS for much longer, like IHS Chief Medical Officer, RADM Michael Toedt (USU 1995). In fact, nearly all the officers commissioned in the past 20 years are still on active duty. Within the IHS, physicians focus on community-oriented practice and improving the health of small-town and rural residents at tribal or federally operated clinics and community hospitals. In addition to performing clinical duties, graduates frequently become leaders within the IHS, advocating for systemwide improvements, performing practice-based research, and improving the overall well-being of AI/AN communities.
Combating the PCP Shortage
It has been well documented that primary care is essential for the prevention and control of chronic disease.8 However, fewer US medical school graduates are choosing to practice in primary care specialties, and the number of PCPs is forecasted to be insufficient for the needs of the American population in the coming years.9,10 This deficit is predicted to be especially pronounced in rural and underserved communities.11
Training PHS officers at the USU can fill this growing need by cultivating PCPs committed to a career of service in areas of high need. PHS medical students who are sponsored to attend USU by the IHS select from 1 of 7 approved primary care residencies: emergency medicine, family medicine, general pediatrics, general internal medicine, general psychiatry, obstetrics/gynecology, and general surgery.7 PHS students are permitted to train at military or civilian graduate medical education programs; permission to pursue combination programs is granted on a case-by-case basis, with consideration for the needs of the agency. Previously, such authorizations have included internal medicine/pediatrics, internal medicine/psychiatry, and family medicine/preventive medicine. This requirement, understood at the time of matriculation, selects for students who are passionate about primary care and are willing to live and practice in rural, underserved areas during their 10-year service commitment to the agency.
During medical school, USU students participate in numerous training activities that prepare doctors for practice in isolated or resource-poor settings, including point-of-care ultrasonography and field exercises in stabilization and transport of critically ill patients. The motto of the SOM, “Learning to Care for Those in Harm’s Way,” thereby applies not only to battlefield medicine, but to those who practice medicine in austere environments of all kinds.
Generating Clinical Researchers
Although IHS currently funds most PHS students, sponsorship also is available through the National Institute of Allergy and Infectious Diseases (NIAID), one of the institutes of the National Institutes of Health (NIH) in Bethesda, Maryland. Students selected for this competitive program complete a residency in either internal medicine or pediatrics, then complete an NIH-sponsored fellowship in either infectious diseases or allergy and immunology. Similar to their IHS counterparts, they incur a debt of service—10 years in the PHS Commissioned Corps; however, their service obligation is served at NIH. This track supports the creation of the next generation of clinical researchers and physician-scientists, critical in this time of ever-increasing threats to public health and national security, like emerging infectious diseases and bioterrorism.
Emergency Response Preparations
Combined training with experts from DoD and HHS prepares junior medical officers to serve as leaders in responding to large-scale emergencies and disasters. According to a memorandum of December 11, 1981, then Surgeon General C. Everett Koop described the importance of this skill set, saying that USU students are “ready for instant mobilization to meet military [needs] and [respond to] national disasters.” He continued, “Students are taught the necessary leadership and management skills to command medical units and organizations in the delivery of health services...They are exposed to the problems of dealing with national medical emergencies such as floods, earthquakes, and mass immigrations to this country.”12 Fittingly, physician graduates of USU have recently led disaster response efforts for Hurricanes Harvey, Irma, and Maria and Typhoon Yutu.
Traditional medical school didactic coursework is supplemented by lectures on disaster response, emergency preparedness, and global health engagement. As training progresses, students translate their knowledge into action with practical fieldwork exercises in mass casualty triage, erection of field hospitals using preventive medicine principles, and containment of infectious disease outbreaks among displaced persons—under the close observation and guidance of military and public health subject matter experts from across the country. Medical students complete their clinical training at military treatment facilities around the country and have elective clerkship opportunities in operational medicine nationally and internationally. PHS graduates of USU are well prepared to interface with their military colleagues, building effective joint mission capacity.
Additional Training Opportunities
In addition to the 4-year, tuition-free MD program, the university offers 7 graduate degree programs in public health and residency programs in preventive medicine specialty areas. Continuing education opportunities and graduate certificates are available in global health, tropical medicine and hygiene, travelers’ health, international and domestic disaster response, and other fields of interest to any public health professional, military or civilian. Many programs are available to federal or uniformed service members at no cost, some incur a degree of service commitment. Furthermore, the university is home to multiple research centers, including the National Center for Disaster Medicine and Public Health, which strive to improve public health through research efforts and education.
Conclusion
Though the emerging public health needs of the nation are both varied and daunting, the USU/PHS partnership trains providers that will heed the call and face the modern public health needs head-on. USU remains an important source for commissioning PHS physicians and producing career officers. The unique training provided at USU educates and enables PHS physicians to ease disparities experienced by AI/AN, combat the shortage of PCPs, generate exceptional clinical researchers, and be prepared and ready to respond to emerging threats to public health.
1. Espey DK, Jim MA, Cobb N, et al. Leading causes of death and all-cause mortality in American Indians and Alaska natives. Am J Public Health . 2014;104(S3):S303-S311.
2. Kunitz SJ, Veazie M, Henderson JA. Historical trends and regional differences in all-cause and amenable mortality among American Indians and Alaska Natives since 1950. Am J Public Health. 2014;104(6)(suppl 3):S268-S277.
3. Sinclair KA, Bogart A, Buchwald D, Henderson JA. The prevalence of metabolic syndrome and associated risk factors in Northern Plains and Southwest American Indians. Diabetes Care. 2011;34(1):118-120.
4. Cobb N, Espey D, King J. Health behaviors and risk factors among American Indians and Alaska Natives, 2000–2010. Am J Public Health. 2014;104(6)(suppl 3):S481-S489.
5. Warne D, Frizzell LB. American Indian health policy: historical trends and contemporary issues. Am J Public Health. 2014;104(6)(suppl 3):S263-S267.
6. Noren J, Kindig D, Sprenger A. Challenges to Native American health care. Public Health Rep. 1998;113(1):22-23.
7. Indian Health Services. Follow Your Path: The Uniformed Services University of the Health Sciences Participant Program Guide. https://www.ihs.gov/careeropps/includes/themes/responsive2017/display_objects/documents/USUHS-IHS-Participant-Program-Guide.pdf. Published October 2015. Accessed August 16, 2018.
8. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q . 2005;83(3):457-502.
9. Health Resources and Services Administration. Projecting the supply and demand for primary care practitioners through 2020. https://bhw.hrsa.gov/health-workforce-analysis/primary-care-2020. Accessed December 14, 2018.
10. Dill MJ, Salsberg ES. The complexities of physician supply and demand: projections through 2025. https://members.aamc.org/eweb/upload/The%20Complexities%20of%20Physician%20Supply.pdf. Published November 2008. Accessed December 14, 2018.
11. Wilson N, Couper I, De Vries E, Reid S, Fish T, Marais B. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural Remote Health . 2009;9(2):1060.
12. Department of Health and Human Services. Memorandum. Continued PHS Participation at USUHS. https://profiles.nlm.nih.gov/ps/access/QQBBZV.pdf. Published December 11, 1981. Accessed December 14, 2018.
1. Espey DK, Jim MA, Cobb N, et al. Leading causes of death and all-cause mortality in American Indians and Alaska natives. Am J Public Health . 2014;104(S3):S303-S311.
2. Kunitz SJ, Veazie M, Henderson JA. Historical trends and regional differences in all-cause and amenable mortality among American Indians and Alaska Natives since 1950. Am J Public Health. 2014;104(6)(suppl 3):S268-S277.
3. Sinclair KA, Bogart A, Buchwald D, Henderson JA. The prevalence of metabolic syndrome and associated risk factors in Northern Plains and Southwest American Indians. Diabetes Care. 2011;34(1):118-120.
4. Cobb N, Espey D, King J. Health behaviors and risk factors among American Indians and Alaska Natives, 2000–2010. Am J Public Health. 2014;104(6)(suppl 3):S481-S489.
5. Warne D, Frizzell LB. American Indian health policy: historical trends and contemporary issues. Am J Public Health. 2014;104(6)(suppl 3):S263-S267.
6. Noren J, Kindig D, Sprenger A. Challenges to Native American health care. Public Health Rep. 1998;113(1):22-23.
7. Indian Health Services. Follow Your Path: The Uniformed Services University of the Health Sciences Participant Program Guide. https://www.ihs.gov/careeropps/includes/themes/responsive2017/display_objects/documents/USUHS-IHS-Participant-Program-Guide.pdf. Published October 2015. Accessed August 16, 2018.
8. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q . 2005;83(3):457-502.
9. Health Resources and Services Administration. Projecting the supply and demand for primary care practitioners through 2020. https://bhw.hrsa.gov/health-workforce-analysis/primary-care-2020. Accessed December 14, 2018.
10. Dill MJ, Salsberg ES. The complexities of physician supply and demand: projections through 2025. https://members.aamc.org/eweb/upload/The%20Complexities%20of%20Physician%20Supply.pdf. Published November 2008. Accessed December 14, 2018.
11. Wilson N, Couper I, De Vries E, Reid S, Fish T, Marais B. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural Remote Health . 2009;9(2):1060.
12. Department of Health and Human Services. Memorandum. Continued PHS Participation at USUHS. https://profiles.nlm.nih.gov/ps/access/QQBBZV.pdf. Published December 11, 1981. Accessed December 14, 2018.
Think outside lower body for pelvic pain
Also today, treating obstructive sleep apnea with positive airway pressure decreased amyloid levels, spending on medical marketing increased by more than $12 billion over that past two decades, and one expert has advice on how you can get your work published.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, treating obstructive sleep apnea with positive airway pressure decreased amyloid levels, spending on medical marketing increased by more than $12 billion over that past two decades, and one expert has advice on how you can get your work published.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, treating obstructive sleep apnea with positive airway pressure decreased amyloid levels, spending on medical marketing increased by more than $12 billion over that past two decades, and one expert has advice on how you can get your work published.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
AAP guidance: How to ask about military service
Knee pathologies predict accelerated knee osteoarthritis, patients with a poor-prognosis cancer have a higher risk of suicide in the first year, and Nuedexta is mainly being prescribed for dementia and Parkinson’s.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Knee pathologies predict accelerated knee osteoarthritis, patients with a poor-prognosis cancer have a higher risk of suicide in the first year, and Nuedexta is mainly being prescribed for dementia and Parkinson’s.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Knee pathologies predict accelerated knee osteoarthritis, patients with a poor-prognosis cancer have a higher risk of suicide in the first year, and Nuedexta is mainly being prescribed for dementia and Parkinson’s.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
AAN publishes position statement on brain death
In a position statement published online ahead of print Jan. 2 in Neurology, Such uniformity would reduce uncertainty and improve patient care, according to the authors. The statement, which was drafted by the AAN’s Brain Death Working Group, also supports the development of uniform policies regarding brain death and its determination within American medical institutions. Finally, the document provides neurologists with guidance for responding to requests for accommodation, including objections to the determination of brain death and to the withdrawal of organ-sustaining technology.
The AAN defines brain death as death resulting from irreversible loss of function of the entire brain. The Uniform Determination of Death Act of 1981 held that brain death and circulatory death (that is, death resulting from irreversible loss of function of the circulatory system) are equivalent, and the AAN acknowledges this equivalence.
The two current medical standards for brain death are the AAN’s 2010 Evidence-Based Guideline Update: Determining Brain Death in Adults and the 2011 Guidelines for the Determination of Brain Death in Infants and Children, which was published by the pediatric section of the Society of Critical Care Medicine, the sections of neurology and critical care of the American Academy of Pediatrics, and the Child Neurology Society. “The AAN is unaware of any cases in which compliant application of the brain death guidelines led to inaccurate determination of death with return of any brain function, including consciousness, brainstem reflexes, or ventilatory effort,” according to their 2019 statement.
The only jurisdiction with laws that specifically defer to these standards, however, is Nevada. The vagueness of most states’ laws has contributed to divergent legal interpretations and idiosyncratic standards for determining brain death, according to the statement.
“The AAN believes that a specific, uniform standard for the determination of brain death is critically important to provide the highest quality patient-centered neurologic and end-of-life care,” said James Russell, DO, MS, a neurologist at Lahey Hospital and Medical Center in Burlington, Mass., and lead author of the position statement. “The AAN supports the development of legislation in every state modeled after the Nevada statute, which specifically defers to these current adult and pediatric brain death guidelines and any future updates.”
In addition to uniform institutional policies for determining brain death within U.S. medical facilities, the AAN calls for the development of training programs and credentialing mechanisms for physicians who determine brain death, regardless of their specialties. The association also supports research that enhances understanding of brain death and enhanced professional and public education.
While expressing respect and sympathy for requests for limited accommodation, the AAN asserts that these requests “must be based on the values of the patient, and not those of loved ones or other surrogate decision makers.” The association further observes that physicians have no ethical obligation to provide medical treatment to a deceased patient. New Jersey is the only state that legally obliges physicians to provide indefinite accommodation and continued application of organ-sustaining technology.
“The AAN believes that its members have both the moral authority and professional responsibility, when lawful, to perform a brain death evaluation, including apnea testing, after informing a patient’s loved ones or lawful surrogates of that intention, but without obligation to obtain informed consent,” according to the statement. “This position is analogous to the authority and responsibility historically granted to the medical profession to determine circulatory death without the requirement for additional informed consent.”
If a dispute about indefinite accommodation cannot be resolved, it is acceptable for a physician to withdraw organ-sustaining technology unilaterally over the objection of loved ones when legally permitted, according to the AAN. Such unilateral action is a measure of last resort and does not apply when the patient is a pregnant woman, said the authors. In the latter case, the ethical analysis should focus mainly on the welfare of the fetus.
The AAN provided financial support for the Brain Death Working Group’s efforts. The statement’s authors reported no relevant disclosures. The American Neurological Association and the Child Neurology Society have endorsed the AAN’s position statement.
SOURCE: Russell JA et al. Neurology. 2018 Jan 2. doi: 10.1212/WNL.0000000000006750.
In a position statement published online ahead of print Jan. 2 in Neurology, Such uniformity would reduce uncertainty and improve patient care, according to the authors. The statement, which was drafted by the AAN’s Brain Death Working Group, also supports the development of uniform policies regarding brain death and its determination within American medical institutions. Finally, the document provides neurologists with guidance for responding to requests for accommodation, including objections to the determination of brain death and to the withdrawal of organ-sustaining technology.
The AAN defines brain death as death resulting from irreversible loss of function of the entire brain. The Uniform Determination of Death Act of 1981 held that brain death and circulatory death (that is, death resulting from irreversible loss of function of the circulatory system) are equivalent, and the AAN acknowledges this equivalence.
The two current medical standards for brain death are the AAN’s 2010 Evidence-Based Guideline Update: Determining Brain Death in Adults and the 2011 Guidelines for the Determination of Brain Death in Infants and Children, which was published by the pediatric section of the Society of Critical Care Medicine, the sections of neurology and critical care of the American Academy of Pediatrics, and the Child Neurology Society. “The AAN is unaware of any cases in which compliant application of the brain death guidelines led to inaccurate determination of death with return of any brain function, including consciousness, brainstem reflexes, or ventilatory effort,” according to their 2019 statement.
The only jurisdiction with laws that specifically defer to these standards, however, is Nevada. The vagueness of most states’ laws has contributed to divergent legal interpretations and idiosyncratic standards for determining brain death, according to the statement.
“The AAN believes that a specific, uniform standard for the determination of brain death is critically important to provide the highest quality patient-centered neurologic and end-of-life care,” said James Russell, DO, MS, a neurologist at Lahey Hospital and Medical Center in Burlington, Mass., and lead author of the position statement. “The AAN supports the development of legislation in every state modeled after the Nevada statute, which specifically defers to these current adult and pediatric brain death guidelines and any future updates.”
In addition to uniform institutional policies for determining brain death within U.S. medical facilities, the AAN calls for the development of training programs and credentialing mechanisms for physicians who determine brain death, regardless of their specialties. The association also supports research that enhances understanding of brain death and enhanced professional and public education.
While expressing respect and sympathy for requests for limited accommodation, the AAN asserts that these requests “must be based on the values of the patient, and not those of loved ones or other surrogate decision makers.” The association further observes that physicians have no ethical obligation to provide medical treatment to a deceased patient. New Jersey is the only state that legally obliges physicians to provide indefinite accommodation and continued application of organ-sustaining technology.
“The AAN believes that its members have both the moral authority and professional responsibility, when lawful, to perform a brain death evaluation, including apnea testing, after informing a patient’s loved ones or lawful surrogates of that intention, but without obligation to obtain informed consent,” according to the statement. “This position is analogous to the authority and responsibility historically granted to the medical profession to determine circulatory death without the requirement for additional informed consent.”
If a dispute about indefinite accommodation cannot be resolved, it is acceptable for a physician to withdraw organ-sustaining technology unilaterally over the objection of loved ones when legally permitted, according to the AAN. Such unilateral action is a measure of last resort and does not apply when the patient is a pregnant woman, said the authors. In the latter case, the ethical analysis should focus mainly on the welfare of the fetus.
The AAN provided financial support for the Brain Death Working Group’s efforts. The statement’s authors reported no relevant disclosures. The American Neurological Association and the Child Neurology Society have endorsed the AAN’s position statement.
SOURCE: Russell JA et al. Neurology. 2018 Jan 2. doi: 10.1212/WNL.0000000000006750.
In a position statement published online ahead of print Jan. 2 in Neurology, Such uniformity would reduce uncertainty and improve patient care, according to the authors. The statement, which was drafted by the AAN’s Brain Death Working Group, also supports the development of uniform policies regarding brain death and its determination within American medical institutions. Finally, the document provides neurologists with guidance for responding to requests for accommodation, including objections to the determination of brain death and to the withdrawal of organ-sustaining technology.
The AAN defines brain death as death resulting from irreversible loss of function of the entire brain. The Uniform Determination of Death Act of 1981 held that brain death and circulatory death (that is, death resulting from irreversible loss of function of the circulatory system) are equivalent, and the AAN acknowledges this equivalence.
The two current medical standards for brain death are the AAN’s 2010 Evidence-Based Guideline Update: Determining Brain Death in Adults and the 2011 Guidelines for the Determination of Brain Death in Infants and Children, which was published by the pediatric section of the Society of Critical Care Medicine, the sections of neurology and critical care of the American Academy of Pediatrics, and the Child Neurology Society. “The AAN is unaware of any cases in which compliant application of the brain death guidelines led to inaccurate determination of death with return of any brain function, including consciousness, brainstem reflexes, or ventilatory effort,” according to their 2019 statement.
The only jurisdiction with laws that specifically defer to these standards, however, is Nevada. The vagueness of most states’ laws has contributed to divergent legal interpretations and idiosyncratic standards for determining brain death, according to the statement.
“The AAN believes that a specific, uniform standard for the determination of brain death is critically important to provide the highest quality patient-centered neurologic and end-of-life care,” said James Russell, DO, MS, a neurologist at Lahey Hospital and Medical Center in Burlington, Mass., and lead author of the position statement. “The AAN supports the development of legislation in every state modeled after the Nevada statute, which specifically defers to these current adult and pediatric brain death guidelines and any future updates.”
In addition to uniform institutional policies for determining brain death within U.S. medical facilities, the AAN calls for the development of training programs and credentialing mechanisms for physicians who determine brain death, regardless of their specialties. The association also supports research that enhances understanding of brain death and enhanced professional and public education.
While expressing respect and sympathy for requests for limited accommodation, the AAN asserts that these requests “must be based on the values of the patient, and not those of loved ones or other surrogate decision makers.” The association further observes that physicians have no ethical obligation to provide medical treatment to a deceased patient. New Jersey is the only state that legally obliges physicians to provide indefinite accommodation and continued application of organ-sustaining technology.
“The AAN believes that its members have both the moral authority and professional responsibility, when lawful, to perform a brain death evaluation, including apnea testing, after informing a patient’s loved ones or lawful surrogates of that intention, but without obligation to obtain informed consent,” according to the statement. “This position is analogous to the authority and responsibility historically granted to the medical profession to determine circulatory death without the requirement for additional informed consent.”
If a dispute about indefinite accommodation cannot be resolved, it is acceptable for a physician to withdraw organ-sustaining technology unilaterally over the objection of loved ones when legally permitted, according to the AAN. Such unilateral action is a measure of last resort and does not apply when the patient is a pregnant woman, said the authors. In the latter case, the ethical analysis should focus mainly on the welfare of the fetus.
The AAN provided financial support for the Brain Death Working Group’s efforts. The statement’s authors reported no relevant disclosures. The American Neurological Association and the Child Neurology Society have endorsed the AAN’s position statement.
SOURCE: Russell JA et al. Neurology. 2018 Jan 2. doi: 10.1212/WNL.0000000000006750.
FROM NEUROLOGY
Key clinical point: The AAN calls for uniform brain death laws, policies, and practices.
Major finding: The association published a position statement online on January 2.
Study details: The AAN’s Brain Death Working Group drafted the statement.
Disclosures: The authors reported no relevant disclosures, and the American Academy of Neurology funded their work.
Source: Russell JA et al. Neurology. 2018 Jan 2. doi: 10.1212/WNL.0000000000006750.
Health care costs matter to patients, and we can do something about it
CASE 1 Huge out-of-pocket cost makes patient forego treatment
Ms. M. is a 28-year-old patient who recently posted this on her Facebook page: “I went to the drugstore this morning to pick up a prescription, and as the pharmacist handed it to me she said, ‘That will be $180.00.’ And that’s after insurance coverage! Wow! I think I’ll pass!”
Our patients probably experience this type of situation more commonly than we know.
CASE 2 Catastrophic medical costs bankrupt family
A middle-class couple who had college degrees and full-time jobs with health insurance had twins at 24 weeks’ gestation. They accrued $450,000 in medical debt after exceeding the $2 million cap of their insurance policy. Having premature twins cost them everything. They liquidated their retirement and savings accounts, sold everything they had, and still ended up filing for bankruptcy.1
Costs indeed matter to patients, and we have a professional responsibility to help our patients navigate the murky waters of health care so that they can maintain financial as well as physical health.
Rising costs, lower yield,and opportunities for change
Rising health care costs are unsustainable for both our patients and our society. Although the United States spends more on health care than any other developed country, our health outcomes are actually worse—ranking at or near the bottom in both prevalence and mortality for multiple diseases, risk factors, and injuries.2
Of the 171 countries included in a study by the United Nations Maternal Mortality Estimation Inter-Agency Group, the United States was 1 of 13 countries that had an increasing maternal mortality and the only developed nation with an increasing maternal mortality rate.3 This tells us that, as our country spends more on health care, our patients’ health is not improving. For individuals, medical bills are now the leading cause of personal bankruptcy in the United States, even for those who are insured.4
ObGyns play an important leadership role in the practice of cost-conscious health care, as 25% of hospitalizations in the United States are pregnancy related.5,6 In addition, the wide scope of ObGyn practice reaches beyond pregnancy-related conditions and provides multiple opportunities to decrease the use of unnecessary tests and treatments.
The good news is that approximately 30% of health care costs are wasted on unnecessary care that could be eliminated without decreasing the quality of care.7
High-value change #1: Eliminate use of expensive products
Embarking on a high-value care improvement project, experts at Greenville Health System examined the cost of different topical pain medications for perineal pain after a vaginal delivery. They found that Epifoam (hydrocortisone acetate/pramoxine hydrochloride) was ordered 2,287 times over the course of a year.
The study intervention consisted of an educational grand rounds and discussion of a Cochrane review, which concluded there was no difference in pain relief with topical anesthetics compared with placebo.8 Less expensive options for pain relief were discussed, and the department agreed to remove Epifoam as a standing order.
After the intervention, Epifoam was ordered 228 times, a 90% reduction. Over the period of a year, this translated to a cost savings of $92,655 for the hospital, with reduced charges passed on to patients.9 Thus, a seemingly small individual cost ($45.00 per can of Epifoam) can add up to a substantial sum in a large health care system.
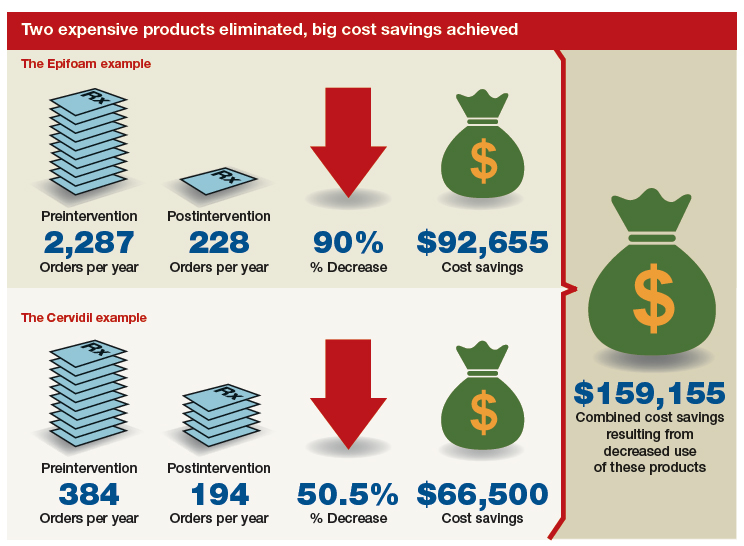
Similarly, practitioners were educated about options for cervical ripening and were given information on the cost and efficacy of various cervical ripening agents. A Cochrane review found that oral misoprostol is as effective as vaginal misoprostol and results in fewer cesarean deliveries than vaginal dinoprostone (Cervidil).10 Practitioners were asked to consider making the transition to oral misoprostol. This action resulted in a 50.5% decrease in Cervidil use, from 384 to 194 cases, producing a cost savings of $66,500. The following year, the department removed Cervidil from the formulary as a high-value decision.9
Both of these examples illustrate what a value-minded department can accomplish by implementing performance improvement projects that focus on high-value care.
Continue to: High-value change #2: Stop ordering unnecessary lab work...
High-value change #2: Stop ordering unnecessary lab work
Another high-value change to consider: Examine each laboratory test order to understand if the test results will really alter the care of a patient. Providers vary, and ordering lab tests to “make sure” can add up as financial expense.
Best practices from the American College of Obstetricians and Gynecologists (ACOG) and other professional societies can help guide decision-making as we order lab tests. Think twice, for example, about whether every evaluation for preeclampsia requires a uric acid test, since ACOG does not endorse that as part of the diagnostic criteria. While a single uric acid test costs only $8.00 to $38.00 (according to Healthcare Bluebook), testing uric acid in many patients over the course of a year can add up to significant dollars.11
High-value change #3: Consider care redesign
In addition to seeking opportunities to use more cost-effective products and reduce the use of unnecessary tests, “care redesign” is an innovative way to provide high-quality care (and increased patient satisfaction) at a lower cost for both the health care system and the patient. A prime example of care redesign is using telehealth to enhance prenatal care.
Several health systems around the country are piloting and implementing remote blood pressure monitoring, app-based prenatal education, and telehealth visits to enhance prenatal care.12,13 Use of a home blood pressure monitor can reduce in-person visits for low-risk prenatal care and open up access for other patients. Additionally, allowing the patient to participate in her own care at home or work can eliminate drives to and waits in the office and reduce absence from work because of a doctor visit.
A systematic review of more than 60,000 women showed that low-risk women who attend 5 to 9 prenatal visits have the same outcomes as women who attend the standard schedule of 13 to 15 visits.14 Although patient satisfaction was higher with more visits, when a bidirectional app or a telehealth visit is offered as an option, then patient satisfaction is equivalent to that in the standard schedule group.12 So why not expand the choice for patients?
The challenge of teaching high-value care: Medical education responds
In a 2010 article in the New England Journal of Medicine, Dr. Molly Cooke commented on medical education’s responsibility regarding cost consciousness in patient care, and she highlighted the importance of teaching medical students and residents about considering cost in treating patients.15 Similarly, the Accreditation Council for Graduate Medical Education asks residents to consider cost and stewardship of medical resources as one of its system-based practice competencies.16 In 2012, the Choosing Wisely campaign, initiated by the American Board of Internal Medicine Foundation, asked specialty society members to identify tests or procedures commonly used in their field whose necessity should be questioned and discussed.17 ACOG and other women’s health specialty societies participate in this campaign.
From an educational standpoint, ACOG’s Council on Resident Education in Obstetrics and Gynecology has developed a curriculum resource, “Cases in High Value Care,” that can be used by any women’s health department to start the conversation on high-value care.18 The web program encourages medical students and residents to submit clinical vignettes that demonstrate examples of low- and high-value care. These cases can be used for discussion and debate and can serve as high-value care performance improvement projects in your own department.
Other useful publications are available outside the ObGyn specialty. Consider the Society of Hospital Medicine’s article series in the Journal of Hospital Medicine, “Choosing Wisely: Things We Do for No Reason”and “Choosing Wisely: Next Steps in Improving Healthcare Value.”19 The former focuses on discussing practices (tests, procedures, supplies, and prescriptions) that may be poorly supported by evidence or are part of standard practice even though other less expensive, higher-value alternatives may be available. The latter highlights perspective pieces that describe health care value initiatives relating to the practice of hospital medicine.
Continue to: The bottom line...
The bottom line
ObGyns and other health care providers are concerned about providing high-value care to patients and are working toward improving performance in this area. We really do care about the health care–related financial burdens that confront Ms. M., the premature twins’ parents, and all our patients.
- Sinconis J. Bankrupted by giving birth: having premature twins cost me everything. The Guardian. January 17, 2018. https://www.theguardian.com/us-news/commentisfree/2018/jan/16/bankrupted-by-giving-birth-having-premature-twins-cost-me-everything. Accessed December 20, 2018.
- Woolf SH, Aron LY. The US health disadvantage relative to other high-income countries: findings from a National Research Council/Institute of Medicine report. JAMA. 2013;309:771-772.
- Ozimek JA, Kilpatrick SJ. Maternal mortality in the twenty-first century. Obstet Gynecol Clin North Am. 2018;45:175-186.
- Himmelstein DU, Thorne D, Warren E, et al. Medical bankruptcy in the United States, 2007: results of a national study. Am J Med. 2009;122:741-746.
- Healthy babies healthy business. March of Dimes website. http://www.marchofdimes.org/hbhb/index.asp. Accessed December 20, 2018.
- Werner EF. Cost matters. Obstet Gynecol. 2014;123:919-920.
- Institute of Medicine (US) Roundtable on Evidence-Based Medicine; Yong PL, Saunders RS, Olsen LA, eds. The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. Washington, DC: National Academies Press; 2010.
- Hedayati H, Parsons J, Crowther CA. Topically applied anaesthetics for treating perineal pain after childbirth. Cochrane Database Syst Rev. 2005;2:CD004223.
- Demosthenes LD, Lane AS, Blackhurst DW. Implementing high-value care. South Med J. 2015;108:645-648.
- Alfirevic Z, Aflaifel N, Weeks A. Oral misoprostol for induction of labour. Cochrane Database Syst Rev. 2014;6:CD001338.
- Lane A. Preeclampsia evaluation. American College of Obstetricians and Gynecologists website. https://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/Cases-in-High-Value-Care/Example-2. Published July 14, 2015. Accessed July 10, 2018.
- Clark EN. Evidence-based prenatal care. University of Utah Health website. https://physicians.utah.edu/echo/pdfs/2018-06-29_evidence-based_prenatal_care.pdf. Accessed August 6, 2018.
- Marko KI, Krapf JM, Meltzer AC, et al. Testing the feasibility of remote patient monitoring in prenatal care using a mobile app and connected devices: a prospective observational trial. JMIR Res Protoc. 2016;5:e200.
- Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2010;10:CD000934.
- Cooke M. Cost consciousness in patient care—what is medical education’s responsibility? N Engl J Med. 2010;362:1253-1255.
- Accreditation Council for Graduate Medical Education. ACGME Common program requirements (residency).https://www.acgme.org/Portals/0/PFAssets/Program Requirements/CPRs_2017-07-01.pdf. Accessed December 19, 2018.
- Choosing Wisely. American Board of Internal Medicine Foundation website. http://www.choosingwisely.org/. Accessed August 7, 2018.
- American College of Obstetricians and Gynecologists Council on Resident Education in Obstetrics and Gynecology. Cases in high value care. https://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/Cases-in-High-Value-Care. Accessed August 8, 2018.
- Journal of Hospital Medicine website. https://www.journalofhospitalmedicine.com/jhospmed/page/author-guidelines. Accessed August 8, 2018.
CASE 1 Huge out-of-pocket cost makes patient forego treatment
Ms. M. is a 28-year-old patient who recently posted this on her Facebook page: “I went to the drugstore this morning to pick up a prescription, and as the pharmacist handed it to me she said, ‘That will be $180.00.’ And that’s after insurance coverage! Wow! I think I’ll pass!”
Our patients probably experience this type of situation more commonly than we know.
CASE 2 Catastrophic medical costs bankrupt family
A middle-class couple who had college degrees and full-time jobs with health insurance had twins at 24 weeks’ gestation. They accrued $450,000 in medical debt after exceeding the $2 million cap of their insurance policy. Having premature twins cost them everything. They liquidated their retirement and savings accounts, sold everything they had, and still ended up filing for bankruptcy.1
Costs indeed matter to patients, and we have a professional responsibility to help our patients navigate the murky waters of health care so that they can maintain financial as well as physical health.
Rising costs, lower yield,and opportunities for change
Rising health care costs are unsustainable for both our patients and our society. Although the United States spends more on health care than any other developed country, our health outcomes are actually worse—ranking at or near the bottom in both prevalence and mortality for multiple diseases, risk factors, and injuries.2
Of the 171 countries included in a study by the United Nations Maternal Mortality Estimation Inter-Agency Group, the United States was 1 of 13 countries that had an increasing maternal mortality and the only developed nation with an increasing maternal mortality rate.3 This tells us that, as our country spends more on health care, our patients’ health is not improving. For individuals, medical bills are now the leading cause of personal bankruptcy in the United States, even for those who are insured.4
ObGyns play an important leadership role in the practice of cost-conscious health care, as 25% of hospitalizations in the United States are pregnancy related.5,6 In addition, the wide scope of ObGyn practice reaches beyond pregnancy-related conditions and provides multiple opportunities to decrease the use of unnecessary tests and treatments.
The good news is that approximately 30% of health care costs are wasted on unnecessary care that could be eliminated without decreasing the quality of care.7
High-value change #1: Eliminate use of expensive products
Embarking on a high-value care improvement project, experts at Greenville Health System examined the cost of different topical pain medications for perineal pain after a vaginal delivery. They found that Epifoam (hydrocortisone acetate/pramoxine hydrochloride) was ordered 2,287 times over the course of a year.
The study intervention consisted of an educational grand rounds and discussion of a Cochrane review, which concluded there was no difference in pain relief with topical anesthetics compared with placebo.8 Less expensive options for pain relief were discussed, and the department agreed to remove Epifoam as a standing order.
After the intervention, Epifoam was ordered 228 times, a 90% reduction. Over the period of a year, this translated to a cost savings of $92,655 for the hospital, with reduced charges passed on to patients.9 Thus, a seemingly small individual cost ($45.00 per can of Epifoam) can add up to a substantial sum in a large health care system.
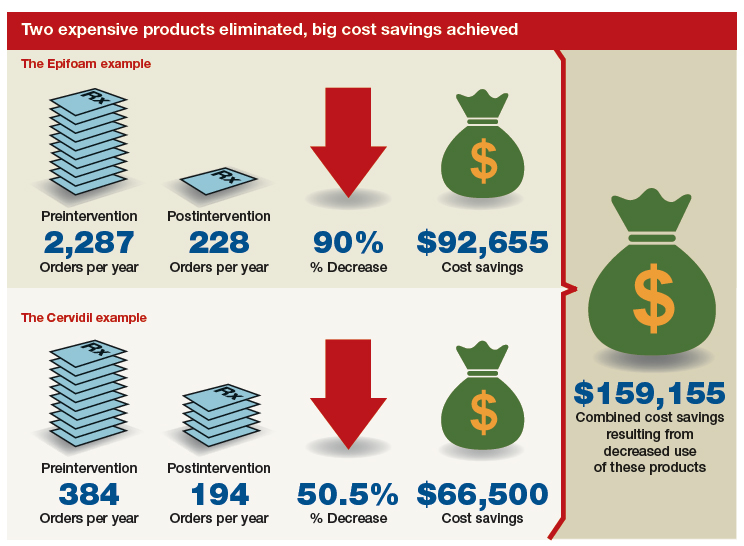
Similarly, practitioners were educated about options for cervical ripening and were given information on the cost and efficacy of various cervical ripening agents. A Cochrane review found that oral misoprostol is as effective as vaginal misoprostol and results in fewer cesarean deliveries than vaginal dinoprostone (Cervidil).10 Practitioners were asked to consider making the transition to oral misoprostol. This action resulted in a 50.5% decrease in Cervidil use, from 384 to 194 cases, producing a cost savings of $66,500. The following year, the department removed Cervidil from the formulary as a high-value decision.9
Both of these examples illustrate what a value-minded department can accomplish by implementing performance improvement projects that focus on high-value care.
Continue to: High-value change #2: Stop ordering unnecessary lab work...
High-value change #2: Stop ordering unnecessary lab work
Another high-value change to consider: Examine each laboratory test order to understand if the test results will really alter the care of a patient. Providers vary, and ordering lab tests to “make sure” can add up as financial expense.
Best practices from the American College of Obstetricians and Gynecologists (ACOG) and other professional societies can help guide decision-making as we order lab tests. Think twice, for example, about whether every evaluation for preeclampsia requires a uric acid test, since ACOG does not endorse that as part of the diagnostic criteria. While a single uric acid test costs only $8.00 to $38.00 (according to Healthcare Bluebook), testing uric acid in many patients over the course of a year can add up to significant dollars.11
High-value change #3: Consider care redesign
In addition to seeking opportunities to use more cost-effective products and reduce the use of unnecessary tests, “care redesign” is an innovative way to provide high-quality care (and increased patient satisfaction) at a lower cost for both the health care system and the patient. A prime example of care redesign is using telehealth to enhance prenatal care.
Several health systems around the country are piloting and implementing remote blood pressure monitoring, app-based prenatal education, and telehealth visits to enhance prenatal care.12,13 Use of a home blood pressure monitor can reduce in-person visits for low-risk prenatal care and open up access for other patients. Additionally, allowing the patient to participate in her own care at home or work can eliminate drives to and waits in the office and reduce absence from work because of a doctor visit.
A systematic review of more than 60,000 women showed that low-risk women who attend 5 to 9 prenatal visits have the same outcomes as women who attend the standard schedule of 13 to 15 visits.14 Although patient satisfaction was higher with more visits, when a bidirectional app or a telehealth visit is offered as an option, then patient satisfaction is equivalent to that in the standard schedule group.12 So why not expand the choice for patients?
The challenge of teaching high-value care: Medical education responds
In a 2010 article in the New England Journal of Medicine, Dr. Molly Cooke commented on medical education’s responsibility regarding cost consciousness in patient care, and she highlighted the importance of teaching medical students and residents about considering cost in treating patients.15 Similarly, the Accreditation Council for Graduate Medical Education asks residents to consider cost and stewardship of medical resources as one of its system-based practice competencies.16 In 2012, the Choosing Wisely campaign, initiated by the American Board of Internal Medicine Foundation, asked specialty society members to identify tests or procedures commonly used in their field whose necessity should be questioned and discussed.17 ACOG and other women’s health specialty societies participate in this campaign.
From an educational standpoint, ACOG’s Council on Resident Education in Obstetrics and Gynecology has developed a curriculum resource, “Cases in High Value Care,” that can be used by any women’s health department to start the conversation on high-value care.18 The web program encourages medical students and residents to submit clinical vignettes that demonstrate examples of low- and high-value care. These cases can be used for discussion and debate and can serve as high-value care performance improvement projects in your own department.
Other useful publications are available outside the ObGyn specialty. Consider the Society of Hospital Medicine’s article series in the Journal of Hospital Medicine, “Choosing Wisely: Things We Do for No Reason”and “Choosing Wisely: Next Steps in Improving Healthcare Value.”19 The former focuses on discussing practices (tests, procedures, supplies, and prescriptions) that may be poorly supported by evidence or are part of standard practice even though other less expensive, higher-value alternatives may be available. The latter highlights perspective pieces that describe health care value initiatives relating to the practice of hospital medicine.
Continue to: The bottom line...
The bottom line
ObGyns and other health care providers are concerned about providing high-value care to patients and are working toward improving performance in this area. We really do care about the health care–related financial burdens that confront Ms. M., the premature twins’ parents, and all our patients.
CASE 1 Huge out-of-pocket cost makes patient forego treatment
Ms. M. is a 28-year-old patient who recently posted this on her Facebook page: “I went to the drugstore this morning to pick up a prescription, and as the pharmacist handed it to me she said, ‘That will be $180.00.’ And that’s after insurance coverage! Wow! I think I’ll pass!”
Our patients probably experience this type of situation more commonly than we know.
CASE 2 Catastrophic medical costs bankrupt family
A middle-class couple who had college degrees and full-time jobs with health insurance had twins at 24 weeks’ gestation. They accrued $450,000 in medical debt after exceeding the $2 million cap of their insurance policy. Having premature twins cost them everything. They liquidated their retirement and savings accounts, sold everything they had, and still ended up filing for bankruptcy.1
Costs indeed matter to patients, and we have a professional responsibility to help our patients navigate the murky waters of health care so that they can maintain financial as well as physical health.
Rising costs, lower yield,and opportunities for change
Rising health care costs are unsustainable for both our patients and our society. Although the United States spends more on health care than any other developed country, our health outcomes are actually worse—ranking at or near the bottom in both prevalence and mortality for multiple diseases, risk factors, and injuries.2
Of the 171 countries included in a study by the United Nations Maternal Mortality Estimation Inter-Agency Group, the United States was 1 of 13 countries that had an increasing maternal mortality and the only developed nation with an increasing maternal mortality rate.3 This tells us that, as our country spends more on health care, our patients’ health is not improving. For individuals, medical bills are now the leading cause of personal bankruptcy in the United States, even for those who are insured.4
ObGyns play an important leadership role in the practice of cost-conscious health care, as 25% of hospitalizations in the United States are pregnancy related.5,6 In addition, the wide scope of ObGyn practice reaches beyond pregnancy-related conditions and provides multiple opportunities to decrease the use of unnecessary tests and treatments.
The good news is that approximately 30% of health care costs are wasted on unnecessary care that could be eliminated without decreasing the quality of care.7
High-value change #1: Eliminate use of expensive products
Embarking on a high-value care improvement project, experts at Greenville Health System examined the cost of different topical pain medications for perineal pain after a vaginal delivery. They found that Epifoam (hydrocortisone acetate/pramoxine hydrochloride) was ordered 2,287 times over the course of a year.
The study intervention consisted of an educational grand rounds and discussion of a Cochrane review, which concluded there was no difference in pain relief with topical anesthetics compared with placebo.8 Less expensive options for pain relief were discussed, and the department agreed to remove Epifoam as a standing order.
After the intervention, Epifoam was ordered 228 times, a 90% reduction. Over the period of a year, this translated to a cost savings of $92,655 for the hospital, with reduced charges passed on to patients.9 Thus, a seemingly small individual cost ($45.00 per can of Epifoam) can add up to a substantial sum in a large health care system.
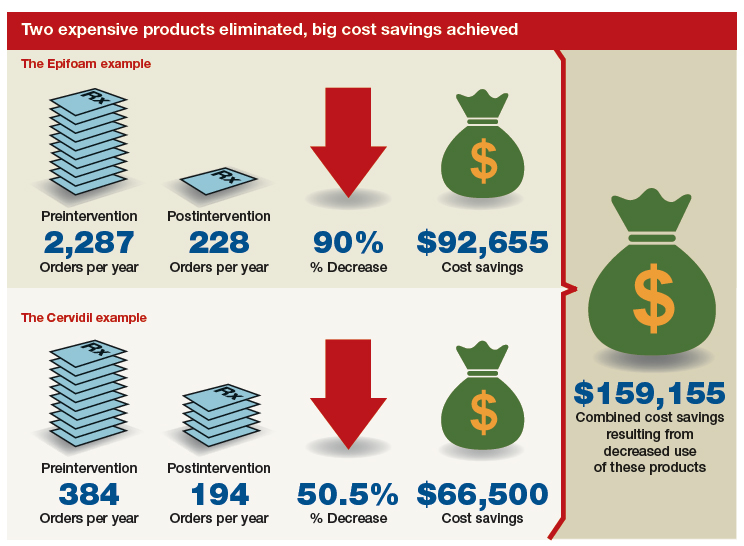
Similarly, practitioners were educated about options for cervical ripening and were given information on the cost and efficacy of various cervical ripening agents. A Cochrane review found that oral misoprostol is as effective as vaginal misoprostol and results in fewer cesarean deliveries than vaginal dinoprostone (Cervidil).10 Practitioners were asked to consider making the transition to oral misoprostol. This action resulted in a 50.5% decrease in Cervidil use, from 384 to 194 cases, producing a cost savings of $66,500. The following year, the department removed Cervidil from the formulary as a high-value decision.9
Both of these examples illustrate what a value-minded department can accomplish by implementing performance improvement projects that focus on high-value care.
Continue to: High-value change #2: Stop ordering unnecessary lab work...
High-value change #2: Stop ordering unnecessary lab work
Another high-value change to consider: Examine each laboratory test order to understand if the test results will really alter the care of a patient. Providers vary, and ordering lab tests to “make sure” can add up as financial expense.
Best practices from the American College of Obstetricians and Gynecologists (ACOG) and other professional societies can help guide decision-making as we order lab tests. Think twice, for example, about whether every evaluation for preeclampsia requires a uric acid test, since ACOG does not endorse that as part of the diagnostic criteria. While a single uric acid test costs only $8.00 to $38.00 (according to Healthcare Bluebook), testing uric acid in many patients over the course of a year can add up to significant dollars.11
High-value change #3: Consider care redesign
In addition to seeking opportunities to use more cost-effective products and reduce the use of unnecessary tests, “care redesign” is an innovative way to provide high-quality care (and increased patient satisfaction) at a lower cost for both the health care system and the patient. A prime example of care redesign is using telehealth to enhance prenatal care.
Several health systems around the country are piloting and implementing remote blood pressure monitoring, app-based prenatal education, and telehealth visits to enhance prenatal care.12,13 Use of a home blood pressure monitor can reduce in-person visits for low-risk prenatal care and open up access for other patients. Additionally, allowing the patient to participate in her own care at home or work can eliminate drives to and waits in the office and reduce absence from work because of a doctor visit.
A systematic review of more than 60,000 women showed that low-risk women who attend 5 to 9 prenatal visits have the same outcomes as women who attend the standard schedule of 13 to 15 visits.14 Although patient satisfaction was higher with more visits, when a bidirectional app or a telehealth visit is offered as an option, then patient satisfaction is equivalent to that in the standard schedule group.12 So why not expand the choice for patients?
The challenge of teaching high-value care: Medical education responds
In a 2010 article in the New England Journal of Medicine, Dr. Molly Cooke commented on medical education’s responsibility regarding cost consciousness in patient care, and she highlighted the importance of teaching medical students and residents about considering cost in treating patients.15 Similarly, the Accreditation Council for Graduate Medical Education asks residents to consider cost and stewardship of medical resources as one of its system-based practice competencies.16 In 2012, the Choosing Wisely campaign, initiated by the American Board of Internal Medicine Foundation, asked specialty society members to identify tests or procedures commonly used in their field whose necessity should be questioned and discussed.17 ACOG and other women’s health specialty societies participate in this campaign.
From an educational standpoint, ACOG’s Council on Resident Education in Obstetrics and Gynecology has developed a curriculum resource, “Cases in High Value Care,” that can be used by any women’s health department to start the conversation on high-value care.18 The web program encourages medical students and residents to submit clinical vignettes that demonstrate examples of low- and high-value care. These cases can be used for discussion and debate and can serve as high-value care performance improvement projects in your own department.
Other useful publications are available outside the ObGyn specialty. Consider the Society of Hospital Medicine’s article series in the Journal of Hospital Medicine, “Choosing Wisely: Things We Do for No Reason”and “Choosing Wisely: Next Steps in Improving Healthcare Value.”19 The former focuses on discussing practices (tests, procedures, supplies, and prescriptions) that may be poorly supported by evidence or are part of standard practice even though other less expensive, higher-value alternatives may be available. The latter highlights perspective pieces that describe health care value initiatives relating to the practice of hospital medicine.
Continue to: The bottom line...
The bottom line
ObGyns and other health care providers are concerned about providing high-value care to patients and are working toward improving performance in this area. We really do care about the health care–related financial burdens that confront Ms. M., the premature twins’ parents, and all our patients.
- Sinconis J. Bankrupted by giving birth: having premature twins cost me everything. The Guardian. January 17, 2018. https://www.theguardian.com/us-news/commentisfree/2018/jan/16/bankrupted-by-giving-birth-having-premature-twins-cost-me-everything. Accessed December 20, 2018.
- Woolf SH, Aron LY. The US health disadvantage relative to other high-income countries: findings from a National Research Council/Institute of Medicine report. JAMA. 2013;309:771-772.
- Ozimek JA, Kilpatrick SJ. Maternal mortality in the twenty-first century. Obstet Gynecol Clin North Am. 2018;45:175-186.
- Himmelstein DU, Thorne D, Warren E, et al. Medical bankruptcy in the United States, 2007: results of a national study. Am J Med. 2009;122:741-746.
- Healthy babies healthy business. March of Dimes website. http://www.marchofdimes.org/hbhb/index.asp. Accessed December 20, 2018.
- Werner EF. Cost matters. Obstet Gynecol. 2014;123:919-920.
- Institute of Medicine (US) Roundtable on Evidence-Based Medicine; Yong PL, Saunders RS, Olsen LA, eds. The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. Washington, DC: National Academies Press; 2010.
- Hedayati H, Parsons J, Crowther CA. Topically applied anaesthetics for treating perineal pain after childbirth. Cochrane Database Syst Rev. 2005;2:CD004223.
- Demosthenes LD, Lane AS, Blackhurst DW. Implementing high-value care. South Med J. 2015;108:645-648.
- Alfirevic Z, Aflaifel N, Weeks A. Oral misoprostol for induction of labour. Cochrane Database Syst Rev. 2014;6:CD001338.
- Lane A. Preeclampsia evaluation. American College of Obstetricians and Gynecologists website. https://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/Cases-in-High-Value-Care/Example-2. Published July 14, 2015. Accessed July 10, 2018.
- Clark EN. Evidence-based prenatal care. University of Utah Health website. https://physicians.utah.edu/echo/pdfs/2018-06-29_evidence-based_prenatal_care.pdf. Accessed August 6, 2018.
- Marko KI, Krapf JM, Meltzer AC, et al. Testing the feasibility of remote patient monitoring in prenatal care using a mobile app and connected devices: a prospective observational trial. JMIR Res Protoc. 2016;5:e200.
- Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2010;10:CD000934.
- Cooke M. Cost consciousness in patient care—what is medical education’s responsibility? N Engl J Med. 2010;362:1253-1255.
- Accreditation Council for Graduate Medical Education. ACGME Common program requirements (residency).https://www.acgme.org/Portals/0/PFAssets/Program Requirements/CPRs_2017-07-01.pdf. Accessed December 19, 2018.
- Choosing Wisely. American Board of Internal Medicine Foundation website. http://www.choosingwisely.org/. Accessed August 7, 2018.
- American College of Obstetricians and Gynecologists Council on Resident Education in Obstetrics and Gynecology. Cases in high value care. https://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/Cases-in-High-Value-Care. Accessed August 8, 2018.
- Journal of Hospital Medicine website. https://www.journalofhospitalmedicine.com/jhospmed/page/author-guidelines. Accessed August 8, 2018.
- Sinconis J. Bankrupted by giving birth: having premature twins cost me everything. The Guardian. January 17, 2018. https://www.theguardian.com/us-news/commentisfree/2018/jan/16/bankrupted-by-giving-birth-having-premature-twins-cost-me-everything. Accessed December 20, 2018.
- Woolf SH, Aron LY. The US health disadvantage relative to other high-income countries: findings from a National Research Council/Institute of Medicine report. JAMA. 2013;309:771-772.
- Ozimek JA, Kilpatrick SJ. Maternal mortality in the twenty-first century. Obstet Gynecol Clin North Am. 2018;45:175-186.
- Himmelstein DU, Thorne D, Warren E, et al. Medical bankruptcy in the United States, 2007: results of a national study. Am J Med. 2009;122:741-746.
- Healthy babies healthy business. March of Dimes website. http://www.marchofdimes.org/hbhb/index.asp. Accessed December 20, 2018.
- Werner EF. Cost matters. Obstet Gynecol. 2014;123:919-920.
- Institute of Medicine (US) Roundtable on Evidence-Based Medicine; Yong PL, Saunders RS, Olsen LA, eds. The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. Washington, DC: National Academies Press; 2010.
- Hedayati H, Parsons J, Crowther CA. Topically applied anaesthetics for treating perineal pain after childbirth. Cochrane Database Syst Rev. 2005;2:CD004223.
- Demosthenes LD, Lane AS, Blackhurst DW. Implementing high-value care. South Med J. 2015;108:645-648.
- Alfirevic Z, Aflaifel N, Weeks A. Oral misoprostol for induction of labour. Cochrane Database Syst Rev. 2014;6:CD001338.
- Lane A. Preeclampsia evaluation. American College of Obstetricians and Gynecologists website. https://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/Cases-in-High-Value-Care/Example-2. Published July 14, 2015. Accessed July 10, 2018.
- Clark EN. Evidence-based prenatal care. University of Utah Health website. https://physicians.utah.edu/echo/pdfs/2018-06-29_evidence-based_prenatal_care.pdf. Accessed August 6, 2018.
- Marko KI, Krapf JM, Meltzer AC, et al. Testing the feasibility of remote patient monitoring in prenatal care using a mobile app and connected devices: a prospective observational trial. JMIR Res Protoc. 2016;5:e200.
- Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2010;10:CD000934.
- Cooke M. Cost consciousness in patient care—what is medical education’s responsibility? N Engl J Med. 2010;362:1253-1255.
- Accreditation Council for Graduate Medical Education. ACGME Common program requirements (residency).https://www.acgme.org/Portals/0/PFAssets/Program Requirements/CPRs_2017-07-01.pdf. Accessed December 19, 2018.
- Choosing Wisely. American Board of Internal Medicine Foundation website. http://www.choosingwisely.org/. Accessed August 7, 2018.
- American College of Obstetricians and Gynecologists Council on Resident Education in Obstetrics and Gynecology. Cases in high value care. https://www.acog.org/About-ACOG/ACOG-Departments/CREOG/CREOG-Search/Cases-in-High-Value-Care. Accessed August 8, 2018.
- Journal of Hospital Medicine website. https://www.journalofhospitalmedicine.com/jhospmed/page/author-guidelines. Accessed August 8, 2018.