User login
Maribavir seen as superior to other antivirals for CMV clearance post transplant
Maribavir, an investigational antiviral agent with a novel mechanism of action, was superior to other antiviral strategies at clearing cytomegalovirus (CMV) viremia and controlling symptoms in hematopoietic cell or solid-organ transplant recipients, results of a phase 3 clinical trial showed.
CMV viremia clearance at study week 8 was seen in 55.7% of all patients randomized to receive maribavir, compared with 23.9% for patients assigned to receive investigator-assigned therapy (IAT), Francisco Marty, MD, from the Dana-Farber Cancer Institute in Boston reported at the Transplant & Cellular Therapies Meetings.
“Maribavir’s benefit was driven by lower incidence of treatment-limiting toxicities, compared with IAT,” he said a late-breaking abstract session during the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
“Available anti-CMV antivirals are limited by development of resistance and toxicities, particularly myelosuppression with the use of valganciclovir and nephrotoxicity with the use of foscarnet and cidofovir. Alternative treatment options are required to address this unmet medical need,” he said.
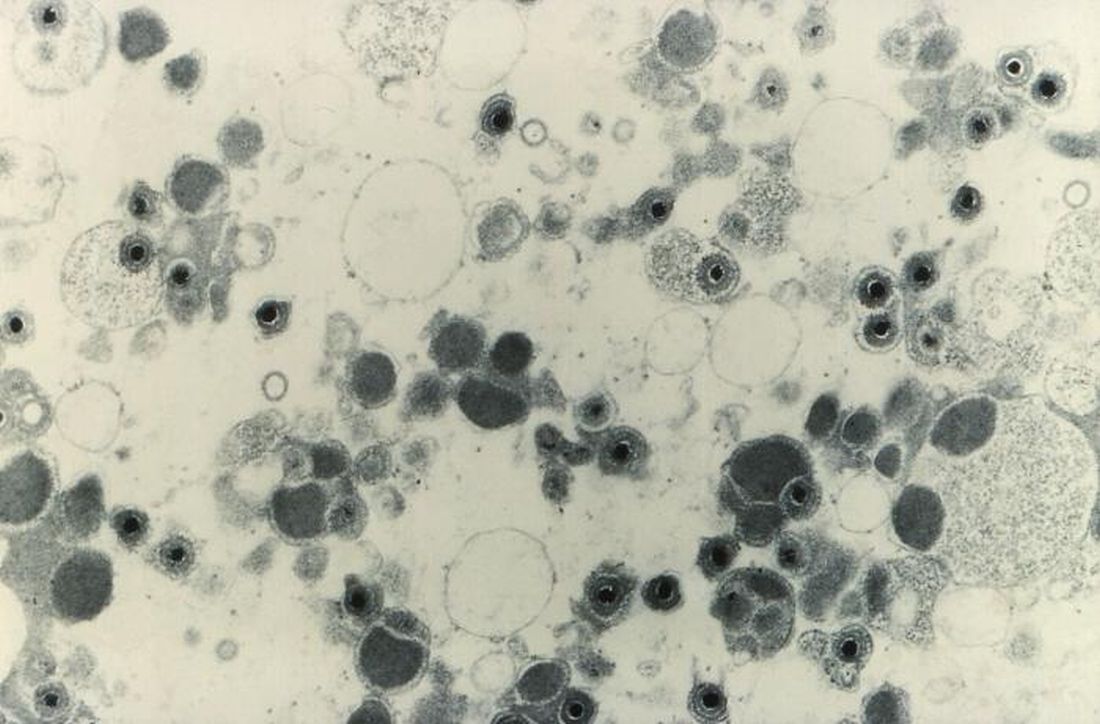
Maribavir inhibits the CMV UL97 protein kinase and is thought to affect several critical processes in CMV replication, including viral DNA synthesis, viral gene expression, encapsidation, and egress of mature capsids from the nucleus.
Details of trial
In the phase 3 SHP620-30e trial (NCT02931539), Dr. Marty and colleagues enrolled patients with relapsed or refractory CMV infections after hematopoietic cell transplant (HCT) or solid-organ transplant (SOT) and after stratification by transplant type and screening CMV DNA level randomly assigned them on a 2:1 basis to receive either maribavir 400 mg twice daily (235 patients) or IAT (117 patients), consisting of either ganciclovir/valganciclovir, foscarnet, cidofovir, or combined foscarnet and val/ganciclovir.
The primary endpoint of viremia clearance at 8 weeks was defined as plasma CMV DNA less than 137 IU/mL in two consecutive tests at a central laboratory at least 5 days apart beginning at the end of week 8.
The trial met its primary endpoint, with a viremia clearance rate of 55.7% with maribavir versus 23.9% with IAT.
The viremia clearance rates were similar in each of the transplant groups: 55.9% versus 20.8%, respectively, in patients who underwent HCT, and 55.6% versus 26.1% in patients who underwent SOT (P < .001).
Clearance rates among patients with CMV DNA below 9,100 IU/mL at baseline were 62.1% with maribavir versus 24.7% with IAT. Among patients with baseline CMV DNA of 9100 IU/mL or above, the respective rates were 43.9% versus 21.9%.
CMV viremia clearance continued from week 8 to week 16 in 18.7% of patients assigned to maribavir and to 10.3% of patients randomized to IAT (P < .013).
The median time to first CMV viremia clearance as 22 days with maribavir versus 27 days with IAT (P = .039).
All-cause mortality was similar between the groups, at 11.5% versus 11.1%, respectively.
The incidences of serious and severe treatment-emergent adverse events (TEAE) were 38.5% and 32.1%, respectively, in the maribavir group, and 37.1% and 37.9% in the IAT group.
Any TEAE leading to study drug discontinuation was less common with maribavir, occurring in 13.2% of patients, compared with 31.9% of patients on IAT. Serious TEAEs leading to drug discontinuation occurred in 8.5% versus 14.7%, respectively.
Serious TEAEs leading to death occurred in 6.8% of patients on maribavir versus 5.2% of those on IAT.
Role of letermovir
In the question-and-answer session following the presentation, comoderator Monalisa Ghosh, MD, from the University of Michigan, Ann Arbor, asked whether any patients in the study were currently on letermovir (Prevymis) prophylaxis, and whether any patients had previously been treated with letermovir but had CMV reactivation and were then treated on study.
Dr. Marty noted that the trial was designed before letermovir was approved for CMV prophylaxis in adults who have undergone an allogeneic HCT.
“Nobody was on letermovir at the beginning of the trial,” he replied, but noted that some patients who were enrolled and had infections that were refractory or resistant to valganciclovir, foscarnet, or a combination of the two received letermovir as secondary prophylaxis.
“I haven’t got the data to tell you how often [letermovir] was used; I think part of the lack of mortality benefit [with maribavir] may be due to the fact that people jumped into secondary prophylaxis with letermovir to minimize the toxicities that we saw,” he said.
Although maribavir has not as of this writing received Food and Drug Administration approval, the drug may be available to some patients through a compassionate-use program from Takeda, Dr. Marty noted.
The study was funded by Shire ViroPharma. Dr. Marty disclosed research funding from Shire and from others. Dr. Ghosh had no relevant disclosures.
Maribavir, an investigational antiviral agent with a novel mechanism of action, was superior to other antiviral strategies at clearing cytomegalovirus (CMV) viremia and controlling symptoms in hematopoietic cell or solid-organ transplant recipients, results of a phase 3 clinical trial showed.
CMV viremia clearance at study week 8 was seen in 55.7% of all patients randomized to receive maribavir, compared with 23.9% for patients assigned to receive investigator-assigned therapy (IAT), Francisco Marty, MD, from the Dana-Farber Cancer Institute in Boston reported at the Transplant & Cellular Therapies Meetings.
“Maribavir’s benefit was driven by lower incidence of treatment-limiting toxicities, compared with IAT,” he said a late-breaking abstract session during the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
“Available anti-CMV antivirals are limited by development of resistance and toxicities, particularly myelosuppression with the use of valganciclovir and nephrotoxicity with the use of foscarnet and cidofovir. Alternative treatment options are required to address this unmet medical need,” he said.
Maribavir inhibits the CMV UL97 protein kinase and is thought to affect several critical processes in CMV replication, including viral DNA synthesis, viral gene expression, encapsidation, and egress of mature capsids from the nucleus.
Details of trial
In the phase 3 SHP620-30e trial (NCT02931539), Dr. Marty and colleagues enrolled patients with relapsed or refractory CMV infections after hematopoietic cell transplant (HCT) or solid-organ transplant (SOT) and after stratification by transplant type and screening CMV DNA level randomly assigned them on a 2:1 basis to receive either maribavir 400 mg twice daily (235 patients) or IAT (117 patients), consisting of either ganciclovir/valganciclovir, foscarnet, cidofovir, or combined foscarnet and val/ganciclovir.
The primary endpoint of viremia clearance at 8 weeks was defined as plasma CMV DNA less than 137 IU/mL in two consecutive tests at a central laboratory at least 5 days apart beginning at the end of week 8.
The trial met its primary endpoint, with a viremia clearance rate of 55.7% with maribavir versus 23.9% with IAT.
The viremia clearance rates were similar in each of the transplant groups: 55.9% versus 20.8%, respectively, in patients who underwent HCT, and 55.6% versus 26.1% in patients who underwent SOT (P < .001).
Clearance rates among patients with CMV DNA below 9,100 IU/mL at baseline were 62.1% with maribavir versus 24.7% with IAT. Among patients with baseline CMV DNA of 9100 IU/mL or above, the respective rates were 43.9% versus 21.9%.
CMV viremia clearance continued from week 8 to week 16 in 18.7% of patients assigned to maribavir and to 10.3% of patients randomized to IAT (P < .013).
The median time to first CMV viremia clearance as 22 days with maribavir versus 27 days with IAT (P = .039).
All-cause mortality was similar between the groups, at 11.5% versus 11.1%, respectively.
The incidences of serious and severe treatment-emergent adverse events (TEAE) were 38.5% and 32.1%, respectively, in the maribavir group, and 37.1% and 37.9% in the IAT group.
Any TEAE leading to study drug discontinuation was less common with maribavir, occurring in 13.2% of patients, compared with 31.9% of patients on IAT. Serious TEAEs leading to drug discontinuation occurred in 8.5% versus 14.7%, respectively.
Serious TEAEs leading to death occurred in 6.8% of patients on maribavir versus 5.2% of those on IAT.
Role of letermovir
In the question-and-answer session following the presentation, comoderator Monalisa Ghosh, MD, from the University of Michigan, Ann Arbor, asked whether any patients in the study were currently on letermovir (Prevymis) prophylaxis, and whether any patients had previously been treated with letermovir but had CMV reactivation and were then treated on study.
Dr. Marty noted that the trial was designed before letermovir was approved for CMV prophylaxis in adults who have undergone an allogeneic HCT.
“Nobody was on letermovir at the beginning of the trial,” he replied, but noted that some patients who were enrolled and had infections that were refractory or resistant to valganciclovir, foscarnet, or a combination of the two received letermovir as secondary prophylaxis.
“I haven’t got the data to tell you how often [letermovir] was used; I think part of the lack of mortality benefit [with maribavir] may be due to the fact that people jumped into secondary prophylaxis with letermovir to minimize the toxicities that we saw,” he said.
Although maribavir has not as of this writing received Food and Drug Administration approval, the drug may be available to some patients through a compassionate-use program from Takeda, Dr. Marty noted.
The study was funded by Shire ViroPharma. Dr. Marty disclosed research funding from Shire and from others. Dr. Ghosh had no relevant disclosures.
Maribavir, an investigational antiviral agent with a novel mechanism of action, was superior to other antiviral strategies at clearing cytomegalovirus (CMV) viremia and controlling symptoms in hematopoietic cell or solid-organ transplant recipients, results of a phase 3 clinical trial showed.
CMV viremia clearance at study week 8 was seen in 55.7% of all patients randomized to receive maribavir, compared with 23.9% for patients assigned to receive investigator-assigned therapy (IAT), Francisco Marty, MD, from the Dana-Farber Cancer Institute in Boston reported at the Transplant & Cellular Therapies Meetings.
“Maribavir’s benefit was driven by lower incidence of treatment-limiting toxicities, compared with IAT,” he said a late-breaking abstract session during the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
“Available anti-CMV antivirals are limited by development of resistance and toxicities, particularly myelosuppression with the use of valganciclovir and nephrotoxicity with the use of foscarnet and cidofovir. Alternative treatment options are required to address this unmet medical need,” he said.
Maribavir inhibits the CMV UL97 protein kinase and is thought to affect several critical processes in CMV replication, including viral DNA synthesis, viral gene expression, encapsidation, and egress of mature capsids from the nucleus.
Details of trial
In the phase 3 SHP620-30e trial (NCT02931539), Dr. Marty and colleagues enrolled patients with relapsed or refractory CMV infections after hematopoietic cell transplant (HCT) or solid-organ transplant (SOT) and after stratification by transplant type and screening CMV DNA level randomly assigned them on a 2:1 basis to receive either maribavir 400 mg twice daily (235 patients) or IAT (117 patients), consisting of either ganciclovir/valganciclovir, foscarnet, cidofovir, or combined foscarnet and val/ganciclovir.
The primary endpoint of viremia clearance at 8 weeks was defined as plasma CMV DNA less than 137 IU/mL in two consecutive tests at a central laboratory at least 5 days apart beginning at the end of week 8.
The trial met its primary endpoint, with a viremia clearance rate of 55.7% with maribavir versus 23.9% with IAT.
The viremia clearance rates were similar in each of the transplant groups: 55.9% versus 20.8%, respectively, in patients who underwent HCT, and 55.6% versus 26.1% in patients who underwent SOT (P < .001).
Clearance rates among patients with CMV DNA below 9,100 IU/mL at baseline were 62.1% with maribavir versus 24.7% with IAT. Among patients with baseline CMV DNA of 9100 IU/mL or above, the respective rates were 43.9% versus 21.9%.
CMV viremia clearance continued from week 8 to week 16 in 18.7% of patients assigned to maribavir and to 10.3% of patients randomized to IAT (P < .013).
The median time to first CMV viremia clearance as 22 days with maribavir versus 27 days with IAT (P = .039).
All-cause mortality was similar between the groups, at 11.5% versus 11.1%, respectively.
The incidences of serious and severe treatment-emergent adverse events (TEAE) were 38.5% and 32.1%, respectively, in the maribavir group, and 37.1% and 37.9% in the IAT group.
Any TEAE leading to study drug discontinuation was less common with maribavir, occurring in 13.2% of patients, compared with 31.9% of patients on IAT. Serious TEAEs leading to drug discontinuation occurred in 8.5% versus 14.7%, respectively.
Serious TEAEs leading to death occurred in 6.8% of patients on maribavir versus 5.2% of those on IAT.
Role of letermovir
In the question-and-answer session following the presentation, comoderator Monalisa Ghosh, MD, from the University of Michigan, Ann Arbor, asked whether any patients in the study were currently on letermovir (Prevymis) prophylaxis, and whether any patients had previously been treated with letermovir but had CMV reactivation and were then treated on study.
Dr. Marty noted that the trial was designed before letermovir was approved for CMV prophylaxis in adults who have undergone an allogeneic HCT.
“Nobody was on letermovir at the beginning of the trial,” he replied, but noted that some patients who were enrolled and had infections that were refractory or resistant to valganciclovir, foscarnet, or a combination of the two received letermovir as secondary prophylaxis.
“I haven’t got the data to tell you how often [letermovir] was used; I think part of the lack of mortality benefit [with maribavir] may be due to the fact that people jumped into secondary prophylaxis with letermovir to minimize the toxicities that we saw,” he said.
Although maribavir has not as of this writing received Food and Drug Administration approval, the drug may be available to some patients through a compassionate-use program from Takeda, Dr. Marty noted.
The study was funded by Shire ViroPharma. Dr. Marty disclosed research funding from Shire and from others. Dr. Ghosh had no relevant disclosures.
FROM TCT 2021
FDA places clinical hold on sickle cell gene therapy
The Food and Drug Administration placed a clinical hold yesterday on two gene therapy trials for sickle cell disease (SCD) after two recent complications: one participant developed acute myeloid leukemia (AML) and another developed myelodysplastic syndrome (MDS). The sponsoring company, bluebird bio, suspended the trials last week upon learning of the cases.
The company has also put the brakes on a treatment for beta thalassemia already approved in the European Union and the United Kingdom, betibeglogene autotemcel (Zynteglo). The treatment hasn’t been associated with problems but uses the same gene delivery vector, a lentivirus, as that used in the SCD trials.
Overall, the company has enrolled 47 SCD patients and 63 with beta thalassemia in trials.
The gene therapy “space” is one with spectacular successes – for a form of retinal blindness and spinal muscular atrophy – rising against a backdrop of recent setbacks and failures – for Duchenne muscular dystrophy, lipoprotein lipase deficiency, and myotubular myopathy.
A lentiviral vector
The retooled lentivirus used in the SCD trials, LentiGlobin, delivers a beta-globin gene with one amino acid replacement to hematopoietic stem cells outside the patient’s body. The modified cells are then infused back into the patient. The gene therapy reshapes red blood cells, enabling them to circulate through narrow blood vessels without sickling and adhering into painful logjams.
What is worrisome is that in the patient who developed AML, and who received the gene therapy more than 5 years ago, the cancer cells contained the vector. Those test results aren’t yet available for the participant who has MDS.
The finding raises suspicion that the gene therapy had a role in the cancer, but is only correlative.
Lentiviral vectors have a good track record, but the two cases evoke memories of 2 decades ago. In 2001, five children being treated for an inherited immunodeficiency (SCID-X1) with a gamma retroviral vector developed leukemia and one died. Those viruses inserted into an oncogene. Happening 2 years after the death of 18-year-old Jesse Gelsinger in another gene therapy trial, the SCID trial had a chilling effect on the field.
Since then, lentiviral vectors have been reinvented to be “self-inactivating,” minimizing the risk for inserting willy-nilly into a genome. “Lentiviral vectors have been expressly designed to avoid insertional oncogenesis, based on prior experience with the gamma retroviruses. We don’t have evidence that the vector is causative, but our studies will shed some light on whether that’s true in these cases,” said bluebird bio chief scientific officer Philip Gregory, DPhil, on a conference call Feb. 16.
Lentiviral vectors have been successful as the backbone of chimeric antigen receptor T-cell (CAR-T) therapy, which directs modified T cells to certain blood cancers. “Among the hundreds to thousands of patients treated with CAR-T cell therapy, lentivirus vector hasn’t been associated with any malignancies,” said bluebird’s chief medical officer, Dave Davidson, MD.
Jeanne Loring, PhD, director of the Center for Regenerative Medicine at Scripps Research, agreed. “Gene therapy is having some extreme highs and lows these days. Most studies use [adeno-associated viral] vectors, which don’t integrate into the genome. But some people have antibodies to AAV vectors, and AAV is diluted out when cells divide. That’s why lentivirus, which integrates into the genome, is used for blood stem cells and T cells in CAR-T therapy.”
Pinpointing causality
At bluebird bio, investigation into the possible “genetic gymnastics” of the lentivirus vector is focusing on where it integrates into the genome – whether it harpoons an oncogene like the gamma retroviral vectors, or affects genome stability, Dr. Gregory explained. To be causative, the affected gene must be a “driver” of the cancer, and not just a “passenger.”
Another suspect is busulfan, a drug used to “condition” the recipient’s bone marrow, making room for modified stem cells. “It’s possible that busulfan is the main problem, as it is a carcinogen unto itself,” said Paul Knoepfler, PhD, a stem cell researcher at the University of California, Davis.
In addition to the two more recent reports of complications, a third trial participant, who had participated in a phase 1/2 trial, developed MDS in 2018 and died of AML in July 2020. The cancer cells from that patient did not contain viral vectors and the MDS was attributed to busulfan conditioning.
Nick Leschly, chief of bluebird, pointed out the importance of clinical context in implicating the vector. Because SCD itself stresses the bone marrow, patients already face an increased risk of developing blood cancer, he said. “Now layer on other risks of the gene therapy. It’s challenging because we’re dealing with patients who have life expectancy in the mid 40s.” Previous treatments, such the antisickling drug hydroxyurea, may also contribute to patient vulnerability.
A patient’s view
SCD affects more than 100,000 people in the United States, and about 20 million globally. Charles Hough is one of them. He can attest to the severity of the disease as well as the promise of gene therapy
Mr. Hough was diagnosed at age 2, and endured the profound fatigue, pain crises, and even coma characteristic of severe cases. He cited his “rebirth” as Sept. 25, 2018, when he received his first modified stem cells at the National Institutes of Health. Mr. Hough told his story a year ago in a webinar for the National Organization for Rare Disorders. This news organization caught up with him in light of the clinical trial hold.
Although the preparative regimens for the gene therapy were tough, his sickle cell symptoms vanished after gene therapy. Even hearing about the current hold on the clinical trial, Mr. Hough doesn’t regret his participation.
“I had a lot of friends who passed because of the complications from sickle cell. I was always worried that I wouldn’t live to see the next day. Now I don’t have that stress hanging over my head and I feel like I can live a normal life. Becoming sickle cell free was my dream.”
A version of this article first appeared on Medscape.com.
The Food and Drug Administration placed a clinical hold yesterday on two gene therapy trials for sickle cell disease (SCD) after two recent complications: one participant developed acute myeloid leukemia (AML) and another developed myelodysplastic syndrome (MDS). The sponsoring company, bluebird bio, suspended the trials last week upon learning of the cases.
The company has also put the brakes on a treatment for beta thalassemia already approved in the European Union and the United Kingdom, betibeglogene autotemcel (Zynteglo). The treatment hasn’t been associated with problems but uses the same gene delivery vector, a lentivirus, as that used in the SCD trials.
Overall, the company has enrolled 47 SCD patients and 63 with beta thalassemia in trials.
The gene therapy “space” is one with spectacular successes – for a form of retinal blindness and spinal muscular atrophy – rising against a backdrop of recent setbacks and failures – for Duchenne muscular dystrophy, lipoprotein lipase deficiency, and myotubular myopathy.
A lentiviral vector
The retooled lentivirus used in the SCD trials, LentiGlobin, delivers a beta-globin gene with one amino acid replacement to hematopoietic stem cells outside the patient’s body. The modified cells are then infused back into the patient. The gene therapy reshapes red blood cells, enabling them to circulate through narrow blood vessels without sickling and adhering into painful logjams.
What is worrisome is that in the patient who developed AML, and who received the gene therapy more than 5 years ago, the cancer cells contained the vector. Those test results aren’t yet available for the participant who has MDS.
The finding raises suspicion that the gene therapy had a role in the cancer, but is only correlative.
Lentiviral vectors have a good track record, but the two cases evoke memories of 2 decades ago. In 2001, five children being treated for an inherited immunodeficiency (SCID-X1) with a gamma retroviral vector developed leukemia and one died. Those viruses inserted into an oncogene. Happening 2 years after the death of 18-year-old Jesse Gelsinger in another gene therapy trial, the SCID trial had a chilling effect on the field.
Since then, lentiviral vectors have been reinvented to be “self-inactivating,” minimizing the risk for inserting willy-nilly into a genome. “Lentiviral vectors have been expressly designed to avoid insertional oncogenesis, based on prior experience with the gamma retroviruses. We don’t have evidence that the vector is causative, but our studies will shed some light on whether that’s true in these cases,” said bluebird bio chief scientific officer Philip Gregory, DPhil, on a conference call Feb. 16.
Lentiviral vectors have been successful as the backbone of chimeric antigen receptor T-cell (CAR-T) therapy, which directs modified T cells to certain blood cancers. “Among the hundreds to thousands of patients treated with CAR-T cell therapy, lentivirus vector hasn’t been associated with any malignancies,” said bluebird’s chief medical officer, Dave Davidson, MD.
Jeanne Loring, PhD, director of the Center for Regenerative Medicine at Scripps Research, agreed. “Gene therapy is having some extreme highs and lows these days. Most studies use [adeno-associated viral] vectors, which don’t integrate into the genome. But some people have antibodies to AAV vectors, and AAV is diluted out when cells divide. That’s why lentivirus, which integrates into the genome, is used for blood stem cells and T cells in CAR-T therapy.”
Pinpointing causality
At bluebird bio, investigation into the possible “genetic gymnastics” of the lentivirus vector is focusing on where it integrates into the genome – whether it harpoons an oncogene like the gamma retroviral vectors, or affects genome stability, Dr. Gregory explained. To be causative, the affected gene must be a “driver” of the cancer, and not just a “passenger.”
Another suspect is busulfan, a drug used to “condition” the recipient’s bone marrow, making room for modified stem cells. “It’s possible that busulfan is the main problem, as it is a carcinogen unto itself,” said Paul Knoepfler, PhD, a stem cell researcher at the University of California, Davis.
In addition to the two more recent reports of complications, a third trial participant, who had participated in a phase 1/2 trial, developed MDS in 2018 and died of AML in July 2020. The cancer cells from that patient did not contain viral vectors and the MDS was attributed to busulfan conditioning.
Nick Leschly, chief of bluebird, pointed out the importance of clinical context in implicating the vector. Because SCD itself stresses the bone marrow, patients already face an increased risk of developing blood cancer, he said. “Now layer on other risks of the gene therapy. It’s challenging because we’re dealing with patients who have life expectancy in the mid 40s.” Previous treatments, such the antisickling drug hydroxyurea, may also contribute to patient vulnerability.
A patient’s view
SCD affects more than 100,000 people in the United States, and about 20 million globally. Charles Hough is one of them. He can attest to the severity of the disease as well as the promise of gene therapy
Mr. Hough was diagnosed at age 2, and endured the profound fatigue, pain crises, and even coma characteristic of severe cases. He cited his “rebirth” as Sept. 25, 2018, when he received his first modified stem cells at the National Institutes of Health. Mr. Hough told his story a year ago in a webinar for the National Organization for Rare Disorders. This news organization caught up with him in light of the clinical trial hold.
Although the preparative regimens for the gene therapy were tough, his sickle cell symptoms vanished after gene therapy. Even hearing about the current hold on the clinical trial, Mr. Hough doesn’t regret his participation.
“I had a lot of friends who passed because of the complications from sickle cell. I was always worried that I wouldn’t live to see the next day. Now I don’t have that stress hanging over my head and I feel like I can live a normal life. Becoming sickle cell free was my dream.”
A version of this article first appeared on Medscape.com.
The Food and Drug Administration placed a clinical hold yesterday on two gene therapy trials for sickle cell disease (SCD) after two recent complications: one participant developed acute myeloid leukemia (AML) and another developed myelodysplastic syndrome (MDS). The sponsoring company, bluebird bio, suspended the trials last week upon learning of the cases.
The company has also put the brakes on a treatment for beta thalassemia already approved in the European Union and the United Kingdom, betibeglogene autotemcel (Zynteglo). The treatment hasn’t been associated with problems but uses the same gene delivery vector, a lentivirus, as that used in the SCD trials.
Overall, the company has enrolled 47 SCD patients and 63 with beta thalassemia in trials.
The gene therapy “space” is one with spectacular successes – for a form of retinal blindness and spinal muscular atrophy – rising against a backdrop of recent setbacks and failures – for Duchenne muscular dystrophy, lipoprotein lipase deficiency, and myotubular myopathy.
A lentiviral vector
The retooled lentivirus used in the SCD trials, LentiGlobin, delivers a beta-globin gene with one amino acid replacement to hematopoietic stem cells outside the patient’s body. The modified cells are then infused back into the patient. The gene therapy reshapes red blood cells, enabling them to circulate through narrow blood vessels without sickling and adhering into painful logjams.
What is worrisome is that in the patient who developed AML, and who received the gene therapy more than 5 years ago, the cancer cells contained the vector. Those test results aren’t yet available for the participant who has MDS.
The finding raises suspicion that the gene therapy had a role in the cancer, but is only correlative.
Lentiviral vectors have a good track record, but the two cases evoke memories of 2 decades ago. In 2001, five children being treated for an inherited immunodeficiency (SCID-X1) with a gamma retroviral vector developed leukemia and one died. Those viruses inserted into an oncogene. Happening 2 years after the death of 18-year-old Jesse Gelsinger in another gene therapy trial, the SCID trial had a chilling effect on the field.
Since then, lentiviral vectors have been reinvented to be “self-inactivating,” minimizing the risk for inserting willy-nilly into a genome. “Lentiviral vectors have been expressly designed to avoid insertional oncogenesis, based on prior experience with the gamma retroviruses. We don’t have evidence that the vector is causative, but our studies will shed some light on whether that’s true in these cases,” said bluebird bio chief scientific officer Philip Gregory, DPhil, on a conference call Feb. 16.
Lentiviral vectors have been successful as the backbone of chimeric antigen receptor T-cell (CAR-T) therapy, which directs modified T cells to certain blood cancers. “Among the hundreds to thousands of patients treated with CAR-T cell therapy, lentivirus vector hasn’t been associated with any malignancies,” said bluebird’s chief medical officer, Dave Davidson, MD.
Jeanne Loring, PhD, director of the Center for Regenerative Medicine at Scripps Research, agreed. “Gene therapy is having some extreme highs and lows these days. Most studies use [adeno-associated viral] vectors, which don’t integrate into the genome. But some people have antibodies to AAV vectors, and AAV is diluted out when cells divide. That’s why lentivirus, which integrates into the genome, is used for blood stem cells and T cells in CAR-T therapy.”
Pinpointing causality
At bluebird bio, investigation into the possible “genetic gymnastics” of the lentivirus vector is focusing on where it integrates into the genome – whether it harpoons an oncogene like the gamma retroviral vectors, or affects genome stability, Dr. Gregory explained. To be causative, the affected gene must be a “driver” of the cancer, and not just a “passenger.”
Another suspect is busulfan, a drug used to “condition” the recipient’s bone marrow, making room for modified stem cells. “It’s possible that busulfan is the main problem, as it is a carcinogen unto itself,” said Paul Knoepfler, PhD, a stem cell researcher at the University of California, Davis.
In addition to the two more recent reports of complications, a third trial participant, who had participated in a phase 1/2 trial, developed MDS in 2018 and died of AML in July 2020. The cancer cells from that patient did not contain viral vectors and the MDS was attributed to busulfan conditioning.
Nick Leschly, chief of bluebird, pointed out the importance of clinical context in implicating the vector. Because SCD itself stresses the bone marrow, patients already face an increased risk of developing blood cancer, he said. “Now layer on other risks of the gene therapy. It’s challenging because we’re dealing with patients who have life expectancy in the mid 40s.” Previous treatments, such the antisickling drug hydroxyurea, may also contribute to patient vulnerability.
A patient’s view
SCD affects more than 100,000 people in the United States, and about 20 million globally. Charles Hough is one of them. He can attest to the severity of the disease as well as the promise of gene therapy
Mr. Hough was diagnosed at age 2, and endured the profound fatigue, pain crises, and even coma characteristic of severe cases. He cited his “rebirth” as Sept. 25, 2018, when he received his first modified stem cells at the National Institutes of Health. Mr. Hough told his story a year ago in a webinar for the National Organization for Rare Disorders. This news organization caught up with him in light of the clinical trial hold.
Although the preparative regimens for the gene therapy were tough, his sickle cell symptoms vanished after gene therapy. Even hearing about the current hold on the clinical trial, Mr. Hough doesn’t regret his participation.
“I had a lot of friends who passed because of the complications from sickle cell. I was always worried that I wouldn’t live to see the next day. Now I don’t have that stress hanging over my head and I feel like I can live a normal life. Becoming sickle cell free was my dream.”
A version of this article first appeared on Medscape.com.
Using engineered T cells reduced acute, chronic GVHD
A novel T-cell engineered product, Orca-T (Orca Bio), was associated with lower incidence of both acute and chronic graft-versus-host disease (GVHD) and more than double the rate of GVHD-free and relapse-free survival, compared with the current standard of care for patients undergoing hematopoietic stem cell transplants (HSCT), investigators said.
In both a multicenter phase 1 trial (NCT04013685) and single-center phase 1/2 trial (NCT01660607) with a total of 50 patients, those who received Orca-T with single-agent GVHD prophylaxis had a 1-year GVHD-free and relapse-free survival rate of 75%, compared with 31% for patients who received standard of care with two-agent prophylaxis, reported Everett H. Meyer, MD, PhD, from the Stanford (Calif.) University.
“Orca-T has good evidence for reduced acute graft-versus-host disease, reduced chromic graft-versus-host disease, and a low nonrelapse mortality,” he said at the Transplant & Cellular Therapies Meetings.
The product can be quickly manufactured and delivered to treatment centers across the continental United States, with “vein-to-vein” time of less than 72 hours, he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Orca-T consists of highly purified, donor-derived T-regulatory (Treg) cells that are sorted and delivered on day 0 with hematopoietic stem cells, without immunosuppressants, followed 2 days later with infusion of a matching dose of conventional T cells.
“The Treg cells are allowed to expand to create the right microenvironment for the [conventional T cells],” he explained.
In preclinical studies, donor-derived, high-purity Tregs delivered prior to adoptive transfer of conventional T cells prevented GVHD while maintaining graft-versus-tumor immunity, he said.
Two T-cell infusions
He reported updated results from current studies on a total of 50 adults, with a cohort of 144 patients treated concurrently with standard of care as controls.
The Orca-T–treated patients had a median age of 47 and 52% were male. Indications for transplant included acute myeloid and acute lymphoblastic leukemia, chronic myeloid leukemia, B-cell lymphoma, myelodysplastic syndrome/myelofibrosis, and other unspecified indications.
In both the Orca-T and control cohorts, patients underwent myeloablative conditioning from 10 to 2 days prior to stem cell infusion.
As noted patients in the experimental arm received infusion of hematopoietic stem/progenitor cells and Tregs, followed 2 days later by conventional T-cell infusion, and, on the day after that, tacrolimus at a target dose of 4.6 ng/mL. The conventional T cells were reserved from donor apheresis and were otherwise unmanipulated prior to infusion into the recipient, Dr. Meyer noted.
Patients in the standard-of-care arm received tacrolimus on the day before standard infusion of the apheresis product, followed by methotrexate prophylaxis on days 1, 3, 6 and 11.
Time to neutrophil engraftment, platelet engraftment, and from day 0 to hospital discharge were all significantly shorter in the Orca-T group, at 12 versus 14 days (P < .0001), 11 vs. 17 days (P < .0001), and 15 vs. 17 days (P = .01) respectively.
At 100 days of follow-up, the rate of grade 2 or greater acute GVHD was 30% among standard-of-care patients versus 10% among Orca-T–treated patients. At 1-year follow-up, respective rates of chronic GVHD were 46% vs. 3%.
Safety
“In general, the protocol is extremely well tolerated by our patients. We’ve seen no exceptional infectious disease complications, and we’ve seen no other major complications,” Dr. Meyer said.
Cytomegalovirus prophylaxis was used variably, depending on the center and on the attending physician. Epstein-Barr virus reactivation occurred in eight patients, with one requiring therapy, but there was no biopsy or radiographic evidence of posttransplant lymphoproliferative disorder.
In all, 18% of patients had serious adverse events during the reporting period, all of which resolved. There were no treatment-related deaths in the Orca-T arm, compared with 11% of controls.
Engraftment differences explored
In the question-and-answer session following the presentation, Christopher J. Gamper, MD, PhD, from the Johns Hopkins Hospital in Baltimore, told Dr. Meyer that “your outcomes from Orca-T look excellent,” and asked about the cost differential, compared with similar, unmanipulated transplants performed with standard GVHD prophylaxis.
“Is this recovered by lower costs for treatment of GVHD?” he asked.
“I have not done an economic cost analysis of course, and I think others may be looking into this,” Dr. Meyer replied. “Graft engineering can be expensive, although it’s an engineering proposition and one could imagine that the costs will go down substantially over time.”
Session moderator Alan Hanash, MD, PhD, from Memorial Sloan Kettering Cancer Center in New York, commented on the differences in engraftment between the experimental controls arms, and asked Dr. Meyer: “Do you think this is due to the difference in prophylaxis? Absence of methotrexate? Do you think that it could be a direct impact of regulatory T cells on hematopoietic engraftment?”
“Certainly not having methotrexate is beneficial for engraftment, and may account for the differences we see, Dr. Meyer said. “However, it is possible that Tregs could be playing a facilitative role. There certainly is good preclinical literature that Tregs, particularly in the bone marrow space, can facilitate bone marrow engraftment.”
The Orca-T trials are sponsored by Orca Bio and Stanford, with support from the National Institutes of Health. Dr. Meyer receives research support from Orca and is a scientific adviser to GigaGen, Triursus, Incyte, and Indee Labs. Dr. Hanash and Dr. Gamper had no relevant disclosures.
A novel T-cell engineered product, Orca-T (Orca Bio), was associated with lower incidence of both acute and chronic graft-versus-host disease (GVHD) and more than double the rate of GVHD-free and relapse-free survival, compared with the current standard of care for patients undergoing hematopoietic stem cell transplants (HSCT), investigators said.
In both a multicenter phase 1 trial (NCT04013685) and single-center phase 1/2 trial (NCT01660607) with a total of 50 patients, those who received Orca-T with single-agent GVHD prophylaxis had a 1-year GVHD-free and relapse-free survival rate of 75%, compared with 31% for patients who received standard of care with two-agent prophylaxis, reported Everett H. Meyer, MD, PhD, from the Stanford (Calif.) University.
“Orca-T has good evidence for reduced acute graft-versus-host disease, reduced chromic graft-versus-host disease, and a low nonrelapse mortality,” he said at the Transplant & Cellular Therapies Meetings.
The product can be quickly manufactured and delivered to treatment centers across the continental United States, with “vein-to-vein” time of less than 72 hours, he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Orca-T consists of highly purified, donor-derived T-regulatory (Treg) cells that are sorted and delivered on day 0 with hematopoietic stem cells, without immunosuppressants, followed 2 days later with infusion of a matching dose of conventional T cells.
“The Treg cells are allowed to expand to create the right microenvironment for the [conventional T cells],” he explained.
In preclinical studies, donor-derived, high-purity Tregs delivered prior to adoptive transfer of conventional T cells prevented GVHD while maintaining graft-versus-tumor immunity, he said.
Two T-cell infusions
He reported updated results from current studies on a total of 50 adults, with a cohort of 144 patients treated concurrently with standard of care as controls.
The Orca-T–treated patients had a median age of 47 and 52% were male. Indications for transplant included acute myeloid and acute lymphoblastic leukemia, chronic myeloid leukemia, B-cell lymphoma, myelodysplastic syndrome/myelofibrosis, and other unspecified indications.
In both the Orca-T and control cohorts, patients underwent myeloablative conditioning from 10 to 2 days prior to stem cell infusion.
As noted patients in the experimental arm received infusion of hematopoietic stem/progenitor cells and Tregs, followed 2 days later by conventional T-cell infusion, and, on the day after that, tacrolimus at a target dose of 4.6 ng/mL. The conventional T cells were reserved from donor apheresis and were otherwise unmanipulated prior to infusion into the recipient, Dr. Meyer noted.
Patients in the standard-of-care arm received tacrolimus on the day before standard infusion of the apheresis product, followed by methotrexate prophylaxis on days 1, 3, 6 and 11.
Time to neutrophil engraftment, platelet engraftment, and from day 0 to hospital discharge were all significantly shorter in the Orca-T group, at 12 versus 14 days (P < .0001), 11 vs. 17 days (P < .0001), and 15 vs. 17 days (P = .01) respectively.
At 100 days of follow-up, the rate of grade 2 or greater acute GVHD was 30% among standard-of-care patients versus 10% among Orca-T–treated patients. At 1-year follow-up, respective rates of chronic GVHD were 46% vs. 3%.
Safety
“In general, the protocol is extremely well tolerated by our patients. We’ve seen no exceptional infectious disease complications, and we’ve seen no other major complications,” Dr. Meyer said.
Cytomegalovirus prophylaxis was used variably, depending on the center and on the attending physician. Epstein-Barr virus reactivation occurred in eight patients, with one requiring therapy, but there was no biopsy or radiographic evidence of posttransplant lymphoproliferative disorder.
In all, 18% of patients had serious adverse events during the reporting period, all of which resolved. There were no treatment-related deaths in the Orca-T arm, compared with 11% of controls.
Engraftment differences explored
In the question-and-answer session following the presentation, Christopher J. Gamper, MD, PhD, from the Johns Hopkins Hospital in Baltimore, told Dr. Meyer that “your outcomes from Orca-T look excellent,” and asked about the cost differential, compared with similar, unmanipulated transplants performed with standard GVHD prophylaxis.
“Is this recovered by lower costs for treatment of GVHD?” he asked.
“I have not done an economic cost analysis of course, and I think others may be looking into this,” Dr. Meyer replied. “Graft engineering can be expensive, although it’s an engineering proposition and one could imagine that the costs will go down substantially over time.”
Session moderator Alan Hanash, MD, PhD, from Memorial Sloan Kettering Cancer Center in New York, commented on the differences in engraftment between the experimental controls arms, and asked Dr. Meyer: “Do you think this is due to the difference in prophylaxis? Absence of methotrexate? Do you think that it could be a direct impact of regulatory T cells on hematopoietic engraftment?”
“Certainly not having methotrexate is beneficial for engraftment, and may account for the differences we see, Dr. Meyer said. “However, it is possible that Tregs could be playing a facilitative role. There certainly is good preclinical literature that Tregs, particularly in the bone marrow space, can facilitate bone marrow engraftment.”
The Orca-T trials are sponsored by Orca Bio and Stanford, with support from the National Institutes of Health. Dr. Meyer receives research support from Orca and is a scientific adviser to GigaGen, Triursus, Incyte, and Indee Labs. Dr. Hanash and Dr. Gamper had no relevant disclosures.
A novel T-cell engineered product, Orca-T (Orca Bio), was associated with lower incidence of both acute and chronic graft-versus-host disease (GVHD) and more than double the rate of GVHD-free and relapse-free survival, compared with the current standard of care for patients undergoing hematopoietic stem cell transplants (HSCT), investigators said.
In both a multicenter phase 1 trial (NCT04013685) and single-center phase 1/2 trial (NCT01660607) with a total of 50 patients, those who received Orca-T with single-agent GVHD prophylaxis had a 1-year GVHD-free and relapse-free survival rate of 75%, compared with 31% for patients who received standard of care with two-agent prophylaxis, reported Everett H. Meyer, MD, PhD, from the Stanford (Calif.) University.
“Orca-T has good evidence for reduced acute graft-versus-host disease, reduced chromic graft-versus-host disease, and a low nonrelapse mortality,” he said at the Transplant & Cellular Therapies Meetings.
The product can be quickly manufactured and delivered to treatment centers across the continental United States, with “vein-to-vein” time of less than 72 hours, he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Orca-T consists of highly purified, donor-derived T-regulatory (Treg) cells that are sorted and delivered on day 0 with hematopoietic stem cells, without immunosuppressants, followed 2 days later with infusion of a matching dose of conventional T cells.
“The Treg cells are allowed to expand to create the right microenvironment for the [conventional T cells],” he explained.
In preclinical studies, donor-derived, high-purity Tregs delivered prior to adoptive transfer of conventional T cells prevented GVHD while maintaining graft-versus-tumor immunity, he said.
Two T-cell infusions
He reported updated results from current studies on a total of 50 adults, with a cohort of 144 patients treated concurrently with standard of care as controls.
The Orca-T–treated patients had a median age of 47 and 52% were male. Indications for transplant included acute myeloid and acute lymphoblastic leukemia, chronic myeloid leukemia, B-cell lymphoma, myelodysplastic syndrome/myelofibrosis, and other unspecified indications.
In both the Orca-T and control cohorts, patients underwent myeloablative conditioning from 10 to 2 days prior to stem cell infusion.
As noted patients in the experimental arm received infusion of hematopoietic stem/progenitor cells and Tregs, followed 2 days later by conventional T-cell infusion, and, on the day after that, tacrolimus at a target dose of 4.6 ng/mL. The conventional T cells were reserved from donor apheresis and were otherwise unmanipulated prior to infusion into the recipient, Dr. Meyer noted.
Patients in the standard-of-care arm received tacrolimus on the day before standard infusion of the apheresis product, followed by methotrexate prophylaxis on days 1, 3, 6 and 11.
Time to neutrophil engraftment, platelet engraftment, and from day 0 to hospital discharge were all significantly shorter in the Orca-T group, at 12 versus 14 days (P < .0001), 11 vs. 17 days (P < .0001), and 15 vs. 17 days (P = .01) respectively.
At 100 days of follow-up, the rate of grade 2 or greater acute GVHD was 30% among standard-of-care patients versus 10% among Orca-T–treated patients. At 1-year follow-up, respective rates of chronic GVHD were 46% vs. 3%.
Safety
“In general, the protocol is extremely well tolerated by our patients. We’ve seen no exceptional infectious disease complications, and we’ve seen no other major complications,” Dr. Meyer said.
Cytomegalovirus prophylaxis was used variably, depending on the center and on the attending physician. Epstein-Barr virus reactivation occurred in eight patients, with one requiring therapy, but there was no biopsy or radiographic evidence of posttransplant lymphoproliferative disorder.
In all, 18% of patients had serious adverse events during the reporting period, all of which resolved. There were no treatment-related deaths in the Orca-T arm, compared with 11% of controls.
Engraftment differences explored
In the question-and-answer session following the presentation, Christopher J. Gamper, MD, PhD, from the Johns Hopkins Hospital in Baltimore, told Dr. Meyer that “your outcomes from Orca-T look excellent,” and asked about the cost differential, compared with similar, unmanipulated transplants performed with standard GVHD prophylaxis.
“Is this recovered by lower costs for treatment of GVHD?” he asked.
“I have not done an economic cost analysis of course, and I think others may be looking into this,” Dr. Meyer replied. “Graft engineering can be expensive, although it’s an engineering proposition and one could imagine that the costs will go down substantially over time.”
Session moderator Alan Hanash, MD, PhD, from Memorial Sloan Kettering Cancer Center in New York, commented on the differences in engraftment between the experimental controls arms, and asked Dr. Meyer: “Do you think this is due to the difference in prophylaxis? Absence of methotrexate? Do you think that it could be a direct impact of regulatory T cells on hematopoietic engraftment?”
“Certainly not having methotrexate is beneficial for engraftment, and may account for the differences we see, Dr. Meyer said. “However, it is possible that Tregs could be playing a facilitative role. There certainly is good preclinical literature that Tregs, particularly in the bone marrow space, can facilitate bone marrow engraftment.”
The Orca-T trials are sponsored by Orca Bio and Stanford, with support from the National Institutes of Health. Dr. Meyer receives research support from Orca and is a scientific adviser to GigaGen, Triursus, Incyte, and Indee Labs. Dr. Hanash and Dr. Gamper had no relevant disclosures.
FROM TCT 2021
Transplant-related mortality higher with CD34 selection
In a clinical trial comparing three graft-versus-host disease (GVHD)–prevention regimens in patients undergoing hematopoietic stem cell transplants, a calcineurin inhibitor (CNI)–free strategy using CD34-selected peripheral blood stem cells (PBSCs) was associated with a nearly twofold increase in transplant-related mortality, compared with either a different CNI-free regimen or tacrolimus plus methotrexate, investigators reported.
In the phase 3 Progress II trial, patients who received CD34-selected PBSCs without post-transplant immune suppression had a hazard ratio for death of 1.74 compared with patients who received T-cell depletion with posttransplant cyclophosphamide, and a HR of 1.78, compared with patients who received tacrolimus and methotrexate after a bone marrow graft, Miguel-Angel Perales , MD, from Memorial Sloan Kettering Cancer Center, New York, reported at the Transplant & Cellular Therapies Meetings.
“CD34 selection was associated with worse overall survival, which offset any benefit from lower rates of moderate to severe chronic GVHD,” he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Neither of the two CNI-free interventions were superior to tacrolimus/methotrexate with bone marrow–derived stem cells for preventing chronic GVHD, and there were no differences in the primary endpoint of chronic GVHD/relapse-free survival, Dr. Perales said.
T-cell depletion vs. CNI
The Progress II trial was designed to see whether either of two CNI-free, T-cell depletion approaches could improve chronic GVHD rates post transplant over a CNI-based regimen.
The investigators enrolled patients aged 65 years or younger with acute leukemia or myelodysplasia with fewer than 5% blasts and a HLA-matched related or unrelated donor.
The patients were randomly assigned to either bone marrow grafts with tacrolimus/methotrexate (118 patients), bone marrow with in vivo posttransplant cyclophosphamide (114), or PBSCs with ex vivo CD34-selected cells (114).
The primary endpoint of chronic GVHD/relapse-free survival (CRFS) was a time-to-event outcome defined as moderate to severe chronic GVHD according to National Institutes of Health consensus criteria, disease relapse or progression, or death from any cause.
As noted before, there were no between-arm differences in the primary CRFS endpoint, and in multivariate analysis controlling for donor type, patient characteristics, disease category and disease risk index, the only factor significantly predictive for CRFS was being aged 50 years or older.
The 2-year posttransplant survival rates were 61.6% in the CD34-selected arm, 76.7% in the posttransplant cyclophosphamide arm, and 74.2% in the tacrolimus/methotrexate arm.
As noted before, the HR for CRFS with CD34 versus tacrolimus/methotrexate was 1.74, and for CD34 versus cyclophosphamide was 1.78 (P = .02 for both comparisons). In contrast, there was no difference in CRFS between posttransplant cyclophosphamide and tacrolimus/methotrexate.
Both relapse-free survival and transplant-related mortality were worse with the CD34-selected group, compared with the other two groups, but there were no significant differences among the arms in disease relapse.
Hematologic recovery was faster in the CD34 arm, but there were no significant differences in graft failure.
In addition, the incidence of grade II-IV acute GVHD was increased in the posttransplant cyclophosphamide group, compared with the other two, while chronic GVHD and moderate to severe chronic GVHD were reduced in the CD34 group.
There were no differences in quality of life measures among the groups, Dr. Perales said.
Practice changing?
In the question-and answer-session following the presentation, comoderator Sarah Nikiforow , MD, PhD, from the Dana-Farber Cancer Institute in Boston, who was not involved in the study, asked whether the trial results could be considered as practice changing for any centers that historically have done CD34 selection, or whether CD34 selection is still a viable approach to GVHD prophylaxis.
“That’s obviously a key question from the study, and a question that we’re asking ourselves,” Dr. Perales said. “I think the lesson that we took from this study as it pertains to CD34 selection is obviously the increased mortality, likely related to regimen toxicity, and I think the use of high-dose radiation is something that we have to reexamine.”
He said that his center is also considering whether to reduce antithymocyte globulin dosing, move it earlier in the process, and to use pharmokinetic-directed ATG as a possible means of decreasing nonrelapse mortality.
“I think it remains a useful platform for adoptive cell therapy, potentially targeting relapsed disease,” he added.
The study was supported by the National Heart, Lung, and Blood Institute. Dr. Perales disclosed advisory board activities and consulting for multiple companies, and receiving research funding for clinical trials from several more. Dr. Nikiforow disclosed a consulting/advisory role for Kite Pharma, and travel accommodations and expense from Celyad Oncology.
In a clinical trial comparing three graft-versus-host disease (GVHD)–prevention regimens in patients undergoing hematopoietic stem cell transplants, a calcineurin inhibitor (CNI)–free strategy using CD34-selected peripheral blood stem cells (PBSCs) was associated with a nearly twofold increase in transplant-related mortality, compared with either a different CNI-free regimen or tacrolimus plus methotrexate, investigators reported.
In the phase 3 Progress II trial, patients who received CD34-selected PBSCs without post-transplant immune suppression had a hazard ratio for death of 1.74 compared with patients who received T-cell depletion with posttransplant cyclophosphamide, and a HR of 1.78, compared with patients who received tacrolimus and methotrexate after a bone marrow graft, Miguel-Angel Perales , MD, from Memorial Sloan Kettering Cancer Center, New York, reported at the Transplant & Cellular Therapies Meetings.
“CD34 selection was associated with worse overall survival, which offset any benefit from lower rates of moderate to severe chronic GVHD,” he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Neither of the two CNI-free interventions were superior to tacrolimus/methotrexate with bone marrow–derived stem cells for preventing chronic GVHD, and there were no differences in the primary endpoint of chronic GVHD/relapse-free survival, Dr. Perales said.
T-cell depletion vs. CNI
The Progress II trial was designed to see whether either of two CNI-free, T-cell depletion approaches could improve chronic GVHD rates post transplant over a CNI-based regimen.
The investigators enrolled patients aged 65 years or younger with acute leukemia or myelodysplasia with fewer than 5% blasts and a HLA-matched related or unrelated donor.
The patients were randomly assigned to either bone marrow grafts with tacrolimus/methotrexate (118 patients), bone marrow with in vivo posttransplant cyclophosphamide (114), or PBSCs with ex vivo CD34-selected cells (114).
The primary endpoint of chronic GVHD/relapse-free survival (CRFS) was a time-to-event outcome defined as moderate to severe chronic GVHD according to National Institutes of Health consensus criteria, disease relapse or progression, or death from any cause.
As noted before, there were no between-arm differences in the primary CRFS endpoint, and in multivariate analysis controlling for donor type, patient characteristics, disease category and disease risk index, the only factor significantly predictive for CRFS was being aged 50 years or older.
The 2-year posttransplant survival rates were 61.6% in the CD34-selected arm, 76.7% in the posttransplant cyclophosphamide arm, and 74.2% in the tacrolimus/methotrexate arm.
As noted before, the HR for CRFS with CD34 versus tacrolimus/methotrexate was 1.74, and for CD34 versus cyclophosphamide was 1.78 (P = .02 for both comparisons). In contrast, there was no difference in CRFS between posttransplant cyclophosphamide and tacrolimus/methotrexate.
Both relapse-free survival and transplant-related mortality were worse with the CD34-selected group, compared with the other two groups, but there were no significant differences among the arms in disease relapse.
Hematologic recovery was faster in the CD34 arm, but there were no significant differences in graft failure.
In addition, the incidence of grade II-IV acute GVHD was increased in the posttransplant cyclophosphamide group, compared with the other two, while chronic GVHD and moderate to severe chronic GVHD were reduced in the CD34 group.
There were no differences in quality of life measures among the groups, Dr. Perales said.
Practice changing?
In the question-and answer-session following the presentation, comoderator Sarah Nikiforow , MD, PhD, from the Dana-Farber Cancer Institute in Boston, who was not involved in the study, asked whether the trial results could be considered as practice changing for any centers that historically have done CD34 selection, or whether CD34 selection is still a viable approach to GVHD prophylaxis.
“That’s obviously a key question from the study, and a question that we’re asking ourselves,” Dr. Perales said. “I think the lesson that we took from this study as it pertains to CD34 selection is obviously the increased mortality, likely related to regimen toxicity, and I think the use of high-dose radiation is something that we have to reexamine.”
He said that his center is also considering whether to reduce antithymocyte globulin dosing, move it earlier in the process, and to use pharmokinetic-directed ATG as a possible means of decreasing nonrelapse mortality.
“I think it remains a useful platform for adoptive cell therapy, potentially targeting relapsed disease,” he added.
The study was supported by the National Heart, Lung, and Blood Institute. Dr. Perales disclosed advisory board activities and consulting for multiple companies, and receiving research funding for clinical trials from several more. Dr. Nikiforow disclosed a consulting/advisory role for Kite Pharma, and travel accommodations and expense from Celyad Oncology.
In a clinical trial comparing three graft-versus-host disease (GVHD)–prevention regimens in patients undergoing hematopoietic stem cell transplants, a calcineurin inhibitor (CNI)–free strategy using CD34-selected peripheral blood stem cells (PBSCs) was associated with a nearly twofold increase in transplant-related mortality, compared with either a different CNI-free regimen or tacrolimus plus methotrexate, investigators reported.
In the phase 3 Progress II trial, patients who received CD34-selected PBSCs without post-transplant immune suppression had a hazard ratio for death of 1.74 compared with patients who received T-cell depletion with posttransplant cyclophosphamide, and a HR of 1.78, compared with patients who received tacrolimus and methotrexate after a bone marrow graft, Miguel-Angel Perales , MD, from Memorial Sloan Kettering Cancer Center, New York, reported at the Transplant & Cellular Therapies Meetings.
“CD34 selection was associated with worse overall survival, which offset any benefit from lower rates of moderate to severe chronic GVHD,” he said at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Neither of the two CNI-free interventions were superior to tacrolimus/methotrexate with bone marrow–derived stem cells for preventing chronic GVHD, and there were no differences in the primary endpoint of chronic GVHD/relapse-free survival, Dr. Perales said.
T-cell depletion vs. CNI
The Progress II trial was designed to see whether either of two CNI-free, T-cell depletion approaches could improve chronic GVHD rates post transplant over a CNI-based regimen.
The investigators enrolled patients aged 65 years or younger with acute leukemia or myelodysplasia with fewer than 5% blasts and a HLA-matched related or unrelated donor.
The patients were randomly assigned to either bone marrow grafts with tacrolimus/methotrexate (118 patients), bone marrow with in vivo posttransplant cyclophosphamide (114), or PBSCs with ex vivo CD34-selected cells (114).
The primary endpoint of chronic GVHD/relapse-free survival (CRFS) was a time-to-event outcome defined as moderate to severe chronic GVHD according to National Institutes of Health consensus criteria, disease relapse or progression, or death from any cause.
As noted before, there were no between-arm differences in the primary CRFS endpoint, and in multivariate analysis controlling for donor type, patient characteristics, disease category and disease risk index, the only factor significantly predictive for CRFS was being aged 50 years or older.
The 2-year posttransplant survival rates were 61.6% in the CD34-selected arm, 76.7% in the posttransplant cyclophosphamide arm, and 74.2% in the tacrolimus/methotrexate arm.
As noted before, the HR for CRFS with CD34 versus tacrolimus/methotrexate was 1.74, and for CD34 versus cyclophosphamide was 1.78 (P = .02 for both comparisons). In contrast, there was no difference in CRFS between posttransplant cyclophosphamide and tacrolimus/methotrexate.
Both relapse-free survival and transplant-related mortality were worse with the CD34-selected group, compared with the other two groups, but there were no significant differences among the arms in disease relapse.
Hematologic recovery was faster in the CD34 arm, but there were no significant differences in graft failure.
In addition, the incidence of grade II-IV acute GVHD was increased in the posttransplant cyclophosphamide group, compared with the other two, while chronic GVHD and moderate to severe chronic GVHD were reduced in the CD34 group.
There were no differences in quality of life measures among the groups, Dr. Perales said.
Practice changing?
In the question-and answer-session following the presentation, comoderator Sarah Nikiforow , MD, PhD, from the Dana-Farber Cancer Institute in Boston, who was not involved in the study, asked whether the trial results could be considered as practice changing for any centers that historically have done CD34 selection, or whether CD34 selection is still a viable approach to GVHD prophylaxis.
“That’s obviously a key question from the study, and a question that we’re asking ourselves,” Dr. Perales said. “I think the lesson that we took from this study as it pertains to CD34 selection is obviously the increased mortality, likely related to regimen toxicity, and I think the use of high-dose radiation is something that we have to reexamine.”
He said that his center is also considering whether to reduce antithymocyte globulin dosing, move it earlier in the process, and to use pharmokinetic-directed ATG as a possible means of decreasing nonrelapse mortality.
“I think it remains a useful platform for adoptive cell therapy, potentially targeting relapsed disease,” he added.
The study was supported by the National Heart, Lung, and Blood Institute. Dr. Perales disclosed advisory board activities and consulting for multiple companies, and receiving research funding for clinical trials from several more. Dr. Nikiforow disclosed a consulting/advisory role for Kite Pharma, and travel accommodations and expense from Celyad Oncology.
FROM TCT 2021
Steroid complications in GVHD common, boost costs of care
Steroids are usually the first choice of therapy for the treatment of patients with graft-vs.-host disease (GVHD), but complications from steroid use may carry a high financial cost, investigators caution.
Among 689 patients with a diagnosis of GVHD following a hematopoietic stem cell transplant (HSCT) who received steroids, 685 (97%) had at least one steroid-related complication, resulting in nearly $165,000 in mean health-care costs over 24 months, said Elizabeth J. Bell, PhD, MPH, an epidemiologist at Optum Inc.
“For both acute and chronic GVHD, the standard of care for first-line treatment is systemic steroids. The complications associated with steroid treatment are well known. However, the health-care resources utilized and the costs incurred by these patients are not well-quantified,” she said at the Transplantation & Cellular Therapies Meetings (Abstract 12).
Dr. Bell reported the results of a retrospective database analysis on costs associated with steroid complications in HSCT recipients at the meeting, which was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
She and colleagues from Optum, Incyte, and the University of Minnesota in Minneapolis looked at data on 689 patients with a diagnosis of GVHD after HSCT who received systemic steroids from July 1, 2010, through Aug. 31, 2019. The data were extracted from the Optum Research database, and included U.S. commercial and Medicare Advantage patients.
They looked at total complications and steroid-associated complications in each of four categories: infections; metabolic or endocrine complications (for example, diabetes, dyslipidemia); gastrointestinal (GI) complications (e.g., peptic ulcer disease); and bone or muscle complications (myopathy, etc).
They estimated costs based on International Classification of Diseases (ICD) codes for any steroid complications during the 24 months after steroid initiation, including those complications that may have been present at the time of GVHD diagnosis.
The median patient age was 55 years, and 60% of the sample were male. The mean Charlson Comorbidity Index score at baseline was 3.
Overall, 22% of patients had only acute GVHD, 21% had only chronic GVHD, and 39% had both acute and chronic disease. The GVHD type was unspecified in the remaining 18%.
The median time from GVHD diagnosis to initiating steroids was 30 days for patients with both acute and chronic disease, as well as those with both presentations. The median time to initiation was 36 days for patients with unspecified GVHD type.
The median cumulative duration of steroid use over 24 months was 62 days for patients with acute GVHD, 208 days for those with chronic GVHD, 166 days for those with both, and 74 days for patients with unspecified GVHD type.
As noted before, complications occurred in 97% of patients, with infections being the most common complications, occurring in 80% of patients, followed by metabolic/endocrine complications in 32%, gastrointestinal in 29%, and bone/muscle complications in 20%.
For the 665 patients who had any steroid-related complication, the mean costs of steroid-associated care in the 24 months after they were started on steroids was $164,787, and the median cost was $50,834.
Health care costs were highest among patients with infections, at a mean of $167,473, and a median of $57,680, followed by bone/muscle conditions ($75,289 and $2,057, respectively), GI conditions ($67,861 and $3,360), and metabolic or endocrine conditions ($47, 101 and $1,164).
In all categories, hospitalizations accounted for the large majority of costs.
Two-thirds (66%) of patients who experienced any steroid-related complication required hospitalization, primarily for infections.
Among all patients with complications, the median cumulative hospital stay over 24 months was 20 days, with bone/muscle complications and infections associated with a median of 19 and 18 days of hospitalization, respectively.
Dr. Bell acknowledged that the study was limited by use of ICD coding to identify steroid complication-related health-care utilization and costs, which can be imprecise, and by the fact that the analysis included only complications resulting in health care use as documented in medical claims. In addition, the investigators noted that they could not control for the possibility that steroids exacerbated conditions that existed at baseline.
“These findings emphasize the need to cautiously evaluate the treatment options for patients with GVHD. Future study with medical records is needed to provide insights on the clinical aspects of the complications (e.g., severity and suspected causality),” Dr. Bell and colleagues concluded in the study’s abstract.
Definitions questioned
An HSCT specialist approached for comment said that the findings of the study made sense, but she had questions regarding the study methodology.
“I would intuitively think that steroid-associated complications are a major cause of health care use in GVHD patients and it’s interesting to see that there is emerging data to support this hypothesis,” HSCT specialist Hélène Schoemans, MD of the University of Leuven, Belgium, said in an interview.
She noted, however, that “it is surprising that the period of steroid initiation was the same for acute and chronic GVHD,” and questioned whether that anomalous finding could be due to the study’s definition of acute and chronic GVHD or to how the period from baseline to steroid initiation was defined.
The questions about the definitions and timing of therapy make it uncertain as to whether the complications reported were caused by steroids or by some other factor, she suggested.
The study was supported by Optum Inc. Dr. Bell is an employee of the company, and a paid consultant of Incyte. Dr. Schoemans has received travel expenses from Celgene, Abbvie, and Incyte; is part of the advisory boards for Incyte; and has received speakers fees from Novartis, Incyte, Jazz Pharmaceuticals, and Takeda.
Steroids are usually the first choice of therapy for the treatment of patients with graft-vs.-host disease (GVHD), but complications from steroid use may carry a high financial cost, investigators caution.
Among 689 patients with a diagnosis of GVHD following a hematopoietic stem cell transplant (HSCT) who received steroids, 685 (97%) had at least one steroid-related complication, resulting in nearly $165,000 in mean health-care costs over 24 months, said Elizabeth J. Bell, PhD, MPH, an epidemiologist at Optum Inc.
“For both acute and chronic GVHD, the standard of care for first-line treatment is systemic steroids. The complications associated with steroid treatment are well known. However, the health-care resources utilized and the costs incurred by these patients are not well-quantified,” she said at the Transplantation & Cellular Therapies Meetings (Abstract 12).
Dr. Bell reported the results of a retrospective database analysis on costs associated with steroid complications in HSCT recipients at the meeting, which was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
She and colleagues from Optum, Incyte, and the University of Minnesota in Minneapolis looked at data on 689 patients with a diagnosis of GVHD after HSCT who received systemic steroids from July 1, 2010, through Aug. 31, 2019. The data were extracted from the Optum Research database, and included U.S. commercial and Medicare Advantage patients.
They looked at total complications and steroid-associated complications in each of four categories: infections; metabolic or endocrine complications (for example, diabetes, dyslipidemia); gastrointestinal (GI) complications (e.g., peptic ulcer disease); and bone or muscle complications (myopathy, etc).
They estimated costs based on International Classification of Diseases (ICD) codes for any steroid complications during the 24 months after steroid initiation, including those complications that may have been present at the time of GVHD diagnosis.
The median patient age was 55 years, and 60% of the sample were male. The mean Charlson Comorbidity Index score at baseline was 3.
Overall, 22% of patients had only acute GVHD, 21% had only chronic GVHD, and 39% had both acute and chronic disease. The GVHD type was unspecified in the remaining 18%.
The median time from GVHD diagnosis to initiating steroids was 30 days for patients with both acute and chronic disease, as well as those with both presentations. The median time to initiation was 36 days for patients with unspecified GVHD type.
The median cumulative duration of steroid use over 24 months was 62 days for patients with acute GVHD, 208 days for those with chronic GVHD, 166 days for those with both, and 74 days for patients with unspecified GVHD type.
As noted before, complications occurred in 97% of patients, with infections being the most common complications, occurring in 80% of patients, followed by metabolic/endocrine complications in 32%, gastrointestinal in 29%, and bone/muscle complications in 20%.
For the 665 patients who had any steroid-related complication, the mean costs of steroid-associated care in the 24 months after they were started on steroids was $164,787, and the median cost was $50,834.
Health care costs were highest among patients with infections, at a mean of $167,473, and a median of $57,680, followed by bone/muscle conditions ($75,289 and $2,057, respectively), GI conditions ($67,861 and $3,360), and metabolic or endocrine conditions ($47, 101 and $1,164).
In all categories, hospitalizations accounted for the large majority of costs.
Two-thirds (66%) of patients who experienced any steroid-related complication required hospitalization, primarily for infections.
Among all patients with complications, the median cumulative hospital stay over 24 months was 20 days, with bone/muscle complications and infections associated with a median of 19 and 18 days of hospitalization, respectively.
Dr. Bell acknowledged that the study was limited by use of ICD coding to identify steroid complication-related health-care utilization and costs, which can be imprecise, and by the fact that the analysis included only complications resulting in health care use as documented in medical claims. In addition, the investigators noted that they could not control for the possibility that steroids exacerbated conditions that existed at baseline.
“These findings emphasize the need to cautiously evaluate the treatment options for patients with GVHD. Future study with medical records is needed to provide insights on the clinical aspects of the complications (e.g., severity and suspected causality),” Dr. Bell and colleagues concluded in the study’s abstract.
Definitions questioned
An HSCT specialist approached for comment said that the findings of the study made sense, but she had questions regarding the study methodology.
“I would intuitively think that steroid-associated complications are a major cause of health care use in GVHD patients and it’s interesting to see that there is emerging data to support this hypothesis,” HSCT specialist Hélène Schoemans, MD of the University of Leuven, Belgium, said in an interview.
She noted, however, that “it is surprising that the period of steroid initiation was the same for acute and chronic GVHD,” and questioned whether that anomalous finding could be due to the study’s definition of acute and chronic GVHD or to how the period from baseline to steroid initiation was defined.
The questions about the definitions and timing of therapy make it uncertain as to whether the complications reported were caused by steroids or by some other factor, she suggested.
The study was supported by Optum Inc. Dr. Bell is an employee of the company, and a paid consultant of Incyte. Dr. Schoemans has received travel expenses from Celgene, Abbvie, and Incyte; is part of the advisory boards for Incyte; and has received speakers fees from Novartis, Incyte, Jazz Pharmaceuticals, and Takeda.
Steroids are usually the first choice of therapy for the treatment of patients with graft-vs.-host disease (GVHD), but complications from steroid use may carry a high financial cost, investigators caution.
Among 689 patients with a diagnosis of GVHD following a hematopoietic stem cell transplant (HSCT) who received steroids, 685 (97%) had at least one steroid-related complication, resulting in nearly $165,000 in mean health-care costs over 24 months, said Elizabeth J. Bell, PhD, MPH, an epidemiologist at Optum Inc.
“For both acute and chronic GVHD, the standard of care for first-line treatment is systemic steroids. The complications associated with steroid treatment are well known. However, the health-care resources utilized and the costs incurred by these patients are not well-quantified,” she said at the Transplantation & Cellular Therapies Meetings (Abstract 12).
Dr. Bell reported the results of a retrospective database analysis on costs associated with steroid complications in HSCT recipients at the meeting, which was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
She and colleagues from Optum, Incyte, and the University of Minnesota in Minneapolis looked at data on 689 patients with a diagnosis of GVHD after HSCT who received systemic steroids from July 1, 2010, through Aug. 31, 2019. The data were extracted from the Optum Research database, and included U.S. commercial and Medicare Advantage patients.
They looked at total complications and steroid-associated complications in each of four categories: infections; metabolic or endocrine complications (for example, diabetes, dyslipidemia); gastrointestinal (GI) complications (e.g., peptic ulcer disease); and bone or muscle complications (myopathy, etc).
They estimated costs based on International Classification of Diseases (ICD) codes for any steroid complications during the 24 months after steroid initiation, including those complications that may have been present at the time of GVHD diagnosis.
The median patient age was 55 years, and 60% of the sample were male. The mean Charlson Comorbidity Index score at baseline was 3.
Overall, 22% of patients had only acute GVHD, 21% had only chronic GVHD, and 39% had both acute and chronic disease. The GVHD type was unspecified in the remaining 18%.
The median time from GVHD diagnosis to initiating steroids was 30 days for patients with both acute and chronic disease, as well as those with both presentations. The median time to initiation was 36 days for patients with unspecified GVHD type.
The median cumulative duration of steroid use over 24 months was 62 days for patients with acute GVHD, 208 days for those with chronic GVHD, 166 days for those with both, and 74 days for patients with unspecified GVHD type.
As noted before, complications occurred in 97% of patients, with infections being the most common complications, occurring in 80% of patients, followed by metabolic/endocrine complications in 32%, gastrointestinal in 29%, and bone/muscle complications in 20%.
For the 665 patients who had any steroid-related complication, the mean costs of steroid-associated care in the 24 months after they were started on steroids was $164,787, and the median cost was $50,834.
Health care costs were highest among patients with infections, at a mean of $167,473, and a median of $57,680, followed by bone/muscle conditions ($75,289 and $2,057, respectively), GI conditions ($67,861 and $3,360), and metabolic or endocrine conditions ($47, 101 and $1,164).
In all categories, hospitalizations accounted for the large majority of costs.
Two-thirds (66%) of patients who experienced any steroid-related complication required hospitalization, primarily for infections.
Among all patients with complications, the median cumulative hospital stay over 24 months was 20 days, with bone/muscle complications and infections associated with a median of 19 and 18 days of hospitalization, respectively.
Dr. Bell acknowledged that the study was limited by use of ICD coding to identify steroid complication-related health-care utilization and costs, which can be imprecise, and by the fact that the analysis included only complications resulting in health care use as documented in medical claims. In addition, the investigators noted that they could not control for the possibility that steroids exacerbated conditions that existed at baseline.
“These findings emphasize the need to cautiously evaluate the treatment options for patients with GVHD. Future study with medical records is needed to provide insights on the clinical aspects of the complications (e.g., severity and suspected causality),” Dr. Bell and colleagues concluded in the study’s abstract.
Definitions questioned
An HSCT specialist approached for comment said that the findings of the study made sense, but she had questions regarding the study methodology.
“I would intuitively think that steroid-associated complications are a major cause of health care use in GVHD patients and it’s interesting to see that there is emerging data to support this hypothesis,” HSCT specialist Hélène Schoemans, MD of the University of Leuven, Belgium, said in an interview.
She noted, however, that “it is surprising that the period of steroid initiation was the same for acute and chronic GVHD,” and questioned whether that anomalous finding could be due to the study’s definition of acute and chronic GVHD or to how the period from baseline to steroid initiation was defined.
The questions about the definitions and timing of therapy make it uncertain as to whether the complications reported were caused by steroids or by some other factor, she suggested.
The study was supported by Optum Inc. Dr. Bell is an employee of the company, and a paid consultant of Incyte. Dr. Schoemans has received travel expenses from Celgene, Abbvie, and Incyte; is part of the advisory boards for Incyte; and has received speakers fees from Novartis, Incyte, Jazz Pharmaceuticals, and Takeda.
FROM TCT 2021
How has the pandemic affected rural and urban cancer patients?
Research has shown that, compared with their urban counterparts, rural cancer patients have higher cancer-related mortality and other negative treatment outcomes.
Among other explanations, the disparity has been attributed to lower education and income levels, medical and behavioral risk factors, differences in health literacy, and lower confidence in the medical system among rural residents (JCO Oncol Pract. 2020 Jul;16(7):422-30).
A new survey has provided some insight into how the COVID-19 pandemic has impacted rural and urban cancer patients differently.
The survey showed that urban patients were more likely to report changes to their daily lives, thought themselves more likely to become infected with SARS-CoV-2, and were more likely to take measures to mitigate the risk of infection. However, there were no major differences between urban and rural patients with regard to changes in social interaction.
Bailee Daniels of the University of Utah in Salt Lake City, presented these results at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S04-03).
The COVID-19 and Oncology Patient Experience Consortium
Ms. Daniels explained that the COVID-19 and Oncology Patient Experience (COPES) Consortium was created to investigate various aspects of the patient experience during the pandemic. Three cancer centers – Moffitt Cancer Center, Huntsman Cancer Institute, and the Sylvester Comprehensive Cancer Center – participate in COPES.
At Huntsman, investigators studied social and health behaviors of cancer patients to assess whether there was a difference between those from rural and urban areas. The researchers looked at the impact of the pandemic on psychosocial outcomes, preventive measures patients implemented, and their perceptions of the risk of SARS-CoV-2 infection.
The team’s hypothesis was that rural patients might be more vulnerable than urban patients to the effects of social isolation, emotional distress, and health-adverse behaviors, but the investigators noted that there has been no prior research on the topic.
Assessing behaviors, attitudes, and outcomes
Between August and September 2020, the researchers surveyed 1,328 adult cancer patients who had visited Huntsman in the previous 4 years and who were enrolled in Huntsman’s Total Cancer Care or Precision Exercise Prescription studies.
Patients completed questionnaires that encompassed demographic and clinical factors, employment status, health behaviors, and infection preventive measures. Questionnaires were provided in electronic, paper, or phone-based formats. Information regarding age, race, ethnicity, and tumor stage was abstracted from Huntsman’s electronic health record.
Modifications in daily life and social interaction were assessed on a 5-point scale. Changes in exercise habits and alcohol consumption were assessed on a 3-point scale. Infection mitigation measures (the use of face masks and hand sanitizer) and perceptions about the likelihood of SARS-CoV-2 infection were measured.
The rural-urban community area codes system, which classifies U.S. census tracts by measures of population density, urbanization, and daily commuting, was utilized to categorize patients into rural and urban residences.
Characteristics of urban and rural cancer patients
There were 997 urban and 331 rural participants. The mean age was 60.1 years in the urban population and 62.6 years in the rural population (P = .01). There were no urban-rural differences in sex, ethnicity, cancer stage, or body mass index.
More urban than rural participants were employed full- or part-time (45% vs. 37%; P = .045). The rural counties had more patients who were not currently employed, primarily due to retirement (77% vs. 69% urban; P < .001).
“No health insurance coverage” was reported by 2% of urban and 4% of rural participants (P = .009), and 85% of all patients reported “good” to “excellent” overall health. Cancer patients in rural counties were significantly more likely to have ever smoked (37% vs. 25% urban; P = .001). In addition, alcohol consumption in the previous year was higher in rural patients. “Every day to less than once monthly” alcohol usage was reported by 44% of urban and 60% of rural patients (P < .001).
Changes in daily life and health-related behavior during the pandemic
Urban patients were more likely to report changes in their daily lives due to the pandemic. Specifically, 35% of urban patients and 26% of rural patients said the pandemic had changed their daily life “a lot” (P = .001).
However, there were no major differences between urban and rural patients when it came to changes in social interaction in the past month or feeling lonely in the past month (P = .45 and P = .88, respectively). Similarly, there were no significant differences for changes in alcohol consumption between the groups (P = .90).
Changes in exercise habits due to the pandemic were more common among patients in urban counties (51% vs. 39% rural; P < .001), though similar percentages of patients reported exercising less (44% urban vs. 45% rural) or more frequently (24% urban vs. 20% rural).
In terms of infection mitigation measures, urban patients were more likely to use face masks “very often” (83% vs. 66% rural; P < .001), while hand sanitizer was used “very often” among 66% of urban and 57% of rural participants (P = .05).
Urban participants were more likely than were their rural counterparts to think themselves “somewhat” or “very” likely to develop COVID-19 (22% vs. 14%; P = .04).
It might be short-sighted for oncology and public health specialists to be dismissive of differences in infection mitigation behaviors and perceptions of vulnerability to SARS-CoV-2 infection. Those behaviors and perceptions of risk could lead to lower vaccination rates in rural areas. If that occurs, there would be major negative consequences for the long-term health of rural communities and their medically vulnerable residents.
Future directions
Although the first 6 months of the COVID-19 pandemic had disparate effects on cancer patients living in rural and urban counties, the reasons for the disparities are complex and not easily explained by this study.
It is possible that sequential administration of the survey during the pandemic would have uncovered greater variances in attitude and health-related behaviors.
As Ms. Daniels noted, when the survey was performed, Utah had not experienced a high frequency of COVID-19 cases. Furthermore, different levels of restrictions were implemented on a county-by-county basis, potentially influencing patients’ behaviors, psychosocial adjustment, and perceptions of risk.
In addition, there may have been differences in unmeasured endpoints (infection rates, medical care utilization via telemedicine, hospitalization rates, late effects, and mortality) between the urban and rural populations.
As the investigators concluded, further research is needed to better characterize the pandemic’s short- and long-term effects on cancer patients in rural and urban settings and appropriate interventions. Such studies may yield insights into the various facets of the well-documented “rural health gap” in cancer outcomes and interventions that could narrow the gap in spheres beyond the COVID-19 pandemic.
Ms. Daniels reported having no relevant disclosures.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Research has shown that, compared with their urban counterparts, rural cancer patients have higher cancer-related mortality and other negative treatment outcomes.
Among other explanations, the disparity has been attributed to lower education and income levels, medical and behavioral risk factors, differences in health literacy, and lower confidence in the medical system among rural residents (JCO Oncol Pract. 2020 Jul;16(7):422-30).
A new survey has provided some insight into how the COVID-19 pandemic has impacted rural and urban cancer patients differently.
The survey showed that urban patients were more likely to report changes to their daily lives, thought themselves more likely to become infected with SARS-CoV-2, and were more likely to take measures to mitigate the risk of infection. However, there were no major differences between urban and rural patients with regard to changes in social interaction.
Bailee Daniels of the University of Utah in Salt Lake City, presented these results at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S04-03).
The COVID-19 and Oncology Patient Experience Consortium
Ms. Daniels explained that the COVID-19 and Oncology Patient Experience (COPES) Consortium was created to investigate various aspects of the patient experience during the pandemic. Three cancer centers – Moffitt Cancer Center, Huntsman Cancer Institute, and the Sylvester Comprehensive Cancer Center – participate in COPES.
At Huntsman, investigators studied social and health behaviors of cancer patients to assess whether there was a difference between those from rural and urban areas. The researchers looked at the impact of the pandemic on psychosocial outcomes, preventive measures patients implemented, and their perceptions of the risk of SARS-CoV-2 infection.
The team’s hypothesis was that rural patients might be more vulnerable than urban patients to the effects of social isolation, emotional distress, and health-adverse behaviors, but the investigators noted that there has been no prior research on the topic.
Assessing behaviors, attitudes, and outcomes
Between August and September 2020, the researchers surveyed 1,328 adult cancer patients who had visited Huntsman in the previous 4 years and who were enrolled in Huntsman’s Total Cancer Care or Precision Exercise Prescription studies.
Patients completed questionnaires that encompassed demographic and clinical factors, employment status, health behaviors, and infection preventive measures. Questionnaires were provided in electronic, paper, or phone-based formats. Information regarding age, race, ethnicity, and tumor stage was abstracted from Huntsman’s electronic health record.
Modifications in daily life and social interaction were assessed on a 5-point scale. Changes in exercise habits and alcohol consumption were assessed on a 3-point scale. Infection mitigation measures (the use of face masks and hand sanitizer) and perceptions about the likelihood of SARS-CoV-2 infection were measured.
The rural-urban community area codes system, which classifies U.S. census tracts by measures of population density, urbanization, and daily commuting, was utilized to categorize patients into rural and urban residences.
Characteristics of urban and rural cancer patients
There were 997 urban and 331 rural participants. The mean age was 60.1 years in the urban population and 62.6 years in the rural population (P = .01). There were no urban-rural differences in sex, ethnicity, cancer stage, or body mass index.
More urban than rural participants were employed full- or part-time (45% vs. 37%; P = .045). The rural counties had more patients who were not currently employed, primarily due to retirement (77% vs. 69% urban; P < .001).
“No health insurance coverage” was reported by 2% of urban and 4% of rural participants (P = .009), and 85% of all patients reported “good” to “excellent” overall health. Cancer patients in rural counties were significantly more likely to have ever smoked (37% vs. 25% urban; P = .001). In addition, alcohol consumption in the previous year was higher in rural patients. “Every day to less than once monthly” alcohol usage was reported by 44% of urban and 60% of rural patients (P < .001).
Changes in daily life and health-related behavior during the pandemic
Urban patients were more likely to report changes in their daily lives due to the pandemic. Specifically, 35% of urban patients and 26% of rural patients said the pandemic had changed their daily life “a lot” (P = .001).
However, there were no major differences between urban and rural patients when it came to changes in social interaction in the past month or feeling lonely in the past month (P = .45 and P = .88, respectively). Similarly, there were no significant differences for changes in alcohol consumption between the groups (P = .90).
Changes in exercise habits due to the pandemic were more common among patients in urban counties (51% vs. 39% rural; P < .001), though similar percentages of patients reported exercising less (44% urban vs. 45% rural) or more frequently (24% urban vs. 20% rural).
In terms of infection mitigation measures, urban patients were more likely to use face masks “very often” (83% vs. 66% rural; P < .001), while hand sanitizer was used “very often” among 66% of urban and 57% of rural participants (P = .05).
Urban participants were more likely than were their rural counterparts to think themselves “somewhat” or “very” likely to develop COVID-19 (22% vs. 14%; P = .04).
It might be short-sighted for oncology and public health specialists to be dismissive of differences in infection mitigation behaviors and perceptions of vulnerability to SARS-CoV-2 infection. Those behaviors and perceptions of risk could lead to lower vaccination rates in rural areas. If that occurs, there would be major negative consequences for the long-term health of rural communities and their medically vulnerable residents.
Future directions
Although the first 6 months of the COVID-19 pandemic had disparate effects on cancer patients living in rural and urban counties, the reasons for the disparities are complex and not easily explained by this study.
It is possible that sequential administration of the survey during the pandemic would have uncovered greater variances in attitude and health-related behaviors.
As Ms. Daniels noted, when the survey was performed, Utah had not experienced a high frequency of COVID-19 cases. Furthermore, different levels of restrictions were implemented on a county-by-county basis, potentially influencing patients’ behaviors, psychosocial adjustment, and perceptions of risk.
In addition, there may have been differences in unmeasured endpoints (infection rates, medical care utilization via telemedicine, hospitalization rates, late effects, and mortality) between the urban and rural populations.
As the investigators concluded, further research is needed to better characterize the pandemic’s short- and long-term effects on cancer patients in rural and urban settings and appropriate interventions. Such studies may yield insights into the various facets of the well-documented “rural health gap” in cancer outcomes and interventions that could narrow the gap in spheres beyond the COVID-19 pandemic.
Ms. Daniels reported having no relevant disclosures.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Research has shown that, compared with their urban counterparts, rural cancer patients have higher cancer-related mortality and other negative treatment outcomes.
Among other explanations, the disparity has been attributed to lower education and income levels, medical and behavioral risk factors, differences in health literacy, and lower confidence in the medical system among rural residents (JCO Oncol Pract. 2020 Jul;16(7):422-30).
A new survey has provided some insight into how the COVID-19 pandemic has impacted rural and urban cancer patients differently.
The survey showed that urban patients were more likely to report changes to their daily lives, thought themselves more likely to become infected with SARS-CoV-2, and were more likely to take measures to mitigate the risk of infection. However, there were no major differences between urban and rural patients with regard to changes in social interaction.
Bailee Daniels of the University of Utah in Salt Lake City, presented these results at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S04-03).
The COVID-19 and Oncology Patient Experience Consortium
Ms. Daniels explained that the COVID-19 and Oncology Patient Experience (COPES) Consortium was created to investigate various aspects of the patient experience during the pandemic. Three cancer centers – Moffitt Cancer Center, Huntsman Cancer Institute, and the Sylvester Comprehensive Cancer Center – participate in COPES.
At Huntsman, investigators studied social and health behaviors of cancer patients to assess whether there was a difference between those from rural and urban areas. The researchers looked at the impact of the pandemic on psychosocial outcomes, preventive measures patients implemented, and their perceptions of the risk of SARS-CoV-2 infection.
The team’s hypothesis was that rural patients might be more vulnerable than urban patients to the effects of social isolation, emotional distress, and health-adverse behaviors, but the investigators noted that there has been no prior research on the topic.
Assessing behaviors, attitudes, and outcomes
Between August and September 2020, the researchers surveyed 1,328 adult cancer patients who had visited Huntsman in the previous 4 years and who were enrolled in Huntsman’s Total Cancer Care or Precision Exercise Prescription studies.
Patients completed questionnaires that encompassed demographic and clinical factors, employment status, health behaviors, and infection preventive measures. Questionnaires were provided in electronic, paper, or phone-based formats. Information regarding age, race, ethnicity, and tumor stage was abstracted from Huntsman’s electronic health record.
Modifications in daily life and social interaction were assessed on a 5-point scale. Changes in exercise habits and alcohol consumption were assessed on a 3-point scale. Infection mitigation measures (the use of face masks and hand sanitizer) and perceptions about the likelihood of SARS-CoV-2 infection were measured.
The rural-urban community area codes system, which classifies U.S. census tracts by measures of population density, urbanization, and daily commuting, was utilized to categorize patients into rural and urban residences.
Characteristics of urban and rural cancer patients
There were 997 urban and 331 rural participants. The mean age was 60.1 years in the urban population and 62.6 years in the rural population (P = .01). There were no urban-rural differences in sex, ethnicity, cancer stage, or body mass index.
More urban than rural participants were employed full- or part-time (45% vs. 37%; P = .045). The rural counties had more patients who were not currently employed, primarily due to retirement (77% vs. 69% urban; P < .001).
“No health insurance coverage” was reported by 2% of urban and 4% of rural participants (P = .009), and 85% of all patients reported “good” to “excellent” overall health. Cancer patients in rural counties were significantly more likely to have ever smoked (37% vs. 25% urban; P = .001). In addition, alcohol consumption in the previous year was higher in rural patients. “Every day to less than once monthly” alcohol usage was reported by 44% of urban and 60% of rural patients (P < .001).
Changes in daily life and health-related behavior during the pandemic
Urban patients were more likely to report changes in their daily lives due to the pandemic. Specifically, 35% of urban patients and 26% of rural patients said the pandemic had changed their daily life “a lot” (P = .001).
However, there were no major differences between urban and rural patients when it came to changes in social interaction in the past month or feeling lonely in the past month (P = .45 and P = .88, respectively). Similarly, there were no significant differences for changes in alcohol consumption between the groups (P = .90).
Changes in exercise habits due to the pandemic were more common among patients in urban counties (51% vs. 39% rural; P < .001), though similar percentages of patients reported exercising less (44% urban vs. 45% rural) or more frequently (24% urban vs. 20% rural).
In terms of infection mitigation measures, urban patients were more likely to use face masks “very often” (83% vs. 66% rural; P < .001), while hand sanitizer was used “very often” among 66% of urban and 57% of rural participants (P = .05).
Urban participants were more likely than were their rural counterparts to think themselves “somewhat” or “very” likely to develop COVID-19 (22% vs. 14%; P = .04).
It might be short-sighted for oncology and public health specialists to be dismissive of differences in infection mitigation behaviors and perceptions of vulnerability to SARS-CoV-2 infection. Those behaviors and perceptions of risk could lead to lower vaccination rates in rural areas. If that occurs, there would be major negative consequences for the long-term health of rural communities and their medically vulnerable residents.
Future directions
Although the first 6 months of the COVID-19 pandemic had disparate effects on cancer patients living in rural and urban counties, the reasons for the disparities are complex and not easily explained by this study.
It is possible that sequential administration of the survey during the pandemic would have uncovered greater variances in attitude and health-related behaviors.
As Ms. Daniels noted, when the survey was performed, Utah had not experienced a high frequency of COVID-19 cases. Furthermore, different levels of restrictions were implemented on a county-by-county basis, potentially influencing patients’ behaviors, psychosocial adjustment, and perceptions of risk.
In addition, there may have been differences in unmeasured endpoints (infection rates, medical care utilization via telemedicine, hospitalization rates, late effects, and mortality) between the urban and rural populations.
As the investigators concluded, further research is needed to better characterize the pandemic’s short- and long-term effects on cancer patients in rural and urban settings and appropriate interventions. Such studies may yield insights into the various facets of the well-documented “rural health gap” in cancer outcomes and interventions that could narrow the gap in spheres beyond the COVID-19 pandemic.
Ms. Daniels reported having no relevant disclosures.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
FROM AACR: COVID-19 AND CANCER 2021
Chronic GVHD therapies offer hope for treating refractory disease
Despite improvements in prevention of graft-versus-host disease, chronic GVHD still occurs in 10%-50% of patients who undergo an allogeneic hematopoietic stem cell transplant, and these patients may require prolonged treatment with multiple lines of therapy, said a hematologist and transplant researcher.
“More effective, less toxic therapies for chronic GVHD are needed,” Stephanie Lee, MD, MPH, from the Fred Hutchinson Cancer Research Center in Seattle said at the Transplant & Cellular Therapies Meetings.
Dr. Lee reviewed clinical trials for chronic GVHD at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Although the incidence of chronic GVHD has gradually declined over the last 40 years and both relapse-free and overall survival following a chronic GVHD diagnosis have improved, “for patients who are diagnosed with chronic GVHD, they still will see many lines of therapy and many years of therapy,” she said.
Among 148 patients with chronic GVHD treated at her center, for example, 66% went on to two lines of therapy, 50% went on to three lines, 37% required four lines of therapy, and 20% needed five lines or more.
Salvage therapies for patients with chronic GVHD have evolved away from immunomodulators and immunosuppressants in the early 1990s, toward monoclonal antibodies such as rituximab in the early 2000s, to interleukin-2 and to tyrosine kinase inhibitors such as ruxolitinib (Jakafi) and ibrutinib (Imbruvica).
There are currently 36 agents that are FDA approved for at least one indication and can also be prescribed for the treatment of chronic GVHD, Dr. Lee noted.
Treatment goals
Dr. Lee laid out six goals for treating patients with chronic GVHD. They include:
- Controlling current signs and symptoms, measured by response rates and patient-reported outcomes
- Preventing further tissue and organ damage
- Minimizing toxicity
- Maintaining graft-versus-tumor effect
- Achieving graft tolerance and stopping immunosuppression
- Decreasing nonrelapse mortality and improving survival
Active trials
Dr. Lee identified 33 trials with chronic GVHD as an indication that are currently recruiting, and an additional 13 trials that are active but closed to recruiting. The trials can be generally grouped by mechanism of action, and involve agents targeting T-regulatory cells, B cells and/or B-cell receptor (BCR) signaling, monocytes/macrophages, costimulatory blockage, a proteasome inhibition, Janus kinase (JAK) 1/2 inhibitors, ROCK2 inhibitors, hedgehog pathway inhibition, cellular therapy, and organ-targeted therapy.
Most of the trials have overall response rate as the primary endpoint, and all but five are currently in phase 1 or 2. The currently active phase 3 trials include two with ibrutinib, one with the investigational agent itacitinib, one with ruxolitinib, and one with mesenchymal stem cells.
“I’ll note that, when results are reported, the denominator really matters for the overall response rate, especially if you’re talking about small trials, because if you require the patient to be treated with an agent for a certain period of time, and you take out all the people who didn’t make it to that time point, then your overall response rate looks better,” she said.
BTK inhibitors
The first-in-class Bruton tyrosine kinase (BTK) inhibitor ibrutinib was the first and thus far only agent approved by the Food and Drug Administration for chronic GVHD. The approval was based on a single-arm, multicenter trial with 42 patients.
The ORR in this trial was 69%, consisting of 31% complete responses and 38% partial responses, with a duration of response longer than 10 months in slightly more than half of all patients. In all, 24% of patients had improvement of symptoms in two consecutive visits, and 29% continued on ibrutinib at the time of the primary analysis in 2017.
Based on these promising results, acalabrutinib, which is more potent and selective for BTK than ibrutinib, with no effect on either platelets or natural killer cells, is currently under investigation in a phase 2 trial in 50 patients at a dose of 100 mg orally twice daily.
JAK1/2 inhibition
The JAK1 inhibitor itacitinib failed to meet its primary ORR endpoint in the phase 3 GRAVITAS-301 study, according to a press release, but the manufacturer (Incyte) said that it is continuing its commitment to JAK inhibitors with ruxolitinib, which has shown activity against acute, steroid-refractory GVHD, and is being explored for prevention of chronic GVHD in the randomized, phase 3 REACH3 study.
The trial met its primary endpoint for a higher ORR at week 24 with ruxolitinib versus best available therapy, at 49.7% versus 25.6%, respectively, which translated into an odds ratio for response with the JAK inhibitor of 2.99 (P < .0001).
Selective T-cell expansion
Efavaleukin alfa is an IL-2-mutated protein (mutein), with a mutation in the IL-2RB-binding portion of IL-2 causing increased selectivity for regulatory T-cell expansion. It is bound to an IgG-Fc domain that is itself mutated, with reduced Fc receptor binding and IgG effector function to give it a longer half life. This agent is being studied in a phase 1/2 trial in a subcutaneous formulation delivered every 1 or 2 weeks to 68 patients.
Monocyte/macrophage depletion
Axatilimab is a high-affinity antibody targeting colony stimulating factor–1 receptor (CSF-1R) expressed on monocytes and macrophages. By blocking CSF-1R, it depletes circulation of nonclassical monocytes and prevents the differentiation and survival of M2 macrophages in tissue.
It is currently being investigated 30 patients in a phase 1/2 study in an intravenous formulation delivered over 30 minutes every 2-4 weeks.
Hedgehog pathway inhibition
There is evidence suggesting that hedgehog pathway inhibition can lessen fibrosis. Glasdegib (Daurismo) a potent selective oral inhibitor of the hedgehog signaling pathway, is approved for use with low-dose cytarabine for patients with newly diagnosed acute myeloid leukemia aged older than 75 years or have comorbidities precluding intensive chemotherapy.
This agent is associated with drug intolerance because of muscle spasms, dysgeusia, and alopecia, however.
The drug is currently in phase 1/2 at a dose of 50 mg orally per day in 20 patients.
ROCK2 inhibition
Belumosudil (formerly KD025) “appears to rebalance the immune system,” Dr. Lee said. Investigators think that the drug dampens an autoaggressive inflammatory response by selective inhibition of ROCK2.
This drug has been studied in a dose-escalation study and a phase 2 trial, in which 132 participants were randomized to receive belumosudil 200 mg either once or twice daily.
At a median follow-up of 8 months, the ORR with belumosudil 200 mg once and twice daily was 73% and 74%, respectively. Similar results were seen in patients who had previously received either ruxolitinib or ibrutinib. High response rates were seen in patients with severe chronic GVHD, involvement of four or more organs and a refractory response to their last line of therapy.
Hard-to-manage patients
“We’re very hopeful for many of these agents, but we have to acknowledge that there are still many management dilemmas, patients that we just don’t really know what to do with,” Dr. Lee said. “These include patients who have bad sclerosis and fasciitis, nonhealing skin ulcers, bronchiolitis obliterans, serositis that can be very difficult to manage, severe keratoconjunctivitis that can be eyesight threatening, nonhealing mouth ulcers, esophageal structures, and always patients who have frequent infections.
“We are hopeful that some these agents will be useful for our patients who have severe manifestations, but often the number of patients with these manifestations in the trials is too low to say something specific about them,” she added.
‘Exciting time’
“It’s an exciting time because there are a lot of different drugs that are being studied for chronic GVHD,” commented Betty Hamilton, MD, a hematologist/oncologist at the Cleveland Clinic.
“I think that where the field is going in terms of treatment is recognizing that chronic GVHD is a pretty heterogeneous disease, and we have to learn even more about the underlying biologic pathways to be able to determine which class of drugs to use and when,” she said in an interview.
She agreed with Dr. Lee that the goals of treating patients with chronic GVHD include improving symptoms and quality, preventing progression, ideally tapering patients off immunosuppression, and achieving a balance between preventing negative consequences of GVHD while maintain the benefits of a graft-versus-leukemia effect.
“In our center, drug choice is based on physician preference and comfort with how often they’ve used the drug, patients’ comorbidities, toxicities of the drug, and logistical considerations,” Dr. Hamilton said.
Dr. Lee disclosed consulting activities for Pfizer and Kadmon, travel and lodging from Amgen, and research funding from those companies and others. Dr. Hamilton disclosed consulting for Syndax and Incyte.
Despite improvements in prevention of graft-versus-host disease, chronic GVHD still occurs in 10%-50% of patients who undergo an allogeneic hematopoietic stem cell transplant, and these patients may require prolonged treatment with multiple lines of therapy, said a hematologist and transplant researcher.
“More effective, less toxic therapies for chronic GVHD are needed,” Stephanie Lee, MD, MPH, from the Fred Hutchinson Cancer Research Center in Seattle said at the Transplant & Cellular Therapies Meetings.
Dr. Lee reviewed clinical trials for chronic GVHD at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Although the incidence of chronic GVHD has gradually declined over the last 40 years and both relapse-free and overall survival following a chronic GVHD diagnosis have improved, “for patients who are diagnosed with chronic GVHD, they still will see many lines of therapy and many years of therapy,” she said.
Among 148 patients with chronic GVHD treated at her center, for example, 66% went on to two lines of therapy, 50% went on to three lines, 37% required four lines of therapy, and 20% needed five lines or more.
Salvage therapies for patients with chronic GVHD have evolved away from immunomodulators and immunosuppressants in the early 1990s, toward monoclonal antibodies such as rituximab in the early 2000s, to interleukin-2 and to tyrosine kinase inhibitors such as ruxolitinib (Jakafi) and ibrutinib (Imbruvica).
There are currently 36 agents that are FDA approved for at least one indication and can also be prescribed for the treatment of chronic GVHD, Dr. Lee noted.
Treatment goals
Dr. Lee laid out six goals for treating patients with chronic GVHD. They include:
- Controlling current signs and symptoms, measured by response rates and patient-reported outcomes
- Preventing further tissue and organ damage
- Minimizing toxicity
- Maintaining graft-versus-tumor effect
- Achieving graft tolerance and stopping immunosuppression
- Decreasing nonrelapse mortality and improving survival
Active trials
Dr. Lee identified 33 trials with chronic GVHD as an indication that are currently recruiting, and an additional 13 trials that are active but closed to recruiting. The trials can be generally grouped by mechanism of action, and involve agents targeting T-regulatory cells, B cells and/or B-cell receptor (BCR) signaling, monocytes/macrophages, costimulatory blockage, a proteasome inhibition, Janus kinase (JAK) 1/2 inhibitors, ROCK2 inhibitors, hedgehog pathway inhibition, cellular therapy, and organ-targeted therapy.
Most of the trials have overall response rate as the primary endpoint, and all but five are currently in phase 1 or 2. The currently active phase 3 trials include two with ibrutinib, one with the investigational agent itacitinib, one with ruxolitinib, and one with mesenchymal stem cells.
“I’ll note that, when results are reported, the denominator really matters for the overall response rate, especially if you’re talking about small trials, because if you require the patient to be treated with an agent for a certain period of time, and you take out all the people who didn’t make it to that time point, then your overall response rate looks better,” she said.
BTK inhibitors
The first-in-class Bruton tyrosine kinase (BTK) inhibitor ibrutinib was the first and thus far only agent approved by the Food and Drug Administration for chronic GVHD. The approval was based on a single-arm, multicenter trial with 42 patients.
The ORR in this trial was 69%, consisting of 31% complete responses and 38% partial responses, with a duration of response longer than 10 months in slightly more than half of all patients. In all, 24% of patients had improvement of symptoms in two consecutive visits, and 29% continued on ibrutinib at the time of the primary analysis in 2017.
Based on these promising results, acalabrutinib, which is more potent and selective for BTK than ibrutinib, with no effect on either platelets or natural killer cells, is currently under investigation in a phase 2 trial in 50 patients at a dose of 100 mg orally twice daily.
JAK1/2 inhibition
The JAK1 inhibitor itacitinib failed to meet its primary ORR endpoint in the phase 3 GRAVITAS-301 study, according to a press release, but the manufacturer (Incyte) said that it is continuing its commitment to JAK inhibitors with ruxolitinib, which has shown activity against acute, steroid-refractory GVHD, and is being explored for prevention of chronic GVHD in the randomized, phase 3 REACH3 study.
The trial met its primary endpoint for a higher ORR at week 24 with ruxolitinib versus best available therapy, at 49.7% versus 25.6%, respectively, which translated into an odds ratio for response with the JAK inhibitor of 2.99 (P < .0001).
Selective T-cell expansion
Efavaleukin alfa is an IL-2-mutated protein (mutein), with a mutation in the IL-2RB-binding portion of IL-2 causing increased selectivity for regulatory T-cell expansion. It is bound to an IgG-Fc domain that is itself mutated, with reduced Fc receptor binding and IgG effector function to give it a longer half life. This agent is being studied in a phase 1/2 trial in a subcutaneous formulation delivered every 1 or 2 weeks to 68 patients.
Monocyte/macrophage depletion
Axatilimab is a high-affinity antibody targeting colony stimulating factor–1 receptor (CSF-1R) expressed on monocytes and macrophages. By blocking CSF-1R, it depletes circulation of nonclassical monocytes and prevents the differentiation and survival of M2 macrophages in tissue.
It is currently being investigated 30 patients in a phase 1/2 study in an intravenous formulation delivered over 30 minutes every 2-4 weeks.
Hedgehog pathway inhibition
There is evidence suggesting that hedgehog pathway inhibition can lessen fibrosis. Glasdegib (Daurismo) a potent selective oral inhibitor of the hedgehog signaling pathway, is approved for use with low-dose cytarabine for patients with newly diagnosed acute myeloid leukemia aged older than 75 years or have comorbidities precluding intensive chemotherapy.
This agent is associated with drug intolerance because of muscle spasms, dysgeusia, and alopecia, however.
The drug is currently in phase 1/2 at a dose of 50 mg orally per day in 20 patients.
ROCK2 inhibition
Belumosudil (formerly KD025) “appears to rebalance the immune system,” Dr. Lee said. Investigators think that the drug dampens an autoaggressive inflammatory response by selective inhibition of ROCK2.
This drug has been studied in a dose-escalation study and a phase 2 trial, in which 132 participants were randomized to receive belumosudil 200 mg either once or twice daily.
At a median follow-up of 8 months, the ORR with belumosudil 200 mg once and twice daily was 73% and 74%, respectively. Similar results were seen in patients who had previously received either ruxolitinib or ibrutinib. High response rates were seen in patients with severe chronic GVHD, involvement of four or more organs and a refractory response to their last line of therapy.
Hard-to-manage patients
“We’re very hopeful for many of these agents, but we have to acknowledge that there are still many management dilemmas, patients that we just don’t really know what to do with,” Dr. Lee said. “These include patients who have bad sclerosis and fasciitis, nonhealing skin ulcers, bronchiolitis obliterans, serositis that can be very difficult to manage, severe keratoconjunctivitis that can be eyesight threatening, nonhealing mouth ulcers, esophageal structures, and always patients who have frequent infections.
“We are hopeful that some these agents will be useful for our patients who have severe manifestations, but often the number of patients with these manifestations in the trials is too low to say something specific about them,” she added.
‘Exciting time’
“It’s an exciting time because there are a lot of different drugs that are being studied for chronic GVHD,” commented Betty Hamilton, MD, a hematologist/oncologist at the Cleveland Clinic.
“I think that where the field is going in terms of treatment is recognizing that chronic GVHD is a pretty heterogeneous disease, and we have to learn even more about the underlying biologic pathways to be able to determine which class of drugs to use and when,” she said in an interview.
She agreed with Dr. Lee that the goals of treating patients with chronic GVHD include improving symptoms and quality, preventing progression, ideally tapering patients off immunosuppression, and achieving a balance between preventing negative consequences of GVHD while maintain the benefits of a graft-versus-leukemia effect.
“In our center, drug choice is based on physician preference and comfort with how often they’ve used the drug, patients’ comorbidities, toxicities of the drug, and logistical considerations,” Dr. Hamilton said.
Dr. Lee disclosed consulting activities for Pfizer and Kadmon, travel and lodging from Amgen, and research funding from those companies and others. Dr. Hamilton disclosed consulting for Syndax and Incyte.
Despite improvements in prevention of graft-versus-host disease, chronic GVHD still occurs in 10%-50% of patients who undergo an allogeneic hematopoietic stem cell transplant, and these patients may require prolonged treatment with multiple lines of therapy, said a hematologist and transplant researcher.
“More effective, less toxic therapies for chronic GVHD are needed,” Stephanie Lee, MD, MPH, from the Fred Hutchinson Cancer Research Center in Seattle said at the Transplant & Cellular Therapies Meetings.
Dr. Lee reviewed clinical trials for chronic GVHD at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Although the incidence of chronic GVHD has gradually declined over the last 40 years and both relapse-free and overall survival following a chronic GVHD diagnosis have improved, “for patients who are diagnosed with chronic GVHD, they still will see many lines of therapy and many years of therapy,” she said.
Among 148 patients with chronic GVHD treated at her center, for example, 66% went on to two lines of therapy, 50% went on to three lines, 37% required four lines of therapy, and 20% needed five lines or more.
Salvage therapies for patients with chronic GVHD have evolved away from immunomodulators and immunosuppressants in the early 1990s, toward monoclonal antibodies such as rituximab in the early 2000s, to interleukin-2 and to tyrosine kinase inhibitors such as ruxolitinib (Jakafi) and ibrutinib (Imbruvica).
There are currently 36 agents that are FDA approved for at least one indication and can also be prescribed for the treatment of chronic GVHD, Dr. Lee noted.
Treatment goals
Dr. Lee laid out six goals for treating patients with chronic GVHD. They include:
- Controlling current signs and symptoms, measured by response rates and patient-reported outcomes
- Preventing further tissue and organ damage
- Minimizing toxicity
- Maintaining graft-versus-tumor effect
- Achieving graft tolerance and stopping immunosuppression
- Decreasing nonrelapse mortality and improving survival
Active trials
Dr. Lee identified 33 trials with chronic GVHD as an indication that are currently recruiting, and an additional 13 trials that are active but closed to recruiting. The trials can be generally grouped by mechanism of action, and involve agents targeting T-regulatory cells, B cells and/or B-cell receptor (BCR) signaling, monocytes/macrophages, costimulatory blockage, a proteasome inhibition, Janus kinase (JAK) 1/2 inhibitors, ROCK2 inhibitors, hedgehog pathway inhibition, cellular therapy, and organ-targeted therapy.
Most of the trials have overall response rate as the primary endpoint, and all but five are currently in phase 1 or 2. The currently active phase 3 trials include two with ibrutinib, one with the investigational agent itacitinib, one with ruxolitinib, and one with mesenchymal stem cells.
“I’ll note that, when results are reported, the denominator really matters for the overall response rate, especially if you’re talking about small trials, because if you require the patient to be treated with an agent for a certain period of time, and you take out all the people who didn’t make it to that time point, then your overall response rate looks better,” she said.
BTK inhibitors
The first-in-class Bruton tyrosine kinase (BTK) inhibitor ibrutinib was the first and thus far only agent approved by the Food and Drug Administration for chronic GVHD. The approval was based on a single-arm, multicenter trial with 42 patients.
The ORR in this trial was 69%, consisting of 31% complete responses and 38% partial responses, with a duration of response longer than 10 months in slightly more than half of all patients. In all, 24% of patients had improvement of symptoms in two consecutive visits, and 29% continued on ibrutinib at the time of the primary analysis in 2017.
Based on these promising results, acalabrutinib, which is more potent and selective for BTK than ibrutinib, with no effect on either platelets or natural killer cells, is currently under investigation in a phase 2 trial in 50 patients at a dose of 100 mg orally twice daily.
JAK1/2 inhibition
The JAK1 inhibitor itacitinib failed to meet its primary ORR endpoint in the phase 3 GRAVITAS-301 study, according to a press release, but the manufacturer (Incyte) said that it is continuing its commitment to JAK inhibitors with ruxolitinib, which has shown activity against acute, steroid-refractory GVHD, and is being explored for prevention of chronic GVHD in the randomized, phase 3 REACH3 study.
The trial met its primary endpoint for a higher ORR at week 24 with ruxolitinib versus best available therapy, at 49.7% versus 25.6%, respectively, which translated into an odds ratio for response with the JAK inhibitor of 2.99 (P < .0001).
Selective T-cell expansion
Efavaleukin alfa is an IL-2-mutated protein (mutein), with a mutation in the IL-2RB-binding portion of IL-2 causing increased selectivity for regulatory T-cell expansion. It is bound to an IgG-Fc domain that is itself mutated, with reduced Fc receptor binding and IgG effector function to give it a longer half life. This agent is being studied in a phase 1/2 trial in a subcutaneous formulation delivered every 1 or 2 weeks to 68 patients.
Monocyte/macrophage depletion
Axatilimab is a high-affinity antibody targeting colony stimulating factor–1 receptor (CSF-1R) expressed on monocytes and macrophages. By blocking CSF-1R, it depletes circulation of nonclassical monocytes and prevents the differentiation and survival of M2 macrophages in tissue.
It is currently being investigated 30 patients in a phase 1/2 study in an intravenous formulation delivered over 30 minutes every 2-4 weeks.
Hedgehog pathway inhibition
There is evidence suggesting that hedgehog pathway inhibition can lessen fibrosis. Glasdegib (Daurismo) a potent selective oral inhibitor of the hedgehog signaling pathway, is approved for use with low-dose cytarabine for patients with newly diagnosed acute myeloid leukemia aged older than 75 years or have comorbidities precluding intensive chemotherapy.
This agent is associated with drug intolerance because of muscle spasms, dysgeusia, and alopecia, however.
The drug is currently in phase 1/2 at a dose of 50 mg orally per day in 20 patients.
ROCK2 inhibition
Belumosudil (formerly KD025) “appears to rebalance the immune system,” Dr. Lee said. Investigators think that the drug dampens an autoaggressive inflammatory response by selective inhibition of ROCK2.
This drug has been studied in a dose-escalation study and a phase 2 trial, in which 132 participants were randomized to receive belumosudil 200 mg either once or twice daily.
At a median follow-up of 8 months, the ORR with belumosudil 200 mg once and twice daily was 73% and 74%, respectively. Similar results were seen in patients who had previously received either ruxolitinib or ibrutinib. High response rates were seen in patients with severe chronic GVHD, involvement of four or more organs and a refractory response to their last line of therapy.
Hard-to-manage patients
“We’re very hopeful for many of these agents, but we have to acknowledge that there are still many management dilemmas, patients that we just don’t really know what to do with,” Dr. Lee said. “These include patients who have bad sclerosis and fasciitis, nonhealing skin ulcers, bronchiolitis obliterans, serositis that can be very difficult to manage, severe keratoconjunctivitis that can be eyesight threatening, nonhealing mouth ulcers, esophageal structures, and always patients who have frequent infections.
“We are hopeful that some these agents will be useful for our patients who have severe manifestations, but often the number of patients with these manifestations in the trials is too low to say something specific about them,” she added.
‘Exciting time’
“It’s an exciting time because there are a lot of different drugs that are being studied for chronic GVHD,” commented Betty Hamilton, MD, a hematologist/oncologist at the Cleveland Clinic.
“I think that where the field is going in terms of treatment is recognizing that chronic GVHD is a pretty heterogeneous disease, and we have to learn even more about the underlying biologic pathways to be able to determine which class of drugs to use and when,” she said in an interview.
She agreed with Dr. Lee that the goals of treating patients with chronic GVHD include improving symptoms and quality, preventing progression, ideally tapering patients off immunosuppression, and achieving a balance between preventing negative consequences of GVHD while maintain the benefits of a graft-versus-leukemia effect.
“In our center, drug choice is based on physician preference and comfort with how often they’ve used the drug, patients’ comorbidities, toxicities of the drug, and logistical considerations,” Dr. Hamilton said.
Dr. Lee disclosed consulting activities for Pfizer and Kadmon, travel and lodging from Amgen, and research funding from those companies and others. Dr. Hamilton disclosed consulting for Syndax and Incyte.
FROM TCT 2021
CXR-Net: An AI-based diagnostic tool for COVID-19
The system, called CXR-Net, was trained to differentiate SARS-CoV-2 chest x-rays (CXRs) from CXRs that are either normal or non–COVID-19 lung pathologies, explained Abdulah Haikal, an MD candidate at Wayne State University, Detroit.
Mr. Haikal described CXR-Net at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S11-04).
CXR-Net is a two-module pipeline, Mr. Haikal explained. Module I is based on Res-CR-Net, a type of neural network originally designed for the semantic segmentation of microscopy images, with the ability to retain the original resolution of the input images in the feature maps of all layers and in the final output.
Module II is a hybrid convolutional neural network in which the first convolutional layer with learned coefficients is replaced by a layer with fixed coefficients provided by the Wavelet Scattering Transform. Module II inputs patients’ CXRs and corresponding lung masks quantified by Module I, and generates as outputs a class assignment (COVID-19 or non–COVID-19) and high-resolution heat maps that detect the severe acute respiratory syndrome–-associated lung regions.
“The system is trained to differentiate COVID and non-COVID pathologies and produces a highly discriminative heat map to point to lung regions where COVID is suspected,” Mr. Haikal said. “The Wavelet Scattering Transform allows for fast determination of COVID versus non-COVID CXRs.”
Preliminary results and implications
CXR-Net was piloted on a small dataset of CXRs from non–COVID-19 and polymerase chain reaction–confirmed COVID-19 patients acquired at a single center in Detroit.
Upon fivefold cross validation of the training set with 2,265 images, 90% accuracy was observed when the training set was tested against the validation set. However, once 1,532 new images were introduced, a 76% accuracy rate was observed.
The F1 scores were 0.81 and 0.70 for the training and test sets, respectively.
“I’m really excited about this new approach, and I think AI will allow us to do more with less, which is exciting,” said Ross L. Levine, MD, of Memorial Sloan Kettering Cancer Center in New York, who led a discussion session with Mr. Haikal about CXR-Net.
One question raised during the discussion was whether the technology will help health care providers be more thoughtful about when and how they image COVID-19 patients.
“The more data you feed into the system, the stronger and more accurate it becomes,” Mr. Haikal said. “However, until we have data sharing from multiple centers, we won’t see improved accuracy results.”
Another question was whether this technology could be integrated with more clinical parameters.
“Some individuals are afraid that AI will replace the job of a professional, but it will only make it better for us,” Mr. Haikal said. “We don’t rely on current imaging techniques to make a definitive diagnosis, but rather have a specificity and sensitivity to establish a diagnosis, and AI can be used in the same way as a diagnostic tool.”
Mr. Haikal and Dr. Levine disclosed no conflicts of interest. No funding sources were reported in the presentation.
The system, called CXR-Net, was trained to differentiate SARS-CoV-2 chest x-rays (CXRs) from CXRs that are either normal or non–COVID-19 lung pathologies, explained Abdulah Haikal, an MD candidate at Wayne State University, Detroit.
Mr. Haikal described CXR-Net at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S11-04).
CXR-Net is a two-module pipeline, Mr. Haikal explained. Module I is based on Res-CR-Net, a type of neural network originally designed for the semantic segmentation of microscopy images, with the ability to retain the original resolution of the input images in the feature maps of all layers and in the final output.
Module II is a hybrid convolutional neural network in which the first convolutional layer with learned coefficients is replaced by a layer with fixed coefficients provided by the Wavelet Scattering Transform. Module II inputs patients’ CXRs and corresponding lung masks quantified by Module I, and generates as outputs a class assignment (COVID-19 or non–COVID-19) and high-resolution heat maps that detect the severe acute respiratory syndrome–-associated lung regions.
“The system is trained to differentiate COVID and non-COVID pathologies and produces a highly discriminative heat map to point to lung regions where COVID is suspected,” Mr. Haikal said. “The Wavelet Scattering Transform allows for fast determination of COVID versus non-COVID CXRs.”
Preliminary results and implications
CXR-Net was piloted on a small dataset of CXRs from non–COVID-19 and polymerase chain reaction–confirmed COVID-19 patients acquired at a single center in Detroit.
Upon fivefold cross validation of the training set with 2,265 images, 90% accuracy was observed when the training set was tested against the validation set. However, once 1,532 new images were introduced, a 76% accuracy rate was observed.
The F1 scores were 0.81 and 0.70 for the training and test sets, respectively.
“I’m really excited about this new approach, and I think AI will allow us to do more with less, which is exciting,” said Ross L. Levine, MD, of Memorial Sloan Kettering Cancer Center in New York, who led a discussion session with Mr. Haikal about CXR-Net.
One question raised during the discussion was whether the technology will help health care providers be more thoughtful about when and how they image COVID-19 patients.
“The more data you feed into the system, the stronger and more accurate it becomes,” Mr. Haikal said. “However, until we have data sharing from multiple centers, we won’t see improved accuracy results.”
Another question was whether this technology could be integrated with more clinical parameters.
“Some individuals are afraid that AI will replace the job of a professional, but it will only make it better for us,” Mr. Haikal said. “We don’t rely on current imaging techniques to make a definitive diagnosis, but rather have a specificity and sensitivity to establish a diagnosis, and AI can be used in the same way as a diagnostic tool.”
Mr. Haikal and Dr. Levine disclosed no conflicts of interest. No funding sources were reported in the presentation.
The system, called CXR-Net, was trained to differentiate SARS-CoV-2 chest x-rays (CXRs) from CXRs that are either normal or non–COVID-19 lung pathologies, explained Abdulah Haikal, an MD candidate at Wayne State University, Detroit.
Mr. Haikal described CXR-Net at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S11-04).
CXR-Net is a two-module pipeline, Mr. Haikal explained. Module I is based on Res-CR-Net, a type of neural network originally designed for the semantic segmentation of microscopy images, with the ability to retain the original resolution of the input images in the feature maps of all layers and in the final output.
Module II is a hybrid convolutional neural network in which the first convolutional layer with learned coefficients is replaced by a layer with fixed coefficients provided by the Wavelet Scattering Transform. Module II inputs patients’ CXRs and corresponding lung masks quantified by Module I, and generates as outputs a class assignment (COVID-19 or non–COVID-19) and high-resolution heat maps that detect the severe acute respiratory syndrome–-associated lung regions.
“The system is trained to differentiate COVID and non-COVID pathologies and produces a highly discriminative heat map to point to lung regions where COVID is suspected,” Mr. Haikal said. “The Wavelet Scattering Transform allows for fast determination of COVID versus non-COVID CXRs.”
Preliminary results and implications
CXR-Net was piloted on a small dataset of CXRs from non–COVID-19 and polymerase chain reaction–confirmed COVID-19 patients acquired at a single center in Detroit.
Upon fivefold cross validation of the training set with 2,265 images, 90% accuracy was observed when the training set was tested against the validation set. However, once 1,532 new images were introduced, a 76% accuracy rate was observed.
The F1 scores were 0.81 and 0.70 for the training and test sets, respectively.
“I’m really excited about this new approach, and I think AI will allow us to do more with less, which is exciting,” said Ross L. Levine, MD, of Memorial Sloan Kettering Cancer Center in New York, who led a discussion session with Mr. Haikal about CXR-Net.
One question raised during the discussion was whether the technology will help health care providers be more thoughtful about when and how they image COVID-19 patients.
“The more data you feed into the system, the stronger and more accurate it becomes,” Mr. Haikal said. “However, until we have data sharing from multiple centers, we won’t see improved accuracy results.”
Another question was whether this technology could be integrated with more clinical parameters.
“Some individuals are afraid that AI will replace the job of a professional, but it will only make it better for us,” Mr. Haikal said. “We don’t rely on current imaging techniques to make a definitive diagnosis, but rather have a specificity and sensitivity to establish a diagnosis, and AI can be used in the same way as a diagnostic tool.”
Mr. Haikal and Dr. Levine disclosed no conflicts of interest. No funding sources were reported in the presentation.
FROM AACR: COVID-19 AND CANCER 2021
CLL, MBL had lower response rates to flu vaccination, compared with healthy adults
Immunogenicity of the high-dose influenza vaccine (HD IIV3) in patients with chronic lymphocytic leukemia (CLL) and monoclonal B-cell lymphocytosis (MBL, the precursor state to CLL) was found lower than reported in healthy adults according to a report in Vaccine.
In addition, immunogenicity to influenza B was found to be greater in those patients with MBL, compared with those with CLL.
“Acute and chronic leukemia patients hospitalized with influenza infection document a case fatality rate of 25%-37%,” according to Jennifer A. Whitaker, MD, of the Mayo Clinic, Rochester, Minn., and colleagues in pointing out the importance of their study.
The prospective pilot study assessed the humoral immune responses of patients to the 2013-2014 and 2014-2015 HD IIV3 (Fluzone High-Dose; Sanofi Pasteur), which was administered as part of routine clinical care in 30 patients (17 with previously untreated CLL and 13 with MBL). The median patient age was 69.5 years.
The primary outcomes were seroconversion and seroprotection, as measured by hemagglutination inhibition assay (HAI).
Lower response rate
At day 28 post vaccination, the seroprotection rates for the overall cohort were 19/30 (63.3%) for A/H1N1, 21/23 (91.3%) for A/H3N2, and 13/30 (43.3%) for influenza B. Patients with MBL achieved significantly higher day 28 HAI geometric mean titers (GMT), compared with CLL patients (54.1 vs. 12.1]; P = .01), In addition, MBL patients achieved higher day 28 seroprotection rates against the influenza B vaccine strain virus than did those with CLL (76.9% vs. 17.6%; P = .002). Seroconversion rates for the overall cohort were 3/30 (10%) for A/H1N1; 5/23 (21.7%) for A/H3N2; and 3/30 (10%) for influenza B. No individual with CLL demonstrated seroconversion for influenza B, according to the researchers.
“Our studies reinforce rigorous adherence to vaccination strategies in patients with hematologic malignancy, including those with CLL, given the increased risk of serious complications among those experiencing influenza infection,” the authors stated.
“Even suboptimal responses to influenza vaccination can provide partial protection, reduce hospitalization rates, and/or prevent serious disease complications. Given the recent major issue with novel and aggressive viruses such COVID-19, we absolutely must continue with larger prospective studies to confirm these findings and evaluate vaccine effectiveness in preventing influenza or other novel viruses in these populations,” the researchers concluded.
This study was funded by the National Institutes of Health. Dr. Whitaker reported having no disclosures. Several of the coauthors reported financial relationships with a variety of pharmaceutical and biotechnology companies.
Immunogenicity of the high-dose influenza vaccine (HD IIV3) in patients with chronic lymphocytic leukemia (CLL) and monoclonal B-cell lymphocytosis (MBL, the precursor state to CLL) was found lower than reported in healthy adults according to a report in Vaccine.
In addition, immunogenicity to influenza B was found to be greater in those patients with MBL, compared with those with CLL.
“Acute and chronic leukemia patients hospitalized with influenza infection document a case fatality rate of 25%-37%,” according to Jennifer A. Whitaker, MD, of the Mayo Clinic, Rochester, Minn., and colleagues in pointing out the importance of their study.
The prospective pilot study assessed the humoral immune responses of patients to the 2013-2014 and 2014-2015 HD IIV3 (Fluzone High-Dose; Sanofi Pasteur), which was administered as part of routine clinical care in 30 patients (17 with previously untreated CLL and 13 with MBL). The median patient age was 69.5 years.
The primary outcomes were seroconversion and seroprotection, as measured by hemagglutination inhibition assay (HAI).
Lower response rate
At day 28 post vaccination, the seroprotection rates for the overall cohort were 19/30 (63.3%) for A/H1N1, 21/23 (91.3%) for A/H3N2, and 13/30 (43.3%) for influenza B. Patients with MBL achieved significantly higher day 28 HAI geometric mean titers (GMT), compared with CLL patients (54.1 vs. 12.1]; P = .01), In addition, MBL patients achieved higher day 28 seroprotection rates against the influenza B vaccine strain virus than did those with CLL (76.9% vs. 17.6%; P = .002). Seroconversion rates for the overall cohort were 3/30 (10%) for A/H1N1; 5/23 (21.7%) for A/H3N2; and 3/30 (10%) for influenza B. No individual with CLL demonstrated seroconversion for influenza B, according to the researchers.
“Our studies reinforce rigorous adherence to vaccination strategies in patients with hematologic malignancy, including those with CLL, given the increased risk of serious complications among those experiencing influenza infection,” the authors stated.
“Even suboptimal responses to influenza vaccination can provide partial protection, reduce hospitalization rates, and/or prevent serious disease complications. Given the recent major issue with novel and aggressive viruses such COVID-19, we absolutely must continue with larger prospective studies to confirm these findings and evaluate vaccine effectiveness in preventing influenza or other novel viruses in these populations,” the researchers concluded.
This study was funded by the National Institutes of Health. Dr. Whitaker reported having no disclosures. Several of the coauthors reported financial relationships with a variety of pharmaceutical and biotechnology companies.
Immunogenicity of the high-dose influenza vaccine (HD IIV3) in patients with chronic lymphocytic leukemia (CLL) and monoclonal B-cell lymphocytosis (MBL, the precursor state to CLL) was found lower than reported in healthy adults according to a report in Vaccine.
In addition, immunogenicity to influenza B was found to be greater in those patients with MBL, compared with those with CLL.
“Acute and chronic leukemia patients hospitalized with influenza infection document a case fatality rate of 25%-37%,” according to Jennifer A. Whitaker, MD, of the Mayo Clinic, Rochester, Minn., and colleagues in pointing out the importance of their study.
The prospective pilot study assessed the humoral immune responses of patients to the 2013-2014 and 2014-2015 HD IIV3 (Fluzone High-Dose; Sanofi Pasteur), which was administered as part of routine clinical care in 30 patients (17 with previously untreated CLL and 13 with MBL). The median patient age was 69.5 years.
The primary outcomes were seroconversion and seroprotection, as measured by hemagglutination inhibition assay (HAI).
Lower response rate
At day 28 post vaccination, the seroprotection rates for the overall cohort were 19/30 (63.3%) for A/H1N1, 21/23 (91.3%) for A/H3N2, and 13/30 (43.3%) for influenza B. Patients with MBL achieved significantly higher day 28 HAI geometric mean titers (GMT), compared with CLL patients (54.1 vs. 12.1]; P = .01), In addition, MBL patients achieved higher day 28 seroprotection rates against the influenza B vaccine strain virus than did those with CLL (76.9% vs. 17.6%; P = .002). Seroconversion rates for the overall cohort were 3/30 (10%) for A/H1N1; 5/23 (21.7%) for A/H3N2; and 3/30 (10%) for influenza B. No individual with CLL demonstrated seroconversion for influenza B, according to the researchers.
“Our studies reinforce rigorous adherence to vaccination strategies in patients with hematologic malignancy, including those with CLL, given the increased risk of serious complications among those experiencing influenza infection,” the authors stated.
“Even suboptimal responses to influenza vaccination can provide partial protection, reduce hospitalization rates, and/or prevent serious disease complications. Given the recent major issue with novel and aggressive viruses such COVID-19, we absolutely must continue with larger prospective studies to confirm these findings and evaluate vaccine effectiveness in preventing influenza or other novel viruses in these populations,” the researchers concluded.
This study was funded by the National Institutes of Health. Dr. Whitaker reported having no disclosures. Several of the coauthors reported financial relationships with a variety of pharmaceutical and biotechnology companies.
FROM VACCINE
Asymptomatic screening for COVID-19 in cancer patients still debated
Of more than 2,000 patients, less than 1% were found to be COVID-19 positive on asymptomatic screening, an investigator reported at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S09-04).
While several models have been proposed to screen for COVID-19 among cancer patients, the optimal strategy remains unknown, said investigator Justin A. Shaya, MD, of the University of California, San Diego.
The most commonly used approach is symptom/exposure-based screening and testing. However, other models have combined this method with polymerase chain reaction (PCR) testing for asymptomatic high-risk patients (such as those undergoing bone marrow transplant, receiving chemotherapy, or with hematologic malignancies) or with PCR testing for all asymptomatic cancer patients.
Dr. Shaya’s institution implemented a novel COVID-19 screening protocol for cancer patients receiving infusional therapy in May 2020.
The protocol required SARS-CoV-2 PCR testing for asymptomatic patients 24-96 hours prior to infusion. However, testing was only required before the administration of anticancer therapy. Infusion visits for supportive care interventions did not require previsit testing.
The researchers retrospectively analyzed data from patients with active cancer receiving infusional anticancer therapy who had at least one asymptomatic SARS-CoV-2 PCR test between June 1 and Dec. 1, 2020. The primary outcome was the rate of COVID-19 positivity among asymptomatic patients.
Results
Among 2,202 patients identified, 21 (0.95%) were found to be COVID-19 positive on asymptomatic screening. Most of these patients (90.5%) had solid tumors, but two (9.5%) had hematologic malignancies.
With respect to treatment, 16 patients (76.2%) received cytotoxic chemotherapy, 2 (9.5%) received targeted therapy, 1 (4.7%) received immunotherapy, and 2 (9.5%) were on a clinical trial.
At a median follow-up of 174 days from a positive PCR test (range, 55-223 days), only two patients (9.5%) developed COVID-related symptoms. Both patients had acute leukemia, and one required hospitalization for COVID-related complications.
In the COVID-19–positive cohort, 20 (95.2%) patients had their anticancer therapy delayed or deferred, with a median delay of 21 days (range, 7-77 days).
In the overall cohort, an additional 26 patients (1.2%) developed symptomatic COVID-19 during the study period.
“These results are particularly interesting because they come from a high-quality center that sees a large number of patients,” said Solange Peters, MD, PhD, of the University of Lausanne (Switzerland), who was not involved in this study.
“As they suggest, it is still a debate on how efficient routine screening is, asking the question whether we’re really detecting COVID-19 infection in our patients. Of course, it depends on the time and environment,” Dr. Peters added.
Dr. Shaya acknowledged that the small sample size was a key limitation of the study. Thus, the results may not be generalizable to other regions.
“One of the most striking things is that asymptomatic patients suffer very few consequences of COVID-19 infection, except for patients with hematologic malignancies,” Dr. Shaya said during a live discussion. “The majority of our patients had solid tumors and failed to develop any signs/symptoms of COVID infection.
“Routine screening provides a lot of security, and our institution is big enough to allow for it, and it seems our teams enjoy the fact of knowing the COVID status for each patient,” he continued.
Dr. Shaya and Dr. Peters disclosed no conflicts of interest. No funding sources were reported in the presentation.
Of more than 2,000 patients, less than 1% were found to be COVID-19 positive on asymptomatic screening, an investigator reported at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S09-04).
While several models have been proposed to screen for COVID-19 among cancer patients, the optimal strategy remains unknown, said investigator Justin A. Shaya, MD, of the University of California, San Diego.
The most commonly used approach is symptom/exposure-based screening and testing. However, other models have combined this method with polymerase chain reaction (PCR) testing for asymptomatic high-risk patients (such as those undergoing bone marrow transplant, receiving chemotherapy, or with hematologic malignancies) or with PCR testing for all asymptomatic cancer patients.
Dr. Shaya’s institution implemented a novel COVID-19 screening protocol for cancer patients receiving infusional therapy in May 2020.
The protocol required SARS-CoV-2 PCR testing for asymptomatic patients 24-96 hours prior to infusion. However, testing was only required before the administration of anticancer therapy. Infusion visits for supportive care interventions did not require previsit testing.
The researchers retrospectively analyzed data from patients with active cancer receiving infusional anticancer therapy who had at least one asymptomatic SARS-CoV-2 PCR test between June 1 and Dec. 1, 2020. The primary outcome was the rate of COVID-19 positivity among asymptomatic patients.
Results
Among 2,202 patients identified, 21 (0.95%) were found to be COVID-19 positive on asymptomatic screening. Most of these patients (90.5%) had solid tumors, but two (9.5%) had hematologic malignancies.
With respect to treatment, 16 patients (76.2%) received cytotoxic chemotherapy, 2 (9.5%) received targeted therapy, 1 (4.7%) received immunotherapy, and 2 (9.5%) were on a clinical trial.
At a median follow-up of 174 days from a positive PCR test (range, 55-223 days), only two patients (9.5%) developed COVID-related symptoms. Both patients had acute leukemia, and one required hospitalization for COVID-related complications.
In the COVID-19–positive cohort, 20 (95.2%) patients had their anticancer therapy delayed or deferred, with a median delay of 21 days (range, 7-77 days).
In the overall cohort, an additional 26 patients (1.2%) developed symptomatic COVID-19 during the study period.
“These results are particularly interesting because they come from a high-quality center that sees a large number of patients,” said Solange Peters, MD, PhD, of the University of Lausanne (Switzerland), who was not involved in this study.
“As they suggest, it is still a debate on how efficient routine screening is, asking the question whether we’re really detecting COVID-19 infection in our patients. Of course, it depends on the time and environment,” Dr. Peters added.
Dr. Shaya acknowledged that the small sample size was a key limitation of the study. Thus, the results may not be generalizable to other regions.
“One of the most striking things is that asymptomatic patients suffer very few consequences of COVID-19 infection, except for patients with hematologic malignancies,” Dr. Shaya said during a live discussion. “The majority of our patients had solid tumors and failed to develop any signs/symptoms of COVID infection.
“Routine screening provides a lot of security, and our institution is big enough to allow for it, and it seems our teams enjoy the fact of knowing the COVID status for each patient,” he continued.
Dr. Shaya and Dr. Peters disclosed no conflicts of interest. No funding sources were reported in the presentation.
Of more than 2,000 patients, less than 1% were found to be COVID-19 positive on asymptomatic screening, an investigator reported at the AACR Virtual Meeting: COVID-19 and Cancer (Abstract S09-04).
While several models have been proposed to screen for COVID-19 among cancer patients, the optimal strategy remains unknown, said investigator Justin A. Shaya, MD, of the University of California, San Diego.
The most commonly used approach is symptom/exposure-based screening and testing. However, other models have combined this method with polymerase chain reaction (PCR) testing for asymptomatic high-risk patients (such as those undergoing bone marrow transplant, receiving chemotherapy, or with hematologic malignancies) or with PCR testing for all asymptomatic cancer patients.
Dr. Shaya’s institution implemented a novel COVID-19 screening protocol for cancer patients receiving infusional therapy in May 2020.
The protocol required SARS-CoV-2 PCR testing for asymptomatic patients 24-96 hours prior to infusion. However, testing was only required before the administration of anticancer therapy. Infusion visits for supportive care interventions did not require previsit testing.
The researchers retrospectively analyzed data from patients with active cancer receiving infusional anticancer therapy who had at least one asymptomatic SARS-CoV-2 PCR test between June 1 and Dec. 1, 2020. The primary outcome was the rate of COVID-19 positivity among asymptomatic patients.
Results
Among 2,202 patients identified, 21 (0.95%) were found to be COVID-19 positive on asymptomatic screening. Most of these patients (90.5%) had solid tumors, but two (9.5%) had hematologic malignancies.
With respect to treatment, 16 patients (76.2%) received cytotoxic chemotherapy, 2 (9.5%) received targeted therapy, 1 (4.7%) received immunotherapy, and 2 (9.5%) were on a clinical trial.
At a median follow-up of 174 days from a positive PCR test (range, 55-223 days), only two patients (9.5%) developed COVID-related symptoms. Both patients had acute leukemia, and one required hospitalization for COVID-related complications.
In the COVID-19–positive cohort, 20 (95.2%) patients had their anticancer therapy delayed or deferred, with a median delay of 21 days (range, 7-77 days).
In the overall cohort, an additional 26 patients (1.2%) developed symptomatic COVID-19 during the study period.
“These results are particularly interesting because they come from a high-quality center that sees a large number of patients,” said Solange Peters, MD, PhD, of the University of Lausanne (Switzerland), who was not involved in this study.
“As they suggest, it is still a debate on how efficient routine screening is, asking the question whether we’re really detecting COVID-19 infection in our patients. Of course, it depends on the time and environment,” Dr. Peters added.
Dr. Shaya acknowledged that the small sample size was a key limitation of the study. Thus, the results may not be generalizable to other regions.
“One of the most striking things is that asymptomatic patients suffer very few consequences of COVID-19 infection, except for patients with hematologic malignancies,” Dr. Shaya said during a live discussion. “The majority of our patients had solid tumors and failed to develop any signs/symptoms of COVID infection.
“Routine screening provides a lot of security, and our institution is big enough to allow for it, and it seems our teams enjoy the fact of knowing the COVID status for each patient,” he continued.
Dr. Shaya and Dr. Peters disclosed no conflicts of interest. No funding sources were reported in the presentation.
FROM AACR: COVID-19 AND CANCER 2021