User login
Socioeconomic Status Linked to Psychiatric Disorders in Older Women Veterans
TOPLINE: Psychiatric disorders affect 37.8% of veteran vs 37.3% of nonveteran in a study of > 42,000 women aged ≥ 65 years. Most differences between veterans and nonveterans were statistically insignificant after removing confounders.
METHODOLOGY:
Researchers analyzed 42,031 Women's Health Initiative (WHI) participants aged > 65 years at enrollment (1993-1998), including 1,512 veterans and 40,519 non-veterans, through linked WHI-Medicare databases with approximately 15 years of follow-up.
Analysis included multivariable logistic and Cox regression models to evaluate characteristics associated with prevalent and incident psychiatric disorders, respectively.
Participants were followed from WHI enrollment until first psychiatric diagnosis, with censoring at death, end of follow-up, or December 31, 2013.
Investigators examined relationships between individual-level and neighborhood-level socioeconomic status indicators with psychiatric disorders before and after stratification by veteran status.
TAKEAWAY:
The overall prevalence of psychiatric disorders was 37.3%, with an incidence rate of 25.5 per 1,000 person-years, showing no significant differences between veterans and non-veterans (odds ratio [OR], 0.95; 95% confidence interval [CI], 0.85-0.06).
There was a higher prevalence of psychiatric disorders for women veterans with technical, sales, or administrative occupations (adjusted OR [aOR], 1.72; 95 % CI, 1.02, 2.89) and those with “other” occupations (aOR, 2.09; 95 % CI, 1.13, 3.88) when compared with women veterans with managerial or professional occupations.
Mood and anxiety disorders emerged as the leading types of psychiatric conditions among both veteran and nonveteran women.
IN PRACTICE: "Although interaction effects by veteran status were nonsignificant,” the authors of the study explained, “lower education, household income, and neighborhood socioeconomic status were associated with higher frequencies of psychiatric disorders only among women non-veterans.”
SOURCE: The study was led by Jack Tsai and the US Department of Veterans Affairs National Center on Homelessness Among Veterans in Washington, DC. It was published online in Journal of Affective Disorders.
LIMITATIONS: The study faced several limitations including potential selection and survival biases, as findings correspond only to Women's Health Initiative participants who survived until age 65 or later. Information bias likely occurred due to self-reported measures and sole reliance on International Classification of Disease, 9th revision, Clinical Modification diagnostic codes from Medicare claims. Additionally, socioeconomic status indicators assessed at enrollment may not reflect early life or midlife exposures that could influence psychiatric diagnoses.
DISCLOSURES: The Women’s Health Initiative program received funding from the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through grants 75N92021D00001, 75N92021D00002, 75N92021D00003, 75N92021D00004, and 75N92021D00005.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
TOPLINE: Psychiatric disorders affect 37.8% of veteran vs 37.3% of nonveteran in a study of > 42,000 women aged ≥ 65 years. Most differences between veterans and nonveterans were statistically insignificant after removing confounders.
METHODOLOGY:
Researchers analyzed 42,031 Women's Health Initiative (WHI) participants aged > 65 years at enrollment (1993-1998), including 1,512 veterans and 40,519 non-veterans, through linked WHI-Medicare databases with approximately 15 years of follow-up.
Analysis included multivariable logistic and Cox regression models to evaluate characteristics associated with prevalent and incident psychiatric disorders, respectively.
Participants were followed from WHI enrollment until first psychiatric diagnosis, with censoring at death, end of follow-up, or December 31, 2013.
Investigators examined relationships between individual-level and neighborhood-level socioeconomic status indicators with psychiatric disorders before and after stratification by veteran status.
TAKEAWAY:
The overall prevalence of psychiatric disorders was 37.3%, with an incidence rate of 25.5 per 1,000 person-years, showing no significant differences between veterans and non-veterans (odds ratio [OR], 0.95; 95% confidence interval [CI], 0.85-0.06).
There was a higher prevalence of psychiatric disorders for women veterans with technical, sales, or administrative occupations (adjusted OR [aOR], 1.72; 95 % CI, 1.02, 2.89) and those with “other” occupations (aOR, 2.09; 95 % CI, 1.13, 3.88) when compared with women veterans with managerial or professional occupations.
Mood and anxiety disorders emerged as the leading types of psychiatric conditions among both veteran and nonveteran women.
IN PRACTICE: "Although interaction effects by veteran status were nonsignificant,” the authors of the study explained, “lower education, household income, and neighborhood socioeconomic status were associated with higher frequencies of psychiatric disorders only among women non-veterans.”
SOURCE: The study was led by Jack Tsai and the US Department of Veterans Affairs National Center on Homelessness Among Veterans in Washington, DC. It was published online in Journal of Affective Disorders.
LIMITATIONS: The study faced several limitations including potential selection and survival biases, as findings correspond only to Women's Health Initiative participants who survived until age 65 or later. Information bias likely occurred due to self-reported measures and sole reliance on International Classification of Disease, 9th revision, Clinical Modification diagnostic codes from Medicare claims. Additionally, socioeconomic status indicators assessed at enrollment may not reflect early life or midlife exposures that could influence psychiatric diagnoses.
DISCLOSURES: The Women’s Health Initiative program received funding from the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through grants 75N92021D00001, 75N92021D00002, 75N92021D00003, 75N92021D00004, and 75N92021D00005.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
TOPLINE: Psychiatric disorders affect 37.8% of veteran vs 37.3% of nonveteran in a study of > 42,000 women aged ≥ 65 years. Most differences between veterans and nonveterans were statistically insignificant after removing confounders.
METHODOLOGY:
Researchers analyzed 42,031 Women's Health Initiative (WHI) participants aged > 65 years at enrollment (1993-1998), including 1,512 veterans and 40,519 non-veterans, through linked WHI-Medicare databases with approximately 15 years of follow-up.
Analysis included multivariable logistic and Cox regression models to evaluate characteristics associated with prevalent and incident psychiatric disorders, respectively.
Participants were followed from WHI enrollment until first psychiatric diagnosis, with censoring at death, end of follow-up, or December 31, 2013.
Investigators examined relationships between individual-level and neighborhood-level socioeconomic status indicators with psychiatric disorders before and after stratification by veteran status.
TAKEAWAY:
The overall prevalence of psychiatric disorders was 37.3%, with an incidence rate of 25.5 per 1,000 person-years, showing no significant differences between veterans and non-veterans (odds ratio [OR], 0.95; 95% confidence interval [CI], 0.85-0.06).
There was a higher prevalence of psychiatric disorders for women veterans with technical, sales, or administrative occupations (adjusted OR [aOR], 1.72; 95 % CI, 1.02, 2.89) and those with “other” occupations (aOR, 2.09; 95 % CI, 1.13, 3.88) when compared with women veterans with managerial or professional occupations.
Mood and anxiety disorders emerged as the leading types of psychiatric conditions among both veteran and nonveteran women.
IN PRACTICE: "Although interaction effects by veteran status were nonsignificant,” the authors of the study explained, “lower education, household income, and neighborhood socioeconomic status were associated with higher frequencies of psychiatric disorders only among women non-veterans.”
SOURCE: The study was led by Jack Tsai and the US Department of Veterans Affairs National Center on Homelessness Among Veterans in Washington, DC. It was published online in Journal of Affective Disorders.
LIMITATIONS: The study faced several limitations including potential selection and survival biases, as findings correspond only to Women's Health Initiative participants who survived until age 65 or later. Information bias likely occurred due to self-reported measures and sole reliance on International Classification of Disease, 9th revision, Clinical Modification diagnostic codes from Medicare claims. Additionally, socioeconomic status indicators assessed at enrollment may not reflect early life or midlife exposures that could influence psychiatric diagnoses.
DISCLOSURES: The Women’s Health Initiative program received funding from the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through grants 75N92021D00001, 75N92021D00002, 75N92021D00003, 75N92021D00004, and 75N92021D00005.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Nine VA Facilities to Open Research Trials for Psychedelics
Nine VA Facilities to Open Research Trials for Psychedelics
On Nov. 22, 2014, 8 years after he came back from Iraq with “crippling” posttraumatic stress disorder (PTSD), Jonathan Lubecky took his first dose of the psychedelic compound methylenedioxymethamphetamine (MDMA). Lubecky, a Marine, Army, and National Guard veteran, described his path to MDMA therapy in in the New Horizons in Health podcast.
After 5 suicide attempts and “the hundreds of times I thought about it or stood on a bridge or had a plan,” he felt he had run out of options. Then, in a counseling session, a psychiatric intern slid a piece of paper across the table to him. It read “Google MDMA PTSD.”
Luckily for Lubecky, a space in a clinical trial opened up, in which he had 8 hours of talk therapy with specially trained therapists, combined with MDMA. “MDMA is a tool that opens up the mind, body and spirit,” he said, “so you can heal and process all those memories and traumas that are causing yourissues. It puts you in a middle place where you can talk about trauma without having panic attacks, without your body betraying you, and look at it from a different perspective.” said he added, “It’s like doing therapy while being hugged by everyone who loves you in a bathtub full of puppies licking your face.” In 2023, 9 years after that first dose, Lubecky said, “I’ve been PTSD free longer than I had it.”
And now, in 2025, the research into psychedelic therapy for veterans like Lubecky is taking another step forward according to a report by Military.com. Nine VA facilities, in the Bronx, Los Angeles, Omaha, Palo Alto, Portland (Oregon), San Diego, San Francisco, West Haven, and White River Junction, are participating in long-term studies to test the safety and clinical impact of psychedelic compounds for PTSD, treatment-resistant depression, and anxiety disorders.
Early trials from Johns Hopkins University, the Multidisciplinary Association for Psychedelic Studies (MAPS), and others found significant symptom reductions for some participants with chronic PTSD. MAPP2, the multisite phase 3 study that extended the findings of MAPP1, found that MDMA-assisted therapy significantly improved PTSD symptoms and functional impairment, compared with placebo-assisted therapy. Notably, of the 52 participants (including 16 veterans) 45 (86%) achieved a clinically meaningful benefit, and 37 (71%) no longer met criteria for PTSD by study end. Despite the promising findings, a US Food and Drug Administration (FDA) advisory panel recommended against approving the treatment.
In 2024 the VA issued a request for applications for proposals from its network of VA researchers and academic institutions to gather “definitive scientific evidence” on the potential efficacy and safety of psychedelic compounds, such as MDMA and psilocybin, when used in conjunction with psychotherapy. It would be the first time since the 1960s that the VA had funded research on such compounds.
Funding proposals for such research have cycled in and out of Congress for years, but have gathered more steam in the last few years. The 2024 National Defense Authorization Act directed the US Department of Defense to establish a process for funding clinical research into the use of certain psychedelic substances to treat PTSD and traumatic brain injury. In April 2024, Representatives Lou Correa (D-CA) and Jack Bergman (R-MI), cochairs of the Psychedelics Advancing Therapies (PATH) caucus, introduced the Innovative Therapies Centers of Excellence Act of 2025, bipartisan legislation that would increase federally funded research on innovative therapies to treat veterans with PTSD, substance use disorder, and depression. It would also, if enacted, direct the VA to create ≥ 5 dedicated centers of excellence to study the therapeutic uses of psychedelic substances. The bill has also been endorsed by the American Legion, Veterans of Foreign Wars, Iraq and Afghanistan Veterans of America, Disabled American Veterans, and the Wounded Warrior Project.
The current administration has two strong high-level supporters of psychedelics research: VA Secretary Doug Collins and US Department of Health and Human Service Secretary Robert F. Kennedy Jr. Sec. Kennedy has castigated the FDA for what he calls “aggressive suppression” of alternative and complementary treatments, including psychedelics. This, although the FDA granted breakthrough therapy status for MDMA for treating PTSD and psilocybin for treating depression in 2018 and 2019, respectively, as well a pivotal draft guidance in 2023 for the development of psychedelic drugs for psychiatric disorders, substance use disorders, and various medical conditions.
Collins, citing an “eye-opening” discussion with Kennedy, enthusiastically backs the research into psychedelics. In a May 2025 hearing that was mainly a series of testy exchanges about his proposed budget slashing, he emphasized the importance of keeping and expanding VA programs and studies on psychedelic treatments, something he has been advocating for since the beginning of his appointment. “We want to make sure we’re not closing off any outlet for a veteran who could be helped by these programs,” he said.
Taking the intern’s advice to look into MDMA, Jonathan Lubecky said, was one of the best decisions he’d ever made. But “it’s not the MDMA that fixes you,” he said. “It’s the therapy. It’s the therapist working with you and you doing the hard work.”
On Nov. 22, 2014, 8 years after he came back from Iraq with “crippling” posttraumatic stress disorder (PTSD), Jonathan Lubecky took his first dose of the psychedelic compound methylenedioxymethamphetamine (MDMA). Lubecky, a Marine, Army, and National Guard veteran, described his path to MDMA therapy in in the New Horizons in Health podcast.
After 5 suicide attempts and “the hundreds of times I thought about it or stood on a bridge or had a plan,” he felt he had run out of options. Then, in a counseling session, a psychiatric intern slid a piece of paper across the table to him. It read “Google MDMA PTSD.”
Luckily for Lubecky, a space in a clinical trial opened up, in which he had 8 hours of talk therapy with specially trained therapists, combined with MDMA. “MDMA is a tool that opens up the mind, body and spirit,” he said, “so you can heal and process all those memories and traumas that are causing yourissues. It puts you in a middle place where you can talk about trauma without having panic attacks, without your body betraying you, and look at it from a different perspective.” said he added, “It’s like doing therapy while being hugged by everyone who loves you in a bathtub full of puppies licking your face.” In 2023, 9 years after that first dose, Lubecky said, “I’ve been PTSD free longer than I had it.”
And now, in 2025, the research into psychedelic therapy for veterans like Lubecky is taking another step forward according to a report by Military.com. Nine VA facilities, in the Bronx, Los Angeles, Omaha, Palo Alto, Portland (Oregon), San Diego, San Francisco, West Haven, and White River Junction, are participating in long-term studies to test the safety and clinical impact of psychedelic compounds for PTSD, treatment-resistant depression, and anxiety disorders.
Early trials from Johns Hopkins University, the Multidisciplinary Association for Psychedelic Studies (MAPS), and others found significant symptom reductions for some participants with chronic PTSD. MAPP2, the multisite phase 3 study that extended the findings of MAPP1, found that MDMA-assisted therapy significantly improved PTSD symptoms and functional impairment, compared with placebo-assisted therapy. Notably, of the 52 participants (including 16 veterans) 45 (86%) achieved a clinically meaningful benefit, and 37 (71%) no longer met criteria for PTSD by study end. Despite the promising findings, a US Food and Drug Administration (FDA) advisory panel recommended against approving the treatment.
In 2024 the VA issued a request for applications for proposals from its network of VA researchers and academic institutions to gather “definitive scientific evidence” on the potential efficacy and safety of psychedelic compounds, such as MDMA and psilocybin, when used in conjunction with psychotherapy. It would be the first time since the 1960s that the VA had funded research on such compounds.
Funding proposals for such research have cycled in and out of Congress for years, but have gathered more steam in the last few years. The 2024 National Defense Authorization Act directed the US Department of Defense to establish a process for funding clinical research into the use of certain psychedelic substances to treat PTSD and traumatic brain injury. In April 2024, Representatives Lou Correa (D-CA) and Jack Bergman (R-MI), cochairs of the Psychedelics Advancing Therapies (PATH) caucus, introduced the Innovative Therapies Centers of Excellence Act of 2025, bipartisan legislation that would increase federally funded research on innovative therapies to treat veterans with PTSD, substance use disorder, and depression. It would also, if enacted, direct the VA to create ≥ 5 dedicated centers of excellence to study the therapeutic uses of psychedelic substances. The bill has also been endorsed by the American Legion, Veterans of Foreign Wars, Iraq and Afghanistan Veterans of America, Disabled American Veterans, and the Wounded Warrior Project.
The current administration has two strong high-level supporters of psychedelics research: VA Secretary Doug Collins and US Department of Health and Human Service Secretary Robert F. Kennedy Jr. Sec. Kennedy has castigated the FDA for what he calls “aggressive suppression” of alternative and complementary treatments, including psychedelics. This, although the FDA granted breakthrough therapy status for MDMA for treating PTSD and psilocybin for treating depression in 2018 and 2019, respectively, as well a pivotal draft guidance in 2023 for the development of psychedelic drugs for psychiatric disorders, substance use disorders, and various medical conditions.
Collins, citing an “eye-opening” discussion with Kennedy, enthusiastically backs the research into psychedelics. In a May 2025 hearing that was mainly a series of testy exchanges about his proposed budget slashing, he emphasized the importance of keeping and expanding VA programs and studies on psychedelic treatments, something he has been advocating for since the beginning of his appointment. “We want to make sure we’re not closing off any outlet for a veteran who could be helped by these programs,” he said.
Taking the intern’s advice to look into MDMA, Jonathan Lubecky said, was one of the best decisions he’d ever made. But “it’s not the MDMA that fixes you,” he said. “It’s the therapy. It’s the therapist working with you and you doing the hard work.”
On Nov. 22, 2014, 8 years after he came back from Iraq with “crippling” posttraumatic stress disorder (PTSD), Jonathan Lubecky took his first dose of the psychedelic compound methylenedioxymethamphetamine (MDMA). Lubecky, a Marine, Army, and National Guard veteran, described his path to MDMA therapy in in the New Horizons in Health podcast.
After 5 suicide attempts and “the hundreds of times I thought about it or stood on a bridge or had a plan,” he felt he had run out of options. Then, in a counseling session, a psychiatric intern slid a piece of paper across the table to him. It read “Google MDMA PTSD.”
Luckily for Lubecky, a space in a clinical trial opened up, in which he had 8 hours of talk therapy with specially trained therapists, combined with MDMA. “MDMA is a tool that opens up the mind, body and spirit,” he said, “so you can heal and process all those memories and traumas that are causing yourissues. It puts you in a middle place where you can talk about trauma without having panic attacks, without your body betraying you, and look at it from a different perspective.” said he added, “It’s like doing therapy while being hugged by everyone who loves you in a bathtub full of puppies licking your face.” In 2023, 9 years after that first dose, Lubecky said, “I’ve been PTSD free longer than I had it.”
And now, in 2025, the research into psychedelic therapy for veterans like Lubecky is taking another step forward according to a report by Military.com. Nine VA facilities, in the Bronx, Los Angeles, Omaha, Palo Alto, Portland (Oregon), San Diego, San Francisco, West Haven, and White River Junction, are participating in long-term studies to test the safety and clinical impact of psychedelic compounds for PTSD, treatment-resistant depression, and anxiety disorders.
Early trials from Johns Hopkins University, the Multidisciplinary Association for Psychedelic Studies (MAPS), and others found significant symptom reductions for some participants with chronic PTSD. MAPP2, the multisite phase 3 study that extended the findings of MAPP1, found that MDMA-assisted therapy significantly improved PTSD symptoms and functional impairment, compared with placebo-assisted therapy. Notably, of the 52 participants (including 16 veterans) 45 (86%) achieved a clinically meaningful benefit, and 37 (71%) no longer met criteria for PTSD by study end. Despite the promising findings, a US Food and Drug Administration (FDA) advisory panel recommended against approving the treatment.
In 2024 the VA issued a request for applications for proposals from its network of VA researchers and academic institutions to gather “definitive scientific evidence” on the potential efficacy and safety of psychedelic compounds, such as MDMA and psilocybin, when used in conjunction with psychotherapy. It would be the first time since the 1960s that the VA had funded research on such compounds.
Funding proposals for such research have cycled in and out of Congress for years, but have gathered more steam in the last few years. The 2024 National Defense Authorization Act directed the US Department of Defense to establish a process for funding clinical research into the use of certain psychedelic substances to treat PTSD and traumatic brain injury. In April 2024, Representatives Lou Correa (D-CA) and Jack Bergman (R-MI), cochairs of the Psychedelics Advancing Therapies (PATH) caucus, introduced the Innovative Therapies Centers of Excellence Act of 2025, bipartisan legislation that would increase federally funded research on innovative therapies to treat veterans with PTSD, substance use disorder, and depression. It would also, if enacted, direct the VA to create ≥ 5 dedicated centers of excellence to study the therapeutic uses of psychedelic substances. The bill has also been endorsed by the American Legion, Veterans of Foreign Wars, Iraq and Afghanistan Veterans of America, Disabled American Veterans, and the Wounded Warrior Project.
The current administration has two strong high-level supporters of psychedelics research: VA Secretary Doug Collins and US Department of Health and Human Service Secretary Robert F. Kennedy Jr. Sec. Kennedy has castigated the FDA for what he calls “aggressive suppression” of alternative and complementary treatments, including psychedelics. This, although the FDA granted breakthrough therapy status for MDMA for treating PTSD and psilocybin for treating depression in 2018 and 2019, respectively, as well a pivotal draft guidance in 2023 for the development of psychedelic drugs for psychiatric disorders, substance use disorders, and various medical conditions.
Collins, citing an “eye-opening” discussion with Kennedy, enthusiastically backs the research into psychedelics. In a May 2025 hearing that was mainly a series of testy exchanges about his proposed budget slashing, he emphasized the importance of keeping and expanding VA programs and studies on psychedelic treatments, something he has been advocating for since the beginning of his appointment. “We want to make sure we’re not closing off any outlet for a veteran who could be helped by these programs,” he said.
Taking the intern’s advice to look into MDMA, Jonathan Lubecky said, was one of the best decisions he’d ever made. But “it’s not the MDMA that fixes you,” he said. “It’s the therapy. It’s the therapist working with you and you doing the hard work.”
Nine VA Facilities to Open Research Trials for Psychedelics
Nine VA Facilities to Open Research Trials for Psychedelics
Process Improvement for Engaging With Trauma-Focused Evidence-Based Psychotherapy for PTSD
Process Improvement for Engaging With Trauma-Focused Evidence-Based Psychotherapy for PTSD
Trauma-focused evidence-based psychotherapies (TF-EBPs), including cognitive processing therapy (CPT) and prolonged exposure therapy (PE), are recommended treatments for posttraumatic stress disorder (PTSD) in clinical practice guidelines.1-3 To increase initiation of these treatments, the US Department of Veterans Affairs (VA) used a large-scale dissemination and implementation effort to improve access to TF-EBP.4,5 These efforts achieved modest success, increasing prevalence of TF-EBP from a handful of veterans in 2004 to an annual prevalence of 14.6% for CPT and 4.3% for PE in 2014.6
Throughout these efforts, qualitative studies have been used to better understand veterans’ perspectives on receiving TF-EBP care.7-18 Barriers to initiation of and engagement in TF-EBP and PTSD care have been identified from these qualitative studies. One identified barrier was lack of knowledge—particularly lack of knowledge about what is meant by a PTSD diagnosis and available treatments.7-10 Stigma (ie, automatic negative associations) toward mental health problems or seeking mental health care also has been identified as a barrier to initiation.7,10-14 Perceptions of poor alignment between treatment and veteran goals, including lack of buy-in for the rationale, served as barriers to initiation and engagement.8,15-18
Using prior qualitative work, numerous initiatives have been developed to reduce stigma, facilitate conversations about how treatment aligns with goals, and fill knowledge gaps, particularly through online resources and shared decision-making.19,20 To better inform the state of veterans’ experiences with TF-EBP, a qualitative investigation was conducted involving veterans who recently initiated TF-EBP. Themes directly related to transitions to TF-EBP were identified; however, all veterans interviewed also described their experiences with TFEBP engagement and mental health care. Consistent with recommendations for qualitative methods, this study extends prior work on transitions to TF-EBP by describing themes with a distinct focus on the experience of engaging with TF-EBP and mental health care.21,22
Methods
The experiences of veterans who were transitioning into TF-EBPs were collected in semistructured interviews and analyzed. The semistructured interview guide was developed and refined in consultation with both qualitative methods experts and PTSD treatment experts to ensure that 6 content domains were appropriately queried: PTSD treatment options, cultural sensitivity of treatment, PTSD treatment selection, transition criteria, beliefs about stabilization treatment, and treatment needs/preferences.
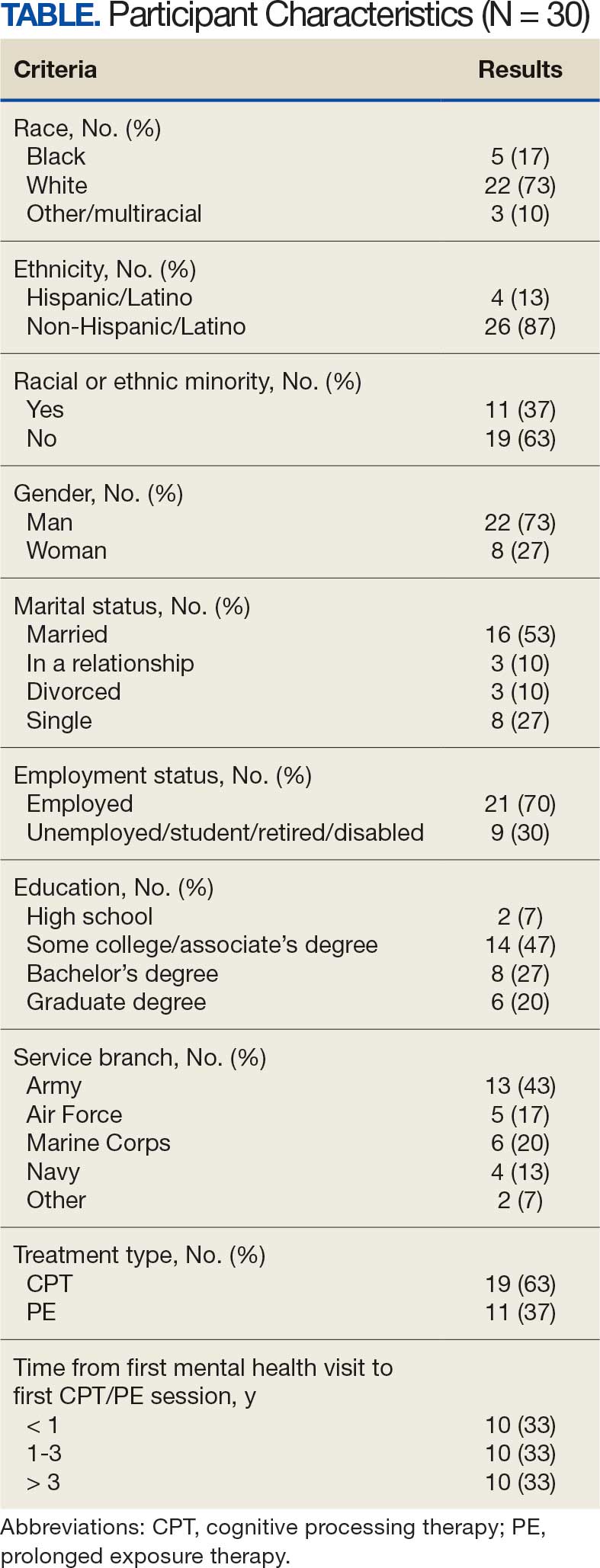
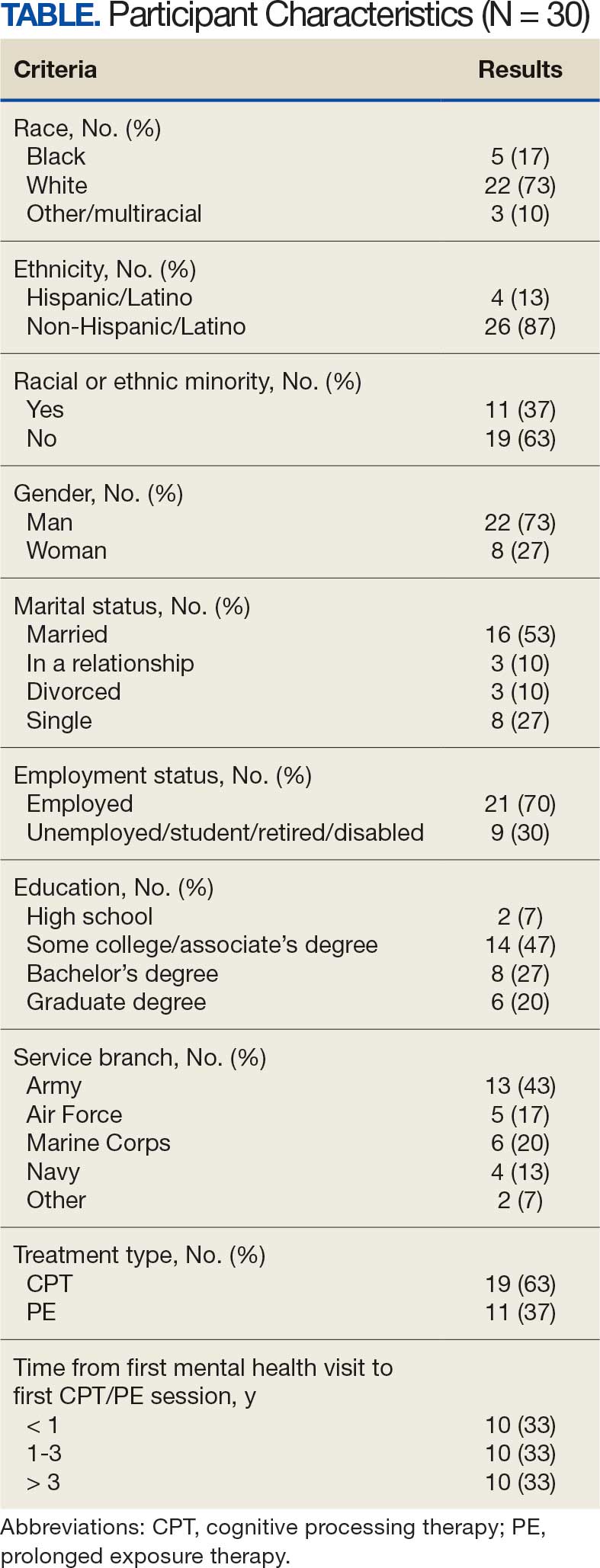
Participants were identified using the VA Corporate Data Warehouse and included post-9/11 veterans who had recently initiated CPT or PE for the first time between September 1, 2021, and September 1, 2022. More details of participant selection are available in Holder et al.21 From a population of 10,814 patients, stratified random sampling generated a recruitment pool of 200 veterans for further outreach. The strata were defined such that this recruitment pool had similar proportions of demographic characteristics (ie, gender, race, ethnicity) to the population of eligible veterans, equivalent distributions of time to CPT or PE initiation (ie, 33.3% < 1 year, 33.3% 1-3 years, and 33.3% > 3 years), and adequate variability in TF-EBP type (ie, 66.7% CPT, 33.3% PE). A manual chart review in the recruitment pool excluded 12 veterans who did not initiate CPT or PE, 1 veteran with evidence of current active psychosis and/or cognitive impairment that would likely preclude comprehension of study materials, and 1 who was deceased.
Eligible veterans from the recruitment pool were contacted in groups of 25. First, a recruitment letter with study information and instructions to opt-out of further contact was mailed or emailed to veterans. After 2 weeks, veterans who had not responded were contacted by phone up to 3 times. Veterans interested in participating were scheduled for a 1-time visit that included verbal consent and the qualitative interview. Metrics were established a priori to ensure an adequately diverse and inclusive sample. Specifically, a minimum number of racial and/or ethnic minority veterans (33%) and women veterans (20%) were sought. Equal distribution across the 3 categories of time from first mental health visit to CPT/PE initiation also was targeted. Throughout enrollment, recruitment efforts were adapted to meet these metrics in the emerging sample. While the goal was to generate a diverse and inclusive sample using these methods, the sample was not intended to be representative of the population.
Of the 186 eligible participants, 21 declined participation and 26 could not be reached. The targeted sample was reached after exhausting contact for 47 veterans and contacting 80 veterans for a final response rate of 40% among fully contacted veterans and 27% among veterans with any contact. The final sample included 30 veterans who received CPT or PE in VA facilities (Table).
After veterans provided verbal consent for study participation, sociodemographic information was verbally reported, and a 30- to 60-minute semistructured qualitative phone interview was recorded and transcribed. Veterans received $40 for participation. All procedures were approved by the University of California San Francisco Institutional Review Board.
Qualitative Data Analysis
Rapid analysis procedures were used to analyze qualitative data. This approach is suitable for focused, moderately structured qualitative analyses in health services research and facilitates rapid dissemination to stakeholders.23 The qualitative analysts were 2 clinical psychologists with expertise in PTSD treatment (NH primary and RR secondary). Consistent with rapid analysis procedures, analysts prepared a templated summary (including relevant quotations) of each interview, organized by the prespecified content domains. Interviews were summarized independently, compared to ensure consistency, and discrepancies were resolved through review of the interview source materials. Individual summary templates were combined into a master analytic matrix to facilitate the identification of patterns and delineation of themes. Analysts routinely met to identify, discuss, and refine preliminary themes, revisiting source materials to reach consensus as needed.
Results
Fifteen themes were identified and organized into 2 distinct focus areas: themes directly related to the transition to TF-EBP (8 themes) and themes related to veterans’ experiences with TF-EBP and general mental health care with potential process-improvement implications (7 themes).21 Seven themes were identified related to experiences with TF-EBP engagement and VA mental health care. The 7 themes related to TF-EBP engagement and VA mental health care themes are summarized with exemplary quotations.
Veterans want a better understanding of psychotherapy and engaging with VA mental health. Veterans reported that they generally had a poor or “nebulous” understanding about the experience of psychotherapy. For example, veterans exhibited confusion about whether certain experiences were equivalent to participating in psychotherapy. They were sometimes unable to distinguish between interactions such as assessment, disability evaluations, peer support, and psychotherapy. One veteran described a conversation with a TFEBP therapist about prior treatment:
She [asked], have you ever been, or gone through a therapy to begin with? And I, I said, well I just chatted with somebody. And she said that’s not, that’s not therapy. So, I was like, oh, it’s not? That’s not what people do?
Veterans were surprised the VA offered a diverse range of psychotherapy interventions, rather than simply therapy. They did not realize there were different types of psychotherapy. As a result, veterans were not aware that some VA mental practitioners have specialty training and certification to provide treatment matched to specific diagnoses or needs. They thought that all clinicians could provide the same care. One veteran described their understanding:
I just figured all mental health people are mental health people. I didn’t have a better understanding of the system and all the different levels and how it plays out and specialties and things like that. Which, I guess, I should have because you have a primary care doctor, but then you have specialists in all these other different sectors that specialize in one particular area. I guess that should’ve been common sense, but it wasn’t.
Stigma was a barrier to seeking and engaging in mental health care. Veterans discovered they had to overcome stigma associated with seeking and engaging in mental health treatment. Military culture was often discussed as promoting stigma regarding mental health treatment. Specifically, veterans described that seeking treatment meant “either, I’m weak or I’m gonna be seen as weak.” In active-duty settings, the strategy for dealing with mental health symptoms was to “leave those feelings, you push ‘em aside,” an approach highly inconsistent with TF-EBP. In some cases, incorrect information about the VA and PTSD was presented as part of discharge from the military, leading to long-term skepticism of the VA and PTSD treatment. One veteran described his experience as part of a class on the VA compensation and pension assessment process for service-connected disabilities during his military discharge:
[A fellow discharging soldier asked] what about like PTSD, gettin’ rated for PTSD. I hear they take our weapons and stuff like we can’t own firearms and all that stuff. And [the instructor] was like, well, yes that’s a thing. He didn’t explain it like if you get compensated for PTSD you don’t lose your rights to carry a firearm or to have, to be able to go hunting.
Importantly, veterans often described how other identities (eg, race, ethnicity, gender, region of origin) interacted with military culture to enhance stigma. Hearing messaging from multiple sources reinforced beliefs that mental health treatment is inappropriate or is associated with weakness:
As a first-generation Italian, I was always taught keep your feelings to yourself. Never talk outside your family. Never bring up problems to other people and stuff like that. Same with the military. And then the old stigma working in [emergency medical services] and public safety, you’re weak if you get help.
The fundamentals of therapy, including rapport and flexibility, were important. Veterans valued nonspecific therapy factors, genuine empathy, building trust, being honest about treatment, personality, and rapport. These characteristics were almost universally described as particularly important:
I liked the fact that she made it personable and she cared. It wasn’t just like, here, we’re gonna start this. She explained it in the ways I could understand, not in medical terms, so to speak, but that’s what I liked about her. She really cared about what she did and helping me.
Flexibility was viewed as an asset, particularly when clinicians acknowledged veteran autonomy. A consistent example was when veterans were able to titrate trauma disclosure. One veteran described this flexible treatment experience: “She was right there in the room, she said, you know, at any time, you know, we could stop, we could debrief.”
Experiences of clinician flexibility and personalization of therapy were contrasted with experiences of overly rigid therapy. Overemphasis on protocols created barriers, often because treatment did not feel personalized. One veteran described how a clinician’s task-oriented approach interfered with their ability to engage in TF-EBP:
They listened, but it just didn’t seem like they were listening, because they really wanted to stay on task… So, I felt like if the person was more concerned, or more sympathetic to the things that was also going on in my life at that present time, I think I would’ve felt more comfortable talking about what was the PTSD part, too.
Veterans valued shared decision-making prior to TF-EBP initiation. Veterans typically described being involved in a shared decision-making process prior to initiating TF-EBP. During these sessions, clinicians discussed treatment options and provided veterans with a variety of materials describing treatments (eg, pamphlets, websites, videos, statistics). Most veterans appreciated being able to reflect on and discuss treatment options with their clinicians. Being given time in and out of session to review was viewed as valuable and increased confidence in treatment choice. One veteran described their experience:
I was given the information, you know, they gave me handouts, PDFs, whatever was available, and let me read over it. I didn’t have to choose anything right then and there, you know, they let me sleep on it. And I got back to them after some thought.
However, some veterans felt overwhelmed by being presented with too much information and did not believe they knew enough to make a final treatment decision. One veteran described being asked to contribute to the treatment decision:
I definitely asked [the clinician] to weigh in on maybe what he thought was best, because—I mean, I don’t know… I’m not necessarily sure I know what I think is best. I think we’re just lucky I’m here, so if you can give me a solid and help me out here by telling me just based on what I’ve said to you and the things that I’ve gone through, what do you think?
Veterans who perceived that their treatment preferences were respected had a positive outlook on TF-EBP. As part of the shared-decision making process, veterans typically described being given choices among PTSD treatments. One way that preferences were respected was through clinicians tailoring treatment descriptions to a veteran’s unique symptoms, experiences, and values. In these cases, clinicians observed specific concerns and clearly linked treatment principles to those concerns. For example, one veteran described their clinician’s recommendation for PE: “The hardest thing for me is to do the normal things like grocery store or getting on a train or anything like that. And so, he suggested that [PE] would be a good idea.”
In other cases, veterans wanted the highest quality of treatment rather than a match between treatment principles and the veteran’s presentation, goals, or strengths. These veterans wanted the best treatment available for PTSD and valued research support, recommendations from clinical practice guidelines, or clinician confidence in the effectiveness of the treatment. One veteran described this perspective:
I just wanted to be able to really tackle it in the best way possible and in the most like aggressive way possible. And it seemed like PE really was going to, they said that it’s a difficult type of therapy, but I really just wanted to kind of do the best that I could to eradicate some of the issues that I was having.
When veterans perceived a lack of respect for their preferences, they were hesitant about TF-EBP. For some veterans, a generic pitch for a TF-EBP was detrimental in the absence of the personal connection between the treatment and their own symptoms, goals, or strengths. These veterans did not question whether the treatment was effective in general but did question whether the treatment was best for them. One veteran described the contrast between their clinician’s perspective and their own.
I felt like they felt very comfortable, very confident in [CPT] being the program, because it was comfortable for them. Because they did it several times. And maybe they had a lot of success with other individuals... but they were very comfortable with that one, as a provider, more than: Is this the best fit for [me]?
Some veterans perceived little concern for their preferences and a lack of choice in available treatments, which tended to perpetuate negative perceptions of TFEBP. These veterans described their lack of choices with frustration. Alternatives to TFEBP were described by these veterans as so undesirable that they did not believe they had a real choice:
[CPT] was the only decision they had. There was nothing else for PTSD. They didn’t offer anything else. So, I mean it wasn’t a decision. It was either … take treatment or don’t take treatment at all… Actually, I need to correct myself. So, there were 2 options, group therapy or CPT. I forgot about that. I’m not a big group guy so I chose the CPT.
Another veteran was offered a choice between therapeutic approaches, but all were delivered via telehealth (consistent with the transition to virtual services during the COVID-19 pandemic). For this veteran, not only was the distinction between approaches unclear, but the choice between approaches was unimportant compared to the mode of delivery.
This happened during COVID-19 and VA stopped seeing anybody physically, face-to-face. So my only option for therapy was [telehealth]… There was like 3 of them, and I tried to figure out, you know, from the layperson’s perspective, like: I don’t know which one to go with.
Veterans wanted to be asked about their cultural identity. Veterans valued when clinicians asked questions about cultural identity as part of their mental health treatment and listened to their cultural context. Cultural identity factors extended beyond factors such as race, ethnicity, gender, and sexual orientation to religion, military culture, and regionality. Veterans often described situations where they wished clinicians would ask the question or initiate conversations about culture. A veteran highlighted the importance of their faith but noted that it was a taboo topic. Their clinician did not say “we don’t go there,” but they “never dove into it either.” Another veteran expressed a desire for their clinician to ask questions about experiences in the National Guard and as an African American veteran:
If a provider was to say like: Oh, you know, it’s a stressful situation being a part of the military, being in the National Guard. You know, just asking questions about that. I think that would really go a long way… Being African American was difficult as well. And more so because of my region, I think… I felt like it would probably be an uncomfortable subject to speak on… I mean, it wasn’t anything that my providers necessarily did, it was more so just because it wasn’t brought up.
One common area of concern for veterans was a match between veteran and therapist demographics. When asked about how their cultural identity influenced treatment, several veterans described the relevance of therapist match. Much like questions about their own cultural identity, veterans valued being asked about identity preferences in clinicians (eg, gender or race matching), rather than having to bring up the preference themselves. One veteran described relief at this question being asked directly: “I was relieved when she had asked [whether I wanted a male or female clinician] primarily because I was going to ask that or bring that up somehow. But her asking that before me was a weight off my shoulders.”
Discussing cultural identity through treatment strengthened veterans’ engagement in therapy. Many veterans appreciated when analogies used in therapy were relevant to their cultural experiences and when clinicians understood their culture (eg, military culture, race, ethnicity, religious beliefs, sexual orientation). One veteran described how their clinician understood military culture and made connections between military culture and the rationale for TF-EBP, which strengthened the veteran’s buy-in for the treatment and alliance with the clinician:
At the beginning when she was explaining PTSD, and I remember she said that your brain needed to think this way when you were in the military because it was a way of protecting and surviving, so your brain was doing that in order for you to survive in whatever areas you were because there was danger. So, your brain had you thinking that way. But now, you’re not in those situations anymore. You’re not in danger. You’re not in the military, but your brain is still thinking you are, and that’s what PTSD generally does to you.
Specific elements of TF-EBP also provided opportunities to discuss and integrate important aspects of identity. This is accomplished in PE by assigning relevant in vivo exercises. In CPT, “connecting the dots” on how prior experiences influenced trauma-related stuck points achieved this element. One veteran described their experience with a clinician who was comfortable discussing the veteran’s sexual orientation and recognized the impacts of prior trauma on intimacy:
They’re very different, and there’s a lot of things that can be accepted in gay relationships that are not in straight ones. With all that said, I think [the PE therapist] did a fantastic job being not—like never once did she laugh or make an uncomfortable comment or say she didn’t wanna talk about something when like part of the reason I wanted to get into therapy is that my partner and I weren’t having sex unless I used alcohol.
Discussion
As part of a larger national qualitative investigation of the experiences of veterans who recently initiated TF-EBP, veterans discussed their experiences with therapy and mental health care that have important implications for continued process improvement.21 Three key areas for continued process improvement were identified: (1) providing information about the diverse range of mental health care services at the VA and the implications of this continuum of care; (2) consideration of veteran preferences in treatment decision-making, including the importance of perceived choice; and (3) incorporating cultural assessment and cultural responsiveness into case conceptualization and treatment.
One area of process improvement identified was increasing knowledge about different types of psychotherapy and the continuum of care available at the VA. Veterans in this study confused or conflated participating in psychotherapy with talking about mental health symptoms with a clinician (eg, assessment, disability evaluation). They were sometimes surprised that psychotherapy is an umbrella term referring to a variety of different modalities. The downstream impact of these misunderstandings was a perception of VA mental health care as nebulous. Veterans were surprised that all mental health practitioners were unable to provide the same care. Confusion may have been compounded by highly variable referral processes across VA.24 To address this, clinicians have developed local educational resources and handouts for both veterans and referring clinicians from nonmental health and general mental health specialties.25 Given the variability in referral processes both between and within VA medical centers, national dissemination of these educational materials may be more difficult compared to materials for TF-EBPs.24 The VA started to use behavioral health interdisciplinary program (BHIP) teams, which are designed to be clinical homes for veterans connected with a central clinician who can explain and coordinate their mental health care as well as bring more consistency to the referral process.26 The ongoing transition toward the BHIP model of mental health care at VA may provide the opportunity to consolidate and integrate knowledge about the VA approach to mental health care, potentially filling knowledge gaps.
A second area of process improvement focused on the shared decision-making process. Consistent with mental health initiatives, veterans generally believed they had received sufficient information about TF-EBP and engaged in shared decision-making with clinicians.20,27 Veterans were given educational materials to review and had the opportunity to discuss these materials with clinicians. However, veterans described variability in the success of shared decision-making. Although veterans valued receiving accurate, comprehensible information to support treatment decisions, some preferred to defer to clinicians’ expertise regarding which treatment to pursue. While these veterans valued information, they also valued the expertise of clinicians in explaining why specific treatments would be beneficial. A key contributor to veterans satisfaction was assessing how veterans wanted to engage in the decision-making process and respecting those preferences.28 Veterans approached shared decision-making differently, from making decisions independently after receiving information to relying solely on clinician recommendation. The process was most successful when clinicians articulated how their recommended treatment aligned with a veteran’s preferences, including recommendations based on specific values (eg, personalized match vs being the best). Another important consideration is ensuring veterans know they can receive a variety of different types of mental health services available in different modalities (eg, virtual vs in-person; group vs individual). When veterans did not perceive choice in treatment aspects important to them (typically despite having choices), they were less satisfied with their TF-EBP experience.
A final area of process improvement identified involves how therapists address important aspects of culture. Veterans often described mental health stigma coming from intersecting cultural identities and expressed appreciation when therapists helped them recognize the impact of these beliefs on treatment. Some veterans did not discuss important aspects of their identity with clinicians, including race/ethnicity, religion, and military culture. Veterans did not report negative interactions with clinicians or experiences suggesting it was inappropriate to discuss identity; however, they were reluctant to independently raise these identity factors. Strategies such as the ADDRESSING framework, a mnemonic acronym that describes a series of potentially relevant characteristics, can help clinicians comprehensively consider different aspects that may be relevant to veterans, modeling that discussion of relevant these characteristics is welcome in TF-EBP.29 Veterans reported that making culturally relevant connections enhanced the TF-EBP experience, most commonly with military culture. These data support that TF-EBP delivery with attention to culture should be an integrated part of treatment, supporting engagement and therapeutic alliance.30 The VA National Center for PTSD consultation program is a resource to support clinicians in assessing and incorporating relevant aspects of cultural identity.31 For example, the National Center for PTSD provides a guide for using case conceptualization to address patient reactions to race-based violence during PTSD treatment.32 Both manualized design and therapist certification training can reinforce that assessing and attending to case conceptualization (including identity factors) is an integral component of TF-EBP.33,34
Limitations
While the current study has numerous strengths (eg, national veteran sampling, robust qualitative methods), results should be considered within the context of study limitations. First, veteran participants all received TF-EBP, and the perspectives of veterans who never initiate TF-EBP may differ. Despite the strong sampling approach, the study design is not intended to be generalizable to all veterans receiving TF-EBP for PTSD. Qualitative analysis yielded 15 themes, described in this study and prior research, consistent with recommendations.21,22 This approach allows rich description of distinct focus areas that would not be possible in a single manuscript. Nonetheless, all veterans interviewed described their experiences in TF-EBP and general mental health care, the focus of the semistructured interview guide was on the experience of transitioning from other treatment to TF-EBP.
Conclusion
This study describes themes related to general mental health and TF-EBP process improvement as part of a larger study on transitions in PTSD care.21,22 Veterans valued the fundamentals of therapy, including rapport and flexibility. Treatment-specific rapport (eg, pointing out treatment progress and effort in completing treatment components) and flexibility within the context of fidelity (ie, personalizing treatment while maintaining core treatment elements) may be most effective at engaging veterans in recommended PTSD treatments.18,34 In addition to successes, themes suggest multiple opportunities for process improvement. Ongoing VA initiatives and priorities (ie, BHIP, shared decision-making, consultation services) aim to improve processes consistent with veteran recommendations. Future research is needed to evaluate the success of these and other programs to optimize access to and engagement in recommended PTSD treatments.
- US Department of Veterans Affairs; US Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. 2023. Updated August 20, 2025. Accessed October 17, 2025. https://www.healthquality.va.gov/guidelines/MH/ptsd/
- International Society for Traumatic Stress Studies. ISTSS PTSD prevention and treatment guidelines: methodology and recommendations. Accessed August 13, 2025. http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-TreatmentGuidelines/ISTSS_PreventionTreatmentGuidelines_FNL-March-19-2019.pdf.aspx
- American Psychological Association. Clinical practice guideline for the treatment of posttraumatic stress disorder in adults. Accessed August 13, 2025. https://www.apa.org/ptsd-guideline/ptsd.pdf
- Karlin BE, Cross G. From the laboratory to the therapy room: National dissemination and implementation of evidence- based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69:19-33. doi:10.1037/a0033888
- Rosen CS, Matthieu MM, Wiltsey Stirman S, et al. A review of studies on the system-wide implementation of evidencebased psychotherapies for posttraumatic stress disorder in the Veterans Health Administration. Adm Policy Ment Health. 2016;43:957-977. doi:10.1007/s10488-016-0755-0
- Maguen S, Holder N, Madden E, et al. Evidence-based psychotherapy trends among posttraumatic stress disorder patients in a national healthcare system, 2001-2014. Depress Anxiety. 2020;37:356-364. doi:10.1002/da.22983
- Cheney AM, Koenig CJ, Miller CJ, et al. Veteran-centered barriers to VA mental healthcare services use. BMC Health Serv Res. 2018;18:591. doi:10.1186/s12913-018-3346-9
- Hundt NE, Mott JM, Miles SR, et al. Veterans’ perspectives on initiating evidence-based psychotherapy for posttraumatic stress disorder. Psychol Trauma. 2015;7:539-546. doi:10.1037/tra0000035
- Hundt NE, Helm A, Smith TL, et al. Failure to engage: a qualitative study of veterans who decline evidence-based psychotherapies for PTSD. Psychol Serv. 2018;15:536- 542. doi:10.1037/ser0000212
- Sayer NA, Friedemann-Sanchez G, Spoont M, et al. A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry. 2009;72:238-255. doi:10.1521/psyc.2009.72.3.238
- Mittal D, Drummond KL, Blevins D, et al. Stigma associated with PTSD: perceptions of treatment seeking combat veterans. Psychiatr Rehabil J. 2013;36:86-92. doi:10.1037/h0094976
- Possemato K, Wray LO, Johnson E, et al. Facilitators and barriers to seeking mental health care among primary care veterans with posttraumatic stress disorder. J Trauma Stress. 2018;31:742-752. doi:10.1002/jts.22327
- Silvestrini M, Chen JA. “It’s a sign of weakness”: Masculinity and help-seeking behaviors among male veterans accessing posttraumatic stress disorder care. Psychol Trauma. 2023;15:665-671. doi:10.1037/tra0001382
- Stecker T, Shiner B, Watts BV, et al. Treatment-seeking barriers for veterans of the Iraq and Afghanistan conflicts who screen positive for PTSD. Psychiatr Serv. 2013;64:280-283. doi:10.1176/appi.ps.001372012
- Etingen B, Grubbs KM, Harik JM. Drivers of preference for evidence-based PTSD treatment: a qualitative assessment. Mil Med. 2020;185:303-310. doi:10.1093/milmed/usz220
- Hundt NE, Ecker AH, Thompson K, et al. “It didn’t fit for me:” A qualitative examination of dropout from prolonged exposure and cognitive processing therapy in veterans. Psychol Serv. 2020;17:414-421. doi:10.1037/ser0000316
- Kehle-Forbes SM, Gerould H, Polusny MA, et al. “It leaves me very skeptical” messaging in marketing prolonged exposure and cognitive processing therapy to veterans with PTSD. Psychol Trauma. 2022;14:849-852. doi:10.1037/tra0000550
- Kehle-Forbes SM, Ackland PE, Spoont MR, et al. Divergent experiences of U.S. veterans who did and did not complete trauma-focused therapies for PTSD: a national qualitative study of treatment dropout. Behav Res Ther. 2022;154:104123. doi:10.1016/j.brat.2022.104123
- Hessinger JD, London MJ, Baer SM. Evaluation of a shared decision-making intervention on the utilization of evidence-based psychotherapy in a VA outpatient PTSD clinic. Psychol Serv. 2018;15:437-441. doi:10.1037/ser0000141
- Hamblen JL, Grubbs KM, Cole B, et al. “Will it work for me?” Developing patient-friendly graphical displays of posttraumatic stress disorder treatment effectiveness. J Trauma Stress. 2022;35:999-1010. doi:10.1002/jts.22808
- Holder N, Ranney RM, Delgado AK, et al. Transitioning into trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatments: a qualitative investigation. Cogn Behav Ther. 2025;54:391-407. doi:10.1080/16506073.2024.2408386
- Levitt HM, Bamberg M, Creswell JW, et al. Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA Publications and Communications Board task force report. Am Psychol. 2018;73:26-46. doi:10.1037/amp0000151
- Palinkas LA, Mendon SJ, Hamilton AB. Innovations in mixed methods evaluations. Annu Rev Public Health. 2019;40:423- 442. doi:10.1146/annurev-publhealth-040218-044215
- Ranney RM, Cordova MJ, Maguen S. A review of the referral process for evidence-based psychotherapies for PTSD among veterans. Prof Psychol Res Pr. 2022;53:276-285. doi:10.1037/pro0000463
- Holder N, Ranney RM, Delgado AK, et al. Transitions to trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatment: a qualitative investigation of clinician’s perspectives. Cogn Behav Ther. 2025;1-19. doi:10.1080/16506073.2025.2481475
- Barry CN, Abraham KM, Weaver KR, et al. Innovating team-based outpatient mental health care in the Veterans Health Administration: staff-perceived benefits and challenges to pilot implementation of the Behavioral Health Interdisciplinary Program (BHIP). Psychol Serv. 2016;13:148-155. doi:10.1037/ser0000072
- Harik JM, Hundt NE, Bernardy NC, et al. Desired involvement in treatment decisions among adults with PTSD symptoms. J Trauma Stress. 2016;29:221-228. doi:10.1002/jts.22102
- Larsen SE, Hooyer K, Kehle-Forbes SM, et al. Patient experiences in making PTSD treatment decisions. Psychol Serv. 2024;21:529-537. doi:10.1037/ser0000817
- Hays PA. Four steps toward intersectionality in psychotherapy using the ADDRESSING framework. Prof Psychol Res Pr. 2024;55:454-462. doi:10.1037/pro0000577
- Galovski TE, Nixon RDV, Kaysen D. Flexible Applications of Cognitive Processing Therapy: Evidence-Based Treatment Methods. Academic Press; 2020.
- Larsen SE, McKee T, Fielstein E, et al. The development of a posttraumatic stress disorder (PTSD) consultation program to support system-wide implementation of high-quality PTSD care for veterans. Psychol Serv. 2025;22:342-348. doi:10.1037/ser0000867
- Galovski T, Kaysen D, McClendon J, et al. Provider guide to addressing patient reactions to race-based violence during PTSD treatment. PTSD.va.gov. Accessed August 3, 2025. www.ptsd.va.gov/professional/treat/specific/patient_reactions_race_violence.asp
- Galovski TE, Nixon RDV, Kehle-Forbes S. Walking the line between fidelity and flexibility: a conceptual review of personalized approaches to manualized treatments for posttraumatic stress disorder. J Trauma Stress. 2024;37:768-774. doi:10.1002/jts.23073
- Galovski TE, McSweeney LB, Nixon RDV, et al. Personalizing cognitive processing therapy with a case formulation approach to intentionally target impairment in psychosocial functioning associated with PTSD. Contemp Clin Trials Commun. 2024;42:101385. doi:10.1016/j.conctc.2024.101385
Trauma-focused evidence-based psychotherapies (TF-EBPs), including cognitive processing therapy (CPT) and prolonged exposure therapy (PE), are recommended treatments for posttraumatic stress disorder (PTSD) in clinical practice guidelines.1-3 To increase initiation of these treatments, the US Department of Veterans Affairs (VA) used a large-scale dissemination and implementation effort to improve access to TF-EBP.4,5 These efforts achieved modest success, increasing prevalence of TF-EBP from a handful of veterans in 2004 to an annual prevalence of 14.6% for CPT and 4.3% for PE in 2014.6
Throughout these efforts, qualitative studies have been used to better understand veterans’ perspectives on receiving TF-EBP care.7-18 Barriers to initiation of and engagement in TF-EBP and PTSD care have been identified from these qualitative studies. One identified barrier was lack of knowledge—particularly lack of knowledge about what is meant by a PTSD diagnosis and available treatments.7-10 Stigma (ie, automatic negative associations) toward mental health problems or seeking mental health care also has been identified as a barrier to initiation.7,10-14 Perceptions of poor alignment between treatment and veteran goals, including lack of buy-in for the rationale, served as barriers to initiation and engagement.8,15-18
Using prior qualitative work, numerous initiatives have been developed to reduce stigma, facilitate conversations about how treatment aligns with goals, and fill knowledge gaps, particularly through online resources and shared decision-making.19,20 To better inform the state of veterans’ experiences with TF-EBP, a qualitative investigation was conducted involving veterans who recently initiated TF-EBP. Themes directly related to transitions to TF-EBP were identified; however, all veterans interviewed also described their experiences with TFEBP engagement and mental health care. Consistent with recommendations for qualitative methods, this study extends prior work on transitions to TF-EBP by describing themes with a distinct focus on the experience of engaging with TF-EBP and mental health care.21,22
Methods
The experiences of veterans who were transitioning into TF-EBPs were collected in semistructured interviews and analyzed. The semistructured interview guide was developed and refined in consultation with both qualitative methods experts and PTSD treatment experts to ensure that 6 content domains were appropriately queried: PTSD treatment options, cultural sensitivity of treatment, PTSD treatment selection, transition criteria, beliefs about stabilization treatment, and treatment needs/preferences.
Participants were identified using the VA Corporate Data Warehouse and included post-9/11 veterans who had recently initiated CPT or PE for the first time between September 1, 2021, and September 1, 2022. More details of participant selection are available in Holder et al.21 From a population of 10,814 patients, stratified random sampling generated a recruitment pool of 200 veterans for further outreach. The strata were defined such that this recruitment pool had similar proportions of demographic characteristics (ie, gender, race, ethnicity) to the population of eligible veterans, equivalent distributions of time to CPT or PE initiation (ie, 33.3% < 1 year, 33.3% 1-3 years, and 33.3% > 3 years), and adequate variability in TF-EBP type (ie, 66.7% CPT, 33.3% PE). A manual chart review in the recruitment pool excluded 12 veterans who did not initiate CPT or PE, 1 veteran with evidence of current active psychosis and/or cognitive impairment that would likely preclude comprehension of study materials, and 1 who was deceased.
Eligible veterans from the recruitment pool were contacted in groups of 25. First, a recruitment letter with study information and instructions to opt-out of further contact was mailed or emailed to veterans. After 2 weeks, veterans who had not responded were contacted by phone up to 3 times. Veterans interested in participating were scheduled for a 1-time visit that included verbal consent and the qualitative interview. Metrics were established a priori to ensure an adequately diverse and inclusive sample. Specifically, a minimum number of racial and/or ethnic minority veterans (33%) and women veterans (20%) were sought. Equal distribution across the 3 categories of time from first mental health visit to CPT/PE initiation also was targeted. Throughout enrollment, recruitment efforts were adapted to meet these metrics in the emerging sample. While the goal was to generate a diverse and inclusive sample using these methods, the sample was not intended to be representative of the population.
Of the 186 eligible participants, 21 declined participation and 26 could not be reached. The targeted sample was reached after exhausting contact for 47 veterans and contacting 80 veterans for a final response rate of 40% among fully contacted veterans and 27% among veterans with any contact. The final sample included 30 veterans who received CPT or PE in VA facilities (Table).
After veterans provided verbal consent for study participation, sociodemographic information was verbally reported, and a 30- to 60-minute semistructured qualitative phone interview was recorded and transcribed. Veterans received $40 for participation. All procedures were approved by the University of California San Francisco Institutional Review Board.
Qualitative Data Analysis
Rapid analysis procedures were used to analyze qualitative data. This approach is suitable for focused, moderately structured qualitative analyses in health services research and facilitates rapid dissemination to stakeholders.23 The qualitative analysts were 2 clinical psychologists with expertise in PTSD treatment (NH primary and RR secondary). Consistent with rapid analysis procedures, analysts prepared a templated summary (including relevant quotations) of each interview, organized by the prespecified content domains. Interviews were summarized independently, compared to ensure consistency, and discrepancies were resolved through review of the interview source materials. Individual summary templates were combined into a master analytic matrix to facilitate the identification of patterns and delineation of themes. Analysts routinely met to identify, discuss, and refine preliminary themes, revisiting source materials to reach consensus as needed.
Results
Fifteen themes were identified and organized into 2 distinct focus areas: themes directly related to the transition to TF-EBP (8 themes) and themes related to veterans’ experiences with TF-EBP and general mental health care with potential process-improvement implications (7 themes).21 Seven themes were identified related to experiences with TF-EBP engagement and VA mental health care. The 7 themes related to TF-EBP engagement and VA mental health care themes are summarized with exemplary quotations.
Veterans want a better understanding of psychotherapy and engaging with VA mental health. Veterans reported that they generally had a poor or “nebulous” understanding about the experience of psychotherapy. For example, veterans exhibited confusion about whether certain experiences were equivalent to participating in psychotherapy. They were sometimes unable to distinguish between interactions such as assessment, disability evaluations, peer support, and psychotherapy. One veteran described a conversation with a TFEBP therapist about prior treatment:
She [asked], have you ever been, or gone through a therapy to begin with? And I, I said, well I just chatted with somebody. And she said that’s not, that’s not therapy. So, I was like, oh, it’s not? That’s not what people do?
Veterans were surprised the VA offered a diverse range of psychotherapy interventions, rather than simply therapy. They did not realize there were different types of psychotherapy. As a result, veterans were not aware that some VA mental practitioners have specialty training and certification to provide treatment matched to specific diagnoses or needs. They thought that all clinicians could provide the same care. One veteran described their understanding:
I just figured all mental health people are mental health people. I didn’t have a better understanding of the system and all the different levels and how it plays out and specialties and things like that. Which, I guess, I should have because you have a primary care doctor, but then you have specialists in all these other different sectors that specialize in one particular area. I guess that should’ve been common sense, but it wasn’t.
Stigma was a barrier to seeking and engaging in mental health care. Veterans discovered they had to overcome stigma associated with seeking and engaging in mental health treatment. Military culture was often discussed as promoting stigma regarding mental health treatment. Specifically, veterans described that seeking treatment meant “either, I’m weak or I’m gonna be seen as weak.” In active-duty settings, the strategy for dealing with mental health symptoms was to “leave those feelings, you push ‘em aside,” an approach highly inconsistent with TF-EBP. In some cases, incorrect information about the VA and PTSD was presented as part of discharge from the military, leading to long-term skepticism of the VA and PTSD treatment. One veteran described his experience as part of a class on the VA compensation and pension assessment process for service-connected disabilities during his military discharge:
[A fellow discharging soldier asked] what about like PTSD, gettin’ rated for PTSD. I hear they take our weapons and stuff like we can’t own firearms and all that stuff. And [the instructor] was like, well, yes that’s a thing. He didn’t explain it like if you get compensated for PTSD you don’t lose your rights to carry a firearm or to have, to be able to go hunting.
Importantly, veterans often described how other identities (eg, race, ethnicity, gender, region of origin) interacted with military culture to enhance stigma. Hearing messaging from multiple sources reinforced beliefs that mental health treatment is inappropriate or is associated with weakness:
As a first-generation Italian, I was always taught keep your feelings to yourself. Never talk outside your family. Never bring up problems to other people and stuff like that. Same with the military. And then the old stigma working in [emergency medical services] and public safety, you’re weak if you get help.
The fundamentals of therapy, including rapport and flexibility, were important. Veterans valued nonspecific therapy factors, genuine empathy, building trust, being honest about treatment, personality, and rapport. These characteristics were almost universally described as particularly important:
I liked the fact that she made it personable and she cared. It wasn’t just like, here, we’re gonna start this. She explained it in the ways I could understand, not in medical terms, so to speak, but that’s what I liked about her. She really cared about what she did and helping me.
Flexibility was viewed as an asset, particularly when clinicians acknowledged veteran autonomy. A consistent example was when veterans were able to titrate trauma disclosure. One veteran described this flexible treatment experience: “She was right there in the room, she said, you know, at any time, you know, we could stop, we could debrief.”
Experiences of clinician flexibility and personalization of therapy were contrasted with experiences of overly rigid therapy. Overemphasis on protocols created barriers, often because treatment did not feel personalized. One veteran described how a clinician’s task-oriented approach interfered with their ability to engage in TF-EBP:
They listened, but it just didn’t seem like they were listening, because they really wanted to stay on task… So, I felt like if the person was more concerned, or more sympathetic to the things that was also going on in my life at that present time, I think I would’ve felt more comfortable talking about what was the PTSD part, too.
Veterans valued shared decision-making prior to TF-EBP initiation. Veterans typically described being involved in a shared decision-making process prior to initiating TF-EBP. During these sessions, clinicians discussed treatment options and provided veterans with a variety of materials describing treatments (eg, pamphlets, websites, videos, statistics). Most veterans appreciated being able to reflect on and discuss treatment options with their clinicians. Being given time in and out of session to review was viewed as valuable and increased confidence in treatment choice. One veteran described their experience:
I was given the information, you know, they gave me handouts, PDFs, whatever was available, and let me read over it. I didn’t have to choose anything right then and there, you know, they let me sleep on it. And I got back to them after some thought.
However, some veterans felt overwhelmed by being presented with too much information and did not believe they knew enough to make a final treatment decision. One veteran described being asked to contribute to the treatment decision:
I definitely asked [the clinician] to weigh in on maybe what he thought was best, because—I mean, I don’t know… I’m not necessarily sure I know what I think is best. I think we’re just lucky I’m here, so if you can give me a solid and help me out here by telling me just based on what I’ve said to you and the things that I’ve gone through, what do you think?
Veterans who perceived that their treatment preferences were respected had a positive outlook on TF-EBP. As part of the shared-decision making process, veterans typically described being given choices among PTSD treatments. One way that preferences were respected was through clinicians tailoring treatment descriptions to a veteran’s unique symptoms, experiences, and values. In these cases, clinicians observed specific concerns and clearly linked treatment principles to those concerns. For example, one veteran described their clinician’s recommendation for PE: “The hardest thing for me is to do the normal things like grocery store or getting on a train or anything like that. And so, he suggested that [PE] would be a good idea.”
In other cases, veterans wanted the highest quality of treatment rather than a match between treatment principles and the veteran’s presentation, goals, or strengths. These veterans wanted the best treatment available for PTSD and valued research support, recommendations from clinical practice guidelines, or clinician confidence in the effectiveness of the treatment. One veteran described this perspective:
I just wanted to be able to really tackle it in the best way possible and in the most like aggressive way possible. And it seemed like PE really was going to, they said that it’s a difficult type of therapy, but I really just wanted to kind of do the best that I could to eradicate some of the issues that I was having.
When veterans perceived a lack of respect for their preferences, they were hesitant about TF-EBP. For some veterans, a generic pitch for a TF-EBP was detrimental in the absence of the personal connection between the treatment and their own symptoms, goals, or strengths. These veterans did not question whether the treatment was effective in general but did question whether the treatment was best for them. One veteran described the contrast between their clinician’s perspective and their own.
I felt like they felt very comfortable, very confident in [CPT] being the program, because it was comfortable for them. Because they did it several times. And maybe they had a lot of success with other individuals... but they were very comfortable with that one, as a provider, more than: Is this the best fit for [me]?
Some veterans perceived little concern for their preferences and a lack of choice in available treatments, which tended to perpetuate negative perceptions of TFEBP. These veterans described their lack of choices with frustration. Alternatives to TFEBP were described by these veterans as so undesirable that they did not believe they had a real choice:
[CPT] was the only decision they had. There was nothing else for PTSD. They didn’t offer anything else. So, I mean it wasn’t a decision. It was either … take treatment or don’t take treatment at all… Actually, I need to correct myself. So, there were 2 options, group therapy or CPT. I forgot about that. I’m not a big group guy so I chose the CPT.
Another veteran was offered a choice between therapeutic approaches, but all were delivered via telehealth (consistent with the transition to virtual services during the COVID-19 pandemic). For this veteran, not only was the distinction between approaches unclear, but the choice between approaches was unimportant compared to the mode of delivery.
This happened during COVID-19 and VA stopped seeing anybody physically, face-to-face. So my only option for therapy was [telehealth]… There was like 3 of them, and I tried to figure out, you know, from the layperson’s perspective, like: I don’t know which one to go with.
Veterans wanted to be asked about their cultural identity. Veterans valued when clinicians asked questions about cultural identity as part of their mental health treatment and listened to their cultural context. Cultural identity factors extended beyond factors such as race, ethnicity, gender, and sexual orientation to religion, military culture, and regionality. Veterans often described situations where they wished clinicians would ask the question or initiate conversations about culture. A veteran highlighted the importance of their faith but noted that it was a taboo topic. Their clinician did not say “we don’t go there,” but they “never dove into it either.” Another veteran expressed a desire for their clinician to ask questions about experiences in the National Guard and as an African American veteran:
If a provider was to say like: Oh, you know, it’s a stressful situation being a part of the military, being in the National Guard. You know, just asking questions about that. I think that would really go a long way… Being African American was difficult as well. And more so because of my region, I think… I felt like it would probably be an uncomfortable subject to speak on… I mean, it wasn’t anything that my providers necessarily did, it was more so just because it wasn’t brought up.
One common area of concern for veterans was a match between veteran and therapist demographics. When asked about how their cultural identity influenced treatment, several veterans described the relevance of therapist match. Much like questions about their own cultural identity, veterans valued being asked about identity preferences in clinicians (eg, gender or race matching), rather than having to bring up the preference themselves. One veteran described relief at this question being asked directly: “I was relieved when she had asked [whether I wanted a male or female clinician] primarily because I was going to ask that or bring that up somehow. But her asking that before me was a weight off my shoulders.”
Discussing cultural identity through treatment strengthened veterans’ engagement in therapy. Many veterans appreciated when analogies used in therapy were relevant to their cultural experiences and when clinicians understood their culture (eg, military culture, race, ethnicity, religious beliefs, sexual orientation). One veteran described how their clinician understood military culture and made connections between military culture and the rationale for TF-EBP, which strengthened the veteran’s buy-in for the treatment and alliance with the clinician:
At the beginning when she was explaining PTSD, and I remember she said that your brain needed to think this way when you were in the military because it was a way of protecting and surviving, so your brain was doing that in order for you to survive in whatever areas you were because there was danger. So, your brain had you thinking that way. But now, you’re not in those situations anymore. You’re not in danger. You’re not in the military, but your brain is still thinking you are, and that’s what PTSD generally does to you.
Specific elements of TF-EBP also provided opportunities to discuss and integrate important aspects of identity. This is accomplished in PE by assigning relevant in vivo exercises. In CPT, “connecting the dots” on how prior experiences influenced trauma-related stuck points achieved this element. One veteran described their experience with a clinician who was comfortable discussing the veteran’s sexual orientation and recognized the impacts of prior trauma on intimacy:
They’re very different, and there’s a lot of things that can be accepted in gay relationships that are not in straight ones. With all that said, I think [the PE therapist] did a fantastic job being not—like never once did she laugh or make an uncomfortable comment or say she didn’t wanna talk about something when like part of the reason I wanted to get into therapy is that my partner and I weren’t having sex unless I used alcohol.
Discussion
As part of a larger national qualitative investigation of the experiences of veterans who recently initiated TF-EBP, veterans discussed their experiences with therapy and mental health care that have important implications for continued process improvement.21 Three key areas for continued process improvement were identified: (1) providing information about the diverse range of mental health care services at the VA and the implications of this continuum of care; (2) consideration of veteran preferences in treatment decision-making, including the importance of perceived choice; and (3) incorporating cultural assessment and cultural responsiveness into case conceptualization and treatment.
One area of process improvement identified was increasing knowledge about different types of psychotherapy and the continuum of care available at the VA. Veterans in this study confused or conflated participating in psychotherapy with talking about mental health symptoms with a clinician (eg, assessment, disability evaluation). They were sometimes surprised that psychotherapy is an umbrella term referring to a variety of different modalities. The downstream impact of these misunderstandings was a perception of VA mental health care as nebulous. Veterans were surprised that all mental health practitioners were unable to provide the same care. Confusion may have been compounded by highly variable referral processes across VA.24 To address this, clinicians have developed local educational resources and handouts for both veterans and referring clinicians from nonmental health and general mental health specialties.25 Given the variability in referral processes both between and within VA medical centers, national dissemination of these educational materials may be more difficult compared to materials for TF-EBPs.24 The VA started to use behavioral health interdisciplinary program (BHIP) teams, which are designed to be clinical homes for veterans connected with a central clinician who can explain and coordinate their mental health care as well as bring more consistency to the referral process.26 The ongoing transition toward the BHIP model of mental health care at VA may provide the opportunity to consolidate and integrate knowledge about the VA approach to mental health care, potentially filling knowledge gaps.
A second area of process improvement focused on the shared decision-making process. Consistent with mental health initiatives, veterans generally believed they had received sufficient information about TF-EBP and engaged in shared decision-making with clinicians.20,27 Veterans were given educational materials to review and had the opportunity to discuss these materials with clinicians. However, veterans described variability in the success of shared decision-making. Although veterans valued receiving accurate, comprehensible information to support treatment decisions, some preferred to defer to clinicians’ expertise regarding which treatment to pursue. While these veterans valued information, they also valued the expertise of clinicians in explaining why specific treatments would be beneficial. A key contributor to veterans satisfaction was assessing how veterans wanted to engage in the decision-making process and respecting those preferences.28 Veterans approached shared decision-making differently, from making decisions independently after receiving information to relying solely on clinician recommendation. The process was most successful when clinicians articulated how their recommended treatment aligned with a veteran’s preferences, including recommendations based on specific values (eg, personalized match vs being the best). Another important consideration is ensuring veterans know they can receive a variety of different types of mental health services available in different modalities (eg, virtual vs in-person; group vs individual). When veterans did not perceive choice in treatment aspects important to them (typically despite having choices), they were less satisfied with their TF-EBP experience.
A final area of process improvement identified involves how therapists address important aspects of culture. Veterans often described mental health stigma coming from intersecting cultural identities and expressed appreciation when therapists helped them recognize the impact of these beliefs on treatment. Some veterans did not discuss important aspects of their identity with clinicians, including race/ethnicity, religion, and military culture. Veterans did not report negative interactions with clinicians or experiences suggesting it was inappropriate to discuss identity; however, they were reluctant to independently raise these identity factors. Strategies such as the ADDRESSING framework, a mnemonic acronym that describes a series of potentially relevant characteristics, can help clinicians comprehensively consider different aspects that may be relevant to veterans, modeling that discussion of relevant these characteristics is welcome in TF-EBP.29 Veterans reported that making culturally relevant connections enhanced the TF-EBP experience, most commonly with military culture. These data support that TF-EBP delivery with attention to culture should be an integrated part of treatment, supporting engagement and therapeutic alliance.30 The VA National Center for PTSD consultation program is a resource to support clinicians in assessing and incorporating relevant aspects of cultural identity.31 For example, the National Center for PTSD provides a guide for using case conceptualization to address patient reactions to race-based violence during PTSD treatment.32 Both manualized design and therapist certification training can reinforce that assessing and attending to case conceptualization (including identity factors) is an integral component of TF-EBP.33,34
Limitations
While the current study has numerous strengths (eg, national veteran sampling, robust qualitative methods), results should be considered within the context of study limitations. First, veteran participants all received TF-EBP, and the perspectives of veterans who never initiate TF-EBP may differ. Despite the strong sampling approach, the study design is not intended to be generalizable to all veterans receiving TF-EBP for PTSD. Qualitative analysis yielded 15 themes, described in this study and prior research, consistent with recommendations.21,22 This approach allows rich description of distinct focus areas that would not be possible in a single manuscript. Nonetheless, all veterans interviewed described their experiences in TF-EBP and general mental health care, the focus of the semistructured interview guide was on the experience of transitioning from other treatment to TF-EBP.
Conclusion
This study describes themes related to general mental health and TF-EBP process improvement as part of a larger study on transitions in PTSD care.21,22 Veterans valued the fundamentals of therapy, including rapport and flexibility. Treatment-specific rapport (eg, pointing out treatment progress and effort in completing treatment components) and flexibility within the context of fidelity (ie, personalizing treatment while maintaining core treatment elements) may be most effective at engaging veterans in recommended PTSD treatments.18,34 In addition to successes, themes suggest multiple opportunities for process improvement. Ongoing VA initiatives and priorities (ie, BHIP, shared decision-making, consultation services) aim to improve processes consistent with veteran recommendations. Future research is needed to evaluate the success of these and other programs to optimize access to and engagement in recommended PTSD treatments.
Trauma-focused evidence-based psychotherapies (TF-EBPs), including cognitive processing therapy (CPT) and prolonged exposure therapy (PE), are recommended treatments for posttraumatic stress disorder (PTSD) in clinical practice guidelines.1-3 To increase initiation of these treatments, the US Department of Veterans Affairs (VA) used a large-scale dissemination and implementation effort to improve access to TF-EBP.4,5 These efforts achieved modest success, increasing prevalence of TF-EBP from a handful of veterans in 2004 to an annual prevalence of 14.6% for CPT and 4.3% for PE in 2014.6
Throughout these efforts, qualitative studies have been used to better understand veterans’ perspectives on receiving TF-EBP care.7-18 Barriers to initiation of and engagement in TF-EBP and PTSD care have been identified from these qualitative studies. One identified barrier was lack of knowledge—particularly lack of knowledge about what is meant by a PTSD diagnosis and available treatments.7-10 Stigma (ie, automatic negative associations) toward mental health problems or seeking mental health care also has been identified as a barrier to initiation.7,10-14 Perceptions of poor alignment between treatment and veteran goals, including lack of buy-in for the rationale, served as barriers to initiation and engagement.8,15-18
Using prior qualitative work, numerous initiatives have been developed to reduce stigma, facilitate conversations about how treatment aligns with goals, and fill knowledge gaps, particularly through online resources and shared decision-making.19,20 To better inform the state of veterans’ experiences with TF-EBP, a qualitative investigation was conducted involving veterans who recently initiated TF-EBP. Themes directly related to transitions to TF-EBP were identified; however, all veterans interviewed also described their experiences with TFEBP engagement and mental health care. Consistent with recommendations for qualitative methods, this study extends prior work on transitions to TF-EBP by describing themes with a distinct focus on the experience of engaging with TF-EBP and mental health care.21,22
Methods
The experiences of veterans who were transitioning into TF-EBPs were collected in semistructured interviews and analyzed. The semistructured interview guide was developed and refined in consultation with both qualitative methods experts and PTSD treatment experts to ensure that 6 content domains were appropriately queried: PTSD treatment options, cultural sensitivity of treatment, PTSD treatment selection, transition criteria, beliefs about stabilization treatment, and treatment needs/preferences.
Participants were identified using the VA Corporate Data Warehouse and included post-9/11 veterans who had recently initiated CPT or PE for the first time between September 1, 2021, and September 1, 2022. More details of participant selection are available in Holder et al.21 From a population of 10,814 patients, stratified random sampling generated a recruitment pool of 200 veterans for further outreach. The strata were defined such that this recruitment pool had similar proportions of demographic characteristics (ie, gender, race, ethnicity) to the population of eligible veterans, equivalent distributions of time to CPT or PE initiation (ie, 33.3% < 1 year, 33.3% 1-3 years, and 33.3% > 3 years), and adequate variability in TF-EBP type (ie, 66.7% CPT, 33.3% PE). A manual chart review in the recruitment pool excluded 12 veterans who did not initiate CPT or PE, 1 veteran with evidence of current active psychosis and/or cognitive impairment that would likely preclude comprehension of study materials, and 1 who was deceased.
Eligible veterans from the recruitment pool were contacted in groups of 25. First, a recruitment letter with study information and instructions to opt-out of further contact was mailed or emailed to veterans. After 2 weeks, veterans who had not responded were contacted by phone up to 3 times. Veterans interested in participating were scheduled for a 1-time visit that included verbal consent and the qualitative interview. Metrics were established a priori to ensure an adequately diverse and inclusive sample. Specifically, a minimum number of racial and/or ethnic minority veterans (33%) and women veterans (20%) were sought. Equal distribution across the 3 categories of time from first mental health visit to CPT/PE initiation also was targeted. Throughout enrollment, recruitment efforts were adapted to meet these metrics in the emerging sample. While the goal was to generate a diverse and inclusive sample using these methods, the sample was not intended to be representative of the population.
Of the 186 eligible participants, 21 declined participation and 26 could not be reached. The targeted sample was reached after exhausting contact for 47 veterans and contacting 80 veterans for a final response rate of 40% among fully contacted veterans and 27% among veterans with any contact. The final sample included 30 veterans who received CPT or PE in VA facilities (Table).
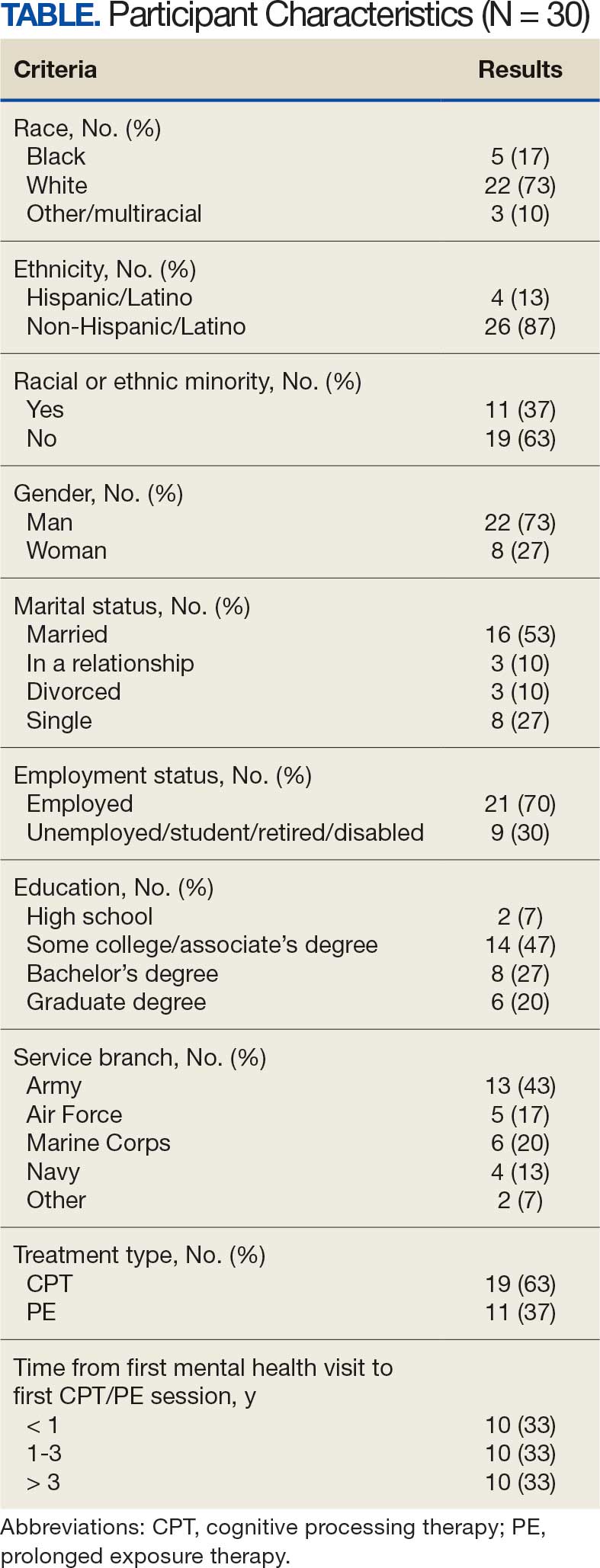
After veterans provided verbal consent for study participation, sociodemographic information was verbally reported, and a 30- to 60-minute semistructured qualitative phone interview was recorded and transcribed. Veterans received $40 for participation. All procedures were approved by the University of California San Francisco Institutional Review Board.
Qualitative Data Analysis
Rapid analysis procedures were used to analyze qualitative data. This approach is suitable for focused, moderately structured qualitative analyses in health services research and facilitates rapid dissemination to stakeholders.23 The qualitative analysts were 2 clinical psychologists with expertise in PTSD treatment (NH primary and RR secondary). Consistent with rapid analysis procedures, analysts prepared a templated summary (including relevant quotations) of each interview, organized by the prespecified content domains. Interviews were summarized independently, compared to ensure consistency, and discrepancies were resolved through review of the interview source materials. Individual summary templates were combined into a master analytic matrix to facilitate the identification of patterns and delineation of themes. Analysts routinely met to identify, discuss, and refine preliminary themes, revisiting source materials to reach consensus as needed.
Results
Fifteen themes were identified and organized into 2 distinct focus areas: themes directly related to the transition to TF-EBP (8 themes) and themes related to veterans’ experiences with TF-EBP and general mental health care with potential process-improvement implications (7 themes).21 Seven themes were identified related to experiences with TF-EBP engagement and VA mental health care. The 7 themes related to TF-EBP engagement and VA mental health care themes are summarized with exemplary quotations.
Veterans want a better understanding of psychotherapy and engaging with VA mental health. Veterans reported that they generally had a poor or “nebulous” understanding about the experience of psychotherapy. For example, veterans exhibited confusion about whether certain experiences were equivalent to participating in psychotherapy. They were sometimes unable to distinguish between interactions such as assessment, disability evaluations, peer support, and psychotherapy. One veteran described a conversation with a TFEBP therapist about prior treatment:
She [asked], have you ever been, or gone through a therapy to begin with? And I, I said, well I just chatted with somebody. And she said that’s not, that’s not therapy. So, I was like, oh, it’s not? That’s not what people do?
Veterans were surprised the VA offered a diverse range of psychotherapy interventions, rather than simply therapy. They did not realize there were different types of psychotherapy. As a result, veterans were not aware that some VA mental practitioners have specialty training and certification to provide treatment matched to specific diagnoses or needs. They thought that all clinicians could provide the same care. One veteran described their understanding:
I just figured all mental health people are mental health people. I didn’t have a better understanding of the system and all the different levels and how it plays out and specialties and things like that. Which, I guess, I should have because you have a primary care doctor, but then you have specialists in all these other different sectors that specialize in one particular area. I guess that should’ve been common sense, but it wasn’t.
Stigma was a barrier to seeking and engaging in mental health care. Veterans discovered they had to overcome stigma associated with seeking and engaging in mental health treatment. Military culture was often discussed as promoting stigma regarding mental health treatment. Specifically, veterans described that seeking treatment meant “either, I’m weak or I’m gonna be seen as weak.” In active-duty settings, the strategy for dealing with mental health symptoms was to “leave those feelings, you push ‘em aside,” an approach highly inconsistent with TF-EBP. In some cases, incorrect information about the VA and PTSD was presented as part of discharge from the military, leading to long-term skepticism of the VA and PTSD treatment. One veteran described his experience as part of a class on the VA compensation and pension assessment process for service-connected disabilities during his military discharge:
[A fellow discharging soldier asked] what about like PTSD, gettin’ rated for PTSD. I hear they take our weapons and stuff like we can’t own firearms and all that stuff. And [the instructor] was like, well, yes that’s a thing. He didn’t explain it like if you get compensated for PTSD you don’t lose your rights to carry a firearm or to have, to be able to go hunting.
Importantly, veterans often described how other identities (eg, race, ethnicity, gender, region of origin) interacted with military culture to enhance stigma. Hearing messaging from multiple sources reinforced beliefs that mental health treatment is inappropriate or is associated with weakness:
As a first-generation Italian, I was always taught keep your feelings to yourself. Never talk outside your family. Never bring up problems to other people and stuff like that. Same with the military. And then the old stigma working in [emergency medical services] and public safety, you’re weak if you get help.
The fundamentals of therapy, including rapport and flexibility, were important. Veterans valued nonspecific therapy factors, genuine empathy, building trust, being honest about treatment, personality, and rapport. These characteristics were almost universally described as particularly important:
I liked the fact that she made it personable and she cared. It wasn’t just like, here, we’re gonna start this. She explained it in the ways I could understand, not in medical terms, so to speak, but that’s what I liked about her. She really cared about what she did and helping me.
Flexibility was viewed as an asset, particularly when clinicians acknowledged veteran autonomy. A consistent example was when veterans were able to titrate trauma disclosure. One veteran described this flexible treatment experience: “She was right there in the room, she said, you know, at any time, you know, we could stop, we could debrief.”
Experiences of clinician flexibility and personalization of therapy were contrasted with experiences of overly rigid therapy. Overemphasis on protocols created barriers, often because treatment did not feel personalized. One veteran described how a clinician’s task-oriented approach interfered with their ability to engage in TF-EBP:
They listened, but it just didn’t seem like they were listening, because they really wanted to stay on task… So, I felt like if the person was more concerned, or more sympathetic to the things that was also going on in my life at that present time, I think I would’ve felt more comfortable talking about what was the PTSD part, too.
Veterans valued shared decision-making prior to TF-EBP initiation. Veterans typically described being involved in a shared decision-making process prior to initiating TF-EBP. During these sessions, clinicians discussed treatment options and provided veterans with a variety of materials describing treatments (eg, pamphlets, websites, videos, statistics). Most veterans appreciated being able to reflect on and discuss treatment options with their clinicians. Being given time in and out of session to review was viewed as valuable and increased confidence in treatment choice. One veteran described their experience:
I was given the information, you know, they gave me handouts, PDFs, whatever was available, and let me read over it. I didn’t have to choose anything right then and there, you know, they let me sleep on it. And I got back to them after some thought.
However, some veterans felt overwhelmed by being presented with too much information and did not believe they knew enough to make a final treatment decision. One veteran described being asked to contribute to the treatment decision:
I definitely asked [the clinician] to weigh in on maybe what he thought was best, because—I mean, I don’t know… I’m not necessarily sure I know what I think is best. I think we’re just lucky I’m here, so if you can give me a solid and help me out here by telling me just based on what I’ve said to you and the things that I’ve gone through, what do you think?
Veterans who perceived that their treatment preferences were respected had a positive outlook on TF-EBP. As part of the shared-decision making process, veterans typically described being given choices among PTSD treatments. One way that preferences were respected was through clinicians tailoring treatment descriptions to a veteran’s unique symptoms, experiences, and values. In these cases, clinicians observed specific concerns and clearly linked treatment principles to those concerns. For example, one veteran described their clinician’s recommendation for PE: “The hardest thing for me is to do the normal things like grocery store or getting on a train or anything like that. And so, he suggested that [PE] would be a good idea.”
In other cases, veterans wanted the highest quality of treatment rather than a match between treatment principles and the veteran’s presentation, goals, or strengths. These veterans wanted the best treatment available for PTSD and valued research support, recommendations from clinical practice guidelines, or clinician confidence in the effectiveness of the treatment. One veteran described this perspective:
I just wanted to be able to really tackle it in the best way possible and in the most like aggressive way possible. And it seemed like PE really was going to, they said that it’s a difficult type of therapy, but I really just wanted to kind of do the best that I could to eradicate some of the issues that I was having.
When veterans perceived a lack of respect for their preferences, they were hesitant about TF-EBP. For some veterans, a generic pitch for a TF-EBP was detrimental in the absence of the personal connection between the treatment and their own symptoms, goals, or strengths. These veterans did not question whether the treatment was effective in general but did question whether the treatment was best for them. One veteran described the contrast between their clinician’s perspective and their own.
I felt like they felt very comfortable, very confident in [CPT] being the program, because it was comfortable for them. Because they did it several times. And maybe they had a lot of success with other individuals... but they were very comfortable with that one, as a provider, more than: Is this the best fit for [me]?
Some veterans perceived little concern for their preferences and a lack of choice in available treatments, which tended to perpetuate negative perceptions of TFEBP. These veterans described their lack of choices with frustration. Alternatives to TFEBP were described by these veterans as so undesirable that they did not believe they had a real choice:
[CPT] was the only decision they had. There was nothing else for PTSD. They didn’t offer anything else. So, I mean it wasn’t a decision. It was either … take treatment or don’t take treatment at all… Actually, I need to correct myself. So, there were 2 options, group therapy or CPT. I forgot about that. I’m not a big group guy so I chose the CPT.
Another veteran was offered a choice between therapeutic approaches, but all were delivered via telehealth (consistent with the transition to virtual services during the COVID-19 pandemic). For this veteran, not only was the distinction between approaches unclear, but the choice between approaches was unimportant compared to the mode of delivery.
This happened during COVID-19 and VA stopped seeing anybody physically, face-to-face. So my only option for therapy was [telehealth]… There was like 3 of them, and I tried to figure out, you know, from the layperson’s perspective, like: I don’t know which one to go with.
Veterans wanted to be asked about their cultural identity. Veterans valued when clinicians asked questions about cultural identity as part of their mental health treatment and listened to their cultural context. Cultural identity factors extended beyond factors such as race, ethnicity, gender, and sexual orientation to religion, military culture, and regionality. Veterans often described situations where they wished clinicians would ask the question or initiate conversations about culture. A veteran highlighted the importance of their faith but noted that it was a taboo topic. Their clinician did not say “we don’t go there,” but they “never dove into it either.” Another veteran expressed a desire for their clinician to ask questions about experiences in the National Guard and as an African American veteran:
If a provider was to say like: Oh, you know, it’s a stressful situation being a part of the military, being in the National Guard. You know, just asking questions about that. I think that would really go a long way… Being African American was difficult as well. And more so because of my region, I think… I felt like it would probably be an uncomfortable subject to speak on… I mean, it wasn’t anything that my providers necessarily did, it was more so just because it wasn’t brought up.
One common area of concern for veterans was a match between veteran and therapist demographics. When asked about how their cultural identity influenced treatment, several veterans described the relevance of therapist match. Much like questions about their own cultural identity, veterans valued being asked about identity preferences in clinicians (eg, gender or race matching), rather than having to bring up the preference themselves. One veteran described relief at this question being asked directly: “I was relieved when she had asked [whether I wanted a male or female clinician] primarily because I was going to ask that or bring that up somehow. But her asking that before me was a weight off my shoulders.”
Discussing cultural identity through treatment strengthened veterans’ engagement in therapy. Many veterans appreciated when analogies used in therapy were relevant to their cultural experiences and when clinicians understood their culture (eg, military culture, race, ethnicity, religious beliefs, sexual orientation). One veteran described how their clinician understood military culture and made connections between military culture and the rationale for TF-EBP, which strengthened the veteran’s buy-in for the treatment and alliance with the clinician:
At the beginning when she was explaining PTSD, and I remember she said that your brain needed to think this way when you were in the military because it was a way of protecting and surviving, so your brain was doing that in order for you to survive in whatever areas you were because there was danger. So, your brain had you thinking that way. But now, you’re not in those situations anymore. You’re not in danger. You’re not in the military, but your brain is still thinking you are, and that’s what PTSD generally does to you.
Specific elements of TF-EBP also provided opportunities to discuss and integrate important aspects of identity. This is accomplished in PE by assigning relevant in vivo exercises. In CPT, “connecting the dots” on how prior experiences influenced trauma-related stuck points achieved this element. One veteran described their experience with a clinician who was comfortable discussing the veteran’s sexual orientation and recognized the impacts of prior trauma on intimacy:
They’re very different, and there’s a lot of things that can be accepted in gay relationships that are not in straight ones. With all that said, I think [the PE therapist] did a fantastic job being not—like never once did she laugh or make an uncomfortable comment or say she didn’t wanna talk about something when like part of the reason I wanted to get into therapy is that my partner and I weren’t having sex unless I used alcohol.
Discussion
As part of a larger national qualitative investigation of the experiences of veterans who recently initiated TF-EBP, veterans discussed their experiences with therapy and mental health care that have important implications for continued process improvement.21 Three key areas for continued process improvement were identified: (1) providing information about the diverse range of mental health care services at the VA and the implications of this continuum of care; (2) consideration of veteran preferences in treatment decision-making, including the importance of perceived choice; and (3) incorporating cultural assessment and cultural responsiveness into case conceptualization and treatment.
One area of process improvement identified was increasing knowledge about different types of psychotherapy and the continuum of care available at the VA. Veterans in this study confused or conflated participating in psychotherapy with talking about mental health symptoms with a clinician (eg, assessment, disability evaluation). They were sometimes surprised that psychotherapy is an umbrella term referring to a variety of different modalities. The downstream impact of these misunderstandings was a perception of VA mental health care as nebulous. Veterans were surprised that all mental health practitioners were unable to provide the same care. Confusion may have been compounded by highly variable referral processes across VA.24 To address this, clinicians have developed local educational resources and handouts for both veterans and referring clinicians from nonmental health and general mental health specialties.25 Given the variability in referral processes both between and within VA medical centers, national dissemination of these educational materials may be more difficult compared to materials for TF-EBPs.24 The VA started to use behavioral health interdisciplinary program (BHIP) teams, which are designed to be clinical homes for veterans connected with a central clinician who can explain and coordinate their mental health care as well as bring more consistency to the referral process.26 The ongoing transition toward the BHIP model of mental health care at VA may provide the opportunity to consolidate and integrate knowledge about the VA approach to mental health care, potentially filling knowledge gaps.
A second area of process improvement focused on the shared decision-making process. Consistent with mental health initiatives, veterans generally believed they had received sufficient information about TF-EBP and engaged in shared decision-making with clinicians.20,27 Veterans were given educational materials to review and had the opportunity to discuss these materials with clinicians. However, veterans described variability in the success of shared decision-making. Although veterans valued receiving accurate, comprehensible information to support treatment decisions, some preferred to defer to clinicians’ expertise regarding which treatment to pursue. While these veterans valued information, they also valued the expertise of clinicians in explaining why specific treatments would be beneficial. A key contributor to veterans satisfaction was assessing how veterans wanted to engage in the decision-making process and respecting those preferences.28 Veterans approached shared decision-making differently, from making decisions independently after receiving information to relying solely on clinician recommendation. The process was most successful when clinicians articulated how their recommended treatment aligned with a veteran’s preferences, including recommendations based on specific values (eg, personalized match vs being the best). Another important consideration is ensuring veterans know they can receive a variety of different types of mental health services available in different modalities (eg, virtual vs in-person; group vs individual). When veterans did not perceive choice in treatment aspects important to them (typically despite having choices), they were less satisfied with their TF-EBP experience.
A final area of process improvement identified involves how therapists address important aspects of culture. Veterans often described mental health stigma coming from intersecting cultural identities and expressed appreciation when therapists helped them recognize the impact of these beliefs on treatment. Some veterans did not discuss important aspects of their identity with clinicians, including race/ethnicity, religion, and military culture. Veterans did not report negative interactions with clinicians or experiences suggesting it was inappropriate to discuss identity; however, they were reluctant to independently raise these identity factors. Strategies such as the ADDRESSING framework, a mnemonic acronym that describes a series of potentially relevant characteristics, can help clinicians comprehensively consider different aspects that may be relevant to veterans, modeling that discussion of relevant these characteristics is welcome in TF-EBP.29 Veterans reported that making culturally relevant connections enhanced the TF-EBP experience, most commonly with military culture. These data support that TF-EBP delivery with attention to culture should be an integrated part of treatment, supporting engagement and therapeutic alliance.30 The VA National Center for PTSD consultation program is a resource to support clinicians in assessing and incorporating relevant aspects of cultural identity.31 For example, the National Center for PTSD provides a guide for using case conceptualization to address patient reactions to race-based violence during PTSD treatment.32 Both manualized design and therapist certification training can reinforce that assessing and attending to case conceptualization (including identity factors) is an integral component of TF-EBP.33,34
Limitations
While the current study has numerous strengths (eg, national veteran sampling, robust qualitative methods), results should be considered within the context of study limitations. First, veteran participants all received TF-EBP, and the perspectives of veterans who never initiate TF-EBP may differ. Despite the strong sampling approach, the study design is not intended to be generalizable to all veterans receiving TF-EBP for PTSD. Qualitative analysis yielded 15 themes, described in this study and prior research, consistent with recommendations.21,22 This approach allows rich description of distinct focus areas that would not be possible in a single manuscript. Nonetheless, all veterans interviewed described their experiences in TF-EBP and general mental health care, the focus of the semistructured interview guide was on the experience of transitioning from other treatment to TF-EBP.
Conclusion
This study describes themes related to general mental health and TF-EBP process improvement as part of a larger study on transitions in PTSD care.21,22 Veterans valued the fundamentals of therapy, including rapport and flexibility. Treatment-specific rapport (eg, pointing out treatment progress and effort in completing treatment components) and flexibility within the context of fidelity (ie, personalizing treatment while maintaining core treatment elements) may be most effective at engaging veterans in recommended PTSD treatments.18,34 In addition to successes, themes suggest multiple opportunities for process improvement. Ongoing VA initiatives and priorities (ie, BHIP, shared decision-making, consultation services) aim to improve processes consistent with veteran recommendations. Future research is needed to evaluate the success of these and other programs to optimize access to and engagement in recommended PTSD treatments.
- US Department of Veterans Affairs; US Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. 2023. Updated August 20, 2025. Accessed October 17, 2025. https://www.healthquality.va.gov/guidelines/MH/ptsd/
- International Society for Traumatic Stress Studies. ISTSS PTSD prevention and treatment guidelines: methodology and recommendations. Accessed August 13, 2025. http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-TreatmentGuidelines/ISTSS_PreventionTreatmentGuidelines_FNL-March-19-2019.pdf.aspx
- American Psychological Association. Clinical practice guideline for the treatment of posttraumatic stress disorder in adults. Accessed August 13, 2025. https://www.apa.org/ptsd-guideline/ptsd.pdf
- Karlin BE, Cross G. From the laboratory to the therapy room: National dissemination and implementation of evidence- based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69:19-33. doi:10.1037/a0033888
- Rosen CS, Matthieu MM, Wiltsey Stirman S, et al. A review of studies on the system-wide implementation of evidencebased psychotherapies for posttraumatic stress disorder in the Veterans Health Administration. Adm Policy Ment Health. 2016;43:957-977. doi:10.1007/s10488-016-0755-0
- Maguen S, Holder N, Madden E, et al. Evidence-based psychotherapy trends among posttraumatic stress disorder patients in a national healthcare system, 2001-2014. Depress Anxiety. 2020;37:356-364. doi:10.1002/da.22983
- Cheney AM, Koenig CJ, Miller CJ, et al. Veteran-centered barriers to VA mental healthcare services use. BMC Health Serv Res. 2018;18:591. doi:10.1186/s12913-018-3346-9
- Hundt NE, Mott JM, Miles SR, et al. Veterans’ perspectives on initiating evidence-based psychotherapy for posttraumatic stress disorder. Psychol Trauma. 2015;7:539-546. doi:10.1037/tra0000035
- Hundt NE, Helm A, Smith TL, et al. Failure to engage: a qualitative study of veterans who decline evidence-based psychotherapies for PTSD. Psychol Serv. 2018;15:536- 542. doi:10.1037/ser0000212
- Sayer NA, Friedemann-Sanchez G, Spoont M, et al. A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry. 2009;72:238-255. doi:10.1521/psyc.2009.72.3.238
- Mittal D, Drummond KL, Blevins D, et al. Stigma associated with PTSD: perceptions of treatment seeking combat veterans. Psychiatr Rehabil J. 2013;36:86-92. doi:10.1037/h0094976
- Possemato K, Wray LO, Johnson E, et al. Facilitators and barriers to seeking mental health care among primary care veterans with posttraumatic stress disorder. J Trauma Stress. 2018;31:742-752. doi:10.1002/jts.22327
- Silvestrini M, Chen JA. “It’s a sign of weakness”: Masculinity and help-seeking behaviors among male veterans accessing posttraumatic stress disorder care. Psychol Trauma. 2023;15:665-671. doi:10.1037/tra0001382
- Stecker T, Shiner B, Watts BV, et al. Treatment-seeking barriers for veterans of the Iraq and Afghanistan conflicts who screen positive for PTSD. Psychiatr Serv. 2013;64:280-283. doi:10.1176/appi.ps.001372012
- Etingen B, Grubbs KM, Harik JM. Drivers of preference for evidence-based PTSD treatment: a qualitative assessment. Mil Med. 2020;185:303-310. doi:10.1093/milmed/usz220
- Hundt NE, Ecker AH, Thompson K, et al. “It didn’t fit for me:” A qualitative examination of dropout from prolonged exposure and cognitive processing therapy in veterans. Psychol Serv. 2020;17:414-421. doi:10.1037/ser0000316
- Kehle-Forbes SM, Gerould H, Polusny MA, et al. “It leaves me very skeptical” messaging in marketing prolonged exposure and cognitive processing therapy to veterans with PTSD. Psychol Trauma. 2022;14:849-852. doi:10.1037/tra0000550
- Kehle-Forbes SM, Ackland PE, Spoont MR, et al. Divergent experiences of U.S. veterans who did and did not complete trauma-focused therapies for PTSD: a national qualitative study of treatment dropout. Behav Res Ther. 2022;154:104123. doi:10.1016/j.brat.2022.104123
- Hessinger JD, London MJ, Baer SM. Evaluation of a shared decision-making intervention on the utilization of evidence-based psychotherapy in a VA outpatient PTSD clinic. Psychol Serv. 2018;15:437-441. doi:10.1037/ser0000141
- Hamblen JL, Grubbs KM, Cole B, et al. “Will it work for me?” Developing patient-friendly graphical displays of posttraumatic stress disorder treatment effectiveness. J Trauma Stress. 2022;35:999-1010. doi:10.1002/jts.22808
- Holder N, Ranney RM, Delgado AK, et al. Transitioning into trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatments: a qualitative investigation. Cogn Behav Ther. 2025;54:391-407. doi:10.1080/16506073.2024.2408386
- Levitt HM, Bamberg M, Creswell JW, et al. Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA Publications and Communications Board task force report. Am Psychol. 2018;73:26-46. doi:10.1037/amp0000151
- Palinkas LA, Mendon SJ, Hamilton AB. Innovations in mixed methods evaluations. Annu Rev Public Health. 2019;40:423- 442. doi:10.1146/annurev-publhealth-040218-044215
- Ranney RM, Cordova MJ, Maguen S. A review of the referral process for evidence-based psychotherapies for PTSD among veterans. Prof Psychol Res Pr. 2022;53:276-285. doi:10.1037/pro0000463
- Holder N, Ranney RM, Delgado AK, et al. Transitions to trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatment: a qualitative investigation of clinician’s perspectives. Cogn Behav Ther. 2025;1-19. doi:10.1080/16506073.2025.2481475
- Barry CN, Abraham KM, Weaver KR, et al. Innovating team-based outpatient mental health care in the Veterans Health Administration: staff-perceived benefits and challenges to pilot implementation of the Behavioral Health Interdisciplinary Program (BHIP). Psychol Serv. 2016;13:148-155. doi:10.1037/ser0000072
- Harik JM, Hundt NE, Bernardy NC, et al. Desired involvement in treatment decisions among adults with PTSD symptoms. J Trauma Stress. 2016;29:221-228. doi:10.1002/jts.22102
- Larsen SE, Hooyer K, Kehle-Forbes SM, et al. Patient experiences in making PTSD treatment decisions. Psychol Serv. 2024;21:529-537. doi:10.1037/ser0000817
- Hays PA. Four steps toward intersectionality in psychotherapy using the ADDRESSING framework. Prof Psychol Res Pr. 2024;55:454-462. doi:10.1037/pro0000577
- Galovski TE, Nixon RDV, Kaysen D. Flexible Applications of Cognitive Processing Therapy: Evidence-Based Treatment Methods. Academic Press; 2020.
- Larsen SE, McKee T, Fielstein E, et al. The development of a posttraumatic stress disorder (PTSD) consultation program to support system-wide implementation of high-quality PTSD care for veterans. Psychol Serv. 2025;22:342-348. doi:10.1037/ser0000867
- Galovski T, Kaysen D, McClendon J, et al. Provider guide to addressing patient reactions to race-based violence during PTSD treatment. PTSD.va.gov. Accessed August 3, 2025. www.ptsd.va.gov/professional/treat/specific/patient_reactions_race_violence.asp
- Galovski TE, Nixon RDV, Kehle-Forbes S. Walking the line between fidelity and flexibility: a conceptual review of personalized approaches to manualized treatments for posttraumatic stress disorder. J Trauma Stress. 2024;37:768-774. doi:10.1002/jts.23073
- Galovski TE, McSweeney LB, Nixon RDV, et al. Personalizing cognitive processing therapy with a case formulation approach to intentionally target impairment in psychosocial functioning associated with PTSD. Contemp Clin Trials Commun. 2024;42:101385. doi:10.1016/j.conctc.2024.101385
- US Department of Veterans Affairs; US Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. 2023. Updated August 20, 2025. Accessed October 17, 2025. https://www.healthquality.va.gov/guidelines/MH/ptsd/
- International Society for Traumatic Stress Studies. ISTSS PTSD prevention and treatment guidelines: methodology and recommendations. Accessed August 13, 2025. http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-TreatmentGuidelines/ISTSS_PreventionTreatmentGuidelines_FNL-March-19-2019.pdf.aspx
- American Psychological Association. Clinical practice guideline for the treatment of posttraumatic stress disorder in adults. Accessed August 13, 2025. https://www.apa.org/ptsd-guideline/ptsd.pdf
- Karlin BE, Cross G. From the laboratory to the therapy room: National dissemination and implementation of evidence- based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69:19-33. doi:10.1037/a0033888
- Rosen CS, Matthieu MM, Wiltsey Stirman S, et al. A review of studies on the system-wide implementation of evidencebased psychotherapies for posttraumatic stress disorder in the Veterans Health Administration. Adm Policy Ment Health. 2016;43:957-977. doi:10.1007/s10488-016-0755-0
- Maguen S, Holder N, Madden E, et al. Evidence-based psychotherapy trends among posttraumatic stress disorder patients in a national healthcare system, 2001-2014. Depress Anxiety. 2020;37:356-364. doi:10.1002/da.22983
- Cheney AM, Koenig CJ, Miller CJ, et al. Veteran-centered barriers to VA mental healthcare services use. BMC Health Serv Res. 2018;18:591. doi:10.1186/s12913-018-3346-9
- Hundt NE, Mott JM, Miles SR, et al. Veterans’ perspectives on initiating evidence-based psychotherapy for posttraumatic stress disorder. Psychol Trauma. 2015;7:539-546. doi:10.1037/tra0000035
- Hundt NE, Helm A, Smith TL, et al. Failure to engage: a qualitative study of veterans who decline evidence-based psychotherapies for PTSD. Psychol Serv. 2018;15:536- 542. doi:10.1037/ser0000212
- Sayer NA, Friedemann-Sanchez G, Spoont M, et al. A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry. 2009;72:238-255. doi:10.1521/psyc.2009.72.3.238
- Mittal D, Drummond KL, Blevins D, et al. Stigma associated with PTSD: perceptions of treatment seeking combat veterans. Psychiatr Rehabil J. 2013;36:86-92. doi:10.1037/h0094976
- Possemato K, Wray LO, Johnson E, et al. Facilitators and barriers to seeking mental health care among primary care veterans with posttraumatic stress disorder. J Trauma Stress. 2018;31:742-752. doi:10.1002/jts.22327
- Silvestrini M, Chen JA. “It’s a sign of weakness”: Masculinity and help-seeking behaviors among male veterans accessing posttraumatic stress disorder care. Psychol Trauma. 2023;15:665-671. doi:10.1037/tra0001382
- Stecker T, Shiner B, Watts BV, et al. Treatment-seeking barriers for veterans of the Iraq and Afghanistan conflicts who screen positive for PTSD. Psychiatr Serv. 2013;64:280-283. doi:10.1176/appi.ps.001372012
- Etingen B, Grubbs KM, Harik JM. Drivers of preference for evidence-based PTSD treatment: a qualitative assessment. Mil Med. 2020;185:303-310. doi:10.1093/milmed/usz220
- Hundt NE, Ecker AH, Thompson K, et al. “It didn’t fit for me:” A qualitative examination of dropout from prolonged exposure and cognitive processing therapy in veterans. Psychol Serv. 2020;17:414-421. doi:10.1037/ser0000316
- Kehle-Forbes SM, Gerould H, Polusny MA, et al. “It leaves me very skeptical” messaging in marketing prolonged exposure and cognitive processing therapy to veterans with PTSD. Psychol Trauma. 2022;14:849-852. doi:10.1037/tra0000550
- Kehle-Forbes SM, Ackland PE, Spoont MR, et al. Divergent experiences of U.S. veterans who did and did not complete trauma-focused therapies for PTSD: a national qualitative study of treatment dropout. Behav Res Ther. 2022;154:104123. doi:10.1016/j.brat.2022.104123
- Hessinger JD, London MJ, Baer SM. Evaluation of a shared decision-making intervention on the utilization of evidence-based psychotherapy in a VA outpatient PTSD clinic. Psychol Serv. 2018;15:437-441. doi:10.1037/ser0000141
- Hamblen JL, Grubbs KM, Cole B, et al. “Will it work for me?” Developing patient-friendly graphical displays of posttraumatic stress disorder treatment effectiveness. J Trauma Stress. 2022;35:999-1010. doi:10.1002/jts.22808
- Holder N, Ranney RM, Delgado AK, et al. Transitioning into trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatments: a qualitative investigation. Cogn Behav Ther. 2025;54:391-407. doi:10.1080/16506073.2024.2408386
- Levitt HM, Bamberg M, Creswell JW, et al. Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA Publications and Communications Board task force report. Am Psychol. 2018;73:26-46. doi:10.1037/amp0000151
- Palinkas LA, Mendon SJ, Hamilton AB. Innovations in mixed methods evaluations. Annu Rev Public Health. 2019;40:423- 442. doi:10.1146/annurev-publhealth-040218-044215
- Ranney RM, Cordova MJ, Maguen S. A review of the referral process for evidence-based psychotherapies for PTSD among veterans. Prof Psychol Res Pr. 2022;53:276-285. doi:10.1037/pro0000463
- Holder N, Ranney RM, Delgado AK, et al. Transitions to trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatment: a qualitative investigation of clinician’s perspectives. Cogn Behav Ther. 2025;1-19. doi:10.1080/16506073.2025.2481475
- Barry CN, Abraham KM, Weaver KR, et al. Innovating team-based outpatient mental health care in the Veterans Health Administration: staff-perceived benefits and challenges to pilot implementation of the Behavioral Health Interdisciplinary Program (BHIP). Psychol Serv. 2016;13:148-155. doi:10.1037/ser0000072
- Harik JM, Hundt NE, Bernardy NC, et al. Desired involvement in treatment decisions among adults with PTSD symptoms. J Trauma Stress. 2016;29:221-228. doi:10.1002/jts.22102
- Larsen SE, Hooyer K, Kehle-Forbes SM, et al. Patient experiences in making PTSD treatment decisions. Psychol Serv. 2024;21:529-537. doi:10.1037/ser0000817
- Hays PA. Four steps toward intersectionality in psychotherapy using the ADDRESSING framework. Prof Psychol Res Pr. 2024;55:454-462. doi:10.1037/pro0000577
- Galovski TE, Nixon RDV, Kaysen D. Flexible Applications of Cognitive Processing Therapy: Evidence-Based Treatment Methods. Academic Press; 2020.
- Larsen SE, McKee T, Fielstein E, et al. The development of a posttraumatic stress disorder (PTSD) consultation program to support system-wide implementation of high-quality PTSD care for veterans. Psychol Serv. 2025;22:342-348. doi:10.1037/ser0000867
- Galovski T, Kaysen D, McClendon J, et al. Provider guide to addressing patient reactions to race-based violence during PTSD treatment. PTSD.va.gov. Accessed August 3, 2025. www.ptsd.va.gov/professional/treat/specific/patient_reactions_race_violence.asp
- Galovski TE, Nixon RDV, Kehle-Forbes S. Walking the line between fidelity and flexibility: a conceptual review of personalized approaches to manualized treatments for posttraumatic stress disorder. J Trauma Stress. 2024;37:768-774. doi:10.1002/jts.23073
- Galovski TE, McSweeney LB, Nixon RDV, et al. Personalizing cognitive processing therapy with a case formulation approach to intentionally target impairment in psychosocial functioning associated with PTSD. Contemp Clin Trials Commun. 2024;42:101385. doi:10.1016/j.conctc.2024.101385
Process Improvement for Engaging With Trauma-Focused Evidence-Based Psychotherapy for PTSD
Process Improvement for Engaging With Trauma-Focused Evidence-Based Psychotherapy for PTSD
Helping Veterans Ease Into Civilian Life
What does a successful military-to-civilian transition look like? How do we know if a veteran is sinking, treading water, or swimming? Two recent studies by the Penn State University Clearinghouse for Military Family Readiness sought to answer to those questions and more while determining how and when is the right time to step in to help a veteran in need.
The research analyzed The Veterans Metrics Initiative data (TVMI). This longitudinal study surveyed 9566 men and women who left active duty in 2016 over 3 years, answering questions about deployment histories, adverse childhood experiences (ACEs) and exposure to combat. They also reported whether they had symptoms related to anxiety and depression.
The TVMI study found that ACEs predicted poor outcomes early on and when combined with warfare experience dramatically increased the likelihood of mental health issues, including posttraumatic stress disorder (PTSD), anxiety, and depression; moral injury impacted adjustment to civilian life (the degree varied by gender); and, many veterans have a “growth outlook” as a result of a trauma or crisis they experienced.
The TVMI study found that almost all veterans use transition resources in the first 2 years after military separation. Beyond that, however, those in high-risk categories (eg, PTSD and cumulative trauma experiences) need continued support. This may come in the form of a universal screener and linking it to a navigation infrastructure (eg, AmericaServes), “thereby identifying risk factors early and providing targeted supports, interventions, and components.”
Veterans often face a series of simultaneous challenges as they return to civilian life. Among them include getting used to family and friends again, finding jobs, losing their military identity, structure, and perhaps leaving military friends behind. In addition, veterans are likely dealing with physical and mental health challenges, which can significantly influence how well they readjust to civilian life and lead to inconsistency experiences for each individual.
A 2019 survey from the Pew Research Center found about 40% of veterans who suffered from PTSD said they frequently had difficulty dealing with the lack of structure in civilian life, compared with 5% of those who do not have PTSD. Another survey cited a large majority (78%) of pre-9/11 veterans said their readjustment was very or somewhat easy. However, 26% said adjusting to civilian life was difficult.
In 2011, 4 variables were identified that predicted easy civilian life re-entry: being an officer; having a consistently clear understanding of the missions while in the service; being a college graduate; and, for post-9/11 veterans, attending religious services frequently. Six variables were associated with a diminished probability of an easy transition: having had a traumatic experience; being seriously injured; serving in the post-9/11 era; serving in a combat zone; serving with someone who was killed or injured; and, for post-9/11 veterans, being married while in the service.
The probabilities of an easy re-entry dropped from 82% for those who did not experience a traumatic event to 56% for those who did—the largest change noted in the 2011 study.
The second Penn State study evaluated a model framework with a lifespan development perspective. The study surveyed veterans on their self-reported satisfaction or symptoms in 7 domains of well-being: employment, education, financial, legal problems, social, physical health, and mental health. Within 3 months of separation , 41% of respondents fell into the “problematic” category for the mental health domain. However, by 30 to 33 months postseparation, this proportion dropped to 34%. During the same period, the proportion of veterans in the at risk category increased from 28% at Wave 1 to 37% at Wave 6. About 30% of veterans fell into the successful category for symptoms across the 3 examined waves. Almost 60% were in the successful category across the 3 time points.
Both Penn State studies emphasize the importance of viewing veterans as individuals on their own timelines.
“These findings underscore that the transition to civilian life is not a single moment, but a process influenced by experiences across the life span,” said Mary M. Mitchell, research professor at the Clearinghouse and lead author on the predictors study. “By following veterans over 3 years, we were able to see how patterns emerge that would be invisible in a one-time survey.”
Current conceptualization “assumes that there are commonalities across veterans when evaluating the success of the transition to civilian life,” according to the authors of the framework study. “However, each veteran likely has his or her view of what a successful transition constitutes, and he or she may weigh domains differently when considering his or her own transition.”
The research highlights the need to find ways to encourage veterans to seek help—and not just in the first year, which is often the most stressful. The Pew Research Center survey identified a “significant break from the past,” in that nearly 70% of post-9/11 veterans said their superiors made them feel comfortable about seeking help with emotional issues resulting from their military service.
However, ≤ 8% veterans in the TVMI study used any health programs, even when they screened positive for mental health problems. Veterans who did use counseling services, however, improved their depression symptoms. Engaging veterans at various time points could help keep mental health problems from worsening during—and beyond—the transition.
What does a successful military-to-civilian transition look like? How do we know if a veteran is sinking, treading water, or swimming? Two recent studies by the Penn State University Clearinghouse for Military Family Readiness sought to answer to those questions and more while determining how and when is the right time to step in to help a veteran in need.
The research analyzed The Veterans Metrics Initiative data (TVMI). This longitudinal study surveyed 9566 men and women who left active duty in 2016 over 3 years, answering questions about deployment histories, adverse childhood experiences (ACEs) and exposure to combat. They also reported whether they had symptoms related to anxiety and depression.
The TVMI study found that ACEs predicted poor outcomes early on and when combined with warfare experience dramatically increased the likelihood of mental health issues, including posttraumatic stress disorder (PTSD), anxiety, and depression; moral injury impacted adjustment to civilian life (the degree varied by gender); and, many veterans have a “growth outlook” as a result of a trauma or crisis they experienced.
The TVMI study found that almost all veterans use transition resources in the first 2 years after military separation. Beyond that, however, those in high-risk categories (eg, PTSD and cumulative trauma experiences) need continued support. This may come in the form of a universal screener and linking it to a navigation infrastructure (eg, AmericaServes), “thereby identifying risk factors early and providing targeted supports, interventions, and components.”
Veterans often face a series of simultaneous challenges as they return to civilian life. Among them include getting used to family and friends again, finding jobs, losing their military identity, structure, and perhaps leaving military friends behind. In addition, veterans are likely dealing with physical and mental health challenges, which can significantly influence how well they readjust to civilian life and lead to inconsistency experiences for each individual.
A 2019 survey from the Pew Research Center found about 40% of veterans who suffered from PTSD said they frequently had difficulty dealing with the lack of structure in civilian life, compared with 5% of those who do not have PTSD. Another survey cited a large majority (78%) of pre-9/11 veterans said their readjustment was very or somewhat easy. However, 26% said adjusting to civilian life was difficult.
In 2011, 4 variables were identified that predicted easy civilian life re-entry: being an officer; having a consistently clear understanding of the missions while in the service; being a college graduate; and, for post-9/11 veterans, attending religious services frequently. Six variables were associated with a diminished probability of an easy transition: having had a traumatic experience; being seriously injured; serving in the post-9/11 era; serving in a combat zone; serving with someone who was killed or injured; and, for post-9/11 veterans, being married while in the service.
The probabilities of an easy re-entry dropped from 82% for those who did not experience a traumatic event to 56% for those who did—the largest change noted in the 2011 study.
The second Penn State study evaluated a model framework with a lifespan development perspective. The study surveyed veterans on their self-reported satisfaction or symptoms in 7 domains of well-being: employment, education, financial, legal problems, social, physical health, and mental health. Within 3 months of separation , 41% of respondents fell into the “problematic” category for the mental health domain. However, by 30 to 33 months postseparation, this proportion dropped to 34%. During the same period, the proportion of veterans in the at risk category increased from 28% at Wave 1 to 37% at Wave 6. About 30% of veterans fell into the successful category for symptoms across the 3 examined waves. Almost 60% were in the successful category across the 3 time points.
Both Penn State studies emphasize the importance of viewing veterans as individuals on their own timelines.
“These findings underscore that the transition to civilian life is not a single moment, but a process influenced by experiences across the life span,” said Mary M. Mitchell, research professor at the Clearinghouse and lead author on the predictors study. “By following veterans over 3 years, we were able to see how patterns emerge that would be invisible in a one-time survey.”
Current conceptualization “assumes that there are commonalities across veterans when evaluating the success of the transition to civilian life,” according to the authors of the framework study. “However, each veteran likely has his or her view of what a successful transition constitutes, and he or she may weigh domains differently when considering his or her own transition.”
The research highlights the need to find ways to encourage veterans to seek help—and not just in the first year, which is often the most stressful. The Pew Research Center survey identified a “significant break from the past,” in that nearly 70% of post-9/11 veterans said their superiors made them feel comfortable about seeking help with emotional issues resulting from their military service.
However, ≤ 8% veterans in the TVMI study used any health programs, even when they screened positive for mental health problems. Veterans who did use counseling services, however, improved their depression symptoms. Engaging veterans at various time points could help keep mental health problems from worsening during—and beyond—the transition.
What does a successful military-to-civilian transition look like? How do we know if a veteran is sinking, treading water, or swimming? Two recent studies by the Penn State University Clearinghouse for Military Family Readiness sought to answer to those questions and more while determining how and when is the right time to step in to help a veteran in need.
The research analyzed The Veterans Metrics Initiative data (TVMI). This longitudinal study surveyed 9566 men and women who left active duty in 2016 over 3 years, answering questions about deployment histories, adverse childhood experiences (ACEs) and exposure to combat. They also reported whether they had symptoms related to anxiety and depression.
The TVMI study found that ACEs predicted poor outcomes early on and when combined with warfare experience dramatically increased the likelihood of mental health issues, including posttraumatic stress disorder (PTSD), anxiety, and depression; moral injury impacted adjustment to civilian life (the degree varied by gender); and, many veterans have a “growth outlook” as a result of a trauma or crisis they experienced.
The TVMI study found that almost all veterans use transition resources in the first 2 years after military separation. Beyond that, however, those in high-risk categories (eg, PTSD and cumulative trauma experiences) need continued support. This may come in the form of a universal screener and linking it to a navigation infrastructure (eg, AmericaServes), “thereby identifying risk factors early and providing targeted supports, interventions, and components.”
Veterans often face a series of simultaneous challenges as they return to civilian life. Among them include getting used to family and friends again, finding jobs, losing their military identity, structure, and perhaps leaving military friends behind. In addition, veterans are likely dealing with physical and mental health challenges, which can significantly influence how well they readjust to civilian life and lead to inconsistency experiences for each individual.
A 2019 survey from the Pew Research Center found about 40% of veterans who suffered from PTSD said they frequently had difficulty dealing with the lack of structure in civilian life, compared with 5% of those who do not have PTSD. Another survey cited a large majority (78%) of pre-9/11 veterans said their readjustment was very or somewhat easy. However, 26% said adjusting to civilian life was difficult.
In 2011, 4 variables were identified that predicted easy civilian life re-entry: being an officer; having a consistently clear understanding of the missions while in the service; being a college graduate; and, for post-9/11 veterans, attending religious services frequently. Six variables were associated with a diminished probability of an easy transition: having had a traumatic experience; being seriously injured; serving in the post-9/11 era; serving in a combat zone; serving with someone who was killed or injured; and, for post-9/11 veterans, being married while in the service.
The probabilities of an easy re-entry dropped from 82% for those who did not experience a traumatic event to 56% for those who did—the largest change noted in the 2011 study.
The second Penn State study evaluated a model framework with a lifespan development perspective. The study surveyed veterans on their self-reported satisfaction or symptoms in 7 domains of well-being: employment, education, financial, legal problems, social, physical health, and mental health. Within 3 months of separation , 41% of respondents fell into the “problematic” category for the mental health domain. However, by 30 to 33 months postseparation, this proportion dropped to 34%. During the same period, the proportion of veterans in the at risk category increased from 28% at Wave 1 to 37% at Wave 6. About 30% of veterans fell into the successful category for symptoms across the 3 examined waves. Almost 60% were in the successful category across the 3 time points.
Both Penn State studies emphasize the importance of viewing veterans as individuals on their own timelines.
“These findings underscore that the transition to civilian life is not a single moment, but a process influenced by experiences across the life span,” said Mary M. Mitchell, research professor at the Clearinghouse and lead author on the predictors study. “By following veterans over 3 years, we were able to see how patterns emerge that would be invisible in a one-time survey.”
Current conceptualization “assumes that there are commonalities across veterans when evaluating the success of the transition to civilian life,” according to the authors of the framework study. “However, each veteran likely has his or her view of what a successful transition constitutes, and he or she may weigh domains differently when considering his or her own transition.”
The research highlights the need to find ways to encourage veterans to seek help—and not just in the first year, which is often the most stressful. The Pew Research Center survey identified a “significant break from the past,” in that nearly 70% of post-9/11 veterans said their superiors made them feel comfortable about seeking help with emotional issues resulting from their military service.
However, ≤ 8% veterans in the TVMI study used any health programs, even when they screened positive for mental health problems. Veterans who did use counseling services, however, improved their depression symptoms. Engaging veterans at various time points could help keep mental health problems from worsening during—and beyond—the transition.
'Energy Insecurity' Tied to Anxiety, Depression Risk
'Energy Insecurity' Tied to Anxiety, Depression Risk
TOPLINE:
Energy insecurity, the inability to meet household energy needs, was associated with more than twice the odds of having depression and anxiety symptoms than energy security in US adults, a new cross-sectional study showed.
METHODOLOGY:
- Using data from the US Census Bureau's online Household Pulse Survey, administered between 2022 and 2024, researchers conducted a cross-sectional study with a weighted population of > 187 million US adults (51% women; 64% White, 16% Hispanic, 10% Black, and 5% Asian). About a quarter of the population was in each of 4 age groups: 18-34 years, 35-49 years, 50-64 years, and ≥ 65 years.
- Three indicators of energy insecurity—inability to pay energy bills, maintaining unsafe/unhealthy home temperatures, and forgoing expenses on basic necessities to pay energy bills—were assessed individually and as a composite measure.
- Mental health was assessed using modified versions of the 2-item Patient Health Questionnaire for depression and the 2-item Generalized Anxiety Disorder scale for anxiety.
- The analysis was adjusted for other social determinants of health, including unemployment, housing instability, and food insecurity. Covariates included a wide range of factors, such as age, educational level, sex, and annual household income.
TAKEAWAY:
- In all, > 43% of the population reported having ≥ 1 form of energy security; around 22% reported being unable to pay energy bills, 22% maintained unsafe home temperatures, and nearly 34% forewent spending on basic necessities to pay energy bills.
- Individuals who gave up spending on basic necessities to pay energy bills had higher odds of anxiety (adjusted odds ratio [aOR], 1.79) and depression (aOR, 1.74) than those who did not.
- Adults with energy insecurity on the composite measure had higher odds for anxiety (aOR, 2.29) and depression (aOR, 2.31) than those with energy security.
- Food insecurity was also associated with poorer mental health, with higher odds for symptoms of depression (aOR, 2.05) and anxiety (aOR, 2.07).
IN PRACTICE:
"Despite its high prevalence, energy insecurity remains underrecognized in public health and policy intervention strategies," the investigators wrote.
"These findings suggest that energy insecurity is a widespread and important factor associated with mental health symptoms and may warrant consideration in efforts to reduce adverse mental health outcomes," they added.
SOURCE:
This study was led by Michelle Graf, PhD, Carter School of Public Policy, Georgia Institute of Technology, Atlanta. It was published online on October 27 in JAMA Network Open.
LIMITATIONS:
The cross-sectional nature of the data limited causal interference and increased the possibility of reverse causality. The questionnaire captured subjective interpretations of unsafe and unhealthy indoor temperatures, which may have varied among respondents. Additionally, the recall periods for energy insecurity and mental health outcomes were different.
DISCLOSURES:
The investigators reported no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
Energy insecurity, the inability to meet household energy needs, was associated with more than twice the odds of having depression and anxiety symptoms than energy security in US adults, a new cross-sectional study showed.
METHODOLOGY:
- Using data from the US Census Bureau's online Household Pulse Survey, administered between 2022 and 2024, researchers conducted a cross-sectional study with a weighted population of > 187 million US adults (51% women; 64% White, 16% Hispanic, 10% Black, and 5% Asian). About a quarter of the population was in each of 4 age groups: 18-34 years, 35-49 years, 50-64 years, and ≥ 65 years.
- Three indicators of energy insecurity—inability to pay energy bills, maintaining unsafe/unhealthy home temperatures, and forgoing expenses on basic necessities to pay energy bills—were assessed individually and as a composite measure.
- Mental health was assessed using modified versions of the 2-item Patient Health Questionnaire for depression and the 2-item Generalized Anxiety Disorder scale for anxiety.
- The analysis was adjusted for other social determinants of health, including unemployment, housing instability, and food insecurity. Covariates included a wide range of factors, such as age, educational level, sex, and annual household income.
TAKEAWAY:
- In all, > 43% of the population reported having ≥ 1 form of energy security; around 22% reported being unable to pay energy bills, 22% maintained unsafe home temperatures, and nearly 34% forewent spending on basic necessities to pay energy bills.
- Individuals who gave up spending on basic necessities to pay energy bills had higher odds of anxiety (adjusted odds ratio [aOR], 1.79) and depression (aOR, 1.74) than those who did not.
- Adults with energy insecurity on the composite measure had higher odds for anxiety (aOR, 2.29) and depression (aOR, 2.31) than those with energy security.
- Food insecurity was also associated with poorer mental health, with higher odds for symptoms of depression (aOR, 2.05) and anxiety (aOR, 2.07).
IN PRACTICE:
"Despite its high prevalence, energy insecurity remains underrecognized in public health and policy intervention strategies," the investigators wrote.
"These findings suggest that energy insecurity is a widespread and important factor associated with mental health symptoms and may warrant consideration in efforts to reduce adverse mental health outcomes," they added.
SOURCE:
This study was led by Michelle Graf, PhD, Carter School of Public Policy, Georgia Institute of Technology, Atlanta. It was published online on October 27 in JAMA Network Open.
LIMITATIONS:
The cross-sectional nature of the data limited causal interference and increased the possibility of reverse causality. The questionnaire captured subjective interpretations of unsafe and unhealthy indoor temperatures, which may have varied among respondents. Additionally, the recall periods for energy insecurity and mental health outcomes were different.
DISCLOSURES:
The investigators reported no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
Energy insecurity, the inability to meet household energy needs, was associated with more than twice the odds of having depression and anxiety symptoms than energy security in US adults, a new cross-sectional study showed.
METHODOLOGY:
- Using data from the US Census Bureau's online Household Pulse Survey, administered between 2022 and 2024, researchers conducted a cross-sectional study with a weighted population of > 187 million US adults (51% women; 64% White, 16% Hispanic, 10% Black, and 5% Asian). About a quarter of the population was in each of 4 age groups: 18-34 years, 35-49 years, 50-64 years, and ≥ 65 years.
- Three indicators of energy insecurity—inability to pay energy bills, maintaining unsafe/unhealthy home temperatures, and forgoing expenses on basic necessities to pay energy bills—were assessed individually and as a composite measure.
- Mental health was assessed using modified versions of the 2-item Patient Health Questionnaire for depression and the 2-item Generalized Anxiety Disorder scale for anxiety.
- The analysis was adjusted for other social determinants of health, including unemployment, housing instability, and food insecurity. Covariates included a wide range of factors, such as age, educational level, sex, and annual household income.
TAKEAWAY:
- In all, > 43% of the population reported having ≥ 1 form of energy security; around 22% reported being unable to pay energy bills, 22% maintained unsafe home temperatures, and nearly 34% forewent spending on basic necessities to pay energy bills.
- Individuals who gave up spending on basic necessities to pay energy bills had higher odds of anxiety (adjusted odds ratio [aOR], 1.79) and depression (aOR, 1.74) than those who did not.
- Adults with energy insecurity on the composite measure had higher odds for anxiety (aOR, 2.29) and depression (aOR, 2.31) than those with energy security.
- Food insecurity was also associated with poorer mental health, with higher odds for symptoms of depression (aOR, 2.05) and anxiety (aOR, 2.07).
IN PRACTICE:
"Despite its high prevalence, energy insecurity remains underrecognized in public health and policy intervention strategies," the investigators wrote.
"These findings suggest that energy insecurity is a widespread and important factor associated with mental health symptoms and may warrant consideration in efforts to reduce adverse mental health outcomes," they added.
SOURCE:
This study was led by Michelle Graf, PhD, Carter School of Public Policy, Georgia Institute of Technology, Atlanta. It was published online on October 27 in JAMA Network Open.
LIMITATIONS:
The cross-sectional nature of the data limited causal interference and increased the possibility of reverse causality. The questionnaire captured subjective interpretations of unsafe and unhealthy indoor temperatures, which may have varied among respondents. Additionally, the recall periods for energy insecurity and mental health outcomes were different.
DISCLOSURES:
The investigators reported no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
'Energy Insecurity' Tied to Anxiety, Depression Risk
'Energy Insecurity' Tied to Anxiety, Depression Risk
Is High Quality VA Psychiatric Care Keeping Readmissions Rates Low?
Repeated and frequent hospitalizations—sometimes referred to as the revolving door phenomenon— are a particular risk for patients during the first month after discharge. Early psychiatric readmission is a standard indicator of adverse outcomes. However, the results
The quality of previous care has long been thought to be a driver of readmission. If that’s the case, a 2025 study suggests that on average veterans received high-quality inpatient psychiatric services at Veterans Health Administration (VHA) facilities across the nation and that may have been key to keeping readmissions down. Analyzing data from 88,954 veterans who received care at VHA Inpatient Mental Health (IMH) services, the researchers found a “relatively low” rate of readmission within 30 days: 7.1% compared with 8% to 31% of other psychiatric patients in the US. With 40,220 unique patients receiving IMH care per year on average between October 2019 and September 2022, a 7.1% readmission rate means > 2800 30-day readmissions annually.
Research has found that veterans who receive care at the VA have better outcomes than those treated in the private sector. Part of that has to do with practitioners who understand the unique needs of their patients. Veterans may have posttraumatic stress disorder or multiple diagnoses, such as depression, panic disorder, and a substance use disorder. Their mental health issues may also coexist with physical health problems, such as traumatic brain injuries due to explosions.
“If you’re trained at the VA, you learn something important about veteran mental health care that you’ll never get if you’re trained someplace else,” Rodney R. Baker, PhD, retired mental health director and chief of psychology for the South Texas VA Health Care System, said recently. Community clinicians may not know how to collect and incorporate information about a patient’s military history, including details about deployments, combat exposure, injuries, military sexual trauma, and unit culture. They may also lack expertise in navigating the transition between military and veteran life, now considered a critical adjustment period.
“This is a unique population,” said Conwell Smith, the American Psychological Association’s deputy chief of military and veteran policy. “Sending veterans out to the community without requiring that mental health care providers understand them is concerning.”
IMH services aim to stabilize mental health crises and improve veterans’ functioning through patient-centered, evidence-based, and recovery-oriented approaches shown to reduce readmission rates. Treatment generally involves a minimum of 4 hours of interdisciplinary, therapeutic programming each day. And upon discharge, the inpatient care team facilitates the patient’s transition to appropriate outpatient services.
Follow-up care, particularly during the first 30 days, has proved critical in reducing readmissions. In studies that have analyzed postdischarge interventions (psychoeducation, mentoring, community-based hospital treatment, use of continuous follow-up and compulsory community treatment), all found fewer hospitalizations when compared to a control group, or a smaller number of admissions after the intervention.
Mental health care for veterans should be provided by experienced practitioners—but those practitioners are leaving VA. According to the VA Office of Inspector General, 57% of medical centers report a shortage of psychologists. And according to the VA’s monthly Workforce Dashboard, the VHA lost 234 psychologists in the first 9 months of 2025. The VA has also announced plans to cut 30,000 jobs by the end of the year and impose caps on staff at every medical center.
“This approach locks in permanent VA understaffing just as demand for mental health services is projected to continue growing through 2030,” said Russell Lemle, PhD, a clinical psychologist and senior policy analyst for the Veterans Healthcare Policy Institute. “The private sector can’t fill this gap either—over a third of Americans live in areas already facing mental health professional shortages. That’s not taking care of our veterans.
“Unless actions are taken quickly to reverse the trend, its mental health services could easily diminish substantially within 10 to 20 years.”
Repeated and frequent hospitalizations—sometimes referred to as the revolving door phenomenon— are a particular risk for patients during the first month after discharge. Early psychiatric readmission is a standard indicator of adverse outcomes. However, the results
The quality of previous care has long been thought to be a driver of readmission. If that’s the case, a 2025 study suggests that on average veterans received high-quality inpatient psychiatric services at Veterans Health Administration (VHA) facilities across the nation and that may have been key to keeping readmissions down. Analyzing data from 88,954 veterans who received care at VHA Inpatient Mental Health (IMH) services, the researchers found a “relatively low” rate of readmission within 30 days: 7.1% compared with 8% to 31% of other psychiatric patients in the US. With 40,220 unique patients receiving IMH care per year on average between October 2019 and September 2022, a 7.1% readmission rate means > 2800 30-day readmissions annually.
Research has found that veterans who receive care at the VA have better outcomes than those treated in the private sector. Part of that has to do with practitioners who understand the unique needs of their patients. Veterans may have posttraumatic stress disorder or multiple diagnoses, such as depression, panic disorder, and a substance use disorder. Their mental health issues may also coexist with physical health problems, such as traumatic brain injuries due to explosions.
“If you’re trained at the VA, you learn something important about veteran mental health care that you’ll never get if you’re trained someplace else,” Rodney R. Baker, PhD, retired mental health director and chief of psychology for the South Texas VA Health Care System, said recently. Community clinicians may not know how to collect and incorporate information about a patient’s military history, including details about deployments, combat exposure, injuries, military sexual trauma, and unit culture. They may also lack expertise in navigating the transition between military and veteran life, now considered a critical adjustment period.
“This is a unique population,” said Conwell Smith, the American Psychological Association’s deputy chief of military and veteran policy. “Sending veterans out to the community without requiring that mental health care providers understand them is concerning.”
IMH services aim to stabilize mental health crises and improve veterans’ functioning through patient-centered, evidence-based, and recovery-oriented approaches shown to reduce readmission rates. Treatment generally involves a minimum of 4 hours of interdisciplinary, therapeutic programming each day. And upon discharge, the inpatient care team facilitates the patient’s transition to appropriate outpatient services.
Follow-up care, particularly during the first 30 days, has proved critical in reducing readmissions. In studies that have analyzed postdischarge interventions (psychoeducation, mentoring, community-based hospital treatment, use of continuous follow-up and compulsory community treatment), all found fewer hospitalizations when compared to a control group, or a smaller number of admissions after the intervention.
Mental health care for veterans should be provided by experienced practitioners—but those practitioners are leaving VA. According to the VA Office of Inspector General, 57% of medical centers report a shortage of psychologists. And according to the VA’s monthly Workforce Dashboard, the VHA lost 234 psychologists in the first 9 months of 2025. The VA has also announced plans to cut 30,000 jobs by the end of the year and impose caps on staff at every medical center.
“This approach locks in permanent VA understaffing just as demand for mental health services is projected to continue growing through 2030,” said Russell Lemle, PhD, a clinical psychologist and senior policy analyst for the Veterans Healthcare Policy Institute. “The private sector can’t fill this gap either—over a third of Americans live in areas already facing mental health professional shortages. That’s not taking care of our veterans.
“Unless actions are taken quickly to reverse the trend, its mental health services could easily diminish substantially within 10 to 20 years.”
Repeated and frequent hospitalizations—sometimes referred to as the revolving door phenomenon— are a particular risk for patients during the first month after discharge. Early psychiatric readmission is a standard indicator of adverse outcomes. However, the results
The quality of previous care has long been thought to be a driver of readmission. If that’s the case, a 2025 study suggests that on average veterans received high-quality inpatient psychiatric services at Veterans Health Administration (VHA) facilities across the nation and that may have been key to keeping readmissions down. Analyzing data from 88,954 veterans who received care at VHA Inpatient Mental Health (IMH) services, the researchers found a “relatively low” rate of readmission within 30 days: 7.1% compared with 8% to 31% of other psychiatric patients in the US. With 40,220 unique patients receiving IMH care per year on average between October 2019 and September 2022, a 7.1% readmission rate means > 2800 30-day readmissions annually.
Research has found that veterans who receive care at the VA have better outcomes than those treated in the private sector. Part of that has to do with practitioners who understand the unique needs of their patients. Veterans may have posttraumatic stress disorder or multiple diagnoses, such as depression, panic disorder, and a substance use disorder. Their mental health issues may also coexist with physical health problems, such as traumatic brain injuries due to explosions.
“If you’re trained at the VA, you learn something important about veteran mental health care that you’ll never get if you’re trained someplace else,” Rodney R. Baker, PhD, retired mental health director and chief of psychology for the South Texas VA Health Care System, said recently. Community clinicians may not know how to collect and incorporate information about a patient’s military history, including details about deployments, combat exposure, injuries, military sexual trauma, and unit culture. They may also lack expertise in navigating the transition between military and veteran life, now considered a critical adjustment period.
“This is a unique population,” said Conwell Smith, the American Psychological Association’s deputy chief of military and veteran policy. “Sending veterans out to the community without requiring that mental health care providers understand them is concerning.”
IMH services aim to stabilize mental health crises and improve veterans’ functioning through patient-centered, evidence-based, and recovery-oriented approaches shown to reduce readmission rates. Treatment generally involves a minimum of 4 hours of interdisciplinary, therapeutic programming each day. And upon discharge, the inpatient care team facilitates the patient’s transition to appropriate outpatient services.
Follow-up care, particularly during the first 30 days, has proved critical in reducing readmissions. In studies that have analyzed postdischarge interventions (psychoeducation, mentoring, community-based hospital treatment, use of continuous follow-up and compulsory community treatment), all found fewer hospitalizations when compared to a control group, or a smaller number of admissions after the intervention.
Mental health care for veterans should be provided by experienced practitioners—but those practitioners are leaving VA. According to the VA Office of Inspector General, 57% of medical centers report a shortage of psychologists. And according to the VA’s monthly Workforce Dashboard, the VHA lost 234 psychologists in the first 9 months of 2025. The VA has also announced plans to cut 30,000 jobs by the end of the year and impose caps on staff at every medical center.
“This approach locks in permanent VA understaffing just as demand for mental health services is projected to continue growing through 2030,” said Russell Lemle, PhD, a clinical psychologist and senior policy analyst for the Veterans Healthcare Policy Institute. “The private sector can’t fill this gap either—over a third of Americans live in areas already facing mental health professional shortages. That’s not taking care of our veterans.
“Unless actions are taken quickly to reverse the trend, its mental health services could easily diminish substantially within 10 to 20 years.”
As Federal Cuts Deepen Mental Health Crisis, Philanthropy Scrambles to Fill the Gap
As Federal Cuts Deepen Mental Health Crisis, Philanthropy Scrambles to Fill the Gap
It's hardly news that the United States is experiencing a mental health crisis -- the CDC says as much. But experts in the field say that the current administration has severely compounded the problem by eliminating agency funding and national programs, slashing research grants and data resources, and creating new barriers to behavioral health care.
Philanthropic foundations aim to do what they can to address the shortfall. The numbers, however, just don't add up.
"Some big foundations and philanthropies have said they're going to increase what they give out in the next 4 years, but they'll never be able to fill the gap," said Morgan F. McDonald, MD, national director of population health at the Milbank Memorial Fund in New York City, which works with states on health policy. "Even if every one of them were to spend down their endowments, they still couldn't."
Given the financial limitations, some foundations are taking a different tack. While looking for ways to join forces with fellow nonprofits, they are providing emergency grants to bridge funding in the short term to keep research from grinding to a halt.
Budget Cuts Reach Far and Wide
Mental health research certainly didn't escape the extensive grant cancellations at the National Institutes of Health and the National Science Foundation.
"It's already affecting our ability to stay on the cutting edge of research, best practices, and treatment approaches," said Zainab Okolo, EdD, senior vice president of policy, advocacy, and government relations at The Jed Foundation in New York City, which focuses on the emotional health of teens and young adults.
The upheaval is evident in an array of government agencies. The Health Resources and Services Administration, which last year awarded $12 billion in grants to community health centers and addiction treatment services, has seen > one-fourth of its staff eliminated. The Substance Abuse and Mental Health Services Administration has lost more than a third of its staff as federal cuts took a $1 billion bite out of its operating budget. The Education Department has halted $1 billion in grants used to hire mental health workers in school districts nationwide.
"We're very, very concerned about cuts to behavioral health systems," said Alonzo Plough, PhD, chief science officer at the Robert Wood Johnson Foundation in Princeton, New Jersey. "Doctors and nurses working in safety-net clinics are seeing tremendous reductions."
All in all, the new tax and spending law means $1 trillion in cuts to health care programs including Medicaid -- the nation's largest payer for mental health services -- Medicare, and Affordable Care Act insurance. An estimated 10 million Americans are expected to lose their health coverage as a result.
"When accessibility to care goes down, there's a chance that more people will die by suicide," said Jill Harkavy-Friedman, PhD, senior vice president of research at the American Foundation for Suicide Prevention. "But it also means people will come into care later in the course of their difficulties. Health professionals will be dealing with worse problems."
Foundations Take Emergency Measures
Even if private dollars can't replace what's been lost, philanthropic and medical foundations are stepping up.
We're seeing a lot of foundations and funders that are shifting their funding," said Alyson Niemann, CEO of Mindful Philanthropy, an organization that works with > 1000 private funders to marshal resources for mental health. This year, in response to federal cuts, "many increased funding to health and well-being, doubling or even tripling it," Niemann noted.
"They're making a great deal of effort to respond with emergency funds, really getting in the trenches and being good partners to their grantees," she said. "We've seen them asking deliberate questions, thinking about where their funding can have the most impact."
The American Psychological Foundation (APF), a longtime supporter of research and innovation, is addressing the current crisis with 2 initiatives, Michelle Quist Ryder, PhD, the organization's CEO, explained in an email. The first is APF Director Action, which funds innovative interventions at the community level. The second, Direct Action Crisis Funding Grants, will help continue research that is at risk of stalling because of budget cuts.
"Studies that are 'paused' or lose funding often cannot simply pick back up where they left off. Having to halt progress on a project can invalidate the work already completed," Ryder wrote. "These Direct Action Crisis Grants help bridge funding gaps and keep research viable."
At the same time, collaboration between foundations is becoming more widespread as they seek to maximize their impact. Philanthropic organizations are sharing ideas and best practices as well as pooling fundings.
"The goal of philanthropy is to help people," Harkavy-Friedman said. "There's strength in numbers and more dollars in numbers."
Some See Hope in Raised Voices
Despite the emergency scrambling, many of those in the trenches remain surprisingly optimistic. Some point out that the current turmoil has put a helpful spotlight on behavioral health care. Practitioners, meanwhile, have an essential role to play.
"There's a reason that things were the way they were: People advocated for many years to get where we've gotten," Harkavy-Friedman said, citing veterans' mental health care, the national violent death reporting system, and 988 as examples. "We have to raise our voices louder -- professionals in particular, because they know the impact a person in the general public many not fully grasp."
As a growing numbers of health professionals call attention to the damage wrought by deep cuts in the federal budget, foundation executives see an opportunity.
"In the mental health field, there's a deficit in the narrative, where there's a lot of focus on crisis. What we're hoping to do is shift the narrative toward 'How do we flourish together?'" Niemann said. "Sometimes deficits are where the most incredible innovations appear."
Debbie Koenig is a health writer whose work has been published by WebMD, The New York Times, and The Washington Post.
A version of this article first appeared on Medscape.com.
It's hardly news that the United States is experiencing a mental health crisis -- the CDC says as much. But experts in the field say that the current administration has severely compounded the problem by eliminating agency funding and national programs, slashing research grants and data resources, and creating new barriers to behavioral health care.
Philanthropic foundations aim to do what they can to address the shortfall. The numbers, however, just don't add up.
"Some big foundations and philanthropies have said they're going to increase what they give out in the next 4 years, but they'll never be able to fill the gap," said Morgan F. McDonald, MD, national director of population health at the Milbank Memorial Fund in New York City, which works with states on health policy. "Even if every one of them were to spend down their endowments, they still couldn't."
Given the financial limitations, some foundations are taking a different tack. While looking for ways to join forces with fellow nonprofits, they are providing emergency grants to bridge funding in the short term to keep research from grinding to a halt.
Budget Cuts Reach Far and Wide
Mental health research certainly didn't escape the extensive grant cancellations at the National Institutes of Health and the National Science Foundation.
"It's already affecting our ability to stay on the cutting edge of research, best practices, and treatment approaches," said Zainab Okolo, EdD, senior vice president of policy, advocacy, and government relations at The Jed Foundation in New York City, which focuses on the emotional health of teens and young adults.
The upheaval is evident in an array of government agencies. The Health Resources and Services Administration, which last year awarded $12 billion in grants to community health centers and addiction treatment services, has seen > one-fourth of its staff eliminated. The Substance Abuse and Mental Health Services Administration has lost more than a third of its staff as federal cuts took a $1 billion bite out of its operating budget. The Education Department has halted $1 billion in grants used to hire mental health workers in school districts nationwide.
"We're very, very concerned about cuts to behavioral health systems," said Alonzo Plough, PhD, chief science officer at the Robert Wood Johnson Foundation in Princeton, New Jersey. "Doctors and nurses working in safety-net clinics are seeing tremendous reductions."
All in all, the new tax and spending law means $1 trillion in cuts to health care programs including Medicaid -- the nation's largest payer for mental health services -- Medicare, and Affordable Care Act insurance. An estimated 10 million Americans are expected to lose their health coverage as a result.
"When accessibility to care goes down, there's a chance that more people will die by suicide," said Jill Harkavy-Friedman, PhD, senior vice president of research at the American Foundation for Suicide Prevention. "But it also means people will come into care later in the course of their difficulties. Health professionals will be dealing with worse problems."
Foundations Take Emergency Measures
Even if private dollars can't replace what's been lost, philanthropic and medical foundations are stepping up.
We're seeing a lot of foundations and funders that are shifting their funding," said Alyson Niemann, CEO of Mindful Philanthropy, an organization that works with > 1000 private funders to marshal resources for mental health. This year, in response to federal cuts, "many increased funding to health and well-being, doubling or even tripling it," Niemann noted.
"They're making a great deal of effort to respond with emergency funds, really getting in the trenches and being good partners to their grantees," she said. "We've seen them asking deliberate questions, thinking about where their funding can have the most impact."
The American Psychological Foundation (APF), a longtime supporter of research and innovation, is addressing the current crisis with 2 initiatives, Michelle Quist Ryder, PhD, the organization's CEO, explained in an email. The first is APF Director Action, which funds innovative interventions at the community level. The second, Direct Action Crisis Funding Grants, will help continue research that is at risk of stalling because of budget cuts.
"Studies that are 'paused' or lose funding often cannot simply pick back up where they left off. Having to halt progress on a project can invalidate the work already completed," Ryder wrote. "These Direct Action Crisis Grants help bridge funding gaps and keep research viable."
At the same time, collaboration between foundations is becoming more widespread as they seek to maximize their impact. Philanthropic organizations are sharing ideas and best practices as well as pooling fundings.
"The goal of philanthropy is to help people," Harkavy-Friedman said. "There's strength in numbers and more dollars in numbers."
Some See Hope in Raised Voices
Despite the emergency scrambling, many of those in the trenches remain surprisingly optimistic. Some point out that the current turmoil has put a helpful spotlight on behavioral health care. Practitioners, meanwhile, have an essential role to play.
"There's a reason that things were the way they were: People advocated for many years to get where we've gotten," Harkavy-Friedman said, citing veterans' mental health care, the national violent death reporting system, and 988 as examples. "We have to raise our voices louder -- professionals in particular, because they know the impact a person in the general public many not fully grasp."
As a growing numbers of health professionals call attention to the damage wrought by deep cuts in the federal budget, foundation executives see an opportunity.
"In the mental health field, there's a deficit in the narrative, where there's a lot of focus on crisis. What we're hoping to do is shift the narrative toward 'How do we flourish together?'" Niemann said. "Sometimes deficits are where the most incredible innovations appear."
Debbie Koenig is a health writer whose work has been published by WebMD, The New York Times, and The Washington Post.
A version of this article first appeared on Medscape.com.
It's hardly news that the United States is experiencing a mental health crisis -- the CDC says as much. But experts in the field say that the current administration has severely compounded the problem by eliminating agency funding and national programs, slashing research grants and data resources, and creating new barriers to behavioral health care.
Philanthropic foundations aim to do what they can to address the shortfall. The numbers, however, just don't add up.
"Some big foundations and philanthropies have said they're going to increase what they give out in the next 4 years, but they'll never be able to fill the gap," said Morgan F. McDonald, MD, national director of population health at the Milbank Memorial Fund in New York City, which works with states on health policy. "Even if every one of them were to spend down their endowments, they still couldn't."
Given the financial limitations, some foundations are taking a different tack. While looking for ways to join forces with fellow nonprofits, they are providing emergency grants to bridge funding in the short term to keep research from grinding to a halt.
Budget Cuts Reach Far and Wide
Mental health research certainly didn't escape the extensive grant cancellations at the National Institutes of Health and the National Science Foundation.
"It's already affecting our ability to stay on the cutting edge of research, best practices, and treatment approaches," said Zainab Okolo, EdD, senior vice president of policy, advocacy, and government relations at The Jed Foundation in New York City, which focuses on the emotional health of teens and young adults.
The upheaval is evident in an array of government agencies. The Health Resources and Services Administration, which last year awarded $12 billion in grants to community health centers and addiction treatment services, has seen > one-fourth of its staff eliminated. The Substance Abuse and Mental Health Services Administration has lost more than a third of its staff as federal cuts took a $1 billion bite out of its operating budget. The Education Department has halted $1 billion in grants used to hire mental health workers in school districts nationwide.
"We're very, very concerned about cuts to behavioral health systems," said Alonzo Plough, PhD, chief science officer at the Robert Wood Johnson Foundation in Princeton, New Jersey. "Doctors and nurses working in safety-net clinics are seeing tremendous reductions."
All in all, the new tax and spending law means $1 trillion in cuts to health care programs including Medicaid -- the nation's largest payer for mental health services -- Medicare, and Affordable Care Act insurance. An estimated 10 million Americans are expected to lose their health coverage as a result.
"When accessibility to care goes down, there's a chance that more people will die by suicide," said Jill Harkavy-Friedman, PhD, senior vice president of research at the American Foundation for Suicide Prevention. "But it also means people will come into care later in the course of their difficulties. Health professionals will be dealing with worse problems."
Foundations Take Emergency Measures
Even if private dollars can't replace what's been lost, philanthropic and medical foundations are stepping up.
We're seeing a lot of foundations and funders that are shifting their funding," said Alyson Niemann, CEO of Mindful Philanthropy, an organization that works with > 1000 private funders to marshal resources for mental health. This year, in response to federal cuts, "many increased funding to health and well-being, doubling or even tripling it," Niemann noted.
"They're making a great deal of effort to respond with emergency funds, really getting in the trenches and being good partners to their grantees," she said. "We've seen them asking deliberate questions, thinking about where their funding can have the most impact."
The American Psychological Foundation (APF), a longtime supporter of research and innovation, is addressing the current crisis with 2 initiatives, Michelle Quist Ryder, PhD, the organization's CEO, explained in an email. The first is APF Director Action, which funds innovative interventions at the community level. The second, Direct Action Crisis Funding Grants, will help continue research that is at risk of stalling because of budget cuts.
"Studies that are 'paused' or lose funding often cannot simply pick back up where they left off. Having to halt progress on a project can invalidate the work already completed," Ryder wrote. "These Direct Action Crisis Grants help bridge funding gaps and keep research viable."
At the same time, collaboration between foundations is becoming more widespread as they seek to maximize their impact. Philanthropic organizations are sharing ideas and best practices as well as pooling fundings.
"The goal of philanthropy is to help people," Harkavy-Friedman said. "There's strength in numbers and more dollars in numbers."
Some See Hope in Raised Voices
Despite the emergency scrambling, many of those in the trenches remain surprisingly optimistic. Some point out that the current turmoil has put a helpful spotlight on behavioral health care. Practitioners, meanwhile, have an essential role to play.
"There's a reason that things were the way they were: People advocated for many years to get where we've gotten," Harkavy-Friedman said, citing veterans' mental health care, the national violent death reporting system, and 988 as examples. "We have to raise our voices louder -- professionals in particular, because they know the impact a person in the general public many not fully grasp."
As a growing numbers of health professionals call attention to the damage wrought by deep cuts in the federal budget, foundation executives see an opportunity.
"In the mental health field, there's a deficit in the narrative, where there's a lot of focus on crisis. What we're hoping to do is shift the narrative toward 'How do we flourish together?'" Niemann said. "Sometimes deficits are where the most incredible innovations appear."
Debbie Koenig is a health writer whose work has been published by WebMD, The New York Times, and The Washington Post.
A version of this article first appeared on Medscape.com.
As Federal Cuts Deepen Mental Health Crisis, Philanthropy Scrambles to Fill the Gap
As Federal Cuts Deepen Mental Health Crisis, Philanthropy Scrambles to Fill the Gap
Taking Therapy Home With Mobile Mental Health Apps
For Kelly, a retired Navy operations specialist, coping with depression and anxiety hindered her ability to enjoy everyday life. Then she elected to enter therapy, a decision she calls “transformative.”
“When I started doing therapy, it was like releasing the toxins, releasing the buildup of the fear or the rage or the overwhelming feelings of shame,” she says. “We can’t just hold on to it. Just telling the truth, it helps me every single day. It is so worth it.”
Kurt, an Army veteran, tried to power through his anxiety, depression, and survivor guilt. He didn’t have much faith in mental health therapy, thinking no one could relate to him. He was surprised, though, once he started treatment, how much his life improved. He now encourages other veterans to face their own mental health challenges, be it through virtual/mental health apps or in-person care.
“From getting help, every day of my life is better,” he says, “and I couldn’t be more grateful for it.”
Stories from Kelly and Kurt are 2 of 7 the US Department of Veterans Affairs (VA) highlighted during National Recovery Month, outlining how their lives were forever changed with the support of mental health care.
But for every Kelly and Kurt, there are thousands of individuals reluctant to seek mental health care. A analysis of 2019-2020 data from the National Health and Resilience in Veterans Study found that 924 (26%) of 4069 veterans met criteria for ≥ 1 psychological disorders, but only 12% reported engagement in mental health care. The researchers considered the role of protective psychosocial characteristics, such as grit (ie, “trait perseverance that extends to one’s decision or commitment to address mental health needs on one’s own; dispositional optimism; and purpose in life”). Veterans who reported mental dysfunction but scored highly on grit were less likely to be engaged in treatment. This pattern suggests higher levels of grit may reduce the likelihood of seeking treatment, “even in the presence of clinically meaningful distress.”
A 2004 study found only 23% to 40% of service members who screened positive for a mental disorder sought care. They often believed they would be seen as weak, or their unit leadership might treat them differently, and unit members would have less confidence in them.
Given that military members and veterans are at increased risk of posttraumatic stress disorder (PTSD) in addition to mood, anxiety, and substance use disorders, any alternatives that increase their access to support and services are crucial. For those who aren’t disposed to office visits and group therapy, the answer may lie in mobile apps.
In a recent randomized controlled trial, 201 veterans who screened positive for PTSD and alcohol use disorder were divided into 2 groups: a mobile mindfulness-based intervention group enhanced with brief alcohol intervention content (Mind Guide), and an active stress management program group. Mind Guide engagement was excellent, according to the study, with averages of > 31 logins and 5 hours of app use. At 16 weeks, the Mind Guide group showed significant reductions in PTSD symptoms (no differences emerged for alcohol use frequency). Mind Guide may be a valuable adjunct to more intensive in-person PTSD treatment by facilitating interest in services, integration into care, and/or sustainment of posttreatment improvements. The VA currently offers 16 apps, including MHA for Veterans, an app designed for patients to complete mental health assessments after their clinician assigned them. Other apps address a variety of issues, such as anger management, insomnia, chronic pain, and PTSD.
Two apps were created with an eye toward specific communities. One, Veterans Wellness Path, was designed for American Indians and Alaska Natives with input from those veterans, their family members, and health care practitioners. It supports the transition from military service to home and encourages balance and connection with self, family, community, and environment. Similarly, WellWithin Coach was designed by the VA National Center for PTSD with input from women veterans and subject matter experts in women’s mental health.
Whatever form it takes—in-person or virtual—finding support that works can make all the difference for veterans. Kelly founded and serves as the executive director of Acta Non Verba: Youth Urban Farm Project, an organization that brings together > 3000 low-income youth and families annually to learn about urban farming, aiming to fill a gap in an area known as a food desert: “We do have the power and the right to wake up the next day and try to do something different,” she said.
For Kelly, a retired Navy operations specialist, coping with depression and anxiety hindered her ability to enjoy everyday life. Then she elected to enter therapy, a decision she calls “transformative.”
“When I started doing therapy, it was like releasing the toxins, releasing the buildup of the fear or the rage or the overwhelming feelings of shame,” she says. “We can’t just hold on to it. Just telling the truth, it helps me every single day. It is so worth it.”
Kurt, an Army veteran, tried to power through his anxiety, depression, and survivor guilt. He didn’t have much faith in mental health therapy, thinking no one could relate to him. He was surprised, though, once he started treatment, how much his life improved. He now encourages other veterans to face their own mental health challenges, be it through virtual/mental health apps or in-person care.
“From getting help, every day of my life is better,” he says, “and I couldn’t be more grateful for it.”
Stories from Kelly and Kurt are 2 of 7 the US Department of Veterans Affairs (VA) highlighted during National Recovery Month, outlining how their lives were forever changed with the support of mental health care.
But for every Kelly and Kurt, there are thousands of individuals reluctant to seek mental health care. A analysis of 2019-2020 data from the National Health and Resilience in Veterans Study found that 924 (26%) of 4069 veterans met criteria for ≥ 1 psychological disorders, but only 12% reported engagement in mental health care. The researchers considered the role of protective psychosocial characteristics, such as grit (ie, “trait perseverance that extends to one’s decision or commitment to address mental health needs on one’s own; dispositional optimism; and purpose in life”). Veterans who reported mental dysfunction but scored highly on grit were less likely to be engaged in treatment. This pattern suggests higher levels of grit may reduce the likelihood of seeking treatment, “even in the presence of clinically meaningful distress.”
A 2004 study found only 23% to 40% of service members who screened positive for a mental disorder sought care. They often believed they would be seen as weak, or their unit leadership might treat them differently, and unit members would have less confidence in them.
Given that military members and veterans are at increased risk of posttraumatic stress disorder (PTSD) in addition to mood, anxiety, and substance use disorders, any alternatives that increase their access to support and services are crucial. For those who aren’t disposed to office visits and group therapy, the answer may lie in mobile apps.
In a recent randomized controlled trial, 201 veterans who screened positive for PTSD and alcohol use disorder were divided into 2 groups: a mobile mindfulness-based intervention group enhanced with brief alcohol intervention content (Mind Guide), and an active stress management program group. Mind Guide engagement was excellent, according to the study, with averages of > 31 logins and 5 hours of app use. At 16 weeks, the Mind Guide group showed significant reductions in PTSD symptoms (no differences emerged for alcohol use frequency). Mind Guide may be a valuable adjunct to more intensive in-person PTSD treatment by facilitating interest in services, integration into care, and/or sustainment of posttreatment improvements. The VA currently offers 16 apps, including MHA for Veterans, an app designed for patients to complete mental health assessments after their clinician assigned them. Other apps address a variety of issues, such as anger management, insomnia, chronic pain, and PTSD.
Two apps were created with an eye toward specific communities. One, Veterans Wellness Path, was designed for American Indians and Alaska Natives with input from those veterans, their family members, and health care practitioners. It supports the transition from military service to home and encourages balance and connection with self, family, community, and environment. Similarly, WellWithin Coach was designed by the VA National Center for PTSD with input from women veterans and subject matter experts in women’s mental health.
Whatever form it takes—in-person or virtual—finding support that works can make all the difference for veterans. Kelly founded and serves as the executive director of Acta Non Verba: Youth Urban Farm Project, an organization that brings together > 3000 low-income youth and families annually to learn about urban farming, aiming to fill a gap in an area known as a food desert: “We do have the power and the right to wake up the next day and try to do something different,” she said.
For Kelly, a retired Navy operations specialist, coping with depression and anxiety hindered her ability to enjoy everyday life. Then she elected to enter therapy, a decision she calls “transformative.”
“When I started doing therapy, it was like releasing the toxins, releasing the buildup of the fear or the rage or the overwhelming feelings of shame,” she says. “We can’t just hold on to it. Just telling the truth, it helps me every single day. It is so worth it.”
Kurt, an Army veteran, tried to power through his anxiety, depression, and survivor guilt. He didn’t have much faith in mental health therapy, thinking no one could relate to him. He was surprised, though, once he started treatment, how much his life improved. He now encourages other veterans to face their own mental health challenges, be it through virtual/mental health apps or in-person care.
“From getting help, every day of my life is better,” he says, “and I couldn’t be more grateful for it.”
Stories from Kelly and Kurt are 2 of 7 the US Department of Veterans Affairs (VA) highlighted during National Recovery Month, outlining how their lives were forever changed with the support of mental health care.
But for every Kelly and Kurt, there are thousands of individuals reluctant to seek mental health care. A analysis of 2019-2020 data from the National Health and Resilience in Veterans Study found that 924 (26%) of 4069 veterans met criteria for ≥ 1 psychological disorders, but only 12% reported engagement in mental health care. The researchers considered the role of protective psychosocial characteristics, such as grit (ie, “trait perseverance that extends to one’s decision or commitment to address mental health needs on one’s own; dispositional optimism; and purpose in life”). Veterans who reported mental dysfunction but scored highly on grit were less likely to be engaged in treatment. This pattern suggests higher levels of grit may reduce the likelihood of seeking treatment, “even in the presence of clinically meaningful distress.”
A 2004 study found only 23% to 40% of service members who screened positive for a mental disorder sought care. They often believed they would be seen as weak, or their unit leadership might treat them differently, and unit members would have less confidence in them.
Given that military members and veterans are at increased risk of posttraumatic stress disorder (PTSD) in addition to mood, anxiety, and substance use disorders, any alternatives that increase their access to support and services are crucial. For those who aren’t disposed to office visits and group therapy, the answer may lie in mobile apps.
In a recent randomized controlled trial, 201 veterans who screened positive for PTSD and alcohol use disorder were divided into 2 groups: a mobile mindfulness-based intervention group enhanced with brief alcohol intervention content (Mind Guide), and an active stress management program group. Mind Guide engagement was excellent, according to the study, with averages of > 31 logins and 5 hours of app use. At 16 weeks, the Mind Guide group showed significant reductions in PTSD symptoms (no differences emerged for alcohol use frequency). Mind Guide may be a valuable adjunct to more intensive in-person PTSD treatment by facilitating interest in services, integration into care, and/or sustainment of posttreatment improvements. The VA currently offers 16 apps, including MHA for Veterans, an app designed for patients to complete mental health assessments after their clinician assigned them. Other apps address a variety of issues, such as anger management, insomnia, chronic pain, and PTSD.
Two apps were created with an eye toward specific communities. One, Veterans Wellness Path, was designed for American Indians and Alaska Natives with input from those veterans, their family members, and health care practitioners. It supports the transition from military service to home and encourages balance and connection with self, family, community, and environment. Similarly, WellWithin Coach was designed by the VA National Center for PTSD with input from women veterans and subject matter experts in women’s mental health.
Whatever form it takes—in-person or virtual—finding support that works can make all the difference for veterans. Kelly founded and serves as the executive director of Acta Non Verba: Youth Urban Farm Project, an organization that brings together > 3000 low-income youth and families annually to learn about urban farming, aiming to fill a gap in an area known as a food desert: “We do have the power and the right to wake up the next day and try to do something different,” she said.
Hospitalists Must Encourage Mental Stimulation for Patients
As a hospitalist, you are in a unique position to notice changes in your hospitalized patients. This frontline perspective can be used to improve inpatient attention and care, and differs from primary care, where a clinician might only see a patient once or twice a year, and subtle, gradual changes may be missed, said George Cao, MD, MBA, a hospitalist at the University of Vermont Medical Center in Burlington and assistant professor at UVM’s Larner College of Medicine.
But in the hospital, Cao said even small shifts — like becoming less active, eating less, or changes in personality — can become much more obvious.
“As hospitalists…we see patients throughout the day, in different situations, and often end up spending more time with them over the course of a week than their primary care provider might in a year,” Cao explained. “This gives us a real advantage in picking up on subtle changes in mental awareness.”
These assessments can also be evaluated with the benefit of daily labs, frequent bedside interactions, and 24–hour observations.
With older adults, Cao said it’s important to go beyond just what’s in the chart.
“I always start by reviewing notes from the primary care provider and previous admissions, but some of the most valuable insights come from talking with family and close friends to get a true sense of the patient’s baseline — how they usually think, move, and interact,” he said.
Why to Watch for Declining Mental Awareness
Declining mental awareness in the inpatient setting is often a sign of an underlying problem — whether that’s a reversible medical condition, unrecognized dementia, or the development of delirium, Cao said.
“On the inpatient side, I pay close attention to more than just memory loss,” he said.
Changes in how patients function day–to–day, shifts in their behavior, or even something as simple as not wanting to get out of bed can be early signs of an aging mind or untreated psychiatric issues, he noted.
“Of course, we always rule out infections and medication side effects, but I also look for other reversible causes like thyroid problems, electrolyte imbalances, low oxygen, pain, urinary retention, constipation, and nutritional deficiencies,” Cao said.
Of note, delirium is the most common cause of sudden mental status changes in the hospital, and “it’s easy to miss if you’re not looking for it.”
He summarized that classic signs are an acute and fluctuating course with changes in alertness, but added there are other red flags too: disorientation, hallucinations, changes in sleep patterns, sporadic unsafe behaviors, mood swings, and changes in activity level, whether that’s agitation or just being unusually quiet.
By combining what he notices bedside and what is learned from the medical record (and from the people who know the patient best), Cao said he’s able to catch these changes early, identify the underlying cause, and work toward the best possible outcome.
“One of the main interventions is providing mental stimulation,” he said.
Why Mental Stimulation Is So Vital
Mental stimulation of the patient is critical to recovery and may prevent prolonged illness, said Meghana R. Medavaram, MD, associate director of consultation liaison and emergency psychiatry at Montefiore Medical Center’s Weiler Hospital in New York City. “Keeping a patient active both physically and mentally can help prevent deconditioning and risks of prolonged immobility,” she said.
It’s important to note that when patients are out of their familiar routines, away from their usual environment and people, and their sleep is fragmented, this can make them even more vulnerable. Keeping patients mentally stimulated during their hospital stay can help maintain their attention, orientation, and a healthy sleep-wake cycle — all things that are easily thrown off in the hospital, Cao said.
“These disruptions hit the pathways that control attention, wakefulness, and the sleep–wake cycle. That’s when you see attention drifting, orientation fading, and circadian rhythms unraveling, especially at night, which is why “sundowning” is so common, Cao said, referring to the syndrome where older adults or people with dementia experience behavioral changes in late afternoon or evening. “Mental stimulation is critical in the hospital because when the brain isn’t active and gets disoriented, it becomes an easy target for delirium.”
He said delirium often develops in older adults when acute stressors like inflammation, low oxygen, metabolic imbalances, or sedating medications disrupt the brain’s arousal systems and networks, especially in older adults.
Therefore, Cao said, encourage your patients to be more engaged during the day through conversation, activities, or regular reorientation. “This supports the brain networks that help prevent inattention and confusion, which are the hallmarks of delirium. Daytime stimulation also helps build up the natural drive for nighttime sleep, so patients are less likely to nap during the day and be awake and disoriented at night.”
To support this, it’s helpful to schedule medications during waking hours instead of around–the–clock dosing that interrupts sleep, and to cluster nighttime care activities to minimize disturbances, Cao explained. Ensuring patients have their glasses, hearing aids, and familiar routines, along with encouraging mobility and hydration, further protects against delirium and supports patients’ cognitive health during hospitalization. “These same principles are just as important in outpatient subacute rehab settings and at home, so it’s essential to take home these strategies after discharge,” he said.
A Family Member or Friend May Help
Hospitalists can suggest straightforward ways to encourage families and friends to keep patients engaged during a hospital stay. Visits and chats can go a long way as conversations are incredibly grounding, Cao said. Other methods could be bringing in favorite foods or snacks, a phone chat or video call, or even showing prerecorded video messages. “These can be effective. Patients respond well to seeing and hearing familiar faces and voices, even if it’s just on a screen,” Cao said.
Beyond that, he said, activities such as watching and discussing the news, reading aloud, using tablets for games, watching movies, doing crossword puzzles, knitting, reminiscing, and playing word games can also be mentally stimulating for patients.
In addition, safe exercises/activities that patients can do in bed — with advice from physical therapy and occupational therapy — are beneficial, Medavaram said. “These often include gentle range–of-motion activities,” she said.
Share Importance of Mental Stimulation With Patients and Caregivers
If a hospitalist wants to motivate patients to keep their minds active, the framing should be simple, positive, and tied directly to their goals of getting better and getting home, said Medavaram. She provided this script suggestion:
“One of the best ways to help your recovery isn’t just taking your medicine, it’s keeping your mind active. When you’re in the hospital, it’s easy to spend the day lying in bed and staring at the TV in your room, but that can make your brain slow down and even cause confusion. Simple things — like reading, talking with visitors, doing puzzles, listening to music you enjoy, or telling a nurse about your favorite memories — can keep your brain sharp. Staying mentally active helps your thinking stay clear and can even help you get home sooner. Think of it like physical therapy for your brain.”
A version of this article first appeared on Medscape.com.
As a hospitalist, you are in a unique position to notice changes in your hospitalized patients. This frontline perspective can be used to improve inpatient attention and care, and differs from primary care, where a clinician might only see a patient once or twice a year, and subtle, gradual changes may be missed, said George Cao, MD, MBA, a hospitalist at the University of Vermont Medical Center in Burlington and assistant professor at UVM’s Larner College of Medicine.
But in the hospital, Cao said even small shifts — like becoming less active, eating less, or changes in personality — can become much more obvious.
“As hospitalists…we see patients throughout the day, in different situations, and often end up spending more time with them over the course of a week than their primary care provider might in a year,” Cao explained. “This gives us a real advantage in picking up on subtle changes in mental awareness.”
These assessments can also be evaluated with the benefit of daily labs, frequent bedside interactions, and 24–hour observations.
With older adults, Cao said it’s important to go beyond just what’s in the chart.
“I always start by reviewing notes from the primary care provider and previous admissions, but some of the most valuable insights come from talking with family and close friends to get a true sense of the patient’s baseline — how they usually think, move, and interact,” he said.
Why to Watch for Declining Mental Awareness
Declining mental awareness in the inpatient setting is often a sign of an underlying problem — whether that’s a reversible medical condition, unrecognized dementia, or the development of delirium, Cao said.
“On the inpatient side, I pay close attention to more than just memory loss,” he said.
Changes in how patients function day–to–day, shifts in their behavior, or even something as simple as not wanting to get out of bed can be early signs of an aging mind or untreated psychiatric issues, he noted.
“Of course, we always rule out infections and medication side effects, but I also look for other reversible causes like thyroid problems, electrolyte imbalances, low oxygen, pain, urinary retention, constipation, and nutritional deficiencies,” Cao said.
Of note, delirium is the most common cause of sudden mental status changes in the hospital, and “it’s easy to miss if you’re not looking for it.”
He summarized that classic signs are an acute and fluctuating course with changes in alertness, but added there are other red flags too: disorientation, hallucinations, changes in sleep patterns, sporadic unsafe behaviors, mood swings, and changes in activity level, whether that’s agitation or just being unusually quiet.
By combining what he notices bedside and what is learned from the medical record (and from the people who know the patient best), Cao said he’s able to catch these changes early, identify the underlying cause, and work toward the best possible outcome.
“One of the main interventions is providing mental stimulation,” he said.
Why Mental Stimulation Is So Vital
Mental stimulation of the patient is critical to recovery and may prevent prolonged illness, said Meghana R. Medavaram, MD, associate director of consultation liaison and emergency psychiatry at Montefiore Medical Center’s Weiler Hospital in New York City. “Keeping a patient active both physically and mentally can help prevent deconditioning and risks of prolonged immobility,” she said.
It’s important to note that when patients are out of their familiar routines, away from their usual environment and people, and their sleep is fragmented, this can make them even more vulnerable. Keeping patients mentally stimulated during their hospital stay can help maintain their attention, orientation, and a healthy sleep-wake cycle — all things that are easily thrown off in the hospital, Cao said.
“These disruptions hit the pathways that control attention, wakefulness, and the sleep–wake cycle. That’s when you see attention drifting, orientation fading, and circadian rhythms unraveling, especially at night, which is why “sundowning” is so common, Cao said, referring to the syndrome where older adults or people with dementia experience behavioral changes in late afternoon or evening. “Mental stimulation is critical in the hospital because when the brain isn’t active and gets disoriented, it becomes an easy target for delirium.”
He said delirium often develops in older adults when acute stressors like inflammation, low oxygen, metabolic imbalances, or sedating medications disrupt the brain’s arousal systems and networks, especially in older adults.
Therefore, Cao said, encourage your patients to be more engaged during the day through conversation, activities, or regular reorientation. “This supports the brain networks that help prevent inattention and confusion, which are the hallmarks of delirium. Daytime stimulation also helps build up the natural drive for nighttime sleep, so patients are less likely to nap during the day and be awake and disoriented at night.”
To support this, it’s helpful to schedule medications during waking hours instead of around–the–clock dosing that interrupts sleep, and to cluster nighttime care activities to minimize disturbances, Cao explained. Ensuring patients have their glasses, hearing aids, and familiar routines, along with encouraging mobility and hydration, further protects against delirium and supports patients’ cognitive health during hospitalization. “These same principles are just as important in outpatient subacute rehab settings and at home, so it’s essential to take home these strategies after discharge,” he said.
A Family Member or Friend May Help
Hospitalists can suggest straightforward ways to encourage families and friends to keep patients engaged during a hospital stay. Visits and chats can go a long way as conversations are incredibly grounding, Cao said. Other methods could be bringing in favorite foods or snacks, a phone chat or video call, or even showing prerecorded video messages. “These can be effective. Patients respond well to seeing and hearing familiar faces and voices, even if it’s just on a screen,” Cao said.
Beyond that, he said, activities such as watching and discussing the news, reading aloud, using tablets for games, watching movies, doing crossword puzzles, knitting, reminiscing, and playing word games can also be mentally stimulating for patients.
In addition, safe exercises/activities that patients can do in bed — with advice from physical therapy and occupational therapy — are beneficial, Medavaram said. “These often include gentle range–of-motion activities,” she said.
Share Importance of Mental Stimulation With Patients and Caregivers
If a hospitalist wants to motivate patients to keep their minds active, the framing should be simple, positive, and tied directly to their goals of getting better and getting home, said Medavaram. She provided this script suggestion:
“One of the best ways to help your recovery isn’t just taking your medicine, it’s keeping your mind active. When you’re in the hospital, it’s easy to spend the day lying in bed and staring at the TV in your room, but that can make your brain slow down and even cause confusion. Simple things — like reading, talking with visitors, doing puzzles, listening to music you enjoy, or telling a nurse about your favorite memories — can keep your brain sharp. Staying mentally active helps your thinking stay clear and can even help you get home sooner. Think of it like physical therapy for your brain.”
A version of this article first appeared on Medscape.com.
As a hospitalist, you are in a unique position to notice changes in your hospitalized patients. This frontline perspective can be used to improve inpatient attention and care, and differs from primary care, where a clinician might only see a patient once or twice a year, and subtle, gradual changes may be missed, said George Cao, MD, MBA, a hospitalist at the University of Vermont Medical Center in Burlington and assistant professor at UVM’s Larner College of Medicine.
But in the hospital, Cao said even small shifts — like becoming less active, eating less, or changes in personality — can become much more obvious.
“As hospitalists…we see patients throughout the day, in different situations, and often end up spending more time with them over the course of a week than their primary care provider might in a year,” Cao explained. “This gives us a real advantage in picking up on subtle changes in mental awareness.”
These assessments can also be evaluated with the benefit of daily labs, frequent bedside interactions, and 24–hour observations.
With older adults, Cao said it’s important to go beyond just what’s in the chart.
“I always start by reviewing notes from the primary care provider and previous admissions, but some of the most valuable insights come from talking with family and close friends to get a true sense of the patient’s baseline — how they usually think, move, and interact,” he said.
Why to Watch for Declining Mental Awareness
Declining mental awareness in the inpatient setting is often a sign of an underlying problem — whether that’s a reversible medical condition, unrecognized dementia, or the development of delirium, Cao said.
“On the inpatient side, I pay close attention to more than just memory loss,” he said.
Changes in how patients function day–to–day, shifts in their behavior, or even something as simple as not wanting to get out of bed can be early signs of an aging mind or untreated psychiatric issues, he noted.
“Of course, we always rule out infections and medication side effects, but I also look for other reversible causes like thyroid problems, electrolyte imbalances, low oxygen, pain, urinary retention, constipation, and nutritional deficiencies,” Cao said.
Of note, delirium is the most common cause of sudden mental status changes in the hospital, and “it’s easy to miss if you’re not looking for it.”
He summarized that classic signs are an acute and fluctuating course with changes in alertness, but added there are other red flags too: disorientation, hallucinations, changes in sleep patterns, sporadic unsafe behaviors, mood swings, and changes in activity level, whether that’s agitation or just being unusually quiet.
By combining what he notices bedside and what is learned from the medical record (and from the people who know the patient best), Cao said he’s able to catch these changes early, identify the underlying cause, and work toward the best possible outcome.
“One of the main interventions is providing mental stimulation,” he said.
Why Mental Stimulation Is So Vital
Mental stimulation of the patient is critical to recovery and may prevent prolonged illness, said Meghana R. Medavaram, MD, associate director of consultation liaison and emergency psychiatry at Montefiore Medical Center’s Weiler Hospital in New York City. “Keeping a patient active both physically and mentally can help prevent deconditioning and risks of prolonged immobility,” she said.
It’s important to note that when patients are out of their familiar routines, away from their usual environment and people, and their sleep is fragmented, this can make them even more vulnerable. Keeping patients mentally stimulated during their hospital stay can help maintain their attention, orientation, and a healthy sleep-wake cycle — all things that are easily thrown off in the hospital, Cao said.
“These disruptions hit the pathways that control attention, wakefulness, and the sleep–wake cycle. That’s when you see attention drifting, orientation fading, and circadian rhythms unraveling, especially at night, which is why “sundowning” is so common, Cao said, referring to the syndrome where older adults or people with dementia experience behavioral changes in late afternoon or evening. “Mental stimulation is critical in the hospital because when the brain isn’t active and gets disoriented, it becomes an easy target for delirium.”
He said delirium often develops in older adults when acute stressors like inflammation, low oxygen, metabolic imbalances, or sedating medications disrupt the brain’s arousal systems and networks, especially in older adults.
Therefore, Cao said, encourage your patients to be more engaged during the day through conversation, activities, or regular reorientation. “This supports the brain networks that help prevent inattention and confusion, which are the hallmarks of delirium. Daytime stimulation also helps build up the natural drive for nighttime sleep, so patients are less likely to nap during the day and be awake and disoriented at night.”
To support this, it’s helpful to schedule medications during waking hours instead of around–the–clock dosing that interrupts sleep, and to cluster nighttime care activities to minimize disturbances, Cao explained. Ensuring patients have their glasses, hearing aids, and familiar routines, along with encouraging mobility and hydration, further protects against delirium and supports patients’ cognitive health during hospitalization. “These same principles are just as important in outpatient subacute rehab settings and at home, so it’s essential to take home these strategies after discharge,” he said.
A Family Member or Friend May Help
Hospitalists can suggest straightforward ways to encourage families and friends to keep patients engaged during a hospital stay. Visits and chats can go a long way as conversations are incredibly grounding, Cao said. Other methods could be bringing in favorite foods or snacks, a phone chat or video call, or even showing prerecorded video messages. “These can be effective. Patients respond well to seeing and hearing familiar faces and voices, even if it’s just on a screen,” Cao said.
Beyond that, he said, activities such as watching and discussing the news, reading aloud, using tablets for games, watching movies, doing crossword puzzles, knitting, reminiscing, and playing word games can also be mentally stimulating for patients.
In addition, safe exercises/activities that patients can do in bed — with advice from physical therapy and occupational therapy — are beneficial, Medavaram said. “These often include gentle range–of-motion activities,” she said.
Share Importance of Mental Stimulation With Patients and Caregivers
If a hospitalist wants to motivate patients to keep their minds active, the framing should be simple, positive, and tied directly to their goals of getting better and getting home, said Medavaram. She provided this script suggestion:
“One of the best ways to help your recovery isn’t just taking your medicine, it’s keeping your mind active. When you’re in the hospital, it’s easy to spend the day lying in bed and staring at the TV in your room, but that can make your brain slow down and even cause confusion. Simple things — like reading, talking with visitors, doing puzzles, listening to music you enjoy, or telling a nurse about your favorite memories — can keep your brain sharp. Staying mentally active helps your thinking stay clear and can even help you get home sooner. Think of it like physical therapy for your brain.”
A version of this article first appeared on Medscape.com.
Signs Your Hospital Patient May Have Lost Some Mental Acuity
Signs Your Hospital Patient May Have Lost Some Mental Acuity
The role of the hospitalist is multidisciplinary and one of the primary responsibilities in your role is to notice and act on the changes you notice regarding your patients, including mental awareness and acuity.
"Evaluation of orientation and level of awareness is a core component of any hospitalist's daily evaluation," said Tara Scribner, MD, an internal medicine hospitalist, The University of Vermont Medical Center; associate program director for POCUS and Procedure Curriculum, UVMMC Internal Medicine Residency Program; and an assistant professor, Robert Larner, M.D. College of Medicine, Burlington, Vermont. "Beyond this, a broader assessment of executive function and functional abilities always occurs at some point during a hospital admission as discharge location and situation depends on this."
While it's relatively easy to identify signs of dementia using information from collateral sources, she also noted it's often difficult to determine whether a patient is experiencing progressive dementia or a more acute encephalopathy such as delirium if collateral sources are not available.
"Once a baseline has been established, hospitalists are in a unique position to identify subtle and acute shifts in mental acuity over the course of a hospital stay," Scribner said. "Unlike our primary care colleagues, who are well-positioned to observe for signs of dementia, we see our patients on a daily basis, sometimes more than once daily, and can track changes which occur over a matter of hours or days."
What Are Signs to Watch
During examinations and assessments, pay attention to shifts in the behavior of patients.
"Subtle signs of delirium and/or declining mental awareness can include disorientation about date, location, reason for admission," said Meghana R. Medavaram, MD, associate director of Consultation Liaison and Emergency Psychiatry, Weiler Hospital at Montefiore Health System in Bronx, New York.
Another sign would be mild inattention, such as drifting off during conversations or even having a hard time understanding and following multistep commands, she also said.
"We can also see sudden irritability or even the opposite, odd politeness or familiarity. We notice these changes occur as fluctuations throughout the day, sometimes with a clinician seeing a different 'personality' in the morning vs afternoon or evening," Medavaram said. "A key message we emphasize for our hospitalist colleagues is to not wait for overt agitation, or hallucinations to step in when assessing a patient and coming up with a treatment plan."
How Would Diet Play a Role
Excess consumption of alcohol is the most common way a patient's diet can affect changes in mental status, said Scribner. "Excess alcohol use has been linked to a significantly increased risk of dementia including both Alzheimer's and to alcohol-related brain damage including Korsakoff syndrome, as well as to the more acute Wernicke encephalopathy through vitamin B1 deficiency."
Also, vitamin deficiencies such as B12 have been linked to development of dementia and other cognitive impairment and can be related to alcohol consumption as well as to dietary habits such as vegetarianism, even in the absence of alcohol intake. Identification and treatment of B12 deficiency is a potentially reversible cause of cognitive impairment, she also said.
Do Medications Affect Mental State
Medications can be a significant cause of acute changes in mental status. "These changes are often reversible and include somnolence and both hypoactive and hyperactive delirium. Adjustment of a patient's usual medications is often necessary in hospitalized patients experiencing acute encephalopathy," Scribner said.
What About Depression
The relationship between dementia and development of dementia is complex and poorly understood, she said, however, those who deal with depression are at a higher risk of developing dementia, and also that patients with dementia are at a higher risk for development of depression.
How to Distinguish Between Short- and Long-term Issues
A thorough hospitalist is typically able to identify the acuity of mental status changes by the time of discharge and therefore predict the likelihood of recovery.
Progressive mental status changes occurring over months to years are almost always representative of dementia and are irreversible, whereas most (but not all) acute encephalopathies are recoverable over days to weeks or months.
Determining which of these is present involves interrogation of collateral sources such as family and friends, assessment of orientation and other signs of delirium, and observation of recovery during the period of hospital admission. It is worth noting that episodes of delirium are associated with a higher risk for long-term cognitive decline and development of dementia.
Written by Erica Lamberg.
A version of this article first appeared on Medscape.com.
The role of the hospitalist is multidisciplinary and one of the primary responsibilities in your role is to notice and act on the changes you notice regarding your patients, including mental awareness and acuity.
"Evaluation of orientation and level of awareness is a core component of any hospitalist's daily evaluation," said Tara Scribner, MD, an internal medicine hospitalist, The University of Vermont Medical Center; associate program director for POCUS and Procedure Curriculum, UVMMC Internal Medicine Residency Program; and an assistant professor, Robert Larner, M.D. College of Medicine, Burlington, Vermont. "Beyond this, a broader assessment of executive function and functional abilities always occurs at some point during a hospital admission as discharge location and situation depends on this."
While it's relatively easy to identify signs of dementia using information from collateral sources, she also noted it's often difficult to determine whether a patient is experiencing progressive dementia or a more acute encephalopathy such as delirium if collateral sources are not available.
"Once a baseline has been established, hospitalists are in a unique position to identify subtle and acute shifts in mental acuity over the course of a hospital stay," Scribner said. "Unlike our primary care colleagues, who are well-positioned to observe for signs of dementia, we see our patients on a daily basis, sometimes more than once daily, and can track changes which occur over a matter of hours or days."
What Are Signs to Watch
During examinations and assessments, pay attention to shifts in the behavior of patients.
"Subtle signs of delirium and/or declining mental awareness can include disorientation about date, location, reason for admission," said Meghana R. Medavaram, MD, associate director of Consultation Liaison and Emergency Psychiatry, Weiler Hospital at Montefiore Health System in Bronx, New York.
Another sign would be mild inattention, such as drifting off during conversations or even having a hard time understanding and following multistep commands, she also said.
"We can also see sudden irritability or even the opposite, odd politeness or familiarity. We notice these changes occur as fluctuations throughout the day, sometimes with a clinician seeing a different 'personality' in the morning vs afternoon or evening," Medavaram said. "A key message we emphasize for our hospitalist colleagues is to not wait for overt agitation, or hallucinations to step in when assessing a patient and coming up with a treatment plan."
How Would Diet Play a Role
Excess consumption of alcohol is the most common way a patient's diet can affect changes in mental status, said Scribner. "Excess alcohol use has been linked to a significantly increased risk of dementia including both Alzheimer's and to alcohol-related brain damage including Korsakoff syndrome, as well as to the more acute Wernicke encephalopathy through vitamin B1 deficiency."
Also, vitamin deficiencies such as B12 have been linked to development of dementia and other cognitive impairment and can be related to alcohol consumption as well as to dietary habits such as vegetarianism, even in the absence of alcohol intake. Identification and treatment of B12 deficiency is a potentially reversible cause of cognitive impairment, she also said.
Do Medications Affect Mental State
Medications can be a significant cause of acute changes in mental status. "These changes are often reversible and include somnolence and both hypoactive and hyperactive delirium. Adjustment of a patient's usual medications is often necessary in hospitalized patients experiencing acute encephalopathy," Scribner said.
What About Depression
The relationship between dementia and development of dementia is complex and poorly understood, she said, however, those who deal with depression are at a higher risk of developing dementia, and also that patients with dementia are at a higher risk for development of depression.
How to Distinguish Between Short- and Long-term Issues
A thorough hospitalist is typically able to identify the acuity of mental status changes by the time of discharge and therefore predict the likelihood of recovery.
Progressive mental status changes occurring over months to years are almost always representative of dementia and are irreversible, whereas most (but not all) acute encephalopathies are recoverable over days to weeks or months.
Determining which of these is present involves interrogation of collateral sources such as family and friends, assessment of orientation and other signs of delirium, and observation of recovery during the period of hospital admission. It is worth noting that episodes of delirium are associated with a higher risk for long-term cognitive decline and development of dementia.
Written by Erica Lamberg.
A version of this article first appeared on Medscape.com.
The role of the hospitalist is multidisciplinary and one of the primary responsibilities in your role is to notice and act on the changes you notice regarding your patients, including mental awareness and acuity.
"Evaluation of orientation and level of awareness is a core component of any hospitalist's daily evaluation," said Tara Scribner, MD, an internal medicine hospitalist, The University of Vermont Medical Center; associate program director for POCUS and Procedure Curriculum, UVMMC Internal Medicine Residency Program; and an assistant professor, Robert Larner, M.D. College of Medicine, Burlington, Vermont. "Beyond this, a broader assessment of executive function and functional abilities always occurs at some point during a hospital admission as discharge location and situation depends on this."
While it's relatively easy to identify signs of dementia using information from collateral sources, she also noted it's often difficult to determine whether a patient is experiencing progressive dementia or a more acute encephalopathy such as delirium if collateral sources are not available.
"Once a baseline has been established, hospitalists are in a unique position to identify subtle and acute shifts in mental acuity over the course of a hospital stay," Scribner said. "Unlike our primary care colleagues, who are well-positioned to observe for signs of dementia, we see our patients on a daily basis, sometimes more than once daily, and can track changes which occur over a matter of hours or days."
What Are Signs to Watch
During examinations and assessments, pay attention to shifts in the behavior of patients.
"Subtle signs of delirium and/or declining mental awareness can include disorientation about date, location, reason for admission," said Meghana R. Medavaram, MD, associate director of Consultation Liaison and Emergency Psychiatry, Weiler Hospital at Montefiore Health System in Bronx, New York.
Another sign would be mild inattention, such as drifting off during conversations or even having a hard time understanding and following multistep commands, she also said.
"We can also see sudden irritability or even the opposite, odd politeness or familiarity. We notice these changes occur as fluctuations throughout the day, sometimes with a clinician seeing a different 'personality' in the morning vs afternoon or evening," Medavaram said. "A key message we emphasize for our hospitalist colleagues is to not wait for overt agitation, or hallucinations to step in when assessing a patient and coming up with a treatment plan."
How Would Diet Play a Role
Excess consumption of alcohol is the most common way a patient's diet can affect changes in mental status, said Scribner. "Excess alcohol use has been linked to a significantly increased risk of dementia including both Alzheimer's and to alcohol-related brain damage including Korsakoff syndrome, as well as to the more acute Wernicke encephalopathy through vitamin B1 deficiency."
Also, vitamin deficiencies such as B12 have been linked to development of dementia and other cognitive impairment and can be related to alcohol consumption as well as to dietary habits such as vegetarianism, even in the absence of alcohol intake. Identification and treatment of B12 deficiency is a potentially reversible cause of cognitive impairment, she also said.
Do Medications Affect Mental State
Medications can be a significant cause of acute changes in mental status. "These changes are often reversible and include somnolence and both hypoactive and hyperactive delirium. Adjustment of a patient's usual medications is often necessary in hospitalized patients experiencing acute encephalopathy," Scribner said.
What About Depression
The relationship between dementia and development of dementia is complex and poorly understood, she said, however, those who deal with depression are at a higher risk of developing dementia, and also that patients with dementia are at a higher risk for development of depression.
How to Distinguish Between Short- and Long-term Issues
A thorough hospitalist is typically able to identify the acuity of mental status changes by the time of discharge and therefore predict the likelihood of recovery.
Progressive mental status changes occurring over months to years are almost always representative of dementia and are irreversible, whereas most (but not all) acute encephalopathies are recoverable over days to weeks or months.
Determining which of these is present involves interrogation of collateral sources such as family and friends, assessment of orientation and other signs of delirium, and observation of recovery during the period of hospital admission. It is worth noting that episodes of delirium are associated with a higher risk for long-term cognitive decline and development of dementia.
Written by Erica Lamberg.
A version of this article first appeared on Medscape.com.
Signs Your Hospital Patient May Have Lost Some Mental Acuity
Signs Your Hospital Patient May Have Lost Some Mental Acuity


