User login
Signs Your Hospital Patient May Have Lost Some Mental Acuity
Signs Your Hospital Patient May Have Lost Some Mental Acuity
The role of the hospitalist is multidisciplinary and one of the primary responsibilities in your role is to notice and act on the changes you notice regarding your patients, including mental awareness and acuity.
"Evaluation of orientation and level of awareness is a core component of any hospitalist's daily evaluation," said Tara Scribner, MD, an internal medicine hospitalist, The University of Vermont Medical Center; associate program director for POCUS and Procedure Curriculum, UVMMC Internal Medicine Residency Program; and an assistant professor, Robert Larner, M.D. College of Medicine, Burlington, Vermont. "Beyond this, a broader assessment of executive function and functional abilities always occurs at some point during a hospital admission as discharge location and situation depends on this."
While it's relatively easy to identify signs of dementia using information from collateral sources, she also noted it's often difficult to determine whether a patient is experiencing progressive dementia or a more acute encephalopathy such as delirium if collateral sources are not available.
"Once a baseline has been established, hospitalists are in a unique position to identify subtle and acute shifts in mental acuity over the course of a hospital stay," Scribner said. "Unlike our primary care colleagues, who are well-positioned to observe for signs of dementia, we see our patients on a daily basis, sometimes more than once daily, and can track changes which occur over a matter of hours or days."
What Are Signs to Watch
During examinations and assessments, pay attention to shifts in the behavior of patients.
"Subtle signs of delirium and/or declining mental awareness can include disorientation about date, location, reason for admission," said Meghana R. Medavaram, MD, associate director of Consultation Liaison and Emergency Psychiatry, Weiler Hospital at Montefiore Health System in Bronx, New York.
Another sign would be mild inattention, such as drifting off during conversations or even having a hard time understanding and following multistep commands, she also said.
"We can also see sudden irritability or even the opposite, odd politeness or familiarity. We notice these changes occur as fluctuations throughout the day, sometimes with a clinician seeing a different 'personality' in the morning vs afternoon or evening," Medavaram said. "A key message we emphasize for our hospitalist colleagues is to not wait for overt agitation, or hallucinations to step in when assessing a patient and coming up with a treatment plan."
How Would Diet Play a Role
Excess consumption of alcohol is the most common way a patient's diet can affect changes in mental status, said Scribner. "Excess alcohol use has been linked to a significantly increased risk of dementia including both Alzheimer's and to alcohol-related brain damage including Korsakoff syndrome, as well as to the more acute Wernicke encephalopathy through vitamin B1 deficiency."
Also, vitamin deficiencies such as B12 have been linked to development of dementia and other cognitive impairment and can be related to alcohol consumption as well as to dietary habits such as vegetarianism, even in the absence of alcohol intake. Identification and treatment of B12 deficiency is a potentially reversible cause of cognitive impairment, she also said.
Do Medications Affect Mental State
Medications can be a significant cause of acute changes in mental status. "These changes are often reversible and include somnolence and both hypoactive and hyperactive delirium. Adjustment of a patient's usual medications is often necessary in hospitalized patients experiencing acute encephalopathy," Scribner said.
What About Depression
The relationship between dementia and development of dementia is complex and poorly understood, she said, however, those who deal with depression are at a higher risk of developing dementia, and also that patients with dementia are at a higher risk for development of depression.
How to Distinguish Between Short- and Long-term Issues
A thorough hospitalist is typically able to identify the acuity of mental status changes by the time of discharge and therefore predict the likelihood of recovery.
Progressive mental status changes occurring over months to years are almost always representative of dementia and are irreversible, whereas most (but not all) acute encephalopathies are recoverable over days to weeks or months.
Determining which of these is present involves interrogation of collateral sources such as family and friends, assessment of orientation and other signs of delirium, and observation of recovery during the period of hospital admission. It is worth noting that episodes of delirium are associated with a higher risk for long-term cognitive decline and development of dementia.
Written by Erica Lamberg.
A version of this article first appeared on Medscape.com.
The role of the hospitalist is multidisciplinary and one of the primary responsibilities in your role is to notice and act on the changes you notice regarding your patients, including mental awareness and acuity.
"Evaluation of orientation and level of awareness is a core component of any hospitalist's daily evaluation," said Tara Scribner, MD, an internal medicine hospitalist, The University of Vermont Medical Center; associate program director for POCUS and Procedure Curriculum, UVMMC Internal Medicine Residency Program; and an assistant professor, Robert Larner, M.D. College of Medicine, Burlington, Vermont. "Beyond this, a broader assessment of executive function and functional abilities always occurs at some point during a hospital admission as discharge location and situation depends on this."
While it's relatively easy to identify signs of dementia using information from collateral sources, she also noted it's often difficult to determine whether a patient is experiencing progressive dementia or a more acute encephalopathy such as delirium if collateral sources are not available.
"Once a baseline has been established, hospitalists are in a unique position to identify subtle and acute shifts in mental acuity over the course of a hospital stay," Scribner said. "Unlike our primary care colleagues, who are well-positioned to observe for signs of dementia, we see our patients on a daily basis, sometimes more than once daily, and can track changes which occur over a matter of hours or days."
What Are Signs to Watch
During examinations and assessments, pay attention to shifts in the behavior of patients.
"Subtle signs of delirium and/or declining mental awareness can include disorientation about date, location, reason for admission," said Meghana R. Medavaram, MD, associate director of Consultation Liaison and Emergency Psychiatry, Weiler Hospital at Montefiore Health System in Bronx, New York.
Another sign would be mild inattention, such as drifting off during conversations or even having a hard time understanding and following multistep commands, she also said.
"We can also see sudden irritability or even the opposite, odd politeness or familiarity. We notice these changes occur as fluctuations throughout the day, sometimes with a clinician seeing a different 'personality' in the morning vs afternoon or evening," Medavaram said. "A key message we emphasize for our hospitalist colleagues is to not wait for overt agitation, or hallucinations to step in when assessing a patient and coming up with a treatment plan."
How Would Diet Play a Role
Excess consumption of alcohol is the most common way a patient's diet can affect changes in mental status, said Scribner. "Excess alcohol use has been linked to a significantly increased risk of dementia including both Alzheimer's and to alcohol-related brain damage including Korsakoff syndrome, as well as to the more acute Wernicke encephalopathy through vitamin B1 deficiency."
Also, vitamin deficiencies such as B12 have been linked to development of dementia and other cognitive impairment and can be related to alcohol consumption as well as to dietary habits such as vegetarianism, even in the absence of alcohol intake. Identification and treatment of B12 deficiency is a potentially reversible cause of cognitive impairment, she also said.
Do Medications Affect Mental State
Medications can be a significant cause of acute changes in mental status. "These changes are often reversible and include somnolence and both hypoactive and hyperactive delirium. Adjustment of a patient's usual medications is often necessary in hospitalized patients experiencing acute encephalopathy," Scribner said.
What About Depression
The relationship between dementia and development of dementia is complex and poorly understood, she said, however, those who deal with depression are at a higher risk of developing dementia, and also that patients with dementia are at a higher risk for development of depression.
How to Distinguish Between Short- and Long-term Issues
A thorough hospitalist is typically able to identify the acuity of mental status changes by the time of discharge and therefore predict the likelihood of recovery.
Progressive mental status changes occurring over months to years are almost always representative of dementia and are irreversible, whereas most (but not all) acute encephalopathies are recoverable over days to weeks or months.
Determining which of these is present involves interrogation of collateral sources such as family and friends, assessment of orientation and other signs of delirium, and observation of recovery during the period of hospital admission. It is worth noting that episodes of delirium are associated with a higher risk for long-term cognitive decline and development of dementia.
Written by Erica Lamberg.
A version of this article first appeared on Medscape.com.
The role of the hospitalist is multidisciplinary and one of the primary responsibilities in your role is to notice and act on the changes you notice regarding your patients, including mental awareness and acuity.
"Evaluation of orientation and level of awareness is a core component of any hospitalist's daily evaluation," said Tara Scribner, MD, an internal medicine hospitalist, The University of Vermont Medical Center; associate program director for POCUS and Procedure Curriculum, UVMMC Internal Medicine Residency Program; and an assistant professor, Robert Larner, M.D. College of Medicine, Burlington, Vermont. "Beyond this, a broader assessment of executive function and functional abilities always occurs at some point during a hospital admission as discharge location and situation depends on this."
While it's relatively easy to identify signs of dementia using information from collateral sources, she also noted it's often difficult to determine whether a patient is experiencing progressive dementia or a more acute encephalopathy such as delirium if collateral sources are not available.
"Once a baseline has been established, hospitalists are in a unique position to identify subtle and acute shifts in mental acuity over the course of a hospital stay," Scribner said. "Unlike our primary care colleagues, who are well-positioned to observe for signs of dementia, we see our patients on a daily basis, sometimes more than once daily, and can track changes which occur over a matter of hours or days."
What Are Signs to Watch
During examinations and assessments, pay attention to shifts in the behavior of patients.
"Subtle signs of delirium and/or declining mental awareness can include disorientation about date, location, reason for admission," said Meghana R. Medavaram, MD, associate director of Consultation Liaison and Emergency Psychiatry, Weiler Hospital at Montefiore Health System in Bronx, New York.
Another sign would be mild inattention, such as drifting off during conversations or even having a hard time understanding and following multistep commands, she also said.
"We can also see sudden irritability or even the opposite, odd politeness or familiarity. We notice these changes occur as fluctuations throughout the day, sometimes with a clinician seeing a different 'personality' in the morning vs afternoon or evening," Medavaram said. "A key message we emphasize for our hospitalist colleagues is to not wait for overt agitation, or hallucinations to step in when assessing a patient and coming up with a treatment plan."
How Would Diet Play a Role
Excess consumption of alcohol is the most common way a patient's diet can affect changes in mental status, said Scribner. "Excess alcohol use has been linked to a significantly increased risk of dementia including both Alzheimer's and to alcohol-related brain damage including Korsakoff syndrome, as well as to the more acute Wernicke encephalopathy through vitamin B1 deficiency."
Also, vitamin deficiencies such as B12 have been linked to development of dementia and other cognitive impairment and can be related to alcohol consumption as well as to dietary habits such as vegetarianism, even in the absence of alcohol intake. Identification and treatment of B12 deficiency is a potentially reversible cause of cognitive impairment, she also said.
Do Medications Affect Mental State
Medications can be a significant cause of acute changes in mental status. "These changes are often reversible and include somnolence and both hypoactive and hyperactive delirium. Adjustment of a patient's usual medications is often necessary in hospitalized patients experiencing acute encephalopathy," Scribner said.
What About Depression
The relationship between dementia and development of dementia is complex and poorly understood, she said, however, those who deal with depression are at a higher risk of developing dementia, and also that patients with dementia are at a higher risk for development of depression.
How to Distinguish Between Short- and Long-term Issues
A thorough hospitalist is typically able to identify the acuity of mental status changes by the time of discharge and therefore predict the likelihood of recovery.
Progressive mental status changes occurring over months to years are almost always representative of dementia and are irreversible, whereas most (but not all) acute encephalopathies are recoverable over days to weeks or months.
Determining which of these is present involves interrogation of collateral sources such as family and friends, assessment of orientation and other signs of delirium, and observation of recovery during the period of hospital admission. It is worth noting that episodes of delirium are associated with a higher risk for long-term cognitive decline and development of dementia.
Written by Erica Lamberg.
A version of this article first appeared on Medscape.com.
Signs Your Hospital Patient May Have Lost Some Mental Acuity
Signs Your Hospital Patient May Have Lost Some Mental Acuity
Veterans and Loneliness: More Than Just Isolation
According to the National Institute on Drug Abuse, > 1 in 10 veterans have been diagnosed with substance use disorder (SUD). Additionally, 7 out of every 100 veterans will have posttraumatic stress disorder (PTSD) at some point in their life, per research from the US Department of Veterans Affairs (VA). However, a common and perhaps unsuspected parallel is found in those statistics: loneliness.
Of the 4069 veterans who participated in the 2019-2020 National Health and Resilience in Veterans Survey, 56.9% reported they felt lonely sometimes or often, while 1 in 5 reported feeling lonely often.
An Epidemic
In his 2023 advisory, Former US Surgeon General Vivek Murthy called it an epidemic noting that when he spoke with veterans during a cross-country listening tour, he heard how they felt “isolated, invisible, and insignificant.” About 1 in 2 adults in America experience loneliness, even before the COVID-19 pandemic isolation.
Loneliness can have individual and synergistic ill effects, including a greater risk of cardiovascular disease, dementia, stroke, depression, anxiety, and premature death. It also can both trigger and exacerbate substance use and PTSD.
A study using data from the RAND Health and Retirement Study Longitudinal File 2020 (N = 5259) found significant associations between loneliness and being unmarried/unpartnered, and greater depressive symptoms for both veterans and civilians, as well as significant negative associations between loneliness and greater life satisfaction and positive affect. Health conditions that limited an individual's ability to work was a “unique risk factor for loneliness among veterans.”
The National Health and Resilience in Veterans Study found that those aged ≤ 50 years were 3 times more likely to screen positive for PTSD compared to older veterans. In a survey of 409 veterans, many who engaged in problematic substance use during the COVID-19 pandemic reported that despite having social supports they still felt lonely. In regression analyses, higher levels of loneliness were associated with more negative impacts of the pandemic, greater substance use, and poorer physical and mental health functioning.
Addressing Loneliness
Researchers believe an answer to some mental health and substance abuse problems may lie in addressing loneliness. Positive psychology is providing promising results in the treatment of SUD. Bryant Stone, from the Johns Hopkins Bloomberg School of Public Health, emphasizes focusing on well-being and quality of life rather than solely on abstinence with “positive psychological interventions,” or activities and behavioral interventions that target positive variables to promote adaptive functioning.
Veterans can face tough challenges as they rejoin civilian life. How successfully they meet and conquer those challenges, especially if they include drug problems, may directly relate to their general feeling of well-being.
The PERMA model outlines 5 core elements to assess well-being: Positive emotions, Engagement, Relationships, Meaning, and Accomplishment. A study based on that model found loneliness to be a “particularly significant factor” among key variables influencing the prevention and treatment of SUDs. The study of 156 veterans with self-reported mental health conditions found the ability to engage in social roles and activities was positively correlated with overall well-being and negatively correlated with degree of problems related to drug abuse.
Rural Veterans
The estimated 4.4 million veterans living in rural communities may benefit most from interventions that tackle isolation. Compared with urban counterparts, they’re more likely to be older, have more complex medical issues, have a service-connected disability, and be unemployed. Those factors, compounded by geographical and social isolation, can have a substantial impact on well-being.
A study centered on the initial validation of a short (5-item) version of PERMA found that individuals who scored higher on the short form tended to report higher levels of optimism, resilience, and happiness. Thus, the short form may be particularly useful for rural veterans who do not always have easy access to health care.
VA has instituted a variety of programs to encourage and support social connection. During the COVID-19 pandemic, telehealth interventions targeted social support and loneliness among veterans—albeit with mixed results. VA CONNECT, a 10-session group telehealth intervention that integrated peer support, did not show significant changes in loneliness, but did significantly reduce perceived stress.
Another initiative, Compassionate Contact Corps, trained volunteers made weekly phone calls aimed at reducing loneliness and fostering social connection. Started in Columbus, Ohio, in 2020, > 80 sites had adopted the initiative by 2021, with 310 volunteers, 5320 visits, and 4757 hours spent with veterans.
In 2014, VA peer specialists developed and co-hosted Veterans Socials through community partnerships between VA, veteran-serving organizations, and veteran community leaders. As of 2025, 178 known Veterans Socials were spread across 26 states and territories.
The researchers say their case examples collectively demonstrate that Veterans Socials have the potential to serve as a vital platform for peer support, resource sharing, and health service use among veterans. Virtual Veterans Socials also provided hosts with a channel to reach potentially isolated veterans who might not otherwise access services while simultaneously offering veterans an opportunity for social connection.
According to the National Institute on Drug Abuse, > 1 in 10 veterans have been diagnosed with substance use disorder (SUD). Additionally, 7 out of every 100 veterans will have posttraumatic stress disorder (PTSD) at some point in their life, per research from the US Department of Veterans Affairs (VA). However, a common and perhaps unsuspected parallel is found in those statistics: loneliness.
Of the 4069 veterans who participated in the 2019-2020 National Health and Resilience in Veterans Survey, 56.9% reported they felt lonely sometimes or often, while 1 in 5 reported feeling lonely often.
An Epidemic
In his 2023 advisory, Former US Surgeon General Vivek Murthy called it an epidemic noting that when he spoke with veterans during a cross-country listening tour, he heard how they felt “isolated, invisible, and insignificant.” About 1 in 2 adults in America experience loneliness, even before the COVID-19 pandemic isolation.
Loneliness can have individual and synergistic ill effects, including a greater risk of cardiovascular disease, dementia, stroke, depression, anxiety, and premature death. It also can both trigger and exacerbate substance use and PTSD.
A study using data from the RAND Health and Retirement Study Longitudinal File 2020 (N = 5259) found significant associations between loneliness and being unmarried/unpartnered, and greater depressive symptoms for both veterans and civilians, as well as significant negative associations between loneliness and greater life satisfaction and positive affect. Health conditions that limited an individual's ability to work was a “unique risk factor for loneliness among veterans.”
The National Health and Resilience in Veterans Study found that those aged ≤ 50 years were 3 times more likely to screen positive for PTSD compared to older veterans. In a survey of 409 veterans, many who engaged in problematic substance use during the COVID-19 pandemic reported that despite having social supports they still felt lonely. In regression analyses, higher levels of loneliness were associated with more negative impacts of the pandemic, greater substance use, and poorer physical and mental health functioning.
Addressing Loneliness
Researchers believe an answer to some mental health and substance abuse problems may lie in addressing loneliness. Positive psychology is providing promising results in the treatment of SUD. Bryant Stone, from the Johns Hopkins Bloomberg School of Public Health, emphasizes focusing on well-being and quality of life rather than solely on abstinence with “positive psychological interventions,” or activities and behavioral interventions that target positive variables to promote adaptive functioning.
Veterans can face tough challenges as they rejoin civilian life. How successfully they meet and conquer those challenges, especially if they include drug problems, may directly relate to their general feeling of well-being.
The PERMA model outlines 5 core elements to assess well-being: Positive emotions, Engagement, Relationships, Meaning, and Accomplishment. A study based on that model found loneliness to be a “particularly significant factor” among key variables influencing the prevention and treatment of SUDs. The study of 156 veterans with self-reported mental health conditions found the ability to engage in social roles and activities was positively correlated with overall well-being and negatively correlated with degree of problems related to drug abuse.
Rural Veterans
The estimated 4.4 million veterans living in rural communities may benefit most from interventions that tackle isolation. Compared with urban counterparts, they’re more likely to be older, have more complex medical issues, have a service-connected disability, and be unemployed. Those factors, compounded by geographical and social isolation, can have a substantial impact on well-being.
A study centered on the initial validation of a short (5-item) version of PERMA found that individuals who scored higher on the short form tended to report higher levels of optimism, resilience, and happiness. Thus, the short form may be particularly useful for rural veterans who do not always have easy access to health care.
VA has instituted a variety of programs to encourage and support social connection. During the COVID-19 pandemic, telehealth interventions targeted social support and loneliness among veterans—albeit with mixed results. VA CONNECT, a 10-session group telehealth intervention that integrated peer support, did not show significant changes in loneliness, but did significantly reduce perceived stress.
Another initiative, Compassionate Contact Corps, trained volunteers made weekly phone calls aimed at reducing loneliness and fostering social connection. Started in Columbus, Ohio, in 2020, > 80 sites had adopted the initiative by 2021, with 310 volunteers, 5320 visits, and 4757 hours spent with veterans.
In 2014, VA peer specialists developed and co-hosted Veterans Socials through community partnerships between VA, veteran-serving organizations, and veteran community leaders. As of 2025, 178 known Veterans Socials were spread across 26 states and territories.
The researchers say their case examples collectively demonstrate that Veterans Socials have the potential to serve as a vital platform for peer support, resource sharing, and health service use among veterans. Virtual Veterans Socials also provided hosts with a channel to reach potentially isolated veterans who might not otherwise access services while simultaneously offering veterans an opportunity for social connection.
According to the National Institute on Drug Abuse, > 1 in 10 veterans have been diagnosed with substance use disorder (SUD). Additionally, 7 out of every 100 veterans will have posttraumatic stress disorder (PTSD) at some point in their life, per research from the US Department of Veterans Affairs (VA). However, a common and perhaps unsuspected parallel is found in those statistics: loneliness.
Of the 4069 veterans who participated in the 2019-2020 National Health and Resilience in Veterans Survey, 56.9% reported they felt lonely sometimes or often, while 1 in 5 reported feeling lonely often.
An Epidemic
In his 2023 advisory, Former US Surgeon General Vivek Murthy called it an epidemic noting that when he spoke with veterans during a cross-country listening tour, he heard how they felt “isolated, invisible, and insignificant.” About 1 in 2 adults in America experience loneliness, even before the COVID-19 pandemic isolation.
Loneliness can have individual and synergistic ill effects, including a greater risk of cardiovascular disease, dementia, stroke, depression, anxiety, and premature death. It also can both trigger and exacerbate substance use and PTSD.
A study using data from the RAND Health and Retirement Study Longitudinal File 2020 (N = 5259) found significant associations between loneliness and being unmarried/unpartnered, and greater depressive symptoms for both veterans and civilians, as well as significant negative associations between loneliness and greater life satisfaction and positive affect. Health conditions that limited an individual's ability to work was a “unique risk factor for loneliness among veterans.”
The National Health and Resilience in Veterans Study found that those aged ≤ 50 years were 3 times more likely to screen positive for PTSD compared to older veterans. In a survey of 409 veterans, many who engaged in problematic substance use during the COVID-19 pandemic reported that despite having social supports they still felt lonely. In regression analyses, higher levels of loneliness were associated with more negative impacts of the pandemic, greater substance use, and poorer physical and mental health functioning.
Addressing Loneliness
Researchers believe an answer to some mental health and substance abuse problems may lie in addressing loneliness. Positive psychology is providing promising results in the treatment of SUD. Bryant Stone, from the Johns Hopkins Bloomberg School of Public Health, emphasizes focusing on well-being and quality of life rather than solely on abstinence with “positive psychological interventions,” or activities and behavioral interventions that target positive variables to promote adaptive functioning.
Veterans can face tough challenges as they rejoin civilian life. How successfully they meet and conquer those challenges, especially if they include drug problems, may directly relate to their general feeling of well-being.
The PERMA model outlines 5 core elements to assess well-being: Positive emotions, Engagement, Relationships, Meaning, and Accomplishment. A study based on that model found loneliness to be a “particularly significant factor” among key variables influencing the prevention and treatment of SUDs. The study of 156 veterans with self-reported mental health conditions found the ability to engage in social roles and activities was positively correlated with overall well-being and negatively correlated with degree of problems related to drug abuse.
Rural Veterans
The estimated 4.4 million veterans living in rural communities may benefit most from interventions that tackle isolation. Compared with urban counterparts, they’re more likely to be older, have more complex medical issues, have a service-connected disability, and be unemployed. Those factors, compounded by geographical and social isolation, can have a substantial impact on well-being.
A study centered on the initial validation of a short (5-item) version of PERMA found that individuals who scored higher on the short form tended to report higher levels of optimism, resilience, and happiness. Thus, the short form may be particularly useful for rural veterans who do not always have easy access to health care.
VA has instituted a variety of programs to encourage and support social connection. During the COVID-19 pandemic, telehealth interventions targeted social support and loneliness among veterans—albeit with mixed results. VA CONNECT, a 10-session group telehealth intervention that integrated peer support, did not show significant changes in loneliness, but did significantly reduce perceived stress.
Another initiative, Compassionate Contact Corps, trained volunteers made weekly phone calls aimed at reducing loneliness and fostering social connection. Started in Columbus, Ohio, in 2020, > 80 sites had adopted the initiative by 2021, with 310 volunteers, 5320 visits, and 4757 hours spent with veterans.
In 2014, VA peer specialists developed and co-hosted Veterans Socials through community partnerships between VA, veteran-serving organizations, and veteran community leaders. As of 2025, 178 known Veterans Socials were spread across 26 states and territories.
The researchers say their case examples collectively demonstrate that Veterans Socials have the potential to serve as a vital platform for peer support, resource sharing, and health service use among veterans. Virtual Veterans Socials also provided hosts with a channel to reach potentially isolated veterans who might not otherwise access services while simultaneously offering veterans an opportunity for social connection.
About Half of Canadian Physicians Report High Burnout Levels
About Half of Canadian Physicians Report High Burnout Levels
Nearly half of physicians in Canada report high levels of burnout, according to preliminary data from the 2025 National Physician Health Survey (NPHS). The new data show that 46% of physicians report high levels of burnout, down from 2021 (53%) but significantly above the level of 2017 (30%), when the first survey was conducted. The full NPHS 2025 Foundational Report will be released later this year.
Other significant findings include the following:
- 74% of physicians reported experiencing bullying, harassment, microaggressions, or discrimination, a slight but meaningful reduction form 78% in 2021.
- 64% of physicians reported spending significant time on electronic medical records outside regular hours.
- 46% of physicians said that their mental health is worse than it was before the start of the pandemic, down 14% from 2021.
- 60% reported being satisfied or very satisfied with work-life balance, an improvement from 49% in 2021, though slightly below 2017 (62%).
- 37% of physicians plan to reduce their clinical hours in the next 2 years.
Margot Burnell, MD, president of the Canadian Medical Association (CMA), told Medscape Medical News that she was "disappointed" with the results.
"I hoped that the burnout numbers would decrease more than they have," she said. "Physicians are still under extreme stress in trying to provide the care for patients that they wish to give."
Reductions in Hours
The most distressing finding is that > one-third of physicians (37%) plan to reduce their hours within 24 hours -- at a time of growing physician shortages -- said Burnell.
"The one positive (finding) that stands out is that physicians are taking care of their own health and wellness and report that it's helping," she said. About 65% of physicians reported having accessed at least 1 wellness support in the past 5 years, up 11% since 2021.
The NPHS includes responses from about 3300 practicing physicians, medical residents, and fellows who were surveyed from March 14 to April 15.
Among the CMA's top priorities is to reduce the administrative burden because that tops the list of what physicians say would help them with burnout, said Burnell.
"The other area is to provide and encourage team-based care," she continued. "That provides some relief for physicians." It also is important to promote the approaches that seem to be helping, such as wellness support and artificial intelligence (AI), she said. In this survey, 59% of respondents who used AI said that it decreased their time spent on administrative tasks.
Burnout by Specialty
Future analyses will examine burnout by specialty, Burnell said. Burnout is particularly high among emergency physicians, regardless of province, according to previous work by Kerstin de Wit, MD, emergency physician and research director for the Department of Emergency Medicine at Queen's University in Kingston, Ontario, and colleagues.
The NPHS findings are not surprising, she told Medscape Medical News. "We resurveyed all our emergency physicians in January and found similar results, in that the levels of burnout were marginally less than they were in 2022 but still significantly higher than they were in 2020. Still, a majority of (emergency department) physicians qualify as having high burnout levels."
The Pandemic's Role
A telling finding of her team's research is that emergency physician burnout levels are now higher than they were in December 2020, the first year of the COVID pandemic, said De Wit. "I don't think you can say burnout is because of COVID. It's because of the problems in the medical system."
Among those problems in hospitals are a shortage of beds, physicians, and nurses and inadequate numbers of physicians in outpatient clinics "so patients are waiting for years" for conditions to be treated, she added.
"We don't have the resources that we need to maintain the standards that we had even 10, 15 years ago. The whole system is collapsing. Government underfunding is huge. Routinely, our emergency department is 100% full of ward patients, so we don't have a room with a door or a curtain to see patients in. All the emergency patients are seen in corridors or the waiting room in full view of everyone else. We have people with serious medical conditions who are dying in waiting rooms because we can't get them in."
The issues are complex, but the overarching problem is chronic underfunding that results in physicians "feeling overworked and powerless to help patients," said De Wit.
Burnell and de Wit reported having no relevant financial relationships.
Marcia Frellick is an independent health care journalist and a regular contributor to Medscape Medical News.
A version of this article first appeared on Medscape.com.
Nearly half of physicians in Canada report high levels of burnout, according to preliminary data from the 2025 National Physician Health Survey (NPHS). The new data show that 46% of physicians report high levels of burnout, down from 2021 (53%) but significantly above the level of 2017 (30%), when the first survey was conducted. The full NPHS 2025 Foundational Report will be released later this year.
Other significant findings include the following:
- 74% of physicians reported experiencing bullying, harassment, microaggressions, or discrimination, a slight but meaningful reduction form 78% in 2021.
- 64% of physicians reported spending significant time on electronic medical records outside regular hours.
- 46% of physicians said that their mental health is worse than it was before the start of the pandemic, down 14% from 2021.
- 60% reported being satisfied or very satisfied with work-life balance, an improvement from 49% in 2021, though slightly below 2017 (62%).
- 37% of physicians plan to reduce their clinical hours in the next 2 years.
Margot Burnell, MD, president of the Canadian Medical Association (CMA), told Medscape Medical News that she was "disappointed" with the results.
"I hoped that the burnout numbers would decrease more than they have," she said. "Physicians are still under extreme stress in trying to provide the care for patients that they wish to give."
Reductions in Hours
The most distressing finding is that > one-third of physicians (37%) plan to reduce their hours within 24 hours -- at a time of growing physician shortages -- said Burnell.
"The one positive (finding) that stands out is that physicians are taking care of their own health and wellness and report that it's helping," she said. About 65% of physicians reported having accessed at least 1 wellness support in the past 5 years, up 11% since 2021.
The NPHS includes responses from about 3300 practicing physicians, medical residents, and fellows who were surveyed from March 14 to April 15.
Among the CMA's top priorities is to reduce the administrative burden because that tops the list of what physicians say would help them with burnout, said Burnell.
"The other area is to provide and encourage team-based care," she continued. "That provides some relief for physicians." It also is important to promote the approaches that seem to be helping, such as wellness support and artificial intelligence (AI), she said. In this survey, 59% of respondents who used AI said that it decreased their time spent on administrative tasks.
Burnout by Specialty
Future analyses will examine burnout by specialty, Burnell said. Burnout is particularly high among emergency physicians, regardless of province, according to previous work by Kerstin de Wit, MD, emergency physician and research director for the Department of Emergency Medicine at Queen's University in Kingston, Ontario, and colleagues.
The NPHS findings are not surprising, she told Medscape Medical News. "We resurveyed all our emergency physicians in January and found similar results, in that the levels of burnout were marginally less than they were in 2022 but still significantly higher than they were in 2020. Still, a majority of (emergency department) physicians qualify as having high burnout levels."
The Pandemic's Role
A telling finding of her team's research is that emergency physician burnout levels are now higher than they were in December 2020, the first year of the COVID pandemic, said De Wit. "I don't think you can say burnout is because of COVID. It's because of the problems in the medical system."
Among those problems in hospitals are a shortage of beds, physicians, and nurses and inadequate numbers of physicians in outpatient clinics "so patients are waiting for years" for conditions to be treated, she added.
"We don't have the resources that we need to maintain the standards that we had even 10, 15 years ago. The whole system is collapsing. Government underfunding is huge. Routinely, our emergency department is 100% full of ward patients, so we don't have a room with a door or a curtain to see patients in. All the emergency patients are seen in corridors or the waiting room in full view of everyone else. We have people with serious medical conditions who are dying in waiting rooms because we can't get them in."
The issues are complex, but the overarching problem is chronic underfunding that results in physicians "feeling overworked and powerless to help patients," said De Wit.
Burnell and de Wit reported having no relevant financial relationships.
Marcia Frellick is an independent health care journalist and a regular contributor to Medscape Medical News.
A version of this article first appeared on Medscape.com.
Nearly half of physicians in Canada report high levels of burnout, according to preliminary data from the 2025 National Physician Health Survey (NPHS). The new data show that 46% of physicians report high levels of burnout, down from 2021 (53%) but significantly above the level of 2017 (30%), when the first survey was conducted. The full NPHS 2025 Foundational Report will be released later this year.
Other significant findings include the following:
- 74% of physicians reported experiencing bullying, harassment, microaggressions, or discrimination, a slight but meaningful reduction form 78% in 2021.
- 64% of physicians reported spending significant time on electronic medical records outside regular hours.
- 46% of physicians said that their mental health is worse than it was before the start of the pandemic, down 14% from 2021.
- 60% reported being satisfied or very satisfied with work-life balance, an improvement from 49% in 2021, though slightly below 2017 (62%).
- 37% of physicians plan to reduce their clinical hours in the next 2 years.
Margot Burnell, MD, president of the Canadian Medical Association (CMA), told Medscape Medical News that she was "disappointed" with the results.
"I hoped that the burnout numbers would decrease more than they have," she said. "Physicians are still under extreme stress in trying to provide the care for patients that they wish to give."
Reductions in Hours
The most distressing finding is that > one-third of physicians (37%) plan to reduce their hours within 24 hours -- at a time of growing physician shortages -- said Burnell.
"The one positive (finding) that stands out is that physicians are taking care of their own health and wellness and report that it's helping," she said. About 65% of physicians reported having accessed at least 1 wellness support in the past 5 years, up 11% since 2021.
The NPHS includes responses from about 3300 practicing physicians, medical residents, and fellows who were surveyed from March 14 to April 15.
Among the CMA's top priorities is to reduce the administrative burden because that tops the list of what physicians say would help them with burnout, said Burnell.
"The other area is to provide and encourage team-based care," she continued. "That provides some relief for physicians." It also is important to promote the approaches that seem to be helping, such as wellness support and artificial intelligence (AI), she said. In this survey, 59% of respondents who used AI said that it decreased their time spent on administrative tasks.
Burnout by Specialty
Future analyses will examine burnout by specialty, Burnell said. Burnout is particularly high among emergency physicians, regardless of province, according to previous work by Kerstin de Wit, MD, emergency physician and research director for the Department of Emergency Medicine at Queen's University in Kingston, Ontario, and colleagues.
The NPHS findings are not surprising, she told Medscape Medical News. "We resurveyed all our emergency physicians in January and found similar results, in that the levels of burnout were marginally less than they were in 2022 but still significantly higher than they were in 2020. Still, a majority of (emergency department) physicians qualify as having high burnout levels."
The Pandemic's Role
A telling finding of her team's research is that emergency physician burnout levels are now higher than they were in December 2020, the first year of the COVID pandemic, said De Wit. "I don't think you can say burnout is because of COVID. It's because of the problems in the medical system."
Among those problems in hospitals are a shortage of beds, physicians, and nurses and inadequate numbers of physicians in outpatient clinics "so patients are waiting for years" for conditions to be treated, she added.
"We don't have the resources that we need to maintain the standards that we had even 10, 15 years ago. The whole system is collapsing. Government underfunding is huge. Routinely, our emergency department is 100% full of ward patients, so we don't have a room with a door or a curtain to see patients in. All the emergency patients are seen in corridors or the waiting room in full view of everyone else. We have people with serious medical conditions who are dying in waiting rooms because we can't get them in."
The issues are complex, but the overarching problem is chronic underfunding that results in physicians "feeling overworked and powerless to help patients," said De Wit.
Burnell and de Wit reported having no relevant financial relationships.
Marcia Frellick is an independent health care journalist and a regular contributor to Medscape Medical News.
A version of this article first appeared on Medscape.com.
About Half of Canadian Physicians Report High Burnout Levels
About Half of Canadian Physicians Report High Burnout Levels
Why Veterans May Conceal Suicidal Thoughts
Veterans at risk of suicide may not share their suicidal ideation with their psychotherapists or may choose not to disclose enough detail to illustrate the depths of those thoughts due to feelings of shame or embarrassment, according to a newly published study. These individuals may view suicidal thoughts as a sign of weakness, fear involuntary hospitalization or prescriptions, or belong to marginalized groups who do not feel comfortable (or safe) to reveal their thoughts or intentions. This can make it difficult for mental health professionals to identify the exact details of a patient’s mindset and provide appropriate care.
A veteran’s first—and sometimes only—stop may be their primary care practitioner (PCPs) rather than a mental health professional. A review of 40 studies found that although 45% of individuals who died by suicide had contact with PCPs within 1 month of their death, only 19% had contact with mental health services. Studies have also found that veterans disclose suicidal ideation during primary care visits closest to the actual suicide less than half the time.
Patients may have an appointment for medical, but not psychological reasons. In a study conducted at Portland Veterans Affairs Medical Center (VAMC), researchers reviewed the medical records of 112 veterans who died by suicide and had contact with a VAMC within 1 year prior to death. Of those last contacts, 32% were patient-initiated for new or exacerbated medical concerns, and 68% were follow-ups.
In that study, health care professionals (HCPs) noted that 41 patients (37%) were experiencing emotional distress at the last contact, but 13 of 18 patients (72%) who were assessed for suicidal ideation at their last contact denied such thoughts. The study says this finding “highlights the complexity of addressing suicidal ideation and associated risk factors in health care settings.” Additionally, a number of veterans who died by suicide either did not have suicidal thoughts at the time of their last contact with HCPs or denied such thoughts even when questioned.
In 2018, the Veterans Health Administration (VHA) implemented the Suicide Risk Identification Strategy (Risk ID), an evidence-informed assessment that includes initial screening and subsequent evaluation. Veterans receiving VHA care are screened annually for suicidal ideation and behaviors. Most screening takes place in primary care and mental health specialty settings, but timely screening may not be enough to assess who is at risk if the patients aren’t being forthcoming about their thoughts and plans.
A recent cross-sectional national survey examined the frequency of self-reported “inaccurate disclosure” of suicidal ideation during initial screening and subsequent evaluation among 734 VHA patients screened in primary care.
Using the Risk ID process with the Columbia Suicide Severity Rating Scale Screener (C-SSRS), the study asked respondents about their previous suicide screening in 2021. Of the 734 respondents, 306 screened positive and 428 screened negative. One survey item asked about the extent to which veterans had accurately responded to the HCP when asked about suicidal thoughts, while another asked how likely they would discuss when they felt suicidal with their PCP.
The study found that inaccurate disclosure is not uncommon: When asked about suicidal thoughts, about one-fifth of screen-negative participants and two-fifths of screen-positive participants said they responded, “less than very accurately.”
In the screen-positive group, women and those who reported more barriers to care were less likely to discuss feeling suicidal. Veterans who had lower ratings of satisfaction with the screening process, patient-staff communication, and the therapeutic relationship reported being less likely to discuss times they were suicidal. Notably, among C-SSRS-negative patients, Black, American Indian/Alaska Native, Hispanic, Asian, and multiracial veterans were more likely than White veterans to inaccurately report suicidal thoughts.
This is consistent with studies on medical mistrust and other research suggesting that veterans who have experienced identity-based discrimination may be less inclined to discuss suicidal thoughts with VHA HCPs. A large 2023 study surveyed veterans about why they might hold back such information. One Gulf War-era veteran, a Black woman, had encountered discrimination when filing her VA benefits claim, leading her to feel like the care system was not interested in helping her.
“It’s one of the main reasons why when I do go in, they don’t get an honest response,” she wrote in her survey response. “I feel that you’re not for me, you’re not trying to help me, you don’t wanna help me, and why even go through it, go through the motions it seems. So, I can come in feeling suicidal and I leave out feeling suicidal then.”
Veterans typically welcome screening for suicidal risk. In a 2023 study, > 90% of veterans reported that it is appropriate to be asked about thoughts of suicide during primary care visits, and about one-half agreed that veterans should be asked about suicidal thoughts at every visit.
For many, though, the level of trust they have with HCPs makes or breaks whether they discuss their suicidal ideation. Higher ratings of the therapeutic relationship with clinicians are associated with more frequent disclosure. However, the screen-positive group demonstrated higher rates of inaccurate disclosure than the screen-negative group. While this may seem counterintuitive, it is possible that screen-positive individuals did not fully disclose their thoughts on the initial screen, or did not fully disclose the severity of their thoughts during follow-up evaluations. Individuals who disclose suicidal thoughts during initial screening may be ambivalent about disclosure and/or become more concerned about consequences of disclosure as additional evaluation ensues.
A 2013 study of 34 Operation Enduring Freedom/Operation Iraqi Freedom veterans found that veterans felt trying to suppress and avoid thoughts of suicide was “burdensome and exhausting.” Despite this, they often failed to disclose severe and pervasive suicidal thoughts when screened. Among the reasons was that they perceived the templated computer reminder process as “perfunctory and disrespectful.”
Research has found that HCPs who focuses on building relationships, demonstrates genuineness and empathy, and uses straightforward and understandable language promotes the trust that can result in more honest disclosure of suicidal thoughts. In the “inaccurate disclosure” study, some veterans reported they did not understand the screening questions, or the questions did not make sense to them. This aligns with prior research, which demonstrates that how HCPs and researchers conceptualize suicidal thoughts may not fit with patients’ experiences. A lack of shared terminology, they note, “may confound how we think about ‘under-disclosure,’ such that perhaps patients may not be trying to hide their thoughts so much as not finding screening questions applicable to their unique situations or experiences.”
Veterans at risk of suicide may not share their suicidal ideation with their psychotherapists or may choose not to disclose enough detail to illustrate the depths of those thoughts due to feelings of shame or embarrassment, according to a newly published study. These individuals may view suicidal thoughts as a sign of weakness, fear involuntary hospitalization or prescriptions, or belong to marginalized groups who do not feel comfortable (or safe) to reveal their thoughts or intentions. This can make it difficult for mental health professionals to identify the exact details of a patient’s mindset and provide appropriate care.
A veteran’s first—and sometimes only—stop may be their primary care practitioner (PCPs) rather than a mental health professional. A review of 40 studies found that although 45% of individuals who died by suicide had contact with PCPs within 1 month of their death, only 19% had contact with mental health services. Studies have also found that veterans disclose suicidal ideation during primary care visits closest to the actual suicide less than half the time.
Patients may have an appointment for medical, but not psychological reasons. In a study conducted at Portland Veterans Affairs Medical Center (VAMC), researchers reviewed the medical records of 112 veterans who died by suicide and had contact with a VAMC within 1 year prior to death. Of those last contacts, 32% were patient-initiated for new or exacerbated medical concerns, and 68% were follow-ups.
In that study, health care professionals (HCPs) noted that 41 patients (37%) were experiencing emotional distress at the last contact, but 13 of 18 patients (72%) who were assessed for suicidal ideation at their last contact denied such thoughts. The study says this finding “highlights the complexity of addressing suicidal ideation and associated risk factors in health care settings.” Additionally, a number of veterans who died by suicide either did not have suicidal thoughts at the time of their last contact with HCPs or denied such thoughts even when questioned.
In 2018, the Veterans Health Administration (VHA) implemented the Suicide Risk Identification Strategy (Risk ID), an evidence-informed assessment that includes initial screening and subsequent evaluation. Veterans receiving VHA care are screened annually for suicidal ideation and behaviors. Most screening takes place in primary care and mental health specialty settings, but timely screening may not be enough to assess who is at risk if the patients aren’t being forthcoming about their thoughts and plans.
A recent cross-sectional national survey examined the frequency of self-reported “inaccurate disclosure” of suicidal ideation during initial screening and subsequent evaluation among 734 VHA patients screened in primary care.
Using the Risk ID process with the Columbia Suicide Severity Rating Scale Screener (C-SSRS), the study asked respondents about their previous suicide screening in 2021. Of the 734 respondents, 306 screened positive and 428 screened negative. One survey item asked about the extent to which veterans had accurately responded to the HCP when asked about suicidal thoughts, while another asked how likely they would discuss when they felt suicidal with their PCP.
The study found that inaccurate disclosure is not uncommon: When asked about suicidal thoughts, about one-fifth of screen-negative participants and two-fifths of screen-positive participants said they responded, “less than very accurately.”
In the screen-positive group, women and those who reported more barriers to care were less likely to discuss feeling suicidal. Veterans who had lower ratings of satisfaction with the screening process, patient-staff communication, and the therapeutic relationship reported being less likely to discuss times they were suicidal. Notably, among C-SSRS-negative patients, Black, American Indian/Alaska Native, Hispanic, Asian, and multiracial veterans were more likely than White veterans to inaccurately report suicidal thoughts.
This is consistent with studies on medical mistrust and other research suggesting that veterans who have experienced identity-based discrimination may be less inclined to discuss suicidal thoughts with VHA HCPs. A large 2023 study surveyed veterans about why they might hold back such information. One Gulf War-era veteran, a Black woman, had encountered discrimination when filing her VA benefits claim, leading her to feel like the care system was not interested in helping her.
“It’s one of the main reasons why when I do go in, they don’t get an honest response,” she wrote in her survey response. “I feel that you’re not for me, you’re not trying to help me, you don’t wanna help me, and why even go through it, go through the motions it seems. So, I can come in feeling suicidal and I leave out feeling suicidal then.”
Veterans typically welcome screening for suicidal risk. In a 2023 study, > 90% of veterans reported that it is appropriate to be asked about thoughts of suicide during primary care visits, and about one-half agreed that veterans should be asked about suicidal thoughts at every visit.
For many, though, the level of trust they have with HCPs makes or breaks whether they discuss their suicidal ideation. Higher ratings of the therapeutic relationship with clinicians are associated with more frequent disclosure. However, the screen-positive group demonstrated higher rates of inaccurate disclosure than the screen-negative group. While this may seem counterintuitive, it is possible that screen-positive individuals did not fully disclose their thoughts on the initial screen, or did not fully disclose the severity of their thoughts during follow-up evaluations. Individuals who disclose suicidal thoughts during initial screening may be ambivalent about disclosure and/or become more concerned about consequences of disclosure as additional evaluation ensues.
A 2013 study of 34 Operation Enduring Freedom/Operation Iraqi Freedom veterans found that veterans felt trying to suppress and avoid thoughts of suicide was “burdensome and exhausting.” Despite this, they often failed to disclose severe and pervasive suicidal thoughts when screened. Among the reasons was that they perceived the templated computer reminder process as “perfunctory and disrespectful.”
Research has found that HCPs who focuses on building relationships, demonstrates genuineness and empathy, and uses straightforward and understandable language promotes the trust that can result in more honest disclosure of suicidal thoughts. In the “inaccurate disclosure” study, some veterans reported they did not understand the screening questions, or the questions did not make sense to them. This aligns with prior research, which demonstrates that how HCPs and researchers conceptualize suicidal thoughts may not fit with patients’ experiences. A lack of shared terminology, they note, “may confound how we think about ‘under-disclosure,’ such that perhaps patients may not be trying to hide their thoughts so much as not finding screening questions applicable to their unique situations or experiences.”
Veterans at risk of suicide may not share their suicidal ideation with their psychotherapists or may choose not to disclose enough detail to illustrate the depths of those thoughts due to feelings of shame or embarrassment, according to a newly published study. These individuals may view suicidal thoughts as a sign of weakness, fear involuntary hospitalization or prescriptions, or belong to marginalized groups who do not feel comfortable (or safe) to reveal their thoughts or intentions. This can make it difficult for mental health professionals to identify the exact details of a patient’s mindset and provide appropriate care.
A veteran’s first—and sometimes only—stop may be their primary care practitioner (PCPs) rather than a mental health professional. A review of 40 studies found that although 45% of individuals who died by suicide had contact with PCPs within 1 month of their death, only 19% had contact with mental health services. Studies have also found that veterans disclose suicidal ideation during primary care visits closest to the actual suicide less than half the time.
Patients may have an appointment for medical, but not psychological reasons. In a study conducted at Portland Veterans Affairs Medical Center (VAMC), researchers reviewed the medical records of 112 veterans who died by suicide and had contact with a VAMC within 1 year prior to death. Of those last contacts, 32% were patient-initiated for new or exacerbated medical concerns, and 68% were follow-ups.
In that study, health care professionals (HCPs) noted that 41 patients (37%) were experiencing emotional distress at the last contact, but 13 of 18 patients (72%) who were assessed for suicidal ideation at their last contact denied such thoughts. The study says this finding “highlights the complexity of addressing suicidal ideation and associated risk factors in health care settings.” Additionally, a number of veterans who died by suicide either did not have suicidal thoughts at the time of their last contact with HCPs or denied such thoughts even when questioned.
In 2018, the Veterans Health Administration (VHA) implemented the Suicide Risk Identification Strategy (Risk ID), an evidence-informed assessment that includes initial screening and subsequent evaluation. Veterans receiving VHA care are screened annually for suicidal ideation and behaviors. Most screening takes place in primary care and mental health specialty settings, but timely screening may not be enough to assess who is at risk if the patients aren’t being forthcoming about their thoughts and plans.
A recent cross-sectional national survey examined the frequency of self-reported “inaccurate disclosure” of suicidal ideation during initial screening and subsequent evaluation among 734 VHA patients screened in primary care.
Using the Risk ID process with the Columbia Suicide Severity Rating Scale Screener (C-SSRS), the study asked respondents about their previous suicide screening in 2021. Of the 734 respondents, 306 screened positive and 428 screened negative. One survey item asked about the extent to which veterans had accurately responded to the HCP when asked about suicidal thoughts, while another asked how likely they would discuss when they felt suicidal with their PCP.
The study found that inaccurate disclosure is not uncommon: When asked about suicidal thoughts, about one-fifth of screen-negative participants and two-fifths of screen-positive participants said they responded, “less than very accurately.”
In the screen-positive group, women and those who reported more barriers to care were less likely to discuss feeling suicidal. Veterans who had lower ratings of satisfaction with the screening process, patient-staff communication, and the therapeutic relationship reported being less likely to discuss times they were suicidal. Notably, among C-SSRS-negative patients, Black, American Indian/Alaska Native, Hispanic, Asian, and multiracial veterans were more likely than White veterans to inaccurately report suicidal thoughts.
This is consistent with studies on medical mistrust and other research suggesting that veterans who have experienced identity-based discrimination may be less inclined to discuss suicidal thoughts with VHA HCPs. A large 2023 study surveyed veterans about why they might hold back such information. One Gulf War-era veteran, a Black woman, had encountered discrimination when filing her VA benefits claim, leading her to feel like the care system was not interested in helping her.
“It’s one of the main reasons why when I do go in, they don’t get an honest response,” she wrote in her survey response. “I feel that you’re not for me, you’re not trying to help me, you don’t wanna help me, and why even go through it, go through the motions it seems. So, I can come in feeling suicidal and I leave out feeling suicidal then.”
Veterans typically welcome screening for suicidal risk. In a 2023 study, > 90% of veterans reported that it is appropriate to be asked about thoughts of suicide during primary care visits, and about one-half agreed that veterans should be asked about suicidal thoughts at every visit.
For many, though, the level of trust they have with HCPs makes or breaks whether they discuss their suicidal ideation. Higher ratings of the therapeutic relationship with clinicians are associated with more frequent disclosure. However, the screen-positive group demonstrated higher rates of inaccurate disclosure than the screen-negative group. While this may seem counterintuitive, it is possible that screen-positive individuals did not fully disclose their thoughts on the initial screen, or did not fully disclose the severity of their thoughts during follow-up evaluations. Individuals who disclose suicidal thoughts during initial screening may be ambivalent about disclosure and/or become more concerned about consequences of disclosure as additional evaluation ensues.
A 2013 study of 34 Operation Enduring Freedom/Operation Iraqi Freedom veterans found that veterans felt trying to suppress and avoid thoughts of suicide was “burdensome and exhausting.” Despite this, they often failed to disclose severe and pervasive suicidal thoughts when screened. Among the reasons was that they perceived the templated computer reminder process as “perfunctory and disrespectful.”
Research has found that HCPs who focuses on building relationships, demonstrates genuineness and empathy, and uses straightforward and understandable language promotes the trust that can result in more honest disclosure of suicidal thoughts. In the “inaccurate disclosure” study, some veterans reported they did not understand the screening questions, or the questions did not make sense to them. This aligns with prior research, which demonstrates that how HCPs and researchers conceptualize suicidal thoughts may not fit with patients’ experiences. A lack of shared terminology, they note, “may confound how we think about ‘under-disclosure,’ such that perhaps patients may not be trying to hide their thoughts so much as not finding screening questions applicable to their unique situations or experiences.”
Mental Health Practitioners Continue to Decrease Despite Aging Vet Population
This article has been updated with a response from the US Department of Veterans Affairs.
The number of US Department of Veterans Affairs (VA) geriatric mental health professionals is failing to keep pace with a growing population of older veterans: nearly 8 million are aged ≥ 65 years. VA psychologists may treat older veterans in primary care settings or community living centers, but many lack formal training in geropsychology.
Some psychologists with the proper training to treat this population are leaving the workforce; a survey by the VA Office of Inspector General found psychology was the most frequently reported severe clinical occupational staffing shortage and the most frequently reported Hybrid Title 38 severe shortage occupation, with 57% of 139 facilities reporting it as a shortage. According to the September Workforce Dashboard, the VA has lost > 200 psychologists in 2025.
Veterans aged ≥ 65 years have higher rates of combined medical and mental health diagnoses than younger veterans and older nonveterans. Nearly 1 of 5 older veterans enrolled in US Department of Veterans Affairs (VA) health care services have confirmed mental health diagnoses, and another 26% have documented mental health concerns without a formal diagnosis in their health record.
Older veterans also tend to have more complex mental health issues than younger adults. Posttraumatic stress nearly doubles their risk of dementia, and their psychiatric diagnoses may be complicated by co-occurring delirium, social isolation/loneliness, and polypharmacy.
According to reporting by The War Horse, the VA has been instituting limits on one-on-one mental health therapy and transitioning veterans to lower levels of treatment after having been told to stop treating them for long, indeterminate periods prior to referring them to group therapy, primary care, or discharging them altogether. In a statement to Federal Practitioner, VA Press Secretary Pete Kasperowicz refuted the reporting from The War Horse.
"The War Horse story is false. VA does not put caps on one-on-one mental health sessions for veterans with clinical care needs," he told Federal Practitioner. "VA works with veterans over an initial eight to 15 mental health sessions, and collaboratively plans any needed follow-on care. As part of this process, veterans and their health care team decide together how to address ongoing needs, including whether to step down to other types of care and self-maintenance, or continue with VA therapy."
The smaller pool of qualified mental health practitioners also may be due to medical students not knowing enough about the category. A study of 136 medical students and 61 internal medicine residents at an academic health center evaluated their beliefs and attitudes regarding 25 content areas essential to the primary care of older adults. Students and residents expressed similar beliefs about the importance of content areas, and attitudes toward aging did not appreciably differ. However, students rated lower in knowledge in areas surrounding general primary care, such as chronic conditions and medications. Residents reported larger gap scores in areas that reflected specialists’ expertise (eg, driving risk, cognition, and psychiatric symptoms).
VA does have channels for filling the gap in geriatric health care. Established in 1975, Geriatric Research, Education, and Clinical Centers (GRECCs), are the department’s centers of excellence focused on aging. Currently, there are 20 GRECCs across the country, each connected with a major research university. Studies focus on aging, for example, examining the effects of Alzheimer’s disease or traumatic brain injuries.
Geriatric Scholars
To specifically fill the gap in mental health care, the Geriatric Scholars Program (GSP) was developed in 2008. Initially focused on primary care physicians, nurse practitioners, physician assistants, and pharmacists, the program later expanded to include other disciplines, including psychiatrists. In 2013, the GSP–Psychology Track (GSP-P) was developed because there were no commercially available training in geropsychology for licensed psychologists. GSP-P is based on an evidence-based educational model for the VA primary care workforce and includes a stepwise curriculum design, pilot implementation, and program evaluation.
A recent survey that assessed the track’s effectiveness found respondents “strongly agreed” that participation in the program improved their geropsychology knowledge and skills. That positive reaction led to shifts in practice that had a positive impact on VA organizational goals. Several GSP-P graduates have become board certified in geropsychology and many proceed to supervise geropsychology-focused clinical rotations for psychology practicum students, predoctoral interns, and postdoctoral fellows.
Whether programs such as GSP-P can adequately address the dwindling number of VA mental health care professionals remains to be seen. More than 160 doctors, psychologists, nurses, and researchers sent a letter to VA Secretary Doug Collins, the VA inspector general, and congressional leaders on Sept. 24 warning that workforce reductions and moves to outsource care will harm veterans.
“We have witnessed these ongoing harms and can provide evidence and testimony of their impacts,” the letter read. By the next day, the number of signees had increased to 350.
Though these shortages may impact their mental health care, older veterans could have an edge in mental resilience. While research in younger adults has found positive linear associations between physical health difficulties and severity of psychiatric symptoms, older veterans may benefit from what researchers have called an “aging paradox,” in which mental health improves later in life despite declining physical and cognitive function. A 2021 study suggests that prevention and treatment strategies designed to foster attachment security, mindfulness, and purpose in life may help enhance psychological resilience to physical health difficulties in older veterans.
This article has been updated with a response from the US Department of Veterans Affairs.
The number of US Department of Veterans Affairs (VA) geriatric mental health professionals is failing to keep pace with a growing population of older veterans: nearly 8 million are aged ≥ 65 years. VA psychologists may treat older veterans in primary care settings or community living centers, but many lack formal training in geropsychology.
Some psychologists with the proper training to treat this population are leaving the workforce; a survey by the VA Office of Inspector General found psychology was the most frequently reported severe clinical occupational staffing shortage and the most frequently reported Hybrid Title 38 severe shortage occupation, with 57% of 139 facilities reporting it as a shortage. According to the September Workforce Dashboard, the VA has lost > 200 psychologists in 2025.
Veterans aged ≥ 65 years have higher rates of combined medical and mental health diagnoses than younger veterans and older nonveterans. Nearly 1 of 5 older veterans enrolled in US Department of Veterans Affairs (VA) health care services have confirmed mental health diagnoses, and another 26% have documented mental health concerns without a formal diagnosis in their health record.
Older veterans also tend to have more complex mental health issues than younger adults. Posttraumatic stress nearly doubles their risk of dementia, and their psychiatric diagnoses may be complicated by co-occurring delirium, social isolation/loneliness, and polypharmacy.
According to reporting by The War Horse, the VA has been instituting limits on one-on-one mental health therapy and transitioning veterans to lower levels of treatment after having been told to stop treating them for long, indeterminate periods prior to referring them to group therapy, primary care, or discharging them altogether. In a statement to Federal Practitioner, VA Press Secretary Pete Kasperowicz refuted the reporting from The War Horse.
"The War Horse story is false. VA does not put caps on one-on-one mental health sessions for veterans with clinical care needs," he told Federal Practitioner. "VA works with veterans over an initial eight to 15 mental health sessions, and collaboratively plans any needed follow-on care. As part of this process, veterans and their health care team decide together how to address ongoing needs, including whether to step down to other types of care and self-maintenance, or continue with VA therapy."
The smaller pool of qualified mental health practitioners also may be due to medical students not knowing enough about the category. A study of 136 medical students and 61 internal medicine residents at an academic health center evaluated their beliefs and attitudes regarding 25 content areas essential to the primary care of older adults. Students and residents expressed similar beliefs about the importance of content areas, and attitudes toward aging did not appreciably differ. However, students rated lower in knowledge in areas surrounding general primary care, such as chronic conditions and medications. Residents reported larger gap scores in areas that reflected specialists’ expertise (eg, driving risk, cognition, and psychiatric symptoms).
VA does have channels for filling the gap in geriatric health care. Established in 1975, Geriatric Research, Education, and Clinical Centers (GRECCs), are the department’s centers of excellence focused on aging. Currently, there are 20 GRECCs across the country, each connected with a major research university. Studies focus on aging, for example, examining the effects of Alzheimer’s disease or traumatic brain injuries.
Geriatric Scholars
To specifically fill the gap in mental health care, the Geriatric Scholars Program (GSP) was developed in 2008. Initially focused on primary care physicians, nurse practitioners, physician assistants, and pharmacists, the program later expanded to include other disciplines, including psychiatrists. In 2013, the GSP–Psychology Track (GSP-P) was developed because there were no commercially available training in geropsychology for licensed psychologists. GSP-P is based on an evidence-based educational model for the VA primary care workforce and includes a stepwise curriculum design, pilot implementation, and program evaluation.
A recent survey that assessed the track’s effectiveness found respondents “strongly agreed” that participation in the program improved their geropsychology knowledge and skills. That positive reaction led to shifts in practice that had a positive impact on VA organizational goals. Several GSP-P graduates have become board certified in geropsychology and many proceed to supervise geropsychology-focused clinical rotations for psychology practicum students, predoctoral interns, and postdoctoral fellows.
Whether programs such as GSP-P can adequately address the dwindling number of VA mental health care professionals remains to be seen. More than 160 doctors, psychologists, nurses, and researchers sent a letter to VA Secretary Doug Collins, the VA inspector general, and congressional leaders on Sept. 24 warning that workforce reductions and moves to outsource care will harm veterans.
“We have witnessed these ongoing harms and can provide evidence and testimony of their impacts,” the letter read. By the next day, the number of signees had increased to 350.
Though these shortages may impact their mental health care, older veterans could have an edge in mental resilience. While research in younger adults has found positive linear associations between physical health difficulties and severity of psychiatric symptoms, older veterans may benefit from what researchers have called an “aging paradox,” in which mental health improves later in life despite declining physical and cognitive function. A 2021 study suggests that prevention and treatment strategies designed to foster attachment security, mindfulness, and purpose in life may help enhance psychological resilience to physical health difficulties in older veterans.
This article has been updated with a response from the US Department of Veterans Affairs.
The number of US Department of Veterans Affairs (VA) geriatric mental health professionals is failing to keep pace with a growing population of older veterans: nearly 8 million are aged ≥ 65 years. VA psychologists may treat older veterans in primary care settings or community living centers, but many lack formal training in geropsychology.
Some psychologists with the proper training to treat this population are leaving the workforce; a survey by the VA Office of Inspector General found psychology was the most frequently reported severe clinical occupational staffing shortage and the most frequently reported Hybrid Title 38 severe shortage occupation, with 57% of 139 facilities reporting it as a shortage. According to the September Workforce Dashboard, the VA has lost > 200 psychologists in 2025.
Veterans aged ≥ 65 years have higher rates of combined medical and mental health diagnoses than younger veterans and older nonveterans. Nearly 1 of 5 older veterans enrolled in US Department of Veterans Affairs (VA) health care services have confirmed mental health diagnoses, and another 26% have documented mental health concerns without a formal diagnosis in their health record.
Older veterans also tend to have more complex mental health issues than younger adults. Posttraumatic stress nearly doubles their risk of dementia, and their psychiatric diagnoses may be complicated by co-occurring delirium, social isolation/loneliness, and polypharmacy.
According to reporting by The War Horse, the VA has been instituting limits on one-on-one mental health therapy and transitioning veterans to lower levels of treatment after having been told to stop treating them for long, indeterminate periods prior to referring them to group therapy, primary care, or discharging them altogether. In a statement to Federal Practitioner, VA Press Secretary Pete Kasperowicz refuted the reporting from The War Horse.
"The War Horse story is false. VA does not put caps on one-on-one mental health sessions for veterans with clinical care needs," he told Federal Practitioner. "VA works with veterans over an initial eight to 15 mental health sessions, and collaboratively plans any needed follow-on care. As part of this process, veterans and their health care team decide together how to address ongoing needs, including whether to step down to other types of care and self-maintenance, or continue with VA therapy."
The smaller pool of qualified mental health practitioners also may be due to medical students not knowing enough about the category. A study of 136 medical students and 61 internal medicine residents at an academic health center evaluated their beliefs and attitudes regarding 25 content areas essential to the primary care of older adults. Students and residents expressed similar beliefs about the importance of content areas, and attitudes toward aging did not appreciably differ. However, students rated lower in knowledge in areas surrounding general primary care, such as chronic conditions and medications. Residents reported larger gap scores in areas that reflected specialists’ expertise (eg, driving risk, cognition, and psychiatric symptoms).
VA does have channels for filling the gap in geriatric health care. Established in 1975, Geriatric Research, Education, and Clinical Centers (GRECCs), are the department’s centers of excellence focused on aging. Currently, there are 20 GRECCs across the country, each connected with a major research university. Studies focus on aging, for example, examining the effects of Alzheimer’s disease or traumatic brain injuries.
Geriatric Scholars
To specifically fill the gap in mental health care, the Geriatric Scholars Program (GSP) was developed in 2008. Initially focused on primary care physicians, nurse practitioners, physician assistants, and pharmacists, the program later expanded to include other disciplines, including psychiatrists. In 2013, the GSP–Psychology Track (GSP-P) was developed because there were no commercially available training in geropsychology for licensed psychologists. GSP-P is based on an evidence-based educational model for the VA primary care workforce and includes a stepwise curriculum design, pilot implementation, and program evaluation.
A recent survey that assessed the track’s effectiveness found respondents “strongly agreed” that participation in the program improved their geropsychology knowledge and skills. That positive reaction led to shifts in practice that had a positive impact on VA organizational goals. Several GSP-P graduates have become board certified in geropsychology and many proceed to supervise geropsychology-focused clinical rotations for psychology practicum students, predoctoral interns, and postdoctoral fellows.
Whether programs such as GSP-P can adequately address the dwindling number of VA mental health care professionals remains to be seen. More than 160 doctors, psychologists, nurses, and researchers sent a letter to VA Secretary Doug Collins, the VA inspector general, and congressional leaders on Sept. 24 warning that workforce reductions and moves to outsource care will harm veterans.
“We have witnessed these ongoing harms and can provide evidence and testimony of their impacts,” the letter read. By the next day, the number of signees had increased to 350.
Though these shortages may impact their mental health care, older veterans could have an edge in mental resilience. While research in younger adults has found positive linear associations between physical health difficulties and severity of psychiatric symptoms, older veterans may benefit from what researchers have called an “aging paradox,” in which mental health improves later in life despite declining physical and cognitive function. A 2021 study suggests that prevention and treatment strategies designed to foster attachment security, mindfulness, and purpose in life may help enhance psychological resilience to physical health difficulties in older veterans.
PET and CPT Show Promise in Veteran PTSD Treatment
Posttraumatic stress disorder (PTSD) guidelines increasingly are recommending prolonged exposure therapy (PET) and cognitive processing therapy (CPT) as first-line treatments, including the 2023 US Department of Veterans Affairs (VA) and US Department of Defense clinical practice guideline.
Since 2006, > 6000 VA therapists have been trained in PET and CPT; the VA requires all veterans to have access to these treatments. However, despite strong clinical trial evidence supporting PET and CPT for the treatment of PTSD, a 2023 study found that only 11.6% of veterans who received a PTSD diagnosis between 2017 and 2019 initiated Trauma-Focused Evidence-Based Psychotherapy (TF-EBP) in their first year of treatment. Of those who initiated TF-EBP, 67% dropped out. Recent VA programs have attempted to expand the reach of PET with video telehealth to reach rural and remote veterans through virtual group programs.
Recent research has suggested ways to maximize the effectiveness of the programs and assist veterans in receiving the full benefits. Studies have found that swapping traditional longer-term treatments (usually spanning 8 to 15 weeks) for intensified, shorter versions (eg, 6 sessions) may enhance engagement and retention.
Intensive PET for PTSD is safe and highly effective. A study involving patients with chronic PTSD and complex trauma showed significant reductions in PTSD symptom severity, with large effect sizes and sustained improvements at 3 and 6 months. Multiple 90-minute sessions over consecutive days, supplemented with in vivo exposure or followed by weekly booster sessions, were found to minimize treatment disruptions.
PET is among the most extensively studied treatments for PTSD and is supported by dozens of clinical trials involving thousands of patients. The intervention was originally developed and validated in civilian samples and includes psychoeducation, relaxation through breathing retraining, and in vivo and imaginal exposure to traumatic memories.
A recent study compared treatment outcomes among military veterans and civilian patients receiving treatment in a community setting. Although some studies have compared PET outcomes for military veterans and civilian participants in community settings, none have directly compared outcomes across trauma type (combat, terror, or civilian trauma) and veteran status (military vs civilian) within the same framework. The study notes that combat-related trauma significantly differs from other forms of trauma exposure, as it is typically more prolonged and severe and therefore is more often resistant to treatment. Military personnel also often find themselves both victims and aggressors, a duality that can intensify guilt, shame, anger, disgust, and emotional reactions to moral injury, complicating treatment.
The study assessed the effects of 8 to 15 PET sessions on PTSD symptoms in 55 civilians and 43 veterans using the PTSD Symptom Scale–Interview Version (PSS-I). Participants showed significant symptom reductions across all trauma types and veteran statuses.
Although veterans and participants in the combat trauma subgroup showed higher levels of baseline symptom severity compared with civilians, all groups experienced similar symptom reductions. These findings differ from some meta-analyses, which have found that PET often produces smaller effect sizes in combat-related PTSD compared to civilian trauma samples.
The study compared treatment outcomes across different groups within the same treatment centers and under consistent supervision. The PET intervention was delivered in community mental health centers to all patients regardless of background. Only 2 prior studies have compared civilian and military veterans within the same locations.
Although the “traditional” number of PET sessions produce evidence-based outcomes, high dropout rates and relapses have catalyzed interest in approaches that boost the power of therapy, such as delivering PET in ever-shorter sequences.
A study in a Swedish psychiatric outpatient clinic compared the effect of an 8-day intensified treatment program with traditionally spaced treatments on 101 participants with PTSD or complex PTSD. The study reported a significant reduction in PTSD symptoms at posttreatment, with large effect sizes in both conditions. Moreover, symptom reduction was maintained at follow-up. Dropout rates were significantly different between treatment groups: 4.3% in the intensified treatment program and 24.1% in the traditional group.
Another study used VA administrative data to assess the impact of sequenced psychotherapy (≥ 8 sessions of not trauma-focused individual or group psychotherapy delivered before trauma-focused care) on initiation and retention in CPT and PET over 2 years. Roughly 13% of 490,097 veterans who entered care for PTSD between 2014 and 2020 initiated VA-disseminated evidence-based treatment within 21 months (9.5% CPT, 3.4% PE). Among those who initiated treatment, retention was 46% and 42%, respectively. Individual therapy was associated with increased CPT and PET retention of 8.0% and 8.2%. For group therapy, retention increases were 3.4% and 8.7%.
Another recent study examined the RESET (Reconsolidation, Exposure, and Short-term Emotional Transformation) clinical protocol, an intensive, structured trauma-focused intervention designed to treat PTSD within 6 daily sessions. The protocol includes psychoeducation, targeted exposure, dynamic case formulation, and guided trauma processing. This novel framework ensures therapy moves beyond symptom reduction, fostering a deep understanding of the patient’s core struggles and their broader psychological patterns, and integrates it with the reconsolidation of the index trauma narrative to form a more cohesive sense of self.”
Clinical studies are ongoing to refine and enhance PET and CPT. They may serve to make therapy more useful and effective in easing—maybe erasing—veterans’ traumatic memories.
Posttraumatic stress disorder (PTSD) guidelines increasingly are recommending prolonged exposure therapy (PET) and cognitive processing therapy (CPT) as first-line treatments, including the 2023 US Department of Veterans Affairs (VA) and US Department of Defense clinical practice guideline.
Since 2006, > 6000 VA therapists have been trained in PET and CPT; the VA requires all veterans to have access to these treatments. However, despite strong clinical trial evidence supporting PET and CPT for the treatment of PTSD, a 2023 study found that only 11.6% of veterans who received a PTSD diagnosis between 2017 and 2019 initiated Trauma-Focused Evidence-Based Psychotherapy (TF-EBP) in their first year of treatment. Of those who initiated TF-EBP, 67% dropped out. Recent VA programs have attempted to expand the reach of PET with video telehealth to reach rural and remote veterans through virtual group programs.
Recent research has suggested ways to maximize the effectiveness of the programs and assist veterans in receiving the full benefits. Studies have found that swapping traditional longer-term treatments (usually spanning 8 to 15 weeks) for intensified, shorter versions (eg, 6 sessions) may enhance engagement and retention.
Intensive PET for PTSD is safe and highly effective. A study involving patients with chronic PTSD and complex trauma showed significant reductions in PTSD symptom severity, with large effect sizes and sustained improvements at 3 and 6 months. Multiple 90-minute sessions over consecutive days, supplemented with in vivo exposure or followed by weekly booster sessions, were found to minimize treatment disruptions.
PET is among the most extensively studied treatments for PTSD and is supported by dozens of clinical trials involving thousands of patients. The intervention was originally developed and validated in civilian samples and includes psychoeducation, relaxation through breathing retraining, and in vivo and imaginal exposure to traumatic memories.
A recent study compared treatment outcomes among military veterans and civilian patients receiving treatment in a community setting. Although some studies have compared PET outcomes for military veterans and civilian participants in community settings, none have directly compared outcomes across trauma type (combat, terror, or civilian trauma) and veteran status (military vs civilian) within the same framework. The study notes that combat-related trauma significantly differs from other forms of trauma exposure, as it is typically more prolonged and severe and therefore is more often resistant to treatment. Military personnel also often find themselves both victims and aggressors, a duality that can intensify guilt, shame, anger, disgust, and emotional reactions to moral injury, complicating treatment.
The study assessed the effects of 8 to 15 PET sessions on PTSD symptoms in 55 civilians and 43 veterans using the PTSD Symptom Scale–Interview Version (PSS-I). Participants showed significant symptom reductions across all trauma types and veteran statuses.
Although veterans and participants in the combat trauma subgroup showed higher levels of baseline symptom severity compared with civilians, all groups experienced similar symptom reductions. These findings differ from some meta-analyses, which have found that PET often produces smaller effect sizes in combat-related PTSD compared to civilian trauma samples.
The study compared treatment outcomes across different groups within the same treatment centers and under consistent supervision. The PET intervention was delivered in community mental health centers to all patients regardless of background. Only 2 prior studies have compared civilian and military veterans within the same locations.
Although the “traditional” number of PET sessions produce evidence-based outcomes, high dropout rates and relapses have catalyzed interest in approaches that boost the power of therapy, such as delivering PET in ever-shorter sequences.
A study in a Swedish psychiatric outpatient clinic compared the effect of an 8-day intensified treatment program with traditionally spaced treatments on 101 participants with PTSD or complex PTSD. The study reported a significant reduction in PTSD symptoms at posttreatment, with large effect sizes in both conditions. Moreover, symptom reduction was maintained at follow-up. Dropout rates were significantly different between treatment groups: 4.3% in the intensified treatment program and 24.1% in the traditional group.
Another study used VA administrative data to assess the impact of sequenced psychotherapy (≥ 8 sessions of not trauma-focused individual or group psychotherapy delivered before trauma-focused care) on initiation and retention in CPT and PET over 2 years. Roughly 13% of 490,097 veterans who entered care for PTSD between 2014 and 2020 initiated VA-disseminated evidence-based treatment within 21 months (9.5% CPT, 3.4% PE). Among those who initiated treatment, retention was 46% and 42%, respectively. Individual therapy was associated with increased CPT and PET retention of 8.0% and 8.2%. For group therapy, retention increases were 3.4% and 8.7%.
Another recent study examined the RESET (Reconsolidation, Exposure, and Short-term Emotional Transformation) clinical protocol, an intensive, structured trauma-focused intervention designed to treat PTSD within 6 daily sessions. The protocol includes psychoeducation, targeted exposure, dynamic case formulation, and guided trauma processing. This novel framework ensures therapy moves beyond symptom reduction, fostering a deep understanding of the patient’s core struggles and their broader psychological patterns, and integrates it with the reconsolidation of the index trauma narrative to form a more cohesive sense of self.”
Clinical studies are ongoing to refine and enhance PET and CPT. They may serve to make therapy more useful and effective in easing—maybe erasing—veterans’ traumatic memories.
Posttraumatic stress disorder (PTSD) guidelines increasingly are recommending prolonged exposure therapy (PET) and cognitive processing therapy (CPT) as first-line treatments, including the 2023 US Department of Veterans Affairs (VA) and US Department of Defense clinical practice guideline.
Since 2006, > 6000 VA therapists have been trained in PET and CPT; the VA requires all veterans to have access to these treatments. However, despite strong clinical trial evidence supporting PET and CPT for the treatment of PTSD, a 2023 study found that only 11.6% of veterans who received a PTSD diagnosis between 2017 and 2019 initiated Trauma-Focused Evidence-Based Psychotherapy (TF-EBP) in their first year of treatment. Of those who initiated TF-EBP, 67% dropped out. Recent VA programs have attempted to expand the reach of PET with video telehealth to reach rural and remote veterans through virtual group programs.
Recent research has suggested ways to maximize the effectiveness of the programs and assist veterans in receiving the full benefits. Studies have found that swapping traditional longer-term treatments (usually spanning 8 to 15 weeks) for intensified, shorter versions (eg, 6 sessions) may enhance engagement and retention.
Intensive PET for PTSD is safe and highly effective. A study involving patients with chronic PTSD and complex trauma showed significant reductions in PTSD symptom severity, with large effect sizes and sustained improvements at 3 and 6 months. Multiple 90-minute sessions over consecutive days, supplemented with in vivo exposure or followed by weekly booster sessions, were found to minimize treatment disruptions.
PET is among the most extensively studied treatments for PTSD and is supported by dozens of clinical trials involving thousands of patients. The intervention was originally developed and validated in civilian samples and includes psychoeducation, relaxation through breathing retraining, and in vivo and imaginal exposure to traumatic memories.
A recent study compared treatment outcomes among military veterans and civilian patients receiving treatment in a community setting. Although some studies have compared PET outcomes for military veterans and civilian participants in community settings, none have directly compared outcomes across trauma type (combat, terror, or civilian trauma) and veteran status (military vs civilian) within the same framework. The study notes that combat-related trauma significantly differs from other forms of trauma exposure, as it is typically more prolonged and severe and therefore is more often resistant to treatment. Military personnel also often find themselves both victims and aggressors, a duality that can intensify guilt, shame, anger, disgust, and emotional reactions to moral injury, complicating treatment.
The study assessed the effects of 8 to 15 PET sessions on PTSD symptoms in 55 civilians and 43 veterans using the PTSD Symptom Scale–Interview Version (PSS-I). Participants showed significant symptom reductions across all trauma types and veteran statuses.
Although veterans and participants in the combat trauma subgroup showed higher levels of baseline symptom severity compared with civilians, all groups experienced similar symptom reductions. These findings differ from some meta-analyses, which have found that PET often produces smaller effect sizes in combat-related PTSD compared to civilian trauma samples.
The study compared treatment outcomes across different groups within the same treatment centers and under consistent supervision. The PET intervention was delivered in community mental health centers to all patients regardless of background. Only 2 prior studies have compared civilian and military veterans within the same locations.
Although the “traditional” number of PET sessions produce evidence-based outcomes, high dropout rates and relapses have catalyzed interest in approaches that boost the power of therapy, such as delivering PET in ever-shorter sequences.
A study in a Swedish psychiatric outpatient clinic compared the effect of an 8-day intensified treatment program with traditionally spaced treatments on 101 participants with PTSD or complex PTSD. The study reported a significant reduction in PTSD symptoms at posttreatment, with large effect sizes in both conditions. Moreover, symptom reduction was maintained at follow-up. Dropout rates were significantly different between treatment groups: 4.3% in the intensified treatment program and 24.1% in the traditional group.
Another study used VA administrative data to assess the impact of sequenced psychotherapy (≥ 8 sessions of not trauma-focused individual or group psychotherapy delivered before trauma-focused care) on initiation and retention in CPT and PET over 2 years. Roughly 13% of 490,097 veterans who entered care for PTSD between 2014 and 2020 initiated VA-disseminated evidence-based treatment within 21 months (9.5% CPT, 3.4% PE). Among those who initiated treatment, retention was 46% and 42%, respectively. Individual therapy was associated with increased CPT and PET retention of 8.0% and 8.2%. For group therapy, retention increases were 3.4% and 8.7%.
Another recent study examined the RESET (Reconsolidation, Exposure, and Short-term Emotional Transformation) clinical protocol, an intensive, structured trauma-focused intervention designed to treat PTSD within 6 daily sessions. The protocol includes psychoeducation, targeted exposure, dynamic case formulation, and guided trauma processing. This novel framework ensures therapy moves beyond symptom reduction, fostering a deep understanding of the patient’s core struggles and their broader psychological patterns, and integrates it with the reconsolidation of the index trauma narrative to form a more cohesive sense of self.”
Clinical studies are ongoing to refine and enhance PET and CPT. They may serve to make therapy more useful and effective in easing—maybe erasing—veterans’ traumatic memories.
Moral Injury-informed Interventions May Enhance Treatment for Combat Veterans
“Moral and mortal stressors may be intertwined in their contribution to the complex symptomatic outcomes” of combat exposure according to a recent study in the European Journal of Psychotraumatology. The study examined the effect moral injury has on Israel Defense Forces (IDF) combat veterans. The resulting trauma may be consolidated in a single category, such as posttraumatic stress disorder (PTSD), but stressors leading to that diagnosis may have been quite different. Properly defining the stressors to assist in better targeted treatment is a challenge.
Moral injury is the emotional distress of being involved in or witnessing actions that conflict with deeply held beliefs. Such experiences could be committing or failing to prevent a transgressive act or learning about or surviving a transgressive act.
The study defines moral injury outcomes as the psychological and emotional consequences that result from exposure to potentially morally injurious events (PMIEs): “This terminology is intended to distinguish the outcomes of moral injury from the broader and sometimes ambiguous use of ‘moral injury’ in the literature, which can refer to either the event, the experience, or the resulting symptoms.”
The study followed 374 male combat veterans for 5 years. Veterans served in the Israel Defense Forces (IDF) in 4 primary combat roles: infantry, armored corps, special forces, and combat engineering. Psychological characteristics were measured 12 months prior to enlistment. PMIE exposure was measured during the final month of military service using the Moral Injury Events Scale. Moral injury outcomes were assessed 6 months postdischarge using the Expressions of Moral Injury Scale-Military Version-Short Form. Posttraumatic stress symptom (PTSS) clusters were evaluated 1 year postdischarge using the PTSD Checklist for the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Nearly half (49%) of participants reported exposure to PMIEs, while 8% met criteria for probable PTSD. The researchers say elevated PMIE rates observed in their sample may be attributed, in part, to participants’ extended deployments in densely populated urban areas, carrying out operations in close proximity to civilians, where it is difficult to distinguish between combatants and noncombatants. PTSD rates were somewhat lower than those reported in US studies (10% to 30%) among veterans; this may be attributed to the cohort not being engaged in a full-scale war, but deployed mostly in peacekeeping missions.
Longitudinal studies have described the effects of wartime atrocities on PTSD symptom severity. Studies have also linked moral injury outcomes and PTSS clusters (including negative alterations in cognition and mood [NACM]), depression, anxiety, and substance abuse. PMIEs can also include perceptions of betrayal from leaders, colleagues, or trusted others. The study of 374 male combat veterans found a direct effect of PMIE-betrayal on arousal and reactivity as well as NACM clusters. Results also showed indirect associations between exposure to all PMIE dimensions and PTSS clusters via moral injury outcomes. Combat exposure and experiencing PMIEs during military service significantly contributed to the emergence of PTSS during the first year after discharge. The study found 2 distinct paths PMIEs may lead to PTSS among veterans: experiencing acts of transgression and encountering betrayal.
Betrayal has been linked to feelings of anger and humiliation, emotions thought to have evolved to trigger adaptive behavioral responses, such as aggression and revenge, to threats or transgressions by others. PMIE-betrayal also demonstrated direct effects on the arousal and reactivity and NACM symptom clusters, suggesting partial mediation. Another study (also on IDF veterans) found significant positive correlations between PMIE-betrayal and the NACM cluster, suggesting PMIE-betrayal as a link between PTSD and moral injury. While the link between betrayal and NACM is readily apparent, its connection to arousal and reactivity, a fear-based physiological symptom, is less evident.
The findings of the study point to the need for assessment tools that separately measure exposure to PMIEs and individual reactions to them. A recent Federal Practitioner study of 100 veterans with a history of incarceration completed the Moral Injury Events Scale and an adapted version for legal-involved persons (MIES-LIP). The authors found that MIES-LIP demonstrated strong psychometric properties, including good reliability and convergent validity for legal-related moral injury.
The study cites a recent review of cognitive-behavioral psychotherapies for individuals experiencing moral injury that challenges the adequacy of existing evidence-based treatments for PTSD for addressing moral injury and its associated symptoms. It is important to evaluate individuals who express feelings of betrayal with tailored, evidence-based interventions such as adaptive disclosure or cognitive-processing therapy. Acceptance and commitment therapy may also help individuals experiencing emotions such as shame, humiliation, guilt, and anger following morally injurious events.
Newer therapy models like Multi-Modal Motion-Assisted Memory Desensitization and Reconsolidation allow clinicians to use personalized trauma cues to facilitate memory processing, reduce avoidance, and aid in emotional reconsolidation. Clinical research has demonstrated this model’s efficacy in reducing PTSD symptoms, depression, and anxiety, with high acceptability and low dropout rates among military personnel, veterans, and first responders.
Regardless of the treatment, the researchers encourage mental health professionals to approach veterans seeking help with the “utmost sensitivity and attentiveness to any expressions of (moral injury) outcomes.”
“Moral and mortal stressors may be intertwined in their contribution to the complex symptomatic outcomes” of combat exposure according to a recent study in the European Journal of Psychotraumatology. The study examined the effect moral injury has on Israel Defense Forces (IDF) combat veterans. The resulting trauma may be consolidated in a single category, such as posttraumatic stress disorder (PTSD), but stressors leading to that diagnosis may have been quite different. Properly defining the stressors to assist in better targeted treatment is a challenge.
Moral injury is the emotional distress of being involved in or witnessing actions that conflict with deeply held beliefs. Such experiences could be committing or failing to prevent a transgressive act or learning about or surviving a transgressive act.
The study defines moral injury outcomes as the psychological and emotional consequences that result from exposure to potentially morally injurious events (PMIEs): “This terminology is intended to distinguish the outcomes of moral injury from the broader and sometimes ambiguous use of ‘moral injury’ in the literature, which can refer to either the event, the experience, or the resulting symptoms.”
The study followed 374 male combat veterans for 5 years. Veterans served in the Israel Defense Forces (IDF) in 4 primary combat roles: infantry, armored corps, special forces, and combat engineering. Psychological characteristics were measured 12 months prior to enlistment. PMIE exposure was measured during the final month of military service using the Moral Injury Events Scale. Moral injury outcomes were assessed 6 months postdischarge using the Expressions of Moral Injury Scale-Military Version-Short Form. Posttraumatic stress symptom (PTSS) clusters were evaluated 1 year postdischarge using the PTSD Checklist for the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Nearly half (49%) of participants reported exposure to PMIEs, while 8% met criteria for probable PTSD. The researchers say elevated PMIE rates observed in their sample may be attributed, in part, to participants’ extended deployments in densely populated urban areas, carrying out operations in close proximity to civilians, where it is difficult to distinguish between combatants and noncombatants. PTSD rates were somewhat lower than those reported in US studies (10% to 30%) among veterans; this may be attributed to the cohort not being engaged in a full-scale war, but deployed mostly in peacekeeping missions.
Longitudinal studies have described the effects of wartime atrocities on PTSD symptom severity. Studies have also linked moral injury outcomes and PTSS clusters (including negative alterations in cognition and mood [NACM]), depression, anxiety, and substance abuse. PMIEs can also include perceptions of betrayal from leaders, colleagues, or trusted others. The study of 374 male combat veterans found a direct effect of PMIE-betrayal on arousal and reactivity as well as NACM clusters. Results also showed indirect associations between exposure to all PMIE dimensions and PTSS clusters via moral injury outcomes. Combat exposure and experiencing PMIEs during military service significantly contributed to the emergence of PTSS during the first year after discharge. The study found 2 distinct paths PMIEs may lead to PTSS among veterans: experiencing acts of transgression and encountering betrayal.
Betrayal has been linked to feelings of anger and humiliation, emotions thought to have evolved to trigger adaptive behavioral responses, such as aggression and revenge, to threats or transgressions by others. PMIE-betrayal also demonstrated direct effects on the arousal and reactivity and NACM symptom clusters, suggesting partial mediation. Another study (also on IDF veterans) found significant positive correlations between PMIE-betrayal and the NACM cluster, suggesting PMIE-betrayal as a link between PTSD and moral injury. While the link between betrayal and NACM is readily apparent, its connection to arousal and reactivity, a fear-based physiological symptom, is less evident.
The findings of the study point to the need for assessment tools that separately measure exposure to PMIEs and individual reactions to them. A recent Federal Practitioner study of 100 veterans with a history of incarceration completed the Moral Injury Events Scale and an adapted version for legal-involved persons (MIES-LIP). The authors found that MIES-LIP demonstrated strong psychometric properties, including good reliability and convergent validity for legal-related moral injury.
The study cites a recent review of cognitive-behavioral psychotherapies for individuals experiencing moral injury that challenges the adequacy of existing evidence-based treatments for PTSD for addressing moral injury and its associated symptoms. It is important to evaluate individuals who express feelings of betrayal with tailored, evidence-based interventions such as adaptive disclosure or cognitive-processing therapy. Acceptance and commitment therapy may also help individuals experiencing emotions such as shame, humiliation, guilt, and anger following morally injurious events.
Newer therapy models like Multi-Modal Motion-Assisted Memory Desensitization and Reconsolidation allow clinicians to use personalized trauma cues to facilitate memory processing, reduce avoidance, and aid in emotional reconsolidation. Clinical research has demonstrated this model’s efficacy in reducing PTSD symptoms, depression, and anxiety, with high acceptability and low dropout rates among military personnel, veterans, and first responders.
Regardless of the treatment, the researchers encourage mental health professionals to approach veterans seeking help with the “utmost sensitivity and attentiveness to any expressions of (moral injury) outcomes.”
“Moral and mortal stressors may be intertwined in their contribution to the complex symptomatic outcomes” of combat exposure according to a recent study in the European Journal of Psychotraumatology. The study examined the effect moral injury has on Israel Defense Forces (IDF) combat veterans. The resulting trauma may be consolidated in a single category, such as posttraumatic stress disorder (PTSD), but stressors leading to that diagnosis may have been quite different. Properly defining the stressors to assist in better targeted treatment is a challenge.
Moral injury is the emotional distress of being involved in or witnessing actions that conflict with deeply held beliefs. Such experiences could be committing or failing to prevent a transgressive act or learning about or surviving a transgressive act.
The study defines moral injury outcomes as the psychological and emotional consequences that result from exposure to potentially morally injurious events (PMIEs): “This terminology is intended to distinguish the outcomes of moral injury from the broader and sometimes ambiguous use of ‘moral injury’ in the literature, which can refer to either the event, the experience, or the resulting symptoms.”
The study followed 374 male combat veterans for 5 years. Veterans served in the Israel Defense Forces (IDF) in 4 primary combat roles: infantry, armored corps, special forces, and combat engineering. Psychological characteristics were measured 12 months prior to enlistment. PMIE exposure was measured during the final month of military service using the Moral Injury Events Scale. Moral injury outcomes were assessed 6 months postdischarge using the Expressions of Moral Injury Scale-Military Version-Short Form. Posttraumatic stress symptom (PTSS) clusters were evaluated 1 year postdischarge using the PTSD Checklist for the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Nearly half (49%) of participants reported exposure to PMIEs, while 8% met criteria for probable PTSD. The researchers say elevated PMIE rates observed in their sample may be attributed, in part, to participants’ extended deployments in densely populated urban areas, carrying out operations in close proximity to civilians, where it is difficult to distinguish between combatants and noncombatants. PTSD rates were somewhat lower than those reported in US studies (10% to 30%) among veterans; this may be attributed to the cohort not being engaged in a full-scale war, but deployed mostly in peacekeeping missions.
Longitudinal studies have described the effects of wartime atrocities on PTSD symptom severity. Studies have also linked moral injury outcomes and PTSS clusters (including negative alterations in cognition and mood [NACM]), depression, anxiety, and substance abuse. PMIEs can also include perceptions of betrayal from leaders, colleagues, or trusted others. The study of 374 male combat veterans found a direct effect of PMIE-betrayal on arousal and reactivity as well as NACM clusters. Results also showed indirect associations between exposure to all PMIE dimensions and PTSS clusters via moral injury outcomes. Combat exposure and experiencing PMIEs during military service significantly contributed to the emergence of PTSS during the first year after discharge. The study found 2 distinct paths PMIEs may lead to PTSS among veterans: experiencing acts of transgression and encountering betrayal.
Betrayal has been linked to feelings of anger and humiliation, emotions thought to have evolved to trigger adaptive behavioral responses, such as aggression and revenge, to threats or transgressions by others. PMIE-betrayal also demonstrated direct effects on the arousal and reactivity and NACM symptom clusters, suggesting partial mediation. Another study (also on IDF veterans) found significant positive correlations between PMIE-betrayal and the NACM cluster, suggesting PMIE-betrayal as a link between PTSD and moral injury. While the link between betrayal and NACM is readily apparent, its connection to arousal and reactivity, a fear-based physiological symptom, is less evident.
The findings of the study point to the need for assessment tools that separately measure exposure to PMIEs and individual reactions to them. A recent Federal Practitioner study of 100 veterans with a history of incarceration completed the Moral Injury Events Scale and an adapted version for legal-involved persons (MIES-LIP). The authors found that MIES-LIP demonstrated strong psychometric properties, including good reliability and convergent validity for legal-related moral injury.
The study cites a recent review of cognitive-behavioral psychotherapies for individuals experiencing moral injury that challenges the adequacy of existing evidence-based treatments for PTSD for addressing moral injury and its associated symptoms. It is important to evaluate individuals who express feelings of betrayal with tailored, evidence-based interventions such as adaptive disclosure or cognitive-processing therapy. Acceptance and commitment therapy may also help individuals experiencing emotions such as shame, humiliation, guilt, and anger following morally injurious events.
Newer therapy models like Multi-Modal Motion-Assisted Memory Desensitization and Reconsolidation allow clinicians to use personalized trauma cues to facilitate memory processing, reduce avoidance, and aid in emotional reconsolidation. Clinical research has demonstrated this model’s efficacy in reducing PTSD symptoms, depression, and anxiety, with high acceptability and low dropout rates among military personnel, veterans, and first responders.
Regardless of the treatment, the researchers encourage mental health professionals to approach veterans seeking help with the “utmost sensitivity and attentiveness to any expressions of (moral injury) outcomes.”
Military Background Shapes Eating Disorders in VA Oncology
Military Background Shapes Eating Disorders in VA Oncology
PHOENIX – Veterans are especially vulnerable to disordered eating because of their military backgrounds, a dietician warned US Department of Veterans Affairs (VA) oncology clinicians at the annual meeting of the Association of VA Hematology/Oncology. In fact, an estimated 15% to 25% of veterans meet diagnostic criteria for eating disorders.
“Their experience in the military probably has really shaped the way that they see weight and the stigma behind it,” said Emily Fasciana, MS, RDN, LDN, a registered dietician with the VA based in Wilkes-Barre, Pennsylvania.
When cancer appears, the risk of eating disorders goes up even more, she said. “If we don’t catch eating disorders early on, severe medical problems can occur. In the cancer population, they’re going through enough medical problems as it is.”
Here are things to know about eating disorders in oncology.
Military Life Can Produce a ‘Perfect Storm’ of Risk Factors
Tightly controlled eating environments and food deprivation are often routine in military life. Along with trauma, these can create a “perfect storm of risk factors for eating disorders,” Fasciana said.
During service, for example, “people often will eat as much as they can when they can, sometimes followed by days of not being able to eat,” she said. These are very much like disordered eating behaviors such as binge eating and restricting, and they can place veterans at greater risk.”
She described how service members can develop specific eating patterns during service, such as “midrats” – midnight rations – “meals served during midnight shifts that were the best meal served all day long that they had access to.”
“When I hear veterans who wake up in the middle of the night, and they’re eating, I ask: ‘Did they practice something similar during their military experience?’ They associate that time of the day with enjoyable comfort foods, and that’s what they go to now.”
Vets Can be Haunted by Stigma of Excess Weight
“Making weight” – meeting weight standards – is routine in the military. The pressure to remain under a certain level can have lasting effects on how veterans think about extra pounds, said Kaitlin Ohde, PhD, a clinical health psychologist with the VA Puget Sound Health Care System in Seattle.
“I’ve heard some veterans tell me about getting kicked out of positions because of not being able to make weight. Then they carry this throughout their life, which is really sad,” Ohde said. “When they gain weight during treatment, sometimes it can be really bothersome for them.”
Regular weigh-ins can trouble patients, she said, so it’s important to explain to them why they’re getting on scales: “I’m getting your weight today because I want to see if this medication is doing XYZ.”
She advised colleagues to “make sure they explicitly know why we’re doing it [measuring weight], and how the things we’re using to treat them can impact their weight. This piece of the puzzle sometimes falls off the radar.”
Eating Disorders Can be Catastrophic in Cancer
Untreated eating disorders cause severe medical complications such as malnutrition, hormone dysregulation, low bone density or fractures, bradycardia, gastroparesis, and even anemia, Fasciana said.
There’s a New Category of Eating Disorder
Fasciana highlighted a condition that is underrecognized in oncology: Avoidant/restrictive food intake disorder (ARFID), which refers to patients who stay away from certain foods but not because they’re worried about body image or weight gain. “Patients with ARFID are clinically distinct from those who have anorexia, bulimia, and binge eating disorder,” she noted.
ARFID diagnosis requires food avoidance that leads to at least 1 of these consequences: significant weight loss, nutritional deficiencies, dependence on supplements or tube feeding, or psychosocial impairment.
“Veterans might have a gagging or retching reflex at the sight or smell of certain foods,” Fasciana explained. “They might have difficulty being in the presence of another person eating a nonpreferred food.”
Some cancer patients may be averse to foods of certain temperatures. “You might need to assess why they don’t like the temperature of that food. Why are those foods something that you can’t go to? Are they hurting your teeth? What are they doing to you?”
ARFID patients may also experience social withdrawal around eating. “With a lot of our head and neck cancer patients, especially those with oral cancers and those on feeding tubes, they might feel embarrassed to be around people while eating,” Fasciana said.
She highlighted a 2021 report about 4 cancer survivors with upper abdominal cancers who developed new-onset eating disorders with malnutrition resembling ARFID.
The patients experienced malabsorption, dumping syndrome, and excessive weight loss for 12 months postoperatively without classic body-image concerns. “This is a case example of how eating disorders can evolve in the oncology population,” Fasciana said.
The report said that none of the patients “returned to a healthy weight and/or healthy eating despite extensive team input… The outcomes were poor; 1 patient died, another required admission to a specialist eating disorder admission with a subsequent relapsing-remitting course, and the remaining 2 had complicated chronic courses.”
Treatment: Start With Screening, Then Reframe Thinking
Fasciana highlighted several screening tools, such as SCOFF, BREDS, and one for ARFID.
“Any screen is going to be better than no screen at all, and any question is going to be better than no question at all,” Fasciana said.
She cautioned that “veterans are not going to be so forthcoming about some of their struggles due to stigma and shame because of their past experiences in the military.”
As for therapy, psychological care may not be required, Ohde said. And it’s especially important to “listen to your patients about what they’re going through, and give them space to share.”
For those who could be helped by psychotherapy, she said, “sometimes I introduce it as therapy that can be really brief. Maybe you just need to talk to someone for a few sessions or just get some support around coping with this.”
One strategy is to focus on bringing enjoyment back to eating, she said. For some patients, “eating becomes a chore,” a task performed without joy, alone in a hospital room.
Fasciana emphasized asking questions over time, perhaps through multiple follow-ups, without expecting answers immediately. And she coaxes patients to consider what they hold dear. “I try to get them to think about the meaning that losing or gaining weight has for them, what their values are, and what really matters to them. I link it back to health, healing, and longevity of life.”
Fasciana and Ohde reported they had no disclosures.
PHOENIX – Veterans are especially vulnerable to disordered eating because of their military backgrounds, a dietician warned US Department of Veterans Affairs (VA) oncology clinicians at the annual meeting of the Association of VA Hematology/Oncology. In fact, an estimated 15% to 25% of veterans meet diagnostic criteria for eating disorders.
“Their experience in the military probably has really shaped the way that they see weight and the stigma behind it,” said Emily Fasciana, MS, RDN, LDN, a registered dietician with the VA based in Wilkes-Barre, Pennsylvania.
When cancer appears, the risk of eating disorders goes up even more, she said. “If we don’t catch eating disorders early on, severe medical problems can occur. In the cancer population, they’re going through enough medical problems as it is.”
Here are things to know about eating disorders in oncology.
Military Life Can Produce a ‘Perfect Storm’ of Risk Factors
Tightly controlled eating environments and food deprivation are often routine in military life. Along with trauma, these can create a “perfect storm of risk factors for eating disorders,” Fasciana said.
During service, for example, “people often will eat as much as they can when they can, sometimes followed by days of not being able to eat,” she said. These are very much like disordered eating behaviors such as binge eating and restricting, and they can place veterans at greater risk.”
She described how service members can develop specific eating patterns during service, such as “midrats” – midnight rations – “meals served during midnight shifts that were the best meal served all day long that they had access to.”
“When I hear veterans who wake up in the middle of the night, and they’re eating, I ask: ‘Did they practice something similar during their military experience?’ They associate that time of the day with enjoyable comfort foods, and that’s what they go to now.”
Vets Can be Haunted by Stigma of Excess Weight
“Making weight” – meeting weight standards – is routine in the military. The pressure to remain under a certain level can have lasting effects on how veterans think about extra pounds, said Kaitlin Ohde, PhD, a clinical health psychologist with the VA Puget Sound Health Care System in Seattle.
“I’ve heard some veterans tell me about getting kicked out of positions because of not being able to make weight. Then they carry this throughout their life, which is really sad,” Ohde said. “When they gain weight during treatment, sometimes it can be really bothersome for them.”
Regular weigh-ins can trouble patients, she said, so it’s important to explain to them why they’re getting on scales: “I’m getting your weight today because I want to see if this medication is doing XYZ.”
She advised colleagues to “make sure they explicitly know why we’re doing it [measuring weight], and how the things we’re using to treat them can impact their weight. This piece of the puzzle sometimes falls off the radar.”
Eating Disorders Can be Catastrophic in Cancer
Untreated eating disorders cause severe medical complications such as malnutrition, hormone dysregulation, low bone density or fractures, bradycardia, gastroparesis, and even anemia, Fasciana said.
There’s a New Category of Eating Disorder
Fasciana highlighted a condition that is underrecognized in oncology: Avoidant/restrictive food intake disorder (ARFID), which refers to patients who stay away from certain foods but not because they’re worried about body image or weight gain. “Patients with ARFID are clinically distinct from those who have anorexia, bulimia, and binge eating disorder,” she noted.
ARFID diagnosis requires food avoidance that leads to at least 1 of these consequences: significant weight loss, nutritional deficiencies, dependence on supplements or tube feeding, or psychosocial impairment.
“Veterans might have a gagging or retching reflex at the sight or smell of certain foods,” Fasciana explained. “They might have difficulty being in the presence of another person eating a nonpreferred food.”
Some cancer patients may be averse to foods of certain temperatures. “You might need to assess why they don’t like the temperature of that food. Why are those foods something that you can’t go to? Are they hurting your teeth? What are they doing to you?”
ARFID patients may also experience social withdrawal around eating. “With a lot of our head and neck cancer patients, especially those with oral cancers and those on feeding tubes, they might feel embarrassed to be around people while eating,” Fasciana said.
She highlighted a 2021 report about 4 cancer survivors with upper abdominal cancers who developed new-onset eating disorders with malnutrition resembling ARFID.
The patients experienced malabsorption, dumping syndrome, and excessive weight loss for 12 months postoperatively without classic body-image concerns. “This is a case example of how eating disorders can evolve in the oncology population,” Fasciana said.
The report said that none of the patients “returned to a healthy weight and/or healthy eating despite extensive team input… The outcomes were poor; 1 patient died, another required admission to a specialist eating disorder admission with a subsequent relapsing-remitting course, and the remaining 2 had complicated chronic courses.”
Treatment: Start With Screening, Then Reframe Thinking
Fasciana highlighted several screening tools, such as SCOFF, BREDS, and one for ARFID.
“Any screen is going to be better than no screen at all, and any question is going to be better than no question at all,” Fasciana said.
She cautioned that “veterans are not going to be so forthcoming about some of their struggles due to stigma and shame because of their past experiences in the military.”
As for therapy, psychological care may not be required, Ohde said. And it’s especially important to “listen to your patients about what they’re going through, and give them space to share.”
For those who could be helped by psychotherapy, she said, “sometimes I introduce it as therapy that can be really brief. Maybe you just need to talk to someone for a few sessions or just get some support around coping with this.”
One strategy is to focus on bringing enjoyment back to eating, she said. For some patients, “eating becomes a chore,” a task performed without joy, alone in a hospital room.
Fasciana emphasized asking questions over time, perhaps through multiple follow-ups, without expecting answers immediately. And she coaxes patients to consider what they hold dear. “I try to get them to think about the meaning that losing or gaining weight has for them, what their values are, and what really matters to them. I link it back to health, healing, and longevity of life.”
Fasciana and Ohde reported they had no disclosures.
PHOENIX – Veterans are especially vulnerable to disordered eating because of their military backgrounds, a dietician warned US Department of Veterans Affairs (VA) oncology clinicians at the annual meeting of the Association of VA Hematology/Oncology. In fact, an estimated 15% to 25% of veterans meet diagnostic criteria for eating disorders.
“Their experience in the military probably has really shaped the way that they see weight and the stigma behind it,” said Emily Fasciana, MS, RDN, LDN, a registered dietician with the VA based in Wilkes-Barre, Pennsylvania.
When cancer appears, the risk of eating disorders goes up even more, she said. “If we don’t catch eating disorders early on, severe medical problems can occur. In the cancer population, they’re going through enough medical problems as it is.”
Here are things to know about eating disorders in oncology.
Military Life Can Produce a ‘Perfect Storm’ of Risk Factors
Tightly controlled eating environments and food deprivation are often routine in military life. Along with trauma, these can create a “perfect storm of risk factors for eating disorders,” Fasciana said.
During service, for example, “people often will eat as much as they can when they can, sometimes followed by days of not being able to eat,” she said. These are very much like disordered eating behaviors such as binge eating and restricting, and they can place veterans at greater risk.”
She described how service members can develop specific eating patterns during service, such as “midrats” – midnight rations – “meals served during midnight shifts that were the best meal served all day long that they had access to.”
“When I hear veterans who wake up in the middle of the night, and they’re eating, I ask: ‘Did they practice something similar during their military experience?’ They associate that time of the day with enjoyable comfort foods, and that’s what they go to now.”
Vets Can be Haunted by Stigma of Excess Weight
“Making weight” – meeting weight standards – is routine in the military. The pressure to remain under a certain level can have lasting effects on how veterans think about extra pounds, said Kaitlin Ohde, PhD, a clinical health psychologist with the VA Puget Sound Health Care System in Seattle.
“I’ve heard some veterans tell me about getting kicked out of positions because of not being able to make weight. Then they carry this throughout their life, which is really sad,” Ohde said. “When they gain weight during treatment, sometimes it can be really bothersome for them.”
Regular weigh-ins can trouble patients, she said, so it’s important to explain to them why they’re getting on scales: “I’m getting your weight today because I want to see if this medication is doing XYZ.”
She advised colleagues to “make sure they explicitly know why we’re doing it [measuring weight], and how the things we’re using to treat them can impact their weight. This piece of the puzzle sometimes falls off the radar.”
Eating Disorders Can be Catastrophic in Cancer
Untreated eating disorders cause severe medical complications such as malnutrition, hormone dysregulation, low bone density or fractures, bradycardia, gastroparesis, and even anemia, Fasciana said.
There’s a New Category of Eating Disorder
Fasciana highlighted a condition that is underrecognized in oncology: Avoidant/restrictive food intake disorder (ARFID), which refers to patients who stay away from certain foods but not because they’re worried about body image or weight gain. “Patients with ARFID are clinically distinct from those who have anorexia, bulimia, and binge eating disorder,” she noted.
ARFID diagnosis requires food avoidance that leads to at least 1 of these consequences: significant weight loss, nutritional deficiencies, dependence on supplements or tube feeding, or psychosocial impairment.
“Veterans might have a gagging or retching reflex at the sight or smell of certain foods,” Fasciana explained. “They might have difficulty being in the presence of another person eating a nonpreferred food.”
Some cancer patients may be averse to foods of certain temperatures. “You might need to assess why they don’t like the temperature of that food. Why are those foods something that you can’t go to? Are they hurting your teeth? What are they doing to you?”
ARFID patients may also experience social withdrawal around eating. “With a lot of our head and neck cancer patients, especially those with oral cancers and those on feeding tubes, they might feel embarrassed to be around people while eating,” Fasciana said.
She highlighted a 2021 report about 4 cancer survivors with upper abdominal cancers who developed new-onset eating disorders with malnutrition resembling ARFID.
The patients experienced malabsorption, dumping syndrome, and excessive weight loss for 12 months postoperatively without classic body-image concerns. “This is a case example of how eating disorders can evolve in the oncology population,” Fasciana said.
The report said that none of the patients “returned to a healthy weight and/or healthy eating despite extensive team input… The outcomes were poor; 1 patient died, another required admission to a specialist eating disorder admission with a subsequent relapsing-remitting course, and the remaining 2 had complicated chronic courses.”
Treatment: Start With Screening, Then Reframe Thinking
Fasciana highlighted several screening tools, such as SCOFF, BREDS, and one for ARFID.
“Any screen is going to be better than no screen at all, and any question is going to be better than no question at all,” Fasciana said.
She cautioned that “veterans are not going to be so forthcoming about some of their struggles due to stigma and shame because of their past experiences in the military.”
As for therapy, psychological care may not be required, Ohde said. And it’s especially important to “listen to your patients about what they’re going through, and give them space to share.”
For those who could be helped by psychotherapy, she said, “sometimes I introduce it as therapy that can be really brief. Maybe you just need to talk to someone for a few sessions or just get some support around coping with this.”
One strategy is to focus on bringing enjoyment back to eating, she said. For some patients, “eating becomes a chore,” a task performed without joy, alone in a hospital room.
Fasciana emphasized asking questions over time, perhaps through multiple follow-ups, without expecting answers immediately. And she coaxes patients to consider what they hold dear. “I try to get them to think about the meaning that losing or gaining weight has for them, what their values are, and what really matters to them. I link it back to health, healing, and longevity of life.”
Fasciana and Ohde reported they had no disclosures.
Military Background Shapes Eating Disorders in VA Oncology
Military Background Shapes Eating Disorders in VA Oncology
VIP Boot Camp: Expanding the Impact of VA Primary Care Mental Health With a Transdiagnostic Modular Group Program
VIP Boot Camp: Expanding the Impact of VA Primary Care Mental Health With a Transdiagnostic Modular Group Program
Since 2007, Primary Care Mental Health Integration (PCMHI) at the Veterans Health Administration (VHA) has improved access to mental health care services for veterans by directly embedding mental health care professionals (HCPs) within primary care teams.1 Veterans referred to PCMHI often have co-occurring physical and mental health disorders.2 Untreated chronic physical and mental comorbidities can diminish the effectiveness of medical and mental health interventions. Growing evidence suggests that treatment of mental health conditions can improve physical health outcomes and management of physical conditions can improve mental health outcomes.2,3
Chronic pain and sleep disorders are common reasons patients present to primary care, and often coexist together with mental health comorbidities.4 Sleep disorders affect 50% to 88% of patients with chronic pain, and 40% of patients with sleep disorders report chronic pain.4 Research has found that chronic pain and sleep disorders increase the risk of suicide attempts and deaths by suicide. Addressing suicide prevention simultaneously with treating chronic pain and insomnia is encouraged.5
Background
PCMHI treats physical and mental health comorbidities with a collaborative framework and a biopsychosocial integrative model.6 PCMHI staff provide mental health services as members of primary care teams. An interdisciplinary PCMHI team can include, but is not limited to, psychologists, mental health social workers, psychiatrists, nurse practitioners, clinical pharmacists, and mental health nurses. Quality of care within this model is elevated, as mental and physical health are recognized as interconnected. Collaboration between primary care and mental health benefits veterans and the VHA by increasing access to mental health care, decreasing stigma associated with mental health treatment, improving health outcomes, and enhancing the likelihood of recovery, resulting in high patient satisfaction.6-8
In the existing PCMHI model, HCPs are encouraged to use short-term, evidence-based psychotherapies (EBPs).9 Veterans referred to PCMHI from primary care are typically able to attend 1 to 6 brief sessions of mental health treatment, often 20 to 30 minutes long. Most EBPs in PCMHI are disorder- specific, providing interventions focused on a single presenting problem (eg, insomnia, chronic pain, or posttraumatic stress disorder [PTSD]). For veterans with a single issue, this model can be very effective. 1,10 However, the high rate of co-occurrence of mental and physical health issues can make it difficult to fully treat interrelated problems if the focus is on 1 specific diagnosis. Veterans with a need for additional (more comprehensive or intensive) mental health treatment are frequently referred to a higher, more resource-intensive level of mental health care, either in the VHA or the community. Examples of higher levels of mental health care include the longer term behavioral health interdisciplinary program (BHIP), sometimes called a mental health clinic (MHC), or a specialty mental health program such as a PTSD clinic.
As PCMHI continues to grow, new challenges have emerged related to staffing shortages and gaps in the clinical delivery of mental health treatment within the VHA. At the same time, demand for VHA mental health treatment has increased. However, a mental health professional shortage severely limits the ability of the VHA to meet this demand. In many systems, this shortage may result in more referrals being made to a higher level of mental health care because of fewer resources to provide comprehensive treatment in a less intensive PCMHI setting.8,10,11 This referral pattern can overburden higher level care, often with long wait times for treatment and lengthy lag times between appointments. Furthermore, these gaps in the clinical delivery of care cannot be effectively addressed by hiring additional mental health professionals. This strain on resources can impede access to care and negatively affect outcomes.10
Recent congressional reports highlight these issues, noting that demand for mental health services continues to outpace the capacity of both PCMHI and higher levels of mental health care, leading to delays in treatment that may negatively affect outcomes.8,10,11 These delays can be particularly detrimental for individuals with conditions requiring timely intervention.8,11 Some veterans are willing to engage with PCMHI in a primary care setting but may be reluctant to engage in general mental health treatment. These veterans might not receive the mental health care they need without PCMHI.
Group Psychotherapy
A group psychotherapy format can address gaps in care delivery and provide advantages for patients, mental health professionals, and the VHA. Group psychotherapy aligns with the US Department of Veterans Affairs (VA) 2018 Blueprint for Excellence and 2018 to 2024 strategic plan, underscoring the need for more timely and efficient mental health services.12,13
Benefits of group psychotherapy include reductions in symptoms, decreased feelings of isolation, increased social support, decreased emotional suppression, and enhanced satisfaction with overall quality of life.14-17 Studies of veterans with PTSD have found less attrition among those who chose group therapy compared with individual therapy.14,18 Group psychotherapy improves access to care by enabling delivery to more patients.14 When compared with individual therapy, the group format allows for a large number of patients to be treated simultaneously, maximizing resources and reducing costs.3,19-21
VISN 9 CRH Innovation
The VA provides care to veterans through regionally distinct administrative systems known as Veterans Integrated Service Networks (VISNs). Clinical resource hubs (CRH) are VISN-based programs created to cover VA staffing shortages by virtually deploying HCPs into local VA systems until vacancies are filled. The national CRH vision of effectively using resources and innovative technologies to meet veterans’ health care needs, along with the above-referenced clinical gaps in the delivery of care, inspired the development of VIP Boot Camp within the VISN 9 CRH.22
Program Description
VIP Boot Camp is an evidence-informed group psychotherapy program designed to provide timely, brief, and comprehensive mental health treatment for veterans. VIP Boot Camp was developed to address the needs of veterans accessing PCMHI services who experience ≥ 1 of the often overlapping problems of anxiety/emotion regulation/stress, sleep difficulties, and chronic pain (Figure). VIP Boot Camp uses an integrative approach to highlight interconnections and similarities among these difficulties and their treatment. A primary vision of the program is to provide this comprehensive treatment within PCMHI (upstream) so additional referrals to higher levels of mental health care (downstream) may not be needed.
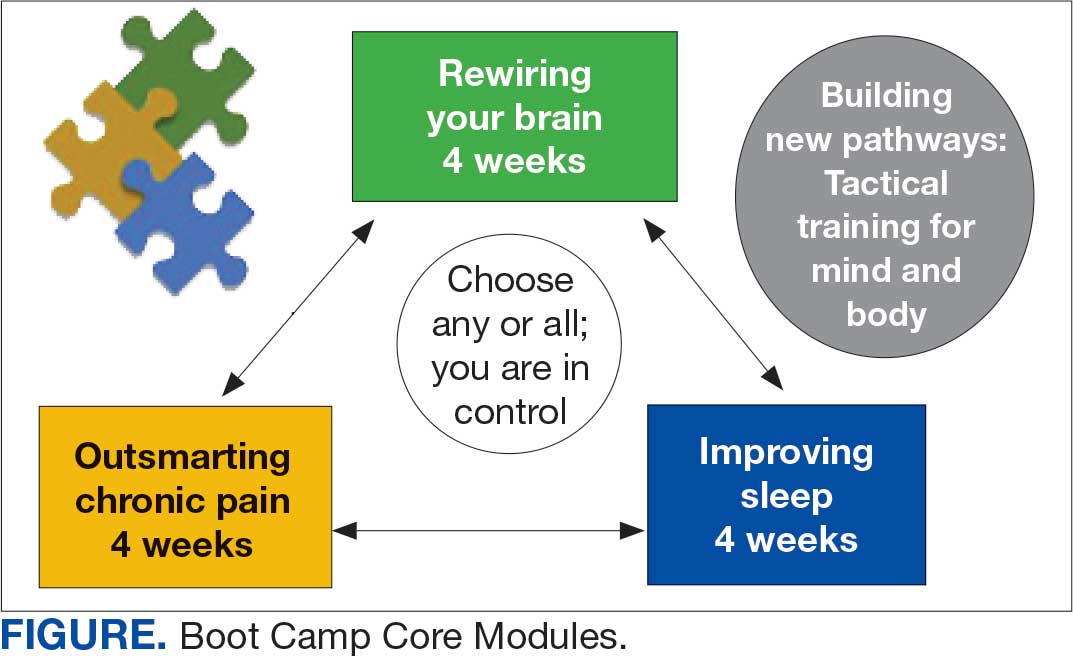
This design is intentional because it increases the number of individuals who can be treated upstream with comprehensive, preventive, and proactive care within PCMHI which, over time, frees up resources in the BHIP for individuals requiring higher levels of care. This approach also aligns with the importance of early treatment for chronic pain and sleep disturbances, which are linked to increased risk of suicide attempts and deaths by suicide for veterans.5 National interest for VIP Boot Camp grew during fiscal year 2024 after it received the Gold Medal Recognition for Most Adoptable and Greatest Potential for Impact during VHA National Access Sprint Wave 3—Mental Health Call of Champions.
History
VIP Boot Camp began in August 2021 at VISN 9 as a 6-week virtual group for veterans with chronic pain. It was established to assist a large VA medical center experiencing PCMHI staffing shortages and lacking available PCMHI groups. Many veterans in the chronic pain group discussed co-occurring issues such as sleep disturbances, anxiety, and stress. The CRH team considered launching 2 separate groups to address these additional PCMHI-level issues; however, in developing the group material which drew from multiple clinical approaches, the team recognized significant overlapping and interconnected themes.
The team discussed EBPs within the VHA and how certain interventions within these treatments could be helpful across many other co-occurring disorders. Integrated tactics (clinical interventions) were drawn from cognitive-behavioral therapy (for depression, insomnia, or chronic pain), acceptance and commitment therapy, prolonged exposure, cognitive processing therapy, dialectical behavior therapy, unified protocol, pain reprocessing therapy, emotional awareness and expression therapy, interpersonal neurobiology, and mindfulness. We collaborated with veterans during VIP Boot Camp groups to determine how to present and discuss complex interventions in ways that were clinically accurate, understandable, relatable, and relevant to their experiences.
To address accessibility issues, the chronic pain group was reduced to 4 weeks. A second 4-week module for anxiety, emotion regulation, and stress was developed, mirroring the tactics, language, and integrative approach of the revised chronic pain module. A similar integrative approach led to the development of the third and final 4-week module for sleep disturbances.
Current Program
The VIP Boot Camp consists of three 4-week integrated modules, each highlighting a critical area: sleep disturbances (Improving Sleep), chronic pain difficulties (Outsmarting Chronic Pain), and emotion regulation difficulties (Rewiring Your Brain). VIP Boot Camp is designed for veterans who are at the PCMHI level of care. Referrals are accepted for patients receiving treatment from primary care or PCMHI.
Guidelines for participation in VIP Boot Camp may differ across sites or VISNs. For example, a veteran who has been referred to the BHIP for medication management only or to a specialty MHC such as a pain clinic or PTSD clinic might also be appropriate and eligible for VIP Boot Camp.
Given the interconnectedness of foundational themes, elements, and practices across the VIP Boot Camp modules, the modules are offered in a rolling format with a veteran-centric “choose your own adventure” approach. Tactics are presented in the modules in a way that allows patients to begin with any 1 of the 3 modules and receive treatment that will help in the other areas. Participants choose their core module and initial treatment focus based on their values, needs, and goals. Individuals who complete a core module can end their VIP Boot Camp experience or continue to the next 4-week module for up to 3 modules.
The group is open to new individuals at the start of any 4-week module and closed for the remainder of its 4-week duration. This innovative rolling modular approach combines elements of open- and closed-group format, allowing for the flexibility and accessibility of an open group with the stability and peer support of a closed group.
Given the complicated and overlapping nature of chronic pain, emotion regulation/ stress, and sleep disturbances, VIP Boot Camp acknowledges that everything is interconnected and difficulties in 1 area may impact other areas. The 3 interconnected modules with repeating themes provide coherence and consistency. Veterans learn how interconnections across difficulties can be leveraged so that tactics learned and practiced in 1 area can assist in other areas, changing the cycle of suffering into a cycle of growth.
VIP Boot Camp sessions are 90 minutes long, once weekly for 4 weeks, with 2 mental health professionals trained to lead a dynamic group psychotherapy experience that aims to be fun for participants. VIP Boot Camp synthesizes evidence-based and evidence-informed interventions, as well as techniques from VHA complementary and integrative health programs, psychoeducation, and interpersonal interventions that model connection, playfulness, and healthy boundaries. These varied strategies combine to equip veterans with practical tactics for self-management outside of sessions, a process described as “finding puzzle pieces.” VIP Boot Camp is built on the idea that people are more likely to adopt and practice any tactic after being taught why that tactic is important, and how it fits into their larger interconnected puzzle. After each session, participants are provided with additional asynchronous educational material to help reinforce their learnings and practices.
Although individuals may hesitate to participate in a group setting, they often find the experience of community enhances and accelerates their treatment and gains. This involvement is highlighted in a core aspect of a VIP Boot Camp session called wins, during which participants learn how others on their Boot Camp team are implementing new skills and moving toward their personal values and objectives in a stepwise manner. Through these shared experiences, veterans discover how tactics working for others may serve as a model for their own personal objectives and plans for practice. The sense of relief described by many upon realizing they are not alone in their experiences, along with the satisfaction felt in discovering their ability to support others in Boot Camp, is described by many participants as deeply meaningful and in line with their personal values.
While developed as a fully virtual group program, VIP Boot Camp can also be conducted in person. The virtual program has been successful and continues to spread across VISN 9. There are 8 virtual VIP Boot Camps running in VISN 9, with plans for continued expansion. In the VISN 9 CRH, Boot Camps typically have 10 to 12 participants. Additionally, as VIP Boot Camp grows within a location there are frequently sufficient referrals to support a second rolling group, which enables staggering of the module offerings to allow for even more timely treatment.
Training Program
VISN 9 CRH also developed a VIP Boot Camp 3-day intensive training program for PCMHI HCPs that consists of learning and practicing VIP Boot Camp material for chronic pain, emotion regulation/ stress, sleep disturbances, mindfulness, and guided imagery, along with gaining experience as a VIP Boot Camp coleader. Feedback received from PCMHI HCPs who completed training has been positive. There is also a private Microsoft Teams channel for HCPs, which allows for resource sharing and community building among coleaders. More than 75 PCMHI HCPs have completed VIP Boot Camp training and > 25 VIP Boot Camps have been established at 4 additional VISNs.
The VISN 9 CRH VIP Boot Camp program initiated an implementation and effectiveness project with the Michael E. DeBakey VA Medical Center and the South Central Mental Illness Research, Education and Clinical Center. The focus of this collaboration is support for implementation and treatment effectiveness research with reports, articles, and a white paper on findings and best practices, alongside continued dissemination of the VIP Boot Camp program and training.
Conclusions
VIP Boot Camp is a PCMHI group program offering readily available, comprehensive, and integrative group psychotherapy services to veterans experiencing . 1 of the following: chronic pain, emotion regulation/ stress, and sleep disturbances. It was launched at the VISN 9 CRH with a goal of addressing clinical gaps in the delivery of mental health care, by increasing the number of patients treated within PCMHI. The VIP Boot Camp model provides veterans the opportunity to transform cycles of suffering into cycles of growth through a single approach that can address multiple presenting and interconnected issues.
A 3-day VIP Boot Camp training program provides a quick and effective path for a PCMHI program to train HCPs to launch a VIP Boot Camp. The VISN 9 CRH will continue to champion VIP Boot Camp as a model for the successful provision of comprehensive and integrative mental health treatment within PCMHI at the VA. Through readily available access to comprehensive mental health treatment in an environment that promotes participant empowerment and social engagement, VIP Boot Camp represents an integrative and innovative model of mental health treatment that offers benefits to veteran participants, HCPs, and the VHA.
- Leung LB, Yoon J, Escarce JJ, et al. Primary care-mental health integration in the VA: shifting mental health services for common mental illnesses to primary care. Psychiatr Serv. 2018;69:403-409. doi:10.1176/appi.ps.201700190
- Zhang A, Park S, Sullivan JE, et al. The effectiveness of problem-solving therapy for primary care patients’ depressive and/or anxiety disorders: a systematic review and meta-analysis. J Am Board Fam Med. 2018;31:139-150. doi:10.3122/jabfm.2018.01.170270
- Hundt NE, Barrera TL, Robinson A, et al. A systematic review of cognitive behavioral therapy for depression in veterans. Mil Med. 2014;179:942-949. doi:10.7205/milmed-d-14-00128
- Jank R, Gallee A, Boeckle M, et al. Chronic pain and sleep disorders in primary care. Pain Res Treat. 2017;2017:1-9. doi:10.1155/2017/9081802
- Ashrafioun L, Bishop TM, Pigeon WR. The relationship between pain severity, insomnia, and suicide attempts among a national veteran sample initiating pain care. Psychosom Med. 2021;83:733- 738. doi:10.1097/psy.0000000000000975
- Ramanuj P, Ferenchik E, Docherty M, et al. Evolving models of integrated behavioral health and primary care. Curr Psychiatry Rep. 2019;21:1. doi:10.1007/s11920-019-0985-4
- Post EP, Metzger M, Dumas P, et al. Integrating mental health into primary care within the Veterans Health Administration. Fam Syst Health. 2010;28:83-90. doi:10.1037/a0020130
- Smith TL, Kim B, Benzer JK, et al. FLOW: early results from a clinical demonstration project to improve the transition of patients with mental health disorders back to primary care. Psychol Serv. 2021;18:23-32. doi:10.1037/ser0000336
- Kearney LK, Post EP, Pomerantz AS, et al. Applying the interprofessional patient aligned care team in the department of veterans affairs transforming primary care. Am Psychol. 2014;69(4):399-408. doi:10.1037/a0035909
- US Government Accountability Office. Veterans health care: staffing challenges persist for fully integrating mental health and primary care services. December 15, 2022. Accessed July 9, 2025. https://www.gao.gov/products/gao-23-105372
- National Academies of Science and Engineering. Evaluation of the Department of Veterans Affairs Mental Health Services. National Academies Press; 2018. Accessed July 9, 2025. https://nap.nationalacademies.org/catalog/24915/evaluation-of-the-department-of-veterans-affairs-mental-health-services
- US Department of Veterans Affairs. Blueprint for excellence: achieving veterans’ excellence. October 6, 2014. Accessed July 9, 2025. https://www.volunteer.va.gov/docs/blueprintforexcellence_factsheet.PDF
- US Department of Veterans Affairs. Department of Veterans Affairs FY 2018-2024 strategic plan. Accessed July 9, 2025. https://www.calvet.ca.gov/Regulations/USDVA%20Strategic%20Plan%202018-2024.pdf
- Sripada RK, Bohnert KM, Ganoczy D, et al. Initial group versus individual therapy for posttraumatic stress disorder and subsequent follow-up treatment adequacy. Psychol Serv. 2016;13:349-355. doi:10.1037/ser0000077
- Burnett-Zeigler IE, Pfeiffer P, Zivin K, et al. Psychotherapy utilization for acute depression within the Veterans Affairs health care system. Psychol Serv. 2012;9:325-335. doi:10.1037/a0027957
- Kim JS, Prins A, Hirschhorn EW, et al. Preliminary investigation into the effectiveness of group webSTAIR for trauma-exposed veterans in primary care. Mil Med. 2024;189:e1403-e1408. doi:10.1093/milmed/usae052
- Jakupcak M, Blais RK, Grossbard J, et al. “Toughness” in association with mental health symptoms among Iraq and Afghanistan war veterans seeking Veterans Affairs health care. Psychol Men Masc. 2014;15:100-104. doi:10.1037/a0031508
- Stoycos SA, Berzenski SR, Beck JG, et al. Predictors of treatment completion in group psychotherapy for male veterans with posttraumatic stress disorder. J Trauma Stress. 2023;36:346-358. doi:10.1002/jts.22915
- Possemato K. The current state of intervention research for posttraumatic stress disorder within the primary care setting. J Clin Psychol Med Settings. 2011;18:268-280. doi:10.1007/s10880-011-9237-4
- Hunt MG, Rosenheck RA. Psychotherapy in mental health clinics of the Department of Veterans Affairs. J Clin Psychol. 2011;67:561-573. doi:10.1002/jclp.20788
- Khatri N, Marziali E, Tchernikov I, et al. Comparing telehealth-based and clinic-based group cognitive behavioral therapy for adults with depression and anxiety: a pilot study. Clin Interv Aging. 2014;9:765. doi:10.2147/cia.s57832
- Dangel J. Clinical resource hub increases veterans' access to care. VA News. January 12, 2025. Accessed September 3, 2025. https://news.va.gov/137439/clinical-resource-hub-increases-access-to-care/
Since 2007, Primary Care Mental Health Integration (PCMHI) at the Veterans Health Administration (VHA) has improved access to mental health care services for veterans by directly embedding mental health care professionals (HCPs) within primary care teams.1 Veterans referred to PCMHI often have co-occurring physical and mental health disorders.2 Untreated chronic physical and mental comorbidities can diminish the effectiveness of medical and mental health interventions. Growing evidence suggests that treatment of mental health conditions can improve physical health outcomes and management of physical conditions can improve mental health outcomes.2,3
Chronic pain and sleep disorders are common reasons patients present to primary care, and often coexist together with mental health comorbidities.4 Sleep disorders affect 50% to 88% of patients with chronic pain, and 40% of patients with sleep disorders report chronic pain.4 Research has found that chronic pain and sleep disorders increase the risk of suicide attempts and deaths by suicide. Addressing suicide prevention simultaneously with treating chronic pain and insomnia is encouraged.5
Background
PCMHI treats physical and mental health comorbidities with a collaborative framework and a biopsychosocial integrative model.6 PCMHI staff provide mental health services as members of primary care teams. An interdisciplinary PCMHI team can include, but is not limited to, psychologists, mental health social workers, psychiatrists, nurse practitioners, clinical pharmacists, and mental health nurses. Quality of care within this model is elevated, as mental and physical health are recognized as interconnected. Collaboration between primary care and mental health benefits veterans and the VHA by increasing access to mental health care, decreasing stigma associated with mental health treatment, improving health outcomes, and enhancing the likelihood of recovery, resulting in high patient satisfaction.6-8
In the existing PCMHI model, HCPs are encouraged to use short-term, evidence-based psychotherapies (EBPs).9 Veterans referred to PCMHI from primary care are typically able to attend 1 to 6 brief sessions of mental health treatment, often 20 to 30 minutes long. Most EBPs in PCMHI are disorder- specific, providing interventions focused on a single presenting problem (eg, insomnia, chronic pain, or posttraumatic stress disorder [PTSD]). For veterans with a single issue, this model can be very effective. 1,10 However, the high rate of co-occurrence of mental and physical health issues can make it difficult to fully treat interrelated problems if the focus is on 1 specific diagnosis. Veterans with a need for additional (more comprehensive or intensive) mental health treatment are frequently referred to a higher, more resource-intensive level of mental health care, either in the VHA or the community. Examples of higher levels of mental health care include the longer term behavioral health interdisciplinary program (BHIP), sometimes called a mental health clinic (MHC), or a specialty mental health program such as a PTSD clinic.
As PCMHI continues to grow, new challenges have emerged related to staffing shortages and gaps in the clinical delivery of mental health treatment within the VHA. At the same time, demand for VHA mental health treatment has increased. However, a mental health professional shortage severely limits the ability of the VHA to meet this demand. In many systems, this shortage may result in more referrals being made to a higher level of mental health care because of fewer resources to provide comprehensive treatment in a less intensive PCMHI setting.8,10,11 This referral pattern can overburden higher level care, often with long wait times for treatment and lengthy lag times between appointments. Furthermore, these gaps in the clinical delivery of care cannot be effectively addressed by hiring additional mental health professionals. This strain on resources can impede access to care and negatively affect outcomes.10
Recent congressional reports highlight these issues, noting that demand for mental health services continues to outpace the capacity of both PCMHI and higher levels of mental health care, leading to delays in treatment that may negatively affect outcomes.8,10,11 These delays can be particularly detrimental for individuals with conditions requiring timely intervention.8,11 Some veterans are willing to engage with PCMHI in a primary care setting but may be reluctant to engage in general mental health treatment. These veterans might not receive the mental health care they need without PCMHI.
Group Psychotherapy
A group psychotherapy format can address gaps in care delivery and provide advantages for patients, mental health professionals, and the VHA. Group psychotherapy aligns with the US Department of Veterans Affairs (VA) 2018 Blueprint for Excellence and 2018 to 2024 strategic plan, underscoring the need for more timely and efficient mental health services.12,13
Benefits of group psychotherapy include reductions in symptoms, decreased feelings of isolation, increased social support, decreased emotional suppression, and enhanced satisfaction with overall quality of life.14-17 Studies of veterans with PTSD have found less attrition among those who chose group therapy compared with individual therapy.14,18 Group psychotherapy improves access to care by enabling delivery to more patients.14 When compared with individual therapy, the group format allows for a large number of patients to be treated simultaneously, maximizing resources and reducing costs.3,19-21
VISN 9 CRH Innovation
The VA provides care to veterans through regionally distinct administrative systems known as Veterans Integrated Service Networks (VISNs). Clinical resource hubs (CRH) are VISN-based programs created to cover VA staffing shortages by virtually deploying HCPs into local VA systems until vacancies are filled. The national CRH vision of effectively using resources and innovative technologies to meet veterans’ health care needs, along with the above-referenced clinical gaps in the delivery of care, inspired the development of VIP Boot Camp within the VISN 9 CRH.22
Program Description
VIP Boot Camp is an evidence-informed group psychotherapy program designed to provide timely, brief, and comprehensive mental health treatment for veterans. VIP Boot Camp was developed to address the needs of veterans accessing PCMHI services who experience ≥ 1 of the often overlapping problems of anxiety/emotion regulation/stress, sleep difficulties, and chronic pain (Figure). VIP Boot Camp uses an integrative approach to highlight interconnections and similarities among these difficulties and their treatment. A primary vision of the program is to provide this comprehensive treatment within PCMHI (upstream) so additional referrals to higher levels of mental health care (downstream) may not be needed.
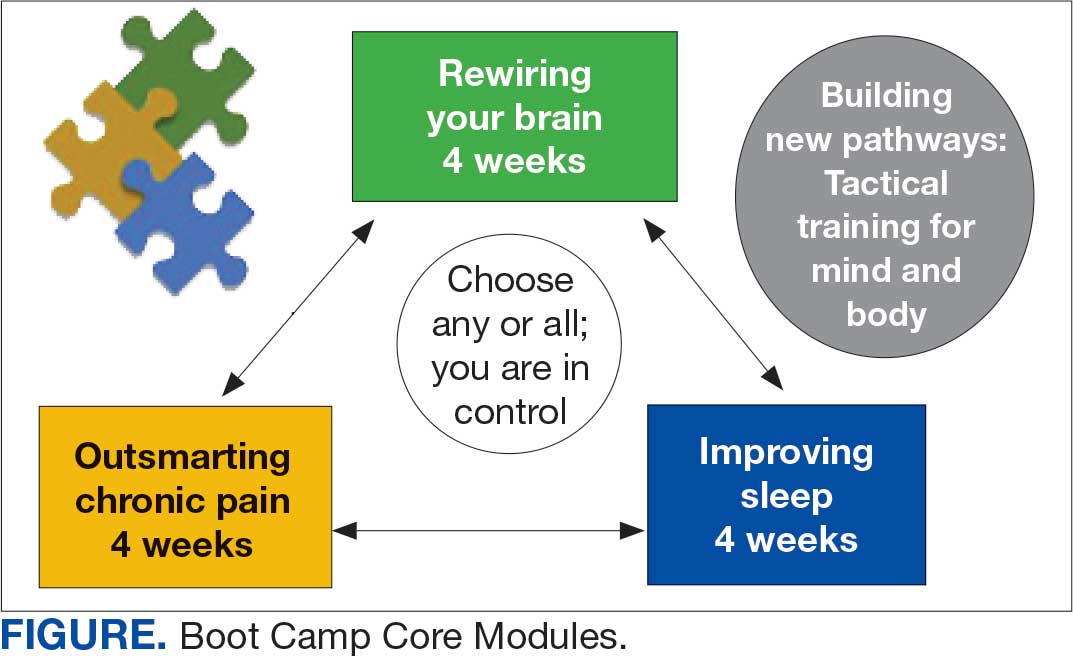
This design is intentional because it increases the number of individuals who can be treated upstream with comprehensive, preventive, and proactive care within PCMHI which, over time, frees up resources in the BHIP for individuals requiring higher levels of care. This approach also aligns with the importance of early treatment for chronic pain and sleep disturbances, which are linked to increased risk of suicide attempts and deaths by suicide for veterans.5 National interest for VIP Boot Camp grew during fiscal year 2024 after it received the Gold Medal Recognition for Most Adoptable and Greatest Potential for Impact during VHA National Access Sprint Wave 3—Mental Health Call of Champions.
History
VIP Boot Camp began in August 2021 at VISN 9 as a 6-week virtual group for veterans with chronic pain. It was established to assist a large VA medical center experiencing PCMHI staffing shortages and lacking available PCMHI groups. Many veterans in the chronic pain group discussed co-occurring issues such as sleep disturbances, anxiety, and stress. The CRH team considered launching 2 separate groups to address these additional PCMHI-level issues; however, in developing the group material which drew from multiple clinical approaches, the team recognized significant overlapping and interconnected themes.
The team discussed EBPs within the VHA and how certain interventions within these treatments could be helpful across many other co-occurring disorders. Integrated tactics (clinical interventions) were drawn from cognitive-behavioral therapy (for depression, insomnia, or chronic pain), acceptance and commitment therapy, prolonged exposure, cognitive processing therapy, dialectical behavior therapy, unified protocol, pain reprocessing therapy, emotional awareness and expression therapy, interpersonal neurobiology, and mindfulness. We collaborated with veterans during VIP Boot Camp groups to determine how to present and discuss complex interventions in ways that were clinically accurate, understandable, relatable, and relevant to their experiences.
To address accessibility issues, the chronic pain group was reduced to 4 weeks. A second 4-week module for anxiety, emotion regulation, and stress was developed, mirroring the tactics, language, and integrative approach of the revised chronic pain module. A similar integrative approach led to the development of the third and final 4-week module for sleep disturbances.
Current Program
The VIP Boot Camp consists of three 4-week integrated modules, each highlighting a critical area: sleep disturbances (Improving Sleep), chronic pain difficulties (Outsmarting Chronic Pain), and emotion regulation difficulties (Rewiring Your Brain). VIP Boot Camp is designed for veterans who are at the PCMHI level of care. Referrals are accepted for patients receiving treatment from primary care or PCMHI.
Guidelines for participation in VIP Boot Camp may differ across sites or VISNs. For example, a veteran who has been referred to the BHIP for medication management only or to a specialty MHC such as a pain clinic or PTSD clinic might also be appropriate and eligible for VIP Boot Camp.
Given the interconnectedness of foundational themes, elements, and practices across the VIP Boot Camp modules, the modules are offered in a rolling format with a veteran-centric “choose your own adventure” approach. Tactics are presented in the modules in a way that allows patients to begin with any 1 of the 3 modules and receive treatment that will help in the other areas. Participants choose their core module and initial treatment focus based on their values, needs, and goals. Individuals who complete a core module can end their VIP Boot Camp experience or continue to the next 4-week module for up to 3 modules.
The group is open to new individuals at the start of any 4-week module and closed for the remainder of its 4-week duration. This innovative rolling modular approach combines elements of open- and closed-group format, allowing for the flexibility and accessibility of an open group with the stability and peer support of a closed group.
Given the complicated and overlapping nature of chronic pain, emotion regulation/ stress, and sleep disturbances, VIP Boot Camp acknowledges that everything is interconnected and difficulties in 1 area may impact other areas. The 3 interconnected modules with repeating themes provide coherence and consistency. Veterans learn how interconnections across difficulties can be leveraged so that tactics learned and practiced in 1 area can assist in other areas, changing the cycle of suffering into a cycle of growth.
VIP Boot Camp sessions are 90 minutes long, once weekly for 4 weeks, with 2 mental health professionals trained to lead a dynamic group psychotherapy experience that aims to be fun for participants. VIP Boot Camp synthesizes evidence-based and evidence-informed interventions, as well as techniques from VHA complementary and integrative health programs, psychoeducation, and interpersonal interventions that model connection, playfulness, and healthy boundaries. These varied strategies combine to equip veterans with practical tactics for self-management outside of sessions, a process described as “finding puzzle pieces.” VIP Boot Camp is built on the idea that people are more likely to adopt and practice any tactic after being taught why that tactic is important, and how it fits into their larger interconnected puzzle. After each session, participants are provided with additional asynchronous educational material to help reinforce their learnings and practices.
Although individuals may hesitate to participate in a group setting, they often find the experience of community enhances and accelerates their treatment and gains. This involvement is highlighted in a core aspect of a VIP Boot Camp session called wins, during which participants learn how others on their Boot Camp team are implementing new skills and moving toward their personal values and objectives in a stepwise manner. Through these shared experiences, veterans discover how tactics working for others may serve as a model for their own personal objectives and plans for practice. The sense of relief described by many upon realizing they are not alone in their experiences, along with the satisfaction felt in discovering their ability to support others in Boot Camp, is described by many participants as deeply meaningful and in line with their personal values.
While developed as a fully virtual group program, VIP Boot Camp can also be conducted in person. The virtual program has been successful and continues to spread across VISN 9. There are 8 virtual VIP Boot Camps running in VISN 9, with plans for continued expansion. In the VISN 9 CRH, Boot Camps typically have 10 to 12 participants. Additionally, as VIP Boot Camp grows within a location there are frequently sufficient referrals to support a second rolling group, which enables staggering of the module offerings to allow for even more timely treatment.
Training Program
VISN 9 CRH also developed a VIP Boot Camp 3-day intensive training program for PCMHI HCPs that consists of learning and practicing VIP Boot Camp material for chronic pain, emotion regulation/ stress, sleep disturbances, mindfulness, and guided imagery, along with gaining experience as a VIP Boot Camp coleader. Feedback received from PCMHI HCPs who completed training has been positive. There is also a private Microsoft Teams channel for HCPs, which allows for resource sharing and community building among coleaders. More than 75 PCMHI HCPs have completed VIP Boot Camp training and > 25 VIP Boot Camps have been established at 4 additional VISNs.
The VISN 9 CRH VIP Boot Camp program initiated an implementation and effectiveness project with the Michael E. DeBakey VA Medical Center and the South Central Mental Illness Research, Education and Clinical Center. The focus of this collaboration is support for implementation and treatment effectiveness research with reports, articles, and a white paper on findings and best practices, alongside continued dissemination of the VIP Boot Camp program and training.
Conclusions
VIP Boot Camp is a PCMHI group program offering readily available, comprehensive, and integrative group psychotherapy services to veterans experiencing . 1 of the following: chronic pain, emotion regulation/ stress, and sleep disturbances. It was launched at the VISN 9 CRH with a goal of addressing clinical gaps in the delivery of mental health care, by increasing the number of patients treated within PCMHI. The VIP Boot Camp model provides veterans the opportunity to transform cycles of suffering into cycles of growth through a single approach that can address multiple presenting and interconnected issues.
A 3-day VIP Boot Camp training program provides a quick and effective path for a PCMHI program to train HCPs to launch a VIP Boot Camp. The VISN 9 CRH will continue to champion VIP Boot Camp as a model for the successful provision of comprehensive and integrative mental health treatment within PCMHI at the VA. Through readily available access to comprehensive mental health treatment in an environment that promotes participant empowerment and social engagement, VIP Boot Camp represents an integrative and innovative model of mental health treatment that offers benefits to veteran participants, HCPs, and the VHA.
Since 2007, Primary Care Mental Health Integration (PCMHI) at the Veterans Health Administration (VHA) has improved access to mental health care services for veterans by directly embedding mental health care professionals (HCPs) within primary care teams.1 Veterans referred to PCMHI often have co-occurring physical and mental health disorders.2 Untreated chronic physical and mental comorbidities can diminish the effectiveness of medical and mental health interventions. Growing evidence suggests that treatment of mental health conditions can improve physical health outcomes and management of physical conditions can improve mental health outcomes.2,3
Chronic pain and sleep disorders are common reasons patients present to primary care, and often coexist together with mental health comorbidities.4 Sleep disorders affect 50% to 88% of patients with chronic pain, and 40% of patients with sleep disorders report chronic pain.4 Research has found that chronic pain and sleep disorders increase the risk of suicide attempts and deaths by suicide. Addressing suicide prevention simultaneously with treating chronic pain and insomnia is encouraged.5
Background
PCMHI treats physical and mental health comorbidities with a collaborative framework and a biopsychosocial integrative model.6 PCMHI staff provide mental health services as members of primary care teams. An interdisciplinary PCMHI team can include, but is not limited to, psychologists, mental health social workers, psychiatrists, nurse practitioners, clinical pharmacists, and mental health nurses. Quality of care within this model is elevated, as mental and physical health are recognized as interconnected. Collaboration between primary care and mental health benefits veterans and the VHA by increasing access to mental health care, decreasing stigma associated with mental health treatment, improving health outcomes, and enhancing the likelihood of recovery, resulting in high patient satisfaction.6-8
In the existing PCMHI model, HCPs are encouraged to use short-term, evidence-based psychotherapies (EBPs).9 Veterans referred to PCMHI from primary care are typically able to attend 1 to 6 brief sessions of mental health treatment, often 20 to 30 minutes long. Most EBPs in PCMHI are disorder- specific, providing interventions focused on a single presenting problem (eg, insomnia, chronic pain, or posttraumatic stress disorder [PTSD]). For veterans with a single issue, this model can be very effective. 1,10 However, the high rate of co-occurrence of mental and physical health issues can make it difficult to fully treat interrelated problems if the focus is on 1 specific diagnosis. Veterans with a need for additional (more comprehensive or intensive) mental health treatment are frequently referred to a higher, more resource-intensive level of mental health care, either in the VHA or the community. Examples of higher levels of mental health care include the longer term behavioral health interdisciplinary program (BHIP), sometimes called a mental health clinic (MHC), or a specialty mental health program such as a PTSD clinic.
As PCMHI continues to grow, new challenges have emerged related to staffing shortages and gaps in the clinical delivery of mental health treatment within the VHA. At the same time, demand for VHA mental health treatment has increased. However, a mental health professional shortage severely limits the ability of the VHA to meet this demand. In many systems, this shortage may result in more referrals being made to a higher level of mental health care because of fewer resources to provide comprehensive treatment in a less intensive PCMHI setting.8,10,11 This referral pattern can overburden higher level care, often with long wait times for treatment and lengthy lag times between appointments. Furthermore, these gaps in the clinical delivery of care cannot be effectively addressed by hiring additional mental health professionals. This strain on resources can impede access to care and negatively affect outcomes.10
Recent congressional reports highlight these issues, noting that demand for mental health services continues to outpace the capacity of both PCMHI and higher levels of mental health care, leading to delays in treatment that may negatively affect outcomes.8,10,11 These delays can be particularly detrimental for individuals with conditions requiring timely intervention.8,11 Some veterans are willing to engage with PCMHI in a primary care setting but may be reluctant to engage in general mental health treatment. These veterans might not receive the mental health care they need without PCMHI.
Group Psychotherapy
A group psychotherapy format can address gaps in care delivery and provide advantages for patients, mental health professionals, and the VHA. Group psychotherapy aligns with the US Department of Veterans Affairs (VA) 2018 Blueprint for Excellence and 2018 to 2024 strategic plan, underscoring the need for more timely and efficient mental health services.12,13
Benefits of group psychotherapy include reductions in symptoms, decreased feelings of isolation, increased social support, decreased emotional suppression, and enhanced satisfaction with overall quality of life.14-17 Studies of veterans with PTSD have found less attrition among those who chose group therapy compared with individual therapy.14,18 Group psychotherapy improves access to care by enabling delivery to more patients.14 When compared with individual therapy, the group format allows for a large number of patients to be treated simultaneously, maximizing resources and reducing costs.3,19-21
VISN 9 CRH Innovation
The VA provides care to veterans through regionally distinct administrative systems known as Veterans Integrated Service Networks (VISNs). Clinical resource hubs (CRH) are VISN-based programs created to cover VA staffing shortages by virtually deploying HCPs into local VA systems until vacancies are filled. The national CRH vision of effectively using resources and innovative technologies to meet veterans’ health care needs, along with the above-referenced clinical gaps in the delivery of care, inspired the development of VIP Boot Camp within the VISN 9 CRH.22
Program Description
VIP Boot Camp is an evidence-informed group psychotherapy program designed to provide timely, brief, and comprehensive mental health treatment for veterans. VIP Boot Camp was developed to address the needs of veterans accessing PCMHI services who experience ≥ 1 of the often overlapping problems of anxiety/emotion regulation/stress, sleep difficulties, and chronic pain (Figure). VIP Boot Camp uses an integrative approach to highlight interconnections and similarities among these difficulties and their treatment. A primary vision of the program is to provide this comprehensive treatment within PCMHI (upstream) so additional referrals to higher levels of mental health care (downstream) may not be needed.
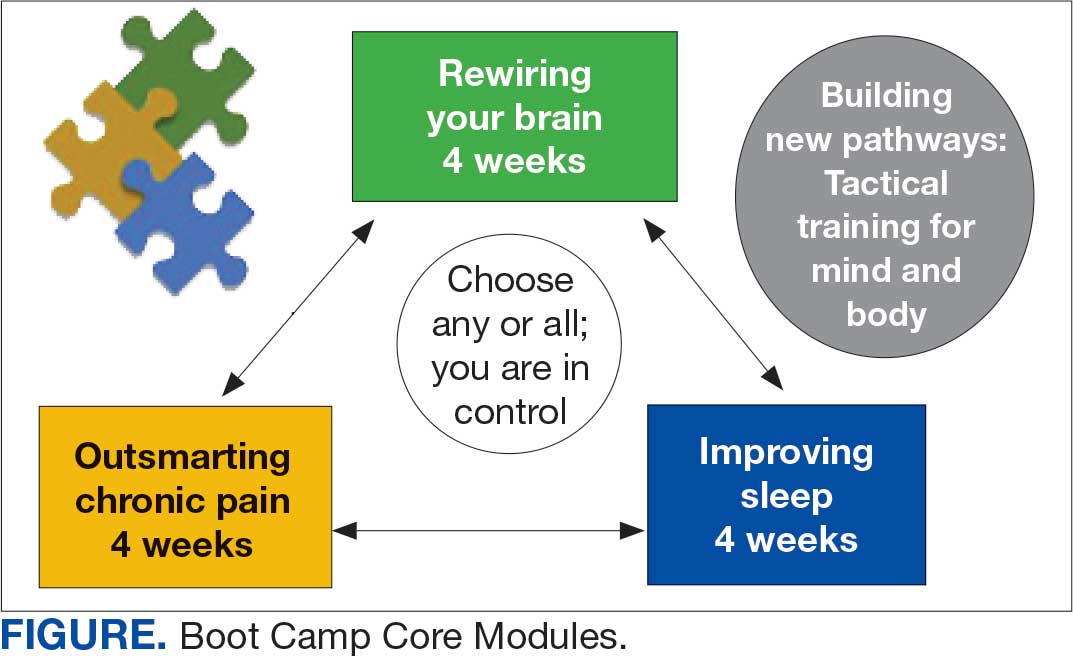
This design is intentional because it increases the number of individuals who can be treated upstream with comprehensive, preventive, and proactive care within PCMHI which, over time, frees up resources in the BHIP for individuals requiring higher levels of care. This approach also aligns with the importance of early treatment for chronic pain and sleep disturbances, which are linked to increased risk of suicide attempts and deaths by suicide for veterans.5 National interest for VIP Boot Camp grew during fiscal year 2024 after it received the Gold Medal Recognition for Most Adoptable and Greatest Potential for Impact during VHA National Access Sprint Wave 3—Mental Health Call of Champions.
History
VIP Boot Camp began in August 2021 at VISN 9 as a 6-week virtual group for veterans with chronic pain. It was established to assist a large VA medical center experiencing PCMHI staffing shortages and lacking available PCMHI groups. Many veterans in the chronic pain group discussed co-occurring issues such as sleep disturbances, anxiety, and stress. The CRH team considered launching 2 separate groups to address these additional PCMHI-level issues; however, in developing the group material which drew from multiple clinical approaches, the team recognized significant overlapping and interconnected themes.
The team discussed EBPs within the VHA and how certain interventions within these treatments could be helpful across many other co-occurring disorders. Integrated tactics (clinical interventions) were drawn from cognitive-behavioral therapy (for depression, insomnia, or chronic pain), acceptance and commitment therapy, prolonged exposure, cognitive processing therapy, dialectical behavior therapy, unified protocol, pain reprocessing therapy, emotional awareness and expression therapy, interpersonal neurobiology, and mindfulness. We collaborated with veterans during VIP Boot Camp groups to determine how to present and discuss complex interventions in ways that were clinically accurate, understandable, relatable, and relevant to their experiences.
To address accessibility issues, the chronic pain group was reduced to 4 weeks. A second 4-week module for anxiety, emotion regulation, and stress was developed, mirroring the tactics, language, and integrative approach of the revised chronic pain module. A similar integrative approach led to the development of the third and final 4-week module for sleep disturbances.
Current Program
The VIP Boot Camp consists of three 4-week integrated modules, each highlighting a critical area: sleep disturbances (Improving Sleep), chronic pain difficulties (Outsmarting Chronic Pain), and emotion regulation difficulties (Rewiring Your Brain). VIP Boot Camp is designed for veterans who are at the PCMHI level of care. Referrals are accepted for patients receiving treatment from primary care or PCMHI.
Guidelines for participation in VIP Boot Camp may differ across sites or VISNs. For example, a veteran who has been referred to the BHIP for medication management only or to a specialty MHC such as a pain clinic or PTSD clinic might also be appropriate and eligible for VIP Boot Camp.
Given the interconnectedness of foundational themes, elements, and practices across the VIP Boot Camp modules, the modules are offered in a rolling format with a veteran-centric “choose your own adventure” approach. Tactics are presented in the modules in a way that allows patients to begin with any 1 of the 3 modules and receive treatment that will help in the other areas. Participants choose their core module and initial treatment focus based on their values, needs, and goals. Individuals who complete a core module can end their VIP Boot Camp experience or continue to the next 4-week module for up to 3 modules.
The group is open to new individuals at the start of any 4-week module and closed for the remainder of its 4-week duration. This innovative rolling modular approach combines elements of open- and closed-group format, allowing for the flexibility and accessibility of an open group with the stability and peer support of a closed group.
Given the complicated and overlapping nature of chronic pain, emotion regulation/ stress, and sleep disturbances, VIP Boot Camp acknowledges that everything is interconnected and difficulties in 1 area may impact other areas. The 3 interconnected modules with repeating themes provide coherence and consistency. Veterans learn how interconnections across difficulties can be leveraged so that tactics learned and practiced in 1 area can assist in other areas, changing the cycle of suffering into a cycle of growth.
VIP Boot Camp sessions are 90 minutes long, once weekly for 4 weeks, with 2 mental health professionals trained to lead a dynamic group psychotherapy experience that aims to be fun for participants. VIP Boot Camp synthesizes evidence-based and evidence-informed interventions, as well as techniques from VHA complementary and integrative health programs, psychoeducation, and interpersonal interventions that model connection, playfulness, and healthy boundaries. These varied strategies combine to equip veterans with practical tactics for self-management outside of sessions, a process described as “finding puzzle pieces.” VIP Boot Camp is built on the idea that people are more likely to adopt and practice any tactic after being taught why that tactic is important, and how it fits into their larger interconnected puzzle. After each session, participants are provided with additional asynchronous educational material to help reinforce their learnings and practices.
Although individuals may hesitate to participate in a group setting, they often find the experience of community enhances and accelerates their treatment and gains. This involvement is highlighted in a core aspect of a VIP Boot Camp session called wins, during which participants learn how others on their Boot Camp team are implementing new skills and moving toward their personal values and objectives in a stepwise manner. Through these shared experiences, veterans discover how tactics working for others may serve as a model for their own personal objectives and plans for practice. The sense of relief described by many upon realizing they are not alone in their experiences, along with the satisfaction felt in discovering their ability to support others in Boot Camp, is described by many participants as deeply meaningful and in line with their personal values.
While developed as a fully virtual group program, VIP Boot Camp can also be conducted in person. The virtual program has been successful and continues to spread across VISN 9. There are 8 virtual VIP Boot Camps running in VISN 9, with plans for continued expansion. In the VISN 9 CRH, Boot Camps typically have 10 to 12 participants. Additionally, as VIP Boot Camp grows within a location there are frequently sufficient referrals to support a second rolling group, which enables staggering of the module offerings to allow for even more timely treatment.
Training Program
VISN 9 CRH also developed a VIP Boot Camp 3-day intensive training program for PCMHI HCPs that consists of learning and practicing VIP Boot Camp material for chronic pain, emotion regulation/ stress, sleep disturbances, mindfulness, and guided imagery, along with gaining experience as a VIP Boot Camp coleader. Feedback received from PCMHI HCPs who completed training has been positive. There is also a private Microsoft Teams channel for HCPs, which allows for resource sharing and community building among coleaders. More than 75 PCMHI HCPs have completed VIP Boot Camp training and > 25 VIP Boot Camps have been established at 4 additional VISNs.
The VISN 9 CRH VIP Boot Camp program initiated an implementation and effectiveness project with the Michael E. DeBakey VA Medical Center and the South Central Mental Illness Research, Education and Clinical Center. The focus of this collaboration is support for implementation and treatment effectiveness research with reports, articles, and a white paper on findings and best practices, alongside continued dissemination of the VIP Boot Camp program and training.
Conclusions
VIP Boot Camp is a PCMHI group program offering readily available, comprehensive, and integrative group psychotherapy services to veterans experiencing . 1 of the following: chronic pain, emotion regulation/ stress, and sleep disturbances. It was launched at the VISN 9 CRH with a goal of addressing clinical gaps in the delivery of mental health care, by increasing the number of patients treated within PCMHI. The VIP Boot Camp model provides veterans the opportunity to transform cycles of suffering into cycles of growth through a single approach that can address multiple presenting and interconnected issues.
A 3-day VIP Boot Camp training program provides a quick and effective path for a PCMHI program to train HCPs to launch a VIP Boot Camp. The VISN 9 CRH will continue to champion VIP Boot Camp as a model for the successful provision of comprehensive and integrative mental health treatment within PCMHI at the VA. Through readily available access to comprehensive mental health treatment in an environment that promotes participant empowerment and social engagement, VIP Boot Camp represents an integrative and innovative model of mental health treatment that offers benefits to veteran participants, HCPs, and the VHA.
- Leung LB, Yoon J, Escarce JJ, et al. Primary care-mental health integration in the VA: shifting mental health services for common mental illnesses to primary care. Psychiatr Serv. 2018;69:403-409. doi:10.1176/appi.ps.201700190
- Zhang A, Park S, Sullivan JE, et al. The effectiveness of problem-solving therapy for primary care patients’ depressive and/or anxiety disorders: a systematic review and meta-analysis. J Am Board Fam Med. 2018;31:139-150. doi:10.3122/jabfm.2018.01.170270
- Hundt NE, Barrera TL, Robinson A, et al. A systematic review of cognitive behavioral therapy for depression in veterans. Mil Med. 2014;179:942-949. doi:10.7205/milmed-d-14-00128
- Jank R, Gallee A, Boeckle M, et al. Chronic pain and sleep disorders in primary care. Pain Res Treat. 2017;2017:1-9. doi:10.1155/2017/9081802
- Ashrafioun L, Bishop TM, Pigeon WR. The relationship between pain severity, insomnia, and suicide attempts among a national veteran sample initiating pain care. Psychosom Med. 2021;83:733- 738. doi:10.1097/psy.0000000000000975
- Ramanuj P, Ferenchik E, Docherty M, et al. Evolving models of integrated behavioral health and primary care. Curr Psychiatry Rep. 2019;21:1. doi:10.1007/s11920-019-0985-4
- Post EP, Metzger M, Dumas P, et al. Integrating mental health into primary care within the Veterans Health Administration. Fam Syst Health. 2010;28:83-90. doi:10.1037/a0020130
- Smith TL, Kim B, Benzer JK, et al. FLOW: early results from a clinical demonstration project to improve the transition of patients with mental health disorders back to primary care. Psychol Serv. 2021;18:23-32. doi:10.1037/ser0000336
- Kearney LK, Post EP, Pomerantz AS, et al. Applying the interprofessional patient aligned care team in the department of veterans affairs transforming primary care. Am Psychol. 2014;69(4):399-408. doi:10.1037/a0035909
- US Government Accountability Office. Veterans health care: staffing challenges persist for fully integrating mental health and primary care services. December 15, 2022. Accessed July 9, 2025. https://www.gao.gov/products/gao-23-105372
- National Academies of Science and Engineering. Evaluation of the Department of Veterans Affairs Mental Health Services. National Academies Press; 2018. Accessed July 9, 2025. https://nap.nationalacademies.org/catalog/24915/evaluation-of-the-department-of-veterans-affairs-mental-health-services
- US Department of Veterans Affairs. Blueprint for excellence: achieving veterans’ excellence. October 6, 2014. Accessed July 9, 2025. https://www.volunteer.va.gov/docs/blueprintforexcellence_factsheet.PDF
- US Department of Veterans Affairs. Department of Veterans Affairs FY 2018-2024 strategic plan. Accessed July 9, 2025. https://www.calvet.ca.gov/Regulations/USDVA%20Strategic%20Plan%202018-2024.pdf
- Sripada RK, Bohnert KM, Ganoczy D, et al. Initial group versus individual therapy for posttraumatic stress disorder and subsequent follow-up treatment adequacy. Psychol Serv. 2016;13:349-355. doi:10.1037/ser0000077
- Burnett-Zeigler IE, Pfeiffer P, Zivin K, et al. Psychotherapy utilization for acute depression within the Veterans Affairs health care system. Psychol Serv. 2012;9:325-335. doi:10.1037/a0027957
- Kim JS, Prins A, Hirschhorn EW, et al. Preliminary investigation into the effectiveness of group webSTAIR for trauma-exposed veterans in primary care. Mil Med. 2024;189:e1403-e1408. doi:10.1093/milmed/usae052
- Jakupcak M, Blais RK, Grossbard J, et al. “Toughness” in association with mental health symptoms among Iraq and Afghanistan war veterans seeking Veterans Affairs health care. Psychol Men Masc. 2014;15:100-104. doi:10.1037/a0031508
- Stoycos SA, Berzenski SR, Beck JG, et al. Predictors of treatment completion in group psychotherapy for male veterans with posttraumatic stress disorder. J Trauma Stress. 2023;36:346-358. doi:10.1002/jts.22915
- Possemato K. The current state of intervention research for posttraumatic stress disorder within the primary care setting. J Clin Psychol Med Settings. 2011;18:268-280. doi:10.1007/s10880-011-9237-4
- Hunt MG, Rosenheck RA. Psychotherapy in mental health clinics of the Department of Veterans Affairs. J Clin Psychol. 2011;67:561-573. doi:10.1002/jclp.20788
- Khatri N, Marziali E, Tchernikov I, et al. Comparing telehealth-based and clinic-based group cognitive behavioral therapy for adults with depression and anxiety: a pilot study. Clin Interv Aging. 2014;9:765. doi:10.2147/cia.s57832
- Dangel J. Clinical resource hub increases veterans' access to care. VA News. January 12, 2025. Accessed September 3, 2025. https://news.va.gov/137439/clinical-resource-hub-increases-access-to-care/
- Leung LB, Yoon J, Escarce JJ, et al. Primary care-mental health integration in the VA: shifting mental health services for common mental illnesses to primary care. Psychiatr Serv. 2018;69:403-409. doi:10.1176/appi.ps.201700190
- Zhang A, Park S, Sullivan JE, et al. The effectiveness of problem-solving therapy for primary care patients’ depressive and/or anxiety disorders: a systematic review and meta-analysis. J Am Board Fam Med. 2018;31:139-150. doi:10.3122/jabfm.2018.01.170270
- Hundt NE, Barrera TL, Robinson A, et al. A systematic review of cognitive behavioral therapy for depression in veterans. Mil Med. 2014;179:942-949. doi:10.7205/milmed-d-14-00128
- Jank R, Gallee A, Boeckle M, et al. Chronic pain and sleep disorders in primary care. Pain Res Treat. 2017;2017:1-9. doi:10.1155/2017/9081802
- Ashrafioun L, Bishop TM, Pigeon WR. The relationship between pain severity, insomnia, and suicide attempts among a national veteran sample initiating pain care. Psychosom Med. 2021;83:733- 738. doi:10.1097/psy.0000000000000975
- Ramanuj P, Ferenchik E, Docherty M, et al. Evolving models of integrated behavioral health and primary care. Curr Psychiatry Rep. 2019;21:1. doi:10.1007/s11920-019-0985-4
- Post EP, Metzger M, Dumas P, et al. Integrating mental health into primary care within the Veterans Health Administration. Fam Syst Health. 2010;28:83-90. doi:10.1037/a0020130
- Smith TL, Kim B, Benzer JK, et al. FLOW: early results from a clinical demonstration project to improve the transition of patients with mental health disorders back to primary care. Psychol Serv. 2021;18:23-32. doi:10.1037/ser0000336
- Kearney LK, Post EP, Pomerantz AS, et al. Applying the interprofessional patient aligned care team in the department of veterans affairs transforming primary care. Am Psychol. 2014;69(4):399-408. doi:10.1037/a0035909
- US Government Accountability Office. Veterans health care: staffing challenges persist for fully integrating mental health and primary care services. December 15, 2022. Accessed July 9, 2025. https://www.gao.gov/products/gao-23-105372
- National Academies of Science and Engineering. Evaluation of the Department of Veterans Affairs Mental Health Services. National Academies Press; 2018. Accessed July 9, 2025. https://nap.nationalacademies.org/catalog/24915/evaluation-of-the-department-of-veterans-affairs-mental-health-services
- US Department of Veterans Affairs. Blueprint for excellence: achieving veterans’ excellence. October 6, 2014. Accessed July 9, 2025. https://www.volunteer.va.gov/docs/blueprintforexcellence_factsheet.PDF
- US Department of Veterans Affairs. Department of Veterans Affairs FY 2018-2024 strategic plan. Accessed July 9, 2025. https://www.calvet.ca.gov/Regulations/USDVA%20Strategic%20Plan%202018-2024.pdf
- Sripada RK, Bohnert KM, Ganoczy D, et al. Initial group versus individual therapy for posttraumatic stress disorder and subsequent follow-up treatment adequacy. Psychol Serv. 2016;13:349-355. doi:10.1037/ser0000077
- Burnett-Zeigler IE, Pfeiffer P, Zivin K, et al. Psychotherapy utilization for acute depression within the Veterans Affairs health care system. Psychol Serv. 2012;9:325-335. doi:10.1037/a0027957
- Kim JS, Prins A, Hirschhorn EW, et al. Preliminary investigation into the effectiveness of group webSTAIR for trauma-exposed veterans in primary care. Mil Med. 2024;189:e1403-e1408. doi:10.1093/milmed/usae052
- Jakupcak M, Blais RK, Grossbard J, et al. “Toughness” in association with mental health symptoms among Iraq and Afghanistan war veterans seeking Veterans Affairs health care. Psychol Men Masc. 2014;15:100-104. doi:10.1037/a0031508
- Stoycos SA, Berzenski SR, Beck JG, et al. Predictors of treatment completion in group psychotherapy for male veterans with posttraumatic stress disorder. J Trauma Stress. 2023;36:346-358. doi:10.1002/jts.22915
- Possemato K. The current state of intervention research for posttraumatic stress disorder within the primary care setting. J Clin Psychol Med Settings. 2011;18:268-280. doi:10.1007/s10880-011-9237-4
- Hunt MG, Rosenheck RA. Psychotherapy in mental health clinics of the Department of Veterans Affairs. J Clin Psychol. 2011;67:561-573. doi:10.1002/jclp.20788
- Khatri N, Marziali E, Tchernikov I, et al. Comparing telehealth-based and clinic-based group cognitive behavioral therapy for adults with depression and anxiety: a pilot study. Clin Interv Aging. 2014;9:765. doi:10.2147/cia.s57832
- Dangel J. Clinical resource hub increases veterans' access to care. VA News. January 12, 2025. Accessed September 3, 2025. https://news.va.gov/137439/clinical-resource-hub-increases-access-to-care/
VIP Boot Camp: Expanding the Impact of VA Primary Care Mental Health With a Transdiagnostic Modular Group Program
VIP Boot Camp: Expanding the Impact of VA Primary Care Mental Health With a Transdiagnostic Modular Group Program
Centralized Psychosocial Distress Screening Led by RN Care Coordinator
Background
Unmet psychosocial health needs negatively impact cancer care and outcomes. The American College of Surgeons’ Commission on Cancer (CoC) accreditation requirements include Psychosocial Distress Screening (PDS) for all newly diagnosed patients. To enhance cancer care and meet CoC standards, the Tibor Rubin Veterans Affairs Medical Center (TRVAMC) developed and implemented a closed-loop, centralized PDS pathway.
Objectives
Develop processes/methods to: (1) identify all newly diagnosed cancer patients; (2) track initiation of first course of treatment; (3) offer and complete PDS at initiation of first course of treatment; and (4) ensure placement of appropriate referrals.
Methods
All staff members were trained in PDS and competency completed. A standard operating procedure (SOP) was created to identify patients meeting criteria for PDS. Newly diagnosed patients were identified from cancer registry lists, tumor boards, radiology and pathology reports. Patients were placed on a tracking tool by the nurse care coordinator (NCC) and monitored to facilitate timely workup and initiation of treatment. Nurses in the cancer program offered and completed PDS and placed all necessary referrals (to > 11 services). Patients were removed from the tracker only after confirmation of PDS and referrals.
Results
Prior to implementation of PDS, no patients received comprehensive screening and referrals. After implementation, data were collected over a 2 year period. In 2023 and 2024, 277/565 (49%) and 256/526 (48.7%) newly diagnosed patients were eligible for PDS, respectively. All eligible patients were offered PDS (100%). Of patients who underwent PDS, 37% scored their distress at a level of 4/10 or higher, underscoring the severity of distress and unmet need. Referrals to various services were indicated and made in 43.8% patients, most frequently to Social Work, Primary Care or Psychology/Mental Health. More recently, nurses in the Infusion Clinic and Radiation Oncology were trained in and also started conducting PDS on patients coming for treatment.
Conclusions
Implementation of comprehensive and timely PDS resulted in early identification and interventions to address diverse facets of distress that are known to interfere with quality of life, compliance with cancer treatments and outcomes. The program also met the CoC standard for accreditation of TRVAMC in 2024.
Background
Unmet psychosocial health needs negatively impact cancer care and outcomes. The American College of Surgeons’ Commission on Cancer (CoC) accreditation requirements include Psychosocial Distress Screening (PDS) for all newly diagnosed patients. To enhance cancer care and meet CoC standards, the Tibor Rubin Veterans Affairs Medical Center (TRVAMC) developed and implemented a closed-loop, centralized PDS pathway.
Objectives
Develop processes/methods to: (1) identify all newly diagnosed cancer patients; (2) track initiation of first course of treatment; (3) offer and complete PDS at initiation of first course of treatment; and (4) ensure placement of appropriate referrals.
Methods
All staff members were trained in PDS and competency completed. A standard operating procedure (SOP) was created to identify patients meeting criteria for PDS. Newly diagnosed patients were identified from cancer registry lists, tumor boards, radiology and pathology reports. Patients were placed on a tracking tool by the nurse care coordinator (NCC) and monitored to facilitate timely workup and initiation of treatment. Nurses in the cancer program offered and completed PDS and placed all necessary referrals (to > 11 services). Patients were removed from the tracker only after confirmation of PDS and referrals.
Results
Prior to implementation of PDS, no patients received comprehensive screening and referrals. After implementation, data were collected over a 2 year period. In 2023 and 2024, 277/565 (49%) and 256/526 (48.7%) newly diagnosed patients were eligible for PDS, respectively. All eligible patients were offered PDS (100%). Of patients who underwent PDS, 37% scored their distress at a level of 4/10 or higher, underscoring the severity of distress and unmet need. Referrals to various services were indicated and made in 43.8% patients, most frequently to Social Work, Primary Care or Psychology/Mental Health. More recently, nurses in the Infusion Clinic and Radiation Oncology were trained in and also started conducting PDS on patients coming for treatment.
Conclusions
Implementation of comprehensive and timely PDS resulted in early identification and interventions to address diverse facets of distress that are known to interfere with quality of life, compliance with cancer treatments and outcomes. The program also met the CoC standard for accreditation of TRVAMC in 2024.
Background
Unmet psychosocial health needs negatively impact cancer care and outcomes. The American College of Surgeons’ Commission on Cancer (CoC) accreditation requirements include Psychosocial Distress Screening (PDS) for all newly diagnosed patients. To enhance cancer care and meet CoC standards, the Tibor Rubin Veterans Affairs Medical Center (TRVAMC) developed and implemented a closed-loop, centralized PDS pathway.
Objectives
Develop processes/methods to: (1) identify all newly diagnosed cancer patients; (2) track initiation of first course of treatment; (3) offer and complete PDS at initiation of first course of treatment; and (4) ensure placement of appropriate referrals.
Methods
All staff members were trained in PDS and competency completed. A standard operating procedure (SOP) was created to identify patients meeting criteria for PDS. Newly diagnosed patients were identified from cancer registry lists, tumor boards, radiology and pathology reports. Patients were placed on a tracking tool by the nurse care coordinator (NCC) and monitored to facilitate timely workup and initiation of treatment. Nurses in the cancer program offered and completed PDS and placed all necessary referrals (to > 11 services). Patients were removed from the tracker only after confirmation of PDS and referrals.
Results
Prior to implementation of PDS, no patients received comprehensive screening and referrals. After implementation, data were collected over a 2 year period. In 2023 and 2024, 277/565 (49%) and 256/526 (48.7%) newly diagnosed patients were eligible for PDS, respectively. All eligible patients were offered PDS (100%). Of patients who underwent PDS, 37% scored their distress at a level of 4/10 or higher, underscoring the severity of distress and unmet need. Referrals to various services were indicated and made in 43.8% patients, most frequently to Social Work, Primary Care or Psychology/Mental Health. More recently, nurses in the Infusion Clinic and Radiation Oncology were trained in and also started conducting PDS on patients coming for treatment.
Conclusions
Implementation of comprehensive and timely PDS resulted in early identification and interventions to address diverse facets of distress that are known to interfere with quality of life, compliance with cancer treatments and outcomes. The program also met the CoC standard for accreditation of TRVAMC in 2024.