User login
When the Next Big Thing Falls Short
Recently, Acadia Pharmaceuticals announced it was stopping trials on Nuplazid for indications outside of Parkinson’s disease psychosis.
I was impressed with what I saw in my office. Although I know there’s some controversy over the drug, the majority of studies do show efficacy, and in my little practice I clearly noticed improvements in patients with Parkinson’s disease who’d previously failed the more standard agents (note - I have no financial affiliation with Acadia Pharmaceuticals).
So, as a lay-neurologist, I expected the drug to work for other kinds of psychosis, particularly Alzheimer’s disease. All of us in practice know how much we need new options for that.
But when the clinical trials came, the drug didn’t work. It didn’t work for schizophrenia, either, Finally, Acadia threw in the towel and gave up.
I have no idea what happened. I’m sure others are wondering the same thing. On paper, I’d have thought it would work for Alzheimer’s psychosis, but in the real world it didn’t.
Is psychosis between the two disorders that different, with different neurotransmitter causes? Are the benefits in my patients with Parkinson’s disease really just from my own selection bias? Or is there just a lot we still don’t know?
Look at the graveyard full of amyloid-targeting drugs. Yeah, I know Leqembi is out there, and donanemab is in the wings, but are they anywhere near as good as we thought they’d be? Not at all.
At the same time, we’ve been waiting for the BTK drugs (not to be confused with a Korean pop band) for multiple sclerosis. They sounded like they were the Next Big Thing.
They may be, but recent data on one of them, evobrutinib, was less than encouraging. Of course, that shouldn’t extrapolate to the group as a whole, but it does leave you wondering why.
Medicine is always improving, but it’s also still a trial-and-error process. Just because something should work doesn’t mean it will, and it may be years before we know why.
It’s just a reminder that, here in 2024, we still have a lot to learn.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, Acadia Pharmaceuticals announced it was stopping trials on Nuplazid for indications outside of Parkinson’s disease psychosis.
I was impressed with what I saw in my office. Although I know there’s some controversy over the drug, the majority of studies do show efficacy, and in my little practice I clearly noticed improvements in patients with Parkinson’s disease who’d previously failed the more standard agents (note - I have no financial affiliation with Acadia Pharmaceuticals).
So, as a lay-neurologist, I expected the drug to work for other kinds of psychosis, particularly Alzheimer’s disease. All of us in practice know how much we need new options for that.
But when the clinical trials came, the drug didn’t work. It didn’t work for schizophrenia, either, Finally, Acadia threw in the towel and gave up.
I have no idea what happened. I’m sure others are wondering the same thing. On paper, I’d have thought it would work for Alzheimer’s psychosis, but in the real world it didn’t.
Is psychosis between the two disorders that different, with different neurotransmitter causes? Are the benefits in my patients with Parkinson’s disease really just from my own selection bias? Or is there just a lot we still don’t know?
Look at the graveyard full of amyloid-targeting drugs. Yeah, I know Leqembi is out there, and donanemab is in the wings, but are they anywhere near as good as we thought they’d be? Not at all.
At the same time, we’ve been waiting for the BTK drugs (not to be confused with a Korean pop band) for multiple sclerosis. They sounded like they were the Next Big Thing.
They may be, but recent data on one of them, evobrutinib, was less than encouraging. Of course, that shouldn’t extrapolate to the group as a whole, but it does leave you wondering why.
Medicine is always improving, but it’s also still a trial-and-error process. Just because something should work doesn’t mean it will, and it may be years before we know why.
It’s just a reminder that, here in 2024, we still have a lot to learn.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, Acadia Pharmaceuticals announced it was stopping trials on Nuplazid for indications outside of Parkinson’s disease psychosis.
I was impressed with what I saw in my office. Although I know there’s some controversy over the drug, the majority of studies do show efficacy, and in my little practice I clearly noticed improvements in patients with Parkinson’s disease who’d previously failed the more standard agents (note - I have no financial affiliation with Acadia Pharmaceuticals).
So, as a lay-neurologist, I expected the drug to work for other kinds of psychosis, particularly Alzheimer’s disease. All of us in practice know how much we need new options for that.
But when the clinical trials came, the drug didn’t work. It didn’t work for schizophrenia, either, Finally, Acadia threw in the towel and gave up.
I have no idea what happened. I’m sure others are wondering the same thing. On paper, I’d have thought it would work for Alzheimer’s psychosis, but in the real world it didn’t.
Is psychosis between the two disorders that different, with different neurotransmitter causes? Are the benefits in my patients with Parkinson’s disease really just from my own selection bias? Or is there just a lot we still don’t know?
Look at the graveyard full of amyloid-targeting drugs. Yeah, I know Leqembi is out there, and donanemab is in the wings, but are they anywhere near as good as we thought they’d be? Not at all.
At the same time, we’ve been waiting for the BTK drugs (not to be confused with a Korean pop band) for multiple sclerosis. They sounded like they were the Next Big Thing.
They may be, but recent data on one of them, evobrutinib, was less than encouraging. Of course, that shouldn’t extrapolate to the group as a whole, but it does leave you wondering why.
Medicine is always improving, but it’s also still a trial-and-error process. Just because something should work doesn’t mean it will, and it may be years before we know why.
It’s just a reminder that, here in 2024, we still have a lot to learn.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Neurological Disorders Now Top Global Cause of Illness, Disability
, a new comprehensive analysis showed.
In 2021, neurological conditions were responsible for 443 million years of healthy life lost due to illness, disability, and premature death — a measurement known as disability-adjusted life years (DALY) — making them the top contributor to the global disease burden, ahead of cardiovascular diseases.
Some 3.4 billion people — 43% of the entire global population — had a neurological illness in 2021, the report noted.
“As the world’s leading cause of overall disease burden, and with case numbers rising 59% globally since 1990, nervous system conditions must be addressed through effective, culturally acceptable, and affordable prevention, treatment, rehabilitation, and long-term care strategies,” lead author Jaimie Steinmetz, PhD, from the Institute of Health Metrics and Evaluation (IHME), University of Washington, Seattle, said in a news release.
The findings, from the Global Burden of Disease, Injuries, and Risk Factors Study (GBD) 2021, “have important health service and policy implications and serve as evidence that global neurological heath loss has been under-recognized and is increasing and unevenly distributed geographically and socioeconomically,” the authors noted.
The study was published online in The Lancet: Neurology.
The Top 10
The top 10 contributors to neurological health loss in 2021 were stroke, neonatal encephalopathy, migraine, Alzheimer’s disease and other dementias, diabetic neuropathy, meningitis, epilepsy, neurological complications from preterm birth, autistic spectrum disorders, and nervous system cancers.
Neurological consequences of COVID-19 ranked 20th out of 37 unique conditions assessed.
In 2021, there were more than 23 million global cases of COVID-19 with long-term cognitive symptoms or Guillain-Barré syndrome, accounting for 57% of all infectious neurological disease cases and contributing to 2.48 million years of healthy life lost, the study found.
The most prevalent neurological disorders were tension-type headache (about 2 billion cases) and migraine (about 1.1 billion cases), while diabetic neuropathy is the fastest-growing of all neurological conditions.
“The number of people with diabetic neuropathy has more than tripled globally since 1990, rising to 206 million in 2021. This is in line with the increase in the global prevalence of diabetes,” co-senior author Liane Ong, PhD, from IHME, said in the release.
The data showed striking differences in the burden of neurological conditions between world regions and national income levels, with over 80% of neurological deaths and health loss occurring in low- and middle-income countries.
Regions with the highest burden of neurological conditions were central and western sub-Saharan Africa, while high-income Asia Pacific and Australasia had the lowest burden.
“Nervous system health loss disproportionately impacts many of the poorest countries partly due to the higher prevalence of conditions affecting neonates and children under 5, especially birth-related complications and infections,” co-senior author Tarun Dua, MD, with the World Health Organization (WHO) brain health unit, noted in the news release.
“Improved infant survival has led to an increase in long-term disability, while limited access to treatment and rehabilitation services is contributing to the much higher proportion of deaths in these countries,” Dr. Dua said.
Prioritize Prevention
The analysis also provides estimates of the proportion of neurological conditions that are potentially preventable by eliminating known risk factors for stroke, dementia, multiple sclerosis, Parkinson’s disease, encephalitis, meningitis, and intellectual disability.
It shows that modifying 18 risk factors over a person’s lifetime — most importantly high systolic blood pressure — could prevent 84% of global DALYs from stroke. Controlling lead exposure could lower intellectual disability cases by 63% and reducing high fasting plasma glucose to normal levels could cut dementia by roughly 15%.
“Because many neurological conditions lack cures, and access to medical care is often limited, understanding modifiable risk factors and the potentially avoidable neurological condition burden is essential to help curb this global health crisis,” co-lead author Katrin Seeher, PhD, mental health specialist with WHO’s brain health unit, said in the release.
It’s important to note that nervous system conditions include infectious and vector-borne diseases and injuries as well as noncommunicable diseases and injuries, Dr. Steinmetz said, “demanding different strategies for prevention and treatment throughout life.”
“We hope that our findings can help policymakers more comprehensively understand the impact of neurological conditions on both adults and children to inform more targeted interventions in individual countries, as well as guide ongoing awareness and advocacy efforts around the world,” Dr. Steinmetz added.
In an accompanying editorial, Wolfgang Grisold, MD, president of the World Federation of Neurology, London, noted that the study builds on previous findings and expands the number of neurological conditions studied from 15 to 37.
“This important new GBD report highlights that the burden of neurological conditions is greater than previously thought,” wrote Dr. Grisold, who was not a part of the study. “In the next iteration, more attention should be given to neuromuscular diseases, the effects of cancer in the nervous system, and neuropathic pain. Comparing the disability caused by conditions with episodic occurrence versus those that cause permanent and progressive disease will remain challenging because the effects on the individuals vary substantially.”
The study was funded by the Bill and Melinda Gates Foundation. Full disclosures are included in the original article.
A version of this article appeared on Medscape.com.
, a new comprehensive analysis showed.
In 2021, neurological conditions were responsible for 443 million years of healthy life lost due to illness, disability, and premature death — a measurement known as disability-adjusted life years (DALY) — making them the top contributor to the global disease burden, ahead of cardiovascular diseases.
Some 3.4 billion people — 43% of the entire global population — had a neurological illness in 2021, the report noted.
“As the world’s leading cause of overall disease burden, and with case numbers rising 59% globally since 1990, nervous system conditions must be addressed through effective, culturally acceptable, and affordable prevention, treatment, rehabilitation, and long-term care strategies,” lead author Jaimie Steinmetz, PhD, from the Institute of Health Metrics and Evaluation (IHME), University of Washington, Seattle, said in a news release.
The findings, from the Global Burden of Disease, Injuries, and Risk Factors Study (GBD) 2021, “have important health service and policy implications and serve as evidence that global neurological heath loss has been under-recognized and is increasing and unevenly distributed geographically and socioeconomically,” the authors noted.
The study was published online in The Lancet: Neurology.
The Top 10
The top 10 contributors to neurological health loss in 2021 were stroke, neonatal encephalopathy, migraine, Alzheimer’s disease and other dementias, diabetic neuropathy, meningitis, epilepsy, neurological complications from preterm birth, autistic spectrum disorders, and nervous system cancers.
Neurological consequences of COVID-19 ranked 20th out of 37 unique conditions assessed.
In 2021, there were more than 23 million global cases of COVID-19 with long-term cognitive symptoms or Guillain-Barré syndrome, accounting for 57% of all infectious neurological disease cases and contributing to 2.48 million years of healthy life lost, the study found.
The most prevalent neurological disorders were tension-type headache (about 2 billion cases) and migraine (about 1.1 billion cases), while diabetic neuropathy is the fastest-growing of all neurological conditions.
“The number of people with diabetic neuropathy has more than tripled globally since 1990, rising to 206 million in 2021. This is in line with the increase in the global prevalence of diabetes,” co-senior author Liane Ong, PhD, from IHME, said in the release.
The data showed striking differences in the burden of neurological conditions between world regions and national income levels, with over 80% of neurological deaths and health loss occurring in low- and middle-income countries.
Regions with the highest burden of neurological conditions were central and western sub-Saharan Africa, while high-income Asia Pacific and Australasia had the lowest burden.
“Nervous system health loss disproportionately impacts many of the poorest countries partly due to the higher prevalence of conditions affecting neonates and children under 5, especially birth-related complications and infections,” co-senior author Tarun Dua, MD, with the World Health Organization (WHO) brain health unit, noted in the news release.
“Improved infant survival has led to an increase in long-term disability, while limited access to treatment and rehabilitation services is contributing to the much higher proportion of deaths in these countries,” Dr. Dua said.
Prioritize Prevention
The analysis also provides estimates of the proportion of neurological conditions that are potentially preventable by eliminating known risk factors for stroke, dementia, multiple sclerosis, Parkinson’s disease, encephalitis, meningitis, and intellectual disability.
It shows that modifying 18 risk factors over a person’s lifetime — most importantly high systolic blood pressure — could prevent 84% of global DALYs from stroke. Controlling lead exposure could lower intellectual disability cases by 63% and reducing high fasting plasma glucose to normal levels could cut dementia by roughly 15%.
“Because many neurological conditions lack cures, and access to medical care is often limited, understanding modifiable risk factors and the potentially avoidable neurological condition burden is essential to help curb this global health crisis,” co-lead author Katrin Seeher, PhD, mental health specialist with WHO’s brain health unit, said in the release.
It’s important to note that nervous system conditions include infectious and vector-borne diseases and injuries as well as noncommunicable diseases and injuries, Dr. Steinmetz said, “demanding different strategies for prevention and treatment throughout life.”
“We hope that our findings can help policymakers more comprehensively understand the impact of neurological conditions on both adults and children to inform more targeted interventions in individual countries, as well as guide ongoing awareness and advocacy efforts around the world,” Dr. Steinmetz added.
In an accompanying editorial, Wolfgang Grisold, MD, president of the World Federation of Neurology, London, noted that the study builds on previous findings and expands the number of neurological conditions studied from 15 to 37.
“This important new GBD report highlights that the burden of neurological conditions is greater than previously thought,” wrote Dr. Grisold, who was not a part of the study. “In the next iteration, more attention should be given to neuromuscular diseases, the effects of cancer in the nervous system, and neuropathic pain. Comparing the disability caused by conditions with episodic occurrence versus those that cause permanent and progressive disease will remain challenging because the effects on the individuals vary substantially.”
The study was funded by the Bill and Melinda Gates Foundation. Full disclosures are included in the original article.
A version of this article appeared on Medscape.com.
, a new comprehensive analysis showed.
In 2021, neurological conditions were responsible for 443 million years of healthy life lost due to illness, disability, and premature death — a measurement known as disability-adjusted life years (DALY) — making them the top contributor to the global disease burden, ahead of cardiovascular diseases.
Some 3.4 billion people — 43% of the entire global population — had a neurological illness in 2021, the report noted.
“As the world’s leading cause of overall disease burden, and with case numbers rising 59% globally since 1990, nervous system conditions must be addressed through effective, culturally acceptable, and affordable prevention, treatment, rehabilitation, and long-term care strategies,” lead author Jaimie Steinmetz, PhD, from the Institute of Health Metrics and Evaluation (IHME), University of Washington, Seattle, said in a news release.
The findings, from the Global Burden of Disease, Injuries, and Risk Factors Study (GBD) 2021, “have important health service and policy implications and serve as evidence that global neurological heath loss has been under-recognized and is increasing and unevenly distributed geographically and socioeconomically,” the authors noted.
The study was published online in The Lancet: Neurology.
The Top 10
The top 10 contributors to neurological health loss in 2021 were stroke, neonatal encephalopathy, migraine, Alzheimer’s disease and other dementias, diabetic neuropathy, meningitis, epilepsy, neurological complications from preterm birth, autistic spectrum disorders, and nervous system cancers.
Neurological consequences of COVID-19 ranked 20th out of 37 unique conditions assessed.
In 2021, there were more than 23 million global cases of COVID-19 with long-term cognitive symptoms or Guillain-Barré syndrome, accounting for 57% of all infectious neurological disease cases and contributing to 2.48 million years of healthy life lost, the study found.
The most prevalent neurological disorders were tension-type headache (about 2 billion cases) and migraine (about 1.1 billion cases), while diabetic neuropathy is the fastest-growing of all neurological conditions.
“The number of people with diabetic neuropathy has more than tripled globally since 1990, rising to 206 million in 2021. This is in line with the increase in the global prevalence of diabetes,” co-senior author Liane Ong, PhD, from IHME, said in the release.
The data showed striking differences in the burden of neurological conditions between world regions and national income levels, with over 80% of neurological deaths and health loss occurring in low- and middle-income countries.
Regions with the highest burden of neurological conditions were central and western sub-Saharan Africa, while high-income Asia Pacific and Australasia had the lowest burden.
“Nervous system health loss disproportionately impacts many of the poorest countries partly due to the higher prevalence of conditions affecting neonates and children under 5, especially birth-related complications and infections,” co-senior author Tarun Dua, MD, with the World Health Organization (WHO) brain health unit, noted in the news release.
“Improved infant survival has led to an increase in long-term disability, while limited access to treatment and rehabilitation services is contributing to the much higher proportion of deaths in these countries,” Dr. Dua said.
Prioritize Prevention
The analysis also provides estimates of the proportion of neurological conditions that are potentially preventable by eliminating known risk factors for stroke, dementia, multiple sclerosis, Parkinson’s disease, encephalitis, meningitis, and intellectual disability.
It shows that modifying 18 risk factors over a person’s lifetime — most importantly high systolic blood pressure — could prevent 84% of global DALYs from stroke. Controlling lead exposure could lower intellectual disability cases by 63% and reducing high fasting plasma glucose to normal levels could cut dementia by roughly 15%.
“Because many neurological conditions lack cures, and access to medical care is often limited, understanding modifiable risk factors and the potentially avoidable neurological condition burden is essential to help curb this global health crisis,” co-lead author Katrin Seeher, PhD, mental health specialist with WHO’s brain health unit, said in the release.
It’s important to note that nervous system conditions include infectious and vector-borne diseases and injuries as well as noncommunicable diseases and injuries, Dr. Steinmetz said, “demanding different strategies for prevention and treatment throughout life.”
“We hope that our findings can help policymakers more comprehensively understand the impact of neurological conditions on both adults and children to inform more targeted interventions in individual countries, as well as guide ongoing awareness and advocacy efforts around the world,” Dr. Steinmetz added.
In an accompanying editorial, Wolfgang Grisold, MD, president of the World Federation of Neurology, London, noted that the study builds on previous findings and expands the number of neurological conditions studied from 15 to 37.
“This important new GBD report highlights that the burden of neurological conditions is greater than previously thought,” wrote Dr. Grisold, who was not a part of the study. “In the next iteration, more attention should be given to neuromuscular diseases, the effects of cancer in the nervous system, and neuropathic pain. Comparing the disability caused by conditions with episodic occurrence versus those that cause permanent and progressive disease will remain challenging because the effects on the individuals vary substantially.”
The study was funded by the Bill and Melinda Gates Foundation. Full disclosures are included in the original article.
A version of this article appeared on Medscape.com.
FROM THE LANCET NEUROLOGY
Social Frailty Linked to Risk for Predementia Syndrome
TOPLINE:
Social frailty, the lack of resources to meet basic social needs, is associated with an increased risk for motoric cognitive risk syndrome (MCR), a predementia syndrome characterized by cognitive complaints and slow gait, results of a large, population-based study suggested.
METHODOLOGY:
- The study used 2011 (Round 1) to 2018 (Round 8) data on a discovery sample of 4657 individuals without MCR or dementia at baseline from the National Health and Aging Trends Study (NHATS), a longitudinal survey of older adult Medicare beneficiaries.
- Researchers also collected data on 3075 newly recruited individuals in Round 5 and followed to Round 8 as an independent validation sample to create a pooled sample of 7732 older adults, mean age 76.06, without MCR at baseline.
- Social frailty, assessed at baseline, included five social items: Going out less, not feeling confident, rarely visiting friends/family, not talking with others, and without live-in partner/spouse (researchers divided participants into normal [zero to one items] and social frailty [two to five items] groups).
- Individuals were considered to have MCR if they had both subjective cognitive complaints and slow gait speed (greater than 1 standard deviation below age-specific level) without dementia or mobility disability.
- Covariates included demographic and lifestyle data, presence of depression and/or anxiety symptoms, and number of chronic diseases.
TAKEAWAY:
- During a median follow-up period of 4 years, 10.35% individuals were diagnosed with MCR.
- After the researchers controlled for confounding factors, those with social frailty had an increased risk for MCR compared with the normal group (pooled sample: hazard ratio [HR], 1.57; 95% CI, 1.34-1.84; P < .001).
- Each additional unfavorable social item was associated with an increased risk for MCR (pooled sample: HR, 1.32; 95% CI, 1.22-1.43; P < .001).
- Results of stratified analyses across subgroups suggested individuals with social frailty had a significantly higher risk for incident MCR than that of those without social frailty, regardless of socioeconomic status, lifestyle factors, chronic diseases, and mental health.
IN PRACTICE:
The findings suggest assessing social frailty using simple questions “is an efficient tool for detecting older individuals with a high risk of MCR,” the authors wrote. They noted that the addition of such a tool in clinical practice may facilitate “timely implementation of prevention strategies.”
SOURCE:
The research was led by Hui Zhang, Human Phenome Institute, Zhangjiang Fudan International Innovation Centre, Fudan University, Shanghai, China. It was published online on January 29, 2024, in Alzheimer’s & Dementia.
LIMITATIONS:
The study was observational, so the association between social frailty and MCR is merely correlational. Due to the lack of genetic information in NHATS data, researchers didn’t evaluate the effect of genetic factors such as apolipoprotein E on the association between social frailty and MCR. Social frailty was assessed at a single time point. In addition, the researchers were unable examine the time sequence between social frailty and MCR and so could not determine the cause of this association.
DISCLOSURES:
The study was supported by the National Natural Science Foundation of China-Youth Science Fund, Shanghai Rising-Star Program, Shanghai Municipal Health Commission and Key Discipline Construction Project of Pudong Health, and Family Planning Commission of Shanghai. The authors reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Social frailty, the lack of resources to meet basic social needs, is associated with an increased risk for motoric cognitive risk syndrome (MCR), a predementia syndrome characterized by cognitive complaints and slow gait, results of a large, population-based study suggested.
METHODOLOGY:
- The study used 2011 (Round 1) to 2018 (Round 8) data on a discovery sample of 4657 individuals without MCR or dementia at baseline from the National Health and Aging Trends Study (NHATS), a longitudinal survey of older adult Medicare beneficiaries.
- Researchers also collected data on 3075 newly recruited individuals in Round 5 and followed to Round 8 as an independent validation sample to create a pooled sample of 7732 older adults, mean age 76.06, without MCR at baseline.
- Social frailty, assessed at baseline, included five social items: Going out less, not feeling confident, rarely visiting friends/family, not talking with others, and without live-in partner/spouse (researchers divided participants into normal [zero to one items] and social frailty [two to five items] groups).
- Individuals were considered to have MCR if they had both subjective cognitive complaints and slow gait speed (greater than 1 standard deviation below age-specific level) without dementia or mobility disability.
- Covariates included demographic and lifestyle data, presence of depression and/or anxiety symptoms, and number of chronic diseases.
TAKEAWAY:
- During a median follow-up period of 4 years, 10.35% individuals were diagnosed with MCR.
- After the researchers controlled for confounding factors, those with social frailty had an increased risk for MCR compared with the normal group (pooled sample: hazard ratio [HR], 1.57; 95% CI, 1.34-1.84; P < .001).
- Each additional unfavorable social item was associated with an increased risk for MCR (pooled sample: HR, 1.32; 95% CI, 1.22-1.43; P < .001).
- Results of stratified analyses across subgroups suggested individuals with social frailty had a significantly higher risk for incident MCR than that of those without social frailty, regardless of socioeconomic status, lifestyle factors, chronic diseases, and mental health.
IN PRACTICE:
The findings suggest assessing social frailty using simple questions “is an efficient tool for detecting older individuals with a high risk of MCR,” the authors wrote. They noted that the addition of such a tool in clinical practice may facilitate “timely implementation of prevention strategies.”
SOURCE:
The research was led by Hui Zhang, Human Phenome Institute, Zhangjiang Fudan International Innovation Centre, Fudan University, Shanghai, China. It was published online on January 29, 2024, in Alzheimer’s & Dementia.
LIMITATIONS:
The study was observational, so the association between social frailty and MCR is merely correlational. Due to the lack of genetic information in NHATS data, researchers didn’t evaluate the effect of genetic factors such as apolipoprotein E on the association between social frailty and MCR. Social frailty was assessed at a single time point. In addition, the researchers were unable examine the time sequence between social frailty and MCR and so could not determine the cause of this association.
DISCLOSURES:
The study was supported by the National Natural Science Foundation of China-Youth Science Fund, Shanghai Rising-Star Program, Shanghai Municipal Health Commission and Key Discipline Construction Project of Pudong Health, and Family Planning Commission of Shanghai. The authors reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Social frailty, the lack of resources to meet basic social needs, is associated with an increased risk for motoric cognitive risk syndrome (MCR), a predementia syndrome characterized by cognitive complaints and slow gait, results of a large, population-based study suggested.
METHODOLOGY:
- The study used 2011 (Round 1) to 2018 (Round 8) data on a discovery sample of 4657 individuals without MCR or dementia at baseline from the National Health and Aging Trends Study (NHATS), a longitudinal survey of older adult Medicare beneficiaries.
- Researchers also collected data on 3075 newly recruited individuals in Round 5 and followed to Round 8 as an independent validation sample to create a pooled sample of 7732 older adults, mean age 76.06, without MCR at baseline.
- Social frailty, assessed at baseline, included five social items: Going out less, not feeling confident, rarely visiting friends/family, not talking with others, and without live-in partner/spouse (researchers divided participants into normal [zero to one items] and social frailty [two to five items] groups).
- Individuals were considered to have MCR if they had both subjective cognitive complaints and slow gait speed (greater than 1 standard deviation below age-specific level) without dementia or mobility disability.
- Covariates included demographic and lifestyle data, presence of depression and/or anxiety symptoms, and number of chronic diseases.
TAKEAWAY:
- During a median follow-up period of 4 years, 10.35% individuals were diagnosed with MCR.
- After the researchers controlled for confounding factors, those with social frailty had an increased risk for MCR compared with the normal group (pooled sample: hazard ratio [HR], 1.57; 95% CI, 1.34-1.84; P < .001).
- Each additional unfavorable social item was associated with an increased risk for MCR (pooled sample: HR, 1.32; 95% CI, 1.22-1.43; P < .001).
- Results of stratified analyses across subgroups suggested individuals with social frailty had a significantly higher risk for incident MCR than that of those without social frailty, regardless of socioeconomic status, lifestyle factors, chronic diseases, and mental health.
IN PRACTICE:
The findings suggest assessing social frailty using simple questions “is an efficient tool for detecting older individuals with a high risk of MCR,” the authors wrote. They noted that the addition of such a tool in clinical practice may facilitate “timely implementation of prevention strategies.”
SOURCE:
The research was led by Hui Zhang, Human Phenome Institute, Zhangjiang Fudan International Innovation Centre, Fudan University, Shanghai, China. It was published online on January 29, 2024, in Alzheimer’s & Dementia.
LIMITATIONS:
The study was observational, so the association between social frailty and MCR is merely correlational. Due to the lack of genetic information in NHATS data, researchers didn’t evaluate the effect of genetic factors such as apolipoprotein E on the association between social frailty and MCR. Social frailty was assessed at a single time point. In addition, the researchers were unable examine the time sequence between social frailty and MCR and so could not determine the cause of this association.
DISCLOSURES:
The study was supported by the National Natural Science Foundation of China-Youth Science Fund, Shanghai Rising-Star Program, Shanghai Municipal Health Commission and Key Discipline Construction Project of Pudong Health, and Family Planning Commission of Shanghai. The authors reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Robotic Garment Improves Stride in Patient With Parkinson’s Disease
A wearable, soft, robotic device could help patients with Parkinson’s disease (PD) walk without experiencing freezing of gait (FoG), early research suggested.
The robotic apparel, worn around the hips and thighs, gently pushes the hips as the leg swings, facilitating a longer stride and preventing FoG, a common disorder in PD that affects nearly all patients over the disease course.
The small, proof-of-concept study included one person with PD. But investigators noted the reduction in freezing and falls and improvement in walking distance and speed was dramatic. Incidence of FoG decreased from 63% to just 6% when the patient wore the robotic garment outdoors. Wearing the device indoors eliminated freezing altogether.
“We demonstrate proof-of-concept that FoG can be averted using a soft robotic device — a machine that aims to apply physical assistance to movement with minimal restriction, a fundamentally different approach to rigid exoskeletons,” lead investigators Conor Walsh, PhD, and Terry Ellis, PhD, PT, told this news organization.
Walsh is a professor at Harvard John A. Paulson School of Engineering and Applied Sciences in Boston, and Ellis is a professor and chair of the physical therapy department and director of the Center for Neurorehabilitation, Boston University, Boston, Massachusetts.
The study was published online on January 5, 2024, in Nature Medicine.
Disabling Disturbance
From a biomechanical perspective, FoG is manifested by an overt breakdown in spatial and temporal mechanics of walking. The impaired limb coordination occurs during the “swing phase” of the gait cycle.
There are currently no interventions that prevent FoG. Available treatment interventions include pharmacotherapy, such as dopamine replacement; deep brain stimulation (DBS) of the subthalamic nucleus; and behavioral interventions, such as cueing strategies. All have shown only modest effects in reducing FoG and, in some cases, might even worsen it, the investigators noted.
“This challenge led us to become interested in leveraging soft wearable robots to deliver mechanical cues to disrupt aberrant gait mechanics and prevent FOG in people with PD,” Dr. Walsh and Dr. Ellis said.
“Wearable robots” have been used to augment kinematics in neurologic conditions, such as stroke, cerebral palsy, and spinal cord injury. Harnessing this technology to address FoG required “a collaboration between engineers, rehabilitation scientists, physical therapists, biomechanists, and apparel designers,” the researchers said.
The wearable robotic device uses cable-driven actuators, which enable physical movement by converting electrical energy into mechanical force, and sensors worn around the waist and thighs. Using motion data collected by the sensors, algorithms estimate the phase of the walking cycle and generate assistive forces in concert with biological muscles.
Real-World Testing
The researchers tested the robotic garment on a 73-year-old man with idiopathic PD of 10-year duration. The man’s ongoing pharmacologic treatment included 1.5 tablets of 25- to 100-mg carbidopa/levodopa taken four times per day, one tablet of 100-mg amantadine twice per day, and one tablet of 200-mg entacapone taken four times per day.
He had also undergone DBS to the globus pallidus internus and utilized behavioral strategies. Despite these interventions, he continued to endure more than 10 episodes of FoG per day and numerous falls.
The patient tended to use walls to stabilize himself when walking. Freezing episodes were observed mostly when he walked in open hallways, turned, walked outdoors, and when he tried to walk and talk simultaneously.
The research was conducted over a 6-month period, with a total of five study sessions that consisted of walking trials. Four were administered in the laboratory. The fifth was conducted in a real-world outdoor community setting.
During the first visit, a biomechanical analysis of walking was performed under single-task conditions during the medication-on phase.
Testing was usually conducted during medication-on phase and under single-task conditions. But testing conditions also included attention-demanding dual tasks and single-task walking during the medication-off phase.
The researchers compared the effects of the assistance of the robotic apparel to no apparel and with the apparel turned off. They measured the percentage of time spent freezing and the total distance walked.
Robust Response
The participant demonstrated a “robust response” to the robotic apparel. With the garment’s assistance, FoG was eliminated when worn indoors, and walking distance increased by 55%. The participant walked faster and had a 25% reduction in gait variability.
These beneficial effects were repeated across multiple days as well as different types of provoking conditions and environmental contexts. When the device was tried outdoors, FoG decreased from 63% to 6% of the time. The patient was also able to simultaneously walk and talk without freezing.
“When the device assisted with hip flexion during the terminal stance phase of walking (when lifting the toe), FoG was instantaneously eliminated during inner walking, accompanied by clinically significant improvement in walking speeds and distance,” Dr. Walsh and Dr. Ellis reported.
The approach “suggests the potential benefits of a ‘bottom-up’ rather than a ‘top-down’ solution to treating gait freezing,” they commented. “We see that restoring almost-normal biomechanics alters the peripheral dynamics of gait and may influence the central processing of gait control.”
Bringing Hope
Rebecca Gilbert MD, PhD, chief mission officer, American Parkinson Disease Association, said this new approach is “exciting.”
Whether the benefits will be as robust in other people with PD “remains to be seen,” said Dr. Gilbert, who was not involved with the study.
“The paper states that multiple experimental variables utilizing the device could potentially be adjusted to serve different people with PD, and these will need to be tested in clinical trials as well,” Dr. Gilbert said.
Additionally, “the device itself is complex and may be challenging to get on and off without help, which may limit its usability in the community,” Dr. Gilbert noted.
Although more work is needed, the study “represents a remarkable proof of concept that brings hope to those with FoG,” she added.
These “promising findings prompt further investigation to validate the effects of the robotic apparel on a broader range of individuals with PD experiencing FoG and across various FoG phenotypes and environments and task contexts, complemented with FoG metrics that include quantification of the severity of the freezing episodes,” Walsh and Ellis added.
This study was based on work supported by the National Science Foundation, the National Institutes of Health, and the Massachusetts Technology Collaborative, Collaborative Research and Development Matching Grant. This work was also partially funded by the John A. Paulson School of Engineering and Applied Sciences at Harvard University as well as received financial support from the Samsung Scholarship.
A version of this article appeared on Medscape.com.
A wearable, soft, robotic device could help patients with Parkinson’s disease (PD) walk without experiencing freezing of gait (FoG), early research suggested.
The robotic apparel, worn around the hips and thighs, gently pushes the hips as the leg swings, facilitating a longer stride and preventing FoG, a common disorder in PD that affects nearly all patients over the disease course.
The small, proof-of-concept study included one person with PD. But investigators noted the reduction in freezing and falls and improvement in walking distance and speed was dramatic. Incidence of FoG decreased from 63% to just 6% when the patient wore the robotic garment outdoors. Wearing the device indoors eliminated freezing altogether.
“We demonstrate proof-of-concept that FoG can be averted using a soft robotic device — a machine that aims to apply physical assistance to movement with minimal restriction, a fundamentally different approach to rigid exoskeletons,” lead investigators Conor Walsh, PhD, and Terry Ellis, PhD, PT, told this news organization.
Walsh is a professor at Harvard John A. Paulson School of Engineering and Applied Sciences in Boston, and Ellis is a professor and chair of the physical therapy department and director of the Center for Neurorehabilitation, Boston University, Boston, Massachusetts.
The study was published online on January 5, 2024, in Nature Medicine.
Disabling Disturbance
From a biomechanical perspective, FoG is manifested by an overt breakdown in spatial and temporal mechanics of walking. The impaired limb coordination occurs during the “swing phase” of the gait cycle.
There are currently no interventions that prevent FoG. Available treatment interventions include pharmacotherapy, such as dopamine replacement; deep brain stimulation (DBS) of the subthalamic nucleus; and behavioral interventions, such as cueing strategies. All have shown only modest effects in reducing FoG and, in some cases, might even worsen it, the investigators noted.
“This challenge led us to become interested in leveraging soft wearable robots to deliver mechanical cues to disrupt aberrant gait mechanics and prevent FOG in people with PD,” Dr. Walsh and Dr. Ellis said.
“Wearable robots” have been used to augment kinematics in neurologic conditions, such as stroke, cerebral palsy, and spinal cord injury. Harnessing this technology to address FoG required “a collaboration between engineers, rehabilitation scientists, physical therapists, biomechanists, and apparel designers,” the researchers said.
The wearable robotic device uses cable-driven actuators, which enable physical movement by converting electrical energy into mechanical force, and sensors worn around the waist and thighs. Using motion data collected by the sensors, algorithms estimate the phase of the walking cycle and generate assistive forces in concert with biological muscles.
Real-World Testing
The researchers tested the robotic garment on a 73-year-old man with idiopathic PD of 10-year duration. The man’s ongoing pharmacologic treatment included 1.5 tablets of 25- to 100-mg carbidopa/levodopa taken four times per day, one tablet of 100-mg amantadine twice per day, and one tablet of 200-mg entacapone taken four times per day.
He had also undergone DBS to the globus pallidus internus and utilized behavioral strategies. Despite these interventions, he continued to endure more than 10 episodes of FoG per day and numerous falls.
The patient tended to use walls to stabilize himself when walking. Freezing episodes were observed mostly when he walked in open hallways, turned, walked outdoors, and when he tried to walk and talk simultaneously.
The research was conducted over a 6-month period, with a total of five study sessions that consisted of walking trials. Four were administered in the laboratory. The fifth was conducted in a real-world outdoor community setting.
During the first visit, a biomechanical analysis of walking was performed under single-task conditions during the medication-on phase.
Testing was usually conducted during medication-on phase and under single-task conditions. But testing conditions also included attention-demanding dual tasks and single-task walking during the medication-off phase.
The researchers compared the effects of the assistance of the robotic apparel to no apparel and with the apparel turned off. They measured the percentage of time spent freezing and the total distance walked.
Robust Response
The participant demonstrated a “robust response” to the robotic apparel. With the garment’s assistance, FoG was eliminated when worn indoors, and walking distance increased by 55%. The participant walked faster and had a 25% reduction in gait variability.
These beneficial effects were repeated across multiple days as well as different types of provoking conditions and environmental contexts. When the device was tried outdoors, FoG decreased from 63% to 6% of the time. The patient was also able to simultaneously walk and talk without freezing.
“When the device assisted with hip flexion during the terminal stance phase of walking (when lifting the toe), FoG was instantaneously eliminated during inner walking, accompanied by clinically significant improvement in walking speeds and distance,” Dr. Walsh and Dr. Ellis reported.
The approach “suggests the potential benefits of a ‘bottom-up’ rather than a ‘top-down’ solution to treating gait freezing,” they commented. “We see that restoring almost-normal biomechanics alters the peripheral dynamics of gait and may influence the central processing of gait control.”
Bringing Hope
Rebecca Gilbert MD, PhD, chief mission officer, American Parkinson Disease Association, said this new approach is “exciting.”
Whether the benefits will be as robust in other people with PD “remains to be seen,” said Dr. Gilbert, who was not involved with the study.
“The paper states that multiple experimental variables utilizing the device could potentially be adjusted to serve different people with PD, and these will need to be tested in clinical trials as well,” Dr. Gilbert said.
Additionally, “the device itself is complex and may be challenging to get on and off without help, which may limit its usability in the community,” Dr. Gilbert noted.
Although more work is needed, the study “represents a remarkable proof of concept that brings hope to those with FoG,” she added.
These “promising findings prompt further investigation to validate the effects of the robotic apparel on a broader range of individuals with PD experiencing FoG and across various FoG phenotypes and environments and task contexts, complemented with FoG metrics that include quantification of the severity of the freezing episodes,” Walsh and Ellis added.
This study was based on work supported by the National Science Foundation, the National Institutes of Health, and the Massachusetts Technology Collaborative, Collaborative Research and Development Matching Grant. This work was also partially funded by the John A. Paulson School of Engineering and Applied Sciences at Harvard University as well as received financial support from the Samsung Scholarship.
A version of this article appeared on Medscape.com.
A wearable, soft, robotic device could help patients with Parkinson’s disease (PD) walk without experiencing freezing of gait (FoG), early research suggested.
The robotic apparel, worn around the hips and thighs, gently pushes the hips as the leg swings, facilitating a longer stride and preventing FoG, a common disorder in PD that affects nearly all patients over the disease course.
The small, proof-of-concept study included one person with PD. But investigators noted the reduction in freezing and falls and improvement in walking distance and speed was dramatic. Incidence of FoG decreased from 63% to just 6% when the patient wore the robotic garment outdoors. Wearing the device indoors eliminated freezing altogether.
“We demonstrate proof-of-concept that FoG can be averted using a soft robotic device — a machine that aims to apply physical assistance to movement with minimal restriction, a fundamentally different approach to rigid exoskeletons,” lead investigators Conor Walsh, PhD, and Terry Ellis, PhD, PT, told this news organization.
Walsh is a professor at Harvard John A. Paulson School of Engineering and Applied Sciences in Boston, and Ellis is a professor and chair of the physical therapy department and director of the Center for Neurorehabilitation, Boston University, Boston, Massachusetts.
The study was published online on January 5, 2024, in Nature Medicine.
Disabling Disturbance
From a biomechanical perspective, FoG is manifested by an overt breakdown in spatial and temporal mechanics of walking. The impaired limb coordination occurs during the “swing phase” of the gait cycle.
There are currently no interventions that prevent FoG. Available treatment interventions include pharmacotherapy, such as dopamine replacement; deep brain stimulation (DBS) of the subthalamic nucleus; and behavioral interventions, such as cueing strategies. All have shown only modest effects in reducing FoG and, in some cases, might even worsen it, the investigators noted.
“This challenge led us to become interested in leveraging soft wearable robots to deliver mechanical cues to disrupt aberrant gait mechanics and prevent FOG in people with PD,” Dr. Walsh and Dr. Ellis said.
“Wearable robots” have been used to augment kinematics in neurologic conditions, such as stroke, cerebral palsy, and spinal cord injury. Harnessing this technology to address FoG required “a collaboration between engineers, rehabilitation scientists, physical therapists, biomechanists, and apparel designers,” the researchers said.
The wearable robotic device uses cable-driven actuators, which enable physical movement by converting electrical energy into mechanical force, and sensors worn around the waist and thighs. Using motion data collected by the sensors, algorithms estimate the phase of the walking cycle and generate assistive forces in concert with biological muscles.
Real-World Testing
The researchers tested the robotic garment on a 73-year-old man with idiopathic PD of 10-year duration. The man’s ongoing pharmacologic treatment included 1.5 tablets of 25- to 100-mg carbidopa/levodopa taken four times per day, one tablet of 100-mg amantadine twice per day, and one tablet of 200-mg entacapone taken four times per day.
He had also undergone DBS to the globus pallidus internus and utilized behavioral strategies. Despite these interventions, he continued to endure more than 10 episodes of FoG per day and numerous falls.
The patient tended to use walls to stabilize himself when walking. Freezing episodes were observed mostly when he walked in open hallways, turned, walked outdoors, and when he tried to walk and talk simultaneously.
The research was conducted over a 6-month period, with a total of five study sessions that consisted of walking trials. Four were administered in the laboratory. The fifth was conducted in a real-world outdoor community setting.
During the first visit, a biomechanical analysis of walking was performed under single-task conditions during the medication-on phase.
Testing was usually conducted during medication-on phase and under single-task conditions. But testing conditions also included attention-demanding dual tasks and single-task walking during the medication-off phase.
The researchers compared the effects of the assistance of the robotic apparel to no apparel and with the apparel turned off. They measured the percentage of time spent freezing and the total distance walked.
Robust Response
The participant demonstrated a “robust response” to the robotic apparel. With the garment’s assistance, FoG was eliminated when worn indoors, and walking distance increased by 55%. The participant walked faster and had a 25% reduction in gait variability.
These beneficial effects were repeated across multiple days as well as different types of provoking conditions and environmental contexts. When the device was tried outdoors, FoG decreased from 63% to 6% of the time. The patient was also able to simultaneously walk and talk without freezing.
“When the device assisted with hip flexion during the terminal stance phase of walking (when lifting the toe), FoG was instantaneously eliminated during inner walking, accompanied by clinically significant improvement in walking speeds and distance,” Dr. Walsh and Dr. Ellis reported.
The approach “suggests the potential benefits of a ‘bottom-up’ rather than a ‘top-down’ solution to treating gait freezing,” they commented. “We see that restoring almost-normal biomechanics alters the peripheral dynamics of gait and may influence the central processing of gait control.”
Bringing Hope
Rebecca Gilbert MD, PhD, chief mission officer, American Parkinson Disease Association, said this new approach is “exciting.”
Whether the benefits will be as robust in other people with PD “remains to be seen,” said Dr. Gilbert, who was not involved with the study.
“The paper states that multiple experimental variables utilizing the device could potentially be adjusted to serve different people with PD, and these will need to be tested in clinical trials as well,” Dr. Gilbert said.
Additionally, “the device itself is complex and may be challenging to get on and off without help, which may limit its usability in the community,” Dr. Gilbert noted.
Although more work is needed, the study “represents a remarkable proof of concept that brings hope to those with FoG,” she added.
These “promising findings prompt further investigation to validate the effects of the robotic apparel on a broader range of individuals with PD experiencing FoG and across various FoG phenotypes and environments and task contexts, complemented with FoG metrics that include quantification of the severity of the freezing episodes,” Walsh and Ellis added.
This study was based on work supported by the National Science Foundation, the National Institutes of Health, and the Massachusetts Technology Collaborative, Collaborative Research and Development Matching Grant. This work was also partially funded by the John A. Paulson School of Engineering and Applied Sciences at Harvard University as well as received financial support from the Samsung Scholarship.
A version of this article appeared on Medscape.com.
Excessive TV-watching tied to elevated risk for dementia, Parkinson’s disease, and depression
TOPLINE:
whereas a limited amount of daily computer use that is not work-related is linked to a lower risk for dementia.
METHODOLOGY:
- Investigators analyzed data on 473,184 people aged 39-72 years from the UK Biobank who were enrolled from 2006 to 2010 and followed until a diagnosis of dementia, PD, depression, death, or study end (2018 for Wales residents; 2021 for residents of England and Scotland).
- Participants reported on the number of hours they spent outside of work exercising, watching television, and using the computer.
- MRI was conducted to determine participants’ brain volume.
TAKEAWAY:
- During the study, 6096 people developed dementia, 3000 developed PD, 23,600 developed depression, 1200 developed dementia and depression, and 486 developed PD and depression.
- Compared with those who watched TV for under 1 hour per day, those who reported watching 4 or more hours per day had a 28% higher risk for dementia (adjusted hazard ratio [aHR], 1.28; 95% CI, 1.17-1.39), a 35% higher risk for depression, (aHR, 1.35; 95% CI, 1.29-1.40) and a 16% greater risk for PD (aHR, 1.16; 95% CI, 1.03-1.29).
- However, moderate computer use outside of work seemed somewhat protective. Participants who used the computer for 30-60 minutes per day had lower risks for dementia (aHR, 0.68; 95% CI, 0.64-0.72), PD, (aHR, 0.86; 95% CI, 0.79-0.93), and depression (aHR, 0.85; 95% CI, 0.83-0.88) compared with those who reported the lowest levels of computer usage.
- Replacing 30 minutes per day of computer time with an equal amount of structured exercise was associated with decreased risk for dementia (aHR, 0.74; 95% CI, 0.85-0.95) and PD (aHR, 0.84; 95% CI, 0.78-0.90).
IN PRACTICE:
The association between extended periods of TV use and higher risk for PD and dementia could be explained by a lack of activity, the authors note. They add that sedentary behavior is, “associated with biomarkers of low-grade inflammation and changes in inflammation markers that could initiate and or worsen neuroinflammation and contribute to neurodegeneration.”
SOURCE:
Hanzhang Wu, PhD, of Tianjin University of Traditional Medicine in Tianjin, China, led the study, which was published online in the International Journal of Behavioral Nutrition and Physical Activity.
LIMITATIONS:
Screen behaviors were assessed using self-report measures, which is subject to recall bias. Also, there may have been variables confounding the findings for which investigators did not account.
DISCLOSURES:
The study was funded by the National Natural Science Foundation of China, the Tianjin Major Public Health Science and Technology Project, the National Health Commission of China, the Food Science and Technology Foundation of Chinese Institute of Food Science and Technology, the China Cohort Consortium, and the Chinese Nutrition Society Nutrition Research Foundation–DSM Research Fund, China. There were no disclosures reported.
Eve Bender has no relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
whereas a limited amount of daily computer use that is not work-related is linked to a lower risk for dementia.
METHODOLOGY:
- Investigators analyzed data on 473,184 people aged 39-72 years from the UK Biobank who were enrolled from 2006 to 2010 and followed until a diagnosis of dementia, PD, depression, death, or study end (2018 for Wales residents; 2021 for residents of England and Scotland).
- Participants reported on the number of hours they spent outside of work exercising, watching television, and using the computer.
- MRI was conducted to determine participants’ brain volume.
TAKEAWAY:
- During the study, 6096 people developed dementia, 3000 developed PD, 23,600 developed depression, 1200 developed dementia and depression, and 486 developed PD and depression.
- Compared with those who watched TV for under 1 hour per day, those who reported watching 4 or more hours per day had a 28% higher risk for dementia (adjusted hazard ratio [aHR], 1.28; 95% CI, 1.17-1.39), a 35% higher risk for depression, (aHR, 1.35; 95% CI, 1.29-1.40) and a 16% greater risk for PD (aHR, 1.16; 95% CI, 1.03-1.29).
- However, moderate computer use outside of work seemed somewhat protective. Participants who used the computer for 30-60 minutes per day had lower risks for dementia (aHR, 0.68; 95% CI, 0.64-0.72), PD, (aHR, 0.86; 95% CI, 0.79-0.93), and depression (aHR, 0.85; 95% CI, 0.83-0.88) compared with those who reported the lowest levels of computer usage.
- Replacing 30 minutes per day of computer time with an equal amount of structured exercise was associated with decreased risk for dementia (aHR, 0.74; 95% CI, 0.85-0.95) and PD (aHR, 0.84; 95% CI, 0.78-0.90).
IN PRACTICE:
The association between extended periods of TV use and higher risk for PD and dementia could be explained by a lack of activity, the authors note. They add that sedentary behavior is, “associated with biomarkers of low-grade inflammation and changes in inflammation markers that could initiate and or worsen neuroinflammation and contribute to neurodegeneration.”
SOURCE:
Hanzhang Wu, PhD, of Tianjin University of Traditional Medicine in Tianjin, China, led the study, which was published online in the International Journal of Behavioral Nutrition and Physical Activity.
LIMITATIONS:
Screen behaviors were assessed using self-report measures, which is subject to recall bias. Also, there may have been variables confounding the findings for which investigators did not account.
DISCLOSURES:
The study was funded by the National Natural Science Foundation of China, the Tianjin Major Public Health Science and Technology Project, the National Health Commission of China, the Food Science and Technology Foundation of Chinese Institute of Food Science and Technology, the China Cohort Consortium, and the Chinese Nutrition Society Nutrition Research Foundation–DSM Research Fund, China. There were no disclosures reported.
Eve Bender has no relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
whereas a limited amount of daily computer use that is not work-related is linked to a lower risk for dementia.
METHODOLOGY:
- Investigators analyzed data on 473,184 people aged 39-72 years from the UK Biobank who were enrolled from 2006 to 2010 and followed until a diagnosis of dementia, PD, depression, death, or study end (2018 for Wales residents; 2021 for residents of England and Scotland).
- Participants reported on the number of hours they spent outside of work exercising, watching television, and using the computer.
- MRI was conducted to determine participants’ brain volume.
TAKEAWAY:
- During the study, 6096 people developed dementia, 3000 developed PD, 23,600 developed depression, 1200 developed dementia and depression, and 486 developed PD and depression.
- Compared with those who watched TV for under 1 hour per day, those who reported watching 4 or more hours per day had a 28% higher risk for dementia (adjusted hazard ratio [aHR], 1.28; 95% CI, 1.17-1.39), a 35% higher risk for depression, (aHR, 1.35; 95% CI, 1.29-1.40) and a 16% greater risk for PD (aHR, 1.16; 95% CI, 1.03-1.29).
- However, moderate computer use outside of work seemed somewhat protective. Participants who used the computer for 30-60 minutes per day had lower risks for dementia (aHR, 0.68; 95% CI, 0.64-0.72), PD, (aHR, 0.86; 95% CI, 0.79-0.93), and depression (aHR, 0.85; 95% CI, 0.83-0.88) compared with those who reported the lowest levels of computer usage.
- Replacing 30 minutes per day of computer time with an equal amount of structured exercise was associated with decreased risk for dementia (aHR, 0.74; 95% CI, 0.85-0.95) and PD (aHR, 0.84; 95% CI, 0.78-0.90).
IN PRACTICE:
The association between extended periods of TV use and higher risk for PD and dementia could be explained by a lack of activity, the authors note. They add that sedentary behavior is, “associated with biomarkers of low-grade inflammation and changes in inflammation markers that could initiate and or worsen neuroinflammation and contribute to neurodegeneration.”
SOURCE:
Hanzhang Wu, PhD, of Tianjin University of Traditional Medicine in Tianjin, China, led the study, which was published online in the International Journal of Behavioral Nutrition and Physical Activity.
LIMITATIONS:
Screen behaviors were assessed using self-report measures, which is subject to recall bias. Also, there may have been variables confounding the findings for which investigators did not account.
DISCLOSURES:
The study was funded by the National Natural Science Foundation of China, the Tianjin Major Public Health Science and Technology Project, the National Health Commission of China, the Food Science and Technology Foundation of Chinese Institute of Food Science and Technology, the China Cohort Consortium, and the Chinese Nutrition Society Nutrition Research Foundation–DSM Research Fund, China. There were no disclosures reported.
Eve Bender has no relevant financial relationships.
A version of this article appeared on Medscape.com.
Spinal cord stimulator restores Parkinson patient’s gait
The neuroprosthesis involves targeted epidural electrical stimulation of areas of the lumbosacral spinal cord that produce walking.
This new therapeutic tool offers hope to patients with PD and, combined with existing approaches, may alleviate a motor sign in PD for which there is currently “no real solution,” study investigator Eduardo Martin Moraud, PhD, who leads PD research at the Defitech Center for Interventional Neurotherapies (NeuroRestore), Lausanne, Switzerland, said in an interview.
“This is exciting for the many patients that develop gait deficits and experience frequent falls, who can only rely on physical therapy to try and minimize the consequences,” he added.
The findings were published online in Nature Medicine.
Personalized stimulation
About 90% of people with advanced PD experience gait and balance problems or freezing-of-gait episodes. These locomotor deficits typically don’t respond well to dopamine replacement therapy or deep brain stimulation (DBS) of the subthalamic nucleus, possibly because the neural origins of these motor problems involve brain circuits not related to dopamine, said Dr. Moraud.
Continuous electrical stimulation over the cervical or thoracic segments of the spinal cord reduces locomotor deficits in some people with PD, but the broader application of this strategy has led to variable and unsatisfying outcomes.
The new approach focuses on correcting abnormal activation of circuits in the lumbar spinal cord, a region that hosts all the neurons that control activation of the leg muscles used for walking.
The stimulating device is placed on the lumbar region of the spinal cord, which sends messages to leg muscles. It is wired to a small impulse generator implanted under the skin of the abdomen. Sensors placed in shoes align the stimulation to the patient’s movement.
The system can detect the beginning of a movement, immediately activate the appropriate electrode, and so facilitate the necessary movement, be that leg flexion, extension, or propulsion, said Dr. Moraud. “This allows for increased walking symmetry, reinforced balance, and increased length of steps.”
The concept of this neuroprosthesis is similar to that used to allow patients with a spinal cord injury (SCI) to walk. But unlike patients with SCI, those with PD can move their legs, indicating that there is a descending command from the brain that needs to interact with the stimulation of the spinal cord, and patients with PD can feel the stimulation.
“Both these elements imply that amplitudes of stimulation need to be much lower in PD than SCI, and that stimulation needs to be fully personalized in PD to synergistically interact with the descending commands from the brain.”
After fine-tuning this new neuroprosthesis in animal models, researchers implanted the device in a 62-year-old man with a 30-year history of PD who presented with severe gait impairments, including marked gait asymmetry, reduced stride length, and balance problems.
Gait restored to near normal
The patient had frequent freezing-of-gait episodes when turning and passing through narrow paths, which led to multiple falls a day. This was despite being treated with DBS and dopaminergic replacement therapies.
But after getting used to the neuroprosthesis, the patient now walks with a gait akin to that of people without PD.
“Our experience in the preclinical animal models and this first patient is that gait can be restored to an almost healthy level, but this, of course, may vary across patients, depending on the severity of their disease progression, and their other motor deficits,” said Dr. Moraud.
When the neuroprosthesis is turned on, freezing of gait nearly vanishes, both with and without DBS.
In addition, the neuroprosthesis augmented the impact of the patient’s rehabilitation program, which involved a variety of regular exercises, including walking on basic and complex terrains, navigating outdoors in community settings, balance training, and basic physical therapy.
Frequent use of the neuroprosthesis during gait rehabilitation also translated into “highly improved” quality of life as reported by the patient (and his wife), said Dr. Moraud.
The patient has now been using the neuroprosthesis about 8 hours a day for nearly 2 years, only switching it off when sitting for long periods of time or while sleeping.
“He regained the capacity to walk in complex or crowded environments such as shops, airports, or his own home, without falling,” said Dr. Moraud. “He went from falling five to six times per day to one or two [falls] every couple of weeks. He’s also much more confident. He can walk for many miles, run, and go on holidays, without the constant fear of falling and having related injuries.”
Dr. Moraud stressed that the device does not replace DBS, which is a “key therapy” that addresses other deficits in PD, such as rigidity or slowness of movement. “What we propose here is a fully complementary approach for the gait problems that are not well addressed by DBS.”
One of the next steps will be to evaluate the efficacy of this approach across a wider spectrum of patient profiles to fully define the best responders, said Dr. Moraud.
A ‘tour de force’
In a comment, Michael S. Okun, MD, director of the Norman Fixel Institute for Neurological Diseases, University of Florida, Gainesville, and medical director of the Parkinson’s Foundation, noted that the researchers used “a smarter device” than past approaches that failed to adequately address progressive walking challenges of patients with PD.
Although it’s “tempting to get excited” about the findings, it’s important to consider that the study included only one human subject and did not target circuits for both walking and balance, said Dr. Okun. “It’s possible that even if future studies revealed a benefit for walking, the device may or may not address falling.”
In an accompanying editorial, Aviv Mizrahi-Kliger, MD, PhD, department of neurology, University of California, San Francisco, and Karunesh Ganguly, MD, PhD, Neurology and Rehabilitation Service, San Francisco Veterans Affairs Health Care System, called the study an “impressive tour de force,” with data from the nonhuman primate model and the individual with PD “jointly” indicating that epidural electrical stimulation (EES) “is a very promising treatment for several aspects of gait, posture and balance impairments in PD.”
But although the effect in the single patient “is quite impressive,” the “next crucial step” is to test this approach in a larger cohort of patients, they said.
They noted the nonhuman model does not exhibit freezing of gait, “which precluded the ability to corroborate or further study the role of EES in alleviating this symptom of PD in an animal model.”
In addition, stimulation parameters in the patient with PD “had to rely on estimated normal activity patterns, owing to the inability to measure pre-disease patterns at the individual level,” they wrote.
The study received funding from the Defitech Foundation, ONWARD Medical, CAMS Innovation Fund for Medical Sciences, National Natural Science Foundation of China, Parkinson Schweiz Foundation, European Community’s Seventh Framework Program (NeuWalk), European Research Council, Wyss Center for Bio and Neuroengineering, Bertarelli Foundation, and Swiss National Science Foundation. Dr. Moraud and other study authors hold various patents or applications in relation to the present work. Dr. Mizrahi-Kliger has no relevant conflicts of interest; Dr. Ganguly has a patent for modulation of sensory inputs to improve motor recovery from stroke and has been a consultant to Cala Health.
A version of this article first appeared on Medscape.com.
The neuroprosthesis involves targeted epidural electrical stimulation of areas of the lumbosacral spinal cord that produce walking.
This new therapeutic tool offers hope to patients with PD and, combined with existing approaches, may alleviate a motor sign in PD for which there is currently “no real solution,” study investigator Eduardo Martin Moraud, PhD, who leads PD research at the Defitech Center for Interventional Neurotherapies (NeuroRestore), Lausanne, Switzerland, said in an interview.
“This is exciting for the many patients that develop gait deficits and experience frequent falls, who can only rely on physical therapy to try and minimize the consequences,” he added.
The findings were published online in Nature Medicine.
Personalized stimulation
About 90% of people with advanced PD experience gait and balance problems or freezing-of-gait episodes. These locomotor deficits typically don’t respond well to dopamine replacement therapy or deep brain stimulation (DBS) of the subthalamic nucleus, possibly because the neural origins of these motor problems involve brain circuits not related to dopamine, said Dr. Moraud.
Continuous electrical stimulation over the cervical or thoracic segments of the spinal cord reduces locomotor deficits in some people with PD, but the broader application of this strategy has led to variable and unsatisfying outcomes.
The new approach focuses on correcting abnormal activation of circuits in the lumbar spinal cord, a region that hosts all the neurons that control activation of the leg muscles used for walking.
The stimulating device is placed on the lumbar region of the spinal cord, which sends messages to leg muscles. It is wired to a small impulse generator implanted under the skin of the abdomen. Sensors placed in shoes align the stimulation to the patient’s movement.
The system can detect the beginning of a movement, immediately activate the appropriate electrode, and so facilitate the necessary movement, be that leg flexion, extension, or propulsion, said Dr. Moraud. “This allows for increased walking symmetry, reinforced balance, and increased length of steps.”
The concept of this neuroprosthesis is similar to that used to allow patients with a spinal cord injury (SCI) to walk. But unlike patients with SCI, those with PD can move their legs, indicating that there is a descending command from the brain that needs to interact with the stimulation of the spinal cord, and patients with PD can feel the stimulation.
“Both these elements imply that amplitudes of stimulation need to be much lower in PD than SCI, and that stimulation needs to be fully personalized in PD to synergistically interact with the descending commands from the brain.”
After fine-tuning this new neuroprosthesis in animal models, researchers implanted the device in a 62-year-old man with a 30-year history of PD who presented with severe gait impairments, including marked gait asymmetry, reduced stride length, and balance problems.
Gait restored to near normal
The patient had frequent freezing-of-gait episodes when turning and passing through narrow paths, which led to multiple falls a day. This was despite being treated with DBS and dopaminergic replacement therapies.
But after getting used to the neuroprosthesis, the patient now walks with a gait akin to that of people without PD.
“Our experience in the preclinical animal models and this first patient is that gait can be restored to an almost healthy level, but this, of course, may vary across patients, depending on the severity of their disease progression, and their other motor deficits,” said Dr. Moraud.
When the neuroprosthesis is turned on, freezing of gait nearly vanishes, both with and without DBS.
In addition, the neuroprosthesis augmented the impact of the patient’s rehabilitation program, which involved a variety of regular exercises, including walking on basic and complex terrains, navigating outdoors in community settings, balance training, and basic physical therapy.
Frequent use of the neuroprosthesis during gait rehabilitation also translated into “highly improved” quality of life as reported by the patient (and his wife), said Dr. Moraud.
The patient has now been using the neuroprosthesis about 8 hours a day for nearly 2 years, only switching it off when sitting for long periods of time or while sleeping.
“He regained the capacity to walk in complex or crowded environments such as shops, airports, or his own home, without falling,” said Dr. Moraud. “He went from falling five to six times per day to one or two [falls] every couple of weeks. He’s also much more confident. He can walk for many miles, run, and go on holidays, without the constant fear of falling and having related injuries.”
Dr. Moraud stressed that the device does not replace DBS, which is a “key therapy” that addresses other deficits in PD, such as rigidity or slowness of movement. “What we propose here is a fully complementary approach for the gait problems that are not well addressed by DBS.”
One of the next steps will be to evaluate the efficacy of this approach across a wider spectrum of patient profiles to fully define the best responders, said Dr. Moraud.
A ‘tour de force’
In a comment, Michael S. Okun, MD, director of the Norman Fixel Institute for Neurological Diseases, University of Florida, Gainesville, and medical director of the Parkinson’s Foundation, noted that the researchers used “a smarter device” than past approaches that failed to adequately address progressive walking challenges of patients with PD.
Although it’s “tempting to get excited” about the findings, it’s important to consider that the study included only one human subject and did not target circuits for both walking and balance, said Dr. Okun. “It’s possible that even if future studies revealed a benefit for walking, the device may or may not address falling.”
In an accompanying editorial, Aviv Mizrahi-Kliger, MD, PhD, department of neurology, University of California, San Francisco, and Karunesh Ganguly, MD, PhD, Neurology and Rehabilitation Service, San Francisco Veterans Affairs Health Care System, called the study an “impressive tour de force,” with data from the nonhuman primate model and the individual with PD “jointly” indicating that epidural electrical stimulation (EES) “is a very promising treatment for several aspects of gait, posture and balance impairments in PD.”
But although the effect in the single patient “is quite impressive,” the “next crucial step” is to test this approach in a larger cohort of patients, they said.
They noted the nonhuman model does not exhibit freezing of gait, “which precluded the ability to corroborate or further study the role of EES in alleviating this symptom of PD in an animal model.”
In addition, stimulation parameters in the patient with PD “had to rely on estimated normal activity patterns, owing to the inability to measure pre-disease patterns at the individual level,” they wrote.
The study received funding from the Defitech Foundation, ONWARD Medical, CAMS Innovation Fund for Medical Sciences, National Natural Science Foundation of China, Parkinson Schweiz Foundation, European Community’s Seventh Framework Program (NeuWalk), European Research Council, Wyss Center for Bio and Neuroengineering, Bertarelli Foundation, and Swiss National Science Foundation. Dr. Moraud and other study authors hold various patents or applications in relation to the present work. Dr. Mizrahi-Kliger has no relevant conflicts of interest; Dr. Ganguly has a patent for modulation of sensory inputs to improve motor recovery from stroke and has been a consultant to Cala Health.
A version of this article first appeared on Medscape.com.
The neuroprosthesis involves targeted epidural electrical stimulation of areas of the lumbosacral spinal cord that produce walking.
This new therapeutic tool offers hope to patients with PD and, combined with existing approaches, may alleviate a motor sign in PD for which there is currently “no real solution,” study investigator Eduardo Martin Moraud, PhD, who leads PD research at the Defitech Center for Interventional Neurotherapies (NeuroRestore), Lausanne, Switzerland, said in an interview.
“This is exciting for the many patients that develop gait deficits and experience frequent falls, who can only rely on physical therapy to try and minimize the consequences,” he added.
The findings were published online in Nature Medicine.
Personalized stimulation
About 90% of people with advanced PD experience gait and balance problems or freezing-of-gait episodes. These locomotor deficits typically don’t respond well to dopamine replacement therapy or deep brain stimulation (DBS) of the subthalamic nucleus, possibly because the neural origins of these motor problems involve brain circuits not related to dopamine, said Dr. Moraud.
Continuous electrical stimulation over the cervical or thoracic segments of the spinal cord reduces locomotor deficits in some people with PD, but the broader application of this strategy has led to variable and unsatisfying outcomes.
The new approach focuses on correcting abnormal activation of circuits in the lumbar spinal cord, a region that hosts all the neurons that control activation of the leg muscles used for walking.
The stimulating device is placed on the lumbar region of the spinal cord, which sends messages to leg muscles. It is wired to a small impulse generator implanted under the skin of the abdomen. Sensors placed in shoes align the stimulation to the patient’s movement.
The system can detect the beginning of a movement, immediately activate the appropriate electrode, and so facilitate the necessary movement, be that leg flexion, extension, or propulsion, said Dr. Moraud. “This allows for increased walking symmetry, reinforced balance, and increased length of steps.”
The concept of this neuroprosthesis is similar to that used to allow patients with a spinal cord injury (SCI) to walk. But unlike patients with SCI, those with PD can move their legs, indicating that there is a descending command from the brain that needs to interact with the stimulation of the spinal cord, and patients with PD can feel the stimulation.
“Both these elements imply that amplitudes of stimulation need to be much lower in PD than SCI, and that stimulation needs to be fully personalized in PD to synergistically interact with the descending commands from the brain.”
After fine-tuning this new neuroprosthesis in animal models, researchers implanted the device in a 62-year-old man with a 30-year history of PD who presented with severe gait impairments, including marked gait asymmetry, reduced stride length, and balance problems.
Gait restored to near normal
The patient had frequent freezing-of-gait episodes when turning and passing through narrow paths, which led to multiple falls a day. This was despite being treated with DBS and dopaminergic replacement therapies.
But after getting used to the neuroprosthesis, the patient now walks with a gait akin to that of people without PD.
“Our experience in the preclinical animal models and this first patient is that gait can be restored to an almost healthy level, but this, of course, may vary across patients, depending on the severity of their disease progression, and their other motor deficits,” said Dr. Moraud.
When the neuroprosthesis is turned on, freezing of gait nearly vanishes, both with and without DBS.
In addition, the neuroprosthesis augmented the impact of the patient’s rehabilitation program, which involved a variety of regular exercises, including walking on basic and complex terrains, navigating outdoors in community settings, balance training, and basic physical therapy.
Frequent use of the neuroprosthesis during gait rehabilitation also translated into “highly improved” quality of life as reported by the patient (and his wife), said Dr. Moraud.
The patient has now been using the neuroprosthesis about 8 hours a day for nearly 2 years, only switching it off when sitting for long periods of time or while sleeping.
“He regained the capacity to walk in complex or crowded environments such as shops, airports, or his own home, without falling,” said Dr. Moraud. “He went from falling five to six times per day to one or two [falls] every couple of weeks. He’s also much more confident. He can walk for many miles, run, and go on holidays, without the constant fear of falling and having related injuries.”
Dr. Moraud stressed that the device does not replace DBS, which is a “key therapy” that addresses other deficits in PD, such as rigidity or slowness of movement. “What we propose here is a fully complementary approach for the gait problems that are not well addressed by DBS.”
One of the next steps will be to evaluate the efficacy of this approach across a wider spectrum of patient profiles to fully define the best responders, said Dr. Moraud.
A ‘tour de force’
In a comment, Michael S. Okun, MD, director of the Norman Fixel Institute for Neurological Diseases, University of Florida, Gainesville, and medical director of the Parkinson’s Foundation, noted that the researchers used “a smarter device” than past approaches that failed to adequately address progressive walking challenges of patients with PD.
Although it’s “tempting to get excited” about the findings, it’s important to consider that the study included only one human subject and did not target circuits for both walking and balance, said Dr. Okun. “It’s possible that even if future studies revealed a benefit for walking, the device may or may not address falling.”
In an accompanying editorial, Aviv Mizrahi-Kliger, MD, PhD, department of neurology, University of California, San Francisco, and Karunesh Ganguly, MD, PhD, Neurology and Rehabilitation Service, San Francisco Veterans Affairs Health Care System, called the study an “impressive tour de force,” with data from the nonhuman primate model and the individual with PD “jointly” indicating that epidural electrical stimulation (EES) “is a very promising treatment for several aspects of gait, posture and balance impairments in PD.”
But although the effect in the single patient “is quite impressive,” the “next crucial step” is to test this approach in a larger cohort of patients, they said.
They noted the nonhuman model does not exhibit freezing of gait, “which precluded the ability to corroborate or further study the role of EES in alleviating this symptom of PD in an animal model.”
In addition, stimulation parameters in the patient with PD “had to rely on estimated normal activity patterns, owing to the inability to measure pre-disease patterns at the individual level,” they wrote.
The study received funding from the Defitech Foundation, ONWARD Medical, CAMS Innovation Fund for Medical Sciences, National Natural Science Foundation of China, Parkinson Schweiz Foundation, European Community’s Seventh Framework Program (NeuWalk), European Research Council, Wyss Center for Bio and Neuroengineering, Bertarelli Foundation, and Swiss National Science Foundation. Dr. Moraud and other study authors hold various patents or applications in relation to the present work. Dr. Mizrahi-Kliger has no relevant conflicts of interest; Dr. Ganguly has a patent for modulation of sensory inputs to improve motor recovery from stroke and has been a consultant to Cala Health.
A version of this article first appeared on Medscape.com.
FROM NATURE MEDICINE
Artificial intelligence presents opportunities, challenges in neurologic practice
PHOENIX – and it presents opportunities for increased production and automation of some tasks. However, it is prone to error and ‘hallucinations’ despite an authoritative tone, so its conclusions must be verified.
Those were some of the messages from a talk by John Morren, MD, an associate professor of neurology at Case Western Reserve University, Cleveland, who spoke about AI at the 2023 annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine (AANEM).
He encouraged attendees to get involved in the conversation of AI, because it is here to stay and will have a big impact on health care. “If we’re not around the table making decisions, decisions will be made for us in our absence and won’t be in our favor,” said Dr. Morren.
He started out his talk by asking if anyone in the room had used AI. After about half raised their hands, he countered that nearly everyone likely had. Voice assistants like SIRI and Alexa, social media with curated feeds, online shopping tools that provide product suggestions, and content recommendations from streaming services like Netflix all rely on AI technology.
Within medicine, AI is already playing a role in various fields, including medical imaging, disease diagnosis, drug discovery and development, predictive analytics, personalized medicine, telemedicine, and health care management.
It also has potential to be used on the job. For example, ChatGPT can generate and refine conversations towards a specific length, format, style, and level of detail. Alternatives include Bing AI from Microsoft, Bard AI from Google, Writesonic, Copy.ai, SpinBot, HIX.AI, and Chatsonic.
Specific to medicine, Consensus is a search engine that uses AI to search for, summarize, and synthesize studies from peer-reviewed literature.
Trust, but verify
Dr. Morren presented some specific use cases, including patient education and responses to patient inquiries, as well as generating letters to insurance companies appealing denial of coverage claims. He also showed an example where he asked Bing AI to explain to a patient, at a sixth- to seventh-grade reading level, the red-flag symptoms of myasthenic crisis.
AI can generate summaries of clinical evidence of previous studies. Asked by this reporter how to trust the accuracies of the summaries if the user hasn’t thoroughly read the papers, he acknowledged the imperfection of AI. “I would say that if you’re going to make a decision that you would not have made normally based on the summary that it’s giving, if you can find the fact that you’re anchoring the decision on, go into the article yourself and make sure that it’s well vetted. The AI is just good to tap you on your shoulder and say, ‘hey, just consider this.’ That’s all it is. You should always trust, but verify. If the AI is forcing you to say something new that you would not say, maybe don’t do it – or at least research it to know that it’s the truth and then you elevate yourself and get yourself to the next level.”
Limitations
The need to verify can create its own burden, according to one attendee. “I often find I end up spending more time verifying [what ChatGPT has provided]. This seems to take more time than a traditional way of going to PubMed or UpToDate or any of the other human generated consensus way,” he said.
Dr. Morren replied that he wouldn’t recommend using ChatGPT to query medical literature. Instead he recommended Consensus, which only searches the peer-reviewed medical literature.
Another key limitation is that most AI programs are date limited: For example, ChatGPT doesn’t include information after September 2021, though this may change with paid subscriptions. He also starkly warned the audience to never enter sensitive information, including patient identifiers.
There are legal and ethical considerations to AI. Dr. Morren warned against overreliance on AI, as this could undermine compassion and lead to erosion of trust, which makes it important to disclose any use of AI-generated content.
Another attendee raised concerns that AI may be generating research content, including slides for presentations, abstracts, titles, or article text. Dr. Morren said that some organizations, such as the International Committee of Medical Journal Editors, have incorporated AI in their recommendations, stating that authors should disclose any contributions of AI to their publications. However, there is little that can be done to identify AI-generated content, leaving it up to the honor code.
Asked to make predictions about how AI will evolve in the clinic over the next 2-3 years, Dr. Morren suggested that it will likely be embedded in electronic medical records. He anticipated that it will save physicians time so that they can spend more time interacting directly with patients. He quoted Eric Topol, MD, professor of medicine at Scripps Research Translational Institute, La Jolla, Calif., as saying that AI could save 20% of a physician’s time, which could be spent with patients. Dr. Morren saw it differently. “I know where that 20% of time liberated is going to go. I’m going to see 20% more patients. I’m a realist,” he said, to audience laughter.
He also predicted that AI will be found in wearables and devices, allowing health care to expand into the patient’s home in real time. “A lot of what we’re wearing is going to be an extension of the doctor’s office,” he said.
For those hoping for more guidance, Dr. Morren noted that he is the chairman of the professional practice committee of AANEM, and the group will be putting out a position statement within the next couple of months. “It will be a little bit of a blueprint for the path going forward. There are specific things that need to be done. In research, for example, you have to ensure that datasets are diverse enough. To do that we need to have inter-institutional collaboration. We have to ensure patient privacy. Consent for this needs to be a little more explicit because this is a novel area. Those are things that need to be stipulated and ratified through a task force.”
Dr. Morren has no relevant financial disclosures.
PHOENIX – and it presents opportunities for increased production and automation of some tasks. However, it is prone to error and ‘hallucinations’ despite an authoritative tone, so its conclusions must be verified.
Those were some of the messages from a talk by John Morren, MD, an associate professor of neurology at Case Western Reserve University, Cleveland, who spoke about AI at the 2023 annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine (AANEM).
He encouraged attendees to get involved in the conversation of AI, because it is here to stay and will have a big impact on health care. “If we’re not around the table making decisions, decisions will be made for us in our absence and won’t be in our favor,” said Dr. Morren.
He started out his talk by asking if anyone in the room had used AI. After about half raised their hands, he countered that nearly everyone likely had. Voice assistants like SIRI and Alexa, social media with curated feeds, online shopping tools that provide product suggestions, and content recommendations from streaming services like Netflix all rely on AI technology.
Within medicine, AI is already playing a role in various fields, including medical imaging, disease diagnosis, drug discovery and development, predictive analytics, personalized medicine, telemedicine, and health care management.
It also has potential to be used on the job. For example, ChatGPT can generate and refine conversations towards a specific length, format, style, and level of detail. Alternatives include Bing AI from Microsoft, Bard AI from Google, Writesonic, Copy.ai, SpinBot, HIX.AI, and Chatsonic.
Specific to medicine, Consensus is a search engine that uses AI to search for, summarize, and synthesize studies from peer-reviewed literature.
Trust, but verify
Dr. Morren presented some specific use cases, including patient education and responses to patient inquiries, as well as generating letters to insurance companies appealing denial of coverage claims. He also showed an example where he asked Bing AI to explain to a patient, at a sixth- to seventh-grade reading level, the red-flag symptoms of myasthenic crisis.
AI can generate summaries of clinical evidence of previous studies. Asked by this reporter how to trust the accuracies of the summaries if the user hasn’t thoroughly read the papers, he acknowledged the imperfection of AI. “I would say that if you’re going to make a decision that you would not have made normally based on the summary that it’s giving, if you can find the fact that you’re anchoring the decision on, go into the article yourself and make sure that it’s well vetted. The AI is just good to tap you on your shoulder and say, ‘hey, just consider this.’ That’s all it is. You should always trust, but verify. If the AI is forcing you to say something new that you would not say, maybe don’t do it – or at least research it to know that it’s the truth and then you elevate yourself and get yourself to the next level.”
Limitations
The need to verify can create its own burden, according to one attendee. “I often find I end up spending more time verifying [what ChatGPT has provided]. This seems to take more time than a traditional way of going to PubMed or UpToDate or any of the other human generated consensus way,” he said.
Dr. Morren replied that he wouldn’t recommend using ChatGPT to query medical literature. Instead he recommended Consensus, which only searches the peer-reviewed medical literature.
Another key limitation is that most AI programs are date limited: For example, ChatGPT doesn’t include information after September 2021, though this may change with paid subscriptions. He also starkly warned the audience to never enter sensitive information, including patient identifiers.
There are legal and ethical considerations to AI. Dr. Morren warned against overreliance on AI, as this could undermine compassion and lead to erosion of trust, which makes it important to disclose any use of AI-generated content.
Another attendee raised concerns that AI may be generating research content, including slides for presentations, abstracts, titles, or article text. Dr. Morren said that some organizations, such as the International Committee of Medical Journal Editors, have incorporated AI in their recommendations, stating that authors should disclose any contributions of AI to their publications. However, there is little that can be done to identify AI-generated content, leaving it up to the honor code.
Asked to make predictions about how AI will evolve in the clinic over the next 2-3 years, Dr. Morren suggested that it will likely be embedded in electronic medical records. He anticipated that it will save physicians time so that they can spend more time interacting directly with patients. He quoted Eric Topol, MD, professor of medicine at Scripps Research Translational Institute, La Jolla, Calif., as saying that AI could save 20% of a physician’s time, which could be spent with patients. Dr. Morren saw it differently. “I know where that 20% of time liberated is going to go. I’m going to see 20% more patients. I’m a realist,” he said, to audience laughter.
He also predicted that AI will be found in wearables and devices, allowing health care to expand into the patient’s home in real time. “A lot of what we’re wearing is going to be an extension of the doctor’s office,” he said.
For those hoping for more guidance, Dr. Morren noted that he is the chairman of the professional practice committee of AANEM, and the group will be putting out a position statement within the next couple of months. “It will be a little bit of a blueprint for the path going forward. There are specific things that need to be done. In research, for example, you have to ensure that datasets are diverse enough. To do that we need to have inter-institutional collaboration. We have to ensure patient privacy. Consent for this needs to be a little more explicit because this is a novel area. Those are things that need to be stipulated and ratified through a task force.”
Dr. Morren has no relevant financial disclosures.
PHOENIX – and it presents opportunities for increased production and automation of some tasks. However, it is prone to error and ‘hallucinations’ despite an authoritative tone, so its conclusions must be verified.
Those were some of the messages from a talk by John Morren, MD, an associate professor of neurology at Case Western Reserve University, Cleveland, who spoke about AI at the 2023 annual meeting of the American Association for Neuromuscular and Electrodiagnostic Medicine (AANEM).
He encouraged attendees to get involved in the conversation of AI, because it is here to stay and will have a big impact on health care. “If we’re not around the table making decisions, decisions will be made for us in our absence and won’t be in our favor,” said Dr. Morren.
He started out his talk by asking if anyone in the room had used AI. After about half raised their hands, he countered that nearly everyone likely had. Voice assistants like SIRI and Alexa, social media with curated feeds, online shopping tools that provide product suggestions, and content recommendations from streaming services like Netflix all rely on AI technology.
Within medicine, AI is already playing a role in various fields, including medical imaging, disease diagnosis, drug discovery and development, predictive analytics, personalized medicine, telemedicine, and health care management.
It also has potential to be used on the job. For example, ChatGPT can generate and refine conversations towards a specific length, format, style, and level of detail. Alternatives include Bing AI from Microsoft, Bard AI from Google, Writesonic, Copy.ai, SpinBot, HIX.AI, and Chatsonic.
Specific to medicine, Consensus is a search engine that uses AI to search for, summarize, and synthesize studies from peer-reviewed literature.
Trust, but verify
Dr. Morren presented some specific use cases, including patient education and responses to patient inquiries, as well as generating letters to insurance companies appealing denial of coverage claims. He also showed an example where he asked Bing AI to explain to a patient, at a sixth- to seventh-grade reading level, the red-flag symptoms of myasthenic crisis.
AI can generate summaries of clinical evidence of previous studies. Asked by this reporter how to trust the accuracies of the summaries if the user hasn’t thoroughly read the papers, he acknowledged the imperfection of AI. “I would say that if you’re going to make a decision that you would not have made normally based on the summary that it’s giving, if you can find the fact that you’re anchoring the decision on, go into the article yourself and make sure that it’s well vetted. The AI is just good to tap you on your shoulder and say, ‘hey, just consider this.’ That’s all it is. You should always trust, but verify. If the AI is forcing you to say something new that you would not say, maybe don’t do it – or at least research it to know that it’s the truth and then you elevate yourself and get yourself to the next level.”
Limitations
The need to verify can create its own burden, according to one attendee. “I often find I end up spending more time verifying [what ChatGPT has provided]. This seems to take more time than a traditional way of going to PubMed or UpToDate or any of the other human generated consensus way,” he said.
Dr. Morren replied that he wouldn’t recommend using ChatGPT to query medical literature. Instead he recommended Consensus, which only searches the peer-reviewed medical literature.
Another key limitation is that most AI programs are date limited: For example, ChatGPT doesn’t include information after September 2021, though this may change with paid subscriptions. He also starkly warned the audience to never enter sensitive information, including patient identifiers.
There are legal and ethical considerations to AI. Dr. Morren warned against overreliance on AI, as this could undermine compassion and lead to erosion of trust, which makes it important to disclose any use of AI-generated content.
Another attendee raised concerns that AI may be generating research content, including slides for presentations, abstracts, titles, or article text. Dr. Morren said that some organizations, such as the International Committee of Medical Journal Editors, have incorporated AI in their recommendations, stating that authors should disclose any contributions of AI to their publications. However, there is little that can be done to identify AI-generated content, leaving it up to the honor code.
Asked to make predictions about how AI will evolve in the clinic over the next 2-3 years, Dr. Morren suggested that it will likely be embedded in electronic medical records. He anticipated that it will save physicians time so that they can spend more time interacting directly with patients. He quoted Eric Topol, MD, professor of medicine at Scripps Research Translational Institute, La Jolla, Calif., as saying that AI could save 20% of a physician’s time, which could be spent with patients. Dr. Morren saw it differently. “I know where that 20% of time liberated is going to go. I’m going to see 20% more patients. I’m a realist,” he said, to audience laughter.
He also predicted that AI will be found in wearables and devices, allowing health care to expand into the patient’s home in real time. “A lot of what we’re wearing is going to be an extension of the doctor’s office,” he said.
For those hoping for more guidance, Dr. Morren noted that he is the chairman of the professional practice committee of AANEM, and the group will be putting out a position statement within the next couple of months. “It will be a little bit of a blueprint for the path going forward. There are specific things that need to be done. In research, for example, you have to ensure that datasets are diverse enough. To do that we need to have inter-institutional collaboration. We have to ensure patient privacy. Consent for this needs to be a little more explicit because this is a novel area. Those are things that need to be stipulated and ratified through a task force.”
Dr. Morren has no relevant financial disclosures.
AT AANEM 2023
Promising new therapies for managing Tourette syndrome
, according to an overview of new therapies presented at the XXVI World Congress of Neurology.
One recent study by University of Nottingham researchers showed a wrist-worn stimulating device significantly reduces the frequency and severity of tics – repetitive movements or vocalizations that can occur several times a day.
“Wearable nerve stimulation holds great promise because it will be good across the age spectrum; adults can wear it to work, and children can go to school with it to help them concentrate on their schoolwork, and then they take it off at night,” Eileen Joyce, PhD, MB BChir, professor of neuropsychiatry at the Institute of Neurology, University College London, told this news organization.
Dr. Joyce, who was not part of the study, discussed this and other new advances in tic therapy at the meeting.
About 24% of children will suffer from tics at some point. The prevalence of Tourette syndrome among males is about four times that of females, Dr. Joyce told delegates. She added the typical age of onset is about 7 years with peak severity at about 12 years.
Predictors of tics persisting into adulthood include comorbid attention deficit hyperactivity disorder (ADHD), obsessive–compulsive disorder, and autism spectrum disorder, said Dr. Joyce, who also discussed the “highly heritable” nature of the syndrome and the numerous related genes identified to date.
Current and emerging treatments
Current treatments include psychological therapy, Botox for focal tics, and medications such as antipsychotics. Emerging therapies included deep brain stimulation and the new median nerve stimulation approach.
A study published earlier this year included 135 patients with moderate to severe tic disorder who were randomly assigned to receive the investigational neuromodulation treatment, a sham treatment, or a wait-list treatment group.
The intervention involves rhythmic pulse trains of median nerve stimulation delivered via a device worn at the wrist. The device was programmed to deliver rhythmic (10 Hz) trains of low-intensity (1-19 mA) electrical stimulation to the median nerve at home once daily, 5 days a week for 4 weeks.
At 4 weeks, tic severity, as measured by the Yale Global Tic Severity Scale-Total Tic Severity Score (YGTSS-TTSS), was reduced by 7.1 points (35% reduction) in the active stimulation group compared to 2.13 points in the sham and 2.11 points in wait-list control groups.
The reduction for active stimulation was substantially larger, clinically meaningful (effect size, 0.5), and statistically significant (P = .02) compared to both the sham stimulation and wait-list control groups, which did not differ from one another.
Tic frequency (tics per minute or TPM) was reduced more in the active than sham stimulation groups (−15.6 TPM vs. −7.7 TPM; P < .03) and the reduction in tic frequency was clinically meaningful (>25% reduction; effect-size, 0.3).
When the active stimulator was turned off, the tics worsened, noted Dr. Joyce.
“The study showed that if you stimulate the median nerve at the wrist, you can train brain oscillations that are linked to the suppression of movement,” Dr. Joyce said. “So based on physiological knowledge, they have developed a median nerve stimulator to entrain cortical rhythms.”
Simple and exciting
The new device is “really exciting”, she added. “It’s not invasive and is quite simple to use and could help a lot of people with Tourette syndrome.”
Asked to comment, Alan Carson, MD, consultant neuropsychiatrist and honorary professor of neuropsychiatry, University of Edinburgh, who co-chaired the neuropsychiatry session featuring this presentation, called the device “promising.”
“Deep brain stimulation appears to be very effective but it’s a major procedure, so a simple wearable device seems highly desirable,” Dr. Carson said.
Dr. Joyce also discussed a study on the efficacy of cannabis (nabiximols; Sativex) as an intervention for tic management in males, those with severe tics, and those with comorbid ADHD.
And a new oral medication, ecopipam, a highly selective D1 receptor antagonist, is also raising hopes, said Dr. Joyce, with results from a randomized controlled trial showing the drug significantly improved tics and had few adverse effects.
Dr. Joyce and Dr. Carson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to an overview of new therapies presented at the XXVI World Congress of Neurology.
One recent study by University of Nottingham researchers showed a wrist-worn stimulating device significantly reduces the frequency and severity of tics – repetitive movements or vocalizations that can occur several times a day.
“Wearable nerve stimulation holds great promise because it will be good across the age spectrum; adults can wear it to work, and children can go to school with it to help them concentrate on their schoolwork, and then they take it off at night,” Eileen Joyce, PhD, MB BChir, professor of neuropsychiatry at the Institute of Neurology, University College London, told this news organization.
Dr. Joyce, who was not part of the study, discussed this and other new advances in tic therapy at the meeting.
About 24% of children will suffer from tics at some point. The prevalence of Tourette syndrome among males is about four times that of females, Dr. Joyce told delegates. She added the typical age of onset is about 7 years with peak severity at about 12 years.
Predictors of tics persisting into adulthood include comorbid attention deficit hyperactivity disorder (ADHD), obsessive–compulsive disorder, and autism spectrum disorder, said Dr. Joyce, who also discussed the “highly heritable” nature of the syndrome and the numerous related genes identified to date.
Current and emerging treatments
Current treatments include psychological therapy, Botox for focal tics, and medications such as antipsychotics. Emerging therapies included deep brain stimulation and the new median nerve stimulation approach.
A study published earlier this year included 135 patients with moderate to severe tic disorder who were randomly assigned to receive the investigational neuromodulation treatment, a sham treatment, or a wait-list treatment group.
The intervention involves rhythmic pulse trains of median nerve stimulation delivered via a device worn at the wrist. The device was programmed to deliver rhythmic (10 Hz) trains of low-intensity (1-19 mA) electrical stimulation to the median nerve at home once daily, 5 days a week for 4 weeks.
At 4 weeks, tic severity, as measured by the Yale Global Tic Severity Scale-Total Tic Severity Score (YGTSS-TTSS), was reduced by 7.1 points (35% reduction) in the active stimulation group compared to 2.13 points in the sham and 2.11 points in wait-list control groups.
The reduction for active stimulation was substantially larger, clinically meaningful (effect size, 0.5), and statistically significant (P = .02) compared to both the sham stimulation and wait-list control groups, which did not differ from one another.
Tic frequency (tics per minute or TPM) was reduced more in the active than sham stimulation groups (−15.6 TPM vs. −7.7 TPM; P < .03) and the reduction in tic frequency was clinically meaningful (>25% reduction; effect-size, 0.3).
When the active stimulator was turned off, the tics worsened, noted Dr. Joyce.
“The study showed that if you stimulate the median nerve at the wrist, you can train brain oscillations that are linked to the suppression of movement,” Dr. Joyce said. “So based on physiological knowledge, they have developed a median nerve stimulator to entrain cortical rhythms.”
Simple and exciting
The new device is “really exciting”, she added. “It’s not invasive and is quite simple to use and could help a lot of people with Tourette syndrome.”
Asked to comment, Alan Carson, MD, consultant neuropsychiatrist and honorary professor of neuropsychiatry, University of Edinburgh, who co-chaired the neuropsychiatry session featuring this presentation, called the device “promising.”
“Deep brain stimulation appears to be very effective but it’s a major procedure, so a simple wearable device seems highly desirable,” Dr. Carson said.
Dr. Joyce also discussed a study on the efficacy of cannabis (nabiximols; Sativex) as an intervention for tic management in males, those with severe tics, and those with comorbid ADHD.
And a new oral medication, ecopipam, a highly selective D1 receptor antagonist, is also raising hopes, said Dr. Joyce, with results from a randomized controlled trial showing the drug significantly improved tics and had few adverse effects.
Dr. Joyce and Dr. Carson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to an overview of new therapies presented at the XXVI World Congress of Neurology.
One recent study by University of Nottingham researchers showed a wrist-worn stimulating device significantly reduces the frequency and severity of tics – repetitive movements or vocalizations that can occur several times a day.
“Wearable nerve stimulation holds great promise because it will be good across the age spectrum; adults can wear it to work, and children can go to school with it to help them concentrate on their schoolwork, and then they take it off at night,” Eileen Joyce, PhD, MB BChir, professor of neuropsychiatry at the Institute of Neurology, University College London, told this news organization.
Dr. Joyce, who was not part of the study, discussed this and other new advances in tic therapy at the meeting.
About 24% of children will suffer from tics at some point. The prevalence of Tourette syndrome among males is about four times that of females, Dr. Joyce told delegates. She added the typical age of onset is about 7 years with peak severity at about 12 years.
Predictors of tics persisting into adulthood include comorbid attention deficit hyperactivity disorder (ADHD), obsessive–compulsive disorder, and autism spectrum disorder, said Dr. Joyce, who also discussed the “highly heritable” nature of the syndrome and the numerous related genes identified to date.
Current and emerging treatments
Current treatments include psychological therapy, Botox for focal tics, and medications such as antipsychotics. Emerging therapies included deep brain stimulation and the new median nerve stimulation approach.
A study published earlier this year included 135 patients with moderate to severe tic disorder who were randomly assigned to receive the investigational neuromodulation treatment, a sham treatment, or a wait-list treatment group.
The intervention involves rhythmic pulse trains of median nerve stimulation delivered via a device worn at the wrist. The device was programmed to deliver rhythmic (10 Hz) trains of low-intensity (1-19 mA) electrical stimulation to the median nerve at home once daily, 5 days a week for 4 weeks.
At 4 weeks, tic severity, as measured by the Yale Global Tic Severity Scale-Total Tic Severity Score (YGTSS-TTSS), was reduced by 7.1 points (35% reduction) in the active stimulation group compared to 2.13 points in the sham and 2.11 points in wait-list control groups.
The reduction for active stimulation was substantially larger, clinically meaningful (effect size, 0.5), and statistically significant (P = .02) compared to both the sham stimulation and wait-list control groups, which did not differ from one another.
Tic frequency (tics per minute or TPM) was reduced more in the active than sham stimulation groups (−15.6 TPM vs. −7.7 TPM; P < .03) and the reduction in tic frequency was clinically meaningful (>25% reduction; effect-size, 0.3).
When the active stimulator was turned off, the tics worsened, noted Dr. Joyce.
“The study showed that if you stimulate the median nerve at the wrist, you can train brain oscillations that are linked to the suppression of movement,” Dr. Joyce said. “So based on physiological knowledge, they have developed a median nerve stimulator to entrain cortical rhythms.”
Simple and exciting
The new device is “really exciting”, she added. “It’s not invasive and is quite simple to use and could help a lot of people with Tourette syndrome.”
Asked to comment, Alan Carson, MD, consultant neuropsychiatrist and honorary professor of neuropsychiatry, University of Edinburgh, who co-chaired the neuropsychiatry session featuring this presentation, called the device “promising.”
“Deep brain stimulation appears to be very effective but it’s a major procedure, so a simple wearable device seems highly desirable,” Dr. Carson said.
Dr. Joyce also discussed a study on the efficacy of cannabis (nabiximols; Sativex) as an intervention for tic management in males, those with severe tics, and those with comorbid ADHD.
And a new oral medication, ecopipam, a highly selective D1 receptor antagonist, is also raising hopes, said Dr. Joyce, with results from a randomized controlled trial showing the drug significantly improved tics and had few adverse effects.
Dr. Joyce and Dr. Carson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM WCN 2023
A new chapter for research on treating Huntington’s disease
The past decade has been a contradictory one for research on Huntington’s disease, marked by breakthroughs in the biology and genetics of this fatal neurodegenerative disease and painful disappointments in trials of novel therapies.
What is Huntington’s disease?
Huntington’s disease is caused by a trinucleotide repeat mutation in the huntingtin gene (HTT) and follows an autosomal dominant pattern of inheritance. In people with more than 39 copies of this CAG repeat tract expansion, the HTT protein misfolds to become toxic, with more repeats linked to earlier disease onset and a more severe course.
Huntington’s disease causes loss of neurons in the striatum and disrupts the cortical-striatal-thalamic pathway, a brain circuit that governs movement. Although behavioral symptoms can emerge earlier, signature symptoms – chorea, dystonia, and cognitive abnormalities – usually present at midlife and progress until the patient’s death.
Huntington’s disease affects an estimated 30,000 people in the United States, and an estimated 10-12 people for every 100,000 worldwide – making it rare enough that neurologists who do not specialize in movement disorders might never treat a Huntington’s patient. Yet Huntington’s disease is sufficiently prevalent to attract robust research interest and sustain large registries, which have led to remarkable findings with implications not just for Huntington’s disease but for other diseases as well.
Right now, the only Food and Drug Administration–approved treatments for Huntington’s disease are symptomatic therapies to help temper disturbances of movement, sleep, and emotions. There are two major avenues of investigation into Huntington’s disease modification:
Reduce levels of mutant HTT protein, whether through small molecules, gene therapies, or antisense oligonucleotides (ASOs) that modulate RNA processing. In March 2021, Roche announced the suspension of its phase 3 trial of tominersen, an ASO.1 Trials of other protein-lowering agents were canceled for lack of target engagement or over safety concerns, in 2021 and 2022, although this approach is still considered viable.
Modify the length of CAG repeats, which involves a more recently encountered mechanism in Huntington’s disease. The strategy is at the preclinical stage. In 2015, a group of scientists reported the game-changing discovery that a large number of genes, associated with some of the same DNA-mismatch repair pathways implicated in cancer, can modify the length of CAG repeats in cells. This gave rise to a new set of therapeutic targets, now being explored.
Neurology Reviews 2023 Rare Neurological Disease Special Report spoke with two frequently collaborating researchers at the forefront of Huntington’s disease science – Cristina Sampaio, MD, PhD, chief medical officer of CHDI Management, Princeton, N.J., and Sarah Tabrizi, MD, PhD, from University College London – about lessons learned from the past several years of Huntington’s disease drug research.
The CHDI Foundation, a nonprofit research organization, was founded in 2003 to facilitate development of Huntington’s disease therapies. Its clinical research platform, Enroll-HD, includes a global registry of some 28,000 patients and a biobank to facilitate biomarker discovery and validation. Dr. Tabrizi’s lab explores Huntington’s disease drug targets in both HTT and DNA mismatch repair, and led two CHDI-funded observational studies, TRACK-HD and TrackOn-HD, to characterize disease progression in people with Huntington’s disease. In 2022, Dr. Tabrizi and Dr. Sampaio were coauthors of a comprehensive review of Huntington’s disease drug development and published a new disease-staging system to help enable trials in presymptomatic Huntington’s disease.
“The story of Huntington’s therapeutics is very informative,” Dr. Sampaio said. “Understanding these mechanisms is relevant for any neurologist – not only for Huntington’s but because they represent a prototype development for a big group of therapies and make us better equipped to think about everything else that is happening in neurology. They’re giving us an understanding of where neurology is going.”
Tackling a tricky protein
Most Huntington’s disease research has focused on ways to attack or lower mutant HTT protein. But HTT has proven a tricky target: HTT is a large protein, present in all cells, and known to interact with more than 100 genes. Healthy HTT is critical to fetal development, but its functions in the adult body remain something of a mystery. Almost all people with Huntington’s disease have both wild-type and mutant HTT.
Tominersen, the investigative ASO developed by Roche, works to block translation of the HTT message, leading to a reduction in both healthy and mutant HTT protein. It is delivered by lumbar injection to reach the brain. Upon halting its phase 3 trial of tominersen in 2021, Roche reported that people in the high-dosage treatment group did measurably worse – although it remains unclear whether this was caused by excess protein lowering or an off-target effect. The tominersen program was the first to clearly show that it is possible to lower HTT with an intervention – a critical first step in the development of this class of drugs.
“I think the problem with the trial was the aggressive loading doses plus exposure-related toxicity,” Dr. Tabrizi said. “Whether that exposure-related toxicity was related to too much wild-type HTT lowering or the proinflammatory effects of the ASO, you can’t yet disentangle.” Roche has not given up: The company is now seeking to test lower dosages of tominersen on a younger subgroup of patients who have fewer CAG repeats, in whom a benefit of protein lowering might be more clearly seen.
Small molecules and gene therapies have also been developed to reduce mutant HTT, although most, as is the case with tominersen, will also reduce healthy protein.
“There is a long and complex debate about how much [lowering] is too much and how much is enough,” Dr. Sampaio said. “And this is a problem that has not been solved.”
Allele-specific therapy. A different class of investigative drugs, called allele-specific therapies, target only mutant HTT, sparing healthy protein. The drugs are tailored to genetic markers, or single-nucleotide polymorphisms (SNPs), that are present in different Huntington’s disease populations worldwide. Because treatments based on SNPs are highly tailored, “you need a new drug for each SNP to cover the global Huntington’s disease population,” Dr. Sampaio said. “This presents challenges from a regulatory perspective, as each drug would have to be evaluated separately.”
Two SNP-based therapies failed clinical trials in 2021, when they did not engage their targets.2 A third trial succeeded in lowering mutant HTT while preserving healthy protein and is being evaluated further in the clinic.2
Other strategies have yielded disappointing or mixed results:
A trial of branaplam, a small molecule, was stopped late in 2022 after patients developed peripheral neuropathy.3 Novartis, the drug’s manufacturer, said it would no longer investigate branaplam for Huntington’s disease.
Months earlier, in August 2022, a trial of a gene therapy to lower HTT protein – injected directly into the striatum of the brain – was halted because of adverse events in its high-dosage arm but has since resumed, with some changes to protocol.4
In neither case was excess protein-lowering thought to be the cause of safety problems.
DNA repair emerges as a promising target
Scientists have understood, since the 1990s, that the number of excess CAG repeats measured in a blood test is not the sole predictor of the onset of motor symptoms or rate of progression of Huntington’s disease.
Since the early 2000s, researchers have also known that the number of CAG repeats in cells is unstable, both in different tissues and cell types, and over time. People with Huntington’s disease turned out to be genetic mosaics, with varying, changing lengths of CAG repeats in cells. Repeats increase as a person ages, most drastically in the spiny medium neurons of the brain.
The process by which CAG repetitions grow in cells, known as somatic instability, remained poorly understood and little investigated until 2015, when a genomewide association study revealed previously unknown mechanisms.5 As it turns out, genes involved in the growth of CAG repeats are related to the DNA mismatch repair pathway, which is also important in cancer.
DNA mismatch repair refers to a complex housekeeping system, involving multiple genes and enzymes, that is fundamental to the functioning of the body as genes are continuously being translated to form proteins. Mismatch repair becomes increasingly error-prone with age: Mistakes that are not repaired become mutations, some of which are irrelevant and others that can be deleterious and lead to cancer.
In Huntington’s disease, enzymes involved in repairing DNA are the same ones that can erroneously add CAG repeats to HTT. A person with Huntington’s disease inherits what can be considered a “dyslexic” DNA repair system, Dr. Sampaio said, that misreads its template and keeps adding CAGs.
After the 2015 genomewide association study, “the DNA mismatch repair pathway became hugely important in Huntington’s disease research, and there is a lot of attention being paid now to its components. The idea is that, if we can intervene in this process, we might stop the somatic instability, the growing of the CAG repetitions, and ameliorate the progression of the disease,” Dr. Sampaio said.
In 2017 Dr. Tabrizi’s team reported that the mismatch repair gene MSH-3 was as a key driver of CAG repeats in people with Huntington’s disease.6 “I’m working really closely now with DNA repair scientists who’ve been working in cancer for 20 years. Cancer and repeat expansion diseases have really come together,” Dr. Tabrizi said.
At CHDI’s April 2023 therapeutics conference in Dubrovnik, Croatia, scientists presented findings on how to target MSH-3 and other mechanisms that underlie somatic instability.7 (Several drug companies are working on small molecules, ASOs, and other ways to inhibit MSH-3.) Researchers also presented extensively on protein lowering. The two treatment strategies are compatible for Huntington’s disease, Dr. Tabrizi said.
“I think the best way to approach Huntington’s is to target the somatic CAG repeat expansion by inhibiting MSH-3 in some way, and also target HTT lowering – but targeting it at the DNA level, as opposed to clearing the protein,” Dr. Tabrizi said. DNA-centered approaches in preclinical testing include CRISPR gene editing to inactivate mutant HTT and zinc finger proteins that allow selective targeting of DNA to reduce mutant HTT.
Recent findings on the mismatch repair pathway in Huntington’s disease have direct implications for other rare neurologic diseases caused by triplet repeat mutations, including myotonic dystrophy and cerebellar ataxias.
“There is very strong basic fundamental research in Huntington’s disease that doesn’t exist for every disease,” Dr. Sampaio said. “The fact that it is monogenic, and an adult disease that progresses relatively slowly, has made it a good disease to study, a kind of model.”
Huntington’s disease research has also generated research strategies of value in neurodegenerative diseases, such as Alzheimer’s and Parkinson’s. It provided key insights about neurofilament light, a biomarker of neuronal damage, and about the ASO drug class, which is being investigated for its utility treating in a range of diseases.
Previously, Huntington’s disease trial cohorts and registries focused on patients with late symptomatic disease. However, researchers are now pivoting to patients with less-severe disease and to preclinical mutation carriers. “We now know you have to treat early,” Dr. Tabrizi said. “This has implications for the whole field.”
Dr. Sampaio disclosed that she is an employee of CHDI Management, the administrative arm of the CHDI foundation. Dr. Tabrizi disclosed serving as a consultant to Alnylam Pharmaceuticals, Annexon, Ascidian Therapeutics, Arrowhead Pharmaceuticals, Atalanta Therapeutics, Design Therapeutics, F. Hoffmann-La Roche, HCD Economics, IQVIA, Iris Medicine, Latus Bio, LifeEdit, Novartis, Pfizer, Prilenia Therapeutics, PTC Therapeutics, Rgenta Therapeutics, Takeda Pharmaceuticals, uniQure, and Vertex Pharmaceuticals.
References
1. Genentech. Genentech Provides Update on Tominersen Program in Manifest Huntington’s Disease. https://www.gene.com/media/press-releases/14902/2021-03-22/genentech-provides-update-on-tominersen-.
2. Wave Life Sciences. Defining a new era of oligonucleotides. https://ir.wavelifesciences.com/news-releases/news-release-details/wave-life-sciences-announces-positive-update-phase-1b2a-select.
3. Novartis. Community update: Status of VIBRANT-HD, the study of branaplam/LMI070 in Huntington’s disease. https://hdsa.org/wp-content/uploads/2022/08/Novartis-FINAL-Community-Letter-8-24-22.pdf.
4. UniQure. Second Quarter 2022 Financial Results. https://uniqure.gcs-web.com/node/10856/pdf.
5. Genetic Modifiers of Huntington’s Disease (GeM-HD) Consortium. Cell. 2015 Jul 30;162(3):516-26. doi: 10.1016/j.cell.2015.07.003.
6. Moss DJH et al. Lancet Neurol. 2017 Sep;16(9):701-11. doi: 10.1016/S1474-4422(17)30161-8.
7. CHDI Foundation. Postcard from Dubrovnik 2023. https://chdifoundation.org/postcard-from-dubrovnik-2023/.
The past decade has been a contradictory one for research on Huntington’s disease, marked by breakthroughs in the biology and genetics of this fatal neurodegenerative disease and painful disappointments in trials of novel therapies.
What is Huntington’s disease?
Huntington’s disease is caused by a trinucleotide repeat mutation in the huntingtin gene (HTT) and follows an autosomal dominant pattern of inheritance. In people with more than 39 copies of this CAG repeat tract expansion, the HTT protein misfolds to become toxic, with more repeats linked to earlier disease onset and a more severe course.
Huntington’s disease causes loss of neurons in the striatum and disrupts the cortical-striatal-thalamic pathway, a brain circuit that governs movement. Although behavioral symptoms can emerge earlier, signature symptoms – chorea, dystonia, and cognitive abnormalities – usually present at midlife and progress until the patient’s death.
Huntington’s disease affects an estimated 30,000 people in the United States, and an estimated 10-12 people for every 100,000 worldwide – making it rare enough that neurologists who do not specialize in movement disorders might never treat a Huntington’s patient. Yet Huntington’s disease is sufficiently prevalent to attract robust research interest and sustain large registries, which have led to remarkable findings with implications not just for Huntington’s disease but for other diseases as well.
Right now, the only Food and Drug Administration–approved treatments for Huntington’s disease are symptomatic therapies to help temper disturbances of movement, sleep, and emotions. There are two major avenues of investigation into Huntington’s disease modification:
Reduce levels of mutant HTT protein, whether through small molecules, gene therapies, or antisense oligonucleotides (ASOs) that modulate RNA processing. In March 2021, Roche announced the suspension of its phase 3 trial of tominersen, an ASO.1 Trials of other protein-lowering agents were canceled for lack of target engagement or over safety concerns, in 2021 and 2022, although this approach is still considered viable.
Modify the length of CAG repeats, which involves a more recently encountered mechanism in Huntington’s disease. The strategy is at the preclinical stage. In 2015, a group of scientists reported the game-changing discovery that a large number of genes, associated with some of the same DNA-mismatch repair pathways implicated in cancer, can modify the length of CAG repeats in cells. This gave rise to a new set of therapeutic targets, now being explored.
Neurology Reviews 2023 Rare Neurological Disease Special Report spoke with two frequently collaborating researchers at the forefront of Huntington’s disease science – Cristina Sampaio, MD, PhD, chief medical officer of CHDI Management, Princeton, N.J., and Sarah Tabrizi, MD, PhD, from University College London – about lessons learned from the past several years of Huntington’s disease drug research.
The CHDI Foundation, a nonprofit research organization, was founded in 2003 to facilitate development of Huntington’s disease therapies. Its clinical research platform, Enroll-HD, includes a global registry of some 28,000 patients and a biobank to facilitate biomarker discovery and validation. Dr. Tabrizi’s lab explores Huntington’s disease drug targets in both HTT and DNA mismatch repair, and led two CHDI-funded observational studies, TRACK-HD and TrackOn-HD, to characterize disease progression in people with Huntington’s disease. In 2022, Dr. Tabrizi and Dr. Sampaio were coauthors of a comprehensive review of Huntington’s disease drug development and published a new disease-staging system to help enable trials in presymptomatic Huntington’s disease.
“The story of Huntington’s therapeutics is very informative,” Dr. Sampaio said. “Understanding these mechanisms is relevant for any neurologist – not only for Huntington’s but because they represent a prototype development for a big group of therapies and make us better equipped to think about everything else that is happening in neurology. They’re giving us an understanding of where neurology is going.”
Tackling a tricky protein
Most Huntington’s disease research has focused on ways to attack or lower mutant HTT protein. But HTT has proven a tricky target: HTT is a large protein, present in all cells, and known to interact with more than 100 genes. Healthy HTT is critical to fetal development, but its functions in the adult body remain something of a mystery. Almost all people with Huntington’s disease have both wild-type and mutant HTT.
Tominersen, the investigative ASO developed by Roche, works to block translation of the HTT message, leading to a reduction in both healthy and mutant HTT protein. It is delivered by lumbar injection to reach the brain. Upon halting its phase 3 trial of tominersen in 2021, Roche reported that people in the high-dosage treatment group did measurably worse – although it remains unclear whether this was caused by excess protein lowering or an off-target effect. The tominersen program was the first to clearly show that it is possible to lower HTT with an intervention – a critical first step in the development of this class of drugs.
“I think the problem with the trial was the aggressive loading doses plus exposure-related toxicity,” Dr. Tabrizi said. “Whether that exposure-related toxicity was related to too much wild-type HTT lowering or the proinflammatory effects of the ASO, you can’t yet disentangle.” Roche has not given up: The company is now seeking to test lower dosages of tominersen on a younger subgroup of patients who have fewer CAG repeats, in whom a benefit of protein lowering might be more clearly seen.
Small molecules and gene therapies have also been developed to reduce mutant HTT, although most, as is the case with tominersen, will also reduce healthy protein.
“There is a long and complex debate about how much [lowering] is too much and how much is enough,” Dr. Sampaio said. “And this is a problem that has not been solved.”
Allele-specific therapy. A different class of investigative drugs, called allele-specific therapies, target only mutant HTT, sparing healthy protein. The drugs are tailored to genetic markers, or single-nucleotide polymorphisms (SNPs), that are present in different Huntington’s disease populations worldwide. Because treatments based on SNPs are highly tailored, “you need a new drug for each SNP to cover the global Huntington’s disease population,” Dr. Sampaio said. “This presents challenges from a regulatory perspective, as each drug would have to be evaluated separately.”
Two SNP-based therapies failed clinical trials in 2021, when they did not engage their targets.2 A third trial succeeded in lowering mutant HTT while preserving healthy protein and is being evaluated further in the clinic.2
Other strategies have yielded disappointing or mixed results:
A trial of branaplam, a small molecule, was stopped late in 2022 after patients developed peripheral neuropathy.3 Novartis, the drug’s manufacturer, said it would no longer investigate branaplam for Huntington’s disease.
Months earlier, in August 2022, a trial of a gene therapy to lower HTT protein – injected directly into the striatum of the brain – was halted because of adverse events in its high-dosage arm but has since resumed, with some changes to protocol.4
In neither case was excess protein-lowering thought to be the cause of safety problems.
DNA repair emerges as a promising target
Scientists have understood, since the 1990s, that the number of excess CAG repeats measured in a blood test is not the sole predictor of the onset of motor symptoms or rate of progression of Huntington’s disease.
Since the early 2000s, researchers have also known that the number of CAG repeats in cells is unstable, both in different tissues and cell types, and over time. People with Huntington’s disease turned out to be genetic mosaics, with varying, changing lengths of CAG repeats in cells. Repeats increase as a person ages, most drastically in the spiny medium neurons of the brain.
The process by which CAG repetitions grow in cells, known as somatic instability, remained poorly understood and little investigated until 2015, when a genomewide association study revealed previously unknown mechanisms.5 As it turns out, genes involved in the growth of CAG repeats are related to the DNA mismatch repair pathway, which is also important in cancer.
DNA mismatch repair refers to a complex housekeeping system, involving multiple genes and enzymes, that is fundamental to the functioning of the body as genes are continuously being translated to form proteins. Mismatch repair becomes increasingly error-prone with age: Mistakes that are not repaired become mutations, some of which are irrelevant and others that can be deleterious and lead to cancer.
In Huntington’s disease, enzymes involved in repairing DNA are the same ones that can erroneously add CAG repeats to HTT. A person with Huntington’s disease inherits what can be considered a “dyslexic” DNA repair system, Dr. Sampaio said, that misreads its template and keeps adding CAGs.
After the 2015 genomewide association study, “the DNA mismatch repair pathway became hugely important in Huntington’s disease research, and there is a lot of attention being paid now to its components. The idea is that, if we can intervene in this process, we might stop the somatic instability, the growing of the CAG repetitions, and ameliorate the progression of the disease,” Dr. Sampaio said.
In 2017 Dr. Tabrizi’s team reported that the mismatch repair gene MSH-3 was as a key driver of CAG repeats in people with Huntington’s disease.6 “I’m working really closely now with DNA repair scientists who’ve been working in cancer for 20 years. Cancer and repeat expansion diseases have really come together,” Dr. Tabrizi said.
At CHDI’s April 2023 therapeutics conference in Dubrovnik, Croatia, scientists presented findings on how to target MSH-3 and other mechanisms that underlie somatic instability.7 (Several drug companies are working on small molecules, ASOs, and other ways to inhibit MSH-3.) Researchers also presented extensively on protein lowering. The two treatment strategies are compatible for Huntington’s disease, Dr. Tabrizi said.
“I think the best way to approach Huntington’s is to target the somatic CAG repeat expansion by inhibiting MSH-3 in some way, and also target HTT lowering – but targeting it at the DNA level, as opposed to clearing the protein,” Dr. Tabrizi said. DNA-centered approaches in preclinical testing include CRISPR gene editing to inactivate mutant HTT and zinc finger proteins that allow selective targeting of DNA to reduce mutant HTT.
Recent findings on the mismatch repair pathway in Huntington’s disease have direct implications for other rare neurologic diseases caused by triplet repeat mutations, including myotonic dystrophy and cerebellar ataxias.
“There is very strong basic fundamental research in Huntington’s disease that doesn’t exist for every disease,” Dr. Sampaio said. “The fact that it is monogenic, and an adult disease that progresses relatively slowly, has made it a good disease to study, a kind of model.”
Huntington’s disease research has also generated research strategies of value in neurodegenerative diseases, such as Alzheimer’s and Parkinson’s. It provided key insights about neurofilament light, a biomarker of neuronal damage, and about the ASO drug class, which is being investigated for its utility treating in a range of diseases.
Previously, Huntington’s disease trial cohorts and registries focused on patients with late symptomatic disease. However, researchers are now pivoting to patients with less-severe disease and to preclinical mutation carriers. “We now know you have to treat early,” Dr. Tabrizi said. “This has implications for the whole field.”
Dr. Sampaio disclosed that she is an employee of CHDI Management, the administrative arm of the CHDI foundation. Dr. Tabrizi disclosed serving as a consultant to Alnylam Pharmaceuticals, Annexon, Ascidian Therapeutics, Arrowhead Pharmaceuticals, Atalanta Therapeutics, Design Therapeutics, F. Hoffmann-La Roche, HCD Economics, IQVIA, Iris Medicine, Latus Bio, LifeEdit, Novartis, Pfizer, Prilenia Therapeutics, PTC Therapeutics, Rgenta Therapeutics, Takeda Pharmaceuticals, uniQure, and Vertex Pharmaceuticals.
References
1. Genentech. Genentech Provides Update on Tominersen Program in Manifest Huntington’s Disease. https://www.gene.com/media/press-releases/14902/2021-03-22/genentech-provides-update-on-tominersen-.
2. Wave Life Sciences. Defining a new era of oligonucleotides. https://ir.wavelifesciences.com/news-releases/news-release-details/wave-life-sciences-announces-positive-update-phase-1b2a-select.
3. Novartis. Community update: Status of VIBRANT-HD, the study of branaplam/LMI070 in Huntington’s disease. https://hdsa.org/wp-content/uploads/2022/08/Novartis-FINAL-Community-Letter-8-24-22.pdf.
4. UniQure. Second Quarter 2022 Financial Results. https://uniqure.gcs-web.com/node/10856/pdf.
5. Genetic Modifiers of Huntington’s Disease (GeM-HD) Consortium. Cell. 2015 Jul 30;162(3):516-26. doi: 10.1016/j.cell.2015.07.003.
6. Moss DJH et al. Lancet Neurol. 2017 Sep;16(9):701-11. doi: 10.1016/S1474-4422(17)30161-8.
7. CHDI Foundation. Postcard from Dubrovnik 2023. https://chdifoundation.org/postcard-from-dubrovnik-2023/.
The past decade has been a contradictory one for research on Huntington’s disease, marked by breakthroughs in the biology and genetics of this fatal neurodegenerative disease and painful disappointments in trials of novel therapies.
What is Huntington’s disease?
Huntington’s disease is caused by a trinucleotide repeat mutation in the huntingtin gene (HTT) and follows an autosomal dominant pattern of inheritance. In people with more than 39 copies of this CAG repeat tract expansion, the HTT protein misfolds to become toxic, with more repeats linked to earlier disease onset and a more severe course.
Huntington’s disease causes loss of neurons in the striatum and disrupts the cortical-striatal-thalamic pathway, a brain circuit that governs movement. Although behavioral symptoms can emerge earlier, signature symptoms – chorea, dystonia, and cognitive abnormalities – usually present at midlife and progress until the patient’s death.
Huntington’s disease affects an estimated 30,000 people in the United States, and an estimated 10-12 people for every 100,000 worldwide – making it rare enough that neurologists who do not specialize in movement disorders might never treat a Huntington’s patient. Yet Huntington’s disease is sufficiently prevalent to attract robust research interest and sustain large registries, which have led to remarkable findings with implications not just for Huntington’s disease but for other diseases as well.
Right now, the only Food and Drug Administration–approved treatments for Huntington’s disease are symptomatic therapies to help temper disturbances of movement, sleep, and emotions. There are two major avenues of investigation into Huntington’s disease modification:
Reduce levels of mutant HTT protein, whether through small molecules, gene therapies, or antisense oligonucleotides (ASOs) that modulate RNA processing. In March 2021, Roche announced the suspension of its phase 3 trial of tominersen, an ASO.1 Trials of other protein-lowering agents were canceled for lack of target engagement or over safety concerns, in 2021 and 2022, although this approach is still considered viable.
Modify the length of CAG repeats, which involves a more recently encountered mechanism in Huntington’s disease. The strategy is at the preclinical stage. In 2015, a group of scientists reported the game-changing discovery that a large number of genes, associated with some of the same DNA-mismatch repair pathways implicated in cancer, can modify the length of CAG repeats in cells. This gave rise to a new set of therapeutic targets, now being explored.
Neurology Reviews 2023 Rare Neurological Disease Special Report spoke with two frequently collaborating researchers at the forefront of Huntington’s disease science – Cristina Sampaio, MD, PhD, chief medical officer of CHDI Management, Princeton, N.J., and Sarah Tabrizi, MD, PhD, from University College London – about lessons learned from the past several years of Huntington’s disease drug research.
The CHDI Foundation, a nonprofit research organization, was founded in 2003 to facilitate development of Huntington’s disease therapies. Its clinical research platform, Enroll-HD, includes a global registry of some 28,000 patients and a biobank to facilitate biomarker discovery and validation. Dr. Tabrizi’s lab explores Huntington’s disease drug targets in both HTT and DNA mismatch repair, and led two CHDI-funded observational studies, TRACK-HD and TrackOn-HD, to characterize disease progression in people with Huntington’s disease. In 2022, Dr. Tabrizi and Dr. Sampaio were coauthors of a comprehensive review of Huntington’s disease drug development and published a new disease-staging system to help enable trials in presymptomatic Huntington’s disease.
“The story of Huntington’s therapeutics is very informative,” Dr. Sampaio said. “Understanding these mechanisms is relevant for any neurologist – not only for Huntington’s but because they represent a prototype development for a big group of therapies and make us better equipped to think about everything else that is happening in neurology. They’re giving us an understanding of where neurology is going.”
Tackling a tricky protein
Most Huntington’s disease research has focused on ways to attack or lower mutant HTT protein. But HTT has proven a tricky target: HTT is a large protein, present in all cells, and known to interact with more than 100 genes. Healthy HTT is critical to fetal development, but its functions in the adult body remain something of a mystery. Almost all people with Huntington’s disease have both wild-type and mutant HTT.
Tominersen, the investigative ASO developed by Roche, works to block translation of the HTT message, leading to a reduction in both healthy and mutant HTT protein. It is delivered by lumbar injection to reach the brain. Upon halting its phase 3 trial of tominersen in 2021, Roche reported that people in the high-dosage treatment group did measurably worse – although it remains unclear whether this was caused by excess protein lowering or an off-target effect. The tominersen program was the first to clearly show that it is possible to lower HTT with an intervention – a critical first step in the development of this class of drugs.
“I think the problem with the trial was the aggressive loading doses plus exposure-related toxicity,” Dr. Tabrizi said. “Whether that exposure-related toxicity was related to too much wild-type HTT lowering or the proinflammatory effects of the ASO, you can’t yet disentangle.” Roche has not given up: The company is now seeking to test lower dosages of tominersen on a younger subgroup of patients who have fewer CAG repeats, in whom a benefit of protein lowering might be more clearly seen.
Small molecules and gene therapies have also been developed to reduce mutant HTT, although most, as is the case with tominersen, will also reduce healthy protein.
“There is a long and complex debate about how much [lowering] is too much and how much is enough,” Dr. Sampaio said. “And this is a problem that has not been solved.”
Allele-specific therapy. A different class of investigative drugs, called allele-specific therapies, target only mutant HTT, sparing healthy protein. The drugs are tailored to genetic markers, or single-nucleotide polymorphisms (SNPs), that are present in different Huntington’s disease populations worldwide. Because treatments based on SNPs are highly tailored, “you need a new drug for each SNP to cover the global Huntington’s disease population,” Dr. Sampaio said. “This presents challenges from a regulatory perspective, as each drug would have to be evaluated separately.”
Two SNP-based therapies failed clinical trials in 2021, when they did not engage their targets.2 A third trial succeeded in lowering mutant HTT while preserving healthy protein and is being evaluated further in the clinic.2
Other strategies have yielded disappointing or mixed results:
A trial of branaplam, a small molecule, was stopped late in 2022 after patients developed peripheral neuropathy.3 Novartis, the drug’s manufacturer, said it would no longer investigate branaplam for Huntington’s disease.
Months earlier, in August 2022, a trial of a gene therapy to lower HTT protein – injected directly into the striatum of the brain – was halted because of adverse events in its high-dosage arm but has since resumed, with some changes to protocol.4
In neither case was excess protein-lowering thought to be the cause of safety problems.
DNA repair emerges as a promising target
Scientists have understood, since the 1990s, that the number of excess CAG repeats measured in a blood test is not the sole predictor of the onset of motor symptoms or rate of progression of Huntington’s disease.
Since the early 2000s, researchers have also known that the number of CAG repeats in cells is unstable, both in different tissues and cell types, and over time. People with Huntington’s disease turned out to be genetic mosaics, with varying, changing lengths of CAG repeats in cells. Repeats increase as a person ages, most drastically in the spiny medium neurons of the brain.
The process by which CAG repetitions grow in cells, known as somatic instability, remained poorly understood and little investigated until 2015, when a genomewide association study revealed previously unknown mechanisms.5 As it turns out, genes involved in the growth of CAG repeats are related to the DNA mismatch repair pathway, which is also important in cancer.
DNA mismatch repair refers to a complex housekeeping system, involving multiple genes and enzymes, that is fundamental to the functioning of the body as genes are continuously being translated to form proteins. Mismatch repair becomes increasingly error-prone with age: Mistakes that are not repaired become mutations, some of which are irrelevant and others that can be deleterious and lead to cancer.
In Huntington’s disease, enzymes involved in repairing DNA are the same ones that can erroneously add CAG repeats to HTT. A person with Huntington’s disease inherits what can be considered a “dyslexic” DNA repair system, Dr. Sampaio said, that misreads its template and keeps adding CAGs.
After the 2015 genomewide association study, “the DNA mismatch repair pathway became hugely important in Huntington’s disease research, and there is a lot of attention being paid now to its components. The idea is that, if we can intervene in this process, we might stop the somatic instability, the growing of the CAG repetitions, and ameliorate the progression of the disease,” Dr. Sampaio said.
In 2017 Dr. Tabrizi’s team reported that the mismatch repair gene MSH-3 was as a key driver of CAG repeats in people with Huntington’s disease.6 “I’m working really closely now with DNA repair scientists who’ve been working in cancer for 20 years. Cancer and repeat expansion diseases have really come together,” Dr. Tabrizi said.
At CHDI’s April 2023 therapeutics conference in Dubrovnik, Croatia, scientists presented findings on how to target MSH-3 and other mechanisms that underlie somatic instability.7 (Several drug companies are working on small molecules, ASOs, and other ways to inhibit MSH-3.) Researchers also presented extensively on protein lowering. The two treatment strategies are compatible for Huntington’s disease, Dr. Tabrizi said.
“I think the best way to approach Huntington’s is to target the somatic CAG repeat expansion by inhibiting MSH-3 in some way, and also target HTT lowering – but targeting it at the DNA level, as opposed to clearing the protein,” Dr. Tabrizi said. DNA-centered approaches in preclinical testing include CRISPR gene editing to inactivate mutant HTT and zinc finger proteins that allow selective targeting of DNA to reduce mutant HTT.
Recent findings on the mismatch repair pathway in Huntington’s disease have direct implications for other rare neurologic diseases caused by triplet repeat mutations, including myotonic dystrophy and cerebellar ataxias.
“There is very strong basic fundamental research in Huntington’s disease that doesn’t exist for every disease,” Dr. Sampaio said. “The fact that it is monogenic, and an adult disease that progresses relatively slowly, has made it a good disease to study, a kind of model.”
Huntington’s disease research has also generated research strategies of value in neurodegenerative diseases, such as Alzheimer’s and Parkinson’s. It provided key insights about neurofilament light, a biomarker of neuronal damage, and about the ASO drug class, which is being investigated for its utility treating in a range of diseases.
Previously, Huntington’s disease trial cohorts and registries focused on patients with late symptomatic disease. However, researchers are now pivoting to patients with less-severe disease and to preclinical mutation carriers. “We now know you have to treat early,” Dr. Tabrizi said. “This has implications for the whole field.”
Dr. Sampaio disclosed that she is an employee of CHDI Management, the administrative arm of the CHDI foundation. Dr. Tabrizi disclosed serving as a consultant to Alnylam Pharmaceuticals, Annexon, Ascidian Therapeutics, Arrowhead Pharmaceuticals, Atalanta Therapeutics, Design Therapeutics, F. Hoffmann-La Roche, HCD Economics, IQVIA, Iris Medicine, Latus Bio, LifeEdit, Novartis, Pfizer, Prilenia Therapeutics, PTC Therapeutics, Rgenta Therapeutics, Takeda Pharmaceuticals, uniQure, and Vertex Pharmaceuticals.
References
1. Genentech. Genentech Provides Update on Tominersen Program in Manifest Huntington’s Disease. https://www.gene.com/media/press-releases/14902/2021-03-22/genentech-provides-update-on-tominersen-.
2. Wave Life Sciences. Defining a new era of oligonucleotides. https://ir.wavelifesciences.com/news-releases/news-release-details/wave-life-sciences-announces-positive-update-phase-1b2a-select.
3. Novartis. Community update: Status of VIBRANT-HD, the study of branaplam/LMI070 in Huntington’s disease. https://hdsa.org/wp-content/uploads/2022/08/Novartis-FINAL-Community-Letter-8-24-22.pdf.
4. UniQure. Second Quarter 2022 Financial Results. https://uniqure.gcs-web.com/node/10856/pdf.
5. Genetic Modifiers of Huntington’s Disease (GeM-HD) Consortium. Cell. 2015 Jul 30;162(3):516-26. doi: 10.1016/j.cell.2015.07.003.
6. Moss DJH et al. Lancet Neurol. 2017 Sep;16(9):701-11. doi: 10.1016/S1474-4422(17)30161-8.
7. CHDI Foundation. Postcard from Dubrovnik 2023. https://chdifoundation.org/postcard-from-dubrovnik-2023/.
The surprising link between loneliness and Parkinson’s disease
This transcript has been edited for clarity.
On May 3, 2023, Surgeon General Vivek Murthy issued an advisory raising an alarm about what he called an “epidemic of loneliness” in the United States.
Now, I am not saying that Vivek Murthy read my book, “How Medicine Works and When It Doesn’t” – released in January and available in bookstores now – where, in chapter 11, I call attention to the problem of loneliness and its relationship to the exponential rise in deaths of despair. But Vivek, if you did, let me know. I could use the publicity.
No, of course the idea that loneliness is a public health issue is not new, but I’m glad to see it finally getting attention. At this point, studies have linked loneliness to heart disease, stroke, dementia, and premature death.
The UK Biobank is really a treasure trove of data for epidemiologists. I must see three to four studies a week coming out of this mega-dataset. This one, appearing in JAMA Neurology, caught my eye for its focus specifically on loneliness as a risk factor – something I’m hoping to see more of in the future.
The study examines data from just under 500,000 individuals in the United Kingdom who answered a survey including the question “Do you often feel lonely?” between 2006 and 2010; 18.4% of people answered yes. Individuals’ electronic health record data were then monitored over time to see who would get a new diagnosis code consistent with Parkinson’s disease. Through 2021, 2822 people did – that’s just over half a percent.
So, now we do the statistics thing. Of the nonlonely folks, 2,273 went on to develop Parkinson’s disease. Of those who said they often feel lonely, 549 people did. The raw numbers here, to be honest, aren’t that compelling. Lonely people had an absolute risk for Parkinson’s disease about 0.03% higher than that of nonlonely people. Put another way, you’d need to take over 3,000 lonely souls and make them not lonely to prevent 1 case of Parkinson’s disease.
Still, the costs of loneliness are not measured exclusively in Parkinson’s disease, and I would argue that the real risks here come from other sources: alcohol abuse, drug abuse, and suicide. Nevertheless, the weak but significant association with Parkinson’s disease reminds us that loneliness is a neurologic phenomenon. There is something about social connection that affects our brain in a way that is not just spiritual; it is actually biological.
Of course, people who say they are often lonely are different in other ways from people who report not being lonely. Lonely people, in this dataset, were younger, more likely to be female, less likely to have a college degree, in worse physical health, and engaged in more high-risk health behaviors like smoking.
The authors adjusted for all of these factors and found that, on the relative scale, lonely people were still about 20%-30% more likely to develop Parkinson’s disease.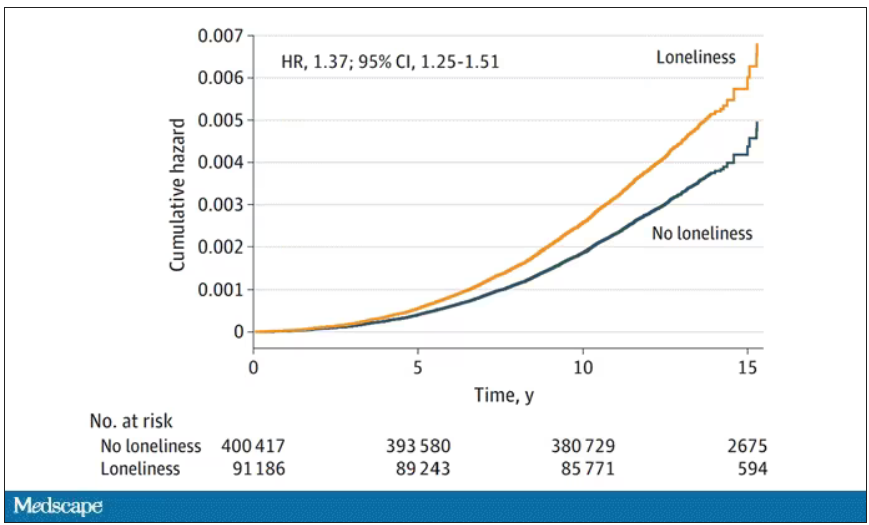
So, what do we do about this? There is no pill for loneliness, and God help us if there ever is. Recognizing the problem is a good start. But there are some policy things we can do to reduce loneliness. We can invest in public spaces that bring people together – parks, museums, libraries – and public transportation. We can deal with tech companies that are so optimized at capturing our attention that we cease to engage with other humans. And, individually, we can just reach out a bit more. We’ve spent the past few pandemic years with our attention focused sharply inward. It’s time to look out again.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
On May 3, 2023, Surgeon General Vivek Murthy issued an advisory raising an alarm about what he called an “epidemic of loneliness” in the United States.
Now, I am not saying that Vivek Murthy read my book, “How Medicine Works and When It Doesn’t” – released in January and available in bookstores now – where, in chapter 11, I call attention to the problem of loneliness and its relationship to the exponential rise in deaths of despair. But Vivek, if you did, let me know. I could use the publicity.
No, of course the idea that loneliness is a public health issue is not new, but I’m glad to see it finally getting attention. At this point, studies have linked loneliness to heart disease, stroke, dementia, and premature death.
The UK Biobank is really a treasure trove of data for epidemiologists. I must see three to four studies a week coming out of this mega-dataset. This one, appearing in JAMA Neurology, caught my eye for its focus specifically on loneliness as a risk factor – something I’m hoping to see more of in the future.
The study examines data from just under 500,000 individuals in the United Kingdom who answered a survey including the question “Do you often feel lonely?” between 2006 and 2010; 18.4% of people answered yes. Individuals’ electronic health record data were then monitored over time to see who would get a new diagnosis code consistent with Parkinson’s disease. Through 2021, 2822 people did – that’s just over half a percent.
So, now we do the statistics thing. Of the nonlonely folks, 2,273 went on to develop Parkinson’s disease. Of those who said they often feel lonely, 549 people did. The raw numbers here, to be honest, aren’t that compelling. Lonely people had an absolute risk for Parkinson’s disease about 0.03% higher than that of nonlonely people. Put another way, you’d need to take over 3,000 lonely souls and make them not lonely to prevent 1 case of Parkinson’s disease.
Still, the costs of loneliness are not measured exclusively in Parkinson’s disease, and I would argue that the real risks here come from other sources: alcohol abuse, drug abuse, and suicide. Nevertheless, the weak but significant association with Parkinson’s disease reminds us that loneliness is a neurologic phenomenon. There is something about social connection that affects our brain in a way that is not just spiritual; it is actually biological.
Of course, people who say they are often lonely are different in other ways from people who report not being lonely. Lonely people, in this dataset, were younger, more likely to be female, less likely to have a college degree, in worse physical health, and engaged in more high-risk health behaviors like smoking.
The authors adjusted for all of these factors and found that, on the relative scale, lonely people were still about 20%-30% more likely to develop Parkinson’s disease.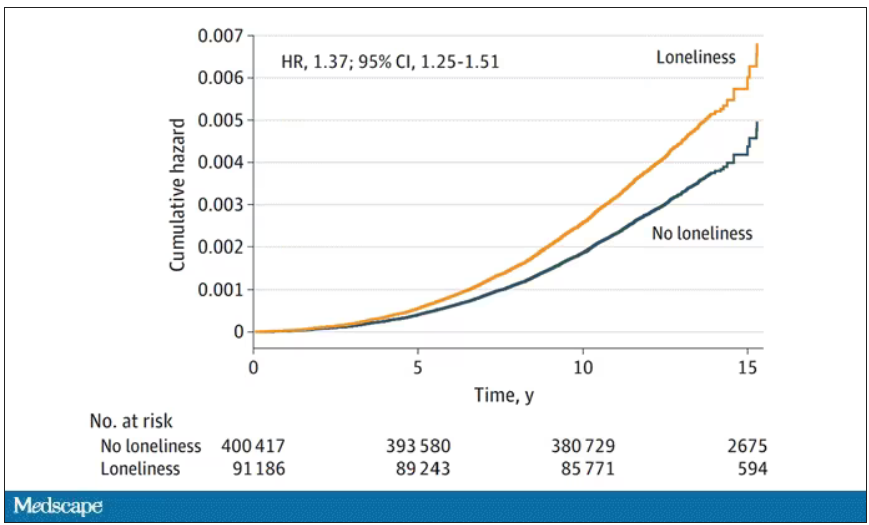
So, what do we do about this? There is no pill for loneliness, and God help us if there ever is. Recognizing the problem is a good start. But there are some policy things we can do to reduce loneliness. We can invest in public spaces that bring people together – parks, museums, libraries – and public transportation. We can deal with tech companies that are so optimized at capturing our attention that we cease to engage with other humans. And, individually, we can just reach out a bit more. We’ve spent the past few pandemic years with our attention focused sharply inward. It’s time to look out again.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
On May 3, 2023, Surgeon General Vivek Murthy issued an advisory raising an alarm about what he called an “epidemic of loneliness” in the United States.
Now, I am not saying that Vivek Murthy read my book, “How Medicine Works and When It Doesn’t” – released in January and available in bookstores now – where, in chapter 11, I call attention to the problem of loneliness and its relationship to the exponential rise in deaths of despair. But Vivek, if you did, let me know. I could use the publicity.
No, of course the idea that loneliness is a public health issue is not new, but I’m glad to see it finally getting attention. At this point, studies have linked loneliness to heart disease, stroke, dementia, and premature death.
The UK Biobank is really a treasure trove of data for epidemiologists. I must see three to four studies a week coming out of this mega-dataset. This one, appearing in JAMA Neurology, caught my eye for its focus specifically on loneliness as a risk factor – something I’m hoping to see more of in the future.
The study examines data from just under 500,000 individuals in the United Kingdom who answered a survey including the question “Do you often feel lonely?” between 2006 and 2010; 18.4% of people answered yes. Individuals’ electronic health record data were then monitored over time to see who would get a new diagnosis code consistent with Parkinson’s disease. Through 2021, 2822 people did – that’s just over half a percent.
So, now we do the statistics thing. Of the nonlonely folks, 2,273 went on to develop Parkinson’s disease. Of those who said they often feel lonely, 549 people did. The raw numbers here, to be honest, aren’t that compelling. Lonely people had an absolute risk for Parkinson’s disease about 0.03% higher than that of nonlonely people. Put another way, you’d need to take over 3,000 lonely souls and make them not lonely to prevent 1 case of Parkinson’s disease.
Still, the costs of loneliness are not measured exclusively in Parkinson’s disease, and I would argue that the real risks here come from other sources: alcohol abuse, drug abuse, and suicide. Nevertheless, the weak but significant association with Parkinson’s disease reminds us that loneliness is a neurologic phenomenon. There is something about social connection that affects our brain in a way that is not just spiritual; it is actually biological.
Of course, people who say they are often lonely are different in other ways from people who report not being lonely. Lonely people, in this dataset, were younger, more likely to be female, less likely to have a college degree, in worse physical health, and engaged in more high-risk health behaviors like smoking.
The authors adjusted for all of these factors and found that, on the relative scale, lonely people were still about 20%-30% more likely to develop Parkinson’s disease.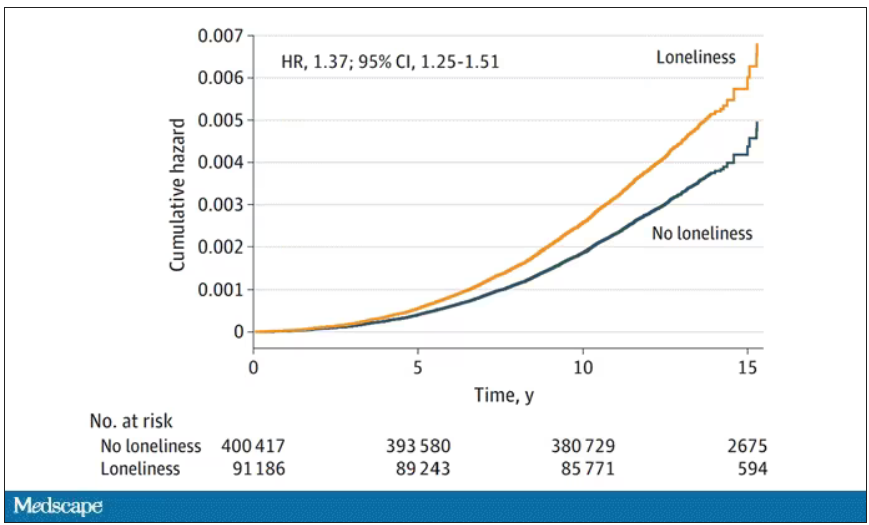
So, what do we do about this? There is no pill for loneliness, and God help us if there ever is. Recognizing the problem is a good start. But there are some policy things we can do to reduce loneliness. We can invest in public spaces that bring people together – parks, museums, libraries – and public transportation. We can deal with tech companies that are so optimized at capturing our attention that we cease to engage with other humans. And, individually, we can just reach out a bit more. We’ve spent the past few pandemic years with our attention focused sharply inward. It’s time to look out again.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.




