User login
No link found between high-potency statins andacute kidney injury
DALLAS – High-potency statin therapy given post acute coronary syndrome did not raise serum creatinine or cause more risk of acute kidney injury than low-potency statin regimens did in a new analysis of two published landmark randomized clinical trials.
"Considering the recently updated AHA/American College of Cardiology lipid guidelines, which call for the use of high-potency statins in millions more patients, these findings provide important reassurance that a high-potency statin regimen will not increase the incidence of adverse renal events," Dr. Amy Sarma said in presenting the study results at the American Heart Association scientific sessions.
She noted that a recent Canadian observational study utilizing Canadian and U.S. administrative databases totaling more than 2 million patients over age 40 who were newly placed on statin therapy showed an adjusted 1.34-fold increased rate of hospitalization for acute kidney injury within the first 120 days in those on a high- as compared to a low-potency regimen, and a 1.11-fold increased risk beyond 120 days through the end of the first year (BMJ 2013;346:f880). Both risk elevations were statistically significant.
However, observational studies such as this are prone to bias in the form of potentially crucial differences between the patients given a prescription for statins and those who aren’t. For this reason, Dr. Sarma and her coinvestigators turned for guidance to two randomized trials of high- versus low-dose statins, since this study design obviates the risks of confounding. The trials were PROVE IT-TIMI 22 (N. Engl. J. Med. 2004;350:1495-504) and the A-to-Z trial (JAMA 2004;292:1307-16).
PROVE IT included 4,122 patients randomized within 10 days post ACS to standard background therapy plus either pravastatin at 40 mg/day or atorvastatin at 80 mg/day. A-to-Z involved 4,497 patients who were placed on simvastatin at either 20 or 80 mg/day within 5 days post ACS. Both trials had a median follow-up of 2 years, and both featured serial measurements of serum creatinine. Two-thirds of subjects in PROVE IT had a baseline estimated glomerular filtration rate below 90 mL/min per 1.73 m2, while two-thirds of those in A-to-Z had a baseline eGFR less than 60, noted Dr. Sarma of Brigham and Women’s Hospital, Boston.
In both studies, mean serum creatinine rose equally during the first 30 days of statin therapy, regardless of treatment potency, and then levels declined. In PROVE IT, for example, serum creatinine in the pravastatin and atorvastatin arms rose by 0.96% and 0.97% above baseline, respectively, at 30 days. Values then dropped by 2.88% and 3.85% from baseline at 4 months, and by 3.88% and 5.83% at 16 months.
In both studies, there was no difference between the high- and low-potency statin groups in the incidence of any increase in serum creatinine of at least 1.5-fold, 2.0-fold, or 3.0-fold greater than baseline. In other words, there was no hint of a safety signal, she added.
Dr. Sarma reported having no financial conflicts of interest.
I’m not convinced by the PROVE IT and A-to-Z data. In the combined analysis, the high-potency statin group had a 15% greater risk of acute kidney injury compared with the low-potency statin group during the first 4 months of treatment. Although that wasn’t a statistically significant difference due to limited patient numbers and broad confidence intervals, it was quite similar to the long-term 11% increased risk seen in the Canadian observational database study with 2 million patients.
Moreover, an even bigger recent observational study led by investigators at the University of North Carolina, Chapel Hill, involving 3.9 million U.S. statin initiators found a 42% greater rate of acute kidney injury during the first year on high- as compared to lower-dose simvastatin in commercially insured patients and a 24% increased risk in the Medicare population. Both risk increases were statistically significant due to the huge patient numbers (Pharmacoepidemiol. Drug Saf. 2013;22:1061-70).

|
|
Also, PROVE IT and A-to-Z featured patient populations who were of a younger average age and less likely to be male and to have diabetes than the general American population of acute MI patients as depicted in the National Cardiovascular Data Registry (J. Am. Coll. Cardiol. 2013;62:1931-47). Advancing age, diabetes, and male gender are predisposing factors for acute kidney disease.
The Canadian observational study defined high-potency statin therapy as at least 20 mg/day of atorvastatin or 40 mg or simvastatin. The University of North Carolina study also defined high-potency simvastatin as at least 40 mg/day as opposed to the 80 mg/day employed in the A-to-Z trial. One wonders whether they would have seen an even larger magnitude of association had they used a higher threshold to define high potency.
I don’t necessarily disagree with Dr. Sarma’s conclusion that for most people after ACS a high-potency statin will be warranted. I just think we need to be cautious and think about the individual patient when we consider the risks and benefits.
It may well be the case that high-potency statin therapy means fewer cardiovascular events at the cost of a greater risk of acute kidney injury and other adverse events. With lower-potency statins, the trade-off may be more cardiovascular events but a lower acute kidney injury risk.
Dr. Tara Chang is a nephrologist at Stanford (Calif.) University. She was the discussant of the paper at the meeting. Dr. Chang disclosed having no financial conflicts.
I’m not convinced by the PROVE IT and A-to-Z data. In the combined analysis, the high-potency statin group had a 15% greater risk of acute kidney injury compared with the low-potency statin group during the first 4 months of treatment. Although that wasn’t a statistically significant difference due to limited patient numbers and broad confidence intervals, it was quite similar to the long-term 11% increased risk seen in the Canadian observational database study with 2 million patients.
Moreover, an even bigger recent observational study led by investigators at the University of North Carolina, Chapel Hill, involving 3.9 million U.S. statin initiators found a 42% greater rate of acute kidney injury during the first year on high- as compared to lower-dose simvastatin in commercially insured patients and a 24% increased risk in the Medicare population. Both risk increases were statistically significant due to the huge patient numbers (Pharmacoepidemiol. Drug Saf. 2013;22:1061-70).

|
|
Also, PROVE IT and A-to-Z featured patient populations who were of a younger average age and less likely to be male and to have diabetes than the general American population of acute MI patients as depicted in the National Cardiovascular Data Registry (J. Am. Coll. Cardiol. 2013;62:1931-47). Advancing age, diabetes, and male gender are predisposing factors for acute kidney disease.
The Canadian observational study defined high-potency statin therapy as at least 20 mg/day of atorvastatin or 40 mg or simvastatin. The University of North Carolina study also defined high-potency simvastatin as at least 40 mg/day as opposed to the 80 mg/day employed in the A-to-Z trial. One wonders whether they would have seen an even larger magnitude of association had they used a higher threshold to define high potency.
I don’t necessarily disagree with Dr. Sarma’s conclusion that for most people after ACS a high-potency statin will be warranted. I just think we need to be cautious and think about the individual patient when we consider the risks and benefits.
It may well be the case that high-potency statin therapy means fewer cardiovascular events at the cost of a greater risk of acute kidney injury and other adverse events. With lower-potency statins, the trade-off may be more cardiovascular events but a lower acute kidney injury risk.
Dr. Tara Chang is a nephrologist at Stanford (Calif.) University. She was the discussant of the paper at the meeting. Dr. Chang disclosed having no financial conflicts.
I’m not convinced by the PROVE IT and A-to-Z data. In the combined analysis, the high-potency statin group had a 15% greater risk of acute kidney injury compared with the low-potency statin group during the first 4 months of treatment. Although that wasn’t a statistically significant difference due to limited patient numbers and broad confidence intervals, it was quite similar to the long-term 11% increased risk seen in the Canadian observational database study with 2 million patients.
Moreover, an even bigger recent observational study led by investigators at the University of North Carolina, Chapel Hill, involving 3.9 million U.S. statin initiators found a 42% greater rate of acute kidney injury during the first year on high- as compared to lower-dose simvastatin in commercially insured patients and a 24% increased risk in the Medicare population. Both risk increases were statistically significant due to the huge patient numbers (Pharmacoepidemiol. Drug Saf. 2013;22:1061-70).

|
|
Also, PROVE IT and A-to-Z featured patient populations who were of a younger average age and less likely to be male and to have diabetes than the general American population of acute MI patients as depicted in the National Cardiovascular Data Registry (J. Am. Coll. Cardiol. 2013;62:1931-47). Advancing age, diabetes, and male gender are predisposing factors for acute kidney disease.
The Canadian observational study defined high-potency statin therapy as at least 20 mg/day of atorvastatin or 40 mg or simvastatin. The University of North Carolina study also defined high-potency simvastatin as at least 40 mg/day as opposed to the 80 mg/day employed in the A-to-Z trial. One wonders whether they would have seen an even larger magnitude of association had they used a higher threshold to define high potency.
I don’t necessarily disagree with Dr. Sarma’s conclusion that for most people after ACS a high-potency statin will be warranted. I just think we need to be cautious and think about the individual patient when we consider the risks and benefits.
It may well be the case that high-potency statin therapy means fewer cardiovascular events at the cost of a greater risk of acute kidney injury and other adverse events. With lower-potency statins, the trade-off may be more cardiovascular events but a lower acute kidney injury risk.
Dr. Tara Chang is a nephrologist at Stanford (Calif.) University. She was the discussant of the paper at the meeting. Dr. Chang disclosed having no financial conflicts.
DALLAS – High-potency statin therapy given post acute coronary syndrome did not raise serum creatinine or cause more risk of acute kidney injury than low-potency statin regimens did in a new analysis of two published landmark randomized clinical trials.
"Considering the recently updated AHA/American College of Cardiology lipid guidelines, which call for the use of high-potency statins in millions more patients, these findings provide important reassurance that a high-potency statin regimen will not increase the incidence of adverse renal events," Dr. Amy Sarma said in presenting the study results at the American Heart Association scientific sessions.
She noted that a recent Canadian observational study utilizing Canadian and U.S. administrative databases totaling more than 2 million patients over age 40 who were newly placed on statin therapy showed an adjusted 1.34-fold increased rate of hospitalization for acute kidney injury within the first 120 days in those on a high- as compared to a low-potency regimen, and a 1.11-fold increased risk beyond 120 days through the end of the first year (BMJ 2013;346:f880). Both risk elevations were statistically significant.
However, observational studies such as this are prone to bias in the form of potentially crucial differences between the patients given a prescription for statins and those who aren’t. For this reason, Dr. Sarma and her coinvestigators turned for guidance to two randomized trials of high- versus low-dose statins, since this study design obviates the risks of confounding. The trials were PROVE IT-TIMI 22 (N. Engl. J. Med. 2004;350:1495-504) and the A-to-Z trial (JAMA 2004;292:1307-16).
PROVE IT included 4,122 patients randomized within 10 days post ACS to standard background therapy plus either pravastatin at 40 mg/day or atorvastatin at 80 mg/day. A-to-Z involved 4,497 patients who were placed on simvastatin at either 20 or 80 mg/day within 5 days post ACS. Both trials had a median follow-up of 2 years, and both featured serial measurements of serum creatinine. Two-thirds of subjects in PROVE IT had a baseline estimated glomerular filtration rate below 90 mL/min per 1.73 m2, while two-thirds of those in A-to-Z had a baseline eGFR less than 60, noted Dr. Sarma of Brigham and Women’s Hospital, Boston.
In both studies, mean serum creatinine rose equally during the first 30 days of statin therapy, regardless of treatment potency, and then levels declined. In PROVE IT, for example, serum creatinine in the pravastatin and atorvastatin arms rose by 0.96% and 0.97% above baseline, respectively, at 30 days. Values then dropped by 2.88% and 3.85% from baseline at 4 months, and by 3.88% and 5.83% at 16 months.
In both studies, there was no difference between the high- and low-potency statin groups in the incidence of any increase in serum creatinine of at least 1.5-fold, 2.0-fold, or 3.0-fold greater than baseline. In other words, there was no hint of a safety signal, she added.
Dr. Sarma reported having no financial conflicts of interest.
DALLAS – High-potency statin therapy given post acute coronary syndrome did not raise serum creatinine or cause more risk of acute kidney injury than low-potency statin regimens did in a new analysis of two published landmark randomized clinical trials.
"Considering the recently updated AHA/American College of Cardiology lipid guidelines, which call for the use of high-potency statins in millions more patients, these findings provide important reassurance that a high-potency statin regimen will not increase the incidence of adverse renal events," Dr. Amy Sarma said in presenting the study results at the American Heart Association scientific sessions.
She noted that a recent Canadian observational study utilizing Canadian and U.S. administrative databases totaling more than 2 million patients over age 40 who were newly placed on statin therapy showed an adjusted 1.34-fold increased rate of hospitalization for acute kidney injury within the first 120 days in those on a high- as compared to a low-potency regimen, and a 1.11-fold increased risk beyond 120 days through the end of the first year (BMJ 2013;346:f880). Both risk elevations were statistically significant.
However, observational studies such as this are prone to bias in the form of potentially crucial differences between the patients given a prescription for statins and those who aren’t. For this reason, Dr. Sarma and her coinvestigators turned for guidance to two randomized trials of high- versus low-dose statins, since this study design obviates the risks of confounding. The trials were PROVE IT-TIMI 22 (N. Engl. J. Med. 2004;350:1495-504) and the A-to-Z trial (JAMA 2004;292:1307-16).
PROVE IT included 4,122 patients randomized within 10 days post ACS to standard background therapy plus either pravastatin at 40 mg/day or atorvastatin at 80 mg/day. A-to-Z involved 4,497 patients who were placed on simvastatin at either 20 or 80 mg/day within 5 days post ACS. Both trials had a median follow-up of 2 years, and both featured serial measurements of serum creatinine. Two-thirds of subjects in PROVE IT had a baseline estimated glomerular filtration rate below 90 mL/min per 1.73 m2, while two-thirds of those in A-to-Z had a baseline eGFR less than 60, noted Dr. Sarma of Brigham and Women’s Hospital, Boston.
In both studies, mean serum creatinine rose equally during the first 30 days of statin therapy, regardless of treatment potency, and then levels declined. In PROVE IT, for example, serum creatinine in the pravastatin and atorvastatin arms rose by 0.96% and 0.97% above baseline, respectively, at 30 days. Values then dropped by 2.88% and 3.85% from baseline at 4 months, and by 3.88% and 5.83% at 16 months.
In both studies, there was no difference between the high- and low-potency statin groups in the incidence of any increase in serum creatinine of at least 1.5-fold, 2.0-fold, or 3.0-fold greater than baseline. In other words, there was no hint of a safety signal, she added.
Dr. Sarma reported having no financial conflicts of interest.
AT THE AHA SCIENTIFIC SESSIONS
Major finding: Patients randomized to a high-potency statin regimen shortly after an acute coronary syndrome did not have higher serum creatinine levels or a greater risk of acute kidney injury than those randomized to a low-potency statin.
Data source: PROVE IT-TIMI 22 and the A-to-Z trial were randomized, double-blind clinical trials in which a total of 8,619 patients with a recent acute coronary syndrome were assigned to high- or lower-potency statin therapy and prospectively followed for a median of 2 years.
Disclosures: Dr. Sarma reported having no financial conflicts of interest.
First-in-man bioengineered graft proves enduring for vascular access
DALLAS – An investigational tissue-engineered vascular graft has enduring potential for vascular access for hemodialysis in patients with end-stage renal disease, based on early clinical results.
Moreover, other potential uses are on the horizon. The big picture involves subsequent extrapolation of this technology from the large-diameter, high-flow bioengineered vessels required for hemodialysis to the creation of small-diameter, low-flow vessels for coronary artery and peripheral arterial graft surgery, Dr. Jeffrey H. Lawson explained at the American Heart Association scientific sessions.
"Our goal is to make a tissue-engineered conduit that could be used widely throughout the body," said Dr. Lawson, professor of surgery and of pathology at Duke University Medical Center, Durham, N.C.
He presented the results from the first-in-man, ongoing phase I clinical experience with the Humacyte graft, which to date has been implanted to provide vascular access for hemodialysis in 28 patients, with 6-month patency as the primary study endpoint. This was a challenging study population, with an average of 4.1 previous access procedure failures per patient. The presentation at the AHA was the first public disclosure of the results of a project Dr. Lawson has been working on for more than 15 years. His surgical colleagues from Poland, who have done the implantations in patients with end-stage renal disease, were in attendance.
The overall 6-month patency was 100%, with no infections, no sign of an immune response, and no aneurysms or other indication of structural degeneration, he said.
Of the 28 patients, 20 had no further interventions, yielding a primary unassisted 6-month patency rate of 71%. Eight patients collectively underwent 10 interventions to maintain patency: eight had thrombectomies for graft- or surgically related thrombosis and two had venous anastomoses. Flow rates have remained suitable for dialysis in all patients, and the grafts are being used for dialysis three times per week. Dr. Lawson described the grafts as easy to cannulate via standard techniques.
He characterized these initial results as "quite remarkable" compared with the outcomes in two large studies of the current benchmark technologies, which are synthetic grafts made of PTFE (polytetrafluoroethyline). In those studies, the primary patency rate at 6 months was less than 50%, with a secondary patency rate of 77% and a 10% infection rate. In other studies, 30%-40% of PTFE grafts are abandoned within 12 months due to loss of patency.
The process of creating the bioengineered grafts begins with harvesting human aortic vascular smooth muscle cells, seeding them on a biodegradable matrix, then culturing them under pulsatile conditions. When the biodegradable matrix melts away, what remains is a tube comprised of vascular smooth muscle cells and extracellular matrix. This is then decellularized, yielding a tube of extracellular matrix that can be shipped off the shelf and around the world.
In primate models, the implanted bioengineered graft has been shown to repopulate with the host’s own vascular smooth muscle cells lined intimally by endothelium.
"Where we implanted an acellular structure, it appears to now be a living tissue, suggesting [the graft] has become their tissue, not ours," Dr. Lawson said.
To date, none of the bioengineered grafts implanted in patients has been explanted, so it’s unknown whether the favorable histologic changes seen in primates’ grafts also occur in humans. Larger clinical trials with longer follow-up are planned in order to assess the bioengineered graft’s durability.
Dr. Lawson’s study is funded by a Department of Defense research grant and by Humacyte. He serves as a consultant to the company.
This work is exciting. The early patency, thrombosis, and infection rates are encouraging.
The unmet clinical need for better ways to provide vascular access for hemodialysis is huge. There are 450,000 U.S. patients with end-stage renal disease on long-term hemodialysis. In this population, hemodialysis access morbidity costs more than $1 billion per year. Although the preferred means of vascular access is an arteriovenous fistula, many hemodialysis patients don’t have suitable veins. And 60% of fistulas become unusable within 6 months.

|
|
We’ve got a conundrum where PTFE grafts have their problems and fistulas have their own problems. We don’t have a good clinical armamentarium.
Synthetic grafts most often lose patency because of venous outflow tract stenosis due to intimal hyperplasia. Balloon angioplasty of the stenotic anastomosis has been the conventional treatment to restore patency, but a landmark randomized trial carried out several years ago (N. Engl. J. Med. 2010;362:494-503) showed the patency rate was a mere 23%, significantly worse than the 51% patency rate with a PTFE-covered stent graft – and even that 51% patency rate, is abysmal.
Dr. Sanjay Misra is professor of radiology at the Mayo Clinic in Rochester, Minn. He was the invited discussant of the paper at the meeting and declared having no relevant financial disclosures.
This work is exciting. The early patency, thrombosis, and infection rates are encouraging.
The unmet clinical need for better ways to provide vascular access for hemodialysis is huge. There are 450,000 U.S. patients with end-stage renal disease on long-term hemodialysis. In this population, hemodialysis access morbidity costs more than $1 billion per year. Although the preferred means of vascular access is an arteriovenous fistula, many hemodialysis patients don’t have suitable veins. And 60% of fistulas become unusable within 6 months.

|
|
We’ve got a conundrum where PTFE grafts have their problems and fistulas have their own problems. We don’t have a good clinical armamentarium.
Synthetic grafts most often lose patency because of venous outflow tract stenosis due to intimal hyperplasia. Balloon angioplasty of the stenotic anastomosis has been the conventional treatment to restore patency, but a landmark randomized trial carried out several years ago (N. Engl. J. Med. 2010;362:494-503) showed the patency rate was a mere 23%, significantly worse than the 51% patency rate with a PTFE-covered stent graft – and even that 51% patency rate, is abysmal.
Dr. Sanjay Misra is professor of radiology at the Mayo Clinic in Rochester, Minn. He was the invited discussant of the paper at the meeting and declared having no relevant financial disclosures.
This work is exciting. The early patency, thrombosis, and infection rates are encouraging.
The unmet clinical need for better ways to provide vascular access for hemodialysis is huge. There are 450,000 U.S. patients with end-stage renal disease on long-term hemodialysis. In this population, hemodialysis access morbidity costs more than $1 billion per year. Although the preferred means of vascular access is an arteriovenous fistula, many hemodialysis patients don’t have suitable veins. And 60% of fistulas become unusable within 6 months.

|
|
We’ve got a conundrum where PTFE grafts have their problems and fistulas have their own problems. We don’t have a good clinical armamentarium.
Synthetic grafts most often lose patency because of venous outflow tract stenosis due to intimal hyperplasia. Balloon angioplasty of the stenotic anastomosis has been the conventional treatment to restore patency, but a landmark randomized trial carried out several years ago (N. Engl. J. Med. 2010;362:494-503) showed the patency rate was a mere 23%, significantly worse than the 51% patency rate with a PTFE-covered stent graft – and even that 51% patency rate, is abysmal.
Dr. Sanjay Misra is professor of radiology at the Mayo Clinic in Rochester, Minn. He was the invited discussant of the paper at the meeting and declared having no relevant financial disclosures.
DALLAS – An investigational tissue-engineered vascular graft has enduring potential for vascular access for hemodialysis in patients with end-stage renal disease, based on early clinical results.
Moreover, other potential uses are on the horizon. The big picture involves subsequent extrapolation of this technology from the large-diameter, high-flow bioengineered vessels required for hemodialysis to the creation of small-diameter, low-flow vessels for coronary artery and peripheral arterial graft surgery, Dr. Jeffrey H. Lawson explained at the American Heart Association scientific sessions.
"Our goal is to make a tissue-engineered conduit that could be used widely throughout the body," said Dr. Lawson, professor of surgery and of pathology at Duke University Medical Center, Durham, N.C.
He presented the results from the first-in-man, ongoing phase I clinical experience with the Humacyte graft, which to date has been implanted to provide vascular access for hemodialysis in 28 patients, with 6-month patency as the primary study endpoint. This was a challenging study population, with an average of 4.1 previous access procedure failures per patient. The presentation at the AHA was the first public disclosure of the results of a project Dr. Lawson has been working on for more than 15 years. His surgical colleagues from Poland, who have done the implantations in patients with end-stage renal disease, were in attendance.
The overall 6-month patency was 100%, with no infections, no sign of an immune response, and no aneurysms or other indication of structural degeneration, he said.
Of the 28 patients, 20 had no further interventions, yielding a primary unassisted 6-month patency rate of 71%. Eight patients collectively underwent 10 interventions to maintain patency: eight had thrombectomies for graft- or surgically related thrombosis and two had venous anastomoses. Flow rates have remained suitable for dialysis in all patients, and the grafts are being used for dialysis three times per week. Dr. Lawson described the grafts as easy to cannulate via standard techniques.
He characterized these initial results as "quite remarkable" compared with the outcomes in two large studies of the current benchmark technologies, which are synthetic grafts made of PTFE (polytetrafluoroethyline). In those studies, the primary patency rate at 6 months was less than 50%, with a secondary patency rate of 77% and a 10% infection rate. In other studies, 30%-40% of PTFE grafts are abandoned within 12 months due to loss of patency.
The process of creating the bioengineered grafts begins with harvesting human aortic vascular smooth muscle cells, seeding them on a biodegradable matrix, then culturing them under pulsatile conditions. When the biodegradable matrix melts away, what remains is a tube comprised of vascular smooth muscle cells and extracellular matrix. This is then decellularized, yielding a tube of extracellular matrix that can be shipped off the shelf and around the world.
In primate models, the implanted bioengineered graft has been shown to repopulate with the host’s own vascular smooth muscle cells lined intimally by endothelium.
"Where we implanted an acellular structure, it appears to now be a living tissue, suggesting [the graft] has become their tissue, not ours," Dr. Lawson said.
To date, none of the bioengineered grafts implanted in patients has been explanted, so it’s unknown whether the favorable histologic changes seen in primates’ grafts also occur in humans. Larger clinical trials with longer follow-up are planned in order to assess the bioengineered graft’s durability.
Dr. Lawson’s study is funded by a Department of Defense research grant and by Humacyte. He serves as a consultant to the company.
DALLAS – An investigational tissue-engineered vascular graft has enduring potential for vascular access for hemodialysis in patients with end-stage renal disease, based on early clinical results.
Moreover, other potential uses are on the horizon. The big picture involves subsequent extrapolation of this technology from the large-diameter, high-flow bioengineered vessels required for hemodialysis to the creation of small-diameter, low-flow vessels for coronary artery and peripheral arterial graft surgery, Dr. Jeffrey H. Lawson explained at the American Heart Association scientific sessions.
"Our goal is to make a tissue-engineered conduit that could be used widely throughout the body," said Dr. Lawson, professor of surgery and of pathology at Duke University Medical Center, Durham, N.C.
He presented the results from the first-in-man, ongoing phase I clinical experience with the Humacyte graft, which to date has been implanted to provide vascular access for hemodialysis in 28 patients, with 6-month patency as the primary study endpoint. This was a challenging study population, with an average of 4.1 previous access procedure failures per patient. The presentation at the AHA was the first public disclosure of the results of a project Dr. Lawson has been working on for more than 15 years. His surgical colleagues from Poland, who have done the implantations in patients with end-stage renal disease, were in attendance.
The overall 6-month patency was 100%, with no infections, no sign of an immune response, and no aneurysms or other indication of structural degeneration, he said.
Of the 28 patients, 20 had no further interventions, yielding a primary unassisted 6-month patency rate of 71%. Eight patients collectively underwent 10 interventions to maintain patency: eight had thrombectomies for graft- or surgically related thrombosis and two had venous anastomoses. Flow rates have remained suitable for dialysis in all patients, and the grafts are being used for dialysis three times per week. Dr. Lawson described the grafts as easy to cannulate via standard techniques.
He characterized these initial results as "quite remarkable" compared with the outcomes in two large studies of the current benchmark technologies, which are synthetic grafts made of PTFE (polytetrafluoroethyline). In those studies, the primary patency rate at 6 months was less than 50%, with a secondary patency rate of 77% and a 10% infection rate. In other studies, 30%-40% of PTFE grafts are abandoned within 12 months due to loss of patency.
The process of creating the bioengineered grafts begins with harvesting human aortic vascular smooth muscle cells, seeding them on a biodegradable matrix, then culturing them under pulsatile conditions. When the biodegradable matrix melts away, what remains is a tube comprised of vascular smooth muscle cells and extracellular matrix. This is then decellularized, yielding a tube of extracellular matrix that can be shipped off the shelf and around the world.
In primate models, the implanted bioengineered graft has been shown to repopulate with the host’s own vascular smooth muscle cells lined intimally by endothelium.
"Where we implanted an acellular structure, it appears to now be a living tissue, suggesting [the graft] has become their tissue, not ours," Dr. Lawson said.
To date, none of the bioengineered grafts implanted in patients has been explanted, so it’s unknown whether the favorable histologic changes seen in primates’ grafts also occur in humans. Larger clinical trials with longer follow-up are planned in order to assess the bioengineered graft’s durability.
Dr. Lawson’s study is funded by a Department of Defense research grant and by Humacyte. He serves as a consultant to the company.
AT THE AHA SCIENTIFIC SESSIONS
Major finding: The 6-month enduring patency rate of an investigational tissue-engineered vascular graft for hemodialysis access was 100%, markedly better than rates achievable with synthetic PTFE grafts, the current benchmark technology.
Data source: An initial report from an ongoing prospective first-in-man study in which, to date, 28 patients with end-stage renal disease have been implanted with a novel tissue-engineered vascular graft for use as a hemodialysis access.
Disclosures: The study was funded by the Department of Defense and Humacyte. The presenter is a consultant to the company.
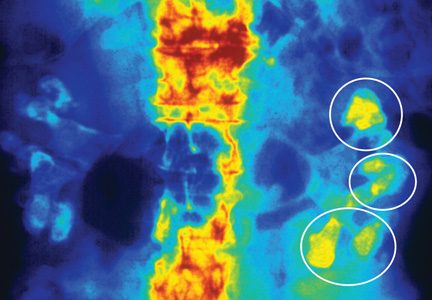
The Modern Realities of Kidney Stones: Diagnosis
Q) I am new to practice and working in urgent care. I was discussing the diagnosis of kidney stones with my supervising physician. He said he does an intravenous pyelogram (IVP) to diagnose stones. He is a little “old school,” and I’m not sure he is right. What is “state of the art” in the work-up and acute treatment for kidney stones?
An IVP involves taking a series of x-rays following the injection of dye into a patient’s vein. As the dye moves through the bloodstream, the anatomy of the urinary system can be better visualized and the stone location identified, as the dye tends to accumulate at areas of obstruction. The downside to this test is that contrast can cause allergic reactions in some patients and can only be used in those with normal renal function. Also, a radiologist is required to be present during the procedure, and the test can take a long time to complete if a severe blockage is present.4
Today, noncontrast CT is considered the gold standard for imaging renal calculi because it is fast, safe (no worries for those with contrast allergy or renal impairment), and nearly 100% accurate.5
There are multiple options for treating kidney stones, though some are more invasive than others. For stones 2 cm or less identified in the upper or middle calyx and renal pelvis, extracorporeal shock wave lithotripsy (ESWL) is the treatment of choice.5,6 The goal of ESWL is to break the stone into small particles that can then be expelled through the urinary system. Adjunct measures, including mechanical percussion, diuresis, and inversion therapy, are often used following lithotripsy to facilitate passage of stone fragments. Medications such as calcium blockers and α-receptor blockers are also used to improve outcomes after lithotripsy. In the past, obese patients had less success with lithotripsy; however, technological advances have improved outcomes in depths up to 17 cm from skin to stone.6
For stones in the lower pole of the kidney (and depending on the size of the stone), ESWL, percutaneous nephrolitholapaxy, retrograde flexible ureteronephroscopy, and partial nephrectomy are options for treatment.3,7 Using an intravenous urogram, measurements and angles are calculated to help determine which procedure would be best for a particular patient.7 In simple terms, narrow angles and longer tube distances make it more difficult for stone particles to exit the urinary system. Therefore, if these problems are identified, an invasive approach may be needed to remove a stone. Other important considerations include stone size, patient symptoms, evidence of infection, or obstruction.7
ESWL is an attractive option for stone removal because it is noninvasive, has a reasonable safety profile, and is less costly than other, more invasive measures. However, advances in endoscopic instrument design are reducing complications previously associated with more invasive approaches, while improving long-term stone-free outcome rates. There may be increased utilization of procedures such as percutaneous nephrolitholapaxy and retrograde flexible ureteronephroscopy in the future.
Kristina Unterseher, CNN-NP
PeaceHealth
St. John Medical Group
Longview, WA
REFERENCES
1. Fink HA, Wilt TJ, Eidman KE, et al. Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline. Ann Intern Med. 2013;158(7):535-543.
2. Hiatt RA, Ettinger B, Caan B, et al. Randomized controlled trial of a low animal protein, high fiber diet in the prevention of recurrent calcium oxalate kidney stones. Am J Epidemiol. 1996;144(1):25-33.
3. Moe OW. Kidney stones: pathophysiology and medical management. Lancet. 2006; 367(9507):333-344.
4. American College of Radiology and Radiological Society of North America. Intravenous pyelogram (2013). www.radiologyinfo.org/en/info.cfm?pg=ivp. Accessed December 16, 2013.
5. Boyce CJ, Pickhardt PJ, Lawrence EM, et al. Prevalence of urolithiasis in asymptomatic adults: objective determination using low dose noncontrast computerized tomography. J Urol. 2010;183(3):1017-1021.
6. Christian C, Thorsten B. The preferred treatment for upper tract stones is extracorporeal shock wave lithotripsy (ESWL) or ureteroscopic: pro ESWL. Urology. 2009;74(2):259-262.
7. Bourdoumis A, Papatsoris AG, Chrisofos M, Deliveliotis C. Lower pole stone management. Med Surg Urol. 2012. www.omicsonline.org/lower-pole-stone-management%20-2168-9857.S4-004.php?aid=7058?abstract _id=7058. Accessed December 16, 2013.
Q) I am new to practice and working in urgent care. I was discussing the diagnosis of kidney stones with my supervising physician. He said he does an intravenous pyelogram (IVP) to diagnose stones. He is a little “old school,” and I’m not sure he is right. What is “state of the art” in the work-up and acute treatment for kidney stones?
An IVP involves taking a series of x-rays following the injection of dye into a patient’s vein. As the dye moves through the bloodstream, the anatomy of the urinary system can be better visualized and the stone location identified, as the dye tends to accumulate at areas of obstruction. The downside to this test is that contrast can cause allergic reactions in some patients and can only be used in those with normal renal function. Also, a radiologist is required to be present during the procedure, and the test can take a long time to complete if a severe blockage is present.4
Today, noncontrast CT is considered the gold standard for imaging renal calculi because it is fast, safe (no worries for those with contrast allergy or renal impairment), and nearly 100% accurate.5
There are multiple options for treating kidney stones, though some are more invasive than others. For stones 2 cm or less identified in the upper or middle calyx and renal pelvis, extracorporeal shock wave lithotripsy (ESWL) is the treatment of choice.5,6 The goal of ESWL is to break the stone into small particles that can then be expelled through the urinary system. Adjunct measures, including mechanical percussion, diuresis, and inversion therapy, are often used following lithotripsy to facilitate passage of stone fragments. Medications such as calcium blockers and α-receptor blockers are also used to improve outcomes after lithotripsy. In the past, obese patients had less success with lithotripsy; however, technological advances have improved outcomes in depths up to 17 cm from skin to stone.6
For stones in the lower pole of the kidney (and depending on the size of the stone), ESWL, percutaneous nephrolitholapaxy, retrograde flexible ureteronephroscopy, and partial nephrectomy are options for treatment.3,7 Using an intravenous urogram, measurements and angles are calculated to help determine which procedure would be best for a particular patient.7 In simple terms, narrow angles and longer tube distances make it more difficult for stone particles to exit the urinary system. Therefore, if these problems are identified, an invasive approach may be needed to remove a stone. Other important considerations include stone size, patient symptoms, evidence of infection, or obstruction.7
ESWL is an attractive option for stone removal because it is noninvasive, has a reasonable safety profile, and is less costly than other, more invasive measures. However, advances in endoscopic instrument design are reducing complications previously associated with more invasive approaches, while improving long-term stone-free outcome rates. There may be increased utilization of procedures such as percutaneous nephrolitholapaxy and retrograde flexible ureteronephroscopy in the future.
Kristina Unterseher, CNN-NP
PeaceHealth
St. John Medical Group
Longview, WA
REFERENCES
1. Fink HA, Wilt TJ, Eidman KE, et al. Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline. Ann Intern Med. 2013;158(7):535-543.
2. Hiatt RA, Ettinger B, Caan B, et al. Randomized controlled trial of a low animal protein, high fiber diet in the prevention of recurrent calcium oxalate kidney stones. Am J Epidemiol. 1996;144(1):25-33.
3. Moe OW. Kidney stones: pathophysiology and medical management. Lancet. 2006; 367(9507):333-344.
4. American College of Radiology and Radiological Society of North America. Intravenous pyelogram (2013). www.radiologyinfo.org/en/info.cfm?pg=ivp. Accessed December 16, 2013.
5. Boyce CJ, Pickhardt PJ, Lawrence EM, et al. Prevalence of urolithiasis in asymptomatic adults: objective determination using low dose noncontrast computerized tomography. J Urol. 2010;183(3):1017-1021.
6. Christian C, Thorsten B. The preferred treatment for upper tract stones is extracorporeal shock wave lithotripsy (ESWL) or ureteroscopic: pro ESWL. Urology. 2009;74(2):259-262.
7. Bourdoumis A, Papatsoris AG, Chrisofos M, Deliveliotis C. Lower pole stone management. Med Surg Urol. 2012. www.omicsonline.org/lower-pole-stone-management%20-2168-9857.S4-004.php?aid=7058?abstract _id=7058. Accessed December 16, 2013.
Q) I am new to practice and working in urgent care. I was discussing the diagnosis of kidney stones with my supervising physician. He said he does an intravenous pyelogram (IVP) to diagnose stones. He is a little “old school,” and I’m not sure he is right. What is “state of the art” in the work-up and acute treatment for kidney stones?
An IVP involves taking a series of x-rays following the injection of dye into a patient’s vein. As the dye moves through the bloodstream, the anatomy of the urinary system can be better visualized and the stone location identified, as the dye tends to accumulate at areas of obstruction. The downside to this test is that contrast can cause allergic reactions in some patients and can only be used in those with normal renal function. Also, a radiologist is required to be present during the procedure, and the test can take a long time to complete if a severe blockage is present.4
Today, noncontrast CT is considered the gold standard for imaging renal calculi because it is fast, safe (no worries for those with contrast allergy or renal impairment), and nearly 100% accurate.5
There are multiple options for treating kidney stones, though some are more invasive than others. For stones 2 cm or less identified in the upper or middle calyx and renal pelvis, extracorporeal shock wave lithotripsy (ESWL) is the treatment of choice.5,6 The goal of ESWL is to break the stone into small particles that can then be expelled through the urinary system. Adjunct measures, including mechanical percussion, diuresis, and inversion therapy, are often used following lithotripsy to facilitate passage of stone fragments. Medications such as calcium blockers and α-receptor blockers are also used to improve outcomes after lithotripsy. In the past, obese patients had less success with lithotripsy; however, technological advances have improved outcomes in depths up to 17 cm from skin to stone.6
For stones in the lower pole of the kidney (and depending on the size of the stone), ESWL, percutaneous nephrolitholapaxy, retrograde flexible ureteronephroscopy, and partial nephrectomy are options for treatment.3,7 Using an intravenous urogram, measurements and angles are calculated to help determine which procedure would be best for a particular patient.7 In simple terms, narrow angles and longer tube distances make it more difficult for stone particles to exit the urinary system. Therefore, if these problems are identified, an invasive approach may be needed to remove a stone. Other important considerations include stone size, patient symptoms, evidence of infection, or obstruction.7
ESWL is an attractive option for stone removal because it is noninvasive, has a reasonable safety profile, and is less costly than other, more invasive measures. However, advances in endoscopic instrument design are reducing complications previously associated with more invasive approaches, while improving long-term stone-free outcome rates. There may be increased utilization of procedures such as percutaneous nephrolitholapaxy and retrograde flexible ureteronephroscopy in the future.
Kristina Unterseher, CNN-NP
PeaceHealth
St. John Medical Group
Longview, WA
REFERENCES
1. Fink HA, Wilt TJ, Eidman KE, et al. Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline. Ann Intern Med. 2013;158(7):535-543.
2. Hiatt RA, Ettinger B, Caan B, et al. Randomized controlled trial of a low animal protein, high fiber diet in the prevention of recurrent calcium oxalate kidney stones. Am J Epidemiol. 1996;144(1):25-33.
3. Moe OW. Kidney stones: pathophysiology and medical management. Lancet. 2006; 367(9507):333-344.
4. American College of Radiology and Radiological Society of North America. Intravenous pyelogram (2013). www.radiologyinfo.org/en/info.cfm?pg=ivp. Accessed December 16, 2013.
5. Boyce CJ, Pickhardt PJ, Lawrence EM, et al. Prevalence of urolithiasis in asymptomatic adults: objective determination using low dose noncontrast computerized tomography. J Urol. 2010;183(3):1017-1021.
6. Christian C, Thorsten B. The preferred treatment for upper tract stones is extracorporeal shock wave lithotripsy (ESWL) or ureteroscopic: pro ESWL. Urology. 2009;74(2):259-262.
7. Bourdoumis A, Papatsoris AG, Chrisofos M, Deliveliotis C. Lower pole stone management. Med Surg Urol. 2012. www.omicsonline.org/lower-pole-stone-management%20-2168-9857.S4-004.php?aid=7058?abstract _id=7058. Accessed December 16, 2013.
The Modern Realities of Kidney Stones: Preventing Reoccurrence
Q) A patient recently came in after an episode of kidney stones. He said he had never experienced such pain before (and this is a former Army Ranger!) and asked if there was anything he could do to keep it from happening again. I told him what I had learned in school (lots of fluids, no organ meats), but is there anything new?
Your patient has some reason for concern. For people who have had a symptomatic kidney stone, the likelihood of developing another within five years is 35% to 50% if no preventive action is taken.1 Certain factors—including family history, younger age at onset, and predisposing medical conditions (eg, hyperparathyroidism, diabetes, obesity, gout)—increase risk for recurrence.2,3
In the past, patients were often advised to restrict their dietary calcium intake to prevent calcium oxalate and/or calcium phosphate stones. However, more recent research has proven the opposite to be true: People with lower dietary calcium intake can be at greater risk for kidney stones.1-3 Therefore, encourage patients to consume about 800 to 1,200 mg/d of dietary calcium. Oral supplementation does not seem to yield the same protective benefits as dietary calcium. This may be related to absorption.1
Diets high in oxalates (eg, chocolate, nuts, spinach) can increase risk for stone formation, particularly in patients who have bowel diseases that cause inflammation or a history of a bowel resection.2 Animal protein in the diet can cause hypercalcinuria and increased uric acid levels, which is particularly problematic for individuals with gout or inflammatory arthritis. High-sodium diets can cause higher urinary calcium oxalate levels, while diets high in phosphorus (particularly dark cola soft drinks) can increase risk for stone formation. Advise your patient to avoid foods high in oxalates, animal proteins, sodium, and phosphorus.2
Dehydration, either due to exercise or poor fluid intake, can result in concentrated urine, which facilitates stone formation. While opinions differ on the benefits of certain dietary restrictions, most research supports the idea that generous fluid intake is the most successful intervention in preventing recurrence of stone formation (regardless of underlying cause). Diluting the urine decreases the concentration of solutes responsible for stone formation.1-3
If the conservative measures of dietary restriction and adequate hydration fail, medications may be beneficial, depending on stone type or underlying metabolic condition. Thiazide diuretics can help lower urinary calcium by enhancing reabsorption of calcium from the distal convoluted tubule and sodium excretion; however, they should be used cautiously due to the risk for adverse effects such as dizziness and lightheadedness.1,3 Allopurinol can lower uric acid levels, decreasing recurrence of both uric acid and calcium oxalate stones. Hypocitraturia is prevalent in 20% to 60% of persons with stones; prescribing potassium citrate can inhibit crystal growth of calcium phosphate and calcium oxalate in urine.2
To help patients prevent stone recurrence, perform a comprehensive assessment of their dietary and lifestyle habits and medical history to identify possible contributing factors. Educate patients on adequate dietary calcium intake, generous water intake to keep urine dilute, and avoidance of dietary triggers.
Nephrolithiasis should be considered a manifestation of another underlying problem. If a patient presents with a kidney stone, attempt to identify the cause—not only to try to prevent recurrence, but also to identify a previously unrecognized disease process.
Kristina Unterseher, CNN-NP
PeaceHealth
St. John Medical Group
Longview, WA
REFERENCES
1. Fink HA, Wilt TJ, Eidman KE, et al. Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline. Ann Intern Med. 2013;158(7):535-543.
2. Hiatt RA, Ettinger B, Caan B, et al. Randomized controlled trial of a low animal protein, high fiber diet in the prevention of recurrent calcium oxalate kidney stones. Am J Epidemiol. 1996;144(1):25-33.
3. Moe OW. Kidney stones: pathophysiology and medical management. Lancet. 2006; 367(9507):333-344.
4. American College of Radiology and Radiological Society of North America. Intravenous pyelogram (2013). www.radiologyinfo.org/en/info.cfm?pg=ivp. Accessed December 16, 2013.
5. Boyce CJ, Pickhardt PJ, Lawrence EM, et al. Prevalence of urolithiasis in asymptomatic adults: objective determination using low dose noncontrast computerized tomography. J Urol. 2010;183(3):1017-1021.
6. Christian C, Thorsten B. The preferred treatment for upper tract stones is extracorporeal shock wave lithotripsy (ESWL) or ureteroscopic: pro ESWL. Urology. 2009;74(2):259-262.
7. Bourdoumis A, Papatsoris AG, Chrisofos M, Deliveliotis C. Lower pole stone management. Med Surg Urol. 2012. www.omicsonline.org/lower-pole-stone-management%20-2168-9857.S4-004.php?aid=7058?abstract _id=7058. Accessed December 16, 2013.
Q) A patient recently came in after an episode of kidney stones. He said he had never experienced such pain before (and this is a former Army Ranger!) and asked if there was anything he could do to keep it from happening again. I told him what I had learned in school (lots of fluids, no organ meats), but is there anything new?
Your patient has some reason for concern. For people who have had a symptomatic kidney stone, the likelihood of developing another within five years is 35% to 50% if no preventive action is taken.1 Certain factors—including family history, younger age at onset, and predisposing medical conditions (eg, hyperparathyroidism, diabetes, obesity, gout)—increase risk for recurrence.2,3
In the past, patients were often advised to restrict their dietary calcium intake to prevent calcium oxalate and/or calcium phosphate stones. However, more recent research has proven the opposite to be true: People with lower dietary calcium intake can be at greater risk for kidney stones.1-3 Therefore, encourage patients to consume about 800 to 1,200 mg/d of dietary calcium. Oral supplementation does not seem to yield the same protective benefits as dietary calcium. This may be related to absorption.1
Diets high in oxalates (eg, chocolate, nuts, spinach) can increase risk for stone formation, particularly in patients who have bowel diseases that cause inflammation or a history of a bowel resection.2 Animal protein in the diet can cause hypercalcinuria and increased uric acid levels, which is particularly problematic for individuals with gout or inflammatory arthritis. High-sodium diets can cause higher urinary calcium oxalate levels, while diets high in phosphorus (particularly dark cola soft drinks) can increase risk for stone formation. Advise your patient to avoid foods high in oxalates, animal proteins, sodium, and phosphorus.2
Dehydration, either due to exercise or poor fluid intake, can result in concentrated urine, which facilitates stone formation. While opinions differ on the benefits of certain dietary restrictions, most research supports the idea that generous fluid intake is the most successful intervention in preventing recurrence of stone formation (regardless of underlying cause). Diluting the urine decreases the concentration of solutes responsible for stone formation.1-3
If the conservative measures of dietary restriction and adequate hydration fail, medications may be beneficial, depending on stone type or underlying metabolic condition. Thiazide diuretics can help lower urinary calcium by enhancing reabsorption of calcium from the distal convoluted tubule and sodium excretion; however, they should be used cautiously due to the risk for adverse effects such as dizziness and lightheadedness.1,3 Allopurinol can lower uric acid levels, decreasing recurrence of both uric acid and calcium oxalate stones. Hypocitraturia is prevalent in 20% to 60% of persons with stones; prescribing potassium citrate can inhibit crystal growth of calcium phosphate and calcium oxalate in urine.2
To help patients prevent stone recurrence, perform a comprehensive assessment of their dietary and lifestyle habits and medical history to identify possible contributing factors. Educate patients on adequate dietary calcium intake, generous water intake to keep urine dilute, and avoidance of dietary triggers.
Nephrolithiasis should be considered a manifestation of another underlying problem. If a patient presents with a kidney stone, attempt to identify the cause—not only to try to prevent recurrence, but also to identify a previously unrecognized disease process.
Kristina Unterseher, CNN-NP
PeaceHealth
St. John Medical Group
Longview, WA
REFERENCES
1. Fink HA, Wilt TJ, Eidman KE, et al. Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline. Ann Intern Med. 2013;158(7):535-543.
2. Hiatt RA, Ettinger B, Caan B, et al. Randomized controlled trial of a low animal protein, high fiber diet in the prevention of recurrent calcium oxalate kidney stones. Am J Epidemiol. 1996;144(1):25-33.
3. Moe OW. Kidney stones: pathophysiology and medical management. Lancet. 2006; 367(9507):333-344.
4. American College of Radiology and Radiological Society of North America. Intravenous pyelogram (2013). www.radiologyinfo.org/en/info.cfm?pg=ivp. Accessed December 16, 2013.
5. Boyce CJ, Pickhardt PJ, Lawrence EM, et al. Prevalence of urolithiasis in asymptomatic adults: objective determination using low dose noncontrast computerized tomography. J Urol. 2010;183(3):1017-1021.
6. Christian C, Thorsten B. The preferred treatment for upper tract stones is extracorporeal shock wave lithotripsy (ESWL) or ureteroscopic: pro ESWL. Urology. 2009;74(2):259-262.
7. Bourdoumis A, Papatsoris AG, Chrisofos M, Deliveliotis C. Lower pole stone management. Med Surg Urol. 2012. www.omicsonline.org/lower-pole-stone-management%20-2168-9857.S4-004.php?aid=7058?abstract _id=7058. Accessed December 16, 2013.
Q) A patient recently came in after an episode of kidney stones. He said he had never experienced such pain before (and this is a former Army Ranger!) and asked if there was anything he could do to keep it from happening again. I told him what I had learned in school (lots of fluids, no organ meats), but is there anything new?
Your patient has some reason for concern. For people who have had a symptomatic kidney stone, the likelihood of developing another within five years is 35% to 50% if no preventive action is taken.1 Certain factors—including family history, younger age at onset, and predisposing medical conditions (eg, hyperparathyroidism, diabetes, obesity, gout)—increase risk for recurrence.2,3
In the past, patients were often advised to restrict their dietary calcium intake to prevent calcium oxalate and/or calcium phosphate stones. However, more recent research has proven the opposite to be true: People with lower dietary calcium intake can be at greater risk for kidney stones.1-3 Therefore, encourage patients to consume about 800 to 1,200 mg/d of dietary calcium. Oral supplementation does not seem to yield the same protective benefits as dietary calcium. This may be related to absorption.1
Diets high in oxalates (eg, chocolate, nuts, spinach) can increase risk for stone formation, particularly in patients who have bowel diseases that cause inflammation or a history of a bowel resection.2 Animal protein in the diet can cause hypercalcinuria and increased uric acid levels, which is particularly problematic for individuals with gout or inflammatory arthritis. High-sodium diets can cause higher urinary calcium oxalate levels, while diets high in phosphorus (particularly dark cola soft drinks) can increase risk for stone formation. Advise your patient to avoid foods high in oxalates, animal proteins, sodium, and phosphorus.2
Dehydration, either due to exercise or poor fluid intake, can result in concentrated urine, which facilitates stone formation. While opinions differ on the benefits of certain dietary restrictions, most research supports the idea that generous fluid intake is the most successful intervention in preventing recurrence of stone formation (regardless of underlying cause). Diluting the urine decreases the concentration of solutes responsible for stone formation.1-3
If the conservative measures of dietary restriction and adequate hydration fail, medications may be beneficial, depending on stone type or underlying metabolic condition. Thiazide diuretics can help lower urinary calcium by enhancing reabsorption of calcium from the distal convoluted tubule and sodium excretion; however, they should be used cautiously due to the risk for adverse effects such as dizziness and lightheadedness.1,3 Allopurinol can lower uric acid levels, decreasing recurrence of both uric acid and calcium oxalate stones. Hypocitraturia is prevalent in 20% to 60% of persons with stones; prescribing potassium citrate can inhibit crystal growth of calcium phosphate and calcium oxalate in urine.2
To help patients prevent stone recurrence, perform a comprehensive assessment of their dietary and lifestyle habits and medical history to identify possible contributing factors. Educate patients on adequate dietary calcium intake, generous water intake to keep urine dilute, and avoidance of dietary triggers.
Nephrolithiasis should be considered a manifestation of another underlying problem. If a patient presents with a kidney stone, attempt to identify the cause—not only to try to prevent recurrence, but also to identify a previously unrecognized disease process.
Kristina Unterseher, CNN-NP
PeaceHealth
St. John Medical Group
Longview, WA
REFERENCES
1. Fink HA, Wilt TJ, Eidman KE, et al. Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline. Ann Intern Med. 2013;158(7):535-543.
2. Hiatt RA, Ettinger B, Caan B, et al. Randomized controlled trial of a low animal protein, high fiber diet in the prevention of recurrent calcium oxalate kidney stones. Am J Epidemiol. 1996;144(1):25-33.
3. Moe OW. Kidney stones: pathophysiology and medical management. Lancet. 2006; 367(9507):333-344.
4. American College of Radiology and Radiological Society of North America. Intravenous pyelogram (2013). www.radiologyinfo.org/en/info.cfm?pg=ivp. Accessed December 16, 2013.
5. Boyce CJ, Pickhardt PJ, Lawrence EM, et al. Prevalence of urolithiasis in asymptomatic adults: objective determination using low dose noncontrast computerized tomography. J Urol. 2010;183(3):1017-1021.
6. Christian C, Thorsten B. The preferred treatment for upper tract stones is extracorporeal shock wave lithotripsy (ESWL) or ureteroscopic: pro ESWL. Urology. 2009;74(2):259-262.
7. Bourdoumis A, Papatsoris AG, Chrisofos M, Deliveliotis C. Lower pole stone management. Med Surg Urol. 2012. www.omicsonline.org/lower-pole-stone-management%20-2168-9857.S4-004.php?aid=7058?abstract _id=7058. Accessed December 16, 2013.
Novel agent appears safe, effective for hyperkalemia
ATLANTA – A novel first-in-class agent that selectively binds cations appears safe and effective for the treatment of hyperkalemia in patients with chronic kidney disease, according to findings from a phase II, dose-ranging proof-of-concept study.
Preliminary data from a phase III study of 753 patients, which was initiated based on the positive findings in the phase II study, similarly demonstrate the safety and efficacy of the selective monovalent cation trap known as ZS-9 (ZS Pharma), Dr. Stephen R. Ash reported at Kidney Week 2013, sponsored by the American Society of Nephrology.
In 90 patients from the phase II study who were randomized to receive either placebo or one of three ZS-9 doses (0.3 g in 12 patients, 3 g in 24 patients, and 10 g in 24 patients), active treatment was associated with significantly greater dose-dependent reductions in serum potassium (K+) than was placebo, said Dr. Ash of Indiana University, Lafayette.
The mean serum K+ level at baseline for both the placebo group and the combined active treatment groups was 5.1 mEq/L. Within 48 hours of treatment initiation, 63% of patients in the 10-g ZS-9 group met the primary end point of at least a 1.0-mEq/L reduction in serum K+, compared with only 17% of patients in the placebo group.
The dose reduction in the 10-g group was "rapid and substantial," with a significant decrease, compared with placebo, occurring within 1 hour of the initial dose. Levels were 0.92-mEq/L lower than baseline after 38 hours (4 hours after the last dose), and 0.68-mEq/L lower than baseline at 48 hours (14 hours after the last dose). The levels remained significantly lower than placebo for an additional 3.5 days after the last dose, Dr. Ash said.
"At every point in the trial for these 10-g–dose patients, the serum potassium was lower in the treatment group than in the control group. ... At 38 hours, almost 90% of the patients who were on the 10-g dose had a serum potassium [level] of less than 4.5," he said.
Participants had mild to moderate chronic kidney disease with a glomerular filtration rate of 30-60 mL/min per 1.73 m2, and mild to moderate hyperkalemia, with serum K+ levels of 5-6 mEq/L.
Treatment with the tasteless, odorless substance, which was delivered orally as a suspension in water three times daily at meal times, was well tolerated. No serious adverse events were reported, and no significant gastrointestinal issues, hypokalemia, hypomagnesemia, or hypocalcemia were observed.
Only one adverse event, a mild case of constipation in the 3-g–dose group, was thought to have a causal relationship to the study drug. No patients withdrew from the study.
The preliminary data from the pivotal randomized, controlled phase III trial also suggest a rapid and dose-dependent reduction in serum K+ in patients treated with ZS-9. In that study, patients were randomized to receive placebo or ZS-9 at doses of 1.25 g, 2.5 g, 5 g, or 10 g three times daily for the initial 48 hours.
Patients whose serum K+ levels normalized during that initial phase of treatment were then randomized to receive placebo or one of the four active drug doses administered daily for 12 days.
Patients in the phase III trial had serum K+ levels of 5-6.5 mEq/L. Those in the 2.5-g, 5-g, and 10-g groups met the primary endpoint, with significantly greater reductions in serum K+, compared with those on placebo, at 48 hours.
The mean serum K+ reduction was 0.73 mEq/L at the 10-g dose at 48 hours. The gastrointestinal adverse event rate was 5.1% in the placebo group patients, and 3.5% in the treatment group.
Final results from the phase III trial are expected in the coming months.
The findings are important because currently only one treatment – sodium polystyrene sulfonate (SPS), an organic polymer resin that nonselectively binds cations – is approved in the United States for the treatment of hyperkalemia – a serious condition that is associated with significant mortality and morbidity in patients with cardiovascular disease or chronic kidney disease.
"Even marginally high potassium levels, such as over 4.5, however, have an increased risk of death and ventricular fibrillation," Dr. Ash explained.
Further, hyperkalemia limits the ability to use cardioprotective and renoprotective agents such as angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, he said.
The efficacy of SPS for lowering serum K+ levels is questionable, and the agent has been associated with several serious adverse effects, including sodium loading, colonic necrosis, and other fatal gastrointestinal effects, Dr. Ash explained.
ZS-9 differs from traditional nonspecific and nonselective cation exchange organic polymer resins in that it is an inorganic cation exchanger – a result of advances in chemistry for the development of highly selective drug therapies.
"ZS-9 was designed and engineered to be highly selective for potassium," he said, noting that ZS-9 has more than nine times the potassium-binding ability of SPS, and is not systemically absorbed; thus, the risk of systemic toxicity is minimized or eliminated.
The findings thus far suggest that ZS-9 is a safe, reliable, fast, effective and well-tolerated therapy for lowering serum K+ levels in patients with hyperkalemia, Dr. Ash concluded.
Dr. Ash disclosed ties with Merit Medical, HemoCleanse (which has a minority share interest in ZS Pharma), Fresenius Medical, Ash Access Technology (in which he has ownership interest), Renal Solutions, and DaVita RMS. He also is editor-in-chief of Seminars in Dialysis, ASKIN section.
ATLANTA – A novel first-in-class agent that selectively binds cations appears safe and effective for the treatment of hyperkalemia in patients with chronic kidney disease, according to findings from a phase II, dose-ranging proof-of-concept study.
Preliminary data from a phase III study of 753 patients, which was initiated based on the positive findings in the phase II study, similarly demonstrate the safety and efficacy of the selective monovalent cation trap known as ZS-9 (ZS Pharma), Dr. Stephen R. Ash reported at Kidney Week 2013, sponsored by the American Society of Nephrology.
In 90 patients from the phase II study who were randomized to receive either placebo or one of three ZS-9 doses (0.3 g in 12 patients, 3 g in 24 patients, and 10 g in 24 patients), active treatment was associated with significantly greater dose-dependent reductions in serum potassium (K+) than was placebo, said Dr. Ash of Indiana University, Lafayette.
The mean serum K+ level at baseline for both the placebo group and the combined active treatment groups was 5.1 mEq/L. Within 48 hours of treatment initiation, 63% of patients in the 10-g ZS-9 group met the primary end point of at least a 1.0-mEq/L reduction in serum K+, compared with only 17% of patients in the placebo group.
The dose reduction in the 10-g group was "rapid and substantial," with a significant decrease, compared with placebo, occurring within 1 hour of the initial dose. Levels were 0.92-mEq/L lower than baseline after 38 hours (4 hours after the last dose), and 0.68-mEq/L lower than baseline at 48 hours (14 hours after the last dose). The levels remained significantly lower than placebo for an additional 3.5 days after the last dose, Dr. Ash said.
"At every point in the trial for these 10-g–dose patients, the serum potassium was lower in the treatment group than in the control group. ... At 38 hours, almost 90% of the patients who were on the 10-g dose had a serum potassium [level] of less than 4.5," he said.
Participants had mild to moderate chronic kidney disease with a glomerular filtration rate of 30-60 mL/min per 1.73 m2, and mild to moderate hyperkalemia, with serum K+ levels of 5-6 mEq/L.
Treatment with the tasteless, odorless substance, which was delivered orally as a suspension in water three times daily at meal times, was well tolerated. No serious adverse events were reported, and no significant gastrointestinal issues, hypokalemia, hypomagnesemia, or hypocalcemia were observed.
Only one adverse event, a mild case of constipation in the 3-g–dose group, was thought to have a causal relationship to the study drug. No patients withdrew from the study.
The preliminary data from the pivotal randomized, controlled phase III trial also suggest a rapid and dose-dependent reduction in serum K+ in patients treated with ZS-9. In that study, patients were randomized to receive placebo or ZS-9 at doses of 1.25 g, 2.5 g, 5 g, or 10 g three times daily for the initial 48 hours.
Patients whose serum K+ levels normalized during that initial phase of treatment were then randomized to receive placebo or one of the four active drug doses administered daily for 12 days.
Patients in the phase III trial had serum K+ levels of 5-6.5 mEq/L. Those in the 2.5-g, 5-g, and 10-g groups met the primary endpoint, with significantly greater reductions in serum K+, compared with those on placebo, at 48 hours.
The mean serum K+ reduction was 0.73 mEq/L at the 10-g dose at 48 hours. The gastrointestinal adverse event rate was 5.1% in the placebo group patients, and 3.5% in the treatment group.
Final results from the phase III trial are expected in the coming months.
The findings are important because currently only one treatment – sodium polystyrene sulfonate (SPS), an organic polymer resin that nonselectively binds cations – is approved in the United States for the treatment of hyperkalemia – a serious condition that is associated with significant mortality and morbidity in patients with cardiovascular disease or chronic kidney disease.
"Even marginally high potassium levels, such as over 4.5, however, have an increased risk of death and ventricular fibrillation," Dr. Ash explained.
Further, hyperkalemia limits the ability to use cardioprotective and renoprotective agents such as angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, he said.
The efficacy of SPS for lowering serum K+ levels is questionable, and the agent has been associated with several serious adverse effects, including sodium loading, colonic necrosis, and other fatal gastrointestinal effects, Dr. Ash explained.
ZS-9 differs from traditional nonspecific and nonselective cation exchange organic polymer resins in that it is an inorganic cation exchanger – a result of advances in chemistry for the development of highly selective drug therapies.
"ZS-9 was designed and engineered to be highly selective for potassium," he said, noting that ZS-9 has more than nine times the potassium-binding ability of SPS, and is not systemically absorbed; thus, the risk of systemic toxicity is minimized or eliminated.
The findings thus far suggest that ZS-9 is a safe, reliable, fast, effective and well-tolerated therapy for lowering serum K+ levels in patients with hyperkalemia, Dr. Ash concluded.
Dr. Ash disclosed ties with Merit Medical, HemoCleanse (which has a minority share interest in ZS Pharma), Fresenius Medical, Ash Access Technology (in which he has ownership interest), Renal Solutions, and DaVita RMS. He also is editor-in-chief of Seminars in Dialysis, ASKIN section.
ATLANTA – A novel first-in-class agent that selectively binds cations appears safe and effective for the treatment of hyperkalemia in patients with chronic kidney disease, according to findings from a phase II, dose-ranging proof-of-concept study.
Preliminary data from a phase III study of 753 patients, which was initiated based on the positive findings in the phase II study, similarly demonstrate the safety and efficacy of the selective monovalent cation trap known as ZS-9 (ZS Pharma), Dr. Stephen R. Ash reported at Kidney Week 2013, sponsored by the American Society of Nephrology.
In 90 patients from the phase II study who were randomized to receive either placebo or one of three ZS-9 doses (0.3 g in 12 patients, 3 g in 24 patients, and 10 g in 24 patients), active treatment was associated with significantly greater dose-dependent reductions in serum potassium (K+) than was placebo, said Dr. Ash of Indiana University, Lafayette.
The mean serum K+ level at baseline for both the placebo group and the combined active treatment groups was 5.1 mEq/L. Within 48 hours of treatment initiation, 63% of patients in the 10-g ZS-9 group met the primary end point of at least a 1.0-mEq/L reduction in serum K+, compared with only 17% of patients in the placebo group.
The dose reduction in the 10-g group was "rapid and substantial," with a significant decrease, compared with placebo, occurring within 1 hour of the initial dose. Levels were 0.92-mEq/L lower than baseline after 38 hours (4 hours after the last dose), and 0.68-mEq/L lower than baseline at 48 hours (14 hours after the last dose). The levels remained significantly lower than placebo for an additional 3.5 days after the last dose, Dr. Ash said.
"At every point in the trial for these 10-g–dose patients, the serum potassium was lower in the treatment group than in the control group. ... At 38 hours, almost 90% of the patients who were on the 10-g dose had a serum potassium [level] of less than 4.5," he said.
Participants had mild to moderate chronic kidney disease with a glomerular filtration rate of 30-60 mL/min per 1.73 m2, and mild to moderate hyperkalemia, with serum K+ levels of 5-6 mEq/L.
Treatment with the tasteless, odorless substance, which was delivered orally as a suspension in water three times daily at meal times, was well tolerated. No serious adverse events were reported, and no significant gastrointestinal issues, hypokalemia, hypomagnesemia, or hypocalcemia were observed.
Only one adverse event, a mild case of constipation in the 3-g–dose group, was thought to have a causal relationship to the study drug. No patients withdrew from the study.
The preliminary data from the pivotal randomized, controlled phase III trial also suggest a rapid and dose-dependent reduction in serum K+ in patients treated with ZS-9. In that study, patients were randomized to receive placebo or ZS-9 at doses of 1.25 g, 2.5 g, 5 g, or 10 g three times daily for the initial 48 hours.
Patients whose serum K+ levels normalized during that initial phase of treatment were then randomized to receive placebo or one of the four active drug doses administered daily for 12 days.
Patients in the phase III trial had serum K+ levels of 5-6.5 mEq/L. Those in the 2.5-g, 5-g, and 10-g groups met the primary endpoint, with significantly greater reductions in serum K+, compared with those on placebo, at 48 hours.
The mean serum K+ reduction was 0.73 mEq/L at the 10-g dose at 48 hours. The gastrointestinal adverse event rate was 5.1% in the placebo group patients, and 3.5% in the treatment group.
Final results from the phase III trial are expected in the coming months.
The findings are important because currently only one treatment – sodium polystyrene sulfonate (SPS), an organic polymer resin that nonselectively binds cations – is approved in the United States for the treatment of hyperkalemia – a serious condition that is associated with significant mortality and morbidity in patients with cardiovascular disease or chronic kidney disease.
"Even marginally high potassium levels, such as over 4.5, however, have an increased risk of death and ventricular fibrillation," Dr. Ash explained.
Further, hyperkalemia limits the ability to use cardioprotective and renoprotective agents such as angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, he said.
The efficacy of SPS for lowering serum K+ levels is questionable, and the agent has been associated with several serious adverse effects, including sodium loading, colonic necrosis, and other fatal gastrointestinal effects, Dr. Ash explained.
ZS-9 differs from traditional nonspecific and nonselective cation exchange organic polymer resins in that it is an inorganic cation exchanger – a result of advances in chemistry for the development of highly selective drug therapies.
"ZS-9 was designed and engineered to be highly selective for potassium," he said, noting that ZS-9 has more than nine times the potassium-binding ability of SPS, and is not systemically absorbed; thus, the risk of systemic toxicity is minimized or eliminated.
The findings thus far suggest that ZS-9 is a safe, reliable, fast, effective and well-tolerated therapy for lowering serum K+ levels in patients with hyperkalemia, Dr. Ash concluded.
Dr. Ash disclosed ties with Merit Medical, HemoCleanse (which has a minority share interest in ZS Pharma), Fresenius Medical, Ash Access Technology (in which he has ownership interest), Renal Solutions, and DaVita RMS. He also is editor-in-chief of Seminars in Dialysis, ASKIN section.
AT KIDNEY WEEK 2013
Major finding: Within 48 hours, 63% of patients in the group who got a 10-g dose of ZS-9 met the primary end point of at least a 1.0-mEq/L reduction in serum K+, compared with only 17% of patients in the placebo group (phase II results).
Data source: A phase II study of 90 patients; a phase III study of 753 patients.
Disclosures: Dr. Ash disclosed ties with Merit Medical, HemoCleanse (which has a minority share interest in ZS Pharma), Fresenius Medical, Ash Access Technology (in which he has ownership interest), Renal Solutions, and DaVita RMS. He also is editor-in-chief of Seminars in Dialysis, ASKIN section.
Only Half of At-risk Adults Being Screened for Diabetes
MELBOURNE – Approximately half of adults who meet the eligibility for glucose testing according to four different guidelines are not being tested for type 2 diabetes, according to data from a large survey of U.S. adults.
Researchers from the Centers for Disease Control and Prevention analyzed data from 3,623 adults without diabetes who participated in the 2007-2010 National Health and Nutrition Examination Survey (NHANES).
They then used four screening and glucose testing guidelines to identify the proportion of adults who met the criteria for glucose testing, and compare this with subjects’ self-reports of glucose testing.
According to data presented at the World Diabetes Congress, the percentage of adults found eligible for glucose testing varied from 36% with the U.S. Preventive Services Task Force (USPSTF) guidelines to 80% using the U.K. National Institute for Health and Clinical Excellence (NICE) guidelines.
The other guidelines examined were the American Diabetes Association (ADA) guidelines, which found 74% were eligible, and the International Diabetes Federation/U.S. National Diabetes Prevention Program (IDF) risk test, which found 43% were eligible.
However, when researchers then examined whether eligible individuals had in fact received glucose testing, they found that approximately half did not recall being tested.
"Of those eligible according to the ADA, USPSTF, IDF, and NICE guidelines, 49.1%, 57.7%, 55.2%, and 48.9%, respectively, reported receiving a glucose test within the past 3 years," according to Dr. Giuseppina Imperatore.
Dr. Imperatore said she was surprised by the significant gap in testing practices.
"You have to take this with caution because maybe there is a recall bias, but definitely, if this is the case, it is a concern because these people should be receiving treatment or they should be receiving lifestyle modification," said Dr. Imperatore of the division of diabetes translation, CDC.
NHANES involves a questionnaire and an at-home interview and assessment, including the taking of a blood sample, which enabled the researchers to measure individuals’ blood glucose levels.
Dr. Imperatore said one of the reasons why some individuals may not have been tested was their health insurance status.
"When we looked at the percentage of tested and nontested in terms of health care insurance, those that were not tested were more likely not to have health insurance, so this is probably one of the reasons they didn’t get tested, although they were at high risk for diabetes or prediabetes," Dr. Imperatore said in an interview.
The study also found a wide range of sensitivities and specificities across the guidelines. The NICE guidelines were the most sensitive at 92% but had the lowest specificity at 31%, while the U.S. Preventive Services Task Force guidelines had the highest specificity (83%) but lowest sensitivity (31%).
Dr. Imperatore said she would opt for the American Diabetes Association guidelines, which had the highest sensitivity of the U.S. guidelines.
There were no conflicts of interest reported.
MELBOURNE – Approximately half of adults who meet the eligibility for glucose testing according to four different guidelines are not being tested for type 2 diabetes, according to data from a large survey of U.S. adults.
Researchers from the Centers for Disease Control and Prevention analyzed data from 3,623 adults without diabetes who participated in the 2007-2010 National Health and Nutrition Examination Survey (NHANES).
They then used four screening and glucose testing guidelines to identify the proportion of adults who met the criteria for glucose testing, and compare this with subjects’ self-reports of glucose testing.
According to data presented at the World Diabetes Congress, the percentage of adults found eligible for glucose testing varied from 36% with the U.S. Preventive Services Task Force (USPSTF) guidelines to 80% using the U.K. National Institute for Health and Clinical Excellence (NICE) guidelines.
The other guidelines examined were the American Diabetes Association (ADA) guidelines, which found 74% were eligible, and the International Diabetes Federation/U.S. National Diabetes Prevention Program (IDF) risk test, which found 43% were eligible.
However, when researchers then examined whether eligible individuals had in fact received glucose testing, they found that approximately half did not recall being tested.
"Of those eligible according to the ADA, USPSTF, IDF, and NICE guidelines, 49.1%, 57.7%, 55.2%, and 48.9%, respectively, reported receiving a glucose test within the past 3 years," according to Dr. Giuseppina Imperatore.
Dr. Imperatore said she was surprised by the significant gap in testing practices.
"You have to take this with caution because maybe there is a recall bias, but definitely, if this is the case, it is a concern because these people should be receiving treatment or they should be receiving lifestyle modification," said Dr. Imperatore of the division of diabetes translation, CDC.
NHANES involves a questionnaire and an at-home interview and assessment, including the taking of a blood sample, which enabled the researchers to measure individuals’ blood glucose levels.
Dr. Imperatore said one of the reasons why some individuals may not have been tested was their health insurance status.
"When we looked at the percentage of tested and nontested in terms of health care insurance, those that were not tested were more likely not to have health insurance, so this is probably one of the reasons they didn’t get tested, although they were at high risk for diabetes or prediabetes," Dr. Imperatore said in an interview.
The study also found a wide range of sensitivities and specificities across the guidelines. The NICE guidelines were the most sensitive at 92% but had the lowest specificity at 31%, while the U.S. Preventive Services Task Force guidelines had the highest specificity (83%) but lowest sensitivity (31%).
Dr. Imperatore said she would opt for the American Diabetes Association guidelines, which had the highest sensitivity of the U.S. guidelines.
There were no conflicts of interest reported.
MELBOURNE – Approximately half of adults who meet the eligibility for glucose testing according to four different guidelines are not being tested for type 2 diabetes, according to data from a large survey of U.S. adults.
Researchers from the Centers for Disease Control and Prevention analyzed data from 3,623 adults without diabetes who participated in the 2007-2010 National Health and Nutrition Examination Survey (NHANES).
They then used four screening and glucose testing guidelines to identify the proportion of adults who met the criteria for glucose testing, and compare this with subjects’ self-reports of glucose testing.
According to data presented at the World Diabetes Congress, the percentage of adults found eligible for glucose testing varied from 36% with the U.S. Preventive Services Task Force (USPSTF) guidelines to 80% using the U.K. National Institute for Health and Clinical Excellence (NICE) guidelines.
The other guidelines examined were the American Diabetes Association (ADA) guidelines, which found 74% were eligible, and the International Diabetes Federation/U.S. National Diabetes Prevention Program (IDF) risk test, which found 43% were eligible.
However, when researchers then examined whether eligible individuals had in fact received glucose testing, they found that approximately half did not recall being tested.
"Of those eligible according to the ADA, USPSTF, IDF, and NICE guidelines, 49.1%, 57.7%, 55.2%, and 48.9%, respectively, reported receiving a glucose test within the past 3 years," according to Dr. Giuseppina Imperatore.
Dr. Imperatore said she was surprised by the significant gap in testing practices.
"You have to take this with caution because maybe there is a recall bias, but definitely, if this is the case, it is a concern because these people should be receiving treatment or they should be receiving lifestyle modification," said Dr. Imperatore of the division of diabetes translation, CDC.
NHANES involves a questionnaire and an at-home interview and assessment, including the taking of a blood sample, which enabled the researchers to measure individuals’ blood glucose levels.
Dr. Imperatore said one of the reasons why some individuals may not have been tested was their health insurance status.
"When we looked at the percentage of tested and nontested in terms of health care insurance, those that were not tested were more likely not to have health insurance, so this is probably one of the reasons they didn’t get tested, although they were at high risk for diabetes or prediabetes," Dr. Imperatore said in an interview.
The study also found a wide range of sensitivities and specificities across the guidelines. The NICE guidelines were the most sensitive at 92% but had the lowest specificity at 31%, while the U.S. Preventive Services Task Force guidelines had the highest specificity (83%) but lowest sensitivity (31%).
Dr. Imperatore said she would opt for the American Diabetes Association guidelines, which had the highest sensitivity of the U.S. guidelines.
There were no conflicts of interest reported.
AT THE WORLD DIABETES CONGRESS
Lower urinary tract symptoms bother obese women more than obese men
LAS VEGAS – Obese women report significantly greater lower urinary tract symptoms and worse overall quality of life than do obese men, results from a single-center study showed.
"Over one-third of U.S. adults are obese and 60% are considered overweight," Dr. Margarita M. Aponte said in a poster presented during the annual meeting of the American Urogynecologic Society. "In women, obesity is an independent risk factor for pelvic floor disorders, and in men, obesity has been associated with an increase in storage symptoms and benign prostatic hypertrophy."
Dr. Aponte and her associates at New York University Langone Medical Center recruited 134 men and women who were planning to undergo laparoscopic-assisted gastric banding (LAGB). They collected demographic information and clinical data, and administered validated questionnaires preoperatively, including the Overactive Bladder Questionnaire (OAB-q), the International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF), the Medical, Epidemiologic and Social aspects of Aging (MESA) scale, and the International Prostate Symptom Score (IPSS), to evaluate lower urinary tract symptoms. The investigators also evaluated quality of life preoperatively with the King’s Health Questionnaire (KHQ). The purpose was to characterize and differentiate baseline lower urinary tract symptoms and quality of life scores in obese men and women who were undergoing LAGB.
Of the 134 patients, 92 (69%) were women and their mean age was 42 years. The researchers reported that on the OAB-Q, women had higher scores in symptom severity (P = .036), concern (P = .002), and health-related quality of life (P = .028) than did men. Increasing body mass index (BMI) was associated with greater concern (P = .024), social effects (P = .021), and total health-related quality of life scores (P = .051). Increasing age and having diabetes were associated with higher scores in almost all OAB-Q domains.
Compared with men, women also had a higher total International Consultation on Incontinence Questionnaire–Short Form score (P = .000) and International Prostate Symptom Score (P = .008), and increasing BMI was associated with incontinence severity in the ICIQ (P = .01).
On the King’s Health Questionnaire, women had higher scores in incontinence impact (P = .045), role limitations (P = .016), and severity (P = .000). Increasing BMI was associated with poor general health perception (P = .006), increased role limitations (P = .005), and severity (P = .002). In men, no association was observed between obesity, age, or the presence of diabetes and any of the KHQ domains.
The researchers said they had no relevant financial disclosures.
LAS VEGAS – Obese women report significantly greater lower urinary tract symptoms and worse overall quality of life than do obese men, results from a single-center study showed.
"Over one-third of U.S. adults are obese and 60% are considered overweight," Dr. Margarita M. Aponte said in a poster presented during the annual meeting of the American Urogynecologic Society. "In women, obesity is an independent risk factor for pelvic floor disorders, and in men, obesity has been associated with an increase in storage symptoms and benign prostatic hypertrophy."
Dr. Aponte and her associates at New York University Langone Medical Center recruited 134 men and women who were planning to undergo laparoscopic-assisted gastric banding (LAGB). They collected demographic information and clinical data, and administered validated questionnaires preoperatively, including the Overactive Bladder Questionnaire (OAB-q), the International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF), the Medical, Epidemiologic and Social aspects of Aging (MESA) scale, and the International Prostate Symptom Score (IPSS), to evaluate lower urinary tract symptoms. The investigators also evaluated quality of life preoperatively with the King’s Health Questionnaire (KHQ). The purpose was to characterize and differentiate baseline lower urinary tract symptoms and quality of life scores in obese men and women who were undergoing LAGB.
Of the 134 patients, 92 (69%) were women and their mean age was 42 years. The researchers reported that on the OAB-Q, women had higher scores in symptom severity (P = .036), concern (P = .002), and health-related quality of life (P = .028) than did men. Increasing body mass index (BMI) was associated with greater concern (P = .024), social effects (P = .021), and total health-related quality of life scores (P = .051). Increasing age and having diabetes were associated with higher scores in almost all OAB-Q domains.
Compared with men, women also had a higher total International Consultation on Incontinence Questionnaire–Short Form score (P = .000) and International Prostate Symptom Score (P = .008), and increasing BMI was associated with incontinence severity in the ICIQ (P = .01).
On the King’s Health Questionnaire, women had higher scores in incontinence impact (P = .045), role limitations (P = .016), and severity (P = .000). Increasing BMI was associated with poor general health perception (P = .006), increased role limitations (P = .005), and severity (P = .002). In men, no association was observed between obesity, age, or the presence of diabetes and any of the KHQ domains.
The researchers said they had no relevant financial disclosures.
LAS VEGAS – Obese women report significantly greater lower urinary tract symptoms and worse overall quality of life than do obese men, results from a single-center study showed.
"Over one-third of U.S. adults are obese and 60% are considered overweight," Dr. Margarita M. Aponte said in a poster presented during the annual meeting of the American Urogynecologic Society. "In women, obesity is an independent risk factor for pelvic floor disorders, and in men, obesity has been associated with an increase in storage symptoms and benign prostatic hypertrophy."
Dr. Aponte and her associates at New York University Langone Medical Center recruited 134 men and women who were planning to undergo laparoscopic-assisted gastric banding (LAGB). They collected demographic information and clinical data, and administered validated questionnaires preoperatively, including the Overactive Bladder Questionnaire (OAB-q), the International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF), the Medical, Epidemiologic and Social aspects of Aging (MESA) scale, and the International Prostate Symptom Score (IPSS), to evaluate lower urinary tract symptoms. The investigators also evaluated quality of life preoperatively with the King’s Health Questionnaire (KHQ). The purpose was to characterize and differentiate baseline lower urinary tract symptoms and quality of life scores in obese men and women who were undergoing LAGB.
Of the 134 patients, 92 (69%) were women and their mean age was 42 years. The researchers reported that on the OAB-Q, women had higher scores in symptom severity (P = .036), concern (P = .002), and health-related quality of life (P = .028) than did men. Increasing body mass index (BMI) was associated with greater concern (P = .024), social effects (P = .021), and total health-related quality of life scores (P = .051). Increasing age and having diabetes were associated with higher scores in almost all OAB-Q domains.
Compared with men, women also had a higher total International Consultation on Incontinence Questionnaire–Short Form score (P = .000) and International Prostate Symptom Score (P = .008), and increasing BMI was associated with incontinence severity in the ICIQ (P = .01).
On the King’s Health Questionnaire, women had higher scores in incontinence impact (P = .045), role limitations (P = .016), and severity (P = .000). Increasing BMI was associated with poor general health perception (P = .006), increased role limitations (P = .005), and severity (P = .002). In men, no association was observed between obesity, age, or the presence of diabetes and any of the KHQ domains.
The researchers said they had no relevant financial disclosures.
AT THE AUGS ANNUAL MEETING
Major finding: On the Overactive Bladder Questionnaire, more obese women than obese men had higher scores in symptom severity (P = .036), concern (P = 0.002), and health-related quality of life (P =.028).
Data source: A study of baseline data from134 men and women who were planning to undergo laparoscopic-assisted gastric banding.
Disclosures: The researchers said they had no relevant financial disclosures.
FDA approves Xiaflex for Peyronie’s disease
The Food and Drug Administration has approved the biologic drug Xiaflex (collagenase clostridium histolyticum) for Peyronie’s disease, making it the first FDA-approved medicine for men with the disease.
Xiaflex, originally approved in 2010 to treat the hand deformity Dupuytren’s contracture, is the first available nonsurgical treatment option for Peyronie’s disease, a condition in which scar tissue develops under the skin of the penis to form a lump. This scar tissue causes an abnormal bend during erection that may cause discomfort during intercourse.
"Xiaflex is believed to work for Peyronie’s disease by breaking down the buildup of collagen that causes the curvature deformity," the FDA said in a statement Dec. 6.
A treatment cycle with Xiaflex consists of two injections directly into the collagen-containing part of the penis and one penile modeling procedure. The patient may undergo a maximum of four treatment cycles.
Xiaflex was studied in two trials of a total of 832 men with Peyronie’s disease and a penile curvature deformity of at least 30 degrees. Patients received either placebo or up to four Xiaflex treatment cycles and were followed over 52 weeks.
The FDA reported that Xiaflex "significantly reduced penile curvature deformity and related bothersome effects" compared with placebo, but warned of possible adverse side effects of the drug, such as penile fracture, hematoma, swelling, and pain.
Because of the risk for adverse reactions, Xiaflex for the treatment of Peyronie’s disease is available only through a restricted program under a Risk Evaluation and Mitigation Strategy. The program requires participating doctors to undergo training and certification in the administration of the drug.
Adverse reactions from the use of Xiaflex should be reported to the FDA’s MedWatch Adverse Event Reporting Program online or by calling 800-FDA-1088.
Xiaflex is marketed by Auxilium Pharmaceuticals.
Xiaflex, scar tissue, under the skin of the penis, lump, abnormal bend during erection, discomfort,
The Food and Drug Administration has approved the biologic drug Xiaflex (collagenase clostridium histolyticum) for Peyronie’s disease, making it the first FDA-approved medicine for men with the disease.
Xiaflex, originally approved in 2010 to treat the hand deformity Dupuytren’s contracture, is the first available nonsurgical treatment option for Peyronie’s disease, a condition in which scar tissue develops under the skin of the penis to form a lump. This scar tissue causes an abnormal bend during erection that may cause discomfort during intercourse.
"Xiaflex is believed to work for Peyronie’s disease by breaking down the buildup of collagen that causes the curvature deformity," the FDA said in a statement Dec. 6.
A treatment cycle with Xiaflex consists of two injections directly into the collagen-containing part of the penis and one penile modeling procedure. The patient may undergo a maximum of four treatment cycles.
Xiaflex was studied in two trials of a total of 832 men with Peyronie’s disease and a penile curvature deformity of at least 30 degrees. Patients received either placebo or up to four Xiaflex treatment cycles and were followed over 52 weeks.
The FDA reported that Xiaflex "significantly reduced penile curvature deformity and related bothersome effects" compared with placebo, but warned of possible adverse side effects of the drug, such as penile fracture, hematoma, swelling, and pain.
Because of the risk for adverse reactions, Xiaflex for the treatment of Peyronie’s disease is available only through a restricted program under a Risk Evaluation and Mitigation Strategy. The program requires participating doctors to undergo training and certification in the administration of the drug.
Adverse reactions from the use of Xiaflex should be reported to the FDA’s MedWatch Adverse Event Reporting Program online or by calling 800-FDA-1088.
Xiaflex is marketed by Auxilium Pharmaceuticals.
The Food and Drug Administration has approved the biologic drug Xiaflex (collagenase clostridium histolyticum) for Peyronie’s disease, making it the first FDA-approved medicine for men with the disease.
Xiaflex, originally approved in 2010 to treat the hand deformity Dupuytren’s contracture, is the first available nonsurgical treatment option for Peyronie’s disease, a condition in which scar tissue develops under the skin of the penis to form a lump. This scar tissue causes an abnormal bend during erection that may cause discomfort during intercourse.
"Xiaflex is believed to work for Peyronie’s disease by breaking down the buildup of collagen that causes the curvature deformity," the FDA said in a statement Dec. 6.
A treatment cycle with Xiaflex consists of two injections directly into the collagen-containing part of the penis and one penile modeling procedure. The patient may undergo a maximum of four treatment cycles.
Xiaflex was studied in two trials of a total of 832 men with Peyronie’s disease and a penile curvature deformity of at least 30 degrees. Patients received either placebo or up to four Xiaflex treatment cycles and were followed over 52 weeks.
The FDA reported that Xiaflex "significantly reduced penile curvature deformity and related bothersome effects" compared with placebo, but warned of possible adverse side effects of the drug, such as penile fracture, hematoma, swelling, and pain.
Because of the risk for adverse reactions, Xiaflex for the treatment of Peyronie’s disease is available only through a restricted program under a Risk Evaluation and Mitigation Strategy. The program requires participating doctors to undergo training and certification in the administration of the drug.
Adverse reactions from the use of Xiaflex should be reported to the FDA’s MedWatch Adverse Event Reporting Program online or by calling 800-FDA-1088.
Xiaflex is marketed by Auxilium Pharmaceuticals.
Xiaflex, scar tissue, under the skin of the penis, lump, abnormal bend during erection, discomfort,
Xiaflex, scar tissue, under the skin of the penis, lump, abnormal bend during erection, discomfort,
With tamsulosin, don’t forget the dip
Benign prostatic hyperplasia is a common condition. An estimated 50% of men over the age of 50 years have BPH. Presenting symptoms include urinary hesitancy, urgency, decreased strength of stream, and double-voiding. In my practice, nocturia is usually what starts the conversation.
First-line therapies include alpha-1 adrenergic receptor antagonists ("alpha-blockers") and 5-alpha-reductase inhibitors ("5-ARIs"). Alpha-blockers are effective, but are associated with orthostasis and syncopal events. Orthostasis has been more commonly associated with medications such as doxazosin and terazosin (in other words, "first-dose phenomenon"). Tamsulosin, a uroselective agent, is supposedly less likely to cause decreases in blood pressure.
But is tamsulosin associated with clinically important dips in blood pressure?
Steven T. Bird, Pharm.D., of the Food and Drug Administration’s Center for Drug Evaluation and Research, and his colleagues published the results from a retrospective, population-based cohort study examining whether tamsulosin is associated with hypotension and hospitalization (i.e., "severe hypotension"). Using information from a database of paid claims from more than 102 health care plans, the authors identified men aged 40-85 years who received alpha-blockers and 5-ARIs. In total, 297,596 new users of tamsulosin and 85,971 new users of 5-ARIs were identified. Median duration of use was 14 weeks for tamsulosin and 34 weeks for 5-ARIs (BMJ 2013;347:f6320).
Patients who took tamsulosin were 2.12 times more likely to experience severe hypotension during the first 4 weeks of therapy (95% confidence interval: 1.29-3.04). During weeks 5-8, severe hypotension was 1.51 times more likely in those who used tamsulosin (95% CI: 1.04-2.18). No significantly increased risk of hypotension was noted during weeks 9-12. Drug restarting (after a 4-week gap) was associated with a significantly increased risk of severe hypotension through 8 weeks of therapy, but not during weeks 9-12. Patients also were at an increased risk of hypotension during maintenance therapy.
In clinical trials of tamsulosin, patients were retained at research sites for 8 hours after the first dose and counseled on the effects of orthostatic hypotension – an environment that "may not apply to treatment practice in the real world," the authors cautioned. The incidence of hypotension in those studies was 12%, compared with 6% for placebo.
We should remind our patients that tamsulosin can cause clinically important dips in blood pressure. Simple instructions about sitting on the edge of the bed when going from supine to standing could make the difference between a better night’s sleep and a worse one in the hospital.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. He reports no conflicts of interest.
Benign prostatic hyperplasia is a common condition. An estimated 50% of men over the age of 50 years have BPH. Presenting symptoms include urinary hesitancy, urgency, decreased strength of stream, and double-voiding. In my practice, nocturia is usually what starts the conversation.
First-line therapies include alpha-1 adrenergic receptor antagonists ("alpha-blockers") and 5-alpha-reductase inhibitors ("5-ARIs"). Alpha-blockers are effective, but are associated with orthostasis and syncopal events. Orthostasis has been more commonly associated with medications such as doxazosin and terazosin (in other words, "first-dose phenomenon"). Tamsulosin, a uroselective agent, is supposedly less likely to cause decreases in blood pressure.
But is tamsulosin associated with clinically important dips in blood pressure?
Steven T. Bird, Pharm.D., of the Food and Drug Administration’s Center for Drug Evaluation and Research, and his colleagues published the results from a retrospective, population-based cohort study examining whether tamsulosin is associated with hypotension and hospitalization (i.e., "severe hypotension"). Using information from a database of paid claims from more than 102 health care plans, the authors identified men aged 40-85 years who received alpha-blockers and 5-ARIs. In total, 297,596 new users of tamsulosin and 85,971 new users of 5-ARIs were identified. Median duration of use was 14 weeks for tamsulosin and 34 weeks for 5-ARIs (BMJ 2013;347:f6320).
Patients who took tamsulosin were 2.12 times more likely to experience severe hypotension during the first 4 weeks of therapy (95% confidence interval: 1.29-3.04). During weeks 5-8, severe hypotension was 1.51 times more likely in those who used tamsulosin (95% CI: 1.04-2.18). No significantly increased risk of hypotension was noted during weeks 9-12. Drug restarting (after a 4-week gap) was associated with a significantly increased risk of severe hypotension through 8 weeks of therapy, but not during weeks 9-12. Patients also were at an increased risk of hypotension during maintenance therapy.
In clinical trials of tamsulosin, patients were retained at research sites for 8 hours after the first dose and counseled on the effects of orthostatic hypotension – an environment that "may not apply to treatment practice in the real world," the authors cautioned. The incidence of hypotension in those studies was 12%, compared with 6% for placebo.
We should remind our patients that tamsulosin can cause clinically important dips in blood pressure. Simple instructions about sitting on the edge of the bed when going from supine to standing could make the difference between a better night’s sleep and a worse one in the hospital.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. He reports no conflicts of interest.
Benign prostatic hyperplasia is a common condition. An estimated 50% of men over the age of 50 years have BPH. Presenting symptoms include urinary hesitancy, urgency, decreased strength of stream, and double-voiding. In my practice, nocturia is usually what starts the conversation.
First-line therapies include alpha-1 adrenergic receptor antagonists ("alpha-blockers") and 5-alpha-reductase inhibitors ("5-ARIs"). Alpha-blockers are effective, but are associated with orthostasis and syncopal events. Orthostasis has been more commonly associated with medications such as doxazosin and terazosin (in other words, "first-dose phenomenon"). Tamsulosin, a uroselective agent, is supposedly less likely to cause decreases in blood pressure.
But is tamsulosin associated with clinically important dips in blood pressure?
Steven T. Bird, Pharm.D., of the Food and Drug Administration’s Center for Drug Evaluation and Research, and his colleagues published the results from a retrospective, population-based cohort study examining whether tamsulosin is associated with hypotension and hospitalization (i.e., "severe hypotension"). Using information from a database of paid claims from more than 102 health care plans, the authors identified men aged 40-85 years who received alpha-blockers and 5-ARIs. In total, 297,596 new users of tamsulosin and 85,971 new users of 5-ARIs were identified. Median duration of use was 14 weeks for tamsulosin and 34 weeks for 5-ARIs (BMJ 2013;347:f6320).
Patients who took tamsulosin were 2.12 times more likely to experience severe hypotension during the first 4 weeks of therapy (95% confidence interval: 1.29-3.04). During weeks 5-8, severe hypotension was 1.51 times more likely in those who used tamsulosin (95% CI: 1.04-2.18). No significantly increased risk of hypotension was noted during weeks 9-12. Drug restarting (after a 4-week gap) was associated with a significantly increased risk of severe hypotension through 8 weeks of therapy, but not during weeks 9-12. Patients also were at an increased risk of hypotension during maintenance therapy.
In clinical trials of tamsulosin, patients were retained at research sites for 8 hours after the first dose and counseled on the effects of orthostatic hypotension – an environment that "may not apply to treatment practice in the real world," the authors cautioned. The incidence of hypotension in those studies was 12%, compared with 6% for placebo.
We should remind our patients that tamsulosin can cause clinically important dips in blood pressure. Simple instructions about sitting on the edge of the bed when going from supine to standing could make the difference between a better night’s sleep and a worse one in the hospital.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. He reports no conflicts of interest.
Single-incision sling may help stress urinary incontinence
NATIONAL HARBOR, MD. – After 12 months, an adjustable, single-incision sling significantly improved clinical and quality of life measures associated with stress urinary incontinence in women.
The Altis sling decreased the Urinary Distress Index (UDI) from a mean of 55 to a mean of 10, Dr. Douglas Van Drie said at a meeting sponsored by the AAGL. The Incontinence Impact Questionnaire (ILQ-7) showed similar improvements at the interim assessment of the device’s 2-year safety and efficacy study.
The study was sponsored by Coloplast, which makes the sling, with input and monitoring by the Food and Drug Administration. Altis was approved in November 2012 based on an investigational device exemption study, which included implant data. The FDA efficacy requirement was a 50% decrease in pad weight by 6 months.
According to the company website, "Altis is a unique, minimally invasive sling that combines integrated two-way tensioning with lightweight sling material to provide strength, security, and adjustability."
Physicians are divided on their thoughts about a single-incision sling, said Dr. Van Drie, a urogynecologist in group practice in Grand Rapids, Mich. "Those [physicians] who use them are advocates for their safety and simplicity, and the ability to insert them in the office. They have been adopted in different areas of the world as an option for doing simplified, less costly incontinence surgery. The argument against is questions about their staying power – will the effect hold up long term?" he said.
Even though the Altis is a single-incision sling, it has a "very secure" anchoring system, Dr. Van Drie said. The anchor not only goes into the obturator internus, but into the membrane and the obturator externus.
The study involved 113 women, with a mean age of 54 years. Their histories included stress incontinence with hypermobility (81%), without hypermobility (19%), mixed incontinence (37%), and overactive bladder (5%).
Most of the procedures were performed during an inpatient hospital stay (59%); however, 24% were performed at an ambulatory surgical center and 17%, in the physician’s office. General anesthesia was used in 52%, spinal in 3%, and local in 45%.
At 12 months, 90% of patients had at least a 50% reduction in pad weight, and 90% had a negative cough stress test result. The UDI decreased by a mean of 46 points, and the IIQ-7 score, by a mean of 47 points.
There were 11 device-related failures in eight patients. These included one each of urinary retention, urinary tract infection, decreased urine stream, dyspareunia, inflammation, worsening of overactive bladder, and voiding dysfunction. There were four mesh extrusions (3.5%), all less than 3 cm. Two patients with extrusion were smokers, and one was diabetic.
Serious adverse events occurred in three patients: One with a hematoma, one patient who needed transfer to the operating room because of anxiety during repair of a 2-mm mesh extrusion, and one patient whose adverse event was changed to a severe adverse event when she moved out of the study. There were no unanticipated device effects, Dr. Van Drie noted.
Dr. Van Drie is a consultant for Coloplast and has received research money and grants from the company.
NATIONAL HARBOR, MD. – After 12 months, an adjustable, single-incision sling significantly improved clinical and quality of life measures associated with stress urinary incontinence in women.
The Altis sling decreased the Urinary Distress Index (UDI) from a mean of 55 to a mean of 10, Dr. Douglas Van Drie said at a meeting sponsored by the AAGL. The Incontinence Impact Questionnaire (ILQ-7) showed similar improvements at the interim assessment of the device’s 2-year safety and efficacy study.
The study was sponsored by Coloplast, which makes the sling, with input and monitoring by the Food and Drug Administration. Altis was approved in November 2012 based on an investigational device exemption study, which included implant data. The FDA efficacy requirement was a 50% decrease in pad weight by 6 months.
According to the company website, "Altis is a unique, minimally invasive sling that combines integrated two-way tensioning with lightweight sling material to provide strength, security, and adjustability."
Physicians are divided on their thoughts about a single-incision sling, said Dr. Van Drie, a urogynecologist in group practice in Grand Rapids, Mich. "Those [physicians] who use them are advocates for their safety and simplicity, and the ability to insert them in the office. They have been adopted in different areas of the world as an option for doing simplified, less costly incontinence surgery. The argument against is questions about their staying power – will the effect hold up long term?" he said.
Even though the Altis is a single-incision sling, it has a "very secure" anchoring system, Dr. Van Drie said. The anchor not only goes into the obturator internus, but into the membrane and the obturator externus.
The study involved 113 women, with a mean age of 54 years. Their histories included stress incontinence with hypermobility (81%), without hypermobility (19%), mixed incontinence (37%), and overactive bladder (5%).
Most of the procedures were performed during an inpatient hospital stay (59%); however, 24% were performed at an ambulatory surgical center and 17%, in the physician’s office. General anesthesia was used in 52%, spinal in 3%, and local in 45%.
At 12 months, 90% of patients had at least a 50% reduction in pad weight, and 90% had a negative cough stress test result. The UDI decreased by a mean of 46 points, and the IIQ-7 score, by a mean of 47 points.
There were 11 device-related failures in eight patients. These included one each of urinary retention, urinary tract infection, decreased urine stream, dyspareunia, inflammation, worsening of overactive bladder, and voiding dysfunction. There were four mesh extrusions (3.5%), all less than 3 cm. Two patients with extrusion were smokers, and one was diabetic.
Serious adverse events occurred in three patients: One with a hematoma, one patient who needed transfer to the operating room because of anxiety during repair of a 2-mm mesh extrusion, and one patient whose adverse event was changed to a severe adverse event when she moved out of the study. There were no unanticipated device effects, Dr. Van Drie noted.
Dr. Van Drie is a consultant for Coloplast and has received research money and grants from the company.
NATIONAL HARBOR, MD. – After 12 months, an adjustable, single-incision sling significantly improved clinical and quality of life measures associated with stress urinary incontinence in women.
The Altis sling decreased the Urinary Distress Index (UDI) from a mean of 55 to a mean of 10, Dr. Douglas Van Drie said at a meeting sponsored by the AAGL. The Incontinence Impact Questionnaire (ILQ-7) showed similar improvements at the interim assessment of the device’s 2-year safety and efficacy study.
The study was sponsored by Coloplast, which makes the sling, with input and monitoring by the Food and Drug Administration. Altis was approved in November 2012 based on an investigational device exemption study, which included implant data. The FDA efficacy requirement was a 50% decrease in pad weight by 6 months.
According to the company website, "Altis is a unique, minimally invasive sling that combines integrated two-way tensioning with lightweight sling material to provide strength, security, and adjustability."
Physicians are divided on their thoughts about a single-incision sling, said Dr. Van Drie, a urogynecologist in group practice in Grand Rapids, Mich. "Those [physicians] who use them are advocates for their safety and simplicity, and the ability to insert them in the office. They have been adopted in different areas of the world as an option for doing simplified, less costly incontinence surgery. The argument against is questions about their staying power – will the effect hold up long term?" he said.
Even though the Altis is a single-incision sling, it has a "very secure" anchoring system, Dr. Van Drie said. The anchor not only goes into the obturator internus, but into the membrane and the obturator externus.
The study involved 113 women, with a mean age of 54 years. Their histories included stress incontinence with hypermobility (81%), without hypermobility (19%), mixed incontinence (37%), and overactive bladder (5%).
Most of the procedures were performed during an inpatient hospital stay (59%); however, 24% were performed at an ambulatory surgical center and 17%, in the physician’s office. General anesthesia was used in 52%, spinal in 3%, and local in 45%.
At 12 months, 90% of patients had at least a 50% reduction in pad weight, and 90% had a negative cough stress test result. The UDI decreased by a mean of 46 points, and the IIQ-7 score, by a mean of 47 points.
There were 11 device-related failures in eight patients. These included one each of urinary retention, urinary tract infection, decreased urine stream, dyspareunia, inflammation, worsening of overactive bladder, and voiding dysfunction. There were four mesh extrusions (3.5%), all less than 3 cm. Two patients with extrusion were smokers, and one was diabetic.
Serious adverse events occurred in three patients: One with a hematoma, one patient who needed transfer to the operating room because of anxiety during repair of a 2-mm mesh extrusion, and one patient whose adverse event was changed to a severe adverse event when she moved out of the study. There were no unanticipated device effects, Dr. Van Drie noted.
Dr. Van Drie is a consultant for Coloplast and has received research money and grants from the company.
AT THE AAGL GLOBAL CONGRESS
Major finding: After receiving a single-incision incontinence sling, 90% of women had significant improvements in clinical and quality of life measures related to stress urinary incontinence.
Data source: A prospective study of 113 women.
Disclosures: Coloplast sponsored the study. Dr. Van Drie is a consultant for Coloplast and has received research money and grants from the company.