User login
Stem cell transplant shows long-term benefit in MS
The benefits of autologous hematopoietic stem cell transplant (AHSCT) for patients with multiple sclerosis (MS) persist for more than 10 years in the majority of patents, new data show. The study reports on 210 Italian patients who underwent AHSCT between 2007 and 2019. Among the entire study cohort, 79.5% of patients had not experienced worsening of disability at 5 years, and 65.5% had not experienced it at 10 years.
Patients with relapsing remitting MS had better results, with 85.5% experiencing no worsening of disability at 5 years, and 71.3% at 10 years. Among patients with progressive MS, 71.0% showed no worsening of disability at 5 years, and 57.2% at 10 years.
“This is the longest follow-up of AHSCT in MS patients so far to be reported,” said study author Matilde Inglese, MD, University of Genoa (Italy). “We have shown AHSCT to be highly effective to prevent long-term disability worsening in most treated patients.”
The study was published online Jan. 20 in Neurology.
“We suggest that AHSCT should be considered as a treatment strategy for MS not responding to conventional therapy,” the authors concluded.
The study had no control group, so a direct comparison is not possible. Nevertheless, Dr. Inglese said she believed these results are better than those that would be achieved with disease-modifying drug therapy for similar patients.
“The best patient candidates for this procedure are those with highly active multiple sclerosis who are not responsive to high-efficacy drugs, such as alemtuzumab or ocrelizumab,” Dr. Inglese commented. “Younger patients with an aggressive form of relapsing remitting MS tend to do the best, although patients with progressive forms of MS who still have active lesions on MRI also benefit.”
Renewing the immune system
The transplant procedure involves giving high-dose cyclophosphamide to stimulate mobilization of bone marrow stem cells, which are collected from peripheral blood. Patients then undergo intense immunosuppression with a cocktail of drugs to remove the autoreactive T cells, and the stem cells, which are not autoreactive, are reinfused.
“We are effectively renewing the immune system,” Dr. Inglese said. “While it is not correct to call it a cure, as we are not eliminating the etiology of the disease, it is the closest to complete suppression of the disease that we can get.”
Other results from the study show that among patients with relapsing remitting MS, rates of relapse-free survival were 78.1% at 5 years and 63.5% at 10 years.
Better results were achieved for patients who received the BEAM+ATG conditioning regimen for immunosuppression. That regimen includes carmustine, cytosine-arabinoside, etoposide, and melphalan, followed by rabbit antithymocyte globulin. Among patients with relapsing remitting disease who were treated with this protocol, rates of relapse-free survival were 86.4% at 5 years and 77.0% at 10 years.
For patients with relapsing remitting MS, the probability of achieving NEDA-3 status (no evidence of disease activity, including the absence of clinical relapses, disability worsening, and MRI inflammatory activity) was 62.2% at 5 years and 40.5% at 10 years.
Among those patients with relapsing remitting MS who received the BEAM+ATG conditioning protocol, NEDA-3 status was achieved in 67.7% at 5 years and in 54.9% at 10 years.
Three deaths occurred within 100 days following AHSCT (1.4% of the entire study population). One patient developed pulmonary thromboembolism, received fibrinolytic treatment, and died 48 hours later after intracranial hemorrhage. The second patient experienced engraftment failure and died 24 days after transplant because of an opportunistic infection. The third patient died 1 month after transplant from Wernicke-like encephalopathy. All the patients who died received the BEAM+ATG conditioning regimen. No transplant-related deaths occurred in patients who underwent transplant after 2007.
Dr. Inglese noted that the mortality rate associated with AHSCT has been greatly reduced in recent years. “We are seeing a very low mortality rate – about 0.3% – thanks to improvements in the procedure and better patient selection. This seems acceptable, given that we are treating patients with very aggressive disease who have a high risk of becoming significantly disabled relatively early in life,” she commented.
However, it is vitally important that the procedure be conducted in a specialized center with a highly experienced multidisciplinary team, she stressed.
In the Neurology article, the authors concluded: “Although patients with RRMS [relapsing remitting MS] are those who benefit the most from transplant, AHSCT has been also shown to prevent disability worsening in a large proportion of patients with active progressive MS.
“The BEAM+ATG conditioning protocol, although associated with a higher transplant mortality rate, was associated with a more pronounced suppression of clinical relapses and MRI inflammatory activity, allowing complete disease control in a higher proportion of patients,” they wrote.
Potent and durable efficacy, with caveats
Commenting on these latest findings, Jeffrey A. Cohen, MD, of the Mellen Center for Multiple Sclerosis at the Cleveland Clinic, said: “AHSCT appears to have potent and durable efficacy in MS but is associated with significant risk and cost.”
The patients who are most likely to benefit are young and have experienced the onset of disease relatively recently. They are still ambulatory with highly active MS and have experienced recent clinical relapses and/or MRI lesion activity, and such activity continues despite disease-modifying therapy, Dr. Cohen noted. He added that “AHSCT is a reasonable option for such patients who have essentially failed the available disease-modifying therapy options.”
He pointed out that the key question is where AHSCT belongs in the overall MS algorithm relative to other high-efficacy therapies. “We need to know whether it should be used more broadly rather than as a last resort.”
To address that question, several randomized trials comparing AHSCT with high-efficacy disease-modifying therapy are in progress, including the National Institutes of Health–sponsored BEAT-MS trial in the United States (for which Dr. Cohen is the lead investigator) and four European trials – NET-MS (for which Dr. Inglese is the lead investigator), STAR-MS, RAM-MS, and COAST-MS.
The current study was partially funded and supported by the Italian Multiple Sclerosis Foundation. Dr. Inglese disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The benefits of autologous hematopoietic stem cell transplant (AHSCT) for patients with multiple sclerosis (MS) persist for more than 10 years in the majority of patents, new data show. The study reports on 210 Italian patients who underwent AHSCT between 2007 and 2019. Among the entire study cohort, 79.5% of patients had not experienced worsening of disability at 5 years, and 65.5% had not experienced it at 10 years.
Patients with relapsing remitting MS had better results, with 85.5% experiencing no worsening of disability at 5 years, and 71.3% at 10 years. Among patients with progressive MS, 71.0% showed no worsening of disability at 5 years, and 57.2% at 10 years.
“This is the longest follow-up of AHSCT in MS patients so far to be reported,” said study author Matilde Inglese, MD, University of Genoa (Italy). “We have shown AHSCT to be highly effective to prevent long-term disability worsening in most treated patients.”
The study was published online Jan. 20 in Neurology.
“We suggest that AHSCT should be considered as a treatment strategy for MS not responding to conventional therapy,” the authors concluded.
The study had no control group, so a direct comparison is not possible. Nevertheless, Dr. Inglese said she believed these results are better than those that would be achieved with disease-modifying drug therapy for similar patients.
“The best patient candidates for this procedure are those with highly active multiple sclerosis who are not responsive to high-efficacy drugs, such as alemtuzumab or ocrelizumab,” Dr. Inglese commented. “Younger patients with an aggressive form of relapsing remitting MS tend to do the best, although patients with progressive forms of MS who still have active lesions on MRI also benefit.”
Renewing the immune system
The transplant procedure involves giving high-dose cyclophosphamide to stimulate mobilization of bone marrow stem cells, which are collected from peripheral blood. Patients then undergo intense immunosuppression with a cocktail of drugs to remove the autoreactive T cells, and the stem cells, which are not autoreactive, are reinfused.
“We are effectively renewing the immune system,” Dr. Inglese said. “While it is not correct to call it a cure, as we are not eliminating the etiology of the disease, it is the closest to complete suppression of the disease that we can get.”
Other results from the study show that among patients with relapsing remitting MS, rates of relapse-free survival were 78.1% at 5 years and 63.5% at 10 years.
Better results were achieved for patients who received the BEAM+ATG conditioning regimen for immunosuppression. That regimen includes carmustine, cytosine-arabinoside, etoposide, and melphalan, followed by rabbit antithymocyte globulin. Among patients with relapsing remitting disease who were treated with this protocol, rates of relapse-free survival were 86.4% at 5 years and 77.0% at 10 years.
For patients with relapsing remitting MS, the probability of achieving NEDA-3 status (no evidence of disease activity, including the absence of clinical relapses, disability worsening, and MRI inflammatory activity) was 62.2% at 5 years and 40.5% at 10 years.
Among those patients with relapsing remitting MS who received the BEAM+ATG conditioning protocol, NEDA-3 status was achieved in 67.7% at 5 years and in 54.9% at 10 years.
Three deaths occurred within 100 days following AHSCT (1.4% of the entire study population). One patient developed pulmonary thromboembolism, received fibrinolytic treatment, and died 48 hours later after intracranial hemorrhage. The second patient experienced engraftment failure and died 24 days after transplant because of an opportunistic infection. The third patient died 1 month after transplant from Wernicke-like encephalopathy. All the patients who died received the BEAM+ATG conditioning regimen. No transplant-related deaths occurred in patients who underwent transplant after 2007.
Dr. Inglese noted that the mortality rate associated with AHSCT has been greatly reduced in recent years. “We are seeing a very low mortality rate – about 0.3% – thanks to improvements in the procedure and better patient selection. This seems acceptable, given that we are treating patients with very aggressive disease who have a high risk of becoming significantly disabled relatively early in life,” she commented.
However, it is vitally important that the procedure be conducted in a specialized center with a highly experienced multidisciplinary team, she stressed.
In the Neurology article, the authors concluded: “Although patients with RRMS [relapsing remitting MS] are those who benefit the most from transplant, AHSCT has been also shown to prevent disability worsening in a large proportion of patients with active progressive MS.
“The BEAM+ATG conditioning protocol, although associated with a higher transplant mortality rate, was associated with a more pronounced suppression of clinical relapses and MRI inflammatory activity, allowing complete disease control in a higher proportion of patients,” they wrote.
Potent and durable efficacy, with caveats
Commenting on these latest findings, Jeffrey A. Cohen, MD, of the Mellen Center for Multiple Sclerosis at the Cleveland Clinic, said: “AHSCT appears to have potent and durable efficacy in MS but is associated with significant risk and cost.”
The patients who are most likely to benefit are young and have experienced the onset of disease relatively recently. They are still ambulatory with highly active MS and have experienced recent clinical relapses and/or MRI lesion activity, and such activity continues despite disease-modifying therapy, Dr. Cohen noted. He added that “AHSCT is a reasonable option for such patients who have essentially failed the available disease-modifying therapy options.”
He pointed out that the key question is where AHSCT belongs in the overall MS algorithm relative to other high-efficacy therapies. “We need to know whether it should be used more broadly rather than as a last resort.”
To address that question, several randomized trials comparing AHSCT with high-efficacy disease-modifying therapy are in progress, including the National Institutes of Health–sponsored BEAT-MS trial in the United States (for which Dr. Cohen is the lead investigator) and four European trials – NET-MS (for which Dr. Inglese is the lead investigator), STAR-MS, RAM-MS, and COAST-MS.
The current study was partially funded and supported by the Italian Multiple Sclerosis Foundation. Dr. Inglese disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The benefits of autologous hematopoietic stem cell transplant (AHSCT) for patients with multiple sclerosis (MS) persist for more than 10 years in the majority of patents, new data show. The study reports on 210 Italian patients who underwent AHSCT between 2007 and 2019. Among the entire study cohort, 79.5% of patients had not experienced worsening of disability at 5 years, and 65.5% had not experienced it at 10 years.
Patients with relapsing remitting MS had better results, with 85.5% experiencing no worsening of disability at 5 years, and 71.3% at 10 years. Among patients with progressive MS, 71.0% showed no worsening of disability at 5 years, and 57.2% at 10 years.
“This is the longest follow-up of AHSCT in MS patients so far to be reported,” said study author Matilde Inglese, MD, University of Genoa (Italy). “We have shown AHSCT to be highly effective to prevent long-term disability worsening in most treated patients.”
The study was published online Jan. 20 in Neurology.
“We suggest that AHSCT should be considered as a treatment strategy for MS not responding to conventional therapy,” the authors concluded.
The study had no control group, so a direct comparison is not possible. Nevertheless, Dr. Inglese said she believed these results are better than those that would be achieved with disease-modifying drug therapy for similar patients.
“The best patient candidates for this procedure are those with highly active multiple sclerosis who are not responsive to high-efficacy drugs, such as alemtuzumab or ocrelizumab,” Dr. Inglese commented. “Younger patients with an aggressive form of relapsing remitting MS tend to do the best, although patients with progressive forms of MS who still have active lesions on MRI also benefit.”
Renewing the immune system
The transplant procedure involves giving high-dose cyclophosphamide to stimulate mobilization of bone marrow stem cells, which are collected from peripheral blood. Patients then undergo intense immunosuppression with a cocktail of drugs to remove the autoreactive T cells, and the stem cells, which are not autoreactive, are reinfused.
“We are effectively renewing the immune system,” Dr. Inglese said. “While it is not correct to call it a cure, as we are not eliminating the etiology of the disease, it is the closest to complete suppression of the disease that we can get.”
Other results from the study show that among patients with relapsing remitting MS, rates of relapse-free survival were 78.1% at 5 years and 63.5% at 10 years.
Better results were achieved for patients who received the BEAM+ATG conditioning regimen for immunosuppression. That regimen includes carmustine, cytosine-arabinoside, etoposide, and melphalan, followed by rabbit antithymocyte globulin. Among patients with relapsing remitting disease who were treated with this protocol, rates of relapse-free survival were 86.4% at 5 years and 77.0% at 10 years.
For patients with relapsing remitting MS, the probability of achieving NEDA-3 status (no evidence of disease activity, including the absence of clinical relapses, disability worsening, and MRI inflammatory activity) was 62.2% at 5 years and 40.5% at 10 years.
Among those patients with relapsing remitting MS who received the BEAM+ATG conditioning protocol, NEDA-3 status was achieved in 67.7% at 5 years and in 54.9% at 10 years.
Three deaths occurred within 100 days following AHSCT (1.4% of the entire study population). One patient developed pulmonary thromboembolism, received fibrinolytic treatment, and died 48 hours later after intracranial hemorrhage. The second patient experienced engraftment failure and died 24 days after transplant because of an opportunistic infection. The third patient died 1 month after transplant from Wernicke-like encephalopathy. All the patients who died received the BEAM+ATG conditioning regimen. No transplant-related deaths occurred in patients who underwent transplant after 2007.
Dr. Inglese noted that the mortality rate associated with AHSCT has been greatly reduced in recent years. “We are seeing a very low mortality rate – about 0.3% – thanks to improvements in the procedure and better patient selection. This seems acceptable, given that we are treating patients with very aggressive disease who have a high risk of becoming significantly disabled relatively early in life,” she commented.
However, it is vitally important that the procedure be conducted in a specialized center with a highly experienced multidisciplinary team, she stressed.
In the Neurology article, the authors concluded: “Although patients with RRMS [relapsing remitting MS] are those who benefit the most from transplant, AHSCT has been also shown to prevent disability worsening in a large proportion of patients with active progressive MS.
“The BEAM+ATG conditioning protocol, although associated with a higher transplant mortality rate, was associated with a more pronounced suppression of clinical relapses and MRI inflammatory activity, allowing complete disease control in a higher proportion of patients,” they wrote.
Potent and durable efficacy, with caveats
Commenting on these latest findings, Jeffrey A. Cohen, MD, of the Mellen Center for Multiple Sclerosis at the Cleveland Clinic, said: “AHSCT appears to have potent and durable efficacy in MS but is associated with significant risk and cost.”
The patients who are most likely to benefit are young and have experienced the onset of disease relatively recently. They are still ambulatory with highly active MS and have experienced recent clinical relapses and/or MRI lesion activity, and such activity continues despite disease-modifying therapy, Dr. Cohen noted. He added that “AHSCT is a reasonable option for such patients who have essentially failed the available disease-modifying therapy options.”
He pointed out that the key question is where AHSCT belongs in the overall MS algorithm relative to other high-efficacy therapies. “We need to know whether it should be used more broadly rather than as a last resort.”
To address that question, several randomized trials comparing AHSCT with high-efficacy disease-modifying therapy are in progress, including the National Institutes of Health–sponsored BEAT-MS trial in the United States (for which Dr. Cohen is the lead investigator) and four European trials – NET-MS (for which Dr. Inglese is the lead investigator), STAR-MS, RAM-MS, and COAST-MS.
The current study was partially funded and supported by the Italian Multiple Sclerosis Foundation. Dr. Inglese disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Blood biomarker may predict Alzheimer’s disease progression
new research suggests.
In a study of more than 1,000 participants, changes over time in levels of p-tau181 were associated with prospective neurodegeneration and cognitive decline characteristic of Alzheimer’s disease. These results have implications for investigative trials as well as clinical practice, the investigators noted.
Like p-tau181, neurofilament light chain (NfL) is associated with imaging markers of degeneration and cognitive decline; in contrast to the findings related to p-tau181, however, the associations between NfL and these outcomes are not specific to Alzheimer’s disease. Using both biomarkers could improve prediction of outcomes and patient monitoring, according to the researchers.
“These findings demonstrate that p-tau181 and NfL in blood have individual and complementary potential roles in the diagnosis and the monitoring of neurodegenerative disease,” said coinvestigator Michael Schöll, PhD, senior lecturer in psychiatry and neurochemistry at the University of Gothenburg (Sweden).
“With the reservation that we did not assess domain-specific cognitive impairment, p-tau181 was also more strongly associated with cognitive decline than was NfL,” Dr. Schöll added.
The findings were published online Jan. 11 in JAMA Neurology.
Biomarker-tracked neurodegeneration
Monitoring a patient’s neurodegenerative changes is important for tracking Alzheimer’s disease progression. Although clinicians can detect amyloid-beta and tau pathology using PET and cerebrospinal fluid (CSF) biomarkers, the widespread use of the latter has been hampered by cost and limited availability of necessary equipment. The use of blood-based biomarkers is not limited in these ways, and so they could aid in diagnosis and patient monitoring.
Previous studies have suggested that p-tau181 is a marker of Alzheimer’s disease status.
In the current study, investigators examined whether baseline and longitudinal levels of p-tau181 in plasma were associated with progressive neurodegeneration related to the disease. They analyzed data from the Alzheimer’s Disease Neuroimaging Initiative, a multicenter study designed to identify biomarkers for the detection and tracking of Alzheimer’s disease.
The researchers selected data for cognitively unimpaired and cognitively impaired participants who participated in the initiative between Feb. 1, 2007, and June 6, 2016. Participants were eligible for inclusion if plasma p-tau181 and NfL data were available for them and if they had undergone at least one 18fluorodeoxyglucose (FDG)–PET scan or structural T1 MRI at the same study visit. Most had also undergone imaging with 18florbetapir, which detects amyloid-beta.
A single-molecule array was used to analyze concentrations of p-tau181 and NfL in participants’ blood samples. Outliers for p-tau181 and NfL concentrations were excluded from further analysis. Using participants’ FDG-PET scans, the investigators measured glucose hypometabolism characteristic of Alzheimer’s disease. They used T1-weighted MRI scans to measure gray-matter volume.
Cognitively unimpaired participants responded to the Preclinical Alzheimer Cognitive Composite, a measure designed to detect early cognitive changes in cognitively normal patients with Alzheimer’s disease pathology. Cognitively impaired participants underwent the Alzheimer Disease Assessment Scale–Cognitive Subscale with 13 tasks to assess the severity of cognitive impairment.
The researchers included 1,113 participants (54% men; 89% non-Hispanic Whites; mean age, 74 years) in their analysis. In all, 378 participants were cognitively unimpaired, and 735 were cognitively impaired. Of the latter group, 73% had mild cognitive impairment, and 27% had Alzheimer’s disease dementia.
Atrophy predictor
Results showed that higher plasma p-tau181 levels at baseline were associated with more rapid progression of hypometabolism and atrophy in areas vulnerable to Alzheimer’s disease among cognitively impaired participants (FDG-PET standardized uptake value ratio change, r = –0.28; P < .001; gray-matter volume change, r = –0.28; P < .001).
The association with atrophy progression in cognitively impaired participants was stronger for p-tau181 than for NfL.
Plasma p-tau181 levels at baseline also predicted atrophy in temporoparietal regions vulnerable to Alzheimer’s disease among cognitively unimpaired participants (r = –0.11; P = .03). NfL, however, was associated with progressive atrophy in frontal regions among cognitively unimpaired participants.
At baseline, plasma p-tau181 levels were associated with prospective cognitive decline in both the cognitively unimpaired group (r = −0.12; P = .04) and the cognitively impaired group (r = 0.35; P < .001). However, plasma NfL was linked to cognitive decline only among those who were cognitively impaired (r = 0.26; P < .001).
Additional analyses showed that p-tau181, unlike NfL, was associated with hypometabolism and atrophy only in participants with amyloid-beta, regardless of cognitive status.
Between 25% and 45% of the association between baseline p-tau181 level and cognitive decline was mediated by baseline imaging markers of neurodegeneration. This finding suggests that another factor, such as regional tau pathology, might have an independent and direct effect on cognition, Dr. Schöll noted.
Furthermore, changes over time in p-tau181 levels were associated with cognitive decline in the cognitively unimpaired (r = –0.24; P < .001) and cognitively impaired (r = 0.34; P < .001) participants. Longitudinal changes in this biomarker also were associated with a prospective decrease in glucose metabolism in cognitively unimpaired (r = –0.05; P = .48) and cognitively impaired (r = –0.27; P < .001) participants, but the association was only significant in the latter group.
Changes over time in p-tau181 levels were linked to prospective decreases in gray-matter volume in brain regions highly characteristic of Alzheimer’s disease in those who were cognitively unimpaired (r = –0.19; P < .001) and those who were cognitively impaired (r = –0.31, P < .001). However, these associations were obtained only in patients with amyloid-beta.
Dr. Schöll noted that blood-based biomarkers that are sensitive to Alzheimer’s disease could greatly expand patients’ access to a diagnostic workup and could improve screening for clinical trials.
“While the final validation of the existence and the monitoring of potential changes of neuropathology in vivo is likely to be conducted using neuroimaging modalities such as PET, our results suggest that at least a part of these examinations could be replaced by regular blood tests,” Dr. Schöll said.
Lead author Alexis Moscoso, PhD, a postdoctoral researcher in psychiatry and neurochemistry at the University of Gothenburg, reported that the researchers will continue validating blood-based biomarkers, especially against established and well-validated neuroimaging methods. “We are also hoping to be able to compare existing and novel blood-based Alzheimer’s disease biomarkers head to head to establish the individual roles each of these play in the research and diagnosis of Alzheimer’s disease,” Dr. Moscoso said.
‘Outstanding study’
Commenting on the findings, David S. Knopman, MD, professor of neurology at Mayo Clinic, Rochester, Minn., said that this is “an outstanding study” because of its large number of participants and because the investigators are “world leaders in the technology of measuring plasma p-tau and NfL.”
Dr. Knopman, who was not involved with the research, noted that the study had no substantive weaknesses.
“The biggest advantages of a blood-based biomarker over CSF- and PET-based biomarkers of Alzheimer disease are the obvious ones of accessibility, cost, portability, and ease of repeatability,” he said.
“As CSF and PET exams are largely limited to major medical centers, valid blood-based biomarkers of Alzheimer disease that are reasonably specific make large-scale epidemiological studies that investigate dementia etiologies in rural or urban and diverse communities feasible,” he added.
Whereas p-tau181 appears to be specific for plaque and tangle disease, NfL is a nonspecific marker of neurodegeneration.
“Each has a role that could be valuable, depending on the circumstance,” said Dr. Knopman. “Plasma NfL has already proved itself useful in frontotemporal degeneration and chronic traumatic encephalopathy, for example.”
He noted that future studies should examine how closely p-tau181 and NfL align with more granular and direct measures of Alzheimer’s disease–related brain pathologies.
“There has got to be some loss of fidelity in detecting abnormality in going from brain tissue to blood, which might siphon off some time-related and severity-related information,” said Dr. Knopman.
“The exact role that plasma p-tau and NfL will play remains to be seen, because the diagnostic information that these biomarkers provide is contingent on the existence of interventions that require specific or nonspecific information about progressive neurodegeneration due to Alzheimer disease,” he added.
The study was funded by grants from the Spanish Instituto de Salud Carlos III, the Brightfocus Foundation, the Swedish Alzheimer Foundation, and the Swedish Brain Foundation. Dr. Schöll reported serving on a scientific advisory board for Servier on matters unrelated to this study. Dr. Moscoso and Dr. Knopman have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
In a study of more than 1,000 participants, changes over time in levels of p-tau181 were associated with prospective neurodegeneration and cognitive decline characteristic of Alzheimer’s disease. These results have implications for investigative trials as well as clinical practice, the investigators noted.
Like p-tau181, neurofilament light chain (NfL) is associated with imaging markers of degeneration and cognitive decline; in contrast to the findings related to p-tau181, however, the associations between NfL and these outcomes are not specific to Alzheimer’s disease. Using both biomarkers could improve prediction of outcomes and patient monitoring, according to the researchers.
“These findings demonstrate that p-tau181 and NfL in blood have individual and complementary potential roles in the diagnosis and the monitoring of neurodegenerative disease,” said coinvestigator Michael Schöll, PhD, senior lecturer in psychiatry and neurochemistry at the University of Gothenburg (Sweden).
“With the reservation that we did not assess domain-specific cognitive impairment, p-tau181 was also more strongly associated with cognitive decline than was NfL,” Dr. Schöll added.
The findings were published online Jan. 11 in JAMA Neurology.
Biomarker-tracked neurodegeneration
Monitoring a patient’s neurodegenerative changes is important for tracking Alzheimer’s disease progression. Although clinicians can detect amyloid-beta and tau pathology using PET and cerebrospinal fluid (CSF) biomarkers, the widespread use of the latter has been hampered by cost and limited availability of necessary equipment. The use of blood-based biomarkers is not limited in these ways, and so they could aid in diagnosis and patient monitoring.
Previous studies have suggested that p-tau181 is a marker of Alzheimer’s disease status.
In the current study, investigators examined whether baseline and longitudinal levels of p-tau181 in plasma were associated with progressive neurodegeneration related to the disease. They analyzed data from the Alzheimer’s Disease Neuroimaging Initiative, a multicenter study designed to identify biomarkers for the detection and tracking of Alzheimer’s disease.
The researchers selected data for cognitively unimpaired and cognitively impaired participants who participated in the initiative between Feb. 1, 2007, and June 6, 2016. Participants were eligible for inclusion if plasma p-tau181 and NfL data were available for them and if they had undergone at least one 18fluorodeoxyglucose (FDG)–PET scan or structural T1 MRI at the same study visit. Most had also undergone imaging with 18florbetapir, which detects amyloid-beta.
A single-molecule array was used to analyze concentrations of p-tau181 and NfL in participants’ blood samples. Outliers for p-tau181 and NfL concentrations were excluded from further analysis. Using participants’ FDG-PET scans, the investigators measured glucose hypometabolism characteristic of Alzheimer’s disease. They used T1-weighted MRI scans to measure gray-matter volume.
Cognitively unimpaired participants responded to the Preclinical Alzheimer Cognitive Composite, a measure designed to detect early cognitive changes in cognitively normal patients with Alzheimer’s disease pathology. Cognitively impaired participants underwent the Alzheimer Disease Assessment Scale–Cognitive Subscale with 13 tasks to assess the severity of cognitive impairment.
The researchers included 1,113 participants (54% men; 89% non-Hispanic Whites; mean age, 74 years) in their analysis. In all, 378 participants were cognitively unimpaired, and 735 were cognitively impaired. Of the latter group, 73% had mild cognitive impairment, and 27% had Alzheimer’s disease dementia.
Atrophy predictor
Results showed that higher plasma p-tau181 levels at baseline were associated with more rapid progression of hypometabolism and atrophy in areas vulnerable to Alzheimer’s disease among cognitively impaired participants (FDG-PET standardized uptake value ratio change, r = –0.28; P < .001; gray-matter volume change, r = –0.28; P < .001).
The association with atrophy progression in cognitively impaired participants was stronger for p-tau181 than for NfL.
Plasma p-tau181 levels at baseline also predicted atrophy in temporoparietal regions vulnerable to Alzheimer’s disease among cognitively unimpaired participants (r = –0.11; P = .03). NfL, however, was associated with progressive atrophy in frontal regions among cognitively unimpaired participants.
At baseline, plasma p-tau181 levels were associated with prospective cognitive decline in both the cognitively unimpaired group (r = −0.12; P = .04) and the cognitively impaired group (r = 0.35; P < .001). However, plasma NfL was linked to cognitive decline only among those who were cognitively impaired (r = 0.26; P < .001).
Additional analyses showed that p-tau181, unlike NfL, was associated with hypometabolism and atrophy only in participants with amyloid-beta, regardless of cognitive status.
Between 25% and 45% of the association between baseline p-tau181 level and cognitive decline was mediated by baseline imaging markers of neurodegeneration. This finding suggests that another factor, such as regional tau pathology, might have an independent and direct effect on cognition, Dr. Schöll noted.
Furthermore, changes over time in p-tau181 levels were associated with cognitive decline in the cognitively unimpaired (r = –0.24; P < .001) and cognitively impaired (r = 0.34; P < .001) participants. Longitudinal changes in this biomarker also were associated with a prospective decrease in glucose metabolism in cognitively unimpaired (r = –0.05; P = .48) and cognitively impaired (r = –0.27; P < .001) participants, but the association was only significant in the latter group.
Changes over time in p-tau181 levels were linked to prospective decreases in gray-matter volume in brain regions highly characteristic of Alzheimer’s disease in those who were cognitively unimpaired (r = –0.19; P < .001) and those who were cognitively impaired (r = –0.31, P < .001). However, these associations were obtained only in patients with amyloid-beta.
Dr. Schöll noted that blood-based biomarkers that are sensitive to Alzheimer’s disease could greatly expand patients’ access to a diagnostic workup and could improve screening for clinical trials.
“While the final validation of the existence and the monitoring of potential changes of neuropathology in vivo is likely to be conducted using neuroimaging modalities such as PET, our results suggest that at least a part of these examinations could be replaced by regular blood tests,” Dr. Schöll said.
Lead author Alexis Moscoso, PhD, a postdoctoral researcher in psychiatry and neurochemistry at the University of Gothenburg, reported that the researchers will continue validating blood-based biomarkers, especially against established and well-validated neuroimaging methods. “We are also hoping to be able to compare existing and novel blood-based Alzheimer’s disease biomarkers head to head to establish the individual roles each of these play in the research and diagnosis of Alzheimer’s disease,” Dr. Moscoso said.
‘Outstanding study’
Commenting on the findings, David S. Knopman, MD, professor of neurology at Mayo Clinic, Rochester, Minn., said that this is “an outstanding study” because of its large number of participants and because the investigators are “world leaders in the technology of measuring plasma p-tau and NfL.”
Dr. Knopman, who was not involved with the research, noted that the study had no substantive weaknesses.
“The biggest advantages of a blood-based biomarker over CSF- and PET-based biomarkers of Alzheimer disease are the obvious ones of accessibility, cost, portability, and ease of repeatability,” he said.
“As CSF and PET exams are largely limited to major medical centers, valid blood-based biomarkers of Alzheimer disease that are reasonably specific make large-scale epidemiological studies that investigate dementia etiologies in rural or urban and diverse communities feasible,” he added.
Whereas p-tau181 appears to be specific for plaque and tangle disease, NfL is a nonspecific marker of neurodegeneration.
“Each has a role that could be valuable, depending on the circumstance,” said Dr. Knopman. “Plasma NfL has already proved itself useful in frontotemporal degeneration and chronic traumatic encephalopathy, for example.”
He noted that future studies should examine how closely p-tau181 and NfL align with more granular and direct measures of Alzheimer’s disease–related brain pathologies.
“There has got to be some loss of fidelity in detecting abnormality in going from brain tissue to blood, which might siphon off some time-related and severity-related information,” said Dr. Knopman.
“The exact role that plasma p-tau and NfL will play remains to be seen, because the diagnostic information that these biomarkers provide is contingent on the existence of interventions that require specific or nonspecific information about progressive neurodegeneration due to Alzheimer disease,” he added.
The study was funded by grants from the Spanish Instituto de Salud Carlos III, the Brightfocus Foundation, the Swedish Alzheimer Foundation, and the Swedish Brain Foundation. Dr. Schöll reported serving on a scientific advisory board for Servier on matters unrelated to this study. Dr. Moscoso and Dr. Knopman have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
In a study of more than 1,000 participants, changes over time in levels of p-tau181 were associated with prospective neurodegeneration and cognitive decline characteristic of Alzheimer’s disease. These results have implications for investigative trials as well as clinical practice, the investigators noted.
Like p-tau181, neurofilament light chain (NfL) is associated with imaging markers of degeneration and cognitive decline; in contrast to the findings related to p-tau181, however, the associations between NfL and these outcomes are not specific to Alzheimer’s disease. Using both biomarkers could improve prediction of outcomes and patient monitoring, according to the researchers.
“These findings demonstrate that p-tau181 and NfL in blood have individual and complementary potential roles in the diagnosis and the monitoring of neurodegenerative disease,” said coinvestigator Michael Schöll, PhD, senior lecturer in psychiatry and neurochemistry at the University of Gothenburg (Sweden).
“With the reservation that we did not assess domain-specific cognitive impairment, p-tau181 was also more strongly associated with cognitive decline than was NfL,” Dr. Schöll added.
The findings were published online Jan. 11 in JAMA Neurology.
Biomarker-tracked neurodegeneration
Monitoring a patient’s neurodegenerative changes is important for tracking Alzheimer’s disease progression. Although clinicians can detect amyloid-beta and tau pathology using PET and cerebrospinal fluid (CSF) biomarkers, the widespread use of the latter has been hampered by cost and limited availability of necessary equipment. The use of blood-based biomarkers is not limited in these ways, and so they could aid in diagnosis and patient monitoring.
Previous studies have suggested that p-tau181 is a marker of Alzheimer’s disease status.
In the current study, investigators examined whether baseline and longitudinal levels of p-tau181 in plasma were associated with progressive neurodegeneration related to the disease. They analyzed data from the Alzheimer’s Disease Neuroimaging Initiative, a multicenter study designed to identify biomarkers for the detection and tracking of Alzheimer’s disease.
The researchers selected data for cognitively unimpaired and cognitively impaired participants who participated in the initiative between Feb. 1, 2007, and June 6, 2016. Participants were eligible for inclusion if plasma p-tau181 and NfL data were available for them and if they had undergone at least one 18fluorodeoxyglucose (FDG)–PET scan or structural T1 MRI at the same study visit. Most had also undergone imaging with 18florbetapir, which detects amyloid-beta.
A single-molecule array was used to analyze concentrations of p-tau181 and NfL in participants’ blood samples. Outliers for p-tau181 and NfL concentrations were excluded from further analysis. Using participants’ FDG-PET scans, the investigators measured glucose hypometabolism characteristic of Alzheimer’s disease. They used T1-weighted MRI scans to measure gray-matter volume.
Cognitively unimpaired participants responded to the Preclinical Alzheimer Cognitive Composite, a measure designed to detect early cognitive changes in cognitively normal patients with Alzheimer’s disease pathology. Cognitively impaired participants underwent the Alzheimer Disease Assessment Scale–Cognitive Subscale with 13 tasks to assess the severity of cognitive impairment.
The researchers included 1,113 participants (54% men; 89% non-Hispanic Whites; mean age, 74 years) in their analysis. In all, 378 participants were cognitively unimpaired, and 735 were cognitively impaired. Of the latter group, 73% had mild cognitive impairment, and 27% had Alzheimer’s disease dementia.
Atrophy predictor
Results showed that higher plasma p-tau181 levels at baseline were associated with more rapid progression of hypometabolism and atrophy in areas vulnerable to Alzheimer’s disease among cognitively impaired participants (FDG-PET standardized uptake value ratio change, r = –0.28; P < .001; gray-matter volume change, r = –0.28; P < .001).
The association with atrophy progression in cognitively impaired participants was stronger for p-tau181 than for NfL.
Plasma p-tau181 levels at baseline also predicted atrophy in temporoparietal regions vulnerable to Alzheimer’s disease among cognitively unimpaired participants (r = –0.11; P = .03). NfL, however, was associated with progressive atrophy in frontal regions among cognitively unimpaired participants.
At baseline, plasma p-tau181 levels were associated with prospective cognitive decline in both the cognitively unimpaired group (r = −0.12; P = .04) and the cognitively impaired group (r = 0.35; P < .001). However, plasma NfL was linked to cognitive decline only among those who were cognitively impaired (r = 0.26; P < .001).
Additional analyses showed that p-tau181, unlike NfL, was associated with hypometabolism and atrophy only in participants with amyloid-beta, regardless of cognitive status.
Between 25% and 45% of the association between baseline p-tau181 level and cognitive decline was mediated by baseline imaging markers of neurodegeneration. This finding suggests that another factor, such as regional tau pathology, might have an independent and direct effect on cognition, Dr. Schöll noted.
Furthermore, changes over time in p-tau181 levels were associated with cognitive decline in the cognitively unimpaired (r = –0.24; P < .001) and cognitively impaired (r = 0.34; P < .001) participants. Longitudinal changes in this biomarker also were associated with a prospective decrease in glucose metabolism in cognitively unimpaired (r = –0.05; P = .48) and cognitively impaired (r = –0.27; P < .001) participants, but the association was only significant in the latter group.
Changes over time in p-tau181 levels were linked to prospective decreases in gray-matter volume in brain regions highly characteristic of Alzheimer’s disease in those who were cognitively unimpaired (r = –0.19; P < .001) and those who were cognitively impaired (r = –0.31, P < .001). However, these associations were obtained only in patients with amyloid-beta.
Dr. Schöll noted that blood-based biomarkers that are sensitive to Alzheimer’s disease could greatly expand patients’ access to a diagnostic workup and could improve screening for clinical trials.
“While the final validation of the existence and the monitoring of potential changes of neuropathology in vivo is likely to be conducted using neuroimaging modalities such as PET, our results suggest that at least a part of these examinations could be replaced by regular blood tests,” Dr. Schöll said.
Lead author Alexis Moscoso, PhD, a postdoctoral researcher in psychiatry and neurochemistry at the University of Gothenburg, reported that the researchers will continue validating blood-based biomarkers, especially against established and well-validated neuroimaging methods. “We are also hoping to be able to compare existing and novel blood-based Alzheimer’s disease biomarkers head to head to establish the individual roles each of these play in the research and diagnosis of Alzheimer’s disease,” Dr. Moscoso said.
‘Outstanding study’
Commenting on the findings, David S. Knopman, MD, professor of neurology at Mayo Clinic, Rochester, Minn., said that this is “an outstanding study” because of its large number of participants and because the investigators are “world leaders in the technology of measuring plasma p-tau and NfL.”
Dr. Knopman, who was not involved with the research, noted that the study had no substantive weaknesses.
“The biggest advantages of a blood-based biomarker over CSF- and PET-based biomarkers of Alzheimer disease are the obvious ones of accessibility, cost, portability, and ease of repeatability,” he said.
“As CSF and PET exams are largely limited to major medical centers, valid blood-based biomarkers of Alzheimer disease that are reasonably specific make large-scale epidemiological studies that investigate dementia etiologies in rural or urban and diverse communities feasible,” he added.
Whereas p-tau181 appears to be specific for plaque and tangle disease, NfL is a nonspecific marker of neurodegeneration.
“Each has a role that could be valuable, depending on the circumstance,” said Dr. Knopman. “Plasma NfL has already proved itself useful in frontotemporal degeneration and chronic traumatic encephalopathy, for example.”
He noted that future studies should examine how closely p-tau181 and NfL align with more granular and direct measures of Alzheimer’s disease–related brain pathologies.
“There has got to be some loss of fidelity in detecting abnormality in going from brain tissue to blood, which might siphon off some time-related and severity-related information,” said Dr. Knopman.
“The exact role that plasma p-tau and NfL will play remains to be seen, because the diagnostic information that these biomarkers provide is contingent on the existence of interventions that require specific or nonspecific information about progressive neurodegeneration due to Alzheimer disease,” he added.
The study was funded by grants from the Spanish Instituto de Salud Carlos III, the Brightfocus Foundation, the Swedish Alzheimer Foundation, and the Swedish Brain Foundation. Dr. Schöll reported serving on a scientific advisory board for Servier on matters unrelated to this study. Dr. Moscoso and Dr. Knopman have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Generalized pruritic blisters and bullous lesions
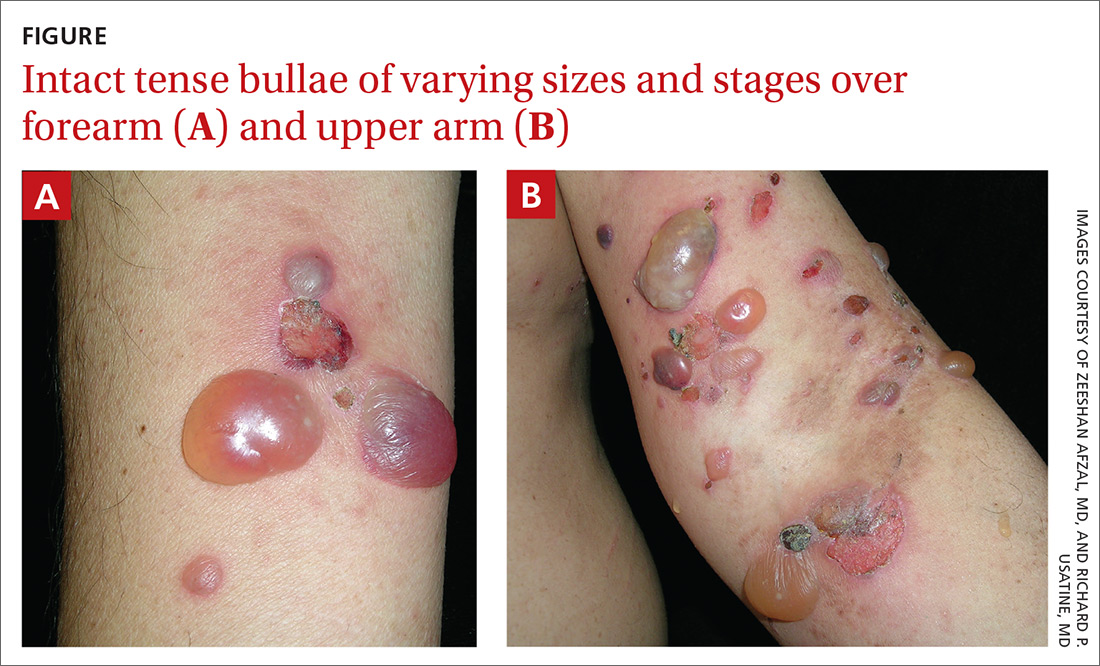
A 62-year-old man presented to our skin clinic with multiple pruritic, tense, bullous lesions that manifested on his arms, abdomen, back, and upper thighs over a 1-month period. There were no lesions in his oral cavity or around his eyes, nose, or penile region. He denied dysphagia.
The patient had multiple comorbidities, including diabetes, hypertension, recent stroke, and end-stage renal disease. He was being prepared for dialysis. His medications included torsemide, warfarin, amiodarone, metoprolol, pantoprozole, atorvastatin, and nifedipine. About 3 months prior to this presentation, he was started on oral linaglipton 5 mg/d, an oral antihyperglycemic medication. He had no history of skin disease or cancer, and his family history was not significant.
Physical examination showed multiple 5-mm to 2-cm blisters and bullae on the flexural surface of both of his arms (FIGURE), back, lower abdomen, and upper thighs. His palms and soles were not involved. The lesions were nontender, tense, and filled with clear fluid. Some were intact and others were rupturing. There was no mucocutaneous involvement. Nikolsky sign was negative. There were no signs of bleeding.
The family physician (FP) obtained a 4-mm punch biopsy at the edge of a 6-mm blister for light microscopy and a 3-mm perilesional punch biopsy for direct immunofluorescence (DIF) microscopy.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Bullous pemphigoid secondary to linagliptin use
DIF of the biopsy sample demonstrated linear deposition of complement 3 (C3) and immunoglobulin (Ig) G along the basement membrane zone. Indirect immunofluorescence on salt-split skin demonstrated linear deposition of IgG and C3 on both the roof and floor of the induced blisters. These findings and the patient’s clinical presentation met the criteria for bullous pemphigoid (BP), which is the most common autoimmune skin-blistering disease.1
BP is associated with subepidermal blistering, which can occur in reaction to a variety of triggers. Pathogenesis of this condition involves IgG anti-basement membrane autoantibody complex formation with the hemidesmosomal antigens BP230 and BP180—a process that activates C3 and the release of proteases that can be destructive to tissue along the dermo-epidermal junction.1
Growing incidence. BP usually occurs in patients > 60 years, with no racial or gender preference.1 The incidence rate of BP ranges from 2.4 to 21.7 new cases per 1 million individuals among various worldwide populations.2 The incidence appears to have increased 1.9- to 4.3-fold over the past 2 decades.2
What you’ll see, who’s at risk
Symptoms of BP include localized areas of erythema or pruritic urticarial plaques that gradually become more extensive. A patient may have pruritis alone for an extended period prior to developing blisters and bullae. The bullae are tense and normally 1 to 7 cm in size.1 Eruption is generalized, mostly affecting the lower abdomen, as well as the flexural parts of the extremities. The palms and soles also can be affected.
FPs should be aware of the atypical clinical variants of BP. In a review by Kridin and Ludwig, variants can be prurigo-like, eczema-like, urticaria-like, dyshidrosiform type, erosive type, and erythema annulare centrifugum–like type.2 At-risk populations, such as elderly patients (> 70 years), whose pruritis manifests with or without bullous formation, should be screened for BP.3,4
Continue to: Risk factors for BP
Risk factors for BP. Certain conditions linked to developing BP include neurologic disorders (dementia and Parkinson disease) and psychiatric disorders (unipolar and bipolar disorder).4 Further, it is important to note any medications that could be the cause of a patient’s BP, including dipeptidyl peptidase-4 (DPP-4) inhibitors, psychotropic medications, spironolactone, furosemide, beta-blockers, and antibiotics.3 This patient was taking a beta-blocker (metoprolol) and a DPP-4 inhibitor (linagliptin). Because he was most recently started on linagliptin, we suspected it may have had a causal role in the development of BP.
The association of DPP-4 inhibitors and BP
FPs are increasingly using DPP-4 inhibitors—including sitagliptin, vildagliptin, and linagliptin—as oral antihyperglycemic agents for type 2 diabetes mellitus. Therefore, it’s important to recognize this medication class’s association with BP.5 In a case-control study of 165 patients with BP, Benzaquen et al reported that 28 patients who were taking DPP-4 inhibitors had an associated increased risk for BP (adjusted odds ratio = 2.64; 95% confidence interval [CI], 1.19-5.85).3
The pathophysiology of BP associated with DPP-4 inhibitors remains unclear, but mechanisms have been proposed. The DPP-4 enzyme is expressed on many cells, including keratinocytes, T cells, and endothelial cells.3 It is possible that DPP-4 inhibition at these cells could stimulate activity of inflammatory cytokines, which can lead to enhanced local eosinophil activation and trigger bullous formation. DPP-4 enzymes are also involved in forming plasmin, which is a protease that cleaves BP180.3 Inhibition of this process can affect proper cleavage of BP180, impacting its function and antigenicity.3,6
Other conditions that also exhibit blisters
There are some skin conditions with similar presentations that need to be ruled out in the work-up.
Bullous diabeticorum is a rare, spontaneous, noninflammatory condition found in patients with diabetes.1 Blisters usually manifest as large, tense, asymmetrical, mildly tender lesions that commonly affect the feet and lower legs but can involve the trunk. These usually develop overnight without preceding trauma. Biopsy would show both intra-epidermal and subepidermal bulla with normal DIF findings.1 This condition usually has an excellent prognosis.
Continue to: Pemphigus vulgaris
Pemphigus vulgaris is characterized by nonpruritic, flaccid, painful blisters. This condition usually begins with manifestation of painful oral lesions that evolve into skin blisters. Some patients can develop mucocutaneous lesions.1 Nikolsky sign is positive in these cases. Light microscopy would show intra-epidermal bullae.
Dermatitis herpetiformis. This condition—usually affecting middle-age patients—is associated with severe pruritis and burning. It may start with a few pruritic papules or vesicles that later evolve into urticarial papules, vesicles, or bullae. Dermatitis herpetiformis can resemble herpes simplex virus. It can also be associated with gluten-sensitive enteropathy and small bowel lymphoma.1 DIF of a biopsy sample would show granular deposition of IgA within the tips of the dermal papillae and along the basement membrane of perilesional skin.1
Epidermolysis bullosa acquisita is a rare, severe, chronic condition with subepidermal mucocutaneous blistering.1 It is associated with skin fragility and spontaneous trauma-induced blisters that heal with scar formation and milia. IgG autoantibodies reacting to proteins in the basement membrane zone can cause the disease. It is also associated with Crohn disease.1 DIF findings are similar in BP, but they are differentiated by location of IgG deposits; they can be found on the dermal side of separation in epidermolysis bullosa acquisita, as compared with the epidermal side in BP.1
How to make the Dx in 3 steps
To effectively diagnose and classify BP, use the following 3-step method:
- Establish the presence of 3 of 4 clinical characteristics: patient’s age > 60 years, absence of atrophic scars, absence of mucosal involvement, and absence of bullous lesions on the head and neck.
- Order light microscopy. Findings should be consistent with eosinophils and neutrophils containing subepidermal bullae.
- Order a punch biopsy to obtain a perilesional specimen. DIF of the biopsy findings should feature linear deposits of IgG with or without C3 along the dermo-epidermal junction. This step is essential for an accurate diagnosis.
There also is benefit in ordering supplemental studies, such as an enzyme-linked immunosorbent assay for the detection of anti-BP180 or anti-BP230 IgG autoantibodies.7 However, for this patient, we did not order this study.
Continue to: Management focuses on steroids
Management focuses on steroids
The offending agent should be discontinued immediately. Depending on the severity of disease, treatment can include the use of potent topical corticosteroids alone or in combination with systemic corticosteroids and anti-inflammatory antibiotics (eg, doxycycline, minocycline, erythromycin).1,7 For patients with resistant or refractory disease, consider azathioprine, methotrexate, dapsone, and chlorambucil.1,7 Exceptional cases may benefit from the use of mycophenolate mofetil, intravenous immunoglobulin, or plasmapheresis.1,7
For this patient, initial treatment included discontinuation of linagliption and introduction of topical clobetasol 0.05% and oral prednisone 40 mg/d for 7 days, followed by prednisone 20 mg for 7 days. He was also started on oral doxycycline 100 mg bid and oral nicotinamide 500 mg bid.
1. Habif TP. Vesicular and bullous diseases. In: Habif TP, ed. Clinical Dermatology: a Color Guide to Diagnosis and Therapy. 6th ed. Elsevier; 2016:635-666.
2. Kridin K, Ludwig RJ. The growing incidence of bullous pemphigoid: overview and potential explanations. Front Med (Lausanne). 2018;5:220.
3. Benzaquen M, Borradori L, Berbis P, et al. Dipeptidyl peptidase IV inhibitors, a risk factor for bullous pemphigoid: retrospective multicenter case-control study from France and Switzerland. J Am Acad Dermatol. 2017;78:1090-1096.
4. Bastuji-Garin S, Joly P, Lemordant P, et al. Risk factors for bullous pemphigoid in the elderly: a prospective case-control study. J Invest Dermatol. 2011;131:637-643.
5. Kridin K, Bergman R. Association of bullous pemphigoid with dipeptidyl-peptidase 4 inhibitors in patients with diabetes: estimating the risk of the new agents and characterizing the patients. JAMA Dermatol. 2018;154:1152-1158.
6. Haber R, Fayad AM, Stephan F, et al. Bullous pemphigoid associated with linagliptin treatment. JAMA Dermatol. 2016;152:224-226.Management of bullous pemphigoid: the European Dermatology Forum consensus in collaboration with the European Academy of Dermatology and Venereology. Br J Dermatol. 2015;172:867-877.
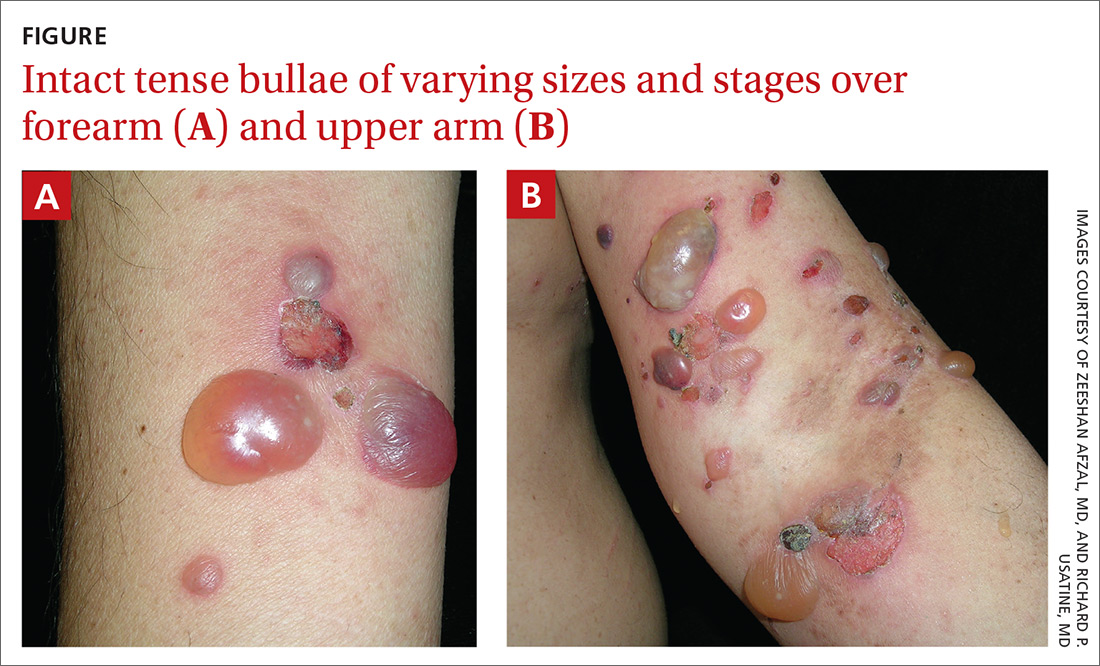
A 62-year-old man presented to our skin clinic with multiple pruritic, tense, bullous lesions that manifested on his arms, abdomen, back, and upper thighs over a 1-month period. There were no lesions in his oral cavity or around his eyes, nose, or penile region. He denied dysphagia.
The patient had multiple comorbidities, including diabetes, hypertension, recent stroke, and end-stage renal disease. He was being prepared for dialysis. His medications included torsemide, warfarin, amiodarone, metoprolol, pantoprozole, atorvastatin, and nifedipine. About 3 months prior to this presentation, he was started on oral linaglipton 5 mg/d, an oral antihyperglycemic medication. He had no history of skin disease or cancer, and his family history was not significant.
Physical examination showed multiple 5-mm to 2-cm blisters and bullae on the flexural surface of both of his arms (FIGURE), back, lower abdomen, and upper thighs. His palms and soles were not involved. The lesions were nontender, tense, and filled with clear fluid. Some were intact and others were rupturing. There was no mucocutaneous involvement. Nikolsky sign was negative. There were no signs of bleeding.
The family physician (FP) obtained a 4-mm punch biopsy at the edge of a 6-mm blister for light microscopy and a 3-mm perilesional punch biopsy for direct immunofluorescence (DIF) microscopy.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Bullous pemphigoid secondary to linagliptin use
DIF of the biopsy sample demonstrated linear deposition of complement 3 (C3) and immunoglobulin (Ig) G along the basement membrane zone. Indirect immunofluorescence on salt-split skin demonstrated linear deposition of IgG and C3 on both the roof and floor of the induced blisters. These findings and the patient’s clinical presentation met the criteria for bullous pemphigoid (BP), which is the most common autoimmune skin-blistering disease.1
BP is associated with subepidermal blistering, which can occur in reaction to a variety of triggers. Pathogenesis of this condition involves IgG anti-basement membrane autoantibody complex formation with the hemidesmosomal antigens BP230 and BP180—a process that activates C3 and the release of proteases that can be destructive to tissue along the dermo-epidermal junction.1
Growing incidence. BP usually occurs in patients > 60 years, with no racial or gender preference.1 The incidence rate of BP ranges from 2.4 to 21.7 new cases per 1 million individuals among various worldwide populations.2 The incidence appears to have increased 1.9- to 4.3-fold over the past 2 decades.2
What you’ll see, who’s at risk
Symptoms of BP include localized areas of erythema or pruritic urticarial plaques that gradually become more extensive. A patient may have pruritis alone for an extended period prior to developing blisters and bullae. The bullae are tense and normally 1 to 7 cm in size.1 Eruption is generalized, mostly affecting the lower abdomen, as well as the flexural parts of the extremities. The palms and soles also can be affected.
FPs should be aware of the atypical clinical variants of BP. In a review by Kridin and Ludwig, variants can be prurigo-like, eczema-like, urticaria-like, dyshidrosiform type, erosive type, and erythema annulare centrifugum–like type.2 At-risk populations, such as elderly patients (> 70 years), whose pruritis manifests with or without bullous formation, should be screened for BP.3,4
Continue to: Risk factors for BP
Risk factors for BP. Certain conditions linked to developing BP include neurologic disorders (dementia and Parkinson disease) and psychiatric disorders (unipolar and bipolar disorder).4 Further, it is important to note any medications that could be the cause of a patient’s BP, including dipeptidyl peptidase-4 (DPP-4) inhibitors, psychotropic medications, spironolactone, furosemide, beta-blockers, and antibiotics.3 This patient was taking a beta-blocker (metoprolol) and a DPP-4 inhibitor (linagliptin). Because he was most recently started on linagliptin, we suspected it may have had a causal role in the development of BP.
The association of DPP-4 inhibitors and BP
FPs are increasingly using DPP-4 inhibitors—including sitagliptin, vildagliptin, and linagliptin—as oral antihyperglycemic agents for type 2 diabetes mellitus. Therefore, it’s important to recognize this medication class’s association with BP.5 In a case-control study of 165 patients with BP, Benzaquen et al reported that 28 patients who were taking DPP-4 inhibitors had an associated increased risk for BP (adjusted odds ratio = 2.64; 95% confidence interval [CI], 1.19-5.85).3
The pathophysiology of BP associated with DPP-4 inhibitors remains unclear, but mechanisms have been proposed. The DPP-4 enzyme is expressed on many cells, including keratinocytes, T cells, and endothelial cells.3 It is possible that DPP-4 inhibition at these cells could stimulate activity of inflammatory cytokines, which can lead to enhanced local eosinophil activation and trigger bullous formation. DPP-4 enzymes are also involved in forming plasmin, which is a protease that cleaves BP180.3 Inhibition of this process can affect proper cleavage of BP180, impacting its function and antigenicity.3,6
Other conditions that also exhibit blisters
There are some skin conditions with similar presentations that need to be ruled out in the work-up.
Bullous diabeticorum is a rare, spontaneous, noninflammatory condition found in patients with diabetes.1 Blisters usually manifest as large, tense, asymmetrical, mildly tender lesions that commonly affect the feet and lower legs but can involve the trunk. These usually develop overnight without preceding trauma. Biopsy would show both intra-epidermal and subepidermal bulla with normal DIF findings.1 This condition usually has an excellent prognosis.
Continue to: Pemphigus vulgaris
Pemphigus vulgaris is characterized by nonpruritic, flaccid, painful blisters. This condition usually begins with manifestation of painful oral lesions that evolve into skin blisters. Some patients can develop mucocutaneous lesions.1 Nikolsky sign is positive in these cases. Light microscopy would show intra-epidermal bullae.
Dermatitis herpetiformis. This condition—usually affecting middle-age patients—is associated with severe pruritis and burning. It may start with a few pruritic papules or vesicles that later evolve into urticarial papules, vesicles, or bullae. Dermatitis herpetiformis can resemble herpes simplex virus. It can also be associated with gluten-sensitive enteropathy and small bowel lymphoma.1 DIF of a biopsy sample would show granular deposition of IgA within the tips of the dermal papillae and along the basement membrane of perilesional skin.1
Epidermolysis bullosa acquisita is a rare, severe, chronic condition with subepidermal mucocutaneous blistering.1 It is associated with skin fragility and spontaneous trauma-induced blisters that heal with scar formation and milia. IgG autoantibodies reacting to proteins in the basement membrane zone can cause the disease. It is also associated with Crohn disease.1 DIF findings are similar in BP, but they are differentiated by location of IgG deposits; they can be found on the dermal side of separation in epidermolysis bullosa acquisita, as compared with the epidermal side in BP.1
How to make the Dx in 3 steps
To effectively diagnose and classify BP, use the following 3-step method:
- Establish the presence of 3 of 4 clinical characteristics: patient’s age > 60 years, absence of atrophic scars, absence of mucosal involvement, and absence of bullous lesions on the head and neck.
- Order light microscopy. Findings should be consistent with eosinophils and neutrophils containing subepidermal bullae.
- Order a punch biopsy to obtain a perilesional specimen. DIF of the biopsy findings should feature linear deposits of IgG with or without C3 along the dermo-epidermal junction. This step is essential for an accurate diagnosis.
There also is benefit in ordering supplemental studies, such as an enzyme-linked immunosorbent assay for the detection of anti-BP180 or anti-BP230 IgG autoantibodies.7 However, for this patient, we did not order this study.
Continue to: Management focuses on steroids
Management focuses on steroids
The offending agent should be discontinued immediately. Depending on the severity of disease, treatment can include the use of potent topical corticosteroids alone or in combination with systemic corticosteroids and anti-inflammatory antibiotics (eg, doxycycline, minocycline, erythromycin).1,7 For patients with resistant or refractory disease, consider azathioprine, methotrexate, dapsone, and chlorambucil.1,7 Exceptional cases may benefit from the use of mycophenolate mofetil, intravenous immunoglobulin, or plasmapheresis.1,7
For this patient, initial treatment included discontinuation of linagliption and introduction of topical clobetasol 0.05% and oral prednisone 40 mg/d for 7 days, followed by prednisone 20 mg for 7 days. He was also started on oral doxycycline 100 mg bid and oral nicotinamide 500 mg bid.
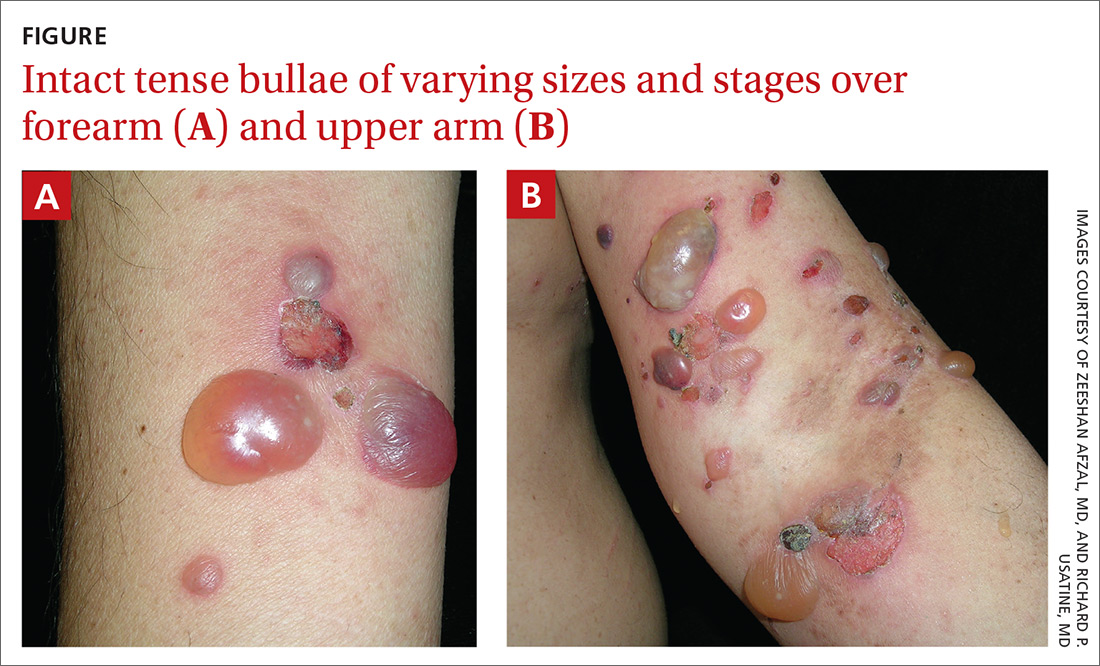
A 62-year-old man presented to our skin clinic with multiple pruritic, tense, bullous lesions that manifested on his arms, abdomen, back, and upper thighs over a 1-month period. There were no lesions in his oral cavity or around his eyes, nose, or penile region. He denied dysphagia.
The patient had multiple comorbidities, including diabetes, hypertension, recent stroke, and end-stage renal disease. He was being prepared for dialysis. His medications included torsemide, warfarin, amiodarone, metoprolol, pantoprozole, atorvastatin, and nifedipine. About 3 months prior to this presentation, he was started on oral linaglipton 5 mg/d, an oral antihyperglycemic medication. He had no history of skin disease or cancer, and his family history was not significant.
Physical examination showed multiple 5-mm to 2-cm blisters and bullae on the flexural surface of both of his arms (FIGURE), back, lower abdomen, and upper thighs. His palms and soles were not involved. The lesions were nontender, tense, and filled with clear fluid. Some were intact and others were rupturing. There was no mucocutaneous involvement. Nikolsky sign was negative. There were no signs of bleeding.
The family physician (FP) obtained a 4-mm punch biopsy at the edge of a 6-mm blister for light microscopy and a 3-mm perilesional punch biopsy for direct immunofluorescence (DIF) microscopy.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Bullous pemphigoid secondary to linagliptin use
DIF of the biopsy sample demonstrated linear deposition of complement 3 (C3) and immunoglobulin (Ig) G along the basement membrane zone. Indirect immunofluorescence on salt-split skin demonstrated linear deposition of IgG and C3 on both the roof and floor of the induced blisters. These findings and the patient’s clinical presentation met the criteria for bullous pemphigoid (BP), which is the most common autoimmune skin-blistering disease.1
BP is associated with subepidermal blistering, which can occur in reaction to a variety of triggers. Pathogenesis of this condition involves IgG anti-basement membrane autoantibody complex formation with the hemidesmosomal antigens BP230 and BP180—a process that activates C3 and the release of proteases that can be destructive to tissue along the dermo-epidermal junction.1
Growing incidence. BP usually occurs in patients > 60 years, with no racial or gender preference.1 The incidence rate of BP ranges from 2.4 to 21.7 new cases per 1 million individuals among various worldwide populations.2 The incidence appears to have increased 1.9- to 4.3-fold over the past 2 decades.2
What you’ll see, who’s at risk
Symptoms of BP include localized areas of erythema or pruritic urticarial plaques that gradually become more extensive. A patient may have pruritis alone for an extended period prior to developing blisters and bullae. The bullae are tense and normally 1 to 7 cm in size.1 Eruption is generalized, mostly affecting the lower abdomen, as well as the flexural parts of the extremities. The palms and soles also can be affected.
FPs should be aware of the atypical clinical variants of BP. In a review by Kridin and Ludwig, variants can be prurigo-like, eczema-like, urticaria-like, dyshidrosiform type, erosive type, and erythema annulare centrifugum–like type.2 At-risk populations, such as elderly patients (> 70 years), whose pruritis manifests with or without bullous formation, should be screened for BP.3,4
Continue to: Risk factors for BP
Risk factors for BP. Certain conditions linked to developing BP include neurologic disorders (dementia and Parkinson disease) and psychiatric disorders (unipolar and bipolar disorder).4 Further, it is important to note any medications that could be the cause of a patient’s BP, including dipeptidyl peptidase-4 (DPP-4) inhibitors, psychotropic medications, spironolactone, furosemide, beta-blockers, and antibiotics.3 This patient was taking a beta-blocker (metoprolol) and a DPP-4 inhibitor (linagliptin). Because he was most recently started on linagliptin, we suspected it may have had a causal role in the development of BP.
The association of DPP-4 inhibitors and BP
FPs are increasingly using DPP-4 inhibitors—including sitagliptin, vildagliptin, and linagliptin—as oral antihyperglycemic agents for type 2 diabetes mellitus. Therefore, it’s important to recognize this medication class’s association with BP.5 In a case-control study of 165 patients with BP, Benzaquen et al reported that 28 patients who were taking DPP-4 inhibitors had an associated increased risk for BP (adjusted odds ratio = 2.64; 95% confidence interval [CI], 1.19-5.85).3
The pathophysiology of BP associated with DPP-4 inhibitors remains unclear, but mechanisms have been proposed. The DPP-4 enzyme is expressed on many cells, including keratinocytes, T cells, and endothelial cells.3 It is possible that DPP-4 inhibition at these cells could stimulate activity of inflammatory cytokines, which can lead to enhanced local eosinophil activation and trigger bullous formation. DPP-4 enzymes are also involved in forming plasmin, which is a protease that cleaves BP180.3 Inhibition of this process can affect proper cleavage of BP180, impacting its function and antigenicity.3,6
Other conditions that also exhibit blisters
There are some skin conditions with similar presentations that need to be ruled out in the work-up.
Bullous diabeticorum is a rare, spontaneous, noninflammatory condition found in patients with diabetes.1 Blisters usually manifest as large, tense, asymmetrical, mildly tender lesions that commonly affect the feet and lower legs but can involve the trunk. These usually develop overnight without preceding trauma. Biopsy would show both intra-epidermal and subepidermal bulla with normal DIF findings.1 This condition usually has an excellent prognosis.
Continue to: Pemphigus vulgaris
Pemphigus vulgaris is characterized by nonpruritic, flaccid, painful blisters. This condition usually begins with manifestation of painful oral lesions that evolve into skin blisters. Some patients can develop mucocutaneous lesions.1 Nikolsky sign is positive in these cases. Light microscopy would show intra-epidermal bullae.
Dermatitis herpetiformis. This condition—usually affecting middle-age patients—is associated with severe pruritis and burning. It may start with a few pruritic papules or vesicles that later evolve into urticarial papules, vesicles, or bullae. Dermatitis herpetiformis can resemble herpes simplex virus. It can also be associated with gluten-sensitive enteropathy and small bowel lymphoma.1 DIF of a biopsy sample would show granular deposition of IgA within the tips of the dermal papillae and along the basement membrane of perilesional skin.1
Epidermolysis bullosa acquisita is a rare, severe, chronic condition with subepidermal mucocutaneous blistering.1 It is associated with skin fragility and spontaneous trauma-induced blisters that heal with scar formation and milia. IgG autoantibodies reacting to proteins in the basement membrane zone can cause the disease. It is also associated with Crohn disease.1 DIF findings are similar in BP, but they are differentiated by location of IgG deposits; they can be found on the dermal side of separation in epidermolysis bullosa acquisita, as compared with the epidermal side in BP.1
How to make the Dx in 3 steps
To effectively diagnose and classify BP, use the following 3-step method:
- Establish the presence of 3 of 4 clinical characteristics: patient’s age > 60 years, absence of atrophic scars, absence of mucosal involvement, and absence of bullous lesions on the head and neck.
- Order light microscopy. Findings should be consistent with eosinophils and neutrophils containing subepidermal bullae.
- Order a punch biopsy to obtain a perilesional specimen. DIF of the biopsy findings should feature linear deposits of IgG with or without C3 along the dermo-epidermal junction. This step is essential for an accurate diagnosis.
There also is benefit in ordering supplemental studies, such as an enzyme-linked immunosorbent assay for the detection of anti-BP180 or anti-BP230 IgG autoantibodies.7 However, for this patient, we did not order this study.
Continue to: Management focuses on steroids
Management focuses on steroids
The offending agent should be discontinued immediately. Depending on the severity of disease, treatment can include the use of potent topical corticosteroids alone or in combination with systemic corticosteroids and anti-inflammatory antibiotics (eg, doxycycline, minocycline, erythromycin).1,7 For patients with resistant or refractory disease, consider azathioprine, methotrexate, dapsone, and chlorambucil.1,7 Exceptional cases may benefit from the use of mycophenolate mofetil, intravenous immunoglobulin, or plasmapheresis.1,7
For this patient, initial treatment included discontinuation of linagliption and introduction of topical clobetasol 0.05% and oral prednisone 40 mg/d for 7 days, followed by prednisone 20 mg for 7 days. He was also started on oral doxycycline 100 mg bid and oral nicotinamide 500 mg bid.
1. Habif TP. Vesicular and bullous diseases. In: Habif TP, ed. Clinical Dermatology: a Color Guide to Diagnosis and Therapy. 6th ed. Elsevier; 2016:635-666.
2. Kridin K, Ludwig RJ. The growing incidence of bullous pemphigoid: overview and potential explanations. Front Med (Lausanne). 2018;5:220.
3. Benzaquen M, Borradori L, Berbis P, et al. Dipeptidyl peptidase IV inhibitors, a risk factor for bullous pemphigoid: retrospective multicenter case-control study from France and Switzerland. J Am Acad Dermatol. 2017;78:1090-1096.
4. Bastuji-Garin S, Joly P, Lemordant P, et al. Risk factors for bullous pemphigoid in the elderly: a prospective case-control study. J Invest Dermatol. 2011;131:637-643.
5. Kridin K, Bergman R. Association of bullous pemphigoid with dipeptidyl-peptidase 4 inhibitors in patients with diabetes: estimating the risk of the new agents and characterizing the patients. JAMA Dermatol. 2018;154:1152-1158.
6. Haber R, Fayad AM, Stephan F, et al. Bullous pemphigoid associated with linagliptin treatment. JAMA Dermatol. 2016;152:224-226.Management of bullous pemphigoid: the European Dermatology Forum consensus in collaboration with the European Academy of Dermatology and Venereology. Br J Dermatol. 2015;172:867-877.
1. Habif TP. Vesicular and bullous diseases. In: Habif TP, ed. Clinical Dermatology: a Color Guide to Diagnosis and Therapy. 6th ed. Elsevier; 2016:635-666.
2. Kridin K, Ludwig RJ. The growing incidence of bullous pemphigoid: overview and potential explanations. Front Med (Lausanne). 2018;5:220.
3. Benzaquen M, Borradori L, Berbis P, et al. Dipeptidyl peptidase IV inhibitors, a risk factor for bullous pemphigoid: retrospective multicenter case-control study from France and Switzerland. J Am Acad Dermatol. 2017;78:1090-1096.
4. Bastuji-Garin S, Joly P, Lemordant P, et al. Risk factors for bullous pemphigoid in the elderly: a prospective case-control study. J Invest Dermatol. 2011;131:637-643.
5. Kridin K, Bergman R. Association of bullous pemphigoid with dipeptidyl-peptidase 4 inhibitors in patients with diabetes: estimating the risk of the new agents and characterizing the patients. JAMA Dermatol. 2018;154:1152-1158.
6. Haber R, Fayad AM, Stephan F, et al. Bullous pemphigoid associated with linagliptin treatment. JAMA Dermatol. 2016;152:224-226.Management of bullous pemphigoid: the European Dermatology Forum consensus in collaboration with the European Academy of Dermatology and Venereology. Br J Dermatol. 2015;172:867-877.
Breaking the cycle of medication overuse headache
Medication overuse headache (MOH), a secondary headache diagnosis, is a prevalent phenomenon that complicates headache diagnosis and treatment, increases the cost of care, and reduces quality of life. Effective abortive medication is essential for the headache sufferer; when an abortive is used too frequently, however, headache frequency increases—potentially beginning a cycle in which the patient then takes more medication to abort the headache. Over time, the patient suffers from an ever-increasing number of headaches, takes even more abortive medication, and so on. In the presence of MOH, there is a reduction in pain response to preventive and abortive treatments; when medication overuse is eliminated, pain response improves.1
Although MOH is well recognized among headache specialists, the condition is often overlooked in primary care. Since headache is a top complaint in primary care, however, and prevention is a major goal in family medicine, the opportunity for you to recognize, treat, and prevent MOH is significant. In fact, a randomized controlled trial showed that brief patient education about headache care and MOH provided by a primary care physician can lead to a significant reduction in headache frequency among patients with MOH.2
This article reviews the recognition and diagnosis of MOH, based on historical features and current criteria; addresses risk factors for abortive medication overuse and how to withdraw an offending agent; and explores the value of bridging and preventive therapies to reduce the overall frequency of headache.
What defines MOH?
Typically, MOH is a chronification of a primary headache disorder. However, in patients with a history of migraine who are undergoing treatment for another chronic pain condition with an opioid or other analgesic, MOH can be induced.3 An increase in the frequency of headache raises the specter of a concomitant increase in the level of disability4; psychiatric comorbidity5; and more headache days, with time lost from school and work.
The Migraine Disability Assessment (MIDAS) questionnaire, a validated instrument that helps the provider (1) measure the impact that headache has on a patient’s life and (2) follow treatment progress, also provides information to employers and insurance companies on treatment coverage and the need for work modification. The MIDAS score is 3 times higher in patients with MOH than in patients with episodic migraine.6,7
The annual associated cost per person of MOH has been estimated at $4000, resulting in billions of dollars in associated costs8; most of these costs are related to absenteeism and disability. After detoxification for MOH, annual outpatient medication costs are reduced by approximately 24%.9
Efforts to solve a common problem create another
Headache affects nearly 50% of the general population worldwide,10 accounting for about 4% of primary care visits11 and approximately 20% of outpatient neurology consultations.12 Although inpatient stays for headache are approximately half the duration of the overall average hospital stay, headache accounts for 3% of admissions.13 According to the Global Burden of Disease study, tension-type headache, migraine, and MOH are the 3 most common headache disorders.10 Headache is the second leading cause of disability among people 15 to 49 years of age.10
Continue to: The prevalence of MOH...
The prevalence of MOH in the general population is 2%.7,14,15 A population-based study showed that the rate of progression from episodic headache (< 15 d/mo) to chronic headache (≥ 15 d/mo) in the general population is 2.5% per year16; however, progression to chronic headache is 14% per year in patients with medication overuse. One-third of the general population with chronic migraine overuses symptomatic medication; in US headache clinics, roughly one-half of patients with chronic headache overuse acute medication.6
Definitions and diagnosis
MOH is a secondary headache diagnosis in the third edition of the International Classification of Headache Disorders (ICHD-3) (TABLE 1),17 which lists diagnostic criteria for recognized headache disorders.
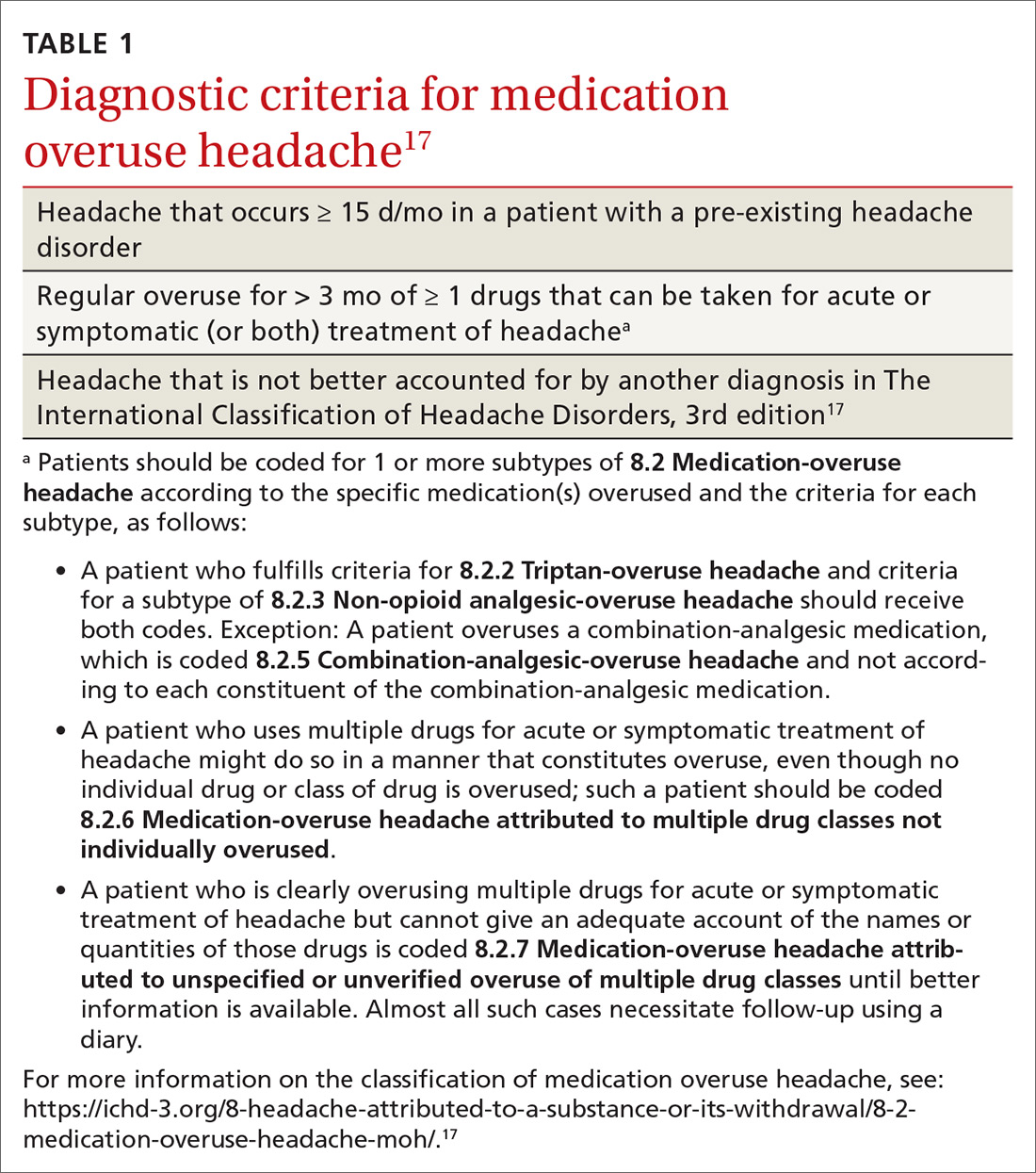
Terminology. MOH has also been called rebound headache, drug-induced headache, and transformed migraine, but these terms are outdated and are not formal diagnoses. Patients sometimes refer to substance-withdrawal headaches (not discussed in this article) as rebound headaches, so clarity is important when discussing headache with patients: namely, that MOH is an exacerbation of an existing headache condition caused by overuse of abortive headache medications, including analgesics, combination analgesics, triptans, barbiturates, and opioids.
MOH was recognized in the early 1950s and fully differentiated as a diagnosis in 2005 in the second edition of the ICHD. The disorder is subcategorized by offending abortive agent (TABLE 217) because the frequency of analgesic use required to develop MOH differs by agent.
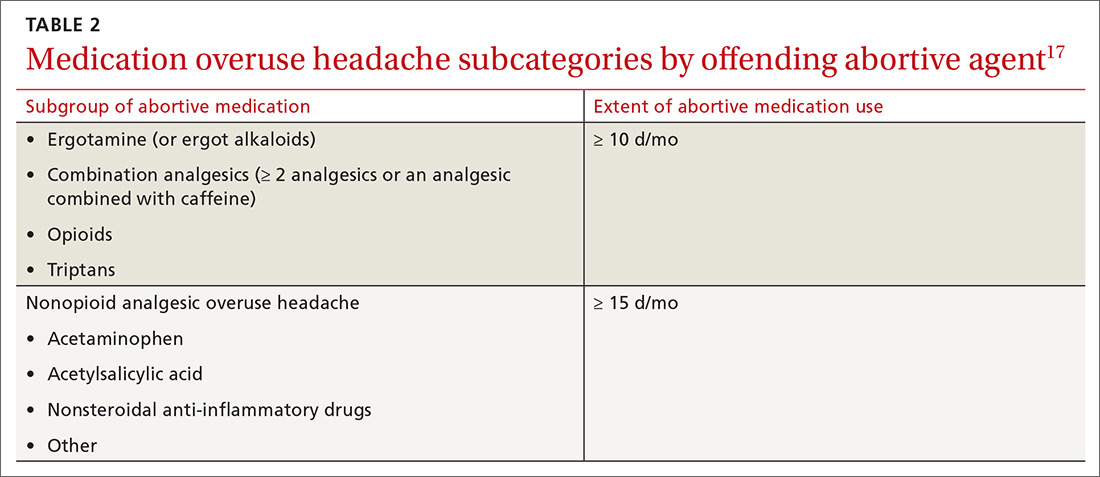
Risk factors for MOH and chronification of a primary headache disorder. There are several risk factors for developing MOH, and others that contribute to increasing headache frequency in general (TABLE 35,14,18-23). Some risk factors are common to each. All are important to address because some are modifiable.
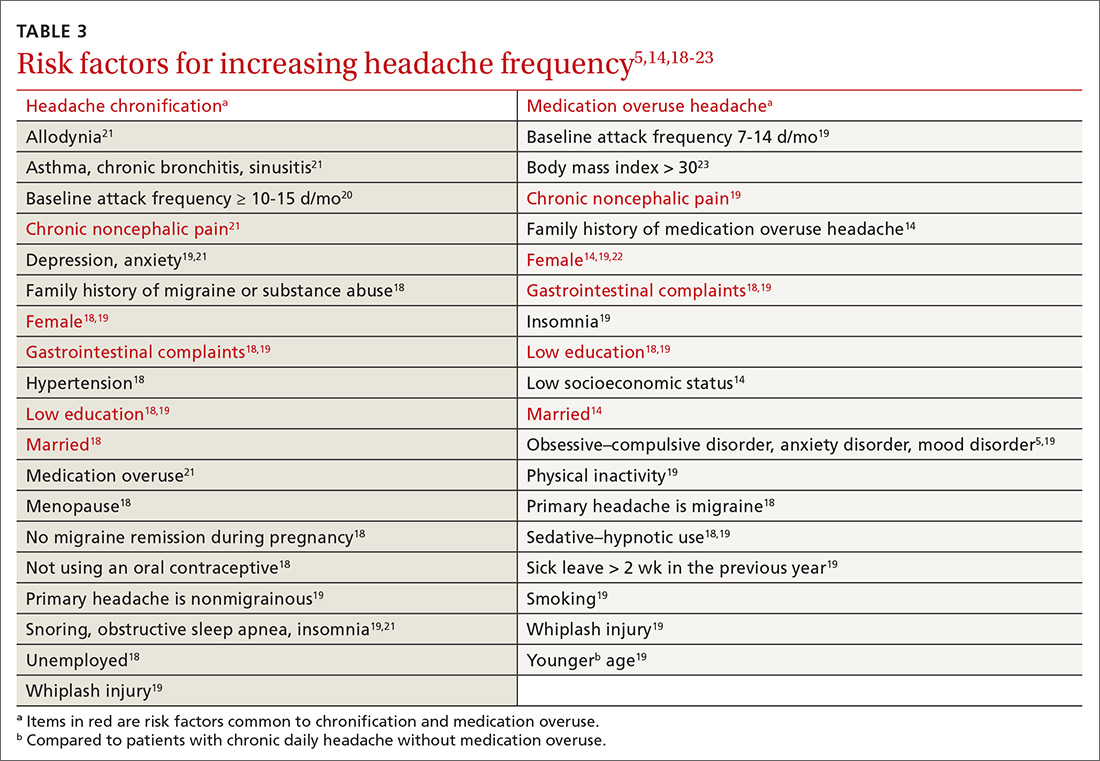
Continue to: Pathophysiology
Pathophysiology. The pathophysiology and psychology behind MOH are largely unknown. Physiologic changes in pain processing and functional imaging changes have been demonstrated in patients with MOH, both of which are reversible upon withdrawal of medication.23 Genetic factors and changes in hormone and neurotransmitter levels are found in MOH patients; this is not the case in patients who have an episodic headache pattern only.24
Presentation. Diagnostic criteria for MOH do not include clinical characteristics. Typically, the phenotype of MOH in a given patient is similar to the underlying primary headache25—although this principle can be complicated to tease out because these medications can suppress some symptoms. Diagnosis of a primary headache disorder should be documented along with the diagnosis of MOH.
Medication overuse can exist without MOH: Not every patient who frequently uses an abortive medication develops MOH.
Treatment is multifaceted—and can become complex
Mainstays of treatment of MOH are education about the disorder and detoxification from the overused agent, although specific treatments can differ depending on the agent involved, the frequency and duration of its use, and a patient’s behavioral patterns and psychiatric comorbidities. Often, a daily medication to prevent headache is considered upon, or after, withdrawal of the offending agent. The timing of introducing a preventive might impact its effectiveness. Some refractory cases require more intensive therapy, including hospitalization at a specialized tertiary center.
But before we look at detoxification from an overused agent, it’s important to review one of the best strategies of all in combatting MOH.
Continue to: First and best strategy
First and best strategy: Avoid onset of MOH
Select an appropriate abortive to reduce the risk of MOH. With regard to specific acute headache medications, some nuances other than type of headache should be considered. Nonsteroidal anti-inflammatory drugs (NSAIDs) are recommended as abortive therapy by the American Headache Society for their efficacy, favorable adverse effect profile, and low cost. NSAIDs are protective against development of MOH if a patient’s baseline headache frequency is < 10/mo; at a frequency of 10 to 14 d/mo, however, the risk of MOH increases when using an NSAID.6 A similar effect has been seen with triptans.16 Longer-acting NSAIDs, such as nabumetone and naproxen, have been proposed as less likely to cause MOH, and are even used as bridging therapy sometimes (as long as neither of these was the overused medication).26
The time it takes to develop MOH is shortest with triptans, followed by ergots, then analgesics.27
Prospective cohort studies6,16 have shown that barbiturates and opioids are more likely to induce MOH; for that reason, agents in these analgesic classes are almost universally avoided unless no other medically acceptable options exist. Using barbiturate-containing compounds or opioids > 4 d/mo exponentially increases the likelihood of MOH.
Promising preclinical data demonstrate that the gepant, or small-molecule calcitonin gene-related peptide (CGRP) receptor antagonist, class of medications used as abortive therapy does not induce medication overuse cutaneous allodynia.28
Provide education. Primary prevention of MOH involves (1) increasing patients’ awareness of how to take medications appropriately and (2) restricting intake of over-the-counter abortive medications. Often, the expert recommendation is to limit abortives to approximately 2 d/wk because more frequent use places patients at risk of further increased use and subsequent MOH.
Continue to: A randomized controlled trial in Norway...
A randomized controlled trial in Norway compared outcomes in 2 groups of patients with MOH: One group was given advice on the disorder by a physician; the other group was not provided with advice. In the “business-as-usual” group, there was no significant improvement; however, when general practitioners provided simple advice (lasting roughly 9 minutes) about reducing abortive medication use to a safe level and cautioned patients that they would be “feeling worse before feeling better,” headache days were reduced by approximately 8 per month and medication days, by 16 per month.2
A subsequent, long-term follow-up study29 of patients from the Norway trial2 who had been given advice and education showed a relapse rate (ie, into overuse of headache medication) of only 8% and sustained reduction of headache days and medication use at 16 months.
Offer support and other nondrug interventions. A recent review of 3 studies23 recommended that extra support for patients from a headache nurse, close follow-up, keeping an electronic diary that provides feedback, and undertaking a short course of psychotherapy can reduce medication overuse and prevent relapse.
If MOH develops, initiate withdrawal, introduce a preventive
Withdraw overused medication. Most current evidence suggests that withdrawal of the offending agent is the most effective factor in reducing headache days and improving quality of life. A randomized controlled trial compared the effects of (1) complete and immediate withdrawal of an abortive medication with (2) reducing its use (ie, limiting intake to 2 d/wk), on headache frequency, disability, and quality of life.30 There was a reduction of headache days in both groups; however, reduction was much greater at 2 months in the complete withdrawal group than in the restricted intake group (respectively, a 41% and a 26% reduction in headache days per month). This effect was sustained at 6 and 12 months in both groups. The study confirmed the results of earlier research2,15: Abrupt withdrawal leads to reversion to an episodic pattern at 2 to 6 months in approximately 40% to 60% of patients.
More studies are needed to determine the most appropriate treatment course for MOH; however, complete withdrawal of the causative drug is the most important intervention.
Continue to: Consider withdrawal plus preventive treatment
Consider withdrawal plus preventive treatment. Use of sodium valproate, in addition to medication overuse detoxification, led to a significant reduction in headache days and improvement in quality of life at 12 weeks but no difference after 24 weeks, compared with detoxification alone in a randomized, double-blind, placebo-controlled study.31
A study of 61 patients showed a larger reduction (by 7.2 d/mo) in headache frequency with any preventive medication in addition to medication withdrawal, compared to withdrawal alone (by 4.1 d/mo) after 3 months; however, the relative benefit was gone at 6 months.32
A study of 98 patients compared immediate and delayed initiation of preventive medication upon withdrawal of overused abortive medication.33 Response was defined as a > 50% reduction in headache frequency and was similar in both groups; results showed a 28% response with immediate initiation of a preventive; a 23% response with delayed (ie, 2 months after withdrawal) initiation; and a 48% response in both groups at 12 months.
Collectively, these studies suggest that adding a preventive medication at the time of withdrawal has the potential to reduce headache frequency more quickly than withdrawal alone. However, after 3 to 6 months, the outcome of reduced headache frequency is the same whether or not a preventive medication is used—as long as the offending agent has been withdrawn.
Do preventives work without withdrawing overused medication? Patients with MOH often show little or no improvement with addition of a preventive medication only; their response to a preventive improves after withdrawal of the overused medication. Patients without previous headache improvement after addition of a preventive, who also did not improve 2 months after withdrawal, then demonstrated an overall reduction in headache by 26% when a preventive was reintroduced after withdrawal.2
Continue to: The research evidence for preventives
The research evidence for preventives. Medications for headache prevention have not been extensively evaluated specifically for treating MOH. Here is what’s known:
- Flunarizine, amitriptyline, and beta-blockers usually are ineffective for MOH.24
- Results for topiramate are mixed: A small, double-blind, placebo-controlled chronic migraine study in Europe showed that, in a subgroup of patients with MOH, topiramate led to a small but significant reduction (3.5 d/mo) in headache frequency, compared to placebo.27 A similar study done in the United States did not show a significant difference between the active-treatment and placebo groups.34
- Findings regarding onabotulinumtoxinA are intriguing: In a posthoc analysis of onabotulinumtoxinA to treat chronic migraine, patients with MOH who did not undergo detoxification had an 8 d/mo greater reduction in headache, compared to placebo.35 However, when compared to placebo in conjunction with detoxification, onabotulinumtoxinA demonstrated no benefit.36
- Newer CGRP antagonist and CGRP receptor antagonist monoclonal antibodies are successful preventive medications that have demonstrated a reduction in acute medication use days per month and headache days per month37; these compounds have not been compared to withdrawal alone.
Reducing the severity and duration of withdrawal symptoms
Withdrawal from overused abortive headache medications can lead to worsening headache, nausea, vomiting, hypotension, tachycardia, sleep disturbances, restlessness, anxiety, and nervousness. Symptoms usually last 2 to 10 days but can persist for as long as 4 weeks; duration of withdrawal symptoms varies with the medication that is being overused. In patients who have used a triptan, for example, mean duration of withdrawal is 4.1 days; ergotamine, 6.7 days; and NSAIDs, 9.5 days.23 Tapered withdrawal is sometimes recommended with opioids and barbiturates to reduce withdrawal symptoms. It is unclear whether starting a preventive medication during withdrawal assists in reducing withdrawal symptoms.38
Bridging therapy to reduce symptoms of withdrawal is often provided despite debatable utility. Available evidence does not favor one agent or method but suggests some strategies that could be helpful:
- A prednisone taper has a potential role during the first 6 days of withdrawal by reducing rebound headache and withdrawal symptoms39; however, oral prednisolone has been shown to have no benefit.40
- Alone, IV methylprednisolone seems not to be of benefit; however, in a retrospective study of 94 patients, IV methylprednisolone plus diazepam for 5 days led to a significant reduction in headache frequency and drug consumption that was sustained after 3 months.41
- Celecoxib was compared to prednisone over a 20-day course: a celecoxib dosage of 400 mg/d for the first 5 days, tapered by 100 mg every 5 days, and an oral prednisone dosage of 75 mg/d for the first 5 days, then tapered every 5 days. Patients taking celecoxib had lower headache intensity but there was no difference in headache frequency and acute medication intake between the groups.42
Other strategies. Using antiemetics and NSAIDs to reduce withdrawal symptoms is widely practiced, but no placebo-controlled trials have been conducted to support this strategy.
Patients in withdrawal might be more likely to benefit from inpatient care if they have a severe comorbidity, such as opioid or barbiturate use; failure to respond to, tolerate, or adhere to treatment; or relapse after withdrawal.38
Continue to: Cognitive behavioral therapy...
Cognitive behavioral therapy, exercise, a headache diary, and biofeedback should be considered in every patient’s treatment strategy because a multidisciplinary approach increases adherence and leads to improvement in headache frequency and a decrease in disability and medication use.43
Predictors of Tx success
A prospective cohort study determined that the rate of MOH relapse is 31% at 6 months, 41% at 1 year, and 45% at 4 years, with the highest risk of relapse during the first year.44 Looking at the correlation between type of medication overused and relapse rate, the research indicates that
- triptans have the lowest risk of relapse,44
- simple analgesics have a higher risk of relapse than triptans,22,44 and
- opioids have the highest risk of relapse.22
Where the data don’t agree. Data on combination analgesics and on ergots are conflicting.22 In addition, data on whether the primary type of headache predicts relapse rate conflict; however, migraine might predict a better outcome than tension-type headache.22
To recap and expand: Management pearls
The major goals of headache management generally are to rule out secondary headache, reach a correct diagnosis, reduce overall headache frequency, and provide effective abortive medication. A large component of reducing headache frequency is addressing and treating medication overuse.
Seek to understand the nature of the patient’s headache disorder. Components of the history are key in identifying the underlying headache diagnosis and ruling out other, more concerning secondary headache diagnoses. The ICHD-3 is an excellent resource for treating headache disorders because the classification lists specific diagnostic criteria for all recognized headache diagnoses.
Continue to: Medication withdrawal...
Medication withdrawal—with or without preventive medication—should reduce the frequency of MOH in 2 or 3 months. If headache does not become less frequent, however, the headache diagnosis might need to be reconsidered. Minimizing the use of abortive medication is generally recommended, but reduction or withdrawal of these medications does not guarantee that patients will revert to an episodic pattern of headache.
Treating withdrawal symptoms is a reasonable approach in some patients, but evidence does not support routinely providing bridging therapy.
Apply preventives carefully. Abortive medication withdrawal should generally be completed before initiating preventive medication; however, over the short term, starting preventive therapy while withdrawing the overused medication could assist in reducing headache frequency rapidly. This strategy can put patients at risk of medication adverse effects and using the medications longer than necessary, yet might be reasonable in certain patients, given their comorbidities, risk of relapse, and physician and patient preference. A preventive medication for an individual patient should generally be chosen in line with recommendations of the American Academy of Neurology45 and on the basis of the history and comorbidities.
Provide education, which is essential to lowering barriers to success. Patients with MOH must be counseled to understand that (1) a headache treatment that is supposed to be making them feel better is, in fact, making them feel worse and (2) they will get worse before they get better. Many patients are afraid to be without medication to use as needed. It is helpful to educate them on the different types of treatments (abortive, preventive); how MOH interferes with headache prophylaxis and medication efficacy; how MOH alters brain function (ie, aforementioned physiologic changes in pain processing and functional imaging changes23); and that such change is reversible when medication is withdrawn.
ACKNOWLEDGEMENT
The author thanks Jeffrey Curtis, MD, MPH, for his support and editing assistance with the manuscript.
CORRESPONDENCE
Allison Crain, MD, 2927 N 7th Avenue, Phoenix, AZ 85013; [email protected].
1. Zeeberg P, Olesen J, Jensen R. Discontinuation of medication overuse in headache patients: recovery of therapeutic responsiveness. Cephalalgia. 2006;26:1192-1198.
2. Kristoffersen ES, Straand J, Vetvik KG, et al. Brief intervention for medication-overuse headache in primary care. The BIMOH study: a double-blind pragmatic cluster randomised parallel controlled trial. J Neurol Neurosurg Psychiatry. 2015;86:505-512.
3. Bahra A, Walsh M, Menon S, et al. Does chronic daily headache arise de novo in association with regular use of analgesics? Headache. 2003;43:179-190.
4. Blumenfeld AM, Varon SF, Wilcox TK, et al. Disability, HRQoL and resource use among chronic and episodic migraineurs: results from the International Burden of Migraine Study (IBMS) Cephalalgia. 2011;31:301-315.
5. Chu H-T, Liang C-S, Lee J-T, et al. Associations between depression/anxiety and headache frequency in migraineurs: a cross-sectional study. Headache. 2018;58:407-415.
6. Bigal ME, Lipton RB. Excessive acute migraine medication use and migraine progression. Neurology. 2008;71:1821-1828.
7. Colás R, Muñoz P, Temprano R, et al. Chronic daily headache with analgesic overuse: epidemiology and impact on quality of life. Neurology. 2004;62:1338-1342.
8. Linde M, Gustavsson A, Stovner LJ, et al. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. 2012;19:703-711.
9. Shah AM, Bendtsen L, Zeeberg P, et al. Reduction of medication costs after detoxification for medication-overuse headache. Headache. 2013;53:665-672.
10. . Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17:954-976.
11. Kernick D, Stapley S, Goadsby PJ, et al. What happens to new-onset headache presenting to primary care? A case–cohort study using electronic primary care records. Cephalalgia. 2008;28:1188-1195.
12. Stone J, Carson A, Duncan R, et al. Who is referred to neurology clinics?—the diagnoses made in 3781 new patients. Clin Neurol Neurosurg. 2010;112:747-751.
13. Munoz-Ceron J, Marin-Careaga V, L, et al. Headache at the emergency room: etiologies, diagnostic usefulness of the ICHD 3 criteria, red and green flags. PloS One. 2019;14:e0208728.
14. Evers S, Marziniak M. Clinical features, pathophysiology, and treatment of medication-overuse headache. Lancet Neurol. 2010;9:391-401.
15. Tassorelli C, Jensen R, Allena M, et al; the . A consensus protocol for the management of medication-overuse headache: evaluation in a multicentric, multinational study. Cephalalgia. 2014;34:645-655.
16. Bigal ME, Serrano D, Buse D, et al. Acute migraine medications and evolution from episodic to chronic migraine: a longitudinal population-based study. Headache. 2008;48:1157-1168.
17. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1-211.
18. Ferrari A, Leone S, Vergoni AV, et al. Similarities and differences between chronic migraine and episodic migraine. Headache. 2007;47:65-72.
19. Hagen K, Linde M, Steiner TJ, et al. Risk factors for medication-overuse headache: an 11-year follow-up study. The Nord-Trøndelag Health Studies. Pain. 2012;153:56-61.
20. Katsarava Z, Schneewiess S, Kurth T, et al. Incidence and predictors for chronicity of headache in patients with episodic migraine. Neurology. 2004;62:788-790.
21. Lipton RB, Fanning KM, Buse DC, et al. Migraine progression in subgroups of migraine based on comorbidities: results of the CaMEO study. Neurology. 2019;93:e2224-e2236.
22. Munksgaard SB, Madsen SK, Wienecke T. Treatment of medication overuse headache—a review. Acta Neurol Scand. 2019;139:405-414.
23. Ferraro S, Grazzi L, Mandelli M, et al. Pain processing in medication overuse headache: a functional magnetic resonance imaging (fMRI) study. Pain Med. 2012;13:255-262.
24. Diener H-C, Holle D, Solbach K, et al. Medication-overuse headache: risk factors, pathophysiology and management. Nat Rev Neurol. 2016;12:575-583.
25. Limmroth V, Katsarava Z, Fritsche G, et al. Features of medication overuse headache following overuse of different acute headache drugs. Neurology. 2002;59:1011-1014.
26. Mauskop A, ed. Migraine and Headache. 2nd ed. Oxford University Press; 2013.
27. Diener H-C, Bussone G, Van Oene JC, et al; . Topiramate reduces headache days in chronic migraine: a randomized, double-blind, placebo-controlled study. Cephalalgia. 2007;27:814-823.
28. Navratilova E, Behravesh S, Oyarzo J, et al. Ubrogepant does not induce latent sensitization in a preclinical model of medication overuse headache Cephalalgia. 2020;40:892-902.
29. Kristoffersen ES, Straand J, Russell MB, et al. Lasting improvement of medication-overuse headache after brief intervention—a long-term follow-up in primary care. Eur J Neurol. 2017;24:883-891.
30. Carlsen LN, Munksgaard SB, Jensen RH, et al. Complete detoxification is the most effective treatment of medication-overuse headache: a randomized controlled open-label trial. Cephalalgia. 2018;38:225-236.
31. Sarchielli P, Messina P, Cupini LM, et al; SAMOHA Study Group. Sodium valproate in migraine without aura and medication overuse headache: a randomized controlled trial. Eur Neuropsychopharmacol. 2014;24:1289-1297.
32. Hagen K, Stovner LJ. A randomized controlled trial on medication-overuse headache: outcome after 1 and 4 years. Acta Neurol Scand Suppl. 2011;124(suppl 191):38-43.
33. Munksgaard SB, Bendtsen L, Jensen RH. Detoxification of medication-overuse headache by a multidisciplinary treatment programme is highly effective: a comparison of two consecutive treatment methods in an open-label design. Cephalalgia. 2012;32:834-844.
34. Silberstein S, Lipton R, Dodick D, et al. Topiramate treatment of chronic migraine: a randomized, placebo-controlled trial of quality of life and other efficacy measures. Headache. 2009;49:1153-1162.
35. Silberstein SD, Blumenfeld AM, Cady RK, et al. OnabotulinumtoxinA for treatment of chronic migraine: PREEMPT 24-week pooled subgroup analysis of patients who had acute headache medication overuse at baseline. J Neurol Sci. 2013;331:48-56.
36. Sandrini G, Perrotta A, Tassorelli C, et al. Botulinum toxin type-A in the prophylactic treatment of medication-overuse headache: a multicenter, double-blind, randomized, placebo-controlled, parallel group study. J Headache Pain. 2011;12:427-433.
37. Tepper SJ. CGRP and headache: a brief review. Neurol Sci. 2019;40(suppl 1):99-105.
38. Diener H-C, Dodick D, Evers S, et al. Pathophysiology, prevention and treatment of medication overuse headache. Lancet Neurol. 2019;18:891-902.
39. Krymchantowski AV, Barbosa JS. Prednisone as initial treatment of analgesic-induced daily headache. Cephalalgia. 2000;20:107-113.
40. Bøe MG, Mygland A, Salvesen R. Prednisolone does not reduce withdrawal headache: a randomized, double-blind study. Neurology. 2007;69:26-31.
41. Paolucci M, Altamura C, Brunelli N, et al. Methylprednisolone plus diazepam i.v. as bridge therapy for medication overuse headache. Neurol Sci. 2017;38:2025-2029.
42. Taghdiri F, Togha M, Razeghi Jahromi S, et al. Celecoxib vs prednisone for the treatment of withdrawal headache in patients with medication overuse headache: a randomized, double-blind clinical trial. Headache. 2015;55:128-135.
43. Ramsey RR, Ryan JL, Hershey AD, et al. Treatment adherence in patients with headache: a systematic review. Headache. 2014;54:795-816.
44. Katsarava Z, Muessig M, Dzagnidze A, et al. Medication overuse headache: rates and predictors for relapse in a 4-year prospective study. Cephalalgia. 2005;25:12-15.
45. Silberstein SD, Holland S, Freitag F, et al; . Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012; 78:1137-1145.
Medication overuse headache (MOH), a secondary headache diagnosis, is a prevalent phenomenon that complicates headache diagnosis and treatment, increases the cost of care, and reduces quality of life. Effective abortive medication is essential for the headache sufferer; when an abortive is used too frequently, however, headache frequency increases—potentially beginning a cycle in which the patient then takes more medication to abort the headache. Over time, the patient suffers from an ever-increasing number of headaches, takes even more abortive medication, and so on. In the presence of MOH, there is a reduction in pain response to preventive and abortive treatments; when medication overuse is eliminated, pain response improves.1
Although MOH is well recognized among headache specialists, the condition is often overlooked in primary care. Since headache is a top complaint in primary care, however, and prevention is a major goal in family medicine, the opportunity for you to recognize, treat, and prevent MOH is significant. In fact, a randomized controlled trial showed that brief patient education about headache care and MOH provided by a primary care physician can lead to a significant reduction in headache frequency among patients with MOH.2
This article reviews the recognition and diagnosis of MOH, based on historical features and current criteria; addresses risk factors for abortive medication overuse and how to withdraw an offending agent; and explores the value of bridging and preventive therapies to reduce the overall frequency of headache.
What defines MOH?
Typically, MOH is a chronification of a primary headache disorder. However, in patients with a history of migraine who are undergoing treatment for another chronic pain condition with an opioid or other analgesic, MOH can be induced.3 An increase in the frequency of headache raises the specter of a concomitant increase in the level of disability4; psychiatric comorbidity5; and more headache days, with time lost from school and work.
The Migraine Disability Assessment (MIDAS) questionnaire, a validated instrument that helps the provider (1) measure the impact that headache has on a patient’s life and (2) follow treatment progress, also provides information to employers and insurance companies on treatment coverage and the need for work modification. The MIDAS score is 3 times higher in patients with MOH than in patients with episodic migraine.6,7
The annual associated cost per person of MOH has been estimated at $4000, resulting in billions of dollars in associated costs8; most of these costs are related to absenteeism and disability. After detoxification for MOH, annual outpatient medication costs are reduced by approximately 24%.9
Efforts to solve a common problem create another
Headache affects nearly 50% of the general population worldwide,10 accounting for about 4% of primary care visits11 and approximately 20% of outpatient neurology consultations.12 Although inpatient stays for headache are approximately half the duration of the overall average hospital stay, headache accounts for 3% of admissions.13 According to the Global Burden of Disease study, tension-type headache, migraine, and MOH are the 3 most common headache disorders.10 Headache is the second leading cause of disability among people 15 to 49 years of age.10
Continue to: The prevalence of MOH...
The prevalence of MOH in the general population is 2%.7,14,15 A population-based study showed that the rate of progression from episodic headache (< 15 d/mo) to chronic headache (≥ 15 d/mo) in the general population is 2.5% per year16; however, progression to chronic headache is 14% per year in patients with medication overuse. One-third of the general population with chronic migraine overuses symptomatic medication; in US headache clinics, roughly one-half of patients with chronic headache overuse acute medication.6
Definitions and diagnosis
MOH is a secondary headache diagnosis in the third edition of the International Classification of Headache Disorders (ICHD-3) (TABLE 1),17 which lists diagnostic criteria for recognized headache disorders.
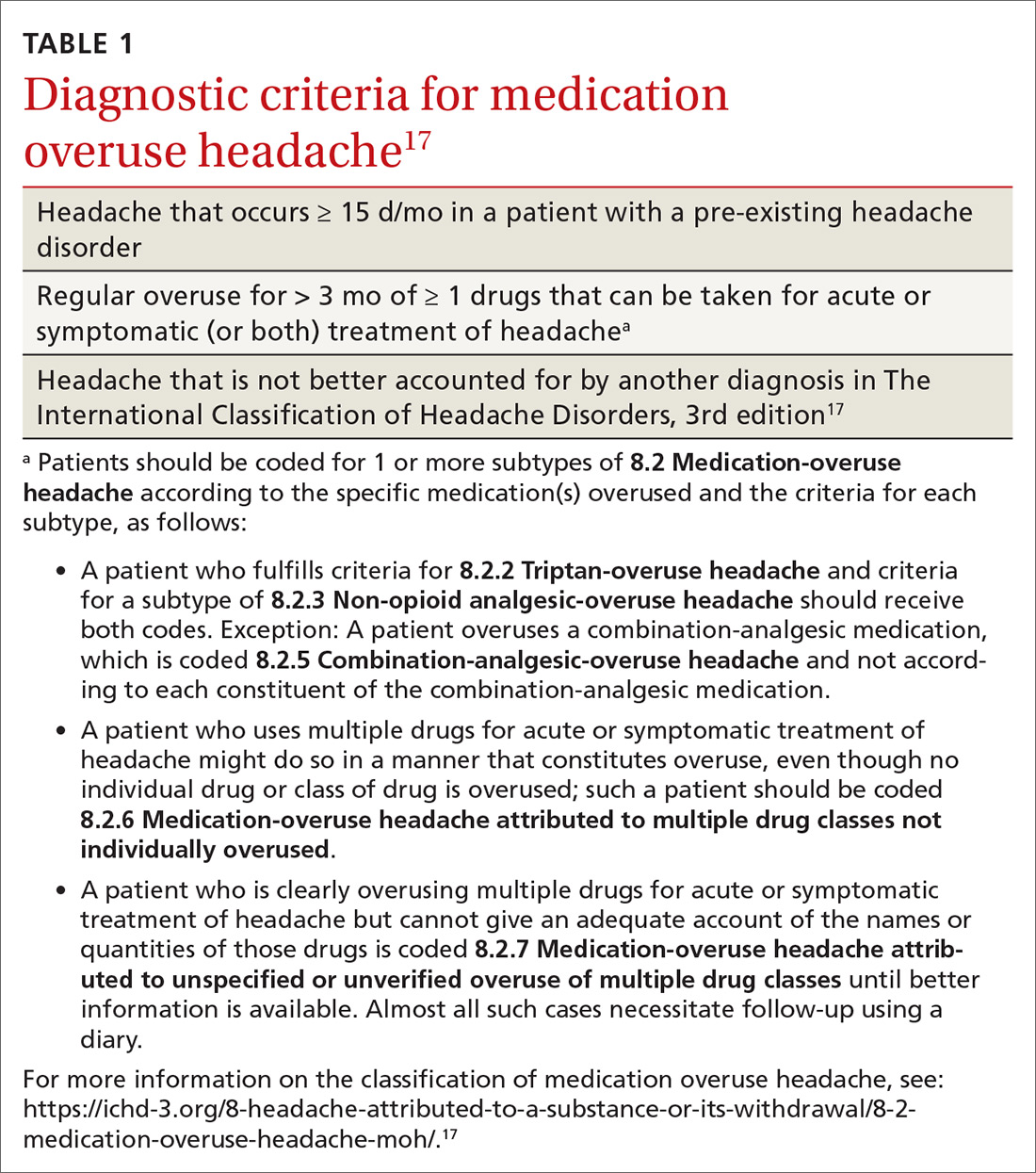
Terminology. MOH has also been called rebound headache, drug-induced headache, and transformed migraine, but these terms are outdated and are not formal diagnoses. Patients sometimes refer to substance-withdrawal headaches (not discussed in this article) as rebound headaches, so clarity is important when discussing headache with patients: namely, that MOH is an exacerbation of an existing headache condition caused by overuse of abortive headache medications, including analgesics, combination analgesics, triptans, barbiturates, and opioids.
MOH was recognized in the early 1950s and fully differentiated as a diagnosis in 2005 in the second edition of the ICHD. The disorder is subcategorized by offending abortive agent (TABLE 217) because the frequency of analgesic use required to develop MOH differs by agent.
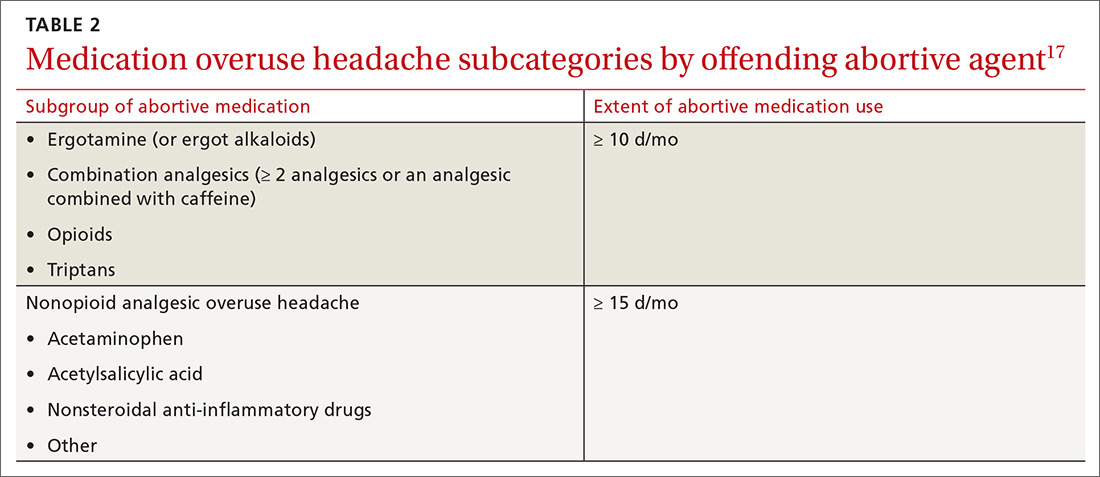
Risk factors for MOH and chronification of a primary headache disorder. There are several risk factors for developing MOH, and others that contribute to increasing headache frequency in general (TABLE 35,14,18-23). Some risk factors are common to each. All are important to address because some are modifiable.
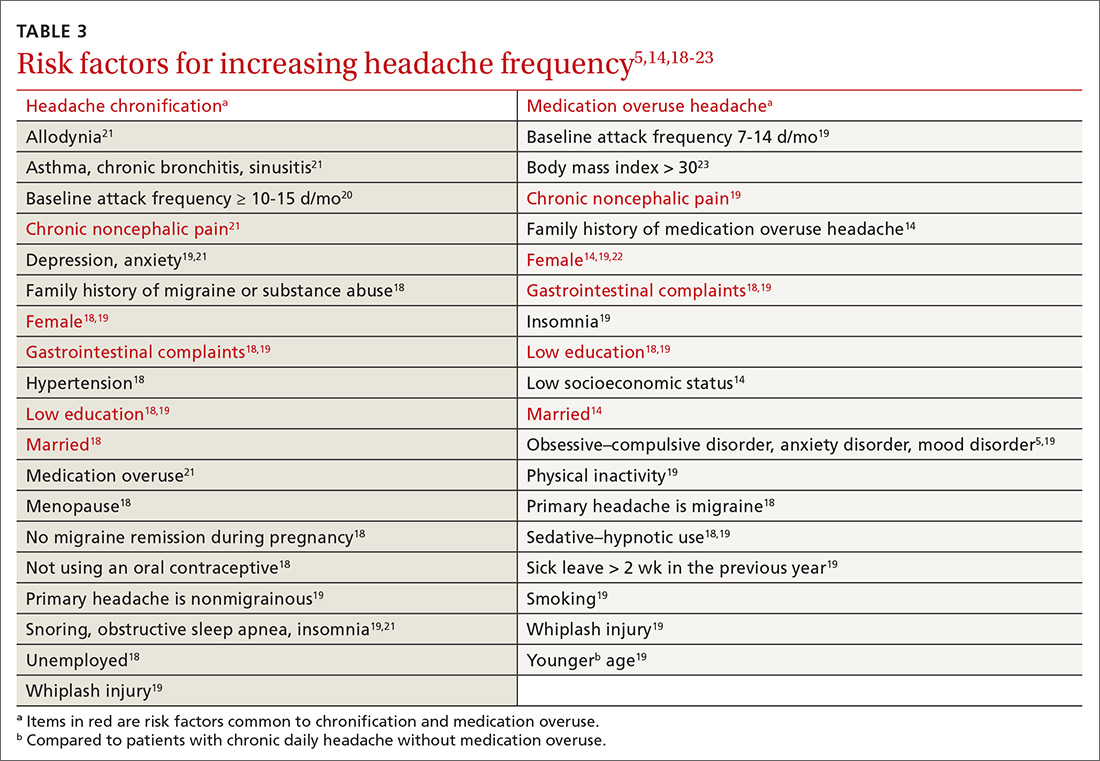
Continue to: Pathophysiology
Pathophysiology. The pathophysiology and psychology behind MOH are largely unknown. Physiologic changes in pain processing and functional imaging changes have been demonstrated in patients with MOH, both of which are reversible upon withdrawal of medication.23 Genetic factors and changes in hormone and neurotransmitter levels are found in MOH patients; this is not the case in patients who have an episodic headache pattern only.24
Presentation. Diagnostic criteria for MOH do not include clinical characteristics. Typically, the phenotype of MOH in a given patient is similar to the underlying primary headache25—although this principle can be complicated to tease out because these medications can suppress some symptoms. Diagnosis of a primary headache disorder should be documented along with the diagnosis of MOH.
Medication overuse can exist without MOH: Not every patient who frequently uses an abortive medication develops MOH.
Treatment is multifaceted—and can become complex
Mainstays of treatment of MOH are education about the disorder and detoxification from the overused agent, although specific treatments can differ depending on the agent involved, the frequency and duration of its use, and a patient’s behavioral patterns and psychiatric comorbidities. Often, a daily medication to prevent headache is considered upon, or after, withdrawal of the offending agent. The timing of introducing a preventive might impact its effectiveness. Some refractory cases require more intensive therapy, including hospitalization at a specialized tertiary center.
But before we look at detoxification from an overused agent, it’s important to review one of the best strategies of all in combatting MOH.
Continue to: First and best strategy
First and best strategy: Avoid onset of MOH
Select an appropriate abortive to reduce the risk of MOH. With regard to specific acute headache medications, some nuances other than type of headache should be considered. Nonsteroidal anti-inflammatory drugs (NSAIDs) are recommended as abortive therapy by the American Headache Society for their efficacy, favorable adverse effect profile, and low cost. NSAIDs are protective against development of MOH if a patient’s baseline headache frequency is < 10/mo; at a frequency of 10 to 14 d/mo, however, the risk of MOH increases when using an NSAID.6 A similar effect has been seen with triptans.16 Longer-acting NSAIDs, such as nabumetone and naproxen, have been proposed as less likely to cause MOH, and are even used as bridging therapy sometimes (as long as neither of these was the overused medication).26
The time it takes to develop MOH is shortest with triptans, followed by ergots, then analgesics.27
Prospective cohort studies6,16 have shown that barbiturates and opioids are more likely to induce MOH; for that reason, agents in these analgesic classes are almost universally avoided unless no other medically acceptable options exist. Using barbiturate-containing compounds or opioids > 4 d/mo exponentially increases the likelihood of MOH.
Promising preclinical data demonstrate that the gepant, or small-molecule calcitonin gene-related peptide (CGRP) receptor antagonist, class of medications used as abortive therapy does not induce medication overuse cutaneous allodynia.28
Provide education. Primary prevention of MOH involves (1) increasing patients’ awareness of how to take medications appropriately and (2) restricting intake of over-the-counter abortive medications. Often, the expert recommendation is to limit abortives to approximately 2 d/wk because more frequent use places patients at risk of further increased use and subsequent MOH.
Continue to: A randomized controlled trial in Norway...
A randomized controlled trial in Norway compared outcomes in 2 groups of patients with MOH: One group was given advice on the disorder by a physician; the other group was not provided with advice. In the “business-as-usual” group, there was no significant improvement; however, when general practitioners provided simple advice (lasting roughly 9 minutes) about reducing abortive medication use to a safe level and cautioned patients that they would be “feeling worse before feeling better,” headache days were reduced by approximately 8 per month and medication days, by 16 per month.2
A subsequent, long-term follow-up study29 of patients from the Norway trial2 who had been given advice and education showed a relapse rate (ie, into overuse of headache medication) of only 8% and sustained reduction of headache days and medication use at 16 months.
Offer support and other nondrug interventions. A recent review of 3 studies23 recommended that extra support for patients from a headache nurse, close follow-up, keeping an electronic diary that provides feedback, and undertaking a short course of psychotherapy can reduce medication overuse and prevent relapse.
If MOH develops, initiate withdrawal, introduce a preventive
Withdraw overused medication. Most current evidence suggests that withdrawal of the offending agent is the most effective factor in reducing headache days and improving quality of life. A randomized controlled trial compared the effects of (1) complete and immediate withdrawal of an abortive medication with (2) reducing its use (ie, limiting intake to 2 d/wk), on headache frequency, disability, and quality of life.30 There was a reduction of headache days in both groups; however, reduction was much greater at 2 months in the complete withdrawal group than in the restricted intake group (respectively, a 41% and a 26% reduction in headache days per month). This effect was sustained at 6 and 12 months in both groups. The study confirmed the results of earlier research2,15: Abrupt withdrawal leads to reversion to an episodic pattern at 2 to 6 months in approximately 40% to 60% of patients.
More studies are needed to determine the most appropriate treatment course for MOH; however, complete withdrawal of the causative drug is the most important intervention.
Continue to: Consider withdrawal plus preventive treatment
Consider withdrawal plus preventive treatment. Use of sodium valproate, in addition to medication overuse detoxification, led to a significant reduction in headache days and improvement in quality of life at 12 weeks but no difference after 24 weeks, compared with detoxification alone in a randomized, double-blind, placebo-controlled study.31
A study of 61 patients showed a larger reduction (by 7.2 d/mo) in headache frequency with any preventive medication in addition to medication withdrawal, compared to withdrawal alone (by 4.1 d/mo) after 3 months; however, the relative benefit was gone at 6 months.32
A study of 98 patients compared immediate and delayed initiation of preventive medication upon withdrawal of overused abortive medication.33 Response was defined as a > 50% reduction in headache frequency and was similar in both groups; results showed a 28% response with immediate initiation of a preventive; a 23% response with delayed (ie, 2 months after withdrawal) initiation; and a 48% response in both groups at 12 months.
Collectively, these studies suggest that adding a preventive medication at the time of withdrawal has the potential to reduce headache frequency more quickly than withdrawal alone. However, after 3 to 6 months, the outcome of reduced headache frequency is the same whether or not a preventive medication is used—as long as the offending agent has been withdrawn.
Do preventives work without withdrawing overused medication? Patients with MOH often show little or no improvement with addition of a preventive medication only; their response to a preventive improves after withdrawal of the overused medication. Patients without previous headache improvement after addition of a preventive, who also did not improve 2 months after withdrawal, then demonstrated an overall reduction in headache by 26% when a preventive was reintroduced after withdrawal.2
Continue to: The research evidence for preventives
The research evidence for preventives. Medications for headache prevention have not been extensively evaluated specifically for treating MOH. Here is what’s known:
- Flunarizine, amitriptyline, and beta-blockers usually are ineffective for MOH.24
- Results for topiramate are mixed: A small, double-blind, placebo-controlled chronic migraine study in Europe showed that, in a subgroup of patients with MOH, topiramate led to a small but significant reduction (3.5 d/mo) in headache frequency, compared to placebo.27 A similar study done in the United States did not show a significant difference between the active-treatment and placebo groups.34
- Findings regarding onabotulinumtoxinA are intriguing: In a posthoc analysis of onabotulinumtoxinA to treat chronic migraine, patients with MOH who did not undergo detoxification had an 8 d/mo greater reduction in headache, compared to placebo.35 However, when compared to placebo in conjunction with detoxification, onabotulinumtoxinA demonstrated no benefit.36
- Newer CGRP antagonist and CGRP receptor antagonist monoclonal antibodies are successful preventive medications that have demonstrated a reduction in acute medication use days per month and headache days per month37; these compounds have not been compared to withdrawal alone.
Reducing the severity and duration of withdrawal symptoms
Withdrawal from overused abortive headache medications can lead to worsening headache, nausea, vomiting, hypotension, tachycardia, sleep disturbances, restlessness, anxiety, and nervousness. Symptoms usually last 2 to 10 days but can persist for as long as 4 weeks; duration of withdrawal symptoms varies with the medication that is being overused. In patients who have used a triptan, for example, mean duration of withdrawal is 4.1 days; ergotamine, 6.7 days; and NSAIDs, 9.5 days.23 Tapered withdrawal is sometimes recommended with opioids and barbiturates to reduce withdrawal symptoms. It is unclear whether starting a preventive medication during withdrawal assists in reducing withdrawal symptoms.38
Bridging therapy to reduce symptoms of withdrawal is often provided despite debatable utility. Available evidence does not favor one agent or method but suggests some strategies that could be helpful:
- A prednisone taper has a potential role during the first 6 days of withdrawal by reducing rebound headache and withdrawal symptoms39; however, oral prednisolone has been shown to have no benefit.40
- Alone, IV methylprednisolone seems not to be of benefit; however, in a retrospective study of 94 patients, IV methylprednisolone plus diazepam for 5 days led to a significant reduction in headache frequency and drug consumption that was sustained after 3 months.41
- Celecoxib was compared to prednisone over a 20-day course: a celecoxib dosage of 400 mg/d for the first 5 days, tapered by 100 mg every 5 days, and an oral prednisone dosage of 75 mg/d for the first 5 days, then tapered every 5 days. Patients taking celecoxib had lower headache intensity but there was no difference in headache frequency and acute medication intake between the groups.42
Other strategies. Using antiemetics and NSAIDs to reduce withdrawal symptoms is widely practiced, but no placebo-controlled trials have been conducted to support this strategy.
Patients in withdrawal might be more likely to benefit from inpatient care if they have a severe comorbidity, such as opioid or barbiturate use; failure to respond to, tolerate, or adhere to treatment; or relapse after withdrawal.38
Continue to: Cognitive behavioral therapy...
Cognitive behavioral therapy, exercise, a headache diary, and biofeedback should be considered in every patient’s treatment strategy because a multidisciplinary approach increases adherence and leads to improvement in headache frequency and a decrease in disability and medication use.43
Predictors of Tx success
A prospective cohort study determined that the rate of MOH relapse is 31% at 6 months, 41% at 1 year, and 45% at 4 years, with the highest risk of relapse during the first year.44 Looking at the correlation between type of medication overused and relapse rate, the research indicates that
- triptans have the lowest risk of relapse,44
- simple analgesics have a higher risk of relapse than triptans,22,44 and
- opioids have the highest risk of relapse.22
Where the data don’t agree. Data on combination analgesics and on ergots are conflicting.22 In addition, data on whether the primary type of headache predicts relapse rate conflict; however, migraine might predict a better outcome than tension-type headache.22
To recap and expand: Management pearls
The major goals of headache management generally are to rule out secondary headache, reach a correct diagnosis, reduce overall headache frequency, and provide effective abortive medication. A large component of reducing headache frequency is addressing and treating medication overuse.
Seek to understand the nature of the patient’s headache disorder. Components of the history are key in identifying the underlying headache diagnosis and ruling out other, more concerning secondary headache diagnoses. The ICHD-3 is an excellent resource for treating headache disorders because the classification lists specific diagnostic criteria for all recognized headache diagnoses.
Continue to: Medication withdrawal...
Medication withdrawal—with or without preventive medication—should reduce the frequency of MOH in 2 or 3 months. If headache does not become less frequent, however, the headache diagnosis might need to be reconsidered. Minimizing the use of abortive medication is generally recommended, but reduction or withdrawal of these medications does not guarantee that patients will revert to an episodic pattern of headache.
Treating withdrawal symptoms is a reasonable approach in some patients, but evidence does not support routinely providing bridging therapy.
Apply preventives carefully. Abortive medication withdrawal should generally be completed before initiating preventive medication; however, over the short term, starting preventive therapy while withdrawing the overused medication could assist in reducing headache frequency rapidly. This strategy can put patients at risk of medication adverse effects and using the medications longer than necessary, yet might be reasonable in certain patients, given their comorbidities, risk of relapse, and physician and patient preference. A preventive medication for an individual patient should generally be chosen in line with recommendations of the American Academy of Neurology45 and on the basis of the history and comorbidities.
Provide education, which is essential to lowering barriers to success. Patients with MOH must be counseled to understand that (1) a headache treatment that is supposed to be making them feel better is, in fact, making them feel worse and (2) they will get worse before they get better. Many patients are afraid to be without medication to use as needed. It is helpful to educate them on the different types of treatments (abortive, preventive); how MOH interferes with headache prophylaxis and medication efficacy; how MOH alters brain function (ie, aforementioned physiologic changes in pain processing and functional imaging changes23); and that such change is reversible when medication is withdrawn.
ACKNOWLEDGEMENT
The author thanks Jeffrey Curtis, MD, MPH, for his support and editing assistance with the manuscript.
CORRESPONDENCE
Allison Crain, MD, 2927 N 7th Avenue, Phoenix, AZ 85013; [email protected].
Medication overuse headache (MOH), a secondary headache diagnosis, is a prevalent phenomenon that complicates headache diagnosis and treatment, increases the cost of care, and reduces quality of life. Effective abortive medication is essential for the headache sufferer; when an abortive is used too frequently, however, headache frequency increases—potentially beginning a cycle in which the patient then takes more medication to abort the headache. Over time, the patient suffers from an ever-increasing number of headaches, takes even more abortive medication, and so on. In the presence of MOH, there is a reduction in pain response to preventive and abortive treatments; when medication overuse is eliminated, pain response improves.1
Although MOH is well recognized among headache specialists, the condition is often overlooked in primary care. Since headache is a top complaint in primary care, however, and prevention is a major goal in family medicine, the opportunity for you to recognize, treat, and prevent MOH is significant. In fact, a randomized controlled trial showed that brief patient education about headache care and MOH provided by a primary care physician can lead to a significant reduction in headache frequency among patients with MOH.2
This article reviews the recognition and diagnosis of MOH, based on historical features and current criteria; addresses risk factors for abortive medication overuse and how to withdraw an offending agent; and explores the value of bridging and preventive therapies to reduce the overall frequency of headache.
What defines MOH?
Typically, MOH is a chronification of a primary headache disorder. However, in patients with a history of migraine who are undergoing treatment for another chronic pain condition with an opioid or other analgesic, MOH can be induced.3 An increase in the frequency of headache raises the specter of a concomitant increase in the level of disability4; psychiatric comorbidity5; and more headache days, with time lost from school and work.
The Migraine Disability Assessment (MIDAS) questionnaire, a validated instrument that helps the provider (1) measure the impact that headache has on a patient’s life and (2) follow treatment progress, also provides information to employers and insurance companies on treatment coverage and the need for work modification. The MIDAS score is 3 times higher in patients with MOH than in patients with episodic migraine.6,7
The annual associated cost per person of MOH has been estimated at $4000, resulting in billions of dollars in associated costs8; most of these costs are related to absenteeism and disability. After detoxification for MOH, annual outpatient medication costs are reduced by approximately 24%.9
Efforts to solve a common problem create another
Headache affects nearly 50% of the general population worldwide,10 accounting for about 4% of primary care visits11 and approximately 20% of outpatient neurology consultations.12 Although inpatient stays for headache are approximately half the duration of the overall average hospital stay, headache accounts for 3% of admissions.13 According to the Global Burden of Disease study, tension-type headache, migraine, and MOH are the 3 most common headache disorders.10 Headache is the second leading cause of disability among people 15 to 49 years of age.10
Continue to: The prevalence of MOH...
The prevalence of MOH in the general population is 2%.7,14,15 A population-based study showed that the rate of progression from episodic headache (< 15 d/mo) to chronic headache (≥ 15 d/mo) in the general population is 2.5% per year16; however, progression to chronic headache is 14% per year in patients with medication overuse. One-third of the general population with chronic migraine overuses symptomatic medication; in US headache clinics, roughly one-half of patients with chronic headache overuse acute medication.6
Definitions and diagnosis
MOH is a secondary headache diagnosis in the third edition of the International Classification of Headache Disorders (ICHD-3) (TABLE 1),17 which lists diagnostic criteria for recognized headache disorders.
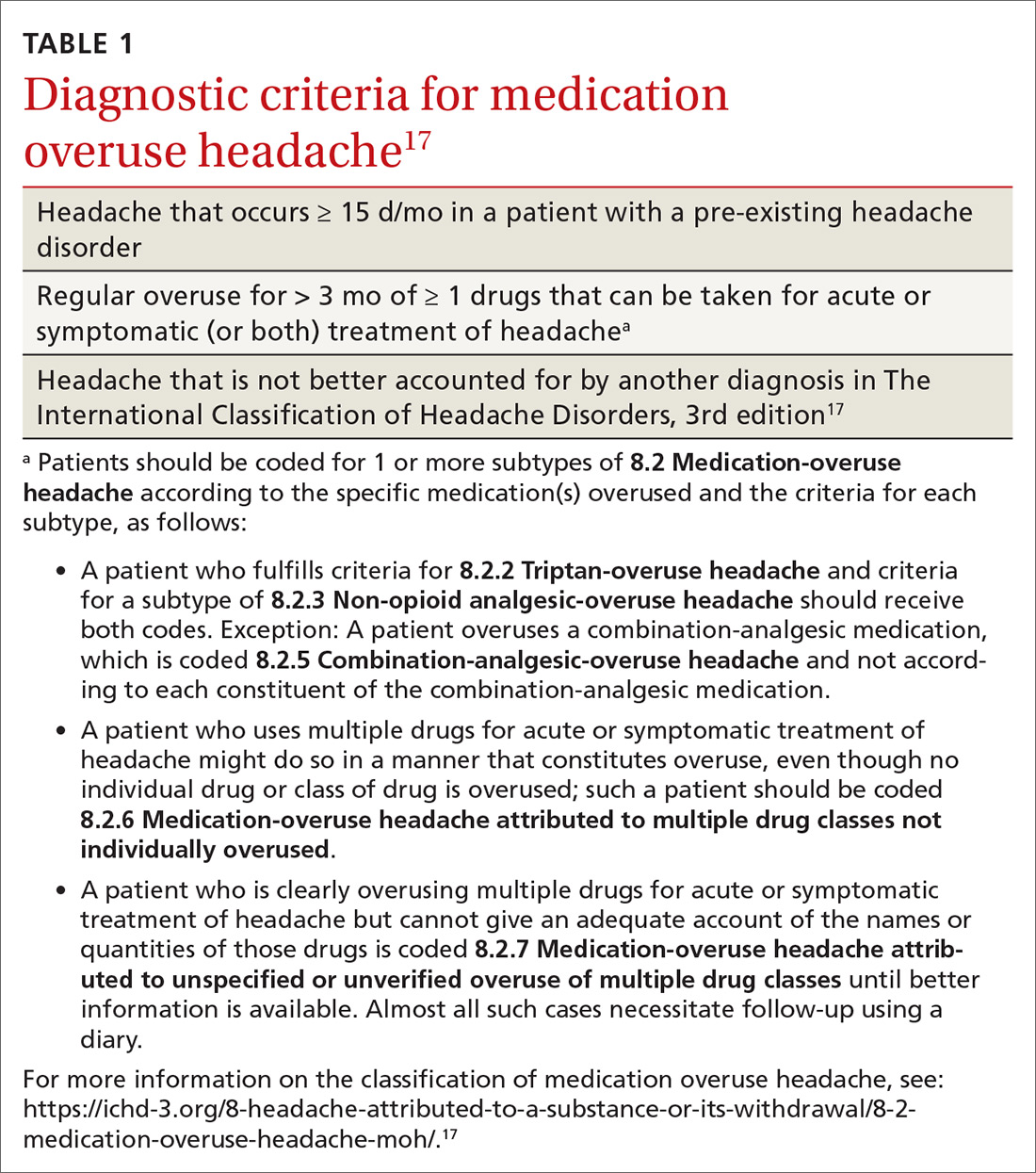
Terminology. MOH has also been called rebound headache, drug-induced headache, and transformed migraine, but these terms are outdated and are not formal diagnoses. Patients sometimes refer to substance-withdrawal headaches (not discussed in this article) as rebound headaches, so clarity is important when discussing headache with patients: namely, that MOH is an exacerbation of an existing headache condition caused by overuse of abortive headache medications, including analgesics, combination analgesics, triptans, barbiturates, and opioids.
MOH was recognized in the early 1950s and fully differentiated as a diagnosis in 2005 in the second edition of the ICHD. The disorder is subcategorized by offending abortive agent (TABLE 217) because the frequency of analgesic use required to develop MOH differs by agent.
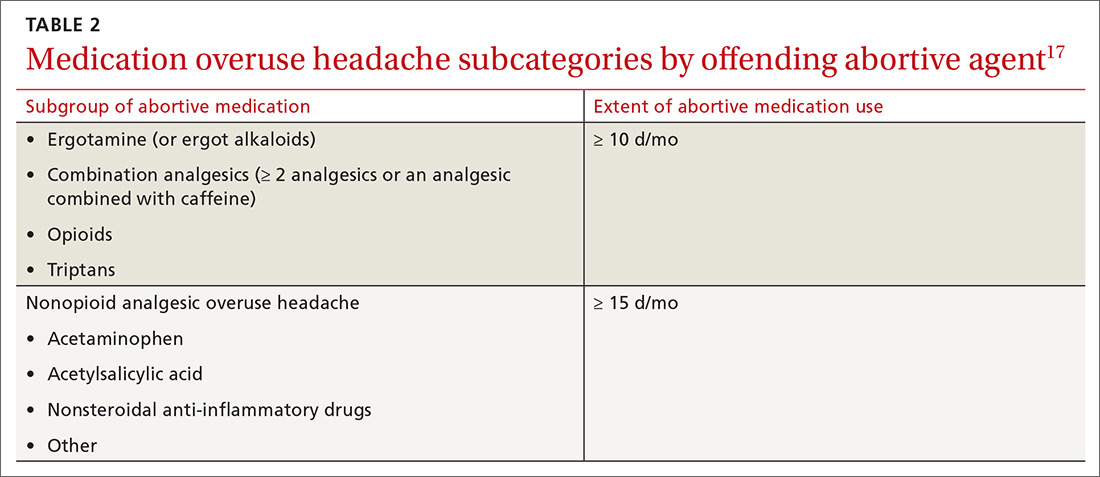
Risk factors for MOH and chronification of a primary headache disorder. There are several risk factors for developing MOH, and others that contribute to increasing headache frequency in general (TABLE 35,14,18-23). Some risk factors are common to each. All are important to address because some are modifiable.
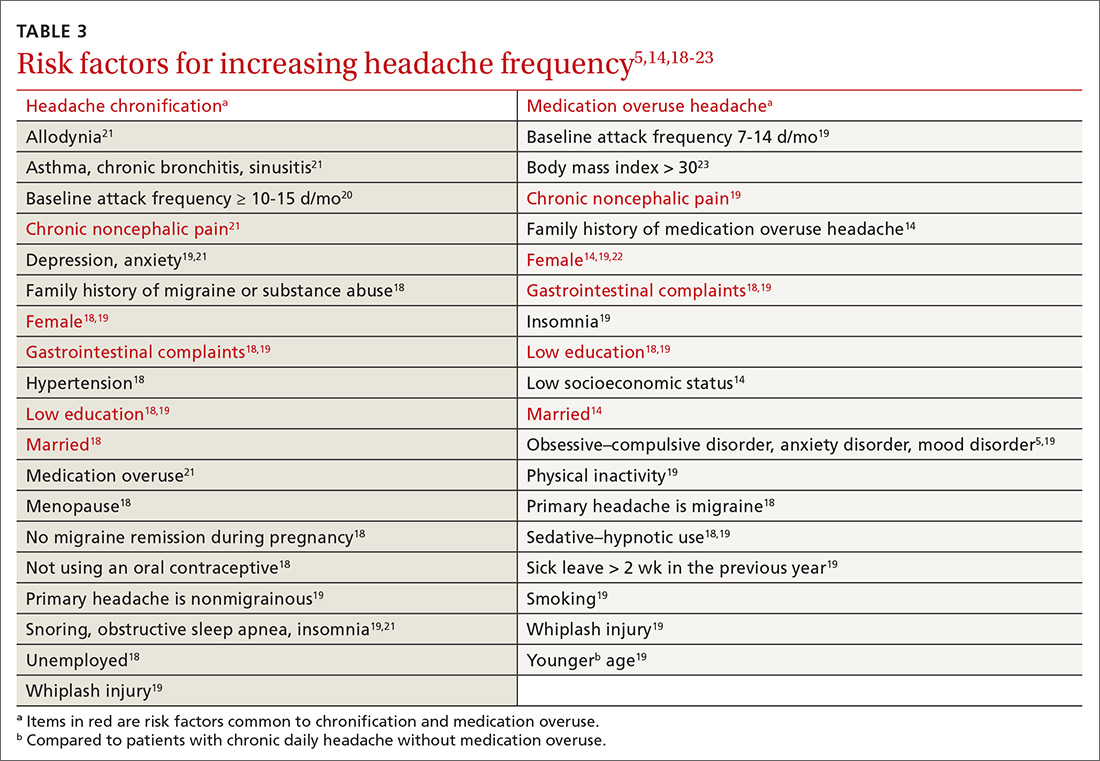
Continue to: Pathophysiology
Pathophysiology. The pathophysiology and psychology behind MOH are largely unknown. Physiologic changes in pain processing and functional imaging changes have been demonstrated in patients with MOH, both of which are reversible upon withdrawal of medication.23 Genetic factors and changes in hormone and neurotransmitter levels are found in MOH patients; this is not the case in patients who have an episodic headache pattern only.24
Presentation. Diagnostic criteria for MOH do not include clinical characteristics. Typically, the phenotype of MOH in a given patient is similar to the underlying primary headache25—although this principle can be complicated to tease out because these medications can suppress some symptoms. Diagnosis of a primary headache disorder should be documented along with the diagnosis of MOH.
Medication overuse can exist without MOH: Not every patient who frequently uses an abortive medication develops MOH.
Treatment is multifaceted—and can become complex
Mainstays of treatment of MOH are education about the disorder and detoxification from the overused agent, although specific treatments can differ depending on the agent involved, the frequency and duration of its use, and a patient’s behavioral patterns and psychiatric comorbidities. Often, a daily medication to prevent headache is considered upon, or after, withdrawal of the offending agent. The timing of introducing a preventive might impact its effectiveness. Some refractory cases require more intensive therapy, including hospitalization at a specialized tertiary center.
But before we look at detoxification from an overused agent, it’s important to review one of the best strategies of all in combatting MOH.
Continue to: First and best strategy
First and best strategy: Avoid onset of MOH
Select an appropriate abortive to reduce the risk of MOH. With regard to specific acute headache medications, some nuances other than type of headache should be considered. Nonsteroidal anti-inflammatory drugs (NSAIDs) are recommended as abortive therapy by the American Headache Society for their efficacy, favorable adverse effect profile, and low cost. NSAIDs are protective against development of MOH if a patient’s baseline headache frequency is < 10/mo; at a frequency of 10 to 14 d/mo, however, the risk of MOH increases when using an NSAID.6 A similar effect has been seen with triptans.16 Longer-acting NSAIDs, such as nabumetone and naproxen, have been proposed as less likely to cause MOH, and are even used as bridging therapy sometimes (as long as neither of these was the overused medication).26
The time it takes to develop MOH is shortest with triptans, followed by ergots, then analgesics.27
Prospective cohort studies6,16 have shown that barbiturates and opioids are more likely to induce MOH; for that reason, agents in these analgesic classes are almost universally avoided unless no other medically acceptable options exist. Using barbiturate-containing compounds or opioids > 4 d/mo exponentially increases the likelihood of MOH.
Promising preclinical data demonstrate that the gepant, or small-molecule calcitonin gene-related peptide (CGRP) receptor antagonist, class of medications used as abortive therapy does not induce medication overuse cutaneous allodynia.28
Provide education. Primary prevention of MOH involves (1) increasing patients’ awareness of how to take medications appropriately and (2) restricting intake of over-the-counter abortive medications. Often, the expert recommendation is to limit abortives to approximately 2 d/wk because more frequent use places patients at risk of further increased use and subsequent MOH.
Continue to: A randomized controlled trial in Norway...
A randomized controlled trial in Norway compared outcomes in 2 groups of patients with MOH: One group was given advice on the disorder by a physician; the other group was not provided with advice. In the “business-as-usual” group, there was no significant improvement; however, when general practitioners provided simple advice (lasting roughly 9 minutes) about reducing abortive medication use to a safe level and cautioned patients that they would be “feeling worse before feeling better,” headache days were reduced by approximately 8 per month and medication days, by 16 per month.2
A subsequent, long-term follow-up study29 of patients from the Norway trial2 who had been given advice and education showed a relapse rate (ie, into overuse of headache medication) of only 8% and sustained reduction of headache days and medication use at 16 months.
Offer support and other nondrug interventions. A recent review of 3 studies23 recommended that extra support for patients from a headache nurse, close follow-up, keeping an electronic diary that provides feedback, and undertaking a short course of psychotherapy can reduce medication overuse and prevent relapse.
If MOH develops, initiate withdrawal, introduce a preventive
Withdraw overused medication. Most current evidence suggests that withdrawal of the offending agent is the most effective factor in reducing headache days and improving quality of life. A randomized controlled trial compared the effects of (1) complete and immediate withdrawal of an abortive medication with (2) reducing its use (ie, limiting intake to 2 d/wk), on headache frequency, disability, and quality of life.30 There was a reduction of headache days in both groups; however, reduction was much greater at 2 months in the complete withdrawal group than in the restricted intake group (respectively, a 41% and a 26% reduction in headache days per month). This effect was sustained at 6 and 12 months in both groups. The study confirmed the results of earlier research2,15: Abrupt withdrawal leads to reversion to an episodic pattern at 2 to 6 months in approximately 40% to 60% of patients.
More studies are needed to determine the most appropriate treatment course for MOH; however, complete withdrawal of the causative drug is the most important intervention.
Continue to: Consider withdrawal plus preventive treatment
Consider withdrawal plus preventive treatment. Use of sodium valproate, in addition to medication overuse detoxification, led to a significant reduction in headache days and improvement in quality of life at 12 weeks but no difference after 24 weeks, compared with detoxification alone in a randomized, double-blind, placebo-controlled study.31
A study of 61 patients showed a larger reduction (by 7.2 d/mo) in headache frequency with any preventive medication in addition to medication withdrawal, compared to withdrawal alone (by 4.1 d/mo) after 3 months; however, the relative benefit was gone at 6 months.32
A study of 98 patients compared immediate and delayed initiation of preventive medication upon withdrawal of overused abortive medication.33 Response was defined as a > 50% reduction in headache frequency and was similar in both groups; results showed a 28% response with immediate initiation of a preventive; a 23% response with delayed (ie, 2 months after withdrawal) initiation; and a 48% response in both groups at 12 months.
Collectively, these studies suggest that adding a preventive medication at the time of withdrawal has the potential to reduce headache frequency more quickly than withdrawal alone. However, after 3 to 6 months, the outcome of reduced headache frequency is the same whether or not a preventive medication is used—as long as the offending agent has been withdrawn.
Do preventives work without withdrawing overused medication? Patients with MOH often show little or no improvement with addition of a preventive medication only; their response to a preventive improves after withdrawal of the overused medication. Patients without previous headache improvement after addition of a preventive, who also did not improve 2 months after withdrawal, then demonstrated an overall reduction in headache by 26% when a preventive was reintroduced after withdrawal.2
Continue to: The research evidence for preventives
The research evidence for preventives. Medications for headache prevention have not been extensively evaluated specifically for treating MOH. Here is what’s known:
- Flunarizine, amitriptyline, and beta-blockers usually are ineffective for MOH.24
- Results for topiramate are mixed: A small, double-blind, placebo-controlled chronic migraine study in Europe showed that, in a subgroup of patients with MOH, topiramate led to a small but significant reduction (3.5 d/mo) in headache frequency, compared to placebo.27 A similar study done in the United States did not show a significant difference between the active-treatment and placebo groups.34
- Findings regarding onabotulinumtoxinA are intriguing: In a posthoc analysis of onabotulinumtoxinA to treat chronic migraine, patients with MOH who did not undergo detoxification had an 8 d/mo greater reduction in headache, compared to placebo.35 However, when compared to placebo in conjunction with detoxification, onabotulinumtoxinA demonstrated no benefit.36
- Newer CGRP antagonist and CGRP receptor antagonist monoclonal antibodies are successful preventive medications that have demonstrated a reduction in acute medication use days per month and headache days per month37; these compounds have not been compared to withdrawal alone.
Reducing the severity and duration of withdrawal symptoms
Withdrawal from overused abortive headache medications can lead to worsening headache, nausea, vomiting, hypotension, tachycardia, sleep disturbances, restlessness, anxiety, and nervousness. Symptoms usually last 2 to 10 days but can persist for as long as 4 weeks; duration of withdrawal symptoms varies with the medication that is being overused. In patients who have used a triptan, for example, mean duration of withdrawal is 4.1 days; ergotamine, 6.7 days; and NSAIDs, 9.5 days.23 Tapered withdrawal is sometimes recommended with opioids and barbiturates to reduce withdrawal symptoms. It is unclear whether starting a preventive medication during withdrawal assists in reducing withdrawal symptoms.38
Bridging therapy to reduce symptoms of withdrawal is often provided despite debatable utility. Available evidence does not favor one agent or method but suggests some strategies that could be helpful:
- A prednisone taper has a potential role during the first 6 days of withdrawal by reducing rebound headache and withdrawal symptoms39; however, oral prednisolone has been shown to have no benefit.40
- Alone, IV methylprednisolone seems not to be of benefit; however, in a retrospective study of 94 patients, IV methylprednisolone plus diazepam for 5 days led to a significant reduction in headache frequency and drug consumption that was sustained after 3 months.41
- Celecoxib was compared to prednisone over a 20-day course: a celecoxib dosage of 400 mg/d for the first 5 days, tapered by 100 mg every 5 days, and an oral prednisone dosage of 75 mg/d for the first 5 days, then tapered every 5 days. Patients taking celecoxib had lower headache intensity but there was no difference in headache frequency and acute medication intake between the groups.42
Other strategies. Using antiemetics and NSAIDs to reduce withdrawal symptoms is widely practiced, but no placebo-controlled trials have been conducted to support this strategy.
Patients in withdrawal might be more likely to benefit from inpatient care if they have a severe comorbidity, such as opioid or barbiturate use; failure to respond to, tolerate, or adhere to treatment; or relapse after withdrawal.38
Continue to: Cognitive behavioral therapy...
Cognitive behavioral therapy, exercise, a headache diary, and biofeedback should be considered in every patient’s treatment strategy because a multidisciplinary approach increases adherence and leads to improvement in headache frequency and a decrease in disability and medication use.43
Predictors of Tx success
A prospective cohort study determined that the rate of MOH relapse is 31% at 6 months, 41% at 1 year, and 45% at 4 years, with the highest risk of relapse during the first year.44 Looking at the correlation between type of medication overused and relapse rate, the research indicates that
- triptans have the lowest risk of relapse,44
- simple analgesics have a higher risk of relapse than triptans,22,44 and
- opioids have the highest risk of relapse.22
Where the data don’t agree. Data on combination analgesics and on ergots are conflicting.22 In addition, data on whether the primary type of headache predicts relapse rate conflict; however, migraine might predict a better outcome than tension-type headache.22
To recap and expand: Management pearls
The major goals of headache management generally are to rule out secondary headache, reach a correct diagnosis, reduce overall headache frequency, and provide effective abortive medication. A large component of reducing headache frequency is addressing and treating medication overuse.
Seek to understand the nature of the patient’s headache disorder. Components of the history are key in identifying the underlying headache diagnosis and ruling out other, more concerning secondary headache diagnoses. The ICHD-3 is an excellent resource for treating headache disorders because the classification lists specific diagnostic criteria for all recognized headache diagnoses.
Continue to: Medication withdrawal...
Medication withdrawal—with or without preventive medication—should reduce the frequency of MOH in 2 or 3 months. If headache does not become less frequent, however, the headache diagnosis might need to be reconsidered. Minimizing the use of abortive medication is generally recommended, but reduction or withdrawal of these medications does not guarantee that patients will revert to an episodic pattern of headache.
Treating withdrawal symptoms is a reasonable approach in some patients, but evidence does not support routinely providing bridging therapy.
Apply preventives carefully. Abortive medication withdrawal should generally be completed before initiating preventive medication; however, over the short term, starting preventive therapy while withdrawing the overused medication could assist in reducing headache frequency rapidly. This strategy can put patients at risk of medication adverse effects and using the medications longer than necessary, yet might be reasonable in certain patients, given their comorbidities, risk of relapse, and physician and patient preference. A preventive medication for an individual patient should generally be chosen in line with recommendations of the American Academy of Neurology45 and on the basis of the history and comorbidities.
Provide education, which is essential to lowering barriers to success. Patients with MOH must be counseled to understand that (1) a headache treatment that is supposed to be making them feel better is, in fact, making them feel worse and (2) they will get worse before they get better. Many patients are afraid to be without medication to use as needed. It is helpful to educate them on the different types of treatments (abortive, preventive); how MOH interferes with headache prophylaxis and medication efficacy; how MOH alters brain function (ie, aforementioned physiologic changes in pain processing and functional imaging changes23); and that such change is reversible when medication is withdrawn.
ACKNOWLEDGEMENT
The author thanks Jeffrey Curtis, MD, MPH, for his support and editing assistance with the manuscript.
CORRESPONDENCE
Allison Crain, MD, 2927 N 7th Avenue, Phoenix, AZ 85013; [email protected].
1. Zeeberg P, Olesen J, Jensen R. Discontinuation of medication overuse in headache patients: recovery of therapeutic responsiveness. Cephalalgia. 2006;26:1192-1198.
2. Kristoffersen ES, Straand J, Vetvik KG, et al. Brief intervention for medication-overuse headache in primary care. The BIMOH study: a double-blind pragmatic cluster randomised parallel controlled trial. J Neurol Neurosurg Psychiatry. 2015;86:505-512.
3. Bahra A, Walsh M, Menon S, et al. Does chronic daily headache arise de novo in association with regular use of analgesics? Headache. 2003;43:179-190.
4. Blumenfeld AM, Varon SF, Wilcox TK, et al. Disability, HRQoL and resource use among chronic and episodic migraineurs: results from the International Burden of Migraine Study (IBMS) Cephalalgia. 2011;31:301-315.
5. Chu H-T, Liang C-S, Lee J-T, et al. Associations between depression/anxiety and headache frequency in migraineurs: a cross-sectional study. Headache. 2018;58:407-415.
6. Bigal ME, Lipton RB. Excessive acute migraine medication use and migraine progression. Neurology. 2008;71:1821-1828.
7. Colás R, Muñoz P, Temprano R, et al. Chronic daily headache with analgesic overuse: epidemiology and impact on quality of life. Neurology. 2004;62:1338-1342.
8. Linde M, Gustavsson A, Stovner LJ, et al. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. 2012;19:703-711.
9. Shah AM, Bendtsen L, Zeeberg P, et al. Reduction of medication costs after detoxification for medication-overuse headache. Headache. 2013;53:665-672.
10. . Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17:954-976.
11. Kernick D, Stapley S, Goadsby PJ, et al. What happens to new-onset headache presenting to primary care? A case–cohort study using electronic primary care records. Cephalalgia. 2008;28:1188-1195.
12. Stone J, Carson A, Duncan R, et al. Who is referred to neurology clinics?—the diagnoses made in 3781 new patients. Clin Neurol Neurosurg. 2010;112:747-751.
13. Munoz-Ceron J, Marin-Careaga V, L, et al. Headache at the emergency room: etiologies, diagnostic usefulness of the ICHD 3 criteria, red and green flags. PloS One. 2019;14:e0208728.
14. Evers S, Marziniak M. Clinical features, pathophysiology, and treatment of medication-overuse headache. Lancet Neurol. 2010;9:391-401.
15. Tassorelli C, Jensen R, Allena M, et al; the . A consensus protocol for the management of medication-overuse headache: evaluation in a multicentric, multinational study. Cephalalgia. 2014;34:645-655.
16. Bigal ME, Serrano D, Buse D, et al. Acute migraine medications and evolution from episodic to chronic migraine: a longitudinal population-based study. Headache. 2008;48:1157-1168.
17. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1-211.
18. Ferrari A, Leone S, Vergoni AV, et al. Similarities and differences between chronic migraine and episodic migraine. Headache. 2007;47:65-72.
19. Hagen K, Linde M, Steiner TJ, et al. Risk factors for medication-overuse headache: an 11-year follow-up study. The Nord-Trøndelag Health Studies. Pain. 2012;153:56-61.
20. Katsarava Z, Schneewiess S, Kurth T, et al. Incidence and predictors for chronicity of headache in patients with episodic migraine. Neurology. 2004;62:788-790.
21. Lipton RB, Fanning KM, Buse DC, et al. Migraine progression in subgroups of migraine based on comorbidities: results of the CaMEO study. Neurology. 2019;93:e2224-e2236.
22. Munksgaard SB, Madsen SK, Wienecke T. Treatment of medication overuse headache—a review. Acta Neurol Scand. 2019;139:405-414.
23. Ferraro S, Grazzi L, Mandelli M, et al. Pain processing in medication overuse headache: a functional magnetic resonance imaging (fMRI) study. Pain Med. 2012;13:255-262.
24. Diener H-C, Holle D, Solbach K, et al. Medication-overuse headache: risk factors, pathophysiology and management. Nat Rev Neurol. 2016;12:575-583.
25. Limmroth V, Katsarava Z, Fritsche G, et al. Features of medication overuse headache following overuse of different acute headache drugs. Neurology. 2002;59:1011-1014.
26. Mauskop A, ed. Migraine and Headache. 2nd ed. Oxford University Press; 2013.
27. Diener H-C, Bussone G, Van Oene JC, et al; . Topiramate reduces headache days in chronic migraine: a randomized, double-blind, placebo-controlled study. Cephalalgia. 2007;27:814-823.
28. Navratilova E, Behravesh S, Oyarzo J, et al. Ubrogepant does not induce latent sensitization in a preclinical model of medication overuse headache Cephalalgia. 2020;40:892-902.
29. Kristoffersen ES, Straand J, Russell MB, et al. Lasting improvement of medication-overuse headache after brief intervention—a long-term follow-up in primary care. Eur J Neurol. 2017;24:883-891.
30. Carlsen LN, Munksgaard SB, Jensen RH, et al. Complete detoxification is the most effective treatment of medication-overuse headache: a randomized controlled open-label trial. Cephalalgia. 2018;38:225-236.
31. Sarchielli P, Messina P, Cupini LM, et al; SAMOHA Study Group. Sodium valproate in migraine without aura and medication overuse headache: a randomized controlled trial. Eur Neuropsychopharmacol. 2014;24:1289-1297.
32. Hagen K, Stovner LJ. A randomized controlled trial on medication-overuse headache: outcome after 1 and 4 years. Acta Neurol Scand Suppl. 2011;124(suppl 191):38-43.
33. Munksgaard SB, Bendtsen L, Jensen RH. Detoxification of medication-overuse headache by a multidisciplinary treatment programme is highly effective: a comparison of two consecutive treatment methods in an open-label design. Cephalalgia. 2012;32:834-844.
34. Silberstein S, Lipton R, Dodick D, et al. Topiramate treatment of chronic migraine: a randomized, placebo-controlled trial of quality of life and other efficacy measures. Headache. 2009;49:1153-1162.
35. Silberstein SD, Blumenfeld AM, Cady RK, et al. OnabotulinumtoxinA for treatment of chronic migraine: PREEMPT 24-week pooled subgroup analysis of patients who had acute headache medication overuse at baseline. J Neurol Sci. 2013;331:48-56.
36. Sandrini G, Perrotta A, Tassorelli C, et al. Botulinum toxin type-A in the prophylactic treatment of medication-overuse headache: a multicenter, double-blind, randomized, placebo-controlled, parallel group study. J Headache Pain. 2011;12:427-433.
37. Tepper SJ. CGRP and headache: a brief review. Neurol Sci. 2019;40(suppl 1):99-105.
38. Diener H-C, Dodick D, Evers S, et al. Pathophysiology, prevention and treatment of medication overuse headache. Lancet Neurol. 2019;18:891-902.
39. Krymchantowski AV, Barbosa JS. Prednisone as initial treatment of analgesic-induced daily headache. Cephalalgia. 2000;20:107-113.
40. Bøe MG, Mygland A, Salvesen R. Prednisolone does not reduce withdrawal headache: a randomized, double-blind study. Neurology. 2007;69:26-31.
41. Paolucci M, Altamura C, Brunelli N, et al. Methylprednisolone plus diazepam i.v. as bridge therapy for medication overuse headache. Neurol Sci. 2017;38:2025-2029.
42. Taghdiri F, Togha M, Razeghi Jahromi S, et al. Celecoxib vs prednisone for the treatment of withdrawal headache in patients with medication overuse headache: a randomized, double-blind clinical trial. Headache. 2015;55:128-135.
43. Ramsey RR, Ryan JL, Hershey AD, et al. Treatment adherence in patients with headache: a systematic review. Headache. 2014;54:795-816.
44. Katsarava Z, Muessig M, Dzagnidze A, et al. Medication overuse headache: rates and predictors for relapse in a 4-year prospective study. Cephalalgia. 2005;25:12-15.
45. Silberstein SD, Holland S, Freitag F, et al; . Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012; 78:1137-1145.
1. Zeeberg P, Olesen J, Jensen R. Discontinuation of medication overuse in headache patients: recovery of therapeutic responsiveness. Cephalalgia. 2006;26:1192-1198.
2. Kristoffersen ES, Straand J, Vetvik KG, et al. Brief intervention for medication-overuse headache in primary care. The BIMOH study: a double-blind pragmatic cluster randomised parallel controlled trial. J Neurol Neurosurg Psychiatry. 2015;86:505-512.
3. Bahra A, Walsh M, Menon S, et al. Does chronic daily headache arise de novo in association with regular use of analgesics? Headache. 2003;43:179-190.
4. Blumenfeld AM, Varon SF, Wilcox TK, et al. Disability, HRQoL and resource use among chronic and episodic migraineurs: results from the International Burden of Migraine Study (IBMS) Cephalalgia. 2011;31:301-315.
5. Chu H-T, Liang C-S, Lee J-T, et al. Associations between depression/anxiety and headache frequency in migraineurs: a cross-sectional study. Headache. 2018;58:407-415.
6. Bigal ME, Lipton RB. Excessive acute migraine medication use and migraine progression. Neurology. 2008;71:1821-1828.
7. Colás R, Muñoz P, Temprano R, et al. Chronic daily headache with analgesic overuse: epidemiology and impact on quality of life. Neurology. 2004;62:1338-1342.
8. Linde M, Gustavsson A, Stovner LJ, et al. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. 2012;19:703-711.
9. Shah AM, Bendtsen L, Zeeberg P, et al. Reduction of medication costs after detoxification for medication-overuse headache. Headache. 2013;53:665-672.
10. . Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17:954-976.
11. Kernick D, Stapley S, Goadsby PJ, et al. What happens to new-onset headache presenting to primary care? A case–cohort study using electronic primary care records. Cephalalgia. 2008;28:1188-1195.
12. Stone J, Carson A, Duncan R, et al. Who is referred to neurology clinics?—the diagnoses made in 3781 new patients. Clin Neurol Neurosurg. 2010;112:747-751.
13. Munoz-Ceron J, Marin-Careaga V, L, et al. Headache at the emergency room: etiologies, diagnostic usefulness of the ICHD 3 criteria, red and green flags. PloS One. 2019;14:e0208728.
14. Evers S, Marziniak M. Clinical features, pathophysiology, and treatment of medication-overuse headache. Lancet Neurol. 2010;9:391-401.
15. Tassorelli C, Jensen R, Allena M, et al; the . A consensus protocol for the management of medication-overuse headache: evaluation in a multicentric, multinational study. Cephalalgia. 2014;34:645-655.
16. Bigal ME, Serrano D, Buse D, et al. Acute migraine medications and evolution from episodic to chronic migraine: a longitudinal population-based study. Headache. 2008;48:1157-1168.
17. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1-211.
18. Ferrari A, Leone S, Vergoni AV, et al. Similarities and differences between chronic migraine and episodic migraine. Headache. 2007;47:65-72.
19. Hagen K, Linde M, Steiner TJ, et al. Risk factors for medication-overuse headache: an 11-year follow-up study. The Nord-Trøndelag Health Studies. Pain. 2012;153:56-61.
20. Katsarava Z, Schneewiess S, Kurth T, et al. Incidence and predictors for chronicity of headache in patients with episodic migraine. Neurology. 2004;62:788-790.
21. Lipton RB, Fanning KM, Buse DC, et al. Migraine progression in subgroups of migraine based on comorbidities: results of the CaMEO study. Neurology. 2019;93:e2224-e2236.
22. Munksgaard SB, Madsen SK, Wienecke T. Treatment of medication overuse headache—a review. Acta Neurol Scand. 2019;139:405-414.
23. Ferraro S, Grazzi L, Mandelli M, et al. Pain processing in medication overuse headache: a functional magnetic resonance imaging (fMRI) study. Pain Med. 2012;13:255-262.
24. Diener H-C, Holle D, Solbach K, et al. Medication-overuse headache: risk factors, pathophysiology and management. Nat Rev Neurol. 2016;12:575-583.
25. Limmroth V, Katsarava Z, Fritsche G, et al. Features of medication overuse headache following overuse of different acute headache drugs. Neurology. 2002;59:1011-1014.
26. Mauskop A, ed. Migraine and Headache. 2nd ed. Oxford University Press; 2013.
27. Diener H-C, Bussone G, Van Oene JC, et al; . Topiramate reduces headache days in chronic migraine: a randomized, double-blind, placebo-controlled study. Cephalalgia. 2007;27:814-823.
28. Navratilova E, Behravesh S, Oyarzo J, et al. Ubrogepant does not induce latent sensitization in a preclinical model of medication overuse headache Cephalalgia. 2020;40:892-902.
29. Kristoffersen ES, Straand J, Russell MB, et al. Lasting improvement of medication-overuse headache after brief intervention—a long-term follow-up in primary care. Eur J Neurol. 2017;24:883-891.
30. Carlsen LN, Munksgaard SB, Jensen RH, et al. Complete detoxification is the most effective treatment of medication-overuse headache: a randomized controlled open-label trial. Cephalalgia. 2018;38:225-236.
31. Sarchielli P, Messina P, Cupini LM, et al; SAMOHA Study Group. Sodium valproate in migraine without aura and medication overuse headache: a randomized controlled trial. Eur Neuropsychopharmacol. 2014;24:1289-1297.
32. Hagen K, Stovner LJ. A randomized controlled trial on medication-overuse headache: outcome after 1 and 4 years. Acta Neurol Scand Suppl. 2011;124(suppl 191):38-43.
33. Munksgaard SB, Bendtsen L, Jensen RH. Detoxification of medication-overuse headache by a multidisciplinary treatment programme is highly effective: a comparison of two consecutive treatment methods in an open-label design. Cephalalgia. 2012;32:834-844.
34. Silberstein S, Lipton R, Dodick D, et al. Topiramate treatment of chronic migraine: a randomized, placebo-controlled trial of quality of life and other efficacy measures. Headache. 2009;49:1153-1162.
35. Silberstein SD, Blumenfeld AM, Cady RK, et al. OnabotulinumtoxinA for treatment of chronic migraine: PREEMPT 24-week pooled subgroup analysis of patients who had acute headache medication overuse at baseline. J Neurol Sci. 2013;331:48-56.
36. Sandrini G, Perrotta A, Tassorelli C, et al. Botulinum toxin type-A in the prophylactic treatment of medication-overuse headache: a multicenter, double-blind, randomized, placebo-controlled, parallel group study. J Headache Pain. 2011;12:427-433.
37. Tepper SJ. CGRP and headache: a brief review. Neurol Sci. 2019;40(suppl 1):99-105.
38. Diener H-C, Dodick D, Evers S, et al. Pathophysiology, prevention and treatment of medication overuse headache. Lancet Neurol. 2019;18:891-902.
39. Krymchantowski AV, Barbosa JS. Prednisone as initial treatment of analgesic-induced daily headache. Cephalalgia. 2000;20:107-113.
40. Bøe MG, Mygland A, Salvesen R. Prednisolone does not reduce withdrawal headache: a randomized, double-blind study. Neurology. 2007;69:26-31.
41. Paolucci M, Altamura C, Brunelli N, et al. Methylprednisolone plus diazepam i.v. as bridge therapy for medication overuse headache. Neurol Sci. 2017;38:2025-2029.
42. Taghdiri F, Togha M, Razeghi Jahromi S, et al. Celecoxib vs prednisone for the treatment of withdrawal headache in patients with medication overuse headache: a randomized, double-blind clinical trial. Headache. 2015;55:128-135.
43. Ramsey RR, Ryan JL, Hershey AD, et al. Treatment adherence in patients with headache: a systematic review. Headache. 2014;54:795-816.
44. Katsarava Z, Muessig M, Dzagnidze A, et al. Medication overuse headache: rates and predictors for relapse in a 4-year prospective study. Cephalalgia. 2005;25:12-15.
45. Silberstein SD, Holland S, Freitag F, et al; . Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012; 78:1137-1145.
PRACTICE RECOMMENDATIONS
› Avoid prescribing barbiturates or opioids for a headache disorder. A
› Limit use of a headache-abortive medication to twice a week when starting a patient on the drug. C
› Consider providing bridging therapy during detoxification of the overused medication. C
› Do not provide a preventive medication without withdrawing the overused agent. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
COVID-19 may damage blood vessels in the brain
Until now, the neurological manifestations of COVID-19 have been believed to be a result of direct damage to nerve cells. However, a new study suggests that the virus might actually damage the brain’s small blood vessels rather than nerve cells themselves.
The findings add further weight to previous research into neurological complications from COVID-19, according to Anna Cervantes, MD. Dr. Cervantes is assistant professor of neurology at the Boston University and has been studying the neurological effects of COVID-19, though she was not involved in this study. “I can tell from my personal experience, and things we’ve published on and the literature that’s out there – there are patients that are having complications like stroke that aren’t even critically ill from COVID. We’re seeing that not in just the acute setting, but also in a delayed fashion. Even though most of the coagulopathy is largely venous and probably microvascular, this does affect the brain through a myriad of ways,” Dr. Cervantes said.
The research was published online Jan. 12 in the New England Journal of Medicine. Myoung‑Hwa Lee, PhD, was the lead author.
The study included high resolution magnetic resonance imaging and histopathological examination of 13 individuals with a median age of 50 years. Among 10 patients with brain alterations, the researchers conducted further studies in 5 individuals using multiplex fluorescence imaging and chromogenic immunostaining in all 10.
The team conducted conventional histopathology on the brains of 18 individuals. Fourteen had a history of chronic illness, including diabetes, and hypertension, and 11 had died unexpectedly or been found dead. Magnetic resonance microscopy revealed punctuate hypo-intensities in nine subjects, indicating microvascular injury and fibrinogen leakage. Histopathology using fluorescence imaging showed the same features. Collagen IV immunostaining showed thinning of the basal lamina of the endothelial cells in five patients. Ten patients had congested blood vessels and surrounding fibrinogen leakage, but comparatively intact vasculature. The researchers interpreted linear hypo-intensities as micro-hemorrhages.
The researchers found little perivascular inflammation, and no vascular occlusion. Thirteen subjects had perivascular-activated microglia, macrophage infiltrates, and hypertrophic astrocytes. Eight had CD3+ and CD8+ T cells in the perivascular spaces and in lumens next to endothelial cells, which could help explain vascular injury.
The researchers found no evidence of the SARS-CoV-2 virus itself, despite efforts using polymerase chain reaction with multiple primer sets, RNA sequencing within the brain, or RNA in situ hybridization and immunostaining. Subjects may have cleared the virus by the time they died, or viral copy numbers could have been below the detection limit of the assays.
The researchers also obtained a convenience sample of subjects who had died from COVID-19. Magnetic resonance microscopy, histopathology, and immunohistochemical analysis of sections revealed microvascular injury in the brain and olfactory bulb, despite no evidence of viral infection. The authors stressed that they could not draw conclusions about the neurological features of COVID-19 because of a lack of clinical information.
Dr. Cervantes noted that limitation: “We’re seeing a lot of patients with encephalopathy or alterations in their mental status. A lot of things can cause that, and some are common in patients who are critically ill, like medications and metabolic derangement.”
Still, the findings could help to inform future medical management. “There’s going to be a large number of patients who don’t have really bad pulmonary disease but still may have encephalopathy. So if there is small vessel involvement because of inflammation that we might not necessarily catch in a lumbar puncture or routine imaging, there’s still somebody we can make better (using) steroids. Having more information on what’s happening on a pathophysiologic level and on pathology is really helpful.”
The study was supported by internal funds from the National Institute of Neurological Disorders and Stroke. Dr. Cervantes has no relevant financial disclosures.
Until now, the neurological manifestations of COVID-19 have been believed to be a result of direct damage to nerve cells. However, a new study suggests that the virus might actually damage the brain’s small blood vessels rather than nerve cells themselves.
The findings add further weight to previous research into neurological complications from COVID-19, according to Anna Cervantes, MD. Dr. Cervantes is assistant professor of neurology at the Boston University and has been studying the neurological effects of COVID-19, though she was not involved in this study. “I can tell from my personal experience, and things we’ve published on and the literature that’s out there – there are patients that are having complications like stroke that aren’t even critically ill from COVID. We’re seeing that not in just the acute setting, but also in a delayed fashion. Even though most of the coagulopathy is largely venous and probably microvascular, this does affect the brain through a myriad of ways,” Dr. Cervantes said.
The research was published online Jan. 12 in the New England Journal of Medicine. Myoung‑Hwa Lee, PhD, was the lead author.
The study included high resolution magnetic resonance imaging and histopathological examination of 13 individuals with a median age of 50 years. Among 10 patients with brain alterations, the researchers conducted further studies in 5 individuals using multiplex fluorescence imaging and chromogenic immunostaining in all 10.
The team conducted conventional histopathology on the brains of 18 individuals. Fourteen had a history of chronic illness, including diabetes, and hypertension, and 11 had died unexpectedly or been found dead. Magnetic resonance microscopy revealed punctuate hypo-intensities in nine subjects, indicating microvascular injury and fibrinogen leakage. Histopathology using fluorescence imaging showed the same features. Collagen IV immunostaining showed thinning of the basal lamina of the endothelial cells in five patients. Ten patients had congested blood vessels and surrounding fibrinogen leakage, but comparatively intact vasculature. The researchers interpreted linear hypo-intensities as micro-hemorrhages.
The researchers found little perivascular inflammation, and no vascular occlusion. Thirteen subjects had perivascular-activated microglia, macrophage infiltrates, and hypertrophic astrocytes. Eight had CD3+ and CD8+ T cells in the perivascular spaces and in lumens next to endothelial cells, which could help explain vascular injury.
The researchers found no evidence of the SARS-CoV-2 virus itself, despite efforts using polymerase chain reaction with multiple primer sets, RNA sequencing within the brain, or RNA in situ hybridization and immunostaining. Subjects may have cleared the virus by the time they died, or viral copy numbers could have been below the detection limit of the assays.
The researchers also obtained a convenience sample of subjects who had died from COVID-19. Magnetic resonance microscopy, histopathology, and immunohistochemical analysis of sections revealed microvascular injury in the brain and olfactory bulb, despite no evidence of viral infection. The authors stressed that they could not draw conclusions about the neurological features of COVID-19 because of a lack of clinical information.
Dr. Cervantes noted that limitation: “We’re seeing a lot of patients with encephalopathy or alterations in their mental status. A lot of things can cause that, and some are common in patients who are critically ill, like medications and metabolic derangement.”
Still, the findings could help to inform future medical management. “There’s going to be a large number of patients who don’t have really bad pulmonary disease but still may have encephalopathy. So if there is small vessel involvement because of inflammation that we might not necessarily catch in a lumbar puncture or routine imaging, there’s still somebody we can make better (using) steroids. Having more information on what’s happening on a pathophysiologic level and on pathology is really helpful.”
The study was supported by internal funds from the National Institute of Neurological Disorders and Stroke. Dr. Cervantes has no relevant financial disclosures.
Until now, the neurological manifestations of COVID-19 have been believed to be a result of direct damage to nerve cells. However, a new study suggests that the virus might actually damage the brain’s small blood vessels rather than nerve cells themselves.
The findings add further weight to previous research into neurological complications from COVID-19, according to Anna Cervantes, MD. Dr. Cervantes is assistant professor of neurology at the Boston University and has been studying the neurological effects of COVID-19, though she was not involved in this study. “I can tell from my personal experience, and things we’ve published on and the literature that’s out there – there are patients that are having complications like stroke that aren’t even critically ill from COVID. We’re seeing that not in just the acute setting, but also in a delayed fashion. Even though most of the coagulopathy is largely venous and probably microvascular, this does affect the brain through a myriad of ways,” Dr. Cervantes said.
The research was published online Jan. 12 in the New England Journal of Medicine. Myoung‑Hwa Lee, PhD, was the lead author.
The study included high resolution magnetic resonance imaging and histopathological examination of 13 individuals with a median age of 50 years. Among 10 patients with brain alterations, the researchers conducted further studies in 5 individuals using multiplex fluorescence imaging and chromogenic immunostaining in all 10.
The team conducted conventional histopathology on the brains of 18 individuals. Fourteen had a history of chronic illness, including diabetes, and hypertension, and 11 had died unexpectedly or been found dead. Magnetic resonance microscopy revealed punctuate hypo-intensities in nine subjects, indicating microvascular injury and fibrinogen leakage. Histopathology using fluorescence imaging showed the same features. Collagen IV immunostaining showed thinning of the basal lamina of the endothelial cells in five patients. Ten patients had congested blood vessels and surrounding fibrinogen leakage, but comparatively intact vasculature. The researchers interpreted linear hypo-intensities as micro-hemorrhages.
The researchers found little perivascular inflammation, and no vascular occlusion. Thirteen subjects had perivascular-activated microglia, macrophage infiltrates, and hypertrophic astrocytes. Eight had CD3+ and CD8+ T cells in the perivascular spaces and in lumens next to endothelial cells, which could help explain vascular injury.
The researchers found no evidence of the SARS-CoV-2 virus itself, despite efforts using polymerase chain reaction with multiple primer sets, RNA sequencing within the brain, or RNA in situ hybridization and immunostaining. Subjects may have cleared the virus by the time they died, or viral copy numbers could have been below the detection limit of the assays.
The researchers also obtained a convenience sample of subjects who had died from COVID-19. Magnetic resonance microscopy, histopathology, and immunohistochemical analysis of sections revealed microvascular injury in the brain and olfactory bulb, despite no evidence of viral infection. The authors stressed that they could not draw conclusions about the neurological features of COVID-19 because of a lack of clinical information.
Dr. Cervantes noted that limitation: “We’re seeing a lot of patients with encephalopathy or alterations in their mental status. A lot of things can cause that, and some are common in patients who are critically ill, like medications and metabolic derangement.”
Still, the findings could help to inform future medical management. “There’s going to be a large number of patients who don’t have really bad pulmonary disease but still may have encephalopathy. So if there is small vessel involvement because of inflammation that we might not necessarily catch in a lumbar puncture or routine imaging, there’s still somebody we can make better (using) steroids. Having more information on what’s happening on a pathophysiologic level and on pathology is really helpful.”
The study was supported by internal funds from the National Institute of Neurological Disorders and Stroke. Dr. Cervantes has no relevant financial disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
HHS will drop buprenorphine waiver rule for most physicians
Federal officials on Thursday announced a plan to largely drop the so-called X-waiver requirement for buprenorphine prescriptions for physicians in a bid to remove an administrative procedure widely seen as a barrier to opioid use disorder (OUD) treatment.
The Department of Health & Human Services unveiled new practice guidelines that include an exemption from current certification requirements. The exemption applies to physicians already registered with the Drug Enforcement Administration.
A restriction included in the new HHS policy is a limit of treating no more than 30 patients with buprenorphine for OUD at any one time. There is an exception to this limit for hospital-based physicians, such as those working in emergency departments, HHS said.
, such as buprenorphine, and does not apply to methadone. The new guidelines say the date on which they will take effect will be added after publication in the Federal Register. HHS did not immediately answer a request from this news organization for a more specific timeline.
Welcomed change
The change in prescribing rule was widely welcomed, with the American Medical Association issuing a statement endorsing the revision. The AMA and many prescribers and researchers had seen the X-waiver as a hurdle to address the nation’s opioid epidemic.
There were more than 83,000 deaths attributed to drug overdoses in the United States in the 12 months ending in June 2020. This is the highest number of overdose deaths ever recorded in a 12-month period, HHS said in a press release, which cited data from the Centers for Disease Control and Prevention.
In a tweet about the new policy, Peter Grinspoon, MD, a Boston internist and author of the memoir “Free Refills: A Doctor Confronts His Addiction,” contrasted the relative ease with which clinicians can give medicines that carry a risk for abuse with the challenge that has existed in trying to provide patients with buprenorphine.
“Absolutely insane that we need a special waiver for buprenorphine to TREAT opioid addiction, but not to prescribe oxycodone, Vicodin, etc., which can get people in trouble in the first place!!” Dr. Grinspoon tweeted.
Patrice Harris, MD, chair of the AMA’s Opioid Task Force and the organization’s immediate past president, said removing the X-waiver requirement can help lessen the stigma associated with this OUD treatment. The AMA had urged HHS to change the regulation.
“With this change, office-based physicians and physician-led teams working with patients to manage their other medical conditions can also treat them for their opioid use disorder without being subjected to a separate and burdensome regulatory regime,” Dr. Harris said in the AMA statement.
Researchers have in recent years sought to highlight what they described as missed opportunities for OUD treatment because of the need for the X-waiver.
Buprenorphine is a cost-effective treatment for opioid use disorder, which reduces the risk of injection-related infections and mortality risk, notes a study published online last month in JAMA Network Open.
However, results showed that fewer than 2% of obstetrician-gynecologists who examined women enrolled in Medicaid were trained to prescribe buprenorphine. The study, which was based on data from 31, 211 ob.gyns. who accepted Medicaid insurance, was created to quantify how many were on the list of Drug Addiction Treatment Act buprenorphine-waived clinicians.
The Drug Addiction Treatment Act has required 8 hours of training for physicians and 24 hours for nurse practitioners and physician assistants for the X-waiver needed to prescribe buprenorphine, the investigators report.
‘X the X-waiver’
Only 10% of recent family residency graduates reported being adequately trained to prescribe buprenorphine and only 7% reported actually prescribing the drug, write Kevin Fiscella, MD, University of Rochester (N.Y.) Medical Center and colleagues in a 2018 Viewpoint article published in JAMA Psychiatry.
In the article, which was subtitled “X the X Waiver,” they called for deregulation of buprenorphine as a way of mainstreaming treatment for OUD.
“The DATA 2000 has failed – too few physicians have obtained X-waivers,” the authors write. “Regulations reinforce the stigma surrounding buprenorphine prescribers and patients who receive it while constraining access and discouraging patient engagement and retention in treatment.”
The change, announced Jan. 14, leaves in place restrictions on prescribing for clinicians other than physicians. On a call with reporters, Adm. Brett P. Giroir, MD, assistant secretary for health, suggested that federal officials should take further steps to remove hurdles to buprenorphine prescriptions.
“Many people will say this has gone too far,” Dr. Giroir said of the drive to end the X-waiver for clinicians. “But I believe more people will say this has not gone far enough.”
A version of this article first appeared on Medscape.com.
Federal officials on Thursday announced a plan to largely drop the so-called X-waiver requirement for buprenorphine prescriptions for physicians in a bid to remove an administrative procedure widely seen as a barrier to opioid use disorder (OUD) treatment.
The Department of Health & Human Services unveiled new practice guidelines that include an exemption from current certification requirements. The exemption applies to physicians already registered with the Drug Enforcement Administration.
A restriction included in the new HHS policy is a limit of treating no more than 30 patients with buprenorphine for OUD at any one time. There is an exception to this limit for hospital-based physicians, such as those working in emergency departments, HHS said.
, such as buprenorphine, and does not apply to methadone. The new guidelines say the date on which they will take effect will be added after publication in the Federal Register. HHS did not immediately answer a request from this news organization for a more specific timeline.
Welcomed change
The change in prescribing rule was widely welcomed, with the American Medical Association issuing a statement endorsing the revision. The AMA and many prescribers and researchers had seen the X-waiver as a hurdle to address the nation’s opioid epidemic.
There were more than 83,000 deaths attributed to drug overdoses in the United States in the 12 months ending in June 2020. This is the highest number of overdose deaths ever recorded in a 12-month period, HHS said in a press release, which cited data from the Centers for Disease Control and Prevention.
In a tweet about the new policy, Peter Grinspoon, MD, a Boston internist and author of the memoir “Free Refills: A Doctor Confronts His Addiction,” contrasted the relative ease with which clinicians can give medicines that carry a risk for abuse with the challenge that has existed in trying to provide patients with buprenorphine.
“Absolutely insane that we need a special waiver for buprenorphine to TREAT opioid addiction, but not to prescribe oxycodone, Vicodin, etc., which can get people in trouble in the first place!!” Dr. Grinspoon tweeted.
Patrice Harris, MD, chair of the AMA’s Opioid Task Force and the organization’s immediate past president, said removing the X-waiver requirement can help lessen the stigma associated with this OUD treatment. The AMA had urged HHS to change the regulation.
“With this change, office-based physicians and physician-led teams working with patients to manage their other medical conditions can also treat them for their opioid use disorder without being subjected to a separate and burdensome regulatory regime,” Dr. Harris said in the AMA statement.
Researchers have in recent years sought to highlight what they described as missed opportunities for OUD treatment because of the need for the X-waiver.
Buprenorphine is a cost-effective treatment for opioid use disorder, which reduces the risk of injection-related infections and mortality risk, notes a study published online last month in JAMA Network Open.
However, results showed that fewer than 2% of obstetrician-gynecologists who examined women enrolled in Medicaid were trained to prescribe buprenorphine. The study, which was based on data from 31, 211 ob.gyns. who accepted Medicaid insurance, was created to quantify how many were on the list of Drug Addiction Treatment Act buprenorphine-waived clinicians.
The Drug Addiction Treatment Act has required 8 hours of training for physicians and 24 hours for nurse practitioners and physician assistants for the X-waiver needed to prescribe buprenorphine, the investigators report.
‘X the X-waiver’
Only 10% of recent family residency graduates reported being adequately trained to prescribe buprenorphine and only 7% reported actually prescribing the drug, write Kevin Fiscella, MD, University of Rochester (N.Y.) Medical Center and colleagues in a 2018 Viewpoint article published in JAMA Psychiatry.
In the article, which was subtitled “X the X Waiver,” they called for deregulation of buprenorphine as a way of mainstreaming treatment for OUD.
“The DATA 2000 has failed – too few physicians have obtained X-waivers,” the authors write. “Regulations reinforce the stigma surrounding buprenorphine prescribers and patients who receive it while constraining access and discouraging patient engagement and retention in treatment.”
The change, announced Jan. 14, leaves in place restrictions on prescribing for clinicians other than physicians. On a call with reporters, Adm. Brett P. Giroir, MD, assistant secretary for health, suggested that federal officials should take further steps to remove hurdles to buprenorphine prescriptions.
“Many people will say this has gone too far,” Dr. Giroir said of the drive to end the X-waiver for clinicians. “But I believe more people will say this has not gone far enough.”
A version of this article first appeared on Medscape.com.
Federal officials on Thursday announced a plan to largely drop the so-called X-waiver requirement for buprenorphine prescriptions for physicians in a bid to remove an administrative procedure widely seen as a barrier to opioid use disorder (OUD) treatment.
The Department of Health & Human Services unveiled new practice guidelines that include an exemption from current certification requirements. The exemption applies to physicians already registered with the Drug Enforcement Administration.
A restriction included in the new HHS policy is a limit of treating no more than 30 patients with buprenorphine for OUD at any one time. There is an exception to this limit for hospital-based physicians, such as those working in emergency departments, HHS said.
, such as buprenorphine, and does not apply to methadone. The new guidelines say the date on which they will take effect will be added after publication in the Federal Register. HHS did not immediately answer a request from this news organization for a more specific timeline.
Welcomed change
The change in prescribing rule was widely welcomed, with the American Medical Association issuing a statement endorsing the revision. The AMA and many prescribers and researchers had seen the X-waiver as a hurdle to address the nation’s opioid epidemic.
There were more than 83,000 deaths attributed to drug overdoses in the United States in the 12 months ending in June 2020. This is the highest number of overdose deaths ever recorded in a 12-month period, HHS said in a press release, which cited data from the Centers for Disease Control and Prevention.
In a tweet about the new policy, Peter Grinspoon, MD, a Boston internist and author of the memoir “Free Refills: A Doctor Confronts His Addiction,” contrasted the relative ease with which clinicians can give medicines that carry a risk for abuse with the challenge that has existed in trying to provide patients with buprenorphine.
“Absolutely insane that we need a special waiver for buprenorphine to TREAT opioid addiction, but not to prescribe oxycodone, Vicodin, etc., which can get people in trouble in the first place!!” Dr. Grinspoon tweeted.
Patrice Harris, MD, chair of the AMA’s Opioid Task Force and the organization’s immediate past president, said removing the X-waiver requirement can help lessen the stigma associated with this OUD treatment. The AMA had urged HHS to change the regulation.
“With this change, office-based physicians and physician-led teams working with patients to manage their other medical conditions can also treat them for their opioid use disorder without being subjected to a separate and burdensome regulatory regime,” Dr. Harris said in the AMA statement.
Researchers have in recent years sought to highlight what they described as missed opportunities for OUD treatment because of the need for the X-waiver.
Buprenorphine is a cost-effective treatment for opioid use disorder, which reduces the risk of injection-related infections and mortality risk, notes a study published online last month in JAMA Network Open.
However, results showed that fewer than 2% of obstetrician-gynecologists who examined women enrolled in Medicaid were trained to prescribe buprenorphine. The study, which was based on data from 31, 211 ob.gyns. who accepted Medicaid insurance, was created to quantify how many were on the list of Drug Addiction Treatment Act buprenorphine-waived clinicians.
The Drug Addiction Treatment Act has required 8 hours of training for physicians and 24 hours for nurse practitioners and physician assistants for the X-waiver needed to prescribe buprenorphine, the investigators report.
‘X the X-waiver’
Only 10% of recent family residency graduates reported being adequately trained to prescribe buprenorphine and only 7% reported actually prescribing the drug, write Kevin Fiscella, MD, University of Rochester (N.Y.) Medical Center and colleagues in a 2018 Viewpoint article published in JAMA Psychiatry.
In the article, which was subtitled “X the X Waiver,” they called for deregulation of buprenorphine as a way of mainstreaming treatment for OUD.
“The DATA 2000 has failed – too few physicians have obtained X-waivers,” the authors write. “Regulations reinforce the stigma surrounding buprenorphine prescribers and patients who receive it while constraining access and discouraging patient engagement and retention in treatment.”
The change, announced Jan. 14, leaves in place restrictions on prescribing for clinicians other than physicians. On a call with reporters, Adm. Brett P. Giroir, MD, assistant secretary for health, suggested that federal officials should take further steps to remove hurdles to buprenorphine prescriptions.
“Many people will say this has gone too far,” Dr. Giroir said of the drive to end the X-waiver for clinicians. “But I believe more people will say this has not gone far enough.”
A version of this article first appeared on Medscape.com.
Covert stroke after noncardiac surgery linked with cognitive decline
Background: Prior studies have established an increased risk of overt stroke after noncardiac surgery, with significant associated morbidity and mortality. Similarly, covert stroke in the nonsurgical population is well described and has been shown to be associated with cognitive decline.
Study design: Prospective cohort study.
Setting: Academic centers in nine countries.
Synopsis: This study evaluated 1,114 patients older than 65 years who were hospitalized for noncardiac surgery, excluding patients with carotid and neurosurgical procedures. All enrolled participants completed diffusion-weight MRI of the brain within 9 days of surgery. Follow-up rates for clinical outcomes (1,112; greater than 99%) were excellent, and the primary outcome measure, follow-up Montreal Cognitive Assessment (MOCA) at 1 year, was defined in 1,001 (90%) of the study subjects.
Covert stroke was detected in 78 (7%) of the study participants. Those with covert stroke had a higher incidence of cognitive decline at 1 year (adjusted odds ratio, 1.98; 95% confidence interval, 1.22-3.2) with an absolute risk increase of 13%. Patients with covert stroke also had a higher rate of delirium within 3 days of surgery (hazard ratio, 2.24; 95% CI, 1.06-4.73) and a higher rate of overt stroke and transient ischemic attack at 1 year (HR, 4.13; 95% CI, 1.14-14.99).
This study helps to establish the incidence of covert stroke after noncardiac surgery and provides support for covert stroke as a risk factor for cognitive impairment.
Bottom line: Covert stroke following noncardiac surgery is common, affecting 1 in 14 patients in this study, and it is associated with an increased risk of cognitive decline, perioperative delirium, and subsequent overt stroke.
Citation: The NeuroVISION Investigators (Mrkobrada M et al.). Perioperative covert stroke in patients undergoing noncardiac surgery (NeuroVISION): a prospective cohort study. Lancet. 2019;394(10203):1022-9.
Dr. Herrle is a hospitalist at Maine Medical Center in Portland and at Stephens Memorial Hospital in Norway, Maine.
Background: Prior studies have established an increased risk of overt stroke after noncardiac surgery, with significant associated morbidity and mortality. Similarly, covert stroke in the nonsurgical population is well described and has been shown to be associated with cognitive decline.
Study design: Prospective cohort study.
Setting: Academic centers in nine countries.
Synopsis: This study evaluated 1,114 patients older than 65 years who were hospitalized for noncardiac surgery, excluding patients with carotid and neurosurgical procedures. All enrolled participants completed diffusion-weight MRI of the brain within 9 days of surgery. Follow-up rates for clinical outcomes (1,112; greater than 99%) were excellent, and the primary outcome measure, follow-up Montreal Cognitive Assessment (MOCA) at 1 year, was defined in 1,001 (90%) of the study subjects.
Covert stroke was detected in 78 (7%) of the study participants. Those with covert stroke had a higher incidence of cognitive decline at 1 year (adjusted odds ratio, 1.98; 95% confidence interval, 1.22-3.2) with an absolute risk increase of 13%. Patients with covert stroke also had a higher rate of delirium within 3 days of surgery (hazard ratio, 2.24; 95% CI, 1.06-4.73) and a higher rate of overt stroke and transient ischemic attack at 1 year (HR, 4.13; 95% CI, 1.14-14.99).
This study helps to establish the incidence of covert stroke after noncardiac surgery and provides support for covert stroke as a risk factor for cognitive impairment.
Bottom line: Covert stroke following noncardiac surgery is common, affecting 1 in 14 patients in this study, and it is associated with an increased risk of cognitive decline, perioperative delirium, and subsequent overt stroke.
Citation: The NeuroVISION Investigators (Mrkobrada M et al.). Perioperative covert stroke in patients undergoing noncardiac surgery (NeuroVISION): a prospective cohort study. Lancet. 2019;394(10203):1022-9.
Dr. Herrle is a hospitalist at Maine Medical Center in Portland and at Stephens Memorial Hospital in Norway, Maine.
Background: Prior studies have established an increased risk of overt stroke after noncardiac surgery, with significant associated morbidity and mortality. Similarly, covert stroke in the nonsurgical population is well described and has been shown to be associated with cognitive decline.
Study design: Prospective cohort study.
Setting: Academic centers in nine countries.
Synopsis: This study evaluated 1,114 patients older than 65 years who were hospitalized for noncardiac surgery, excluding patients with carotid and neurosurgical procedures. All enrolled participants completed diffusion-weight MRI of the brain within 9 days of surgery. Follow-up rates for clinical outcomes (1,112; greater than 99%) were excellent, and the primary outcome measure, follow-up Montreal Cognitive Assessment (MOCA) at 1 year, was defined in 1,001 (90%) of the study subjects.
Covert stroke was detected in 78 (7%) of the study participants. Those with covert stroke had a higher incidence of cognitive decline at 1 year (adjusted odds ratio, 1.98; 95% confidence interval, 1.22-3.2) with an absolute risk increase of 13%. Patients with covert stroke also had a higher rate of delirium within 3 days of surgery (hazard ratio, 2.24; 95% CI, 1.06-4.73) and a higher rate of overt stroke and transient ischemic attack at 1 year (HR, 4.13; 95% CI, 1.14-14.99).
This study helps to establish the incidence of covert stroke after noncardiac surgery and provides support for covert stroke as a risk factor for cognitive impairment.
Bottom line: Covert stroke following noncardiac surgery is common, affecting 1 in 14 patients in this study, and it is associated with an increased risk of cognitive decline, perioperative delirium, and subsequent overt stroke.
Citation: The NeuroVISION Investigators (Mrkobrada M et al.). Perioperative covert stroke in patients undergoing noncardiac surgery (NeuroVISION): a prospective cohort study. Lancet. 2019;394(10203):1022-9.
Dr. Herrle is a hospitalist at Maine Medical Center in Portland and at Stephens Memorial Hospital in Norway, Maine.
Overcoming the challenges of COVID-19 for Alzheimer’s patients in long-term care, research
An alarming number of additional Alzheimer’s disease (AD) deaths have been reported across various states within the past several months, according to the Alzheimer’s Association. Centers for Disease Control and Prevention data indicate that no less than 31,000 additional people with the neurodegenerative condition had died from the beginning of the pandemic through the end of September 2020. We know that long-term care facilities have been hit hardest, and access to adequate and/or prompt testing has been cited as the most pressing issue during the onset of the pandemic.1
When ADLs become a matter of survival
For individuals affected with Alzheimer’s disease and other types of dementia, performing routine tasks may seem cumbersome and overwhelming. Many of these patients are dependent upon caregivers and family support to facilitate their activities of daily living (ADLs).
Transitioning into the “new normal” set by the pandemic milieu is not an easy task for the average AD individual, because they are now expected to comply with numerous safety instructions (for example, maintaining hygiene, social distancing, etc.). They are also expected to monitor and communicate information about the onset of any suspected symptom to their caregiver or health care clinician.
The additional tasks added to their list of ADLs are particularly distressing given their already compromised short-term memory and overall cognitive decline. Individuals with AD may also be dealing with a host of psychobehavioral challenges, such as the presence of depression, anxiety, and/or agitation amid self-isolation. Enforced social isolation tied to COVID-19 may compound those issues.
Resource diversion and mitigation strategies
Unfortunately, any disruption in services within a long-term care setting may lead to a suboptimal therapeutic environment for patients. The Washington State LTC, for example, reported experiencing a case fatality rate (CFR) exceeding more than a third of its residents; essential staff and health care clinicians were duly affected from exposure to the virus (the risk of transmission increases considerably during transport between facilities). Access to personal protective equipment (PPE) might have been hindered by availability.
Another issue with far-reaching consequences is diversion of resources for urgent care. Health care professionals may simply not be readily available for those with chronic care needs because of the enormous scale of the impact of COVID-19 upon health care systems.
Continuity of therapy might include evaluations or follow-up services via teleconferencing modalities, but an exhaustive initial onsite physical examination is often necessary for accurate diagnostics and care. Medication management for the newly diagnosed AD or dementia patient necessitates a thorough screening process involving appropriate in-person blood or laboratory work. It is for this reason that clinicians will need to plan ahead by preparing a contingency plan with the corresponding mitigation strategies (for example, telemedicine, proposed solutions to anticipated disruption of services, extended support, and feedback from family members, etc.).2
Resilience and recovery in a retrospective study
A research team from Wuhan Red Cross Hospital in China performed a retrospective cohort study on a sample of patients (n = 42) to determine the severity and prognostic features of COVID-19 pneumonia; 19 AD patients (as per National Institute on Aging/Alzheimer’s Association diagnostic guidelines) were directly compared with 23 age-matched non-AD COVID-19 patients in a similar treatment context.
The study yielded some rather unexpected findings, namely, AD patients experienced remarkably shorter hospital stays and better appetites, especially with respect to their non-AD counterparts. This is even more puzzling when considering that previous studies indicated that dementia patients with concomitant COVID-19 pneumonia are twice as likely to die as those without neurodegenerative compromise.
Aside from a seemingly inexplicable interest in food, the observable positive changes may be attributable to such factors that are particular to the nursing home – residents have immediate access to health care services, which generally allows for timely diagnosis and care. However, the authors of the study speculate that the pathophysiological response of angiotensin-converting enzyme 2 (ACE2) confers to AD patients a therapeutic advantage as they have reduced expression.3 Despite the notoriously high mortality rates of COVID-19 pneumonia among the elderly population, , which underscores the importance of early diagnosis and intervention.
Genetic and environmental susceptibility
One of the more devastating observations about the ongoing pandemic environment is that a whopping 80% of dying patients committed to a long-term facility also include those with AD; it has been reported that almost half of all patients in nursing homes and related services have the neurodegenerative condition. The grim scenario is brought about by several factors, chief of which is the proximity of shared living arrangements within the context of a residential care setting. It should be noted that patients with AD exhibit comorbid conditions (for example, diabetes, cardiovascular disease, and/or respiratory issues) that immediately put them at high risk for COVID exposure. Interestingly enough, the ApoE4 genotype, which is associated with an increased susceptibility for AD, is also correlated with COVID-19 prognosis and severity. Although exact numbers are difficult to come by, it is of utmost importance for clinicians to evaluate the overall scope of the situation, identify at-risk patients such as individuals with AD and related dementias, and work with caregivers to afford care to patients who need it the most.4
Transcending research design
The elderly population, unsurprisingly, experiences the highest COVID-19 mortality rate because of the presence of multiple risk factors, namely, compromised immunity and difficulties maintaining ADLs, and thereby adhering to safety protocols. As far as Alzheimer’s patients are concerned, numerous hurdles affect the domain of neurodegenerative research.
To safeguard the health and well-being of the participants and caregivers, site sponsors and investigators must explore various communication avenues with the goal of facilitating health education (for example, mitigation strategies, adverse effects monitoring, etc.), as well as implementing contingency plans in the event that a site becomes inaccessible (for example, site closure, traveling regulations, lockdowns, etc.).
Alternatives such as telemedicine present viable solutions for ensuring completion of studies. Given the nature of the pandemic, there is a possibility that a research participant may contract the virus, necessitating a break from the established protocol. It is for this reason that site sponsors and corresponding regulatory bodies are advised to proactively engage in dialogue and transparent communications with respect to ensuing protocol deviations. Institutional Review Boards can expedite the review process by making the necessary changes in a timely manner.5
References
1. Ritchie K. KJZZ. 2020 Nov 16.
2. Brown EE et al. Am J Geriatr Psychiatry. 2020 Jul;28(7):712-21.
3. Li J et al. J Alzheimers Dis. 2020;77(1):67-73.
4. Perry G. J Alzheimers Dis. 2020 Jan 1;76(1):1.
5. Alzheimers Dement. 2020 Apr;16(4):587-8.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation, Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Dr. Dhillon is a staff neurologist at Brigham and Women’s Hospital in Boston. Dr. Dhillon is currently on the speaker bureau/advisory board for Biogen, Bristol Myers Squibb, Genzyme, and Teva Neuroscience.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the International Maternal and Child Health Foundation. He has no disclosures.
An alarming number of additional Alzheimer’s disease (AD) deaths have been reported across various states within the past several months, according to the Alzheimer’s Association. Centers for Disease Control and Prevention data indicate that no less than 31,000 additional people with the neurodegenerative condition had died from the beginning of the pandemic through the end of September 2020. We know that long-term care facilities have been hit hardest, and access to adequate and/or prompt testing has been cited as the most pressing issue during the onset of the pandemic.1
When ADLs become a matter of survival
For individuals affected with Alzheimer’s disease and other types of dementia, performing routine tasks may seem cumbersome and overwhelming. Many of these patients are dependent upon caregivers and family support to facilitate their activities of daily living (ADLs).
Transitioning into the “new normal” set by the pandemic milieu is not an easy task for the average AD individual, because they are now expected to comply with numerous safety instructions (for example, maintaining hygiene, social distancing, etc.). They are also expected to monitor and communicate information about the onset of any suspected symptom to their caregiver or health care clinician.
The additional tasks added to their list of ADLs are particularly distressing given their already compromised short-term memory and overall cognitive decline. Individuals with AD may also be dealing with a host of psychobehavioral challenges, such as the presence of depression, anxiety, and/or agitation amid self-isolation. Enforced social isolation tied to COVID-19 may compound those issues.
Resource diversion and mitigation strategies
Unfortunately, any disruption in services within a long-term care setting may lead to a suboptimal therapeutic environment for patients. The Washington State LTC, for example, reported experiencing a case fatality rate (CFR) exceeding more than a third of its residents; essential staff and health care clinicians were duly affected from exposure to the virus (the risk of transmission increases considerably during transport between facilities). Access to personal protective equipment (PPE) might have been hindered by availability.
Another issue with far-reaching consequences is diversion of resources for urgent care. Health care professionals may simply not be readily available for those with chronic care needs because of the enormous scale of the impact of COVID-19 upon health care systems.
Continuity of therapy might include evaluations or follow-up services via teleconferencing modalities, but an exhaustive initial onsite physical examination is often necessary for accurate diagnostics and care. Medication management for the newly diagnosed AD or dementia patient necessitates a thorough screening process involving appropriate in-person blood or laboratory work. It is for this reason that clinicians will need to plan ahead by preparing a contingency plan with the corresponding mitigation strategies (for example, telemedicine, proposed solutions to anticipated disruption of services, extended support, and feedback from family members, etc.).2
Resilience and recovery in a retrospective study
A research team from Wuhan Red Cross Hospital in China performed a retrospective cohort study on a sample of patients (n = 42) to determine the severity and prognostic features of COVID-19 pneumonia; 19 AD patients (as per National Institute on Aging/Alzheimer’s Association diagnostic guidelines) were directly compared with 23 age-matched non-AD COVID-19 patients in a similar treatment context.
The study yielded some rather unexpected findings, namely, AD patients experienced remarkably shorter hospital stays and better appetites, especially with respect to their non-AD counterparts. This is even more puzzling when considering that previous studies indicated that dementia patients with concomitant COVID-19 pneumonia are twice as likely to die as those without neurodegenerative compromise.
Aside from a seemingly inexplicable interest in food, the observable positive changes may be attributable to such factors that are particular to the nursing home – residents have immediate access to health care services, which generally allows for timely diagnosis and care. However, the authors of the study speculate that the pathophysiological response of angiotensin-converting enzyme 2 (ACE2) confers to AD patients a therapeutic advantage as they have reduced expression.3 Despite the notoriously high mortality rates of COVID-19 pneumonia among the elderly population, , which underscores the importance of early diagnosis and intervention.
Genetic and environmental susceptibility
One of the more devastating observations about the ongoing pandemic environment is that a whopping 80% of dying patients committed to a long-term facility also include those with AD; it has been reported that almost half of all patients in nursing homes and related services have the neurodegenerative condition. The grim scenario is brought about by several factors, chief of which is the proximity of shared living arrangements within the context of a residential care setting. It should be noted that patients with AD exhibit comorbid conditions (for example, diabetes, cardiovascular disease, and/or respiratory issues) that immediately put them at high risk for COVID exposure. Interestingly enough, the ApoE4 genotype, which is associated with an increased susceptibility for AD, is also correlated with COVID-19 prognosis and severity. Although exact numbers are difficult to come by, it is of utmost importance for clinicians to evaluate the overall scope of the situation, identify at-risk patients such as individuals with AD and related dementias, and work with caregivers to afford care to patients who need it the most.4
Transcending research design
The elderly population, unsurprisingly, experiences the highest COVID-19 mortality rate because of the presence of multiple risk factors, namely, compromised immunity and difficulties maintaining ADLs, and thereby adhering to safety protocols. As far as Alzheimer’s patients are concerned, numerous hurdles affect the domain of neurodegenerative research.
To safeguard the health and well-being of the participants and caregivers, site sponsors and investigators must explore various communication avenues with the goal of facilitating health education (for example, mitigation strategies, adverse effects monitoring, etc.), as well as implementing contingency plans in the event that a site becomes inaccessible (for example, site closure, traveling regulations, lockdowns, etc.).
Alternatives such as telemedicine present viable solutions for ensuring completion of studies. Given the nature of the pandemic, there is a possibility that a research participant may contract the virus, necessitating a break from the established protocol. It is for this reason that site sponsors and corresponding regulatory bodies are advised to proactively engage in dialogue and transparent communications with respect to ensuing protocol deviations. Institutional Review Boards can expedite the review process by making the necessary changes in a timely manner.5
References
1. Ritchie K. KJZZ. 2020 Nov 16.
2. Brown EE et al. Am J Geriatr Psychiatry. 2020 Jul;28(7):712-21.
3. Li J et al. J Alzheimers Dis. 2020;77(1):67-73.
4. Perry G. J Alzheimers Dis. 2020 Jan 1;76(1):1.
5. Alzheimers Dement. 2020 Apr;16(4):587-8.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation, Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Dr. Dhillon is a staff neurologist at Brigham and Women’s Hospital in Boston. Dr. Dhillon is currently on the speaker bureau/advisory board for Biogen, Bristol Myers Squibb, Genzyme, and Teva Neuroscience.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the International Maternal and Child Health Foundation. He has no disclosures.
An alarming number of additional Alzheimer’s disease (AD) deaths have been reported across various states within the past several months, according to the Alzheimer’s Association. Centers for Disease Control and Prevention data indicate that no less than 31,000 additional people with the neurodegenerative condition had died from the beginning of the pandemic through the end of September 2020. We know that long-term care facilities have been hit hardest, and access to adequate and/or prompt testing has been cited as the most pressing issue during the onset of the pandemic.1
When ADLs become a matter of survival
For individuals affected with Alzheimer’s disease and other types of dementia, performing routine tasks may seem cumbersome and overwhelming. Many of these patients are dependent upon caregivers and family support to facilitate their activities of daily living (ADLs).
Transitioning into the “new normal” set by the pandemic milieu is not an easy task for the average AD individual, because they are now expected to comply with numerous safety instructions (for example, maintaining hygiene, social distancing, etc.). They are also expected to monitor and communicate information about the onset of any suspected symptom to their caregiver or health care clinician.
The additional tasks added to their list of ADLs are particularly distressing given their already compromised short-term memory and overall cognitive decline. Individuals with AD may also be dealing with a host of psychobehavioral challenges, such as the presence of depression, anxiety, and/or agitation amid self-isolation. Enforced social isolation tied to COVID-19 may compound those issues.
Resource diversion and mitigation strategies
Unfortunately, any disruption in services within a long-term care setting may lead to a suboptimal therapeutic environment for patients. The Washington State LTC, for example, reported experiencing a case fatality rate (CFR) exceeding more than a third of its residents; essential staff and health care clinicians were duly affected from exposure to the virus (the risk of transmission increases considerably during transport between facilities). Access to personal protective equipment (PPE) might have been hindered by availability.
Another issue with far-reaching consequences is diversion of resources for urgent care. Health care professionals may simply not be readily available for those with chronic care needs because of the enormous scale of the impact of COVID-19 upon health care systems.
Continuity of therapy might include evaluations or follow-up services via teleconferencing modalities, but an exhaustive initial onsite physical examination is often necessary for accurate diagnostics and care. Medication management for the newly diagnosed AD or dementia patient necessitates a thorough screening process involving appropriate in-person blood or laboratory work. It is for this reason that clinicians will need to plan ahead by preparing a contingency plan with the corresponding mitigation strategies (for example, telemedicine, proposed solutions to anticipated disruption of services, extended support, and feedback from family members, etc.).2
Resilience and recovery in a retrospective study
A research team from Wuhan Red Cross Hospital in China performed a retrospective cohort study on a sample of patients (n = 42) to determine the severity and prognostic features of COVID-19 pneumonia; 19 AD patients (as per National Institute on Aging/Alzheimer’s Association diagnostic guidelines) were directly compared with 23 age-matched non-AD COVID-19 patients in a similar treatment context.
The study yielded some rather unexpected findings, namely, AD patients experienced remarkably shorter hospital stays and better appetites, especially with respect to their non-AD counterparts. This is even more puzzling when considering that previous studies indicated that dementia patients with concomitant COVID-19 pneumonia are twice as likely to die as those without neurodegenerative compromise.
Aside from a seemingly inexplicable interest in food, the observable positive changes may be attributable to such factors that are particular to the nursing home – residents have immediate access to health care services, which generally allows for timely diagnosis and care. However, the authors of the study speculate that the pathophysiological response of angiotensin-converting enzyme 2 (ACE2) confers to AD patients a therapeutic advantage as they have reduced expression.3 Despite the notoriously high mortality rates of COVID-19 pneumonia among the elderly population, , which underscores the importance of early diagnosis and intervention.
Genetic and environmental susceptibility
One of the more devastating observations about the ongoing pandemic environment is that a whopping 80% of dying patients committed to a long-term facility also include those with AD; it has been reported that almost half of all patients in nursing homes and related services have the neurodegenerative condition. The grim scenario is brought about by several factors, chief of which is the proximity of shared living arrangements within the context of a residential care setting. It should be noted that patients with AD exhibit comorbid conditions (for example, diabetes, cardiovascular disease, and/or respiratory issues) that immediately put them at high risk for COVID exposure. Interestingly enough, the ApoE4 genotype, which is associated with an increased susceptibility for AD, is also correlated with COVID-19 prognosis and severity. Although exact numbers are difficult to come by, it is of utmost importance for clinicians to evaluate the overall scope of the situation, identify at-risk patients such as individuals with AD and related dementias, and work with caregivers to afford care to patients who need it the most.4
Transcending research design
The elderly population, unsurprisingly, experiences the highest COVID-19 mortality rate because of the presence of multiple risk factors, namely, compromised immunity and difficulties maintaining ADLs, and thereby adhering to safety protocols. As far as Alzheimer’s patients are concerned, numerous hurdles affect the domain of neurodegenerative research.
To safeguard the health and well-being of the participants and caregivers, site sponsors and investigators must explore various communication avenues with the goal of facilitating health education (for example, mitigation strategies, adverse effects monitoring, etc.), as well as implementing contingency plans in the event that a site becomes inaccessible (for example, site closure, traveling regulations, lockdowns, etc.).
Alternatives such as telemedicine present viable solutions for ensuring completion of studies. Given the nature of the pandemic, there is a possibility that a research participant may contract the virus, necessitating a break from the established protocol. It is for this reason that site sponsors and corresponding regulatory bodies are advised to proactively engage in dialogue and transparent communications with respect to ensuing protocol deviations. Institutional Review Boards can expedite the review process by making the necessary changes in a timely manner.5
References
1. Ritchie K. KJZZ. 2020 Nov 16.
2. Brown EE et al. Am J Geriatr Psychiatry. 2020 Jul;28(7):712-21.
3. Li J et al. J Alzheimers Dis. 2020;77(1):67-73.
4. Perry G. J Alzheimers Dis. 2020 Jan 1;76(1):1.
5. Alzheimers Dement. 2020 Apr;16(4):587-8.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation, Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Dr. Dhillon is a staff neurologist at Brigham and Women’s Hospital in Boston. Dr. Dhillon is currently on the speaker bureau/advisory board for Biogen, Bristol Myers Squibb, Genzyme, and Teva Neuroscience.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the International Maternal and Child Health Foundation. He has no disclosures.
Microvascular injury of brain, olfactory bulb seen in COVID-19
new research suggests.
Postmortem MRI brain scans of 13 patients who died from COVID-19 showed abnormalities in 10 of the participants. Of these, nine showed punctate hyperintensities, “which represented areas of microvascular injury and fibrinogen leakage,” the investigators reported. Immunostaining also showed a thinning of the basal lamina in five of these patients.
Further analyses showed punctate hypointensities linked to congested blood vessels in 10 patients. These areas were “interpreted as microhemorrhages,” the researchers noted.
There was no evidence of viral infection, including SARS-CoV-2.
“These findings may inform the interpretation of changes observed on [MRI] of punctate hyperintensities and linear hypointensities in patients with COVID-19,” wrote Myoung-Hwa Lee, PhD, a research fellow at the National Institute of Neurological Disorders and Stroke, and colleagues. The findings were published online Dec. 30 in a “correspondence” piece in the New England Journal of Medicine.
Interpret with caution
The investigators examined brains from a convenience sample of 19 patients (mean age, 50 years), all of whom died from COVID-19 between March and July 2020.
An 11.7-tesla scanner was used to obtain magnetic resonance microscopy images for 13 of the patients. In order to scan the olfactory bulb, the scanner was set at a resolution of 25 mcm; for the brain, it was set at 100 mcm.
Chromogenic immunostaining was used to assess brain abnormalities found in 10 of the patients. Multiplex fluorescence imaging was also used for some of the patients.
For 18 study participants, a histopathological brain examination was performed. In the patients who also had medical histories available to the researchers, five had mild respiratory syndrome, four had acute respiratory distress syndrome, two had pulmonary embolism, one had delirium, and three had unknown symptoms.
The punctate hyperintensities found on magnetic resonance microscopy were also found on histopathological exam. Collagen IV immunostaining showed a thinning in the basal lamina of endothelial cells in these areas.
In addition to congested blood vessels, punctate hypointensities were linked to areas of fibrinogen leakage – but also to “relatively intact vasculature,” the investigators reported.
“There was minimal perivascular inflammation in the specimens examined, but there was no vascular occlusion,” they added.
SARS-CoV-2 was also not found in any of the participants. “It is possible that the virus was cleared by the time of death or that viral copy numbers were below the level of detection by our assays,” the researchers noted.
In 13 of the patients, hypertrophic astrocytes, macrophage infiltrates, and perivascular-activated microglia were found. Eight patients showed CD3+ and CD8+ T cells in spaces and lumens next to endothelial cells.
Finally, five patients showed activated microglia next to neurons. This is “suggestive of neuronophagia in the olfactory bulb, substantial nigra, dorsal motor nucleus of the vagal nerve, and the pre-Bötzinger complex in the medulla, which is involved in the generation of spontaneous rhythmic breathing,” wrote the investigators.
In summary, vascular pathology was found in 10 cases, perivascular infiltrates were present in 13 cases, acute ischemic hypoxic neurons were present in 6 cases, and changes suggestive of neuronophagia were present in 5 cases.
The researchers noted that, although the study findings may be helpful when interpreting brain changes on MRI scan in this patient population, availability of clinical information for the participants was limited.
Therefore, “no conclusions can be drawn in relation to neurologic features of COVID-19,” they wrote.
The study was funded by NINDS. Dr. Lee and all but one of the other investigators reported no relevant financial relationships; the remaining investigator reported having received grants from NINDS during the conduct of this study.
A version of this article first appeared on Medscape.com.
new research suggests.
Postmortem MRI brain scans of 13 patients who died from COVID-19 showed abnormalities in 10 of the participants. Of these, nine showed punctate hyperintensities, “which represented areas of microvascular injury and fibrinogen leakage,” the investigators reported. Immunostaining also showed a thinning of the basal lamina in five of these patients.
Further analyses showed punctate hypointensities linked to congested blood vessels in 10 patients. These areas were “interpreted as microhemorrhages,” the researchers noted.
There was no evidence of viral infection, including SARS-CoV-2.
“These findings may inform the interpretation of changes observed on [MRI] of punctate hyperintensities and linear hypointensities in patients with COVID-19,” wrote Myoung-Hwa Lee, PhD, a research fellow at the National Institute of Neurological Disorders and Stroke, and colleagues. The findings were published online Dec. 30 in a “correspondence” piece in the New England Journal of Medicine.
Interpret with caution
The investigators examined brains from a convenience sample of 19 patients (mean age, 50 years), all of whom died from COVID-19 between March and July 2020.
An 11.7-tesla scanner was used to obtain magnetic resonance microscopy images for 13 of the patients. In order to scan the olfactory bulb, the scanner was set at a resolution of 25 mcm; for the brain, it was set at 100 mcm.
Chromogenic immunostaining was used to assess brain abnormalities found in 10 of the patients. Multiplex fluorescence imaging was also used for some of the patients.
For 18 study participants, a histopathological brain examination was performed. In the patients who also had medical histories available to the researchers, five had mild respiratory syndrome, four had acute respiratory distress syndrome, two had pulmonary embolism, one had delirium, and three had unknown symptoms.
The punctate hyperintensities found on magnetic resonance microscopy were also found on histopathological exam. Collagen IV immunostaining showed a thinning in the basal lamina of endothelial cells in these areas.
In addition to congested blood vessels, punctate hypointensities were linked to areas of fibrinogen leakage – but also to “relatively intact vasculature,” the investigators reported.
“There was minimal perivascular inflammation in the specimens examined, but there was no vascular occlusion,” they added.
SARS-CoV-2 was also not found in any of the participants. “It is possible that the virus was cleared by the time of death or that viral copy numbers were below the level of detection by our assays,” the researchers noted.
In 13 of the patients, hypertrophic astrocytes, macrophage infiltrates, and perivascular-activated microglia were found. Eight patients showed CD3+ and CD8+ T cells in spaces and lumens next to endothelial cells.
Finally, five patients showed activated microglia next to neurons. This is “suggestive of neuronophagia in the olfactory bulb, substantial nigra, dorsal motor nucleus of the vagal nerve, and the pre-Bötzinger complex in the medulla, which is involved in the generation of spontaneous rhythmic breathing,” wrote the investigators.
In summary, vascular pathology was found in 10 cases, perivascular infiltrates were present in 13 cases, acute ischemic hypoxic neurons were present in 6 cases, and changes suggestive of neuronophagia were present in 5 cases.
The researchers noted that, although the study findings may be helpful when interpreting brain changes on MRI scan in this patient population, availability of clinical information for the participants was limited.
Therefore, “no conclusions can be drawn in relation to neurologic features of COVID-19,” they wrote.
The study was funded by NINDS. Dr. Lee and all but one of the other investigators reported no relevant financial relationships; the remaining investigator reported having received grants from NINDS during the conduct of this study.
A version of this article first appeared on Medscape.com.
new research suggests.
Postmortem MRI brain scans of 13 patients who died from COVID-19 showed abnormalities in 10 of the participants. Of these, nine showed punctate hyperintensities, “which represented areas of microvascular injury and fibrinogen leakage,” the investigators reported. Immunostaining also showed a thinning of the basal lamina in five of these patients.
Further analyses showed punctate hypointensities linked to congested blood vessels in 10 patients. These areas were “interpreted as microhemorrhages,” the researchers noted.
There was no evidence of viral infection, including SARS-CoV-2.
“These findings may inform the interpretation of changes observed on [MRI] of punctate hyperintensities and linear hypointensities in patients with COVID-19,” wrote Myoung-Hwa Lee, PhD, a research fellow at the National Institute of Neurological Disorders and Stroke, and colleagues. The findings were published online Dec. 30 in a “correspondence” piece in the New England Journal of Medicine.
Interpret with caution
The investigators examined brains from a convenience sample of 19 patients (mean age, 50 years), all of whom died from COVID-19 between March and July 2020.
An 11.7-tesla scanner was used to obtain magnetic resonance microscopy images for 13 of the patients. In order to scan the olfactory bulb, the scanner was set at a resolution of 25 mcm; for the brain, it was set at 100 mcm.
Chromogenic immunostaining was used to assess brain abnormalities found in 10 of the patients. Multiplex fluorescence imaging was also used for some of the patients.
For 18 study participants, a histopathological brain examination was performed. In the patients who also had medical histories available to the researchers, five had mild respiratory syndrome, four had acute respiratory distress syndrome, two had pulmonary embolism, one had delirium, and three had unknown symptoms.
The punctate hyperintensities found on magnetic resonance microscopy were also found on histopathological exam. Collagen IV immunostaining showed a thinning in the basal lamina of endothelial cells in these areas.
In addition to congested blood vessels, punctate hypointensities were linked to areas of fibrinogen leakage – but also to “relatively intact vasculature,” the investigators reported.
“There was minimal perivascular inflammation in the specimens examined, but there was no vascular occlusion,” they added.
SARS-CoV-2 was also not found in any of the participants. “It is possible that the virus was cleared by the time of death or that viral copy numbers were below the level of detection by our assays,” the researchers noted.
In 13 of the patients, hypertrophic astrocytes, macrophage infiltrates, and perivascular-activated microglia were found. Eight patients showed CD3+ and CD8+ T cells in spaces and lumens next to endothelial cells.
Finally, five patients showed activated microglia next to neurons. This is “suggestive of neuronophagia in the olfactory bulb, substantial nigra, dorsal motor nucleus of the vagal nerve, and the pre-Bötzinger complex in the medulla, which is involved in the generation of spontaneous rhythmic breathing,” wrote the investigators.
In summary, vascular pathology was found in 10 cases, perivascular infiltrates were present in 13 cases, acute ischemic hypoxic neurons were present in 6 cases, and changes suggestive of neuronophagia were present in 5 cases.
The researchers noted that, although the study findings may be helpful when interpreting brain changes on MRI scan in this patient population, availability of clinical information for the participants was limited.
Therefore, “no conclusions can be drawn in relation to neurologic features of COVID-19,” they wrote.
The study was funded by NINDS. Dr. Lee and all but one of the other investigators reported no relevant financial relationships; the remaining investigator reported having received grants from NINDS during the conduct of this study.
A version of this article first appeared on Medscape.com.
The top pediatric articles of 2019
Updates in pediatric hospital medicine
The expansion of the field of pediatric hospital medicine in the past 30 years has resulted in improved health care outcomes for hospitalized children1,2 and has been accompanied by a robust increase in the amount of scholarly work related to the field.3 We performed a review of the literature published in 2019 to identify the 10 articles that had the most impact on pediatric hospital medicine, and presented the findings at HM20 Virtual, the 2020 annual conference of the Society of Hospital Medicine. Five of the selected articles are highlighted here.
STUDY 1
Wechsler ME et al. Step-up therapy in black children and adults with poorly controlled asthma. N Engl J Med. 2019 Sep 26;381(13):1227-39.
Background
Current pediatric asthma guidelines suggest adding a long-acting beta-agonist (LABA) to inhaled corticosteroid (ICS) therapy, rather than increasing the ICS dose, for children with poorly controlled asthma. However, these data are based on trials with disproportionately few Black subjects. This study aimed to determine the best step-up therapy for Black patients whose asthma was poorly controlled on ICS monotherapy.
Study overview and results
The authors reported two parallel double-blind, randomized, controlled trials, one in children and one in adolescents and adults. The study of children included 280 subjects ranging in age from 5 to 11, with at least one Black grandparent, and with poorly controlled asthma on low-dose ICS therapy. It used a four-way crossover design in which each subject was treated with four different 14-week treatment regimens: either double (medium-dose) or quintuple (high-dose) their baseline ICS dose, with or without the addition of a LABA. A superior response was defined by the composite outcome of at least one fewer asthma exacerbation, more asthma-control days, or a 5–percentage point difference in predicted FEV1. Forty-six percent of children had improved asthma outcomes when the ICS dose was increased rather than with the addition of a LABA. In contrast, Black adolescents and Black adults had superior responses to the addition of a LABA. There was no significant interaction between the percentage of African ancestry as determined by DNA genotyping and the primary composite outcome. High-dose ICS was associated with a decrease in the ratio of urinary cortisol to creatinine in children younger than 8 years.
Limitations
Approximately 25% of children dropped out of the study, with disproportionately more children dropping out while on a high-dose ICS regimen. Additionally, the difference in the composite outcome was primarily driven by differences in FEV1, with few subjects demonstrating a difference in asthma exacerbations or asthma-control days. Although a decrease in urinary cortisol to creatinine ratio was noted in children under 8 on high-dose ICS, the study period was not long enough to determine the clinical implications of this finding.
Important findings and implications
While studies with a majority of white children have suggested a superior response from adding a LABA compared to increasing the dose of an ICS, almost half of Black children showed a superior response when the dose of an ICS was increased rather than adding a LABA. It is important to note that current guidelines are based on studies with a disproportionate majority of white subjects and may not accurately reflect optimal care for patients in other racial groups. This study underscores the need to include a diverse patient population in research studies.
STUDY 2
Chang PW, Newman TB. A simpler prediction rule for rebound hyperbilirubinemia. Pediatrics. 2019 Jul;144(1):e20183712.
Background
Hyperbilirubinemia (jaundice) is estimated to affect 50%-60% of all newborns. Rebound hyperbilirubinemia – a rise in bilirubin after cessation of phototherapy – is common and can lead to recently discharged infants being readmitted for additional therapy. Lack of clear guidelines regarding when to discharge infants with hyperbilirubinemia has likely contributed to practice variation and some trepidation regarding whether a bilirubin level is “low enough” to discontinue therapy.
Study overview and results
The authors had previously proposed a three-factor hyperbilirubinemia risk model and sought to simplify their rule further.4 They examined a retrospective cohort of 7,048 infants greater than or equal to 35 weeks’ gestation using a random split sample. The authors derived a two-factor model using the same methods and compared its performance to the three-factor model. The two-factor formula was shown to be a good fit as a logistic regression model (Hosmer-Lemeshow test 9.21; P = .33), and the AUROC (area under the receiver operating characteristic) curves for the derivation and validation cohorts were similar between the two-factor (0.877 and 0.876, respectively) and three-factor risk models (0.887 and 0.881, respectively).
Limitations
These data are limited to infants receiving their first treatment of phototherapy and have not been externally validated. An important variable, serum bilirubin at phototherapy termination, was estimated in most subjects, which may have affected the accuracy of the prediction rule. Whether infants received home phototherapy was based only on equipment orders, and some infants may have received phototherapy unbeknownst to investigators. Last, infants with rebound hyperbilirubinemia at less than 72 hours after phototherapy discontinuation may have been missed.
Important findings and implications
This prediction model provides evidence-based, concrete data that can be used in making joint decisions with families regarding discharge timing of infants with hyperbilirubinemia. It also could be beneficial when deciding appropriate follow-up time after discharge.
STUDY 3
Ramgopal S et al. Risk of serious bacterial infection in infants aged ≤60 days presenting to emergency departments with a history of fever only. J Pediatr. 2019 Jan;204:191-195. doi: 10.1016/j.jpeds.2018.08.043.
Background
Febrile infants aged 60 days and younger are at risk for serious bacterial infections (SBI) including urinary tract infections (UTI), bacteremia, and meningitis. As physical exam is a poor discriminator of SBI in this age group, providers frequently rely on laboratory values and risk factors to guide management. Infants presenting with documented fevers by caregivers but found to have no fever in the emergency department are a challenge, and there are limited data regarding SBI frequency in this population.
Study overview and results
The authors performed a secondary analysis of a prospectively gathered cohort of infants aged 60 days and younger within the Pediatric Emergency Care Applied Research Network (PECARN) who had blood, urine, and CSF data available. Notable exclusions included infants who were premature, had a focal infection, were clinically ill, had recent antibiotic use, did not have blood, urine, and CSF data available, or were lost to telephone follow-up at 7 days to ensure wellness. The study cohort included 6,014 infants, 1,233 (32%) who were febrile by history alone. Rates of overall SBI were lower in the afebrile group (8.8% vs. 12.8%). For infants 0-28 days, rates of UTI were lower for the afebrile group (9.5% vs. 14.5%), but there was no difference in the rates of bacteremia or meningitis. For infants 29-60 days, rates of UTI (6.6% vs. 9.3%) and bacteremia (.5% vs. 1.7%) were lower in the afebrile group.
Limitations
Neither the use of home antipyretics nor the method of temperature taking at home were studied. Also, as this was a secondary analysis, it is possible that not all infants who presented with history of fever only were captured, as work-up was dictated by individual treating providers who may have chosen not to work up certain afebrile infants.
Important findings and implications
Nearly one-third of infants presenting for fever evaluation are afebrile on arrival. Although overall rates of SBI were lower in the group with fever by history only, this difference is largely accounted for by differing rates of UTI. Rates of bacteremia and meningitis remained substantial between groups, particularly for infants aged 0-28 days. Because of the significant morbidity associated with these infections, it is reasonable to suggest that absence of fever on presentation alone should not alter clinical or laboratory work-up, particularly in infants 0-28 days.
STUDY 4
Humphrey-Murto S et al. The influence of prior performance information on ratings of current performance and implications for learner handover: A scoping review. Acad Med. 2019 Jul;94(7):1050-7.
Background
Learner Handover (LH) or “forward feeding” occurs when information about trainees is shared between faculty supervisors. Although this can be helpful to tailor educational experiences and build upon previous assessments, it risks stigmatizing trainees and adding bias to future feedback and assessments as the trainee never really has a “clean slate.” In this study, the authors sought to uncover the key concepts of how prior performance information (PPI) influences assessments and any implications for medical education.
Study overview and results
The authors performed a cross-disciplinary scoping review looking at over 17,000 articles published between 1980 and 2017 across the domains of psychology, sports, business, and education. Seven themes were identified with the following notable findings. Raters exposed to positive PPI scored a learner’s performance higher, and vice versa. There was a dose-response relationship with more positive and more negative PPI resulting in higher and lower assessments, respectively. General standards, such as a direction to complete all work in a timely manner, caused an assimilation effect, while specific standards, such as a direction to complete a certain task by a certain day, did not. More motivated and more experienced raters are less affected by PPI, and those who believe that people can change (incremental theorists) are less affected by PPI while those who believe personal attributes are fixed (entity theorists) are more affected.
Limitations
The heterogeneity of the studies and the fact that they were largely conducted in experimental settings may limit generalizability to medical education. Slightly less than half of the studies included a control arm. Last, most of the studies looked at the ratings of only one target performance, not multiple performances over time.
Important findings and implications
Ratings of current performance displace toward PPI direction, with negative PPI more influential than positive PPI. In a formative setting, PPI may help the assessor focus on areas of possible weakness. In contrast, for a summative assessment, PPI may be prejudicial and have an impact on the rating given to the student. Clinicians should be mindful of the information they share with future raters about learners and the potential bias on future assessments that can manifest as a result.
STUDY 5
McCann ME et al. Neurodevelopmental outcome at 5 years of age after general anaesthesia or awake-regional anaesthesia in infancy (GAS): An international, multicentre, randomised, controlled equivalence trial. The Lancet. 2019 Feb;393:664-77.
Background
Animal models and observational studies have suggested a link between early anesthesia exposure and adverse neurocognitive outcomes; however, findings have been mixed and studies are prone to confounding. This study is the first randomized controlled trial to compare neurocognitive outcomes for infants exposed to general anesthesia versus awake-regional anesthesia.
Study overview and results
In this international, multicenter, assessor-masked trial, 722 infants undergoing inguinal hernia repair were randomized to awake-regional anesthesia or single-agent sevoflurane-based general anesthesia. Infants born at greater than 26 weeks’ gestational age were eligible, while those with prior anesthesia exposure or risks for neurocognitive delay were excluded. The primary outcome was full-scale intelligence quotient (FSIQ) testing at 5 years of age on the Wechsler Preschool and Primary Scale of Intelligence, third edition (WPPSI-III). Seven additional neurodevelopmental assessments and parental questionnaires regarding behavior were administered as secondary outcomes. Average anesthesia exposure was 54 minutes and no infant had exposure greater than 120 minutes. There was no significant difference in mean scores on WPPSI-III FSIQ testing, and no difference in the additional neurocognitive assessments or parent-reported outcomes used as secondary outcomes.
Limitations
This study was limited to single, short periods of single-agent anesthesia exposure in children with no additional neurologic risk factors, so caution should be used in extrapolating these data to children with medical complexity and children undergoing multiple procedures, longer surgeries, or multidrug anesthetic regimens. The study population was majority male because of the surgical pathology selected and included only children in the narrow range of postmenstrual age 60 weeks or less. While this population represents a suspected a period of high cerebral vulnerability based on animal models, the implications of anesthesia exposure at other ages are unclear.
Important findings and implications
An estimated 10% of children from developed countries are exposed to general anesthesia during the first 3 years of life. While hospitalists do not typically select the route of anesthesia, they frequently care for patients undergoing procedures and must address parental concerns regarding the safety of anesthesia exposure. Given the rigorous study methods and long-term follow up in the current study, these data should provide reassurance that, for healthy infants undergoing short, single-agent anesthetic exposure, there is no evidence of future adverse neurologic outcomes.
Dr. Russo is director of pediatrics, medical director for quality and innovation, at WellSpan Health, York, Pa. Dr. Money is a pediatric hospitalist at Primary Children’s Hospital, University of Utah School of Medicine, Salt Lake City. Dr. Steed is instructor of hospital medicine, Northwestern Memorial Hospital and Ann and Robert H. Lurie Children’s Hospital of Chicago, Northwestern University School of Medicine, Chicago. The authors would like to thank Dr. Klint M. Schwenk and the Society for Hospital Medicine Pediatric Special Interest Group Executive Council.
References
1. Roberts KB, Fisher ER, and Rauch DA. The history of pediatric hospital medicine in the United States, 1996-2019. J Hosp Med. 2020 Jul;15(7):424-7.
2. Mussman GM and Conway PH. Pediatric hospitalist systems versus traditional models of care: Effect on quality and cost outcomes. J Hosp Med. 2012 Apr;7(4):350-7.
3. Wang ME, Shaughnessy EE, and Leyenaar JK. The future of pediatric hospital medicine: Challenges and opportunities. J Hosp Med. 2020 Jul;15(7):428-30.
4. Chang PW et al. A clinical prediction rule for rebound hyperbilirubinemia following inpatient phototherapy. Pediatrics. 2017;139 Mar;139(3):e20162896.
Updates in pediatric hospital medicine
Updates in pediatric hospital medicine
The expansion of the field of pediatric hospital medicine in the past 30 years has resulted in improved health care outcomes for hospitalized children1,2 and has been accompanied by a robust increase in the amount of scholarly work related to the field.3 We performed a review of the literature published in 2019 to identify the 10 articles that had the most impact on pediatric hospital medicine, and presented the findings at HM20 Virtual, the 2020 annual conference of the Society of Hospital Medicine. Five of the selected articles are highlighted here.
STUDY 1
Wechsler ME et al. Step-up therapy in black children and adults with poorly controlled asthma. N Engl J Med. 2019 Sep 26;381(13):1227-39.
Background
Current pediatric asthma guidelines suggest adding a long-acting beta-agonist (LABA) to inhaled corticosteroid (ICS) therapy, rather than increasing the ICS dose, for children with poorly controlled asthma. However, these data are based on trials with disproportionately few Black subjects. This study aimed to determine the best step-up therapy for Black patients whose asthma was poorly controlled on ICS monotherapy.
Study overview and results
The authors reported two parallel double-blind, randomized, controlled trials, one in children and one in adolescents and adults. The study of children included 280 subjects ranging in age from 5 to 11, with at least one Black grandparent, and with poorly controlled asthma on low-dose ICS therapy. It used a four-way crossover design in which each subject was treated with four different 14-week treatment regimens: either double (medium-dose) or quintuple (high-dose) their baseline ICS dose, with or without the addition of a LABA. A superior response was defined by the composite outcome of at least one fewer asthma exacerbation, more asthma-control days, or a 5–percentage point difference in predicted FEV1. Forty-six percent of children had improved asthma outcomes when the ICS dose was increased rather than with the addition of a LABA. In contrast, Black adolescents and Black adults had superior responses to the addition of a LABA. There was no significant interaction between the percentage of African ancestry as determined by DNA genotyping and the primary composite outcome. High-dose ICS was associated with a decrease in the ratio of urinary cortisol to creatinine in children younger than 8 years.
Limitations
Approximately 25% of children dropped out of the study, with disproportionately more children dropping out while on a high-dose ICS regimen. Additionally, the difference in the composite outcome was primarily driven by differences in FEV1, with few subjects demonstrating a difference in asthma exacerbations or asthma-control days. Although a decrease in urinary cortisol to creatinine ratio was noted in children under 8 on high-dose ICS, the study period was not long enough to determine the clinical implications of this finding.
Important findings and implications
While studies with a majority of white children have suggested a superior response from adding a LABA compared to increasing the dose of an ICS, almost half of Black children showed a superior response when the dose of an ICS was increased rather than adding a LABA. It is important to note that current guidelines are based on studies with a disproportionate majority of white subjects and may not accurately reflect optimal care for patients in other racial groups. This study underscores the need to include a diverse patient population in research studies.
STUDY 2
Chang PW, Newman TB. A simpler prediction rule for rebound hyperbilirubinemia. Pediatrics. 2019 Jul;144(1):e20183712.
Background
Hyperbilirubinemia (jaundice) is estimated to affect 50%-60% of all newborns. Rebound hyperbilirubinemia – a rise in bilirubin after cessation of phototherapy – is common and can lead to recently discharged infants being readmitted for additional therapy. Lack of clear guidelines regarding when to discharge infants with hyperbilirubinemia has likely contributed to practice variation and some trepidation regarding whether a bilirubin level is “low enough” to discontinue therapy.
Study overview and results
The authors had previously proposed a three-factor hyperbilirubinemia risk model and sought to simplify their rule further.4 They examined a retrospective cohort of 7,048 infants greater than or equal to 35 weeks’ gestation using a random split sample. The authors derived a two-factor model using the same methods and compared its performance to the three-factor model. The two-factor formula was shown to be a good fit as a logistic regression model (Hosmer-Lemeshow test 9.21; P = .33), and the AUROC (area under the receiver operating characteristic) curves for the derivation and validation cohorts were similar between the two-factor (0.877 and 0.876, respectively) and three-factor risk models (0.887 and 0.881, respectively).
Limitations
These data are limited to infants receiving their first treatment of phototherapy and have not been externally validated. An important variable, serum bilirubin at phototherapy termination, was estimated in most subjects, which may have affected the accuracy of the prediction rule. Whether infants received home phototherapy was based only on equipment orders, and some infants may have received phototherapy unbeknownst to investigators. Last, infants with rebound hyperbilirubinemia at less than 72 hours after phototherapy discontinuation may have been missed.
Important findings and implications
This prediction model provides evidence-based, concrete data that can be used in making joint decisions with families regarding discharge timing of infants with hyperbilirubinemia. It also could be beneficial when deciding appropriate follow-up time after discharge.
STUDY 3
Ramgopal S et al. Risk of serious bacterial infection in infants aged ≤60 days presenting to emergency departments with a history of fever only. J Pediatr. 2019 Jan;204:191-195. doi: 10.1016/j.jpeds.2018.08.043.
Background
Febrile infants aged 60 days and younger are at risk for serious bacterial infections (SBI) including urinary tract infections (UTI), bacteremia, and meningitis. As physical exam is a poor discriminator of SBI in this age group, providers frequently rely on laboratory values and risk factors to guide management. Infants presenting with documented fevers by caregivers but found to have no fever in the emergency department are a challenge, and there are limited data regarding SBI frequency in this population.
Study overview and results
The authors performed a secondary analysis of a prospectively gathered cohort of infants aged 60 days and younger within the Pediatric Emergency Care Applied Research Network (PECARN) who had blood, urine, and CSF data available. Notable exclusions included infants who were premature, had a focal infection, were clinically ill, had recent antibiotic use, did not have blood, urine, and CSF data available, or were lost to telephone follow-up at 7 days to ensure wellness. The study cohort included 6,014 infants, 1,233 (32%) who were febrile by history alone. Rates of overall SBI were lower in the afebrile group (8.8% vs. 12.8%). For infants 0-28 days, rates of UTI were lower for the afebrile group (9.5% vs. 14.5%), but there was no difference in the rates of bacteremia or meningitis. For infants 29-60 days, rates of UTI (6.6% vs. 9.3%) and bacteremia (.5% vs. 1.7%) were lower in the afebrile group.
Limitations
Neither the use of home antipyretics nor the method of temperature taking at home were studied. Also, as this was a secondary analysis, it is possible that not all infants who presented with history of fever only were captured, as work-up was dictated by individual treating providers who may have chosen not to work up certain afebrile infants.
Important findings and implications
Nearly one-third of infants presenting for fever evaluation are afebrile on arrival. Although overall rates of SBI were lower in the group with fever by history only, this difference is largely accounted for by differing rates of UTI. Rates of bacteremia and meningitis remained substantial between groups, particularly for infants aged 0-28 days. Because of the significant morbidity associated with these infections, it is reasonable to suggest that absence of fever on presentation alone should not alter clinical or laboratory work-up, particularly in infants 0-28 days.
STUDY 4
Humphrey-Murto S et al. The influence of prior performance information on ratings of current performance and implications for learner handover: A scoping review. Acad Med. 2019 Jul;94(7):1050-7.
Background
Learner Handover (LH) or “forward feeding” occurs when information about trainees is shared between faculty supervisors. Although this can be helpful to tailor educational experiences and build upon previous assessments, it risks stigmatizing trainees and adding bias to future feedback and assessments as the trainee never really has a “clean slate.” In this study, the authors sought to uncover the key concepts of how prior performance information (PPI) influences assessments and any implications for medical education.
Study overview and results
The authors performed a cross-disciplinary scoping review looking at over 17,000 articles published between 1980 and 2017 across the domains of psychology, sports, business, and education. Seven themes were identified with the following notable findings. Raters exposed to positive PPI scored a learner’s performance higher, and vice versa. There was a dose-response relationship with more positive and more negative PPI resulting in higher and lower assessments, respectively. General standards, such as a direction to complete all work in a timely manner, caused an assimilation effect, while specific standards, such as a direction to complete a certain task by a certain day, did not. More motivated and more experienced raters are less affected by PPI, and those who believe that people can change (incremental theorists) are less affected by PPI while those who believe personal attributes are fixed (entity theorists) are more affected.
Limitations
The heterogeneity of the studies and the fact that they were largely conducted in experimental settings may limit generalizability to medical education. Slightly less than half of the studies included a control arm. Last, most of the studies looked at the ratings of only one target performance, not multiple performances over time.
Important findings and implications
Ratings of current performance displace toward PPI direction, with negative PPI more influential than positive PPI. In a formative setting, PPI may help the assessor focus on areas of possible weakness. In contrast, for a summative assessment, PPI may be prejudicial and have an impact on the rating given to the student. Clinicians should be mindful of the information they share with future raters about learners and the potential bias on future assessments that can manifest as a result.
STUDY 5
McCann ME et al. Neurodevelopmental outcome at 5 years of age after general anaesthesia or awake-regional anaesthesia in infancy (GAS): An international, multicentre, randomised, controlled equivalence trial. The Lancet. 2019 Feb;393:664-77.
Background
Animal models and observational studies have suggested a link between early anesthesia exposure and adverse neurocognitive outcomes; however, findings have been mixed and studies are prone to confounding. This study is the first randomized controlled trial to compare neurocognitive outcomes for infants exposed to general anesthesia versus awake-regional anesthesia.
Study overview and results
In this international, multicenter, assessor-masked trial, 722 infants undergoing inguinal hernia repair were randomized to awake-regional anesthesia or single-agent sevoflurane-based general anesthesia. Infants born at greater than 26 weeks’ gestational age were eligible, while those with prior anesthesia exposure or risks for neurocognitive delay were excluded. The primary outcome was full-scale intelligence quotient (FSIQ) testing at 5 years of age on the Wechsler Preschool and Primary Scale of Intelligence, third edition (WPPSI-III). Seven additional neurodevelopmental assessments and parental questionnaires regarding behavior were administered as secondary outcomes. Average anesthesia exposure was 54 minutes and no infant had exposure greater than 120 minutes. There was no significant difference in mean scores on WPPSI-III FSIQ testing, and no difference in the additional neurocognitive assessments or parent-reported outcomes used as secondary outcomes.
Limitations
This study was limited to single, short periods of single-agent anesthesia exposure in children with no additional neurologic risk factors, so caution should be used in extrapolating these data to children with medical complexity and children undergoing multiple procedures, longer surgeries, or multidrug anesthetic regimens. The study population was majority male because of the surgical pathology selected and included only children in the narrow range of postmenstrual age 60 weeks or less. While this population represents a suspected a period of high cerebral vulnerability based on animal models, the implications of anesthesia exposure at other ages are unclear.
Important findings and implications
An estimated 10% of children from developed countries are exposed to general anesthesia during the first 3 years of life. While hospitalists do not typically select the route of anesthesia, they frequently care for patients undergoing procedures and must address parental concerns regarding the safety of anesthesia exposure. Given the rigorous study methods and long-term follow up in the current study, these data should provide reassurance that, for healthy infants undergoing short, single-agent anesthetic exposure, there is no evidence of future adverse neurologic outcomes.
Dr. Russo is director of pediatrics, medical director for quality and innovation, at WellSpan Health, York, Pa. Dr. Money is a pediatric hospitalist at Primary Children’s Hospital, University of Utah School of Medicine, Salt Lake City. Dr. Steed is instructor of hospital medicine, Northwestern Memorial Hospital and Ann and Robert H. Lurie Children’s Hospital of Chicago, Northwestern University School of Medicine, Chicago. The authors would like to thank Dr. Klint M. Schwenk and the Society for Hospital Medicine Pediatric Special Interest Group Executive Council.
References
1. Roberts KB, Fisher ER, and Rauch DA. The history of pediatric hospital medicine in the United States, 1996-2019. J Hosp Med. 2020 Jul;15(7):424-7.
2. Mussman GM and Conway PH. Pediatric hospitalist systems versus traditional models of care: Effect on quality and cost outcomes. J Hosp Med. 2012 Apr;7(4):350-7.
3. Wang ME, Shaughnessy EE, and Leyenaar JK. The future of pediatric hospital medicine: Challenges and opportunities. J Hosp Med. 2020 Jul;15(7):428-30.
4. Chang PW et al. A clinical prediction rule for rebound hyperbilirubinemia following inpatient phototherapy. Pediatrics. 2017;139 Mar;139(3):e20162896.
The expansion of the field of pediatric hospital medicine in the past 30 years has resulted in improved health care outcomes for hospitalized children1,2 and has been accompanied by a robust increase in the amount of scholarly work related to the field.3 We performed a review of the literature published in 2019 to identify the 10 articles that had the most impact on pediatric hospital medicine, and presented the findings at HM20 Virtual, the 2020 annual conference of the Society of Hospital Medicine. Five of the selected articles are highlighted here.
STUDY 1
Wechsler ME et al. Step-up therapy in black children and adults with poorly controlled asthma. N Engl J Med. 2019 Sep 26;381(13):1227-39.
Background
Current pediatric asthma guidelines suggest adding a long-acting beta-agonist (LABA) to inhaled corticosteroid (ICS) therapy, rather than increasing the ICS dose, for children with poorly controlled asthma. However, these data are based on trials with disproportionately few Black subjects. This study aimed to determine the best step-up therapy for Black patients whose asthma was poorly controlled on ICS monotherapy.
Study overview and results
The authors reported two parallel double-blind, randomized, controlled trials, one in children and one in adolescents and adults. The study of children included 280 subjects ranging in age from 5 to 11, with at least one Black grandparent, and with poorly controlled asthma on low-dose ICS therapy. It used a four-way crossover design in which each subject was treated with four different 14-week treatment regimens: either double (medium-dose) or quintuple (high-dose) their baseline ICS dose, with or without the addition of a LABA. A superior response was defined by the composite outcome of at least one fewer asthma exacerbation, more asthma-control days, or a 5–percentage point difference in predicted FEV1. Forty-six percent of children had improved asthma outcomes when the ICS dose was increased rather than with the addition of a LABA. In contrast, Black adolescents and Black adults had superior responses to the addition of a LABA. There was no significant interaction between the percentage of African ancestry as determined by DNA genotyping and the primary composite outcome. High-dose ICS was associated with a decrease in the ratio of urinary cortisol to creatinine in children younger than 8 years.
Limitations
Approximately 25% of children dropped out of the study, with disproportionately more children dropping out while on a high-dose ICS regimen. Additionally, the difference in the composite outcome was primarily driven by differences in FEV1, with few subjects demonstrating a difference in asthma exacerbations or asthma-control days. Although a decrease in urinary cortisol to creatinine ratio was noted in children under 8 on high-dose ICS, the study period was not long enough to determine the clinical implications of this finding.
Important findings and implications
While studies with a majority of white children have suggested a superior response from adding a LABA compared to increasing the dose of an ICS, almost half of Black children showed a superior response when the dose of an ICS was increased rather than adding a LABA. It is important to note that current guidelines are based on studies with a disproportionate majority of white subjects and may not accurately reflect optimal care for patients in other racial groups. This study underscores the need to include a diverse patient population in research studies.
STUDY 2
Chang PW, Newman TB. A simpler prediction rule for rebound hyperbilirubinemia. Pediatrics. 2019 Jul;144(1):e20183712.
Background
Hyperbilirubinemia (jaundice) is estimated to affect 50%-60% of all newborns. Rebound hyperbilirubinemia – a rise in bilirubin after cessation of phototherapy – is common and can lead to recently discharged infants being readmitted for additional therapy. Lack of clear guidelines regarding when to discharge infants with hyperbilirubinemia has likely contributed to practice variation and some trepidation regarding whether a bilirubin level is “low enough” to discontinue therapy.
Study overview and results
The authors had previously proposed a three-factor hyperbilirubinemia risk model and sought to simplify their rule further.4 They examined a retrospective cohort of 7,048 infants greater than or equal to 35 weeks’ gestation using a random split sample. The authors derived a two-factor model using the same methods and compared its performance to the three-factor model. The two-factor formula was shown to be a good fit as a logistic regression model (Hosmer-Lemeshow test 9.21; P = .33), and the AUROC (area under the receiver operating characteristic) curves for the derivation and validation cohorts were similar between the two-factor (0.877 and 0.876, respectively) and three-factor risk models (0.887 and 0.881, respectively).
Limitations
These data are limited to infants receiving their first treatment of phototherapy and have not been externally validated. An important variable, serum bilirubin at phototherapy termination, was estimated in most subjects, which may have affected the accuracy of the prediction rule. Whether infants received home phototherapy was based only on equipment orders, and some infants may have received phototherapy unbeknownst to investigators. Last, infants with rebound hyperbilirubinemia at less than 72 hours after phototherapy discontinuation may have been missed.
Important findings and implications
This prediction model provides evidence-based, concrete data that can be used in making joint decisions with families regarding discharge timing of infants with hyperbilirubinemia. It also could be beneficial when deciding appropriate follow-up time after discharge.
STUDY 3
Ramgopal S et al. Risk of serious bacterial infection in infants aged ≤60 days presenting to emergency departments with a history of fever only. J Pediatr. 2019 Jan;204:191-195. doi: 10.1016/j.jpeds.2018.08.043.
Background
Febrile infants aged 60 days and younger are at risk for serious bacterial infections (SBI) including urinary tract infections (UTI), bacteremia, and meningitis. As physical exam is a poor discriminator of SBI in this age group, providers frequently rely on laboratory values and risk factors to guide management. Infants presenting with documented fevers by caregivers but found to have no fever in the emergency department are a challenge, and there are limited data regarding SBI frequency in this population.
Study overview and results
The authors performed a secondary analysis of a prospectively gathered cohort of infants aged 60 days and younger within the Pediatric Emergency Care Applied Research Network (PECARN) who had blood, urine, and CSF data available. Notable exclusions included infants who were premature, had a focal infection, were clinically ill, had recent antibiotic use, did not have blood, urine, and CSF data available, or were lost to telephone follow-up at 7 days to ensure wellness. The study cohort included 6,014 infants, 1,233 (32%) who were febrile by history alone. Rates of overall SBI were lower in the afebrile group (8.8% vs. 12.8%). For infants 0-28 days, rates of UTI were lower for the afebrile group (9.5% vs. 14.5%), but there was no difference in the rates of bacteremia or meningitis. For infants 29-60 days, rates of UTI (6.6% vs. 9.3%) and bacteremia (.5% vs. 1.7%) were lower in the afebrile group.
Limitations
Neither the use of home antipyretics nor the method of temperature taking at home were studied. Also, as this was a secondary analysis, it is possible that not all infants who presented with history of fever only were captured, as work-up was dictated by individual treating providers who may have chosen not to work up certain afebrile infants.
Important findings and implications
Nearly one-third of infants presenting for fever evaluation are afebrile on arrival. Although overall rates of SBI were lower in the group with fever by history only, this difference is largely accounted for by differing rates of UTI. Rates of bacteremia and meningitis remained substantial between groups, particularly for infants aged 0-28 days. Because of the significant morbidity associated with these infections, it is reasonable to suggest that absence of fever on presentation alone should not alter clinical or laboratory work-up, particularly in infants 0-28 days.
STUDY 4
Humphrey-Murto S et al. The influence of prior performance information on ratings of current performance and implications for learner handover: A scoping review. Acad Med. 2019 Jul;94(7):1050-7.
Background
Learner Handover (LH) or “forward feeding” occurs when information about trainees is shared between faculty supervisors. Although this can be helpful to tailor educational experiences and build upon previous assessments, it risks stigmatizing trainees and adding bias to future feedback and assessments as the trainee never really has a “clean slate.” In this study, the authors sought to uncover the key concepts of how prior performance information (PPI) influences assessments and any implications for medical education.
Study overview and results
The authors performed a cross-disciplinary scoping review looking at over 17,000 articles published between 1980 and 2017 across the domains of psychology, sports, business, and education. Seven themes were identified with the following notable findings. Raters exposed to positive PPI scored a learner’s performance higher, and vice versa. There was a dose-response relationship with more positive and more negative PPI resulting in higher and lower assessments, respectively. General standards, such as a direction to complete all work in a timely manner, caused an assimilation effect, while specific standards, such as a direction to complete a certain task by a certain day, did not. More motivated and more experienced raters are less affected by PPI, and those who believe that people can change (incremental theorists) are less affected by PPI while those who believe personal attributes are fixed (entity theorists) are more affected.
Limitations
The heterogeneity of the studies and the fact that they were largely conducted in experimental settings may limit generalizability to medical education. Slightly less than half of the studies included a control arm. Last, most of the studies looked at the ratings of only one target performance, not multiple performances over time.
Important findings and implications
Ratings of current performance displace toward PPI direction, with negative PPI more influential than positive PPI. In a formative setting, PPI may help the assessor focus on areas of possible weakness. In contrast, for a summative assessment, PPI may be prejudicial and have an impact on the rating given to the student. Clinicians should be mindful of the information they share with future raters about learners and the potential bias on future assessments that can manifest as a result.
STUDY 5
McCann ME et al. Neurodevelopmental outcome at 5 years of age after general anaesthesia or awake-regional anaesthesia in infancy (GAS): An international, multicentre, randomised, controlled equivalence trial. The Lancet. 2019 Feb;393:664-77.
Background
Animal models and observational studies have suggested a link between early anesthesia exposure and adverse neurocognitive outcomes; however, findings have been mixed and studies are prone to confounding. This study is the first randomized controlled trial to compare neurocognitive outcomes for infants exposed to general anesthesia versus awake-regional anesthesia.
Study overview and results
In this international, multicenter, assessor-masked trial, 722 infants undergoing inguinal hernia repair were randomized to awake-regional anesthesia or single-agent sevoflurane-based general anesthesia. Infants born at greater than 26 weeks’ gestational age were eligible, while those with prior anesthesia exposure or risks for neurocognitive delay were excluded. The primary outcome was full-scale intelligence quotient (FSIQ) testing at 5 years of age on the Wechsler Preschool and Primary Scale of Intelligence, third edition (WPPSI-III). Seven additional neurodevelopmental assessments and parental questionnaires regarding behavior were administered as secondary outcomes. Average anesthesia exposure was 54 minutes and no infant had exposure greater than 120 minutes. There was no significant difference in mean scores on WPPSI-III FSIQ testing, and no difference in the additional neurocognitive assessments or parent-reported outcomes used as secondary outcomes.
Limitations
This study was limited to single, short periods of single-agent anesthesia exposure in children with no additional neurologic risk factors, so caution should be used in extrapolating these data to children with medical complexity and children undergoing multiple procedures, longer surgeries, or multidrug anesthetic regimens. The study population was majority male because of the surgical pathology selected and included only children in the narrow range of postmenstrual age 60 weeks or less. While this population represents a suspected a period of high cerebral vulnerability based on animal models, the implications of anesthesia exposure at other ages are unclear.
Important findings and implications
An estimated 10% of children from developed countries are exposed to general anesthesia during the first 3 years of life. While hospitalists do not typically select the route of anesthesia, they frequently care for patients undergoing procedures and must address parental concerns regarding the safety of anesthesia exposure. Given the rigorous study methods and long-term follow up in the current study, these data should provide reassurance that, for healthy infants undergoing short, single-agent anesthetic exposure, there is no evidence of future adverse neurologic outcomes.
Dr. Russo is director of pediatrics, medical director for quality and innovation, at WellSpan Health, York, Pa. Dr. Money is a pediatric hospitalist at Primary Children’s Hospital, University of Utah School of Medicine, Salt Lake City. Dr. Steed is instructor of hospital medicine, Northwestern Memorial Hospital and Ann and Robert H. Lurie Children’s Hospital of Chicago, Northwestern University School of Medicine, Chicago. The authors would like to thank Dr. Klint M. Schwenk and the Society for Hospital Medicine Pediatric Special Interest Group Executive Council.
References
1. Roberts KB, Fisher ER, and Rauch DA. The history of pediatric hospital medicine in the United States, 1996-2019. J Hosp Med. 2020 Jul;15(7):424-7.
2. Mussman GM and Conway PH. Pediatric hospitalist systems versus traditional models of care: Effect on quality and cost outcomes. J Hosp Med. 2012 Apr;7(4):350-7.
3. Wang ME, Shaughnessy EE, and Leyenaar JK. The future of pediatric hospital medicine: Challenges and opportunities. J Hosp Med. 2020 Jul;15(7):428-30.
4. Chang PW et al. A clinical prediction rule for rebound hyperbilirubinemia following inpatient phototherapy. Pediatrics. 2017;139 Mar;139(3):e20162896.