User login
Economic burden of migraine increases with the number of treatment failures
, researchers wrote. Utilization of health care resources and associated costs are greater among patients with three or more treatment failures, compared with patients with fewer treatment failures. This research was presented online as part of the 2020 American Academy of Neurology Science Highlights.
Migraine entails a significant economic burden, including direct costs (e.g., medical costs) and indirect costs (e.g., lost productivity). Information about the burden associated with failed preventive treatments among migraineurs is limited, however. Lawrence C. Newman, MD, director of the division of headache at NYU Langone Health in New York, and colleagues conducted a study to characterize health care resource utilization (HCRU) and its associated costs among migraineurs, stratified by the number of preventive treatment failures.
About one quarter of patients had two treatment failures
Using data from the IBM MarketScan Commercial and Medicare Supplemental database, Dr. Newman and colleagues identified patients who received a new diagnosis of migraine between Jan. 1, 2011, and June 30, 2015. Next, they identified the number of treatment failures during the 2 years following the initial migraine diagnosis. They assessed HCRU and associated costs during the 12 months following an index event. The index was the date of initiation of the second preventive treatment for patients with one treatment failure, the date of initiation of the third treatment for patients with two treatment failures, and the date of initiation of the fourth treatment for patients with three or more treatment failures.
Dr. Newman’s group identified 44,181 patients with incident migraine who had failed preventive treatments. Of this population, 27,112 patients (61.4%) had one treatment failure, 10,583 (24%) had two treatment failures, and 6,486 (14.7%) had three or more treatment failures.
The total medical cost per patient, including emergency room (ER), inpatient (IP), and outpatient (OP) care, increased with increasing number of treatment failures ($10,329 for one, $13,774 for two, and $35,392 for three or more). When the investigators added prescription drug costs, the total health care costs also increased with number of treatment failures ($13,946 for one, $18,685 for two, and $41,864 for three or more).
Similarly, the per-patient annual health care provider visits increased with increasing numbers of treatment failures. The number of ER visits per year was 0.54, 0.69, and 1.02 for patients with one, two, and three or more treatment failures, respectively. The annual number of IP visits was 0.46, 0.59, and 0.97, for patients with one, two, and three or more treatment failures, respectively. OP visits showed a similar trend. The annual number of office visits was 9.47 for patients with one, 11.24 for patients with two, and 14.26 for patients with three or more treatment failures. The annual number of other visits was 13.15 for patients with one, 15.73 for patients with two, and 19.96 for patients with three or more treatment failures.
Guidelines could enable appropriate treatment
Reasons for treatment failure include misdiagnosis of the headache disorder, failure to identify and account for comorbidities, overlooking concurrent acute medication overuse, and inappropriate dose or formulation, said Dr. Newman. “Common pitfalls in prevention that lead to treatment failure include not using evidence-based treatments, starting at too low of a dose and not increasing, starting too high or increasing the dose too quickly, discontinuing the medication before an effect can be seen (before 8 weeks), patient nonadherence, and not establishing realistic expectations.”
Available resources could help clinicians treat migraine effectively. “The American Headache Society (AHS)/AAN preventive guidelines have been retired, yet they offered several levels of effectiveness of pharmacologic treatments that were evidence-based,” said Dr. Newman. “Furthermore, in 2019, the AHS published a consensus statement on integrating new migraine treatments into clinical practice. This statement offered advice about the new anti-CGRP agents, onabotulinum toxin, and neuromodulation devices. I think this is a good starting point for neurologists to be familiar with to choose appropriate therapeutic options for people living with migraine.”
Earlier treatment may reduce patients’ economic burden
The study’s weaknesses included its observational design and its reliance on diagnostic codes, which raised the possibility that comorbidities were inadequately recognized, said Dr. Newman. The reasons that patients changed medications are unknown, and the results are not generalizable to patients aged 65 years or older, he added.
Major strengths of Dr. Newman’s study are its large sample size and wealth of available data, said Alan M. Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles. “The multiple subcategories suggest that this was a carefully organized and implemented study,” he added. If any diagnoses of migraine were provided by general practitioners with little knowledge of migraine, this would weaken the study, said Dr. Rapoport, editor-in-chief of Neurology Reviews.
“We can ease the economic burden of migraineurs by improving acute care therapy with better selection and earlier starting of effective preventive therapy,” he continued. “Going for migraine-specific acute care therapy is better than pain medications or other nonspecific therapies. If you do not stop a migraine attack with effective therapy, you increase the odds that the patient will go on to chronic migraine. It is always important to effectively teach doctors and nurses to improve their diagnostic skills and use the optimal acute and preventive therapy.” For their next trial, maximizing an accurate diagnosis and performing a prospective study measuring treatment outcomes will be particularly valuable, Dr. Rapoport concluded.
Dr. Newman’s study was supported by Novartis Pharma in Basel, Switzerland. Together with Amgen, Novartis developed erenumab. Dr. Newman has received compensation from Allergan, Alder, Amgen, Biohaven, Novartis, Teva, Supernus, and Theranica for consulting, serving on a scientific advisory board, speaking, or other activities. He has received compensation from Springer Scientific for editorial services.
SOURCE: Newman L et al. AAN 2020, Abstract S47.009.
, researchers wrote. Utilization of health care resources and associated costs are greater among patients with three or more treatment failures, compared with patients with fewer treatment failures. This research was presented online as part of the 2020 American Academy of Neurology Science Highlights.
Migraine entails a significant economic burden, including direct costs (e.g., medical costs) and indirect costs (e.g., lost productivity). Information about the burden associated with failed preventive treatments among migraineurs is limited, however. Lawrence C. Newman, MD, director of the division of headache at NYU Langone Health in New York, and colleagues conducted a study to characterize health care resource utilization (HCRU) and its associated costs among migraineurs, stratified by the number of preventive treatment failures.
About one quarter of patients had two treatment failures
Using data from the IBM MarketScan Commercial and Medicare Supplemental database, Dr. Newman and colleagues identified patients who received a new diagnosis of migraine between Jan. 1, 2011, and June 30, 2015. Next, they identified the number of treatment failures during the 2 years following the initial migraine diagnosis. They assessed HCRU and associated costs during the 12 months following an index event. The index was the date of initiation of the second preventive treatment for patients with one treatment failure, the date of initiation of the third treatment for patients with two treatment failures, and the date of initiation of the fourth treatment for patients with three or more treatment failures.
Dr. Newman’s group identified 44,181 patients with incident migraine who had failed preventive treatments. Of this population, 27,112 patients (61.4%) had one treatment failure, 10,583 (24%) had two treatment failures, and 6,486 (14.7%) had three or more treatment failures.
The total medical cost per patient, including emergency room (ER), inpatient (IP), and outpatient (OP) care, increased with increasing number of treatment failures ($10,329 for one, $13,774 for two, and $35,392 for three or more). When the investigators added prescription drug costs, the total health care costs also increased with number of treatment failures ($13,946 for one, $18,685 for two, and $41,864 for three or more).
Similarly, the per-patient annual health care provider visits increased with increasing numbers of treatment failures. The number of ER visits per year was 0.54, 0.69, and 1.02 for patients with one, two, and three or more treatment failures, respectively. The annual number of IP visits was 0.46, 0.59, and 0.97, for patients with one, two, and three or more treatment failures, respectively. OP visits showed a similar trend. The annual number of office visits was 9.47 for patients with one, 11.24 for patients with two, and 14.26 for patients with three or more treatment failures. The annual number of other visits was 13.15 for patients with one, 15.73 for patients with two, and 19.96 for patients with three or more treatment failures.
Guidelines could enable appropriate treatment
Reasons for treatment failure include misdiagnosis of the headache disorder, failure to identify and account for comorbidities, overlooking concurrent acute medication overuse, and inappropriate dose or formulation, said Dr. Newman. “Common pitfalls in prevention that lead to treatment failure include not using evidence-based treatments, starting at too low of a dose and not increasing, starting too high or increasing the dose too quickly, discontinuing the medication before an effect can be seen (before 8 weeks), patient nonadherence, and not establishing realistic expectations.”
Available resources could help clinicians treat migraine effectively. “The American Headache Society (AHS)/AAN preventive guidelines have been retired, yet they offered several levels of effectiveness of pharmacologic treatments that were evidence-based,” said Dr. Newman. “Furthermore, in 2019, the AHS published a consensus statement on integrating new migraine treatments into clinical practice. This statement offered advice about the new anti-CGRP agents, onabotulinum toxin, and neuromodulation devices. I think this is a good starting point for neurologists to be familiar with to choose appropriate therapeutic options for people living with migraine.”
Earlier treatment may reduce patients’ economic burden
The study’s weaknesses included its observational design and its reliance on diagnostic codes, which raised the possibility that comorbidities were inadequately recognized, said Dr. Newman. The reasons that patients changed medications are unknown, and the results are not generalizable to patients aged 65 years or older, he added.
Major strengths of Dr. Newman’s study are its large sample size and wealth of available data, said Alan M. Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles. “The multiple subcategories suggest that this was a carefully organized and implemented study,” he added. If any diagnoses of migraine were provided by general practitioners with little knowledge of migraine, this would weaken the study, said Dr. Rapoport, editor-in-chief of Neurology Reviews.
“We can ease the economic burden of migraineurs by improving acute care therapy with better selection and earlier starting of effective preventive therapy,” he continued. “Going for migraine-specific acute care therapy is better than pain medications or other nonspecific therapies. If you do not stop a migraine attack with effective therapy, you increase the odds that the patient will go on to chronic migraine. It is always important to effectively teach doctors and nurses to improve their diagnostic skills and use the optimal acute and preventive therapy.” For their next trial, maximizing an accurate diagnosis and performing a prospective study measuring treatment outcomes will be particularly valuable, Dr. Rapoport concluded.
Dr. Newman’s study was supported by Novartis Pharma in Basel, Switzerland. Together with Amgen, Novartis developed erenumab. Dr. Newman has received compensation from Allergan, Alder, Amgen, Biohaven, Novartis, Teva, Supernus, and Theranica for consulting, serving on a scientific advisory board, speaking, or other activities. He has received compensation from Springer Scientific for editorial services.
SOURCE: Newman L et al. AAN 2020, Abstract S47.009.
, researchers wrote. Utilization of health care resources and associated costs are greater among patients with three or more treatment failures, compared with patients with fewer treatment failures. This research was presented online as part of the 2020 American Academy of Neurology Science Highlights.
Migraine entails a significant economic burden, including direct costs (e.g., medical costs) and indirect costs (e.g., lost productivity). Information about the burden associated with failed preventive treatments among migraineurs is limited, however. Lawrence C. Newman, MD, director of the division of headache at NYU Langone Health in New York, and colleagues conducted a study to characterize health care resource utilization (HCRU) and its associated costs among migraineurs, stratified by the number of preventive treatment failures.
About one quarter of patients had two treatment failures
Using data from the IBM MarketScan Commercial and Medicare Supplemental database, Dr. Newman and colleagues identified patients who received a new diagnosis of migraine between Jan. 1, 2011, and June 30, 2015. Next, they identified the number of treatment failures during the 2 years following the initial migraine diagnosis. They assessed HCRU and associated costs during the 12 months following an index event. The index was the date of initiation of the second preventive treatment for patients with one treatment failure, the date of initiation of the third treatment for patients with two treatment failures, and the date of initiation of the fourth treatment for patients with three or more treatment failures.
Dr. Newman’s group identified 44,181 patients with incident migraine who had failed preventive treatments. Of this population, 27,112 patients (61.4%) had one treatment failure, 10,583 (24%) had two treatment failures, and 6,486 (14.7%) had three or more treatment failures.
The total medical cost per patient, including emergency room (ER), inpatient (IP), and outpatient (OP) care, increased with increasing number of treatment failures ($10,329 for one, $13,774 for two, and $35,392 for three or more). When the investigators added prescription drug costs, the total health care costs also increased with number of treatment failures ($13,946 for one, $18,685 for two, and $41,864 for three or more).
Similarly, the per-patient annual health care provider visits increased with increasing numbers of treatment failures. The number of ER visits per year was 0.54, 0.69, and 1.02 for patients with one, two, and three or more treatment failures, respectively. The annual number of IP visits was 0.46, 0.59, and 0.97, for patients with one, two, and three or more treatment failures, respectively. OP visits showed a similar trend. The annual number of office visits was 9.47 for patients with one, 11.24 for patients with two, and 14.26 for patients with three or more treatment failures. The annual number of other visits was 13.15 for patients with one, 15.73 for patients with two, and 19.96 for patients with three or more treatment failures.
Guidelines could enable appropriate treatment
Reasons for treatment failure include misdiagnosis of the headache disorder, failure to identify and account for comorbidities, overlooking concurrent acute medication overuse, and inappropriate dose or formulation, said Dr. Newman. “Common pitfalls in prevention that lead to treatment failure include not using evidence-based treatments, starting at too low of a dose and not increasing, starting too high or increasing the dose too quickly, discontinuing the medication before an effect can be seen (before 8 weeks), patient nonadherence, and not establishing realistic expectations.”
Available resources could help clinicians treat migraine effectively. “The American Headache Society (AHS)/AAN preventive guidelines have been retired, yet they offered several levels of effectiveness of pharmacologic treatments that were evidence-based,” said Dr. Newman. “Furthermore, in 2019, the AHS published a consensus statement on integrating new migraine treatments into clinical practice. This statement offered advice about the new anti-CGRP agents, onabotulinum toxin, and neuromodulation devices. I think this is a good starting point for neurologists to be familiar with to choose appropriate therapeutic options for people living with migraine.”
Earlier treatment may reduce patients’ economic burden
The study’s weaknesses included its observational design and its reliance on diagnostic codes, which raised the possibility that comorbidities were inadequately recognized, said Dr. Newman. The reasons that patients changed medications are unknown, and the results are not generalizable to patients aged 65 years or older, he added.
Major strengths of Dr. Newman’s study are its large sample size and wealth of available data, said Alan M. Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles. “The multiple subcategories suggest that this was a carefully organized and implemented study,” he added. If any diagnoses of migraine were provided by general practitioners with little knowledge of migraine, this would weaken the study, said Dr. Rapoport, editor-in-chief of Neurology Reviews.
“We can ease the economic burden of migraineurs by improving acute care therapy with better selection and earlier starting of effective preventive therapy,” he continued. “Going for migraine-specific acute care therapy is better than pain medications or other nonspecific therapies. If you do not stop a migraine attack with effective therapy, you increase the odds that the patient will go on to chronic migraine. It is always important to effectively teach doctors and nurses to improve their diagnostic skills and use the optimal acute and preventive therapy.” For their next trial, maximizing an accurate diagnosis and performing a prospective study measuring treatment outcomes will be particularly valuable, Dr. Rapoport concluded.
Dr. Newman’s study was supported by Novartis Pharma in Basel, Switzerland. Together with Amgen, Novartis developed erenumab. Dr. Newman has received compensation from Allergan, Alder, Amgen, Biohaven, Novartis, Teva, Supernus, and Theranica for consulting, serving on a scientific advisory board, speaking, or other activities. He has received compensation from Springer Scientific for editorial services.
SOURCE: Newman L et al. AAN 2020, Abstract S47.009.
From AAN 2020
Predictors of ICH after thrombectomy identified
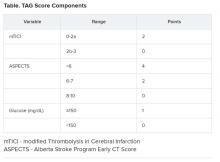
(ICH), new research suggests. In a study of nearly 600 patients undergoing thrombectomy, investigators combined a modified Thrombolysis in Cerebral Ischemia (TICI) score, an Alberta Stroke Program Early Computed Tomography Score (ASPECTS), and glucose levels (the “TAG score”) to predict risk. Results showed that each unit increase in the combination score was associated with a significant, nearly twofold greater likelihood of symptomatic ICH.
“It is very easy” to calculate the new score in a clinical setting, lead author Mayra Johana Montalvo Perero, MD, Department of Neurology, Brown University and Rhode Island Hospital, Providence, said. “You just need three variables.”
The findings were presented online as part of the 2020 American Academy of Neurology Science Highlights.
Limited data
High TAG scores are associated with symptomatic ICH in patients receiving mechanical thrombectomy, Dr. Montalvo Perero and colleagues said.
Although clinical predictors of symptomatic ICH are well established, “there is limited data in patients who underwent mechanical thrombectomy,” the researchers noted.
To learn more, they assessed 578 patients (52% women; mean age, 73 years) who had mechanical thrombectomy for acute ischemic stroke at a comprehensive stroke center. Within this cohort, 19 patients (3.3%) developed symptomatic ICH.
The investigators compared clinical and radiographic findings between patients who experienced symptomatic ICH and those who did not.
The TICI score emerged as a predictor when each unit decrease in this score was associated with greater risk for symptomatic ICH (odds ratio, 5.13; 95% confidence interval, 1.84-14.29; P = .002).
Each one-point decrease in the ASPECTS score also predicted increased risk (OR, 1.52; 95% CI, 1.1-2.0; P = .003).
“The main driver is the size of the stroke core, which is correlated with the ASPECTS score,” Dr. Montalvo Perero said.
Each 10 mg/dL increase in glucose level also correlated with increased risk (OR, 1.07; 95% CI, 1.01-1.13; P = .018).
Twice the risk
The investigators then combined these three independent variables into a weighted TAG score based on a multivariate analysis. Each unit increase in this composite score was associated with increased risk of symptomatic ICH (OR, 1.98; 95% CI, 1.48-2.66; P < .001).
There was no association between patients who received tissue plasminogen activator (tPA) and risk of symptomatic ICH, which Dr. Montalvo Perero said was surprising.
However, “that may be due to a small number” of patients with symptomatic ICH included in the study, she said. “Therefore, that would be an interesting question to ask in future studies with bigger cohorts.”
Larger studies are also needed to validate this scoring system and to test strategies to reduce risk of symptomatic ICH and make thrombectomy safer in patients with elevated TAG scores, Dr. Montalvo Perero said.
A step in the right direction?
Commenting on the study, Jeremy Payne, MD, PhD, director of the Stroke Center at Banner Health’s University Medicine Neuroscience Institute in Phoenix, Arizona, noted the importance of predicting which patients might have secondary bleeding after interventional treatment of a large vessel occlusion stroke
“In aggregate, the role of endovascular thrombectomy is quite clear, but we still struggle to predict at the individual patient level who will benefit,” said Dr. Payne, who was not involved with the research.
Transfer and treatment of these patients also carries an economic cost. “Just getting patients to our center, where about 80% of the complex stroke patients come by helicopter, costs upwards of $30,000,” Dr. Payne said. “The financial argument isn’t one we like to talk much about, but we’re committing to spending probably $100,000-$200,000 on each person’s care.”
This study “attempts to address an important issue,” he said.
Predicting who is more likely to benefit leads to the assumption that if that were to happen, “we could skip all the rigamarole of helicopters and procedures, avoid the extra expense and particularly not make things worse than they already are,” explained Dr. Payne.
Potential limitations include that this is a single-center study and is based on an analysis of 19 patients out of 578. As a result, it is not clear that these findings will necessarily be generalizable to other centers, said Dr. Payne.
The TICI and ASPECTS “are pretty obvious markers of risk,” he noted. “The glucose levels, however, are more subtly interesting.”
He also pointed out that an association between diabetes and worse stroke outcomes is well established.
“The mechanisms are poorly understood, but the role of glucose keeps popping up as a potential marker of risk, and so it’s interesting that it bubbles up in their work too,” Dr. Payne said.
Furthermore, unlike TICI and ASPECTS, glucose levels are modifiable.
“Overall, then, we will continue to study this,” Dr. Payne said. “It’s very important to refine our ability to predict which patients may receive benefit versus harm from such procedures, and this is a step in the right direction.”
Some findings were also published December 2019 in the Journal of Neurology, Neurosurgery & Psychiatry.
Montalvo Perero and Payne have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
SOURCE: Motalvo Perero MJ et al. AAN 2020, Abstract S20.001.
(ICH), new research suggests. In a study of nearly 600 patients undergoing thrombectomy, investigators combined a modified Thrombolysis in Cerebral Ischemia (TICI) score, an Alberta Stroke Program Early Computed Tomography Score (ASPECTS), and glucose levels (the “TAG score”) to predict risk. Results showed that each unit increase in the combination score was associated with a significant, nearly twofold greater likelihood of symptomatic ICH.
“It is very easy” to calculate the new score in a clinical setting, lead author Mayra Johana Montalvo Perero, MD, Department of Neurology, Brown University and Rhode Island Hospital, Providence, said. “You just need three variables.”
The findings were presented online as part of the 2020 American Academy of Neurology Science Highlights.
Limited data
High TAG scores are associated with symptomatic ICH in patients receiving mechanical thrombectomy, Dr. Montalvo Perero and colleagues said.
Although clinical predictors of symptomatic ICH are well established, “there is limited data in patients who underwent mechanical thrombectomy,” the researchers noted.
To learn more, they assessed 578 patients (52% women; mean age, 73 years) who had mechanical thrombectomy for acute ischemic stroke at a comprehensive stroke center. Within this cohort, 19 patients (3.3%) developed symptomatic ICH.
The investigators compared clinical and radiographic findings between patients who experienced symptomatic ICH and those who did not.
The TICI score emerged as a predictor when each unit decrease in this score was associated with greater risk for symptomatic ICH (odds ratio, 5.13; 95% confidence interval, 1.84-14.29; P = .002).
Each one-point decrease in the ASPECTS score also predicted increased risk (OR, 1.52; 95% CI, 1.1-2.0; P = .003).
“The main driver is the size of the stroke core, which is correlated with the ASPECTS score,” Dr. Montalvo Perero said.
Each 10 mg/dL increase in glucose level also correlated with increased risk (OR, 1.07; 95% CI, 1.01-1.13; P = .018).
Twice the risk
The investigators then combined these three independent variables into a weighted TAG score based on a multivariate analysis. Each unit increase in this composite score was associated with increased risk of symptomatic ICH (OR, 1.98; 95% CI, 1.48-2.66; P < .001).
There was no association between patients who received tissue plasminogen activator (tPA) and risk of symptomatic ICH, which Dr. Montalvo Perero said was surprising.
However, “that may be due to a small number” of patients with symptomatic ICH included in the study, she said. “Therefore, that would be an interesting question to ask in future studies with bigger cohorts.”
Larger studies are also needed to validate this scoring system and to test strategies to reduce risk of symptomatic ICH and make thrombectomy safer in patients with elevated TAG scores, Dr. Montalvo Perero said.
A step in the right direction?
Commenting on the study, Jeremy Payne, MD, PhD, director of the Stroke Center at Banner Health’s University Medicine Neuroscience Institute in Phoenix, Arizona, noted the importance of predicting which patients might have secondary bleeding after interventional treatment of a large vessel occlusion stroke
“In aggregate, the role of endovascular thrombectomy is quite clear, but we still struggle to predict at the individual patient level who will benefit,” said Dr. Payne, who was not involved with the research.
Transfer and treatment of these patients also carries an economic cost. “Just getting patients to our center, where about 80% of the complex stroke patients come by helicopter, costs upwards of $30,000,” Dr. Payne said. “The financial argument isn’t one we like to talk much about, but we’re committing to spending probably $100,000-$200,000 on each person’s care.”
This study “attempts to address an important issue,” he said.
Predicting who is more likely to benefit leads to the assumption that if that were to happen, “we could skip all the rigamarole of helicopters and procedures, avoid the extra expense and particularly not make things worse than they already are,” explained Dr. Payne.
Potential limitations include that this is a single-center study and is based on an analysis of 19 patients out of 578. As a result, it is not clear that these findings will necessarily be generalizable to other centers, said Dr. Payne.
The TICI and ASPECTS “are pretty obvious markers of risk,” he noted. “The glucose levels, however, are more subtly interesting.”
He also pointed out that an association between diabetes and worse stroke outcomes is well established.
“The mechanisms are poorly understood, but the role of glucose keeps popping up as a potential marker of risk, and so it’s interesting that it bubbles up in their work too,” Dr. Payne said.
Furthermore, unlike TICI and ASPECTS, glucose levels are modifiable.
“Overall, then, we will continue to study this,” Dr. Payne said. “It’s very important to refine our ability to predict which patients may receive benefit versus harm from such procedures, and this is a step in the right direction.”
Some findings were also published December 2019 in the Journal of Neurology, Neurosurgery & Psychiatry.
Montalvo Perero and Payne have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
SOURCE: Motalvo Perero MJ et al. AAN 2020, Abstract S20.001.
(ICH), new research suggests. In a study of nearly 600 patients undergoing thrombectomy, investigators combined a modified Thrombolysis in Cerebral Ischemia (TICI) score, an Alberta Stroke Program Early Computed Tomography Score (ASPECTS), and glucose levels (the “TAG score”) to predict risk. Results showed that each unit increase in the combination score was associated with a significant, nearly twofold greater likelihood of symptomatic ICH.
“It is very easy” to calculate the new score in a clinical setting, lead author Mayra Johana Montalvo Perero, MD, Department of Neurology, Brown University and Rhode Island Hospital, Providence, said. “You just need three variables.”
The findings were presented online as part of the 2020 American Academy of Neurology Science Highlights.
Limited data
High TAG scores are associated with symptomatic ICH in patients receiving mechanical thrombectomy, Dr. Montalvo Perero and colleagues said.
Although clinical predictors of symptomatic ICH are well established, “there is limited data in patients who underwent mechanical thrombectomy,” the researchers noted.
To learn more, they assessed 578 patients (52% women; mean age, 73 years) who had mechanical thrombectomy for acute ischemic stroke at a comprehensive stroke center. Within this cohort, 19 patients (3.3%) developed symptomatic ICH.
The investigators compared clinical and radiographic findings between patients who experienced symptomatic ICH and those who did not.
The TICI score emerged as a predictor when each unit decrease in this score was associated with greater risk for symptomatic ICH (odds ratio, 5.13; 95% confidence interval, 1.84-14.29; P = .002).
Each one-point decrease in the ASPECTS score also predicted increased risk (OR, 1.52; 95% CI, 1.1-2.0; P = .003).
“The main driver is the size of the stroke core, which is correlated with the ASPECTS score,” Dr. Montalvo Perero said.
Each 10 mg/dL increase in glucose level also correlated with increased risk (OR, 1.07; 95% CI, 1.01-1.13; P = .018).
Twice the risk
The investigators then combined these three independent variables into a weighted TAG score based on a multivariate analysis. Each unit increase in this composite score was associated with increased risk of symptomatic ICH (OR, 1.98; 95% CI, 1.48-2.66; P < .001).
There was no association between patients who received tissue plasminogen activator (tPA) and risk of symptomatic ICH, which Dr. Montalvo Perero said was surprising.
However, “that may be due to a small number” of patients with symptomatic ICH included in the study, she said. “Therefore, that would be an interesting question to ask in future studies with bigger cohorts.”
Larger studies are also needed to validate this scoring system and to test strategies to reduce risk of symptomatic ICH and make thrombectomy safer in patients with elevated TAG scores, Dr. Montalvo Perero said.
A step in the right direction?
Commenting on the study, Jeremy Payne, MD, PhD, director of the Stroke Center at Banner Health’s University Medicine Neuroscience Institute in Phoenix, Arizona, noted the importance of predicting which patients might have secondary bleeding after interventional treatment of a large vessel occlusion stroke
“In aggregate, the role of endovascular thrombectomy is quite clear, but we still struggle to predict at the individual patient level who will benefit,” said Dr. Payne, who was not involved with the research.
Transfer and treatment of these patients also carries an economic cost. “Just getting patients to our center, where about 80% of the complex stroke patients come by helicopter, costs upwards of $30,000,” Dr. Payne said. “The financial argument isn’t one we like to talk much about, but we’re committing to spending probably $100,000-$200,000 on each person’s care.”
This study “attempts to address an important issue,” he said.
Predicting who is more likely to benefit leads to the assumption that if that were to happen, “we could skip all the rigamarole of helicopters and procedures, avoid the extra expense and particularly not make things worse than they already are,” explained Dr. Payne.
Potential limitations include that this is a single-center study and is based on an analysis of 19 patients out of 578. As a result, it is not clear that these findings will necessarily be generalizable to other centers, said Dr. Payne.
The TICI and ASPECTS “are pretty obvious markers of risk,” he noted. “The glucose levels, however, are more subtly interesting.”
He also pointed out that an association between diabetes and worse stroke outcomes is well established.
“The mechanisms are poorly understood, but the role of glucose keeps popping up as a potential marker of risk, and so it’s interesting that it bubbles up in their work too,” Dr. Payne said.
Furthermore, unlike TICI and ASPECTS, glucose levels are modifiable.
“Overall, then, we will continue to study this,” Dr. Payne said. “It’s very important to refine our ability to predict which patients may receive benefit versus harm from such procedures, and this is a step in the right direction.”
Some findings were also published December 2019 in the Journal of Neurology, Neurosurgery & Psychiatry.
Montalvo Perero and Payne have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
SOURCE: Motalvo Perero MJ et al. AAN 2020, Abstract S20.001.
AAN 2020
CGRP inhibitors receive reassuring real-world safety report
Stephen D. Silberstein, MD, reported online as part of the 2020 American Academy of Neurology Science Highlights.
He presented a retrospective analysis of spontaneous postmarketing reports to the Food and Drug Administration Adverse Events Reporting System (FAERS) for Aimovig (erenumab-aooe), Ajovy (fremanezumab-vfrm), and Emgality (galcanezumab-gnlm).
The top-10 lists of adverse events for all three monoclonal antibodies targeting CGRP were skewed heavily towards injection-site reactions, such as injection-site pain, itching, swelling, and erythema. The rates were relatively low. For example, injection-site pain was reported at a rate of 2.94 cases per 1,000 patients exposed to erenumab, 0.8/1,000 for fremanezumab, and 4.9/1,000 for galcanezumab, according to Dr. Silberstein, professor of neurology and director of the headache center at Sidney Kimmel Medical College, Philadelphia.
Migraine, headache, and drug ineffectiveness were in the top 10 for all three medications, as is typical in FAERS reports, since no drug is effective in everyone. These events were reported at rates of 1-5/1,000 exposed patients. Constipation was reported in association with the use of erenumab at a rate of 4.9 cases/1,000 patients, but did not reach the top-10 lists for the other two CGRP antagonists.
Notably, cardiovascular events were not among the top-10 adverse events reported for any of the novel preventive agents.
“These results will be practice changing, since some physicians have been holding back from prescribing these drugs pending the results of this sort of longer-term safety data,” Dr. Silberstein predicted in an interview.
Asked to comment on the FAERS study, neurologist Holly Yancy, DO, said that she found the findings unsurprising because the adverse effects were essentially as expected based upon the earlier favorable clinical trials experience.
“These medications are living up to the expectations for good tolerability that were in place when they were initially approved by the FDA just under 2 years ago,” said Dr. Yancy, a headache specialist at the Banner–University Medicine Neuroscience Institute in Phoenix.
“Injection-site reactions were anticipated. Clinically, I’ve found that if the medications reduce migraine days and severity, patients find the risk of temporary pain, redness, or itching at the injection site is an easy trade off,” she added.
CGRP is a vasoactive peptide. There has been a theoretic concern that its pharmacologic inhibition for prevention of migraine could lead to an increased risk of adverse cardiovascular events, especially in individuals with coronary disease or a history of stroke. The absence of any such signal during the first 6 months of widespread clinical use of the CGRP inhibitors is highly encouraging, although this is an issue that warrants longer-term study, Dr. Yancy continued.
These drugs, which were expressly designed for migraine prevention, are a considerable advance over what was previously available in her view. They’re equally or more effective and considerably better tolerated than the preventive medications physicians had long been using off label, including antidepressants, antiepileptics, and cardiac drugs.
Dr. Silberstein reported financial relationships with close to two dozen pharmaceutical companies. Dr. Yancy reported serving on speakers’ bureaus for Amgen and Novartis.
SOURCE: Silverstein SD et al. AAN 2020, Abstract S58.008.
Stephen D. Silberstein, MD, reported online as part of the 2020 American Academy of Neurology Science Highlights.
He presented a retrospective analysis of spontaneous postmarketing reports to the Food and Drug Administration Adverse Events Reporting System (FAERS) for Aimovig (erenumab-aooe), Ajovy (fremanezumab-vfrm), and Emgality (galcanezumab-gnlm).
The top-10 lists of adverse events for all three monoclonal antibodies targeting CGRP were skewed heavily towards injection-site reactions, such as injection-site pain, itching, swelling, and erythema. The rates were relatively low. For example, injection-site pain was reported at a rate of 2.94 cases per 1,000 patients exposed to erenumab, 0.8/1,000 for fremanezumab, and 4.9/1,000 for galcanezumab, according to Dr. Silberstein, professor of neurology and director of the headache center at Sidney Kimmel Medical College, Philadelphia.
Migraine, headache, and drug ineffectiveness were in the top 10 for all three medications, as is typical in FAERS reports, since no drug is effective in everyone. These events were reported at rates of 1-5/1,000 exposed patients. Constipation was reported in association with the use of erenumab at a rate of 4.9 cases/1,000 patients, but did not reach the top-10 lists for the other two CGRP antagonists.
Notably, cardiovascular events were not among the top-10 adverse events reported for any of the novel preventive agents.
“These results will be practice changing, since some physicians have been holding back from prescribing these drugs pending the results of this sort of longer-term safety data,” Dr. Silberstein predicted in an interview.
Asked to comment on the FAERS study, neurologist Holly Yancy, DO, said that she found the findings unsurprising because the adverse effects were essentially as expected based upon the earlier favorable clinical trials experience.
“These medications are living up to the expectations for good tolerability that were in place when they were initially approved by the FDA just under 2 years ago,” said Dr. Yancy, a headache specialist at the Banner–University Medicine Neuroscience Institute in Phoenix.
“Injection-site reactions were anticipated. Clinically, I’ve found that if the medications reduce migraine days and severity, patients find the risk of temporary pain, redness, or itching at the injection site is an easy trade off,” she added.
CGRP is a vasoactive peptide. There has been a theoretic concern that its pharmacologic inhibition for prevention of migraine could lead to an increased risk of adverse cardiovascular events, especially in individuals with coronary disease or a history of stroke. The absence of any such signal during the first 6 months of widespread clinical use of the CGRP inhibitors is highly encouraging, although this is an issue that warrants longer-term study, Dr. Yancy continued.
These drugs, which were expressly designed for migraine prevention, are a considerable advance over what was previously available in her view. They’re equally or more effective and considerably better tolerated than the preventive medications physicians had long been using off label, including antidepressants, antiepileptics, and cardiac drugs.
Dr. Silberstein reported financial relationships with close to two dozen pharmaceutical companies. Dr. Yancy reported serving on speakers’ bureaus for Amgen and Novartis.
SOURCE: Silverstein SD et al. AAN 2020, Abstract S58.008.
Stephen D. Silberstein, MD, reported online as part of the 2020 American Academy of Neurology Science Highlights.
He presented a retrospective analysis of spontaneous postmarketing reports to the Food and Drug Administration Adverse Events Reporting System (FAERS) for Aimovig (erenumab-aooe), Ajovy (fremanezumab-vfrm), and Emgality (galcanezumab-gnlm).
The top-10 lists of adverse events for all three monoclonal antibodies targeting CGRP were skewed heavily towards injection-site reactions, such as injection-site pain, itching, swelling, and erythema. The rates were relatively low. For example, injection-site pain was reported at a rate of 2.94 cases per 1,000 patients exposed to erenumab, 0.8/1,000 for fremanezumab, and 4.9/1,000 for galcanezumab, according to Dr. Silberstein, professor of neurology and director of the headache center at Sidney Kimmel Medical College, Philadelphia.
Migraine, headache, and drug ineffectiveness were in the top 10 for all three medications, as is typical in FAERS reports, since no drug is effective in everyone. These events were reported at rates of 1-5/1,000 exposed patients. Constipation was reported in association with the use of erenumab at a rate of 4.9 cases/1,000 patients, but did not reach the top-10 lists for the other two CGRP antagonists.
Notably, cardiovascular events were not among the top-10 adverse events reported for any of the novel preventive agents.
“These results will be practice changing, since some physicians have been holding back from prescribing these drugs pending the results of this sort of longer-term safety data,” Dr. Silberstein predicted in an interview.
Asked to comment on the FAERS study, neurologist Holly Yancy, DO, said that she found the findings unsurprising because the adverse effects were essentially as expected based upon the earlier favorable clinical trials experience.
“These medications are living up to the expectations for good tolerability that were in place when they were initially approved by the FDA just under 2 years ago,” said Dr. Yancy, a headache specialist at the Banner–University Medicine Neuroscience Institute in Phoenix.
“Injection-site reactions were anticipated. Clinically, I’ve found that if the medications reduce migraine days and severity, patients find the risk of temporary pain, redness, or itching at the injection site is an easy trade off,” she added.
CGRP is a vasoactive peptide. There has been a theoretic concern that its pharmacologic inhibition for prevention of migraine could lead to an increased risk of adverse cardiovascular events, especially in individuals with coronary disease or a history of stroke. The absence of any such signal during the first 6 months of widespread clinical use of the CGRP inhibitors is highly encouraging, although this is an issue that warrants longer-term study, Dr. Yancy continued.
These drugs, which were expressly designed for migraine prevention, are a considerable advance over what was previously available in her view. They’re equally or more effective and considerably better tolerated than the preventive medications physicians had long been using off label, including antidepressants, antiepileptics, and cardiac drugs.
Dr. Silberstein reported financial relationships with close to two dozen pharmaceutical companies. Dr. Yancy reported serving on speakers’ bureaus for Amgen and Novartis.
SOURCE: Silverstein SD et al. AAN 2020, Abstract S58.008.
FROM AAN 2020
Anti-NMDAR encephalitis or primary psychiatric disorder?
New insights and ‘red flags’ provide clues to diagnosis
It remains difficult to distinguish anti-NMDA receptor encephalitis from a primary psychiatric disorder, but recent studies have identified clinical features and proposed screening criteria that could make it easier to identify these patients who would benefit from immunotherapy, according to an expert in the neurologic disease.
Most patients with confirmed anti-NMDA receptor encephalitis will experience substantial improvement after treatment with immunotherapy and other modalities, said Josep Dalmau, MD, PhD, professor at the Catalan Institute for Research and Advanced Studies at the University of Barcelona and adjunct professor of neurology at the University of Pennsylvania, Philadelphia.
“In our experience, being aggressive with immune therapy ... the patients do quite well, which means that basically 85%-90% of the patients substantially improved over the next few months,” Dr. Dalmau said at the annual meeting of the American Psychiatric Association, which was held as a virtual live event.
Identified for the first time a little more than a decade ago, anti-NMDA receptor encephalitis is a rare, immune-mediated disease that is usually found in children and young adults and is more common among women. It is frequently associated with ovarian tumors and teratomas, said Dr. Dalmau, and in about 90% of cases, patients will have prominent psychiatric and behavioral symptoms.
Patients develop IgG antibodies against the GluN1 subunit of the NMDA receptor. These autoantibodies represent not only a diagnostic marker of the disease, but are also pathogenic, altering NMDA receptor–related synaptic transmission, Dr. Dalmau said.
In several recent studies, investigators have attempted to cobble together a distinct phenotype on anti-NMDA receptor encephalitis to aid psychiatrists who might encounter patients with the disease, he said.
In one of the most recent studies, researchers combed the medical literature and found that, among 544 individuals with the disease, the most common psychiatric symptoms were agitation, seen in 59%, and psychotic symptoms (particularly visual-auditory hallucinations and disorganized behavior) in 54%; catatonia was seen in 42% of adults and 35% of children.
according to a report from researchers in Berlin, Dr. Dalmau added. By picking up on those clinical signs, which included seizures, catatonia, autonomic instability, or hyperkinesia, the time from symptom onset to diagnosis could be cut in half, the researchers found.
There’s also a handy acronym that could serve as a mnemonic to pick up on “diagnostic clues” of anti-NMDA receptor encephalitis among patients with new-onset psychiatric symptoms, Dr. Dalmau said.
That acronym, published in a review article by Dr. Dalmau and colleagues, is SEARCH For NMDAR-A, covering, in order: sleep dysfunction, excitement, agitation, rapid onset, child and young adult predominance, history of psychiatric disease (absent), fluctuating catatonia, negative and positive symptoms, memory deficit, decreased verbal output, antipsychotic intolerance, rule out neuroleptic malignant syndrome, and of course, antibodies (though the final “A” also stands for additional testing, including magnetic resonance imaging, cerebrospinal fluid studies, and electroencephalogram).
While the disease can be lethal, Dr. Dalmau said most patients respond to immunotherapy, and if applicable, treatment of the underlying tumor can help. The most common first-line treatments include steroids, intravenous immunoglobulin, and plasma exchange, he said, while second-line treatments include the monoclonal anti-CD20 antibody rituximab and cyclophosphamide.
Beyond immunotherapy, patients may benefit from supportive care and psychiatric treatment. Benzodiazepines are well tolerated, but Dr. Dalmau said antipsychotic intolerance is frequent, and electroconvulsive therapy has “mixed results” in these patients.
The recovery process can take months and may be complicated by hypersomnia, hyperphagia, and hypersexuality, he added.
“Some patients improve dramatically in 1 month, but this is uncommon, really,” he said, adding that an early recovery may be a “red flag” that the underlying condition is something other than anti-NMDA receptor encephalitis.
Dr. Dalmau provided disclosures related to Cellex Foundation, Safra Foundation, Caixa Health Project Foundation, and Sage Therapeutics.
SOURCE: Dalmau J. APA 2020, Abstract.
New insights and ‘red flags’ provide clues to diagnosis
New insights and ‘red flags’ provide clues to diagnosis
It remains difficult to distinguish anti-NMDA receptor encephalitis from a primary psychiatric disorder, but recent studies have identified clinical features and proposed screening criteria that could make it easier to identify these patients who would benefit from immunotherapy, according to an expert in the neurologic disease.
Most patients with confirmed anti-NMDA receptor encephalitis will experience substantial improvement after treatment with immunotherapy and other modalities, said Josep Dalmau, MD, PhD, professor at the Catalan Institute for Research and Advanced Studies at the University of Barcelona and adjunct professor of neurology at the University of Pennsylvania, Philadelphia.
“In our experience, being aggressive with immune therapy ... the patients do quite well, which means that basically 85%-90% of the patients substantially improved over the next few months,” Dr. Dalmau said at the annual meeting of the American Psychiatric Association, which was held as a virtual live event.
Identified for the first time a little more than a decade ago, anti-NMDA receptor encephalitis is a rare, immune-mediated disease that is usually found in children and young adults and is more common among women. It is frequently associated with ovarian tumors and teratomas, said Dr. Dalmau, and in about 90% of cases, patients will have prominent psychiatric and behavioral symptoms.
Patients develop IgG antibodies against the GluN1 subunit of the NMDA receptor. These autoantibodies represent not only a diagnostic marker of the disease, but are also pathogenic, altering NMDA receptor–related synaptic transmission, Dr. Dalmau said.
In several recent studies, investigators have attempted to cobble together a distinct phenotype on anti-NMDA receptor encephalitis to aid psychiatrists who might encounter patients with the disease, he said.
In one of the most recent studies, researchers combed the medical literature and found that, among 544 individuals with the disease, the most common psychiatric symptoms were agitation, seen in 59%, and psychotic symptoms (particularly visual-auditory hallucinations and disorganized behavior) in 54%; catatonia was seen in 42% of adults and 35% of children.
according to a report from researchers in Berlin, Dr. Dalmau added. By picking up on those clinical signs, which included seizures, catatonia, autonomic instability, or hyperkinesia, the time from symptom onset to diagnosis could be cut in half, the researchers found.
There’s also a handy acronym that could serve as a mnemonic to pick up on “diagnostic clues” of anti-NMDA receptor encephalitis among patients with new-onset psychiatric symptoms, Dr. Dalmau said.
That acronym, published in a review article by Dr. Dalmau and colleagues, is SEARCH For NMDAR-A, covering, in order: sleep dysfunction, excitement, agitation, rapid onset, child and young adult predominance, history of psychiatric disease (absent), fluctuating catatonia, negative and positive symptoms, memory deficit, decreased verbal output, antipsychotic intolerance, rule out neuroleptic malignant syndrome, and of course, antibodies (though the final “A” also stands for additional testing, including magnetic resonance imaging, cerebrospinal fluid studies, and electroencephalogram).
While the disease can be lethal, Dr. Dalmau said most patients respond to immunotherapy, and if applicable, treatment of the underlying tumor can help. The most common first-line treatments include steroids, intravenous immunoglobulin, and plasma exchange, he said, while second-line treatments include the monoclonal anti-CD20 antibody rituximab and cyclophosphamide.
Beyond immunotherapy, patients may benefit from supportive care and psychiatric treatment. Benzodiazepines are well tolerated, but Dr. Dalmau said antipsychotic intolerance is frequent, and electroconvulsive therapy has “mixed results” in these patients.
The recovery process can take months and may be complicated by hypersomnia, hyperphagia, and hypersexuality, he added.
“Some patients improve dramatically in 1 month, but this is uncommon, really,” he said, adding that an early recovery may be a “red flag” that the underlying condition is something other than anti-NMDA receptor encephalitis.
Dr. Dalmau provided disclosures related to Cellex Foundation, Safra Foundation, Caixa Health Project Foundation, and Sage Therapeutics.
SOURCE: Dalmau J. APA 2020, Abstract.
It remains difficult to distinguish anti-NMDA receptor encephalitis from a primary psychiatric disorder, but recent studies have identified clinical features and proposed screening criteria that could make it easier to identify these patients who would benefit from immunotherapy, according to an expert in the neurologic disease.
Most patients with confirmed anti-NMDA receptor encephalitis will experience substantial improvement after treatment with immunotherapy and other modalities, said Josep Dalmau, MD, PhD, professor at the Catalan Institute for Research and Advanced Studies at the University of Barcelona and adjunct professor of neurology at the University of Pennsylvania, Philadelphia.
“In our experience, being aggressive with immune therapy ... the patients do quite well, which means that basically 85%-90% of the patients substantially improved over the next few months,” Dr. Dalmau said at the annual meeting of the American Psychiatric Association, which was held as a virtual live event.
Identified for the first time a little more than a decade ago, anti-NMDA receptor encephalitis is a rare, immune-mediated disease that is usually found in children and young adults and is more common among women. It is frequently associated with ovarian tumors and teratomas, said Dr. Dalmau, and in about 90% of cases, patients will have prominent psychiatric and behavioral symptoms.
Patients develop IgG antibodies against the GluN1 subunit of the NMDA receptor. These autoantibodies represent not only a diagnostic marker of the disease, but are also pathogenic, altering NMDA receptor–related synaptic transmission, Dr. Dalmau said.
In several recent studies, investigators have attempted to cobble together a distinct phenotype on anti-NMDA receptor encephalitis to aid psychiatrists who might encounter patients with the disease, he said.
In one of the most recent studies, researchers combed the medical literature and found that, among 544 individuals with the disease, the most common psychiatric symptoms were agitation, seen in 59%, and psychotic symptoms (particularly visual-auditory hallucinations and disorganized behavior) in 54%; catatonia was seen in 42% of adults and 35% of children.
according to a report from researchers in Berlin, Dr. Dalmau added. By picking up on those clinical signs, which included seizures, catatonia, autonomic instability, or hyperkinesia, the time from symptom onset to diagnosis could be cut in half, the researchers found.
There’s also a handy acronym that could serve as a mnemonic to pick up on “diagnostic clues” of anti-NMDA receptor encephalitis among patients with new-onset psychiatric symptoms, Dr. Dalmau said.
That acronym, published in a review article by Dr. Dalmau and colleagues, is SEARCH For NMDAR-A, covering, in order: sleep dysfunction, excitement, agitation, rapid onset, child and young adult predominance, history of psychiatric disease (absent), fluctuating catatonia, negative and positive symptoms, memory deficit, decreased verbal output, antipsychotic intolerance, rule out neuroleptic malignant syndrome, and of course, antibodies (though the final “A” also stands for additional testing, including magnetic resonance imaging, cerebrospinal fluid studies, and electroencephalogram).
While the disease can be lethal, Dr. Dalmau said most patients respond to immunotherapy, and if applicable, treatment of the underlying tumor can help. The most common first-line treatments include steroids, intravenous immunoglobulin, and plasma exchange, he said, while second-line treatments include the monoclonal anti-CD20 antibody rituximab and cyclophosphamide.
Beyond immunotherapy, patients may benefit from supportive care and psychiatric treatment. Benzodiazepines are well tolerated, but Dr. Dalmau said antipsychotic intolerance is frequent, and electroconvulsive therapy has “mixed results” in these patients.
The recovery process can take months and may be complicated by hypersomnia, hyperphagia, and hypersexuality, he added.
“Some patients improve dramatically in 1 month, but this is uncommon, really,” he said, adding that an early recovery may be a “red flag” that the underlying condition is something other than anti-NMDA receptor encephalitis.
Dr. Dalmau provided disclosures related to Cellex Foundation, Safra Foundation, Caixa Health Project Foundation, and Sage Therapeutics.
SOURCE: Dalmau J. APA 2020, Abstract.
FROM APA 2020
Trials and tribulations: Neurology research during COVID-19
However, researchers remain determined to forge ahead – with many redesigning their studies, at least in part to optimize the safety of their participants and research staff.
Keeping people engaged while protocols are on hold; expanding normal safety considerations; and re-enlisting statisticians to keep their findings as significant as possible are just some of study survival strategies underway.
Alzheimer’s disease research on hold
The pandemic is having a significant impact on Alzheimer’s disease research, and medical research in general, says Heather Snyder, PhD, vice president, Medical & Scientific Relations at the Alzheimer’s Association.
“Many clinical trials worldwide are pausing, changing, or halting the testing of the drug or the intervention,” she told Medscape Medical News. “How the teams have adapted depends on the study,” she added. “As you can imagine, things are changing on a daily basis.”
The US Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk (U.S. POINTER) trial, for example, is on hold until at least May 31. The Alzheimer’s Association is helping to implement and fund the study along with Wake Forest University Medical Center.
“We’re not randomizing participants at this point in time and the intervention — which is based on a team meeting, and there is a social aspect to that — has been paused,” Dr. Snyder said.
Another pivotal study underway is the Anti-Amyloid Treatment in Asymptomatic Alzheimer’s study (the A4 Study). Investigators are evaluating if an anti-amyloid antibody, solanezumab (Eli Lilly), can slow memory loss among people with amyloid on imaging but no symptoms of cognitive decline at baseline.
“The A4 Study is definitely continuing. However, in an effort to minimize risk to participants, site staff and study integrity, we have implemented an optional study hiatus for both the double-blind and open-label extension phases,” lead investigator Reisa Anne Sperling, MD, told Medscape Medical News.
“We wanted to prioritize the safety of our participants as well as the ability of participants to remain in the study … despite disruptions from the COVID-19 pandemic,” said Dr. Sperling, who is professor of neurology at Harvard Medical School and director of the Center for Alzheimer Research and Treatment at Brigham and Women’s Hospital and Massachusetts General Hospital in Boston.
The ultimate goal is for A4 participants to receive the full number of planned infusions and assessments, even if it takes longer, she added.
Many Alzheimer’s disease researchers outside the United States face similar challenges. “As you probably are well aware, Spain is now in a complete lockdown. This has affected research centers like ours, the Barcelona Brain Research Center, and the way we work,” José Luís Molinuevo Guix, MD, PhD, told Medscape Medical News.
All participants in observational studies like the ALFA+ study and initiatives, as well as those in trials including PENSA and AB1601, “are not allowed, by law, to come in, hence from a safety perspective we are on good grounds,” added Dr. Molinuevo Guix, who directs the Alzheimer’s disease and other cognitive disorders unit at the Hospital Clinic de Barcelona.
The investigators are creating protocols for communicating with participants during the pandemic and for restarting visits safely after the lockdown has ended.
Stroke studies amended or suspended
A similar situation is occurring in stroke trials. Stroke is “obviously an acute disease, as well as a disease that requires secondary prevention,” Mitchell Elkind, MD, president-elect of the American Heart Association, told Medscape Medical News.
“One could argue that patients with stroke are going to be in the hospital anyway – why not enroll them in a study? They’re not incurring any additional risk,” he said. “But the staff have to come in to see them, and we’re really trying to avoid exposure.”
One ongoing trial, the Atrial Cardiopathy and Antithrombotic Drugs In Prevention After Cryptogenic Stroke (ARCADIA), stopped randomly assigning new participants to secondary prevention with apixaban or aspirin because of COVID-19. However, Dr. Elkind and colleagues plan to provide medication to the 440 people already in the trial.
“Wherever possible, the study coordinators are shipping the drug to people and doing follow-up visits by phone or video,” said Dr. Elkind, chief of the Division of Neurology Clinical Outcomes Research and Population Sciences at Columbia University in New York City.
Protecting patients, staff, and ultimately society is a “major driving force in stopping the randomizations,” he stressed.
ARCADIA is part of the StrokeNet prevention trials network, run by the NIH’s National Institute of Neurologic Disorders and Stroke (NINDS). Additional pivotal trials include the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST) and the Multi-arm Optimization of Stroke Thrombolysis (MOST) studies, he said.
Joseph Broderick, MD, director of the national NIH StrokeNet, agreed that safety comes first. “It was the decision of the StrokeNet leadership and the principal investigators of the trials that we needed to hold recruitment of new patients while we worked on adapting processes of enrollment to ensure the safety of both patients and researchers interacting with study patients,” he told Medscape Medical News.
Potential risks vary based on the study intervention and the need for in-person interactions. Trials that include stimulation devices or physical therapy, for example, might be most affected, added Dr. Broderick, professor and director of the UC Gardner Neuroscience Institute at the University of Cincinnati in Ohio.
Nevertheless, “there are potential ways … to move as much as possible toward telemedicine and digital interactions during this time.”
Multiple challenges in multiple sclerosis
At the national level, the COVID-19 pandemic has had an “unprecedented impact on almost all the clinical trials funded by NINDS,” said Clinton Wright, MD, director of the Division of Clinical Research at NINDS. “Investigators have had to adapt quickly.”
Supplementing existing grants with money to conduct research on COVID-19 and pursuing research opportunities from different institutes are “some of the creative approaches [that] have come from the NIH [National Institutes of Health] itself,” Dr. Wright said. “Other creative approaches have come from investigators trying to keep their studies and trials going during the pandemic.”
In clinical trials, “everything from electronic consent to in-home research drug delivery is being brought to bear.”
“A few ongoing trials have been able to modify their protocols to obtain consent and carry out evaluations remotely by telephone or videoconferencing,” Dr. Wright said. “This is especially critical for trials that involve medical management of specific risk factors or conditions, where suspension of the trial could itself have adverse consequences due to reduced engagement with research participants.”
For participants already in MS studies, “each upcoming visit is assessed for whether it’s critical or could be done virtually or just skipped. If a person needs a treatment that cannot be postponed or skipped, they come in,” Jeffrey Cohen, MD, director of the Experimental Therapeutics Program at the Mellen Center for Multiple Sclerosis Treatment and Research at the Cleveland Clinic, Ohio, told Medscape Medical News.
New study enrollment is largely on hold and study visits for existing participants are limited, said Dr. Cohen, who is also president of the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS).
Some of the major ongoing trials in MS are “looking at very fundamental questions in the field,” Dr. Cohen said. The Determining the Effectiveness of earLy Intensive Versus Escalation Approaches for RRMS (DELIVER-MS) and Traditional Versus Early Aggressive Therapy for Multiple Sclerosis (TREAT-MS) trials, for example, evaluate whether treatment should be initiated with one of the less efficacious agents with escalation as needed, or whether treatment should begin with a high-efficacy agent.
Both trials are currently on hold because of the pandemic, as is the Best Available Therapy Versus Autologous Hematopoietic Stem Cell Transplant for Multiple Sclerosis (BEAT-MS) study.
“There has been a lot of interest in hematopoietic stem cell transplants and where they fit into our overall treatment strategy, and this is intended to provide a more definitive answer,” Dr. Cohen said.
Making the most of down time
“The pandemic has been challenging” in terms of ongoing MS research, said Benjamin M. Segal, MD, chair of the Department of Neurology and director of the Neuroscience Research Institute at the Ohio State University Wexner Medical Center, Columbus.
“With regard to the lab, our animal model experiments have been placed on hold. We have stopped collecting samples from clinical subjects for biomarker studies.
“However, my research team has been taking advantage of the time that has been freed up from bench work by analyzing data sets that had been placed aside, delving more deeply into the literature, and writing new grant proposals and articles,” he added.
Two of Dr. Segal’s trainees are writing review articles on the immunopathogenesis of MS and its treatment. Another postdoctoral candidate is writing a grant proposal to investigate how coinfection with a coronavirus modulates CNS pathology and the clinical course of an animal model of MS.
“I am asking my trainees to plan out experiments further in advance than they ever have before, so they are as prepared as possible to resume their research agendas once we are up and running again,” Dr. Segal said.
Confronting current challenges while planning for a future less disrupted by the pandemic is a common theme that emerges.
“The duration of this [pandemic] will dictate how we analyze the data at the end [for the US POINTER study]. There is a large group of statisticians working on this,” Dr. Snyder said.
Dr. Sperling of Harvard Medical School also remains undeterred. “This is definitely a challenging time, as we must not allow the COVID-19 to interfere with our essential mission to find a successful treatment to prevent cognitive decline in AD. We do need, however, to be as flexible as possible to protect our participants and minimize the impact to our overall study integrity,” she said.
NIH guidance
Dr. Molinuevo Guix, of the Barcelona Brain Research Center, is also determined to continue his Alzheimer’s disease research. “I am aware that after the crisis, there will be less [risk] but still a COVID-19 infection risk, so apart from trying to generate part of our visits virtually, we want to make sure we have all necessary safety measures in place. We remain very active to preserve the work we have done to keep up the fight against Alzheimer’s and dementia,” he said.
Such forward thinking also applies to major stroke trials, said Dr. Broderick of the University of Cincinnati. “As soon as we shut down enrollment in stroke trials, we immediately began to make plans about how and when we can restart our stroke trials,” he explained. “One of our trials can do every step of the trial process remotely without direct in-person interactions and will be able to restart soon.”
An individualized approach is needed, Dr. Broderick added. “For trials involving necessary in-person and hands-on assessments, we will need to consider how best to use protective equipment and expanded testing that will likely match the ongoing clinical care and requirements at a given institution.
“Even if a trial officially reopens enrollment, the decision to enroll locally will need to follow local institutional environment and guidelines. Thus, restart of trial enrollment will not likely be uniform, similar to how trials often start in the first place,” Dr. Broderick said.
The NIH published uniform standards for researchers across its institutes to help guide them during the pandemic. Future contingency plans also are underway at the NINDS.
“As the pandemic wanes and in-person research activities restart, it will be important to have in place safety measures that prevent a resurgence of the virus, such as proper personal protective equipment for staff and research participants, said Dr. Wright, the clinical research director at NINDS.
For clinical trials, NINDS is prepared to provide supplemental funds to trial investigators to help support additional activities undertaken as a result of the pandemic.
“This has been an instructive experience. The pandemic will end, and we will resume much of our old patterns of behavior,” said Ohio State’s Dr. Segal. “But some of the strategies that we have employed to get through this time will continue to influence the way we communicate information, plan experiments, and prioritize research activities in the future, to good effect.”
Drs. Snyder, Sperling, Molinuevo Guix, Elkind, Broderick, Wright, Cohen, and Segal have disclosed no relevant disclosures.
This story first appeared on Medscape.com.
However, researchers remain determined to forge ahead – with many redesigning their studies, at least in part to optimize the safety of their participants and research staff.
Keeping people engaged while protocols are on hold; expanding normal safety considerations; and re-enlisting statisticians to keep their findings as significant as possible are just some of study survival strategies underway.
Alzheimer’s disease research on hold
The pandemic is having a significant impact on Alzheimer’s disease research, and medical research in general, says Heather Snyder, PhD, vice president, Medical & Scientific Relations at the Alzheimer’s Association.
“Many clinical trials worldwide are pausing, changing, or halting the testing of the drug or the intervention,” she told Medscape Medical News. “How the teams have adapted depends on the study,” she added. “As you can imagine, things are changing on a daily basis.”
The US Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk (U.S. POINTER) trial, for example, is on hold until at least May 31. The Alzheimer’s Association is helping to implement and fund the study along with Wake Forest University Medical Center.
“We’re not randomizing participants at this point in time and the intervention — which is based on a team meeting, and there is a social aspect to that — has been paused,” Dr. Snyder said.
Another pivotal study underway is the Anti-Amyloid Treatment in Asymptomatic Alzheimer’s study (the A4 Study). Investigators are evaluating if an anti-amyloid antibody, solanezumab (Eli Lilly), can slow memory loss among people with amyloid on imaging but no symptoms of cognitive decline at baseline.
“The A4 Study is definitely continuing. However, in an effort to minimize risk to participants, site staff and study integrity, we have implemented an optional study hiatus for both the double-blind and open-label extension phases,” lead investigator Reisa Anne Sperling, MD, told Medscape Medical News.
“We wanted to prioritize the safety of our participants as well as the ability of participants to remain in the study … despite disruptions from the COVID-19 pandemic,” said Dr. Sperling, who is professor of neurology at Harvard Medical School and director of the Center for Alzheimer Research and Treatment at Brigham and Women’s Hospital and Massachusetts General Hospital in Boston.
The ultimate goal is for A4 participants to receive the full number of planned infusions and assessments, even if it takes longer, she added.
Many Alzheimer’s disease researchers outside the United States face similar challenges. “As you probably are well aware, Spain is now in a complete lockdown. This has affected research centers like ours, the Barcelona Brain Research Center, and the way we work,” José Luís Molinuevo Guix, MD, PhD, told Medscape Medical News.
All participants in observational studies like the ALFA+ study and initiatives, as well as those in trials including PENSA and AB1601, “are not allowed, by law, to come in, hence from a safety perspective we are on good grounds,” added Dr. Molinuevo Guix, who directs the Alzheimer’s disease and other cognitive disorders unit at the Hospital Clinic de Barcelona.
The investigators are creating protocols for communicating with participants during the pandemic and for restarting visits safely after the lockdown has ended.
Stroke studies amended or suspended
A similar situation is occurring in stroke trials. Stroke is “obviously an acute disease, as well as a disease that requires secondary prevention,” Mitchell Elkind, MD, president-elect of the American Heart Association, told Medscape Medical News.
“One could argue that patients with stroke are going to be in the hospital anyway – why not enroll them in a study? They’re not incurring any additional risk,” he said. “But the staff have to come in to see them, and we’re really trying to avoid exposure.”
One ongoing trial, the Atrial Cardiopathy and Antithrombotic Drugs In Prevention After Cryptogenic Stroke (ARCADIA), stopped randomly assigning new participants to secondary prevention with apixaban or aspirin because of COVID-19. However, Dr. Elkind and colleagues plan to provide medication to the 440 people already in the trial.
“Wherever possible, the study coordinators are shipping the drug to people and doing follow-up visits by phone or video,” said Dr. Elkind, chief of the Division of Neurology Clinical Outcomes Research and Population Sciences at Columbia University in New York City.
Protecting patients, staff, and ultimately society is a “major driving force in stopping the randomizations,” he stressed.
ARCADIA is part of the StrokeNet prevention trials network, run by the NIH’s National Institute of Neurologic Disorders and Stroke (NINDS). Additional pivotal trials include the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST) and the Multi-arm Optimization of Stroke Thrombolysis (MOST) studies, he said.
Joseph Broderick, MD, director of the national NIH StrokeNet, agreed that safety comes first. “It was the decision of the StrokeNet leadership and the principal investigators of the trials that we needed to hold recruitment of new patients while we worked on adapting processes of enrollment to ensure the safety of both patients and researchers interacting with study patients,” he told Medscape Medical News.
Potential risks vary based on the study intervention and the need for in-person interactions. Trials that include stimulation devices or physical therapy, for example, might be most affected, added Dr. Broderick, professor and director of the UC Gardner Neuroscience Institute at the University of Cincinnati in Ohio.
Nevertheless, “there are potential ways … to move as much as possible toward telemedicine and digital interactions during this time.”
Multiple challenges in multiple sclerosis
At the national level, the COVID-19 pandemic has had an “unprecedented impact on almost all the clinical trials funded by NINDS,” said Clinton Wright, MD, director of the Division of Clinical Research at NINDS. “Investigators have had to adapt quickly.”
Supplementing existing grants with money to conduct research on COVID-19 and pursuing research opportunities from different institutes are “some of the creative approaches [that] have come from the NIH [National Institutes of Health] itself,” Dr. Wright said. “Other creative approaches have come from investigators trying to keep their studies and trials going during the pandemic.”
In clinical trials, “everything from electronic consent to in-home research drug delivery is being brought to bear.”
“A few ongoing trials have been able to modify their protocols to obtain consent and carry out evaluations remotely by telephone or videoconferencing,” Dr. Wright said. “This is especially critical for trials that involve medical management of specific risk factors or conditions, where suspension of the trial could itself have adverse consequences due to reduced engagement with research participants.”
For participants already in MS studies, “each upcoming visit is assessed for whether it’s critical or could be done virtually or just skipped. If a person needs a treatment that cannot be postponed or skipped, they come in,” Jeffrey Cohen, MD, director of the Experimental Therapeutics Program at the Mellen Center for Multiple Sclerosis Treatment and Research at the Cleveland Clinic, Ohio, told Medscape Medical News.
New study enrollment is largely on hold and study visits for existing participants are limited, said Dr. Cohen, who is also president of the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS).
Some of the major ongoing trials in MS are “looking at very fundamental questions in the field,” Dr. Cohen said. The Determining the Effectiveness of earLy Intensive Versus Escalation Approaches for RRMS (DELIVER-MS) and Traditional Versus Early Aggressive Therapy for Multiple Sclerosis (TREAT-MS) trials, for example, evaluate whether treatment should be initiated with one of the less efficacious agents with escalation as needed, or whether treatment should begin with a high-efficacy agent.
Both trials are currently on hold because of the pandemic, as is the Best Available Therapy Versus Autologous Hematopoietic Stem Cell Transplant for Multiple Sclerosis (BEAT-MS) study.
“There has been a lot of interest in hematopoietic stem cell transplants and where they fit into our overall treatment strategy, and this is intended to provide a more definitive answer,” Dr. Cohen said.
Making the most of down time
“The pandemic has been challenging” in terms of ongoing MS research, said Benjamin M. Segal, MD, chair of the Department of Neurology and director of the Neuroscience Research Institute at the Ohio State University Wexner Medical Center, Columbus.
“With regard to the lab, our animal model experiments have been placed on hold. We have stopped collecting samples from clinical subjects for biomarker studies.
“However, my research team has been taking advantage of the time that has been freed up from bench work by analyzing data sets that had been placed aside, delving more deeply into the literature, and writing new grant proposals and articles,” he added.
Two of Dr. Segal’s trainees are writing review articles on the immunopathogenesis of MS and its treatment. Another postdoctoral candidate is writing a grant proposal to investigate how coinfection with a coronavirus modulates CNS pathology and the clinical course of an animal model of MS.
“I am asking my trainees to plan out experiments further in advance than they ever have before, so they are as prepared as possible to resume their research agendas once we are up and running again,” Dr. Segal said.
Confronting current challenges while planning for a future less disrupted by the pandemic is a common theme that emerges.
“The duration of this [pandemic] will dictate how we analyze the data at the end [for the US POINTER study]. There is a large group of statisticians working on this,” Dr. Snyder said.
Dr. Sperling of Harvard Medical School also remains undeterred. “This is definitely a challenging time, as we must not allow the COVID-19 to interfere with our essential mission to find a successful treatment to prevent cognitive decline in AD. We do need, however, to be as flexible as possible to protect our participants and minimize the impact to our overall study integrity,” she said.
NIH guidance
Dr. Molinuevo Guix, of the Barcelona Brain Research Center, is also determined to continue his Alzheimer’s disease research. “I am aware that after the crisis, there will be less [risk] but still a COVID-19 infection risk, so apart from trying to generate part of our visits virtually, we want to make sure we have all necessary safety measures in place. We remain very active to preserve the work we have done to keep up the fight against Alzheimer’s and dementia,” he said.
Such forward thinking also applies to major stroke trials, said Dr. Broderick of the University of Cincinnati. “As soon as we shut down enrollment in stroke trials, we immediately began to make plans about how and when we can restart our stroke trials,” he explained. “One of our trials can do every step of the trial process remotely without direct in-person interactions and will be able to restart soon.”
An individualized approach is needed, Dr. Broderick added. “For trials involving necessary in-person and hands-on assessments, we will need to consider how best to use protective equipment and expanded testing that will likely match the ongoing clinical care and requirements at a given institution.
“Even if a trial officially reopens enrollment, the decision to enroll locally will need to follow local institutional environment and guidelines. Thus, restart of trial enrollment will not likely be uniform, similar to how trials often start in the first place,” Dr. Broderick said.
The NIH published uniform standards for researchers across its institutes to help guide them during the pandemic. Future contingency plans also are underway at the NINDS.
“As the pandemic wanes and in-person research activities restart, it will be important to have in place safety measures that prevent a resurgence of the virus, such as proper personal protective equipment for staff and research participants, said Dr. Wright, the clinical research director at NINDS.
For clinical trials, NINDS is prepared to provide supplemental funds to trial investigators to help support additional activities undertaken as a result of the pandemic.
“This has been an instructive experience. The pandemic will end, and we will resume much of our old patterns of behavior,” said Ohio State’s Dr. Segal. “But some of the strategies that we have employed to get through this time will continue to influence the way we communicate information, plan experiments, and prioritize research activities in the future, to good effect.”
Drs. Snyder, Sperling, Molinuevo Guix, Elkind, Broderick, Wright, Cohen, and Segal have disclosed no relevant disclosures.
This story first appeared on Medscape.com.
However, researchers remain determined to forge ahead – with many redesigning their studies, at least in part to optimize the safety of their participants and research staff.
Keeping people engaged while protocols are on hold; expanding normal safety considerations; and re-enlisting statisticians to keep their findings as significant as possible are just some of study survival strategies underway.
Alzheimer’s disease research on hold
The pandemic is having a significant impact on Alzheimer’s disease research, and medical research in general, says Heather Snyder, PhD, vice president, Medical & Scientific Relations at the Alzheimer’s Association.
“Many clinical trials worldwide are pausing, changing, or halting the testing of the drug or the intervention,” she told Medscape Medical News. “How the teams have adapted depends on the study,” she added. “As you can imagine, things are changing on a daily basis.”
The US Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk (U.S. POINTER) trial, for example, is on hold until at least May 31. The Alzheimer’s Association is helping to implement and fund the study along with Wake Forest University Medical Center.
“We’re not randomizing participants at this point in time and the intervention — which is based on a team meeting, and there is a social aspect to that — has been paused,” Dr. Snyder said.
Another pivotal study underway is the Anti-Amyloid Treatment in Asymptomatic Alzheimer’s study (the A4 Study). Investigators are evaluating if an anti-amyloid antibody, solanezumab (Eli Lilly), can slow memory loss among people with amyloid on imaging but no symptoms of cognitive decline at baseline.
“The A4 Study is definitely continuing. However, in an effort to minimize risk to participants, site staff and study integrity, we have implemented an optional study hiatus for both the double-blind and open-label extension phases,” lead investigator Reisa Anne Sperling, MD, told Medscape Medical News.
“We wanted to prioritize the safety of our participants as well as the ability of participants to remain in the study … despite disruptions from the COVID-19 pandemic,” said Dr. Sperling, who is professor of neurology at Harvard Medical School and director of the Center for Alzheimer Research and Treatment at Brigham and Women’s Hospital and Massachusetts General Hospital in Boston.
The ultimate goal is for A4 participants to receive the full number of planned infusions and assessments, even if it takes longer, she added.
Many Alzheimer’s disease researchers outside the United States face similar challenges. “As you probably are well aware, Spain is now in a complete lockdown. This has affected research centers like ours, the Barcelona Brain Research Center, and the way we work,” José Luís Molinuevo Guix, MD, PhD, told Medscape Medical News.
All participants in observational studies like the ALFA+ study and initiatives, as well as those in trials including PENSA and AB1601, “are not allowed, by law, to come in, hence from a safety perspective we are on good grounds,” added Dr. Molinuevo Guix, who directs the Alzheimer’s disease and other cognitive disorders unit at the Hospital Clinic de Barcelona.
The investigators are creating protocols for communicating with participants during the pandemic and for restarting visits safely after the lockdown has ended.
Stroke studies amended or suspended
A similar situation is occurring in stroke trials. Stroke is “obviously an acute disease, as well as a disease that requires secondary prevention,” Mitchell Elkind, MD, president-elect of the American Heart Association, told Medscape Medical News.
“One could argue that patients with stroke are going to be in the hospital anyway – why not enroll them in a study? They’re not incurring any additional risk,” he said. “But the staff have to come in to see them, and we’re really trying to avoid exposure.”
One ongoing trial, the Atrial Cardiopathy and Antithrombotic Drugs In Prevention After Cryptogenic Stroke (ARCADIA), stopped randomly assigning new participants to secondary prevention with apixaban or aspirin because of COVID-19. However, Dr. Elkind and colleagues plan to provide medication to the 440 people already in the trial.
“Wherever possible, the study coordinators are shipping the drug to people and doing follow-up visits by phone or video,” said Dr. Elkind, chief of the Division of Neurology Clinical Outcomes Research and Population Sciences at Columbia University in New York City.
Protecting patients, staff, and ultimately society is a “major driving force in stopping the randomizations,” he stressed.
ARCADIA is part of the StrokeNet prevention trials network, run by the NIH’s National Institute of Neurologic Disorders and Stroke (NINDS). Additional pivotal trials include the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST) and the Multi-arm Optimization of Stroke Thrombolysis (MOST) studies, he said.
Joseph Broderick, MD, director of the national NIH StrokeNet, agreed that safety comes first. “It was the decision of the StrokeNet leadership and the principal investigators of the trials that we needed to hold recruitment of new patients while we worked on adapting processes of enrollment to ensure the safety of both patients and researchers interacting with study patients,” he told Medscape Medical News.
Potential risks vary based on the study intervention and the need for in-person interactions. Trials that include stimulation devices or physical therapy, for example, might be most affected, added Dr. Broderick, professor and director of the UC Gardner Neuroscience Institute at the University of Cincinnati in Ohio.
Nevertheless, “there are potential ways … to move as much as possible toward telemedicine and digital interactions during this time.”
Multiple challenges in multiple sclerosis
At the national level, the COVID-19 pandemic has had an “unprecedented impact on almost all the clinical trials funded by NINDS,” said Clinton Wright, MD, director of the Division of Clinical Research at NINDS. “Investigators have had to adapt quickly.”
Supplementing existing grants with money to conduct research on COVID-19 and pursuing research opportunities from different institutes are “some of the creative approaches [that] have come from the NIH [National Institutes of Health] itself,” Dr. Wright said. “Other creative approaches have come from investigators trying to keep their studies and trials going during the pandemic.”
In clinical trials, “everything from electronic consent to in-home research drug delivery is being brought to bear.”
“A few ongoing trials have been able to modify their protocols to obtain consent and carry out evaluations remotely by telephone or videoconferencing,” Dr. Wright said. “This is especially critical for trials that involve medical management of specific risk factors or conditions, where suspension of the trial could itself have adverse consequences due to reduced engagement with research participants.”
For participants already in MS studies, “each upcoming visit is assessed for whether it’s critical or could be done virtually or just skipped. If a person needs a treatment that cannot be postponed or skipped, they come in,” Jeffrey Cohen, MD, director of the Experimental Therapeutics Program at the Mellen Center for Multiple Sclerosis Treatment and Research at the Cleveland Clinic, Ohio, told Medscape Medical News.
New study enrollment is largely on hold and study visits for existing participants are limited, said Dr. Cohen, who is also president of the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS).
Some of the major ongoing trials in MS are “looking at very fundamental questions in the field,” Dr. Cohen said. The Determining the Effectiveness of earLy Intensive Versus Escalation Approaches for RRMS (DELIVER-MS) and Traditional Versus Early Aggressive Therapy for Multiple Sclerosis (TREAT-MS) trials, for example, evaluate whether treatment should be initiated with one of the less efficacious agents with escalation as needed, or whether treatment should begin with a high-efficacy agent.
Both trials are currently on hold because of the pandemic, as is the Best Available Therapy Versus Autologous Hematopoietic Stem Cell Transplant for Multiple Sclerosis (BEAT-MS) study.
“There has been a lot of interest in hematopoietic stem cell transplants and where they fit into our overall treatment strategy, and this is intended to provide a more definitive answer,” Dr. Cohen said.
Making the most of down time
“The pandemic has been challenging” in terms of ongoing MS research, said Benjamin M. Segal, MD, chair of the Department of Neurology and director of the Neuroscience Research Institute at the Ohio State University Wexner Medical Center, Columbus.
“With regard to the lab, our animal model experiments have been placed on hold. We have stopped collecting samples from clinical subjects for biomarker studies.
“However, my research team has been taking advantage of the time that has been freed up from bench work by analyzing data sets that had been placed aside, delving more deeply into the literature, and writing new grant proposals and articles,” he added.
Two of Dr. Segal’s trainees are writing review articles on the immunopathogenesis of MS and its treatment. Another postdoctoral candidate is writing a grant proposal to investigate how coinfection with a coronavirus modulates CNS pathology and the clinical course of an animal model of MS.
“I am asking my trainees to plan out experiments further in advance than they ever have before, so they are as prepared as possible to resume their research agendas once we are up and running again,” Dr. Segal said.
Confronting current challenges while planning for a future less disrupted by the pandemic is a common theme that emerges.
“The duration of this [pandemic] will dictate how we analyze the data at the end [for the US POINTER study]. There is a large group of statisticians working on this,” Dr. Snyder said.
Dr. Sperling of Harvard Medical School also remains undeterred. “This is definitely a challenging time, as we must not allow the COVID-19 to interfere with our essential mission to find a successful treatment to prevent cognitive decline in AD. We do need, however, to be as flexible as possible to protect our participants and minimize the impact to our overall study integrity,” she said.
NIH guidance
Dr. Molinuevo Guix, of the Barcelona Brain Research Center, is also determined to continue his Alzheimer’s disease research. “I am aware that after the crisis, there will be less [risk] but still a COVID-19 infection risk, so apart from trying to generate part of our visits virtually, we want to make sure we have all necessary safety measures in place. We remain very active to preserve the work we have done to keep up the fight against Alzheimer’s and dementia,” he said.
Such forward thinking also applies to major stroke trials, said Dr. Broderick of the University of Cincinnati. “As soon as we shut down enrollment in stroke trials, we immediately began to make plans about how and when we can restart our stroke trials,” he explained. “One of our trials can do every step of the trial process remotely without direct in-person interactions and will be able to restart soon.”
An individualized approach is needed, Dr. Broderick added. “For trials involving necessary in-person and hands-on assessments, we will need to consider how best to use protective equipment and expanded testing that will likely match the ongoing clinical care and requirements at a given institution.
“Even if a trial officially reopens enrollment, the decision to enroll locally will need to follow local institutional environment and guidelines. Thus, restart of trial enrollment will not likely be uniform, similar to how trials often start in the first place,” Dr. Broderick said.
The NIH published uniform standards for researchers across its institutes to help guide them during the pandemic. Future contingency plans also are underway at the NINDS.
“As the pandemic wanes and in-person research activities restart, it will be important to have in place safety measures that prevent a resurgence of the virus, such as proper personal protective equipment for staff and research participants, said Dr. Wright, the clinical research director at NINDS.
For clinical trials, NINDS is prepared to provide supplemental funds to trial investigators to help support additional activities undertaken as a result of the pandemic.
“This has been an instructive experience. The pandemic will end, and we will resume much of our old patterns of behavior,” said Ohio State’s Dr. Segal. “But some of the strategies that we have employed to get through this time will continue to influence the way we communicate information, plan experiments, and prioritize research activities in the future, to good effect.”
Drs. Snyder, Sperling, Molinuevo Guix, Elkind, Broderick, Wright, Cohen, and Segal have disclosed no relevant disclosures.
This story first appeared on Medscape.com.
Acetaminophen plus ibuprofen cut patient-controlled morphine after total hip arthroplasty
Background: The use of multimodal non-opioid analgesics is a common practice to minimize postoperative pain and opioid analgesic use. There is limited high-quality evidence to confirm the synergistic effect and safety of acetaminophen and ibuprofen in the peripostoperative setting. The Paracetamol and NSAID in combination (PANSAID) trial investigated the analgesic efficacy and safety of four multimodal analgesic regimens after total hip arthroplasty.
Study design: Multicenter, randomized, blinded trial.
Setting: A total of six hospitals in Denmark, which represented regional and large university settings.
Synopsis: A total of 559 patients who underwent total hip arthroplasty were randomized to receive one of the following oral regimens: acetaminophen (1,000 mg) and ibuprofen (400 mg), acetaminophen (1,000 mg) and placebo, ibuprofen (400 mg) and placebo, and half-strength acetaminophen (500 mg) and ibuprofen (200 mg). One of the regimens was initiated 1 hour before surgery and continued every 6 hours for a total of 4 doses on the first postoperative day. The mean age was 67 years, and half of the patients were women.
The median morphine consumption in the 24 hours after surgery was significantly lower with full-strength acetaminophen-ibuprofen compared with acetaminophen monotherapy (20 mg vs. 36 mg, 99.6% confidence interval, 6.5-24; P < .001), which exceeded the prespecified 10-mg threshold for a minimal clinically important difference (MCID). The difference between acetaminophen-ibuprofen and ibuprofen monotherapy (20 mg vs. 26 mg) did not exceed the MCID, and was not clinically meaningful. The differences in morphine consumption with full-strength acetaminophen-ibuprofen compared to half-strength acetaminophen-ibuprofen (28 mg) and ibuprofen compared to acetaminophen monotherapy were not statistically significant.
Serious adverse events, the other primary outcome, within 90 days after surgery (15% in the ibuprofen group and 11% in the acetaminophen group, relative risk, 1.44; 97.5% CI, 0.79-2.64; P = .18) did not differ between acetaminophen monotherapy and ibuprofen monotherapy. Secondary outcomes included statistically significant analgesia (lower pain scores) at rest and with mobilization at 24 hours in the acetaminophen-ibuprofen group compared to the other groups.
An interesting observation was that acetaminophen-ibuprofen did not exceed the MCID compared to ibuprofen, which suggests that ibuprofen monotherapy may be a reasonable option for early postoperative analgesia.
Bottom line: Acetaminophen-ibuprofen reduced postoperative morphine use and had improved analgesia 24 hours after total hip arthroplasty, and was not associated with an increased 3-month risk of serious adverse events.
Citation: Thybo KH et al. Effect of combination of paracetamol (acetaminophen) and ibuprofen vs. either alone on patient-controlled morphine consumption in the first 24 hours after total hip arthroplasty. The PANSAID randomized clinical trial. JAMA. 2019;321(6):562-71.
Dr. Lambert is a hospital medicine clinician and addiction medicine specialist in the division of hospital medicine at Massachusetts General Hospital.
Background: The use of multimodal non-opioid analgesics is a common practice to minimize postoperative pain and opioid analgesic use. There is limited high-quality evidence to confirm the synergistic effect and safety of acetaminophen and ibuprofen in the peripostoperative setting. The Paracetamol and NSAID in combination (PANSAID) trial investigated the analgesic efficacy and safety of four multimodal analgesic regimens after total hip arthroplasty.
Study design: Multicenter, randomized, blinded trial.
Setting: A total of six hospitals in Denmark, which represented regional and large university settings.
Synopsis: A total of 559 patients who underwent total hip arthroplasty were randomized to receive one of the following oral regimens: acetaminophen (1,000 mg) and ibuprofen (400 mg), acetaminophen (1,000 mg) and placebo, ibuprofen (400 mg) and placebo, and half-strength acetaminophen (500 mg) and ibuprofen (200 mg). One of the regimens was initiated 1 hour before surgery and continued every 6 hours for a total of 4 doses on the first postoperative day. The mean age was 67 years, and half of the patients were women.
The median morphine consumption in the 24 hours after surgery was significantly lower with full-strength acetaminophen-ibuprofen compared with acetaminophen monotherapy (20 mg vs. 36 mg, 99.6% confidence interval, 6.5-24; P < .001), which exceeded the prespecified 10-mg threshold for a minimal clinically important difference (MCID). The difference between acetaminophen-ibuprofen and ibuprofen monotherapy (20 mg vs. 26 mg) did not exceed the MCID, and was not clinically meaningful. The differences in morphine consumption with full-strength acetaminophen-ibuprofen compared to half-strength acetaminophen-ibuprofen (28 mg) and ibuprofen compared to acetaminophen monotherapy were not statistically significant.
Serious adverse events, the other primary outcome, within 90 days after surgery (15% in the ibuprofen group and 11% in the acetaminophen group, relative risk, 1.44; 97.5% CI, 0.79-2.64; P = .18) did not differ between acetaminophen monotherapy and ibuprofen monotherapy. Secondary outcomes included statistically significant analgesia (lower pain scores) at rest and with mobilization at 24 hours in the acetaminophen-ibuprofen group compared to the other groups.
An interesting observation was that acetaminophen-ibuprofen did not exceed the MCID compared to ibuprofen, which suggests that ibuprofen monotherapy may be a reasonable option for early postoperative analgesia.
Bottom line: Acetaminophen-ibuprofen reduced postoperative morphine use and had improved analgesia 24 hours after total hip arthroplasty, and was not associated with an increased 3-month risk of serious adverse events.
Citation: Thybo KH et al. Effect of combination of paracetamol (acetaminophen) and ibuprofen vs. either alone on patient-controlled morphine consumption in the first 24 hours after total hip arthroplasty. The PANSAID randomized clinical trial. JAMA. 2019;321(6):562-71.
Dr. Lambert is a hospital medicine clinician and addiction medicine specialist in the division of hospital medicine at Massachusetts General Hospital.
Background: The use of multimodal non-opioid analgesics is a common practice to minimize postoperative pain and opioid analgesic use. There is limited high-quality evidence to confirm the synergistic effect and safety of acetaminophen and ibuprofen in the peripostoperative setting. The Paracetamol and NSAID in combination (PANSAID) trial investigated the analgesic efficacy and safety of four multimodal analgesic regimens after total hip arthroplasty.
Study design: Multicenter, randomized, blinded trial.
Setting: A total of six hospitals in Denmark, which represented regional and large university settings.
Synopsis: A total of 559 patients who underwent total hip arthroplasty were randomized to receive one of the following oral regimens: acetaminophen (1,000 mg) and ibuprofen (400 mg), acetaminophen (1,000 mg) and placebo, ibuprofen (400 mg) and placebo, and half-strength acetaminophen (500 mg) and ibuprofen (200 mg). One of the regimens was initiated 1 hour before surgery and continued every 6 hours for a total of 4 doses on the first postoperative day. The mean age was 67 years, and half of the patients were women.
The median morphine consumption in the 24 hours after surgery was significantly lower with full-strength acetaminophen-ibuprofen compared with acetaminophen monotherapy (20 mg vs. 36 mg, 99.6% confidence interval, 6.5-24; P < .001), which exceeded the prespecified 10-mg threshold for a minimal clinically important difference (MCID). The difference between acetaminophen-ibuprofen and ibuprofen monotherapy (20 mg vs. 26 mg) did not exceed the MCID, and was not clinically meaningful. The differences in morphine consumption with full-strength acetaminophen-ibuprofen compared to half-strength acetaminophen-ibuprofen (28 mg) and ibuprofen compared to acetaminophen monotherapy were not statistically significant.
Serious adverse events, the other primary outcome, within 90 days after surgery (15% in the ibuprofen group and 11% in the acetaminophen group, relative risk, 1.44; 97.5% CI, 0.79-2.64; P = .18) did not differ between acetaminophen monotherapy and ibuprofen monotherapy. Secondary outcomes included statistically significant analgesia (lower pain scores) at rest and with mobilization at 24 hours in the acetaminophen-ibuprofen group compared to the other groups.
An interesting observation was that acetaminophen-ibuprofen did not exceed the MCID compared to ibuprofen, which suggests that ibuprofen monotherapy may be a reasonable option for early postoperative analgesia.
Bottom line: Acetaminophen-ibuprofen reduced postoperative morphine use and had improved analgesia 24 hours after total hip arthroplasty, and was not associated with an increased 3-month risk of serious adverse events.
Citation: Thybo KH et al. Effect of combination of paracetamol (acetaminophen) and ibuprofen vs. either alone on patient-controlled morphine consumption in the first 24 hours after total hip arthroplasty. The PANSAID randomized clinical trial. JAMA. 2019;321(6):562-71.
Dr. Lambert is a hospital medicine clinician and addiction medicine specialist in the division of hospital medicine at Massachusetts General Hospital.
Compounded analgesic topical creams offer no benefit in treatment of localized chronic pain
Background: Federal health system programs, including TRICARE for military personnel, spent $259 million in 2013 and $746 million in 2014 for compounded analgesic medications despite a dearth of efficacy data. The purpose of this trial was to evaluate the efficacy and functional impact of this class of medications for chronic localized pain.
Study design: Randomized, double-blind, parallel trial.
Setting: Walter Reed National Military Medical Center.
Synopsis: A total of 339 patients with at least mild, chronic localized pain were allocated to three subgroups of 133 patients based on pain type; neuropathic, nociceptive, or mixed pain. The patients in the neuropathic pain arm received a compounded formulation containing 10% ketamine, 6% gabapentin, 0.2% clonidine, and 2% lidocaine; in the nociceptive pain arm, a formulation containing 10% ketoprofen, 2% baclofen, 2% cyclobenzaprine, and 2% lidocaine; and in the mixed pain arm, a formulation containing 10% ketamine, 6% gabapentin, 3% diclofenac, 2% baclofen, 2% cyclobenzaprine, and 2% lidocaine. Half of the patients in each subgroup received the compounded formulation and the other half received placebo.
The primary outcome was the average pain score at 1 month follow-up, based on self-recorded arithmetic mean pain scores in the preceding week. Secondary outcomes included mean worst pain over the past week, functional improvement (assessed by validated Short-Form 36 Health Survey scores), and satisfaction (measured on a 1 to 5 Likert scale) with the individual treatment regimen.
Patients had small improvements in average pain scores at 1 month in the compounded formulation and placebo subgroups in all pain type categories. No significant differences were noted in the average pain scores compared to baseline, functional improvement or satisfaction in the compounded formulation and placebo groups of the total cohort or in any of the subgroups.
Bottom line: Compounded topical analgesics are costly and ineffective in the treatment of all types of chronic localized pain.
Citation: Brutcher RE et al. Compounded topical pain creams to treat localized chronic pain. Ann Intern Med. 2019;170(5):309-18.
Dr. Lambert is a hospital medicine clinician and addiction medicine specialist in the division of hospital medicine at Massachusetts General Hospital.
Background: Federal health system programs, including TRICARE for military personnel, spent $259 million in 2013 and $746 million in 2014 for compounded analgesic medications despite a dearth of efficacy data. The purpose of this trial was to evaluate the efficacy and functional impact of this class of medications for chronic localized pain.
Study design: Randomized, double-blind, parallel trial.
Setting: Walter Reed National Military Medical Center.
Synopsis: A total of 339 patients with at least mild, chronic localized pain were allocated to three subgroups of 133 patients based on pain type; neuropathic, nociceptive, or mixed pain. The patients in the neuropathic pain arm received a compounded formulation containing 10% ketamine, 6% gabapentin, 0.2% clonidine, and 2% lidocaine; in the nociceptive pain arm, a formulation containing 10% ketoprofen, 2% baclofen, 2% cyclobenzaprine, and 2% lidocaine; and in the mixed pain arm, a formulation containing 10% ketamine, 6% gabapentin, 3% diclofenac, 2% baclofen, 2% cyclobenzaprine, and 2% lidocaine. Half of the patients in each subgroup received the compounded formulation and the other half received placebo.
The primary outcome was the average pain score at 1 month follow-up, based on self-recorded arithmetic mean pain scores in the preceding week. Secondary outcomes included mean worst pain over the past week, functional improvement (assessed by validated Short-Form 36 Health Survey scores), and satisfaction (measured on a 1 to 5 Likert scale) with the individual treatment regimen.
Patients had small improvements in average pain scores at 1 month in the compounded formulation and placebo subgroups in all pain type categories. No significant differences were noted in the average pain scores compared to baseline, functional improvement or satisfaction in the compounded formulation and placebo groups of the total cohort or in any of the subgroups.
Bottom line: Compounded topical analgesics are costly and ineffective in the treatment of all types of chronic localized pain.
Citation: Brutcher RE et al. Compounded topical pain creams to treat localized chronic pain. Ann Intern Med. 2019;170(5):309-18.
Dr. Lambert is a hospital medicine clinician and addiction medicine specialist in the division of hospital medicine at Massachusetts General Hospital.
Background: Federal health system programs, including TRICARE for military personnel, spent $259 million in 2013 and $746 million in 2014 for compounded analgesic medications despite a dearth of efficacy data. The purpose of this trial was to evaluate the efficacy and functional impact of this class of medications for chronic localized pain.
Study design: Randomized, double-blind, parallel trial.
Setting: Walter Reed National Military Medical Center.
Synopsis: A total of 339 patients with at least mild, chronic localized pain were allocated to three subgroups of 133 patients based on pain type; neuropathic, nociceptive, or mixed pain. The patients in the neuropathic pain arm received a compounded formulation containing 10% ketamine, 6% gabapentin, 0.2% clonidine, and 2% lidocaine; in the nociceptive pain arm, a formulation containing 10% ketoprofen, 2% baclofen, 2% cyclobenzaprine, and 2% lidocaine; and in the mixed pain arm, a formulation containing 10% ketamine, 6% gabapentin, 3% diclofenac, 2% baclofen, 2% cyclobenzaprine, and 2% lidocaine. Half of the patients in each subgroup received the compounded formulation and the other half received placebo.
The primary outcome was the average pain score at 1 month follow-up, based on self-recorded arithmetic mean pain scores in the preceding week. Secondary outcomes included mean worst pain over the past week, functional improvement (assessed by validated Short-Form 36 Health Survey scores), and satisfaction (measured on a 1 to 5 Likert scale) with the individual treatment regimen.
Patients had small improvements in average pain scores at 1 month in the compounded formulation and placebo subgroups in all pain type categories. No significant differences were noted in the average pain scores compared to baseline, functional improvement or satisfaction in the compounded formulation and placebo groups of the total cohort or in any of the subgroups.
Bottom line: Compounded topical analgesics are costly and ineffective in the treatment of all types of chronic localized pain.
Citation: Brutcher RE et al. Compounded topical pain creams to treat localized chronic pain. Ann Intern Med. 2019;170(5):309-18.
Dr. Lambert is a hospital medicine clinician and addiction medicine specialist in the division of hospital medicine at Massachusetts General Hospital.
Seniors with COVID-19 show unusual symptoms, doctors say
complicating efforts to ensure they get timely and appropriate treatment, according to physicians.
COVID-19 is typically signaled by three symptoms: a fever, an insistent cough, and shortness of breath. But older adults – the age group most at risk of severe complications or death from this condition – may have none of these characteristics.
Instead, seniors may seem “off” – not acting like themselves – early on after being infected by the coronavirus. They may sleep more than usual or stop eating. They may seem unusually apathetic or confused, losing orientation to their surroundings. They may become dizzy and fall. Sometimes, seniors stop speaking or simply collapse.
“With a lot of conditions, older adults don’t present in a typical way, and we’re seeing that with COVID-19 as well,” said Camille Vaughan, MD, section chief of geriatrics and gerontology at Emory University, Atlanta.
The reason has to do with how older bodies respond to illness and infection.
At advanced ages, “someone’s immune response may be blunted and their ability to regulate temperature may be altered,” said Dr. Joseph Ouslander, a professor of geriatric medicine at Florida Atlantic University in Boca Raton.
“Underlying chronic illnesses can mask or interfere with signs of infection,” he said. “Some older people, whether from age-related changes or previous neurologic issues such as a stroke, may have altered cough reflexes. Others with cognitive impairment may not be able to communicate their symptoms.”
Recognizing danger signs is important: If early signs of COVID-19 are missed, seniors may deteriorate before getting needed care. And people may go in and out of their homes without adequate protective measures, risking the spread of infection.
Quratulain Syed, MD, an Atlanta geriatrician, describes a man in his 80s whom she treated in mid-March. Over a period of days, this patient, who had heart disease, diabetes and moderate cognitive impairment, stopped walking and became incontinent and profoundly lethargic. But he didn’t have a fever or a cough. His only respiratory symptom: sneezing off and on.
The man’s elderly spouse called 911 twice. Both times, paramedics checked his vital signs and declared he was OK. After another worried call from the overwhelmed spouse, Dr. Syed insisted the patient be taken to the hospital, where he tested positive for COVID-19.
“I was quite concerned about the paramedics and health aides who’d been in the house and who hadn’t used PPE [personal protective equipment],” Dr. Syed said.
Dr. Sam Torbati, medical director of the emergency department at Cedars-Sinai Medical Center, Los Angeles, describes treating seniors who initially appear to be trauma patients but are found to have COVID-19.
“They get weak and dehydrated,” he said, “and when they stand to walk, they collapse and injure themselves badly.”
Dr. Torbati has seen older adults who are profoundly disoriented and unable to speak and who appear at first to have suffered strokes.
“When we test them, we discover that what’s producing these changes is a central nervous system effect of coronavirus,” he said.
Laura Perry, MD, of the University of California, San Francisco, saw a patient like this several weeks ago. The woman, in her 80s, had what seemed to be a cold before becoming very confused. In the hospital, she couldn’t identify where she was or stay awake during an examination. Dr. Perry diagnosed hypoactive delirium, an altered mental state in which people become inactive and drowsy. The patient tested positive for coronavirus and is still in the ICU.
Anthony Perry, MD, of the department of geriatric medicine at Rush University Medical Center in Chicago, tells of an 81-year-old woman with nausea, vomiting, and diarrhea who tested positive for COVID-19 in the emergency room. After receiving intravenous fluids, oxygen, and medication for her intestinal upset, she returned home after 2 days and is doing well.
Another 80-year-old Rush patient with similar symptoms – nausea and vomiting, but no cough, fever, or shortness of breath – is in intensive care after getting a positive COVID-19 test and due to be put on a ventilator. The difference? This patient is frail with “a lot of cardiovascular disease,” Dr. Perry said. Other than that, it’s not yet clear why some older patients do well while others do not.
So far, reports of cases like these have been anecdotal. But a few physicians are trying to gather more systematic information.
In Switzerland, Sylvain Nguyen, MD, a geriatrician at the University of Lausanne Hospital Center, put together a list of typical and atypical symptoms in older COVID-19 patients for a paper to be published in the Revue Médicale Suisse. Included on the atypical list are changes in a patient’s usual status, delirium, falls, fatigue, lethargy, low blood pressure, painful swallowing, fainting, diarrhea, nausea, vomiting, abdominal pain, and the loss of smell and taste.
Data come from hospitals and nursing homes in Switzerland, Italy, and France, Dr. Nguyen said in an email.
On the front lines, physicians need to make sure they carefully assess an older patient’s symptoms.
“While we have to have a high suspicion of COVID-19 because it’s so dangerous in the older population, there are many other things to consider,” said Kathleen Unroe, MD, a geriatrician at Indiana University, Indianapolis.
Seniors may also do poorly because their routines have changed. In nursing homes and most assisted living centers, activities have stopped and “residents are going to get weaker and more deconditioned because they’re not walking to and from the dining hall,” she said.
At home, isolated seniors may not be getting as much help with medication management or other essential needs from family members who are keeping their distance, other experts suggested. Or they may have become apathetic or depressed.
“I’d want to know ‘What’s the potential this person has had an exposure [to the coronavirus], especially in the last 2 weeks?’ ” said Dr. Vaughan of Emory. “Do they have home health personnel coming in? Have they gotten together with other family members? Are chronic conditions being controlled? Is there another diagnosis that seems more likely?”
“Someone may be just having a bad day. But if they’re not themselves for a couple of days, absolutely reach out to a primary care doctor or a local health system hotline to see if they meet the threshold for [coronavirus] testing,” Dr. Vaughan advised. “Be persistent. If you get a ‘no’ the first time and things aren’t improving, call back and ask again.”
Kaiser Health News (khn.org) is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
complicating efforts to ensure they get timely and appropriate treatment, according to physicians.
COVID-19 is typically signaled by three symptoms: a fever, an insistent cough, and shortness of breath. But older adults – the age group most at risk of severe complications or death from this condition – may have none of these characteristics.
Instead, seniors may seem “off” – not acting like themselves – early on after being infected by the coronavirus. They may sleep more than usual or stop eating. They may seem unusually apathetic or confused, losing orientation to their surroundings. They may become dizzy and fall. Sometimes, seniors stop speaking or simply collapse.
“With a lot of conditions, older adults don’t present in a typical way, and we’re seeing that with COVID-19 as well,” said Camille Vaughan, MD, section chief of geriatrics and gerontology at Emory University, Atlanta.
The reason has to do with how older bodies respond to illness and infection.
At advanced ages, “someone’s immune response may be blunted and their ability to regulate temperature may be altered,” said Dr. Joseph Ouslander, a professor of geriatric medicine at Florida Atlantic University in Boca Raton.
“Underlying chronic illnesses can mask or interfere with signs of infection,” he said. “Some older people, whether from age-related changes or previous neurologic issues such as a stroke, may have altered cough reflexes. Others with cognitive impairment may not be able to communicate their symptoms.”
Recognizing danger signs is important: If early signs of COVID-19 are missed, seniors may deteriorate before getting needed care. And people may go in and out of their homes without adequate protective measures, risking the spread of infection.
Quratulain Syed, MD, an Atlanta geriatrician, describes a man in his 80s whom she treated in mid-March. Over a period of days, this patient, who had heart disease, diabetes and moderate cognitive impairment, stopped walking and became incontinent and profoundly lethargic. But he didn’t have a fever or a cough. His only respiratory symptom: sneezing off and on.
The man’s elderly spouse called 911 twice. Both times, paramedics checked his vital signs and declared he was OK. After another worried call from the overwhelmed spouse, Dr. Syed insisted the patient be taken to the hospital, where he tested positive for COVID-19.
“I was quite concerned about the paramedics and health aides who’d been in the house and who hadn’t used PPE [personal protective equipment],” Dr. Syed said.
Dr. Sam Torbati, medical director of the emergency department at Cedars-Sinai Medical Center, Los Angeles, describes treating seniors who initially appear to be trauma patients but are found to have COVID-19.
“They get weak and dehydrated,” he said, “and when they stand to walk, they collapse and injure themselves badly.”
Dr. Torbati has seen older adults who are profoundly disoriented and unable to speak and who appear at first to have suffered strokes.
“When we test them, we discover that what’s producing these changes is a central nervous system effect of coronavirus,” he said.
Laura Perry, MD, of the University of California, San Francisco, saw a patient like this several weeks ago. The woman, in her 80s, had what seemed to be a cold before becoming very confused. In the hospital, she couldn’t identify where she was or stay awake during an examination. Dr. Perry diagnosed hypoactive delirium, an altered mental state in which people become inactive and drowsy. The patient tested positive for coronavirus and is still in the ICU.
Anthony Perry, MD, of the department of geriatric medicine at Rush University Medical Center in Chicago, tells of an 81-year-old woman with nausea, vomiting, and diarrhea who tested positive for COVID-19 in the emergency room. After receiving intravenous fluids, oxygen, and medication for her intestinal upset, she returned home after 2 days and is doing well.
Another 80-year-old Rush patient with similar symptoms – nausea and vomiting, but no cough, fever, or shortness of breath – is in intensive care after getting a positive COVID-19 test and due to be put on a ventilator. The difference? This patient is frail with “a lot of cardiovascular disease,” Dr. Perry said. Other than that, it’s not yet clear why some older patients do well while others do not.
So far, reports of cases like these have been anecdotal. But a few physicians are trying to gather more systematic information.
In Switzerland, Sylvain Nguyen, MD, a geriatrician at the University of Lausanne Hospital Center, put together a list of typical and atypical symptoms in older COVID-19 patients for a paper to be published in the Revue Médicale Suisse. Included on the atypical list are changes in a patient’s usual status, delirium, falls, fatigue, lethargy, low blood pressure, painful swallowing, fainting, diarrhea, nausea, vomiting, abdominal pain, and the loss of smell and taste.
Data come from hospitals and nursing homes in Switzerland, Italy, and France, Dr. Nguyen said in an email.
On the front lines, physicians need to make sure they carefully assess an older patient’s symptoms.
“While we have to have a high suspicion of COVID-19 because it’s so dangerous in the older population, there are many other things to consider,” said Kathleen Unroe, MD, a geriatrician at Indiana University, Indianapolis.
Seniors may also do poorly because their routines have changed. In nursing homes and most assisted living centers, activities have stopped and “residents are going to get weaker and more deconditioned because they’re not walking to and from the dining hall,” she said.
At home, isolated seniors may not be getting as much help with medication management or other essential needs from family members who are keeping their distance, other experts suggested. Or they may have become apathetic or depressed.
“I’d want to know ‘What’s the potential this person has had an exposure [to the coronavirus], especially in the last 2 weeks?’ ” said Dr. Vaughan of Emory. “Do they have home health personnel coming in? Have they gotten together with other family members? Are chronic conditions being controlled? Is there another diagnosis that seems more likely?”
“Someone may be just having a bad day. But if they’re not themselves for a couple of days, absolutely reach out to a primary care doctor or a local health system hotline to see if they meet the threshold for [coronavirus] testing,” Dr. Vaughan advised. “Be persistent. If you get a ‘no’ the first time and things aren’t improving, call back and ask again.”
Kaiser Health News (khn.org) is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
complicating efforts to ensure they get timely and appropriate treatment, according to physicians.
COVID-19 is typically signaled by three symptoms: a fever, an insistent cough, and shortness of breath. But older adults – the age group most at risk of severe complications or death from this condition – may have none of these characteristics.
Instead, seniors may seem “off” – not acting like themselves – early on after being infected by the coronavirus. They may sleep more than usual or stop eating. They may seem unusually apathetic or confused, losing orientation to their surroundings. They may become dizzy and fall. Sometimes, seniors stop speaking or simply collapse.
“With a lot of conditions, older adults don’t present in a typical way, and we’re seeing that with COVID-19 as well,” said Camille Vaughan, MD, section chief of geriatrics and gerontology at Emory University, Atlanta.
The reason has to do with how older bodies respond to illness and infection.
At advanced ages, “someone’s immune response may be blunted and their ability to regulate temperature may be altered,” said Dr. Joseph Ouslander, a professor of geriatric medicine at Florida Atlantic University in Boca Raton.
“Underlying chronic illnesses can mask or interfere with signs of infection,” he said. “Some older people, whether from age-related changes or previous neurologic issues such as a stroke, may have altered cough reflexes. Others with cognitive impairment may not be able to communicate their symptoms.”
Recognizing danger signs is important: If early signs of COVID-19 are missed, seniors may deteriorate before getting needed care. And people may go in and out of their homes without adequate protective measures, risking the spread of infection.
Quratulain Syed, MD, an Atlanta geriatrician, describes a man in his 80s whom she treated in mid-March. Over a period of days, this patient, who had heart disease, diabetes and moderate cognitive impairment, stopped walking and became incontinent and profoundly lethargic. But he didn’t have a fever or a cough. His only respiratory symptom: sneezing off and on.
The man’s elderly spouse called 911 twice. Both times, paramedics checked his vital signs and declared he was OK. After another worried call from the overwhelmed spouse, Dr. Syed insisted the patient be taken to the hospital, where he tested positive for COVID-19.
“I was quite concerned about the paramedics and health aides who’d been in the house and who hadn’t used PPE [personal protective equipment],” Dr. Syed said.
Dr. Sam Torbati, medical director of the emergency department at Cedars-Sinai Medical Center, Los Angeles, describes treating seniors who initially appear to be trauma patients but are found to have COVID-19.
“They get weak and dehydrated,” he said, “and when they stand to walk, they collapse and injure themselves badly.”
Dr. Torbati has seen older adults who are profoundly disoriented and unable to speak and who appear at first to have suffered strokes.
“When we test them, we discover that what’s producing these changes is a central nervous system effect of coronavirus,” he said.
Laura Perry, MD, of the University of California, San Francisco, saw a patient like this several weeks ago. The woman, in her 80s, had what seemed to be a cold before becoming very confused. In the hospital, she couldn’t identify where she was or stay awake during an examination. Dr. Perry diagnosed hypoactive delirium, an altered mental state in which people become inactive and drowsy. The patient tested positive for coronavirus and is still in the ICU.
Anthony Perry, MD, of the department of geriatric medicine at Rush University Medical Center in Chicago, tells of an 81-year-old woman with nausea, vomiting, and diarrhea who tested positive for COVID-19 in the emergency room. After receiving intravenous fluids, oxygen, and medication for her intestinal upset, she returned home after 2 days and is doing well.
Another 80-year-old Rush patient with similar symptoms – nausea and vomiting, but no cough, fever, or shortness of breath – is in intensive care after getting a positive COVID-19 test and due to be put on a ventilator. The difference? This patient is frail with “a lot of cardiovascular disease,” Dr. Perry said. Other than that, it’s not yet clear why some older patients do well while others do not.
So far, reports of cases like these have been anecdotal. But a few physicians are trying to gather more systematic information.
In Switzerland, Sylvain Nguyen, MD, a geriatrician at the University of Lausanne Hospital Center, put together a list of typical and atypical symptoms in older COVID-19 patients for a paper to be published in the Revue Médicale Suisse. Included on the atypical list are changes in a patient’s usual status, delirium, falls, fatigue, lethargy, low blood pressure, painful swallowing, fainting, diarrhea, nausea, vomiting, abdominal pain, and the loss of smell and taste.
Data come from hospitals and nursing homes in Switzerland, Italy, and France, Dr. Nguyen said in an email.
On the front lines, physicians need to make sure they carefully assess an older patient’s symptoms.
“While we have to have a high suspicion of COVID-19 because it’s so dangerous in the older population, there are many other things to consider,” said Kathleen Unroe, MD, a geriatrician at Indiana University, Indianapolis.
Seniors may also do poorly because their routines have changed. In nursing homes and most assisted living centers, activities have stopped and “residents are going to get weaker and more deconditioned because they’re not walking to and from the dining hall,” she said.
At home, isolated seniors may not be getting as much help with medication management or other essential needs from family members who are keeping their distance, other experts suggested. Or they may have become apathetic or depressed.
“I’d want to know ‘What’s the potential this person has had an exposure [to the coronavirus], especially in the last 2 weeks?’ ” said Dr. Vaughan of Emory. “Do they have home health personnel coming in? Have they gotten together with other family members? Are chronic conditions being controlled? Is there another diagnosis that seems more likely?”
“Someone may be just having a bad day. But if they’re not themselves for a couple of days, absolutely reach out to a primary care doctor or a local health system hotline to see if they meet the threshold for [coronavirus] testing,” Dr. Vaughan advised. “Be persistent. If you get a ‘no’ the first time and things aren’t improving, call back and ask again.”
Kaiser Health News (khn.org) is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
COVID-19 linked to large vessel stroke in young adults
In a rapid communication to be published online April 29 in the New England Journal of Medicine, investigators led by Thomas Oxley, MD, PhD, of the department of neurosurgery at Mount Sinai Health System, reported five cases of large vessel stroke over a 2-week period in COVID-19 patients under age 50 years. This represents a sevenfold increase in what would normally be expected.
The five cases had either no, or mild, COVID-19 symptoms.
“It’s been surprising to learn that the virus appears to cause disease through a process of blood clotting,” Dr. Oxley said in an interview.
The message for neurologists and other physicians is “we’re learning that this can disproportionally affect large vessels more than small vessels in terms of presentation of stroke,” he said.
Inflammation in the blood vessel walls may be driving thrombosis formation, Dr. Oxley added. This report joins other research pointing to this emerging phenomenon.
Recently, investigators in the Netherlands found a “remarkably high” 31% rate of thrombotic complications among 184 critical care patients with COVID-19 pneumonia.
Dr. Oxley and colleagues also suggested that, since the onset of the pandemic, fewer patients may be calling emergency services when they experience signs of a stroke. The physicians noted that two of the five cases in the report delayed calling an ambulance.
“I understand why people do not want to leave the household. I think people are more willing to ignore other [non–COVID-19] symptoms in this environment,” he said.
As previously reported, physicians in hospitals across the United States and elsewhere have reported a significant drop in stroke patients since the COVID-19 pandemic took hold, which suggests that patients may indeed be foregoing emergency care.
The observations from Dr. Oxley and colleagues call for greater awareness of the association between COVID-19 and large vessel strokes in this age group, they add.
One patient in the case series died, one remains hospitalized, two are undergoing rehabilitation, and one was discharged home as of April 24.
Dr. Oxley and colleagues dedicated their report to “our inspiring colleague Gary Sclar, MD, a stroke physician who succumbed to COVID-19 while caring for his patients.”
Dr. Oxley has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In a rapid communication to be published online April 29 in the New England Journal of Medicine, investigators led by Thomas Oxley, MD, PhD, of the department of neurosurgery at Mount Sinai Health System, reported five cases of large vessel stroke over a 2-week period in COVID-19 patients under age 50 years. This represents a sevenfold increase in what would normally be expected.
The five cases had either no, or mild, COVID-19 symptoms.
“It’s been surprising to learn that the virus appears to cause disease through a process of blood clotting,” Dr. Oxley said in an interview.
The message for neurologists and other physicians is “we’re learning that this can disproportionally affect large vessels more than small vessels in terms of presentation of stroke,” he said.
Inflammation in the blood vessel walls may be driving thrombosis formation, Dr. Oxley added. This report joins other research pointing to this emerging phenomenon.
Recently, investigators in the Netherlands found a “remarkably high” 31% rate of thrombotic complications among 184 critical care patients with COVID-19 pneumonia.
Dr. Oxley and colleagues also suggested that, since the onset of the pandemic, fewer patients may be calling emergency services when they experience signs of a stroke. The physicians noted that two of the five cases in the report delayed calling an ambulance.
“I understand why people do not want to leave the household. I think people are more willing to ignore other [non–COVID-19] symptoms in this environment,” he said.
As previously reported, physicians in hospitals across the United States and elsewhere have reported a significant drop in stroke patients since the COVID-19 pandemic took hold, which suggests that patients may indeed be foregoing emergency care.
The observations from Dr. Oxley and colleagues call for greater awareness of the association between COVID-19 and large vessel strokes in this age group, they add.
One patient in the case series died, one remains hospitalized, two are undergoing rehabilitation, and one was discharged home as of April 24.
Dr. Oxley and colleagues dedicated their report to “our inspiring colleague Gary Sclar, MD, a stroke physician who succumbed to COVID-19 while caring for his patients.”
Dr. Oxley has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In a rapid communication to be published online April 29 in the New England Journal of Medicine, investigators led by Thomas Oxley, MD, PhD, of the department of neurosurgery at Mount Sinai Health System, reported five cases of large vessel stroke over a 2-week period in COVID-19 patients under age 50 years. This represents a sevenfold increase in what would normally be expected.
The five cases had either no, or mild, COVID-19 symptoms.
“It’s been surprising to learn that the virus appears to cause disease through a process of blood clotting,” Dr. Oxley said in an interview.
The message for neurologists and other physicians is “we’re learning that this can disproportionally affect large vessels more than small vessels in terms of presentation of stroke,” he said.
Inflammation in the blood vessel walls may be driving thrombosis formation, Dr. Oxley added. This report joins other research pointing to this emerging phenomenon.
Recently, investigators in the Netherlands found a “remarkably high” 31% rate of thrombotic complications among 184 critical care patients with COVID-19 pneumonia.
Dr. Oxley and colleagues also suggested that, since the onset of the pandemic, fewer patients may be calling emergency services when they experience signs of a stroke. The physicians noted that two of the five cases in the report delayed calling an ambulance.
“I understand why people do not want to leave the household. I think people are more willing to ignore other [non–COVID-19] symptoms in this environment,” he said.
As previously reported, physicians in hospitals across the United States and elsewhere have reported a significant drop in stroke patients since the COVID-19 pandemic took hold, which suggests that patients may indeed be foregoing emergency care.
The observations from Dr. Oxley and colleagues call for greater awareness of the association between COVID-19 and large vessel strokes in this age group, they add.
One patient in the case series died, one remains hospitalized, two are undergoing rehabilitation, and one was discharged home as of April 24.
Dr. Oxley and colleagues dedicated their report to “our inspiring colleague Gary Sclar, MD, a stroke physician who succumbed to COVID-19 while caring for his patients.”
Dr. Oxley has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Brant Oliver, PhD, on patient-reported outcomes in MS
Brant Oliver, PhD, MS, MPH, APRN-BC, is a health care improvement and implementation scientist, educator, and board-certified family and psychiatric nurse practitioner (FNP-BC, PMHNP-BC). Dr. Oliver's work focuses on applied health care improvement science research, with a focus on "3C" (complex, costly, and chronic) conditions including MS, IBD, CF, RA, and others; coproduction; learning health systems; and shared decision making. He is Associate Professor at the Geisel School of Medicine at Dartmouth and also has been in clinical practice since 2003, working primarily as a certified MS specialist (MSCN) and a MS neurobehavioral nurse practitioner.
Which patient-reported outcomes (PROs) are commonly assessed in the care of patients with multiple sclerosis (MS)?
BRANT OLIVER, PhD: The current reality is that PROs are not being used routinely in MS clinical care in most settings. They are most commonly being used in research settings, either as part of clinical trials of new treatments, or in epidemiologic studies looking at the prevalence, incidence, and severity of certain symptoms or functional impairments in MS at the population level. A good example is the NARCOMS registry, which has been used to conduct high-quality epidemiologic studies of MS-related symptoms using self-report questionnaires.
We are starting to see some use of MS PROs in select clinical settings. Oftentimes these are measures of highly prevalent comorbid conditions that have an impact on quality of life, treatment adherence (depression severity and anxiety), and self-efficacy, which is a measure of perceived coping ability related to self-management of a chronic illness. Also, measures of patient experience are being employed in hospital-based clinics, such as the CG-CAHPS satisfaction measures.
The PROMIS (Patient-Reported Outcomes Measurement Information System) battery is a promising set of PRO measures that are being utilized across a number of conditions and that contain some MS-specific measures, such as the Fatigue MS measure. Fatigue is the most common and disabling symptom in MS, so having a good measure of fatigue is of critical importance. Having a sense of a patient’s experience with fatigue over time can also be very helpful from a clinical perspective. The PROMIS measure performs much better than its predecessor, the Modified Fatigue Impact Scale (MFIS). Another strength of the PROMIS measures is that they tend to do well correlating with other conditions. In certain research and improvement settings, PROMIS can help us understand the burden a particular disease or population places on total health system resources. For example, is fatigue burden in MS similar in severity to that in another 3C condition, such as inflammatory bowel disease?
There are other PRO measures that have not been used in MS but which I think we will see used in the future. One of these is called Collaborate, which falls into the category of patient-reported experience measures (PREMs). Collaborate measures the degree of shared decision-making that occurs in a clinical encounter, which becomes especially important as the complexity of disease-modifying treatment decisions increases as more disease-modifying therapies are introduced, each with their own profile of risks and benefits. I anticipate that the ability of clinics to facilitate effective shared decision-making will be of increasing interest to clinicians, patients, and also payers in the future.
What are some of the potential benefits of using PRO measures in terms of clinician/patient communication and clinical decision-making?
BRANT OLIVER, PhD: I think the most important benefit of measuring PROs is that it can make care more patient-centered. The big push for PROs in the first place was to incorporate more of the patient’s voice into their own care. Standard clinical measures, such as magnetic resonance imaging (MRI) or relapse rates, can be very precise and provide a good clinical picture of how the disease is behaving. But if we rely solely on that kind of information, we can lose sight of the person who is experiencing the disease.
PROs, be they just regular PROs (instruments that gather qualitative and/or quantitative patient-reported information) or PROMs (validated and standardized PRO measures) or PREMs (standardized and validated patient-reported experience measures), all aim to improve the ability to get a better story of the person who's experiencing the illness and how that condition affects them. We can also gain insight on what's most important to them regarding how their illness is managed, and what their experience of care is.
Sometimes the PRO picture and the clinical picture don't necessarily align. I'll tell a story about one a person, who's given me permission to share the story. She is an established professional, and her PRO measures concerning her quality of life, support from her workplace environment, and her ability to function in society are very high. She's very high functioning according to the PRO picture. However, her clinical measures suggest that she is significantly impaired. Her MRI burden is quite high, and her disability due to the MS, her EDSS (Expanded Disability Status Scale), is also quite high. So there are 2 very different stories provided by 2 different sets of data. The inclusion of PROs data, in connection with clinical data, can provide a more holistic view of this person, who is functioning well despite significant disease burden.
As a clinician working with patients with MS, this gives me much more to work with in trying to help people, not only treating the disease, but also trying to see where the person is most in need of help. A person could be very well controlled on MRI in terms of relapse rate, but have fatigue severity that is through the roof. If I weren't paying closer attention to that with a validated scale that measures fatigue severity over time, like the PROMIS Fatigue MS, I may not have a sense of how well treatment is helping that person's fatigue longitudinally, beyond what I can glean from the history and clinical examination.
PROs can also be helpful in terms of conditions that are harder to quantify. Depression is a significant cause of disability and a significant factor contributing to poor treatment adherence in MS. Also, the suicide rate in persons with MS is much higher than that in the general population. But there is no blood test for depression severity, and oftentimes a patient’s report on exam can be incomplete or misleading. Accompanying the mental status exam and the clinical evaluation with a validated depression severity measure (such as the PHQ9 [Patient Health Questionnaire-9], CES-D [Center for Epidemiologic Studies Depression Scale], or others) can help to determine whether treatments are having an initial effect, and this can also help with self-monitoring and treatment adherence.
That brings us to the second area where PROs show real promise in MS care: the learning health system (LHS) approach, which uses feed forward information to either predict the needs of people before they come to the office or optimize decision-making at the point of care (as discussed in our review article published in JCOM).1
PROs can play a significant role in the LHS approach in 2 ways. For example, if I have a good sense before a visit that the person has stable symptoms but is having a lot of trouble coping with MS, that may change how I allocate resources and focus the time at the visit to target the primary concern of the person before the visit even occurs. Over time I'd be able to monitor if those coping scores increase in response to the work we’re doing with the person.
The second part of this approach is a feedback mechanism. These measures can be aggregated at the population level and fed back to clinical MS centers to help clinicians who are trying to improve overall population health outcomes of people with MS to see how well they're doing on things like fatigue management, depression management, coping ability, and pain control, which can't be tested for with biologic methods. So in addition to looking at the MRI scan trends across the population and relapse rate annualized for the population over time, I'd also be able to see fatigue severity and depression severity at a clinic population level and assess the change in these severity levels over time, which I could then use to inform efforts to change how my system (clinic) provides MS care.
This capability of PROs could be of significant interest to payers, especially those who are looking to optimize the value of care that is being provided, given the high cost of MS care. MS treatments are very expensive, and MS care is multidisciplinary and requires a lot of resources. Payers, I think, will have an increasing interest in assessing the value of high-cost care. PROs could help to demonstrate that value, especially if they can help quantify that outcomes can be improved over time at the population level.
The third area where PROs are beneficial is population health research, especially in terms of the major improvement movements going on in the country, such as those advocated for by the Institute for Healthcare Improvement via the Triple Aim: improve population health outcomes, improve the experience of care, and minimize per capita cost. PROs can really help with the first 2 of those Triple Aim categories.
What are some of the factors that limit the use of PRO measures in MS research and clinical practice?
BRANT OLIVER, PhD: In our JCOM paper,1 we outlined major barriers or constraints or challenges to implementing PRO measures. One is time and technology in clinical care. It's busy. It's fast. A PRO measure requires patients to complete a questionnaire. And to do that, you need some time and space during the clinical visit, or before the visit, to collect this data. In the absence of appropriate technology, this is done using paper-based methods, which can be challenging. Technology can help. Examples include smart phone app-based collection systems, tablet PCs, or an online mechanism. But there are barriers to technology, too. Is the technology good enough? Is the interface with the people using it working well? Do you have an equal amount of access to and understanding of the technology from the people across your population? Is it only being used by a certain subset that is wealthier and more educated, or maybe who has English as a first language? Such constraints can be overcome, but they’re present in any situation where you are gathering PRO data.
Software constraints also extend to the electronic health record (EHR) capability of the clinics. If you can collect PRO data, does the EHR have the capability to present that data in a useful way during a 20- or 30-minute clinical visit? In other words, does it improve the quality of the visit, or does it generate just one more distraction during the visit? Some approaches, such as feed forward dashboards, provide easy visual displays that can quickly and easily add information at the point of care and can get around this limitation. However, a lot of MS care centers in private practice settings may not have the informatics capability of a large academic center.
Academic centers often have more EHR capability, but can also move much slower in implementation than more nimble private practice or community clinics. With many competing demands, it can sometimes take months to build one of these surveys into an EHR, for a task that takes just a day or so. But because other departments are in the queue for these changes, implementation often takes longer than we would intuitively think.
A second barrier is the burden on the individuals themselves. As much as we feel that PROs can make a difference, and the growing literature suggests that they really can, this is counterbalanced with the burden they may place on the patient. For example, a person may arrive at a clinic visit already with a lot on their mind, and then they get a questionnaire to complete in the waiting room before their visit (or perhaps they get asked to do it at home before the visit). The patient, rather than perceiving this as beneficial, may instead perceive it as an extra task or stressor. Explaining the purpose of the PRO measures, encouraging their use, and then actually using the results meaningfully during the visit can substantially improve their perceived value.
It’s important to limit the total amount of PROs used. In research, as well as in clinical settings, too many measures can lead to too little data. It's similar to an overly complex treatment plan: the chance that a person will adhere to all of it decreases with each level of complexity added. This can lead to decreased engagement by patients, and gradually they'll move away from participating in the PROs in general. Research and clinical efforts around PROs strive to get to a parsimonious set of critical measures, which will minimize the burden, but maximize the potential benefit.
A third challenge is interpretability. This gets into the psychometric properties of the PRO measures and setting appropriate clinical thresholds for what constitutes a “positive” or “actionable” result. What is a clinically significant level of fatigue severity on the PROMIS MS Fatigue? We know that the mean range of that instrument is somewhere between 50 and 60. Does that mean that scores above 60 suggest higher than average fatigue levels, or is it more complicated than that? In many cases, the instruments don't have extensive population level research for the populations in which they are used. Setting clinical thresholds can be difficult, and I suspect that this will be a major area of research in the coming years.
Another example is setting appropriate depression thresholds. We know that on the CES-D, for example, the positive threshold for active depression in a patient with MS may be different from that in a patient without MS, because fatigue is a contributing factor to the neurovegetative symptoms that are scored on the CES-D.
So even if we can incorporate PROs into general practice and minimize burden, we also have to pay attention to factors that limit their interpretability and employ them in a way whereby they provide clinically meaningful results that can help inform care. The good news is, for many PROs, even with these limitations, this can be done.
Following directly from this is error risk. Many PRO measures were designed for large-sample epidemiologic research, not for a smaller sample clinical practice, which can lead to a higher error risk, especially when following single individuals over time. Adjustments in how these scales are interpreted are required in many cases.
The limitations of many of the respondents completing questionnaires needs to be taken into account. Fatigue and cognitive impairment are very common in MS. Respondents may be selecting answers that are not entirely accurate if they're getting fatigued while doing the surveys, or if they have a comprehension deficit or a short-term memory deficit.
A final challenge is demonstrating, just like any treatment or assessment approach, that the benefit outweighs the burden. PRO measures that are fairly reliable, validated, and quick and easy to complete suddenly become quite valuable because their benefit far outweighs the potential constraints. I think as PROs and the ways of assessing them continue to develop, that will become a bigger issue. The question will be, okay, you can do this, but what is the value added by doing this? That added value could be demonstrated in terms of better clinical outcomes, reduced costs, reduced hospitalizations, better treatment adherence, and so on.
How do you see the use of patient-reported outcomes in MS care evolving over time?
BRANT OLIVER, PhD: I tend to be optimistic regarding PROs. I think they will become part of the new reality, especially in LHS-oriented models of care. As mentioned, LHSs use feed forward data to predict the needs of people or optimize shared decision-making. I think we're going to see more shared decision-making rather than less over time in complex chronic illnesses care.
In environments where there's an increasing focus on value for high-cost, such as complex chronic conditions like MS and inflammatory bowel disease, systems will have to justify the high cost of treatment. PROs will be a critical piece in making that value assessment, especially since that value assessment is coming from the voice of patients rather than only from clinicians or other stakeholders. Arguably, patients may be able to contribute the most to making the value proposition because it is their outcomes and their experiences that matter to payers. Because experience matters (and not just outcomes), I think we'll see more PREMs used over time, including in MS.
I also think over time we'll see studies working to optimize PROs in the clinical environment and for improvement and research. An early example of that is the MS Continuous Quality Improvement (MS-CQI) Collaborative. It is a prospective randomized multicenter study using patient-reported and clinical data in a LHS approach to study population health outcomes and the effect of quality improvement interventions on those outcomes. It's also optimizing how these PRO measures are actually used at the point of care. Studies like MS-CQI will help to better articulate how, when, and for what purpose PROs should best be used and also when they should be avoided.
I think over time the predictive analytics component of PROs will be emphasized. There is a big push in the MS field in developing biomarkers to help predict disease progression over time. From the predictive analytics or machine learning perspective, imagine a situation where PROs could be used to predict a person's trajectory over time: if they were more likely to be lost to follow-up, to be hospitalized, or to have a relapse in the next year or 2. Reliable PROs generating population health data at scale can inform the development of risk and outcome predictive models.
Dr. Oliver discloses that he has received research grant support (MS-CQI research study mentioned in interview). He is the principal investigator and developer of the MS-CQI study, which is grant funded by Biogen under a Sponsored Research Agreement.
1. Manohar N, Perkins T, Laurion R, Oliver B. Patient-reported outcomes in multiple sclerosis: an overview. J Clin Outcomes Manage. 2019;26:277-288.
Brant Oliver, PhD, MS, MPH, APRN-BC, is a health care improvement and implementation scientist, educator, and board-certified family and psychiatric nurse practitioner (FNP-BC, PMHNP-BC). Dr. Oliver's work focuses on applied health care improvement science research, with a focus on "3C" (complex, costly, and chronic) conditions including MS, IBD, CF, RA, and others; coproduction; learning health systems; and shared decision making. He is Associate Professor at the Geisel School of Medicine at Dartmouth and also has been in clinical practice since 2003, working primarily as a certified MS specialist (MSCN) and a MS neurobehavioral nurse practitioner.
Which patient-reported outcomes (PROs) are commonly assessed in the care of patients with multiple sclerosis (MS)?
BRANT OLIVER, PhD: The current reality is that PROs are not being used routinely in MS clinical care in most settings. They are most commonly being used in research settings, either as part of clinical trials of new treatments, or in epidemiologic studies looking at the prevalence, incidence, and severity of certain symptoms or functional impairments in MS at the population level. A good example is the NARCOMS registry, which has been used to conduct high-quality epidemiologic studies of MS-related symptoms using self-report questionnaires.
We are starting to see some use of MS PROs in select clinical settings. Oftentimes these are measures of highly prevalent comorbid conditions that have an impact on quality of life, treatment adherence (depression severity and anxiety), and self-efficacy, which is a measure of perceived coping ability related to self-management of a chronic illness. Also, measures of patient experience are being employed in hospital-based clinics, such as the CG-CAHPS satisfaction measures.
The PROMIS (Patient-Reported Outcomes Measurement Information System) battery is a promising set of PRO measures that are being utilized across a number of conditions and that contain some MS-specific measures, such as the Fatigue MS measure. Fatigue is the most common and disabling symptom in MS, so having a good measure of fatigue is of critical importance. Having a sense of a patient’s experience with fatigue over time can also be very helpful from a clinical perspective. The PROMIS measure performs much better than its predecessor, the Modified Fatigue Impact Scale (MFIS). Another strength of the PROMIS measures is that they tend to do well correlating with other conditions. In certain research and improvement settings, PROMIS can help us understand the burden a particular disease or population places on total health system resources. For example, is fatigue burden in MS similar in severity to that in another 3C condition, such as inflammatory bowel disease?
There are other PRO measures that have not been used in MS but which I think we will see used in the future. One of these is called Collaborate, which falls into the category of patient-reported experience measures (PREMs). Collaborate measures the degree of shared decision-making that occurs in a clinical encounter, which becomes especially important as the complexity of disease-modifying treatment decisions increases as more disease-modifying therapies are introduced, each with their own profile of risks and benefits. I anticipate that the ability of clinics to facilitate effective shared decision-making will be of increasing interest to clinicians, patients, and also payers in the future.
What are some of the potential benefits of using PRO measures in terms of clinician/patient communication and clinical decision-making?
BRANT OLIVER, PhD: I think the most important benefit of measuring PROs is that it can make care more patient-centered. The big push for PROs in the first place was to incorporate more of the patient’s voice into their own care. Standard clinical measures, such as magnetic resonance imaging (MRI) or relapse rates, can be very precise and provide a good clinical picture of how the disease is behaving. But if we rely solely on that kind of information, we can lose sight of the person who is experiencing the disease.
PROs, be they just regular PROs (instruments that gather qualitative and/or quantitative patient-reported information) or PROMs (validated and standardized PRO measures) or PREMs (standardized and validated patient-reported experience measures), all aim to improve the ability to get a better story of the person who's experiencing the illness and how that condition affects them. We can also gain insight on what's most important to them regarding how their illness is managed, and what their experience of care is.
Sometimes the PRO picture and the clinical picture don't necessarily align. I'll tell a story about one a person, who's given me permission to share the story. She is an established professional, and her PRO measures concerning her quality of life, support from her workplace environment, and her ability to function in society are very high. She's very high functioning according to the PRO picture. However, her clinical measures suggest that she is significantly impaired. Her MRI burden is quite high, and her disability due to the MS, her EDSS (Expanded Disability Status Scale), is also quite high. So there are 2 very different stories provided by 2 different sets of data. The inclusion of PROs data, in connection with clinical data, can provide a more holistic view of this person, who is functioning well despite significant disease burden.
As a clinician working with patients with MS, this gives me much more to work with in trying to help people, not only treating the disease, but also trying to see where the person is most in need of help. A person could be very well controlled on MRI in terms of relapse rate, but have fatigue severity that is through the roof. If I weren't paying closer attention to that with a validated scale that measures fatigue severity over time, like the PROMIS Fatigue MS, I may not have a sense of how well treatment is helping that person's fatigue longitudinally, beyond what I can glean from the history and clinical examination.
PROs can also be helpful in terms of conditions that are harder to quantify. Depression is a significant cause of disability and a significant factor contributing to poor treatment adherence in MS. Also, the suicide rate in persons with MS is much higher than that in the general population. But there is no blood test for depression severity, and oftentimes a patient’s report on exam can be incomplete or misleading. Accompanying the mental status exam and the clinical evaluation with a validated depression severity measure (such as the PHQ9 [Patient Health Questionnaire-9], CES-D [Center for Epidemiologic Studies Depression Scale], or others) can help to determine whether treatments are having an initial effect, and this can also help with self-monitoring and treatment adherence.
That brings us to the second area where PROs show real promise in MS care: the learning health system (LHS) approach, which uses feed forward information to either predict the needs of people before they come to the office or optimize decision-making at the point of care (as discussed in our review article published in JCOM).1
PROs can play a significant role in the LHS approach in 2 ways. For example, if I have a good sense before a visit that the person has stable symptoms but is having a lot of trouble coping with MS, that may change how I allocate resources and focus the time at the visit to target the primary concern of the person before the visit even occurs. Over time I'd be able to monitor if those coping scores increase in response to the work we’re doing with the person.
The second part of this approach is a feedback mechanism. These measures can be aggregated at the population level and fed back to clinical MS centers to help clinicians who are trying to improve overall population health outcomes of people with MS to see how well they're doing on things like fatigue management, depression management, coping ability, and pain control, which can't be tested for with biologic methods. So in addition to looking at the MRI scan trends across the population and relapse rate annualized for the population over time, I'd also be able to see fatigue severity and depression severity at a clinic population level and assess the change in these severity levels over time, which I could then use to inform efforts to change how my system (clinic) provides MS care.
This capability of PROs could be of significant interest to payers, especially those who are looking to optimize the value of care that is being provided, given the high cost of MS care. MS treatments are very expensive, and MS care is multidisciplinary and requires a lot of resources. Payers, I think, will have an increasing interest in assessing the value of high-cost care. PROs could help to demonstrate that value, especially if they can help quantify that outcomes can be improved over time at the population level.
The third area where PROs are beneficial is population health research, especially in terms of the major improvement movements going on in the country, such as those advocated for by the Institute for Healthcare Improvement via the Triple Aim: improve population health outcomes, improve the experience of care, and minimize per capita cost. PROs can really help with the first 2 of those Triple Aim categories.
What are some of the factors that limit the use of PRO measures in MS research and clinical practice?
BRANT OLIVER, PhD: In our JCOM paper,1 we outlined major barriers or constraints or challenges to implementing PRO measures. One is time and technology in clinical care. It's busy. It's fast. A PRO measure requires patients to complete a questionnaire. And to do that, you need some time and space during the clinical visit, or before the visit, to collect this data. In the absence of appropriate technology, this is done using paper-based methods, which can be challenging. Technology can help. Examples include smart phone app-based collection systems, tablet PCs, or an online mechanism. But there are barriers to technology, too. Is the technology good enough? Is the interface with the people using it working well? Do you have an equal amount of access to and understanding of the technology from the people across your population? Is it only being used by a certain subset that is wealthier and more educated, or maybe who has English as a first language? Such constraints can be overcome, but they’re present in any situation where you are gathering PRO data.
Software constraints also extend to the electronic health record (EHR) capability of the clinics. If you can collect PRO data, does the EHR have the capability to present that data in a useful way during a 20- or 30-minute clinical visit? In other words, does it improve the quality of the visit, or does it generate just one more distraction during the visit? Some approaches, such as feed forward dashboards, provide easy visual displays that can quickly and easily add information at the point of care and can get around this limitation. However, a lot of MS care centers in private practice settings may not have the informatics capability of a large academic center.
Academic centers often have more EHR capability, but can also move much slower in implementation than more nimble private practice or community clinics. With many competing demands, it can sometimes take months to build one of these surveys into an EHR, for a task that takes just a day or so. But because other departments are in the queue for these changes, implementation often takes longer than we would intuitively think.
A second barrier is the burden on the individuals themselves. As much as we feel that PROs can make a difference, and the growing literature suggests that they really can, this is counterbalanced with the burden they may place on the patient. For example, a person may arrive at a clinic visit already with a lot on their mind, and then they get a questionnaire to complete in the waiting room before their visit (or perhaps they get asked to do it at home before the visit). The patient, rather than perceiving this as beneficial, may instead perceive it as an extra task or stressor. Explaining the purpose of the PRO measures, encouraging their use, and then actually using the results meaningfully during the visit can substantially improve their perceived value.
It’s important to limit the total amount of PROs used. In research, as well as in clinical settings, too many measures can lead to too little data. It's similar to an overly complex treatment plan: the chance that a person will adhere to all of it decreases with each level of complexity added. This can lead to decreased engagement by patients, and gradually they'll move away from participating in the PROs in general. Research and clinical efforts around PROs strive to get to a parsimonious set of critical measures, which will minimize the burden, but maximize the potential benefit.
A third challenge is interpretability. This gets into the psychometric properties of the PRO measures and setting appropriate clinical thresholds for what constitutes a “positive” or “actionable” result. What is a clinically significant level of fatigue severity on the PROMIS MS Fatigue? We know that the mean range of that instrument is somewhere between 50 and 60. Does that mean that scores above 60 suggest higher than average fatigue levels, or is it more complicated than that? In many cases, the instruments don't have extensive population level research for the populations in which they are used. Setting clinical thresholds can be difficult, and I suspect that this will be a major area of research in the coming years.
Another example is setting appropriate depression thresholds. We know that on the CES-D, for example, the positive threshold for active depression in a patient with MS may be different from that in a patient without MS, because fatigue is a contributing factor to the neurovegetative symptoms that are scored on the CES-D.
So even if we can incorporate PROs into general practice and minimize burden, we also have to pay attention to factors that limit their interpretability and employ them in a way whereby they provide clinically meaningful results that can help inform care. The good news is, for many PROs, even with these limitations, this can be done.
Following directly from this is error risk. Many PRO measures were designed for large-sample epidemiologic research, not for a smaller sample clinical practice, which can lead to a higher error risk, especially when following single individuals over time. Adjustments in how these scales are interpreted are required in many cases.
The limitations of many of the respondents completing questionnaires needs to be taken into account. Fatigue and cognitive impairment are very common in MS. Respondents may be selecting answers that are not entirely accurate if they're getting fatigued while doing the surveys, or if they have a comprehension deficit or a short-term memory deficit.
A final challenge is demonstrating, just like any treatment or assessment approach, that the benefit outweighs the burden. PRO measures that are fairly reliable, validated, and quick and easy to complete suddenly become quite valuable because their benefit far outweighs the potential constraints. I think as PROs and the ways of assessing them continue to develop, that will become a bigger issue. The question will be, okay, you can do this, but what is the value added by doing this? That added value could be demonstrated in terms of better clinical outcomes, reduced costs, reduced hospitalizations, better treatment adherence, and so on.
How do you see the use of patient-reported outcomes in MS care evolving over time?
BRANT OLIVER, PhD: I tend to be optimistic regarding PROs. I think they will become part of the new reality, especially in LHS-oriented models of care. As mentioned, LHSs use feed forward data to predict the needs of people or optimize shared decision-making. I think we're going to see more shared decision-making rather than less over time in complex chronic illnesses care.
In environments where there's an increasing focus on value for high-cost, such as complex chronic conditions like MS and inflammatory bowel disease, systems will have to justify the high cost of treatment. PROs will be a critical piece in making that value assessment, especially since that value assessment is coming from the voice of patients rather than only from clinicians or other stakeholders. Arguably, patients may be able to contribute the most to making the value proposition because it is their outcomes and their experiences that matter to payers. Because experience matters (and not just outcomes), I think we'll see more PREMs used over time, including in MS.
I also think over time we'll see studies working to optimize PROs in the clinical environment and for improvement and research. An early example of that is the MS Continuous Quality Improvement (MS-CQI) Collaborative. It is a prospective randomized multicenter study using patient-reported and clinical data in a LHS approach to study population health outcomes and the effect of quality improvement interventions on those outcomes. It's also optimizing how these PRO measures are actually used at the point of care. Studies like MS-CQI will help to better articulate how, when, and for what purpose PROs should best be used and also when they should be avoided.
I think over time the predictive analytics component of PROs will be emphasized. There is a big push in the MS field in developing biomarkers to help predict disease progression over time. From the predictive analytics or machine learning perspective, imagine a situation where PROs could be used to predict a person's trajectory over time: if they were more likely to be lost to follow-up, to be hospitalized, or to have a relapse in the next year or 2. Reliable PROs generating population health data at scale can inform the development of risk and outcome predictive models.
Dr. Oliver discloses that he has received research grant support (MS-CQI research study mentioned in interview). He is the principal investigator and developer of the MS-CQI study, which is grant funded by Biogen under a Sponsored Research Agreement.
Brant Oliver, PhD, MS, MPH, APRN-BC, is a health care improvement and implementation scientist, educator, and board-certified family and psychiatric nurse practitioner (FNP-BC, PMHNP-BC). Dr. Oliver's work focuses on applied health care improvement science research, with a focus on "3C" (complex, costly, and chronic) conditions including MS, IBD, CF, RA, and others; coproduction; learning health systems; and shared decision making. He is Associate Professor at the Geisel School of Medicine at Dartmouth and also has been in clinical practice since 2003, working primarily as a certified MS specialist (MSCN) and a MS neurobehavioral nurse practitioner.
Which patient-reported outcomes (PROs) are commonly assessed in the care of patients with multiple sclerosis (MS)?
BRANT OLIVER, PhD: The current reality is that PROs are not being used routinely in MS clinical care in most settings. They are most commonly being used in research settings, either as part of clinical trials of new treatments, or in epidemiologic studies looking at the prevalence, incidence, and severity of certain symptoms or functional impairments in MS at the population level. A good example is the NARCOMS registry, which has been used to conduct high-quality epidemiologic studies of MS-related symptoms using self-report questionnaires.
We are starting to see some use of MS PROs in select clinical settings. Oftentimes these are measures of highly prevalent comorbid conditions that have an impact on quality of life, treatment adherence (depression severity and anxiety), and self-efficacy, which is a measure of perceived coping ability related to self-management of a chronic illness. Also, measures of patient experience are being employed in hospital-based clinics, such as the CG-CAHPS satisfaction measures.
The PROMIS (Patient-Reported Outcomes Measurement Information System) battery is a promising set of PRO measures that are being utilized across a number of conditions and that contain some MS-specific measures, such as the Fatigue MS measure. Fatigue is the most common and disabling symptom in MS, so having a good measure of fatigue is of critical importance. Having a sense of a patient’s experience with fatigue over time can also be very helpful from a clinical perspective. The PROMIS measure performs much better than its predecessor, the Modified Fatigue Impact Scale (MFIS). Another strength of the PROMIS measures is that they tend to do well correlating with other conditions. In certain research and improvement settings, PROMIS can help us understand the burden a particular disease or population places on total health system resources. For example, is fatigue burden in MS similar in severity to that in another 3C condition, such as inflammatory bowel disease?
There are other PRO measures that have not been used in MS but which I think we will see used in the future. One of these is called Collaborate, which falls into the category of patient-reported experience measures (PREMs). Collaborate measures the degree of shared decision-making that occurs in a clinical encounter, which becomes especially important as the complexity of disease-modifying treatment decisions increases as more disease-modifying therapies are introduced, each with their own profile of risks and benefits. I anticipate that the ability of clinics to facilitate effective shared decision-making will be of increasing interest to clinicians, patients, and also payers in the future.
What are some of the potential benefits of using PRO measures in terms of clinician/patient communication and clinical decision-making?
BRANT OLIVER, PhD: I think the most important benefit of measuring PROs is that it can make care more patient-centered. The big push for PROs in the first place was to incorporate more of the patient’s voice into their own care. Standard clinical measures, such as magnetic resonance imaging (MRI) or relapse rates, can be very precise and provide a good clinical picture of how the disease is behaving. But if we rely solely on that kind of information, we can lose sight of the person who is experiencing the disease.
PROs, be they just regular PROs (instruments that gather qualitative and/or quantitative patient-reported information) or PROMs (validated and standardized PRO measures) or PREMs (standardized and validated patient-reported experience measures), all aim to improve the ability to get a better story of the person who's experiencing the illness and how that condition affects them. We can also gain insight on what's most important to them regarding how their illness is managed, and what their experience of care is.
Sometimes the PRO picture and the clinical picture don't necessarily align. I'll tell a story about one a person, who's given me permission to share the story. She is an established professional, and her PRO measures concerning her quality of life, support from her workplace environment, and her ability to function in society are very high. She's very high functioning according to the PRO picture. However, her clinical measures suggest that she is significantly impaired. Her MRI burden is quite high, and her disability due to the MS, her EDSS (Expanded Disability Status Scale), is also quite high. So there are 2 very different stories provided by 2 different sets of data. The inclusion of PROs data, in connection with clinical data, can provide a more holistic view of this person, who is functioning well despite significant disease burden.
As a clinician working with patients with MS, this gives me much more to work with in trying to help people, not only treating the disease, but also trying to see where the person is most in need of help. A person could be very well controlled on MRI in terms of relapse rate, but have fatigue severity that is through the roof. If I weren't paying closer attention to that with a validated scale that measures fatigue severity over time, like the PROMIS Fatigue MS, I may not have a sense of how well treatment is helping that person's fatigue longitudinally, beyond what I can glean from the history and clinical examination.
PROs can also be helpful in terms of conditions that are harder to quantify. Depression is a significant cause of disability and a significant factor contributing to poor treatment adherence in MS. Also, the suicide rate in persons with MS is much higher than that in the general population. But there is no blood test for depression severity, and oftentimes a patient’s report on exam can be incomplete or misleading. Accompanying the mental status exam and the clinical evaluation with a validated depression severity measure (such as the PHQ9 [Patient Health Questionnaire-9], CES-D [Center for Epidemiologic Studies Depression Scale], or others) can help to determine whether treatments are having an initial effect, and this can also help with self-monitoring and treatment adherence.
That brings us to the second area where PROs show real promise in MS care: the learning health system (LHS) approach, which uses feed forward information to either predict the needs of people before they come to the office or optimize decision-making at the point of care (as discussed in our review article published in JCOM).1
PROs can play a significant role in the LHS approach in 2 ways. For example, if I have a good sense before a visit that the person has stable symptoms but is having a lot of trouble coping with MS, that may change how I allocate resources and focus the time at the visit to target the primary concern of the person before the visit even occurs. Over time I'd be able to monitor if those coping scores increase in response to the work we’re doing with the person.
The second part of this approach is a feedback mechanism. These measures can be aggregated at the population level and fed back to clinical MS centers to help clinicians who are trying to improve overall population health outcomes of people with MS to see how well they're doing on things like fatigue management, depression management, coping ability, and pain control, which can't be tested for with biologic methods. So in addition to looking at the MRI scan trends across the population and relapse rate annualized for the population over time, I'd also be able to see fatigue severity and depression severity at a clinic population level and assess the change in these severity levels over time, which I could then use to inform efforts to change how my system (clinic) provides MS care.
This capability of PROs could be of significant interest to payers, especially those who are looking to optimize the value of care that is being provided, given the high cost of MS care. MS treatments are very expensive, and MS care is multidisciplinary and requires a lot of resources. Payers, I think, will have an increasing interest in assessing the value of high-cost care. PROs could help to demonstrate that value, especially if they can help quantify that outcomes can be improved over time at the population level.
The third area where PROs are beneficial is population health research, especially in terms of the major improvement movements going on in the country, such as those advocated for by the Institute for Healthcare Improvement via the Triple Aim: improve population health outcomes, improve the experience of care, and minimize per capita cost. PROs can really help with the first 2 of those Triple Aim categories.
What are some of the factors that limit the use of PRO measures in MS research and clinical practice?
BRANT OLIVER, PhD: In our JCOM paper,1 we outlined major barriers or constraints or challenges to implementing PRO measures. One is time and technology in clinical care. It's busy. It's fast. A PRO measure requires patients to complete a questionnaire. And to do that, you need some time and space during the clinical visit, or before the visit, to collect this data. In the absence of appropriate technology, this is done using paper-based methods, which can be challenging. Technology can help. Examples include smart phone app-based collection systems, tablet PCs, or an online mechanism. But there are barriers to technology, too. Is the technology good enough? Is the interface with the people using it working well? Do you have an equal amount of access to and understanding of the technology from the people across your population? Is it only being used by a certain subset that is wealthier and more educated, or maybe who has English as a first language? Such constraints can be overcome, but they’re present in any situation where you are gathering PRO data.
Software constraints also extend to the electronic health record (EHR) capability of the clinics. If you can collect PRO data, does the EHR have the capability to present that data in a useful way during a 20- or 30-minute clinical visit? In other words, does it improve the quality of the visit, or does it generate just one more distraction during the visit? Some approaches, such as feed forward dashboards, provide easy visual displays that can quickly and easily add information at the point of care and can get around this limitation. However, a lot of MS care centers in private practice settings may not have the informatics capability of a large academic center.
Academic centers often have more EHR capability, but can also move much slower in implementation than more nimble private practice or community clinics. With many competing demands, it can sometimes take months to build one of these surveys into an EHR, for a task that takes just a day or so. But because other departments are in the queue for these changes, implementation often takes longer than we would intuitively think.
A second barrier is the burden on the individuals themselves. As much as we feel that PROs can make a difference, and the growing literature suggests that they really can, this is counterbalanced with the burden they may place on the patient. For example, a person may arrive at a clinic visit already with a lot on their mind, and then they get a questionnaire to complete in the waiting room before their visit (or perhaps they get asked to do it at home before the visit). The patient, rather than perceiving this as beneficial, may instead perceive it as an extra task or stressor. Explaining the purpose of the PRO measures, encouraging their use, and then actually using the results meaningfully during the visit can substantially improve their perceived value.
It’s important to limit the total amount of PROs used. In research, as well as in clinical settings, too many measures can lead to too little data. It's similar to an overly complex treatment plan: the chance that a person will adhere to all of it decreases with each level of complexity added. This can lead to decreased engagement by patients, and gradually they'll move away from participating in the PROs in general. Research and clinical efforts around PROs strive to get to a parsimonious set of critical measures, which will minimize the burden, but maximize the potential benefit.
A third challenge is interpretability. This gets into the psychometric properties of the PRO measures and setting appropriate clinical thresholds for what constitutes a “positive” or “actionable” result. What is a clinically significant level of fatigue severity on the PROMIS MS Fatigue? We know that the mean range of that instrument is somewhere between 50 and 60. Does that mean that scores above 60 suggest higher than average fatigue levels, or is it more complicated than that? In many cases, the instruments don't have extensive population level research for the populations in which they are used. Setting clinical thresholds can be difficult, and I suspect that this will be a major area of research in the coming years.
Another example is setting appropriate depression thresholds. We know that on the CES-D, for example, the positive threshold for active depression in a patient with MS may be different from that in a patient without MS, because fatigue is a contributing factor to the neurovegetative symptoms that are scored on the CES-D.
So even if we can incorporate PROs into general practice and minimize burden, we also have to pay attention to factors that limit their interpretability and employ them in a way whereby they provide clinically meaningful results that can help inform care. The good news is, for many PROs, even with these limitations, this can be done.
Following directly from this is error risk. Many PRO measures were designed for large-sample epidemiologic research, not for a smaller sample clinical practice, which can lead to a higher error risk, especially when following single individuals over time. Adjustments in how these scales are interpreted are required in many cases.
The limitations of many of the respondents completing questionnaires needs to be taken into account. Fatigue and cognitive impairment are very common in MS. Respondents may be selecting answers that are not entirely accurate if they're getting fatigued while doing the surveys, or if they have a comprehension deficit or a short-term memory deficit.
A final challenge is demonstrating, just like any treatment or assessment approach, that the benefit outweighs the burden. PRO measures that are fairly reliable, validated, and quick and easy to complete suddenly become quite valuable because their benefit far outweighs the potential constraints. I think as PROs and the ways of assessing them continue to develop, that will become a bigger issue. The question will be, okay, you can do this, but what is the value added by doing this? That added value could be demonstrated in terms of better clinical outcomes, reduced costs, reduced hospitalizations, better treatment adherence, and so on.
How do you see the use of patient-reported outcomes in MS care evolving over time?
BRANT OLIVER, PhD: I tend to be optimistic regarding PROs. I think they will become part of the new reality, especially in LHS-oriented models of care. As mentioned, LHSs use feed forward data to predict the needs of people or optimize shared decision-making. I think we're going to see more shared decision-making rather than less over time in complex chronic illnesses care.
In environments where there's an increasing focus on value for high-cost, such as complex chronic conditions like MS and inflammatory bowel disease, systems will have to justify the high cost of treatment. PROs will be a critical piece in making that value assessment, especially since that value assessment is coming from the voice of patients rather than only from clinicians or other stakeholders. Arguably, patients may be able to contribute the most to making the value proposition because it is their outcomes and their experiences that matter to payers. Because experience matters (and not just outcomes), I think we'll see more PREMs used over time, including in MS.
I also think over time we'll see studies working to optimize PROs in the clinical environment and for improvement and research. An early example of that is the MS Continuous Quality Improvement (MS-CQI) Collaborative. It is a prospective randomized multicenter study using patient-reported and clinical data in a LHS approach to study population health outcomes and the effect of quality improvement interventions on those outcomes. It's also optimizing how these PRO measures are actually used at the point of care. Studies like MS-CQI will help to better articulate how, when, and for what purpose PROs should best be used and also when they should be avoided.
I think over time the predictive analytics component of PROs will be emphasized. There is a big push in the MS field in developing biomarkers to help predict disease progression over time. From the predictive analytics or machine learning perspective, imagine a situation where PROs could be used to predict a person's trajectory over time: if they were more likely to be lost to follow-up, to be hospitalized, or to have a relapse in the next year or 2. Reliable PROs generating population health data at scale can inform the development of risk and outcome predictive models.
Dr. Oliver discloses that he has received research grant support (MS-CQI research study mentioned in interview). He is the principal investigator and developer of the MS-CQI study, which is grant funded by Biogen under a Sponsored Research Agreement.
1. Manohar N, Perkins T, Laurion R, Oliver B. Patient-reported outcomes in multiple sclerosis: an overview. J Clin Outcomes Manage. 2019;26:277-288.
1. Manohar N, Perkins T, Laurion R, Oliver B. Patient-reported outcomes in multiple sclerosis: an overview. J Clin Outcomes Manage. 2019;26:277-288.