User login
Newborn’s pulmonary hypertension risk up slightly after SSRI exposure in pregnancy
Exposure to selective serotonin reuptake inhibitor therapy in the last trimester of pregnancy may raise the risk of persistent pulmonary hypertension of the newborn, but that risk is smaller than previous studies have suggested, according to a report published June 2 in JAMA.
Persistent pulmonary hypertension of the newborn (PPHN) is grave, with up to 20% of affected infants dying from the disorder and survivors facing serious long-term sequelae such as chronic lung disease, seizures, and neurodevelopmental problems. The Food and Drug Administration released a public health advisory in 2006 warning that SSRI exposure during late pregnancy may raise the risk of PPHN, based on a single epidemiologic study. Subsequent studies with conflicting findings prompted an update of the advisory in 2011, which concluded that it is not yet possible to determine whether such a link exists.
To examine the possible association, researchers analyzed information concerning 3,789,330 eligible pregnancies during a 10-year period in a Medicaid database covering 46 states and the District of Columbia. A total of 128,950 of these mothers (3.4%) used an antidepressant in the final trimester: 102,179 used an SSRI and 26,771 used a non-SSRI.
After the data were adjusted to account for the substantial differences between women who used antidepressants and women who did not, the adjusted odds ratio for having a neonate with PPHN was 1.10 for women who used SSRIs and 1.02 for those who used non-SSRIs, compared with nonusers.
This indicates that SSRI exposure “may be” associated with an increased risk of PPHN, but the magnitude of that risk – if present – is smaller than previous studies have reported, Krista F. Huybrechts, Ph.D., of the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital and of Harvard Medical School, both in Boston, and her associates reported (JAMA 2015;313:2142-51 [doi:10.1001/jama.2015.5605]).
“Clinicians and patients need to balance the potential small increase in the risk of PPHN, along with other risks that have been attributed to SSRI use during pregnancy, with the benefits attributable to these drugs in improving maternal health and well-being,” they wrote.
This study was supported by the Agency for Healthcare Research and Quality and the National Institutes of Health. The researchers reported having no financial disclosures.
Exposure to selective serotonin reuptake inhibitor therapy in the last trimester of pregnancy may raise the risk of persistent pulmonary hypertension of the newborn, but that risk is smaller than previous studies have suggested, according to a report published June 2 in JAMA.
Persistent pulmonary hypertension of the newborn (PPHN) is grave, with up to 20% of affected infants dying from the disorder and survivors facing serious long-term sequelae such as chronic lung disease, seizures, and neurodevelopmental problems. The Food and Drug Administration released a public health advisory in 2006 warning that SSRI exposure during late pregnancy may raise the risk of PPHN, based on a single epidemiologic study. Subsequent studies with conflicting findings prompted an update of the advisory in 2011, which concluded that it is not yet possible to determine whether such a link exists.
To examine the possible association, researchers analyzed information concerning 3,789,330 eligible pregnancies during a 10-year period in a Medicaid database covering 46 states and the District of Columbia. A total of 128,950 of these mothers (3.4%) used an antidepressant in the final trimester: 102,179 used an SSRI and 26,771 used a non-SSRI.
After the data were adjusted to account for the substantial differences between women who used antidepressants and women who did not, the adjusted odds ratio for having a neonate with PPHN was 1.10 for women who used SSRIs and 1.02 for those who used non-SSRIs, compared with nonusers.
This indicates that SSRI exposure “may be” associated with an increased risk of PPHN, but the magnitude of that risk – if present – is smaller than previous studies have reported, Krista F. Huybrechts, Ph.D., of the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital and of Harvard Medical School, both in Boston, and her associates reported (JAMA 2015;313:2142-51 [doi:10.1001/jama.2015.5605]).
“Clinicians and patients need to balance the potential small increase in the risk of PPHN, along with other risks that have been attributed to SSRI use during pregnancy, with the benefits attributable to these drugs in improving maternal health and well-being,” they wrote.
This study was supported by the Agency for Healthcare Research and Quality and the National Institutes of Health. The researchers reported having no financial disclosures.
Exposure to selective serotonin reuptake inhibitor therapy in the last trimester of pregnancy may raise the risk of persistent pulmonary hypertension of the newborn, but that risk is smaller than previous studies have suggested, according to a report published June 2 in JAMA.
Persistent pulmonary hypertension of the newborn (PPHN) is grave, with up to 20% of affected infants dying from the disorder and survivors facing serious long-term sequelae such as chronic lung disease, seizures, and neurodevelopmental problems. The Food and Drug Administration released a public health advisory in 2006 warning that SSRI exposure during late pregnancy may raise the risk of PPHN, based on a single epidemiologic study. Subsequent studies with conflicting findings prompted an update of the advisory in 2011, which concluded that it is not yet possible to determine whether such a link exists.
To examine the possible association, researchers analyzed information concerning 3,789,330 eligible pregnancies during a 10-year period in a Medicaid database covering 46 states and the District of Columbia. A total of 128,950 of these mothers (3.4%) used an antidepressant in the final trimester: 102,179 used an SSRI and 26,771 used a non-SSRI.
After the data were adjusted to account for the substantial differences between women who used antidepressants and women who did not, the adjusted odds ratio for having a neonate with PPHN was 1.10 for women who used SSRIs and 1.02 for those who used non-SSRIs, compared with nonusers.
This indicates that SSRI exposure “may be” associated with an increased risk of PPHN, but the magnitude of that risk – if present – is smaller than previous studies have reported, Krista F. Huybrechts, Ph.D., of the division of pharmacoepidemiology and pharmacoeconomics at Brigham and Women’s Hospital and of Harvard Medical School, both in Boston, and her associates reported (JAMA 2015;313:2142-51 [doi:10.1001/jama.2015.5605]).
“Clinicians and patients need to balance the potential small increase in the risk of PPHN, along with other risks that have been attributed to SSRI use during pregnancy, with the benefits attributable to these drugs in improving maternal health and well-being,” they wrote.
This study was supported by the Agency for Healthcare Research and Quality and the National Institutes of Health. The researchers reported having no financial disclosures.
FROM JAMA
Key clinical point: Exposure to SSRI therapy in the last trimester may raise the risk of persistent pulmonary hypertension of the newborn, but only to a small degree.
Major finding: The adjusted odds ratio for having a neonate with PPHN was 1.10 for women who used SSRIs and 1.02 for those who used non-SSRIs, compared with nonusers.
Data source: A large cohort study involving 3,789,330 completed pregnancies in 46 states during a 10-year period.
Disclosures: This study was supported by the Agency for Healthcare Research and Quality and the National Institutes of Health. The researchers reported having no financial disclosures.
Ebola in the United States: Management considerations during pregnancy
“[Pregnant patients infected with the Ebola virus in West Africa] aren’t given preferential treatment...They aren’t even given beds.…They are assumed to die. Priority is given to the patients whom the health-care workers believe they can save. In effect, pregnant women are being triaged last.”
—Joshua Lang1
Ebola is a rare and potentially deadly disease caused by infection with a strain of the Ebola virus. First described in 1967,2 the Ebola virus has caused significant morbidity and mortality in many parts of sub-Saharan Africa. Awareness about this disease has increased dramatically in the United States as a result of the largest Ebola epidemic in history, which broke out in West Africa in 2014. The 3 countries most widely affected include Sierra Leone, Liberia, and Guinea. As of May 15, 2015, there were 26,798 cases of Ebola in this epidemic (with 14,971 laboratory confirmed), of whom 11,089 have died.3 There have been a total of 868 confirmed health care worker infections reported in Guinea, Liberia, and Sierra Leone since the start of the outbreak, with 507 reported deaths.4
It is highly unlikely that an Ebola epidemic of similar proportion will break out in any developed nation. However, isolated cases of Ebola have been identified among high-risk individuals in the United States (such as those who had recently served as medical volunteers in West Africa), which has raised concern about Ebola infection prevention and management in this country.
Little is known about Ebola infection in pregnancy. The few reports available suggest that pregnant women who become infected are highly contagious, with a maternal and perinatal mortality rate near 100%.5 Significant efforts were put in place in hospitals around the United States, including in labor and delivery units, to care for potentially or actively infected individuals, to protect health care workers, and to contain the spread of any new infections. It is important that clinicians be aware of the efforts and the recommended protocols—especially for the unique circumstance of infection during pregnancy. We review these protocols, as well as provide details on viral transmission and treatment.
What is Ebola virus and why are humans affected?
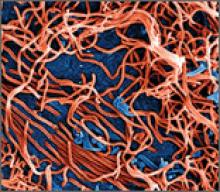
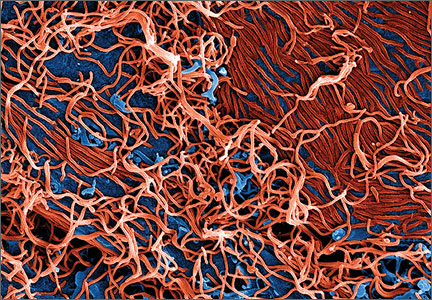
Ebola virus is a single-stranded RNA filovirus (FIGURE) with 5 independently identified species named after the countries or regions in which they were identified. Four of these are known to cause disease in humans, including Zaire Ebola virus, Sudan virus, Tai Forest virus (isolated in Ivory Coast), and Bundibugyo virus.1 Zaire Ebola virus is the most virulent species and has been responsible for most of the outbreaks in sub-Saharan Africa, with an overall mortality rate of around 70%.2 Sudan virus was responsible for outbreaks in the 1970s, 2000, and 2004; Bundibugyo virus caused a single outbreak in 2007, which had a lower mortality rate of around 30%. The fifth virus, Reston virus, does not appear to cause infection in humans, but does infect pigs and nonhuman primates.1
The natural reservoir of the Ebola virus is not known. It is unlikely to be primates, since the virus typically kills its primate host within a matter of days. Recent studies suggest that the natural host may be bats.3 Initial infections in humans may result from preparing and eating infected bush meat or from exposure to infected bat droppings during such activities as mining and spelunking.
References
- Bray M. Filoviridae. In: Clinical Virology, 2nd ed. Richman DD, Whitley RJ, Hayden FG, eds. Washington, DC: ASM Press; 2002:875.
- WHO Ebola Response Team. Ebola virus disease in West Africa—the first 9 months of the epidemic and forward projections. N Engl J Med. 2014;371:1481–1495.
- Centers for Disease Control and Prevention. Epidemiologic risk factors to consider when evaluating a person for exposure to Ebola virus. http://www.cdc.gov/vhf/ebola/exposure/risk-factors-when-evaluating-person-for-exposure.html. Updated May 1, 2015. Accessed May 14, 2015.
Transmission and clinical presentation
Ebola is not spread through air, water supply, food, or by mosquitoes.6 The Ebola virus is spread from person to person through direct contact with blood or bodily fluids from an infected individual who has developed disease symptoms. It is generally accepted that asymptomatic individuals are not infectious, likely due to their low circulating viral load. The incubation period is between 2 and 21 days.6,7
Sexual transmission. The Centers for Disease Control and Prevention (CDC) now recommends that contact with semen from male Ebola survivors be avoided “until more information regarding the duration and infectiousness of viral shedding in body fluids is known.” They recommend a condom be used (correctly and consistently) when male survivors have oral, vaginal, or anal sex.8
Following the initial inoculation, the virus spreads rapidly throughout the body, infecting many cell types, although it primarily targets macrophages (including the Kupffer cells of the liver), dendritic cells, and endothelial cells. Infected cells die and release more viral particles as well as proinflammatory mediators (tumor-necrosis-factor−a, interleukins, nitric oxide) leading to a massive systemic inflammatory response. Impaired dendritic cells are unable to mount an effective immune response to fight the infection.9
Symptoms develop rapidly, starting with fever and malaise, and progressing within a few days to vomiting, diarrhea, loss of appetite, abdominal pain, and rash. Signs include hypotension (due to vasodilation and increased vascular permeability), shock, multisystem organ failure, and coagulopathy (which occurs in 20% of cases due to activation of tissue factor). Leukopenia, thrombocytopenia, transaminitis, coagulation abnormalities, proteinuria, renal failure, and electrolyte abnormalities are commonly seen on laboratory analysis.10,11 Interestingly, the Ebola virus gains entry into human cells using the Niemann-Pick C1 cholesterol transporter, and cells from patients with Niemann-Pick type C disease are immune to infection with the Ebola virus.12
Ebola in pregnancy
Information about the true incidence and complications of Ebola disease is limited. Most infected patients have been cared for in community-based health care facilities in Africa with little access to diagnostic testing and unreliable medical records. The data we do have about risks factors, disease transmission, and mortality rates come mainly from epidemiologic studies conducted in the midst of an Ebola epidemic or from studies in nonhuman primates. Data on Ebola infection in pregnancy are even more limited.
Pregnant women are more vulnerable to and may have more complications as a result of certain infections, including malaria, varicella, and seasonal influenza. While data are limited, pregnant women and their fetuses infected with the Ebola virus also appear to have worse outcomes, with a maternal and perinatal mortality rate that approaches 100%.5 Under normal conditions, pregnant women are given priority within the medical system. However, given the overall poor prognosis, their increased infectivity, and concerns about the well-being of health care providers, many pregnant women infected with the Ebola virus during the recent epidemic were set aside and denied basic health care needs, including hospital admission. Whether improved infection control and more intensive medical care would improve the survival rate of infected pregnant women is not clear.
Most of what we know about Ebola infection in pregnancy comes from the 1995 epidemic in the Kikwit area of the Democratic Republic of the Congo (Zaire). Of the 202 people infected during that epidemic, 105 were women and 15 were pregnant (4 in the first trimester, 6 in the second trimester, and 5 in the third trimester). Pregnant women presented with vaginal bleeding and occasionally bleeding from other sites, including gum bleeding, hematemesis, hematuria, and melena. Of note, the diagnosis of Ebola during the Kikwit epidemic was based on clinical examination alone.5 Fourteen of these 15 women died, giving a mortality rate of 93.3%, with death occurring within 10 days in all instances. One woman delivered a live-born child, but both she and the baby died within 3 days. The woman who did survivehad a miscarriage in the first trimester.5
In the 1976 epidemic centered in Yambuku, Zaire, pregnant women fared slightly better, with a mortality rate of 89% (73/82), which was similar to the mortality rate for the population as a whole of 88%.5 Nineteen women (23%) had a spontaneous abortion. Ten women (12%) delivered live-born babies, but all died within 19 days. It is assumed that these infants contracted the Ebola virus, but whether this was indeed the case and when and how they contracted the infection is not known. The combined perinatal and infant mortality rate in these 2 epidemics was 100%.
During the recent epidemic in Guinea, there were 2 pregnant patients, both of whom presented with fetal demise in the third trimester. Their labors were induced and both mothers survived.13 During the height of the recent Liberian epidemic (between August and October 2014), 700 infected patients were admitted to the largest treatment center. Four women were pregnant, all in the latter half of gestation. Of these, 3 died (75% mortality rate). The remaining woman survived, but her fetus died.9 Taken together, the prevailing evidence suggests that maternal and perinatal outcomes of pregnant women infected with the Ebola virus are dismal, with mortality rates approaching 100%.
Protecting health care workers
Transmission of the Ebola virus to health care workers has emerged as a major concern during the most recent outbreak in West Africa. Frontline health care workers are usually the first to see such patients and are at high risk of exposure to infected bodily fluids. This is especially true of health care professionals working on labor and delivery units, where exposure to blood and amniotic fluid is commonplace at the time of delivery.
Contaminated needles and syringes also may play a role in transmission.14,15 And, in Africa, a large number of transmissions have been attributed to ritual washing of the body at funerals, since viral load is maximal at the time of death, but this is unlikely to play a significant role in transmission of the virus in developed countries. Ebola virus has been isolated from breast milk.16 While direct transmission of the virus through breastfeeding has not been documented, breast milk from infected individuals should be disposed of carefully.
Prophylaxis
Is a vaccine on the way?
Development of an Ebola vaccine is under way. The most promising vaccine to date is cAd3-ZEBOV (GlaxoSmithKline, Brentford, London, United Kingdom). This vaccine is derived from a chimpanzee adenovirus, called Chimp Adenovirus type 3 (ChAd3), which has been genetically engineered to express proteins from both the Zaire and Sudan species of Ebola virus to provoke an immune response against them. Phase 1 trials of this vaccine began in September 2014.17
Appropriate precautions
Until an effective vaccine is available, a number of recommendations have been put in place in an effort to prevent Ebola infection:
- Avoid all nonessential travel to West Africa, especially to Sierre Leone, Guinea, and Liberia.7
- Avoid exposure to bodily fluids of patients who have been exposed to or are at high risk of having Ebola. This includes individuals who are febrile or feeling unwell and who have traveled to West Africa within the previous 21 days, especially if they visited 1 of the 3 countries with the highest Ebola infection rates (Sierre Leone, Guinea, and Liberia).
- Introduce universal screening of all patients, family members, and employees entering labor and delivery units.
Classifying risk and risk-associated protocols
If an at-risk patient is identified, she should be placed in isolation and consultation with an infectious disease specialist should occur. Using appropriate personal protective equipment (PPE), a detailed history and physical examination should be performed, and the patient should be classified according to risk14,15:
- No risk—defined as those who traveled to an Ebola-affected country more than 21 days previously, those in contact with an asymptomatic person prior to them being diagnosed with Ebola, and those in contact with an asymptomatic person who in turn had contact with an infected individual.
- Low risk—including those who traveled to an Ebola-affected country within 21 days but are asymptomatic, those with brief contact with asymptomatic infected individuals, those exposed to infected individuals in countries without widespread disease while wearing PPE, and those in brief proximity to a symptomatic individual, such as being in the same room or on the same airplane.
- Some (moderate) risk—including those in close contact (within 1 m) with a symptomatic individual or those exposed to an infected individual in a country with widespread disease while wearing PPE.
- High risk—defined as those exposed to the bodily fluids of an infected individual without PPE.
When should a patient be tested for Ebola, and what does that testing entail?
Patients found to be at no risk should not be tested or monitored, regardless of whether or not they are symptomatic. Asymptomatic patients with risk factors should not be tested for the Ebola virus. However, they do need to be followed for signs and symptoms of infection. At this time, the CDC has decided that it will take on the responsibility of monitoring all such patients until they are out of the 21-day window.14,15
Symptomatic patients with risk factors should be tested for the Ebola virus, regardless of whether they are designated as being at low, moderate, or high risk of infection. Strict infection control precautions should be followed for such patients, and local/state health departments should be notified. Laboratory testing includes RT-PCR or Ebola immunoassay. A negative RT-PCR test result obtained more than 72 hours after the onset of symptoms effectively rules out Ebola infection. In general, patients can be discharged from the hospital if they are asymptomatic and have 2 negative RT-PCR test results within 48 hours.14,15
Other diagnoses that should be considered in these patients include influenza, malaria, Lassa fever, meningococcal infection, and typhoid. If a patient is asymptomatic but at risk, all nonemergent medical care should be deferred until they are out of the 21-day window. Repeat testing may be warranted in certain clinical scenarios.
Management of infected patients in a maternity ward
While no pregnant patient has yet been diagnosed with Ebola infection in the United States, it remains a possibility, and clinicians should be aware of appropriate management actions. Once the diagnosis is confirmed, patients and their families should be placed in strict isolation. In some states, specific regional centers have been designated to care for these patients. They should be cared for by a small, dedicated team of clinicians dressed in state-of-the-art PPE and fully trained in the technique of donning and doffing the gear. Some institutions have mandated that no medical students or residents be involved directly in the care of these patients. Infectious disease specialists should be actively involved. All medical equipment (such as stethoscopes, blood pressure cuffs, thermometers, and fetal heart rate monitors) should be dedicated to the care of this patient alone and should remain in the room, as the virus can remain viable on surfaces for “a few hours or days.”18
Treatment itself is largely supportive, with significant intravascular expansion and treatment of fever, nausea, vomiting, and diarrhea. Patients typically require 5 to 10 L of fluid replacement each day, along with regular electrolyte repletion. The development of coagulopathy is a real concern and should be carefully monitored for and corrected as needed. Since blood is highly infectious, every effort should be made to perform only critical blood tests and to do so at the bedside, if possible. Mobile devices are available that can be stationed in the room and provide basic hematologic and electrolyte measurements, thereby avoiding the need to transport the blood and the risk of potentially contaminating laboratory equipment. Dedicated staff should be trained on the use of such equipment. In all likelihood, radiologic imaging will not be available and management decisions will need to be made on the basis of clinical examination alone.
Treatment of the virus and the conditions it can cause
A number of experimental treatments are under investigation. These include some antiviral agents (such as the CMV antiviral drug brincidofovir and the influenza antiviral favipiravir), immune sera from Ebola survivors, and RNA interference agents (such as TKM-Ebola). Zmapp, a cocktail of 3 anti-Ebola monoclonal antibodies, has been shown to be protective in macaque monkeys in the late stages of the disease and has been given to 4 infected patients in the United States, with variable results.19 All of these options should be considered on an individual basis.
Some patients may experience renal or respiratory failure requiring advanced life support measures such as dialysis, mechanical ventilation, or cardiorespiratory resuscitation (CPR). The decision of whether or not to proceed with such interventions should be left to the discretion of the attending physician staff. Given the extremely poor prognosis for the patient and the attendant risks to the health care staff and potentially to subsequent patients using these same pieces of medical equipment, it would seem reasonable to withhold such interventions.
Unique considerations during pregnancy. In pregnant patients with Ebola, it may be reasonable to withhold the option of cesarean and offer only vaginal delivery in the event of labor. This is not just a theoretic concern. In 1 case in Zaire in 1995, an entire surgical team was infected after operating on an infected patient, with the infection spreading to outside hospital staff and family members.20
Survival rates are dismal
Reported survival rates are extremely low, especially for pregnant women. Patients who are younger, have lower viral loads, and do not have diarrhea or severe dehydration have a higher likelihood of surviving. Whether survival rates are higher in developed countries with more health care resources has yet to be confirmed. If patients do survive, the recovery period is long, with prolonged weakness, fatigue, and weight loss. While sexual transmission of the Ebola virus has not been documented, the CDC has recommended sexual abstinence for at least 3 months after recovery.14,15 Ebola survivors are thought to be immune to subsequent infections.
Education is the most important factor for most of us
In November 2014, the American College of Obstetricians and Gynecologists (ACOG) published a practice advisory on the care of obstetric patients during an Ebola virus outbreak.21 While the number of Ebola cases in the United States has been, and likely will continue to be low, especially among pregnant women, we should continue to focus on education and screening. Only providers who have undergone Ebola training and have proper PPE should be involved in the care of potentially infected or confirmed cases. The greatest potential for harm is suboptimal obstetric care leading to an adverse event in a patient suspected of having Ebola who subsequently tests negative. Once an Ebola infection has been confirmed, patients—regardless of whether or not they are pregnant—should be hospitalized in institutions with the requisite resources, protocols, and expertise to deal with such highly infectious patients.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Lang J. Ebola in the maternity ward. http://www.newyorker.com/tech/elements/ebola-maternity-ward. Published October 29, 2014. Accessed May 16, 2015.
2. Martini GA. Marburg agent disease in man. Trans R Soc Trop Med Hyg. 1969;63(3):295–302.
3. Centers for Disease Control and Prevention. 2014 Ebola Outbreak in West Africa - Case Counts. http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/case-counts.html. Updated May 15, 2015. Accessed May 17, 2015.
4. Centers for Disease Control and Prevention. 2014 Ebola outbreak in West Africa. http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/index.html. Updated May 15, 2015. Accessed May 17, 2015.
5. Mupapa K, Mukundu W, Bwaka MA, et al. Ebola hemorrhagic fever and pregnancy. J Infect Dis. 1999;179(suppl 1):S11–S12.
6. Centers for Disease Control and Prevention. Epidemiologic risk factors to consider when evaluating a person for exposure to Ebola virus. http://www.cdc.gov/vhf/ebola/exposure/risk-factors-when-evaluating-person-for-exposure.html. Updated May 1, 2015. Accessed May 16, 2015.
7. Centers for Disease Control and Prevention. Ebola (Ebola virus disease). http://www.cdc.gov/vhf/ebola/. Updated May 15, 2015. Accessed May 16, 2015.
8. Christie A, Davies-Wayne GJ, Cordier-Lasalle T, et al. Possible sexual transmission of Ebola virus — Liberia, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(17):479–481.
9. Chertow DS, Kleine C, Edwards JK, et al. Ebola virus disease in West Africa—clinical manifestations and management. N Engl J Med. 2014;371(22):2054–2057.
10. Mahanty S, Bray M. Pathogenesis of filoviral haemorrhagic fevers. Lancet Infect Dis. 2004;4(8):487–498.
11. Bray M. Pathogenesis of viral hemorrhagic fever. Curr Opin Immunol. 2005;17(4):399–403.
12. Carette JE, Raaben M, Wong AC, et al. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature. 2011;477(7364):340–343.
13. Baggi FM, Taybi A, Kurth A, et al. Management of pregnant women infected with Ebola virus in a treatment centre in Guinea, June 2014. Euro Surveill. 2014;19(49). pii: 20983.
14. Centers for Disease Control and Prevention. Review of human-to-human transmission of Ebola virus. http://www.cdc.gov/vhf/ebola/transmission/human-transmission.html. Updated October 29, 2014. Accessed May 16, 2015.
15. Centers for Disease Control and Prevention. Ebola virus disease (EVD) information for clinicians in U.S. healthcare settings. http://www.cdc.gov/vhf/ebola/healthcare-us/preparing/clinicians.html. Updated April 1, 2015. Accessed May 16, 2015.
16. Bausch DG, Towner JS, Dowell SF, et al. Assessment of the risk of Ebola virus transmission from bodily fluids and fomites. J Infect Dis. 2007;196(suppl 2):S142–S147.
17. Ledgerwood JE, DeZure AD, Stanley DA, et al; VRC 207 Study Team. Chimpanzee adenovirus vector Ebola vaccine — preliminary report [published online ahead of print November 26, 2014]. N Engl J Med. http://www.nejm.org/doi/full/10.1056/NEJMoa1410863. Accessed May 17, 2015.
18. Centers for Disease Control and Prevention. Q&As on transmission. http://www.cdc.gov/vhf/ebola/transmission/qas.html. Updated April 24, 2015. Accessed May 17, 2015.
19. Lyon GM, Mehta AK, Varkey JB, et al; Emory Serious Communicable Diseases Unit. Clinical care of two patients with Ebola virus disease in the United States. N Engl J Med. 2014;371(25):2402–2409.
20. Khan AS, Tshioko FK, Heymann DL, et al. The reemergence of Ebola hemorrhagic fever, Democratic Republic of the Congo, 1995. Commission de Lutte contre les Epidémies à Kikwit. J Infect Dis. 1999;179(suppl 1):S76.
21. American College of Obstetricians and Gynecologists. Practice Advisory: Care of obstetric patients during an Ebola virus outbreak. http://www.acog.org/About-ACOG/News-Room/Practice-Advisories/ACOG-Practice-Advisory-Care-of-Obstetric-Patients-During-an-Ebola-Virus-Outbreak. Published November 3, 2014. Accessed May 17, 2015.
“[Pregnant patients infected with the Ebola virus in West Africa] aren’t given preferential treatment...They aren’t even given beds.…They are assumed to die. Priority is given to the patients whom the health-care workers believe they can save. In effect, pregnant women are being triaged last.”
—Joshua Lang1
Ebola is a rare and potentially deadly disease caused by infection with a strain of the Ebola virus. First described in 1967,2 the Ebola virus has caused significant morbidity and mortality in many parts of sub-Saharan Africa. Awareness about this disease has increased dramatically in the United States as a result of the largest Ebola epidemic in history, which broke out in West Africa in 2014. The 3 countries most widely affected include Sierra Leone, Liberia, and Guinea. As of May 15, 2015, there were 26,798 cases of Ebola in this epidemic (with 14,971 laboratory confirmed), of whom 11,089 have died.3 There have been a total of 868 confirmed health care worker infections reported in Guinea, Liberia, and Sierra Leone since the start of the outbreak, with 507 reported deaths.4
It is highly unlikely that an Ebola epidemic of similar proportion will break out in any developed nation. However, isolated cases of Ebola have been identified among high-risk individuals in the United States (such as those who had recently served as medical volunteers in West Africa), which has raised concern about Ebola infection prevention and management in this country.
Little is known about Ebola infection in pregnancy. The few reports available suggest that pregnant women who become infected are highly contagious, with a maternal and perinatal mortality rate near 100%.5 Significant efforts were put in place in hospitals around the United States, including in labor and delivery units, to care for potentially or actively infected individuals, to protect health care workers, and to contain the spread of any new infections. It is important that clinicians be aware of the efforts and the recommended protocols—especially for the unique circumstance of infection during pregnancy. We review these protocols, as well as provide details on viral transmission and treatment.
What is Ebola virus and why are humans affected?
Ebola virus is a single-stranded RNA filovirus (FIGURE) with 5 independently identified species named after the countries or regions in which they were identified. Four of these are known to cause disease in humans, including Zaire Ebola virus, Sudan virus, Tai Forest virus (isolated in Ivory Coast), and Bundibugyo virus.1 Zaire Ebola virus is the most virulent species and has been responsible for most of the outbreaks in sub-Saharan Africa, with an overall mortality rate of around 70%.2 Sudan virus was responsible for outbreaks in the 1970s, 2000, and 2004; Bundibugyo virus caused a single outbreak in 2007, which had a lower mortality rate of around 30%. The fifth virus, Reston virus, does not appear to cause infection in humans, but does infect pigs and nonhuman primates.1
The natural reservoir of the Ebola virus is not known. It is unlikely to be primates, since the virus typically kills its primate host within a matter of days. Recent studies suggest that the natural host may be bats.3 Initial infections in humans may result from preparing and eating infected bush meat or from exposure to infected bat droppings during such activities as mining and spelunking.
References
- Bray M. Filoviridae. In: Clinical Virology, 2nd ed. Richman DD, Whitley RJ, Hayden FG, eds. Washington, DC: ASM Press; 2002:875.
- WHO Ebola Response Team. Ebola virus disease in West Africa—the first 9 months of the epidemic and forward projections. N Engl J Med. 2014;371:1481–1495.
- Centers for Disease Control and Prevention. Epidemiologic risk factors to consider when evaluating a person for exposure to Ebola virus. http://www.cdc.gov/vhf/ebola/exposure/risk-factors-when-evaluating-person-for-exposure.html. Updated May 1, 2015. Accessed May 14, 2015.
Transmission and clinical presentation
Ebola is not spread through air, water supply, food, or by mosquitoes.6 The Ebola virus is spread from person to person through direct contact with blood or bodily fluids from an infected individual who has developed disease symptoms. It is generally accepted that asymptomatic individuals are not infectious, likely due to their low circulating viral load. The incubation period is between 2 and 21 days.6,7
Sexual transmission. The Centers for Disease Control and Prevention (CDC) now recommends that contact with semen from male Ebola survivors be avoided “until more information regarding the duration and infectiousness of viral shedding in body fluids is known.” They recommend a condom be used (correctly and consistently) when male survivors have oral, vaginal, or anal sex.8
Following the initial inoculation, the virus spreads rapidly throughout the body, infecting many cell types, although it primarily targets macrophages (including the Kupffer cells of the liver), dendritic cells, and endothelial cells. Infected cells die and release more viral particles as well as proinflammatory mediators (tumor-necrosis-factor−a, interleukins, nitric oxide) leading to a massive systemic inflammatory response. Impaired dendritic cells are unable to mount an effective immune response to fight the infection.9
Symptoms develop rapidly, starting with fever and malaise, and progressing within a few days to vomiting, diarrhea, loss of appetite, abdominal pain, and rash. Signs include hypotension (due to vasodilation and increased vascular permeability), shock, multisystem organ failure, and coagulopathy (which occurs in 20% of cases due to activation of tissue factor). Leukopenia, thrombocytopenia, transaminitis, coagulation abnormalities, proteinuria, renal failure, and electrolyte abnormalities are commonly seen on laboratory analysis.10,11 Interestingly, the Ebola virus gains entry into human cells using the Niemann-Pick C1 cholesterol transporter, and cells from patients with Niemann-Pick type C disease are immune to infection with the Ebola virus.12
Ebola in pregnancy
Information about the true incidence and complications of Ebola disease is limited. Most infected patients have been cared for in community-based health care facilities in Africa with little access to diagnostic testing and unreliable medical records. The data we do have about risks factors, disease transmission, and mortality rates come mainly from epidemiologic studies conducted in the midst of an Ebola epidemic or from studies in nonhuman primates. Data on Ebola infection in pregnancy are even more limited.
Pregnant women are more vulnerable to and may have more complications as a result of certain infections, including malaria, varicella, and seasonal influenza. While data are limited, pregnant women and their fetuses infected with the Ebola virus also appear to have worse outcomes, with a maternal and perinatal mortality rate that approaches 100%.5 Under normal conditions, pregnant women are given priority within the medical system. However, given the overall poor prognosis, their increased infectivity, and concerns about the well-being of health care providers, many pregnant women infected with the Ebola virus during the recent epidemic were set aside and denied basic health care needs, including hospital admission. Whether improved infection control and more intensive medical care would improve the survival rate of infected pregnant women is not clear.
Most of what we know about Ebola infection in pregnancy comes from the 1995 epidemic in the Kikwit area of the Democratic Republic of the Congo (Zaire). Of the 202 people infected during that epidemic, 105 were women and 15 were pregnant (4 in the first trimester, 6 in the second trimester, and 5 in the third trimester). Pregnant women presented with vaginal bleeding and occasionally bleeding from other sites, including gum bleeding, hematemesis, hematuria, and melena. Of note, the diagnosis of Ebola during the Kikwit epidemic was based on clinical examination alone.5 Fourteen of these 15 women died, giving a mortality rate of 93.3%, with death occurring within 10 days in all instances. One woman delivered a live-born child, but both she and the baby died within 3 days. The woman who did survivehad a miscarriage in the first trimester.5
In the 1976 epidemic centered in Yambuku, Zaire, pregnant women fared slightly better, with a mortality rate of 89% (73/82), which was similar to the mortality rate for the population as a whole of 88%.5 Nineteen women (23%) had a spontaneous abortion. Ten women (12%) delivered live-born babies, but all died within 19 days. It is assumed that these infants contracted the Ebola virus, but whether this was indeed the case and when and how they contracted the infection is not known. The combined perinatal and infant mortality rate in these 2 epidemics was 100%.
During the recent epidemic in Guinea, there were 2 pregnant patients, both of whom presented with fetal demise in the third trimester. Their labors were induced and both mothers survived.13 During the height of the recent Liberian epidemic (between August and October 2014), 700 infected patients were admitted to the largest treatment center. Four women were pregnant, all in the latter half of gestation. Of these, 3 died (75% mortality rate). The remaining woman survived, but her fetus died.9 Taken together, the prevailing evidence suggests that maternal and perinatal outcomes of pregnant women infected with the Ebola virus are dismal, with mortality rates approaching 100%.
Protecting health care workers
Transmission of the Ebola virus to health care workers has emerged as a major concern during the most recent outbreak in West Africa. Frontline health care workers are usually the first to see such patients and are at high risk of exposure to infected bodily fluids. This is especially true of health care professionals working on labor and delivery units, where exposure to blood and amniotic fluid is commonplace at the time of delivery.
Contaminated needles and syringes also may play a role in transmission.14,15 And, in Africa, a large number of transmissions have been attributed to ritual washing of the body at funerals, since viral load is maximal at the time of death, but this is unlikely to play a significant role in transmission of the virus in developed countries. Ebola virus has been isolated from breast milk.16 While direct transmission of the virus through breastfeeding has not been documented, breast milk from infected individuals should be disposed of carefully.
Prophylaxis
Is a vaccine on the way?
Development of an Ebola vaccine is under way. The most promising vaccine to date is cAd3-ZEBOV (GlaxoSmithKline, Brentford, London, United Kingdom). This vaccine is derived from a chimpanzee adenovirus, called Chimp Adenovirus type 3 (ChAd3), which has been genetically engineered to express proteins from both the Zaire and Sudan species of Ebola virus to provoke an immune response against them. Phase 1 trials of this vaccine began in September 2014.17
Appropriate precautions
Until an effective vaccine is available, a number of recommendations have been put in place in an effort to prevent Ebola infection:
- Avoid all nonessential travel to West Africa, especially to Sierre Leone, Guinea, and Liberia.7
- Avoid exposure to bodily fluids of patients who have been exposed to or are at high risk of having Ebola. This includes individuals who are febrile or feeling unwell and who have traveled to West Africa within the previous 21 days, especially if they visited 1 of the 3 countries with the highest Ebola infection rates (Sierre Leone, Guinea, and Liberia).
- Introduce universal screening of all patients, family members, and employees entering labor and delivery units.
Classifying risk and risk-associated protocols
If an at-risk patient is identified, she should be placed in isolation and consultation with an infectious disease specialist should occur. Using appropriate personal protective equipment (PPE), a detailed history and physical examination should be performed, and the patient should be classified according to risk14,15:
- No risk—defined as those who traveled to an Ebola-affected country more than 21 days previously, those in contact with an asymptomatic person prior to them being diagnosed with Ebola, and those in contact with an asymptomatic person who in turn had contact with an infected individual.
- Low risk—including those who traveled to an Ebola-affected country within 21 days but are asymptomatic, those with brief contact with asymptomatic infected individuals, those exposed to infected individuals in countries without widespread disease while wearing PPE, and those in brief proximity to a symptomatic individual, such as being in the same room or on the same airplane.
- Some (moderate) risk—including those in close contact (within 1 m) with a symptomatic individual or those exposed to an infected individual in a country with widespread disease while wearing PPE.
- High risk—defined as those exposed to the bodily fluids of an infected individual without PPE.
When should a patient be tested for Ebola, and what does that testing entail?
Patients found to be at no risk should not be tested or monitored, regardless of whether or not they are symptomatic. Asymptomatic patients with risk factors should not be tested for the Ebola virus. However, they do need to be followed for signs and symptoms of infection. At this time, the CDC has decided that it will take on the responsibility of monitoring all such patients until they are out of the 21-day window.14,15
Symptomatic patients with risk factors should be tested for the Ebola virus, regardless of whether they are designated as being at low, moderate, or high risk of infection. Strict infection control precautions should be followed for such patients, and local/state health departments should be notified. Laboratory testing includes RT-PCR or Ebola immunoassay. A negative RT-PCR test result obtained more than 72 hours after the onset of symptoms effectively rules out Ebola infection. In general, patients can be discharged from the hospital if they are asymptomatic and have 2 negative RT-PCR test results within 48 hours.14,15
Other diagnoses that should be considered in these patients include influenza, malaria, Lassa fever, meningococcal infection, and typhoid. If a patient is asymptomatic but at risk, all nonemergent medical care should be deferred until they are out of the 21-day window. Repeat testing may be warranted in certain clinical scenarios.
Management of infected patients in a maternity ward
While no pregnant patient has yet been diagnosed with Ebola infection in the United States, it remains a possibility, and clinicians should be aware of appropriate management actions. Once the diagnosis is confirmed, patients and their families should be placed in strict isolation. In some states, specific regional centers have been designated to care for these patients. They should be cared for by a small, dedicated team of clinicians dressed in state-of-the-art PPE and fully trained in the technique of donning and doffing the gear. Some institutions have mandated that no medical students or residents be involved directly in the care of these patients. Infectious disease specialists should be actively involved. All medical equipment (such as stethoscopes, blood pressure cuffs, thermometers, and fetal heart rate monitors) should be dedicated to the care of this patient alone and should remain in the room, as the virus can remain viable on surfaces for “a few hours or days.”18
Treatment itself is largely supportive, with significant intravascular expansion and treatment of fever, nausea, vomiting, and diarrhea. Patients typically require 5 to 10 L of fluid replacement each day, along with regular electrolyte repletion. The development of coagulopathy is a real concern and should be carefully monitored for and corrected as needed. Since blood is highly infectious, every effort should be made to perform only critical blood tests and to do so at the bedside, if possible. Mobile devices are available that can be stationed in the room and provide basic hematologic and electrolyte measurements, thereby avoiding the need to transport the blood and the risk of potentially contaminating laboratory equipment. Dedicated staff should be trained on the use of such equipment. In all likelihood, radiologic imaging will not be available and management decisions will need to be made on the basis of clinical examination alone.
Treatment of the virus and the conditions it can cause
A number of experimental treatments are under investigation. These include some antiviral agents (such as the CMV antiviral drug brincidofovir and the influenza antiviral favipiravir), immune sera from Ebola survivors, and RNA interference agents (such as TKM-Ebola). Zmapp, a cocktail of 3 anti-Ebola monoclonal antibodies, has been shown to be protective in macaque monkeys in the late stages of the disease and has been given to 4 infected patients in the United States, with variable results.19 All of these options should be considered on an individual basis.
Some patients may experience renal or respiratory failure requiring advanced life support measures such as dialysis, mechanical ventilation, or cardiorespiratory resuscitation (CPR). The decision of whether or not to proceed with such interventions should be left to the discretion of the attending physician staff. Given the extremely poor prognosis for the patient and the attendant risks to the health care staff and potentially to subsequent patients using these same pieces of medical equipment, it would seem reasonable to withhold such interventions.
Unique considerations during pregnancy. In pregnant patients with Ebola, it may be reasonable to withhold the option of cesarean and offer only vaginal delivery in the event of labor. This is not just a theoretic concern. In 1 case in Zaire in 1995, an entire surgical team was infected after operating on an infected patient, with the infection spreading to outside hospital staff and family members.20
Survival rates are dismal
Reported survival rates are extremely low, especially for pregnant women. Patients who are younger, have lower viral loads, and do not have diarrhea or severe dehydration have a higher likelihood of surviving. Whether survival rates are higher in developed countries with more health care resources has yet to be confirmed. If patients do survive, the recovery period is long, with prolonged weakness, fatigue, and weight loss. While sexual transmission of the Ebola virus has not been documented, the CDC has recommended sexual abstinence for at least 3 months after recovery.14,15 Ebola survivors are thought to be immune to subsequent infections.
Education is the most important factor for most of us
In November 2014, the American College of Obstetricians and Gynecologists (ACOG) published a practice advisory on the care of obstetric patients during an Ebola virus outbreak.21 While the number of Ebola cases in the United States has been, and likely will continue to be low, especially among pregnant women, we should continue to focus on education and screening. Only providers who have undergone Ebola training and have proper PPE should be involved in the care of potentially infected or confirmed cases. The greatest potential for harm is suboptimal obstetric care leading to an adverse event in a patient suspected of having Ebola who subsequently tests negative. Once an Ebola infection has been confirmed, patients—regardless of whether or not they are pregnant—should be hospitalized in institutions with the requisite resources, protocols, and expertise to deal with such highly infectious patients.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
“[Pregnant patients infected with the Ebola virus in West Africa] aren’t given preferential treatment...They aren’t even given beds.…They are assumed to die. Priority is given to the patients whom the health-care workers believe they can save. In effect, pregnant women are being triaged last.”
—Joshua Lang1
Ebola is a rare and potentially deadly disease caused by infection with a strain of the Ebola virus. First described in 1967,2 the Ebola virus has caused significant morbidity and mortality in many parts of sub-Saharan Africa. Awareness about this disease has increased dramatically in the United States as a result of the largest Ebola epidemic in history, which broke out in West Africa in 2014. The 3 countries most widely affected include Sierra Leone, Liberia, and Guinea. As of May 15, 2015, there were 26,798 cases of Ebola in this epidemic (with 14,971 laboratory confirmed), of whom 11,089 have died.3 There have been a total of 868 confirmed health care worker infections reported in Guinea, Liberia, and Sierra Leone since the start of the outbreak, with 507 reported deaths.4
It is highly unlikely that an Ebola epidemic of similar proportion will break out in any developed nation. However, isolated cases of Ebola have been identified among high-risk individuals in the United States (such as those who had recently served as medical volunteers in West Africa), which has raised concern about Ebola infection prevention and management in this country.
Little is known about Ebola infection in pregnancy. The few reports available suggest that pregnant women who become infected are highly contagious, with a maternal and perinatal mortality rate near 100%.5 Significant efforts were put in place in hospitals around the United States, including in labor and delivery units, to care for potentially or actively infected individuals, to protect health care workers, and to contain the spread of any new infections. It is important that clinicians be aware of the efforts and the recommended protocols—especially for the unique circumstance of infection during pregnancy. We review these protocols, as well as provide details on viral transmission and treatment.
What is Ebola virus and why are humans affected?
Ebola virus is a single-stranded RNA filovirus (FIGURE) with 5 independently identified species named after the countries or regions in which they were identified. Four of these are known to cause disease in humans, including Zaire Ebola virus, Sudan virus, Tai Forest virus (isolated in Ivory Coast), and Bundibugyo virus.1 Zaire Ebola virus is the most virulent species and has been responsible for most of the outbreaks in sub-Saharan Africa, with an overall mortality rate of around 70%.2 Sudan virus was responsible for outbreaks in the 1970s, 2000, and 2004; Bundibugyo virus caused a single outbreak in 2007, which had a lower mortality rate of around 30%. The fifth virus, Reston virus, does not appear to cause infection in humans, but does infect pigs and nonhuman primates.1
The natural reservoir of the Ebola virus is not known. It is unlikely to be primates, since the virus typically kills its primate host within a matter of days. Recent studies suggest that the natural host may be bats.3 Initial infections in humans may result from preparing and eating infected bush meat or from exposure to infected bat droppings during such activities as mining and spelunking.
References
- Bray M. Filoviridae. In: Clinical Virology, 2nd ed. Richman DD, Whitley RJ, Hayden FG, eds. Washington, DC: ASM Press; 2002:875.
- WHO Ebola Response Team. Ebola virus disease in West Africa—the first 9 months of the epidemic and forward projections. N Engl J Med. 2014;371:1481–1495.
- Centers for Disease Control and Prevention. Epidemiologic risk factors to consider when evaluating a person for exposure to Ebola virus. http://www.cdc.gov/vhf/ebola/exposure/risk-factors-when-evaluating-person-for-exposure.html. Updated May 1, 2015. Accessed May 14, 2015.
Transmission and clinical presentation
Ebola is not spread through air, water supply, food, or by mosquitoes.6 The Ebola virus is spread from person to person through direct contact with blood or bodily fluids from an infected individual who has developed disease symptoms. It is generally accepted that asymptomatic individuals are not infectious, likely due to their low circulating viral load. The incubation period is between 2 and 21 days.6,7
Sexual transmission. The Centers for Disease Control and Prevention (CDC) now recommends that contact with semen from male Ebola survivors be avoided “until more information regarding the duration and infectiousness of viral shedding in body fluids is known.” They recommend a condom be used (correctly and consistently) when male survivors have oral, vaginal, or anal sex.8
Following the initial inoculation, the virus spreads rapidly throughout the body, infecting many cell types, although it primarily targets macrophages (including the Kupffer cells of the liver), dendritic cells, and endothelial cells. Infected cells die and release more viral particles as well as proinflammatory mediators (tumor-necrosis-factor−a, interleukins, nitric oxide) leading to a massive systemic inflammatory response. Impaired dendritic cells are unable to mount an effective immune response to fight the infection.9
Symptoms develop rapidly, starting with fever and malaise, and progressing within a few days to vomiting, diarrhea, loss of appetite, abdominal pain, and rash. Signs include hypotension (due to vasodilation and increased vascular permeability), shock, multisystem organ failure, and coagulopathy (which occurs in 20% of cases due to activation of tissue factor). Leukopenia, thrombocytopenia, transaminitis, coagulation abnormalities, proteinuria, renal failure, and electrolyte abnormalities are commonly seen on laboratory analysis.10,11 Interestingly, the Ebola virus gains entry into human cells using the Niemann-Pick C1 cholesterol transporter, and cells from patients with Niemann-Pick type C disease are immune to infection with the Ebola virus.12
Ebola in pregnancy
Information about the true incidence and complications of Ebola disease is limited. Most infected patients have been cared for in community-based health care facilities in Africa with little access to diagnostic testing and unreliable medical records. The data we do have about risks factors, disease transmission, and mortality rates come mainly from epidemiologic studies conducted in the midst of an Ebola epidemic or from studies in nonhuman primates. Data on Ebola infection in pregnancy are even more limited.
Pregnant women are more vulnerable to and may have more complications as a result of certain infections, including malaria, varicella, and seasonal influenza. While data are limited, pregnant women and their fetuses infected with the Ebola virus also appear to have worse outcomes, with a maternal and perinatal mortality rate that approaches 100%.5 Under normal conditions, pregnant women are given priority within the medical system. However, given the overall poor prognosis, their increased infectivity, and concerns about the well-being of health care providers, many pregnant women infected with the Ebola virus during the recent epidemic were set aside and denied basic health care needs, including hospital admission. Whether improved infection control and more intensive medical care would improve the survival rate of infected pregnant women is not clear.
Most of what we know about Ebola infection in pregnancy comes from the 1995 epidemic in the Kikwit area of the Democratic Republic of the Congo (Zaire). Of the 202 people infected during that epidemic, 105 were women and 15 were pregnant (4 in the first trimester, 6 in the second trimester, and 5 in the third trimester). Pregnant women presented with vaginal bleeding and occasionally bleeding from other sites, including gum bleeding, hematemesis, hematuria, and melena. Of note, the diagnosis of Ebola during the Kikwit epidemic was based on clinical examination alone.5 Fourteen of these 15 women died, giving a mortality rate of 93.3%, with death occurring within 10 days in all instances. One woman delivered a live-born child, but both she and the baby died within 3 days. The woman who did survivehad a miscarriage in the first trimester.5
In the 1976 epidemic centered in Yambuku, Zaire, pregnant women fared slightly better, with a mortality rate of 89% (73/82), which was similar to the mortality rate for the population as a whole of 88%.5 Nineteen women (23%) had a spontaneous abortion. Ten women (12%) delivered live-born babies, but all died within 19 days. It is assumed that these infants contracted the Ebola virus, but whether this was indeed the case and when and how they contracted the infection is not known. The combined perinatal and infant mortality rate in these 2 epidemics was 100%.
During the recent epidemic in Guinea, there were 2 pregnant patients, both of whom presented with fetal demise in the third trimester. Their labors were induced and both mothers survived.13 During the height of the recent Liberian epidemic (between August and October 2014), 700 infected patients were admitted to the largest treatment center. Four women were pregnant, all in the latter half of gestation. Of these, 3 died (75% mortality rate). The remaining woman survived, but her fetus died.9 Taken together, the prevailing evidence suggests that maternal and perinatal outcomes of pregnant women infected with the Ebola virus are dismal, with mortality rates approaching 100%.
Protecting health care workers
Transmission of the Ebola virus to health care workers has emerged as a major concern during the most recent outbreak in West Africa. Frontline health care workers are usually the first to see such patients and are at high risk of exposure to infected bodily fluids. This is especially true of health care professionals working on labor and delivery units, where exposure to blood and amniotic fluid is commonplace at the time of delivery.
Contaminated needles and syringes also may play a role in transmission.14,15 And, in Africa, a large number of transmissions have been attributed to ritual washing of the body at funerals, since viral load is maximal at the time of death, but this is unlikely to play a significant role in transmission of the virus in developed countries. Ebola virus has been isolated from breast milk.16 While direct transmission of the virus through breastfeeding has not been documented, breast milk from infected individuals should be disposed of carefully.
Prophylaxis
Is a vaccine on the way?
Development of an Ebola vaccine is under way. The most promising vaccine to date is cAd3-ZEBOV (GlaxoSmithKline, Brentford, London, United Kingdom). This vaccine is derived from a chimpanzee adenovirus, called Chimp Adenovirus type 3 (ChAd3), which has been genetically engineered to express proteins from both the Zaire and Sudan species of Ebola virus to provoke an immune response against them. Phase 1 trials of this vaccine began in September 2014.17
Appropriate precautions
Until an effective vaccine is available, a number of recommendations have been put in place in an effort to prevent Ebola infection:
- Avoid all nonessential travel to West Africa, especially to Sierre Leone, Guinea, and Liberia.7
- Avoid exposure to bodily fluids of patients who have been exposed to or are at high risk of having Ebola. This includes individuals who are febrile or feeling unwell and who have traveled to West Africa within the previous 21 days, especially if they visited 1 of the 3 countries with the highest Ebola infection rates (Sierre Leone, Guinea, and Liberia).
- Introduce universal screening of all patients, family members, and employees entering labor and delivery units.
Classifying risk and risk-associated protocols
If an at-risk patient is identified, she should be placed in isolation and consultation with an infectious disease specialist should occur. Using appropriate personal protective equipment (PPE), a detailed history and physical examination should be performed, and the patient should be classified according to risk14,15:
- No risk—defined as those who traveled to an Ebola-affected country more than 21 days previously, those in contact with an asymptomatic person prior to them being diagnosed with Ebola, and those in contact with an asymptomatic person who in turn had contact with an infected individual.
- Low risk—including those who traveled to an Ebola-affected country within 21 days but are asymptomatic, those with brief contact with asymptomatic infected individuals, those exposed to infected individuals in countries without widespread disease while wearing PPE, and those in brief proximity to a symptomatic individual, such as being in the same room or on the same airplane.
- Some (moderate) risk—including those in close contact (within 1 m) with a symptomatic individual or those exposed to an infected individual in a country with widespread disease while wearing PPE.
- High risk—defined as those exposed to the bodily fluids of an infected individual without PPE.
When should a patient be tested for Ebola, and what does that testing entail?
Patients found to be at no risk should not be tested or monitored, regardless of whether or not they are symptomatic. Asymptomatic patients with risk factors should not be tested for the Ebola virus. However, they do need to be followed for signs and symptoms of infection. At this time, the CDC has decided that it will take on the responsibility of monitoring all such patients until they are out of the 21-day window.14,15
Symptomatic patients with risk factors should be tested for the Ebola virus, regardless of whether they are designated as being at low, moderate, or high risk of infection. Strict infection control precautions should be followed for such patients, and local/state health departments should be notified. Laboratory testing includes RT-PCR or Ebola immunoassay. A negative RT-PCR test result obtained more than 72 hours after the onset of symptoms effectively rules out Ebola infection. In general, patients can be discharged from the hospital if they are asymptomatic and have 2 negative RT-PCR test results within 48 hours.14,15
Other diagnoses that should be considered in these patients include influenza, malaria, Lassa fever, meningococcal infection, and typhoid. If a patient is asymptomatic but at risk, all nonemergent medical care should be deferred until they are out of the 21-day window. Repeat testing may be warranted in certain clinical scenarios.
Management of infected patients in a maternity ward
While no pregnant patient has yet been diagnosed with Ebola infection in the United States, it remains a possibility, and clinicians should be aware of appropriate management actions. Once the diagnosis is confirmed, patients and their families should be placed in strict isolation. In some states, specific regional centers have been designated to care for these patients. They should be cared for by a small, dedicated team of clinicians dressed in state-of-the-art PPE and fully trained in the technique of donning and doffing the gear. Some institutions have mandated that no medical students or residents be involved directly in the care of these patients. Infectious disease specialists should be actively involved. All medical equipment (such as stethoscopes, blood pressure cuffs, thermometers, and fetal heart rate monitors) should be dedicated to the care of this patient alone and should remain in the room, as the virus can remain viable on surfaces for “a few hours or days.”18
Treatment itself is largely supportive, with significant intravascular expansion and treatment of fever, nausea, vomiting, and diarrhea. Patients typically require 5 to 10 L of fluid replacement each day, along with regular electrolyte repletion. The development of coagulopathy is a real concern and should be carefully monitored for and corrected as needed. Since blood is highly infectious, every effort should be made to perform only critical blood tests and to do so at the bedside, if possible. Mobile devices are available that can be stationed in the room and provide basic hematologic and electrolyte measurements, thereby avoiding the need to transport the blood and the risk of potentially contaminating laboratory equipment. Dedicated staff should be trained on the use of such equipment. In all likelihood, radiologic imaging will not be available and management decisions will need to be made on the basis of clinical examination alone.
Treatment of the virus and the conditions it can cause
A number of experimental treatments are under investigation. These include some antiviral agents (such as the CMV antiviral drug brincidofovir and the influenza antiviral favipiravir), immune sera from Ebola survivors, and RNA interference agents (such as TKM-Ebola). Zmapp, a cocktail of 3 anti-Ebola monoclonal antibodies, has been shown to be protective in macaque monkeys in the late stages of the disease and has been given to 4 infected patients in the United States, with variable results.19 All of these options should be considered on an individual basis.
Some patients may experience renal or respiratory failure requiring advanced life support measures such as dialysis, mechanical ventilation, or cardiorespiratory resuscitation (CPR). The decision of whether or not to proceed with such interventions should be left to the discretion of the attending physician staff. Given the extremely poor prognosis for the patient and the attendant risks to the health care staff and potentially to subsequent patients using these same pieces of medical equipment, it would seem reasonable to withhold such interventions.
Unique considerations during pregnancy. In pregnant patients with Ebola, it may be reasonable to withhold the option of cesarean and offer only vaginal delivery in the event of labor. This is not just a theoretic concern. In 1 case in Zaire in 1995, an entire surgical team was infected after operating on an infected patient, with the infection spreading to outside hospital staff and family members.20
Survival rates are dismal
Reported survival rates are extremely low, especially for pregnant women. Patients who are younger, have lower viral loads, and do not have diarrhea or severe dehydration have a higher likelihood of surviving. Whether survival rates are higher in developed countries with more health care resources has yet to be confirmed. If patients do survive, the recovery period is long, with prolonged weakness, fatigue, and weight loss. While sexual transmission of the Ebola virus has not been documented, the CDC has recommended sexual abstinence for at least 3 months after recovery.14,15 Ebola survivors are thought to be immune to subsequent infections.
Education is the most important factor for most of us
In November 2014, the American College of Obstetricians and Gynecologists (ACOG) published a practice advisory on the care of obstetric patients during an Ebola virus outbreak.21 While the number of Ebola cases in the United States has been, and likely will continue to be low, especially among pregnant women, we should continue to focus on education and screening. Only providers who have undergone Ebola training and have proper PPE should be involved in the care of potentially infected or confirmed cases. The greatest potential for harm is suboptimal obstetric care leading to an adverse event in a patient suspected of having Ebola who subsequently tests negative. Once an Ebola infection has been confirmed, patients—regardless of whether or not they are pregnant—should be hospitalized in institutions with the requisite resources, protocols, and expertise to deal with such highly infectious patients.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Lang J. Ebola in the maternity ward. http://www.newyorker.com/tech/elements/ebola-maternity-ward. Published October 29, 2014. Accessed May 16, 2015.
2. Martini GA. Marburg agent disease in man. Trans R Soc Trop Med Hyg. 1969;63(3):295–302.
3. Centers for Disease Control and Prevention. 2014 Ebola Outbreak in West Africa - Case Counts. http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/case-counts.html. Updated May 15, 2015. Accessed May 17, 2015.
4. Centers for Disease Control and Prevention. 2014 Ebola outbreak in West Africa. http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/index.html. Updated May 15, 2015. Accessed May 17, 2015.
5. Mupapa K, Mukundu W, Bwaka MA, et al. Ebola hemorrhagic fever and pregnancy. J Infect Dis. 1999;179(suppl 1):S11–S12.
6. Centers for Disease Control and Prevention. Epidemiologic risk factors to consider when evaluating a person for exposure to Ebola virus. http://www.cdc.gov/vhf/ebola/exposure/risk-factors-when-evaluating-person-for-exposure.html. Updated May 1, 2015. Accessed May 16, 2015.
7. Centers for Disease Control and Prevention. Ebola (Ebola virus disease). http://www.cdc.gov/vhf/ebola/. Updated May 15, 2015. Accessed May 16, 2015.
8. Christie A, Davies-Wayne GJ, Cordier-Lasalle T, et al. Possible sexual transmission of Ebola virus — Liberia, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(17):479–481.
9. Chertow DS, Kleine C, Edwards JK, et al. Ebola virus disease in West Africa—clinical manifestations and management. N Engl J Med. 2014;371(22):2054–2057.
10. Mahanty S, Bray M. Pathogenesis of filoviral haemorrhagic fevers. Lancet Infect Dis. 2004;4(8):487–498.
11. Bray M. Pathogenesis of viral hemorrhagic fever. Curr Opin Immunol. 2005;17(4):399–403.
12. Carette JE, Raaben M, Wong AC, et al. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature. 2011;477(7364):340–343.
13. Baggi FM, Taybi A, Kurth A, et al. Management of pregnant women infected with Ebola virus in a treatment centre in Guinea, June 2014. Euro Surveill. 2014;19(49). pii: 20983.
14. Centers for Disease Control and Prevention. Review of human-to-human transmission of Ebola virus. http://www.cdc.gov/vhf/ebola/transmission/human-transmission.html. Updated October 29, 2014. Accessed May 16, 2015.
15. Centers for Disease Control and Prevention. Ebola virus disease (EVD) information for clinicians in U.S. healthcare settings. http://www.cdc.gov/vhf/ebola/healthcare-us/preparing/clinicians.html. Updated April 1, 2015. Accessed May 16, 2015.
16. Bausch DG, Towner JS, Dowell SF, et al. Assessment of the risk of Ebola virus transmission from bodily fluids and fomites. J Infect Dis. 2007;196(suppl 2):S142–S147.
17. Ledgerwood JE, DeZure AD, Stanley DA, et al; VRC 207 Study Team. Chimpanzee adenovirus vector Ebola vaccine — preliminary report [published online ahead of print November 26, 2014]. N Engl J Med. http://www.nejm.org/doi/full/10.1056/NEJMoa1410863. Accessed May 17, 2015.
18. Centers for Disease Control and Prevention. Q&As on transmission. http://www.cdc.gov/vhf/ebola/transmission/qas.html. Updated April 24, 2015. Accessed May 17, 2015.
19. Lyon GM, Mehta AK, Varkey JB, et al; Emory Serious Communicable Diseases Unit. Clinical care of two patients with Ebola virus disease in the United States. N Engl J Med. 2014;371(25):2402–2409.
20. Khan AS, Tshioko FK, Heymann DL, et al. The reemergence of Ebola hemorrhagic fever, Democratic Republic of the Congo, 1995. Commission de Lutte contre les Epidémies à Kikwit. J Infect Dis. 1999;179(suppl 1):S76.
21. American College of Obstetricians and Gynecologists. Practice Advisory: Care of obstetric patients during an Ebola virus outbreak. http://www.acog.org/About-ACOG/News-Room/Practice-Advisories/ACOG-Practice-Advisory-Care-of-Obstetric-Patients-During-an-Ebola-Virus-Outbreak. Published November 3, 2014. Accessed May 17, 2015.
1. Lang J. Ebola in the maternity ward. http://www.newyorker.com/tech/elements/ebola-maternity-ward. Published October 29, 2014. Accessed May 16, 2015.
2. Martini GA. Marburg agent disease in man. Trans R Soc Trop Med Hyg. 1969;63(3):295–302.
3. Centers for Disease Control and Prevention. 2014 Ebola Outbreak in West Africa - Case Counts. http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/case-counts.html. Updated May 15, 2015. Accessed May 17, 2015.
4. Centers for Disease Control and Prevention. 2014 Ebola outbreak in West Africa. http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/index.html. Updated May 15, 2015. Accessed May 17, 2015.
5. Mupapa K, Mukundu W, Bwaka MA, et al. Ebola hemorrhagic fever and pregnancy. J Infect Dis. 1999;179(suppl 1):S11–S12.
6. Centers for Disease Control and Prevention. Epidemiologic risk factors to consider when evaluating a person for exposure to Ebola virus. http://www.cdc.gov/vhf/ebola/exposure/risk-factors-when-evaluating-person-for-exposure.html. Updated May 1, 2015. Accessed May 16, 2015.
7. Centers for Disease Control and Prevention. Ebola (Ebola virus disease). http://www.cdc.gov/vhf/ebola/. Updated May 15, 2015. Accessed May 16, 2015.
8. Christie A, Davies-Wayne GJ, Cordier-Lasalle T, et al. Possible sexual transmission of Ebola virus — Liberia, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(17):479–481.
9. Chertow DS, Kleine C, Edwards JK, et al. Ebola virus disease in West Africa—clinical manifestations and management. N Engl J Med. 2014;371(22):2054–2057.
10. Mahanty S, Bray M. Pathogenesis of filoviral haemorrhagic fevers. Lancet Infect Dis. 2004;4(8):487–498.
11. Bray M. Pathogenesis of viral hemorrhagic fever. Curr Opin Immunol. 2005;17(4):399–403.
12. Carette JE, Raaben M, Wong AC, et al. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature. 2011;477(7364):340–343.
13. Baggi FM, Taybi A, Kurth A, et al. Management of pregnant women infected with Ebola virus in a treatment centre in Guinea, June 2014. Euro Surveill. 2014;19(49). pii: 20983.
14. Centers for Disease Control and Prevention. Review of human-to-human transmission of Ebola virus. http://www.cdc.gov/vhf/ebola/transmission/human-transmission.html. Updated October 29, 2014. Accessed May 16, 2015.
15. Centers for Disease Control and Prevention. Ebola virus disease (EVD) information for clinicians in U.S. healthcare settings. http://www.cdc.gov/vhf/ebola/healthcare-us/preparing/clinicians.html. Updated April 1, 2015. Accessed May 16, 2015.
16. Bausch DG, Towner JS, Dowell SF, et al. Assessment of the risk of Ebola virus transmission from bodily fluids and fomites. J Infect Dis. 2007;196(suppl 2):S142–S147.
17. Ledgerwood JE, DeZure AD, Stanley DA, et al; VRC 207 Study Team. Chimpanzee adenovirus vector Ebola vaccine — preliminary report [published online ahead of print November 26, 2014]. N Engl J Med. http://www.nejm.org/doi/full/10.1056/NEJMoa1410863. Accessed May 17, 2015.
18. Centers for Disease Control and Prevention. Q&As on transmission. http://www.cdc.gov/vhf/ebola/transmission/qas.html. Updated April 24, 2015. Accessed May 17, 2015.
19. Lyon GM, Mehta AK, Varkey JB, et al; Emory Serious Communicable Diseases Unit. Clinical care of two patients with Ebola virus disease in the United States. N Engl J Med. 2014;371(25):2402–2409.
20. Khan AS, Tshioko FK, Heymann DL, et al. The reemergence of Ebola hemorrhagic fever, Democratic Republic of the Congo, 1995. Commission de Lutte contre les Epidémies à Kikwit. J Infect Dis. 1999;179(suppl 1):S76.
21. American College of Obstetricians and Gynecologists. Practice Advisory: Care of obstetric patients during an Ebola virus outbreak. http://www.acog.org/About-ACOG/News-Room/Practice-Advisories/ACOG-Practice-Advisory-Care-of-Obstetric-Patients-During-an-Ebola-Virus-Outbreak. Published November 3, 2014. Accessed May 17, 2015.
In this article
- What we know about Ebola in pregnancy
- Is a vaccine on the way?
- Unique treatment considerations in pregnancy
How can electronic fetal heart-rate monitoring best improve neonatal outcomes during induction of labor?
In this prospective cohort study of women undergoing induction of labor of a singleton fetus at term (≥37 weeks), Clark and colleagues examined each patient chart for adherence to 6 clinical practices:
- fetal weight estimated prior to induction
- clinical assessment of pelvic adequacy prior to induction
- completion of a safety checklist prior to induction
- completion of a safety checklist every 30 minutes during induction
- oxytocin infusion rate decreased if the fetal heart rate did not meet defined requirements
- oxytocin infusion rate decreased if uterine activity did not meet defined requirements.
Defined requirements for fetal heart rate included at least 1 acceleration of 15 bpm x 15 seconds in 30 minutes, or adequate variability for 10 of the previous 30 minutes. There should have been no more than 1 late deceleration in the previous 30 minutes. And there should have been no more than 2 variable decelerations exceeding 60 seconds and decreasing more than 60 bpm from baseline in the previous 30 minutes.
Defined requirements for uterine activity included no more than 5 contractions in 10 minutes for any 20-minute interval. There should have been no 2 contractions longer than 120 seconds in duration. In addition, the uterus should have been soft upon palpation between contractions. If an intrauterine pressure catheter was in place, measurement in Montevideo units should have been less than 300 mm Hg, with baseline resting tone of less than 25 mm Hg.
Outcome measures included admission to a neonatal intensive care unit (NICU), 1- and 5-minute Apgar scores of less than 7, and primary cesarean delivery.
Study findings underscore value of a checklist
The study found that completion of a safety checklist every 30 minutes during labor was associated with a significantly reduced rate of NICU admission and cesarean delivery. When the clinician stopped or reduced oxytocin for failure to meet specific uterine activity requirements, the rate of NICU admission also was reduced, but there were no differences in other outcomes. When the clinician stopped or reduced oxytocin for a failure to meet specific fetal heart-rate requirements, the rate of NICU admission was significantly reduced, as was the rate of low Apgar scores at birth, but there was a significantly higher rate of cesarean delivery (26.6% vs 17.5%).
Strengths include size of the study
This is a large study in a population with demographics that likely reflect those of the general US population. The study size permitted detection of relatively small differences in outcome.
The data clearly support the conclusions that “electronic fetal heart-rate monitoring improves neonatal outcomes when unambiguous definitions of abnormal fetal heart rate and tachysystole are coupled with specific interventions” and that “utilization of a checklist for oxytocin monitoring is associated with improved neonatal outcomes.” However, data were conflicting regarding the impact of a standard oxytocin checklist on the rate of cesarean delivery.
What this evidence means for practice
Implementation of a conservative intrapartum checklist has been shown to improve specific measures of newborn outcome. Further study is needed to define the impact on the rate of cesarean delivery.
—David A. Miller, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In this prospective cohort study of women undergoing induction of labor of a singleton fetus at term (≥37 weeks), Clark and colleagues examined each patient chart for adherence to 6 clinical practices:
- fetal weight estimated prior to induction
- clinical assessment of pelvic adequacy prior to induction
- completion of a safety checklist prior to induction
- completion of a safety checklist every 30 minutes during induction
- oxytocin infusion rate decreased if the fetal heart rate did not meet defined requirements
- oxytocin infusion rate decreased if uterine activity did not meet defined requirements.
Defined requirements for fetal heart rate included at least 1 acceleration of 15 bpm x 15 seconds in 30 minutes, or adequate variability for 10 of the previous 30 minutes. There should have been no more than 1 late deceleration in the previous 30 minutes. And there should have been no more than 2 variable decelerations exceeding 60 seconds and decreasing more than 60 bpm from baseline in the previous 30 minutes.
Defined requirements for uterine activity included no more than 5 contractions in 10 minutes for any 20-minute interval. There should have been no 2 contractions longer than 120 seconds in duration. In addition, the uterus should have been soft upon palpation between contractions. If an intrauterine pressure catheter was in place, measurement in Montevideo units should have been less than 300 mm Hg, with baseline resting tone of less than 25 mm Hg.
Outcome measures included admission to a neonatal intensive care unit (NICU), 1- and 5-minute Apgar scores of less than 7, and primary cesarean delivery.
Study findings underscore value of a checklist
The study found that completion of a safety checklist every 30 minutes during labor was associated with a significantly reduced rate of NICU admission and cesarean delivery. When the clinician stopped or reduced oxytocin for failure to meet specific uterine activity requirements, the rate of NICU admission also was reduced, but there were no differences in other outcomes. When the clinician stopped or reduced oxytocin for a failure to meet specific fetal heart-rate requirements, the rate of NICU admission was significantly reduced, as was the rate of low Apgar scores at birth, but there was a significantly higher rate of cesarean delivery (26.6% vs 17.5%).
Strengths include size of the study
This is a large study in a population with demographics that likely reflect those of the general US population. The study size permitted detection of relatively small differences in outcome.
The data clearly support the conclusions that “electronic fetal heart-rate monitoring improves neonatal outcomes when unambiguous definitions of abnormal fetal heart rate and tachysystole are coupled with specific interventions” and that “utilization of a checklist for oxytocin monitoring is associated with improved neonatal outcomes.” However, data were conflicting regarding the impact of a standard oxytocin checklist on the rate of cesarean delivery.
What this evidence means for practice
Implementation of a conservative intrapartum checklist has been shown to improve specific measures of newborn outcome. Further study is needed to define the impact on the rate of cesarean delivery.
—David A. Miller, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In this prospective cohort study of women undergoing induction of labor of a singleton fetus at term (≥37 weeks), Clark and colleagues examined each patient chart for adherence to 6 clinical practices:
- fetal weight estimated prior to induction
- clinical assessment of pelvic adequacy prior to induction
- completion of a safety checklist prior to induction
- completion of a safety checklist every 30 minutes during induction
- oxytocin infusion rate decreased if the fetal heart rate did not meet defined requirements
- oxytocin infusion rate decreased if uterine activity did not meet defined requirements.
Defined requirements for fetal heart rate included at least 1 acceleration of 15 bpm x 15 seconds in 30 minutes, or adequate variability for 10 of the previous 30 minutes. There should have been no more than 1 late deceleration in the previous 30 minutes. And there should have been no more than 2 variable decelerations exceeding 60 seconds and decreasing more than 60 bpm from baseline in the previous 30 minutes.
Defined requirements for uterine activity included no more than 5 contractions in 10 minutes for any 20-minute interval. There should have been no 2 contractions longer than 120 seconds in duration. In addition, the uterus should have been soft upon palpation between contractions. If an intrauterine pressure catheter was in place, measurement in Montevideo units should have been less than 300 mm Hg, with baseline resting tone of less than 25 mm Hg.
Outcome measures included admission to a neonatal intensive care unit (NICU), 1- and 5-minute Apgar scores of less than 7, and primary cesarean delivery.
Study findings underscore value of a checklist
The study found that completion of a safety checklist every 30 minutes during labor was associated with a significantly reduced rate of NICU admission and cesarean delivery. When the clinician stopped or reduced oxytocin for failure to meet specific uterine activity requirements, the rate of NICU admission also was reduced, but there were no differences in other outcomes. When the clinician stopped or reduced oxytocin for a failure to meet specific fetal heart-rate requirements, the rate of NICU admission was significantly reduced, as was the rate of low Apgar scores at birth, but there was a significantly higher rate of cesarean delivery (26.6% vs 17.5%).
Strengths include size of the study
This is a large study in a population with demographics that likely reflect those of the general US population. The study size permitted detection of relatively small differences in outcome.
The data clearly support the conclusions that “electronic fetal heart-rate monitoring improves neonatal outcomes when unambiguous definitions of abnormal fetal heart rate and tachysystole are coupled with specific interventions” and that “utilization of a checklist for oxytocin monitoring is associated with improved neonatal outcomes.” However, data were conflicting regarding the impact of a standard oxytocin checklist on the rate of cesarean delivery.
What this evidence means for practice
Implementation of a conservative intrapartum checklist has been shown to improve specific measures of newborn outcome. Further study is needed to define the impact on the rate of cesarean delivery.
—David A. Miller, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Report IDs insurance barriers to breastfeeding services
Dr. Holly S. Puritz, an ob.gyn. in Norfolk, Va., wasn’t surprised by the findings of a recent report that claims insurers are failing to cover breastfeeding services as required by the Affordable Care Act.
“If I’m being charitable, I would say lots of the new rules are confusing and difficult for anyone to sort out,” said Dr. Puritz, who is in private practice and is also medical director for labor and delivery at Sentara Leigh Hospital. “However, my gut tells me that anything a company can put off paying for any amount of time equals profit, and most insurance companies have shareholders they answer to.”
The National Women’s Law Center (NWLC) found that at least 20 insurance companies are disregarding some ACA requirements by limiting coverage of breast pump purchases or failing to provide in-network lactation counselors.
For its report, published on May 21, NWLC analyzed coverage of breastfeeding support and supplies offered in the health insurance marketplaces of 15 states during 2014 and 2015. Researchers also reviewed personal accounts from patients collected from emails and calls to the center’s hotline.
The NWLC found that some health plans are placing improper coverage limits on breastfeeding benefits, including only allowing women to receive lactation services within 2 months of delivery; failing to cover breast pumps until after a baby is born; and denying claims for out-of-network lactation consultants even when in-network services are not available.
The ACA requires that insurers cover breastfeeding supplies and counseling without copays, deductibles, or coinsurance.
“The Affordable Care Act has made dramatic improvements in women’s health coverage,” Gretchen Borchelt, vice president for health and reproductive rights at NWLC, said in a statement. “If insurance companies fail to comply, they are illegally blocking further progress toward helping women breastfeed successfully. Everyone involved, from insurance companies to federal regulators, must work together to ensure that breastfeeding coverage fulfills the promise of the ACA.”
But America’s Health Insurance Plans (AHIP), a trade group representing the insurance industry, criticized the report, calling the study unscientific and lacking hard data.
“This report presents a distorted picture of reality,” AHIP President and CEO Karen Ignagni said in an interview. “Health plans provide access to care for millions of women each day and receive high marks in customer satisfaction surveys. To use highly selective anecdotes to draw sweeping conclusions about consumers’ coverage does nothing to improve the quality, accessibility, or affordability of health care for individuals and families.”
During its study, NWLC researchers found that physicians were generally very supportive in getting their patients’ help from trained lactation providers when possible, said Anna C. Benyo, NWLC senior health policy analyst. In some cases, pediatricians’ offices had a registered nurse who was also a trained lactation consultant and who could provide some education and support during well-child visits, Ms. Benyo said in an interview.
“But, for the most part, the pediatrician wants women to get help, and then [patients] try to find a provider who takes their insurance, and that’s where things start to fall apart,” Ms. Benyo said. “Their insurance company hasn’t set up a network and when they try to go out-of-network as allowed by federal rules, the plans deny coverage.”
In cases where the type of pump is an issue, Ms. Benyo said physicians sometimes write prescriptions for hospital-grade pumps to help patients get the needed equipment. Under the ACA, insurance plans are not required to cover a certain type of pump, leading some plans to cover only manual pumps and exclude electronic or hospital-grade pumps.
Dr. Puritz said she and her colleagues have written prescriptions for hospital-grade pumps.
“The hospital-grade breast pumps that are now covered [by prescription] are a huge improvement for women who want to breastfeed [versus] the less expensive ones that many women would try as that was what they could afford,” she said in an interview. “They didn’t work well and discouraged many of my patients from continuing to nurse.”
For physicians, seeing patients struggle to obtain insurance coverage for needed medical supplies is frustrating, Dr. Puritz added. She said she has not seen any specific cases involving coverage denials for breastfeeding services, but in general, the problem is troublesome.
“Coverage improves access plain and simple,” Dr. Purtiz said. “The problem is when physicians get denials, it’s lots of extra work for them and their staff. They have to be really committed to make it work.”
On Twitter @legal_med
Dr. Holly S. Puritz, an ob.gyn. in Norfolk, Va., wasn’t surprised by the findings of a recent report that claims insurers are failing to cover breastfeeding services as required by the Affordable Care Act.
“If I’m being charitable, I would say lots of the new rules are confusing and difficult for anyone to sort out,” said Dr. Puritz, who is in private practice and is also medical director for labor and delivery at Sentara Leigh Hospital. “However, my gut tells me that anything a company can put off paying for any amount of time equals profit, and most insurance companies have shareholders they answer to.”
The National Women’s Law Center (NWLC) found that at least 20 insurance companies are disregarding some ACA requirements by limiting coverage of breast pump purchases or failing to provide in-network lactation counselors.
For its report, published on May 21, NWLC analyzed coverage of breastfeeding support and supplies offered in the health insurance marketplaces of 15 states during 2014 and 2015. Researchers also reviewed personal accounts from patients collected from emails and calls to the center’s hotline.
The NWLC found that some health plans are placing improper coverage limits on breastfeeding benefits, including only allowing women to receive lactation services within 2 months of delivery; failing to cover breast pumps until after a baby is born; and denying claims for out-of-network lactation consultants even when in-network services are not available.
The ACA requires that insurers cover breastfeeding supplies and counseling without copays, deductibles, or coinsurance.
“The Affordable Care Act has made dramatic improvements in women’s health coverage,” Gretchen Borchelt, vice president for health and reproductive rights at NWLC, said in a statement. “If insurance companies fail to comply, they are illegally blocking further progress toward helping women breastfeed successfully. Everyone involved, from insurance companies to federal regulators, must work together to ensure that breastfeeding coverage fulfills the promise of the ACA.”
But America’s Health Insurance Plans (AHIP), a trade group representing the insurance industry, criticized the report, calling the study unscientific and lacking hard data.
“This report presents a distorted picture of reality,” AHIP President and CEO Karen Ignagni said in an interview. “Health plans provide access to care for millions of women each day and receive high marks in customer satisfaction surveys. To use highly selective anecdotes to draw sweeping conclusions about consumers’ coverage does nothing to improve the quality, accessibility, or affordability of health care for individuals and families.”
During its study, NWLC researchers found that physicians were generally very supportive in getting their patients’ help from trained lactation providers when possible, said Anna C. Benyo, NWLC senior health policy analyst. In some cases, pediatricians’ offices had a registered nurse who was also a trained lactation consultant and who could provide some education and support during well-child visits, Ms. Benyo said in an interview.
“But, for the most part, the pediatrician wants women to get help, and then [patients] try to find a provider who takes their insurance, and that’s where things start to fall apart,” Ms. Benyo said. “Their insurance company hasn’t set up a network and when they try to go out-of-network as allowed by federal rules, the plans deny coverage.”
In cases where the type of pump is an issue, Ms. Benyo said physicians sometimes write prescriptions for hospital-grade pumps to help patients get the needed equipment. Under the ACA, insurance plans are not required to cover a certain type of pump, leading some plans to cover only manual pumps and exclude electronic or hospital-grade pumps.
Dr. Puritz said she and her colleagues have written prescriptions for hospital-grade pumps.
“The hospital-grade breast pumps that are now covered [by prescription] are a huge improvement for women who want to breastfeed [versus] the less expensive ones that many women would try as that was what they could afford,” she said in an interview. “They didn’t work well and discouraged many of my patients from continuing to nurse.”
For physicians, seeing patients struggle to obtain insurance coverage for needed medical supplies is frustrating, Dr. Puritz added. She said she has not seen any specific cases involving coverage denials for breastfeeding services, but in general, the problem is troublesome.
“Coverage improves access plain and simple,” Dr. Purtiz said. “The problem is when physicians get denials, it’s lots of extra work for them and their staff. They have to be really committed to make it work.”
On Twitter @legal_med
Dr. Holly S. Puritz, an ob.gyn. in Norfolk, Va., wasn’t surprised by the findings of a recent report that claims insurers are failing to cover breastfeeding services as required by the Affordable Care Act.
“If I’m being charitable, I would say lots of the new rules are confusing and difficult for anyone to sort out,” said Dr. Puritz, who is in private practice and is also medical director for labor and delivery at Sentara Leigh Hospital. “However, my gut tells me that anything a company can put off paying for any amount of time equals profit, and most insurance companies have shareholders they answer to.”
The National Women’s Law Center (NWLC) found that at least 20 insurance companies are disregarding some ACA requirements by limiting coverage of breast pump purchases or failing to provide in-network lactation counselors.
For its report, published on May 21, NWLC analyzed coverage of breastfeeding support and supplies offered in the health insurance marketplaces of 15 states during 2014 and 2015. Researchers also reviewed personal accounts from patients collected from emails and calls to the center’s hotline.
The NWLC found that some health plans are placing improper coverage limits on breastfeeding benefits, including only allowing women to receive lactation services within 2 months of delivery; failing to cover breast pumps until after a baby is born; and denying claims for out-of-network lactation consultants even when in-network services are not available.
The ACA requires that insurers cover breastfeeding supplies and counseling without copays, deductibles, or coinsurance.
“The Affordable Care Act has made dramatic improvements in women’s health coverage,” Gretchen Borchelt, vice president for health and reproductive rights at NWLC, said in a statement. “If insurance companies fail to comply, they are illegally blocking further progress toward helping women breastfeed successfully. Everyone involved, from insurance companies to federal regulators, must work together to ensure that breastfeeding coverage fulfills the promise of the ACA.”
But America’s Health Insurance Plans (AHIP), a trade group representing the insurance industry, criticized the report, calling the study unscientific and lacking hard data.
“This report presents a distorted picture of reality,” AHIP President and CEO Karen Ignagni said in an interview. “Health plans provide access to care for millions of women each day and receive high marks in customer satisfaction surveys. To use highly selective anecdotes to draw sweeping conclusions about consumers’ coverage does nothing to improve the quality, accessibility, or affordability of health care for individuals and families.”
During its study, NWLC researchers found that physicians were generally very supportive in getting their patients’ help from trained lactation providers when possible, said Anna C. Benyo, NWLC senior health policy analyst. In some cases, pediatricians’ offices had a registered nurse who was also a trained lactation consultant and who could provide some education and support during well-child visits, Ms. Benyo said in an interview.
“But, for the most part, the pediatrician wants women to get help, and then [patients] try to find a provider who takes their insurance, and that’s where things start to fall apart,” Ms. Benyo said. “Their insurance company hasn’t set up a network and when they try to go out-of-network as allowed by federal rules, the plans deny coverage.”
In cases where the type of pump is an issue, Ms. Benyo said physicians sometimes write prescriptions for hospital-grade pumps to help patients get the needed equipment. Under the ACA, insurance plans are not required to cover a certain type of pump, leading some plans to cover only manual pumps and exclude electronic or hospital-grade pumps.
Dr. Puritz said she and her colleagues have written prescriptions for hospital-grade pumps.
“The hospital-grade breast pumps that are now covered [by prescription] are a huge improvement for women who want to breastfeed [versus] the less expensive ones that many women would try as that was what they could afford,” she said in an interview. “They didn’t work well and discouraged many of my patients from continuing to nurse.”
For physicians, seeing patients struggle to obtain insurance coverage for needed medical supplies is frustrating, Dr. Puritz added. She said she has not seen any specific cases involving coverage denials for breastfeeding services, but in general, the problem is troublesome.
“Coverage improves access plain and simple,” Dr. Purtiz said. “The problem is when physicians get denials, it’s lots of extra work for them and their staff. They have to be really committed to make it work.”
On Twitter @legal_med
Newer Oral Contraceptives Pose Higher VTE Risk
The risk of developing venous thromboembolism is generally greater for women using oral contraceptives with newer types of progestogen hormones than for those taking older, second-generation birth control pills, study results showed.
“Women exposed to drospirenone, gestodene, cyproterone, and desogestrel within the last 28 days had around a four times increased risk of venous thromboembolism,” the investigators found. Women exposed to levonorgestrel, norethisterone, and norgestimate had about a 2.5 times greater risk of venous thromboembolism than did women not exposed in the past year, said Yana Vinogradova and her colleagues at the University of Nottingham (England) (BMJ. 2015 May 26 [doi:10.1136/bmj.h2135]).
The researchers conducted two nested case-control studies using data from 618 primary care practices in the Clinical Practice Research Datalink (CPRD) and 722 practices in the QResearch primary care database. A total of 5,062 cases from CPRD and 5,500 cases from QResearch were matched one to five with 19,638 and 22,396 controls, respectively.
Approximately 29% of CPRD patients and 26% of QResearch patients used oral contraceptives, most commonly levonorgestrel. Overall, any use of combined oral contraceptives resulted in a three times increased risk for venous thromboembolism, compared with no use in the past year.
After accounting for smoking, obesity, a wide range of other health conditions, alcohol consumption, polycystic ovary syndrome and recent infections, surgeries, leg/hip fractures, and hospital admission, the researchers calculated an increased odds ratio for each hormone: desogestrel (4.28), cyproterone (4.27), drospirenone (4.12), gestodene (3.64), levonorgestrel (2.38), norgestimate (2.53), and norethisterone (2.56). The increased VTE risk in patients on these hormones was compared with no exposure to oral contraceptives in the previous year.
In terms of numbers needed to harm, the researchers estimated that use of levonorgestrel and norgestimate resulted in 6 extra cases of VTE each year per 10,000 treated women aged 15-49, and 7 extra cases for women aged 25-49.
Desogestrel and cyproterone each contributed 14 additional cases of VTE each year per 10,000 treated women aged 15-49, and drospirenone, desogestrel, and cyproterone each contributed to an extra 17 cases of VTE each year per 10,000 women aged 25-49.
“We believe this study has the statistical power and sufficient adjustment for relevant confounders to be regarded as an important clarifying study, which has produced the most reliable possible risk estimates using currently available U.K. prescription data,” the researchers wrote.
There was no external funding for the study. Julia Hippisley-Cox is the unpaid director of QResearch, a not-for-profit organization that is a joint partnership between the University of Nottingham and EMIS, a commercial IT supplier. She is also a paid director of ClinRisk, which produces clinical risk algorithm-related software.
The risk of developing venous thromboembolism is generally greater for women using oral contraceptives with newer types of progestogen hormones than for those taking older, second-generation birth control pills, study results showed.
“Women exposed to drospirenone, gestodene, cyproterone, and desogestrel within the last 28 days had around a four times increased risk of venous thromboembolism,” the investigators found. Women exposed to levonorgestrel, norethisterone, and norgestimate had about a 2.5 times greater risk of venous thromboembolism than did women not exposed in the past year, said Yana Vinogradova and her colleagues at the University of Nottingham (England) (BMJ. 2015 May 26 [doi:10.1136/bmj.h2135]).
The researchers conducted two nested case-control studies using data from 618 primary care practices in the Clinical Practice Research Datalink (CPRD) and 722 practices in the QResearch primary care database. A total of 5,062 cases from CPRD and 5,500 cases from QResearch were matched one to five with 19,638 and 22,396 controls, respectively.
Approximately 29% of CPRD patients and 26% of QResearch patients used oral contraceptives, most commonly levonorgestrel. Overall, any use of combined oral contraceptives resulted in a three times increased risk for venous thromboembolism, compared with no use in the past year.
After accounting for smoking, obesity, a wide range of other health conditions, alcohol consumption, polycystic ovary syndrome and recent infections, surgeries, leg/hip fractures, and hospital admission, the researchers calculated an increased odds ratio for each hormone: desogestrel (4.28), cyproterone (4.27), drospirenone (4.12), gestodene (3.64), levonorgestrel (2.38), norgestimate (2.53), and norethisterone (2.56). The increased VTE risk in patients on these hormones was compared with no exposure to oral contraceptives in the previous year.
In terms of numbers needed to harm, the researchers estimated that use of levonorgestrel and norgestimate resulted in 6 extra cases of VTE each year per 10,000 treated women aged 15-49, and 7 extra cases for women aged 25-49.
Desogestrel and cyproterone each contributed 14 additional cases of VTE each year per 10,000 treated women aged 15-49, and drospirenone, desogestrel, and cyproterone each contributed to an extra 17 cases of VTE each year per 10,000 women aged 25-49.
“We believe this study has the statistical power and sufficient adjustment for relevant confounders to be regarded as an important clarifying study, which has produced the most reliable possible risk estimates using currently available U.K. prescription data,” the researchers wrote.
There was no external funding for the study. Julia Hippisley-Cox is the unpaid director of QResearch, a not-for-profit organization that is a joint partnership between the University of Nottingham and EMIS, a commercial IT supplier. She is also a paid director of ClinRisk, which produces clinical risk algorithm-related software.
The risk of developing venous thromboembolism is generally greater for women using oral contraceptives with newer types of progestogen hormones than for those taking older, second-generation birth control pills, study results showed.
“Women exposed to drospirenone, gestodene, cyproterone, and desogestrel within the last 28 days had around a four times increased risk of venous thromboembolism,” the investigators found. Women exposed to levonorgestrel, norethisterone, and norgestimate had about a 2.5 times greater risk of venous thromboembolism than did women not exposed in the past year, said Yana Vinogradova and her colleagues at the University of Nottingham (England) (BMJ. 2015 May 26 [doi:10.1136/bmj.h2135]).
The researchers conducted two nested case-control studies using data from 618 primary care practices in the Clinical Practice Research Datalink (CPRD) and 722 practices in the QResearch primary care database. A total of 5,062 cases from CPRD and 5,500 cases from QResearch were matched one to five with 19,638 and 22,396 controls, respectively.
Approximately 29% of CPRD patients and 26% of QResearch patients used oral contraceptives, most commonly levonorgestrel. Overall, any use of combined oral contraceptives resulted in a three times increased risk for venous thromboembolism, compared with no use in the past year.
After accounting for smoking, obesity, a wide range of other health conditions, alcohol consumption, polycystic ovary syndrome and recent infections, surgeries, leg/hip fractures, and hospital admission, the researchers calculated an increased odds ratio for each hormone: desogestrel (4.28), cyproterone (4.27), drospirenone (4.12), gestodene (3.64), levonorgestrel (2.38), norgestimate (2.53), and norethisterone (2.56). The increased VTE risk in patients on these hormones was compared with no exposure to oral contraceptives in the previous year.
In terms of numbers needed to harm, the researchers estimated that use of levonorgestrel and norgestimate resulted in 6 extra cases of VTE each year per 10,000 treated women aged 15-49, and 7 extra cases for women aged 25-49.
Desogestrel and cyproterone each contributed 14 additional cases of VTE each year per 10,000 treated women aged 15-49, and drospirenone, desogestrel, and cyproterone each contributed to an extra 17 cases of VTE each year per 10,000 women aged 25-49.
“We believe this study has the statistical power and sufficient adjustment for relevant confounders to be regarded as an important clarifying study, which has produced the most reliable possible risk estimates using currently available U.K. prescription data,” the researchers wrote.
There was no external funding for the study. Julia Hippisley-Cox is the unpaid director of QResearch, a not-for-profit organization that is a joint partnership between the University of Nottingham and EMIS, a commercial IT supplier. She is also a paid director of ClinRisk, which produces clinical risk algorithm-related software.
FROM BMJ
Is azithromycin a good alternative to erythromycin for PPROM prophylaxis?
The objective of this investigation by Pierson and colleagues was to determine if there was any significant difference between erythyromycin and azithromycin, used in combination with ampicillin, for prophylaxis in women with PPROM.
Details of the study
The authors conducted a retrospective study of 168 women at 24 to 34 weeks’ gestation. At the discretion of the attending physician, patients received either ampicillin plus erythromycin or ampicillin plus azithromycin as their prophylactic antibiotic regimen. Patients were excluded from the study if they had a cerclage, a multiple gestation, a history of amniocentesis or fetal surgery, a history of abdominal trauma, or if they had a fetus with a lethal anomaly.
The primary study end point was the duration of the latency period between rupture of membranes and onset of labor. The secondary outcomes were gestational age at delivery, adverse drug effects, neonatal birth weight, Apgar scores, and rates of neonatal death, respiratory distress syndrome, and sepsis.
The mean (SD) duration of the latent period was 9.4 (10.4) days in the azithromycin group and 9.6 (13.2) days in the erythromycin group (P = .4). There also were no significant differences in any of the secondary outcome measures. Accordingly, the authors concluded that azithromycin was an acceptable alternative to erythromycin in the prophylactic antibiotic regimen for patients with PPROM.
Several factors make azithromycin the favored PPROM prophylactic option
In the original Maternal-Fetal Medicine Network trial of prophylactic antibiotics for PPROM, Mercer and colleagues1 used the combination regimen of ampicillin plus erythromycin. In this regimen, ampicillin primarily targets group B streptococci and Escherichia coli. Erythromycin specifically targets mycoplasma organisms, which can be part of the polymicrobial flora that causes chorioamnionitis. The drug also is effective against chlamydia.
However, erythromycin may cause troublesome gastrointestinal adverse effects, notably diarrhea, in some patients. Therefore, in recent years, several investigators have advocated use of azithromycin in lieu of erythromycin. Azithromycin has a similar spectrum of activity as erythromycin, but it has a more favorable pharmacokinetic profile. When given in a single oral dose of 1,000 mg, it has a half-life of 68 hours, compared with erythromycin’s half-life of 1.6 hours. Thus, it is much easier to administer. Moreover, it is usually much better tolerated than erythromycin and, now that generic versions of the drug are available, it is relatively inexpensive.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Although this study is retrospective (Level II evidence), it is the first to demonstrate that, from the perspective of clinical effectiveness, azithromycin is comparable to erythromycin when used in combination with ampicillin for prophylaxis in patients with PPROM. For the reasons outlined above, I strongly favor azithromycin in lieu of erythromycin.
At our center we administer the drug in a single 1,000-mg oral dose. If the patient cannot tolerate oral medication at the time of admission, the drug can be administered intravenously.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
- Mercer BM, Miodovnik M, Thurnau GR, et al. Antibiotic therapy for reduction of infant morbidity after preterm premature rupture of the membranes. A randomized controlled trial. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. JAMA. 1997;278(12):989–995.
The objective of this investigation by Pierson and colleagues was to determine if there was any significant difference between erythyromycin and azithromycin, used in combination with ampicillin, for prophylaxis in women with PPROM.
Details of the study
The authors conducted a retrospective study of 168 women at 24 to 34 weeks’ gestation. At the discretion of the attending physician, patients received either ampicillin plus erythromycin or ampicillin plus azithromycin as their prophylactic antibiotic regimen. Patients were excluded from the study if they had a cerclage, a multiple gestation, a history of amniocentesis or fetal surgery, a history of abdominal trauma, or if they had a fetus with a lethal anomaly.
The primary study end point was the duration of the latency period between rupture of membranes and onset of labor. The secondary outcomes were gestational age at delivery, adverse drug effects, neonatal birth weight, Apgar scores, and rates of neonatal death, respiratory distress syndrome, and sepsis.
The mean (SD) duration of the latent period was 9.4 (10.4) days in the azithromycin group and 9.6 (13.2) days in the erythromycin group (P = .4). There also were no significant differences in any of the secondary outcome measures. Accordingly, the authors concluded that azithromycin was an acceptable alternative to erythromycin in the prophylactic antibiotic regimen for patients with PPROM.
Several factors make azithromycin the favored PPROM prophylactic option
In the original Maternal-Fetal Medicine Network trial of prophylactic antibiotics for PPROM, Mercer and colleagues1 used the combination regimen of ampicillin plus erythromycin. In this regimen, ampicillin primarily targets group B streptococci and Escherichia coli. Erythromycin specifically targets mycoplasma organisms, which can be part of the polymicrobial flora that causes chorioamnionitis. The drug also is effective against chlamydia.
However, erythromycin may cause troublesome gastrointestinal adverse effects, notably diarrhea, in some patients. Therefore, in recent years, several investigators have advocated use of azithromycin in lieu of erythromycin. Azithromycin has a similar spectrum of activity as erythromycin, but it has a more favorable pharmacokinetic profile. When given in a single oral dose of 1,000 mg, it has a half-life of 68 hours, compared with erythromycin’s half-life of 1.6 hours. Thus, it is much easier to administer. Moreover, it is usually much better tolerated than erythromycin and, now that generic versions of the drug are available, it is relatively inexpensive.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Although this study is retrospective (Level II evidence), it is the first to demonstrate that, from the perspective of clinical effectiveness, azithromycin is comparable to erythromycin when used in combination with ampicillin for prophylaxis in patients with PPROM. For the reasons outlined above, I strongly favor azithromycin in lieu of erythromycin.
At our center we administer the drug in a single 1,000-mg oral dose. If the patient cannot tolerate oral medication at the time of admission, the drug can be administered intravenously.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The objective of this investigation by Pierson and colleagues was to determine if there was any significant difference between erythyromycin and azithromycin, used in combination with ampicillin, for prophylaxis in women with PPROM.
Details of the study
The authors conducted a retrospective study of 168 women at 24 to 34 weeks’ gestation. At the discretion of the attending physician, patients received either ampicillin plus erythromycin or ampicillin plus azithromycin as their prophylactic antibiotic regimen. Patients were excluded from the study if they had a cerclage, a multiple gestation, a history of amniocentesis or fetal surgery, a history of abdominal trauma, or if they had a fetus with a lethal anomaly.
The primary study end point was the duration of the latency period between rupture of membranes and onset of labor. The secondary outcomes were gestational age at delivery, adverse drug effects, neonatal birth weight, Apgar scores, and rates of neonatal death, respiratory distress syndrome, and sepsis.
The mean (SD) duration of the latent period was 9.4 (10.4) days in the azithromycin group and 9.6 (13.2) days in the erythromycin group (P = .4). There also were no significant differences in any of the secondary outcome measures. Accordingly, the authors concluded that azithromycin was an acceptable alternative to erythromycin in the prophylactic antibiotic regimen for patients with PPROM.
Several factors make azithromycin the favored PPROM prophylactic option
In the original Maternal-Fetal Medicine Network trial of prophylactic antibiotics for PPROM, Mercer and colleagues1 used the combination regimen of ampicillin plus erythromycin. In this regimen, ampicillin primarily targets group B streptococci and Escherichia coli. Erythromycin specifically targets mycoplasma organisms, which can be part of the polymicrobial flora that causes chorioamnionitis. The drug also is effective against chlamydia.
However, erythromycin may cause troublesome gastrointestinal adverse effects, notably diarrhea, in some patients. Therefore, in recent years, several investigators have advocated use of azithromycin in lieu of erythromycin. Azithromycin has a similar spectrum of activity as erythromycin, but it has a more favorable pharmacokinetic profile. When given in a single oral dose of 1,000 mg, it has a half-life of 68 hours, compared with erythromycin’s half-life of 1.6 hours. Thus, it is much easier to administer. Moreover, it is usually much better tolerated than erythromycin and, now that generic versions of the drug are available, it is relatively inexpensive.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Although this study is retrospective (Level II evidence), it is the first to demonstrate that, from the perspective of clinical effectiveness, azithromycin is comparable to erythromycin when used in combination with ampicillin for prophylaxis in patients with PPROM. For the reasons outlined above, I strongly favor azithromycin in lieu of erythromycin.
At our center we administer the drug in a single 1,000-mg oral dose. If the patient cannot tolerate oral medication at the time of admission, the drug can be administered intravenously.
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Reference
- Mercer BM, Miodovnik M, Thurnau GR, et al. Antibiotic therapy for reduction of infant morbidity after preterm premature rupture of the membranes. A randomized controlled trial. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. JAMA. 1997;278(12):989–995.
Reference
- Mercer BM, Miodovnik M, Thurnau GR, et al. Antibiotic therapy for reduction of infant morbidity after preterm premature rupture of the membranes. A randomized controlled trial. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. JAMA. 1997;278(12):989–995.
Buprenorphine is best for opioid-addicted pregnant women
Buprenorphine is the treatment of choice for opioid addiction during pregnancy, according to Dr. Marjorie Meyer, of the department of maternal fetal medicine at the University of Vermont in Burlington.
As an in-office prescription, buprenorphine is easier to access than methadone, and a large, randomized trial that pitted methadone against buprenorphine found that women treated with buprenorphine have fewer delivery complications (N. Engl. J. Med. 2010;363:2320-31). Their babies are also born heavier and at greater gestational age than those born to mothers on methadone, and require less morphine for neonatal abstinence syndrome and recover from it sooner, Dr. Meyer said during a webinar sponsored by Premier Inc., a health care performance improvement alliance of about 3,400 U.S. hospitals and 110,000 other providers.
The evidence from the trial – the most rigorous to date comparing the two options – all favors buprenorphine, she said.
“The concerning thing about this study was that a third of women dropped out during buprenorphine induction; the way they induced I think might precipitate a little bit of withdrawal,” she said. If that’s avoided, “you can get the dropout rate down.”
In general, treatment for addicted mothers “improves pregnancy outcomes, and should be offered,” but traditional detox is not optimal therapy, Dr. Meyer said. It can help prevent neonatal abstinence, but the dropout rate is high, perhaps about 50%. Even if women stick with the program, “what you have is a very sick mother who is unable to parent,” she said.
There are still many questions about what physicians can do for pain when women on methadone or buprenorphine go into labor. Full-agonist opioid or regional analgesia are good options, but not nalbuphine and butorphanol, Dr. Meyer said. As partial opioid agonists, they can throw women into withdrawal.
“One thing that is very reassuring is that spinals and epidurals actually work just as well,” she said.
There’s no need to increase pain control after vaginal delivery in women on buprenorphine or methadone maintenance. Routine postpartum orders with p.r.n. opioids for 24 hours should be effective, Dr. Meyer said.
After cesarean delivery, however, these women need more opioids for the first few days, generally about 50%-70% more.
“We tend to go ahead and give them higher doses of p.o. dilaudid and it seems to work very well” dosed at 4-6 mg every 4-6 hours. Treatment doesn’t need to last longer than in other women, only about a week. Transversus abdominis plane (TAP) blocks have also very effective, Dr. Meyer said.
If women receive nalbuphine and butorphanol by mistake at some point during labor and delivery, Dr. Meyer said she’s seen IV morphine work well for rescue.
Patients on maintenance therapy often ask if there’s something they can do to help prevent their baby from going into withdrawal. “The obvious answer is ‘yes, stop smoking,’” she said.
The vast majority of opioid abusers smoke cigarettes, and smoking has been shown to be “a very important contributor to neonatal abstinence syndrome,” she said. “I use this [fact] as a tool to really encourage smoking cessation, or even smoking reduction.”
Dr. Meyer reported having no relevant financial disclosures.
Buprenorphine is the treatment of choice for opioid addiction during pregnancy, according to Dr. Marjorie Meyer, of the department of maternal fetal medicine at the University of Vermont in Burlington.
As an in-office prescription, buprenorphine is easier to access than methadone, and a large, randomized trial that pitted methadone against buprenorphine found that women treated with buprenorphine have fewer delivery complications (N. Engl. J. Med. 2010;363:2320-31). Their babies are also born heavier and at greater gestational age than those born to mothers on methadone, and require less morphine for neonatal abstinence syndrome and recover from it sooner, Dr. Meyer said during a webinar sponsored by Premier Inc., a health care performance improvement alliance of about 3,400 U.S. hospitals and 110,000 other providers.
The evidence from the trial – the most rigorous to date comparing the two options – all favors buprenorphine, she said.
“The concerning thing about this study was that a third of women dropped out during buprenorphine induction; the way they induced I think might precipitate a little bit of withdrawal,” she said. If that’s avoided, “you can get the dropout rate down.”
In general, treatment for addicted mothers “improves pregnancy outcomes, and should be offered,” but traditional detox is not optimal therapy, Dr. Meyer said. It can help prevent neonatal abstinence, but the dropout rate is high, perhaps about 50%. Even if women stick with the program, “what you have is a very sick mother who is unable to parent,” she said.
There are still many questions about what physicians can do for pain when women on methadone or buprenorphine go into labor. Full-agonist opioid or regional analgesia are good options, but not nalbuphine and butorphanol, Dr. Meyer said. As partial opioid agonists, they can throw women into withdrawal.
“One thing that is very reassuring is that spinals and epidurals actually work just as well,” she said.
There’s no need to increase pain control after vaginal delivery in women on buprenorphine or methadone maintenance. Routine postpartum orders with p.r.n. opioids for 24 hours should be effective, Dr. Meyer said.
After cesarean delivery, however, these women need more opioids for the first few days, generally about 50%-70% more.
“We tend to go ahead and give them higher doses of p.o. dilaudid and it seems to work very well” dosed at 4-6 mg every 4-6 hours. Treatment doesn’t need to last longer than in other women, only about a week. Transversus abdominis plane (TAP) blocks have also very effective, Dr. Meyer said.
If women receive nalbuphine and butorphanol by mistake at some point during labor and delivery, Dr. Meyer said she’s seen IV morphine work well for rescue.
Patients on maintenance therapy often ask if there’s something they can do to help prevent their baby from going into withdrawal. “The obvious answer is ‘yes, stop smoking,’” she said.
The vast majority of opioid abusers smoke cigarettes, and smoking has been shown to be “a very important contributor to neonatal abstinence syndrome,” she said. “I use this [fact] as a tool to really encourage smoking cessation, or even smoking reduction.”
Dr. Meyer reported having no relevant financial disclosures.
Buprenorphine is the treatment of choice for opioid addiction during pregnancy, according to Dr. Marjorie Meyer, of the department of maternal fetal medicine at the University of Vermont in Burlington.
As an in-office prescription, buprenorphine is easier to access than methadone, and a large, randomized trial that pitted methadone against buprenorphine found that women treated with buprenorphine have fewer delivery complications (N. Engl. J. Med. 2010;363:2320-31). Their babies are also born heavier and at greater gestational age than those born to mothers on methadone, and require less morphine for neonatal abstinence syndrome and recover from it sooner, Dr. Meyer said during a webinar sponsored by Premier Inc., a health care performance improvement alliance of about 3,400 U.S. hospitals and 110,000 other providers.
The evidence from the trial – the most rigorous to date comparing the two options – all favors buprenorphine, she said.
“The concerning thing about this study was that a third of women dropped out during buprenorphine induction; the way they induced I think might precipitate a little bit of withdrawal,” she said. If that’s avoided, “you can get the dropout rate down.”
In general, treatment for addicted mothers “improves pregnancy outcomes, and should be offered,” but traditional detox is not optimal therapy, Dr. Meyer said. It can help prevent neonatal abstinence, but the dropout rate is high, perhaps about 50%. Even if women stick with the program, “what you have is a very sick mother who is unable to parent,” she said.
There are still many questions about what physicians can do for pain when women on methadone or buprenorphine go into labor. Full-agonist opioid or regional analgesia are good options, but not nalbuphine and butorphanol, Dr. Meyer said. As partial opioid agonists, they can throw women into withdrawal.
“One thing that is very reassuring is that spinals and epidurals actually work just as well,” she said.
There’s no need to increase pain control after vaginal delivery in women on buprenorphine or methadone maintenance. Routine postpartum orders with p.r.n. opioids for 24 hours should be effective, Dr. Meyer said.
After cesarean delivery, however, these women need more opioids for the first few days, generally about 50%-70% more.
“We tend to go ahead and give them higher doses of p.o. dilaudid and it seems to work very well” dosed at 4-6 mg every 4-6 hours. Treatment doesn’t need to last longer than in other women, only about a week. Transversus abdominis plane (TAP) blocks have also very effective, Dr. Meyer said.
If women receive nalbuphine and butorphanol by mistake at some point during labor and delivery, Dr. Meyer said she’s seen IV morphine work well for rescue.
Patients on maintenance therapy often ask if there’s something they can do to help prevent their baby from going into withdrawal. “The obvious answer is ‘yes, stop smoking,’” she said.
The vast majority of opioid abusers smoke cigarettes, and smoking has been shown to be “a very important contributor to neonatal abstinence syndrome,” she said. “I use this [fact] as a tool to really encourage smoking cessation, or even smoking reduction.”
Dr. Meyer reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM PREMIER, INC.
Delayed cord clamping linked to better neurodevelopmental outcomes
Delaying the clamping of the umbilical cord at least 3 minutes after birth appears to improve social and fine motor skills in children at age 4 years, a follow-up study showed.
No differences in IQ were found, however, between those with early vs. delayed cord clamping.
“The included children constitute a group of low-risk children born in a high-income country with a low prevalence of iron deficiency,” Dr. Ola Andersson of Uppsala (Sweden) University and her associates wrote (JAMA Pediatr. 2015 May 26 [doi:10.1001/jamapediatrics.2015.0358]). “Still, differences between the groups were found, indicating that there are positive, and in no instance harmful, effects from delayed cord clamping,” they added. “Delaying umbilical cord clamping by 2-3 minutes after delivery allows fetal blood remaining in the placental circulation to be transfused to the newborn.”
In the original trial, 382 term infants from low-risk pregnancies were randomized to have their umbilical cords clamped within 10 seconds after birth or else at least 3 minutes after birth at a Swedish county hospital between April 2008 and May 2010. Four years later, 263 children underwent IQ testing with the Wechsler Preschool and Primary Scale of Intelligence and motor skills testing with the Movement Assessment Battery for Children. In addition, parents filled out questionnaires regarding the children’s behavior and developmental stages.
Average IQ scores did not differ between the two groups, but fewer children in the delayed cord-clamping group had an immature pencil grip: 13.2% percent, compared with 25.6% of those who had immediate cord clamping. Further, 3.8% of children who had delayed clamping and 12.9% of children who had immediate clamping fell below average on another fine motor test (the bicycle-trail task).
“In girls, there were no differences between the groups for any of the assessments. An at-risk result in the bicycle-trail task was less prevalent in boys who received delayed cord clamping, compared with those who received early cord clamping (3.6% vs. 23.1%); findings were similar in the Ages and Stages Questionnaire, Third Edition, fine-motor domain (8.9% vs 23.6%),” Dr. Andersson and her associates wrote.
“The effect by sex is consistent with previous results from the same study population at 12 months,” they said, because past studies have shown lower iron stores in boys, compared with girls, at birth and in infancy.
The research was funded by the Regional Scientific Council of Halland, the Linnéa and Josef Carlsson Foundation, the Southern Health care Region, H.R.H. Crown Princess Lovisa’s Society for Child Care, Uppsala University, the Little Childs Foundation, and the Swedish Research Council for Health, Working Life, and Welfare. The authors reported no relevant financial disclosures.
Early clamping of the cord was introduced in the past to avoid maternal hemorrhage without considering potential neonatal adverse effects. A meta-analysis by McDonald et al. (Cochrane Database Syst. Rev. 2013;7:CD004074) found no significant differences in postpartum hemorrhage rates when comparing early vs. late cord-clamping groups in five trials that included 2,260 women. In the current issue of JAMA Pediatrics, Andersson et al. describe the long-term follow-up of the same cohort of healthy term newborns at 4 years of age.
Until now, data on long-term follow-up of preterm and term infants who have been randomized to early vs. delayed cord clamping have been limited. While many physicians have incorporated delayed cord clamping into practice, there remains a hesitation to implement delayed cord clamping, particularly with term infants. As evidence of the safety and benefits of delayed cord clamping are demonstrated, this hesitation should disappear.
We applaud Dr. Andersson and colleagues for their persistence because their study closes the knowledge gap regarding the long-term safety of delayed cord clamping in healthy term newborns. Their important findings suggest that there is an absence of harm that lasts until 4 years of age.
Since 2000, no randomized clinical trials have substantiated prior concerns of symptomatic polycythemia or hyperbilirubinemia needing treatment. Physicians need to appreciate the significant risk of lower iron stores and iron-deficiency anemia on the early developing brain. The potential benefit of improving maternal and neonatal care by a simple no-cost intervention of delayed cord clamping should be championed by the international community beginning now and leading into the next decade.
These comments were excerpted from a commentary by Dr. Heike Rabe of the academic department of paediatrics at Brighton and Sussex Medical School and University Hospitals in England, and Debra A. Erickson-Owens, , Ph.D., and Judith S. Mercer, Ph.D., both of the College of Nursing at the University of Rhode Island, Kingston (JAMA Pediatr. 2015 May 26 [doi:10.1001/jamapediatrics.2015.0431]). The authors reported no relevant financial disclosures.
Early clamping of the cord was introduced in the past to avoid maternal hemorrhage without considering potential neonatal adverse effects. A meta-analysis by McDonald et al. (Cochrane Database Syst. Rev. 2013;7:CD004074) found no significant differences in postpartum hemorrhage rates when comparing early vs. late cord-clamping groups in five trials that included 2,260 women. In the current issue of JAMA Pediatrics, Andersson et al. describe the long-term follow-up of the same cohort of healthy term newborns at 4 years of age.
Until now, data on long-term follow-up of preterm and term infants who have been randomized to early vs. delayed cord clamping have been limited. While many physicians have incorporated delayed cord clamping into practice, there remains a hesitation to implement delayed cord clamping, particularly with term infants. As evidence of the safety and benefits of delayed cord clamping are demonstrated, this hesitation should disappear.
We applaud Dr. Andersson and colleagues for their persistence because their study closes the knowledge gap regarding the long-term safety of delayed cord clamping in healthy term newborns. Their important findings suggest that there is an absence of harm that lasts until 4 years of age.
Since 2000, no randomized clinical trials have substantiated prior concerns of symptomatic polycythemia or hyperbilirubinemia needing treatment. Physicians need to appreciate the significant risk of lower iron stores and iron-deficiency anemia on the early developing brain. The potential benefit of improving maternal and neonatal care by a simple no-cost intervention of delayed cord clamping should be championed by the international community beginning now and leading into the next decade.
These comments were excerpted from a commentary by Dr. Heike Rabe of the academic department of paediatrics at Brighton and Sussex Medical School and University Hospitals in England, and Debra A. Erickson-Owens, , Ph.D., and Judith S. Mercer, Ph.D., both of the College of Nursing at the University of Rhode Island, Kingston (JAMA Pediatr. 2015 May 26 [doi:10.1001/jamapediatrics.2015.0431]). The authors reported no relevant financial disclosures.
Early clamping of the cord was introduced in the past to avoid maternal hemorrhage without considering potential neonatal adverse effects. A meta-analysis by McDonald et al. (Cochrane Database Syst. Rev. 2013;7:CD004074) found no significant differences in postpartum hemorrhage rates when comparing early vs. late cord-clamping groups in five trials that included 2,260 women. In the current issue of JAMA Pediatrics, Andersson et al. describe the long-term follow-up of the same cohort of healthy term newborns at 4 years of age.
Until now, data on long-term follow-up of preterm and term infants who have been randomized to early vs. delayed cord clamping have been limited. While many physicians have incorporated delayed cord clamping into practice, there remains a hesitation to implement delayed cord clamping, particularly with term infants. As evidence of the safety and benefits of delayed cord clamping are demonstrated, this hesitation should disappear.
We applaud Dr. Andersson and colleagues for their persistence because their study closes the knowledge gap regarding the long-term safety of delayed cord clamping in healthy term newborns. Their important findings suggest that there is an absence of harm that lasts until 4 years of age.
Since 2000, no randomized clinical trials have substantiated prior concerns of symptomatic polycythemia or hyperbilirubinemia needing treatment. Physicians need to appreciate the significant risk of lower iron stores and iron-deficiency anemia on the early developing brain. The potential benefit of improving maternal and neonatal care by a simple no-cost intervention of delayed cord clamping should be championed by the international community beginning now and leading into the next decade.
These comments were excerpted from a commentary by Dr. Heike Rabe of the academic department of paediatrics at Brighton and Sussex Medical School and University Hospitals in England, and Debra A. Erickson-Owens, , Ph.D., and Judith S. Mercer, Ph.D., both of the College of Nursing at the University of Rhode Island, Kingston (JAMA Pediatr. 2015 May 26 [doi:10.1001/jamapediatrics.2015.0431]). The authors reported no relevant financial disclosures.
Delaying the clamping of the umbilical cord at least 3 minutes after birth appears to improve social and fine motor skills in children at age 4 years, a follow-up study showed.
No differences in IQ were found, however, between those with early vs. delayed cord clamping.
“The included children constitute a group of low-risk children born in a high-income country with a low prevalence of iron deficiency,” Dr. Ola Andersson of Uppsala (Sweden) University and her associates wrote (JAMA Pediatr. 2015 May 26 [doi:10.1001/jamapediatrics.2015.0358]). “Still, differences between the groups were found, indicating that there are positive, and in no instance harmful, effects from delayed cord clamping,” they added. “Delaying umbilical cord clamping by 2-3 minutes after delivery allows fetal blood remaining in the placental circulation to be transfused to the newborn.”
In the original trial, 382 term infants from low-risk pregnancies were randomized to have their umbilical cords clamped within 10 seconds after birth or else at least 3 minutes after birth at a Swedish county hospital between April 2008 and May 2010. Four years later, 263 children underwent IQ testing with the Wechsler Preschool and Primary Scale of Intelligence and motor skills testing with the Movement Assessment Battery for Children. In addition, parents filled out questionnaires regarding the children’s behavior and developmental stages.
Average IQ scores did not differ between the two groups, but fewer children in the delayed cord-clamping group had an immature pencil grip: 13.2% percent, compared with 25.6% of those who had immediate cord clamping. Further, 3.8% of children who had delayed clamping and 12.9% of children who had immediate clamping fell below average on another fine motor test (the bicycle-trail task).
“In girls, there were no differences between the groups for any of the assessments. An at-risk result in the bicycle-trail task was less prevalent in boys who received delayed cord clamping, compared with those who received early cord clamping (3.6% vs. 23.1%); findings were similar in the Ages and Stages Questionnaire, Third Edition, fine-motor domain (8.9% vs 23.6%),” Dr. Andersson and her associates wrote.
“The effect by sex is consistent with previous results from the same study population at 12 months,” they said, because past studies have shown lower iron stores in boys, compared with girls, at birth and in infancy.
The research was funded by the Regional Scientific Council of Halland, the Linnéa and Josef Carlsson Foundation, the Southern Health care Region, H.R.H. Crown Princess Lovisa’s Society for Child Care, Uppsala University, the Little Childs Foundation, and the Swedish Research Council for Health, Working Life, and Welfare. The authors reported no relevant financial disclosures.
Delaying the clamping of the umbilical cord at least 3 minutes after birth appears to improve social and fine motor skills in children at age 4 years, a follow-up study showed.
No differences in IQ were found, however, between those with early vs. delayed cord clamping.
“The included children constitute a group of low-risk children born in a high-income country with a low prevalence of iron deficiency,” Dr. Ola Andersson of Uppsala (Sweden) University and her associates wrote (JAMA Pediatr. 2015 May 26 [doi:10.1001/jamapediatrics.2015.0358]). “Still, differences between the groups were found, indicating that there are positive, and in no instance harmful, effects from delayed cord clamping,” they added. “Delaying umbilical cord clamping by 2-3 minutes after delivery allows fetal blood remaining in the placental circulation to be transfused to the newborn.”
In the original trial, 382 term infants from low-risk pregnancies were randomized to have their umbilical cords clamped within 10 seconds after birth or else at least 3 minutes after birth at a Swedish county hospital between April 2008 and May 2010. Four years later, 263 children underwent IQ testing with the Wechsler Preschool and Primary Scale of Intelligence and motor skills testing with the Movement Assessment Battery for Children. In addition, parents filled out questionnaires regarding the children’s behavior and developmental stages.
Average IQ scores did not differ between the two groups, but fewer children in the delayed cord-clamping group had an immature pencil grip: 13.2% percent, compared with 25.6% of those who had immediate cord clamping. Further, 3.8% of children who had delayed clamping and 12.9% of children who had immediate clamping fell below average on another fine motor test (the bicycle-trail task).
“In girls, there were no differences between the groups for any of the assessments. An at-risk result in the bicycle-trail task was less prevalent in boys who received delayed cord clamping, compared with those who received early cord clamping (3.6% vs. 23.1%); findings were similar in the Ages and Stages Questionnaire, Third Edition, fine-motor domain (8.9% vs 23.6%),” Dr. Andersson and her associates wrote.
“The effect by sex is consistent with previous results from the same study population at 12 months,” they said, because past studies have shown lower iron stores in boys, compared with girls, at birth and in infancy.
The research was funded by the Regional Scientific Council of Halland, the Linnéa and Josef Carlsson Foundation, the Southern Health care Region, H.R.H. Crown Princess Lovisa’s Society for Child Care, Uppsala University, the Little Childs Foundation, and the Swedish Research Council for Health, Working Life, and Welfare. The authors reported no relevant financial disclosures.
Key clinical point: Delayed cord clamping improved social and fine motor skills at age 4.
Major finding: The average mean difference in personal-social skills and fine motor skills was 2.8 and 2.1 points higher, respectively, among those with delayed cord clamping.
Data source: The findings are based on the follow-up of 263 term infants, 4 years after a randomized clinical trial conducted from April 2008 to May 2010 at a Swedish county hospital.
Disclosures: The research was funded by the Regional Scientific Council of Halland, the Linnéa and Josef Carlsson Foundation, the Southern Health care Region, H.R.H. Crown Princess Lovisa’s Society for Child Care, Uppsala University, the Little Childs Foundation and the Swedish Research Council for Health, Working Life, and Welfare. The authors reported no relevant financial disclosures.
Call to action: Saving 100,000 U.S. mothers in 5 years
The United States now ranks 60th in the world, and worst among developed nations, in maternal mortality. Each year more than 600 women in the United States die from pregnancy and childbirth, and more than 50,000 suffer a life-threatening complication (“severe maternal morbidity”).
The maternal mortality ratio doubled between 1987 and 2011, from 7.2 to 17.8 deaths per 100,000 live births; severe maternal morbidity doubled between 1998 and 2011, from 74 to 163 per 10,000 delivery hospitalizations. There continues to be large and persistent disparities; for example, a black woman is more than three times as likely to die from pregnancy and childbirth as a white woman, a gap we haven’t been able to close in decades.
The Maternal and Child Health Bureau is partnering with the American College of Obstetricians and Gynecologists and the Council on Patient Safety in Women’s Health Care (“the Council”) in launching a new national campaign to reduce maternal mortality and severe morbidity in the United States. The goal of the campaign is to prevent 100,000 maternal deaths or severe morbidities in the next 5 years by doing three things:
• Improving women’s health before pregnancy, with a focus on promoting preventive services including preconception, interconception, and postpartum care.
• Reducing primary cesarean deliveries, with an immediate focus on developing an evidence-based patient safety bundle to reduce low-risk, nulliparous, term, spontaneous, and vertex (NTSV) cesarean deliveries.
• Improving the quality and safety of maternity care, with a focus on implementing patient safety bundles to reduce mortality and morbidity associated with hemorrhage, preeclampsia, and thromboembolism in every birthing hospital and facility across the country in the next 3 years.
Safety bundles are small, straightforward sets of evidence-based practices that, when performed collectively and reliably, have improved patient outcomes. Several states have begun to pilot these safety bundles. In New York, ob.gyn. leaders such as Dr. Mary D’Alton are working with more than 1,000 health care providers to implement these safety bundles in 118 hospitals throughout the state.
In California, under the leadership of Dr. Elliott Main and other clinical and public health leaders, and in partnership with California Department of Public Health, the maternal mortality ratio decreased from a high of 16.9 in 2006 to 6.2 deaths per 100,000 live births in 2012.
If we are going to move the needle on maternal mortality and severe morbidity in this country, we are going to need an ob.gyn. champion in every hospital and every state. To learn more about the campaign and to find out how you can help, please visit the Council’s website at safehealthcareforeverywoman.org and click on the AIM Program.
Dr. Lu is the director of the Maternal and Child Health Bureau at the Health Resources and Services Administration, and an associate professor of obstetrics, gynecology, and public health at the University of California, Los Angeles.
The United States now ranks 60th in the world, and worst among developed nations, in maternal mortality. Each year more than 600 women in the United States die from pregnancy and childbirth, and more than 50,000 suffer a life-threatening complication (“severe maternal morbidity”).
The maternal mortality ratio doubled between 1987 and 2011, from 7.2 to 17.8 deaths per 100,000 live births; severe maternal morbidity doubled between 1998 and 2011, from 74 to 163 per 10,000 delivery hospitalizations. There continues to be large and persistent disparities; for example, a black woman is more than three times as likely to die from pregnancy and childbirth as a white woman, a gap we haven’t been able to close in decades.
The Maternal and Child Health Bureau is partnering with the American College of Obstetricians and Gynecologists and the Council on Patient Safety in Women’s Health Care (“the Council”) in launching a new national campaign to reduce maternal mortality and severe morbidity in the United States. The goal of the campaign is to prevent 100,000 maternal deaths or severe morbidities in the next 5 years by doing three things:
• Improving women’s health before pregnancy, with a focus on promoting preventive services including preconception, interconception, and postpartum care.
• Reducing primary cesarean deliveries, with an immediate focus on developing an evidence-based patient safety bundle to reduce low-risk, nulliparous, term, spontaneous, and vertex (NTSV) cesarean deliveries.
• Improving the quality and safety of maternity care, with a focus on implementing patient safety bundles to reduce mortality and morbidity associated with hemorrhage, preeclampsia, and thromboembolism in every birthing hospital and facility across the country in the next 3 years.
Safety bundles are small, straightforward sets of evidence-based practices that, when performed collectively and reliably, have improved patient outcomes. Several states have begun to pilot these safety bundles. In New York, ob.gyn. leaders such as Dr. Mary D’Alton are working with more than 1,000 health care providers to implement these safety bundles in 118 hospitals throughout the state.
In California, under the leadership of Dr. Elliott Main and other clinical and public health leaders, and in partnership with California Department of Public Health, the maternal mortality ratio decreased from a high of 16.9 in 2006 to 6.2 deaths per 100,000 live births in 2012.
If we are going to move the needle on maternal mortality and severe morbidity in this country, we are going to need an ob.gyn. champion in every hospital and every state. To learn more about the campaign and to find out how you can help, please visit the Council’s website at safehealthcareforeverywoman.org and click on the AIM Program.
Dr. Lu is the director of the Maternal and Child Health Bureau at the Health Resources and Services Administration, and an associate professor of obstetrics, gynecology, and public health at the University of California, Los Angeles.
The United States now ranks 60th in the world, and worst among developed nations, in maternal mortality. Each year more than 600 women in the United States die from pregnancy and childbirth, and more than 50,000 suffer a life-threatening complication (“severe maternal morbidity”).
The maternal mortality ratio doubled between 1987 and 2011, from 7.2 to 17.8 deaths per 100,000 live births; severe maternal morbidity doubled between 1998 and 2011, from 74 to 163 per 10,000 delivery hospitalizations. There continues to be large and persistent disparities; for example, a black woman is more than three times as likely to die from pregnancy and childbirth as a white woman, a gap we haven’t been able to close in decades.
The Maternal and Child Health Bureau is partnering with the American College of Obstetricians and Gynecologists and the Council on Patient Safety in Women’s Health Care (“the Council”) in launching a new national campaign to reduce maternal mortality and severe morbidity in the United States. The goal of the campaign is to prevent 100,000 maternal deaths or severe morbidities in the next 5 years by doing three things:
• Improving women’s health before pregnancy, with a focus on promoting preventive services including preconception, interconception, and postpartum care.
• Reducing primary cesarean deliveries, with an immediate focus on developing an evidence-based patient safety bundle to reduce low-risk, nulliparous, term, spontaneous, and vertex (NTSV) cesarean deliveries.
• Improving the quality and safety of maternity care, with a focus on implementing patient safety bundles to reduce mortality and morbidity associated with hemorrhage, preeclampsia, and thromboembolism in every birthing hospital and facility across the country in the next 3 years.
Safety bundles are small, straightforward sets of evidence-based practices that, when performed collectively and reliably, have improved patient outcomes. Several states have begun to pilot these safety bundles. In New York, ob.gyn. leaders such as Dr. Mary D’Alton are working with more than 1,000 health care providers to implement these safety bundles in 118 hospitals throughout the state.
In California, under the leadership of Dr. Elliott Main and other clinical and public health leaders, and in partnership with California Department of Public Health, the maternal mortality ratio decreased from a high of 16.9 in 2006 to 6.2 deaths per 100,000 live births in 2012.
If we are going to move the needle on maternal mortality and severe morbidity in this country, we are going to need an ob.gyn. champion in every hospital and every state. To learn more about the campaign and to find out how you can help, please visit the Council’s website at safehealthcareforeverywoman.org and click on the AIM Program.
Dr. Lu is the director of the Maternal and Child Health Bureau at the Health Resources and Services Administration, and an associate professor of obstetrics, gynecology, and public health at the University of California, Los Angeles.
CDC: Tdap vaccine coverage during pregnancy is low
Most women who receive the Tetanus-diphtheria-acellular pertussis (Tdap) vaccine do so after delivery, contrary to recommendations from the Advisory Committee on Immunizations Practices, which calls for vaccination during pregnancy.
Data from the Pregnancy Risk Assessment Monitoring System show that among 6,852 survey respondents in 16 states and New York City who had a live birth between September and December 2011, 20.8% did not know their vaccination status. Of the 5,499 who did know their status, more than half reported being vaccinated with Tdap (13.9% before pregnancy, 9.9% during pregnancy, and 30.5% after delivery).
The findings were published May 21 in Morbidity and Mortality Weekly Report (MMWR. 2015;64:522-6).
ACIP guidelines suggest the optimal time for vaccination is at 27-36 weeks’ gestation, according to the report.
Until 2011, it was recommended that women receive the vaccine either before pregnancy or postpartum. In June 2011, the ACIP changed its recommendation to one dose of the vaccine during pregnancy in women who had never received it before. ACIP further expanded this recommendation in 2012 to recommend vaccination during each pregnancy to provide maternal antibodies for each infant.
“Results from this analysis might reflect the early transition from a policy of vaccinating women postpartum to a policy of vaccinating them during pregnancy,” wrote Indu B. Ahluwalia, Ph.D., and coauthors from the CDC’s Division of Reproductive Health at the National Center for Chronic Disease Prevention and Health Promotion.
Physicians can also “assist pregnant women by providing specific information about where to obtain Tdap vaccination, or offering to provide the vaccination, and also to write a prescription in case it is needed,” the authors wrote.
Most women who receive the Tetanus-diphtheria-acellular pertussis (Tdap) vaccine do so after delivery, contrary to recommendations from the Advisory Committee on Immunizations Practices, which calls for vaccination during pregnancy.
Data from the Pregnancy Risk Assessment Monitoring System show that among 6,852 survey respondents in 16 states and New York City who had a live birth between September and December 2011, 20.8% did not know their vaccination status. Of the 5,499 who did know their status, more than half reported being vaccinated with Tdap (13.9% before pregnancy, 9.9% during pregnancy, and 30.5% after delivery).
The findings were published May 21 in Morbidity and Mortality Weekly Report (MMWR. 2015;64:522-6).
ACIP guidelines suggest the optimal time for vaccination is at 27-36 weeks’ gestation, according to the report.
Until 2011, it was recommended that women receive the vaccine either before pregnancy or postpartum. In June 2011, the ACIP changed its recommendation to one dose of the vaccine during pregnancy in women who had never received it before. ACIP further expanded this recommendation in 2012 to recommend vaccination during each pregnancy to provide maternal antibodies for each infant.
“Results from this analysis might reflect the early transition from a policy of vaccinating women postpartum to a policy of vaccinating them during pregnancy,” wrote Indu B. Ahluwalia, Ph.D., and coauthors from the CDC’s Division of Reproductive Health at the National Center for Chronic Disease Prevention and Health Promotion.
Physicians can also “assist pregnant women by providing specific information about where to obtain Tdap vaccination, or offering to provide the vaccination, and also to write a prescription in case it is needed,” the authors wrote.
Most women who receive the Tetanus-diphtheria-acellular pertussis (Tdap) vaccine do so after delivery, contrary to recommendations from the Advisory Committee on Immunizations Practices, which calls for vaccination during pregnancy.
Data from the Pregnancy Risk Assessment Monitoring System show that among 6,852 survey respondents in 16 states and New York City who had a live birth between September and December 2011, 20.8% did not know their vaccination status. Of the 5,499 who did know their status, more than half reported being vaccinated with Tdap (13.9% before pregnancy, 9.9% during pregnancy, and 30.5% after delivery).
The findings were published May 21 in Morbidity and Mortality Weekly Report (MMWR. 2015;64:522-6).
ACIP guidelines suggest the optimal time for vaccination is at 27-36 weeks’ gestation, according to the report.
Until 2011, it was recommended that women receive the vaccine either before pregnancy or postpartum. In June 2011, the ACIP changed its recommendation to one dose of the vaccine during pregnancy in women who had never received it before. ACIP further expanded this recommendation in 2012 to recommend vaccination during each pregnancy to provide maternal antibodies for each infant.
“Results from this analysis might reflect the early transition from a policy of vaccinating women postpartum to a policy of vaccinating them during pregnancy,” wrote Indu B. Ahluwalia, Ph.D., and coauthors from the CDC’s Division of Reproductive Health at the National Center for Chronic Disease Prevention and Health Promotion.
Physicians can also “assist pregnant women by providing specific information about where to obtain Tdap vaccination, or offering to provide the vaccination, and also to write a prescription in case it is needed,” the authors wrote.