User login
Late summer heat may bring increased risk of miscarriage
Summer heat is notorious for making the strain of pregnancy worse. But for many pregnant people, sweltering temperatures are much worse than a sweaty annoyance.
In late August, for example, the risk of losing a pregnancy is 44% higher than in February, according to the findings.
“One of our hypotheses is that heat may trigger miscarriage, which is something that we are now exploring further,” says Amelia Wesselink, PhD, an assistant professor of epidemiology at Boston University School of Public Health, who led the study team. “Our next step is to dig into drivers of this seasonal pattern.”
She and her colleagues analyzed seasonal differences and pregnancy outcomes for over 12,000 women. Spontaneous abortion rates peaked in late August, especially for those living in the southern and midwestern United States.
Spontaneous abortion was defined as miscarriage, chemical pregnancy (a very early miscarriage where the embryo stops growing), or blighted ovum (the embryo stops developing or never develops).
From 2013 to 2020, 12,197 women living in the United States and Canada were followed for up to 1 year using Pregnancy Study Online (PRESTO), an internet-based fertility study from the Boston University School of Public Health. Those in the study answered questions about their income, education, race/ethnicity, and lifestyle, as well as follow-up questions about their pregnancy and/or loss of pregnancy.
Most of the people studied were non-Hispanic White (86%) and had at least a college degree (79%). Almost half earned more than $100,000 annually (47%). Those seeking fertility treatments were excluded from the study.
Half of the women (6,104) said they conceived in the first 12 months of trying to get pregnant, and almost one in five (19.5%) of those who conceived miscarried.
The risk of miscarriage was 44% higher in late August than it was in late February, the month with the lowest rate of lost pregnancies. This trend was almost exclusively seen for pregnancies in their first 8 weeks. The risk of miscarriage increased 31% in late August for pregnancies at any stage.
The link between miscarriage and extreme heat was strongest in the South and Midwest, with peaks in late August and early September, respectively.
“We know so little about the causes of miscarriage that it’s difficult to tie seasonal variation in risk to any particular cause,” says David Savitz, PhD, a professor of epidemiology and obstetrics, gynecology & pediatrics at Brown University, Providence, R.I., who helped conduct the study. “Exposures vary by summer, including a lower risk of respiratory infection in the warm season, changes in diet and physical activity, and physical factors such as temperature and sunlight.”
But another expert warned that extreme heat may not be the only culprit in summer’s observed miscarriage rates.
“You need to be careful when linking summer months to miscarriage, as women may pursue more outdoor activities during summer,” says Saifuddin Ahmed PhD, a researcher at Johns Hopkins Bloomberg School of Public Health, Baltimore.
Although the paper suggested physical activity may play a role in miscarriage frequency, no analysis supported this claim, Dr. Ahmed says.
Also, participants in the study were mostly White and tended to be wealthier than the general population, so the findings may not apply to everyone, Dr. Wesselink says. Although the researchers saw some similarities between participants with income above $100,000 a year and those who earned less, socioeconomic status plays an important role in environmental exposures – including heat – so the results may not hold among lower-income populations, Dr. Wesselink says.
Dr. Wesselink and her colleagues published their findings in the journal Epidemiology.
A version of this article first appeared on WebMD.com.
Summer heat is notorious for making the strain of pregnancy worse. But for many pregnant people, sweltering temperatures are much worse than a sweaty annoyance.
In late August, for example, the risk of losing a pregnancy is 44% higher than in February, according to the findings.
“One of our hypotheses is that heat may trigger miscarriage, which is something that we are now exploring further,” says Amelia Wesselink, PhD, an assistant professor of epidemiology at Boston University School of Public Health, who led the study team. “Our next step is to dig into drivers of this seasonal pattern.”
She and her colleagues analyzed seasonal differences and pregnancy outcomes for over 12,000 women. Spontaneous abortion rates peaked in late August, especially for those living in the southern and midwestern United States.
Spontaneous abortion was defined as miscarriage, chemical pregnancy (a very early miscarriage where the embryo stops growing), or blighted ovum (the embryo stops developing or never develops).
From 2013 to 2020, 12,197 women living in the United States and Canada were followed for up to 1 year using Pregnancy Study Online (PRESTO), an internet-based fertility study from the Boston University School of Public Health. Those in the study answered questions about their income, education, race/ethnicity, and lifestyle, as well as follow-up questions about their pregnancy and/or loss of pregnancy.
Most of the people studied were non-Hispanic White (86%) and had at least a college degree (79%). Almost half earned more than $100,000 annually (47%). Those seeking fertility treatments were excluded from the study.
Half of the women (6,104) said they conceived in the first 12 months of trying to get pregnant, and almost one in five (19.5%) of those who conceived miscarried.
The risk of miscarriage was 44% higher in late August than it was in late February, the month with the lowest rate of lost pregnancies. This trend was almost exclusively seen for pregnancies in their first 8 weeks. The risk of miscarriage increased 31% in late August for pregnancies at any stage.
The link between miscarriage and extreme heat was strongest in the South and Midwest, with peaks in late August and early September, respectively.
“We know so little about the causes of miscarriage that it’s difficult to tie seasonal variation in risk to any particular cause,” says David Savitz, PhD, a professor of epidemiology and obstetrics, gynecology & pediatrics at Brown University, Providence, R.I., who helped conduct the study. “Exposures vary by summer, including a lower risk of respiratory infection in the warm season, changes in diet and physical activity, and physical factors such as temperature and sunlight.”
But another expert warned that extreme heat may not be the only culprit in summer’s observed miscarriage rates.
“You need to be careful when linking summer months to miscarriage, as women may pursue more outdoor activities during summer,” says Saifuddin Ahmed PhD, a researcher at Johns Hopkins Bloomberg School of Public Health, Baltimore.
Although the paper suggested physical activity may play a role in miscarriage frequency, no analysis supported this claim, Dr. Ahmed says.
Also, participants in the study were mostly White and tended to be wealthier than the general population, so the findings may not apply to everyone, Dr. Wesselink says. Although the researchers saw some similarities between participants with income above $100,000 a year and those who earned less, socioeconomic status plays an important role in environmental exposures – including heat – so the results may not hold among lower-income populations, Dr. Wesselink says.
Dr. Wesselink and her colleagues published their findings in the journal Epidemiology.
A version of this article first appeared on WebMD.com.
Summer heat is notorious for making the strain of pregnancy worse. But for many pregnant people, sweltering temperatures are much worse than a sweaty annoyance.
In late August, for example, the risk of losing a pregnancy is 44% higher than in February, according to the findings.
“One of our hypotheses is that heat may trigger miscarriage, which is something that we are now exploring further,” says Amelia Wesselink, PhD, an assistant professor of epidemiology at Boston University School of Public Health, who led the study team. “Our next step is to dig into drivers of this seasonal pattern.”
She and her colleagues analyzed seasonal differences and pregnancy outcomes for over 12,000 women. Spontaneous abortion rates peaked in late August, especially for those living in the southern and midwestern United States.
Spontaneous abortion was defined as miscarriage, chemical pregnancy (a very early miscarriage where the embryo stops growing), or blighted ovum (the embryo stops developing or never develops).
From 2013 to 2020, 12,197 women living in the United States and Canada were followed for up to 1 year using Pregnancy Study Online (PRESTO), an internet-based fertility study from the Boston University School of Public Health. Those in the study answered questions about their income, education, race/ethnicity, and lifestyle, as well as follow-up questions about their pregnancy and/or loss of pregnancy.
Most of the people studied were non-Hispanic White (86%) and had at least a college degree (79%). Almost half earned more than $100,000 annually (47%). Those seeking fertility treatments were excluded from the study.
Half of the women (6,104) said they conceived in the first 12 months of trying to get pregnant, and almost one in five (19.5%) of those who conceived miscarried.
The risk of miscarriage was 44% higher in late August than it was in late February, the month with the lowest rate of lost pregnancies. This trend was almost exclusively seen for pregnancies in their first 8 weeks. The risk of miscarriage increased 31% in late August for pregnancies at any stage.
The link between miscarriage and extreme heat was strongest in the South and Midwest, with peaks in late August and early September, respectively.
“We know so little about the causes of miscarriage that it’s difficult to tie seasonal variation in risk to any particular cause,” says David Savitz, PhD, a professor of epidemiology and obstetrics, gynecology & pediatrics at Brown University, Providence, R.I., who helped conduct the study. “Exposures vary by summer, including a lower risk of respiratory infection in the warm season, changes in diet and physical activity, and physical factors such as temperature and sunlight.”
But another expert warned that extreme heat may not be the only culprit in summer’s observed miscarriage rates.
“You need to be careful when linking summer months to miscarriage, as women may pursue more outdoor activities during summer,” says Saifuddin Ahmed PhD, a researcher at Johns Hopkins Bloomberg School of Public Health, Baltimore.
Although the paper suggested physical activity may play a role in miscarriage frequency, no analysis supported this claim, Dr. Ahmed says.
Also, participants in the study were mostly White and tended to be wealthier than the general population, so the findings may not apply to everyone, Dr. Wesselink says. Although the researchers saw some similarities between participants with income above $100,000 a year and those who earned less, socioeconomic status plays an important role in environmental exposures – including heat – so the results may not hold among lower-income populations, Dr. Wesselink says.
Dr. Wesselink and her colleagues published their findings in the journal Epidemiology.
A version of this article first appeared on WebMD.com.
Fertility doctors, IVF families, post Roe: ‘We’re anxious’
Married for nearly 5 years, Jessica King, 34, and her wife, Sarah, agreed on some things right from the start. “We always knew kids were in the equation,” Jessica says.
Now, Jessica is nearly 20 weeks pregnant, thanks to in vitro fertilization, or IVF. They did “reciprocal” IVF, with Sarah’s egg mixed with donor sperm and the embryo transferred into Jessica. “We’re excited – and terrified,” Jessica says.
But that terror goes beyond the typical concerns of excess weight gain and long labors. They live in Missouri, one of 13 states with so-called trigger laws that went into effect after the Supreme Court overturned Roe v. Wade and the constitutional right to abortion, giving states the power to regulate it. States with trigger laws either banned abortion immediately or within a specified time frame after the ruling. In all, 26 states are expected to have abortion restrictions.
Missouri now allows abortion only for medical emergencies. If her upcoming ultrasound shows serious issues, Jessica says they could easily travel to another state and pay for an abortion. She realizes not everyone can.
However, the concern about trigger laws goes well beyond abortion. Many experts worry about the “spill-over” effects the abortion laws – both the existing ones and future proposals – may have on fertility care and treatments.
‘Personhood’ laws drive the concern
“The current trigger laws on the books are not impacting people’s access to IVF,” says Barbara Collura, president and CEO of RESOLVE, an advocacy group for those with fertility issues. “What we are concerned about is they will come back and make them stronger.”
The chief concern for reproductive rights advocates is so-called “personhood” legislation. According to the Guttmacher Institute, at least six bills about personhood have been introduced in five states, including Iowa, Oklahoma, South Carolina, Vermont, and West Virginia. One of the two Oklahoma bills has gone the farthest, passed by one chamber.
Since the Guttmacher report, Ohio introduced its own personhood legislation July 11, recognizing the personhood of an unborn person from conception.
Personhood legislation defines a fertilized egg or embryo as a legal human entity, says Sean Tipton, chief policy and advocacy officer for the Washington-based American Society of Reproductive Medicine, a nonprofit advocacy group.
“If the legal status of fertilized eggs or early embryos is codified, in vitro fertilization procedures may become legally risky for patients, physicians and staff,” Mr. Tipton wrote in late June in Contemporary OB/GYN Journal. The American Society for Reproductive Medicine has posted a report on state abortion trigger laws and their potential implications for reproductive medicine. Of the 13 with trigger laws in effect, the report found concern about the potential effect on IVF only with Utah’s.
‘Safe’ states?
Even in states without trigger laws or personhood bills, IVF patients say they are anxious about how the Supreme Court ruling may ultimately affect care. Thanks to IVF, Shelly Battista and her husband Robert are expecting twins in December, little sisters to their daughter Emilia, who is 2½.
They live in Illinois, where abortion is legal. “Even though we are safe now, I think the overturning of Roe has made it clear to all of us that none of our freedoms are safe, especially reproductive rights,” Ms. Shelly says.
About one in eight U.S. couples are infertile, according to RESOLVE, In 2019, 2% of all babies born in the United States, or about 78,000 infants, were conceived with the use of assisted reproductive technologies, according to the Centers for Disease Control and Prevention. The most common assisted reproductive technology is IVF, in which the sperm fertilizes the egg outside the body and an embryo is then transferred. The standard of practice is to transfer a single embryo, freezing others for future use.
Trigger state doctors weigh in
Some fertility doctors in those “trigger” states are keeping a close eye on proposed legislation and talking to legislators for interpretation of current and proposed laws.
Eli Reshef, MD, a reproductive endocrinologist and fertility specialist at Bennett Fertility Institute in Oklahoma City, notes that his state has “the strictest abortion law in the land.” The law prohibits all abortions with few exceptions, such as the removal of an ectopic pregnancy (when a fertilized egg implants outside the uterus, such as in the fallopian tubes).
While IVF will not be affected for now, he worries that the Oklahoma law allows a private citizen to sue a health care provider that they feel is performing abortion. The Oklahoma law leaves interpretation of abortion up to the general public, who may be unfamiliar with the language of the law, House Bill 4327.
Dean Moutos, MD, a reproductive endocrinologist and medical director of Arkansas Fertility and Gynecology in Little Rock, says his state’s current trigger law should not affect IVF. “When you read the bill, it says abortion means to terminate the pregnancy of a woman.” Still, he says, “we are concerned about what might happen in the future” and the possibility that some legislators may interpret that differently.
A minority approach
John David Gordon, MD, a reproductive endocrinologist and medical director of Southeastern Fertility Center for Fertility and Reproductive Surgery in Knoxville, Tenn., is also in a trigger state. However, it’s not likely any personhood laws would affect his practice.
That’s because his center, which he acknowledges is clearly in the minority, only performs natural-cycle IVF, which usually results in a single egg, or “mini-stim IVF,” which usually results in three to eight eggs in order to limit the number that may be potentially fertilized. Often, he says, patients choose to freeze unfertilized eggs (alone) to avoid creating an excessive number of embryos. He has a “no discard” program, with any viable embryos frozen or transferred. Abandoned embryos are donated to others.
“This may work for young women,” says Marcelle Cedars, MD, director of reproductive endocrinology at the University of California, San Francisco, and president of the American Society of Reproductive Medicine. However, she says, it will be very inefficient for older patients, since they have a higher percentage of abnormal eggs.
Overall, that approach will also drive up costs, especially for older women, Dr. Cedars says. An average cycle of IVF costs $12,400, and most Americans’ insurance plans don’t cover IVF, according to Mr. Tipton.
Top concerns for IVF
“Personhood” legislation has the potential to upend many common IVF practices, experts say.
Of greatest concern to fertility practices are potential restrictions on the freezing or discarding of embryos, Dr. Cedars says. “This could have a critical impact on practicing the safest, most evidence-based medicine,” she says.
Most children born in the United States as a result of IVF procedures are born from frozen embryos, according to the Society for Assisted Reproductive Technology, an organization for reproductive specialists.
“The practice of IVF really requires that we generate more embryos than will be used in a given [IVF] cycle,” agrees Kara Goldman, MD, associate professor of obstetrics and gynecology and medical director of the fertility preservation program at Northwestern University, Chicago. She performed the embryo transfer for the Battistas.
In nature, she says, it’s known that only a small number of eggs will be competent to generate a baby. “We see the same thing in IVF.” In a single cycle, 20 eggs may be retrieved, but many fewer typically reach successful fertilization and are able to be implanted.
When patients have completed their family, unused embryos are donated to research, donated for adoption, or destroyed. If embryo destruction is outlawed, Dr. Goldman says, it will have serious ramifications for the practice of IVF.
And if personhood legislation prohibits destroying any embryos, others wonder: Would a lab technician who accidentally dropped and destroyed an embryo be subject to charges? If laws prohibit destruction of embryos, others wonder if will families be forced to pay the embryo storage fees, generally $500-$1,000 a year, in perpetuity.
If an embryo is declared a person, it could also affect a practice called preimplantation genetic testing, or PGT. In PGT, cells are retrieved from an embryo and checked for genetic disorders such as sickle cell anemia and cystic fibrosis, with some parents choosing to discard embryos that are found to be affected.
Some potential parents choose this testing because they know they are carriers for genetic diseases that are serious and even incompatible with life, says Art Caplan, PhD, head of the division of medical ethics at New York University. They may choose to discard embryos that show evidence of the diseases.
Also under fire could be “selective reduction,” reducing multiple fetuses to a single or twin, to reduce risks to babies and mother.
Dr. Caplan predicts if states have many restrictions, some providers will adopt the attitude that “if no one reports, it did not happen.” And those prospective parents with the means, he says, will go to court and fight restrictions. “When they do it, they are saying, ‘You say you are pro-life; I’m trying to have a child. What are you doing getting in my way?’”
IVF families: Tough decisions, emotional times
The Battistas, of Illinois, have had an especially rough road. Shelly was diagnosed with a fast-growing breast cancer in 2020, when Emilia was just an infant. Warned that the chemotherapy she needed would suppress her ovaries, Shelly underwent egg retrieval before starting the cancer treatment.
She opted to have a double mastectomy and her ovaries removed after learning she carried the BRCA1 genetic mutation, boosting the risk of both breast and ovarian cancer.
Once she was cancer-free, she was cleared to start IVF. The first two embryo transfers failed. The third transfer, of a single embryo, was successful. But it split, a rare occurrence, producing two embryos. “It was a big shock, but in the best way,” she says about learning they were having twins. “Now we are over the moon.”
Five frozen embryos remain. At the start, the Battistas decided to discard unused embryos. She and Robert are discussing what to do next. If they decide they are done building their family after the twins’ birth, she wonders, “do we need to discard our [other] embryos before that becomes something that isn’t eligible [possible] for us any longer?” She doesn’t want to be rushed into that decision, however, especially with her medical history.
Jessica King and Sarah have 20 more embryos.
The couple had decided to donate unused embryos for research, when the time comes, and for different reasons. Her wife’s decision is based on her belief in science, while Jessica cites her faith. “As a Jew, it is part of our faith, that we should be doing everything we can to advance humanity,” she says.
In the midst of all the uncertainty, Jessica says, only half-jokingly, that she is tempted to claim the frozen embryos as dependents. “If you are truly going to claim these are precious human lives, you should be giving me all the benefits from having children,” she says.
Shelly knows that having one daughter, with two more on the way, affects her thinking about the court’s ruling. “My overall wish would be that Roe v. Wade is reinstated, and my daughters have the same rights and options that I have … or I did have until my current 36 years of life.”
A version of this article first appeared on WebMD.com.
Married for nearly 5 years, Jessica King, 34, and her wife, Sarah, agreed on some things right from the start. “We always knew kids were in the equation,” Jessica says.
Now, Jessica is nearly 20 weeks pregnant, thanks to in vitro fertilization, or IVF. They did “reciprocal” IVF, with Sarah’s egg mixed with donor sperm and the embryo transferred into Jessica. “We’re excited – and terrified,” Jessica says.
But that terror goes beyond the typical concerns of excess weight gain and long labors. They live in Missouri, one of 13 states with so-called trigger laws that went into effect after the Supreme Court overturned Roe v. Wade and the constitutional right to abortion, giving states the power to regulate it. States with trigger laws either banned abortion immediately or within a specified time frame after the ruling. In all, 26 states are expected to have abortion restrictions.
Missouri now allows abortion only for medical emergencies. If her upcoming ultrasound shows serious issues, Jessica says they could easily travel to another state and pay for an abortion. She realizes not everyone can.
However, the concern about trigger laws goes well beyond abortion. Many experts worry about the “spill-over” effects the abortion laws – both the existing ones and future proposals – may have on fertility care and treatments.
‘Personhood’ laws drive the concern
“The current trigger laws on the books are not impacting people’s access to IVF,” says Barbara Collura, president and CEO of RESOLVE, an advocacy group for those with fertility issues. “What we are concerned about is they will come back and make them stronger.”
The chief concern for reproductive rights advocates is so-called “personhood” legislation. According to the Guttmacher Institute, at least six bills about personhood have been introduced in five states, including Iowa, Oklahoma, South Carolina, Vermont, and West Virginia. One of the two Oklahoma bills has gone the farthest, passed by one chamber.
Since the Guttmacher report, Ohio introduced its own personhood legislation July 11, recognizing the personhood of an unborn person from conception.
Personhood legislation defines a fertilized egg or embryo as a legal human entity, says Sean Tipton, chief policy and advocacy officer for the Washington-based American Society of Reproductive Medicine, a nonprofit advocacy group.
“If the legal status of fertilized eggs or early embryos is codified, in vitro fertilization procedures may become legally risky for patients, physicians and staff,” Mr. Tipton wrote in late June in Contemporary OB/GYN Journal. The American Society for Reproductive Medicine has posted a report on state abortion trigger laws and their potential implications for reproductive medicine. Of the 13 with trigger laws in effect, the report found concern about the potential effect on IVF only with Utah’s.
‘Safe’ states?
Even in states without trigger laws or personhood bills, IVF patients say they are anxious about how the Supreme Court ruling may ultimately affect care. Thanks to IVF, Shelly Battista and her husband Robert are expecting twins in December, little sisters to their daughter Emilia, who is 2½.
They live in Illinois, where abortion is legal. “Even though we are safe now, I think the overturning of Roe has made it clear to all of us that none of our freedoms are safe, especially reproductive rights,” Ms. Shelly says.
About one in eight U.S. couples are infertile, according to RESOLVE, In 2019, 2% of all babies born in the United States, or about 78,000 infants, were conceived with the use of assisted reproductive technologies, according to the Centers for Disease Control and Prevention. The most common assisted reproductive technology is IVF, in which the sperm fertilizes the egg outside the body and an embryo is then transferred. The standard of practice is to transfer a single embryo, freezing others for future use.
Trigger state doctors weigh in
Some fertility doctors in those “trigger” states are keeping a close eye on proposed legislation and talking to legislators for interpretation of current and proposed laws.
Eli Reshef, MD, a reproductive endocrinologist and fertility specialist at Bennett Fertility Institute in Oklahoma City, notes that his state has “the strictest abortion law in the land.” The law prohibits all abortions with few exceptions, such as the removal of an ectopic pregnancy (when a fertilized egg implants outside the uterus, such as in the fallopian tubes).
While IVF will not be affected for now, he worries that the Oklahoma law allows a private citizen to sue a health care provider that they feel is performing abortion. The Oklahoma law leaves interpretation of abortion up to the general public, who may be unfamiliar with the language of the law, House Bill 4327.
Dean Moutos, MD, a reproductive endocrinologist and medical director of Arkansas Fertility and Gynecology in Little Rock, says his state’s current trigger law should not affect IVF. “When you read the bill, it says abortion means to terminate the pregnancy of a woman.” Still, he says, “we are concerned about what might happen in the future” and the possibility that some legislators may interpret that differently.
A minority approach
John David Gordon, MD, a reproductive endocrinologist and medical director of Southeastern Fertility Center for Fertility and Reproductive Surgery in Knoxville, Tenn., is also in a trigger state. However, it’s not likely any personhood laws would affect his practice.
That’s because his center, which he acknowledges is clearly in the minority, only performs natural-cycle IVF, which usually results in a single egg, or “mini-stim IVF,” which usually results in three to eight eggs in order to limit the number that may be potentially fertilized. Often, he says, patients choose to freeze unfertilized eggs (alone) to avoid creating an excessive number of embryos. He has a “no discard” program, with any viable embryos frozen or transferred. Abandoned embryos are donated to others.
“This may work for young women,” says Marcelle Cedars, MD, director of reproductive endocrinology at the University of California, San Francisco, and president of the American Society of Reproductive Medicine. However, she says, it will be very inefficient for older patients, since they have a higher percentage of abnormal eggs.
Overall, that approach will also drive up costs, especially for older women, Dr. Cedars says. An average cycle of IVF costs $12,400, and most Americans’ insurance plans don’t cover IVF, according to Mr. Tipton.
Top concerns for IVF
“Personhood” legislation has the potential to upend many common IVF practices, experts say.
Of greatest concern to fertility practices are potential restrictions on the freezing or discarding of embryos, Dr. Cedars says. “This could have a critical impact on practicing the safest, most evidence-based medicine,” she says.
Most children born in the United States as a result of IVF procedures are born from frozen embryos, according to the Society for Assisted Reproductive Technology, an organization for reproductive specialists.
“The practice of IVF really requires that we generate more embryos than will be used in a given [IVF] cycle,” agrees Kara Goldman, MD, associate professor of obstetrics and gynecology and medical director of the fertility preservation program at Northwestern University, Chicago. She performed the embryo transfer for the Battistas.
In nature, she says, it’s known that only a small number of eggs will be competent to generate a baby. “We see the same thing in IVF.” In a single cycle, 20 eggs may be retrieved, but many fewer typically reach successful fertilization and are able to be implanted.
When patients have completed their family, unused embryos are donated to research, donated for adoption, or destroyed. If embryo destruction is outlawed, Dr. Goldman says, it will have serious ramifications for the practice of IVF.
And if personhood legislation prohibits destroying any embryos, others wonder: Would a lab technician who accidentally dropped and destroyed an embryo be subject to charges? If laws prohibit destruction of embryos, others wonder if will families be forced to pay the embryo storage fees, generally $500-$1,000 a year, in perpetuity.
If an embryo is declared a person, it could also affect a practice called preimplantation genetic testing, or PGT. In PGT, cells are retrieved from an embryo and checked for genetic disorders such as sickle cell anemia and cystic fibrosis, with some parents choosing to discard embryos that are found to be affected.
Some potential parents choose this testing because they know they are carriers for genetic diseases that are serious and even incompatible with life, says Art Caplan, PhD, head of the division of medical ethics at New York University. They may choose to discard embryos that show evidence of the diseases.
Also under fire could be “selective reduction,” reducing multiple fetuses to a single or twin, to reduce risks to babies and mother.
Dr. Caplan predicts if states have many restrictions, some providers will adopt the attitude that “if no one reports, it did not happen.” And those prospective parents with the means, he says, will go to court and fight restrictions. “When they do it, they are saying, ‘You say you are pro-life; I’m trying to have a child. What are you doing getting in my way?’”
IVF families: Tough decisions, emotional times
The Battistas, of Illinois, have had an especially rough road. Shelly was diagnosed with a fast-growing breast cancer in 2020, when Emilia was just an infant. Warned that the chemotherapy she needed would suppress her ovaries, Shelly underwent egg retrieval before starting the cancer treatment.
She opted to have a double mastectomy and her ovaries removed after learning she carried the BRCA1 genetic mutation, boosting the risk of both breast and ovarian cancer.
Once she was cancer-free, she was cleared to start IVF. The first two embryo transfers failed. The third transfer, of a single embryo, was successful. But it split, a rare occurrence, producing two embryos. “It was a big shock, but in the best way,” she says about learning they were having twins. “Now we are over the moon.”
Five frozen embryos remain. At the start, the Battistas decided to discard unused embryos. She and Robert are discussing what to do next. If they decide they are done building their family after the twins’ birth, she wonders, “do we need to discard our [other] embryos before that becomes something that isn’t eligible [possible] for us any longer?” She doesn’t want to be rushed into that decision, however, especially with her medical history.
Jessica King and Sarah have 20 more embryos.
The couple had decided to donate unused embryos for research, when the time comes, and for different reasons. Her wife’s decision is based on her belief in science, while Jessica cites her faith. “As a Jew, it is part of our faith, that we should be doing everything we can to advance humanity,” she says.
In the midst of all the uncertainty, Jessica says, only half-jokingly, that she is tempted to claim the frozen embryos as dependents. “If you are truly going to claim these are precious human lives, you should be giving me all the benefits from having children,” she says.
Shelly knows that having one daughter, with two more on the way, affects her thinking about the court’s ruling. “My overall wish would be that Roe v. Wade is reinstated, and my daughters have the same rights and options that I have … or I did have until my current 36 years of life.”
A version of this article first appeared on WebMD.com.
Married for nearly 5 years, Jessica King, 34, and her wife, Sarah, agreed on some things right from the start. “We always knew kids were in the equation,” Jessica says.
Now, Jessica is nearly 20 weeks pregnant, thanks to in vitro fertilization, or IVF. They did “reciprocal” IVF, with Sarah’s egg mixed with donor sperm and the embryo transferred into Jessica. “We’re excited – and terrified,” Jessica says.
But that terror goes beyond the typical concerns of excess weight gain and long labors. They live in Missouri, one of 13 states with so-called trigger laws that went into effect after the Supreme Court overturned Roe v. Wade and the constitutional right to abortion, giving states the power to regulate it. States with trigger laws either banned abortion immediately or within a specified time frame after the ruling. In all, 26 states are expected to have abortion restrictions.
Missouri now allows abortion only for medical emergencies. If her upcoming ultrasound shows serious issues, Jessica says they could easily travel to another state and pay for an abortion. She realizes not everyone can.
However, the concern about trigger laws goes well beyond abortion. Many experts worry about the “spill-over” effects the abortion laws – both the existing ones and future proposals – may have on fertility care and treatments.
‘Personhood’ laws drive the concern
“The current trigger laws on the books are not impacting people’s access to IVF,” says Barbara Collura, president and CEO of RESOLVE, an advocacy group for those with fertility issues. “What we are concerned about is they will come back and make them stronger.”
The chief concern for reproductive rights advocates is so-called “personhood” legislation. According to the Guttmacher Institute, at least six bills about personhood have been introduced in five states, including Iowa, Oklahoma, South Carolina, Vermont, and West Virginia. One of the two Oklahoma bills has gone the farthest, passed by one chamber.
Since the Guttmacher report, Ohio introduced its own personhood legislation July 11, recognizing the personhood of an unborn person from conception.
Personhood legislation defines a fertilized egg or embryo as a legal human entity, says Sean Tipton, chief policy and advocacy officer for the Washington-based American Society of Reproductive Medicine, a nonprofit advocacy group.
“If the legal status of fertilized eggs or early embryos is codified, in vitro fertilization procedures may become legally risky for patients, physicians and staff,” Mr. Tipton wrote in late June in Contemporary OB/GYN Journal. The American Society for Reproductive Medicine has posted a report on state abortion trigger laws and their potential implications for reproductive medicine. Of the 13 with trigger laws in effect, the report found concern about the potential effect on IVF only with Utah’s.
‘Safe’ states?
Even in states without trigger laws or personhood bills, IVF patients say they are anxious about how the Supreme Court ruling may ultimately affect care. Thanks to IVF, Shelly Battista and her husband Robert are expecting twins in December, little sisters to their daughter Emilia, who is 2½.
They live in Illinois, where abortion is legal. “Even though we are safe now, I think the overturning of Roe has made it clear to all of us that none of our freedoms are safe, especially reproductive rights,” Ms. Shelly says.
About one in eight U.S. couples are infertile, according to RESOLVE, In 2019, 2% of all babies born in the United States, or about 78,000 infants, were conceived with the use of assisted reproductive technologies, according to the Centers for Disease Control and Prevention. The most common assisted reproductive technology is IVF, in which the sperm fertilizes the egg outside the body and an embryo is then transferred. The standard of practice is to transfer a single embryo, freezing others for future use.
Trigger state doctors weigh in
Some fertility doctors in those “trigger” states are keeping a close eye on proposed legislation and talking to legislators for interpretation of current and proposed laws.
Eli Reshef, MD, a reproductive endocrinologist and fertility specialist at Bennett Fertility Institute in Oklahoma City, notes that his state has “the strictest abortion law in the land.” The law prohibits all abortions with few exceptions, such as the removal of an ectopic pregnancy (when a fertilized egg implants outside the uterus, such as in the fallopian tubes).
While IVF will not be affected for now, he worries that the Oklahoma law allows a private citizen to sue a health care provider that they feel is performing abortion. The Oklahoma law leaves interpretation of abortion up to the general public, who may be unfamiliar with the language of the law, House Bill 4327.
Dean Moutos, MD, a reproductive endocrinologist and medical director of Arkansas Fertility and Gynecology in Little Rock, says his state’s current trigger law should not affect IVF. “When you read the bill, it says abortion means to terminate the pregnancy of a woman.” Still, he says, “we are concerned about what might happen in the future” and the possibility that some legislators may interpret that differently.
A minority approach
John David Gordon, MD, a reproductive endocrinologist and medical director of Southeastern Fertility Center for Fertility and Reproductive Surgery in Knoxville, Tenn., is also in a trigger state. However, it’s not likely any personhood laws would affect his practice.
That’s because his center, which he acknowledges is clearly in the minority, only performs natural-cycle IVF, which usually results in a single egg, or “mini-stim IVF,” which usually results in three to eight eggs in order to limit the number that may be potentially fertilized. Often, he says, patients choose to freeze unfertilized eggs (alone) to avoid creating an excessive number of embryos. He has a “no discard” program, with any viable embryos frozen or transferred. Abandoned embryos are donated to others.
“This may work for young women,” says Marcelle Cedars, MD, director of reproductive endocrinology at the University of California, San Francisco, and president of the American Society of Reproductive Medicine. However, she says, it will be very inefficient for older patients, since they have a higher percentage of abnormal eggs.
Overall, that approach will also drive up costs, especially for older women, Dr. Cedars says. An average cycle of IVF costs $12,400, and most Americans’ insurance plans don’t cover IVF, according to Mr. Tipton.
Top concerns for IVF
“Personhood” legislation has the potential to upend many common IVF practices, experts say.
Of greatest concern to fertility practices are potential restrictions on the freezing or discarding of embryos, Dr. Cedars says. “This could have a critical impact on practicing the safest, most evidence-based medicine,” she says.
Most children born in the United States as a result of IVF procedures are born from frozen embryos, according to the Society for Assisted Reproductive Technology, an organization for reproductive specialists.
“The practice of IVF really requires that we generate more embryos than will be used in a given [IVF] cycle,” agrees Kara Goldman, MD, associate professor of obstetrics and gynecology and medical director of the fertility preservation program at Northwestern University, Chicago. She performed the embryo transfer for the Battistas.
In nature, she says, it’s known that only a small number of eggs will be competent to generate a baby. “We see the same thing in IVF.” In a single cycle, 20 eggs may be retrieved, but many fewer typically reach successful fertilization and are able to be implanted.
When patients have completed their family, unused embryos are donated to research, donated for adoption, or destroyed. If embryo destruction is outlawed, Dr. Goldman says, it will have serious ramifications for the practice of IVF.
And if personhood legislation prohibits destroying any embryos, others wonder: Would a lab technician who accidentally dropped and destroyed an embryo be subject to charges? If laws prohibit destruction of embryos, others wonder if will families be forced to pay the embryo storage fees, generally $500-$1,000 a year, in perpetuity.
If an embryo is declared a person, it could also affect a practice called preimplantation genetic testing, or PGT. In PGT, cells are retrieved from an embryo and checked for genetic disorders such as sickle cell anemia and cystic fibrosis, with some parents choosing to discard embryos that are found to be affected.
Some potential parents choose this testing because they know they are carriers for genetic diseases that are serious and even incompatible with life, says Art Caplan, PhD, head of the division of medical ethics at New York University. They may choose to discard embryos that show evidence of the diseases.
Also under fire could be “selective reduction,” reducing multiple fetuses to a single or twin, to reduce risks to babies and mother.
Dr. Caplan predicts if states have many restrictions, some providers will adopt the attitude that “if no one reports, it did not happen.” And those prospective parents with the means, he says, will go to court and fight restrictions. “When they do it, they are saying, ‘You say you are pro-life; I’m trying to have a child. What are you doing getting in my way?’”
IVF families: Tough decisions, emotional times
The Battistas, of Illinois, have had an especially rough road. Shelly was diagnosed with a fast-growing breast cancer in 2020, when Emilia was just an infant. Warned that the chemotherapy she needed would suppress her ovaries, Shelly underwent egg retrieval before starting the cancer treatment.
She opted to have a double mastectomy and her ovaries removed after learning she carried the BRCA1 genetic mutation, boosting the risk of both breast and ovarian cancer.
Once she was cancer-free, she was cleared to start IVF. The first two embryo transfers failed. The third transfer, of a single embryo, was successful. But it split, a rare occurrence, producing two embryos. “It was a big shock, but in the best way,” she says about learning they were having twins. “Now we are over the moon.”
Five frozen embryos remain. At the start, the Battistas decided to discard unused embryos. She and Robert are discussing what to do next. If they decide they are done building their family after the twins’ birth, she wonders, “do we need to discard our [other] embryos before that becomes something that isn’t eligible [possible] for us any longer?” She doesn’t want to be rushed into that decision, however, especially with her medical history.
Jessica King and Sarah have 20 more embryos.
The couple had decided to donate unused embryos for research, when the time comes, and for different reasons. Her wife’s decision is based on her belief in science, while Jessica cites her faith. “As a Jew, it is part of our faith, that we should be doing everything we can to advance humanity,” she says.
In the midst of all the uncertainty, Jessica says, only half-jokingly, that she is tempted to claim the frozen embryos as dependents. “If you are truly going to claim these are precious human lives, you should be giving me all the benefits from having children,” she says.
Shelly knows that having one daughter, with two more on the way, affects her thinking about the court’s ruling. “My overall wish would be that Roe v. Wade is reinstated, and my daughters have the same rights and options that I have … or I did have until my current 36 years of life.”
A version of this article first appeared on WebMD.com.
Three things to know about insurance coverage for abortion
Will your health plan pay for an abortion now that the Supreme Court has overturned Roe v. Wade?
Even before the June 24 ruling, insurance coverage for abortion varied widely. Now the issue is even more complex as states set varying rules – about half are expected to limit or ban abortion in almost all circumstances.
To be clear, though, the question of whether an insurance plan covers abortion is not the same as whether abortion is allowed in a state. Coverage issues are more complicated and governed by a wide variety of factors, including the level of abortion access a state allows.
How dense a thicket is it? Abortion may be covered by a health plan, but if no providers are available, patients don’t have access. However, people with insurance that does not cover abortion can still get one – but only if it’s available in their states or they can afford to travel and pay out of pocket. There are also a host of unanswered questions about whether states that restrict abortion will have the legal authority to target abortion coverage in employer plans.
The issues will likely be before the courts for years to come.
“States will pass laws, there will be some conflict, and then it goes to the courts,” said Erin Fuse Brown, director of the Center for Law, Health & Society at the Georgia State University, Atlanta. “It could be a while.”
In the meantime, here are answers to three common questions.
Are health plans – or employers – required to offer coverage for elective abortions?
The simple answer is “no.”
“There’s no law that requires any health plan, employer-based or anything else, to cover an elective abortion,” Ms. Fuse Brown said.
Whether they do is more complicated.
Some job-based health plans cover elective abortions. Patients can search their plan documents or call their insurers directly to check.
Coverage is more likely in plans offered by self-insured employers because a federal pensions law generally preempts state regulation of those health plans. Self-funded employers, which tend to be the larger ones, pay the medical bills, although they generally hire third parties, sometimes health insurers, to handle claims and administrative work.
Still, millions of Americans work for smaller employers, which tend to buy plans directly from health insurers, which then pay the medical bills. Those plans, known as “fully insured,” are subject to state laws, whose approaches to abortion coverage have long varied.
Eleven states bar those private plans from covering abortion in most circumstances, according to KFF, although some of the states allow consumers to purchase an insurance rider that would cover abortion costs.
If you’re not sure what type of health plan you have, ask the administrators.
“There is no way to tell from the face of your insurance card if you are fully insured or self-funded,” Ms. Fuse Brown said.
For the more than 14 million Americans who buy their coverage through the Affordable Care Act marketplaces, their state of residence is key.
Twenty-six states restrict abortion coverage in ACA plans, while seven states require it as a plan benefit, according to KFF. Those states are California, Illinois, Maine, Maryland, New York, Oregon, and Washington.
The rules for Medicaid, the federal-state health program for people with low incomes, also vary. Thirty-four states and the District of Columbia follow the so-called Hyde Amendment, which bars federal funds from paying for abortions, except in cases of rape or incest or to save the life of the mother, although some states allow coverage for other medically necessary abortions.
For all those reasons, it’s not surprising that research published in the journal Health Affairs noted that patients paid out-of-pocket for the majority of abortions (69% in one study). The researchers found that the median cost of a medication abortion was $560 and that abortion procedures ranged from a median of $575 in the first trimester to $895 in the second.
What about coverage for pregnancy-related complications that require treatment similar to abortion?
Insurance policies must cover care for essential health services, including medically necessary pregnancy care and abortion when carrying a pregnancy to term would endanger a patient’s life.
Under the Pregnancy Discrimination Act of 1978 and other rules, Ms. Fuse Brown said, “pregnancy and prenatal care, including high-risk pregnancies, and obstetric care in general is required to be covered.”
In an ectopic pregnancy – when a fertilized egg implants outside the uterus – the embryo is not viable, and the condition is generally life-threatening to the mother without medical treatment. Many other scenarios could come into play, including situations in which a woman has a miscarriage but not all the tissue is expelled, potentially leading to a dangerous infection.
Although all state laws that currently restrict abortion include an exception to save the life of the mother, what constitutes a life-threatening scenario is not always clear. That means physicians in abortion-ban states may have to weigh the pregnant person’s medical risk against possible legal ramifications.
“This is less of a coverage question and more of a question of whether providers in the states that ban abortion are going to provide the care,” said Katie Keith, a research faculty member at the Center on Health Insurance Reforms at Georgetown University, Washington. “All of these laws are designed to chill behavior, to make it so unattractive or scary to providers to keep them from doing it at all.”
Can residents of states where abortion is illegal get coverage in other states or help with travel costs?
In recent weeks, many large employers – including Microsoft, Bank of America, Disney, and Netflix – have said they will set up programs to help pay travel costs so workers or other beneficiaries in states with bans can travel to get an abortion elsewhere.
But it isn’t as straightforward as it sounds. Employers will have to figure out whether workers will access this benefit through the health plan or some other reimbursement method. Protecting privacy, too, may be an issue. Some consultants also said employers will need to consider whether their travel reimbursement benefit conflicts with other rules. If an employer, for example, covers travel for abortion procedures but not for an eating disorder clinic, does that violate the Mental Health Parity and Addiction Equity Act? If a plan has no providers willing or able to do abortions, does it violate any state or federal network adequacy rules?
Lawmakers need to think about these conflicts, said Jessica Waltman, vice president for compliance at employee benefits company MZQ Consulting. “They could be putting all the employer group plans in their state in a very precarious position if that state law would prohibit them from complying with federal law,” particularly if they restrict access to benefits called for in the Pregnancy Discrimination Act.
There are other potential conflicts if an employer is in a state that allows abortion but a worker is in a state that restricts it. “If I’m an Oregon-based company, my insurance plan must provide for abortion coverage, but what do I do about an Oklahoma employee? I don’t know the answer,” said René Thorne, a principal at Jackson Lewis, where she oversees litigation that involves self-insured firms.
Also uncertain is whether state laws will take aim at insurers, employers, or others that offer benefits, including travel or televisits, for abortion services.
Laws that restrict abortion, Ms. Thorne wrote in a white paper for clients, generally apply to the medical provider and sometimes those who “aid or abet” the abortion. Some states, including Texas, allow private citizens to sue for $10,000 anyone who provides an illegal abortion or helps a person access an abortion.
Whether those laws will be applied to employers or insurers will undoubtedly end up in the courts.
“We are in uncharted territory here, as we’ve never before been in a situation where plans, as well as their employer sponsors and those administering the plans, might face criminal liability in connection with a plan benefit,” said Seth Perretta, a principal at the Groom Law Group, which advises employers.
Answers won’t come soon, but “there will be so much litigation around this,” said Ms. Thorne.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Will your health plan pay for an abortion now that the Supreme Court has overturned Roe v. Wade?
Even before the June 24 ruling, insurance coverage for abortion varied widely. Now the issue is even more complex as states set varying rules – about half are expected to limit or ban abortion in almost all circumstances.
To be clear, though, the question of whether an insurance plan covers abortion is not the same as whether abortion is allowed in a state. Coverage issues are more complicated and governed by a wide variety of factors, including the level of abortion access a state allows.
How dense a thicket is it? Abortion may be covered by a health plan, but if no providers are available, patients don’t have access. However, people with insurance that does not cover abortion can still get one – but only if it’s available in their states or they can afford to travel and pay out of pocket. There are also a host of unanswered questions about whether states that restrict abortion will have the legal authority to target abortion coverage in employer plans.
The issues will likely be before the courts for years to come.
“States will pass laws, there will be some conflict, and then it goes to the courts,” said Erin Fuse Brown, director of the Center for Law, Health & Society at the Georgia State University, Atlanta. “It could be a while.”
In the meantime, here are answers to three common questions.
Are health plans – or employers – required to offer coverage for elective abortions?
The simple answer is “no.”
“There’s no law that requires any health plan, employer-based or anything else, to cover an elective abortion,” Ms. Fuse Brown said.
Whether they do is more complicated.
Some job-based health plans cover elective abortions. Patients can search their plan documents or call their insurers directly to check.
Coverage is more likely in plans offered by self-insured employers because a federal pensions law generally preempts state regulation of those health plans. Self-funded employers, which tend to be the larger ones, pay the medical bills, although they generally hire third parties, sometimes health insurers, to handle claims and administrative work.
Still, millions of Americans work for smaller employers, which tend to buy plans directly from health insurers, which then pay the medical bills. Those plans, known as “fully insured,” are subject to state laws, whose approaches to abortion coverage have long varied.
Eleven states bar those private plans from covering abortion in most circumstances, according to KFF, although some of the states allow consumers to purchase an insurance rider that would cover abortion costs.
If you’re not sure what type of health plan you have, ask the administrators.
“There is no way to tell from the face of your insurance card if you are fully insured or self-funded,” Ms. Fuse Brown said.
For the more than 14 million Americans who buy their coverage through the Affordable Care Act marketplaces, their state of residence is key.
Twenty-six states restrict abortion coverage in ACA plans, while seven states require it as a plan benefit, according to KFF. Those states are California, Illinois, Maine, Maryland, New York, Oregon, and Washington.
The rules for Medicaid, the federal-state health program for people with low incomes, also vary. Thirty-four states and the District of Columbia follow the so-called Hyde Amendment, which bars federal funds from paying for abortions, except in cases of rape or incest or to save the life of the mother, although some states allow coverage for other medically necessary abortions.
For all those reasons, it’s not surprising that research published in the journal Health Affairs noted that patients paid out-of-pocket for the majority of abortions (69% in one study). The researchers found that the median cost of a medication abortion was $560 and that abortion procedures ranged from a median of $575 in the first trimester to $895 in the second.
What about coverage for pregnancy-related complications that require treatment similar to abortion?
Insurance policies must cover care for essential health services, including medically necessary pregnancy care and abortion when carrying a pregnancy to term would endanger a patient’s life.
Under the Pregnancy Discrimination Act of 1978 and other rules, Ms. Fuse Brown said, “pregnancy and prenatal care, including high-risk pregnancies, and obstetric care in general is required to be covered.”
In an ectopic pregnancy – when a fertilized egg implants outside the uterus – the embryo is not viable, and the condition is generally life-threatening to the mother without medical treatment. Many other scenarios could come into play, including situations in which a woman has a miscarriage but not all the tissue is expelled, potentially leading to a dangerous infection.
Although all state laws that currently restrict abortion include an exception to save the life of the mother, what constitutes a life-threatening scenario is not always clear. That means physicians in abortion-ban states may have to weigh the pregnant person’s medical risk against possible legal ramifications.
“This is less of a coverage question and more of a question of whether providers in the states that ban abortion are going to provide the care,” said Katie Keith, a research faculty member at the Center on Health Insurance Reforms at Georgetown University, Washington. “All of these laws are designed to chill behavior, to make it so unattractive or scary to providers to keep them from doing it at all.”
Can residents of states where abortion is illegal get coverage in other states or help with travel costs?
In recent weeks, many large employers – including Microsoft, Bank of America, Disney, and Netflix – have said they will set up programs to help pay travel costs so workers or other beneficiaries in states with bans can travel to get an abortion elsewhere.
But it isn’t as straightforward as it sounds. Employers will have to figure out whether workers will access this benefit through the health plan or some other reimbursement method. Protecting privacy, too, may be an issue. Some consultants also said employers will need to consider whether their travel reimbursement benefit conflicts with other rules. If an employer, for example, covers travel for abortion procedures but not for an eating disorder clinic, does that violate the Mental Health Parity and Addiction Equity Act? If a plan has no providers willing or able to do abortions, does it violate any state or federal network adequacy rules?
Lawmakers need to think about these conflicts, said Jessica Waltman, vice president for compliance at employee benefits company MZQ Consulting. “They could be putting all the employer group plans in their state in a very precarious position if that state law would prohibit them from complying with federal law,” particularly if they restrict access to benefits called for in the Pregnancy Discrimination Act.
There are other potential conflicts if an employer is in a state that allows abortion but a worker is in a state that restricts it. “If I’m an Oregon-based company, my insurance plan must provide for abortion coverage, but what do I do about an Oklahoma employee? I don’t know the answer,” said René Thorne, a principal at Jackson Lewis, where she oversees litigation that involves self-insured firms.
Also uncertain is whether state laws will take aim at insurers, employers, or others that offer benefits, including travel or televisits, for abortion services.
Laws that restrict abortion, Ms. Thorne wrote in a white paper for clients, generally apply to the medical provider and sometimes those who “aid or abet” the abortion. Some states, including Texas, allow private citizens to sue for $10,000 anyone who provides an illegal abortion or helps a person access an abortion.
Whether those laws will be applied to employers or insurers will undoubtedly end up in the courts.
“We are in uncharted territory here, as we’ve never before been in a situation where plans, as well as their employer sponsors and those administering the plans, might face criminal liability in connection with a plan benefit,” said Seth Perretta, a principal at the Groom Law Group, which advises employers.
Answers won’t come soon, but “there will be so much litigation around this,” said Ms. Thorne.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Will your health plan pay for an abortion now that the Supreme Court has overturned Roe v. Wade?
Even before the June 24 ruling, insurance coverage for abortion varied widely. Now the issue is even more complex as states set varying rules – about half are expected to limit or ban abortion in almost all circumstances.
To be clear, though, the question of whether an insurance plan covers abortion is not the same as whether abortion is allowed in a state. Coverage issues are more complicated and governed by a wide variety of factors, including the level of abortion access a state allows.
How dense a thicket is it? Abortion may be covered by a health plan, but if no providers are available, patients don’t have access. However, people with insurance that does not cover abortion can still get one – but only if it’s available in their states or they can afford to travel and pay out of pocket. There are also a host of unanswered questions about whether states that restrict abortion will have the legal authority to target abortion coverage in employer plans.
The issues will likely be before the courts for years to come.
“States will pass laws, there will be some conflict, and then it goes to the courts,” said Erin Fuse Brown, director of the Center for Law, Health & Society at the Georgia State University, Atlanta. “It could be a while.”
In the meantime, here are answers to three common questions.
Are health plans – or employers – required to offer coverage for elective abortions?
The simple answer is “no.”
“There’s no law that requires any health plan, employer-based or anything else, to cover an elective abortion,” Ms. Fuse Brown said.
Whether they do is more complicated.
Some job-based health plans cover elective abortions. Patients can search their plan documents or call their insurers directly to check.
Coverage is more likely in plans offered by self-insured employers because a federal pensions law generally preempts state regulation of those health plans. Self-funded employers, which tend to be the larger ones, pay the medical bills, although they generally hire third parties, sometimes health insurers, to handle claims and administrative work.
Still, millions of Americans work for smaller employers, which tend to buy plans directly from health insurers, which then pay the medical bills. Those plans, known as “fully insured,” are subject to state laws, whose approaches to abortion coverage have long varied.
Eleven states bar those private plans from covering abortion in most circumstances, according to KFF, although some of the states allow consumers to purchase an insurance rider that would cover abortion costs.
If you’re not sure what type of health plan you have, ask the administrators.
“There is no way to tell from the face of your insurance card if you are fully insured or self-funded,” Ms. Fuse Brown said.
For the more than 14 million Americans who buy their coverage through the Affordable Care Act marketplaces, their state of residence is key.
Twenty-six states restrict abortion coverage in ACA plans, while seven states require it as a plan benefit, according to KFF. Those states are California, Illinois, Maine, Maryland, New York, Oregon, and Washington.
The rules for Medicaid, the federal-state health program for people with low incomes, also vary. Thirty-four states and the District of Columbia follow the so-called Hyde Amendment, which bars federal funds from paying for abortions, except in cases of rape or incest or to save the life of the mother, although some states allow coverage for other medically necessary abortions.
For all those reasons, it’s not surprising that research published in the journal Health Affairs noted that patients paid out-of-pocket for the majority of abortions (69% in one study). The researchers found that the median cost of a medication abortion was $560 and that abortion procedures ranged from a median of $575 in the first trimester to $895 in the second.
What about coverage for pregnancy-related complications that require treatment similar to abortion?
Insurance policies must cover care for essential health services, including medically necessary pregnancy care and abortion when carrying a pregnancy to term would endanger a patient’s life.
Under the Pregnancy Discrimination Act of 1978 and other rules, Ms. Fuse Brown said, “pregnancy and prenatal care, including high-risk pregnancies, and obstetric care in general is required to be covered.”
In an ectopic pregnancy – when a fertilized egg implants outside the uterus – the embryo is not viable, and the condition is generally life-threatening to the mother without medical treatment. Many other scenarios could come into play, including situations in which a woman has a miscarriage but not all the tissue is expelled, potentially leading to a dangerous infection.
Although all state laws that currently restrict abortion include an exception to save the life of the mother, what constitutes a life-threatening scenario is not always clear. That means physicians in abortion-ban states may have to weigh the pregnant person’s medical risk against possible legal ramifications.
“This is less of a coverage question and more of a question of whether providers in the states that ban abortion are going to provide the care,” said Katie Keith, a research faculty member at the Center on Health Insurance Reforms at Georgetown University, Washington. “All of these laws are designed to chill behavior, to make it so unattractive or scary to providers to keep them from doing it at all.”
Can residents of states where abortion is illegal get coverage in other states or help with travel costs?
In recent weeks, many large employers – including Microsoft, Bank of America, Disney, and Netflix – have said they will set up programs to help pay travel costs so workers or other beneficiaries in states with bans can travel to get an abortion elsewhere.
But it isn’t as straightforward as it sounds. Employers will have to figure out whether workers will access this benefit through the health plan or some other reimbursement method. Protecting privacy, too, may be an issue. Some consultants also said employers will need to consider whether their travel reimbursement benefit conflicts with other rules. If an employer, for example, covers travel for abortion procedures but not for an eating disorder clinic, does that violate the Mental Health Parity and Addiction Equity Act? If a plan has no providers willing or able to do abortions, does it violate any state or federal network adequacy rules?
Lawmakers need to think about these conflicts, said Jessica Waltman, vice president for compliance at employee benefits company MZQ Consulting. “They could be putting all the employer group plans in their state in a very precarious position if that state law would prohibit them from complying with federal law,” particularly if they restrict access to benefits called for in the Pregnancy Discrimination Act.
There are other potential conflicts if an employer is in a state that allows abortion but a worker is in a state that restricts it. “If I’m an Oregon-based company, my insurance plan must provide for abortion coverage, but what do I do about an Oklahoma employee? I don’t know the answer,” said René Thorne, a principal at Jackson Lewis, where she oversees litigation that involves self-insured firms.
Also uncertain is whether state laws will take aim at insurers, employers, or others that offer benefits, including travel or televisits, for abortion services.
Laws that restrict abortion, Ms. Thorne wrote in a white paper for clients, generally apply to the medical provider and sometimes those who “aid or abet” the abortion. Some states, including Texas, allow private citizens to sue for $10,000 anyone who provides an illegal abortion or helps a person access an abortion.
Whether those laws will be applied to employers or insurers will undoubtedly end up in the courts.
“We are in uncharted territory here, as we’ve never before been in a situation where plans, as well as their employer sponsors and those administering the plans, might face criminal liability in connection with a plan benefit,” said Seth Perretta, a principal at the Groom Law Group, which advises employers.
Answers won’t come soon, but “there will be so much litigation around this,” said Ms. Thorne.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Feds warn pharmacists: Don’t refuse to provide abortion pills
The Department of Health & Human Services listed several conditions that are commonly treated with drugs that can induce abortion, warning that withholding the pills could violate civil rights laws and could be considered discrimination based on sex or disability.
“We are committed to ensuring that everyone can access health care, free of discrimination,” Xavier Becerra, the U.S. health and human services secretary, said in a statement. “This includes access to prescription medications for reproductive health and other types of care.”
On July 11, Mr. Becerra issued other guidance to remind hospitals that federal law requires doctors to provide stabilizing treatment for patients with emergency medical conditions, which could include an abortion for those who arrive at emergency departments with a life-threatening issue.
Both actions by the Biden administration assert that federal laws override state laws that have banned or restricted abortion access since the Supreme Court overturned Roe v. Wade, according to The New York Times.
The guidance focuses on Section 1557 of the Affordable Care Act and related federal regulations, which state that recipients of federal financial assistance – including pharmacies that get Medicare and Medicaid payments – can’t discriminate based on race, color, national origin, sex, age, and disability. The guidance highlights that pregnancy discrimination includes discrimination based on current pregnancy, past pregnancy, potential or intended pregnancy, and medical conditions related to pregnancy or childbirth.
Three drugs in particular – mifepristone, misoprostol, and methotrexate – are often prescribed for other medical conditions but can also induce abortions in certain cases. Methotrexate, for example, is used for cancer and autoimmune disorders, such as rheumatoid arthritis.
Mifepristone is often used for patients with Cushing’s syndrome, while misoprostol is often prescribed for ulcers. When used in combination, the two drugs are authorized by the Food and Drug Administration to terminate a pregnancy during the first 10 weeks and after a miscarriage.
Since Roe was overturned, women have posted on social media that they were denied the drugs for their medical conditions due to being of “childbearing age.”
“These are very legitimate issues in terms of people being concerned about having access to the basic medications that they have been receiving for years, just because those medications have the capacity to end a pregnancy,” Alina Salganicoff, PhD, the director of women’s health policy at the Kaiser Family Foundation, told the Times.
“It doesn’t sound like [pharmacies] are blocking this for men,” she said.
The Biden administration’s guidance will likely be challenged in court, the newspaper reported. The update is cautiously written and doesn’t directly say that pharmacies must provide the drugs for the purpose of medication abortion.
In the meantime, pharmacists could feel stuck in the middle. Pharmacists who “believe they are acting in good faith in accordance with their state’s laws on abortion shouldn’t be left without a clear pathway forward,” the National Community Pharmacists Association said in a statement on July 13.
The association, which represents about 19,400 independent pharmacies across the United States, said pharmacies are regulated by states, and most states haven’t advised pharmacists on how to dispense the drugs in question.
“States have provided very little clarity on how pharmacists should proceed in light of conflicting state and federal laws and regulations,” B. Douglas Hoey, the association’s CEO, said in the statement.
“It is highly unfair for state and federal governments to threaten aggressive action against pharmacists who are just trying to serve their patients within new legal boundaries that are still taking shape,” he said.
A version of this article first appeared on WebMD.com.
The Department of Health & Human Services listed several conditions that are commonly treated with drugs that can induce abortion, warning that withholding the pills could violate civil rights laws and could be considered discrimination based on sex or disability.
“We are committed to ensuring that everyone can access health care, free of discrimination,” Xavier Becerra, the U.S. health and human services secretary, said in a statement. “This includes access to prescription medications for reproductive health and other types of care.”
On July 11, Mr. Becerra issued other guidance to remind hospitals that federal law requires doctors to provide stabilizing treatment for patients with emergency medical conditions, which could include an abortion for those who arrive at emergency departments with a life-threatening issue.
Both actions by the Biden administration assert that federal laws override state laws that have banned or restricted abortion access since the Supreme Court overturned Roe v. Wade, according to The New York Times.
The guidance focuses on Section 1557 of the Affordable Care Act and related federal regulations, which state that recipients of federal financial assistance – including pharmacies that get Medicare and Medicaid payments – can’t discriminate based on race, color, national origin, sex, age, and disability. The guidance highlights that pregnancy discrimination includes discrimination based on current pregnancy, past pregnancy, potential or intended pregnancy, and medical conditions related to pregnancy or childbirth.
Three drugs in particular – mifepristone, misoprostol, and methotrexate – are often prescribed for other medical conditions but can also induce abortions in certain cases. Methotrexate, for example, is used for cancer and autoimmune disorders, such as rheumatoid arthritis.
Mifepristone is often used for patients with Cushing’s syndrome, while misoprostol is often prescribed for ulcers. When used in combination, the two drugs are authorized by the Food and Drug Administration to terminate a pregnancy during the first 10 weeks and after a miscarriage.
Since Roe was overturned, women have posted on social media that they were denied the drugs for their medical conditions due to being of “childbearing age.”
“These are very legitimate issues in terms of people being concerned about having access to the basic medications that they have been receiving for years, just because those medications have the capacity to end a pregnancy,” Alina Salganicoff, PhD, the director of women’s health policy at the Kaiser Family Foundation, told the Times.
“It doesn’t sound like [pharmacies] are blocking this for men,” she said.
The Biden administration’s guidance will likely be challenged in court, the newspaper reported. The update is cautiously written and doesn’t directly say that pharmacies must provide the drugs for the purpose of medication abortion.
In the meantime, pharmacists could feel stuck in the middle. Pharmacists who “believe they are acting in good faith in accordance with their state’s laws on abortion shouldn’t be left without a clear pathway forward,” the National Community Pharmacists Association said in a statement on July 13.
The association, which represents about 19,400 independent pharmacies across the United States, said pharmacies are regulated by states, and most states haven’t advised pharmacists on how to dispense the drugs in question.
“States have provided very little clarity on how pharmacists should proceed in light of conflicting state and federal laws and regulations,” B. Douglas Hoey, the association’s CEO, said in the statement.
“It is highly unfair for state and federal governments to threaten aggressive action against pharmacists who are just trying to serve their patients within new legal boundaries that are still taking shape,” he said.
A version of this article first appeared on WebMD.com.
The Department of Health & Human Services listed several conditions that are commonly treated with drugs that can induce abortion, warning that withholding the pills could violate civil rights laws and could be considered discrimination based on sex or disability.
“We are committed to ensuring that everyone can access health care, free of discrimination,” Xavier Becerra, the U.S. health and human services secretary, said in a statement. “This includes access to prescription medications for reproductive health and other types of care.”
On July 11, Mr. Becerra issued other guidance to remind hospitals that federal law requires doctors to provide stabilizing treatment for patients with emergency medical conditions, which could include an abortion for those who arrive at emergency departments with a life-threatening issue.
Both actions by the Biden administration assert that federal laws override state laws that have banned or restricted abortion access since the Supreme Court overturned Roe v. Wade, according to The New York Times.
The guidance focuses on Section 1557 of the Affordable Care Act and related federal regulations, which state that recipients of federal financial assistance – including pharmacies that get Medicare and Medicaid payments – can’t discriminate based on race, color, national origin, sex, age, and disability. The guidance highlights that pregnancy discrimination includes discrimination based on current pregnancy, past pregnancy, potential or intended pregnancy, and medical conditions related to pregnancy or childbirth.
Three drugs in particular – mifepristone, misoprostol, and methotrexate – are often prescribed for other medical conditions but can also induce abortions in certain cases. Methotrexate, for example, is used for cancer and autoimmune disorders, such as rheumatoid arthritis.
Mifepristone is often used for patients with Cushing’s syndrome, while misoprostol is often prescribed for ulcers. When used in combination, the two drugs are authorized by the Food and Drug Administration to terminate a pregnancy during the first 10 weeks and after a miscarriage.
Since Roe was overturned, women have posted on social media that they were denied the drugs for their medical conditions due to being of “childbearing age.”
“These are very legitimate issues in terms of people being concerned about having access to the basic medications that they have been receiving for years, just because those medications have the capacity to end a pregnancy,” Alina Salganicoff, PhD, the director of women’s health policy at the Kaiser Family Foundation, told the Times.
“It doesn’t sound like [pharmacies] are blocking this for men,” she said.
The Biden administration’s guidance will likely be challenged in court, the newspaper reported. The update is cautiously written and doesn’t directly say that pharmacies must provide the drugs for the purpose of medication abortion.
In the meantime, pharmacists could feel stuck in the middle. Pharmacists who “believe they are acting in good faith in accordance with their state’s laws on abortion shouldn’t be left without a clear pathway forward,” the National Community Pharmacists Association said in a statement on July 13.
The association, which represents about 19,400 independent pharmacies across the United States, said pharmacies are regulated by states, and most states haven’t advised pharmacists on how to dispense the drugs in question.
“States have provided very little clarity on how pharmacists should proceed in light of conflicting state and federal laws and regulations,” B. Douglas Hoey, the association’s CEO, said in the statement.
“It is highly unfair for state and federal governments to threaten aggressive action against pharmacists who are just trying to serve their patients within new legal boundaries that are still taking shape,” he said.
A version of this article first appeared on WebMD.com.
Should treatment be initiated for mild chronic hypertension in pregnancy to improve outcomes?
Tita AT, Szychowski JM, Boggess K, et al. Treatment for mild chronic hypertension during pregnancy. N Engl J Med. 2022;386:1781-1792. doi: 10.1056/NEJMoa2201295.
Expert Commentary
In the nonpregnant population, medical management of hypertension >140/90 mm Hg is standard practice. By contrast, much higher blood pressures (BPs; up to 160/110 mm Hg) traditionally have been tolerated in pregnant patients with chronic hypertension without initiating treatment, and existing medications are often discontinued during pregnancy. Concern for impaired fetal growth as well as lack of data on improved outcomes have led to different recommendations for the management of mild chronic hypertension in pregnancy. However, chronic hypertension affects a substantial number of pregnant patients and is known to be a risk factor for severe short-term pregnancy and long-term health complications. With preliminary data suggesting that BPs >140/90 mm Hg prior to 20 weeks’ gestation are associated with an increase in adverse outcomes, Tita and colleagues sought to determine the effects of decreasing BP in pregnant patients with mild chronic hypertension.
Details about the study
This is an investigator-initiated, multicenter, pragmatic, open-label, randomized control trial of 2,408 patients with mild chronic hypertension. The active treatment group was treated with antihypertensive medication (including titration of existing medication), targeting a BP of <140/90 mm Hg. The control group only received medication for severe hypertension (≥160 mm Hg systolic or ≥105 mm Hg diastolic). The primary outcome of the study was a composite of preeclampsia with severe features, medically indicated preterm delivery prior to 35 weeks’ gestation (not spontaneous labor or rupture of membranes), placental abruption, and fetal or neonatal death. Birthweight that was less than the 10th percentile was used as a safety outcome. The hypothesis was that treatment would decrease the rate of adverse pregnancy and fetal/neonatal outcomes.
The patient population of singleton pregnancies at a gestational age of less than 23 weeks included 56% with known chronic hypertension on medications, 22% with known chronic hypertension without medications, and 22% with newly diagnosed (during pregnancy) chronic hypertension. The treatment group primarily received labetalol (61.7%) or nifedipine (35.6%); the maximum dose of a single agent was used as tolerated prior to adding a second agent. The control group only received an antihypertensive medication for severe hypertension.
Treatment of chronic hypertension demonstrated a decreased risk of the composite adverse outcome with an adjusted risk ratio of 0.82 (95% confidence interval [CI], 0.74 to 0.92; P<.001) and a number needed to treat (NNT) of 14.7. When analyzed separately, a similar risk reduction was noted for both preeclampsia with severe features and medically indicated preterm birth <35 weeks’ gestation. There was no statistical difference between the groups for birth weight <10th percentile and <5th percentile (adjusted risk ratio, 1.04 [0.82–1.31] vs 0.89 [0.62–1.26], respectively).
Planned subgroup analysis by type of chronic hypertension, race/ethnic group, diabetes status, gestational age at baseline, and body mass index (BMI) demonstrated a similar treatment effect to the overall composite primary outcome, with the exception of patients with newly diagn
Study strengths and weaknesses
The study strengths cited are a large sample size, multiple study sites, an independent data and safety monitoring board with close oversight, and centralized blinded confirmation of outcomes. Another strength is that the patient population of the study was similar to the overall population of pregnant patients in the United States with chronic hypertension in terms of age, race, and ethnicity.
The weaknesses of the study include the open-label design and the high ratio of screened to enrolled patients. Both of these issues appear related to the study design (ethics and logistics of a blinded treatment and gestational age cutoff) and the physiology of pregnancy (expected decrease in BP in the second trimester rendering patients ineligible due to lower BP). The study was also not powered to assess treatment effect in all of the subgroups, and further evaluation of patients with newly diagnosed chronic hypertension and BMI ≥ 40 kg/m2 is needed. ●
Pregnant patients with chronic hypertension should continue or initiate antihypertensive medication to target a BP goal of <140/90 mm Hg. This substantial practice change is supported by the significant decrease demonstrated in this study in adverse outcomes such as preeclampsia with severe features and medically indicated preterm birth <35 weeks’ gestation without an increase in small-for-gestational-age newborns.
Tita AT, Szychowski JM, Boggess K, et al. Treatment for mild chronic hypertension during pregnancy. N Engl J Med. 2022;386:1781-1792. doi: 10.1056/NEJMoa2201295.
Expert Commentary
In the nonpregnant population, medical management of hypertension >140/90 mm Hg is standard practice. By contrast, much higher blood pressures (BPs; up to 160/110 mm Hg) traditionally have been tolerated in pregnant patients with chronic hypertension without initiating treatment, and existing medications are often discontinued during pregnancy. Concern for impaired fetal growth as well as lack of data on improved outcomes have led to different recommendations for the management of mild chronic hypertension in pregnancy. However, chronic hypertension affects a substantial number of pregnant patients and is known to be a risk factor for severe short-term pregnancy and long-term health complications. With preliminary data suggesting that BPs >140/90 mm Hg prior to 20 weeks’ gestation are associated with an increase in adverse outcomes, Tita and colleagues sought to determine the effects of decreasing BP in pregnant patients with mild chronic hypertension.
Details about the study
This is an investigator-initiated, multicenter, pragmatic, open-label, randomized control trial of 2,408 patients with mild chronic hypertension. The active treatment group was treated with antihypertensive medication (including titration of existing medication), targeting a BP of <140/90 mm Hg. The control group only received medication for severe hypertension (≥160 mm Hg systolic or ≥105 mm Hg diastolic). The primary outcome of the study was a composite of preeclampsia with severe features, medically indicated preterm delivery prior to 35 weeks’ gestation (not spontaneous labor or rupture of membranes), placental abruption, and fetal or neonatal death. Birthweight that was less than the 10th percentile was used as a safety outcome. The hypothesis was that treatment would decrease the rate of adverse pregnancy and fetal/neonatal outcomes.
The patient population of singleton pregnancies at a gestational age of less than 23 weeks included 56% with known chronic hypertension on medications, 22% with known chronic hypertension without medications, and 22% with newly diagnosed (during pregnancy) chronic hypertension. The treatment group primarily received labetalol (61.7%) or nifedipine (35.6%); the maximum dose of a single agent was used as tolerated prior to adding a second agent. The control group only received an antihypertensive medication for severe hypertension.
Treatment of chronic hypertension demonstrated a decreased risk of the composite adverse outcome with an adjusted risk ratio of 0.82 (95% confidence interval [CI], 0.74 to 0.92; P<.001) and a number needed to treat (NNT) of 14.7. When analyzed separately, a similar risk reduction was noted for both preeclampsia with severe features and medically indicated preterm birth <35 weeks’ gestation. There was no statistical difference between the groups for birth weight <10th percentile and <5th percentile (adjusted risk ratio, 1.04 [0.82–1.31] vs 0.89 [0.62–1.26], respectively).
Planned subgroup analysis by type of chronic hypertension, race/ethnic group, diabetes status, gestational age at baseline, and body mass index (BMI) demonstrated a similar treatment effect to the overall composite primary outcome, with the exception of patients with newly diagn
Study strengths and weaknesses
The study strengths cited are a large sample size, multiple study sites, an independent data and safety monitoring board with close oversight, and centralized blinded confirmation of outcomes. Another strength is that the patient population of the study was similar to the overall population of pregnant patients in the United States with chronic hypertension in terms of age, race, and ethnicity.
The weaknesses of the study include the open-label design and the high ratio of screened to enrolled patients. Both of these issues appear related to the study design (ethics and logistics of a blinded treatment and gestational age cutoff) and the physiology of pregnancy (expected decrease in BP in the second trimester rendering patients ineligible due to lower BP). The study was also not powered to assess treatment effect in all of the subgroups, and further evaluation of patients with newly diagnosed chronic hypertension and BMI ≥ 40 kg/m2 is needed. ●
Pregnant patients with chronic hypertension should continue or initiate antihypertensive medication to target a BP goal of <140/90 mm Hg. This substantial practice change is supported by the significant decrease demonstrated in this study in adverse outcomes such as preeclampsia with severe features and medically indicated preterm birth <35 weeks’ gestation without an increase in small-for-gestational-age newborns.
Tita AT, Szychowski JM, Boggess K, et al. Treatment for mild chronic hypertension during pregnancy. N Engl J Med. 2022;386:1781-1792. doi: 10.1056/NEJMoa2201295.
Expert Commentary
In the nonpregnant population, medical management of hypertension >140/90 mm Hg is standard practice. By contrast, much higher blood pressures (BPs; up to 160/110 mm Hg) traditionally have been tolerated in pregnant patients with chronic hypertension without initiating treatment, and existing medications are often discontinued during pregnancy. Concern for impaired fetal growth as well as lack of data on improved outcomes have led to different recommendations for the management of mild chronic hypertension in pregnancy. However, chronic hypertension affects a substantial number of pregnant patients and is known to be a risk factor for severe short-term pregnancy and long-term health complications. With preliminary data suggesting that BPs >140/90 mm Hg prior to 20 weeks’ gestation are associated with an increase in adverse outcomes, Tita and colleagues sought to determine the effects of decreasing BP in pregnant patients with mild chronic hypertension.
Details about the study
This is an investigator-initiated, multicenter, pragmatic, open-label, randomized control trial of 2,408 patients with mild chronic hypertension. The active treatment group was treated with antihypertensive medication (including titration of existing medication), targeting a BP of <140/90 mm Hg. The control group only received medication for severe hypertension (≥160 mm Hg systolic or ≥105 mm Hg diastolic). The primary outcome of the study was a composite of preeclampsia with severe features, medically indicated preterm delivery prior to 35 weeks’ gestation (not spontaneous labor or rupture of membranes), placental abruption, and fetal or neonatal death. Birthweight that was less than the 10th percentile was used as a safety outcome. The hypothesis was that treatment would decrease the rate of adverse pregnancy and fetal/neonatal outcomes.
The patient population of singleton pregnancies at a gestational age of less than 23 weeks included 56% with known chronic hypertension on medications, 22% with known chronic hypertension without medications, and 22% with newly diagnosed (during pregnancy) chronic hypertension. The treatment group primarily received labetalol (61.7%) or nifedipine (35.6%); the maximum dose of a single agent was used as tolerated prior to adding a second agent. The control group only received an antihypertensive medication for severe hypertension.
Treatment of chronic hypertension demonstrated a decreased risk of the composite adverse outcome with an adjusted risk ratio of 0.82 (95% confidence interval [CI], 0.74 to 0.92; P<.001) and a number needed to treat (NNT) of 14.7. When analyzed separately, a similar risk reduction was noted for both preeclampsia with severe features and medically indicated preterm birth <35 weeks’ gestation. There was no statistical difference between the groups for birth weight <10th percentile and <5th percentile (adjusted risk ratio, 1.04 [0.82–1.31] vs 0.89 [0.62–1.26], respectively).
Planned subgroup analysis by type of chronic hypertension, race/ethnic group, diabetes status, gestational age at baseline, and body mass index (BMI) demonstrated a similar treatment effect to the overall composite primary outcome, with the exception of patients with newly diagn
Study strengths and weaknesses
The study strengths cited are a large sample size, multiple study sites, an independent data and safety monitoring board with close oversight, and centralized blinded confirmation of outcomes. Another strength is that the patient population of the study was similar to the overall population of pregnant patients in the United States with chronic hypertension in terms of age, race, and ethnicity.
The weaknesses of the study include the open-label design and the high ratio of screened to enrolled patients. Both of these issues appear related to the study design (ethics and logistics of a blinded treatment and gestational age cutoff) and the physiology of pregnancy (expected decrease in BP in the second trimester rendering patients ineligible due to lower BP). The study was also not powered to assess treatment effect in all of the subgroups, and further evaluation of patients with newly diagnosed chronic hypertension and BMI ≥ 40 kg/m2 is needed. ●
Pregnant patients with chronic hypertension should continue or initiate antihypertensive medication to target a BP goal of <140/90 mm Hg. This substantial practice change is supported by the significant decrease demonstrated in this study in adverse outcomes such as preeclampsia with severe features and medically indicated preterm birth <35 weeks’ gestation without an increase in small-for-gestational-age newborns.
Misoprostol: Clinical pharmacology in obstetrics and gynecology
Oxytocin and prostaglandins are critically important regulators of uterine contraction. Obstetrician-gynecologists commonly prescribe oxytocin and prostaglandin agonists (misoprostol, dinoprostone) to stimulate uterine contraction for the induction of labor, prevention and treatment of postpartum hemorrhage, and treatment of miscarriage and fetal demise. The focus of this editorial is the clinical pharmacology of misoprostol.
Misoprostol is approved by the US Food and Drug Administration (FDA) for the prevention and treatment of nonsteroidal anti-inflammatory drug–induced gastric ulcers and for patients at high risk for gastric ulcers, including those with a history of gastric ulcers. The approved misoprostol route and dose for this indication is oral administration of 200 µg four times daily with food.1 Recent food intake and antacid use reduces the absorption of orally administered misoprostol. There are no FDA-approved indications for the use of misoprostol as a single agent in obstetrics and gynecology. The FDA has approved the combination of mifepristone and misoprostol for medication abortion in the first trimester. In contrast to misoprostol, PGE2 (dinoprostone) is approved by the FDA as a vaginal insert containing 10 mg of dinoprostone for the initiation and/or continuation of cervical ripening in patients at or near term in whom there is a medical or obstetric indication for induction of labor (Cervidil; Ferring Pharmaceuticals Inc, Parsippany, New Jersey).2
Pharmacology of misoprostol
Misoprostol is a prostaglandin E1 (PGE1) agonist analogue. Prostaglandin E1 (alprostadil) is rapidly metabolized, has a half-life in the range of minutes and is not orally active, requiring administration by intravenous infusion or injection. It is indicated to maintain a patent ductus arteriosus in newborns with ductal-dependent circulation and to treat erectile dysfunction.3 In contrast to PGE1, misoprostol has a methyl ester group at carbon-1 (C-1) that increases potency and duration of action. Misoprostol also has no hydroxyl group at C-15, replacing that moiety with the addition of both a methyl- and hydroxyl- group at C-16 (FIGURE). These molecular changes improve oral activity and increase duration of action.4 Pure misoprostol is a viscous oil. It is formulated into tables by dispersing the oil on hydroxypropyl methyl cellulose before compounding into tablets. Unlike naturally occurring prostaglandins (PGE1), misoprostol tablets are stabile at room temperature for years.4
Following absorption, the methyl ester at C-1 is enzymatically cleaved, yielding misoprostol acid, the active drug.4 Misoprostol binds to the E prostanoid receptor 3 (EP-3).5 Activation of myometrial EP-3 receptor induces an increase in intracellular phosphoinositol turnover and calcium mobilization, resulting in an increase in intracellular-free calcium, triggering actin-myosin contractility.6 The increase in free calcium is propagated cell-to-cell through gap junctions that link the myometrial cells to facilitate the generation of a coordinated contraction.
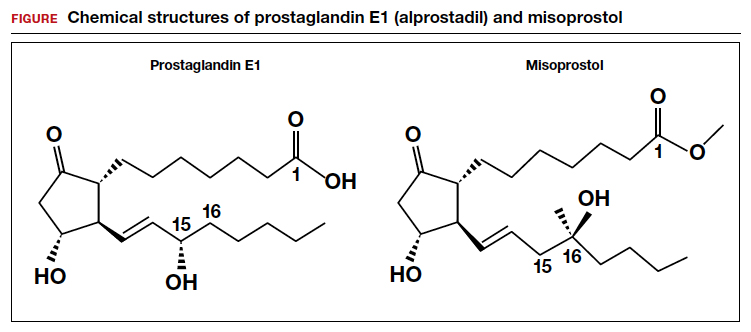
Misoprostol: Various routes of administration are not equal
Misoprostol can be given by an oral, buccal, vaginal, or rectal route of administration. To study the effect of the route of administration on uterine tone and contractility, investigators randomly assigned patients at 8 to 11 weeks’ gestation to receive misoprostol 400 µg as a single dose by the oral or vaginal route. Uterine tone and contractility were measured using an intrauterine pressure transducer. Compared to vaginal administration, oral administration of misprostol was associated with rapid attainment of peak plasma level at 30 minutes, followed by a decline in concentration by 60 minutes. This rapid onset and rapid offset of plasma concentration was paralleled by the onset of uterine tone within 8 minutes, but surprisingly no sustained uterine contractions.7 By contrast, following vaginal administration of misoprostol, serum levels rose slowly and peaked in 1 to 2 hours. Uterine tone increased within 21 minutes, and sustained uterine contractions were recorded for 4 hours.7 The rapid rise and fall in plasma misoprostol following oral administration and the more sustained plasma misoprostol concentration over 4 hours has been previously reported.8 In a second study involving patients 8 to 11 weeks’ gestation, the effect of a single dose of misoprostol 400 µg by an oral or vaginal route on uterine contractility was compared using an intrauterine pressure transducer.9 Confirming previous results, the time from misoprostol administration to increased uterine tone was more rapid with oral than with vaginal administration (8 min vs 19 min). Over the course of 4 hours, uterine contraction activity was greater with vaginal than with oral administration (454 vs 166 Montevideo units).9
Both studies reported that oral administration of misoprostol resulted in more rapid onset and offset of action than vaginal administration. Oral administration of a single dose of misoprostol 400 µg did not result in sustained uterine contractions in most patients in the first trimester. Vaginal administration produced a slower onset of increased uterine tone but sustained uterine contractions over 4 hours. Compared with vaginal administration of misoprostol, the rapid onset and offset of action of oral misoprostol may reduce the rate of tachysystole and changes in fetal heart rate observed with vaginal administration.10
An important finding is that buccal and vaginal administration of misoprostol have similar effects on uterine tone in the first trimester.11 To study the effect of buccal and vaginal administration of misoprostol on uterine tone, patients 6 to 13 weeks’ gestation were randomly allocated to receive a single dose of misoprostol 400 µg by a buccal or vaginal route.11 Uterine activity over 5 hours following administration was assessed using an intrauterine pressure transducer. Uterine tone 20 to 30 minutes after buccal or vaginal administration of misoprostol (400 µg) was 27 and 28 mm Hg, respectively. Peak uterine tone, as measured by an intrauterine pressure transducer, for buccal and vaginal administration of misoprostol was 49 mm Hg and 54 mm Hg, respectively. Total Alexandria units (AU) over 5 hours following buccal or vaginal administration was 6,537 AU and 6,090 AU, respectively.11
An AU is calculated as the average amplitude of the contractions (mm Hg) multiplied by the average duration of the contractions (min) multiplied by average frequency of contraction over 10 minutes.12 By contrast, a Montevideo unit does not include an assessment of contraction duration and is calculated as average amplitude of contractions (mm Hg) multiplied by frequency of uterine contractions over 10 minutes.12
In contrast to buccal or vaginal administration, rectal administration of misoprostol resulted in much lower peak uterine tone and contractility as measured by a pressure transducer. Uterine tone 20 to 30 minutes after vaginal and rectal administration of misoprostol (400 µg) was 28 and 19 mm Hg, respectively.11 Peak uterine tone, as measured by an intrauterine pressure transducer, for vaginal and rectal administration of misoprostol was 54 and 31 mm Hg, respectively. AUs over 5 hours following vaginal and rectal administration was 6,090 AU and 2,768 AU, respectively.11 Compared with buccal and vaginal administration of misoprostol, rectal administration produced less sustained uterine contractions in the first trimester of pregnancy. To achieve maximal sustained uterine contractions, buccal and vaginal routes of administration are superior to oral and rectal administration.
Continue to: Misoprostol and cervical ripening...
Misoprostol and cervical ripening
Misoprostol is commonly used to soften and ripen the cervix. Some of the cervical ripening effects of misoprostol are likely due to increased uterine tone. In addition, misoprostol may have a direct effect on the collagen structure of the cervix. To study the effect of misoprostol on the cervix, pregnant patients in the first trimester were randomly assigned to receive misoprostol 200 µg by vaginal self-administration, isosorbide mononitrate (IMN) 40 mg by vaginal self-administration or no treatment the evening prior to pregnancy termination.13 The following day, before uterine evacuation, a cervical biopsy was obtained for electron microscopy studies and immunohistochemistry to assess the presence of enzymes involved in collagen degradation, including matrix metalloproteinase 1 (MMP-1) and matrix metalloproteinase 9 (MMP-9). Electron microscopy demonstrated that pretreatment with misoprostol resulted in a pronounced splitting and disorganization of collagen fibers.13 Compared with misoprostol treatment, IMN produced less splitting and disorganization of collagen fibers, and in the no treatment group, no marked changes in the collagen framework were observed.
Compared with no treatment, misoprostol and IMN pretreatment were associated with marked increases in MMP-1 and MMP-9 as assessed by immunohistochemistry. Misoprostol pretreatment also resulted in a significant increase in interleukin-8 concentration compared with IMN pretreatment and no treatment (8.8 vs 2.7 vs 2.4 pg/mg tissue), respectively.13 Other investigators have also reported that misoprostol increased cervical leukocyte influx and collagen disrupting enzymes MMP-8 and MMP-9.14,15
An open-label clinical trial compared the efficacy of misoprostol versus Foley catheter for labor induction at term in 1,859 patients ≥ 37 weeks’ gestation with a Bishop score <6.16 Patients were randomly allocated to misoprostol (50 µg orally every 4 hours up to 3 times in 24 hours) versus placement of a 16 F or 18 F Foley catheter introduced through the cervix, filled with 30 mL of sodium chloride or water. The investigators reported that oral misoprostol and Foley catheter cervical ripening had similar safety and effectiveness for cervical ripening as a prelude to induction of labor, including no statistically significant differences in 5-minute Apgar score <7, umbilical cord artery pH ≤ 7.05, postpartum hemorrhage, or cesarean birth rate.16
Bottom line
Misoprostol and oxytocin are commonly prescribed in obstetric practice for cervical ripening and induction of labor, respectively. The dose and route of administration of misoprostol influences the effect on the uterus. For cervical ripening, where rapid onset and offset may help to reduce the risk of uterine tachysystole and worrisome fetal heart rate changes, low-dose (50 µg) oral administration of misoprostol may be a preferred dose and route. For the treatment of miscarriage and fetal demise, to stimulate sustained uterine contractions over many hours, buccal and vaginal administration of misoprostol are preferred. Rectal administration is generally inferior to buccal and vaginal administration for stimulating sustained uterine contractions and its uses should be limited. ●
Common side effects of misoprostol are abdominal cramping, diarrhea, nausea, vomiting, headache, and fever. Elevated temperature following misoprostol administration is a concerning side effect that may require further investigation to rule out an infection, especially if the elevated temperature persists for > 4 hours. The preoptic area of the anterior hypothalamus (POAH) plays a major role in thermoregulation. When an infection causes an increase in endogenous pyrogens, including interleukin-1β, interleukin-6 and tumor necrosis factor, prostaglandins are generated in the region of the POAH, increasing the thermoregulatory set point, triggering cutaneous vasoconstriction and shivering and non-shivering thermogenesis.1 Misoprostol, especially at doses >400 µg commonly causes both patient-reported chills and temperature elevation >38° C.
In a study comparing misoprostol and oxytocin for the management of the third stage of labor, 597 patients were randomly allocated to receive oxytocin 10 units by intramuscular injection or misoprostol 400 µg or 600 µg by the oral route.2 Patient-reported shivering occurred in 13%, 19%, and 28% of patients receiving oxytocin, misoprostol 400 µg and misoprostol 800 µg, respectively. A recorded temperature >38° C occurred within 1 hour of medication administration in approximately 3%, 2%, and 7.5% of patients receiving oxytocin, misoprostol 400 µg, and misoprostol 800 µg, respectively. In another study, 453 patients scheduled for a cesarean birth were randomly allocated to receive 1 of 3 doses of rectal misoprostol 200 μg, 400 μg, or 600 μg before incision. Fever was detected in 2.6%, 9.9%, and 5.1% of the patients receiving misoprostol 200 μg, 400 μg, or 600 μg, respectively.3
References
1. Aronoff DM, Neilson EG. Antipyretics: mechanisms of action and clinical use in fever suppression. Am J Med. 2001;111:304-315. doi: 10.1016/s0002-9343(01)00834-8.
2. Lumbiganon P, Hofmeyr J, Gumezoglu AM, et al. Misoprostol dose-related shivering and pyrexia in the third stage of labor. WHO Collaborative Trial of Misoprostol in the Management of the Third Stage of Labor. Br J Obstet Gynaecol. 1999;106:304-308. doi: 10.1111/j.1471-0528.1999.tb08266.x.
3. Sweed M, El-Said M, Abou-Gamrah AA, et al. Comparison between 200, 400 and 600 microgram rectal misoprostol before cesarean section: a randomized clinical trial. J Obstet Gynaecol Res. 2019;45:585-591. doi: 10.1111 /jog.13883.
- Cytotec [package insert]. Chicago, IL: GD Searle & Co. https://www.accessdata.fda.gov/drugsatfda_docs/label/2002/19268slr037.pdf. Accessed June 20, 2022.
- Cervidil [package insert]. St Louis, MO: Forrest Pharmaceuticals Inc.; May 2006. Accessed June 20, 2022.
- Caverject [package insert]. New York, NY: Pfizer Inc.; March 2014. Accessed June 20, 2022.
- Collins PW. Misoprostol: discovery, development and clinical applications. Med Res Rev. 1990;10:149-172. doi: 10.1002/med.2610100202.
- Audit M, White KI, Breton B, et al. Crystal structure of misoprostol bound to the labor inducer prostaglandin E2 receptor. Nat Chem Biol. 2019;15:11-17. doi: 10.1038/s41589-018-0160-y.
- Pallliser KH, Hirst JJ, Ooi G, et al. Prostaglandin E and F receptor expression and myometrial sensitivity in labor onset in the sheep. Biol Reprod. 2005;72:937-943. doi: 10.1095/biolreprod.104.035311.
- Gemzell-Danilesson K, Marions L, Rodriguez A, et al. Comparison between oral and vaginal administration of misoprostol on uterine contractility. Obstet Gynecol. 1999;93:275-280. doi: 10.1016/s0029-7844(98)00436-0.
- Zieman M, Fong SK, Benowitz NL, et al. Absorption kinetics of misoprostol with oral or vaginal administration. Obstet Gynecol. 1997;90:88-92. doi: 10.1016/S0029-7844(97)00111-7.
- Aronsson A, Bygdeman M, Gemzell-Danielsson K. Effects of misoprostol on uterine contractility following different routes of administration. Hum Reprod. 2004;19:81-84. doi: 10.1093/humrep/deh005.
- Young DC, Delaney T, Armson BA, et al. Oral misoprostol, low dose vaginal misoprostol and vaginal dinoprostone for labor induction: randomized controlled trial. PLOS One. 2020;15:e0227245. doi: 10.1371/journal.pone.0227245.
- Meckstroth KR, Whitaker AK, Bertisch S, et al. Misoprostol administered by epithelial routes. Drug absorption and uterine response. Obstet Gynecol. 2006;108:582-590. doi: 10.1097/01.AOG.0000230398.32794.9d.
- el-Sahwi S, Gaafar AA, Toppozada HK. A new unit for evaluation of uterine activity. Am J Obstet Gynecol. 1967;98:900-903. doi: 10.1016/0002-9378(67)90074-9.
- Vukas N, Ekerhovd E, Abrahamsson G, et al. Cervical priming in the first trimester: morphological and biochemical effects of misoprostol and isosorbide mononitrate. Acta Obstet Gyecol. 2009;88:43-51. doi: 10.1080/00016340802585440.
- Aronsson A, Ulfgren AK, Stabi B, et al. The effect of orally and vaginally administered misoprostol on inflammatory mediators and cervical ripening during early pregnancy. Contraception. 2005;72:33-39. doi: 10.1016/j.contraception.2005.02.012.
- Denison FC, Riley SC, Elliott CL, et al. The effect of mifepristone administration on leukocyte populations, matrix metalloproteinases and inflammatory mediators in the first trimester cervix. Mol Hum Reprod. 2000;6:541-548. doi: 10.1093/molehr/6.6.541.
- ten Eikelder MLG, Rengerink KO, Jozwiak M, et al. Induction of labour at term with oral misoprostol versus a Foley catheter (PROBAAT-II): a multicentre randomised controlled non-inferiority trial. Lancet. 2016;387:1619-1628. doi: 10.1016 /S0140-6736(16)00084-2.
Oxytocin and prostaglandins are critically important regulators of uterine contraction. Obstetrician-gynecologists commonly prescribe oxytocin and prostaglandin agonists (misoprostol, dinoprostone) to stimulate uterine contraction for the induction of labor, prevention and treatment of postpartum hemorrhage, and treatment of miscarriage and fetal demise. The focus of this editorial is the clinical pharmacology of misoprostol.
Misoprostol is approved by the US Food and Drug Administration (FDA) for the prevention and treatment of nonsteroidal anti-inflammatory drug–induced gastric ulcers and for patients at high risk for gastric ulcers, including those with a history of gastric ulcers. The approved misoprostol route and dose for this indication is oral administration of 200 µg four times daily with food.1 Recent food intake and antacid use reduces the absorption of orally administered misoprostol. There are no FDA-approved indications for the use of misoprostol as a single agent in obstetrics and gynecology. The FDA has approved the combination of mifepristone and misoprostol for medication abortion in the first trimester. In contrast to misoprostol, PGE2 (dinoprostone) is approved by the FDA as a vaginal insert containing 10 mg of dinoprostone for the initiation and/or continuation of cervical ripening in patients at or near term in whom there is a medical or obstetric indication for induction of labor (Cervidil; Ferring Pharmaceuticals Inc, Parsippany, New Jersey).2
Pharmacology of misoprostol
Misoprostol is a prostaglandin E1 (PGE1) agonist analogue. Prostaglandin E1 (alprostadil) is rapidly metabolized, has a half-life in the range of minutes and is not orally active, requiring administration by intravenous infusion or injection. It is indicated to maintain a patent ductus arteriosus in newborns with ductal-dependent circulation and to treat erectile dysfunction.3 In contrast to PGE1, misoprostol has a methyl ester group at carbon-1 (C-1) that increases potency and duration of action. Misoprostol also has no hydroxyl group at C-15, replacing that moiety with the addition of both a methyl- and hydroxyl- group at C-16 (FIGURE). These molecular changes improve oral activity and increase duration of action.4 Pure misoprostol is a viscous oil. It is formulated into tables by dispersing the oil on hydroxypropyl methyl cellulose before compounding into tablets. Unlike naturally occurring prostaglandins (PGE1), misoprostol tablets are stabile at room temperature for years.4
Following absorption, the methyl ester at C-1 is enzymatically cleaved, yielding misoprostol acid, the active drug.4 Misoprostol binds to the E prostanoid receptor 3 (EP-3).5 Activation of myometrial EP-3 receptor induces an increase in intracellular phosphoinositol turnover and calcium mobilization, resulting in an increase in intracellular-free calcium, triggering actin-myosin contractility.6 The increase in free calcium is propagated cell-to-cell through gap junctions that link the myometrial cells to facilitate the generation of a coordinated contraction.
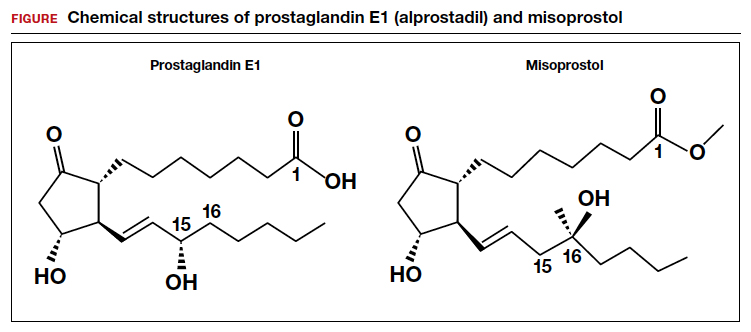
Misoprostol: Various routes of administration are not equal
Misoprostol can be given by an oral, buccal, vaginal, or rectal route of administration. To study the effect of the route of administration on uterine tone and contractility, investigators randomly assigned patients at 8 to 11 weeks’ gestation to receive misoprostol 400 µg as a single dose by the oral or vaginal route. Uterine tone and contractility were measured using an intrauterine pressure transducer. Compared to vaginal administration, oral administration of misprostol was associated with rapid attainment of peak plasma level at 30 minutes, followed by a decline in concentration by 60 minutes. This rapid onset and rapid offset of plasma concentration was paralleled by the onset of uterine tone within 8 minutes, but surprisingly no sustained uterine contractions.7 By contrast, following vaginal administration of misoprostol, serum levels rose slowly and peaked in 1 to 2 hours. Uterine tone increased within 21 minutes, and sustained uterine contractions were recorded for 4 hours.7 The rapid rise and fall in plasma misoprostol following oral administration and the more sustained plasma misoprostol concentration over 4 hours has been previously reported.8 In a second study involving patients 8 to 11 weeks’ gestation, the effect of a single dose of misoprostol 400 µg by an oral or vaginal route on uterine contractility was compared using an intrauterine pressure transducer.9 Confirming previous results, the time from misoprostol administration to increased uterine tone was more rapid with oral than with vaginal administration (8 min vs 19 min). Over the course of 4 hours, uterine contraction activity was greater with vaginal than with oral administration (454 vs 166 Montevideo units).9
Both studies reported that oral administration of misoprostol resulted in more rapid onset and offset of action than vaginal administration. Oral administration of a single dose of misoprostol 400 µg did not result in sustained uterine contractions in most patients in the first trimester. Vaginal administration produced a slower onset of increased uterine tone but sustained uterine contractions over 4 hours. Compared with vaginal administration of misoprostol, the rapid onset and offset of action of oral misoprostol may reduce the rate of tachysystole and changes in fetal heart rate observed with vaginal administration.10
An important finding is that buccal and vaginal administration of misoprostol have similar effects on uterine tone in the first trimester.11 To study the effect of buccal and vaginal administration of misoprostol on uterine tone, patients 6 to 13 weeks’ gestation were randomly allocated to receive a single dose of misoprostol 400 µg by a buccal or vaginal route.11 Uterine activity over 5 hours following administration was assessed using an intrauterine pressure transducer. Uterine tone 20 to 30 minutes after buccal or vaginal administration of misoprostol (400 µg) was 27 and 28 mm Hg, respectively. Peak uterine tone, as measured by an intrauterine pressure transducer, for buccal and vaginal administration of misoprostol was 49 mm Hg and 54 mm Hg, respectively. Total Alexandria units (AU) over 5 hours following buccal or vaginal administration was 6,537 AU and 6,090 AU, respectively.11
An AU is calculated as the average amplitude of the contractions (mm Hg) multiplied by the average duration of the contractions (min) multiplied by average frequency of contraction over 10 minutes.12 By contrast, a Montevideo unit does not include an assessment of contraction duration and is calculated as average amplitude of contractions (mm Hg) multiplied by frequency of uterine contractions over 10 minutes.12
In contrast to buccal or vaginal administration, rectal administration of misoprostol resulted in much lower peak uterine tone and contractility as measured by a pressure transducer. Uterine tone 20 to 30 minutes after vaginal and rectal administration of misoprostol (400 µg) was 28 and 19 mm Hg, respectively.11 Peak uterine tone, as measured by an intrauterine pressure transducer, for vaginal and rectal administration of misoprostol was 54 and 31 mm Hg, respectively. AUs over 5 hours following vaginal and rectal administration was 6,090 AU and 2,768 AU, respectively.11 Compared with buccal and vaginal administration of misoprostol, rectal administration produced less sustained uterine contractions in the first trimester of pregnancy. To achieve maximal sustained uterine contractions, buccal and vaginal routes of administration are superior to oral and rectal administration.
Continue to: Misoprostol and cervical ripening...
Misoprostol and cervical ripening
Misoprostol is commonly used to soften and ripen the cervix. Some of the cervical ripening effects of misoprostol are likely due to increased uterine tone. In addition, misoprostol may have a direct effect on the collagen structure of the cervix. To study the effect of misoprostol on the cervix, pregnant patients in the first trimester were randomly assigned to receive misoprostol 200 µg by vaginal self-administration, isosorbide mononitrate (IMN) 40 mg by vaginal self-administration or no treatment the evening prior to pregnancy termination.13 The following day, before uterine evacuation, a cervical biopsy was obtained for electron microscopy studies and immunohistochemistry to assess the presence of enzymes involved in collagen degradation, including matrix metalloproteinase 1 (MMP-1) and matrix metalloproteinase 9 (MMP-9). Electron microscopy demonstrated that pretreatment with misoprostol resulted in a pronounced splitting and disorganization of collagen fibers.13 Compared with misoprostol treatment, IMN produced less splitting and disorganization of collagen fibers, and in the no treatment group, no marked changes in the collagen framework were observed.
Compared with no treatment, misoprostol and IMN pretreatment were associated with marked increases in MMP-1 and MMP-9 as assessed by immunohistochemistry. Misoprostol pretreatment also resulted in a significant increase in interleukin-8 concentration compared with IMN pretreatment and no treatment (8.8 vs 2.7 vs 2.4 pg/mg tissue), respectively.13 Other investigators have also reported that misoprostol increased cervical leukocyte influx and collagen disrupting enzymes MMP-8 and MMP-9.14,15
An open-label clinical trial compared the efficacy of misoprostol versus Foley catheter for labor induction at term in 1,859 patients ≥ 37 weeks’ gestation with a Bishop score <6.16 Patients were randomly allocated to misoprostol (50 µg orally every 4 hours up to 3 times in 24 hours) versus placement of a 16 F or 18 F Foley catheter introduced through the cervix, filled with 30 mL of sodium chloride or water. The investigators reported that oral misoprostol and Foley catheter cervical ripening had similar safety and effectiveness for cervical ripening as a prelude to induction of labor, including no statistically significant differences in 5-minute Apgar score <7, umbilical cord artery pH ≤ 7.05, postpartum hemorrhage, or cesarean birth rate.16
Bottom line
Misoprostol and oxytocin are commonly prescribed in obstetric practice for cervical ripening and induction of labor, respectively. The dose and route of administration of misoprostol influences the effect on the uterus. For cervical ripening, where rapid onset and offset may help to reduce the risk of uterine tachysystole and worrisome fetal heart rate changes, low-dose (50 µg) oral administration of misoprostol may be a preferred dose and route. For the treatment of miscarriage and fetal demise, to stimulate sustained uterine contractions over many hours, buccal and vaginal administration of misoprostol are preferred. Rectal administration is generally inferior to buccal and vaginal administration for stimulating sustained uterine contractions and its uses should be limited. ●
Common side effects of misoprostol are abdominal cramping, diarrhea, nausea, vomiting, headache, and fever. Elevated temperature following misoprostol administration is a concerning side effect that may require further investigation to rule out an infection, especially if the elevated temperature persists for > 4 hours. The preoptic area of the anterior hypothalamus (POAH) plays a major role in thermoregulation. When an infection causes an increase in endogenous pyrogens, including interleukin-1β, interleukin-6 and tumor necrosis factor, prostaglandins are generated in the region of the POAH, increasing the thermoregulatory set point, triggering cutaneous vasoconstriction and shivering and non-shivering thermogenesis.1 Misoprostol, especially at doses >400 µg commonly causes both patient-reported chills and temperature elevation >38° C.
In a study comparing misoprostol and oxytocin for the management of the third stage of labor, 597 patients were randomly allocated to receive oxytocin 10 units by intramuscular injection or misoprostol 400 µg or 600 µg by the oral route.2 Patient-reported shivering occurred in 13%, 19%, and 28% of patients receiving oxytocin, misoprostol 400 µg and misoprostol 800 µg, respectively. A recorded temperature >38° C occurred within 1 hour of medication administration in approximately 3%, 2%, and 7.5% of patients receiving oxytocin, misoprostol 400 µg, and misoprostol 800 µg, respectively. In another study, 453 patients scheduled for a cesarean birth were randomly allocated to receive 1 of 3 doses of rectal misoprostol 200 μg, 400 μg, or 600 μg before incision. Fever was detected in 2.6%, 9.9%, and 5.1% of the patients receiving misoprostol 200 μg, 400 μg, or 600 μg, respectively.3
References
1. Aronoff DM, Neilson EG. Antipyretics: mechanisms of action and clinical use in fever suppression. Am J Med. 2001;111:304-315. doi: 10.1016/s0002-9343(01)00834-8.
2. Lumbiganon P, Hofmeyr J, Gumezoglu AM, et al. Misoprostol dose-related shivering and pyrexia in the third stage of labor. WHO Collaborative Trial of Misoprostol in the Management of the Third Stage of Labor. Br J Obstet Gynaecol. 1999;106:304-308. doi: 10.1111/j.1471-0528.1999.tb08266.x.
3. Sweed M, El-Said M, Abou-Gamrah AA, et al. Comparison between 200, 400 and 600 microgram rectal misoprostol before cesarean section: a randomized clinical trial. J Obstet Gynaecol Res. 2019;45:585-591. doi: 10.1111 /jog.13883.
Oxytocin and prostaglandins are critically important regulators of uterine contraction. Obstetrician-gynecologists commonly prescribe oxytocin and prostaglandin agonists (misoprostol, dinoprostone) to stimulate uterine contraction for the induction of labor, prevention and treatment of postpartum hemorrhage, and treatment of miscarriage and fetal demise. The focus of this editorial is the clinical pharmacology of misoprostol.
Misoprostol is approved by the US Food and Drug Administration (FDA) for the prevention and treatment of nonsteroidal anti-inflammatory drug–induced gastric ulcers and for patients at high risk for gastric ulcers, including those with a history of gastric ulcers. The approved misoprostol route and dose for this indication is oral administration of 200 µg four times daily with food.1 Recent food intake and antacid use reduces the absorption of orally administered misoprostol. There are no FDA-approved indications for the use of misoprostol as a single agent in obstetrics and gynecology. The FDA has approved the combination of mifepristone and misoprostol for medication abortion in the first trimester. In contrast to misoprostol, PGE2 (dinoprostone) is approved by the FDA as a vaginal insert containing 10 mg of dinoprostone for the initiation and/or continuation of cervical ripening in patients at or near term in whom there is a medical or obstetric indication for induction of labor (Cervidil; Ferring Pharmaceuticals Inc, Parsippany, New Jersey).2
Pharmacology of misoprostol
Misoprostol is a prostaglandin E1 (PGE1) agonist analogue. Prostaglandin E1 (alprostadil) is rapidly metabolized, has a half-life in the range of minutes and is not orally active, requiring administration by intravenous infusion or injection. It is indicated to maintain a patent ductus arteriosus in newborns with ductal-dependent circulation and to treat erectile dysfunction.3 In contrast to PGE1, misoprostol has a methyl ester group at carbon-1 (C-1) that increases potency and duration of action. Misoprostol also has no hydroxyl group at C-15, replacing that moiety with the addition of both a methyl- and hydroxyl- group at C-16 (FIGURE). These molecular changes improve oral activity and increase duration of action.4 Pure misoprostol is a viscous oil. It is formulated into tables by dispersing the oil on hydroxypropyl methyl cellulose before compounding into tablets. Unlike naturally occurring prostaglandins (PGE1), misoprostol tablets are stabile at room temperature for years.4
Following absorption, the methyl ester at C-1 is enzymatically cleaved, yielding misoprostol acid, the active drug.4 Misoprostol binds to the E prostanoid receptor 3 (EP-3).5 Activation of myometrial EP-3 receptor induces an increase in intracellular phosphoinositol turnover and calcium mobilization, resulting in an increase in intracellular-free calcium, triggering actin-myosin contractility.6 The increase in free calcium is propagated cell-to-cell through gap junctions that link the myometrial cells to facilitate the generation of a coordinated contraction.
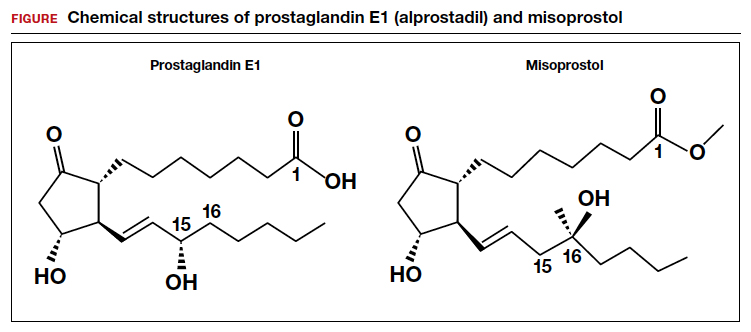
Misoprostol: Various routes of administration are not equal
Misoprostol can be given by an oral, buccal, vaginal, or rectal route of administration. To study the effect of the route of administration on uterine tone and contractility, investigators randomly assigned patients at 8 to 11 weeks’ gestation to receive misoprostol 400 µg as a single dose by the oral or vaginal route. Uterine tone and contractility were measured using an intrauterine pressure transducer. Compared to vaginal administration, oral administration of misprostol was associated with rapid attainment of peak plasma level at 30 minutes, followed by a decline in concentration by 60 minutes. This rapid onset and rapid offset of plasma concentration was paralleled by the onset of uterine tone within 8 minutes, but surprisingly no sustained uterine contractions.7 By contrast, following vaginal administration of misoprostol, serum levels rose slowly and peaked in 1 to 2 hours. Uterine tone increased within 21 minutes, and sustained uterine contractions were recorded for 4 hours.7 The rapid rise and fall in plasma misoprostol following oral administration and the more sustained plasma misoprostol concentration over 4 hours has been previously reported.8 In a second study involving patients 8 to 11 weeks’ gestation, the effect of a single dose of misoprostol 400 µg by an oral or vaginal route on uterine contractility was compared using an intrauterine pressure transducer.9 Confirming previous results, the time from misoprostol administration to increased uterine tone was more rapid with oral than with vaginal administration (8 min vs 19 min). Over the course of 4 hours, uterine contraction activity was greater with vaginal than with oral administration (454 vs 166 Montevideo units).9
Both studies reported that oral administration of misoprostol resulted in more rapid onset and offset of action than vaginal administration. Oral administration of a single dose of misoprostol 400 µg did not result in sustained uterine contractions in most patients in the first trimester. Vaginal administration produced a slower onset of increased uterine tone but sustained uterine contractions over 4 hours. Compared with vaginal administration of misoprostol, the rapid onset and offset of action of oral misoprostol may reduce the rate of tachysystole and changes in fetal heart rate observed with vaginal administration.10
An important finding is that buccal and vaginal administration of misoprostol have similar effects on uterine tone in the first trimester.11 To study the effect of buccal and vaginal administration of misoprostol on uterine tone, patients 6 to 13 weeks’ gestation were randomly allocated to receive a single dose of misoprostol 400 µg by a buccal or vaginal route.11 Uterine activity over 5 hours following administration was assessed using an intrauterine pressure transducer. Uterine tone 20 to 30 minutes after buccal or vaginal administration of misoprostol (400 µg) was 27 and 28 mm Hg, respectively. Peak uterine tone, as measured by an intrauterine pressure transducer, for buccal and vaginal administration of misoprostol was 49 mm Hg and 54 mm Hg, respectively. Total Alexandria units (AU) over 5 hours following buccal or vaginal administration was 6,537 AU and 6,090 AU, respectively.11
An AU is calculated as the average amplitude of the contractions (mm Hg) multiplied by the average duration of the contractions (min) multiplied by average frequency of contraction over 10 minutes.12 By contrast, a Montevideo unit does not include an assessment of contraction duration and is calculated as average amplitude of contractions (mm Hg) multiplied by frequency of uterine contractions over 10 minutes.12
In contrast to buccal or vaginal administration, rectal administration of misoprostol resulted in much lower peak uterine tone and contractility as measured by a pressure transducer. Uterine tone 20 to 30 minutes after vaginal and rectal administration of misoprostol (400 µg) was 28 and 19 mm Hg, respectively.11 Peak uterine tone, as measured by an intrauterine pressure transducer, for vaginal and rectal administration of misoprostol was 54 and 31 mm Hg, respectively. AUs over 5 hours following vaginal and rectal administration was 6,090 AU and 2,768 AU, respectively.11 Compared with buccal and vaginal administration of misoprostol, rectal administration produced less sustained uterine contractions in the first trimester of pregnancy. To achieve maximal sustained uterine contractions, buccal and vaginal routes of administration are superior to oral and rectal administration.
Continue to: Misoprostol and cervical ripening...
Misoprostol and cervical ripening
Misoprostol is commonly used to soften and ripen the cervix. Some of the cervical ripening effects of misoprostol are likely due to increased uterine tone. In addition, misoprostol may have a direct effect on the collagen structure of the cervix. To study the effect of misoprostol on the cervix, pregnant patients in the first trimester were randomly assigned to receive misoprostol 200 µg by vaginal self-administration, isosorbide mononitrate (IMN) 40 mg by vaginal self-administration or no treatment the evening prior to pregnancy termination.13 The following day, before uterine evacuation, a cervical biopsy was obtained for electron microscopy studies and immunohistochemistry to assess the presence of enzymes involved in collagen degradation, including matrix metalloproteinase 1 (MMP-1) and matrix metalloproteinase 9 (MMP-9). Electron microscopy demonstrated that pretreatment with misoprostol resulted in a pronounced splitting and disorganization of collagen fibers.13 Compared with misoprostol treatment, IMN produced less splitting and disorganization of collagen fibers, and in the no treatment group, no marked changes in the collagen framework were observed.
Compared with no treatment, misoprostol and IMN pretreatment were associated with marked increases in MMP-1 and MMP-9 as assessed by immunohistochemistry. Misoprostol pretreatment also resulted in a significant increase in interleukin-8 concentration compared with IMN pretreatment and no treatment (8.8 vs 2.7 vs 2.4 pg/mg tissue), respectively.13 Other investigators have also reported that misoprostol increased cervical leukocyte influx and collagen disrupting enzymes MMP-8 and MMP-9.14,15
An open-label clinical trial compared the efficacy of misoprostol versus Foley catheter for labor induction at term in 1,859 patients ≥ 37 weeks’ gestation with a Bishop score <6.16 Patients were randomly allocated to misoprostol (50 µg orally every 4 hours up to 3 times in 24 hours) versus placement of a 16 F or 18 F Foley catheter introduced through the cervix, filled with 30 mL of sodium chloride or water. The investigators reported that oral misoprostol and Foley catheter cervical ripening had similar safety and effectiveness for cervical ripening as a prelude to induction of labor, including no statistically significant differences in 5-minute Apgar score <7, umbilical cord artery pH ≤ 7.05, postpartum hemorrhage, or cesarean birth rate.16
Bottom line
Misoprostol and oxytocin are commonly prescribed in obstetric practice for cervical ripening and induction of labor, respectively. The dose and route of administration of misoprostol influences the effect on the uterus. For cervical ripening, where rapid onset and offset may help to reduce the risk of uterine tachysystole and worrisome fetal heart rate changes, low-dose (50 µg) oral administration of misoprostol may be a preferred dose and route. For the treatment of miscarriage and fetal demise, to stimulate sustained uterine contractions over many hours, buccal and vaginal administration of misoprostol are preferred. Rectal administration is generally inferior to buccal and vaginal administration for stimulating sustained uterine contractions and its uses should be limited. ●
Common side effects of misoprostol are abdominal cramping, diarrhea, nausea, vomiting, headache, and fever. Elevated temperature following misoprostol administration is a concerning side effect that may require further investigation to rule out an infection, especially if the elevated temperature persists for > 4 hours. The preoptic area of the anterior hypothalamus (POAH) plays a major role in thermoregulation. When an infection causes an increase in endogenous pyrogens, including interleukin-1β, interleukin-6 and tumor necrosis factor, prostaglandins are generated in the region of the POAH, increasing the thermoregulatory set point, triggering cutaneous vasoconstriction and shivering and non-shivering thermogenesis.1 Misoprostol, especially at doses >400 µg commonly causes both patient-reported chills and temperature elevation >38° C.
In a study comparing misoprostol and oxytocin for the management of the third stage of labor, 597 patients were randomly allocated to receive oxytocin 10 units by intramuscular injection or misoprostol 400 µg or 600 µg by the oral route.2 Patient-reported shivering occurred in 13%, 19%, and 28% of patients receiving oxytocin, misoprostol 400 µg and misoprostol 800 µg, respectively. A recorded temperature >38° C occurred within 1 hour of medication administration in approximately 3%, 2%, and 7.5% of patients receiving oxytocin, misoprostol 400 µg, and misoprostol 800 µg, respectively. In another study, 453 patients scheduled for a cesarean birth were randomly allocated to receive 1 of 3 doses of rectal misoprostol 200 μg, 400 μg, or 600 μg before incision. Fever was detected in 2.6%, 9.9%, and 5.1% of the patients receiving misoprostol 200 μg, 400 μg, or 600 μg, respectively.3
References
1. Aronoff DM, Neilson EG. Antipyretics: mechanisms of action and clinical use in fever suppression. Am J Med. 2001;111:304-315. doi: 10.1016/s0002-9343(01)00834-8.
2. Lumbiganon P, Hofmeyr J, Gumezoglu AM, et al. Misoprostol dose-related shivering and pyrexia in the third stage of labor. WHO Collaborative Trial of Misoprostol in the Management of the Third Stage of Labor. Br J Obstet Gynaecol. 1999;106:304-308. doi: 10.1111/j.1471-0528.1999.tb08266.x.
3. Sweed M, El-Said M, Abou-Gamrah AA, et al. Comparison between 200, 400 and 600 microgram rectal misoprostol before cesarean section: a randomized clinical trial. J Obstet Gynaecol Res. 2019;45:585-591. doi: 10.1111 /jog.13883.
- Cytotec [package insert]. Chicago, IL: GD Searle & Co. https://www.accessdata.fda.gov/drugsatfda_docs/label/2002/19268slr037.pdf. Accessed June 20, 2022.
- Cervidil [package insert]. St Louis, MO: Forrest Pharmaceuticals Inc.; May 2006. Accessed June 20, 2022.
- Caverject [package insert]. New York, NY: Pfizer Inc.; March 2014. Accessed June 20, 2022.
- Collins PW. Misoprostol: discovery, development and clinical applications. Med Res Rev. 1990;10:149-172. doi: 10.1002/med.2610100202.
- Audit M, White KI, Breton B, et al. Crystal structure of misoprostol bound to the labor inducer prostaglandin E2 receptor. Nat Chem Biol. 2019;15:11-17. doi: 10.1038/s41589-018-0160-y.
- Pallliser KH, Hirst JJ, Ooi G, et al. Prostaglandin E and F receptor expression and myometrial sensitivity in labor onset in the sheep. Biol Reprod. 2005;72:937-943. doi: 10.1095/biolreprod.104.035311.
- Gemzell-Danilesson K, Marions L, Rodriguez A, et al. Comparison between oral and vaginal administration of misoprostol on uterine contractility. Obstet Gynecol. 1999;93:275-280. doi: 10.1016/s0029-7844(98)00436-0.
- Zieman M, Fong SK, Benowitz NL, et al. Absorption kinetics of misoprostol with oral or vaginal administration. Obstet Gynecol. 1997;90:88-92. doi: 10.1016/S0029-7844(97)00111-7.
- Aronsson A, Bygdeman M, Gemzell-Danielsson K. Effects of misoprostol on uterine contractility following different routes of administration. Hum Reprod. 2004;19:81-84. doi: 10.1093/humrep/deh005.
- Young DC, Delaney T, Armson BA, et al. Oral misoprostol, low dose vaginal misoprostol and vaginal dinoprostone for labor induction: randomized controlled trial. PLOS One. 2020;15:e0227245. doi: 10.1371/journal.pone.0227245.
- Meckstroth KR, Whitaker AK, Bertisch S, et al. Misoprostol administered by epithelial routes. Drug absorption and uterine response. Obstet Gynecol. 2006;108:582-590. doi: 10.1097/01.AOG.0000230398.32794.9d.
- el-Sahwi S, Gaafar AA, Toppozada HK. A new unit for evaluation of uterine activity. Am J Obstet Gynecol. 1967;98:900-903. doi: 10.1016/0002-9378(67)90074-9.
- Vukas N, Ekerhovd E, Abrahamsson G, et al. Cervical priming in the first trimester: morphological and biochemical effects of misoprostol and isosorbide mononitrate. Acta Obstet Gyecol. 2009;88:43-51. doi: 10.1080/00016340802585440.
- Aronsson A, Ulfgren AK, Stabi B, et al. The effect of orally and vaginally administered misoprostol on inflammatory mediators and cervical ripening during early pregnancy. Contraception. 2005;72:33-39. doi: 10.1016/j.contraception.2005.02.012.
- Denison FC, Riley SC, Elliott CL, et al. The effect of mifepristone administration on leukocyte populations, matrix metalloproteinases and inflammatory mediators in the first trimester cervix. Mol Hum Reprod. 2000;6:541-548. doi: 10.1093/molehr/6.6.541.
- ten Eikelder MLG, Rengerink KO, Jozwiak M, et al. Induction of labour at term with oral misoprostol versus a Foley catheter (PROBAAT-II): a multicentre randomised controlled non-inferiority trial. Lancet. 2016;387:1619-1628. doi: 10.1016 /S0140-6736(16)00084-2.
- Cytotec [package insert]. Chicago, IL: GD Searle & Co. https://www.accessdata.fda.gov/drugsatfda_docs/label/2002/19268slr037.pdf. Accessed June 20, 2022.
- Cervidil [package insert]. St Louis, MO: Forrest Pharmaceuticals Inc.; May 2006. Accessed June 20, 2022.
- Caverject [package insert]. New York, NY: Pfizer Inc.; March 2014. Accessed June 20, 2022.
- Collins PW. Misoprostol: discovery, development and clinical applications. Med Res Rev. 1990;10:149-172. doi: 10.1002/med.2610100202.
- Audit M, White KI, Breton B, et al. Crystal structure of misoprostol bound to the labor inducer prostaglandin E2 receptor. Nat Chem Biol. 2019;15:11-17. doi: 10.1038/s41589-018-0160-y.
- Pallliser KH, Hirst JJ, Ooi G, et al. Prostaglandin E and F receptor expression and myometrial sensitivity in labor onset in the sheep. Biol Reprod. 2005;72:937-943. doi: 10.1095/biolreprod.104.035311.
- Gemzell-Danilesson K, Marions L, Rodriguez A, et al. Comparison between oral and vaginal administration of misoprostol on uterine contractility. Obstet Gynecol. 1999;93:275-280. doi: 10.1016/s0029-7844(98)00436-0.
- Zieman M, Fong SK, Benowitz NL, et al. Absorption kinetics of misoprostol with oral or vaginal administration. Obstet Gynecol. 1997;90:88-92. doi: 10.1016/S0029-7844(97)00111-7.
- Aronsson A, Bygdeman M, Gemzell-Danielsson K. Effects of misoprostol on uterine contractility following different routes of administration. Hum Reprod. 2004;19:81-84. doi: 10.1093/humrep/deh005.
- Young DC, Delaney T, Armson BA, et al. Oral misoprostol, low dose vaginal misoprostol and vaginal dinoprostone for labor induction: randomized controlled trial. PLOS One. 2020;15:e0227245. doi: 10.1371/journal.pone.0227245.
- Meckstroth KR, Whitaker AK, Bertisch S, et al. Misoprostol administered by epithelial routes. Drug absorption and uterine response. Obstet Gynecol. 2006;108:582-590. doi: 10.1097/01.AOG.0000230398.32794.9d.
- el-Sahwi S, Gaafar AA, Toppozada HK. A new unit for evaluation of uterine activity. Am J Obstet Gynecol. 1967;98:900-903. doi: 10.1016/0002-9378(67)90074-9.
- Vukas N, Ekerhovd E, Abrahamsson G, et al. Cervical priming in the first trimester: morphological and biochemical effects of misoprostol and isosorbide mononitrate. Acta Obstet Gyecol. 2009;88:43-51. doi: 10.1080/00016340802585440.
- Aronsson A, Ulfgren AK, Stabi B, et al. The effect of orally and vaginally administered misoprostol on inflammatory mediators and cervical ripening during early pregnancy. Contraception. 2005;72:33-39. doi: 10.1016/j.contraception.2005.02.012.
- Denison FC, Riley SC, Elliott CL, et al. The effect of mifepristone administration on leukocyte populations, matrix metalloproteinases and inflammatory mediators in the first trimester cervix. Mol Hum Reprod. 2000;6:541-548. doi: 10.1093/molehr/6.6.541.
- ten Eikelder MLG, Rengerink KO, Jozwiak M, et al. Induction of labour at term with oral misoprostol versus a Foley catheter (PROBAAT-II): a multicentre randomised controlled non-inferiority trial. Lancet. 2016;387:1619-1628. doi: 10.1016 /S0140-6736(16)00084-2.
Appropriate antibiotic selection for 12 common infections in obstetric patients
For the infections we most commonly encounter in obstetric practice, I review in this article the selection of specific antibiotics. I focus on the key pathogens that cause these infections, the most useful diagnostic tests, and the most cost-effective antibiotic therapy. Relative cost estimates (high vs low) for drugs are based on information published on the GoodRx website (https://www.goodrx.com/). Actual charges to patients, of course, may vary widely depending on contractual relationships between hospitals, insurance companies, and wholesale vendors. The infections are listed in alphabetical order, not in order of frequency or severity.
1. Bacterial vaginosis
Bacterial vaginosis (BV) is a polymicrobial infection that results from perturbation of the normal vaginal flora due to conditions such as pregnancy, hormonal therapy, and changes in the menstrual cycle. It is characterized by a decrease in the vaginal concentration of Lactobacillus crispatus, followed by an increase in Prevotella bivia, Gardnerella vaginalis, Mobiluncus species, Atopobium vaginae, and Megasphaera type 1.1,2
BV is characterized by a thin, white-gray malodorous (fishlike smell) discharge. The vaginal pH is >4.5. Clue cells are apparent on saline microscopy, and the whiff (amine) test is positive when potassium hydroxide is added to a drop of vaginal secretions. Diagnostic accuracy can be improved using one of the new vaginal panel assays such as BD MAX Vaginal Panel (Becton, Dickinson and Company).3
Antibiotic selection
Antibiotic treatment of BV is directed primarily at the anaerobic component of the infection. The preferred treatment is oral metronidazole 500 mg twice daily for 7 days. If the patient cannot tolerate metronidazole, oral clindamycin 300 mg twice daily for 7 days, can be used, although it is more expensive than metronidazole. Topical metronidazole vaginal gel (0.75%), 1 applicatorful daily for 5 days, is effective in treating the local vaginal infection, but it is not effective in preventing systemic complications such as preterm labor, chorioamnionitis, and puerperal endometritis.2 It also is significantly more expensive than the oral formulation of metronidazole. Topical clindamycin cream, 1 applicatorful daily for 5 days, is even more expensive.
Tinidazole 2 g orally daily for 2 days is an effective alternative to oral metronidazole. Single-dose therapy with oral secnidazole (2 g), a 5-nitroimidazole with a longer half-life than metronidazole, has been effective in small studies, but experience with this drug in the United States is limited. Secnidazole is also very expensive.4
2. Candidiasis
Vulvovaginal candidiasis usually is caused by Candida albicans. Other less common species include C tropicalis, C glabrata, C auris, C lusitaniae, and C krusei. The most common clinical findings are vulvovaginal pruritus in association with a curdlike white vaginal discharge. The diagnosis can be established by confirmation of a normal vaginal pH and identification of budding yeast and hyphae on a potassium hydroxide preparation. As noted above for BV, the vaginal panel assay improves the accuracy of clinical diagnosis.3 Culture usually is indicated only in patients with infections that are refractory to therapy.
Continue to: Antibiotic selection...
Antibiotic selection
In the first trimester of pregnancy, vulvovaginal candidiasis should be treated with a topical medication such as clotrimazole cream 1% (50 mg intravaginally daily for 7 days), miconazole cream 2% (100 mg intravaginally daily for 7 days), or terconazole cream 0.4% (50 g intravaginally daily for 7 days). Single-dose formulations or 3-day courses of treatment may not be quite as effective in pregnant patients, but they do offer a more convenient dosing schedule.2,5
Oral fluconazole should not be used in the first trimester of pregnancy because it has been associated with an increased risk for spontaneous abortion and with fetal cardiac septal defects. Beyond the first trimester, oral fluconazole offers an attractive option for treatment of vulvovaginal candidiasis. The appropriate dose is 150 mg initially, with a repeat dose in 3 days if symptoms persist.2,5
Ibrexafungerp (300 mg twice daily for 1 day) was recently approved by the US Food and Drug Administration (FDA) for oral treatment of vulvovaginal candidiasis. However, this drug is teratogenic and is contraindicated during pregnancy and lactation. It also is significantly more expensive than fluconazole.6
3. Cesarean delivery prophylaxis
All women having a cesarean delivery (CD) should receive antibiotic prophylaxis to reduce the risk of endometritis and wound infection.
Antibiotic selection
In my opinion, the preferred regimen is intravenous cefazolin 2 g plus azithromycin 500 mg administered preoperatively.7 Cefazolin can be administered in a rapid bolus; azithromycin should be administered over 1 hour.
In an exceptionally rigorous investigation called the C/SOAP trial (Cesarean Section Optimal Antibiotic Prophylaxis trial), Tita and colleagues showed that the combination of cefazolin plus azithromycin was superior to single-agent prophylaxis (usually with cefazolin) in preventing the composite of endometritis, wound infection, or other infection occurring within 6 weeks of surgery.8 The additive effect of azithromycin was particularly pronounced in patients having CD after labor and rupture of membranes. Harper and associates subsequently validated the cost-effectiveness of this combination regimen using a decision analytic model.9
If the patient has a serious allergy to β-lactam antibiotics, the best alternative regimen for prophylaxis is clindamycin plus gentamicin. The appropriate single intravenous dose of clindamycin is 900 mg; the single dose of gentamicin should be 5 mg/kg of ideal body weight (IBW).7
4. Chlamydia
Chlamydia trachomatis is an obligate intracellular bacterium. In pregnant women, it typically causes urethritis, endocervicitis, and inflammatory proctitis. Along with gonorrhea, it is the cause of an unusual infection/inflammation of the liver capsule, termed Fitz-Hugh-Curtis syndrome (perihepatitis). The diagnosis of chlamydia infection is best confirmed with a nucleic acid amplification test (NAAT). The NAAT simultaneously tests for chlamydia and gonorrhea in urine or in secretions obtained from the urethra, endocervix, and rectum.2
Antibiotic selection
The drug of choice for treating chlamydia in pregnancy is azithromycin 1,000 mg orally in a single dose. Erythromycin can be used as an alternative to azithromycin, but it usually is not well tolerated because of gastrointestinal adverse effects. In my practice, the preferred alternative for a patient who cannot tolerate azithromycin is amoxicillin 500 mg orally 3 times daily for 7 days.2,10
Continue to: 5. Chorioamnionitis...
5. Chorioamnionitis
Chorioamnionitis is a polymicrobial infection caused by anaerobes, aerobic gram-negative bacilli (predominantly Escherichia coli), and aerobic gram-positive cocci (primarily group B streptococci [GBS]). The diagnosis usually is made based on clinical examination: maternal fever, maternal and fetal tachycardia, and no other localizing sign of infection. The diagnosis can be confirmed by obtaining a sample of amniotic fluid via amniocentesis or via aspiration through the intrauterine pressure catheter and demonstrating a positive Gram stain, low glucose concentration (<20 mg/dL), positive nitrites, positive leukocyte esterase, and ultimately, a positive bacteriologic culture.2
Antibiotic selection
The initial treatment of chorioamnionitis specifically targets the 2 major organisms that cause neonatal pneumonia, meningitis, and sepsis: GBS and E coli. For many years, the drugs of choice have been intravenous ampicillin (2 g every 6 hours) plus intravenous gentamicin (5 mg/kg of IBW every 24 hours). Gentamicin also can be administered intravenously at a dose of 1.5 mg/kg every 8 hours. I prefer the once-daily dosing for 3 reasons:
- Gentamicin works by a concentration-dependent mechanism; the higher the initial serum concentration, the better the killing effect.
- Once-daily dosing preserves long periods with low trough levels, an effect that minimizes ototoxicity and nephrotoxicity.
- Once-daily dosing is more convenient.
In a patient who has a contraindication to use of an aminoglycoside, aztreonam (2 g intravenously every 8 hours) may be combined with ampicillin.2
If the patient delivers vaginally, 1 dose of each drug should be administered postpartum, and then the antibiotics should be discontinued. If the patient delivers by cesarean, a single dose of a medication with strong anaerobic coverage should be administered immediately after the infant’s umbilical cord is clamped. Options include clindamycin (900 mg intravenously) or metronidazole (500 mg intravenously).11
There are 2 key exceptions to the single postpartum dose rule, however. If the patient is obese (body mass index [BMI] >30 kg/m2) or if the membranes have been ruptured for more than 24 hours, antibiotics should be continued until she has been afebrile and asymptomatic for 24 hours.12
Two single agents are excellent alternatives to the combination ampicillin-gentamicin regimen. One is ampicillin-sulbactam, 3 g intravenously every 6 hours. The other is piperacillin-tazobactam, 3.375 g intravenously every 6 hours. These extended-spectrum penicillins provide exceptionally good coverage against the major pathogens that cause chorioamnionitis. Although more expensive than the combination regimen, they avoid the potential ototoxicity and nephrotoxicity associated with gentamicin.2
6. Endometritis
Puerperal endometritis is significantly more common after CD than after vaginal delivery. The infection is polymicrobial, and the principal pathogens are anaerobic gram-positive cocci, anaerobic gram-negative bacilli, aerobic gram-negative bacilli, and aerobic gram-positive cocci. The diagnosis usually is made almost exclusively based on clinical findings: fever within 24 to 36 hours of delivery, tachycardia, mild tachypnea, and lower abdominal/pelvic pain and tenderness in the absence of any other localizing sign of infection.13
Antibiotic selection
Effective treatment of endometritis requires administration of antibiotics that provide coverage against the broad range of pelvic pathogens. For many years, the gold standard of treatment has been the combination regimens of clindamycin plus gentamicin or metronidazole plus ampicillin plus gentamicin. These drugs are available in generic form and are relatively inexpensive. However, several broad-spectrum single agents are now available for treatment of endometritis. Although they are moderately more expensive than the generic combination regimens, they usually are very well tolerated, and they avoid the potential nephrotoxicity and ototoxicity associated with gentamicin. TABLE 1 summarizes the dosing regimens of these various agents and their potential weaknesses in coverage.2,13
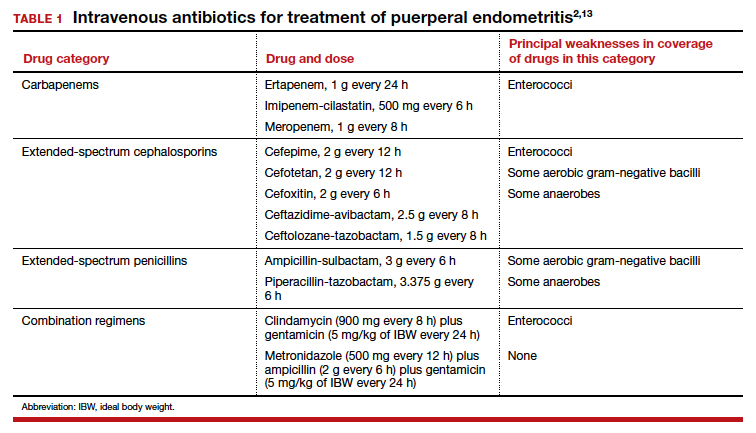
7. Gonorrhea
Gonorrhea is caused by the gram-negative diplococcus, Neisseria gonorrhoeae. The organism has a propensity to infect columnar epithelium and uroepithelium, and, typically, it causes a localized infection of the urethra, endocervix, and rectum. The organism also can cause an oropharyngeal infection, a disseminated infection (most commonly manifested by dermatitis and arthritis), and perihepatitis.
The diagnosis is best confirmed by a NAAT that can simultaneously test for gonorrhea and chlamydia in urine or in secretions obtained from the urethra, endocervix, and rectum.2,10
Antibiotic selection
The drugs of choice for treating uncomplicated gonococcal infection in pregnancy are a single dose of ceftriaxone 500 mg intramuscularly, or cefixime 800 mg orally. If the patient is allergic to β-lactam antibiotics, the recommended treatment is gentamicin 240 mg intramuscularly in a single dose, combined with azithromycin 2,000 mg orally.14
8. Group B streptococci prophylaxis
The first-line agents for GBS prophylaxis are penicillin and ampicillin. Resistance of GBS to either of these antibiotics is extremely rare. The appropriate penicillin dose is 3 million U intravenously every 4 hours; the intravenous dose of ampicillin is 2 g initially, then 1 g every 4 hours. I prefer penicillin for prophylaxis because it has a narrower spectrum of activity and is less likely to cause antibiotic-associated diarrhea. The antibiotic should be continued until delivery of the neonate.2,15,16
If the patient has a mild allergy to penicillin, the drug of choice is cefazolin 2 g intravenously initially, then 1 g every 8 hours. If the patient’s allergy to β-lactam antibiotics is severe, the alternative agents are vancomycin (20 mg/kg intravenously every 8 hours infused over 1–2 hours; maximum single dose of 2 g) and clindamycin (900 mg intravenously every 8 hours). The latter drug should be used only if sensitivity testing has confirmed that the GBS strain is sensitive to clindamycin. Resistance to clindamycin usually ranges from 10% to 15%.2,15,16
9. Puerperal mastitis
The principal microorganisms that cause puerperal mastitis are the aerobic streptococci and staphylococci that form part of the normal skin flora. The diagnosis usually is made based on the characteristic clinical findings: erythema, tenderness, and warmth in an area of the breast accompanied by a purulent nipple discharge and fever and chills. The vast majority of cases can be treated with oral antibiotics on an outpatient basis. The key indications for hospitalization are severe illness, particularly in an immunocompromised patient, and suspicion of a breast abscess.2
Continue to: Antibiotic selection...
Antibiotic selection
The initial drug of choice for treatment of mastitis is dicloxacillin sodium 500 mg every 6 hours for 7 to 10 days. If the patient has a mild allergy to penicillin, the appropriate alternative is cephalexin 500 mg every 8 hours for 7 to 10 days. If the patient’s allergy to penicillin is severe, 2 alternatives are possible. One is clindamycin 300 mg twice daily for 7 to 10 days; the other is trimethoprim-sulfamethoxazole double strength (800 mg/160 mg), twice daily for 7 to 10 days. The latter 2 drugs are also of great value if the patient fails to respond to initial therapy and/or infection with methicillin-resistant Staphylococcus aureus (MRSA) is suspected.2 I prefer the latter agent because it is less expensive than clindamycin and is less likely to cause antibiotic-induced diarrhea.
If hospitalization is required, the drug of choice is intravenous vancomycin. The appropriate dosage is 20 mg/kg every 8 to 12 hours (maximum single dose of 2 g).2
10. Syphilis
Syphilis is caused by the spirochete bacterium, Treponema pallidum. The diagnosis can be made by clinical examination if the characteristic findings listed in TABLE 2 are present.2,17 However, most patients in our practice will have latent syphilis, and the diagnosis must be established based on serologic screening.17
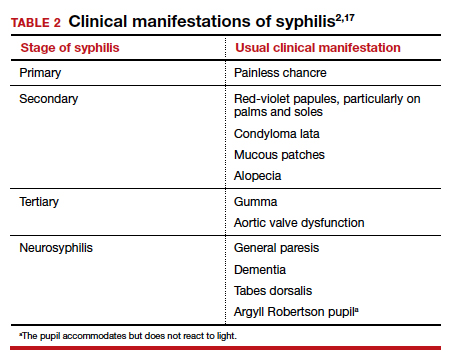
Antibiotic selection
In pregnancy, the treatment of choice for syphilis is penicillin (TABLE 3).2,10,17 Only penicillin has been proven effective in treating both maternal and fetal infection. If the patient has a history of allergy to penicillin, she should undergo skin testing to determine if she is truly allergic. If hypersensitivity is confirmed, the patient should be desensitized and then treated with the appropriate regimen outlined in TABLE 3. Of interest, within a short period of time after treatment, the patient’s sensitivity to penicillin will be reestablished, and she should not be treated again with penicillin unless she undergoes another desensitization process.2,17
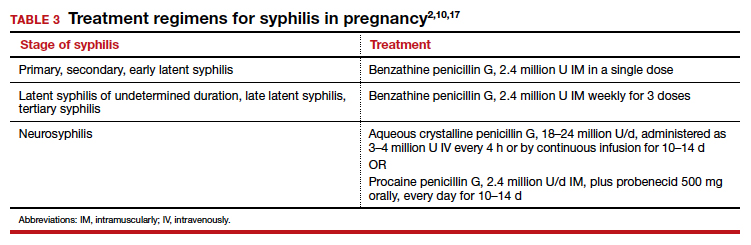
11. Trichomoniasis
Trichomoniasis is caused by the flagellated protozoan, Trichomonas vaginalis. The condition is characterized by a distinct yellowish-green vaginal discharge. The vaginal pH is >4.5, and motile flagellated organisms are easily visualized on saline microscopy. The vaginal panel assay also is a valuable diagnostic test.3
Antibiotic selection
The drug of choice for trichomoniasis is oral metronidazole 500 mg twice daily for 7 days. The patient’s sexual partner(s) should be treated concurrently to prevent reinfection. Most treatment failures are due to poor compliance with therapy on the part of either the patient or her partner(s); true drug resistance is uncommon. When antibiotic resistance is strongly suspected, the patient may be treated with a single 2-g oral dose of tinidazole.2
12. Urinary tract infections
Urethritis
Acute urethritis usually is caused by C trachomatis or N gonorrhoeae. The treatment of infections with these 2 organisms is discussed above.
Asymptomatic bacteriuria and acute cystitis
Bladder infections are caused primarily by E coli, Klebsiella pneumoniae, and Proteus species. Gram-positive cocci such as enterococci, Staphylococcus saprophyticus, and GBS are less common pathogens.18
The key diagnostic criterion for asymptomatic bacteriuria is a colony count greater than 100,000 organisms/mL of a single uropathogen on a clean-catch midstream urine specimen.18
The usual clinical manifestations of acute cystitis include frequency, urgency, hesitancy, suprapubic discomfort, and a low-grade fever. The diagnosis is most effectively confirmed by obtaining urine by catheterization and demonstrating a positive nitrite and positive leukocyte esterase reaction on dipstick examination. The finding of a urine pH of 8 or greater usually indicates an infection caused by Proteus species. When urine is obtained by catheterization, the criterion for defining a positive culture is greater than 100 colonies/mL.18
Antibiotic selection. In the first trimester, the preferred agents for treatment of a lower urinary tract infection are oral amoxicillin (875 mg twice daily) or cephalexin (500 mg every 8 hours). For an initial infection, a 3-day course of therapy usually is adequate. For a recurrent infection, a 7- to 10-day course is indicated.
Beyond the first trimester, nitrofurantoin monohydrate macrocrystals (100 mg orally twice daily) or trimethoprim-sulfamethoxazole double strength (800 mg/160 mg twice daily) are the preferred agents. Unless no other oral drug is likely to be effective, these 2 drugs should be avoided in the first trimester. The former has been associated with eye, heart, and cleft defects. The latter has been associated with neural tube defects, cardiac anomalies, choanal atresia, and diaphragmatic hernia.18
Acute pyelonephritis
Acute infections of the kidney usually are caused by the aerobic gram-negative bacilli: E coli, K pneumoniae, and Proteus species. Enterococci, S saprophyticus, and GBS are less likely to cause upper tract infection as opposed to bladder infection.
The typical clinical manifestations of acute pyelonephritis include high fever and chills in association with flank pain and tenderness. The diagnosis is best confirmed by obtaining urine by catheterization and documenting the presence of a positive nitrite and leukocyte esterase reaction. Again, an elevated urine pH is indicative of an infection secondary to Proteus species. The criterion for defining a positive culture from catheterized urine is greater than 100 colonies/mL.2,18
Antibiotic selection. Patients in the first half of pregnancy who are hemodynamically stable and who show no signs of preterm labor may be treated with oral antibiotics as outpatients. The 2 drugs of choice are amoxicillin-clavulanate (875 mg twice daily for 7 to 10 days) or trimethoprim-sulfamethoxazole double strength (800 mg/160 mg twice daily for 7 to 10 days).
For unstable patients in the first half of pregnancy and for essentially all patients in the second half of pregnancy, parenteral treatment should be administered on an inpatient basis. My preference for treatment is ceftriaxone, 2 g intravenously every 24 hours. The drug provides excellent coverage against almost all the uropathogens. It has a convenient dosing schedule, and it usually is very well tolerated. Parenteral therapy should be continued until the patient has been afebrile and asymptomatic for 24 to 48 hours. At this point, the patient can be transitioned to one of the oral regimens listed above and managed as an outpatient. If the patient is allergic to β-lactam antibiotics, an excellent alternative is aztreonam, 2 g intravenously every 8 hours.2,18 ●
- Reeder CF, Duff P. A case of BV during pregnancy: best management approach. OBG Manag. 2021;33(2):38-42.
- Duff P. Maternal and perinatal infection in pregnancy: bacterial. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe’s Obstetrics: Normal and Problem Pregnancies, 8th ed. Elsevier; 2021:1124-1145.
- Broache M, Cammarata CL, Stonebraker E, et al. Performance of a vaginal panel assay compared with the clinical diagnosis of vaginitis. Obstet Gynecol. 2021;138:853-859.
- Hiller SL, Nyirjesy P, Waldbaum AS, et al. Secnidazole treatment of bacterial vaginosis: a randomized controlled trial. Obstet Gynecol. 2017;130:379-386.
- Kirkpatrick K, Duff P. Candidiasis: the essentials of diagnosis and treatment. OBG Manag. 2020;32(8):27-29, 34.
- Ibrexafungerp (Brexafemme) for vulvovaginal candidiasis. Med Lett Drugs Ther. 2021;63:141-143.
- Duff P. Prevention of infection after cesarean delivery. Clin Obstet Gynecol. 2019;62:758-770.
- Tita AT, Szychowski JM, Boggess K, et al; for the C/SOAP Trial Consortium. Adjunctive azithromycin prophylaxis for cesarean delivery. N Engl J Med. 2016;375:1231-1241.
- Harper LM, Kilgore M, Szychowski JM, et al. Economic evaluation of adjunctive azithromycin prophylaxis for cesarean delivery. Obstet Gynecol. 2017;130:328-334.
- Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Morbid Mortal Wkly Rep. 2015;64(RR3):1-137.
- Edwards RK, Duff P. Single additional dose postpartum therapy for women with chorioamnionitis. Obstet Gynecol. 2003;102(5 pt 1):957-961.
- Black LP, Hinson L, Duff P. Limited course of antibiotic treatment for chorioamnionitis. Obstet Gynecol. 2012;119:1102-1105.
- Duff P. Fever following cesarean delivery: what are your steps for management? OBG Manag. 2021;33(12):26-30, 35.
- St Cyr S, Barbee L, Warkowski KA, et al. Update to CDC’s treatment guidelines for gonococcal infection, 2020. MMWR Morbid Mortal Wkly Rep. 2020;69:1911-1916.
- Prevention of group B streptococcal early-onset disease in newborns: ACOG committee opinion summary, number 782. Obstet Gynecol. 2019;134:1.
- Duff P. Preventing early-onset group B streptococcal disease in newborns. OBG Manag. 2019;31(12):26, 28-31.
- Finley TA, Duff P. Syphilis: cutting risk through primary prevention and prenatal screening. OBG Manag. 2020;32(11):20, 22-27.
- Duff P. UTIs in pregnancy: managing urethritis, asymptomatic bacteriuria, cystitis, and pyelonephritis. OBG Manag. 2022;34(1):42-46.
For the infections we most commonly encounter in obstetric practice, I review in this article the selection of specific antibiotics. I focus on the key pathogens that cause these infections, the most useful diagnostic tests, and the most cost-effective antibiotic therapy. Relative cost estimates (high vs low) for drugs are based on information published on the GoodRx website (https://www.goodrx.com/). Actual charges to patients, of course, may vary widely depending on contractual relationships between hospitals, insurance companies, and wholesale vendors. The infections are listed in alphabetical order, not in order of frequency or severity.
1. Bacterial vaginosis
Bacterial vaginosis (BV) is a polymicrobial infection that results from perturbation of the normal vaginal flora due to conditions such as pregnancy, hormonal therapy, and changes in the menstrual cycle. It is characterized by a decrease in the vaginal concentration of Lactobacillus crispatus, followed by an increase in Prevotella bivia, Gardnerella vaginalis, Mobiluncus species, Atopobium vaginae, and Megasphaera type 1.1,2
BV is characterized by a thin, white-gray malodorous (fishlike smell) discharge. The vaginal pH is >4.5. Clue cells are apparent on saline microscopy, and the whiff (amine) test is positive when potassium hydroxide is added to a drop of vaginal secretions. Diagnostic accuracy can be improved using one of the new vaginal panel assays such as BD MAX Vaginal Panel (Becton, Dickinson and Company).3
Antibiotic selection
Antibiotic treatment of BV is directed primarily at the anaerobic component of the infection. The preferred treatment is oral metronidazole 500 mg twice daily for 7 days. If the patient cannot tolerate metronidazole, oral clindamycin 300 mg twice daily for 7 days, can be used, although it is more expensive than metronidazole. Topical metronidazole vaginal gel (0.75%), 1 applicatorful daily for 5 days, is effective in treating the local vaginal infection, but it is not effective in preventing systemic complications such as preterm labor, chorioamnionitis, and puerperal endometritis.2 It also is significantly more expensive than the oral formulation of metronidazole. Topical clindamycin cream, 1 applicatorful daily for 5 days, is even more expensive.
Tinidazole 2 g orally daily for 2 days is an effective alternative to oral metronidazole. Single-dose therapy with oral secnidazole (2 g), a 5-nitroimidazole with a longer half-life than metronidazole, has been effective in small studies, but experience with this drug in the United States is limited. Secnidazole is also very expensive.4
2. Candidiasis
Vulvovaginal candidiasis usually is caused by Candida albicans. Other less common species include C tropicalis, C glabrata, C auris, C lusitaniae, and C krusei. The most common clinical findings are vulvovaginal pruritus in association with a curdlike white vaginal discharge. The diagnosis can be established by confirmation of a normal vaginal pH and identification of budding yeast and hyphae on a potassium hydroxide preparation. As noted above for BV, the vaginal panel assay improves the accuracy of clinical diagnosis.3 Culture usually is indicated only in patients with infections that are refractory to therapy.
Continue to: Antibiotic selection...
Antibiotic selection
In the first trimester of pregnancy, vulvovaginal candidiasis should be treated with a topical medication such as clotrimazole cream 1% (50 mg intravaginally daily for 7 days), miconazole cream 2% (100 mg intravaginally daily for 7 days), or terconazole cream 0.4% (50 g intravaginally daily for 7 days). Single-dose formulations or 3-day courses of treatment may not be quite as effective in pregnant patients, but they do offer a more convenient dosing schedule.2,5
Oral fluconazole should not be used in the first trimester of pregnancy because it has been associated with an increased risk for spontaneous abortion and with fetal cardiac septal defects. Beyond the first trimester, oral fluconazole offers an attractive option for treatment of vulvovaginal candidiasis. The appropriate dose is 150 mg initially, with a repeat dose in 3 days if symptoms persist.2,5
Ibrexafungerp (300 mg twice daily for 1 day) was recently approved by the US Food and Drug Administration (FDA) for oral treatment of vulvovaginal candidiasis. However, this drug is teratogenic and is contraindicated during pregnancy and lactation. It also is significantly more expensive than fluconazole.6
3. Cesarean delivery prophylaxis
All women having a cesarean delivery (CD) should receive antibiotic prophylaxis to reduce the risk of endometritis and wound infection.
Antibiotic selection
In my opinion, the preferred regimen is intravenous cefazolin 2 g plus azithromycin 500 mg administered preoperatively.7 Cefazolin can be administered in a rapid bolus; azithromycin should be administered over 1 hour.
In an exceptionally rigorous investigation called the C/SOAP trial (Cesarean Section Optimal Antibiotic Prophylaxis trial), Tita and colleagues showed that the combination of cefazolin plus azithromycin was superior to single-agent prophylaxis (usually with cefazolin) in preventing the composite of endometritis, wound infection, or other infection occurring within 6 weeks of surgery.8 The additive effect of azithromycin was particularly pronounced in patients having CD after labor and rupture of membranes. Harper and associates subsequently validated the cost-effectiveness of this combination regimen using a decision analytic model.9
If the patient has a serious allergy to β-lactam antibiotics, the best alternative regimen for prophylaxis is clindamycin plus gentamicin. The appropriate single intravenous dose of clindamycin is 900 mg; the single dose of gentamicin should be 5 mg/kg of ideal body weight (IBW).7
4. Chlamydia
Chlamydia trachomatis is an obligate intracellular bacterium. In pregnant women, it typically causes urethritis, endocervicitis, and inflammatory proctitis. Along with gonorrhea, it is the cause of an unusual infection/inflammation of the liver capsule, termed Fitz-Hugh-Curtis syndrome (perihepatitis). The diagnosis of chlamydia infection is best confirmed with a nucleic acid amplification test (NAAT). The NAAT simultaneously tests for chlamydia and gonorrhea in urine or in secretions obtained from the urethra, endocervix, and rectum.2
Antibiotic selection
The drug of choice for treating chlamydia in pregnancy is azithromycin 1,000 mg orally in a single dose. Erythromycin can be used as an alternative to azithromycin, but it usually is not well tolerated because of gastrointestinal adverse effects. In my practice, the preferred alternative for a patient who cannot tolerate azithromycin is amoxicillin 500 mg orally 3 times daily for 7 days.2,10
Continue to: 5. Chorioamnionitis...
5. Chorioamnionitis
Chorioamnionitis is a polymicrobial infection caused by anaerobes, aerobic gram-negative bacilli (predominantly Escherichia coli), and aerobic gram-positive cocci (primarily group B streptococci [GBS]). The diagnosis usually is made based on clinical examination: maternal fever, maternal and fetal tachycardia, and no other localizing sign of infection. The diagnosis can be confirmed by obtaining a sample of amniotic fluid via amniocentesis or via aspiration through the intrauterine pressure catheter and demonstrating a positive Gram stain, low glucose concentration (<20 mg/dL), positive nitrites, positive leukocyte esterase, and ultimately, a positive bacteriologic culture.2
Antibiotic selection
The initial treatment of chorioamnionitis specifically targets the 2 major organisms that cause neonatal pneumonia, meningitis, and sepsis: GBS and E coli. For many years, the drugs of choice have been intravenous ampicillin (2 g every 6 hours) plus intravenous gentamicin (5 mg/kg of IBW every 24 hours). Gentamicin also can be administered intravenously at a dose of 1.5 mg/kg every 8 hours. I prefer the once-daily dosing for 3 reasons:
- Gentamicin works by a concentration-dependent mechanism; the higher the initial serum concentration, the better the killing effect.
- Once-daily dosing preserves long periods with low trough levels, an effect that minimizes ototoxicity and nephrotoxicity.
- Once-daily dosing is more convenient.
In a patient who has a contraindication to use of an aminoglycoside, aztreonam (2 g intravenously every 8 hours) may be combined with ampicillin.2
If the patient delivers vaginally, 1 dose of each drug should be administered postpartum, and then the antibiotics should be discontinued. If the patient delivers by cesarean, a single dose of a medication with strong anaerobic coverage should be administered immediately after the infant’s umbilical cord is clamped. Options include clindamycin (900 mg intravenously) or metronidazole (500 mg intravenously).11
There are 2 key exceptions to the single postpartum dose rule, however. If the patient is obese (body mass index [BMI] >30 kg/m2) or if the membranes have been ruptured for more than 24 hours, antibiotics should be continued until she has been afebrile and asymptomatic for 24 hours.12
Two single agents are excellent alternatives to the combination ampicillin-gentamicin regimen. One is ampicillin-sulbactam, 3 g intravenously every 6 hours. The other is piperacillin-tazobactam, 3.375 g intravenously every 6 hours. These extended-spectrum penicillins provide exceptionally good coverage against the major pathogens that cause chorioamnionitis. Although more expensive than the combination regimen, they avoid the potential ototoxicity and nephrotoxicity associated with gentamicin.2
6. Endometritis
Puerperal endometritis is significantly more common after CD than after vaginal delivery. The infection is polymicrobial, and the principal pathogens are anaerobic gram-positive cocci, anaerobic gram-negative bacilli, aerobic gram-negative bacilli, and aerobic gram-positive cocci. The diagnosis usually is made almost exclusively based on clinical findings: fever within 24 to 36 hours of delivery, tachycardia, mild tachypnea, and lower abdominal/pelvic pain and tenderness in the absence of any other localizing sign of infection.13
Antibiotic selection
Effective treatment of endometritis requires administration of antibiotics that provide coverage against the broad range of pelvic pathogens. For many years, the gold standard of treatment has been the combination regimens of clindamycin plus gentamicin or metronidazole plus ampicillin plus gentamicin. These drugs are available in generic form and are relatively inexpensive. However, several broad-spectrum single agents are now available for treatment of endometritis. Although they are moderately more expensive than the generic combination regimens, they usually are very well tolerated, and they avoid the potential nephrotoxicity and ototoxicity associated with gentamicin. TABLE 1 summarizes the dosing regimens of these various agents and their potential weaknesses in coverage.2,13
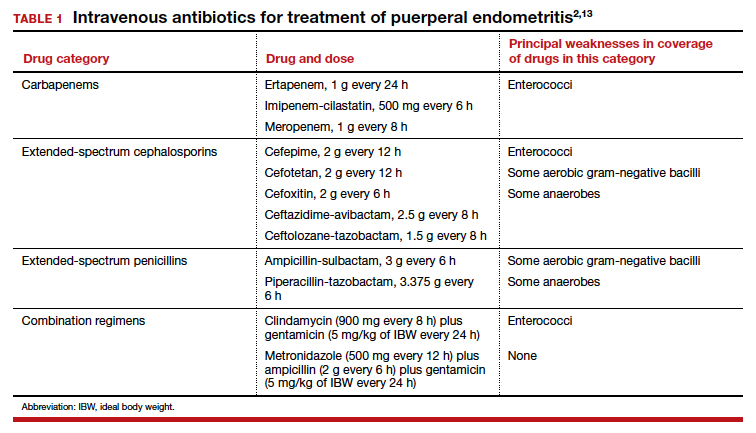
7. Gonorrhea
Gonorrhea is caused by the gram-negative diplococcus, Neisseria gonorrhoeae. The organism has a propensity to infect columnar epithelium and uroepithelium, and, typically, it causes a localized infection of the urethra, endocervix, and rectum. The organism also can cause an oropharyngeal infection, a disseminated infection (most commonly manifested by dermatitis and arthritis), and perihepatitis.
The diagnosis is best confirmed by a NAAT that can simultaneously test for gonorrhea and chlamydia in urine or in secretions obtained from the urethra, endocervix, and rectum.2,10
Antibiotic selection
The drugs of choice for treating uncomplicated gonococcal infection in pregnancy are a single dose of ceftriaxone 500 mg intramuscularly, or cefixime 800 mg orally. If the patient is allergic to β-lactam antibiotics, the recommended treatment is gentamicin 240 mg intramuscularly in a single dose, combined with azithromycin 2,000 mg orally.14
8. Group B streptococci prophylaxis
The first-line agents for GBS prophylaxis are penicillin and ampicillin. Resistance of GBS to either of these antibiotics is extremely rare. The appropriate penicillin dose is 3 million U intravenously every 4 hours; the intravenous dose of ampicillin is 2 g initially, then 1 g every 4 hours. I prefer penicillin for prophylaxis because it has a narrower spectrum of activity and is less likely to cause antibiotic-associated diarrhea. The antibiotic should be continued until delivery of the neonate.2,15,16
If the patient has a mild allergy to penicillin, the drug of choice is cefazolin 2 g intravenously initially, then 1 g every 8 hours. If the patient’s allergy to β-lactam antibiotics is severe, the alternative agents are vancomycin (20 mg/kg intravenously every 8 hours infused over 1–2 hours; maximum single dose of 2 g) and clindamycin (900 mg intravenously every 8 hours). The latter drug should be used only if sensitivity testing has confirmed that the GBS strain is sensitive to clindamycin. Resistance to clindamycin usually ranges from 10% to 15%.2,15,16
9. Puerperal mastitis
The principal microorganisms that cause puerperal mastitis are the aerobic streptococci and staphylococci that form part of the normal skin flora. The diagnosis usually is made based on the characteristic clinical findings: erythema, tenderness, and warmth in an area of the breast accompanied by a purulent nipple discharge and fever and chills. The vast majority of cases can be treated with oral antibiotics on an outpatient basis. The key indications for hospitalization are severe illness, particularly in an immunocompromised patient, and suspicion of a breast abscess.2
Continue to: Antibiotic selection...
Antibiotic selection
The initial drug of choice for treatment of mastitis is dicloxacillin sodium 500 mg every 6 hours for 7 to 10 days. If the patient has a mild allergy to penicillin, the appropriate alternative is cephalexin 500 mg every 8 hours for 7 to 10 days. If the patient’s allergy to penicillin is severe, 2 alternatives are possible. One is clindamycin 300 mg twice daily for 7 to 10 days; the other is trimethoprim-sulfamethoxazole double strength (800 mg/160 mg), twice daily for 7 to 10 days. The latter 2 drugs are also of great value if the patient fails to respond to initial therapy and/or infection with methicillin-resistant Staphylococcus aureus (MRSA) is suspected.2 I prefer the latter agent because it is less expensive than clindamycin and is less likely to cause antibiotic-induced diarrhea.
If hospitalization is required, the drug of choice is intravenous vancomycin. The appropriate dosage is 20 mg/kg every 8 to 12 hours (maximum single dose of 2 g).2
10. Syphilis
Syphilis is caused by the spirochete bacterium, Treponema pallidum. The diagnosis can be made by clinical examination if the characteristic findings listed in TABLE 2 are present.2,17 However, most patients in our practice will have latent syphilis, and the diagnosis must be established based on serologic screening.17
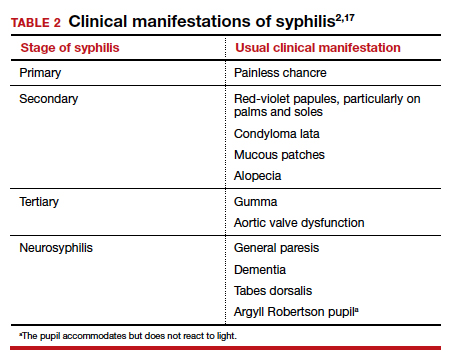
Antibiotic selection
In pregnancy, the treatment of choice for syphilis is penicillin (TABLE 3).2,10,17 Only penicillin has been proven effective in treating both maternal and fetal infection. If the patient has a history of allergy to penicillin, she should undergo skin testing to determine if she is truly allergic. If hypersensitivity is confirmed, the patient should be desensitized and then treated with the appropriate regimen outlined in TABLE 3. Of interest, within a short period of time after treatment, the patient’s sensitivity to penicillin will be reestablished, and she should not be treated again with penicillin unless she undergoes another desensitization process.2,17
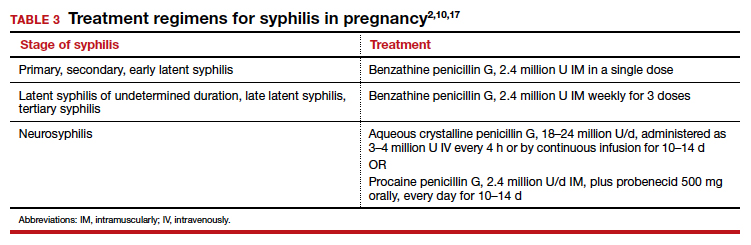
11. Trichomoniasis
Trichomoniasis is caused by the flagellated protozoan, Trichomonas vaginalis. The condition is characterized by a distinct yellowish-green vaginal discharge. The vaginal pH is >4.5, and motile flagellated organisms are easily visualized on saline microscopy. The vaginal panel assay also is a valuable diagnostic test.3
Antibiotic selection
The drug of choice for trichomoniasis is oral metronidazole 500 mg twice daily for 7 days. The patient’s sexual partner(s) should be treated concurrently to prevent reinfection. Most treatment failures are due to poor compliance with therapy on the part of either the patient or her partner(s); true drug resistance is uncommon. When antibiotic resistance is strongly suspected, the patient may be treated with a single 2-g oral dose of tinidazole.2
12. Urinary tract infections
Urethritis
Acute urethritis usually is caused by C trachomatis or N gonorrhoeae. The treatment of infections with these 2 organisms is discussed above.
Asymptomatic bacteriuria and acute cystitis
Bladder infections are caused primarily by E coli, Klebsiella pneumoniae, and Proteus species. Gram-positive cocci such as enterococci, Staphylococcus saprophyticus, and GBS are less common pathogens.18
The key diagnostic criterion for asymptomatic bacteriuria is a colony count greater than 100,000 organisms/mL of a single uropathogen on a clean-catch midstream urine specimen.18
The usual clinical manifestations of acute cystitis include frequency, urgency, hesitancy, suprapubic discomfort, and a low-grade fever. The diagnosis is most effectively confirmed by obtaining urine by catheterization and demonstrating a positive nitrite and positive leukocyte esterase reaction on dipstick examination. The finding of a urine pH of 8 or greater usually indicates an infection caused by Proteus species. When urine is obtained by catheterization, the criterion for defining a positive culture is greater than 100 colonies/mL.18
Antibiotic selection. In the first trimester, the preferred agents for treatment of a lower urinary tract infection are oral amoxicillin (875 mg twice daily) or cephalexin (500 mg every 8 hours). For an initial infection, a 3-day course of therapy usually is adequate. For a recurrent infection, a 7- to 10-day course is indicated.
Beyond the first trimester, nitrofurantoin monohydrate macrocrystals (100 mg orally twice daily) or trimethoprim-sulfamethoxazole double strength (800 mg/160 mg twice daily) are the preferred agents. Unless no other oral drug is likely to be effective, these 2 drugs should be avoided in the first trimester. The former has been associated with eye, heart, and cleft defects. The latter has been associated with neural tube defects, cardiac anomalies, choanal atresia, and diaphragmatic hernia.18
Acute pyelonephritis
Acute infections of the kidney usually are caused by the aerobic gram-negative bacilli: E coli, K pneumoniae, and Proteus species. Enterococci, S saprophyticus, and GBS are less likely to cause upper tract infection as opposed to bladder infection.
The typical clinical manifestations of acute pyelonephritis include high fever and chills in association with flank pain and tenderness. The diagnosis is best confirmed by obtaining urine by catheterization and documenting the presence of a positive nitrite and leukocyte esterase reaction. Again, an elevated urine pH is indicative of an infection secondary to Proteus species. The criterion for defining a positive culture from catheterized urine is greater than 100 colonies/mL.2,18
Antibiotic selection. Patients in the first half of pregnancy who are hemodynamically stable and who show no signs of preterm labor may be treated with oral antibiotics as outpatients. The 2 drugs of choice are amoxicillin-clavulanate (875 mg twice daily for 7 to 10 days) or trimethoprim-sulfamethoxazole double strength (800 mg/160 mg twice daily for 7 to 10 days).
For unstable patients in the first half of pregnancy and for essentially all patients in the second half of pregnancy, parenteral treatment should be administered on an inpatient basis. My preference for treatment is ceftriaxone, 2 g intravenously every 24 hours. The drug provides excellent coverage against almost all the uropathogens. It has a convenient dosing schedule, and it usually is very well tolerated. Parenteral therapy should be continued until the patient has been afebrile and asymptomatic for 24 to 48 hours. At this point, the patient can be transitioned to one of the oral regimens listed above and managed as an outpatient. If the patient is allergic to β-lactam antibiotics, an excellent alternative is aztreonam, 2 g intravenously every 8 hours.2,18 ●
For the infections we most commonly encounter in obstetric practice, I review in this article the selection of specific antibiotics. I focus on the key pathogens that cause these infections, the most useful diagnostic tests, and the most cost-effective antibiotic therapy. Relative cost estimates (high vs low) for drugs are based on information published on the GoodRx website (https://www.goodrx.com/). Actual charges to patients, of course, may vary widely depending on contractual relationships between hospitals, insurance companies, and wholesale vendors. The infections are listed in alphabetical order, not in order of frequency or severity.
1. Bacterial vaginosis
Bacterial vaginosis (BV) is a polymicrobial infection that results from perturbation of the normal vaginal flora due to conditions such as pregnancy, hormonal therapy, and changes in the menstrual cycle. It is characterized by a decrease in the vaginal concentration of Lactobacillus crispatus, followed by an increase in Prevotella bivia, Gardnerella vaginalis, Mobiluncus species, Atopobium vaginae, and Megasphaera type 1.1,2
BV is characterized by a thin, white-gray malodorous (fishlike smell) discharge. The vaginal pH is >4.5. Clue cells are apparent on saline microscopy, and the whiff (amine) test is positive when potassium hydroxide is added to a drop of vaginal secretions. Diagnostic accuracy can be improved using one of the new vaginal panel assays such as BD MAX Vaginal Panel (Becton, Dickinson and Company).3
Antibiotic selection
Antibiotic treatment of BV is directed primarily at the anaerobic component of the infection. The preferred treatment is oral metronidazole 500 mg twice daily for 7 days. If the patient cannot tolerate metronidazole, oral clindamycin 300 mg twice daily for 7 days, can be used, although it is more expensive than metronidazole. Topical metronidazole vaginal gel (0.75%), 1 applicatorful daily for 5 days, is effective in treating the local vaginal infection, but it is not effective in preventing systemic complications such as preterm labor, chorioamnionitis, and puerperal endometritis.2 It also is significantly more expensive than the oral formulation of metronidazole. Topical clindamycin cream, 1 applicatorful daily for 5 days, is even more expensive.
Tinidazole 2 g orally daily for 2 days is an effective alternative to oral metronidazole. Single-dose therapy with oral secnidazole (2 g), a 5-nitroimidazole with a longer half-life than metronidazole, has been effective in small studies, but experience with this drug in the United States is limited. Secnidazole is also very expensive.4
2. Candidiasis
Vulvovaginal candidiasis usually is caused by Candida albicans. Other less common species include C tropicalis, C glabrata, C auris, C lusitaniae, and C krusei. The most common clinical findings are vulvovaginal pruritus in association with a curdlike white vaginal discharge. The diagnosis can be established by confirmation of a normal vaginal pH and identification of budding yeast and hyphae on a potassium hydroxide preparation. As noted above for BV, the vaginal panel assay improves the accuracy of clinical diagnosis.3 Culture usually is indicated only in patients with infections that are refractory to therapy.
Continue to: Antibiotic selection...
Antibiotic selection
In the first trimester of pregnancy, vulvovaginal candidiasis should be treated with a topical medication such as clotrimazole cream 1% (50 mg intravaginally daily for 7 days), miconazole cream 2% (100 mg intravaginally daily for 7 days), or terconazole cream 0.4% (50 g intravaginally daily for 7 days). Single-dose formulations or 3-day courses of treatment may not be quite as effective in pregnant patients, but they do offer a more convenient dosing schedule.2,5
Oral fluconazole should not be used in the first trimester of pregnancy because it has been associated with an increased risk for spontaneous abortion and with fetal cardiac septal defects. Beyond the first trimester, oral fluconazole offers an attractive option for treatment of vulvovaginal candidiasis. The appropriate dose is 150 mg initially, with a repeat dose in 3 days if symptoms persist.2,5
Ibrexafungerp (300 mg twice daily for 1 day) was recently approved by the US Food and Drug Administration (FDA) for oral treatment of vulvovaginal candidiasis. However, this drug is teratogenic and is contraindicated during pregnancy and lactation. It also is significantly more expensive than fluconazole.6
3. Cesarean delivery prophylaxis
All women having a cesarean delivery (CD) should receive antibiotic prophylaxis to reduce the risk of endometritis and wound infection.
Antibiotic selection
In my opinion, the preferred regimen is intravenous cefazolin 2 g plus azithromycin 500 mg administered preoperatively.7 Cefazolin can be administered in a rapid bolus; azithromycin should be administered over 1 hour.
In an exceptionally rigorous investigation called the C/SOAP trial (Cesarean Section Optimal Antibiotic Prophylaxis trial), Tita and colleagues showed that the combination of cefazolin plus azithromycin was superior to single-agent prophylaxis (usually with cefazolin) in preventing the composite of endometritis, wound infection, or other infection occurring within 6 weeks of surgery.8 The additive effect of azithromycin was particularly pronounced in patients having CD after labor and rupture of membranes. Harper and associates subsequently validated the cost-effectiveness of this combination regimen using a decision analytic model.9
If the patient has a serious allergy to β-lactam antibiotics, the best alternative regimen for prophylaxis is clindamycin plus gentamicin. The appropriate single intravenous dose of clindamycin is 900 mg; the single dose of gentamicin should be 5 mg/kg of ideal body weight (IBW).7
4. Chlamydia
Chlamydia trachomatis is an obligate intracellular bacterium. In pregnant women, it typically causes urethritis, endocervicitis, and inflammatory proctitis. Along with gonorrhea, it is the cause of an unusual infection/inflammation of the liver capsule, termed Fitz-Hugh-Curtis syndrome (perihepatitis). The diagnosis of chlamydia infection is best confirmed with a nucleic acid amplification test (NAAT). The NAAT simultaneously tests for chlamydia and gonorrhea in urine or in secretions obtained from the urethra, endocervix, and rectum.2
Antibiotic selection
The drug of choice for treating chlamydia in pregnancy is azithromycin 1,000 mg orally in a single dose. Erythromycin can be used as an alternative to azithromycin, but it usually is not well tolerated because of gastrointestinal adverse effects. In my practice, the preferred alternative for a patient who cannot tolerate azithromycin is amoxicillin 500 mg orally 3 times daily for 7 days.2,10
Continue to: 5. Chorioamnionitis...
5. Chorioamnionitis
Chorioamnionitis is a polymicrobial infection caused by anaerobes, aerobic gram-negative bacilli (predominantly Escherichia coli), and aerobic gram-positive cocci (primarily group B streptococci [GBS]). The diagnosis usually is made based on clinical examination: maternal fever, maternal and fetal tachycardia, and no other localizing sign of infection. The diagnosis can be confirmed by obtaining a sample of amniotic fluid via amniocentesis or via aspiration through the intrauterine pressure catheter and demonstrating a positive Gram stain, low glucose concentration (<20 mg/dL), positive nitrites, positive leukocyte esterase, and ultimately, a positive bacteriologic culture.2
Antibiotic selection
The initial treatment of chorioamnionitis specifically targets the 2 major organisms that cause neonatal pneumonia, meningitis, and sepsis: GBS and E coli. For many years, the drugs of choice have been intravenous ampicillin (2 g every 6 hours) plus intravenous gentamicin (5 mg/kg of IBW every 24 hours). Gentamicin also can be administered intravenously at a dose of 1.5 mg/kg every 8 hours. I prefer the once-daily dosing for 3 reasons:
- Gentamicin works by a concentration-dependent mechanism; the higher the initial serum concentration, the better the killing effect.
- Once-daily dosing preserves long periods with low trough levels, an effect that minimizes ototoxicity and nephrotoxicity.
- Once-daily dosing is more convenient.
In a patient who has a contraindication to use of an aminoglycoside, aztreonam (2 g intravenously every 8 hours) may be combined with ampicillin.2
If the patient delivers vaginally, 1 dose of each drug should be administered postpartum, and then the antibiotics should be discontinued. If the patient delivers by cesarean, a single dose of a medication with strong anaerobic coverage should be administered immediately after the infant’s umbilical cord is clamped. Options include clindamycin (900 mg intravenously) or metronidazole (500 mg intravenously).11
There are 2 key exceptions to the single postpartum dose rule, however. If the patient is obese (body mass index [BMI] >30 kg/m2) or if the membranes have been ruptured for more than 24 hours, antibiotics should be continued until she has been afebrile and asymptomatic for 24 hours.12
Two single agents are excellent alternatives to the combination ampicillin-gentamicin regimen. One is ampicillin-sulbactam, 3 g intravenously every 6 hours. The other is piperacillin-tazobactam, 3.375 g intravenously every 6 hours. These extended-spectrum penicillins provide exceptionally good coverage against the major pathogens that cause chorioamnionitis. Although more expensive than the combination regimen, they avoid the potential ototoxicity and nephrotoxicity associated with gentamicin.2
6. Endometritis
Puerperal endometritis is significantly more common after CD than after vaginal delivery. The infection is polymicrobial, and the principal pathogens are anaerobic gram-positive cocci, anaerobic gram-negative bacilli, aerobic gram-negative bacilli, and aerobic gram-positive cocci. The diagnosis usually is made almost exclusively based on clinical findings: fever within 24 to 36 hours of delivery, tachycardia, mild tachypnea, and lower abdominal/pelvic pain and tenderness in the absence of any other localizing sign of infection.13
Antibiotic selection
Effective treatment of endometritis requires administration of antibiotics that provide coverage against the broad range of pelvic pathogens. For many years, the gold standard of treatment has been the combination regimens of clindamycin plus gentamicin or metronidazole plus ampicillin plus gentamicin. These drugs are available in generic form and are relatively inexpensive. However, several broad-spectrum single agents are now available for treatment of endometritis. Although they are moderately more expensive than the generic combination regimens, they usually are very well tolerated, and they avoid the potential nephrotoxicity and ototoxicity associated with gentamicin. TABLE 1 summarizes the dosing regimens of these various agents and their potential weaknesses in coverage.2,13
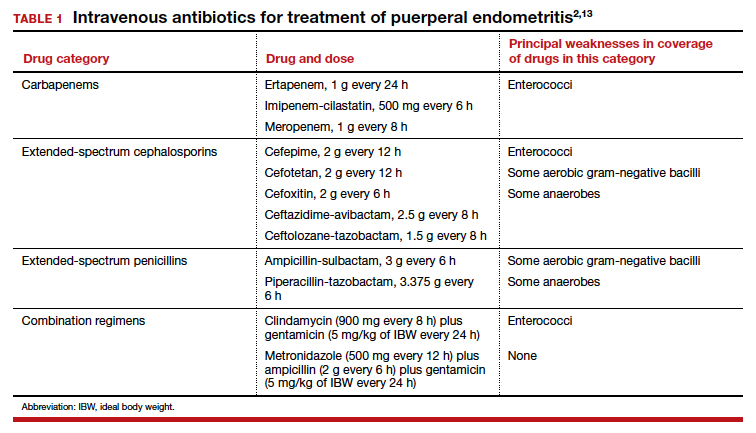
7. Gonorrhea
Gonorrhea is caused by the gram-negative diplococcus, Neisseria gonorrhoeae. The organism has a propensity to infect columnar epithelium and uroepithelium, and, typically, it causes a localized infection of the urethra, endocervix, and rectum. The organism also can cause an oropharyngeal infection, a disseminated infection (most commonly manifested by dermatitis and arthritis), and perihepatitis.
The diagnosis is best confirmed by a NAAT that can simultaneously test for gonorrhea and chlamydia in urine or in secretions obtained from the urethra, endocervix, and rectum.2,10
Antibiotic selection
The drugs of choice for treating uncomplicated gonococcal infection in pregnancy are a single dose of ceftriaxone 500 mg intramuscularly, or cefixime 800 mg orally. If the patient is allergic to β-lactam antibiotics, the recommended treatment is gentamicin 240 mg intramuscularly in a single dose, combined with azithromycin 2,000 mg orally.14
8. Group B streptococci prophylaxis
The first-line agents for GBS prophylaxis are penicillin and ampicillin. Resistance of GBS to either of these antibiotics is extremely rare. The appropriate penicillin dose is 3 million U intravenously every 4 hours; the intravenous dose of ampicillin is 2 g initially, then 1 g every 4 hours. I prefer penicillin for prophylaxis because it has a narrower spectrum of activity and is less likely to cause antibiotic-associated diarrhea. The antibiotic should be continued until delivery of the neonate.2,15,16
If the patient has a mild allergy to penicillin, the drug of choice is cefazolin 2 g intravenously initially, then 1 g every 8 hours. If the patient’s allergy to β-lactam antibiotics is severe, the alternative agents are vancomycin (20 mg/kg intravenously every 8 hours infused over 1–2 hours; maximum single dose of 2 g) and clindamycin (900 mg intravenously every 8 hours). The latter drug should be used only if sensitivity testing has confirmed that the GBS strain is sensitive to clindamycin. Resistance to clindamycin usually ranges from 10% to 15%.2,15,16
9. Puerperal mastitis
The principal microorganisms that cause puerperal mastitis are the aerobic streptococci and staphylococci that form part of the normal skin flora. The diagnosis usually is made based on the characteristic clinical findings: erythema, tenderness, and warmth in an area of the breast accompanied by a purulent nipple discharge and fever and chills. The vast majority of cases can be treated with oral antibiotics on an outpatient basis. The key indications for hospitalization are severe illness, particularly in an immunocompromised patient, and suspicion of a breast abscess.2
Continue to: Antibiotic selection...
Antibiotic selection
The initial drug of choice for treatment of mastitis is dicloxacillin sodium 500 mg every 6 hours for 7 to 10 days. If the patient has a mild allergy to penicillin, the appropriate alternative is cephalexin 500 mg every 8 hours for 7 to 10 days. If the patient’s allergy to penicillin is severe, 2 alternatives are possible. One is clindamycin 300 mg twice daily for 7 to 10 days; the other is trimethoprim-sulfamethoxazole double strength (800 mg/160 mg), twice daily for 7 to 10 days. The latter 2 drugs are also of great value if the patient fails to respond to initial therapy and/or infection with methicillin-resistant Staphylococcus aureus (MRSA) is suspected.2 I prefer the latter agent because it is less expensive than clindamycin and is less likely to cause antibiotic-induced diarrhea.
If hospitalization is required, the drug of choice is intravenous vancomycin. The appropriate dosage is 20 mg/kg every 8 to 12 hours (maximum single dose of 2 g).2
10. Syphilis
Syphilis is caused by the spirochete bacterium, Treponema pallidum. The diagnosis can be made by clinical examination if the characteristic findings listed in TABLE 2 are present.2,17 However, most patients in our practice will have latent syphilis, and the diagnosis must be established based on serologic screening.17
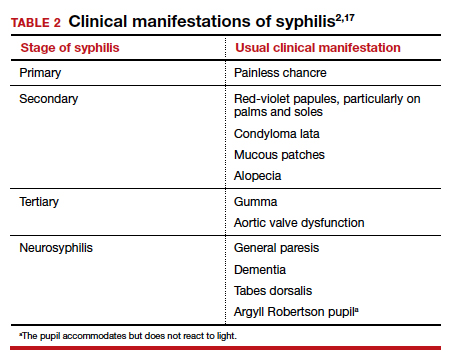
Antibiotic selection
In pregnancy, the treatment of choice for syphilis is penicillin (TABLE 3).2,10,17 Only penicillin has been proven effective in treating both maternal and fetal infection. If the patient has a history of allergy to penicillin, she should undergo skin testing to determine if she is truly allergic. If hypersensitivity is confirmed, the patient should be desensitized and then treated with the appropriate regimen outlined in TABLE 3. Of interest, within a short period of time after treatment, the patient’s sensitivity to penicillin will be reestablished, and she should not be treated again with penicillin unless she undergoes another desensitization process.2,17
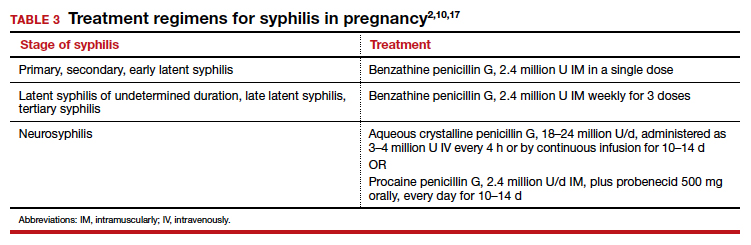
11. Trichomoniasis
Trichomoniasis is caused by the flagellated protozoan, Trichomonas vaginalis. The condition is characterized by a distinct yellowish-green vaginal discharge. The vaginal pH is >4.5, and motile flagellated organisms are easily visualized on saline microscopy. The vaginal panel assay also is a valuable diagnostic test.3
Antibiotic selection
The drug of choice for trichomoniasis is oral metronidazole 500 mg twice daily for 7 days. The patient’s sexual partner(s) should be treated concurrently to prevent reinfection. Most treatment failures are due to poor compliance with therapy on the part of either the patient or her partner(s); true drug resistance is uncommon. When antibiotic resistance is strongly suspected, the patient may be treated with a single 2-g oral dose of tinidazole.2
12. Urinary tract infections
Urethritis
Acute urethritis usually is caused by C trachomatis or N gonorrhoeae. The treatment of infections with these 2 organisms is discussed above.
Asymptomatic bacteriuria and acute cystitis
Bladder infections are caused primarily by E coli, Klebsiella pneumoniae, and Proteus species. Gram-positive cocci such as enterococci, Staphylococcus saprophyticus, and GBS are less common pathogens.18
The key diagnostic criterion for asymptomatic bacteriuria is a colony count greater than 100,000 organisms/mL of a single uropathogen on a clean-catch midstream urine specimen.18
The usual clinical manifestations of acute cystitis include frequency, urgency, hesitancy, suprapubic discomfort, and a low-grade fever. The diagnosis is most effectively confirmed by obtaining urine by catheterization and demonstrating a positive nitrite and positive leukocyte esterase reaction on dipstick examination. The finding of a urine pH of 8 or greater usually indicates an infection caused by Proteus species. When urine is obtained by catheterization, the criterion for defining a positive culture is greater than 100 colonies/mL.18
Antibiotic selection. In the first trimester, the preferred agents for treatment of a lower urinary tract infection are oral amoxicillin (875 mg twice daily) or cephalexin (500 mg every 8 hours). For an initial infection, a 3-day course of therapy usually is adequate. For a recurrent infection, a 7- to 10-day course is indicated.
Beyond the first trimester, nitrofurantoin monohydrate macrocrystals (100 mg orally twice daily) or trimethoprim-sulfamethoxazole double strength (800 mg/160 mg twice daily) are the preferred agents. Unless no other oral drug is likely to be effective, these 2 drugs should be avoided in the first trimester. The former has been associated with eye, heart, and cleft defects. The latter has been associated with neural tube defects, cardiac anomalies, choanal atresia, and diaphragmatic hernia.18
Acute pyelonephritis
Acute infections of the kidney usually are caused by the aerobic gram-negative bacilli: E coli, K pneumoniae, and Proteus species. Enterococci, S saprophyticus, and GBS are less likely to cause upper tract infection as opposed to bladder infection.
The typical clinical manifestations of acute pyelonephritis include high fever and chills in association with flank pain and tenderness. The diagnosis is best confirmed by obtaining urine by catheterization and documenting the presence of a positive nitrite and leukocyte esterase reaction. Again, an elevated urine pH is indicative of an infection secondary to Proteus species. The criterion for defining a positive culture from catheterized urine is greater than 100 colonies/mL.2,18
Antibiotic selection. Patients in the first half of pregnancy who are hemodynamically stable and who show no signs of preterm labor may be treated with oral antibiotics as outpatients. The 2 drugs of choice are amoxicillin-clavulanate (875 mg twice daily for 7 to 10 days) or trimethoprim-sulfamethoxazole double strength (800 mg/160 mg twice daily for 7 to 10 days).
For unstable patients in the first half of pregnancy and for essentially all patients in the second half of pregnancy, parenteral treatment should be administered on an inpatient basis. My preference for treatment is ceftriaxone, 2 g intravenously every 24 hours. The drug provides excellent coverage against almost all the uropathogens. It has a convenient dosing schedule, and it usually is very well tolerated. Parenteral therapy should be continued until the patient has been afebrile and asymptomatic for 24 to 48 hours. At this point, the patient can be transitioned to one of the oral regimens listed above and managed as an outpatient. If the patient is allergic to β-lactam antibiotics, an excellent alternative is aztreonam, 2 g intravenously every 8 hours.2,18 ●
- Reeder CF, Duff P. A case of BV during pregnancy: best management approach. OBG Manag. 2021;33(2):38-42.
- Duff P. Maternal and perinatal infection in pregnancy: bacterial. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe’s Obstetrics: Normal and Problem Pregnancies, 8th ed. Elsevier; 2021:1124-1145.
- Broache M, Cammarata CL, Stonebraker E, et al. Performance of a vaginal panel assay compared with the clinical diagnosis of vaginitis. Obstet Gynecol. 2021;138:853-859.
- Hiller SL, Nyirjesy P, Waldbaum AS, et al. Secnidazole treatment of bacterial vaginosis: a randomized controlled trial. Obstet Gynecol. 2017;130:379-386.
- Kirkpatrick K, Duff P. Candidiasis: the essentials of diagnosis and treatment. OBG Manag. 2020;32(8):27-29, 34.
- Ibrexafungerp (Brexafemme) for vulvovaginal candidiasis. Med Lett Drugs Ther. 2021;63:141-143.
- Duff P. Prevention of infection after cesarean delivery. Clin Obstet Gynecol. 2019;62:758-770.
- Tita AT, Szychowski JM, Boggess K, et al; for the C/SOAP Trial Consortium. Adjunctive azithromycin prophylaxis for cesarean delivery. N Engl J Med. 2016;375:1231-1241.
- Harper LM, Kilgore M, Szychowski JM, et al. Economic evaluation of adjunctive azithromycin prophylaxis for cesarean delivery. Obstet Gynecol. 2017;130:328-334.
- Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Morbid Mortal Wkly Rep. 2015;64(RR3):1-137.
- Edwards RK, Duff P. Single additional dose postpartum therapy for women with chorioamnionitis. Obstet Gynecol. 2003;102(5 pt 1):957-961.
- Black LP, Hinson L, Duff P. Limited course of antibiotic treatment for chorioamnionitis. Obstet Gynecol. 2012;119:1102-1105.
- Duff P. Fever following cesarean delivery: what are your steps for management? OBG Manag. 2021;33(12):26-30, 35.
- St Cyr S, Barbee L, Warkowski KA, et al. Update to CDC’s treatment guidelines for gonococcal infection, 2020. MMWR Morbid Mortal Wkly Rep. 2020;69:1911-1916.
- Prevention of group B streptococcal early-onset disease in newborns: ACOG committee opinion summary, number 782. Obstet Gynecol. 2019;134:1.
- Duff P. Preventing early-onset group B streptococcal disease in newborns. OBG Manag. 2019;31(12):26, 28-31.
- Finley TA, Duff P. Syphilis: cutting risk through primary prevention and prenatal screening. OBG Manag. 2020;32(11):20, 22-27.
- Duff P. UTIs in pregnancy: managing urethritis, asymptomatic bacteriuria, cystitis, and pyelonephritis. OBG Manag. 2022;34(1):42-46.
- Reeder CF, Duff P. A case of BV during pregnancy: best management approach. OBG Manag. 2021;33(2):38-42.
- Duff P. Maternal and perinatal infection in pregnancy: bacterial. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe’s Obstetrics: Normal and Problem Pregnancies, 8th ed. Elsevier; 2021:1124-1145.
- Broache M, Cammarata CL, Stonebraker E, et al. Performance of a vaginal panel assay compared with the clinical diagnosis of vaginitis. Obstet Gynecol. 2021;138:853-859.
- Hiller SL, Nyirjesy P, Waldbaum AS, et al. Secnidazole treatment of bacterial vaginosis: a randomized controlled trial. Obstet Gynecol. 2017;130:379-386.
- Kirkpatrick K, Duff P. Candidiasis: the essentials of diagnosis and treatment. OBG Manag. 2020;32(8):27-29, 34.
- Ibrexafungerp (Brexafemme) for vulvovaginal candidiasis. Med Lett Drugs Ther. 2021;63:141-143.
- Duff P. Prevention of infection after cesarean delivery. Clin Obstet Gynecol. 2019;62:758-770.
- Tita AT, Szychowski JM, Boggess K, et al; for the C/SOAP Trial Consortium. Adjunctive azithromycin prophylaxis for cesarean delivery. N Engl J Med. 2016;375:1231-1241.
- Harper LM, Kilgore M, Szychowski JM, et al. Economic evaluation of adjunctive azithromycin prophylaxis for cesarean delivery. Obstet Gynecol. 2017;130:328-334.
- Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Morbid Mortal Wkly Rep. 2015;64(RR3):1-137.
- Edwards RK, Duff P. Single additional dose postpartum therapy for women with chorioamnionitis. Obstet Gynecol. 2003;102(5 pt 1):957-961.
- Black LP, Hinson L, Duff P. Limited course of antibiotic treatment for chorioamnionitis. Obstet Gynecol. 2012;119:1102-1105.
- Duff P. Fever following cesarean delivery: what are your steps for management? OBG Manag. 2021;33(12):26-30, 35.
- St Cyr S, Barbee L, Warkowski KA, et al. Update to CDC’s treatment guidelines for gonococcal infection, 2020. MMWR Morbid Mortal Wkly Rep. 2020;69:1911-1916.
- Prevention of group B streptococcal early-onset disease in newborns: ACOG committee opinion summary, number 782. Obstet Gynecol. 2019;134:1.
- Duff P. Preventing early-onset group B streptococcal disease in newborns. OBG Manag. 2019;31(12):26, 28-31.
- Finley TA, Duff P. Syphilis: cutting risk through primary prevention and prenatal screening. OBG Manag. 2020;32(11):20, 22-27.
- Duff P. UTIs in pregnancy: managing urethritis, asymptomatic bacteriuria, cystitis, and pyelonephritis. OBG Manag. 2022;34(1):42-46.
Amniotic fluid embolism: Management using a checklist
CASE Part 1: CPR initiated during induction of labor
A 32-year-old gravida 4 para 3-0-0-3 is undergoing induction of labor with intravenous (IV) oxytocin at 39 weeks of gestation. She has no significant medical or obstetric history. Fifteen minutes after reaching complete cervical dilation, she says “I don’t feel right,” then suddenly loses consciousness. The nurse finds no detectable pulse, calls a “code blue,” and initiates cardiopulmonary resuscitation (CPR). The obstetrician is notified, appears promptly, assesses the situation, and delivers a 3.6-kg baby via vacuum extraction. Apgar score is 2/10 at 1 minute and 6/10 at 5 minutes. After delivery of the placenta, there is uterine atony and brisk hemorrhage with 2 L of blood loss.
Management of AFE: A rare complication
This case demonstrates a classic presentation of amniotic fluid embolism (AFE) syndrome—a patient in labor or within 30 minutes after delivery has sudden onset of cardiorespiratory collapse followed by disseminated intravascular coagulation (DIC). AFE is rare, affecting only about 2 to 6 per 100,000 births, but classic cases have a reported maternal mortality rate that exceeds 50%.1 It is thought to reflect a complex, systemic proinflammatory response to maternal intravasation of pregnancy material, such as trophoblast, thromboplastins, fetal cells, or amniotic fluid. Because the syndrome is not necessarily directly caused by emboli or by amniotic fluid per se,2 it has been proposed that AFE be called “anaphylactoid syndrome of pregnancy,” but this terminology has not yet been widely adopted.3
Guidelines from the Society for Maternal-Fetal Medicine (SMFM) recommend several time-critical steps for the initial stabilization and management of patients with AFE.4 However, because AFE is rare, most obstetric providers may not encounter a case for many years or even decades after they have received training, so it is unrealistic to expect that they will remember these guidelines when they are needed. For this reason, when AFE occurs, it is important to have a readily accessible cognitive aid, such as a checklist that summarizes the key management steps. The SMFM provides a checklist for initial management of AFE that can be used at your institution; it is presented in the FIGURE and provides the outline for this discussion.5

Provide CPR immediately
Most AFE cases are accompanied by cardiorespiratory arrest. If the patient has no pulse, call a “code” to mobilize additional help and immediately start CPR. Use a backboard to make cardiac compressions most effective and manually displace the uterus or tilt the patient to avoid supine hypotension. Designate a timekeeper to call out 1-minute intervals and record critical data, such as medication administration and laboratory orders/results.
Expedite delivery
Immediate delivery is needed if maternal cardiac activity is not restored within 4 minutes of starting CPR, with a target to have delivery completed within 5 minutes. Operative vaginal delivery may be an option if delivery is imminent, as in the case presented, but cesarean delivery (CD) will be needed in most cases. This was previously called “perimortem cesarean” delivery, but the term “resuscitative hysterotomy” has been proposed because the primary goal is to improve the effectiveness of CPR6 and prevent both maternal and perinatal death. CPR is less effective in pregnant women because the pregnant uterus takes a substantial fraction of the maternal cardiac output, as well as compresses the vena cava. Some experts suggest that, rather than waiting 4 minutes, CD should be started as soon as an obstetrician or other surgeon is present, unless there is an immediate response to electrical cardioversion.6,7
In most cases, immediate CD should be performed wherever the patient is located rather than using precious minutes to move the patient to an operating room. Antiseptic preparation is expedited by simply pouring povidone-iodine or chlorhexidine over the lower abdomen if readily available; if not available, skip this step. Enter the abdomen and uterus as rapidly as possible using only a scalpel to make generous midline incisions.
If CPR is not required, proceed with cesarean or operative vaginal delivery as soon as the mother has been stabilized. These procedures should be performed using standard safety precautions outlined in the SMFM patient safety checklists for cesarean or operative vaginal delivery.8,9
Continue to: Anticipate hemorrhage...
Anticipate hemorrhage
Be prepared for uterine atony, coagulopathy, and catastrophic hemorrhage. Initiate IV oxytocin prophylaxis as soon as the infant is delivered. Have a low threshold for giving other uterotonic agents such as methylergonovine, carboprost, or misoprostol. If hemorrhage or DIC occurs, give tranexamic acid. Have the anesthesiologist or trauma team (if available) insert an intraosseous line for fluid resuscitation if peripheral IV access is inadequate.
Massive transfusion is often needed to treat DIC, which occurs in most AFE cases. Anticipate—do not wait—for DIC to occur. We propose activating your hospital’s massive transfusion protocol (MTP) as soon as you diagnose AFE so that blood products will be available as soon as possible. A typical MTP provides several units of red blood cells, a pheresis pack of platelets, and fresh/frozen plasma (FFP). If clinically indicated, administer cryoprecipitate instead of FFP to minimize volume overload, which may occur with FFP.
CASE Part 2: MTP initiated to treat DIC
The MTP is initiated. Laboratory results immediately pre-transfusion include hemoglobin 11.3 g/dL, platelet count 46,000 per mm3, fibrinogen 87 mg/dL, and an elevated prothrombin time international normalized ratio.
Expect heart failure
The initial hemodynamic picture in AFE is right heart failure, which should optimally be managed by a specialist from anesthesiology, cardiology, or critical care as soon as they are available. An emergency department physician may manage the hemodynamics until a specialist arrives. Avoidance of fluid overload is one important principle. If fluid challenges are needed for hypovolemic shock, boluses should be restricted to 500 mL rather than the traditional 1000 mL.
Pharmacologic treatment may include vasopressors, inotropic agents, and pulmonary vasodilators. Example medications and dosages recommended by SMFM are summarized in the checklist (FIGURE).5
After the initial phase of recovery, the hemodynamic picture often changes from right heart failure to left heart failure. Management of left heart failure is not covered in the SMFM checklist because, by the time it appears, the patient will usually be in the intensive care unit, managed by the critical care team. Management of left heart failure generally includes diuresis as needed for cardiogenic pulmonary edema, optimization of cardiac preload, and inotropic agents or vasopressors if needed to maintain cardiac output or perfusion pressure.4
Debrief, learning opportunities
Complex emergencies such as AFE are rarely handled 100% perfectly, even those with a good outcome, so they present opportunities for team learning and improvement. The team should conduct a 10- to 15-minute debrief soon after the patient is stabilized. Make an explicit statement that the main goal of the debrief is to gather suggestions as to how systems and processes could be improved for next time, not to find fault or lay blame on individuals. Encourage all personnel involved in the initial management to attend and discuss what went well and what did not. Another goal is to provide support for individuals who may feel traumatized by the dramatic, frightening events surrounding an AFE and by the poor patient outcome or guarded prognosis that frequently follows. Another goal is to discuss the plan for providing support and disclosure to the patient and family.
The vast majority of AFE cases meet criteria to be designated as “sentinel events,” because of patient transfer to the intensive care unit, multi-unit blood transfusion, other severe maternal morbidities, or maternal death. Therefore, most AFE cases will trigger a root cause analysis (RCA) or other formal sentinel event analysis conducted by the hospital’s Safety or Quality Department. As with the immediate post-event debrief, the first goal of the RCA is to identify systems issues that may have resulted in suboptimal care and that can be modified to improve future care. Specific issues regarding the checklist should also be addressed:
- Was the checklist used?
- Was the checklist available?
- Are there items on the checklist that need to be modified, added, or deleted?
The RCA concludes with the development of a performance improvement plan.
Ultimately, we encourage all AFE cases be reported to the registry maintained by the Amniotic Fluid Embolism Foundation at https://www.afesupport.org/, regardless of whether the outcome was favorable for the mother and newborn. The registry includes over 130 AFE cases since 2013 from around the world. Researchers periodically report on the registry findings.10 If providers report cases with both good and bad outcomes, the registry may provide future insights regarding which adjunctive or empiric treatments may or may not be promising.
Continue to: Empiric treatments...
Empiric treatments
From time-to-time, new regimens for empiric treatment of AFE are reported. It is important to recognize that these reports are generally uncontrolled case reports of favorable outcomes and that, without a control group, it is impossible to determine to what extent the treatment contributed to the outcome or was merely incidental. Given the rarity of AFE, it seems unlikely that there will ever be a randomized clinical trial or even a controlled prospective study comparing treatment regimens.
The “A-OK” regimen is an empiric treatment that has garnered some interest after an initial case report.11 It consists of an anticholinergic agent (atropine 0.2 mg IV), a selective 5-HT3 receptor antagonist (ondansetron 8 mg IV), and a nonsteroidal anti-inflammatory drug (ketorolac 15 mg IV). We have some reservations about this regimen, however, because atropine is relatively contraindicated if the patient has tachycardia (which is common in patients with hemorrhage) and ketorolac may suppress platelet function, which might be harmful for patients with DIC or thrombocytopenia.
Another empiric treatment is the “50-50-500” regimen, which includes an H1 antihistamine (diphenhydramine 50 mg IV), an H2 antihistamine (famotidine 50 mg IV), and a corticosteroid (hydrocortisone 500 mg IV). This regimen aims to suppress histamine-mediated and cell-mediated inflammatory responses, based on the notion that proinflammatory responses likely mediate much of the underlying pathophysiology of the AFE syndrome.
We would emphasize that these empiric regimens are not clinically validated, US Food and Drug Administration approved for treatment of AFE, or considered standard of care. Future reports of these and other regimens will be needed to evaluate their efficacy, limitations, and risks. Again, we encourage providers to report all AFE cases to the AFE Foundation registry, regardless of whether the treatments are successful.
CASE Conclusion
The hemorrhage stops after administration of oxytocin, carboprost, 6 units of cryoprecipitate, and a 6-unit platelet pheresis pack. The patient is transferred to the intensive care unit where she eventually requires a total of 10 units of red cells, 8 more units of cryoprecipitate, and another platelet pheresis pack. She is discharged to home in stable condition on postpartum day 4.
Be prepared, have the checklist ready
Because AFE is rare, most members of the health care team will have no prior experience managing a real case. It may have been years or decades since they had any education on AFE or they last read a review article such as this one. It is even possible the anesthesiologist, cardiologist, or critical care specialist has never heard of AFE. Thus if they rely on memory alone, there is substantial risk of forgetting items, getting dosages wrong, or other errors. With this in mind, what is the best way to prepare the team to expeditiously employ the management steps outlined here?
Use of a checklist that summarizes these key steps for early management, such as the SMFM checklist in the FIGURE, will help ensure that all relevant steps are performed in every AFE case. It is designed to be printed on a single sheet of letter-sized paper, and we propose that every labor and delivery (L&D) unit keep laminated copies of this checklist in several places where they will be immediately available should an AFE occur. Copies can be kept on the anesthesia carts in the L&D operating rooms, in an emergency procedures binder on the unit, and on the “crash carts” and hemorrhage supply carts in the L&D unit. Effective implementation of an AFE checklist requires all personnel know where to readily find it and have some familiarity with its contents.
An interdisciplinary team comprising representatives from nursing, obstetrics, and anesthesia should meet to discuss whether the checklist needs to be modified to fit the local hospital formulary or other unique local circumstances. The team should develop an implementation plan that includes where to keep checklist copies, a process to periodically ensure that the copies are still present and readable, a roll-out plan to inform all personnel about the checklist process, and most importantly a training plan that includes incorporating AFE cases into the schedule of multidisciplinary simulations and drills for obstetric emergencies. Other implementation strategies are outlined in the SMFM document.5
Ultimately an organized, systematic approach is recommended for management of AFE. There is no single best treatment of AFE; it is supportive and directed toward the underlying pathophysiology, which may vary from patient to patient. Therefore, although a checklist, in conjunction with regular education and simulation activities, may help optimize care and improve outcomes, there is still a high risk of maternal morbidity and mortality from AFE. ●
- Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014;123(2 Pt 1):337-348. doi:10.1097/AOG.0000000000000107.
- Funk M, Damron A, Bandi V, et al. Pulmonary vascular obstruction by squamous cells is not involved in amniotic fluid embolism. Am J Obstet Gynecol. 2018;218:460-461. doi:10.1016/j.ajog.2017.12.225.
- Gilmore DA, Wakim J, Secrest J, et al. Anaphylactoid syndrome of pregnancy: a review of the literature with latest management and outcome data. AANA J. 2003;71:120-126.
- Society for Maternal-Fetal Medicine, Pacheco LD, Saade G, et al. Amniotic fluid embolism: diagnosis and management. Am J Obstet Gynecol. 2016;215:B16-24. doi:10.1016/j.ajog.2016.03.012.
- Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine; Combs CA, Montgomery DM, et al. Society for Maternal-Fetal Medicine Special Statement: checklist for initial management of amniotic fluid embolism. Am J Obstet Gynecol. 2021;224:B29-B32. doi:10.1016/j.ajog.2021.01.001.
- Rose CH, Faksh A, Traynor KD, et al. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2015;213:653-6, 653.e1. doi:10.1016/j.ajog.2015.07.019.
- Pacheco LD, Clark SL, Klassen M, et al. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol. 2020;222:48-52. doi:10.1016/j.ajog.2019.07.036.
- Combs CA, Einerson BD, Toner LE, SMFM Patient Safety and Quality Committee. SMFM Special Statement: surgical safety checklists for cesarean delivery. Am J Obstet Gynecol. 2021;225:B43-B49. doi:10.1016/j.ajog.2021.07.011.
- SMFM Patient Safety and Quality Committee, Staat B, Combs CA. SMFM Special Statement: operative vaginal delivery: checklists for performance and documentation. Am J Obstet Gynecol. 2020;222:B15-B21. doi:10.1016/j.ajog.2020.02.011.
- Stafford IA, Moaddab A, Dildy GA, et al. Amniotic fluid embolism syndrome: analysis of the United States international registry. Am J Obstet Gynecol MFM. 2020;2:100083. doi:10.1016/j.ajogmf.2019.100083.
- Rezai S, Hughes AZC, Larsen TB, et al. Atypical amniotic f luid embolism managed with a novel therapeutic regimen. Case Rep Obstet Gynecol. 2017; 2017:8458375. doi:10.1155/2017/8458375.
CASE Part 1: CPR initiated during induction of labor
A 32-year-old gravida 4 para 3-0-0-3 is undergoing induction of labor with intravenous (IV) oxytocin at 39 weeks of gestation. She has no significant medical or obstetric history. Fifteen minutes after reaching complete cervical dilation, she says “I don’t feel right,” then suddenly loses consciousness. The nurse finds no detectable pulse, calls a “code blue,” and initiates cardiopulmonary resuscitation (CPR). The obstetrician is notified, appears promptly, assesses the situation, and delivers a 3.6-kg baby via vacuum extraction. Apgar score is 2/10 at 1 minute and 6/10 at 5 minutes. After delivery of the placenta, there is uterine atony and brisk hemorrhage with 2 L of blood loss.
Management of AFE: A rare complication
This case demonstrates a classic presentation of amniotic fluid embolism (AFE) syndrome—a patient in labor or within 30 minutes after delivery has sudden onset of cardiorespiratory collapse followed by disseminated intravascular coagulation (DIC). AFE is rare, affecting only about 2 to 6 per 100,000 births, but classic cases have a reported maternal mortality rate that exceeds 50%.1 It is thought to reflect a complex, systemic proinflammatory response to maternal intravasation of pregnancy material, such as trophoblast, thromboplastins, fetal cells, or amniotic fluid. Because the syndrome is not necessarily directly caused by emboli or by amniotic fluid per se,2 it has been proposed that AFE be called “anaphylactoid syndrome of pregnancy,” but this terminology has not yet been widely adopted.3
Guidelines from the Society for Maternal-Fetal Medicine (SMFM) recommend several time-critical steps for the initial stabilization and management of patients with AFE.4 However, because AFE is rare, most obstetric providers may not encounter a case for many years or even decades after they have received training, so it is unrealistic to expect that they will remember these guidelines when they are needed. For this reason, when AFE occurs, it is important to have a readily accessible cognitive aid, such as a checklist that summarizes the key management steps. The SMFM provides a checklist for initial management of AFE that can be used at your institution; it is presented in the FIGURE and provides the outline for this discussion.5

Provide CPR immediately
Most AFE cases are accompanied by cardiorespiratory arrest. If the patient has no pulse, call a “code” to mobilize additional help and immediately start CPR. Use a backboard to make cardiac compressions most effective and manually displace the uterus or tilt the patient to avoid supine hypotension. Designate a timekeeper to call out 1-minute intervals and record critical data, such as medication administration and laboratory orders/results.
Expedite delivery
Immediate delivery is needed if maternal cardiac activity is not restored within 4 minutes of starting CPR, with a target to have delivery completed within 5 minutes. Operative vaginal delivery may be an option if delivery is imminent, as in the case presented, but cesarean delivery (CD) will be needed in most cases. This was previously called “perimortem cesarean” delivery, but the term “resuscitative hysterotomy” has been proposed because the primary goal is to improve the effectiveness of CPR6 and prevent both maternal and perinatal death. CPR is less effective in pregnant women because the pregnant uterus takes a substantial fraction of the maternal cardiac output, as well as compresses the vena cava. Some experts suggest that, rather than waiting 4 minutes, CD should be started as soon as an obstetrician or other surgeon is present, unless there is an immediate response to electrical cardioversion.6,7
In most cases, immediate CD should be performed wherever the patient is located rather than using precious minutes to move the patient to an operating room. Antiseptic preparation is expedited by simply pouring povidone-iodine or chlorhexidine over the lower abdomen if readily available; if not available, skip this step. Enter the abdomen and uterus as rapidly as possible using only a scalpel to make generous midline incisions.
If CPR is not required, proceed with cesarean or operative vaginal delivery as soon as the mother has been stabilized. These procedures should be performed using standard safety precautions outlined in the SMFM patient safety checklists for cesarean or operative vaginal delivery.8,9
Continue to: Anticipate hemorrhage...
Anticipate hemorrhage
Be prepared for uterine atony, coagulopathy, and catastrophic hemorrhage. Initiate IV oxytocin prophylaxis as soon as the infant is delivered. Have a low threshold for giving other uterotonic agents such as methylergonovine, carboprost, or misoprostol. If hemorrhage or DIC occurs, give tranexamic acid. Have the anesthesiologist or trauma team (if available) insert an intraosseous line for fluid resuscitation if peripheral IV access is inadequate.
Massive transfusion is often needed to treat DIC, which occurs in most AFE cases. Anticipate—do not wait—for DIC to occur. We propose activating your hospital’s massive transfusion protocol (MTP) as soon as you diagnose AFE so that blood products will be available as soon as possible. A typical MTP provides several units of red blood cells, a pheresis pack of platelets, and fresh/frozen plasma (FFP). If clinically indicated, administer cryoprecipitate instead of FFP to minimize volume overload, which may occur with FFP.
CASE Part 2: MTP initiated to treat DIC
The MTP is initiated. Laboratory results immediately pre-transfusion include hemoglobin 11.3 g/dL, platelet count 46,000 per mm3, fibrinogen 87 mg/dL, and an elevated prothrombin time international normalized ratio.
Expect heart failure
The initial hemodynamic picture in AFE is right heart failure, which should optimally be managed by a specialist from anesthesiology, cardiology, or critical care as soon as they are available. An emergency department physician may manage the hemodynamics until a specialist arrives. Avoidance of fluid overload is one important principle. If fluid challenges are needed for hypovolemic shock, boluses should be restricted to 500 mL rather than the traditional 1000 mL.
Pharmacologic treatment may include vasopressors, inotropic agents, and pulmonary vasodilators. Example medications and dosages recommended by SMFM are summarized in the checklist (FIGURE).5
After the initial phase of recovery, the hemodynamic picture often changes from right heart failure to left heart failure. Management of left heart failure is not covered in the SMFM checklist because, by the time it appears, the patient will usually be in the intensive care unit, managed by the critical care team. Management of left heart failure generally includes diuresis as needed for cardiogenic pulmonary edema, optimization of cardiac preload, and inotropic agents or vasopressors if needed to maintain cardiac output or perfusion pressure.4
Debrief, learning opportunities
Complex emergencies such as AFE are rarely handled 100% perfectly, even those with a good outcome, so they present opportunities for team learning and improvement. The team should conduct a 10- to 15-minute debrief soon after the patient is stabilized. Make an explicit statement that the main goal of the debrief is to gather suggestions as to how systems and processes could be improved for next time, not to find fault or lay blame on individuals. Encourage all personnel involved in the initial management to attend and discuss what went well and what did not. Another goal is to provide support for individuals who may feel traumatized by the dramatic, frightening events surrounding an AFE and by the poor patient outcome or guarded prognosis that frequently follows. Another goal is to discuss the plan for providing support and disclosure to the patient and family.
The vast majority of AFE cases meet criteria to be designated as “sentinel events,” because of patient transfer to the intensive care unit, multi-unit blood transfusion, other severe maternal morbidities, or maternal death. Therefore, most AFE cases will trigger a root cause analysis (RCA) or other formal sentinel event analysis conducted by the hospital’s Safety or Quality Department. As with the immediate post-event debrief, the first goal of the RCA is to identify systems issues that may have resulted in suboptimal care and that can be modified to improve future care. Specific issues regarding the checklist should also be addressed:
- Was the checklist used?
- Was the checklist available?
- Are there items on the checklist that need to be modified, added, or deleted?
The RCA concludes with the development of a performance improvement plan.
Ultimately, we encourage all AFE cases be reported to the registry maintained by the Amniotic Fluid Embolism Foundation at https://www.afesupport.org/, regardless of whether the outcome was favorable for the mother and newborn. The registry includes over 130 AFE cases since 2013 from around the world. Researchers periodically report on the registry findings.10 If providers report cases with both good and bad outcomes, the registry may provide future insights regarding which adjunctive or empiric treatments may or may not be promising.
Continue to: Empiric treatments...
Empiric treatments
From time-to-time, new regimens for empiric treatment of AFE are reported. It is important to recognize that these reports are generally uncontrolled case reports of favorable outcomes and that, without a control group, it is impossible to determine to what extent the treatment contributed to the outcome or was merely incidental. Given the rarity of AFE, it seems unlikely that there will ever be a randomized clinical trial or even a controlled prospective study comparing treatment regimens.
The “A-OK” regimen is an empiric treatment that has garnered some interest after an initial case report.11 It consists of an anticholinergic agent (atropine 0.2 mg IV), a selective 5-HT3 receptor antagonist (ondansetron 8 mg IV), and a nonsteroidal anti-inflammatory drug (ketorolac 15 mg IV). We have some reservations about this regimen, however, because atropine is relatively contraindicated if the patient has tachycardia (which is common in patients with hemorrhage) and ketorolac may suppress platelet function, which might be harmful for patients with DIC or thrombocytopenia.
Another empiric treatment is the “50-50-500” regimen, which includes an H1 antihistamine (diphenhydramine 50 mg IV), an H2 antihistamine (famotidine 50 mg IV), and a corticosteroid (hydrocortisone 500 mg IV). This regimen aims to suppress histamine-mediated and cell-mediated inflammatory responses, based on the notion that proinflammatory responses likely mediate much of the underlying pathophysiology of the AFE syndrome.
We would emphasize that these empiric regimens are not clinically validated, US Food and Drug Administration approved for treatment of AFE, or considered standard of care. Future reports of these and other regimens will be needed to evaluate their efficacy, limitations, and risks. Again, we encourage providers to report all AFE cases to the AFE Foundation registry, regardless of whether the treatments are successful.
CASE Conclusion
The hemorrhage stops after administration of oxytocin, carboprost, 6 units of cryoprecipitate, and a 6-unit platelet pheresis pack. The patient is transferred to the intensive care unit where she eventually requires a total of 10 units of red cells, 8 more units of cryoprecipitate, and another platelet pheresis pack. She is discharged to home in stable condition on postpartum day 4.
Be prepared, have the checklist ready
Because AFE is rare, most members of the health care team will have no prior experience managing a real case. It may have been years or decades since they had any education on AFE or they last read a review article such as this one. It is even possible the anesthesiologist, cardiologist, or critical care specialist has never heard of AFE. Thus if they rely on memory alone, there is substantial risk of forgetting items, getting dosages wrong, or other errors. With this in mind, what is the best way to prepare the team to expeditiously employ the management steps outlined here?
Use of a checklist that summarizes these key steps for early management, such as the SMFM checklist in the FIGURE, will help ensure that all relevant steps are performed in every AFE case. It is designed to be printed on a single sheet of letter-sized paper, and we propose that every labor and delivery (L&D) unit keep laminated copies of this checklist in several places where they will be immediately available should an AFE occur. Copies can be kept on the anesthesia carts in the L&D operating rooms, in an emergency procedures binder on the unit, and on the “crash carts” and hemorrhage supply carts in the L&D unit. Effective implementation of an AFE checklist requires all personnel know where to readily find it and have some familiarity with its contents.
An interdisciplinary team comprising representatives from nursing, obstetrics, and anesthesia should meet to discuss whether the checklist needs to be modified to fit the local hospital formulary or other unique local circumstances. The team should develop an implementation plan that includes where to keep checklist copies, a process to periodically ensure that the copies are still present and readable, a roll-out plan to inform all personnel about the checklist process, and most importantly a training plan that includes incorporating AFE cases into the schedule of multidisciplinary simulations and drills for obstetric emergencies. Other implementation strategies are outlined in the SMFM document.5
Ultimately an organized, systematic approach is recommended for management of AFE. There is no single best treatment of AFE; it is supportive and directed toward the underlying pathophysiology, which may vary from patient to patient. Therefore, although a checklist, in conjunction with regular education and simulation activities, may help optimize care and improve outcomes, there is still a high risk of maternal morbidity and mortality from AFE. ●
CASE Part 1: CPR initiated during induction of labor
A 32-year-old gravida 4 para 3-0-0-3 is undergoing induction of labor with intravenous (IV) oxytocin at 39 weeks of gestation. She has no significant medical or obstetric history. Fifteen minutes after reaching complete cervical dilation, she says “I don’t feel right,” then suddenly loses consciousness. The nurse finds no detectable pulse, calls a “code blue,” and initiates cardiopulmonary resuscitation (CPR). The obstetrician is notified, appears promptly, assesses the situation, and delivers a 3.6-kg baby via vacuum extraction. Apgar score is 2/10 at 1 minute and 6/10 at 5 minutes. After delivery of the placenta, there is uterine atony and brisk hemorrhage with 2 L of blood loss.
Management of AFE: A rare complication
This case demonstrates a classic presentation of amniotic fluid embolism (AFE) syndrome—a patient in labor or within 30 minutes after delivery has sudden onset of cardiorespiratory collapse followed by disseminated intravascular coagulation (DIC). AFE is rare, affecting only about 2 to 6 per 100,000 births, but classic cases have a reported maternal mortality rate that exceeds 50%.1 It is thought to reflect a complex, systemic proinflammatory response to maternal intravasation of pregnancy material, such as trophoblast, thromboplastins, fetal cells, or amniotic fluid. Because the syndrome is not necessarily directly caused by emboli or by amniotic fluid per se,2 it has been proposed that AFE be called “anaphylactoid syndrome of pregnancy,” but this terminology has not yet been widely adopted.3
Guidelines from the Society for Maternal-Fetal Medicine (SMFM) recommend several time-critical steps for the initial stabilization and management of patients with AFE.4 However, because AFE is rare, most obstetric providers may not encounter a case for many years or even decades after they have received training, so it is unrealistic to expect that they will remember these guidelines when they are needed. For this reason, when AFE occurs, it is important to have a readily accessible cognitive aid, such as a checklist that summarizes the key management steps. The SMFM provides a checklist for initial management of AFE that can be used at your institution; it is presented in the FIGURE and provides the outline for this discussion.5

Provide CPR immediately
Most AFE cases are accompanied by cardiorespiratory arrest. If the patient has no pulse, call a “code” to mobilize additional help and immediately start CPR. Use a backboard to make cardiac compressions most effective and manually displace the uterus or tilt the patient to avoid supine hypotension. Designate a timekeeper to call out 1-minute intervals and record critical data, such as medication administration and laboratory orders/results.
Expedite delivery
Immediate delivery is needed if maternal cardiac activity is not restored within 4 minutes of starting CPR, with a target to have delivery completed within 5 minutes. Operative vaginal delivery may be an option if delivery is imminent, as in the case presented, but cesarean delivery (CD) will be needed in most cases. This was previously called “perimortem cesarean” delivery, but the term “resuscitative hysterotomy” has been proposed because the primary goal is to improve the effectiveness of CPR6 and prevent both maternal and perinatal death. CPR is less effective in pregnant women because the pregnant uterus takes a substantial fraction of the maternal cardiac output, as well as compresses the vena cava. Some experts suggest that, rather than waiting 4 minutes, CD should be started as soon as an obstetrician or other surgeon is present, unless there is an immediate response to electrical cardioversion.6,7
In most cases, immediate CD should be performed wherever the patient is located rather than using precious minutes to move the patient to an operating room. Antiseptic preparation is expedited by simply pouring povidone-iodine or chlorhexidine over the lower abdomen if readily available; if not available, skip this step. Enter the abdomen and uterus as rapidly as possible using only a scalpel to make generous midline incisions.
If CPR is not required, proceed with cesarean or operative vaginal delivery as soon as the mother has been stabilized. These procedures should be performed using standard safety precautions outlined in the SMFM patient safety checklists for cesarean or operative vaginal delivery.8,9
Continue to: Anticipate hemorrhage...
Anticipate hemorrhage
Be prepared for uterine atony, coagulopathy, and catastrophic hemorrhage. Initiate IV oxytocin prophylaxis as soon as the infant is delivered. Have a low threshold for giving other uterotonic agents such as methylergonovine, carboprost, or misoprostol. If hemorrhage or DIC occurs, give tranexamic acid. Have the anesthesiologist or trauma team (if available) insert an intraosseous line for fluid resuscitation if peripheral IV access is inadequate.
Massive transfusion is often needed to treat DIC, which occurs in most AFE cases. Anticipate—do not wait—for DIC to occur. We propose activating your hospital’s massive transfusion protocol (MTP) as soon as you diagnose AFE so that blood products will be available as soon as possible. A typical MTP provides several units of red blood cells, a pheresis pack of platelets, and fresh/frozen plasma (FFP). If clinically indicated, administer cryoprecipitate instead of FFP to minimize volume overload, which may occur with FFP.
CASE Part 2: MTP initiated to treat DIC
The MTP is initiated. Laboratory results immediately pre-transfusion include hemoglobin 11.3 g/dL, platelet count 46,000 per mm3, fibrinogen 87 mg/dL, and an elevated prothrombin time international normalized ratio.
Expect heart failure
The initial hemodynamic picture in AFE is right heart failure, which should optimally be managed by a specialist from anesthesiology, cardiology, or critical care as soon as they are available. An emergency department physician may manage the hemodynamics until a specialist arrives. Avoidance of fluid overload is one important principle. If fluid challenges are needed for hypovolemic shock, boluses should be restricted to 500 mL rather than the traditional 1000 mL.
Pharmacologic treatment may include vasopressors, inotropic agents, and pulmonary vasodilators. Example medications and dosages recommended by SMFM are summarized in the checklist (FIGURE).5
After the initial phase of recovery, the hemodynamic picture often changes from right heart failure to left heart failure. Management of left heart failure is not covered in the SMFM checklist because, by the time it appears, the patient will usually be in the intensive care unit, managed by the critical care team. Management of left heart failure generally includes diuresis as needed for cardiogenic pulmonary edema, optimization of cardiac preload, and inotropic agents or vasopressors if needed to maintain cardiac output or perfusion pressure.4
Debrief, learning opportunities
Complex emergencies such as AFE are rarely handled 100% perfectly, even those with a good outcome, so they present opportunities for team learning and improvement. The team should conduct a 10- to 15-minute debrief soon after the patient is stabilized. Make an explicit statement that the main goal of the debrief is to gather suggestions as to how systems and processes could be improved for next time, not to find fault or lay blame on individuals. Encourage all personnel involved in the initial management to attend and discuss what went well and what did not. Another goal is to provide support for individuals who may feel traumatized by the dramatic, frightening events surrounding an AFE and by the poor patient outcome or guarded prognosis that frequently follows. Another goal is to discuss the plan for providing support and disclosure to the patient and family.
The vast majority of AFE cases meet criteria to be designated as “sentinel events,” because of patient transfer to the intensive care unit, multi-unit blood transfusion, other severe maternal morbidities, or maternal death. Therefore, most AFE cases will trigger a root cause analysis (RCA) or other formal sentinel event analysis conducted by the hospital’s Safety or Quality Department. As with the immediate post-event debrief, the first goal of the RCA is to identify systems issues that may have resulted in suboptimal care and that can be modified to improve future care. Specific issues regarding the checklist should also be addressed:
- Was the checklist used?
- Was the checklist available?
- Are there items on the checklist that need to be modified, added, or deleted?
The RCA concludes with the development of a performance improvement plan.
Ultimately, we encourage all AFE cases be reported to the registry maintained by the Amniotic Fluid Embolism Foundation at https://www.afesupport.org/, regardless of whether the outcome was favorable for the mother and newborn. The registry includes over 130 AFE cases since 2013 from around the world. Researchers periodically report on the registry findings.10 If providers report cases with both good and bad outcomes, the registry may provide future insights regarding which adjunctive or empiric treatments may or may not be promising.
Continue to: Empiric treatments...
Empiric treatments
From time-to-time, new regimens for empiric treatment of AFE are reported. It is important to recognize that these reports are generally uncontrolled case reports of favorable outcomes and that, without a control group, it is impossible to determine to what extent the treatment contributed to the outcome or was merely incidental. Given the rarity of AFE, it seems unlikely that there will ever be a randomized clinical trial or even a controlled prospective study comparing treatment regimens.
The “A-OK” regimen is an empiric treatment that has garnered some interest after an initial case report.11 It consists of an anticholinergic agent (atropine 0.2 mg IV), a selective 5-HT3 receptor antagonist (ondansetron 8 mg IV), and a nonsteroidal anti-inflammatory drug (ketorolac 15 mg IV). We have some reservations about this regimen, however, because atropine is relatively contraindicated if the patient has tachycardia (which is common in patients with hemorrhage) and ketorolac may suppress platelet function, which might be harmful for patients with DIC or thrombocytopenia.
Another empiric treatment is the “50-50-500” regimen, which includes an H1 antihistamine (diphenhydramine 50 mg IV), an H2 antihistamine (famotidine 50 mg IV), and a corticosteroid (hydrocortisone 500 mg IV). This regimen aims to suppress histamine-mediated and cell-mediated inflammatory responses, based on the notion that proinflammatory responses likely mediate much of the underlying pathophysiology of the AFE syndrome.
We would emphasize that these empiric regimens are not clinically validated, US Food and Drug Administration approved for treatment of AFE, or considered standard of care. Future reports of these and other regimens will be needed to evaluate their efficacy, limitations, and risks. Again, we encourage providers to report all AFE cases to the AFE Foundation registry, regardless of whether the treatments are successful.
CASE Conclusion
The hemorrhage stops after administration of oxytocin, carboprost, 6 units of cryoprecipitate, and a 6-unit platelet pheresis pack. The patient is transferred to the intensive care unit where she eventually requires a total of 10 units of red cells, 8 more units of cryoprecipitate, and another platelet pheresis pack. She is discharged to home in stable condition on postpartum day 4.
Be prepared, have the checklist ready
Because AFE is rare, most members of the health care team will have no prior experience managing a real case. It may have been years or decades since they had any education on AFE or they last read a review article such as this one. It is even possible the anesthesiologist, cardiologist, or critical care specialist has never heard of AFE. Thus if they rely on memory alone, there is substantial risk of forgetting items, getting dosages wrong, or other errors. With this in mind, what is the best way to prepare the team to expeditiously employ the management steps outlined here?
Use of a checklist that summarizes these key steps for early management, such as the SMFM checklist in the FIGURE, will help ensure that all relevant steps are performed in every AFE case. It is designed to be printed on a single sheet of letter-sized paper, and we propose that every labor and delivery (L&D) unit keep laminated copies of this checklist in several places where they will be immediately available should an AFE occur. Copies can be kept on the anesthesia carts in the L&D operating rooms, in an emergency procedures binder on the unit, and on the “crash carts” and hemorrhage supply carts in the L&D unit. Effective implementation of an AFE checklist requires all personnel know where to readily find it and have some familiarity with its contents.
An interdisciplinary team comprising representatives from nursing, obstetrics, and anesthesia should meet to discuss whether the checklist needs to be modified to fit the local hospital formulary or other unique local circumstances. The team should develop an implementation plan that includes where to keep checklist copies, a process to periodically ensure that the copies are still present and readable, a roll-out plan to inform all personnel about the checklist process, and most importantly a training plan that includes incorporating AFE cases into the schedule of multidisciplinary simulations and drills for obstetric emergencies. Other implementation strategies are outlined in the SMFM document.5
Ultimately an organized, systematic approach is recommended for management of AFE. There is no single best treatment of AFE; it is supportive and directed toward the underlying pathophysiology, which may vary from patient to patient. Therefore, although a checklist, in conjunction with regular education and simulation activities, may help optimize care and improve outcomes, there is still a high risk of maternal morbidity and mortality from AFE. ●
- Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014;123(2 Pt 1):337-348. doi:10.1097/AOG.0000000000000107.
- Funk M, Damron A, Bandi V, et al. Pulmonary vascular obstruction by squamous cells is not involved in amniotic fluid embolism. Am J Obstet Gynecol. 2018;218:460-461. doi:10.1016/j.ajog.2017.12.225.
- Gilmore DA, Wakim J, Secrest J, et al. Anaphylactoid syndrome of pregnancy: a review of the literature with latest management and outcome data. AANA J. 2003;71:120-126.
- Society for Maternal-Fetal Medicine, Pacheco LD, Saade G, et al. Amniotic fluid embolism: diagnosis and management. Am J Obstet Gynecol. 2016;215:B16-24. doi:10.1016/j.ajog.2016.03.012.
- Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine; Combs CA, Montgomery DM, et al. Society for Maternal-Fetal Medicine Special Statement: checklist for initial management of amniotic fluid embolism. Am J Obstet Gynecol. 2021;224:B29-B32. doi:10.1016/j.ajog.2021.01.001.
- Rose CH, Faksh A, Traynor KD, et al. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2015;213:653-6, 653.e1. doi:10.1016/j.ajog.2015.07.019.
- Pacheco LD, Clark SL, Klassen M, et al. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol. 2020;222:48-52. doi:10.1016/j.ajog.2019.07.036.
- Combs CA, Einerson BD, Toner LE, SMFM Patient Safety and Quality Committee. SMFM Special Statement: surgical safety checklists for cesarean delivery. Am J Obstet Gynecol. 2021;225:B43-B49. doi:10.1016/j.ajog.2021.07.011.
- SMFM Patient Safety and Quality Committee, Staat B, Combs CA. SMFM Special Statement: operative vaginal delivery: checklists for performance and documentation. Am J Obstet Gynecol. 2020;222:B15-B21. doi:10.1016/j.ajog.2020.02.011.
- Stafford IA, Moaddab A, Dildy GA, et al. Amniotic fluid embolism syndrome: analysis of the United States international registry. Am J Obstet Gynecol MFM. 2020;2:100083. doi:10.1016/j.ajogmf.2019.100083.
- Rezai S, Hughes AZC, Larsen TB, et al. Atypical amniotic f luid embolism managed with a novel therapeutic regimen. Case Rep Obstet Gynecol. 2017; 2017:8458375. doi:10.1155/2017/8458375.
- Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014;123(2 Pt 1):337-348. doi:10.1097/AOG.0000000000000107.
- Funk M, Damron A, Bandi V, et al. Pulmonary vascular obstruction by squamous cells is not involved in amniotic fluid embolism. Am J Obstet Gynecol. 2018;218:460-461. doi:10.1016/j.ajog.2017.12.225.
- Gilmore DA, Wakim J, Secrest J, et al. Anaphylactoid syndrome of pregnancy: a review of the literature with latest management and outcome data. AANA J. 2003;71:120-126.
- Society for Maternal-Fetal Medicine, Pacheco LD, Saade G, et al. Amniotic fluid embolism: diagnosis and management. Am J Obstet Gynecol. 2016;215:B16-24. doi:10.1016/j.ajog.2016.03.012.
- Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine; Combs CA, Montgomery DM, et al. Society for Maternal-Fetal Medicine Special Statement: checklist for initial management of amniotic fluid embolism. Am J Obstet Gynecol. 2021;224:B29-B32. doi:10.1016/j.ajog.2021.01.001.
- Rose CH, Faksh A, Traynor KD, et al. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2015;213:653-6, 653.e1. doi:10.1016/j.ajog.2015.07.019.
- Pacheco LD, Clark SL, Klassen M, et al. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol. 2020;222:48-52. doi:10.1016/j.ajog.2019.07.036.
- Combs CA, Einerson BD, Toner LE, SMFM Patient Safety and Quality Committee. SMFM Special Statement: surgical safety checklists for cesarean delivery. Am J Obstet Gynecol. 2021;225:B43-B49. doi:10.1016/j.ajog.2021.07.011.
- SMFM Patient Safety and Quality Committee, Staat B, Combs CA. SMFM Special Statement: operative vaginal delivery: checklists for performance and documentation. Am J Obstet Gynecol. 2020;222:B15-B21. doi:10.1016/j.ajog.2020.02.011.
- Stafford IA, Moaddab A, Dildy GA, et al. Amniotic fluid embolism syndrome: analysis of the United States international registry. Am J Obstet Gynecol MFM. 2020;2:100083. doi:10.1016/j.ajogmf.2019.100083.
- Rezai S, Hughes AZC, Larsen TB, et al. Atypical amniotic f luid embolism managed with a novel therapeutic regimen. Case Rep Obstet Gynecol. 2017; 2017:8458375. doi:10.1155/2017/8458375.
Medical management of miscarriage curbs costs and maintains quality of care
Medical management of early pregnancy loss costs less and offers similar quality of life to uterine aspiration, based on data from an analytical model.
Early pregnancy loss (EPL) occurs in more than 1 million women in the United States each year, and many patients are diagnosed before they show symptoms, wrote Divyah Nagendra, MD, of Cambridge Health Alliance, Mass., and colleagues.
A 2018 study showed that medical management of EPL with mifepristone added to misoprostol increased effectiveness and reduced the need for additional medication or subsequent uterine procedures, but the cost of mifepristone is perceived as a barrier, and the cost-effectiveness of its use, compared with surgical or expectant management, has not been well studied, the researchers noted.
“We already know that adding mifepristone to the medical management of early pregnancy loss increases the effectiveness of the regimen,” coauthor Courtney A. Schreiber, MD, of the University of Pennsylvania, Philadelphia, said in an interview. “Procedural uterine aspiration is highly effective as well, so patients and providers may consider the cost when deciding on a treatment strategy,” she added.
“If medication management is preferred by many patients, decreases the need to access in-person clinical care during a pandemic, and is found to be cost-effective, clinicians and policymakers should increase efforts to improve mifepristone availability and reduce access burdens,” the researchers wrote.
In a study published in the American Journal of Obstetrics & Gynecology, the researchers created a decision-analytic model using data from published literature and the Pregnancy Failure Regiments Trial (PreFaiR) to compare office-based uterine aspiration to medical management with mifepristone pretreatment followed by misoprostol for EPL.
The PrFaiR study randomized 300 women who experienced EPL before 12 weeks’ gestation to medication management with 800 mcg misoprostol vaginally, with or without pretreatment of 200 mg mifeprestone orally. The average age of the participants was 30.7 years, and demographics were similar between the groups.
The researchers used the PrFaiR data for medical management and patient-level data from published literature for uterine aspiration.
The primary outcome was the cost per quality-adjusted life year (QALY) gained. QALY was based on a modified utility score from the published literature. Effectiveness was based on QALY gained and the rate of complete expulsion of the gestational sac without additional intervention.
Overall, the mean costs per person were significantly higher for uterine aspiration, compared with medical management ($828 vs. $661, P = .004). Uterine aspiration was significantly more effective for complete gestational sac expulsion (97.3% vs. 83.8%, P = .0001). However, the QALYs were significantly higher for medical management, compared with uterine aspiration (0.082 vs. 0.079, P < .0001).
Cost-effectiveness was greater for medical management from a health care sector perspective, with lower costs and higher QALYs than uterine aspiration, the researchers noted.
They also evaluated the effect of mifepristone pretreatment on cost-effectiveness and found that medical management would remain cost effective, compared with uterine aspiration even if uterine aspiration procedures decreased in cost and mifepristone increased in cost, and even if medication management had a decreased completion rate and utility score, compared with uterine aspiration.
“Our analysis demonstrates that the incremental cost-effectiveness ratio (ICER) for medical management is well below the maximum willingness-to-pay threshold of approximately $100,000 per QALY gained,” the researchers wrote in their discussion of the findings.
Potential savings, uncertain access
Despite the potential savings and patient benefits, access to mifepristone remains a barrier, the researchers said.
Although the FDA lifted some restrictions on mifepristone in 2021 in the wake of the ongoing COVID-19 pandemic, the effect of new abortion-related restrictions remains to be seen.
The study findings were limited by several factors, including the use of 2018 National Medicare reimbursement rates to calculate costs, though actual costs vary by region and payer, the researchers noted. Other limitations include variations in cost of mifepristone by region and time and the differences in data sources between the uterine aspiration and medical management groups. More research is needed to assess QALYs for early pregnancy loss to establish standard measures and to assess the societal perspective of ESL as well as the health care perspective, they added.
However, the current results support medical management of EPL with mifepristone pretreatment followed by misoprostol as a “high-value care alternative” to office-based uterine aspiration, they said. “Increasing access to mifepristone and eliminating unnecessary restrictions will improve early pregnancy care,” they concluded.
“Given how effective procedural management is, we were slightly surprised that medical management remains cost effective,” Dr. Schreiber said in an interview.
Looking ahead in the wake of new restrictions on use for abortion, “patients may have difficulty accessing either medical or procedural management for early pregnancy loss,” Dr. Schreiber noted. “We support the accessibility of all evidence-based care and hope that our data will help overcome perceived financial barriers,” she said. Additional research needs include improved implementation and access to evidence-based early pregnancy loss care, she added.
Reasons to lift regulations
“Given the recent overturning of Roe v. Wade, any medications that are associated with abortion have increased scrutiny, especially mifepristone and misoprostol, even though these medications are also used for managing early pregnancy loss,” Sarah W. Prager, MD, of the University of Washington, Seattle, said in an interview. “Demonstrating that medication management of EPL with mifepristone/misoprostol is less expensive and has increased QALYs associated with it is yet another reason to deregulate mifepristone so it can also be more accessible for management of EPL,” said Dr. Prager, who was not involved in the study.
Dr. Prager said she was not surprised by the findings, as effective medication should be less expensive than a procedure. “I would caution that the increased QALYs found in this study should not be interpreted as a reason to restrict surgical management of EPL but to increase access also to medication management, even though medication has a slightly lower rate of complete gestational sac expulsion,” she noted. “Mode of management should be up to the patient, unless there is a clear medical reason for one or the other.”
Going forward, “the FDA has it in its power to remove the REMS, which would immediately make mifepristone a medication that can be prescribed through a pharmacy and therefore much more available,” said Dr. Prager. “Restrictions for both medication and surgical management of EPL will likely increase in states where abortion is illegal, and it could possibly lead to patients having less choice as to mode of management,” she explained.
“There are many studies showing that all modes of EPL management are safe and effective and should be supported with respect to patient choice,” Dr. Prager noted. “There are also substantial data supporting the overall safety of mifepristone, and there are no scientific or medical data suggesting the REMS increases safety in any way. Frankly, there are no good, evidence-based reasons to continue to keep the REMS in place,” she said.
The study was supported by the National Institute of Child Health and Human Development of the National Institutes of Health and a Society of Family Planning Research Fund Midcareer Mentor Award. The researchers had no financial conflicts to disclose. Dr. Prager had no financial conflicts to disclose and serves on the Editorial Advisory Board of Ob.Gyn. News.
Medical management of early pregnancy loss costs less and offers similar quality of life to uterine aspiration, based on data from an analytical model.
Early pregnancy loss (EPL) occurs in more than 1 million women in the United States each year, and many patients are diagnosed before they show symptoms, wrote Divyah Nagendra, MD, of Cambridge Health Alliance, Mass., and colleagues.
A 2018 study showed that medical management of EPL with mifepristone added to misoprostol increased effectiveness and reduced the need for additional medication or subsequent uterine procedures, but the cost of mifepristone is perceived as a barrier, and the cost-effectiveness of its use, compared with surgical or expectant management, has not been well studied, the researchers noted.
“We already know that adding mifepristone to the medical management of early pregnancy loss increases the effectiveness of the regimen,” coauthor Courtney A. Schreiber, MD, of the University of Pennsylvania, Philadelphia, said in an interview. “Procedural uterine aspiration is highly effective as well, so patients and providers may consider the cost when deciding on a treatment strategy,” she added.
“If medication management is preferred by many patients, decreases the need to access in-person clinical care during a pandemic, and is found to be cost-effective, clinicians and policymakers should increase efforts to improve mifepristone availability and reduce access burdens,” the researchers wrote.
In a study published in the American Journal of Obstetrics & Gynecology, the researchers created a decision-analytic model using data from published literature and the Pregnancy Failure Regiments Trial (PreFaiR) to compare office-based uterine aspiration to medical management with mifepristone pretreatment followed by misoprostol for EPL.
The PrFaiR study randomized 300 women who experienced EPL before 12 weeks’ gestation to medication management with 800 mcg misoprostol vaginally, with or without pretreatment of 200 mg mifeprestone orally. The average age of the participants was 30.7 years, and demographics were similar between the groups.
The researchers used the PrFaiR data for medical management and patient-level data from published literature for uterine aspiration.
The primary outcome was the cost per quality-adjusted life year (QALY) gained. QALY was based on a modified utility score from the published literature. Effectiveness was based on QALY gained and the rate of complete expulsion of the gestational sac without additional intervention.
Overall, the mean costs per person were significantly higher for uterine aspiration, compared with medical management ($828 vs. $661, P = .004). Uterine aspiration was significantly more effective for complete gestational sac expulsion (97.3% vs. 83.8%, P = .0001). However, the QALYs were significantly higher for medical management, compared with uterine aspiration (0.082 vs. 0.079, P < .0001).
Cost-effectiveness was greater for medical management from a health care sector perspective, with lower costs and higher QALYs than uterine aspiration, the researchers noted.
They also evaluated the effect of mifepristone pretreatment on cost-effectiveness and found that medical management would remain cost effective, compared with uterine aspiration even if uterine aspiration procedures decreased in cost and mifepristone increased in cost, and even if medication management had a decreased completion rate and utility score, compared with uterine aspiration.
“Our analysis demonstrates that the incremental cost-effectiveness ratio (ICER) for medical management is well below the maximum willingness-to-pay threshold of approximately $100,000 per QALY gained,” the researchers wrote in their discussion of the findings.
Potential savings, uncertain access
Despite the potential savings and patient benefits, access to mifepristone remains a barrier, the researchers said.
Although the FDA lifted some restrictions on mifepristone in 2021 in the wake of the ongoing COVID-19 pandemic, the effect of new abortion-related restrictions remains to be seen.
The study findings were limited by several factors, including the use of 2018 National Medicare reimbursement rates to calculate costs, though actual costs vary by region and payer, the researchers noted. Other limitations include variations in cost of mifepristone by region and time and the differences in data sources between the uterine aspiration and medical management groups. More research is needed to assess QALYs for early pregnancy loss to establish standard measures and to assess the societal perspective of ESL as well as the health care perspective, they added.
However, the current results support medical management of EPL with mifepristone pretreatment followed by misoprostol as a “high-value care alternative” to office-based uterine aspiration, they said. “Increasing access to mifepristone and eliminating unnecessary restrictions will improve early pregnancy care,” they concluded.
“Given how effective procedural management is, we were slightly surprised that medical management remains cost effective,” Dr. Schreiber said in an interview.
Looking ahead in the wake of new restrictions on use for abortion, “patients may have difficulty accessing either medical or procedural management for early pregnancy loss,” Dr. Schreiber noted. “We support the accessibility of all evidence-based care and hope that our data will help overcome perceived financial barriers,” she said. Additional research needs include improved implementation and access to evidence-based early pregnancy loss care, she added.
Reasons to lift regulations
“Given the recent overturning of Roe v. Wade, any medications that are associated with abortion have increased scrutiny, especially mifepristone and misoprostol, even though these medications are also used for managing early pregnancy loss,” Sarah W. Prager, MD, of the University of Washington, Seattle, said in an interview. “Demonstrating that medication management of EPL with mifepristone/misoprostol is less expensive and has increased QALYs associated with it is yet another reason to deregulate mifepristone so it can also be more accessible for management of EPL,” said Dr. Prager, who was not involved in the study.
Dr. Prager said she was not surprised by the findings, as effective medication should be less expensive than a procedure. “I would caution that the increased QALYs found in this study should not be interpreted as a reason to restrict surgical management of EPL but to increase access also to medication management, even though medication has a slightly lower rate of complete gestational sac expulsion,” she noted. “Mode of management should be up to the patient, unless there is a clear medical reason for one or the other.”
Going forward, “the FDA has it in its power to remove the REMS, which would immediately make mifepristone a medication that can be prescribed through a pharmacy and therefore much more available,” said Dr. Prager. “Restrictions for both medication and surgical management of EPL will likely increase in states where abortion is illegal, and it could possibly lead to patients having less choice as to mode of management,” she explained.
“There are many studies showing that all modes of EPL management are safe and effective and should be supported with respect to patient choice,” Dr. Prager noted. “There are also substantial data supporting the overall safety of mifepristone, and there are no scientific or medical data suggesting the REMS increases safety in any way. Frankly, there are no good, evidence-based reasons to continue to keep the REMS in place,” she said.
The study was supported by the National Institute of Child Health and Human Development of the National Institutes of Health and a Society of Family Planning Research Fund Midcareer Mentor Award. The researchers had no financial conflicts to disclose. Dr. Prager had no financial conflicts to disclose and serves on the Editorial Advisory Board of Ob.Gyn. News.
Medical management of early pregnancy loss costs less and offers similar quality of life to uterine aspiration, based on data from an analytical model.
Early pregnancy loss (EPL) occurs in more than 1 million women in the United States each year, and many patients are diagnosed before they show symptoms, wrote Divyah Nagendra, MD, of Cambridge Health Alliance, Mass., and colleagues.
A 2018 study showed that medical management of EPL with mifepristone added to misoprostol increased effectiveness and reduced the need for additional medication or subsequent uterine procedures, but the cost of mifepristone is perceived as a barrier, and the cost-effectiveness of its use, compared with surgical or expectant management, has not been well studied, the researchers noted.
“We already know that adding mifepristone to the medical management of early pregnancy loss increases the effectiveness of the regimen,” coauthor Courtney A. Schreiber, MD, of the University of Pennsylvania, Philadelphia, said in an interview. “Procedural uterine aspiration is highly effective as well, so patients and providers may consider the cost when deciding on a treatment strategy,” she added.
“If medication management is preferred by many patients, decreases the need to access in-person clinical care during a pandemic, and is found to be cost-effective, clinicians and policymakers should increase efforts to improve mifepristone availability and reduce access burdens,” the researchers wrote.
In a study published in the American Journal of Obstetrics & Gynecology, the researchers created a decision-analytic model using data from published literature and the Pregnancy Failure Regiments Trial (PreFaiR) to compare office-based uterine aspiration to medical management with mifepristone pretreatment followed by misoprostol for EPL.
The PrFaiR study randomized 300 women who experienced EPL before 12 weeks’ gestation to medication management with 800 mcg misoprostol vaginally, with or without pretreatment of 200 mg mifeprestone orally. The average age of the participants was 30.7 years, and demographics were similar between the groups.
The researchers used the PrFaiR data for medical management and patient-level data from published literature for uterine aspiration.
The primary outcome was the cost per quality-adjusted life year (QALY) gained. QALY was based on a modified utility score from the published literature. Effectiveness was based on QALY gained and the rate of complete expulsion of the gestational sac without additional intervention.
Overall, the mean costs per person were significantly higher for uterine aspiration, compared with medical management ($828 vs. $661, P = .004). Uterine aspiration was significantly more effective for complete gestational sac expulsion (97.3% vs. 83.8%, P = .0001). However, the QALYs were significantly higher for medical management, compared with uterine aspiration (0.082 vs. 0.079, P < .0001).
Cost-effectiveness was greater for medical management from a health care sector perspective, with lower costs and higher QALYs than uterine aspiration, the researchers noted.
They also evaluated the effect of mifepristone pretreatment on cost-effectiveness and found that medical management would remain cost effective, compared with uterine aspiration even if uterine aspiration procedures decreased in cost and mifepristone increased in cost, and even if medication management had a decreased completion rate and utility score, compared with uterine aspiration.
“Our analysis demonstrates that the incremental cost-effectiveness ratio (ICER) for medical management is well below the maximum willingness-to-pay threshold of approximately $100,000 per QALY gained,” the researchers wrote in their discussion of the findings.
Potential savings, uncertain access
Despite the potential savings and patient benefits, access to mifepristone remains a barrier, the researchers said.
Although the FDA lifted some restrictions on mifepristone in 2021 in the wake of the ongoing COVID-19 pandemic, the effect of new abortion-related restrictions remains to be seen.
The study findings were limited by several factors, including the use of 2018 National Medicare reimbursement rates to calculate costs, though actual costs vary by region and payer, the researchers noted. Other limitations include variations in cost of mifepristone by region and time and the differences in data sources between the uterine aspiration and medical management groups. More research is needed to assess QALYs for early pregnancy loss to establish standard measures and to assess the societal perspective of ESL as well as the health care perspective, they added.
However, the current results support medical management of EPL with mifepristone pretreatment followed by misoprostol as a “high-value care alternative” to office-based uterine aspiration, they said. “Increasing access to mifepristone and eliminating unnecessary restrictions will improve early pregnancy care,” they concluded.
“Given how effective procedural management is, we were slightly surprised that medical management remains cost effective,” Dr. Schreiber said in an interview.
Looking ahead in the wake of new restrictions on use for abortion, “patients may have difficulty accessing either medical or procedural management for early pregnancy loss,” Dr. Schreiber noted. “We support the accessibility of all evidence-based care and hope that our data will help overcome perceived financial barriers,” she said. Additional research needs include improved implementation and access to evidence-based early pregnancy loss care, she added.
Reasons to lift regulations
“Given the recent overturning of Roe v. Wade, any medications that are associated with abortion have increased scrutiny, especially mifepristone and misoprostol, even though these medications are also used for managing early pregnancy loss,” Sarah W. Prager, MD, of the University of Washington, Seattle, said in an interview. “Demonstrating that medication management of EPL with mifepristone/misoprostol is less expensive and has increased QALYs associated with it is yet another reason to deregulate mifepristone so it can also be more accessible for management of EPL,” said Dr. Prager, who was not involved in the study.
Dr. Prager said she was not surprised by the findings, as effective medication should be less expensive than a procedure. “I would caution that the increased QALYs found in this study should not be interpreted as a reason to restrict surgical management of EPL but to increase access also to medication management, even though medication has a slightly lower rate of complete gestational sac expulsion,” she noted. “Mode of management should be up to the patient, unless there is a clear medical reason for one or the other.”
Going forward, “the FDA has it in its power to remove the REMS, which would immediately make mifepristone a medication that can be prescribed through a pharmacy and therefore much more available,” said Dr. Prager. “Restrictions for both medication and surgical management of EPL will likely increase in states where abortion is illegal, and it could possibly lead to patients having less choice as to mode of management,” she explained.
“There are many studies showing that all modes of EPL management are safe and effective and should be supported with respect to patient choice,” Dr. Prager noted. “There are also substantial data supporting the overall safety of mifepristone, and there are no scientific or medical data suggesting the REMS increases safety in any way. Frankly, there are no good, evidence-based reasons to continue to keep the REMS in place,” she said.
The study was supported by the National Institute of Child Health and Human Development of the National Institutes of Health and a Society of Family Planning Research Fund Midcareer Mentor Award. The researchers had no financial conflicts to disclose. Dr. Prager had no financial conflicts to disclose and serves on the Editorial Advisory Board of Ob.Gyn. News.
FROM THE AMERICAN JOURNAL OF OBSTETRICS & GYNECOLOGY
Roe v. Wade overturned: A family medicine resident reacts
I remember how small and shy she looked, curled into herself in her too-large hospital gown. I remember thinking that it was autumn, and she should have been at her first homecoming dance, not sitting in the ER staring mutely at the hospital-issued safety socks on her feet. Her mother, puffy-eyed from crying, was sitting on the bed beside her, stroking her hair.
Together, my patients and I talked about the pregnancy. She told me how scared she was, how she didn’t want to “kill her baby”, but that she also wasn’t sure she could take care of a child. She told me that she was terrified of childbirth, that she didn’t want her friends at school to know and to judge her. We talked about how she was a victim; how she was an innocent child, too. I reassured her, and her mom emphatically agreed – her body was still her own.
The man who hurt her did not take that from her. She could make any choice she wanted, and it would be the right choice.
Eventually, she was able to make a decision which was best for her. I don’t know what became of her, but I hope she is well now, and I hope she’s thriving and happy. I also hope that she doesn’t see the news about Roe v. Wade and feel stripped of her personhood, as many women did.
When I heard about the Supreme Court decision I thought of her, and how important our conversation was to the trajectory of her life. I wondered if across the country these conversations might be silenced, and patients might be left to navigate this important facet of their health alone.
Some version of the conversation I had with my young patient occurs in exam rooms across the country countless times a day. Sometimes these conversations are cut and dry. Other times, they are accompanied by heartbreak and tears.
These conversations are common – one in four women in the United States have had an abortion. I have had many friends who were faced with deciding what to do after an unexpectedly positive pregnancy test. The reasons were different for each person – one was raped at a party, another’s birth control failed, the boyfriend of a third friend wouldn’t wear a condom – but the underlying sentiments were the same for each woman. They thought: “This is a difficult choice, but it’s a choice I’m ready to make. I’m not ready to have a baby at this point in my life.”
My friends talked to their doctors, who assisted them in making an informed choice. Some of them chose abortion. Others chose to deliver their baby. All were helped along in their decision by a physician who was there to support them and assist them in making a well-considered choice for their individual circumstance.
Economic and health consequences of restricting access to abortion
The facts are clear: Nearly half of all pregnancies in American women in 2011 were unplanned, and about 4 in 10 of them ended in an elective abortion, according to the Guttmacher Institute.1 Restricting access to abortions does not stop abortions from happening; it limits the opportunity for women to seek advice from trusted friends and professionals and it reduces access to safe abortions.
The people who will be most harmed by these restrictions are the most socially and economically vulnerable. Wealthy, mobile women with the ability to travel to other states or countries will always be able to access abortion care; low-income, work-tethered women and women with other children to care for at home will struggle to do so.
Denying women abortion services puts them at increased risk for lifelong, multigenerational economic hardship. Women who sought abortions but were unable to obtain them experienced an increase in household poverty which lasted years relative to women who were able to receive an abortion, according to the authors of The Turnaway Study.2 They were less socially, geographically, and economically mobile, and were less likely to go on to receive a higher education.
In a country where citizens do not have paid maternity leave, affordable and accessible childcare services, or universal health care, raising a child is an enormous financial burden. Women who are denied abortions also are much more likely to end up as a single parent, shouldering that burden alone.
Additionally, low socioeconomic status is associated with increased all-cause mortality. People who live in poverty are disproportionately affected by diabetes and other chronic health conditions, and have lower life expectancies overall.
The reversal of Roe v. Wade is not only going to lead directly to patient death by decreasing access to safe abortion, causing women to pursue unsafe alternatives; it will also indirectly result in more women being driven into and remaining in poverty and suffering the health consequences.
In addition to risking a woman’s life medically, pregnancy also significantly increases that individual’s risk of being a victim of intimate partner violence. The number one cause of death in pregnant women is homicide, most often by their sexual partner, said an article published in Nature in 2021.3 Therefore, restricting a woman’s ability to control if and when she has children could put her at risk for death from serious pregnancy-related complications and unsafe abortion consequences and increase her likelihood of dying by domestic violence.
Patient-physicians interactions are changed
As a physician I hope that I am able to convey my intense respect for and support of a woman’s autonomy into every family planning visit I conduct. Unfortunately, this ruling will not only have an immediate impact on the lives of women across the country – it will also alter the way many of us interact with our patients on a day-to-day basis. When patients can report doctors to authorities in some states for offering terminations, and doctors can report patients for seeking them, there will be absolutely no trust in the therapeutic relationship.
With this ruling, the content of private and protected conversations between patients and their physicians will be subject to censure and potentially criminal consequences.
Regardless of where I eventually practice medicine, I should not be in the position of talking to a patient and telling them that they do not have any agency over their body unless they have the money and resources to travel to a state where abortion is legal. I should not have to tell a child that she must carry and birth another child just to appease the often-fickle whims of lawmakers.
The conversation I had with my pediatric patient was important to her health and to her future, and she deserved to have the chance to discuss her feelings with a trusted physician. Every woman has the right to make her own decisions within the sanctity of the exam room, not from the distance of a courtroom.
Dr. Persampiere is a resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at [email protected] or via [email protected].
References
1. Unintended pregnancy in the United States. Guttmacher Institute. 2019 Jan 9. https://www.guttmacher.org/fact-sheet/unintended-pregnancy-united-states
2. Foster D et al. The harms of denying a woman a wanted abortion - ANSIRH. https://www.ansirh.org/sites/default/files/publications/files/the_harms_of_denying_a_woman_a_wanted_abortion_4-16-2020.pdf
3. Subbaraman N. 2021 Nov 12. Homicide is a top cause of maternal death in the United States. Nature News. https://www.nature.com/articles/d41586-021-03392-8
I remember how small and shy she looked, curled into herself in her too-large hospital gown. I remember thinking that it was autumn, and she should have been at her first homecoming dance, not sitting in the ER staring mutely at the hospital-issued safety socks on her feet. Her mother, puffy-eyed from crying, was sitting on the bed beside her, stroking her hair.
Together, my patients and I talked about the pregnancy. She told me how scared she was, how she didn’t want to “kill her baby”, but that she also wasn’t sure she could take care of a child. She told me that she was terrified of childbirth, that she didn’t want her friends at school to know and to judge her. We talked about how she was a victim; how she was an innocent child, too. I reassured her, and her mom emphatically agreed – her body was still her own.
The man who hurt her did not take that from her. She could make any choice she wanted, and it would be the right choice.
Eventually, she was able to make a decision which was best for her. I don’t know what became of her, but I hope she is well now, and I hope she’s thriving and happy. I also hope that she doesn’t see the news about Roe v. Wade and feel stripped of her personhood, as many women did.
When I heard about the Supreme Court decision I thought of her, and how important our conversation was to the trajectory of her life. I wondered if across the country these conversations might be silenced, and patients might be left to navigate this important facet of their health alone.
Some version of the conversation I had with my young patient occurs in exam rooms across the country countless times a day. Sometimes these conversations are cut and dry. Other times, they are accompanied by heartbreak and tears.
These conversations are common – one in four women in the United States have had an abortion. I have had many friends who were faced with deciding what to do after an unexpectedly positive pregnancy test. The reasons were different for each person – one was raped at a party, another’s birth control failed, the boyfriend of a third friend wouldn’t wear a condom – but the underlying sentiments were the same for each woman. They thought: “This is a difficult choice, but it’s a choice I’m ready to make. I’m not ready to have a baby at this point in my life.”
My friends talked to their doctors, who assisted them in making an informed choice. Some of them chose abortion. Others chose to deliver their baby. All were helped along in their decision by a physician who was there to support them and assist them in making a well-considered choice for their individual circumstance.
Economic and health consequences of restricting access to abortion
The facts are clear: Nearly half of all pregnancies in American women in 2011 were unplanned, and about 4 in 10 of them ended in an elective abortion, according to the Guttmacher Institute.1 Restricting access to abortions does not stop abortions from happening; it limits the opportunity for women to seek advice from trusted friends and professionals and it reduces access to safe abortions.
The people who will be most harmed by these restrictions are the most socially and economically vulnerable. Wealthy, mobile women with the ability to travel to other states or countries will always be able to access abortion care; low-income, work-tethered women and women with other children to care for at home will struggle to do so.
Denying women abortion services puts them at increased risk for lifelong, multigenerational economic hardship. Women who sought abortions but were unable to obtain them experienced an increase in household poverty which lasted years relative to women who were able to receive an abortion, according to the authors of The Turnaway Study.2 They were less socially, geographically, and economically mobile, and were less likely to go on to receive a higher education.
In a country where citizens do not have paid maternity leave, affordable and accessible childcare services, or universal health care, raising a child is an enormous financial burden. Women who are denied abortions also are much more likely to end up as a single parent, shouldering that burden alone.
Additionally, low socioeconomic status is associated with increased all-cause mortality. People who live in poverty are disproportionately affected by diabetes and other chronic health conditions, and have lower life expectancies overall.
The reversal of Roe v. Wade is not only going to lead directly to patient death by decreasing access to safe abortion, causing women to pursue unsafe alternatives; it will also indirectly result in more women being driven into and remaining in poverty and suffering the health consequences.
In addition to risking a woman’s life medically, pregnancy also significantly increases that individual’s risk of being a victim of intimate partner violence. The number one cause of death in pregnant women is homicide, most often by their sexual partner, said an article published in Nature in 2021.3 Therefore, restricting a woman’s ability to control if and when she has children could put her at risk for death from serious pregnancy-related complications and unsafe abortion consequences and increase her likelihood of dying by domestic violence.
Patient-physicians interactions are changed
As a physician I hope that I am able to convey my intense respect for and support of a woman’s autonomy into every family planning visit I conduct. Unfortunately, this ruling will not only have an immediate impact on the lives of women across the country – it will also alter the way many of us interact with our patients on a day-to-day basis. When patients can report doctors to authorities in some states for offering terminations, and doctors can report patients for seeking them, there will be absolutely no trust in the therapeutic relationship.
With this ruling, the content of private and protected conversations between patients and their physicians will be subject to censure and potentially criminal consequences.
Regardless of where I eventually practice medicine, I should not be in the position of talking to a patient and telling them that they do not have any agency over their body unless they have the money and resources to travel to a state where abortion is legal. I should not have to tell a child that she must carry and birth another child just to appease the often-fickle whims of lawmakers.
The conversation I had with my pediatric patient was important to her health and to her future, and she deserved to have the chance to discuss her feelings with a trusted physician. Every woman has the right to make her own decisions within the sanctity of the exam room, not from the distance of a courtroom.
Dr. Persampiere is a resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at [email protected] or via [email protected].
References
1. Unintended pregnancy in the United States. Guttmacher Institute. 2019 Jan 9. https://www.guttmacher.org/fact-sheet/unintended-pregnancy-united-states
2. Foster D et al. The harms of denying a woman a wanted abortion - ANSIRH. https://www.ansirh.org/sites/default/files/publications/files/the_harms_of_denying_a_woman_a_wanted_abortion_4-16-2020.pdf
3. Subbaraman N. 2021 Nov 12. Homicide is a top cause of maternal death in the United States. Nature News. https://www.nature.com/articles/d41586-021-03392-8
I remember how small and shy she looked, curled into herself in her too-large hospital gown. I remember thinking that it was autumn, and she should have been at her first homecoming dance, not sitting in the ER staring mutely at the hospital-issued safety socks on her feet. Her mother, puffy-eyed from crying, was sitting on the bed beside her, stroking her hair.
Together, my patients and I talked about the pregnancy. She told me how scared she was, how she didn’t want to “kill her baby”, but that she also wasn’t sure she could take care of a child. She told me that she was terrified of childbirth, that she didn’t want her friends at school to know and to judge her. We talked about how she was a victim; how she was an innocent child, too. I reassured her, and her mom emphatically agreed – her body was still her own.
The man who hurt her did not take that from her. She could make any choice she wanted, and it would be the right choice.
Eventually, she was able to make a decision which was best for her. I don’t know what became of her, but I hope she is well now, and I hope she’s thriving and happy. I also hope that she doesn’t see the news about Roe v. Wade and feel stripped of her personhood, as many women did.
When I heard about the Supreme Court decision I thought of her, and how important our conversation was to the trajectory of her life. I wondered if across the country these conversations might be silenced, and patients might be left to navigate this important facet of their health alone.
Some version of the conversation I had with my young patient occurs in exam rooms across the country countless times a day. Sometimes these conversations are cut and dry. Other times, they are accompanied by heartbreak and tears.
These conversations are common – one in four women in the United States have had an abortion. I have had many friends who were faced with deciding what to do after an unexpectedly positive pregnancy test. The reasons were different for each person – one was raped at a party, another’s birth control failed, the boyfriend of a third friend wouldn’t wear a condom – but the underlying sentiments were the same for each woman. They thought: “This is a difficult choice, but it’s a choice I’m ready to make. I’m not ready to have a baby at this point in my life.”
My friends talked to their doctors, who assisted them in making an informed choice. Some of them chose abortion. Others chose to deliver their baby. All were helped along in their decision by a physician who was there to support them and assist them in making a well-considered choice for their individual circumstance.
Economic and health consequences of restricting access to abortion
The facts are clear: Nearly half of all pregnancies in American women in 2011 were unplanned, and about 4 in 10 of them ended in an elective abortion, according to the Guttmacher Institute.1 Restricting access to abortions does not stop abortions from happening; it limits the opportunity for women to seek advice from trusted friends and professionals and it reduces access to safe abortions.
The people who will be most harmed by these restrictions are the most socially and economically vulnerable. Wealthy, mobile women with the ability to travel to other states or countries will always be able to access abortion care; low-income, work-tethered women and women with other children to care for at home will struggle to do so.
Denying women abortion services puts them at increased risk for lifelong, multigenerational economic hardship. Women who sought abortions but were unable to obtain them experienced an increase in household poverty which lasted years relative to women who were able to receive an abortion, according to the authors of The Turnaway Study.2 They were less socially, geographically, and economically mobile, and were less likely to go on to receive a higher education.
In a country where citizens do not have paid maternity leave, affordable and accessible childcare services, or universal health care, raising a child is an enormous financial burden. Women who are denied abortions also are much more likely to end up as a single parent, shouldering that burden alone.
Additionally, low socioeconomic status is associated with increased all-cause mortality. People who live in poverty are disproportionately affected by diabetes and other chronic health conditions, and have lower life expectancies overall.
The reversal of Roe v. Wade is not only going to lead directly to patient death by decreasing access to safe abortion, causing women to pursue unsafe alternatives; it will also indirectly result in more women being driven into and remaining in poverty and suffering the health consequences.
In addition to risking a woman’s life medically, pregnancy also significantly increases that individual’s risk of being a victim of intimate partner violence. The number one cause of death in pregnant women is homicide, most often by their sexual partner, said an article published in Nature in 2021.3 Therefore, restricting a woman’s ability to control if and when she has children could put her at risk for death from serious pregnancy-related complications and unsafe abortion consequences and increase her likelihood of dying by domestic violence.
Patient-physicians interactions are changed
As a physician I hope that I am able to convey my intense respect for and support of a woman’s autonomy into every family planning visit I conduct. Unfortunately, this ruling will not only have an immediate impact on the lives of women across the country – it will also alter the way many of us interact with our patients on a day-to-day basis. When patients can report doctors to authorities in some states for offering terminations, and doctors can report patients for seeking them, there will be absolutely no trust in the therapeutic relationship.
With this ruling, the content of private and protected conversations between patients and their physicians will be subject to censure and potentially criminal consequences.
Regardless of where I eventually practice medicine, I should not be in the position of talking to a patient and telling them that they do not have any agency over their body unless they have the money and resources to travel to a state where abortion is legal. I should not have to tell a child that she must carry and birth another child just to appease the often-fickle whims of lawmakers.
The conversation I had with my pediatric patient was important to her health and to her future, and she deserved to have the chance to discuss her feelings with a trusted physician. Every woman has the right to make her own decisions within the sanctity of the exam room, not from the distance of a courtroom.
Dr. Persampiere is a resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at [email protected] or via [email protected].
References
1. Unintended pregnancy in the United States. Guttmacher Institute. 2019 Jan 9. https://www.guttmacher.org/fact-sheet/unintended-pregnancy-united-states
2. Foster D et al. The harms of denying a woman a wanted abortion - ANSIRH. https://www.ansirh.org/sites/default/files/publications/files/the_harms_of_denying_a_woman_a_wanted_abortion_4-16-2020.pdf
3. Subbaraman N. 2021 Nov 12. Homicide is a top cause of maternal death in the United States. Nature News. https://www.nature.com/articles/d41586-021-03392-8