User login
Babies are dying of syphilis. It’s 100% preventable.
This story was originally published on ProPublica and was co-published with NPR.
When Mai Yang is looking for a patient, she travels light. She dresses deliberately — not too formal, so she won’t be mistaken for a police officer; not too casual, so people will look past her tiny 4-foot-10 stature and youthful face and trust her with sensitive health information. Always, she wears closed-toed shoes, “just in case I need to run.”
Yang carries a stack of cards issued by the Centers for Disease Control and Prevention that show what happens when the Treponema pallidum bacteria invades a patient’s body. There’s a photo of an angry red sore on a penis. There’s one of a tongue, marred by mucus-lined lesions. And there’s one of a newborn baby, its belly, torso and thighs dotted in a rash, its mouth open, as if caught midcry.
It was because of the prospect of one such baby that Yang found herself walking through a homeless encampment on a blazing July day in Huron, Calif., an hour’s drive southwest of her office at the Fresno County Department of Public Health. She was looking for a pregnant woman named Angelica, whose visit to a community clinic had triggered a report to the health department’s sexually transmitted disease program. Angelica had tested positive for syphilis. If she was not treated, her baby could end up like the one in the picture or worse — there was a 40% chance the baby would die.
Ms. Yang knew, though, that if she helped Angelica get treated with three weekly shots of penicillin at least 30 days before she gave birth, it was likely that the infection would be wiped out and her baby would be born without any symptoms at all. Every case of congenital syphilis, when a baby is born with the disease, is avoidable. Each is considered a “sentinel event,” a warning that the public health system is failing.
The alarms are now clamoring. In the United States, more than 129,800 syphilis cases were recorded in 2019, double the case count of five years prior. In the same time period, cases of congenital syphilis quadrupled: 1,870 babies were born with the disease; 128 died. Case counts from 2020 are still being finalized, but the CDC has said that reported cases of congenital syphilis have already exceeded the prior year. Black, Hispanic, and Native American babies are disproportionately at risk.
There was a time, not too long ago, when CDC officials thought they could eliminate the centuries-old scourge from the United States, for adults and babies. But the effort lost steam and cases soon crept up again. Syphilis is not an outlier. The United States goes through what former CDC director Dr. Tom Frieden calls “a deadly cycle of panic and neglect” in which emergencies propel officials to scramble and throw money at a problem — whether that’s Ebola, Zika, or COVID-19. Then, as fear ebbs, so does the attention and motivation to finish the task.
The last fraction of cases can be the hardest to solve, whether that’s eradicating a bug or getting vaccines into arms, yet too often, that’s exactly when political attention gets diverted to the next alarm. The result: The hardest to reach and most vulnerable populations are the ones left suffering, after everyone else looks away.
Ms. Yang first received Angelica’s lab report on June 17. The address listed was a P.O. box, and the phone number belonged to her sister, who said Angelica was living in Huron. That was a piece of luck: Huron is tiny; the city spans just 1.6 square miles. On her first visit, a worker at the Alamo Motel said she knew Angelica and directed Ms. Yang to a nearby homeless encampment. Angelica wasn’t there, so Ms. Yang returned a second time, bringing one of the health department nurses who could serve as an interpreter.
They made their way to the barren patch of land behind Huron Valley Foods, the local grocery store, where people took shelter in makeshift lean-tos composed of cardboard boxes, scrap wood ,and scavenged furniture, draped with sheets that served as ceilings and curtains. Yang stopped outside one of the structures, calling a greeting.
“Hi, I’m from the health department, I’m looking for Angelica.”
The nurse echoed her in Spanish.
Angelica emerged, squinting in the sunlight. Ms. Yang couldn’t tell if she was visibly pregnant yet, as her body was obscured by an oversized shirt. The two women were about the same age: Ms. Yang 26 and Angelica 27. Ms. Yang led her away from the tent, so they could speak privately. Angelica seemed reticent, surprised by the sudden appearance of the two health officers. “You’re not in trouble,” Ms. Yang said, before revealing the results of her blood test.
Angelica had never heard of syphilis.
“Have you been to prenatal care?”
Angelica shook her head. The local clinic had referred her to an obstetrician in Hanford, a 30-minute drive away. She had no car. She also mentioned that she didn’t intend to raise her baby; her two oldest children lived with her mother, and this one likely would, too.
Ms. Yang pulled out the CDC cards, showing them to Angelica and asking if she had experienced any of the symptoms illustrated. No, Angelica said, her lips pursed with disgust.
“Right now you still feel healthy, but this bacteria is still in your body,” Ms. Yang pressed. “You need to get the infection treated to prevent further health complications to yourself and your baby.”
The community clinic was just across the street. “Can we walk you over to the clinic and make sure you get seen so we can get this taken care of?”
Angelica demurred. She said she hadn’t showered for a week and wanted to wash up first. She said she’d go later.
Ms. Yang tried once more to extract a promise: “What time do you think you’ll go?”
“Today, for sure.”
Syphilis is called The Great Imitator: It can look like any number of diseases. In its first stage, the only evidence of infection is a painless sore at the bacteria’s point of entry. Weeks later, as the bacteria multiplies, skin rashes bloom on the palms of the hands and bottoms of the feet. Other traits of this stage include fever, headaches, muscle aches, sore throat, and fatigue. These symptoms eventually disappear and the patient progresses into the latent phase, which betrays no external signs. But if left untreated, after a decade or more, syphilis will reemerge in up to 30% of patients, capable of wreaking horror on a wide range of organ systems. Dr. Marion Sims, president of the American Medical Association in 1876, called it a “terrible scourge, which begins with lamb-like mildness and ends with lion-like rage that ruthlessly destroys everything in its way.”
The corkscrew-shaped bacteria can infiltrate the nervous system at any stage of the infection. Ms. Yang is haunted by her memory of interviewing a young man whose dementia was so severe that he didn’t know why he was in the hospital or how old he was. And regardless of symptoms or stage, the bacteria can penetrate the placenta to infect a fetus. Even in these cases the infection is unpredictable: Many babies are born with normal physical features, but others can have deformed bones or damaged brains, and they can struggle to hear, see, or breathe.
From its earliest days, syphilis has been shrouded in stigma. The first recorded outbreak was in the late 15th century, when Charles VIII led the French army to invade Naples. Italian physicians described French soldiers covered with pustules, dying from a sexually transmitted disease. As the affliction spread, Italians called it the French Disease. The French blamed the Neopolitans. It was also called the German, Polish, or Spanish disease, depending on which neighbor one wanted to blame. Even its name bears the taint of divine judgement: It comes from a 16th-century poem that tells of a shepherd, Syphilus, who offended the god Apollo and was punished with a hideous disease.
By 1937 in America, when former Surgeon General Thomas Parran wrote the book “Shadow on the Land,” he estimated some 680,000 people were under treatment for syphilis; about 60,000 babies were being born annually with congenital syphilis. There was no cure, and the stigma was so strong that public health officials feared even properly documenting cases.
Thanks to Dr. Parran’s ardent advocacy, Congress in 1938 passed the National Venereal Disease Control Act, which created grants for states to set up clinics and support testing and treatment. Other than a short-lived funding effort during World War I, this was the first coordinated federal push to respond to the disease.
Around the same time, the Public Health Service launched an effort to record the natural history of syphilis. Situated in Tuskegee, Ala., the infamous study recruited 600 black men. By the early 1940s, penicillin became widely available and was found to be a reliable cure, but the treatment was withheld from the study participants. Outrage over the ethical violations would cast a stain across syphilis research for decades to come and fuel generations of mistrust in the medical system among Black Americans that continues to this day.
With the introduction of penicillin, cases began to plummet. Twice, the CDC has announced efforts to wipe out the disease — once in the 1960s and again in 1999.
In the latest effort, the CDC announced that the United States had “a unique opportunity to eliminate syphilis within its borders,” thanks to historically low rates, with 80% of counties reporting zero cases. The concentration of cases in the South “identifies communities in which there is a fundamental failure of public health capacity,” the agency noted, adding that elimination — which it defined as fewer than 1,000 cases a year — would “decrease one of our most glaring racial disparities in health.”
Two years after the campaign began, cases started climbing, first among gay men and later, heterosexuals. Cases in women started accelerating in 2013, followed shortly by increasing numbers of babies born with syphilis.The reasons for failure are complex; people relaxed safer sex practices after the advent of potent HIV combination therapies, increased methamphetamine use drove riskier behavior and an explosion of online dating made it hard to track and test sexual partners, according to Dr. Ina Park, medical director of the California Prevention Training Center at the University of California San Francisco.
But federal and state public health efforts were hamstrung from the get-go. In 1999, the CDC said it would need about $35 million to $39 million in new federal funds annually for at least five years to eliminate syphilis. The agency got less than half of what it asked for, according to Jo Valentine, former program coordinator of the CDC’s Syphilis Elimination Effort. As cases rose, the CDC modified its goals in 2006 from 0.4 primary and secondary syphilis cases per 100,000 in population to 2.2 cases per 100,000. By 2013, as elimination seemed less and less viable, the CDC changed its focus to ending congenital syphilis only.
Since then, funding has remained anemic. From 2015 to 2020, the CDC’s budget for preventing sexually transmitted infections grew by 2.2%. Taking inflation into account, that’s a 7.4% reduction in purchasing power. In the same period, cases of syphilis, gonorrhea and chlamydia — the three STDs that have federally funded control programs — increased by nearly 30%.
“We have a long history of nearly eradicating something, then changing our attention, and seeing a resurgence in numbers,” said David Harvey, executive director of the National Coalition of STD Directors. “We have more congenital syphilis cases today in America than we ever had pediatric AIDS at the height of the AIDS epidemic. It’s heartbreaking.”
Adriane Casalotti, chief of government and public affairs at the National Association of County and City Health Officials, warns that the United States should not be surprised to see case counts continue to climb. “The bugs don’t go away,” she said. “They’re just waiting for the next opportunity, when you’re not paying attention.”
Ms. Yang waited until the end of the day, then called the clinic to see if Angelica had gone for her shot. She had not. Ms. Yang would have to block off another half day to visit Huron again, but she had three dozen other cases to deal with.
States in the South and West have seen the highest syphilis rates in recent years. In 2017, 64 babies in Fresno County were born with syphilis at a rate of 440 babies per 100,000 live births — about 19 times the national rate. While the county had managed to lower case counts in the two years that followed, the pandemic threatened to unravel that progress, forcing STD staffers to do COVID-19 contact tracing, pausing field visits to find infected people, and scaring patients from seeking care. Ms. Yang’s colleague handled three cases of stillbirth in 2020; in each, the woman was never diagnosed with syphilis because she feared catching the coronavirus and skipped prenatal care.
Ms. Yang, whose caseload peaked at 70 during a COVID-19 surge, knew she would not be able handle them all as thoroughly as she’d like to. “When I was being mentored by another investigator, he said: ‘You’re not a superhero. You can’t save everybody,’” she said. She prioritizes men who have sex with men, because there’s a higher prevalence of syphilis in that population, and pregnant people, because of the horrific consequences for babies.
The job of a disease intervention specialist isn’t for everyone: It means meeting patients whenever and wherever they are available — in the mop closet of a bus station, in a quiet parking lot — to inform them about the disease, to extract names of sex partners and to encourage treatment. Patients are often reluctant to talk. They can get belligerent, upset that “the government” has their personal information or shattered at the thought that a partner is likely cheating on them. Salaries typically start in the low $40,000s.
Jena Adams, Ms. Yang’s supervisor, has eight investigators working on HIV and syphilis. In the middle of 2020, she lost two and replaced them only recently. “It’s been exhausting,” Ms. Adams said. She has only one specialist who is trained to take blood samples in the field, crucial for guaranteeing that the partners of those who test positive for syphilis also get tested. Ms. Adams wants to get phlebotomy training for the rest of her staff, but it’s $2,000 per person. The department also doesn’t have anyone who can administer penicillin injections in the field; that would have been key when Ms. Yang met Angelica. For a while, a nurse who worked in the tuberculosis program would ride along to give penicillin shots on a volunteer basis. Then he, too, left the health department.
Much of the resources in public health trickle down from the CDC, which distributes money to states, which then parcel it out to counties. The CDC gets its budget from Congress, which tells the agency, by line item, exactly how much money it can spend to fight a disease or virus, in an uncommonly specific manner not seen in many other agencies. The decisions are often politically driven and can be detached from actual health needs.
When the House and Senate appropriations committees meet to decide how much the CDC will get for each line item, they are barraged by lobbyists for individual disease interests. Stephanie Arnold Pang, senior director of policy and government relations at the National Coalition of STD Directors, can pick out the groups by sight: breast cancer wears pink, Alzheimer’s goes in purple, multiple sclerosis comes in orange, HIV in red. STD prevention advocates, like herself, don a green ribbon, but they’re far outnumbered.
And unlike diseases that might already be familiar to lawmakers, or have patient and family spokespeople who can tell their own powerful stories, syphilis doesn’t have many willing poster children. “Congressmen don’t wake up one day and say, ‘Oh hey, there’s congenital syphilis in my jurisdiction.’ You have to raise awareness,” Arnold Pang said. It can be hard jockeying for a meeting. “Some offices might say, ‘I don’t have time for you because we’ve just seen HIV.’ ... Sometimes, it feels like you’re talking into a void.”
The consequences of the political nature of public health funding have become more obvious during the coronavirus pandemic. The 2014 Ebola epidemic was seen as a “global wakeup call” that the world wasn’t prepared for a major pandemic, yet in 2018, the CDC scaled back its epidemic prevention work as money ran out. “If you’ve got to choose between Alzheimer’s research and stopping an outbreak that may not happen? Stopping an outbreak that might not happen doesn’t do well,” said Dr. Frieden, the former CDC director. “The CDC needs to have more money and more flexible money. Otherwise, we’re going to be in this situation long term.”
In May 2021, President Joe Biden’s administration announced it would set aside $7.4 billion over the next five years to hire and train public health workers, including $1.1 billion for more disease intervention specialists like Ms. Yang. Public health officials are thrilled to have the chance to expand their workforce, but some worry the time horizon may be too short. “We’ve seen this movie before, right?” Dr. Frieden said. “Everyone gets concerned when there’s an outbreak, and when that outbreak stops, the headlines stop, and an economic downturn happens, the budget gets cut.”
Fresno’s STD clinic was shuttered in 2010 amid the Great Recession. Many others have vanished since the passage of the Affordable Care Act. Health leaders thought “by magically beefing up the primary care system, that we would do a better job of catching STIs and treating them,” said Mr. Harvey, the executive director of the National Coalition of STD Directors. That hasn’t worked out; people want access to anonymous services, and primary care doctors often don’t have STDs top of mind. The coalition is lobbying Congress for funding to support STD clinical services, proposing a three-year demonstration project funded at $600 million.
It’s one of Ms. Adams’ dreams to see Fresno’s STD clinic restored as it was. “You could come in for an HIV test and get other STDs checked,” she said. “And if a patient is positive, you can give a first injection on the spot.”
On Aug. 12, Ms. Yang set out for Huron again, speeding past groves of almond trees and fields of grapes in the department’s white Chevy Cruze. She brought along a colleague, Jorge Sevilla, who had recently transferred to the STD program from COVID-19 contact tracing. Ms. Yang was anxious to find Angelica again. “She’s probably in her second trimester now,” she said.
They found her outside of a pale yellow house a few blocks from the homeless encampment; the owner was letting her stay in a shed tucked in the corner of the dirt yard. This time, it was evident that she was pregnant. Ms. Yang noted that Angelica was wearing a wig; hair loss is a symptom of syphilis.
“Do you remember me?” Ms. Yang asked.
Angelica nodded. She didn’t seem surprised to see Ms. Yang again. (I came along, and Mr. Sevilla explained who I was and that I was writing about syphilis and the people affected by it. Angelica signed a release for me to report about her case, and she said she had no problem with me writing about her or even using her full name. ProPublica chose to only print her first name.)
“How are you doing? How’s the baby?”
“Bien.”
“So the last time we talked, we were going to have you go to United Healthcare Center to get treatment. Have you gone since?”
Angelica shook her head.
“We brought some gift cards...” Mr. Sevilla started in Spanish. The department uses them as incentives for completing injections. But Angelica was already shaking her head. The nearest Walmart was the next town over.
Ms. Yang turned to her partner. “Tell her: So the reason why we’re coming out here again is because we really need her to go in for treatment. ... We really are concerned for the baby’s health especially since she’s had the infection for quite a while.”
Angelica listened while Mr. Sevilla interpreted, her eyes on the ground. Then she looked up. “Orita?” she asked. Right now?
“I’ll walk with you,” Ms. Yang offered. Angelica shook her head. “She said she wants to shower first before she goes over there,” Mr. Sevilla said.
Ms. Yang made a face. “She said that to me last time.” Ms. Yang offered to wait, but Angelica didn’t want the health officers to linger by the house. She said she would meet them by the clinic in 15 minutes.
Ms. Yang was reluctant to let her go but again had no other option. She and Mr. Sevilla drove to the clinic, then stood on the corner of the parking lot, staring down the road.
Talk to the pediatricians, obstetricians, and families on the front lines of the congenital syphilis surge and it becomes clear why Ms. Yang and others are trying so desperately to prevent cases. Dr. J. B. Cantey, associate professor in pediatrics at UT Health San Antonio, remembers a baby girl born at 25 weeks gestation who weighed a pound and a half. Syphilis had spread through her bones and lungs. She spent five months in the neonatal intensive care unit, breathing through a ventilator, and was still eating through a tube when she was discharged.
Then, there are the miscarriages, the stillbirths and the inconsolable parents. Dr. Irene Stafford, an associate professor and maternal-fetal medicine specialist at UT Health in Houston, cannot forget a patient who came in at 36 weeks for a routine checkup, pregnant with her first child. Dr. Stafford realized that there was no heartbeat. “She could see on my face that something was really wrong,” Dr. Stafford recalled. She had to let the patient know that syphilis had killed her baby. “She was hysterical, just bawling,” Dr. Stafford said. “I’ve seen people’s families ripped apart and I’ve seen beautiful babies die.” Fewer than 10% of patients who experience a stillbirth are tested for syphilis, suggesting that cases are underdiagnosed.
A Texas grandmother named Solidad Odunuga offers a glimpse into what the future could hold for Angelica’s mother, who may wind up raising her baby.
In February of last year, Ms. Odunuga got a call from the Lyndon B. Johnson Hospital in Houston. A nurse told her that her daughter was about to give birth and that child protective services had been called. Ms. Odunuga had lost contact with her daughter, who struggled with homelessness and substance abuse. She arrived in time to see her grandson delivered, premature at 30 weeks old, weighing 2.7 pounds. He tested positive for syphilis.
When a child protective worker asked Ms. Odunuga to take custody of the infant, she felt a wave of dread. “I was in denial,” she recalled. “I did not plan to be a mom again.” The baby’s medical problems were daunting: “Global developmental delays ... concerns for visual impairments ... high risk of cerebral palsy,” read a note from the doctor at the time.
Still, Ms. Odunuga visited her grandson every day for three months, driving to the NICU from her job at the University of Houston. “I’d put him in my shirt to keep him warm and hold him there.” She fell in love. She named him Emmanuel.
Once Emmanuel was discharged, Ms. Odunuga realized she had no choice but to quit her job. While Medicaid covered the costs of Emmanuel’s treatment, it was on her to care for him. From infancy, Emmanuel’s life has been a whirlwind of constant therapy. Today, at 20 months old, Odunuga brings him to physical, occupational, speech, and developmental therapy, each a different appointment on a different day of the week.
Emmanuel has thrived beyond what his doctors predicted, toddling so fast that Ms. Odunuga can’t look away for a minute and beaming as he waves his favorite toy phone. Yet he still suffers from gagging issues, which means Ms. Odunuga can’t feed him any solid foods. Liquid gets into his lungs when he aspirates; it has led to pneumonia three times. Emmanuel has a special stroller that helps keep his head in a position that won’t aggravate his persistent reflux, but Odunuga said she still has to pull over on the side of the road sometimes when she hears him projectile vomiting from the backseat.
The days are endless. Once she puts Emmanuel to bed, Ms. Odunuga starts planning the next day’s appointments. “I’ve had to cry alone, scream out alone,” she said. “Sometimes I wake up and think, Is this real? And then I hear him in the next room.”
Putting aside the challenge of eliminating syphilis entirely, everyone agrees it’s both doable and necessary to prevent newborn cases. “There was a crisis in perinatal HIV almost 30 years ago and people stood up and said this is not OK — it’s not acceptable for babies to be born in that condition. ... [We] brought it down from 1,700 babies born each year with perinatal HIV to less than 40 per year today,” said Virginia Bowen, an epidemiologist at the CDC. “Now here we are with a slightly different condition. We can also stand up and say, ‘This is not acceptable.’” Belarus, Bermuda, Cuba, Malaysia, Thailand, and Sri Lanka are among countries recognized by the World Health Organization for eliminating congenital syphilis.
Success starts with filling gaps across the health care system.
For almost a century, public health experts have advocated for testing pregnant patients more than once for syphilis in order to catch the infection. But policies nationwide still don’t reflect this best practice. Six states have no prenatal screening requirement at all. Even in states that require three tests, public health officials say that many physicians aren’t aware of the requirements. Dr. Stafford, the maternal-fetal medicine specialist in Houston, says she’s tired of hearing her own peers in medicine tell her, “Oh, syphilis is a problem?”
It costs public health departments less than 25 cents a dose to buy penicillin, but for a private practice, it’s more than $1,000, according to Dr. Park of the University of California San Francisco. “There’s no incentive for a private physician to stock a dose that could expire before it’s used, so they often don’t have it. So a woman comes in, they say, ‘We’ll send you to the emergency department or health department to get it,’ then [the patients] don’t show up.”
A vaccine would be invaluable for preventing spread among people at high risk for reinfection. But there is none. Scientists only recently figured out how to grow the bacteria in the lab, prompting grants from the National Institutes of Health to fund research into a vaccine. Dr. Justin Radolf, a researcher at the University of Connecticut School of Medicine, said he hopes his team will have a vaccine candidate by the end of its five-year grant. But it’ll likely take years more to find a manufacturer and run human trials.
Public health agencies also need to recognize that many of the hurdles to getting pregnant people treated involve access to care, economic stability, safe housing and transportation. In Fresno, Ms. Adams has been working on ways her department can collaborate with mental health services. Recently, one of her disease intervention specialists managed to get a pregnant woman treated with penicillin shots and, at the patient’s request, connected her with an addiction treatment center.
Gaining a patient’s cooperation means seeing them as complex humans instead of just a case to solve. “There may be past traumas with the health care system,” said Cynthia Deverson, project manager of the Houston Fetal Infant Morbidity Review. “There’s the fear of being discovered if she’s doing something illegal to survive. ... She may need to be in a certain place at a certain time so she can get something to eat, or maybe it’s the only time of the day that’s safe for her to sleep. They’re not going to tell you that. Yes, they understand there’s a problem, but it’s not an immediate threat, maybe they don’t feel bad yet, so obviously this is not urgent. ...
“What helps to gain trust is consistency,” she said. “Literally, it’s seeing that [disease specialist] constantly, daily. ... The woman can see that you’re not going to harm her, you’re saying, ‘I’m here at this time if you need me.’”
Ms. Yang stood outside the clinic, waiting for Angelica to show up, baking in the 90-degree heat. Her feelings ranged from irritation — Why didn’t she just go? I’d have more energy for other cases — to an appreciation for the parts of Angelica’s story that she didn’t know — She’s in survival mode. I need to be more patient.
Fifteen minutes ticked by, then 20.
“OK,” Ms. Yang announced. “We’re going back.”
She asked Sevilla if he would be OK if they drove Angelica to the clinic; they technically weren’t supposed to because of coronavirus precautions, but Ms. Yang wasn’t sure she could convince Angelica to walk. Mr. Sevilla gave her the thumbs up.
When they pulled up, they saw Angelica sitting in the backyard, chatting with a friend. She now wore a fresh T-shirt and had shoes on her feet. Angelica sat silently in the back seat as Ms. Yang drove to the clinic. A few minutes later, they pulled up to the parking lot.
Finally, Ms. Yang thought. We got her here.
The clinic was packed with people waiting for COVID-19 tests and vaccinations. A worker there had previously told Ms. Yang that a walk-in would be fine, but a receptionist now said they were too busy to treat Angelica. She would have to return.
Ms. Yang felt a surge of frustration, sensing that her hard-fought opportunity was slipping away. She tried to talk to the nurse supervisor, but he wasn’t available. She tried to leave the gift cards at the office to reward Angelica if she came, but the receptionist said she couldn’t hold them. While Ms. Yang negotiated, Mr. Sevilla sat with Angelica in the car, waiting.
Finally, Ms. Yang accepted this was yet another thing she couldn’t control.
She drove Angelica back to the yellow house. As they arrived, she tried once more to impress on her just how important it was to get treated, asking Mr. Sevilla to interpret. “We don’t want it to get any more serious, because she can go blind, she could go deaf, she could lose her baby.”
Angelica already had the door halfway open.
“So on a scale from one to 10, how important is this to get treated?” Ms. Yang asked.
“Ten,” Angelica said. Ms. Yang reminded her of the appointment that afternoon. Then Angelica stepped out and returned to the dusty yard.
Ms. Yang lingered for a moment, watching Angelica go. Then she turned the car back onto the highway and set off toward Fresno, knowing, already, that she’d be back.
Postscript: A reporter visited Huron twice more in the months that followed, including once independently to try to interview Angelica, but she wasn’t in town. Ms. Yang has visited Huron twice more as well — six times in total thus far. In October, a couple of men at the yellow house said Angelica was still in town, still pregnant. Ms. Yang and Mr. Sevilla spent an hour driving around, talking to residents, hoping to catch Angelica. But she was nowhere to be found.
ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive their biggest stories as soon as they’re published.
This story was originally published on ProPublica and was co-published with NPR.
When Mai Yang is looking for a patient, she travels light. She dresses deliberately — not too formal, so she won’t be mistaken for a police officer; not too casual, so people will look past her tiny 4-foot-10 stature and youthful face and trust her with sensitive health information. Always, she wears closed-toed shoes, “just in case I need to run.”
Yang carries a stack of cards issued by the Centers for Disease Control and Prevention that show what happens when the Treponema pallidum bacteria invades a patient’s body. There’s a photo of an angry red sore on a penis. There’s one of a tongue, marred by mucus-lined lesions. And there’s one of a newborn baby, its belly, torso and thighs dotted in a rash, its mouth open, as if caught midcry.
It was because of the prospect of one such baby that Yang found herself walking through a homeless encampment on a blazing July day in Huron, Calif., an hour’s drive southwest of her office at the Fresno County Department of Public Health. She was looking for a pregnant woman named Angelica, whose visit to a community clinic had triggered a report to the health department’s sexually transmitted disease program. Angelica had tested positive for syphilis. If she was not treated, her baby could end up like the one in the picture or worse — there was a 40% chance the baby would die.
Ms. Yang knew, though, that if she helped Angelica get treated with three weekly shots of penicillin at least 30 days before she gave birth, it was likely that the infection would be wiped out and her baby would be born without any symptoms at all. Every case of congenital syphilis, when a baby is born with the disease, is avoidable. Each is considered a “sentinel event,” a warning that the public health system is failing.
The alarms are now clamoring. In the United States, more than 129,800 syphilis cases were recorded in 2019, double the case count of five years prior. In the same time period, cases of congenital syphilis quadrupled: 1,870 babies were born with the disease; 128 died. Case counts from 2020 are still being finalized, but the CDC has said that reported cases of congenital syphilis have already exceeded the prior year. Black, Hispanic, and Native American babies are disproportionately at risk.
There was a time, not too long ago, when CDC officials thought they could eliminate the centuries-old scourge from the United States, for adults and babies. But the effort lost steam and cases soon crept up again. Syphilis is not an outlier. The United States goes through what former CDC director Dr. Tom Frieden calls “a deadly cycle of panic and neglect” in which emergencies propel officials to scramble and throw money at a problem — whether that’s Ebola, Zika, or COVID-19. Then, as fear ebbs, so does the attention and motivation to finish the task.
The last fraction of cases can be the hardest to solve, whether that’s eradicating a bug or getting vaccines into arms, yet too often, that’s exactly when political attention gets diverted to the next alarm. The result: The hardest to reach and most vulnerable populations are the ones left suffering, after everyone else looks away.
Ms. Yang first received Angelica’s lab report on June 17. The address listed was a P.O. box, and the phone number belonged to her sister, who said Angelica was living in Huron. That was a piece of luck: Huron is tiny; the city spans just 1.6 square miles. On her first visit, a worker at the Alamo Motel said she knew Angelica and directed Ms. Yang to a nearby homeless encampment. Angelica wasn’t there, so Ms. Yang returned a second time, bringing one of the health department nurses who could serve as an interpreter.
They made their way to the barren patch of land behind Huron Valley Foods, the local grocery store, where people took shelter in makeshift lean-tos composed of cardboard boxes, scrap wood ,and scavenged furniture, draped with sheets that served as ceilings and curtains. Yang stopped outside one of the structures, calling a greeting.
“Hi, I’m from the health department, I’m looking for Angelica.”
The nurse echoed her in Spanish.
Angelica emerged, squinting in the sunlight. Ms. Yang couldn’t tell if she was visibly pregnant yet, as her body was obscured by an oversized shirt. The two women were about the same age: Ms. Yang 26 and Angelica 27. Ms. Yang led her away from the tent, so they could speak privately. Angelica seemed reticent, surprised by the sudden appearance of the two health officers. “You’re not in trouble,” Ms. Yang said, before revealing the results of her blood test.
Angelica had never heard of syphilis.
“Have you been to prenatal care?”
Angelica shook her head. The local clinic had referred her to an obstetrician in Hanford, a 30-minute drive away. She had no car. She also mentioned that she didn’t intend to raise her baby; her two oldest children lived with her mother, and this one likely would, too.
Ms. Yang pulled out the CDC cards, showing them to Angelica and asking if she had experienced any of the symptoms illustrated. No, Angelica said, her lips pursed with disgust.
“Right now you still feel healthy, but this bacteria is still in your body,” Ms. Yang pressed. “You need to get the infection treated to prevent further health complications to yourself and your baby.”
The community clinic was just across the street. “Can we walk you over to the clinic and make sure you get seen so we can get this taken care of?”
Angelica demurred. She said she hadn’t showered for a week and wanted to wash up first. She said she’d go later.
Ms. Yang tried once more to extract a promise: “What time do you think you’ll go?”
“Today, for sure.”
Syphilis is called The Great Imitator: It can look like any number of diseases. In its first stage, the only evidence of infection is a painless sore at the bacteria’s point of entry. Weeks later, as the bacteria multiplies, skin rashes bloom on the palms of the hands and bottoms of the feet. Other traits of this stage include fever, headaches, muscle aches, sore throat, and fatigue. These symptoms eventually disappear and the patient progresses into the latent phase, which betrays no external signs. But if left untreated, after a decade or more, syphilis will reemerge in up to 30% of patients, capable of wreaking horror on a wide range of organ systems. Dr. Marion Sims, president of the American Medical Association in 1876, called it a “terrible scourge, which begins with lamb-like mildness and ends with lion-like rage that ruthlessly destroys everything in its way.”
The corkscrew-shaped bacteria can infiltrate the nervous system at any stage of the infection. Ms. Yang is haunted by her memory of interviewing a young man whose dementia was so severe that he didn’t know why he was in the hospital or how old he was. And regardless of symptoms or stage, the bacteria can penetrate the placenta to infect a fetus. Even in these cases the infection is unpredictable: Many babies are born with normal physical features, but others can have deformed bones or damaged brains, and they can struggle to hear, see, or breathe.
From its earliest days, syphilis has been shrouded in stigma. The first recorded outbreak was in the late 15th century, when Charles VIII led the French army to invade Naples. Italian physicians described French soldiers covered with pustules, dying from a sexually transmitted disease. As the affliction spread, Italians called it the French Disease. The French blamed the Neopolitans. It was also called the German, Polish, or Spanish disease, depending on which neighbor one wanted to blame. Even its name bears the taint of divine judgement: It comes from a 16th-century poem that tells of a shepherd, Syphilus, who offended the god Apollo and was punished with a hideous disease.
By 1937 in America, when former Surgeon General Thomas Parran wrote the book “Shadow on the Land,” he estimated some 680,000 people were under treatment for syphilis; about 60,000 babies were being born annually with congenital syphilis. There was no cure, and the stigma was so strong that public health officials feared even properly documenting cases.
Thanks to Dr. Parran’s ardent advocacy, Congress in 1938 passed the National Venereal Disease Control Act, which created grants for states to set up clinics and support testing and treatment. Other than a short-lived funding effort during World War I, this was the first coordinated federal push to respond to the disease.
Around the same time, the Public Health Service launched an effort to record the natural history of syphilis. Situated in Tuskegee, Ala., the infamous study recruited 600 black men. By the early 1940s, penicillin became widely available and was found to be a reliable cure, but the treatment was withheld from the study participants. Outrage over the ethical violations would cast a stain across syphilis research for decades to come and fuel generations of mistrust in the medical system among Black Americans that continues to this day.
With the introduction of penicillin, cases began to plummet. Twice, the CDC has announced efforts to wipe out the disease — once in the 1960s and again in 1999.
In the latest effort, the CDC announced that the United States had “a unique opportunity to eliminate syphilis within its borders,” thanks to historically low rates, with 80% of counties reporting zero cases. The concentration of cases in the South “identifies communities in which there is a fundamental failure of public health capacity,” the agency noted, adding that elimination — which it defined as fewer than 1,000 cases a year — would “decrease one of our most glaring racial disparities in health.”
Two years after the campaign began, cases started climbing, first among gay men and later, heterosexuals. Cases in women started accelerating in 2013, followed shortly by increasing numbers of babies born with syphilis.The reasons for failure are complex; people relaxed safer sex practices after the advent of potent HIV combination therapies, increased methamphetamine use drove riskier behavior and an explosion of online dating made it hard to track and test sexual partners, according to Dr. Ina Park, medical director of the California Prevention Training Center at the University of California San Francisco.
But federal and state public health efforts were hamstrung from the get-go. In 1999, the CDC said it would need about $35 million to $39 million in new federal funds annually for at least five years to eliminate syphilis. The agency got less than half of what it asked for, according to Jo Valentine, former program coordinator of the CDC’s Syphilis Elimination Effort. As cases rose, the CDC modified its goals in 2006 from 0.4 primary and secondary syphilis cases per 100,000 in population to 2.2 cases per 100,000. By 2013, as elimination seemed less and less viable, the CDC changed its focus to ending congenital syphilis only.
Since then, funding has remained anemic. From 2015 to 2020, the CDC’s budget for preventing sexually transmitted infections grew by 2.2%. Taking inflation into account, that’s a 7.4% reduction in purchasing power. In the same period, cases of syphilis, gonorrhea and chlamydia — the three STDs that have federally funded control programs — increased by nearly 30%.
“We have a long history of nearly eradicating something, then changing our attention, and seeing a resurgence in numbers,” said David Harvey, executive director of the National Coalition of STD Directors. “We have more congenital syphilis cases today in America than we ever had pediatric AIDS at the height of the AIDS epidemic. It’s heartbreaking.”
Adriane Casalotti, chief of government and public affairs at the National Association of County and City Health Officials, warns that the United States should not be surprised to see case counts continue to climb. “The bugs don’t go away,” she said. “They’re just waiting for the next opportunity, when you’re not paying attention.”
Ms. Yang waited until the end of the day, then called the clinic to see if Angelica had gone for her shot. She had not. Ms. Yang would have to block off another half day to visit Huron again, but she had three dozen other cases to deal with.
States in the South and West have seen the highest syphilis rates in recent years. In 2017, 64 babies in Fresno County were born with syphilis at a rate of 440 babies per 100,000 live births — about 19 times the national rate. While the county had managed to lower case counts in the two years that followed, the pandemic threatened to unravel that progress, forcing STD staffers to do COVID-19 contact tracing, pausing field visits to find infected people, and scaring patients from seeking care. Ms. Yang’s colleague handled three cases of stillbirth in 2020; in each, the woman was never diagnosed with syphilis because she feared catching the coronavirus and skipped prenatal care.
Ms. Yang, whose caseload peaked at 70 during a COVID-19 surge, knew she would not be able handle them all as thoroughly as she’d like to. “When I was being mentored by another investigator, he said: ‘You’re not a superhero. You can’t save everybody,’” she said. She prioritizes men who have sex with men, because there’s a higher prevalence of syphilis in that population, and pregnant people, because of the horrific consequences for babies.
The job of a disease intervention specialist isn’t for everyone: It means meeting patients whenever and wherever they are available — in the mop closet of a bus station, in a quiet parking lot — to inform them about the disease, to extract names of sex partners and to encourage treatment. Patients are often reluctant to talk. They can get belligerent, upset that “the government” has their personal information or shattered at the thought that a partner is likely cheating on them. Salaries typically start in the low $40,000s.
Jena Adams, Ms. Yang’s supervisor, has eight investigators working on HIV and syphilis. In the middle of 2020, she lost two and replaced them only recently. “It’s been exhausting,” Ms. Adams said. She has only one specialist who is trained to take blood samples in the field, crucial for guaranteeing that the partners of those who test positive for syphilis also get tested. Ms. Adams wants to get phlebotomy training for the rest of her staff, but it’s $2,000 per person. The department also doesn’t have anyone who can administer penicillin injections in the field; that would have been key when Ms. Yang met Angelica. For a while, a nurse who worked in the tuberculosis program would ride along to give penicillin shots on a volunteer basis. Then he, too, left the health department.
Much of the resources in public health trickle down from the CDC, which distributes money to states, which then parcel it out to counties. The CDC gets its budget from Congress, which tells the agency, by line item, exactly how much money it can spend to fight a disease or virus, in an uncommonly specific manner not seen in many other agencies. The decisions are often politically driven and can be detached from actual health needs.
When the House and Senate appropriations committees meet to decide how much the CDC will get for each line item, they are barraged by lobbyists for individual disease interests. Stephanie Arnold Pang, senior director of policy and government relations at the National Coalition of STD Directors, can pick out the groups by sight: breast cancer wears pink, Alzheimer’s goes in purple, multiple sclerosis comes in orange, HIV in red. STD prevention advocates, like herself, don a green ribbon, but they’re far outnumbered.
And unlike diseases that might already be familiar to lawmakers, or have patient and family spokespeople who can tell their own powerful stories, syphilis doesn’t have many willing poster children. “Congressmen don’t wake up one day and say, ‘Oh hey, there’s congenital syphilis in my jurisdiction.’ You have to raise awareness,” Arnold Pang said. It can be hard jockeying for a meeting. “Some offices might say, ‘I don’t have time for you because we’ve just seen HIV.’ ... Sometimes, it feels like you’re talking into a void.”
The consequences of the political nature of public health funding have become more obvious during the coronavirus pandemic. The 2014 Ebola epidemic was seen as a “global wakeup call” that the world wasn’t prepared for a major pandemic, yet in 2018, the CDC scaled back its epidemic prevention work as money ran out. “If you’ve got to choose between Alzheimer’s research and stopping an outbreak that may not happen? Stopping an outbreak that might not happen doesn’t do well,” said Dr. Frieden, the former CDC director. “The CDC needs to have more money and more flexible money. Otherwise, we’re going to be in this situation long term.”
In May 2021, President Joe Biden’s administration announced it would set aside $7.4 billion over the next five years to hire and train public health workers, including $1.1 billion for more disease intervention specialists like Ms. Yang. Public health officials are thrilled to have the chance to expand their workforce, but some worry the time horizon may be too short. “We’ve seen this movie before, right?” Dr. Frieden said. “Everyone gets concerned when there’s an outbreak, and when that outbreak stops, the headlines stop, and an economic downturn happens, the budget gets cut.”
Fresno’s STD clinic was shuttered in 2010 amid the Great Recession. Many others have vanished since the passage of the Affordable Care Act. Health leaders thought “by magically beefing up the primary care system, that we would do a better job of catching STIs and treating them,” said Mr. Harvey, the executive director of the National Coalition of STD Directors. That hasn’t worked out; people want access to anonymous services, and primary care doctors often don’t have STDs top of mind. The coalition is lobbying Congress for funding to support STD clinical services, proposing a three-year demonstration project funded at $600 million.
It’s one of Ms. Adams’ dreams to see Fresno’s STD clinic restored as it was. “You could come in for an HIV test and get other STDs checked,” she said. “And if a patient is positive, you can give a first injection on the spot.”
On Aug. 12, Ms. Yang set out for Huron again, speeding past groves of almond trees and fields of grapes in the department’s white Chevy Cruze. She brought along a colleague, Jorge Sevilla, who had recently transferred to the STD program from COVID-19 contact tracing. Ms. Yang was anxious to find Angelica again. “She’s probably in her second trimester now,” she said.
They found her outside of a pale yellow house a few blocks from the homeless encampment; the owner was letting her stay in a shed tucked in the corner of the dirt yard. This time, it was evident that she was pregnant. Ms. Yang noted that Angelica was wearing a wig; hair loss is a symptom of syphilis.
“Do you remember me?” Ms. Yang asked.
Angelica nodded. She didn’t seem surprised to see Ms. Yang again. (I came along, and Mr. Sevilla explained who I was and that I was writing about syphilis and the people affected by it. Angelica signed a release for me to report about her case, and she said she had no problem with me writing about her or even using her full name. ProPublica chose to only print her first name.)
“How are you doing? How’s the baby?”
“Bien.”
“So the last time we talked, we were going to have you go to United Healthcare Center to get treatment. Have you gone since?”
Angelica shook her head.
“We brought some gift cards...” Mr. Sevilla started in Spanish. The department uses them as incentives for completing injections. But Angelica was already shaking her head. The nearest Walmart was the next town over.
Ms. Yang turned to her partner. “Tell her: So the reason why we’re coming out here again is because we really need her to go in for treatment. ... We really are concerned for the baby’s health especially since she’s had the infection for quite a while.”
Angelica listened while Mr. Sevilla interpreted, her eyes on the ground. Then she looked up. “Orita?” she asked. Right now?
“I’ll walk with you,” Ms. Yang offered. Angelica shook her head. “She said she wants to shower first before she goes over there,” Mr. Sevilla said.
Ms. Yang made a face. “She said that to me last time.” Ms. Yang offered to wait, but Angelica didn’t want the health officers to linger by the house. She said she would meet them by the clinic in 15 minutes.
Ms. Yang was reluctant to let her go but again had no other option. She and Mr. Sevilla drove to the clinic, then stood on the corner of the parking lot, staring down the road.
Talk to the pediatricians, obstetricians, and families on the front lines of the congenital syphilis surge and it becomes clear why Ms. Yang and others are trying so desperately to prevent cases. Dr. J. B. Cantey, associate professor in pediatrics at UT Health San Antonio, remembers a baby girl born at 25 weeks gestation who weighed a pound and a half. Syphilis had spread through her bones and lungs. She spent five months in the neonatal intensive care unit, breathing through a ventilator, and was still eating through a tube when she was discharged.
Then, there are the miscarriages, the stillbirths and the inconsolable parents. Dr. Irene Stafford, an associate professor and maternal-fetal medicine specialist at UT Health in Houston, cannot forget a patient who came in at 36 weeks for a routine checkup, pregnant with her first child. Dr. Stafford realized that there was no heartbeat. “She could see on my face that something was really wrong,” Dr. Stafford recalled. She had to let the patient know that syphilis had killed her baby. “She was hysterical, just bawling,” Dr. Stafford said. “I’ve seen people’s families ripped apart and I’ve seen beautiful babies die.” Fewer than 10% of patients who experience a stillbirth are tested for syphilis, suggesting that cases are underdiagnosed.
A Texas grandmother named Solidad Odunuga offers a glimpse into what the future could hold for Angelica’s mother, who may wind up raising her baby.
In February of last year, Ms. Odunuga got a call from the Lyndon B. Johnson Hospital in Houston. A nurse told her that her daughter was about to give birth and that child protective services had been called. Ms. Odunuga had lost contact with her daughter, who struggled with homelessness and substance abuse. She arrived in time to see her grandson delivered, premature at 30 weeks old, weighing 2.7 pounds. He tested positive for syphilis.
When a child protective worker asked Ms. Odunuga to take custody of the infant, she felt a wave of dread. “I was in denial,” she recalled. “I did not plan to be a mom again.” The baby’s medical problems were daunting: “Global developmental delays ... concerns for visual impairments ... high risk of cerebral palsy,” read a note from the doctor at the time.
Still, Ms. Odunuga visited her grandson every day for three months, driving to the NICU from her job at the University of Houston. “I’d put him in my shirt to keep him warm and hold him there.” She fell in love. She named him Emmanuel.
Once Emmanuel was discharged, Ms. Odunuga realized she had no choice but to quit her job. While Medicaid covered the costs of Emmanuel’s treatment, it was on her to care for him. From infancy, Emmanuel’s life has been a whirlwind of constant therapy. Today, at 20 months old, Odunuga brings him to physical, occupational, speech, and developmental therapy, each a different appointment on a different day of the week.
Emmanuel has thrived beyond what his doctors predicted, toddling so fast that Ms. Odunuga can’t look away for a minute and beaming as he waves his favorite toy phone. Yet he still suffers from gagging issues, which means Ms. Odunuga can’t feed him any solid foods. Liquid gets into his lungs when he aspirates; it has led to pneumonia three times. Emmanuel has a special stroller that helps keep his head in a position that won’t aggravate his persistent reflux, but Odunuga said she still has to pull over on the side of the road sometimes when she hears him projectile vomiting from the backseat.
The days are endless. Once she puts Emmanuel to bed, Ms. Odunuga starts planning the next day’s appointments. “I’ve had to cry alone, scream out alone,” she said. “Sometimes I wake up and think, Is this real? And then I hear him in the next room.”
Putting aside the challenge of eliminating syphilis entirely, everyone agrees it’s both doable and necessary to prevent newborn cases. “There was a crisis in perinatal HIV almost 30 years ago and people stood up and said this is not OK — it’s not acceptable for babies to be born in that condition. ... [We] brought it down from 1,700 babies born each year with perinatal HIV to less than 40 per year today,” said Virginia Bowen, an epidemiologist at the CDC. “Now here we are with a slightly different condition. We can also stand up and say, ‘This is not acceptable.’” Belarus, Bermuda, Cuba, Malaysia, Thailand, and Sri Lanka are among countries recognized by the World Health Organization for eliminating congenital syphilis.
Success starts with filling gaps across the health care system.
For almost a century, public health experts have advocated for testing pregnant patients more than once for syphilis in order to catch the infection. But policies nationwide still don’t reflect this best practice. Six states have no prenatal screening requirement at all. Even in states that require three tests, public health officials say that many physicians aren’t aware of the requirements. Dr. Stafford, the maternal-fetal medicine specialist in Houston, says she’s tired of hearing her own peers in medicine tell her, “Oh, syphilis is a problem?”
It costs public health departments less than 25 cents a dose to buy penicillin, but for a private practice, it’s more than $1,000, according to Dr. Park of the University of California San Francisco. “There’s no incentive for a private physician to stock a dose that could expire before it’s used, so they often don’t have it. So a woman comes in, they say, ‘We’ll send you to the emergency department or health department to get it,’ then [the patients] don’t show up.”
A vaccine would be invaluable for preventing spread among people at high risk for reinfection. But there is none. Scientists only recently figured out how to grow the bacteria in the lab, prompting grants from the National Institutes of Health to fund research into a vaccine. Dr. Justin Radolf, a researcher at the University of Connecticut School of Medicine, said he hopes his team will have a vaccine candidate by the end of its five-year grant. But it’ll likely take years more to find a manufacturer and run human trials.
Public health agencies also need to recognize that many of the hurdles to getting pregnant people treated involve access to care, economic stability, safe housing and transportation. In Fresno, Ms. Adams has been working on ways her department can collaborate with mental health services. Recently, one of her disease intervention specialists managed to get a pregnant woman treated with penicillin shots and, at the patient’s request, connected her with an addiction treatment center.
Gaining a patient’s cooperation means seeing them as complex humans instead of just a case to solve. “There may be past traumas with the health care system,” said Cynthia Deverson, project manager of the Houston Fetal Infant Morbidity Review. “There’s the fear of being discovered if she’s doing something illegal to survive. ... She may need to be in a certain place at a certain time so she can get something to eat, or maybe it’s the only time of the day that’s safe for her to sleep. They’re not going to tell you that. Yes, they understand there’s a problem, but it’s not an immediate threat, maybe they don’t feel bad yet, so obviously this is not urgent. ...
“What helps to gain trust is consistency,” she said. “Literally, it’s seeing that [disease specialist] constantly, daily. ... The woman can see that you’re not going to harm her, you’re saying, ‘I’m here at this time if you need me.’”
Ms. Yang stood outside the clinic, waiting for Angelica to show up, baking in the 90-degree heat. Her feelings ranged from irritation — Why didn’t she just go? I’d have more energy for other cases — to an appreciation for the parts of Angelica’s story that she didn’t know — She’s in survival mode. I need to be more patient.
Fifteen minutes ticked by, then 20.
“OK,” Ms. Yang announced. “We’re going back.”
She asked Sevilla if he would be OK if they drove Angelica to the clinic; they technically weren’t supposed to because of coronavirus precautions, but Ms. Yang wasn’t sure she could convince Angelica to walk. Mr. Sevilla gave her the thumbs up.
When they pulled up, they saw Angelica sitting in the backyard, chatting with a friend. She now wore a fresh T-shirt and had shoes on her feet. Angelica sat silently in the back seat as Ms. Yang drove to the clinic. A few minutes later, they pulled up to the parking lot.
Finally, Ms. Yang thought. We got her here.
The clinic was packed with people waiting for COVID-19 tests and vaccinations. A worker there had previously told Ms. Yang that a walk-in would be fine, but a receptionist now said they were too busy to treat Angelica. She would have to return.
Ms. Yang felt a surge of frustration, sensing that her hard-fought opportunity was slipping away. She tried to talk to the nurse supervisor, but he wasn’t available. She tried to leave the gift cards at the office to reward Angelica if she came, but the receptionist said she couldn’t hold them. While Ms. Yang negotiated, Mr. Sevilla sat with Angelica in the car, waiting.
Finally, Ms. Yang accepted this was yet another thing she couldn’t control.
She drove Angelica back to the yellow house. As they arrived, she tried once more to impress on her just how important it was to get treated, asking Mr. Sevilla to interpret. “We don’t want it to get any more serious, because she can go blind, she could go deaf, she could lose her baby.”
Angelica already had the door halfway open.
“So on a scale from one to 10, how important is this to get treated?” Ms. Yang asked.
“Ten,” Angelica said. Ms. Yang reminded her of the appointment that afternoon. Then Angelica stepped out and returned to the dusty yard.
Ms. Yang lingered for a moment, watching Angelica go. Then she turned the car back onto the highway and set off toward Fresno, knowing, already, that she’d be back.
Postscript: A reporter visited Huron twice more in the months that followed, including once independently to try to interview Angelica, but she wasn’t in town. Ms. Yang has visited Huron twice more as well — six times in total thus far. In October, a couple of men at the yellow house said Angelica was still in town, still pregnant. Ms. Yang and Mr. Sevilla spent an hour driving around, talking to residents, hoping to catch Angelica. But she was nowhere to be found.
ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive their biggest stories as soon as they’re published.
This story was originally published on ProPublica and was co-published with NPR.
When Mai Yang is looking for a patient, she travels light. She dresses deliberately — not too formal, so she won’t be mistaken for a police officer; not too casual, so people will look past her tiny 4-foot-10 stature and youthful face and trust her with sensitive health information. Always, she wears closed-toed shoes, “just in case I need to run.”
Yang carries a stack of cards issued by the Centers for Disease Control and Prevention that show what happens when the Treponema pallidum bacteria invades a patient’s body. There’s a photo of an angry red sore on a penis. There’s one of a tongue, marred by mucus-lined lesions. And there’s one of a newborn baby, its belly, torso and thighs dotted in a rash, its mouth open, as if caught midcry.
It was because of the prospect of one such baby that Yang found herself walking through a homeless encampment on a blazing July day in Huron, Calif., an hour’s drive southwest of her office at the Fresno County Department of Public Health. She was looking for a pregnant woman named Angelica, whose visit to a community clinic had triggered a report to the health department’s sexually transmitted disease program. Angelica had tested positive for syphilis. If she was not treated, her baby could end up like the one in the picture or worse — there was a 40% chance the baby would die.
Ms. Yang knew, though, that if she helped Angelica get treated with three weekly shots of penicillin at least 30 days before she gave birth, it was likely that the infection would be wiped out and her baby would be born without any symptoms at all. Every case of congenital syphilis, when a baby is born with the disease, is avoidable. Each is considered a “sentinel event,” a warning that the public health system is failing.
The alarms are now clamoring. In the United States, more than 129,800 syphilis cases were recorded in 2019, double the case count of five years prior. In the same time period, cases of congenital syphilis quadrupled: 1,870 babies were born with the disease; 128 died. Case counts from 2020 are still being finalized, but the CDC has said that reported cases of congenital syphilis have already exceeded the prior year. Black, Hispanic, and Native American babies are disproportionately at risk.
There was a time, not too long ago, when CDC officials thought they could eliminate the centuries-old scourge from the United States, for adults and babies. But the effort lost steam and cases soon crept up again. Syphilis is not an outlier. The United States goes through what former CDC director Dr. Tom Frieden calls “a deadly cycle of panic and neglect” in which emergencies propel officials to scramble and throw money at a problem — whether that’s Ebola, Zika, or COVID-19. Then, as fear ebbs, so does the attention and motivation to finish the task.
The last fraction of cases can be the hardest to solve, whether that’s eradicating a bug or getting vaccines into arms, yet too often, that’s exactly when political attention gets diverted to the next alarm. The result: The hardest to reach and most vulnerable populations are the ones left suffering, after everyone else looks away.
Ms. Yang first received Angelica’s lab report on June 17. The address listed was a P.O. box, and the phone number belonged to her sister, who said Angelica was living in Huron. That was a piece of luck: Huron is tiny; the city spans just 1.6 square miles. On her first visit, a worker at the Alamo Motel said she knew Angelica and directed Ms. Yang to a nearby homeless encampment. Angelica wasn’t there, so Ms. Yang returned a second time, bringing one of the health department nurses who could serve as an interpreter.
They made their way to the barren patch of land behind Huron Valley Foods, the local grocery store, where people took shelter in makeshift lean-tos composed of cardboard boxes, scrap wood ,and scavenged furniture, draped with sheets that served as ceilings and curtains. Yang stopped outside one of the structures, calling a greeting.
“Hi, I’m from the health department, I’m looking for Angelica.”
The nurse echoed her in Spanish.
Angelica emerged, squinting in the sunlight. Ms. Yang couldn’t tell if she was visibly pregnant yet, as her body was obscured by an oversized shirt. The two women were about the same age: Ms. Yang 26 and Angelica 27. Ms. Yang led her away from the tent, so they could speak privately. Angelica seemed reticent, surprised by the sudden appearance of the two health officers. “You’re not in trouble,” Ms. Yang said, before revealing the results of her blood test.
Angelica had never heard of syphilis.
“Have you been to prenatal care?”
Angelica shook her head. The local clinic had referred her to an obstetrician in Hanford, a 30-minute drive away. She had no car. She also mentioned that she didn’t intend to raise her baby; her two oldest children lived with her mother, and this one likely would, too.
Ms. Yang pulled out the CDC cards, showing them to Angelica and asking if she had experienced any of the symptoms illustrated. No, Angelica said, her lips pursed with disgust.
“Right now you still feel healthy, but this bacteria is still in your body,” Ms. Yang pressed. “You need to get the infection treated to prevent further health complications to yourself and your baby.”
The community clinic was just across the street. “Can we walk you over to the clinic and make sure you get seen so we can get this taken care of?”
Angelica demurred. She said she hadn’t showered for a week and wanted to wash up first. She said she’d go later.
Ms. Yang tried once more to extract a promise: “What time do you think you’ll go?”
“Today, for sure.”
Syphilis is called The Great Imitator: It can look like any number of diseases. In its first stage, the only evidence of infection is a painless sore at the bacteria’s point of entry. Weeks later, as the bacteria multiplies, skin rashes bloom on the palms of the hands and bottoms of the feet. Other traits of this stage include fever, headaches, muscle aches, sore throat, and fatigue. These symptoms eventually disappear and the patient progresses into the latent phase, which betrays no external signs. But if left untreated, after a decade or more, syphilis will reemerge in up to 30% of patients, capable of wreaking horror on a wide range of organ systems. Dr. Marion Sims, president of the American Medical Association in 1876, called it a “terrible scourge, which begins with lamb-like mildness and ends with lion-like rage that ruthlessly destroys everything in its way.”
The corkscrew-shaped bacteria can infiltrate the nervous system at any stage of the infection. Ms. Yang is haunted by her memory of interviewing a young man whose dementia was so severe that he didn’t know why he was in the hospital or how old he was. And regardless of symptoms or stage, the bacteria can penetrate the placenta to infect a fetus. Even in these cases the infection is unpredictable: Many babies are born with normal physical features, but others can have deformed bones or damaged brains, and they can struggle to hear, see, or breathe.
From its earliest days, syphilis has been shrouded in stigma. The first recorded outbreak was in the late 15th century, when Charles VIII led the French army to invade Naples. Italian physicians described French soldiers covered with pustules, dying from a sexually transmitted disease. As the affliction spread, Italians called it the French Disease. The French blamed the Neopolitans. It was also called the German, Polish, or Spanish disease, depending on which neighbor one wanted to blame. Even its name bears the taint of divine judgement: It comes from a 16th-century poem that tells of a shepherd, Syphilus, who offended the god Apollo and was punished with a hideous disease.
By 1937 in America, when former Surgeon General Thomas Parran wrote the book “Shadow on the Land,” he estimated some 680,000 people were under treatment for syphilis; about 60,000 babies were being born annually with congenital syphilis. There was no cure, and the stigma was so strong that public health officials feared even properly documenting cases.
Thanks to Dr. Parran’s ardent advocacy, Congress in 1938 passed the National Venereal Disease Control Act, which created grants for states to set up clinics and support testing and treatment. Other than a short-lived funding effort during World War I, this was the first coordinated federal push to respond to the disease.
Around the same time, the Public Health Service launched an effort to record the natural history of syphilis. Situated in Tuskegee, Ala., the infamous study recruited 600 black men. By the early 1940s, penicillin became widely available and was found to be a reliable cure, but the treatment was withheld from the study participants. Outrage over the ethical violations would cast a stain across syphilis research for decades to come and fuel generations of mistrust in the medical system among Black Americans that continues to this day.
With the introduction of penicillin, cases began to plummet. Twice, the CDC has announced efforts to wipe out the disease — once in the 1960s and again in 1999.
In the latest effort, the CDC announced that the United States had “a unique opportunity to eliminate syphilis within its borders,” thanks to historically low rates, with 80% of counties reporting zero cases. The concentration of cases in the South “identifies communities in which there is a fundamental failure of public health capacity,” the agency noted, adding that elimination — which it defined as fewer than 1,000 cases a year — would “decrease one of our most glaring racial disparities in health.”
Two years after the campaign began, cases started climbing, first among gay men and later, heterosexuals. Cases in women started accelerating in 2013, followed shortly by increasing numbers of babies born with syphilis.The reasons for failure are complex; people relaxed safer sex practices after the advent of potent HIV combination therapies, increased methamphetamine use drove riskier behavior and an explosion of online dating made it hard to track and test sexual partners, according to Dr. Ina Park, medical director of the California Prevention Training Center at the University of California San Francisco.
But federal and state public health efforts were hamstrung from the get-go. In 1999, the CDC said it would need about $35 million to $39 million in new federal funds annually for at least five years to eliminate syphilis. The agency got less than half of what it asked for, according to Jo Valentine, former program coordinator of the CDC’s Syphilis Elimination Effort. As cases rose, the CDC modified its goals in 2006 from 0.4 primary and secondary syphilis cases per 100,000 in population to 2.2 cases per 100,000. By 2013, as elimination seemed less and less viable, the CDC changed its focus to ending congenital syphilis only.
Since then, funding has remained anemic. From 2015 to 2020, the CDC’s budget for preventing sexually transmitted infections grew by 2.2%. Taking inflation into account, that’s a 7.4% reduction in purchasing power. In the same period, cases of syphilis, gonorrhea and chlamydia — the three STDs that have federally funded control programs — increased by nearly 30%.
“We have a long history of nearly eradicating something, then changing our attention, and seeing a resurgence in numbers,” said David Harvey, executive director of the National Coalition of STD Directors. “We have more congenital syphilis cases today in America than we ever had pediatric AIDS at the height of the AIDS epidemic. It’s heartbreaking.”
Adriane Casalotti, chief of government and public affairs at the National Association of County and City Health Officials, warns that the United States should not be surprised to see case counts continue to climb. “The bugs don’t go away,” she said. “They’re just waiting for the next opportunity, when you’re not paying attention.”
Ms. Yang waited until the end of the day, then called the clinic to see if Angelica had gone for her shot. She had not. Ms. Yang would have to block off another half day to visit Huron again, but she had three dozen other cases to deal with.
States in the South and West have seen the highest syphilis rates in recent years. In 2017, 64 babies in Fresno County were born with syphilis at a rate of 440 babies per 100,000 live births — about 19 times the national rate. While the county had managed to lower case counts in the two years that followed, the pandemic threatened to unravel that progress, forcing STD staffers to do COVID-19 contact tracing, pausing field visits to find infected people, and scaring patients from seeking care. Ms. Yang’s colleague handled three cases of stillbirth in 2020; in each, the woman was never diagnosed with syphilis because she feared catching the coronavirus and skipped prenatal care.
Ms. Yang, whose caseload peaked at 70 during a COVID-19 surge, knew she would not be able handle them all as thoroughly as she’d like to. “When I was being mentored by another investigator, he said: ‘You’re not a superhero. You can’t save everybody,’” she said. She prioritizes men who have sex with men, because there’s a higher prevalence of syphilis in that population, and pregnant people, because of the horrific consequences for babies.
The job of a disease intervention specialist isn’t for everyone: It means meeting patients whenever and wherever they are available — in the mop closet of a bus station, in a quiet parking lot — to inform them about the disease, to extract names of sex partners and to encourage treatment. Patients are often reluctant to talk. They can get belligerent, upset that “the government” has their personal information or shattered at the thought that a partner is likely cheating on them. Salaries typically start in the low $40,000s.
Jena Adams, Ms. Yang’s supervisor, has eight investigators working on HIV and syphilis. In the middle of 2020, she lost two and replaced them only recently. “It’s been exhausting,” Ms. Adams said. She has only one specialist who is trained to take blood samples in the field, crucial for guaranteeing that the partners of those who test positive for syphilis also get tested. Ms. Adams wants to get phlebotomy training for the rest of her staff, but it’s $2,000 per person. The department also doesn’t have anyone who can administer penicillin injections in the field; that would have been key when Ms. Yang met Angelica. For a while, a nurse who worked in the tuberculosis program would ride along to give penicillin shots on a volunteer basis. Then he, too, left the health department.
Much of the resources in public health trickle down from the CDC, which distributes money to states, which then parcel it out to counties. The CDC gets its budget from Congress, which tells the agency, by line item, exactly how much money it can spend to fight a disease or virus, in an uncommonly specific manner not seen in many other agencies. The decisions are often politically driven and can be detached from actual health needs.
When the House and Senate appropriations committees meet to decide how much the CDC will get for each line item, they are barraged by lobbyists for individual disease interests. Stephanie Arnold Pang, senior director of policy and government relations at the National Coalition of STD Directors, can pick out the groups by sight: breast cancer wears pink, Alzheimer’s goes in purple, multiple sclerosis comes in orange, HIV in red. STD prevention advocates, like herself, don a green ribbon, but they’re far outnumbered.
And unlike diseases that might already be familiar to lawmakers, or have patient and family spokespeople who can tell their own powerful stories, syphilis doesn’t have many willing poster children. “Congressmen don’t wake up one day and say, ‘Oh hey, there’s congenital syphilis in my jurisdiction.’ You have to raise awareness,” Arnold Pang said. It can be hard jockeying for a meeting. “Some offices might say, ‘I don’t have time for you because we’ve just seen HIV.’ ... Sometimes, it feels like you’re talking into a void.”
The consequences of the political nature of public health funding have become more obvious during the coronavirus pandemic. The 2014 Ebola epidemic was seen as a “global wakeup call” that the world wasn’t prepared for a major pandemic, yet in 2018, the CDC scaled back its epidemic prevention work as money ran out. “If you’ve got to choose between Alzheimer’s research and stopping an outbreak that may not happen? Stopping an outbreak that might not happen doesn’t do well,” said Dr. Frieden, the former CDC director. “The CDC needs to have more money and more flexible money. Otherwise, we’re going to be in this situation long term.”
In May 2021, President Joe Biden’s administration announced it would set aside $7.4 billion over the next five years to hire and train public health workers, including $1.1 billion for more disease intervention specialists like Ms. Yang. Public health officials are thrilled to have the chance to expand their workforce, but some worry the time horizon may be too short. “We’ve seen this movie before, right?” Dr. Frieden said. “Everyone gets concerned when there’s an outbreak, and when that outbreak stops, the headlines stop, and an economic downturn happens, the budget gets cut.”
Fresno’s STD clinic was shuttered in 2010 amid the Great Recession. Many others have vanished since the passage of the Affordable Care Act. Health leaders thought “by magically beefing up the primary care system, that we would do a better job of catching STIs and treating them,” said Mr. Harvey, the executive director of the National Coalition of STD Directors. That hasn’t worked out; people want access to anonymous services, and primary care doctors often don’t have STDs top of mind. The coalition is lobbying Congress for funding to support STD clinical services, proposing a three-year demonstration project funded at $600 million.
It’s one of Ms. Adams’ dreams to see Fresno’s STD clinic restored as it was. “You could come in for an HIV test and get other STDs checked,” she said. “And if a patient is positive, you can give a first injection on the spot.”
On Aug. 12, Ms. Yang set out for Huron again, speeding past groves of almond trees and fields of grapes in the department’s white Chevy Cruze. She brought along a colleague, Jorge Sevilla, who had recently transferred to the STD program from COVID-19 contact tracing. Ms. Yang was anxious to find Angelica again. “She’s probably in her second trimester now,” she said.
They found her outside of a pale yellow house a few blocks from the homeless encampment; the owner was letting her stay in a shed tucked in the corner of the dirt yard. This time, it was evident that she was pregnant. Ms. Yang noted that Angelica was wearing a wig; hair loss is a symptom of syphilis.
“Do you remember me?” Ms. Yang asked.
Angelica nodded. She didn’t seem surprised to see Ms. Yang again. (I came along, and Mr. Sevilla explained who I was and that I was writing about syphilis and the people affected by it. Angelica signed a release for me to report about her case, and she said she had no problem with me writing about her or even using her full name. ProPublica chose to only print her first name.)
“How are you doing? How’s the baby?”
“Bien.”
“So the last time we talked, we were going to have you go to United Healthcare Center to get treatment. Have you gone since?”
Angelica shook her head.
“We brought some gift cards...” Mr. Sevilla started in Spanish. The department uses them as incentives for completing injections. But Angelica was already shaking her head. The nearest Walmart was the next town over.
Ms. Yang turned to her partner. “Tell her: So the reason why we’re coming out here again is because we really need her to go in for treatment. ... We really are concerned for the baby’s health especially since she’s had the infection for quite a while.”
Angelica listened while Mr. Sevilla interpreted, her eyes on the ground. Then she looked up. “Orita?” she asked. Right now?
“I’ll walk with you,” Ms. Yang offered. Angelica shook her head. “She said she wants to shower first before she goes over there,” Mr. Sevilla said.
Ms. Yang made a face. “She said that to me last time.” Ms. Yang offered to wait, but Angelica didn’t want the health officers to linger by the house. She said she would meet them by the clinic in 15 minutes.
Ms. Yang was reluctant to let her go but again had no other option. She and Mr. Sevilla drove to the clinic, then stood on the corner of the parking lot, staring down the road.
Talk to the pediatricians, obstetricians, and families on the front lines of the congenital syphilis surge and it becomes clear why Ms. Yang and others are trying so desperately to prevent cases. Dr. J. B. Cantey, associate professor in pediatrics at UT Health San Antonio, remembers a baby girl born at 25 weeks gestation who weighed a pound and a half. Syphilis had spread through her bones and lungs. She spent five months in the neonatal intensive care unit, breathing through a ventilator, and was still eating through a tube when she was discharged.
Then, there are the miscarriages, the stillbirths and the inconsolable parents. Dr. Irene Stafford, an associate professor and maternal-fetal medicine specialist at UT Health in Houston, cannot forget a patient who came in at 36 weeks for a routine checkup, pregnant with her first child. Dr. Stafford realized that there was no heartbeat. “She could see on my face that something was really wrong,” Dr. Stafford recalled. She had to let the patient know that syphilis had killed her baby. “She was hysterical, just bawling,” Dr. Stafford said. “I’ve seen people’s families ripped apart and I’ve seen beautiful babies die.” Fewer than 10% of patients who experience a stillbirth are tested for syphilis, suggesting that cases are underdiagnosed.
A Texas grandmother named Solidad Odunuga offers a glimpse into what the future could hold for Angelica’s mother, who may wind up raising her baby.
In February of last year, Ms. Odunuga got a call from the Lyndon B. Johnson Hospital in Houston. A nurse told her that her daughter was about to give birth and that child protective services had been called. Ms. Odunuga had lost contact with her daughter, who struggled with homelessness and substance abuse. She arrived in time to see her grandson delivered, premature at 30 weeks old, weighing 2.7 pounds. He tested positive for syphilis.
When a child protective worker asked Ms. Odunuga to take custody of the infant, she felt a wave of dread. “I was in denial,” she recalled. “I did not plan to be a mom again.” The baby’s medical problems were daunting: “Global developmental delays ... concerns for visual impairments ... high risk of cerebral palsy,” read a note from the doctor at the time.
Still, Ms. Odunuga visited her grandson every day for three months, driving to the NICU from her job at the University of Houston. “I’d put him in my shirt to keep him warm and hold him there.” She fell in love. She named him Emmanuel.
Once Emmanuel was discharged, Ms. Odunuga realized she had no choice but to quit her job. While Medicaid covered the costs of Emmanuel’s treatment, it was on her to care for him. From infancy, Emmanuel’s life has been a whirlwind of constant therapy. Today, at 20 months old, Odunuga brings him to physical, occupational, speech, and developmental therapy, each a different appointment on a different day of the week.
Emmanuel has thrived beyond what his doctors predicted, toddling so fast that Ms. Odunuga can’t look away for a minute and beaming as he waves his favorite toy phone. Yet he still suffers from gagging issues, which means Ms. Odunuga can’t feed him any solid foods. Liquid gets into his lungs when he aspirates; it has led to pneumonia three times. Emmanuel has a special stroller that helps keep his head in a position that won’t aggravate his persistent reflux, but Odunuga said she still has to pull over on the side of the road sometimes when she hears him projectile vomiting from the backseat.
The days are endless. Once she puts Emmanuel to bed, Ms. Odunuga starts planning the next day’s appointments. “I’ve had to cry alone, scream out alone,” she said. “Sometimes I wake up and think, Is this real? And then I hear him in the next room.”
Putting aside the challenge of eliminating syphilis entirely, everyone agrees it’s both doable and necessary to prevent newborn cases. “There was a crisis in perinatal HIV almost 30 years ago and people stood up and said this is not OK — it’s not acceptable for babies to be born in that condition. ... [We] brought it down from 1,700 babies born each year with perinatal HIV to less than 40 per year today,” said Virginia Bowen, an epidemiologist at the CDC. “Now here we are with a slightly different condition. We can also stand up and say, ‘This is not acceptable.’” Belarus, Bermuda, Cuba, Malaysia, Thailand, and Sri Lanka are among countries recognized by the World Health Organization for eliminating congenital syphilis.
Success starts with filling gaps across the health care system.
For almost a century, public health experts have advocated for testing pregnant patients more than once for syphilis in order to catch the infection. But policies nationwide still don’t reflect this best practice. Six states have no prenatal screening requirement at all. Even in states that require three tests, public health officials say that many physicians aren’t aware of the requirements. Dr. Stafford, the maternal-fetal medicine specialist in Houston, says she’s tired of hearing her own peers in medicine tell her, “Oh, syphilis is a problem?”
It costs public health departments less than 25 cents a dose to buy penicillin, but for a private practice, it’s more than $1,000, according to Dr. Park of the University of California San Francisco. “There’s no incentive for a private physician to stock a dose that could expire before it’s used, so they often don’t have it. So a woman comes in, they say, ‘We’ll send you to the emergency department or health department to get it,’ then [the patients] don’t show up.”
A vaccine would be invaluable for preventing spread among people at high risk for reinfection. But there is none. Scientists only recently figured out how to grow the bacteria in the lab, prompting grants from the National Institutes of Health to fund research into a vaccine. Dr. Justin Radolf, a researcher at the University of Connecticut School of Medicine, said he hopes his team will have a vaccine candidate by the end of its five-year grant. But it’ll likely take years more to find a manufacturer and run human trials.
Public health agencies also need to recognize that many of the hurdles to getting pregnant people treated involve access to care, economic stability, safe housing and transportation. In Fresno, Ms. Adams has been working on ways her department can collaborate with mental health services. Recently, one of her disease intervention specialists managed to get a pregnant woman treated with penicillin shots and, at the patient’s request, connected her with an addiction treatment center.
Gaining a patient’s cooperation means seeing them as complex humans instead of just a case to solve. “There may be past traumas with the health care system,” said Cynthia Deverson, project manager of the Houston Fetal Infant Morbidity Review. “There’s the fear of being discovered if she’s doing something illegal to survive. ... She may need to be in a certain place at a certain time so she can get something to eat, or maybe it’s the only time of the day that’s safe for her to sleep. They’re not going to tell you that. Yes, they understand there’s a problem, but it’s not an immediate threat, maybe they don’t feel bad yet, so obviously this is not urgent. ...
“What helps to gain trust is consistency,” she said. “Literally, it’s seeing that [disease specialist] constantly, daily. ... The woman can see that you’re not going to harm her, you’re saying, ‘I’m here at this time if you need me.’”
Ms. Yang stood outside the clinic, waiting for Angelica to show up, baking in the 90-degree heat. Her feelings ranged from irritation — Why didn’t she just go? I’d have more energy for other cases — to an appreciation for the parts of Angelica’s story that she didn’t know — She’s in survival mode. I need to be more patient.
Fifteen minutes ticked by, then 20.
“OK,” Ms. Yang announced. “We’re going back.”
She asked Sevilla if he would be OK if they drove Angelica to the clinic; they technically weren’t supposed to because of coronavirus precautions, but Ms. Yang wasn’t sure she could convince Angelica to walk. Mr. Sevilla gave her the thumbs up.
When they pulled up, they saw Angelica sitting in the backyard, chatting with a friend. She now wore a fresh T-shirt and had shoes on her feet. Angelica sat silently in the back seat as Ms. Yang drove to the clinic. A few minutes later, they pulled up to the parking lot.
Finally, Ms. Yang thought. We got her here.
The clinic was packed with people waiting for COVID-19 tests and vaccinations. A worker there had previously told Ms. Yang that a walk-in would be fine, but a receptionist now said they were too busy to treat Angelica. She would have to return.
Ms. Yang felt a surge of frustration, sensing that her hard-fought opportunity was slipping away. She tried to talk to the nurse supervisor, but he wasn’t available. She tried to leave the gift cards at the office to reward Angelica if she came, but the receptionist said she couldn’t hold them. While Ms. Yang negotiated, Mr. Sevilla sat with Angelica in the car, waiting.
Finally, Ms. Yang accepted this was yet another thing she couldn’t control.
She drove Angelica back to the yellow house. As they arrived, she tried once more to impress on her just how important it was to get treated, asking Mr. Sevilla to interpret. “We don’t want it to get any more serious, because she can go blind, she could go deaf, she could lose her baby.”
Angelica already had the door halfway open.
“So on a scale from one to 10, how important is this to get treated?” Ms. Yang asked.
“Ten,” Angelica said. Ms. Yang reminded her of the appointment that afternoon. Then Angelica stepped out and returned to the dusty yard.
Ms. Yang lingered for a moment, watching Angelica go. Then she turned the car back onto the highway and set off toward Fresno, knowing, already, that she’d be back.
Postscript: A reporter visited Huron twice more in the months that followed, including once independently to try to interview Angelica, but she wasn’t in town. Ms. Yang has visited Huron twice more as well — six times in total thus far. In October, a couple of men at the yellow house said Angelica was still in town, still pregnant. Ms. Yang and Mr. Sevilla spent an hour driving around, talking to residents, hoping to catch Angelica. But she was nowhere to be found.
ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive their biggest stories as soon as they’re published.
Q&A: Meeting the challenge of giving COVID vaccines to younger kids
This news organization spoke to several pediatric experts to get answers.
More than 6 million children and adolescents (up to age 18 years) in the United States have been infected with SARS-CoV-2. Children represent about 17% of all cases, and an estimated 0.1%-2% of infected children end up hospitalized, according to Oct. 28 data from the American Academy of Pediatrics.
Physicians and other health care practitioners are gearing up for what could be an influx of patients. “Pediatricians are standing by to talk with families about the vaccine and to administer the vaccine to children as soon as possible,” Lee Savio Beers, MD, FAAP, president of the AAP, said in a statement.
In this Q&A, this news organization asked for additional advice from Sara “Sally” Goza, MD, a pediatrician in Fayetteville, Georgia, and immediate past president of the AAP; Peter Hotez, MD, PhD, dean of the National School of Tropical Medicine at Baylor College of Medicine and codirector of the Texas Children’s Hospital Center for Vaccine Development, both in Houston; and Danielle M. Zerr, MD, professor and chief of the division of pediatric infectious disease at the University of Washington, Seattle, and medical director of infection prevention at Seattle Children’s Hospital.
Q: How are smaller pediatric practices and solo practitioners going to handle the additional vaccinations?
Dr. Goza: It’s a scheduling challenge with this rollout and all the people who want it and want it right now. They’re going to want it this week.
I’ve actually had some children asking their moms: “When can I get it? When can I get it?” It’s been very interesting – they are chomping at the bit.
If I give the vaccine to a patient this week, in 3 weeks the second dose will be right around Thanksgiving. No one in my office is going to want to be here to give the shot on Thanksgiving, and no patient is going to want to come in on Thanksgiving weekend. So I’m trying to delay those parents – saying, let’s do it next week. That way we’re not messing up a holiday.
Children are going to need two doses, and they won’t be fully protected until 2 weeks after their second dose. So they won’t get full protection for Thanksgiving, but they will have full protection for Christmas.
I know there are a lot of pediatricians who have preordered the vaccine. I know in our office they sent us an email ... to let us know our vaccines are being shipped. So I think a lot of pediatricians are going to have the vaccine.
Q: How should pediatricians counsel parents who are fearful or hesitant?
Dr. Hotez: It’s important to emphasize the severity of the 2021 summer Delta epidemic in children. We need to get beyond this false narrative that COVID only produces a mild disease in children. It’s caused thousands of pediatric hospitalizations, not to mention long COVID.
Dr. Zerr: It is key to find out what concerns parents have and then focus on answering their specific questions. It is helpful to emphasize the safety and efficacy of the vaccine and to explain the rigorous processes that the vaccine went through to receive Food and Drug Administration approval.
Q: How should pediatricians counter any misinformation/disinformation out there about the COVID-19 vaccines?
Dr. Goza: The most important thing is not to discount what they are saying. Don’t say: “That’s crazy” or “That’s not true.” Don’t roll your eyes and say: “Really, you’re going to believe all that?”
Instead, have a conversation with them about why we think that is not true, or why we know that’s not true. We really have to have that relationship and ask: “Well, what are your concerns?” And then really counter (any misinformation) with facts, with science, and based on your experience.
Q: Do the data presented to the FDA and the CDC about the safety and effectiveness of the COVID-19 vaccine for 5- to 11-year-olds seem robust to you?
Dr. Zerr: Yes, and data collection will be ongoing.
Dr. Hotez: I’ve only seen what’s publicly available so far, and it seems to support moving forward with emergency use authorization. The only shortfall is the size, roughly 2,200 children, which would not be of sufficient size to detect a rare safety signal.
Q: Do previous controversies around pediatric vaccines (for example, the MMR vaccine and autism) give pediatricians some background and experience so they can address any pushback on the COVID-19 vaccines?
Dr. Goza: Pediatricians have been dealing with vaccine hesitancy for a while now, ever since the MMR and autism controversy started. Even before then, there were certain groups of people who didn’t want vaccines.
We’ve really worked hard at helping teach pediatricians how to deal with the misinformation, how to counter it, and how to help parents understand the vaccines are safe and effective – and that they save lives.
That (experience) will help us in some ways. Unfortunately, there is more misinformation out there – there is almost a concerted effort on misinformation. It’s big.
Pediatricians will do everything we can, but we need help countering it. We need the misinformation to quit getting spread on social media. We can talk one on one with patients and families, but if all they are hearing on social media is the misinformation, it’s really hard.
Q: Are pediatricians, especially solo practitioners or pediatricians at smaller practices, going to face challenges with multidose vials and not wasting vaccine product?
Dr. Goza: I’m at a small practice. We have 3.5 FTEs (full-time equivalents) of MDs and three FTEs of nurse practitioners. So we’re not that big – about six providers.
You know, it is a challenge. We’re not going to buy the super-duper freezer, and we’re not going to be able to store these vaccines for a long period of time.
So when we order, we need smaller amounts. For the 12- to 18-year-olds, [maximum storage] was 45 days. Now for the 5- to 11-year-olds, we’re going to be able to store the vaccine in the refrigerator for 10 weeks, which gives us more leeway there.
We try to do all of vaccinations on 1 day, so we know how many people are coming in, and we are not going to waste too many doses.
Our Department of Public Health in Georgia has said: “We want these vaccines in the arms of kids, and if you have to waste some doses, don’t worry about it.” But it’s a 10-dose vial. It’s going to be hard for me to open it up for one child. I just don’t like wasting anything like this.
Our main goal is to get this vaccine in to the arms of children whose parents want it.
Q: What are some additional sources of information for pediatricians?
Dr. Zerr: There are a lot of great resources on vaccine hesitancy from reputable sources, including these from the CDC and from the National Academies of Sciences, Engineering, and Medicine:
- Building Confidence With OVID-19 Vaccines
- How to Talk With Parents About COVID-19 Vaccination
- Strategies for Building Confidence in the COVID-19 Vaccines
- Communication Strategies for Building Confidence in COVID-19 Vaccines: Addressing Variants and Childhood Vaccinations
A version of this article first appeared on Medscape.com.
This news organization spoke to several pediatric experts to get answers.
More than 6 million children and adolescents (up to age 18 years) in the United States have been infected with SARS-CoV-2. Children represent about 17% of all cases, and an estimated 0.1%-2% of infected children end up hospitalized, according to Oct. 28 data from the American Academy of Pediatrics.
Physicians and other health care practitioners are gearing up for what could be an influx of patients. “Pediatricians are standing by to talk with families about the vaccine and to administer the vaccine to children as soon as possible,” Lee Savio Beers, MD, FAAP, president of the AAP, said in a statement.
In this Q&A, this news organization asked for additional advice from Sara “Sally” Goza, MD, a pediatrician in Fayetteville, Georgia, and immediate past president of the AAP; Peter Hotez, MD, PhD, dean of the National School of Tropical Medicine at Baylor College of Medicine and codirector of the Texas Children’s Hospital Center for Vaccine Development, both in Houston; and Danielle M. Zerr, MD, professor and chief of the division of pediatric infectious disease at the University of Washington, Seattle, and medical director of infection prevention at Seattle Children’s Hospital.
Q: How are smaller pediatric practices and solo practitioners going to handle the additional vaccinations?
Dr. Goza: It’s a scheduling challenge with this rollout and all the people who want it and want it right now. They’re going to want it this week.
I’ve actually had some children asking their moms: “When can I get it? When can I get it?” It’s been very interesting – they are chomping at the bit.
If I give the vaccine to a patient this week, in 3 weeks the second dose will be right around Thanksgiving. No one in my office is going to want to be here to give the shot on Thanksgiving, and no patient is going to want to come in on Thanksgiving weekend. So I’m trying to delay those parents – saying, let’s do it next week. That way we’re not messing up a holiday.
Children are going to need two doses, and they won’t be fully protected until 2 weeks after their second dose. So they won’t get full protection for Thanksgiving, but they will have full protection for Christmas.
I know there are a lot of pediatricians who have preordered the vaccine. I know in our office they sent us an email ... to let us know our vaccines are being shipped. So I think a lot of pediatricians are going to have the vaccine.
Q: How should pediatricians counsel parents who are fearful or hesitant?
Dr. Hotez: It’s important to emphasize the severity of the 2021 summer Delta epidemic in children. We need to get beyond this false narrative that COVID only produces a mild disease in children. It’s caused thousands of pediatric hospitalizations, not to mention long COVID.
Dr. Zerr: It is key to find out what concerns parents have and then focus on answering their specific questions. It is helpful to emphasize the safety and efficacy of the vaccine and to explain the rigorous processes that the vaccine went through to receive Food and Drug Administration approval.
Q: How should pediatricians counter any misinformation/disinformation out there about the COVID-19 vaccines?
Dr. Goza: The most important thing is not to discount what they are saying. Don’t say: “That’s crazy” or “That’s not true.” Don’t roll your eyes and say: “Really, you’re going to believe all that?”
Instead, have a conversation with them about why we think that is not true, or why we know that’s not true. We really have to have that relationship and ask: “Well, what are your concerns?” And then really counter (any misinformation) with facts, with science, and based on your experience.
Q: Do the data presented to the FDA and the CDC about the safety and effectiveness of the COVID-19 vaccine for 5- to 11-year-olds seem robust to you?
Dr. Zerr: Yes, and data collection will be ongoing.
Dr. Hotez: I’ve only seen what’s publicly available so far, and it seems to support moving forward with emergency use authorization. The only shortfall is the size, roughly 2,200 children, which would not be of sufficient size to detect a rare safety signal.
Q: Do previous controversies around pediatric vaccines (for example, the MMR vaccine and autism) give pediatricians some background and experience so they can address any pushback on the COVID-19 vaccines?
Dr. Goza: Pediatricians have been dealing with vaccine hesitancy for a while now, ever since the MMR and autism controversy started. Even before then, there were certain groups of people who didn’t want vaccines.
We’ve really worked hard at helping teach pediatricians how to deal with the misinformation, how to counter it, and how to help parents understand the vaccines are safe and effective – and that they save lives.
That (experience) will help us in some ways. Unfortunately, there is more misinformation out there – there is almost a concerted effort on misinformation. It’s big.
Pediatricians will do everything we can, but we need help countering it. We need the misinformation to quit getting spread on social media. We can talk one on one with patients and families, but if all they are hearing on social media is the misinformation, it’s really hard.
Q: Are pediatricians, especially solo practitioners or pediatricians at smaller practices, going to face challenges with multidose vials and not wasting vaccine product?
Dr. Goza: I’m at a small practice. We have 3.5 FTEs (full-time equivalents) of MDs and three FTEs of nurse practitioners. So we’re not that big – about six providers.
You know, it is a challenge. We’re not going to buy the super-duper freezer, and we’re not going to be able to store these vaccines for a long period of time.
So when we order, we need smaller amounts. For the 12- to 18-year-olds, [maximum storage] was 45 days. Now for the 5- to 11-year-olds, we’re going to be able to store the vaccine in the refrigerator for 10 weeks, which gives us more leeway there.
We try to do all of vaccinations on 1 day, so we know how many people are coming in, and we are not going to waste too many doses.
Our Department of Public Health in Georgia has said: “We want these vaccines in the arms of kids, and if you have to waste some doses, don’t worry about it.” But it’s a 10-dose vial. It’s going to be hard for me to open it up for one child. I just don’t like wasting anything like this.
Our main goal is to get this vaccine in to the arms of children whose parents want it.
Q: What are some additional sources of information for pediatricians?
Dr. Zerr: There are a lot of great resources on vaccine hesitancy from reputable sources, including these from the CDC and from the National Academies of Sciences, Engineering, and Medicine:
- Building Confidence With OVID-19 Vaccines
- How to Talk With Parents About COVID-19 Vaccination
- Strategies for Building Confidence in the COVID-19 Vaccines
- Communication Strategies for Building Confidence in COVID-19 Vaccines: Addressing Variants and Childhood Vaccinations
A version of this article first appeared on Medscape.com.
This news organization spoke to several pediatric experts to get answers.
More than 6 million children and adolescents (up to age 18 years) in the United States have been infected with SARS-CoV-2. Children represent about 17% of all cases, and an estimated 0.1%-2% of infected children end up hospitalized, according to Oct. 28 data from the American Academy of Pediatrics.
Physicians and other health care practitioners are gearing up for what could be an influx of patients. “Pediatricians are standing by to talk with families about the vaccine and to administer the vaccine to children as soon as possible,” Lee Savio Beers, MD, FAAP, president of the AAP, said in a statement.
In this Q&A, this news organization asked for additional advice from Sara “Sally” Goza, MD, a pediatrician in Fayetteville, Georgia, and immediate past president of the AAP; Peter Hotez, MD, PhD, dean of the National School of Tropical Medicine at Baylor College of Medicine and codirector of the Texas Children’s Hospital Center for Vaccine Development, both in Houston; and Danielle M. Zerr, MD, professor and chief of the division of pediatric infectious disease at the University of Washington, Seattle, and medical director of infection prevention at Seattle Children’s Hospital.
Q: How are smaller pediatric practices and solo practitioners going to handle the additional vaccinations?
Dr. Goza: It’s a scheduling challenge with this rollout and all the people who want it and want it right now. They’re going to want it this week.
I’ve actually had some children asking their moms: “When can I get it? When can I get it?” It’s been very interesting – they are chomping at the bit.
If I give the vaccine to a patient this week, in 3 weeks the second dose will be right around Thanksgiving. No one in my office is going to want to be here to give the shot on Thanksgiving, and no patient is going to want to come in on Thanksgiving weekend. So I’m trying to delay those parents – saying, let’s do it next week. That way we’re not messing up a holiday.
Children are going to need two doses, and they won’t be fully protected until 2 weeks after their second dose. So they won’t get full protection for Thanksgiving, but they will have full protection for Christmas.
I know there are a lot of pediatricians who have preordered the vaccine. I know in our office they sent us an email ... to let us know our vaccines are being shipped. So I think a lot of pediatricians are going to have the vaccine.
Q: How should pediatricians counsel parents who are fearful or hesitant?
Dr. Hotez: It’s important to emphasize the severity of the 2021 summer Delta epidemic in children. We need to get beyond this false narrative that COVID only produces a mild disease in children. It’s caused thousands of pediatric hospitalizations, not to mention long COVID.
Dr. Zerr: It is key to find out what concerns parents have and then focus on answering their specific questions. It is helpful to emphasize the safety and efficacy of the vaccine and to explain the rigorous processes that the vaccine went through to receive Food and Drug Administration approval.
Q: How should pediatricians counter any misinformation/disinformation out there about the COVID-19 vaccines?
Dr. Goza: The most important thing is not to discount what they are saying. Don’t say: “That’s crazy” or “That’s not true.” Don’t roll your eyes and say: “Really, you’re going to believe all that?”
Instead, have a conversation with them about why we think that is not true, or why we know that’s not true. We really have to have that relationship and ask: “Well, what are your concerns?” And then really counter (any misinformation) with facts, with science, and based on your experience.
Q: Do the data presented to the FDA and the CDC about the safety and effectiveness of the COVID-19 vaccine for 5- to 11-year-olds seem robust to you?
Dr. Zerr: Yes, and data collection will be ongoing.
Dr. Hotez: I’ve only seen what’s publicly available so far, and it seems to support moving forward with emergency use authorization. The only shortfall is the size, roughly 2,200 children, which would not be of sufficient size to detect a rare safety signal.
Q: Do previous controversies around pediatric vaccines (for example, the MMR vaccine and autism) give pediatricians some background and experience so they can address any pushback on the COVID-19 vaccines?
Dr. Goza: Pediatricians have been dealing with vaccine hesitancy for a while now, ever since the MMR and autism controversy started. Even before then, there were certain groups of people who didn’t want vaccines.
We’ve really worked hard at helping teach pediatricians how to deal with the misinformation, how to counter it, and how to help parents understand the vaccines are safe and effective – and that they save lives.
That (experience) will help us in some ways. Unfortunately, there is more misinformation out there – there is almost a concerted effort on misinformation. It’s big.
Pediatricians will do everything we can, but we need help countering it. We need the misinformation to quit getting spread on social media. We can talk one on one with patients and families, but if all they are hearing on social media is the misinformation, it’s really hard.
Q: Are pediatricians, especially solo practitioners or pediatricians at smaller practices, going to face challenges with multidose vials and not wasting vaccine product?
Dr. Goza: I’m at a small practice. We have 3.5 FTEs (full-time equivalents) of MDs and three FTEs of nurse practitioners. So we’re not that big – about six providers.
You know, it is a challenge. We’re not going to buy the super-duper freezer, and we’re not going to be able to store these vaccines for a long period of time.
So when we order, we need smaller amounts. For the 12- to 18-year-olds, [maximum storage] was 45 days. Now for the 5- to 11-year-olds, we’re going to be able to store the vaccine in the refrigerator for 10 weeks, which gives us more leeway there.
We try to do all of vaccinations on 1 day, so we know how many people are coming in, and we are not going to waste too many doses.
Our Department of Public Health in Georgia has said: “We want these vaccines in the arms of kids, and if you have to waste some doses, don’t worry about it.” But it’s a 10-dose vial. It’s going to be hard for me to open it up for one child. I just don’t like wasting anything like this.
Our main goal is to get this vaccine in to the arms of children whose parents want it.
Q: What are some additional sources of information for pediatricians?
Dr. Zerr: There are a lot of great resources on vaccine hesitancy from reputable sources, including these from the CDC and from the National Academies of Sciences, Engineering, and Medicine:
- Building Confidence With OVID-19 Vaccines
- How to Talk With Parents About COVID-19 Vaccination
- Strategies for Building Confidence in the COVID-19 Vaccines
- Communication Strategies for Building Confidence in COVID-19 Vaccines: Addressing Variants and Childhood Vaccinations
A version of this article first appeared on Medscape.com.
Can adjunct corticosteroids help in childrens’ eye and throat infections?
Adding anti-inflammatory corticosteroids to antibiotics for certain pediatric throat and ocular infections may have some benefit, according to results from two recent database studies, but their benefit remains unclear.
Using steroids in this setting is a practice many pediatricians consider, although no clear guidance exists.
Drawing on data from a registry of 51 free-standing children’s hospitals in the Pediatric Health Information System (PHIS), and published online in Pediatrics, the analyses looked, respectively, at retro- and parapharyngeal abscesses (RPAs/PPAs) and acute orbital cellulitis.
Throat abscesses
In the first study, pediatrician Pratichi K. Goenka, MD, of Cohen Children’s Medical Center–Northwell Health and an assistant professor at Hofstra University, both in New Hyde Park, N.Y., and colleagues reported on the effect of systemic corticosteroids on several outcomes in RPAs/PPAs in 2,259 well-matched patients. The patients, aged 2 months to 8 years, were treated at 46 hospitals during the period from January 2016 to December 2019.
The data revealed that the 582 (25.8%) who received steroids had a significantly lower rate of surgical drainage, the study’s primary endpoint (odds ratio, 0.28; 95% confidence interval, 0.22-0.36). There was no difference, however, in length of hospital stay (rate ratio, 0.97; 95% CI, 0.92-1.02).
Those in the steroid group also had lower overall hospital costs and were less likely to be given opioid medications for pain. They were, however, more likely to undergo repeat CT imaging and also had a higher 7-day ED revisit rate but no increase in readmission 30 days after discharge: 4% versus 3% in the nonsteroid group (P = .29).
“As hospitalists, we share the care of young children with RPAs and PPAs with our otolaryngology colleagues. The primary therapy is antibiotics but there was no clear guidance on the next step, and the current literature had no answers as to how systemic corticosteroids might impact the care of these children,” Dr. Goenka said in an interview. “So we wanted to leverage the PHIS data to better understand the association with the need for surgery and length of stay. Surgery is painful and often involves IV administration of opioid painkillers. It’s something we may be able to avoid if we can optimize medical treatment.”
Pending results from randomized trials, what immediate impact could these registry findings have? “We hope that physicians will think about the best initial medical treatment plan for these children,” Dr. Goenka said. ”Given these data, I would be more likely to incorporate steroids early on in medical treatment.”
She emphasized, however, that before routine adoption prospective studies are needed to clearly identify which patients will have a strong benefit and which will not benefit. “That is the nuanced discussion that will happen with more prospective work.”
Dr. Goenka and associates explained that the rising incidence of RPAs and PPAs over the past 20 years has been attributed to more cases of tonsillitis because of a shift away from tonsillectomies, as well as the changing epidemiology of methicillin-resistant Staphylococcus aureus.
In an accompanying editorial, Ellen R. Wald, MD, and Jens C. Eickhoff, PhD, of the University of Wisconsin–Madison, stated that the use of corticosteroids in bacterial meningitis is often cited as an example of the benefits of steroids in infection. “The specific rationale for use of corticosteroids is [their] anti-inflammatory effects, which may result in decreases of swelling and/ or edema to facilitate drainage, perfusion, reduction in pain, and healing.”
They cautioned, however, that the pharmacologic effects of steroids are myriad and complicated, and include potential masking of the clinical course of disease, thereby delaying appropriate therapy for unrecognized deterioration, as well potential immunosuppression.
Acute orbital cellulitis
In the second retrospective analysis, a group led by pediatrician Maria Anna Leszczynska, MD, of Johns Hopkins All Children’s Hospital in Baltimore, analyzed a retrospective PHIS cohort of 5,645 children younger than 18 years with a primary diagnosis of orbital cellulitis treated at 51 hospitals from January 2007 to December 2018.
Of these, 1,347 (24%) received steroids, but, contrary to earlier reports, the data showed no reduction in length of stay associated with these drugs after adjustment for age, meningitis, abscess, or vision issues (ebeta, 1.01; 95% CI, 0.97-1.06). Corticosteroid exposure was, however, associated with operative episodes after 2 days’ hospitalization (OR, 2.05; 95% CI, 1.29-3.27) and 30-day readmission (OR, 2.40; 95% CI, 1.52-3.78).
“Among children hospitalized for orbital cellulitis, we did not observe the reduction in LOS [length of stay] for patients prescribed systemic corticosteroids as described previously in the literature,” the authors wrote.
In terms of surgical procedures, 52.0% of corticosteroid recipients versus 14.0% of nonrecipients underwent surgery (P < .001), and more were hospitalized in the pediatric ICU (4.4% vs 2.6%; P < .001).
According to the editorialists: “Both observations suggest that children who received steroids may have been a sicker group of patients.”
Dr. Wald and Dr. Eickhoff pointed out that the effect of steroids is ultimately unclear because of the retrospective study’s inherent potential for bias because of unobserved confounders. Were steroids prescribed more often when children were perceived to be sicker with more severe disease, or did these medications cause worse outcomes?
The authors agreed that the study could not determine causality. “Although we used all available markers of disease severity, there does not exist a validated disease severity clinical score for pediatric orbital cellulitis,” they wrote.
According to Ricardo A. Quinonez, MD, an associate professor of pediatrics and division and service chief of pediatric hospital medicine at Baylor College of Medicine and Texas Children’s Hospital, both in Houston, “orbital cellulitis is a not very common thing in children so we don’t treat many patients with this. But having said that, there is usually some debate among providers about whether to use steroids.”
Some centers use them routinely for central nervous system and eye infections or extensions of sinusitis, he said, but there is variability in the prescribing of corticosteroids. “There’s ongoing discussion as to whether they‘re as helpful in orbital cellulitis as they are in similar conditions,” Dr. Quinonez said in an interview. “At our institution we don’t typically prescribe them – not never but not routinely. Children who are sicker tend to get steroids, as they do in other conditions.”
In the context of PPA as in the first study, he added, “I think the evidence favoring the use of steroids in infections that affect the airway is stronger, and their use is definitely more prevalent in those instances.”
While both PHIS analyses suggested some benefit from steroids, he continued, some children may not benefit and there may be harms. “The evidence is still mostly retrospective and observational with no multicenter randomized controlled data. Without those data the evidence is difficult to interpret and subject to all the biases that observational and retrospective data is subject to and the current evidence should not lead physicians to change their practice until controlled, randomized evidence is available.”
The editorialists concurred with the study authors and Dr. Quinonez that large, controlled, prospective clinical trials are needed to ascertain the effect of steroids and to standardize the approach to diagnosis and management. “Use of administrative databases are not optimal to answer questions related to outcome,” they wrote.
The study by Dr. Goenka and associates received no external funding; the study by Dr. Leszczynska and associates also received no external funding. None of the authors declared potential competing interests. Dr. Quinonez had no competing interests to declare. Dr. Wald and Dr. Eickhoff disclosed no competing interests with regard to their editorial.
Adding anti-inflammatory corticosteroids to antibiotics for certain pediatric throat and ocular infections may have some benefit, according to results from two recent database studies, but their benefit remains unclear.
Using steroids in this setting is a practice many pediatricians consider, although no clear guidance exists.
Drawing on data from a registry of 51 free-standing children’s hospitals in the Pediatric Health Information System (PHIS), and published online in Pediatrics, the analyses looked, respectively, at retro- and parapharyngeal abscesses (RPAs/PPAs) and acute orbital cellulitis.
Throat abscesses
In the first study, pediatrician Pratichi K. Goenka, MD, of Cohen Children’s Medical Center–Northwell Health and an assistant professor at Hofstra University, both in New Hyde Park, N.Y., and colleagues reported on the effect of systemic corticosteroids on several outcomes in RPAs/PPAs in 2,259 well-matched patients. The patients, aged 2 months to 8 years, were treated at 46 hospitals during the period from January 2016 to December 2019.
The data revealed that the 582 (25.8%) who received steroids had a significantly lower rate of surgical drainage, the study’s primary endpoint (odds ratio, 0.28; 95% confidence interval, 0.22-0.36). There was no difference, however, in length of hospital stay (rate ratio, 0.97; 95% CI, 0.92-1.02).
Those in the steroid group also had lower overall hospital costs and were less likely to be given opioid medications for pain. They were, however, more likely to undergo repeat CT imaging and also had a higher 7-day ED revisit rate but no increase in readmission 30 days after discharge: 4% versus 3% in the nonsteroid group (P = .29).
“As hospitalists, we share the care of young children with RPAs and PPAs with our otolaryngology colleagues. The primary therapy is antibiotics but there was no clear guidance on the next step, and the current literature had no answers as to how systemic corticosteroids might impact the care of these children,” Dr. Goenka said in an interview. “So we wanted to leverage the PHIS data to better understand the association with the need for surgery and length of stay. Surgery is painful and often involves IV administration of opioid painkillers. It’s something we may be able to avoid if we can optimize medical treatment.”
Pending results from randomized trials, what immediate impact could these registry findings have? “We hope that physicians will think about the best initial medical treatment plan for these children,” Dr. Goenka said. ”Given these data, I would be more likely to incorporate steroids early on in medical treatment.”
She emphasized, however, that before routine adoption prospective studies are needed to clearly identify which patients will have a strong benefit and which will not benefit. “That is the nuanced discussion that will happen with more prospective work.”
Dr. Goenka and associates explained that the rising incidence of RPAs and PPAs over the past 20 years has been attributed to more cases of tonsillitis because of a shift away from tonsillectomies, as well as the changing epidemiology of methicillin-resistant Staphylococcus aureus.
In an accompanying editorial, Ellen R. Wald, MD, and Jens C. Eickhoff, PhD, of the University of Wisconsin–Madison, stated that the use of corticosteroids in bacterial meningitis is often cited as an example of the benefits of steroids in infection. “The specific rationale for use of corticosteroids is [their] anti-inflammatory effects, which may result in decreases of swelling and/ or edema to facilitate drainage, perfusion, reduction in pain, and healing.”
They cautioned, however, that the pharmacologic effects of steroids are myriad and complicated, and include potential masking of the clinical course of disease, thereby delaying appropriate therapy for unrecognized deterioration, as well potential immunosuppression.
Acute orbital cellulitis
In the second retrospective analysis, a group led by pediatrician Maria Anna Leszczynska, MD, of Johns Hopkins All Children’s Hospital in Baltimore, analyzed a retrospective PHIS cohort of 5,645 children younger than 18 years with a primary diagnosis of orbital cellulitis treated at 51 hospitals from January 2007 to December 2018.
Of these, 1,347 (24%) received steroids, but, contrary to earlier reports, the data showed no reduction in length of stay associated with these drugs after adjustment for age, meningitis, abscess, or vision issues (ebeta, 1.01; 95% CI, 0.97-1.06). Corticosteroid exposure was, however, associated with operative episodes after 2 days’ hospitalization (OR, 2.05; 95% CI, 1.29-3.27) and 30-day readmission (OR, 2.40; 95% CI, 1.52-3.78).
“Among children hospitalized for orbital cellulitis, we did not observe the reduction in LOS [length of stay] for patients prescribed systemic corticosteroids as described previously in the literature,” the authors wrote.
In terms of surgical procedures, 52.0% of corticosteroid recipients versus 14.0% of nonrecipients underwent surgery (P < .001), and more were hospitalized in the pediatric ICU (4.4% vs 2.6%; P < .001).
According to the editorialists: “Both observations suggest that children who received steroids may have been a sicker group of patients.”
Dr. Wald and Dr. Eickhoff pointed out that the effect of steroids is ultimately unclear because of the retrospective study’s inherent potential for bias because of unobserved confounders. Were steroids prescribed more often when children were perceived to be sicker with more severe disease, or did these medications cause worse outcomes?
The authors agreed that the study could not determine causality. “Although we used all available markers of disease severity, there does not exist a validated disease severity clinical score for pediatric orbital cellulitis,” they wrote.
According to Ricardo A. Quinonez, MD, an associate professor of pediatrics and division and service chief of pediatric hospital medicine at Baylor College of Medicine and Texas Children’s Hospital, both in Houston, “orbital cellulitis is a not very common thing in children so we don’t treat many patients with this. But having said that, there is usually some debate among providers about whether to use steroids.”
Some centers use them routinely for central nervous system and eye infections or extensions of sinusitis, he said, but there is variability in the prescribing of corticosteroids. “There’s ongoing discussion as to whether they‘re as helpful in orbital cellulitis as they are in similar conditions,” Dr. Quinonez said in an interview. “At our institution we don’t typically prescribe them – not never but not routinely. Children who are sicker tend to get steroids, as they do in other conditions.”
In the context of PPA as in the first study, he added, “I think the evidence favoring the use of steroids in infections that affect the airway is stronger, and their use is definitely more prevalent in those instances.”
While both PHIS analyses suggested some benefit from steroids, he continued, some children may not benefit and there may be harms. “The evidence is still mostly retrospective and observational with no multicenter randomized controlled data. Without those data the evidence is difficult to interpret and subject to all the biases that observational and retrospective data is subject to and the current evidence should not lead physicians to change their practice until controlled, randomized evidence is available.”
The editorialists concurred with the study authors and Dr. Quinonez that large, controlled, prospective clinical trials are needed to ascertain the effect of steroids and to standardize the approach to diagnosis and management. “Use of administrative databases are not optimal to answer questions related to outcome,” they wrote.
The study by Dr. Goenka and associates received no external funding; the study by Dr. Leszczynska and associates also received no external funding. None of the authors declared potential competing interests. Dr. Quinonez had no competing interests to declare. Dr. Wald and Dr. Eickhoff disclosed no competing interests with regard to their editorial.
Adding anti-inflammatory corticosteroids to antibiotics for certain pediatric throat and ocular infections may have some benefit, according to results from two recent database studies, but their benefit remains unclear.
Using steroids in this setting is a practice many pediatricians consider, although no clear guidance exists.
Drawing on data from a registry of 51 free-standing children’s hospitals in the Pediatric Health Information System (PHIS), and published online in Pediatrics, the analyses looked, respectively, at retro- and parapharyngeal abscesses (RPAs/PPAs) and acute orbital cellulitis.
Throat abscesses
In the first study, pediatrician Pratichi K. Goenka, MD, of Cohen Children’s Medical Center–Northwell Health and an assistant professor at Hofstra University, both in New Hyde Park, N.Y., and colleagues reported on the effect of systemic corticosteroids on several outcomes in RPAs/PPAs in 2,259 well-matched patients. The patients, aged 2 months to 8 years, were treated at 46 hospitals during the period from January 2016 to December 2019.
The data revealed that the 582 (25.8%) who received steroids had a significantly lower rate of surgical drainage, the study’s primary endpoint (odds ratio, 0.28; 95% confidence interval, 0.22-0.36). There was no difference, however, in length of hospital stay (rate ratio, 0.97; 95% CI, 0.92-1.02).
Those in the steroid group also had lower overall hospital costs and were less likely to be given opioid medications for pain. They were, however, more likely to undergo repeat CT imaging and also had a higher 7-day ED revisit rate but no increase in readmission 30 days after discharge: 4% versus 3% in the nonsteroid group (P = .29).
“As hospitalists, we share the care of young children with RPAs and PPAs with our otolaryngology colleagues. The primary therapy is antibiotics but there was no clear guidance on the next step, and the current literature had no answers as to how systemic corticosteroids might impact the care of these children,” Dr. Goenka said in an interview. “So we wanted to leverage the PHIS data to better understand the association with the need for surgery and length of stay. Surgery is painful and often involves IV administration of opioid painkillers. It’s something we may be able to avoid if we can optimize medical treatment.”
Pending results from randomized trials, what immediate impact could these registry findings have? “We hope that physicians will think about the best initial medical treatment plan for these children,” Dr. Goenka said. ”Given these data, I would be more likely to incorporate steroids early on in medical treatment.”
She emphasized, however, that before routine adoption prospective studies are needed to clearly identify which patients will have a strong benefit and which will not benefit. “That is the nuanced discussion that will happen with more prospective work.”
Dr. Goenka and associates explained that the rising incidence of RPAs and PPAs over the past 20 years has been attributed to more cases of tonsillitis because of a shift away from tonsillectomies, as well as the changing epidemiology of methicillin-resistant Staphylococcus aureus.
In an accompanying editorial, Ellen R. Wald, MD, and Jens C. Eickhoff, PhD, of the University of Wisconsin–Madison, stated that the use of corticosteroids in bacterial meningitis is often cited as an example of the benefits of steroids in infection. “The specific rationale for use of corticosteroids is [their] anti-inflammatory effects, which may result in decreases of swelling and/ or edema to facilitate drainage, perfusion, reduction in pain, and healing.”
They cautioned, however, that the pharmacologic effects of steroids are myriad and complicated, and include potential masking of the clinical course of disease, thereby delaying appropriate therapy for unrecognized deterioration, as well potential immunosuppression.
Acute orbital cellulitis
In the second retrospective analysis, a group led by pediatrician Maria Anna Leszczynska, MD, of Johns Hopkins All Children’s Hospital in Baltimore, analyzed a retrospective PHIS cohort of 5,645 children younger than 18 years with a primary diagnosis of orbital cellulitis treated at 51 hospitals from January 2007 to December 2018.
Of these, 1,347 (24%) received steroids, but, contrary to earlier reports, the data showed no reduction in length of stay associated with these drugs after adjustment for age, meningitis, abscess, or vision issues (ebeta, 1.01; 95% CI, 0.97-1.06). Corticosteroid exposure was, however, associated with operative episodes after 2 days’ hospitalization (OR, 2.05; 95% CI, 1.29-3.27) and 30-day readmission (OR, 2.40; 95% CI, 1.52-3.78).
“Among children hospitalized for orbital cellulitis, we did not observe the reduction in LOS [length of stay] for patients prescribed systemic corticosteroids as described previously in the literature,” the authors wrote.
In terms of surgical procedures, 52.0% of corticosteroid recipients versus 14.0% of nonrecipients underwent surgery (P < .001), and more were hospitalized in the pediatric ICU (4.4% vs 2.6%; P < .001).
According to the editorialists: “Both observations suggest that children who received steroids may have been a sicker group of patients.”
Dr. Wald and Dr. Eickhoff pointed out that the effect of steroids is ultimately unclear because of the retrospective study’s inherent potential for bias because of unobserved confounders. Were steroids prescribed more often when children were perceived to be sicker with more severe disease, or did these medications cause worse outcomes?
The authors agreed that the study could not determine causality. “Although we used all available markers of disease severity, there does not exist a validated disease severity clinical score for pediatric orbital cellulitis,” they wrote.
According to Ricardo A. Quinonez, MD, an associate professor of pediatrics and division and service chief of pediatric hospital medicine at Baylor College of Medicine and Texas Children’s Hospital, both in Houston, “orbital cellulitis is a not very common thing in children so we don’t treat many patients with this. But having said that, there is usually some debate among providers about whether to use steroids.”
Some centers use them routinely for central nervous system and eye infections or extensions of sinusitis, he said, but there is variability in the prescribing of corticosteroids. “There’s ongoing discussion as to whether they‘re as helpful in orbital cellulitis as they are in similar conditions,” Dr. Quinonez said in an interview. “At our institution we don’t typically prescribe them – not never but not routinely. Children who are sicker tend to get steroids, as they do in other conditions.”
In the context of PPA as in the first study, he added, “I think the evidence favoring the use of steroids in infections that affect the airway is stronger, and their use is definitely more prevalent in those instances.”
While both PHIS analyses suggested some benefit from steroids, he continued, some children may not benefit and there may be harms. “The evidence is still mostly retrospective and observational with no multicenter randomized controlled data. Without those data the evidence is difficult to interpret and subject to all the biases that observational and retrospective data is subject to and the current evidence should not lead physicians to change their practice until controlled, randomized evidence is available.”
The editorialists concurred with the study authors and Dr. Quinonez that large, controlled, prospective clinical trials are needed to ascertain the effect of steroids and to standardize the approach to diagnosis and management. “Use of administrative databases are not optimal to answer questions related to outcome,” they wrote.
The study by Dr. Goenka and associates received no external funding; the study by Dr. Leszczynska and associates also received no external funding. None of the authors declared potential competing interests. Dr. Quinonez had no competing interests to declare. Dr. Wald and Dr. Eickhoff disclosed no competing interests with regard to their editorial.
FROM PEDIATRICS
Health care unaffordability common for pregnant/postpartum women
Financial hardship remains prevalent among pregnant and postpartum women, despite the implementation of the Affordable Care Act (ACA), according to new findings published in JAMA Network Open.
Nearly a quarter (24%) of pregnant and postpartum women reported having unmet health care needs, 60% had health care unaffordability, and 54% reported general financial stress. Notably, the type of insurance was associated with the ability to afford health care.
Those with private insurance, along with women with lower incomes, were more likely to experience unaffordable health care, compared to those covered by public insurance or who had higher incomes.
Senior study author Michelle H. Moniz, MD, assistant professor in the department of obstetrics and gynecology at the University of Michigan, Ann Arbor, was surprised by multiple study findings. “The prevalence of financial hardship overall, and the three individual indicators of hardship, did not change over time from 2013 to 2018,” she said. “The ACA was enacted just prior to the study period, and while this policy had many benefits for women – especially around increasing insurance coverage – it does not seem to have improved financial hardship among pregnant and postpartum women.”
She emphasized that two groups were at the highest risk of health care unaffordability: those with private insurance and those living on low incomes. “This is notable, as we often think of private insurance as offering ‘Cadillac coverage,’ but our prior work suggests that privately insured women have strikingly high out-of-pocket costs for pregnancy and childbirth-related care,” Dr. Moniz said.
These expenses include deductibles, copays, and coinsurance payments, which come to about $4,500 on average. Medicaid plans, in contrast, have exceedingly low out-of-pocket costs for pregnant and postpartum women. “Findings from the current study call for targeted policy interventions to alleviate financial strain and remove financial barriers to health care access for privately insured families,” she said. “Similarly, families living on lower incomes were also at high risk of health care unaffordability. This may be because even small out-of-pocket costs, or health care–associated costs, account for a larger share of the family’s income.”
This finding for lower-income women calls for targeted policy interventions. “Sliding-scale deductibles, for example, are one solution that might mitigate economic hardship and remove cost-related barriers to health care for pregnant and postpartum women,” Dr. Moniz added.
Health care unaffordability high
In this study, Dr. Moniz and colleagues evaluated the prevalence of financial hardship among peripartum women over time, and how it was affected by their income level and the type of insurance coverage.
They conducted a cross-sectional study that included peripartum women between the ages of 18 and 45 years who reported being currently pregnant or pregnant in the past 12 months. The women were all participants in the National Health Interview Survey, which covers the period from 2013 to 2018, and the data were analyzed from January to May 2021.
The cohort included 3,509 peripartum women, and was weighted to represent 1,050,789 women, with a mean age of 29 years. In 2018, an estimated 39,017 of 184,018 (21.2%) were Black; 36,045 (19.6%) were Hispanic; and 97,366 (52.9%) were White. In the latter years of the study period, the participants tended to be older, more highly educated, and less likely to lack insurance.
When the authors compared the unadjusted reported financial hardship outcome by each study year, unmet health care need (2013: 27.9% [95% confidence interval, 24.4%-31.7%]; 2018: 23.7% [95% CI, 19.5%-28.6%]), health care unaffordability (2013: 65.7% [95% CI, 61.1%-70.0%]; 2018: 58.8% [95% CI, 53.4%-64.0%]), and general financial stress (2013: 60.6% [95% CI, 55.2%-65.8%]; 2018: 53.8% [95% CI, 47.8%-59.8%]) remained largely unchanged between 2013 and 2018.
When they looked at the relationship between insurance type, income, and financial difficulties, some degree of financial hardship was common across all groups; private insurance: 63.8% [95% CI, 61.1%-66.6%]; with public insurance: 49.9% [95% CI, 46.4%-53.4%]; with no insurance: 81.8% [95% CI, 76.4%-87.3%]; with income < 400% of the federal poverty level (FPL): 65.5% [95% CI, 62.1%-66.9%]; with income at least 400% of the FPL: 49.3% [95% CI,44.7%-53.9%]).
Those without any insurance had the highest odds of reporting unmet health care needs (adjusted OR [aOR], 4.40; 95% CI, 3.23-6.00) and health care unaffordability (aOR, 5.18; 95% CI, 3.49-7.70) compared with women who received public insurance.
But while women with private insurance had lower odds of reporting unmet health care needs (aOR, 0.67; 95% CI, 0.52-0.87), they faced higher odds of reporting health care unaffordability (aOR, 1.88; 95% CI, 1.49-2.36) compared to women who had public insurance.
Those with household incomes of less than 400% of the FPL had higher odds of reporting unmet health care need (aOR,1.50; 95% CI, 1.08-2.08) and health care unaffordability (aOR, 1.98; 95% CI, 1.54-2.55) versus women whose household incomes were at least 400% of FPL. The odds of general financial stress did not significantly differ by insurance status/type or income level.
Weighing in on the data
Jamie Daw, PhD, assistant professor of health policy and management, Columbia University Mailman School of Public Health, New York, noted that many people think of private insurance as “good coverage.”
“But the portion of medical costs that patients are required to pay under private plans has risen dramatically over the past decade,” she said. “Over half of the U.S. workforce is now enrolled in high-deductible plans, where the average deductible was $4,500 in 2020. The private insurance of today does not provide sufficient financial protection for most families, who would need to have the liquid assets to cover childbirth.”
Another expert agreed that the high out-of-pocket costs for women with private health insurance were probably responsible for making peripartum health care more unaffordable. These included costs for pregnancy care as well as for maternal and infant care during and after childbirth.
“This study reporting the high unmet medical needs and unaffordability of health care for peripartum women further underscores that the U.S. health care system is not meeting the needs of pregnant women, mothers, and their newborn infants,” said Lois K. Lee, MD, associate professor of pediatrics and emergency medicine at Harvard Medical School and associate director for public policy at the Sandra L. Fenwick Institute for Pediatric Health Equity and Inclusion, Boston.
“It is imperative to optimize the health of pregnant mothers to optimize the health of infants, who are our future society,” she said. “Policies which would expand Medicaid coverage to a full 1-year postpartum across all states is one important strategy to improve health care access and affordability to peripartum women. However, this must be part of a multipronged approach addressing the social determinants of health, as insurance coverage alone will not fully address this important health issue of peripartum women, and their children.”
Dr Moniz reported receiving personal fees from the RAND Corporation, the Society of Family Planning outside the submitted work and grant K08 HS025465 from the Agency for Healthcare Research and Quality. Dr. Daw has no disclosures. Dr. Lee reports speaker fees from the American Academy of Pediatrics and SUNY Upstate Medical University. Coauthor Dr. Taylor was supported by the National Clinician Scholars Program at the University of Michigan. Dr Dalton was supported by grant R01 HS023784 from the Agency for Healthcare Research and Quality.
Financial hardship remains prevalent among pregnant and postpartum women, despite the implementation of the Affordable Care Act (ACA), according to new findings published in JAMA Network Open.
Nearly a quarter (24%) of pregnant and postpartum women reported having unmet health care needs, 60% had health care unaffordability, and 54% reported general financial stress. Notably, the type of insurance was associated with the ability to afford health care.
Those with private insurance, along with women with lower incomes, were more likely to experience unaffordable health care, compared to those covered by public insurance or who had higher incomes.
Senior study author Michelle H. Moniz, MD, assistant professor in the department of obstetrics and gynecology at the University of Michigan, Ann Arbor, was surprised by multiple study findings. “The prevalence of financial hardship overall, and the three individual indicators of hardship, did not change over time from 2013 to 2018,” she said. “The ACA was enacted just prior to the study period, and while this policy had many benefits for women – especially around increasing insurance coverage – it does not seem to have improved financial hardship among pregnant and postpartum women.”
She emphasized that two groups were at the highest risk of health care unaffordability: those with private insurance and those living on low incomes. “This is notable, as we often think of private insurance as offering ‘Cadillac coverage,’ but our prior work suggests that privately insured women have strikingly high out-of-pocket costs for pregnancy and childbirth-related care,” Dr. Moniz said.
These expenses include deductibles, copays, and coinsurance payments, which come to about $4,500 on average. Medicaid plans, in contrast, have exceedingly low out-of-pocket costs for pregnant and postpartum women. “Findings from the current study call for targeted policy interventions to alleviate financial strain and remove financial barriers to health care access for privately insured families,” she said. “Similarly, families living on lower incomes were also at high risk of health care unaffordability. This may be because even small out-of-pocket costs, or health care–associated costs, account for a larger share of the family’s income.”
This finding for lower-income women calls for targeted policy interventions. “Sliding-scale deductibles, for example, are one solution that might mitigate economic hardship and remove cost-related barriers to health care for pregnant and postpartum women,” Dr. Moniz added.
Health care unaffordability high
In this study, Dr. Moniz and colleagues evaluated the prevalence of financial hardship among peripartum women over time, and how it was affected by their income level and the type of insurance coverage.
They conducted a cross-sectional study that included peripartum women between the ages of 18 and 45 years who reported being currently pregnant or pregnant in the past 12 months. The women were all participants in the National Health Interview Survey, which covers the period from 2013 to 2018, and the data were analyzed from January to May 2021.
The cohort included 3,509 peripartum women, and was weighted to represent 1,050,789 women, with a mean age of 29 years. In 2018, an estimated 39,017 of 184,018 (21.2%) were Black; 36,045 (19.6%) were Hispanic; and 97,366 (52.9%) were White. In the latter years of the study period, the participants tended to be older, more highly educated, and less likely to lack insurance.
When the authors compared the unadjusted reported financial hardship outcome by each study year, unmet health care need (2013: 27.9% [95% confidence interval, 24.4%-31.7%]; 2018: 23.7% [95% CI, 19.5%-28.6%]), health care unaffordability (2013: 65.7% [95% CI, 61.1%-70.0%]; 2018: 58.8% [95% CI, 53.4%-64.0%]), and general financial stress (2013: 60.6% [95% CI, 55.2%-65.8%]; 2018: 53.8% [95% CI, 47.8%-59.8%]) remained largely unchanged between 2013 and 2018.
When they looked at the relationship between insurance type, income, and financial difficulties, some degree of financial hardship was common across all groups; private insurance: 63.8% [95% CI, 61.1%-66.6%]; with public insurance: 49.9% [95% CI, 46.4%-53.4%]; with no insurance: 81.8% [95% CI, 76.4%-87.3%]; with income < 400% of the federal poverty level (FPL): 65.5% [95% CI, 62.1%-66.9%]; with income at least 400% of the FPL: 49.3% [95% CI,44.7%-53.9%]).
Those without any insurance had the highest odds of reporting unmet health care needs (adjusted OR [aOR], 4.40; 95% CI, 3.23-6.00) and health care unaffordability (aOR, 5.18; 95% CI, 3.49-7.70) compared with women who received public insurance.
But while women with private insurance had lower odds of reporting unmet health care needs (aOR, 0.67; 95% CI, 0.52-0.87), they faced higher odds of reporting health care unaffordability (aOR, 1.88; 95% CI, 1.49-2.36) compared to women who had public insurance.
Those with household incomes of less than 400% of the FPL had higher odds of reporting unmet health care need (aOR,1.50; 95% CI, 1.08-2.08) and health care unaffordability (aOR, 1.98; 95% CI, 1.54-2.55) versus women whose household incomes were at least 400% of FPL. The odds of general financial stress did not significantly differ by insurance status/type or income level.
Weighing in on the data
Jamie Daw, PhD, assistant professor of health policy and management, Columbia University Mailman School of Public Health, New York, noted that many people think of private insurance as “good coverage.”
“But the portion of medical costs that patients are required to pay under private plans has risen dramatically over the past decade,” she said. “Over half of the U.S. workforce is now enrolled in high-deductible plans, where the average deductible was $4,500 in 2020. The private insurance of today does not provide sufficient financial protection for most families, who would need to have the liquid assets to cover childbirth.”
Another expert agreed that the high out-of-pocket costs for women with private health insurance were probably responsible for making peripartum health care more unaffordable. These included costs for pregnancy care as well as for maternal and infant care during and after childbirth.
“This study reporting the high unmet medical needs and unaffordability of health care for peripartum women further underscores that the U.S. health care system is not meeting the needs of pregnant women, mothers, and their newborn infants,” said Lois K. Lee, MD, associate professor of pediatrics and emergency medicine at Harvard Medical School and associate director for public policy at the Sandra L. Fenwick Institute for Pediatric Health Equity and Inclusion, Boston.
“It is imperative to optimize the health of pregnant mothers to optimize the health of infants, who are our future society,” she said. “Policies which would expand Medicaid coverage to a full 1-year postpartum across all states is one important strategy to improve health care access and affordability to peripartum women. However, this must be part of a multipronged approach addressing the social determinants of health, as insurance coverage alone will not fully address this important health issue of peripartum women, and their children.”
Dr Moniz reported receiving personal fees from the RAND Corporation, the Society of Family Planning outside the submitted work and grant K08 HS025465 from the Agency for Healthcare Research and Quality. Dr. Daw has no disclosures. Dr. Lee reports speaker fees from the American Academy of Pediatrics and SUNY Upstate Medical University. Coauthor Dr. Taylor was supported by the National Clinician Scholars Program at the University of Michigan. Dr Dalton was supported by grant R01 HS023784 from the Agency for Healthcare Research and Quality.
Financial hardship remains prevalent among pregnant and postpartum women, despite the implementation of the Affordable Care Act (ACA), according to new findings published in JAMA Network Open.
Nearly a quarter (24%) of pregnant and postpartum women reported having unmet health care needs, 60% had health care unaffordability, and 54% reported general financial stress. Notably, the type of insurance was associated with the ability to afford health care.
Those with private insurance, along with women with lower incomes, were more likely to experience unaffordable health care, compared to those covered by public insurance or who had higher incomes.
Senior study author Michelle H. Moniz, MD, assistant professor in the department of obstetrics and gynecology at the University of Michigan, Ann Arbor, was surprised by multiple study findings. “The prevalence of financial hardship overall, and the three individual indicators of hardship, did not change over time from 2013 to 2018,” she said. “The ACA was enacted just prior to the study period, and while this policy had many benefits for women – especially around increasing insurance coverage – it does not seem to have improved financial hardship among pregnant and postpartum women.”
She emphasized that two groups were at the highest risk of health care unaffordability: those with private insurance and those living on low incomes. “This is notable, as we often think of private insurance as offering ‘Cadillac coverage,’ but our prior work suggests that privately insured women have strikingly high out-of-pocket costs for pregnancy and childbirth-related care,” Dr. Moniz said.
These expenses include deductibles, copays, and coinsurance payments, which come to about $4,500 on average. Medicaid plans, in contrast, have exceedingly low out-of-pocket costs for pregnant and postpartum women. “Findings from the current study call for targeted policy interventions to alleviate financial strain and remove financial barriers to health care access for privately insured families,” she said. “Similarly, families living on lower incomes were also at high risk of health care unaffordability. This may be because even small out-of-pocket costs, or health care–associated costs, account for a larger share of the family’s income.”
This finding for lower-income women calls for targeted policy interventions. “Sliding-scale deductibles, for example, are one solution that might mitigate economic hardship and remove cost-related barriers to health care for pregnant and postpartum women,” Dr. Moniz added.
Health care unaffordability high
In this study, Dr. Moniz and colleagues evaluated the prevalence of financial hardship among peripartum women over time, and how it was affected by their income level and the type of insurance coverage.
They conducted a cross-sectional study that included peripartum women between the ages of 18 and 45 years who reported being currently pregnant or pregnant in the past 12 months. The women were all participants in the National Health Interview Survey, which covers the period from 2013 to 2018, and the data were analyzed from January to May 2021.
The cohort included 3,509 peripartum women, and was weighted to represent 1,050,789 women, with a mean age of 29 years. In 2018, an estimated 39,017 of 184,018 (21.2%) were Black; 36,045 (19.6%) were Hispanic; and 97,366 (52.9%) were White. In the latter years of the study period, the participants tended to be older, more highly educated, and less likely to lack insurance.
When the authors compared the unadjusted reported financial hardship outcome by each study year, unmet health care need (2013: 27.9% [95% confidence interval, 24.4%-31.7%]; 2018: 23.7% [95% CI, 19.5%-28.6%]), health care unaffordability (2013: 65.7% [95% CI, 61.1%-70.0%]; 2018: 58.8% [95% CI, 53.4%-64.0%]), and general financial stress (2013: 60.6% [95% CI, 55.2%-65.8%]; 2018: 53.8% [95% CI, 47.8%-59.8%]) remained largely unchanged between 2013 and 2018.
When they looked at the relationship between insurance type, income, and financial difficulties, some degree of financial hardship was common across all groups; private insurance: 63.8% [95% CI, 61.1%-66.6%]; with public insurance: 49.9% [95% CI, 46.4%-53.4%]; with no insurance: 81.8% [95% CI, 76.4%-87.3%]; with income < 400% of the federal poverty level (FPL): 65.5% [95% CI, 62.1%-66.9%]; with income at least 400% of the FPL: 49.3% [95% CI,44.7%-53.9%]).
Those without any insurance had the highest odds of reporting unmet health care needs (adjusted OR [aOR], 4.40; 95% CI, 3.23-6.00) and health care unaffordability (aOR, 5.18; 95% CI, 3.49-7.70) compared with women who received public insurance.
But while women with private insurance had lower odds of reporting unmet health care needs (aOR, 0.67; 95% CI, 0.52-0.87), they faced higher odds of reporting health care unaffordability (aOR, 1.88; 95% CI, 1.49-2.36) compared to women who had public insurance.
Those with household incomes of less than 400% of the FPL had higher odds of reporting unmet health care need (aOR,1.50; 95% CI, 1.08-2.08) and health care unaffordability (aOR, 1.98; 95% CI, 1.54-2.55) versus women whose household incomes were at least 400% of FPL. The odds of general financial stress did not significantly differ by insurance status/type or income level.
Weighing in on the data
Jamie Daw, PhD, assistant professor of health policy and management, Columbia University Mailman School of Public Health, New York, noted that many people think of private insurance as “good coverage.”
“But the portion of medical costs that patients are required to pay under private plans has risen dramatically over the past decade,” she said. “Over half of the U.S. workforce is now enrolled in high-deductible plans, where the average deductible was $4,500 in 2020. The private insurance of today does not provide sufficient financial protection for most families, who would need to have the liquid assets to cover childbirth.”
Another expert agreed that the high out-of-pocket costs for women with private health insurance were probably responsible for making peripartum health care more unaffordable. These included costs for pregnancy care as well as for maternal and infant care during and after childbirth.
“This study reporting the high unmet medical needs and unaffordability of health care for peripartum women further underscores that the U.S. health care system is not meeting the needs of pregnant women, mothers, and their newborn infants,” said Lois K. Lee, MD, associate professor of pediatrics and emergency medicine at Harvard Medical School and associate director for public policy at the Sandra L. Fenwick Institute for Pediatric Health Equity and Inclusion, Boston.
“It is imperative to optimize the health of pregnant mothers to optimize the health of infants, who are our future society,” she said. “Policies which would expand Medicaid coverage to a full 1-year postpartum across all states is one important strategy to improve health care access and affordability to peripartum women. However, this must be part of a multipronged approach addressing the social determinants of health, as insurance coverage alone will not fully address this important health issue of peripartum women, and their children.”
Dr Moniz reported receiving personal fees from the RAND Corporation, the Society of Family Planning outside the submitted work and grant K08 HS025465 from the Agency for Healthcare Research and Quality. Dr. Daw has no disclosures. Dr. Lee reports speaker fees from the American Academy of Pediatrics and SUNY Upstate Medical University. Coauthor Dr. Taylor was supported by the National Clinician Scholars Program at the University of Michigan. Dr Dalton was supported by grant R01 HS023784 from the Agency for Healthcare Research and Quality.
FROM JAMA NETWORK OPEN
Time to attack hypoactivity in our children
My 50th medical school reunion has come and gone. This milestone offered me another opportunity to look back over the last 5 decades of pediatrics that I have watched pass under the bridge. Triggered by the discovery of two recently published studies, this particular view back over my shoulder induced a wave of sadness, anger, and frustration that I have had trouble shaking.
The first study demonstrated a strong positive effect of exercise on academic achievement, the other found that children who were more physically active have weathered the pandemic with fewer mental health problems.
These studies are just two pieces of a growing body of evidence that our sedentary lifestyles are shortening our lives and launching our children into adulthood burdened with a raft of health risks they could possibly have avoided by being more physically active. Encountering these two papers just as the alumni office was inviting me to engage in an orgy of retrospection and introspection made me consider how little I and others in my profession have done to substantially address this scourge on our young people.
Yes, I have tried to encourage my patients to be less sedentary and more active. Yes, I have tried to set a very visible example by bicycling and walking around town. Yes, I have coached youth sports teams. All of my children and grandchildren are leading active lives and appear to be reaping the benefits. But in the grander scheme of things I feel that neither I nor the American Academy of Pediatrics has made a difference.
In March of 2020 the AAP published a clinical report that lists the numerous positive associations between activity and health that includes a comprehensive collection of suggestions for providers on how we might assess the problem of inactivity and then play a role in addressing it with our patients and our communities. Unfortunately, the message’s importance was lost in the glut of pandemic news.
While the AAP’s report should have been published many decades ago, I doubt the delay lessened its impact significantly because the report is primarily a compendium of recommendations that in the long run will be seen as just another example of us believers preaching to the choir.
Making lifestyle changes on the order of magnitude necessary to convert an increasingly sedentary population into one that unconsciously becomes physically active requires more than recommendations. It is only natural that folks have trouble saying “No.”
No to the entertainment of electronic devices. No to the comforts of all-weather enclosed transportation. No to hours on the couch. Overcoming the inertia built into our society is going to require more than encouragement, recommendations, and professional sports–sponsored presidential initiatives.
Mandate has become a politically charged dirty word. But our current experience with the COVID-19 vaccines should help us realize that there is a significant segment of the population that doesn’t like being told what to do even if the outcome is in their best interest. Education and rewards have fallen short, but the evidence is mounting that mandates can work.
There was a time when physical activity was built into every child’s school day. For a variety of bad reasons, vigorous physical education classes and once- or twice-daily outdoor recesses have disappeared from the educational landscape. It is time to return to them in a robust form. Unfortunately, because activity isn’t happening at home it will take a government mandate.
There will be pushback. Even from some educators whose observations should have shown them the critical role of physical activity in health and academic success. We must move the distraction of the phenomenon once known simply as hyperactivity to the back burner and tackle the real epidemic of hypoactivity that is destroying our children.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
My 50th medical school reunion has come and gone. This milestone offered me another opportunity to look back over the last 5 decades of pediatrics that I have watched pass under the bridge. Triggered by the discovery of two recently published studies, this particular view back over my shoulder induced a wave of sadness, anger, and frustration that I have had trouble shaking.
The first study demonstrated a strong positive effect of exercise on academic achievement, the other found that children who were more physically active have weathered the pandemic with fewer mental health problems.
These studies are just two pieces of a growing body of evidence that our sedentary lifestyles are shortening our lives and launching our children into adulthood burdened with a raft of health risks they could possibly have avoided by being more physically active. Encountering these two papers just as the alumni office was inviting me to engage in an orgy of retrospection and introspection made me consider how little I and others in my profession have done to substantially address this scourge on our young people.
Yes, I have tried to encourage my patients to be less sedentary and more active. Yes, I have tried to set a very visible example by bicycling and walking around town. Yes, I have coached youth sports teams. All of my children and grandchildren are leading active lives and appear to be reaping the benefits. But in the grander scheme of things I feel that neither I nor the American Academy of Pediatrics has made a difference.
In March of 2020 the AAP published a clinical report that lists the numerous positive associations between activity and health that includes a comprehensive collection of suggestions for providers on how we might assess the problem of inactivity and then play a role in addressing it with our patients and our communities. Unfortunately, the message’s importance was lost in the glut of pandemic news.
While the AAP’s report should have been published many decades ago, I doubt the delay lessened its impact significantly because the report is primarily a compendium of recommendations that in the long run will be seen as just another example of us believers preaching to the choir.
Making lifestyle changes on the order of magnitude necessary to convert an increasingly sedentary population into one that unconsciously becomes physically active requires more than recommendations. It is only natural that folks have trouble saying “No.”
No to the entertainment of electronic devices. No to the comforts of all-weather enclosed transportation. No to hours on the couch. Overcoming the inertia built into our society is going to require more than encouragement, recommendations, and professional sports–sponsored presidential initiatives.
Mandate has become a politically charged dirty word. But our current experience with the COVID-19 vaccines should help us realize that there is a significant segment of the population that doesn’t like being told what to do even if the outcome is in their best interest. Education and rewards have fallen short, but the evidence is mounting that mandates can work.
There was a time when physical activity was built into every child’s school day. For a variety of bad reasons, vigorous physical education classes and once- or twice-daily outdoor recesses have disappeared from the educational landscape. It is time to return to them in a robust form. Unfortunately, because activity isn’t happening at home it will take a government mandate.
There will be pushback. Even from some educators whose observations should have shown them the critical role of physical activity in health and academic success. We must move the distraction of the phenomenon once known simply as hyperactivity to the back burner and tackle the real epidemic of hypoactivity that is destroying our children.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
My 50th medical school reunion has come and gone. This milestone offered me another opportunity to look back over the last 5 decades of pediatrics that I have watched pass under the bridge. Triggered by the discovery of two recently published studies, this particular view back over my shoulder induced a wave of sadness, anger, and frustration that I have had trouble shaking.
The first study demonstrated a strong positive effect of exercise on academic achievement, the other found that children who were more physically active have weathered the pandemic with fewer mental health problems.
These studies are just two pieces of a growing body of evidence that our sedentary lifestyles are shortening our lives and launching our children into adulthood burdened with a raft of health risks they could possibly have avoided by being more physically active. Encountering these two papers just as the alumni office was inviting me to engage in an orgy of retrospection and introspection made me consider how little I and others in my profession have done to substantially address this scourge on our young people.
Yes, I have tried to encourage my patients to be less sedentary and more active. Yes, I have tried to set a very visible example by bicycling and walking around town. Yes, I have coached youth sports teams. All of my children and grandchildren are leading active lives and appear to be reaping the benefits. But in the grander scheme of things I feel that neither I nor the American Academy of Pediatrics has made a difference.
In March of 2020 the AAP published a clinical report that lists the numerous positive associations between activity and health that includes a comprehensive collection of suggestions for providers on how we might assess the problem of inactivity and then play a role in addressing it with our patients and our communities. Unfortunately, the message’s importance was lost in the glut of pandemic news.
While the AAP’s report should have been published many decades ago, I doubt the delay lessened its impact significantly because the report is primarily a compendium of recommendations that in the long run will be seen as just another example of us believers preaching to the choir.
Making lifestyle changes on the order of magnitude necessary to convert an increasingly sedentary population into one that unconsciously becomes physically active requires more than recommendations. It is only natural that folks have trouble saying “No.”
No to the entertainment of electronic devices. No to the comforts of all-weather enclosed transportation. No to hours on the couch. Overcoming the inertia built into our society is going to require more than encouragement, recommendations, and professional sports–sponsored presidential initiatives.
Mandate has become a politically charged dirty word. But our current experience with the COVID-19 vaccines should help us realize that there is a significant segment of the population that doesn’t like being told what to do even if the outcome is in their best interest. Education and rewards have fallen short, but the evidence is mounting that mandates can work.
There was a time when physical activity was built into every child’s school day. For a variety of bad reasons, vigorous physical education classes and once- or twice-daily outdoor recesses have disappeared from the educational landscape. It is time to return to them in a robust form. Unfortunately, because activity isn’t happening at home it will take a government mandate.
There will be pushback. Even from some educators whose observations should have shown them the critical role of physical activity in health and academic success. We must move the distraction of the phenomenon once known simply as hyperactivity to the back burner and tackle the real epidemic of hypoactivity that is destroying our children.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Lesbian, gay, bisexual youth miss out on health care
Youth identifying as lesbian, gay, or bisexual were significantly less likely than were their peers to communicate with a physician or utilize health care in the past 12 months, according to data from a cohort study of approximately 4,000 adolescents.
Disparities in physical and mental health outcomes for individuals who identify as lesbian, gay, or bisexual (LGB) persist in the United States, and emerge in adolescents and young adults, wrote Sari L. Reisner, ScD, of Boston Children’s Hospital, and colleagues.
“LGB adult research indicates substantial unmet medical needs, including needed care and preventive care,” for reasons including “reluctance to disclose sexual identity to clinicians, lower health insurance rates, lack of culturally appropriate preventive services, and lack of clinician LGB care competence,” they said.
However, health use trends by adolescents who identify as LGB have not been well studied, they noted.
In a study published in JAMA Network Open, the researchers analyzed data from 4,256 participants in the third wave (10th grade) of adolescents in Healthy Passages, a longitudinal, observational cohort study of diverse public school students in Birmingham, Ala.; Houston; and Los Angeles County. Data were collected in grades 5, 7, and 10.
The study population included 640 youth who identified as LGB, and 3,616 non-LGB youth. Sexual status was based on responses to questions in the grade 10 youth survey. Health care use was based on the responses to questions about routine care, such as a regular checkup, and other care, such as a sick visit. Data on delayed care were collected from parents and youth. At baseline, the average age of the study participants in fifth grade was 11 years, 48.9% were female, 44.5% were Hispanic or Latino, and 28.9% were Black.
Overall, more LGB youth reported not receiving needed medical care when they thought they needed it within the past 12 months compared with non-LGB youth (42.4% of LGB vs. 30.2% of non-LGB youth; adjusted odds ratio 1.68). The most common conditions for which LGB youth did not seek care were sexually transmitted infections, contraception, and substance use.
Overall, the main reason given for not seeking medical care was that they thought the problem would go away (approximately 26% for LGB and non-LGB). Approximately twice as many LGB youth as non-LGB youth said they avoided medical care because they did not want their parents to know (14.5% vs. 9.4%).
Significantly more LGB youth than non-LGB youth reported difficulty communicating with their physicians in the past 12 months (15.3% vs. 9.4%; aOR 1.71). The main reasons for not communicating with a clinician about a topic of concern were that the adolescent did not want parents to know (40.7% of LGB and 30.2% of non-LGB) and that they were too embarrassed to talk about the topic (37.5% of LGB and 25.9% of non-LGB).
The researchers were not surprised that “LGB youth self-reported greater difficulty communicating with a clinician about topics they wanted to discuss,” but they found no significant differences in reasons for communication difficulty based on sexual orientation.
Approximately two-thirds (65.8%) of LGB youth reported feeling “a little or not at all comfortable” talking to a health care clinician about their sexual attractions, compared with approximately one-third (37.8%) of non-LGB youth.
Only 12.5% of the LGB youth said that their clinicians knew their sexual orientation, the researchers noted. However, clinicians need to know youths’ sexual orientation to provide appropriate and comprehensive care, they said, especially in light of the known negative health consequences of LGB internalized stigma, as well as the pertinence of certain sexual behaviors to preventive care and screening.
The study findings were limited by several factors including the cross-sectional design and inability to show causality, and by the incongruence of different dimensions of sexual orientation, the researchers noted. Other limitations included the use only of English and Spanish language, and a lack of complete information on disclosure of sexual orientation to parents, the researchers noted.
The results were strengthened by the diverse demographics, although they may not be generalizable to a wider population, they added.
However, the data show that responsive health care is needed to reduce disparities for LGB youth, they emphasized. “Care should be sensitive and respectful to sexual orientation for all youth, with clinicians taking time to ask adolescents about their sexual identity, attractions, and behaviors, particularly in sexual and reproductive health,” they concluded.
Adolescents suffer barriers similar to those of adults
“We know that significant health disparities exist for LGBTQ adults and adolescents,” Kelly Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, said in an interview. “LGBTQ adults often have had poor experiences during health care encounters – ranging from poor interactions with inadequately trained clinicians to frank discrimination,” she said. “These experiences can prevent individuals from seeking health care in the future or disclosing important information during a medical visit, both of which can contribute to worsened health outcomes,” she emphasized.
Prior to this study, data to confirm similar patterns of decreased health care utilization in LGB youth were limited, Dr. Curran said. “Identifying and understanding barriers to health care for LGBTQ youth are essential to help address the disparities in this population,” she said.
Dr. Curran said she was not surprised by the study findings for adolescents, which reflect patterns seen in LGBTQ adults.
Overcoming barriers to encourage LGB youth to seek regular medical care involves “training health care professionals about LGBTQ health, teaching the skill of taking a nonjudgmental, inclusive history, and making health care facilities welcoming and inclusive, such as displaying a pride flag in clinic, and using forms asking for pronouns,” Dr. Curran said.
Dr. Curran said she thinks the trends in decreased health care use are similar for transgender youth. “I suspect, if anything, that transgender youth will have even further decreased health care utilization when compared to cisgender heterosexual peers and LGB peers,” she noted.
Going forward, it will be important to understand the reasons behind decreased health care use among LGB youth, such as poor experiences, discrimination, or fears about confidentiality, said Dr. Curran. “Additionally, it would be important to understand if this decreased health utilization also occurs with transgender youth,” she said.
The Healthy Passages Study was funded by the Centers for Disease Control and Prevention. One of the study coauthors disclosed funding from the Agency for Healthcare Research and Quality as part of the Harvard-wide Pediatric Health Services Research Fellowship Program. The researchers had no financial conflicts to disclose. Dr. Curran had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
Youth identifying as lesbian, gay, or bisexual were significantly less likely than were their peers to communicate with a physician or utilize health care in the past 12 months, according to data from a cohort study of approximately 4,000 adolescents.
Disparities in physical and mental health outcomes for individuals who identify as lesbian, gay, or bisexual (LGB) persist in the United States, and emerge in adolescents and young adults, wrote Sari L. Reisner, ScD, of Boston Children’s Hospital, and colleagues.
“LGB adult research indicates substantial unmet medical needs, including needed care and preventive care,” for reasons including “reluctance to disclose sexual identity to clinicians, lower health insurance rates, lack of culturally appropriate preventive services, and lack of clinician LGB care competence,” they said.
However, health use trends by adolescents who identify as LGB have not been well studied, they noted.
In a study published in JAMA Network Open, the researchers analyzed data from 4,256 participants in the third wave (10th grade) of adolescents in Healthy Passages, a longitudinal, observational cohort study of diverse public school students in Birmingham, Ala.; Houston; and Los Angeles County. Data were collected in grades 5, 7, and 10.
The study population included 640 youth who identified as LGB, and 3,616 non-LGB youth. Sexual status was based on responses to questions in the grade 10 youth survey. Health care use was based on the responses to questions about routine care, such as a regular checkup, and other care, such as a sick visit. Data on delayed care were collected from parents and youth. At baseline, the average age of the study participants in fifth grade was 11 years, 48.9% were female, 44.5% were Hispanic or Latino, and 28.9% were Black.
Overall, more LGB youth reported not receiving needed medical care when they thought they needed it within the past 12 months compared with non-LGB youth (42.4% of LGB vs. 30.2% of non-LGB youth; adjusted odds ratio 1.68). The most common conditions for which LGB youth did not seek care were sexually transmitted infections, contraception, and substance use.
Overall, the main reason given for not seeking medical care was that they thought the problem would go away (approximately 26% for LGB and non-LGB). Approximately twice as many LGB youth as non-LGB youth said they avoided medical care because they did not want their parents to know (14.5% vs. 9.4%).
Significantly more LGB youth than non-LGB youth reported difficulty communicating with their physicians in the past 12 months (15.3% vs. 9.4%; aOR 1.71). The main reasons for not communicating with a clinician about a topic of concern were that the adolescent did not want parents to know (40.7% of LGB and 30.2% of non-LGB) and that they were too embarrassed to talk about the topic (37.5% of LGB and 25.9% of non-LGB).
The researchers were not surprised that “LGB youth self-reported greater difficulty communicating with a clinician about topics they wanted to discuss,” but they found no significant differences in reasons for communication difficulty based on sexual orientation.
Approximately two-thirds (65.8%) of LGB youth reported feeling “a little or not at all comfortable” talking to a health care clinician about their sexual attractions, compared with approximately one-third (37.8%) of non-LGB youth.
Only 12.5% of the LGB youth said that their clinicians knew their sexual orientation, the researchers noted. However, clinicians need to know youths’ sexual orientation to provide appropriate and comprehensive care, they said, especially in light of the known negative health consequences of LGB internalized stigma, as well as the pertinence of certain sexual behaviors to preventive care and screening.
The study findings were limited by several factors including the cross-sectional design and inability to show causality, and by the incongruence of different dimensions of sexual orientation, the researchers noted. Other limitations included the use only of English and Spanish language, and a lack of complete information on disclosure of sexual orientation to parents, the researchers noted.
The results were strengthened by the diverse demographics, although they may not be generalizable to a wider population, they added.
However, the data show that responsive health care is needed to reduce disparities for LGB youth, they emphasized. “Care should be sensitive and respectful to sexual orientation for all youth, with clinicians taking time to ask adolescents about their sexual identity, attractions, and behaviors, particularly in sexual and reproductive health,” they concluded.
Adolescents suffer barriers similar to those of adults
“We know that significant health disparities exist for LGBTQ adults and adolescents,” Kelly Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, said in an interview. “LGBTQ adults often have had poor experiences during health care encounters – ranging from poor interactions with inadequately trained clinicians to frank discrimination,” she said. “These experiences can prevent individuals from seeking health care in the future or disclosing important information during a medical visit, both of which can contribute to worsened health outcomes,” she emphasized.
Prior to this study, data to confirm similar patterns of decreased health care utilization in LGB youth were limited, Dr. Curran said. “Identifying and understanding barriers to health care for LGBTQ youth are essential to help address the disparities in this population,” she said.
Dr. Curran said she was not surprised by the study findings for adolescents, which reflect patterns seen in LGBTQ adults.
Overcoming barriers to encourage LGB youth to seek regular medical care involves “training health care professionals about LGBTQ health, teaching the skill of taking a nonjudgmental, inclusive history, and making health care facilities welcoming and inclusive, such as displaying a pride flag in clinic, and using forms asking for pronouns,” Dr. Curran said.
Dr. Curran said she thinks the trends in decreased health care use are similar for transgender youth. “I suspect, if anything, that transgender youth will have even further decreased health care utilization when compared to cisgender heterosexual peers and LGB peers,” she noted.
Going forward, it will be important to understand the reasons behind decreased health care use among LGB youth, such as poor experiences, discrimination, or fears about confidentiality, said Dr. Curran. “Additionally, it would be important to understand if this decreased health utilization also occurs with transgender youth,” she said.
The Healthy Passages Study was funded by the Centers for Disease Control and Prevention. One of the study coauthors disclosed funding from the Agency for Healthcare Research and Quality as part of the Harvard-wide Pediatric Health Services Research Fellowship Program. The researchers had no financial conflicts to disclose. Dr. Curran had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
Youth identifying as lesbian, gay, or bisexual were significantly less likely than were their peers to communicate with a physician or utilize health care in the past 12 months, according to data from a cohort study of approximately 4,000 adolescents.
Disparities in physical and mental health outcomes for individuals who identify as lesbian, gay, or bisexual (LGB) persist in the United States, and emerge in adolescents and young adults, wrote Sari L. Reisner, ScD, of Boston Children’s Hospital, and colleagues.
“LGB adult research indicates substantial unmet medical needs, including needed care and preventive care,” for reasons including “reluctance to disclose sexual identity to clinicians, lower health insurance rates, lack of culturally appropriate preventive services, and lack of clinician LGB care competence,” they said.
However, health use trends by adolescents who identify as LGB have not been well studied, they noted.
In a study published in JAMA Network Open, the researchers analyzed data from 4,256 participants in the third wave (10th grade) of adolescents in Healthy Passages, a longitudinal, observational cohort study of diverse public school students in Birmingham, Ala.; Houston; and Los Angeles County. Data were collected in grades 5, 7, and 10.
The study population included 640 youth who identified as LGB, and 3,616 non-LGB youth. Sexual status was based on responses to questions in the grade 10 youth survey. Health care use was based on the responses to questions about routine care, such as a regular checkup, and other care, such as a sick visit. Data on delayed care were collected from parents and youth. At baseline, the average age of the study participants in fifth grade was 11 years, 48.9% were female, 44.5% were Hispanic or Latino, and 28.9% were Black.
Overall, more LGB youth reported not receiving needed medical care when they thought they needed it within the past 12 months compared with non-LGB youth (42.4% of LGB vs. 30.2% of non-LGB youth; adjusted odds ratio 1.68). The most common conditions for which LGB youth did not seek care were sexually transmitted infections, contraception, and substance use.
Overall, the main reason given for not seeking medical care was that they thought the problem would go away (approximately 26% for LGB and non-LGB). Approximately twice as many LGB youth as non-LGB youth said they avoided medical care because they did not want their parents to know (14.5% vs. 9.4%).
Significantly more LGB youth than non-LGB youth reported difficulty communicating with their physicians in the past 12 months (15.3% vs. 9.4%; aOR 1.71). The main reasons for not communicating with a clinician about a topic of concern were that the adolescent did not want parents to know (40.7% of LGB and 30.2% of non-LGB) and that they were too embarrassed to talk about the topic (37.5% of LGB and 25.9% of non-LGB).
The researchers were not surprised that “LGB youth self-reported greater difficulty communicating with a clinician about topics they wanted to discuss,” but they found no significant differences in reasons for communication difficulty based on sexual orientation.
Approximately two-thirds (65.8%) of LGB youth reported feeling “a little or not at all comfortable” talking to a health care clinician about their sexual attractions, compared with approximately one-third (37.8%) of non-LGB youth.
Only 12.5% of the LGB youth said that their clinicians knew their sexual orientation, the researchers noted. However, clinicians need to know youths’ sexual orientation to provide appropriate and comprehensive care, they said, especially in light of the known negative health consequences of LGB internalized stigma, as well as the pertinence of certain sexual behaviors to preventive care and screening.
The study findings were limited by several factors including the cross-sectional design and inability to show causality, and by the incongruence of different dimensions of sexual orientation, the researchers noted. Other limitations included the use only of English and Spanish language, and a lack of complete information on disclosure of sexual orientation to parents, the researchers noted.
The results were strengthened by the diverse demographics, although they may not be generalizable to a wider population, they added.
However, the data show that responsive health care is needed to reduce disparities for LGB youth, they emphasized. “Care should be sensitive and respectful to sexual orientation for all youth, with clinicians taking time to ask adolescents about their sexual identity, attractions, and behaviors, particularly in sexual and reproductive health,” they concluded.
Adolescents suffer barriers similar to those of adults
“We know that significant health disparities exist for LGBTQ adults and adolescents,” Kelly Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, said in an interview. “LGBTQ adults often have had poor experiences during health care encounters – ranging from poor interactions with inadequately trained clinicians to frank discrimination,” she said. “These experiences can prevent individuals from seeking health care in the future or disclosing important information during a medical visit, both of which can contribute to worsened health outcomes,” she emphasized.
Prior to this study, data to confirm similar patterns of decreased health care utilization in LGB youth were limited, Dr. Curran said. “Identifying and understanding barriers to health care for LGBTQ youth are essential to help address the disparities in this population,” she said.
Dr. Curran said she was not surprised by the study findings for adolescents, which reflect patterns seen in LGBTQ adults.
Overcoming barriers to encourage LGB youth to seek regular medical care involves “training health care professionals about LGBTQ health, teaching the skill of taking a nonjudgmental, inclusive history, and making health care facilities welcoming and inclusive, such as displaying a pride flag in clinic, and using forms asking for pronouns,” Dr. Curran said.
Dr. Curran said she thinks the trends in decreased health care use are similar for transgender youth. “I suspect, if anything, that transgender youth will have even further decreased health care utilization when compared to cisgender heterosexual peers and LGB peers,” she noted.
Going forward, it will be important to understand the reasons behind decreased health care use among LGB youth, such as poor experiences, discrimination, or fears about confidentiality, said Dr. Curran. “Additionally, it would be important to understand if this decreased health utilization also occurs with transgender youth,” she said.
The Healthy Passages Study was funded by the Centers for Disease Control and Prevention. One of the study coauthors disclosed funding from the Agency for Healthcare Research and Quality as part of the Harvard-wide Pediatric Health Services Research Fellowship Program. The researchers had no financial conflicts to disclose. Dr. Curran had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
FROM JAMA NETWORK OPEN
HCV in pregnancy: One piece of a bigger problem
Mirroring the opioid crisis, maternal and newborn hepatitis C infections (HCV) more than doubled in the United States between 2009 and 2019, with disproportionate increases in people of White, American Indian, and Alaska Native race, especially those with less education, according to a cross-sectional study published in JAMA Health Forum. However, the level of risk within these populations was mitigated in counties with higher employment, reported Stephen W. Patrick, MD, of Vanderbilt University, in Nashville, Tenn., and coauthors.
“As we develop public health approaches to prevent HCV infections, connect to treatment, and monitor exposed infants, understanding these factors can be of critical importance to tailoring interventions,” Dr. Patrick said in an interview. “HCV is one more complication of the opioid crisis,” he added. “These data also enable us to step back a bit from HCV and look at the landscape of how the opioid crisis continues to grow in complexity and scope. Throughout the opioid crisis we have often failed to recognize and address the unique needs of pregnant people and infants.”
The study authors used data from the National Center for Health Statistics at the Centers for Disease Control and Prevention, and from the Area Health Resource File to examine maternal-infant HCV infection among all U.S. births between 2009 and 2019. The researchers also examined community-level risk factors including rurality, employment, and access to medical care.
In counties reporting HCV, there were 39,380,122 people who had live births, of whom 138,343 (0.4%) were diagnosed with HCV. The overall rate of maternal HCV infection increased from 1.8 to 5.1 per 1,000 live births between 2009 and 2019.
Infection rates were highest in American Indian/Alaska Native (AI/AN) and White people (adjusted odds ratio [aOR] 7.94 and 7.37, respectively) compared with Black people. They were higher among individuals without a 4-year degree compared to those with higher education (aOR, 3.19).
Among these groups considered to be at higher risk for HCV infection, high employment rates somewhat mitigated the risk. Specifically, in counties in the 10th percentile of employment, the predicted probability of HCV increased from 0.16% to 1.37%, between 2009 and 2019, whereas in counties at the 90th percentile of employment, the predicted probability remained similar, at 0.36% in 2009 and 0.48% in 2019.
“With constrained national resources, understanding both individual and community-level factors associated with HCV infections in pregnant people could inform strategies to mitigate its spread, such as harm reduction efforts (e.g., syringe service programs), improving access to treatment for [opioid use disorder] or increasing the obstetrical workforce in high-risk communities, HCV testing strategies in pregnant people and people of childbearing age, and treatment with novel antiviral therapies,” wrote the authors.
In the time since the authors began the study, universal HCV screening for every pregnancy has been recommended by a number of groups, including the U.S. Preventive Services Task Force, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine (SMFM). However, Dr. Patrick says even though such recommendations are now adopted, it will be some time before they are fully operational, making knowledge of HCV risk factors important for obstetricians as well as pediatricians and family physicians. “We don’t know how if hospitals and clinicians have started universal screening for HCV and even when it is completely adopted, understanding individual and community-level factors associated with HCV in pregnant people is still of critical importance,” he explained. “In some of our previous work we have found that non-White HCV-exposed infants are less likely to be tested for HCV than are White infants, even after accounting for multiple individual and hospital-level factors. The pattern we are seeing in our research and in research in other groups is one of unequal treatment of pregnant people with substance use disorder in terms of being given evidence-based treatments, being tested for HCV, and even in child welfare outcomes like foster placement. It is important to know these issues are occurring, but we need specific equitable approaches to ensuring optimal outcomes for all families.
Jeffrey A. Kuller, MD, one of the authors of the SMFM’s new recommendations for universal HCV screening in pregnancy, agreed that until universal screening is widely adopted, awareness of maternal HCV risk factors is important, “to better determine who is at highest risk for hep C, barriers to care, and patients to better target.” This information also affects procedure at the time of delivery, added Dr. Kuller, professor of obstetrics and gynecology in the division of maternal-fetal medicine at Duke University, Durham, N.C. “We do not perform C-sections for the presence of hep C,” he told this publication. However, in labor, “we try to avoid internal fetal monitoring when possible, and early artificial rupture of membranes when possible, and avoid the use of routine episiotomy,” he said. “Hep C–positive patients should also be assessed for other sexually transmitted diseases including HIV, syphilis, gonorrhea, chlamydia, and hep B. “Although we do not typically treat hep C pharmacologically during pregnancy, we try to get the patient placed with a hepatologist for long-term management.”
The study has important implications for pediatric patients, added Audrey R. Lloyd, MD, a med-peds infectious disease fellow who is studying HCV in pregnancy at the University of Alabama at Birmingham. “In the setting of maternal HCV viremia, maternal-fetal transmission occurs in around 6% of exposed infants and around 10% if there is maternal HIV-HCV coinfection,” she said in an interview. “With the increasing rates of HCV in pregnant women described by Dr. Patrick et al., HCV infections among infants will also rise. Even when maternal HCV infection is documented, we often do not do a good job screening the infants for infection and linking them to treatment. This new data makes me worried we may see more complications of pediatric HCV infection in the future,” she added. She explained that safe and effective treatments for HCV infection are approved down to 3 years of age, but patients must first be diagnosed to receive treatment.
From whichever angle you approach it, tackling both the opioid epidemic and HCV infection in pregnancy will inevitably end up helping both parts of the mother-infant dyad, said Dr. Patrick. “Not too long ago I was caring for an opioid-exposed infant at the hospital where I practice who had transferred in from another center hours away. The mother had not been tested for HCV, so I tested the infant for HCV antibodies which were positive. Imagine that, determining a mother is HCV positive by testing the infant. There are so many layers of systems that should be fixed to make this not happen. And what are the chances the mother, after she found out, was able to access treatment for HCV? What about the infant being tested? The systems are just fragmented and we need to do better.”
The study was funded by the National Institute on Drug Abuse of the National Institutes of Health. Neither Dr. Patrick, Dr. Kuller, nor Dr. Lloyd reported any conflicts of interest.
Mirroring the opioid crisis, maternal and newborn hepatitis C infections (HCV) more than doubled in the United States between 2009 and 2019, with disproportionate increases in people of White, American Indian, and Alaska Native race, especially those with less education, according to a cross-sectional study published in JAMA Health Forum. However, the level of risk within these populations was mitigated in counties with higher employment, reported Stephen W. Patrick, MD, of Vanderbilt University, in Nashville, Tenn., and coauthors.
“As we develop public health approaches to prevent HCV infections, connect to treatment, and monitor exposed infants, understanding these factors can be of critical importance to tailoring interventions,” Dr. Patrick said in an interview. “HCV is one more complication of the opioid crisis,” he added. “These data also enable us to step back a bit from HCV and look at the landscape of how the opioid crisis continues to grow in complexity and scope. Throughout the opioid crisis we have often failed to recognize and address the unique needs of pregnant people and infants.”
The study authors used data from the National Center for Health Statistics at the Centers for Disease Control and Prevention, and from the Area Health Resource File to examine maternal-infant HCV infection among all U.S. births between 2009 and 2019. The researchers also examined community-level risk factors including rurality, employment, and access to medical care.
In counties reporting HCV, there were 39,380,122 people who had live births, of whom 138,343 (0.4%) were diagnosed with HCV. The overall rate of maternal HCV infection increased from 1.8 to 5.1 per 1,000 live births between 2009 and 2019.
Infection rates were highest in American Indian/Alaska Native (AI/AN) and White people (adjusted odds ratio [aOR] 7.94 and 7.37, respectively) compared with Black people. They were higher among individuals without a 4-year degree compared to those with higher education (aOR, 3.19).
Among these groups considered to be at higher risk for HCV infection, high employment rates somewhat mitigated the risk. Specifically, in counties in the 10th percentile of employment, the predicted probability of HCV increased from 0.16% to 1.37%, between 2009 and 2019, whereas in counties at the 90th percentile of employment, the predicted probability remained similar, at 0.36% in 2009 and 0.48% in 2019.
“With constrained national resources, understanding both individual and community-level factors associated with HCV infections in pregnant people could inform strategies to mitigate its spread, such as harm reduction efforts (e.g., syringe service programs), improving access to treatment for [opioid use disorder] or increasing the obstetrical workforce in high-risk communities, HCV testing strategies in pregnant people and people of childbearing age, and treatment with novel antiviral therapies,” wrote the authors.
In the time since the authors began the study, universal HCV screening for every pregnancy has been recommended by a number of groups, including the U.S. Preventive Services Task Force, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine (SMFM). However, Dr. Patrick says even though such recommendations are now adopted, it will be some time before they are fully operational, making knowledge of HCV risk factors important for obstetricians as well as pediatricians and family physicians. “We don’t know how if hospitals and clinicians have started universal screening for HCV and even when it is completely adopted, understanding individual and community-level factors associated with HCV in pregnant people is still of critical importance,” he explained. “In some of our previous work we have found that non-White HCV-exposed infants are less likely to be tested for HCV than are White infants, even after accounting for multiple individual and hospital-level factors. The pattern we are seeing in our research and in research in other groups is one of unequal treatment of pregnant people with substance use disorder in terms of being given evidence-based treatments, being tested for HCV, and even in child welfare outcomes like foster placement. It is important to know these issues are occurring, but we need specific equitable approaches to ensuring optimal outcomes for all families.
Jeffrey A. Kuller, MD, one of the authors of the SMFM’s new recommendations for universal HCV screening in pregnancy, agreed that until universal screening is widely adopted, awareness of maternal HCV risk factors is important, “to better determine who is at highest risk for hep C, barriers to care, and patients to better target.” This information also affects procedure at the time of delivery, added Dr. Kuller, professor of obstetrics and gynecology in the division of maternal-fetal medicine at Duke University, Durham, N.C. “We do not perform C-sections for the presence of hep C,” he told this publication. However, in labor, “we try to avoid internal fetal monitoring when possible, and early artificial rupture of membranes when possible, and avoid the use of routine episiotomy,” he said. “Hep C–positive patients should also be assessed for other sexually transmitted diseases including HIV, syphilis, gonorrhea, chlamydia, and hep B. “Although we do not typically treat hep C pharmacologically during pregnancy, we try to get the patient placed with a hepatologist for long-term management.”
The study has important implications for pediatric patients, added Audrey R. Lloyd, MD, a med-peds infectious disease fellow who is studying HCV in pregnancy at the University of Alabama at Birmingham. “In the setting of maternal HCV viremia, maternal-fetal transmission occurs in around 6% of exposed infants and around 10% if there is maternal HIV-HCV coinfection,” she said in an interview. “With the increasing rates of HCV in pregnant women described by Dr. Patrick et al., HCV infections among infants will also rise. Even when maternal HCV infection is documented, we often do not do a good job screening the infants for infection and linking them to treatment. This new data makes me worried we may see more complications of pediatric HCV infection in the future,” she added. She explained that safe and effective treatments for HCV infection are approved down to 3 years of age, but patients must first be diagnosed to receive treatment.
From whichever angle you approach it, tackling both the opioid epidemic and HCV infection in pregnancy will inevitably end up helping both parts of the mother-infant dyad, said Dr. Patrick. “Not too long ago I was caring for an opioid-exposed infant at the hospital where I practice who had transferred in from another center hours away. The mother had not been tested for HCV, so I tested the infant for HCV antibodies which were positive. Imagine that, determining a mother is HCV positive by testing the infant. There are so many layers of systems that should be fixed to make this not happen. And what are the chances the mother, after she found out, was able to access treatment for HCV? What about the infant being tested? The systems are just fragmented and we need to do better.”
The study was funded by the National Institute on Drug Abuse of the National Institutes of Health. Neither Dr. Patrick, Dr. Kuller, nor Dr. Lloyd reported any conflicts of interest.
Mirroring the opioid crisis, maternal and newborn hepatitis C infections (HCV) more than doubled in the United States between 2009 and 2019, with disproportionate increases in people of White, American Indian, and Alaska Native race, especially those with less education, according to a cross-sectional study published in JAMA Health Forum. However, the level of risk within these populations was mitigated in counties with higher employment, reported Stephen W. Patrick, MD, of Vanderbilt University, in Nashville, Tenn., and coauthors.
“As we develop public health approaches to prevent HCV infections, connect to treatment, and monitor exposed infants, understanding these factors can be of critical importance to tailoring interventions,” Dr. Patrick said in an interview. “HCV is one more complication of the opioid crisis,” he added. “These data also enable us to step back a bit from HCV and look at the landscape of how the opioid crisis continues to grow in complexity and scope. Throughout the opioid crisis we have often failed to recognize and address the unique needs of pregnant people and infants.”
The study authors used data from the National Center for Health Statistics at the Centers for Disease Control and Prevention, and from the Area Health Resource File to examine maternal-infant HCV infection among all U.S. births between 2009 and 2019. The researchers also examined community-level risk factors including rurality, employment, and access to medical care.
In counties reporting HCV, there were 39,380,122 people who had live births, of whom 138,343 (0.4%) were diagnosed with HCV. The overall rate of maternal HCV infection increased from 1.8 to 5.1 per 1,000 live births between 2009 and 2019.
Infection rates were highest in American Indian/Alaska Native (AI/AN) and White people (adjusted odds ratio [aOR] 7.94 and 7.37, respectively) compared with Black people. They were higher among individuals without a 4-year degree compared to those with higher education (aOR, 3.19).
Among these groups considered to be at higher risk for HCV infection, high employment rates somewhat mitigated the risk. Specifically, in counties in the 10th percentile of employment, the predicted probability of HCV increased from 0.16% to 1.37%, between 2009 and 2019, whereas in counties at the 90th percentile of employment, the predicted probability remained similar, at 0.36% in 2009 and 0.48% in 2019.
“With constrained national resources, understanding both individual and community-level factors associated with HCV infections in pregnant people could inform strategies to mitigate its spread, such as harm reduction efforts (e.g., syringe service programs), improving access to treatment for [opioid use disorder] or increasing the obstetrical workforce in high-risk communities, HCV testing strategies in pregnant people and people of childbearing age, and treatment with novel antiviral therapies,” wrote the authors.
In the time since the authors began the study, universal HCV screening for every pregnancy has been recommended by a number of groups, including the U.S. Preventive Services Task Force, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine (SMFM). However, Dr. Patrick says even though such recommendations are now adopted, it will be some time before they are fully operational, making knowledge of HCV risk factors important for obstetricians as well as pediatricians and family physicians. “We don’t know how if hospitals and clinicians have started universal screening for HCV and even when it is completely adopted, understanding individual and community-level factors associated with HCV in pregnant people is still of critical importance,” he explained. “In some of our previous work we have found that non-White HCV-exposed infants are less likely to be tested for HCV than are White infants, even after accounting for multiple individual and hospital-level factors. The pattern we are seeing in our research and in research in other groups is one of unequal treatment of pregnant people with substance use disorder in terms of being given evidence-based treatments, being tested for HCV, and even in child welfare outcomes like foster placement. It is important to know these issues are occurring, but we need specific equitable approaches to ensuring optimal outcomes for all families.
Jeffrey A. Kuller, MD, one of the authors of the SMFM’s new recommendations for universal HCV screening in pregnancy, agreed that until universal screening is widely adopted, awareness of maternal HCV risk factors is important, “to better determine who is at highest risk for hep C, barriers to care, and patients to better target.” This information also affects procedure at the time of delivery, added Dr. Kuller, professor of obstetrics and gynecology in the division of maternal-fetal medicine at Duke University, Durham, N.C. “We do not perform C-sections for the presence of hep C,” he told this publication. However, in labor, “we try to avoid internal fetal monitoring when possible, and early artificial rupture of membranes when possible, and avoid the use of routine episiotomy,” he said. “Hep C–positive patients should also be assessed for other sexually transmitted diseases including HIV, syphilis, gonorrhea, chlamydia, and hep B. “Although we do not typically treat hep C pharmacologically during pregnancy, we try to get the patient placed with a hepatologist for long-term management.”
The study has important implications for pediatric patients, added Audrey R. Lloyd, MD, a med-peds infectious disease fellow who is studying HCV in pregnancy at the University of Alabama at Birmingham. “In the setting of maternal HCV viremia, maternal-fetal transmission occurs in around 6% of exposed infants and around 10% if there is maternal HIV-HCV coinfection,” she said in an interview. “With the increasing rates of HCV in pregnant women described by Dr. Patrick et al., HCV infections among infants will also rise. Even when maternal HCV infection is documented, we often do not do a good job screening the infants for infection and linking them to treatment. This new data makes me worried we may see more complications of pediatric HCV infection in the future,” she added. She explained that safe and effective treatments for HCV infection are approved down to 3 years of age, but patients must first be diagnosed to receive treatment.
From whichever angle you approach it, tackling both the opioid epidemic and HCV infection in pregnancy will inevitably end up helping both parts of the mother-infant dyad, said Dr. Patrick. “Not too long ago I was caring for an opioid-exposed infant at the hospital where I practice who had transferred in from another center hours away. The mother had not been tested for HCV, so I tested the infant for HCV antibodies which were positive. Imagine that, determining a mother is HCV positive by testing the infant. There are so many layers of systems that should be fixed to make this not happen. And what are the chances the mother, after she found out, was able to access treatment for HCV? What about the infant being tested? The systems are just fragmented and we need to do better.”
The study was funded by the National Institute on Drug Abuse of the National Institutes of Health. Neither Dr. Patrick, Dr. Kuller, nor Dr. Lloyd reported any conflicts of interest.
FROM JAMA HEALTH FORUM
Children and COVID: A look at the pace of vaccination
With children aged 5-11 years about to enter the battle-of-the-COVID-vaccine phase of the war on COVID, there are many questions. MDedge takes a look at one: How long will it take to get 5- to 11-year-olds vaccinated?
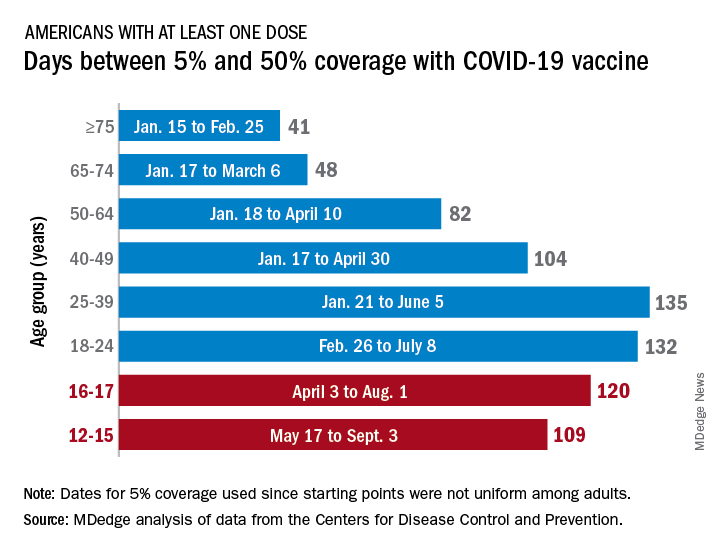
Previous experience may provide some guidance. The vaccine was approved by the Centers for Disease Control and Prevention for the closest group in age, 12- to 15-year-olds, on May 12, 2021, and according to data from the CDC.
(Use of the 5% figure acknowledges the uneven start after approval – the vaccine became available to different age groups at different times, even though it had been approved for all adults aged 18 years and older.)
The 16- to 17-year-olds, despite being a smaller group of less than 7.6 million individuals, took 120 days to go from 5% to 50% coverage. For those aged 18-24 years, the corresponding time was 132 days, while the 24- to 36-year-olds took longer than any other age group, 135 days, to reach the 50%-with-at-least-one-dose milestone. The time, in turn, decreased for each group as age increased, with those aged 75 and older taking just 41 days to get at least one dose in 50% of individuals, the CDC data show.
That trend also applies to full vaccination, for the most part. The oldest group, 75 and older, had the shortest time to 50% being fully vaccinated at 69 days, and the 25- to 39-year-olds had the longest time at 206 days, with the length rising as age decreased and dropping for groups younger than 25-39. Except for the 12- to 15-year-olds. It has been 160 days (as of Nov. 2) since the 5% mark was reached on May 17, but only 47.4% of the group is fully vaccinated, making it unlikely that the 50% mark will be reached earlier than the 169 days it took the 16- to 17-year-olds.
So where does that put the 5- to 11-year-olds?
The White House said on Nov. 1 that vaccinations could start the first week of November, pending approval from the CDC’s Advisory Committee on Immunization Practices, which meets on Nov. 2. “This is an important step forward in our nation’s fight against the virus,” Jeff Zients, the White House COVID-19 Response Coordinator, said in a briefing. “As we await the CDC decision, we are not waiting on the operations and logistics. In fact, we’ve been preparing for weeks.”
Availability, of course, is not the only factor involved. In a survey conducted Oct. 14-24, the Kaiser Family Foundation found that only 27% of parents of children aged 5-11 years are planning to have them vaccinated against COVID-19 “right away” once the vaccine is available, and that 33% would “wait and see” how the vaccine works.
“Parents of 5-11 year-olds cite a range of concerns when it comes to vaccinating their children for COVID-19, with safety issues topping off the list,” and “two-thirds say they are concerned the vaccine may negatively impact their child’s fertility in the future,” Kaiser said.
With children aged 5-11 years about to enter the battle-of-the-COVID-vaccine phase of the war on COVID, there are many questions. MDedge takes a look at one: How long will it take to get 5- to 11-year-olds vaccinated?
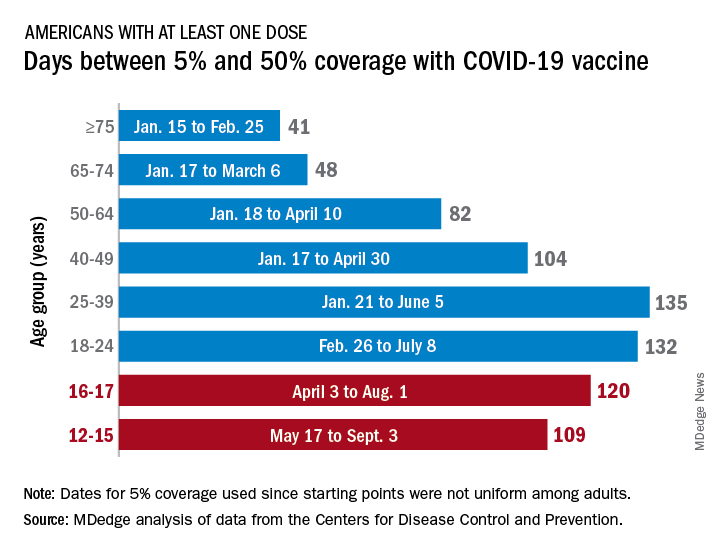
Previous experience may provide some guidance. The vaccine was approved by the Centers for Disease Control and Prevention for the closest group in age, 12- to 15-year-olds, on May 12, 2021, and according to data from the CDC.
(Use of the 5% figure acknowledges the uneven start after approval – the vaccine became available to different age groups at different times, even though it had been approved for all adults aged 18 years and older.)
The 16- to 17-year-olds, despite being a smaller group of less than 7.6 million individuals, took 120 days to go from 5% to 50% coverage. For those aged 18-24 years, the corresponding time was 132 days, while the 24- to 36-year-olds took longer than any other age group, 135 days, to reach the 50%-with-at-least-one-dose milestone. The time, in turn, decreased for each group as age increased, with those aged 75 and older taking just 41 days to get at least one dose in 50% of individuals, the CDC data show.
That trend also applies to full vaccination, for the most part. The oldest group, 75 and older, had the shortest time to 50% being fully vaccinated at 69 days, and the 25- to 39-year-olds had the longest time at 206 days, with the length rising as age decreased and dropping for groups younger than 25-39. Except for the 12- to 15-year-olds. It has been 160 days (as of Nov. 2) since the 5% mark was reached on May 17, but only 47.4% of the group is fully vaccinated, making it unlikely that the 50% mark will be reached earlier than the 169 days it took the 16- to 17-year-olds.
So where does that put the 5- to 11-year-olds?
The White House said on Nov. 1 that vaccinations could start the first week of November, pending approval from the CDC’s Advisory Committee on Immunization Practices, which meets on Nov. 2. “This is an important step forward in our nation’s fight against the virus,” Jeff Zients, the White House COVID-19 Response Coordinator, said in a briefing. “As we await the CDC decision, we are not waiting on the operations and logistics. In fact, we’ve been preparing for weeks.”
Availability, of course, is not the only factor involved. In a survey conducted Oct. 14-24, the Kaiser Family Foundation found that only 27% of parents of children aged 5-11 years are planning to have them vaccinated against COVID-19 “right away” once the vaccine is available, and that 33% would “wait and see” how the vaccine works.
“Parents of 5-11 year-olds cite a range of concerns when it comes to vaccinating their children for COVID-19, with safety issues topping off the list,” and “two-thirds say they are concerned the vaccine may negatively impact their child’s fertility in the future,” Kaiser said.
With children aged 5-11 years about to enter the battle-of-the-COVID-vaccine phase of the war on COVID, there are many questions. MDedge takes a look at one: How long will it take to get 5- to 11-year-olds vaccinated?
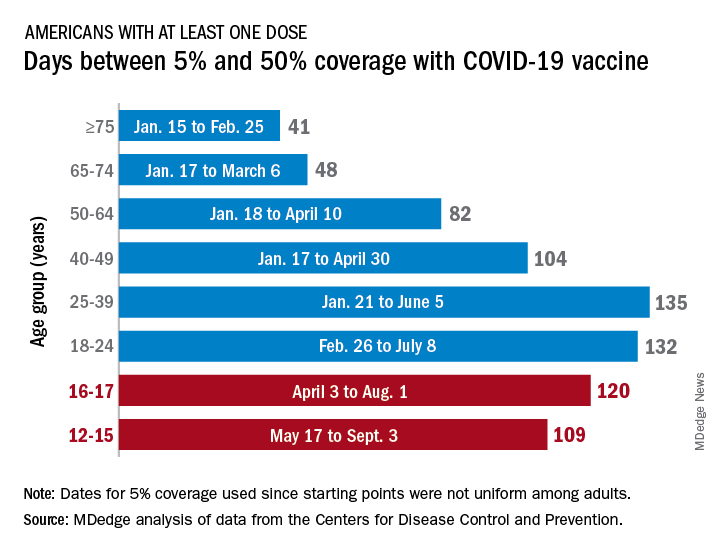
Previous experience may provide some guidance. The vaccine was approved by the Centers for Disease Control and Prevention for the closest group in age, 12- to 15-year-olds, on May 12, 2021, and according to data from the CDC.
(Use of the 5% figure acknowledges the uneven start after approval – the vaccine became available to different age groups at different times, even though it had been approved for all adults aged 18 years and older.)
The 16- to 17-year-olds, despite being a smaller group of less than 7.6 million individuals, took 120 days to go from 5% to 50% coverage. For those aged 18-24 years, the corresponding time was 132 days, while the 24- to 36-year-olds took longer than any other age group, 135 days, to reach the 50%-with-at-least-one-dose milestone. The time, in turn, decreased for each group as age increased, with those aged 75 and older taking just 41 days to get at least one dose in 50% of individuals, the CDC data show.
That trend also applies to full vaccination, for the most part. The oldest group, 75 and older, had the shortest time to 50% being fully vaccinated at 69 days, and the 25- to 39-year-olds had the longest time at 206 days, with the length rising as age decreased and dropping for groups younger than 25-39. Except for the 12- to 15-year-olds. It has been 160 days (as of Nov. 2) since the 5% mark was reached on May 17, but only 47.4% of the group is fully vaccinated, making it unlikely that the 50% mark will be reached earlier than the 169 days it took the 16- to 17-year-olds.
So where does that put the 5- to 11-year-olds?
The White House said on Nov. 1 that vaccinations could start the first week of November, pending approval from the CDC’s Advisory Committee on Immunization Practices, which meets on Nov. 2. “This is an important step forward in our nation’s fight against the virus,” Jeff Zients, the White House COVID-19 Response Coordinator, said in a briefing. “As we await the CDC decision, we are not waiting on the operations and logistics. In fact, we’ve been preparing for weeks.”
Availability, of course, is not the only factor involved. In a survey conducted Oct. 14-24, the Kaiser Family Foundation found that only 27% of parents of children aged 5-11 years are planning to have them vaccinated against COVID-19 “right away” once the vaccine is available, and that 33% would “wait and see” how the vaccine works.
“Parents of 5-11 year-olds cite a range of concerns when it comes to vaccinating their children for COVID-19, with safety issues topping off the list,” and “two-thirds say they are concerned the vaccine may negatively impact their child’s fertility in the future,” Kaiser said.
The impact of modifiable risk factors such as diet and obesity in Pediatric MS patients
James Nicholas Brenton, M.D., is the director of the University of Virginia’s Pediatric and Young Adult MS and Related Disorders Clinic. He is also associate professor of neurology and pediatrics for clinical research and performs collaborative clinical research within the field of pediatric MS. His research focuses on pediatric demyelinating disease and autoimmune epilepsies.
As the director of a clinic focusing on pediatric and young adults MS and related disorders, how do modifiable risk factors such as obesity, smoking, et cetera, increase the risk of MS in general?
Dr. Brenton: There are several risk factors for pediatric-onset MS. When I say pediatric-onset, I'm referring to patients with clinical onset of MS prior to the age of 18 years. Some MS risk factors are not considered “modifiable,” such as genetic risks. The greatest genetic risk for MS is related to specific haplotypes in the HLA-DRB1 gene. Another risk factor that is less amenable to modification is early exposure to certain viruses, like the Epstein-Barr virus (Makhani, et al 2016).
On the other hand, there are several potentially modifiable risk factors for MS. This includes smoking - either first or second-hand smoke. In the case of pediatric MS patients, it is most often related to second-hand (or passive) smoke exposure (Lavery, et al 2019). Another example of a modifiable MS risk factor is vitamin D deficiency. Vitamin D levels are influenced significantly by duration and intensity of direct exposure to sunlight, which depends (in part) on the geographic location of where you grow up. For example, those who live at higher latitudes (e.g. live further away from the equator) have less exposure to direct sunlight than a child who lives at lower latitudes (e.g. closer to the equator) (Banwell, et al 2011).
Obesity during childhood or adolescence is another modifiable risk factor for MS. Obesity’s risk for MS (like smoking) is dose-dependent – meaning, the more obese that you are, the higher your overall risk for future development of MS. In fact, the BMI in children with MS is markedly higher than their non-MS peers, and begins in early childhood, years before the clinical onset of the disease (Brenton, et al 2019).
There is mixed evidence regarding the impact of certain perinatal factors on future risk for MS. For example, some literature suggests that Caesarean delivery increases the risk of MS (Maghzi, et al 2012). Our research has found that infantile breastfeeding is associated with a lower future risk of pediatric-onset MS (Brenton, et al 2017).
Children are two to three times more likely to experience MS relapses compared with adults. How likely is it for the childhood obesity epidemic to lead to increased morbidity from MS or CIS, particularly in adolescent girls?
Dr. Brenton: Obesity is a systemic disease that manifests as excessive or abnormal accumulation of body fat. We know that chronic obesity leads to higher overall morbidity, lower quality of life, and reduced life expectancy. There are several common co-morbidities associated with obesity - like cardiovascular disease, type II diabetes mellitus, hypertension, polycystic ovarian syndrome, dyslipidemia, infertility, and some cancers (Abdelaal, et al 2017). Certainly, all these implications for the general population would pertain to those with MS who exhibit chronic obesity.
While we have fairly good evidence that obesity is a causal risk factor for the development of MS, there actually is a paucity of literature that has studied the impact of persistent obesity on an already established MS disease state. Several recent studies show that obesity is associated with a pro-inflammatory state in the blood and cerebrospinal fluid of MS patients (Stampanoni, et al 2019). There are other studies that shown a direct association between MS-related neurologic disability and obesity – such that those with a greater waist circumference exhibit higher rates of neurologic disability (Fitzgerald, et al 2019).
Recent studies have assessed whether SNAP factors are associated with health outcomes. How does a modifiable SNAP risk score in people with multiple sclerosis impacts the likelihood of disability worsening??
Dr. Brenton: SNAP factors may not be as well known to some people in this field. SNAP factors refer to smoking (“S”), poor nutrition (“N”), alcohol consumption (“A”) and insufficient physical activity (“P”). These four factors appear to be the most preventable causes of morbidity within the general population. SNAP factors are common in people with MS. The most common SNAP factors in MS patients are poor nutrition and insufficient physical activity. Cross-sectionally, these factors appear to be associated with worsening neurologic disability (Marck, et al 2019).
There is data suggesting that SNAP factors, particularly those that increase over time, can associate with worsening disability when followed over several years. Importantly, your baseline SNAP score does not appear to predict your future level of disability (Marck, et al 2019). Collective SNAP scores have not yet been well-studied in pediatric MS patients, but are important to study - particularly given that children with MS reach maximum neurologic disability at a younger age than adult-onset MS patients (Renoux, et al 2007).
What are some of the best practices MS health care providers can engage in to promote exercise and rehabilitative protocols to significantly impact the physical and cognitive performance of MS patients?
Dr. Brenton: Even though pediatric MS patients exhibit relatively low levels of physical neurologic disability early in their disease, the physical activity levels of youth with MS are quite low. These patients engage in less moderate and vigorous physical activity when you compare them to their non-MS peers (Grover, et al 2016), but we still don't fully understand why this is the case. In fact, it may be related to several different factors - including pain, fatigue, sleep quality, MS disease activity, and psychological factors (such as depression, social anxiety, and perceptions of self-efficacy). In order to truly provide patient-specific interventions that positively impact physical activity we need to better understand what factors to study and how these factors play into the individual patient. For example, if high levels of fatigue are inhibiting a patient from being physically active, the provider should explore sources of fatigue: “how are sleep patterns?”, “are they napping throughout the day?”, “does the fatigue occur only after a period of physical activity, or is it persistent despite how active they are?” These are examples of questions that may lead a neurologist to different approaches for managing reduced physical activity.
Generally speaking however, pediatric and adult MS providers would ideally provide healthy nutrition guidance and counseling to all patients, regardless of their weight. Though there is no particular proven “MS diet,” in general, we recommend a balanced diet that is lower in saturated fats and processed sugars and higher in fruits and vegetables. In the case of a pediatric MS patient, it's important to have the family on board with consuming a healthier diet, as parental involvement increases the likelihood of healthy behavioral changes in the child.
It is important to ask patients targeted questions about their physical activity and assist with goal setting toward achievable targets. If the patient is receptive, a provider can advise on the use of digital interventions, like apps or internet-based social groups that incorporate education, accountability, and self-monitoring. What we do not know yet, but hope to know soon, is if physical activity and/or reducing obesity/improving diet can serve as a modifier of disease in kids and adults with MS. My current research is focused on studying the role of obesity and diet on the clinical course of children with MS. Many others are studying the role of physical activity on the disease course of children with MS. Suffice to say, there is much more to learn on the role of diet, body composition, and physical activity in youth with MS.
Lavery AM, Collins BN, Waldman AT, Hart CN, Bar-Or A, Marrie RA, Arnold D, O'Mahony J, Banwell B. The contribution of secondhand tobacco smoke exposure to pediatric multiple sclerosis risk. Mult Scler. 2019 Apr;25(4):515-522.
Maghzi AH, Etemadifar M, Heshmat-Ghahdarijani K, Nonahal S, Minagar A, Moradi V. Cesarean delivery may increase the risk of multiple sclerosis. Mult Scler. 2012;18:468-471.
Marck CH, Aitken Z, Simpson S, Weiland TJ, Jelinek GA. Does a modifiable risk factor score predict disability worsening in people with multiple sclerosis? Mult Scler J Exp Transl Clin. 2019 Oct 11;5(4):2055217319881769.
Stampanoni Bassi M, Iezzi E, Buttari F, et al. Obesity worsens central inflammation and disability in multiple sclerosis. Mult Scler. 2019:1352458519853473.
James Nicholas Brenton, M.D., is the director of the University of Virginia’s Pediatric and Young Adult MS and Related Disorders Clinic. He is also associate professor of neurology and pediatrics for clinical research and performs collaborative clinical research within the field of pediatric MS. His research focuses on pediatric demyelinating disease and autoimmune epilepsies.
As the director of a clinic focusing on pediatric and young adults MS and related disorders, how do modifiable risk factors such as obesity, smoking, et cetera, increase the risk of MS in general?
Dr. Brenton: There are several risk factors for pediatric-onset MS. When I say pediatric-onset, I'm referring to patients with clinical onset of MS prior to the age of 18 years. Some MS risk factors are not considered “modifiable,” such as genetic risks. The greatest genetic risk for MS is related to specific haplotypes in the HLA-DRB1 gene. Another risk factor that is less amenable to modification is early exposure to certain viruses, like the Epstein-Barr virus (Makhani, et al 2016).
On the other hand, there are several potentially modifiable risk factors for MS. This includes smoking - either first or second-hand smoke. In the case of pediatric MS patients, it is most often related to second-hand (or passive) smoke exposure (Lavery, et al 2019). Another example of a modifiable MS risk factor is vitamin D deficiency. Vitamin D levels are influenced significantly by duration and intensity of direct exposure to sunlight, which depends (in part) on the geographic location of where you grow up. For example, those who live at higher latitudes (e.g. live further away from the equator) have less exposure to direct sunlight than a child who lives at lower latitudes (e.g. closer to the equator) (Banwell, et al 2011).
Obesity during childhood or adolescence is another modifiable risk factor for MS. Obesity’s risk for MS (like smoking) is dose-dependent – meaning, the more obese that you are, the higher your overall risk for future development of MS. In fact, the BMI in children with MS is markedly higher than their non-MS peers, and begins in early childhood, years before the clinical onset of the disease (Brenton, et al 2019).
There is mixed evidence regarding the impact of certain perinatal factors on future risk for MS. For example, some literature suggests that Caesarean delivery increases the risk of MS (Maghzi, et al 2012). Our research has found that infantile breastfeeding is associated with a lower future risk of pediatric-onset MS (Brenton, et al 2017).
Children are two to three times more likely to experience MS relapses compared with adults. How likely is it for the childhood obesity epidemic to lead to increased morbidity from MS or CIS, particularly in adolescent girls?
Dr. Brenton: Obesity is a systemic disease that manifests as excessive or abnormal accumulation of body fat. We know that chronic obesity leads to higher overall morbidity, lower quality of life, and reduced life expectancy. There are several common co-morbidities associated with obesity - like cardiovascular disease, type II diabetes mellitus, hypertension, polycystic ovarian syndrome, dyslipidemia, infertility, and some cancers (Abdelaal, et al 2017). Certainly, all these implications for the general population would pertain to those with MS who exhibit chronic obesity.
While we have fairly good evidence that obesity is a causal risk factor for the development of MS, there actually is a paucity of literature that has studied the impact of persistent obesity on an already established MS disease state. Several recent studies show that obesity is associated with a pro-inflammatory state in the blood and cerebrospinal fluid of MS patients (Stampanoni, et al 2019). There are other studies that shown a direct association between MS-related neurologic disability and obesity – such that those with a greater waist circumference exhibit higher rates of neurologic disability (Fitzgerald, et al 2019).
Recent studies have assessed whether SNAP factors are associated with health outcomes. How does a modifiable SNAP risk score in people with multiple sclerosis impacts the likelihood of disability worsening??
Dr. Brenton: SNAP factors may not be as well known to some people in this field. SNAP factors refer to smoking (“S”), poor nutrition (“N”), alcohol consumption (“A”) and insufficient physical activity (“P”). These four factors appear to be the most preventable causes of morbidity within the general population. SNAP factors are common in people with MS. The most common SNAP factors in MS patients are poor nutrition and insufficient physical activity. Cross-sectionally, these factors appear to be associated with worsening neurologic disability (Marck, et al 2019).
There is data suggesting that SNAP factors, particularly those that increase over time, can associate with worsening disability when followed over several years. Importantly, your baseline SNAP score does not appear to predict your future level of disability (Marck, et al 2019). Collective SNAP scores have not yet been well-studied in pediatric MS patients, but are important to study - particularly given that children with MS reach maximum neurologic disability at a younger age than adult-onset MS patients (Renoux, et al 2007).
What are some of the best practices MS health care providers can engage in to promote exercise and rehabilitative protocols to significantly impact the physical and cognitive performance of MS patients?
Dr. Brenton: Even though pediatric MS patients exhibit relatively low levels of physical neurologic disability early in their disease, the physical activity levels of youth with MS are quite low. These patients engage in less moderate and vigorous physical activity when you compare them to their non-MS peers (Grover, et al 2016), but we still don't fully understand why this is the case. In fact, it may be related to several different factors - including pain, fatigue, sleep quality, MS disease activity, and psychological factors (such as depression, social anxiety, and perceptions of self-efficacy). In order to truly provide patient-specific interventions that positively impact physical activity we need to better understand what factors to study and how these factors play into the individual patient. For example, if high levels of fatigue are inhibiting a patient from being physically active, the provider should explore sources of fatigue: “how are sleep patterns?”, “are they napping throughout the day?”, “does the fatigue occur only after a period of physical activity, or is it persistent despite how active they are?” These are examples of questions that may lead a neurologist to different approaches for managing reduced physical activity.
Generally speaking however, pediatric and adult MS providers would ideally provide healthy nutrition guidance and counseling to all patients, regardless of their weight. Though there is no particular proven “MS diet,” in general, we recommend a balanced diet that is lower in saturated fats and processed sugars and higher in fruits and vegetables. In the case of a pediatric MS patient, it's important to have the family on board with consuming a healthier diet, as parental involvement increases the likelihood of healthy behavioral changes in the child.
It is important to ask patients targeted questions about their physical activity and assist with goal setting toward achievable targets. If the patient is receptive, a provider can advise on the use of digital interventions, like apps or internet-based social groups that incorporate education, accountability, and self-monitoring. What we do not know yet, but hope to know soon, is if physical activity and/or reducing obesity/improving diet can serve as a modifier of disease in kids and adults with MS. My current research is focused on studying the role of obesity and diet on the clinical course of children with MS. Many others are studying the role of physical activity on the disease course of children with MS. Suffice to say, there is much more to learn on the role of diet, body composition, and physical activity in youth with MS.
James Nicholas Brenton, M.D., is the director of the University of Virginia’s Pediatric and Young Adult MS and Related Disorders Clinic. He is also associate professor of neurology and pediatrics for clinical research and performs collaborative clinical research within the field of pediatric MS. His research focuses on pediatric demyelinating disease and autoimmune epilepsies.
As the director of a clinic focusing on pediatric and young adults MS and related disorders, how do modifiable risk factors such as obesity, smoking, et cetera, increase the risk of MS in general?
Dr. Brenton: There are several risk factors for pediatric-onset MS. When I say pediatric-onset, I'm referring to patients with clinical onset of MS prior to the age of 18 years. Some MS risk factors are not considered “modifiable,” such as genetic risks. The greatest genetic risk for MS is related to specific haplotypes in the HLA-DRB1 gene. Another risk factor that is less amenable to modification is early exposure to certain viruses, like the Epstein-Barr virus (Makhani, et al 2016).
On the other hand, there are several potentially modifiable risk factors for MS. This includes smoking - either first or second-hand smoke. In the case of pediatric MS patients, it is most often related to second-hand (or passive) smoke exposure (Lavery, et al 2019). Another example of a modifiable MS risk factor is vitamin D deficiency. Vitamin D levels are influenced significantly by duration and intensity of direct exposure to sunlight, which depends (in part) on the geographic location of where you grow up. For example, those who live at higher latitudes (e.g. live further away from the equator) have less exposure to direct sunlight than a child who lives at lower latitudes (e.g. closer to the equator) (Banwell, et al 2011).
Obesity during childhood or adolescence is another modifiable risk factor for MS. Obesity’s risk for MS (like smoking) is dose-dependent – meaning, the more obese that you are, the higher your overall risk for future development of MS. In fact, the BMI in children with MS is markedly higher than their non-MS peers, and begins in early childhood, years before the clinical onset of the disease (Brenton, et al 2019).
There is mixed evidence regarding the impact of certain perinatal factors on future risk for MS. For example, some literature suggests that Caesarean delivery increases the risk of MS (Maghzi, et al 2012). Our research has found that infantile breastfeeding is associated with a lower future risk of pediatric-onset MS (Brenton, et al 2017).
Children are two to three times more likely to experience MS relapses compared with adults. How likely is it for the childhood obesity epidemic to lead to increased morbidity from MS or CIS, particularly in adolescent girls?
Dr. Brenton: Obesity is a systemic disease that manifests as excessive or abnormal accumulation of body fat. We know that chronic obesity leads to higher overall morbidity, lower quality of life, and reduced life expectancy. There are several common co-morbidities associated with obesity - like cardiovascular disease, type II diabetes mellitus, hypertension, polycystic ovarian syndrome, dyslipidemia, infertility, and some cancers (Abdelaal, et al 2017). Certainly, all these implications for the general population would pertain to those with MS who exhibit chronic obesity.
While we have fairly good evidence that obesity is a causal risk factor for the development of MS, there actually is a paucity of literature that has studied the impact of persistent obesity on an already established MS disease state. Several recent studies show that obesity is associated with a pro-inflammatory state in the blood and cerebrospinal fluid of MS patients (Stampanoni, et al 2019). There are other studies that shown a direct association between MS-related neurologic disability and obesity – such that those with a greater waist circumference exhibit higher rates of neurologic disability (Fitzgerald, et al 2019).
Recent studies have assessed whether SNAP factors are associated with health outcomes. How does a modifiable SNAP risk score in people with multiple sclerosis impacts the likelihood of disability worsening??
Dr. Brenton: SNAP factors may not be as well known to some people in this field. SNAP factors refer to smoking (“S”), poor nutrition (“N”), alcohol consumption (“A”) and insufficient physical activity (“P”). These four factors appear to be the most preventable causes of morbidity within the general population. SNAP factors are common in people with MS. The most common SNAP factors in MS patients are poor nutrition and insufficient physical activity. Cross-sectionally, these factors appear to be associated with worsening neurologic disability (Marck, et al 2019).
There is data suggesting that SNAP factors, particularly those that increase over time, can associate with worsening disability when followed over several years. Importantly, your baseline SNAP score does not appear to predict your future level of disability (Marck, et al 2019). Collective SNAP scores have not yet been well-studied in pediatric MS patients, but are important to study - particularly given that children with MS reach maximum neurologic disability at a younger age than adult-onset MS patients (Renoux, et al 2007).
What are some of the best practices MS health care providers can engage in to promote exercise and rehabilitative protocols to significantly impact the physical and cognitive performance of MS patients?
Dr. Brenton: Even though pediatric MS patients exhibit relatively low levels of physical neurologic disability early in their disease, the physical activity levels of youth with MS are quite low. These patients engage in less moderate and vigorous physical activity when you compare them to their non-MS peers (Grover, et al 2016), but we still don't fully understand why this is the case. In fact, it may be related to several different factors - including pain, fatigue, sleep quality, MS disease activity, and psychological factors (such as depression, social anxiety, and perceptions of self-efficacy). In order to truly provide patient-specific interventions that positively impact physical activity we need to better understand what factors to study and how these factors play into the individual patient. For example, if high levels of fatigue are inhibiting a patient from being physically active, the provider should explore sources of fatigue: “how are sleep patterns?”, “are they napping throughout the day?”, “does the fatigue occur only after a period of physical activity, or is it persistent despite how active they are?” These are examples of questions that may lead a neurologist to different approaches for managing reduced physical activity.
Generally speaking however, pediatric and adult MS providers would ideally provide healthy nutrition guidance and counseling to all patients, regardless of their weight. Though there is no particular proven “MS diet,” in general, we recommend a balanced diet that is lower in saturated fats and processed sugars and higher in fruits and vegetables. In the case of a pediatric MS patient, it's important to have the family on board with consuming a healthier diet, as parental involvement increases the likelihood of healthy behavioral changes in the child.
It is important to ask patients targeted questions about their physical activity and assist with goal setting toward achievable targets. If the patient is receptive, a provider can advise on the use of digital interventions, like apps or internet-based social groups that incorporate education, accountability, and self-monitoring. What we do not know yet, but hope to know soon, is if physical activity and/or reducing obesity/improving diet can serve as a modifier of disease in kids and adults with MS. My current research is focused on studying the role of obesity and diet on the clinical course of children with MS. Many others are studying the role of physical activity on the disease course of children with MS. Suffice to say, there is much more to learn on the role of diet, body composition, and physical activity in youth with MS.
Lavery AM, Collins BN, Waldman AT, Hart CN, Bar-Or A, Marrie RA, Arnold D, O'Mahony J, Banwell B. The contribution of secondhand tobacco smoke exposure to pediatric multiple sclerosis risk. Mult Scler. 2019 Apr;25(4):515-522.
Maghzi AH, Etemadifar M, Heshmat-Ghahdarijani K, Nonahal S, Minagar A, Moradi V. Cesarean delivery may increase the risk of multiple sclerosis. Mult Scler. 2012;18:468-471.
Marck CH, Aitken Z, Simpson S, Weiland TJ, Jelinek GA. Does a modifiable risk factor score predict disability worsening in people with multiple sclerosis? Mult Scler J Exp Transl Clin. 2019 Oct 11;5(4):2055217319881769.
Stampanoni Bassi M, Iezzi E, Buttari F, et al. Obesity worsens central inflammation and disability in multiple sclerosis. Mult Scler. 2019:1352458519853473.
Lavery AM, Collins BN, Waldman AT, Hart CN, Bar-Or A, Marrie RA, Arnold D, O'Mahony J, Banwell B. The contribution of secondhand tobacco smoke exposure to pediatric multiple sclerosis risk. Mult Scler. 2019 Apr;25(4):515-522.
Maghzi AH, Etemadifar M, Heshmat-Ghahdarijani K, Nonahal S, Minagar A, Moradi V. Cesarean delivery may increase the risk of multiple sclerosis. Mult Scler. 2012;18:468-471.
Marck CH, Aitken Z, Simpson S, Weiland TJ, Jelinek GA. Does a modifiable risk factor score predict disability worsening in people with multiple sclerosis? Mult Scler J Exp Transl Clin. 2019 Oct 11;5(4):2055217319881769.
Stampanoni Bassi M, Iezzi E, Buttari F, et al. Obesity worsens central inflammation and disability in multiple sclerosis. Mult Scler. 2019:1352458519853473.
FDA authorizes Pfizer’s COVID-19 vaccine for kids
The move brings families with young children a step closer to resuming their normal activities, and it should help further slow transmission of the coronavirus virus in the United States.
States have already placed their orders for initial doses of the vaccines. The Oct. 29 FDA authorization triggers the shipment of millions of doses to pediatricians, family practice doctors, children’s hospitals, community health centers, and pharmacies.
Next, a panel of experts known as the Advisory Committee on Immunization Practices, or ACIP, will meet Nov. 2 to vote on recommendations for use of the vaccine.
As soon as the Centers for Disease Control and Prevention’s director signs off on those recommendations, children can get the shots, perhaps as early as Nov. 3.
Pfizer’s vaccine for children is 10 micrograms, or one-third of the dose given to teens and adults. Kids get two doses of the vaccine 3 weeks apart. In clinical trials, the most common side effects were pain at the injection site, fatigue, and headache. These side effects were mild and disappeared quickly. There were no serious adverse events detected in the studies, which included about 3,100 children. In one study, the vaccine was 90% effective at preventing COVID-19 infections with symptoms in younger children.
There are about 28 million children in the United States between the ages of 5 and 12.
“As a mother and a physician, I know that parents, caregivers, school staff, and children have been waiting for today’s authorization. Vaccinating younger children against COVID-19 will bring us closer to returning to a sense of normalcy,” Acting FDA Commissioner Janet Woodcock, MD, said in an FDA news release.
“Our comprehensive and rigorous evaluation of the data pertaining to the vaccine’s safety and effectiveness should help assure parents and guardians that this vaccine meets our high standards,” she said.
A version of this article first appeared on WebMD.com.
The move brings families with young children a step closer to resuming their normal activities, and it should help further slow transmission of the coronavirus virus in the United States.
States have already placed their orders for initial doses of the vaccines. The Oct. 29 FDA authorization triggers the shipment of millions of doses to pediatricians, family practice doctors, children’s hospitals, community health centers, and pharmacies.
Next, a panel of experts known as the Advisory Committee on Immunization Practices, or ACIP, will meet Nov. 2 to vote on recommendations for use of the vaccine.
As soon as the Centers for Disease Control and Prevention’s director signs off on those recommendations, children can get the shots, perhaps as early as Nov. 3.
Pfizer’s vaccine for children is 10 micrograms, or one-third of the dose given to teens and adults. Kids get two doses of the vaccine 3 weeks apart. In clinical trials, the most common side effects were pain at the injection site, fatigue, and headache. These side effects were mild and disappeared quickly. There were no serious adverse events detected in the studies, which included about 3,100 children. In one study, the vaccine was 90% effective at preventing COVID-19 infections with symptoms in younger children.
There are about 28 million children in the United States between the ages of 5 and 12.
“As a mother and a physician, I know that parents, caregivers, school staff, and children have been waiting for today’s authorization. Vaccinating younger children against COVID-19 will bring us closer to returning to a sense of normalcy,” Acting FDA Commissioner Janet Woodcock, MD, said in an FDA news release.
“Our comprehensive and rigorous evaluation of the data pertaining to the vaccine’s safety and effectiveness should help assure parents and guardians that this vaccine meets our high standards,” she said.
A version of this article first appeared on WebMD.com.
The move brings families with young children a step closer to resuming their normal activities, and it should help further slow transmission of the coronavirus virus in the United States.
States have already placed their orders for initial doses of the vaccines. The Oct. 29 FDA authorization triggers the shipment of millions of doses to pediatricians, family practice doctors, children’s hospitals, community health centers, and pharmacies.
Next, a panel of experts known as the Advisory Committee on Immunization Practices, or ACIP, will meet Nov. 2 to vote on recommendations for use of the vaccine.
As soon as the Centers for Disease Control and Prevention’s director signs off on those recommendations, children can get the shots, perhaps as early as Nov. 3.
Pfizer’s vaccine for children is 10 micrograms, or one-third of the dose given to teens and adults. Kids get two doses of the vaccine 3 weeks apart. In clinical trials, the most common side effects were pain at the injection site, fatigue, and headache. These side effects were mild and disappeared quickly. There were no serious adverse events detected in the studies, which included about 3,100 children. In one study, the vaccine was 90% effective at preventing COVID-19 infections with symptoms in younger children.
There are about 28 million children in the United States between the ages of 5 and 12.
“As a mother and a physician, I know that parents, caregivers, school staff, and children have been waiting for today’s authorization. Vaccinating younger children against COVID-19 will bring us closer to returning to a sense of normalcy,” Acting FDA Commissioner Janet Woodcock, MD, said in an FDA news release.
“Our comprehensive and rigorous evaluation of the data pertaining to the vaccine’s safety and effectiveness should help assure parents and guardians that this vaccine meets our high standards,” she said.
A version of this article first appeared on WebMD.com.





