User login
How telehealth can work best for our patients
Social distancing measures instituted during the COVID-19 pandemic challenged the usual way of operating in primary care. To continue delivering medical services, physicians had to transition quickly to forms of remote interaction with patients. Use of technology appeared to be the answer. And it gave clinicians the ability to do what many had long hoped for: offer patients the option of telehealth.
The terms telemedicine and telehealth have similar definitions and are commonly used interchangeably. We think most practices probably would have adopted telehealth earlier were it not for reimbursement barriers. In this article, we adopt the World Health Organization’s definition of telemedicine as: “The delivery of healthcare services, where distance is a critical factor, by all healthcare professionals using information and communication technologies for the exchange of valid information for the diagnosis, treatment, and prevention of disease and injuries, research and evaluation, and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities.”1
To provide family medicine clinicians with evidence-based recommendations about telehealth, we conducted a critical review of the literature published through April 30, 2021. The scope of this review includes studies found using the PubMed and Google Scholar databases. In addition, we used the keywords “telehealth,” “telemedicine,” “family medicine,” and “primary care.” We divided this review into 6 sections, including focus areas on implementation in primary care, remote diagnostic accuracy, conditions lending themselves to telehealth, physician and patient perceptions, disparities in telehealth, and finally, the conclusions.
Telehealth implementation in primary care
Telehealth in various forms had been around for years before the pandemic, mainly in the form of commercial telehealth businesses. Telehealth was being used in rural and remote areas where it could be difficult to see a primary care provider—let alone a specialist. The family medicine department of the University of Colorado was an early adopter of telehealth and had navigated this transition since 2017, with clinical champions guiding the process. By 2019, 54% of their clinicians were conducting telehealth encounters.2
However, telehealth implementation elsewhere was not accepted so readily. Before the pandemic, a cross-sectional study of more than 1.1 million patients in Northern California showed that 86% preferred in-person care over video.3 Even as the pandemic began and social distancing measures were implemented, a quality improvement project at a family medicine residency clinic in Florida documented that clinicians still preferred telephone interviews despite the capacity for video visits.4 And many primary care systems were simply unprepared to adopt telehealth technologies.
With time, however, family physicians began to improvise using popular videoconferencing technologies (eg, Zoom) that were readily available and familiar to patients, and medical centers began to repurpose their existing videoconferencing systems.5 The Ohio State University Wexner Medical Center launched a virtual health initiative just before the pandemic struck, at which time fewer than 5% of patient visits were conducted through telehealth. Weeks later, nearly 93% of patient visits were offered through telehealth.6
Reimbursement. Another significant impediment to early telehealth uptake was the late reaction by the Centers for Medicare and Medicaid Services (CMS) in changing the payment system. Hectic expansion of telehealth in response to the crisis pointed to the lack of policies that supported primary care with payments based on outcomes rather than fee-for-service models.7 By the end of April 2020, CMS finally announced that video visits would be reimbursed at the same rate as in-person visits. However, telephone-only visits are still very limited in coverage, and appropriate codes should be verified with payers.
Continue to: Remote diagnosis comes with a caveat
Remote diagnosis comes with a caveat
Some primary care practices have found that images of skin lesions submitted by patients (usually by cell phone) suffice for accurate diagnosis in lieu of office visits.8 With chronic conditions, home-based remote monitoring of vital signs may assist in diagnosing and managing acute issues. More efficient triage of patients is increasingly possible with the receipt of still images or video files of concerning lesions (eg, burns, rash, chronic wounds) sent from smartphones alone9,10 or with devices attached to smartphones (eg, parent-managed otoscopes).11,12
Family physicians historically have relied on in-person visits for holistic assessment and diagnosis. Telehealth video visits have the potential to assist with this goal, but there are risks. For example, one patient cut her foot while swimming and the wound became infected.
Specific conditions usually suitable for telehealth evaluation
The pandemic helped us understand that some situations and conditions are better suited than others to coverage by telehealth. The National Ambulatory Medical Care Survey examined 850 million patient–physician encounters and found that 66% of all ambulatory primary care visits required in-office care,15 suggesting that about one-third of patient encounters could be treated via telehealth.
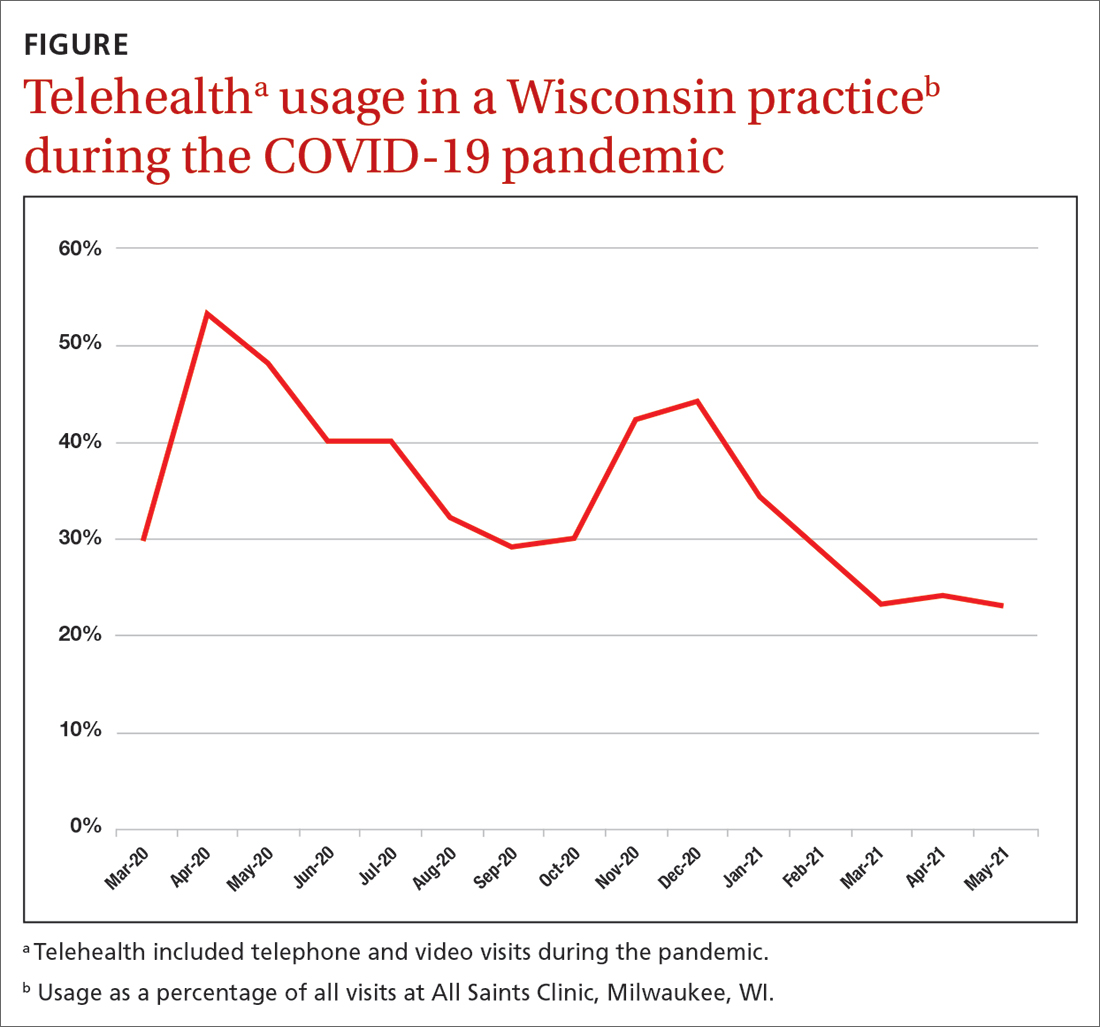
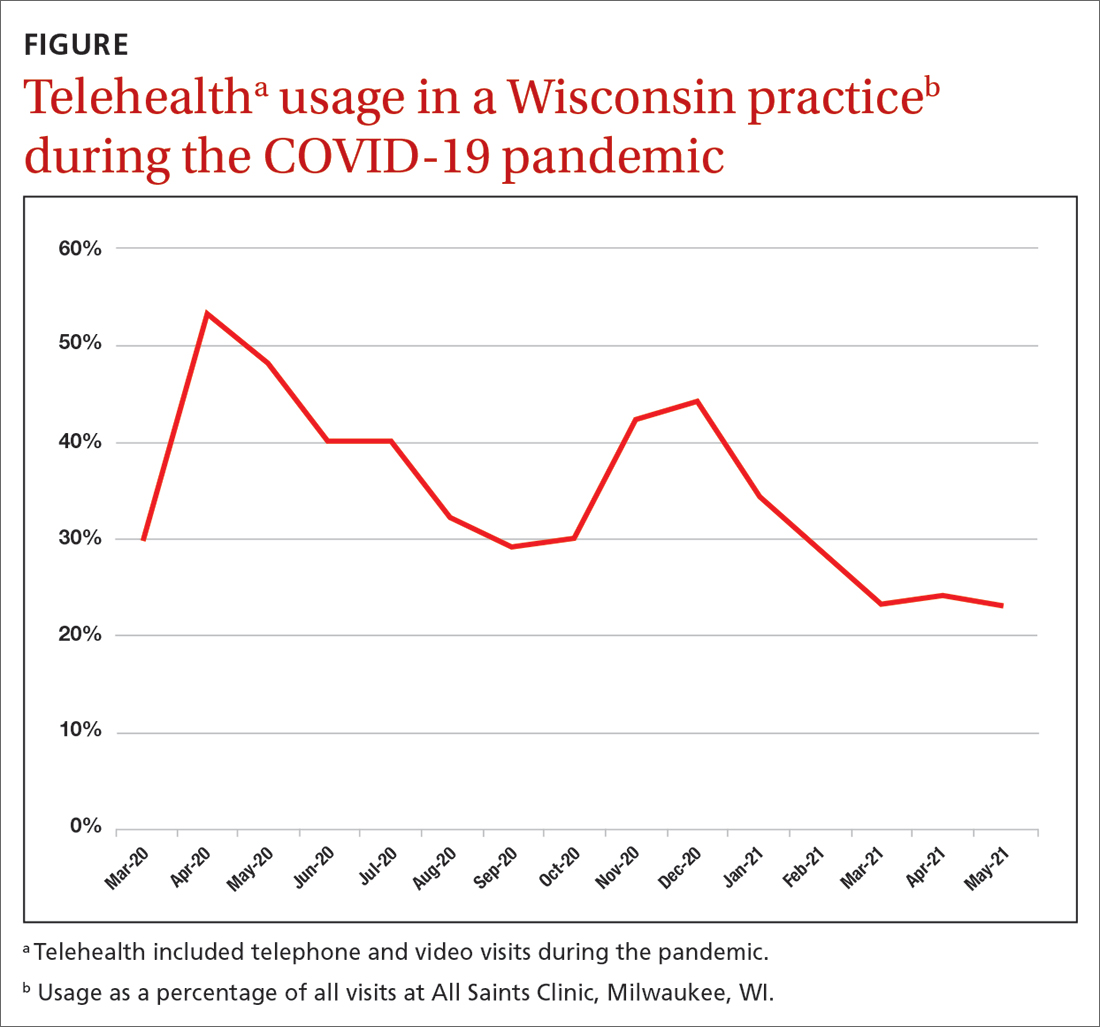
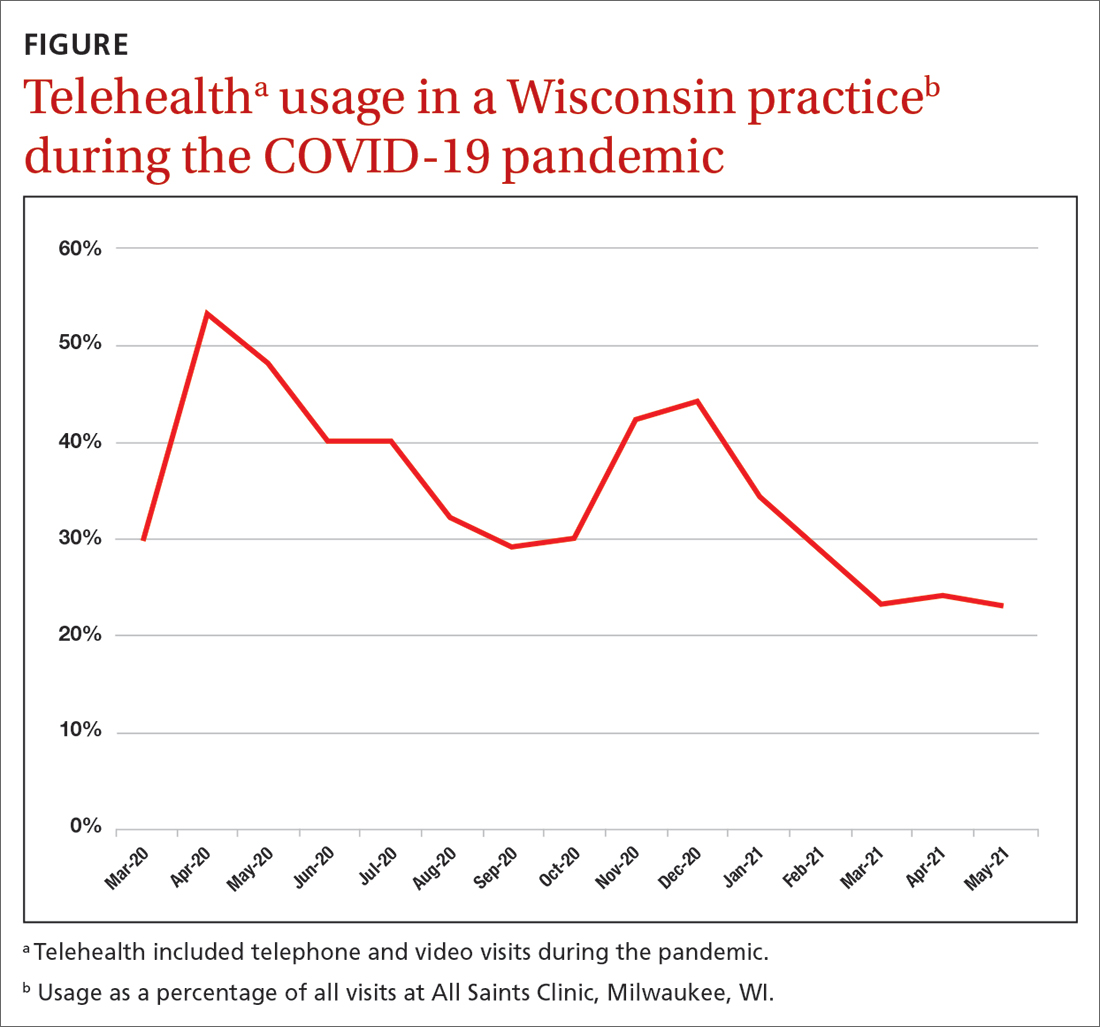
As an example, our southeastern Wisconsin urban clinic has about 20,000 office visits per year. We launched telehealth in March 2020 in direct response to the pandemic. Telehealth usage peaked at the beginning of the pandemic (FIGURE), fell gradually, hit a lower peak in November and December as COVID case counts increased, and then decreased again as our community changed from a “quarantine/lockdown” mentality to “opening up/back to new normal.
Some conditions can be managed favorably with the telehealth format:
Infectious diseases may be treatable remotely.16,17 Following an initial telehealth visit, the physician can evaluate and recommend further care.
Stable, chronic conditions. Telehealth can be used for stable, chronic conditions such as diabetes, chronic obstructive pulmonary disease, and heart failure when lab or imaging studies are not needed.18
Mental health. Telehealth can be useful in counseling and providing mental health and social support.18 Safeguards can be put in place to protect patient privacy in this setting.19
Behavioral change. Telehealth can be effective in providing support for patients actively trying to quit smoking or lose weight, and for caregivers. A physician who “checks in” can be a positive motivator and can promote a patient’s continued success.20
Continue to: Telehealth is less beneficial...
Telehealth is less beneficial when a physical exam is needed to assess pain, tenderness, strength, or other sensations. Office visits also are required for lab assays and imaging, as in periodic checks of A1C levels in patients with diabetes. As technology advances, home-based laboratory kits and sensors likely will change this picture. New patients may be better served through an initial office visit to develop the patient–physician relationship.
Visual assessment of conditions may be limited by telehealth depending on the quality of the devices used. For example, rashes may be difficult to assess given the clarity of the picture on the device and the ability to see only in 2D. There is still a need for more controlled trials to clarify which conditions can be evaluated and managed by telehealth and which ones need in-person care.21
Physician and patient perceptions of telehealth encounters
Research into family physicians’ perceptions of telehealth is scant. However, 3 studies published in 2021 reveal some advantages and challenges for telehealth adoption.
- A qualitative study found that physicians valued the increased access to care for some patients, changes to reimbursement practices not covered before, and the opportunity to see patients’ home environments.22 Disadvantages included an inability to examine the patient, problems with diagnostic accuracy, hindrances to developing personal connections, and the potential for burnout with on-demand care.22 The researchers suggested that telehealth might better serve to augment in-person care.
- A second study found that clinicians are satisfied with the use of telehealth in general. However, it also noted that the lack of physical examination could hinder accurate diagnosis and treatment.23
- A third study surveyed 109 family physicians, reinforcing the importance of physical exams and highlighting the lack of body language as another barrier.24
In addition, all 3 studies noted that video visits are typically briefer than in-person visits. Previous research predominantly done in specialty and mental health care showed that the benefits of telehealth for physicians include an increase in efficiency, reduced commute time, and improved work-life balance.25
Patient perspectives. Many patients have reported that they prefer telehealth because of lower costs, decreased travel time, and faster health care access.26,27 However, patients also have expressed concerns that the telehealth environment may reduce physician attention, can limit personal interaction (and impart a sense of being rushed), and lacks the physical examination that may be key to an adequate diagnosis.28
Continue to: A survey of 223 patients showed...
A survey of 223 patients showed that sicker patients choose in-person care because they want more in-depth visits with more attention to detail than healthier patients do.29 In a Veterans Affairs health care system qualitative study, patients voiced concerns about communicating with physicians via telehealth, including the potential for errors, less attention paid to their needs, audio difficulties, and challenges to establishing a physician–patient relationship.30 Some patients thought telehealth inhibited their personal expression or that the clinician was not attentive enough. These patient reports underscore the importance of patient–clinician relationships developed in person.31 The perceived level of complexity involved in a visit appears to be an essential factor in a patient opting for telehealth—or not.
In light of these known physician and patient perspectives, it seems wise to develop a hybrid model approach in which visits alternate between telehealth and office.
Patient disparities that may limit the use of telehealth
Race and ethnicity is a major factor in telehealth use. Patients who are Black or Hispanic use telehealth services less often than patients who are White.32,33 A study that looked at patients with chronic conditions—hypertension and diabetes—that disproportionately affect Black and Hispanic patients found that patients in these populations with either of these conditions had a lower prevalence of Internet use when compared with White patients.34 However, subpopulations can vary in their usage. For example, a study in East Harlem, New York, found that Hispanic pregnant women used telehealth frequently for prenatal care and perceived the care as satisfactory.35
Age is also a significant variable in the adoption of telehealth, with pre-COVID-19 studies finding lower use of technology among older adults. However, a study performed at the University of Missouri during the first months of the pandemic found an increase in telehealth use in seniors,32 although the increase was in telephone use and not full video sessions.
Many patients in need of health care services may have older devices and/or low-speed or no Internet access; they also may lack the technical know-how to conduct a telehealth visit.4,36 For example, regardless of race or ethnicity, patients on government insurance (Medicaid and Medicare) have been shown to complete more telephone than video visits,37 underscoring the importance of telehealth practice flexibility and the need for increased technology support to decrease the digital divide. Even with adequate technological support and patient training, telehealth may be more complicated if patients have such comorbidities as hearing, visual, or cognitive impairment.31 Patients from a lower socioeconomic status may feel uncomfortable with providers seeing their home environment on video.38
Overall, incorporating telehealth for the care of older and/or vulnerable patients will present a unique set of challenges that organizations must address. Efforts must be made to understand the available technologies and patients’ comfort in using them. A hybrid model offering telehealth and in-office encounters may be the best solution.
Hernan Barenboim, PhD, KPC Health Group, 301 North San Jacinto Street, Hemet, CA 92543; [email protected]
1. WHO. A health telematics policy: in support of WHO’s Health-for-All strategy for global health development. 1997. Accessed February 8, 2023. https://apps.who.int/iris/bitstream/handle/10665/63857/WHO_DGO_98.1.pdf?sequence=1&isAllowed=y
2. Knierim K, Palmer C, Kramer ES, et al. Lessons learned during COVID-19 that can move telehealth in primary care forward. J Am Board Fam Med. Supplement 2021;34(suppl):S196-S202. doi: 10.3122/jabfm.2021.S1.200419
3. Reed ME, Huang J, Graetz I, et al. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw Open. 2020;3:e205873. doi: 10.1001/jamanetworkopen.2020.5873
4. Silver SL, Lewis MN, Ledford CJ. A stepwise transition to telemedicine in response to COVID-19. J Am Board Fam Med. 2021;34(suppl):S152-S161. doi: 10.3122/jabfm.2021.S1.200358
5. Hron JD, Parsons CR, Williams LA, et al. Rapid implementation of an inpatient telehealth program during the COVID-19 pandemic. Appl Clin Inform. 2020;3:452-459. doi: 10.1055/s-0040-1713635
6. Olayiwola JN, Magaña C, Harmon A, et al. Telehealth as a bright spot of the COVID-19 pandemic: recommendations from the virtual frontlines (“Frontweb”). JMIR Public Health Surveill. 2020;6:e19045. doi: 10.2196/19045
7. Gausvik C, Jabbarpour Y. COVID-19 timeline: Centers for Medicare and Medicaid Services (CMS) changes and primary care support were not enough to prevent practice losses. J Am Board Fam Med. 2021;34(suppl):S7-S9. doi: 10.3122/jabfm.2021.S1.200305
8. Marin-Gomez FX, Vidal-Alaball J, Poch PR, et al. Diagnosis of skin lesions using photographs taken with a mobile phone: an online survey of primary care physicians. J Prim Care Community Health. 2020;11:2150132720937831. doi: 10.1177/2150132720937831
9. Garber RN, Garcia E, Goodwin CW, et al. (2020). Pictures do influence the decision to transfer: outcomes of a telemedicine program serving an eight-state rural population. J Burn Care Res. 2020;41:690-694. doi: 10.1093/jbcr/iraa017
10. Felix F, Greenblatt M, Shin L. Saving limbs in the time of COVID. 2020. Accessed February 8, 2023. https://podiatrym.com/pdf/2020/7/FelixGreenblattShin820web.pdf
11. Erkkola-Anttinen N, Irjala H, Laine MK, et al. Smartphone otoscopy performed by parents. Telemed J E Health. 2019;25:477-484. doi: 10.1089/tmj.2018.0062
12. Verzantvoort NC, Teunis T, Verheij TJ, et al. Self-triage for acute primary care via a smartphone application: practical, safe and efficient? PLoS One. 2018;13:e0199284. doi: 10.1371/journal.pone.0199284
13. Hickner J. When patients don’t get the care they should. J Fam Pract. 2020;69:427.
14. Pappan N, Benkhadra R, Papincak D, et al. Values and limits of telemedicine: a case report. SN Compr Clin Med. 2021;3:317-319. doi: 10.1007/s42399-020-00725-y
15. Jabbarpour Y, Jetty A, Westfall M, et al. Not telehealth: which primary care visits need in-person care? J Am Board Fam Med. 2021;34(suppl):S162-S169. doi: 10.3122/jabfm.2021.S1.200247
16. Parmar P, Mackie D, Varghese S, et al. Use of telemedicine technologies in the management of infectious diseases: a review. Clin Infect Dis. 2015;60:1084-1094. doi: 10.1093/cid/ciu1143
17. Young JD, Abdel-Massih R, Herchline T, et al. Infectious Diseases Society of America position statement on Telehealth and Telemedicine as Applied to the Practice of Infectious Diseases. Clin Infect Dis. 2019;68:1437-1443. doi: 10.1093/cid/ciy907
18. ARHQ. Telehealth: mapping the evidence for patient outcomes from systematic reviews. 2016. Accessed March 27, 2023. https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/telehealth_technical-brief.pdf
19. Lustgarten SD, Garrison YL, Sinnard MT, et al. Digital privacy in mental healthcare: current issues and recommendations for technology use. Curr Opin Psychol. 2020;36:25-31. doi: 10.1016/j.copsyc.2020.03.012
20. Baird A, Xia Y, Cheng Y. Consumer perceptions of telehealth for mental health or substance abuse: a Twitter-based topic modeling analysis. JAMIA Open. 2022;5:ooac028. doi: 10.1093/jamiaopen/ooac028
21. Flumignan CD, da Rocha AP, Pinto AC, et al. What do Cochrane systematic reviews say about telemedicine for healthcare? Sao Paulo Med J. 2019;137:184-192. doi: 10.1590/1516-3180.0177240419
22. Gomez T, Anaya YB, Shih KJ, et al. A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19. J Am Board Fam Med. 2021;34(suppl):S61-S70. doi: 10.3122/jabfm.2021.S1.200517
23. Malliaras P, Merolli M, Williams CM, et al. ‘It’s not hands-on therapy, so it’s very limited’: telehealth use and views among allied health clinicians during the coronavirus pandemic. Musculoskelet Sci Pract. 2021;52:102340. doi: 10.1016/j.msksp.2021.102340
24. Gold KJ, Laurie AR, Kinney DR, et al. Video visits: family physician experiences with uptake during the COVID-19 pandemic. Fam Med. 53:207-210. doi: 10.22454/FamMed.2021.613099
25. Björndell C, Premberg A. Physicians’ experiences of video consultation with patients at a public virtual primary care clinic: a qualitative interview study. Scand J Prim Health Care. 2021;39:67-76. doi: 10.1080/02813432.2021.1882082
26. Powell RE, Henstenburg JM, Cooper G, et al. Patient perceptions of telehealth primary care video visits. Ann Fam Med. 2017;15:225-229. doi: 10.1370/afm.2095
27. Imlach F, McKinlay E, Middleton L, et al. Telehealth consultations in general practice during a pandemic lockdown: survey and interviews on patient experiences and preferences. BMC Fam Pract. 2020;21:1-14. doi: 10.1186/s12875-020-01336-1
28. Gordon HS, Solanki P, Bokhour BG, et al. “I’m not feeling like I’m part of the conversation” patients’ perspectives on communicating in clinical video telehealth visits. J Gen Intern Med. 2020;35:1751-1758. doi: 10.1007/s11606-020-05673-w
29. Volcy J, Smith W, Mills K, et al. Assessment of patient and provider satisfaction with the change to telehealth from in-person visits at an academic safety net institution during the COVID-19 pandemic. J Am Board Fam Med. 2021;34(suppl):S71-S76. doi: 10.3122/jabfm.2021.S1.200393
30. Gopal RK, Solanki P, Bokhour BG, et al. Provider, staff, and patient perspectives on medical visits using clinical video telehealth: a foundation for educational initiatives to improve medical care in telehealth. J Nurse Pract. 2021;17:582-587. doi: 10.1016/j.nurpra.2021.02.020
31. Edgoose JY. Exploring the face-to-face: revisiting patient-doctor relationships in a time of expanding telemedicine. J Am Board Fam Med. 2021;34(suppl):S252-S254. doi: 10.3122/jabfm.2021.S1.200398
32. Pierce RP, Stevermer JJ. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. 2023;29:3-9. doi: 10.1177/1357633X20963893
33. Lame M, Leyden D, Platt SL. Geocode maps spotlight disparities in telehealth utilization during the COVID-19 pandemic in New York City. Telemed J E Health. 2021;27:251-253. doi: 10.1089/tmj.2020.0297
34. Jain V, Al Rifai M, Lee MT, et al. Racial and geographic disparities in internet use in the US among patients with hypertension or diabetes: implications for telehealth in the era of COVID-19. Diabetes Care. 2021;44:e15-e17. doi: 10.2337/dc20-2016
35. Futterman I, Rosenfeld E, Toaff M, et al. Addressing disparities in prenatal care via telehealth during COVID-19: prenatal satisfaction survey in East Harlem. Am J Perinatol. 2021;38:88-92. doi: 10.1055/s-0040-1718695
36. Wegermann K, Wilder JM, Parish A, et al. Racial and socioeconomic disparities in utilization of telehealth in patients with liver disease during COVID-19. Dig Dis Sci. 2022;67:93-99. doi: 10.1007/s10620-021-06842-5.
37. ASPE. National survey trends in telehealth use in 2021: disparities in utilization and audio vs. video services. Issue brief: February 21, 2022. Accessed March 27, 2023. https://aspe.hhs.gov/sites/default/files/documents/4e1853c0b4885112b2994680a58af9ed/telehealth-hps-ib.pdf
38. Ukoha EP, Davis K, Yinger M, et al. Ensuring equitable implementation of telemedicine in perinatal care. Obstet Gynecol. 2021;137:487-492. doi: 10.1097/AOG.0000000000004276
Social distancing measures instituted during the COVID-19 pandemic challenged the usual way of operating in primary care. To continue delivering medical services, physicians had to transition quickly to forms of remote interaction with patients. Use of technology appeared to be the answer. And it gave clinicians the ability to do what many had long hoped for: offer patients the option of telehealth.
The terms telemedicine and telehealth have similar definitions and are commonly used interchangeably. We think most practices probably would have adopted telehealth earlier were it not for reimbursement barriers. In this article, we adopt the World Health Organization’s definition of telemedicine as: “The delivery of healthcare services, where distance is a critical factor, by all healthcare professionals using information and communication technologies for the exchange of valid information for the diagnosis, treatment, and prevention of disease and injuries, research and evaluation, and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities.”1
To provide family medicine clinicians with evidence-based recommendations about telehealth, we conducted a critical review of the literature published through April 30, 2021. The scope of this review includes studies found using the PubMed and Google Scholar databases. In addition, we used the keywords “telehealth,” “telemedicine,” “family medicine,” and “primary care.” We divided this review into 6 sections, including focus areas on implementation in primary care, remote diagnostic accuracy, conditions lending themselves to telehealth, physician and patient perceptions, disparities in telehealth, and finally, the conclusions.
Telehealth implementation in primary care
Telehealth in various forms had been around for years before the pandemic, mainly in the form of commercial telehealth businesses. Telehealth was being used in rural and remote areas where it could be difficult to see a primary care provider—let alone a specialist. The family medicine department of the University of Colorado was an early adopter of telehealth and had navigated this transition since 2017, with clinical champions guiding the process. By 2019, 54% of their clinicians were conducting telehealth encounters.2
However, telehealth implementation elsewhere was not accepted so readily. Before the pandemic, a cross-sectional study of more than 1.1 million patients in Northern California showed that 86% preferred in-person care over video.3 Even as the pandemic began and social distancing measures were implemented, a quality improvement project at a family medicine residency clinic in Florida documented that clinicians still preferred telephone interviews despite the capacity for video visits.4 And many primary care systems were simply unprepared to adopt telehealth technologies.
With time, however, family physicians began to improvise using popular videoconferencing technologies (eg, Zoom) that were readily available and familiar to patients, and medical centers began to repurpose their existing videoconferencing systems.5 The Ohio State University Wexner Medical Center launched a virtual health initiative just before the pandemic struck, at which time fewer than 5% of patient visits were conducted through telehealth. Weeks later, nearly 93% of patient visits were offered through telehealth.6
Reimbursement. Another significant impediment to early telehealth uptake was the late reaction by the Centers for Medicare and Medicaid Services (CMS) in changing the payment system. Hectic expansion of telehealth in response to the crisis pointed to the lack of policies that supported primary care with payments based on outcomes rather than fee-for-service models.7 By the end of April 2020, CMS finally announced that video visits would be reimbursed at the same rate as in-person visits. However, telephone-only visits are still very limited in coverage, and appropriate codes should be verified with payers.
Continue to: Remote diagnosis comes with a caveat
Remote diagnosis comes with a caveat
Some primary care practices have found that images of skin lesions submitted by patients (usually by cell phone) suffice for accurate diagnosis in lieu of office visits.8 With chronic conditions, home-based remote monitoring of vital signs may assist in diagnosing and managing acute issues. More efficient triage of patients is increasingly possible with the receipt of still images or video files of concerning lesions (eg, burns, rash, chronic wounds) sent from smartphones alone9,10 or with devices attached to smartphones (eg, parent-managed otoscopes).11,12
Family physicians historically have relied on in-person visits for holistic assessment and diagnosis. Telehealth video visits have the potential to assist with this goal, but there are risks. For example, one patient cut her foot while swimming and the wound became infected.
Specific conditions usually suitable for telehealth evaluation
The pandemic helped us understand that some situations and conditions are better suited than others to coverage by telehealth. The National Ambulatory Medical Care Survey examined 850 million patient–physician encounters and found that 66% of all ambulatory primary care visits required in-office care,15 suggesting that about one-third of patient encounters could be treated via telehealth.
As an example, our southeastern Wisconsin urban clinic has about 20,000 office visits per year. We launched telehealth in March 2020 in direct response to the pandemic. Telehealth usage peaked at the beginning of the pandemic (FIGURE), fell gradually, hit a lower peak in November and December as COVID case counts increased, and then decreased again as our community changed from a “quarantine/lockdown” mentality to “opening up/back to new normal.
Some conditions can be managed favorably with the telehealth format:
Infectious diseases may be treatable remotely.16,17 Following an initial telehealth visit, the physician can evaluate and recommend further care.
Stable, chronic conditions. Telehealth can be used for stable, chronic conditions such as diabetes, chronic obstructive pulmonary disease, and heart failure when lab or imaging studies are not needed.18
Mental health. Telehealth can be useful in counseling and providing mental health and social support.18 Safeguards can be put in place to protect patient privacy in this setting.19
Behavioral change. Telehealth can be effective in providing support for patients actively trying to quit smoking or lose weight, and for caregivers. A physician who “checks in” can be a positive motivator and can promote a patient’s continued success.20
Continue to: Telehealth is less beneficial...
Telehealth is less beneficial when a physical exam is needed to assess pain, tenderness, strength, or other sensations. Office visits also are required for lab assays and imaging, as in periodic checks of A1C levels in patients with diabetes. As technology advances, home-based laboratory kits and sensors likely will change this picture. New patients may be better served through an initial office visit to develop the patient–physician relationship.
Visual assessment of conditions may be limited by telehealth depending on the quality of the devices used. For example, rashes may be difficult to assess given the clarity of the picture on the device and the ability to see only in 2D. There is still a need for more controlled trials to clarify which conditions can be evaluated and managed by telehealth and which ones need in-person care.21
Physician and patient perceptions of telehealth encounters
Research into family physicians’ perceptions of telehealth is scant. However, 3 studies published in 2021 reveal some advantages and challenges for telehealth adoption.
- A qualitative study found that physicians valued the increased access to care for some patients, changes to reimbursement practices not covered before, and the opportunity to see patients’ home environments.22 Disadvantages included an inability to examine the patient, problems with diagnostic accuracy, hindrances to developing personal connections, and the potential for burnout with on-demand care.22 The researchers suggested that telehealth might better serve to augment in-person care.
- A second study found that clinicians are satisfied with the use of telehealth in general. However, it also noted that the lack of physical examination could hinder accurate diagnosis and treatment.23
- A third study surveyed 109 family physicians, reinforcing the importance of physical exams and highlighting the lack of body language as another barrier.24
In addition, all 3 studies noted that video visits are typically briefer than in-person visits. Previous research predominantly done in specialty and mental health care showed that the benefits of telehealth for physicians include an increase in efficiency, reduced commute time, and improved work-life balance.25
Patient perspectives. Many patients have reported that they prefer telehealth because of lower costs, decreased travel time, and faster health care access.26,27 However, patients also have expressed concerns that the telehealth environment may reduce physician attention, can limit personal interaction (and impart a sense of being rushed), and lacks the physical examination that may be key to an adequate diagnosis.28
Continue to: A survey of 223 patients showed...
A survey of 223 patients showed that sicker patients choose in-person care because they want more in-depth visits with more attention to detail than healthier patients do.29 In a Veterans Affairs health care system qualitative study, patients voiced concerns about communicating with physicians via telehealth, including the potential for errors, less attention paid to their needs, audio difficulties, and challenges to establishing a physician–patient relationship.30 Some patients thought telehealth inhibited their personal expression or that the clinician was not attentive enough. These patient reports underscore the importance of patient–clinician relationships developed in person.31 The perceived level of complexity involved in a visit appears to be an essential factor in a patient opting for telehealth—or not.
In light of these known physician and patient perspectives, it seems wise to develop a hybrid model approach in which visits alternate between telehealth and office.
Patient disparities that may limit the use of telehealth
Race and ethnicity is a major factor in telehealth use. Patients who are Black or Hispanic use telehealth services less often than patients who are White.32,33 A study that looked at patients with chronic conditions—hypertension and diabetes—that disproportionately affect Black and Hispanic patients found that patients in these populations with either of these conditions had a lower prevalence of Internet use when compared with White patients.34 However, subpopulations can vary in their usage. For example, a study in East Harlem, New York, found that Hispanic pregnant women used telehealth frequently for prenatal care and perceived the care as satisfactory.35
Age is also a significant variable in the adoption of telehealth, with pre-COVID-19 studies finding lower use of technology among older adults. However, a study performed at the University of Missouri during the first months of the pandemic found an increase in telehealth use in seniors,32 although the increase was in telephone use and not full video sessions.
Many patients in need of health care services may have older devices and/or low-speed or no Internet access; they also may lack the technical know-how to conduct a telehealth visit.4,36 For example, regardless of race or ethnicity, patients on government insurance (Medicaid and Medicare) have been shown to complete more telephone than video visits,37 underscoring the importance of telehealth practice flexibility and the need for increased technology support to decrease the digital divide. Even with adequate technological support and patient training, telehealth may be more complicated if patients have such comorbidities as hearing, visual, or cognitive impairment.31 Patients from a lower socioeconomic status may feel uncomfortable with providers seeing their home environment on video.38
Overall, incorporating telehealth for the care of older and/or vulnerable patients will present a unique set of challenges that organizations must address. Efforts must be made to understand the available technologies and patients’ comfort in using them. A hybrid model offering telehealth and in-office encounters may be the best solution.
Hernan Barenboim, PhD, KPC Health Group, 301 North San Jacinto Street, Hemet, CA 92543; [email protected]
Social distancing measures instituted during the COVID-19 pandemic challenged the usual way of operating in primary care. To continue delivering medical services, physicians had to transition quickly to forms of remote interaction with patients. Use of technology appeared to be the answer. And it gave clinicians the ability to do what many had long hoped for: offer patients the option of telehealth.
The terms telemedicine and telehealth have similar definitions and are commonly used interchangeably. We think most practices probably would have adopted telehealth earlier were it not for reimbursement barriers. In this article, we adopt the World Health Organization’s definition of telemedicine as: “The delivery of healthcare services, where distance is a critical factor, by all healthcare professionals using information and communication technologies for the exchange of valid information for the diagnosis, treatment, and prevention of disease and injuries, research and evaluation, and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities.”1
To provide family medicine clinicians with evidence-based recommendations about telehealth, we conducted a critical review of the literature published through April 30, 2021. The scope of this review includes studies found using the PubMed and Google Scholar databases. In addition, we used the keywords “telehealth,” “telemedicine,” “family medicine,” and “primary care.” We divided this review into 6 sections, including focus areas on implementation in primary care, remote diagnostic accuracy, conditions lending themselves to telehealth, physician and patient perceptions, disparities in telehealth, and finally, the conclusions.
Telehealth implementation in primary care
Telehealth in various forms had been around for years before the pandemic, mainly in the form of commercial telehealth businesses. Telehealth was being used in rural and remote areas where it could be difficult to see a primary care provider—let alone a specialist. The family medicine department of the University of Colorado was an early adopter of telehealth and had navigated this transition since 2017, with clinical champions guiding the process. By 2019, 54% of their clinicians were conducting telehealth encounters.2
However, telehealth implementation elsewhere was not accepted so readily. Before the pandemic, a cross-sectional study of more than 1.1 million patients in Northern California showed that 86% preferred in-person care over video.3 Even as the pandemic began and social distancing measures were implemented, a quality improvement project at a family medicine residency clinic in Florida documented that clinicians still preferred telephone interviews despite the capacity for video visits.4 And many primary care systems were simply unprepared to adopt telehealth technologies.
With time, however, family physicians began to improvise using popular videoconferencing technologies (eg, Zoom) that were readily available and familiar to patients, and medical centers began to repurpose their existing videoconferencing systems.5 The Ohio State University Wexner Medical Center launched a virtual health initiative just before the pandemic struck, at which time fewer than 5% of patient visits were conducted through telehealth. Weeks later, nearly 93% of patient visits were offered through telehealth.6
Reimbursement. Another significant impediment to early telehealth uptake was the late reaction by the Centers for Medicare and Medicaid Services (CMS) in changing the payment system. Hectic expansion of telehealth in response to the crisis pointed to the lack of policies that supported primary care with payments based on outcomes rather than fee-for-service models.7 By the end of April 2020, CMS finally announced that video visits would be reimbursed at the same rate as in-person visits. However, telephone-only visits are still very limited in coverage, and appropriate codes should be verified with payers.
Continue to: Remote diagnosis comes with a caveat
Remote diagnosis comes with a caveat
Some primary care practices have found that images of skin lesions submitted by patients (usually by cell phone) suffice for accurate diagnosis in lieu of office visits.8 With chronic conditions, home-based remote monitoring of vital signs may assist in diagnosing and managing acute issues. More efficient triage of patients is increasingly possible with the receipt of still images or video files of concerning lesions (eg, burns, rash, chronic wounds) sent from smartphones alone9,10 or with devices attached to smartphones (eg, parent-managed otoscopes).11,12
Family physicians historically have relied on in-person visits for holistic assessment and diagnosis. Telehealth video visits have the potential to assist with this goal, but there are risks. For example, one patient cut her foot while swimming and the wound became infected.
Specific conditions usually suitable for telehealth evaluation
The pandemic helped us understand that some situations and conditions are better suited than others to coverage by telehealth. The National Ambulatory Medical Care Survey examined 850 million patient–physician encounters and found that 66% of all ambulatory primary care visits required in-office care,15 suggesting that about one-third of patient encounters could be treated via telehealth.
As an example, our southeastern Wisconsin urban clinic has about 20,000 office visits per year. We launched telehealth in March 2020 in direct response to the pandemic. Telehealth usage peaked at the beginning of the pandemic (FIGURE), fell gradually, hit a lower peak in November and December as COVID case counts increased, and then decreased again as our community changed from a “quarantine/lockdown” mentality to “opening up/back to new normal.
Some conditions can be managed favorably with the telehealth format:
Infectious diseases may be treatable remotely.16,17 Following an initial telehealth visit, the physician can evaluate and recommend further care.
Stable, chronic conditions. Telehealth can be used for stable, chronic conditions such as diabetes, chronic obstructive pulmonary disease, and heart failure when lab or imaging studies are not needed.18
Mental health. Telehealth can be useful in counseling and providing mental health and social support.18 Safeguards can be put in place to protect patient privacy in this setting.19
Behavioral change. Telehealth can be effective in providing support for patients actively trying to quit smoking or lose weight, and for caregivers. A physician who “checks in” can be a positive motivator and can promote a patient’s continued success.20
Continue to: Telehealth is less beneficial...
Telehealth is less beneficial when a physical exam is needed to assess pain, tenderness, strength, or other sensations. Office visits also are required for lab assays and imaging, as in periodic checks of A1C levels in patients with diabetes. As technology advances, home-based laboratory kits and sensors likely will change this picture. New patients may be better served through an initial office visit to develop the patient–physician relationship.
Visual assessment of conditions may be limited by telehealth depending on the quality of the devices used. For example, rashes may be difficult to assess given the clarity of the picture on the device and the ability to see only in 2D. There is still a need for more controlled trials to clarify which conditions can be evaluated and managed by telehealth and which ones need in-person care.21
Physician and patient perceptions of telehealth encounters
Research into family physicians’ perceptions of telehealth is scant. However, 3 studies published in 2021 reveal some advantages and challenges for telehealth adoption.
- A qualitative study found that physicians valued the increased access to care for some patients, changes to reimbursement practices not covered before, and the opportunity to see patients’ home environments.22 Disadvantages included an inability to examine the patient, problems with diagnostic accuracy, hindrances to developing personal connections, and the potential for burnout with on-demand care.22 The researchers suggested that telehealth might better serve to augment in-person care.
- A second study found that clinicians are satisfied with the use of telehealth in general. However, it also noted that the lack of physical examination could hinder accurate diagnosis and treatment.23
- A third study surveyed 109 family physicians, reinforcing the importance of physical exams and highlighting the lack of body language as another barrier.24
In addition, all 3 studies noted that video visits are typically briefer than in-person visits. Previous research predominantly done in specialty and mental health care showed that the benefits of telehealth for physicians include an increase in efficiency, reduced commute time, and improved work-life balance.25
Patient perspectives. Many patients have reported that they prefer telehealth because of lower costs, decreased travel time, and faster health care access.26,27 However, patients also have expressed concerns that the telehealth environment may reduce physician attention, can limit personal interaction (and impart a sense of being rushed), and lacks the physical examination that may be key to an adequate diagnosis.28
Continue to: A survey of 223 patients showed...
A survey of 223 patients showed that sicker patients choose in-person care because they want more in-depth visits with more attention to detail than healthier patients do.29 In a Veterans Affairs health care system qualitative study, patients voiced concerns about communicating with physicians via telehealth, including the potential for errors, less attention paid to their needs, audio difficulties, and challenges to establishing a physician–patient relationship.30 Some patients thought telehealth inhibited their personal expression or that the clinician was not attentive enough. These patient reports underscore the importance of patient–clinician relationships developed in person.31 The perceived level of complexity involved in a visit appears to be an essential factor in a patient opting for telehealth—or not.
In light of these known physician and patient perspectives, it seems wise to develop a hybrid model approach in which visits alternate between telehealth and office.
Patient disparities that may limit the use of telehealth
Race and ethnicity is a major factor in telehealth use. Patients who are Black or Hispanic use telehealth services less often than patients who are White.32,33 A study that looked at patients with chronic conditions—hypertension and diabetes—that disproportionately affect Black and Hispanic patients found that patients in these populations with either of these conditions had a lower prevalence of Internet use when compared with White patients.34 However, subpopulations can vary in their usage. For example, a study in East Harlem, New York, found that Hispanic pregnant women used telehealth frequently for prenatal care and perceived the care as satisfactory.35
Age is also a significant variable in the adoption of telehealth, with pre-COVID-19 studies finding lower use of technology among older adults. However, a study performed at the University of Missouri during the first months of the pandemic found an increase in telehealth use in seniors,32 although the increase was in telephone use and not full video sessions.
Many patients in need of health care services may have older devices and/or low-speed or no Internet access; they also may lack the technical know-how to conduct a telehealth visit.4,36 For example, regardless of race or ethnicity, patients on government insurance (Medicaid and Medicare) have been shown to complete more telephone than video visits,37 underscoring the importance of telehealth practice flexibility and the need for increased technology support to decrease the digital divide. Even with adequate technological support and patient training, telehealth may be more complicated if patients have such comorbidities as hearing, visual, or cognitive impairment.31 Patients from a lower socioeconomic status may feel uncomfortable with providers seeing their home environment on video.38
Overall, incorporating telehealth for the care of older and/or vulnerable patients will present a unique set of challenges that organizations must address. Efforts must be made to understand the available technologies and patients’ comfort in using them. A hybrid model offering telehealth and in-office encounters may be the best solution.
Hernan Barenboim, PhD, KPC Health Group, 301 North San Jacinto Street, Hemet, CA 92543; [email protected]
1. WHO. A health telematics policy: in support of WHO’s Health-for-All strategy for global health development. 1997. Accessed February 8, 2023. https://apps.who.int/iris/bitstream/handle/10665/63857/WHO_DGO_98.1.pdf?sequence=1&isAllowed=y
2. Knierim K, Palmer C, Kramer ES, et al. Lessons learned during COVID-19 that can move telehealth in primary care forward. J Am Board Fam Med. Supplement 2021;34(suppl):S196-S202. doi: 10.3122/jabfm.2021.S1.200419
3. Reed ME, Huang J, Graetz I, et al. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw Open. 2020;3:e205873. doi: 10.1001/jamanetworkopen.2020.5873
4. Silver SL, Lewis MN, Ledford CJ. A stepwise transition to telemedicine in response to COVID-19. J Am Board Fam Med. 2021;34(suppl):S152-S161. doi: 10.3122/jabfm.2021.S1.200358
5. Hron JD, Parsons CR, Williams LA, et al. Rapid implementation of an inpatient telehealth program during the COVID-19 pandemic. Appl Clin Inform. 2020;3:452-459. doi: 10.1055/s-0040-1713635
6. Olayiwola JN, Magaña C, Harmon A, et al. Telehealth as a bright spot of the COVID-19 pandemic: recommendations from the virtual frontlines (“Frontweb”). JMIR Public Health Surveill. 2020;6:e19045. doi: 10.2196/19045
7. Gausvik C, Jabbarpour Y. COVID-19 timeline: Centers for Medicare and Medicaid Services (CMS) changes and primary care support were not enough to prevent practice losses. J Am Board Fam Med. 2021;34(suppl):S7-S9. doi: 10.3122/jabfm.2021.S1.200305
8. Marin-Gomez FX, Vidal-Alaball J, Poch PR, et al. Diagnosis of skin lesions using photographs taken with a mobile phone: an online survey of primary care physicians. J Prim Care Community Health. 2020;11:2150132720937831. doi: 10.1177/2150132720937831
9. Garber RN, Garcia E, Goodwin CW, et al. (2020). Pictures do influence the decision to transfer: outcomes of a telemedicine program serving an eight-state rural population. J Burn Care Res. 2020;41:690-694. doi: 10.1093/jbcr/iraa017
10. Felix F, Greenblatt M, Shin L. Saving limbs in the time of COVID. 2020. Accessed February 8, 2023. https://podiatrym.com/pdf/2020/7/FelixGreenblattShin820web.pdf
11. Erkkola-Anttinen N, Irjala H, Laine MK, et al. Smartphone otoscopy performed by parents. Telemed J E Health. 2019;25:477-484. doi: 10.1089/tmj.2018.0062
12. Verzantvoort NC, Teunis T, Verheij TJ, et al. Self-triage for acute primary care via a smartphone application: practical, safe and efficient? PLoS One. 2018;13:e0199284. doi: 10.1371/journal.pone.0199284
13. Hickner J. When patients don’t get the care they should. J Fam Pract. 2020;69:427.
14. Pappan N, Benkhadra R, Papincak D, et al. Values and limits of telemedicine: a case report. SN Compr Clin Med. 2021;3:317-319. doi: 10.1007/s42399-020-00725-y
15. Jabbarpour Y, Jetty A, Westfall M, et al. Not telehealth: which primary care visits need in-person care? J Am Board Fam Med. 2021;34(suppl):S162-S169. doi: 10.3122/jabfm.2021.S1.200247
16. Parmar P, Mackie D, Varghese S, et al. Use of telemedicine technologies in the management of infectious diseases: a review. Clin Infect Dis. 2015;60:1084-1094. doi: 10.1093/cid/ciu1143
17. Young JD, Abdel-Massih R, Herchline T, et al. Infectious Diseases Society of America position statement on Telehealth and Telemedicine as Applied to the Practice of Infectious Diseases. Clin Infect Dis. 2019;68:1437-1443. doi: 10.1093/cid/ciy907
18. ARHQ. Telehealth: mapping the evidence for patient outcomes from systematic reviews. 2016. Accessed March 27, 2023. https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/telehealth_technical-brief.pdf
19. Lustgarten SD, Garrison YL, Sinnard MT, et al. Digital privacy in mental healthcare: current issues and recommendations for technology use. Curr Opin Psychol. 2020;36:25-31. doi: 10.1016/j.copsyc.2020.03.012
20. Baird A, Xia Y, Cheng Y. Consumer perceptions of telehealth for mental health or substance abuse: a Twitter-based topic modeling analysis. JAMIA Open. 2022;5:ooac028. doi: 10.1093/jamiaopen/ooac028
21. Flumignan CD, da Rocha AP, Pinto AC, et al. What do Cochrane systematic reviews say about telemedicine for healthcare? Sao Paulo Med J. 2019;137:184-192. doi: 10.1590/1516-3180.0177240419
22. Gomez T, Anaya YB, Shih KJ, et al. A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19. J Am Board Fam Med. 2021;34(suppl):S61-S70. doi: 10.3122/jabfm.2021.S1.200517
23. Malliaras P, Merolli M, Williams CM, et al. ‘It’s not hands-on therapy, so it’s very limited’: telehealth use and views among allied health clinicians during the coronavirus pandemic. Musculoskelet Sci Pract. 2021;52:102340. doi: 10.1016/j.msksp.2021.102340
24. Gold KJ, Laurie AR, Kinney DR, et al. Video visits: family physician experiences with uptake during the COVID-19 pandemic. Fam Med. 53:207-210. doi: 10.22454/FamMed.2021.613099
25. Björndell C, Premberg A. Physicians’ experiences of video consultation with patients at a public virtual primary care clinic: a qualitative interview study. Scand J Prim Health Care. 2021;39:67-76. doi: 10.1080/02813432.2021.1882082
26. Powell RE, Henstenburg JM, Cooper G, et al. Patient perceptions of telehealth primary care video visits. Ann Fam Med. 2017;15:225-229. doi: 10.1370/afm.2095
27. Imlach F, McKinlay E, Middleton L, et al. Telehealth consultations in general practice during a pandemic lockdown: survey and interviews on patient experiences and preferences. BMC Fam Pract. 2020;21:1-14. doi: 10.1186/s12875-020-01336-1
28. Gordon HS, Solanki P, Bokhour BG, et al. “I’m not feeling like I’m part of the conversation” patients’ perspectives on communicating in clinical video telehealth visits. J Gen Intern Med. 2020;35:1751-1758. doi: 10.1007/s11606-020-05673-w
29. Volcy J, Smith W, Mills K, et al. Assessment of patient and provider satisfaction with the change to telehealth from in-person visits at an academic safety net institution during the COVID-19 pandemic. J Am Board Fam Med. 2021;34(suppl):S71-S76. doi: 10.3122/jabfm.2021.S1.200393
30. Gopal RK, Solanki P, Bokhour BG, et al. Provider, staff, and patient perspectives on medical visits using clinical video telehealth: a foundation for educational initiatives to improve medical care in telehealth. J Nurse Pract. 2021;17:582-587. doi: 10.1016/j.nurpra.2021.02.020
31. Edgoose JY. Exploring the face-to-face: revisiting patient-doctor relationships in a time of expanding telemedicine. J Am Board Fam Med. 2021;34(suppl):S252-S254. doi: 10.3122/jabfm.2021.S1.200398
32. Pierce RP, Stevermer JJ. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. 2023;29:3-9. doi: 10.1177/1357633X20963893
33. Lame M, Leyden D, Platt SL. Geocode maps spotlight disparities in telehealth utilization during the COVID-19 pandemic in New York City. Telemed J E Health. 2021;27:251-253. doi: 10.1089/tmj.2020.0297
34. Jain V, Al Rifai M, Lee MT, et al. Racial and geographic disparities in internet use in the US among patients with hypertension or diabetes: implications for telehealth in the era of COVID-19. Diabetes Care. 2021;44:e15-e17. doi: 10.2337/dc20-2016
35. Futterman I, Rosenfeld E, Toaff M, et al. Addressing disparities in prenatal care via telehealth during COVID-19: prenatal satisfaction survey in East Harlem. Am J Perinatol. 2021;38:88-92. doi: 10.1055/s-0040-1718695
36. Wegermann K, Wilder JM, Parish A, et al. Racial and socioeconomic disparities in utilization of telehealth in patients with liver disease during COVID-19. Dig Dis Sci. 2022;67:93-99. doi: 10.1007/s10620-021-06842-5.
37. ASPE. National survey trends in telehealth use in 2021: disparities in utilization and audio vs. video services. Issue brief: February 21, 2022. Accessed March 27, 2023. https://aspe.hhs.gov/sites/default/files/documents/4e1853c0b4885112b2994680a58af9ed/telehealth-hps-ib.pdf
38. Ukoha EP, Davis K, Yinger M, et al. Ensuring equitable implementation of telemedicine in perinatal care. Obstet Gynecol. 2021;137:487-492. doi: 10.1097/AOG.0000000000004276
1. WHO. A health telematics policy: in support of WHO’s Health-for-All strategy for global health development. 1997. Accessed February 8, 2023. https://apps.who.int/iris/bitstream/handle/10665/63857/WHO_DGO_98.1.pdf?sequence=1&isAllowed=y
2. Knierim K, Palmer C, Kramer ES, et al. Lessons learned during COVID-19 that can move telehealth in primary care forward. J Am Board Fam Med. Supplement 2021;34(suppl):S196-S202. doi: 10.3122/jabfm.2021.S1.200419
3. Reed ME, Huang J, Graetz I, et al. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw Open. 2020;3:e205873. doi: 10.1001/jamanetworkopen.2020.5873
4. Silver SL, Lewis MN, Ledford CJ. A stepwise transition to telemedicine in response to COVID-19. J Am Board Fam Med. 2021;34(suppl):S152-S161. doi: 10.3122/jabfm.2021.S1.200358
5. Hron JD, Parsons CR, Williams LA, et al. Rapid implementation of an inpatient telehealth program during the COVID-19 pandemic. Appl Clin Inform. 2020;3:452-459. doi: 10.1055/s-0040-1713635
6. Olayiwola JN, Magaña C, Harmon A, et al. Telehealth as a bright spot of the COVID-19 pandemic: recommendations from the virtual frontlines (“Frontweb”). JMIR Public Health Surveill. 2020;6:e19045. doi: 10.2196/19045
7. Gausvik C, Jabbarpour Y. COVID-19 timeline: Centers for Medicare and Medicaid Services (CMS) changes and primary care support were not enough to prevent practice losses. J Am Board Fam Med. 2021;34(suppl):S7-S9. doi: 10.3122/jabfm.2021.S1.200305
8. Marin-Gomez FX, Vidal-Alaball J, Poch PR, et al. Diagnosis of skin lesions using photographs taken with a mobile phone: an online survey of primary care physicians. J Prim Care Community Health. 2020;11:2150132720937831. doi: 10.1177/2150132720937831
9. Garber RN, Garcia E, Goodwin CW, et al. (2020). Pictures do influence the decision to transfer: outcomes of a telemedicine program serving an eight-state rural population. J Burn Care Res. 2020;41:690-694. doi: 10.1093/jbcr/iraa017
10. Felix F, Greenblatt M, Shin L. Saving limbs in the time of COVID. 2020. Accessed February 8, 2023. https://podiatrym.com/pdf/2020/7/FelixGreenblattShin820web.pdf
11. Erkkola-Anttinen N, Irjala H, Laine MK, et al. Smartphone otoscopy performed by parents. Telemed J E Health. 2019;25:477-484. doi: 10.1089/tmj.2018.0062
12. Verzantvoort NC, Teunis T, Verheij TJ, et al. Self-triage for acute primary care via a smartphone application: practical, safe and efficient? PLoS One. 2018;13:e0199284. doi: 10.1371/journal.pone.0199284
13. Hickner J. When patients don’t get the care they should. J Fam Pract. 2020;69:427.
14. Pappan N, Benkhadra R, Papincak D, et al. Values and limits of telemedicine: a case report. SN Compr Clin Med. 2021;3:317-319. doi: 10.1007/s42399-020-00725-y
15. Jabbarpour Y, Jetty A, Westfall M, et al. Not telehealth: which primary care visits need in-person care? J Am Board Fam Med. 2021;34(suppl):S162-S169. doi: 10.3122/jabfm.2021.S1.200247
16. Parmar P, Mackie D, Varghese S, et al. Use of telemedicine technologies in the management of infectious diseases: a review. Clin Infect Dis. 2015;60:1084-1094. doi: 10.1093/cid/ciu1143
17. Young JD, Abdel-Massih R, Herchline T, et al. Infectious Diseases Society of America position statement on Telehealth and Telemedicine as Applied to the Practice of Infectious Diseases. Clin Infect Dis. 2019;68:1437-1443. doi: 10.1093/cid/ciy907
18. ARHQ. Telehealth: mapping the evidence for patient outcomes from systematic reviews. 2016. Accessed March 27, 2023. https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/telehealth_technical-brief.pdf
19. Lustgarten SD, Garrison YL, Sinnard MT, et al. Digital privacy in mental healthcare: current issues and recommendations for technology use. Curr Opin Psychol. 2020;36:25-31. doi: 10.1016/j.copsyc.2020.03.012
20. Baird A, Xia Y, Cheng Y. Consumer perceptions of telehealth for mental health or substance abuse: a Twitter-based topic modeling analysis. JAMIA Open. 2022;5:ooac028. doi: 10.1093/jamiaopen/ooac028
21. Flumignan CD, da Rocha AP, Pinto AC, et al. What do Cochrane systematic reviews say about telemedicine for healthcare? Sao Paulo Med J. 2019;137:184-192. doi: 10.1590/1516-3180.0177240419
22. Gomez T, Anaya YB, Shih KJ, et al. A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19. J Am Board Fam Med. 2021;34(suppl):S61-S70. doi: 10.3122/jabfm.2021.S1.200517
23. Malliaras P, Merolli M, Williams CM, et al. ‘It’s not hands-on therapy, so it’s very limited’: telehealth use and views among allied health clinicians during the coronavirus pandemic. Musculoskelet Sci Pract. 2021;52:102340. doi: 10.1016/j.msksp.2021.102340
24. Gold KJ, Laurie AR, Kinney DR, et al. Video visits: family physician experiences with uptake during the COVID-19 pandemic. Fam Med. 53:207-210. doi: 10.22454/FamMed.2021.613099
25. Björndell C, Premberg A. Physicians’ experiences of video consultation with patients at a public virtual primary care clinic: a qualitative interview study. Scand J Prim Health Care. 2021;39:67-76. doi: 10.1080/02813432.2021.1882082
26. Powell RE, Henstenburg JM, Cooper G, et al. Patient perceptions of telehealth primary care video visits. Ann Fam Med. 2017;15:225-229. doi: 10.1370/afm.2095
27. Imlach F, McKinlay E, Middleton L, et al. Telehealth consultations in general practice during a pandemic lockdown: survey and interviews on patient experiences and preferences. BMC Fam Pract. 2020;21:1-14. doi: 10.1186/s12875-020-01336-1
28. Gordon HS, Solanki P, Bokhour BG, et al. “I’m not feeling like I’m part of the conversation” patients’ perspectives on communicating in clinical video telehealth visits. J Gen Intern Med. 2020;35:1751-1758. doi: 10.1007/s11606-020-05673-w
29. Volcy J, Smith W, Mills K, et al. Assessment of patient and provider satisfaction with the change to telehealth from in-person visits at an academic safety net institution during the COVID-19 pandemic. J Am Board Fam Med. 2021;34(suppl):S71-S76. doi: 10.3122/jabfm.2021.S1.200393
30. Gopal RK, Solanki P, Bokhour BG, et al. Provider, staff, and patient perspectives on medical visits using clinical video telehealth: a foundation for educational initiatives to improve medical care in telehealth. J Nurse Pract. 2021;17:582-587. doi: 10.1016/j.nurpra.2021.02.020
31. Edgoose JY. Exploring the face-to-face: revisiting patient-doctor relationships in a time of expanding telemedicine. J Am Board Fam Med. 2021;34(suppl):S252-S254. doi: 10.3122/jabfm.2021.S1.200398
32. Pierce RP, Stevermer JJ. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. 2023;29:3-9. doi: 10.1177/1357633X20963893
33. Lame M, Leyden D, Platt SL. Geocode maps spotlight disparities in telehealth utilization during the COVID-19 pandemic in New York City. Telemed J E Health. 2021;27:251-253. doi: 10.1089/tmj.2020.0297
34. Jain V, Al Rifai M, Lee MT, et al. Racial and geographic disparities in internet use in the US among patients with hypertension or diabetes: implications for telehealth in the era of COVID-19. Diabetes Care. 2021;44:e15-e17. doi: 10.2337/dc20-2016
35. Futterman I, Rosenfeld E, Toaff M, et al. Addressing disparities in prenatal care via telehealth during COVID-19: prenatal satisfaction survey in East Harlem. Am J Perinatol. 2021;38:88-92. doi: 10.1055/s-0040-1718695
36. Wegermann K, Wilder JM, Parish A, et al. Racial and socioeconomic disparities in utilization of telehealth in patients with liver disease during COVID-19. Dig Dis Sci. 2022;67:93-99. doi: 10.1007/s10620-021-06842-5.
37. ASPE. National survey trends in telehealth use in 2021: disparities in utilization and audio vs. video services. Issue brief: February 21, 2022. Accessed March 27, 2023. https://aspe.hhs.gov/sites/default/files/documents/4e1853c0b4885112b2994680a58af9ed/telehealth-hps-ib.pdf
38. Ukoha EP, Davis K, Yinger M, et al. Ensuring equitable implementation of telemedicine in perinatal care. Obstet Gynecol. 2021;137:487-492. doi: 10.1097/AOG.0000000000004276
PRACTICE RECOMMENDATIONS
› Consider using telehealth encounters for diagnosing and treating infectious diseases and for monitoring stable chronic conditions. C
› Consider telehealth “check-ins” to encourage patients working on behavioral change, such as smoking cessation. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Widespread carboplatin, cisplatin shortages: NCCN survey
The survey, which included responses from 27 NCCN member institutions, revealed that 93% are experiencing a shortage of carboplatin and that 70% have reported a shortage of cisplatin.
“This is an unacceptable situation,” Robert W. Carlson, MD, NCCN’s chief executive offer, said in the statement released by the network.
“We are hearing from oncologists and pharmacists across the country who have to scramble to find appropriate alternatives for treating their patients with cancer right now,” Dr. Carlson said. And while the survey results show patients are still able to get lifesaving care, “it comes at a burden to our overtaxed medical facilities.”
The NCCN called on the federal government, the pharmaceutical industry, providers, and payers to take steps to “help mitigate any impacts” from this cancer drug shortage.
“We need to work together to improve the current situation and prevent it from happening again in the future,” Dr. Carlson stressed.
Carboplatin and cisplatin, which are frequently used together for systemic treatment, are highly effective therapies prescribed to treat many cancer types, including lung, breast, and prostate cancers, as well as leukemias and lymphomas. An estimated 500,000 new patients with cancer receive these agents each year.
The current survey, conducted over the last week of May, found that 100% of responding centers are able to continue to treat patients who need cisplatin without delays.
The same cannot be said for carboplatin: only 64% of centers said they are still able to continue treating all current patients receiving the platinum-based therapy. Among 19 responding centers, 20% reported that they were continuing carboplatin regimens for some but not all patients. And 16% reported treatment delays from having to obtain prior authorization for modified treatment plans, though none reported denials.
“Carboplatin has been in short supply for months but in the last 4 weeks has reached a critical stage,” according to one survey comment. “Without additional inventory many of our sites will be out of drug by early next week.”
In response to the survey question, “Is your center experiencing a shortage of carboplatin,” others made similar comments:
- “Current shipments from established manufacturers have been paused.”
- “The supply of carboplatin available is not meeting our demands.”
- “Without additional supply in early June, we will have to implement several shortage mitigation strategies.”
Survey respondents also addressed whether manufacturers or suppliers have provided any indication of when these drugs will become readily available again. For both drugs, about 60% of respondents said no. And for those who do receive updates, many noted that the “information is tentative and variable.”
Respondents indicated that other cancer agents, including methotrexate (67%) and 5FU (26%), are also in short supply at their centers.
The shortage and the uncertainty as to when it will end are forcing some centers to develop conservation and mitigation strategies.
The NCCN has broadly outlined how the federal government, the pharmaceutical industry, providers, and payers can help with prevention and mitigation. The NCCN has called on the federal government and the pharmaceutical industry to work to secure a steady supply of core anticancer drugs and has asked payers to “put patients first and provide flexible and efficient systems of providing coverage for alternative therapies replacing anti-cancer drugs that are unavailable or in shortage.”
Overall, the survey results “demonstrate the widespread impact of the chemotherapy shortage,” said Alyssa Schatz, MSW, senior director of policy and advocacy for NCCN. “We hope that by sharing this survey and calling for united action across the oncology community, we can come together to prevent future drug shortages and ensure quality, effective, equitable, and accessible cancer care for all.”
A version of this article first appeared on Medscape.com.
The survey, which included responses from 27 NCCN member institutions, revealed that 93% are experiencing a shortage of carboplatin and that 70% have reported a shortage of cisplatin.
“This is an unacceptable situation,” Robert W. Carlson, MD, NCCN’s chief executive offer, said in the statement released by the network.
“We are hearing from oncologists and pharmacists across the country who have to scramble to find appropriate alternatives for treating their patients with cancer right now,” Dr. Carlson said. And while the survey results show patients are still able to get lifesaving care, “it comes at a burden to our overtaxed medical facilities.”
The NCCN called on the federal government, the pharmaceutical industry, providers, and payers to take steps to “help mitigate any impacts” from this cancer drug shortage.
“We need to work together to improve the current situation and prevent it from happening again in the future,” Dr. Carlson stressed.
Carboplatin and cisplatin, which are frequently used together for systemic treatment, are highly effective therapies prescribed to treat many cancer types, including lung, breast, and prostate cancers, as well as leukemias and lymphomas. An estimated 500,000 new patients with cancer receive these agents each year.
The current survey, conducted over the last week of May, found that 100% of responding centers are able to continue to treat patients who need cisplatin without delays.
The same cannot be said for carboplatin: only 64% of centers said they are still able to continue treating all current patients receiving the platinum-based therapy. Among 19 responding centers, 20% reported that they were continuing carboplatin regimens for some but not all patients. And 16% reported treatment delays from having to obtain prior authorization for modified treatment plans, though none reported denials.
“Carboplatin has been in short supply for months but in the last 4 weeks has reached a critical stage,” according to one survey comment. “Without additional inventory many of our sites will be out of drug by early next week.”
In response to the survey question, “Is your center experiencing a shortage of carboplatin,” others made similar comments:
- “Current shipments from established manufacturers have been paused.”
- “The supply of carboplatin available is not meeting our demands.”
- “Without additional supply in early June, we will have to implement several shortage mitigation strategies.”
Survey respondents also addressed whether manufacturers or suppliers have provided any indication of when these drugs will become readily available again. For both drugs, about 60% of respondents said no. And for those who do receive updates, many noted that the “information is tentative and variable.”
Respondents indicated that other cancer agents, including methotrexate (67%) and 5FU (26%), are also in short supply at their centers.
The shortage and the uncertainty as to when it will end are forcing some centers to develop conservation and mitigation strategies.
The NCCN has broadly outlined how the federal government, the pharmaceutical industry, providers, and payers can help with prevention and mitigation. The NCCN has called on the federal government and the pharmaceutical industry to work to secure a steady supply of core anticancer drugs and has asked payers to “put patients first and provide flexible and efficient systems of providing coverage for alternative therapies replacing anti-cancer drugs that are unavailable or in shortage.”
Overall, the survey results “demonstrate the widespread impact of the chemotherapy shortage,” said Alyssa Schatz, MSW, senior director of policy and advocacy for NCCN. “We hope that by sharing this survey and calling for united action across the oncology community, we can come together to prevent future drug shortages and ensure quality, effective, equitable, and accessible cancer care for all.”
A version of this article first appeared on Medscape.com.
The survey, which included responses from 27 NCCN member institutions, revealed that 93% are experiencing a shortage of carboplatin and that 70% have reported a shortage of cisplatin.
“This is an unacceptable situation,” Robert W. Carlson, MD, NCCN’s chief executive offer, said in the statement released by the network.
“We are hearing from oncologists and pharmacists across the country who have to scramble to find appropriate alternatives for treating their patients with cancer right now,” Dr. Carlson said. And while the survey results show patients are still able to get lifesaving care, “it comes at a burden to our overtaxed medical facilities.”
The NCCN called on the federal government, the pharmaceutical industry, providers, and payers to take steps to “help mitigate any impacts” from this cancer drug shortage.
“We need to work together to improve the current situation and prevent it from happening again in the future,” Dr. Carlson stressed.
Carboplatin and cisplatin, which are frequently used together for systemic treatment, are highly effective therapies prescribed to treat many cancer types, including lung, breast, and prostate cancers, as well as leukemias and lymphomas. An estimated 500,000 new patients with cancer receive these agents each year.
The current survey, conducted over the last week of May, found that 100% of responding centers are able to continue to treat patients who need cisplatin without delays.
The same cannot be said for carboplatin: only 64% of centers said they are still able to continue treating all current patients receiving the platinum-based therapy. Among 19 responding centers, 20% reported that they were continuing carboplatin regimens for some but not all patients. And 16% reported treatment delays from having to obtain prior authorization for modified treatment plans, though none reported denials.
“Carboplatin has been in short supply for months but in the last 4 weeks has reached a critical stage,” according to one survey comment. “Without additional inventory many of our sites will be out of drug by early next week.”
In response to the survey question, “Is your center experiencing a shortage of carboplatin,” others made similar comments:
- “Current shipments from established manufacturers have been paused.”
- “The supply of carboplatin available is not meeting our demands.”
- “Without additional supply in early June, we will have to implement several shortage mitigation strategies.”
Survey respondents also addressed whether manufacturers or suppliers have provided any indication of when these drugs will become readily available again. For both drugs, about 60% of respondents said no. And for those who do receive updates, many noted that the “information is tentative and variable.”
Respondents indicated that other cancer agents, including methotrexate (67%) and 5FU (26%), are also in short supply at their centers.
The shortage and the uncertainty as to when it will end are forcing some centers to develop conservation and mitigation strategies.
The NCCN has broadly outlined how the federal government, the pharmaceutical industry, providers, and payers can help with prevention and mitigation. The NCCN has called on the federal government and the pharmaceutical industry to work to secure a steady supply of core anticancer drugs and has asked payers to “put patients first and provide flexible and efficient systems of providing coverage for alternative therapies replacing anti-cancer drugs that are unavailable or in shortage.”
Overall, the survey results “demonstrate the widespread impact of the chemotherapy shortage,” said Alyssa Schatz, MSW, senior director of policy and advocacy for NCCN. “We hope that by sharing this survey and calling for united action across the oncology community, we can come together to prevent future drug shortages and ensure quality, effective, equitable, and accessible cancer care for all.”
A version of this article first appeared on Medscape.com.
Is ChatGPT a friend or foe of medical publishing?
. These tools should not be listed as authors, and researchers must denote how AI-assisted technologies were used, the committee said.
These new guidelines are the latest effort for medical journals to define policies for using these large-scale language models (LLMs) in scientific publication. While these AI-assisted tools can help with tasks such as writing, analyzing data, catching mistakes, and much more, they are also prone to errors, noted Casey Greene, PhD, a professor of biomedical informatics at the University of Colorado at Denver, Aurora. It is also not totally clear how information is stored and processed in these kinds of tools, and who has access to that information, he noted.
At the same time, experts argue that these AI tools could have a positive impact on the field by limiting some of the linguistic disparities in scientific publishing as well as alleviating the burden of some monotonous or mechanical tasks that come along with manuscript writing.
What experts can agree on, though, is that the use of AI tools is here to stay. “This is going to become a common tool,” Dr. Greene said. “I don’t think there’s a way out of that at this point.”
A change in medical publishing
OpenAI released ChatGPT in November 2022. In its own words, ChatGPT is “a deep learning model that has been trained on a massive amount of text data to understand and generate humanlike text.” Enter a question or a prompt, and it will respond. For example, when asked how the AI tool can be used in scientific publishing, ChatGPT responded:
“ChatGPT can aid scientific publishing by generating ideas, clarifying concepts, conducting preliminary literature reviews, providing proofreading and editing suggestions, and assisting with outlining and organizing scientific papers. However, it should be used as a supportive tool alongside domain expertise and validation from trusted scientific sources.”
Just a few months after ChatGPT became available, researchers began using this tool in their own work. One individual, Som Biswas, MD, a radiologist at the University of Tennessee Health Science Center in Memphis, reportedly used ChatGPT to author 16 scientific articles in just 4 months, according to the Daily Beast. Five of these articles have been published in four different journals. Dr. Biswas declined to be interviewed for this article.
There were also reports of papers with ChatGPT as one of the listed authors, which sparked backlash. In response, JAMA, Nature, and Science all published editorials in January outlining their policies for using ChatGPT and other large language models in the scientific authoring process. Editors from the journals of the American College of Cardiology and the American College of Rheumatology also updated their policies to reflect the influence of AI authoring tools.
The consensus is that AI has no place on the author byline.
“We think that’s not appropriate, because coauthorship means that you are taking responsibility for the analysis and the generation of data that are included in a manuscript. A machine that is dictated by AI can’t take responsibility,” said Daniel Solomon, MD, MPH, a rheumatologist at Brigham and Women’s Hospital, Boston, and the editor in chief of the ACR journal Arthritis & Rheumatology.
Issues with AI
One of the big concerns around using AI in writing is that it can generate text that seems plausible but is untrue or not supported by data. For example, Dr. Greene and colleague Milton Pividori, PhD, also of the University of Colorado, were writing a journal article about new software they developed that uses a large language model to revise scientific manuscripts.
“We used the same software to revise that article and at one point, it added a line that noted that the large language model had been fine-tuned on a data set of manuscripts from within the same field. This makes a lot of sense, and is absolutely something you could do, but was not something that we did,” Dr. Greene said. “Without a really careful review of the content, it becomes possible to invent things that were not actually done.”
In another case, ChatGPT falsely stated that a prominent law professor had been accused of sexual assault, citing a Washington Post article that did not exist.
“We live in a society where we are extremely concerned about fake news,” Dr. Pividori added, “and [these kinds of errors] could certainly exacerbate that in the scientific community, which is very concerning because science informs public policy.”
Another issue is the lack of transparency around how large language models like ChatGPT process and store data used to make queries.
“We have no idea how they are recording all the prompts and things that we input into ChatGPT and their systems,” Dr. Pividori said.
OpenAI recently addressed some privacy concerns by allowing users to turn off their chat history with the AI chatbot, so conversations cannot be used to train or improve the company’s models. But Dr. Greene noted that the terms of service “still remain pretty nebulous.”
Dr. Solomon is also concerned with researchers using these AI tools in authoring without knowing how they work. “The thing we are really concerned about is that fact that [LLMs] are a bit of a black box – people don’t really understand the methodologies,” he said.
A positive tool?
But despite these concerns, many think that these types of AI-assisted tools could have a positive impact on medical publishing, particularly for researchers for whom English is not their first language, noted Catherine Gao, MD, a pulmonary and critical care instructor at Northwestern University, Chicago. She recently led research comparing scientific abstracts written by ChatGPT and real abstracts and discovered that reviewers found it “surprisingly difficult” to differentiate the two.
“The majority of research is published in English,” she said in an email. “Responsible use of LLMs can potentially reduce the burden of writing for busy scientists and improve equity for those who are not native English speakers.”
Dr. Pividori agreed, adding that as a non-native English speaker, he spends much more time working on the structure and grammar of sentences when authoring a manuscript, compared with people who speak English as a first language. He noted that these tools can also be used to automate some of the more monotonous tasks that come along with writing manuscripts and allow researchers to focus on the more creative aspects.
In the future, “I want to focus more on the things that only a human can do and let these tools do all the rest of it,” he said.
New rules
But despite how individual researchers feel about LLMs, they agree that these AI tools are here to stay.
“I think that we should anticipate that they will become part of the medical research establishment over time, when we figure out how to use them appropriately,” Dr. Solomon said.
While the debate of how to best use AI in medical publications will continue, journal editors agree that all authors of a manuscript are solely responsible for content in articles that used AI-assisted technology.
“Authors should carefully review and edit the result because AI can generate authoritative-sounding output that can be incorrect, incomplete, or biased,” the ICMJE guidelines state. “Authors should be able to assert that there is no plagiarism in their paper, including in text and images produced by the AI.” This includes appropriate attribution of all cited materials.
The committee also recommends that authors write in both the cover letter and submitted work how AI was used in the manuscript writing process. Recently updated guidelines from the World Association of Medical Editors recommend that all prompts used to generate new text or analytical work should be provided in submitted work. Dr. Greene also noted that if authors used an AI tool to revise their work, they can include a version of the manuscript untouched by LLMs.
It is similar to a preprint, he said, but rather than publishing a version of a paper prior to peer review, someone is showing a version of a manuscript before it was reviewed and revised by AI. “This type of practice could be a path that lets us benefit from these models,” he said, “without having the drawbacks that many are concerned about.”
Dr. Solomon has financial relationships with AbbVie, Amgen, Janssen, CorEvitas, and Moderna. Both Dr. Greene and Dr. Pividori are inventors in the U.S. Provisional Patent Application No. 63/486,706 that the University of Colorado has filed for the “Publishing Infrastructure For AI-Assisted Academic Authoring” invention with the U.S. Patent and Trademark Office. Dr. Greene and Dr. Pividori also received a grant from the Alfred P. Sloan Foundation to improve their AI-based manuscript revision tool. Dr. Gao reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
. These tools should not be listed as authors, and researchers must denote how AI-assisted technologies were used, the committee said.
These new guidelines are the latest effort for medical journals to define policies for using these large-scale language models (LLMs) in scientific publication. While these AI-assisted tools can help with tasks such as writing, analyzing data, catching mistakes, and much more, they are also prone to errors, noted Casey Greene, PhD, a professor of biomedical informatics at the University of Colorado at Denver, Aurora. It is also not totally clear how information is stored and processed in these kinds of tools, and who has access to that information, he noted.
At the same time, experts argue that these AI tools could have a positive impact on the field by limiting some of the linguistic disparities in scientific publishing as well as alleviating the burden of some monotonous or mechanical tasks that come along with manuscript writing.
What experts can agree on, though, is that the use of AI tools is here to stay. “This is going to become a common tool,” Dr. Greene said. “I don’t think there’s a way out of that at this point.”
A change in medical publishing
OpenAI released ChatGPT in November 2022. In its own words, ChatGPT is “a deep learning model that has been trained on a massive amount of text data to understand and generate humanlike text.” Enter a question or a prompt, and it will respond. For example, when asked how the AI tool can be used in scientific publishing, ChatGPT responded:
“ChatGPT can aid scientific publishing by generating ideas, clarifying concepts, conducting preliminary literature reviews, providing proofreading and editing suggestions, and assisting with outlining and organizing scientific papers. However, it should be used as a supportive tool alongside domain expertise and validation from trusted scientific sources.”
Just a few months after ChatGPT became available, researchers began using this tool in their own work. One individual, Som Biswas, MD, a radiologist at the University of Tennessee Health Science Center in Memphis, reportedly used ChatGPT to author 16 scientific articles in just 4 months, according to the Daily Beast. Five of these articles have been published in four different journals. Dr. Biswas declined to be interviewed for this article.
There were also reports of papers with ChatGPT as one of the listed authors, which sparked backlash. In response, JAMA, Nature, and Science all published editorials in January outlining their policies for using ChatGPT and other large language models in the scientific authoring process. Editors from the journals of the American College of Cardiology and the American College of Rheumatology also updated their policies to reflect the influence of AI authoring tools.
The consensus is that AI has no place on the author byline.
“We think that’s not appropriate, because coauthorship means that you are taking responsibility for the analysis and the generation of data that are included in a manuscript. A machine that is dictated by AI can’t take responsibility,” said Daniel Solomon, MD, MPH, a rheumatologist at Brigham and Women’s Hospital, Boston, and the editor in chief of the ACR journal Arthritis & Rheumatology.
Issues with AI
One of the big concerns around using AI in writing is that it can generate text that seems plausible but is untrue or not supported by data. For example, Dr. Greene and colleague Milton Pividori, PhD, also of the University of Colorado, were writing a journal article about new software they developed that uses a large language model to revise scientific manuscripts.
“We used the same software to revise that article and at one point, it added a line that noted that the large language model had been fine-tuned on a data set of manuscripts from within the same field. This makes a lot of sense, and is absolutely something you could do, but was not something that we did,” Dr. Greene said. “Without a really careful review of the content, it becomes possible to invent things that were not actually done.”
In another case, ChatGPT falsely stated that a prominent law professor had been accused of sexual assault, citing a Washington Post article that did not exist.
“We live in a society where we are extremely concerned about fake news,” Dr. Pividori added, “and [these kinds of errors] could certainly exacerbate that in the scientific community, which is very concerning because science informs public policy.”
Another issue is the lack of transparency around how large language models like ChatGPT process and store data used to make queries.
“We have no idea how they are recording all the prompts and things that we input into ChatGPT and their systems,” Dr. Pividori said.
OpenAI recently addressed some privacy concerns by allowing users to turn off their chat history with the AI chatbot, so conversations cannot be used to train or improve the company’s models. But Dr. Greene noted that the terms of service “still remain pretty nebulous.”
Dr. Solomon is also concerned with researchers using these AI tools in authoring without knowing how they work. “The thing we are really concerned about is that fact that [LLMs] are a bit of a black box – people don’t really understand the methodologies,” he said.
A positive tool?
But despite these concerns, many think that these types of AI-assisted tools could have a positive impact on medical publishing, particularly for researchers for whom English is not their first language, noted Catherine Gao, MD, a pulmonary and critical care instructor at Northwestern University, Chicago. She recently led research comparing scientific abstracts written by ChatGPT and real abstracts and discovered that reviewers found it “surprisingly difficult” to differentiate the two.
“The majority of research is published in English,” she said in an email. “Responsible use of LLMs can potentially reduce the burden of writing for busy scientists and improve equity for those who are not native English speakers.”
Dr. Pividori agreed, adding that as a non-native English speaker, he spends much more time working on the structure and grammar of sentences when authoring a manuscript, compared with people who speak English as a first language. He noted that these tools can also be used to automate some of the more monotonous tasks that come along with writing manuscripts and allow researchers to focus on the more creative aspects.
In the future, “I want to focus more on the things that only a human can do and let these tools do all the rest of it,” he said.
New rules
But despite how individual researchers feel about LLMs, they agree that these AI tools are here to stay.
“I think that we should anticipate that they will become part of the medical research establishment over time, when we figure out how to use them appropriately,” Dr. Solomon said.
While the debate of how to best use AI in medical publications will continue, journal editors agree that all authors of a manuscript are solely responsible for content in articles that used AI-assisted technology.
“Authors should carefully review and edit the result because AI can generate authoritative-sounding output that can be incorrect, incomplete, or biased,” the ICMJE guidelines state. “Authors should be able to assert that there is no plagiarism in their paper, including in text and images produced by the AI.” This includes appropriate attribution of all cited materials.
The committee also recommends that authors write in both the cover letter and submitted work how AI was used in the manuscript writing process. Recently updated guidelines from the World Association of Medical Editors recommend that all prompts used to generate new text or analytical work should be provided in submitted work. Dr. Greene also noted that if authors used an AI tool to revise their work, they can include a version of the manuscript untouched by LLMs.
It is similar to a preprint, he said, but rather than publishing a version of a paper prior to peer review, someone is showing a version of a manuscript before it was reviewed and revised by AI. “This type of practice could be a path that lets us benefit from these models,” he said, “without having the drawbacks that many are concerned about.”
Dr. Solomon has financial relationships with AbbVie, Amgen, Janssen, CorEvitas, and Moderna. Both Dr. Greene and Dr. Pividori are inventors in the U.S. Provisional Patent Application No. 63/486,706 that the University of Colorado has filed for the “Publishing Infrastructure For AI-Assisted Academic Authoring” invention with the U.S. Patent and Trademark Office. Dr. Greene and Dr. Pividori also received a grant from the Alfred P. Sloan Foundation to improve their AI-based manuscript revision tool. Dr. Gao reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
. These tools should not be listed as authors, and researchers must denote how AI-assisted technologies were used, the committee said.
These new guidelines are the latest effort for medical journals to define policies for using these large-scale language models (LLMs) in scientific publication. While these AI-assisted tools can help with tasks such as writing, analyzing data, catching mistakes, and much more, they are also prone to errors, noted Casey Greene, PhD, a professor of biomedical informatics at the University of Colorado at Denver, Aurora. It is also not totally clear how information is stored and processed in these kinds of tools, and who has access to that information, he noted.
At the same time, experts argue that these AI tools could have a positive impact on the field by limiting some of the linguistic disparities in scientific publishing as well as alleviating the burden of some monotonous or mechanical tasks that come along with manuscript writing.
What experts can agree on, though, is that the use of AI tools is here to stay. “This is going to become a common tool,” Dr. Greene said. “I don’t think there’s a way out of that at this point.”
A change in medical publishing
OpenAI released ChatGPT in November 2022. In its own words, ChatGPT is “a deep learning model that has been trained on a massive amount of text data to understand and generate humanlike text.” Enter a question or a prompt, and it will respond. For example, when asked how the AI tool can be used in scientific publishing, ChatGPT responded:
“ChatGPT can aid scientific publishing by generating ideas, clarifying concepts, conducting preliminary literature reviews, providing proofreading and editing suggestions, and assisting with outlining and organizing scientific papers. However, it should be used as a supportive tool alongside domain expertise and validation from trusted scientific sources.”
Just a few months after ChatGPT became available, researchers began using this tool in their own work. One individual, Som Biswas, MD, a radiologist at the University of Tennessee Health Science Center in Memphis, reportedly used ChatGPT to author 16 scientific articles in just 4 months, according to the Daily Beast. Five of these articles have been published in four different journals. Dr. Biswas declined to be interviewed for this article.
There were also reports of papers with ChatGPT as one of the listed authors, which sparked backlash. In response, JAMA, Nature, and Science all published editorials in January outlining their policies for using ChatGPT and other large language models in the scientific authoring process. Editors from the journals of the American College of Cardiology and the American College of Rheumatology also updated their policies to reflect the influence of AI authoring tools.
The consensus is that AI has no place on the author byline.
“We think that’s not appropriate, because coauthorship means that you are taking responsibility for the analysis and the generation of data that are included in a manuscript. A machine that is dictated by AI can’t take responsibility,” said Daniel Solomon, MD, MPH, a rheumatologist at Brigham and Women’s Hospital, Boston, and the editor in chief of the ACR journal Arthritis & Rheumatology.
Issues with AI
One of the big concerns around using AI in writing is that it can generate text that seems plausible but is untrue or not supported by data. For example, Dr. Greene and colleague Milton Pividori, PhD, also of the University of Colorado, were writing a journal article about new software they developed that uses a large language model to revise scientific manuscripts.
“We used the same software to revise that article and at one point, it added a line that noted that the large language model had been fine-tuned on a data set of manuscripts from within the same field. This makes a lot of sense, and is absolutely something you could do, but was not something that we did,” Dr. Greene said. “Without a really careful review of the content, it becomes possible to invent things that were not actually done.”
In another case, ChatGPT falsely stated that a prominent law professor had been accused of sexual assault, citing a Washington Post article that did not exist.
“We live in a society where we are extremely concerned about fake news,” Dr. Pividori added, “and [these kinds of errors] could certainly exacerbate that in the scientific community, which is very concerning because science informs public policy.”
Another issue is the lack of transparency around how large language models like ChatGPT process and store data used to make queries.
“We have no idea how they are recording all the prompts and things that we input into ChatGPT and their systems,” Dr. Pividori said.
OpenAI recently addressed some privacy concerns by allowing users to turn off their chat history with the AI chatbot, so conversations cannot be used to train or improve the company’s models. But Dr. Greene noted that the terms of service “still remain pretty nebulous.”
Dr. Solomon is also concerned with researchers using these AI tools in authoring without knowing how they work. “The thing we are really concerned about is that fact that [LLMs] are a bit of a black box – people don’t really understand the methodologies,” he said.
A positive tool?
But despite these concerns, many think that these types of AI-assisted tools could have a positive impact on medical publishing, particularly for researchers for whom English is not their first language, noted Catherine Gao, MD, a pulmonary and critical care instructor at Northwestern University, Chicago. She recently led research comparing scientific abstracts written by ChatGPT and real abstracts and discovered that reviewers found it “surprisingly difficult” to differentiate the two.
“The majority of research is published in English,” she said in an email. “Responsible use of LLMs can potentially reduce the burden of writing for busy scientists and improve equity for those who are not native English speakers.”
Dr. Pividori agreed, adding that as a non-native English speaker, he spends much more time working on the structure and grammar of sentences when authoring a manuscript, compared with people who speak English as a first language. He noted that these tools can also be used to automate some of the more monotonous tasks that come along with writing manuscripts and allow researchers to focus on the more creative aspects.
In the future, “I want to focus more on the things that only a human can do and let these tools do all the rest of it,” he said.
New rules
But despite how individual researchers feel about LLMs, they agree that these AI tools are here to stay.
“I think that we should anticipate that they will become part of the medical research establishment over time, when we figure out how to use them appropriately,” Dr. Solomon said.
While the debate of how to best use AI in medical publications will continue, journal editors agree that all authors of a manuscript are solely responsible for content in articles that used AI-assisted technology.
“Authors should carefully review and edit the result because AI can generate authoritative-sounding output that can be incorrect, incomplete, or biased,” the ICMJE guidelines state. “Authors should be able to assert that there is no plagiarism in their paper, including in text and images produced by the AI.” This includes appropriate attribution of all cited materials.
The committee also recommends that authors write in both the cover letter and submitted work how AI was used in the manuscript writing process. Recently updated guidelines from the World Association of Medical Editors recommend that all prompts used to generate new text or analytical work should be provided in submitted work. Dr. Greene also noted that if authors used an AI tool to revise their work, they can include a version of the manuscript untouched by LLMs.
It is similar to a preprint, he said, but rather than publishing a version of a paper prior to peer review, someone is showing a version of a manuscript before it was reviewed and revised by AI. “This type of practice could be a path that lets us benefit from these models,” he said, “without having the drawbacks that many are concerned about.”
Dr. Solomon has financial relationships with AbbVie, Amgen, Janssen, CorEvitas, and Moderna. Both Dr. Greene and Dr. Pividori are inventors in the U.S. Provisional Patent Application No. 63/486,706 that the University of Colorado has filed for the “Publishing Infrastructure For AI-Assisted Academic Authoring” invention with the U.S. Patent and Trademark Office. Dr. Greene and Dr. Pividori also received a grant from the Alfred P. Sloan Foundation to improve their AI-based manuscript revision tool. Dr. Gao reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
When could you be sued for AI malpractice? You’re likely using it now
The ways in which artificial intelligence (AI) may transform the future of medicine is making headlines across the globe. But chances are, you’re already using AI in your practice every day – you may just not realize it.
And whether you recognize the presence of AI or not, the technology could be putting you in danger of a lawsuit, legal experts say.
“For physicians, AI has also not yet drastically changed or improved the way care is provided or consumed,” said Michael LeTang, chief nursing informatics officer and vice president of risk management and patient safety at Healthcare Risk Advisors, part of TDC Group. “Consequently, it may seem like AI is not present in their work streams, but in reality, it has been utilized in health care for several years. As AI technologies continue to develop and become more sophisticated, we can expect them to play an increasingly significant role in health care.”
Today, most AI applications in health care use narrow AI, which is designed to complete a single task without human assistance, as opposed to artificial general intelligence (AGI), which pertains to human-level reasoning and problem solving across a broad spectrum. Here are some ways doctors are using AI throughout the day – sometimes being aware of its assistance, and sometimes being unaware:
- Many doctors use electronic health records (EHRs) with integrated AI that include computerized clinical decision support tools designed to reduce the risk of diagnostic error and to integrate decision-making in the medication ordering function.
- Cardiologists, pathologists, and dermatologists use AI in the interpretation of vast amounts of images, tracings, and complex patterns.
- Surgeons are using AI-enhanced surgical robotics for orthopedic surgeries, such as joint replacement and spine surgery.
- A growing number of doctors are using ChatGPT to assist in drafting prior authorization letters for insurers. Experts say more doctors are also experimenting with ChatGPT to support medical decision-making.
- Within oncology, physicians use machine learning techniques in the form of computer-aided detection systems for early breast cancer detection.
- AI algorithms are often used by health systems for workflow, staffing optimization, population management, and care coordination.
- Some systems within EHRs use AI to indicate high-risk patients.
- Physicians are using AI applications for the early recognition of sepsis, including EHR-integrated decision tools, such as the Hospital Corporation of America Healthcare’s Sepsis Prediction and Optimization Therapy and the Sepsis Early Risk Assessment algorithm.
- About 30% of radiologists use AI in their practice to analyze x-rays and CT scans.
- Epic Systems recently announced a partnership with Microsoft to integrate ChatGPT into MyChart, Epic’s patient portal system. Pilot hospitals will utilize ChatGPT to automatically generate responses to patient-generated questions sent via the portal.
The growth of AI in health care has been enormous, and it’s only going to continue, said Ravi B. Parikh, MD, an assistant professor in the department of medical ethics and health policy and medicine at the University of Pennsylvania, Philadelphia.
“What’s really critical is that physicians, clinicians, and nurses using AI are provided with the tools to understand how artificial intelligence works and, most importantly, understand that they are still accountable for making the ultimate decision,” Mr. LeTang said, “The information is not always going to be the right thing to do or the most accurate thing to do. They’re still liable for making a bad decision, even if AI is driving that.”
What are the top AI legal dangers of today?
A pressing legal risk is becoming too reliant on the suggestions that AI-based systems provide, which can lead to poor care decisions, said Kenneth Rashbaum, a New York–based cybersecurity attorney with more than 25 years of experience in medical malpractice defense.
This can occur, for example, when using clinical support systems that leverage AI, machine learning, or statistical pattern recognition. Today, clinical support systems are commonly administered through EHRs and other computerized clinical workflows. In general, such systems match a patient’s characteristics to a computerized clinical knowledge base. An assessment or recommendation is then presented to the physician for a decision.
“If the clinician blindly accepts it without considering whether it’s appropriate for this patient at this time with this presentation, the clinician may bear some responsibility if there is an untoward result,” Mr. Rashbaum said.
“A common claim even in the days before the EMR [electronic medical record] and AI, was that the clinician did not take all available information into account in rendering treatment, including history of past and present condition, as reflected in the records, communication with past and other present treating clinicians, lab and radiology results, discussions with the patient, and physical examination findings,” he said. “So, if the clinician relied upon the support prompt to the exclusion of these other sources of information, that could be a very strong argument for the plaintiff.”
Chatbots, such OpenAI’s ChatGPT, are another form of AI raising legal red flags. ChatGPT, trained on a massive set of text data, can carry out conversations, write code, draft emails, and answer any question posed. The chatbot has gained considerable credibility for accurately diagnosing rare conditions in seconds, and it recently passed the U.S. Medical Licensing Examination.
It’s unclear how many doctors are signing onto the ChatGPT website daily, but physicians are actively using the chatbot, particularly for assistance with prior authorization letters and to support decision-making processes in their practices, said Mr. LeTang.
When physicians ask ChatGPT a question, however, they should be mindful that ChatGPT could “hallucinate,” a term that refers to a generated response that sounds plausible but is factually incorrect or is unrelated to the context, explains Harvey Castro, MD, an emergency physician, ChatGPT health care expert, and author of the 2023 book “ChatGPT and Healthcare: Unlocking the Potential of Patient Empowerment.”
Acting on ChatGPT’s response without vetting the information places doctors at serious risk of a lawsuit, he said.
“Sometimes, the response is half true and half false,” he said. “Say, I go outside my specialty of emergency medicine and ask it about a pediatric surgical procedure. It could give me a response that sounds medically correct, but then I ask a pediatric cardiologist, and he says, ‘We don’t even do this. This doesn’t even exist!’ Physicians really have to make sure they are vetting the information provided.”
In response to ChatGPT’s growing usage by health care professionals, hospitals and practices are quickly implementing guidelines, policies, and restrictions that caution physicians about the accuracy of ChatGPT-generated information, adds Mr. LeTang.
Emerging best practices include avoiding the input of patient health information, personally identifiable information, or any data that could be commercially valuable or considered the intellectual property of a hospital or health system, he said.
“Another crucial guideline is not to rely solely on ChatGPT as a definitive source for clinical decision-making; physicians must exercise their professional judgment,” he said. “If best practices are not adhered to, the associated risks are present today. However, these risks may become more significant as AI technologies continue to evolve and become increasingly integrated into health care.”
The potential for misdiagnosis by AI systems and the risk of unnecessary procedures if physicians do not thoroughly evaluate and validate AI predictions are other dangers.
As an example, Mr. LeTang described a case in which a physician documents in the EHR that a patient has presented to the emergency department with chest pains and other signs of a heart attack, and an AI algorithm predicts that the patient is experiencing an active myocardial infarction. If the physician then sends the patient for stenting or an angioplasty without other concrete evidence or tests to confirm the diagnosis, the doctor could later face a misdiagnosis complaint if the costly procedures were unnecessary.
“That’s one of the risks of using artificial intelligence,” he said. “A large percentage of malpractice claims is failure to diagnose, delayed diagnosis, or inaccurate diagnosis. What falls in the category of failure to diagnose is sending a patient for an unnecessary procedure or having an adverse event or bad outcome because of the failure to diagnose.”
So far, no AI lawsuits have been filed, but they may make an appearance soon, said Sue Boisvert, senior patient safety risk manager at The Doctors Company, a national medical liability insurer.
“There are hundreds of AI programs currently in use in health care,” she said. “At some point, a provider will make a decision that is contrary to what the AI recommended. The AI may be wrong, or the provider may be wrong. Either way, the provider will neglect to document their clinical reasoning, a patient will be harmed, and we will have the first AI claim.”
Upcoming AI legal risks to watch for
Lawsuits that allege biased patient care by physicians on the basis of algorithmic bias may also be forthcoming, analysts warn.
Much has been written about algorithmic bias that compounds and worsens inequities in socioeconomic status, ethnicity, sexual orientation, and gender in health systems. In 2019, a groundbreaking article in Science shed light on commonly used algorithms that are considered racially biased and how health care professionals often use such information to make medical decisions.
No claims involving AI bias have come down the pipeline yet, but it’s an area to watch, said Ms. Boisvert. She noted a website that highlights complaints and accusations of AI bias, including in health care.
“We need to be sure the training of the AI is appropriate, current, and broad enough so that there is no bias in the AI when it’s participating in the decision-making,” said Ms. Boisvert. “Imagine if the AI is diagnosing based on a dataset that is not local. It doesn’t represent the population at that particular hospital, and it’s providing inaccurate information to the physicians who are then making decisions about treatment.”
In pain management, for example, there are known differences in how patients experience pain, Ms. Boisvert said. If AI was being used to develop an algorithm for how a particular patient’s postoperative pain should be managed, and the algorithm did not include the differences, the pain control for a certain patient could be inappropriate. A poor outcome resulting from the treatment could lead to a claim against the physician or hospital that used the biased AI system, she said.
In the future, as AI becomes more integrated and accepted in medicine, there may be a risk of legal complaints against doctors for not using AI, said Saurabh Jha, MD, an associate professor of radiology at the University of Pennsylvania, Philadelphia, and a scholar of AI in radiology.
“Ultimately, we might get to a place where AI starts helping physicians detect more or reduce the miss of certain conditions, and it becomes the standard of care,” Dr. Jha said. “For example, if it became part of the standard of care for pulmonary embolism [PE] detection, and you didn’t use it for PE detection, and there was a miss. That could put you at legal risk. We’re not at that stage yet, but that is one future possibility.”
Dr. Parikh envisions an even cloudier liability landscape as the potential grows for AI to control patient care decisions. In such a scenario, rather than just issuing an alert or prediction to a physician, the AI system could trigger an action.
For instance, if an algorithm is trained to predict sepsis and, once triggered, the AI could initiate a nurse-led rapid response or a change in patient care outside the clinician’s control, said Dr. Parikh, who coauthored a recent article on AI and medical liability in The Milbank Quarterly.
“That’s still very much the minority of how AI is being used, but as evidence is growing that AI-based diagnostic tools perform equivalent or even superior to physicians, these autonomous workflows are being considered,” Dr. Parikh said. “When the ultimate action upon the patient is more determined by the AI than what the clinician does, then I think the liability picture gets murkier, and we should be thinking about how we can respond to that from a liability framework.”
How you can prevent AI-related lawsuits
The first step to preventing an AI-related claim is being aware of when and how you are using AI.
Ensure you’re informed about how the AI was trained, Ms. Boisvert stresses.
“Ask questions!” she said. “Is the AI safe? Are the recommendations accurate? Does the AI perform better than current systems? In what way? What databases were used, and did the programmers consider bias? Do I understand how to use the results?”
Never blindly trust the AI but rather view it as a data point in a medical decision, said Dr. Parikh. Ensure that other sources of medical information are properly accessed and that best practices for your specialty are still being followed.
When using any form of AI, document your usage, adds Mr. Rashbaum. A record that clearly outlines how the physician incorporated the AI is critical if a claim later arises in which the doctor is accused of AI-related malpractice, he said.
“Indicating how the AI tool was used, why it was used, and that it was used in conjunction with available clinical information and the clinician’s best judgment could reduce the risk of being found responsible as a result of AI use in a particular case,” he said.
Use chatbots, such as ChatGPT, the way they were intended, as support tools, rather than definitive diagnostic instruments, adds Dr. Castro.
“Doctors should also be well-trained in interpreting and understanding the suggestions provided by ChatGPT and should use their clinical judgment and experience alongside the AI tool for more accurate decision-making,” he said.
In addition, because no AI insurance product exists on the market, physicians and organizations using AI – particularly for direct health care – should evaluate their current insurance or insurance-like products to determine where a claim involving AI might fall and whether the policy would respond, said Ms. Boisvert. The AI vendor/manufacturer will likely have indemnified themselves in the purchase and sale agreement or contract, she said.
It will also become increasingly important for medical practices, hospitals, and health systems to put in place strong data governance strategies, Mr. LeTang said.
“AI relies on good data,” he said. “A data governance strategy is a key component to making sure we understand where the data is coming from, what is represents, how accurate it is, if it’s reproducible, what controls are in place to ensure the right people have the right access, and that if we’re starting to use it to build algorithms, that it’s deidentified.”
While no malpractice claims associated with the use of AI have yet surfaced, this may change as legal courts catch up on the backlog of malpractice claims that were delayed because of COVID-19, and even more so as AI becomes more prevalent in health care, Mr. LeTang said.
“Similar to the attention that autonomous driving systems, like Tesla, receive when the system fails and accidents occur, we can be assured that media outlets will widely publicize AI-related medical adverse events,” he said. “It is crucial for health care professionals, AI developers, and regulatory authorities to work together to ensure the responsible use of AI in health care, with patient safety as the top priority. By doing so, they can mitigate the risks associated with AI implementation and minimize the potential for legal disputes arising from AI-related medical errors.”
A version of this article first appeared on Medscape.com.
The ways in which artificial intelligence (AI) may transform the future of medicine is making headlines across the globe. But chances are, you’re already using AI in your practice every day – you may just not realize it.
And whether you recognize the presence of AI or not, the technology could be putting you in danger of a lawsuit, legal experts say.
“For physicians, AI has also not yet drastically changed or improved the way care is provided or consumed,” said Michael LeTang, chief nursing informatics officer and vice president of risk management and patient safety at Healthcare Risk Advisors, part of TDC Group. “Consequently, it may seem like AI is not present in their work streams, but in reality, it has been utilized in health care for several years. As AI technologies continue to develop and become more sophisticated, we can expect them to play an increasingly significant role in health care.”
Today, most AI applications in health care use narrow AI, which is designed to complete a single task without human assistance, as opposed to artificial general intelligence (AGI), which pertains to human-level reasoning and problem solving across a broad spectrum. Here are some ways doctors are using AI throughout the day – sometimes being aware of its assistance, and sometimes being unaware:
- Many doctors use electronic health records (EHRs) with integrated AI that include computerized clinical decision support tools designed to reduce the risk of diagnostic error and to integrate decision-making in the medication ordering function.
- Cardiologists, pathologists, and dermatologists use AI in the interpretation of vast amounts of images, tracings, and complex patterns.
- Surgeons are using AI-enhanced surgical robotics for orthopedic surgeries, such as joint replacement and spine surgery.
- A growing number of doctors are using ChatGPT to assist in drafting prior authorization letters for insurers. Experts say more doctors are also experimenting with ChatGPT to support medical decision-making.
- Within oncology, physicians use machine learning techniques in the form of computer-aided detection systems for early breast cancer detection.
- AI algorithms are often used by health systems for workflow, staffing optimization, population management, and care coordination.
- Some systems within EHRs use AI to indicate high-risk patients.
- Physicians are using AI applications for the early recognition of sepsis, including EHR-integrated decision tools, such as the Hospital Corporation of America Healthcare’s Sepsis Prediction and Optimization Therapy and the Sepsis Early Risk Assessment algorithm.
- About 30% of radiologists use AI in their practice to analyze x-rays and CT scans.
- Epic Systems recently announced a partnership with Microsoft to integrate ChatGPT into MyChart, Epic’s patient portal system. Pilot hospitals will utilize ChatGPT to automatically generate responses to patient-generated questions sent via the portal.
The growth of AI in health care has been enormous, and it’s only going to continue, said Ravi B. Parikh, MD, an assistant professor in the department of medical ethics and health policy and medicine at the University of Pennsylvania, Philadelphia.
“What’s really critical is that physicians, clinicians, and nurses using AI are provided with the tools to understand how artificial intelligence works and, most importantly, understand that they are still accountable for making the ultimate decision,” Mr. LeTang said, “The information is not always going to be the right thing to do or the most accurate thing to do. They’re still liable for making a bad decision, even if AI is driving that.”
What are the top AI legal dangers of today?
A pressing legal risk is becoming too reliant on the suggestions that AI-based systems provide, which can lead to poor care decisions, said Kenneth Rashbaum, a New York–based cybersecurity attorney with more than 25 years of experience in medical malpractice defense.
This can occur, for example, when using clinical support systems that leverage AI, machine learning, or statistical pattern recognition. Today, clinical support systems are commonly administered through EHRs and other computerized clinical workflows. In general, such systems match a patient’s characteristics to a computerized clinical knowledge base. An assessment or recommendation is then presented to the physician for a decision.
“If the clinician blindly accepts it without considering whether it’s appropriate for this patient at this time with this presentation, the clinician may bear some responsibility if there is an untoward result,” Mr. Rashbaum said.
“A common claim even in the days before the EMR [electronic medical record] and AI, was that the clinician did not take all available information into account in rendering treatment, including history of past and present condition, as reflected in the records, communication with past and other present treating clinicians, lab and radiology results, discussions with the patient, and physical examination findings,” he said. “So, if the clinician relied upon the support prompt to the exclusion of these other sources of information, that could be a very strong argument for the plaintiff.”
Chatbots, such OpenAI’s ChatGPT, are another form of AI raising legal red flags. ChatGPT, trained on a massive set of text data, can carry out conversations, write code, draft emails, and answer any question posed. The chatbot has gained considerable credibility for accurately diagnosing rare conditions in seconds, and it recently passed the U.S. Medical Licensing Examination.
It’s unclear how many doctors are signing onto the ChatGPT website daily, but physicians are actively using the chatbot, particularly for assistance with prior authorization letters and to support decision-making processes in their practices, said Mr. LeTang.
When physicians ask ChatGPT a question, however, they should be mindful that ChatGPT could “hallucinate,” a term that refers to a generated response that sounds plausible but is factually incorrect or is unrelated to the context, explains Harvey Castro, MD, an emergency physician, ChatGPT health care expert, and author of the 2023 book “ChatGPT and Healthcare: Unlocking the Potential of Patient Empowerment.”
Acting on ChatGPT’s response without vetting the information places doctors at serious risk of a lawsuit, he said.
“Sometimes, the response is half true and half false,” he said. “Say, I go outside my specialty of emergency medicine and ask it about a pediatric surgical procedure. It could give me a response that sounds medically correct, but then I ask a pediatric cardiologist, and he says, ‘We don’t even do this. This doesn’t even exist!’ Physicians really have to make sure they are vetting the information provided.”
In response to ChatGPT’s growing usage by health care professionals, hospitals and practices are quickly implementing guidelines, policies, and restrictions that caution physicians about the accuracy of ChatGPT-generated information, adds Mr. LeTang.
Emerging best practices include avoiding the input of patient health information, personally identifiable information, or any data that could be commercially valuable or considered the intellectual property of a hospital or health system, he said.
“Another crucial guideline is not to rely solely on ChatGPT as a definitive source for clinical decision-making; physicians must exercise their professional judgment,” he said. “If best practices are not adhered to, the associated risks are present today. However, these risks may become more significant as AI technologies continue to evolve and become increasingly integrated into health care.”
The potential for misdiagnosis by AI systems and the risk of unnecessary procedures if physicians do not thoroughly evaluate and validate AI predictions are other dangers.
As an example, Mr. LeTang described a case in which a physician documents in the EHR that a patient has presented to the emergency department with chest pains and other signs of a heart attack, and an AI algorithm predicts that the patient is experiencing an active myocardial infarction. If the physician then sends the patient for stenting or an angioplasty without other concrete evidence or tests to confirm the diagnosis, the doctor could later face a misdiagnosis complaint if the costly procedures were unnecessary.
“That’s one of the risks of using artificial intelligence,” he said. “A large percentage of malpractice claims is failure to diagnose, delayed diagnosis, or inaccurate diagnosis. What falls in the category of failure to diagnose is sending a patient for an unnecessary procedure or having an adverse event or bad outcome because of the failure to diagnose.”
So far, no AI lawsuits have been filed, but they may make an appearance soon, said Sue Boisvert, senior patient safety risk manager at The Doctors Company, a national medical liability insurer.
“There are hundreds of AI programs currently in use in health care,” she said. “At some point, a provider will make a decision that is contrary to what the AI recommended. The AI may be wrong, or the provider may be wrong. Either way, the provider will neglect to document their clinical reasoning, a patient will be harmed, and we will have the first AI claim.”
Upcoming AI legal risks to watch for
Lawsuits that allege biased patient care by physicians on the basis of algorithmic bias may also be forthcoming, analysts warn.
Much has been written about algorithmic bias that compounds and worsens inequities in socioeconomic status, ethnicity, sexual orientation, and gender in health systems. In 2019, a groundbreaking article in Science shed light on commonly used algorithms that are considered racially biased and how health care professionals often use such information to make medical decisions.
No claims involving AI bias have come down the pipeline yet, but it’s an area to watch, said Ms. Boisvert. She noted a website that highlights complaints and accusations of AI bias, including in health care.
“We need to be sure the training of the AI is appropriate, current, and broad enough so that there is no bias in the AI when it’s participating in the decision-making,” said Ms. Boisvert. “Imagine if the AI is diagnosing based on a dataset that is not local. It doesn’t represent the population at that particular hospital, and it’s providing inaccurate information to the physicians who are then making decisions about treatment.”
In pain management, for example, there are known differences in how patients experience pain, Ms. Boisvert said. If AI was being used to develop an algorithm for how a particular patient’s postoperative pain should be managed, and the algorithm did not include the differences, the pain control for a certain patient could be inappropriate. A poor outcome resulting from the treatment could lead to a claim against the physician or hospital that used the biased AI system, she said.
In the future, as AI becomes more integrated and accepted in medicine, there may be a risk of legal complaints against doctors for not using AI, said Saurabh Jha, MD, an associate professor of radiology at the University of Pennsylvania, Philadelphia, and a scholar of AI in radiology.
“Ultimately, we might get to a place where AI starts helping physicians detect more or reduce the miss of certain conditions, and it becomes the standard of care,” Dr. Jha said. “For example, if it became part of the standard of care for pulmonary embolism [PE] detection, and you didn’t use it for PE detection, and there was a miss. That could put you at legal risk. We’re not at that stage yet, but that is one future possibility.”
Dr. Parikh envisions an even cloudier liability landscape as the potential grows for AI to control patient care decisions. In such a scenario, rather than just issuing an alert or prediction to a physician, the AI system could trigger an action.
For instance, if an algorithm is trained to predict sepsis and, once triggered, the AI could initiate a nurse-led rapid response or a change in patient care outside the clinician’s control, said Dr. Parikh, who coauthored a recent article on AI and medical liability in The Milbank Quarterly.
“That’s still very much the minority of how AI is being used, but as evidence is growing that AI-based diagnostic tools perform equivalent or even superior to physicians, these autonomous workflows are being considered,” Dr. Parikh said. “When the ultimate action upon the patient is more determined by the AI than what the clinician does, then I think the liability picture gets murkier, and we should be thinking about how we can respond to that from a liability framework.”
How you can prevent AI-related lawsuits
The first step to preventing an AI-related claim is being aware of when and how you are using AI.
Ensure you’re informed about how the AI was trained, Ms. Boisvert stresses.
“Ask questions!” she said. “Is the AI safe? Are the recommendations accurate? Does the AI perform better than current systems? In what way? What databases were used, and did the programmers consider bias? Do I understand how to use the results?”
Never blindly trust the AI but rather view it as a data point in a medical decision, said Dr. Parikh. Ensure that other sources of medical information are properly accessed and that best practices for your specialty are still being followed.
When using any form of AI, document your usage, adds Mr. Rashbaum. A record that clearly outlines how the physician incorporated the AI is critical if a claim later arises in which the doctor is accused of AI-related malpractice, he said.
“Indicating how the AI tool was used, why it was used, and that it was used in conjunction with available clinical information and the clinician’s best judgment could reduce the risk of being found responsible as a result of AI use in a particular case,” he said.
Use chatbots, such as ChatGPT, the way they were intended, as support tools, rather than definitive diagnostic instruments, adds Dr. Castro.
“Doctors should also be well-trained in interpreting and understanding the suggestions provided by ChatGPT and should use their clinical judgment and experience alongside the AI tool for more accurate decision-making,” he said.
In addition, because no AI insurance product exists on the market, physicians and organizations using AI – particularly for direct health care – should evaluate their current insurance or insurance-like products to determine where a claim involving AI might fall and whether the policy would respond, said Ms. Boisvert. The AI vendor/manufacturer will likely have indemnified themselves in the purchase and sale agreement or contract, she said.
It will also become increasingly important for medical practices, hospitals, and health systems to put in place strong data governance strategies, Mr. LeTang said.
“AI relies on good data,” he said. “A data governance strategy is a key component to making sure we understand where the data is coming from, what is represents, how accurate it is, if it’s reproducible, what controls are in place to ensure the right people have the right access, and that if we’re starting to use it to build algorithms, that it’s deidentified.”
While no malpractice claims associated with the use of AI have yet surfaced, this may change as legal courts catch up on the backlog of malpractice claims that were delayed because of COVID-19, and even more so as AI becomes more prevalent in health care, Mr. LeTang said.
“Similar to the attention that autonomous driving systems, like Tesla, receive when the system fails and accidents occur, we can be assured that media outlets will widely publicize AI-related medical adverse events,” he said. “It is crucial for health care professionals, AI developers, and regulatory authorities to work together to ensure the responsible use of AI in health care, with patient safety as the top priority. By doing so, they can mitigate the risks associated with AI implementation and minimize the potential for legal disputes arising from AI-related medical errors.”
A version of this article first appeared on Medscape.com.
The ways in which artificial intelligence (AI) may transform the future of medicine is making headlines across the globe. But chances are, you’re already using AI in your practice every day – you may just not realize it.
And whether you recognize the presence of AI or not, the technology could be putting you in danger of a lawsuit, legal experts say.
“For physicians, AI has also not yet drastically changed or improved the way care is provided or consumed,” said Michael LeTang, chief nursing informatics officer and vice president of risk management and patient safety at Healthcare Risk Advisors, part of TDC Group. “Consequently, it may seem like AI is not present in their work streams, but in reality, it has been utilized in health care for several years. As AI technologies continue to develop and become more sophisticated, we can expect them to play an increasingly significant role in health care.”
Today, most AI applications in health care use narrow AI, which is designed to complete a single task without human assistance, as opposed to artificial general intelligence (AGI), which pertains to human-level reasoning and problem solving across a broad spectrum. Here are some ways doctors are using AI throughout the day – sometimes being aware of its assistance, and sometimes being unaware:
- Many doctors use electronic health records (EHRs) with integrated AI that include computerized clinical decision support tools designed to reduce the risk of diagnostic error and to integrate decision-making in the medication ordering function.
- Cardiologists, pathologists, and dermatologists use AI in the interpretation of vast amounts of images, tracings, and complex patterns.
- Surgeons are using AI-enhanced surgical robotics for orthopedic surgeries, such as joint replacement and spine surgery.
- A growing number of doctors are using ChatGPT to assist in drafting prior authorization letters for insurers. Experts say more doctors are also experimenting with ChatGPT to support medical decision-making.
- Within oncology, physicians use machine learning techniques in the form of computer-aided detection systems for early breast cancer detection.
- AI algorithms are often used by health systems for workflow, staffing optimization, population management, and care coordination.
- Some systems within EHRs use AI to indicate high-risk patients.
- Physicians are using AI applications for the early recognition of sepsis, including EHR-integrated decision tools, such as the Hospital Corporation of America Healthcare’s Sepsis Prediction and Optimization Therapy and the Sepsis Early Risk Assessment algorithm.
- About 30% of radiologists use AI in their practice to analyze x-rays and CT scans.
- Epic Systems recently announced a partnership with Microsoft to integrate ChatGPT into MyChart, Epic’s patient portal system. Pilot hospitals will utilize ChatGPT to automatically generate responses to patient-generated questions sent via the portal.
The growth of AI in health care has been enormous, and it’s only going to continue, said Ravi B. Parikh, MD, an assistant professor in the department of medical ethics and health policy and medicine at the University of Pennsylvania, Philadelphia.
“What’s really critical is that physicians, clinicians, and nurses using AI are provided with the tools to understand how artificial intelligence works and, most importantly, understand that they are still accountable for making the ultimate decision,” Mr. LeTang said, “The information is not always going to be the right thing to do or the most accurate thing to do. They’re still liable for making a bad decision, even if AI is driving that.”
What are the top AI legal dangers of today?
A pressing legal risk is becoming too reliant on the suggestions that AI-based systems provide, which can lead to poor care decisions, said Kenneth Rashbaum, a New York–based cybersecurity attorney with more than 25 years of experience in medical malpractice defense.
This can occur, for example, when using clinical support systems that leverage AI, machine learning, or statistical pattern recognition. Today, clinical support systems are commonly administered through EHRs and other computerized clinical workflows. In general, such systems match a patient’s characteristics to a computerized clinical knowledge base. An assessment or recommendation is then presented to the physician for a decision.
“If the clinician blindly accepts it without considering whether it’s appropriate for this patient at this time with this presentation, the clinician may bear some responsibility if there is an untoward result,” Mr. Rashbaum said.
“A common claim even in the days before the EMR [electronic medical record] and AI, was that the clinician did not take all available information into account in rendering treatment, including history of past and present condition, as reflected in the records, communication with past and other present treating clinicians, lab and radiology results, discussions with the patient, and physical examination findings,” he said. “So, if the clinician relied upon the support prompt to the exclusion of these other sources of information, that could be a very strong argument for the plaintiff.”
Chatbots, such OpenAI’s ChatGPT, are another form of AI raising legal red flags. ChatGPT, trained on a massive set of text data, can carry out conversations, write code, draft emails, and answer any question posed. The chatbot has gained considerable credibility for accurately diagnosing rare conditions in seconds, and it recently passed the U.S. Medical Licensing Examination.
It’s unclear how many doctors are signing onto the ChatGPT website daily, but physicians are actively using the chatbot, particularly for assistance with prior authorization letters and to support decision-making processes in their practices, said Mr. LeTang.
When physicians ask ChatGPT a question, however, they should be mindful that ChatGPT could “hallucinate,” a term that refers to a generated response that sounds plausible but is factually incorrect or is unrelated to the context, explains Harvey Castro, MD, an emergency physician, ChatGPT health care expert, and author of the 2023 book “ChatGPT and Healthcare: Unlocking the Potential of Patient Empowerment.”
Acting on ChatGPT’s response without vetting the information places doctors at serious risk of a lawsuit, he said.
“Sometimes, the response is half true and half false,” he said. “Say, I go outside my specialty of emergency medicine and ask it about a pediatric surgical procedure. It could give me a response that sounds medically correct, but then I ask a pediatric cardiologist, and he says, ‘We don’t even do this. This doesn’t even exist!’ Physicians really have to make sure they are vetting the information provided.”
In response to ChatGPT’s growing usage by health care professionals, hospitals and practices are quickly implementing guidelines, policies, and restrictions that caution physicians about the accuracy of ChatGPT-generated information, adds Mr. LeTang.
Emerging best practices include avoiding the input of patient health information, personally identifiable information, or any data that could be commercially valuable or considered the intellectual property of a hospital or health system, he said.
“Another crucial guideline is not to rely solely on ChatGPT as a definitive source for clinical decision-making; physicians must exercise their professional judgment,” he said. “If best practices are not adhered to, the associated risks are present today. However, these risks may become more significant as AI technologies continue to evolve and become increasingly integrated into health care.”
The potential for misdiagnosis by AI systems and the risk of unnecessary procedures if physicians do not thoroughly evaluate and validate AI predictions are other dangers.
As an example, Mr. LeTang described a case in which a physician documents in the EHR that a patient has presented to the emergency department with chest pains and other signs of a heart attack, and an AI algorithm predicts that the patient is experiencing an active myocardial infarction. If the physician then sends the patient for stenting or an angioplasty without other concrete evidence or tests to confirm the diagnosis, the doctor could later face a misdiagnosis complaint if the costly procedures were unnecessary.
“That’s one of the risks of using artificial intelligence,” he said. “A large percentage of malpractice claims is failure to diagnose, delayed diagnosis, or inaccurate diagnosis. What falls in the category of failure to diagnose is sending a patient for an unnecessary procedure or having an adverse event or bad outcome because of the failure to diagnose.”
So far, no AI lawsuits have been filed, but they may make an appearance soon, said Sue Boisvert, senior patient safety risk manager at The Doctors Company, a national medical liability insurer.
“There are hundreds of AI programs currently in use in health care,” she said. “At some point, a provider will make a decision that is contrary to what the AI recommended. The AI may be wrong, or the provider may be wrong. Either way, the provider will neglect to document their clinical reasoning, a patient will be harmed, and we will have the first AI claim.”
Upcoming AI legal risks to watch for
Lawsuits that allege biased patient care by physicians on the basis of algorithmic bias may also be forthcoming, analysts warn.
Much has been written about algorithmic bias that compounds and worsens inequities in socioeconomic status, ethnicity, sexual orientation, and gender in health systems. In 2019, a groundbreaking article in Science shed light on commonly used algorithms that are considered racially biased and how health care professionals often use such information to make medical decisions.
No claims involving AI bias have come down the pipeline yet, but it’s an area to watch, said Ms. Boisvert. She noted a website that highlights complaints and accusations of AI bias, including in health care.
“We need to be sure the training of the AI is appropriate, current, and broad enough so that there is no bias in the AI when it’s participating in the decision-making,” said Ms. Boisvert. “Imagine if the AI is diagnosing based on a dataset that is not local. It doesn’t represent the population at that particular hospital, and it’s providing inaccurate information to the physicians who are then making decisions about treatment.”
In pain management, for example, there are known differences in how patients experience pain, Ms. Boisvert said. If AI was being used to develop an algorithm for how a particular patient’s postoperative pain should be managed, and the algorithm did not include the differences, the pain control for a certain patient could be inappropriate. A poor outcome resulting from the treatment could lead to a claim against the physician or hospital that used the biased AI system, she said.
In the future, as AI becomes more integrated and accepted in medicine, there may be a risk of legal complaints against doctors for not using AI, said Saurabh Jha, MD, an associate professor of radiology at the University of Pennsylvania, Philadelphia, and a scholar of AI in radiology.
“Ultimately, we might get to a place where AI starts helping physicians detect more or reduce the miss of certain conditions, and it becomes the standard of care,” Dr. Jha said. “For example, if it became part of the standard of care for pulmonary embolism [PE] detection, and you didn’t use it for PE detection, and there was a miss. That could put you at legal risk. We’re not at that stage yet, but that is one future possibility.”
Dr. Parikh envisions an even cloudier liability landscape as the potential grows for AI to control patient care decisions. In such a scenario, rather than just issuing an alert or prediction to a physician, the AI system could trigger an action.
For instance, if an algorithm is trained to predict sepsis and, once triggered, the AI could initiate a nurse-led rapid response or a change in patient care outside the clinician’s control, said Dr. Parikh, who coauthored a recent article on AI and medical liability in The Milbank Quarterly.
“That’s still very much the minority of how AI is being used, but as evidence is growing that AI-based diagnostic tools perform equivalent or even superior to physicians, these autonomous workflows are being considered,” Dr. Parikh said. “When the ultimate action upon the patient is more determined by the AI than what the clinician does, then I think the liability picture gets murkier, and we should be thinking about how we can respond to that from a liability framework.”
How you can prevent AI-related lawsuits
The first step to preventing an AI-related claim is being aware of when and how you are using AI.
Ensure you’re informed about how the AI was trained, Ms. Boisvert stresses.
“Ask questions!” she said. “Is the AI safe? Are the recommendations accurate? Does the AI perform better than current systems? In what way? What databases were used, and did the programmers consider bias? Do I understand how to use the results?”
Never blindly trust the AI but rather view it as a data point in a medical decision, said Dr. Parikh. Ensure that other sources of medical information are properly accessed and that best practices for your specialty are still being followed.
When using any form of AI, document your usage, adds Mr. Rashbaum. A record that clearly outlines how the physician incorporated the AI is critical if a claim later arises in which the doctor is accused of AI-related malpractice, he said.
“Indicating how the AI tool was used, why it was used, and that it was used in conjunction with available clinical information and the clinician’s best judgment could reduce the risk of being found responsible as a result of AI use in a particular case,” he said.
Use chatbots, such as ChatGPT, the way they were intended, as support tools, rather than definitive diagnostic instruments, adds Dr. Castro.
“Doctors should also be well-trained in interpreting and understanding the suggestions provided by ChatGPT and should use their clinical judgment and experience alongside the AI tool for more accurate decision-making,” he said.
In addition, because no AI insurance product exists on the market, physicians and organizations using AI – particularly for direct health care – should evaluate their current insurance or insurance-like products to determine where a claim involving AI might fall and whether the policy would respond, said Ms. Boisvert. The AI vendor/manufacturer will likely have indemnified themselves in the purchase and sale agreement or contract, she said.
It will also become increasingly important for medical practices, hospitals, and health systems to put in place strong data governance strategies, Mr. LeTang said.
“AI relies on good data,” he said. “A data governance strategy is a key component to making sure we understand where the data is coming from, what is represents, how accurate it is, if it’s reproducible, what controls are in place to ensure the right people have the right access, and that if we’re starting to use it to build algorithms, that it’s deidentified.”
While no malpractice claims associated with the use of AI have yet surfaced, this may change as legal courts catch up on the backlog of malpractice claims that were delayed because of COVID-19, and even more so as AI becomes more prevalent in health care, Mr. LeTang said.
“Similar to the attention that autonomous driving systems, like Tesla, receive when the system fails and accidents occur, we can be assured that media outlets will widely publicize AI-related medical adverse events,” he said. “It is crucial for health care professionals, AI developers, and regulatory authorities to work together to ensure the responsible use of AI in health care, with patient safety as the top priority. By doing so, they can mitigate the risks associated with AI implementation and minimize the potential for legal disputes arising from AI-related medical errors.”
A version of this article first appeared on Medscape.com.
How can we make medical training less ‘toxic’?
This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining me to discuss ways to address and reform the toxic culture associated with medical training is Dr. Amy Faith Ho, senior vice president of clinical informatics and analytics at Integrative Emergency Services in Dallas. Also joining us is Dr. Júlia Loyola Ferreira, a pediatric surgeon originally from Brazil, now practicing at Montreal Children’s and focused on advocacy for gender equity and patient-centered care.
Welcome to both of you. Thanks so much for joining me.
Amy Faith Ho, MD, MPH: Thanks so much for having us, Rob.
Dr. Glatter: Amy, I noticed a tweet recently where you talked about how your career choice was affected by the toxic environment in medical school, affecting your choice of residency. Can you elaborate on that?
Dr. Ho: In this instance, what we’re talking about is gender, but it can be directed toward any number of other groups as well.
What you’re alluding to is a tweet by Stanford Surgery Group showing the next residency class, and what was really stunning about this residency class was that it was almost all females. And this was something that took off on social media.
When I saw this, I was really brought back to one of my personal experiences that I chose to share, which was basically that, as a medical student, I really wanted to be a surgeon. I’m an emergency medicine doctor now, so you know that didn’t happen.
The story that I was sharing was that when I was a third-year medical student rotating on surgery, we had a male attending who was very well known at that school at the time who basically would take the female medical students, and instead of clinic, he would round us up. He would have us sit around him in the workplace room while everyone else was seeing patients, and he would have you look at news clippings of himself. He would tell you stories about himself, like he was holding court for the ladies.
It was this very weird culture where my takeaway as a med student was like, “Wow, this is kind of abusive patriarchy that is supported,” because everyone knew about it and was complicit. Even though I really liked surgery, this was just one instance and one example of where you see this culture that really resonates into the rest of life that I didn’t really want to be a part of.
I went into emergency medicine and loved it. It’s also highly procedural, and I was very happy with where I was. What was really interesting about this tweet to me, though, is that it really took off and garnered hundreds of thousands of views on a very niche topic, because what was most revealing is that everyone has a story like this.
It is not just surgery. It is definitely not just one specialty and it is not just one school. It is an endemic problem in medicine. Not only does it change the lives of young women, but it also says so much about the complicity and the culture that we have in medicine that many people were upset about just the same way I was.
Medical training experience in other countries vs. the United States
Dr. Glatter: Júlia, I want to hear about your experience in medical school, surgery, and then fellowship training and up to the present, if possible.
Júlia Loyola Ferreira, MD: In Brazil, as in many countries now, women have made up the majority of the medical students since 2010. It’s a more female-friendly environment when you’re going through medical school, and I was lucky enough to do rotations in areas of surgery where people were friendly to women.
I lived in this tiny bubble that also gave me the privilege of not facing some things that I can imagine that people in Brazil in different areas and smaller towns face. In Brazil, people try to not talk about this gender agenda. This is something that’s being talked about outside Brazil. But in Brazil, we are years back. People are not really engaging on this conversation. I thought it was going to be hard for me as a woman, because Brazil has around 20% female surgeons.
I knew it was going to be challenging, but I had no idea how bad it was. When I started and things started happening, the list was big. I have an example of everything that is written about – microaggression, implicit bias, discrimination, harassment.
Every time I would try to speak about it and talk to someone, I would be strongly gaslighted. It was the whole training, the whole 5 years. People would say, “Oh, I don’t think it was like that. I think you were overreacting.” People would come with all these different answers for what I was experiencing, and that was frustrating. That was even harder because I had to cope with everything that was happening and I had no one to turn to. I had no mentors.
When I looked up to women who were in surgery, they would be tougher on us young surgeons than the men and they would tell us that we should not complain because in their time it was even harder. Now, it’s getting better and we are supposed to accept whatever comes.
That was at least a little bit of what I experienced in my training. It was only after I finished and started to do research about it that I really encountered a field of people who would echo what I was trying to say to many people in different hospitals that I attended to.
That was the key for me to get out of that situation of being gaslighted and of not being able to really talk about it. Suddenly, I started to publish things about Brazil that nobody was even writing or studying. That gave me a large amount of responsibility, but also motivation to keep going and to see the change.
Valuing women in medicine
Dr. Glatter: This is a very important point that you’re raising about the environment of women being hard on other women. We know that men can be very difficult on and also judgmental toward their trainees.
Amy, how would you respond to that? Was your experience similar in emergency medicine training?
Dr. Ho: I actually don’t feel like it was. I think what Júlia is alluding to is this “mean girls” idea, of “I went through it and thus you have to go through it.” I think you do see this in many specialties. One of the classic ones we hear about, and I don’t want to speak to it too much because it’s not my specialty, is ob.gyn., where it is a very female-dominant surgery group. There’s almost a hazing level that you hear about in some of the more malignant workplaces.
I think that you speak to two really important things. Number one is the numbers game. As you were saying, Brazil actually has many women. That’s awesome. That’s actually different from the United States, especially for the historic, existing workplace and less so for the medical students and for residents. I think step one is having minorities like women just present and there.
Step two is actually including and valuing them. While I think it’s really easy to move away from the women discussion, because there are women when you look around in medicine, it doesn’t mean that women are actually being heard, that they’re actually being accepted, or that their viewpoints are being listened to. A big part of it is normalizing not only seeing women in medicine but also normalizing the narrative of women in medicine.
It’s not just about motherhood; it’s about things like normalizing talking about advancement, academic promotions, pay, culture, being called things like “too reactive,” “anxious,” or “too assertive.” These are all classic things that we hear about when we talk about women.
That’s why we’re looking to not only conversations like this, but also structured ways for women to discuss being women in medicine. There are many women in medicine groups in emergency medicine, including: Females Working in Emergency Medicine (FemInEM); the American College of Emergency Physicians (ACEP) and Society for Academic Emergency Medicine (SAEM) women’s groups, which are American Association of Women Emergency Physicians (AAWEP) and Academy for Women in Academic Emergency Medicine (AWAEM), respectively; and the American Medical Women’s Association (AMWA), which is the American Medical Association’s offshoot.
All of these groups are geared toward normalizing women in medicine, normalizing the narrative of women in medicine, and then working on mentoring and educating so that we can advance our initiatives.
Gender balance is not gender equity
Dr. Glatter: Amy, you bring up a very critical point that mentoring is sort of the antidote to gender-based discrimination. Júlia had written a paper back in November of 2022 that was published in the Journal of Surgical Research talking exactly about this and how important it is to develop mentoring. Part of her research showed that about 20% of medical students who took the survey, about 1,000 people, had mentors, which was very disturbing.
Dr. Loyola Ferreira: Mentorship is one of the ways of changing the reality about gender-based discrimination. Amy’s comment was very strong and we need to really keep saying it, which is that gender balance is not gender equity.
The idea of having more women is not the same as women being recognized as equals, as able as men, and as valued as men. To change this very long culture of male domination, we need support, and this support comes from mentorship.
Although I didn’t have one, I feel that since I started being a mentor for some students, it changed not only them but myself. It gave me strength to keep going, studying, publishing, and going further with this discussion. I feel like the relationship was as good for them as it is for me. That’s how things change.
Diversity, equity, and inclusion training
Dr. Glatter: We’re talking about the reality of gender equity in terms of the ability to have equal respect, recognition, opportunities, and access. That’s really an important point to realize, and for our audience, to understand that gender equity is not gender balance.
Amy, I want to talk about medical school curriculums. Are there advances that you’re aware of being made at certain schools, programs, even in residencies, to enforce these things and make it a priority?
Dr. Ho: We’re really lucky that, as a culture in the United States, medical training is certainly very geared toward diversity. Some of that is certainly unofficial. Some of that just means when they’re looking at a medical school class or looking at rank lists for residency, that they’re cognizant of the different backgrounds that people have. That’s still a step. That is a step, that we’re at least acknowledging it.
There are multiple medical schools and residencies that have more formal unconscious-bias training or diversity, equity, and inclusion (DEI) training, both of which are excellent not only for us in the workplace but also for our patients. Almost all of us will see patients of highly diverse backgrounds. I think the biggest push is looking toward the criteria that we use for selecting trainees and students into our programs. Historically, it’s been MCAT, GPA, and so on.
We’ve really started to ask the question of, are these sorts of “objective criteria” actually biased in institutional ways? They talk about this all the time where GPAs will bias against students from underrepresented minorities (URM). I think all medical students and residencies have really acknowledged that. Although there are still test cutoffs, we are putting an inquisitive eye to what those mean, why they exist, and what are the other things that we should consider. This is all very heartening from what I’m seeing in medical training.
Dr. Glatter: There’s no formal rating system for DEI curriculums right now, like ranking of this school, or this program has more advanced recognition in terms of DEI?
Dr. Ho: No, but on the flip side, the U.S. News & World Report was classically one of the major rankings for medical schools. What we saw fairly recently was that very high-tier schools like Harvard and University of Chicago pulled out of that ranking because that ranking did not acknowledge the value of diversity. That was an incredible stance for medical schools to take, to say, “Hey, you are not evaluating an important criterion of ours.”
Dr. Glatter: That’s a great point. Júlia, where are we now in Brazil in terms of awareness of DEI and curriculum in schools and training programs?
Dr. Loyola Ferreira: Our reality is not as good as in the U.S., unfortunately. I don’t see much discussion on residency programs or medical schools at the moment. I see many students bringing it out and trying to make their schools engage in that discussion. This is something that is coming from the bottom up and not from the top down. I think it can lead to change as well. It is a step and it’s a beginning. Institutions should take the responsibility of doing this from the beginning. This is something where Brazil is still years behind you guys.
Dr. Glatter: It’s unfortunate, but certainly it’s important to hear that. What about in Canada and certainly your institution, McGill, where you just completed a master’s degree?
Dr. Loyola Ferreira: Canada is very much like the U.S. This is something that is really happening and it’s happening fast. I see, at least at McGill, a large amount of DEI inclusion and everything on this discussion. They have institutional courses for us to do as students, and we are all obliged to do many courses, which I think is really educating, especially for people with different cultures and backgrounds.
Dr. Glatter: Amy, where do you think we are in emergency medicine to look at the other side of it? Comparing surgery with emergency medicine, do you think we’re well advanced in terms of DEI, inclusion criteria, respect, and dignity, or are we really far off?
Dr. Ho: I may be biased, but I think emergency medicine is one of the best in terms of this, and I think there are a couple of reasons for it. One is that we are an inherently team-based organization. The attending, the residents, and the students all work in line with one another. There’s less of a hierarchy.
The same is true for our nurses, pharmacists, techs, and EMS. We all work together as a team. Because of that fairly flat structure, it’s really easy for us to value one another as individuals with our diverse backgrounds. In a way, that’s harder for specialties that are more hierarchical, and I think surgery is certainly one of the most hierarchical.
The second reason why emergency medicine is fairly well off in this is that we’re, by nature, a safety-net specialty. We see patients of all-comers, all walks, all backgrounds. I think we both recognize the value of physician-patient concordance. When we share characteristics with our patients, we recognize that value immediately at the bedside.
It exposes us to so much diversity. I see a refugee one day and the next patient is someone who is incarcerated. The next patient after that is an important businessman in society. That diversity and whiplash in the type of patients that we see back-to-back helps us see the playing field in a really flat, diverse way. Because of that, I think our culture is much better, as is our understanding of the value and importance of diversity not only for our programs, but also for our patients.
Do female doctors have better patient outcomes?
Dr. Glatter: Specialties working together in the emergency department is so important. Building that team and that togetherness is so critical. Júlia, would you agree?
Dr. Loyola Ferreira: Definitely. Something Amy said that is beautiful is that you recognize yourself in these patients. In surgery, we are taught to try to be away from the patients and not to put ourselves in the same position. We are taught to be less engaging, and this is not good. The good thing is when we really have patient-centered care, when we listen to them, and when we are involved with them.
I saw a publication showing that female and male surgeons treating similar patients had the same surgical outcomes. Women are as good as men technically to do surgery and have the same surgical outcomes. However, there is research showing that surgical teams with greater representation of women have improved surgical outcomes because of patient-centered care and the way women conduct bedside attention to patients. And they have better patient experience measures afterward. That is not only from the women who are treating the patients, but the whole environment. Women end up bringing men [into the conversation] and this better improves patient-centered care, and that makes the whole team a better team attending patients. Definitely, we are in the moment of patient experience and satisfaction, and increasing women is a way of achieving better patient satisfaction and experience.
Dr. Ho: There’s much to be said about having female clinicians available for patients. It doesn’t have to be just for female patients, although again, concordance between physicians and patients is certainly beneficial. Besides outcomes benefit, there’s even just a communication benefit. The way that women and men communicate is inherently different. The way women and men experience certain things is also inherently different.
A classic example of this is women who are experiencing a heart attack may not actually have chest pain but present with nausea. As a female who’s sensitive to this, when I see a woman throwing up, I am very attuned to something actually being wrong, knowing that they may not present with classic pain for a syndrome, but actually may be presenting with nausea instead. It doesn’t have to be a woman who takes that knowledge and turns it into something at the bedside. It certainly doesn’t have to, but it is just a natural, easy thing to step into as a female.
While I’m really careful to not step into this “women are better than men” or “men are better than women” argument, there’s something to be said about how the availability of female clinicians for all patients, not just female patients, can have benefit. Again, it’s shown in studies with cardiovascular outcomes and cardiologists, it’s certainly shown in ob.gyn., particularly for underrepresented minorities as well for maternal outcomes of Black mothers. It’s certainly shown again in patient satisfaction, which is concordance.
There is a profound level of research already on this that goes beyond just the idea of stacking the bench and putting more women in there. That’s not the value. We’re not just here to check off the box. We’re here to actually lend some value to our patients and, again, to one another as well.
Dr. Glatter: Absolutely. These are excellent points. The point you make about patient presentation is so vital. The fact that women have nausea sometimes in ACS presentations, the research never was really attentive to this. It was biased. The symptoms that women may have that are not “typical” for ACS weren’t included in patient presentations. Educating everyone about, overall, the types of presentations that we can recognize is vital and important.
Dr. Ho: Yes. It’s worth saying that, when you look at how medicine and research developed, classically, who were the research participants? They were often White men. They were college students who, historically, because women were not allowed to go to college, were men.
I say that not to fault the institution, because that was the culture of our history, but to just say it is okay to question things. It is okay to realize that someone’s presenting outside of the box and that maybe we actually need to reframe what even created the walls of the box in the first place.
Dr. Glatter: Thank you again for joining us. I truly appreciate your insight and expertise.
Dr. Glatter is assistant professor of emergency medicine, department of emergency medicine, Hofstra/Northwell, New York. Dr. Ho is senior vice president of clinical informatics & analytics, department of emergency medicine, Integrative Emergency Services, Dallas. Dr. Loyola Ferreira is a master of science candidate, department of experimental surgery, McGill University, Montreal. They reported that they had no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining me to discuss ways to address and reform the toxic culture associated with medical training is Dr. Amy Faith Ho, senior vice president of clinical informatics and analytics at Integrative Emergency Services in Dallas. Also joining us is Dr. Júlia Loyola Ferreira, a pediatric surgeon originally from Brazil, now practicing at Montreal Children’s and focused on advocacy for gender equity and patient-centered care.
Welcome to both of you. Thanks so much for joining me.
Amy Faith Ho, MD, MPH: Thanks so much for having us, Rob.
Dr. Glatter: Amy, I noticed a tweet recently where you talked about how your career choice was affected by the toxic environment in medical school, affecting your choice of residency. Can you elaborate on that?
Dr. Ho: In this instance, what we’re talking about is gender, but it can be directed toward any number of other groups as well.
What you’re alluding to is a tweet by Stanford Surgery Group showing the next residency class, and what was really stunning about this residency class was that it was almost all females. And this was something that took off on social media.
When I saw this, I was really brought back to one of my personal experiences that I chose to share, which was basically that, as a medical student, I really wanted to be a surgeon. I’m an emergency medicine doctor now, so you know that didn’t happen.
The story that I was sharing was that when I was a third-year medical student rotating on surgery, we had a male attending who was very well known at that school at the time who basically would take the female medical students, and instead of clinic, he would round us up. He would have us sit around him in the workplace room while everyone else was seeing patients, and he would have you look at news clippings of himself. He would tell you stories about himself, like he was holding court for the ladies.
It was this very weird culture where my takeaway as a med student was like, “Wow, this is kind of abusive patriarchy that is supported,” because everyone knew about it and was complicit. Even though I really liked surgery, this was just one instance and one example of where you see this culture that really resonates into the rest of life that I didn’t really want to be a part of.
I went into emergency medicine and loved it. It’s also highly procedural, and I was very happy with where I was. What was really interesting about this tweet to me, though, is that it really took off and garnered hundreds of thousands of views on a very niche topic, because what was most revealing is that everyone has a story like this.
It is not just surgery. It is definitely not just one specialty and it is not just one school. It is an endemic problem in medicine. Not only does it change the lives of young women, but it also says so much about the complicity and the culture that we have in medicine that many people were upset about just the same way I was.
Medical training experience in other countries vs. the United States
Dr. Glatter: Júlia, I want to hear about your experience in medical school, surgery, and then fellowship training and up to the present, if possible.
Júlia Loyola Ferreira, MD: In Brazil, as in many countries now, women have made up the majority of the medical students since 2010. It’s a more female-friendly environment when you’re going through medical school, and I was lucky enough to do rotations in areas of surgery where people were friendly to women.
I lived in this tiny bubble that also gave me the privilege of not facing some things that I can imagine that people in Brazil in different areas and smaller towns face. In Brazil, people try to not talk about this gender agenda. This is something that’s being talked about outside Brazil. But in Brazil, we are years back. People are not really engaging on this conversation. I thought it was going to be hard for me as a woman, because Brazil has around 20% female surgeons.
I knew it was going to be challenging, but I had no idea how bad it was. When I started and things started happening, the list was big. I have an example of everything that is written about – microaggression, implicit bias, discrimination, harassment.
Every time I would try to speak about it and talk to someone, I would be strongly gaslighted. It was the whole training, the whole 5 years. People would say, “Oh, I don’t think it was like that. I think you were overreacting.” People would come with all these different answers for what I was experiencing, and that was frustrating. That was even harder because I had to cope with everything that was happening and I had no one to turn to. I had no mentors.
When I looked up to women who were in surgery, they would be tougher on us young surgeons than the men and they would tell us that we should not complain because in their time it was even harder. Now, it’s getting better and we are supposed to accept whatever comes.
That was at least a little bit of what I experienced in my training. It was only after I finished and started to do research about it that I really encountered a field of people who would echo what I was trying to say to many people in different hospitals that I attended to.
That was the key for me to get out of that situation of being gaslighted and of not being able to really talk about it. Suddenly, I started to publish things about Brazil that nobody was even writing or studying. That gave me a large amount of responsibility, but also motivation to keep going and to see the change.
Valuing women in medicine
Dr. Glatter: This is a very important point that you’re raising about the environment of women being hard on other women. We know that men can be very difficult on and also judgmental toward their trainees.
Amy, how would you respond to that? Was your experience similar in emergency medicine training?
Dr. Ho: I actually don’t feel like it was. I think what Júlia is alluding to is this “mean girls” idea, of “I went through it and thus you have to go through it.” I think you do see this in many specialties. One of the classic ones we hear about, and I don’t want to speak to it too much because it’s not my specialty, is ob.gyn., where it is a very female-dominant surgery group. There’s almost a hazing level that you hear about in some of the more malignant workplaces.
I think that you speak to two really important things. Number one is the numbers game. As you were saying, Brazil actually has many women. That’s awesome. That’s actually different from the United States, especially for the historic, existing workplace and less so for the medical students and for residents. I think step one is having minorities like women just present and there.
Step two is actually including and valuing them. While I think it’s really easy to move away from the women discussion, because there are women when you look around in medicine, it doesn’t mean that women are actually being heard, that they’re actually being accepted, or that their viewpoints are being listened to. A big part of it is normalizing not only seeing women in medicine but also normalizing the narrative of women in medicine.
It’s not just about motherhood; it’s about things like normalizing talking about advancement, academic promotions, pay, culture, being called things like “too reactive,” “anxious,” or “too assertive.” These are all classic things that we hear about when we talk about women.
That’s why we’re looking to not only conversations like this, but also structured ways for women to discuss being women in medicine. There are many women in medicine groups in emergency medicine, including: Females Working in Emergency Medicine (FemInEM); the American College of Emergency Physicians (ACEP) and Society for Academic Emergency Medicine (SAEM) women’s groups, which are American Association of Women Emergency Physicians (AAWEP) and Academy for Women in Academic Emergency Medicine (AWAEM), respectively; and the American Medical Women’s Association (AMWA), which is the American Medical Association’s offshoot.
All of these groups are geared toward normalizing women in medicine, normalizing the narrative of women in medicine, and then working on mentoring and educating so that we can advance our initiatives.
Gender balance is not gender equity
Dr. Glatter: Amy, you bring up a very critical point that mentoring is sort of the antidote to gender-based discrimination. Júlia had written a paper back in November of 2022 that was published in the Journal of Surgical Research talking exactly about this and how important it is to develop mentoring. Part of her research showed that about 20% of medical students who took the survey, about 1,000 people, had mentors, which was very disturbing.
Dr. Loyola Ferreira: Mentorship is one of the ways of changing the reality about gender-based discrimination. Amy’s comment was very strong and we need to really keep saying it, which is that gender balance is not gender equity.
The idea of having more women is not the same as women being recognized as equals, as able as men, and as valued as men. To change this very long culture of male domination, we need support, and this support comes from mentorship.
Although I didn’t have one, I feel that since I started being a mentor for some students, it changed not only them but myself. It gave me strength to keep going, studying, publishing, and going further with this discussion. I feel like the relationship was as good for them as it is for me. That’s how things change.
Diversity, equity, and inclusion training
Dr. Glatter: We’re talking about the reality of gender equity in terms of the ability to have equal respect, recognition, opportunities, and access. That’s really an important point to realize, and for our audience, to understand that gender equity is not gender balance.
Amy, I want to talk about medical school curriculums. Are there advances that you’re aware of being made at certain schools, programs, even in residencies, to enforce these things and make it a priority?
Dr. Ho: We’re really lucky that, as a culture in the United States, medical training is certainly very geared toward diversity. Some of that is certainly unofficial. Some of that just means when they’re looking at a medical school class or looking at rank lists for residency, that they’re cognizant of the different backgrounds that people have. That’s still a step. That is a step, that we’re at least acknowledging it.
There are multiple medical schools and residencies that have more formal unconscious-bias training or diversity, equity, and inclusion (DEI) training, both of which are excellent not only for us in the workplace but also for our patients. Almost all of us will see patients of highly diverse backgrounds. I think the biggest push is looking toward the criteria that we use for selecting trainees and students into our programs. Historically, it’s been MCAT, GPA, and so on.
We’ve really started to ask the question of, are these sorts of “objective criteria” actually biased in institutional ways? They talk about this all the time where GPAs will bias against students from underrepresented minorities (URM). I think all medical students and residencies have really acknowledged that. Although there are still test cutoffs, we are putting an inquisitive eye to what those mean, why they exist, and what are the other things that we should consider. This is all very heartening from what I’m seeing in medical training.
Dr. Glatter: There’s no formal rating system for DEI curriculums right now, like ranking of this school, or this program has more advanced recognition in terms of DEI?
Dr. Ho: No, but on the flip side, the U.S. News & World Report was classically one of the major rankings for medical schools. What we saw fairly recently was that very high-tier schools like Harvard and University of Chicago pulled out of that ranking because that ranking did not acknowledge the value of diversity. That was an incredible stance for medical schools to take, to say, “Hey, you are not evaluating an important criterion of ours.”
Dr. Glatter: That’s a great point. Júlia, where are we now in Brazil in terms of awareness of DEI and curriculum in schools and training programs?
Dr. Loyola Ferreira: Our reality is not as good as in the U.S., unfortunately. I don’t see much discussion on residency programs or medical schools at the moment. I see many students bringing it out and trying to make their schools engage in that discussion. This is something that is coming from the bottom up and not from the top down. I think it can lead to change as well. It is a step and it’s a beginning. Institutions should take the responsibility of doing this from the beginning. This is something where Brazil is still years behind you guys.
Dr. Glatter: It’s unfortunate, but certainly it’s important to hear that. What about in Canada and certainly your institution, McGill, where you just completed a master’s degree?
Dr. Loyola Ferreira: Canada is very much like the U.S. This is something that is really happening and it’s happening fast. I see, at least at McGill, a large amount of DEI inclusion and everything on this discussion. They have institutional courses for us to do as students, and we are all obliged to do many courses, which I think is really educating, especially for people with different cultures and backgrounds.
Dr. Glatter: Amy, where do you think we are in emergency medicine to look at the other side of it? Comparing surgery with emergency medicine, do you think we’re well advanced in terms of DEI, inclusion criteria, respect, and dignity, or are we really far off?
Dr. Ho: I may be biased, but I think emergency medicine is one of the best in terms of this, and I think there are a couple of reasons for it. One is that we are an inherently team-based organization. The attending, the residents, and the students all work in line with one another. There’s less of a hierarchy.
The same is true for our nurses, pharmacists, techs, and EMS. We all work together as a team. Because of that fairly flat structure, it’s really easy for us to value one another as individuals with our diverse backgrounds. In a way, that’s harder for specialties that are more hierarchical, and I think surgery is certainly one of the most hierarchical.
The second reason why emergency medicine is fairly well off in this is that we’re, by nature, a safety-net specialty. We see patients of all-comers, all walks, all backgrounds. I think we both recognize the value of physician-patient concordance. When we share characteristics with our patients, we recognize that value immediately at the bedside.
It exposes us to so much diversity. I see a refugee one day and the next patient is someone who is incarcerated. The next patient after that is an important businessman in society. That diversity and whiplash in the type of patients that we see back-to-back helps us see the playing field in a really flat, diverse way. Because of that, I think our culture is much better, as is our understanding of the value and importance of diversity not only for our programs, but also for our patients.
Do female doctors have better patient outcomes?
Dr. Glatter: Specialties working together in the emergency department is so important. Building that team and that togetherness is so critical. Júlia, would you agree?
Dr. Loyola Ferreira: Definitely. Something Amy said that is beautiful is that you recognize yourself in these patients. In surgery, we are taught to try to be away from the patients and not to put ourselves in the same position. We are taught to be less engaging, and this is not good. The good thing is when we really have patient-centered care, when we listen to them, and when we are involved with them.
I saw a publication showing that female and male surgeons treating similar patients had the same surgical outcomes. Women are as good as men technically to do surgery and have the same surgical outcomes. However, there is research showing that surgical teams with greater representation of women have improved surgical outcomes because of patient-centered care and the way women conduct bedside attention to patients. And they have better patient experience measures afterward. That is not only from the women who are treating the patients, but the whole environment. Women end up bringing men [into the conversation] and this better improves patient-centered care, and that makes the whole team a better team attending patients. Definitely, we are in the moment of patient experience and satisfaction, and increasing women is a way of achieving better patient satisfaction and experience.
Dr. Ho: There’s much to be said about having female clinicians available for patients. It doesn’t have to be just for female patients, although again, concordance between physicians and patients is certainly beneficial. Besides outcomes benefit, there’s even just a communication benefit. The way that women and men communicate is inherently different. The way women and men experience certain things is also inherently different.
A classic example of this is women who are experiencing a heart attack may not actually have chest pain but present with nausea. As a female who’s sensitive to this, when I see a woman throwing up, I am very attuned to something actually being wrong, knowing that they may not present with classic pain for a syndrome, but actually may be presenting with nausea instead. It doesn’t have to be a woman who takes that knowledge and turns it into something at the bedside. It certainly doesn’t have to, but it is just a natural, easy thing to step into as a female.
While I’m really careful to not step into this “women are better than men” or “men are better than women” argument, there’s something to be said about how the availability of female clinicians for all patients, not just female patients, can have benefit. Again, it’s shown in studies with cardiovascular outcomes and cardiologists, it’s certainly shown in ob.gyn., particularly for underrepresented minorities as well for maternal outcomes of Black mothers. It’s certainly shown again in patient satisfaction, which is concordance.
There is a profound level of research already on this that goes beyond just the idea of stacking the bench and putting more women in there. That’s not the value. We’re not just here to check off the box. We’re here to actually lend some value to our patients and, again, to one another as well.
Dr. Glatter: Absolutely. These are excellent points. The point you make about patient presentation is so vital. The fact that women have nausea sometimes in ACS presentations, the research never was really attentive to this. It was biased. The symptoms that women may have that are not “typical” for ACS weren’t included in patient presentations. Educating everyone about, overall, the types of presentations that we can recognize is vital and important.
Dr. Ho: Yes. It’s worth saying that, when you look at how medicine and research developed, classically, who were the research participants? They were often White men. They were college students who, historically, because women were not allowed to go to college, were men.
I say that not to fault the institution, because that was the culture of our history, but to just say it is okay to question things. It is okay to realize that someone’s presenting outside of the box and that maybe we actually need to reframe what even created the walls of the box in the first place.
Dr. Glatter: Thank you again for joining us. I truly appreciate your insight and expertise.
Dr. Glatter is assistant professor of emergency medicine, department of emergency medicine, Hofstra/Northwell, New York. Dr. Ho is senior vice president of clinical informatics & analytics, department of emergency medicine, Integrative Emergency Services, Dallas. Dr. Loyola Ferreira is a master of science candidate, department of experimental surgery, McGill University, Montreal. They reported that they had no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining me to discuss ways to address and reform the toxic culture associated with medical training is Dr. Amy Faith Ho, senior vice president of clinical informatics and analytics at Integrative Emergency Services in Dallas. Also joining us is Dr. Júlia Loyola Ferreira, a pediatric surgeon originally from Brazil, now practicing at Montreal Children’s and focused on advocacy for gender equity and patient-centered care.
Welcome to both of you. Thanks so much for joining me.
Amy Faith Ho, MD, MPH: Thanks so much for having us, Rob.
Dr. Glatter: Amy, I noticed a tweet recently where you talked about how your career choice was affected by the toxic environment in medical school, affecting your choice of residency. Can you elaborate on that?
Dr. Ho: In this instance, what we’re talking about is gender, but it can be directed toward any number of other groups as well.
What you’re alluding to is a tweet by Stanford Surgery Group showing the next residency class, and what was really stunning about this residency class was that it was almost all females. And this was something that took off on social media.
When I saw this, I was really brought back to one of my personal experiences that I chose to share, which was basically that, as a medical student, I really wanted to be a surgeon. I’m an emergency medicine doctor now, so you know that didn’t happen.
The story that I was sharing was that when I was a third-year medical student rotating on surgery, we had a male attending who was very well known at that school at the time who basically would take the female medical students, and instead of clinic, he would round us up. He would have us sit around him in the workplace room while everyone else was seeing patients, and he would have you look at news clippings of himself. He would tell you stories about himself, like he was holding court for the ladies.
It was this very weird culture where my takeaway as a med student was like, “Wow, this is kind of abusive patriarchy that is supported,” because everyone knew about it and was complicit. Even though I really liked surgery, this was just one instance and one example of where you see this culture that really resonates into the rest of life that I didn’t really want to be a part of.
I went into emergency medicine and loved it. It’s also highly procedural, and I was very happy with where I was. What was really interesting about this tweet to me, though, is that it really took off and garnered hundreds of thousands of views on a very niche topic, because what was most revealing is that everyone has a story like this.
It is not just surgery. It is definitely not just one specialty and it is not just one school. It is an endemic problem in medicine. Not only does it change the lives of young women, but it also says so much about the complicity and the culture that we have in medicine that many people were upset about just the same way I was.
Medical training experience in other countries vs. the United States
Dr. Glatter: Júlia, I want to hear about your experience in medical school, surgery, and then fellowship training and up to the present, if possible.
Júlia Loyola Ferreira, MD: In Brazil, as in many countries now, women have made up the majority of the medical students since 2010. It’s a more female-friendly environment when you’re going through medical school, and I was lucky enough to do rotations in areas of surgery where people were friendly to women.
I lived in this tiny bubble that also gave me the privilege of not facing some things that I can imagine that people in Brazil in different areas and smaller towns face. In Brazil, people try to not talk about this gender agenda. This is something that’s being talked about outside Brazil. But in Brazil, we are years back. People are not really engaging on this conversation. I thought it was going to be hard for me as a woman, because Brazil has around 20% female surgeons.
I knew it was going to be challenging, but I had no idea how bad it was. When I started and things started happening, the list was big. I have an example of everything that is written about – microaggression, implicit bias, discrimination, harassment.
Every time I would try to speak about it and talk to someone, I would be strongly gaslighted. It was the whole training, the whole 5 years. People would say, “Oh, I don’t think it was like that. I think you were overreacting.” People would come with all these different answers for what I was experiencing, and that was frustrating. That was even harder because I had to cope with everything that was happening and I had no one to turn to. I had no mentors.
When I looked up to women who were in surgery, they would be tougher on us young surgeons than the men and they would tell us that we should not complain because in their time it was even harder. Now, it’s getting better and we are supposed to accept whatever comes.
That was at least a little bit of what I experienced in my training. It was only after I finished and started to do research about it that I really encountered a field of people who would echo what I was trying to say to many people in different hospitals that I attended to.
That was the key for me to get out of that situation of being gaslighted and of not being able to really talk about it. Suddenly, I started to publish things about Brazil that nobody was even writing or studying. That gave me a large amount of responsibility, but also motivation to keep going and to see the change.
Valuing women in medicine
Dr. Glatter: This is a very important point that you’re raising about the environment of women being hard on other women. We know that men can be very difficult on and also judgmental toward their trainees.
Amy, how would you respond to that? Was your experience similar in emergency medicine training?
Dr. Ho: I actually don’t feel like it was. I think what Júlia is alluding to is this “mean girls” idea, of “I went through it and thus you have to go through it.” I think you do see this in many specialties. One of the classic ones we hear about, and I don’t want to speak to it too much because it’s not my specialty, is ob.gyn., where it is a very female-dominant surgery group. There’s almost a hazing level that you hear about in some of the more malignant workplaces.
I think that you speak to two really important things. Number one is the numbers game. As you were saying, Brazil actually has many women. That’s awesome. That’s actually different from the United States, especially for the historic, existing workplace and less so for the medical students and for residents. I think step one is having minorities like women just present and there.
Step two is actually including and valuing them. While I think it’s really easy to move away from the women discussion, because there are women when you look around in medicine, it doesn’t mean that women are actually being heard, that they’re actually being accepted, or that their viewpoints are being listened to. A big part of it is normalizing not only seeing women in medicine but also normalizing the narrative of women in medicine.
It’s not just about motherhood; it’s about things like normalizing talking about advancement, academic promotions, pay, culture, being called things like “too reactive,” “anxious,” or “too assertive.” These are all classic things that we hear about when we talk about women.
That’s why we’re looking to not only conversations like this, but also structured ways for women to discuss being women in medicine. There are many women in medicine groups in emergency medicine, including: Females Working in Emergency Medicine (FemInEM); the American College of Emergency Physicians (ACEP) and Society for Academic Emergency Medicine (SAEM) women’s groups, which are American Association of Women Emergency Physicians (AAWEP) and Academy for Women in Academic Emergency Medicine (AWAEM), respectively; and the American Medical Women’s Association (AMWA), which is the American Medical Association’s offshoot.
All of these groups are geared toward normalizing women in medicine, normalizing the narrative of women in medicine, and then working on mentoring and educating so that we can advance our initiatives.
Gender balance is not gender equity
Dr. Glatter: Amy, you bring up a very critical point that mentoring is sort of the antidote to gender-based discrimination. Júlia had written a paper back in November of 2022 that was published in the Journal of Surgical Research talking exactly about this and how important it is to develop mentoring. Part of her research showed that about 20% of medical students who took the survey, about 1,000 people, had mentors, which was very disturbing.
Dr. Loyola Ferreira: Mentorship is one of the ways of changing the reality about gender-based discrimination. Amy’s comment was very strong and we need to really keep saying it, which is that gender balance is not gender equity.
The idea of having more women is not the same as women being recognized as equals, as able as men, and as valued as men. To change this very long culture of male domination, we need support, and this support comes from mentorship.
Although I didn’t have one, I feel that since I started being a mentor for some students, it changed not only them but myself. It gave me strength to keep going, studying, publishing, and going further with this discussion. I feel like the relationship was as good for them as it is for me. That’s how things change.
Diversity, equity, and inclusion training
Dr. Glatter: We’re talking about the reality of gender equity in terms of the ability to have equal respect, recognition, opportunities, and access. That’s really an important point to realize, and for our audience, to understand that gender equity is not gender balance.
Amy, I want to talk about medical school curriculums. Are there advances that you’re aware of being made at certain schools, programs, even in residencies, to enforce these things and make it a priority?
Dr. Ho: We’re really lucky that, as a culture in the United States, medical training is certainly very geared toward diversity. Some of that is certainly unofficial. Some of that just means when they’re looking at a medical school class or looking at rank lists for residency, that they’re cognizant of the different backgrounds that people have. That’s still a step. That is a step, that we’re at least acknowledging it.
There are multiple medical schools and residencies that have more formal unconscious-bias training or diversity, equity, and inclusion (DEI) training, both of which are excellent not only for us in the workplace but also for our patients. Almost all of us will see patients of highly diverse backgrounds. I think the biggest push is looking toward the criteria that we use for selecting trainees and students into our programs. Historically, it’s been MCAT, GPA, and so on.
We’ve really started to ask the question of, are these sorts of “objective criteria” actually biased in institutional ways? They talk about this all the time where GPAs will bias against students from underrepresented minorities (URM). I think all medical students and residencies have really acknowledged that. Although there are still test cutoffs, we are putting an inquisitive eye to what those mean, why they exist, and what are the other things that we should consider. This is all very heartening from what I’m seeing in medical training.
Dr. Glatter: There’s no formal rating system for DEI curriculums right now, like ranking of this school, or this program has more advanced recognition in terms of DEI?
Dr. Ho: No, but on the flip side, the U.S. News & World Report was classically one of the major rankings for medical schools. What we saw fairly recently was that very high-tier schools like Harvard and University of Chicago pulled out of that ranking because that ranking did not acknowledge the value of diversity. That was an incredible stance for medical schools to take, to say, “Hey, you are not evaluating an important criterion of ours.”
Dr. Glatter: That’s a great point. Júlia, where are we now in Brazil in terms of awareness of DEI and curriculum in schools and training programs?
Dr. Loyola Ferreira: Our reality is not as good as in the U.S., unfortunately. I don’t see much discussion on residency programs or medical schools at the moment. I see many students bringing it out and trying to make their schools engage in that discussion. This is something that is coming from the bottom up and not from the top down. I think it can lead to change as well. It is a step and it’s a beginning. Institutions should take the responsibility of doing this from the beginning. This is something where Brazil is still years behind you guys.
Dr. Glatter: It’s unfortunate, but certainly it’s important to hear that. What about in Canada and certainly your institution, McGill, where you just completed a master’s degree?
Dr. Loyola Ferreira: Canada is very much like the U.S. This is something that is really happening and it’s happening fast. I see, at least at McGill, a large amount of DEI inclusion and everything on this discussion. They have institutional courses for us to do as students, and we are all obliged to do many courses, which I think is really educating, especially for people with different cultures and backgrounds.
Dr. Glatter: Amy, where do you think we are in emergency medicine to look at the other side of it? Comparing surgery with emergency medicine, do you think we’re well advanced in terms of DEI, inclusion criteria, respect, and dignity, or are we really far off?
Dr. Ho: I may be biased, but I think emergency medicine is one of the best in terms of this, and I think there are a couple of reasons for it. One is that we are an inherently team-based organization. The attending, the residents, and the students all work in line with one another. There’s less of a hierarchy.
The same is true for our nurses, pharmacists, techs, and EMS. We all work together as a team. Because of that fairly flat structure, it’s really easy for us to value one another as individuals with our diverse backgrounds. In a way, that’s harder for specialties that are more hierarchical, and I think surgery is certainly one of the most hierarchical.
The second reason why emergency medicine is fairly well off in this is that we’re, by nature, a safety-net specialty. We see patients of all-comers, all walks, all backgrounds. I think we both recognize the value of physician-patient concordance. When we share characteristics with our patients, we recognize that value immediately at the bedside.
It exposes us to so much diversity. I see a refugee one day and the next patient is someone who is incarcerated. The next patient after that is an important businessman in society. That diversity and whiplash in the type of patients that we see back-to-back helps us see the playing field in a really flat, diverse way. Because of that, I think our culture is much better, as is our understanding of the value and importance of diversity not only for our programs, but also for our patients.
Do female doctors have better patient outcomes?
Dr. Glatter: Specialties working together in the emergency department is so important. Building that team and that togetherness is so critical. Júlia, would you agree?
Dr. Loyola Ferreira: Definitely. Something Amy said that is beautiful is that you recognize yourself in these patients. In surgery, we are taught to try to be away from the patients and not to put ourselves in the same position. We are taught to be less engaging, and this is not good. The good thing is when we really have patient-centered care, when we listen to them, and when we are involved with them.
I saw a publication showing that female and male surgeons treating similar patients had the same surgical outcomes. Women are as good as men technically to do surgery and have the same surgical outcomes. However, there is research showing that surgical teams with greater representation of women have improved surgical outcomes because of patient-centered care and the way women conduct bedside attention to patients. And they have better patient experience measures afterward. That is not only from the women who are treating the patients, but the whole environment. Women end up bringing men [into the conversation] and this better improves patient-centered care, and that makes the whole team a better team attending patients. Definitely, we are in the moment of patient experience and satisfaction, and increasing women is a way of achieving better patient satisfaction and experience.
Dr. Ho: There’s much to be said about having female clinicians available for patients. It doesn’t have to be just for female patients, although again, concordance between physicians and patients is certainly beneficial. Besides outcomes benefit, there’s even just a communication benefit. The way that women and men communicate is inherently different. The way women and men experience certain things is also inherently different.
A classic example of this is women who are experiencing a heart attack may not actually have chest pain but present with nausea. As a female who’s sensitive to this, when I see a woman throwing up, I am very attuned to something actually being wrong, knowing that they may not present with classic pain for a syndrome, but actually may be presenting with nausea instead. It doesn’t have to be a woman who takes that knowledge and turns it into something at the bedside. It certainly doesn’t have to, but it is just a natural, easy thing to step into as a female.
While I’m really careful to not step into this “women are better than men” or “men are better than women” argument, there’s something to be said about how the availability of female clinicians for all patients, not just female patients, can have benefit. Again, it’s shown in studies with cardiovascular outcomes and cardiologists, it’s certainly shown in ob.gyn., particularly for underrepresented minorities as well for maternal outcomes of Black mothers. It’s certainly shown again in patient satisfaction, which is concordance.
There is a profound level of research already on this that goes beyond just the idea of stacking the bench and putting more women in there. That’s not the value. We’re not just here to check off the box. We’re here to actually lend some value to our patients and, again, to one another as well.
Dr. Glatter: Absolutely. These are excellent points. The point you make about patient presentation is so vital. The fact that women have nausea sometimes in ACS presentations, the research never was really attentive to this. It was biased. The symptoms that women may have that are not “typical” for ACS weren’t included in patient presentations. Educating everyone about, overall, the types of presentations that we can recognize is vital and important.
Dr. Ho: Yes. It’s worth saying that, when you look at how medicine and research developed, classically, who were the research participants? They were often White men. They were college students who, historically, because women were not allowed to go to college, were men.
I say that not to fault the institution, because that was the culture of our history, but to just say it is okay to question things. It is okay to realize that someone’s presenting outside of the box and that maybe we actually need to reframe what even created the walls of the box in the first place.
Dr. Glatter: Thank you again for joining us. I truly appreciate your insight and expertise.
Dr. Glatter is assistant professor of emergency medicine, department of emergency medicine, Hofstra/Northwell, New York. Dr. Ho is senior vice president of clinical informatics & analytics, department of emergency medicine, Integrative Emergency Services, Dallas. Dr. Loyola Ferreira is a master of science candidate, department of experimental surgery, McGill University, Montreal. They reported that they had no conflicts of interest.
A version of this article first appeared on Medscape.com.
Coding the “Spot Check”: Part 2
When the Current Procedural Terminology (CPT) evaluation and management (E/M) reporting rules changed dramatically in January 2021, “bullet counting” became unnecessary and the coding level became based on either the new medical decision making (MDM) table or time spent on all activities relating to the care of the patient on the day of the encounter. 1
To make your documentation more likely to pass audits, explicitly link parts of your documentation to CPT MDM descriptors. Part 1 of this series discussed how to approach the “spot check,” a commonly encountered chief concern (CC) within dermatology, with 2 scenarios presented.2 The American Medical Association3 and American Academy of Dermatology4 have provided education that focuses on how to report a given vignette, but specific examples of documentation with commentary are uncommon. In part 2, we describe how to best code an encounter that includes a “spot check” with other concerns.
Scenario 3: By the Way, Doc
A 34-year-old presents with a new spot on the left cheek that seems to be growing and changing shape rapidly. You examine the patient and discuss treatment options. The documentation reads as follows:
- CC: New spot on left cheek that seems to be growing and changing shape rapidly.
- History: No family history of skin cancer; concerned about scarring, no blood thinner.
- Examination: Irregular tan to brown to black 8-mm macule. No lymphadenopathy.
- Impression: Rule out melanoma (undiagnosed new problem with uncertain prognosis).
- Plan: Discuss risks, benefits, and alternatives, including biopsy (decision regarding minor surgery with identified patient or procedure risk factors) vs a noninvasive gene expression profiling (GEP) melanoma rule-out test. (Based on the decision you and the patient make, you also would document which option was chosen, so a biopsy would include your standard documentation, and if the GEP is chosen, you would simply state that this was chosen and performed.)
As you turn to leave the room, the patient says:“By the way, Doc, can you do anything about these
How would it be best to approach this scenario? It depends on which treatment option the patient chooses.
If you performed a noninvasive GEP melanoma rule-out test, the CPT reporting does not change with the addition of the new problem, and only the codes 99204 (new patient office or other outpatient visit) or 99214 (established patient office or other outpatient visit) would be reported. This would be because, with the original documentation, the number and complexity of problems would be an “undiagnosed new problem with uncertain prognosis,” which would be moderate complexity (column 1, level 4). There are no data that are reviewed or analyzed, which would be straightforward (column 2, level 2). For risk, the discussion of the biopsy as a diagnostic choice should include possible scarring, bleeding, pain, and infection, which would be best described as a decision regarding minor surgery with identified patient or procedure risk factors, given the identified patient concerns, making this of moderate complexity (column 3, level 4).1
Importantly, even if the procedure is not chosen as the final treatment plan, the discussion regarding the surgery, including the risks, benefits, and alternatives, can still count toward this category in the MDM table. Therefore, in this scenario, documentation would best fit with CPT code 99204 for a new patient or 99214 for an established patient. The addition of the psoriasis diagnosis would not change the level of service but also should include documentation of the psoriasis as medically necessary.
However, if you perform the biopsy, then the documentation above would only allow reporting the biopsy, as the decision to perform a 0- or 10-day global procedure is “bundled” with the procedure if performed on the same date of service. Therefore, with the addition of the psoriasis diagnosis, you would now use a separate E/M code to report the psoriasis. You must append a modifier −25 to the E/M code to certify that you are dealing with a separate and discrete problem with no overlap in physician work.
Clearly you also have an E/M to report. But what level? Is this chronic? Yes, as CPT clearly defines chronic as “[a] problem with an expected duration of at least one year or until the death of the patient.”1,5
But is this stable progressive or showing side effects of treatment? “‘Stable’ for the purposes of categorizing MDM is defined by the specific treatment goals for an individual patient. A patient who is not at his or her treatment goal is not stable, even if the condition has not changed and there is no short-term threat to life or function,” according to the CPT descriptors. Therefore, in this scenario, the documentation would best fit a chronic illness with exacerbation, progression, or side effects of treatment (column 1, level 4), which is of moderate complexity.1
But what about column 3, where we look at risks of testing and treatment? This would depend on the type of treatment given. If an over-the-counter product such as a tar gel is recommended, this is a low risk (column 3, level 3), which would mean this lower value determines the E/M code to be 99213 or 99203 depending on whether this is an established or new patient, respectively. If we treat with a prescription medication such as a topical corticosteroid, we are providing prescription drug management (column 3, level 4), which is moderate risk, and we would use codes 99204 or 99214, assuming we document appropriately. Again, including the CPT terminology of “not at treatment goal” in your impression and “prescription drug management” in your plan tells an auditor what you are thinking and doing.1,5
The Takeaway—Clearly if a GEP is performed, there is a single CPT code used—99204 or 99214. If the biopsy is performed, there would be a biopsy code and an E/M code with a modifier −25 attached to the latter. For the documentation below, a 99204 or 99214 would be the chosen E/M code:
- CC: (1) New spot on left cheek that seems to be growing and changing shape rapidly; (2) Silvery spots on elbows, knees, and buttocks for which patient desires treatment.
- History: No family history of skin cancer; concerned about scarring, no blood thinner. Mom has psoriasis. Tried petroleum jelly on scaly areas but no better.
- Examination: Irregular tan to brown to black 8-mm macule. No lymphadenopathy. Silver scaly erythematous plaques on elbows, knees, sacrum.
- Impression: (1) Rule out melanoma (undiagnosed new problem with uncertain prognosis); (2) Psoriasis (chronic disease not at treatment goal).
- Plan: (1) Discuss risks, benefits, and alternatives, including biopsy (decision regarding minor surgery with identified patient or procedure risk factors) vs a noninvasive GEP melanoma rule-out test. Patient wants biopsy. Consent, biopsy via shave technique. Lidocaine hydrochloride 1% with epinephrine 1 cc, prepare and drape, aluminum chloride for hemostasis, ointment and bandage applied, care instructions provided; (2) Discuss options. Calcipotriene cream daily; triamcinolone ointment 0.1% twice a day (prescription drug management). Review bathing, avoiding trauma to site, no picking.
Scenario 4: Here for a Total-Body Screening Examination
Medicare does not cover skin cancer screenings as a primary CC. Being worried or knowing someone with melanoma are not CCs that are covered. However, “spot of concern,” “changing mole,” or ”new growth” would be. Conversely, if the patient has a history of skin cancer, actinic keratoses, or other premalignant lesions, and/or is immunosuppressed or has a high-risk genetic syndrome, the visit may be covered if these factors are documented in the note.6
For the diagnosis, the International Classification of Diseases, Tenth Revision, code Z12.83—“encounter for screening for malignant neoplasm of skin”—is not an appropriate primary billing code. However, D48.5—“neoplasm of behavior of skin”—can be, unless there is a specific diagnosis you are able to make (eg, melanocytic nevus, seborrheic keratosis).6
Let’s look at documentation examples:
- CC: 1-year follow-up on basal cell carcinoma (BCC) excision and concern about a new spot on the nose.
- History: Notice new spot on the nose; due for annual follow-up and came early for nose lesion.
- Examination: Left ala with flesh-colored papule dermoscopically banal. Prior left back BCC excision site soft and supple. Total-body examination performed, except perianal and external genitalia, and is unremarkable.
- Impression: Fibrous papule of nose and prior BCC treatment site with no sign of recurrence.
- Plan: Reassure. Annual surveillance in 1 year.
Using what we have previously discussed, this would likely be considered CPT code 99212 (established patient office visit). However, it is important to ensure all concerns and treatment interventions are fully documented. Consider this fuller documentation with bolded additions:
- CC: 1-year follow-up on BCC excision and concern about a new spot on the nose.
- History: Notice new spot on the nose; due for annual follow-up and came early for nose lesion. Also unhappy with generally looking older.
- Examination: Left ala with flesh-colored papule dermoscopically banal. Prior left back BCC excision site soft and supple. Diffuse changes of chronic sun damage. Total-body examination performed, except perianal and external genitalia, and is unremarkable.
- Impression: Fibrous papule of nose and prior BCC treatment site with no sign of recurrence and heliodermatosis/chronic sun damage not at treat-ment goal.
- Plan: Reassure. Annual surveillance in 1 year. Over-the-counter broad-spectrum sun protection factor 30+ sunscreen daily.
This is better but still possibly confusing to an auditor. Consider instead with bolded additions to the changes to the impression:
- CC: 1-year follow-up on BCC excision and concern about a new spot on the nose.
- History: Notice new spot on the nose; due for annual follow-up and came early for nose lesion. Also unhappy with generally looking older.
- Examination: Left ala with flesh-colored papule dermoscopically banal. Prior left back BCC excision site soft and supple. Diffuse changes of chronic sun damage. Total-body examination performed, except perianal and external genitalia, and is unremarkable.
- Impression: Fibrous papule of nose (D22.39)7 and prior BCC treatment site with no sign of recurrence (Z85.828: “personal history of other malignant neoplasm of skin) and heliodermatosis/chronic sun damage not at treatment goal (L57.8: “other skin changes due to chronic exposure to nonionizing radiation”).
- Plan: Reassure. Annual surveillance 1 year. Over-the-counter broad-spectrum sun protection factor 30+ sunscreen daily.
We now have chronic heliodermatitis not at treatment goal, which is moderate (column 1, level 4), and the over-the-counter broad-spectrum sun protection factor 30+ sunscreen (column 1, low) would be best coded as CPT code 99213.
Final Thoughts
“Spot check” encounters are common dermatologic visits, both on their own and in combination with other concerns. With the updated E/M guidelines, it is crucial to clarify and streamline your documentation. In particular, utilize language clearly defining the number and complexity of problems, data to be reviewed and/or analyzed, and appropriate risk stratification to ensure appropriate reimbursement and minimize your difficulties with audits.
- American Medical Association. CPT evaluation and management (E/M) code and guideline changes; 2023. Accessed May 15, 2023. https://www.ama-assn.org/system/files/2023-e-m-descriptors-guidelines.pdf
- Flamm A, Siegel DM. Coding the “spot check”: part 1. Cutis. 2023;111:224-226. doi:10.12788/cutis.0762
- American Medical Association. Evaluation and management (E/M) coding. Accessed May 15, 2023. https://www.ama-assn.org/topics/evaluation-and-management-em-coding
- American Academy of Dermatology Association. Coding resource center. Accessed May 15, 2023. https://www.aad.org/member/practice/coding
- American Medical Association. CPT Professional Edition 2023. American Medical Association; 2022.
- Elizey Coding Solutions, Inc. Dermatology preventive/screening exam visit caution. Updated September 18, 2016. Accessed May 2, 2023. https://www.ellzeycodingsolutions.com/kb_results.asp?ID=9
- 2023 ICD-10-CM diagnosis code D22.39: melanocytic nevi of other parts of the face. Accessed May 2, 2023. https://www.icd10data.com/ICD10CM/Codes/C00-D49/D10-D36/D22-/D22.39
When the Current Procedural Terminology (CPT) evaluation and management (E/M) reporting rules changed dramatically in January 2021, “bullet counting” became unnecessary and the coding level became based on either the new medical decision making (MDM) table or time spent on all activities relating to the care of the patient on the day of the encounter. 1
To make your documentation more likely to pass audits, explicitly link parts of your documentation to CPT MDM descriptors. Part 1 of this series discussed how to approach the “spot check,” a commonly encountered chief concern (CC) within dermatology, with 2 scenarios presented.2 The American Medical Association3 and American Academy of Dermatology4 have provided education that focuses on how to report a given vignette, but specific examples of documentation with commentary are uncommon. In part 2, we describe how to best code an encounter that includes a “spot check” with other concerns.
Scenario 3: By the Way, Doc
A 34-year-old presents with a new spot on the left cheek that seems to be growing and changing shape rapidly. You examine the patient and discuss treatment options. The documentation reads as follows:
- CC: New spot on left cheek that seems to be growing and changing shape rapidly.
- History: No family history of skin cancer; concerned about scarring, no blood thinner.
- Examination: Irregular tan to brown to black 8-mm macule. No lymphadenopathy.
- Impression: Rule out melanoma (undiagnosed new problem with uncertain prognosis).
- Plan: Discuss risks, benefits, and alternatives, including biopsy (decision regarding minor surgery with identified patient or procedure risk factors) vs a noninvasive gene expression profiling (GEP) melanoma rule-out test. (Based on the decision you and the patient make, you also would document which option was chosen, so a biopsy would include your standard documentation, and if the GEP is chosen, you would simply state that this was chosen and performed.)
As you turn to leave the room, the patient says:“By the way, Doc, can you do anything about these
How would it be best to approach this scenario? It depends on which treatment option the patient chooses.
If you performed a noninvasive GEP melanoma rule-out test, the CPT reporting does not change with the addition of the new problem, and only the codes 99204 (new patient office or other outpatient visit) or 99214 (established patient office or other outpatient visit) would be reported. This would be because, with the original documentation, the number and complexity of problems would be an “undiagnosed new problem with uncertain prognosis,” which would be moderate complexity (column 1, level 4). There are no data that are reviewed or analyzed, which would be straightforward (column 2, level 2). For risk, the discussion of the biopsy as a diagnostic choice should include possible scarring, bleeding, pain, and infection, which would be best described as a decision regarding minor surgery with identified patient or procedure risk factors, given the identified patient concerns, making this of moderate complexity (column 3, level 4).1
Importantly, even if the procedure is not chosen as the final treatment plan, the discussion regarding the surgery, including the risks, benefits, and alternatives, can still count toward this category in the MDM table. Therefore, in this scenario, documentation would best fit with CPT code 99204 for a new patient or 99214 for an established patient. The addition of the psoriasis diagnosis would not change the level of service but also should include documentation of the psoriasis as medically necessary.
However, if you perform the biopsy, then the documentation above would only allow reporting the biopsy, as the decision to perform a 0- or 10-day global procedure is “bundled” with the procedure if performed on the same date of service. Therefore, with the addition of the psoriasis diagnosis, you would now use a separate E/M code to report the psoriasis. You must append a modifier −25 to the E/M code to certify that you are dealing with a separate and discrete problem with no overlap in physician work.
Clearly you also have an E/M to report. But what level? Is this chronic? Yes, as CPT clearly defines chronic as “[a] problem with an expected duration of at least one year or until the death of the patient.”1,5
But is this stable progressive or showing side effects of treatment? “‘Stable’ for the purposes of categorizing MDM is defined by the specific treatment goals for an individual patient. A patient who is not at his or her treatment goal is not stable, even if the condition has not changed and there is no short-term threat to life or function,” according to the CPT descriptors. Therefore, in this scenario, the documentation would best fit a chronic illness with exacerbation, progression, or side effects of treatment (column 1, level 4), which is of moderate complexity.1
But what about column 3, where we look at risks of testing and treatment? This would depend on the type of treatment given. If an over-the-counter product such as a tar gel is recommended, this is a low risk (column 3, level 3), which would mean this lower value determines the E/M code to be 99213 or 99203 depending on whether this is an established or new patient, respectively. If we treat with a prescription medication such as a topical corticosteroid, we are providing prescription drug management (column 3, level 4), which is moderate risk, and we would use codes 99204 or 99214, assuming we document appropriately. Again, including the CPT terminology of “not at treatment goal” in your impression and “prescription drug management” in your plan tells an auditor what you are thinking and doing.1,5
The Takeaway—Clearly if a GEP is performed, there is a single CPT code used—99204 or 99214. If the biopsy is performed, there would be a biopsy code and an E/M code with a modifier −25 attached to the latter. For the documentation below, a 99204 or 99214 would be the chosen E/M code:
- CC: (1) New spot on left cheek that seems to be growing and changing shape rapidly; (2) Silvery spots on elbows, knees, and buttocks for which patient desires treatment.
- History: No family history of skin cancer; concerned about scarring, no blood thinner. Mom has psoriasis. Tried petroleum jelly on scaly areas but no better.
- Examination: Irregular tan to brown to black 8-mm macule. No lymphadenopathy. Silver scaly erythematous plaques on elbows, knees, sacrum.
- Impression: (1) Rule out melanoma (undiagnosed new problem with uncertain prognosis); (2) Psoriasis (chronic disease not at treatment goal).
- Plan: (1) Discuss risks, benefits, and alternatives, including biopsy (decision regarding minor surgery with identified patient or procedure risk factors) vs a noninvasive GEP melanoma rule-out test. Patient wants biopsy. Consent, biopsy via shave technique. Lidocaine hydrochloride 1% with epinephrine 1 cc, prepare and drape, aluminum chloride for hemostasis, ointment and bandage applied, care instructions provided; (2) Discuss options. Calcipotriene cream daily; triamcinolone ointment 0.1% twice a day (prescription drug management). Review bathing, avoiding trauma to site, no picking.
Scenario 4: Here for a Total-Body Screening Examination
Medicare does not cover skin cancer screenings as a primary CC. Being worried or knowing someone with melanoma are not CCs that are covered. However, “spot of concern,” “changing mole,” or ”new growth” would be. Conversely, if the patient has a history of skin cancer, actinic keratoses, or other premalignant lesions, and/or is immunosuppressed or has a high-risk genetic syndrome, the visit may be covered if these factors are documented in the note.6
For the diagnosis, the International Classification of Diseases, Tenth Revision, code Z12.83—“encounter for screening for malignant neoplasm of skin”—is not an appropriate primary billing code. However, D48.5—“neoplasm of behavior of skin”—can be, unless there is a specific diagnosis you are able to make (eg, melanocytic nevus, seborrheic keratosis).6
Let’s look at documentation examples:
- CC: 1-year follow-up on basal cell carcinoma (BCC) excision and concern about a new spot on the nose.
- History: Notice new spot on the nose; due for annual follow-up and came early for nose lesion.
- Examination: Left ala with flesh-colored papule dermoscopically banal. Prior left back BCC excision site soft and supple. Total-body examination performed, except perianal and external genitalia, and is unremarkable.
- Impression: Fibrous papule of nose and prior BCC treatment site with no sign of recurrence.
- Plan: Reassure. Annual surveillance in 1 year.
Using what we have previously discussed, this would likely be considered CPT code 99212 (established patient office visit). However, it is important to ensure all concerns and treatment interventions are fully documented. Consider this fuller documentation with bolded additions:
- CC: 1-year follow-up on BCC excision and concern about a new spot on the nose.
- History: Notice new spot on the nose; due for annual follow-up and came early for nose lesion. Also unhappy with generally looking older.
- Examination: Left ala with flesh-colored papule dermoscopically banal. Prior left back BCC excision site soft and supple. Diffuse changes of chronic sun damage. Total-body examination performed, except perianal and external genitalia, and is unremarkable.
- Impression: Fibrous papule of nose and prior BCC treatment site with no sign of recurrence and heliodermatosis/chronic sun damage not at treat-ment goal.
- Plan: Reassure. Annual surveillance in 1 year. Over-the-counter broad-spectrum sun protection factor 30+ sunscreen daily.
This is better but still possibly confusing to an auditor. Consider instead with bolded additions to the changes to the impression:
- CC: 1-year follow-up on BCC excision and concern about a new spot on the nose.
- History: Notice new spot on the nose; due for annual follow-up and came early for nose lesion. Also unhappy with generally looking older.
- Examination: Left ala with flesh-colored papule dermoscopically banal. Prior left back BCC excision site soft and supple. Diffuse changes of chronic sun damage. Total-body examination performed, except perianal and external genitalia, and is unremarkable.
- Impression: Fibrous papule of nose (D22.39)7 and prior BCC treatment site with no sign of recurrence (Z85.828: “personal history of other malignant neoplasm of skin) and heliodermatosis/chronic sun damage not at treatment goal (L57.8: “other skin changes due to chronic exposure to nonionizing radiation”).
- Plan: Reassure. Annual surveillance 1 year. Over-the-counter broad-spectrum sun protection factor 30+ sunscreen daily.
We now have chronic heliodermatitis not at treatment goal, which is moderate (column 1, level 4), and the over-the-counter broad-spectrum sun protection factor 30+ sunscreen (column 1, low) would be best coded as CPT code 99213.
Final Thoughts
“Spot check” encounters are common dermatologic visits, both on their own and in combination with other concerns. With the updated E/M guidelines, it is crucial to clarify and streamline your documentation. In particular, utilize language clearly defining the number and complexity of problems, data to be reviewed and/or analyzed, and appropriate risk stratification to ensure appropriate reimbursement and minimize your difficulties with audits.
When the Current Procedural Terminology (CPT) evaluation and management (E/M) reporting rules changed dramatically in January 2021, “bullet counting” became unnecessary and the coding level became based on either the new medical decision making (MDM) table or time spent on all activities relating to the care of the patient on the day of the encounter. 1
To make your documentation more likely to pass audits, explicitly link parts of your documentation to CPT MDM descriptors. Part 1 of this series discussed how to approach the “spot check,” a commonly encountered chief concern (CC) within dermatology, with 2 scenarios presented.2 The American Medical Association3 and American Academy of Dermatology4 have provided education that focuses on how to report a given vignette, but specific examples of documentation with commentary are uncommon. In part 2, we describe how to best code an encounter that includes a “spot check” with other concerns.
Scenario 3: By the Way, Doc
A 34-year-old presents with a new spot on the left cheek that seems to be growing and changing shape rapidly. You examine the patient and discuss treatment options. The documentation reads as follows:
- CC: New spot on left cheek that seems to be growing and changing shape rapidly.
- History: No family history of skin cancer; concerned about scarring, no blood thinner.
- Examination: Irregular tan to brown to black 8-mm macule. No lymphadenopathy.
- Impression: Rule out melanoma (undiagnosed new problem with uncertain prognosis).
- Plan: Discuss risks, benefits, and alternatives, including biopsy (decision regarding minor surgery with identified patient or procedure risk factors) vs a noninvasive gene expression profiling (GEP) melanoma rule-out test. (Based on the decision you and the patient make, you also would document which option was chosen, so a biopsy would include your standard documentation, and if the GEP is chosen, you would simply state that this was chosen and performed.)
As you turn to leave the room, the patient says:“By the way, Doc, can you do anything about these
How would it be best to approach this scenario? It depends on which treatment option the patient chooses.
If you performed a noninvasive GEP melanoma rule-out test, the CPT reporting does not change with the addition of the new problem, and only the codes 99204 (new patient office or other outpatient visit) or 99214 (established patient office or other outpatient visit) would be reported. This would be because, with the original documentation, the number and complexity of problems would be an “undiagnosed new problem with uncertain prognosis,” which would be moderate complexity (column 1, level 4). There are no data that are reviewed or analyzed, which would be straightforward (column 2, level 2). For risk, the discussion of the biopsy as a diagnostic choice should include possible scarring, bleeding, pain, and infection, which would be best described as a decision regarding minor surgery with identified patient or procedure risk factors, given the identified patient concerns, making this of moderate complexity (column 3, level 4).1
Importantly, even if the procedure is not chosen as the final treatment plan, the discussion regarding the surgery, including the risks, benefits, and alternatives, can still count toward this category in the MDM table. Therefore, in this scenario, documentation would best fit with CPT code 99204 for a new patient or 99214 for an established patient. The addition of the psoriasis diagnosis would not change the level of service but also should include documentation of the psoriasis as medically necessary.
However, if you perform the biopsy, then the documentation above would only allow reporting the biopsy, as the decision to perform a 0- or 10-day global procedure is “bundled” with the procedure if performed on the same date of service. Therefore, with the addition of the psoriasis diagnosis, you would now use a separate E/M code to report the psoriasis. You must append a modifier −25 to the E/M code to certify that you are dealing with a separate and discrete problem with no overlap in physician work.
Clearly you also have an E/M to report. But what level? Is this chronic? Yes, as CPT clearly defines chronic as “[a] problem with an expected duration of at least one year or until the death of the patient.”1,5
But is this stable progressive or showing side effects of treatment? “‘Stable’ for the purposes of categorizing MDM is defined by the specific treatment goals for an individual patient. A patient who is not at his or her treatment goal is not stable, even if the condition has not changed and there is no short-term threat to life or function,” according to the CPT descriptors. Therefore, in this scenario, the documentation would best fit a chronic illness with exacerbation, progression, or side effects of treatment (column 1, level 4), which is of moderate complexity.1
But what about column 3, where we look at risks of testing and treatment? This would depend on the type of treatment given. If an over-the-counter product such as a tar gel is recommended, this is a low risk (column 3, level 3), which would mean this lower value determines the E/M code to be 99213 or 99203 depending on whether this is an established or new patient, respectively. If we treat with a prescription medication such as a topical corticosteroid, we are providing prescription drug management (column 3, level 4), which is moderate risk, and we would use codes 99204 or 99214, assuming we document appropriately. Again, including the CPT terminology of “not at treatment goal” in your impression and “prescription drug management” in your plan tells an auditor what you are thinking and doing.1,5
The Takeaway—Clearly if a GEP is performed, there is a single CPT code used—99204 or 99214. If the biopsy is performed, there would be a biopsy code and an E/M code with a modifier −25 attached to the latter. For the documentation below, a 99204 or 99214 would be the chosen E/M code:
- CC: (1) New spot on left cheek that seems to be growing and changing shape rapidly; (2) Silvery spots on elbows, knees, and buttocks for which patient desires treatment.
- History: No family history of skin cancer; concerned about scarring, no blood thinner. Mom has psoriasis. Tried petroleum jelly on scaly areas but no better.
- Examination: Irregular tan to brown to black 8-mm macule. No lymphadenopathy. Silver scaly erythematous plaques on elbows, knees, sacrum.
- Impression: (1) Rule out melanoma (undiagnosed new problem with uncertain prognosis); (2) Psoriasis (chronic disease not at treatment goal).
- Plan: (1) Discuss risks, benefits, and alternatives, including biopsy (decision regarding minor surgery with identified patient or procedure risk factors) vs a noninvasive GEP melanoma rule-out test. Patient wants biopsy. Consent, biopsy via shave technique. Lidocaine hydrochloride 1% with epinephrine 1 cc, prepare and drape, aluminum chloride for hemostasis, ointment and bandage applied, care instructions provided; (2) Discuss options. Calcipotriene cream daily; triamcinolone ointment 0.1% twice a day (prescription drug management). Review bathing, avoiding trauma to site, no picking.
Scenario 4: Here for a Total-Body Screening Examination
Medicare does not cover skin cancer screenings as a primary CC. Being worried or knowing someone with melanoma are not CCs that are covered. However, “spot of concern,” “changing mole,” or ”new growth” would be. Conversely, if the patient has a history of skin cancer, actinic keratoses, or other premalignant lesions, and/or is immunosuppressed or has a high-risk genetic syndrome, the visit may be covered if these factors are documented in the note.6
For the diagnosis, the International Classification of Diseases, Tenth Revision, code Z12.83—“encounter for screening for malignant neoplasm of skin”—is not an appropriate primary billing code. However, D48.5—“neoplasm of behavior of skin”—can be, unless there is a specific diagnosis you are able to make (eg, melanocytic nevus, seborrheic keratosis).6
Let’s look at documentation examples:
- CC: 1-year follow-up on basal cell carcinoma (BCC) excision and concern about a new spot on the nose.
- History: Notice new spot on the nose; due for annual follow-up and came early for nose lesion.
- Examination: Left ala with flesh-colored papule dermoscopically banal. Prior left back BCC excision site soft and supple. Total-body examination performed, except perianal and external genitalia, and is unremarkable.
- Impression: Fibrous papule of nose and prior BCC treatment site with no sign of recurrence.
- Plan: Reassure. Annual surveillance in 1 year.
Using what we have previously discussed, this would likely be considered CPT code 99212 (established patient office visit). However, it is important to ensure all concerns and treatment interventions are fully documented. Consider this fuller documentation with bolded additions:
- CC: 1-year follow-up on BCC excision and concern about a new spot on the nose.
- History: Notice new spot on the nose; due for annual follow-up and came early for nose lesion. Also unhappy with generally looking older.
- Examination: Left ala with flesh-colored papule dermoscopically banal. Prior left back BCC excision site soft and supple. Diffuse changes of chronic sun damage. Total-body examination performed, except perianal and external genitalia, and is unremarkable.
- Impression: Fibrous papule of nose and prior BCC treatment site with no sign of recurrence and heliodermatosis/chronic sun damage not at treat-ment goal.
- Plan: Reassure. Annual surveillance in 1 year. Over-the-counter broad-spectrum sun protection factor 30+ sunscreen daily.
This is better but still possibly confusing to an auditor. Consider instead with bolded additions to the changes to the impression:
- CC: 1-year follow-up on BCC excision and concern about a new spot on the nose.
- History: Notice new spot on the nose; due for annual follow-up and came early for nose lesion. Also unhappy with generally looking older.
- Examination: Left ala with flesh-colored papule dermoscopically banal. Prior left back BCC excision site soft and supple. Diffuse changes of chronic sun damage. Total-body examination performed, except perianal and external genitalia, and is unremarkable.
- Impression: Fibrous papule of nose (D22.39)7 and prior BCC treatment site with no sign of recurrence (Z85.828: “personal history of other malignant neoplasm of skin) and heliodermatosis/chronic sun damage not at treatment goal (L57.8: “other skin changes due to chronic exposure to nonionizing radiation”).
- Plan: Reassure. Annual surveillance 1 year. Over-the-counter broad-spectrum sun protection factor 30+ sunscreen daily.
We now have chronic heliodermatitis not at treatment goal, which is moderate (column 1, level 4), and the over-the-counter broad-spectrum sun protection factor 30+ sunscreen (column 1, low) would be best coded as CPT code 99213.
Final Thoughts
“Spot check” encounters are common dermatologic visits, both on their own and in combination with other concerns. With the updated E/M guidelines, it is crucial to clarify and streamline your documentation. In particular, utilize language clearly defining the number and complexity of problems, data to be reviewed and/or analyzed, and appropriate risk stratification to ensure appropriate reimbursement and minimize your difficulties with audits.
- American Medical Association. CPT evaluation and management (E/M) code and guideline changes; 2023. Accessed May 15, 2023. https://www.ama-assn.org/system/files/2023-e-m-descriptors-guidelines.pdf
- Flamm A, Siegel DM. Coding the “spot check”: part 1. Cutis. 2023;111:224-226. doi:10.12788/cutis.0762
- American Medical Association. Evaluation and management (E/M) coding. Accessed May 15, 2023. https://www.ama-assn.org/topics/evaluation-and-management-em-coding
- American Academy of Dermatology Association. Coding resource center. Accessed May 15, 2023. https://www.aad.org/member/practice/coding
- American Medical Association. CPT Professional Edition 2023. American Medical Association; 2022.
- Elizey Coding Solutions, Inc. Dermatology preventive/screening exam visit caution. Updated September 18, 2016. Accessed May 2, 2023. https://www.ellzeycodingsolutions.com/kb_results.asp?ID=9
- 2023 ICD-10-CM diagnosis code D22.39: melanocytic nevi of other parts of the face. Accessed May 2, 2023. https://www.icd10data.com/ICD10CM/Codes/C00-D49/D10-D36/D22-/D22.39
- American Medical Association. CPT evaluation and management (E/M) code and guideline changes; 2023. Accessed May 15, 2023. https://www.ama-assn.org/system/files/2023-e-m-descriptors-guidelines.pdf
- Flamm A, Siegel DM. Coding the “spot check”: part 1. Cutis. 2023;111:224-226. doi:10.12788/cutis.0762
- American Medical Association. Evaluation and management (E/M) coding. Accessed May 15, 2023. https://www.ama-assn.org/topics/evaluation-and-management-em-coding
- American Academy of Dermatology Association. Coding resource center. Accessed May 15, 2023. https://www.aad.org/member/practice/coding
- American Medical Association. CPT Professional Edition 2023. American Medical Association; 2022.
- Elizey Coding Solutions, Inc. Dermatology preventive/screening exam visit caution. Updated September 18, 2016. Accessed May 2, 2023. https://www.ellzeycodingsolutions.com/kb_results.asp?ID=9
- 2023 ICD-10-CM diagnosis code D22.39: melanocytic nevi of other parts of the face. Accessed May 2, 2023. https://www.icd10data.com/ICD10CM/Codes/C00-D49/D10-D36/D22-/D22.39
Practice Points
- Clear documentation that reflects your thought process is an important component of effective coding and billing.
- Include Current Procedural Terminology–defined language within documentation to help ensure appropriate reimbursement and decrease the risk of audits.
Oncologist pleads guilty to prescription drug fraud
, according to a press release from the U.S. Attorney’s Office for the District of New Jersey.
Instead, the drug purchases were part of a fraudulent profit-making scheme.
Anise Kachadourian, MD, of Towaco, N.J. – located about 20 miles from Manhattan – now faces a maximum of 3 years in prison and a $10,000 fine. Her sentencing is scheduled for Feb. 6, 2024.
Overall, “Kachadourian was paid more than $170,000 for purchasing and allowing others to purchase in her name millions of dollars in prescription drugs during the scheme, which ran from October 2016 through January 2019,” the office said in the release.
The scheme involved Dr. Kachadourian and others making “numerous false and misleading representations to the pharmaceutical manufacturers and authorized distributors, including that Dr. Kachadourian purchased the drugs to use to treat her patients, and that the drugs would not be resold or redistributed,” the office said.
However, none of the drugs were administered to any of Dr. Kachadourian’s patients.
The press release explained that while working in her medical practice’s offices in various parts of New Jersey, Dr. Kachadourian was recruited by an individual who owned a pharmacy as well as two wholesale prescription drug distributors.
At this individual’s request and at the request of others who worked for him, Dr. Kachadourian used her medical license and allowed others to use it to purchase expensive drugs. The drugs primarily included cold-chain biologic infusion medications, such as trastuzumab and rituximab, often use to treat cancer, macular degeneration, and autoimmune diseases.
In return, Dr. Kachadourian received a kickback of approximately $5,000 per month.
“By recruiting and using Kachadourian and her medical license to purchase the drugs, these individuals were able to obtain prescription drugs from the pharmaceutical manufacturers’ authorized distributors that they would not otherwise have been permitted to purchase,” the DA’s office said.
The drugs were ultimately sold to customers of the two wholesale distributor businesses “at a significant profit.”
For example, according to a court document, on April 26, 2018, trastuzumab 150 mg was purchased for $254,189.04 and then sold by the wholesale distributor businesses at $336,000, for a profit of $81,810.95.
Dr. Kachadourian is the third doctor to plead guilty to the scheme. The press release didn’t name the other two doctors or the pharmacy owner and their two businesses. A court document did name a coconspirator, Jon Paul Dadaian, MD, a board-certified anesthesiologist and pain management specialist who had offices at several locations in New Jersey.
A version of this article first appeared on Medscape.com.
, according to a press release from the U.S. Attorney’s Office for the District of New Jersey.
Instead, the drug purchases were part of a fraudulent profit-making scheme.
Anise Kachadourian, MD, of Towaco, N.J. – located about 20 miles from Manhattan – now faces a maximum of 3 years in prison and a $10,000 fine. Her sentencing is scheduled for Feb. 6, 2024.
Overall, “Kachadourian was paid more than $170,000 for purchasing and allowing others to purchase in her name millions of dollars in prescription drugs during the scheme, which ran from October 2016 through January 2019,” the office said in the release.
The scheme involved Dr. Kachadourian and others making “numerous false and misleading representations to the pharmaceutical manufacturers and authorized distributors, including that Dr. Kachadourian purchased the drugs to use to treat her patients, and that the drugs would not be resold or redistributed,” the office said.
However, none of the drugs were administered to any of Dr. Kachadourian’s patients.
The press release explained that while working in her medical practice’s offices in various parts of New Jersey, Dr. Kachadourian was recruited by an individual who owned a pharmacy as well as two wholesale prescription drug distributors.
At this individual’s request and at the request of others who worked for him, Dr. Kachadourian used her medical license and allowed others to use it to purchase expensive drugs. The drugs primarily included cold-chain biologic infusion medications, such as trastuzumab and rituximab, often use to treat cancer, macular degeneration, and autoimmune diseases.
In return, Dr. Kachadourian received a kickback of approximately $5,000 per month.
“By recruiting and using Kachadourian and her medical license to purchase the drugs, these individuals were able to obtain prescription drugs from the pharmaceutical manufacturers’ authorized distributors that they would not otherwise have been permitted to purchase,” the DA’s office said.
The drugs were ultimately sold to customers of the two wholesale distributor businesses “at a significant profit.”
For example, according to a court document, on April 26, 2018, trastuzumab 150 mg was purchased for $254,189.04 and then sold by the wholesale distributor businesses at $336,000, for a profit of $81,810.95.
Dr. Kachadourian is the third doctor to plead guilty to the scheme. The press release didn’t name the other two doctors or the pharmacy owner and their two businesses. A court document did name a coconspirator, Jon Paul Dadaian, MD, a board-certified anesthesiologist and pain management specialist who had offices at several locations in New Jersey.
A version of this article first appeared on Medscape.com.
, according to a press release from the U.S. Attorney’s Office for the District of New Jersey.
Instead, the drug purchases were part of a fraudulent profit-making scheme.
Anise Kachadourian, MD, of Towaco, N.J. – located about 20 miles from Manhattan – now faces a maximum of 3 years in prison and a $10,000 fine. Her sentencing is scheduled for Feb. 6, 2024.
Overall, “Kachadourian was paid more than $170,000 for purchasing and allowing others to purchase in her name millions of dollars in prescription drugs during the scheme, which ran from October 2016 through January 2019,” the office said in the release.
The scheme involved Dr. Kachadourian and others making “numerous false and misleading representations to the pharmaceutical manufacturers and authorized distributors, including that Dr. Kachadourian purchased the drugs to use to treat her patients, and that the drugs would not be resold or redistributed,” the office said.
However, none of the drugs were administered to any of Dr. Kachadourian’s patients.
The press release explained that while working in her medical practice’s offices in various parts of New Jersey, Dr. Kachadourian was recruited by an individual who owned a pharmacy as well as two wholesale prescription drug distributors.
At this individual’s request and at the request of others who worked for him, Dr. Kachadourian used her medical license and allowed others to use it to purchase expensive drugs. The drugs primarily included cold-chain biologic infusion medications, such as trastuzumab and rituximab, often use to treat cancer, macular degeneration, and autoimmune diseases.
In return, Dr. Kachadourian received a kickback of approximately $5,000 per month.
“By recruiting and using Kachadourian and her medical license to purchase the drugs, these individuals were able to obtain prescription drugs from the pharmaceutical manufacturers’ authorized distributors that they would not otherwise have been permitted to purchase,” the DA’s office said.
The drugs were ultimately sold to customers of the two wholesale distributor businesses “at a significant profit.”
For example, according to a court document, on April 26, 2018, trastuzumab 150 mg was purchased for $254,189.04 and then sold by the wholesale distributor businesses at $336,000, for a profit of $81,810.95.
Dr. Kachadourian is the third doctor to plead guilty to the scheme. The press release didn’t name the other two doctors or the pharmacy owner and their two businesses. A court document did name a coconspirator, Jon Paul Dadaian, MD, a board-certified anesthesiologist and pain management specialist who had offices at several locations in New Jersey.
A version of this article first appeared on Medscape.com.
Omitting radiation in rectal cancer: ‘Less is more’
“This study establishes preoperative therapy with FOLFOX and only selective use of chemoradiation for patients with locally advanced rectal cancer,” commented principal investigator Deborah Schrag, MD, MPH, gastrointestinal oncologist at Memorial Sloan Kettering Cancer Center, New York.
“Having this option is important for several reasons,” she said. “First, in many parts of the world, radiation therapy is not readily accessible. An all-chemotherapy approach may make curative intent treatment accessible for patients in these resource-constrained settings. Additionally, given the rising rates of colorectal cancer in young patients, this provides an option for patients who wish to preserve fertility or avoid early menopause.”
Reacting to the findings, Pamela Kunz, MD, leader of the gastrointestinal cancers program at Yale Cancer Center, New Haven, Conn., commented: “What’s important here is that radiation can be safely omitted in many patients with clinically advanced rectal cancer – this is really ‘less is more.’ ”
“We can spare select patients from receiving radiation without compromising efficacy,” she said. “This leads to improved quality of life, and reduced side effects, including things like early menopause and infertility.”
Dr. Kunz spoke at a press briefing where the results were highlighted prior to being presented at a plenary session at the annual meeting of the American Society of Clinical Oncology.
She said the trial was “practice changing, and it aligns incredibly well with the theme at this year’s annual meeting around de-escalation of therapy and partnering with patients.”
Julie R. Gralow, MD, ASCO chief medical officer and executive vice president, added that the theme may be de-escalation, but in this case it is “really more accurately optimization, because you were able to de-escalate in 91%, but you found the 9% who really needed that escalation, if you will.”
The efficacy results were published simultaneously in the New England Journal of Medicine, while the patient-reported outcomes were published in the Journal of Clinical Oncology.
Chemoradiation is standard approach
Presenting the findings, Dr. Schrag began by noting that approximately half of all new rectal cancer diagnoses have locally advanced disease, which in the United States represents 48,000 cases per year.
She explained that the “standard approach” to treatment is 5½ weeks of daily chemoradiation, comprising radiation to the pelvis alongside sensitizing chemotherapy with a fluoropyrimidine, followed by surgery, and then approximately 16 weeks of adjuvant chemotherapy.
“This way, we have achieved very good outcomes,” Dr. Schrag noted, with the inclusion of radiation in the 1980s a “critically important advance” in slowing rates of recurrence, which is a “cause of enormous suffering.”
However, the treatment is “long and hard,” and the pelvic radiation causes “real toxicities,” she said. These can include impaired bowel, bladder, and sexual function, and an increase in late effects, such as increased risk of pelvic fractures and secondary cancers, as well as infertility and early menopause, and impaired bone marrow function.
This depressed bone marrow function can “become a problem for people going into chemotherapy into the future,” while infertility and early menopause are “a big deal because we’re seeing increasing diagnosis of rectal cancer in people before the age of 50 years.”
Dr. Schrag said that, since chemoradiotherapy became the standard of care, there has been “so much progress,” with better chemotherapy, better surgical techniques, and more screening, so we’re finding more tumors when they are smaller and easier to treat.”
The impetus for the PROSPECT trial, Dr. Schrag said, was therefore: “Could we use radiotherapy more selectively, and only give it to people who don’t respond to chemotherapy rather than giving [it] to everybody?”
The trial enrolled 1,128 patients with rectal cancer with clinically staged T2 node–positive, T3 node–negative, or T3 node–positive disease and who were candidates for sphincter-sparing surgery.
They were randomly assigned to receive either a modified chemotherapy regimen (n = 585) or standard chemoradiation (n = 543). The mean age of the patients was 57 years; 34.5% were female. The majority (85%) were White.
All patients then underwent surgery, with low anterior resection with total mesorectal excision.
The standard chemoradiotherapy consisted of pelvic radiotherapy at 50.4 Gy over 28 fractions alongside sensitizing chemotherapy with either fluorouracil or capecitabine.
The modified chemotherapy regimen consisted of mFOLFOX6, which included modified oxaliplatin with l-leucovorin, and bolus/continuous infusion of 5-fluorouracil.
Patients in the mFOLFOX6 group whose primary tumor decreased in size by at least 20% after the six cycles proceeded straight to surgery, while were rest given the chemoradiotherapy before surgery (9% ended up receiving chemoradiotherapy).
Postoperative adjuvant chemotherapy with six cycles in the mFOLFOX6 group, or eight cycles in the chemoradiotherapy group, was suggested but not mandated.
Dr. Schrag said in an interview that the team chose to use mFOLFOX6 because of their long experience in using it.
FOLFOX first became available in 2002, and randomized controlled trials showed that it was more effective than 5-fluorouracil alone in colon cancer trials.
She explained that locally advanced rectal cancer patients were “never included” in those trials because they were already receiving chemoradiotherapy, but that its use in metastatic rectal cancer, coupled with the data in colon cancer, led them to try it in the current setting.
“It’s also quite tolerable, it’s given every 2 weeks, and it’s familiar to oncologists everywhere,” Dr. Schrag added.
She noted that it’s “not risk free,” with an increased risk of neuropathy, “which is not a great side effect, but we’re able to modulate that.”
Trial results
After a median follow-up of 58 months, mFOLFOX6 was found to be noninferior to chemoradiotherapy for disease-free survival, at a hazard ratio for disease recurrence or death of 0.92 (P = .005 for noninferiority).
The 5-year disease-free survival was 80.8% in the mFOLFOX6 group and 78.6% among patients assigned to chemoradiotherapy, while 5-year overall survival was 89.5% versus 90.2%, at a nonsignificant HR for death of 1.04.
Rates of local recurrence at 5 years were low, at 1.8% with mFOLFOX6 and 1.6% with chemoradiotherapy.
Grade 3 or higher adverse effects were twice as common in the mFOLFOX6 group than among patients who received chemoradiotherapy, at 41% versus 22.8%, although the researchers noted that the treatment period was also twice as long in the chemotherapy arm.
The most common grade 3 or higher adverse effects with mFOLFOX6 were neutropenia (20.3%), pain (3.1%), and hypertension (2.9%), while those with chemoradiotherapy were lymphopenia (8.3%), diarrhea (6.4%), and hypertension (1.7%).
In terms of patient reported outcomes, patients receiving mFOLFOX6 reported lower rates of diarrhea and better overall bowel function during the neoadjuvant phase than those given chemoradiotherapy (P < .05 for all).
However, those assigned to chemoradiotherapy experienced lower rates of anxiety, appetite loss, constipation, depression, dysphagia, dyspnea, edema, fatigue, mucositis, nausea, neuropathy, and vomiting during treatment (P < .05 for all).
At 12-month postoperative follow-up, however, those differences had disappeared, and patients originally assigned to mFOLFOX6 had lower rates of fatigue and neuropathy, and better sexual function, than those given chemoradiotherapy (P < .05 for all).
“During the treatment itself, multiple symptoms were worse with chemotherapy, but a year after treatment ended, those symptoms resolved and the pattern flipped so that patients who received radiation exhibited lingering symptoms,” said coinvestigator Ethan Basch, MD, MSc, chief of medical oncology, and director of the cancer outcomes research program at University of North Carolina Lineberger Comprehensive Cancer Center, Chapel Hill.
“Patients ideally will understand the potential impact of treatments on how they feel and function when making choices, so as oncologists we need to talk with our patients about their options and the consequences of those options,” he said in a statement.
The study was funded by the National Cancer Institute of the National Institutes of Health. Dr. Schrag reported relationships with Merck, JAMA, the American Association for Cancer Research, and Grail. Dr. Basch reported relationships with AstraZeneca, Navigating Cancer, Resilience Care, SIVAN Innovation, ASCO, Centers for Medicare & Medicaid Services, JAMA, the National Cancer Institute, and the Patient-Centered Outcomes Research Institute. Dr. Kunz reported relationships with Novartis, Genentech/Roche, Amgen, Crinetics Pharmaceuticals, Natera, HUTCHMED, and Isotope Technologies Munich. Dr. Gralow reported relationships with Genentech/Roche.
A version of this article first appeared on Medscape.com.
“This study establishes preoperative therapy with FOLFOX and only selective use of chemoradiation for patients with locally advanced rectal cancer,” commented principal investigator Deborah Schrag, MD, MPH, gastrointestinal oncologist at Memorial Sloan Kettering Cancer Center, New York.
“Having this option is important for several reasons,” she said. “First, in many parts of the world, radiation therapy is not readily accessible. An all-chemotherapy approach may make curative intent treatment accessible for patients in these resource-constrained settings. Additionally, given the rising rates of colorectal cancer in young patients, this provides an option for patients who wish to preserve fertility or avoid early menopause.”
Reacting to the findings, Pamela Kunz, MD, leader of the gastrointestinal cancers program at Yale Cancer Center, New Haven, Conn., commented: “What’s important here is that radiation can be safely omitted in many patients with clinically advanced rectal cancer – this is really ‘less is more.’ ”
“We can spare select patients from receiving radiation without compromising efficacy,” she said. “This leads to improved quality of life, and reduced side effects, including things like early menopause and infertility.”
Dr. Kunz spoke at a press briefing where the results were highlighted prior to being presented at a plenary session at the annual meeting of the American Society of Clinical Oncology.
She said the trial was “practice changing, and it aligns incredibly well with the theme at this year’s annual meeting around de-escalation of therapy and partnering with patients.”
Julie R. Gralow, MD, ASCO chief medical officer and executive vice president, added that the theme may be de-escalation, but in this case it is “really more accurately optimization, because you were able to de-escalate in 91%, but you found the 9% who really needed that escalation, if you will.”
The efficacy results were published simultaneously in the New England Journal of Medicine, while the patient-reported outcomes were published in the Journal of Clinical Oncology.
Chemoradiation is standard approach
Presenting the findings, Dr. Schrag began by noting that approximately half of all new rectal cancer diagnoses have locally advanced disease, which in the United States represents 48,000 cases per year.
She explained that the “standard approach” to treatment is 5½ weeks of daily chemoradiation, comprising radiation to the pelvis alongside sensitizing chemotherapy with a fluoropyrimidine, followed by surgery, and then approximately 16 weeks of adjuvant chemotherapy.
“This way, we have achieved very good outcomes,” Dr. Schrag noted, with the inclusion of radiation in the 1980s a “critically important advance” in slowing rates of recurrence, which is a “cause of enormous suffering.”
However, the treatment is “long and hard,” and the pelvic radiation causes “real toxicities,” she said. These can include impaired bowel, bladder, and sexual function, and an increase in late effects, such as increased risk of pelvic fractures and secondary cancers, as well as infertility and early menopause, and impaired bone marrow function.
This depressed bone marrow function can “become a problem for people going into chemotherapy into the future,” while infertility and early menopause are “a big deal because we’re seeing increasing diagnosis of rectal cancer in people before the age of 50 years.”
Dr. Schrag said that, since chemoradiotherapy became the standard of care, there has been “so much progress,” with better chemotherapy, better surgical techniques, and more screening, so we’re finding more tumors when they are smaller and easier to treat.”
The impetus for the PROSPECT trial, Dr. Schrag said, was therefore: “Could we use radiotherapy more selectively, and only give it to people who don’t respond to chemotherapy rather than giving [it] to everybody?”
The trial enrolled 1,128 patients with rectal cancer with clinically staged T2 node–positive, T3 node–negative, or T3 node–positive disease and who were candidates for sphincter-sparing surgery.
They were randomly assigned to receive either a modified chemotherapy regimen (n = 585) or standard chemoradiation (n = 543). The mean age of the patients was 57 years; 34.5% were female. The majority (85%) were White.
All patients then underwent surgery, with low anterior resection with total mesorectal excision.
The standard chemoradiotherapy consisted of pelvic radiotherapy at 50.4 Gy over 28 fractions alongside sensitizing chemotherapy with either fluorouracil or capecitabine.
The modified chemotherapy regimen consisted of mFOLFOX6, which included modified oxaliplatin with l-leucovorin, and bolus/continuous infusion of 5-fluorouracil.
Patients in the mFOLFOX6 group whose primary tumor decreased in size by at least 20% after the six cycles proceeded straight to surgery, while were rest given the chemoradiotherapy before surgery (9% ended up receiving chemoradiotherapy).
Postoperative adjuvant chemotherapy with six cycles in the mFOLFOX6 group, or eight cycles in the chemoradiotherapy group, was suggested but not mandated.
Dr. Schrag said in an interview that the team chose to use mFOLFOX6 because of their long experience in using it.
FOLFOX first became available in 2002, and randomized controlled trials showed that it was more effective than 5-fluorouracil alone in colon cancer trials.
She explained that locally advanced rectal cancer patients were “never included” in those trials because they were already receiving chemoradiotherapy, but that its use in metastatic rectal cancer, coupled with the data in colon cancer, led them to try it in the current setting.
“It’s also quite tolerable, it’s given every 2 weeks, and it’s familiar to oncologists everywhere,” Dr. Schrag added.
She noted that it’s “not risk free,” with an increased risk of neuropathy, “which is not a great side effect, but we’re able to modulate that.”
Trial results
After a median follow-up of 58 months, mFOLFOX6 was found to be noninferior to chemoradiotherapy for disease-free survival, at a hazard ratio for disease recurrence or death of 0.92 (P = .005 for noninferiority).
The 5-year disease-free survival was 80.8% in the mFOLFOX6 group and 78.6% among patients assigned to chemoradiotherapy, while 5-year overall survival was 89.5% versus 90.2%, at a nonsignificant HR for death of 1.04.
Rates of local recurrence at 5 years were low, at 1.8% with mFOLFOX6 and 1.6% with chemoradiotherapy.
Grade 3 or higher adverse effects were twice as common in the mFOLFOX6 group than among patients who received chemoradiotherapy, at 41% versus 22.8%, although the researchers noted that the treatment period was also twice as long in the chemotherapy arm.
The most common grade 3 or higher adverse effects with mFOLFOX6 were neutropenia (20.3%), pain (3.1%), and hypertension (2.9%), while those with chemoradiotherapy were lymphopenia (8.3%), diarrhea (6.4%), and hypertension (1.7%).
In terms of patient reported outcomes, patients receiving mFOLFOX6 reported lower rates of diarrhea and better overall bowel function during the neoadjuvant phase than those given chemoradiotherapy (P < .05 for all).
However, those assigned to chemoradiotherapy experienced lower rates of anxiety, appetite loss, constipation, depression, dysphagia, dyspnea, edema, fatigue, mucositis, nausea, neuropathy, and vomiting during treatment (P < .05 for all).
At 12-month postoperative follow-up, however, those differences had disappeared, and patients originally assigned to mFOLFOX6 had lower rates of fatigue and neuropathy, and better sexual function, than those given chemoradiotherapy (P < .05 for all).
“During the treatment itself, multiple symptoms were worse with chemotherapy, but a year after treatment ended, those symptoms resolved and the pattern flipped so that patients who received radiation exhibited lingering symptoms,” said coinvestigator Ethan Basch, MD, MSc, chief of medical oncology, and director of the cancer outcomes research program at University of North Carolina Lineberger Comprehensive Cancer Center, Chapel Hill.
“Patients ideally will understand the potential impact of treatments on how they feel and function when making choices, so as oncologists we need to talk with our patients about their options and the consequences of those options,” he said in a statement.
The study was funded by the National Cancer Institute of the National Institutes of Health. Dr. Schrag reported relationships with Merck, JAMA, the American Association for Cancer Research, and Grail. Dr. Basch reported relationships with AstraZeneca, Navigating Cancer, Resilience Care, SIVAN Innovation, ASCO, Centers for Medicare & Medicaid Services, JAMA, the National Cancer Institute, and the Patient-Centered Outcomes Research Institute. Dr. Kunz reported relationships with Novartis, Genentech/Roche, Amgen, Crinetics Pharmaceuticals, Natera, HUTCHMED, and Isotope Technologies Munich. Dr. Gralow reported relationships with Genentech/Roche.
A version of this article first appeared on Medscape.com.
“This study establishes preoperative therapy with FOLFOX and only selective use of chemoradiation for patients with locally advanced rectal cancer,” commented principal investigator Deborah Schrag, MD, MPH, gastrointestinal oncologist at Memorial Sloan Kettering Cancer Center, New York.
“Having this option is important for several reasons,” she said. “First, in many parts of the world, radiation therapy is not readily accessible. An all-chemotherapy approach may make curative intent treatment accessible for patients in these resource-constrained settings. Additionally, given the rising rates of colorectal cancer in young patients, this provides an option for patients who wish to preserve fertility or avoid early menopause.”
Reacting to the findings, Pamela Kunz, MD, leader of the gastrointestinal cancers program at Yale Cancer Center, New Haven, Conn., commented: “What’s important here is that radiation can be safely omitted in many patients with clinically advanced rectal cancer – this is really ‘less is more.’ ”
“We can spare select patients from receiving radiation without compromising efficacy,” she said. “This leads to improved quality of life, and reduced side effects, including things like early menopause and infertility.”
Dr. Kunz spoke at a press briefing where the results were highlighted prior to being presented at a plenary session at the annual meeting of the American Society of Clinical Oncology.
She said the trial was “practice changing, and it aligns incredibly well with the theme at this year’s annual meeting around de-escalation of therapy and partnering with patients.”
Julie R. Gralow, MD, ASCO chief medical officer and executive vice president, added that the theme may be de-escalation, but in this case it is “really more accurately optimization, because you were able to de-escalate in 91%, but you found the 9% who really needed that escalation, if you will.”
The efficacy results were published simultaneously in the New England Journal of Medicine, while the patient-reported outcomes were published in the Journal of Clinical Oncology.
Chemoradiation is standard approach
Presenting the findings, Dr. Schrag began by noting that approximately half of all new rectal cancer diagnoses have locally advanced disease, which in the United States represents 48,000 cases per year.
She explained that the “standard approach” to treatment is 5½ weeks of daily chemoradiation, comprising radiation to the pelvis alongside sensitizing chemotherapy with a fluoropyrimidine, followed by surgery, and then approximately 16 weeks of adjuvant chemotherapy.
“This way, we have achieved very good outcomes,” Dr. Schrag noted, with the inclusion of radiation in the 1980s a “critically important advance” in slowing rates of recurrence, which is a “cause of enormous suffering.”
However, the treatment is “long and hard,” and the pelvic radiation causes “real toxicities,” she said. These can include impaired bowel, bladder, and sexual function, and an increase in late effects, such as increased risk of pelvic fractures and secondary cancers, as well as infertility and early menopause, and impaired bone marrow function.
This depressed bone marrow function can “become a problem for people going into chemotherapy into the future,” while infertility and early menopause are “a big deal because we’re seeing increasing diagnosis of rectal cancer in people before the age of 50 years.”
Dr. Schrag said that, since chemoradiotherapy became the standard of care, there has been “so much progress,” with better chemotherapy, better surgical techniques, and more screening, so we’re finding more tumors when they are smaller and easier to treat.”
The impetus for the PROSPECT trial, Dr. Schrag said, was therefore: “Could we use radiotherapy more selectively, and only give it to people who don’t respond to chemotherapy rather than giving [it] to everybody?”
The trial enrolled 1,128 patients with rectal cancer with clinically staged T2 node–positive, T3 node–negative, or T3 node–positive disease and who were candidates for sphincter-sparing surgery.
They were randomly assigned to receive either a modified chemotherapy regimen (n = 585) or standard chemoradiation (n = 543). The mean age of the patients was 57 years; 34.5% were female. The majority (85%) were White.
All patients then underwent surgery, with low anterior resection with total mesorectal excision.
The standard chemoradiotherapy consisted of pelvic radiotherapy at 50.4 Gy over 28 fractions alongside sensitizing chemotherapy with either fluorouracil or capecitabine.
The modified chemotherapy regimen consisted of mFOLFOX6, which included modified oxaliplatin with l-leucovorin, and bolus/continuous infusion of 5-fluorouracil.
Patients in the mFOLFOX6 group whose primary tumor decreased in size by at least 20% after the six cycles proceeded straight to surgery, while were rest given the chemoradiotherapy before surgery (9% ended up receiving chemoradiotherapy).
Postoperative adjuvant chemotherapy with six cycles in the mFOLFOX6 group, or eight cycles in the chemoradiotherapy group, was suggested but not mandated.
Dr. Schrag said in an interview that the team chose to use mFOLFOX6 because of their long experience in using it.
FOLFOX first became available in 2002, and randomized controlled trials showed that it was more effective than 5-fluorouracil alone in colon cancer trials.
She explained that locally advanced rectal cancer patients were “never included” in those trials because they were already receiving chemoradiotherapy, but that its use in metastatic rectal cancer, coupled with the data in colon cancer, led them to try it in the current setting.
“It’s also quite tolerable, it’s given every 2 weeks, and it’s familiar to oncologists everywhere,” Dr. Schrag added.
She noted that it’s “not risk free,” with an increased risk of neuropathy, “which is not a great side effect, but we’re able to modulate that.”
Trial results
After a median follow-up of 58 months, mFOLFOX6 was found to be noninferior to chemoradiotherapy for disease-free survival, at a hazard ratio for disease recurrence or death of 0.92 (P = .005 for noninferiority).
The 5-year disease-free survival was 80.8% in the mFOLFOX6 group and 78.6% among patients assigned to chemoradiotherapy, while 5-year overall survival was 89.5% versus 90.2%, at a nonsignificant HR for death of 1.04.
Rates of local recurrence at 5 years were low, at 1.8% with mFOLFOX6 and 1.6% with chemoradiotherapy.
Grade 3 or higher adverse effects were twice as common in the mFOLFOX6 group than among patients who received chemoradiotherapy, at 41% versus 22.8%, although the researchers noted that the treatment period was also twice as long in the chemotherapy arm.
The most common grade 3 or higher adverse effects with mFOLFOX6 were neutropenia (20.3%), pain (3.1%), and hypertension (2.9%), while those with chemoradiotherapy were lymphopenia (8.3%), diarrhea (6.4%), and hypertension (1.7%).
In terms of patient reported outcomes, patients receiving mFOLFOX6 reported lower rates of diarrhea and better overall bowel function during the neoadjuvant phase than those given chemoradiotherapy (P < .05 for all).
However, those assigned to chemoradiotherapy experienced lower rates of anxiety, appetite loss, constipation, depression, dysphagia, dyspnea, edema, fatigue, mucositis, nausea, neuropathy, and vomiting during treatment (P < .05 for all).
At 12-month postoperative follow-up, however, those differences had disappeared, and patients originally assigned to mFOLFOX6 had lower rates of fatigue and neuropathy, and better sexual function, than those given chemoradiotherapy (P < .05 for all).
“During the treatment itself, multiple symptoms were worse with chemotherapy, but a year after treatment ended, those symptoms resolved and the pattern flipped so that patients who received radiation exhibited lingering symptoms,” said coinvestigator Ethan Basch, MD, MSc, chief of medical oncology, and director of the cancer outcomes research program at University of North Carolina Lineberger Comprehensive Cancer Center, Chapel Hill.
“Patients ideally will understand the potential impact of treatments on how they feel and function when making choices, so as oncologists we need to talk with our patients about their options and the consequences of those options,” he said in a statement.
The study was funded by the National Cancer Institute of the National Institutes of Health. Dr. Schrag reported relationships with Merck, JAMA, the American Association for Cancer Research, and Grail. Dr. Basch reported relationships with AstraZeneca, Navigating Cancer, Resilience Care, SIVAN Innovation, ASCO, Centers for Medicare & Medicaid Services, JAMA, the National Cancer Institute, and the Patient-Centered Outcomes Research Institute. Dr. Kunz reported relationships with Novartis, Genentech/Roche, Amgen, Crinetics Pharmaceuticals, Natera, HUTCHMED, and Isotope Technologies Munich. Dr. Gralow reported relationships with Genentech/Roche.
A version of this article first appeared on Medscape.com.
AT ASCO 2023
Medicaid expansion closing racial gap in GI cancer deaths
Across the United States, minority patients with cancer often have worse outcomes than White patients, with Black patients more likely to die sooner.
But new data suggest that these racial disparities are lessening. They come from a cross-sectional cohort study of patients with gastrointestinal cancers and show that the gap in mortality rates was reduced in Medicaid expansion states, compared with nonexpansion states.
The results were particularly notable for Black patients, for whom there was a consistent increase in receiving therapy (chemotherapy or surgery) and a decrease in mortality from stomach, colorectal, and pancreatic cancer, the investigators commented.
The study was highlighted at a press briefing held in advance of the annual meeting of the American Society of Clinical Oncology.
“The findings of this study provide a solid step for closing the gap, showing that the Medicaid expansion opportunity offered by the Affordable Care Act, which allows participating states to improve health care access for disadvantaged populations, results in better cancer outcomes and mitigation of racial disparities in cancer survival,” commented Julie Gralow, MD, chief medical officer and executive vice president of ASCO.
The study included 86,052 patients from the National Cancer Database who, from 2009 to 2019, were diagnosed with pancreatic cancer, colorectal cancer, or stomach cancer. Just over 22,000 patients (25.7%) were Black; the remainder 63,943 (74.3%) were White.
In Medicaid expansion states, there was a greater absolute reduction in 2-year mortality among Black patients with pancreatic cancer of –11.8%, compared with nonexpansion states, at –2.4%, a difference-in-difference (DID) of –9.4%. Additionally, there was an increase in treatment with chemotherapy for patients with stage III-IV pancreatic cancer (4.5% for Black patients and 3.2% for White), compared with patients in nonexpansion states (0.8% for Black patients and 0.4% for White; DID, 3.7% for Black patients and DID, 2.7% for White).
“We found similar results in colorectal cancer, but this effect is primarily observed among the stage IV patients,” commented lead author Naveen Manisundaram, MD, a research fellow at the University of Texas MD Anderson Cancer Center, Houston. “Black patients with advanced stage disease experienced a 12.6% reduction in mortality in expansion states.”
Among Black patients with stage IV colorectal cancer, there was an increase in rates of surgery in expansion states, compared with nonexpansion states (DID, 5.7%). However, there was no increase in treatment with chemotherapy (DID, 1%; P = .66).
Mortality rates for Black patients with stomach cancer also decreased. In expansion states, there was a –13% absolute decrease in mortality, compared with a –5.2% decrease in nonexpansion states.
The investigators noted that Medicaid coverage was a key component in access to care through the Affordable Care Act. About two-thirds (66.7%) of Black patients had Medicaid; 33.3% were uninsured. Coverage was similar among White patients; 64.1% had Medicaid and 35.9% were uninsured.
“Our study provides compelling data that show Medicaid expansion was associated with improvement in survival for both Black and White patients with gastrointestinal cancers. Additionally, it suggests that Medicaid expansion is one potential avenue to mitigate existing racial survival disparities among these patients,” Dr. Manisundaram concluded.
The study was funded by the National Institutes of Health. One coauthor reported an advisory role with Medicaroid. Dr. Gralow has had a consulting or advisory role with Genentech and Roche.
A version of this article first appeared on Medscape.com.
Across the United States, minority patients with cancer often have worse outcomes than White patients, with Black patients more likely to die sooner.
But new data suggest that these racial disparities are lessening. They come from a cross-sectional cohort study of patients with gastrointestinal cancers and show that the gap in mortality rates was reduced in Medicaid expansion states, compared with nonexpansion states.
The results were particularly notable for Black patients, for whom there was a consistent increase in receiving therapy (chemotherapy or surgery) and a decrease in mortality from stomach, colorectal, and pancreatic cancer, the investigators commented.
The study was highlighted at a press briefing held in advance of the annual meeting of the American Society of Clinical Oncology.
“The findings of this study provide a solid step for closing the gap, showing that the Medicaid expansion opportunity offered by the Affordable Care Act, which allows participating states to improve health care access for disadvantaged populations, results in better cancer outcomes and mitigation of racial disparities in cancer survival,” commented Julie Gralow, MD, chief medical officer and executive vice president of ASCO.
The study included 86,052 patients from the National Cancer Database who, from 2009 to 2019, were diagnosed with pancreatic cancer, colorectal cancer, or stomach cancer. Just over 22,000 patients (25.7%) were Black; the remainder 63,943 (74.3%) were White.
In Medicaid expansion states, there was a greater absolute reduction in 2-year mortality among Black patients with pancreatic cancer of –11.8%, compared with nonexpansion states, at –2.4%, a difference-in-difference (DID) of –9.4%. Additionally, there was an increase in treatment with chemotherapy for patients with stage III-IV pancreatic cancer (4.5% for Black patients and 3.2% for White), compared with patients in nonexpansion states (0.8% for Black patients and 0.4% for White; DID, 3.7% for Black patients and DID, 2.7% for White).
“We found similar results in colorectal cancer, but this effect is primarily observed among the stage IV patients,” commented lead author Naveen Manisundaram, MD, a research fellow at the University of Texas MD Anderson Cancer Center, Houston. “Black patients with advanced stage disease experienced a 12.6% reduction in mortality in expansion states.”
Among Black patients with stage IV colorectal cancer, there was an increase in rates of surgery in expansion states, compared with nonexpansion states (DID, 5.7%). However, there was no increase in treatment with chemotherapy (DID, 1%; P = .66).
Mortality rates for Black patients with stomach cancer also decreased. In expansion states, there was a –13% absolute decrease in mortality, compared with a –5.2% decrease in nonexpansion states.
The investigators noted that Medicaid coverage was a key component in access to care through the Affordable Care Act. About two-thirds (66.7%) of Black patients had Medicaid; 33.3% were uninsured. Coverage was similar among White patients; 64.1% had Medicaid and 35.9% were uninsured.
“Our study provides compelling data that show Medicaid expansion was associated with improvement in survival for both Black and White patients with gastrointestinal cancers. Additionally, it suggests that Medicaid expansion is one potential avenue to mitigate existing racial survival disparities among these patients,” Dr. Manisundaram concluded.
The study was funded by the National Institutes of Health. One coauthor reported an advisory role with Medicaroid. Dr. Gralow has had a consulting or advisory role with Genentech and Roche.
A version of this article first appeared on Medscape.com.
Across the United States, minority patients with cancer often have worse outcomes than White patients, with Black patients more likely to die sooner.
But new data suggest that these racial disparities are lessening. They come from a cross-sectional cohort study of patients with gastrointestinal cancers and show that the gap in mortality rates was reduced in Medicaid expansion states, compared with nonexpansion states.
The results were particularly notable for Black patients, for whom there was a consistent increase in receiving therapy (chemotherapy or surgery) and a decrease in mortality from stomach, colorectal, and pancreatic cancer, the investigators commented.
The study was highlighted at a press briefing held in advance of the annual meeting of the American Society of Clinical Oncology.
“The findings of this study provide a solid step for closing the gap, showing that the Medicaid expansion opportunity offered by the Affordable Care Act, which allows participating states to improve health care access for disadvantaged populations, results in better cancer outcomes and mitigation of racial disparities in cancer survival,” commented Julie Gralow, MD, chief medical officer and executive vice president of ASCO.
The study included 86,052 patients from the National Cancer Database who, from 2009 to 2019, were diagnosed with pancreatic cancer, colorectal cancer, or stomach cancer. Just over 22,000 patients (25.7%) were Black; the remainder 63,943 (74.3%) were White.
In Medicaid expansion states, there was a greater absolute reduction in 2-year mortality among Black patients with pancreatic cancer of –11.8%, compared with nonexpansion states, at –2.4%, a difference-in-difference (DID) of –9.4%. Additionally, there was an increase in treatment with chemotherapy for patients with stage III-IV pancreatic cancer (4.5% for Black patients and 3.2% for White), compared with patients in nonexpansion states (0.8% for Black patients and 0.4% for White; DID, 3.7% for Black patients and DID, 2.7% for White).
“We found similar results in colorectal cancer, but this effect is primarily observed among the stage IV patients,” commented lead author Naveen Manisundaram, MD, a research fellow at the University of Texas MD Anderson Cancer Center, Houston. “Black patients with advanced stage disease experienced a 12.6% reduction in mortality in expansion states.”
Among Black patients with stage IV colorectal cancer, there was an increase in rates of surgery in expansion states, compared with nonexpansion states (DID, 5.7%). However, there was no increase in treatment with chemotherapy (DID, 1%; P = .66).
Mortality rates for Black patients with stomach cancer also decreased. In expansion states, there was a –13% absolute decrease in mortality, compared with a –5.2% decrease in nonexpansion states.
The investigators noted that Medicaid coverage was a key component in access to care through the Affordable Care Act. About two-thirds (66.7%) of Black patients had Medicaid; 33.3% were uninsured. Coverage was similar among White patients; 64.1% had Medicaid and 35.9% were uninsured.
“Our study provides compelling data that show Medicaid expansion was associated with improvement in survival for both Black and White patients with gastrointestinal cancers. Additionally, it suggests that Medicaid expansion is one potential avenue to mitigate existing racial survival disparities among these patients,” Dr. Manisundaram concluded.
The study was funded by the National Institutes of Health. One coauthor reported an advisory role with Medicaroid. Dr. Gralow has had a consulting or advisory role with Genentech and Roche.
A version of this article first appeared on Medscape.com.
FROM ASCO 2023
Cross-border U.S.-Mexican collaboration drives up ALL survival
A team from a hospital in San Diego combined a previously established training program from the World Health Organization with a new collaboration, which resulted in improvements in care standards and sustainability of care in a center in Tijuana, Mexico, just 23 miles away.
Implementation of the program in 2013 led to a significant 6% improvement in 5-year overall survival for children with ALL.
For patients at standard risk, 5-year overall survival increased from 73% to 100% after implementation of the program.
“This is really remarkable because this survival is the same as we have here in San Diego,” commented Paula Aristizabal, MD, MAS, a pediatric hematologist/oncologist at Rady Children’s Hospital, San Diego, at a press briefing before the annual meeting of the American Society of Clinical Oncology.
The findings show that “sustained improvements in cancer outcomes in low- and middle-income countries [LMICs] are feasible with innovative cross-border programs, particularly in borders that are shared” between a high- and low-income country, she commented. In other words, “it takes a village in both countries” to drive up standards.
Dr. Aristizabal also noted that the partnership will continue with a particularly focus on improving survival among patients with high-risk disease.
“We like to call it ‘twinning,’ because that means we are twins forever,” she said. “This is not a marriage that can be dissolved.”
‘Huge survival gap’
“The burden of childhood cancer has increased globally, but unfortunately, survival in low- and middle-income countries has not improved at the same level as in high-income countries,” Dr. Aristizabal commented.
This has resulted in a “huge survival gap” between high-income countries and the LMICs. ALL is now a leading cause of death among children in these countries, she commented.
“This study illustrates collaborative strategies that can be put into place today that could greatly improve outcomes for children with cancer globally,” commented Julie R. Gralow, MD, ASCO chief medical officer and executive vice president.
Speaking at the press conference, she added: “As I’ve heard Princess Dina Mired of Jordan say many times: ‘Your ZIP code should not determine if you survive cancer.’ ”
She said the differences in ALL survival between the United States and Mexico are an “example of children being so close in terms of proximity not having the same advantages.”
Also commenting, ASCO President Eric Winer, MD, from the Yale Cancer Center, New Haven, Conn., asked whether the proximity of the hospitals in San Diego and Tijuana “makes a difference, or do you think this is something that done ... at a distance?”
Dr. Aristizabal said that the proximity between the institutions “has been extremely helpful,” as they can go between hospitals in just 30 minutes.
However, “one of the things that we learned with COVID is that we can do a lot of things remotely,” she answered.
“Some of the projects that we started in Tijuana, through our collaboration with St. Jude Children’s Research Hospital, we have been able to implement in many other centers in Mexico,” she said.
Study details
Rady Children’s Hospital partnered with the public sector in Baja California, with the aim of improving outcomes in children’s cancer, she explained.
In 2008, the team collaborated with St. Jude Children’s Research Hospital, Memphis, to establish a training program in the Hospital General Tijuana in Tijuana that shared knowledge, technology, and organizational skills.
The team also consulted on clinical cases and set up education and research programs, all with the aim of building capacity and sustainability in Mexico.
“As the number of leukemia patients increased, we wanted to decrease depending on their international collaborators in the U.S. and ensure long-term sustainability,” Dr. Aristizabal explained.
This led in 2013 to the implementation of the WHO Framework for Action HSS training model, which has several components, including health service delivery.
Combined with the previously established model, the overall goals of the program were to improve health outcomes, systems efficiency, timely access to care, and social and financial risk protection.
Dr. Aristizabal said in an interview that this involved developing highly specific leukemia treatment guidelines, which have now gone through three iterations, as well as guidelines for supportive care.
Working with a local foundation, the team has also “focused on providing psychosocial support, nutritional support, a shelter for families that live 12-14 hours away from the pediatric cancer center, as well as food subsidies, trying to address financial toxicity and food insecurity in these families.”
Impact of the collaboration
To assess the impact of the WHO framework, the researchers conducted a study that involved 109 children with ALL who were treated at Hospital General Tijuana over the preimplementation phase in 2008-2012 and the postimplementation phase in 2013-2017.
The mean age of the patients was 7.04 years, and 50.4% were girls. The majority (67%) were classified as having high-risk disease.
Over the entire study period, the 5-year overall survival rate was 65%. Analysis revealed that between the pre- and postimplementation periods, 5-year overall survival increased from 59% to 65%, which Dr. Aristizabal described as “a significant improvement.”
Among high-risk patients, the improvement in 5-year survival between the pre- and postimplementation period went from 48% to 55%.
“This is an area for improvement,” Dr. Aristizabal said, “and we’re working on additional strategies to help improve survival for high-risk patients.
The study was funded by Rady Children’s Hospital, the Mexican Secretary of Health, and the Patronato Foundation. Dr. Aristizabal and coauthors reported no relevant financial relationships. Dr. Gralow reported relationships with Genentech and Roche. Dr. Winer reported relationships with Leap Therapeutics, Jounce Therapeutics, Carrick Therapeutics, and Genentech.
A version of this article first appeared on Medscape.com.
A team from a hospital in San Diego combined a previously established training program from the World Health Organization with a new collaboration, which resulted in improvements in care standards and sustainability of care in a center in Tijuana, Mexico, just 23 miles away.
Implementation of the program in 2013 led to a significant 6% improvement in 5-year overall survival for children with ALL.
For patients at standard risk, 5-year overall survival increased from 73% to 100% after implementation of the program.
“This is really remarkable because this survival is the same as we have here in San Diego,” commented Paula Aristizabal, MD, MAS, a pediatric hematologist/oncologist at Rady Children’s Hospital, San Diego, at a press briefing before the annual meeting of the American Society of Clinical Oncology.
The findings show that “sustained improvements in cancer outcomes in low- and middle-income countries [LMICs] are feasible with innovative cross-border programs, particularly in borders that are shared” between a high- and low-income country, she commented. In other words, “it takes a village in both countries” to drive up standards.
Dr. Aristizabal also noted that the partnership will continue with a particularly focus on improving survival among patients with high-risk disease.
“We like to call it ‘twinning,’ because that means we are twins forever,” she said. “This is not a marriage that can be dissolved.”
‘Huge survival gap’
“The burden of childhood cancer has increased globally, but unfortunately, survival in low- and middle-income countries has not improved at the same level as in high-income countries,” Dr. Aristizabal commented.
This has resulted in a “huge survival gap” between high-income countries and the LMICs. ALL is now a leading cause of death among children in these countries, she commented.
“This study illustrates collaborative strategies that can be put into place today that could greatly improve outcomes for children with cancer globally,” commented Julie R. Gralow, MD, ASCO chief medical officer and executive vice president.
Speaking at the press conference, she added: “As I’ve heard Princess Dina Mired of Jordan say many times: ‘Your ZIP code should not determine if you survive cancer.’ ”
She said the differences in ALL survival between the United States and Mexico are an “example of children being so close in terms of proximity not having the same advantages.”
Also commenting, ASCO President Eric Winer, MD, from the Yale Cancer Center, New Haven, Conn., asked whether the proximity of the hospitals in San Diego and Tijuana “makes a difference, or do you think this is something that done ... at a distance?”
Dr. Aristizabal said that the proximity between the institutions “has been extremely helpful,” as they can go between hospitals in just 30 minutes.
However, “one of the things that we learned with COVID is that we can do a lot of things remotely,” she answered.
“Some of the projects that we started in Tijuana, through our collaboration with St. Jude Children’s Research Hospital, we have been able to implement in many other centers in Mexico,” she said.
Study details
Rady Children’s Hospital partnered with the public sector in Baja California, with the aim of improving outcomes in children’s cancer, she explained.
In 2008, the team collaborated with St. Jude Children’s Research Hospital, Memphis, to establish a training program in the Hospital General Tijuana in Tijuana that shared knowledge, technology, and organizational skills.
The team also consulted on clinical cases and set up education and research programs, all with the aim of building capacity and sustainability in Mexico.
“As the number of leukemia patients increased, we wanted to decrease depending on their international collaborators in the U.S. and ensure long-term sustainability,” Dr. Aristizabal explained.
This led in 2013 to the implementation of the WHO Framework for Action HSS training model, which has several components, including health service delivery.
Combined with the previously established model, the overall goals of the program were to improve health outcomes, systems efficiency, timely access to care, and social and financial risk protection.
Dr. Aristizabal said in an interview that this involved developing highly specific leukemia treatment guidelines, which have now gone through three iterations, as well as guidelines for supportive care.
Working with a local foundation, the team has also “focused on providing psychosocial support, nutritional support, a shelter for families that live 12-14 hours away from the pediatric cancer center, as well as food subsidies, trying to address financial toxicity and food insecurity in these families.”
Impact of the collaboration
To assess the impact of the WHO framework, the researchers conducted a study that involved 109 children with ALL who were treated at Hospital General Tijuana over the preimplementation phase in 2008-2012 and the postimplementation phase in 2013-2017.
The mean age of the patients was 7.04 years, and 50.4% were girls. The majority (67%) were classified as having high-risk disease.
Over the entire study period, the 5-year overall survival rate was 65%. Analysis revealed that between the pre- and postimplementation periods, 5-year overall survival increased from 59% to 65%, which Dr. Aristizabal described as “a significant improvement.”
Among high-risk patients, the improvement in 5-year survival between the pre- and postimplementation period went from 48% to 55%.
“This is an area for improvement,” Dr. Aristizabal said, “and we’re working on additional strategies to help improve survival for high-risk patients.
The study was funded by Rady Children’s Hospital, the Mexican Secretary of Health, and the Patronato Foundation. Dr. Aristizabal and coauthors reported no relevant financial relationships. Dr. Gralow reported relationships with Genentech and Roche. Dr. Winer reported relationships with Leap Therapeutics, Jounce Therapeutics, Carrick Therapeutics, and Genentech.
A version of this article first appeared on Medscape.com.
A team from a hospital in San Diego combined a previously established training program from the World Health Organization with a new collaboration, which resulted in improvements in care standards and sustainability of care in a center in Tijuana, Mexico, just 23 miles away.
Implementation of the program in 2013 led to a significant 6% improvement in 5-year overall survival for children with ALL.
For patients at standard risk, 5-year overall survival increased from 73% to 100% after implementation of the program.
“This is really remarkable because this survival is the same as we have here in San Diego,” commented Paula Aristizabal, MD, MAS, a pediatric hematologist/oncologist at Rady Children’s Hospital, San Diego, at a press briefing before the annual meeting of the American Society of Clinical Oncology.
The findings show that “sustained improvements in cancer outcomes in low- and middle-income countries [LMICs] are feasible with innovative cross-border programs, particularly in borders that are shared” between a high- and low-income country, she commented. In other words, “it takes a village in both countries” to drive up standards.
Dr. Aristizabal also noted that the partnership will continue with a particularly focus on improving survival among patients with high-risk disease.
“We like to call it ‘twinning,’ because that means we are twins forever,” she said. “This is not a marriage that can be dissolved.”
‘Huge survival gap’
“The burden of childhood cancer has increased globally, but unfortunately, survival in low- and middle-income countries has not improved at the same level as in high-income countries,” Dr. Aristizabal commented.
This has resulted in a “huge survival gap” between high-income countries and the LMICs. ALL is now a leading cause of death among children in these countries, she commented.
“This study illustrates collaborative strategies that can be put into place today that could greatly improve outcomes for children with cancer globally,” commented Julie R. Gralow, MD, ASCO chief medical officer and executive vice president.
Speaking at the press conference, she added: “As I’ve heard Princess Dina Mired of Jordan say many times: ‘Your ZIP code should not determine if you survive cancer.’ ”
She said the differences in ALL survival between the United States and Mexico are an “example of children being so close in terms of proximity not having the same advantages.”
Also commenting, ASCO President Eric Winer, MD, from the Yale Cancer Center, New Haven, Conn., asked whether the proximity of the hospitals in San Diego and Tijuana “makes a difference, or do you think this is something that done ... at a distance?”
Dr. Aristizabal said that the proximity between the institutions “has been extremely helpful,” as they can go between hospitals in just 30 minutes.
However, “one of the things that we learned with COVID is that we can do a lot of things remotely,” she answered.
“Some of the projects that we started in Tijuana, through our collaboration with St. Jude Children’s Research Hospital, we have been able to implement in many other centers in Mexico,” she said.
Study details
Rady Children’s Hospital partnered with the public sector in Baja California, with the aim of improving outcomes in children’s cancer, she explained.
In 2008, the team collaborated with St. Jude Children’s Research Hospital, Memphis, to establish a training program in the Hospital General Tijuana in Tijuana that shared knowledge, technology, and organizational skills.
The team also consulted on clinical cases and set up education and research programs, all with the aim of building capacity and sustainability in Mexico.
“As the number of leukemia patients increased, we wanted to decrease depending on their international collaborators in the U.S. and ensure long-term sustainability,” Dr. Aristizabal explained.
This led in 2013 to the implementation of the WHO Framework for Action HSS training model, which has several components, including health service delivery.
Combined with the previously established model, the overall goals of the program were to improve health outcomes, systems efficiency, timely access to care, and social and financial risk protection.
Dr. Aristizabal said in an interview that this involved developing highly specific leukemia treatment guidelines, which have now gone through three iterations, as well as guidelines for supportive care.
Working with a local foundation, the team has also “focused on providing psychosocial support, nutritional support, a shelter for families that live 12-14 hours away from the pediatric cancer center, as well as food subsidies, trying to address financial toxicity and food insecurity in these families.”
Impact of the collaboration
To assess the impact of the WHO framework, the researchers conducted a study that involved 109 children with ALL who were treated at Hospital General Tijuana over the preimplementation phase in 2008-2012 and the postimplementation phase in 2013-2017.
The mean age of the patients was 7.04 years, and 50.4% were girls. The majority (67%) were classified as having high-risk disease.
Over the entire study period, the 5-year overall survival rate was 65%. Analysis revealed that between the pre- and postimplementation periods, 5-year overall survival increased from 59% to 65%, which Dr. Aristizabal described as “a significant improvement.”
Among high-risk patients, the improvement in 5-year survival between the pre- and postimplementation period went from 48% to 55%.
“This is an area for improvement,” Dr. Aristizabal said, “and we’re working on additional strategies to help improve survival for high-risk patients.
The study was funded by Rady Children’s Hospital, the Mexican Secretary of Health, and the Patronato Foundation. Dr. Aristizabal and coauthors reported no relevant financial relationships. Dr. Gralow reported relationships with Genentech and Roche. Dr. Winer reported relationships with Leap Therapeutics, Jounce Therapeutics, Carrick Therapeutics, and Genentech.
A version of this article first appeared on Medscape.com.
FROM ASCO 2023

