User login
Clinical Guidelines Hub only
Endocarditis in dental patients rises after guidelines discourage prophylaxis
The number of prescriptions for antibiotic prophylaxis before invasive dental procedures has dropped sharply in England since 2008, while the incidence of infective endocarditis has risen significantly in the same time period, researchers found.
A study led by Dr. Martin Thornhill of the University of Sheffield (England) School of Clinical Dentistry, and published online Nov. 18 in the Lancet (doi: 10.1016/S0140-6736(14)62007-9) showed that after the National Institute for Health and Care Excellence issued guidelines against antibiotic prophylaxis, even for patients at high risk of endocarditis, prescriptions fell precipitously from a mean 10,900 per month in 2004-2008 in England to a mean 2,236 a month between April 2008 and April 2013, with only 1,235 issued in the last month of the study period. The NICE guidance, which went further than other published recommendations that have aimed to limit, but not eliminate, the use of antibiotic prophylaxis as a form of endocarditis prevention, cited the absence of a robust evidence base supporting its effectiveness, and also the risk of adverse drug reactions.
Dr. Thornhill and his colleagues reviewed both national prescription records and hospital discharge records for patients with a primary diagnosis of infective endocarditis. Prescriptions of antibiotic prophylaxis for the prevention of infective endocarditis fell significantly after introduction of the NICE guidance.
The incidence of infective endocarditis, in contrast, rose by 0.11 cases per 10 million people per month following the 2008 guidance (95% confidence interval, 0.05-0.16; P < .0001). By March 2013, the researchers found that there were 34.9 more cases per month than would have been expected had the previous trend continued (95% CI, 7.9-61.9). Moreover, the increase was significant for patients determined to be at low or moderate risk as well as for those deemed high risk. The researchers did not find a statistically significant increase in endocarditis-related mortality corresponding to the drop in prescriptions.
Dr. Thornhill and his colleagues cautioned that their results did not establish a causal association between the drop in prescriptions and the rise in cases, and that further investigations were now warranted.
The study was funded by Heart Research UK, Simplyhealth, and the U.S. National Institutes of Health. Two of its authors were involved in guidelines on infective endocarditis issued by the American Heart Association in 2007. One author helped produce European Society of Cardiology endocarditis guidelines in 2009, and also acted as a consultant to NICE during the drafting of the 2008 guidelines on antibiotic prophylaxis in endocarditis.
The number of prescriptions for antibiotic prophylaxis before invasive dental procedures has dropped sharply in England since 2008, while the incidence of infective endocarditis has risen significantly in the same time period, researchers found.
A study led by Dr. Martin Thornhill of the University of Sheffield (England) School of Clinical Dentistry, and published online Nov. 18 in the Lancet (doi: 10.1016/S0140-6736(14)62007-9) showed that after the National Institute for Health and Care Excellence issued guidelines against antibiotic prophylaxis, even for patients at high risk of endocarditis, prescriptions fell precipitously from a mean 10,900 per month in 2004-2008 in England to a mean 2,236 a month between April 2008 and April 2013, with only 1,235 issued in the last month of the study period. The NICE guidance, which went further than other published recommendations that have aimed to limit, but not eliminate, the use of antibiotic prophylaxis as a form of endocarditis prevention, cited the absence of a robust evidence base supporting its effectiveness, and also the risk of adverse drug reactions.
Dr. Thornhill and his colleagues reviewed both national prescription records and hospital discharge records for patients with a primary diagnosis of infective endocarditis. Prescriptions of antibiotic prophylaxis for the prevention of infective endocarditis fell significantly after introduction of the NICE guidance.
The incidence of infective endocarditis, in contrast, rose by 0.11 cases per 10 million people per month following the 2008 guidance (95% confidence interval, 0.05-0.16; P < .0001). By March 2013, the researchers found that there were 34.9 more cases per month than would have been expected had the previous trend continued (95% CI, 7.9-61.9). Moreover, the increase was significant for patients determined to be at low or moderate risk as well as for those deemed high risk. The researchers did not find a statistically significant increase in endocarditis-related mortality corresponding to the drop in prescriptions.
Dr. Thornhill and his colleagues cautioned that their results did not establish a causal association between the drop in prescriptions and the rise in cases, and that further investigations were now warranted.
The study was funded by Heart Research UK, Simplyhealth, and the U.S. National Institutes of Health. Two of its authors were involved in guidelines on infective endocarditis issued by the American Heart Association in 2007. One author helped produce European Society of Cardiology endocarditis guidelines in 2009, and also acted as a consultant to NICE during the drafting of the 2008 guidelines on antibiotic prophylaxis in endocarditis.
The number of prescriptions for antibiotic prophylaxis before invasive dental procedures has dropped sharply in England since 2008, while the incidence of infective endocarditis has risen significantly in the same time period, researchers found.
A study led by Dr. Martin Thornhill of the University of Sheffield (England) School of Clinical Dentistry, and published online Nov. 18 in the Lancet (doi: 10.1016/S0140-6736(14)62007-9) showed that after the National Institute for Health and Care Excellence issued guidelines against antibiotic prophylaxis, even for patients at high risk of endocarditis, prescriptions fell precipitously from a mean 10,900 per month in 2004-2008 in England to a mean 2,236 a month between April 2008 and April 2013, with only 1,235 issued in the last month of the study period. The NICE guidance, which went further than other published recommendations that have aimed to limit, but not eliminate, the use of antibiotic prophylaxis as a form of endocarditis prevention, cited the absence of a robust evidence base supporting its effectiveness, and also the risk of adverse drug reactions.
Dr. Thornhill and his colleagues reviewed both national prescription records and hospital discharge records for patients with a primary diagnosis of infective endocarditis. Prescriptions of antibiotic prophylaxis for the prevention of infective endocarditis fell significantly after introduction of the NICE guidance.
The incidence of infective endocarditis, in contrast, rose by 0.11 cases per 10 million people per month following the 2008 guidance (95% confidence interval, 0.05-0.16; P < .0001). By March 2013, the researchers found that there were 34.9 more cases per month than would have been expected had the previous trend continued (95% CI, 7.9-61.9). Moreover, the increase was significant for patients determined to be at low or moderate risk as well as for those deemed high risk. The researchers did not find a statistically significant increase in endocarditis-related mortality corresponding to the drop in prescriptions.
Dr. Thornhill and his colleagues cautioned that their results did not establish a causal association between the drop in prescriptions and the rise in cases, and that further investigations were now warranted.
The study was funded by Heart Research UK, Simplyhealth, and the U.S. National Institutes of Health. Two of its authors were involved in guidelines on infective endocarditis issued by the American Heart Association in 2007. One author helped produce European Society of Cardiology endocarditis guidelines in 2009, and also acted as a consultant to NICE during the drafting of the 2008 guidelines on antibiotic prophylaxis in endocarditis.
FROM THE LANCET
Key clinical point: Antibiotic prophylaxis before invasive dental procedures dropped sharply while the incidence of infective endocarditis rose significantly.
Major finding: The incidence of infective endocarditis rose by 0.11 cases per 10 million people per month following the 2008 guidance.
Data source: Researchers reviewed both national prescription records and hospital discharge records for patients with a primary diagnosis of infective endocarditis in the United Kingdom.
Disclosures: The study was funded by Heart Research UK, Simplyhealth, and the U.S. National Institutes of Health. Two of its authors were involved in guidelines on infective endocarditis issued by the American Heart Association in 2007. One author helped produce European Society of Cardiology endocarditis guidelines in 2009, and also acted as a consultant to NICE during the drafting of the 2008 guidelines on antibiotic prophylaxis in endocarditis.
Guideline: Bi-level positive airway pressure (BPAP) devices
Recommendations
- Appropriate for patients with obstructive sleep apnea (OSA) who have failed continuous positive airway pressure (CPAP)/auto-titrating positive airway pressure (APAP) or require supplemental ventilatory support due to a hypoventilation syndrome
BPAP (with back-up rate feature)
- Appropriate for patients with established central sleep apnea (CSA) diagnosed by an in-lab sleep study demonstrating all of the following:
- OSA has been excluded or treated
- Oxygen saturation level is 88% or less for at least five (5) continuous minutes while the patient breathes his/her usual fraction of inspired oxygen (FiO2) OR the patient demonstrates Cheyne-Stokes respiration for five (5) continuous minutes with oxygen saturation falling to 88% or less at least once during that 5 minute interval
- A titration study (split-night or whole-night) has demonstrated significant improvement of sleep-related hypoventilation adjusted to the settings that will be prescribed for home use (while breathing the individual's usual FiO2)
BPAP (with or without back-up rate feature)
- Appropriate in the management of patients with severe chronic obstructive pulmonary disease (COPD) demonstrating either of the following:
- Partial pressure of arterial carbon dioxide (PaCO2) measured by arterial blood gas drawn while the patient is awake and breathing his/her usual FiO2 is 45 mmHg or greater; OR
- Sleep oximetry demonstrates oxygen saturation of 88% or less for at least five continuous minutes while the patient breathes oxygen at 2 L per minute or his/her usual FiO2 (whichever is higher)
BPAP (with or without back-up rate feature)
- Appropriate in the management of patients with certain restrictive thoracic disorders when both a and b below are true:
- The patient has an established diagnosis of a progressive neuromuscular disease (e.g., amyotrophic lateral sclerosis [ALS]) OR a severe thoracic cage abnormality; AND
- One of the following statements is true:
- PaCO2 measured by arterial blood gas drawn while the patient is awake and breathing his/her usual FiO2 is 45 mmHg or greater.
- Sleep oximetry demonstrates oxygen saturation of 88% or less for at least five continuous minutes while the patient breathes his/her usual FiO2
- Maximal inspiratory pressure is less than 60 cm H2O or forced vital capacity is less than 50% of predicted (applies to patients with progressive neuromuscular disease only)
Ongoing Treatment with BPAP
Ongoing treatment is indicated for patients who demonstrate compliance with therapy. Demonstration of compliance is required every 90 days for the first year of treatment and annually thereafter. Compliance is defined as:
- Use of the BPAP device for greater than or equal to four (4) hours per night on 70% of nights during a consecutive thirty (30) day period within the preceding 90 days; OR
- There is clinical evidence submitted by the treating provider that demonstrates continued clinical benefit from use of the positive airway pressure device.
Recommendations
- Appropriate for patients with obstructive sleep apnea (OSA) who have failed continuous positive airway pressure (CPAP)/auto-titrating positive airway pressure (APAP) or require supplemental ventilatory support due to a hypoventilation syndrome
BPAP (with back-up rate feature)
- Appropriate for patients with established central sleep apnea (CSA) diagnosed by an in-lab sleep study demonstrating all of the following:
- OSA has been excluded or treated
- Oxygen saturation level is 88% or less for at least five (5) continuous minutes while the patient breathes his/her usual fraction of inspired oxygen (FiO2) OR the patient demonstrates Cheyne-Stokes respiration for five (5) continuous minutes with oxygen saturation falling to 88% or less at least once during that 5 minute interval
- A titration study (split-night or whole-night) has demonstrated significant improvement of sleep-related hypoventilation adjusted to the settings that will be prescribed for home use (while breathing the individual's usual FiO2)
BPAP (with or without back-up rate feature)
- Appropriate in the management of patients with severe chronic obstructive pulmonary disease (COPD) demonstrating either of the following:
- Partial pressure of arterial carbon dioxide (PaCO2) measured by arterial blood gas drawn while the patient is awake and breathing his/her usual FiO2 is 45 mmHg or greater; OR
- Sleep oximetry demonstrates oxygen saturation of 88% or less for at least five continuous minutes while the patient breathes oxygen at 2 L per minute or his/her usual FiO2 (whichever is higher)
BPAP (with or without back-up rate feature)
- Appropriate in the management of patients with certain restrictive thoracic disorders when both a and b below are true:
- The patient has an established diagnosis of a progressive neuromuscular disease (e.g., amyotrophic lateral sclerosis [ALS]) OR a severe thoracic cage abnormality; AND
- One of the following statements is true:
- PaCO2 measured by arterial blood gas drawn while the patient is awake and breathing his/her usual FiO2 is 45 mmHg or greater.
- Sleep oximetry demonstrates oxygen saturation of 88% or less for at least five continuous minutes while the patient breathes his/her usual FiO2
- Maximal inspiratory pressure is less than 60 cm H2O or forced vital capacity is less than 50% of predicted (applies to patients with progressive neuromuscular disease only)
Ongoing Treatment with BPAP
Ongoing treatment is indicated for patients who demonstrate compliance with therapy. Demonstration of compliance is required every 90 days for the first year of treatment and annually thereafter. Compliance is defined as:
- Use of the BPAP device for greater than or equal to four (4) hours per night on 70% of nights during a consecutive thirty (30) day period within the preceding 90 days; OR
- There is clinical evidence submitted by the treating provider that demonstrates continued clinical benefit from use of the positive airway pressure device.
Recommendations
- Appropriate for patients with obstructive sleep apnea (OSA) who have failed continuous positive airway pressure (CPAP)/auto-titrating positive airway pressure (APAP) or require supplemental ventilatory support due to a hypoventilation syndrome
BPAP (with back-up rate feature)
- Appropriate for patients with established central sleep apnea (CSA) diagnosed by an in-lab sleep study demonstrating all of the following:
- OSA has been excluded or treated
- Oxygen saturation level is 88% or less for at least five (5) continuous minutes while the patient breathes his/her usual fraction of inspired oxygen (FiO2) OR the patient demonstrates Cheyne-Stokes respiration for five (5) continuous minutes with oxygen saturation falling to 88% or less at least once during that 5 minute interval
- A titration study (split-night or whole-night) has demonstrated significant improvement of sleep-related hypoventilation adjusted to the settings that will be prescribed for home use (while breathing the individual's usual FiO2)
BPAP (with or without back-up rate feature)
- Appropriate in the management of patients with severe chronic obstructive pulmonary disease (COPD) demonstrating either of the following:
- Partial pressure of arterial carbon dioxide (PaCO2) measured by arterial blood gas drawn while the patient is awake and breathing his/her usual FiO2 is 45 mmHg or greater; OR
- Sleep oximetry demonstrates oxygen saturation of 88% or less for at least five continuous minutes while the patient breathes oxygen at 2 L per minute or his/her usual FiO2 (whichever is higher)
BPAP (with or without back-up rate feature)
- Appropriate in the management of patients with certain restrictive thoracic disorders when both a and b below are true:
- The patient has an established diagnosis of a progressive neuromuscular disease (e.g., amyotrophic lateral sclerosis [ALS]) OR a severe thoracic cage abnormality; AND
- One of the following statements is true:
- PaCO2 measured by arterial blood gas drawn while the patient is awake and breathing his/her usual FiO2 is 45 mmHg or greater.
- Sleep oximetry demonstrates oxygen saturation of 88% or less for at least five continuous minutes while the patient breathes his/her usual FiO2
- Maximal inspiratory pressure is less than 60 cm H2O or forced vital capacity is less than 50% of predicted (applies to patients with progressive neuromuscular disease only)
Ongoing Treatment with BPAP
Ongoing treatment is indicated for patients who demonstrate compliance with therapy. Demonstration of compliance is required every 90 days for the first year of treatment and annually thereafter. Compliance is defined as:
- Use of the BPAP device for greater than or equal to four (4) hours per night on 70% of nights during a consecutive thirty (30) day period within the preceding 90 days; OR
- There is clinical evidence submitted by the treating provider that demonstrates continued clinical benefit from use of the positive airway pressure device.
RA draft guidelines: Treat to target
BOSTON – Treat to target in both early and established rheumatoid arthritis, recommended the authors of American College of Rheumatology draft guidelines on the management of RA.
The new ACR guidelines, expected to be finalized and published by the spring of 2015, also focus on the care of those patients whom most rheumatologists see in day-to-day practice, and they call for patience when trying a new therapy or new dose of an existing drug, Dr. Jasvinder Singh, of the division of clinical immunology and rheumatology at the University of Alabama, Birmingham, said to a standing-room-only crowd at the annual meeting of the American College of Rheumatology.
One of the guiding principles of the proposed recommendations is that “if a patient is doing well and the RA is under control, switching from one therapy to another should be done by a physician in consultation and agreement with the patient, and arbitrary switching between therapies should not be done,” he said.
Overall, the evidence-based guidelines emphasize several important aspects of RA care, including the following:
• Focus on the common patient and not exceptional cases.
• Give optimal doses of medications for 3 months before escalating or switching therapy.
• Assess disease activity using one of ACR’s recommended measures at a majority of encounters with RA patients.
• Consider methotrexate as the initial therapy in most RA patients.
• Methotrexate is the preferred monotherapy with a disease-modifying antirheumatic drug (DMARD), but other options include sulfasalazine, hydroxychloroquine, or leflunomide.
• A rheumatologist is the clinician of first choice for all patients with RA.
• Limit glucocorticoid treatment to the lowest possible dose for the shortest possible time to offer the best ratio of benefit to risk.
• Routinely assess patients’ functional status with standardized validated measures at least once yearly, or more frequently when RA is active.
The draft guidelines strongly recommend “using a treat-to-target strategy rather than a nontargeted approach” in both early and established RA.
Ideally, the target to be determined by the clinician and patient, should be remission or low disease activity. The guidelines acknowledge, however, that in some cases risk tolerance or comorbidities may require choice of a different and presumably less aggressive target.
Early RA
For early RA in treatment-naive patients, the guidelines offer an algorithm suggesting DMARD monotherapy for patients with low disease activity and, if the disease flares, recourse to short-term glucocorticoids.
For patients with moderately or highly active early RA, DMARD monotherapy can be followed with either short-term glucocorticoids, or in the case of DMARD failure, to either combination traditional DMARDs, a tumor necrosis factor inhibitor (TNFi) with or without methotrexate, or a non-TNF biologic agent with or without methotrexate, and with or without low-dose glucocorticoids. If the above therapies fail, the clinician and patient should consider a treatment course used for established RA.
Established RA
As with early RA, DMARD-naive patients with low disease activity may be started on DMARD monotherapy and proceed to traditional DMARD combinations, a TNFi with/without methotrexate, or non-TNF biologic with/without methotrexate, or tofacitinib with methotrexate. The guidelines offer a less robust recommendation about adding low-dose glucocorticoids, or short-term glucocorticoids for flares.
Patients who have not responded to treatment with single TNFi can move to a non-TNF biologic plus or minus methotrexate, or a different TNFi with/without methotrexate.
Patients who have not responded to treatment with multiple TNFi can try a non-TNF biologic plus/minus methotrexate, or tofacitinib with or without methotrexate.
Patients who have not responded to treatment with a single non-TNF biologic agent can try a different non-TNF biologic with/without methotrexate.
When both a TNFi and non-TNF biologic fail to help, the patient can try another non-TNF biologic plus/minus methotrexate, or tofacitinib plus/minus methotrexate.
Patients for whom multiple non-TNF biologic agents have failed can try either tofacitinib plus/minus methotrexate, or, if the patient is TNFi naive, a TNFi plus/minus methotrexate.
Special considerations
The guidelines make recommendations about treating patients with previously treated or untreated melanoma (TNFi preferable to tofacitinib) or nonmelanoma skin cancer (combination DMARD or non-TNF biologic preferable to TNFi) or a previously treated lymphoproliferative disorder (combination DMARD or non-TNF biologic such as abatacept, tocilizumab or rituximab over a TNFi). Patients with treated solid-organ malignancies, however, can be treated as other patients with RA are treated.
For patients with active hepatitis B or C virus infection who are receiving effective antiviral therapy, a DMARD, TNFi, non-TNF biologic, or tofacitinib can be prescribed, based on American Association for the Study of Liver Diseases case series and clinical experience, Dr. Singh said.
For patients with established RA and heart failure (HF), the guidelines recommend combination DMARD, non-TNF biologic, or tofacitinib over a TNFi, and if the patient has established or worsening HF on a TNFi, the three drug options above are preferable to switching the patient to another TNFi.
For patients with previous serious infections, however, there was less agreement on the optimal course. The guidelines, as currently planned, recommend a DMARD combination or abatacept over a TNFi in these patients, but there was no consensus about either rituximab or tocilizumab over a TNFi, Dr. Singh noted.
Tapering therapy
Finally, the proposed guidelines deal with therapeutic tapers. Specifically, for patients with established RA and low disease activity on maintenance methotrexate, the guidelines strongly recommend continuing on a traditional DMARD, TNFi, non-TNF biologic, or tofacitinib.
There is a conditional recommendation that patients with established RA in remission continuing on methotrexate can taper traditional DMARD therapy, TNFi, non-TNF biologic, or tofacitinib. But the guidelines strongly recommend against discontinuing all therapies in these patients, Dr. Singh emphasized.
“The strong recommendation is based on clinical experience that only a very small minority of patients are able to discontinue all therapies. Conditional recommendations here, supported by low-level evidence, are largely based upon expert opinion and clinical experience,” said Dr. Singh, who disclosed financial relationships with Allergan, Regeneron, Savient, and Takeda.
Join the queue
The proposed guidelines follow up on ACR’s 2012 guidelines, and will join an already crowded field of clinical practice recommendations, including those published in 2013 by the European League Against Rheumatism.
BOSTON – Treat to target in both early and established rheumatoid arthritis, recommended the authors of American College of Rheumatology draft guidelines on the management of RA.
The new ACR guidelines, expected to be finalized and published by the spring of 2015, also focus on the care of those patients whom most rheumatologists see in day-to-day practice, and they call for patience when trying a new therapy or new dose of an existing drug, Dr. Jasvinder Singh, of the division of clinical immunology and rheumatology at the University of Alabama, Birmingham, said to a standing-room-only crowd at the annual meeting of the American College of Rheumatology.
One of the guiding principles of the proposed recommendations is that “if a patient is doing well and the RA is under control, switching from one therapy to another should be done by a physician in consultation and agreement with the patient, and arbitrary switching between therapies should not be done,” he said.
Overall, the evidence-based guidelines emphasize several important aspects of RA care, including the following:
• Focus on the common patient and not exceptional cases.
• Give optimal doses of medications for 3 months before escalating or switching therapy.
• Assess disease activity using one of ACR’s recommended measures at a majority of encounters with RA patients.
• Consider methotrexate as the initial therapy in most RA patients.
• Methotrexate is the preferred monotherapy with a disease-modifying antirheumatic drug (DMARD), but other options include sulfasalazine, hydroxychloroquine, or leflunomide.
• A rheumatologist is the clinician of first choice for all patients with RA.
• Limit glucocorticoid treatment to the lowest possible dose for the shortest possible time to offer the best ratio of benefit to risk.
• Routinely assess patients’ functional status with standardized validated measures at least once yearly, or more frequently when RA is active.
The draft guidelines strongly recommend “using a treat-to-target strategy rather than a nontargeted approach” in both early and established RA.
Ideally, the target to be determined by the clinician and patient, should be remission or low disease activity. The guidelines acknowledge, however, that in some cases risk tolerance or comorbidities may require choice of a different and presumably less aggressive target.
Early RA
For early RA in treatment-naive patients, the guidelines offer an algorithm suggesting DMARD monotherapy for patients with low disease activity and, if the disease flares, recourse to short-term glucocorticoids.
For patients with moderately or highly active early RA, DMARD monotherapy can be followed with either short-term glucocorticoids, or in the case of DMARD failure, to either combination traditional DMARDs, a tumor necrosis factor inhibitor (TNFi) with or without methotrexate, or a non-TNF biologic agent with or without methotrexate, and with or without low-dose glucocorticoids. If the above therapies fail, the clinician and patient should consider a treatment course used for established RA.
Established RA
As with early RA, DMARD-naive patients with low disease activity may be started on DMARD monotherapy and proceed to traditional DMARD combinations, a TNFi with/without methotrexate, or non-TNF biologic with/without methotrexate, or tofacitinib with methotrexate. The guidelines offer a less robust recommendation about adding low-dose glucocorticoids, or short-term glucocorticoids for flares.
Patients who have not responded to treatment with single TNFi can move to a non-TNF biologic plus or minus methotrexate, or a different TNFi with/without methotrexate.
Patients who have not responded to treatment with multiple TNFi can try a non-TNF biologic plus/minus methotrexate, or tofacitinib with or without methotrexate.
Patients who have not responded to treatment with a single non-TNF biologic agent can try a different non-TNF biologic with/without methotrexate.
When both a TNFi and non-TNF biologic fail to help, the patient can try another non-TNF biologic plus/minus methotrexate, or tofacitinib plus/minus methotrexate.
Patients for whom multiple non-TNF biologic agents have failed can try either tofacitinib plus/minus methotrexate, or, if the patient is TNFi naive, a TNFi plus/minus methotrexate.
Special considerations
The guidelines make recommendations about treating patients with previously treated or untreated melanoma (TNFi preferable to tofacitinib) or nonmelanoma skin cancer (combination DMARD or non-TNF biologic preferable to TNFi) or a previously treated lymphoproliferative disorder (combination DMARD or non-TNF biologic such as abatacept, tocilizumab or rituximab over a TNFi). Patients with treated solid-organ malignancies, however, can be treated as other patients with RA are treated.
For patients with active hepatitis B or C virus infection who are receiving effective antiviral therapy, a DMARD, TNFi, non-TNF biologic, or tofacitinib can be prescribed, based on American Association for the Study of Liver Diseases case series and clinical experience, Dr. Singh said.
For patients with established RA and heart failure (HF), the guidelines recommend combination DMARD, non-TNF biologic, or tofacitinib over a TNFi, and if the patient has established or worsening HF on a TNFi, the three drug options above are preferable to switching the patient to another TNFi.
For patients with previous serious infections, however, there was less agreement on the optimal course. The guidelines, as currently planned, recommend a DMARD combination or abatacept over a TNFi in these patients, but there was no consensus about either rituximab or tocilizumab over a TNFi, Dr. Singh noted.
Tapering therapy
Finally, the proposed guidelines deal with therapeutic tapers. Specifically, for patients with established RA and low disease activity on maintenance methotrexate, the guidelines strongly recommend continuing on a traditional DMARD, TNFi, non-TNF biologic, or tofacitinib.
There is a conditional recommendation that patients with established RA in remission continuing on methotrexate can taper traditional DMARD therapy, TNFi, non-TNF biologic, or tofacitinib. But the guidelines strongly recommend against discontinuing all therapies in these patients, Dr. Singh emphasized.
“The strong recommendation is based on clinical experience that only a very small minority of patients are able to discontinue all therapies. Conditional recommendations here, supported by low-level evidence, are largely based upon expert opinion and clinical experience,” said Dr. Singh, who disclosed financial relationships with Allergan, Regeneron, Savient, and Takeda.
Join the queue
The proposed guidelines follow up on ACR’s 2012 guidelines, and will join an already crowded field of clinical practice recommendations, including those published in 2013 by the European League Against Rheumatism.
BOSTON – Treat to target in both early and established rheumatoid arthritis, recommended the authors of American College of Rheumatology draft guidelines on the management of RA.
The new ACR guidelines, expected to be finalized and published by the spring of 2015, also focus on the care of those patients whom most rheumatologists see in day-to-day practice, and they call for patience when trying a new therapy or new dose of an existing drug, Dr. Jasvinder Singh, of the division of clinical immunology and rheumatology at the University of Alabama, Birmingham, said to a standing-room-only crowd at the annual meeting of the American College of Rheumatology.
One of the guiding principles of the proposed recommendations is that “if a patient is doing well and the RA is under control, switching from one therapy to another should be done by a physician in consultation and agreement with the patient, and arbitrary switching between therapies should not be done,” he said.
Overall, the evidence-based guidelines emphasize several important aspects of RA care, including the following:
• Focus on the common patient and not exceptional cases.
• Give optimal doses of medications for 3 months before escalating or switching therapy.
• Assess disease activity using one of ACR’s recommended measures at a majority of encounters with RA patients.
• Consider methotrexate as the initial therapy in most RA patients.
• Methotrexate is the preferred monotherapy with a disease-modifying antirheumatic drug (DMARD), but other options include sulfasalazine, hydroxychloroquine, or leflunomide.
• A rheumatologist is the clinician of first choice for all patients with RA.
• Limit glucocorticoid treatment to the lowest possible dose for the shortest possible time to offer the best ratio of benefit to risk.
• Routinely assess patients’ functional status with standardized validated measures at least once yearly, or more frequently when RA is active.
The draft guidelines strongly recommend “using a treat-to-target strategy rather than a nontargeted approach” in both early and established RA.
Ideally, the target to be determined by the clinician and patient, should be remission or low disease activity. The guidelines acknowledge, however, that in some cases risk tolerance or comorbidities may require choice of a different and presumably less aggressive target.
Early RA
For early RA in treatment-naive patients, the guidelines offer an algorithm suggesting DMARD monotherapy for patients with low disease activity and, if the disease flares, recourse to short-term glucocorticoids.
For patients with moderately or highly active early RA, DMARD monotherapy can be followed with either short-term glucocorticoids, or in the case of DMARD failure, to either combination traditional DMARDs, a tumor necrosis factor inhibitor (TNFi) with or without methotrexate, or a non-TNF biologic agent with or without methotrexate, and with or without low-dose glucocorticoids. If the above therapies fail, the clinician and patient should consider a treatment course used for established RA.
Established RA
As with early RA, DMARD-naive patients with low disease activity may be started on DMARD monotherapy and proceed to traditional DMARD combinations, a TNFi with/without methotrexate, or non-TNF biologic with/without methotrexate, or tofacitinib with methotrexate. The guidelines offer a less robust recommendation about adding low-dose glucocorticoids, or short-term glucocorticoids for flares.
Patients who have not responded to treatment with single TNFi can move to a non-TNF biologic plus or minus methotrexate, or a different TNFi with/without methotrexate.
Patients who have not responded to treatment with multiple TNFi can try a non-TNF biologic plus/minus methotrexate, or tofacitinib with or without methotrexate.
Patients who have not responded to treatment with a single non-TNF biologic agent can try a different non-TNF biologic with/without methotrexate.
When both a TNFi and non-TNF biologic fail to help, the patient can try another non-TNF biologic plus/minus methotrexate, or tofacitinib plus/minus methotrexate.
Patients for whom multiple non-TNF biologic agents have failed can try either tofacitinib plus/minus methotrexate, or, if the patient is TNFi naive, a TNFi plus/minus methotrexate.
Special considerations
The guidelines make recommendations about treating patients with previously treated or untreated melanoma (TNFi preferable to tofacitinib) or nonmelanoma skin cancer (combination DMARD or non-TNF biologic preferable to TNFi) or a previously treated lymphoproliferative disorder (combination DMARD or non-TNF biologic such as abatacept, tocilizumab or rituximab over a TNFi). Patients with treated solid-organ malignancies, however, can be treated as other patients with RA are treated.
For patients with active hepatitis B or C virus infection who are receiving effective antiviral therapy, a DMARD, TNFi, non-TNF biologic, or tofacitinib can be prescribed, based on American Association for the Study of Liver Diseases case series and clinical experience, Dr. Singh said.
For patients with established RA and heart failure (HF), the guidelines recommend combination DMARD, non-TNF biologic, or tofacitinib over a TNFi, and if the patient has established or worsening HF on a TNFi, the three drug options above are preferable to switching the patient to another TNFi.
For patients with previous serious infections, however, there was less agreement on the optimal course. The guidelines, as currently planned, recommend a DMARD combination or abatacept over a TNFi in these patients, but there was no consensus about either rituximab or tocilizumab over a TNFi, Dr. Singh noted.
Tapering therapy
Finally, the proposed guidelines deal with therapeutic tapers. Specifically, for patients with established RA and low disease activity on maintenance methotrexate, the guidelines strongly recommend continuing on a traditional DMARD, TNFi, non-TNF biologic, or tofacitinib.
There is a conditional recommendation that patients with established RA in remission continuing on methotrexate can taper traditional DMARD therapy, TNFi, non-TNF biologic, or tofacitinib. But the guidelines strongly recommend against discontinuing all therapies in these patients, Dr. Singh emphasized.
“The strong recommendation is based on clinical experience that only a very small minority of patients are able to discontinue all therapies. Conditional recommendations here, supported by low-level evidence, are largely based upon expert opinion and clinical experience,” said Dr. Singh, who disclosed financial relationships with Allergan, Regeneron, Savient, and Takeda.
Join the queue
The proposed guidelines follow up on ACR’s 2012 guidelines, and will join an already crowded field of clinical practice recommendations, including those published in 2013 by the European League Against Rheumatism.
AT THE ACR ANNUAL MEETING
Telephone CPR training boosts cardiac arrest survival
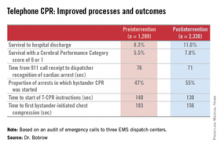
CHICAGO – Systematic implementation of a comprehensive telephone CPR bundle of care targeting EMS dispatch services resulted in substantial improvements in rates of survival to hospital discharge with good neurologic outcomes in patients with out-of-hospital cardiac arrest in a major Arizona statewide public health initiative.
How big was the intervention’s impact? The rate of survival to hospital discharge showed a 33% relative increase compared to preintervention, and survival with a favorable Cerebral Performance Category score of 0 or 1 increased by 42%, Dr. Bentley J. Bobrow reported at the American Heart Association Scientific Sessions.
“These results suggest that when deliberately implemented and measured, telephone CPR is a targeted, effective method to increase bystander CPR and survival on a vast scale with minimal capital expense. This is why we believe telephone CPR along with public training may be the most efficient way to move the needle on cardiac arrest survival,” declared Dr. Bobrow, professor of emergency medicine at the University of Arizona College of Medicine-Phoenix Campus and chair of the AHA Basic Life Support Subcommittee.
Telephone CPR (T-CPR) entails the provision of CPR instruction to bystanders who have called 911 regarding an out of hospital cardiac arrest (OHCA). It’s well established that bystander CPR commenced before EMS personnel arrive on the scene doubles or even triples OHCA survival, but it is provided in only about one-third of OHCA events. And while T-CPR is independently associated with increased rates of bystander CPR as well as patient survival, its utilization varies widely throughout the country and few EMS services measure performance.
Dr. Bobrow reported on an ambitious undertaking that involved systematic training in T-CPR for dispatchers, 911 managers, and medical directors at all nine of the regional emergency dispatch centers in Arizona, which together with 190 EMS agencies and 40 cardiac care hospitals participate in a statewide resuscitation program.
The training was designed to implement the latest AHA guidelines on T-CPR (Circulation 2012;125:648-55). The program entailed a half-day in-person training session plus completion of a 1-hour web-based interactive video. The protocol emphasizes asking two key questions of the 911 caller: “Is the patient conscious?” and “Is the patient breathing normally?” If the response is no to both, the dispatcher is to start issuing bystander CPR instructions without delay – no further questions – and continue the coaching until EMS personnel arrive on the scene to take over.
A core aspect of the T-CPR bundle is performance measurement for quality improvement, with auditing of 911 calls to learn the time from the start of the call to the bystander’s first chest compression and five other key performance metrics. Feedback is provided to the 911 call center regarding system- and case-level performance reports in a continuing education, quality improvement process. Individual dispatchers are singled out for exemplary performance, Dr. Bobrow explained.
He presented a prospective before-and-after study conducted at the three EMS dispatch centers serving Arizona’s Maricopa County, home to two-thirds of the state’s population. The study entailed auditing nearly 6,000 911 calls, each averaging 6.5 minutes in length. After excluding calls where CPR wasn’t indicated or the OHCA involved a patient less than 8 years old, investigators were left with two groups for comparison comprised of 1,289 pre- and 2,330 post-intervention events.
The improvements in process and clinical outcomes were dramatic. In 2012, after introduction of the T-CPR training program, the bystander CPR rate crossed the 50% threshold for the first time ever in Maricopa County. The rate of survival of OHCA to hospital discharge improved from 8.3% to 11%, a highly statistically significant 33% relative increase. Survival with a Cerebral Performance Category score of 0 or 1 climbed from 5.5% to 7.8%, a 42% relative increase. In a multivariate analysis adjusted for potential confounders, the adjusted odds ratio for survival of OHCA was 2.25-fold greater for all cases after implementation of the T-CPR program and similarly increased for arrests of cardiac origin.
Dr. Bobrow observed that this was not a randomized trial, which he considered would be both unethical and impractical.
“We controlled for known risk factors and confounders, and while we cannot prove that better outcomes resulted directly from the process improvements, the two are independently associated in this controlled study,” said the emergency physician, who is medical director of the Bureau of Emergency Medical Services and Trauma Systems at the Arizona Dept. of Health Services.
Audience members rose to praise the “fantastic” achievements in Arizona and ask why they’re not having similar success rates in their own districts, given that the AHA guidelines are readily available.
“A lot of places say they’re doing this,” Dr. Bobrow replied, “but when they realize what ‘this’ is, they understand that they really weren’t doing it in this type of depth. When we showed them the data on how marginal their performance was, I think that really made the difference.”
“I think that once most dispatch centers really understand the issues and their importance and the power that they have, and you can engage them, I’m confident that people would see the same changes,” he added.
His study was honored as the best oral abstract presentation at the AHA resuscitation science symposium.
Dr. Bobrow reported serving as co-principal investigator of the HeartRescue Project, funded by Medtronic Philanthropy.
CHICAGO – Systematic implementation of a comprehensive telephone CPR bundle of care targeting EMS dispatch services resulted in substantial improvements in rates of survival to hospital discharge with good neurologic outcomes in patients with out-of-hospital cardiac arrest in a major Arizona statewide public health initiative.
How big was the intervention’s impact? The rate of survival to hospital discharge showed a 33% relative increase compared to preintervention, and survival with a favorable Cerebral Performance Category score of 0 or 1 increased by 42%, Dr. Bentley J. Bobrow reported at the American Heart Association Scientific Sessions.
“These results suggest that when deliberately implemented and measured, telephone CPR is a targeted, effective method to increase bystander CPR and survival on a vast scale with minimal capital expense. This is why we believe telephone CPR along with public training may be the most efficient way to move the needle on cardiac arrest survival,” declared Dr. Bobrow, professor of emergency medicine at the University of Arizona College of Medicine-Phoenix Campus and chair of the AHA Basic Life Support Subcommittee.
Telephone CPR (T-CPR) entails the provision of CPR instruction to bystanders who have called 911 regarding an out of hospital cardiac arrest (OHCA). It’s well established that bystander CPR commenced before EMS personnel arrive on the scene doubles or even triples OHCA survival, but it is provided in only about one-third of OHCA events. And while T-CPR is independently associated with increased rates of bystander CPR as well as patient survival, its utilization varies widely throughout the country and few EMS services measure performance.
Dr. Bobrow reported on an ambitious undertaking that involved systematic training in T-CPR for dispatchers, 911 managers, and medical directors at all nine of the regional emergency dispatch centers in Arizona, which together with 190 EMS agencies and 40 cardiac care hospitals participate in a statewide resuscitation program.
The training was designed to implement the latest AHA guidelines on T-CPR (Circulation 2012;125:648-55). The program entailed a half-day in-person training session plus completion of a 1-hour web-based interactive video. The protocol emphasizes asking two key questions of the 911 caller: “Is the patient conscious?” and “Is the patient breathing normally?” If the response is no to both, the dispatcher is to start issuing bystander CPR instructions without delay – no further questions – and continue the coaching until EMS personnel arrive on the scene to take over.
A core aspect of the T-CPR bundle is performance measurement for quality improvement, with auditing of 911 calls to learn the time from the start of the call to the bystander’s first chest compression and five other key performance metrics. Feedback is provided to the 911 call center regarding system- and case-level performance reports in a continuing education, quality improvement process. Individual dispatchers are singled out for exemplary performance, Dr. Bobrow explained.
He presented a prospective before-and-after study conducted at the three EMS dispatch centers serving Arizona’s Maricopa County, home to two-thirds of the state’s population. The study entailed auditing nearly 6,000 911 calls, each averaging 6.5 minutes in length. After excluding calls where CPR wasn’t indicated or the OHCA involved a patient less than 8 years old, investigators were left with two groups for comparison comprised of 1,289 pre- and 2,330 post-intervention events.
The improvements in process and clinical outcomes were dramatic. In 2012, after introduction of the T-CPR training program, the bystander CPR rate crossed the 50% threshold for the first time ever in Maricopa County. The rate of survival of OHCA to hospital discharge improved from 8.3% to 11%, a highly statistically significant 33% relative increase. Survival with a Cerebral Performance Category score of 0 or 1 climbed from 5.5% to 7.8%, a 42% relative increase. In a multivariate analysis adjusted for potential confounders, the adjusted odds ratio for survival of OHCA was 2.25-fold greater for all cases after implementation of the T-CPR program and similarly increased for arrests of cardiac origin.
Dr. Bobrow observed that this was not a randomized trial, which he considered would be both unethical and impractical.
“We controlled for known risk factors and confounders, and while we cannot prove that better outcomes resulted directly from the process improvements, the two are independently associated in this controlled study,” said the emergency physician, who is medical director of the Bureau of Emergency Medical Services and Trauma Systems at the Arizona Dept. of Health Services.
Audience members rose to praise the “fantastic” achievements in Arizona and ask why they’re not having similar success rates in their own districts, given that the AHA guidelines are readily available.
“A lot of places say they’re doing this,” Dr. Bobrow replied, “but when they realize what ‘this’ is, they understand that they really weren’t doing it in this type of depth. When we showed them the data on how marginal their performance was, I think that really made the difference.”
“I think that once most dispatch centers really understand the issues and their importance and the power that they have, and you can engage them, I’m confident that people would see the same changes,” he added.
His study was honored as the best oral abstract presentation at the AHA resuscitation science symposium.
Dr. Bobrow reported serving as co-principal investigator of the HeartRescue Project, funded by Medtronic Philanthropy.
CHICAGO – Systematic implementation of a comprehensive telephone CPR bundle of care targeting EMS dispatch services resulted in substantial improvements in rates of survival to hospital discharge with good neurologic outcomes in patients with out-of-hospital cardiac arrest in a major Arizona statewide public health initiative.
How big was the intervention’s impact? The rate of survival to hospital discharge showed a 33% relative increase compared to preintervention, and survival with a favorable Cerebral Performance Category score of 0 or 1 increased by 42%, Dr. Bentley J. Bobrow reported at the American Heart Association Scientific Sessions.
“These results suggest that when deliberately implemented and measured, telephone CPR is a targeted, effective method to increase bystander CPR and survival on a vast scale with minimal capital expense. This is why we believe telephone CPR along with public training may be the most efficient way to move the needle on cardiac arrest survival,” declared Dr. Bobrow, professor of emergency medicine at the University of Arizona College of Medicine-Phoenix Campus and chair of the AHA Basic Life Support Subcommittee.
Telephone CPR (T-CPR) entails the provision of CPR instruction to bystanders who have called 911 regarding an out of hospital cardiac arrest (OHCA). It’s well established that bystander CPR commenced before EMS personnel arrive on the scene doubles or even triples OHCA survival, but it is provided in only about one-third of OHCA events. And while T-CPR is independently associated with increased rates of bystander CPR as well as patient survival, its utilization varies widely throughout the country and few EMS services measure performance.
Dr. Bobrow reported on an ambitious undertaking that involved systematic training in T-CPR for dispatchers, 911 managers, and medical directors at all nine of the regional emergency dispatch centers in Arizona, which together with 190 EMS agencies and 40 cardiac care hospitals participate in a statewide resuscitation program.
The training was designed to implement the latest AHA guidelines on T-CPR (Circulation 2012;125:648-55). The program entailed a half-day in-person training session plus completion of a 1-hour web-based interactive video. The protocol emphasizes asking two key questions of the 911 caller: “Is the patient conscious?” and “Is the patient breathing normally?” If the response is no to both, the dispatcher is to start issuing bystander CPR instructions without delay – no further questions – and continue the coaching until EMS personnel arrive on the scene to take over.
A core aspect of the T-CPR bundle is performance measurement for quality improvement, with auditing of 911 calls to learn the time from the start of the call to the bystander’s first chest compression and five other key performance metrics. Feedback is provided to the 911 call center regarding system- and case-level performance reports in a continuing education, quality improvement process. Individual dispatchers are singled out for exemplary performance, Dr. Bobrow explained.
He presented a prospective before-and-after study conducted at the three EMS dispatch centers serving Arizona’s Maricopa County, home to two-thirds of the state’s population. The study entailed auditing nearly 6,000 911 calls, each averaging 6.5 minutes in length. After excluding calls where CPR wasn’t indicated or the OHCA involved a patient less than 8 years old, investigators were left with two groups for comparison comprised of 1,289 pre- and 2,330 post-intervention events.
The improvements in process and clinical outcomes were dramatic. In 2012, after introduction of the T-CPR training program, the bystander CPR rate crossed the 50% threshold for the first time ever in Maricopa County. The rate of survival of OHCA to hospital discharge improved from 8.3% to 11%, a highly statistically significant 33% relative increase. Survival with a Cerebral Performance Category score of 0 or 1 climbed from 5.5% to 7.8%, a 42% relative increase. In a multivariate analysis adjusted for potential confounders, the adjusted odds ratio for survival of OHCA was 2.25-fold greater for all cases after implementation of the T-CPR program and similarly increased for arrests of cardiac origin.
Dr. Bobrow observed that this was not a randomized trial, which he considered would be both unethical and impractical.
“We controlled for known risk factors and confounders, and while we cannot prove that better outcomes resulted directly from the process improvements, the two are independently associated in this controlled study,” said the emergency physician, who is medical director of the Bureau of Emergency Medical Services and Trauma Systems at the Arizona Dept. of Health Services.
Audience members rose to praise the “fantastic” achievements in Arizona and ask why they’re not having similar success rates in their own districts, given that the AHA guidelines are readily available.
“A lot of places say they’re doing this,” Dr. Bobrow replied, “but when they realize what ‘this’ is, they understand that they really weren’t doing it in this type of depth. When we showed them the data on how marginal their performance was, I think that really made the difference.”
“I think that once most dispatch centers really understand the issues and their importance and the power that they have, and you can engage them, I’m confident that people would see the same changes,” he added.
His study was honored as the best oral abstract presentation at the AHA resuscitation science symposium.
Dr. Bobrow reported serving as co-principal investigator of the HeartRescue Project, funded by Medtronic Philanthropy.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Adoption of the most recent AHA guidelines on telephone CPR by EMS dispatchers will lead to vast improvement in survival for patients with out-of-hospital cardiac arrest.
Major finding: Following implementation of an Arizona statewide program to improve telephone CPR by 911 dispatchers to bystanders at the scene of out-of-hospital cardiac arrest, survival to hospital discharge climbed from 8.3% to 11.0%.
Data source: This was a prospective study comparing the outcomes of 1,289 calls to Arizona 911 centers regarding out-of-hospital cardiac arrests before introduction of a comprehensive statewide telephone CPR program to 2,330 calls received post-intervention.
Disclosures: The study was financially supported by Medtronic Philanthropy as part of the HeartRescue Project. The presenter is co-principal investigator of the project.
Enhanced thyroid cancer guidelines expected in 2015
CORONADO, CALIF. – Expect significant enhancements to the updated thyroid cancer management guidelines from the American Thyroid Association, due to be released in early 2015.
Last updated in 2009, the goal of the new guidelines is to “be evidence based and helpful,” guidelines task force chair Dr. Bryan R. Haugen said at the annual meeting of the American Thyroid Association. For example, the new guidelines will contain 101 recommendations, up from 80 in the 2009 version; 175 subrecommendations, up from 103; and 998 references, up from 437. “Still, 59 of the existing 80 recommendations are not substantially changed, showing a general stability in our field over the past 5 to 6 years,” he said.
One enhancement is a definition of risk of structural disease recurrence in patients without structurally identifiable disease after initial therapy for thyroid cancer. Low risk is defined as intrathyroidal differentiated thyroid cancer involving up to five metastases less than 0.2 cm in size. Intermediate risk is defined as the presence of aggressive histology, minor extrathyroidal extension, vascular invasion, or more than five involved lymph nodes with metastases 0.2-0.3 cm in size. High risk is defined as the presence of gross extrathyroidal extension, incomplete tumor resection, distant metastases, or lymph node metastases greater than 3 cm in size.
The guidelines also include a table that defines a patient’s response to therapy as a dynamic risk assessment. “This best applies to the low- to intermediate-risk patients, although it definitely applies to high risk as well,” said Dr. Haugen, who heads the division of endocrinology, metabolism, and diabetes at the University of Colorado Health Sciences Center, Denver. “It’s [a] strong recommendation based on low-quality evidence to use this risk-based response to therapy. A lot of this data is generated from patients who’ve had a thyroidectomy and have received radioiodine. So we’re on a bit more shaky ground right now in a patient who’s had a thyroidectomy but no radioiodine, or a patient who’s had a lobectomy.”
Other changes include the concept that it’s not necessary to biopsy every nodule more than 1 cm in size. “We’re going to be guided by the sonographic pattern in who we biopsy and how we monitor them,” Dr. Haugen explained. “A new recommendation adds follow-up guidance for nodules that do not meet FNA [fine-needle aspiration] criteria. We’re also recommending use of the Bethesda Cytology Classification System for cytology.”
Changes in the initial management of thyroid cancer include a recommendation for cross-sectional imaging with contrast for higher-risk disease and the consideration of lobectomy for some patients with tumors 1-4 cm in size. “This is a controversial recommendation,” Dr. Haugen said. “We got some feedback from members asking if you do it, what’s the TSH target? Should we give them synthetic levothyroxine? We are revising the guidelines based on this feedback to help guide clinicians.”
The new guidelines also call for more detailed/standardized pathology reports, with inclusion of lymph node size, extranodal invasion, and the number of invaded vessels. “I’ve talked to a number of pathologists and clinicians who are very happy about this guidance,” he said. “We also need to look at tumor stage, recurrence risk, and response to therapy in our patients, and the use of selective radioiodine. There is some more information on considering lower administered activities, especially in the lower-risk patients.”
For the first time, the guidelines include a section on radioiodine treatment for refractory differentiated thyroid cancer, including tips on directed therapy, clinical trials, systemic therapy, and bone-specific therapy.
Dr. Haugen disclosed that he has received grants and research support from Veracyte and Genzyme.
On Twitter @dougbrunk
CORONADO, CALIF. – Expect significant enhancements to the updated thyroid cancer management guidelines from the American Thyroid Association, due to be released in early 2015.
Last updated in 2009, the goal of the new guidelines is to “be evidence based and helpful,” guidelines task force chair Dr. Bryan R. Haugen said at the annual meeting of the American Thyroid Association. For example, the new guidelines will contain 101 recommendations, up from 80 in the 2009 version; 175 subrecommendations, up from 103; and 998 references, up from 437. “Still, 59 of the existing 80 recommendations are not substantially changed, showing a general stability in our field over the past 5 to 6 years,” he said.
One enhancement is a definition of risk of structural disease recurrence in patients without structurally identifiable disease after initial therapy for thyroid cancer. Low risk is defined as intrathyroidal differentiated thyroid cancer involving up to five metastases less than 0.2 cm in size. Intermediate risk is defined as the presence of aggressive histology, minor extrathyroidal extension, vascular invasion, or more than five involved lymph nodes with metastases 0.2-0.3 cm in size. High risk is defined as the presence of gross extrathyroidal extension, incomplete tumor resection, distant metastases, or lymph node metastases greater than 3 cm in size.
The guidelines also include a table that defines a patient’s response to therapy as a dynamic risk assessment. “This best applies to the low- to intermediate-risk patients, although it definitely applies to high risk as well,” said Dr. Haugen, who heads the division of endocrinology, metabolism, and diabetes at the University of Colorado Health Sciences Center, Denver. “It’s [a] strong recommendation based on low-quality evidence to use this risk-based response to therapy. A lot of this data is generated from patients who’ve had a thyroidectomy and have received radioiodine. So we’re on a bit more shaky ground right now in a patient who’s had a thyroidectomy but no radioiodine, or a patient who’s had a lobectomy.”
Other changes include the concept that it’s not necessary to biopsy every nodule more than 1 cm in size. “We’re going to be guided by the sonographic pattern in who we biopsy and how we monitor them,” Dr. Haugen explained. “A new recommendation adds follow-up guidance for nodules that do not meet FNA [fine-needle aspiration] criteria. We’re also recommending use of the Bethesda Cytology Classification System for cytology.”
Changes in the initial management of thyroid cancer include a recommendation for cross-sectional imaging with contrast for higher-risk disease and the consideration of lobectomy for some patients with tumors 1-4 cm in size. “This is a controversial recommendation,” Dr. Haugen said. “We got some feedback from members asking if you do it, what’s the TSH target? Should we give them synthetic levothyroxine? We are revising the guidelines based on this feedback to help guide clinicians.”
The new guidelines also call for more detailed/standardized pathology reports, with inclusion of lymph node size, extranodal invasion, and the number of invaded vessels. “I’ve talked to a number of pathologists and clinicians who are very happy about this guidance,” he said. “We also need to look at tumor stage, recurrence risk, and response to therapy in our patients, and the use of selective radioiodine. There is some more information on considering lower administered activities, especially in the lower-risk patients.”
For the first time, the guidelines include a section on radioiodine treatment for refractory differentiated thyroid cancer, including tips on directed therapy, clinical trials, systemic therapy, and bone-specific therapy.
Dr. Haugen disclosed that he has received grants and research support from Veracyte and Genzyme.
On Twitter @dougbrunk
CORONADO, CALIF. – Expect significant enhancements to the updated thyroid cancer management guidelines from the American Thyroid Association, due to be released in early 2015.
Last updated in 2009, the goal of the new guidelines is to “be evidence based and helpful,” guidelines task force chair Dr. Bryan R. Haugen said at the annual meeting of the American Thyroid Association. For example, the new guidelines will contain 101 recommendations, up from 80 in the 2009 version; 175 subrecommendations, up from 103; and 998 references, up from 437. “Still, 59 of the existing 80 recommendations are not substantially changed, showing a general stability in our field over the past 5 to 6 years,” he said.
One enhancement is a definition of risk of structural disease recurrence in patients without structurally identifiable disease after initial therapy for thyroid cancer. Low risk is defined as intrathyroidal differentiated thyroid cancer involving up to five metastases less than 0.2 cm in size. Intermediate risk is defined as the presence of aggressive histology, minor extrathyroidal extension, vascular invasion, or more than five involved lymph nodes with metastases 0.2-0.3 cm in size. High risk is defined as the presence of gross extrathyroidal extension, incomplete tumor resection, distant metastases, or lymph node metastases greater than 3 cm in size.
The guidelines also include a table that defines a patient’s response to therapy as a dynamic risk assessment. “This best applies to the low- to intermediate-risk patients, although it definitely applies to high risk as well,” said Dr. Haugen, who heads the division of endocrinology, metabolism, and diabetes at the University of Colorado Health Sciences Center, Denver. “It’s [a] strong recommendation based on low-quality evidence to use this risk-based response to therapy. A lot of this data is generated from patients who’ve had a thyroidectomy and have received radioiodine. So we’re on a bit more shaky ground right now in a patient who’s had a thyroidectomy but no radioiodine, or a patient who’s had a lobectomy.”
Other changes include the concept that it’s not necessary to biopsy every nodule more than 1 cm in size. “We’re going to be guided by the sonographic pattern in who we biopsy and how we monitor them,” Dr. Haugen explained. “A new recommendation adds follow-up guidance for nodules that do not meet FNA [fine-needle aspiration] criteria. We’re also recommending use of the Bethesda Cytology Classification System for cytology.”
Changes in the initial management of thyroid cancer include a recommendation for cross-sectional imaging with contrast for higher-risk disease and the consideration of lobectomy for some patients with tumors 1-4 cm in size. “This is a controversial recommendation,” Dr. Haugen said. “We got some feedback from members asking if you do it, what’s the TSH target? Should we give them synthetic levothyroxine? We are revising the guidelines based on this feedback to help guide clinicians.”
The new guidelines also call for more detailed/standardized pathology reports, with inclusion of lymph node size, extranodal invasion, and the number of invaded vessels. “I’ve talked to a number of pathologists and clinicians who are very happy about this guidance,” he said. “We also need to look at tumor stage, recurrence risk, and response to therapy in our patients, and the use of selective radioiodine. There is some more information on considering lower administered activities, especially in the lower-risk patients.”
For the first time, the guidelines include a section on radioiodine treatment for refractory differentiated thyroid cancer, including tips on directed therapy, clinical trials, systemic therapy, and bone-specific therapy.
Dr. Haugen disclosed that he has received grants and research support from Veracyte and Genzyme.
On Twitter @dougbrunk
EXPERT ANALYSIS FROM THE ATA ANNUAL MEETING
VIDEO: Hepatitis C screening recommendations falling on deaf ears
BOSTON – The call to screen Baby Boomers for hepatitis C virus infections appears to have gone unheeded so far, results from a Chicago primary care clinic show.
Screening increased by only 2% among some 25,000 patients seen in the primary care clinic of the University of Chicago after the 2012 Centers for Disease Control and Prevention recommendation to screen adults born between 1945 and 1965, Dr. Mansi Kothari reported at the annual meeting of the American Association for the Study of Liver Diseases.
On a positive note, Dr. Kothari of the University of Chicago Medical Center noted in an interview that if a patient tested positive for hepatitis C virus, rates of additional testing and referral to a hepatologist remained high.
Dr. Kothari reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – The call to screen Baby Boomers for hepatitis C virus infections appears to have gone unheeded so far, results from a Chicago primary care clinic show.
Screening increased by only 2% among some 25,000 patients seen in the primary care clinic of the University of Chicago after the 2012 Centers for Disease Control and Prevention recommendation to screen adults born between 1945 and 1965, Dr. Mansi Kothari reported at the annual meeting of the American Association for the Study of Liver Diseases.
On a positive note, Dr. Kothari of the University of Chicago Medical Center noted in an interview that if a patient tested positive for hepatitis C virus, rates of additional testing and referral to a hepatologist remained high.
Dr. Kothari reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – The call to screen Baby Boomers for hepatitis C virus infections appears to have gone unheeded so far, results from a Chicago primary care clinic show.
Screening increased by only 2% among some 25,000 patients seen in the primary care clinic of the University of Chicago after the 2012 Centers for Disease Control and Prevention recommendation to screen adults born between 1945 and 1965, Dr. Mansi Kothari reported at the annual meeting of the American Association for the Study of Liver Diseases.
On a positive note, Dr. Kothari of the University of Chicago Medical Center noted in an interview that if a patient tested positive for hepatitis C virus, rates of additional testing and referral to a hepatologist remained high.
Dr. Kothari reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE LIVER MEETING 2014
VIDEO: Most baby boomers didn’t know their hep C status
BOSTON– Almost two-thirds of baby boomers presenting to Alabama emergency departments were unaware of their hepatitis C virus status, despite having such high-risk factors as past intravenous drug use or receipt of a blood transfusion prior to 1992.
Equally concerning, only 48% of patients who knew they were HCV positive were aware of some of the highly efficacious treatments now available, study author and medical student Derek Wells of the University of Alabama-Birmingham said in a video interview at the annual meeting of the American Association for the Study of Liver Diseases.
Mr. Wells called for increased awareness among front-line providers to improve screening and help eradicate HCV in the United States.
Mr. Wells reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON– Almost two-thirds of baby boomers presenting to Alabama emergency departments were unaware of their hepatitis C virus status, despite having such high-risk factors as past intravenous drug use or receipt of a blood transfusion prior to 1992.
Equally concerning, only 48% of patients who knew they were HCV positive were aware of some of the highly efficacious treatments now available, study author and medical student Derek Wells of the University of Alabama-Birmingham said in a video interview at the annual meeting of the American Association for the Study of Liver Diseases.
Mr. Wells called for increased awareness among front-line providers to improve screening and help eradicate HCV in the United States.
Mr. Wells reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON– Almost two-thirds of baby boomers presenting to Alabama emergency departments were unaware of their hepatitis C virus status, despite having such high-risk factors as past intravenous drug use or receipt of a blood transfusion prior to 1992.
Equally concerning, only 48% of patients who knew they were HCV positive were aware of some of the highly efficacious treatments now available, study author and medical student Derek Wells of the University of Alabama-Birmingham said in a video interview at the annual meeting of the American Association for the Study of Liver Diseases.
Mr. Wells called for increased awareness among front-line providers to improve screening and help eradicate HCV in the United States.
Mr. Wells reported no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE LIVER MEETING 2014
VIDEO: EMR reminder reduces unnecessary transfusions
SAN FRANCISCO – To reduce unnecessary transfusions, all it takes is a reminder in the electronic medical record system that they aren’t generally necessary if surgery patients have hemoglobins greater than 10 g/dL, according to investigators from Emory University in Atlanta.
A reminder in Emory’s EMR dropped transfusion rates in cardiothoracic patients without increasing negative outcomes. It also saved money and reduced the number of surgical site infections. Emory is now rolling it out systemwide (J. Am. Coll. Surg. 2014 June 25 [doi: 10.1016/j.jamcollsurg.2014.06.012]). Lead investigator Dr. Seyed Razavi explained the initiative in a video interview at the annual clinical congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Hossein Almassi, FCCP, comments: By their nature, cardiac operations are associated with higher transfusion rates than other surgical procedures. The negative impact of blood transfusion on short term hospital outcomes and mortality is well known. Any effort in reducing the adverse outcomes is a step in the right direction, especially in this era of 'pay per performance". A "reminder in the EMR" is but one such step.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: By their nature, cardiac operations are associated with higher transfusion rates than other surgical procedures. The negative impact of blood transfusion on short term hospital outcomes and mortality is well known. Any effort in reducing the adverse outcomes is a step in the right direction, especially in this era of 'pay per performance". A "reminder in the EMR" is but one such step.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
Dr. Hossein Almassi, FCCP, comments: By their nature, cardiac operations are associated with higher transfusion rates than other surgical procedures. The negative impact of blood transfusion on short term hospital outcomes and mortality is well known. Any effort in reducing the adverse outcomes is a step in the right direction, especially in this era of 'pay per performance". A "reminder in the EMR" is but one such step.
Dr. Almassi specializes in cardiothoracic surgery at the Medical College of Wisconsin in Milwaukee, Wisconsin.
SAN FRANCISCO – To reduce unnecessary transfusions, all it takes is a reminder in the electronic medical record system that they aren’t generally necessary if surgery patients have hemoglobins greater than 10 g/dL, according to investigators from Emory University in Atlanta.
A reminder in Emory’s EMR dropped transfusion rates in cardiothoracic patients without increasing negative outcomes. It also saved money and reduced the number of surgical site infections. Emory is now rolling it out systemwide (J. Am. Coll. Surg. 2014 June 25 [doi: 10.1016/j.jamcollsurg.2014.06.012]). Lead investigator Dr. Seyed Razavi explained the initiative in a video interview at the annual clinical congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN FRANCISCO – To reduce unnecessary transfusions, all it takes is a reminder in the electronic medical record system that they aren’t generally necessary if surgery patients have hemoglobins greater than 10 g/dL, according to investigators from Emory University in Atlanta.
A reminder in Emory’s EMR dropped transfusion rates in cardiothoracic patients without increasing negative outcomes. It also saved money and reduced the number of surgical site infections. Emory is now rolling it out systemwide (J. Am. Coll. Surg. 2014 June 25 [doi: 10.1016/j.jamcollsurg.2014.06.012]). Lead investigator Dr. Seyed Razavi explained the initiative in a video interview at the annual clinical congress of the American College of Surgeons.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACS CLINICAL CONGRESS
Guidelines: Urinate 2 liters daily to stop kidney stones’ return
Patients who have had kidney stones at least once should increase their fluid consumption to produce at least 2 L of urine per day to prevent the condition from recurring, according to new guidelines published by the American College of Physicians.
If increased fluid intake doesn’t prevent recurrent nephrolithiasis, the updated ACP guidelines recommend adding treatment with a thiazide diuretic, citrate, or allopurinol. “Increased fluid intake spread throughout the day can decrease stone recurrence by at least half with virtually no side effects,” said Dr. David A. Fleming, ACP president, in a statement. “However, people who already drink the recommended amount of liquids, or when increased fluid intake is contraindicated, should not increase their fluid intake.”
The guidelines are based on a review of nephrolithiasis studies, in which the ACP’s director of clinical policy, Dr. Amir Qaseem, and his associates examined baseline stone composition, blood and urine chemistries, and final health outcomes, among other factors. Only English-language trials were used, and research was collected through searches of MEDLINE, the Cochrane Database of Systematic Reviews, Google Scholar, ClinicalTrials.gov, and Web of Science (Ann. Intern. Med. 2014;161:659-67).
Thiazide diuretics, citrates, or allopurinol significantly reduced recurrence of calcium-based stones (the most common type of kidney stone) in patients who had nephrolithiasis at least twice before, according to the analysis.
The ACP guidelines also caution against consuming non-fruit–flavored sodas and carbonated beverages, because they are acidified by phosphoric acid, and dietary animal protein and purines.
However, the guidelines encourage consumption of dietary oxalate – commonly found in chocolate, beets, nuts, rhubarb, spinach, strawberries, tea, and wheat bran – and support maintaining normal dietary calcium. There was no evidence to suggest a risk reduction advantage in drinking tap water rather than mineral water.
The recommendations do not apply to “patients with suspected hyperparathyroidism or other rare cases,” the guidelines authors noted.
Financial support for the guidelines came from the ACP operating budget. The authors had no other relevant financial disclosures.
Patients who have had kidney stones at least once should increase their fluid consumption to produce at least 2 L of urine per day to prevent the condition from recurring, according to new guidelines published by the American College of Physicians.
If increased fluid intake doesn’t prevent recurrent nephrolithiasis, the updated ACP guidelines recommend adding treatment with a thiazide diuretic, citrate, or allopurinol. “Increased fluid intake spread throughout the day can decrease stone recurrence by at least half with virtually no side effects,” said Dr. David A. Fleming, ACP president, in a statement. “However, people who already drink the recommended amount of liquids, or when increased fluid intake is contraindicated, should not increase their fluid intake.”
The guidelines are based on a review of nephrolithiasis studies, in which the ACP’s director of clinical policy, Dr. Amir Qaseem, and his associates examined baseline stone composition, blood and urine chemistries, and final health outcomes, among other factors. Only English-language trials were used, and research was collected through searches of MEDLINE, the Cochrane Database of Systematic Reviews, Google Scholar, ClinicalTrials.gov, and Web of Science (Ann. Intern. Med. 2014;161:659-67).
Thiazide diuretics, citrates, or allopurinol significantly reduced recurrence of calcium-based stones (the most common type of kidney stone) in patients who had nephrolithiasis at least twice before, according to the analysis.
The ACP guidelines also caution against consuming non-fruit–flavored sodas and carbonated beverages, because they are acidified by phosphoric acid, and dietary animal protein and purines.
However, the guidelines encourage consumption of dietary oxalate – commonly found in chocolate, beets, nuts, rhubarb, spinach, strawberries, tea, and wheat bran – and support maintaining normal dietary calcium. There was no evidence to suggest a risk reduction advantage in drinking tap water rather than mineral water.
The recommendations do not apply to “patients with suspected hyperparathyroidism or other rare cases,” the guidelines authors noted.
Financial support for the guidelines came from the ACP operating budget. The authors had no other relevant financial disclosures.
Patients who have had kidney stones at least once should increase their fluid consumption to produce at least 2 L of urine per day to prevent the condition from recurring, according to new guidelines published by the American College of Physicians.
If increased fluid intake doesn’t prevent recurrent nephrolithiasis, the updated ACP guidelines recommend adding treatment with a thiazide diuretic, citrate, or allopurinol. “Increased fluid intake spread throughout the day can decrease stone recurrence by at least half with virtually no side effects,” said Dr. David A. Fleming, ACP president, in a statement. “However, people who already drink the recommended amount of liquids, or when increased fluid intake is contraindicated, should not increase their fluid intake.”
The guidelines are based on a review of nephrolithiasis studies, in which the ACP’s director of clinical policy, Dr. Amir Qaseem, and his associates examined baseline stone composition, blood and urine chemistries, and final health outcomes, among other factors. Only English-language trials were used, and research was collected through searches of MEDLINE, the Cochrane Database of Systematic Reviews, Google Scholar, ClinicalTrials.gov, and Web of Science (Ann. Intern. Med. 2014;161:659-67).
Thiazide diuretics, citrates, or allopurinol significantly reduced recurrence of calcium-based stones (the most common type of kidney stone) in patients who had nephrolithiasis at least twice before, according to the analysis.
The ACP guidelines also caution against consuming non-fruit–flavored sodas and carbonated beverages, because they are acidified by phosphoric acid, and dietary animal protein and purines.
However, the guidelines encourage consumption of dietary oxalate – commonly found in chocolate, beets, nuts, rhubarb, spinach, strawberries, tea, and wheat bran – and support maintaining normal dietary calcium. There was no evidence to suggest a risk reduction advantage in drinking tap water rather than mineral water.
The recommendations do not apply to “patients with suspected hyperparathyroidism or other rare cases,” the guidelines authors noted.
Financial support for the guidelines came from the ACP operating budget. The authors had no other relevant financial disclosures.
FROM THE ANNALS OF INTERNAL MEDICINE
AHA guidelines recommend Mediterranean diet to prevent stroke
Lifestyle modifications, including eating a Mediterranean or DASH-style diet, should be encouraged to lower an individual’s risk of first-time stroke, according to new guidelines for the primary prevention of stroke from the American Heart Association and American Stroke Association.
Mediterranean and DASH (Dietary Approaches to Stop Hypertension) dietary plans are characterized by their emphasis on fruits, vegetables, whole grains, legumes, nuts, seeds, poultry, and fish, while limiting red meats, sweets, and any foods with saturated fats. This new guidelines – which have been endorsed by the American Academy of Neurology, American Association of Neurological Surgeons, Congress of Neurological Surgeons, and Preventive Cardiovascular Nurses Association – suggest that adopting either of these diets in addition to a few other healthy living habits can dramatically reduce an individual’s odds of suffering a stroke (Stroke 2014;45 [doi: 10.1161/STR.0000000000000046]).
“We have a huge opportunity to improve how we prevent new strokes, because risk factors that can be changed or controlled – especially high blood pressure – account for 90% of strokes,” said Dr. James Meschia, chair of the writing committee and chairman of neurology at the Mayo Clinic in Jacksonville, Fla., in a statement. The last such guidelines were released 3 years ago (Stroke 2011;42:517-84)
The writing committee gathered data pertaining to the age, birth weight, race/ethnicity, and genetic factors, among several others. Studies examined included a U.S. Nationwide Inpatient Sample, which showed that stroke hospitalizations increased between 1998 and 2007 for individuals aged 25-34 years and 35-44 years; the Framingham Heart Study, which estimated that the odds of a middle-aged adult suffering a stroke are 1 in 6; an analysis of South Carolina Medicaid beneficiaries under age 50, which revealed that individuals born weighing less than 2,500 g were twice as likely to have a stroke as those born heavier; and an Atherosclerosis Risk in Communities (ARIC) study that showed Latino and African American populations being at higher risk for stroke due to hypertension, obesity, and diabetes.
Because blood pressure, hypertension, diabetes, and obesity are so commonly linked to stroke risk, the new American Heart Association/American Stroke Association (AHA/ASA) guidelines highly recommend a Mediterranean or DASH-style diet supplemented with nuts. Additionally, the guidelines advise health care professionals to advise patients to cut down on sodium intake, regularly monitor their blood pressure, talk to their physicians immediately if any medication does not do what it is intended to or creates negative side effects, and quit smoking, and, for women, consider an alternative to oral birth control pills.
Hypertension, “the most important, well-documented, modifiable stroke risk factor,” should be treated with antihypertensive medication to a target blood pressure of less than 140/90 mm Hg, the guidelines state.
Furthermore, the ASA/AHA guidelines continue to recommend regular physical exercise and acute monitoring of individuals’ cholesterol levels, such as LDL, HDL, and triglycerides, as failure to keep these numbers in check can easily lead to a serious stroke. The guidelines also state that although heavy alcohol consumption can increase the chance of stroke, “light to moderate” alcohol consumption can actually decrease the odds of suffering a stroke.
The AHA/ASA guidelines also examine factors such as migraines, which are associated with stroke in women under age 55, and hyperhomocysteinemia, which is also associated with an increased risk of stroke. Other factors like hypercoagulability and sleep apnea were not shown to have any identifiable relationship with an increased risk of stroke.
“As health professionals, we must ensure that progress in preventing stroke does not lead to complacency,” say the guidelines. “We must acknowledge that several recommendations remain vague because of suboptimal clinical trial evidence or, even more concerning, may be out of date and therefore irrelevant.”
Dr. Meschia and his associates warn that although medications are helpful, the best way to safeguard against a stroke is to change a person’s lifestyle into one of healthy eating and exercise habits. Unfortunately, say the authors, “it is easier to convince a patient to take a pill than to radically change his or her lifestyle, [but] we must expect the same standards of evidence for lifestyle interventions.”
Dr. Meschia disclosed that his research grant comes from the National Institute of Neurological Disorders and Stroke. He had no other relevant financial disclosures of interest. Several of the guidelines’ coauthors had disclosures of their own, which are listed in the statement.
Lifestyle modifications, including eating a Mediterranean or DASH-style diet, should be encouraged to lower an individual’s risk of first-time stroke, according to new guidelines for the primary prevention of stroke from the American Heart Association and American Stroke Association.
Mediterranean and DASH (Dietary Approaches to Stop Hypertension) dietary plans are characterized by their emphasis on fruits, vegetables, whole grains, legumes, nuts, seeds, poultry, and fish, while limiting red meats, sweets, and any foods with saturated fats. This new guidelines – which have been endorsed by the American Academy of Neurology, American Association of Neurological Surgeons, Congress of Neurological Surgeons, and Preventive Cardiovascular Nurses Association – suggest that adopting either of these diets in addition to a few other healthy living habits can dramatically reduce an individual’s odds of suffering a stroke (Stroke 2014;45 [doi: 10.1161/STR.0000000000000046]).
“We have a huge opportunity to improve how we prevent new strokes, because risk factors that can be changed or controlled – especially high blood pressure – account for 90% of strokes,” said Dr. James Meschia, chair of the writing committee and chairman of neurology at the Mayo Clinic in Jacksonville, Fla., in a statement. The last such guidelines were released 3 years ago (Stroke 2011;42:517-84)
The writing committee gathered data pertaining to the age, birth weight, race/ethnicity, and genetic factors, among several others. Studies examined included a U.S. Nationwide Inpatient Sample, which showed that stroke hospitalizations increased between 1998 and 2007 for individuals aged 25-34 years and 35-44 years; the Framingham Heart Study, which estimated that the odds of a middle-aged adult suffering a stroke are 1 in 6; an analysis of South Carolina Medicaid beneficiaries under age 50, which revealed that individuals born weighing less than 2,500 g were twice as likely to have a stroke as those born heavier; and an Atherosclerosis Risk in Communities (ARIC) study that showed Latino and African American populations being at higher risk for stroke due to hypertension, obesity, and diabetes.
Because blood pressure, hypertension, diabetes, and obesity are so commonly linked to stroke risk, the new American Heart Association/American Stroke Association (AHA/ASA) guidelines highly recommend a Mediterranean or DASH-style diet supplemented with nuts. Additionally, the guidelines advise health care professionals to advise patients to cut down on sodium intake, regularly monitor their blood pressure, talk to their physicians immediately if any medication does not do what it is intended to or creates negative side effects, and quit smoking, and, for women, consider an alternative to oral birth control pills.
Hypertension, “the most important, well-documented, modifiable stroke risk factor,” should be treated with antihypertensive medication to a target blood pressure of less than 140/90 mm Hg, the guidelines state.
Furthermore, the ASA/AHA guidelines continue to recommend regular physical exercise and acute monitoring of individuals’ cholesterol levels, such as LDL, HDL, and triglycerides, as failure to keep these numbers in check can easily lead to a serious stroke. The guidelines also state that although heavy alcohol consumption can increase the chance of stroke, “light to moderate” alcohol consumption can actually decrease the odds of suffering a stroke.
The AHA/ASA guidelines also examine factors such as migraines, which are associated with stroke in women under age 55, and hyperhomocysteinemia, which is also associated with an increased risk of stroke. Other factors like hypercoagulability and sleep apnea were not shown to have any identifiable relationship with an increased risk of stroke.
“As health professionals, we must ensure that progress in preventing stroke does not lead to complacency,” say the guidelines. “We must acknowledge that several recommendations remain vague because of suboptimal clinical trial evidence or, even more concerning, may be out of date and therefore irrelevant.”
Dr. Meschia and his associates warn that although medications are helpful, the best way to safeguard against a stroke is to change a person’s lifestyle into one of healthy eating and exercise habits. Unfortunately, say the authors, “it is easier to convince a patient to take a pill than to radically change his or her lifestyle, [but] we must expect the same standards of evidence for lifestyle interventions.”
Dr. Meschia disclosed that his research grant comes from the National Institute of Neurological Disorders and Stroke. He had no other relevant financial disclosures of interest. Several of the guidelines’ coauthors had disclosures of their own, which are listed in the statement.
Lifestyle modifications, including eating a Mediterranean or DASH-style diet, should be encouraged to lower an individual’s risk of first-time stroke, according to new guidelines for the primary prevention of stroke from the American Heart Association and American Stroke Association.
Mediterranean and DASH (Dietary Approaches to Stop Hypertension) dietary plans are characterized by their emphasis on fruits, vegetables, whole grains, legumes, nuts, seeds, poultry, and fish, while limiting red meats, sweets, and any foods with saturated fats. This new guidelines – which have been endorsed by the American Academy of Neurology, American Association of Neurological Surgeons, Congress of Neurological Surgeons, and Preventive Cardiovascular Nurses Association – suggest that adopting either of these diets in addition to a few other healthy living habits can dramatically reduce an individual’s odds of suffering a stroke (Stroke 2014;45 [doi: 10.1161/STR.0000000000000046]).
“We have a huge opportunity to improve how we prevent new strokes, because risk factors that can be changed or controlled – especially high blood pressure – account for 90% of strokes,” said Dr. James Meschia, chair of the writing committee and chairman of neurology at the Mayo Clinic in Jacksonville, Fla., in a statement. The last such guidelines were released 3 years ago (Stroke 2011;42:517-84)
The writing committee gathered data pertaining to the age, birth weight, race/ethnicity, and genetic factors, among several others. Studies examined included a U.S. Nationwide Inpatient Sample, which showed that stroke hospitalizations increased between 1998 and 2007 for individuals aged 25-34 years and 35-44 years; the Framingham Heart Study, which estimated that the odds of a middle-aged adult suffering a stroke are 1 in 6; an analysis of South Carolina Medicaid beneficiaries under age 50, which revealed that individuals born weighing less than 2,500 g were twice as likely to have a stroke as those born heavier; and an Atherosclerosis Risk in Communities (ARIC) study that showed Latino and African American populations being at higher risk for stroke due to hypertension, obesity, and diabetes.
Because blood pressure, hypertension, diabetes, and obesity are so commonly linked to stroke risk, the new American Heart Association/American Stroke Association (AHA/ASA) guidelines highly recommend a Mediterranean or DASH-style diet supplemented with nuts. Additionally, the guidelines advise health care professionals to advise patients to cut down on sodium intake, regularly monitor their blood pressure, talk to their physicians immediately if any medication does not do what it is intended to or creates negative side effects, and quit smoking, and, for women, consider an alternative to oral birth control pills.
Hypertension, “the most important, well-documented, modifiable stroke risk factor,” should be treated with antihypertensive medication to a target blood pressure of less than 140/90 mm Hg, the guidelines state.
Furthermore, the ASA/AHA guidelines continue to recommend regular physical exercise and acute monitoring of individuals’ cholesterol levels, such as LDL, HDL, and triglycerides, as failure to keep these numbers in check can easily lead to a serious stroke. The guidelines also state that although heavy alcohol consumption can increase the chance of stroke, “light to moderate” alcohol consumption can actually decrease the odds of suffering a stroke.
The AHA/ASA guidelines also examine factors such as migraines, which are associated with stroke in women under age 55, and hyperhomocysteinemia, which is also associated with an increased risk of stroke. Other factors like hypercoagulability and sleep apnea were not shown to have any identifiable relationship with an increased risk of stroke.
“As health professionals, we must ensure that progress in preventing stroke does not lead to complacency,” say the guidelines. “We must acknowledge that several recommendations remain vague because of suboptimal clinical trial evidence or, even more concerning, may be out of date and therefore irrelevant.”
Dr. Meschia and his associates warn that although medications are helpful, the best way to safeguard against a stroke is to change a person’s lifestyle into one of healthy eating and exercise habits. Unfortunately, say the authors, “it is easier to convince a patient to take a pill than to radically change his or her lifestyle, [but] we must expect the same standards of evidence for lifestyle interventions.”
Dr. Meschia disclosed that his research grant comes from the National Institute of Neurological Disorders and Stroke. He had no other relevant financial disclosures of interest. Several of the guidelines’ coauthors had disclosures of their own, which are listed in the statement.
FROM THE AMERICAN HEART ASSOCIATION AND THE AMERICAN STROKE ASSOCIATION