User login
Cosmetic Corner: Dermatologists Weigh in on Redness-Reducing Products
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top redness-reducing products. Consideration must be given to:
• CeraVe Facial Moisturizing Lotion AM
Valeant Consumer Products, a division of Valeant Pharmaceuticals North America LLC
“Sunscreen is a must. I recommend CeraVe.”—Gary Goldenberg, MD, New York, New York
• Oxymetazoline such as Afrin Nasal Spray
MSD Consumer Care, Inc
“The mechanism is sympathomimetic/vasoconstrictive. I tell patients to take the nozzle off and apply to red areas of the face with a cotton ball if they want to get a few hours of decreased redness. It works on only a short-term basis for things like an event/wedding/photo to decrease erythema/flushing for many patients. Rebound redness can occur with overuse, similar to rebound congestion when it is used intranasally.”—Lorraine L. Rosamilia, MD, State College, Pennsylvania
• PÊCHE Redness Control
Neocutis Inc
“Patients have found [this product] to be soothing. Patients with rosacea have tolerated it well and found a decrease in redness.”—Mary P. Lupo, MD, New Orleans, Louisiana
“ROSAPLEX [in this product] is an exclusive redness-balancing complex with dextran sulfate, zinc, caffeine, and glycerin, which helps to eliminate the appearance of blotchiness and blemishes, and improve overall skin tone. PÊCHE is a very versatile cream and can be used alone or in conjunction with prescription products for rosacea.”—Marta I. Rendon, MD, Boca Raton, Florida
• Redness Solutions Daily Relief Cream
Clinique Laboratories, LLC
“This cream is safe for patients with rosacea to use as a general moisturizer and it has an underlying green base, which cuts the appearance of red.”—Anthony M. Rossi, MD, New York, New York
• Redness Solutions Soothing Cleanser
Clinique Laboratories, LLC
“[I recommend that patients] use the Redness Solutions Soothing Cleanser, then apply the Redness Solutions Daily Relief Cream.”—Gary Goldenberg, MD, New York, New York
Cutis invites readers to send us their recommendations. Sunscreens, body moisturizers, and face washes will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to [email protected].
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top redness-reducing products. Consideration must be given to:
• CeraVe Facial Moisturizing Lotion AM
Valeant Consumer Products, a division of Valeant Pharmaceuticals North America LLC
“Sunscreen is a must. I recommend CeraVe.”—Gary Goldenberg, MD, New York, New York
• Oxymetazoline such as Afrin Nasal Spray
MSD Consumer Care, Inc
“The mechanism is sympathomimetic/vasoconstrictive. I tell patients to take the nozzle off and apply to red areas of the face with a cotton ball if they want to get a few hours of decreased redness. It works on only a short-term basis for things like an event/wedding/photo to decrease erythema/flushing for many patients. Rebound redness can occur with overuse, similar to rebound congestion when it is used intranasally.”—Lorraine L. Rosamilia, MD, State College, Pennsylvania
• PÊCHE Redness Control
Neocutis Inc
“Patients have found [this product] to be soothing. Patients with rosacea have tolerated it well and found a decrease in redness.”—Mary P. Lupo, MD, New Orleans, Louisiana
“ROSAPLEX [in this product] is an exclusive redness-balancing complex with dextran sulfate, zinc, caffeine, and glycerin, which helps to eliminate the appearance of blotchiness and blemishes, and improve overall skin tone. PÊCHE is a very versatile cream and can be used alone or in conjunction with prescription products for rosacea.”—Marta I. Rendon, MD, Boca Raton, Florida
• Redness Solutions Daily Relief Cream
Clinique Laboratories, LLC
“This cream is safe for patients with rosacea to use as a general moisturizer and it has an underlying green base, which cuts the appearance of red.”—Anthony M. Rossi, MD, New York, New York
• Redness Solutions Soothing Cleanser
Clinique Laboratories, LLC
“[I recommend that patients] use the Redness Solutions Soothing Cleanser, then apply the Redness Solutions Daily Relief Cream.”—Gary Goldenberg, MD, New York, New York
Cutis invites readers to send us their recommendations. Sunscreens, body moisturizers, and face washes will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to [email protected].
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top redness-reducing products. Consideration must be given to:
• CeraVe Facial Moisturizing Lotion AM
Valeant Consumer Products, a division of Valeant Pharmaceuticals North America LLC
“Sunscreen is a must. I recommend CeraVe.”—Gary Goldenberg, MD, New York, New York
• Oxymetazoline such as Afrin Nasal Spray
MSD Consumer Care, Inc
“The mechanism is sympathomimetic/vasoconstrictive. I tell patients to take the nozzle off and apply to red areas of the face with a cotton ball if they want to get a few hours of decreased redness. It works on only a short-term basis for things like an event/wedding/photo to decrease erythema/flushing for many patients. Rebound redness can occur with overuse, similar to rebound congestion when it is used intranasally.”—Lorraine L. Rosamilia, MD, State College, Pennsylvania
• PÊCHE Redness Control
Neocutis Inc
“Patients have found [this product] to be soothing. Patients with rosacea have tolerated it well and found a decrease in redness.”—Mary P. Lupo, MD, New Orleans, Louisiana
“ROSAPLEX [in this product] is an exclusive redness-balancing complex with dextran sulfate, zinc, caffeine, and glycerin, which helps to eliminate the appearance of blotchiness and blemishes, and improve overall skin tone. PÊCHE is a very versatile cream and can be used alone or in conjunction with prescription products for rosacea.”—Marta I. Rendon, MD, Boca Raton, Florida
• Redness Solutions Daily Relief Cream
Clinique Laboratories, LLC
“This cream is safe for patients with rosacea to use as a general moisturizer and it has an underlying green base, which cuts the appearance of red.”—Anthony M. Rossi, MD, New York, New York
• Redness Solutions Soothing Cleanser
Clinique Laboratories, LLC
“[I recommend that patients] use the Redness Solutions Soothing Cleanser, then apply the Redness Solutions Daily Relief Cream.”—Gary Goldenberg, MD, New York, New York
Cutis invites readers to send us their recommendations. Sunscreens, body moisturizers, and face washes will be featured in upcoming editions of Cosmetic Corner. Please e-mail your recommendation(s) to [email protected].
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cutis or Frontline Medical Communications Inc and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cutis or Frontline Medical Communications Inc endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
Rosacea Fulminans
Test your knowledge on rosacea with MD-IQ: the medical intelligence quiz. Click here to answer 5 questions.
Probiotics in Acne and Rosacea
Diagnosis and treatment of pediatric acne
Acne is a common skin disorder among young people, affecting up to 85% of adolescents, often causing a significant amount of distress, and, when severe, it can have long-lasting effects.
Pathophysiology
Acne vulgaris involves four processes: sebaceous hyperplasia driven by increased androgen levels; alterations of follicular growth and differentiation; colonization of follicle by Propionibacterium acnes; and immune response and inflammation.
Categorization
Categorizing acne on the basis of morphology and severity of lesions is useful. The three basic morphologies are comedonal, inflammatory, and mixed. Comedones are closed (whitehead) or open (blackhead). Closed comedones result from cell proliferation mixing with sebum and partially clogging the follicular lumen. Open comedones result when the follicle has a broader opening with visible keratin buildup that darkens. Inflammation manifests as papules, pustules, nodules, or pseudocysts and may include scarring or sinus tracts. The inflammation results from P. acne colonization, with release of inflammatory mediators. Severity is classified as mild, moderate, and severe. This assessment is subjective but should be based on number and type of lesions, amount of skin involved, scarring, and risk of dyspigmentation, which is greater in darker skin.
Age-specific considerations
The differential diagnosis and work-up of acne varies by age group. Neonatal (birth-6 weeks) acne has a prevalence of 20%, though these lesions actually may represent acneiform conditions such as self-limited neonatal cephalic pustulosis or transient neonatal pustular melanosis.
Infantile (6 weeks to 12 months, or uncommonly up to a few years old) acne is more common in males, usually is comedonal and inflammatory, and presents with papules, pustules, or nodules. A work-up usually is not necessary unless growth is abnormal or signs of hirsutism/virilization exist, in which case referral to endocrinology is made for a possible hormonal anomaly. Of note, true infantile acne may portend an increased risk of severe adolescent acne.
Mid-childhood (1-7 years) acne is not common since this age group does not produce significant levels of adrenal or gonadal androgens. If it does occur, a work-up by an endocrinologist is recommended.
Preadolescent (7-12 years) acne is common and may be the first sign of pubertal maturation. Such acne usually is comedonal with a "T-zone" distribution (forehead and central face), and may appear on the ears. Inflammatory lesions are sparse. No work-up beyond history and physical is needed unless there is concern for endocrinologic abnormalities (for example, PCOS), which may manifest as very severe or refractory acne.
Treatment
Goals of treatment involve addressing pathogenic factors and using the least aggressive but effective regimen, while avoiding bacterial resistance development. Additionally, side effects and expectations of results (in other words, noticeable results may take 4-8 weeks for any acne treatment) should be discussed in order to enhance compliance.
Various over-the-counter (OTC) products and prescription agents are available for the treatment of acne. OTC agents that have been tested include salicylic acid and benzoyl peroxide (BP). BP is effective, safe, and inexpensive. It can be used as monotherapy and, when used in combination with topical or systemic antibiotics, may minimize antibiotic-resistant P. acnes development.
Prescription options include topical retinoids, topical antibiotics, topical dapsone, oral antibiotics (typically tetracycline, doxycycline, or minocycline), oral isotretinoin, fixed-dose combination topical agents (BP/topical antibiotic, BP/topical retinoid, and topical retinoid/antibiotic), and hormonal therapy. The recommendations address the treatment of mild, moderate, and severe pediatric acne.
Mild acne usually presents as comedonal or mixed. Initial treatment can include BP monotherapy, topical retinoids, or combinations of topical retinoids, antibiotics, and BP. In patients of color, where there is a greater risk of scarring and dyspigmentation, initial therapy might also include a topical or oral antibiotic. In cases of inadequate response, the concentration, type, or formulation of topical retinoid can be changed or the topical combination can be modified.
Moderate acne may require an aggressive regimen of combination topical therapy that includes a retinoid and BP with or without topical dapsone, with the likely addition of an oral antibiotic. If lesions are moderate to severe inflammatory or mixed, oral antibiotics are effective, with maximal response taking 3-6 months. If an inadequate response and adherence assured, the strength, type, and formulation of topical regimens can be adjusted, although referral to a specialist may be considered.
Severe acne requires prompt initiation of treatment to avoid scarring and permanent skin changes. Treatment should include oral antibiotics with topical retinoids plus BP, with or without topical antibiotics. Strong consideration should be given to adding hormonal therapy to the treatment regimen of young menstruating women who have severe acne. In addition, for both males and females, oral isotretinoin and referral to a specialist may be considered.
Some recommend refraining from oral contraceptives until 1 year after menarche because of concerns about growth and bone density. When considering oral isotretinoin, remember it is teratogenic and that it causes questionable changes to bone health, mood, and bowel disorders, which may cause more issues in the pediatric population.
If there is an inadequate response after combination therapy with isotretinoin, physicians can try oral antibiotics with topical retinoids plus BP. If acne persists, consideration can be given to switch to a different oral antibiotic to address possible resistant organisms.
Remember that tetracyclines should not be used in ages younger than 8 years. Erythromycin, azithromycin, and trimethoprim/sulfamethoxazole are options for children younger than 8 years or those with a tetracycline allergy, as long as there is close monitoring for adverse events with any oral antibiotics in children.
Bottom line
The diagnosis, work-up, and management of pediatric acne vary depending upon age and pubertal onset. When approaching acne therapy, the best treatment is determined by assessment of type and severity of lesions. Use of topical BP, retinoids, antibiotics, and oral antibiotics are the base of therapy, with strength and combination of agents determined by type and severity of the acne.
Reference
Eichenfield, L.F., Krakowski, A.C., Piggott, C., Del Rosso, J., Baldwin, H., Friedlander, S.F., Levy, M., Lucky, A., Mancini, A.J., Orlow, S.J., Yan, A.C., Vaux, K.K., Webster, G., Zaenglein, A.L., Thiboutot, D.M. (2013). Evidence-Based Recommendations for the Diagnosis and Treatment of Pediatric Acne. (Pediatrics 2013;131:S163 [doi:10.1542/peds.2013-0490B]).
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. Dr. Lee is a third-year and chief resident in the family medicine residency program at Abington Memorial Hospital.
Acne is a common skin disorder among young people, affecting up to 85% of adolescents, often causing a significant amount of distress, and, when severe, it can have long-lasting effects.
Pathophysiology
Acne vulgaris involves four processes: sebaceous hyperplasia driven by increased androgen levels; alterations of follicular growth and differentiation; colonization of follicle by Propionibacterium acnes; and immune response and inflammation.
Categorization
Categorizing acne on the basis of morphology and severity of lesions is useful. The three basic morphologies are comedonal, inflammatory, and mixed. Comedones are closed (whitehead) or open (blackhead). Closed comedones result from cell proliferation mixing with sebum and partially clogging the follicular lumen. Open comedones result when the follicle has a broader opening with visible keratin buildup that darkens. Inflammation manifests as papules, pustules, nodules, or pseudocysts and may include scarring or sinus tracts. The inflammation results from P. acne colonization, with release of inflammatory mediators. Severity is classified as mild, moderate, and severe. This assessment is subjective but should be based on number and type of lesions, amount of skin involved, scarring, and risk of dyspigmentation, which is greater in darker skin.
Age-specific considerations
The differential diagnosis and work-up of acne varies by age group. Neonatal (birth-6 weeks) acne has a prevalence of 20%, though these lesions actually may represent acneiform conditions such as self-limited neonatal cephalic pustulosis or transient neonatal pustular melanosis.
Infantile (6 weeks to 12 months, or uncommonly up to a few years old) acne is more common in males, usually is comedonal and inflammatory, and presents with papules, pustules, or nodules. A work-up usually is not necessary unless growth is abnormal or signs of hirsutism/virilization exist, in which case referral to endocrinology is made for a possible hormonal anomaly. Of note, true infantile acne may portend an increased risk of severe adolescent acne.
Mid-childhood (1-7 years) acne is not common since this age group does not produce significant levels of adrenal or gonadal androgens. If it does occur, a work-up by an endocrinologist is recommended.
Preadolescent (7-12 years) acne is common and may be the first sign of pubertal maturation. Such acne usually is comedonal with a "T-zone" distribution (forehead and central face), and may appear on the ears. Inflammatory lesions are sparse. No work-up beyond history and physical is needed unless there is concern for endocrinologic abnormalities (for example, PCOS), which may manifest as very severe or refractory acne.
Treatment
Goals of treatment involve addressing pathogenic factors and using the least aggressive but effective regimen, while avoiding bacterial resistance development. Additionally, side effects and expectations of results (in other words, noticeable results may take 4-8 weeks for any acne treatment) should be discussed in order to enhance compliance.
Various over-the-counter (OTC) products and prescription agents are available for the treatment of acne. OTC agents that have been tested include salicylic acid and benzoyl peroxide (BP). BP is effective, safe, and inexpensive. It can be used as monotherapy and, when used in combination with topical or systemic antibiotics, may minimize antibiotic-resistant P. acnes development.
Prescription options include topical retinoids, topical antibiotics, topical dapsone, oral antibiotics (typically tetracycline, doxycycline, or minocycline), oral isotretinoin, fixed-dose combination topical agents (BP/topical antibiotic, BP/topical retinoid, and topical retinoid/antibiotic), and hormonal therapy. The recommendations address the treatment of mild, moderate, and severe pediatric acne.
Mild acne usually presents as comedonal or mixed. Initial treatment can include BP monotherapy, topical retinoids, or combinations of topical retinoids, antibiotics, and BP. In patients of color, where there is a greater risk of scarring and dyspigmentation, initial therapy might also include a topical or oral antibiotic. In cases of inadequate response, the concentration, type, or formulation of topical retinoid can be changed or the topical combination can be modified.
Moderate acne may require an aggressive regimen of combination topical therapy that includes a retinoid and BP with or without topical dapsone, with the likely addition of an oral antibiotic. If lesions are moderate to severe inflammatory or mixed, oral antibiotics are effective, with maximal response taking 3-6 months. If an inadequate response and adherence assured, the strength, type, and formulation of topical regimens can be adjusted, although referral to a specialist may be considered.
Severe acne requires prompt initiation of treatment to avoid scarring and permanent skin changes. Treatment should include oral antibiotics with topical retinoids plus BP, with or without topical antibiotics. Strong consideration should be given to adding hormonal therapy to the treatment regimen of young menstruating women who have severe acne. In addition, for both males and females, oral isotretinoin and referral to a specialist may be considered.
Some recommend refraining from oral contraceptives until 1 year after menarche because of concerns about growth and bone density. When considering oral isotretinoin, remember it is teratogenic and that it causes questionable changes to bone health, mood, and bowel disorders, which may cause more issues in the pediatric population.
If there is an inadequate response after combination therapy with isotretinoin, physicians can try oral antibiotics with topical retinoids plus BP. If acne persists, consideration can be given to switch to a different oral antibiotic to address possible resistant organisms.
Remember that tetracyclines should not be used in ages younger than 8 years. Erythromycin, azithromycin, and trimethoprim/sulfamethoxazole are options for children younger than 8 years or those with a tetracycline allergy, as long as there is close monitoring for adverse events with any oral antibiotics in children.
Bottom line
The diagnosis, work-up, and management of pediatric acne vary depending upon age and pubertal onset. When approaching acne therapy, the best treatment is determined by assessment of type and severity of lesions. Use of topical BP, retinoids, antibiotics, and oral antibiotics are the base of therapy, with strength and combination of agents determined by type and severity of the acne.
Reference
Eichenfield, L.F., Krakowski, A.C., Piggott, C., Del Rosso, J., Baldwin, H., Friedlander, S.F., Levy, M., Lucky, A., Mancini, A.J., Orlow, S.J., Yan, A.C., Vaux, K.K., Webster, G., Zaenglein, A.L., Thiboutot, D.M. (2013). Evidence-Based Recommendations for the Diagnosis and Treatment of Pediatric Acne. (Pediatrics 2013;131:S163 [doi:10.1542/peds.2013-0490B]).
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. Dr. Lee is a third-year and chief resident in the family medicine residency program at Abington Memorial Hospital.
Acne is a common skin disorder among young people, affecting up to 85% of adolescents, often causing a significant amount of distress, and, when severe, it can have long-lasting effects.
Pathophysiology
Acne vulgaris involves four processes: sebaceous hyperplasia driven by increased androgen levels; alterations of follicular growth and differentiation; colonization of follicle by Propionibacterium acnes; and immune response and inflammation.
Categorization
Categorizing acne on the basis of morphology and severity of lesions is useful. The three basic morphologies are comedonal, inflammatory, and mixed. Comedones are closed (whitehead) or open (blackhead). Closed comedones result from cell proliferation mixing with sebum and partially clogging the follicular lumen. Open comedones result when the follicle has a broader opening with visible keratin buildup that darkens. Inflammation manifests as papules, pustules, nodules, or pseudocysts and may include scarring or sinus tracts. The inflammation results from P. acne colonization, with release of inflammatory mediators. Severity is classified as mild, moderate, and severe. This assessment is subjective but should be based on number and type of lesions, amount of skin involved, scarring, and risk of dyspigmentation, which is greater in darker skin.
Age-specific considerations
The differential diagnosis and work-up of acne varies by age group. Neonatal (birth-6 weeks) acne has a prevalence of 20%, though these lesions actually may represent acneiform conditions such as self-limited neonatal cephalic pustulosis or transient neonatal pustular melanosis.
Infantile (6 weeks to 12 months, or uncommonly up to a few years old) acne is more common in males, usually is comedonal and inflammatory, and presents with papules, pustules, or nodules. A work-up usually is not necessary unless growth is abnormal or signs of hirsutism/virilization exist, in which case referral to endocrinology is made for a possible hormonal anomaly. Of note, true infantile acne may portend an increased risk of severe adolescent acne.
Mid-childhood (1-7 years) acne is not common since this age group does not produce significant levels of adrenal or gonadal androgens. If it does occur, a work-up by an endocrinologist is recommended.
Preadolescent (7-12 years) acne is common and may be the first sign of pubertal maturation. Such acne usually is comedonal with a "T-zone" distribution (forehead and central face), and may appear on the ears. Inflammatory lesions are sparse. No work-up beyond history and physical is needed unless there is concern for endocrinologic abnormalities (for example, PCOS), which may manifest as very severe or refractory acne.
Treatment
Goals of treatment involve addressing pathogenic factors and using the least aggressive but effective regimen, while avoiding bacterial resistance development. Additionally, side effects and expectations of results (in other words, noticeable results may take 4-8 weeks for any acne treatment) should be discussed in order to enhance compliance.
Various over-the-counter (OTC) products and prescription agents are available for the treatment of acne. OTC agents that have been tested include salicylic acid and benzoyl peroxide (BP). BP is effective, safe, and inexpensive. It can be used as monotherapy and, when used in combination with topical or systemic antibiotics, may minimize antibiotic-resistant P. acnes development.
Prescription options include topical retinoids, topical antibiotics, topical dapsone, oral antibiotics (typically tetracycline, doxycycline, or minocycline), oral isotretinoin, fixed-dose combination topical agents (BP/topical antibiotic, BP/topical retinoid, and topical retinoid/antibiotic), and hormonal therapy. The recommendations address the treatment of mild, moderate, and severe pediatric acne.
Mild acne usually presents as comedonal or mixed. Initial treatment can include BP monotherapy, topical retinoids, or combinations of topical retinoids, antibiotics, and BP. In patients of color, where there is a greater risk of scarring and dyspigmentation, initial therapy might also include a topical or oral antibiotic. In cases of inadequate response, the concentration, type, or formulation of topical retinoid can be changed or the topical combination can be modified.
Moderate acne may require an aggressive regimen of combination topical therapy that includes a retinoid and BP with or without topical dapsone, with the likely addition of an oral antibiotic. If lesions are moderate to severe inflammatory or mixed, oral antibiotics are effective, with maximal response taking 3-6 months. If an inadequate response and adherence assured, the strength, type, and formulation of topical regimens can be adjusted, although referral to a specialist may be considered.
Severe acne requires prompt initiation of treatment to avoid scarring and permanent skin changes. Treatment should include oral antibiotics with topical retinoids plus BP, with or without topical antibiotics. Strong consideration should be given to adding hormonal therapy to the treatment regimen of young menstruating women who have severe acne. In addition, for both males and females, oral isotretinoin and referral to a specialist may be considered.
Some recommend refraining from oral contraceptives until 1 year after menarche because of concerns about growth and bone density. When considering oral isotretinoin, remember it is teratogenic and that it causes questionable changes to bone health, mood, and bowel disorders, which may cause more issues in the pediatric population.
If there is an inadequate response after combination therapy with isotretinoin, physicians can try oral antibiotics with topical retinoids plus BP. If acne persists, consideration can be given to switch to a different oral antibiotic to address possible resistant organisms.
Remember that tetracyclines should not be used in ages younger than 8 years. Erythromycin, azithromycin, and trimethoprim/sulfamethoxazole are options for children younger than 8 years or those with a tetracycline allergy, as long as there is close monitoring for adverse events with any oral antibiotics in children.
Bottom line
The diagnosis, work-up, and management of pediatric acne vary depending upon age and pubertal onset. When approaching acne therapy, the best treatment is determined by assessment of type and severity of lesions. Use of topical BP, retinoids, antibiotics, and oral antibiotics are the base of therapy, with strength and combination of agents determined by type and severity of the acne.
Reference
Eichenfield, L.F., Krakowski, A.C., Piggott, C., Del Rosso, J., Baldwin, H., Friedlander, S.F., Levy, M., Lucky, A., Mancini, A.J., Orlow, S.J., Yan, A.C., Vaux, K.K., Webster, G., Zaenglein, A.L., Thiboutot, D.M. (2013). Evidence-Based Recommendations for the Diagnosis and Treatment of Pediatric Acne. (Pediatrics 2013;131:S163 [doi:10.1542/peds.2013-0490B]).
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. Dr. Lee is a third-year and chief resident in the family medicine residency program at Abington Memorial Hospital.
Tweeting the truth about acne
The truth about acne is out there, but it isn’t always on Twitter.
As the popular social-networking platform continues to grow as a forum for health information, clinicians should be aware of the acne myths, misinformation, and miscellaneous home remedies being shared, and take the opportunity to tweak their patient-education strategies in the clinic setting and online, according to information published in a research letter in JAMA Dermatology.
Health care providers who are comfortable with Twitter can use it to follow acne-related tweets and share reliable medical information and resources, Dr. Kamal Jethwani of the Center for Connected Health, Boston, and his colleagues suggested.
During a 2-week period in June 2012, Dr. Jethwani and his colleagues identified more than 8,000 "high-impact" tweets related to acne. High-impact tweets were defined as those with one or more retweets during the study period, and contained at least one of five keywords: acne, pimple, pimples, zit, or zits.
They used the Twitter Streaming Application Programming Interface to determine how Twitter users share information (and misinformation) about acne.
The researchers sorted the tweets into four categories: personal, celebrity (because stars like Jessica Simpson get acne, too), education, and irrelevant/excluded.
Overall, the researchers examined 8,192 English-language high-impact tweets. Of these, 43% were personal, 20% were about celebrities (the researchers didn’t mention any names), 27% were educational, and 9% were excluded or irrelevant. Of the education tweets, 17% were related to disease information and 9% were treatment-related.
Approximately two-thirds of the disease tweets were variations on the theme of "Why does acne exist?" Not surprisingly, the most often tweeted treatment-related question was a variation of "How do I get rid of my acne?"
"There were a large variety of acne home remedies suggested, including topical food-based remedies ranging from eggs to herbs to fruit," the researchers noted. In addition, 3% of tweeters recommended the topical use of over-the-counter products including baking soda, aloe vera gel, and crushed aspirin (for salicylic acid).
The researchers then compared the word frequency of the selected tweets to the word choices on the American Academy of Dermatology website. Tweeters were more likely to use nonmedical terms such as pimple or pimples vs. terms like pores, skin, or cells used on the AAD website.
"In addition, the AAD website did not address topics that are commonly discussed on Twitter, like makeup, stress, and the efficacy of diet, toothpaste, or other home remedies on acne," the researchers noted.
So, doctors who tweet, you have 140 characters to say whether toothpaste works on zits.
One of the study coauthors, Dr. Joseph Kvedar, reported serving as a consultant for and holding stock in Healthrageous. The other researchers had no financial conflicts to disclose.
The truth about acne is out there, but it isn’t always on Twitter.
As the popular social-networking platform continues to grow as a forum for health information, clinicians should be aware of the acne myths, misinformation, and miscellaneous home remedies being shared, and take the opportunity to tweak their patient-education strategies in the clinic setting and online, according to information published in a research letter in JAMA Dermatology.
Health care providers who are comfortable with Twitter can use it to follow acne-related tweets and share reliable medical information and resources, Dr. Kamal Jethwani of the Center for Connected Health, Boston, and his colleagues suggested.
During a 2-week period in June 2012, Dr. Jethwani and his colleagues identified more than 8,000 "high-impact" tweets related to acne. High-impact tweets were defined as those with one or more retweets during the study period, and contained at least one of five keywords: acne, pimple, pimples, zit, or zits.
They used the Twitter Streaming Application Programming Interface to determine how Twitter users share information (and misinformation) about acne.
The researchers sorted the tweets into four categories: personal, celebrity (because stars like Jessica Simpson get acne, too), education, and irrelevant/excluded.
Overall, the researchers examined 8,192 English-language high-impact tweets. Of these, 43% were personal, 20% were about celebrities (the researchers didn’t mention any names), 27% were educational, and 9% were excluded or irrelevant. Of the education tweets, 17% were related to disease information and 9% were treatment-related.
Approximately two-thirds of the disease tweets were variations on the theme of "Why does acne exist?" Not surprisingly, the most often tweeted treatment-related question was a variation of "How do I get rid of my acne?"
"There were a large variety of acne home remedies suggested, including topical food-based remedies ranging from eggs to herbs to fruit," the researchers noted. In addition, 3% of tweeters recommended the topical use of over-the-counter products including baking soda, aloe vera gel, and crushed aspirin (for salicylic acid).
The researchers then compared the word frequency of the selected tweets to the word choices on the American Academy of Dermatology website. Tweeters were more likely to use nonmedical terms such as pimple or pimples vs. terms like pores, skin, or cells used on the AAD website.
"In addition, the AAD website did not address topics that are commonly discussed on Twitter, like makeup, stress, and the efficacy of diet, toothpaste, or other home remedies on acne," the researchers noted.
So, doctors who tweet, you have 140 characters to say whether toothpaste works on zits.
One of the study coauthors, Dr. Joseph Kvedar, reported serving as a consultant for and holding stock in Healthrageous. The other researchers had no financial conflicts to disclose.
The truth about acne is out there, but it isn’t always on Twitter.
As the popular social-networking platform continues to grow as a forum for health information, clinicians should be aware of the acne myths, misinformation, and miscellaneous home remedies being shared, and take the opportunity to tweak their patient-education strategies in the clinic setting and online, according to information published in a research letter in JAMA Dermatology.
Health care providers who are comfortable with Twitter can use it to follow acne-related tweets and share reliable medical information and resources, Dr. Kamal Jethwani of the Center for Connected Health, Boston, and his colleagues suggested.
During a 2-week period in June 2012, Dr. Jethwani and his colleagues identified more than 8,000 "high-impact" tweets related to acne. High-impact tweets were defined as those with one or more retweets during the study period, and contained at least one of five keywords: acne, pimple, pimples, zit, or zits.
They used the Twitter Streaming Application Programming Interface to determine how Twitter users share information (and misinformation) about acne.
The researchers sorted the tweets into four categories: personal, celebrity (because stars like Jessica Simpson get acne, too), education, and irrelevant/excluded.
Overall, the researchers examined 8,192 English-language high-impact tweets. Of these, 43% were personal, 20% were about celebrities (the researchers didn’t mention any names), 27% were educational, and 9% were excluded or irrelevant. Of the education tweets, 17% were related to disease information and 9% were treatment-related.
Approximately two-thirds of the disease tweets were variations on the theme of "Why does acne exist?" Not surprisingly, the most often tweeted treatment-related question was a variation of "How do I get rid of my acne?"
"There were a large variety of acne home remedies suggested, including topical food-based remedies ranging from eggs to herbs to fruit," the researchers noted. In addition, 3% of tweeters recommended the topical use of over-the-counter products including baking soda, aloe vera gel, and crushed aspirin (for salicylic acid).
The researchers then compared the word frequency of the selected tweets to the word choices on the American Academy of Dermatology website. Tweeters were more likely to use nonmedical terms such as pimple or pimples vs. terms like pores, skin, or cells used on the AAD website.
"In addition, the AAD website did not address topics that are commonly discussed on Twitter, like makeup, stress, and the efficacy of diet, toothpaste, or other home remedies on acne," the researchers noted.
So, doctors who tweet, you have 140 characters to say whether toothpaste works on zits.
One of the study coauthors, Dr. Joseph Kvedar, reported serving as a consultant for and holding stock in Healthrageous. The other researchers had no financial conflicts to disclose.
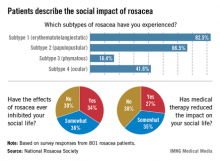
Social inhibition stings rosacea patients
The phymatous form of rosacea (subtype 3) has the most profound negative effect on patients’ social lives, compared with other subtypes, according to a survey by the National Rosacea Society.
More than 82% of those surveyed said that they had experienced erythematotelangiectatic rosacea (subtype 1), compared with 66.5% reporting symptoms of papulopustular (subtype 2), 16.4% reporting phymatous (subtype 3), and 41.6% reporting ocular (subtype 4) rosacea, the society said.
When analyzed by subtype, those patients with subtype 3 were most likely (85%) to have their social lives negatively affected. Those with subtype 2 were the next most likely to be negatively affected (77%), followed by subtype 4 (71%) and subtype 1 (61%), according to the survey data.
However, approximately two-thirds (62%) of the respondents said that medical therapy had at least somewhat reduced the negative impact of rosacea on their social lives.
The phymatous form of rosacea (subtype 3) has the most profound negative effect on patients’ social lives, compared with other subtypes, according to a survey by the National Rosacea Society.
More than 82% of those surveyed said that they had experienced erythematotelangiectatic rosacea (subtype 1), compared with 66.5% reporting symptoms of papulopustular (subtype 2), 16.4% reporting phymatous (subtype 3), and 41.6% reporting ocular (subtype 4) rosacea, the society said.
When analyzed by subtype, those patients with subtype 3 were most likely (85%) to have their social lives negatively affected. Those with subtype 2 were the next most likely to be negatively affected (77%), followed by subtype 4 (71%) and subtype 1 (61%), according to the survey data.
However, approximately two-thirds (62%) of the respondents said that medical therapy had at least somewhat reduced the negative impact of rosacea on their social lives.
The phymatous form of rosacea (subtype 3) has the most profound negative effect on patients’ social lives, compared with other subtypes, according to a survey by the National Rosacea Society.
More than 82% of those surveyed said that they had experienced erythematotelangiectatic rosacea (subtype 1), compared with 66.5% reporting symptoms of papulopustular (subtype 2), 16.4% reporting phymatous (subtype 3), and 41.6% reporting ocular (subtype 4) rosacea, the society said.
When analyzed by subtype, those patients with subtype 3 were most likely (85%) to have their social lives negatively affected. Those with subtype 2 were the next most likely to be negatively affected (77%), followed by subtype 4 (71%) and subtype 1 (61%), according to the survey data.
However, approximately two-thirds (62%) of the respondents said that medical therapy had at least somewhat reduced the negative impact of rosacea on their social lives.
Maximize your resources for treating rosacea
MAUI, HAWAII – Within the next year or two, two promising new topical medications may join the roster of products for managing rosacea, according to Dr. Joseph F. Fowler Jr.
The two coming attractions are brimonidine tartrate 0.5% gel and oxymetazoline cream. Brimonidine is further along in development; Galderma has submitted an application for Food and Drug Administration marketing approval of the product. Phase II studies of oxymetazoline cream are ongoing.
"Having seen both of these drugs in studies, I think both are going to be effective," said Dr. Fowler, of the University of Louisville (Ky.). "I have no idea if one will be more effective than the other, but I can tell you that both of them are probably going to be a lot better than anything else we have now for the erythema of rosacea," he noted.
"It usually takes around a year after that for a drug to reach the market, assuming no problems arise," Dr. Fowler said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
Both drugs are vasoconstrictors; they are already marketed in other formulations for indications other than rosacea. Oxymetazoline is used as a decongestant in some versions of Afrin nasal spray. Brimonidine is an alpha-2 agonist formulated as a prescription eye drop for the treatment of glaucoma, said Dr. Fowler, who was codirector of the seminar.
The only two topical therapies currently approved for treatment of rosacea – metronidazole and azelaic acid – don’t do much at all to improve the erythematous component of rosacea, in Dr. Fowler’s view. They do reduce inflammatory lesion counts, but not the background redness, he said.
In a separate presentation during the seminar, Dr. Guy W. Webster described his off-label experience in treating rosacea using oxymetazoline and brimonidine in their current formulations.
"These are two off-label products that really work," he said. "I have rosacea patients who are such spectacular flushers that they can’t go outside in the wintertime, but many of them do great with one of these two off-label medicines. It’s something to think about" when other efforts to improve erythema and flushing fail, said Dr. Webster of Thomas Jefferson University, Philadelphia.
Of the two products, the brimonidine eye drops work better when applied to the skin, said Dr. Webster. In fact, the eye drops are so effective that patients require careful instruction in off-label use or they will end up with white streaking on a background of untreated redness that may last for 4-8 hours, he said. Dr. Webster also recommends a preemptive phone call to a patient’s pharmacist to confirm that the "apply to cheeks" instruction on the prescription for the glaucoma medication is in fact correct.
Alternatively, the version of Afrin that contains oxymetazoline can be sprayed on the cheeks for temporary relief of rosacea. However, the investigational cream formulation works better, Dr. Webster said.
Dr. Webster also discussed the use of the two approved topical agents for rosacea and several other drugs with well-established off-label use.
Topical metronidazole 0.75% was the first the original concentration approved for rosacea, but the more recently approved 1% concentration is "vastly superior," in Dr. Webster’s view.
"Unfortunately, a lot of our insurers make patients get the old generic form, which I find is like a placebo," he noted.
Dr. Webster said that some of his patients respond to azelaic acid – the other FDA-approved topical drug – but not to metronidazole, and vice versa.
Topical benzoyl peroxide/clindamycin products often improve papular inflammatory rosacea, although the mechanism of action is unclear, he added.
Dr. Webster said he is unimpressed with the efficacy of sodium sulfacetamide/sulfur for rosacea. "For the amount of activity it gives, it’s almost not worth the expense," he said.
In Dr. Webster’s experience, tacrolimus and pimecrolimus are not useful in uncomplicated rosacea, but he said he finds the topical calcineurin inhibitors invaluable in patients whose rosacea is exacerbated by comorbid atopic dermatitis or seborrheic dermatitis.
"I find I can’t get the rosacea better when it’s being tweaked by a coexisting inflammatory disease unless I get the atopic dermatitis or seborrheic dermatitis better. These two drugs, off label, are critical to getting the rosacea to be able to respond because rosacea is provoked by other inflammation," he explained.
Dr. Webster serves as a consultant to half a dozen pharmaceutical companies, including Galderma and Allergan, which are developing brimonidine gel and oxymetazoline cream, respectively, as rosacea drugs.
Dr. Fowler is a consultant to multiple pharmaceutical companies, including Galderma, and is a research investigator for multiple companies including Galderma and Allergan.
SDEF and this news organization are owned by the same parent company.
MAUI, HAWAII – Within the next year or two, two promising new topical medications may join the roster of products for managing rosacea, according to Dr. Joseph F. Fowler Jr.
The two coming attractions are brimonidine tartrate 0.5% gel and oxymetazoline cream. Brimonidine is further along in development; Galderma has submitted an application for Food and Drug Administration marketing approval of the product. Phase II studies of oxymetazoline cream are ongoing.
"Having seen both of these drugs in studies, I think both are going to be effective," said Dr. Fowler, of the University of Louisville (Ky.). "I have no idea if one will be more effective than the other, but I can tell you that both of them are probably going to be a lot better than anything else we have now for the erythema of rosacea," he noted.
"It usually takes around a year after that for a drug to reach the market, assuming no problems arise," Dr. Fowler said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
Both drugs are vasoconstrictors; they are already marketed in other formulations for indications other than rosacea. Oxymetazoline is used as a decongestant in some versions of Afrin nasal spray. Brimonidine is an alpha-2 agonist formulated as a prescription eye drop for the treatment of glaucoma, said Dr. Fowler, who was codirector of the seminar.
The only two topical therapies currently approved for treatment of rosacea – metronidazole and azelaic acid – don’t do much at all to improve the erythematous component of rosacea, in Dr. Fowler’s view. They do reduce inflammatory lesion counts, but not the background redness, he said.
In a separate presentation during the seminar, Dr. Guy W. Webster described his off-label experience in treating rosacea using oxymetazoline and brimonidine in their current formulations.
"These are two off-label products that really work," he said. "I have rosacea patients who are such spectacular flushers that they can’t go outside in the wintertime, but many of them do great with one of these two off-label medicines. It’s something to think about" when other efforts to improve erythema and flushing fail, said Dr. Webster of Thomas Jefferson University, Philadelphia.
Of the two products, the brimonidine eye drops work better when applied to the skin, said Dr. Webster. In fact, the eye drops are so effective that patients require careful instruction in off-label use or they will end up with white streaking on a background of untreated redness that may last for 4-8 hours, he said. Dr. Webster also recommends a preemptive phone call to a patient’s pharmacist to confirm that the "apply to cheeks" instruction on the prescription for the glaucoma medication is in fact correct.
Alternatively, the version of Afrin that contains oxymetazoline can be sprayed on the cheeks for temporary relief of rosacea. However, the investigational cream formulation works better, Dr. Webster said.
Dr. Webster also discussed the use of the two approved topical agents for rosacea and several other drugs with well-established off-label use.
Topical metronidazole 0.75% was the first the original concentration approved for rosacea, but the more recently approved 1% concentration is "vastly superior," in Dr. Webster’s view.
"Unfortunately, a lot of our insurers make patients get the old generic form, which I find is like a placebo," he noted.
Dr. Webster said that some of his patients respond to azelaic acid – the other FDA-approved topical drug – but not to metronidazole, and vice versa.
Topical benzoyl peroxide/clindamycin products often improve papular inflammatory rosacea, although the mechanism of action is unclear, he added.
Dr. Webster said he is unimpressed with the efficacy of sodium sulfacetamide/sulfur for rosacea. "For the amount of activity it gives, it’s almost not worth the expense," he said.
In Dr. Webster’s experience, tacrolimus and pimecrolimus are not useful in uncomplicated rosacea, but he said he finds the topical calcineurin inhibitors invaluable in patients whose rosacea is exacerbated by comorbid atopic dermatitis or seborrheic dermatitis.
"I find I can’t get the rosacea better when it’s being tweaked by a coexisting inflammatory disease unless I get the atopic dermatitis or seborrheic dermatitis better. These two drugs, off label, are critical to getting the rosacea to be able to respond because rosacea is provoked by other inflammation," he explained.
Dr. Webster serves as a consultant to half a dozen pharmaceutical companies, including Galderma and Allergan, which are developing brimonidine gel and oxymetazoline cream, respectively, as rosacea drugs.
Dr. Fowler is a consultant to multiple pharmaceutical companies, including Galderma, and is a research investigator for multiple companies including Galderma and Allergan.
SDEF and this news organization are owned by the same parent company.
MAUI, HAWAII – Within the next year or two, two promising new topical medications may join the roster of products for managing rosacea, according to Dr. Joseph F. Fowler Jr.
The two coming attractions are brimonidine tartrate 0.5% gel and oxymetazoline cream. Brimonidine is further along in development; Galderma has submitted an application for Food and Drug Administration marketing approval of the product. Phase II studies of oxymetazoline cream are ongoing.
"Having seen both of these drugs in studies, I think both are going to be effective," said Dr. Fowler, of the University of Louisville (Ky.). "I have no idea if one will be more effective than the other, but I can tell you that both of them are probably going to be a lot better than anything else we have now for the erythema of rosacea," he noted.
"It usually takes around a year after that for a drug to reach the market, assuming no problems arise," Dr. Fowler said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
Both drugs are vasoconstrictors; they are already marketed in other formulations for indications other than rosacea. Oxymetazoline is used as a decongestant in some versions of Afrin nasal spray. Brimonidine is an alpha-2 agonist formulated as a prescription eye drop for the treatment of glaucoma, said Dr. Fowler, who was codirector of the seminar.
The only two topical therapies currently approved for treatment of rosacea – metronidazole and azelaic acid – don’t do much at all to improve the erythematous component of rosacea, in Dr. Fowler’s view. They do reduce inflammatory lesion counts, but not the background redness, he said.
In a separate presentation during the seminar, Dr. Guy W. Webster described his off-label experience in treating rosacea using oxymetazoline and brimonidine in their current formulations.
"These are two off-label products that really work," he said. "I have rosacea patients who are such spectacular flushers that they can’t go outside in the wintertime, but many of them do great with one of these two off-label medicines. It’s something to think about" when other efforts to improve erythema and flushing fail, said Dr. Webster of Thomas Jefferson University, Philadelphia.
Of the two products, the brimonidine eye drops work better when applied to the skin, said Dr. Webster. In fact, the eye drops are so effective that patients require careful instruction in off-label use or they will end up with white streaking on a background of untreated redness that may last for 4-8 hours, he said. Dr. Webster also recommends a preemptive phone call to a patient’s pharmacist to confirm that the "apply to cheeks" instruction on the prescription for the glaucoma medication is in fact correct.
Alternatively, the version of Afrin that contains oxymetazoline can be sprayed on the cheeks for temporary relief of rosacea. However, the investigational cream formulation works better, Dr. Webster said.
Dr. Webster also discussed the use of the two approved topical agents for rosacea and several other drugs with well-established off-label use.
Topical metronidazole 0.75% was the first the original concentration approved for rosacea, but the more recently approved 1% concentration is "vastly superior," in Dr. Webster’s view.
"Unfortunately, a lot of our insurers make patients get the old generic form, which I find is like a placebo," he noted.
Dr. Webster said that some of his patients respond to azelaic acid – the other FDA-approved topical drug – but not to metronidazole, and vice versa.
Topical benzoyl peroxide/clindamycin products often improve papular inflammatory rosacea, although the mechanism of action is unclear, he added.
Dr. Webster said he is unimpressed with the efficacy of sodium sulfacetamide/sulfur for rosacea. "For the amount of activity it gives, it’s almost not worth the expense," he said.
In Dr. Webster’s experience, tacrolimus and pimecrolimus are not useful in uncomplicated rosacea, but he said he finds the topical calcineurin inhibitors invaluable in patients whose rosacea is exacerbated by comorbid atopic dermatitis or seborrheic dermatitis.
"I find I can’t get the rosacea better when it’s being tweaked by a coexisting inflammatory disease unless I get the atopic dermatitis or seborrheic dermatitis better. These two drugs, off label, are critical to getting the rosacea to be able to respond because rosacea is provoked by other inflammation," he explained.
Dr. Webster serves as a consultant to half a dozen pharmaceutical companies, including Galderma and Allergan, which are developing brimonidine gel and oxymetazoline cream, respectively, as rosacea drugs.
Dr. Fowler is a consultant to multiple pharmaceutical companies, including Galderma, and is a research investigator for multiple companies including Galderma and Allergan.
SDEF and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Eat fish and avoid acne?
MAUI, HAWAII – The relationship between diet and acne risk has grown more intriguing as a consequence of a recent Italian study linking milk consumption to an increased risk, while eating fish had a protective effect.
"This was a well-done, very large, multicenter case-control study," said Dr. Lawrence F. Eichenfield, who presented highlights of the Italian investigation at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
A diet-acne link has been an endless topic of debate for many years among dermatologists and dieticians, with the public looking on attentively. Conventional wisdom formerly held that chocolate and greasy foods exacerbated acne, a notion that later was dispelled. A recent literature review of 27 published studies implicated high-glycemic-index foods and milk (J. Acad. Nutr. Diet. 2013;113:416-30).
The Italian study Dr. Eichenfield spotlighted included 205 consecutive patients aged 10-24 years who were newly diagnosed with moderate to severe acne. The control group consisted of 358 patients with no or only mild acne who consulted a dermatologist for a concern other than acne. Investigators inquired about family history, diet, personal habits, and menstrual history.
Family history of acne emerged as a strong risk factor. A history of acne in a first-degree relative was associated with a 3.4-fold increased risk of moderate to severe acne.
Drinking milk more than three times per week was associated with a 1.8-fold increased risk of significant acne. The risk was more pronounced in skim-milk drinkers than whole-milk drinkers, with consumption of more than three servings per week of nonfat milk being associated with a 2.2-fold increased risk of moderate to severe acne (J. Am. Acad. Dermatol. 2012;67:1129-35).
In contrast, regular consumption of fish was associated with a 32% reduction in the likelihood of having moderate to severe acne.
Body mass index was *directly associated with acne: Adolescents and young adults with a BMI greater than 18.5 kg/m2 were at 1.9-fold greater risk of significant acne than those with a smaller BMI. This protective effect of a low BMI was stronger in male than female subjects.
Neither menstrual factors nor smoking showed any relationship with acne risk in the Italian study, noted Dr. Eichenfield, professor of clinical pediatrics and medicine at the University of California, San Diego.
"How do I take this new information and use it in the clinic? The answer is, I don’t, because I really don’t know what the impact will be of dietary changes in my actual care of individuals with acne who come to me. But this whole issue of diet and acne is a really fascinating one," the pediatric dermatologist commented.
SDEF and this news organization are owned by the same parent company.
Dr. Eichenfield reported receiving research grants for clinical investigations from half a dozen pharmaceutical companies.
*Correction (04/09/13): A previous version of this story mischaracterized the association between BMI and acne in one instance. This story has been updated.
MAUI, HAWAII – The relationship between diet and acne risk has grown more intriguing as a consequence of a recent Italian study linking milk consumption to an increased risk, while eating fish had a protective effect.
"This was a well-done, very large, multicenter case-control study," said Dr. Lawrence F. Eichenfield, who presented highlights of the Italian investigation at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
A diet-acne link has been an endless topic of debate for many years among dermatologists and dieticians, with the public looking on attentively. Conventional wisdom formerly held that chocolate and greasy foods exacerbated acne, a notion that later was dispelled. A recent literature review of 27 published studies implicated high-glycemic-index foods and milk (J. Acad. Nutr. Diet. 2013;113:416-30).
The Italian study Dr. Eichenfield spotlighted included 205 consecutive patients aged 10-24 years who were newly diagnosed with moderate to severe acne. The control group consisted of 358 patients with no or only mild acne who consulted a dermatologist for a concern other than acne. Investigators inquired about family history, diet, personal habits, and menstrual history.
Family history of acne emerged as a strong risk factor. A history of acne in a first-degree relative was associated with a 3.4-fold increased risk of moderate to severe acne.
Drinking milk more than three times per week was associated with a 1.8-fold increased risk of significant acne. The risk was more pronounced in skim-milk drinkers than whole-milk drinkers, with consumption of more than three servings per week of nonfat milk being associated with a 2.2-fold increased risk of moderate to severe acne (J. Am. Acad. Dermatol. 2012;67:1129-35).
In contrast, regular consumption of fish was associated with a 32% reduction in the likelihood of having moderate to severe acne.
Body mass index was *directly associated with acne: Adolescents and young adults with a BMI greater than 18.5 kg/m2 were at 1.9-fold greater risk of significant acne than those with a smaller BMI. This protective effect of a low BMI was stronger in male than female subjects.
Neither menstrual factors nor smoking showed any relationship with acne risk in the Italian study, noted Dr. Eichenfield, professor of clinical pediatrics and medicine at the University of California, San Diego.
"How do I take this new information and use it in the clinic? The answer is, I don’t, because I really don’t know what the impact will be of dietary changes in my actual care of individuals with acne who come to me. But this whole issue of diet and acne is a really fascinating one," the pediatric dermatologist commented.
SDEF and this news organization are owned by the same parent company.
Dr. Eichenfield reported receiving research grants for clinical investigations from half a dozen pharmaceutical companies.
*Correction (04/09/13): A previous version of this story mischaracterized the association between BMI and acne in one instance. This story has been updated.
MAUI, HAWAII – The relationship between diet and acne risk has grown more intriguing as a consequence of a recent Italian study linking milk consumption to an increased risk, while eating fish had a protective effect.
"This was a well-done, very large, multicenter case-control study," said Dr. Lawrence F. Eichenfield, who presented highlights of the Italian investigation at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
A diet-acne link has been an endless topic of debate for many years among dermatologists and dieticians, with the public looking on attentively. Conventional wisdom formerly held that chocolate and greasy foods exacerbated acne, a notion that later was dispelled. A recent literature review of 27 published studies implicated high-glycemic-index foods and milk (J. Acad. Nutr. Diet. 2013;113:416-30).
The Italian study Dr. Eichenfield spotlighted included 205 consecutive patients aged 10-24 years who were newly diagnosed with moderate to severe acne. The control group consisted of 358 patients with no or only mild acne who consulted a dermatologist for a concern other than acne. Investigators inquired about family history, diet, personal habits, and menstrual history.
Family history of acne emerged as a strong risk factor. A history of acne in a first-degree relative was associated with a 3.4-fold increased risk of moderate to severe acne.
Drinking milk more than three times per week was associated with a 1.8-fold increased risk of significant acne. The risk was more pronounced in skim-milk drinkers than whole-milk drinkers, with consumption of more than three servings per week of nonfat milk being associated with a 2.2-fold increased risk of moderate to severe acne (J. Am. Acad. Dermatol. 2012;67:1129-35).
In contrast, regular consumption of fish was associated with a 32% reduction in the likelihood of having moderate to severe acne.
Body mass index was *directly associated with acne: Adolescents and young adults with a BMI greater than 18.5 kg/m2 were at 1.9-fold greater risk of significant acne than those with a smaller BMI. This protective effect of a low BMI was stronger in male than female subjects.
Neither menstrual factors nor smoking showed any relationship with acne risk in the Italian study, noted Dr. Eichenfield, professor of clinical pediatrics and medicine at the University of California, San Diego.
"How do I take this new information and use it in the clinic? The answer is, I don’t, because I really don’t know what the impact will be of dietary changes in my actual care of individuals with acne who come to me. But this whole issue of diet and acne is a really fascinating one," the pediatric dermatologist commented.
SDEF and this news organization are owned by the same parent company.
Dr. Eichenfield reported receiving research grants for clinical investigations from half a dozen pharmaceutical companies.
*Correction (04/09/13): A previous version of this story mischaracterized the association between BMI and acne in one instance. This story has been updated.
EXPERT OPINION FROM SDEF HAWAII DERMATOLOGY SEMINAR
Childhood acne: When to worry
WAILEA, HAWAII – Acne arising in a 1- to 7-year-old means "it’s time to worry," according to Dr. Lawrence F. Eichenfield.
Acne originating in this midchildhood age range is very uncommon. It signals the need for a detailed endocrinologic work-up. Possible underlying causes include precocious adrenarche, congenital adrenal hyperplasia, Cushing’s syndrome, precocious puberty, and a gonadal or adrenal tumor, he noted at the Hawaii Dermatology Seminar sponsored by the Global Academy for Medical Education/Skin Disease Education Foundation.
"If you want to take it on yourself you can, but the standard is going to be an evaluation that includes a growth chart, a bone age assessment, Tanner staging, and measurement of total and free testosterone, LH [luteinizing hormone], FSH [follicle-stimulating hormone], prolactin, DHEAS [dehydroepiandrosterone sulfate], andrestenedione, and 17-hydroxyprogesterone. Generally we say refer to a pediatric endocrinologist," said Dr. Eichenfield, professor of clinical pediatrics and medicine (dermatology) at the University of California, San Diego.
He noted that acne occurring at age 1-7 is prominently identified as a red flag in guidelines for the management of pediatric acne developed by the American Acne and Rosacea Society and subsequently approved by the American Academy of Pediatrics. Dr. Eichenfield was cochair of the expert panel that crafted the guidelines.
The comprehensive guidelines – the first ever to specifically address acne in the pediatric age range – include a general acne categorization scheme based upon age. While acne in a 1- to 7-year-old is characterized as a cause for concern, acne arising in a seemingly healthy slightly older preadolescent – roughly age 7-12 – is not.
"Acne in a child in this age group who otherwise looks well and has no signs or history that would make you suspicious of an underlying endocrinopathy is essentially a normal variant we now call preadolescent acne. You do not need to refer that patient for further evaluation," the pediatric dermatologist explained.
Nonworrisome preadolescent acne presents as comedone-predominant disease typically concentrated on the forehead and midface, with truncal involvement much less frequent. The acne may precede other signs of puberty. There is solid evidence that the more pronounced the expression of early preadolescent acne – that is, the greater the number of facial comedones present – the more severe the acne will be in adolescence. Indeed, severe preadolescent acne is often a harbinger of the later need for isotretinoin.
Acne developing within the first 6 weeks of life is most often an erythematous papulopustular eruption categorized in the guidelines as neonatal acne, also known as neonatal cephalic pustulosis. It is not true acne, but rather a self-limited condition associated with Malassezia globosa and M. sympodialis.
In contrast, infantile acne is true acne, mainly comedonal, which typically doesn’t show up until a baby is several months old and lasts for up to about a year.
The guidelines put forth detailed treatment algorithms featuring multiple options available for each acne age category and degree of severity. Of note, benzoyl peroxide is listed as a first-line treatment across the board, either as monotherapy or in combination with an antibiotic or topical retinoid.
"There is a theme that whenever one is using an antibiotic – whether a systemic drug or a topical product like clindamycin – benzoyl peroxide is advised in the regimen of care because of the feeling that if you use an unopposed antibiotic, you can have the development of bacterial resistance," Dr. Eichenfield noted.
He reported receiving research grants for clinical investigations from half a dozen pharmaceutical companies.
SDEF and this news organization are owned by the same parent company.
WAILEA, HAWAII – Acne arising in a 1- to 7-year-old means "it’s time to worry," according to Dr. Lawrence F. Eichenfield.
Acne originating in this midchildhood age range is very uncommon. It signals the need for a detailed endocrinologic work-up. Possible underlying causes include precocious adrenarche, congenital adrenal hyperplasia, Cushing’s syndrome, precocious puberty, and a gonadal or adrenal tumor, he noted at the Hawaii Dermatology Seminar sponsored by the Global Academy for Medical Education/Skin Disease Education Foundation.
"If you want to take it on yourself you can, but the standard is going to be an evaluation that includes a growth chart, a bone age assessment, Tanner staging, and measurement of total and free testosterone, LH [luteinizing hormone], FSH [follicle-stimulating hormone], prolactin, DHEAS [dehydroepiandrosterone sulfate], andrestenedione, and 17-hydroxyprogesterone. Generally we say refer to a pediatric endocrinologist," said Dr. Eichenfield, professor of clinical pediatrics and medicine (dermatology) at the University of California, San Diego.
He noted that acne occurring at age 1-7 is prominently identified as a red flag in guidelines for the management of pediatric acne developed by the American Acne and Rosacea Society and subsequently approved by the American Academy of Pediatrics. Dr. Eichenfield was cochair of the expert panel that crafted the guidelines.
The comprehensive guidelines – the first ever to specifically address acne in the pediatric age range – include a general acne categorization scheme based upon age. While acne in a 1- to 7-year-old is characterized as a cause for concern, acne arising in a seemingly healthy slightly older preadolescent – roughly age 7-12 – is not.
"Acne in a child in this age group who otherwise looks well and has no signs or history that would make you suspicious of an underlying endocrinopathy is essentially a normal variant we now call preadolescent acne. You do not need to refer that patient for further evaluation," the pediatric dermatologist explained.
Nonworrisome preadolescent acne presents as comedone-predominant disease typically concentrated on the forehead and midface, with truncal involvement much less frequent. The acne may precede other signs of puberty. There is solid evidence that the more pronounced the expression of early preadolescent acne – that is, the greater the number of facial comedones present – the more severe the acne will be in adolescence. Indeed, severe preadolescent acne is often a harbinger of the later need for isotretinoin.
Acne developing within the first 6 weeks of life is most often an erythematous papulopustular eruption categorized in the guidelines as neonatal acne, also known as neonatal cephalic pustulosis. It is not true acne, but rather a self-limited condition associated with Malassezia globosa and M. sympodialis.
In contrast, infantile acne is true acne, mainly comedonal, which typically doesn’t show up until a baby is several months old and lasts for up to about a year.
The guidelines put forth detailed treatment algorithms featuring multiple options available for each acne age category and degree of severity. Of note, benzoyl peroxide is listed as a first-line treatment across the board, either as monotherapy or in combination with an antibiotic or topical retinoid.
"There is a theme that whenever one is using an antibiotic – whether a systemic drug or a topical product like clindamycin – benzoyl peroxide is advised in the regimen of care because of the feeling that if you use an unopposed antibiotic, you can have the development of bacterial resistance," Dr. Eichenfield noted.
He reported receiving research grants for clinical investigations from half a dozen pharmaceutical companies.
SDEF and this news organization are owned by the same parent company.
WAILEA, HAWAII – Acne arising in a 1- to 7-year-old means "it’s time to worry," according to Dr. Lawrence F. Eichenfield.
Acne originating in this midchildhood age range is very uncommon. It signals the need for a detailed endocrinologic work-up. Possible underlying causes include precocious adrenarche, congenital adrenal hyperplasia, Cushing’s syndrome, precocious puberty, and a gonadal or adrenal tumor, he noted at the Hawaii Dermatology Seminar sponsored by the Global Academy for Medical Education/Skin Disease Education Foundation.
"If you want to take it on yourself you can, but the standard is going to be an evaluation that includes a growth chart, a bone age assessment, Tanner staging, and measurement of total and free testosterone, LH [luteinizing hormone], FSH [follicle-stimulating hormone], prolactin, DHEAS [dehydroepiandrosterone sulfate], andrestenedione, and 17-hydroxyprogesterone. Generally we say refer to a pediatric endocrinologist," said Dr. Eichenfield, professor of clinical pediatrics and medicine (dermatology) at the University of California, San Diego.
He noted that acne occurring at age 1-7 is prominently identified as a red flag in guidelines for the management of pediatric acne developed by the American Acne and Rosacea Society and subsequently approved by the American Academy of Pediatrics. Dr. Eichenfield was cochair of the expert panel that crafted the guidelines.
The comprehensive guidelines – the first ever to specifically address acne in the pediatric age range – include a general acne categorization scheme based upon age. While acne in a 1- to 7-year-old is characterized as a cause for concern, acne arising in a seemingly healthy slightly older preadolescent – roughly age 7-12 – is not.
"Acne in a child in this age group who otherwise looks well and has no signs or history that would make you suspicious of an underlying endocrinopathy is essentially a normal variant we now call preadolescent acne. You do not need to refer that patient for further evaluation," the pediatric dermatologist explained.
Nonworrisome preadolescent acne presents as comedone-predominant disease typically concentrated on the forehead and midface, with truncal involvement much less frequent. The acne may precede other signs of puberty. There is solid evidence that the more pronounced the expression of early preadolescent acne – that is, the greater the number of facial comedones present – the more severe the acne will be in adolescence. Indeed, severe preadolescent acne is often a harbinger of the later need for isotretinoin.
Acne developing within the first 6 weeks of life is most often an erythematous papulopustular eruption categorized in the guidelines as neonatal acne, also known as neonatal cephalic pustulosis. It is not true acne, but rather a self-limited condition associated with Malassezia globosa and M. sympodialis.
In contrast, infantile acne is true acne, mainly comedonal, which typically doesn’t show up until a baby is several months old and lasts for up to about a year.
The guidelines put forth detailed treatment algorithms featuring multiple options available for each acne age category and degree of severity. Of note, benzoyl peroxide is listed as a first-line treatment across the board, either as monotherapy or in combination with an antibiotic or topical retinoid.
"There is a theme that whenever one is using an antibiotic – whether a systemic drug or a topical product like clindamycin – benzoyl peroxide is advised in the regimen of care because of the feeling that if you use an unopposed antibiotic, you can have the development of bacterial resistance," Dr. Eichenfield noted.
He reported receiving research grants for clinical investigations from half a dozen pharmaceutical companies.
SDEF and this news organization are owned by the same parent company.
EXPERT OPINION FROM SDEF HAWAII DERMATOLOGY SEMINAR
Actual acne treatment lasts longer than studies suggest
MIAMI BEACH – In practice, acne patients are treated three times longer than clinical trials suggest, based on data from more than 2,000 patients at an academic medical center.
The findings have implications both for setting patients’ treatment expectations and for designing future clinical trials, said Karen Huang of Wake Forest University, Winston-Salem, N.C., said at the annual meeting of the American Academy of Dermatology.
Ms. Huang and her colleagues reviewed electronic records for patients who were treated at an academic medical practice between Jan. 1, 2009, and Nov. 15, 2012. Overall, 2,250 patients had at least one acne-related visit with a dermatologist. Of these, 57% had only one visit and 43% had multiple visits.
For patients who had multiple visits, the mean duration of treatment from the first to the last visit was approximately 9 months (0.79 years). Approximately 25% continued seeing their dermatologists for about a year, and half continued treatment for nearly 5 months (0.4 years).
Not unexpectedly, patients treated with oral medication, including isotretinoin and other oral treatments, were more likely than those treated with topical medications to have multiple visits. In addition, the number of visits by patients who received isotretinoin slowed gradually at first, then declined more rapidly over time compared with patients who received topical treatments.
Approximately 90% of individuals experience acne during their lifetimes, but the actual duration of acne episodes has not been well characterized in the literature, said Ms. Huang. The duration of treatment seen in 40 recent studies of acne treatment identified at clinicaltrials.gov was about 12 weeks, she added.
The current findings represent a lower limit on the duration of acne treatment because of a lack of data on which patients may have discontinued treatment prematurely or continued treatment elsewhere, such as with a primary care physician, she said.
The study findings may be of interest not only for clinical trial design (in that researchers might want to simulate average treatment duration), but also for physicians who want to set realistic expectations about treatment for their patients.
"It has been shown that if you help set patients’ expectations of what their treatment will be like, it may help improve adherence," she said.
Ms. Huang had no financial conflicts to disclose.
MIAMI BEACH – In practice, acne patients are treated three times longer than clinical trials suggest, based on data from more than 2,000 patients at an academic medical center.
The findings have implications both for setting patients’ treatment expectations and for designing future clinical trials, said Karen Huang of Wake Forest University, Winston-Salem, N.C., said at the annual meeting of the American Academy of Dermatology.
Ms. Huang and her colleagues reviewed electronic records for patients who were treated at an academic medical practice between Jan. 1, 2009, and Nov. 15, 2012. Overall, 2,250 patients had at least one acne-related visit with a dermatologist. Of these, 57% had only one visit and 43% had multiple visits.
For patients who had multiple visits, the mean duration of treatment from the first to the last visit was approximately 9 months (0.79 years). Approximately 25% continued seeing their dermatologists for about a year, and half continued treatment for nearly 5 months (0.4 years).
Not unexpectedly, patients treated with oral medication, including isotretinoin and other oral treatments, were more likely than those treated with topical medications to have multiple visits. In addition, the number of visits by patients who received isotretinoin slowed gradually at first, then declined more rapidly over time compared with patients who received topical treatments.
Approximately 90% of individuals experience acne during their lifetimes, but the actual duration of acne episodes has not been well characterized in the literature, said Ms. Huang. The duration of treatment seen in 40 recent studies of acne treatment identified at clinicaltrials.gov was about 12 weeks, she added.
The current findings represent a lower limit on the duration of acne treatment because of a lack of data on which patients may have discontinued treatment prematurely or continued treatment elsewhere, such as with a primary care physician, she said.
The study findings may be of interest not only for clinical trial design (in that researchers might want to simulate average treatment duration), but also for physicians who want to set realistic expectations about treatment for their patients.
"It has been shown that if you help set patients’ expectations of what their treatment will be like, it may help improve adherence," she said.
Ms. Huang had no financial conflicts to disclose.
MIAMI BEACH – In practice, acne patients are treated three times longer than clinical trials suggest, based on data from more than 2,000 patients at an academic medical center.
The findings have implications both for setting patients’ treatment expectations and for designing future clinical trials, said Karen Huang of Wake Forest University, Winston-Salem, N.C., said at the annual meeting of the American Academy of Dermatology.
Ms. Huang and her colleagues reviewed electronic records for patients who were treated at an academic medical practice between Jan. 1, 2009, and Nov. 15, 2012. Overall, 2,250 patients had at least one acne-related visit with a dermatologist. Of these, 57% had only one visit and 43% had multiple visits.
For patients who had multiple visits, the mean duration of treatment from the first to the last visit was approximately 9 months (0.79 years). Approximately 25% continued seeing their dermatologists for about a year, and half continued treatment for nearly 5 months (0.4 years).
Not unexpectedly, patients treated with oral medication, including isotretinoin and other oral treatments, were more likely than those treated with topical medications to have multiple visits. In addition, the number of visits by patients who received isotretinoin slowed gradually at first, then declined more rapidly over time compared with patients who received topical treatments.
Approximately 90% of individuals experience acne during their lifetimes, but the actual duration of acne episodes has not been well characterized in the literature, said Ms. Huang. The duration of treatment seen in 40 recent studies of acne treatment identified at clinicaltrials.gov was about 12 weeks, she added.
The current findings represent a lower limit on the duration of acne treatment because of a lack of data on which patients may have discontinued treatment prematurely or continued treatment elsewhere, such as with a primary care physician, she said.
The study findings may be of interest not only for clinical trial design (in that researchers might want to simulate average treatment duration), but also for physicians who want to set realistic expectations about treatment for their patients.
"It has been shown that if you help set patients’ expectations of what their treatment will be like, it may help improve adherence," she said.
Ms. Huang had no financial conflicts to disclose.
AT THE AAD ANNUAL MEETING
Major finding: The mean duration of acne treatment was approximately 9 months in clinical practice vs. 3 months in clinical trials.
Data source: A retrospective review of data from 2,250 patients seen at an academic practice.
Disclosures: Dr. Huang reported having no disclosures.