User login
Medical transition in transgender patients
Medical transition in transgender patients
I just read the article “Writing letters for transgender patients undergoing medical transition” by Dr. Amy Riese (Pearls,
I would like to use her piece as an opportunity to highlight what has become a chasm in psychiatric care. Dr. Riese’s article was on the letter itself and not the assessment of a patient with possible gender dysphoria, but assessment is barely mentioned, and is the single most important part of a gender transition process. Assessment has become the huge chasm in treatment. In my community, both personally and professionally, I have witnessed very little assessment taking place, yet a lot of transitioning is happening.
Concerned and caring family members take their child (or self-present if the patient is an adult) to gender specialists for their expertise. What is happening during these evaluations are brief conversations during which the gender specialist accepts a patient’s (sometimes a minor’s) self-diagnosis of gender dysphoria. There is discussion of the importance of being gender-affirming, and the beginning of a discussion of hormone therapy. During these discussions of hormone therapy, there is very little disclosure of some of the untoward effects. I understand this is a generalization, and there are some gender specialists who are doing excellent, thorough assessments. But this is what I am seeing in my community, to the point that I have no local specialists to whom I feel comfortable sending my patients who may have gender dysphoria.
During discussions, some of the significant medical outcomes of hormone therapy (immunosuppression, loss of bone density, sterility, increased risk of certain types of cancer, etc.) are not mentioned, or are mentioned in passing. Clinicians have begun using euphemisms such as “top surgery” or “upper body surgery,” as used in Dr. Riese’s article, rather than the medically accurate term, which is “bilateral mastectomy.” These behaviors are being manifested by mostly well-meaning clinicians, and start the process of ushering a patient down a one-way street toward a medical transition.
In April of this year, a prestigious institution in my state did a training on aspects of treating transgender and nonbinary youth. The training advocated giving less information to transgender youth regarding the effects of treatment on fertility, arguing that giving adequate information would disrupt the normal course of development. However, we are allowing these same youth to consent for treatment.
This is a very destructive phenomenon, and only time will tell what the psychiatric outcomes will be for patients who medically transition who did not have an adequate assessment. After so much loss under the auspices of treatment, one would hope that at the very least, these children and young adults would be in a better place psychologically, that they would finally be happy and fulfilled in their new reality, that their mental anguish would evaporate, and with it, their risk of suicide. And this may be true if the patient had gender dysphoria.
But what about the patients who did not have an adequate assessment, whose self-diagnosis was accepted without question, the gender-affirming model immediately implemented, and referrals quickly made for medical treatment? For those patients, once everything has been done, every hormone taken, every surgery performed, but still not male enough, not convincingly male in every aspect, now what? Where does one go from there?
Only time will tell what the psychiatric outcomes will be for these patients, who are primarily youth and young adults at this point. What about the psychological pain that brought them to identify as transgender in the first place? Since the patient was colluded with in the diagnosis of gender dysphoria, that pain was never identified and addressed. What will the suicide rate be of these fully transitioned patients who never had gender dysphoria?
And what shall become of the clinicians who treated them without pause or careful consideration, who bypassed informed consent, treating teens as if they had the judgment and psychological maturity of an adult? What will be their defense when the malpractice lawsuits begin to mount against them, when patients and their families emerge on the other side of the medical transition to find that life, identity, intimacy, and the most basic biological functions have been altered forever based on the capricious and suggestible whims of children?
According to the DSM-5, the prevalence of gender dysphoria is very low. Even if we were to double the DSM-5 estimate, it is still very low. As psychiatrists, we are leaders in the mental health field, and need to set the tone and guide nonphysician clinicians toward extremely careful assessment of these patients.
While Dr. Riese gives excellent information about how to write a letter for a patient who needs transition, far fewer of these letters should be written. The upward trend in the numbers of patients receiving a diagnosis, and subsequently letters, is largely imposed by clinicians who disregard the DSM-5 and fail to apply critical thought to this assessments.
Medical transition in transgender patients
I just read the article “Writing letters for transgender patients undergoing medical transition” by Dr. Amy Riese (Pearls,
I would like to use her piece as an opportunity to highlight what has become a chasm in psychiatric care. Dr. Riese’s article was on the letter itself and not the assessment of a patient with possible gender dysphoria, but assessment is barely mentioned, and is the single most important part of a gender transition process. Assessment has become the huge chasm in treatment. In my community, both personally and professionally, I have witnessed very little assessment taking place, yet a lot of transitioning is happening.
Concerned and caring family members take their child (or self-present if the patient is an adult) to gender specialists for their expertise. What is happening during these evaluations are brief conversations during which the gender specialist accepts a patient’s (sometimes a minor’s) self-diagnosis of gender dysphoria. There is discussion of the importance of being gender-affirming, and the beginning of a discussion of hormone therapy. During these discussions of hormone therapy, there is very little disclosure of some of the untoward effects. I understand this is a generalization, and there are some gender specialists who are doing excellent, thorough assessments. But this is what I am seeing in my community, to the point that I have no local specialists to whom I feel comfortable sending my patients who may have gender dysphoria.
During discussions, some of the significant medical outcomes of hormone therapy (immunosuppression, loss of bone density, sterility, increased risk of certain types of cancer, etc.) are not mentioned, or are mentioned in passing. Clinicians have begun using euphemisms such as “top surgery” or “upper body surgery,” as used in Dr. Riese’s article, rather than the medically accurate term, which is “bilateral mastectomy.” These behaviors are being manifested by mostly well-meaning clinicians, and start the process of ushering a patient down a one-way street toward a medical transition.
In April of this year, a prestigious institution in my state did a training on aspects of treating transgender and nonbinary youth. The training advocated giving less information to transgender youth regarding the effects of treatment on fertility, arguing that giving adequate information would disrupt the normal course of development. However, we are allowing these same youth to consent for treatment.
This is a very destructive phenomenon, and only time will tell what the psychiatric outcomes will be for patients who medically transition who did not have an adequate assessment. After so much loss under the auspices of treatment, one would hope that at the very least, these children and young adults would be in a better place psychologically, that they would finally be happy and fulfilled in their new reality, that their mental anguish would evaporate, and with it, their risk of suicide. And this may be true if the patient had gender dysphoria.
But what about the patients who did not have an adequate assessment, whose self-diagnosis was accepted without question, the gender-affirming model immediately implemented, and referrals quickly made for medical treatment? For those patients, once everything has been done, every hormone taken, every surgery performed, but still not male enough, not convincingly male in every aspect, now what? Where does one go from there?
Only time will tell what the psychiatric outcomes will be for these patients, who are primarily youth and young adults at this point. What about the psychological pain that brought them to identify as transgender in the first place? Since the patient was colluded with in the diagnosis of gender dysphoria, that pain was never identified and addressed. What will the suicide rate be of these fully transitioned patients who never had gender dysphoria?
And what shall become of the clinicians who treated them without pause or careful consideration, who bypassed informed consent, treating teens as if they had the judgment and psychological maturity of an adult? What will be their defense when the malpractice lawsuits begin to mount against them, when patients and their families emerge on the other side of the medical transition to find that life, identity, intimacy, and the most basic biological functions have been altered forever based on the capricious and suggestible whims of children?
According to the DSM-5, the prevalence of gender dysphoria is very low. Even if we were to double the DSM-5 estimate, it is still very low. As psychiatrists, we are leaders in the mental health field, and need to set the tone and guide nonphysician clinicians toward extremely careful assessment of these patients.
While Dr. Riese gives excellent information about how to write a letter for a patient who needs transition, far fewer of these letters should be written. The upward trend in the numbers of patients receiving a diagnosis, and subsequently letters, is largely imposed by clinicians who disregard the DSM-5 and fail to apply critical thought to this assessments.
Medical transition in transgender patients
I just read the article “Writing letters for transgender patients undergoing medical transition” by Dr. Amy Riese (Pearls,
I would like to use her piece as an opportunity to highlight what has become a chasm in psychiatric care. Dr. Riese’s article was on the letter itself and not the assessment of a patient with possible gender dysphoria, but assessment is barely mentioned, and is the single most important part of a gender transition process. Assessment has become the huge chasm in treatment. In my community, both personally and professionally, I have witnessed very little assessment taking place, yet a lot of transitioning is happening.
Concerned and caring family members take their child (or self-present if the patient is an adult) to gender specialists for their expertise. What is happening during these evaluations are brief conversations during which the gender specialist accepts a patient’s (sometimes a minor’s) self-diagnosis of gender dysphoria. There is discussion of the importance of being gender-affirming, and the beginning of a discussion of hormone therapy. During these discussions of hormone therapy, there is very little disclosure of some of the untoward effects. I understand this is a generalization, and there are some gender specialists who are doing excellent, thorough assessments. But this is what I am seeing in my community, to the point that I have no local specialists to whom I feel comfortable sending my patients who may have gender dysphoria.
During discussions, some of the significant medical outcomes of hormone therapy (immunosuppression, loss of bone density, sterility, increased risk of certain types of cancer, etc.) are not mentioned, or are mentioned in passing. Clinicians have begun using euphemisms such as “top surgery” or “upper body surgery,” as used in Dr. Riese’s article, rather than the medically accurate term, which is “bilateral mastectomy.” These behaviors are being manifested by mostly well-meaning clinicians, and start the process of ushering a patient down a one-way street toward a medical transition.
In April of this year, a prestigious institution in my state did a training on aspects of treating transgender and nonbinary youth. The training advocated giving less information to transgender youth regarding the effects of treatment on fertility, arguing that giving adequate information would disrupt the normal course of development. However, we are allowing these same youth to consent for treatment.
This is a very destructive phenomenon, and only time will tell what the psychiatric outcomes will be for patients who medically transition who did not have an adequate assessment. After so much loss under the auspices of treatment, one would hope that at the very least, these children and young adults would be in a better place psychologically, that they would finally be happy and fulfilled in their new reality, that their mental anguish would evaporate, and with it, their risk of suicide. And this may be true if the patient had gender dysphoria.
But what about the patients who did not have an adequate assessment, whose self-diagnosis was accepted without question, the gender-affirming model immediately implemented, and referrals quickly made for medical treatment? For those patients, once everything has been done, every hormone taken, every surgery performed, but still not male enough, not convincingly male in every aspect, now what? Where does one go from there?
Only time will tell what the psychiatric outcomes will be for these patients, who are primarily youth and young adults at this point. What about the psychological pain that brought them to identify as transgender in the first place? Since the patient was colluded with in the diagnosis of gender dysphoria, that pain was never identified and addressed. What will the suicide rate be of these fully transitioned patients who never had gender dysphoria?
And what shall become of the clinicians who treated them without pause or careful consideration, who bypassed informed consent, treating teens as if they had the judgment and psychological maturity of an adult? What will be their defense when the malpractice lawsuits begin to mount against them, when patients and their families emerge on the other side of the medical transition to find that life, identity, intimacy, and the most basic biological functions have been altered forever based on the capricious and suggestible whims of children?
According to the DSM-5, the prevalence of gender dysphoria is very low. Even if we were to double the DSM-5 estimate, it is still very low. As psychiatrists, we are leaders in the mental health field, and need to set the tone and guide nonphysician clinicians toward extremely careful assessment of these patients.
While Dr. Riese gives excellent information about how to write a letter for a patient who needs transition, far fewer of these letters should be written. The upward trend in the numbers of patients receiving a diagnosis, and subsequently letters, is largely imposed by clinicians who disregard the DSM-5 and fail to apply critical thought to this assessments.
FDA issues stronger safety requirements for breast implants
The Food and Drug Administration on Oct. 27 announced stronger safety requirements for breast implants, restricting sales of implants only to providers and health facilities that review potential risks of the devices with patients before surgery, via a “Patient Decision Checklist.” The agency also placed a boxed warning – the strongest warning that the FDA requires – on all legally marketed breast implants.
“Protecting patients’ health when they are treated with a medical device is our most important priority,” Binita Ashar, MD, director of the Office of Surgical and Infection Control Devices in the FDA’s Center for Devices and Radiological Health, said in a press release. “In recent years, the FDA has sought more ways to increase patients’ access to clear and understandable information about the benefits and risks of breast implants. By strengthening the safety requirements for manufacturers, the FDA is working to close information gaps for anyone who may be considering breast implant surgery.”
This announcement comes 10 years after the FDA issued a comprehensive safety update on silicone gel–filled implants, which reported a possible association between these devices and anaplastic large cell lymphoma (ALCL). The studies reviewed in the 2011 document also noted that a “significant percentage of women who receive silicone gel–filled breast implants experience complications and adverse outcomes,” the most common being repeat operation, implant removal, rupture, or capsular contracture (scar tissue tightening around the implant).
Breast augmentation has been one of the top five cosmetic procedures in the United States since 2006, according to the American Society for Plastic Surgery, with more than 400,000 people getting breast implants in 2019. Nearly 300,000 were for cosmetic reasons, and more than 100,000 were for breast reconstruction after mastectomies.
In 2019, the FDA proposed adding a boxed warning for breast implants, stating that the devices do not last an entire lifetime; that over time the risk for complications increases; and that breast implants have been associated with ALCL, and also may be associated with systemic symptoms such as fatigue, joint pain, and brain fog. The Oct. 27 FDA action now requires that manufacturers update breast implant packaging to include that information in a boxed warning, as well as the following:
- A patient-decision checklist
- Updated silicone gel–filled breast implant rupture screening recommendations
- A device description including materials used in the device
- Patient device ID cards
The updated label changes must be present on manufacturers’ websites in 30 days, the FDA said.
The new requirements have received largely positive reactions from both physicians and patient organizations. In an emailed statement to this news organization, Lynn Jeffers, MD, MBA, the immediate past president of the American Society of Plastic Surgeons, said that “ASPS has always supported patients being fully informed about their choices and the risks, benefits, and alternatives of the options available. “We look forward to our continued collaboration with the FDA on the safety of implants and other devices.”
Maria Gmitro, president and cofounder of the Breast Implant Safety Alliance, an all-volunteer nonprofit based in Charleston, S.C., said that some of the language in the patient checklist could be stronger, especially when referring to breast implant–associated ALCL.
To inform patients of risks more clearly, “it’s the words like ‘associated with’ that we feel need to be stronger” she said in an interview. She also noted that women who already have breast implants may not be aware of these potential complications, which these new FDA requirements do not address.
But overall, the nonprofit was “thrilled” with the announcement, Ms. Gmitro said. “Placing restrictions on breast implants is a really big step, and we applaud the FDA’s efforts. This is information that every patient considering breast implants should know, and we’ve been advocating for better informed consent.”
A version of this article first appeared on Medscape.com.
The Food and Drug Administration on Oct. 27 announced stronger safety requirements for breast implants, restricting sales of implants only to providers and health facilities that review potential risks of the devices with patients before surgery, via a “Patient Decision Checklist.” The agency also placed a boxed warning – the strongest warning that the FDA requires – on all legally marketed breast implants.
“Protecting patients’ health when they are treated with a medical device is our most important priority,” Binita Ashar, MD, director of the Office of Surgical and Infection Control Devices in the FDA’s Center for Devices and Radiological Health, said in a press release. “In recent years, the FDA has sought more ways to increase patients’ access to clear and understandable information about the benefits and risks of breast implants. By strengthening the safety requirements for manufacturers, the FDA is working to close information gaps for anyone who may be considering breast implant surgery.”
This announcement comes 10 years after the FDA issued a comprehensive safety update on silicone gel–filled implants, which reported a possible association between these devices and anaplastic large cell lymphoma (ALCL). The studies reviewed in the 2011 document also noted that a “significant percentage of women who receive silicone gel–filled breast implants experience complications and adverse outcomes,” the most common being repeat operation, implant removal, rupture, or capsular contracture (scar tissue tightening around the implant).
Breast augmentation has been one of the top five cosmetic procedures in the United States since 2006, according to the American Society for Plastic Surgery, with more than 400,000 people getting breast implants in 2019. Nearly 300,000 were for cosmetic reasons, and more than 100,000 were for breast reconstruction after mastectomies.
In 2019, the FDA proposed adding a boxed warning for breast implants, stating that the devices do not last an entire lifetime; that over time the risk for complications increases; and that breast implants have been associated with ALCL, and also may be associated with systemic symptoms such as fatigue, joint pain, and brain fog. The Oct. 27 FDA action now requires that manufacturers update breast implant packaging to include that information in a boxed warning, as well as the following:
- A patient-decision checklist
- Updated silicone gel–filled breast implant rupture screening recommendations
- A device description including materials used in the device
- Patient device ID cards
The updated label changes must be present on manufacturers’ websites in 30 days, the FDA said.
The new requirements have received largely positive reactions from both physicians and patient organizations. In an emailed statement to this news organization, Lynn Jeffers, MD, MBA, the immediate past president of the American Society of Plastic Surgeons, said that “ASPS has always supported patients being fully informed about their choices and the risks, benefits, and alternatives of the options available. “We look forward to our continued collaboration with the FDA on the safety of implants and other devices.”
Maria Gmitro, president and cofounder of the Breast Implant Safety Alliance, an all-volunteer nonprofit based in Charleston, S.C., said that some of the language in the patient checklist could be stronger, especially when referring to breast implant–associated ALCL.
To inform patients of risks more clearly, “it’s the words like ‘associated with’ that we feel need to be stronger” she said in an interview. She also noted that women who already have breast implants may not be aware of these potential complications, which these new FDA requirements do not address.
But overall, the nonprofit was “thrilled” with the announcement, Ms. Gmitro said. “Placing restrictions on breast implants is a really big step, and we applaud the FDA’s efforts. This is information that every patient considering breast implants should know, and we’ve been advocating for better informed consent.”
A version of this article first appeared on Medscape.com.
The Food and Drug Administration on Oct. 27 announced stronger safety requirements for breast implants, restricting sales of implants only to providers and health facilities that review potential risks of the devices with patients before surgery, via a “Patient Decision Checklist.” The agency also placed a boxed warning – the strongest warning that the FDA requires – on all legally marketed breast implants.
“Protecting patients’ health when they are treated with a medical device is our most important priority,” Binita Ashar, MD, director of the Office of Surgical and Infection Control Devices in the FDA’s Center for Devices and Radiological Health, said in a press release. “In recent years, the FDA has sought more ways to increase patients’ access to clear and understandable information about the benefits and risks of breast implants. By strengthening the safety requirements for manufacturers, the FDA is working to close information gaps for anyone who may be considering breast implant surgery.”
This announcement comes 10 years after the FDA issued a comprehensive safety update on silicone gel–filled implants, which reported a possible association between these devices and anaplastic large cell lymphoma (ALCL). The studies reviewed in the 2011 document also noted that a “significant percentage of women who receive silicone gel–filled breast implants experience complications and adverse outcomes,” the most common being repeat operation, implant removal, rupture, or capsular contracture (scar tissue tightening around the implant).
Breast augmentation has been one of the top five cosmetic procedures in the United States since 2006, according to the American Society for Plastic Surgery, with more than 400,000 people getting breast implants in 2019. Nearly 300,000 were for cosmetic reasons, and more than 100,000 were for breast reconstruction after mastectomies.
In 2019, the FDA proposed adding a boxed warning for breast implants, stating that the devices do not last an entire lifetime; that over time the risk for complications increases; and that breast implants have been associated with ALCL, and also may be associated with systemic symptoms such as fatigue, joint pain, and brain fog. The Oct. 27 FDA action now requires that manufacturers update breast implant packaging to include that information in a boxed warning, as well as the following:
- A patient-decision checklist
- Updated silicone gel–filled breast implant rupture screening recommendations
- A device description including materials used in the device
- Patient device ID cards
The updated label changes must be present on manufacturers’ websites in 30 days, the FDA said.
The new requirements have received largely positive reactions from both physicians and patient organizations. In an emailed statement to this news organization, Lynn Jeffers, MD, MBA, the immediate past president of the American Society of Plastic Surgeons, said that “ASPS has always supported patients being fully informed about their choices and the risks, benefits, and alternatives of the options available. “We look forward to our continued collaboration with the FDA on the safety of implants and other devices.”
Maria Gmitro, president and cofounder of the Breast Implant Safety Alliance, an all-volunteer nonprofit based in Charleston, S.C., said that some of the language in the patient checklist could be stronger, especially when referring to breast implant–associated ALCL.
To inform patients of risks more clearly, “it’s the words like ‘associated with’ that we feel need to be stronger” she said in an interview. She also noted that women who already have breast implants may not be aware of these potential complications, which these new FDA requirements do not address.
But overall, the nonprofit was “thrilled” with the announcement, Ms. Gmitro said. “Placing restrictions on breast implants is a really big step, and we applaud the FDA’s efforts. This is information that every patient considering breast implants should know, and we’ve been advocating for better informed consent.”
A version of this article first appeared on Medscape.com.
Transgender use of dermatologic procedures has strong gender tilt
, according to the results of a recent survey.
Transfeminine persons – those assigned male at birth – were much more likely to report a previous dermatologic procedure, compared with transmasculine respondents, by a margin of 64.9%-7.5%, Laura Ragmanauskaite, MD, and associates reported.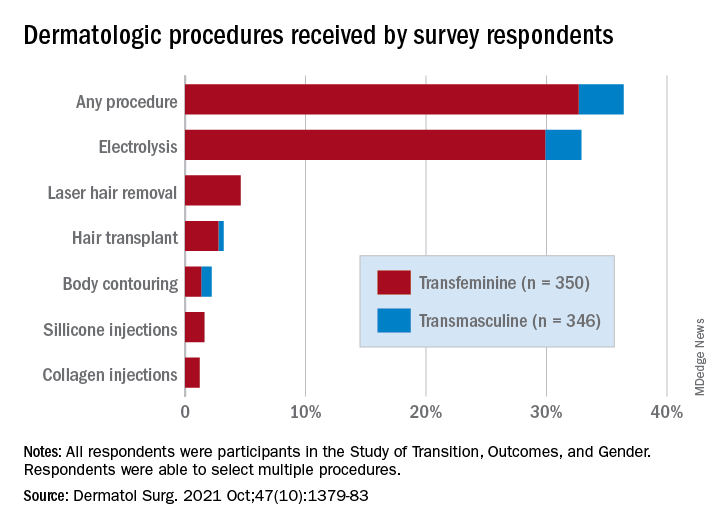
“Hair removal was the most frequently reported procedure type, with electrolysis being more common than laser hair removal,” they said, noting that “previous research on hair removal treatments among gender minority persons did not detect differences in the use of electrolysis and laser hair removal.”
Just under one-third of all respondents (32.9%) said that they had undergone electrolysis and 4.6% reported previous laser hair removal. For electrolysis, that works out to 59.4% of transfeminine and 6.1% of transmasculine respondents, while 9.1% of all transfeminine and no transmasculine persons had received laser hair removal, Dr. Ragmanauskaite of the department of dermatology, Emory University, Atlanta, and her coauthors said.
Those who had undergone gender-affirming surgery were significantly more likely to report electrolysis (78.6%) than were persons who had received no gender-affirming surgery or hormone therapy alone (47.4%), a statistically significant difference (P < .01). All of the other, less common procedures included in the online survey – 696 responses were received from 350 transfeminine and 346 transmasculine persons participating in the Study of Transition, Outcomes, and Gender – were reported more often by the transfeminine respondents. The procedure with the closest gender distribution was body contouring, reported by nine transfeminine and six transmasculine persons, the researchers said.
Use of dermal fillers was even less common (2.8% among all respondents, all transfeminine persons), with just 11 reporting having received silicone and 8 reporting having received collagen, although the survey did not ask about how the injections were obtained. In a previous study, the prevalence of illicit filler injection in transgender women was 16.9%, they pointed out.
These types of noninvasive, gender-affirming procedures “may contribute to higher levels of self-confidence and [reduce] gender dysphoria. Future studies should examine motivations, barriers, and optimal timing” for such procedures in transgender persons, Dr. Ragmanauskaite and associates wrote.
The authors reported that they had no relevant disclosures.
, according to the results of a recent survey.
Transfeminine persons – those assigned male at birth – were much more likely to report a previous dermatologic procedure, compared with transmasculine respondents, by a margin of 64.9%-7.5%, Laura Ragmanauskaite, MD, and associates reported.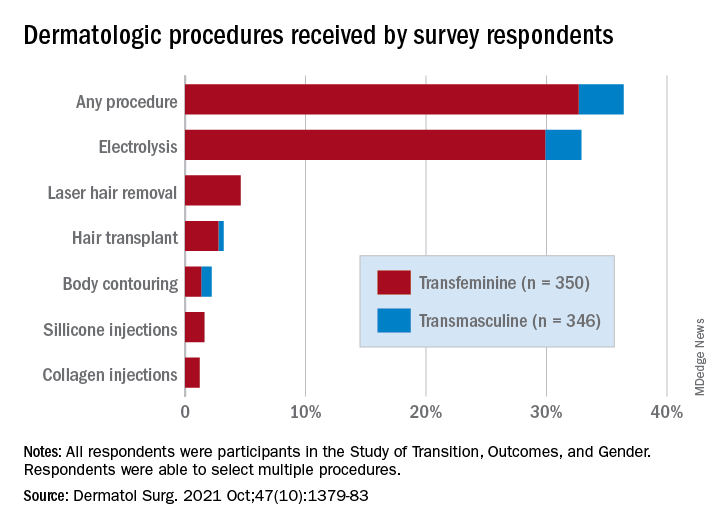
“Hair removal was the most frequently reported procedure type, with electrolysis being more common than laser hair removal,” they said, noting that “previous research on hair removal treatments among gender minority persons did not detect differences in the use of electrolysis and laser hair removal.”
Just under one-third of all respondents (32.9%) said that they had undergone electrolysis and 4.6% reported previous laser hair removal. For electrolysis, that works out to 59.4% of transfeminine and 6.1% of transmasculine respondents, while 9.1% of all transfeminine and no transmasculine persons had received laser hair removal, Dr. Ragmanauskaite of the department of dermatology, Emory University, Atlanta, and her coauthors said.
Those who had undergone gender-affirming surgery were significantly more likely to report electrolysis (78.6%) than were persons who had received no gender-affirming surgery or hormone therapy alone (47.4%), a statistically significant difference (P < .01). All of the other, less common procedures included in the online survey – 696 responses were received from 350 transfeminine and 346 transmasculine persons participating in the Study of Transition, Outcomes, and Gender – were reported more often by the transfeminine respondents. The procedure with the closest gender distribution was body contouring, reported by nine transfeminine and six transmasculine persons, the researchers said.
Use of dermal fillers was even less common (2.8% among all respondents, all transfeminine persons), with just 11 reporting having received silicone and 8 reporting having received collagen, although the survey did not ask about how the injections were obtained. In a previous study, the prevalence of illicit filler injection in transgender women was 16.9%, they pointed out.
These types of noninvasive, gender-affirming procedures “may contribute to higher levels of self-confidence and [reduce] gender dysphoria. Future studies should examine motivations, barriers, and optimal timing” for such procedures in transgender persons, Dr. Ragmanauskaite and associates wrote.
The authors reported that they had no relevant disclosures.
, according to the results of a recent survey.
Transfeminine persons – those assigned male at birth – were much more likely to report a previous dermatologic procedure, compared with transmasculine respondents, by a margin of 64.9%-7.5%, Laura Ragmanauskaite, MD, and associates reported.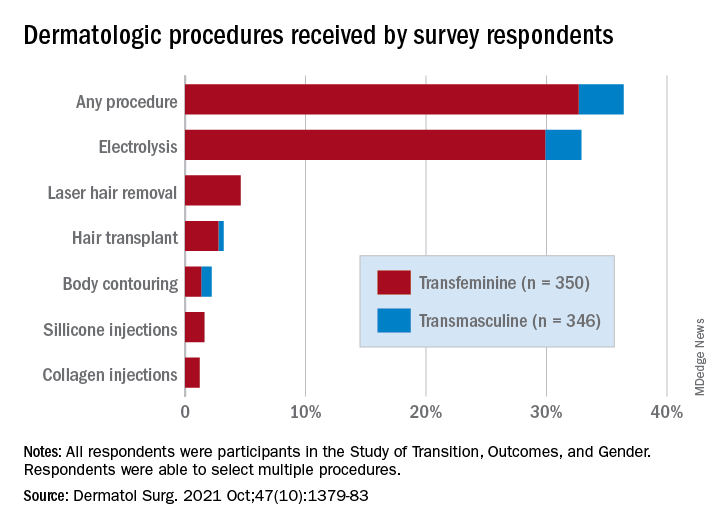
“Hair removal was the most frequently reported procedure type, with electrolysis being more common than laser hair removal,” they said, noting that “previous research on hair removal treatments among gender minority persons did not detect differences in the use of electrolysis and laser hair removal.”
Just under one-third of all respondents (32.9%) said that they had undergone electrolysis and 4.6% reported previous laser hair removal. For electrolysis, that works out to 59.4% of transfeminine and 6.1% of transmasculine respondents, while 9.1% of all transfeminine and no transmasculine persons had received laser hair removal, Dr. Ragmanauskaite of the department of dermatology, Emory University, Atlanta, and her coauthors said.
Those who had undergone gender-affirming surgery were significantly more likely to report electrolysis (78.6%) than were persons who had received no gender-affirming surgery or hormone therapy alone (47.4%), a statistically significant difference (P < .01). All of the other, less common procedures included in the online survey – 696 responses were received from 350 transfeminine and 346 transmasculine persons participating in the Study of Transition, Outcomes, and Gender – were reported more often by the transfeminine respondents. The procedure with the closest gender distribution was body contouring, reported by nine transfeminine and six transmasculine persons, the researchers said.
Use of dermal fillers was even less common (2.8% among all respondents, all transfeminine persons), with just 11 reporting having received silicone and 8 reporting having received collagen, although the survey did not ask about how the injections were obtained. In a previous study, the prevalence of illicit filler injection in transgender women was 16.9%, they pointed out.
These types of noninvasive, gender-affirming procedures “may contribute to higher levels of self-confidence and [reduce] gender dysphoria. Future studies should examine motivations, barriers, and optimal timing” for such procedures in transgender persons, Dr. Ragmanauskaite and associates wrote.
The authors reported that they had no relevant disclosures.
FROM DERMATOLOGIC SURGERY
Overview of guidelines for patients seeking gender-affirmation surgery
Gender-affirmation surgery refers to a collection of procedures by which a transgender individual physically alters characteristics to align with their gender identity. While not all patients who identify as transgender will choose to undergo surgery, the surgeries are considered medically necessary and lead to significant improvements in emotional and psychological well-being.1 With increasing insurance coverage and improved access to care, more and more patients are seeking gender-affirming surgery, and it is incumbent for providers to familiarize themselves with preoperative recommendations and requirements.
Ob.gyns. play a key role in patients seeking surgical treatment as patients may inquire about available procedures and what steps are necessary prior to scheduling a visit with the appropriate surgeon. The World Professional Association of Transgender Health has established standards of care that provide multidisciplinary, evidence-based guidance for patients seeking a variety of gender-affirming services ranging from mental health, hormone therapy, and surgery.
Basic preoperative surgical prerequisites set forth by WPATH include being a patient with well-documented gender dysphoria, being the age of majority, and having the ability to provide informed consent.1
As with any surgical candidate, it is also equally important for a patient to have well-controlled medical and psychiatric comorbidities, which should also include smoking cessation. A variety of surgical procedures are available to patients and include breast/chest surgery, genital (bottom) surgery, and nongenital surgery (facial feminization, pectoral implant placement, thyroid chondroplasty, lipofilling/liposuction, body contouring, and voice modification). Patients may choose to undergo chest/breast surgery and/or bottom surgery or forgo surgical procedures altogether.
For transmasculine patients, breast/chest surgery, otherwise known as top surgery, is the most common and desired procedure. According to a recent survey, approximately 97% of transmasculine patients had or wanted masculinizing chest surgery.2 In addition to patients meeting the basic requirements set forth by WPATH, one referral from a mental health provider specializing in gender-affirming care is also needed prior to this procedure. It is also important to note that testosterone use is no longer a needed prior to masculinizing chest surgery.
Transmasculine bottom surgery, which includes hysterectomy, bilateral salpingo-oophorectomy, metoidioplasty, vaginectomy, scrotoplasty, testicular implant placement, and/or phalloplasty have additional nuances. Compared with transmasculine individuals seeking top surgery, the number of patients who have had or desire metoidioplasty and phalloplasty is much lower, which is mainly because of the high complication rates of these procedures. In the same survey, only 4% of patients had undergone a metoidioplasty procedure and 2% of patients had undergone a phalloplasty.2
In evaluating rates of hysterectomy with or without salpingo-oophorectomy, approximately 21% of transgender men underwent hysterectomy, with 58% desiring it in the future.2 Unlike patients pursuing top surgery, patients who desire any form of bottom surgery need to be on 12 months of continuous hormone therapy.1 They also must provide two letters from two different mental health providers, one of whom must have either an MD/DO or PhD. In cases in which a patient requests a hysterectomy for reasons other than gender dysphoria, such as pelvic pain or abnormal uterine bleeding, these criteria do not apply.
For transfeminine individuals, augmentation mammoplasty is performed following 12 months of continuous hormone therapy. This is to allow maximum breast growth, which occurs approximately 2-3 months after hormone initiation and peaks at 1-2 years.3 Rates of transfeminine individuals seeking augmentation mammoplasty is similar to that of their transmasculine counterparts at 74%.2 One referral letter from a mental health provider is also needed prior to augmentation mammoplasty.
Transfeminine patients who desire bottom surgery, which can involve an orchiectomy or vaginoplasty (single-stage penile inversion, peritoneal, or colonic interposition), have the same additional requirements as transmasculine individuals seeking bottom surgery. Furthermore, it is interesting to note that 25% of transfeminine individuals had already undergone orchiectomy and 87% had either undergone or desired a vaginoplasty in the future.2 This is in stark contrast to transmasculine patients and rates of bottom surgery.
Unless there is a specific medical contraindication to hormone therapy, emphasis is placed on 12 months of continuous hormone usage. Additional emphasis is placed on patients seeking bottom surgery to live for a minimum of 12 months in their congruent gender role. This also allows patients to further explore their gender identity and make appropriate preparations for surgery.
As with any surgical procedure, obtaining informed consent and reviewing patient expectations are key. In my clinical practice, I discuss with patients that the general surgical goals are to achieve both function and good aesthetic outcome but that their results are also tailored to their individual bodies. Assessing a patient’s support system and social factors is also equally important in the preoperative planning period. As this field continues to grow, it is essential for providers to understand the evolving distinctions in surgical care to improve access to patients.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. She has no conflicts. Email her at [email protected].
References
1. The World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. https://www.wpath.org/publications/soc.
2. James SE et al. The report of the 2015 U.S. Transgender survey. Washington, D.C.: National Center for Transgender Equality. 2016.
3. Thomas TN. Overview of surgery for transgender patients, in “Comprehensive care for the transgender patient.” Philadelphia: Elsevier, 2020. pp. 48-53.
Gender-affirmation surgery refers to a collection of procedures by which a transgender individual physically alters characteristics to align with their gender identity. While not all patients who identify as transgender will choose to undergo surgery, the surgeries are considered medically necessary and lead to significant improvements in emotional and psychological well-being.1 With increasing insurance coverage and improved access to care, more and more patients are seeking gender-affirming surgery, and it is incumbent for providers to familiarize themselves with preoperative recommendations and requirements.
Ob.gyns. play a key role in patients seeking surgical treatment as patients may inquire about available procedures and what steps are necessary prior to scheduling a visit with the appropriate surgeon. The World Professional Association of Transgender Health has established standards of care that provide multidisciplinary, evidence-based guidance for patients seeking a variety of gender-affirming services ranging from mental health, hormone therapy, and surgery.
Basic preoperative surgical prerequisites set forth by WPATH include being a patient with well-documented gender dysphoria, being the age of majority, and having the ability to provide informed consent.1
As with any surgical candidate, it is also equally important for a patient to have well-controlled medical and psychiatric comorbidities, which should also include smoking cessation. A variety of surgical procedures are available to patients and include breast/chest surgery, genital (bottom) surgery, and nongenital surgery (facial feminization, pectoral implant placement, thyroid chondroplasty, lipofilling/liposuction, body contouring, and voice modification). Patients may choose to undergo chest/breast surgery and/or bottom surgery or forgo surgical procedures altogether.
For transmasculine patients, breast/chest surgery, otherwise known as top surgery, is the most common and desired procedure. According to a recent survey, approximately 97% of transmasculine patients had or wanted masculinizing chest surgery.2 In addition to patients meeting the basic requirements set forth by WPATH, one referral from a mental health provider specializing in gender-affirming care is also needed prior to this procedure. It is also important to note that testosterone use is no longer a needed prior to masculinizing chest surgery.
Transmasculine bottom surgery, which includes hysterectomy, bilateral salpingo-oophorectomy, metoidioplasty, vaginectomy, scrotoplasty, testicular implant placement, and/or phalloplasty have additional nuances. Compared with transmasculine individuals seeking top surgery, the number of patients who have had or desire metoidioplasty and phalloplasty is much lower, which is mainly because of the high complication rates of these procedures. In the same survey, only 4% of patients had undergone a metoidioplasty procedure and 2% of patients had undergone a phalloplasty.2
In evaluating rates of hysterectomy with or without salpingo-oophorectomy, approximately 21% of transgender men underwent hysterectomy, with 58% desiring it in the future.2 Unlike patients pursuing top surgery, patients who desire any form of bottom surgery need to be on 12 months of continuous hormone therapy.1 They also must provide two letters from two different mental health providers, one of whom must have either an MD/DO or PhD. In cases in which a patient requests a hysterectomy for reasons other than gender dysphoria, such as pelvic pain or abnormal uterine bleeding, these criteria do not apply.
For transfeminine individuals, augmentation mammoplasty is performed following 12 months of continuous hormone therapy. This is to allow maximum breast growth, which occurs approximately 2-3 months after hormone initiation and peaks at 1-2 years.3 Rates of transfeminine individuals seeking augmentation mammoplasty is similar to that of their transmasculine counterparts at 74%.2 One referral letter from a mental health provider is also needed prior to augmentation mammoplasty.
Transfeminine patients who desire bottom surgery, which can involve an orchiectomy or vaginoplasty (single-stage penile inversion, peritoneal, or colonic interposition), have the same additional requirements as transmasculine individuals seeking bottom surgery. Furthermore, it is interesting to note that 25% of transfeminine individuals had already undergone orchiectomy and 87% had either undergone or desired a vaginoplasty in the future.2 This is in stark contrast to transmasculine patients and rates of bottom surgery.
Unless there is a specific medical contraindication to hormone therapy, emphasis is placed on 12 months of continuous hormone usage. Additional emphasis is placed on patients seeking bottom surgery to live for a minimum of 12 months in their congruent gender role. This also allows patients to further explore their gender identity and make appropriate preparations for surgery.
As with any surgical procedure, obtaining informed consent and reviewing patient expectations are key. In my clinical practice, I discuss with patients that the general surgical goals are to achieve both function and good aesthetic outcome but that their results are also tailored to their individual bodies. Assessing a patient’s support system and social factors is also equally important in the preoperative planning period. As this field continues to grow, it is essential for providers to understand the evolving distinctions in surgical care to improve access to patients.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. She has no conflicts. Email her at [email protected].
References
1. The World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. https://www.wpath.org/publications/soc.
2. James SE et al. The report of the 2015 U.S. Transgender survey. Washington, D.C.: National Center for Transgender Equality. 2016.
3. Thomas TN. Overview of surgery for transgender patients, in “Comprehensive care for the transgender patient.” Philadelphia: Elsevier, 2020. pp. 48-53.
Gender-affirmation surgery refers to a collection of procedures by which a transgender individual physically alters characteristics to align with their gender identity. While not all patients who identify as transgender will choose to undergo surgery, the surgeries are considered medically necessary and lead to significant improvements in emotional and psychological well-being.1 With increasing insurance coverage and improved access to care, more and more patients are seeking gender-affirming surgery, and it is incumbent for providers to familiarize themselves with preoperative recommendations and requirements.
Ob.gyns. play a key role in patients seeking surgical treatment as patients may inquire about available procedures and what steps are necessary prior to scheduling a visit with the appropriate surgeon. The World Professional Association of Transgender Health has established standards of care that provide multidisciplinary, evidence-based guidance for patients seeking a variety of gender-affirming services ranging from mental health, hormone therapy, and surgery.
Basic preoperative surgical prerequisites set forth by WPATH include being a patient with well-documented gender dysphoria, being the age of majority, and having the ability to provide informed consent.1
As with any surgical candidate, it is also equally important for a patient to have well-controlled medical and psychiatric comorbidities, which should also include smoking cessation. A variety of surgical procedures are available to patients and include breast/chest surgery, genital (bottom) surgery, and nongenital surgery (facial feminization, pectoral implant placement, thyroid chondroplasty, lipofilling/liposuction, body contouring, and voice modification). Patients may choose to undergo chest/breast surgery and/or bottom surgery or forgo surgical procedures altogether.
For transmasculine patients, breast/chest surgery, otherwise known as top surgery, is the most common and desired procedure. According to a recent survey, approximately 97% of transmasculine patients had or wanted masculinizing chest surgery.2 In addition to patients meeting the basic requirements set forth by WPATH, one referral from a mental health provider specializing in gender-affirming care is also needed prior to this procedure. It is also important to note that testosterone use is no longer a needed prior to masculinizing chest surgery.
Transmasculine bottom surgery, which includes hysterectomy, bilateral salpingo-oophorectomy, metoidioplasty, vaginectomy, scrotoplasty, testicular implant placement, and/or phalloplasty have additional nuances. Compared with transmasculine individuals seeking top surgery, the number of patients who have had or desire metoidioplasty and phalloplasty is much lower, which is mainly because of the high complication rates of these procedures. In the same survey, only 4% of patients had undergone a metoidioplasty procedure and 2% of patients had undergone a phalloplasty.2
In evaluating rates of hysterectomy with or without salpingo-oophorectomy, approximately 21% of transgender men underwent hysterectomy, with 58% desiring it in the future.2 Unlike patients pursuing top surgery, patients who desire any form of bottom surgery need to be on 12 months of continuous hormone therapy.1 They also must provide two letters from two different mental health providers, one of whom must have either an MD/DO or PhD. In cases in which a patient requests a hysterectomy for reasons other than gender dysphoria, such as pelvic pain or abnormal uterine bleeding, these criteria do not apply.
For transfeminine individuals, augmentation mammoplasty is performed following 12 months of continuous hormone therapy. This is to allow maximum breast growth, which occurs approximately 2-3 months after hormone initiation and peaks at 1-2 years.3 Rates of transfeminine individuals seeking augmentation mammoplasty is similar to that of their transmasculine counterparts at 74%.2 One referral letter from a mental health provider is also needed prior to augmentation mammoplasty.
Transfeminine patients who desire bottom surgery, which can involve an orchiectomy or vaginoplasty (single-stage penile inversion, peritoneal, or colonic interposition), have the same additional requirements as transmasculine individuals seeking bottom surgery. Furthermore, it is interesting to note that 25% of transfeminine individuals had already undergone orchiectomy and 87% had either undergone or desired a vaginoplasty in the future.2 This is in stark contrast to transmasculine patients and rates of bottom surgery.
Unless there is a specific medical contraindication to hormone therapy, emphasis is placed on 12 months of continuous hormone usage. Additional emphasis is placed on patients seeking bottom surgery to live for a minimum of 12 months in their congruent gender role. This also allows patients to further explore their gender identity and make appropriate preparations for surgery.
As with any surgical procedure, obtaining informed consent and reviewing patient expectations are key. In my clinical practice, I discuss with patients that the general surgical goals are to achieve both function and good aesthetic outcome but that their results are also tailored to their individual bodies. Assessing a patient’s support system and social factors is also equally important in the preoperative planning period. As this field continues to grow, it is essential for providers to understand the evolving distinctions in surgical care to improve access to patients.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. She has no conflicts. Email her at [email protected].
References
1. The World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. https://www.wpath.org/publications/soc.
2. James SE et al. The report of the 2015 U.S. Transgender survey. Washington, D.C.: National Center for Transgender Equality. 2016.
3. Thomas TN. Overview of surgery for transgender patients, in “Comprehensive care for the transgender patient.” Philadelphia: Elsevier, 2020. pp. 48-53.
Gender-affirming care ‘can save lives,’ new research shows
Transgender and nonbinary young people experienced less depression and fewer suicidal thoughts after a year of gender-affirming care with hormones or puberty blockers, according to new research.
“Given the high rates of adverse mental health comorbidities, these data provide critical evidence that expansion of gender-affirming care can save lives,” said David J. Inwards-Breland, MD, MPH, chief of adolescent and young adult medicine and codirector of the Center for Gender-Affirming Care at Rady Children’s Hospital in San Diego, during his presentation.
The findings, presented October 11 at the American Academy of Pediatrics 2021 National Conference, were not at all surprising to Cora Breuner, MD, MPH, professor of pediatrics at Seattle Children’s Hospital.
“The younger we can provide gender-affirming care, the less likely they’re going to have depression, and then the negative outcomes from untreated depression, which includes suicide intent or even suicide completion,” Dr. Breuner told this news organization. “It’s so obvious that we are saving lives by providing gender-affirming care.”
For their study, Dr. Inwards-Breland and his colleagues tracked depression, anxiety, and suicidality in 104 trans and nonbinary people 13 to 21 years of age who received care at the Seattle Children’s gender clinic between August 2017 and June 2018.
The study population consisted of 63 transgender male or male participants, 27 transgender female or female participants, 10 nonbinary participants, and four participants who had not defined their gender identity. Of this cohort, 62.5% were receiving mental health therapy, and 34.7% reported some substance use.
Participants completed the nine-item Patient Health Questionnaire (PHQ-9) and the seven-item Generalized Anxiety Disorder scale (GAD-7) at baseline and then at 3, 6, and 12 months. The researchers defined severe depression and severe anxiety as a score of 10 or greater on either scale.
At baseline, 56.7% of the participants had moderate to severe depression, 43.3% reported thoughts of self-harm or suicidal in the previous 2 weeks, and 50.0% had moderate to severe anxiety.
After 12 months of care, participants experienced a 60% decrease in depression (adjusted odds ratio, 0.4) and a 73% decrease in suicidality (aOR, 0.27), after adjustment for temporal trends and sex assigned at birth, race/ethnicity, level of parental support, ongoing mental health therapy, substance use, and victimization, including bullying, interpersonal violence, neglect, and abuse.
Although the decline in depression and suicidality after gender-affirming treatment was not a surprise, “those drops are huge,” Dr. Inwards-Breland said in an interview.
He said he attributes the improvement to a health care system that “affirms who these young people are” and enables changes that allow their outward appearance to reflect “who they know they are inside.”
There were no significant changes in anxiety during the study period. “Anxiety, I think, is just a little harder to treat, and it takes a little longer to treat,” he explained. And a lot of factors can trigger anxiety, and those can continue during treatment.
The slow pace of changes to gender identity can have an effect on people’s moods. “Since they’re not happening quickly, these young people are still being misgendered, they’re still seeing the body that they don’t feel like they should have, and they have to go to school and go out in public. I think that continues to fuel anxiety with a lot of these young people.”
Family support is important in reducing depression and suicidal thoughts in this population. Parents will often see positive changes after their child receives gender-affirming care, which can help contribute to positive changes in parents’ attitudes, Dr. Inwards-Breland said.
Such changes reinforce “that protective factor of connectedness with family,” he noted. “Families are crucial for any health care, and if there’s that connectedness with families, we know that, clinically, patients do better.”
Balancing risks
Although there are risks associated with gender-affirming hormones and puberty blockers, the risks of not receiving treatment must also be considered.
“Our young people are killing themselves,” he said. “Our young people are developing severe eating disorders that are killing them. Our young people are increasing their substance abuse, homelessness, depression. The list just goes on.”
For trans-masculine and nonbinary masculine patients, the potential permanent changes of hormone therapy include a deeper voice, hair growth, enlargement of the clitoris, and, in some patients, the development of male pattern baldness. In trans and nonbinary feminine patients, potential long-term effects include breast development and an increased risk for fertility issues.
The consent forms required for young people who want gender-affirming hormones or puberty blockers are extensive, with every possible reversible and irreversible effect described in detail, Dr. Breuner said.
“Parents sign them because they want their child to stay alive,” she explained. “When you compare the cost of someone who has severe debilitating depression and dying by suicide with some of the risks associated with gender-affirming hormone therapy, that’s a no-brainer to me.”
This study is limited by the fact that screening tests, not diagnostic tests, were used to identify depression, anxiety, and suicidality, and the fact that the use of antidepression or antianxiety medications was not taken into account, Dr. Inwards-Breland acknowledged.
“I think future studies should look at a mental health evaluation and diagnosis by a mental health provider,” he added. And mental health, gender dysphoria, suicidality, and self-harm should be tracked over the course of treatment.
He also acknowledged the study’s selection bias. All participants sought care at a multidisciplinary gender clinic, so were likely to be privileged and to have supportive families. “There’s a good chance that if we had more trans and nonbinary youth of color, we may have different findings,” he said.
More qualitative research is needed to assess the effect of gender-affirming therapy on the mental health of these patients, Dr. Breuner said.
“Being able to finally come into who you think you are and enjoy expressing who you are in a gender-affirming way has to be positive in such a way that you’re not depressed anymore,” she added. “It has to be tragic for people who cannot stand the body they’re in and cannot talk about it to anybody or express themselves without fear of recourse, to the point that they would be so devastated that they’d want to die by suicide.”
This research was funded by the Seattle Children’s Center for Diversity and Health Equity and the Pacific Hospital Development and Port Authority. Dr. Inwards-Breland and Dr. Breuner have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender and nonbinary young people experienced less depression and fewer suicidal thoughts after a year of gender-affirming care with hormones or puberty blockers, according to new research.
“Given the high rates of adverse mental health comorbidities, these data provide critical evidence that expansion of gender-affirming care can save lives,” said David J. Inwards-Breland, MD, MPH, chief of adolescent and young adult medicine and codirector of the Center for Gender-Affirming Care at Rady Children’s Hospital in San Diego, during his presentation.
The findings, presented October 11 at the American Academy of Pediatrics 2021 National Conference, were not at all surprising to Cora Breuner, MD, MPH, professor of pediatrics at Seattle Children’s Hospital.
“The younger we can provide gender-affirming care, the less likely they’re going to have depression, and then the negative outcomes from untreated depression, which includes suicide intent or even suicide completion,” Dr. Breuner told this news organization. “It’s so obvious that we are saving lives by providing gender-affirming care.”
For their study, Dr. Inwards-Breland and his colleagues tracked depression, anxiety, and suicidality in 104 trans and nonbinary people 13 to 21 years of age who received care at the Seattle Children’s gender clinic between August 2017 and June 2018.
The study population consisted of 63 transgender male or male participants, 27 transgender female or female participants, 10 nonbinary participants, and four participants who had not defined their gender identity. Of this cohort, 62.5% were receiving mental health therapy, and 34.7% reported some substance use.
Participants completed the nine-item Patient Health Questionnaire (PHQ-9) and the seven-item Generalized Anxiety Disorder scale (GAD-7) at baseline and then at 3, 6, and 12 months. The researchers defined severe depression and severe anxiety as a score of 10 or greater on either scale.
At baseline, 56.7% of the participants had moderate to severe depression, 43.3% reported thoughts of self-harm or suicidal in the previous 2 weeks, and 50.0% had moderate to severe anxiety.
After 12 months of care, participants experienced a 60% decrease in depression (adjusted odds ratio, 0.4) and a 73% decrease in suicidality (aOR, 0.27), after adjustment for temporal trends and sex assigned at birth, race/ethnicity, level of parental support, ongoing mental health therapy, substance use, and victimization, including bullying, interpersonal violence, neglect, and abuse.
Although the decline in depression and suicidality after gender-affirming treatment was not a surprise, “those drops are huge,” Dr. Inwards-Breland said in an interview.
He said he attributes the improvement to a health care system that “affirms who these young people are” and enables changes that allow their outward appearance to reflect “who they know they are inside.”
There were no significant changes in anxiety during the study period. “Anxiety, I think, is just a little harder to treat, and it takes a little longer to treat,” he explained. And a lot of factors can trigger anxiety, and those can continue during treatment.
The slow pace of changes to gender identity can have an effect on people’s moods. “Since they’re not happening quickly, these young people are still being misgendered, they’re still seeing the body that they don’t feel like they should have, and they have to go to school and go out in public. I think that continues to fuel anxiety with a lot of these young people.”
Family support is important in reducing depression and suicidal thoughts in this population. Parents will often see positive changes after their child receives gender-affirming care, which can help contribute to positive changes in parents’ attitudes, Dr. Inwards-Breland said.
Such changes reinforce “that protective factor of connectedness with family,” he noted. “Families are crucial for any health care, and if there’s that connectedness with families, we know that, clinically, patients do better.”
Balancing risks
Although there are risks associated with gender-affirming hormones and puberty blockers, the risks of not receiving treatment must also be considered.
“Our young people are killing themselves,” he said. “Our young people are developing severe eating disorders that are killing them. Our young people are increasing their substance abuse, homelessness, depression. The list just goes on.”
For trans-masculine and nonbinary masculine patients, the potential permanent changes of hormone therapy include a deeper voice, hair growth, enlargement of the clitoris, and, in some patients, the development of male pattern baldness. In trans and nonbinary feminine patients, potential long-term effects include breast development and an increased risk for fertility issues.
The consent forms required for young people who want gender-affirming hormones or puberty blockers are extensive, with every possible reversible and irreversible effect described in detail, Dr. Breuner said.
“Parents sign them because they want their child to stay alive,” she explained. “When you compare the cost of someone who has severe debilitating depression and dying by suicide with some of the risks associated with gender-affirming hormone therapy, that’s a no-brainer to me.”
This study is limited by the fact that screening tests, not diagnostic tests, were used to identify depression, anxiety, and suicidality, and the fact that the use of antidepression or antianxiety medications was not taken into account, Dr. Inwards-Breland acknowledged.
“I think future studies should look at a mental health evaluation and diagnosis by a mental health provider,” he added. And mental health, gender dysphoria, suicidality, and self-harm should be tracked over the course of treatment.
He also acknowledged the study’s selection bias. All participants sought care at a multidisciplinary gender clinic, so were likely to be privileged and to have supportive families. “There’s a good chance that if we had more trans and nonbinary youth of color, we may have different findings,” he said.
More qualitative research is needed to assess the effect of gender-affirming therapy on the mental health of these patients, Dr. Breuner said.
“Being able to finally come into who you think you are and enjoy expressing who you are in a gender-affirming way has to be positive in such a way that you’re not depressed anymore,” she added. “It has to be tragic for people who cannot stand the body they’re in and cannot talk about it to anybody or express themselves without fear of recourse, to the point that they would be so devastated that they’d want to die by suicide.”
This research was funded by the Seattle Children’s Center for Diversity and Health Equity and the Pacific Hospital Development and Port Authority. Dr. Inwards-Breland and Dr. Breuner have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender and nonbinary young people experienced less depression and fewer suicidal thoughts after a year of gender-affirming care with hormones or puberty blockers, according to new research.
“Given the high rates of adverse mental health comorbidities, these data provide critical evidence that expansion of gender-affirming care can save lives,” said David J. Inwards-Breland, MD, MPH, chief of adolescent and young adult medicine and codirector of the Center for Gender-Affirming Care at Rady Children’s Hospital in San Diego, during his presentation.
The findings, presented October 11 at the American Academy of Pediatrics 2021 National Conference, were not at all surprising to Cora Breuner, MD, MPH, professor of pediatrics at Seattle Children’s Hospital.
“The younger we can provide gender-affirming care, the less likely they’re going to have depression, and then the negative outcomes from untreated depression, which includes suicide intent or even suicide completion,” Dr. Breuner told this news organization. “It’s so obvious that we are saving lives by providing gender-affirming care.”
For their study, Dr. Inwards-Breland and his colleagues tracked depression, anxiety, and suicidality in 104 trans and nonbinary people 13 to 21 years of age who received care at the Seattle Children’s gender clinic between August 2017 and June 2018.
The study population consisted of 63 transgender male or male participants, 27 transgender female or female participants, 10 nonbinary participants, and four participants who had not defined their gender identity. Of this cohort, 62.5% were receiving mental health therapy, and 34.7% reported some substance use.
Participants completed the nine-item Patient Health Questionnaire (PHQ-9) and the seven-item Generalized Anxiety Disorder scale (GAD-7) at baseline and then at 3, 6, and 12 months. The researchers defined severe depression and severe anxiety as a score of 10 or greater on either scale.
At baseline, 56.7% of the participants had moderate to severe depression, 43.3% reported thoughts of self-harm or suicidal in the previous 2 weeks, and 50.0% had moderate to severe anxiety.
After 12 months of care, participants experienced a 60% decrease in depression (adjusted odds ratio, 0.4) and a 73% decrease in suicidality (aOR, 0.27), after adjustment for temporal trends and sex assigned at birth, race/ethnicity, level of parental support, ongoing mental health therapy, substance use, and victimization, including bullying, interpersonal violence, neglect, and abuse.
Although the decline in depression and suicidality after gender-affirming treatment was not a surprise, “those drops are huge,” Dr. Inwards-Breland said in an interview.
He said he attributes the improvement to a health care system that “affirms who these young people are” and enables changes that allow their outward appearance to reflect “who they know they are inside.”
There were no significant changes in anxiety during the study period. “Anxiety, I think, is just a little harder to treat, and it takes a little longer to treat,” he explained. And a lot of factors can trigger anxiety, and those can continue during treatment.
The slow pace of changes to gender identity can have an effect on people’s moods. “Since they’re not happening quickly, these young people are still being misgendered, they’re still seeing the body that they don’t feel like they should have, and they have to go to school and go out in public. I think that continues to fuel anxiety with a lot of these young people.”
Family support is important in reducing depression and suicidal thoughts in this population. Parents will often see positive changes after their child receives gender-affirming care, which can help contribute to positive changes in parents’ attitudes, Dr. Inwards-Breland said.
Such changes reinforce “that protective factor of connectedness with family,” he noted. “Families are crucial for any health care, and if there’s that connectedness with families, we know that, clinically, patients do better.”
Balancing risks
Although there are risks associated with gender-affirming hormones and puberty blockers, the risks of not receiving treatment must also be considered.
“Our young people are killing themselves,” he said. “Our young people are developing severe eating disorders that are killing them. Our young people are increasing their substance abuse, homelessness, depression. The list just goes on.”
For trans-masculine and nonbinary masculine patients, the potential permanent changes of hormone therapy include a deeper voice, hair growth, enlargement of the clitoris, and, in some patients, the development of male pattern baldness. In trans and nonbinary feminine patients, potential long-term effects include breast development and an increased risk for fertility issues.
The consent forms required for young people who want gender-affirming hormones or puberty blockers are extensive, with every possible reversible and irreversible effect described in detail, Dr. Breuner said.
“Parents sign them because they want their child to stay alive,” she explained. “When you compare the cost of someone who has severe debilitating depression and dying by suicide with some of the risks associated with gender-affirming hormone therapy, that’s a no-brainer to me.”
This study is limited by the fact that screening tests, not diagnostic tests, were used to identify depression, anxiety, and suicidality, and the fact that the use of antidepression or antianxiety medications was not taken into account, Dr. Inwards-Breland acknowledged.
“I think future studies should look at a mental health evaluation and diagnosis by a mental health provider,” he added. And mental health, gender dysphoria, suicidality, and self-harm should be tracked over the course of treatment.
He also acknowledged the study’s selection bias. All participants sought care at a multidisciplinary gender clinic, so were likely to be privileged and to have supportive families. “There’s a good chance that if we had more trans and nonbinary youth of color, we may have different findings,” he said.
More qualitative research is needed to assess the effect of gender-affirming therapy on the mental health of these patients, Dr. Breuner said.
“Being able to finally come into who you think you are and enjoy expressing who you are in a gender-affirming way has to be positive in such a way that you’re not depressed anymore,” she added. “It has to be tragic for people who cannot stand the body they’re in and cannot talk about it to anybody or express themselves without fear of recourse, to the point that they would be so devastated that they’d want to die by suicide.”
This research was funded by the Seattle Children’s Center for Diversity and Health Equity and the Pacific Hospital Development and Port Authority. Dr. Inwards-Breland and Dr. Breuner have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Call them by their names in your office
Given that approximately 9.5% of youth aged 13-17 in the United States identify as lesbian, gay, bisexual, transgender, or queer (LGBTQ),1 it is likely that a general pediatrician or pediatric subspecialist is going to encounter at least one LGBTQ patient during the course of the average workweek. By having an easy way to identify these patients and store this data in a user-friendly manner, you can ensure that your practice is LGBTQ friendly and an affirming environment for all sexual- and gender-minority youth.
One way to do this is to look over any paper or electronic forms your practice uses and make sure that they provide patients and families a range of options to identify themselves. For example, you could provide more options for gender, other than male or female, including a nonbinary or “other” (with a free text line) option. This allows your patients to give you an accurate description of what their affirmed gender is. Instead of having a space for mother’s name and father’s name, you could list these fields as “parent/guardian #1” and “parent/guardian #2.” These labels allow for more inclusivity and to reflect the diverse makeup of modern families. Providing a space for a patient to put the name and pronouns that they use allows your staff to make sure that you are calling a patient by the correct name and using the correct pronouns.
Within your EMR, there may be editable fields that allow for you or your staff to list the patient’s affirmed name and pronouns. Making this small change allows any staff member who accesses the chart to have that information displayed correctly for them and reduces the chances of staff misgendering or dead-naming a patient. Underscoring the importance of this, Sequeira et al. found that in a sample of youth from a gender clinic, only 9% of those adolescents reported that they were asked their name/pronouns outside of the gender clinic.2 If those fields are not there, you may check with your IT staff or your EMR vendor to see if these fields may be added in. However, staff needs to make sure that they check with the child/adolescent first to discern with whom the patient has discussed their gender identity. If you were to put a patient’s affirmed name into the chart and then call the patient by that name in front of the parent/guardian, the parent/guardian may look at you quizzically about why you are calling their child by that name. This could then cause an uncomfortable conversation in the exam room or result in harm to the patient after the visit.
It is not just good clinical practice to ensure that you use a patient’s affirmed name and pronouns. Russell et al. looked at the relationship between depressive symptoms and suicidal ideation and whether an adolescent’s name/pronouns were used in the context of their home, school, work, and/or friend group. They found that use of an adolescent’s affirmed name in at least one of these contexts was associated with a decrease in depressive symptoms and a 29% decrease in suicidal ideation.3 Therefore, the use of an adolescent’s affirmed name and pronouns in your office contributes to the overall mental well-being of your patients.
Fortunately, there are many guides to help you and your practice be successful at implementing some of these changes. The Gay, Lesbian, Bisexual and Transgender Health Access Project put together its “Community Standards of Practice for the Provision of Quality Health Care Services to Lesbian, Gay, Bisexual, and Transgender Clients” to aid practices in developing environments that are LGBTQ affirming. The National LGBTQIA+ Health Education Center, a part of the Fenway Institute, has a series of learning modules that you and your staff can view for interactive training and tips for best practices. These resources offer pediatricians and their practices free resources to improve their policies and procedures. By instituting these small changes, you can ensure that your practice continues to be an affirming environment for your LGBTQ children and adolescents.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Conran KJ. LGBT youth population in the United States, UCLA School of Law, Williams Institute, 2020 Sep.
2. Sequeira GM et al. Affirming transgender youths’ names and pronouns in the electronic medical record. JAMA Pediatr. 2020;174(5):501-3.
3. Russell ST et al. Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. J Adolesc Health. 2018;63(4):503-5.
Given that approximately 9.5% of youth aged 13-17 in the United States identify as lesbian, gay, bisexual, transgender, or queer (LGBTQ),1 it is likely that a general pediatrician or pediatric subspecialist is going to encounter at least one LGBTQ patient during the course of the average workweek. By having an easy way to identify these patients and store this data in a user-friendly manner, you can ensure that your practice is LGBTQ friendly and an affirming environment for all sexual- and gender-minority youth.
One way to do this is to look over any paper or electronic forms your practice uses and make sure that they provide patients and families a range of options to identify themselves. For example, you could provide more options for gender, other than male or female, including a nonbinary or “other” (with a free text line) option. This allows your patients to give you an accurate description of what their affirmed gender is. Instead of having a space for mother’s name and father’s name, you could list these fields as “parent/guardian #1” and “parent/guardian #2.” These labels allow for more inclusivity and to reflect the diverse makeup of modern families. Providing a space for a patient to put the name and pronouns that they use allows your staff to make sure that you are calling a patient by the correct name and using the correct pronouns.
Within your EMR, there may be editable fields that allow for you or your staff to list the patient’s affirmed name and pronouns. Making this small change allows any staff member who accesses the chart to have that information displayed correctly for them and reduces the chances of staff misgendering or dead-naming a patient. Underscoring the importance of this, Sequeira et al. found that in a sample of youth from a gender clinic, only 9% of those adolescents reported that they were asked their name/pronouns outside of the gender clinic.2 If those fields are not there, you may check with your IT staff or your EMR vendor to see if these fields may be added in. However, staff needs to make sure that they check with the child/adolescent first to discern with whom the patient has discussed their gender identity. If you were to put a patient’s affirmed name into the chart and then call the patient by that name in front of the parent/guardian, the parent/guardian may look at you quizzically about why you are calling their child by that name. This could then cause an uncomfortable conversation in the exam room or result in harm to the patient after the visit.
It is not just good clinical practice to ensure that you use a patient’s affirmed name and pronouns. Russell et al. looked at the relationship between depressive symptoms and suicidal ideation and whether an adolescent’s name/pronouns were used in the context of their home, school, work, and/or friend group. They found that use of an adolescent’s affirmed name in at least one of these contexts was associated with a decrease in depressive symptoms and a 29% decrease in suicidal ideation.3 Therefore, the use of an adolescent’s affirmed name and pronouns in your office contributes to the overall mental well-being of your patients.
Fortunately, there are many guides to help you and your practice be successful at implementing some of these changes. The Gay, Lesbian, Bisexual and Transgender Health Access Project put together its “Community Standards of Practice for the Provision of Quality Health Care Services to Lesbian, Gay, Bisexual, and Transgender Clients” to aid practices in developing environments that are LGBTQ affirming. The National LGBTQIA+ Health Education Center, a part of the Fenway Institute, has a series of learning modules that you and your staff can view for interactive training and tips for best practices. These resources offer pediatricians and their practices free resources to improve their policies and procedures. By instituting these small changes, you can ensure that your practice continues to be an affirming environment for your LGBTQ children and adolescents.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Conran KJ. LGBT youth population in the United States, UCLA School of Law, Williams Institute, 2020 Sep.
2. Sequeira GM et al. Affirming transgender youths’ names and pronouns in the electronic medical record. JAMA Pediatr. 2020;174(5):501-3.
3. Russell ST et al. Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. J Adolesc Health. 2018;63(4):503-5.
Given that approximately 9.5% of youth aged 13-17 in the United States identify as lesbian, gay, bisexual, transgender, or queer (LGBTQ),1 it is likely that a general pediatrician or pediatric subspecialist is going to encounter at least one LGBTQ patient during the course of the average workweek. By having an easy way to identify these patients and store this data in a user-friendly manner, you can ensure that your practice is LGBTQ friendly and an affirming environment for all sexual- and gender-minority youth.
One way to do this is to look over any paper or electronic forms your practice uses and make sure that they provide patients and families a range of options to identify themselves. For example, you could provide more options for gender, other than male or female, including a nonbinary or “other” (with a free text line) option. This allows your patients to give you an accurate description of what their affirmed gender is. Instead of having a space for mother’s name and father’s name, you could list these fields as “parent/guardian #1” and “parent/guardian #2.” These labels allow for more inclusivity and to reflect the diverse makeup of modern families. Providing a space for a patient to put the name and pronouns that they use allows your staff to make sure that you are calling a patient by the correct name and using the correct pronouns.
Within your EMR, there may be editable fields that allow for you or your staff to list the patient’s affirmed name and pronouns. Making this small change allows any staff member who accesses the chart to have that information displayed correctly for them and reduces the chances of staff misgendering or dead-naming a patient. Underscoring the importance of this, Sequeira et al. found that in a sample of youth from a gender clinic, only 9% of those adolescents reported that they were asked their name/pronouns outside of the gender clinic.2 If those fields are not there, you may check with your IT staff or your EMR vendor to see if these fields may be added in. However, staff needs to make sure that they check with the child/adolescent first to discern with whom the patient has discussed their gender identity. If you were to put a patient’s affirmed name into the chart and then call the patient by that name in front of the parent/guardian, the parent/guardian may look at you quizzically about why you are calling their child by that name. This could then cause an uncomfortable conversation in the exam room or result in harm to the patient after the visit.
It is not just good clinical practice to ensure that you use a patient’s affirmed name and pronouns. Russell et al. looked at the relationship between depressive symptoms and suicidal ideation and whether an adolescent’s name/pronouns were used in the context of their home, school, work, and/or friend group. They found that use of an adolescent’s affirmed name in at least one of these contexts was associated with a decrease in depressive symptoms and a 29% decrease in suicidal ideation.3 Therefore, the use of an adolescent’s affirmed name and pronouns in your office contributes to the overall mental well-being of your patients.
Fortunately, there are many guides to help you and your practice be successful at implementing some of these changes. The Gay, Lesbian, Bisexual and Transgender Health Access Project put together its “Community Standards of Practice for the Provision of Quality Health Care Services to Lesbian, Gay, Bisexual, and Transgender Clients” to aid practices in developing environments that are LGBTQ affirming. The National LGBTQIA+ Health Education Center, a part of the Fenway Institute, has a series of learning modules that you and your staff can view for interactive training and tips for best practices. These resources offer pediatricians and their practices free resources to improve their policies and procedures. By instituting these small changes, you can ensure that your practice continues to be an affirming environment for your LGBTQ children and adolescents.
Dr. Cooper is assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Conran KJ. LGBT youth population in the United States, UCLA School of Law, Williams Institute, 2020 Sep.
2. Sequeira GM et al. Affirming transgender youths’ names and pronouns in the electronic medical record. JAMA Pediatr. 2020;174(5):501-3.
3. Russell ST et al. Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. J Adolesc Health. 2018;63(4):503-5.
HHS okays first U.S. pilot to mandate coverage of gender-affirming care
The approval means transgender-related care must be included as part of the essential benefits offered on the state’s Affordable Care Act marketplace, which includes private individual and small group insurance plans. The coverage will start Jan. 1, 2023. Colorado is the first state in the United States to require such coverage.
The HHS notes that gender-affirming treatments to be covered include eye and lid modifications, face tightening, facial bone remodeling for facial feminization, breast/chest construction and reductions, and laser hair removal.
“I am proud to stand with Colorado to remove barriers that have historically made it difficult for transgender people to access health coverage and medical care,” said HHS Secretary Xavier Becerra in a statement.
“Colorado’s expansion of their essential health benefits to include gender-affirming surgery and other treatments is a model for other states to follow, and we invite other states to follow suit,” said Centers for Medicare & Medicaid Services Administrator Chiquita Brooks-LaSure in the statement.
Medicaid already covers comprehensive transgender care in Colorado.
The LGBTQ+ advocacy group One Colorado estimated that, thanks to the Affordable Care Act, only 5% of the state’s LGBTQ+ community was uninsured in 2019, compared to 10% in 2011.
However, 34% of transgender respondents to a One Colorado poll in 2018 said they had been denied coverage for an LGBTQ-specific medical service, such as gender-affirming care. Sixty-two percent said that a lack of insurance or limited insurance was a barrier to care; 84% said another barrier was the lack of adequately trained mental and behavioral health professionals.
Mental health also covered
The Colorado plan requires individual and small group plans to cover an annual 45- to 60-minute mental health wellness exam with a qualified mental health care practitioner. The visit can include behavioral health screening, education and consultation about healthy lifestyle changes, referrals to mental health treatment, and discussion of potential medication options.
The plans also must cover an additional 15 medications as alternatives to opioids and up to six acupuncture visits annually.
“This plan expands access to mental health services for Coloradans while helping those fighting substance abuse to overcome their addiction,” said Governor Jared Polis in a statement.
“This improves care for Coloradans and ensures that even more Coloradans have access to help when they need it,” he said.
A version of this article first appeared on Medscape.com.
The approval means transgender-related care must be included as part of the essential benefits offered on the state’s Affordable Care Act marketplace, which includes private individual and small group insurance plans. The coverage will start Jan. 1, 2023. Colorado is the first state in the United States to require such coverage.
The HHS notes that gender-affirming treatments to be covered include eye and lid modifications, face tightening, facial bone remodeling for facial feminization, breast/chest construction and reductions, and laser hair removal.
“I am proud to stand with Colorado to remove barriers that have historically made it difficult for transgender people to access health coverage and medical care,” said HHS Secretary Xavier Becerra in a statement.
“Colorado’s expansion of their essential health benefits to include gender-affirming surgery and other treatments is a model for other states to follow, and we invite other states to follow suit,” said Centers for Medicare & Medicaid Services Administrator Chiquita Brooks-LaSure in the statement.
Medicaid already covers comprehensive transgender care in Colorado.
The LGBTQ+ advocacy group One Colorado estimated that, thanks to the Affordable Care Act, only 5% of the state’s LGBTQ+ community was uninsured in 2019, compared to 10% in 2011.
However, 34% of transgender respondents to a One Colorado poll in 2018 said they had been denied coverage for an LGBTQ-specific medical service, such as gender-affirming care. Sixty-two percent said that a lack of insurance or limited insurance was a barrier to care; 84% said another barrier was the lack of adequately trained mental and behavioral health professionals.
Mental health also covered
The Colorado plan requires individual and small group plans to cover an annual 45- to 60-minute mental health wellness exam with a qualified mental health care practitioner. The visit can include behavioral health screening, education and consultation about healthy lifestyle changes, referrals to mental health treatment, and discussion of potential medication options.
The plans also must cover an additional 15 medications as alternatives to opioids and up to six acupuncture visits annually.
“This plan expands access to mental health services for Coloradans while helping those fighting substance abuse to overcome their addiction,” said Governor Jared Polis in a statement.
“This improves care for Coloradans and ensures that even more Coloradans have access to help when they need it,” he said.
A version of this article first appeared on Medscape.com.
The approval means transgender-related care must be included as part of the essential benefits offered on the state’s Affordable Care Act marketplace, which includes private individual and small group insurance plans. The coverage will start Jan. 1, 2023. Colorado is the first state in the United States to require such coverage.
The HHS notes that gender-affirming treatments to be covered include eye and lid modifications, face tightening, facial bone remodeling for facial feminization, breast/chest construction and reductions, and laser hair removal.
“I am proud to stand with Colorado to remove barriers that have historically made it difficult for transgender people to access health coverage and medical care,” said HHS Secretary Xavier Becerra in a statement.
“Colorado’s expansion of their essential health benefits to include gender-affirming surgery and other treatments is a model for other states to follow, and we invite other states to follow suit,” said Centers for Medicare & Medicaid Services Administrator Chiquita Brooks-LaSure in the statement.
Medicaid already covers comprehensive transgender care in Colorado.
The LGBTQ+ advocacy group One Colorado estimated that, thanks to the Affordable Care Act, only 5% of the state’s LGBTQ+ community was uninsured in 2019, compared to 10% in 2011.
However, 34% of transgender respondents to a One Colorado poll in 2018 said they had been denied coverage for an LGBTQ-specific medical service, such as gender-affirming care. Sixty-two percent said that a lack of insurance or limited insurance was a barrier to care; 84% said another barrier was the lack of adequately trained mental and behavioral health professionals.
Mental health also covered
The Colorado plan requires individual and small group plans to cover an annual 45- to 60-minute mental health wellness exam with a qualified mental health care practitioner. The visit can include behavioral health screening, education and consultation about healthy lifestyle changes, referrals to mental health treatment, and discussion of potential medication options.
The plans also must cover an additional 15 medications as alternatives to opioids and up to six acupuncture visits annually.
“This plan expands access to mental health services for Coloradans while helping those fighting substance abuse to overcome their addiction,” said Governor Jared Polis in a statement.
“This improves care for Coloradans and ensures that even more Coloradans have access to help when they need it,” he said.
A version of this article first appeared on Medscape.com.
FDA OKs iPLEDGE change for gender-neutral language
The Food and Drug Administration has approved a modification to the isotretinoin risk-mitigation program to make it more inclusive for transgender patients.
Beginning on Dec. 13, 2021, Previously, there were three risk categories: females of reproductive potential, females not of reproductive potential, and males.
In recent years, dermatologists and others have advocated for the change, hoping to make the process more inclusive and less intrusive for their transgender patients.
Isotretinoin (Accutane, Absorica, Amnesteem, Claravis, others) has a high risk of severe birth defects, and has been linked with other health issues, making it crucial for those with the ability to become pregnant to take contraceptive precautions while on the medication. Under the iPLEDGE program, physicians, patients, and pharmacies prescribing, using, or dispensing the drug must all be registered, with requirements that include the use of two forms of an effective contraceptive and regular pregnancy testing for patients who can become pregnant.
The FDA had given notification in June 2018 that the REMS modification and labeling change would be required, replacing the gender-specific language with gender-neutral language, according to an FDA spokesperson. The change was based on feedback that the gender-specific language can be a barrier to access for some patients. The FDA approved the modification on Oct. 8.
Expert reactions
“This is an exciting and welcome change from the FDA on iPLEDGE that many dermatologists, myself included, have advocated for quite a few years,” Howa Yeung, MD, MSc, assistant professor of dermatology at Emory University, Atlanta, said in an interview.
In a report on the dermatologic care for lesbian, gay, bisexual, and transgender persons published in the Journal of the American Academy of Dermatology, Dr. Yeung and his colleagues noted that more than 10 million lesbian, gay, bisexual and transgender people live in the United States and that improving their health is a public health priority.
“For cisgender patients, nothing has changed – patients will continue to receive appropriate educational material related to isotretinoin based on their pregnancy potential,” Dr. Yeung said. “For transgender and gender diverse patients, this is a huge step forward.”
Under the previous system, doctors were asked to register patients using gender binary categories, “which were confusing when they did not reflect reality” for these patients, Dr. Yeung said. The new system, Dr. Yeung added, “will make my job easier. I no longer have to struggle between respecting the patient’s gender identity and providing medically necessary care for patients with severe acne.”
“The new terminology is not just respectful, it also is simpler and makes more sense,” agreed Joshua D. Safer, MD, executive director of the Center for Transgender Medicine and Surgery at Mount Sinai Health System and professor of medicine at the Icahn School of Medicine at Mount Sinai, New York. “As it stood, a transgender man with his uterus and ovaries in place might be missed in the pregnancy surveillance system because he could simply be labeled a man and not followed further. At the same time, both transgender women and cisgender women who were at no risk of pregnancy could be subject to more medical scrutiny that might have been consider intrusive.”
The change “validates the important point that pregnancy potential is not exclusively defined by sociocultural constructs of gender and allow dermatologists to focus purely on what matters when prescribing isotretinoin – whether an individual is able to become pregnant or not, regardless of their gender identity,” Klint Peebles, MD, a dermatologist at Kaiser Permanente in Washington, D.C., and suburban Maryland, who has also advocated for the change, said in an interview.
FDA elaborates
The modification includes important changes for doctors, pharmacists, and patients alike, according to the FDA.
Health care providers must assign and confirm their currently enrolled patient’s risk category when they first log in to the IPLEDGE REMS website on or after Dec. 13, the effective date. They should be sure any patient whose prescription RMA (iPLEDGE authorization) expires on Dec. 11-12 is told to obtain their prescription before midnight, Eastern time, Dec. 10.
Pharmacists will be affected, too, since the iPLEDGE REMS changed to a new platform vendor and the current “switch” pharmacy management system will be removed as a method to verify authorization to dispense isotretinoin. With these changes, as of Dec. 13, pharmacists can’t use the switch system to obtain a predispense authorization, or RMA (risk management authorization). They will need to obtain an RMA online by accessing the iPLEDGE REMS website or via telephone to the PLEDGE REMS center, 866-495-0654, before dispensing the prescription.
Patients, beginning Dec. 13, will have the option of presenting a unique QR code at the pharmacy on their smartphone rather than providing the iPLEDGE identification number. The code can be accessed by logging into their account on the iPLEDGE REMS website.
Patients with an isotretinoin prescription RMA that expires Dec. 11-12, must obtain the prescription before 11:59 p.m. Eastern time on Dec. 10. If the RMA expires before the prescription is picked up, the patient must begin the authorization process all over again.
Dr. Safer, Dr. Yeung, and Dr. Peebles have no relevant disclosures.
More information on the update and the isotretinoin REMS program is available on the FDA website.
The Food and Drug Administration has approved a modification to the isotretinoin risk-mitigation program to make it more inclusive for transgender patients.
Beginning on Dec. 13, 2021, Previously, there were three risk categories: females of reproductive potential, females not of reproductive potential, and males.
In recent years, dermatologists and others have advocated for the change, hoping to make the process more inclusive and less intrusive for their transgender patients.
Isotretinoin (Accutane, Absorica, Amnesteem, Claravis, others) has a high risk of severe birth defects, and has been linked with other health issues, making it crucial for those with the ability to become pregnant to take contraceptive precautions while on the medication. Under the iPLEDGE program, physicians, patients, and pharmacies prescribing, using, or dispensing the drug must all be registered, with requirements that include the use of two forms of an effective contraceptive and regular pregnancy testing for patients who can become pregnant.
The FDA had given notification in June 2018 that the REMS modification and labeling change would be required, replacing the gender-specific language with gender-neutral language, according to an FDA spokesperson. The change was based on feedback that the gender-specific language can be a barrier to access for some patients. The FDA approved the modification on Oct. 8.
Expert reactions
“This is an exciting and welcome change from the FDA on iPLEDGE that many dermatologists, myself included, have advocated for quite a few years,” Howa Yeung, MD, MSc, assistant professor of dermatology at Emory University, Atlanta, said in an interview.
In a report on the dermatologic care for lesbian, gay, bisexual, and transgender persons published in the Journal of the American Academy of Dermatology, Dr. Yeung and his colleagues noted that more than 10 million lesbian, gay, bisexual and transgender people live in the United States and that improving their health is a public health priority.
“For cisgender patients, nothing has changed – patients will continue to receive appropriate educational material related to isotretinoin based on their pregnancy potential,” Dr. Yeung said. “For transgender and gender diverse patients, this is a huge step forward.”
Under the previous system, doctors were asked to register patients using gender binary categories, “which were confusing when they did not reflect reality” for these patients, Dr. Yeung said. The new system, Dr. Yeung added, “will make my job easier. I no longer have to struggle between respecting the patient’s gender identity and providing medically necessary care for patients with severe acne.”
“The new terminology is not just respectful, it also is simpler and makes more sense,” agreed Joshua D. Safer, MD, executive director of the Center for Transgender Medicine and Surgery at Mount Sinai Health System and professor of medicine at the Icahn School of Medicine at Mount Sinai, New York. “As it stood, a transgender man with his uterus and ovaries in place might be missed in the pregnancy surveillance system because he could simply be labeled a man and not followed further. At the same time, both transgender women and cisgender women who were at no risk of pregnancy could be subject to more medical scrutiny that might have been consider intrusive.”
The change “validates the important point that pregnancy potential is not exclusively defined by sociocultural constructs of gender and allow dermatologists to focus purely on what matters when prescribing isotretinoin – whether an individual is able to become pregnant or not, regardless of their gender identity,” Klint Peebles, MD, a dermatologist at Kaiser Permanente in Washington, D.C., and suburban Maryland, who has also advocated for the change, said in an interview.
FDA elaborates
The modification includes important changes for doctors, pharmacists, and patients alike, according to the FDA.
Health care providers must assign and confirm their currently enrolled patient’s risk category when they first log in to the IPLEDGE REMS website on or after Dec. 13, the effective date. They should be sure any patient whose prescription RMA (iPLEDGE authorization) expires on Dec. 11-12 is told to obtain their prescription before midnight, Eastern time, Dec. 10.
Pharmacists will be affected, too, since the iPLEDGE REMS changed to a new platform vendor and the current “switch” pharmacy management system will be removed as a method to verify authorization to dispense isotretinoin. With these changes, as of Dec. 13, pharmacists can’t use the switch system to obtain a predispense authorization, or RMA (risk management authorization). They will need to obtain an RMA online by accessing the iPLEDGE REMS website or via telephone to the PLEDGE REMS center, 866-495-0654, before dispensing the prescription.
Patients, beginning Dec. 13, will have the option of presenting a unique QR code at the pharmacy on their smartphone rather than providing the iPLEDGE identification number. The code can be accessed by logging into their account on the iPLEDGE REMS website.
Patients with an isotretinoin prescription RMA that expires Dec. 11-12, must obtain the prescription before 11:59 p.m. Eastern time on Dec. 10. If the RMA expires before the prescription is picked up, the patient must begin the authorization process all over again.
Dr. Safer, Dr. Yeung, and Dr. Peebles have no relevant disclosures.
More information on the update and the isotretinoin REMS program is available on the FDA website.
The Food and Drug Administration has approved a modification to the isotretinoin risk-mitigation program to make it more inclusive for transgender patients.
Beginning on Dec. 13, 2021, Previously, there were three risk categories: females of reproductive potential, females not of reproductive potential, and males.
In recent years, dermatologists and others have advocated for the change, hoping to make the process more inclusive and less intrusive for their transgender patients.
Isotretinoin (Accutane, Absorica, Amnesteem, Claravis, others) has a high risk of severe birth defects, and has been linked with other health issues, making it crucial for those with the ability to become pregnant to take contraceptive precautions while on the medication. Under the iPLEDGE program, physicians, patients, and pharmacies prescribing, using, or dispensing the drug must all be registered, with requirements that include the use of two forms of an effective contraceptive and regular pregnancy testing for patients who can become pregnant.
The FDA had given notification in June 2018 that the REMS modification and labeling change would be required, replacing the gender-specific language with gender-neutral language, according to an FDA spokesperson. The change was based on feedback that the gender-specific language can be a barrier to access for some patients. The FDA approved the modification on Oct. 8.
Expert reactions
“This is an exciting and welcome change from the FDA on iPLEDGE that many dermatologists, myself included, have advocated for quite a few years,” Howa Yeung, MD, MSc, assistant professor of dermatology at Emory University, Atlanta, said in an interview.
In a report on the dermatologic care for lesbian, gay, bisexual, and transgender persons published in the Journal of the American Academy of Dermatology, Dr. Yeung and his colleagues noted that more than 10 million lesbian, gay, bisexual and transgender people live in the United States and that improving their health is a public health priority.
“For cisgender patients, nothing has changed – patients will continue to receive appropriate educational material related to isotretinoin based on their pregnancy potential,” Dr. Yeung said. “For transgender and gender diverse patients, this is a huge step forward.”
Under the previous system, doctors were asked to register patients using gender binary categories, “which were confusing when they did not reflect reality” for these patients, Dr. Yeung said. The new system, Dr. Yeung added, “will make my job easier. I no longer have to struggle between respecting the patient’s gender identity and providing medically necessary care for patients with severe acne.”
“The new terminology is not just respectful, it also is simpler and makes more sense,” agreed Joshua D. Safer, MD, executive director of the Center for Transgender Medicine and Surgery at Mount Sinai Health System and professor of medicine at the Icahn School of Medicine at Mount Sinai, New York. “As it stood, a transgender man with his uterus and ovaries in place might be missed in the pregnancy surveillance system because he could simply be labeled a man and not followed further. At the same time, both transgender women and cisgender women who were at no risk of pregnancy could be subject to more medical scrutiny that might have been consider intrusive.”
The change “validates the important point that pregnancy potential is not exclusively defined by sociocultural constructs of gender and allow dermatologists to focus purely on what matters when prescribing isotretinoin – whether an individual is able to become pregnant or not, regardless of their gender identity,” Klint Peebles, MD, a dermatologist at Kaiser Permanente in Washington, D.C., and suburban Maryland, who has also advocated for the change, said in an interview.
FDA elaborates
The modification includes important changes for doctors, pharmacists, and patients alike, according to the FDA.
Health care providers must assign and confirm their currently enrolled patient’s risk category when they first log in to the IPLEDGE REMS website on or after Dec. 13, the effective date. They should be sure any patient whose prescription RMA (iPLEDGE authorization) expires on Dec. 11-12 is told to obtain their prescription before midnight, Eastern time, Dec. 10.
Pharmacists will be affected, too, since the iPLEDGE REMS changed to a new platform vendor and the current “switch” pharmacy management system will be removed as a method to verify authorization to dispense isotretinoin. With these changes, as of Dec. 13, pharmacists can’t use the switch system to obtain a predispense authorization, or RMA (risk management authorization). They will need to obtain an RMA online by accessing the iPLEDGE REMS website or via telephone to the PLEDGE REMS center, 866-495-0654, before dispensing the prescription.
Patients, beginning Dec. 13, will have the option of presenting a unique QR code at the pharmacy on their smartphone rather than providing the iPLEDGE identification number. The code can be accessed by logging into their account on the iPLEDGE REMS website.
Patients with an isotretinoin prescription RMA that expires Dec. 11-12, must obtain the prescription before 11:59 p.m. Eastern time on Dec. 10. If the RMA expires before the prescription is picked up, the patient must begin the authorization process all over again.
Dr. Safer, Dr. Yeung, and Dr. Peebles have no relevant disclosures.
More information on the update and the isotretinoin REMS program is available on the FDA website.
Psychiatrists shift stance on gender dysphoria, recommend therapy
A new position statement from the Royal Australian and New Zealand College of Psychiatrists (RANZCP) stresses the importance of a mental health evaluation for people with gender dysphoria – in particular for children and adolescents – before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries, often referred to as “gender-affirming care.”
“There is a paucity of quality evidence on the outcomes of those presenting with gender dysphoria. In particular, there is a need for better evidence in relation to outcomes for children and young people,” the guidance states.
Because gender dysphoria “is associated with significant distress ... each case should be assessed by a mental health professional, which will frequently be a psychiatrist, with the person at the center of care. It is important the psychological state and context in which gender dysphoria has arisen is explored to assess the most appropriate treatment,” it adds.
The move by the psychiatry body represents a big shift in the landscape regarding recommendations for the treatment of gender dysphoria in Australia and New Zealand.
Asked to explain the new RANZCP position, Philip Morris, MBBS, FRANZCP, said: “The College acknowledged the complexity of the issues and the legitimacy of different approaches.”
Exploration of a patient’s reasons for identifying as transgender is essential, he said in an interview, especially when it comes to young people.
“There may be other reasons for doing it, and we need to look for those, identify them and treat them. This needs to be done before initiating hormones and changing the whole physical nature of the child,” he said.
“A cautious psychotherapy-first approach makes sense. If we can do that with adolescents, then we will take a big step in the right direction,” stressed Dr. Morris, who is president of the National Association of Practising Psychiatrists in Australia.
Keira Bell case and Scandinavian stance lead to more open discussion
The rapid rise in gender dysphoria among adolescents in the Western world, referred to as “rapid-onset” or “late-onset” gender dysphoria, has seen a huge increase in the number of natal girls presenting and created frenzied debate that has intensified worldwide in the last 12 months about how to best treat youth with gender dysphoria.
Concerns have arisen that some transgender identification is due to social contagion, and there is a growing number of “detransitioners” – people who identified as transgender, transitioned to the opposite gender, but then regretted their decision, changed their minds, and “detransitioned” back to their birth sex. If they have had hormone therapy, and in some cases surgery, they are left with irreversible changes to their bodies.
As a result, Scandinavian countries, most notably Finland, once eager advocates of the gender-affirmative approach, have pulled back and issued new treatment guidelines in 2020 stating that psychotherapy, rather than gender reassignment, should be the first line of treatment for gender-dysphoric youth.
This, along with a landmark High Court decision in the U.K. regarding the use of puberty-blocking drugs for children with gender dysphoria, brought by detransitioner Keira Bell, which was recently overturned by the Appeal Court, but which Ms. Bell now says she will take to the Supreme Court, has led to a considerable shift in the conversation around treating transgender adolescents with hormonal therapy, says Dr. Morris.
“This [has moved from] ... a topic that could previously not be talked about freely to one that we can discuss more openly now. This is a big improvement. Previously, everyone thought it was all settled, but it’s not, certainly not from a medical angle,” he states.
At odds with prior Australian recommendations
The RANZCP had previously endorsed the standard guidelines of the Royal Children’s Hospital (RCH) Melbourne, followed by most gender-identity services in Australia and similar guidance from New Zealand, which both recommend gender-affirming care.
“Increasing evidence demonstrates that with supportive, gender-affirming care during childhood and adolescence, harms can be ameliorated and mental health and well-being outcomes can be significantly improved,” state the RCH guidelines.
But in 2019, RANZCP removed its endorsement of the RCH guidelines and started a consultation, which resulted in the new position statement.
However, Ken Pang, MD, of the Murdoch Children’s Research Institute in Melbourne and an author of the RCH guidelines, says the key recommendations of the new RANZCP position statement are consistent with their own guidelines.
The former note “the need for a skilled mental health clinician in providing comprehensive exploration of a child or adolescent’s biopsychosocial context,” Dr. Pang says.
However, it’s difficult not to see the contrast in stance when the new RANZCP statement maintains: “Research on gender dysphoria is still emerging. There are polarized views and mixed evidence regarding treatment options for people presenting with gender identity concerns, especially children and young people.”
Dr. Pang says the RCH guidelines do, however, recognize the need for further research in the field.
“I look forward to being able to incorporate such research, including from our own Trans20 study, into future revisions of our guidelines,” he told this news organization.
Watch your backs with affirmative therapy: Will there be a compromise?
Dr. Morris says there will obviously be cases where “the child might transition with a medical intervention, but that wouldn’t be the first step.”
And yet, he adds, “There are those who push the pro-trans view that everyone should be allowed to transition, and the doctors are only technicians that provide hormones with no questions asked.”
But from a doctor’s perspective, clinicians will still be held responsible in medical and legal terms for the treatments given, he stressed.
“I don’t think they will ever not be accountable for that. They will always need to determine in their own mind whether their actions have positive value that outweigh any disadvantages,” Dr. Morris continues.
The RANZCP statement does, in fact, stress just this.
All health care professionals need to “be aware of ethical and medicolegal dilemmas” pertaining to affirmative therapy, it indicates. “Psychiatrists should practice within the relevant laws and accepted professional standards in relation to assessing capacity and obtaining consent...”
Dr. Morris hopes there will ultimately be many more checks and balances in place and that courts and clinicians will need to step back and not assume every child who seeks to transition is doing it as a result of pure gender dysphoria.
He predicts that things will end in a compromise.
“In my view, this compromise will treat children with respect and approach them like any other patient that presents with a condition that requires proper assessment and treatment.”
“In the end, some cases will be transitioned, but there will be fewer than [are] transitioned at the moment,” he predicts.
Dr. Morris has reported no relevant financial relationships. Dr. Pang is a member of the Australian Professional Association for Trans Health and its research committee.
A version of this article first appeared on Medscape.com.
A new position statement from the Royal Australian and New Zealand College of Psychiatrists (RANZCP) stresses the importance of a mental health evaluation for people with gender dysphoria – in particular for children and adolescents – before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries, often referred to as “gender-affirming care.”
“There is a paucity of quality evidence on the outcomes of those presenting with gender dysphoria. In particular, there is a need for better evidence in relation to outcomes for children and young people,” the guidance states.
Because gender dysphoria “is associated with significant distress ... each case should be assessed by a mental health professional, which will frequently be a psychiatrist, with the person at the center of care. It is important the psychological state and context in which gender dysphoria has arisen is explored to assess the most appropriate treatment,” it adds.
The move by the psychiatry body represents a big shift in the landscape regarding recommendations for the treatment of gender dysphoria in Australia and New Zealand.
Asked to explain the new RANZCP position, Philip Morris, MBBS, FRANZCP, said: “The College acknowledged the complexity of the issues and the legitimacy of different approaches.”
Exploration of a patient’s reasons for identifying as transgender is essential, he said in an interview, especially when it comes to young people.
“There may be other reasons for doing it, and we need to look for those, identify them and treat them. This needs to be done before initiating hormones and changing the whole physical nature of the child,” he said.
“A cautious psychotherapy-first approach makes sense. If we can do that with adolescents, then we will take a big step in the right direction,” stressed Dr. Morris, who is president of the National Association of Practising Psychiatrists in Australia.
Keira Bell case and Scandinavian stance lead to more open discussion
The rapid rise in gender dysphoria among adolescents in the Western world, referred to as “rapid-onset” or “late-onset” gender dysphoria, has seen a huge increase in the number of natal girls presenting and created frenzied debate that has intensified worldwide in the last 12 months about how to best treat youth with gender dysphoria.
Concerns have arisen that some transgender identification is due to social contagion, and there is a growing number of “detransitioners” – people who identified as transgender, transitioned to the opposite gender, but then regretted their decision, changed their minds, and “detransitioned” back to their birth sex. If they have had hormone therapy, and in some cases surgery, they are left with irreversible changes to their bodies.
As a result, Scandinavian countries, most notably Finland, once eager advocates of the gender-affirmative approach, have pulled back and issued new treatment guidelines in 2020 stating that psychotherapy, rather than gender reassignment, should be the first line of treatment for gender-dysphoric youth.
This, along with a landmark High Court decision in the U.K. regarding the use of puberty-blocking drugs for children with gender dysphoria, brought by detransitioner Keira Bell, which was recently overturned by the Appeal Court, but which Ms. Bell now says she will take to the Supreme Court, has led to a considerable shift in the conversation around treating transgender adolescents with hormonal therapy, says Dr. Morris.
“This [has moved from] ... a topic that could previously not be talked about freely to one that we can discuss more openly now. This is a big improvement. Previously, everyone thought it was all settled, but it’s not, certainly not from a medical angle,” he states.
At odds with prior Australian recommendations
The RANZCP had previously endorsed the standard guidelines of the Royal Children’s Hospital (RCH) Melbourne, followed by most gender-identity services in Australia and similar guidance from New Zealand, which both recommend gender-affirming care.
“Increasing evidence demonstrates that with supportive, gender-affirming care during childhood and adolescence, harms can be ameliorated and mental health and well-being outcomes can be significantly improved,” state the RCH guidelines.
But in 2019, RANZCP removed its endorsement of the RCH guidelines and started a consultation, which resulted in the new position statement.
However, Ken Pang, MD, of the Murdoch Children’s Research Institute in Melbourne and an author of the RCH guidelines, says the key recommendations of the new RANZCP position statement are consistent with their own guidelines.
The former note “the need for a skilled mental health clinician in providing comprehensive exploration of a child or adolescent’s biopsychosocial context,” Dr. Pang says.
However, it’s difficult not to see the contrast in stance when the new RANZCP statement maintains: “Research on gender dysphoria is still emerging. There are polarized views and mixed evidence regarding treatment options for people presenting with gender identity concerns, especially children and young people.”
Dr. Pang says the RCH guidelines do, however, recognize the need for further research in the field.
“I look forward to being able to incorporate such research, including from our own Trans20 study, into future revisions of our guidelines,” he told this news organization.
Watch your backs with affirmative therapy: Will there be a compromise?
Dr. Morris says there will obviously be cases where “the child might transition with a medical intervention, but that wouldn’t be the first step.”
And yet, he adds, “There are those who push the pro-trans view that everyone should be allowed to transition, and the doctors are only technicians that provide hormones with no questions asked.”
But from a doctor’s perspective, clinicians will still be held responsible in medical and legal terms for the treatments given, he stressed.
“I don’t think they will ever not be accountable for that. They will always need to determine in their own mind whether their actions have positive value that outweigh any disadvantages,” Dr. Morris continues.
The RANZCP statement does, in fact, stress just this.
All health care professionals need to “be aware of ethical and medicolegal dilemmas” pertaining to affirmative therapy, it indicates. “Psychiatrists should practice within the relevant laws and accepted professional standards in relation to assessing capacity and obtaining consent...”
Dr. Morris hopes there will ultimately be many more checks and balances in place and that courts and clinicians will need to step back and not assume every child who seeks to transition is doing it as a result of pure gender dysphoria.
He predicts that things will end in a compromise.
“In my view, this compromise will treat children with respect and approach them like any other patient that presents with a condition that requires proper assessment and treatment.”
“In the end, some cases will be transitioned, but there will be fewer than [are] transitioned at the moment,” he predicts.
Dr. Morris has reported no relevant financial relationships. Dr. Pang is a member of the Australian Professional Association for Trans Health and its research committee.
A version of this article first appeared on Medscape.com.
A new position statement from the Royal Australian and New Zealand College of Psychiatrists (RANZCP) stresses the importance of a mental health evaluation for people with gender dysphoria – in particular for children and adolescents – before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries, often referred to as “gender-affirming care.”
“There is a paucity of quality evidence on the outcomes of those presenting with gender dysphoria. In particular, there is a need for better evidence in relation to outcomes for children and young people,” the guidance states.
Because gender dysphoria “is associated with significant distress ... each case should be assessed by a mental health professional, which will frequently be a psychiatrist, with the person at the center of care. It is important the psychological state and context in which gender dysphoria has arisen is explored to assess the most appropriate treatment,” it adds.
The move by the psychiatry body represents a big shift in the landscape regarding recommendations for the treatment of gender dysphoria in Australia and New Zealand.
Asked to explain the new RANZCP position, Philip Morris, MBBS, FRANZCP, said: “The College acknowledged the complexity of the issues and the legitimacy of different approaches.”
Exploration of a patient’s reasons for identifying as transgender is essential, he said in an interview, especially when it comes to young people.
“There may be other reasons for doing it, and we need to look for those, identify them and treat them. This needs to be done before initiating hormones and changing the whole physical nature of the child,” he said.
“A cautious psychotherapy-first approach makes sense. If we can do that with adolescents, then we will take a big step in the right direction,” stressed Dr. Morris, who is president of the National Association of Practising Psychiatrists in Australia.
Keira Bell case and Scandinavian stance lead to more open discussion
The rapid rise in gender dysphoria among adolescents in the Western world, referred to as “rapid-onset” or “late-onset” gender dysphoria, has seen a huge increase in the number of natal girls presenting and created frenzied debate that has intensified worldwide in the last 12 months about how to best treat youth with gender dysphoria.
Concerns have arisen that some transgender identification is due to social contagion, and there is a growing number of “detransitioners” – people who identified as transgender, transitioned to the opposite gender, but then regretted their decision, changed their minds, and “detransitioned” back to their birth sex. If they have had hormone therapy, and in some cases surgery, they are left with irreversible changes to their bodies.
As a result, Scandinavian countries, most notably Finland, once eager advocates of the gender-affirmative approach, have pulled back and issued new treatment guidelines in 2020 stating that psychotherapy, rather than gender reassignment, should be the first line of treatment for gender-dysphoric youth.
This, along with a landmark High Court decision in the U.K. regarding the use of puberty-blocking drugs for children with gender dysphoria, brought by detransitioner Keira Bell, which was recently overturned by the Appeal Court, but which Ms. Bell now says she will take to the Supreme Court, has led to a considerable shift in the conversation around treating transgender adolescents with hormonal therapy, says Dr. Morris.
“This [has moved from] ... a topic that could previously not be talked about freely to one that we can discuss more openly now. This is a big improvement. Previously, everyone thought it was all settled, but it’s not, certainly not from a medical angle,” he states.
At odds with prior Australian recommendations
The RANZCP had previously endorsed the standard guidelines of the Royal Children’s Hospital (RCH) Melbourne, followed by most gender-identity services in Australia and similar guidance from New Zealand, which both recommend gender-affirming care.
“Increasing evidence demonstrates that with supportive, gender-affirming care during childhood and adolescence, harms can be ameliorated and mental health and well-being outcomes can be significantly improved,” state the RCH guidelines.
But in 2019, RANZCP removed its endorsement of the RCH guidelines and started a consultation, which resulted in the new position statement.
However, Ken Pang, MD, of the Murdoch Children’s Research Institute in Melbourne and an author of the RCH guidelines, says the key recommendations of the new RANZCP position statement are consistent with their own guidelines.
The former note “the need for a skilled mental health clinician in providing comprehensive exploration of a child or adolescent’s biopsychosocial context,” Dr. Pang says.
However, it’s difficult not to see the contrast in stance when the new RANZCP statement maintains: “Research on gender dysphoria is still emerging. There are polarized views and mixed evidence regarding treatment options for people presenting with gender identity concerns, especially children and young people.”
Dr. Pang says the RCH guidelines do, however, recognize the need for further research in the field.
“I look forward to being able to incorporate such research, including from our own Trans20 study, into future revisions of our guidelines,” he told this news organization.
Watch your backs with affirmative therapy: Will there be a compromise?
Dr. Morris says there will obviously be cases where “the child might transition with a medical intervention, but that wouldn’t be the first step.”
And yet, he adds, “There are those who push the pro-trans view that everyone should be allowed to transition, and the doctors are only technicians that provide hormones with no questions asked.”
But from a doctor’s perspective, clinicians will still be held responsible in medical and legal terms for the treatments given, he stressed.
“I don’t think they will ever not be accountable for that. They will always need to determine in their own mind whether their actions have positive value that outweigh any disadvantages,” Dr. Morris continues.
The RANZCP statement does, in fact, stress just this.
All health care professionals need to “be aware of ethical and medicolegal dilemmas” pertaining to affirmative therapy, it indicates. “Psychiatrists should practice within the relevant laws and accepted professional standards in relation to assessing capacity and obtaining consent...”
Dr. Morris hopes there will ultimately be many more checks and balances in place and that courts and clinicians will need to step back and not assume every child who seeks to transition is doing it as a result of pure gender dysphoria.
He predicts that things will end in a compromise.
“In my view, this compromise will treat children with respect and approach them like any other patient that presents with a condition that requires proper assessment and treatment.”
“In the end, some cases will be transitioned, but there will be fewer than [are] transitioned at the moment,” he predicts.
Dr. Morris has reported no relevant financial relationships. Dr. Pang is a member of the Australian Professional Association for Trans Health and its research committee.
A version of this article first appeared on Medscape.com.
Why Texas Senate Bill 8 will negatively affect LGBTQ patients
On Sept. 1, Texas enacted astonishing legislation that effectively bans abortion after a fetal heartbeat is detected. In addition, it further empowers private citizens to sue anyone “aiding and abetting” patients who seek abortion services. Many organizations, including Planned Parenthood and the American College of Obstetricians and Gynecologists, have issued formalized statements condemning the bill. While we as obstetrician/gynecologists try to remain as nonpartisan as humanly possible in our patient care, unfortunately our specialty is inarguably one of the few in the medical field that is routinely significantly affected by federal and state politics.
It is no secret that Texas Senate Bill 8, otherwise referred to the “Texas Heartbeat Act,” will have devastating consequences for women, particularly women of color, but it will also have potentially catastrophic repercussions for patients who identify as LGBTQ. Overall, the LGBTQ population faces higher rates of poverty, unemployment, insurance coverage barriers, and provider discrimination because of their gender identity or sexual orientation, which can make access to abortion services challenging. Furthermore, they are more susceptible to hate-motivated violence and sexual assault and as a result, may seek to terminate pregnancies that result from these traumatic experiences.
A survey conducted by the Centers for Disease Control and Prevention examining rates of intimate partner violence and sexual violence found that 44% of lesbians and 61% of bisexual women experience rape and physical violence, compared with 35% of straight women.1 A separate survey revealed that 47% of transgender people are sexually assaulted at some point in their lifetime, with rates reaching as high as 65% among transgender people of color.2 Furthermore, many members of the LGBTQ population are misinformed or have misconceptions regarding their need for contraceptives and experience unintended pregnancies. As discussed in a previous column, one-third of pregnancies in transgender men were unplanned, and 20% of those patients were amenorrheic on testosterone at the time of conception.3
Current studies estimate that approximately 25% of all cisgender women will have an abortion. No corresponding data exist to describe the abortion rates of transgender and gender diverse patients.4,5 Bills such as Texas SB8 make accessing safe abortions for patients virtually impossible and interferes with the ability for physicians to provide patients with much needed health care services. It further delegitimizes rape and incest victims and is almost punitive in requiring such victims to carry the unintended pregnancies resulting from these heinous acts to term.
Regardless of a provider’s feelings toward abortion or even gender-affirming care, it is undeniable that access to these services is necessary and should be readily available to patients seeking them. As we all took an oath in medical school to “do no harm,” we must not only abide by that solemn decree in everyday patient interactions, but also live by those words to advocate for our patients when politics prohibit appropriate care. While discussions surrounding abortion are often limited to cisgender, heterosexual patients, providers must also be aware that abortion access spans across a wider spectrum that includes the LGBTQ community. Our patients, and all patients, deserve equal access to abortion. This harmful law sets a dangerous precedent that could continue to threaten these services with detrimental effects to our patients.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Black MC et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2011.
2. James SE et al. The Report of the 2015 U.S. Transgender Survey. Washington, DC: National Center for Transgender Equality; 2016.
3. Abern L, Maguire K. Obstet Gynecol 2018;131:65S.
4. Jones RK et al. Abortion incidence and service availability in the Unites States, 2017. New York, NY: Guttmacher Institute: 2019.
5. Moseson H et al. Am J Obstet Gynecol 2021;224:376.e1-11.
On Sept. 1, Texas enacted astonishing legislation that effectively bans abortion after a fetal heartbeat is detected. In addition, it further empowers private citizens to sue anyone “aiding and abetting” patients who seek abortion services. Many organizations, including Planned Parenthood and the American College of Obstetricians and Gynecologists, have issued formalized statements condemning the bill. While we as obstetrician/gynecologists try to remain as nonpartisan as humanly possible in our patient care, unfortunately our specialty is inarguably one of the few in the medical field that is routinely significantly affected by federal and state politics.
It is no secret that Texas Senate Bill 8, otherwise referred to the “Texas Heartbeat Act,” will have devastating consequences for women, particularly women of color, but it will also have potentially catastrophic repercussions for patients who identify as LGBTQ. Overall, the LGBTQ population faces higher rates of poverty, unemployment, insurance coverage barriers, and provider discrimination because of their gender identity or sexual orientation, which can make access to abortion services challenging. Furthermore, they are more susceptible to hate-motivated violence and sexual assault and as a result, may seek to terminate pregnancies that result from these traumatic experiences.
A survey conducted by the Centers for Disease Control and Prevention examining rates of intimate partner violence and sexual violence found that 44% of lesbians and 61% of bisexual women experience rape and physical violence, compared with 35% of straight women.1 A separate survey revealed that 47% of transgender people are sexually assaulted at some point in their lifetime, with rates reaching as high as 65% among transgender people of color.2 Furthermore, many members of the LGBTQ population are misinformed or have misconceptions regarding their need for contraceptives and experience unintended pregnancies. As discussed in a previous column, one-third of pregnancies in transgender men were unplanned, and 20% of those patients were amenorrheic on testosterone at the time of conception.3
Current studies estimate that approximately 25% of all cisgender women will have an abortion. No corresponding data exist to describe the abortion rates of transgender and gender diverse patients.4,5 Bills such as Texas SB8 make accessing safe abortions for patients virtually impossible and interferes with the ability for physicians to provide patients with much needed health care services. It further delegitimizes rape and incest victims and is almost punitive in requiring such victims to carry the unintended pregnancies resulting from these heinous acts to term.
Regardless of a provider’s feelings toward abortion or even gender-affirming care, it is undeniable that access to these services is necessary and should be readily available to patients seeking them. As we all took an oath in medical school to “do no harm,” we must not only abide by that solemn decree in everyday patient interactions, but also live by those words to advocate for our patients when politics prohibit appropriate care. While discussions surrounding abortion are often limited to cisgender, heterosexual patients, providers must also be aware that abortion access spans across a wider spectrum that includes the LGBTQ community. Our patients, and all patients, deserve equal access to abortion. This harmful law sets a dangerous precedent that could continue to threaten these services with detrimental effects to our patients.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Black MC et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2011.
2. James SE et al. The Report of the 2015 U.S. Transgender Survey. Washington, DC: National Center for Transgender Equality; 2016.
3. Abern L, Maguire K. Obstet Gynecol 2018;131:65S.
4. Jones RK et al. Abortion incidence and service availability in the Unites States, 2017. New York, NY: Guttmacher Institute: 2019.
5. Moseson H et al. Am J Obstet Gynecol 2021;224:376.e1-11.
On Sept. 1, Texas enacted astonishing legislation that effectively bans abortion after a fetal heartbeat is detected. In addition, it further empowers private citizens to sue anyone “aiding and abetting” patients who seek abortion services. Many organizations, including Planned Parenthood and the American College of Obstetricians and Gynecologists, have issued formalized statements condemning the bill. While we as obstetrician/gynecologists try to remain as nonpartisan as humanly possible in our patient care, unfortunately our specialty is inarguably one of the few in the medical field that is routinely significantly affected by federal and state politics.
It is no secret that Texas Senate Bill 8, otherwise referred to the “Texas Heartbeat Act,” will have devastating consequences for women, particularly women of color, but it will also have potentially catastrophic repercussions for patients who identify as LGBTQ. Overall, the LGBTQ population faces higher rates of poverty, unemployment, insurance coverage barriers, and provider discrimination because of their gender identity or sexual orientation, which can make access to abortion services challenging. Furthermore, they are more susceptible to hate-motivated violence and sexual assault and as a result, may seek to terminate pregnancies that result from these traumatic experiences.
A survey conducted by the Centers for Disease Control and Prevention examining rates of intimate partner violence and sexual violence found that 44% of lesbians and 61% of bisexual women experience rape and physical violence, compared with 35% of straight women.1 A separate survey revealed that 47% of transgender people are sexually assaulted at some point in their lifetime, with rates reaching as high as 65% among transgender people of color.2 Furthermore, many members of the LGBTQ population are misinformed or have misconceptions regarding their need for contraceptives and experience unintended pregnancies. As discussed in a previous column, one-third of pregnancies in transgender men were unplanned, and 20% of those patients were amenorrheic on testosterone at the time of conception.3
Current studies estimate that approximately 25% of all cisgender women will have an abortion. No corresponding data exist to describe the abortion rates of transgender and gender diverse patients.4,5 Bills such as Texas SB8 make accessing safe abortions for patients virtually impossible and interferes with the ability for physicians to provide patients with much needed health care services. It further delegitimizes rape and incest victims and is almost punitive in requiring such victims to carry the unintended pregnancies resulting from these heinous acts to term.
Regardless of a provider’s feelings toward abortion or even gender-affirming care, it is undeniable that access to these services is necessary and should be readily available to patients seeking them. As we all took an oath in medical school to “do no harm,” we must not only abide by that solemn decree in everyday patient interactions, but also live by those words to advocate for our patients when politics prohibit appropriate care. While discussions surrounding abortion are often limited to cisgender, heterosexual patients, providers must also be aware that abortion access spans across a wider spectrum that includes the LGBTQ community. Our patients, and all patients, deserve equal access to abortion. This harmful law sets a dangerous precedent that could continue to threaten these services with detrimental effects to our patients.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Black MC et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2011.
2. James SE et al. The Report of the 2015 U.S. Transgender Survey. Washington, DC: National Center for Transgender Equality; 2016.
3. Abern L, Maguire K. Obstet Gynecol 2018;131:65S.
4. Jones RK et al. Abortion incidence and service availability in the Unites States, 2017. New York, NY: Guttmacher Institute: 2019.
5. Moseson H et al. Am J Obstet Gynecol 2021;224:376.e1-11.



