User login
Official Newspaper of the American College of Surgeons
Health exchanges could bring unpleasant surprises
SAN FRANCISCO – Stand by for some unexpected and potentially nasty surprises when the health insurance exchanges start up in 2014.
The exchanges will start enrolling patients this fall and begin sending information to patients and physicians as soon as this summer. Health insurers will begin sending new contracts to physicians at around the same time.
But there’s information available now that should send shivers up physicians’ spines, Elizabeth McNeil, vice president of the center for federal government relations at the California Medical Association, said at the annual meeting of the American College of Physicians.
A little-noticed provision of the Affordable Care Act gives exchange participants a 90-day grace period to pay their premiums. This was designed to provide a cushion for people who might not be used to paying health insurance premiums.
Insurers have to pay all claims incurred by the patient in the first month, but in the second month, if the patient is still delinquent, all claims can be held as pending. By the third month, if the patient still has not paid, the insurer can terminate him or her.
The physician then has to collect payment for all outstanding claims from the patient.
"This is going to put you at a lot of risk," Ms. McNeil said. "You’re going to have to be very vigilant with the exchange patients in watching what’s going on."
Ms. McNeil added in an interview later, "Why would a doctor sign up if they are going to be completely at risk and have to collect from the patient for the care?"
The CMA is seeking a change in the federal regulation on the grace period, which was included in the overall health insurance regulations issued in November 2012.
So far, none of the California insurers who have issued materials about their health insurance exchange plans have mentioned the grace period, Ms. McNeil said. She added that 33 health plans have said they were interested in participating in the California exchange, which is called Covered California.
Many patients who get insurance coverage through the health insurance exchanges will also have much larger out-of-pocket costs than they are used to paying, Ms. McNeil said. In California, the CMA estimates that an individual could face as much as $6,400 in uncovered expenses, and a family, up to $12,800.
Physicians also will need to pay close attention to the contracts they sign with health insurers that are participating in the exchanges. The exchange could bring a large number of new patients to the practice and physicians need to think about how many additional patients they can actually accommodate, she said.
Another thing to keep in mind: Does the contract have an all-payer clause that requires your practice to accept exchange patients? Can the practice opt in or out of a network? Many plans in California still have not determined their premiums or benefits for the exchange policies, which means they also have not set their reimbursement rates, Ms. McNeil said.
When negotiating rates, be aware that many of the patients who gain coverage via the health insurance exchanges will have pent-up demand for health care because they have previously been uninsured or underinsured, Ms. McNeil advised. Their care could be more complex and time consuming, so doctors will want to be sure that reimbursement rates are adequate to cover this care.
"There are a lot of issues here. You’re going to have to watch your practice and the big picture," she said.
On Twitter @aliciaault
SAN FRANCISCO – Stand by for some unexpected and potentially nasty surprises when the health insurance exchanges start up in 2014.
The exchanges will start enrolling patients this fall and begin sending information to patients and physicians as soon as this summer. Health insurers will begin sending new contracts to physicians at around the same time.
But there’s information available now that should send shivers up physicians’ spines, Elizabeth McNeil, vice president of the center for federal government relations at the California Medical Association, said at the annual meeting of the American College of Physicians.
A little-noticed provision of the Affordable Care Act gives exchange participants a 90-day grace period to pay their premiums. This was designed to provide a cushion for people who might not be used to paying health insurance premiums.
Insurers have to pay all claims incurred by the patient in the first month, but in the second month, if the patient is still delinquent, all claims can be held as pending. By the third month, if the patient still has not paid, the insurer can terminate him or her.
The physician then has to collect payment for all outstanding claims from the patient.
"This is going to put you at a lot of risk," Ms. McNeil said. "You’re going to have to be very vigilant with the exchange patients in watching what’s going on."
Ms. McNeil added in an interview later, "Why would a doctor sign up if they are going to be completely at risk and have to collect from the patient for the care?"
The CMA is seeking a change in the federal regulation on the grace period, which was included in the overall health insurance regulations issued in November 2012.
So far, none of the California insurers who have issued materials about their health insurance exchange plans have mentioned the grace period, Ms. McNeil said. She added that 33 health plans have said they were interested in participating in the California exchange, which is called Covered California.
Many patients who get insurance coverage through the health insurance exchanges will also have much larger out-of-pocket costs than they are used to paying, Ms. McNeil said. In California, the CMA estimates that an individual could face as much as $6,400 in uncovered expenses, and a family, up to $12,800.
Physicians also will need to pay close attention to the contracts they sign with health insurers that are participating in the exchanges. The exchange could bring a large number of new patients to the practice and physicians need to think about how many additional patients they can actually accommodate, she said.
Another thing to keep in mind: Does the contract have an all-payer clause that requires your practice to accept exchange patients? Can the practice opt in or out of a network? Many plans in California still have not determined their premiums or benefits for the exchange policies, which means they also have not set their reimbursement rates, Ms. McNeil said.
When negotiating rates, be aware that many of the patients who gain coverage via the health insurance exchanges will have pent-up demand for health care because they have previously been uninsured or underinsured, Ms. McNeil advised. Their care could be more complex and time consuming, so doctors will want to be sure that reimbursement rates are adequate to cover this care.
"There are a lot of issues here. You’re going to have to watch your practice and the big picture," she said.
On Twitter @aliciaault
SAN FRANCISCO – Stand by for some unexpected and potentially nasty surprises when the health insurance exchanges start up in 2014.
The exchanges will start enrolling patients this fall and begin sending information to patients and physicians as soon as this summer. Health insurers will begin sending new contracts to physicians at around the same time.
But there’s information available now that should send shivers up physicians’ spines, Elizabeth McNeil, vice president of the center for federal government relations at the California Medical Association, said at the annual meeting of the American College of Physicians.
A little-noticed provision of the Affordable Care Act gives exchange participants a 90-day grace period to pay their premiums. This was designed to provide a cushion for people who might not be used to paying health insurance premiums.
Insurers have to pay all claims incurred by the patient in the first month, but in the second month, if the patient is still delinquent, all claims can be held as pending. By the third month, if the patient still has not paid, the insurer can terminate him or her.
The physician then has to collect payment for all outstanding claims from the patient.
"This is going to put you at a lot of risk," Ms. McNeil said. "You’re going to have to be very vigilant with the exchange patients in watching what’s going on."
Ms. McNeil added in an interview later, "Why would a doctor sign up if they are going to be completely at risk and have to collect from the patient for the care?"
The CMA is seeking a change in the federal regulation on the grace period, which was included in the overall health insurance regulations issued in November 2012.
So far, none of the California insurers who have issued materials about their health insurance exchange plans have mentioned the grace period, Ms. McNeil said. She added that 33 health plans have said they were interested in participating in the California exchange, which is called Covered California.
Many patients who get insurance coverage through the health insurance exchanges will also have much larger out-of-pocket costs than they are used to paying, Ms. McNeil said. In California, the CMA estimates that an individual could face as much as $6,400 in uncovered expenses, and a family, up to $12,800.
Physicians also will need to pay close attention to the contracts they sign with health insurers that are participating in the exchanges. The exchange could bring a large number of new patients to the practice and physicians need to think about how many additional patients they can actually accommodate, she said.
Another thing to keep in mind: Does the contract have an all-payer clause that requires your practice to accept exchange patients? Can the practice opt in or out of a network? Many plans in California still have not determined their premiums or benefits for the exchange policies, which means they also have not set their reimbursement rates, Ms. McNeil said.
When negotiating rates, be aware that many of the patients who gain coverage via the health insurance exchanges will have pent-up demand for health care because they have previously been uninsured or underinsured, Ms. McNeil advised. Their care could be more complex and time consuming, so doctors will want to be sure that reimbursement rates are adequate to cover this care.
"There are a lot of issues here. You’re going to have to watch your practice and the big picture," she said.
On Twitter @aliciaault
AT ACP INTERNAL MEDICINE 2013
Adjuvant therapy selection in gastric cancer still more art than science
NATIONAL HARBOR, MD. – There are no hard and fast rules when it comes to selecting neoadjuvant or adjuvant therapy for patients with gastric cancer, according to Dr. Daniel G. Coit.
"Clinical trials of adjuvant therapy describe the impact of treatment on one group relative to another group. They do not predict the impact of treatment on an individual patient," said Dr. Coit, a surgical oncologist at Memorial Sloan-Kettering Cancer Center, New York.
Patient selection is a multi-step process that must incorporate an understanding of the risk of recurrence, the absolute benefit of treatment, strategies to improve the odds for achieving a benefit, and individual patient comorbidities and preferences, Dr. Coit said at the annual Society of Surgical Oncology Cancer Symposium.
Where oncologists often run into trouble is in the interpretation of data on benefits from clinical trials, and on the question of neoadjuvant vs. adjuvant therapy, both, or neither, he said.
Therapy delivered prior to surgery is likely to be better tolerated and improve the chance of R0 or "clean" resections. Neoadjuvant therapy can also help to identify, before surgery, those patients unlikely to respond metabolically or histologically to therapy, which can serve as both a prognostic factor for poor outcomes, and as a guide for additional pre- or postoperative therapy, Dr. Coit said.
Adjuvant therapy, on the other hand, allows treatment decisions to be based on an accurate estimate of recurrence risk using postoperative pathologic staging, he added.
"If we’re going to even consider preoperative therapy, neoadjuvant chemotherapy, we need to have some sense for how good our preoperative or pretreatment risk-assessment tools are. They’re not all that good," he said.
He noted that in a 2001 study (J. Clin. Gastroenterol. 2001;32:41-4) of 549 patients who were tested for carcinoembryonic antigen (CEA) and cancer antigen 19-9 (CA-19-9) before gastrectomy for gastric cancer, elevated levels of both markers were associated with "increased depth of invasion, more extensive nodal metastases, liver metastases, and less ‘curability.’ "
However, the authors found on multivariate analysis that a doubling of the normal threshold CEA was the only preoperative factor predictive of prognosis.
Endoscopic ultrasound (EUS), which is about 75% accurate at identifying node-positive vs. node-negative disease and at distinguishing early- from late-stage disease, is "very poorly predictive of outcome."
"The same thing happens with N stage: the endoscopic observation of node positivity is a terrible predictor of outcome," Dr. Coit said.
There are a few published nomograms that are fairly good at predicting disease-specific survival after R0 resections for gastric cancer, he noted, but these are all based on postoperative pathology findings, and "as yet we do not have a good nomogram for preoperative risk assessment."
Preventing recurrence
The goal of current therapy is to prevent recurrence at all costs, because few patients who experience recurrence will be salvageable, Dr. Coit said.
Studies of adjuvant therapy for gastric cancer with either postoperative 5-fluorauracil (5FU) and radiation (N. Engl. J. Med. 2001;345:725-30), postoperative epirubicin, cisplatin, and continuous 5FU infusion (ECF) (N. Engl. J. Med. 2006;355:11-20), or the oral fluoropyrimidine agent S-1, which is not available in the United States (N. Engl. J. Med. 2007:357:1810-20) all show about a 10% benefit, meaning that 10 patients would need to be treated for 1 to benefit.
More recently, in the CLASSIC trial (Lancet 2012;379:315-21) 1,035 patients with stage II-III gastric cancer who underwent curative resections with D2 extended lymph node dissection who were randomized to adjuvant capecitabine (Xeloda) and oxaliplatin had a 74% 3-year disease-free survival rate, compared with 59% for patients managed with postoperative observation only (hazard ratio 0.56, P less than .0001).
This trial showed that if patients are determined to have high-risk disease on postoperative pathology, "you have a very legitimate option available to you for postoperative treatment," Dr. Coit said.
In the ARTIST trial (J. Clin. Oncol. 2011;30:268-73), 458 patients underwent curative surgery with D2 lymph node dissection and were randomized to postoperative Xeloda/cisplatin (XP) or XP plus concurrent capecitabine radio therapy. The researchers found no statistically significant difference in 3-year disease-free survival among all patients, although there was some evidence of a benefit for XP plus radiation in patients with node-positive disease (P = .04).
Enriching the population
"It’s very clear that clinical trials do show a modest improvement in survival among the group of patients receiving adjuvant chemotherapy. The adjuvant therapy has no impact whatsoever in virtually 90% of the patients who are being treated, and we need to enrich this population that’s likely to benefit," he stated.
One strategy available for better selection of patients for adjuvant therapy is genetic tumor profiling to indentify targetable mutations such as HER-2 which is overexpressed in some gastric cancers.
A promising approach for identifying patients who might benefit from neoadjuvant therapy involves tumor uptake of fluorodeoxyglucose on positron-emission tomography (FDG-PET). In the MUNICON phase II trial (Lancet Oncol 2007;8:797-805), patients deemed to be responders, defined by decreases in tumor glucose standard uptake values (SUVs), had a median event-free survival of 29.7 months compared with 14.1 months in nonresponders (hazard ratio 2.18, P = .002), and 29 of 29 of 50 metabolic responders (58% ) had major histologic remissions, whereas none of the metabolic nonresponders did.
Dr. Coit reported having no financial disclosures.
NATIONAL HARBOR, MD. – There are no hard and fast rules when it comes to selecting neoadjuvant or adjuvant therapy for patients with gastric cancer, according to Dr. Daniel G. Coit.
"Clinical trials of adjuvant therapy describe the impact of treatment on one group relative to another group. They do not predict the impact of treatment on an individual patient," said Dr. Coit, a surgical oncologist at Memorial Sloan-Kettering Cancer Center, New York.
Patient selection is a multi-step process that must incorporate an understanding of the risk of recurrence, the absolute benefit of treatment, strategies to improve the odds for achieving a benefit, and individual patient comorbidities and preferences, Dr. Coit said at the annual Society of Surgical Oncology Cancer Symposium.
Where oncologists often run into trouble is in the interpretation of data on benefits from clinical trials, and on the question of neoadjuvant vs. adjuvant therapy, both, or neither, he said.
Therapy delivered prior to surgery is likely to be better tolerated and improve the chance of R0 or "clean" resections. Neoadjuvant therapy can also help to identify, before surgery, those patients unlikely to respond metabolically or histologically to therapy, which can serve as both a prognostic factor for poor outcomes, and as a guide for additional pre- or postoperative therapy, Dr. Coit said.
Adjuvant therapy, on the other hand, allows treatment decisions to be based on an accurate estimate of recurrence risk using postoperative pathologic staging, he added.
"If we’re going to even consider preoperative therapy, neoadjuvant chemotherapy, we need to have some sense for how good our preoperative or pretreatment risk-assessment tools are. They’re not all that good," he said.
He noted that in a 2001 study (J. Clin. Gastroenterol. 2001;32:41-4) of 549 patients who were tested for carcinoembryonic antigen (CEA) and cancer antigen 19-9 (CA-19-9) before gastrectomy for gastric cancer, elevated levels of both markers were associated with "increased depth of invasion, more extensive nodal metastases, liver metastases, and less ‘curability.’ "
However, the authors found on multivariate analysis that a doubling of the normal threshold CEA was the only preoperative factor predictive of prognosis.
Endoscopic ultrasound (EUS), which is about 75% accurate at identifying node-positive vs. node-negative disease and at distinguishing early- from late-stage disease, is "very poorly predictive of outcome."
"The same thing happens with N stage: the endoscopic observation of node positivity is a terrible predictor of outcome," Dr. Coit said.
There are a few published nomograms that are fairly good at predicting disease-specific survival after R0 resections for gastric cancer, he noted, but these are all based on postoperative pathology findings, and "as yet we do not have a good nomogram for preoperative risk assessment."
Preventing recurrence
The goal of current therapy is to prevent recurrence at all costs, because few patients who experience recurrence will be salvageable, Dr. Coit said.
Studies of adjuvant therapy for gastric cancer with either postoperative 5-fluorauracil (5FU) and radiation (N. Engl. J. Med. 2001;345:725-30), postoperative epirubicin, cisplatin, and continuous 5FU infusion (ECF) (N. Engl. J. Med. 2006;355:11-20), or the oral fluoropyrimidine agent S-1, which is not available in the United States (N. Engl. J. Med. 2007:357:1810-20) all show about a 10% benefit, meaning that 10 patients would need to be treated for 1 to benefit.
More recently, in the CLASSIC trial (Lancet 2012;379:315-21) 1,035 patients with stage II-III gastric cancer who underwent curative resections with D2 extended lymph node dissection who were randomized to adjuvant capecitabine (Xeloda) and oxaliplatin had a 74% 3-year disease-free survival rate, compared with 59% for patients managed with postoperative observation only (hazard ratio 0.56, P less than .0001).
This trial showed that if patients are determined to have high-risk disease on postoperative pathology, "you have a very legitimate option available to you for postoperative treatment," Dr. Coit said.
In the ARTIST trial (J. Clin. Oncol. 2011;30:268-73), 458 patients underwent curative surgery with D2 lymph node dissection and were randomized to postoperative Xeloda/cisplatin (XP) or XP plus concurrent capecitabine radio therapy. The researchers found no statistically significant difference in 3-year disease-free survival among all patients, although there was some evidence of a benefit for XP plus radiation in patients with node-positive disease (P = .04).
Enriching the population
"It’s very clear that clinical trials do show a modest improvement in survival among the group of patients receiving adjuvant chemotherapy. The adjuvant therapy has no impact whatsoever in virtually 90% of the patients who are being treated, and we need to enrich this population that’s likely to benefit," he stated.
One strategy available for better selection of patients for adjuvant therapy is genetic tumor profiling to indentify targetable mutations such as HER-2 which is overexpressed in some gastric cancers.
A promising approach for identifying patients who might benefit from neoadjuvant therapy involves tumor uptake of fluorodeoxyglucose on positron-emission tomography (FDG-PET). In the MUNICON phase II trial (Lancet Oncol 2007;8:797-805), patients deemed to be responders, defined by decreases in tumor glucose standard uptake values (SUVs), had a median event-free survival of 29.7 months compared with 14.1 months in nonresponders (hazard ratio 2.18, P = .002), and 29 of 29 of 50 metabolic responders (58% ) had major histologic remissions, whereas none of the metabolic nonresponders did.
Dr. Coit reported having no financial disclosures.
NATIONAL HARBOR, MD. – There are no hard and fast rules when it comes to selecting neoadjuvant or adjuvant therapy for patients with gastric cancer, according to Dr. Daniel G. Coit.
"Clinical trials of adjuvant therapy describe the impact of treatment on one group relative to another group. They do not predict the impact of treatment on an individual patient," said Dr. Coit, a surgical oncologist at Memorial Sloan-Kettering Cancer Center, New York.
Patient selection is a multi-step process that must incorporate an understanding of the risk of recurrence, the absolute benefit of treatment, strategies to improve the odds for achieving a benefit, and individual patient comorbidities and preferences, Dr. Coit said at the annual Society of Surgical Oncology Cancer Symposium.
Where oncologists often run into trouble is in the interpretation of data on benefits from clinical trials, and on the question of neoadjuvant vs. adjuvant therapy, both, or neither, he said.
Therapy delivered prior to surgery is likely to be better tolerated and improve the chance of R0 or "clean" resections. Neoadjuvant therapy can also help to identify, before surgery, those patients unlikely to respond metabolically or histologically to therapy, which can serve as both a prognostic factor for poor outcomes, and as a guide for additional pre- or postoperative therapy, Dr. Coit said.
Adjuvant therapy, on the other hand, allows treatment decisions to be based on an accurate estimate of recurrence risk using postoperative pathologic staging, he added.
"If we’re going to even consider preoperative therapy, neoadjuvant chemotherapy, we need to have some sense for how good our preoperative or pretreatment risk-assessment tools are. They’re not all that good," he said.
He noted that in a 2001 study (J. Clin. Gastroenterol. 2001;32:41-4) of 549 patients who were tested for carcinoembryonic antigen (CEA) and cancer antigen 19-9 (CA-19-9) before gastrectomy for gastric cancer, elevated levels of both markers were associated with "increased depth of invasion, more extensive nodal metastases, liver metastases, and less ‘curability.’ "
However, the authors found on multivariate analysis that a doubling of the normal threshold CEA was the only preoperative factor predictive of prognosis.
Endoscopic ultrasound (EUS), which is about 75% accurate at identifying node-positive vs. node-negative disease and at distinguishing early- from late-stage disease, is "very poorly predictive of outcome."
"The same thing happens with N stage: the endoscopic observation of node positivity is a terrible predictor of outcome," Dr. Coit said.
There are a few published nomograms that are fairly good at predicting disease-specific survival after R0 resections for gastric cancer, he noted, but these are all based on postoperative pathology findings, and "as yet we do not have a good nomogram for preoperative risk assessment."
Preventing recurrence
The goal of current therapy is to prevent recurrence at all costs, because few patients who experience recurrence will be salvageable, Dr. Coit said.
Studies of adjuvant therapy for gastric cancer with either postoperative 5-fluorauracil (5FU) and radiation (N. Engl. J. Med. 2001;345:725-30), postoperative epirubicin, cisplatin, and continuous 5FU infusion (ECF) (N. Engl. J. Med. 2006;355:11-20), or the oral fluoropyrimidine agent S-1, which is not available in the United States (N. Engl. J. Med. 2007:357:1810-20) all show about a 10% benefit, meaning that 10 patients would need to be treated for 1 to benefit.
More recently, in the CLASSIC trial (Lancet 2012;379:315-21) 1,035 patients with stage II-III gastric cancer who underwent curative resections with D2 extended lymph node dissection who were randomized to adjuvant capecitabine (Xeloda) and oxaliplatin had a 74% 3-year disease-free survival rate, compared with 59% for patients managed with postoperative observation only (hazard ratio 0.56, P less than .0001).
This trial showed that if patients are determined to have high-risk disease on postoperative pathology, "you have a very legitimate option available to you for postoperative treatment," Dr. Coit said.
In the ARTIST trial (J. Clin. Oncol. 2011;30:268-73), 458 patients underwent curative surgery with D2 lymph node dissection and were randomized to postoperative Xeloda/cisplatin (XP) or XP plus concurrent capecitabine radio therapy. The researchers found no statistically significant difference in 3-year disease-free survival among all patients, although there was some evidence of a benefit for XP plus radiation in patients with node-positive disease (P = .04).
Enriching the population
"It’s very clear that clinical trials do show a modest improvement in survival among the group of patients receiving adjuvant chemotherapy. The adjuvant therapy has no impact whatsoever in virtually 90% of the patients who are being treated, and we need to enrich this population that’s likely to benefit," he stated.
One strategy available for better selection of patients for adjuvant therapy is genetic tumor profiling to indentify targetable mutations such as HER-2 which is overexpressed in some gastric cancers.
A promising approach for identifying patients who might benefit from neoadjuvant therapy involves tumor uptake of fluorodeoxyglucose on positron-emission tomography (FDG-PET). In the MUNICON phase II trial (Lancet Oncol 2007;8:797-805), patients deemed to be responders, defined by decreases in tumor glucose standard uptake values (SUVs), had a median event-free survival of 29.7 months compared with 14.1 months in nonresponders (hazard ratio 2.18, P = .002), and 29 of 29 of 50 metabolic responders (58% ) had major histologic remissions, whereas none of the metabolic nonresponders did.
Dr. Coit reported having no financial disclosures.
AT SSO 2013
Obesity's price tag calculated in surgical patients
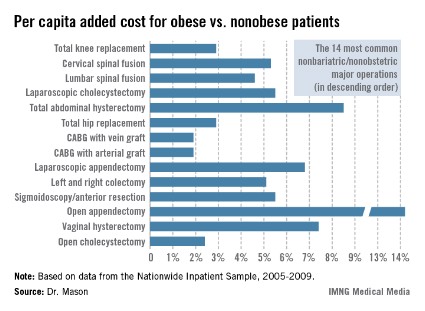
INDIANAPOLIS – Obesity adds an estimated $164 million annually to the total hospital cost of major nonbariatric/nonobstetric operative procedures, Dr. Rodney J. Mason reported at the annual meeting of the American Surgical Association.
And that figure, audience members were swift to point out, is a very, very conservative estimate.
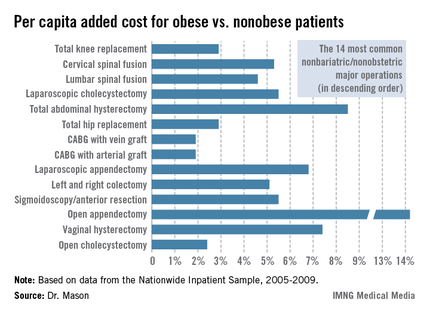
Dr. Mason presented an analysis of national cost estimates for obese vs. nonobese patients who underwent the 14 most common nonbariatric/nonobstetric major surgical procedures in the United States during 2005-2009 (see chart). He used data from the Nationwide Inpatient Sample (NIS) database sponsored by the Agency for Healthcare Research and Quality. The database provides detailed case information, including inpatient charges, from 20% of the nation’s hospitals.
One-quarter of the roughly 48 million hospitalized patients in the NIS database for this 5-year period underwent a major surgical procedure. Ten percent of patients who had 1 of the top 14 surgeries were obese. Dr. Mason and coworkers matched each of the 219,906 obese patients undergoing one of these operations to a nonobese patient who had the same operation; the tight one-to-one matching was based upon demographics and 28 defined comorbid conditions.
Because the NIS database records hospital charges, these charges had to be converted to estimated costs using a widely accepted formula. Once that was accomplished, the resultant annual total national estimated cost for the initial inpatient stay – not including physician costs – for patients undergoing one of the 14 surgical procedures was calculated at $4.38 billion in nonobese patients, compared with $4.55 billion in obese patients, for a $163,609,328 excess (3.7%) in the obese group, according to Dr. Mason of the University of Southern California, Los Angeles.
The mean per capita costs were $648 higher in obese than in nonobese surgical patients. To Dr. Mason’s surprise, this higher inpatient cost in the obese group was not driven by more postoperative complications; indeed, complication rates were equivalent in obese and nonobese patients. Instead, the explanation for the increased costs in the obese group was that they averaged a 0.025-day longer length of stay and they got significantly more secondary therapeutic, but not diagnostic, procedures.
Discussant Edward H. Livingston was sympathetic to the difficulties inherent in reliance upon the NIS database in conducting research, but he pointed out that the NIS is notoriously unreliable in recording obesity. This administrative database relies upon ICD-9 codes for obesity, and there’s good evidence that those codes often simply don’t get entered into the patient’s medical record. He noted that a mere 10% of the millions of surgical patients in the NIS database during the study years were categorized as obese, yet it’s well recognized that fully one-third of Americans are obese and another one-third are overweight. Clearly, then, a great many obese surgery patients were not captured in the study.
As for the study’s conclusion that the increased hospital costs in obese surgical patients were because of greater resource utilization and length of stay, Dr. Livingston said he thinks that’s probably all to the good.
"It may be that obese people do need more time in the hospital to recover and that they may need more resources to avoid more serious complications. We’ve learned how to better manage obese patients, and if those resources hadn’t been invested, then those patients might have done even worse," asserted Dr. Livingston, professor of surgery at the University of Texas Southwestern Medical Center, Dallas.
Taking care of obese patients is the reality of what physicians and surgeons deal with in hospitals now, he observed.
"Bariatric surgery has become the fifth most common operation in general surgery, and because of that we bariatric surgeons have taught everyone in the hospital how to take care of obese patients. We’ve learned over the years that there’s utility in using certain kinds of beds or having lifts available to move patients from one place to another. We’ve developed long instruments for facilitating laparoscopic surgery in obese patients. One of my own greatest learning experiences has been the utility of CPAP to manage morbidly obese patients in the postoperative period to help counter the effects of opiates and respiratory depression. The staff has become aware of how to take care of obese people and how to use medications appropriately in those people. All of that costs money," he said.
"Future research should aim to demonstrate that such costs are appropriate before Medicare does to us what it did with the so-called preventable complications, making a unilateral determination that we have too many complications or are spending too much money," the surgeon cautioned.
Dr. Mason responded that he’d like to see his study data shared with health policy makers in Washington.
"Hospitals get paid by [diagnosis-related group]. But if it costs more to manage obese patients, surely we should get more money to look after them. And right now we are not," he said.
Dr. Mason reported having no financial conflicts.
INDIANAPOLIS – Obesity adds an estimated $164 million annually to the total hospital cost of major nonbariatric/nonobstetric operative procedures, Dr. Rodney J. Mason reported at the annual meeting of the American Surgical Association.
And that figure, audience members were swift to point out, is a very, very conservative estimate.
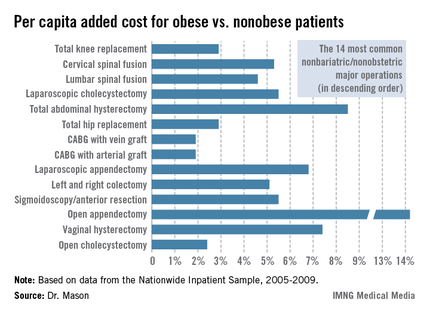
Dr. Mason presented an analysis of national cost estimates for obese vs. nonobese patients who underwent the 14 most common nonbariatric/nonobstetric major surgical procedures in the United States during 2005-2009 (see chart). He used data from the Nationwide Inpatient Sample (NIS) database sponsored by the Agency for Healthcare Research and Quality. The database provides detailed case information, including inpatient charges, from 20% of the nation’s hospitals.
One-quarter of the roughly 48 million hospitalized patients in the NIS database for this 5-year period underwent a major surgical procedure. Ten percent of patients who had 1 of the top 14 surgeries were obese. Dr. Mason and coworkers matched each of the 219,906 obese patients undergoing one of these operations to a nonobese patient who had the same operation; the tight one-to-one matching was based upon demographics and 28 defined comorbid conditions.
Because the NIS database records hospital charges, these charges had to be converted to estimated costs using a widely accepted formula. Once that was accomplished, the resultant annual total national estimated cost for the initial inpatient stay – not including physician costs – for patients undergoing one of the 14 surgical procedures was calculated at $4.38 billion in nonobese patients, compared with $4.55 billion in obese patients, for a $163,609,328 excess (3.7%) in the obese group, according to Dr. Mason of the University of Southern California, Los Angeles.
The mean per capita costs were $648 higher in obese than in nonobese surgical patients. To Dr. Mason’s surprise, this higher inpatient cost in the obese group was not driven by more postoperative complications; indeed, complication rates were equivalent in obese and nonobese patients. Instead, the explanation for the increased costs in the obese group was that they averaged a 0.025-day longer length of stay and they got significantly more secondary therapeutic, but not diagnostic, procedures.
Discussant Edward H. Livingston was sympathetic to the difficulties inherent in reliance upon the NIS database in conducting research, but he pointed out that the NIS is notoriously unreliable in recording obesity. This administrative database relies upon ICD-9 codes for obesity, and there’s good evidence that those codes often simply don’t get entered into the patient’s medical record. He noted that a mere 10% of the millions of surgical patients in the NIS database during the study years were categorized as obese, yet it’s well recognized that fully one-third of Americans are obese and another one-third are overweight. Clearly, then, a great many obese surgery patients were not captured in the study.
As for the study’s conclusion that the increased hospital costs in obese surgical patients were because of greater resource utilization and length of stay, Dr. Livingston said he thinks that’s probably all to the good.
"It may be that obese people do need more time in the hospital to recover and that they may need more resources to avoid more serious complications. We’ve learned how to better manage obese patients, and if those resources hadn’t been invested, then those patients might have done even worse," asserted Dr. Livingston, professor of surgery at the University of Texas Southwestern Medical Center, Dallas.
Taking care of obese patients is the reality of what physicians and surgeons deal with in hospitals now, he observed.
"Bariatric surgery has become the fifth most common operation in general surgery, and because of that we bariatric surgeons have taught everyone in the hospital how to take care of obese patients. We’ve learned over the years that there’s utility in using certain kinds of beds or having lifts available to move patients from one place to another. We’ve developed long instruments for facilitating laparoscopic surgery in obese patients. One of my own greatest learning experiences has been the utility of CPAP to manage morbidly obese patients in the postoperative period to help counter the effects of opiates and respiratory depression. The staff has become aware of how to take care of obese people and how to use medications appropriately in those people. All of that costs money," he said.
"Future research should aim to demonstrate that such costs are appropriate before Medicare does to us what it did with the so-called preventable complications, making a unilateral determination that we have too many complications or are spending too much money," the surgeon cautioned.
Dr. Mason responded that he’d like to see his study data shared with health policy makers in Washington.
"Hospitals get paid by [diagnosis-related group]. But if it costs more to manage obese patients, surely we should get more money to look after them. And right now we are not," he said.
Dr. Mason reported having no financial conflicts.
INDIANAPOLIS – Obesity adds an estimated $164 million annually to the total hospital cost of major nonbariatric/nonobstetric operative procedures, Dr. Rodney J. Mason reported at the annual meeting of the American Surgical Association.
And that figure, audience members were swift to point out, is a very, very conservative estimate.
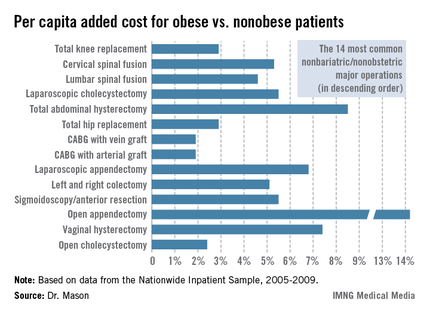
Dr. Mason presented an analysis of national cost estimates for obese vs. nonobese patients who underwent the 14 most common nonbariatric/nonobstetric major surgical procedures in the United States during 2005-2009 (see chart). He used data from the Nationwide Inpatient Sample (NIS) database sponsored by the Agency for Healthcare Research and Quality. The database provides detailed case information, including inpatient charges, from 20% of the nation’s hospitals.
One-quarter of the roughly 48 million hospitalized patients in the NIS database for this 5-year period underwent a major surgical procedure. Ten percent of patients who had 1 of the top 14 surgeries were obese. Dr. Mason and coworkers matched each of the 219,906 obese patients undergoing one of these operations to a nonobese patient who had the same operation; the tight one-to-one matching was based upon demographics and 28 defined comorbid conditions.
Because the NIS database records hospital charges, these charges had to be converted to estimated costs using a widely accepted formula. Once that was accomplished, the resultant annual total national estimated cost for the initial inpatient stay – not including physician costs – for patients undergoing one of the 14 surgical procedures was calculated at $4.38 billion in nonobese patients, compared with $4.55 billion in obese patients, for a $163,609,328 excess (3.7%) in the obese group, according to Dr. Mason of the University of Southern California, Los Angeles.
The mean per capita costs were $648 higher in obese than in nonobese surgical patients. To Dr. Mason’s surprise, this higher inpatient cost in the obese group was not driven by more postoperative complications; indeed, complication rates were equivalent in obese and nonobese patients. Instead, the explanation for the increased costs in the obese group was that they averaged a 0.025-day longer length of stay and they got significantly more secondary therapeutic, but not diagnostic, procedures.
Discussant Edward H. Livingston was sympathetic to the difficulties inherent in reliance upon the NIS database in conducting research, but he pointed out that the NIS is notoriously unreliable in recording obesity. This administrative database relies upon ICD-9 codes for obesity, and there’s good evidence that those codes often simply don’t get entered into the patient’s medical record. He noted that a mere 10% of the millions of surgical patients in the NIS database during the study years were categorized as obese, yet it’s well recognized that fully one-third of Americans are obese and another one-third are overweight. Clearly, then, a great many obese surgery patients were not captured in the study.
As for the study’s conclusion that the increased hospital costs in obese surgical patients were because of greater resource utilization and length of stay, Dr. Livingston said he thinks that’s probably all to the good.
"It may be that obese people do need more time in the hospital to recover and that they may need more resources to avoid more serious complications. We’ve learned how to better manage obese patients, and if those resources hadn’t been invested, then those patients might have done even worse," asserted Dr. Livingston, professor of surgery at the University of Texas Southwestern Medical Center, Dallas.
Taking care of obese patients is the reality of what physicians and surgeons deal with in hospitals now, he observed.
"Bariatric surgery has become the fifth most common operation in general surgery, and because of that we bariatric surgeons have taught everyone in the hospital how to take care of obese patients. We’ve learned over the years that there’s utility in using certain kinds of beds or having lifts available to move patients from one place to another. We’ve developed long instruments for facilitating laparoscopic surgery in obese patients. One of my own greatest learning experiences has been the utility of CPAP to manage morbidly obese patients in the postoperative period to help counter the effects of opiates and respiratory depression. The staff has become aware of how to take care of obese people and how to use medications appropriately in those people. All of that costs money," he said.
"Future research should aim to demonstrate that such costs are appropriate before Medicare does to us what it did with the so-called preventable complications, making a unilateral determination that we have too many complications or are spending too much money," the surgeon cautioned.
Dr. Mason responded that he’d like to see his study data shared with health policy makers in Washington.
"Hospitals get paid by [diagnosis-related group]. But if it costs more to manage obese patients, surely we should get more money to look after them. And right now we are not," he said.
Dr. Mason reported having no financial conflicts.
AT THE ASA ANNUAL MEETING
Major Finding: Obese patients undergoing 1 of the 14 most common nonbariatric/nonobstetric major surgical procedures had a mean average total hospital cost excluding physician fees that was $648 higher than for tightly matched nonobese patients undergoing the same operation. That added up to a national cost of roughly $164 million/year annually
Data Source: A matched pair analysis of data on 219,906 and an equal number of nonobese patients obtained from the Nationwide Inpatient Sample.
Disclosures: The Nationwide Inpatient Sample is sponsored by the Agency for Healthcare Research and Quality. The study presenter reported having no conflicts of interest.
Early cholecystectomy beats delayed in acute cholecystitis
INDIANAPOLIS – Acute cholecystitis patients fared significantly better with early rather than delayed laparoscopic cholecystectomy in the largest-ever randomized trial addressing surgical timing for this common condition.
Patients assigned to early cholecystectomy – that is, surgery within 24 hours of presentation to the hospital – had one-third the morbidity, markedly shorter hospital lengths of stay, and correspondingly lower hospital costs compared with patients who underwent surgery on day 7-45, according to Dr. Markus W. Buchler of Heidelberg (Ger.) University.
"Early cholecystectomy in patients fit for surgery and in hospitals experienced in doing difficult laparoscopic cholecystectomies should become the standard of care in acute cholecystitis," he declared in presenting the results of the ACDC (Acute Cholecystitis: Early Versus Delayed Cholecystectomy) trial at the annual meeting of the American Surgical Association.
The optimal timing of surgical intervention in acute cholecystitis is a subject of long-standing controversy. The ACDC trial was conducted because in a Cochrane review of five smaller randomized trials totaling 451 acute cholecystitis patients, researchers concluded there was insufficient evidence to say which surgical strategy was best (Cochrane Database Syst. Rev. 2006 Oct 18;4:CD005440).
Dr. Buchler noted that surveys indicate many American surgeons prefer to delay laparoscopic cholecystectomy, while in Germany the surgical preference is for immediate surgery in patients with uncomplicated acute cholecystitis.
The ACDC trial involved 618 patients with uncomplicated acute cholecystitis who were placed on the same antibiotic – moxifloxacin – and randomized to early laparoscopic cholecystectomy or to delayed surgery on day 7-45. Pregnant patients were excluded from the trial, which was conducted at 35 European hospitals, including seven German university medical centers. All participating hospitals were staffed by surgical teams experienced in performing difficult laparoscopic cholecystectomies.
The primary endpoint was total morbidity within 75 days. This included cholangitis, pancreatitis, biliary leak, stroke, myocardial infarction, abscess, bleeding, peritonitis, infection, and renal failure. The rate was 11.6% in the early cholecystectomy group compared with 31.3% with delayed surgery. Among less challenging patients with an ASA score of 2 or less, the rates were 9.7% and 28.6%, respectively. Patients with an ASA score above 2 had an overall morbidity rate of 20% with early surgery compared with 47% with delayed laparoscopic cholecystectomy.
The rate of conversion to open surgery was 9.9% in the early laparoscopic cholecystectomy group and similar at 11.9% in the delayed surgery group. This came as a surprise to Dr. Buchler and his coinvestigators. They expected a significantly higher conversion rate in conjunction with delayed laparoscopic cholecystectomy.
"I think what this tells us is surgeons have gotten really good at laparoscopic cholecystectomy even in more difficult situations," he observed.
Total hospital stays averaged 5.4 days in the early surgery group compared with 10.0 days with delayed surgery. Mean total hospital costs calculated via the German DRG system were 2,919 euro in the early cholecystectomy group and 4,261 euro with delayed surgery.
Discussant Dr. Andrew L. Warshaw praised Dr. Buchler and his coworkers in the German surgical clinical trials study group for their "leadership in determining evidence-based standards of care."
"There’s no doubt in my mind that immediate cholecystectomy is superior in this patient population," said Dr. Warshaw, professor and chairman of the department of surgery at Harvard Medical School, Boston.
Noting that most acute cholecystitis patients are first seen by an internist or gastroenterologist who then makes the initial treatment decision, Dr. Warshaw asked Dr. Buchler if German internists and gastroenterologists have gotten on board this immediate surgery treatment pathway.
"Convincing internists and gastroenterologists will take a long time, at least in Germany," the surgeon replied. "It is much easier to convince the emergency department physicians to refer patients early to surgery; they’re much closer to the surgeons."
He noted that German surgical practice differs from that in the United States in several respects. For one, German patients routinely stay in the hospital longer, even if they don’t experience complications. That’s why the mean length of stay after cholecystectomy in ACDC was 4.68 days in the early surgery group and closely similar at 4.89 days in the delayed surgery group, even though the delayed surgery group had a threefold higher complication rate.
Another difference is that, unlike in this country, intraoperative cholangiography is rarely done in Germany.
"It’s the absolute exception that intraoperative cholangiography is used. It is used only when there’s a reason for it, such as jaundice. There was probably less than a 3% intraoperative cholangiography rate in this trial," said Dr. Buchler.
The ACDC trial was funded with government research grants. Dr. Buchler reported having no financial conflicts.
INDIANAPOLIS – Acute cholecystitis patients fared significantly better with early rather than delayed laparoscopic cholecystectomy in the largest-ever randomized trial addressing surgical timing for this common condition.
Patients assigned to early cholecystectomy – that is, surgery within 24 hours of presentation to the hospital – had one-third the morbidity, markedly shorter hospital lengths of stay, and correspondingly lower hospital costs compared with patients who underwent surgery on day 7-45, according to Dr. Markus W. Buchler of Heidelberg (Ger.) University.
"Early cholecystectomy in patients fit for surgery and in hospitals experienced in doing difficult laparoscopic cholecystectomies should become the standard of care in acute cholecystitis," he declared in presenting the results of the ACDC (Acute Cholecystitis: Early Versus Delayed Cholecystectomy) trial at the annual meeting of the American Surgical Association.
The optimal timing of surgical intervention in acute cholecystitis is a subject of long-standing controversy. The ACDC trial was conducted because in a Cochrane review of five smaller randomized trials totaling 451 acute cholecystitis patients, researchers concluded there was insufficient evidence to say which surgical strategy was best (Cochrane Database Syst. Rev. 2006 Oct 18;4:CD005440).
Dr. Buchler noted that surveys indicate many American surgeons prefer to delay laparoscopic cholecystectomy, while in Germany the surgical preference is for immediate surgery in patients with uncomplicated acute cholecystitis.
The ACDC trial involved 618 patients with uncomplicated acute cholecystitis who were placed on the same antibiotic – moxifloxacin – and randomized to early laparoscopic cholecystectomy or to delayed surgery on day 7-45. Pregnant patients were excluded from the trial, which was conducted at 35 European hospitals, including seven German university medical centers. All participating hospitals were staffed by surgical teams experienced in performing difficult laparoscopic cholecystectomies.
The primary endpoint was total morbidity within 75 days. This included cholangitis, pancreatitis, biliary leak, stroke, myocardial infarction, abscess, bleeding, peritonitis, infection, and renal failure. The rate was 11.6% in the early cholecystectomy group compared with 31.3% with delayed surgery. Among less challenging patients with an ASA score of 2 or less, the rates were 9.7% and 28.6%, respectively. Patients with an ASA score above 2 had an overall morbidity rate of 20% with early surgery compared with 47% with delayed laparoscopic cholecystectomy.
The rate of conversion to open surgery was 9.9% in the early laparoscopic cholecystectomy group and similar at 11.9% in the delayed surgery group. This came as a surprise to Dr. Buchler and his coinvestigators. They expected a significantly higher conversion rate in conjunction with delayed laparoscopic cholecystectomy.
"I think what this tells us is surgeons have gotten really good at laparoscopic cholecystectomy even in more difficult situations," he observed.
Total hospital stays averaged 5.4 days in the early surgery group compared with 10.0 days with delayed surgery. Mean total hospital costs calculated via the German DRG system were 2,919 euro in the early cholecystectomy group and 4,261 euro with delayed surgery.
Discussant Dr. Andrew L. Warshaw praised Dr. Buchler and his coworkers in the German surgical clinical trials study group for their "leadership in determining evidence-based standards of care."
"There’s no doubt in my mind that immediate cholecystectomy is superior in this patient population," said Dr. Warshaw, professor and chairman of the department of surgery at Harvard Medical School, Boston.
Noting that most acute cholecystitis patients are first seen by an internist or gastroenterologist who then makes the initial treatment decision, Dr. Warshaw asked Dr. Buchler if German internists and gastroenterologists have gotten on board this immediate surgery treatment pathway.
"Convincing internists and gastroenterologists will take a long time, at least in Germany," the surgeon replied. "It is much easier to convince the emergency department physicians to refer patients early to surgery; they’re much closer to the surgeons."
He noted that German surgical practice differs from that in the United States in several respects. For one, German patients routinely stay in the hospital longer, even if they don’t experience complications. That’s why the mean length of stay after cholecystectomy in ACDC was 4.68 days in the early surgery group and closely similar at 4.89 days in the delayed surgery group, even though the delayed surgery group had a threefold higher complication rate.
Another difference is that, unlike in this country, intraoperative cholangiography is rarely done in Germany.
"It’s the absolute exception that intraoperative cholangiography is used. It is used only when there’s a reason for it, such as jaundice. There was probably less than a 3% intraoperative cholangiography rate in this trial," said Dr. Buchler.
The ACDC trial was funded with government research grants. Dr. Buchler reported having no financial conflicts.
INDIANAPOLIS – Acute cholecystitis patients fared significantly better with early rather than delayed laparoscopic cholecystectomy in the largest-ever randomized trial addressing surgical timing for this common condition.
Patients assigned to early cholecystectomy – that is, surgery within 24 hours of presentation to the hospital – had one-third the morbidity, markedly shorter hospital lengths of stay, and correspondingly lower hospital costs compared with patients who underwent surgery on day 7-45, according to Dr. Markus W. Buchler of Heidelberg (Ger.) University.
"Early cholecystectomy in patients fit for surgery and in hospitals experienced in doing difficult laparoscopic cholecystectomies should become the standard of care in acute cholecystitis," he declared in presenting the results of the ACDC (Acute Cholecystitis: Early Versus Delayed Cholecystectomy) trial at the annual meeting of the American Surgical Association.
The optimal timing of surgical intervention in acute cholecystitis is a subject of long-standing controversy. The ACDC trial was conducted because in a Cochrane review of five smaller randomized trials totaling 451 acute cholecystitis patients, researchers concluded there was insufficient evidence to say which surgical strategy was best (Cochrane Database Syst. Rev. 2006 Oct 18;4:CD005440).
Dr. Buchler noted that surveys indicate many American surgeons prefer to delay laparoscopic cholecystectomy, while in Germany the surgical preference is for immediate surgery in patients with uncomplicated acute cholecystitis.
The ACDC trial involved 618 patients with uncomplicated acute cholecystitis who were placed on the same antibiotic – moxifloxacin – and randomized to early laparoscopic cholecystectomy or to delayed surgery on day 7-45. Pregnant patients were excluded from the trial, which was conducted at 35 European hospitals, including seven German university medical centers. All participating hospitals were staffed by surgical teams experienced in performing difficult laparoscopic cholecystectomies.
The primary endpoint was total morbidity within 75 days. This included cholangitis, pancreatitis, biliary leak, stroke, myocardial infarction, abscess, bleeding, peritonitis, infection, and renal failure. The rate was 11.6% in the early cholecystectomy group compared with 31.3% with delayed surgery. Among less challenging patients with an ASA score of 2 or less, the rates were 9.7% and 28.6%, respectively. Patients with an ASA score above 2 had an overall morbidity rate of 20% with early surgery compared with 47% with delayed laparoscopic cholecystectomy.
The rate of conversion to open surgery was 9.9% in the early laparoscopic cholecystectomy group and similar at 11.9% in the delayed surgery group. This came as a surprise to Dr. Buchler and his coinvestigators. They expected a significantly higher conversion rate in conjunction with delayed laparoscopic cholecystectomy.
"I think what this tells us is surgeons have gotten really good at laparoscopic cholecystectomy even in more difficult situations," he observed.
Total hospital stays averaged 5.4 days in the early surgery group compared with 10.0 days with delayed surgery. Mean total hospital costs calculated via the German DRG system were 2,919 euro in the early cholecystectomy group and 4,261 euro with delayed surgery.
Discussant Dr. Andrew L. Warshaw praised Dr. Buchler and his coworkers in the German surgical clinical trials study group for their "leadership in determining evidence-based standards of care."
"There’s no doubt in my mind that immediate cholecystectomy is superior in this patient population," said Dr. Warshaw, professor and chairman of the department of surgery at Harvard Medical School, Boston.
Noting that most acute cholecystitis patients are first seen by an internist or gastroenterologist who then makes the initial treatment decision, Dr. Warshaw asked Dr. Buchler if German internists and gastroenterologists have gotten on board this immediate surgery treatment pathway.
"Convincing internists and gastroenterologists will take a long time, at least in Germany," the surgeon replied. "It is much easier to convince the emergency department physicians to refer patients early to surgery; they’re much closer to the surgeons."
He noted that German surgical practice differs from that in the United States in several respects. For one, German patients routinely stay in the hospital longer, even if they don’t experience complications. That’s why the mean length of stay after cholecystectomy in ACDC was 4.68 days in the early surgery group and closely similar at 4.89 days in the delayed surgery group, even though the delayed surgery group had a threefold higher complication rate.
Another difference is that, unlike in this country, intraoperative cholangiography is rarely done in Germany.
"It’s the absolute exception that intraoperative cholangiography is used. It is used only when there’s a reason for it, such as jaundice. There was probably less than a 3% intraoperative cholangiography rate in this trial," said Dr. Buchler.
The ACDC trial was funded with government research grants. Dr. Buchler reported having no financial conflicts.
AT THE ASA ANNUAL MEETING
Major Finding: Acute cholecystitis patients randomized to laparoscopic cholecystectomy within 24 hours of hospital arrival had a 75-day total morbidity rate of 11.6% compared with 31.3% for those randomized to delayed laparoscopic cholecystectomy on days 7-45. Mean total hospital costs were one-third less in the early cholecystectomy group.
Data Source: ACDC trial of 618 randomized patients at 35 European medical centers.
Disclosures: The trial was funded by a German governmental research grant. The presenter reported having no conflict of interest.
ACP and FSMB offer social media guidelines
SAN FRANCISCO – Tempted to "friend" a patient on your personal Facebook page? That’s probably not a good idea, according to new guidelines issued by the American College of Physicians and the Federation of State Medical Boards.
The ACP and federation guidelines outline many benefits from use of e-mail and social media, including improving access to care, but "the boundaries between professional and social spheres can blur online," said Dr. Humayun J. Chaudhry, president and chief executive officer of the Federation of State Medical Boards (FSMB) and an author of the guidelines. "Physicians should keep the spheres separate and comport themselves professionally online."
Opportunities for misadventure abound with online communications and texting, Dr. Chaudhry said at the annual meeting of the American College of Physicians. Confidentiality can be breached, as can the patient-physician relationship; the communications can be taken out of context or be spread widely beyond the original conversation.
And disciplinary actions are likely to increase. In a recent study of state medical boards, 92% reported that they had dealt with at least one case of unprofessional online behavior that led to punishment, including license revocation (Ann. Intern. Med. 2013;158:124-30).
The ACP and FSMB guidelines, published online Apr. 11 in the Annals of Internal Medicine, are meant "to serve as a wake-up call to physicians, to make them aware of some of the dangers that are out there," he said. Aside from not "friending" patients, the guidelines also recommend the following to physicians:
• Don’t use text messaging for medical interactions, even with established patients, except with caution and the patient’s consent.
• Only use e-mail within the context of an established relationship with a patient, and with that patient’s consent.
• Establish a professional online profile so that it appears at the top of a web-based search, above any physician rating site.
• Discourage e-mail or on-line communications with individuals who are not patients, instead referring them to make an appointment or visit an appropriate health provider.
• Manage their digital image, including refraining from posting about personal social activities that might not reflect positively or providing less-than-measured comments on Twitter, blogs, or in response to online articles.
E-mail presents several dangers, said Dr. David A. Fleming, a member of the ACP Board of Regents and chairman of the ACP Ethics, Professionalism, and Human Rights Committee. The new guidelines urge e-mail communications only with established patients who have a relationship with the physician and understand that the communication might not be secure, he said, adding that information sent via e-mail also can be discoverable for legal purposes.
An e-mail from a patient in a crisis situation presents a different present challenge. "As soon as we respond in any way, then the relationship forms and we have a fiduciary responsibility to, first of all, know our limits, but also the extent to which an intervention is needed," Dr. Fleming said. If the crisis warrants intervention, then the physician is obligated to help the patient.
Social media can be a great way to encourage patients to get vaccinated or exercise or watch their weight, but postings on Twitter or Facebook can still be fraught with peril, Dr. Fleming and Dr. Chaudhry said. Physicians need to be clear when they are expressing their personal opinion or representing a professional organization, for instance.
Both physicians said that the ACP and the FSMB are not advocating censorship.
"We’re not telling people what to say, what not to say, we’re just asking them to think before you press send," said Dr. Chaudhry.
On Twitter @aliciaault
SAN FRANCISCO – Tempted to "friend" a patient on your personal Facebook page? That’s probably not a good idea, according to new guidelines issued by the American College of Physicians and the Federation of State Medical Boards.
The ACP and federation guidelines outline many benefits from use of e-mail and social media, including improving access to care, but "the boundaries between professional and social spheres can blur online," said Dr. Humayun J. Chaudhry, president and chief executive officer of the Federation of State Medical Boards (FSMB) and an author of the guidelines. "Physicians should keep the spheres separate and comport themselves professionally online."
Opportunities for misadventure abound with online communications and texting, Dr. Chaudhry said at the annual meeting of the American College of Physicians. Confidentiality can be breached, as can the patient-physician relationship; the communications can be taken out of context or be spread widely beyond the original conversation.
And disciplinary actions are likely to increase. In a recent study of state medical boards, 92% reported that they had dealt with at least one case of unprofessional online behavior that led to punishment, including license revocation (Ann. Intern. Med. 2013;158:124-30).
The ACP and FSMB guidelines, published online Apr. 11 in the Annals of Internal Medicine, are meant "to serve as a wake-up call to physicians, to make them aware of some of the dangers that are out there," he said. Aside from not "friending" patients, the guidelines also recommend the following to physicians:
• Don’t use text messaging for medical interactions, even with established patients, except with caution and the patient’s consent.
• Only use e-mail within the context of an established relationship with a patient, and with that patient’s consent.
• Establish a professional online profile so that it appears at the top of a web-based search, above any physician rating site.
• Discourage e-mail or on-line communications with individuals who are not patients, instead referring them to make an appointment or visit an appropriate health provider.
• Manage their digital image, including refraining from posting about personal social activities that might not reflect positively or providing less-than-measured comments on Twitter, blogs, or in response to online articles.
E-mail presents several dangers, said Dr. David A. Fleming, a member of the ACP Board of Regents and chairman of the ACP Ethics, Professionalism, and Human Rights Committee. The new guidelines urge e-mail communications only with established patients who have a relationship with the physician and understand that the communication might not be secure, he said, adding that information sent via e-mail also can be discoverable for legal purposes.
An e-mail from a patient in a crisis situation presents a different present challenge. "As soon as we respond in any way, then the relationship forms and we have a fiduciary responsibility to, first of all, know our limits, but also the extent to which an intervention is needed," Dr. Fleming said. If the crisis warrants intervention, then the physician is obligated to help the patient.
Social media can be a great way to encourage patients to get vaccinated or exercise or watch their weight, but postings on Twitter or Facebook can still be fraught with peril, Dr. Fleming and Dr. Chaudhry said. Physicians need to be clear when they are expressing their personal opinion or representing a professional organization, for instance.
Both physicians said that the ACP and the FSMB are not advocating censorship.
"We’re not telling people what to say, what not to say, we’re just asking them to think before you press send," said Dr. Chaudhry.
On Twitter @aliciaault
SAN FRANCISCO – Tempted to "friend" a patient on your personal Facebook page? That’s probably not a good idea, according to new guidelines issued by the American College of Physicians and the Federation of State Medical Boards.
The ACP and federation guidelines outline many benefits from use of e-mail and social media, including improving access to care, but "the boundaries between professional and social spheres can blur online," said Dr. Humayun J. Chaudhry, president and chief executive officer of the Federation of State Medical Boards (FSMB) and an author of the guidelines. "Physicians should keep the spheres separate and comport themselves professionally online."
Opportunities for misadventure abound with online communications and texting, Dr. Chaudhry said at the annual meeting of the American College of Physicians. Confidentiality can be breached, as can the patient-physician relationship; the communications can be taken out of context or be spread widely beyond the original conversation.
And disciplinary actions are likely to increase. In a recent study of state medical boards, 92% reported that they had dealt with at least one case of unprofessional online behavior that led to punishment, including license revocation (Ann. Intern. Med. 2013;158:124-30).
The ACP and FSMB guidelines, published online Apr. 11 in the Annals of Internal Medicine, are meant "to serve as a wake-up call to physicians, to make them aware of some of the dangers that are out there," he said. Aside from not "friending" patients, the guidelines also recommend the following to physicians:
• Don’t use text messaging for medical interactions, even with established patients, except with caution and the patient’s consent.
• Only use e-mail within the context of an established relationship with a patient, and with that patient’s consent.
• Establish a professional online profile so that it appears at the top of a web-based search, above any physician rating site.
• Discourage e-mail or on-line communications with individuals who are not patients, instead referring them to make an appointment or visit an appropriate health provider.
• Manage their digital image, including refraining from posting about personal social activities that might not reflect positively or providing less-than-measured comments on Twitter, blogs, or in response to online articles.
E-mail presents several dangers, said Dr. David A. Fleming, a member of the ACP Board of Regents and chairman of the ACP Ethics, Professionalism, and Human Rights Committee. The new guidelines urge e-mail communications only with established patients who have a relationship with the physician and understand that the communication might not be secure, he said, adding that information sent via e-mail also can be discoverable for legal purposes.
An e-mail from a patient in a crisis situation presents a different present challenge. "As soon as we respond in any way, then the relationship forms and we have a fiduciary responsibility to, first of all, know our limits, but also the extent to which an intervention is needed," Dr. Fleming said. If the crisis warrants intervention, then the physician is obligated to help the patient.
Social media can be a great way to encourage patients to get vaccinated or exercise or watch their weight, but postings on Twitter or Facebook can still be fraught with peril, Dr. Fleming and Dr. Chaudhry said. Physicians need to be clear when they are expressing their personal opinion or representing a professional organization, for instance.
Both physicians said that the ACP and the FSMB are not advocating censorship.
"We’re not telling people what to say, what not to say, we’re just asking them to think before you press send," said Dr. Chaudhry.
On Twitter @aliciaault
AT ACP INTERNAL MEDICINE 2013
Only doctors can save America
Dr. Ezekiel J. Emanuel, one of the brains behind Obamacare, has a blunt message for his fellow physicians:
Only you can save America.
He's not just talking about medicine. As might befit someone who holds a faculty title at the business-oriented Wharton School at the University of Pennsylvania, Dr. Emanuel spent much of his keynote address here at the American College of Physicians' annual meeting in San Francisco talking about the U.S. economy. The enormous impact of runaway spending on U.S. health care threatens "everything we care about," including access to health care, state funds available for education, corporate wages for the middle class, and the fiscal health of the nation, he said.
"More than any other group in America, doctors have the power to solve our long-term economic challenges to ensure a prosperous future," Dr. Emanuel said.
If the U.S. health care system were a country, its nearly $3 trillion economy in 2012 would be the fifth largest in the world, behind only the U.S. as a whole, China, Japan, and Germany. "We spend more on health care in this country than the 66 million French spend on everything in their society," he said. "It is an astounding number how much we spend on health care."
Take just the federal portions of Medicare and Medicaid, excluding state spending, and you've still got the 16th largest economy in the world, bigger than the economies of Switzerland, Turkey, or the Netherlands, for example. The impact of any other fiscal variable on the U.S. economy, including Social Security, is swamped by the impact of health care costs, said Dr. Emanuel, who is also chair of medical ethics and health policy at the University of Pennsylvania, Philadelphia.
Per person, the United States far outspends other countries when it comes to health care, and the proportion of the gross domestic product consumed by health care keeps getting larger and larger.
Dr. Emanuel served as a special adviser for health policy to the director of the federal Office of Management and Budget in 2009-2011 - during the design, passage, and first steps to implementation of the Patient Protection and Affordable Care Act (commonly known as Obamacare) - and he seemed to address some critics in absentia who have claimed that health care reform will lead to unwanted rationing of care. There's no need to ration, Dr. Emanuel said. Switzerland doesn't ration care, and it spends far less per capita for what is considered quality health care. "We can do a better job in this country of controlling costs without the need to ration care," he said.
The only way to really control costs is to transform the way U.S. health care is delivered, he said. Ten percent of U.S. patients account for 63% of dollars spent on health care. "You know who they are - people with congestive heart failure, COPD, diabetes, adult asthma, coronary artery disease, cancer. People with chronic multiple chronic illnesses. That's where the money's going. That's where the uneven quality is," and that's where health care delivery needs to improve, he said.
Dr. Emanuel proposed six essential components to transforming the health care system. Among them: The focus needs to be on cost according to value, and getting rid of services with no value. The system must focus on patients' needs, not on physicians' schedules or other concerns. And the system must evolve toward clinicians working as teams including allied health professionals, not as individuals. "We are not going to be, going forward, one-sies and two-sies in practice" anymore, he said.
Greater emphasis on delivering health care via organizations and systems, standardization of processes, and transparency around price and quality will be essential, he added.
Transparency in pricing and quality isn't just something consumers will want. Physicians will want it in order to refer patients to quality care and set prices appropriately, Dr. Emanuel argued. "I think this is inevitable, and I think it's going to happen faster than you think," he said.
Most U.S. physicians are stuck in fee-for-service payment systems, which don't provide the incentives needed for change, he said. Doctors "as a group" should push for changes to the payment system, which will increase physician autonomy but also will assign more financial risk to physicians. "I see no way of getting out of that," Dr. Emanuel said.
In his eyes, if doctors don't push for changes in how health care is delivered, we basically can kiss the U.S. economy and future prosperity good-bye. "Doctors are the only people who can re-engineer the delivery system," he said. "If you don't do it, it ain't gonna happen. It's that simple," he said. All previous reform efforts that did not have physician leadership have failed.
"You have to lead this," he explained.
No one should expect that reforming the fifth-largest economy in the world could be accomplished in just a few years, however. "It's going to take this decade," Dr. Emanuel predicted.
Dr. Emanuel reported having no financial disclosures.
Twitter: @sherryboschert
Dr. Ezekiel J. Emanuel, one of the brains behind Obamacare, has a blunt message for his fellow physicians:
Only you can save America.
He's not just talking about medicine. As might befit someone who holds a faculty title at the business-oriented Wharton School at the University of Pennsylvania, Dr. Emanuel spent much of his keynote address here at the American College of Physicians' annual meeting in San Francisco talking about the U.S. economy. The enormous impact of runaway spending on U.S. health care threatens "everything we care about," including access to health care, state funds available for education, corporate wages for the middle class, and the fiscal health of the nation, he said.
"More than any other group in America, doctors have the power to solve our long-term economic challenges to ensure a prosperous future," Dr. Emanuel said.
If the U.S. health care system were a country, its nearly $3 trillion economy in 2012 would be the fifth largest in the world, behind only the U.S. as a whole, China, Japan, and Germany. "We spend more on health care in this country than the 66 million French spend on everything in their society," he said. "It is an astounding number how much we spend on health care."
Take just the federal portions of Medicare and Medicaid, excluding state spending, and you've still got the 16th largest economy in the world, bigger than the economies of Switzerland, Turkey, or the Netherlands, for example. The impact of any other fiscal variable on the U.S. economy, including Social Security, is swamped by the impact of health care costs, said Dr. Emanuel, who is also chair of medical ethics and health policy at the University of Pennsylvania, Philadelphia.
Per person, the United States far outspends other countries when it comes to health care, and the proportion of the gross domestic product consumed by health care keeps getting larger and larger.
Dr. Emanuel served as a special adviser for health policy to the director of the federal Office of Management and Budget in 2009-2011 - during the design, passage, and first steps to implementation of the Patient Protection and Affordable Care Act (commonly known as Obamacare) - and he seemed to address some critics in absentia who have claimed that health care reform will lead to unwanted rationing of care. There's no need to ration, Dr. Emanuel said. Switzerland doesn't ration care, and it spends far less per capita for what is considered quality health care. "We can do a better job in this country of controlling costs without the need to ration care," he said.
The only way to really control costs is to transform the way U.S. health care is delivered, he said. Ten percent of U.S. patients account for 63% of dollars spent on health care. "You know who they are - people with congestive heart failure, COPD, diabetes, adult asthma, coronary artery disease, cancer. People with chronic multiple chronic illnesses. That's where the money's going. That's where the uneven quality is," and that's where health care delivery needs to improve, he said.
Dr. Emanuel proposed six essential components to transforming the health care system. Among them: The focus needs to be on cost according to value, and getting rid of services with no value. The system must focus on patients' needs, not on physicians' schedules or other concerns. And the system must evolve toward clinicians working as teams including allied health professionals, not as individuals. "We are not going to be, going forward, one-sies and two-sies in practice" anymore, he said.
Greater emphasis on delivering health care via organizations and systems, standardization of processes, and transparency around price and quality will be essential, he added.
Transparency in pricing and quality isn't just something consumers will want. Physicians will want it in order to refer patients to quality care and set prices appropriately, Dr. Emanuel argued. "I think this is inevitable, and I think it's going to happen faster than you think," he said.
Most U.S. physicians are stuck in fee-for-service payment systems, which don't provide the incentives needed for change, he said. Doctors "as a group" should push for changes to the payment system, which will increase physician autonomy but also will assign more financial risk to physicians. "I see no way of getting out of that," Dr. Emanuel said.
In his eyes, if doctors don't push for changes in how health care is delivered, we basically can kiss the U.S. economy and future prosperity good-bye. "Doctors are the only people who can re-engineer the delivery system," he said. "If you don't do it, it ain't gonna happen. It's that simple," he said. All previous reform efforts that did not have physician leadership have failed.
"You have to lead this," he explained.
No one should expect that reforming the fifth-largest economy in the world could be accomplished in just a few years, however. "It's going to take this decade," Dr. Emanuel predicted.
Dr. Emanuel reported having no financial disclosures.
Twitter: @sherryboschert
Dr. Ezekiel J. Emanuel, one of the brains behind Obamacare, has a blunt message for his fellow physicians:
Only you can save America.
He's not just talking about medicine. As might befit someone who holds a faculty title at the business-oriented Wharton School at the University of Pennsylvania, Dr. Emanuel spent much of his keynote address here at the American College of Physicians' annual meeting in San Francisco talking about the U.S. economy. The enormous impact of runaway spending on U.S. health care threatens "everything we care about," including access to health care, state funds available for education, corporate wages for the middle class, and the fiscal health of the nation, he said.
"More than any other group in America, doctors have the power to solve our long-term economic challenges to ensure a prosperous future," Dr. Emanuel said.
If the U.S. health care system were a country, its nearly $3 trillion economy in 2012 would be the fifth largest in the world, behind only the U.S. as a whole, China, Japan, and Germany. "We spend more on health care in this country than the 66 million French spend on everything in their society," he said. "It is an astounding number how much we spend on health care."
Take just the federal portions of Medicare and Medicaid, excluding state spending, and you've still got the 16th largest economy in the world, bigger than the economies of Switzerland, Turkey, or the Netherlands, for example. The impact of any other fiscal variable on the U.S. economy, including Social Security, is swamped by the impact of health care costs, said Dr. Emanuel, who is also chair of medical ethics and health policy at the University of Pennsylvania, Philadelphia.
Per person, the United States far outspends other countries when it comes to health care, and the proportion of the gross domestic product consumed by health care keeps getting larger and larger.
Dr. Emanuel served as a special adviser for health policy to the director of the federal Office of Management and Budget in 2009-2011 - during the design, passage, and first steps to implementation of the Patient Protection and Affordable Care Act (commonly known as Obamacare) - and he seemed to address some critics in absentia who have claimed that health care reform will lead to unwanted rationing of care. There's no need to ration, Dr. Emanuel said. Switzerland doesn't ration care, and it spends far less per capita for what is considered quality health care. "We can do a better job in this country of controlling costs without the need to ration care," he said.
The only way to really control costs is to transform the way U.S. health care is delivered, he said. Ten percent of U.S. patients account for 63% of dollars spent on health care. "You know who they are - people with congestive heart failure, COPD, diabetes, adult asthma, coronary artery disease, cancer. People with chronic multiple chronic illnesses. That's where the money's going. That's where the uneven quality is," and that's where health care delivery needs to improve, he said.
Dr. Emanuel proposed six essential components to transforming the health care system. Among them: The focus needs to be on cost according to value, and getting rid of services with no value. The system must focus on patients' needs, not on physicians' schedules or other concerns. And the system must evolve toward clinicians working as teams including allied health professionals, not as individuals. "We are not going to be, going forward, one-sies and two-sies in practice" anymore, he said.
Greater emphasis on delivering health care via organizations and systems, standardization of processes, and transparency around price and quality will be essential, he added.
Transparency in pricing and quality isn't just something consumers will want. Physicians will want it in order to refer patients to quality care and set prices appropriately, Dr. Emanuel argued. "I think this is inevitable, and I think it's going to happen faster than you think," he said.
Most U.S. physicians are stuck in fee-for-service payment systems, which don't provide the incentives needed for change, he said. Doctors "as a group" should push for changes to the payment system, which will increase physician autonomy but also will assign more financial risk to physicians. "I see no way of getting out of that," Dr. Emanuel said.
In his eyes, if doctors don't push for changes in how health care is delivered, we basically can kiss the U.S. economy and future prosperity good-bye. "Doctors are the only people who can re-engineer the delivery system," he said. "If you don't do it, it ain't gonna happen. It's that simple," he said. All previous reform efforts that did not have physician leadership have failed.
"You have to lead this," he explained.
No one should expect that reforming the fifth-largest economy in the world could be accomplished in just a few years, however. "It's going to take this decade," Dr. Emanuel predicted.
Dr. Emanuel reported having no financial disclosures.
Twitter: @sherryboschert
Obama's budget proposal gives more power to IPAB
President Obama is proposing to cut more than $370 billion from the Medicare program over the next decade, a move aimed at reducing the federal deficit and putting the program on firmer financial footing.
The president’s fiscal year 2014 budget proposal, sent to Congress April 10, includes cuts for physicians, drug companies, hospitals, and long-term facilities, as well as increased cost-sharing for some Medicare beneficiaries.
The part of the budget with the potential to have the biggest impact on doctors is the increased authority for the Independent Payment Advisory Board (IPAB). The 15-member board was created under the Affordable Care Act (ACA) and is charged with recommending to Congress how to reduce spending growth in Medicare. Under current law, IPAB would make recommendations only if the projected Medicare per capita growth rate exceeded the gross domestic product (GDP) plus 1%. In the president’s budget proposal, that target would be triggered early, when Medicare spending was projected to exceed GDP plus 0.5%.
| Source: U.S. Dept. of Health and Human Services |
This change is projected to save the federal government $4.1 billion over the next decade.
The bulk of the Medicare savings will come from proposals to cut payments to drug companies, long-term care facilities, and increases in cost sharing by beneficiaries.
For instance, the administration estimates it will save about $123 billion over 10 years by allowing the Medicare Part D program to pay the lower Medicaid rate for prescription drugs for its low-income beneficiaries.
A change involving post–acute care providers would save $79 billion. The administration wants to reduce the market basket updates for inpatient rehabilitation facilities, long-term care hospitals, skilled nursing facilities, and home health agencies by 1.1% starting in 2014 and running through 2023.
Beneficiaries also would contribute more for their Medicare premiums under the Obama budget proposal. Starting in 2017, certain Medicare beneficiaries will pay more for their Part B and D premiums, which is expected to generate $50 billion in savings over 10 years.
The budget also includes about $22.1 billion in cuts to Medicaid over 10 years.
The budget also includes a little good news for physicians: It assumes that the Congress will eliminate the Sustainable Growth Rate (SGR) formula used in setting Medicare physician payments.
The American Medical Association praised the administration for its commitment to move toward new ways to pay for health care. "The President’s proposals align with many of the principles developed by the AMA and 110 other physician organizations on transitioning Medicare to include an array of accountable payment models," Dr. Jeremy A. Lazarus, AMA president, said in a statement. "It is critical for physicians to have a period of stability and the flexibility to choose options that will help them lower costs and improve the quality of care for their patients. We are encouraged that the president and members of Congress are focused this year on eliminating this failed formula and strengthening Medicare for patients now and in the future."
The cost-cutting proposals aren’t new; President Obama included some of them in last year’s budget proposal. He also called for cuts to Medicare when negotiating for a deficit reduction deal with House Speaker John Boehner (R-Ohio) late last year.
President Obama said his proposed budget would lower the federal deficit in a "balanced way," allowing more targeted cuts to replace the across-the-board budget cuts set out in the sequester, which took effect in March. Overall, the Obama administration estimates that the new budget would achieve $1.8 trillion in deficit reduction over the next 10 years.
But the budget is already getting a cool reception from Republicans on Capitol Hill. House Budget Committee Chairman Paul Ryan (R-Wisc.) said that after eliminating the sequester, there is only about $119 billion in deficit reduction over the next decade in the president’s proposed budget. "I’m disappointed by the president’s proposal because it merely ratifies the status quo," Rep. Ryan said in a statement. "It doesn’t break new ground; it goes over old ground."
Both the House and the Senate have already passed their own budget proposals for fiscal year 2014.
In addition to the Medicare and Medicaid cuts, the President’s budget offers some targeted increases.
For instance, the Centers for Medicare and Medicaid Services is seeking about $1.5 billion in new funding to help support operations and outreach related to the ACA’s health insurance exchanges. The funds would support the federally operated exchanges and offer assistance to states that are running their own exchanges. The exchanges will open for enrollment on Oct. 1, 2013, the first day of fiscal year 2014. Coverage under the exchanges is set to begin on Jan. 1, 2014.
Health and Human Services Secretary Kathleen Sebelius said she is hopeful that Congress will come through with the money to help launch the new program. "We intend to implement the law," she said at a press conference April 10.
The budget also includes funding for mental health. The proposal invests $130 million to add 5,000 mental health professionals to the behavioral health workforce. The money will also fund Project AWARE (Advancing Wellness and Resilience in Education), which trains teachers to detect and respond to mental illness in their students.
The Centers for Disease Control and Prevention would get an additional $30 million to track gun violence and research ways to prevent it under the budget proposal sent to Congress.
The American Psychiatric Association supported the administration’s effort to identify at-risk individuals early through Project AWARE. But the APA said in a statement that it was concerned that the effort to expand the supply of mental health professionals seems to stop at nonphysician providers.
"We recognize the growing need for mental health providers; however, providing a small amount of training to lesser-qualified health professionals at the expense of utilizing veteran medical psychiatrists will only serve to exacerbate the problem we are trying to solve," the APA wrote. "As a nation, we should ensure that patients have access to the full range of services, from physician care to hospital care to outpatient clinics and long-term follow-up."
The National Institutes of Health would receive a $471 million funding increase over its fiscal year 2012 funding, bringing its total budget to $31.1 billion. That includes about $40 billion toward an effort to map the human brain. The agency will also invest $80 million to speed up drug development and the testing of new therapies for Alzheimer’s disease.
President Obama is proposing to cut more than $370 billion from the Medicare program over the next decade, a move aimed at reducing the federal deficit and putting the program on firmer financial footing.
The president’s fiscal year 2014 budget proposal, sent to Congress April 10, includes cuts for physicians, drug companies, hospitals, and long-term facilities, as well as increased cost-sharing for some Medicare beneficiaries.
The part of the budget with the potential to have the biggest impact on doctors is the increased authority for the Independent Payment Advisory Board (IPAB). The 15-member board was created under the Affordable Care Act (ACA) and is charged with recommending to Congress how to reduce spending growth in Medicare. Under current law, IPAB would make recommendations only if the projected Medicare per capita growth rate exceeded the gross domestic product (GDP) plus 1%. In the president’s budget proposal, that target would be triggered early, when Medicare spending was projected to exceed GDP plus 0.5%.
| Source: U.S. Dept. of Health and Human Services |
This change is projected to save the federal government $4.1 billion over the next decade.
The bulk of the Medicare savings will come from proposals to cut payments to drug companies, long-term care facilities, and increases in cost sharing by beneficiaries.
For instance, the administration estimates it will save about $123 billion over 10 years by allowing the Medicare Part D program to pay the lower Medicaid rate for prescription drugs for its low-income beneficiaries.
A change involving post–acute care providers would save $79 billion. The administration wants to reduce the market basket updates for inpatient rehabilitation facilities, long-term care hospitals, skilled nursing facilities, and home health agencies by 1.1% starting in 2014 and running through 2023.
Beneficiaries also would contribute more for their Medicare premiums under the Obama budget proposal. Starting in 2017, certain Medicare beneficiaries will pay more for their Part B and D premiums, which is expected to generate $50 billion in savings over 10 years.
The budget also includes about $22.1 billion in cuts to Medicaid over 10 years.
The budget also includes a little good news for physicians: It assumes that the Congress will eliminate the Sustainable Growth Rate (SGR) formula used in setting Medicare physician payments.
The American Medical Association praised the administration for its commitment to move toward new ways to pay for health care. "The President’s proposals align with many of the principles developed by the AMA and 110 other physician organizations on transitioning Medicare to include an array of accountable payment models," Dr. Jeremy A. Lazarus, AMA president, said in a statement. "It is critical for physicians to have a period of stability and the flexibility to choose options that will help them lower costs and improve the quality of care for their patients. We are encouraged that the president and members of Congress are focused this year on eliminating this failed formula and strengthening Medicare for patients now and in the future."
The cost-cutting proposals aren’t new; President Obama included some of them in last year’s budget proposal. He also called for cuts to Medicare when negotiating for a deficit reduction deal with House Speaker John Boehner (R-Ohio) late last year.
President Obama said his proposed budget would lower the federal deficit in a "balanced way," allowing more targeted cuts to replace the across-the-board budget cuts set out in the sequester, which took effect in March. Overall, the Obama administration estimates that the new budget would achieve $1.8 trillion in deficit reduction over the next 10 years.
But the budget is already getting a cool reception from Republicans on Capitol Hill. House Budget Committee Chairman Paul Ryan (R-Wisc.) said that after eliminating the sequester, there is only about $119 billion in deficit reduction over the next decade in the president’s proposed budget. "I’m disappointed by the president’s proposal because it merely ratifies the status quo," Rep. Ryan said in a statement. "It doesn’t break new ground; it goes over old ground."
Both the House and the Senate have already passed their own budget proposals for fiscal year 2014.
In addition to the Medicare and Medicaid cuts, the President’s budget offers some targeted increases.
For instance, the Centers for Medicare and Medicaid Services is seeking about $1.5 billion in new funding to help support operations and outreach related to the ACA’s health insurance exchanges. The funds would support the federally operated exchanges and offer assistance to states that are running their own exchanges. The exchanges will open for enrollment on Oct. 1, 2013, the first day of fiscal year 2014. Coverage under the exchanges is set to begin on Jan. 1, 2014.
Health and Human Services Secretary Kathleen Sebelius said she is hopeful that Congress will come through with the money to help launch the new program. "We intend to implement the law," she said at a press conference April 10.
The budget also includes funding for mental health. The proposal invests $130 million to add 5,000 mental health professionals to the behavioral health workforce. The money will also fund Project AWARE (Advancing Wellness and Resilience in Education), which trains teachers to detect and respond to mental illness in their students.
The Centers for Disease Control and Prevention would get an additional $30 million to track gun violence and research ways to prevent it under the budget proposal sent to Congress.
The American Psychiatric Association supported the administration’s effort to identify at-risk individuals early through Project AWARE. But the APA said in a statement that it was concerned that the effort to expand the supply of mental health professionals seems to stop at nonphysician providers.
"We recognize the growing need for mental health providers; however, providing a small amount of training to lesser-qualified health professionals at the expense of utilizing veteran medical psychiatrists will only serve to exacerbate the problem we are trying to solve," the APA wrote. "As a nation, we should ensure that patients have access to the full range of services, from physician care to hospital care to outpatient clinics and long-term follow-up."
The National Institutes of Health would receive a $471 million funding increase over its fiscal year 2012 funding, bringing its total budget to $31.1 billion. That includes about $40 billion toward an effort to map the human brain. The agency will also invest $80 million to speed up drug development and the testing of new therapies for Alzheimer’s disease.
President Obama is proposing to cut more than $370 billion from the Medicare program over the next decade, a move aimed at reducing the federal deficit and putting the program on firmer financial footing.
The president’s fiscal year 2014 budget proposal, sent to Congress April 10, includes cuts for physicians, drug companies, hospitals, and long-term facilities, as well as increased cost-sharing for some Medicare beneficiaries.
The part of the budget with the potential to have the biggest impact on doctors is the increased authority for the Independent Payment Advisory Board (IPAB). The 15-member board was created under the Affordable Care Act (ACA) and is charged with recommending to Congress how to reduce spending growth in Medicare. Under current law, IPAB would make recommendations only if the projected Medicare per capita growth rate exceeded the gross domestic product (GDP) plus 1%. In the president’s budget proposal, that target would be triggered early, when Medicare spending was projected to exceed GDP plus 0.5%.
| Source: U.S. Dept. of Health and Human Services |
This change is projected to save the federal government $4.1 billion over the next decade.
The bulk of the Medicare savings will come from proposals to cut payments to drug companies, long-term care facilities, and increases in cost sharing by beneficiaries.
For instance, the administration estimates it will save about $123 billion over 10 years by allowing the Medicare Part D program to pay the lower Medicaid rate for prescription drugs for its low-income beneficiaries.
A change involving post–acute care providers would save $79 billion. The administration wants to reduce the market basket updates for inpatient rehabilitation facilities, long-term care hospitals, skilled nursing facilities, and home health agencies by 1.1% starting in 2014 and running through 2023.
Beneficiaries also would contribute more for their Medicare premiums under the Obama budget proposal. Starting in 2017, certain Medicare beneficiaries will pay more for their Part B and D premiums, which is expected to generate $50 billion in savings over 10 years.
The budget also includes about $22.1 billion in cuts to Medicaid over 10 years.
The budget also includes a little good news for physicians: It assumes that the Congress will eliminate the Sustainable Growth Rate (SGR) formula used in setting Medicare physician payments.
The American Medical Association praised the administration for its commitment to move toward new ways to pay for health care. "The President’s proposals align with many of the principles developed by the AMA and 110 other physician organizations on transitioning Medicare to include an array of accountable payment models," Dr. Jeremy A. Lazarus, AMA president, said in a statement. "It is critical for physicians to have a period of stability and the flexibility to choose options that will help them lower costs and improve the quality of care for their patients. We are encouraged that the president and members of Congress are focused this year on eliminating this failed formula and strengthening Medicare for patients now and in the future."
The cost-cutting proposals aren’t new; President Obama included some of them in last year’s budget proposal. He also called for cuts to Medicare when negotiating for a deficit reduction deal with House Speaker John Boehner (R-Ohio) late last year.
President Obama said his proposed budget would lower the federal deficit in a "balanced way," allowing more targeted cuts to replace the across-the-board budget cuts set out in the sequester, which took effect in March. Overall, the Obama administration estimates that the new budget would achieve $1.8 trillion in deficit reduction over the next 10 years.
But the budget is already getting a cool reception from Republicans on Capitol Hill. House Budget Committee Chairman Paul Ryan (R-Wisc.) said that after eliminating the sequester, there is only about $119 billion in deficit reduction over the next decade in the president’s proposed budget. "I’m disappointed by the president’s proposal because it merely ratifies the status quo," Rep. Ryan said in a statement. "It doesn’t break new ground; it goes over old ground."
Both the House and the Senate have already passed their own budget proposals for fiscal year 2014.
In addition to the Medicare and Medicaid cuts, the President’s budget offers some targeted increases.
For instance, the Centers for Medicare and Medicaid Services is seeking about $1.5 billion in new funding to help support operations and outreach related to the ACA’s health insurance exchanges. The funds would support the federally operated exchanges and offer assistance to states that are running their own exchanges. The exchanges will open for enrollment on Oct. 1, 2013, the first day of fiscal year 2014. Coverage under the exchanges is set to begin on Jan. 1, 2014.
Health and Human Services Secretary Kathleen Sebelius said she is hopeful that Congress will come through with the money to help launch the new program. "We intend to implement the law," she said at a press conference April 10.
The budget also includes funding for mental health. The proposal invests $130 million to add 5,000 mental health professionals to the behavioral health workforce. The money will also fund Project AWARE (Advancing Wellness and Resilience in Education), which trains teachers to detect and respond to mental illness in their students.
The Centers for Disease Control and Prevention would get an additional $30 million to track gun violence and research ways to prevent it under the budget proposal sent to Congress.
The American Psychiatric Association supported the administration’s effort to identify at-risk individuals early through Project AWARE. But the APA said in a statement that it was concerned that the effort to expand the supply of mental health professionals seems to stop at nonphysician providers.
"We recognize the growing need for mental health providers; however, providing a small amount of training to lesser-qualified health professionals at the expense of utilizing veteran medical psychiatrists will only serve to exacerbate the problem we are trying to solve," the APA wrote. "As a nation, we should ensure that patients have access to the full range of services, from physician care to hospital care to outpatient clinics and long-term follow-up."
The National Institutes of Health would receive a $471 million funding increase over its fiscal year 2012 funding, bringing its total budget to $31.1 billion. That includes about $40 billion toward an effort to map the human brain. The agency will also invest $80 million to speed up drug development and the testing of new therapies for Alzheimer’s disease.
CA125 level predicts microscopic residual disease in ovarian cancer
LOS ANGELES – Preoperative levels of cancer antigen 125 (CA125) predict surgical and disease outcomes in women with advanced epithelial ovarian cancer who are able to undergo optimal debulking surgery, new data show, and may therefore help guide treatment decisions.
A team led by Dr. Neil S. Horowitz of Brigham and Women’s Hospital and the Dana Farber Cancer Institute in Boston assessed levels of the biomarker among nearly 1,000 women who had stage III or IV disease that was optimally debulked to less than 1 cm of residual disease and who received adjuvant paclitaxel- and platinum-containing chemotherapy.
Results showed that no cutoff value of preoperative CA125 levels clearly separated women in whom microscopic residual disease was achieved surgically from women in whom a greater volume of disease remained, he reported at the annual meeting of the Society of Gynecologic Oncology.
But the probability of achieving microscopic status decreased with increasing CA125 levels. For example, it fell from 33% in women with a level of 500 U/mL to 27% in women with a level of 1,000 U/mL.
"Although a strict CA125 value to predict microscopic residual cannot be made, these data are helpful for counseling patients regarding surgical results and outcome, and should influence decisions regarding primary debulking surgery and possibly use of other ... treatment options like neoadjuvant chemotherapy," Dr. Horowitz said. "Each surgeon and [his or her] patient have to decide for themselves what is an acceptable probability of successful surgical outcome to microscopic residual disease.
Additional study findings showed that women with higher preoperative CA125 levels and women with smaller reductions in CA125 levels between the preoperative period and the pretreatment period, before starting chemotherapy, had significantly worse progression-free and overall survival.
One session attendee asked, "What impact do you think surgical expertise has on the ability to predict the extent of cytoreduction?"
"Most trained gyn oncologists have the ability and training to take somebody to microscopic residual disease. What it takes to get to that place obviously varies from patient to patient and the disease that they have at the time that they present. Ultimately, what has to be decided between the patient and the physician is what’s going to be the best possibility for them and using CA125 as a potential guide, say, taking everything into consideration – age, where their disease is, what their CA125 is, what my comfort level is doing certain procedures being able to get them down to microscopic disease," Dr. Horowitz replied. "So I don’t think it’s a one-size-fits-all [objective] based just on the surgical expertise. Most gyn oncologists are trained adequately to be able to do this. It’s just, because you can do it, the question is, should you be doing it on everybody."
Another attendee said, "In follow-up to that, do you think that the difference in the behavior of the presurgical and the pretreatment CA125 could be confounded, the latter by surgical decisions or surgical intervention?"
"It’s potentially confounded; whether it’s surgical skill or some people would say, I don’t want to use the term honesty, but it may be a reflection of what truly is left behind versus not left behind, if it didn’t really follow the way it should. It may be a window into how accurate our predictions or our estimates of what we left behind really are," Dr. Horowitz explained. "Pretreatment CA125, it is difficult to really get a good understanding of this number because obviously the patients who start with the highest CA125 have the greatest chance to fall ... So it’s a little tricky trying to figure out what to make of that number, whereas patients who start with a lower one, although they didn’t fall with the same percentile, you still may have done just as good a job surgically."
The 998 women studied were from Gynecologic Oncology Group (GOG) trial 182. "This is the largest reported series to evaluate the ability of preoperative CA125 to predict surgical cytoreductive outcomes and survival in a population of women with optimally cytoreduced primary ovarian or peritoneal cancer," Dr. Horowitz noted.
Overall, 33% had microscopic residual disease, while the other 67% had more extensive residual disease but still measuring less than 1 cm.
The median preoperative CA125 level was 346 U/mL in the former group and 870 U/mL in the latter, reported Dr. Horowitz, who disclosed no conflicts of interest related to the research.
"Despite the difference in median preoperative CA125 values, the distributions of the preoperative CA125s in those with microscopic and less than 1 cm residual overlapped almost completely," Dr. Horowitz reported. "This suggests that there is not a preoperative CA125 beyond which one cannot achieve a complete cytoreductive surgery."
However, the higher the preoperative CA125 level, the lower the predicted probability of achieving microscopic residual disease (P less than .01). For example, the probability was 33%, 27%, and 19% for women having a level of 500, 1,000, and 2,500 U/mL, respectively.
"It is important to remember that these curves only reflect data from women who achieved optimal cytoreduction and do not include those with suboptimal primary debulking. Therefore, the estimated predictions and probabilities are likely to decrease when applied to a preoperative population of unknown surgical outcome," he said. "But if one assumes a priori that you can achieve and will achieve optimal cytoreduction, then preoperative CA125 can estimate the likelihood of obtaining either microscopic or less than 1-cm residual."
In adjusted analyses, preoperative CA125 levels and extent of residual disease jointly predicted both progression-free survival (P less than .001) and overall survival (P = .04). For example, median overall survival ranged from 82 months in women having microscopic residual disease and a CA125 level of 35 U/mL to just 39 months in their counterparts with more residual disease and a CA125 level of 1,000 U/mL.
The change from preoperative to pretreatment CA125 levels predicted both progression-free survival (P less than .0001) and overall survival (P less than .0001). For example, median overall survival ranged from 60 months in women having a reduction in levels exceeding 80% to 45 months in their counterparts having stable or increasing levels.
In addition, among the group having a greater than 80% decline in CA125 level, survival was almost twice as long among those achieving microscopic residual disease, at 82 months, as among those with greater residual disease, at 48 months, "suggesting that residual disease rather than change in CA125 is more important to survival," Dr. Horowitz said.
LOS ANGELES – Preoperative levels of cancer antigen 125 (CA125) predict surgical and disease outcomes in women with advanced epithelial ovarian cancer who are able to undergo optimal debulking surgery, new data show, and may therefore help guide treatment decisions.
A team led by Dr. Neil S. Horowitz of Brigham and Women’s Hospital and the Dana Farber Cancer Institute in Boston assessed levels of the biomarker among nearly 1,000 women who had stage III or IV disease that was optimally debulked to less than 1 cm of residual disease and who received adjuvant paclitaxel- and platinum-containing chemotherapy.
Results showed that no cutoff value of preoperative CA125 levels clearly separated women in whom microscopic residual disease was achieved surgically from women in whom a greater volume of disease remained, he reported at the annual meeting of the Society of Gynecologic Oncology.
But the probability of achieving microscopic status decreased with increasing CA125 levels. For example, it fell from 33% in women with a level of 500 U/mL to 27% in women with a level of 1,000 U/mL.
"Although a strict CA125 value to predict microscopic residual cannot be made, these data are helpful for counseling patients regarding surgical results and outcome, and should influence decisions regarding primary debulking surgery and possibly use of other ... treatment options like neoadjuvant chemotherapy," Dr. Horowitz said. "Each surgeon and [his or her] patient have to decide for themselves what is an acceptable probability of successful surgical outcome to microscopic residual disease.
Additional study findings showed that women with higher preoperative CA125 levels and women with smaller reductions in CA125 levels between the preoperative period and the pretreatment period, before starting chemotherapy, had significantly worse progression-free and overall survival.
One session attendee asked, "What impact do you think surgical expertise has on the ability to predict the extent of cytoreduction?"
"Most trained gyn oncologists have the ability and training to take somebody to microscopic residual disease. What it takes to get to that place obviously varies from patient to patient and the disease that they have at the time that they present. Ultimately, what has to be decided between the patient and the physician is what’s going to be the best possibility for them and using CA125 as a potential guide, say, taking everything into consideration – age, where their disease is, what their CA125 is, what my comfort level is doing certain procedures being able to get them down to microscopic disease," Dr. Horowitz replied. "So I don’t think it’s a one-size-fits-all [objective] based just on the surgical expertise. Most gyn oncologists are trained adequately to be able to do this. It’s just, because you can do it, the question is, should you be doing it on everybody."
Another attendee said, "In follow-up to that, do you think that the difference in the behavior of the presurgical and the pretreatment CA125 could be confounded, the latter by surgical decisions or surgical intervention?"
"It’s potentially confounded; whether it’s surgical skill or some people would say, I don’t want to use the term honesty, but it may be a reflection of what truly is left behind versus not left behind, if it didn’t really follow the way it should. It may be a window into how accurate our predictions or our estimates of what we left behind really are," Dr. Horowitz explained. "Pretreatment CA125, it is difficult to really get a good understanding of this number because obviously the patients who start with the highest CA125 have the greatest chance to fall ... So it’s a little tricky trying to figure out what to make of that number, whereas patients who start with a lower one, although they didn’t fall with the same percentile, you still may have done just as good a job surgically."
The 998 women studied were from Gynecologic Oncology Group (GOG) trial 182. "This is the largest reported series to evaluate the ability of preoperative CA125 to predict surgical cytoreductive outcomes and survival in a population of women with optimally cytoreduced primary ovarian or peritoneal cancer," Dr. Horowitz noted.
Overall, 33% had microscopic residual disease, while the other 67% had more extensive residual disease but still measuring less than 1 cm.
The median preoperative CA125 level was 346 U/mL in the former group and 870 U/mL in the latter, reported Dr. Horowitz, who disclosed no conflicts of interest related to the research.
"Despite the difference in median preoperative CA125 values, the distributions of the preoperative CA125s in those with microscopic and less than 1 cm residual overlapped almost completely," Dr. Horowitz reported. "This suggests that there is not a preoperative CA125 beyond which one cannot achieve a complete cytoreductive surgery."
However, the higher the preoperative CA125 level, the lower the predicted probability of achieving microscopic residual disease (P less than .01). For example, the probability was 33%, 27%, and 19% for women having a level of 500, 1,000, and 2,500 U/mL, respectively.
"It is important to remember that these curves only reflect data from women who achieved optimal cytoreduction and do not include those with suboptimal primary debulking. Therefore, the estimated predictions and probabilities are likely to decrease when applied to a preoperative population of unknown surgical outcome," he said. "But if one assumes a priori that you can achieve and will achieve optimal cytoreduction, then preoperative CA125 can estimate the likelihood of obtaining either microscopic or less than 1-cm residual."
In adjusted analyses, preoperative CA125 levels and extent of residual disease jointly predicted both progression-free survival (P less than .001) and overall survival (P = .04). For example, median overall survival ranged from 82 months in women having microscopic residual disease and a CA125 level of 35 U/mL to just 39 months in their counterparts with more residual disease and a CA125 level of 1,000 U/mL.
The change from preoperative to pretreatment CA125 levels predicted both progression-free survival (P less than .0001) and overall survival (P less than .0001). For example, median overall survival ranged from 60 months in women having a reduction in levels exceeding 80% to 45 months in their counterparts having stable or increasing levels.
In addition, among the group having a greater than 80% decline in CA125 level, survival was almost twice as long among those achieving microscopic residual disease, at 82 months, as among those with greater residual disease, at 48 months, "suggesting that residual disease rather than change in CA125 is more important to survival," Dr. Horowitz said.
LOS ANGELES – Preoperative levels of cancer antigen 125 (CA125) predict surgical and disease outcomes in women with advanced epithelial ovarian cancer who are able to undergo optimal debulking surgery, new data show, and may therefore help guide treatment decisions.
A team led by Dr. Neil S. Horowitz of Brigham and Women’s Hospital and the Dana Farber Cancer Institute in Boston assessed levels of the biomarker among nearly 1,000 women who had stage III or IV disease that was optimally debulked to less than 1 cm of residual disease and who received adjuvant paclitaxel- and platinum-containing chemotherapy.
Results showed that no cutoff value of preoperative CA125 levels clearly separated women in whom microscopic residual disease was achieved surgically from women in whom a greater volume of disease remained, he reported at the annual meeting of the Society of Gynecologic Oncology.
But the probability of achieving microscopic status decreased with increasing CA125 levels. For example, it fell from 33% in women with a level of 500 U/mL to 27% in women with a level of 1,000 U/mL.
"Although a strict CA125 value to predict microscopic residual cannot be made, these data are helpful for counseling patients regarding surgical results and outcome, and should influence decisions regarding primary debulking surgery and possibly use of other ... treatment options like neoadjuvant chemotherapy," Dr. Horowitz said. "Each surgeon and [his or her] patient have to decide for themselves what is an acceptable probability of successful surgical outcome to microscopic residual disease.
Additional study findings showed that women with higher preoperative CA125 levels and women with smaller reductions in CA125 levels between the preoperative period and the pretreatment period, before starting chemotherapy, had significantly worse progression-free and overall survival.
One session attendee asked, "What impact do you think surgical expertise has on the ability to predict the extent of cytoreduction?"
"Most trained gyn oncologists have the ability and training to take somebody to microscopic residual disease. What it takes to get to that place obviously varies from patient to patient and the disease that they have at the time that they present. Ultimately, what has to be decided between the patient and the physician is what’s going to be the best possibility for them and using CA125 as a potential guide, say, taking everything into consideration – age, where their disease is, what their CA125 is, what my comfort level is doing certain procedures being able to get them down to microscopic disease," Dr. Horowitz replied. "So I don’t think it’s a one-size-fits-all [objective] based just on the surgical expertise. Most gyn oncologists are trained adequately to be able to do this. It’s just, because you can do it, the question is, should you be doing it on everybody."
Another attendee said, "In follow-up to that, do you think that the difference in the behavior of the presurgical and the pretreatment CA125 could be confounded, the latter by surgical decisions or surgical intervention?"
"It’s potentially confounded; whether it’s surgical skill or some people would say, I don’t want to use the term honesty, but it may be a reflection of what truly is left behind versus not left behind, if it didn’t really follow the way it should. It may be a window into how accurate our predictions or our estimates of what we left behind really are," Dr. Horowitz explained. "Pretreatment CA125, it is difficult to really get a good understanding of this number because obviously the patients who start with the highest CA125 have the greatest chance to fall ... So it’s a little tricky trying to figure out what to make of that number, whereas patients who start with a lower one, although they didn’t fall with the same percentile, you still may have done just as good a job surgically."
The 998 women studied were from Gynecologic Oncology Group (GOG) trial 182. "This is the largest reported series to evaluate the ability of preoperative CA125 to predict surgical cytoreductive outcomes and survival in a population of women with optimally cytoreduced primary ovarian or peritoneal cancer," Dr. Horowitz noted.
Overall, 33% had microscopic residual disease, while the other 67% had more extensive residual disease but still measuring less than 1 cm.
The median preoperative CA125 level was 346 U/mL in the former group and 870 U/mL in the latter, reported Dr. Horowitz, who disclosed no conflicts of interest related to the research.
"Despite the difference in median preoperative CA125 values, the distributions of the preoperative CA125s in those with microscopic and less than 1 cm residual overlapped almost completely," Dr. Horowitz reported. "This suggests that there is not a preoperative CA125 beyond which one cannot achieve a complete cytoreductive surgery."
However, the higher the preoperative CA125 level, the lower the predicted probability of achieving microscopic residual disease (P less than .01). For example, the probability was 33%, 27%, and 19% for women having a level of 500, 1,000, and 2,500 U/mL, respectively.
"It is important to remember that these curves only reflect data from women who achieved optimal cytoreduction and do not include those with suboptimal primary debulking. Therefore, the estimated predictions and probabilities are likely to decrease when applied to a preoperative population of unknown surgical outcome," he said. "But if one assumes a priori that you can achieve and will achieve optimal cytoreduction, then preoperative CA125 can estimate the likelihood of obtaining either microscopic or less than 1-cm residual."
In adjusted analyses, preoperative CA125 levels and extent of residual disease jointly predicted both progression-free survival (P less than .001) and overall survival (P = .04). For example, median overall survival ranged from 82 months in women having microscopic residual disease and a CA125 level of 35 U/mL to just 39 months in their counterparts with more residual disease and a CA125 level of 1,000 U/mL.
The change from preoperative to pretreatment CA125 levels predicted both progression-free survival (P less than .0001) and overall survival (P less than .0001). For example, median overall survival ranged from 60 months in women having a reduction in levels exceeding 80% to 45 months in their counterparts having stable or increasing levels.
In addition, among the group having a greater than 80% decline in CA125 level, survival was almost twice as long among those achieving microscopic residual disease, at 82 months, as among those with greater residual disease, at 48 months, "suggesting that residual disease rather than change in CA125 is more important to survival," Dr. Horowitz said.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Major finding: The higher the preoperative CA125 level, the lower the predicted probability of achieving microscopic residual disease. Probability was 33%, 27%, and 19% for levels of 500, 1,000, and 2,500 U/mL, respectively.
Data source: An ancillary study among 998 women with optimally debulked advanced epithelial ovarian cancer or primary peritoneal cancer from the GOG 182 trial.
Disclosures: Dr. Horowitz disclosed no relevant conflicts of interest.
Cyberknife therapy offers benefits for recurring gyn cancers
LOS ANGELES – Robotic Cyberknife radiation therapy will likely expand the treatment options for patients whose gynecologic malignancies recur, researchers reported at the annual meeting of the Society of Gynecologic Oncologists.
A total of 50 patients with recurrent gynecologic (mainly ovarian and endometrial) cancers underwent Cyberknife treatment, which allows targeting of high doses of radiation to the tumor while largely sparing adjacent healthy tissue. In this case, patients received an 8-Gy treatment on each of 3 consecutive days.
Results showed that two-thirds of the patients had a complete response, a partial response, or stable disease 6 months after treatment. Higher-severity acute adverse events were uncommon and consisted of single cases of diarrhea and hyperbilirubinemia.
"This is the first phase II clinical trial of robotic radiosurgery in the gynecologic oncology space. Robotic Cyberknife radiation therapy does definitely provide clinical benefit to your patients," commented lead author Dr. Charles Kunos, a radiation oncologist with the Case Comprehensive Cancer Center in Cleveland and the Summa Cancer Institute in Akron, Ohio.
However, the majority of women ultimately had progression in nontargeted areas of disease, and this progression was the cause of death in 40%. Therefore, the investigators have initiated a phase I trial combining Cyberknife therapy with systemic chemotherapy.
One attendee noted, "As I think we all know, many of these patients who have recurrent side-wall disease from gynecologic cancers have a loop of bowel that’s sitting immediately adjacent to the potential target. And we have always felt that you needed to adjust the dose per fraction depending on that in patients with recurrent disease who have been previously irradiated. How do you select your patients for these 8-Gy-fraction treatments?"
"Patient selection is mostly based on target volume and the number of sites that are going to be treated during the course of therapy. ... We find that the 8-Gy dose is extremely well tolerated," he noted. The team is currently performing analyses to determine maximum tissue tolerances and optimally guide patient selection.
Another attendee had a similar question, asking whether any of the lesions treated were located in a previously irradiated field.
"More than 60% of those patients had received prior radiation therapy. Almost all the cervical cancer patients in the trial, as well as the majority of those patients with endometrial cancer, had received prior radiation therapy," Dr. Kunos replied. "The prior radiation therapy is not a barrier for delivering this form of treatment at these doses. Our toxicity rates are extraordinarily low, even in the cases with the prior radiation, so with selection of the patient who has a relatively good performing health status, as well as considering the time of when the previous radiation therapy dose was delivered, I think you can adequately select patients for this type of therapy."
A third attendee posed bigger-picture questions: "Can you tell us a little bit about the cost-effectiveness of the Cyberknife therapy and, given that you have an ongoing phase I trial looking at this in dual-modality [treatment] with chemotherapy, what is the future of this therapeutic approach for gyn malignancies?"
"The NCI [National Cancer Institute] is interested in exploring the radiosurgery platform as a way of testing novel therapeutics as radiation sensitizers, but because the radiation therapy is so exquisitely tuned to the actual cancer target, there is an opportunity to study whether or not there are systemic effects of the novel drugs as well. So I think at some level, the future is relatively bright," Dr. Kunos explained.
"Regarding the cost or the expense of therapy, we are condensing 5, 6, 7 weeks of radiation therapy into 3 days on the trial, so there are considerable savings in that regard to patient travel and other, social aspects of treatment in trying to get patients back and forth for several weeks of therapy in a palliative situation," he continued. "The radiosurgery itself is expensive; that part of the cost structure will probably continue to come down in the future with the way that patients will be managed."
The cohort enrolled in the trial included 25 patients with ovarian cancer, 14 with endometrial cancer, 9 with cervical cancer, and 2 with vulvar cancer. All had received at least one chemotherapy or radiation therapy regimen previously.
The patients had up to four targets of disease to be treated. They underwent implantation of gold seeds for target tracking during treatment, and co-registered computed tomography and positron emission tomography scans were used to generate the radiation therapy plan.
The patients received a total of 24 Gy of radiation delivered in three daily doses of 8 Gy each. The median duration of follow-up was 15 months.
Study results, reported at the meeting and recently published (Front. Oncol. 2012;2:181), showed that 3 months after treatment, 50% of patients had a complete response, 46% had a partial response, and 4% had stable disease, according to Dr. Kunos.
At 6 months, the rate of clinical benefit – capturing patients with a complete response, partial response, or stable disease – was 68%.
Ultimately, 62% of patients had progression in a nontargeted disease site, and 40% died from disease progression.
"Reversible fatigue lasting up to 1 week after treatment was the most noticeable toxicity," Dr. Kunos said. In the first 30 days after treatment, the most common adverse effects were grade 2 fatigue, seen in 16% of patients, and grade 2 nausea, seen in 8%. Only 2% of patients had grade 3 diarrhea, and only 2% had grade 4 hyperbilirubinemia.
Dr. Kunos disclosed that he had no relevant conflicts of interest.
LOS ANGELES – Robotic Cyberknife radiation therapy will likely expand the treatment options for patients whose gynecologic malignancies recur, researchers reported at the annual meeting of the Society of Gynecologic Oncologists.
A total of 50 patients with recurrent gynecologic (mainly ovarian and endometrial) cancers underwent Cyberknife treatment, which allows targeting of high doses of radiation to the tumor while largely sparing adjacent healthy tissue. In this case, patients received an 8-Gy treatment on each of 3 consecutive days.
Results showed that two-thirds of the patients had a complete response, a partial response, or stable disease 6 months after treatment. Higher-severity acute adverse events were uncommon and consisted of single cases of diarrhea and hyperbilirubinemia.
"This is the first phase II clinical trial of robotic radiosurgery in the gynecologic oncology space. Robotic Cyberknife radiation therapy does definitely provide clinical benefit to your patients," commented lead author Dr. Charles Kunos, a radiation oncologist with the Case Comprehensive Cancer Center in Cleveland and the Summa Cancer Institute in Akron, Ohio.
However, the majority of women ultimately had progression in nontargeted areas of disease, and this progression was the cause of death in 40%. Therefore, the investigators have initiated a phase I trial combining Cyberknife therapy with systemic chemotherapy.
One attendee noted, "As I think we all know, many of these patients who have recurrent side-wall disease from gynecologic cancers have a loop of bowel that’s sitting immediately adjacent to the potential target. And we have always felt that you needed to adjust the dose per fraction depending on that in patients with recurrent disease who have been previously irradiated. How do you select your patients for these 8-Gy-fraction treatments?"
"Patient selection is mostly based on target volume and the number of sites that are going to be treated during the course of therapy. ... We find that the 8-Gy dose is extremely well tolerated," he noted. The team is currently performing analyses to determine maximum tissue tolerances and optimally guide patient selection.
Another attendee had a similar question, asking whether any of the lesions treated were located in a previously irradiated field.
"More than 60% of those patients had received prior radiation therapy. Almost all the cervical cancer patients in the trial, as well as the majority of those patients with endometrial cancer, had received prior radiation therapy," Dr. Kunos replied. "The prior radiation therapy is not a barrier for delivering this form of treatment at these doses. Our toxicity rates are extraordinarily low, even in the cases with the prior radiation, so with selection of the patient who has a relatively good performing health status, as well as considering the time of when the previous radiation therapy dose was delivered, I think you can adequately select patients for this type of therapy."
A third attendee posed bigger-picture questions: "Can you tell us a little bit about the cost-effectiveness of the Cyberknife therapy and, given that you have an ongoing phase I trial looking at this in dual-modality [treatment] with chemotherapy, what is the future of this therapeutic approach for gyn malignancies?"
"The NCI [National Cancer Institute] is interested in exploring the radiosurgery platform as a way of testing novel therapeutics as radiation sensitizers, but because the radiation therapy is so exquisitely tuned to the actual cancer target, there is an opportunity to study whether or not there are systemic effects of the novel drugs as well. So I think at some level, the future is relatively bright," Dr. Kunos explained.
"Regarding the cost or the expense of therapy, we are condensing 5, 6, 7 weeks of radiation therapy into 3 days on the trial, so there are considerable savings in that regard to patient travel and other, social aspects of treatment in trying to get patients back and forth for several weeks of therapy in a palliative situation," he continued. "The radiosurgery itself is expensive; that part of the cost structure will probably continue to come down in the future with the way that patients will be managed."
The cohort enrolled in the trial included 25 patients with ovarian cancer, 14 with endometrial cancer, 9 with cervical cancer, and 2 with vulvar cancer. All had received at least one chemotherapy or radiation therapy regimen previously.
The patients had up to four targets of disease to be treated. They underwent implantation of gold seeds for target tracking during treatment, and co-registered computed tomography and positron emission tomography scans were used to generate the radiation therapy plan.
The patients received a total of 24 Gy of radiation delivered in three daily doses of 8 Gy each. The median duration of follow-up was 15 months.
Study results, reported at the meeting and recently published (Front. Oncol. 2012;2:181), showed that 3 months after treatment, 50% of patients had a complete response, 46% had a partial response, and 4% had stable disease, according to Dr. Kunos.
At 6 months, the rate of clinical benefit – capturing patients with a complete response, partial response, or stable disease – was 68%.
Ultimately, 62% of patients had progression in a nontargeted disease site, and 40% died from disease progression.
"Reversible fatigue lasting up to 1 week after treatment was the most noticeable toxicity," Dr. Kunos said. In the first 30 days after treatment, the most common adverse effects were grade 2 fatigue, seen in 16% of patients, and grade 2 nausea, seen in 8%. Only 2% of patients had grade 3 diarrhea, and only 2% had grade 4 hyperbilirubinemia.
Dr. Kunos disclosed that he had no relevant conflicts of interest.
LOS ANGELES – Robotic Cyberknife radiation therapy will likely expand the treatment options for patients whose gynecologic malignancies recur, researchers reported at the annual meeting of the Society of Gynecologic Oncologists.
A total of 50 patients with recurrent gynecologic (mainly ovarian and endometrial) cancers underwent Cyberknife treatment, which allows targeting of high doses of radiation to the tumor while largely sparing adjacent healthy tissue. In this case, patients received an 8-Gy treatment on each of 3 consecutive days.
Results showed that two-thirds of the patients had a complete response, a partial response, or stable disease 6 months after treatment. Higher-severity acute adverse events were uncommon and consisted of single cases of diarrhea and hyperbilirubinemia.
"This is the first phase II clinical trial of robotic radiosurgery in the gynecologic oncology space. Robotic Cyberknife radiation therapy does definitely provide clinical benefit to your patients," commented lead author Dr. Charles Kunos, a radiation oncologist with the Case Comprehensive Cancer Center in Cleveland and the Summa Cancer Institute in Akron, Ohio.
However, the majority of women ultimately had progression in nontargeted areas of disease, and this progression was the cause of death in 40%. Therefore, the investigators have initiated a phase I trial combining Cyberknife therapy with systemic chemotherapy.
One attendee noted, "As I think we all know, many of these patients who have recurrent side-wall disease from gynecologic cancers have a loop of bowel that’s sitting immediately adjacent to the potential target. And we have always felt that you needed to adjust the dose per fraction depending on that in patients with recurrent disease who have been previously irradiated. How do you select your patients for these 8-Gy-fraction treatments?"
"Patient selection is mostly based on target volume and the number of sites that are going to be treated during the course of therapy. ... We find that the 8-Gy dose is extremely well tolerated," he noted. The team is currently performing analyses to determine maximum tissue tolerances and optimally guide patient selection.
Another attendee had a similar question, asking whether any of the lesions treated were located in a previously irradiated field.
"More than 60% of those patients had received prior radiation therapy. Almost all the cervical cancer patients in the trial, as well as the majority of those patients with endometrial cancer, had received prior radiation therapy," Dr. Kunos replied. "The prior radiation therapy is not a barrier for delivering this form of treatment at these doses. Our toxicity rates are extraordinarily low, even in the cases with the prior radiation, so with selection of the patient who has a relatively good performing health status, as well as considering the time of when the previous radiation therapy dose was delivered, I think you can adequately select patients for this type of therapy."
A third attendee posed bigger-picture questions: "Can you tell us a little bit about the cost-effectiveness of the Cyberknife therapy and, given that you have an ongoing phase I trial looking at this in dual-modality [treatment] with chemotherapy, what is the future of this therapeutic approach for gyn malignancies?"
"The NCI [National Cancer Institute] is interested in exploring the radiosurgery platform as a way of testing novel therapeutics as radiation sensitizers, but because the radiation therapy is so exquisitely tuned to the actual cancer target, there is an opportunity to study whether or not there are systemic effects of the novel drugs as well. So I think at some level, the future is relatively bright," Dr. Kunos explained.
"Regarding the cost or the expense of therapy, we are condensing 5, 6, 7 weeks of radiation therapy into 3 days on the trial, so there are considerable savings in that regard to patient travel and other, social aspects of treatment in trying to get patients back and forth for several weeks of therapy in a palliative situation," he continued. "The radiosurgery itself is expensive; that part of the cost structure will probably continue to come down in the future with the way that patients will be managed."
The cohort enrolled in the trial included 25 patients with ovarian cancer, 14 with endometrial cancer, 9 with cervical cancer, and 2 with vulvar cancer. All had received at least one chemotherapy or radiation therapy regimen previously.
The patients had up to four targets of disease to be treated. They underwent implantation of gold seeds for target tracking during treatment, and co-registered computed tomography and positron emission tomography scans were used to generate the radiation therapy plan.
The patients received a total of 24 Gy of radiation delivered in three daily doses of 8 Gy each. The median duration of follow-up was 15 months.
Study results, reported at the meeting and recently published (Front. Oncol. 2012;2:181), showed that 3 months after treatment, 50% of patients had a complete response, 46% had a partial response, and 4% had stable disease, according to Dr. Kunos.
At 6 months, the rate of clinical benefit – capturing patients with a complete response, partial response, or stable disease – was 68%.
Ultimately, 62% of patients had progression in a nontargeted disease site, and 40% died from disease progression.
"Reversible fatigue lasting up to 1 week after treatment was the most noticeable toxicity," Dr. Kunos said. In the first 30 days after treatment, the most common adverse effects were grade 2 fatigue, seen in 16% of patients, and grade 2 nausea, seen in 8%. Only 2% of patients had grade 3 diarrhea, and only 2% had grade 4 hyperbilirubinemia.
Dr. Kunos disclosed that he had no relevant conflicts of interest.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Major finding: The 6-month clinical benefit rate was 68%. Higher-severity acute adverse events were uncommon.
Data source: A phase II trial among 50 patients with recurrent gynecologic cancers.
Disclosures: Dr. Kunos disclosed that he had no relevant conflicts of interest.
Mammography screening at 75 may have value
WASHINGTON – For women aged 75 years and older, a span of 5 or more years between mammograms translated into a threefold increased risk of death from breast cancer, compared with women in the same age group who had yearly exams.
While the exact reasons for the finding can’t be pinpointed, it should at least reawaken the discussion about whether older women should get a regular mammogram, Dr. Michael Simon noted at the annual meeting of the American Association for Cancer Research.
In 2009, the U.S. Preventive Services Task Force changed its recommendation on screening exams for women aged 75 and older, noting that there was insufficient evidence to recommend for or against breast cancer screening in this population (Ann. Intern. Med. 2009;151:716-26).
However, the absence of evidence does not automatically translate into absence of benefit, Dr. Simon said in an interview. "You can’t assume that at 75, it’s not worth screening anymore. Yes, there’s no evidence from randomized trials of women older than 75, and the recommendations are based on this kind of evidence. But just because there are no trials doesn’t mean there is no benefit."
Dr. Simon and his coinvestigators extracted data from the 15-year Women’s Health Initiative study. The cohort comprised 9,057 women who had been diagnosed with breast cancer over a 12-year period.
The multivariate analysis examined the relationship between death from breast cancer and mammography screening intervals. The screening intervals studied were from 6 months to 1 year, 1 to 2 years, 2 to 5 years, and more than 5 years or never. The study cohort was divided into women by age: 50-74 years (6,497) and 75 years or older (2,560).
Baseline characteristics showed that the older group of women presented with dangerous breast cancers almost as often as did the younger group, including moderately differentiated (22% vs. 21%, respectively) and poorly differentiated tumors (28% vs. 31%). Older women were more likely to have hormone receptor–positive tumors (75% vs. 67%), and just as likely to have hormone receptor–negative tumors (12% of each group).
Stage was also similar between the older and younger groups: in situ (18% vs. 20%, respectively); localized (62% vs. 59%); regional (17% vs. 19%); and distant (1% in both groups).
Significant differences occurred when the investigators broke the group of more than 9,000 women out by mammogram intervals.
Overall, an interval of 5 or more years between a woman’s last mammogram and breast cancer diagnosis was associated with advanced-stage disease in 23%, compared with 20% in women with an interval of 1 year or less – a statistically significant difference, which could affect large numbers of women, said Dr. Simon, head of the breast multidisciplinary team at Barbara Ann Karmanos Cancer Institute in Detroit.
"We also saw significantly more aggressive cancers that were hormone receptor negative in the group with the longest interval between mammograms," he said (22% vs. 16%).
The multivariate analysis adjusted for age at enrollment in the WHI study and the trial component in which subjects enrolled, age at diagnosis, race and ethnicity, insurance and marital status, comorbidities, and body mass index at baseline.
In this analysis, women aged 75 years and older who went at least 5 years between mammograms were 67% more likely to die from a breast cancer than were those who had yearly exams. Older women who went 5 or more years between mammograms were three times more likely to die than were those who had yearly screening, Dr. Simon said.
The results show a need for stronger emphasis on regular mammograms for older women, he said. "Women are living longer and living vitally longer. If we have a test that can identify an early cancer ... we should take advantage of it."
For women of any age, mammograms have their downsides, including anxiety while waiting for results, overdiagnosis, and treatment of indolent, in situ tumors that may never progress to serious cancers – especially in women with a shorter lifespan ahead of them. Dr. Simon said those risks are small compared with the benefit of finding and treating a potentially lethal tumor.
Cost, however, is the sticking point, admitted Dr. Simon, who is also a public health expert.
"Resource allocation is something we can’t ignore. We know that it takes 1,700 mammograms to benefit one woman. That sounds like a lot, but when you think about it in a global perspective – how many women there are in this country – you see it in a different light. What we’re paying for mammograms is small potatoes."
Dr. Simon had no financial disclosures.
WASHINGTON – For women aged 75 years and older, a span of 5 or more years between mammograms translated into a threefold increased risk of death from breast cancer, compared with women in the same age group who had yearly exams.
While the exact reasons for the finding can’t be pinpointed, it should at least reawaken the discussion about whether older women should get a regular mammogram, Dr. Michael Simon noted at the annual meeting of the American Association for Cancer Research.
In 2009, the U.S. Preventive Services Task Force changed its recommendation on screening exams for women aged 75 and older, noting that there was insufficient evidence to recommend for or against breast cancer screening in this population (Ann. Intern. Med. 2009;151:716-26).
However, the absence of evidence does not automatically translate into absence of benefit, Dr. Simon said in an interview. "You can’t assume that at 75, it’s not worth screening anymore. Yes, there’s no evidence from randomized trials of women older than 75, and the recommendations are based on this kind of evidence. But just because there are no trials doesn’t mean there is no benefit."
Dr. Simon and his coinvestigators extracted data from the 15-year Women’s Health Initiative study. The cohort comprised 9,057 women who had been diagnosed with breast cancer over a 12-year period.
The multivariate analysis examined the relationship between death from breast cancer and mammography screening intervals. The screening intervals studied were from 6 months to 1 year, 1 to 2 years, 2 to 5 years, and more than 5 years or never. The study cohort was divided into women by age: 50-74 years (6,497) and 75 years or older (2,560).
Baseline characteristics showed that the older group of women presented with dangerous breast cancers almost as often as did the younger group, including moderately differentiated (22% vs. 21%, respectively) and poorly differentiated tumors (28% vs. 31%). Older women were more likely to have hormone receptor–positive tumors (75% vs. 67%), and just as likely to have hormone receptor–negative tumors (12% of each group).
Stage was also similar between the older and younger groups: in situ (18% vs. 20%, respectively); localized (62% vs. 59%); regional (17% vs. 19%); and distant (1% in both groups).
Significant differences occurred when the investigators broke the group of more than 9,000 women out by mammogram intervals.
Overall, an interval of 5 or more years between a woman’s last mammogram and breast cancer diagnosis was associated with advanced-stage disease in 23%, compared with 20% in women with an interval of 1 year or less – a statistically significant difference, which could affect large numbers of women, said Dr. Simon, head of the breast multidisciplinary team at Barbara Ann Karmanos Cancer Institute in Detroit.
"We also saw significantly more aggressive cancers that were hormone receptor negative in the group with the longest interval between mammograms," he said (22% vs. 16%).
The multivariate analysis adjusted for age at enrollment in the WHI study and the trial component in which subjects enrolled, age at diagnosis, race and ethnicity, insurance and marital status, comorbidities, and body mass index at baseline.
In this analysis, women aged 75 years and older who went at least 5 years between mammograms were 67% more likely to die from a breast cancer than were those who had yearly exams. Older women who went 5 or more years between mammograms were three times more likely to die than were those who had yearly screening, Dr. Simon said.
The results show a need for stronger emphasis on regular mammograms for older women, he said. "Women are living longer and living vitally longer. If we have a test that can identify an early cancer ... we should take advantage of it."
For women of any age, mammograms have their downsides, including anxiety while waiting for results, overdiagnosis, and treatment of indolent, in situ tumors that may never progress to serious cancers – especially in women with a shorter lifespan ahead of them. Dr. Simon said those risks are small compared with the benefit of finding and treating a potentially lethal tumor.
Cost, however, is the sticking point, admitted Dr. Simon, who is also a public health expert.
"Resource allocation is something we can’t ignore. We know that it takes 1,700 mammograms to benefit one woman. That sounds like a lot, but when you think about it in a global perspective – how many women there are in this country – you see it in a different light. What we’re paying for mammograms is small potatoes."
Dr. Simon had no financial disclosures.
WASHINGTON – For women aged 75 years and older, a span of 5 or more years between mammograms translated into a threefold increased risk of death from breast cancer, compared with women in the same age group who had yearly exams.
While the exact reasons for the finding can’t be pinpointed, it should at least reawaken the discussion about whether older women should get a regular mammogram, Dr. Michael Simon noted at the annual meeting of the American Association for Cancer Research.
In 2009, the U.S. Preventive Services Task Force changed its recommendation on screening exams for women aged 75 and older, noting that there was insufficient evidence to recommend for or against breast cancer screening in this population (Ann. Intern. Med. 2009;151:716-26).
However, the absence of evidence does not automatically translate into absence of benefit, Dr. Simon said in an interview. "You can’t assume that at 75, it’s not worth screening anymore. Yes, there’s no evidence from randomized trials of women older than 75, and the recommendations are based on this kind of evidence. But just because there are no trials doesn’t mean there is no benefit."
Dr. Simon and his coinvestigators extracted data from the 15-year Women’s Health Initiative study. The cohort comprised 9,057 women who had been diagnosed with breast cancer over a 12-year period.
The multivariate analysis examined the relationship between death from breast cancer and mammography screening intervals. The screening intervals studied were from 6 months to 1 year, 1 to 2 years, 2 to 5 years, and more than 5 years or never. The study cohort was divided into women by age: 50-74 years (6,497) and 75 years or older (2,560).
Baseline characteristics showed that the older group of women presented with dangerous breast cancers almost as often as did the younger group, including moderately differentiated (22% vs. 21%, respectively) and poorly differentiated tumors (28% vs. 31%). Older women were more likely to have hormone receptor–positive tumors (75% vs. 67%), and just as likely to have hormone receptor–negative tumors (12% of each group).
Stage was also similar between the older and younger groups: in situ (18% vs. 20%, respectively); localized (62% vs. 59%); regional (17% vs. 19%); and distant (1% in both groups).
Significant differences occurred when the investigators broke the group of more than 9,000 women out by mammogram intervals.
Overall, an interval of 5 or more years between a woman’s last mammogram and breast cancer diagnosis was associated with advanced-stage disease in 23%, compared with 20% in women with an interval of 1 year or less – a statistically significant difference, which could affect large numbers of women, said Dr. Simon, head of the breast multidisciplinary team at Barbara Ann Karmanos Cancer Institute in Detroit.
"We also saw significantly more aggressive cancers that were hormone receptor negative in the group with the longest interval between mammograms," he said (22% vs. 16%).
The multivariate analysis adjusted for age at enrollment in the WHI study and the trial component in which subjects enrolled, age at diagnosis, race and ethnicity, insurance and marital status, comorbidities, and body mass index at baseline.
In this analysis, women aged 75 years and older who went at least 5 years between mammograms were 67% more likely to die from a breast cancer than were those who had yearly exams. Older women who went 5 or more years between mammograms were three times more likely to die than were those who had yearly screening, Dr. Simon said.
The results show a need for stronger emphasis on regular mammograms for older women, he said. "Women are living longer and living vitally longer. If we have a test that can identify an early cancer ... we should take advantage of it."
For women of any age, mammograms have their downsides, including anxiety while waiting for results, overdiagnosis, and treatment of indolent, in situ tumors that may never progress to serious cancers – especially in women with a shorter lifespan ahead of them. Dr. Simon said those risks are small compared with the benefit of finding and treating a potentially lethal tumor.
Cost, however, is the sticking point, admitted Dr. Simon, who is also a public health expert.
"Resource allocation is something we can’t ignore. We know that it takes 1,700 mammograms to benefit one woman. That sounds like a lot, but when you think about it in a global perspective – how many women there are in this country – you see it in a different light. What we’re paying for mammograms is small potatoes."
Dr. Simon had no financial disclosures.
AT THE AACR ANNUAL MEETING
Major finding: Women aged 75 years and older were 3 times more likely to die from breast cancer if they went 5 or more years between mammograms, compared with those who had a yearly screening.
Data source: Women’s Health Initiative data on more than 9,000 women diagnosed with breast cancer.
Disclosures: Dr. Simon had no financial disclosures.