User login
Official Newspaper of the American College of Surgeons
FDA backs abuse-deterring OxyContin, thwarts generics
In an eleventh-hour action that derailed the possibility of generic formulations of controlled-release oxycodone (OxyContin) from appearing on the U.S. market anytime soon, the Food and Drug Administration announced April 16 that it withdrew its approval of the original, conventional formulation of OxyContin.
Acting on the very day that the patent on the original formulation of OxyContin, held by Purdue Pharma, was set to expire, the FDA took an additional step to support the newer formulation of OxyContin that Purdue has marketed exclusively since August 2010. The newer version includes a polymer so that, when a pill is crushed and then mixed with water it turns into a gel rather than remaining a more easily manipulated powder. The FDA approved updated labeling for OxyContin that highlights the abuse-deterring features of the newer formulation, which means that Purdue can now cite these attributes when marketing the drug.
The FDA "approved labeling for reformulated OxyContin stating that it possesses physiochemical properties that are expected to: (1) make abuse via injection difficult, and (2) reduce abuse via the intranasal route. This is the first opioid product for which FDA has approved labeling that includes statements regarding abuse-deterrence," according to a letter from FDA Commissioner Margaret A. Hamburg sent April 16 to Rep. Fred Upton (R-Mich.) and Sen. Tom Coburn (R-Okla).
"We applaud FDA Commissioner Hamburg’s announcement that the FDA will not approve any abbreviated new drug applications that rely upon the approval of original OxyContin which did not have abuse-deterrent properties," the lawmakers said in a statement. "With more than 16,000 Americans dying from opioid drug overdoses each year, Commissioner Hamburg’s announcement is a significant step forward in the federal government’s effort to reduce opioid drug abuse and protect consumers. For too long, drug abusers have been able to crush or dissolve opioid drug products in order to defeat their time-release mechanisms for snorting or injecting the drugs."
For patients, the major downside of the FDA’s action is economic. OxyContin retails for about $7.50 per tablet and had roughly $2.7 billion in U.S. sales in 2012. The patent on the abuse-deterring formulation of the drug lasts until 2025.
On Twitter @mitchelzoler
In an eleventh-hour action that derailed the possibility of generic formulations of controlled-release oxycodone (OxyContin) from appearing on the U.S. market anytime soon, the Food and Drug Administration announced April 16 that it withdrew its approval of the original, conventional formulation of OxyContin.
Acting on the very day that the patent on the original formulation of OxyContin, held by Purdue Pharma, was set to expire, the FDA took an additional step to support the newer formulation of OxyContin that Purdue has marketed exclusively since August 2010. The newer version includes a polymer so that, when a pill is crushed and then mixed with water it turns into a gel rather than remaining a more easily manipulated powder. The FDA approved updated labeling for OxyContin that highlights the abuse-deterring features of the newer formulation, which means that Purdue can now cite these attributes when marketing the drug.
The FDA "approved labeling for reformulated OxyContin stating that it possesses physiochemical properties that are expected to: (1) make abuse via injection difficult, and (2) reduce abuse via the intranasal route. This is the first opioid product for which FDA has approved labeling that includes statements regarding abuse-deterrence," according to a letter from FDA Commissioner Margaret A. Hamburg sent April 16 to Rep. Fred Upton (R-Mich.) and Sen. Tom Coburn (R-Okla).
"We applaud FDA Commissioner Hamburg’s announcement that the FDA will not approve any abbreviated new drug applications that rely upon the approval of original OxyContin which did not have abuse-deterrent properties," the lawmakers said in a statement. "With more than 16,000 Americans dying from opioid drug overdoses each year, Commissioner Hamburg’s announcement is a significant step forward in the federal government’s effort to reduce opioid drug abuse and protect consumers. For too long, drug abusers have been able to crush or dissolve opioid drug products in order to defeat their time-release mechanisms for snorting or injecting the drugs."
For patients, the major downside of the FDA’s action is economic. OxyContin retails for about $7.50 per tablet and had roughly $2.7 billion in U.S. sales in 2012. The patent on the abuse-deterring formulation of the drug lasts until 2025.
On Twitter @mitchelzoler
In an eleventh-hour action that derailed the possibility of generic formulations of controlled-release oxycodone (OxyContin) from appearing on the U.S. market anytime soon, the Food and Drug Administration announced April 16 that it withdrew its approval of the original, conventional formulation of OxyContin.
Acting on the very day that the patent on the original formulation of OxyContin, held by Purdue Pharma, was set to expire, the FDA took an additional step to support the newer formulation of OxyContin that Purdue has marketed exclusively since August 2010. The newer version includes a polymer so that, when a pill is crushed and then mixed with water it turns into a gel rather than remaining a more easily manipulated powder. The FDA approved updated labeling for OxyContin that highlights the abuse-deterring features of the newer formulation, which means that Purdue can now cite these attributes when marketing the drug.
The FDA "approved labeling for reformulated OxyContin stating that it possesses physiochemical properties that are expected to: (1) make abuse via injection difficult, and (2) reduce abuse via the intranasal route. This is the first opioid product for which FDA has approved labeling that includes statements regarding abuse-deterrence," according to a letter from FDA Commissioner Margaret A. Hamburg sent April 16 to Rep. Fred Upton (R-Mich.) and Sen. Tom Coburn (R-Okla).
"We applaud FDA Commissioner Hamburg’s announcement that the FDA will not approve any abbreviated new drug applications that rely upon the approval of original OxyContin which did not have abuse-deterrent properties," the lawmakers said in a statement. "With more than 16,000 Americans dying from opioid drug overdoses each year, Commissioner Hamburg’s announcement is a significant step forward in the federal government’s effort to reduce opioid drug abuse and protect consumers. For too long, drug abusers have been able to crush or dissolve opioid drug products in order to defeat their time-release mechanisms for snorting or injecting the drugs."
For patients, the major downside of the FDA’s action is economic. OxyContin retails for about $7.50 per tablet and had roughly $2.7 billion in U.S. sales in 2012. The patent on the abuse-deterring formulation of the drug lasts until 2025.
On Twitter @mitchelzoler
Watchful waiting doesn't pay for asymptomatic inguinal hernias
INDIANAPOLIS – The luster has suddenly worn off the time-honored strategy of nonoperative watchful waiting in men with minimally symptomatic inguinal hernias.
New evidence indicates the vast majority of men with asymptomatic or minimally symptomatic inguinal hernias will eventually come to surgery. This may not occur until years down the road, when their advanced age may render surgery more arduous.
"Although watchful waiting remains a safe strategy, even on long-term follow-up, patients who present to their physician to have their hernia evaluated, especially if elderly, should be informed that almost certainly they will come to surgery eventually ... The logical assumption is that watchful waiting is not an effective strategy, as with time almost all men cross over," Dr. Robert J. Fitzgibbons Jr. explained at the annual meeting of the American Surgical Association.
He presented an extended follow-up of patients enrolled in a landmark randomized multicenter clinical trial, one of only two randomized studies ever done comparing watchful waiting versus routine surgical repair for men with minimally symptomatic inguinal hernia. In the earlier report by Dr. Fitzgibbons and coworkers, watchful waiting was deemed "an acceptable option" because only 23% of patients crossed over to surgery due to increased pain during the first 2 years of follow-up (JAMA 2006;295:285-92).
At the ASA meeting, however, he presented updated 10-year follow-up data on 167 patients from the cohort initially assigned to watchful waiting. The rate of crossover to surgery was 68% by 10 years, with a marked age-based divergence. Patients below age 65 had a 62% crossover rate, while those above that age had a 79% crossover rate, according to Dr. Fitzgibbons, professor of surgery and chief of the division of general surgery at Creighton University, Omaha, Neb.
The good news was that hernia incarceration was a rare event, occurring at a rate of just 0.2% per year over the course of 10 years.
"We as surgeons have been taught for many years that we must repair all our hernias to prevent hernia accidents. Well, only three patients in our whole study developed incarceration, for which they underwent surgery with no mortality," Dr. Fitzgibbons noted. "The risk of a hernia accident should not be considered an indication for surgery. Older studies in the literature which would suggest otherwise can no longer be considered relevant."
He offered a caveat regarding the study findings: Participants were enrolled after they sought medical attention because of their hernias, even though they were asymptomatic or only minimally symptomatic. So the study results are most applicable to men concerned enough about their hernias that they visit a physician for that reason.
"It’s probably not valid to extrapolate the conclusions in this study to the entire population of minimally symptomatic inguinal hernia patients," the surgeon said. "Physicians have been observing elderly patients for years and would be loath to believe a crossover rate this high."
Nevertheless, the results of this study are virtually identical to those of the only other randomized trial of watchful waiting, which was conducted by surgeons at the University of Glasgow. The most recent update from that study showed an estimated crossover rate in the watchful waiting group of 16% at 1 year, 54% at 5 years, and 72% at 7.5 years. As in the American study, the rate of acute incarceration was reassuringly small. The investigators concluded that watchful waiting appears pointless, and they recommended surgical repair for medically fit patients (Br. J. Surg. 2011;98:596-9).
Discussant Dr. Michael E. Zenilman commented that his own approach is to individualize patient management based in large part upon activity level.
"When I see patients who are 80 years old in the office with an asymptomatic hernia, my conversation with them is about what their lifestyle is like. If they’re an active golfer I know that they’re going to end up getting their hernia fixed. If they’re sedentary, sitting at home in retirement, they don’t. So I think the next step in your research project should be to find out what the activity level is of these patients who are getting older and have asymptomatic hernias," said Dr. Zenilman, vice chair and regional director of surgery for the Washington, D.C., region, Johns Hopkins Medicine.
Dr. Fitzgibbons’ trial was funded by the Agency for Healthcare Research and Quality with support from the American College of Surgeons. He reported having no financial conflicts.
This report is finally a victory for surgeons who plead for common sense in the pursuit of evidence-based practice. Dr. Robert J. Fitzgibbons, recognized as one of surgery's foremost experts in hernia repair, presents long-term follow-up of patients with inguinal hernia who are treated expectantly. There are three very significant results. First, complications are very rare (0.5% per year, and these patients did OK with urgent management). Second, most patients will decide to have their hernias repaired, eventually (68% at 10 years). Finally, older patients are the ones most likely to come to repair.
Dr. Savarise |
What this means for the thousands of surgeons who see these patients on a regular basis is that shared clinical decision making with our patients, based on the surgeon's judgment of operative risks and benefits, is the correct clinical pathway. Nonoperative management, when in the opinion of the surgeon and in the patient to be in the patient's best interest, is safe. Immediate operation, even in patients with asymptomatic hernias, is standard of care. And it would be perfectly reasonable for any good-risk patient to schedule an elective hernia repair at his convenience.
Dr. Mark Savarise is an ACS Fellow and clinical assistant professor of surgery, University of Utah, Salt Lake City.
This report is finally a victory for surgeons who plead for common sense in the pursuit of evidence-based practice. Dr. Robert J. Fitzgibbons, recognized as one of surgery's foremost experts in hernia repair, presents long-term follow-up of patients with inguinal hernia who are treated expectantly. There are three very significant results. First, complications are very rare (0.5% per year, and these patients did OK with urgent management). Second, most patients will decide to have their hernias repaired, eventually (68% at 10 years). Finally, older patients are the ones most likely to come to repair.
Dr. Savarise |
What this means for the thousands of surgeons who see these patients on a regular basis is that shared clinical decision making with our patients, based on the surgeon's judgment of operative risks and benefits, is the correct clinical pathway. Nonoperative management, when in the opinion of the surgeon and in the patient to be in the patient's best interest, is safe. Immediate operation, even in patients with asymptomatic hernias, is standard of care. And it would be perfectly reasonable for any good-risk patient to schedule an elective hernia repair at his convenience.
Dr. Mark Savarise is an ACS Fellow and clinical assistant professor of surgery, University of Utah, Salt Lake City.
This report is finally a victory for surgeons who plead for common sense in the pursuit of evidence-based practice. Dr. Robert J. Fitzgibbons, recognized as one of surgery's foremost experts in hernia repair, presents long-term follow-up of patients with inguinal hernia who are treated expectantly. There are three very significant results. First, complications are very rare (0.5% per year, and these patients did OK with urgent management). Second, most patients will decide to have their hernias repaired, eventually (68% at 10 years). Finally, older patients are the ones most likely to come to repair.
Dr. Savarise |
What this means for the thousands of surgeons who see these patients on a regular basis is that shared clinical decision making with our patients, based on the surgeon's judgment of operative risks and benefits, is the correct clinical pathway. Nonoperative management, when in the opinion of the surgeon and in the patient to be in the patient's best interest, is safe. Immediate operation, even in patients with asymptomatic hernias, is standard of care. And it would be perfectly reasonable for any good-risk patient to schedule an elective hernia repair at his convenience.
Dr. Mark Savarise is an ACS Fellow and clinical assistant professor of surgery, University of Utah, Salt Lake City.
INDIANAPOLIS – The luster has suddenly worn off the time-honored strategy of nonoperative watchful waiting in men with minimally symptomatic inguinal hernias.
New evidence indicates the vast majority of men with asymptomatic or minimally symptomatic inguinal hernias will eventually come to surgery. This may not occur until years down the road, when their advanced age may render surgery more arduous.
"Although watchful waiting remains a safe strategy, even on long-term follow-up, patients who present to their physician to have their hernia evaluated, especially if elderly, should be informed that almost certainly they will come to surgery eventually ... The logical assumption is that watchful waiting is not an effective strategy, as with time almost all men cross over," Dr. Robert J. Fitzgibbons Jr. explained at the annual meeting of the American Surgical Association.
He presented an extended follow-up of patients enrolled in a landmark randomized multicenter clinical trial, one of only two randomized studies ever done comparing watchful waiting versus routine surgical repair for men with minimally symptomatic inguinal hernia. In the earlier report by Dr. Fitzgibbons and coworkers, watchful waiting was deemed "an acceptable option" because only 23% of patients crossed over to surgery due to increased pain during the first 2 years of follow-up (JAMA 2006;295:285-92).
At the ASA meeting, however, he presented updated 10-year follow-up data on 167 patients from the cohort initially assigned to watchful waiting. The rate of crossover to surgery was 68% by 10 years, with a marked age-based divergence. Patients below age 65 had a 62% crossover rate, while those above that age had a 79% crossover rate, according to Dr. Fitzgibbons, professor of surgery and chief of the division of general surgery at Creighton University, Omaha, Neb.
The good news was that hernia incarceration was a rare event, occurring at a rate of just 0.2% per year over the course of 10 years.
"We as surgeons have been taught for many years that we must repair all our hernias to prevent hernia accidents. Well, only three patients in our whole study developed incarceration, for which they underwent surgery with no mortality," Dr. Fitzgibbons noted. "The risk of a hernia accident should not be considered an indication for surgery. Older studies in the literature which would suggest otherwise can no longer be considered relevant."
He offered a caveat regarding the study findings: Participants were enrolled after they sought medical attention because of their hernias, even though they were asymptomatic or only minimally symptomatic. So the study results are most applicable to men concerned enough about their hernias that they visit a physician for that reason.
"It’s probably not valid to extrapolate the conclusions in this study to the entire population of minimally symptomatic inguinal hernia patients," the surgeon said. "Physicians have been observing elderly patients for years and would be loath to believe a crossover rate this high."
Nevertheless, the results of this study are virtually identical to those of the only other randomized trial of watchful waiting, which was conducted by surgeons at the University of Glasgow. The most recent update from that study showed an estimated crossover rate in the watchful waiting group of 16% at 1 year, 54% at 5 years, and 72% at 7.5 years. As in the American study, the rate of acute incarceration was reassuringly small. The investigators concluded that watchful waiting appears pointless, and they recommended surgical repair for medically fit patients (Br. J. Surg. 2011;98:596-9).
Discussant Dr. Michael E. Zenilman commented that his own approach is to individualize patient management based in large part upon activity level.
"When I see patients who are 80 years old in the office with an asymptomatic hernia, my conversation with them is about what their lifestyle is like. If they’re an active golfer I know that they’re going to end up getting their hernia fixed. If they’re sedentary, sitting at home in retirement, they don’t. So I think the next step in your research project should be to find out what the activity level is of these patients who are getting older and have asymptomatic hernias," said Dr. Zenilman, vice chair and regional director of surgery for the Washington, D.C., region, Johns Hopkins Medicine.
Dr. Fitzgibbons’ trial was funded by the Agency for Healthcare Research and Quality with support from the American College of Surgeons. He reported having no financial conflicts.
INDIANAPOLIS – The luster has suddenly worn off the time-honored strategy of nonoperative watchful waiting in men with minimally symptomatic inguinal hernias.
New evidence indicates the vast majority of men with asymptomatic or minimally symptomatic inguinal hernias will eventually come to surgery. This may not occur until years down the road, when their advanced age may render surgery more arduous.
"Although watchful waiting remains a safe strategy, even on long-term follow-up, patients who present to their physician to have their hernia evaluated, especially if elderly, should be informed that almost certainly they will come to surgery eventually ... The logical assumption is that watchful waiting is not an effective strategy, as with time almost all men cross over," Dr. Robert J. Fitzgibbons Jr. explained at the annual meeting of the American Surgical Association.
He presented an extended follow-up of patients enrolled in a landmark randomized multicenter clinical trial, one of only two randomized studies ever done comparing watchful waiting versus routine surgical repair for men with minimally symptomatic inguinal hernia. In the earlier report by Dr. Fitzgibbons and coworkers, watchful waiting was deemed "an acceptable option" because only 23% of patients crossed over to surgery due to increased pain during the first 2 years of follow-up (JAMA 2006;295:285-92).
At the ASA meeting, however, he presented updated 10-year follow-up data on 167 patients from the cohort initially assigned to watchful waiting. The rate of crossover to surgery was 68% by 10 years, with a marked age-based divergence. Patients below age 65 had a 62% crossover rate, while those above that age had a 79% crossover rate, according to Dr. Fitzgibbons, professor of surgery and chief of the division of general surgery at Creighton University, Omaha, Neb.
The good news was that hernia incarceration was a rare event, occurring at a rate of just 0.2% per year over the course of 10 years.
"We as surgeons have been taught for many years that we must repair all our hernias to prevent hernia accidents. Well, only three patients in our whole study developed incarceration, for which they underwent surgery with no mortality," Dr. Fitzgibbons noted. "The risk of a hernia accident should not be considered an indication for surgery. Older studies in the literature which would suggest otherwise can no longer be considered relevant."
He offered a caveat regarding the study findings: Participants were enrolled after they sought medical attention because of their hernias, even though they were asymptomatic or only minimally symptomatic. So the study results are most applicable to men concerned enough about their hernias that they visit a physician for that reason.
"It’s probably not valid to extrapolate the conclusions in this study to the entire population of minimally symptomatic inguinal hernia patients," the surgeon said. "Physicians have been observing elderly patients for years and would be loath to believe a crossover rate this high."
Nevertheless, the results of this study are virtually identical to those of the only other randomized trial of watchful waiting, which was conducted by surgeons at the University of Glasgow. The most recent update from that study showed an estimated crossover rate in the watchful waiting group of 16% at 1 year, 54% at 5 years, and 72% at 7.5 years. As in the American study, the rate of acute incarceration was reassuringly small. The investigators concluded that watchful waiting appears pointless, and they recommended surgical repair for medically fit patients (Br. J. Surg. 2011;98:596-9).
Discussant Dr. Michael E. Zenilman commented that his own approach is to individualize patient management based in large part upon activity level.
"When I see patients who are 80 years old in the office with an asymptomatic hernia, my conversation with them is about what their lifestyle is like. If they’re an active golfer I know that they’re going to end up getting their hernia fixed. If they’re sedentary, sitting at home in retirement, they don’t. So I think the next step in your research project should be to find out what the activity level is of these patients who are getting older and have asymptomatic hernias," said Dr. Zenilman, vice chair and regional director of surgery for the Washington, D.C., region, Johns Hopkins Medicine.
Dr. Fitzgibbons’ trial was funded by the Agency for Healthcare Research and Quality with support from the American College of Surgeons. He reported having no financial conflicts.
AT THE ASA ANNUAL MEETING
Major finding: Sixty-eight percent of men randomized to nonoperative observation of their asymptomatic or minimally symptomatic inguinal hernia crossed over to surgical repair within 10 years.
Data source: This was an open registry long-term extension of a randomized trial in which 720 men with minimally symptomatic inguinal hernia were assigned to watchful waiting or routine surgical repair.
Disclosures: The sponsor was the Agency for Healthcare Research and Quality. The presenter reported having no conflicts of interest.
Supplemental glutamine may harm critically ill patients
Early supplemental glutamine appears to harm rather than benefit critically ill patients who have multiorgan failure, according to a report published online April 18 in the New England Journal of Medicine.
In an international randomized controlled trial, in-hospital mortality and 6-month mortality were significantly increased in patients given intravenous glutamine within 24 hours of presentation to the ICU, compared with those given placebo, said Dr. Daren Heyland of Kingston (Ont.) General Hospital and his associates. A nonsignificant increase was seen in 28-day mortality.
Most of the patients in this study showed no glutamine deficiency at study entry. This observation, together with the primary finding that glutamine therapy may actually be harmful in this setting, "challenges the prevailing concept that glutamine is an essential nutrient that is deficient in critically ill patients and requires immediate supplementation," Dr. Heyland and his colleagues said.
The researchers also assessed whether supplemental antioxidants improved mortality or other outcomes in this study population and found that they did not.
Dr. Heyland and his associates performed this study because glutamine is thought to be rapidly depleted in critical illness and low levels of glutamine have been linked to increased mortality in ICU patients. Metaanalyses of small randomized trials suggested that both glutamine and antioxidant supplementation might improve survival in critically ill patients, but more recent and larger studies failed to confirm such a benefit.
This study included 1,223 consecutive adults who presented to 40 ICUs in the United States, Canada, and Europe during a 6-year period and required mechanical ventilation and had two or more organ failures related to their acute illness. The average patient age was 63 years. Primary diagnoses included cardiovascular, respiratory, gastrointestinal, neurologic, metabolic, and gynecologic disorders as well as sepsis and trauma.
The patients were randomly assigned in a double-blind fashion to receive daily intravenous glutamine, intravenous plus enteral antioxidants, glutamine plus antioxidants, or placebo fluids. The antioxidants included selenium, zinc, beta carotene, vitamin E, and vitamin C.
The primary outcome measure was 28-day mortality. There was a nonsignificant trend toward higher mortality in the patients given glutamine (32.4%) compared with those not given glutamine (27.2%). However, two secondary outcomes – in-hospital mortality and 6-month mortality – both were significantly higher in patients given glutamine than in those not given glutamine. In hospital mortality was 37.2% vs. 31%, respectively; 6-month mortality was 43.7% vs. 37.2%, respectively.
Other secondary outcomes – median time from randomization to ICU discharge and median time to hospital discharge – also were significantly longer for patients who received glutamine (17.1 vs. 13.1 days and 51.1 vs. 40.1 days, respectively), the investigators said (N. Engl. J. Med. 2013 April 18 [doi:10.1056/NEJMoa1212722]).
These results were confirmed in a sensitivity analysis that included only patients who received their assigned intervention for a minimum of 5 days. They also remained the same in several subgroup analyses and in an intention-to-treat analysis.
Glutamine showed no effect on the secondary outcomes of organ failure or infections.
Antioxidants had no significant effect on any outcome, either in the study population as a whole or in any subgroups of patients. "This finding may reflect the true lack of usefulness of antioxidants; alternatively, it may be due to the characteristics of the study population or to the dose and method of administration in this trial," Dr. Heyland and his associates said.
Rates of serious adverse events were similar across all the study groups, but the frequency of excessively high urea levels was greater in patients who received glutamine (13.4%) than in those who did not (4.0%).
There may be several reasons why the findings of this clinical trial are so different from those of previous trials.
The earlier trials were smaller and less methodologically robust, and their results had to be pooled in metaanalyses. Patients in this trial received the highest dose of glutamine currently prescribed for critically ill patients, which is higher than the maximal doses used in previous studies. The agents were administered through both intravenous and enteral routes in this study, while in previous studies the subjects received either exclusively intravenous or exclusively enteral administration.
In addition, "we targeted critically ill patients with multiorgan failure, the majority of whom were in shock, whereas previous studies typically excluded such patients," Dr. Heyland and his colleagues said.
Treatment was initiated within 24 hours of admission to the ICU in this study, but in earlier studies it was given later in the course of critical illness. And finally, most of the patients in this study received enteral nutrition, while those in previous trials received parenteral nutrition.
This study was supported by the Canadian Institutes of Health Research. Fresenius Kabi provided the glutamine supplements and Biosyn provided the selenium to the participating European sites. Dr. Heyland and his associates reported ties to numerous industry sources.
With its exceptionally good design, execution, and analysis, this study "ticks all the boxes for quality," said Dr. Greet Van den Berghe.
The findings allow clinicians "to reject with confidence the hypothesis that glutamine supplementation in very ill patients in the ICU improves outcome," she said.
"Probably the most important contribution of the present trial is that it provides firm support for the need for large, adequately powered, randomized, controlled trials in critical care medicine to investigate whether what we intuitively consider to be the best treatment for our patients also is truly effective and without harm," she wrote.
Dr. Van den Berghe is with the department of cellular and molecular medicine at Leuven (Belgium) Catholic University. She reported receiving a research grant from Baxter Healthcare. These remarks were taken from her editorial accompanying Dr. Heyland’s report (N. Engl. J. Med. 2013 April 18 [doi:10.1056/NEJMe1302301]).
With its exceptionally good design, execution, and analysis, this study "ticks all the boxes for quality," said Dr. Greet Van den Berghe.
The findings allow clinicians "to reject with confidence the hypothesis that glutamine supplementation in very ill patients in the ICU improves outcome," she said.
"Probably the most important contribution of the present trial is that it provides firm support for the need for large, adequately powered, randomized, controlled trials in critical care medicine to investigate whether what we intuitively consider to be the best treatment for our patients also is truly effective and without harm," she wrote.
Dr. Van den Berghe is with the department of cellular and molecular medicine at Leuven (Belgium) Catholic University. She reported receiving a research grant from Baxter Healthcare. These remarks were taken from her editorial accompanying Dr. Heyland’s report (N. Engl. J. Med. 2013 April 18 [doi:10.1056/NEJMe1302301]).
With its exceptionally good design, execution, and analysis, this study "ticks all the boxes for quality," said Dr. Greet Van den Berghe.
The findings allow clinicians "to reject with confidence the hypothesis that glutamine supplementation in very ill patients in the ICU improves outcome," she said.
"Probably the most important contribution of the present trial is that it provides firm support for the need for large, adequately powered, randomized, controlled trials in critical care medicine to investigate whether what we intuitively consider to be the best treatment for our patients also is truly effective and without harm," she wrote.
Dr. Van den Berghe is with the department of cellular and molecular medicine at Leuven (Belgium) Catholic University. She reported receiving a research grant from Baxter Healthcare. These remarks were taken from her editorial accompanying Dr. Heyland’s report (N. Engl. J. Med. 2013 April 18 [doi:10.1056/NEJMe1302301]).
Early supplemental glutamine appears to harm rather than benefit critically ill patients who have multiorgan failure, according to a report published online April 18 in the New England Journal of Medicine.
In an international randomized controlled trial, in-hospital mortality and 6-month mortality were significantly increased in patients given intravenous glutamine within 24 hours of presentation to the ICU, compared with those given placebo, said Dr. Daren Heyland of Kingston (Ont.) General Hospital and his associates. A nonsignificant increase was seen in 28-day mortality.
Most of the patients in this study showed no glutamine deficiency at study entry. This observation, together with the primary finding that glutamine therapy may actually be harmful in this setting, "challenges the prevailing concept that glutamine is an essential nutrient that is deficient in critically ill patients and requires immediate supplementation," Dr. Heyland and his colleagues said.
The researchers also assessed whether supplemental antioxidants improved mortality or other outcomes in this study population and found that they did not.
Dr. Heyland and his associates performed this study because glutamine is thought to be rapidly depleted in critical illness and low levels of glutamine have been linked to increased mortality in ICU patients. Metaanalyses of small randomized trials suggested that both glutamine and antioxidant supplementation might improve survival in critically ill patients, but more recent and larger studies failed to confirm such a benefit.
This study included 1,223 consecutive adults who presented to 40 ICUs in the United States, Canada, and Europe during a 6-year period and required mechanical ventilation and had two or more organ failures related to their acute illness. The average patient age was 63 years. Primary diagnoses included cardiovascular, respiratory, gastrointestinal, neurologic, metabolic, and gynecologic disorders as well as sepsis and trauma.
The patients were randomly assigned in a double-blind fashion to receive daily intravenous glutamine, intravenous plus enteral antioxidants, glutamine plus antioxidants, or placebo fluids. The antioxidants included selenium, zinc, beta carotene, vitamin E, and vitamin C.
The primary outcome measure was 28-day mortality. There was a nonsignificant trend toward higher mortality in the patients given glutamine (32.4%) compared with those not given glutamine (27.2%). However, two secondary outcomes – in-hospital mortality and 6-month mortality – both were significantly higher in patients given glutamine than in those not given glutamine. In hospital mortality was 37.2% vs. 31%, respectively; 6-month mortality was 43.7% vs. 37.2%, respectively.
Other secondary outcomes – median time from randomization to ICU discharge and median time to hospital discharge – also were significantly longer for patients who received glutamine (17.1 vs. 13.1 days and 51.1 vs. 40.1 days, respectively), the investigators said (N. Engl. J. Med. 2013 April 18 [doi:10.1056/NEJMoa1212722]).
These results were confirmed in a sensitivity analysis that included only patients who received their assigned intervention for a minimum of 5 days. They also remained the same in several subgroup analyses and in an intention-to-treat analysis.
Glutamine showed no effect on the secondary outcomes of organ failure or infections.
Antioxidants had no significant effect on any outcome, either in the study population as a whole or in any subgroups of patients. "This finding may reflect the true lack of usefulness of antioxidants; alternatively, it may be due to the characteristics of the study population or to the dose and method of administration in this trial," Dr. Heyland and his associates said.
Rates of serious adverse events were similar across all the study groups, but the frequency of excessively high urea levels was greater in patients who received glutamine (13.4%) than in those who did not (4.0%).
There may be several reasons why the findings of this clinical trial are so different from those of previous trials.
The earlier trials were smaller and less methodologically robust, and their results had to be pooled in metaanalyses. Patients in this trial received the highest dose of glutamine currently prescribed for critically ill patients, which is higher than the maximal doses used in previous studies. The agents were administered through both intravenous and enteral routes in this study, while in previous studies the subjects received either exclusively intravenous or exclusively enteral administration.
In addition, "we targeted critically ill patients with multiorgan failure, the majority of whom were in shock, whereas previous studies typically excluded such patients," Dr. Heyland and his colleagues said.
Treatment was initiated within 24 hours of admission to the ICU in this study, but in earlier studies it was given later in the course of critical illness. And finally, most of the patients in this study received enteral nutrition, while those in previous trials received parenteral nutrition.
This study was supported by the Canadian Institutes of Health Research. Fresenius Kabi provided the glutamine supplements and Biosyn provided the selenium to the participating European sites. Dr. Heyland and his associates reported ties to numerous industry sources.
Early supplemental glutamine appears to harm rather than benefit critically ill patients who have multiorgan failure, according to a report published online April 18 in the New England Journal of Medicine.
In an international randomized controlled trial, in-hospital mortality and 6-month mortality were significantly increased in patients given intravenous glutamine within 24 hours of presentation to the ICU, compared with those given placebo, said Dr. Daren Heyland of Kingston (Ont.) General Hospital and his associates. A nonsignificant increase was seen in 28-day mortality.
Most of the patients in this study showed no glutamine deficiency at study entry. This observation, together with the primary finding that glutamine therapy may actually be harmful in this setting, "challenges the prevailing concept that glutamine is an essential nutrient that is deficient in critically ill patients and requires immediate supplementation," Dr. Heyland and his colleagues said.
The researchers also assessed whether supplemental antioxidants improved mortality or other outcomes in this study population and found that they did not.
Dr. Heyland and his associates performed this study because glutamine is thought to be rapidly depleted in critical illness and low levels of glutamine have been linked to increased mortality in ICU patients. Metaanalyses of small randomized trials suggested that both glutamine and antioxidant supplementation might improve survival in critically ill patients, but more recent and larger studies failed to confirm such a benefit.
This study included 1,223 consecutive adults who presented to 40 ICUs in the United States, Canada, and Europe during a 6-year period and required mechanical ventilation and had two or more organ failures related to their acute illness. The average patient age was 63 years. Primary diagnoses included cardiovascular, respiratory, gastrointestinal, neurologic, metabolic, and gynecologic disorders as well as sepsis and trauma.
The patients were randomly assigned in a double-blind fashion to receive daily intravenous glutamine, intravenous plus enteral antioxidants, glutamine plus antioxidants, or placebo fluids. The antioxidants included selenium, zinc, beta carotene, vitamin E, and vitamin C.
The primary outcome measure was 28-day mortality. There was a nonsignificant trend toward higher mortality in the patients given glutamine (32.4%) compared with those not given glutamine (27.2%). However, two secondary outcomes – in-hospital mortality and 6-month mortality – both were significantly higher in patients given glutamine than in those not given glutamine. In hospital mortality was 37.2% vs. 31%, respectively; 6-month mortality was 43.7% vs. 37.2%, respectively.
Other secondary outcomes – median time from randomization to ICU discharge and median time to hospital discharge – also were significantly longer for patients who received glutamine (17.1 vs. 13.1 days and 51.1 vs. 40.1 days, respectively), the investigators said (N. Engl. J. Med. 2013 April 18 [doi:10.1056/NEJMoa1212722]).
These results were confirmed in a sensitivity analysis that included only patients who received their assigned intervention for a minimum of 5 days. They also remained the same in several subgroup analyses and in an intention-to-treat analysis.
Glutamine showed no effect on the secondary outcomes of organ failure or infections.
Antioxidants had no significant effect on any outcome, either in the study population as a whole or in any subgroups of patients. "This finding may reflect the true lack of usefulness of antioxidants; alternatively, it may be due to the characteristics of the study population or to the dose and method of administration in this trial," Dr. Heyland and his associates said.
Rates of serious adverse events were similar across all the study groups, but the frequency of excessively high urea levels was greater in patients who received glutamine (13.4%) than in those who did not (4.0%).
There may be several reasons why the findings of this clinical trial are so different from those of previous trials.
The earlier trials were smaller and less methodologically robust, and their results had to be pooled in metaanalyses. Patients in this trial received the highest dose of glutamine currently prescribed for critically ill patients, which is higher than the maximal doses used in previous studies. The agents were administered through both intravenous and enteral routes in this study, while in previous studies the subjects received either exclusively intravenous or exclusively enteral administration.
In addition, "we targeted critically ill patients with multiorgan failure, the majority of whom were in shock, whereas previous studies typically excluded such patients," Dr. Heyland and his colleagues said.
Treatment was initiated within 24 hours of admission to the ICU in this study, but in earlier studies it was given later in the course of critical illness. And finally, most of the patients in this study received enteral nutrition, while those in previous trials received parenteral nutrition.
This study was supported by the Canadian Institutes of Health Research. Fresenius Kabi provided the glutamine supplements and Biosyn provided the selenium to the participating European sites. Dr. Heyland and his associates reported ties to numerous industry sources.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major Finding: In-hospital mortality was higher (37.2% vs. 31%) in patients receiving glutamine therapy compared with placebo, as was 6-month mortality (43.7% vs. 37.2%).
Data source: An international randomized, double-blind, placebo-controlled trial involving 1,223 critically ill adults in 40 ICUs who were followed for 6 months.
Disclosures: This study was supported by the Canadian Institutes of Health Research. Dr. Heyland and his associates reported ties to numerous industry sources.
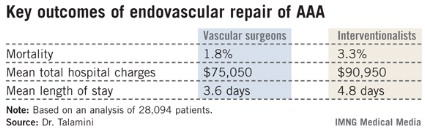
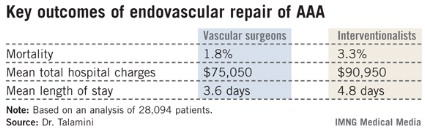
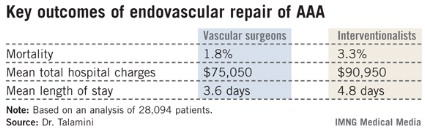
Vascular surgeons get superior outcomes in aortic aneurysm repair
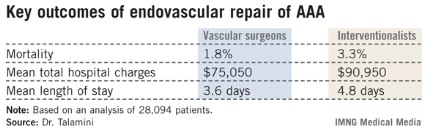
INDIANAPOLIS – Major outcomes in patients undergoing endovascular repair of abdominal aortic aneurysm are superior in terms of mortality, length of stay, and total hospital charges when the procedure is done by vascular surgeons rather than cardiologists or interventional radiologists, according to an analysis of a comprehensive national hospital database.
"Obviously these are striking findings," Dr. Mark A. Talamini noted in presenting the study results at the annual meeting of the American Surgical Association. "We believe that health policy in support of selective referrals for aneurysm repair, or integrating interventionalists and vascular surgeons more effectively, should be considered."
He presented an outcomes analysis involving 28,094 patients who underwent endovascular implantation of a graft for an abdominal aortic aneurysm within the Nationwide Inpatient Sample during 2001-2009. This database, sponsored by the Agency for Healthcare Research and Quality, receives input from a representative cross-section composed of 20% of U.S. hospitals. Dr. Talamini and coworkers were able to reliably determine whether an operator was a vascular surgeon, a cardiologist, or an interventional radiologist. Vascular surgeons performed 78.1% of the cases, while nonsurgeon interventionalists did the rest. Ninety-seven percent of patients presented with a nonruptured aneurysm.
The unadjusted differences in key outcomes between vascular surgeons and interventionalists were striking. Perhaps even more impressive were the differences following adjustment for operator volume, comorbid conditions, aneurysm rupture status, patient demographics and socioeconomic status, and hospital location and teaching status. The interventionalists’ patients had a 39% greater risk of mortality, an average of $20,000 more in total hospital charges, and a 1.4-day longer length of stay, reported Dr. Talamini, a nonvascular surgeon who is professor and chairman of the department of surgery at the University of California, San Diego.
Additional findings of interest were that the patients of high-volume operators (defined as those who performed more than 10 cases per year) had a 31% reduction in mortality risk regardless of operator specialty. In addition, high-volume operators averaged $10,000 per patient less in total hospital charges and shorter hospital length of stay by 1 full day. Undergoing aneurysm repair in a teaching hospital had no impact upon mortality or total charges, but was associated with an average 0.4-day greater length of stay, he continued.
Dr. Talamini offered two potential explanations for the disparate outcomes. One is that perhaps the patient populations of vascular surgeons and interventionalists differ in ways that were not accounted for in the multivariate analysis. The other possibility is that vascular surgeons achieve better outcomes because their training and experience are superior, allowing them to make better judgments about treatment than those of interventionalists.
"Obviously, this is the ‘we’re better than they are’ argument, and I hardly think we can assume that this is the case until we exhaust all other potential explanations. Further work using longitudinal databases with more detail hopefully will allow us to do just that," said Dr. Talamini.
Discussant Dr. K. Craig Kent called the study findings "very provocative."
"The moral of the story is expertise in disease is far more important than expertise in technology," declared Dr. Kent, professor and chairman of the department of surgery at the University of Wisconsin, Madison.
"When I first became a vascular surgeon 25 years ago it was difficult to recruit to the specialty. There were few that wanted to care for a group of patients for whom procedures were long and tedious, reoperations were common, and outcomes weren’t always favorable," Dr. Kent recalled. "Fast forward to 2013, where everybody wants to be a vascular surgeon: cardiologists, interventional radiologists, nephrologists, dermatologists, vascular medicine physicians, and many others. Why the dramatic change? For the nonsurgeons, the reason is the development of minimally invasive technology that has allowed any specialist with catheter-based skills to participate in vascular care. But is it appropriate for nonsurgical specialists to treat vascular patients? The answer from this study is a resounding no."
Dr. Samuel E. Wilson, a vascular surgeon who was Dr. Talamini’s coinvestigator in the study, said he thinks patient selection is the key to understanding the outcome disparities.
"If you think about it, the vascular surgeon in his office has the ability to make an elective decision, carefully considered, and decide whether or not he’s going to actually do the procedure. The hospital-based radiologist may not have that opportunity; he receives a call, a procedure on an inpatient is requested, and he feels obligated to proceed. Another key aspect may be postoperative care. Vascular surgery patients receive their postoperative care under the direction of the surgeon," observed Dr. Wilson of the University of California, Irvine.
It’s worth noting, he added, that the outcomes for both vascular surgeons and interventionalists improved over the years of the study. The results are coming closer together over time, although significant differences remain.
Dr. Robert S. Rhodes said that general surgeons should be included in any further comparative effectiveness studies focused on endovascular repair of abdominal aortic aneurysms.
"Our data at the American Board of Surgery suggests that general surgeons who perform vascular surgery actually do so in substantial volume, so it may be that they’ve also acquired endovascular skills," said Dr. Rhodes, associate executive director for vascular surgery at the ABS.
None of the speakers reported having any financial conflicts.
INDIANAPOLIS – Major outcomes in patients undergoing endovascular repair of abdominal aortic aneurysm are superior in terms of mortality, length of stay, and total hospital charges when the procedure is done by vascular surgeons rather than cardiologists or interventional radiologists, according to an analysis of a comprehensive national hospital database.
"Obviously these are striking findings," Dr. Mark A. Talamini noted in presenting the study results at the annual meeting of the American Surgical Association. "We believe that health policy in support of selective referrals for aneurysm repair, or integrating interventionalists and vascular surgeons more effectively, should be considered."
He presented an outcomes analysis involving 28,094 patients who underwent endovascular implantation of a graft for an abdominal aortic aneurysm within the Nationwide Inpatient Sample during 2001-2009. This database, sponsored by the Agency for Healthcare Research and Quality, receives input from a representative cross-section composed of 20% of U.S. hospitals. Dr. Talamini and coworkers were able to reliably determine whether an operator was a vascular surgeon, a cardiologist, or an interventional radiologist. Vascular surgeons performed 78.1% of the cases, while nonsurgeon interventionalists did the rest. Ninety-seven percent of patients presented with a nonruptured aneurysm.
The unadjusted differences in key outcomes between vascular surgeons and interventionalists were striking. Perhaps even more impressive were the differences following adjustment for operator volume, comorbid conditions, aneurysm rupture status, patient demographics and socioeconomic status, and hospital location and teaching status. The interventionalists’ patients had a 39% greater risk of mortality, an average of $20,000 more in total hospital charges, and a 1.4-day longer length of stay, reported Dr. Talamini, a nonvascular surgeon who is professor and chairman of the department of surgery at the University of California, San Diego.
Additional findings of interest were that the patients of high-volume operators (defined as those who performed more than 10 cases per year) had a 31% reduction in mortality risk regardless of operator specialty. In addition, high-volume operators averaged $10,000 per patient less in total hospital charges and shorter hospital length of stay by 1 full day. Undergoing aneurysm repair in a teaching hospital had no impact upon mortality or total charges, but was associated with an average 0.4-day greater length of stay, he continued.
Dr. Talamini offered two potential explanations for the disparate outcomes. One is that perhaps the patient populations of vascular surgeons and interventionalists differ in ways that were not accounted for in the multivariate analysis. The other possibility is that vascular surgeons achieve better outcomes because their training and experience are superior, allowing them to make better judgments about treatment than those of interventionalists.
"Obviously, this is the ‘we’re better than they are’ argument, and I hardly think we can assume that this is the case until we exhaust all other potential explanations. Further work using longitudinal databases with more detail hopefully will allow us to do just that," said Dr. Talamini.
Discussant Dr. K. Craig Kent called the study findings "very provocative."
"The moral of the story is expertise in disease is far more important than expertise in technology," declared Dr. Kent, professor and chairman of the department of surgery at the University of Wisconsin, Madison.
"When I first became a vascular surgeon 25 years ago it was difficult to recruit to the specialty. There were few that wanted to care for a group of patients for whom procedures were long and tedious, reoperations were common, and outcomes weren’t always favorable," Dr. Kent recalled. "Fast forward to 2013, where everybody wants to be a vascular surgeon: cardiologists, interventional radiologists, nephrologists, dermatologists, vascular medicine physicians, and many others. Why the dramatic change? For the nonsurgeons, the reason is the development of minimally invasive technology that has allowed any specialist with catheter-based skills to participate in vascular care. But is it appropriate for nonsurgical specialists to treat vascular patients? The answer from this study is a resounding no."
Dr. Samuel E. Wilson, a vascular surgeon who was Dr. Talamini’s coinvestigator in the study, said he thinks patient selection is the key to understanding the outcome disparities.
"If you think about it, the vascular surgeon in his office has the ability to make an elective decision, carefully considered, and decide whether or not he’s going to actually do the procedure. The hospital-based radiologist may not have that opportunity; he receives a call, a procedure on an inpatient is requested, and he feels obligated to proceed. Another key aspect may be postoperative care. Vascular surgery patients receive their postoperative care under the direction of the surgeon," observed Dr. Wilson of the University of California, Irvine.
It’s worth noting, he added, that the outcomes for both vascular surgeons and interventionalists improved over the years of the study. The results are coming closer together over time, although significant differences remain.
Dr. Robert S. Rhodes said that general surgeons should be included in any further comparative effectiveness studies focused on endovascular repair of abdominal aortic aneurysms.
"Our data at the American Board of Surgery suggests that general surgeons who perform vascular surgery actually do so in substantial volume, so it may be that they’ve also acquired endovascular skills," said Dr. Rhodes, associate executive director for vascular surgery at the ABS.
None of the speakers reported having any financial conflicts.
INDIANAPOLIS – Major outcomes in patients undergoing endovascular repair of abdominal aortic aneurysm are superior in terms of mortality, length of stay, and total hospital charges when the procedure is done by vascular surgeons rather than cardiologists or interventional radiologists, according to an analysis of a comprehensive national hospital database.
"Obviously these are striking findings," Dr. Mark A. Talamini noted in presenting the study results at the annual meeting of the American Surgical Association. "We believe that health policy in support of selective referrals for aneurysm repair, or integrating interventionalists and vascular surgeons more effectively, should be considered."
He presented an outcomes analysis involving 28,094 patients who underwent endovascular implantation of a graft for an abdominal aortic aneurysm within the Nationwide Inpatient Sample during 2001-2009. This database, sponsored by the Agency for Healthcare Research and Quality, receives input from a representative cross-section composed of 20% of U.S. hospitals. Dr. Talamini and coworkers were able to reliably determine whether an operator was a vascular surgeon, a cardiologist, or an interventional radiologist. Vascular surgeons performed 78.1% of the cases, while nonsurgeon interventionalists did the rest. Ninety-seven percent of patients presented with a nonruptured aneurysm.
The unadjusted differences in key outcomes between vascular surgeons and interventionalists were striking. Perhaps even more impressive were the differences following adjustment for operator volume, comorbid conditions, aneurysm rupture status, patient demographics and socioeconomic status, and hospital location and teaching status. The interventionalists’ patients had a 39% greater risk of mortality, an average of $20,000 more in total hospital charges, and a 1.4-day longer length of stay, reported Dr. Talamini, a nonvascular surgeon who is professor and chairman of the department of surgery at the University of California, San Diego.
Additional findings of interest were that the patients of high-volume operators (defined as those who performed more than 10 cases per year) had a 31% reduction in mortality risk regardless of operator specialty. In addition, high-volume operators averaged $10,000 per patient less in total hospital charges and shorter hospital length of stay by 1 full day. Undergoing aneurysm repair in a teaching hospital had no impact upon mortality or total charges, but was associated with an average 0.4-day greater length of stay, he continued.
Dr. Talamini offered two potential explanations for the disparate outcomes. One is that perhaps the patient populations of vascular surgeons and interventionalists differ in ways that were not accounted for in the multivariate analysis. The other possibility is that vascular surgeons achieve better outcomes because their training and experience are superior, allowing them to make better judgments about treatment than those of interventionalists.
"Obviously, this is the ‘we’re better than they are’ argument, and I hardly think we can assume that this is the case until we exhaust all other potential explanations. Further work using longitudinal databases with more detail hopefully will allow us to do just that," said Dr. Talamini.
Discussant Dr. K. Craig Kent called the study findings "very provocative."
"The moral of the story is expertise in disease is far more important than expertise in technology," declared Dr. Kent, professor and chairman of the department of surgery at the University of Wisconsin, Madison.
"When I first became a vascular surgeon 25 years ago it was difficult to recruit to the specialty. There were few that wanted to care for a group of patients for whom procedures were long and tedious, reoperations were common, and outcomes weren’t always favorable," Dr. Kent recalled. "Fast forward to 2013, where everybody wants to be a vascular surgeon: cardiologists, interventional radiologists, nephrologists, dermatologists, vascular medicine physicians, and many others. Why the dramatic change? For the nonsurgeons, the reason is the development of minimally invasive technology that has allowed any specialist with catheter-based skills to participate in vascular care. But is it appropriate for nonsurgical specialists to treat vascular patients? The answer from this study is a resounding no."
Dr. Samuel E. Wilson, a vascular surgeon who was Dr. Talamini’s coinvestigator in the study, said he thinks patient selection is the key to understanding the outcome disparities.
"If you think about it, the vascular surgeon in his office has the ability to make an elective decision, carefully considered, and decide whether or not he’s going to actually do the procedure. The hospital-based radiologist may not have that opportunity; he receives a call, a procedure on an inpatient is requested, and he feels obligated to proceed. Another key aspect may be postoperative care. Vascular surgery patients receive their postoperative care under the direction of the surgeon," observed Dr. Wilson of the University of California, Irvine.
It’s worth noting, he added, that the outcomes for both vascular surgeons and interventionalists improved over the years of the study. The results are coming closer together over time, although significant differences remain.
Dr. Robert S. Rhodes said that general surgeons should be included in any further comparative effectiveness studies focused on endovascular repair of abdominal aortic aneurysms.
"Our data at the American Board of Surgery suggests that general surgeons who perform vascular surgery actually do so in substantial volume, so it may be that they’ve also acquired endovascular skills," said Dr. Rhodes, associate executive director for vascular surgery at the ABS.
None of the speakers reported having any financial conflicts.
AT THE ASA ANNUAL MEETING
Major Finding: The mortality rate in patients undergoing endovascular repair of an abdominal aortic aneurysm was 1.8% when vascular surgeons did the procedure compared to 3.3% when it was performed by an interventional radiologist or cardiologist.
Data Source: An analysis of 28,094 patients who underwent endovascular repair of an abdominal aortic aneurysm in 2001-2009 and were included in the Nationwide Inpatient Sample.
Disclosures: The Nationwide Inpatient Sample is sponsored by the Agency for Healthcare Research and Quality. The presenter reported having no conflicts of interest.
Manage most SEGAs with rapamycin analogs, not surgery
SAN DIEGO – Medical management with sirolimus or everolimus for pediatric patients with tuberous sclerosis complex and subependymal giant cell astrocytomas is more effective and safer than surgery, researchers from the University of Cincinnati and University of California, Los Angeles, have found.
Although the benign tumors have traditionally been left to surgeons, it’s become clear in recent years that rapamycin analogs are effective, too. The question has been "which [approach] is best? Medical management "is known to be pretty mild compared to the surgery," but it’s not curative, explained lead investigator Susanne Yoon, the University of Cincinnati medical student who presented the results at the annual meeting of the American Academy of Neurology.
The team compared outcomes for 23 SEGA (subependymal giant cell astrocytoma) patients who underwent surgery, 81 who took sirolimus or everolimus, and 9 who got both. The surgery patients were diagnosed when they were about 10 years old and were followed for a median of 8.9 years; the medical patients were about 7 years old when diagnosed, and were followed for a median of 2.8 years. Boys made up the majority of both groups.
None of the children who took a rapamycin analog needed surgery; tumors shrank by more than half in 61% (45). The drugs caused infections, weight change, or hyperlipidemia in some, but only 13% (11) needed to stop the drug or go to the hospital because of side effects.
Meanwhile, surgery cured just 39% (9) of the children who got it, sometimes after two or three operations; 61% (14) of those patients had prolonged hospitalizations or were hospitalized due to postoperative complications that included intracranial hemorrhage in 8, hydrocephalus/shunt malfunction in 6, neurologic impairment, and seizures.
"Not only does medical management win in efficacy, but it also wins in the safety issues. Rapalog [rapamycin] therapy, alone or in combination, is becoming a cornerstone of tumor management" in neurocutaneous disorders, said Dr. David H. Viskochil, professor of pediatrics at the University of Utah, Salt Lake City, commenting on the study.
"Of course, there are emergent situations where you’ve just got to go in and get the tumor out; you can’t wait 3 months to see" if drugs work. "But if a child is just starting to show some symptoms and not deteriorating, then you can start with medicine first and see what happens," he said.
"The question is if you got [SEGAs] really early, would surgical cure be much more likely? The studies aren’t quite there yet," he said in an interview.
Ms. Yoon and Dr. Viskochil said they have no disclosures.
SAN DIEGO – Medical management with sirolimus or everolimus for pediatric patients with tuberous sclerosis complex and subependymal giant cell astrocytomas is more effective and safer than surgery, researchers from the University of Cincinnati and University of California, Los Angeles, have found.
Although the benign tumors have traditionally been left to surgeons, it’s become clear in recent years that rapamycin analogs are effective, too. The question has been "which [approach] is best? Medical management "is known to be pretty mild compared to the surgery," but it’s not curative, explained lead investigator Susanne Yoon, the University of Cincinnati medical student who presented the results at the annual meeting of the American Academy of Neurology.
The team compared outcomes for 23 SEGA (subependymal giant cell astrocytoma) patients who underwent surgery, 81 who took sirolimus or everolimus, and 9 who got both. The surgery patients were diagnosed when they were about 10 years old and were followed for a median of 8.9 years; the medical patients were about 7 years old when diagnosed, and were followed for a median of 2.8 years. Boys made up the majority of both groups.
None of the children who took a rapamycin analog needed surgery; tumors shrank by more than half in 61% (45). The drugs caused infections, weight change, or hyperlipidemia in some, but only 13% (11) needed to stop the drug or go to the hospital because of side effects.
Meanwhile, surgery cured just 39% (9) of the children who got it, sometimes after two or three operations; 61% (14) of those patients had prolonged hospitalizations or were hospitalized due to postoperative complications that included intracranial hemorrhage in 8, hydrocephalus/shunt malfunction in 6, neurologic impairment, and seizures.
"Not only does medical management win in efficacy, but it also wins in the safety issues. Rapalog [rapamycin] therapy, alone or in combination, is becoming a cornerstone of tumor management" in neurocutaneous disorders, said Dr. David H. Viskochil, professor of pediatrics at the University of Utah, Salt Lake City, commenting on the study.
"Of course, there are emergent situations where you’ve just got to go in and get the tumor out; you can’t wait 3 months to see" if drugs work. "But if a child is just starting to show some symptoms and not deteriorating, then you can start with medicine first and see what happens," he said.
"The question is if you got [SEGAs] really early, would surgical cure be much more likely? The studies aren’t quite there yet," he said in an interview.
Ms. Yoon and Dr. Viskochil said they have no disclosures.
SAN DIEGO – Medical management with sirolimus or everolimus for pediatric patients with tuberous sclerosis complex and subependymal giant cell astrocytomas is more effective and safer than surgery, researchers from the University of Cincinnati and University of California, Los Angeles, have found.
Although the benign tumors have traditionally been left to surgeons, it’s become clear in recent years that rapamycin analogs are effective, too. The question has been "which [approach] is best? Medical management "is known to be pretty mild compared to the surgery," but it’s not curative, explained lead investigator Susanne Yoon, the University of Cincinnati medical student who presented the results at the annual meeting of the American Academy of Neurology.
The team compared outcomes for 23 SEGA (subependymal giant cell astrocytoma) patients who underwent surgery, 81 who took sirolimus or everolimus, and 9 who got both. The surgery patients were diagnosed when they were about 10 years old and were followed for a median of 8.9 years; the medical patients were about 7 years old when diagnosed, and were followed for a median of 2.8 years. Boys made up the majority of both groups.
None of the children who took a rapamycin analog needed surgery; tumors shrank by more than half in 61% (45). The drugs caused infections, weight change, or hyperlipidemia in some, but only 13% (11) needed to stop the drug or go to the hospital because of side effects.
Meanwhile, surgery cured just 39% (9) of the children who got it, sometimes after two or three operations; 61% (14) of those patients had prolonged hospitalizations or were hospitalized due to postoperative complications that included intracranial hemorrhage in 8, hydrocephalus/shunt malfunction in 6, neurologic impairment, and seizures.
"Not only does medical management win in efficacy, but it also wins in the safety issues. Rapalog [rapamycin] therapy, alone or in combination, is becoming a cornerstone of tumor management" in neurocutaneous disorders, said Dr. David H. Viskochil, professor of pediatrics at the University of Utah, Salt Lake City, commenting on the study.
"Of course, there are emergent situations where you’ve just got to go in and get the tumor out; you can’t wait 3 months to see" if drugs work. "But if a child is just starting to show some symptoms and not deteriorating, then you can start with medicine first and see what happens," he said.
"The question is if you got [SEGAs] really early, would surgical cure be much more likely? The studies aren’t quite there yet," he said in an interview.
Ms. Yoon and Dr. Viskochil said they have no disclosures.
AT THE 2013 AAN ANNUAL MEETING
Major finding: Rapamycin analogs shrink SEGA tumors by more than 50% in a majority of children, and obviate the need for surgery.
Data source: Comparison of surgical and medical treatment of SEGA tumors in 113 children.
Disclosures: Ms. Yoon and Dr. Viskochil said they have no disclosures.
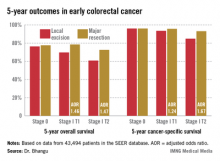
Radical resection trumps local excision in stage I CRC
INDIANAPOLIS – Local excision of early invasive stage I colon or rectal carcinoma confers significantly worse 5-year overall and cancer-specific survival than does radical resection, according to analysis of a large national database.
This was true for stage I T1 and T2 disease; that is, for patients with tumor invading the submucosa as well as for those with tumor invading the muscularis propria, Dr. Aneel Bhangu reported at the annual meeting of the American Surgical Association.
In contrast, 5-year survival rates were equivalent with local excision compared with radical resection in patients with stage 0 disease, also known as carcinoma in situ, added Dr. Bhangu of Royal Marsden Hospital, London.
"We recommend that it is safe to perform local excision for stage 0 lesions – that is, carcinoma in situ or severely dysplastic polyps. Refined selection criteria for T1 cancers are required and should be the focus of further research. The use of local excision as a definitive treatment should be carefully considered for patients with T2 colorectal cancer, especially when treating younger, fit patients," he said.
The surgical oncologist presented an analysis of 43,494 patients with surgically treated stage 0 or I adenocarcinoma of the colon or rectum in the Surveillance, Epidemiology, and End Results (SEER) database for 1998-2009. He noted as an aside that the National Cancer Institute’s SEER database is "an open-access and free resource which is the envy of the worldwide oncological community and a shining example of how open-access data can be used by the global community to forward research."
Seventy percent of patients had colonic cancers, 30% rectal. Stage 0 cancer was present in 8.2%, while 91.8% of patients had stage I cancers, 51% of which were T1, 49% T2. Eighteen percent of subjects underwent local excision, while the rest had major resections.
Five-year overall survival was nearly an absolute 8% better in patients with stage I disease treated by radical resection, an advantage that grew even more dramatic in a multivariate analysis adjusted for age and other potential confounders.
Dr. Bhangu observed that these findings take on added import because the number of patients presenting with early colorectal cancer is climbing as a consequence of effective population-based colorectal cancer screening programs. The use of local excision as treatment for such cancers is growing as well. Yet the availability of high-tech tools and techniques for endoscopic local excision of these malignancies has created a dilemma: Such surgery spares the patient from a major operation with all its attendant hazards and morbidity, but when recurrences of these initially small cancers happen they may be inoperable in 10% of cases, and even when they are operable they require extensive visceral resection up to 50% of the time.
Discussant Dr. Genevieve Melton-Meaux of the University of Minnesota, Minneapolis, noted that a surprisingly large percentage of younger patients with stage I disease in this series – that is, patients under age 60 – were treated via local excision.
"We, too, were surprised by this," Dr. Bhangu replied. "If I were to speculate why, I’d say that it may be an issue of clinician equipoise. Some surgeons and endoscopists are true believers in this technology and they may be applying it to a wide scope of patients."
This same lack of equipoise explains the glacially slow recruitment rates into ongoing clinical trials badly needed to establish evidence-based therapy for early-stage colorectal cancer, he added.
He and his coworkers recommended directing future research in this field toward determining which patients with stage I disease are appropriate for local excision. Potentially relevant pathologic markers include depth of invasion and the degree of tumor differentiation. Biomarkers predictive of recurrence also are sorely needed.
Discussant Edward M. Copeland III noted that in light of Dr. Bhangu’s findings it makes sense to offer patients with T2 lesions neoadjuvant radiation and/or chemotherapy.
"You’d probably downstage a lot of them to T0 and you could then locally excise them, doing away with that 8% difference in survival between local excision and major resection you found in the SEER database," said Dr. Copeland, professor and chairman of the department of surgery at the University of Florida, Gainesville.
"I would venture to say if you had a patient with a T2 rectal lesion and offered neoadjuvant therapy followed by local excision, without a major operation, and with virtually zero chance of recurrence, I would take that, personally," he added.
Dr. Bhangu responded that it’s an intriguing notion, but the supporting evidence simply doesn’t exist. However, an ongoing U.K. randomized trial is evaluating just such an approach in patients with stage I T1 and T2 rectal cancer.
"I think this will provide the high-quality evidence that we require to treat these patients with evidence-based principles," he added.
Discussant Dr. Conor P. Delaney praised Dr. Bhangu for presenting "a great study." He placed the findings in perspective.
"It’s important to remember that the disadvantage that you’re showing with local therapy is very similar in size to the benefit that all of medical oncology gives us, with all of the effort that we invest in medical oncology. So this is actually a very significant result," declared Dr. Delaney, professor of surgery and chief of the division of colorectal surgery at Case Western Reserve University, Cleveland.
Dr. Bhangu reported having no financial conflicts.
INDIANAPOLIS – Local excision of early invasive stage I colon or rectal carcinoma confers significantly worse 5-year overall and cancer-specific survival than does radical resection, according to analysis of a large national database.
This was true for stage I T1 and T2 disease; that is, for patients with tumor invading the submucosa as well as for those with tumor invading the muscularis propria, Dr. Aneel Bhangu reported at the annual meeting of the American Surgical Association.
In contrast, 5-year survival rates were equivalent with local excision compared with radical resection in patients with stage 0 disease, also known as carcinoma in situ, added Dr. Bhangu of Royal Marsden Hospital, London.
"We recommend that it is safe to perform local excision for stage 0 lesions – that is, carcinoma in situ or severely dysplastic polyps. Refined selection criteria for T1 cancers are required and should be the focus of further research. The use of local excision as a definitive treatment should be carefully considered for patients with T2 colorectal cancer, especially when treating younger, fit patients," he said.
The surgical oncologist presented an analysis of 43,494 patients with surgically treated stage 0 or I adenocarcinoma of the colon or rectum in the Surveillance, Epidemiology, and End Results (SEER) database for 1998-2009. He noted as an aside that the National Cancer Institute’s SEER database is "an open-access and free resource which is the envy of the worldwide oncological community and a shining example of how open-access data can be used by the global community to forward research."
Seventy percent of patients had colonic cancers, 30% rectal. Stage 0 cancer was present in 8.2%, while 91.8% of patients had stage I cancers, 51% of which were T1, 49% T2. Eighteen percent of subjects underwent local excision, while the rest had major resections.
Five-year overall survival was nearly an absolute 8% better in patients with stage I disease treated by radical resection, an advantage that grew even more dramatic in a multivariate analysis adjusted for age and other potential confounders.
Dr. Bhangu observed that these findings take on added import because the number of patients presenting with early colorectal cancer is climbing as a consequence of effective population-based colorectal cancer screening programs. The use of local excision as treatment for such cancers is growing as well. Yet the availability of high-tech tools and techniques for endoscopic local excision of these malignancies has created a dilemma: Such surgery spares the patient from a major operation with all its attendant hazards and morbidity, but when recurrences of these initially small cancers happen they may be inoperable in 10% of cases, and even when they are operable they require extensive visceral resection up to 50% of the time.
Discussant Dr. Genevieve Melton-Meaux of the University of Minnesota, Minneapolis, noted that a surprisingly large percentage of younger patients with stage I disease in this series – that is, patients under age 60 – were treated via local excision.
"We, too, were surprised by this," Dr. Bhangu replied. "If I were to speculate why, I’d say that it may be an issue of clinician equipoise. Some surgeons and endoscopists are true believers in this technology and they may be applying it to a wide scope of patients."
This same lack of equipoise explains the glacially slow recruitment rates into ongoing clinical trials badly needed to establish evidence-based therapy for early-stage colorectal cancer, he added.
He and his coworkers recommended directing future research in this field toward determining which patients with stage I disease are appropriate for local excision. Potentially relevant pathologic markers include depth of invasion and the degree of tumor differentiation. Biomarkers predictive of recurrence also are sorely needed.
Discussant Edward M. Copeland III noted that in light of Dr. Bhangu’s findings it makes sense to offer patients with T2 lesions neoadjuvant radiation and/or chemotherapy.
"You’d probably downstage a lot of them to T0 and you could then locally excise them, doing away with that 8% difference in survival between local excision and major resection you found in the SEER database," said Dr. Copeland, professor and chairman of the department of surgery at the University of Florida, Gainesville.
"I would venture to say if you had a patient with a T2 rectal lesion and offered neoadjuvant therapy followed by local excision, without a major operation, and with virtually zero chance of recurrence, I would take that, personally," he added.
Dr. Bhangu responded that it’s an intriguing notion, but the supporting evidence simply doesn’t exist. However, an ongoing U.K. randomized trial is evaluating just such an approach in patients with stage I T1 and T2 rectal cancer.
"I think this will provide the high-quality evidence that we require to treat these patients with evidence-based principles," he added.
Discussant Dr. Conor P. Delaney praised Dr. Bhangu for presenting "a great study." He placed the findings in perspective.
"It’s important to remember that the disadvantage that you’re showing with local therapy is very similar in size to the benefit that all of medical oncology gives us, with all of the effort that we invest in medical oncology. So this is actually a very significant result," declared Dr. Delaney, professor of surgery and chief of the division of colorectal surgery at Case Western Reserve University, Cleveland.
Dr. Bhangu reported having no financial conflicts.
INDIANAPOLIS – Local excision of early invasive stage I colon or rectal carcinoma confers significantly worse 5-year overall and cancer-specific survival than does radical resection, according to analysis of a large national database.
This was true for stage I T1 and T2 disease; that is, for patients with tumor invading the submucosa as well as for those with tumor invading the muscularis propria, Dr. Aneel Bhangu reported at the annual meeting of the American Surgical Association.
In contrast, 5-year survival rates were equivalent with local excision compared with radical resection in patients with stage 0 disease, also known as carcinoma in situ, added Dr. Bhangu of Royal Marsden Hospital, London.
"We recommend that it is safe to perform local excision for stage 0 lesions – that is, carcinoma in situ or severely dysplastic polyps. Refined selection criteria for T1 cancers are required and should be the focus of further research. The use of local excision as a definitive treatment should be carefully considered for patients with T2 colorectal cancer, especially when treating younger, fit patients," he said.
The surgical oncologist presented an analysis of 43,494 patients with surgically treated stage 0 or I adenocarcinoma of the colon or rectum in the Surveillance, Epidemiology, and End Results (SEER) database for 1998-2009. He noted as an aside that the National Cancer Institute’s SEER database is "an open-access and free resource which is the envy of the worldwide oncological community and a shining example of how open-access data can be used by the global community to forward research."
Seventy percent of patients had colonic cancers, 30% rectal. Stage 0 cancer was present in 8.2%, while 91.8% of patients had stage I cancers, 51% of which were T1, 49% T2. Eighteen percent of subjects underwent local excision, while the rest had major resections.
Five-year overall survival was nearly an absolute 8% better in patients with stage I disease treated by radical resection, an advantage that grew even more dramatic in a multivariate analysis adjusted for age and other potential confounders.
Dr. Bhangu observed that these findings take on added import because the number of patients presenting with early colorectal cancer is climbing as a consequence of effective population-based colorectal cancer screening programs. The use of local excision as treatment for such cancers is growing as well. Yet the availability of high-tech tools and techniques for endoscopic local excision of these malignancies has created a dilemma: Such surgery spares the patient from a major operation with all its attendant hazards and morbidity, but when recurrences of these initially small cancers happen they may be inoperable in 10% of cases, and even when they are operable they require extensive visceral resection up to 50% of the time.
Discussant Dr. Genevieve Melton-Meaux of the University of Minnesota, Minneapolis, noted that a surprisingly large percentage of younger patients with stage I disease in this series – that is, patients under age 60 – were treated via local excision.
"We, too, were surprised by this," Dr. Bhangu replied. "If I were to speculate why, I’d say that it may be an issue of clinician equipoise. Some surgeons and endoscopists are true believers in this technology and they may be applying it to a wide scope of patients."
This same lack of equipoise explains the glacially slow recruitment rates into ongoing clinical trials badly needed to establish evidence-based therapy for early-stage colorectal cancer, he added.
He and his coworkers recommended directing future research in this field toward determining which patients with stage I disease are appropriate for local excision. Potentially relevant pathologic markers include depth of invasion and the degree of tumor differentiation. Biomarkers predictive of recurrence also are sorely needed.
Discussant Edward M. Copeland III noted that in light of Dr. Bhangu’s findings it makes sense to offer patients with T2 lesions neoadjuvant radiation and/or chemotherapy.
"You’d probably downstage a lot of them to T0 and you could then locally excise them, doing away with that 8% difference in survival between local excision and major resection you found in the SEER database," said Dr. Copeland, professor and chairman of the department of surgery at the University of Florida, Gainesville.
"I would venture to say if you had a patient with a T2 rectal lesion and offered neoadjuvant therapy followed by local excision, without a major operation, and with virtually zero chance of recurrence, I would take that, personally," he added.
Dr. Bhangu responded that it’s an intriguing notion, but the supporting evidence simply doesn’t exist. However, an ongoing U.K. randomized trial is evaluating just such an approach in patients with stage I T1 and T2 rectal cancer.
"I think this will provide the high-quality evidence that we require to treat these patients with evidence-based principles," he added.
Discussant Dr. Conor P. Delaney praised Dr. Bhangu for presenting "a great study." He placed the findings in perspective.
"It’s important to remember that the disadvantage that you’re showing with local therapy is very similar in size to the benefit that all of medical oncology gives us, with all of the effort that we invest in medical oncology. So this is actually a very significant result," declared Dr. Delaney, professor of surgery and chief of the division of colorectal surgery at Case Western Reserve University, Cleveland.
Dr. Bhangu reported having no financial conflicts.
AT THE ASA ANNUAL MEETING
Major Finding: Five-year overall survival in patients with stage I colorectal carcinoma treated via local excision was 68.4% compared to 75.2% with radical resection. Survival rates did not differ between the two surgical strategies in patients with stage 0 cancer.
Data Source: A retrospective analysis of data on nearly 44,000 patients with stage 0 or I colorectal cancer in the SEER database.
Disclosures: The SEER database is sponsored by the National Cancer Institute. The study presenter reported having no financial conflicts.
More than 23% of uninsured didn't take medications as prescribed
To save money, almost a quarter of uninsured American adults did not take medications as prescribed or asked physicians for lower-cost medications, according to a report from the National Center for Health Statistics.
Data from the 2011 National Health Interview Survey show that 23.1% of uninsured respondents aged 18-64 years skipped doses, took less medicine, or delayed filling prescriptions and that 24.3% asked a doctor for a lower-cost alternative. Among the uninsured, 11.9% used alternative therapies to save money and 4.9% bought prescription drugs from another country, the NCHS said.
Among respondents aged 18-64 years with private insurance, 18.9% asked a doctor for a lower-cost medication, compared with 15.1% of those on Medicaid; however, more Medicaid recipients (13.6%) did not take medication as prescribed, compared with those who had private coverage (8.7%), the report noted.
To save money, almost a quarter of uninsured American adults did not take medications as prescribed or asked physicians for lower-cost medications, according to a report from the National Center for Health Statistics.
Data from the 2011 National Health Interview Survey show that 23.1% of uninsured respondents aged 18-64 years skipped doses, took less medicine, or delayed filling prescriptions and that 24.3% asked a doctor for a lower-cost alternative. Among the uninsured, 11.9% used alternative therapies to save money and 4.9% bought prescription drugs from another country, the NCHS said.
Among respondents aged 18-64 years with private insurance, 18.9% asked a doctor for a lower-cost medication, compared with 15.1% of those on Medicaid; however, more Medicaid recipients (13.6%) did not take medication as prescribed, compared with those who had private coverage (8.7%), the report noted.
To save money, almost a quarter of uninsured American adults did not take medications as prescribed or asked physicians for lower-cost medications, according to a report from the National Center for Health Statistics.
Data from the 2011 National Health Interview Survey show that 23.1% of uninsured respondents aged 18-64 years skipped doses, took less medicine, or delayed filling prescriptions and that 24.3% asked a doctor for a lower-cost alternative. Among the uninsured, 11.9% used alternative therapies to save money and 4.9% bought prescription drugs from another country, the NCHS said.
Among respondents aged 18-64 years with private insurance, 18.9% asked a doctor for a lower-cost medication, compared with 15.1% of those on Medicaid; however, more Medicaid recipients (13.6%) did not take medication as prescribed, compared with those who had private coverage (8.7%), the report noted.
Providers order fewer tests when fees are listed
Providers order slightly fewer laboratory tests when presented with cost information at the time of ordering, and adopting this tactic on a widespread basis might help reduce the number of inappropriately ordered diagnostic tests, researchers from Johns Hopkins University found.
Dr. Leonard S. Feldman and his colleagues compared ordering behavior among all providers, including nonphysicians, who ordered 61 lab tests through the computerized order entry system at the Johns Hopkins Hospital in Baltimore during a baseline period and an intervention period. During the intervention period, Medicare-allowable fees were displayed for 30 of the 61 lab tests.
Orders for the tests with cost data displayed fell 9% during the intervention period, and the number of tests per patient-day decreased as well, from 3.72 to 3.40 (about 9%), the researchers found. Meanwhile, orders for the 31 tests without cost data rose 5% during the intervention period when compared with the baseline period, and tests per patient-day increased nearly 6% (JAMA Intern. Med. [doi:10.1001/jamainternmed.2013.232]).
Overall, the hospital saved $400,000 in lab charges during the 6-month intervention.
"Although the overall financial impact is modest, our study offers evidence that presenting providers with associated test fees as they order is a simple and unobtrusive way to alter behavior," the researchers concluded. "Unlike the process in previous studies, no extra steps were added to the ordering process and no large-scale educational efforts accompanied this exportable intervention."
The study was supported in part by the Johns Hopkins Hospitalist Scholars Program. The authors reported no relevant conflicts of interest.
Providers order slightly fewer laboratory tests when presented with cost information at the time of ordering, and adopting this tactic on a widespread basis might help reduce the number of inappropriately ordered diagnostic tests, researchers from Johns Hopkins University found.
Dr. Leonard S. Feldman and his colleagues compared ordering behavior among all providers, including nonphysicians, who ordered 61 lab tests through the computerized order entry system at the Johns Hopkins Hospital in Baltimore during a baseline period and an intervention period. During the intervention period, Medicare-allowable fees were displayed for 30 of the 61 lab tests.
Orders for the tests with cost data displayed fell 9% during the intervention period, and the number of tests per patient-day decreased as well, from 3.72 to 3.40 (about 9%), the researchers found. Meanwhile, orders for the 31 tests without cost data rose 5% during the intervention period when compared with the baseline period, and tests per patient-day increased nearly 6% (JAMA Intern. Med. [doi:10.1001/jamainternmed.2013.232]).
Overall, the hospital saved $400,000 in lab charges during the 6-month intervention.
"Although the overall financial impact is modest, our study offers evidence that presenting providers with associated test fees as they order is a simple and unobtrusive way to alter behavior," the researchers concluded. "Unlike the process in previous studies, no extra steps were added to the ordering process and no large-scale educational efforts accompanied this exportable intervention."
The study was supported in part by the Johns Hopkins Hospitalist Scholars Program. The authors reported no relevant conflicts of interest.
Providers order slightly fewer laboratory tests when presented with cost information at the time of ordering, and adopting this tactic on a widespread basis might help reduce the number of inappropriately ordered diagnostic tests, researchers from Johns Hopkins University found.
Dr. Leonard S. Feldman and his colleagues compared ordering behavior among all providers, including nonphysicians, who ordered 61 lab tests through the computerized order entry system at the Johns Hopkins Hospital in Baltimore during a baseline period and an intervention period. During the intervention period, Medicare-allowable fees were displayed for 30 of the 61 lab tests.
Orders for the tests with cost data displayed fell 9% during the intervention period, and the number of tests per patient-day decreased as well, from 3.72 to 3.40 (about 9%), the researchers found. Meanwhile, orders for the 31 tests without cost data rose 5% during the intervention period when compared with the baseline period, and tests per patient-day increased nearly 6% (JAMA Intern. Med. [doi:10.1001/jamainternmed.2013.232]).
Overall, the hospital saved $400,000 in lab charges during the 6-month intervention.
"Although the overall financial impact is modest, our study offers evidence that presenting providers with associated test fees as they order is a simple and unobtrusive way to alter behavior," the researchers concluded. "Unlike the process in previous studies, no extra steps were added to the ordering process and no large-scale educational efforts accompanied this exportable intervention."
The study was supported in part by the Johns Hopkins Hospitalist Scholars Program. The authors reported no relevant conflicts of interest.
The case for robotic-assisted hysterectomy
During my address as president of the Board of Trustees of the AAGL in 2008, I noted that essentially 95% of all cholecystectomies, 95% of all bariatric surgery, and 70% of all appendectomies in the United States were performed laparoscopically. Unfortunately, less than 20% of hysterectomies were performed via a minimally invasive route.
Subsequently, at the time of my 2012 presidential address for the International Society for Gynecologic Endoscopy (ISGE), I noted that the percentage of minimally invasive hysterectomies performed in the United States now reached 50%, while the percentage of laparoscopic and vaginal hysterectomies was still mired at 18% and 14%, respectively. The increase in a minimally invasive approach to hysterectomy appeared to be due to the newest method of hysterectomy; that is, robotic-assisted hysterectomy.
On March 14, 2013, Dr. James T. Breeden, president of the American College of Obstetricians and Gynecologists, released a statement regarding robotic surgery. In that, he noted, "While there may be some advantages to the use of robotics in complex hysterectomies ... studies have shown that adding this expensive technology for routine surgical care does not improve patient outcomes. Consequently, there is no good data proving that robotic hysterectomy is even as good as – let alone better than – existing, and far less costly, minimally invasive alternatives."
Dr. Breeden then went on to refer to a recent article in the Journal of the American Medical Association (JAMA 2013;309:689-98) to make the point that, in a study of 264,758 patients undergoing hysterectomy in 441 hospitals in the Premier hospital group, robotics added an average of $2,000/procedure without any demonstrable benefit.
Interestingly, however, the authors of the JAMA article acknowledge that while uptake of laparoscopic hysterectomy has been slow since its inception in the early 1990s, accounting for only 14% of hysterectomies in 2005, within 3 years of the introduction of the adoption of robotics for hysterectomy, nearly 10% of all cases were completed by this enabling technology. Furthermore, the authors comment that, "The introduction of robotic gynecologic surgery was associated with a decrease in the rate of abdominal hysterectomy and an increase in the use of minimally invasive surgery as a whole, including both laparoscopic and robotic hysterectomy." The authors acknowledge that robotic surgery may be easier to learn and that robotic assistance may allow for the completion of more technically demanding cases. In addition, they note that the increase in numbers of laparoscopic hysterectomy may have occurred because of competitive pressures or an increased awareness and appreciation of minimally invasive surgical options.
In comparison, the authors found that in hospitals at which robotic surgery was not performed as of the first quarter of 2010, nearly 50% of all hysterectomies were performed via an open abdominal route, while less than 40% of hysterectomies were performed with a laparotomy incision when robotic hysterectomy was performed at the hospital. With the future adoption of the robotics in gynecologic surgery, I am sure there will be a continued reduction in open abdominal hysterectomy. Benefit ... a resounding yes!
Another fascinating finding of the JAMA study was the fact that overall complication rates were similar for robotic-assisted and laparoscopic hysterectomy (5.5% vs. 5.3%; relative risk, 1.03; 95% confidence interval, 0.86-1.24). Moreover, patients who underwent a robotic-assisted hysterectomy were less likely to have a length of stay longer than 2 days (19.6% vs. 24.9%; RR, 0.78; 95% CI, 0.67-0.92).
Despite no differences in complications in the JAMA study, given the fact that robotics is an emerging technology, one can easily extrapolate that the percentage of cases performed in the study by relatively inexperienced robotic surgeons, as compared with laparoscopic surgeons, was higher. Therefore, with increased surgeon experience, as with any new technology, the rate of complications would be expected to be further decreased. To this end, one must remember that early in its inception, the New York Assembly voiced concerns with laparoscopic cholecystectomy secondary to complications. Now, virtually 95% of all cholecystectomies in the United States are performed via a laparoscopic route. Currently, what is the latest focus in cholecystectomy ... robotic assisted single site cholecystectomy that is being rapidly adopted throughout the country.
While one must acknowledge that, at present, robotic-assisted surgery would appear to be more expensive to perform than laparoscopic surgery is, it is difficult to ascertain what that cost differential is truly. Furthermore, one would anticipate with increased experience and efficiency that cost would, indeed, decrease. While in 1996, Dr. James H. Dorsey published an article on the higher costs associated with laparoscopic surgery (N. Engl. J. Med. 1996;335:476-82), more recent studies by Warren L., et al. (J. Minim. Invasive Gynecol. 2009;16:581-8), and Jonsdottir G.M., et al. (Obstet. Gynecol. 2011;117:1142-9) actually show that the laparoscopic route can be more cost effective.
In this era of cost containment, it is imperative that surgical innovation thrive. Where would all specialties involved in minimally invasive surgery be if surgical pioneer and visionary Professor Kurt Semm were not allowed to perform early operative laparoscopic cases in Kiel, Germany? As chronicled by his associate, Professor Lisolette Mettler, in the July-September 2003 NewsScope of the AAGL, "Kurt endured much resistance, including a request for him to undergo a brain scan to rule out brain damage when attempting to introduce operative laparoscopy; the laughter of general surgeons when he recommended laparoscopic cholecystectomy in the late 1970s; a call for suspension by the president of the German Surgical Society after a 1981 lecture on laparoscopic appendectomy; and rejection of a paper on laparoscopic appendectomy to the American Journal of Obstetrics & Gynecology as unethical." Where would the cholecystectomy market be if general surgeons headed the randomized controlled trial of open vs. laparoscopic cholecystectomy published in Lancet in 1996 (Lancet 1996;347:989-94)? The study concluded that the open procedure was superior because there was no difference in hospital stay or recovery, compared with the laparoscopic route. Where would minimally invasive gynecologic surgery be if our specialty fell in line behind Dr. Roy Pitkin, then president of ACOG, who in 1992 entitled an editorial in Obstetrics & Gynecology "Operative Laparoscopy: Surgical Advance or Technical Gimmick?" (Obstet. Gynecol. 1992;79:441-2). In this editorial he questioned operative laparoscopy on the following:
• How does one separate technical feasibility from therapeutic appropriateness?
• What is the nature of "quality assurance"?
• How can appropriate credentialing criteria be established for procedures not taught in residency and for which no present member of the medical staff can claim experience?
• To what extent are these procedures "experimental," requiring review by an institutional body charged with protection of human subjects, and how should truly informed consent be obtained?
• What about fees? When the procedure is not part of established clinical care, is it ethical to charge for professional services?
Dr. Pitkin concluded by commenting, "Our approach to evaluation of these newer surgical techniques is not something of which we can be proud." Many of these same concerns are currently being voiced by those who do not see the brilliant potential of robotics in gynecologic surgery.
Eighteen years later, in a subsequent editorial (Obstet. Gynecol. 2010;115:890-1), Dr. Pitkin acknowledged that "A substantial body of evidence has accumulated in the recent years to support the laparoscopic approach to various gynecologic operations. ... From this extensive literature, it is now clear that many, if not most gynecologic operations traditionally done by laparotomy are amenable to a laparoscopic approach. Further, the studies are consistent in indicating that operative laparoscopy confers unequivocal advantages over older surgical approaches."
Dr. Pitkin and his coauthor, Dr. William Parker, then go on to discuss the issue of cost, "All health care financial studies are complicated by inconsistencies and uncertainties regarding the meaning of cost. ... Increase in operating time with laparoscopic surgery and disposable instruments are offset, by decreased charges reflecting shortened postoperative hospital stays. If a societal cost that included financial results from early return to work or full home activity were calculated, the advantage of endoscopic surgery would be even greater."
Just as it is imperative that our surgical specialty must remain innovative, we must remember, as can be learned with Dr. Pitkin’s two editorials, that scientific evidence behind the innovation takes time. The fact that, in its infancy, robotic assisted surgery has enabled more gynecologic surgeons to perform minimally invasive surgery for more patients cannot be denied. As seen by the JAMA article, even early on, it can be performed safely and effectively. Data collected in the final decade of the 20th century and the first decade of the 21st have enabled operative laparoscopy to enter mainstream surgical care. One can foresee, with the accumulation of knowledge and experience, that robotics will have a similar – if not even greater – role within our specialty. We must learn from William Shakespeare, who provided Marc Anthony the words, "I have come to bury Caesar, not to praise him." We must not come here to bury robotic assisted surgery, but to praise it!
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, immediate past president of the International Society for Gynecologic Endoscopy, and a past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville, Ill., and Schaumburg, Ill.; the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill; and the medical editor of this column. Dr. Miller has received grants from Intuitive Surgical Inc. He also has served as a consultant for and served on the speakers bureau for Intuitive.
During my address as president of the Board of Trustees of the AAGL in 2008, I noted that essentially 95% of all cholecystectomies, 95% of all bariatric surgery, and 70% of all appendectomies in the United States were performed laparoscopically. Unfortunately, less than 20% of hysterectomies were performed via a minimally invasive route.
Subsequently, at the time of my 2012 presidential address for the International Society for Gynecologic Endoscopy (ISGE), I noted that the percentage of minimally invasive hysterectomies performed in the United States now reached 50%, while the percentage of laparoscopic and vaginal hysterectomies was still mired at 18% and 14%, respectively. The increase in a minimally invasive approach to hysterectomy appeared to be due to the newest method of hysterectomy; that is, robotic-assisted hysterectomy.
On March 14, 2013, Dr. James T. Breeden, president of the American College of Obstetricians and Gynecologists, released a statement regarding robotic surgery. In that, he noted, "While there may be some advantages to the use of robotics in complex hysterectomies ... studies have shown that adding this expensive technology for routine surgical care does not improve patient outcomes. Consequently, there is no good data proving that robotic hysterectomy is even as good as – let alone better than – existing, and far less costly, minimally invasive alternatives."
Dr. Breeden then went on to refer to a recent article in the Journal of the American Medical Association (JAMA 2013;309:689-98) to make the point that, in a study of 264,758 patients undergoing hysterectomy in 441 hospitals in the Premier hospital group, robotics added an average of $2,000/procedure without any demonstrable benefit.
Interestingly, however, the authors of the JAMA article acknowledge that while uptake of laparoscopic hysterectomy has been slow since its inception in the early 1990s, accounting for only 14% of hysterectomies in 2005, within 3 years of the introduction of the adoption of robotics for hysterectomy, nearly 10% of all cases were completed by this enabling technology. Furthermore, the authors comment that, "The introduction of robotic gynecologic surgery was associated with a decrease in the rate of abdominal hysterectomy and an increase in the use of minimally invasive surgery as a whole, including both laparoscopic and robotic hysterectomy." The authors acknowledge that robotic surgery may be easier to learn and that robotic assistance may allow for the completion of more technically demanding cases. In addition, they note that the increase in numbers of laparoscopic hysterectomy may have occurred because of competitive pressures or an increased awareness and appreciation of minimally invasive surgical options.
In comparison, the authors found that in hospitals at which robotic surgery was not performed as of the first quarter of 2010, nearly 50% of all hysterectomies were performed via an open abdominal route, while less than 40% of hysterectomies were performed with a laparotomy incision when robotic hysterectomy was performed at the hospital. With the future adoption of the robotics in gynecologic surgery, I am sure there will be a continued reduction in open abdominal hysterectomy. Benefit ... a resounding yes!
Another fascinating finding of the JAMA study was the fact that overall complication rates were similar for robotic-assisted and laparoscopic hysterectomy (5.5% vs. 5.3%; relative risk, 1.03; 95% confidence interval, 0.86-1.24). Moreover, patients who underwent a robotic-assisted hysterectomy were less likely to have a length of stay longer than 2 days (19.6% vs. 24.9%; RR, 0.78; 95% CI, 0.67-0.92).
Despite no differences in complications in the JAMA study, given the fact that robotics is an emerging technology, one can easily extrapolate that the percentage of cases performed in the study by relatively inexperienced robotic surgeons, as compared with laparoscopic surgeons, was higher. Therefore, with increased surgeon experience, as with any new technology, the rate of complications would be expected to be further decreased. To this end, one must remember that early in its inception, the New York Assembly voiced concerns with laparoscopic cholecystectomy secondary to complications. Now, virtually 95% of all cholecystectomies in the United States are performed via a laparoscopic route. Currently, what is the latest focus in cholecystectomy ... robotic assisted single site cholecystectomy that is being rapidly adopted throughout the country.
While one must acknowledge that, at present, robotic-assisted surgery would appear to be more expensive to perform than laparoscopic surgery is, it is difficult to ascertain what that cost differential is truly. Furthermore, one would anticipate with increased experience and efficiency that cost would, indeed, decrease. While in 1996, Dr. James H. Dorsey published an article on the higher costs associated with laparoscopic surgery (N. Engl. J. Med. 1996;335:476-82), more recent studies by Warren L., et al. (J. Minim. Invasive Gynecol. 2009;16:581-8), and Jonsdottir G.M., et al. (Obstet. Gynecol. 2011;117:1142-9) actually show that the laparoscopic route can be more cost effective.
In this era of cost containment, it is imperative that surgical innovation thrive. Where would all specialties involved in minimally invasive surgery be if surgical pioneer and visionary Professor Kurt Semm were not allowed to perform early operative laparoscopic cases in Kiel, Germany? As chronicled by his associate, Professor Lisolette Mettler, in the July-September 2003 NewsScope of the AAGL, "Kurt endured much resistance, including a request for him to undergo a brain scan to rule out brain damage when attempting to introduce operative laparoscopy; the laughter of general surgeons when he recommended laparoscopic cholecystectomy in the late 1970s; a call for suspension by the president of the German Surgical Society after a 1981 lecture on laparoscopic appendectomy; and rejection of a paper on laparoscopic appendectomy to the American Journal of Obstetrics & Gynecology as unethical." Where would the cholecystectomy market be if general surgeons headed the randomized controlled trial of open vs. laparoscopic cholecystectomy published in Lancet in 1996 (Lancet 1996;347:989-94)? The study concluded that the open procedure was superior because there was no difference in hospital stay or recovery, compared with the laparoscopic route. Where would minimally invasive gynecologic surgery be if our specialty fell in line behind Dr. Roy Pitkin, then president of ACOG, who in 1992 entitled an editorial in Obstetrics & Gynecology "Operative Laparoscopy: Surgical Advance or Technical Gimmick?" (Obstet. Gynecol. 1992;79:441-2). In this editorial he questioned operative laparoscopy on the following:
• How does one separate technical feasibility from therapeutic appropriateness?
• What is the nature of "quality assurance"?
• How can appropriate credentialing criteria be established for procedures not taught in residency and for which no present member of the medical staff can claim experience?
• To what extent are these procedures "experimental," requiring review by an institutional body charged with protection of human subjects, and how should truly informed consent be obtained?
• What about fees? When the procedure is not part of established clinical care, is it ethical to charge for professional services?
Dr. Pitkin concluded by commenting, "Our approach to evaluation of these newer surgical techniques is not something of which we can be proud." Many of these same concerns are currently being voiced by those who do not see the brilliant potential of robotics in gynecologic surgery.
Eighteen years later, in a subsequent editorial (Obstet. Gynecol. 2010;115:890-1), Dr. Pitkin acknowledged that "A substantial body of evidence has accumulated in the recent years to support the laparoscopic approach to various gynecologic operations. ... From this extensive literature, it is now clear that many, if not most gynecologic operations traditionally done by laparotomy are amenable to a laparoscopic approach. Further, the studies are consistent in indicating that operative laparoscopy confers unequivocal advantages over older surgical approaches."
Dr. Pitkin and his coauthor, Dr. William Parker, then go on to discuss the issue of cost, "All health care financial studies are complicated by inconsistencies and uncertainties regarding the meaning of cost. ... Increase in operating time with laparoscopic surgery and disposable instruments are offset, by decreased charges reflecting shortened postoperative hospital stays. If a societal cost that included financial results from early return to work or full home activity were calculated, the advantage of endoscopic surgery would be even greater."
Just as it is imperative that our surgical specialty must remain innovative, we must remember, as can be learned with Dr. Pitkin’s two editorials, that scientific evidence behind the innovation takes time. The fact that, in its infancy, robotic assisted surgery has enabled more gynecologic surgeons to perform minimally invasive surgery for more patients cannot be denied. As seen by the JAMA article, even early on, it can be performed safely and effectively. Data collected in the final decade of the 20th century and the first decade of the 21st have enabled operative laparoscopy to enter mainstream surgical care. One can foresee, with the accumulation of knowledge and experience, that robotics will have a similar – if not even greater – role within our specialty. We must learn from William Shakespeare, who provided Marc Anthony the words, "I have come to bury Caesar, not to praise him." We must not come here to bury robotic assisted surgery, but to praise it!
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, immediate past president of the International Society for Gynecologic Endoscopy, and a past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville, Ill., and Schaumburg, Ill.; the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill; and the medical editor of this column. Dr. Miller has received grants from Intuitive Surgical Inc. He also has served as a consultant for and served on the speakers bureau for Intuitive.
During my address as president of the Board of Trustees of the AAGL in 2008, I noted that essentially 95% of all cholecystectomies, 95% of all bariatric surgery, and 70% of all appendectomies in the United States were performed laparoscopically. Unfortunately, less than 20% of hysterectomies were performed via a minimally invasive route.
Subsequently, at the time of my 2012 presidential address for the International Society for Gynecologic Endoscopy (ISGE), I noted that the percentage of minimally invasive hysterectomies performed in the United States now reached 50%, while the percentage of laparoscopic and vaginal hysterectomies was still mired at 18% and 14%, respectively. The increase in a minimally invasive approach to hysterectomy appeared to be due to the newest method of hysterectomy; that is, robotic-assisted hysterectomy.
On March 14, 2013, Dr. James T. Breeden, president of the American College of Obstetricians and Gynecologists, released a statement regarding robotic surgery. In that, he noted, "While there may be some advantages to the use of robotics in complex hysterectomies ... studies have shown that adding this expensive technology for routine surgical care does not improve patient outcomes. Consequently, there is no good data proving that robotic hysterectomy is even as good as – let alone better than – existing, and far less costly, minimally invasive alternatives."
Dr. Breeden then went on to refer to a recent article in the Journal of the American Medical Association (JAMA 2013;309:689-98) to make the point that, in a study of 264,758 patients undergoing hysterectomy in 441 hospitals in the Premier hospital group, robotics added an average of $2,000/procedure without any demonstrable benefit.
Interestingly, however, the authors of the JAMA article acknowledge that while uptake of laparoscopic hysterectomy has been slow since its inception in the early 1990s, accounting for only 14% of hysterectomies in 2005, within 3 years of the introduction of the adoption of robotics for hysterectomy, nearly 10% of all cases were completed by this enabling technology. Furthermore, the authors comment that, "The introduction of robotic gynecologic surgery was associated with a decrease in the rate of abdominal hysterectomy and an increase in the use of minimally invasive surgery as a whole, including both laparoscopic and robotic hysterectomy." The authors acknowledge that robotic surgery may be easier to learn and that robotic assistance may allow for the completion of more technically demanding cases. In addition, they note that the increase in numbers of laparoscopic hysterectomy may have occurred because of competitive pressures or an increased awareness and appreciation of minimally invasive surgical options.
In comparison, the authors found that in hospitals at which robotic surgery was not performed as of the first quarter of 2010, nearly 50% of all hysterectomies were performed via an open abdominal route, while less than 40% of hysterectomies were performed with a laparotomy incision when robotic hysterectomy was performed at the hospital. With the future adoption of the robotics in gynecologic surgery, I am sure there will be a continued reduction in open abdominal hysterectomy. Benefit ... a resounding yes!
Another fascinating finding of the JAMA study was the fact that overall complication rates were similar for robotic-assisted and laparoscopic hysterectomy (5.5% vs. 5.3%; relative risk, 1.03; 95% confidence interval, 0.86-1.24). Moreover, patients who underwent a robotic-assisted hysterectomy were less likely to have a length of stay longer than 2 days (19.6% vs. 24.9%; RR, 0.78; 95% CI, 0.67-0.92).
Despite no differences in complications in the JAMA study, given the fact that robotics is an emerging technology, one can easily extrapolate that the percentage of cases performed in the study by relatively inexperienced robotic surgeons, as compared with laparoscopic surgeons, was higher. Therefore, with increased surgeon experience, as with any new technology, the rate of complications would be expected to be further decreased. To this end, one must remember that early in its inception, the New York Assembly voiced concerns with laparoscopic cholecystectomy secondary to complications. Now, virtually 95% of all cholecystectomies in the United States are performed via a laparoscopic route. Currently, what is the latest focus in cholecystectomy ... robotic assisted single site cholecystectomy that is being rapidly adopted throughout the country.
While one must acknowledge that, at present, robotic-assisted surgery would appear to be more expensive to perform than laparoscopic surgery is, it is difficult to ascertain what that cost differential is truly. Furthermore, one would anticipate with increased experience and efficiency that cost would, indeed, decrease. While in 1996, Dr. James H. Dorsey published an article on the higher costs associated with laparoscopic surgery (N. Engl. J. Med. 1996;335:476-82), more recent studies by Warren L., et al. (J. Minim. Invasive Gynecol. 2009;16:581-8), and Jonsdottir G.M., et al. (Obstet. Gynecol. 2011;117:1142-9) actually show that the laparoscopic route can be more cost effective.
In this era of cost containment, it is imperative that surgical innovation thrive. Where would all specialties involved in minimally invasive surgery be if surgical pioneer and visionary Professor Kurt Semm were not allowed to perform early operative laparoscopic cases in Kiel, Germany? As chronicled by his associate, Professor Lisolette Mettler, in the July-September 2003 NewsScope of the AAGL, "Kurt endured much resistance, including a request for him to undergo a brain scan to rule out brain damage when attempting to introduce operative laparoscopy; the laughter of general surgeons when he recommended laparoscopic cholecystectomy in the late 1970s; a call for suspension by the president of the German Surgical Society after a 1981 lecture on laparoscopic appendectomy; and rejection of a paper on laparoscopic appendectomy to the American Journal of Obstetrics & Gynecology as unethical." Where would the cholecystectomy market be if general surgeons headed the randomized controlled trial of open vs. laparoscopic cholecystectomy published in Lancet in 1996 (Lancet 1996;347:989-94)? The study concluded that the open procedure was superior because there was no difference in hospital stay or recovery, compared with the laparoscopic route. Where would minimally invasive gynecologic surgery be if our specialty fell in line behind Dr. Roy Pitkin, then president of ACOG, who in 1992 entitled an editorial in Obstetrics & Gynecology "Operative Laparoscopy: Surgical Advance or Technical Gimmick?" (Obstet. Gynecol. 1992;79:441-2). In this editorial he questioned operative laparoscopy on the following:
• How does one separate technical feasibility from therapeutic appropriateness?
• What is the nature of "quality assurance"?
• How can appropriate credentialing criteria be established for procedures not taught in residency and for which no present member of the medical staff can claim experience?
• To what extent are these procedures "experimental," requiring review by an institutional body charged with protection of human subjects, and how should truly informed consent be obtained?
• What about fees? When the procedure is not part of established clinical care, is it ethical to charge for professional services?
Dr. Pitkin concluded by commenting, "Our approach to evaluation of these newer surgical techniques is not something of which we can be proud." Many of these same concerns are currently being voiced by those who do not see the brilliant potential of robotics in gynecologic surgery.
Eighteen years later, in a subsequent editorial (Obstet. Gynecol. 2010;115:890-1), Dr. Pitkin acknowledged that "A substantial body of evidence has accumulated in the recent years to support the laparoscopic approach to various gynecologic operations. ... From this extensive literature, it is now clear that many, if not most gynecologic operations traditionally done by laparotomy are amenable to a laparoscopic approach. Further, the studies are consistent in indicating that operative laparoscopy confers unequivocal advantages over older surgical approaches."
Dr. Pitkin and his coauthor, Dr. William Parker, then go on to discuss the issue of cost, "All health care financial studies are complicated by inconsistencies and uncertainties regarding the meaning of cost. ... Increase in operating time with laparoscopic surgery and disposable instruments are offset, by decreased charges reflecting shortened postoperative hospital stays. If a societal cost that included financial results from early return to work or full home activity were calculated, the advantage of endoscopic surgery would be even greater."
Just as it is imperative that our surgical specialty must remain innovative, we must remember, as can be learned with Dr. Pitkin’s two editorials, that scientific evidence behind the innovation takes time. The fact that, in its infancy, robotic assisted surgery has enabled more gynecologic surgeons to perform minimally invasive surgery for more patients cannot be denied. As seen by the JAMA article, even early on, it can be performed safely and effectively. Data collected in the final decade of the 20th century and the first decade of the 21st have enabled operative laparoscopy to enter mainstream surgical care. One can foresee, with the accumulation of knowledge and experience, that robotics will have a similar – if not even greater – role within our specialty. We must learn from William Shakespeare, who provided Marc Anthony the words, "I have come to bury Caesar, not to praise him." We must not come here to bury robotic assisted surgery, but to praise it!
Dr. Miller is clinical associate professor at the University of Illinois at Chicago, immediate past president of the International Society for Gynecologic Endoscopy, and a past president of the AAGL. He is a reproductive endocrinologist and minimally invasive gynecologic surgeon in private practice in Naperville, Ill., and Schaumburg, Ill.; the director of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital, Park Ridge, Ill; and the medical editor of this column. Dr. Miller has received grants from Intuitive Surgical Inc. He also has served as a consultant for and served on the speakers bureau for Intuitive.
Battling over the budget: The Policy & Practice Podcast
With the release of President Obama’s fiscal year 2014 budget, the wrangling on Capitol Hill can begin in earnest.
Both the House and the Senate have approved their own versions of next year’s federal budget, but the president’s proposal will begin those discussions anew. Most of his health care proposals don’t break new ground. For instance, the president is proposing policies estimated to save $370 billion from the Medicare program over the next decade. Those policies, which have been proposed before, include cutting payments to drug companies and long-term care facilities, and some increases in cost sharing by beneficiaries.
But there’s also some new spending on health priorities. For instance, the budget proposal calls for spending $100 million to fund a wide-ranging initiative to map the human brain. It also includes a $130 million investment in mental health. That proposal calls for adding 5,000 mental health professionals to the behavioral health workforce and training teachers to recognize the early signs of mental illness.
The president may have a tougher time getting the $1.5 billion he’s seeking to help jumpstart the health insurance exchanges that are part of the Affordable Care Act. The budget proposal includes funding to support operations and outreach related to the federally operated exchanges. The money would also go to assist states who are running their own exchanges. The exchanges are set to open for enrollment on Oct. 1 and coverage will begin Jan. 1, 2014.
Check out this week’s Policy & Practice podcast for all the budget news, plus more on the sequester and the pending nomination of Marilyn Tavenner to head the Centers for Medicare and Medicaid Services.
On Twitter @MaryEllenNY
With the release of President Obama’s fiscal year 2014 budget, the wrangling on Capitol Hill can begin in earnest.
Both the House and the Senate have approved their own versions of next year’s federal budget, but the president’s proposal will begin those discussions anew. Most of his health care proposals don’t break new ground. For instance, the president is proposing policies estimated to save $370 billion from the Medicare program over the next decade. Those policies, which have been proposed before, include cutting payments to drug companies and long-term care facilities, and some increases in cost sharing by beneficiaries.
But there’s also some new spending on health priorities. For instance, the budget proposal calls for spending $100 million to fund a wide-ranging initiative to map the human brain. It also includes a $130 million investment in mental health. That proposal calls for adding 5,000 mental health professionals to the behavioral health workforce and training teachers to recognize the early signs of mental illness.
The president may have a tougher time getting the $1.5 billion he’s seeking to help jumpstart the health insurance exchanges that are part of the Affordable Care Act. The budget proposal includes funding to support operations and outreach related to the federally operated exchanges. The money would also go to assist states who are running their own exchanges. The exchanges are set to open for enrollment on Oct. 1 and coverage will begin Jan. 1, 2014.
Check out this week’s Policy & Practice podcast for all the budget news, plus more on the sequester and the pending nomination of Marilyn Tavenner to head the Centers for Medicare and Medicaid Services.
On Twitter @MaryEllenNY
With the release of President Obama’s fiscal year 2014 budget, the wrangling on Capitol Hill can begin in earnest.
Both the House and the Senate have approved their own versions of next year’s federal budget, but the president’s proposal will begin those discussions anew. Most of his health care proposals don’t break new ground. For instance, the president is proposing policies estimated to save $370 billion from the Medicare program over the next decade. Those policies, which have been proposed before, include cutting payments to drug companies and long-term care facilities, and some increases in cost sharing by beneficiaries.
But there’s also some new spending on health priorities. For instance, the budget proposal calls for spending $100 million to fund a wide-ranging initiative to map the human brain. It also includes a $130 million investment in mental health. That proposal calls for adding 5,000 mental health professionals to the behavioral health workforce and training teachers to recognize the early signs of mental illness.
The president may have a tougher time getting the $1.5 billion he’s seeking to help jumpstart the health insurance exchanges that are part of the Affordable Care Act. The budget proposal includes funding to support operations and outreach related to the federally operated exchanges. The money would also go to assist states who are running their own exchanges. The exchanges are set to open for enrollment on Oct. 1 and coverage will begin Jan. 1, 2014.
Check out this week’s Policy & Practice podcast for all the budget news, plus more on the sequester and the pending nomination of Marilyn Tavenner to head the Centers for Medicare and Medicaid Services.
On Twitter @MaryEllenNY