User login
Official Newspaper of the American College of Surgeons
FDA warns kratom vendors about unproven claims
The Food and Drug Administration has issued letters of warning to – and therefore breaking federal law – according to a statement from FDA commissioner Scott Gottlieb, MD. These vendors both claimed that their kratom products could, among other things, “relieve” or “treat” opium/opioid withdrawal.
“To date, there have been no adequate and well-controlled studies involving the use of kratom as a treatment for opioid use withdrawal or other diseases in humans,” noted Dr. Gottlieb.
As Dr. Gottlieb pointed out in his statement, not only can fraudulent health claims pose direct health risks, they can also, in the case of kratom, deter or delay people who’re suffering from opioid use disorder from seeking FDA-approved treatments that have been demonstrated to be safe and effective.
Kratom, also known more formally as Mitragyna speciosa, is a plant native to Thailand, Malaysia, Indonesia, and Papua New Guinea. Some compounds in the plant are believed to be opioids, some of which may have the potential for abuse. As Dr. Gottlieb pointed out in his statement, the substance is illegal or controlled in several countries and banned in some states and municipalities in the United States.
Find out more in Dr. Gottlieb’s full statement on the FDA website.
The Food and Drug Administration has issued letters of warning to – and therefore breaking federal law – according to a statement from FDA commissioner Scott Gottlieb, MD. These vendors both claimed that their kratom products could, among other things, “relieve” or “treat” opium/opioid withdrawal.
“To date, there have been no adequate and well-controlled studies involving the use of kratom as a treatment for opioid use withdrawal or other diseases in humans,” noted Dr. Gottlieb.
As Dr. Gottlieb pointed out in his statement, not only can fraudulent health claims pose direct health risks, they can also, in the case of kratom, deter or delay people who’re suffering from opioid use disorder from seeking FDA-approved treatments that have been demonstrated to be safe and effective.
Kratom, also known more formally as Mitragyna speciosa, is a plant native to Thailand, Malaysia, Indonesia, and Papua New Guinea. Some compounds in the plant are believed to be opioids, some of which may have the potential for abuse. As Dr. Gottlieb pointed out in his statement, the substance is illegal or controlled in several countries and banned in some states and municipalities in the United States.
Find out more in Dr. Gottlieb’s full statement on the FDA website.
The Food and Drug Administration has issued letters of warning to – and therefore breaking federal law – according to a statement from FDA commissioner Scott Gottlieb, MD. These vendors both claimed that their kratom products could, among other things, “relieve” or “treat” opium/opioid withdrawal.
“To date, there have been no adequate and well-controlled studies involving the use of kratom as a treatment for opioid use withdrawal or other diseases in humans,” noted Dr. Gottlieb.
As Dr. Gottlieb pointed out in his statement, not only can fraudulent health claims pose direct health risks, they can also, in the case of kratom, deter or delay people who’re suffering from opioid use disorder from seeking FDA-approved treatments that have been demonstrated to be safe and effective.
Kratom, also known more formally as Mitragyna speciosa, is a plant native to Thailand, Malaysia, Indonesia, and Papua New Guinea. Some compounds in the plant are believed to be opioids, some of which may have the potential for abuse. As Dr. Gottlieb pointed out in his statement, the substance is illegal or controlled in several countries and banned in some states and municipalities in the United States.
Find out more in Dr. Gottlieb’s full statement on the FDA website.
New stroke intervention guidelines stress volume
A consensus working group from numerous international societies has published new guidelines for standards of practice in the treatment of acute ischemic stroke (AIS). The new guidelines differ somewhat from the Joint Commission guideline, released in 2015, primarily by raising the bar for the number of mechanical thrombectomy (MT) procedures that level 1 and level 2 stroke centers should perform annually in order to maintain a minimum safety threshold.
Previous studies have shown lower mortality in high-volume centers, but setting minimum standards can be a challenge, especially in under-served countries and localities. The authors, led by first author Laurent Pierot, MD, PhD, of University Hospital Reims (France), acknowledge that newly established level 2 centers may struggle to meet the minimum requirement for MT procedures, but that this is acceptable as long as the volume is expected to meet the minimum within 12-24 months.
The guidelines were created by a working group of delegates from 13 international societies, including the American Society of Neuroradiology, European Stroke Organization, World Stroke Organization, and the Society of NeuroInterventional Surgery.
The publication in 2015 of studies showing the efficacy of MT in anterior circulation emergent large-vessel occlusion (ELVO) stroke patients reverberated through the stroke care community, but posed a challenge in delivering this therapy to populations in diverse localities that have no access to level 1 stroke centers.
The guidelines, published online in the Journal of NeuroInterventional Surgery, aim to ensure that facilities can handle not only the MT procedure, but also the medical management before, during, and after the procedure.
According to the new guidelines, level 2 centers should handle cases when a level 1 center cannot be reached within 2 hours. Level 2 centers should care for at least 100 AIS patients per year and should also have a relationship with a level 1 center to maintain staff training, teleconsultations, referrals, and other collaborations.
Previous studies have identified 35 or 36 MT procedures annually as a threshold to be considered “high volume,” a category that led to lower mortality. The new recommendations fall below that threshold because they are intended to apply broadly, to regions that may be under-served. In highly developed countries, stroke centers should follow regional or national guidelines that have higher limits.
Level 2 centers should perform at least 50 intracranial thrombectomy procedures for ELVO, and a total of 120 diagnostic or interventional neuroendovascular procedures per year. Individual interventionists should conduct at least 15 intracranial thrombectomy and 50 interventional neuroendovascular procedures per year.
Other recommendations cover additional details about personnel, as well as community and emergency medical services outreach.
In many ways, the recommendations are in line with the Joint Commission (TJC), according to David Tirschwell, MD, who is the medical director for the UW Medicine* Comprehensive Stroke Center at Harborview Medical Center, Seattle. He was not involved in the development of the new guidelines.
Dr. Tirschwell noted one key difference with respect to the number of MT procedures required to qualify. TJC offered no minimum annual procedures for Comprehensive Stroke Centers (equivalent to level 1), and only 15 for Thrombectomy Capable Stroke Centers (level 2), versus 50 in the new guidelines. The minimum procedure numbers are also higher for individual clinicians.
The guidelines also recommend that level 2 centers have at least three interventionalists on staff available at all times, while TJC does not address this element of staffing.
“The higher minimum number of procedures in the new international recommendations is a substantial difference and would make it harder for many hospitals to qualify, compared to the TJC requirements. As such, a lower number of hospitals may qualify, and such a barrier could prevent access to mechanical thrombectomy for many patients. On the other hand, the higher minimum number may ensure a higher quality of care, which can be seen as a strong positive feature,” Dr. Tirschwell said.
A spokesman for the Joint Commission and the American Heart Association indicated that they will review the new guidelines and consider whether to make changes to their 2015 guidelines.
SOURCE: Pierot Laurent et al. J Neurointervent Surg. 2018 Aug 28. doi: 10.1136/neurintsurg-2018-014287.
*Updated Sept. 14, 2018.
A consensus working group from numerous international societies has published new guidelines for standards of practice in the treatment of acute ischemic stroke (AIS). The new guidelines differ somewhat from the Joint Commission guideline, released in 2015, primarily by raising the bar for the number of mechanical thrombectomy (MT) procedures that level 1 and level 2 stroke centers should perform annually in order to maintain a minimum safety threshold.
Previous studies have shown lower mortality in high-volume centers, but setting minimum standards can be a challenge, especially in under-served countries and localities. The authors, led by first author Laurent Pierot, MD, PhD, of University Hospital Reims (France), acknowledge that newly established level 2 centers may struggle to meet the minimum requirement for MT procedures, but that this is acceptable as long as the volume is expected to meet the minimum within 12-24 months.
The guidelines were created by a working group of delegates from 13 international societies, including the American Society of Neuroradiology, European Stroke Organization, World Stroke Organization, and the Society of NeuroInterventional Surgery.
The publication in 2015 of studies showing the efficacy of MT in anterior circulation emergent large-vessel occlusion (ELVO) stroke patients reverberated through the stroke care community, but posed a challenge in delivering this therapy to populations in diverse localities that have no access to level 1 stroke centers.
The guidelines, published online in the Journal of NeuroInterventional Surgery, aim to ensure that facilities can handle not only the MT procedure, but also the medical management before, during, and after the procedure.
According to the new guidelines, level 2 centers should handle cases when a level 1 center cannot be reached within 2 hours. Level 2 centers should care for at least 100 AIS patients per year and should also have a relationship with a level 1 center to maintain staff training, teleconsultations, referrals, and other collaborations.
Previous studies have identified 35 or 36 MT procedures annually as a threshold to be considered “high volume,” a category that led to lower mortality. The new recommendations fall below that threshold because they are intended to apply broadly, to regions that may be under-served. In highly developed countries, stroke centers should follow regional or national guidelines that have higher limits.
Level 2 centers should perform at least 50 intracranial thrombectomy procedures for ELVO, and a total of 120 diagnostic or interventional neuroendovascular procedures per year. Individual interventionists should conduct at least 15 intracranial thrombectomy and 50 interventional neuroendovascular procedures per year.
Other recommendations cover additional details about personnel, as well as community and emergency medical services outreach.
In many ways, the recommendations are in line with the Joint Commission (TJC), according to David Tirschwell, MD, who is the medical director for the UW Medicine* Comprehensive Stroke Center at Harborview Medical Center, Seattle. He was not involved in the development of the new guidelines.
Dr. Tirschwell noted one key difference with respect to the number of MT procedures required to qualify. TJC offered no minimum annual procedures for Comprehensive Stroke Centers (equivalent to level 1), and only 15 for Thrombectomy Capable Stroke Centers (level 2), versus 50 in the new guidelines. The minimum procedure numbers are also higher for individual clinicians.
The guidelines also recommend that level 2 centers have at least three interventionalists on staff available at all times, while TJC does not address this element of staffing.
“The higher minimum number of procedures in the new international recommendations is a substantial difference and would make it harder for many hospitals to qualify, compared to the TJC requirements. As such, a lower number of hospitals may qualify, and such a barrier could prevent access to mechanical thrombectomy for many patients. On the other hand, the higher minimum number may ensure a higher quality of care, which can be seen as a strong positive feature,” Dr. Tirschwell said.
A spokesman for the Joint Commission and the American Heart Association indicated that they will review the new guidelines and consider whether to make changes to their 2015 guidelines.
SOURCE: Pierot Laurent et al. J Neurointervent Surg. 2018 Aug 28. doi: 10.1136/neurintsurg-2018-014287.
*Updated Sept. 14, 2018.
A consensus working group from numerous international societies has published new guidelines for standards of practice in the treatment of acute ischemic stroke (AIS). The new guidelines differ somewhat from the Joint Commission guideline, released in 2015, primarily by raising the bar for the number of mechanical thrombectomy (MT) procedures that level 1 and level 2 stroke centers should perform annually in order to maintain a minimum safety threshold.
Previous studies have shown lower mortality in high-volume centers, but setting minimum standards can be a challenge, especially in under-served countries and localities. The authors, led by first author Laurent Pierot, MD, PhD, of University Hospital Reims (France), acknowledge that newly established level 2 centers may struggle to meet the minimum requirement for MT procedures, but that this is acceptable as long as the volume is expected to meet the minimum within 12-24 months.
The guidelines were created by a working group of delegates from 13 international societies, including the American Society of Neuroradiology, European Stroke Organization, World Stroke Organization, and the Society of NeuroInterventional Surgery.
The publication in 2015 of studies showing the efficacy of MT in anterior circulation emergent large-vessel occlusion (ELVO) stroke patients reverberated through the stroke care community, but posed a challenge in delivering this therapy to populations in diverse localities that have no access to level 1 stroke centers.
The guidelines, published online in the Journal of NeuroInterventional Surgery, aim to ensure that facilities can handle not only the MT procedure, but also the medical management before, during, and after the procedure.
According to the new guidelines, level 2 centers should handle cases when a level 1 center cannot be reached within 2 hours. Level 2 centers should care for at least 100 AIS patients per year and should also have a relationship with a level 1 center to maintain staff training, teleconsultations, referrals, and other collaborations.
Previous studies have identified 35 or 36 MT procedures annually as a threshold to be considered “high volume,” a category that led to lower mortality. The new recommendations fall below that threshold because they are intended to apply broadly, to regions that may be under-served. In highly developed countries, stroke centers should follow regional or national guidelines that have higher limits.
Level 2 centers should perform at least 50 intracranial thrombectomy procedures for ELVO, and a total of 120 diagnostic or interventional neuroendovascular procedures per year. Individual interventionists should conduct at least 15 intracranial thrombectomy and 50 interventional neuroendovascular procedures per year.
Other recommendations cover additional details about personnel, as well as community and emergency medical services outreach.
In many ways, the recommendations are in line with the Joint Commission (TJC), according to David Tirschwell, MD, who is the medical director for the UW Medicine* Comprehensive Stroke Center at Harborview Medical Center, Seattle. He was not involved in the development of the new guidelines.
Dr. Tirschwell noted one key difference with respect to the number of MT procedures required to qualify. TJC offered no minimum annual procedures for Comprehensive Stroke Centers (equivalent to level 1), and only 15 for Thrombectomy Capable Stroke Centers (level 2), versus 50 in the new guidelines. The minimum procedure numbers are also higher for individual clinicians.
The guidelines also recommend that level 2 centers have at least three interventionalists on staff available at all times, while TJC does not address this element of staffing.
“The higher minimum number of procedures in the new international recommendations is a substantial difference and would make it harder for many hospitals to qualify, compared to the TJC requirements. As such, a lower number of hospitals may qualify, and such a barrier could prevent access to mechanical thrombectomy for many patients. On the other hand, the higher minimum number may ensure a higher quality of care, which can be seen as a strong positive feature,” Dr. Tirschwell said.
A spokesman for the Joint Commission and the American Heart Association indicated that they will review the new guidelines and consider whether to make changes to their 2015 guidelines.
SOURCE: Pierot Laurent et al. J Neurointervent Surg. 2018 Aug 28. doi: 10.1136/neurintsurg-2018-014287.
*Updated Sept. 14, 2018.
FROM THE JOURNAL OF NEUROINTERVENTIONAL SURGERY
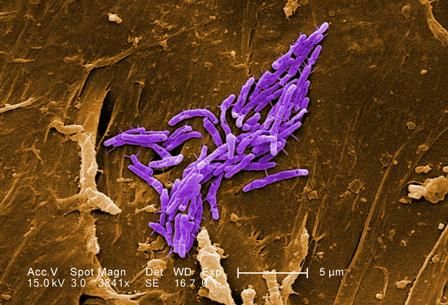
NYC outbreak of Candida auris linked to 45% mortality
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
FROM EMERGING INFECTIOUS DISEASES
One-quarter of ED sprained ankle diagnoses result in opioid prescription
One-quarter of patients who present at the ED with a , according to the findings of a large study using a national insurance claims database.
M. Kit Delgado, MD, of the Center for Emergency Care Policy and Research at the Perelman School of Medicine, University of Pennsylvania, Philadelphia, and his coauthors analyzed private insurance claims for 30,832 opioid-naive patients who were treated in the emergency department for ankle sprains.
The researchers looked at the initial opioid prescription intensity and duration of subsequent opioid use. The study, published online in Annals of Emergency Medicine, also found a wide variation in prescribing by hospital and geographic region, and an association between higher-potency opioid prescriptions (hydrocodone and oxycodone) and likelihood of extended or prolonged opioid use.
Overall, 25.1% of patients received an opioid prescription, the median tablet quantity was 15 tablets, and median days of opioids supplied was 3 days. Only 5% of patients were prescribed more than 30 tablets, which suggested that the majority of prescriptions written were in agreement with guidelines, the authors wrote.
They noted that nonsteroidal anti-inflammatory drugs are the first-line treatment for ankle sprains, rather than opioids, and are as effective for pain reduction.
Among patients prescribed the equivalent of more than 30 tabs of oxycodone 5 mg, 4.9% of them showed prolonged opioid use – defined as filling four or more subsequent opioid prescriptions in the 30-180 days after the index visit – compared with 1.1% of patients who received fewer than 10 tabs, and 0.5% of those who did not fill an opioid prescription. This represented a nearly fivefold increased probability of transition to prolonged use. For every 26 patients exposed to the higher intensity prescription, 1 would go on to prolonged opioid use.
“We confirmed that the majority of subsequent prescriptions were unlikely to be related to the initial ankle sprain or chronic ankle pain,” the researchers wrote. “This suggests that association between larger prescriptions and increased likelihood of prolonged use could be due to other factors such as patients requesting opioids as default pain control, or the development of dependence or misuse.”
The most commonly prescribed opioid was hydrocodone (64.9%), followed by tramadol (16.2%), oxycodone (14.4%), and codeine (5.5%). The analysis found that patients prescribed higher-potency drugs – namely hydrocodone and oxycodone – were at even greater risk of developing prolonged use.
The researchers noted significant geographic differences in prescribing habits, with 40% of study participants in Arkansas receiving an opioid prescription, compared with 2.8% in North Dakota. Overall, southern states were more likely to overprescribe, and northern states more likely to underprescribe.
Women were at greater risk of transitioning to high-risk prolonged use, as were individuals aged 35-44 years, those with a higher comorbidity burden, or those with a history of drug abuse.
The study was supported by the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, and the Leonard Davis Institute of Health Economics at the University of Pennsylvania. One author declared an honorarium from the United Health Group.
SOURCE: Delgado MK et al. Ann Emerg Med. 2018. Jul 24. doi: 10.1016/j.annemergmed.2018.06.003.
One-quarter of patients who present at the ED with a , according to the findings of a large study using a national insurance claims database.
M. Kit Delgado, MD, of the Center for Emergency Care Policy and Research at the Perelman School of Medicine, University of Pennsylvania, Philadelphia, and his coauthors analyzed private insurance claims for 30,832 opioid-naive patients who were treated in the emergency department for ankle sprains.
The researchers looked at the initial opioid prescription intensity and duration of subsequent opioid use. The study, published online in Annals of Emergency Medicine, also found a wide variation in prescribing by hospital and geographic region, and an association between higher-potency opioid prescriptions (hydrocodone and oxycodone) and likelihood of extended or prolonged opioid use.
Overall, 25.1% of patients received an opioid prescription, the median tablet quantity was 15 tablets, and median days of opioids supplied was 3 days. Only 5% of patients were prescribed more than 30 tablets, which suggested that the majority of prescriptions written were in agreement with guidelines, the authors wrote.
They noted that nonsteroidal anti-inflammatory drugs are the first-line treatment for ankle sprains, rather than opioids, and are as effective for pain reduction.
Among patients prescribed the equivalent of more than 30 tabs of oxycodone 5 mg, 4.9% of them showed prolonged opioid use – defined as filling four or more subsequent opioid prescriptions in the 30-180 days after the index visit – compared with 1.1% of patients who received fewer than 10 tabs, and 0.5% of those who did not fill an opioid prescription. This represented a nearly fivefold increased probability of transition to prolonged use. For every 26 patients exposed to the higher intensity prescription, 1 would go on to prolonged opioid use.
“We confirmed that the majority of subsequent prescriptions were unlikely to be related to the initial ankle sprain or chronic ankle pain,” the researchers wrote. “This suggests that association between larger prescriptions and increased likelihood of prolonged use could be due to other factors such as patients requesting opioids as default pain control, or the development of dependence or misuse.”
The most commonly prescribed opioid was hydrocodone (64.9%), followed by tramadol (16.2%), oxycodone (14.4%), and codeine (5.5%). The analysis found that patients prescribed higher-potency drugs – namely hydrocodone and oxycodone – were at even greater risk of developing prolonged use.
The researchers noted significant geographic differences in prescribing habits, with 40% of study participants in Arkansas receiving an opioid prescription, compared with 2.8% in North Dakota. Overall, southern states were more likely to overprescribe, and northern states more likely to underprescribe.
Women were at greater risk of transitioning to high-risk prolonged use, as were individuals aged 35-44 years, those with a higher comorbidity burden, or those with a history of drug abuse.
The study was supported by the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, and the Leonard Davis Institute of Health Economics at the University of Pennsylvania. One author declared an honorarium from the United Health Group.
SOURCE: Delgado MK et al. Ann Emerg Med. 2018. Jul 24. doi: 10.1016/j.annemergmed.2018.06.003.
One-quarter of patients who present at the ED with a , according to the findings of a large study using a national insurance claims database.
M. Kit Delgado, MD, of the Center for Emergency Care Policy and Research at the Perelman School of Medicine, University of Pennsylvania, Philadelphia, and his coauthors analyzed private insurance claims for 30,832 opioid-naive patients who were treated in the emergency department for ankle sprains.
The researchers looked at the initial opioid prescription intensity and duration of subsequent opioid use. The study, published online in Annals of Emergency Medicine, also found a wide variation in prescribing by hospital and geographic region, and an association between higher-potency opioid prescriptions (hydrocodone and oxycodone) and likelihood of extended or prolonged opioid use.
Overall, 25.1% of patients received an opioid prescription, the median tablet quantity was 15 tablets, and median days of opioids supplied was 3 days. Only 5% of patients were prescribed more than 30 tablets, which suggested that the majority of prescriptions written were in agreement with guidelines, the authors wrote.
They noted that nonsteroidal anti-inflammatory drugs are the first-line treatment for ankle sprains, rather than opioids, and are as effective for pain reduction.
Among patients prescribed the equivalent of more than 30 tabs of oxycodone 5 mg, 4.9% of them showed prolonged opioid use – defined as filling four or more subsequent opioid prescriptions in the 30-180 days after the index visit – compared with 1.1% of patients who received fewer than 10 tabs, and 0.5% of those who did not fill an opioid prescription. This represented a nearly fivefold increased probability of transition to prolonged use. For every 26 patients exposed to the higher intensity prescription, 1 would go on to prolonged opioid use.
“We confirmed that the majority of subsequent prescriptions were unlikely to be related to the initial ankle sprain or chronic ankle pain,” the researchers wrote. “This suggests that association between larger prescriptions and increased likelihood of prolonged use could be due to other factors such as patients requesting opioids as default pain control, or the development of dependence or misuse.”
The most commonly prescribed opioid was hydrocodone (64.9%), followed by tramadol (16.2%), oxycodone (14.4%), and codeine (5.5%). The analysis found that patients prescribed higher-potency drugs – namely hydrocodone and oxycodone – were at even greater risk of developing prolonged use.
The researchers noted significant geographic differences in prescribing habits, with 40% of study participants in Arkansas receiving an opioid prescription, compared with 2.8% in North Dakota. Overall, southern states were more likely to overprescribe, and northern states more likely to underprescribe.
Women were at greater risk of transitioning to high-risk prolonged use, as were individuals aged 35-44 years, those with a higher comorbidity burden, or those with a history of drug abuse.
The study was supported by the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, and the Leonard Davis Institute of Health Economics at the University of Pennsylvania. One author declared an honorarium from the United Health Group.
SOURCE: Delgado MK et al. Ann Emerg Med. 2018. Jul 24. doi: 10.1016/j.annemergmed.2018.06.003.
FROM ANNALS OF EMERGENCY MEDICINE
Key clinical point: Opioids prescribed for sprained ankles increase the risk of prolonged use.
Major finding: High-intensity opioid prescriptions after a sprained ankle were linked to a fivefold higher risk of prolonged use.
Study details: Analysis of health insurance data from 30,832 patients treated in the emergency department for ankle sprains.
Disclosures: The study was supported by the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, and the Leonard Davis Institute of Health Economics at the University of Pennsylvania. One author declared an honorarium from the United Health Group.
Source: Delgado MK et al. Ann Emerg Med. 2018 Jul 24. doi: 10.1016/j.annemergmed.2018.06.003.
Review protocols, follow reprocessing guidelines to cut device-related HAIs
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
[email protected]
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
[email protected]
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
[email protected]
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
REPORTING FROM ICEID 2018
Key clinical point: Medical devices can be reservoirs and transmission vectors for health care–associated infections.
Major finding: Of 285 consultations, 48 involved medical devices or device reprocessing.
Study details: A review of records from 285 consultations
Disclosures: Dr. Benowitz reported having no disclosures
Source: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
Penalties not necessary to save money in some Medicare ACOs
The Centers for Medicare & Medicaid Services may be able to reduce spending through the Medicare Shared Savings Program (MSSP) without asking for health care professionals and organizations to take on penalties or so-called downside risk, according to a study published in Sept. 5 in the New England Journal of Medicine.
Researchers, using fee-for-service claims from 2009 through 2015 and performing difference-in-difference analyses to compare changes in Medicare spending, found that Accountable Care Organizations (ACOs) formed from physician practices were able to save money while hospital-based ACOs were not.
“Our results also suggest that shared-savings contracts that do not impose a downside risk of financial losses for spending above benchmarks – which may appeal to smaller organizations without sufficient reserves to withstand potential losses – may be effective in lowering Medicare spending,” J. Michael McWilliams, MD, PhD, of Harvard Medical School, Boston, and his colleagues wrote.
Researchers found that by 2015, groups participating in MSSP, as compared with those who did not participate, were “associated with a mean differential reduction of $302 in total Medicare spending per beneficiary in the 2012 entry of cohorts of ACOs,” without accounting for bonus payments.
“Accounting for shared-savings bonus payments, we determined that the differential spending reductions in the entry cohorts of physician-group ACOs from 2012 through 2014 constituted a net savings to Medicare of $256.4 million in 2015,” Dr. McWilliams and his colleagues wrote. “For hospital-integrated ACOs, bonus payments more than offset annual spending reductions.”
Dr. McWilliams and his colleagues noted that their findings were limited by a narrow focus on organizational structure (financial independence from hospitals), so other factors could have held to differences in savings; changes in coding practices for ACOs coming in as of 2013; lack of data on costs to ACOs or efforts to lower spending or improve quality; and the inability to assess the effects of the MSSP on many aspects of quality of care because of the nature of using claims-based measures.
“Our results probably underestimate savings to Medicare because they do not account for spillover effects of ACO efforts on nonattributed patients or effects of lower fee-for-service Medicare spending on payments to Medicare Advantage plans,” the researchers added.
The study was funded by a grant from the National Institute on Aging. Dr. McWilliams and Michael Chernew, PhD, also of Harvard Medical School, both have received consulting fees related to ACO research.
SOURCE: McWilliams JM et al. N Engl J Med. 2018 Sep 5. doi: 10.1056/NEJMsa1803388.
The Centers for Medicare & Medicaid Services may be able to reduce spending through the Medicare Shared Savings Program (MSSP) without asking for health care professionals and organizations to take on penalties or so-called downside risk, according to a study published in Sept. 5 in the New England Journal of Medicine.
Researchers, using fee-for-service claims from 2009 through 2015 and performing difference-in-difference analyses to compare changes in Medicare spending, found that Accountable Care Organizations (ACOs) formed from physician practices were able to save money while hospital-based ACOs were not.
“Our results also suggest that shared-savings contracts that do not impose a downside risk of financial losses for spending above benchmarks – which may appeal to smaller organizations without sufficient reserves to withstand potential losses – may be effective in lowering Medicare spending,” J. Michael McWilliams, MD, PhD, of Harvard Medical School, Boston, and his colleagues wrote.
Researchers found that by 2015, groups participating in MSSP, as compared with those who did not participate, were “associated with a mean differential reduction of $302 in total Medicare spending per beneficiary in the 2012 entry of cohorts of ACOs,” without accounting for bonus payments.
“Accounting for shared-savings bonus payments, we determined that the differential spending reductions in the entry cohorts of physician-group ACOs from 2012 through 2014 constituted a net savings to Medicare of $256.4 million in 2015,” Dr. McWilliams and his colleagues wrote. “For hospital-integrated ACOs, bonus payments more than offset annual spending reductions.”
Dr. McWilliams and his colleagues noted that their findings were limited by a narrow focus on organizational structure (financial independence from hospitals), so other factors could have held to differences in savings; changes in coding practices for ACOs coming in as of 2013; lack of data on costs to ACOs or efforts to lower spending or improve quality; and the inability to assess the effects of the MSSP on many aspects of quality of care because of the nature of using claims-based measures.
“Our results probably underestimate savings to Medicare because they do not account for spillover effects of ACO efforts on nonattributed patients or effects of lower fee-for-service Medicare spending on payments to Medicare Advantage plans,” the researchers added.
The study was funded by a grant from the National Institute on Aging. Dr. McWilliams and Michael Chernew, PhD, also of Harvard Medical School, both have received consulting fees related to ACO research.
SOURCE: McWilliams JM et al. N Engl J Med. 2018 Sep 5. doi: 10.1056/NEJMsa1803388.
The Centers for Medicare & Medicaid Services may be able to reduce spending through the Medicare Shared Savings Program (MSSP) without asking for health care professionals and organizations to take on penalties or so-called downside risk, according to a study published in Sept. 5 in the New England Journal of Medicine.
Researchers, using fee-for-service claims from 2009 through 2015 and performing difference-in-difference analyses to compare changes in Medicare spending, found that Accountable Care Organizations (ACOs) formed from physician practices were able to save money while hospital-based ACOs were not.
“Our results also suggest that shared-savings contracts that do not impose a downside risk of financial losses for spending above benchmarks – which may appeal to smaller organizations without sufficient reserves to withstand potential losses – may be effective in lowering Medicare spending,” J. Michael McWilliams, MD, PhD, of Harvard Medical School, Boston, and his colleagues wrote.
Researchers found that by 2015, groups participating in MSSP, as compared with those who did not participate, were “associated with a mean differential reduction of $302 in total Medicare spending per beneficiary in the 2012 entry of cohorts of ACOs,” without accounting for bonus payments.
“Accounting for shared-savings bonus payments, we determined that the differential spending reductions in the entry cohorts of physician-group ACOs from 2012 through 2014 constituted a net savings to Medicare of $256.4 million in 2015,” Dr. McWilliams and his colleagues wrote. “For hospital-integrated ACOs, bonus payments more than offset annual spending reductions.”
Dr. McWilliams and his colleagues noted that their findings were limited by a narrow focus on organizational structure (financial independence from hospitals), so other factors could have held to differences in savings; changes in coding practices for ACOs coming in as of 2013; lack of data on costs to ACOs or efforts to lower spending or improve quality; and the inability to assess the effects of the MSSP on many aspects of quality of care because of the nature of using claims-based measures.
“Our results probably underestimate savings to Medicare because they do not account for spillover effects of ACO efforts on nonattributed patients or effects of lower fee-for-service Medicare spending on payments to Medicare Advantage plans,” the researchers added.
The study was funded by a grant from the National Institute on Aging. Dr. McWilliams and Michael Chernew, PhD, also of Harvard Medical School, both have received consulting fees related to ACO research.
SOURCE: McWilliams JM et al. N Engl J Med. 2018 Sep 5. doi: 10.1056/NEJMsa1803388.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Physician group ACOs in the Medicare Shared Savings Program (MSSP) generated more savings than did hospital-led ACO groups.
Major finding: Physician group ACOs joining the MSSP in 2012-2014 generated $256.4 million in Medicare savings in 2015.
Study details: Analysis of fee-for-service Medicare claims during 2009-2015.
Disclosures: The study was funded by the National Institute on Aging. Dr. McWilliams and Dr. Chernew disclosed consulting fees related to ACO research.
Source: McWilliams JM et al. N Engl J Med. doi: 10.1056/NEJMsa1803388.
POEM effective for more than achalasia
.
The procedure was clinically successful and relieved chest pain in most patients, reported Mouen A. Khashab, MD, director of therapeutic endoscopy at Johns Hopkins Hospital in Baltimore.
POEM was introduced in 2008 as a less invasive alternative to laparoscopic Heller myotomy. During the procedure, submucosal tunneling is performed through the lower esophageal sphincter to the gastric cardia, thereby weakening the lower esophageal sphincter to allow passage of food.
POEM is clinically successful in 80%-90% of patients with achalasia. Although the procedure is regarded as safe and effective for achalasia, it has not been thoroughly researched for treatment of other esophageal motility disorders, including junction outflow obstruction (EGJOO), jackhammer esophagus (JE), or esophagogastric distal esophageal spasm (DES). EGJOO is similar to achalasia, but with peristalsis and a mean integrated relaxation pressure (IRP) greater than 15 mm Hg. Both JE and DES are spastic esophageal disorders. Patients with JE exhibit extreme esophageal hypercontractility, whereas patients with DES have a normal mean IRP and at least 20% premature contractions.
“The role POEM plays in management of these disorders is not clear, mainly due to scarcity of studies on this topic,” the authors wrote in Endoscopy International Open. “A previous multicenter study investigated the role of POEM in 73 patients with spastic esophageal disorders. However, the vast majority of patients (n = 54) in that study had type III (spastic) achalasia.” Since therapies such as botulinum toxin injections and calcium channel blockers are ineffective for many patients with nonachalasia esophageal motility disorders, “POEM is potentially an ideal treatment.”
The international, multicenter study involved 11 treatment centers and 50 patients. Patients with JE (n = 18), EGJOO (n = 15), and DES (n = 17) were included, each diagnosed according to the Chicago classification of esophageal motility disorders. Patients with type III achalasia were excluded.
Outcomes included technical success (completion of myotomy) and clinical success (Eckardt score at least 3 and symptom improvement). Prior to the procedure, the mean Eckardt score was 6.9 and chest pain was reported by almost three-quarters of the patients (72%).
Technical success was achieved in all patients. Myotomy thickness varied between cases; approximately half had a selective inner circular myotomy (48%), slightly less had a full-thickness myotomy (44%), and several were undefined (8%). Mean esophageal myotomy length was 12.5 cm and mean gastric myotomy length was 2.5 cm. Mean procedure time was approximately 90 minutes. Median duration of hospital stay was 2 days.
Nine adverse events (AEs) occurred in 8 patients, including submucosal hematoma, aspiration pneumonia, inadvertent mucosotomy, postprocedure pain, esophageal leak, bleed, and symptomatic capno-thorax/peritoneum.
“Although AEs occurred in 18% of patients,” the authors noted, “55.6% were rated as mild and 44.4% as moderate with no severe events. Most AEs can be managed intraprocedurally.”
Median follow-up time was approximately 8 months, during which 42 patients (87.5%) achieved clinical success, with many dramatically improved; over half of the patients (52%) had Eckardt scores of 0 or 1. From the group of patients who had chest pain prior to the procedure, 87% had resolution of chest pain. Although reflux developed in almost a quarter of the patients (22.2%), this was successfully managed with proton pump inhibitors in all instances. Most patients (82.9%) who underwent postoperative manometry had resolution of preoperative abnormalities.
Subgroup analysis was also performed. Clinical success was achieved in 94.1% of patients with DES, 93.3% of patients with EGJOO, and 75.0% with JE. Collectively, the spastic disorders (DES/JE) had a lower numerical response than EGJOO. However, the authors noted that “the difference was not statistically significant (P = .41), likely a type II error due to the relatively small number of included patients.” In all subgroups, postprocedural mean Eckardt scores decreased to less than 2. Patients with EGJOO were most likely to achieve Eckardt scores of 0 or 1. AEs were similar between subgroups.
“Remarkably, chest pain improved in more than 85% of patients,” the authors wrote. “Chest pain is frequently the major presenting symptom in these disorders and is difficult to treat.”
“It is important to mention that a long esophageal myotomy is essential to ensure that proximal esophageal spasms are effectively covered and treated,” the authors wrote. “Mean length of esophageal myotomy in patients with DES and JE in the current study was about 14 cm, which is more than twice the length of a typical endoscopic or surgical myotomy performed in achalasia patients.”
Even with the need for an extended myotomy, “results from the current study along with published data suggest POEM as an effective technique” for nonachalasia esophageal motility disorders, the authors concluded.
Since retrospective studies are inherently limited by design, the authors encouraged randomized trials to clarify the primary role of POEM in the management of nonachalasia esophageal motility disorders.
The authors reported compensation from Olympus, Boston Scientific, and Cook Medical.
SOURCE: Khashab MA et al. Endosc Int Open. 2018 Aug 10. doi: 10.1055/a-0625-6288.
.
The procedure was clinically successful and relieved chest pain in most patients, reported Mouen A. Khashab, MD, director of therapeutic endoscopy at Johns Hopkins Hospital in Baltimore.
POEM was introduced in 2008 as a less invasive alternative to laparoscopic Heller myotomy. During the procedure, submucosal tunneling is performed through the lower esophageal sphincter to the gastric cardia, thereby weakening the lower esophageal sphincter to allow passage of food.
POEM is clinically successful in 80%-90% of patients with achalasia. Although the procedure is regarded as safe and effective for achalasia, it has not been thoroughly researched for treatment of other esophageal motility disorders, including junction outflow obstruction (EGJOO), jackhammer esophagus (JE), or esophagogastric distal esophageal spasm (DES). EGJOO is similar to achalasia, but with peristalsis and a mean integrated relaxation pressure (IRP) greater than 15 mm Hg. Both JE and DES are spastic esophageal disorders. Patients with JE exhibit extreme esophageal hypercontractility, whereas patients with DES have a normal mean IRP and at least 20% premature contractions.
“The role POEM plays in management of these disorders is not clear, mainly due to scarcity of studies on this topic,” the authors wrote in Endoscopy International Open. “A previous multicenter study investigated the role of POEM in 73 patients with spastic esophageal disorders. However, the vast majority of patients (n = 54) in that study had type III (spastic) achalasia.” Since therapies such as botulinum toxin injections and calcium channel blockers are ineffective for many patients with nonachalasia esophageal motility disorders, “POEM is potentially an ideal treatment.”
The international, multicenter study involved 11 treatment centers and 50 patients. Patients with JE (n = 18), EGJOO (n = 15), and DES (n = 17) were included, each diagnosed according to the Chicago classification of esophageal motility disorders. Patients with type III achalasia were excluded.
Outcomes included technical success (completion of myotomy) and clinical success (Eckardt score at least 3 and symptom improvement). Prior to the procedure, the mean Eckardt score was 6.9 and chest pain was reported by almost three-quarters of the patients (72%).
Technical success was achieved in all patients. Myotomy thickness varied between cases; approximately half had a selective inner circular myotomy (48%), slightly less had a full-thickness myotomy (44%), and several were undefined (8%). Mean esophageal myotomy length was 12.5 cm and mean gastric myotomy length was 2.5 cm. Mean procedure time was approximately 90 minutes. Median duration of hospital stay was 2 days.
Nine adverse events (AEs) occurred in 8 patients, including submucosal hematoma, aspiration pneumonia, inadvertent mucosotomy, postprocedure pain, esophageal leak, bleed, and symptomatic capno-thorax/peritoneum.
“Although AEs occurred in 18% of patients,” the authors noted, “55.6% were rated as mild and 44.4% as moderate with no severe events. Most AEs can be managed intraprocedurally.”
Median follow-up time was approximately 8 months, during which 42 patients (87.5%) achieved clinical success, with many dramatically improved; over half of the patients (52%) had Eckardt scores of 0 or 1. From the group of patients who had chest pain prior to the procedure, 87% had resolution of chest pain. Although reflux developed in almost a quarter of the patients (22.2%), this was successfully managed with proton pump inhibitors in all instances. Most patients (82.9%) who underwent postoperative manometry had resolution of preoperative abnormalities.
Subgroup analysis was also performed. Clinical success was achieved in 94.1% of patients with DES, 93.3% of patients with EGJOO, and 75.0% with JE. Collectively, the spastic disorders (DES/JE) had a lower numerical response than EGJOO. However, the authors noted that “the difference was not statistically significant (P = .41), likely a type II error due to the relatively small number of included patients.” In all subgroups, postprocedural mean Eckardt scores decreased to less than 2. Patients with EGJOO were most likely to achieve Eckardt scores of 0 or 1. AEs were similar between subgroups.
“Remarkably, chest pain improved in more than 85% of patients,” the authors wrote. “Chest pain is frequently the major presenting symptom in these disorders and is difficult to treat.”
“It is important to mention that a long esophageal myotomy is essential to ensure that proximal esophageal spasms are effectively covered and treated,” the authors wrote. “Mean length of esophageal myotomy in patients with DES and JE in the current study was about 14 cm, which is more than twice the length of a typical endoscopic or surgical myotomy performed in achalasia patients.”
Even with the need for an extended myotomy, “results from the current study along with published data suggest POEM as an effective technique” for nonachalasia esophageal motility disorders, the authors concluded.
Since retrospective studies are inherently limited by design, the authors encouraged randomized trials to clarify the primary role of POEM in the management of nonachalasia esophageal motility disorders.
The authors reported compensation from Olympus, Boston Scientific, and Cook Medical.
SOURCE: Khashab MA et al. Endosc Int Open. 2018 Aug 10. doi: 10.1055/a-0625-6288.
.
The procedure was clinically successful and relieved chest pain in most patients, reported Mouen A. Khashab, MD, director of therapeutic endoscopy at Johns Hopkins Hospital in Baltimore.
POEM was introduced in 2008 as a less invasive alternative to laparoscopic Heller myotomy. During the procedure, submucosal tunneling is performed through the lower esophageal sphincter to the gastric cardia, thereby weakening the lower esophageal sphincter to allow passage of food.
POEM is clinically successful in 80%-90% of patients with achalasia. Although the procedure is regarded as safe and effective for achalasia, it has not been thoroughly researched for treatment of other esophageal motility disorders, including junction outflow obstruction (EGJOO), jackhammer esophagus (JE), or esophagogastric distal esophageal spasm (DES). EGJOO is similar to achalasia, but with peristalsis and a mean integrated relaxation pressure (IRP) greater than 15 mm Hg. Both JE and DES are spastic esophageal disorders. Patients with JE exhibit extreme esophageal hypercontractility, whereas patients with DES have a normal mean IRP and at least 20% premature contractions.
“The role POEM plays in management of these disorders is not clear, mainly due to scarcity of studies on this topic,” the authors wrote in Endoscopy International Open. “A previous multicenter study investigated the role of POEM in 73 patients with spastic esophageal disorders. However, the vast majority of patients (n = 54) in that study had type III (spastic) achalasia.” Since therapies such as botulinum toxin injections and calcium channel blockers are ineffective for many patients with nonachalasia esophageal motility disorders, “POEM is potentially an ideal treatment.”
The international, multicenter study involved 11 treatment centers and 50 patients. Patients with JE (n = 18), EGJOO (n = 15), and DES (n = 17) were included, each diagnosed according to the Chicago classification of esophageal motility disorders. Patients with type III achalasia were excluded.
Outcomes included technical success (completion of myotomy) and clinical success (Eckardt score at least 3 and symptom improvement). Prior to the procedure, the mean Eckardt score was 6.9 and chest pain was reported by almost three-quarters of the patients (72%).
Technical success was achieved in all patients. Myotomy thickness varied between cases; approximately half had a selective inner circular myotomy (48%), slightly less had a full-thickness myotomy (44%), and several were undefined (8%). Mean esophageal myotomy length was 12.5 cm and mean gastric myotomy length was 2.5 cm. Mean procedure time was approximately 90 minutes. Median duration of hospital stay was 2 days.
Nine adverse events (AEs) occurred in 8 patients, including submucosal hematoma, aspiration pneumonia, inadvertent mucosotomy, postprocedure pain, esophageal leak, bleed, and symptomatic capno-thorax/peritoneum.
“Although AEs occurred in 18% of patients,” the authors noted, “55.6% were rated as mild and 44.4% as moderate with no severe events. Most AEs can be managed intraprocedurally.”
Median follow-up time was approximately 8 months, during which 42 patients (87.5%) achieved clinical success, with many dramatically improved; over half of the patients (52%) had Eckardt scores of 0 or 1. From the group of patients who had chest pain prior to the procedure, 87% had resolution of chest pain. Although reflux developed in almost a quarter of the patients (22.2%), this was successfully managed with proton pump inhibitors in all instances. Most patients (82.9%) who underwent postoperative manometry had resolution of preoperative abnormalities.
Subgroup analysis was also performed. Clinical success was achieved in 94.1% of patients with DES, 93.3% of patients with EGJOO, and 75.0% with JE. Collectively, the spastic disorders (DES/JE) had a lower numerical response than EGJOO. However, the authors noted that “the difference was not statistically significant (P = .41), likely a type II error due to the relatively small number of included patients.” In all subgroups, postprocedural mean Eckardt scores decreased to less than 2. Patients with EGJOO were most likely to achieve Eckardt scores of 0 or 1. AEs were similar between subgroups.
“Remarkably, chest pain improved in more than 85% of patients,” the authors wrote. “Chest pain is frequently the major presenting symptom in these disorders and is difficult to treat.”
“It is important to mention that a long esophageal myotomy is essential to ensure that proximal esophageal spasms are effectively covered and treated,” the authors wrote. “Mean length of esophageal myotomy in patients with DES and JE in the current study was about 14 cm, which is more than twice the length of a typical endoscopic or surgical myotomy performed in achalasia patients.”
Even with the need for an extended myotomy, “results from the current study along with published data suggest POEM as an effective technique” for nonachalasia esophageal motility disorders, the authors concluded.
Since retrospective studies are inherently limited by design, the authors encouraged randomized trials to clarify the primary role of POEM in the management of nonachalasia esophageal motility disorders.
The authors reported compensation from Olympus, Boston Scientific, and Cook Medical.
SOURCE: Khashab MA et al. Endosc Int Open. 2018 Aug 10. doi: 10.1055/a-0625-6288.
FROM ENDOSCOPY INTERNATIONAL OPEN
Key clinical point: Peroral endoscopic myotomy (POEM) is safe and effective for jackhammer esophagus (JE), esophagogastric junction outflow obstruction (EGJOO), and distal esophageal spasm (DES).
Major finding: POEM was clinically successful in approximately 90% of patients with nonachalasia esophageal motility disorders.
Study details: A retrospective, multicenter study involving 50 patients with nonachalasia esophageal motility disorders.
Disclosures: Authors reported compensation from Olympus, Boston Scientific, and Cook Medical.
Source: Khashab MA et al. Endosc Int Open. 2018 Aug 10. doi: 10.1055/a-0625-6288
Diclofenac’s cardiovascular risk confirmed in novel Nordic study
Those beginning diclofenac had a 50% increased 30-day risk for a composite outcome of major adverse cardiovascular events (MACE) compared with individuals who didn’t initiate an NSAID or acetaminophen (95% confidence interval for incidence rate ratio, 1.4-1.7).
The risk was still significantly elevated when the study’s first author, Morten Schmidt, MD, and his colleagues compared diclofenac initiation with beginning other NSAIDs or acetaminophen. Compared with those starting ibuprofen or acetaminophen, the MACE risk was elevated 20% in diclofenac initiators (95% CI, 1.1-1.3 for both). Initiating diclofenac was associated with 30% greater risk for MACE compared with initiating naproxen (95% CI, 1.1-1.5).
“Diclofenac is the most frequently used NSAID in low-, middle-, and high-income countries and is available over the counter in most countries; therefore, its cardiovascular risk profile is of major clinical and public health importance,” wrote Dr. Schmidt and his coauthors.
In all, the study included 1,370,832 individuals who initiated diclofenac, 3,878,454 ibuprofen initiators, 291,490 naproxen initiators, and 764,781 acetaminophen initiators. Those starting diclofenac were compared with those starting other medications, and with 1,303,209 individuals who sought health care but did not start one of the medications.
The researchers used the longstanding and complete Danish health registry system to their advantage in designing a cohort trial that was modeled to resemble a clinical trial. For each month, beginning in 1996 and continuing through 2016, Dr. Schmidt and his collaborators assembled propensity-matched cohorts of individuals to compare each study group. The study design achieved many of the aims of a clinical trial while working within the ethical constraints of studying medications now known to elevate cardiovascular risk.
For each 30-day period, the investigators were then able to track and compare cardiovascular outcomes for each group. Each month, data for a new cohort were collected, beginning a new “clinical trial.” Individuals could be included in more than one month’s worth of “trial” data as long as they continued to meet inclusion criteria.
The completeness of Danish health data meant that the researchers were confident in data about comorbidities, other prescription medications, and outcomes.
Dr. Schmidt and his colleagues performed subgroup and sensitivity analyses to look at the extent to which preexisting risks for cardiovascular disease mediated MACE risk on diclofenac initiation. They found that diclofenac initiators in the highest risk group had up to 40 excess cardiovascular events per year – about half of them fatal – that were attributable to starting the medication. Although that group had the highest absolute risk, however, “the relative risks were highest in those with the lowest baseline risk,” wrote the investigators.
In addition to looking at rates of MACE, secondary outcomes for the study included evaluating the association between medication use or non-use and each individual component of the composite primary outcome. These included first-time occurrences of the nonfatal endpoints of atrial fibrillation or flutter, ischemic (but not hemorrhagic) stroke, heart failure, and myocardial infarction. Cardiac death was death from any cardiac cause.
“Supporting use of a combined endpoint, event rates consistently increased for all individual outcomes” for diclofenac initiators compared with those who did not start an NSAID, wrote Dr. Schmidt and his colleagues.
Individuals were excluded if they had known cardiovascular, kidney, liver, or ulcer disease, and if they had malignancy or serious mental health diagnoses such as dementia or schizophrenia. Participants, aged a mean 48-56 years, had to be at least 18 years of age and could not have filled a prescription for an NSAID within the previous 12 months. Men made up 36.6%-46.3% of the cohorts.
Dr. Schmidt, of Aarhus (Denmark) University, and his collaborators said that in comparison with other NSAIDs, the short half-life of diclofenac means that a supratherapeutic plasma concentration of diclofenac soon after initiation achieves not just cyclooxygenase-2 (COX-2), but also COX-1 inhibition. However, after those high levels fall, patients taking diclofenac spend a substantial period of time with unopposed COX-2 inhibition, a state that is known to be prothrombotic, and also associated with blood pressure elevation, atherogenesis, and worsening of heart failure.
Diclofenac and ibuprofen had similar gastrointestinal bleeding risks, and both medications were associated with a higher risk of bleeding than were ibuprofen, acetaminophen, or no medication.
“Comparing diclofenac initiation with no NSAID initiation, the consistency between our results and those of previous meta-analyses of both trial and observational data provides strong evidence to guide clinical decision making,” said Dr. Schmidt and his coauthors.
“Considering its cardiovascular and gastrointestinal risks, however, there is little justification to initiate diclofenac treatment before other traditional NSAIDs,” noted the investigators. “It is time to acknowledge the potential health risk of diclofenac and to reduce its use.”
The study was funded by the Department of Clinical Epidemiology Research Foundation, University of Aarhus, and by the Program for Clinical Research Infrastructure, funded by the Lundbeck Foundation, Novo Nordisk Foundation, and the Danish Research Council. The authors reported that they had no relevant conflicts of interest.
SOURCE: Schmidt M et al. BMJ 2018;362:k3426
Those beginning diclofenac had a 50% increased 30-day risk for a composite outcome of major adverse cardiovascular events (MACE) compared with individuals who didn’t initiate an NSAID or acetaminophen (95% confidence interval for incidence rate ratio, 1.4-1.7).
The risk was still significantly elevated when the study’s first author, Morten Schmidt, MD, and his colleagues compared diclofenac initiation with beginning other NSAIDs or acetaminophen. Compared with those starting ibuprofen or acetaminophen, the MACE risk was elevated 20% in diclofenac initiators (95% CI, 1.1-1.3 for both). Initiating diclofenac was associated with 30% greater risk for MACE compared with initiating naproxen (95% CI, 1.1-1.5).
“Diclofenac is the most frequently used NSAID in low-, middle-, and high-income countries and is available over the counter in most countries; therefore, its cardiovascular risk profile is of major clinical and public health importance,” wrote Dr. Schmidt and his coauthors.
In all, the study included 1,370,832 individuals who initiated diclofenac, 3,878,454 ibuprofen initiators, 291,490 naproxen initiators, and 764,781 acetaminophen initiators. Those starting diclofenac were compared with those starting other medications, and with 1,303,209 individuals who sought health care but did not start one of the medications.
The researchers used the longstanding and complete Danish health registry system to their advantage in designing a cohort trial that was modeled to resemble a clinical trial. For each month, beginning in 1996 and continuing through 2016, Dr. Schmidt and his collaborators assembled propensity-matched cohorts of individuals to compare each study group. The study design achieved many of the aims of a clinical trial while working within the ethical constraints of studying medications now known to elevate cardiovascular risk.
For each 30-day period, the investigators were then able to track and compare cardiovascular outcomes for each group. Each month, data for a new cohort were collected, beginning a new “clinical trial.” Individuals could be included in more than one month’s worth of “trial” data as long as they continued to meet inclusion criteria.
The completeness of Danish health data meant that the researchers were confident in data about comorbidities, other prescription medications, and outcomes.
Dr. Schmidt and his colleagues performed subgroup and sensitivity analyses to look at the extent to which preexisting risks for cardiovascular disease mediated MACE risk on diclofenac initiation. They found that diclofenac initiators in the highest risk group had up to 40 excess cardiovascular events per year – about half of them fatal – that were attributable to starting the medication. Although that group had the highest absolute risk, however, “the relative risks were highest in those with the lowest baseline risk,” wrote the investigators.
In addition to looking at rates of MACE, secondary outcomes for the study included evaluating the association between medication use or non-use and each individual component of the composite primary outcome. These included first-time occurrences of the nonfatal endpoints of atrial fibrillation or flutter, ischemic (but not hemorrhagic) stroke, heart failure, and myocardial infarction. Cardiac death was death from any cardiac cause.
“Supporting use of a combined endpoint, event rates consistently increased for all individual outcomes” for diclofenac initiators compared with those who did not start an NSAID, wrote Dr. Schmidt and his colleagues.
Individuals were excluded if they had known cardiovascular, kidney, liver, or ulcer disease, and if they had malignancy or serious mental health diagnoses such as dementia or schizophrenia. Participants, aged a mean 48-56 years, had to be at least 18 years of age and could not have filled a prescription for an NSAID within the previous 12 months. Men made up 36.6%-46.3% of the cohorts.
Dr. Schmidt, of Aarhus (Denmark) University, and his collaborators said that in comparison with other NSAIDs, the short half-life of diclofenac means that a supratherapeutic plasma concentration of diclofenac soon after initiation achieves not just cyclooxygenase-2 (COX-2), but also COX-1 inhibition. However, after those high levels fall, patients taking diclofenac spend a substantial period of time with unopposed COX-2 inhibition, a state that is known to be prothrombotic, and also associated with blood pressure elevation, atherogenesis, and worsening of heart failure.
Diclofenac and ibuprofen had similar gastrointestinal bleeding risks, and both medications were associated with a higher risk of bleeding than were ibuprofen, acetaminophen, or no medication.
“Comparing diclofenac initiation with no NSAID initiation, the consistency between our results and those of previous meta-analyses of both trial and observational data provides strong evidence to guide clinical decision making,” said Dr. Schmidt and his coauthors.
“Considering its cardiovascular and gastrointestinal risks, however, there is little justification to initiate diclofenac treatment before other traditional NSAIDs,” noted the investigators. “It is time to acknowledge the potential health risk of diclofenac and to reduce its use.”
The study was funded by the Department of Clinical Epidemiology Research Foundation, University of Aarhus, and by the Program for Clinical Research Infrastructure, funded by the Lundbeck Foundation, Novo Nordisk Foundation, and the Danish Research Council. The authors reported that they had no relevant conflicts of interest.
SOURCE: Schmidt M et al. BMJ 2018;362:k3426
Those beginning diclofenac had a 50% increased 30-day risk for a composite outcome of major adverse cardiovascular events (MACE) compared with individuals who didn’t initiate an NSAID or acetaminophen (95% confidence interval for incidence rate ratio, 1.4-1.7).
The risk was still significantly elevated when the study’s first author, Morten Schmidt, MD, and his colleagues compared diclofenac initiation with beginning other NSAIDs or acetaminophen. Compared with those starting ibuprofen or acetaminophen, the MACE risk was elevated 20% in diclofenac initiators (95% CI, 1.1-1.3 for both). Initiating diclofenac was associated with 30% greater risk for MACE compared with initiating naproxen (95% CI, 1.1-1.5).
“Diclofenac is the most frequently used NSAID in low-, middle-, and high-income countries and is available over the counter in most countries; therefore, its cardiovascular risk profile is of major clinical and public health importance,” wrote Dr. Schmidt and his coauthors.
In all, the study included 1,370,832 individuals who initiated diclofenac, 3,878,454 ibuprofen initiators, 291,490 naproxen initiators, and 764,781 acetaminophen initiators. Those starting diclofenac were compared with those starting other medications, and with 1,303,209 individuals who sought health care but did not start one of the medications.
The researchers used the longstanding and complete Danish health registry system to their advantage in designing a cohort trial that was modeled to resemble a clinical trial. For each month, beginning in 1996 and continuing through 2016, Dr. Schmidt and his collaborators assembled propensity-matched cohorts of individuals to compare each study group. The study design achieved many of the aims of a clinical trial while working within the ethical constraints of studying medications now known to elevate cardiovascular risk.
For each 30-day period, the investigators were then able to track and compare cardiovascular outcomes for each group. Each month, data for a new cohort were collected, beginning a new “clinical trial.” Individuals could be included in more than one month’s worth of “trial” data as long as they continued to meet inclusion criteria.
The completeness of Danish health data meant that the researchers were confident in data about comorbidities, other prescription medications, and outcomes.
Dr. Schmidt and his colleagues performed subgroup and sensitivity analyses to look at the extent to which preexisting risks for cardiovascular disease mediated MACE risk on diclofenac initiation. They found that diclofenac initiators in the highest risk group had up to 40 excess cardiovascular events per year – about half of them fatal – that were attributable to starting the medication. Although that group had the highest absolute risk, however, “the relative risks were highest in those with the lowest baseline risk,” wrote the investigators.
In addition to looking at rates of MACE, secondary outcomes for the study included evaluating the association between medication use or non-use and each individual component of the composite primary outcome. These included first-time occurrences of the nonfatal endpoints of atrial fibrillation or flutter, ischemic (but not hemorrhagic) stroke, heart failure, and myocardial infarction. Cardiac death was death from any cardiac cause.
“Supporting use of a combined endpoint, event rates consistently increased for all individual outcomes” for diclofenac initiators compared with those who did not start an NSAID, wrote Dr. Schmidt and his colleagues.
Individuals were excluded if they had known cardiovascular, kidney, liver, or ulcer disease, and if they had malignancy or serious mental health diagnoses such as dementia or schizophrenia. Participants, aged a mean 48-56 years, had to be at least 18 years of age and could not have filled a prescription for an NSAID within the previous 12 months. Men made up 36.6%-46.3% of the cohorts.
Dr. Schmidt, of Aarhus (Denmark) University, and his collaborators said that in comparison with other NSAIDs, the short half-life of diclofenac means that a supratherapeutic plasma concentration of diclofenac soon after initiation achieves not just cyclooxygenase-2 (COX-2), but also COX-1 inhibition. However, after those high levels fall, patients taking diclofenac spend a substantial period of time with unopposed COX-2 inhibition, a state that is known to be prothrombotic, and also associated with blood pressure elevation, atherogenesis, and worsening of heart failure.
Diclofenac and ibuprofen had similar gastrointestinal bleeding risks, and both medications were associated with a higher risk of bleeding than were ibuprofen, acetaminophen, or no medication.
“Comparing diclofenac initiation with no NSAID initiation, the consistency between our results and those of previous meta-analyses of both trial and observational data provides strong evidence to guide clinical decision making,” said Dr. Schmidt and his coauthors.
“Considering its cardiovascular and gastrointestinal risks, however, there is little justification to initiate diclofenac treatment before other traditional NSAIDs,” noted the investigators. “It is time to acknowledge the potential health risk of diclofenac and to reduce its use.”
The study was funded by the Department of Clinical Epidemiology Research Foundation, University of Aarhus, and by the Program for Clinical Research Infrastructure, funded by the Lundbeck Foundation, Novo Nordisk Foundation, and the Danish Research Council. The authors reported that they had no relevant conflicts of interest.
SOURCE: Schmidt M et al. BMJ 2018;362:k3426
FROM BMJ
Key clinical point: Those starting diclofenac had increased risk for cardiovascular events or cardiac death.
Major finding: Risk for major adverse cardiovascular events was increased by 50% compared with noninitiators.
Study details: Retrospective propensity-matched cohort study using national databases and registries.
Disclosures: The study was supported by the Department of Clinical Epidemiology Research Foundation of the University of Aarhus, Denmark, and by the Program for Clinical Research Infrastructure, funded by the Lundbeck Foundation, Novo Nordisk Foundation, and the Danish Research Council. The authors reported that they had no relevant conflicts of interest.
Source: Schmidt M et al. BMJ 2018;362:k3426.
United Kingdom experience provides important lessons for controlling C. auris outbreaks
ATLANTA – The persistence and transmission of Candida auris in health care settings appears to be dependent on environmental survival, underscoring the need for careful investigation of the environment – and, in particular, multiuse patient equipment.
That’s the key lesson from one of the largest outbreaks of the emerging, multidrug-resistant pathogen to date, David Eyre, DPhil, said at the International Conference on Emerging Infectious Diseases.
“Our experience at Oxford began with a Public Health England alert, which closely followed a similar alert from the [Centers for Disease Control and Prevention] in the summer of 2016,” Dr. Eyre of the University of Oxford (England) said during an update on the epidemiology of the outbreak and the successful, multipronged effort to control it.
The outbreak, which occurred in the neurosciences intensive care unit of Oxford University Hospitals beginning in early 2015, was detected in 2016 when a cluster of C. auris infections was identified and traced to the unit. An intensive patient and environmental screening program was established, isolation protocols were used for patients who tested positive, enhanced cleaning processes were initiated, and equipment was removed and replaced with single-use equipment when possible.
“We also worked quite closely with our staff to raise awareness,” he said, adding that colonized patients who were undergoing a surgical procedure received single-dose antifungal prophylaxis prior to the procedure.
A case-control study was conducted, and after the researchers used multivariate logistic regression to control for length of stay, patient physiology, and biomarkers, exposure to multiuse skin surface axillary temperature monitoring was shown to be one of the strongest independent predictors of C. auris colonization and infection (odds ratio 6.80), he said, adding that antifungal exposure was also a significant risk factor, but only 5% of patients had received antifungals.
The axillary probes were then removed from the environment. As of April 2017 (when the probes were removed), 66 patients had been colonized or infected, and an additional 10 cases occurred after the probes were removed, with the last case occurring in November 2017.
Seven of the 76 cases involved invasive infection, and 1 patient died several months after hospital discharge, Dr. Eyre said.
The patient screening processes allowed for estimation of colonization time (approximately 2 months), and also allowed for whole-genome sequencing of 79 samples from 43 patients, 6 environmental isolates, and 2 isolates from regional surveillance, Dr. Eyre said.
All outbreak sequences formed a single genetic cluster within the C. auris South African clade, and were found to have been introduced to Oxford around 2012 or 2013, with about six mutations per year, or “roughly 12 million base pairs in total,” he said, adding that both patients and temperature probes were colonized with multiple strains, and there was “close mixing” between the two.
This pattern changed following removal of the temperature probes, but it took some time.
“However, from November [2017] onward – so that’s now 291 days ... we’ve not had another new patient isolate, and that’s not only no invasive infection, but also no colonization despite continuing the screening program,” he said.
According to the CDC, C. auris is “an emerging fungus that presents a serious global health threat” because of its often multidrug-resistant nature, difficulty identifying the pathogen using standard laboratory methods, and the risk for misidentification in labs without specific technology, which could lead to inappropriate management.
“It has caused outbreaks in health care settings. For this reason, it is important to quickly identify C. auris in a hospitalized patient so that health care facilities can take special precautions to stop its spread,” a CDC page on C. auris states. “CDC encourages all U.S. laboratory staff who identify C. auris to notify their state or local public health authorities and CDC at [email protected].”
Dr. Eyre reported having no disclosures.
SOURCE: Eyre D et al. ICEID 2018 Oral Abstract Presentation.
ATLANTA – The persistence and transmission of Candida auris in health care settings appears to be dependent on environmental survival, underscoring the need for careful investigation of the environment – and, in particular, multiuse patient equipment.
That’s the key lesson from one of the largest outbreaks of the emerging, multidrug-resistant pathogen to date, David Eyre, DPhil, said at the International Conference on Emerging Infectious Diseases.
“Our experience at Oxford began with a Public Health England alert, which closely followed a similar alert from the [Centers for Disease Control and Prevention] in the summer of 2016,” Dr. Eyre of the University of Oxford (England) said during an update on the epidemiology of the outbreak and the successful, multipronged effort to control it.
The outbreak, which occurred in the neurosciences intensive care unit of Oxford University Hospitals beginning in early 2015, was detected in 2016 when a cluster of C. auris infections was identified and traced to the unit. An intensive patient and environmental screening program was established, isolation protocols were used for patients who tested positive, enhanced cleaning processes were initiated, and equipment was removed and replaced with single-use equipment when possible.
“We also worked quite closely with our staff to raise awareness,” he said, adding that colonized patients who were undergoing a surgical procedure received single-dose antifungal prophylaxis prior to the procedure.
A case-control study was conducted, and after the researchers used multivariate logistic regression to control for length of stay, patient physiology, and biomarkers, exposure to multiuse skin surface axillary temperature monitoring was shown to be one of the strongest independent predictors of C. auris colonization and infection (odds ratio 6.80), he said, adding that antifungal exposure was also a significant risk factor, but only 5% of patients had received antifungals.
The axillary probes were then removed from the environment. As of April 2017 (when the probes were removed), 66 patients had been colonized or infected, and an additional 10 cases occurred after the probes were removed, with the last case occurring in November 2017.
Seven of the 76 cases involved invasive infection, and 1 patient died several months after hospital discharge, Dr. Eyre said.
The patient screening processes allowed for estimation of colonization time (approximately 2 months), and also allowed for whole-genome sequencing of 79 samples from 43 patients, 6 environmental isolates, and 2 isolates from regional surveillance, Dr. Eyre said.
All outbreak sequences formed a single genetic cluster within the C. auris South African clade, and were found to have been introduced to Oxford around 2012 or 2013, with about six mutations per year, or “roughly 12 million base pairs in total,” he said, adding that both patients and temperature probes were colonized with multiple strains, and there was “close mixing” between the two.
This pattern changed following removal of the temperature probes, but it took some time.
“However, from November [2017] onward – so that’s now 291 days ... we’ve not had another new patient isolate, and that’s not only no invasive infection, but also no colonization despite continuing the screening program,” he said.
According to the CDC, C. auris is “an emerging fungus that presents a serious global health threat” because of its often multidrug-resistant nature, difficulty identifying the pathogen using standard laboratory methods, and the risk for misidentification in labs without specific technology, which could lead to inappropriate management.
“It has caused outbreaks in health care settings. For this reason, it is important to quickly identify C. auris in a hospitalized patient so that health care facilities can take special precautions to stop its spread,” a CDC page on C. auris states. “CDC encourages all U.S. laboratory staff who identify C. auris to notify their state or local public health authorities and CDC at [email protected].”
Dr. Eyre reported having no disclosures.
SOURCE: Eyre D et al. ICEID 2018 Oral Abstract Presentation.
ATLANTA – The persistence and transmission of Candida auris in health care settings appears to be dependent on environmental survival, underscoring the need for careful investigation of the environment – and, in particular, multiuse patient equipment.
That’s the key lesson from one of the largest outbreaks of the emerging, multidrug-resistant pathogen to date, David Eyre, DPhil, said at the International Conference on Emerging Infectious Diseases.
“Our experience at Oxford began with a Public Health England alert, which closely followed a similar alert from the [Centers for Disease Control and Prevention] in the summer of 2016,” Dr. Eyre of the University of Oxford (England) said during an update on the epidemiology of the outbreak and the successful, multipronged effort to control it.
The outbreak, which occurred in the neurosciences intensive care unit of Oxford University Hospitals beginning in early 2015, was detected in 2016 when a cluster of C. auris infections was identified and traced to the unit. An intensive patient and environmental screening program was established, isolation protocols were used for patients who tested positive, enhanced cleaning processes were initiated, and equipment was removed and replaced with single-use equipment when possible.
“We also worked quite closely with our staff to raise awareness,” he said, adding that colonized patients who were undergoing a surgical procedure received single-dose antifungal prophylaxis prior to the procedure.
A case-control study was conducted, and after the researchers used multivariate logistic regression to control for length of stay, patient physiology, and biomarkers, exposure to multiuse skin surface axillary temperature monitoring was shown to be one of the strongest independent predictors of C. auris colonization and infection (odds ratio 6.80), he said, adding that antifungal exposure was also a significant risk factor, but only 5% of patients had received antifungals.
The axillary probes were then removed from the environment. As of April 2017 (when the probes were removed), 66 patients had been colonized or infected, and an additional 10 cases occurred after the probes were removed, with the last case occurring in November 2017.
Seven of the 76 cases involved invasive infection, and 1 patient died several months after hospital discharge, Dr. Eyre said.
The patient screening processes allowed for estimation of colonization time (approximately 2 months), and also allowed for whole-genome sequencing of 79 samples from 43 patients, 6 environmental isolates, and 2 isolates from regional surveillance, Dr. Eyre said.
All outbreak sequences formed a single genetic cluster within the C. auris South African clade, and were found to have been introduced to Oxford around 2012 or 2013, with about six mutations per year, or “roughly 12 million base pairs in total,” he said, adding that both patients and temperature probes were colonized with multiple strains, and there was “close mixing” between the two.
This pattern changed following removal of the temperature probes, but it took some time.
“However, from November [2017] onward – so that’s now 291 days ... we’ve not had another new patient isolate, and that’s not only no invasive infection, but also no colonization despite continuing the screening program,” he said.
According to the CDC, C. auris is “an emerging fungus that presents a serious global health threat” because of its often multidrug-resistant nature, difficulty identifying the pathogen using standard laboratory methods, and the risk for misidentification in labs without specific technology, which could lead to inappropriate management.
“It has caused outbreaks in health care settings. For this reason, it is important to quickly identify C. auris in a hospitalized patient so that health care facilities can take special precautions to stop its spread,” a CDC page on C. auris states. “CDC encourages all U.S. laboratory staff who identify C. auris to notify their state or local public health authorities and CDC at [email protected].”
Dr. Eyre reported having no disclosures.
SOURCE: Eyre D et al. ICEID 2018 Oral Abstract Presentation.
REPORTING FROM ICEID 2018
Key clinical point:
Major finding: Ten additional cases occurred in the 7 months after the axillary probes were removed from the environment.
Study details: A review of the epidemiology and control of a C. auris outbreak affecting 76 patients.
Disclosures: Dr. Eyre reported having no disclosures.
Source: Eyre D et al. ICEID 2018 Oral Abstract Presentation.
Physician groups call for CMS to drop E/M proposal
More than 170 physician groups are calling on the Centers for Medicare & Medicaid Services to withdraw a provision in the proposed 2019 physician fee schedule that would flatten evaluation and management payments.
The controversial proposal would set the payment rate for a level 1 evaluation and management (E/M) office visit for a new patient at $44, down from the $45 using the current methodology. Payment for levels 2-5 would be $135. Currently, payments for level 2 new patient visits are set at $76, level 3 at $110, level 4 at $167, and level 5 at $211.
For E/M office visits with established patients, the proposed rate would be $24 for level 1, up from the current payment of $22. Payment for levels 2-5 would be $93. Under the current methodology, payments for established patient level 2 visits are set at $45, level 3 at $74, level 4 at $109, and level 5 at $148.
In an Aug. 28 letter to the CMS, led by the American College of Rheumatology, physician groups applauded CMS recognition of the problems with the current E/M documentation guidelines and codes, but urged them to reconsider plans to “cut and consolidate evaluation and management services.” Doing so would “severely reduce Medicare patients’ access to care by cutting payments for complex office visits, adversely effecting the care and treatment of patients with complex conditions, and potentially exacerbate physician workforce shortages.”
A separate letter, led by the American Medical Association, made similar assertions that the current proposal has the potential to “hurt physicians and other health care professionals in specialties that treat the sickest patients, as well as those who provide comprehensive primary care, ultimately jeopardizing patients’ access to care.”
Daniel P. McQuillen, MD, of Lahey Hospital and Medical Center, Burlington, Mass. and member of the Infectious Diseases Society of America, said that IDSA is “worried that the implementation is being pushed ahead too fast without really considering whether it’s the right way of doing it and whether there might be some alternative ways of doing it that make more sense.”
Another concern related to the implementation of this proposal is the financial impact on physicians.
Implementation of the CMS proposal, as currently written, “would be amazingly expensive for private practice [doctors] and really for anyone else because we would have to change our EMRs,” Barbara Levy, MD, cochair of the CPT/RUC Work Group at the AMA.
“We would have to reprogram our billing software. All of that comes with a significant cost,” said Dr. Levy, who also serves as vice president of health policy at the American College of Obstetricians and Gynecologists.
Part of the selling point of the CMS proposal is the reduction in documentation that accompanies the E/M payment changes. The goal, according to the CMS, is to reduce time spent on paperwork and free up physicians to devote more time to patient care. But some physicians are skeptical it would work out that way.
“I don’t think it is going to change my documentation burden very much,” Jeffery Ward, MD, chair of the American Society of Clinical Oncology Government Relations Committee, said in an interview. “Their assumption is that I write my notes in order to meet a billing requirement and if I don’t have that billing requirement, I won’t have to write nearly as detailed notes. My notes are written so that if someone else needs to take care of my patient when I am not there, they can step in, read my notes, know what’s going on, and follow the patient.”
Dr. Ward suggested that the real purpose of the proposal is to shift more money to primary care, and raised the concern that the CMS is using this proposal “as a vehicle to take money away from specialists who take care of very complicated patients in order to give it to other people, particularly to primary care.”
ASCO and the Community Oncology Alliance both anticipate a 7%-8% reduction in payments to cancer specialists if this provision takes effect, Dr. Ward said.
Another element of the proposal that is raising concerns among physician groups is a proposed payment reduction when a visit involves more than one service. For example, when a single office visit includes both an E/M code and a procedure code, the proposal calls for the E/M code to be cut in half.
“From the patients’ perspective, the potential threat is that doctors could be incentivized to spend less time with patients or potentially bring patients back for subsequent visits to handle multiple problems,” Angus Worthing, MD, chair of the American College of Rheumatology’s Committee on Government Affairs, said in an interview.
Comments on the proposed update to the 2019 Medicare physician fee schedule are due Sept. 10.
More than 170 physician groups are calling on the Centers for Medicare & Medicaid Services to withdraw a provision in the proposed 2019 physician fee schedule that would flatten evaluation and management payments.
The controversial proposal would set the payment rate for a level 1 evaluation and management (E/M) office visit for a new patient at $44, down from the $45 using the current methodology. Payment for levels 2-5 would be $135. Currently, payments for level 2 new patient visits are set at $76, level 3 at $110, level 4 at $167, and level 5 at $211.
For E/M office visits with established patients, the proposed rate would be $24 for level 1, up from the current payment of $22. Payment for levels 2-5 would be $93. Under the current methodology, payments for established patient level 2 visits are set at $45, level 3 at $74, level 4 at $109, and level 5 at $148.
In an Aug. 28 letter to the CMS, led by the American College of Rheumatology, physician groups applauded CMS recognition of the problems with the current E/M documentation guidelines and codes, but urged them to reconsider plans to “cut and consolidate evaluation and management services.” Doing so would “severely reduce Medicare patients’ access to care by cutting payments for complex office visits, adversely effecting the care and treatment of patients with complex conditions, and potentially exacerbate physician workforce shortages.”
A separate letter, led by the American Medical Association, made similar assertions that the current proposal has the potential to “hurt physicians and other health care professionals in specialties that treat the sickest patients, as well as those who provide comprehensive primary care, ultimately jeopardizing patients’ access to care.”
Daniel P. McQuillen, MD, of Lahey Hospital and Medical Center, Burlington, Mass. and member of the Infectious Diseases Society of America, said that IDSA is “worried that the implementation is being pushed ahead too fast without really considering whether it’s the right way of doing it and whether there might be some alternative ways of doing it that make more sense.”
Another concern related to the implementation of this proposal is the financial impact on physicians.
Implementation of the CMS proposal, as currently written, “would be amazingly expensive for private practice [doctors] and really for anyone else because we would have to change our EMRs,” Barbara Levy, MD, cochair of the CPT/RUC Work Group at the AMA.
“We would have to reprogram our billing software. All of that comes with a significant cost,” said Dr. Levy, who also serves as vice president of health policy at the American College of Obstetricians and Gynecologists.
Part of the selling point of the CMS proposal is the reduction in documentation that accompanies the E/M payment changes. The goal, according to the CMS, is to reduce time spent on paperwork and free up physicians to devote more time to patient care. But some physicians are skeptical it would work out that way.
“I don’t think it is going to change my documentation burden very much,” Jeffery Ward, MD, chair of the American Society of Clinical Oncology Government Relations Committee, said in an interview. “Their assumption is that I write my notes in order to meet a billing requirement and if I don’t have that billing requirement, I won’t have to write nearly as detailed notes. My notes are written so that if someone else needs to take care of my patient when I am not there, they can step in, read my notes, know what’s going on, and follow the patient.”
Dr. Ward suggested that the real purpose of the proposal is to shift more money to primary care, and raised the concern that the CMS is using this proposal “as a vehicle to take money away from specialists who take care of very complicated patients in order to give it to other people, particularly to primary care.”
ASCO and the Community Oncology Alliance both anticipate a 7%-8% reduction in payments to cancer specialists if this provision takes effect, Dr. Ward said.
Another element of the proposal that is raising concerns among physician groups is a proposed payment reduction when a visit involves more than one service. For example, when a single office visit includes both an E/M code and a procedure code, the proposal calls for the E/M code to be cut in half.
“From the patients’ perspective, the potential threat is that doctors could be incentivized to spend less time with patients or potentially bring patients back for subsequent visits to handle multiple problems,” Angus Worthing, MD, chair of the American College of Rheumatology’s Committee on Government Affairs, said in an interview.
Comments on the proposed update to the 2019 Medicare physician fee schedule are due Sept. 10.
More than 170 physician groups are calling on the Centers for Medicare & Medicaid Services to withdraw a provision in the proposed 2019 physician fee schedule that would flatten evaluation and management payments.
The controversial proposal would set the payment rate for a level 1 evaluation and management (E/M) office visit for a new patient at $44, down from the $45 using the current methodology. Payment for levels 2-5 would be $135. Currently, payments for level 2 new patient visits are set at $76, level 3 at $110, level 4 at $167, and level 5 at $211.
For E/M office visits with established patients, the proposed rate would be $24 for level 1, up from the current payment of $22. Payment for levels 2-5 would be $93. Under the current methodology, payments for established patient level 2 visits are set at $45, level 3 at $74, level 4 at $109, and level 5 at $148.
In an Aug. 28 letter to the CMS, led by the American College of Rheumatology, physician groups applauded CMS recognition of the problems with the current E/M documentation guidelines and codes, but urged them to reconsider plans to “cut and consolidate evaluation and management services.” Doing so would “severely reduce Medicare patients’ access to care by cutting payments for complex office visits, adversely effecting the care and treatment of patients with complex conditions, and potentially exacerbate physician workforce shortages.”
A separate letter, led by the American Medical Association, made similar assertions that the current proposal has the potential to “hurt physicians and other health care professionals in specialties that treat the sickest patients, as well as those who provide comprehensive primary care, ultimately jeopardizing patients’ access to care.”
Daniel P. McQuillen, MD, of Lahey Hospital and Medical Center, Burlington, Mass. and member of the Infectious Diseases Society of America, said that IDSA is “worried that the implementation is being pushed ahead too fast without really considering whether it’s the right way of doing it and whether there might be some alternative ways of doing it that make more sense.”
Another concern related to the implementation of this proposal is the financial impact on physicians.
Implementation of the CMS proposal, as currently written, “would be amazingly expensive for private practice [doctors] and really for anyone else because we would have to change our EMRs,” Barbara Levy, MD, cochair of the CPT/RUC Work Group at the AMA.
“We would have to reprogram our billing software. All of that comes with a significant cost,” said Dr. Levy, who also serves as vice president of health policy at the American College of Obstetricians and Gynecologists.
Part of the selling point of the CMS proposal is the reduction in documentation that accompanies the E/M payment changes. The goal, according to the CMS, is to reduce time spent on paperwork and free up physicians to devote more time to patient care. But some physicians are skeptical it would work out that way.
“I don’t think it is going to change my documentation burden very much,” Jeffery Ward, MD, chair of the American Society of Clinical Oncology Government Relations Committee, said in an interview. “Their assumption is that I write my notes in order to meet a billing requirement and if I don’t have that billing requirement, I won’t have to write nearly as detailed notes. My notes are written so that if someone else needs to take care of my patient when I am not there, they can step in, read my notes, know what’s going on, and follow the patient.”
Dr. Ward suggested that the real purpose of the proposal is to shift more money to primary care, and raised the concern that the CMS is using this proposal “as a vehicle to take money away from specialists who take care of very complicated patients in order to give it to other people, particularly to primary care.”
ASCO and the Community Oncology Alliance both anticipate a 7%-8% reduction in payments to cancer specialists if this provision takes effect, Dr. Ward said.
Another element of the proposal that is raising concerns among physician groups is a proposed payment reduction when a visit involves more than one service. For example, when a single office visit includes both an E/M code and a procedure code, the proposal calls for the E/M code to be cut in half.
“From the patients’ perspective, the potential threat is that doctors could be incentivized to spend less time with patients or potentially bring patients back for subsequent visits to handle multiple problems,” Angus Worthing, MD, chair of the American College of Rheumatology’s Committee on Government Affairs, said in an interview.
Comments on the proposed update to the 2019 Medicare physician fee schedule are due Sept. 10.