User login
Azithromycin and doxycycline effective for urogenital chlamydia*
BRISBANE, AUSTRALIA – Azithromycin and doxycycline have been shown to still be highly effective treatments for urogenital chlamydia in a randomized clinical trial conducted in a youth correctional facility.*
The study, presented at the World STI & HIV Congress 2015, found a 7-day, twice-daily regimen of 100 mg of doxycycline achieved a 100% cure rate, compared with a 96.8% success rate with a single 1-g dose of azithromycin.
However, noninferiority of azithromycin to doxycycline was not established, said Dr. William Geisler of the division of infectious diseases at the University of Alabama at Birmingham.
“I think the big finding from the study was that both drugs still work quite well, and I think it puts to rest a lot of the concerns about azithromycin for urogenital chlamydia,” said Dr. Geisler.
The study enrolled 310 males and nonpregnant females (median age 17 years) who tested positive for chlamydia when screened upon arrival at the correctional facility.
They were then randomized to receive either doxycycline or azithromycin, and followed up with chlamydia testing 28 days after treatment, which included genotyping to distinguish between treatment failure and infection with a new chlamydia strain.
Of the five treatment failures, four were males and one female; the researchers noted that painful urination occurred more often in azithromycin-treated males who failed treatment versus those cured, although the difference was not statistically significant.
Commenting on this finding, a member of the audience asked whether Dr. Geisler would therefore reconsider treating a symptomatic man with azithromycin.
Dr. Geisler said that while he did have concerns about the efficacy of azithromycin in symptomatic men, adherence also was a factor to be taken into consideration.
“In general, most of the males I see, I don’t feel that great about their likelihood for full adherence [with doxycycline], so I would still feel very comfortable about giving azithromycin to a symptomatic male,” he said.
About three-quarters of the males who were positive for chlamydia at randomization were asymptomatic, compared with nearly 40% of the females.
Adherence was a nonissue for azithromycin, because the single dose could be taken under observation, Dr. Geisler noted. There were greater variations in adherence with the doxycycline, with participants taking between 11 and 16 doses, although about 80% took the prescribed 14 doses.
The study was conducted in correctional facilities in an attempt to limit the possibility of reinfection, and to help improve the likelihood of adherence – both issues that have plagued previous studies.
“These residents, once they get in the facilities, are not typically re-exposed to the untreated partner who’s outside of the facility, so whatever exposures they would have would be new partners in the facility,” Dr. Geisler said at the conference. “The facility that we used for this study, there were really minimal opportunities for re-exposure to chlamydia because everybody who entered the facility got routinely screened and treated for chlamydia.”
While it was challenging to get approval to conduct the study in the correctional facility, Dr. Geisler said it was worth considering.
“Maybe this will pave the way for other studies in these facilities, ones that have low-risk type of procedures [because] controlling for sex is a lot easier in these settings,” he said in an interview.
The National Institutes of Health funded the study. There were no conflicts of interest declared.
*Correction, 11/3/2015: An earlier version of this story incorrectly stated the study's major finding. Although the cure rates were high for both treatments, noninferiority of azithromycin to doxycycline was not established in the study.
BRISBANE, AUSTRALIA – Azithromycin and doxycycline have been shown to still be highly effective treatments for urogenital chlamydia in a randomized clinical trial conducted in a youth correctional facility.*
The study, presented at the World STI & HIV Congress 2015, found a 7-day, twice-daily regimen of 100 mg of doxycycline achieved a 100% cure rate, compared with a 96.8% success rate with a single 1-g dose of azithromycin.
However, noninferiority of azithromycin to doxycycline was not established, said Dr. William Geisler of the division of infectious diseases at the University of Alabama at Birmingham.
“I think the big finding from the study was that both drugs still work quite well, and I think it puts to rest a lot of the concerns about azithromycin for urogenital chlamydia,” said Dr. Geisler.
The study enrolled 310 males and nonpregnant females (median age 17 years) who tested positive for chlamydia when screened upon arrival at the correctional facility.
They were then randomized to receive either doxycycline or azithromycin, and followed up with chlamydia testing 28 days after treatment, which included genotyping to distinguish between treatment failure and infection with a new chlamydia strain.
Of the five treatment failures, four were males and one female; the researchers noted that painful urination occurred more often in azithromycin-treated males who failed treatment versus those cured, although the difference was not statistically significant.
Commenting on this finding, a member of the audience asked whether Dr. Geisler would therefore reconsider treating a symptomatic man with azithromycin.
Dr. Geisler said that while he did have concerns about the efficacy of azithromycin in symptomatic men, adherence also was a factor to be taken into consideration.
“In general, most of the males I see, I don’t feel that great about their likelihood for full adherence [with doxycycline], so I would still feel very comfortable about giving azithromycin to a symptomatic male,” he said.
About three-quarters of the males who were positive for chlamydia at randomization were asymptomatic, compared with nearly 40% of the females.
Adherence was a nonissue for azithromycin, because the single dose could be taken under observation, Dr. Geisler noted. There were greater variations in adherence with the doxycycline, with participants taking between 11 and 16 doses, although about 80% took the prescribed 14 doses.
The study was conducted in correctional facilities in an attempt to limit the possibility of reinfection, and to help improve the likelihood of adherence – both issues that have plagued previous studies.
“These residents, once they get in the facilities, are not typically re-exposed to the untreated partner who’s outside of the facility, so whatever exposures they would have would be new partners in the facility,” Dr. Geisler said at the conference. “The facility that we used for this study, there were really minimal opportunities for re-exposure to chlamydia because everybody who entered the facility got routinely screened and treated for chlamydia.”
While it was challenging to get approval to conduct the study in the correctional facility, Dr. Geisler said it was worth considering.
“Maybe this will pave the way for other studies in these facilities, ones that have low-risk type of procedures [because] controlling for sex is a lot easier in these settings,” he said in an interview.
The National Institutes of Health funded the study. There were no conflicts of interest declared.
*Correction, 11/3/2015: An earlier version of this story incorrectly stated the study's major finding. Although the cure rates were high for both treatments, noninferiority of azithromycin to doxycycline was not established in the study.
BRISBANE, AUSTRALIA – Azithromycin and doxycycline have been shown to still be highly effective treatments for urogenital chlamydia in a randomized clinical trial conducted in a youth correctional facility.*
The study, presented at the World STI & HIV Congress 2015, found a 7-day, twice-daily regimen of 100 mg of doxycycline achieved a 100% cure rate, compared with a 96.8% success rate with a single 1-g dose of azithromycin.
However, noninferiority of azithromycin to doxycycline was not established, said Dr. William Geisler of the division of infectious diseases at the University of Alabama at Birmingham.
“I think the big finding from the study was that both drugs still work quite well, and I think it puts to rest a lot of the concerns about azithromycin for urogenital chlamydia,” said Dr. Geisler.
The study enrolled 310 males and nonpregnant females (median age 17 years) who tested positive for chlamydia when screened upon arrival at the correctional facility.
They were then randomized to receive either doxycycline or azithromycin, and followed up with chlamydia testing 28 days after treatment, which included genotyping to distinguish between treatment failure and infection with a new chlamydia strain.
Of the five treatment failures, four were males and one female; the researchers noted that painful urination occurred more often in azithromycin-treated males who failed treatment versus those cured, although the difference was not statistically significant.
Commenting on this finding, a member of the audience asked whether Dr. Geisler would therefore reconsider treating a symptomatic man with azithromycin.
Dr. Geisler said that while he did have concerns about the efficacy of azithromycin in symptomatic men, adherence also was a factor to be taken into consideration.
“In general, most of the males I see, I don’t feel that great about their likelihood for full adherence [with doxycycline], so I would still feel very comfortable about giving azithromycin to a symptomatic male,” he said.
About three-quarters of the males who were positive for chlamydia at randomization were asymptomatic, compared with nearly 40% of the females.
Adherence was a nonissue for azithromycin, because the single dose could be taken under observation, Dr. Geisler noted. There were greater variations in adherence with the doxycycline, with participants taking between 11 and 16 doses, although about 80% took the prescribed 14 doses.
The study was conducted in correctional facilities in an attempt to limit the possibility of reinfection, and to help improve the likelihood of adherence – both issues that have plagued previous studies.
“These residents, once they get in the facilities, are not typically re-exposed to the untreated partner who’s outside of the facility, so whatever exposures they would have would be new partners in the facility,” Dr. Geisler said at the conference. “The facility that we used for this study, there were really minimal opportunities for re-exposure to chlamydia because everybody who entered the facility got routinely screened and treated for chlamydia.”
While it was challenging to get approval to conduct the study in the correctional facility, Dr. Geisler said it was worth considering.
“Maybe this will pave the way for other studies in these facilities, ones that have low-risk type of procedures [because] controlling for sex is a lot easier in these settings,” he said in an interview.
The National Institutes of Health funded the study. There were no conflicts of interest declared.
*Correction, 11/3/2015: An earlier version of this story incorrectly stated the study's major finding. Although the cure rates were high for both treatments, noninferiority of azithromycin to doxycycline was not established in the study.
FROM THE WORLD STI & HIV CONGRESS 2015
Key clinical point: Azithromycin and doxycycline remain highly effective for the treatment of urogenital chlamydia with cure rates greater than 95%.
Major finding: Azithromycin achieved a 96.8% cure rate for chlamydia, compared with a 100% cure rate with doxycycline. Although the cure rates were high for both treatments, noninferiority of azithromycin to doxycycline was not established in the study.
Data source: Randomized clinical trial of 310 males and females in a youth correctional facility.
Disclosures: The National Institutes of Health funded the study. There were no conflicts of interest declared.
Smartphone app can pick up covert hepatic encephalopathy
Researchers have road-tested an app based on the Stroop test, which is designed to detect covert hepatic encephalopathy, with results suggesting it achieves results similar to those of a paper-based Stroop test.
The smartphone-based EncephalApp was tested in 167 patients with cirrhosis and 114 healthy age-matched controls, and showed significant correlation with individual paper/pen test and with crashes and illegal turns in driving simulation tests, as well as high test/retest reliability at 1 and 3 months.
The study also found that patients with prior overt hepatic encephalopathy had significantly worse response times with the EncephalApp compared to controls (Clin Gastroenterol Hepatol. 2015;13:1828-35).
“Although these [gold standard paper-pencil] measures are used to diagnose CHE [covert hepatic encephalopathy] in research studies, they have not found traction in clinical practice because of their copyrighted nature, need for psychological expertise, and time requirements,” wrote Dr. Jasmohan S. Bajaj of Virginia Commonwealth University and McGuire VA Hospital, both in Richmond, Va.
“Our results are in sync with the prior experience with the old Stroop App in that in similar prior HE [hepatic encephalopathy] studies, we found that the psychomotor function, i.e., the time required to complete tasks, was much more predictive than the errors committed (number of runs required) and the cognitive flexibility measures (OnTime-OffTime) in differentiating groups,” wrote Dr. Bajaj and colleagues.
The National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Advancing Translational Research and the McGuire Research Institute funded the study. There were no other conflicts of interest declared.
Researchers have road-tested an app based on the Stroop test, which is designed to detect covert hepatic encephalopathy, with results suggesting it achieves results similar to those of a paper-based Stroop test.
The smartphone-based EncephalApp was tested in 167 patients with cirrhosis and 114 healthy age-matched controls, and showed significant correlation with individual paper/pen test and with crashes and illegal turns in driving simulation tests, as well as high test/retest reliability at 1 and 3 months.
The study also found that patients with prior overt hepatic encephalopathy had significantly worse response times with the EncephalApp compared to controls (Clin Gastroenterol Hepatol. 2015;13:1828-35).
“Although these [gold standard paper-pencil] measures are used to diagnose CHE [covert hepatic encephalopathy] in research studies, they have not found traction in clinical practice because of their copyrighted nature, need for psychological expertise, and time requirements,” wrote Dr. Jasmohan S. Bajaj of Virginia Commonwealth University and McGuire VA Hospital, both in Richmond, Va.
“Our results are in sync with the prior experience with the old Stroop App in that in similar prior HE [hepatic encephalopathy] studies, we found that the psychomotor function, i.e., the time required to complete tasks, was much more predictive than the errors committed (number of runs required) and the cognitive flexibility measures (OnTime-OffTime) in differentiating groups,” wrote Dr. Bajaj and colleagues.
The National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Advancing Translational Research and the McGuire Research Institute funded the study. There were no other conflicts of interest declared.
Researchers have road-tested an app based on the Stroop test, which is designed to detect covert hepatic encephalopathy, with results suggesting it achieves results similar to those of a paper-based Stroop test.
The smartphone-based EncephalApp was tested in 167 patients with cirrhosis and 114 healthy age-matched controls, and showed significant correlation with individual paper/pen test and with crashes and illegal turns in driving simulation tests, as well as high test/retest reliability at 1 and 3 months.
The study also found that patients with prior overt hepatic encephalopathy had significantly worse response times with the EncephalApp compared to controls (Clin Gastroenterol Hepatol. 2015;13:1828-35).
“Although these [gold standard paper-pencil] measures are used to diagnose CHE [covert hepatic encephalopathy] in research studies, they have not found traction in clinical practice because of their copyrighted nature, need for psychological expertise, and time requirements,” wrote Dr. Jasmohan S. Bajaj of Virginia Commonwealth University and McGuire VA Hospital, both in Richmond, Va.
“Our results are in sync with the prior experience with the old Stroop App in that in similar prior HE [hepatic encephalopathy] studies, we found that the psychomotor function, i.e., the time required to complete tasks, was much more predictive than the errors committed (number of runs required) and the cognitive flexibility measures (OnTime-OffTime) in differentiating groups,” wrote Dr. Bajaj and colleagues.
The National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Advancing Translational Research and the McGuire Research Institute funded the study. There were no other conflicts of interest declared.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point:A smartphone-based app has achieved results in detecting covert hepatic encephalopathy similar to those of a paper/pen–based Stroop test.
Major finding: EncephalApp showed significant correlation with individual paper/pen test and with crashes and illegal turns in driving simulation tests, as well as high test/retest reliability.
Data source: Controlled study of 167 patients with cirrhosis and 114 healthy age-matched controls.
Disclosures: The National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Advancing Translational Research, and the McGuire Research Institute funded the study. There were no other conflicts of interest declared.
Integrated care overcomes HCV treatment barriers
Patients with hepatitis C and psychiatric disorders or substance abuse problems benefit significantly from an integrated care model of treatment, with a randomized controlled trial showing such an approach is linked to greater rates of antiviral therapy and treatment response.
The prospective trial of integrated care versus usual care involved 363 patients attending three hepatitis C (HCV) clinics, with the integrated care being delivered by a midlevel mental health provider within the clinic who served as the regular contact and case manager.
Patients randomized to integrated care, which included brief psychological interventions and case management, were more than twice as likely to start antiviral therapy earlier and achieve a sustained virologic response than those who received usual care, according to Dr. Samuel B. Ho of the VA San Diego Healthcare System and his coauthors.
While individuals with a history of prior psychiatric disorder or active drug use were significantly less likely to achieve sustained virologic response, the integrated-care approach had particularly positive effects on treatment initiative and response for individuals with a risk for active psychiatric disease at baseline, they said (Clin Gastroenterol Hepatol. 2015. doi: 10.1016/j.cgh.2015.02.022).
“To optimize the public health impact of antiviral treatments for HCV, the number of patients who are able to receive these treatments must be expanded,” wrote Dr. Ho and his associates, adding that “new interferon-free regimens have fewer side effects and are expected to expand treatment populations to include a broader range of patients, many with very significant psychiatric and substance abuse disorders.”
The study was supported by VA Health Services Research and Development. Three authors declared research support, grants, advisory board positions or speakers bureau roles with the pharmaceutical industry.
AGA Resource
Through the AGA Roadmap to the Future of Practice, AGA offers a Hepatitis C Clinical Service line to support high-quality patient care at www.gastro.org/patient-care/conditions-diseases/hepatitis-c.
Patients with hepatitis C and psychiatric disorders or substance abuse problems benefit significantly from an integrated care model of treatment, with a randomized controlled trial showing such an approach is linked to greater rates of antiviral therapy and treatment response.
The prospective trial of integrated care versus usual care involved 363 patients attending three hepatitis C (HCV) clinics, with the integrated care being delivered by a midlevel mental health provider within the clinic who served as the regular contact and case manager.
Patients randomized to integrated care, which included brief psychological interventions and case management, were more than twice as likely to start antiviral therapy earlier and achieve a sustained virologic response than those who received usual care, according to Dr. Samuel B. Ho of the VA San Diego Healthcare System and his coauthors.
While individuals with a history of prior psychiatric disorder or active drug use were significantly less likely to achieve sustained virologic response, the integrated-care approach had particularly positive effects on treatment initiative and response for individuals with a risk for active psychiatric disease at baseline, they said (Clin Gastroenterol Hepatol. 2015. doi: 10.1016/j.cgh.2015.02.022).
“To optimize the public health impact of antiviral treatments for HCV, the number of patients who are able to receive these treatments must be expanded,” wrote Dr. Ho and his associates, adding that “new interferon-free regimens have fewer side effects and are expected to expand treatment populations to include a broader range of patients, many with very significant psychiatric and substance abuse disorders.”
The study was supported by VA Health Services Research and Development. Three authors declared research support, grants, advisory board positions or speakers bureau roles with the pharmaceutical industry.
AGA Resource
Through the AGA Roadmap to the Future of Practice, AGA offers a Hepatitis C Clinical Service line to support high-quality patient care at www.gastro.org/patient-care/conditions-diseases/hepatitis-c.
Patients with hepatitis C and psychiatric disorders or substance abuse problems benefit significantly from an integrated care model of treatment, with a randomized controlled trial showing such an approach is linked to greater rates of antiviral therapy and treatment response.
The prospective trial of integrated care versus usual care involved 363 patients attending three hepatitis C (HCV) clinics, with the integrated care being delivered by a midlevel mental health provider within the clinic who served as the regular contact and case manager.
Patients randomized to integrated care, which included brief psychological interventions and case management, were more than twice as likely to start antiviral therapy earlier and achieve a sustained virologic response than those who received usual care, according to Dr. Samuel B. Ho of the VA San Diego Healthcare System and his coauthors.
While individuals with a history of prior psychiatric disorder or active drug use were significantly less likely to achieve sustained virologic response, the integrated-care approach had particularly positive effects on treatment initiative and response for individuals with a risk for active psychiatric disease at baseline, they said (Clin Gastroenterol Hepatol. 2015. doi: 10.1016/j.cgh.2015.02.022).
“To optimize the public health impact of antiviral treatments for HCV, the number of patients who are able to receive these treatments must be expanded,” wrote Dr. Ho and his associates, adding that “new interferon-free regimens have fewer side effects and are expected to expand treatment populations to include a broader range of patients, many with very significant psychiatric and substance abuse disorders.”
The study was supported by VA Health Services Research and Development. Three authors declared research support, grants, advisory board positions or speakers bureau roles with the pharmaceutical industry.
AGA Resource
Through the AGA Roadmap to the Future of Practice, AGA offers a Hepatitis C Clinical Service line to support high-quality patient care at www.gastro.org/patient-care/conditions-diseases/hepatitis-c.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point:Patients with hepatitis C and psychiatric disorders or substance abuse problems benefit significantly from an integrated care model of treatment.
Major finding: Integrated care was associated with a more than twofold increase in early initiation of antiviral therapy and sustained virologic response.
Data source: A prospective, randomized controlled trial in 363 patients with hepatitis C and psychiatric disorders or substance abuse problems.
Disclosures: The study was supported by VA Health Services Research and Development. Three authors declared research support, grants, advisory board positions, or speakers bureau roles with the pharmaceutical industry.
Integrated care overcomes HCV treatment barriers
Patients with hepatitis C and psychiatric disorders or substance abuse problems benefit significantly from an integrated care model of treatment, with a randomized controlled trial showing such an approach is linked to greater rates of antiviral therapy and treatment response.
The prospective trial of integrated care versus usual care involved 363 patients attending three hepatitis C (HCV) clinics, with the integrated care being delivered by a midlevel mental health provider within the clinic who served as the regular contact and case manager.
Patients randomized to integrated care, which included brief psychological interventions and case management, were more than twice as likely to start antiviral therapy earlier and achieve a sustained virologic response than those who received usual care, according to Dr. Samuel B. Ho of the VA San Diego Healthcare System and his coauthors.
While individuals with a history of prior psychiatric disorder or active drug use were significantly less likely to achieve sustained virologic response, the integrated-care approach had particularly positive effects on treatment initiative and response for individuals with a risk for active psychiatric disease at baseline, they said (Clin Gastroenterol Hepatol. 2015. doi: 10.1016/j.cgh.2015.02.022).
“To optimize the public health impact of antiviral treatments for HCV, the number of patients who are able to receive these treatments must be expanded,” wrote Dr. Ho and his associates, adding that “new interferon-free regimens have fewer side effects and are expected to expand treatment populations to include a broader range of patients, many with very significant psychiatric and substance abuse disorders.”
The study was supported by VA Health Services Research and Development. Three authors declared research support, grants, advisory board positions or speakers bureau roles with the pharmaceutical industry.
Patients with hepatitis C and psychiatric disorders or substance abuse problems benefit significantly from an integrated care model of treatment, with a randomized controlled trial showing such an approach is linked to greater rates of antiviral therapy and treatment response.
The prospective trial of integrated care versus usual care involved 363 patients attending three hepatitis C (HCV) clinics, with the integrated care being delivered by a midlevel mental health provider within the clinic who served as the regular contact and case manager.
Patients randomized to integrated care, which included brief psychological interventions and case management, were more than twice as likely to start antiviral therapy earlier and achieve a sustained virologic response than those who received usual care, according to Dr. Samuel B. Ho of the VA San Diego Healthcare System and his coauthors.
While individuals with a history of prior psychiatric disorder or active drug use were significantly less likely to achieve sustained virologic response, the integrated-care approach had particularly positive effects on treatment initiative and response for individuals with a risk for active psychiatric disease at baseline, they said (Clin Gastroenterol Hepatol. 2015. doi: 10.1016/j.cgh.2015.02.022).
“To optimize the public health impact of antiviral treatments for HCV, the number of patients who are able to receive these treatments must be expanded,” wrote Dr. Ho and his associates, adding that “new interferon-free regimens have fewer side effects and are expected to expand treatment populations to include a broader range of patients, many with very significant psychiatric and substance abuse disorders.”
The study was supported by VA Health Services Research and Development. Three authors declared research support, grants, advisory board positions or speakers bureau roles with the pharmaceutical industry.
Patients with hepatitis C and psychiatric disorders or substance abuse problems benefit significantly from an integrated care model of treatment, with a randomized controlled trial showing such an approach is linked to greater rates of antiviral therapy and treatment response.
The prospective trial of integrated care versus usual care involved 363 patients attending three hepatitis C (HCV) clinics, with the integrated care being delivered by a midlevel mental health provider within the clinic who served as the regular contact and case manager.
Patients randomized to integrated care, which included brief psychological interventions and case management, were more than twice as likely to start antiviral therapy earlier and achieve a sustained virologic response than those who received usual care, according to Dr. Samuel B. Ho of the VA San Diego Healthcare System and his coauthors.
While individuals with a history of prior psychiatric disorder or active drug use were significantly less likely to achieve sustained virologic response, the integrated-care approach had particularly positive effects on treatment initiative and response for individuals with a risk for active psychiatric disease at baseline, they said (Clin Gastroenterol Hepatol. 2015. doi: 10.1016/j.cgh.2015.02.022).
“To optimize the public health impact of antiviral treatments for HCV, the number of patients who are able to receive these treatments must be expanded,” wrote Dr. Ho and his associates, adding that “new interferon-free regimens have fewer side effects and are expected to expand treatment populations to include a broader range of patients, many with very significant psychiatric and substance abuse disorders.”
The study was supported by VA Health Services Research and Development. Three authors declared research support, grants, advisory board positions or speakers bureau roles with the pharmaceutical industry.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point:Patients with hepatitis C and psychiatric disorders or substance abuse problems benefit significantly from an integrated care model of treatment.
Major finding: Integrated care was associated with a more than twofold increase in early initiation of antiviral therapy and sustained virologic response.
Data source: A prospective, randomized controlled trial in 363 patients with hepatitis C and psychiatric disorders or substance abuse problems.
Disclosures: The study was supported by VA Health Services Research and Development. Three authors declared research support, grants, advisory board positions, or speakers bureau roles with the pharmaceutical industry.
One in 20 students using e-cigarettes for cannabis
Significant numbers of high school students are using e-cigarettes to vaporize cannabis, new data suggest.
An anonymous survey of 3,847 Connecticut high school students found that, overall, 5.4% of the total sample reported using e-cigarettes or vaporizers to vaporize cannabis, either in the form of hash oil, THC-infused wax, or dried leaves.
Among students who had ever used an e-cigarette, 18% said that they had used it for cannabis, while 18.4% of cannabis users reported using e-cigarettes for cannabis.
More than one-quarter of students who reported using both cannabis and e-cigarettes said they had used e-cigarettes as a delivery mechanism for cannabis, according to a study published online Sept. 7 in Pediatrics.
Males and younger students were significantly more likely than females or older students to use e-cigarettes for cannabis, and the researchers found that the students’ socioeconomic status (SES) was not related to their tendency to use e-cigarettes to vaporize cannabis. The study did find significantly different rates of cannabis e-cigarette use between the five schools included in the study.
“These results indicate that factors such as the acceptability of cannabis use within a school (i.e., ‘cannabis culture’) or the extent to which a school has explicit policies prohibiting e-cigarette use may play a more important role in encouraging or deterring vaporizing cannabis than students’ SES,” wrote Meghan E. Morean, Ph.D., of Oberlin College, Ohio, and her coauthors.
Dried cannabis leaves were the most popular form of cannabis used in portable vaporizers, and hash oil was more commonly used with e-cigarettes than THC-infused wax (Pediatrics. 2015 Sept. 7. doi: 10.1542/peds.2015-1727).
While acknowledging that the results might be an underestimation of true figures because of the limitations of self-reporting, the authors said that further research is needed to determine whether e-cigarette use might serve as a gateway to cannabis use and the health impact of vaporized cannabis.
“At this time, the relative safety of using e-cigarettes for vaping cannabis versus smoking combustible cannabis is not well established,” Dr. Morean and her coauthors wrote. “However, a recent study indicated that adults who vaporize hash oil experience greater subjective tolerance and evidence of dependence compared with those smoking combustible cannabis.”
Cannabis consumed through e-cigarettes is particularly challenging for parents, teachers, and police to detect because the device does not produce the characteristic pungent aroma of smoked cannabis, the researchers reported.
“As e-cigarettes and related devices continue to gain popularity among youth, it will be important to monitor rates of using these products to vaporize cannabis.”
When asked about the findings, Dr. Robert L. DuPont said in an interview that American drug markets are changing rapidly, making more drugs available through highly potent routes of administration such as vaporization.
“This effective and convenient way of delivering THC has much appeal, especially to youth, being new, cool, and smoke-free as the rate of cannabis passes cigarettes for youth,” said Dr. DuPont, president of the Institute for Behavior and Health in Rockville, Md., and the first director of the National Institute on Drug Abuse.
The study was funded by the National Institutes of Health. No conflicts of interest were declared.
We have previously studied the process by which a child or adolescent becomes a regular smoker or binge drinker, but in our work we extended the gateway hypothesis on teen use to suggest that learning how to smoke or inhale drug vapors was the critical gateway event.
A young person who learns to inhibit a natural aversion to smoke or smoke-filled environments and suppress his or her cough reflex to inhale cigarettes has learned a particularly dangerous behavior, and as the gateway drugs have shifted from tobacco and alcohol to cannabis, it is deja vu for experts who trained and worked in the 1960s and 1970s.
Dr. Mark S. Gold is an adjunct professor of psychiatry at Washington University in St. Louis and is the former chairman of the department of psychiatry at the University of Florida, Gainesville. No conflicts of interest were declared.
We have previously studied the process by which a child or adolescent becomes a regular smoker or binge drinker, but in our work we extended the gateway hypothesis on teen use to suggest that learning how to smoke or inhale drug vapors was the critical gateway event.
A young person who learns to inhibit a natural aversion to smoke or smoke-filled environments and suppress his or her cough reflex to inhale cigarettes has learned a particularly dangerous behavior, and as the gateway drugs have shifted from tobacco and alcohol to cannabis, it is deja vu for experts who trained and worked in the 1960s and 1970s.
Dr. Mark S. Gold is an adjunct professor of psychiatry at Washington University in St. Louis and is the former chairman of the department of psychiatry at the University of Florida, Gainesville. No conflicts of interest were declared.
We have previously studied the process by which a child or adolescent becomes a regular smoker or binge drinker, but in our work we extended the gateway hypothesis on teen use to suggest that learning how to smoke or inhale drug vapors was the critical gateway event.
A young person who learns to inhibit a natural aversion to smoke or smoke-filled environments and suppress his or her cough reflex to inhale cigarettes has learned a particularly dangerous behavior, and as the gateway drugs have shifted from tobacco and alcohol to cannabis, it is deja vu for experts who trained and worked in the 1960s and 1970s.
Dr. Mark S. Gold is an adjunct professor of psychiatry at Washington University in St. Louis and is the former chairman of the department of psychiatry at the University of Florida, Gainesville. No conflicts of interest were declared.
Significant numbers of high school students are using e-cigarettes to vaporize cannabis, new data suggest.
An anonymous survey of 3,847 Connecticut high school students found that, overall, 5.4% of the total sample reported using e-cigarettes or vaporizers to vaporize cannabis, either in the form of hash oil, THC-infused wax, or dried leaves.
Among students who had ever used an e-cigarette, 18% said that they had used it for cannabis, while 18.4% of cannabis users reported using e-cigarettes for cannabis.
More than one-quarter of students who reported using both cannabis and e-cigarettes said they had used e-cigarettes as a delivery mechanism for cannabis, according to a study published online Sept. 7 in Pediatrics.
Males and younger students were significantly more likely than females or older students to use e-cigarettes for cannabis, and the researchers found that the students’ socioeconomic status (SES) was not related to their tendency to use e-cigarettes to vaporize cannabis. The study did find significantly different rates of cannabis e-cigarette use between the five schools included in the study.
“These results indicate that factors such as the acceptability of cannabis use within a school (i.e., ‘cannabis culture’) or the extent to which a school has explicit policies prohibiting e-cigarette use may play a more important role in encouraging or deterring vaporizing cannabis than students’ SES,” wrote Meghan E. Morean, Ph.D., of Oberlin College, Ohio, and her coauthors.
Dried cannabis leaves were the most popular form of cannabis used in portable vaporizers, and hash oil was more commonly used with e-cigarettes than THC-infused wax (Pediatrics. 2015 Sept. 7. doi: 10.1542/peds.2015-1727).
While acknowledging that the results might be an underestimation of true figures because of the limitations of self-reporting, the authors said that further research is needed to determine whether e-cigarette use might serve as a gateway to cannabis use and the health impact of vaporized cannabis.
“At this time, the relative safety of using e-cigarettes for vaping cannabis versus smoking combustible cannabis is not well established,” Dr. Morean and her coauthors wrote. “However, a recent study indicated that adults who vaporize hash oil experience greater subjective tolerance and evidence of dependence compared with those smoking combustible cannabis.”
Cannabis consumed through e-cigarettes is particularly challenging for parents, teachers, and police to detect because the device does not produce the characteristic pungent aroma of smoked cannabis, the researchers reported.
“As e-cigarettes and related devices continue to gain popularity among youth, it will be important to monitor rates of using these products to vaporize cannabis.”
When asked about the findings, Dr. Robert L. DuPont said in an interview that American drug markets are changing rapidly, making more drugs available through highly potent routes of administration such as vaporization.
“This effective and convenient way of delivering THC has much appeal, especially to youth, being new, cool, and smoke-free as the rate of cannabis passes cigarettes for youth,” said Dr. DuPont, president of the Institute for Behavior and Health in Rockville, Md., and the first director of the National Institute on Drug Abuse.
The study was funded by the National Institutes of Health. No conflicts of interest were declared.
Significant numbers of high school students are using e-cigarettes to vaporize cannabis, new data suggest.
An anonymous survey of 3,847 Connecticut high school students found that, overall, 5.4% of the total sample reported using e-cigarettes or vaporizers to vaporize cannabis, either in the form of hash oil, THC-infused wax, or dried leaves.
Among students who had ever used an e-cigarette, 18% said that they had used it for cannabis, while 18.4% of cannabis users reported using e-cigarettes for cannabis.
More than one-quarter of students who reported using both cannabis and e-cigarettes said they had used e-cigarettes as a delivery mechanism for cannabis, according to a study published online Sept. 7 in Pediatrics.
Males and younger students were significantly more likely than females or older students to use e-cigarettes for cannabis, and the researchers found that the students’ socioeconomic status (SES) was not related to their tendency to use e-cigarettes to vaporize cannabis. The study did find significantly different rates of cannabis e-cigarette use between the five schools included in the study.
“These results indicate that factors such as the acceptability of cannabis use within a school (i.e., ‘cannabis culture’) or the extent to which a school has explicit policies prohibiting e-cigarette use may play a more important role in encouraging or deterring vaporizing cannabis than students’ SES,” wrote Meghan E. Morean, Ph.D., of Oberlin College, Ohio, and her coauthors.
Dried cannabis leaves were the most popular form of cannabis used in portable vaporizers, and hash oil was more commonly used with e-cigarettes than THC-infused wax (Pediatrics. 2015 Sept. 7. doi: 10.1542/peds.2015-1727).
While acknowledging that the results might be an underestimation of true figures because of the limitations of self-reporting, the authors said that further research is needed to determine whether e-cigarette use might serve as a gateway to cannabis use and the health impact of vaporized cannabis.
“At this time, the relative safety of using e-cigarettes for vaping cannabis versus smoking combustible cannabis is not well established,” Dr. Morean and her coauthors wrote. “However, a recent study indicated that adults who vaporize hash oil experience greater subjective tolerance and evidence of dependence compared with those smoking combustible cannabis.”
Cannabis consumed through e-cigarettes is particularly challenging for parents, teachers, and police to detect because the device does not produce the characteristic pungent aroma of smoked cannabis, the researchers reported.
“As e-cigarettes and related devices continue to gain popularity among youth, it will be important to monitor rates of using these products to vaporize cannabis.”
When asked about the findings, Dr. Robert L. DuPont said in an interview that American drug markets are changing rapidly, making more drugs available through highly potent routes of administration such as vaporization.
“This effective and convenient way of delivering THC has much appeal, especially to youth, being new, cool, and smoke-free as the rate of cannabis passes cigarettes for youth,” said Dr. DuPont, president of the Institute for Behavior and Health in Rockville, Md., and the first director of the National Institute on Drug Abuse.
The study was funded by the National Institutes of Health. No conflicts of interest were declared.
FROM PEDIATRICS
Key clinical point: Significant numbers of high school students are using e-cigarettes and vaporizing devices to vaporize cannabis.
Major finding: One in 20 students reported using e-cigarettes to vaporize cannabis, particularly those who had used e-cigarettes or cannabis before.
Data source: An anonymous survey of 3,847 Connecticut high school students.
Disclosures: The study was funded by the National Institutes of Health. No conflicts of interest were declared.
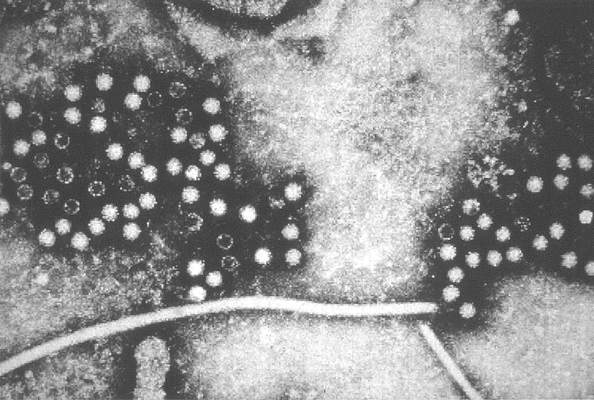
Hepatitis E linked to 1 in 10 liver failure cases in Europe
A significant number of cases of acute liver failure may be caused by the hepatitis E virus, which a new study suggests may not necessarily be identified or excluded using serologic tests.
A retrospective analysis of 80 European patients with acute liver failure or acute hepatitis found that, while 12 patients (15%) tested positive for hepatitis E virus (HEV) IgG antibodies, seven of these patients were negative for IgM antibodies or HEV RNA, according to a study published in Clinical Gastroenterology and Hepatology.
Eight patients (10%) tested positive for HEV RNA, but only four of these were definitely positive for HEV IgG and five for HEV IgM.
Four were initially diagnosed as having idiosyncratic drug-induced liver injury, with other diagnoses being acetaminophen intoxication, amanita intoxication, and Wilson’s disease; one patient who had received a hematopoietic stem cell transplant was initially diagnosed with graft-versus-host disease.
One patient died, two received liver transplants, and the remaining patients survived (Clin Gastro Hepatol. 2015. doi: 10.1016/j.cgh.2015.04.014).
“Our data confirms recent descriptions of cases of severe liver injury in Europe, and underlines the necessity to consider hepatitis E as an underlying or additional cause for ALF [acute liver failure],” wrote Dr. Paul Manka of the University Duisburg-Essen in Essen, Germany, and coauthors.
The study was supported by the Deutsche Forschungsgemeinschaft (German Research Foundation) and by the Wilhelm-Laupitz Foundation. There were no other conflicts of interest declared.
A significant number of cases of acute liver failure may be caused by the hepatitis E virus, which a new study suggests may not necessarily be identified or excluded using serologic tests.
A retrospective analysis of 80 European patients with acute liver failure or acute hepatitis found that, while 12 patients (15%) tested positive for hepatitis E virus (HEV) IgG antibodies, seven of these patients were negative for IgM antibodies or HEV RNA, according to a study published in Clinical Gastroenterology and Hepatology.
Eight patients (10%) tested positive for HEV RNA, but only four of these were definitely positive for HEV IgG and five for HEV IgM.
Four were initially diagnosed as having idiosyncratic drug-induced liver injury, with other diagnoses being acetaminophen intoxication, amanita intoxication, and Wilson’s disease; one patient who had received a hematopoietic stem cell transplant was initially diagnosed with graft-versus-host disease.
One patient died, two received liver transplants, and the remaining patients survived (Clin Gastro Hepatol. 2015. doi: 10.1016/j.cgh.2015.04.014).
“Our data confirms recent descriptions of cases of severe liver injury in Europe, and underlines the necessity to consider hepatitis E as an underlying or additional cause for ALF [acute liver failure],” wrote Dr. Paul Manka of the University Duisburg-Essen in Essen, Germany, and coauthors.
The study was supported by the Deutsche Forschungsgemeinschaft (German Research Foundation) and by the Wilhelm-Laupitz Foundation. There were no other conflicts of interest declared.
A significant number of cases of acute liver failure may be caused by the hepatitis E virus, which a new study suggests may not necessarily be identified or excluded using serologic tests.
A retrospective analysis of 80 European patients with acute liver failure or acute hepatitis found that, while 12 patients (15%) tested positive for hepatitis E virus (HEV) IgG antibodies, seven of these patients were negative for IgM antibodies or HEV RNA, according to a study published in Clinical Gastroenterology and Hepatology.
Eight patients (10%) tested positive for HEV RNA, but only four of these were definitely positive for HEV IgG and five for HEV IgM.
Four were initially diagnosed as having idiosyncratic drug-induced liver injury, with other diagnoses being acetaminophen intoxication, amanita intoxication, and Wilson’s disease; one patient who had received a hematopoietic stem cell transplant was initially diagnosed with graft-versus-host disease.
One patient died, two received liver transplants, and the remaining patients survived (Clin Gastro Hepatol. 2015. doi: 10.1016/j.cgh.2015.04.014).
“Our data confirms recent descriptions of cases of severe liver injury in Europe, and underlines the necessity to consider hepatitis E as an underlying or additional cause for ALF [acute liver failure],” wrote Dr. Paul Manka of the University Duisburg-Essen in Essen, Germany, and coauthors.
The study was supported by the Deutsche Forschungsgemeinschaft (German Research Foundation) and by the Wilhelm-Laupitz Foundation. There were no other conflicts of interest declared.
Key clinical point: A significant number of cases of acute liver failure may be caused by the hepatitis E virus.
Major finding: 10% of patients with acute liver failure or acute hepatitis tested positive for hepatitis E virus RNA.
Data source: A retrospective analysis of 80 patients with acute liver failure or acute hepatitis.
Disclosures: The study was supported by the Deutsche Forschungsgemeinschaft (German Research Foundation) and by the Wilhelm-Laupitz Foundation. There were no other conflicts of interest declared.
Melanoma regression a positive prognostic indicator
Histologic regression in melanoma is associated with a significantly lower risk of sentinel lymph node positivity and may serve as a prognostic factor when deciding whether to perform a sentinel lymph node biopsy, according to a study published online Sept. 2 in JAMA Dermatology.
Researchers conducted a meta-analysis of 14 studies in 10,098 patients who showed histologic regression of a primary melanoma and whose sentinel lymph node status was available. In the 14 studies combined, the analysis showed patients with histologic regression had a 44% lower likelihood of having a positive sentinel lymph node than patients without regression, reported Dr. Simone Ribero of the University of Turin (Italy), and coauthors (JAMA Dermatol. 2015 Sep 2. doi: 10.1001/jamadermatol.2015.2235).
This figure was even lower for patients enrolled in high-quality studies, compared with lower-quality studies, they said. In the nine studies considered high quality, patients with regression had a 52% lower likelihood of having a positive sentinel lymph node, while those enrolled in the five studies considered low quality had a 27% lower likelihood of having a positive sentinel lymph node.
The prognostic significance of regression in primary melanoma has been confounded by the fact that disappearance of part of the tumor can result in an underestimation of the original Breslow thickness. Some previous studies have found an increase in sentinel lymph node positivity associated with regression, while other studies suggested that regression was in fact a protective factor against sentinel lymph node metastasis.
Although the studies used different definitions of histologic regression and all were observational (counted among the limitations of the studies), the authors concluded that regression was prognostically favorable. “The results of this meta-analysis may be useful when deciding to offer SLNB [sentinel lymph node biopsy] to patients with regressions of melanomas,” they wrote, adding: “It may help clinicians make a final selection of the most appropriate patients for this procedure.”
The authors had no conflicts of interest to declare.
The finding that patients with histologic regression have half the risk for micrometastases in sentinel lymph node biopsy, compared with patients without regression gives a clear answer to the question of whether patients with thin melanoma and regression should undergo SLNB, and that answer is “No.”

|
Dr. Claus Garbe |
These findings underline that fact that prognosis of patients with melanoma does not depend only on the characteristics of the tumor itself, such as tumor thickness, ulceration, and mitosis, but also on the immune response of the host.
Dr. Claus Garbe is from the Department of Dermatology, University Hospital Tübingen (Germany). These comments are taken from an accompanying editorial (JAMA Dermatol. 2015 Sep 2. doi: 10.1001/jamadermatol.2015.2235). No conflicts of interest were declared.
The finding that patients with histologic regression have half the risk for micrometastases in sentinel lymph node biopsy, compared with patients without regression gives a clear answer to the question of whether patients with thin melanoma and regression should undergo SLNB, and that answer is “No.”

|
Dr. Claus Garbe |
These findings underline that fact that prognosis of patients with melanoma does not depend only on the characteristics of the tumor itself, such as tumor thickness, ulceration, and mitosis, but also on the immune response of the host.
Dr. Claus Garbe is from the Department of Dermatology, University Hospital Tübingen (Germany). These comments are taken from an accompanying editorial (JAMA Dermatol. 2015 Sep 2. doi: 10.1001/jamadermatol.2015.2235). No conflicts of interest were declared.
The finding that patients with histologic regression have half the risk for micrometastases in sentinel lymph node biopsy, compared with patients without regression gives a clear answer to the question of whether patients with thin melanoma and regression should undergo SLNB, and that answer is “No.”

|
Dr. Claus Garbe |
These findings underline that fact that prognosis of patients with melanoma does not depend only on the characteristics of the tumor itself, such as tumor thickness, ulceration, and mitosis, but also on the immune response of the host.
Dr. Claus Garbe is from the Department of Dermatology, University Hospital Tübingen (Germany). These comments are taken from an accompanying editorial (JAMA Dermatol. 2015 Sep 2. doi: 10.1001/jamadermatol.2015.2235). No conflicts of interest were declared.
Histologic regression in melanoma is associated with a significantly lower risk of sentinel lymph node positivity and may serve as a prognostic factor when deciding whether to perform a sentinel lymph node biopsy, according to a study published online Sept. 2 in JAMA Dermatology.
Researchers conducted a meta-analysis of 14 studies in 10,098 patients who showed histologic regression of a primary melanoma and whose sentinel lymph node status was available. In the 14 studies combined, the analysis showed patients with histologic regression had a 44% lower likelihood of having a positive sentinel lymph node than patients without regression, reported Dr. Simone Ribero of the University of Turin (Italy), and coauthors (JAMA Dermatol. 2015 Sep 2. doi: 10.1001/jamadermatol.2015.2235).
This figure was even lower for patients enrolled in high-quality studies, compared with lower-quality studies, they said. In the nine studies considered high quality, patients with regression had a 52% lower likelihood of having a positive sentinel lymph node, while those enrolled in the five studies considered low quality had a 27% lower likelihood of having a positive sentinel lymph node.
The prognostic significance of regression in primary melanoma has been confounded by the fact that disappearance of part of the tumor can result in an underestimation of the original Breslow thickness. Some previous studies have found an increase in sentinel lymph node positivity associated with regression, while other studies suggested that regression was in fact a protective factor against sentinel lymph node metastasis.
Although the studies used different definitions of histologic regression and all were observational (counted among the limitations of the studies), the authors concluded that regression was prognostically favorable. “The results of this meta-analysis may be useful when deciding to offer SLNB [sentinel lymph node biopsy] to patients with regressions of melanomas,” they wrote, adding: “It may help clinicians make a final selection of the most appropriate patients for this procedure.”
The authors had no conflicts of interest to declare.
Histologic regression in melanoma is associated with a significantly lower risk of sentinel lymph node positivity and may serve as a prognostic factor when deciding whether to perform a sentinel lymph node biopsy, according to a study published online Sept. 2 in JAMA Dermatology.
Researchers conducted a meta-analysis of 14 studies in 10,098 patients who showed histologic regression of a primary melanoma and whose sentinel lymph node status was available. In the 14 studies combined, the analysis showed patients with histologic regression had a 44% lower likelihood of having a positive sentinel lymph node than patients without regression, reported Dr. Simone Ribero of the University of Turin (Italy), and coauthors (JAMA Dermatol. 2015 Sep 2. doi: 10.1001/jamadermatol.2015.2235).
This figure was even lower for patients enrolled in high-quality studies, compared with lower-quality studies, they said. In the nine studies considered high quality, patients with regression had a 52% lower likelihood of having a positive sentinel lymph node, while those enrolled in the five studies considered low quality had a 27% lower likelihood of having a positive sentinel lymph node.
The prognostic significance of regression in primary melanoma has been confounded by the fact that disappearance of part of the tumor can result in an underestimation of the original Breslow thickness. Some previous studies have found an increase in sentinel lymph node positivity associated with regression, while other studies suggested that regression was in fact a protective factor against sentinel lymph node metastasis.
Although the studies used different definitions of histologic regression and all were observational (counted among the limitations of the studies), the authors concluded that regression was prognostically favorable. “The results of this meta-analysis may be useful when deciding to offer SLNB [sentinel lymph node biopsy] to patients with regressions of melanomas,” they wrote, adding: “It may help clinicians make a final selection of the most appropriate patients for this procedure.”
The authors had no conflicts of interest to declare.
FROM JAMA DERMATOLOGY
Key clinical point: Histologic regression in melanoma is associated with a significantly lower risk of sentinel lymph node positivity.
Major finding: Individuals with histologic regression in melanoma had a 44% lower likelihood of having a positive sentinel lymph node than patients without regression.
Data source: A meta-analysis evaluated 14 studies in 10,098 patients.
Disclosures: None of the authors had conflicts of interest to disclose.
Heart attack risk rises in first month after knee, hip arthroplasty
Total knee and hip arthroplasty were associated with a significantly increased risk of myocardial infarction in the first month after surgery, but not at 6 months after surgery, a cohort study showed.
The finding challenges other studies suggesting that total knee or hip arthroplasty surgery reduces the risk of serious cardiovascular events among individuals with osteoarthritis.
Analysis of data from 13,849 British patients who underwent a total knee arthroplasty, 6,063 patients who received total hip arthroplasty, and an equal number of matched controls showed a greater than eightfold increase in the risk of myocardial infarction in the first postoperative month in the knee arthroplasty group (hazard ratio, 8.75), and a fourfold increase in risk in the hip arthroplasty group (HR, 4.33), compared with controls.
However, the hazard ratio declined to insignificance after 6 months, in contrast to the risk of venous thromboembolism – a known complication of arthroplasty – according to a paper published online in the Aug. 31 edition of Arthritis & Rheumatology.
“The major difference between the previous study and ours is that cardiovascular events occurring shortly after total joint arthroplasty were excluded from the previous study,” wrote Na Lu and his colleagues from Boston University.
The study observed 306 cases of myocardial infarction among individuals who underwent total knee arthroplasty and 128 cases in those who underwent total hip arthroplasty (Arthritis Rheumatol. 2015; August 31 [doi:10.1002/art.39246]).
The study was partly support by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. There were no other conflicts of interest declared.
Total knee and hip arthroplasty were associated with a significantly increased risk of myocardial infarction in the first month after surgery, but not at 6 months after surgery, a cohort study showed.
The finding challenges other studies suggesting that total knee or hip arthroplasty surgery reduces the risk of serious cardiovascular events among individuals with osteoarthritis.
Analysis of data from 13,849 British patients who underwent a total knee arthroplasty, 6,063 patients who received total hip arthroplasty, and an equal number of matched controls showed a greater than eightfold increase in the risk of myocardial infarction in the first postoperative month in the knee arthroplasty group (hazard ratio, 8.75), and a fourfold increase in risk in the hip arthroplasty group (HR, 4.33), compared with controls.
However, the hazard ratio declined to insignificance after 6 months, in contrast to the risk of venous thromboembolism – a known complication of arthroplasty – according to a paper published online in the Aug. 31 edition of Arthritis & Rheumatology.
“The major difference between the previous study and ours is that cardiovascular events occurring shortly after total joint arthroplasty were excluded from the previous study,” wrote Na Lu and his colleagues from Boston University.
The study observed 306 cases of myocardial infarction among individuals who underwent total knee arthroplasty and 128 cases in those who underwent total hip arthroplasty (Arthritis Rheumatol. 2015; August 31 [doi:10.1002/art.39246]).
The study was partly support by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. There were no other conflicts of interest declared.
Total knee and hip arthroplasty were associated with a significantly increased risk of myocardial infarction in the first month after surgery, but not at 6 months after surgery, a cohort study showed.
The finding challenges other studies suggesting that total knee or hip arthroplasty surgery reduces the risk of serious cardiovascular events among individuals with osteoarthritis.
Analysis of data from 13,849 British patients who underwent a total knee arthroplasty, 6,063 patients who received total hip arthroplasty, and an equal number of matched controls showed a greater than eightfold increase in the risk of myocardial infarction in the first postoperative month in the knee arthroplasty group (hazard ratio, 8.75), and a fourfold increase in risk in the hip arthroplasty group (HR, 4.33), compared with controls.
However, the hazard ratio declined to insignificance after 6 months, in contrast to the risk of venous thromboembolism – a known complication of arthroplasty – according to a paper published online in the Aug. 31 edition of Arthritis & Rheumatology.
“The major difference between the previous study and ours is that cardiovascular events occurring shortly after total joint arthroplasty were excluded from the previous study,” wrote Na Lu and his colleagues from Boston University.
The study observed 306 cases of myocardial infarction among individuals who underwent total knee arthroplasty and 128 cases in those who underwent total hip arthroplasty (Arthritis Rheumatol. 2015; August 31 [doi:10.1002/art.39246]).
The study was partly support by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. There were no other conflicts of interest declared.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: Total knee and hip arthroplasty were associated with a significantly increased risk of myocardial infarction in the first month after surgery.
Major finding: Patients undergoing total knee arthroplasty have an eightfold increase in the risk of myocardial infarction in the month after surgery.
Data source: Cohort study of 13,849 total knee arthroplasty patients and 6,063 total hip arthroplasty patients and an equal number of matched controls.
Disclosures: The study was partly support by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. There were no conflicts of interest declared.
Topical timolol reduces facial angiofibromas in tuberous sclerosis
Topical beta-blockers could be an alternative to rapamycin for the treatment of angiofibromas after traditional destructive procedures such as ablative laser resurfacing, according to a case study published in the Aug. 24 edition of Pediatrics.
A 26-year-old woman with tuberous sclerosis complex had her facial angiofibromas treated with ablative fractional laser resurfacing and pulsed-dye laser, with topical timolol 0.5% gel applied to one side of her face twice a day for 2 weeks presurgery and from day 5 after surgery.
At 4 months, there was markedly reduced erythema, and a reduced number and size of angiofibromas on the timolol-treated cheek, compared with the untreated cheek (Pediatrics 2015 Aug 24. [doi: 10.1542/peds.2015-0025]).
“Because angiofibromas are known to contain a highly vascular component expressing angiogenic factors such as VEGF [vascular endothelial growth factor], it is likely the patient’s right cheek improved due to the antiangiogenic and proapoptotic effects of the topically administered beta-blocker,” wrote Dr. Andrew C. Krakowski of the University of California, San Diego, and Tuyet A. Nguyen of the Rady Children’s Hospital, San Diego.
An ideal treatment for angiofibromas remains elusive, with destructive treatments such as cryotherapy, dermabrasion, and radiofrequency or laser ablation associated with complications such as pain, postoperative hyperpigmentation, and scarring, and topical rapamycin being of limited accessibility because of cost and availability.
“Consequently, beta-blockers could prove a useful adjuvant to rapamycin and more traditional directly destructive procedures,” the authors wrote.
Dr. Krakowski and Ms. Nguyen said they had no financial disclosures.
Topical beta-blockers could be an alternative to rapamycin for the treatment of angiofibromas after traditional destructive procedures such as ablative laser resurfacing, according to a case study published in the Aug. 24 edition of Pediatrics.
A 26-year-old woman with tuberous sclerosis complex had her facial angiofibromas treated with ablative fractional laser resurfacing and pulsed-dye laser, with topical timolol 0.5% gel applied to one side of her face twice a day for 2 weeks presurgery and from day 5 after surgery.
At 4 months, there was markedly reduced erythema, and a reduced number and size of angiofibromas on the timolol-treated cheek, compared with the untreated cheek (Pediatrics 2015 Aug 24. [doi: 10.1542/peds.2015-0025]).
“Because angiofibromas are known to contain a highly vascular component expressing angiogenic factors such as VEGF [vascular endothelial growth factor], it is likely the patient’s right cheek improved due to the antiangiogenic and proapoptotic effects of the topically administered beta-blocker,” wrote Dr. Andrew C. Krakowski of the University of California, San Diego, and Tuyet A. Nguyen of the Rady Children’s Hospital, San Diego.
An ideal treatment for angiofibromas remains elusive, with destructive treatments such as cryotherapy, dermabrasion, and radiofrequency or laser ablation associated with complications such as pain, postoperative hyperpigmentation, and scarring, and topical rapamycin being of limited accessibility because of cost and availability.
“Consequently, beta-blockers could prove a useful adjuvant to rapamycin and more traditional directly destructive procedures,” the authors wrote.
Dr. Krakowski and Ms. Nguyen said they had no financial disclosures.
Topical beta-blockers could be an alternative to rapamycin for the treatment of angiofibromas after traditional destructive procedures such as ablative laser resurfacing, according to a case study published in the Aug. 24 edition of Pediatrics.
A 26-year-old woman with tuberous sclerosis complex had her facial angiofibromas treated with ablative fractional laser resurfacing and pulsed-dye laser, with topical timolol 0.5% gel applied to one side of her face twice a day for 2 weeks presurgery and from day 5 after surgery.
At 4 months, there was markedly reduced erythema, and a reduced number and size of angiofibromas on the timolol-treated cheek, compared with the untreated cheek (Pediatrics 2015 Aug 24. [doi: 10.1542/peds.2015-0025]).
“Because angiofibromas are known to contain a highly vascular component expressing angiogenic factors such as VEGF [vascular endothelial growth factor], it is likely the patient’s right cheek improved due to the antiangiogenic and proapoptotic effects of the topically administered beta-blocker,” wrote Dr. Andrew C. Krakowski of the University of California, San Diego, and Tuyet A. Nguyen of the Rady Children’s Hospital, San Diego.
An ideal treatment for angiofibromas remains elusive, with destructive treatments such as cryotherapy, dermabrasion, and radiofrequency or laser ablation associated with complications such as pain, postoperative hyperpigmentation, and scarring, and topical rapamycin being of limited accessibility because of cost and availability.
“Consequently, beta-blockers could prove a useful adjuvant to rapamycin and more traditional directly destructive procedures,” the authors wrote.
Dr. Krakowski and Ms. Nguyen said they had no financial disclosures.
FROM PEDIATRICS
Key clinical point: Topical beta-blockers could be an alternative to rapamycin for the treatment of angiofibromas after traditional destructive procedures.
Major finding: Treatment with topical timolol after laser resurfacing significantly reduced erythema and the number and size of angiofibromas in a woman with tuberous sclerosis complex.
Data source: A case study 26-year-old woman with tuberous sclerosis complex.
Disclosures: Dr. Krakowski and Ms. Nguyen said they had no financial disclosures.
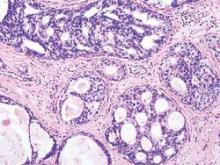
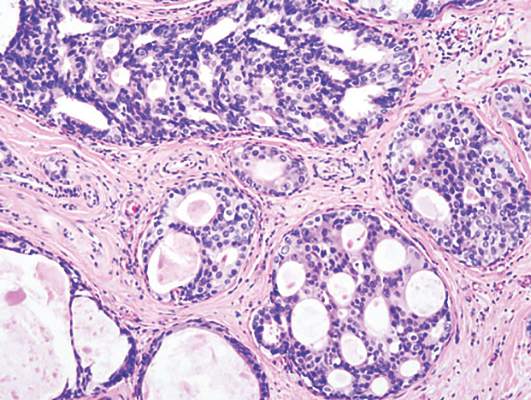
Reduced invasive recurrence after DCIS does not reduce mortality
Radiotherapy after breast-conserving surgery for ductal carcinoma in situ reduces the risk of ipsilateral invasive recurrence but does not reduce breast cancer mortality, new research shows.
Analysis of data from 108,196 women diagnosed with ductal carcinoma in situ (DCIS), who were included in the Surveillance, Epidemiology, and End Results (SEER) 18 registries database, showed radiotherapy significantly reduced the risk of ipsilateral invasive recurrence at 10 years (adjusted hazard, 0.47; 95% confidence interval, 0.42-0.53; P less than .001) but only achieved a nonsignificant reduction in breast cancer mortality (adjusted HR, 0.81; 95% CI, 0.63-1.04; P = .10).
“The finding of greatest clinical importance was that prevention of ipsilateral invasive recurrence did not prevent death from breast cancer,” wrote Dr. Steven A. Narod and his colleagues from the Women’s College Hospital and the University of Toronto.
Though it is often stated that DCIS is a preinvasive neoplastic lesion that is not lethal in itself, these results suggest that this interpretation should be revisited, they said in the report, published online August 20 in JAMA Oncology.
“Some cases of DCIS have an inherent potential for distant metastatic spread. It is therefore appropriate to consider these as de facto breast cancers and not as preinvasive markers predictive of a subsequent invasive cancer,” they said.
The mean age at diagnosis of DCIS for the women in the database was 53.8 (range, 15-69) years, and the mean duration of follow-up was 7.5 (range, 0-23.9) years. Overall, the 20-year breast cancer–specific mortality rate following a diagnosis of DCIS was 3.3% (95% CI, 3.0%-3.6%).
Just over 1% of the 42,250 women treated with lumpectomy and radiotherapy developed an ipsilateral invasive recurrence in the follow-up period and 163 women (0.4%) died of breast cancer. Of the 19,762 women who were treated with lumpectomy without radiotherapy, 595 women (3%) developed an ipsilateral invasive recurrence and 102 women (0.5%) died of breast cancer, Dr. Narod and his associates reported (JAMA Oncology. 2015 Aug. 20 doi: 10.1001/jamaoncol.2015.2510).
Among the 956 women who died of breast cancer in the follow-up period, over half (517) did not experience an in-breast invasive recurrence prior to death. Of the 163 women who were treated with lumpectomy and radiotherapy and then died of breast cancer, 57.7% (94) did not experience an in-breast invasive recurrence prior to death. Among the 102 women treated with lumpectomy without radiotherapy who died of breast cancer, 51 did not experience an in-breast invasive recurrence prior to death (50.0%). Among the 154 women treated with a mastectomy (unilateral or bilateral) who died of breast cancer, 112 did not experience an in-breast invasive recurrence prior to death (72.7%), the investigators reported.
They found that young age at diagnosis and black ethnicity were predictors of breast cancer mortality. Young women diagnosed with ductal carcinoma in situ before the age of 35 years had a more than twofold greater risk of dying from breast cancer than older women (7.8% vs. 3.2%; HR 2.58, 95% CI, 1.85-3.60; P less than .001). Black women also had a much greater risk of dying from breast cancer than non-Hispanic whites (7.0% vs. 3.0%; HR, 2.55, 95% CI, 2.17-3.01; P less than .001).
“If DCIS were truly a (noninvasive) precursor of breast cancer, then a woman with DCIS should not die of breast cancer without first experiencing an invasive breast cancer (ipsilateral or contralateral), and the prevention of an invasive recurrence should prevent her death from breast cancer. Surprisingly, the majority of women with DCIS in the cohort who died of breast cancer did not experience an invasive in-breast recurrence (ipsilateral or contralateral) prior to death (54.1%),” the investigators said.
“The outcome of breast cancer mortality for DCIS patients is of importance in itself and potential treatments that affect mortality are deserving of study,” they concluded.
No relevant conflicts of interest were declared.
The analysis by Dr. Narod and his associates fuels a growing concern that we should rethink our strategy for the detection and treatment of DCIS. Given the low breast cancer mortality risk, we should stop telling women that DCIS is an emergency and that they should schedule definitive surgery within 2 weeks of diagnosis. For the lowest-risk lesions, observation and prevention interventions alone should be tested. High-risk lesions (such as HER2 positive, those in patients aged less than 40 years, hormone-receptor negative, large size) should still be aggressively treated, but this analysis suggests that our current approach of surgical removal and radiation therapy may not suffice for the rare cases that lead to breast cancer mortality, so new approaches are needed.
We should continue to better understand the biological characteristics of the highest-risk DCIS and test targeted approaches to reduce death from breast cancer.
Dr. Laura Esserman and Christina Yau, Ph.D., are with the department of surgery at the University of California, San Francisco. These comments were taken from an accompanying editorial (JAMA Oncology. 2015 Aug. 20 doi: 10.1001/jamaoncol.2015.2607). No conflicts of interest were declared.
The analysis by Dr. Narod and his associates fuels a growing concern that we should rethink our strategy for the detection and treatment of DCIS. Given the low breast cancer mortality risk, we should stop telling women that DCIS is an emergency and that they should schedule definitive surgery within 2 weeks of diagnosis. For the lowest-risk lesions, observation and prevention interventions alone should be tested. High-risk lesions (such as HER2 positive, those in patients aged less than 40 years, hormone-receptor negative, large size) should still be aggressively treated, but this analysis suggests that our current approach of surgical removal and radiation therapy may not suffice for the rare cases that lead to breast cancer mortality, so new approaches are needed.
We should continue to better understand the biological characteristics of the highest-risk DCIS and test targeted approaches to reduce death from breast cancer.
Dr. Laura Esserman and Christina Yau, Ph.D., are with the department of surgery at the University of California, San Francisco. These comments were taken from an accompanying editorial (JAMA Oncology. 2015 Aug. 20 doi: 10.1001/jamaoncol.2015.2607). No conflicts of interest were declared.
The analysis by Dr. Narod and his associates fuels a growing concern that we should rethink our strategy for the detection and treatment of DCIS. Given the low breast cancer mortality risk, we should stop telling women that DCIS is an emergency and that they should schedule definitive surgery within 2 weeks of diagnosis. For the lowest-risk lesions, observation and prevention interventions alone should be tested. High-risk lesions (such as HER2 positive, those in patients aged less than 40 years, hormone-receptor negative, large size) should still be aggressively treated, but this analysis suggests that our current approach of surgical removal and radiation therapy may not suffice for the rare cases that lead to breast cancer mortality, so new approaches are needed.
We should continue to better understand the biological characteristics of the highest-risk DCIS and test targeted approaches to reduce death from breast cancer.
Dr. Laura Esserman and Christina Yau, Ph.D., are with the department of surgery at the University of California, San Francisco. These comments were taken from an accompanying editorial (JAMA Oncology. 2015 Aug. 20 doi: 10.1001/jamaoncol.2015.2607). No conflicts of interest were declared.
Radiotherapy after breast-conserving surgery for ductal carcinoma in situ reduces the risk of ipsilateral invasive recurrence but does not reduce breast cancer mortality, new research shows.
Analysis of data from 108,196 women diagnosed with ductal carcinoma in situ (DCIS), who were included in the Surveillance, Epidemiology, and End Results (SEER) 18 registries database, showed radiotherapy significantly reduced the risk of ipsilateral invasive recurrence at 10 years (adjusted hazard, 0.47; 95% confidence interval, 0.42-0.53; P less than .001) but only achieved a nonsignificant reduction in breast cancer mortality (adjusted HR, 0.81; 95% CI, 0.63-1.04; P = .10).
“The finding of greatest clinical importance was that prevention of ipsilateral invasive recurrence did not prevent death from breast cancer,” wrote Dr. Steven A. Narod and his colleagues from the Women’s College Hospital and the University of Toronto.
Though it is often stated that DCIS is a preinvasive neoplastic lesion that is not lethal in itself, these results suggest that this interpretation should be revisited, they said in the report, published online August 20 in JAMA Oncology.
“Some cases of DCIS have an inherent potential for distant metastatic spread. It is therefore appropriate to consider these as de facto breast cancers and not as preinvasive markers predictive of a subsequent invasive cancer,” they said.
The mean age at diagnosis of DCIS for the women in the database was 53.8 (range, 15-69) years, and the mean duration of follow-up was 7.5 (range, 0-23.9) years. Overall, the 20-year breast cancer–specific mortality rate following a diagnosis of DCIS was 3.3% (95% CI, 3.0%-3.6%).
Just over 1% of the 42,250 women treated with lumpectomy and radiotherapy developed an ipsilateral invasive recurrence in the follow-up period and 163 women (0.4%) died of breast cancer. Of the 19,762 women who were treated with lumpectomy without radiotherapy, 595 women (3%) developed an ipsilateral invasive recurrence and 102 women (0.5%) died of breast cancer, Dr. Narod and his associates reported (JAMA Oncology. 2015 Aug. 20 doi: 10.1001/jamaoncol.2015.2510).
Among the 956 women who died of breast cancer in the follow-up period, over half (517) did not experience an in-breast invasive recurrence prior to death. Of the 163 women who were treated with lumpectomy and radiotherapy and then died of breast cancer, 57.7% (94) did not experience an in-breast invasive recurrence prior to death. Among the 102 women treated with lumpectomy without radiotherapy who died of breast cancer, 51 did not experience an in-breast invasive recurrence prior to death (50.0%). Among the 154 women treated with a mastectomy (unilateral or bilateral) who died of breast cancer, 112 did not experience an in-breast invasive recurrence prior to death (72.7%), the investigators reported.
They found that young age at diagnosis and black ethnicity were predictors of breast cancer mortality. Young women diagnosed with ductal carcinoma in situ before the age of 35 years had a more than twofold greater risk of dying from breast cancer than older women (7.8% vs. 3.2%; HR 2.58, 95% CI, 1.85-3.60; P less than .001). Black women also had a much greater risk of dying from breast cancer than non-Hispanic whites (7.0% vs. 3.0%; HR, 2.55, 95% CI, 2.17-3.01; P less than .001).
“If DCIS were truly a (noninvasive) precursor of breast cancer, then a woman with DCIS should not die of breast cancer without first experiencing an invasive breast cancer (ipsilateral or contralateral), and the prevention of an invasive recurrence should prevent her death from breast cancer. Surprisingly, the majority of women with DCIS in the cohort who died of breast cancer did not experience an invasive in-breast recurrence (ipsilateral or contralateral) prior to death (54.1%),” the investigators said.
“The outcome of breast cancer mortality for DCIS patients is of importance in itself and potential treatments that affect mortality are deserving of study,” they concluded.
No relevant conflicts of interest were declared.
Radiotherapy after breast-conserving surgery for ductal carcinoma in situ reduces the risk of ipsilateral invasive recurrence but does not reduce breast cancer mortality, new research shows.
Analysis of data from 108,196 women diagnosed with ductal carcinoma in situ (DCIS), who were included in the Surveillance, Epidemiology, and End Results (SEER) 18 registries database, showed radiotherapy significantly reduced the risk of ipsilateral invasive recurrence at 10 years (adjusted hazard, 0.47; 95% confidence interval, 0.42-0.53; P less than .001) but only achieved a nonsignificant reduction in breast cancer mortality (adjusted HR, 0.81; 95% CI, 0.63-1.04; P = .10).
“The finding of greatest clinical importance was that prevention of ipsilateral invasive recurrence did not prevent death from breast cancer,” wrote Dr. Steven A. Narod and his colleagues from the Women’s College Hospital and the University of Toronto.
Though it is often stated that DCIS is a preinvasive neoplastic lesion that is not lethal in itself, these results suggest that this interpretation should be revisited, they said in the report, published online August 20 in JAMA Oncology.
“Some cases of DCIS have an inherent potential for distant metastatic spread. It is therefore appropriate to consider these as de facto breast cancers and not as preinvasive markers predictive of a subsequent invasive cancer,” they said.
The mean age at diagnosis of DCIS for the women in the database was 53.8 (range, 15-69) years, and the mean duration of follow-up was 7.5 (range, 0-23.9) years. Overall, the 20-year breast cancer–specific mortality rate following a diagnosis of DCIS was 3.3% (95% CI, 3.0%-3.6%).
Just over 1% of the 42,250 women treated with lumpectomy and radiotherapy developed an ipsilateral invasive recurrence in the follow-up period and 163 women (0.4%) died of breast cancer. Of the 19,762 women who were treated with lumpectomy without radiotherapy, 595 women (3%) developed an ipsilateral invasive recurrence and 102 women (0.5%) died of breast cancer, Dr. Narod and his associates reported (JAMA Oncology. 2015 Aug. 20 doi: 10.1001/jamaoncol.2015.2510).
Among the 956 women who died of breast cancer in the follow-up period, over half (517) did not experience an in-breast invasive recurrence prior to death. Of the 163 women who were treated with lumpectomy and radiotherapy and then died of breast cancer, 57.7% (94) did not experience an in-breast invasive recurrence prior to death. Among the 102 women treated with lumpectomy without radiotherapy who died of breast cancer, 51 did not experience an in-breast invasive recurrence prior to death (50.0%). Among the 154 women treated with a mastectomy (unilateral or bilateral) who died of breast cancer, 112 did not experience an in-breast invasive recurrence prior to death (72.7%), the investigators reported.
They found that young age at diagnosis and black ethnicity were predictors of breast cancer mortality. Young women diagnosed with ductal carcinoma in situ before the age of 35 years had a more than twofold greater risk of dying from breast cancer than older women (7.8% vs. 3.2%; HR 2.58, 95% CI, 1.85-3.60; P less than .001). Black women also had a much greater risk of dying from breast cancer than non-Hispanic whites (7.0% vs. 3.0%; HR, 2.55, 95% CI, 2.17-3.01; P less than .001).
“If DCIS were truly a (noninvasive) precursor of breast cancer, then a woman with DCIS should not die of breast cancer without first experiencing an invasive breast cancer (ipsilateral or contralateral), and the prevention of an invasive recurrence should prevent her death from breast cancer. Surprisingly, the majority of women with DCIS in the cohort who died of breast cancer did not experience an invasive in-breast recurrence (ipsilateral or contralateral) prior to death (54.1%),” the investigators said.
“The outcome of breast cancer mortality for DCIS patients is of importance in itself and potential treatments that affect mortality are deserving of study,” they concluded.
No relevant conflicts of interest were declared.
FROM JAMA ONCOLOGY
Key clinical point: Radiotherapy after ductal carcinoma in situ reduces the risk of ipsilateral invasive recurrence but does not reduce breast cancer mortality.
Major finding: Radiotherapy after DCIS halves the risk of recurrence but does not significantly impact the risk of death from breast cancer.
Data source: Observational study of data from 108,196 women diagnosed with ductal carcinoma in situ in the SEER18 registries.
Disclosures: No conflicts of interest were declared.