User login
Very-low-volume vascular surgery practice linked to worse outcomes
The very-low-volume practice of surgeons performing no more than one open abdominal aortic aneurysm repair (OAR) or carotid endarterectomy (CEA) per year has persisted in New York State and was associated with worse postoperative outcomes and longer lengths of stay in a cohort study of statewide hospital data.
The study examined inpatient data on elective OARs and CEAs performed from 2000 to 2014 in every hospital in the state.
While the numbers and proportions of very-low-volume surgeons decreased (44.6%-23% for OAR and 35.2%-18.1% for CEA) and the number of procedures performed by these surgeons also decreased (QAR, 346-47; CEA, 395-90), the data are “concerning” and elucidate the “persistence” of very-low-volume practice in open vascular surgery, said Jialin Mao, MD, of Cornell University, New York, and associates (JAMA Surg. doi: 10:1001/jamasurg.2017.1100).
Very-low-volume surgeons were significantly less likely to be vascular surgeons, compared with higher-volume surgeons for both OAR (23.9% vs. 63.9%) and CEA (14.6% vs. 51.7%), they reported.
Compared with patients treated by higher-volume surgeons, those whose OAR was performed by very-low-volume surgeons had a twofold higher risk of postoperative death (6.7% vs. 3.5%) after adjusting for patient risk factors, surgeon specialty, and facility characteristics. Patients of very-low-volume surgeons also had significantly higher odds of sepsis or shock (odds ratio, 1.45), prolonged length of stay (OR, 1.37) and 30-day readmission (OR, 1.19), although the latter was not significant.
Similarly, patients whose CEA was performed by very-low-volume surgeons had a significant 1.8-fold higher odds of experiencing postoperative acute myocardial infarction (1.5% vs. 0.5%) and stroke (3.5% vs. 2.1%). They also were significantly more likely to have 30-day readmission (OR, 1.30).
With both procedures, patients treated by very-low-volume surgeons tended to be younger and healthier (less likely to have two or more comorbidities). They also were more likely to be nonwhite or insured by Medicaid.
“It is reasonable to speculate,” the researchers wrote, “that those treated by very-low-volume surgeons were more likely to be socioeconomically disadvantaged.”
Notably, 30% of the very-low-volume practice occurred in New York City, “where accessibility to high-volume practitioners should generally be higher,” they said.
The findings “indicate the need to eliminate this type of practice, to restrict the practice of these very-low-volume surgeons or to force referrals to higher-volume and specialized surgeons, and to improve disparity in access to high-quality care for all patients,” they said.
The study was funded in part by the U.S. Food and Drug Administration. The researchers reported having no relevant conflicts of interest.
The delineation of a threshold number of cases of OAR and CEA below which surgeons should not be credentialed remains unclear, despite much discussion of the volume-outcome relationship in vascular surgery.
In the current endovascular era, OAR in particular has become increasingly less frequent, with a dramatic effect on trainee experiences. It is often proposed that these cases be limited to high-volume surgeons. Some are concerned, however, that this action will leave rural surgeons unprepared to deal with ruptured abdominal aortic aneurysm and will force patients to travel long distances.
Sarah E. Deery, MD, and Marc L. Schermerhorn, MD, are in the division of vascular and endovascular surgery at Beth Israel Deaconess Medical Center in Boston. These remarks are adapted from an editorial accompanying the study. They reported having no disclosures.
The delineation of a threshold number of cases of OAR and CEA below which surgeons should not be credentialed remains unclear, despite much discussion of the volume-outcome relationship in vascular surgery.
In the current endovascular era, OAR in particular has become increasingly less frequent, with a dramatic effect on trainee experiences. It is often proposed that these cases be limited to high-volume surgeons. Some are concerned, however, that this action will leave rural surgeons unprepared to deal with ruptured abdominal aortic aneurysm and will force patients to travel long distances.
Sarah E. Deery, MD, and Marc L. Schermerhorn, MD, are in the division of vascular and endovascular surgery at Beth Israel Deaconess Medical Center in Boston. These remarks are adapted from an editorial accompanying the study. They reported having no disclosures.
The delineation of a threshold number of cases of OAR and CEA below which surgeons should not be credentialed remains unclear, despite much discussion of the volume-outcome relationship in vascular surgery.
In the current endovascular era, OAR in particular has become increasingly less frequent, with a dramatic effect on trainee experiences. It is often proposed that these cases be limited to high-volume surgeons. Some are concerned, however, that this action will leave rural surgeons unprepared to deal with ruptured abdominal aortic aneurysm and will force patients to travel long distances.
Sarah E. Deery, MD, and Marc L. Schermerhorn, MD, are in the division of vascular and endovascular surgery at Beth Israel Deaconess Medical Center in Boston. These remarks are adapted from an editorial accompanying the study. They reported having no disclosures.
The very-low-volume practice of surgeons performing no more than one open abdominal aortic aneurysm repair (OAR) or carotid endarterectomy (CEA) per year has persisted in New York State and was associated with worse postoperative outcomes and longer lengths of stay in a cohort study of statewide hospital data.
The study examined inpatient data on elective OARs and CEAs performed from 2000 to 2014 in every hospital in the state.
While the numbers and proportions of very-low-volume surgeons decreased (44.6%-23% for OAR and 35.2%-18.1% for CEA) and the number of procedures performed by these surgeons also decreased (QAR, 346-47; CEA, 395-90), the data are “concerning” and elucidate the “persistence” of very-low-volume practice in open vascular surgery, said Jialin Mao, MD, of Cornell University, New York, and associates (JAMA Surg. doi: 10:1001/jamasurg.2017.1100).
Very-low-volume surgeons were significantly less likely to be vascular surgeons, compared with higher-volume surgeons for both OAR (23.9% vs. 63.9%) and CEA (14.6% vs. 51.7%), they reported.
Compared with patients treated by higher-volume surgeons, those whose OAR was performed by very-low-volume surgeons had a twofold higher risk of postoperative death (6.7% vs. 3.5%) after adjusting for patient risk factors, surgeon specialty, and facility characteristics. Patients of very-low-volume surgeons also had significantly higher odds of sepsis or shock (odds ratio, 1.45), prolonged length of stay (OR, 1.37) and 30-day readmission (OR, 1.19), although the latter was not significant.
Similarly, patients whose CEA was performed by very-low-volume surgeons had a significant 1.8-fold higher odds of experiencing postoperative acute myocardial infarction (1.5% vs. 0.5%) and stroke (3.5% vs. 2.1%). They also were significantly more likely to have 30-day readmission (OR, 1.30).
With both procedures, patients treated by very-low-volume surgeons tended to be younger and healthier (less likely to have two or more comorbidities). They also were more likely to be nonwhite or insured by Medicaid.
“It is reasonable to speculate,” the researchers wrote, “that those treated by very-low-volume surgeons were more likely to be socioeconomically disadvantaged.”
Notably, 30% of the very-low-volume practice occurred in New York City, “where accessibility to high-volume practitioners should generally be higher,” they said.
The findings “indicate the need to eliminate this type of practice, to restrict the practice of these very-low-volume surgeons or to force referrals to higher-volume and specialized surgeons, and to improve disparity in access to high-quality care for all patients,” they said.
The study was funded in part by the U.S. Food and Drug Administration. The researchers reported having no relevant conflicts of interest.
The very-low-volume practice of surgeons performing no more than one open abdominal aortic aneurysm repair (OAR) or carotid endarterectomy (CEA) per year has persisted in New York State and was associated with worse postoperative outcomes and longer lengths of stay in a cohort study of statewide hospital data.
The study examined inpatient data on elective OARs and CEAs performed from 2000 to 2014 in every hospital in the state.
While the numbers and proportions of very-low-volume surgeons decreased (44.6%-23% for OAR and 35.2%-18.1% for CEA) and the number of procedures performed by these surgeons also decreased (QAR, 346-47; CEA, 395-90), the data are “concerning” and elucidate the “persistence” of very-low-volume practice in open vascular surgery, said Jialin Mao, MD, of Cornell University, New York, and associates (JAMA Surg. doi: 10:1001/jamasurg.2017.1100).
Very-low-volume surgeons were significantly less likely to be vascular surgeons, compared with higher-volume surgeons for both OAR (23.9% vs. 63.9%) and CEA (14.6% vs. 51.7%), they reported.
Compared with patients treated by higher-volume surgeons, those whose OAR was performed by very-low-volume surgeons had a twofold higher risk of postoperative death (6.7% vs. 3.5%) after adjusting for patient risk factors, surgeon specialty, and facility characteristics. Patients of very-low-volume surgeons also had significantly higher odds of sepsis or shock (odds ratio, 1.45), prolonged length of stay (OR, 1.37) and 30-day readmission (OR, 1.19), although the latter was not significant.
Similarly, patients whose CEA was performed by very-low-volume surgeons had a significant 1.8-fold higher odds of experiencing postoperative acute myocardial infarction (1.5% vs. 0.5%) and stroke (3.5% vs. 2.1%). They also were significantly more likely to have 30-day readmission (OR, 1.30).
With both procedures, patients treated by very-low-volume surgeons tended to be younger and healthier (less likely to have two or more comorbidities). They also were more likely to be nonwhite or insured by Medicaid.
“It is reasonable to speculate,” the researchers wrote, “that those treated by very-low-volume surgeons were more likely to be socioeconomically disadvantaged.”
Notably, 30% of the very-low-volume practice occurred in New York City, “where accessibility to high-volume practitioners should generally be higher,” they said.
The findings “indicate the need to eliminate this type of practice, to restrict the practice of these very-low-volume surgeons or to force referrals to higher-volume and specialized surgeons, and to improve disparity in access to high-quality care for all patients,” they said.
The study was funded in part by the U.S. Food and Drug Administration. The researchers reported having no relevant conflicts of interest.
FROM JAMA SURGERY
Key clinical point: The very-low-volume practice of open abdominal aortic aneurysm repair and carotid endarterectomy (one or fewer annual procedures) is associated with worse postoperative outcomes and greater length of stay.
Major finding: Patients whose procedure was performed by very-low-volume surgeons had a twofold higher risk of postoperative death after OAR or 1.8-fold higher odds of experiencing postoperative acute myocardial infarction or stroke after CEA.
Data source: The study was funded in part by the U.S. Food and Drug Administration.
Disclosures: The researchers reported having no relevant conflicts of interest.
Spotlight shifts to active treatment for concussions
The prevailing notion that concussions should be managed solely or primarily with prescribed cognitive and physical rest is shifting.
Experts in concussion management are increasingly in agreement that concussion is a much more heterogeneous injury than previously believed, and that “active” approaches targeting specific symptoms and impairments can be initiated early and may improve recovery for patients who have concussions from sports as well as from falls, motor vehicle accidents, or other accidents.
Evidence for such active approaches to rehabilitation – including vestibular, vision, and behavioral therapies, and submaximal aerobic training – is deemed “preliminary” by experts and comes from small, mostly single-center studies.
“There’s emerging evidence that strict or prolonged rest is not good, and there’s emerging consensus that we need to start looking at concussion subtypes” and then target treatments to those clinical profiles, he said. “We’re at the cusp of dramatic changes [in management].”
An article published recently in Neurosurgery and coauthored by several dozen concussion experts details 16 “statements of agreement” on targeted evaluation and active management. The experts – from neuropsychology, sports medicine, neurology and neurosurgery, athletic training, and other fields – convened in Pittsburgh in late 2015 at the invitation of Michael W. Collins, PhD, and his colleagues at the University of Pittsburgh Medical Center (UPMC), where the Sports Medicine Concussion Program was established in 2000 (Neurosurgery. 2016 Dec;79[6]:912-29).
Thus far, guidelines and statements on concussion in sport have advised a rest-based approach to management that’s dependent on the spontaneous resolution of symptoms. In some documents, rest is recommended until patients are asymptomatic. Other statements mention the possibility of symptom-based approaches after initial rest, but offer little if any guidance.
The theory of prescribed rest has been twofold, driven both by concern about re-injury in sport and by the belief that cognitive and physical activity can exacerbate symptoms and concussion-associated impairments, thus prolonging recovery, the Pittsburgh paper says.
However, “avoiding contact during the vulnerable period after concussion and prescribed rest represent two separate strategies,” the experts wrote. Avoiding contact “is always recommended to avoid further head impacts,” they say, but monitored activity does not appear to worsen injury.
Recent research suggests, moreover, that prolonged physical and cognitive rest – not activity – is associated with increased symptoms and delayed recovery. And strict rest – avoidance of nearly all brain stimulation – is “not empirically supported ... and may have unintended adverse effects,” the experts wrote.
Physicians and others “have to avoid treating concussion as a punishment,” said Dr. Halstead of St. Louis Children’s Hospital in Chesterfield, Mo., who coauthored a recent editorial entitled “Rethinking Cognitive Rest” (Br J Sports Med. 2017;51:147).
“It’s been taken to the extreme. When we talk about not texting or not going out or not doing anything physically active until you’re without symptoms ... students can develop symptoms of depression and anxiety that then just complicate the injury altogether,” he said.
Physicians also need to dig beneath symptom checklists and perform multidomain assessments to better understand root contributors of symptoms that, without active treatment, can persist for weeks upon weeks in some patients. “There could be neck injuries, sleep issues, vestibular issues, oculomotor issues” and different types of headache, Dr. Halstead said. “If we can identify these things, we can actually be doing rehabilitation to fix these injuries.”
At UPMC’s Sports Medicine Concussion Program, concussions are generally categorized into six clinical profiles – vestibular, ocular-motor, cognitive/fatigue, posttraumatic migraine, cervical, and anxiety/mood. The profiles are not mutually exclusive, but each drives particular rehabilitation recommendations. Clinicians at other concussion programs and centers are similarly attempting to classify concussions.
“We still need to come to agreement as to what exactly the clinical profiles are,” said UPMC’s Dr. Collins, who directs the concussion program and is the lead author of the Neurosurgery paper. “But I think the big concept to come out of our meeting is that we now agree there are different profiles and that we have to match treatment.”
Additional research is needed to determine and validate concussion clinical profiles, to identify biomarkers to assess recovery and determine the effectiveness of treatments, and to determine the best timing of specific active treatments, he and his coauthors said.
Applying individualized and active treatments after concussion is consistent with approaches taken for other injuries and conditions, noted Dr. Hainline, who attended both the UPMC conference and the 5th International Conference on Concussion in Sport.
“It’s rare that prolonged rest is the answer. Look at stroke – you don’t have patients resting indefinitely. You have to get their nervous systems re-engaged,” he said.
“If you keep [concussion] patients with predominantly vestibular symptoms at rest [for example], the vestibular symptoms can become more centralized, and that then becomes the behavior of the nervous system,” he said. “Another example is convergence insufficiencies – if you keep resting [the vision system] and don’t rehabilitate it,” symptoms perpetuate.
Prolonged rest also may lead to deconditioning that lowers tolerance for physical activity. Randomized clinical trials are needed to compare the benefits of physical rest with those of more physically active treatments, but “emerging clinical research” suggests that exposing patients to supervised low-level physical activity (for example, submaximal aerobic training) after an initial period of rest is “not only safe but effective,” the Pittsburgh conference paper says.
The Pittsburgh conference paper “rang a bell with me,” Dr. Wergin said. “Rest is still important, but prolonged rest may not be best for all patients, and maybe it’s possible to do some interventions. We need to stay tuned as we get more of an evidence base.”
The conference – coined the TEAM (for targeted evaluation and active management) Approaches to Treating Concussion Meeting – was attended by staff from the National Institutes of Health, the Centers for Disease Control and Prevention, the Department of Defense, and the National Football League (NFL) and other sporting organizations, Dr. Collins said. It was sponsored by UPMC and the NFL. Coauthors reported numerous disclosures, including various advising and consulting roles with the NFL.
The prevailing notion that concussions should be managed solely or primarily with prescribed cognitive and physical rest is shifting.
Experts in concussion management are increasingly in agreement that concussion is a much more heterogeneous injury than previously believed, and that “active” approaches targeting specific symptoms and impairments can be initiated early and may improve recovery for patients who have concussions from sports as well as from falls, motor vehicle accidents, or other accidents.
Evidence for such active approaches to rehabilitation – including vestibular, vision, and behavioral therapies, and submaximal aerobic training – is deemed “preliminary” by experts and comes from small, mostly single-center studies.
“There’s emerging evidence that strict or prolonged rest is not good, and there’s emerging consensus that we need to start looking at concussion subtypes” and then target treatments to those clinical profiles, he said. “We’re at the cusp of dramatic changes [in management].”
An article published recently in Neurosurgery and coauthored by several dozen concussion experts details 16 “statements of agreement” on targeted evaluation and active management. The experts – from neuropsychology, sports medicine, neurology and neurosurgery, athletic training, and other fields – convened in Pittsburgh in late 2015 at the invitation of Michael W. Collins, PhD, and his colleagues at the University of Pittsburgh Medical Center (UPMC), where the Sports Medicine Concussion Program was established in 2000 (Neurosurgery. 2016 Dec;79[6]:912-29).
Thus far, guidelines and statements on concussion in sport have advised a rest-based approach to management that’s dependent on the spontaneous resolution of symptoms. In some documents, rest is recommended until patients are asymptomatic. Other statements mention the possibility of symptom-based approaches after initial rest, but offer little if any guidance.
The theory of prescribed rest has been twofold, driven both by concern about re-injury in sport and by the belief that cognitive and physical activity can exacerbate symptoms and concussion-associated impairments, thus prolonging recovery, the Pittsburgh paper says.
However, “avoiding contact during the vulnerable period after concussion and prescribed rest represent two separate strategies,” the experts wrote. Avoiding contact “is always recommended to avoid further head impacts,” they say, but monitored activity does not appear to worsen injury.
Recent research suggests, moreover, that prolonged physical and cognitive rest – not activity – is associated with increased symptoms and delayed recovery. And strict rest – avoidance of nearly all brain stimulation – is “not empirically supported ... and may have unintended adverse effects,” the experts wrote.
Physicians and others “have to avoid treating concussion as a punishment,” said Dr. Halstead of St. Louis Children’s Hospital in Chesterfield, Mo., who coauthored a recent editorial entitled “Rethinking Cognitive Rest” (Br J Sports Med. 2017;51:147).
“It’s been taken to the extreme. When we talk about not texting or not going out or not doing anything physically active until you’re without symptoms ... students can develop symptoms of depression and anxiety that then just complicate the injury altogether,” he said.
Physicians also need to dig beneath symptom checklists and perform multidomain assessments to better understand root contributors of symptoms that, without active treatment, can persist for weeks upon weeks in some patients. “There could be neck injuries, sleep issues, vestibular issues, oculomotor issues” and different types of headache, Dr. Halstead said. “If we can identify these things, we can actually be doing rehabilitation to fix these injuries.”
At UPMC’s Sports Medicine Concussion Program, concussions are generally categorized into six clinical profiles – vestibular, ocular-motor, cognitive/fatigue, posttraumatic migraine, cervical, and anxiety/mood. The profiles are not mutually exclusive, but each drives particular rehabilitation recommendations. Clinicians at other concussion programs and centers are similarly attempting to classify concussions.
“We still need to come to agreement as to what exactly the clinical profiles are,” said UPMC’s Dr. Collins, who directs the concussion program and is the lead author of the Neurosurgery paper. “But I think the big concept to come out of our meeting is that we now agree there are different profiles and that we have to match treatment.”
Additional research is needed to determine and validate concussion clinical profiles, to identify biomarkers to assess recovery and determine the effectiveness of treatments, and to determine the best timing of specific active treatments, he and his coauthors said.
Applying individualized and active treatments after concussion is consistent with approaches taken for other injuries and conditions, noted Dr. Hainline, who attended both the UPMC conference and the 5th International Conference on Concussion in Sport.
“It’s rare that prolonged rest is the answer. Look at stroke – you don’t have patients resting indefinitely. You have to get their nervous systems re-engaged,” he said.
“If you keep [concussion] patients with predominantly vestibular symptoms at rest [for example], the vestibular symptoms can become more centralized, and that then becomes the behavior of the nervous system,” he said. “Another example is convergence insufficiencies – if you keep resting [the vision system] and don’t rehabilitate it,” symptoms perpetuate.
Prolonged rest also may lead to deconditioning that lowers tolerance for physical activity. Randomized clinical trials are needed to compare the benefits of physical rest with those of more physically active treatments, but “emerging clinical research” suggests that exposing patients to supervised low-level physical activity (for example, submaximal aerobic training) after an initial period of rest is “not only safe but effective,” the Pittsburgh conference paper says.
The Pittsburgh conference paper “rang a bell with me,” Dr. Wergin said. “Rest is still important, but prolonged rest may not be best for all patients, and maybe it’s possible to do some interventions. We need to stay tuned as we get more of an evidence base.”
The conference – coined the TEAM (for targeted evaluation and active management) Approaches to Treating Concussion Meeting – was attended by staff from the National Institutes of Health, the Centers for Disease Control and Prevention, the Department of Defense, and the National Football League (NFL) and other sporting organizations, Dr. Collins said. It was sponsored by UPMC and the NFL. Coauthors reported numerous disclosures, including various advising and consulting roles with the NFL.
The prevailing notion that concussions should be managed solely or primarily with prescribed cognitive and physical rest is shifting.
Experts in concussion management are increasingly in agreement that concussion is a much more heterogeneous injury than previously believed, and that “active” approaches targeting specific symptoms and impairments can be initiated early and may improve recovery for patients who have concussions from sports as well as from falls, motor vehicle accidents, or other accidents.
Evidence for such active approaches to rehabilitation – including vestibular, vision, and behavioral therapies, and submaximal aerobic training – is deemed “preliminary” by experts and comes from small, mostly single-center studies.
“There’s emerging evidence that strict or prolonged rest is not good, and there’s emerging consensus that we need to start looking at concussion subtypes” and then target treatments to those clinical profiles, he said. “We’re at the cusp of dramatic changes [in management].”
An article published recently in Neurosurgery and coauthored by several dozen concussion experts details 16 “statements of agreement” on targeted evaluation and active management. The experts – from neuropsychology, sports medicine, neurology and neurosurgery, athletic training, and other fields – convened in Pittsburgh in late 2015 at the invitation of Michael W. Collins, PhD, and his colleagues at the University of Pittsburgh Medical Center (UPMC), where the Sports Medicine Concussion Program was established in 2000 (Neurosurgery. 2016 Dec;79[6]:912-29).
Thus far, guidelines and statements on concussion in sport have advised a rest-based approach to management that’s dependent on the spontaneous resolution of symptoms. In some documents, rest is recommended until patients are asymptomatic. Other statements mention the possibility of symptom-based approaches after initial rest, but offer little if any guidance.
The theory of prescribed rest has been twofold, driven both by concern about re-injury in sport and by the belief that cognitive and physical activity can exacerbate symptoms and concussion-associated impairments, thus prolonging recovery, the Pittsburgh paper says.
However, “avoiding contact during the vulnerable period after concussion and prescribed rest represent two separate strategies,” the experts wrote. Avoiding contact “is always recommended to avoid further head impacts,” they say, but monitored activity does not appear to worsen injury.
Recent research suggests, moreover, that prolonged physical and cognitive rest – not activity – is associated with increased symptoms and delayed recovery. And strict rest – avoidance of nearly all brain stimulation – is “not empirically supported ... and may have unintended adverse effects,” the experts wrote.
Physicians and others “have to avoid treating concussion as a punishment,” said Dr. Halstead of St. Louis Children’s Hospital in Chesterfield, Mo., who coauthored a recent editorial entitled “Rethinking Cognitive Rest” (Br J Sports Med. 2017;51:147).
“It’s been taken to the extreme. When we talk about not texting or not going out or not doing anything physically active until you’re without symptoms ... students can develop symptoms of depression and anxiety that then just complicate the injury altogether,” he said.
Physicians also need to dig beneath symptom checklists and perform multidomain assessments to better understand root contributors of symptoms that, without active treatment, can persist for weeks upon weeks in some patients. “There could be neck injuries, sleep issues, vestibular issues, oculomotor issues” and different types of headache, Dr. Halstead said. “If we can identify these things, we can actually be doing rehabilitation to fix these injuries.”
At UPMC’s Sports Medicine Concussion Program, concussions are generally categorized into six clinical profiles – vestibular, ocular-motor, cognitive/fatigue, posttraumatic migraine, cervical, and anxiety/mood. The profiles are not mutually exclusive, but each drives particular rehabilitation recommendations. Clinicians at other concussion programs and centers are similarly attempting to classify concussions.
“We still need to come to agreement as to what exactly the clinical profiles are,” said UPMC’s Dr. Collins, who directs the concussion program and is the lead author of the Neurosurgery paper. “But I think the big concept to come out of our meeting is that we now agree there are different profiles and that we have to match treatment.”
Additional research is needed to determine and validate concussion clinical profiles, to identify biomarkers to assess recovery and determine the effectiveness of treatments, and to determine the best timing of specific active treatments, he and his coauthors said.
Applying individualized and active treatments after concussion is consistent with approaches taken for other injuries and conditions, noted Dr. Hainline, who attended both the UPMC conference and the 5th International Conference on Concussion in Sport.
“It’s rare that prolonged rest is the answer. Look at stroke – you don’t have patients resting indefinitely. You have to get their nervous systems re-engaged,” he said.
“If you keep [concussion] patients with predominantly vestibular symptoms at rest [for example], the vestibular symptoms can become more centralized, and that then becomes the behavior of the nervous system,” he said. “Another example is convergence insufficiencies – if you keep resting [the vision system] and don’t rehabilitate it,” symptoms perpetuate.
Prolonged rest also may lead to deconditioning that lowers tolerance for physical activity. Randomized clinical trials are needed to compare the benefits of physical rest with those of more physically active treatments, but “emerging clinical research” suggests that exposing patients to supervised low-level physical activity (for example, submaximal aerobic training) after an initial period of rest is “not only safe but effective,” the Pittsburgh conference paper says.
The Pittsburgh conference paper “rang a bell with me,” Dr. Wergin said. “Rest is still important, but prolonged rest may not be best for all patients, and maybe it’s possible to do some interventions. We need to stay tuned as we get more of an evidence base.”
The conference – coined the TEAM (for targeted evaluation and active management) Approaches to Treating Concussion Meeting – was attended by staff from the National Institutes of Health, the Centers for Disease Control and Prevention, the Department of Defense, and the National Football League (NFL) and other sporting organizations, Dr. Collins said. It was sponsored by UPMC and the NFL. Coauthors reported numerous disclosures, including various advising and consulting roles with the NFL.
Well-child care: Steady growth in breadth and content
Fifty years ago in 1967, the American Academy of Pediatrics published a “Suggested Schedule for Preventive Child Health Care.” It was, in essence, the first periodicity schedule for well-child visits.
Described by AAP officials at the time as an “amalgamation of schedules used in various clinics and private offices,” it charted out the frequency and basic content of visits from 1 month through 6 years of age, and offered a simple list of items to be considered for guidance and discussion in all visits from 6 years on.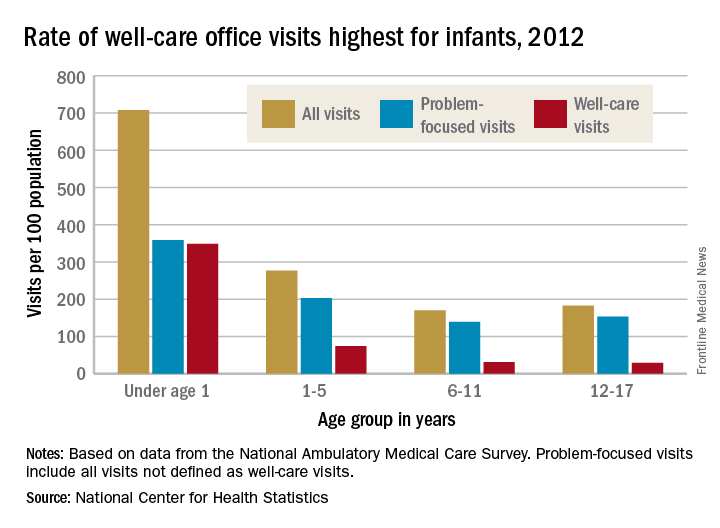
It is updated in real time, and is accompanied by an expansive package of Bright Futures recommendations, guidelines, and tools (including forms, handouts, and questionnaires) for health promotion and guidance. Together, the Periodicity Schedule and Bright Futures guidance reflect decades of steady change in the breadth and content of well-child care – and more recently, in some of its processes.
“When I started practicing [in 1979], developmental surveillance meant asking a few questions about developmental milestones, observing, and maybe lifting a few questions from the Denver Scale [the Denver Developmental Screening Test] to support our surveillance,” said Joseph F. Hagan, Jr., MD, a pediatrician in Burlington, Vt., and coeditor of Bright Futures.
Jack Swanson, MD, a pediatrician in Ames, Iowa, and a member of the Bright Futures Steering Committee, has similar recollections of well-child care in the early 1970s. “The developmental milestones were just questions and nothing more formal. Nutrition was a big [anticipatory guidance] issue, and some safety,” he recalled.
In early pediatric visits, “parents were interested in Dr. [Benjamin] Spock’s recommendations about feeding and raising their baby… and we used to make our own [anticipatory guidance] handouts,” he said. And in the later years, “an adolescent visit used to be every 2 or 3 years.”
“During the Vietnam War, there weren’t enough people who were healthy enough, physically fit enough, to be mustered into the Army,” said Peter Rappo, MD, a pediatrician in Brockton, Mass., who chaired the AAP’s Committee on Practice and Ambulatory Medicine in the late 1990s.
Dr. Rappo became interested in the history of preventive pediatric care after discovering a Children’s Year Campaign (1918-1919) poster in an antiques market. The poster’s message – “The Health of the Child is the Power of the Nation” – remained relevant through the Vietnam War. “I’d like to think that [childhood preventive services] were all about the kids,” he said, “but at the end of the day, it was about military issues too.”
Still, interest in the 1960s in the long-term implications of early-life development fed research that eventually led to an explosion of new science in the 1990s on the importance of early brain development and early life experiences. This scientific literature combined with greater societal interest in school readiness helped drive development of research-based instruments for developmental screening, said pediatrician Edward L. Schor, MD, formerly a vice president at the Commonwealth Fund and now a senior vice president for programs and partnerships at Lucile Packard Foundation for Children’s Health.
“Development was the first topic … of screening instruments,” he said. The tools have “not only increased the quality of care, they also have increased the efficiency of care, because the time to ask and answer these questions was shifted to the waiting room.”
Their use is far from universal, but increasing. Results of the Periodic Surveys administered to a national random sample of AAP members show that pediatricians’ use of at least one formal screening instrument to identify children through 36 months of age at risk for developmental delay increased from 23% in 2002 to 45% in 2009 and 63% in 2016. (And in 2016, 81% reported “always/almost always” using at least one formal screening tool for autism.) The data was presented at the annual meeting of the Society of Developmental and Behavioral Pediatrics September 2016.
For Dr. Rappo’s practice in Massachusetts, the adoption of developmental and behavioral health screening questionnaires for all ages was spurred by a 2007 mandate requiring formal screening for children and adolescents in MassHealth, the state’s combined Medicaid–Children’s Health Insurance Program.
“We all knew intuitively this is what we should be doing, so we also sat down with insurers to talk about why this is important for kids,” he said. Reimbursement improved, and most importantly, he said, use of the tools “has tremendously improved our opportunities for opening up discussions with parents about developmental-behavioral issues.”
The well-child visit of 50 years ago was much more of “a physician-generated, physician-led visit,” said Dr. Swanson. “The pediatrician knew what was needed, and at the end, we’d ask if there were any questions. Today, the first question recommended by Bright Futures is ‘Do you have any questions for the visit?’”
According to a 2009 focus group study involving 282 pediatricians and 41 nurse-practitioners, clinicians agree that eliciting and prioritizing parent concerns is a top priority in well-child care. Yet there’s also some unease. Some said in the focus group discussions that they feel constrained by the Periodicity Schedule, for instance, or feel tension between inviting parents’ concerns while simultaneously addressing the content recommended by professional guidelines (Pediatrics. 2009 Sep;124[3]:849-57).
Indeed, policies and recommendations for health promotion and anticipatory guidance (some consensus-based, some evidence-based or evidence-informed) mushroomed throughout the 1980s and 1990s, Dr. Swanson said. Combined with the increase in recommended screenings through the 1990s and 2000s – and in recent years, the increasing need for discussions to address vaccine concerns, mental and behavioral health issues, and obesity and overweight problems – there are real pulls and tugs.
The time allotted to well-child visits may have increased slightly for some pediatricians – to just over 20 minutes – but overall, visit length hasn’t changed much over the past few decades. “It has pretty much stayed the same, averaging between 15 and 20 minutes,” said Dr. Schor.
Offering guidance to clinicians in prioritizing questions and issues has been a goal in the last two editions (2008 and 2016) of the Bright Futures recommendations – formally called the Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. “The joke was that if you did a Bright Futures well-child visit according to the old Bright Futures, you’d do one in the morning and one in the afternoon,” said Dr. Hagan.
The first edition came out in 1994, after a multidisciplinary group convened by the Maternal and Child Health Bureau at the Health Resources and Services Administration, and the Medicaid Bureau (then part of the Health Care Financing Administration) established the Bright Futures Children’s Health Charter to improve children’s health. The second edition was released in 2000 and updated in 2002, at which point the AAP established the Bright Futures National Center.
Previsit screening tools included in the new edition are aimed at assessing and prioritizing anticipatory guidance issues, Dr. Hagan said, noting too that the Periodicity Schedule and Bright Futures recommendations make distinctions between universal and selective screening. “By design,” he emphasized, “there’s more anticipatory guidance than you might ever accomplish in one visit, because we want to be thorough enough to provide a context – a schema – to deal with the issues.”
Oftentimes, he said, “what parents want to talk about is what you want to talk about.” And pediatricians “develop a skill set to temporize, to figure out what needs to be covered today, and what can be dealt with better at a later time,” Dr. Hagan said. “If you tell kids, for instance, ‘I can help you with this, I just have to get more information,’ they hear that there’s help on the way. Then you follow through.”
Overall, his well-child visits “have gotten much more involved with the emotional well-being of children.” Given that emotional issues and behavioral issues “tend to take a longer time to discuss and unravel,” he sets aside consultation times near the end of the day for families who need to discuss these issues.
And he routinely devotes time – starting at the 2-month visit – to discuss screen time and media use. “I believe that technology is making our children sick,” he said, noting that in his nearly 17 years of practice he has seen increasing numbers of children and adolescents with depression, anxiety, anger, and attention deficit/hyperactivity disorder. “The AAP has done a pretty good job of raising the point, but I don’t think it has hit home with parents yet.”
For Dr. Chung, electronic medical records and systems have enabled him to better flag issues for follow-up over the course of well-child visits, leading to “better longitudinal care.”
Surveys and questionnaires filled out by parents in his practice’s waiting room are scanned into charts, he noted, and adolescents can mark answers on a proprietary confidential risk questionnaire that subsequently gets scrambled so that no one but the provider can understand the responses.
Other potential impacts of electronic systems have yet to be realized, he and others said. Some pediatric practices, Dr. Schor said, have begun engaging with families ahead of well-child visits through the use of a computerized questionnaire that elicits areas and issues of interest. Such outreach may help families feel more invested and committed to attending the visits, particularly those that don’t involve immunizations or school/sport forms, he said.
Families are “not [always] buying what we’re selling [for well-child care],” said Dr. Schor, who has served on AAP committees and has written several well-cited articles on preventive pediatrics care.
Insurance coverage for well-child care got a boost in 2010 when Bright Futures was cited in the Affordable Care Act as the standard of what well-child care should accomplish, and its recommended screenings and services were required to be covered by insurers without cost-sharing.
In the long-run, he said, rethinking the roles of nonphysicians in anticipatory guidance and developmental and psychosocial screening – in interpreting results of questionnaires, for instance – may be essential for well-child care. Outside of large health care systems, “the use of personnel [has been] pretty much been unchanged over the years,” he said. “We need to ask, how can we use each individual’s skills and training most efficiently? How can we retrain and reorganize our patient flow?”
This may be especially important as well-child care increasingly considers family psychosocial issues such as housing, food insecurity, family violence, and other family social stressors. Maternal depression screening made its way into the Periodicity Schedule in February 2016, and Dr. Schor predicts that the schedule will include “family psychosocial risk screening” in another several years.
For now, the newly revised Bright Futures guidelines – and much of well-child care – places an increased emphasis on the social determinants of health, which Dr. Hagan said reflects the “long-standing, logical conclusion that we reached back in the 1990s – that if families are healthy, kids will be healthy … and that family health is also linked to community health.”
Fifty years ago in 1967, the American Academy of Pediatrics published a “Suggested Schedule for Preventive Child Health Care.” It was, in essence, the first periodicity schedule for well-child visits.
Described by AAP officials at the time as an “amalgamation of schedules used in various clinics and private offices,” it charted out the frequency and basic content of visits from 1 month through 6 years of age, and offered a simple list of items to be considered for guidance and discussion in all visits from 6 years on.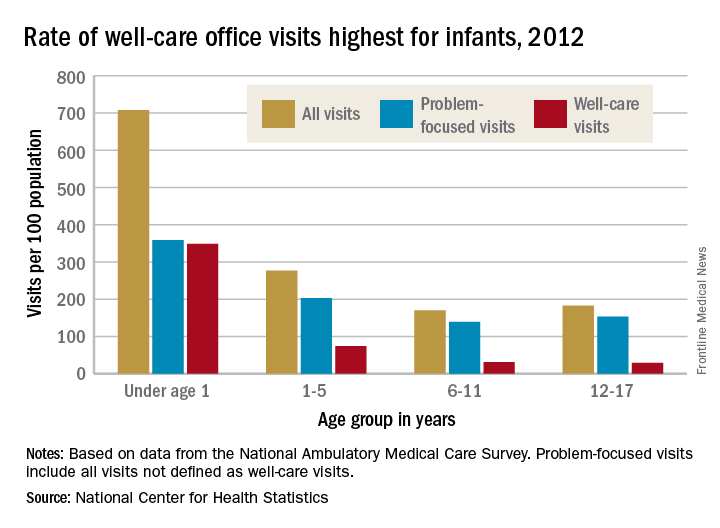
It is updated in real time, and is accompanied by an expansive package of Bright Futures recommendations, guidelines, and tools (including forms, handouts, and questionnaires) for health promotion and guidance. Together, the Periodicity Schedule and Bright Futures guidance reflect decades of steady change in the breadth and content of well-child care – and more recently, in some of its processes.
“When I started practicing [in 1979], developmental surveillance meant asking a few questions about developmental milestones, observing, and maybe lifting a few questions from the Denver Scale [the Denver Developmental Screening Test] to support our surveillance,” said Joseph F. Hagan, Jr., MD, a pediatrician in Burlington, Vt., and coeditor of Bright Futures.
Jack Swanson, MD, a pediatrician in Ames, Iowa, and a member of the Bright Futures Steering Committee, has similar recollections of well-child care in the early 1970s. “The developmental milestones were just questions and nothing more formal. Nutrition was a big [anticipatory guidance] issue, and some safety,” he recalled.
In early pediatric visits, “parents were interested in Dr. [Benjamin] Spock’s recommendations about feeding and raising their baby… and we used to make our own [anticipatory guidance] handouts,” he said. And in the later years, “an adolescent visit used to be every 2 or 3 years.”
“During the Vietnam War, there weren’t enough people who were healthy enough, physically fit enough, to be mustered into the Army,” said Peter Rappo, MD, a pediatrician in Brockton, Mass., who chaired the AAP’s Committee on Practice and Ambulatory Medicine in the late 1990s.
Dr. Rappo became interested in the history of preventive pediatric care after discovering a Children’s Year Campaign (1918-1919) poster in an antiques market. The poster’s message – “The Health of the Child is the Power of the Nation” – remained relevant through the Vietnam War. “I’d like to think that [childhood preventive services] were all about the kids,” he said, “but at the end of the day, it was about military issues too.”
Still, interest in the 1960s in the long-term implications of early-life development fed research that eventually led to an explosion of new science in the 1990s on the importance of early brain development and early life experiences. This scientific literature combined with greater societal interest in school readiness helped drive development of research-based instruments for developmental screening, said pediatrician Edward L. Schor, MD, formerly a vice president at the Commonwealth Fund and now a senior vice president for programs and partnerships at Lucile Packard Foundation for Children’s Health.
“Development was the first topic … of screening instruments,” he said. The tools have “not only increased the quality of care, they also have increased the efficiency of care, because the time to ask and answer these questions was shifted to the waiting room.”
Their use is far from universal, but increasing. Results of the Periodic Surveys administered to a national random sample of AAP members show that pediatricians’ use of at least one formal screening instrument to identify children through 36 months of age at risk for developmental delay increased from 23% in 2002 to 45% in 2009 and 63% in 2016. (And in 2016, 81% reported “always/almost always” using at least one formal screening tool for autism.) The data was presented at the annual meeting of the Society of Developmental and Behavioral Pediatrics September 2016.
For Dr. Rappo’s practice in Massachusetts, the adoption of developmental and behavioral health screening questionnaires for all ages was spurred by a 2007 mandate requiring formal screening for children and adolescents in MassHealth, the state’s combined Medicaid–Children’s Health Insurance Program.
“We all knew intuitively this is what we should be doing, so we also sat down with insurers to talk about why this is important for kids,” he said. Reimbursement improved, and most importantly, he said, use of the tools “has tremendously improved our opportunities for opening up discussions with parents about developmental-behavioral issues.”
The well-child visit of 50 years ago was much more of “a physician-generated, physician-led visit,” said Dr. Swanson. “The pediatrician knew what was needed, and at the end, we’d ask if there were any questions. Today, the first question recommended by Bright Futures is ‘Do you have any questions for the visit?’”
According to a 2009 focus group study involving 282 pediatricians and 41 nurse-practitioners, clinicians agree that eliciting and prioritizing parent concerns is a top priority in well-child care. Yet there’s also some unease. Some said in the focus group discussions that they feel constrained by the Periodicity Schedule, for instance, or feel tension between inviting parents’ concerns while simultaneously addressing the content recommended by professional guidelines (Pediatrics. 2009 Sep;124[3]:849-57).
Indeed, policies and recommendations for health promotion and anticipatory guidance (some consensus-based, some evidence-based or evidence-informed) mushroomed throughout the 1980s and 1990s, Dr. Swanson said. Combined with the increase in recommended screenings through the 1990s and 2000s – and in recent years, the increasing need for discussions to address vaccine concerns, mental and behavioral health issues, and obesity and overweight problems – there are real pulls and tugs.
The time allotted to well-child visits may have increased slightly for some pediatricians – to just over 20 minutes – but overall, visit length hasn’t changed much over the past few decades. “It has pretty much stayed the same, averaging between 15 and 20 minutes,” said Dr. Schor.
Offering guidance to clinicians in prioritizing questions and issues has been a goal in the last two editions (2008 and 2016) of the Bright Futures recommendations – formally called the Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. “The joke was that if you did a Bright Futures well-child visit according to the old Bright Futures, you’d do one in the morning and one in the afternoon,” said Dr. Hagan.
The first edition came out in 1994, after a multidisciplinary group convened by the Maternal and Child Health Bureau at the Health Resources and Services Administration, and the Medicaid Bureau (then part of the Health Care Financing Administration) established the Bright Futures Children’s Health Charter to improve children’s health. The second edition was released in 2000 and updated in 2002, at which point the AAP established the Bright Futures National Center.
Previsit screening tools included in the new edition are aimed at assessing and prioritizing anticipatory guidance issues, Dr. Hagan said, noting too that the Periodicity Schedule and Bright Futures recommendations make distinctions between universal and selective screening. “By design,” he emphasized, “there’s more anticipatory guidance than you might ever accomplish in one visit, because we want to be thorough enough to provide a context – a schema – to deal with the issues.”
Oftentimes, he said, “what parents want to talk about is what you want to talk about.” And pediatricians “develop a skill set to temporize, to figure out what needs to be covered today, and what can be dealt with better at a later time,” Dr. Hagan said. “If you tell kids, for instance, ‘I can help you with this, I just have to get more information,’ they hear that there’s help on the way. Then you follow through.”
Overall, his well-child visits “have gotten much more involved with the emotional well-being of children.” Given that emotional issues and behavioral issues “tend to take a longer time to discuss and unravel,” he sets aside consultation times near the end of the day for families who need to discuss these issues.
And he routinely devotes time – starting at the 2-month visit – to discuss screen time and media use. “I believe that technology is making our children sick,” he said, noting that in his nearly 17 years of practice he has seen increasing numbers of children and adolescents with depression, anxiety, anger, and attention deficit/hyperactivity disorder. “The AAP has done a pretty good job of raising the point, but I don’t think it has hit home with parents yet.”
For Dr. Chung, electronic medical records and systems have enabled him to better flag issues for follow-up over the course of well-child visits, leading to “better longitudinal care.”
Surveys and questionnaires filled out by parents in his practice’s waiting room are scanned into charts, he noted, and adolescents can mark answers on a proprietary confidential risk questionnaire that subsequently gets scrambled so that no one but the provider can understand the responses.
Other potential impacts of electronic systems have yet to be realized, he and others said. Some pediatric practices, Dr. Schor said, have begun engaging with families ahead of well-child visits through the use of a computerized questionnaire that elicits areas and issues of interest. Such outreach may help families feel more invested and committed to attending the visits, particularly those that don’t involve immunizations or school/sport forms, he said.
Families are “not [always] buying what we’re selling [for well-child care],” said Dr. Schor, who has served on AAP committees and has written several well-cited articles on preventive pediatrics care.
Insurance coverage for well-child care got a boost in 2010 when Bright Futures was cited in the Affordable Care Act as the standard of what well-child care should accomplish, and its recommended screenings and services were required to be covered by insurers without cost-sharing.
In the long-run, he said, rethinking the roles of nonphysicians in anticipatory guidance and developmental and psychosocial screening – in interpreting results of questionnaires, for instance – may be essential for well-child care. Outside of large health care systems, “the use of personnel [has been] pretty much been unchanged over the years,” he said. “We need to ask, how can we use each individual’s skills and training most efficiently? How can we retrain and reorganize our patient flow?”
This may be especially important as well-child care increasingly considers family psychosocial issues such as housing, food insecurity, family violence, and other family social stressors. Maternal depression screening made its way into the Periodicity Schedule in February 2016, and Dr. Schor predicts that the schedule will include “family psychosocial risk screening” in another several years.
For now, the newly revised Bright Futures guidelines – and much of well-child care – places an increased emphasis on the social determinants of health, which Dr. Hagan said reflects the “long-standing, logical conclusion that we reached back in the 1990s – that if families are healthy, kids will be healthy … and that family health is also linked to community health.”
Fifty years ago in 1967, the American Academy of Pediatrics published a “Suggested Schedule for Preventive Child Health Care.” It was, in essence, the first periodicity schedule for well-child visits.
Described by AAP officials at the time as an “amalgamation of schedules used in various clinics and private offices,” it charted out the frequency and basic content of visits from 1 month through 6 years of age, and offered a simple list of items to be considered for guidance and discussion in all visits from 6 years on.
It is updated in real time, and is accompanied by an expansive package of Bright Futures recommendations, guidelines, and tools (including forms, handouts, and questionnaires) for health promotion and guidance. Together, the Periodicity Schedule and Bright Futures guidance reflect decades of steady change in the breadth and content of well-child care – and more recently, in some of its processes.
“When I started practicing [in 1979], developmental surveillance meant asking a few questions about developmental milestones, observing, and maybe lifting a few questions from the Denver Scale [the Denver Developmental Screening Test] to support our surveillance,” said Joseph F. Hagan, Jr., MD, a pediatrician in Burlington, Vt., and coeditor of Bright Futures.
Jack Swanson, MD, a pediatrician in Ames, Iowa, and a member of the Bright Futures Steering Committee, has similar recollections of well-child care in the early 1970s. “The developmental milestones were just questions and nothing more formal. Nutrition was a big [anticipatory guidance] issue, and some safety,” he recalled.
In early pediatric visits, “parents were interested in Dr. [Benjamin] Spock’s recommendations about feeding and raising their baby… and we used to make our own [anticipatory guidance] handouts,” he said. And in the later years, “an adolescent visit used to be every 2 or 3 years.”
“During the Vietnam War, there weren’t enough people who were healthy enough, physically fit enough, to be mustered into the Army,” said Peter Rappo, MD, a pediatrician in Brockton, Mass., who chaired the AAP’s Committee on Practice and Ambulatory Medicine in the late 1990s.
Dr. Rappo became interested in the history of preventive pediatric care after discovering a Children’s Year Campaign (1918-1919) poster in an antiques market. The poster’s message – “The Health of the Child is the Power of the Nation” – remained relevant through the Vietnam War. “I’d like to think that [childhood preventive services] were all about the kids,” he said, “but at the end of the day, it was about military issues too.”
Still, interest in the 1960s in the long-term implications of early-life development fed research that eventually led to an explosion of new science in the 1990s on the importance of early brain development and early life experiences. This scientific literature combined with greater societal interest in school readiness helped drive development of research-based instruments for developmental screening, said pediatrician Edward L. Schor, MD, formerly a vice president at the Commonwealth Fund and now a senior vice president for programs and partnerships at Lucile Packard Foundation for Children’s Health.
“Development was the first topic … of screening instruments,” he said. The tools have “not only increased the quality of care, they also have increased the efficiency of care, because the time to ask and answer these questions was shifted to the waiting room.”
Their use is far from universal, but increasing. Results of the Periodic Surveys administered to a national random sample of AAP members show that pediatricians’ use of at least one formal screening instrument to identify children through 36 months of age at risk for developmental delay increased from 23% in 2002 to 45% in 2009 and 63% in 2016. (And in 2016, 81% reported “always/almost always” using at least one formal screening tool for autism.) The data was presented at the annual meeting of the Society of Developmental and Behavioral Pediatrics September 2016.
For Dr. Rappo’s practice in Massachusetts, the adoption of developmental and behavioral health screening questionnaires for all ages was spurred by a 2007 mandate requiring formal screening for children and adolescents in MassHealth, the state’s combined Medicaid–Children’s Health Insurance Program.
“We all knew intuitively this is what we should be doing, so we also sat down with insurers to talk about why this is important for kids,” he said. Reimbursement improved, and most importantly, he said, use of the tools “has tremendously improved our opportunities for opening up discussions with parents about developmental-behavioral issues.”
The well-child visit of 50 years ago was much more of “a physician-generated, physician-led visit,” said Dr. Swanson. “The pediatrician knew what was needed, and at the end, we’d ask if there were any questions. Today, the first question recommended by Bright Futures is ‘Do you have any questions for the visit?’”
According to a 2009 focus group study involving 282 pediatricians and 41 nurse-practitioners, clinicians agree that eliciting and prioritizing parent concerns is a top priority in well-child care. Yet there’s also some unease. Some said in the focus group discussions that they feel constrained by the Periodicity Schedule, for instance, or feel tension between inviting parents’ concerns while simultaneously addressing the content recommended by professional guidelines (Pediatrics. 2009 Sep;124[3]:849-57).
Indeed, policies and recommendations for health promotion and anticipatory guidance (some consensus-based, some evidence-based or evidence-informed) mushroomed throughout the 1980s and 1990s, Dr. Swanson said. Combined with the increase in recommended screenings through the 1990s and 2000s – and in recent years, the increasing need for discussions to address vaccine concerns, mental and behavioral health issues, and obesity and overweight problems – there are real pulls and tugs.
The time allotted to well-child visits may have increased slightly for some pediatricians – to just over 20 minutes – but overall, visit length hasn’t changed much over the past few decades. “It has pretty much stayed the same, averaging between 15 and 20 minutes,” said Dr. Schor.
Offering guidance to clinicians in prioritizing questions and issues has been a goal in the last two editions (2008 and 2016) of the Bright Futures recommendations – formally called the Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. “The joke was that if you did a Bright Futures well-child visit according to the old Bright Futures, you’d do one in the morning and one in the afternoon,” said Dr. Hagan.
The first edition came out in 1994, after a multidisciplinary group convened by the Maternal and Child Health Bureau at the Health Resources and Services Administration, and the Medicaid Bureau (then part of the Health Care Financing Administration) established the Bright Futures Children’s Health Charter to improve children’s health. The second edition was released in 2000 and updated in 2002, at which point the AAP established the Bright Futures National Center.
Previsit screening tools included in the new edition are aimed at assessing and prioritizing anticipatory guidance issues, Dr. Hagan said, noting too that the Periodicity Schedule and Bright Futures recommendations make distinctions between universal and selective screening. “By design,” he emphasized, “there’s more anticipatory guidance than you might ever accomplish in one visit, because we want to be thorough enough to provide a context – a schema – to deal with the issues.”
Oftentimes, he said, “what parents want to talk about is what you want to talk about.” And pediatricians “develop a skill set to temporize, to figure out what needs to be covered today, and what can be dealt with better at a later time,” Dr. Hagan said. “If you tell kids, for instance, ‘I can help you with this, I just have to get more information,’ they hear that there’s help on the way. Then you follow through.”
Overall, his well-child visits “have gotten much more involved with the emotional well-being of children.” Given that emotional issues and behavioral issues “tend to take a longer time to discuss and unravel,” he sets aside consultation times near the end of the day for families who need to discuss these issues.
And he routinely devotes time – starting at the 2-month visit – to discuss screen time and media use. “I believe that technology is making our children sick,” he said, noting that in his nearly 17 years of practice he has seen increasing numbers of children and adolescents with depression, anxiety, anger, and attention deficit/hyperactivity disorder. “The AAP has done a pretty good job of raising the point, but I don’t think it has hit home with parents yet.”
For Dr. Chung, electronic medical records and systems have enabled him to better flag issues for follow-up over the course of well-child visits, leading to “better longitudinal care.”
Surveys and questionnaires filled out by parents in his practice’s waiting room are scanned into charts, he noted, and adolescents can mark answers on a proprietary confidential risk questionnaire that subsequently gets scrambled so that no one but the provider can understand the responses.
Other potential impacts of electronic systems have yet to be realized, he and others said. Some pediatric practices, Dr. Schor said, have begun engaging with families ahead of well-child visits through the use of a computerized questionnaire that elicits areas and issues of interest. Such outreach may help families feel more invested and committed to attending the visits, particularly those that don’t involve immunizations or school/sport forms, he said.
Families are “not [always] buying what we’re selling [for well-child care],” said Dr. Schor, who has served on AAP committees and has written several well-cited articles on preventive pediatrics care.
Insurance coverage for well-child care got a boost in 2010 when Bright Futures was cited in the Affordable Care Act as the standard of what well-child care should accomplish, and its recommended screenings and services were required to be covered by insurers without cost-sharing.
In the long-run, he said, rethinking the roles of nonphysicians in anticipatory guidance and developmental and psychosocial screening – in interpreting results of questionnaires, for instance – may be essential for well-child care. Outside of large health care systems, “the use of personnel [has been] pretty much been unchanged over the years,” he said. “We need to ask, how can we use each individual’s skills and training most efficiently? How can we retrain and reorganize our patient flow?”
This may be especially important as well-child care increasingly considers family psychosocial issues such as housing, food insecurity, family violence, and other family social stressors. Maternal depression screening made its way into the Periodicity Schedule in February 2016, and Dr. Schor predicts that the schedule will include “family psychosocial risk screening” in another several years.
For now, the newly revised Bright Futures guidelines – and much of well-child care – places an increased emphasis on the social determinants of health, which Dr. Hagan said reflects the “long-standing, logical conclusion that we reached back in the 1990s – that if families are healthy, kids will be healthy … and that family health is also linked to community health.”
The culture change of assessing parents for ACEs
Several years ago, pediatricians R.J. Gillespie, MD, MHPE, and Teri Pettersen, MD, piloted the use of a questionnaire about adverse childhood experiences (ACEs) and resilience at the 4-month well-child visit.
They and six other pediatricians at The Children’s Clinic in Portland, Ore., explained in a cover letter why they were posing the questions of parents, and they ended the survey by asking them about their interest in potential resources.
[[{"fid":"172157","view_mode":"medstat_image_flush_left","fields":{"format":"medstat_image_flush_left","field_file_image_alt_text[und][0][value]":"R.J. Gillespie, MD, MHPE","field_file_image_credit[und][0][value]":"Courtesy The Children's Clinic","field_file_image_caption[und][0][value]":"Dr. R.J. Gillespie "},"type":"media","attributes":{"class":"media-element file-medstat_image_flush_left"}}]]Today, all 28 of the pediatricians at the clinic screen for ACEs and resilience, and Dr. Pettersen, now retired from the practice, travels through the state conducting training for the Oregon Pediatric Society about the impact of ACEs in parents and their children, and how to go about identifying and addressing them.
“So many of our visits are about behavioral problems or emotional disturbances, and so often at the root of these issues is some sort of trauma the child is experiencing,” Dr. Gillespie said in an interview. “What we’re seeing in many of these cases really are coping strategies for that child to deal with the toxic stress in his or her life.”
By assessing parents’ exposure to ACEs, briefly talking with them about how ACEs might impact their parenting, and tailoring their counseling and anticipatory guidance, the pediatricians hope to prevent ACEs and consequent toxic stress from developing in children.
The driving science
The term ACEs entered the medical lexicon after 1998, when a landmark study called the Adverse Childhood Experiences Study showed that traumatic experiences in childhood – abuse, neglect, and other severe dysfunctions in a household – not only are common among American adults but are associated with numerous poor health outcomes.
In the study and subsequent analyses, Dr. Vincent Felitti of Kaiser Permanente in San Diego and Dr. Robert Anda of the Centers for Disease Control and Prevention surveyed more than 17,000 patients about 10 types of ACEs and their current health status and behaviors. About two-thirds reported having at least one ACE, and one in eight reported four or more (Am J Prev Med. 1998;14[4]:245-58, www.cdc.gov/violenceprevention/acestudy/about.html).
Adults with four or more ACEs were not only significantly more likely to report health risk behaviors (smoking, substance abuse) and poor mental health outcomes (depression, suicide attempt); they were also significantly more likely to have poor physical health outcomes, with 2.2 times the risk of ischemic heart disease, 1.9 times the risk of cancer, and 3.9 times the risk of chronic bronchitis or emphysema, for instance. There was a strong dose-response relationship between ACEs and poor outcomes.
The Felitti study spawned dozens of analyses and additional research – in children as well as adults – on the associations between early-life adversity and the incidence of poor behavioral, mental, and physical outcomes, as well as on potential mechanisms.
Some research suggested a direct link between ACEs and negative outcomes, independent of whether individuals adopt risky behavior. Other studies suggested what experts in child development and mental health have long argued – that the more ACEs a parent has, the more ACEs their child will have.
And a growing body of biomedical literature linked the extreme, frequent, or prolonged activation of the body’s stress response in childhood – what has come to be known as “toxic stress” – with disruptions of the developing nervous, cardiovascular, immune, and metabolic systems.
While precise connections and mechanisms need to be clarified, “we now know that the repeated activation of the stress response leads to [negative] changes in the neuroendocrine immune pathways,” said Dr. Burke Harris, who coauthored a recent review of toxic stress in children and adolescents (Adv Pediatr. 2016;63[1]:403-28).
In January 2012, the American Academy of Pediatrics published a policy statement titled “Early Childhood Adversity, Toxic Stress, and the Role of the Pediatrician: Translating Developmental Science into Lifelong Health,” in which it urged pediatricians to consider actively screening for precipitants of toxic stress that are common in their communities (Pediatrics. 2011 Dec. doi: 10.1542/peds.2011-2662). But it stopped short of recommending particular tools or methods.
Dr. Gillespie and Dr. Pettersen did not want to wait for tools to be validated and approaches to be proven. “We’re building the plane as we fly,” Dr. Pettersen said.
The clinic’s roll-out
Dr. Pettersen learned about the ACE study and related research about 8 years ago while on a sabbatical to learn more about mental health issues. It “changed everything” about the way she viewed children and families and adversity. “I knew (we) didn’t have the infrastructure at the clinic, or the clinic’s support, to really start assessing children for what was happening to them,” she said, so she began thinking about ACE prevention and a focus on parenting.
Dr. Gillespie, in the meantime, was active in various quality improvement efforts at the state and national level, and had also become increasingly bothered by visits in which he saw children affected by maternal depression, abnormal attachment, and other problems. “I was seeing the consequences of ACEs, but I didn’t know specifically what was going on or how to talk about it,” he said.
The two pediatricians agreed to ask parents about ACEs at the 4-month well visit – a time when the families “knew us a little bit” and when “we could still influence parenting styles.”
In March 2013, they and their colleagues in the pilot group began giving parents a questionnaire that included the 10 ACE questions from Felitti’s study, questions about resilience from the Children’s Resilience Initiative, and a list of potential resources so they could understand parents’ needs.
They created a confidential field in their electronic medical record for documentation that appears during a visit, but does not print into notes and therefore will not be inadvertently released.
As they moved through the pilot phase, the pediatricians used various approaches to follow up on the assessment face-to-face. Eventually, they chose three particular questions as nonthreatening and helpful for conversation: Are there any experiences that still bother you? Of those experiences that don’t bother you, how did you get to the point where they don’t bother you? And how do these experiences affect your parenting now?
“It’s a motivational interviewing sort of style,” said Dr. Gillespie. “Parents can start identifying for themselves the solutions for the problems they’ve experienced, and they can start thinking about how their parenting might be impacted by things that have happened [or are still happening] to them.”
As the project rolled out, the physicians tweaked their process. They added four more ACE questions to address issues – community violence, extreme bullying, racism and prejudice, and foster care exposure – that they thought might lead to toxic stress in their population, for instance. And rather than ask on the written questionnaire for a “yes” or “no” to each of the ACE questions, they began asking the parent how many of the ACE questions applied to them. Moving away from the yes-no format to asking for a total count has led to more disclosures, Dr. Gillespie said.
To “keep the conversation going” in subsequent well-child visits, they developed a few questions to ask high-risk parents, like “How do you and your partner resolve conflict?” and “How did your parents resolve conflict in your household when you were a child?” And they provided training to all of the clinic’s staff on trauma-informed care and the need for support and compassion in their interactions with family members.
In the 3-plus years since incorporating ACEs assessments, the clinic’s pediatricians have made soft referrals to mental health professionals in only several cases – in each case, by suggesting that the parent contact their primary care physician. What most parents have wanted, says Dr. Gillespie, is recommendations for parenting classes and support groups. The clinic’s care manager assists the pediatricians in maintaining and providing links and handouts for various resources.
For Dr. Gillespie, the impact of the culture shift has been dramatic. “I’ve had 8-10 moms spontaneously reveal domestic violence to me in a subsequent visit, and say that they need a little help, because they’ve gotten the message that this is a safe place to talk about their experiences,” he said. “That had never happened to me in the previous 12 years of so of my career.”
Dr. Pettersen’s relationships with parents became “more intimate and more honest.” There was more trust. “If we can talk with parents [about ACEs] and not judge them for it,” she said, “then nothing is off the table.”
The ‘Two-Gen’ approach
“But I’d push back and say, parents know they have toxic stress but they don’t name it,” she said. “What we can do as trusted providers who want to advocate for families is to bear witness to their history by asking about it. Once they realize it’s not what’s wrong with [them], it’s what’s happened to [them], a shift occurs. That’s extremely validating for parents.”
That validation is part of a two-generation approach that she and Dr. Burke Harris see as part of a movement to break cycles of ACEs and toxic stress. At the California Pacific Medical Center’s Bayview Child Health Center in San Francisco, Dr. Burke Harris uses three ACE questionnaires – two of them ask parents (of children or teens) to report how many adverse experience types, or categories, apply to them and/or their child or teen, and one surveys adolescents themselves.
With the resources and clinical support of the Center for Youth Wellness, whose major funders include Google, Dr. Burke Harris can initiate a “warm hand-off” of patients with a high ACE score to a care coordinator or therapist. (The Center for Youth Wellness is beginning research to validate its ACE screening tools.) And in the meantime, the medical care she provides is trauma-informed.
“If a patient comes in for ADHD [attention-deficit/hyperactivity disorder] and has an ACE score of 6, my differential diagnosis and assessment will be different than if I see a patient sent by the school who has an ACE score of 0,” she said.
At the Portland Clinic, even though ACEs screening is now tied with the 4-month visit, pediatricians are much more attentive across the board to possible ACEs and toxic stress, and feel better able to converse with families, Dr. Gillespie said. One of his partners recently saw a 12-year-old boy who was failing in school and not making friends. Trauma-informed history-taking revealed at least several ACEs, and conversation turned to “all the resilience pieces… the connections he was missing and what he needed to cope,” he said.
References
• Resilience Project: This AAP project houses a “trauma toolkit” for primary care, case studies, and a variety of other tools.
• Center for Youth Wellness: The ACEs screening tools used by Dr. Burke Harris may be accessed at this website, along with a user guide containing sample scripts, and two white papers on ACEs and toxic stress.
• Resilience: The Biology of Stress and the Science of Hope: This documentary film, released in September 2016, is about ACEs and “a new movement” to treat and prevent toxic stress; it features the work of Dr. Burke Harris and others.
• Academy on Violence & Abuse: Various papers on ACEs screening and case finding in practice may be accessed here.
Several years ago, pediatricians R.J. Gillespie, MD, MHPE, and Teri Pettersen, MD, piloted the use of a questionnaire about adverse childhood experiences (ACEs) and resilience at the 4-month well-child visit.
They and six other pediatricians at The Children’s Clinic in Portland, Ore., explained in a cover letter why they were posing the questions of parents, and they ended the survey by asking them about their interest in potential resources.
[[{"fid":"172157","view_mode":"medstat_image_flush_left","fields":{"format":"medstat_image_flush_left","field_file_image_alt_text[und][0][value]":"R.J. Gillespie, MD, MHPE","field_file_image_credit[und][0][value]":"Courtesy The Children's Clinic","field_file_image_caption[und][0][value]":"Dr. R.J. Gillespie "},"type":"media","attributes":{"class":"media-element file-medstat_image_flush_left"}}]]Today, all 28 of the pediatricians at the clinic screen for ACEs and resilience, and Dr. Pettersen, now retired from the practice, travels through the state conducting training for the Oregon Pediatric Society about the impact of ACEs in parents and their children, and how to go about identifying and addressing them.
“So many of our visits are about behavioral problems or emotional disturbances, and so often at the root of these issues is some sort of trauma the child is experiencing,” Dr. Gillespie said in an interview. “What we’re seeing in many of these cases really are coping strategies for that child to deal with the toxic stress in his or her life.”
By assessing parents’ exposure to ACEs, briefly talking with them about how ACEs might impact their parenting, and tailoring their counseling and anticipatory guidance, the pediatricians hope to prevent ACEs and consequent toxic stress from developing in children.
The driving science
The term ACEs entered the medical lexicon after 1998, when a landmark study called the Adverse Childhood Experiences Study showed that traumatic experiences in childhood – abuse, neglect, and other severe dysfunctions in a household – not only are common among American adults but are associated with numerous poor health outcomes.
In the study and subsequent analyses, Dr. Vincent Felitti of Kaiser Permanente in San Diego and Dr. Robert Anda of the Centers for Disease Control and Prevention surveyed more than 17,000 patients about 10 types of ACEs and their current health status and behaviors. About two-thirds reported having at least one ACE, and one in eight reported four or more (Am J Prev Med. 1998;14[4]:245-58, www.cdc.gov/violenceprevention/acestudy/about.html).
Adults with four or more ACEs were not only significantly more likely to report health risk behaviors (smoking, substance abuse) and poor mental health outcomes (depression, suicide attempt); they were also significantly more likely to have poor physical health outcomes, with 2.2 times the risk of ischemic heart disease, 1.9 times the risk of cancer, and 3.9 times the risk of chronic bronchitis or emphysema, for instance. There was a strong dose-response relationship between ACEs and poor outcomes.
The Felitti study spawned dozens of analyses and additional research – in children as well as adults – on the associations between early-life adversity and the incidence of poor behavioral, mental, and physical outcomes, as well as on potential mechanisms.
Some research suggested a direct link between ACEs and negative outcomes, independent of whether individuals adopt risky behavior. Other studies suggested what experts in child development and mental health have long argued – that the more ACEs a parent has, the more ACEs their child will have.
And a growing body of biomedical literature linked the extreme, frequent, or prolonged activation of the body’s stress response in childhood – what has come to be known as “toxic stress” – with disruptions of the developing nervous, cardiovascular, immune, and metabolic systems.
While precise connections and mechanisms need to be clarified, “we now know that the repeated activation of the stress response leads to [negative] changes in the neuroendocrine immune pathways,” said Dr. Burke Harris, who coauthored a recent review of toxic stress in children and adolescents (Adv Pediatr. 2016;63[1]:403-28).
In January 2012, the American Academy of Pediatrics published a policy statement titled “Early Childhood Adversity, Toxic Stress, and the Role of the Pediatrician: Translating Developmental Science into Lifelong Health,” in which it urged pediatricians to consider actively screening for precipitants of toxic stress that are common in their communities (Pediatrics. 2011 Dec. doi: 10.1542/peds.2011-2662). But it stopped short of recommending particular tools or methods.
Dr. Gillespie and Dr. Pettersen did not want to wait for tools to be validated and approaches to be proven. “We’re building the plane as we fly,” Dr. Pettersen said.
The clinic’s roll-out
Dr. Pettersen learned about the ACE study and related research about 8 years ago while on a sabbatical to learn more about mental health issues. It “changed everything” about the way she viewed children and families and adversity. “I knew (we) didn’t have the infrastructure at the clinic, or the clinic’s support, to really start assessing children for what was happening to them,” she said, so she began thinking about ACE prevention and a focus on parenting.
Dr. Gillespie, in the meantime, was active in various quality improvement efforts at the state and national level, and had also become increasingly bothered by visits in which he saw children affected by maternal depression, abnormal attachment, and other problems. “I was seeing the consequences of ACEs, but I didn’t know specifically what was going on or how to talk about it,” he said.
The two pediatricians agreed to ask parents about ACEs at the 4-month well visit – a time when the families “knew us a little bit” and when “we could still influence parenting styles.”
In March 2013, they and their colleagues in the pilot group began giving parents a questionnaire that included the 10 ACE questions from Felitti’s study, questions about resilience from the Children’s Resilience Initiative, and a list of potential resources so they could understand parents’ needs.
They created a confidential field in their electronic medical record for documentation that appears during a visit, but does not print into notes and therefore will not be inadvertently released.
As they moved through the pilot phase, the pediatricians used various approaches to follow up on the assessment face-to-face. Eventually, they chose three particular questions as nonthreatening and helpful for conversation: Are there any experiences that still bother you? Of those experiences that don’t bother you, how did you get to the point where they don’t bother you? And how do these experiences affect your parenting now?
“It’s a motivational interviewing sort of style,” said Dr. Gillespie. “Parents can start identifying for themselves the solutions for the problems they’ve experienced, and they can start thinking about how their parenting might be impacted by things that have happened [or are still happening] to them.”
As the project rolled out, the physicians tweaked their process. They added four more ACE questions to address issues – community violence, extreme bullying, racism and prejudice, and foster care exposure – that they thought might lead to toxic stress in their population, for instance. And rather than ask on the written questionnaire for a “yes” or “no” to each of the ACE questions, they began asking the parent how many of the ACE questions applied to them. Moving away from the yes-no format to asking for a total count has led to more disclosures, Dr. Gillespie said.
To “keep the conversation going” in subsequent well-child visits, they developed a few questions to ask high-risk parents, like “How do you and your partner resolve conflict?” and “How did your parents resolve conflict in your household when you were a child?” And they provided training to all of the clinic’s staff on trauma-informed care and the need for support and compassion in their interactions with family members.
In the 3-plus years since incorporating ACEs assessments, the clinic’s pediatricians have made soft referrals to mental health professionals in only several cases – in each case, by suggesting that the parent contact their primary care physician. What most parents have wanted, says Dr. Gillespie, is recommendations for parenting classes and support groups. The clinic’s care manager assists the pediatricians in maintaining and providing links and handouts for various resources.
For Dr. Gillespie, the impact of the culture shift has been dramatic. “I’ve had 8-10 moms spontaneously reveal domestic violence to me in a subsequent visit, and say that they need a little help, because they’ve gotten the message that this is a safe place to talk about their experiences,” he said. “That had never happened to me in the previous 12 years of so of my career.”
Dr. Pettersen’s relationships with parents became “more intimate and more honest.” There was more trust. “If we can talk with parents [about ACEs] and not judge them for it,” she said, “then nothing is off the table.”
The ‘Two-Gen’ approach
“But I’d push back and say, parents know they have toxic stress but they don’t name it,” she said. “What we can do as trusted providers who want to advocate for families is to bear witness to their history by asking about it. Once they realize it’s not what’s wrong with [them], it’s what’s happened to [them], a shift occurs. That’s extremely validating for parents.”
That validation is part of a two-generation approach that she and Dr. Burke Harris see as part of a movement to break cycles of ACEs and toxic stress. At the California Pacific Medical Center’s Bayview Child Health Center in San Francisco, Dr. Burke Harris uses three ACE questionnaires – two of them ask parents (of children or teens) to report how many adverse experience types, or categories, apply to them and/or their child or teen, and one surveys adolescents themselves.
With the resources and clinical support of the Center for Youth Wellness, whose major funders include Google, Dr. Burke Harris can initiate a “warm hand-off” of patients with a high ACE score to a care coordinator or therapist. (The Center for Youth Wellness is beginning research to validate its ACE screening tools.) And in the meantime, the medical care she provides is trauma-informed.
“If a patient comes in for ADHD [attention-deficit/hyperactivity disorder] and has an ACE score of 6, my differential diagnosis and assessment will be different than if I see a patient sent by the school who has an ACE score of 0,” she said.
At the Portland Clinic, even though ACEs screening is now tied with the 4-month visit, pediatricians are much more attentive across the board to possible ACEs and toxic stress, and feel better able to converse with families, Dr. Gillespie said. One of his partners recently saw a 12-year-old boy who was failing in school and not making friends. Trauma-informed history-taking revealed at least several ACEs, and conversation turned to “all the resilience pieces… the connections he was missing and what he needed to cope,” he said.
References
• Resilience Project: This AAP project houses a “trauma toolkit” for primary care, case studies, and a variety of other tools.
• Center for Youth Wellness: The ACEs screening tools used by Dr. Burke Harris may be accessed at this website, along with a user guide containing sample scripts, and two white papers on ACEs and toxic stress.
• Resilience: The Biology of Stress and the Science of Hope: This documentary film, released in September 2016, is about ACEs and “a new movement” to treat and prevent toxic stress; it features the work of Dr. Burke Harris and others.
• Academy on Violence & Abuse: Various papers on ACEs screening and case finding in practice may be accessed here.
Several years ago, pediatricians R.J. Gillespie, MD, MHPE, and Teri Pettersen, MD, piloted the use of a questionnaire about adverse childhood experiences (ACEs) and resilience at the 4-month well-child visit.
They and six other pediatricians at The Children’s Clinic in Portland, Ore., explained in a cover letter why they were posing the questions of parents, and they ended the survey by asking them about their interest in potential resources.
[[{"fid":"172157","view_mode":"medstat_image_flush_left","fields":{"format":"medstat_image_flush_left","field_file_image_alt_text[und][0][value]":"R.J. Gillespie, MD, MHPE","field_file_image_credit[und][0][value]":"Courtesy The Children's Clinic","field_file_image_caption[und][0][value]":"Dr. R.J. Gillespie "},"type":"media","attributes":{"class":"media-element file-medstat_image_flush_left"}}]]Today, all 28 of the pediatricians at the clinic screen for ACEs and resilience, and Dr. Pettersen, now retired from the practice, travels through the state conducting training for the Oregon Pediatric Society about the impact of ACEs in parents and their children, and how to go about identifying and addressing them.
“So many of our visits are about behavioral problems or emotional disturbances, and so often at the root of these issues is some sort of trauma the child is experiencing,” Dr. Gillespie said in an interview. “What we’re seeing in many of these cases really are coping strategies for that child to deal with the toxic stress in his or her life.”
By assessing parents’ exposure to ACEs, briefly talking with them about how ACEs might impact their parenting, and tailoring their counseling and anticipatory guidance, the pediatricians hope to prevent ACEs and consequent toxic stress from developing in children.
The driving science
The term ACEs entered the medical lexicon after 1998, when a landmark study called the Adverse Childhood Experiences Study showed that traumatic experiences in childhood – abuse, neglect, and other severe dysfunctions in a household – not only are common among American adults but are associated with numerous poor health outcomes.
In the study and subsequent analyses, Dr. Vincent Felitti of Kaiser Permanente in San Diego and Dr. Robert Anda of the Centers for Disease Control and Prevention surveyed more than 17,000 patients about 10 types of ACEs and their current health status and behaviors. About two-thirds reported having at least one ACE, and one in eight reported four or more (Am J Prev Med. 1998;14[4]:245-58, www.cdc.gov/violenceprevention/acestudy/about.html).
Adults with four or more ACEs were not only significantly more likely to report health risk behaviors (smoking, substance abuse) and poor mental health outcomes (depression, suicide attempt); they were also significantly more likely to have poor physical health outcomes, with 2.2 times the risk of ischemic heart disease, 1.9 times the risk of cancer, and 3.9 times the risk of chronic bronchitis or emphysema, for instance. There was a strong dose-response relationship between ACEs and poor outcomes.
The Felitti study spawned dozens of analyses and additional research – in children as well as adults – on the associations between early-life adversity and the incidence of poor behavioral, mental, and physical outcomes, as well as on potential mechanisms.
Some research suggested a direct link between ACEs and negative outcomes, independent of whether individuals adopt risky behavior. Other studies suggested what experts in child development and mental health have long argued – that the more ACEs a parent has, the more ACEs their child will have.
And a growing body of biomedical literature linked the extreme, frequent, or prolonged activation of the body’s stress response in childhood – what has come to be known as “toxic stress” – with disruptions of the developing nervous, cardiovascular, immune, and metabolic systems.
While precise connections and mechanisms need to be clarified, “we now know that the repeated activation of the stress response leads to [negative] changes in the neuroendocrine immune pathways,” said Dr. Burke Harris, who coauthored a recent review of toxic stress in children and adolescents (Adv Pediatr. 2016;63[1]:403-28).
In January 2012, the American Academy of Pediatrics published a policy statement titled “Early Childhood Adversity, Toxic Stress, and the Role of the Pediatrician: Translating Developmental Science into Lifelong Health,” in which it urged pediatricians to consider actively screening for precipitants of toxic stress that are common in their communities (Pediatrics. 2011 Dec. doi: 10.1542/peds.2011-2662). But it stopped short of recommending particular tools or methods.
Dr. Gillespie and Dr. Pettersen did not want to wait for tools to be validated and approaches to be proven. “We’re building the plane as we fly,” Dr. Pettersen said.
The clinic’s roll-out
Dr. Pettersen learned about the ACE study and related research about 8 years ago while on a sabbatical to learn more about mental health issues. It “changed everything” about the way she viewed children and families and adversity. “I knew (we) didn’t have the infrastructure at the clinic, or the clinic’s support, to really start assessing children for what was happening to them,” she said, so she began thinking about ACE prevention and a focus on parenting.
Dr. Gillespie, in the meantime, was active in various quality improvement efforts at the state and national level, and had also become increasingly bothered by visits in which he saw children affected by maternal depression, abnormal attachment, and other problems. “I was seeing the consequences of ACEs, but I didn’t know specifically what was going on or how to talk about it,” he said.
The two pediatricians agreed to ask parents about ACEs at the 4-month well visit – a time when the families “knew us a little bit” and when “we could still influence parenting styles.”
In March 2013, they and their colleagues in the pilot group began giving parents a questionnaire that included the 10 ACE questions from Felitti’s study, questions about resilience from the Children’s Resilience Initiative, and a list of potential resources so they could understand parents’ needs.
They created a confidential field in their electronic medical record for documentation that appears during a visit, but does not print into notes and therefore will not be inadvertently released.
As they moved through the pilot phase, the pediatricians used various approaches to follow up on the assessment face-to-face. Eventually, they chose three particular questions as nonthreatening and helpful for conversation: Are there any experiences that still bother you? Of those experiences that don’t bother you, how did you get to the point where they don’t bother you? And how do these experiences affect your parenting now?
“It’s a motivational interviewing sort of style,” said Dr. Gillespie. “Parents can start identifying for themselves the solutions for the problems they’ve experienced, and they can start thinking about how their parenting might be impacted by things that have happened [or are still happening] to them.”
As the project rolled out, the physicians tweaked their process. They added four more ACE questions to address issues – community violence, extreme bullying, racism and prejudice, and foster care exposure – that they thought might lead to toxic stress in their population, for instance. And rather than ask on the written questionnaire for a “yes” or “no” to each of the ACE questions, they began asking the parent how many of the ACE questions applied to them. Moving away from the yes-no format to asking for a total count has led to more disclosures, Dr. Gillespie said.
To “keep the conversation going” in subsequent well-child visits, they developed a few questions to ask high-risk parents, like “How do you and your partner resolve conflict?” and “How did your parents resolve conflict in your household when you were a child?” And they provided training to all of the clinic’s staff on trauma-informed care and the need for support and compassion in their interactions with family members.
In the 3-plus years since incorporating ACEs assessments, the clinic’s pediatricians have made soft referrals to mental health professionals in only several cases – in each case, by suggesting that the parent contact their primary care physician. What most parents have wanted, says Dr. Gillespie, is recommendations for parenting classes and support groups. The clinic’s care manager assists the pediatricians in maintaining and providing links and handouts for various resources.
For Dr. Gillespie, the impact of the culture shift has been dramatic. “I’ve had 8-10 moms spontaneously reveal domestic violence to me in a subsequent visit, and say that they need a little help, because they’ve gotten the message that this is a safe place to talk about their experiences,” he said. “That had never happened to me in the previous 12 years of so of my career.”
Dr. Pettersen’s relationships with parents became “more intimate and more honest.” There was more trust. “If we can talk with parents [about ACEs] and not judge them for it,” she said, “then nothing is off the table.”
The ‘Two-Gen’ approach
“But I’d push back and say, parents know they have toxic stress but they don’t name it,” she said. “What we can do as trusted providers who want to advocate for families is to bear witness to their history by asking about it. Once they realize it’s not what’s wrong with [them], it’s what’s happened to [them], a shift occurs. That’s extremely validating for parents.”
That validation is part of a two-generation approach that she and Dr. Burke Harris see as part of a movement to break cycles of ACEs and toxic stress. At the California Pacific Medical Center’s Bayview Child Health Center in San Francisco, Dr. Burke Harris uses three ACE questionnaires – two of them ask parents (of children or teens) to report how many adverse experience types, or categories, apply to them and/or their child or teen, and one surveys adolescents themselves.
With the resources and clinical support of the Center for Youth Wellness, whose major funders include Google, Dr. Burke Harris can initiate a “warm hand-off” of patients with a high ACE score to a care coordinator or therapist. (The Center for Youth Wellness is beginning research to validate its ACE screening tools.) And in the meantime, the medical care she provides is trauma-informed.
“If a patient comes in for ADHD [attention-deficit/hyperactivity disorder] and has an ACE score of 6, my differential diagnosis and assessment will be different than if I see a patient sent by the school who has an ACE score of 0,” she said.
At the Portland Clinic, even though ACEs screening is now tied with the 4-month visit, pediatricians are much more attentive across the board to possible ACEs and toxic stress, and feel better able to converse with families, Dr. Gillespie said. One of his partners recently saw a 12-year-old boy who was failing in school and not making friends. Trauma-informed history-taking revealed at least several ACEs, and conversation turned to “all the resilience pieces… the connections he was missing and what he needed to cope,” he said.
References
• Resilience Project: This AAP project houses a “trauma toolkit” for primary care, case studies, and a variety of other tools.
• Center for Youth Wellness: The ACEs screening tools used by Dr. Burke Harris may be accessed at this website, along with a user guide containing sample scripts, and two white papers on ACEs and toxic stress.
• Resilience: The Biology of Stress and the Science of Hope: This documentary film, released in September 2016, is about ACEs and “a new movement” to treat and prevent toxic stress; it features the work of Dr. Burke Harris and others.
• Academy on Violence & Abuse: Various papers on ACEs screening and case finding in practice may be accessed here.
Well-woman care: Reshaping the routine visit
From her vantage point in medical education, Christine M. Peterson, MD, is acutely aware that well-woman care is at a turning point.
“We’re at an interesting crossroads between tradition and evidence-based practice,” said Dr. Peterson, who practiced obstetrics and gynecology in the 1980s and now serves as associate professor of ob.gyn. and assistant dean for student affairs at the University of Virginia’s School of Medicine in Charlottesville.
“Even young trainees are aware of the traditions for the annual well-woman visit – the Pap, the pelvic, the breast exam,” she said. “But the evidence is pointing us in a different direction ... toward doing only those things that are effective for prevention and early detection of disease, or that have [demonstrated] value in one way or another.”
If all goes as planned at a national level, Dr. Peterson’s students who become ob.gyns., family physicians, and general internists will practice under a reshaped and well-defined umbrella of well-woman care – one that includes a broad array of insurer-covered screening and counseling services.
That umbrella already includes HPV testing, and screening and/or counseling on intimate partner violence, sexually transmitted infections, and HIV, in addition to contraception counseling. These preventive services were described in the Women’s Preventive Services Guidelines and adopted as covered benefits by the Department of Health & Human Services in 2011.
And more change is on the way. In March, the American College of Obstetricians and Gynecologists (ACOG) launched the Women’s Preventive Services Initiative (WPSI) – a broad coalition tasked with recommending updates to the 2011 guidelines and developing new recommendations for the scope and implementation of women’s preventive health care services.
The effort is funded through a 5-year cooperative agreement with the Health Resources & Services Administration (HRSA). It’s similar to the American Academy of Pediatrics’ approach in developing the HRSA-supported Bright Futures guidelines almost 25 years ago. Under the Affordable Care Act, all HRSA-recommended preventive services must be covered by most private insurers without patient cost sharing.
“Over the years, we’ve gone from an emphasis on the Pap and pelvic to well-woman care that assesses the whole woman,” said Jeanne A. Conry, MD, assistant physician-in-chief at the Permanente Medical Group in Roseville, Calif., and a past president of ACOG.
Ob.gyns. have long provided preventive care, but today more than ever before, Dr. Conry said, “my emphasis is on helping women to get well and stay well.”
The evolution
Fifty years ago, in 1966, use of the Pap test was being widely promoted, modern mammography techniques were on the cusp of advancement, and ob.gyns. were prescribing the first birth control pill approved by the Food and Drug Administration. ACOG’s main practice guidance book, “Standards for Obstetric-Gynecologic Hospital Services,” addressed the general physical examination but otherwise focused on obstetrics and reproductive health.
Thirty years later, women’s health care as described in the first edition of ACOG’s “Guidelines for Women’s Health Care” (1996) had grown to include distinct categories of “primary and preventive care” and “evaluation and counseling” that were separate from gynecologic services and broken down by age.
What was referred to as the “women’s health exam” through the 1990s gradually took on the “well-woman” label in the 2000s. Ob.gyns. were encouraged to address a growing range of preventive issues, but the annual Pap test remained a focus and, in many ways, drove women’s visits.
“Women would say, ‘I’m going for my Pap,’” Dr. Conry said.
Most recently, new technology and evidence-based reviews have changed the framework for well-woman visits to one with longer intervals for cervical cancer screening (every 3-5 years) and a move away from performing internal pelvic exams in all women (ACOG recommends pelvic exams annually for patients aged 21 and older but advises shared decision making for complete pelvic exams in asymptomatic patients).
Recent evidence reviews have also added some uncertainty about the role of annual breast exams in all women, as well as the role of breast self-exams, particularly for women not at high risk.
Maintaining patient relationships
One of the biggest and most immediate challenges for ob.gyns in the face of changing guidelines lies in maintaining the physician-patient relationship and “continuing communication” about the importance of regular well-woman visits, said Jill Rabin, MD, cochief of the division of ambulatory care, women’s health programs–prenatal care assistance program services at Northwell Health, New Hyde Park, N.Y.
“We want patients to understand that, even though they no longer need the Pap every year, they still should see us for good, comprehensive care ... that we can help them achieve their health care goals,” she said.
How often well-woman visits should occur has been a subject of much discussion. The HRSA-supported preventive services guidelines call for well-woman preventive care annually but note that “several visits may be needed to obtain all the necessary recommended services.”
And, in its first set of draft recommendations for HRSA, WPSI offered clarifications, saying there’s a need for “at least one annual preventive care visit for women beginning in adolescence and continuing across the lifespan to ensure that women obtain recommended preventive services” as determined by age and risk factors.
The draft recommendations, aimed at reviewing and updating the 2011 HRSA-sponsored guidelines, will be finalized by the end of 2016. WPSI will submit additional recommendations over the next 4 years.
Carol S. Weisman, PhD, a sociologist and health services researcher who sat on the Institute of Medicine committee that wrote the Women’s Preventive Services Guidelines, said the IOM’s recommendation for well-women visits – “in plural” form – recognizes “that historically many women have patched together their well-woman care from multiple providers, getting some of their preventive care from their generalist, and some from their ob.gyn.”
What’s more, the current list of preventive services covered under the Affordable Care Act is “enormous” – too long to address in one visit for many patients, said Dr. Weisman of the Penn State Center for Women’s Health Research in Hershey.
In addition to the women’s preventive services, the Affordable Care Act requires plans to cover services recommended with a grade A or B rating by the U.S. Preventive Services Task Force (counseling and screening for cancer, cardiovascular disease, and more) as well as vaccines recommended by the Advisory Committee on Immunization Practices, and HRSA’s Bright Futures services (for adolescents as well as children).
Beyond gynecology
How much further ob.gyns. will reach outside the gynecologic realm to offer additional preventive care services is an open question, but it’s likely to be based mainly on comfort levels, sources said.
“The changing needs of the gynecologic visit enable us to spend more time on other things,” said Hal C. Lawrence III, MD, ACOG’s executive vice president and chief executive officer. “But within the specialty, there’s going to be variation as to what level of expanded services ob.gyns. provide. Some will provide a lot of what women need, others not as much.”
Heather Johnson, MD, practices with a large ob.gyn. group in Chevy Chase, Md. and provides well-woman care largely to women in their 50s and 60s, whose children she delivered. She’s comfortable, she said, with screening for and treating osteoporosis and mild depression, for instance. She regularly performs lipid testing but refers out for management of high cholesterol levels or high blood pressure.
“I encourage all my patients to have a primary care physician of record,” she said, “but I still am happy to discuss the issues with them.”
What’s key, according to Dr. Lawrence and Dr. Conry, is coordination.
“We know there will be different individuals providing different components [of well-woman care],” Dr. Conry said. “I may see a woman for various things. Then she may go to her internist. But we should be able to collaborate to hit all the preventive health goals for her.”
Dr. Conry emphasized that the ob.gyn.’s expertise in reproductive health is critical to well-woman care planning, especially given medicine’s growing knowledge of how obstetric health and pregnancy complications can have long-term impacts on cardiovascular disease and other conditions. “It’s important for all providers to realize this,” she said.
Primary care status?
Intertwined with the future of well-women care is the issue of primary care status for ob.gyns. ACOG continues to advocate for ob.gyns. to be listed as primary care providers and part of primary care payment policies. Leaders are also pushing for projects on ob.gyn.–led medical homes.
At the same time, ACOG has been taking a broad collaborative approach to shaping well-woman care, aiming to develop comprehensive, age-specific recommendations for use by any provider who cares for adolescent girls and women.
Representatives of the American Academy of Family Physicians, the American College of Physicians, and the National Association of Nurse Practitioners in Women’s Health were involved in a Well-Woman Task Force that Dr. Conry appointed while serving as ACOG president in 2013-2014. These organizations now sit on WPSI’s advisory panel with ACOG.
Representatives from the American Academy of Pediatrics have also been close partners, as ACOG officials view the HRSA-sponsored Bright Futures guidelines (which includes the “Periodicity Schedule”) as a potential model for well-woman care. The guidelines are comprehensive, well-organized, and user-friendly, ACOG officials said.
At the University of Virginia, in the meantime, Dr. Peterson is arming the next generation of ob.gyns. with the skills needed for a team-based approach to well-woman visits. She said nurse practitioners and physician assistants will provide much more of the education and “more of the truly individualized conversations with patients” that will increasingly be part of well-woman care.
This is already happening. All of the nurse practitioners in Dr. Johnson’s group practice perform well-woman visits, “referring to the gynecologists for complicated gyn problems and out to the patient’s primary care physician for complicated medical problems,” Dr. Johnson said.
Even as the tools and recommendations for women’s preventive care become more evidence-based, the scope of well-woman visits will be based on risk factors, shared decision making, and other issues, Dr. Peterson said. “We will be telling patients, this is your path for your well-woman care,” she said.
Throughout 2016, Ob.Gyn. News is celebrating its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and whether the practice environment is better or worse.
From her vantage point in medical education, Christine M. Peterson, MD, is acutely aware that well-woman care is at a turning point.
“We’re at an interesting crossroads between tradition and evidence-based practice,” said Dr. Peterson, who practiced obstetrics and gynecology in the 1980s and now serves as associate professor of ob.gyn. and assistant dean for student affairs at the University of Virginia’s School of Medicine in Charlottesville.
“Even young trainees are aware of the traditions for the annual well-woman visit – the Pap, the pelvic, the breast exam,” she said. “But the evidence is pointing us in a different direction ... toward doing only those things that are effective for prevention and early detection of disease, or that have [demonstrated] value in one way or another.”
If all goes as planned at a national level, Dr. Peterson’s students who become ob.gyns., family physicians, and general internists will practice under a reshaped and well-defined umbrella of well-woman care – one that includes a broad array of insurer-covered screening and counseling services.
That umbrella already includes HPV testing, and screening and/or counseling on intimate partner violence, sexually transmitted infections, and HIV, in addition to contraception counseling. These preventive services were described in the Women’s Preventive Services Guidelines and adopted as covered benefits by the Department of Health & Human Services in 2011.
And more change is on the way. In March, the American College of Obstetricians and Gynecologists (ACOG) launched the Women’s Preventive Services Initiative (WPSI) – a broad coalition tasked with recommending updates to the 2011 guidelines and developing new recommendations for the scope and implementation of women’s preventive health care services.
The effort is funded through a 5-year cooperative agreement with the Health Resources & Services Administration (HRSA). It’s similar to the American Academy of Pediatrics’ approach in developing the HRSA-supported Bright Futures guidelines almost 25 years ago. Under the Affordable Care Act, all HRSA-recommended preventive services must be covered by most private insurers without patient cost sharing.
“Over the years, we’ve gone from an emphasis on the Pap and pelvic to well-woman care that assesses the whole woman,” said Jeanne A. Conry, MD, assistant physician-in-chief at the Permanente Medical Group in Roseville, Calif., and a past president of ACOG.
Ob.gyns. have long provided preventive care, but today more than ever before, Dr. Conry said, “my emphasis is on helping women to get well and stay well.”
The evolution
Fifty years ago, in 1966, use of the Pap test was being widely promoted, modern mammography techniques were on the cusp of advancement, and ob.gyns. were prescribing the first birth control pill approved by the Food and Drug Administration. ACOG’s main practice guidance book, “Standards for Obstetric-Gynecologic Hospital Services,” addressed the general physical examination but otherwise focused on obstetrics and reproductive health.
Thirty years later, women’s health care as described in the first edition of ACOG’s “Guidelines for Women’s Health Care” (1996) had grown to include distinct categories of “primary and preventive care” and “evaluation and counseling” that were separate from gynecologic services and broken down by age.
What was referred to as the “women’s health exam” through the 1990s gradually took on the “well-woman” label in the 2000s. Ob.gyns. were encouraged to address a growing range of preventive issues, but the annual Pap test remained a focus and, in many ways, drove women’s visits.
“Women would say, ‘I’m going for my Pap,’” Dr. Conry said.
Most recently, new technology and evidence-based reviews have changed the framework for well-woman visits to one with longer intervals for cervical cancer screening (every 3-5 years) and a move away from performing internal pelvic exams in all women (ACOG recommends pelvic exams annually for patients aged 21 and older but advises shared decision making for complete pelvic exams in asymptomatic patients).
Recent evidence reviews have also added some uncertainty about the role of annual breast exams in all women, as well as the role of breast self-exams, particularly for women not at high risk.
Maintaining patient relationships
One of the biggest and most immediate challenges for ob.gyns in the face of changing guidelines lies in maintaining the physician-patient relationship and “continuing communication” about the importance of regular well-woman visits, said Jill Rabin, MD, cochief of the division of ambulatory care, women’s health programs–prenatal care assistance program services at Northwell Health, New Hyde Park, N.Y.
“We want patients to understand that, even though they no longer need the Pap every year, they still should see us for good, comprehensive care ... that we can help them achieve their health care goals,” she said.
How often well-woman visits should occur has been a subject of much discussion. The HRSA-supported preventive services guidelines call for well-woman preventive care annually but note that “several visits may be needed to obtain all the necessary recommended services.”
And, in its first set of draft recommendations for HRSA, WPSI offered clarifications, saying there’s a need for “at least one annual preventive care visit for women beginning in adolescence and continuing across the lifespan to ensure that women obtain recommended preventive services” as determined by age and risk factors.
The draft recommendations, aimed at reviewing and updating the 2011 HRSA-sponsored guidelines, will be finalized by the end of 2016. WPSI will submit additional recommendations over the next 4 years.
Carol S. Weisman, PhD, a sociologist and health services researcher who sat on the Institute of Medicine committee that wrote the Women’s Preventive Services Guidelines, said the IOM’s recommendation for well-women visits – “in plural” form – recognizes “that historically many women have patched together their well-woman care from multiple providers, getting some of their preventive care from their generalist, and some from their ob.gyn.”
What’s more, the current list of preventive services covered under the Affordable Care Act is “enormous” – too long to address in one visit for many patients, said Dr. Weisman of the Penn State Center for Women’s Health Research in Hershey.
In addition to the women’s preventive services, the Affordable Care Act requires plans to cover services recommended with a grade A or B rating by the U.S. Preventive Services Task Force (counseling and screening for cancer, cardiovascular disease, and more) as well as vaccines recommended by the Advisory Committee on Immunization Practices, and HRSA’s Bright Futures services (for adolescents as well as children).
Beyond gynecology
How much further ob.gyns. will reach outside the gynecologic realm to offer additional preventive care services is an open question, but it’s likely to be based mainly on comfort levels, sources said.
“The changing needs of the gynecologic visit enable us to spend more time on other things,” said Hal C. Lawrence III, MD, ACOG’s executive vice president and chief executive officer. “But within the specialty, there’s going to be variation as to what level of expanded services ob.gyns. provide. Some will provide a lot of what women need, others not as much.”
Heather Johnson, MD, practices with a large ob.gyn. group in Chevy Chase, Md. and provides well-woman care largely to women in their 50s and 60s, whose children she delivered. She’s comfortable, she said, with screening for and treating osteoporosis and mild depression, for instance. She regularly performs lipid testing but refers out for management of high cholesterol levels or high blood pressure.
“I encourage all my patients to have a primary care physician of record,” she said, “but I still am happy to discuss the issues with them.”
What’s key, according to Dr. Lawrence and Dr. Conry, is coordination.
“We know there will be different individuals providing different components [of well-woman care],” Dr. Conry said. “I may see a woman for various things. Then she may go to her internist. But we should be able to collaborate to hit all the preventive health goals for her.”
Dr. Conry emphasized that the ob.gyn.’s expertise in reproductive health is critical to well-woman care planning, especially given medicine’s growing knowledge of how obstetric health and pregnancy complications can have long-term impacts on cardiovascular disease and other conditions. “It’s important for all providers to realize this,” she said.
Primary care status?
Intertwined with the future of well-women care is the issue of primary care status for ob.gyns. ACOG continues to advocate for ob.gyns. to be listed as primary care providers and part of primary care payment policies. Leaders are also pushing for projects on ob.gyn.–led medical homes.
At the same time, ACOG has been taking a broad collaborative approach to shaping well-woman care, aiming to develop comprehensive, age-specific recommendations for use by any provider who cares for adolescent girls and women.
Representatives of the American Academy of Family Physicians, the American College of Physicians, and the National Association of Nurse Practitioners in Women’s Health were involved in a Well-Woman Task Force that Dr. Conry appointed while serving as ACOG president in 2013-2014. These organizations now sit on WPSI’s advisory panel with ACOG.
Representatives from the American Academy of Pediatrics have also been close partners, as ACOG officials view the HRSA-sponsored Bright Futures guidelines (which includes the “Periodicity Schedule”) as a potential model for well-woman care. The guidelines are comprehensive, well-organized, and user-friendly, ACOG officials said.
At the University of Virginia, in the meantime, Dr. Peterson is arming the next generation of ob.gyns. with the skills needed for a team-based approach to well-woman visits. She said nurse practitioners and physician assistants will provide much more of the education and “more of the truly individualized conversations with patients” that will increasingly be part of well-woman care.
This is already happening. All of the nurse practitioners in Dr. Johnson’s group practice perform well-woman visits, “referring to the gynecologists for complicated gyn problems and out to the patient’s primary care physician for complicated medical problems,” Dr. Johnson said.
Even as the tools and recommendations for women’s preventive care become more evidence-based, the scope of well-woman visits will be based on risk factors, shared decision making, and other issues, Dr. Peterson said. “We will be telling patients, this is your path for your well-woman care,” she said.
Throughout 2016, Ob.Gyn. News is celebrating its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and whether the practice environment is better or worse.
From her vantage point in medical education, Christine M. Peterson, MD, is acutely aware that well-woman care is at a turning point.
“We’re at an interesting crossroads between tradition and evidence-based practice,” said Dr. Peterson, who practiced obstetrics and gynecology in the 1980s and now serves as associate professor of ob.gyn. and assistant dean for student affairs at the University of Virginia’s School of Medicine in Charlottesville.
“Even young trainees are aware of the traditions for the annual well-woman visit – the Pap, the pelvic, the breast exam,” she said. “But the evidence is pointing us in a different direction ... toward doing only those things that are effective for prevention and early detection of disease, or that have [demonstrated] value in one way or another.”
If all goes as planned at a national level, Dr. Peterson’s students who become ob.gyns., family physicians, and general internists will practice under a reshaped and well-defined umbrella of well-woman care – one that includes a broad array of insurer-covered screening and counseling services.
That umbrella already includes HPV testing, and screening and/or counseling on intimate partner violence, sexually transmitted infections, and HIV, in addition to contraception counseling. These preventive services were described in the Women’s Preventive Services Guidelines and adopted as covered benefits by the Department of Health & Human Services in 2011.
And more change is on the way. In March, the American College of Obstetricians and Gynecologists (ACOG) launched the Women’s Preventive Services Initiative (WPSI) – a broad coalition tasked with recommending updates to the 2011 guidelines and developing new recommendations for the scope and implementation of women’s preventive health care services.
The effort is funded through a 5-year cooperative agreement with the Health Resources & Services Administration (HRSA). It’s similar to the American Academy of Pediatrics’ approach in developing the HRSA-supported Bright Futures guidelines almost 25 years ago. Under the Affordable Care Act, all HRSA-recommended preventive services must be covered by most private insurers without patient cost sharing.
“Over the years, we’ve gone from an emphasis on the Pap and pelvic to well-woman care that assesses the whole woman,” said Jeanne A. Conry, MD, assistant physician-in-chief at the Permanente Medical Group in Roseville, Calif., and a past president of ACOG.
Ob.gyns. have long provided preventive care, but today more than ever before, Dr. Conry said, “my emphasis is on helping women to get well and stay well.”
The evolution
Fifty years ago, in 1966, use of the Pap test was being widely promoted, modern mammography techniques were on the cusp of advancement, and ob.gyns. were prescribing the first birth control pill approved by the Food and Drug Administration. ACOG’s main practice guidance book, “Standards for Obstetric-Gynecologic Hospital Services,” addressed the general physical examination but otherwise focused on obstetrics and reproductive health.
Thirty years later, women’s health care as described in the first edition of ACOG’s “Guidelines for Women’s Health Care” (1996) had grown to include distinct categories of “primary and preventive care” and “evaluation and counseling” that were separate from gynecologic services and broken down by age.
What was referred to as the “women’s health exam” through the 1990s gradually took on the “well-woman” label in the 2000s. Ob.gyns. were encouraged to address a growing range of preventive issues, but the annual Pap test remained a focus and, in many ways, drove women’s visits.
“Women would say, ‘I’m going for my Pap,’” Dr. Conry said.
Most recently, new technology and evidence-based reviews have changed the framework for well-woman visits to one with longer intervals for cervical cancer screening (every 3-5 years) and a move away from performing internal pelvic exams in all women (ACOG recommends pelvic exams annually for patients aged 21 and older but advises shared decision making for complete pelvic exams in asymptomatic patients).
Recent evidence reviews have also added some uncertainty about the role of annual breast exams in all women, as well as the role of breast self-exams, particularly for women not at high risk.
Maintaining patient relationships
One of the biggest and most immediate challenges for ob.gyns in the face of changing guidelines lies in maintaining the physician-patient relationship and “continuing communication” about the importance of regular well-woman visits, said Jill Rabin, MD, cochief of the division of ambulatory care, women’s health programs–prenatal care assistance program services at Northwell Health, New Hyde Park, N.Y.
“We want patients to understand that, even though they no longer need the Pap every year, they still should see us for good, comprehensive care ... that we can help them achieve their health care goals,” she said.
How often well-woman visits should occur has been a subject of much discussion. The HRSA-supported preventive services guidelines call for well-woman preventive care annually but note that “several visits may be needed to obtain all the necessary recommended services.”
And, in its first set of draft recommendations for HRSA, WPSI offered clarifications, saying there’s a need for “at least one annual preventive care visit for women beginning in adolescence and continuing across the lifespan to ensure that women obtain recommended preventive services” as determined by age and risk factors.
The draft recommendations, aimed at reviewing and updating the 2011 HRSA-sponsored guidelines, will be finalized by the end of 2016. WPSI will submit additional recommendations over the next 4 years.
Carol S. Weisman, PhD, a sociologist and health services researcher who sat on the Institute of Medicine committee that wrote the Women’s Preventive Services Guidelines, said the IOM’s recommendation for well-women visits – “in plural” form – recognizes “that historically many women have patched together their well-woman care from multiple providers, getting some of their preventive care from their generalist, and some from their ob.gyn.”
What’s more, the current list of preventive services covered under the Affordable Care Act is “enormous” – too long to address in one visit for many patients, said Dr. Weisman of the Penn State Center for Women’s Health Research in Hershey.
In addition to the women’s preventive services, the Affordable Care Act requires plans to cover services recommended with a grade A or B rating by the U.S. Preventive Services Task Force (counseling and screening for cancer, cardiovascular disease, and more) as well as vaccines recommended by the Advisory Committee on Immunization Practices, and HRSA’s Bright Futures services (for adolescents as well as children).
Beyond gynecology
How much further ob.gyns. will reach outside the gynecologic realm to offer additional preventive care services is an open question, but it’s likely to be based mainly on comfort levels, sources said.
“The changing needs of the gynecologic visit enable us to spend more time on other things,” said Hal C. Lawrence III, MD, ACOG’s executive vice president and chief executive officer. “But within the specialty, there’s going to be variation as to what level of expanded services ob.gyns. provide. Some will provide a lot of what women need, others not as much.”
Heather Johnson, MD, practices with a large ob.gyn. group in Chevy Chase, Md. and provides well-woman care largely to women in their 50s and 60s, whose children she delivered. She’s comfortable, she said, with screening for and treating osteoporosis and mild depression, for instance. She regularly performs lipid testing but refers out for management of high cholesterol levels or high blood pressure.
“I encourage all my patients to have a primary care physician of record,” she said, “but I still am happy to discuss the issues with them.”
What’s key, according to Dr. Lawrence and Dr. Conry, is coordination.
“We know there will be different individuals providing different components [of well-woman care],” Dr. Conry said. “I may see a woman for various things. Then she may go to her internist. But we should be able to collaborate to hit all the preventive health goals for her.”
Dr. Conry emphasized that the ob.gyn.’s expertise in reproductive health is critical to well-woman care planning, especially given medicine’s growing knowledge of how obstetric health and pregnancy complications can have long-term impacts on cardiovascular disease and other conditions. “It’s important for all providers to realize this,” she said.
Primary care status?
Intertwined with the future of well-women care is the issue of primary care status for ob.gyns. ACOG continues to advocate for ob.gyns. to be listed as primary care providers and part of primary care payment policies. Leaders are also pushing for projects on ob.gyn.–led medical homes.
At the same time, ACOG has been taking a broad collaborative approach to shaping well-woman care, aiming to develop comprehensive, age-specific recommendations for use by any provider who cares for adolescent girls and women.
Representatives of the American Academy of Family Physicians, the American College of Physicians, and the National Association of Nurse Practitioners in Women’s Health were involved in a Well-Woman Task Force that Dr. Conry appointed while serving as ACOG president in 2013-2014. These organizations now sit on WPSI’s advisory panel with ACOG.
Representatives from the American Academy of Pediatrics have also been close partners, as ACOG officials view the HRSA-sponsored Bright Futures guidelines (which includes the “Periodicity Schedule”) as a potential model for well-woman care. The guidelines are comprehensive, well-organized, and user-friendly, ACOG officials said.
At the University of Virginia, in the meantime, Dr. Peterson is arming the next generation of ob.gyns. with the skills needed for a team-based approach to well-woman visits. She said nurse practitioners and physician assistants will provide much more of the education and “more of the truly individualized conversations with patients” that will increasingly be part of well-woman care.
This is already happening. All of the nurse practitioners in Dr. Johnson’s group practice perform well-woman visits, “referring to the gynecologists for complicated gyn problems and out to the patient’s primary care physician for complicated medical problems,” Dr. Johnson said.
Even as the tools and recommendations for women’s preventive care become more evidence-based, the scope of well-woman visits will be based on risk factors, shared decision making, and other issues, Dr. Peterson said. “We will be telling patients, this is your path for your well-woman care,” she said.
Throughout 2016, Ob.Gyn. News is celebrating its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and whether the practice environment is better or worse.
Meta-analysis suggests earlier twin delivery to prevent stillbirth
Delivery for uncomplicated dichorionic twin pregnancies should be considered at 37 weeks’ gestation, a week earlier than is generally recommended in the United States, according to a systematic review and meta-analysis of studies that reported rates of stillbirth and neonatal mortality at various gestational ages.
The researchers assessed the competing risks in twin pregnancies of stillbirth from expectant management versus neonatal death from early delivery, looking for an optimal gestational age at which these risks were balanced.
In dichorionic pregnancies continuing beyond 34 weeks, these perinatal risks were balanced at 37 weeks. Beyond that, “the risks of stillbirth significantly outweighed the risk of neonatal death from delivery,” with a 1-week delay in delivery (to 38 weeks’ gestation) leading to an additional 8.8 perinatal deaths per 1,000 pregnancies due to an increase in stillbirth, Fiona Cheong-See, MD, of the Queen Mary University of London and her colleagues reported (BMJ 2016;354:i4353. doi: 10.1136/bmj.i4353).
The review included 32 studies published in the past 10 years (observational cohort studies and cohorts nested in randomized studies) that reported rates of stillbirth and/or neonatal outcomes, including neonatal mortality, in monochorionic and/or dichorionic twins. Neonatal death was defined as death up to 28 days after delivery.
The study authors shared unpublished aggregate and individual patient data with the meta-analysis researchers, which enabled an analysis at weekly intervals. The data included in the review covered 35,171 women with twin gestations (29,685 dichorionic and 5,486 monochorionic pregnancies).
Pregnancies with unclear chorionicity, monoamnionity, and twin-to-twin transfusion syndrome were excluded from the analysis.
In monochorionic pregnancies continuing beyond 34 weeks (2,149 pregnancies), there was a trend after 36 weeks toward stillbirth risk being higher than the risk of neonatal death, but the risk difference was not significant.
More data are needed, the researchers said, but “based on our findings, there is no clear evidence to recommend early preterm delivery routinely before 36 weeks in monochorionic pregnancies.”
A committee opinion published by the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine (ACOG-SMFM) on medically indicated late-preterm and early-term deliveries states that decisions regarding the timing of delivery should be individualized and should take into account relative maternal and newborn risks, practice environment, and patient preferences (Obstet Gynecol. 2013;121:908-10).
Still, the ACOG-SMFM document offers delivery recommendations: 38 0/7-38 6/7 weeks of gestation for dichorionic-diamniotic pregnancies, and 34 0/7-36 6/7 weeks of gestation for monochorionic-diamniotic pregnancies.
The opinion was published in 2013 and reflects recommendations made 2 years earlier by the National Institute of Child Health and Human Development and SMFM after a workshop on indicated preterm birth (Obstet Gynecol 2011;118:323-33). ACOG and SMFM reaffirmed their document in 2015.
Brigid McCue, MD, chief of ob.gyn. at Beth Israel Deaconess Hospital–Plymouth (Mass.) and a member of ACOG’s Committee on Obstetric Practice, said the meta-analysis is of “high quality,” with “helpful and valid” findings for dichorionic twins.
The risk of stillbirth was 1.2/1,000 pregnancies at 34 weeks’ gestation, while the risk of neonatal death from delivery was 6.7/1,000 pregnancies. The risk of stillbirth remained significantly lower than the risk of neonatal death from delivery at 35 weeks, and was lower at 36 weeks as well. At 37 weeks, the two categories of perinatal death risk were basically balanced, with the risk of stillbirth at 3.4/1,000 pregnancies.
Beyond that, at 38 weeks’ gestation, the risk of stillbirth (10.6/1,000) significantly outweighed the risk of neonatal death from delivery (1.5/1,000) for a pooled risk difference of 8.8.
“The finding that stillbirth risk is higher when you allow someone to go from 37 to 38 weeks – I think this is true,” Dr. McCue said in an interview.
Further research needs to account, however, for the risks of neonatal morbidity at 37 and 38 weeks. “The next question in coming up with a point of inflection is to ask, What are other contributors to the balance of timing of the delivery?” Dr. McCue said. “There’s a bigger picture that needs more analysis.”
“We don’t induce singletons prior to 39 weeks because they can have more respiratory distress, more hypoglycemia, more temperature instability, and less success breastfeeding, for example,” she added. “These complications pale in comparison to a stillbirth, but the numbers of stillbirth are so low and the numbers for [these other morbidities] are much higher.”
The authors of the meta-analysis noted that their findings were limited by the common policy of planned delivery beyond 37 and 38 weeks’ gestation. “This reduced the sample size near term, particularly in monochorionic pregnancies, and could have led to underestimation of risk of stillbirth in the last weeks of pregnancy,” they wrote.
The rates of assisted ventilation, respiratory distress syndrome, admission to the neonatal intensive care unit, and septicemia showed a consistent reduction with increasing gestational age in babies of both monochorionic and dichorionic pregnancies, the researchers noted.
The researchers reported that they received no funding support from any organization and had no relevant financial disclosures.
Delivery for uncomplicated dichorionic twin pregnancies should be considered at 37 weeks’ gestation, a week earlier than is generally recommended in the United States, according to a systematic review and meta-analysis of studies that reported rates of stillbirth and neonatal mortality at various gestational ages.
The researchers assessed the competing risks in twin pregnancies of stillbirth from expectant management versus neonatal death from early delivery, looking for an optimal gestational age at which these risks were balanced.
In dichorionic pregnancies continuing beyond 34 weeks, these perinatal risks were balanced at 37 weeks. Beyond that, “the risks of stillbirth significantly outweighed the risk of neonatal death from delivery,” with a 1-week delay in delivery (to 38 weeks’ gestation) leading to an additional 8.8 perinatal deaths per 1,000 pregnancies due to an increase in stillbirth, Fiona Cheong-See, MD, of the Queen Mary University of London and her colleagues reported (BMJ 2016;354:i4353. doi: 10.1136/bmj.i4353).
The review included 32 studies published in the past 10 years (observational cohort studies and cohorts nested in randomized studies) that reported rates of stillbirth and/or neonatal outcomes, including neonatal mortality, in monochorionic and/or dichorionic twins. Neonatal death was defined as death up to 28 days after delivery.
The study authors shared unpublished aggregate and individual patient data with the meta-analysis researchers, which enabled an analysis at weekly intervals. The data included in the review covered 35,171 women with twin gestations (29,685 dichorionic and 5,486 monochorionic pregnancies).
Pregnancies with unclear chorionicity, monoamnionity, and twin-to-twin transfusion syndrome were excluded from the analysis.
In monochorionic pregnancies continuing beyond 34 weeks (2,149 pregnancies), there was a trend after 36 weeks toward stillbirth risk being higher than the risk of neonatal death, but the risk difference was not significant.
More data are needed, the researchers said, but “based on our findings, there is no clear evidence to recommend early preterm delivery routinely before 36 weeks in monochorionic pregnancies.”
A committee opinion published by the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine (ACOG-SMFM) on medically indicated late-preterm and early-term deliveries states that decisions regarding the timing of delivery should be individualized and should take into account relative maternal and newborn risks, practice environment, and patient preferences (Obstet Gynecol. 2013;121:908-10).
Still, the ACOG-SMFM document offers delivery recommendations: 38 0/7-38 6/7 weeks of gestation for dichorionic-diamniotic pregnancies, and 34 0/7-36 6/7 weeks of gestation for monochorionic-diamniotic pregnancies.
The opinion was published in 2013 and reflects recommendations made 2 years earlier by the National Institute of Child Health and Human Development and SMFM after a workshop on indicated preterm birth (Obstet Gynecol 2011;118:323-33). ACOG and SMFM reaffirmed their document in 2015.
Brigid McCue, MD, chief of ob.gyn. at Beth Israel Deaconess Hospital–Plymouth (Mass.) and a member of ACOG’s Committee on Obstetric Practice, said the meta-analysis is of “high quality,” with “helpful and valid” findings for dichorionic twins.
The risk of stillbirth was 1.2/1,000 pregnancies at 34 weeks’ gestation, while the risk of neonatal death from delivery was 6.7/1,000 pregnancies. The risk of stillbirth remained significantly lower than the risk of neonatal death from delivery at 35 weeks, and was lower at 36 weeks as well. At 37 weeks, the two categories of perinatal death risk were basically balanced, with the risk of stillbirth at 3.4/1,000 pregnancies.
Beyond that, at 38 weeks’ gestation, the risk of stillbirth (10.6/1,000) significantly outweighed the risk of neonatal death from delivery (1.5/1,000) for a pooled risk difference of 8.8.
“The finding that stillbirth risk is higher when you allow someone to go from 37 to 38 weeks – I think this is true,” Dr. McCue said in an interview.
Further research needs to account, however, for the risks of neonatal morbidity at 37 and 38 weeks. “The next question in coming up with a point of inflection is to ask, What are other contributors to the balance of timing of the delivery?” Dr. McCue said. “There’s a bigger picture that needs more analysis.”
“We don’t induce singletons prior to 39 weeks because they can have more respiratory distress, more hypoglycemia, more temperature instability, and less success breastfeeding, for example,” she added. “These complications pale in comparison to a stillbirth, but the numbers of stillbirth are so low and the numbers for [these other morbidities] are much higher.”
The authors of the meta-analysis noted that their findings were limited by the common policy of planned delivery beyond 37 and 38 weeks’ gestation. “This reduced the sample size near term, particularly in monochorionic pregnancies, and could have led to underestimation of risk of stillbirth in the last weeks of pregnancy,” they wrote.
The rates of assisted ventilation, respiratory distress syndrome, admission to the neonatal intensive care unit, and septicemia showed a consistent reduction with increasing gestational age in babies of both monochorionic and dichorionic pregnancies, the researchers noted.
The researchers reported that they received no funding support from any organization and had no relevant financial disclosures.
Delivery for uncomplicated dichorionic twin pregnancies should be considered at 37 weeks’ gestation, a week earlier than is generally recommended in the United States, according to a systematic review and meta-analysis of studies that reported rates of stillbirth and neonatal mortality at various gestational ages.
The researchers assessed the competing risks in twin pregnancies of stillbirth from expectant management versus neonatal death from early delivery, looking for an optimal gestational age at which these risks were balanced.
In dichorionic pregnancies continuing beyond 34 weeks, these perinatal risks were balanced at 37 weeks. Beyond that, “the risks of stillbirth significantly outweighed the risk of neonatal death from delivery,” with a 1-week delay in delivery (to 38 weeks’ gestation) leading to an additional 8.8 perinatal deaths per 1,000 pregnancies due to an increase in stillbirth, Fiona Cheong-See, MD, of the Queen Mary University of London and her colleagues reported (BMJ 2016;354:i4353. doi: 10.1136/bmj.i4353).
The review included 32 studies published in the past 10 years (observational cohort studies and cohorts nested in randomized studies) that reported rates of stillbirth and/or neonatal outcomes, including neonatal mortality, in monochorionic and/or dichorionic twins. Neonatal death was defined as death up to 28 days after delivery.
The study authors shared unpublished aggregate and individual patient data with the meta-analysis researchers, which enabled an analysis at weekly intervals. The data included in the review covered 35,171 women with twin gestations (29,685 dichorionic and 5,486 monochorionic pregnancies).
Pregnancies with unclear chorionicity, monoamnionity, and twin-to-twin transfusion syndrome were excluded from the analysis.
In monochorionic pregnancies continuing beyond 34 weeks (2,149 pregnancies), there was a trend after 36 weeks toward stillbirth risk being higher than the risk of neonatal death, but the risk difference was not significant.
More data are needed, the researchers said, but “based on our findings, there is no clear evidence to recommend early preterm delivery routinely before 36 weeks in monochorionic pregnancies.”
A committee opinion published by the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine (ACOG-SMFM) on medically indicated late-preterm and early-term deliveries states that decisions regarding the timing of delivery should be individualized and should take into account relative maternal and newborn risks, practice environment, and patient preferences (Obstet Gynecol. 2013;121:908-10).
Still, the ACOG-SMFM document offers delivery recommendations: 38 0/7-38 6/7 weeks of gestation for dichorionic-diamniotic pregnancies, and 34 0/7-36 6/7 weeks of gestation for monochorionic-diamniotic pregnancies.
The opinion was published in 2013 and reflects recommendations made 2 years earlier by the National Institute of Child Health and Human Development and SMFM after a workshop on indicated preterm birth (Obstet Gynecol 2011;118:323-33). ACOG and SMFM reaffirmed their document in 2015.
Brigid McCue, MD, chief of ob.gyn. at Beth Israel Deaconess Hospital–Plymouth (Mass.) and a member of ACOG’s Committee on Obstetric Practice, said the meta-analysis is of “high quality,” with “helpful and valid” findings for dichorionic twins.
The risk of stillbirth was 1.2/1,000 pregnancies at 34 weeks’ gestation, while the risk of neonatal death from delivery was 6.7/1,000 pregnancies. The risk of stillbirth remained significantly lower than the risk of neonatal death from delivery at 35 weeks, and was lower at 36 weeks as well. At 37 weeks, the two categories of perinatal death risk were basically balanced, with the risk of stillbirth at 3.4/1,000 pregnancies.
Beyond that, at 38 weeks’ gestation, the risk of stillbirth (10.6/1,000) significantly outweighed the risk of neonatal death from delivery (1.5/1,000) for a pooled risk difference of 8.8.
“The finding that stillbirth risk is higher when you allow someone to go from 37 to 38 weeks – I think this is true,” Dr. McCue said in an interview.
Further research needs to account, however, for the risks of neonatal morbidity at 37 and 38 weeks. “The next question in coming up with a point of inflection is to ask, What are other contributors to the balance of timing of the delivery?” Dr. McCue said. “There’s a bigger picture that needs more analysis.”
“We don’t induce singletons prior to 39 weeks because they can have more respiratory distress, more hypoglycemia, more temperature instability, and less success breastfeeding, for example,” she added. “These complications pale in comparison to a stillbirth, but the numbers of stillbirth are so low and the numbers for [these other morbidities] are much higher.”
The authors of the meta-analysis noted that their findings were limited by the common policy of planned delivery beyond 37 and 38 weeks’ gestation. “This reduced the sample size near term, particularly in monochorionic pregnancies, and could have led to underestimation of risk of stillbirth in the last weeks of pregnancy,” they wrote.
The rates of assisted ventilation, respiratory distress syndrome, admission to the neonatal intensive care unit, and septicemia showed a consistent reduction with increasing gestational age in babies of both monochorionic and dichorionic pregnancies, the researchers noted.
The researchers reported that they received no funding support from any organization and had no relevant financial disclosures.
FROM BMJ
Key clinical point: Delivery of uncomplicated dichorionic twin pregnancies at 37 weeks’ gestation could minimize perinatal deaths.
Major finding: A delay in delivery to 38 weeks’ gestation led to an additional 8.8 perinatal deaths per 1,000 pregnancies because of an increase in stillbirth.
Data source: A systematic review and meta-analysis of 32 studies.
Disclosures: The researchers reported that they received no funding support from any organization and had no relevant financial disclosures.
AAP report warns against early single-sport specialization
Delaying single-sport specialization until late adolescence not only minimizes the risks of overuse injuries and burnout, but it increases the likelihood of athletic success, according to a new clinical report from the American Academy of Pediatrics.
The new report gives pediatricians a current knowledge base to draw upon in well checks and sports injury visits, author Joel S. Brenner, MD, MPH, of the AAP’s Council on Sports Medicine and Fitness, said in an interview.
Specializing in a single sport at younger ages – and playing intensively year-round – has become increasingly common, and is often driven by aspirations for college scholarships or elite athletic status. Yet evidence suggests that early specialization may actually work against such goals.
Studies of top college athletes and reviews of other elite athletes and their specialization history show that “for the majority of sports, late specialization with early diversification [playing multiple sports early] is most likely to lead to elite status,” the report states (Pediatrics. 2016;138[3]:e20162148).
Youth who participate in a variety of sports until late adolescence (about 15-16 years of age) also have fewer injuries and a higher chance of remaining engaged in sports for the long term than do children who specialize early, according to the guideline. “Unfortunately, 70% of children drop out of organized sports by 13 years of age.”
If a young athlete has decided to specialize in a single sport, you should discuss his or her goals to determine if they are appropriate and realistic. A mere 1% of high school athletes receive athletic scholarships and only 3%-11% go on to compete at college level; of high school athletes, only 0.03%-0.5% proceed to the professional sports level, the report notes.
Having at least 1-2 days off per week from the focal sport can decrease the chance of injury, and taking 1 month off at least 3 times a year “will allow for athletes’ physical and psychological recovery.”
An estimated 50% of athletic injuries are related to overuse. The physiologic and psychological effects of intensive training in young athletes are detailed in other articles by the AAP (Pediatrics. 2007;119[6]:1242-5) and the American Medical Society for Sports Medicine (Clin J Sport Med. 2014;24[1]:3-20).
According to a 2008 report from the National Council of Youth Sports, 27% of the youth active in adult-led organized sports participated in only 1 sport. “There is increased pressure to participate at a high level, to specialize in one sport early, and to play year-round, often on multiple teams,” the guideline notes.
This clinical report replaces the academy’s 2000 policy statement on sports specialization and intensive training and provides “concrete guidance” for pediatricians, said Dr. Brenner, who is medical director of Children’s Hospital of the King’s Daughters’ sports medicine and adolescent medicine programs and the director of CHKD’s sports concussion program, in Norfolk, Va.
There was no external funding for this report and the authors had no relevant financial disclosures.
Delaying single-sport specialization until late adolescence not only minimizes the risks of overuse injuries and burnout, but it increases the likelihood of athletic success, according to a new clinical report from the American Academy of Pediatrics.
The new report gives pediatricians a current knowledge base to draw upon in well checks and sports injury visits, author Joel S. Brenner, MD, MPH, of the AAP’s Council on Sports Medicine and Fitness, said in an interview.
Specializing in a single sport at younger ages – and playing intensively year-round – has become increasingly common, and is often driven by aspirations for college scholarships or elite athletic status. Yet evidence suggests that early specialization may actually work against such goals.
Studies of top college athletes and reviews of other elite athletes and their specialization history show that “for the majority of sports, late specialization with early diversification [playing multiple sports early] is most likely to lead to elite status,” the report states (Pediatrics. 2016;138[3]:e20162148).
Youth who participate in a variety of sports until late adolescence (about 15-16 years of age) also have fewer injuries and a higher chance of remaining engaged in sports for the long term than do children who specialize early, according to the guideline. “Unfortunately, 70% of children drop out of organized sports by 13 years of age.”
If a young athlete has decided to specialize in a single sport, you should discuss his or her goals to determine if they are appropriate and realistic. A mere 1% of high school athletes receive athletic scholarships and only 3%-11% go on to compete at college level; of high school athletes, only 0.03%-0.5% proceed to the professional sports level, the report notes.
Having at least 1-2 days off per week from the focal sport can decrease the chance of injury, and taking 1 month off at least 3 times a year “will allow for athletes’ physical and psychological recovery.”
An estimated 50% of athletic injuries are related to overuse. The physiologic and psychological effects of intensive training in young athletes are detailed in other articles by the AAP (Pediatrics. 2007;119[6]:1242-5) and the American Medical Society for Sports Medicine (Clin J Sport Med. 2014;24[1]:3-20).
According to a 2008 report from the National Council of Youth Sports, 27% of the youth active in adult-led organized sports participated in only 1 sport. “There is increased pressure to participate at a high level, to specialize in one sport early, and to play year-round, often on multiple teams,” the guideline notes.
This clinical report replaces the academy’s 2000 policy statement on sports specialization and intensive training and provides “concrete guidance” for pediatricians, said Dr. Brenner, who is medical director of Children’s Hospital of the King’s Daughters’ sports medicine and adolescent medicine programs and the director of CHKD’s sports concussion program, in Norfolk, Va.
There was no external funding for this report and the authors had no relevant financial disclosures.
Delaying single-sport specialization until late adolescence not only minimizes the risks of overuse injuries and burnout, but it increases the likelihood of athletic success, according to a new clinical report from the American Academy of Pediatrics.
The new report gives pediatricians a current knowledge base to draw upon in well checks and sports injury visits, author Joel S. Brenner, MD, MPH, of the AAP’s Council on Sports Medicine and Fitness, said in an interview.
Specializing in a single sport at younger ages – and playing intensively year-round – has become increasingly common, and is often driven by aspirations for college scholarships or elite athletic status. Yet evidence suggests that early specialization may actually work against such goals.
Studies of top college athletes and reviews of other elite athletes and their specialization history show that “for the majority of sports, late specialization with early diversification [playing multiple sports early] is most likely to lead to elite status,” the report states (Pediatrics. 2016;138[3]:e20162148).
Youth who participate in a variety of sports until late adolescence (about 15-16 years of age) also have fewer injuries and a higher chance of remaining engaged in sports for the long term than do children who specialize early, according to the guideline. “Unfortunately, 70% of children drop out of organized sports by 13 years of age.”
If a young athlete has decided to specialize in a single sport, you should discuss his or her goals to determine if they are appropriate and realistic. A mere 1% of high school athletes receive athletic scholarships and only 3%-11% go on to compete at college level; of high school athletes, only 0.03%-0.5% proceed to the professional sports level, the report notes.
Having at least 1-2 days off per week from the focal sport can decrease the chance of injury, and taking 1 month off at least 3 times a year “will allow for athletes’ physical and psychological recovery.”
An estimated 50% of athletic injuries are related to overuse. The physiologic and psychological effects of intensive training in young athletes are detailed in other articles by the AAP (Pediatrics. 2007;119[6]:1242-5) and the American Medical Society for Sports Medicine (Clin J Sport Med. 2014;24[1]:3-20).
According to a 2008 report from the National Council of Youth Sports, 27% of the youth active in adult-led organized sports participated in only 1 sport. “There is increased pressure to participate at a high level, to specialize in one sport early, and to play year-round, often on multiple teams,” the guideline notes.
This clinical report replaces the academy’s 2000 policy statement on sports specialization and intensive training and provides “concrete guidance” for pediatricians, said Dr. Brenner, who is medical director of Children’s Hospital of the King’s Daughters’ sports medicine and adolescent medicine programs and the director of CHKD’s sports concussion program, in Norfolk, Va.
There was no external funding for this report and the authors had no relevant financial disclosures.
FROM PEDIATRICS
Collaborative depression care model offers promise in rural practice
An ob.gyn. practice in rural Washington state has successfully implemented a collaborative care model for depression management that relies on “depression care managers” and a consulting psychiatrist to aid ob.gyns. in providing effective depression care.
The initiative was a rural test run of the DAWN (Depression Attention for Women Now) intervention that was shown in a randomized controlled trial 2 years ago to improve depression outcomes for women in two urban ob.gyn. clinics affiliated with the University of Washington in Seattle. Both the trial and the pilot project were funded by the National Institute of Mental Health.
Nearly 75% of the 25 women enrolled in the rural pilot project had a significant improvement in their Patient Health Questionnaire-9 (PHQ-9) scores, and more than half improved their depression symptoms by at least 50%, Roger Rowles, MD, of the Generations practice in Yakima, Wash., and Susan D. Reed, MD, a coinvestigator of the original DAWN trial, reported at the annual meeting of the American College of Obstetricians and Gynecologists.
They urged others to consider taking a similar collaborative approach to depression care, especially now that the U.S. Preventive Services Task Force has recommended depression screening for all adults, including pregnant and postpartum women.
Previously, “when we identified someone with perinatal depression, we’d need a 30-minute initial consultation and then 15-20 minutes on a regular basis,” Dr. Rowles said. “We didn’t have the time to do that. ... And I had no training. Most of us felt we weren’t capable [of providing quality depression care].”
In the DAWN model, a social worker, nurse, medical assistant, or other staff member is trained to provide collaborative depression care and takes charge of this care, regularly meeting in-person or by phone with the patient to promote engagement and to closely monitor treatment progress.
Patients choose their initial treatment, including medication and Problem-Solving Treatment in Primary Care (PST-PC) therapy, an evidence-based brief behavioral intervention that helps identify stressors and improve problem solving. The depression care manager delivers the PST-PC therapy, tracks treatment response and compliance, and participates in weekly structured case reviews with the ob.gyn. and a consulting psychiatrist.
Results then and now
The original DAWN trial randomized women at two urban clinics to either 12 months of collaborative depression care or to usual care. Usual care included educational material, access to the clinic social worker, and possible psychiatry referral and prescriptions from the ob.gyn.
At 6 months, the reduction in depression scores as measured by the 20-item Hopkins Symptom Checklist was similar between the two groups, but at 12 months and at 18 months follow-up, the intervention group had significantly lower scores. They were more likely to have at least a 50% decrease in depressive symptoms at 12 months and were significantly more satisfied with their depression care (Obstet Gynecol. 2014 Jun;123[6]:1237-46).
The pilot project in Yakima, a farming community of 80,000 people, was of shorter duration than the randomized trial and focused on women coming for periconception, pregnancy, and postpartum care.
The majority – 74% – had significant improvement in their PHQ scores (a final score of less than 10), and almost one-third had a final score of less than 5. A score of 10 or more indicates the likelihood of having major depression. More than half – 59% – had at least a 50% improvement in depressive symptoms.
Unlike in the original DAWN trial, depression care managers in the Yakima project used text messaging in addition to phone calls to stay engaged with patients and monitor treatment. Almost all of the 25 enrolled women received PST-PC, and approximately 56% received antidepressants, for a mean treatment time of 14 weeks.
“Given that short duration of follow-up, the improvement we saw was very good,” said Amritha Bhat, MD, MBBS, the University of Washington psychiatrist who served as the consulting psychiatrist for the project.
Without a placebo-controlled arm, the researchers don’t know how much of the improvement was due to the collaborative care, Dr. Bhat said in an interview. “But we know now that it’s feasible in a rural setting.”
Depression care needs
Women have two times the rate of major depression as men, with prevalence rates of 13% annually and 21% over a lifetime, and low-income and minority women are at highest risk of depression and are also more likely to seek routine care from ob.gyns., according to Dr. Reed, who is a professor of ob.gyn at the University of Washington, Seattle, and chief of ob.gyn. at Harborview Medical Center.
Dr. Rowles said he was “astounded” that 30% of the screened patients in his practice had positive results. Many “either didn’t want to participate in the project or had exclusions, but even so we enrolled [our cohort] quickly,” he said.
The DAWN model stipulates that depression care managers support women as much as possible with social service interventions, facilitating financial assistance for medications, and serving as a “point person” for assistance with housing, food, domestic abuse, and other issues.
The task of integrating a social service element into depression care is necessary but can be daunting, Dr. Rowles said. In Yakima, he said, the significant need for basic assistance was a “big frustration” to the depression care managers involved in the project. “They wanted to do more, because they’d identified these problems and had a rapport [with the women], but our resources in Yakima are not that great.”
To prepare the Yakima practice for the intervention, a University of Washington team visited the clinic to educate staff about collaborative care, and three depression care managers were trained to deliver PST-PC and manage care. The depression care managers – a nurse employed by the local hospital, a nurse employed by another clinic for farm workers, and a local psychologist – “were the glue for this program,” Dr. Rowles said.
In other settings, depression care managers might more likely be clinic social workers or other members of the practice.
A psychiatrist’s involvement is also crucial, particularly when it comes to prescribing antidepressant medications at their full effective doses, Dr. Reed stressed. “You won’t feel comfortable pushing those doses to the max without [a psychiatrist to consult with],” Dr. Reed said at the ACOG meeting.
In the DAWN trial, similar numbers of patients in the collaborative care group and the usual care group were prescribed antidepressants, but more patients in the intervention group had their doses increased to an effective therapeutic range, and more patients adhered to their medication regimens, she said.
The 12-month DAWN intervention was provided at a cost per patient of up to $1,000.
Dr. Reed’s clinic has sustained funding for the intervention since the National Institute of Mental Health grant expired, and Dr. Rowles said he was seeking funding to continue DAWN at his Yakima clinic. Funding sources for ob.gyn. practices interested in implementing the model may include state funding agencies and organizations such as the March of Dimes, Dr. Reed said, noting that some states offer maternal services support that could be helpful for integrating collaborative depression care.
While the pilot project focused on pregnancy care, Dr. Reed urged ob.gyns. to think broadly. “Do you know when you catch these women? When they come in for their Pap smears and their routine care, before they become pregnant,” she said. “If you help them with their mood disorder early, they’ll do so much better with pregnancy.”
Information about DAWN – including resources on PST-PC and antidepressant medication, and an intervention manual – can be found at www.dawncare.org.
An ob.gyn. practice in rural Washington state has successfully implemented a collaborative care model for depression management that relies on “depression care managers” and a consulting psychiatrist to aid ob.gyns. in providing effective depression care.
The initiative was a rural test run of the DAWN (Depression Attention for Women Now) intervention that was shown in a randomized controlled trial 2 years ago to improve depression outcomes for women in two urban ob.gyn. clinics affiliated with the University of Washington in Seattle. Both the trial and the pilot project were funded by the National Institute of Mental Health.
Nearly 75% of the 25 women enrolled in the rural pilot project had a significant improvement in their Patient Health Questionnaire-9 (PHQ-9) scores, and more than half improved their depression symptoms by at least 50%, Roger Rowles, MD, of the Generations practice in Yakima, Wash., and Susan D. Reed, MD, a coinvestigator of the original DAWN trial, reported at the annual meeting of the American College of Obstetricians and Gynecologists.
They urged others to consider taking a similar collaborative approach to depression care, especially now that the U.S. Preventive Services Task Force has recommended depression screening for all adults, including pregnant and postpartum women.
Previously, “when we identified someone with perinatal depression, we’d need a 30-minute initial consultation and then 15-20 minutes on a regular basis,” Dr. Rowles said. “We didn’t have the time to do that. ... And I had no training. Most of us felt we weren’t capable [of providing quality depression care].”
In the DAWN model, a social worker, nurse, medical assistant, or other staff member is trained to provide collaborative depression care and takes charge of this care, regularly meeting in-person or by phone with the patient to promote engagement and to closely monitor treatment progress.
Patients choose their initial treatment, including medication and Problem-Solving Treatment in Primary Care (PST-PC) therapy, an evidence-based brief behavioral intervention that helps identify stressors and improve problem solving. The depression care manager delivers the PST-PC therapy, tracks treatment response and compliance, and participates in weekly structured case reviews with the ob.gyn. and a consulting psychiatrist.
Results then and now
The original DAWN trial randomized women at two urban clinics to either 12 months of collaborative depression care or to usual care. Usual care included educational material, access to the clinic social worker, and possible psychiatry referral and prescriptions from the ob.gyn.
At 6 months, the reduction in depression scores as measured by the 20-item Hopkins Symptom Checklist was similar between the two groups, but at 12 months and at 18 months follow-up, the intervention group had significantly lower scores. They were more likely to have at least a 50% decrease in depressive symptoms at 12 months and were significantly more satisfied with their depression care (Obstet Gynecol. 2014 Jun;123[6]:1237-46).
The pilot project in Yakima, a farming community of 80,000 people, was of shorter duration than the randomized trial and focused on women coming for periconception, pregnancy, and postpartum care.
The majority – 74% – had significant improvement in their PHQ scores (a final score of less than 10), and almost one-third had a final score of less than 5. A score of 10 or more indicates the likelihood of having major depression. More than half – 59% – had at least a 50% improvement in depressive symptoms.
Unlike in the original DAWN trial, depression care managers in the Yakima project used text messaging in addition to phone calls to stay engaged with patients and monitor treatment. Almost all of the 25 enrolled women received PST-PC, and approximately 56% received antidepressants, for a mean treatment time of 14 weeks.
“Given that short duration of follow-up, the improvement we saw was very good,” said Amritha Bhat, MD, MBBS, the University of Washington psychiatrist who served as the consulting psychiatrist for the project.
Without a placebo-controlled arm, the researchers don’t know how much of the improvement was due to the collaborative care, Dr. Bhat said in an interview. “But we know now that it’s feasible in a rural setting.”
Depression care needs
Women have two times the rate of major depression as men, with prevalence rates of 13% annually and 21% over a lifetime, and low-income and minority women are at highest risk of depression and are also more likely to seek routine care from ob.gyns., according to Dr. Reed, who is a professor of ob.gyn at the University of Washington, Seattle, and chief of ob.gyn. at Harborview Medical Center.
Dr. Rowles said he was “astounded” that 30% of the screened patients in his practice had positive results. Many “either didn’t want to participate in the project or had exclusions, but even so we enrolled [our cohort] quickly,” he said.
The DAWN model stipulates that depression care managers support women as much as possible with social service interventions, facilitating financial assistance for medications, and serving as a “point person” for assistance with housing, food, domestic abuse, and other issues.
The task of integrating a social service element into depression care is necessary but can be daunting, Dr. Rowles said. In Yakima, he said, the significant need for basic assistance was a “big frustration” to the depression care managers involved in the project. “They wanted to do more, because they’d identified these problems and had a rapport [with the women], but our resources in Yakima are not that great.”
To prepare the Yakima practice for the intervention, a University of Washington team visited the clinic to educate staff about collaborative care, and three depression care managers were trained to deliver PST-PC and manage care. The depression care managers – a nurse employed by the local hospital, a nurse employed by another clinic for farm workers, and a local psychologist – “were the glue for this program,” Dr. Rowles said.
In other settings, depression care managers might more likely be clinic social workers or other members of the practice.
A psychiatrist’s involvement is also crucial, particularly when it comes to prescribing antidepressant medications at their full effective doses, Dr. Reed stressed. “You won’t feel comfortable pushing those doses to the max without [a psychiatrist to consult with],” Dr. Reed said at the ACOG meeting.
In the DAWN trial, similar numbers of patients in the collaborative care group and the usual care group were prescribed antidepressants, but more patients in the intervention group had their doses increased to an effective therapeutic range, and more patients adhered to their medication regimens, she said.
The 12-month DAWN intervention was provided at a cost per patient of up to $1,000.
Dr. Reed’s clinic has sustained funding for the intervention since the National Institute of Mental Health grant expired, and Dr. Rowles said he was seeking funding to continue DAWN at his Yakima clinic. Funding sources for ob.gyn. practices interested in implementing the model may include state funding agencies and organizations such as the March of Dimes, Dr. Reed said, noting that some states offer maternal services support that could be helpful for integrating collaborative depression care.
While the pilot project focused on pregnancy care, Dr. Reed urged ob.gyns. to think broadly. “Do you know when you catch these women? When they come in for their Pap smears and their routine care, before they become pregnant,” she said. “If you help them with their mood disorder early, they’ll do so much better with pregnancy.”
Information about DAWN – including resources on PST-PC and antidepressant medication, and an intervention manual – can be found at www.dawncare.org.
An ob.gyn. practice in rural Washington state has successfully implemented a collaborative care model for depression management that relies on “depression care managers” and a consulting psychiatrist to aid ob.gyns. in providing effective depression care.
The initiative was a rural test run of the DAWN (Depression Attention for Women Now) intervention that was shown in a randomized controlled trial 2 years ago to improve depression outcomes for women in two urban ob.gyn. clinics affiliated with the University of Washington in Seattle. Both the trial and the pilot project were funded by the National Institute of Mental Health.
Nearly 75% of the 25 women enrolled in the rural pilot project had a significant improvement in their Patient Health Questionnaire-9 (PHQ-9) scores, and more than half improved their depression symptoms by at least 50%, Roger Rowles, MD, of the Generations practice in Yakima, Wash., and Susan D. Reed, MD, a coinvestigator of the original DAWN trial, reported at the annual meeting of the American College of Obstetricians and Gynecologists.
They urged others to consider taking a similar collaborative approach to depression care, especially now that the U.S. Preventive Services Task Force has recommended depression screening for all adults, including pregnant and postpartum women.
Previously, “when we identified someone with perinatal depression, we’d need a 30-minute initial consultation and then 15-20 minutes on a regular basis,” Dr. Rowles said. “We didn’t have the time to do that. ... And I had no training. Most of us felt we weren’t capable [of providing quality depression care].”
In the DAWN model, a social worker, nurse, medical assistant, or other staff member is trained to provide collaborative depression care and takes charge of this care, regularly meeting in-person or by phone with the patient to promote engagement and to closely monitor treatment progress.
Patients choose their initial treatment, including medication and Problem-Solving Treatment in Primary Care (PST-PC) therapy, an evidence-based brief behavioral intervention that helps identify stressors and improve problem solving. The depression care manager delivers the PST-PC therapy, tracks treatment response and compliance, and participates in weekly structured case reviews with the ob.gyn. and a consulting psychiatrist.
Results then and now
The original DAWN trial randomized women at two urban clinics to either 12 months of collaborative depression care or to usual care. Usual care included educational material, access to the clinic social worker, and possible psychiatry referral and prescriptions from the ob.gyn.
At 6 months, the reduction in depression scores as measured by the 20-item Hopkins Symptom Checklist was similar between the two groups, but at 12 months and at 18 months follow-up, the intervention group had significantly lower scores. They were more likely to have at least a 50% decrease in depressive symptoms at 12 months and were significantly more satisfied with their depression care (Obstet Gynecol. 2014 Jun;123[6]:1237-46).
The pilot project in Yakima, a farming community of 80,000 people, was of shorter duration than the randomized trial and focused on women coming for periconception, pregnancy, and postpartum care.
The majority – 74% – had significant improvement in their PHQ scores (a final score of less than 10), and almost one-third had a final score of less than 5. A score of 10 or more indicates the likelihood of having major depression. More than half – 59% – had at least a 50% improvement in depressive symptoms.
Unlike in the original DAWN trial, depression care managers in the Yakima project used text messaging in addition to phone calls to stay engaged with patients and monitor treatment. Almost all of the 25 enrolled women received PST-PC, and approximately 56% received antidepressants, for a mean treatment time of 14 weeks.
“Given that short duration of follow-up, the improvement we saw was very good,” said Amritha Bhat, MD, MBBS, the University of Washington psychiatrist who served as the consulting psychiatrist for the project.
Without a placebo-controlled arm, the researchers don’t know how much of the improvement was due to the collaborative care, Dr. Bhat said in an interview. “But we know now that it’s feasible in a rural setting.”
Depression care needs
Women have two times the rate of major depression as men, with prevalence rates of 13% annually and 21% over a lifetime, and low-income and minority women are at highest risk of depression and are also more likely to seek routine care from ob.gyns., according to Dr. Reed, who is a professor of ob.gyn at the University of Washington, Seattle, and chief of ob.gyn. at Harborview Medical Center.
Dr. Rowles said he was “astounded” that 30% of the screened patients in his practice had positive results. Many “either didn’t want to participate in the project or had exclusions, but even so we enrolled [our cohort] quickly,” he said.
The DAWN model stipulates that depression care managers support women as much as possible with social service interventions, facilitating financial assistance for medications, and serving as a “point person” for assistance with housing, food, domestic abuse, and other issues.
The task of integrating a social service element into depression care is necessary but can be daunting, Dr. Rowles said. In Yakima, he said, the significant need for basic assistance was a “big frustration” to the depression care managers involved in the project. “They wanted to do more, because they’d identified these problems and had a rapport [with the women], but our resources in Yakima are not that great.”
To prepare the Yakima practice for the intervention, a University of Washington team visited the clinic to educate staff about collaborative care, and three depression care managers were trained to deliver PST-PC and manage care. The depression care managers – a nurse employed by the local hospital, a nurse employed by another clinic for farm workers, and a local psychologist – “were the glue for this program,” Dr. Rowles said.
In other settings, depression care managers might more likely be clinic social workers or other members of the practice.
A psychiatrist’s involvement is also crucial, particularly when it comes to prescribing antidepressant medications at their full effective doses, Dr. Reed stressed. “You won’t feel comfortable pushing those doses to the max without [a psychiatrist to consult with],” Dr. Reed said at the ACOG meeting.
In the DAWN trial, similar numbers of patients in the collaborative care group and the usual care group were prescribed antidepressants, but more patients in the intervention group had their doses increased to an effective therapeutic range, and more patients adhered to their medication regimens, she said.
The 12-month DAWN intervention was provided at a cost per patient of up to $1,000.
Dr. Reed’s clinic has sustained funding for the intervention since the National Institute of Mental Health grant expired, and Dr. Rowles said he was seeking funding to continue DAWN at his Yakima clinic. Funding sources for ob.gyn. practices interested in implementing the model may include state funding agencies and organizations such as the March of Dimes, Dr. Reed said, noting that some states offer maternal services support that could be helpful for integrating collaborative depression care.
While the pilot project focused on pregnancy care, Dr. Reed urged ob.gyns. to think broadly. “Do you know when you catch these women? When they come in for their Pap smears and their routine care, before they become pregnant,” she said. “If you help them with their mood disorder early, they’ll do so much better with pregnancy.”
Information about DAWN – including resources on PST-PC and antidepressant medication, and an intervention manual – can be found at www.dawncare.org.
Study helps set upper boundary for leukocytosis after prenatal corticosteroids
WASHINGTON – Maternal leukocytosis after prenatal corticosteroid administration peaks at up to 24 hours after therapy, with the highest second standard deviation from the mean being 18.3 x 109/L, according to a systematic review and meta-analysis.
There has been limited data available on the magnitude and timing of leukocytosis after corticosteroid administration, making it difficult to interpret the significance of elevated white blood cell counts, Dr. Samuel Bauer, of Beaumont Health, Royal Oak, Mich., said at the annual meeting of the American College of Obstetricians and Gynecologists.
“We know corticosteroids cause leukocytosis, but we haven’t really known what the upper boundary is,” he said.
Driven by concerns about maternal sepsis and the ability to recognize early signs, Dr. Bauer and his colleagues identified six studies that reported white blood cell counts prior to corticosteroid administration, and between 24 and 96 hours afterward in healthy women with singleton gestations. The studies also met the inclusion criterion of having “excluded infected parturients between 23 and 34 weeks of gestation,” he said.
Mean maternal white blood cell count values prior to corticosteroid administration and up to 24 hours, 48 hours, 72 hours, and 96 hours after corticosteroid administration were 10.2, 13.7, 12.8, 11.5, and 11.1 x 109/L, respectively.
The highest second standard deviation from the mean of 18.3 x 109/L did not occur after 24 hours, he emphasized, and by 72 hours, mean values had returned to 11.5 x 109/L.
The findings need to be applied “cautiously” in practice, Dr. Bauer said, since the analysis did not include women with signs of infection and because some women who develop serious infections “have a very low white blood cell count.”
Still, the findings “establish a temporal trend and give us an upper boundary” for the level of leukocytosis that can be expected with prenatal corticosteroids. This can be helpful – along with other considerations – in determining whether an infectious workup is needed when white blood cell counts are high, he said in an interview.
It is not uncommon in clinical practice for maternal leukocytosis at 5-6 days or a week after corticosteroid administration to be attributed to the corticosteroids, he said. But the parameters drawn by this analysis of healthy, non-infected patients show this is a faulty assumption, he added.
The analysis covered 524 patients and 1,406 observations. Dr. Bauer and his coinvestigators did not report any financial disclosures.
WASHINGTON – Maternal leukocytosis after prenatal corticosteroid administration peaks at up to 24 hours after therapy, with the highest second standard deviation from the mean being 18.3 x 109/L, according to a systematic review and meta-analysis.
There has been limited data available on the magnitude and timing of leukocytosis after corticosteroid administration, making it difficult to interpret the significance of elevated white blood cell counts, Dr. Samuel Bauer, of Beaumont Health, Royal Oak, Mich., said at the annual meeting of the American College of Obstetricians and Gynecologists.
“We know corticosteroids cause leukocytosis, but we haven’t really known what the upper boundary is,” he said.
Driven by concerns about maternal sepsis and the ability to recognize early signs, Dr. Bauer and his colleagues identified six studies that reported white blood cell counts prior to corticosteroid administration, and between 24 and 96 hours afterward in healthy women with singleton gestations. The studies also met the inclusion criterion of having “excluded infected parturients between 23 and 34 weeks of gestation,” he said.
Mean maternal white blood cell count values prior to corticosteroid administration and up to 24 hours, 48 hours, 72 hours, and 96 hours after corticosteroid administration were 10.2, 13.7, 12.8, 11.5, and 11.1 x 109/L, respectively.
The highest second standard deviation from the mean of 18.3 x 109/L did not occur after 24 hours, he emphasized, and by 72 hours, mean values had returned to 11.5 x 109/L.
The findings need to be applied “cautiously” in practice, Dr. Bauer said, since the analysis did not include women with signs of infection and because some women who develop serious infections “have a very low white blood cell count.”
Still, the findings “establish a temporal trend and give us an upper boundary” for the level of leukocytosis that can be expected with prenatal corticosteroids. This can be helpful – along with other considerations – in determining whether an infectious workup is needed when white blood cell counts are high, he said in an interview.
It is not uncommon in clinical practice for maternal leukocytosis at 5-6 days or a week after corticosteroid administration to be attributed to the corticosteroids, he said. But the parameters drawn by this analysis of healthy, non-infected patients show this is a faulty assumption, he added.
The analysis covered 524 patients and 1,406 observations. Dr. Bauer and his coinvestigators did not report any financial disclosures.
WASHINGTON – Maternal leukocytosis after prenatal corticosteroid administration peaks at up to 24 hours after therapy, with the highest second standard deviation from the mean being 18.3 x 109/L, according to a systematic review and meta-analysis.
There has been limited data available on the magnitude and timing of leukocytosis after corticosteroid administration, making it difficult to interpret the significance of elevated white blood cell counts, Dr. Samuel Bauer, of Beaumont Health, Royal Oak, Mich., said at the annual meeting of the American College of Obstetricians and Gynecologists.
“We know corticosteroids cause leukocytosis, but we haven’t really known what the upper boundary is,” he said.
Driven by concerns about maternal sepsis and the ability to recognize early signs, Dr. Bauer and his colleagues identified six studies that reported white blood cell counts prior to corticosteroid administration, and between 24 and 96 hours afterward in healthy women with singleton gestations. The studies also met the inclusion criterion of having “excluded infected parturients between 23 and 34 weeks of gestation,” he said.
Mean maternal white blood cell count values prior to corticosteroid administration and up to 24 hours, 48 hours, 72 hours, and 96 hours after corticosteroid administration were 10.2, 13.7, 12.8, 11.5, and 11.1 x 109/L, respectively.
The highest second standard deviation from the mean of 18.3 x 109/L did not occur after 24 hours, he emphasized, and by 72 hours, mean values had returned to 11.5 x 109/L.
The findings need to be applied “cautiously” in practice, Dr. Bauer said, since the analysis did not include women with signs of infection and because some women who develop serious infections “have a very low white blood cell count.”
Still, the findings “establish a temporal trend and give us an upper boundary” for the level of leukocytosis that can be expected with prenatal corticosteroids. This can be helpful – along with other considerations – in determining whether an infectious workup is needed when white blood cell counts are high, he said in an interview.
It is not uncommon in clinical practice for maternal leukocytosis at 5-6 days or a week after corticosteroid administration to be attributed to the corticosteroids, he said. But the parameters drawn by this analysis of healthy, non-infected patients show this is a faulty assumption, he added.
The analysis covered 524 patients and 1,406 observations. Dr. Bauer and his coinvestigators did not report any financial disclosures.
AT ACOG 2016
Key clinical point: Leukocytosis attributable to prenatal corticosteroids, rather than infection, has a definable upper boundary.
Major finding: Maternal leukocytosis peaks at up to 24 hours after administration of antenatal corticosteroids. The highest second standard deviation from the mean was 18.3 x 109/L.
Data source: A systematic review and meta-analysis.
Disclosures: Dr. Bauer reported that he and his coinvestigators had no financial disclosures.
Remote prenatal care monitoring is a hit with patients
WASHINGTON – Is it time to reconsider the standard prenatal care model of 12-14 in-office prenatal visits?
As pregnant women increasingly use digital technology, and as the array of available health monitoring tools grows larger and smarter, the question looms.
Research findings reported at the annual meeting of the American College of Obstetricians and Gynecologists suggest that women with low-risk pregnancies have equivalent outcomes but are more satisfied with models that reduce the number of office visits and utilize remote monitoring.
At the Mayo Clinic in Rochester, Minn., 300 women deemed to have low-risk pregnancies were randomized to either 12 planned office visits with a physician or midwife, or to the clinic’s “OB Nest” model of care consisting of 8 planned clinic visits with a physician or midwife, 6 virtual visits with a nurse (by phone or email), home monitoring with an automatic blood pressure cuff and a hand-held fetal Doppler monitor, and access to an online prenatal care community.
The clinic’s OB Nest model “was born out of concern that the traditional model no longer met the needs of our patients,” said Dr. Yvonne S. Butler Tobah, a senior associate consultant to the department of obstetrics and gynecology at Mayo.
The goal, she said, is to “shift our prenatal clinic’s culture … to a wellness care model and to strengthen the autonomy, confidence, self-awareness and empowerment of our patients.”
Patients in the OB Nest group were encouraged to get blood pressure readings once a week, and weekly Doppler readings of fetal heart rate between weeks 12 and 28. They could use the cuff and monitor anytime they chose, however.
Values were recorded in a pregnancy journal – along with weight – and reported during the scheduled virtual visits. The patients could send in concerning readings or otherwise communicate with dedicated OB Nest nurses at any time they chose by phone or via an online portal. Emergencies were to be reported immediately.
The online prenatal care community is an invitation-only, Mayo-specific social platform, monitored by the OB Nest nurses, which gave patients the opportunity to share and discuss issues.
Patient satisfaction, as measured at 36 weeks with a 16-item validated satisfaction scale, was significantly higher in the OB Nest group; these patients had a mean score of 93.9 on a 1-100 point scale, compared with a mean score of 78.9 in the usual care group.
Levels of pregnancy-related stress – measured at three points in time with a 9-item prenatal maternal stress survey – were also significantly lower at 14 weeks and lower at 36 weeks in the OB Nest group compared with usual care. Stress levels were similar in both groups at 24 weeks.
Perceived quality of care was assessed at 36 weeks using a modified version of a prenatal processes-of-care scale that addressed communication and decision making, and no differences were observed.
“OB Nest significantly improved patient satisfaction with care and reduced maternal stress,” Dr. Tobah said. “And it did this while maintaining perceived quality of care and maintaining [safe] outcomes.”
The study was not sufficiently powered to detect statistically significant differences in clinical outcomes, which were the study’s secondary outcomes. However, there were no differences observed in maternal-fetal events or delivery outcomes, with the exception of a 4.5% rate of gestational diabetes in the OB Nest group, compared with none in the usual care group, Dr. Tobah explained.
Of the 150 patients randomized to each group, 19 and 20 were lost to follow-up in the OB Nest group and usual care group, respectively. Patients in the study had a mean age of 29, and the majority were white and married. “It was a highly educated, low-risk group,” she said. “Patients said [at the end] that they liked the general accessibility and consistent communication with a provider on an ongoing basis.”
While patients in the OB Nest group ultimately had 3.4 fewer in-office appointments than did usual care patients, they required more out-of-office nursing time and the length of in-office visits was significantly higher, Dr. Tobah noted.
In another study of remote prenatal care monitoring reported at the ACOG meeting, low-risk patients assigned to an alternative prenatal care schedule of 8 in-office visits supplemented with digital monitoring of blood pressure and weight similarly had higher patient satisfaction scores than did low-risk patients assigned to 14 prenatal visits.
Patient satisfaction was measured several times during pregnancy. Scores were significantly higher at 20 weeks in the 49-patient alternative care group “and evened out [with the 41-patient usual-care group] at the tail end of pregnancy,” said Dr. Nihar Ganju of George Washington University, Washington. “And there was no difference in pregnancy outcomes.”
This study used the Babyscripts mobile app connected to a wireless weight scale and a wireless blood pressure cuff. Patients were instructed to check their weight and blood pressure at least once a week.
They were “highly engaged,” Dr. Ganju said, checking their blood pressure a mean of 1.4 times weekly and their weight almost twice weekly. Providers received “four notifications of abnormal values,” he said.
Dr. Ganju and his colleagues are hopeful that the digital health tool “can really be effective in addressing the issue of excessive weight gain,” he said at the ACOG meeting. They are also beginning a study on remote monitoring for patients with chronic hypertension.
Findings on the effectiveness of remote personalized weight management are also expected to come from the soon-to-be-completed LIFE-Moms study, a national project looking at how overweight and obese women can best manage weight gain in pregnancy and improve their maternal and fetal outcomes.
Dr. Ganju reported having no disclosures. Two coauthors reported a nonfinancial advisory relationship with 1Eq Inc., the mobile app company that developed Babyscripts and helped fund the study. Another author is an employee of 1Eq. Dr. Tobah reported that she had no disclosures.
WASHINGTON – Is it time to reconsider the standard prenatal care model of 12-14 in-office prenatal visits?
As pregnant women increasingly use digital technology, and as the array of available health monitoring tools grows larger and smarter, the question looms.
Research findings reported at the annual meeting of the American College of Obstetricians and Gynecologists suggest that women with low-risk pregnancies have equivalent outcomes but are more satisfied with models that reduce the number of office visits and utilize remote monitoring.
At the Mayo Clinic in Rochester, Minn., 300 women deemed to have low-risk pregnancies were randomized to either 12 planned office visits with a physician or midwife, or to the clinic’s “OB Nest” model of care consisting of 8 planned clinic visits with a physician or midwife, 6 virtual visits with a nurse (by phone or email), home monitoring with an automatic blood pressure cuff and a hand-held fetal Doppler monitor, and access to an online prenatal care community.
The clinic’s OB Nest model “was born out of concern that the traditional model no longer met the needs of our patients,” said Dr. Yvonne S. Butler Tobah, a senior associate consultant to the department of obstetrics and gynecology at Mayo.
The goal, she said, is to “shift our prenatal clinic’s culture … to a wellness care model and to strengthen the autonomy, confidence, self-awareness and empowerment of our patients.”
Patients in the OB Nest group were encouraged to get blood pressure readings once a week, and weekly Doppler readings of fetal heart rate between weeks 12 and 28. They could use the cuff and monitor anytime they chose, however.
Values were recorded in a pregnancy journal – along with weight – and reported during the scheduled virtual visits. The patients could send in concerning readings or otherwise communicate with dedicated OB Nest nurses at any time they chose by phone or via an online portal. Emergencies were to be reported immediately.
The online prenatal care community is an invitation-only, Mayo-specific social platform, monitored by the OB Nest nurses, which gave patients the opportunity to share and discuss issues.
Patient satisfaction, as measured at 36 weeks with a 16-item validated satisfaction scale, was significantly higher in the OB Nest group; these patients had a mean score of 93.9 on a 1-100 point scale, compared with a mean score of 78.9 in the usual care group.
Levels of pregnancy-related stress – measured at three points in time with a 9-item prenatal maternal stress survey – were also significantly lower at 14 weeks and lower at 36 weeks in the OB Nest group compared with usual care. Stress levels were similar in both groups at 24 weeks.
Perceived quality of care was assessed at 36 weeks using a modified version of a prenatal processes-of-care scale that addressed communication and decision making, and no differences were observed.
“OB Nest significantly improved patient satisfaction with care and reduced maternal stress,” Dr. Tobah said. “And it did this while maintaining perceived quality of care and maintaining [safe] outcomes.”
The study was not sufficiently powered to detect statistically significant differences in clinical outcomes, which were the study’s secondary outcomes. However, there were no differences observed in maternal-fetal events or delivery outcomes, with the exception of a 4.5% rate of gestational diabetes in the OB Nest group, compared with none in the usual care group, Dr. Tobah explained.
Of the 150 patients randomized to each group, 19 and 20 were lost to follow-up in the OB Nest group and usual care group, respectively. Patients in the study had a mean age of 29, and the majority were white and married. “It was a highly educated, low-risk group,” she said. “Patients said [at the end] that they liked the general accessibility and consistent communication with a provider on an ongoing basis.”
While patients in the OB Nest group ultimately had 3.4 fewer in-office appointments than did usual care patients, they required more out-of-office nursing time and the length of in-office visits was significantly higher, Dr. Tobah noted.
In another study of remote prenatal care monitoring reported at the ACOG meeting, low-risk patients assigned to an alternative prenatal care schedule of 8 in-office visits supplemented with digital monitoring of blood pressure and weight similarly had higher patient satisfaction scores than did low-risk patients assigned to 14 prenatal visits.
Patient satisfaction was measured several times during pregnancy. Scores were significantly higher at 20 weeks in the 49-patient alternative care group “and evened out [with the 41-patient usual-care group] at the tail end of pregnancy,” said Dr. Nihar Ganju of George Washington University, Washington. “And there was no difference in pregnancy outcomes.”
This study used the Babyscripts mobile app connected to a wireless weight scale and a wireless blood pressure cuff. Patients were instructed to check their weight and blood pressure at least once a week.
They were “highly engaged,” Dr. Ganju said, checking their blood pressure a mean of 1.4 times weekly and their weight almost twice weekly. Providers received “four notifications of abnormal values,” he said.
Dr. Ganju and his colleagues are hopeful that the digital health tool “can really be effective in addressing the issue of excessive weight gain,” he said at the ACOG meeting. They are also beginning a study on remote monitoring for patients with chronic hypertension.
Findings on the effectiveness of remote personalized weight management are also expected to come from the soon-to-be-completed LIFE-Moms study, a national project looking at how overweight and obese women can best manage weight gain in pregnancy and improve their maternal and fetal outcomes.
Dr. Ganju reported having no disclosures. Two coauthors reported a nonfinancial advisory relationship with 1Eq Inc., the mobile app company that developed Babyscripts and helped fund the study. Another author is an employee of 1Eq. Dr. Tobah reported that she had no disclosures.
WASHINGTON – Is it time to reconsider the standard prenatal care model of 12-14 in-office prenatal visits?
As pregnant women increasingly use digital technology, and as the array of available health monitoring tools grows larger and smarter, the question looms.
Research findings reported at the annual meeting of the American College of Obstetricians and Gynecologists suggest that women with low-risk pregnancies have equivalent outcomes but are more satisfied with models that reduce the number of office visits and utilize remote monitoring.
At the Mayo Clinic in Rochester, Minn., 300 women deemed to have low-risk pregnancies were randomized to either 12 planned office visits with a physician or midwife, or to the clinic’s “OB Nest” model of care consisting of 8 planned clinic visits with a physician or midwife, 6 virtual visits with a nurse (by phone or email), home monitoring with an automatic blood pressure cuff and a hand-held fetal Doppler monitor, and access to an online prenatal care community.
The clinic’s OB Nest model “was born out of concern that the traditional model no longer met the needs of our patients,” said Dr. Yvonne S. Butler Tobah, a senior associate consultant to the department of obstetrics and gynecology at Mayo.
The goal, she said, is to “shift our prenatal clinic’s culture … to a wellness care model and to strengthen the autonomy, confidence, self-awareness and empowerment of our patients.”
Patients in the OB Nest group were encouraged to get blood pressure readings once a week, and weekly Doppler readings of fetal heart rate between weeks 12 and 28. They could use the cuff and monitor anytime they chose, however.
Values were recorded in a pregnancy journal – along with weight – and reported during the scheduled virtual visits. The patients could send in concerning readings or otherwise communicate with dedicated OB Nest nurses at any time they chose by phone or via an online portal. Emergencies were to be reported immediately.
The online prenatal care community is an invitation-only, Mayo-specific social platform, monitored by the OB Nest nurses, which gave patients the opportunity to share and discuss issues.
Patient satisfaction, as measured at 36 weeks with a 16-item validated satisfaction scale, was significantly higher in the OB Nest group; these patients had a mean score of 93.9 on a 1-100 point scale, compared with a mean score of 78.9 in the usual care group.
Levels of pregnancy-related stress – measured at three points in time with a 9-item prenatal maternal stress survey – were also significantly lower at 14 weeks and lower at 36 weeks in the OB Nest group compared with usual care. Stress levels were similar in both groups at 24 weeks.
Perceived quality of care was assessed at 36 weeks using a modified version of a prenatal processes-of-care scale that addressed communication and decision making, and no differences were observed.
“OB Nest significantly improved patient satisfaction with care and reduced maternal stress,” Dr. Tobah said. “And it did this while maintaining perceived quality of care and maintaining [safe] outcomes.”
The study was not sufficiently powered to detect statistically significant differences in clinical outcomes, which were the study’s secondary outcomes. However, there were no differences observed in maternal-fetal events or delivery outcomes, with the exception of a 4.5% rate of gestational diabetes in the OB Nest group, compared with none in the usual care group, Dr. Tobah explained.
Of the 150 patients randomized to each group, 19 and 20 were lost to follow-up in the OB Nest group and usual care group, respectively. Patients in the study had a mean age of 29, and the majority were white and married. “It was a highly educated, low-risk group,” she said. “Patients said [at the end] that they liked the general accessibility and consistent communication with a provider on an ongoing basis.”
While patients in the OB Nest group ultimately had 3.4 fewer in-office appointments than did usual care patients, they required more out-of-office nursing time and the length of in-office visits was significantly higher, Dr. Tobah noted.
In another study of remote prenatal care monitoring reported at the ACOG meeting, low-risk patients assigned to an alternative prenatal care schedule of 8 in-office visits supplemented with digital monitoring of blood pressure and weight similarly had higher patient satisfaction scores than did low-risk patients assigned to 14 prenatal visits.
Patient satisfaction was measured several times during pregnancy. Scores were significantly higher at 20 weeks in the 49-patient alternative care group “and evened out [with the 41-patient usual-care group] at the tail end of pregnancy,” said Dr. Nihar Ganju of George Washington University, Washington. “And there was no difference in pregnancy outcomes.”
This study used the Babyscripts mobile app connected to a wireless weight scale and a wireless blood pressure cuff. Patients were instructed to check their weight and blood pressure at least once a week.
They were “highly engaged,” Dr. Ganju said, checking their blood pressure a mean of 1.4 times weekly and their weight almost twice weekly. Providers received “four notifications of abnormal values,” he said.
Dr. Ganju and his colleagues are hopeful that the digital health tool “can really be effective in addressing the issue of excessive weight gain,” he said at the ACOG meeting. They are also beginning a study on remote monitoring for patients with chronic hypertension.
Findings on the effectiveness of remote personalized weight management are also expected to come from the soon-to-be-completed LIFE-Moms study, a national project looking at how overweight and obese women can best manage weight gain in pregnancy and improve their maternal and fetal outcomes.
Dr. Ganju reported having no disclosures. Two coauthors reported a nonfinancial advisory relationship with 1Eq Inc., the mobile app company that developed Babyscripts and helped fund the study. Another author is an employee of 1Eq. Dr. Tobah reported that she had no disclosures.
AT ACOG 2016
Key clinical point: Patient satisfaction improves with reduced clinic visits supplemented with remote monitoring.
Major finding: Patient satisfaction scores were significantly higher in alternative care groups, compared with usual care groups (12-14 in-office visits) in two studies.
Data source: A 300-patient randomized controlled trial of the OB Nest model at the Mayo Clinic, Rochester, Minn., and a 90-patient controlled study involving the Babyscripts tool at George Washington University, Washington.
Disclosures: Dr. Ganju reported having no disclosures. Two coauthors reported a nonfinancial advisory relationship with 1Eq Inc., the mobile app company that developed Babyscripts and helped fund the study. Another author is an employee of 1Eq. Dr. Tobah reported that she had no disclosures.