User login
Jeff Evans has been editor of Rheumatology News/MDedge Rheumatology and the EULAR Congress News since 2013. He started at Frontline Medical Communications in 2001 and was a reporter for 8 years before serving as editor of Clinical Neurology News and World Neurology, and briefly as editor of GI & Hepatology News. He graduated cum laude from Cornell University (New York) with a BA in biological sciences, concentrating in neurobiology and behavior.
Novel mutations point to new genetic etiologies of Dravet syndrome
Mutations in two newly identified genes appear to cause Dravet syndrome in a substantial proportion of patients who do not have SCN1A gene mutations, which are known to cause the epilepsy syndrome in about 75% of affected individuals, according to a study of whole-exome sequencing in 13 patients and targeted resequencing in an additional 67 patients.
Besides four other genes that have been implicated in causing Dravet syndrome in rare cases, the genetic etiology of Dravet syndrome patients without an SCN1A mutation was previously unknown, reported lead author Gemma L. Carvill, Ph.D., of the division of genetic medicine in the department of pediatrics at the University of Washington, Seattle, and her colleagues. Now the investigators have extended the genetic causes of Dravet syndrome to mutations in the genes GABRA1 and STXBP1, as well as new SCN1A mutations that previously have not been reported and went undetected with conventional mutation detection techniques (Neurology 2014 March 12 [doi:10.1212/WNL.0000000000000291]) .
Among four patients with novel GABRA1 mutations, three of the mutations were de novo, and the inheritance of the fourth could not be determined because parents were not available. In vitro experiments with one GABRA1 mutation indicated that it reduced sensitivity to gamma-aminobutyric acid in the brain. These four patients had a typical Dravet syndrome presentation, with the only uncommon feature being atonic drop attacks in two patients.
Three patients with Dravet syndrome onset at an age of 6-12 months had de novo STXBP1mutations. Two of the patients had both tonic and atonic seizures early in the course of the disease, which is uncommon, but tonic seizures have been reported in older Dravet syndrome patients, according to Dr. Carvill and her associates.
GABRA1 and STXBP1 mutations have been reported in other epilepsies but not previously in Dravet syndrome.
"GABRA1 and STXBP1 are significant contributors to SCN1A-negative Dravet syndrome that should be tested in patients with Dravet syndrome negative for SCN1A mutations. With identification of further cases with Dravet syndrome due to these genes, specific phenotypic patterns may emerge that distinguish these rarer causes of Dravet syndrome from those due to SCN1A mutations," the investigators wrote.
In an accompanying comment to the study, Mingxuan Xu, Ph.D., of the department of neurology at Baylor College of Medicine, Houston, wrote that the discovery provides "insights for developing new diagnostic testing and drug targets and possibly leading to individualized therapeutic strategies for [Dravet syndrome] patients with different genotypes" (Neurology 2014 March 12 [doi:10.1212/WNL.0000000000000300]).
The study was supported by a variety of governmental and nongovernmental funding sources from Australia, New Zealand, Belgium, the European Union, and the United States, including the National Institute of Neurological Disorders and Stroke. Most of the authors reported having no relevant disclosures, but some reported financial ties to companies manufacturing antiepileptic drugs and epilepsy diagnostic tests.
Mutations in two newly identified genes appear to cause Dravet syndrome in a substantial proportion of patients who do not have SCN1A gene mutations, which are known to cause the epilepsy syndrome in about 75% of affected individuals, according to a study of whole-exome sequencing in 13 patients and targeted resequencing in an additional 67 patients.
Besides four other genes that have been implicated in causing Dravet syndrome in rare cases, the genetic etiology of Dravet syndrome patients without an SCN1A mutation was previously unknown, reported lead author Gemma L. Carvill, Ph.D., of the division of genetic medicine in the department of pediatrics at the University of Washington, Seattle, and her colleagues. Now the investigators have extended the genetic causes of Dravet syndrome to mutations in the genes GABRA1 and STXBP1, as well as new SCN1A mutations that previously have not been reported and went undetected with conventional mutation detection techniques (Neurology 2014 March 12 [doi:10.1212/WNL.0000000000000291]) .
Among four patients with novel GABRA1 mutations, three of the mutations were de novo, and the inheritance of the fourth could not be determined because parents were not available. In vitro experiments with one GABRA1 mutation indicated that it reduced sensitivity to gamma-aminobutyric acid in the brain. These four patients had a typical Dravet syndrome presentation, with the only uncommon feature being atonic drop attacks in two patients.
Three patients with Dravet syndrome onset at an age of 6-12 months had de novo STXBP1mutations. Two of the patients had both tonic and atonic seizures early in the course of the disease, which is uncommon, but tonic seizures have been reported in older Dravet syndrome patients, according to Dr. Carvill and her associates.
GABRA1 and STXBP1 mutations have been reported in other epilepsies but not previously in Dravet syndrome.
"GABRA1 and STXBP1 are significant contributors to SCN1A-negative Dravet syndrome that should be tested in patients with Dravet syndrome negative for SCN1A mutations. With identification of further cases with Dravet syndrome due to these genes, specific phenotypic patterns may emerge that distinguish these rarer causes of Dravet syndrome from those due to SCN1A mutations," the investigators wrote.
In an accompanying comment to the study, Mingxuan Xu, Ph.D., of the department of neurology at Baylor College of Medicine, Houston, wrote that the discovery provides "insights for developing new diagnostic testing and drug targets and possibly leading to individualized therapeutic strategies for [Dravet syndrome] patients with different genotypes" (Neurology 2014 March 12 [doi:10.1212/WNL.0000000000000300]).
The study was supported by a variety of governmental and nongovernmental funding sources from Australia, New Zealand, Belgium, the European Union, and the United States, including the National Institute of Neurological Disorders and Stroke. Most of the authors reported having no relevant disclosures, but some reported financial ties to companies manufacturing antiepileptic drugs and epilepsy diagnostic tests.
Mutations in two newly identified genes appear to cause Dravet syndrome in a substantial proportion of patients who do not have SCN1A gene mutations, which are known to cause the epilepsy syndrome in about 75% of affected individuals, according to a study of whole-exome sequencing in 13 patients and targeted resequencing in an additional 67 patients.
Besides four other genes that have been implicated in causing Dravet syndrome in rare cases, the genetic etiology of Dravet syndrome patients without an SCN1A mutation was previously unknown, reported lead author Gemma L. Carvill, Ph.D., of the division of genetic medicine in the department of pediatrics at the University of Washington, Seattle, and her colleagues. Now the investigators have extended the genetic causes of Dravet syndrome to mutations in the genes GABRA1 and STXBP1, as well as new SCN1A mutations that previously have not been reported and went undetected with conventional mutation detection techniques (Neurology 2014 March 12 [doi:10.1212/WNL.0000000000000291]) .
Among four patients with novel GABRA1 mutations, three of the mutations were de novo, and the inheritance of the fourth could not be determined because parents were not available. In vitro experiments with one GABRA1 mutation indicated that it reduced sensitivity to gamma-aminobutyric acid in the brain. These four patients had a typical Dravet syndrome presentation, with the only uncommon feature being atonic drop attacks in two patients.
Three patients with Dravet syndrome onset at an age of 6-12 months had de novo STXBP1mutations. Two of the patients had both tonic and atonic seizures early in the course of the disease, which is uncommon, but tonic seizures have been reported in older Dravet syndrome patients, according to Dr. Carvill and her associates.
GABRA1 and STXBP1 mutations have been reported in other epilepsies but not previously in Dravet syndrome.
"GABRA1 and STXBP1 are significant contributors to SCN1A-negative Dravet syndrome that should be tested in patients with Dravet syndrome negative for SCN1A mutations. With identification of further cases with Dravet syndrome due to these genes, specific phenotypic patterns may emerge that distinguish these rarer causes of Dravet syndrome from those due to SCN1A mutations," the investigators wrote.
In an accompanying comment to the study, Mingxuan Xu, Ph.D., of the department of neurology at Baylor College of Medicine, Houston, wrote that the discovery provides "insights for developing new diagnostic testing and drug targets and possibly leading to individualized therapeutic strategies for [Dravet syndrome] patients with different genotypes" (Neurology 2014 March 12 [doi:10.1212/WNL.0000000000000300]).
The study was supported by a variety of governmental and nongovernmental funding sources from Australia, New Zealand, Belgium, the European Union, and the United States, including the National Institute of Neurological Disorders and Stroke. Most of the authors reported having no relevant disclosures, but some reported financial ties to companies manufacturing antiepileptic drugs and epilepsy diagnostic tests.
FROM NEUROLOGY
Major finding: New disease-causing mutations were detected in novel genes for Dravet syndrome, including mutations in GABRA1 in four cases and in STXBP1 in three, and three patients had previously undetected SCN1A mutations.
Data source: A study of whole-exome sequencing in 13 patients with Dravet syndrome and targeted resequencing in an additional 67.
Disclosures: The study was supported by a variety of governmental and nongovernmental funding sources from Australia, New Zealand, Belgium, the European Union, and the United States, including the National Institute for Neurological Disorders and Stroke. Most of the authors reported having no relevant disclosures, but some reported financial ties to companies manufacturing antiepileptic drugs and epilepsy diagnostic tests.
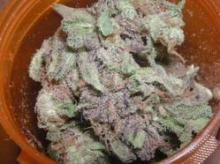
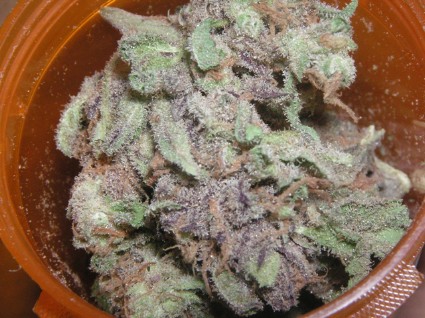
Orphan drug designation spurs trials for cannabidiol in Dravet syndrome
The development of a purified oral liquid formulation of a nonpsychoactive molecule found in marijuana, cannabidiol, for the treatment of drug-resistant epilepsy received a boost in winning orphan drug designations from the Food and Drug Administration for the indications of treating patients with Dravet and Lennox-Gastaut syndromes.
GW Pharmaceuticals, which is developing the purified cannabidiol product, so far has several trials slated to test the refined cannabidiol product in patients with Dravet syndrome. The company also received permission from the agency to allow U.S. physicians to treat up to 125 pediatric patients with pediatric epilepsy syndromes, including Dravet and Lennox-Gastaut, under an expanded access to investigational drugs protocol.
The orphan drug designation provides a 7-year exclusive marketing period in the United States for the first new drug application that receives approval for an indication to treat a rare disease or condition – generally a disease or condition that affects fewer than 200,000 individuals in the United States.
In a survey and other anecdotal reports, parents of children with drug-refractory epilepsy syndromes have reported successful treatment with cannabidiol-enriched marijuana. But little high-quality evidence is available about the efficacy and safety of cannabidiol in patients with Dravet, Lennox-Gastaux, and other pediatric epilepsy syndromes, as shown by a recent Cochrane Collaboration review of four randomized trials totaling 48 patients with epilepsy that found no adverse effects with 200-300 mg daily over short periods but did not report on the efficacy of the drug.
One double-blind, randomized placebo-controlled trial that GW has planned will test the safety of an oral solution containing either 25 mg/mL or 100 mg/mL cannabidiol during a 7-week period and single-dose pharmacokinetics with or without concomitant use of clobazam in 30 patients with Dravet syndrome.
Another double-blind, randomized placebo-controlled trial will test 25 mg/mL cannabidiol in 60 children and young adults with Dravet syndrome during a 12-week period to measure its effects on convulsive seizure frequency as the primary endpoint. Secondary endpoints will include the number of patients with a 50% or greater reduction in convulsive seizures from baseline, the change in nonconvulsive seizure frequency, the degree of sleep disruption, the degree of sleepiness, and caregiver impression of change.
The development of a purified oral liquid formulation of a nonpsychoactive molecule found in marijuana, cannabidiol, for the treatment of drug-resistant epilepsy received a boost in winning orphan drug designations from the Food and Drug Administration for the indications of treating patients with Dravet and Lennox-Gastaut syndromes.
GW Pharmaceuticals, which is developing the purified cannabidiol product, so far has several trials slated to test the refined cannabidiol product in patients with Dravet syndrome. The company also received permission from the agency to allow U.S. physicians to treat up to 125 pediatric patients with pediatric epilepsy syndromes, including Dravet and Lennox-Gastaut, under an expanded access to investigational drugs protocol.
The orphan drug designation provides a 7-year exclusive marketing period in the United States for the first new drug application that receives approval for an indication to treat a rare disease or condition – generally a disease or condition that affects fewer than 200,000 individuals in the United States.
In a survey and other anecdotal reports, parents of children with drug-refractory epilepsy syndromes have reported successful treatment with cannabidiol-enriched marijuana. But little high-quality evidence is available about the efficacy and safety of cannabidiol in patients with Dravet, Lennox-Gastaux, and other pediatric epilepsy syndromes, as shown by a recent Cochrane Collaboration review of four randomized trials totaling 48 patients with epilepsy that found no adverse effects with 200-300 mg daily over short periods but did not report on the efficacy of the drug.
One double-blind, randomized placebo-controlled trial that GW has planned will test the safety of an oral solution containing either 25 mg/mL or 100 mg/mL cannabidiol during a 7-week period and single-dose pharmacokinetics with or without concomitant use of clobazam in 30 patients with Dravet syndrome.
Another double-blind, randomized placebo-controlled trial will test 25 mg/mL cannabidiol in 60 children and young adults with Dravet syndrome during a 12-week period to measure its effects on convulsive seizure frequency as the primary endpoint. Secondary endpoints will include the number of patients with a 50% or greater reduction in convulsive seizures from baseline, the change in nonconvulsive seizure frequency, the degree of sleep disruption, the degree of sleepiness, and caregiver impression of change.
The development of a purified oral liquid formulation of a nonpsychoactive molecule found in marijuana, cannabidiol, for the treatment of drug-resistant epilepsy received a boost in winning orphan drug designations from the Food and Drug Administration for the indications of treating patients with Dravet and Lennox-Gastaut syndromes.
GW Pharmaceuticals, which is developing the purified cannabidiol product, so far has several trials slated to test the refined cannabidiol product in patients with Dravet syndrome. The company also received permission from the agency to allow U.S. physicians to treat up to 125 pediatric patients with pediatric epilepsy syndromes, including Dravet and Lennox-Gastaut, under an expanded access to investigational drugs protocol.
The orphan drug designation provides a 7-year exclusive marketing period in the United States for the first new drug application that receives approval for an indication to treat a rare disease or condition – generally a disease or condition that affects fewer than 200,000 individuals in the United States.
In a survey and other anecdotal reports, parents of children with drug-refractory epilepsy syndromes have reported successful treatment with cannabidiol-enriched marijuana. But little high-quality evidence is available about the efficacy and safety of cannabidiol in patients with Dravet, Lennox-Gastaux, and other pediatric epilepsy syndromes, as shown by a recent Cochrane Collaboration review of four randomized trials totaling 48 patients with epilepsy that found no adverse effects with 200-300 mg daily over short periods but did not report on the efficacy of the drug.
One double-blind, randomized placebo-controlled trial that GW has planned will test the safety of an oral solution containing either 25 mg/mL or 100 mg/mL cannabidiol during a 7-week period and single-dose pharmacokinetics with or without concomitant use of clobazam in 30 patients with Dravet syndrome.
Another double-blind, randomized placebo-controlled trial will test 25 mg/mL cannabidiol in 60 children and young adults with Dravet syndrome during a 12-week period to measure its effects on convulsive seizure frequency as the primary endpoint. Secondary endpoints will include the number of patients with a 50% or greater reduction in convulsive seizures from baseline, the change in nonconvulsive seizure frequency, the degree of sleep disruption, the degree of sleepiness, and caregiver impression of change.
New interleukin-17 inhibitor improved RA in phase II trial
The investigational anti-interleukin-17 monoclonal antibody ixekizumab proved efficacious and as safe as other biologic therapies in treating rheumatoid arthritis both in patients who had never received a biologic and in patients who had an inadequate response to previous treatment with a tumor necrosis factor–alpha inhibitor, in a study recently published in Arthritis & Rheumatology.
The 12-week, phase II trial, whose results were previously reported by Dr. Mark C. Genovese at the 2012 European Congress of Rheumatology, tested five different doses of ixekizumab against placebo and found that each dose produced significantly better rates of American College of Rheumatology (ACR) 20 responses after 12 weeks than did placebo.
The ACR 20 response rates were significantly different from those produced by placebo in both biologic-naive patients and those with an inadequate response to a TNF-alpha inhibitor. The ACR 20 response rates also followed a dose-response relationship in biologic-naive patients. ACR 20 responses, as well as decreases in 28-joint Disease Activity Score and C-reactive protein levels, occurred within 3 days of starting ixekizumab. No unforeseen adverse events occurred, according to first author Dr. Genovese, of the division of immunology and rheumatology at Stanford (Calif.) University, and his coinvestigators (Arthritis Rheumatol. 2014 March 12 [doi: 10.1002/art.38617]).
More recently, investigators at the 2013 ACR annual meeting presented data from an open-label extension of the trial out to 64 weeks. ACR 20 response rates were maintained or improved after patients went on a treatment hiatus during weeks 10-16 and then restarted ixekizumab at 160 mg once every 4 weeks out through 64 weeks. In the 202 biologic-naive patients who completed the extension phase, 89% of the 107 who had an ACR 20 response at 16 weeks maintained it through 64 weeks. The corresponding rate in 99 patients formerly on TNF-alpha inhibitors was 76% of 41 patients. Those who were formerly assigned to placebo treatment had responses that were similar to those observed in patients who were originally randomized to ixekizumab in the randomized trial (Arthritis Rheum. 2013;65[Suppl. S10]:S188).
Eli Lilly sponsored the trial. Dr. Genovese reported receiving research funding and consulting compensation from Eli Lilly. Another two investigators reported receiving research grants from the company. Other investigators are or were employees of Eli Lilly.
The investigational anti-interleukin-17 monoclonal antibody ixekizumab proved efficacious and as safe as other biologic therapies in treating rheumatoid arthritis both in patients who had never received a biologic and in patients who had an inadequate response to previous treatment with a tumor necrosis factor–alpha inhibitor, in a study recently published in Arthritis & Rheumatology.
The 12-week, phase II trial, whose results were previously reported by Dr. Mark C. Genovese at the 2012 European Congress of Rheumatology, tested five different doses of ixekizumab against placebo and found that each dose produced significantly better rates of American College of Rheumatology (ACR) 20 responses after 12 weeks than did placebo.
The ACR 20 response rates were significantly different from those produced by placebo in both biologic-naive patients and those with an inadequate response to a TNF-alpha inhibitor. The ACR 20 response rates also followed a dose-response relationship in biologic-naive patients. ACR 20 responses, as well as decreases in 28-joint Disease Activity Score and C-reactive protein levels, occurred within 3 days of starting ixekizumab. No unforeseen adverse events occurred, according to first author Dr. Genovese, of the division of immunology and rheumatology at Stanford (Calif.) University, and his coinvestigators (Arthritis Rheumatol. 2014 March 12 [doi: 10.1002/art.38617]).
More recently, investigators at the 2013 ACR annual meeting presented data from an open-label extension of the trial out to 64 weeks. ACR 20 response rates were maintained or improved after patients went on a treatment hiatus during weeks 10-16 and then restarted ixekizumab at 160 mg once every 4 weeks out through 64 weeks. In the 202 biologic-naive patients who completed the extension phase, 89% of the 107 who had an ACR 20 response at 16 weeks maintained it through 64 weeks. The corresponding rate in 99 patients formerly on TNF-alpha inhibitors was 76% of 41 patients. Those who were formerly assigned to placebo treatment had responses that were similar to those observed in patients who were originally randomized to ixekizumab in the randomized trial (Arthritis Rheum. 2013;65[Suppl. S10]:S188).
Eli Lilly sponsored the trial. Dr. Genovese reported receiving research funding and consulting compensation from Eli Lilly. Another two investigators reported receiving research grants from the company. Other investigators are or were employees of Eli Lilly.
The investigational anti-interleukin-17 monoclonal antibody ixekizumab proved efficacious and as safe as other biologic therapies in treating rheumatoid arthritis both in patients who had never received a biologic and in patients who had an inadequate response to previous treatment with a tumor necrosis factor–alpha inhibitor, in a study recently published in Arthritis & Rheumatology.
The 12-week, phase II trial, whose results were previously reported by Dr. Mark C. Genovese at the 2012 European Congress of Rheumatology, tested five different doses of ixekizumab against placebo and found that each dose produced significantly better rates of American College of Rheumatology (ACR) 20 responses after 12 weeks than did placebo.
The ACR 20 response rates were significantly different from those produced by placebo in both biologic-naive patients and those with an inadequate response to a TNF-alpha inhibitor. The ACR 20 response rates also followed a dose-response relationship in biologic-naive patients. ACR 20 responses, as well as decreases in 28-joint Disease Activity Score and C-reactive protein levels, occurred within 3 days of starting ixekizumab. No unforeseen adverse events occurred, according to first author Dr. Genovese, of the division of immunology and rheumatology at Stanford (Calif.) University, and his coinvestigators (Arthritis Rheumatol. 2014 March 12 [doi: 10.1002/art.38617]).
More recently, investigators at the 2013 ACR annual meeting presented data from an open-label extension of the trial out to 64 weeks. ACR 20 response rates were maintained or improved after patients went on a treatment hiatus during weeks 10-16 and then restarted ixekizumab at 160 mg once every 4 weeks out through 64 weeks. In the 202 biologic-naive patients who completed the extension phase, 89% of the 107 who had an ACR 20 response at 16 weeks maintained it through 64 weeks. The corresponding rate in 99 patients formerly on TNF-alpha inhibitors was 76% of 41 patients. Those who were formerly assigned to placebo treatment had responses that were similar to those observed in patients who were originally randomized to ixekizumab in the randomized trial (Arthritis Rheum. 2013;65[Suppl. S10]:S188).
Eli Lilly sponsored the trial. Dr. Genovese reported receiving research funding and consulting compensation from Eli Lilly. Another two investigators reported receiving research grants from the company. Other investigators are or were employees of Eli Lilly.
FROM ARTHRITIS & RHEUMATOLOGY
Methotrexate alone or with etanercept have equal efficacy for early inflammatory arthritis
Methotrexate alone appears to be just as good as when it is combined with etanercept in reducing tender and swollen joints in patients with early inflammatory arthritis who have at least one joint with clinical synovitis, according to results from a randomized, controlled trial.
However, the combination of etanercept (Enbrel) and methotrexate (MTX) gave a more rapid clinical response that was maintained, along with responses on various imaging outcomes, in the majority of patients who stopped taking etanercept if they had no tender or swollen joints for 26 weeks or if they had reached week 52 of treatment when the primary outcome of no tender or swollen joints was measured.
A previous study has shown that the combination of methotrexate and etanercept produced greater rates of remission in patients with early rheumatoid arthritis of 4 months or less duration, but the current study, conducted by Dr. Jackie L. Nam, a clinical research fellow at the University of Leeds (England) Musculoskeletal Biomedical Research Unit and her associates, is the first to test the combination in early inflammatory arthritis (Ann. Rheum. Dis. 2014 March 11 [doi:10.1136/annrheumdis-2013-204882]).
The investigators enrolled a total of 110 patients at four centers into the trial during October 2006-May 2009. They had a mean age of 48.6 years and median symptom duration of 7 months, although all had been diagnosed within 3 months of receiving treatment in the trial. None had been treated with a synthetic or biologic disease-modifying antirheumatic drug. Most of the patients were female (76%) and many tested positive for rheumatoid factor (53%), anti-citrullinated peptide antibodies (77%), and shared epitope (82%). Most (94%) also met the 2010 ACR-EULAR (American College of Rheumatology–European League Against Rheumatism) classification criteria for rheumatoid arthritis (RA), whereas 41% met the 1987 ACR RA classification criteria. At baseline, the patients had a mean C-reactive protein Disease Activity Score (DAS28-CRP) of about 4.13 and a DAS44-CRP of 2.94.
Both groups received MTX starting at 10 mg weekly, which could then be increased by 5 mg every 4 weeks up to 20 mg and then up to a final dose of 25 mg/week if the primary outcome of no swollen or tender joints had not been reached by week 12 or thereafter. After week 52, patients could take other conventional disease-modifying antirheumatic drugs if there was ongoing disease activity. NSAIDs also were permitted throughout the trial. A single intramuscular or intra-articular corticosteroid injection equivalent to 120 mg methylprednisolone was permitted on one occasion during the first 9 months of the trial and as clinically indicated afterward.
MTX plus etanercept or MTX plus placebo led to similar rates of no tender or swollen joints at 52 weeks in patients with early inflammatory arthritis diagnosed within 3 months of treatment (32.5% vs. 28.1%, respectively). But in exploratory analyses, a significantly higher proportion of patients in the combination therapy group achieved a 28-joint, DAS28-CRP of less than 2.6 at 2 weeks than did those taking MTX monotherapy (38.5% vs. 9.2%) as well as for DAS28-CRP of 3.2 or lower (55.5% vs. 22.2%).
Initially, the investigators had hypothesized that the combination therapy group would have a 60% response rate in no tender or swollen joints at 52 weeks and the MTX monotherapy group would have a 30% response rate, but they noted that "It is likely that [no tender or swollen joints] was too strict a target and that the achievement of no swollen joints alone may have been a more realistic outcome."
There were no surprises in adverse events among the two groups, with comparable numbers occurring in the patients on combination therapy and in those on monotherapy (451.6/100 patient-years vs. 417.3, respectively) and more serious adverse events occurring among patients treated with etanercept (16.4/100 patient-years vs. 3.7), although the investigators said that many were related to medical or surgical procedures that the patients underwent.
Pfizer provided the study drug and unrestricted grant funding. Seven of the 13 investigators reported potential conflicts of interest with numerous pharmaceutical companies, including Pfizer and other companies marketing treatments for inflammatory arthritis.
Methotrexate alone appears to be just as good as when it is combined with etanercept in reducing tender and swollen joints in patients with early inflammatory arthritis who have at least one joint with clinical synovitis, according to results from a randomized, controlled trial.
However, the combination of etanercept (Enbrel) and methotrexate (MTX) gave a more rapid clinical response that was maintained, along with responses on various imaging outcomes, in the majority of patients who stopped taking etanercept if they had no tender or swollen joints for 26 weeks or if they had reached week 52 of treatment when the primary outcome of no tender or swollen joints was measured.
A previous study has shown that the combination of methotrexate and etanercept produced greater rates of remission in patients with early rheumatoid arthritis of 4 months or less duration, but the current study, conducted by Dr. Jackie L. Nam, a clinical research fellow at the University of Leeds (England) Musculoskeletal Biomedical Research Unit and her associates, is the first to test the combination in early inflammatory arthritis (Ann. Rheum. Dis. 2014 March 11 [doi:10.1136/annrheumdis-2013-204882]).
The investigators enrolled a total of 110 patients at four centers into the trial during October 2006-May 2009. They had a mean age of 48.6 years and median symptom duration of 7 months, although all had been diagnosed within 3 months of receiving treatment in the trial. None had been treated with a synthetic or biologic disease-modifying antirheumatic drug. Most of the patients were female (76%) and many tested positive for rheumatoid factor (53%), anti-citrullinated peptide antibodies (77%), and shared epitope (82%). Most (94%) also met the 2010 ACR-EULAR (American College of Rheumatology–European League Against Rheumatism) classification criteria for rheumatoid arthritis (RA), whereas 41% met the 1987 ACR RA classification criteria. At baseline, the patients had a mean C-reactive protein Disease Activity Score (DAS28-CRP) of about 4.13 and a DAS44-CRP of 2.94.
Both groups received MTX starting at 10 mg weekly, which could then be increased by 5 mg every 4 weeks up to 20 mg and then up to a final dose of 25 mg/week if the primary outcome of no swollen or tender joints had not been reached by week 12 or thereafter. After week 52, patients could take other conventional disease-modifying antirheumatic drugs if there was ongoing disease activity. NSAIDs also were permitted throughout the trial. A single intramuscular or intra-articular corticosteroid injection equivalent to 120 mg methylprednisolone was permitted on one occasion during the first 9 months of the trial and as clinically indicated afterward.
MTX plus etanercept or MTX plus placebo led to similar rates of no tender or swollen joints at 52 weeks in patients with early inflammatory arthritis diagnosed within 3 months of treatment (32.5% vs. 28.1%, respectively). But in exploratory analyses, a significantly higher proportion of patients in the combination therapy group achieved a 28-joint, DAS28-CRP of less than 2.6 at 2 weeks than did those taking MTX monotherapy (38.5% vs. 9.2%) as well as for DAS28-CRP of 3.2 or lower (55.5% vs. 22.2%).
Initially, the investigators had hypothesized that the combination therapy group would have a 60% response rate in no tender or swollen joints at 52 weeks and the MTX monotherapy group would have a 30% response rate, but they noted that "It is likely that [no tender or swollen joints] was too strict a target and that the achievement of no swollen joints alone may have been a more realistic outcome."
There were no surprises in adverse events among the two groups, with comparable numbers occurring in the patients on combination therapy and in those on monotherapy (451.6/100 patient-years vs. 417.3, respectively) and more serious adverse events occurring among patients treated with etanercept (16.4/100 patient-years vs. 3.7), although the investigators said that many were related to medical or surgical procedures that the patients underwent.
Pfizer provided the study drug and unrestricted grant funding. Seven of the 13 investigators reported potential conflicts of interest with numerous pharmaceutical companies, including Pfizer and other companies marketing treatments for inflammatory arthritis.
Methotrexate alone appears to be just as good as when it is combined with etanercept in reducing tender and swollen joints in patients with early inflammatory arthritis who have at least one joint with clinical synovitis, according to results from a randomized, controlled trial.
However, the combination of etanercept (Enbrel) and methotrexate (MTX) gave a more rapid clinical response that was maintained, along with responses on various imaging outcomes, in the majority of patients who stopped taking etanercept if they had no tender or swollen joints for 26 weeks or if they had reached week 52 of treatment when the primary outcome of no tender or swollen joints was measured.
A previous study has shown that the combination of methotrexate and etanercept produced greater rates of remission in patients with early rheumatoid arthritis of 4 months or less duration, but the current study, conducted by Dr. Jackie L. Nam, a clinical research fellow at the University of Leeds (England) Musculoskeletal Biomedical Research Unit and her associates, is the first to test the combination in early inflammatory arthritis (Ann. Rheum. Dis. 2014 March 11 [doi:10.1136/annrheumdis-2013-204882]).
The investigators enrolled a total of 110 patients at four centers into the trial during October 2006-May 2009. They had a mean age of 48.6 years and median symptom duration of 7 months, although all had been diagnosed within 3 months of receiving treatment in the trial. None had been treated with a synthetic or biologic disease-modifying antirheumatic drug. Most of the patients were female (76%) and many tested positive for rheumatoid factor (53%), anti-citrullinated peptide antibodies (77%), and shared epitope (82%). Most (94%) also met the 2010 ACR-EULAR (American College of Rheumatology–European League Against Rheumatism) classification criteria for rheumatoid arthritis (RA), whereas 41% met the 1987 ACR RA classification criteria. At baseline, the patients had a mean C-reactive protein Disease Activity Score (DAS28-CRP) of about 4.13 and a DAS44-CRP of 2.94.
Both groups received MTX starting at 10 mg weekly, which could then be increased by 5 mg every 4 weeks up to 20 mg and then up to a final dose of 25 mg/week if the primary outcome of no swollen or tender joints had not been reached by week 12 or thereafter. After week 52, patients could take other conventional disease-modifying antirheumatic drugs if there was ongoing disease activity. NSAIDs also were permitted throughout the trial. A single intramuscular or intra-articular corticosteroid injection equivalent to 120 mg methylprednisolone was permitted on one occasion during the first 9 months of the trial and as clinically indicated afterward.
MTX plus etanercept or MTX plus placebo led to similar rates of no tender or swollen joints at 52 weeks in patients with early inflammatory arthritis diagnosed within 3 months of treatment (32.5% vs. 28.1%, respectively). But in exploratory analyses, a significantly higher proportion of patients in the combination therapy group achieved a 28-joint, DAS28-CRP of less than 2.6 at 2 weeks than did those taking MTX monotherapy (38.5% vs. 9.2%) as well as for DAS28-CRP of 3.2 or lower (55.5% vs. 22.2%).
Initially, the investigators had hypothesized that the combination therapy group would have a 60% response rate in no tender or swollen joints at 52 weeks and the MTX monotherapy group would have a 30% response rate, but they noted that "It is likely that [no tender or swollen joints] was too strict a target and that the achievement of no swollen joints alone may have been a more realistic outcome."
There were no surprises in adverse events among the two groups, with comparable numbers occurring in the patients on combination therapy and in those on monotherapy (451.6/100 patient-years vs. 417.3, respectively) and more serious adverse events occurring among patients treated with etanercept (16.4/100 patient-years vs. 3.7), although the investigators said that many were related to medical or surgical procedures that the patients underwent.
Pfizer provided the study drug and unrestricted grant funding. Seven of the 13 investigators reported potential conflicts of interest with numerous pharmaceutical companies, including Pfizer and other companies marketing treatments for inflammatory arthritis.
FROM ANNALS OF THE RHEUMATIC DISEASES
Major finding: Methotrexate plus etanercept or methotrexate plus placebo for 52 weeks led to similar rates of no tender or swollen joints in patients with early inflammatory arthritis diagnosed within 3 months of treatment (32.5% vs. 28.1%, respectively).
Data source: A multicenter, randomized, double-blind, placebo-controlled trial in patients with early inflammatory arthritis diagnosed within 3 months of treatment who had not been treated with any synthetic or biologic disease-modifying antirheumatic drug.
Disclosures: Pfizer provided the study drug and unrestricted grant funding. Seven of the 13 investigators reported potential conflicts of interest with numerous pharmaceutical companies, including Pfizer and other companies marketing treatments for inflammatory arthritis.
DEPDC5 mutations discovered in rolandic epilepsy and other focal childhood epilepsies
Rolandic epilepsy and other genetic focal childhood epilepsies, some occurring with focal cortical dysplasia, are part of the phenotypic spectrum of inherited focal epilepsy syndromes caused by mutations in the recently described DEPDC5 gene, according to studies on families and unrelated individuals with the disorders by two separate groups of investigators.
The researchers described truncating and nonsense mutations in DEPDC5 (Dishevelled, Egl-10, and Pleckstrin-domain-containing protein 5) that would likely prevent its encoded protein from being translated or cause it to lose its functional abilities, as well as missense mutations, which were of uncertain significance. However, these mutations appeared to have low penetrance in some instances in the families of affected index patients.
DEPDC5 is a member of a complex of proteins involved in controlling mTOR (mammalian target of rapamycin) signaling, which regulates processes involved in cell growth and homeostasis and is involved in other forms of epilepsy, such as tuberous sclerosis. Individuals with mutations in DEPDC5, which normally acts as a repressor of mTOR activity, could be responsive to treatment with drugs in the rapamycin family of drugs, such as sirolimus, according to study investigators.
In one study, senior investigator Dr. Bernd A. Neubauer and first author Dennis Lal, Ph.D., of the department of neuropediatrics at University Medical Center Giessen and Marburg, Germany, and their colleagues reported finding five DEPDC5 mutations in 207 patients with rolandic epilepsy (also known as benign epilepsy with centrotemporal spikes). In all, 87 of these patients were index patients in families with at least two affected siblings, and 120 were unrelated. The 87 index patients from multiplex families had either rolandic epilepsy (72), an atypical form of rolandic epilepsy (12), or electrical status epilepticus of sleep (3). The investigators also found two mutations in 82 unrelated patients with genetic focal or cryptogenic epilepsy who had variable degrees of intellectual disability and had been referred to centers in the study for diagnosis (Ann. Neurol. 2014 March 1 [doi: 10.1002/ana.24127]).
The researchers tracked the segregation of the mutations in families of six of the seven patients in whom DEPDC5 mutations were discovered. In one family, 4 of 18 carriers of a mutation were affected by rolandic epilepsy (one with centrotemporal spikes without seizures, and two with focal genetic epilepsy with centrotemporal spikes that persisted into adulthood). Another family had four members with unclassified focal childhood epilepsies, one of whom had a "relatively benign course." The father of the index individual in another family was homozygous for DEPDC5 mutations but was unaffected. But throughout all the families, those who had seizures carried a mutation in DEPDC5.
The other study described a family with six affected males with focal epilepsy and a truncation mutation in DEPDC5. Frontal focal cortical dysplasia was present in two of the affected individuals in the family, as well as in two other patients from the original two families in whom mutations in DEPDC5 were first described (Nat. Genet. 2013;45:546-51).
Magnetic resonance imaging showed in three of the individuals a bottom-of-the-sulcus dysplasia in a distinct region of the frontal lobe. In the fourth individual, there was unilateral, subtle band heterotopia in the white matter adjacent to dysplastic cortex in the left frontal lobe, Dr. Ingrid E. Scheffer of the Epilepsy Research Centre at the University of Melbourne and her associates reported (Ann. Neurol. 2014 March 1 [doi: 10.1002/ana.24126]).
"The concept that a single gene mutation may produce nonlesional focal epilepsy in one family member and focal cortical dysplasia in another challenges previous notions of the separation of genetic malformation syndromes from nonlesional epilepsy syndromes," the authors wrote, making one wonder whether more powerful imaging techniques could detect subtle dysgenesis in the patients without dysplasia detected by MRI. They noted that while "rare individuals with genetic malformation syndromes have no visible lesion on imaging (e.g., mildly affected subjects with DCX mutations), the inverse, where a proportion of subjects with a genetic epilepsy syndrome have a subtle malformation, has not previously been described."
Dr. Lal’s and Dr. Neubauer’s study was funded by grants from the EuroEPINOMICS Programme within the European Science Foundation. The study by Dr. Scheffer and her colleagues was supported by the National Health and Medical Research Council of Australia. No financial disclosures were made.
Rolandic epilepsy and other genetic focal childhood epilepsies, some occurring with focal cortical dysplasia, are part of the phenotypic spectrum of inherited focal epilepsy syndromes caused by mutations in the recently described DEPDC5 gene, according to studies on families and unrelated individuals with the disorders by two separate groups of investigators.
The researchers described truncating and nonsense mutations in DEPDC5 (Dishevelled, Egl-10, and Pleckstrin-domain-containing protein 5) that would likely prevent its encoded protein from being translated or cause it to lose its functional abilities, as well as missense mutations, which were of uncertain significance. However, these mutations appeared to have low penetrance in some instances in the families of affected index patients.
DEPDC5 is a member of a complex of proteins involved in controlling mTOR (mammalian target of rapamycin) signaling, which regulates processes involved in cell growth and homeostasis and is involved in other forms of epilepsy, such as tuberous sclerosis. Individuals with mutations in DEPDC5, which normally acts as a repressor of mTOR activity, could be responsive to treatment with drugs in the rapamycin family of drugs, such as sirolimus, according to study investigators.
In one study, senior investigator Dr. Bernd A. Neubauer and first author Dennis Lal, Ph.D., of the department of neuropediatrics at University Medical Center Giessen and Marburg, Germany, and their colleagues reported finding five DEPDC5 mutations in 207 patients with rolandic epilepsy (also known as benign epilepsy with centrotemporal spikes). In all, 87 of these patients were index patients in families with at least two affected siblings, and 120 were unrelated. The 87 index patients from multiplex families had either rolandic epilepsy (72), an atypical form of rolandic epilepsy (12), or electrical status epilepticus of sleep (3). The investigators also found two mutations in 82 unrelated patients with genetic focal or cryptogenic epilepsy who had variable degrees of intellectual disability and had been referred to centers in the study for diagnosis (Ann. Neurol. 2014 March 1 [doi: 10.1002/ana.24127]).
The researchers tracked the segregation of the mutations in families of six of the seven patients in whom DEPDC5 mutations were discovered. In one family, 4 of 18 carriers of a mutation were affected by rolandic epilepsy (one with centrotemporal spikes without seizures, and two with focal genetic epilepsy with centrotemporal spikes that persisted into adulthood). Another family had four members with unclassified focal childhood epilepsies, one of whom had a "relatively benign course." The father of the index individual in another family was homozygous for DEPDC5 mutations but was unaffected. But throughout all the families, those who had seizures carried a mutation in DEPDC5.
The other study described a family with six affected males with focal epilepsy and a truncation mutation in DEPDC5. Frontal focal cortical dysplasia was present in two of the affected individuals in the family, as well as in two other patients from the original two families in whom mutations in DEPDC5 were first described (Nat. Genet. 2013;45:546-51).
Magnetic resonance imaging showed in three of the individuals a bottom-of-the-sulcus dysplasia in a distinct region of the frontal lobe. In the fourth individual, there was unilateral, subtle band heterotopia in the white matter adjacent to dysplastic cortex in the left frontal lobe, Dr. Ingrid E. Scheffer of the Epilepsy Research Centre at the University of Melbourne and her associates reported (Ann. Neurol. 2014 March 1 [doi: 10.1002/ana.24126]).
"The concept that a single gene mutation may produce nonlesional focal epilepsy in one family member and focal cortical dysplasia in another challenges previous notions of the separation of genetic malformation syndromes from nonlesional epilepsy syndromes," the authors wrote, making one wonder whether more powerful imaging techniques could detect subtle dysgenesis in the patients without dysplasia detected by MRI. They noted that while "rare individuals with genetic malformation syndromes have no visible lesion on imaging (e.g., mildly affected subjects with DCX mutations), the inverse, where a proportion of subjects with a genetic epilepsy syndrome have a subtle malformation, has not previously been described."
Dr. Lal’s and Dr. Neubauer’s study was funded by grants from the EuroEPINOMICS Programme within the European Science Foundation. The study by Dr. Scheffer and her colleagues was supported by the National Health and Medical Research Council of Australia. No financial disclosures were made.
Rolandic epilepsy and other genetic focal childhood epilepsies, some occurring with focal cortical dysplasia, are part of the phenotypic spectrum of inherited focal epilepsy syndromes caused by mutations in the recently described DEPDC5 gene, according to studies on families and unrelated individuals with the disorders by two separate groups of investigators.
The researchers described truncating and nonsense mutations in DEPDC5 (Dishevelled, Egl-10, and Pleckstrin-domain-containing protein 5) that would likely prevent its encoded protein from being translated or cause it to lose its functional abilities, as well as missense mutations, which were of uncertain significance. However, these mutations appeared to have low penetrance in some instances in the families of affected index patients.
DEPDC5 is a member of a complex of proteins involved in controlling mTOR (mammalian target of rapamycin) signaling, which regulates processes involved in cell growth and homeostasis and is involved in other forms of epilepsy, such as tuberous sclerosis. Individuals with mutations in DEPDC5, which normally acts as a repressor of mTOR activity, could be responsive to treatment with drugs in the rapamycin family of drugs, such as sirolimus, according to study investigators.
In one study, senior investigator Dr. Bernd A. Neubauer and first author Dennis Lal, Ph.D., of the department of neuropediatrics at University Medical Center Giessen and Marburg, Germany, and their colleagues reported finding five DEPDC5 mutations in 207 patients with rolandic epilepsy (also known as benign epilepsy with centrotemporal spikes). In all, 87 of these patients were index patients in families with at least two affected siblings, and 120 were unrelated. The 87 index patients from multiplex families had either rolandic epilepsy (72), an atypical form of rolandic epilepsy (12), or electrical status epilepticus of sleep (3). The investigators also found two mutations in 82 unrelated patients with genetic focal or cryptogenic epilepsy who had variable degrees of intellectual disability and had been referred to centers in the study for diagnosis (Ann. Neurol. 2014 March 1 [doi: 10.1002/ana.24127]).
The researchers tracked the segregation of the mutations in families of six of the seven patients in whom DEPDC5 mutations were discovered. In one family, 4 of 18 carriers of a mutation were affected by rolandic epilepsy (one with centrotemporal spikes without seizures, and two with focal genetic epilepsy with centrotemporal spikes that persisted into adulthood). Another family had four members with unclassified focal childhood epilepsies, one of whom had a "relatively benign course." The father of the index individual in another family was homozygous for DEPDC5 mutations but was unaffected. But throughout all the families, those who had seizures carried a mutation in DEPDC5.
The other study described a family with six affected males with focal epilepsy and a truncation mutation in DEPDC5. Frontal focal cortical dysplasia was present in two of the affected individuals in the family, as well as in two other patients from the original two families in whom mutations in DEPDC5 were first described (Nat. Genet. 2013;45:546-51).
Magnetic resonance imaging showed in three of the individuals a bottom-of-the-sulcus dysplasia in a distinct region of the frontal lobe. In the fourth individual, there was unilateral, subtle band heterotopia in the white matter adjacent to dysplastic cortex in the left frontal lobe, Dr. Ingrid E. Scheffer of the Epilepsy Research Centre at the University of Melbourne and her associates reported (Ann. Neurol. 2014 March 1 [doi: 10.1002/ana.24126]).
"The concept that a single gene mutation may produce nonlesional focal epilepsy in one family member and focal cortical dysplasia in another challenges previous notions of the separation of genetic malformation syndromes from nonlesional epilepsy syndromes," the authors wrote, making one wonder whether more powerful imaging techniques could detect subtle dysgenesis in the patients without dysplasia detected by MRI. They noted that while "rare individuals with genetic malformation syndromes have no visible lesion on imaging (e.g., mildly affected subjects with DCX mutations), the inverse, where a proportion of subjects with a genetic epilepsy syndrome have a subtle malformation, has not previously been described."
Dr. Lal’s and Dr. Neubauer’s study was funded by grants from the EuroEPINOMICS Programme within the European Science Foundation. The study by Dr. Scheffer and her colleagues was supported by the National Health and Medical Research Council of Australia. No financial disclosures were made.
FROM ANNALS OF NEUROLOGY
Polyarteritis nodosa gene discovery raises new possibilities for field
Autosomal recessive mutations in the gene CECR1 cause an inflammatory vasculopathy with a highly varied clinical presentation that often meets the criteria for polyarteritis nodosa and can occur with early-onset strokes, according to findings from two separate reports on families with several affected members as well as unrelated affected persons.
All but 2 of the combined total of 33 patients in both studies were younger than 18 years at the onset of disease, including 13 with a history of lacunar strokes and 12 who met criteria for polyarteritis nodosa (PAN) from the Paediatric Rheumatology European Society and the European League Against Rheumatism for those with an onset before 18 years of age or from the American College of Rheumatology at an onset of 18 years of age or older.
The studies identified 12 CECR1 (cat eye syndrome chromosome region, candidate 1) variants that encoded dysfunctional adenosine deaminase 2 (ADA2) proteins. In one report, Israeli and German researchers described individuals who presented primarily with features of polyarteritis nodosa. They identified mutations in 16 patients from five families of Georgian Jewish ancestry and four siblings from one family of German ancestry, as well as single cases in three unrelated patients of Georgian Jewish ancestry and 1 Turkish patient who had been referred to them (N. Engl. J. Med. 2014;370:921-31).
In the other report, researchers from the National Institutes of Health studied nine patients with pediatric onset of disease, including five patients from the United States, one from the United Kingdom, and three from Turkey, including one pair of siblings. Eight of the patients presented with a history of lacunar strokes (N. Engl. J. Med. 2014;370:911-20).
Both reports used whole-exome sequencing in most cases and candidate-gene sequencing in others to detect autosomally recessive mutations in CECR1 (cat’s eye syndrome chromosome region, candidate 1) that cause a deficiency in adenosine deaminase 2 (ADA2), including cases with heterozygous compound mutations. Cell culture experiments indicated that ADA2 is a growth factor for endothelial and leukocyte development and differentiation, and modeling of the mutations’ effects in zebrafish resulted in intracranial hemorrhages.
One of the main differences between the two studies was in the differing presentation of patients, with mainly strokes in the NIH study but more PAN-like disease and peripheral nervous system involvement in the Israeli and German study.
All of the patients in the Israeli and German study had highly variable disease severity, even within families. Of the 19 Georgian Jewish patients, 18 had cutaneous manifestation of the disease, mainly livedo reticularis, although some had ischemia and necrosis of the fingers and toes. Fever was present in 11, and myalgia and/or arthralgia occurred in 12. Ten had visceral features, six of which were gastrointestinal, and eight had neurologic disease, most of which occurred peripherally. Among the four German siblings, all had peripheral neuropathy, three had symptomatic or subclinical brain infarctions, three had cutaneous manifestations, and three had myalgia and/or arthralgia, but none had visceral involvement. The single Turkish patient had most of these clinical manifestations except for peripheral or central nervous system involvement. Not all of the 24 patients in the Israeli and German study were fully evaluated for PAN, but nearly all were suspected of having the disease.
The NIH team compiled cases that were most striking for the history of early-onset ischemic lacunar stroke in eight of the nine patients, including five from the United States who had strokes before the age of 5 years but showed no signs of cerebral vasculitis on MR angiography. Three patients also had hemorrhagic stroke or hemorrhagic transformation. All patients had recurrent fever, eight had livedo racemosa, and five had ophthalmologic involvement. Only the two Turkish siblings had a diagnosis of PAN.
The spectrum of disease observed in the studies could be related to what CECR1 mutation is present, with 12 overall reported in the two studies, according to one of the NIH study investigators, Dr. Daniel L. Kastner, a rheumatologist and scientific director of the National Human Genome Research Institute. He also is head of the inflammatory diseases section in the medical genetics branch of the Institute.
"It wouldn’t be surprising to me if certain mutations are associated with certain clinical presentations," he said in an interview.
The most common mutation reported among the Georgian Jewish patients – all of whom were diagnosed with PAN – was also found in the NIH study’s three Turkish patients, two of whom had a PAN diagnosis. This variant had a carrier frequency of about 10% in a control group of 246 unrelated Georgian Jewish controls, which would predict based on Mendelian genetic principles that 1 in 400 individuals in the Georgian Jewish population in Israel would carry two copies of the variant. The individuals who were homozygous for that variant in the Israeli and German study showed variability in phenotype, ranging from a diagnosis of diagnosed PAN to milder disease not meeting the full criteria for PAN. Given the relative commonality of the variant, ADA2-associated disease in Georgian Jewish people and other populations is likely underdiagnosed or being misdiagnosed for other conditions because of the clinical variability, Dr. Kastner said.
NIH investigators have talked with Dr. Peter Merkel, principal investigator and director of the Vasculitis Clinical Research Consortium, about conducting collaborative studies to look for variants of ADA2 in others who have nonfamilial PAN and did not have early-onset disease. "Even if they don’t [have variants in ADA2], it may still be the case that the pathway is somehow important and studies of biopsies from those patients would in some way allow us to connect that pathway to their disease. But that’s unknown," Dr. Kastner said.
When Dr. Kastner and his associates were looking for the mutations in other genetics databases, they found that whole-exome sequencing of 47 pairs of siblings with late-onset ischemic stroke in the Siblings With Ischemic Stroke Study had detected two brothers who each were heterozygous carriers of one of the mutations discovered in the study. Their ischemic strokes were similar in distribution to those seen in children with two mutations. "So it’s at least possible, although at this point it’s not formally proven, [that] that perhaps carrying one copy of this mutation, as opposed to having two as these kids have, could put you at some risk for having stroke later on in life. And it may be that, similarly, having one copy of a variant in this gene would predispose to other forms of vasculitis as well."
In three of the patients in the NIH study, treatment with low doses of fresh frozen plasma as a replacement therapy for ADA2 deficiency has appeared to be safe, but getting enough of it into patients and knowing whether it will last long enough are questions that the investigators are currently trying to answer, Dr. Kastner said. Initially, Dr. Kastner said his group was hesitant to use anti–tumor necrosis factor-alpha agents to treat patients because of the known, but small risk of demyelination with their use, which would not have been appropriate to try in patients who already had neurologic problems, because it would be very hard to tell if further lesions would be caused by underlying disease or the drug. However, when the Israeli group reported success with anti-TNF-alpha agents in their patients (and ultimately reported that 10 patients had a clinically significant therapeutic response), the NIH investigators decided to try them. Treatment with etanercept in five patients has reduced the occurrence of fevers in all and improved urticarial papules and plaques observed in three patients.
Pediatric rheumatologists who have patients with vasculitis or are suspected of having vasculitis should keep CECR1 mutations in mind now that the cause and some of the natural history and possible treatments for early-onset disease are known. Rheumatologists seeing adult patients with PAN could consider these mutations as a possible cause and at least note that some of these pathways may be important in their patients even if they don’t have mutations in CECR1, advised Dr. Kastner. He had no financial conflicts to disclose.
Autosomal recessive mutations in the gene CECR1 cause an inflammatory vasculopathy with a highly varied clinical presentation that often meets the criteria for polyarteritis nodosa and can occur with early-onset strokes, according to findings from two separate reports on families with several affected members as well as unrelated affected persons.
All but 2 of the combined total of 33 patients in both studies were younger than 18 years at the onset of disease, including 13 with a history of lacunar strokes and 12 who met criteria for polyarteritis nodosa (PAN) from the Paediatric Rheumatology European Society and the European League Against Rheumatism for those with an onset before 18 years of age or from the American College of Rheumatology at an onset of 18 years of age or older.
The studies identified 12 CECR1 (cat eye syndrome chromosome region, candidate 1) variants that encoded dysfunctional adenosine deaminase 2 (ADA2) proteins. In one report, Israeli and German researchers described individuals who presented primarily with features of polyarteritis nodosa. They identified mutations in 16 patients from five families of Georgian Jewish ancestry and four siblings from one family of German ancestry, as well as single cases in three unrelated patients of Georgian Jewish ancestry and 1 Turkish patient who had been referred to them (N. Engl. J. Med. 2014;370:921-31).
In the other report, researchers from the National Institutes of Health studied nine patients with pediatric onset of disease, including five patients from the United States, one from the United Kingdom, and three from Turkey, including one pair of siblings. Eight of the patients presented with a history of lacunar strokes (N. Engl. J. Med. 2014;370:911-20).
Both reports used whole-exome sequencing in most cases and candidate-gene sequencing in others to detect autosomally recessive mutations in CECR1 (cat’s eye syndrome chromosome region, candidate 1) that cause a deficiency in adenosine deaminase 2 (ADA2), including cases with heterozygous compound mutations. Cell culture experiments indicated that ADA2 is a growth factor for endothelial and leukocyte development and differentiation, and modeling of the mutations’ effects in zebrafish resulted in intracranial hemorrhages.
One of the main differences between the two studies was in the differing presentation of patients, with mainly strokes in the NIH study but more PAN-like disease and peripheral nervous system involvement in the Israeli and German study.
All of the patients in the Israeli and German study had highly variable disease severity, even within families. Of the 19 Georgian Jewish patients, 18 had cutaneous manifestation of the disease, mainly livedo reticularis, although some had ischemia and necrosis of the fingers and toes. Fever was present in 11, and myalgia and/or arthralgia occurred in 12. Ten had visceral features, six of which were gastrointestinal, and eight had neurologic disease, most of which occurred peripherally. Among the four German siblings, all had peripheral neuropathy, three had symptomatic or subclinical brain infarctions, three had cutaneous manifestations, and three had myalgia and/or arthralgia, but none had visceral involvement. The single Turkish patient had most of these clinical manifestations except for peripheral or central nervous system involvement. Not all of the 24 patients in the Israeli and German study were fully evaluated for PAN, but nearly all were suspected of having the disease.
The NIH team compiled cases that were most striking for the history of early-onset ischemic lacunar stroke in eight of the nine patients, including five from the United States who had strokes before the age of 5 years but showed no signs of cerebral vasculitis on MR angiography. Three patients also had hemorrhagic stroke or hemorrhagic transformation. All patients had recurrent fever, eight had livedo racemosa, and five had ophthalmologic involvement. Only the two Turkish siblings had a diagnosis of PAN.
The spectrum of disease observed in the studies could be related to what CECR1 mutation is present, with 12 overall reported in the two studies, according to one of the NIH study investigators, Dr. Daniel L. Kastner, a rheumatologist and scientific director of the National Human Genome Research Institute. He also is head of the inflammatory diseases section in the medical genetics branch of the Institute.
"It wouldn’t be surprising to me if certain mutations are associated with certain clinical presentations," he said in an interview.
The most common mutation reported among the Georgian Jewish patients – all of whom were diagnosed with PAN – was also found in the NIH study’s three Turkish patients, two of whom had a PAN diagnosis. This variant had a carrier frequency of about 10% in a control group of 246 unrelated Georgian Jewish controls, which would predict based on Mendelian genetic principles that 1 in 400 individuals in the Georgian Jewish population in Israel would carry two copies of the variant. The individuals who were homozygous for that variant in the Israeli and German study showed variability in phenotype, ranging from a diagnosis of diagnosed PAN to milder disease not meeting the full criteria for PAN. Given the relative commonality of the variant, ADA2-associated disease in Georgian Jewish people and other populations is likely underdiagnosed or being misdiagnosed for other conditions because of the clinical variability, Dr. Kastner said.
NIH investigators have talked with Dr. Peter Merkel, principal investigator and director of the Vasculitis Clinical Research Consortium, about conducting collaborative studies to look for variants of ADA2 in others who have nonfamilial PAN and did not have early-onset disease. "Even if they don’t [have variants in ADA2], it may still be the case that the pathway is somehow important and studies of biopsies from those patients would in some way allow us to connect that pathway to their disease. But that’s unknown," Dr. Kastner said.
When Dr. Kastner and his associates were looking for the mutations in other genetics databases, they found that whole-exome sequencing of 47 pairs of siblings with late-onset ischemic stroke in the Siblings With Ischemic Stroke Study had detected two brothers who each were heterozygous carriers of one of the mutations discovered in the study. Their ischemic strokes were similar in distribution to those seen in children with two mutations. "So it’s at least possible, although at this point it’s not formally proven, [that] that perhaps carrying one copy of this mutation, as opposed to having two as these kids have, could put you at some risk for having stroke later on in life. And it may be that, similarly, having one copy of a variant in this gene would predispose to other forms of vasculitis as well."
In three of the patients in the NIH study, treatment with low doses of fresh frozen plasma as a replacement therapy for ADA2 deficiency has appeared to be safe, but getting enough of it into patients and knowing whether it will last long enough are questions that the investigators are currently trying to answer, Dr. Kastner said. Initially, Dr. Kastner said his group was hesitant to use anti–tumor necrosis factor-alpha agents to treat patients because of the known, but small risk of demyelination with their use, which would not have been appropriate to try in patients who already had neurologic problems, because it would be very hard to tell if further lesions would be caused by underlying disease or the drug. However, when the Israeli group reported success with anti-TNF-alpha agents in their patients (and ultimately reported that 10 patients had a clinically significant therapeutic response), the NIH investigators decided to try them. Treatment with etanercept in five patients has reduced the occurrence of fevers in all and improved urticarial papules and plaques observed in three patients.
Pediatric rheumatologists who have patients with vasculitis or are suspected of having vasculitis should keep CECR1 mutations in mind now that the cause and some of the natural history and possible treatments for early-onset disease are known. Rheumatologists seeing adult patients with PAN could consider these mutations as a possible cause and at least note that some of these pathways may be important in their patients even if they don’t have mutations in CECR1, advised Dr. Kastner. He had no financial conflicts to disclose.
Autosomal recessive mutations in the gene CECR1 cause an inflammatory vasculopathy with a highly varied clinical presentation that often meets the criteria for polyarteritis nodosa and can occur with early-onset strokes, according to findings from two separate reports on families with several affected members as well as unrelated affected persons.
All but 2 of the combined total of 33 patients in both studies were younger than 18 years at the onset of disease, including 13 with a history of lacunar strokes and 12 who met criteria for polyarteritis nodosa (PAN) from the Paediatric Rheumatology European Society and the European League Against Rheumatism for those with an onset before 18 years of age or from the American College of Rheumatology at an onset of 18 years of age or older.
The studies identified 12 CECR1 (cat eye syndrome chromosome region, candidate 1) variants that encoded dysfunctional adenosine deaminase 2 (ADA2) proteins. In one report, Israeli and German researchers described individuals who presented primarily with features of polyarteritis nodosa. They identified mutations in 16 patients from five families of Georgian Jewish ancestry and four siblings from one family of German ancestry, as well as single cases in three unrelated patients of Georgian Jewish ancestry and 1 Turkish patient who had been referred to them (N. Engl. J. Med. 2014;370:921-31).
In the other report, researchers from the National Institutes of Health studied nine patients with pediatric onset of disease, including five patients from the United States, one from the United Kingdom, and three from Turkey, including one pair of siblings. Eight of the patients presented with a history of lacunar strokes (N. Engl. J. Med. 2014;370:911-20).
Both reports used whole-exome sequencing in most cases and candidate-gene sequencing in others to detect autosomally recessive mutations in CECR1 (cat’s eye syndrome chromosome region, candidate 1) that cause a deficiency in adenosine deaminase 2 (ADA2), including cases with heterozygous compound mutations. Cell culture experiments indicated that ADA2 is a growth factor for endothelial and leukocyte development and differentiation, and modeling of the mutations’ effects in zebrafish resulted in intracranial hemorrhages.
One of the main differences between the two studies was in the differing presentation of patients, with mainly strokes in the NIH study but more PAN-like disease and peripheral nervous system involvement in the Israeli and German study.
All of the patients in the Israeli and German study had highly variable disease severity, even within families. Of the 19 Georgian Jewish patients, 18 had cutaneous manifestation of the disease, mainly livedo reticularis, although some had ischemia and necrosis of the fingers and toes. Fever was present in 11, and myalgia and/or arthralgia occurred in 12. Ten had visceral features, six of which were gastrointestinal, and eight had neurologic disease, most of which occurred peripherally. Among the four German siblings, all had peripheral neuropathy, three had symptomatic or subclinical brain infarctions, three had cutaneous manifestations, and three had myalgia and/or arthralgia, but none had visceral involvement. The single Turkish patient had most of these clinical manifestations except for peripheral or central nervous system involvement. Not all of the 24 patients in the Israeli and German study were fully evaluated for PAN, but nearly all were suspected of having the disease.
The NIH team compiled cases that were most striking for the history of early-onset ischemic lacunar stroke in eight of the nine patients, including five from the United States who had strokes before the age of 5 years but showed no signs of cerebral vasculitis on MR angiography. Three patients also had hemorrhagic stroke or hemorrhagic transformation. All patients had recurrent fever, eight had livedo racemosa, and five had ophthalmologic involvement. Only the two Turkish siblings had a diagnosis of PAN.
The spectrum of disease observed in the studies could be related to what CECR1 mutation is present, with 12 overall reported in the two studies, according to one of the NIH study investigators, Dr. Daniel L. Kastner, a rheumatologist and scientific director of the National Human Genome Research Institute. He also is head of the inflammatory diseases section in the medical genetics branch of the Institute.
"It wouldn’t be surprising to me if certain mutations are associated with certain clinical presentations," he said in an interview.
The most common mutation reported among the Georgian Jewish patients – all of whom were diagnosed with PAN – was also found in the NIH study’s three Turkish patients, two of whom had a PAN diagnosis. This variant had a carrier frequency of about 10% in a control group of 246 unrelated Georgian Jewish controls, which would predict based on Mendelian genetic principles that 1 in 400 individuals in the Georgian Jewish population in Israel would carry two copies of the variant. The individuals who were homozygous for that variant in the Israeli and German study showed variability in phenotype, ranging from a diagnosis of diagnosed PAN to milder disease not meeting the full criteria for PAN. Given the relative commonality of the variant, ADA2-associated disease in Georgian Jewish people and other populations is likely underdiagnosed or being misdiagnosed for other conditions because of the clinical variability, Dr. Kastner said.
NIH investigators have talked with Dr. Peter Merkel, principal investigator and director of the Vasculitis Clinical Research Consortium, about conducting collaborative studies to look for variants of ADA2 in others who have nonfamilial PAN and did not have early-onset disease. "Even if they don’t [have variants in ADA2], it may still be the case that the pathway is somehow important and studies of biopsies from those patients would in some way allow us to connect that pathway to their disease. But that’s unknown," Dr. Kastner said.
When Dr. Kastner and his associates were looking for the mutations in other genetics databases, they found that whole-exome sequencing of 47 pairs of siblings with late-onset ischemic stroke in the Siblings With Ischemic Stroke Study had detected two brothers who each were heterozygous carriers of one of the mutations discovered in the study. Their ischemic strokes were similar in distribution to those seen in children with two mutations. "So it’s at least possible, although at this point it’s not formally proven, [that] that perhaps carrying one copy of this mutation, as opposed to having two as these kids have, could put you at some risk for having stroke later on in life. And it may be that, similarly, having one copy of a variant in this gene would predispose to other forms of vasculitis as well."
In three of the patients in the NIH study, treatment with low doses of fresh frozen plasma as a replacement therapy for ADA2 deficiency has appeared to be safe, but getting enough of it into patients and knowing whether it will last long enough are questions that the investigators are currently trying to answer, Dr. Kastner said. Initially, Dr. Kastner said his group was hesitant to use anti–tumor necrosis factor-alpha agents to treat patients because of the known, but small risk of demyelination with their use, which would not have been appropriate to try in patients who already had neurologic problems, because it would be very hard to tell if further lesions would be caused by underlying disease or the drug. However, when the Israeli group reported success with anti-TNF-alpha agents in their patients (and ultimately reported that 10 patients had a clinically significant therapeutic response), the NIH investigators decided to try them. Treatment with etanercept in five patients has reduced the occurrence of fevers in all and improved urticarial papules and plaques observed in three patients.
Pediatric rheumatologists who have patients with vasculitis or are suspected of having vasculitis should keep CECR1 mutations in mind now that the cause and some of the natural history and possible treatments for early-onset disease are known. Rheumatologists seeing adult patients with PAN could consider these mutations as a possible cause and at least note that some of these pathways may be important in their patients even if they don’t have mutations in CECR1, advised Dr. Kastner. He had no financial conflicts to disclose.
FROM NEW ENGLAND JOURNAL OF MEDICINE
NIH and pharma partner on RA, lupus, diabetes, Alzheimer’s research
The National Institutes of Health, 10 biopharmaceutical companies, and several nonprofit organizations have partnered to transform the current model for identifying and validating the most promising biological targets of disease for new diagnostics and drug development.
The Accelerating Medicines Partnership aims to pinpoint biological targets that are most likely to respond to new therapies. Partners in this initiative, which include major drug makers such as GlaxoSmithKline and Merck, along with nonprofits such as the Rheumatology Research Foundation, the Lupus Foundation of America, the American Diabetes Association, and the Alzheimer’s Association, are expected to invest more than $230 million over 5 years in the first projects, which will focus on rheumatoid arthritis and systemic lupus erythematosus (total funding of $41.6 million), type 2 diabetes ($58.4 million), and Alzheimer’s disease ($129.5 million).
Data and analyses generated by these projects will be made publicly available to the broad biomedical community through an Internet-based information portal, and the initial projects could set the stage for broadening the initiative into other diseases and conditions, the NIH says.
For rheumatoid arthritis and lupus, the project will focus on collecting and analyzing tissue and blood samples from patients to see how changes at the single-cell and systems levels can provide insight into the disease process and inform comparisons across diseases, as well as identify differences between patients in response to treatment.
The type 2 diabetes project will aim "to use and supplement the substantial amount of human genetic data available from people with type 2 diabetes – or at risk for developing type 2 diabetes – to identify and validate novel molecules and pathways as targets for therapeutic development." Researchers also will build a type 2 diabetes knowledge portal for academic and industry researchers that will contain DNA sequences, functional genomic and epigenomic information, and clinical data from studies on type 2 diabetes and its cardiac and renal complications totaling 100,000-150,000 individuals.
The Alzheimer’s project will seek to increase the amount of data available from clinical trials to increase support for therapeutic target validation in humans. This will be done by using selected biomarkers in four NIH- and industry-supported clinical trials that are designed to delay or prevent disease onset, as well as performing a large-scale analysis of brain tissue samples from Alzheimer’s disease patients to validate biological targets previously shown to play key roles in disease progression and increase understanding of the molecular pathways involved in the disease, in order to identify new potential therapeutic targets.
The National Institutes of Health, 10 biopharmaceutical companies, and several nonprofit organizations have partnered to transform the current model for identifying and validating the most promising biological targets of disease for new diagnostics and drug development.
The Accelerating Medicines Partnership aims to pinpoint biological targets that are most likely to respond to new therapies. Partners in this initiative, which include major drug makers such as GlaxoSmithKline and Merck, along with nonprofits such as the Rheumatology Research Foundation, the Lupus Foundation of America, the American Diabetes Association, and the Alzheimer’s Association, are expected to invest more than $230 million over 5 years in the first projects, which will focus on rheumatoid arthritis and systemic lupus erythematosus (total funding of $41.6 million), type 2 diabetes ($58.4 million), and Alzheimer’s disease ($129.5 million).
Data and analyses generated by these projects will be made publicly available to the broad biomedical community through an Internet-based information portal, and the initial projects could set the stage for broadening the initiative into other diseases and conditions, the NIH says.
For rheumatoid arthritis and lupus, the project will focus on collecting and analyzing tissue and blood samples from patients to see how changes at the single-cell and systems levels can provide insight into the disease process and inform comparisons across diseases, as well as identify differences between patients in response to treatment.
The type 2 diabetes project will aim "to use and supplement the substantial amount of human genetic data available from people with type 2 diabetes – or at risk for developing type 2 diabetes – to identify and validate novel molecules and pathways as targets for therapeutic development." Researchers also will build a type 2 diabetes knowledge portal for academic and industry researchers that will contain DNA sequences, functional genomic and epigenomic information, and clinical data from studies on type 2 diabetes and its cardiac and renal complications totaling 100,000-150,000 individuals.
The Alzheimer’s project will seek to increase the amount of data available from clinical trials to increase support for therapeutic target validation in humans. This will be done by using selected biomarkers in four NIH- and industry-supported clinical trials that are designed to delay or prevent disease onset, as well as performing a large-scale analysis of brain tissue samples from Alzheimer’s disease patients to validate biological targets previously shown to play key roles in disease progression and increase understanding of the molecular pathways involved in the disease, in order to identify new potential therapeutic targets.
The National Institutes of Health, 10 biopharmaceutical companies, and several nonprofit organizations have partnered to transform the current model for identifying and validating the most promising biological targets of disease for new diagnostics and drug development.
The Accelerating Medicines Partnership aims to pinpoint biological targets that are most likely to respond to new therapies. Partners in this initiative, which include major drug makers such as GlaxoSmithKline and Merck, along with nonprofits such as the Rheumatology Research Foundation, the Lupus Foundation of America, the American Diabetes Association, and the Alzheimer’s Association, are expected to invest more than $230 million over 5 years in the first projects, which will focus on rheumatoid arthritis and systemic lupus erythematosus (total funding of $41.6 million), type 2 diabetes ($58.4 million), and Alzheimer’s disease ($129.5 million).
Data and analyses generated by these projects will be made publicly available to the broad biomedical community through an Internet-based information portal, and the initial projects could set the stage for broadening the initiative into other diseases and conditions, the NIH says.
For rheumatoid arthritis and lupus, the project will focus on collecting and analyzing tissue and blood samples from patients to see how changes at the single-cell and systems levels can provide insight into the disease process and inform comparisons across diseases, as well as identify differences between patients in response to treatment.
The type 2 diabetes project will aim "to use and supplement the substantial amount of human genetic data available from people with type 2 diabetes – or at risk for developing type 2 diabetes – to identify and validate novel molecules and pathways as targets for therapeutic development." Researchers also will build a type 2 diabetes knowledge portal for academic and industry researchers that will contain DNA sequences, functional genomic and epigenomic information, and clinical data from studies on type 2 diabetes and its cardiac and renal complications totaling 100,000-150,000 individuals.
The Alzheimer’s project will seek to increase the amount of data available from clinical trials to increase support for therapeutic target validation in humans. This will be done by using selected biomarkers in four NIH- and industry-supported clinical trials that are designed to delay or prevent disease onset, as well as performing a large-scale analysis of brain tissue samples from Alzheimer’s disease patients to validate biological targets previously shown to play key roles in disease progression and increase understanding of the molecular pathways involved in the disease, in order to identify new potential therapeutic targets.
Higher-dose glatiramer acetate formulation approved for MS
The Food and Drug Administration has approved a new higher-dose subcutaneous injection formulation of glatiramer acetate that is injected three times per week instead of daily, according to the manufacturer, Teva.
The approval, announced Jan. 28, is based on the randomized, blinded, placebo-controlled GALA (Glatiramer Acetate Low Frequency Administration) study, in which 943 relapsing-remitting multiple sclerosis patients were randomized to 40 mg of subcutaneous glatiramer acetate (Copaxone) three times weekly and 461 patients to matched placebo injections. (Read about the trial’s results in a report out of the 2013 American Academy of Neurology annual meeting).
Teva said that it is shipping the 40-mg dose to distribution outlets immediately and it should be available to patients "within days." The new label information can be found here.
The daily 20-mg/mL subcutaneous injection formulation, approved in 1996, will continue to be available.
The Food and Drug Administration has approved a new higher-dose subcutaneous injection formulation of glatiramer acetate that is injected three times per week instead of daily, according to the manufacturer, Teva.
The approval, announced Jan. 28, is based on the randomized, blinded, placebo-controlled GALA (Glatiramer Acetate Low Frequency Administration) study, in which 943 relapsing-remitting multiple sclerosis patients were randomized to 40 mg of subcutaneous glatiramer acetate (Copaxone) three times weekly and 461 patients to matched placebo injections. (Read about the trial’s results in a report out of the 2013 American Academy of Neurology annual meeting).
Teva said that it is shipping the 40-mg dose to distribution outlets immediately and it should be available to patients "within days." The new label information can be found here.
The daily 20-mg/mL subcutaneous injection formulation, approved in 1996, will continue to be available.
The Food and Drug Administration has approved a new higher-dose subcutaneous injection formulation of glatiramer acetate that is injected three times per week instead of daily, according to the manufacturer, Teva.
The approval, announced Jan. 28, is based on the randomized, blinded, placebo-controlled GALA (Glatiramer Acetate Low Frequency Administration) study, in which 943 relapsing-remitting multiple sclerosis patients were randomized to 40 mg of subcutaneous glatiramer acetate (Copaxone) three times weekly and 461 patients to matched placebo injections. (Read about the trial’s results in a report out of the 2013 American Academy of Neurology annual meeting).
Teva said that it is shipping the 40-mg dose to distribution outlets immediately and it should be available to patients "within days." The new label information can be found here.
The daily 20-mg/mL subcutaneous injection formulation, approved in 1996, will continue to be available.
Hyaluronic acid injection for knee OA as effective as NSAIDs in short term
Treatment of osteoarthritis with intra-articular injections of hyaluronic acid over a 5-week period provided symptomatic relief that had noninferior efficacy and was safer than treatment with an oral NSAID in an open-label, multicenter randomized trial of older Japanese adults.
Intra-articular injections of hyaluronic acid (IA-HA) have been shown to reduce pain and improve joint function in knee osteoarthritis (OA), but studies also have reported a relatively slow speed of therapeutic onset and "considerable heterogeneity" in outcomes. NSAIDs have long been regarded as effective for symptomatic relief of knee OA, but carry the risk of serious gastrointestinal adverse events. The lack of data on the short-term effects of IA-HA compared with widely used NSAIDs spurred Dr. Muneaki Ishijima of Juntendo University, Tokyo, and colleagues to conduct the first trial to directly compare efficacy and safety of the two treatments for knee OA (Arthritis Res. Ther. 2014 Jan. 21 [doi:10.1186/ar4446]).
The investigators randomized 200 patients to 5 weeks of either weekly IA-HA or the nonselective cyclo-oxygenase inhibitor loxoprofen in three 60-mg tablets daily and evaluated patients’ percent change from baseline on the patient-reported Japanese Knee Osteoarthritis Measure (JKOM, primary endpoint) and their percent change from baseline in pain as rated on a 0- to 100-point visual analog scale (VAS, secondary endpoint). (Loxoprofen is not approved in the United States.)
After the 5 weeks of therapy, the investigators analyzed data from 98 patients who underwent IA-HA and 86 patients who received loxoprofen who had final JKOM scores available. In the IA-HA group, one patient withdrew consent before undergoing IA-HA, and one was lost to follow-up before the final JKOM analysis. In the NSAID group, six patients withdrew consent before receiving treatment, one patient was excluded because of duplicate entry into the trial before receiving treatment, and another seven were lost to follow-up before the final analysis.
The trial participants had a mean age of about 68 years, and approximately 72% were women. The patients had OA of the medial femorotibial joint with a Kellgren-Lawrence grade of 1-3.
The mean JKOM score declined 32.2% (from 32.0 to 22.0) with NSAID treatment and 34.7% (from 33.8 to 21.5) with IA-HA. This difference of –2.5% and its 95% confidence interval of –14.0% to 9.1% meant that the two treatments had similar efficacy based on the trial’s prespecified definition of noninferiority as a 10% difference or less in the upper limit of the confidence interval. The result did not change after adjustment for age, Kellgren-Lawrence grade, body mass index, and medical center.
Pain on the VAS dropped by 36.0% (from 55.5 to 31.9) with NSAID therapy and by 41.2% (from 60.1 to 31.8) with IA-HA, a nonsignificant difference.
There also were no differences in the percentage of responders in each group based on Outcome Measures in Rheumatology clinical trials and Osteoarthritis Research Society International (OMERACT-OARSI) response criteria, with 69.7% in the IA-HA group and 62.4% in the NSAID group. For this trial, the responder criteria were partly modified by use of the JKOM score. Response was defined as a decrease in joint pain or improvement in function based on at least a 50% reduction in score and a decrease of at least 20 mm on the VAS or clinical improvement on two of three measures: at least a 20% decline in joint pain and at least 10 mm on the VAS; functional improvement of at least 20% and a drop of at least 4 points on the 40-point JKOM functional subcategory scale; and a decrease of at least 20% on the patient’s global assessment score and a drop of at least 10 points from the total JKOM score.
No serious adverse events occurred in either group, but in the NSAID group, seven patients had symptoms related to a GI tract disorder, and three had allergy to loxoprofen, compared with one patient who received IA-HA who had stiffness in the treated knee after injection, a significant difference.
"The present study suggests that future randomized trials should thus be carried out with a longer duration of follow-up and larger samples, in order to identify optimal knee OA treatment alternatives," the investigators wrote.
They acknowledged the problems inherent with the potential of the trial’s open-label design to introduce bias into the results and the use of a 10% difference in the change in JKOM score to define noninferiority, although this margin was supported by a pilot study.
The authors reported no relevant financial disclosures.
In this interesting, multicenter, Japanese noninferiority trial, 200 patients with symptomatic knee osteoarthritis were randomized to either intra-articular hyaluronic acid (once per week for 5 weeks) or an oral NSAID (three times daily for 5 weeks). For both the primary (Japanese Knee Osteoarthritis Measure) and secondary (pain visual analog scale) outcomes, there was no significant difference in treatment response between the two groups. In addition, a similar proportion in each group (60%-70%) attained OMERACT-OARSI responder status.
There were fewer withdrawals in the IA-HA group, and no serious adverse events were seen in either arm. This trial was of very short duration with all outcomes assessed immediately after treatment at 5 weeks. There was no placebo arm, and the approximately 30% response rate for both treatments is similar to the placebo response in many clinical trials of OA, so while both therapies were equally efficacious, it may be that neither was more effective than placebo. In addition, there is no information in the literature regarding a minimal clinically important difference in the JKOM, making the 10-point difference before and after treatment difficult to interpret.

|
|
Investigators and patients were masked to initial randomization, but not for actual treatment, which could also have introduced some bias. Finally, given the very short trial duration, no information is available regarding longer-term efficacy or adverse events.
This study supports a lack of difference between IA-HA and oral NSAIDs over a period of 5 weeks, and should be applauded for the attempt at direct comparison of two commonly used treatment modalities. However, the clinical relevance of this finding is unclear, as much of the difficulty in the treatment of OA stems from the need for safe treatments that are effective over the many years’ duration of this chronic condition.
Dr. Amanda E. Nelson is with the division of rheumatology, allergy, and immunology at the Thurston Arthritis Research Center, University of North Carolina at Chapel Hill, and is an investigator in the Johnston County (N.C.) Osteoarthritis Project. She reported no relevant financial disclosures.
In this interesting, multicenter, Japanese noninferiority trial, 200 patients with symptomatic knee osteoarthritis were randomized to either intra-articular hyaluronic acid (once per week for 5 weeks) or an oral NSAID (three times daily for 5 weeks). For both the primary (Japanese Knee Osteoarthritis Measure) and secondary (pain visual analog scale) outcomes, there was no significant difference in treatment response between the two groups. In addition, a similar proportion in each group (60%-70%) attained OMERACT-OARSI responder status.
There were fewer withdrawals in the IA-HA group, and no serious adverse events were seen in either arm. This trial was of very short duration with all outcomes assessed immediately after treatment at 5 weeks. There was no placebo arm, and the approximately 30% response rate for both treatments is similar to the placebo response in many clinical trials of OA, so while both therapies were equally efficacious, it may be that neither was more effective than placebo. In addition, there is no information in the literature regarding a minimal clinically important difference in the JKOM, making the 10-point difference before and after treatment difficult to interpret.

|
|
Investigators and patients were masked to initial randomization, but not for actual treatment, which could also have introduced some bias. Finally, given the very short trial duration, no information is available regarding longer-term efficacy or adverse events.
This study supports a lack of difference between IA-HA and oral NSAIDs over a period of 5 weeks, and should be applauded for the attempt at direct comparison of two commonly used treatment modalities. However, the clinical relevance of this finding is unclear, as much of the difficulty in the treatment of OA stems from the need for safe treatments that are effective over the many years’ duration of this chronic condition.
Dr. Amanda E. Nelson is with the division of rheumatology, allergy, and immunology at the Thurston Arthritis Research Center, University of North Carolina at Chapel Hill, and is an investigator in the Johnston County (N.C.) Osteoarthritis Project. She reported no relevant financial disclosures.
In this interesting, multicenter, Japanese noninferiority trial, 200 patients with symptomatic knee osteoarthritis were randomized to either intra-articular hyaluronic acid (once per week for 5 weeks) or an oral NSAID (three times daily for 5 weeks). For both the primary (Japanese Knee Osteoarthritis Measure) and secondary (pain visual analog scale) outcomes, there was no significant difference in treatment response between the two groups. In addition, a similar proportion in each group (60%-70%) attained OMERACT-OARSI responder status.
There were fewer withdrawals in the IA-HA group, and no serious adverse events were seen in either arm. This trial was of very short duration with all outcomes assessed immediately after treatment at 5 weeks. There was no placebo arm, and the approximately 30% response rate for both treatments is similar to the placebo response in many clinical trials of OA, so while both therapies were equally efficacious, it may be that neither was more effective than placebo. In addition, there is no information in the literature regarding a minimal clinically important difference in the JKOM, making the 10-point difference before and after treatment difficult to interpret.

|
|
Investigators and patients were masked to initial randomization, but not for actual treatment, which could also have introduced some bias. Finally, given the very short trial duration, no information is available regarding longer-term efficacy or adverse events.
This study supports a lack of difference between IA-HA and oral NSAIDs over a period of 5 weeks, and should be applauded for the attempt at direct comparison of two commonly used treatment modalities. However, the clinical relevance of this finding is unclear, as much of the difficulty in the treatment of OA stems from the need for safe treatments that are effective over the many years’ duration of this chronic condition.
Dr. Amanda E. Nelson is with the division of rheumatology, allergy, and immunology at the Thurston Arthritis Research Center, University of North Carolina at Chapel Hill, and is an investigator in the Johnston County (N.C.) Osteoarthritis Project. She reported no relevant financial disclosures.
Treatment of osteoarthritis with intra-articular injections of hyaluronic acid over a 5-week period provided symptomatic relief that had noninferior efficacy and was safer than treatment with an oral NSAID in an open-label, multicenter randomized trial of older Japanese adults.
Intra-articular injections of hyaluronic acid (IA-HA) have been shown to reduce pain and improve joint function in knee osteoarthritis (OA), but studies also have reported a relatively slow speed of therapeutic onset and "considerable heterogeneity" in outcomes. NSAIDs have long been regarded as effective for symptomatic relief of knee OA, but carry the risk of serious gastrointestinal adverse events. The lack of data on the short-term effects of IA-HA compared with widely used NSAIDs spurred Dr. Muneaki Ishijima of Juntendo University, Tokyo, and colleagues to conduct the first trial to directly compare efficacy and safety of the two treatments for knee OA (Arthritis Res. Ther. 2014 Jan. 21 [doi:10.1186/ar4446]).
The investigators randomized 200 patients to 5 weeks of either weekly IA-HA or the nonselective cyclo-oxygenase inhibitor loxoprofen in three 60-mg tablets daily and evaluated patients’ percent change from baseline on the patient-reported Japanese Knee Osteoarthritis Measure (JKOM, primary endpoint) and their percent change from baseline in pain as rated on a 0- to 100-point visual analog scale (VAS, secondary endpoint). (Loxoprofen is not approved in the United States.)
After the 5 weeks of therapy, the investigators analyzed data from 98 patients who underwent IA-HA and 86 patients who received loxoprofen who had final JKOM scores available. In the IA-HA group, one patient withdrew consent before undergoing IA-HA, and one was lost to follow-up before the final JKOM analysis. In the NSAID group, six patients withdrew consent before receiving treatment, one patient was excluded because of duplicate entry into the trial before receiving treatment, and another seven were lost to follow-up before the final analysis.
The trial participants had a mean age of about 68 years, and approximately 72% were women. The patients had OA of the medial femorotibial joint with a Kellgren-Lawrence grade of 1-3.
The mean JKOM score declined 32.2% (from 32.0 to 22.0) with NSAID treatment and 34.7% (from 33.8 to 21.5) with IA-HA. This difference of –2.5% and its 95% confidence interval of –14.0% to 9.1% meant that the two treatments had similar efficacy based on the trial’s prespecified definition of noninferiority as a 10% difference or less in the upper limit of the confidence interval. The result did not change after adjustment for age, Kellgren-Lawrence grade, body mass index, and medical center.
Pain on the VAS dropped by 36.0% (from 55.5 to 31.9) with NSAID therapy and by 41.2% (from 60.1 to 31.8) with IA-HA, a nonsignificant difference.
There also were no differences in the percentage of responders in each group based on Outcome Measures in Rheumatology clinical trials and Osteoarthritis Research Society International (OMERACT-OARSI) response criteria, with 69.7% in the IA-HA group and 62.4% in the NSAID group. For this trial, the responder criteria were partly modified by use of the JKOM score. Response was defined as a decrease in joint pain or improvement in function based on at least a 50% reduction in score and a decrease of at least 20 mm on the VAS or clinical improvement on two of three measures: at least a 20% decline in joint pain and at least 10 mm on the VAS; functional improvement of at least 20% and a drop of at least 4 points on the 40-point JKOM functional subcategory scale; and a decrease of at least 20% on the patient’s global assessment score and a drop of at least 10 points from the total JKOM score.
No serious adverse events occurred in either group, but in the NSAID group, seven patients had symptoms related to a GI tract disorder, and three had allergy to loxoprofen, compared with one patient who received IA-HA who had stiffness in the treated knee after injection, a significant difference.
"The present study suggests that future randomized trials should thus be carried out with a longer duration of follow-up and larger samples, in order to identify optimal knee OA treatment alternatives," the investigators wrote.
They acknowledged the problems inherent with the potential of the trial’s open-label design to introduce bias into the results and the use of a 10% difference in the change in JKOM score to define noninferiority, although this margin was supported by a pilot study.
The authors reported no relevant financial disclosures.
Treatment of osteoarthritis with intra-articular injections of hyaluronic acid over a 5-week period provided symptomatic relief that had noninferior efficacy and was safer than treatment with an oral NSAID in an open-label, multicenter randomized trial of older Japanese adults.
Intra-articular injections of hyaluronic acid (IA-HA) have been shown to reduce pain and improve joint function in knee osteoarthritis (OA), but studies also have reported a relatively slow speed of therapeutic onset and "considerable heterogeneity" in outcomes. NSAIDs have long been regarded as effective for symptomatic relief of knee OA, but carry the risk of serious gastrointestinal adverse events. The lack of data on the short-term effects of IA-HA compared with widely used NSAIDs spurred Dr. Muneaki Ishijima of Juntendo University, Tokyo, and colleagues to conduct the first trial to directly compare efficacy and safety of the two treatments for knee OA (Arthritis Res. Ther. 2014 Jan. 21 [doi:10.1186/ar4446]).
The investigators randomized 200 patients to 5 weeks of either weekly IA-HA or the nonselective cyclo-oxygenase inhibitor loxoprofen in three 60-mg tablets daily and evaluated patients’ percent change from baseline on the patient-reported Japanese Knee Osteoarthritis Measure (JKOM, primary endpoint) and their percent change from baseline in pain as rated on a 0- to 100-point visual analog scale (VAS, secondary endpoint). (Loxoprofen is not approved in the United States.)
After the 5 weeks of therapy, the investigators analyzed data from 98 patients who underwent IA-HA and 86 patients who received loxoprofen who had final JKOM scores available. In the IA-HA group, one patient withdrew consent before undergoing IA-HA, and one was lost to follow-up before the final JKOM analysis. In the NSAID group, six patients withdrew consent before receiving treatment, one patient was excluded because of duplicate entry into the trial before receiving treatment, and another seven were lost to follow-up before the final analysis.
The trial participants had a mean age of about 68 years, and approximately 72% were women. The patients had OA of the medial femorotibial joint with a Kellgren-Lawrence grade of 1-3.
The mean JKOM score declined 32.2% (from 32.0 to 22.0) with NSAID treatment and 34.7% (from 33.8 to 21.5) with IA-HA. This difference of –2.5% and its 95% confidence interval of –14.0% to 9.1% meant that the two treatments had similar efficacy based on the trial’s prespecified definition of noninferiority as a 10% difference or less in the upper limit of the confidence interval. The result did not change after adjustment for age, Kellgren-Lawrence grade, body mass index, and medical center.
Pain on the VAS dropped by 36.0% (from 55.5 to 31.9) with NSAID therapy and by 41.2% (from 60.1 to 31.8) with IA-HA, a nonsignificant difference.
There also were no differences in the percentage of responders in each group based on Outcome Measures in Rheumatology clinical trials and Osteoarthritis Research Society International (OMERACT-OARSI) response criteria, with 69.7% in the IA-HA group and 62.4% in the NSAID group. For this trial, the responder criteria were partly modified by use of the JKOM score. Response was defined as a decrease in joint pain or improvement in function based on at least a 50% reduction in score and a decrease of at least 20 mm on the VAS or clinical improvement on two of three measures: at least a 20% decline in joint pain and at least 10 mm on the VAS; functional improvement of at least 20% and a drop of at least 4 points on the 40-point JKOM functional subcategory scale; and a decrease of at least 20% on the patient’s global assessment score and a drop of at least 10 points from the total JKOM score.
No serious adverse events occurred in either group, but in the NSAID group, seven patients had symptoms related to a GI tract disorder, and three had allergy to loxoprofen, compared with one patient who received IA-HA who had stiffness in the treated knee after injection, a significant difference.
"The present study suggests that future randomized trials should thus be carried out with a longer duration of follow-up and larger samples, in order to identify optimal knee OA treatment alternatives," the investigators wrote.
They acknowledged the problems inherent with the potential of the trial’s open-label design to introduce bias into the results and the use of a 10% difference in the change in JKOM score to define noninferiority, although this margin was supported by a pilot study.
The authors reported no relevant financial disclosures.
FROM ARTHRITIS RESEARCH & THERAPY
Major finding: The mean JKOM score declined 32.2% (from 32.0 to 22.0) with NSAID treatment and 34.7% (from 33.8 to 21.5) with IA-HA.
Data source: A multicenter, randomized, open-label noninferiority trial of 184 older Japanese adults with osteoarthritis.
Disclosures: The authors reported no relevant financial disclosures.
Dental infection didn’t raise rheumatoid arthritis risk
Arthralgia patients who later developed rheumatoid arthritis were no more likely to show signs of dental infection with Porphyromonas gingivalis than were those who didn’t develop the disease, according to a small case-control study.
Previous studies have suggested an association between periodontitis and rheumatoid arthritis (RA), which has been theorized to occur potentially through the ability of P. gingivalis to convert the amino acid arginine to citrulline. This interaction might thereby lead to the production of anticitrullinated protein antibodies (ACPA), which are known to precede the development of RA.
Dr. Menke de Smit of the Center for Dentistry and Oral Hygiene at the University of Groningen, the Netherlands, and associates studied the prognostic potential of using anti–P. gingivalis antibody levels to predict the development of RA in a cohort of 289 adults with a mean age of 50 years (79% women) who were at risk for RA by virtue of having arthralgia with seropositivity for immunoglobulin M–rheumatoid factor (IgM-RF) and/or ACPA. They had a median follow-up period of 30 months (Ann. Rheum. Dis. 2014 Jan. 13 [doi:10.1136/annrheumdis-2013-204594]).
The investigators used reference groups for anti–P. gingivalis antibody levels, including 36 healthy control patients and 117 severe periodontitis patients without systemic disease. Cultures for P. gingivalis tested positive in 42% of the reference group patients with periodontitis, but in none of the healthy controls. IgM levels of anti–P. gingivalis did not differ between the two reference groups, but culture-positive patients with periodontitis had significantly higher levels of IgA and IgG anti–P. gingivalis than did healthy controls and culture-negative patients with periodontitis.
The 33% of seropositive arthralgia patients who developed RA after a follow-up period of 12 months did not have higher anti–P. gingivalis levels than seropositive arthralgia patients who didn’t develop the disease.
Significantly more seropositive arthralgia patients who did not develop RA had elevated levels of IgA (25%) and IgG anti–P. gingivalis (37%), based on a cut-off value of twice the standard deviation of levels found in healthy controls, compared with those who did have RA (11% and 26%, respectively).
However, there was a weak yet statistically significant correlation (r = .23) between IgM anti–P. gingivalis and ACPA levels in seropositive arthralgia patients who later developed RA.
In all seropositive arthralgia patients combined, IgA and IgG anti–P. gingivalis levels were higher than in healthy controls, but were lower than in patients with periodontitis. IgM anti–P. gingivalis levels were similar across all three groups. In the seropositive arthralgia patients, none of the anti–P. gingivalis immunoglobulin levels differed according to ACPA status.
Positivity for anti–P. gingivalis did not significantly predict the development of RA in a multivariate Cox proportional hazards model, but ACPA positivity, IgM-RF positivity, number of tender joints, and HLA-DRB1 SE carrier status all were independent predictors of RA.
"Within the limitations of this study, we conclude that anti–P. gingivalis antibody levels are not prognostic for development of RA," they wrote.
The study was funded by the authors’ institutions. The authors had no financial conflicts of interest to disclose.
Arthralgia patients who later developed rheumatoid arthritis were no more likely to show signs of dental infection with Porphyromonas gingivalis than were those who didn’t develop the disease, according to a small case-control study.
Previous studies have suggested an association between periodontitis and rheumatoid arthritis (RA), which has been theorized to occur potentially through the ability of P. gingivalis to convert the amino acid arginine to citrulline. This interaction might thereby lead to the production of anticitrullinated protein antibodies (ACPA), which are known to precede the development of RA.
Dr. Menke de Smit of the Center for Dentistry and Oral Hygiene at the University of Groningen, the Netherlands, and associates studied the prognostic potential of using anti–P. gingivalis antibody levels to predict the development of RA in a cohort of 289 adults with a mean age of 50 years (79% women) who were at risk for RA by virtue of having arthralgia with seropositivity for immunoglobulin M–rheumatoid factor (IgM-RF) and/or ACPA. They had a median follow-up period of 30 months (Ann. Rheum. Dis. 2014 Jan. 13 [doi:10.1136/annrheumdis-2013-204594]).
The investigators used reference groups for anti–P. gingivalis antibody levels, including 36 healthy control patients and 117 severe periodontitis patients without systemic disease. Cultures for P. gingivalis tested positive in 42% of the reference group patients with periodontitis, but in none of the healthy controls. IgM levels of anti–P. gingivalis did not differ between the two reference groups, but culture-positive patients with periodontitis had significantly higher levels of IgA and IgG anti–P. gingivalis than did healthy controls and culture-negative patients with periodontitis.
The 33% of seropositive arthralgia patients who developed RA after a follow-up period of 12 months did not have higher anti–P. gingivalis levels than seropositive arthralgia patients who didn’t develop the disease.
Significantly more seropositive arthralgia patients who did not develop RA had elevated levels of IgA (25%) and IgG anti–P. gingivalis (37%), based on a cut-off value of twice the standard deviation of levels found in healthy controls, compared with those who did have RA (11% and 26%, respectively).
However, there was a weak yet statistically significant correlation (r = .23) between IgM anti–P. gingivalis and ACPA levels in seropositive arthralgia patients who later developed RA.
In all seropositive arthralgia patients combined, IgA and IgG anti–P. gingivalis levels were higher than in healthy controls, but were lower than in patients with periodontitis. IgM anti–P. gingivalis levels were similar across all three groups. In the seropositive arthralgia patients, none of the anti–P. gingivalis immunoglobulin levels differed according to ACPA status.
Positivity for anti–P. gingivalis did not significantly predict the development of RA in a multivariate Cox proportional hazards model, but ACPA positivity, IgM-RF positivity, number of tender joints, and HLA-DRB1 SE carrier status all were independent predictors of RA.
"Within the limitations of this study, we conclude that anti–P. gingivalis antibody levels are not prognostic for development of RA," they wrote.
The study was funded by the authors’ institutions. The authors had no financial conflicts of interest to disclose.
Arthralgia patients who later developed rheumatoid arthritis were no more likely to show signs of dental infection with Porphyromonas gingivalis than were those who didn’t develop the disease, according to a small case-control study.
Previous studies have suggested an association between periodontitis and rheumatoid arthritis (RA), which has been theorized to occur potentially through the ability of P. gingivalis to convert the amino acid arginine to citrulline. This interaction might thereby lead to the production of anticitrullinated protein antibodies (ACPA), which are known to precede the development of RA.
Dr. Menke de Smit of the Center for Dentistry and Oral Hygiene at the University of Groningen, the Netherlands, and associates studied the prognostic potential of using anti–P. gingivalis antibody levels to predict the development of RA in a cohort of 289 adults with a mean age of 50 years (79% women) who were at risk for RA by virtue of having arthralgia with seropositivity for immunoglobulin M–rheumatoid factor (IgM-RF) and/or ACPA. They had a median follow-up period of 30 months (Ann. Rheum. Dis. 2014 Jan. 13 [doi:10.1136/annrheumdis-2013-204594]).
The investigators used reference groups for anti–P. gingivalis antibody levels, including 36 healthy control patients and 117 severe periodontitis patients without systemic disease. Cultures for P. gingivalis tested positive in 42% of the reference group patients with periodontitis, but in none of the healthy controls. IgM levels of anti–P. gingivalis did not differ between the two reference groups, but culture-positive patients with periodontitis had significantly higher levels of IgA and IgG anti–P. gingivalis than did healthy controls and culture-negative patients with periodontitis.
The 33% of seropositive arthralgia patients who developed RA after a follow-up period of 12 months did not have higher anti–P. gingivalis levels than seropositive arthralgia patients who didn’t develop the disease.
Significantly more seropositive arthralgia patients who did not develop RA had elevated levels of IgA (25%) and IgG anti–P. gingivalis (37%), based on a cut-off value of twice the standard deviation of levels found in healthy controls, compared with those who did have RA (11% and 26%, respectively).
However, there was a weak yet statistically significant correlation (r = .23) between IgM anti–P. gingivalis and ACPA levels in seropositive arthralgia patients who later developed RA.
In all seropositive arthralgia patients combined, IgA and IgG anti–P. gingivalis levels were higher than in healthy controls, but were lower than in patients with periodontitis. IgM anti–P. gingivalis levels were similar across all three groups. In the seropositive arthralgia patients, none of the anti–P. gingivalis immunoglobulin levels differed according to ACPA status.
Positivity for anti–P. gingivalis did not significantly predict the development of RA in a multivariate Cox proportional hazards model, but ACPA positivity, IgM-RF positivity, number of tender joints, and HLA-DRB1 SE carrier status all were independent predictors of RA.
"Within the limitations of this study, we conclude that anti–P. gingivalis antibody levels are not prognostic for development of RA," they wrote.
The study was funded by the authors’ institutions. The authors had no financial conflicts of interest to disclose.
FROM ANNALS OF THE RHEUMATIC DISEASES
Major finding: Significantly more seropositive arthralgia patients who did not develop rheumatoid arthritis had elevated levels of IgA (25%) and IgG anti-P. gingivalis (37%), compared with those who did have RA (11% and 26%, respectively).
Data source: A case-control study of 289 patients who were at risk for RA.
Disclosures: The study was funded by the authors’ institutions. The authors had no financial conflicts of interest to disclose.