User login
Young children with leukemia are outliving teens
“Outcomes are improving. However, additional efforts, support, and resources are needed to further improve short- and long-term survival for acute leukemia survivors. Targeted efforts focused on populations that face greater disparities in their survival are needed to move the needle faster,” Michael Roth, MD, codirector of the Adolescent and Young Adult Oncology Program at the University of Texas M.D. Anderson Cancer Center, said in an interview.
In one study, released in The Lancet Child & Adolescent Health, an international team of researchers tracked survival outcomes from various types of leukemia in 61 nations. The study focused on the years 2000-2014 and followed patients aged 0-24.
“Age-standardized 5-year net survival in children, adolescents, and young adults for all leukemias combined during 2010-14 varied widely, ranging from 46% in Mexico to more than 85% in Canada, Cyprus, Belgium, Denmark, Finland, and Australia,” the researchers wrote. “Throughout 2000-14, survival from all leukemias combined remained consistently higher for children than adolescents and young adults, and minimal improvement was seen for adolescents and young adults in most countries.”
The U.S. data came from 41 states that cover 86% of the nation’s population, lead author Naomi Ssenyonga, a research fellow at London School of Hygiene & Tropical Medicine, said in an interview.
The 5-year survival rate for acute lymphoid leukemia (ALL) rose from 80% during 2000-2004 to 86% during 2010-2014. Survival in patients with acute myeloid leukemia (AML) was lower than for other subtypes: 66% in 2010-2014 vs. 57% in 2000-2004.
In regard to all leukemias, “we noted a steady increase in the U.S. of 6 percentage points in 5-year survival, up from 77% for patients diagnosed during 2000-2004 to 83% for those diagnosed during 2010-2014,” Ms. Ssenyonga said. “The gains were largely driven by the improvements seen among children.”
Why haven’t adolescents and young adults gained as much ground in survival?
“They often have unique clinical needs,” Ms. Ssenyonga said. “Over the past few years, adolescents and young adults with leukemia in some parts of the world, including the U.S., have increasingly been treated under pediatric protocols. This has led to higher survival. However, this approach has not been adopted consistently, and survival for adolescents and young adults with leukemia is still generally lower than survival for children.”
Gwen Nichols, MD, chief medical officer of the Leukemia & Lymphoma Society, agreed that pediatric treatment protocols hold promise as treatments for young adults. However, “because we arbitrarily set an age cutoff for being an adult, many of these patients are treated by an adult [nonpediatric] hematologist/oncologist, and some patients in the 20-39 age group do not receive the more intensive treatment regimens given to children,” she said in an interview.
In another study, published in Cancer Epidemiology, Biomarkers, & Prevention, M.D. Anderson Cancer Center’s Dr. Roth and colleagues tracked 1,938 patients with ALL and 2,350 with AML who were diagnosed at ages 15-39 from 1980 to 2009. All lived at least 5 years after diagnosis. In both groups, about 58% were White, and most of the rest were Hispanic. The median age of diagnosis for ALL was 23 (range: 15-39) and 28 years for AML (range: 15-39).
“For ALL, 10-year survival for those diagnosed in the 1980s, 1990s, and 2000s was 83%, 88%, and 88%, respectively,” the researchers reported. “Ten-year survival for AML was 82%, 90%, and 90% for those diagnosed in the 1980s, 1990s, and 2000s, respectively.”
“Early mortality within 10 years of diagnosis was mostly secondary to leukemia progressing or recurring. We believe that later mortality is secondary to the development of late side effects from their cancer treatment,” Dr. Roth said.
He noted that many adolescents and young adults with ALL or AML receive stem-cell transplants. “This treatment approach is effective. However, it is associated with short- and long-term toxicity that impacts patients’ health for many years after treatment.”
Indeed, up to 80% of acute leukemia survivors have significant health complications after therapy, said the Leukemia & Lymphoma Society’s Dr. Nichols, who wasn’t surprised by the findings. According to the society, “even when treatments are effective, more than 70% of childhood cancer survivors have a chronic health condition and 42% have a severe, disabling or life-threatening condition 30 years after diagnosis.”
“It would be interesting to understand the male predominance better,” she added, noting that the study found that male patients had worse long-term survival than females (survival time ratio: 0.61, 95% confidence interval, 0.45-0.82). “While it is tempting to suggest it is due to difference in cardiac disease, I am not aware of data to support why there is this survival difference.”
What’s next? “In ALL, we now have a number of new modalities to treat high-risk and relapsed disease such as antibodies and CAR-T,” Dr. Nichols said. “We anticipate that 5-year survival can improve utilizing these modalities due to getting more patients into remission, hopefully while reducing chemotherapeutic toxicity.”
Dr. Nichol’s also highlighted the society’s new genomic-led Pediatric Acute Leukemia (PedAL) Master Clinical Trial, which began enrolling children with acute leukemia in the United States and Canada this year, in an effort to transform medicine’s traditional high-level chemotherapy strategy to their care. The project was launched in collaboration with the National Cancer Institute, Children’s Oncology Group, and the European Pediatric Acute Leukemia Foundation.
As part of the screening process, the biology of each child’s cancer will be identified, and families will be encouraged to enroll them in appropriate targeted therapy trials.
“Until we are able to decrease the toxicity of leukemia regimens, we won’t see a dramatic shift in late effects and thus in morbidity and mortality,” Dr. Nichols said. “The trial is an effort to test newer, less toxic regimens to begin to change that cycle.”
The 5-year survival study was funded by Children with Cancer UK, Institut National du Cancer, La Ligue Contre le Cancer, Centers for Disease Control and Prevention, Swiss Re, Swiss Cancer Research foundation, Swiss Cancer League, Rossy Family Foundation, National Cancer Institute, and the American Cancer Society. One author reports a grant from Macmillan Cancer Support, consultancy fees from Pfizer, and unsolicited small gifts from Moondance Cancer Initiative for philanthropic work. The other authors report no disclosures.
The long-term survival study was funded by the National Cancer Institute, the Archer Foundation and LyondellBasell Industries. Dr. Roth reports no disclosures; other authors report various disclosures. Dr. Nichols reports no disclosures.
“Outcomes are improving. However, additional efforts, support, and resources are needed to further improve short- and long-term survival for acute leukemia survivors. Targeted efforts focused on populations that face greater disparities in their survival are needed to move the needle faster,” Michael Roth, MD, codirector of the Adolescent and Young Adult Oncology Program at the University of Texas M.D. Anderson Cancer Center, said in an interview.
In one study, released in The Lancet Child & Adolescent Health, an international team of researchers tracked survival outcomes from various types of leukemia in 61 nations. The study focused on the years 2000-2014 and followed patients aged 0-24.
“Age-standardized 5-year net survival in children, adolescents, and young adults for all leukemias combined during 2010-14 varied widely, ranging from 46% in Mexico to more than 85% in Canada, Cyprus, Belgium, Denmark, Finland, and Australia,” the researchers wrote. “Throughout 2000-14, survival from all leukemias combined remained consistently higher for children than adolescents and young adults, and minimal improvement was seen for adolescents and young adults in most countries.”
The U.S. data came from 41 states that cover 86% of the nation’s population, lead author Naomi Ssenyonga, a research fellow at London School of Hygiene & Tropical Medicine, said in an interview.
The 5-year survival rate for acute lymphoid leukemia (ALL) rose from 80% during 2000-2004 to 86% during 2010-2014. Survival in patients with acute myeloid leukemia (AML) was lower than for other subtypes: 66% in 2010-2014 vs. 57% in 2000-2004.
In regard to all leukemias, “we noted a steady increase in the U.S. of 6 percentage points in 5-year survival, up from 77% for patients diagnosed during 2000-2004 to 83% for those diagnosed during 2010-2014,” Ms. Ssenyonga said. “The gains were largely driven by the improvements seen among children.”
Why haven’t adolescents and young adults gained as much ground in survival?
“They often have unique clinical needs,” Ms. Ssenyonga said. “Over the past few years, adolescents and young adults with leukemia in some parts of the world, including the U.S., have increasingly been treated under pediatric protocols. This has led to higher survival. However, this approach has not been adopted consistently, and survival for adolescents and young adults with leukemia is still generally lower than survival for children.”
Gwen Nichols, MD, chief medical officer of the Leukemia & Lymphoma Society, agreed that pediatric treatment protocols hold promise as treatments for young adults. However, “because we arbitrarily set an age cutoff for being an adult, many of these patients are treated by an adult [nonpediatric] hematologist/oncologist, and some patients in the 20-39 age group do not receive the more intensive treatment regimens given to children,” she said in an interview.
In another study, published in Cancer Epidemiology, Biomarkers, & Prevention, M.D. Anderson Cancer Center’s Dr. Roth and colleagues tracked 1,938 patients with ALL and 2,350 with AML who were diagnosed at ages 15-39 from 1980 to 2009. All lived at least 5 years after diagnosis. In both groups, about 58% were White, and most of the rest were Hispanic. The median age of diagnosis for ALL was 23 (range: 15-39) and 28 years for AML (range: 15-39).
“For ALL, 10-year survival for those diagnosed in the 1980s, 1990s, and 2000s was 83%, 88%, and 88%, respectively,” the researchers reported. “Ten-year survival for AML was 82%, 90%, and 90% for those diagnosed in the 1980s, 1990s, and 2000s, respectively.”
“Early mortality within 10 years of diagnosis was mostly secondary to leukemia progressing or recurring. We believe that later mortality is secondary to the development of late side effects from their cancer treatment,” Dr. Roth said.
He noted that many adolescents and young adults with ALL or AML receive stem-cell transplants. “This treatment approach is effective. However, it is associated with short- and long-term toxicity that impacts patients’ health for many years after treatment.”
Indeed, up to 80% of acute leukemia survivors have significant health complications after therapy, said the Leukemia & Lymphoma Society’s Dr. Nichols, who wasn’t surprised by the findings. According to the society, “even when treatments are effective, more than 70% of childhood cancer survivors have a chronic health condition and 42% have a severe, disabling or life-threatening condition 30 years after diagnosis.”
“It would be interesting to understand the male predominance better,” she added, noting that the study found that male patients had worse long-term survival than females (survival time ratio: 0.61, 95% confidence interval, 0.45-0.82). “While it is tempting to suggest it is due to difference in cardiac disease, I am not aware of data to support why there is this survival difference.”
What’s next? “In ALL, we now have a number of new modalities to treat high-risk and relapsed disease such as antibodies and CAR-T,” Dr. Nichols said. “We anticipate that 5-year survival can improve utilizing these modalities due to getting more patients into remission, hopefully while reducing chemotherapeutic toxicity.”
Dr. Nichol’s also highlighted the society’s new genomic-led Pediatric Acute Leukemia (PedAL) Master Clinical Trial, which began enrolling children with acute leukemia in the United States and Canada this year, in an effort to transform medicine’s traditional high-level chemotherapy strategy to their care. The project was launched in collaboration with the National Cancer Institute, Children’s Oncology Group, and the European Pediatric Acute Leukemia Foundation.
As part of the screening process, the biology of each child’s cancer will be identified, and families will be encouraged to enroll them in appropriate targeted therapy trials.
“Until we are able to decrease the toxicity of leukemia regimens, we won’t see a dramatic shift in late effects and thus in morbidity and mortality,” Dr. Nichols said. “The trial is an effort to test newer, less toxic regimens to begin to change that cycle.”
The 5-year survival study was funded by Children with Cancer UK, Institut National du Cancer, La Ligue Contre le Cancer, Centers for Disease Control and Prevention, Swiss Re, Swiss Cancer Research foundation, Swiss Cancer League, Rossy Family Foundation, National Cancer Institute, and the American Cancer Society. One author reports a grant from Macmillan Cancer Support, consultancy fees from Pfizer, and unsolicited small gifts from Moondance Cancer Initiative for philanthropic work. The other authors report no disclosures.
The long-term survival study was funded by the National Cancer Institute, the Archer Foundation and LyondellBasell Industries. Dr. Roth reports no disclosures; other authors report various disclosures. Dr. Nichols reports no disclosures.
“Outcomes are improving. However, additional efforts, support, and resources are needed to further improve short- and long-term survival for acute leukemia survivors. Targeted efforts focused on populations that face greater disparities in their survival are needed to move the needle faster,” Michael Roth, MD, codirector of the Adolescent and Young Adult Oncology Program at the University of Texas M.D. Anderson Cancer Center, said in an interview.
In one study, released in The Lancet Child & Adolescent Health, an international team of researchers tracked survival outcomes from various types of leukemia in 61 nations. The study focused on the years 2000-2014 and followed patients aged 0-24.
“Age-standardized 5-year net survival in children, adolescents, and young adults for all leukemias combined during 2010-14 varied widely, ranging from 46% in Mexico to more than 85% in Canada, Cyprus, Belgium, Denmark, Finland, and Australia,” the researchers wrote. “Throughout 2000-14, survival from all leukemias combined remained consistently higher for children than adolescents and young adults, and minimal improvement was seen for adolescents and young adults in most countries.”
The U.S. data came from 41 states that cover 86% of the nation’s population, lead author Naomi Ssenyonga, a research fellow at London School of Hygiene & Tropical Medicine, said in an interview.
The 5-year survival rate for acute lymphoid leukemia (ALL) rose from 80% during 2000-2004 to 86% during 2010-2014. Survival in patients with acute myeloid leukemia (AML) was lower than for other subtypes: 66% in 2010-2014 vs. 57% in 2000-2004.
In regard to all leukemias, “we noted a steady increase in the U.S. of 6 percentage points in 5-year survival, up from 77% for patients diagnosed during 2000-2004 to 83% for those diagnosed during 2010-2014,” Ms. Ssenyonga said. “The gains were largely driven by the improvements seen among children.”
Why haven’t adolescents and young adults gained as much ground in survival?
“They often have unique clinical needs,” Ms. Ssenyonga said. “Over the past few years, adolescents and young adults with leukemia in some parts of the world, including the U.S., have increasingly been treated under pediatric protocols. This has led to higher survival. However, this approach has not been adopted consistently, and survival for adolescents and young adults with leukemia is still generally lower than survival for children.”
Gwen Nichols, MD, chief medical officer of the Leukemia & Lymphoma Society, agreed that pediatric treatment protocols hold promise as treatments for young adults. However, “because we arbitrarily set an age cutoff for being an adult, many of these patients are treated by an adult [nonpediatric] hematologist/oncologist, and some patients in the 20-39 age group do not receive the more intensive treatment regimens given to children,” she said in an interview.
In another study, published in Cancer Epidemiology, Biomarkers, & Prevention, M.D. Anderson Cancer Center’s Dr. Roth and colleagues tracked 1,938 patients with ALL and 2,350 with AML who were diagnosed at ages 15-39 from 1980 to 2009. All lived at least 5 years after diagnosis. In both groups, about 58% were White, and most of the rest were Hispanic. The median age of diagnosis for ALL was 23 (range: 15-39) and 28 years for AML (range: 15-39).
“For ALL, 10-year survival for those diagnosed in the 1980s, 1990s, and 2000s was 83%, 88%, and 88%, respectively,” the researchers reported. “Ten-year survival for AML was 82%, 90%, and 90% for those diagnosed in the 1980s, 1990s, and 2000s, respectively.”
“Early mortality within 10 years of diagnosis was mostly secondary to leukemia progressing or recurring. We believe that later mortality is secondary to the development of late side effects from their cancer treatment,” Dr. Roth said.
He noted that many adolescents and young adults with ALL or AML receive stem-cell transplants. “This treatment approach is effective. However, it is associated with short- and long-term toxicity that impacts patients’ health for many years after treatment.”
Indeed, up to 80% of acute leukemia survivors have significant health complications after therapy, said the Leukemia & Lymphoma Society’s Dr. Nichols, who wasn’t surprised by the findings. According to the society, “even when treatments are effective, more than 70% of childhood cancer survivors have a chronic health condition and 42% have a severe, disabling or life-threatening condition 30 years after diagnosis.”
“It would be interesting to understand the male predominance better,” she added, noting that the study found that male patients had worse long-term survival than females (survival time ratio: 0.61, 95% confidence interval, 0.45-0.82). “While it is tempting to suggest it is due to difference in cardiac disease, I am not aware of data to support why there is this survival difference.”
What’s next? “In ALL, we now have a number of new modalities to treat high-risk and relapsed disease such as antibodies and CAR-T,” Dr. Nichols said. “We anticipate that 5-year survival can improve utilizing these modalities due to getting more patients into remission, hopefully while reducing chemotherapeutic toxicity.”
Dr. Nichol’s also highlighted the society’s new genomic-led Pediatric Acute Leukemia (PedAL) Master Clinical Trial, which began enrolling children with acute leukemia in the United States and Canada this year, in an effort to transform medicine’s traditional high-level chemotherapy strategy to their care. The project was launched in collaboration with the National Cancer Institute, Children’s Oncology Group, and the European Pediatric Acute Leukemia Foundation.
As part of the screening process, the biology of each child’s cancer will be identified, and families will be encouraged to enroll them in appropriate targeted therapy trials.
“Until we are able to decrease the toxicity of leukemia regimens, we won’t see a dramatic shift in late effects and thus in morbidity and mortality,” Dr. Nichols said. “The trial is an effort to test newer, less toxic regimens to begin to change that cycle.”
The 5-year survival study was funded by Children with Cancer UK, Institut National du Cancer, La Ligue Contre le Cancer, Centers for Disease Control and Prevention, Swiss Re, Swiss Cancer Research foundation, Swiss Cancer League, Rossy Family Foundation, National Cancer Institute, and the American Cancer Society. One author reports a grant from Macmillan Cancer Support, consultancy fees from Pfizer, and unsolicited small gifts from Moondance Cancer Initiative for philanthropic work. The other authors report no disclosures.
The long-term survival study was funded by the National Cancer Institute, the Archer Foundation and LyondellBasell Industries. Dr. Roth reports no disclosures; other authors report various disclosures. Dr. Nichols reports no disclosures.
Digital therapy may ‘rewire’ the brain to improve tinnitus
, new research suggests. In a randomized controlled trial, results at 12 weeks showed patients with tinnitus reported clinically meaningful reductions in ratings of annoyance, inability to ignore, unpleasantness, and loudness after using a digital polytherapeutic app prototype that focuses on relief, relaxation, and attention-focused retraining. In addition, their improvements were significantly greater than for the control group, which received a common white noise app.
Researchers called the results “promising” for a condition that has no cure and few successful treatments. “What this therapy does is essentially rewire the brain in a way that de-emphasizes the sound of the tinnitus to a background noise that has no meaning or relevance to the listener,” lead author Grant Searchfield, PhD, associate professor of audiology at the University of Auckland, New Zealand, said in a press release.
The findings were published online in Frontiers in Neurology.
Worldwide problem
A recent study showed more than 740 million adults worldwide (nearly 15% of the population) have experienced at least one symptom of tinnitus – and about 120 million are severely affected. Tinnitus is the perception of a ringing, buzzing, whistling, or hissing noise in one or both ears when no external source of the sound is present. Often caused by damage to the auditory system, tinnitus can also be a symptom of a wide range of medical conditions and has been identified as a side effect of COVID-19 vaccination. In its most severe form, which is associated with hearing loss, tinnitus can also affect a patient’s mental, emotional, and social health.
For the current study, participants with tinnitus were randomly assigned to a popular app that uses white noise (control group, n = 30) or to the UpSilent app (n = 31). The UpSilent group received a smartphone app, Bluetooth bone conduction headphones, a Bluetooth neck pillow speaker for sleep, and written counseling materials. Participants in the control group received a widely available app called “White Noise” and in-ear wired headphones.
‘Quicker and more effective’
Both groups reported reductions in ratings of annoyance, inability to ignore, unpleasantness, and loudness at 12 weeks. But significantly more of the UpSilent group reported clinically meaningful improvement compared with the control group (65% vs. 43%, respectively; P = .049).
“Earlier trials have found white noise, goal-based counseling, goal-oriented games, and other technology-based therapies are effective for some people some of the time,” Dr. Searchfield said. “This is quicker and more effective, taking 12 weeks rather than 12 months for more individuals to gain some control,” he added.
The investigators noted that the study was not designed to determine which of the app’s functions of passive listening, active listening, or counseling contributed to symptom improvement.
The next step will be to refine the prototype and proceed to larger local and international trials with a view toward approval by the U.S. Food and Drug Administration, they reported.
The researchers hope the app will be clinically available in about 6 months.
The study was funded by Return on Science, Auckland UniServices. Dr. Searchfield is a founder and scientific officer for TrueSilence, a spinout company of the University of Auckland, and has a financial interest in TrueSilence. His coauthor has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests. In a randomized controlled trial, results at 12 weeks showed patients with tinnitus reported clinically meaningful reductions in ratings of annoyance, inability to ignore, unpleasantness, and loudness after using a digital polytherapeutic app prototype that focuses on relief, relaxation, and attention-focused retraining. In addition, their improvements were significantly greater than for the control group, which received a common white noise app.
Researchers called the results “promising” for a condition that has no cure and few successful treatments. “What this therapy does is essentially rewire the brain in a way that de-emphasizes the sound of the tinnitus to a background noise that has no meaning or relevance to the listener,” lead author Grant Searchfield, PhD, associate professor of audiology at the University of Auckland, New Zealand, said in a press release.
The findings were published online in Frontiers in Neurology.
Worldwide problem
A recent study showed more than 740 million adults worldwide (nearly 15% of the population) have experienced at least one symptom of tinnitus – and about 120 million are severely affected. Tinnitus is the perception of a ringing, buzzing, whistling, or hissing noise in one or both ears when no external source of the sound is present. Often caused by damage to the auditory system, tinnitus can also be a symptom of a wide range of medical conditions and has been identified as a side effect of COVID-19 vaccination. In its most severe form, which is associated with hearing loss, tinnitus can also affect a patient’s mental, emotional, and social health.
For the current study, participants with tinnitus were randomly assigned to a popular app that uses white noise (control group, n = 30) or to the UpSilent app (n = 31). The UpSilent group received a smartphone app, Bluetooth bone conduction headphones, a Bluetooth neck pillow speaker for sleep, and written counseling materials. Participants in the control group received a widely available app called “White Noise” and in-ear wired headphones.
‘Quicker and more effective’
Both groups reported reductions in ratings of annoyance, inability to ignore, unpleasantness, and loudness at 12 weeks. But significantly more of the UpSilent group reported clinically meaningful improvement compared with the control group (65% vs. 43%, respectively; P = .049).
“Earlier trials have found white noise, goal-based counseling, goal-oriented games, and other technology-based therapies are effective for some people some of the time,” Dr. Searchfield said. “This is quicker and more effective, taking 12 weeks rather than 12 months for more individuals to gain some control,” he added.
The investigators noted that the study was not designed to determine which of the app’s functions of passive listening, active listening, or counseling contributed to symptom improvement.
The next step will be to refine the prototype and proceed to larger local and international trials with a view toward approval by the U.S. Food and Drug Administration, they reported.
The researchers hope the app will be clinically available in about 6 months.
The study was funded by Return on Science, Auckland UniServices. Dr. Searchfield is a founder and scientific officer for TrueSilence, a spinout company of the University of Auckland, and has a financial interest in TrueSilence. His coauthor has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests. In a randomized controlled trial, results at 12 weeks showed patients with tinnitus reported clinically meaningful reductions in ratings of annoyance, inability to ignore, unpleasantness, and loudness after using a digital polytherapeutic app prototype that focuses on relief, relaxation, and attention-focused retraining. In addition, their improvements were significantly greater than for the control group, which received a common white noise app.
Researchers called the results “promising” for a condition that has no cure and few successful treatments. “What this therapy does is essentially rewire the brain in a way that de-emphasizes the sound of the tinnitus to a background noise that has no meaning or relevance to the listener,” lead author Grant Searchfield, PhD, associate professor of audiology at the University of Auckland, New Zealand, said in a press release.
The findings were published online in Frontiers in Neurology.
Worldwide problem
A recent study showed more than 740 million adults worldwide (nearly 15% of the population) have experienced at least one symptom of tinnitus – and about 120 million are severely affected. Tinnitus is the perception of a ringing, buzzing, whistling, or hissing noise in one or both ears when no external source of the sound is present. Often caused by damage to the auditory system, tinnitus can also be a symptom of a wide range of medical conditions and has been identified as a side effect of COVID-19 vaccination. In its most severe form, which is associated with hearing loss, tinnitus can also affect a patient’s mental, emotional, and social health.
For the current study, participants with tinnitus were randomly assigned to a popular app that uses white noise (control group, n = 30) or to the UpSilent app (n = 31). The UpSilent group received a smartphone app, Bluetooth bone conduction headphones, a Bluetooth neck pillow speaker for sleep, and written counseling materials. Participants in the control group received a widely available app called “White Noise” and in-ear wired headphones.
‘Quicker and more effective’
Both groups reported reductions in ratings of annoyance, inability to ignore, unpleasantness, and loudness at 12 weeks. But significantly more of the UpSilent group reported clinically meaningful improvement compared with the control group (65% vs. 43%, respectively; P = .049).
“Earlier trials have found white noise, goal-based counseling, goal-oriented games, and other technology-based therapies are effective for some people some of the time,” Dr. Searchfield said. “This is quicker and more effective, taking 12 weeks rather than 12 months for more individuals to gain some control,” he added.
The investigators noted that the study was not designed to determine which of the app’s functions of passive listening, active listening, or counseling contributed to symptom improvement.
The next step will be to refine the prototype and proceed to larger local and international trials with a view toward approval by the U.S. Food and Drug Administration, they reported.
The researchers hope the app will be clinically available in about 6 months.
The study was funded by Return on Science, Auckland UniServices. Dr. Searchfield is a founder and scientific officer for TrueSilence, a spinout company of the University of Auckland, and has a financial interest in TrueSilence. His coauthor has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM FRONTIERS IN NEUROLOGY
Gender and Patient Satisfaction in a Veterans Health Administration Outpatient Chemotherapy Unit
Gender differences in patient satisfaction with medical care have been evaluated in multiple settings; however, studies specific to the unique population of women veterans with cancer are lacking. Women are reported to value privacy, psychosocial support, and communication to a higher degree compared with men.1 Factors affecting satisfaction include the following: discomfort in sharing treatment rooms with the opposite gender, a desire for privacy with treatment and restroom use, anatomic or illness differences, and a personal history of abuse.2-4 Regrettably, up to 1 in 3 women in the United States are victims of sexual trauma in their lifetimes, and up to 1 in 4 women in the military are victims of military sexual trauma. Incidence in both settings is suspected to be higher due to underreporting.5,6
Chemotherapy treatment units are often uniquely designed as an open space, with several patients sharing a treatment area. The design reduces isolation and facilitates quick nurse-patient access during potentially toxic treatments known to have frequent adverse effects. Data suggest that nursing staff prefer open models to facilitate quick patient assessments and interventions as needed; however, patients and families prefer private treatment rooms, especially among women patients or those receiving longer infusions.7
The Veterans Health Administration (VHA) patient population is male predominant, comprised only of 10% female patients.8 Although the proportion of female patients in the VHA is expected to rise annually to about 16% by 2043, the low percentage of female veterans will persist for the foreseeable future.8 This low percentage of female veterans is reflected in the Veterans Affairs Portland Health Care System (VAPHCS) cancer patient population and in the use of the chemotherapy infusion unit, which is used for the ambulatory treatment of veterans undergoing cancer therapy.
The VHA has previously explored gender differences in health care, such as with cardiovascular disease, transgender care, and access to mental health.9-11 However, to the best of our knowledge, no analysis has explored gender differences within the outpatient cancer treatment experience. Patient satisfaction with outpatient cancer care may be magnified in the VHA setting due to the uniquely unequal gender populations, shared treatment space design, and high incidence of sexual abuse among women veterans. Given this, we aimed to identify gender-related preferences in outpatient cancer care in our chemotherapy infusion unit.
In our study, we used the terms male and female to reflect statistical data from the literature or labeled data from the electronic health record (EHR); whereas the terms men and women were used to describe and encompass the cultural implications and context of gender.12
Methods
This study was designated as a quality improvement (QI) project by the VAPHCS research office and Institutional Review Board in accordance with VHA policies.
The VAPHCS outpatient chemotherapy infusion unit is designed with 6 rooms for chemotherapy administration. One room is a large open space with 6 chairs for patients. The other rooms are smaller with glass dividers between the rooms, and 3 chairs inside each for patients. There are 2 private bathrooms, each gender neutral. Direct patient care is provided by physicians, nurse practitioners (NPs), infusion unit nurses, and nurse coordinators. Men represent the majority of hematology and oncology physicians (13 of 20 total: 5 women fellow physicians and 2 women attending physicians), and 2 of 4 NPs. Women represent 10 of 12 infusion unit and cancer coordinator nurses. We used the VHA Computerized Patient Record System (CPRS) EHR, to create a list of veterans treated at the VAPHCS outpatient chemotherapy infusion unit for a 2-year period (January 1, 2018, to December 31, 2020).
Male and female patient lists were first generated based on CPRS categorization. We identified all female veterans treated in the ambulatory infusion unit during the study period. Male patients were then chosen at random, recording the most recent names for each year until a matched number per year compared with the female cohort was reached. Patients were recorded only once even though they had multiple infusion unit visits. Patients were excluded who were deceased, on hospice care, lost to follow-up, could not be reached by phone, refused to take the survey, had undeliverable email addresses, or lacked internet or email access.
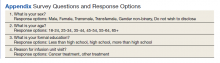
After filing the appropriate request through the VAPHCS Institutional Review Board committee in January 2021, patient records were reviewed for demographics data, contact information, and infusion treatment history. The survey was then conducted over a 2-week period during January and February 2021. Each patient was invited by phone to complete a 25-question anonymous online survey. The survey questions were created from patient-relayed experiences, then modeled into survey questions in a format similar to other patient satisfaction questionnaires described in cancer care and gender differences.2,13,14 The survey included self-identification of gender and was multiple choice for all except 2 questions, which allowed an open-ended response (Appendix). Only 1 answer per question was permitted. Only 1 survey link was sent to each veteran who gave permission for the survey. To protect anonymity for the small patient population, we excluded those identifying as gender nonbinary or transgender.
Statistical Analysis
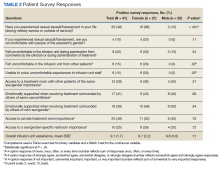
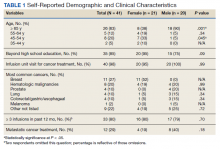
Patient, disease, and treatment features are separated by male and female cohorts to reflect information from the EHR (Table 1). Survey percentages were calculated to reflect the affirmative response of the question asked (Table 2). Questions with answer options of not important, minimally important, important, or very important were calculated to reflect the sum of any importance in both cohorts. Questions with answer options of never, once, often, or every time were calculated to reflect any occurrence (sum of once, often, or every time) in both patient groups. Questions with answer options of strongly agree, somewhat agree, somewhat disagree, and strongly disagree were calculated to reflect any agreement (somewhat agree and strongly agree summed together) for both groups. Comparisons between cohorts were then conducted using a Fisher exact test. A Welch t test was used to calculate the significance of the continuous variable and overall ranking of the infusion unit experience between groups.
Results
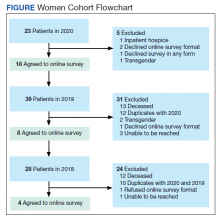
In 2020, 414 individual patients were treated at the VAPAHCS outpatient infusion unit. Of these, 23 (5.6%) were female, and 18 agreed to take the survey. After deceased and duplicate names from 2020 were removed, another 14 eligible 2019 female patients were invited and 6 agreed to participate; 6 eligible 2018 female patients were invited and 4 agreed to take the survey (Figure). Thirty female veterans were sent a survey link and 21 (70%) responses were collected. Twenty-one male 2020 patients were contacted and 18 agreed to take the survey. After removing duplicate names and deceased individuals, 17 of 21 eligible 2019 male patients and 4 of 6 eligible 2018 patients agreed to take the survey. Five additional male veterans declined the online-based survey method. In total, 39 male veterans were reached who agreed to have the survey link emailed, and 20 (51%) total responses were collected.
Most respondents answered all questions in the survey. The most frequently skipped questions included 3 questions that were contingent on a yes answer to a prior question, and 2 openended questions asking for a write-in response. Percentages for female and male respondents were adjusted for number of responses when applicable.
Thirteen (62%) female patients were aged < 65 years, while 18 (90%) of male patients were aged ≥ 65 years. Education beyond high school was reported in 20 female and 15 male respondents. Almost all treatment administered in the infusion unit was for cancer-directed treatment, with only 1 reporting a noncancer treatment (IV iron). The most common malignancy among female patients was breast cancer (n = 11, 52%); for male patients prostate cancer (n = 4, 20%) and hematologic malignancy (n = 4, 20%) were most common. Four (19%) female and 8 (40%) male respondents reported having a metastatic diagnosis. Overall patient satisfaction ranked high with an average score of 9.1 on a 10-point scale. The mean (SD) satisfaction score for female respondents was 1 point lower than that for men: 8.7 (2.2) vs 9.6 (0.6) in men (P = .11).
Eighteen (86%) women reported a history of sexual abuse or harassment compared with 2 (10%) men (P < .001). The sexual abuse assailant was a different gender for 17 of 18 female respondents and of the same gender for both male respondents. Of those with sexual abuse history, 4 women reported feeling uncomfortable around their assailant’s gender vs no men (P = .11), but this difference was not statistically significant. Six women (29%) and 2 (10%) men reported feeling uncomfortable during clinical examinations from comments made by the clinician or during treatment administration (P = .24). Six (29%) women and no men reported that they “felt uncomfortable in the infusion unit by other patients” (P = .02). Six (29%) women and no men reported feeling unable to “voice uncomfortable experiences” to the infusion unit clinician (P = .02).
Ten (48%) women and 6 (30%) men reported emotional support when receiving treatments provided by staff of the same gender (P = .34). Eight (38%) women and 4 (20%) men noted that access to treatment with the same gender was important (P = .31). Six (29%) women and 4 (20%) men indicated that access to a sex or gender-specific restroom was important (P = .72). No gender preferences were identified in the survey questions regarding importance of private treatment room access and level of emotional support when receiving treatment with others of the same malignancy. These relationships were not statistically significant.
In addition, 2 open-ended questions were asked. Seventeen women and 14 men responded. Contact the corresponding author for more information on the questions and responses.
Discussion
Overall patient satisfaction was high among the men and women veterans with cancer who received treatment in our outpatient infusion unit; however, notable gender differences existed. Three items in the survey revealed statistically significant differences in the patient experience between men and women veterans: history of sexual abuse or harassment, uncomfortable feelings among other patients, and discomfort in relaying uncomfortable feelings to a clinician. Other items in the survey did not reach statistical significance; however, we have included discussion of the findings as they may highlight important trends and be of clinical significance.
We suspect differences among genders in patient satisfaction to be related to the high incidence of sexual abuse or harassment history reported by women, much higher at 86% than the one-third to one-fourth incidence rates estimated by the existing literature for civilian or military sexual abuse in women.5,6 These high sexual abuse or harassment rates are present in a majority of women who receive cancer-directed treatment toward a gender-specific breast malignancy, surrounded predominantly among men in a shared treatment space. Together, these factors are likely key reasons behind the differences in satisfaction observed. This sentiment is expressed in our cohort, where one-fifth of women with a sexual abuse or harassment history continue to remain uncomfortable around men, and 29% of women reporting some uncomfortable feelings during their treatment experience compared with none of the men. Additionally, 6 (29%) women vs no men felt uncomfortable in reporting an uncomfortable experience with a clinician; this represents a significant barrier in providing care for these patients.
A key gender preference among women included access to shared treatment rooms with other women and that sharing a treatment space with other women resulted in feeling more emotional support during treatments. Access to gender-specific restrooms was also preferred by women more than men. Key findings in both genders were that about half of men and women valued access to a private treatment room and would derive more emotional support when surrounded by others with the same cancer.
Prior studies on gender and patient satisfaction in general medical care and cancer care have found women value privacy more than men.1-3 Wessels and colleagues performed an analysis of 386 patients with cancer in Europe and found gender to be the strongest influence in patient preferences within cancer care. Specifically, the highest statically significant association in care preferences among women included privacy, support/counseling/rehabilitation access, and decreased wait times.2 These findings were most pronounced in those with breast cancer compared with other malignancy type and highlights that malignancy type and gender predominance impact care satisfaction.
Traditionally a shared treatment space design has been used in outpatient chemotherapy units, similar to the design of the VAPHCS. However, recent data report on the patient preference for a private treatment space, which was especially prominent among women and those receiving longer infusions.7 In another study that evaluated 225 patients with cancer preferences in sharing a treatment space with those of a different sexual orientation or gender identify, differences were found. Both men and women had a similar level of comfort in sharing a treatment room with someone of a different sexual orientation; however, more women reported discomfort in sharing a treatment space with a transgender woman compared with men who felt more comfortable sharing a space with a transgender man.4 We noted a gender preference may be present to explain the difference. Within our cohort, women valued access to treatment with other women and derived more emotional support when with other women; however, we did not inquire about feelings in sharing a treatment space among transgender individuals or differing sexual orientation.
Gender differences for privacy and in shared room preferences may result from the lasting impacts of prior sexual abuse or harassment. A history of sexual abuse negatively impacts later medical care access and use.15 Those veterans who experienced sexual abuse/harrassment reported higher feelings of lack of control, vulnerability, depression, and pursued less medical care.15,16 Within cancer care, these feelings are most pronounced among women with gender-specific malignancies, such as gynecologic cancers or breast cancer. Treatment, screening, and physical examinations by clinicians who are of the same gender as the sexual abuse/harassment assailant can recreate traumatic feelings.15,16
A majority of women (n = 18, 86%) in our cohort reported a history of sexual abuse or harassment and breast malignancy was the most common cancer among women. However women represent just 5.6% of the VAPHCS infusion unit treatment population. This combination of factors may explain the reasons for women veterans’ preference for privacy during treatments, access to gender-specific restrooms, and feeling more emotional support when surrounded by other women. Strategies to help patients with a history of abuse have been described and include discussions from the clinician asking about abuse history, allowing time for the patient to express fears with an examination or test, and training on how to deliver sensitive care for those with trauma.17,18
Quality Improvement
Project In the VAPHCS infusion unit, several low-cost interventions have been undertaken as a result of our survey findings. We presented our survey data to the VAPHCS Cancer Committee, accredited through the national American College of Surgeons Commission on Cancer. The committee awarded support for a yearlong QI project, including a formal framework of quarterly multidisciplinary meetings to discuss project updates, challenges, and resources. The QI project centers on education to raise awareness of survey results as well as specific interventions for improvement.
Education efforts have been applied through multiple department-wide emails, in-person education to our chemotherapy unit staff, abstract submission to national oncology conferences, and grand rounds department presentations at VAPHCS and at other VHA-affiliated university programs. Additionally, education to clinicians with specific contact information for psychology and women’s health to support mental health, trauma, and sexual abuse histories has been given to each clinician who cares for veterans in the chemotherapy unit.
We also have implemented a mandatory cancer care navigation consultation for all women veterans who have a new cancer or infusion need. The cancer care navigator has received specialized training in sensitive history-taking and provides women veterans with a direct number to reach the cancer care navigation nurse. Cancer care navigation also provides a continuum of support and referral access for psychosocial needs as indicated between infusion or health care visits. Our hope is that these resources may help offset the sentiment reflected in our cohort of women feeling unable to voice concerns to a clinician.
Other interventions underway include offering designated scheduling time each week to women so they can receive infusions in an area with other women. This may help mitigate the finding that women veterans felt more uncomfortable around other patients during infusion treatments compared with how men felt in the chemotherapy unit. We also have implemented gender-specific restrooms labeled with a sign on each bathroom door so men and women can have access to a designated restroom. Offering private or semiprivate treatment rooms is currently limited by space and capacity; however, these may offer the greatest opportunity to improve patient satisfaction, especially among women veterans. Working with the support of the VAPHCS Cancer Committee, we aim to reevaluate the impact of the education and QI efforts on gender differences and patient satisfaction at completion of the 1-year award.
Limitations
Limitations to our study include the overall small sample size. This is due to the combination of the low number of women treated at VAPHCS and many with advanced cancer who, unfortunately, have a limited overall survival and hinders accrual of a larger sample size. Other limitations included age as a possible confounder in our findings, with women representing a younger demographic compared with men. We did not collect responses on duration of infusion time, which also may impact overall satisfaction and patient experience. We also acknowledge that biologic male or female sex may not correspond to a specific individual’s gender. Use of CPRS to obtain a matched number of male and female patients through random selection relied on labeled data from the EHR. This potentially may have excluded male patients who identify as another gender that would have been captured on the anonymous survey.
Last, we restricted survey responses to online only, which excluded a small percentage who declined this approach.
Conclusions
Our findings may have broad applications to other VHA facilities and other cancer-directed treatment centers where the patient demographic and open shared infusion unit design may be similar. The study also may serve as a model of survey design and implementation from which other centers may consider improving patient satisfaction. We hope these survey results and interventions can provide insight and be used to improve patient satisfaction among all cancer patients at infusion units serving veterans and nonveterans.
Acknowledgments
We are very thankful to our cancer patients who took the time to take the survey. We also are very grateful to the VHA infusion unit nurses, staff, nurse practitioners, and physicians who have embraced this project and welcomed any changes that may positively impact treatment of veterans. Also, thank you to Tia Kohs for statistical support and Sophie West for gender discussions. Last, we specifically thank Barbara, for her pursuit of better care for women and for all veterans.
1. Clarke SA, Booth L, Velikova G, Hewison J. Social support: gender differences in cancer patients in the United Kingdom. Cancer Nurs. 2006;29(1):66-72. doi:10.1097/00002820-200601000-00012
2. Wessels H, de Graeff A, Wynia K, et al. Gender-related needs and preferences in cancer care indicate the need for an individualized approach to cancer patients. Oncologist. 2010;15(6):648-655. doi:10.1634/theoncologist.2009-0337
3. Hartigan SM, Bonnet K, Chisholm L, et al. Why do women not use the bathroom? Women’s attitudes and beliefs on using public restrooms. Int J Environ Res Public Health. 2020;17(6):2053. doi:10.3390/ijerph17062053
4. Alexander K, Walters CB, Banerjee SC. Oncology patients’ preferences regarding sexual orientation and gender identity (SOGI) disclosure and room sharing sharing. Patient Educ Couns. 2020;103(5):1041-1048. doi:10.1016/j.pec.2019.12.006
5. Centers for Disease Control and Prevention. Facts about sexual violence. Updated July 5, 2022. Accessed July 13, 2022. https://www.cdc.gov/injury/features /sexual-violence/index.html
6. US Department of Veterans Affairs. Military sexual trauma. Updated May 16, 2022. Accessed July 13, 2022. https:// www.mentalhealth.va.gov/mentalhealth/msthome/index.asp
7. Wang Z, Pukszta M. Private Rooms, Semi-open areas, or open areas for chemotherapy care: perspectives of cancer patients, families, and nursing staff. HERD. 2018;11(3):94- 108. doi:10.1177/1937586718758445
8. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Women veterans report: the past, present, and future of women veterans. Accessed July 13, 2022. https://www.va.gov/vetdata /docs/specialreports/women_veterans_2015_final.pdf
9. Driscoll MA, Higgins DM, Seng EK, et al. Trauma, social support, family conflict, and chronic pain in recent service veterans: does gender matter? Pain Med. 2015;16(6):1101- 1111. doi:10.1111/pme.12744
10. Fox AB, Meyer EC, Vogt D. Attitudes about the VA healthcare setting, mental illness, and mental health treatment and their relationship with VA mental health service use among female and male OEF/OIF veterans. Psychol Serv. 2015;12(1):49-58. doi:10.1037/a0038269
11. Virani SS, Woodard LD, Ramsey DJ, et al. Gender disparities in evidence-based statin therapy in patients with cardiovascular disease. Am J Cardiol. 2015;115(1):21-26. doi:10.1016/j.amjcard.2014.09.041
12. Tseng J. Sex, gender, and why the differences matter. Virtual Mentor. 2008;10(7):427-428. doi:10.1001/virtualmentor.2008.10.7.fred1-0807
13. Booij JC, Zegers M, Evers PMPJ, Hendricks M, Delnoij DMJ, Rademakers JJDJM. Improving cancer patient care: development of a generic cancer consumer quality index questionnaire for cancer patients. BMC Cancer. 2013;13(203). doi:10.1186/1471-2407-13-203
14. Meropol NJ, Egleston BL, Buzaglo JS, et al. Cancer patient preferences for quality and length of life. Cancer. 2008;113(12):3459-3466. doi:10.1002/cncr.23968 1
5. Schnur JB, Dillon MJ, Goldsmith RE, Montgomery GH. Cancer treatment experiences among survivors of childhood sexual abuse: a qualitative investigation of triggers and reactions to cumulative trauma. Palliat Support Care. 2018;16(6):767-776. doi:10.1017/S147895151700075X
16. Cadman L, Waller J, Ashdown-Barr L, Szarewski A. Barriers to cervical screening in women who have experienced sexual abuse: an exploratory study. J Fam Plann Reprod Health Care. 2012;38(4):214-220. doi:10.1136/jfprhc-2012-100378
17. Kelly S. The effects of childhood sexual abuse on women’s lives and their attitudes to cervical screening. J Fam Plann Reprod Health Care. 2012;38(4):212-213. doi:10.1136/jfprhc-2012-100418
18. McCloskey LA, Lichter E, Williams C, Gerber M, Wittenberg E, Ganz M. Assessing intimate partner violence in health care settings leads to women’s receipt of interventions and improved health. Public Health Rep. 2006;121(4):435-444. doi:10.1177/003335490612100412
Gender differences in patient satisfaction with medical care have been evaluated in multiple settings; however, studies specific to the unique population of women veterans with cancer are lacking. Women are reported to value privacy, psychosocial support, and communication to a higher degree compared with men.1 Factors affecting satisfaction include the following: discomfort in sharing treatment rooms with the opposite gender, a desire for privacy with treatment and restroom use, anatomic or illness differences, and a personal history of abuse.2-4 Regrettably, up to 1 in 3 women in the United States are victims of sexual trauma in their lifetimes, and up to 1 in 4 women in the military are victims of military sexual trauma. Incidence in both settings is suspected to be higher due to underreporting.5,6
Chemotherapy treatment units are often uniquely designed as an open space, with several patients sharing a treatment area. The design reduces isolation and facilitates quick nurse-patient access during potentially toxic treatments known to have frequent adverse effects. Data suggest that nursing staff prefer open models to facilitate quick patient assessments and interventions as needed; however, patients and families prefer private treatment rooms, especially among women patients or those receiving longer infusions.7
The Veterans Health Administration (VHA) patient population is male predominant, comprised only of 10% female patients.8 Although the proportion of female patients in the VHA is expected to rise annually to about 16% by 2043, the low percentage of female veterans will persist for the foreseeable future.8 This low percentage of female veterans is reflected in the Veterans Affairs Portland Health Care System (VAPHCS) cancer patient population and in the use of the chemotherapy infusion unit, which is used for the ambulatory treatment of veterans undergoing cancer therapy.
The VHA has previously explored gender differences in health care, such as with cardiovascular disease, transgender care, and access to mental health.9-11 However, to the best of our knowledge, no analysis has explored gender differences within the outpatient cancer treatment experience. Patient satisfaction with outpatient cancer care may be magnified in the VHA setting due to the uniquely unequal gender populations, shared treatment space design, and high incidence of sexual abuse among women veterans. Given this, we aimed to identify gender-related preferences in outpatient cancer care in our chemotherapy infusion unit.
In our study, we used the terms male and female to reflect statistical data from the literature or labeled data from the electronic health record (EHR); whereas the terms men and women were used to describe and encompass the cultural implications and context of gender.12
Methods
This study was designated as a quality improvement (QI) project by the VAPHCS research office and Institutional Review Board in accordance with VHA policies.
The VAPHCS outpatient chemotherapy infusion unit is designed with 6 rooms for chemotherapy administration. One room is a large open space with 6 chairs for patients. The other rooms are smaller with glass dividers between the rooms, and 3 chairs inside each for patients. There are 2 private bathrooms, each gender neutral. Direct patient care is provided by physicians, nurse practitioners (NPs), infusion unit nurses, and nurse coordinators. Men represent the majority of hematology and oncology physicians (13 of 20 total: 5 women fellow physicians and 2 women attending physicians), and 2 of 4 NPs. Women represent 10 of 12 infusion unit and cancer coordinator nurses. We used the VHA Computerized Patient Record System (CPRS) EHR, to create a list of veterans treated at the VAPHCS outpatient chemotherapy infusion unit for a 2-year period (January 1, 2018, to December 31, 2020).
Male and female patient lists were first generated based on CPRS categorization. We identified all female veterans treated in the ambulatory infusion unit during the study period. Male patients were then chosen at random, recording the most recent names for each year until a matched number per year compared with the female cohort was reached. Patients were recorded only once even though they had multiple infusion unit visits. Patients were excluded who were deceased, on hospice care, lost to follow-up, could not be reached by phone, refused to take the survey, had undeliverable email addresses, or lacked internet or email access.
After filing the appropriate request through the VAPHCS Institutional Review Board committee in January 2021, patient records were reviewed for demographics data, contact information, and infusion treatment history. The survey was then conducted over a 2-week period during January and February 2021. Each patient was invited by phone to complete a 25-question anonymous online survey. The survey questions were created from patient-relayed experiences, then modeled into survey questions in a format similar to other patient satisfaction questionnaires described in cancer care and gender differences.2,13,14 The survey included self-identification of gender and was multiple choice for all except 2 questions, which allowed an open-ended response (Appendix). Only 1 answer per question was permitted. Only 1 survey link was sent to each veteran who gave permission for the survey. To protect anonymity for the small patient population, we excluded those identifying as gender nonbinary or transgender.
Statistical Analysis
Patient, disease, and treatment features are separated by male and female cohorts to reflect information from the EHR (Table 1). Survey percentages were calculated to reflect the affirmative response of the question asked (Table 2). Questions with answer options of not important, minimally important, important, or very important were calculated to reflect the sum of any importance in both cohorts. Questions with answer options of never, once, often, or every time were calculated to reflect any occurrence (sum of once, often, or every time) in both patient groups. Questions with answer options of strongly agree, somewhat agree, somewhat disagree, and strongly disagree were calculated to reflect any agreement (somewhat agree and strongly agree summed together) for both groups. Comparisons between cohorts were then conducted using a Fisher exact test. A Welch t test was used to calculate the significance of the continuous variable and overall ranking of the infusion unit experience between groups.
Results
In 2020, 414 individual patients were treated at the VAPAHCS outpatient infusion unit. Of these, 23 (5.6%) were female, and 18 agreed to take the survey. After deceased and duplicate names from 2020 were removed, another 14 eligible 2019 female patients were invited and 6 agreed to participate; 6 eligible 2018 female patients were invited and 4 agreed to take the survey (Figure). Thirty female veterans were sent a survey link and 21 (70%) responses were collected. Twenty-one male 2020 patients were contacted and 18 agreed to take the survey. After removing duplicate names and deceased individuals, 17 of 21 eligible 2019 male patients and 4 of 6 eligible 2018 patients agreed to take the survey. Five additional male veterans declined the online-based survey method. In total, 39 male veterans were reached who agreed to have the survey link emailed, and 20 (51%) total responses were collected.
Most respondents answered all questions in the survey. The most frequently skipped questions included 3 questions that were contingent on a yes answer to a prior question, and 2 openended questions asking for a write-in response. Percentages for female and male respondents were adjusted for number of responses when applicable.
Thirteen (62%) female patients were aged < 65 years, while 18 (90%) of male patients were aged ≥ 65 years. Education beyond high school was reported in 20 female and 15 male respondents. Almost all treatment administered in the infusion unit was for cancer-directed treatment, with only 1 reporting a noncancer treatment (IV iron). The most common malignancy among female patients was breast cancer (n = 11, 52%); for male patients prostate cancer (n = 4, 20%) and hematologic malignancy (n = 4, 20%) were most common. Four (19%) female and 8 (40%) male respondents reported having a metastatic diagnosis. Overall patient satisfaction ranked high with an average score of 9.1 on a 10-point scale. The mean (SD) satisfaction score for female respondents was 1 point lower than that for men: 8.7 (2.2) vs 9.6 (0.6) in men (P = .11).
Eighteen (86%) women reported a history of sexual abuse or harassment compared with 2 (10%) men (P < .001). The sexual abuse assailant was a different gender for 17 of 18 female respondents and of the same gender for both male respondents. Of those with sexual abuse history, 4 women reported feeling uncomfortable around their assailant’s gender vs no men (P = .11), but this difference was not statistically significant. Six women (29%) and 2 (10%) men reported feeling uncomfortable during clinical examinations from comments made by the clinician or during treatment administration (P = .24). Six (29%) women and no men reported that they “felt uncomfortable in the infusion unit by other patients” (P = .02). Six (29%) women and no men reported feeling unable to “voice uncomfortable experiences” to the infusion unit clinician (P = .02).
Ten (48%) women and 6 (30%) men reported emotional support when receiving treatments provided by staff of the same gender (P = .34). Eight (38%) women and 4 (20%) men noted that access to treatment with the same gender was important (P = .31). Six (29%) women and 4 (20%) men indicated that access to a sex or gender-specific restroom was important (P = .72). No gender preferences were identified in the survey questions regarding importance of private treatment room access and level of emotional support when receiving treatment with others of the same malignancy. These relationships were not statistically significant.
In addition, 2 open-ended questions were asked. Seventeen women and 14 men responded. Contact the corresponding author for more information on the questions and responses.
Discussion
Overall patient satisfaction was high among the men and women veterans with cancer who received treatment in our outpatient infusion unit; however, notable gender differences existed. Three items in the survey revealed statistically significant differences in the patient experience between men and women veterans: history of sexual abuse or harassment, uncomfortable feelings among other patients, and discomfort in relaying uncomfortable feelings to a clinician. Other items in the survey did not reach statistical significance; however, we have included discussion of the findings as they may highlight important trends and be of clinical significance.
We suspect differences among genders in patient satisfaction to be related to the high incidence of sexual abuse or harassment history reported by women, much higher at 86% than the one-third to one-fourth incidence rates estimated by the existing literature for civilian or military sexual abuse in women.5,6 These high sexual abuse or harassment rates are present in a majority of women who receive cancer-directed treatment toward a gender-specific breast malignancy, surrounded predominantly among men in a shared treatment space. Together, these factors are likely key reasons behind the differences in satisfaction observed. This sentiment is expressed in our cohort, where one-fifth of women with a sexual abuse or harassment history continue to remain uncomfortable around men, and 29% of women reporting some uncomfortable feelings during their treatment experience compared with none of the men. Additionally, 6 (29%) women vs no men felt uncomfortable in reporting an uncomfortable experience with a clinician; this represents a significant barrier in providing care for these patients.
A key gender preference among women included access to shared treatment rooms with other women and that sharing a treatment space with other women resulted in feeling more emotional support during treatments. Access to gender-specific restrooms was also preferred by women more than men. Key findings in both genders were that about half of men and women valued access to a private treatment room and would derive more emotional support when surrounded by others with the same cancer.
Prior studies on gender and patient satisfaction in general medical care and cancer care have found women value privacy more than men.1-3 Wessels and colleagues performed an analysis of 386 patients with cancer in Europe and found gender to be the strongest influence in patient preferences within cancer care. Specifically, the highest statically significant association in care preferences among women included privacy, support/counseling/rehabilitation access, and decreased wait times.2 These findings were most pronounced in those with breast cancer compared with other malignancy type and highlights that malignancy type and gender predominance impact care satisfaction.
Traditionally a shared treatment space design has been used in outpatient chemotherapy units, similar to the design of the VAPHCS. However, recent data report on the patient preference for a private treatment space, which was especially prominent among women and those receiving longer infusions.7 In another study that evaluated 225 patients with cancer preferences in sharing a treatment space with those of a different sexual orientation or gender identify, differences were found. Both men and women had a similar level of comfort in sharing a treatment room with someone of a different sexual orientation; however, more women reported discomfort in sharing a treatment space with a transgender woman compared with men who felt more comfortable sharing a space with a transgender man.4 We noted a gender preference may be present to explain the difference. Within our cohort, women valued access to treatment with other women and derived more emotional support when with other women; however, we did not inquire about feelings in sharing a treatment space among transgender individuals or differing sexual orientation.
Gender differences for privacy and in shared room preferences may result from the lasting impacts of prior sexual abuse or harassment. A history of sexual abuse negatively impacts later medical care access and use.15 Those veterans who experienced sexual abuse/harrassment reported higher feelings of lack of control, vulnerability, depression, and pursued less medical care.15,16 Within cancer care, these feelings are most pronounced among women with gender-specific malignancies, such as gynecologic cancers or breast cancer. Treatment, screening, and physical examinations by clinicians who are of the same gender as the sexual abuse/harassment assailant can recreate traumatic feelings.15,16
A majority of women (n = 18, 86%) in our cohort reported a history of sexual abuse or harassment and breast malignancy was the most common cancer among women. However women represent just 5.6% of the VAPHCS infusion unit treatment population. This combination of factors may explain the reasons for women veterans’ preference for privacy during treatments, access to gender-specific restrooms, and feeling more emotional support when surrounded by other women. Strategies to help patients with a history of abuse have been described and include discussions from the clinician asking about abuse history, allowing time for the patient to express fears with an examination or test, and training on how to deliver sensitive care for those with trauma.17,18
Quality Improvement
Project In the VAPHCS infusion unit, several low-cost interventions have been undertaken as a result of our survey findings. We presented our survey data to the VAPHCS Cancer Committee, accredited through the national American College of Surgeons Commission on Cancer. The committee awarded support for a yearlong QI project, including a formal framework of quarterly multidisciplinary meetings to discuss project updates, challenges, and resources. The QI project centers on education to raise awareness of survey results as well as specific interventions for improvement.
Education efforts have been applied through multiple department-wide emails, in-person education to our chemotherapy unit staff, abstract submission to national oncology conferences, and grand rounds department presentations at VAPHCS and at other VHA-affiliated university programs. Additionally, education to clinicians with specific contact information for psychology and women’s health to support mental health, trauma, and sexual abuse histories has been given to each clinician who cares for veterans in the chemotherapy unit.
We also have implemented a mandatory cancer care navigation consultation for all women veterans who have a new cancer or infusion need. The cancer care navigator has received specialized training in sensitive history-taking and provides women veterans with a direct number to reach the cancer care navigation nurse. Cancer care navigation also provides a continuum of support and referral access for psychosocial needs as indicated between infusion or health care visits. Our hope is that these resources may help offset the sentiment reflected in our cohort of women feeling unable to voice concerns to a clinician.
Other interventions underway include offering designated scheduling time each week to women so they can receive infusions in an area with other women. This may help mitigate the finding that women veterans felt more uncomfortable around other patients during infusion treatments compared with how men felt in the chemotherapy unit. We also have implemented gender-specific restrooms labeled with a sign on each bathroom door so men and women can have access to a designated restroom. Offering private or semiprivate treatment rooms is currently limited by space and capacity; however, these may offer the greatest opportunity to improve patient satisfaction, especially among women veterans. Working with the support of the VAPHCS Cancer Committee, we aim to reevaluate the impact of the education and QI efforts on gender differences and patient satisfaction at completion of the 1-year award.
Limitations
Limitations to our study include the overall small sample size. This is due to the combination of the low number of women treated at VAPHCS and many with advanced cancer who, unfortunately, have a limited overall survival and hinders accrual of a larger sample size. Other limitations included age as a possible confounder in our findings, with women representing a younger demographic compared with men. We did not collect responses on duration of infusion time, which also may impact overall satisfaction and patient experience. We also acknowledge that biologic male or female sex may not correspond to a specific individual’s gender. Use of CPRS to obtain a matched number of male and female patients through random selection relied on labeled data from the EHR. This potentially may have excluded male patients who identify as another gender that would have been captured on the anonymous survey.
Last, we restricted survey responses to online only, which excluded a small percentage who declined this approach.
Conclusions
Our findings may have broad applications to other VHA facilities and other cancer-directed treatment centers where the patient demographic and open shared infusion unit design may be similar. The study also may serve as a model of survey design and implementation from which other centers may consider improving patient satisfaction. We hope these survey results and interventions can provide insight and be used to improve patient satisfaction among all cancer patients at infusion units serving veterans and nonveterans.
Acknowledgments
We are very thankful to our cancer patients who took the time to take the survey. We also are very grateful to the VHA infusion unit nurses, staff, nurse practitioners, and physicians who have embraced this project and welcomed any changes that may positively impact treatment of veterans. Also, thank you to Tia Kohs for statistical support and Sophie West for gender discussions. Last, we specifically thank Barbara, for her pursuit of better care for women and for all veterans.
Gender differences in patient satisfaction with medical care have been evaluated in multiple settings; however, studies specific to the unique population of women veterans with cancer are lacking. Women are reported to value privacy, psychosocial support, and communication to a higher degree compared with men.1 Factors affecting satisfaction include the following: discomfort in sharing treatment rooms with the opposite gender, a desire for privacy with treatment and restroom use, anatomic or illness differences, and a personal history of abuse.2-4 Regrettably, up to 1 in 3 women in the United States are victims of sexual trauma in their lifetimes, and up to 1 in 4 women in the military are victims of military sexual trauma. Incidence in both settings is suspected to be higher due to underreporting.5,6
Chemotherapy treatment units are often uniquely designed as an open space, with several patients sharing a treatment area. The design reduces isolation and facilitates quick nurse-patient access during potentially toxic treatments known to have frequent adverse effects. Data suggest that nursing staff prefer open models to facilitate quick patient assessments and interventions as needed; however, patients and families prefer private treatment rooms, especially among women patients or those receiving longer infusions.7
The Veterans Health Administration (VHA) patient population is male predominant, comprised only of 10% female patients.8 Although the proportion of female patients in the VHA is expected to rise annually to about 16% by 2043, the low percentage of female veterans will persist for the foreseeable future.8 This low percentage of female veterans is reflected in the Veterans Affairs Portland Health Care System (VAPHCS) cancer patient population and in the use of the chemotherapy infusion unit, which is used for the ambulatory treatment of veterans undergoing cancer therapy.
The VHA has previously explored gender differences in health care, such as with cardiovascular disease, transgender care, and access to mental health.9-11 However, to the best of our knowledge, no analysis has explored gender differences within the outpatient cancer treatment experience. Patient satisfaction with outpatient cancer care may be magnified in the VHA setting due to the uniquely unequal gender populations, shared treatment space design, and high incidence of sexual abuse among women veterans. Given this, we aimed to identify gender-related preferences in outpatient cancer care in our chemotherapy infusion unit.
In our study, we used the terms male and female to reflect statistical data from the literature or labeled data from the electronic health record (EHR); whereas the terms men and women were used to describe and encompass the cultural implications and context of gender.12
Methods
This study was designated as a quality improvement (QI) project by the VAPHCS research office and Institutional Review Board in accordance with VHA policies.
The VAPHCS outpatient chemotherapy infusion unit is designed with 6 rooms for chemotherapy administration. One room is a large open space with 6 chairs for patients. The other rooms are smaller with glass dividers between the rooms, and 3 chairs inside each for patients. There are 2 private bathrooms, each gender neutral. Direct patient care is provided by physicians, nurse practitioners (NPs), infusion unit nurses, and nurse coordinators. Men represent the majority of hematology and oncology physicians (13 of 20 total: 5 women fellow physicians and 2 women attending physicians), and 2 of 4 NPs. Women represent 10 of 12 infusion unit and cancer coordinator nurses. We used the VHA Computerized Patient Record System (CPRS) EHR, to create a list of veterans treated at the VAPHCS outpatient chemotherapy infusion unit for a 2-year period (January 1, 2018, to December 31, 2020).
Male and female patient lists were first generated based on CPRS categorization. We identified all female veterans treated in the ambulatory infusion unit during the study period. Male patients were then chosen at random, recording the most recent names for each year until a matched number per year compared with the female cohort was reached. Patients were recorded only once even though they had multiple infusion unit visits. Patients were excluded who were deceased, on hospice care, lost to follow-up, could not be reached by phone, refused to take the survey, had undeliverable email addresses, or lacked internet or email access.
After filing the appropriate request through the VAPHCS Institutional Review Board committee in January 2021, patient records were reviewed for demographics data, contact information, and infusion treatment history. The survey was then conducted over a 2-week period during January and February 2021. Each patient was invited by phone to complete a 25-question anonymous online survey. The survey questions were created from patient-relayed experiences, then modeled into survey questions in a format similar to other patient satisfaction questionnaires described in cancer care and gender differences.2,13,14 The survey included self-identification of gender and was multiple choice for all except 2 questions, which allowed an open-ended response (Appendix). Only 1 answer per question was permitted. Only 1 survey link was sent to each veteran who gave permission for the survey. To protect anonymity for the small patient population, we excluded those identifying as gender nonbinary or transgender.
Statistical Analysis
Patient, disease, and treatment features are separated by male and female cohorts to reflect information from the EHR (Table 1). Survey percentages were calculated to reflect the affirmative response of the question asked (Table 2). Questions with answer options of not important, minimally important, important, or very important were calculated to reflect the sum of any importance in both cohorts. Questions with answer options of never, once, often, or every time were calculated to reflect any occurrence (sum of once, often, or every time) in both patient groups. Questions with answer options of strongly agree, somewhat agree, somewhat disagree, and strongly disagree were calculated to reflect any agreement (somewhat agree and strongly agree summed together) for both groups. Comparisons between cohorts were then conducted using a Fisher exact test. A Welch t test was used to calculate the significance of the continuous variable and overall ranking of the infusion unit experience between groups.
Results
In 2020, 414 individual patients were treated at the VAPAHCS outpatient infusion unit. Of these, 23 (5.6%) were female, and 18 agreed to take the survey. After deceased and duplicate names from 2020 were removed, another 14 eligible 2019 female patients were invited and 6 agreed to participate; 6 eligible 2018 female patients were invited and 4 agreed to take the survey (Figure). Thirty female veterans were sent a survey link and 21 (70%) responses were collected. Twenty-one male 2020 patients were contacted and 18 agreed to take the survey. After removing duplicate names and deceased individuals, 17 of 21 eligible 2019 male patients and 4 of 6 eligible 2018 patients agreed to take the survey. Five additional male veterans declined the online-based survey method. In total, 39 male veterans were reached who agreed to have the survey link emailed, and 20 (51%) total responses were collected.
Most respondents answered all questions in the survey. The most frequently skipped questions included 3 questions that were contingent on a yes answer to a prior question, and 2 openended questions asking for a write-in response. Percentages for female and male respondents were adjusted for number of responses when applicable.
Thirteen (62%) female patients were aged < 65 years, while 18 (90%) of male patients were aged ≥ 65 years. Education beyond high school was reported in 20 female and 15 male respondents. Almost all treatment administered in the infusion unit was for cancer-directed treatment, with only 1 reporting a noncancer treatment (IV iron). The most common malignancy among female patients was breast cancer (n = 11, 52%); for male patients prostate cancer (n = 4, 20%) and hematologic malignancy (n = 4, 20%) were most common. Four (19%) female and 8 (40%) male respondents reported having a metastatic diagnosis. Overall patient satisfaction ranked high with an average score of 9.1 on a 10-point scale. The mean (SD) satisfaction score for female respondents was 1 point lower than that for men: 8.7 (2.2) vs 9.6 (0.6) in men (P = .11).
Eighteen (86%) women reported a history of sexual abuse or harassment compared with 2 (10%) men (P < .001). The sexual abuse assailant was a different gender for 17 of 18 female respondents and of the same gender for both male respondents. Of those with sexual abuse history, 4 women reported feeling uncomfortable around their assailant’s gender vs no men (P = .11), but this difference was not statistically significant. Six women (29%) and 2 (10%) men reported feeling uncomfortable during clinical examinations from comments made by the clinician or during treatment administration (P = .24). Six (29%) women and no men reported that they “felt uncomfortable in the infusion unit by other patients” (P = .02). Six (29%) women and no men reported feeling unable to “voice uncomfortable experiences” to the infusion unit clinician (P = .02).
Ten (48%) women and 6 (30%) men reported emotional support when receiving treatments provided by staff of the same gender (P = .34). Eight (38%) women and 4 (20%) men noted that access to treatment with the same gender was important (P = .31). Six (29%) women and 4 (20%) men indicated that access to a sex or gender-specific restroom was important (P = .72). No gender preferences were identified in the survey questions regarding importance of private treatment room access and level of emotional support when receiving treatment with others of the same malignancy. These relationships were not statistically significant.
In addition, 2 open-ended questions were asked. Seventeen women and 14 men responded. Contact the corresponding author for more information on the questions and responses.
Discussion
Overall patient satisfaction was high among the men and women veterans with cancer who received treatment in our outpatient infusion unit; however, notable gender differences existed. Three items in the survey revealed statistically significant differences in the patient experience between men and women veterans: history of sexual abuse or harassment, uncomfortable feelings among other patients, and discomfort in relaying uncomfortable feelings to a clinician. Other items in the survey did not reach statistical significance; however, we have included discussion of the findings as they may highlight important trends and be of clinical significance.
We suspect differences among genders in patient satisfaction to be related to the high incidence of sexual abuse or harassment history reported by women, much higher at 86% than the one-third to one-fourth incidence rates estimated by the existing literature for civilian or military sexual abuse in women.5,6 These high sexual abuse or harassment rates are present in a majority of women who receive cancer-directed treatment toward a gender-specific breast malignancy, surrounded predominantly among men in a shared treatment space. Together, these factors are likely key reasons behind the differences in satisfaction observed. This sentiment is expressed in our cohort, where one-fifth of women with a sexual abuse or harassment history continue to remain uncomfortable around men, and 29% of women reporting some uncomfortable feelings during their treatment experience compared with none of the men. Additionally, 6 (29%) women vs no men felt uncomfortable in reporting an uncomfortable experience with a clinician; this represents a significant barrier in providing care for these patients.
A key gender preference among women included access to shared treatment rooms with other women and that sharing a treatment space with other women resulted in feeling more emotional support during treatments. Access to gender-specific restrooms was also preferred by women more than men. Key findings in both genders were that about half of men and women valued access to a private treatment room and would derive more emotional support when surrounded by others with the same cancer.
Prior studies on gender and patient satisfaction in general medical care and cancer care have found women value privacy more than men.1-3 Wessels and colleagues performed an analysis of 386 patients with cancer in Europe and found gender to be the strongest influence in patient preferences within cancer care. Specifically, the highest statically significant association in care preferences among women included privacy, support/counseling/rehabilitation access, and decreased wait times.2 These findings were most pronounced in those with breast cancer compared with other malignancy type and highlights that malignancy type and gender predominance impact care satisfaction.
Traditionally a shared treatment space design has been used in outpatient chemotherapy units, similar to the design of the VAPHCS. However, recent data report on the patient preference for a private treatment space, which was especially prominent among women and those receiving longer infusions.7 In another study that evaluated 225 patients with cancer preferences in sharing a treatment space with those of a different sexual orientation or gender identify, differences were found. Both men and women had a similar level of comfort in sharing a treatment room with someone of a different sexual orientation; however, more women reported discomfort in sharing a treatment space with a transgender woman compared with men who felt more comfortable sharing a space with a transgender man.4 We noted a gender preference may be present to explain the difference. Within our cohort, women valued access to treatment with other women and derived more emotional support when with other women; however, we did not inquire about feelings in sharing a treatment space among transgender individuals or differing sexual orientation.
Gender differences for privacy and in shared room preferences may result from the lasting impacts of prior sexual abuse or harassment. A history of sexual abuse negatively impacts later medical care access and use.15 Those veterans who experienced sexual abuse/harrassment reported higher feelings of lack of control, vulnerability, depression, and pursued less medical care.15,16 Within cancer care, these feelings are most pronounced among women with gender-specific malignancies, such as gynecologic cancers or breast cancer. Treatment, screening, and physical examinations by clinicians who are of the same gender as the sexual abuse/harassment assailant can recreate traumatic feelings.15,16
A majority of women (n = 18, 86%) in our cohort reported a history of sexual abuse or harassment and breast malignancy was the most common cancer among women. However women represent just 5.6% of the VAPHCS infusion unit treatment population. This combination of factors may explain the reasons for women veterans’ preference for privacy during treatments, access to gender-specific restrooms, and feeling more emotional support when surrounded by other women. Strategies to help patients with a history of abuse have been described and include discussions from the clinician asking about abuse history, allowing time for the patient to express fears with an examination or test, and training on how to deliver sensitive care for those with trauma.17,18
Quality Improvement
Project In the VAPHCS infusion unit, several low-cost interventions have been undertaken as a result of our survey findings. We presented our survey data to the VAPHCS Cancer Committee, accredited through the national American College of Surgeons Commission on Cancer. The committee awarded support for a yearlong QI project, including a formal framework of quarterly multidisciplinary meetings to discuss project updates, challenges, and resources. The QI project centers on education to raise awareness of survey results as well as specific interventions for improvement.
Education efforts have been applied through multiple department-wide emails, in-person education to our chemotherapy unit staff, abstract submission to national oncology conferences, and grand rounds department presentations at VAPHCS and at other VHA-affiliated university programs. Additionally, education to clinicians with specific contact information for psychology and women’s health to support mental health, trauma, and sexual abuse histories has been given to each clinician who cares for veterans in the chemotherapy unit.
We also have implemented a mandatory cancer care navigation consultation for all women veterans who have a new cancer or infusion need. The cancer care navigator has received specialized training in sensitive history-taking and provides women veterans with a direct number to reach the cancer care navigation nurse. Cancer care navigation also provides a continuum of support and referral access for psychosocial needs as indicated between infusion or health care visits. Our hope is that these resources may help offset the sentiment reflected in our cohort of women feeling unable to voice concerns to a clinician.
Other interventions underway include offering designated scheduling time each week to women so they can receive infusions in an area with other women. This may help mitigate the finding that women veterans felt more uncomfortable around other patients during infusion treatments compared with how men felt in the chemotherapy unit. We also have implemented gender-specific restrooms labeled with a sign on each bathroom door so men and women can have access to a designated restroom. Offering private or semiprivate treatment rooms is currently limited by space and capacity; however, these may offer the greatest opportunity to improve patient satisfaction, especially among women veterans. Working with the support of the VAPHCS Cancer Committee, we aim to reevaluate the impact of the education and QI efforts on gender differences and patient satisfaction at completion of the 1-year award.
Limitations
Limitations to our study include the overall small sample size. This is due to the combination of the low number of women treated at VAPHCS and many with advanced cancer who, unfortunately, have a limited overall survival and hinders accrual of a larger sample size. Other limitations included age as a possible confounder in our findings, with women representing a younger demographic compared with men. We did not collect responses on duration of infusion time, which also may impact overall satisfaction and patient experience. We also acknowledge that biologic male or female sex may not correspond to a specific individual’s gender. Use of CPRS to obtain a matched number of male and female patients through random selection relied on labeled data from the EHR. This potentially may have excluded male patients who identify as another gender that would have been captured on the anonymous survey.
Last, we restricted survey responses to online only, which excluded a small percentage who declined this approach.
Conclusions
Our findings may have broad applications to other VHA facilities and other cancer-directed treatment centers where the patient demographic and open shared infusion unit design may be similar. The study also may serve as a model of survey design and implementation from which other centers may consider improving patient satisfaction. We hope these survey results and interventions can provide insight and be used to improve patient satisfaction among all cancer patients at infusion units serving veterans and nonveterans.
Acknowledgments
We are very thankful to our cancer patients who took the time to take the survey. We also are very grateful to the VHA infusion unit nurses, staff, nurse practitioners, and physicians who have embraced this project and welcomed any changes that may positively impact treatment of veterans. Also, thank you to Tia Kohs for statistical support and Sophie West for gender discussions. Last, we specifically thank Barbara, for her pursuit of better care for women and for all veterans.
1. Clarke SA, Booth L, Velikova G, Hewison J. Social support: gender differences in cancer patients in the United Kingdom. Cancer Nurs. 2006;29(1):66-72. doi:10.1097/00002820-200601000-00012
2. Wessels H, de Graeff A, Wynia K, et al. Gender-related needs and preferences in cancer care indicate the need for an individualized approach to cancer patients. Oncologist. 2010;15(6):648-655. doi:10.1634/theoncologist.2009-0337
3. Hartigan SM, Bonnet K, Chisholm L, et al. Why do women not use the bathroom? Women’s attitudes and beliefs on using public restrooms. Int J Environ Res Public Health. 2020;17(6):2053. doi:10.3390/ijerph17062053
4. Alexander K, Walters CB, Banerjee SC. Oncology patients’ preferences regarding sexual orientation and gender identity (SOGI) disclosure and room sharing sharing. Patient Educ Couns. 2020;103(5):1041-1048. doi:10.1016/j.pec.2019.12.006
5. Centers for Disease Control and Prevention. Facts about sexual violence. Updated July 5, 2022. Accessed July 13, 2022. https://www.cdc.gov/injury/features /sexual-violence/index.html
6. US Department of Veterans Affairs. Military sexual trauma. Updated May 16, 2022. Accessed July 13, 2022. https:// www.mentalhealth.va.gov/mentalhealth/msthome/index.asp
7. Wang Z, Pukszta M. Private Rooms, Semi-open areas, or open areas for chemotherapy care: perspectives of cancer patients, families, and nursing staff. HERD. 2018;11(3):94- 108. doi:10.1177/1937586718758445
8. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Women veterans report: the past, present, and future of women veterans. Accessed July 13, 2022. https://www.va.gov/vetdata /docs/specialreports/women_veterans_2015_final.pdf
9. Driscoll MA, Higgins DM, Seng EK, et al. Trauma, social support, family conflict, and chronic pain in recent service veterans: does gender matter? Pain Med. 2015;16(6):1101- 1111. doi:10.1111/pme.12744
10. Fox AB, Meyer EC, Vogt D. Attitudes about the VA healthcare setting, mental illness, and mental health treatment and their relationship with VA mental health service use among female and male OEF/OIF veterans. Psychol Serv. 2015;12(1):49-58. doi:10.1037/a0038269
11. Virani SS, Woodard LD, Ramsey DJ, et al. Gender disparities in evidence-based statin therapy in patients with cardiovascular disease. Am J Cardiol. 2015;115(1):21-26. doi:10.1016/j.amjcard.2014.09.041
12. Tseng J. Sex, gender, and why the differences matter. Virtual Mentor. 2008;10(7):427-428. doi:10.1001/virtualmentor.2008.10.7.fred1-0807
13. Booij JC, Zegers M, Evers PMPJ, Hendricks M, Delnoij DMJ, Rademakers JJDJM. Improving cancer patient care: development of a generic cancer consumer quality index questionnaire for cancer patients. BMC Cancer. 2013;13(203). doi:10.1186/1471-2407-13-203
14. Meropol NJ, Egleston BL, Buzaglo JS, et al. Cancer patient preferences for quality and length of life. Cancer. 2008;113(12):3459-3466. doi:10.1002/cncr.23968 1
5. Schnur JB, Dillon MJ, Goldsmith RE, Montgomery GH. Cancer treatment experiences among survivors of childhood sexual abuse: a qualitative investigation of triggers and reactions to cumulative trauma. Palliat Support Care. 2018;16(6):767-776. doi:10.1017/S147895151700075X
16. Cadman L, Waller J, Ashdown-Barr L, Szarewski A. Barriers to cervical screening in women who have experienced sexual abuse: an exploratory study. J Fam Plann Reprod Health Care. 2012;38(4):214-220. doi:10.1136/jfprhc-2012-100378
17. Kelly S. The effects of childhood sexual abuse on women’s lives and their attitudes to cervical screening. J Fam Plann Reprod Health Care. 2012;38(4):212-213. doi:10.1136/jfprhc-2012-100418
18. McCloskey LA, Lichter E, Williams C, Gerber M, Wittenberg E, Ganz M. Assessing intimate partner violence in health care settings leads to women’s receipt of interventions and improved health. Public Health Rep. 2006;121(4):435-444. doi:10.1177/003335490612100412
1. Clarke SA, Booth L, Velikova G, Hewison J. Social support: gender differences in cancer patients in the United Kingdom. Cancer Nurs. 2006;29(1):66-72. doi:10.1097/00002820-200601000-00012
2. Wessels H, de Graeff A, Wynia K, et al. Gender-related needs and preferences in cancer care indicate the need for an individualized approach to cancer patients. Oncologist. 2010;15(6):648-655. doi:10.1634/theoncologist.2009-0337
3. Hartigan SM, Bonnet K, Chisholm L, et al. Why do women not use the bathroom? Women’s attitudes and beliefs on using public restrooms. Int J Environ Res Public Health. 2020;17(6):2053. doi:10.3390/ijerph17062053
4. Alexander K, Walters CB, Banerjee SC. Oncology patients’ preferences regarding sexual orientation and gender identity (SOGI) disclosure and room sharing sharing. Patient Educ Couns. 2020;103(5):1041-1048. doi:10.1016/j.pec.2019.12.006
5. Centers for Disease Control and Prevention. Facts about sexual violence. Updated July 5, 2022. Accessed July 13, 2022. https://www.cdc.gov/injury/features /sexual-violence/index.html
6. US Department of Veterans Affairs. Military sexual trauma. Updated May 16, 2022. Accessed July 13, 2022. https:// www.mentalhealth.va.gov/mentalhealth/msthome/index.asp
7. Wang Z, Pukszta M. Private Rooms, Semi-open areas, or open areas for chemotherapy care: perspectives of cancer patients, families, and nursing staff. HERD. 2018;11(3):94- 108. doi:10.1177/1937586718758445
8. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Women veterans report: the past, present, and future of women veterans. Accessed July 13, 2022. https://www.va.gov/vetdata /docs/specialreports/women_veterans_2015_final.pdf
9. Driscoll MA, Higgins DM, Seng EK, et al. Trauma, social support, family conflict, and chronic pain in recent service veterans: does gender matter? Pain Med. 2015;16(6):1101- 1111. doi:10.1111/pme.12744
10. Fox AB, Meyer EC, Vogt D. Attitudes about the VA healthcare setting, mental illness, and mental health treatment and their relationship with VA mental health service use among female and male OEF/OIF veterans. Psychol Serv. 2015;12(1):49-58. doi:10.1037/a0038269
11. Virani SS, Woodard LD, Ramsey DJ, et al. Gender disparities in evidence-based statin therapy in patients with cardiovascular disease. Am J Cardiol. 2015;115(1):21-26. doi:10.1016/j.amjcard.2014.09.041
12. Tseng J. Sex, gender, and why the differences matter. Virtual Mentor. 2008;10(7):427-428. doi:10.1001/virtualmentor.2008.10.7.fred1-0807
13. Booij JC, Zegers M, Evers PMPJ, Hendricks M, Delnoij DMJ, Rademakers JJDJM. Improving cancer patient care: development of a generic cancer consumer quality index questionnaire for cancer patients. BMC Cancer. 2013;13(203). doi:10.1186/1471-2407-13-203
14. Meropol NJ, Egleston BL, Buzaglo JS, et al. Cancer patient preferences for quality and length of life. Cancer. 2008;113(12):3459-3466. doi:10.1002/cncr.23968 1
5. Schnur JB, Dillon MJ, Goldsmith RE, Montgomery GH. Cancer treatment experiences among survivors of childhood sexual abuse: a qualitative investigation of triggers and reactions to cumulative trauma. Palliat Support Care. 2018;16(6):767-776. doi:10.1017/S147895151700075X
16. Cadman L, Waller J, Ashdown-Barr L, Szarewski A. Barriers to cervical screening in women who have experienced sexual abuse: an exploratory study. J Fam Plann Reprod Health Care. 2012;38(4):214-220. doi:10.1136/jfprhc-2012-100378
17. Kelly S. The effects of childhood sexual abuse on women’s lives and their attitudes to cervical screening. J Fam Plann Reprod Health Care. 2012;38(4):212-213. doi:10.1136/jfprhc-2012-100418
18. McCloskey LA, Lichter E, Williams C, Gerber M, Wittenberg E, Ganz M. Assessing intimate partner violence in health care settings leads to women’s receipt of interventions and improved health. Public Health Rep. 2006;121(4):435-444. doi:10.1177/003335490612100412
Incomplete recovery common 6 months after mild TBI
, new data from the TRACK-TBI study shows.
“Seeing that more than half of the GCS [Glasgow Coma Score] 15, CT-negative TBI cohort in our study were not back to their preinjury baseline at 6 months was surprising and impacts the millions of Americans who suffer from concussions annually,” said lead author Debbie Madhok, MD, with department of emergency medicine, University of California, San Francisco.
“These results highlight the importance of improving care pathways for concussion, particularly from the emergency department,” Dr. Madhok said.
The findings were published online in JAMA Network Open.
The short- and long-term outcomes in the large group of patients who come into the ED with TBI, a GCS of 15, and without acute intracranial traumatic injury (defined as a negative head CT scan) remain poorly understood, the investigators noted. To investigate further, they evaluated outcomes at 2 weeks and 6 months in 991 of these patients (mean age, 38 years; 64% men) from the TRACK-TBI study.
Among the 751 (76%) participants followed up at 2 weeks after the injury, only 204 (27%) had functional recovery – with a Glasgow Outcome Scale-Extended (GOS-E) score of 8. The remaining 547 (73%) had incomplete recovery (GOS-E scores < 8).
Among the 659 patients (66%) followed up at 6 months after the injury, 287 (44%) had functional recovery and 372 (56%) had incomplete recovery.
Most patients who failed to recover completely reported they had not returned to their preinjury life (88%). They described trouble returning to social activities outside the home and disruptions in family relationships and friendships.
The researchers noted that the study population had a high rate of preinjury psychiatric comorbidities, and these patients were more likely to have incomplete recovery than those without psychiatric comorbidities. This aligns with results from previous studies, they added.
The investigators also noted that patients with mild TBI without acute intracranial trauma are typically managed by ED personnel.
“These findings highlight the importance of ED clinicians being aware of the risk of incomplete recovery for patients with a mild TBI (that is, GCS score of 15 and negative head CT scan) and providing accurate education and timely referral information before ED discharge,” they wrote.
The study was funded by grants from the National Foundation of Emergency Medicine, the National Institute of Neurological Disorders and Stroke, and the U.S. Department of Defense Traumatic Brain Injury Endpoints Development Initiative. Dr. Madhok has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new data from the TRACK-TBI study shows.
“Seeing that more than half of the GCS [Glasgow Coma Score] 15, CT-negative TBI cohort in our study were not back to their preinjury baseline at 6 months was surprising and impacts the millions of Americans who suffer from concussions annually,” said lead author Debbie Madhok, MD, with department of emergency medicine, University of California, San Francisco.
“These results highlight the importance of improving care pathways for concussion, particularly from the emergency department,” Dr. Madhok said.
The findings were published online in JAMA Network Open.
The short- and long-term outcomes in the large group of patients who come into the ED with TBI, a GCS of 15, and without acute intracranial traumatic injury (defined as a negative head CT scan) remain poorly understood, the investigators noted. To investigate further, they evaluated outcomes at 2 weeks and 6 months in 991 of these patients (mean age, 38 years; 64% men) from the TRACK-TBI study.
Among the 751 (76%) participants followed up at 2 weeks after the injury, only 204 (27%) had functional recovery – with a Glasgow Outcome Scale-Extended (GOS-E) score of 8. The remaining 547 (73%) had incomplete recovery (GOS-E scores < 8).
Among the 659 patients (66%) followed up at 6 months after the injury, 287 (44%) had functional recovery and 372 (56%) had incomplete recovery.
Most patients who failed to recover completely reported they had not returned to their preinjury life (88%). They described trouble returning to social activities outside the home and disruptions in family relationships and friendships.
The researchers noted that the study population had a high rate of preinjury psychiatric comorbidities, and these patients were more likely to have incomplete recovery than those without psychiatric comorbidities. This aligns with results from previous studies, they added.
The investigators also noted that patients with mild TBI without acute intracranial trauma are typically managed by ED personnel.
“These findings highlight the importance of ED clinicians being aware of the risk of incomplete recovery for patients with a mild TBI (that is, GCS score of 15 and negative head CT scan) and providing accurate education and timely referral information before ED discharge,” they wrote.
The study was funded by grants from the National Foundation of Emergency Medicine, the National Institute of Neurological Disorders and Stroke, and the U.S. Department of Defense Traumatic Brain Injury Endpoints Development Initiative. Dr. Madhok has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new data from the TRACK-TBI study shows.
“Seeing that more than half of the GCS [Glasgow Coma Score] 15, CT-negative TBI cohort in our study were not back to their preinjury baseline at 6 months was surprising and impacts the millions of Americans who suffer from concussions annually,” said lead author Debbie Madhok, MD, with department of emergency medicine, University of California, San Francisco.
“These results highlight the importance of improving care pathways for concussion, particularly from the emergency department,” Dr. Madhok said.
The findings were published online in JAMA Network Open.
The short- and long-term outcomes in the large group of patients who come into the ED with TBI, a GCS of 15, and without acute intracranial traumatic injury (defined as a negative head CT scan) remain poorly understood, the investigators noted. To investigate further, they evaluated outcomes at 2 weeks and 6 months in 991 of these patients (mean age, 38 years; 64% men) from the TRACK-TBI study.
Among the 751 (76%) participants followed up at 2 weeks after the injury, only 204 (27%) had functional recovery – with a Glasgow Outcome Scale-Extended (GOS-E) score of 8. The remaining 547 (73%) had incomplete recovery (GOS-E scores < 8).
Among the 659 patients (66%) followed up at 6 months after the injury, 287 (44%) had functional recovery and 372 (56%) had incomplete recovery.
Most patients who failed to recover completely reported they had not returned to their preinjury life (88%). They described trouble returning to social activities outside the home and disruptions in family relationships and friendships.
The researchers noted that the study population had a high rate of preinjury psychiatric comorbidities, and these patients were more likely to have incomplete recovery than those without psychiatric comorbidities. This aligns with results from previous studies, they added.
The investigators also noted that patients with mild TBI without acute intracranial trauma are typically managed by ED personnel.
“These findings highlight the importance of ED clinicians being aware of the risk of incomplete recovery for patients with a mild TBI (that is, GCS score of 15 and negative head CT scan) and providing accurate education and timely referral information before ED discharge,” they wrote.
The study was funded by grants from the National Foundation of Emergency Medicine, the National Institute of Neurological Disorders and Stroke, and the U.S. Department of Defense Traumatic Brain Injury Endpoints Development Initiative. Dr. Madhok has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Leukemia rates two to three times higher in children born near fracking
Children born near fracking and other “unconventional” drilling sites are at two to three times greater risk of developing childhood leukemia, according to new research.
The study, published in the journal Environmental Health Perspectives, compared proximity of homes to unconventional oil and gas development (UOGD) sites and risk of the most common form of childhood leukemia, acute lymphoblastic leukemia (ALL).
Researchers looked at 405 children aged 2-7 diagnosed with ALL in Pennsylvania from 2009 to 2017. These children were compared to a control group of 2,080 without the disease matched on the year of birth.
“Unconventional oil and gas development can both use and release chemicals that have been linked to cancer,” study coauthor Nicole Deziel, PhD, of the Yale School of Public Health, New Haven, Conn., said in a statement . She noted that the possibility that children living in close proximity to such sites are “exposed to these chemical carcinogens is a major public health concern.”
About 17 million Americans live within a half-mile of active oil and gas production, according to the Oil & Gas Threat Map, Common Dreams reports. That number includes 4 million children.
The Yale study also found that drinking water could be an important pathway of exposure to oil- and gas-related chemicals used in the UOGD methods of extraction.
Researchers used a new metric that measures exposure to contaminated drinking water and distance to a well. They were able to identify UOGD-affected wells that fell within watersheds where children and their families likely obtained their water.
“Previous health studies have found links between proximity to oil and gas drilling and various children’s health outcomes,” said Dr. Deziel. “This study is among the few to focus on drinking water specifically and the first to apply a novel metric designed to capture potential exposure through this pathway.”
A version of this article first appeared on WebMD.com.
Children born near fracking and other “unconventional” drilling sites are at two to three times greater risk of developing childhood leukemia, according to new research.
The study, published in the journal Environmental Health Perspectives, compared proximity of homes to unconventional oil and gas development (UOGD) sites and risk of the most common form of childhood leukemia, acute lymphoblastic leukemia (ALL).
Researchers looked at 405 children aged 2-7 diagnosed with ALL in Pennsylvania from 2009 to 2017. These children were compared to a control group of 2,080 without the disease matched on the year of birth.
“Unconventional oil and gas development can both use and release chemicals that have been linked to cancer,” study coauthor Nicole Deziel, PhD, of the Yale School of Public Health, New Haven, Conn., said in a statement . She noted that the possibility that children living in close proximity to such sites are “exposed to these chemical carcinogens is a major public health concern.”
About 17 million Americans live within a half-mile of active oil and gas production, according to the Oil & Gas Threat Map, Common Dreams reports. That number includes 4 million children.
The Yale study also found that drinking water could be an important pathway of exposure to oil- and gas-related chemicals used in the UOGD methods of extraction.
Researchers used a new metric that measures exposure to contaminated drinking water and distance to a well. They were able to identify UOGD-affected wells that fell within watersheds where children and their families likely obtained their water.
“Previous health studies have found links between proximity to oil and gas drilling and various children’s health outcomes,” said Dr. Deziel. “This study is among the few to focus on drinking water specifically and the first to apply a novel metric designed to capture potential exposure through this pathway.”
A version of this article first appeared on WebMD.com.
Children born near fracking and other “unconventional” drilling sites are at two to three times greater risk of developing childhood leukemia, according to new research.
The study, published in the journal Environmental Health Perspectives, compared proximity of homes to unconventional oil and gas development (UOGD) sites and risk of the most common form of childhood leukemia, acute lymphoblastic leukemia (ALL).
Researchers looked at 405 children aged 2-7 diagnosed with ALL in Pennsylvania from 2009 to 2017. These children were compared to a control group of 2,080 without the disease matched on the year of birth.
“Unconventional oil and gas development can both use and release chemicals that have been linked to cancer,” study coauthor Nicole Deziel, PhD, of the Yale School of Public Health, New Haven, Conn., said in a statement . She noted that the possibility that children living in close proximity to such sites are “exposed to these chemical carcinogens is a major public health concern.”
About 17 million Americans live within a half-mile of active oil and gas production, according to the Oil & Gas Threat Map, Common Dreams reports. That number includes 4 million children.
The Yale study also found that drinking water could be an important pathway of exposure to oil- and gas-related chemicals used in the UOGD methods of extraction.
Researchers used a new metric that measures exposure to contaminated drinking water and distance to a well. They were able to identify UOGD-affected wells that fell within watersheds where children and their families likely obtained their water.
“Previous health studies have found links between proximity to oil and gas drilling and various children’s health outcomes,” said Dr. Deziel. “This study is among the few to focus on drinking water specifically and the first to apply a novel metric designed to capture potential exposure through this pathway.”
A version of this article first appeared on WebMD.com.
Are artificial sweeteners really harmless?
New research discounts the long-held notion that aspartame and other nonnutritive sweeteners (NNS) have no effect on the human body.
Researchers found that these sugar substitutes are not metabolically inert and can alter the gut microbiome in a way that can influence blood glucose levels.
The study was published online in the journal Cell.
Gut reaction?
Several years ago, a team led by Eran Elinav, MD, PhD, an immunologist and microbiome researcher at the Weizmann Institute of Science, Rehovot, Israel, observed that these sweeteners affect the microbiome of mice in ways that could affect glycemic responses.
They have now confirmed this observation in a randomized controlled trial with 120 healthy adults.
Each sweetener “significantly and distinctly” altered stool and oral microbiome, and two of them (saccharin and sucralose) significantly impaired glucose tolerance, the researchers reported.
“Importantly, by performing extensive fecal transplantation of human microbiomes into germ-free mice, we demonstrate a causal and individualized link between NNS-altered microbiomes and glucose intolerance developing in non–NNS-consuming recipient mice,” they said.
They noted that the effects of these sweeteners will likely vary from person to person because of the unique composition of an individual’s microbiome.
“We need to raise awareness of the fact that NNS are not inert to the human body as we originally believed. With that said, the clinical health implications of the changes they may elicit in humans remain unknown and merit future long-term studies,” Dr. Elinav said in a news release.
For now, Dr. Elinav said it’s his personal view that “drinking only water seems to be the best solution.”
Weighing the evidence
Several experts weighed in on the results in a statement from the U.K. nonprofit organization, Science Media Centre.
Duane Mellor, PhD, RD, RNutr, registered dietitian and senior teaching fellow, Aston University, Birmingham, England, notes that the study does not show a link between all NNS and higher blood glucose levels in the long term (only after a glucose tolerance test).
“It did suggest, though, that some individuals who do not normally consume sweeteners may not tolerate glucose as well after consuming six sachets of either saccharin or sucralose mixed with glucose per day,” Dr. Mellor says.
Kim Barrett, PhD, distinguished professor of physiology and membrane biology, University of California, Davis, concurs, saying “this well-designed study indicates the potential for NNS to have adverse effects in at least some individuals.”
The study also does not provide any information about how people who normally consume sweeteners or people with either type 1 or type 2 diabetes respond to NNS.
“Therefore, for some people, it is likely to be a better option and more sustainable approach to use sweeteners as a ‘stepping stone’ allowing them to reduce the amount of added sugar in foods and drinks, to reduce their sugar intake and still enjoy what they eat and drink, on the way to reducing both added sugar and sweeteners in their diet,” Dr. Mellor suggests.
Kevin McConway, PhD, with the Open University, Milton Keynes, England, said it’s “important to understand that the research is not saying that these sweeteners are worse for us, in heath terms, than sugar.
“But exactly what the health consequences of all this, if any, might be is a subject for future research,” Dr. McConway added.
Kathy Redfern, PhD, lecturer in human nutrition, University of Plymouth (England) agrees.
“We still have a lot to learn about the human microbiome, and although this study suggests two of the sweeteners tested in this study (sucralose and saccharin) significantly affected glucose tolerance, these deviations were small,” she says.
The International Sweeteners Association also weighs in, saying, “No conclusions about the effects of low/no calorie sweeteners on glucose control or overall health can be extrapolated from this study for the general population or for people who typically consume sweeteners, including people living with diabetes.”
They add “a recent review of the literature concluded that there is clear evidence that changes in the diet unrelated to low/no calorie sweeteners consumption are likely the major determinants of change in gut microbiota.”
Nevertheless, Dr. Redfern says the results “warrant further investigation to assess how small changes in glucose tolerance in response to NNS consumption may influence longer-term glucose tolerance and risk for metabolic complications, such as type 2 diabetes.”
The study had no specific funding. Dr. Elinav is a scientific founder of DayTwo and BiomX, a paid consultant to Hello Inside and Aposense, and a member of the scientific advisory board of Cell. Dr. Mellor has provided consultancy to the International Sweetener Agency and has worked on projects funded by the Food Standards Agency that investigated the health effects of aspartame. Dr. Barrett, Dr. McConway, and Dr. Redfern report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This article was updated 8/29/22.
New research discounts the long-held notion that aspartame and other nonnutritive sweeteners (NNS) have no effect on the human body.
Researchers found that these sugar substitutes are not metabolically inert and can alter the gut microbiome in a way that can influence blood glucose levels.
The study was published online in the journal Cell.
Gut reaction?
Several years ago, a team led by Eran Elinav, MD, PhD, an immunologist and microbiome researcher at the Weizmann Institute of Science, Rehovot, Israel, observed that these sweeteners affect the microbiome of mice in ways that could affect glycemic responses.
They have now confirmed this observation in a randomized controlled trial with 120 healthy adults.
Each sweetener “significantly and distinctly” altered stool and oral microbiome, and two of them (saccharin and sucralose) significantly impaired glucose tolerance, the researchers reported.
“Importantly, by performing extensive fecal transplantation of human microbiomes into germ-free mice, we demonstrate a causal and individualized link between NNS-altered microbiomes and glucose intolerance developing in non–NNS-consuming recipient mice,” they said.
They noted that the effects of these sweeteners will likely vary from person to person because of the unique composition of an individual’s microbiome.
“We need to raise awareness of the fact that NNS are not inert to the human body as we originally believed. With that said, the clinical health implications of the changes they may elicit in humans remain unknown and merit future long-term studies,” Dr. Elinav said in a news release.
For now, Dr. Elinav said it’s his personal view that “drinking only water seems to be the best solution.”
Weighing the evidence
Several experts weighed in on the results in a statement from the U.K. nonprofit organization, Science Media Centre.
Duane Mellor, PhD, RD, RNutr, registered dietitian and senior teaching fellow, Aston University, Birmingham, England, notes that the study does not show a link between all NNS and higher blood glucose levels in the long term (only after a glucose tolerance test).
“It did suggest, though, that some individuals who do not normally consume sweeteners may not tolerate glucose as well after consuming six sachets of either saccharin or sucralose mixed with glucose per day,” Dr. Mellor says.
Kim Barrett, PhD, distinguished professor of physiology and membrane biology, University of California, Davis, concurs, saying “this well-designed study indicates the potential for NNS to have adverse effects in at least some individuals.”
The study also does not provide any information about how people who normally consume sweeteners or people with either type 1 or type 2 diabetes respond to NNS.
“Therefore, for some people, it is likely to be a better option and more sustainable approach to use sweeteners as a ‘stepping stone’ allowing them to reduce the amount of added sugar in foods and drinks, to reduce their sugar intake and still enjoy what they eat and drink, on the way to reducing both added sugar and sweeteners in their diet,” Dr. Mellor suggests.
Kevin McConway, PhD, with the Open University, Milton Keynes, England, said it’s “important to understand that the research is not saying that these sweeteners are worse for us, in heath terms, than sugar.
“But exactly what the health consequences of all this, if any, might be is a subject for future research,” Dr. McConway added.
Kathy Redfern, PhD, lecturer in human nutrition, University of Plymouth (England) agrees.
“We still have a lot to learn about the human microbiome, and although this study suggests two of the sweeteners tested in this study (sucralose and saccharin) significantly affected glucose tolerance, these deviations were small,” she says.
The International Sweeteners Association also weighs in, saying, “No conclusions about the effects of low/no calorie sweeteners on glucose control or overall health can be extrapolated from this study for the general population or for people who typically consume sweeteners, including people living with diabetes.”
They add “a recent review of the literature concluded that there is clear evidence that changes in the diet unrelated to low/no calorie sweeteners consumption are likely the major determinants of change in gut microbiota.”
Nevertheless, Dr. Redfern says the results “warrant further investigation to assess how small changes in glucose tolerance in response to NNS consumption may influence longer-term glucose tolerance and risk for metabolic complications, such as type 2 diabetes.”
The study had no specific funding. Dr. Elinav is a scientific founder of DayTwo and BiomX, a paid consultant to Hello Inside and Aposense, and a member of the scientific advisory board of Cell. Dr. Mellor has provided consultancy to the International Sweetener Agency and has worked on projects funded by the Food Standards Agency that investigated the health effects of aspartame. Dr. Barrett, Dr. McConway, and Dr. Redfern report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This article was updated 8/29/22.
New research discounts the long-held notion that aspartame and other nonnutritive sweeteners (NNS) have no effect on the human body.
Researchers found that these sugar substitutes are not metabolically inert and can alter the gut microbiome in a way that can influence blood glucose levels.
The study was published online in the journal Cell.
Gut reaction?
Several years ago, a team led by Eran Elinav, MD, PhD, an immunologist and microbiome researcher at the Weizmann Institute of Science, Rehovot, Israel, observed that these sweeteners affect the microbiome of mice in ways that could affect glycemic responses.
They have now confirmed this observation in a randomized controlled trial with 120 healthy adults.
Each sweetener “significantly and distinctly” altered stool and oral microbiome, and two of them (saccharin and sucralose) significantly impaired glucose tolerance, the researchers reported.
“Importantly, by performing extensive fecal transplantation of human microbiomes into germ-free mice, we demonstrate a causal and individualized link between NNS-altered microbiomes and glucose intolerance developing in non–NNS-consuming recipient mice,” they said.
They noted that the effects of these sweeteners will likely vary from person to person because of the unique composition of an individual’s microbiome.
“We need to raise awareness of the fact that NNS are not inert to the human body as we originally believed. With that said, the clinical health implications of the changes they may elicit in humans remain unknown and merit future long-term studies,” Dr. Elinav said in a news release.
For now, Dr. Elinav said it’s his personal view that “drinking only water seems to be the best solution.”
Weighing the evidence
Several experts weighed in on the results in a statement from the U.K. nonprofit organization, Science Media Centre.
Duane Mellor, PhD, RD, RNutr, registered dietitian and senior teaching fellow, Aston University, Birmingham, England, notes that the study does not show a link between all NNS and higher blood glucose levels in the long term (only after a glucose tolerance test).
“It did suggest, though, that some individuals who do not normally consume sweeteners may not tolerate glucose as well after consuming six sachets of either saccharin or sucralose mixed with glucose per day,” Dr. Mellor says.
Kim Barrett, PhD, distinguished professor of physiology and membrane biology, University of California, Davis, concurs, saying “this well-designed study indicates the potential for NNS to have adverse effects in at least some individuals.”
The study also does not provide any information about how people who normally consume sweeteners or people with either type 1 or type 2 diabetes respond to NNS.
“Therefore, for some people, it is likely to be a better option and more sustainable approach to use sweeteners as a ‘stepping stone’ allowing them to reduce the amount of added sugar in foods and drinks, to reduce their sugar intake and still enjoy what they eat and drink, on the way to reducing both added sugar and sweeteners in their diet,” Dr. Mellor suggests.
Kevin McConway, PhD, with the Open University, Milton Keynes, England, said it’s “important to understand that the research is not saying that these sweeteners are worse for us, in heath terms, than sugar.
“But exactly what the health consequences of all this, if any, might be is a subject for future research,” Dr. McConway added.
Kathy Redfern, PhD, lecturer in human nutrition, University of Plymouth (England) agrees.
“We still have a lot to learn about the human microbiome, and although this study suggests two of the sweeteners tested in this study (sucralose and saccharin) significantly affected glucose tolerance, these deviations were small,” she says.
The International Sweeteners Association also weighs in, saying, “No conclusions about the effects of low/no calorie sweeteners on glucose control or overall health can be extrapolated from this study for the general population or for people who typically consume sweeteners, including people living with diabetes.”
They add “a recent review of the literature concluded that there is clear evidence that changes in the diet unrelated to low/no calorie sweeteners consumption are likely the major determinants of change in gut microbiota.”
Nevertheless, Dr. Redfern says the results “warrant further investigation to assess how small changes in glucose tolerance in response to NNS consumption may influence longer-term glucose tolerance and risk for metabolic complications, such as type 2 diabetes.”
The study had no specific funding. Dr. Elinav is a scientific founder of DayTwo and BiomX, a paid consultant to Hello Inside and Aposense, and a member of the scientific advisory board of Cell. Dr. Mellor has provided consultancy to the International Sweetener Agency and has worked on projects funded by the Food Standards Agency that investigated the health effects of aspartame. Dr. Barrett, Dr. McConway, and Dr. Redfern report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This article was updated 8/29/22.
Where women’s voices still get heard less
“Our study provides the first analysis of gender and early-career faculty disparities in speakers at hematology and medical oncology board review meetings,” the authors reported in research published in Blood Advances.
“We covered six major board reviews over the last 5 years that are either conducted yearly or every other year, [and] the general trend across all meetings showed skewness toward men speakers,” the authors reported.
Recent data from 2021 suggests a closing of the gender gap in oncology, with women making up 44.6% of oncologists in training. However, they still only represented 35.2% of practicing oncologists and are underrepresented in leadership positions in academic oncology, the authors reported.
With speaking roles at academic meetings potentially marking a key step in career advancement and improved opportunities, the authors sought to investigate the balance of gender, as well as early-career faculty among speakers at prominent hematology and/or oncology board review lecture series taking place in the United States between 2017 and 2021.
The five institutions and one society presenting the board review lecture series included Baylor College of Medicine/MD Anderson Cancer Center, both in Houston; Dana-Farber Brigham Cancer Center, Boston; George Washington University, Washington; Memorial Sloan Kettering Cancer Center, New York; Seattle Cancer Care Alliance; and the hematology board review series from the American Society of Hematology.
During the period in question, among 1,224 board review lectures presented, women constituted only 37.7% of the speakers. In lectures presented by American Board of Internal Medicine–certified speakers (n = 1,016, 83%), women were found to have made up fewer than 50% of speakers in five of six courses.
Men were also more likely to be recurrent speakers; across all courses, 13 men but only 2 women conducted 10 or more lectures. And while 35 men gave six or more lectures across all courses, only 12 women did so.
The lecture topics with the lowest rates of women presenters included malignant hematology (24.8%), solid tumors (38.9%), and benign hematology lectures (44.1%).
“We suspected [the imbalance in malignant hematology] since multiple recurrent roles were concentrated in the malignant hematology,” senior author Samer Al Hadidi, MD, of the Myeloma Center, Winthrop P. Rockefeller Cancer Institute, University of Arkansas for Medical Sciences, Little Rock, AK, said in an interview.
He noted that “there are no regulations that such courses need to follow to ensure certain proportions of women and junior faculty are involved.”
Early-career faculty
In terms of early-career representation, more than 50% of lectures were given by faculty who had received their initial certifications more than 15 years earlier. The median time from initial certification was 12.5 years for hematology and 14 years for medical oncology.
The findings that more than half of the board review lectures were presented by faculty with more than 15 years’ experience since initial certification “reflects a lack of appropriate involvement of early-career faculty, who arguably may have more recent experience with board certification,” the authors wrote.
While being underrepresented in such roles is detrimental, there are no regulations that such courses follow to ensure certain proportions of women and junior faculty are involved, Dr. Al Hadidi noted.
Equal representation remains elusive
The study does suggest some notable gains. In a previous study of 181 academic conferences in the United States and Canada between 2007 and 2017, the rate of women speakers was only 15%, compared with 37.7% in the new study.
And an overall trend analysis in the study shows an approximately 10% increase in representation of women in all of the board reviews. However, only the ASH hematology board review achieved more than 50% women in their two courses.
“Overall, the proportion of women speakers is improving over the years, though it remains suboptimal,” Dr. Al Hadidi said.
The authors noted that oncology is clearly not the only specialty with gender disparities. They documented a lack of women speakers at conferences involving otolaryngology head and neck meetings, radiation oncology, emergency medicine, and research conferences.
They pointed to the work of ASH’s Women in Hematology Working Group as an important example of the needed effort to improve the balance of women hematologists.
Ariela Marshall, MD, director of women’s thrombosis and hemostasis at Penn Medicine in Philadelphia and a leader of ASH’s Women in Hematology Working Group, agreed that more efforts are needed to address both gender disparities as well as those of early career speakers. She asserted that the two disparities appear to be connected.
“If you broke down gender representation over time and the faculty/time since initial certification, the findings may mirror the percent of women in hematology-oncology at that given point in time,” Dr. Marshall said in an interview.
“If an institution is truly committed to taking action on gender equity, it needs to look at gender and experience equity of speakers,” she said. “Perhaps it’s the time to say ‘Dr. X has been doing this review course for 15 years. Let’s give someone else a chance.’
“This is not even just from a gender equity perspective but from a career development perspective overall,” she added. “Junior faculty need these speaking engagements a lot more than senior faculty.”
Meanwhile, the higher number of female trainees is a trend that ideally will be sustained as those trainees move into positions of leadership, Dr. Marshall noted.
“We do see that over time, we have achieved gender equity in the percent of women matriculating to medical school. And my hope is that, 20 years down the line, we will see the effects of this reflected in increased equity in leadership positions such as division/department chair, dean, and hospital CEO,” she said. “However, we have a lot of work to do because there are still huge inequities in the culture of medicine (institutional and more broadly), including gender-based discrimination, maternal discrimination, and high attrition rates for women physicians, compared to male physicians.
“It’s not enough to simply say ‘well, we have fixed the problem because our incoming medical student classes are now equitable in gender distribution,’ ”
The authors and Dr. Marshall had no disclosures to report.
“Our study provides the first analysis of gender and early-career faculty disparities in speakers at hematology and medical oncology board review meetings,” the authors reported in research published in Blood Advances.
“We covered six major board reviews over the last 5 years that are either conducted yearly or every other year, [and] the general trend across all meetings showed skewness toward men speakers,” the authors reported.
Recent data from 2021 suggests a closing of the gender gap in oncology, with women making up 44.6% of oncologists in training. However, they still only represented 35.2% of practicing oncologists and are underrepresented in leadership positions in academic oncology, the authors reported.
With speaking roles at academic meetings potentially marking a key step in career advancement and improved opportunities, the authors sought to investigate the balance of gender, as well as early-career faculty among speakers at prominent hematology and/or oncology board review lecture series taking place in the United States between 2017 and 2021.
The five institutions and one society presenting the board review lecture series included Baylor College of Medicine/MD Anderson Cancer Center, both in Houston; Dana-Farber Brigham Cancer Center, Boston; George Washington University, Washington; Memorial Sloan Kettering Cancer Center, New York; Seattle Cancer Care Alliance; and the hematology board review series from the American Society of Hematology.
During the period in question, among 1,224 board review lectures presented, women constituted only 37.7% of the speakers. In lectures presented by American Board of Internal Medicine–certified speakers (n = 1,016, 83%), women were found to have made up fewer than 50% of speakers in five of six courses.
Men were also more likely to be recurrent speakers; across all courses, 13 men but only 2 women conducted 10 or more lectures. And while 35 men gave six or more lectures across all courses, only 12 women did so.
The lecture topics with the lowest rates of women presenters included malignant hematology (24.8%), solid tumors (38.9%), and benign hematology lectures (44.1%).
“We suspected [the imbalance in malignant hematology] since multiple recurrent roles were concentrated in the malignant hematology,” senior author Samer Al Hadidi, MD, of the Myeloma Center, Winthrop P. Rockefeller Cancer Institute, University of Arkansas for Medical Sciences, Little Rock, AK, said in an interview.
He noted that “there are no regulations that such courses need to follow to ensure certain proportions of women and junior faculty are involved.”
Early-career faculty
In terms of early-career representation, more than 50% of lectures were given by faculty who had received their initial certifications more than 15 years earlier. The median time from initial certification was 12.5 years for hematology and 14 years for medical oncology.
The findings that more than half of the board review lectures were presented by faculty with more than 15 years’ experience since initial certification “reflects a lack of appropriate involvement of early-career faculty, who arguably may have more recent experience with board certification,” the authors wrote.
While being underrepresented in such roles is detrimental, there are no regulations that such courses follow to ensure certain proportions of women and junior faculty are involved, Dr. Al Hadidi noted.
Equal representation remains elusive
The study does suggest some notable gains. In a previous study of 181 academic conferences in the United States and Canada between 2007 and 2017, the rate of women speakers was only 15%, compared with 37.7% in the new study.
And an overall trend analysis in the study shows an approximately 10% increase in representation of women in all of the board reviews. However, only the ASH hematology board review achieved more than 50% women in their two courses.
“Overall, the proportion of women speakers is improving over the years, though it remains suboptimal,” Dr. Al Hadidi said.
The authors noted that oncology is clearly not the only specialty with gender disparities. They documented a lack of women speakers at conferences involving otolaryngology head and neck meetings, radiation oncology, emergency medicine, and research conferences.
They pointed to the work of ASH’s Women in Hematology Working Group as an important example of the needed effort to improve the balance of women hematologists.
Ariela Marshall, MD, director of women’s thrombosis and hemostasis at Penn Medicine in Philadelphia and a leader of ASH’s Women in Hematology Working Group, agreed that more efforts are needed to address both gender disparities as well as those of early career speakers. She asserted that the two disparities appear to be connected.
“If you broke down gender representation over time and the faculty/time since initial certification, the findings may mirror the percent of women in hematology-oncology at that given point in time,” Dr. Marshall said in an interview.
“If an institution is truly committed to taking action on gender equity, it needs to look at gender and experience equity of speakers,” she said. “Perhaps it’s the time to say ‘Dr. X has been doing this review course for 15 years. Let’s give someone else a chance.’
“This is not even just from a gender equity perspective but from a career development perspective overall,” she added. “Junior faculty need these speaking engagements a lot more than senior faculty.”
Meanwhile, the higher number of female trainees is a trend that ideally will be sustained as those trainees move into positions of leadership, Dr. Marshall noted.
“We do see that over time, we have achieved gender equity in the percent of women matriculating to medical school. And my hope is that, 20 years down the line, we will see the effects of this reflected in increased equity in leadership positions such as division/department chair, dean, and hospital CEO,” she said. “However, we have a lot of work to do because there are still huge inequities in the culture of medicine (institutional and more broadly), including gender-based discrimination, maternal discrimination, and high attrition rates for women physicians, compared to male physicians.
“It’s not enough to simply say ‘well, we have fixed the problem because our incoming medical student classes are now equitable in gender distribution,’ ”
The authors and Dr. Marshall had no disclosures to report.
“Our study provides the first analysis of gender and early-career faculty disparities in speakers at hematology and medical oncology board review meetings,” the authors reported in research published in Blood Advances.
“We covered six major board reviews over the last 5 years that are either conducted yearly or every other year, [and] the general trend across all meetings showed skewness toward men speakers,” the authors reported.
Recent data from 2021 suggests a closing of the gender gap in oncology, with women making up 44.6% of oncologists in training. However, they still only represented 35.2% of practicing oncologists and are underrepresented in leadership positions in academic oncology, the authors reported.
With speaking roles at academic meetings potentially marking a key step in career advancement and improved opportunities, the authors sought to investigate the balance of gender, as well as early-career faculty among speakers at prominent hematology and/or oncology board review lecture series taking place in the United States between 2017 and 2021.
The five institutions and one society presenting the board review lecture series included Baylor College of Medicine/MD Anderson Cancer Center, both in Houston; Dana-Farber Brigham Cancer Center, Boston; George Washington University, Washington; Memorial Sloan Kettering Cancer Center, New York; Seattle Cancer Care Alliance; and the hematology board review series from the American Society of Hematology.
During the period in question, among 1,224 board review lectures presented, women constituted only 37.7% of the speakers. In lectures presented by American Board of Internal Medicine–certified speakers (n = 1,016, 83%), women were found to have made up fewer than 50% of speakers in five of six courses.
Men were also more likely to be recurrent speakers; across all courses, 13 men but only 2 women conducted 10 or more lectures. And while 35 men gave six or more lectures across all courses, only 12 women did so.
The lecture topics with the lowest rates of women presenters included malignant hematology (24.8%), solid tumors (38.9%), and benign hematology lectures (44.1%).
“We suspected [the imbalance in malignant hematology] since multiple recurrent roles were concentrated in the malignant hematology,” senior author Samer Al Hadidi, MD, of the Myeloma Center, Winthrop P. Rockefeller Cancer Institute, University of Arkansas for Medical Sciences, Little Rock, AK, said in an interview.
He noted that “there are no regulations that such courses need to follow to ensure certain proportions of women and junior faculty are involved.”
Early-career faculty
In terms of early-career representation, more than 50% of lectures were given by faculty who had received their initial certifications more than 15 years earlier. The median time from initial certification was 12.5 years for hematology and 14 years for medical oncology.
The findings that more than half of the board review lectures were presented by faculty with more than 15 years’ experience since initial certification “reflects a lack of appropriate involvement of early-career faculty, who arguably may have more recent experience with board certification,” the authors wrote.
While being underrepresented in such roles is detrimental, there are no regulations that such courses follow to ensure certain proportions of women and junior faculty are involved, Dr. Al Hadidi noted.
Equal representation remains elusive
The study does suggest some notable gains. In a previous study of 181 academic conferences in the United States and Canada between 2007 and 2017, the rate of women speakers was only 15%, compared with 37.7% in the new study.
And an overall trend analysis in the study shows an approximately 10% increase in representation of women in all of the board reviews. However, only the ASH hematology board review achieved more than 50% women in their two courses.
“Overall, the proportion of women speakers is improving over the years, though it remains suboptimal,” Dr. Al Hadidi said.
The authors noted that oncology is clearly not the only specialty with gender disparities. They documented a lack of women speakers at conferences involving otolaryngology head and neck meetings, radiation oncology, emergency medicine, and research conferences.
They pointed to the work of ASH’s Women in Hematology Working Group as an important example of the needed effort to improve the balance of women hematologists.
Ariela Marshall, MD, director of women’s thrombosis and hemostasis at Penn Medicine in Philadelphia and a leader of ASH’s Women in Hematology Working Group, agreed that more efforts are needed to address both gender disparities as well as those of early career speakers. She asserted that the two disparities appear to be connected.
“If you broke down gender representation over time and the faculty/time since initial certification, the findings may mirror the percent of women in hematology-oncology at that given point in time,” Dr. Marshall said in an interview.
“If an institution is truly committed to taking action on gender equity, it needs to look at gender and experience equity of speakers,” she said. “Perhaps it’s the time to say ‘Dr. X has been doing this review course for 15 years. Let’s give someone else a chance.’
“This is not even just from a gender equity perspective but from a career development perspective overall,” she added. “Junior faculty need these speaking engagements a lot more than senior faculty.”
Meanwhile, the higher number of female trainees is a trend that ideally will be sustained as those trainees move into positions of leadership, Dr. Marshall noted.
“We do see that over time, we have achieved gender equity in the percent of women matriculating to medical school. And my hope is that, 20 years down the line, we will see the effects of this reflected in increased equity in leadership positions such as division/department chair, dean, and hospital CEO,” she said. “However, we have a lot of work to do because there are still huge inequities in the culture of medicine (institutional and more broadly), including gender-based discrimination, maternal discrimination, and high attrition rates for women physicians, compared to male physicians.
“It’s not enough to simply say ‘well, we have fixed the problem because our incoming medical student classes are now equitable in gender distribution,’ ”
The authors and Dr. Marshall had no disclosures to report.
FROM BLOOD ADVANCES
AML’s seasonal peak suggests viral or environmental etiology
Most diagnoses of acute myeloid leukemia (AML) are made during January. This finding strongly implies that seasonal factors, such as infectious agents or environmental triggers, influence the development or proliferation of the disease, which points to prevention opportunities. This was the conclusion of an international study led by a team from the Jiménez Díaz Foundation University Hospital Health Research Institute (IIS-FJD) in Madrid, in collaboration with colleagues from the University of Bristol, England. Their work was published in the British Journal of Haematology.
The study’s aim was to investigate the potential seasonal and long-term trends in AML diagnosis in an overall population and in subgroups according to sex and age. To do so, the researchers examined 26,472 cases of AML diagnosed in Spain between 2004 and 2015. They found seasonality in the diagnosis of this type of leukemia. This “could point to there being an underlying seasonal etiology at play,” noted one of the main authors of the study, Juan Manuel Alonso, MD, a physician in the IIS-FJD’s department of hematology and hemotherapy.
“The environmental triggers involved could be radiation, pollution, allergens, or infectious agents like viruses. We’re leaning toward viruses, because there are already distinct solid tumor and hematologic cancers that are caused by them and because, in the winter months, there’s an increased incidence of cancers due to viral infections,” Dr. Alonso said in an interview. “The etiological mechanism should be different from that exerted by chronic viral pressure, because here we’re dealing with an acute and aggressive disease that probably needs a short incubation period.”
Various hypotheses
In an interview, David Martínez, MD, a hematologist at La Fe University Hospital in Valencia, Spain, described the research as “an extremely well done and much-discussed study on AML, a disease that appears to be diagnosed more frequently at a certain time of year – namely, January.
“There’s no clear explanation for this finding,” Dr. Martínez said. “Several possible reasons have been put forward and are being talked about. The one that seems to hold the most water is the hypothesis that infectious agents and environmental factors may have a greater influence. This is because the idea that they’re involved in neoplastic diseases is nothing new. In fact, there are a lot of publications and a good amount of scientific evidence that link viral infections and environmental factors with the development of oncologic diseases.”
AML is a rare disease yet is responsible for many cancer-related deaths. Mutations that cause AML can occur due to an inherited mutant gene or exposure to certain carcinogens, such as chemotherapy, radiotherapy, ionizing radiation, tobacco, and benzene. These findings are broadly similar to those of a large U.S.-based study by Calip et al., who found a peak of adult AML diagnoses during December and January from 1992 to 2008. Previous smaller studies have provided conflicting evidence, likely due to lower power or to the use of less advanced statistical approaches.
Seasonal factors involved?
Demonstration of seasonal variation in the occurrence of AML would, firstly, provide supportive evidence of etiology by seasonal factors, such as infectious agents or environmental factors, and, secondly, focus research onto the etiologic role of such factors.
The current study used population-based data on cases of AML occurring in Spain from a nationwide hospital discharge registry for the years 2004 to 2015. “This is, to our knowledge, the largest study aimed at investigating the potential seasonal and long-term trends in AML incidence in an overall population and in subgroups according to sex and age while employing novel statistical models with serial dependence for discrete-valued time series,” wrote the researchers.
They extracted information from the register of each case about the date of admission, discharge date, the anonymous identifier for each patient, International Classification of Diseases (ICD)–9 codes, sex, and date of birth, from which they derived age groups as described for the at-risk population. For patients hospitalized on more than one occasion, only the record corresponding to their first diagnosis of AML was selected.
AML cases per month were standardized to months of equal length.
Age/sex-standardized monthly incidence rates of AML were calculated using the census of Spanish population in 2010 as a “standard” population. Age-standardized and sex-standardized monthly incidence rates of AML were calculated.
Nine separate time-series decompositions were performed as an initial exploratory analysis on the monthly incidence rates of AML using data for all cases and data for each sex and age group. Nine separate Poisson generalized linear autoregressive moving average (GLARMA) models were fitted to evaluate the temporal dynamics in AML incidence using data for all cases, and data for each sex and age group.
Long-term trend
A total of 26,472 patients with a first diagnosis of active AML were hospitalized in Spain and registered at the country’s Minimum Basic Data Set (CMBD) during 2004-2015. In the end, there were 26,475 patients in the study population; a greater proportion of cases were male (56.0%), and the median age at diagnosis was 67 years.
Seasonal and trend decomposition using Loess decomposition of the incidence rates observed in the overall population exhibited seasonal fluctuation with a peak in January. A slight upward trend was apparent from visual inspection with an upturn in early 2005 and a downturn at the end of 2013. As for the differences by sex groups and age groups, Dr. Alonso said, “For both sexes and in age groups 5-19, 20-49, and 50-64 years, we found that the results were identical to those found in the overall population.”
The final model included an upward linear long-term trend, as well as the variables monthly seasonality and December 2015. The estimated monthly long-term trend implies that the monthly incidence rates of AML diagnoses annually increased by 0.4% (95% confidence interval [CI], 0.2%-0.6%; P = .0011), given that the other covariates are held constant.
January displayed the highest incidence rate of AML, with a minimum average difference of 7%, when compared with February (95% CI, 2%-12%; P = .0143) and a maximum average difference of 16%, compared with November (95% CI, 11%-21%; P < .0001) and August (95% CI, 10%-21%; P < .0001).
The incidence rate of AML for December 2015 was 0.43 (95% CI, 0.34-0.54; P < .0001) times the average incidence rate for the rest of the study period.
Potential role of viruses
“We have to keep in mind that infectious agents (viral infections) and environmental factors (allergens) don’t disappear in the warmer months,” Dr. Martínez added. “There are just other viruses and different factors. We don’t know the role or the weight that each one of the factors has, either individually or specifically, in the development of AML. In addition, we know that AML is a very heterogeneous disease and that various factors, including genetic ones, can be involved in its etiopathogenesis.”
With respect to the stem cell theory in this leukemia, Dr. Alonso emphasized that, “in theory, the virus could fit into it with no problem. That said, any other environmental agent could also produce the described phenomenon where the rapid proliferation of quiescent leukemic stem cells is stimulated, thereby hastening the diagnosis.”
“Should the etiological factor be found,” Dr. Martínez noted, “we can try to reduce exposure and thereby decrease the incidence of AML. On the other hand, discovering how the environmental factor stimulates the proliferation of quiescent leukemic [stem] cells could enhance our knowledge about the regulation of that.”
As to whether there is evidence for the involvement of infections in other hematologic malignancies, Dr. Martínez reported, “This has already been seen. And this study shows other examples (Epstein-Barr virus and human T-cell lymphotropic virus type 1 with lymphomas), and there could also be Helicobacter pylori and lymphomas.”
Outside of hematology, human papillomavirus has been associated with cervical cancer, tobacco with lung cancer, sun with skin cancer, and diet with the development of some solid neoplasms.
“The study speaks about the concept of a latency period. To accept the idea that a factor or virus that’s more prevalent in winter produces, on its own, AML in a few weeks or months means accepting the idea of a very short latency period – something that’s not usually the case. For that, another explanation is given: An abnormal immune response or that a seasonal infectious agent can be capable of promoting leukemogenesis. These are also hypotheses to be explored in the future,” suggested Dr. Martínez.
New research network
Several potential limitations of this study should be considered. One limitation is that AML cases were obtained from the CMBD registry as defined by ICD-9, and no other AML classifications were available. Another limitation is that information on the date of onset of clinical symptoms was not available for analysis. In addition, a further limitation related to the source of their data may have led the researchers to underestimate the incidence rates of AML in older patients, as only hospitalized patients were captured in their study.
As for continuing the research, the results make it necessary to carry out complementary epidemiologic studies that will examine the association between seasonal risk factors and the increased diagnosis of AML during winter months.
To go forward, the first step would be to secure funding. For this purpose, a network is being put together featuring collaborators from other world-renowned research groups that are at the top of their respective disciplines. Through this network, they hope to be able to apply together for public research grants from countries in Europe and elsewhere as well as to establish collaborations with various companies in the private sector.
“This could open up new therapeutic avenues in the future, as we could try to force leukemic stem cells to divide, thereby reducing the resistance that the standard treatments usually demonstrate,” Dr. Alonso concluded.
Dr. Alonso received research funding from Incyte, Pfizer International, and Astellas Pharma outside the present work. Dr. Martínez disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish edition. A version of the article appeared on Medscape.com.
Most diagnoses of acute myeloid leukemia (AML) are made during January. This finding strongly implies that seasonal factors, such as infectious agents or environmental triggers, influence the development or proliferation of the disease, which points to prevention opportunities. This was the conclusion of an international study led by a team from the Jiménez Díaz Foundation University Hospital Health Research Institute (IIS-FJD) in Madrid, in collaboration with colleagues from the University of Bristol, England. Their work was published in the British Journal of Haematology.
The study’s aim was to investigate the potential seasonal and long-term trends in AML diagnosis in an overall population and in subgroups according to sex and age. To do so, the researchers examined 26,472 cases of AML diagnosed in Spain between 2004 and 2015. They found seasonality in the diagnosis of this type of leukemia. This “could point to there being an underlying seasonal etiology at play,” noted one of the main authors of the study, Juan Manuel Alonso, MD, a physician in the IIS-FJD’s department of hematology and hemotherapy.
“The environmental triggers involved could be radiation, pollution, allergens, or infectious agents like viruses. We’re leaning toward viruses, because there are already distinct solid tumor and hematologic cancers that are caused by them and because, in the winter months, there’s an increased incidence of cancers due to viral infections,” Dr. Alonso said in an interview. “The etiological mechanism should be different from that exerted by chronic viral pressure, because here we’re dealing with an acute and aggressive disease that probably needs a short incubation period.”
Various hypotheses
In an interview, David Martínez, MD, a hematologist at La Fe University Hospital in Valencia, Spain, described the research as “an extremely well done and much-discussed study on AML, a disease that appears to be diagnosed more frequently at a certain time of year – namely, January.
“There’s no clear explanation for this finding,” Dr. Martínez said. “Several possible reasons have been put forward and are being talked about. The one that seems to hold the most water is the hypothesis that infectious agents and environmental factors may have a greater influence. This is because the idea that they’re involved in neoplastic diseases is nothing new. In fact, there are a lot of publications and a good amount of scientific evidence that link viral infections and environmental factors with the development of oncologic diseases.”
AML is a rare disease yet is responsible for many cancer-related deaths. Mutations that cause AML can occur due to an inherited mutant gene or exposure to certain carcinogens, such as chemotherapy, radiotherapy, ionizing radiation, tobacco, and benzene. These findings are broadly similar to those of a large U.S.-based study by Calip et al., who found a peak of adult AML diagnoses during December and January from 1992 to 2008. Previous smaller studies have provided conflicting evidence, likely due to lower power or to the use of less advanced statistical approaches.
Seasonal factors involved?
Demonstration of seasonal variation in the occurrence of AML would, firstly, provide supportive evidence of etiology by seasonal factors, such as infectious agents or environmental factors, and, secondly, focus research onto the etiologic role of such factors.
The current study used population-based data on cases of AML occurring in Spain from a nationwide hospital discharge registry for the years 2004 to 2015. “This is, to our knowledge, the largest study aimed at investigating the potential seasonal and long-term trends in AML incidence in an overall population and in subgroups according to sex and age while employing novel statistical models with serial dependence for discrete-valued time series,” wrote the researchers.
They extracted information from the register of each case about the date of admission, discharge date, the anonymous identifier for each patient, International Classification of Diseases (ICD)–9 codes, sex, and date of birth, from which they derived age groups as described for the at-risk population. For patients hospitalized on more than one occasion, only the record corresponding to their first diagnosis of AML was selected.
AML cases per month were standardized to months of equal length.
Age/sex-standardized monthly incidence rates of AML were calculated using the census of Spanish population in 2010 as a “standard” population. Age-standardized and sex-standardized monthly incidence rates of AML were calculated.
Nine separate time-series decompositions were performed as an initial exploratory analysis on the monthly incidence rates of AML using data for all cases and data for each sex and age group. Nine separate Poisson generalized linear autoregressive moving average (GLARMA) models were fitted to evaluate the temporal dynamics in AML incidence using data for all cases, and data for each sex and age group.
Long-term trend
A total of 26,472 patients with a first diagnosis of active AML were hospitalized in Spain and registered at the country’s Minimum Basic Data Set (CMBD) during 2004-2015. In the end, there were 26,475 patients in the study population; a greater proportion of cases were male (56.0%), and the median age at diagnosis was 67 years.
Seasonal and trend decomposition using Loess decomposition of the incidence rates observed in the overall population exhibited seasonal fluctuation with a peak in January. A slight upward trend was apparent from visual inspection with an upturn in early 2005 and a downturn at the end of 2013. As for the differences by sex groups and age groups, Dr. Alonso said, “For both sexes and in age groups 5-19, 20-49, and 50-64 years, we found that the results were identical to those found in the overall population.”
The final model included an upward linear long-term trend, as well as the variables monthly seasonality and December 2015. The estimated monthly long-term trend implies that the monthly incidence rates of AML diagnoses annually increased by 0.4% (95% confidence interval [CI], 0.2%-0.6%; P = .0011), given that the other covariates are held constant.
January displayed the highest incidence rate of AML, with a minimum average difference of 7%, when compared with February (95% CI, 2%-12%; P = .0143) and a maximum average difference of 16%, compared with November (95% CI, 11%-21%; P < .0001) and August (95% CI, 10%-21%; P < .0001).
The incidence rate of AML for December 2015 was 0.43 (95% CI, 0.34-0.54; P < .0001) times the average incidence rate for the rest of the study period.
Potential role of viruses
“We have to keep in mind that infectious agents (viral infections) and environmental factors (allergens) don’t disappear in the warmer months,” Dr. Martínez added. “There are just other viruses and different factors. We don’t know the role or the weight that each one of the factors has, either individually or specifically, in the development of AML. In addition, we know that AML is a very heterogeneous disease and that various factors, including genetic ones, can be involved in its etiopathogenesis.”
With respect to the stem cell theory in this leukemia, Dr. Alonso emphasized that, “in theory, the virus could fit into it with no problem. That said, any other environmental agent could also produce the described phenomenon where the rapid proliferation of quiescent leukemic stem cells is stimulated, thereby hastening the diagnosis.”
“Should the etiological factor be found,” Dr. Martínez noted, “we can try to reduce exposure and thereby decrease the incidence of AML. On the other hand, discovering how the environmental factor stimulates the proliferation of quiescent leukemic [stem] cells could enhance our knowledge about the regulation of that.”
As to whether there is evidence for the involvement of infections in other hematologic malignancies, Dr. Martínez reported, “This has already been seen. And this study shows other examples (Epstein-Barr virus and human T-cell lymphotropic virus type 1 with lymphomas), and there could also be Helicobacter pylori and lymphomas.”
Outside of hematology, human papillomavirus has been associated with cervical cancer, tobacco with lung cancer, sun with skin cancer, and diet with the development of some solid neoplasms.
“The study speaks about the concept of a latency period. To accept the idea that a factor or virus that’s more prevalent in winter produces, on its own, AML in a few weeks or months means accepting the idea of a very short latency period – something that’s not usually the case. For that, another explanation is given: An abnormal immune response or that a seasonal infectious agent can be capable of promoting leukemogenesis. These are also hypotheses to be explored in the future,” suggested Dr. Martínez.
New research network
Several potential limitations of this study should be considered. One limitation is that AML cases were obtained from the CMBD registry as defined by ICD-9, and no other AML classifications were available. Another limitation is that information on the date of onset of clinical symptoms was not available for analysis. In addition, a further limitation related to the source of their data may have led the researchers to underestimate the incidence rates of AML in older patients, as only hospitalized patients were captured in their study.
As for continuing the research, the results make it necessary to carry out complementary epidemiologic studies that will examine the association between seasonal risk factors and the increased diagnosis of AML during winter months.
To go forward, the first step would be to secure funding. For this purpose, a network is being put together featuring collaborators from other world-renowned research groups that are at the top of their respective disciplines. Through this network, they hope to be able to apply together for public research grants from countries in Europe and elsewhere as well as to establish collaborations with various companies in the private sector.
“This could open up new therapeutic avenues in the future, as we could try to force leukemic stem cells to divide, thereby reducing the resistance that the standard treatments usually demonstrate,” Dr. Alonso concluded.
Dr. Alonso received research funding from Incyte, Pfizer International, and Astellas Pharma outside the present work. Dr. Martínez disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish edition. A version of the article appeared on Medscape.com.
Most diagnoses of acute myeloid leukemia (AML) are made during January. This finding strongly implies that seasonal factors, such as infectious agents or environmental triggers, influence the development or proliferation of the disease, which points to prevention opportunities. This was the conclusion of an international study led by a team from the Jiménez Díaz Foundation University Hospital Health Research Institute (IIS-FJD) in Madrid, in collaboration with colleagues from the University of Bristol, England. Their work was published in the British Journal of Haematology.
The study’s aim was to investigate the potential seasonal and long-term trends in AML diagnosis in an overall population and in subgroups according to sex and age. To do so, the researchers examined 26,472 cases of AML diagnosed in Spain between 2004 and 2015. They found seasonality in the diagnosis of this type of leukemia. This “could point to there being an underlying seasonal etiology at play,” noted one of the main authors of the study, Juan Manuel Alonso, MD, a physician in the IIS-FJD’s department of hematology and hemotherapy.
“The environmental triggers involved could be radiation, pollution, allergens, or infectious agents like viruses. We’re leaning toward viruses, because there are already distinct solid tumor and hematologic cancers that are caused by them and because, in the winter months, there’s an increased incidence of cancers due to viral infections,” Dr. Alonso said in an interview. “The etiological mechanism should be different from that exerted by chronic viral pressure, because here we’re dealing with an acute and aggressive disease that probably needs a short incubation period.”
Various hypotheses
In an interview, David Martínez, MD, a hematologist at La Fe University Hospital in Valencia, Spain, described the research as “an extremely well done and much-discussed study on AML, a disease that appears to be diagnosed more frequently at a certain time of year – namely, January.
“There’s no clear explanation for this finding,” Dr. Martínez said. “Several possible reasons have been put forward and are being talked about. The one that seems to hold the most water is the hypothesis that infectious agents and environmental factors may have a greater influence. This is because the idea that they’re involved in neoplastic diseases is nothing new. In fact, there are a lot of publications and a good amount of scientific evidence that link viral infections and environmental factors with the development of oncologic diseases.”
AML is a rare disease yet is responsible for many cancer-related deaths. Mutations that cause AML can occur due to an inherited mutant gene or exposure to certain carcinogens, such as chemotherapy, radiotherapy, ionizing radiation, tobacco, and benzene. These findings are broadly similar to those of a large U.S.-based study by Calip et al., who found a peak of adult AML diagnoses during December and January from 1992 to 2008. Previous smaller studies have provided conflicting evidence, likely due to lower power or to the use of less advanced statistical approaches.
Seasonal factors involved?
Demonstration of seasonal variation in the occurrence of AML would, firstly, provide supportive evidence of etiology by seasonal factors, such as infectious agents or environmental factors, and, secondly, focus research onto the etiologic role of such factors.
The current study used population-based data on cases of AML occurring in Spain from a nationwide hospital discharge registry for the years 2004 to 2015. “This is, to our knowledge, the largest study aimed at investigating the potential seasonal and long-term trends in AML incidence in an overall population and in subgroups according to sex and age while employing novel statistical models with serial dependence for discrete-valued time series,” wrote the researchers.
They extracted information from the register of each case about the date of admission, discharge date, the anonymous identifier for each patient, International Classification of Diseases (ICD)–9 codes, sex, and date of birth, from which they derived age groups as described for the at-risk population. For patients hospitalized on more than one occasion, only the record corresponding to their first diagnosis of AML was selected.
AML cases per month were standardized to months of equal length.
Age/sex-standardized monthly incidence rates of AML were calculated using the census of Spanish population in 2010 as a “standard” population. Age-standardized and sex-standardized monthly incidence rates of AML were calculated.
Nine separate time-series decompositions were performed as an initial exploratory analysis on the monthly incidence rates of AML using data for all cases and data for each sex and age group. Nine separate Poisson generalized linear autoregressive moving average (GLARMA) models were fitted to evaluate the temporal dynamics in AML incidence using data for all cases, and data for each sex and age group.
Long-term trend
A total of 26,472 patients with a first diagnosis of active AML were hospitalized in Spain and registered at the country’s Minimum Basic Data Set (CMBD) during 2004-2015. In the end, there were 26,475 patients in the study population; a greater proportion of cases were male (56.0%), and the median age at diagnosis was 67 years.
Seasonal and trend decomposition using Loess decomposition of the incidence rates observed in the overall population exhibited seasonal fluctuation with a peak in January. A slight upward trend was apparent from visual inspection with an upturn in early 2005 and a downturn at the end of 2013. As for the differences by sex groups and age groups, Dr. Alonso said, “For both sexes and in age groups 5-19, 20-49, and 50-64 years, we found that the results were identical to those found in the overall population.”
The final model included an upward linear long-term trend, as well as the variables monthly seasonality and December 2015. The estimated monthly long-term trend implies that the monthly incidence rates of AML diagnoses annually increased by 0.4% (95% confidence interval [CI], 0.2%-0.6%; P = .0011), given that the other covariates are held constant.
January displayed the highest incidence rate of AML, with a minimum average difference of 7%, when compared with February (95% CI, 2%-12%; P = .0143) and a maximum average difference of 16%, compared with November (95% CI, 11%-21%; P < .0001) and August (95% CI, 10%-21%; P < .0001).
The incidence rate of AML for December 2015 was 0.43 (95% CI, 0.34-0.54; P < .0001) times the average incidence rate for the rest of the study period.
Potential role of viruses
“We have to keep in mind that infectious agents (viral infections) and environmental factors (allergens) don’t disappear in the warmer months,” Dr. Martínez added. “There are just other viruses and different factors. We don’t know the role or the weight that each one of the factors has, either individually or specifically, in the development of AML. In addition, we know that AML is a very heterogeneous disease and that various factors, including genetic ones, can be involved in its etiopathogenesis.”
With respect to the stem cell theory in this leukemia, Dr. Alonso emphasized that, “in theory, the virus could fit into it with no problem. That said, any other environmental agent could also produce the described phenomenon where the rapid proliferation of quiescent leukemic stem cells is stimulated, thereby hastening the diagnosis.”
“Should the etiological factor be found,” Dr. Martínez noted, “we can try to reduce exposure and thereby decrease the incidence of AML. On the other hand, discovering how the environmental factor stimulates the proliferation of quiescent leukemic [stem] cells could enhance our knowledge about the regulation of that.”
As to whether there is evidence for the involvement of infections in other hematologic malignancies, Dr. Martínez reported, “This has already been seen. And this study shows other examples (Epstein-Barr virus and human T-cell lymphotropic virus type 1 with lymphomas), and there could also be Helicobacter pylori and lymphomas.”
Outside of hematology, human papillomavirus has been associated with cervical cancer, tobacco with lung cancer, sun with skin cancer, and diet with the development of some solid neoplasms.
“The study speaks about the concept of a latency period. To accept the idea that a factor or virus that’s more prevalent in winter produces, on its own, AML in a few weeks or months means accepting the idea of a very short latency period – something that’s not usually the case. For that, another explanation is given: An abnormal immune response or that a seasonal infectious agent can be capable of promoting leukemogenesis. These are also hypotheses to be explored in the future,” suggested Dr. Martínez.
New research network
Several potential limitations of this study should be considered. One limitation is that AML cases were obtained from the CMBD registry as defined by ICD-9, and no other AML classifications were available. Another limitation is that information on the date of onset of clinical symptoms was not available for analysis. In addition, a further limitation related to the source of their data may have led the researchers to underestimate the incidence rates of AML in older patients, as only hospitalized patients were captured in their study.
As for continuing the research, the results make it necessary to carry out complementary epidemiologic studies that will examine the association between seasonal risk factors and the increased diagnosis of AML during winter months.
To go forward, the first step would be to secure funding. For this purpose, a network is being put together featuring collaborators from other world-renowned research groups that are at the top of their respective disciplines. Through this network, they hope to be able to apply together for public research grants from countries in Europe and elsewhere as well as to establish collaborations with various companies in the private sector.
“This could open up new therapeutic avenues in the future, as we could try to force leukemic stem cells to divide, thereby reducing the resistance that the standard treatments usually demonstrate,” Dr. Alonso concluded.
Dr. Alonso received research funding from Incyte, Pfizer International, and Astellas Pharma outside the present work. Dr. Martínez disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish edition. A version of the article appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF HEMATOLOGY
Annual PSA screening important for Black men
, new data suggest.
The data come from a review of 45,834 veterans (aged 55-69 years) who had been diagnosed with prostate cancer. About one-third of these men self-identified as non-Hispanic Black, and the rest were White.
During the study period (2004-2017), 2,465 men (5.4%) died of the disease.
The review found that annual prostate-specific antigen (PSA) screening significantly reduced the risk of dying from prostate cancer among Black men but not White men.
The study was published online in JAMA Oncology.
“These results may be biologically plausible because a shorter screening interval may be valuable for detecting aggressive disease, which is more common in Black men,” say investigators, led by University of California, San Diego, radiation oncology resident Michael Sherer, MD.
“Given that Black men are younger at diagnosis and have worse prostate cancer survival compared with White men,” more intensive screening recommendations “may benefit Black patients,” they write.
The study “conclusions are reasonable,” said Christopher Wallis, MD, PhD, a urologic oncologist at Mount Sinai Hospital in Toronto, when asked for comment.
Annual screening may well have “a greater potential to benefit” Black men, he said. “While we would ideally see randomized data supporting this, those data are unlikely to ever be forthcoming. Thus, this study provides a strong rationale to support the recommendations from many guideline panels (including those from the American Urological Association) that Black men, in the context of shared decision-making, may benefit more from PSA-based prostate cancer screening than the population at large,” he added.
Overall, the findings could help inform screening discussions with Black men, the investigators comments. In its most recent guidance, the U.S. Preventive Services Task Force recommends shared decision-making regarding PSA screening for men aged 55-69 years.
Similar screening frequency
For their study, the team reviewed Veterans Health Administration data to assess PSA screening patterns – which they categorized as no screening, less than annual screening, or annual screening – in the 5 years leading up to diagnosis.
They then correlated screening behaviors with the subsequent risk of dying from prostate cancer.
Overall, the reduction in risk of prostate cancer–specific mortality (PCSM) associated with screening was similar among Black men (subdistribution hazard ratio, 0.56; P = .001) and White men (sHR, 0.58; P = .001).
However, on multivariable regression, annual screening, in comparison with some screening, was associated with a significant reduction in the risk of dying from prostate cancer only among Black men (sHR, 0.65; P = .02), not among White men (sHR, 0.91; P = .35).
The cumulative incidence of PCSM among Black men was 4.7% with annual screening but 7.3% with only some screening.
Among White men, the cumulative incidence of PCSM with annual screening was 5.9% vs. 6.9% with less than annual screening.
Screening frequency was similar between Black men and White men. Black men were younger on average (61.8 vs. 63.1 years) and had slightly higher PSA levels at diagnosis but were not more likely to have regional or metastatic disease.
No funding was reported for this study. The investigators have disclosed no relevant financial relationships. Dr. Wallis has received personal fees from Janssen Canada.
A version of this article first appeared on Medscape.com.
, new data suggest.
The data come from a review of 45,834 veterans (aged 55-69 years) who had been diagnosed with prostate cancer. About one-third of these men self-identified as non-Hispanic Black, and the rest were White.
During the study period (2004-2017), 2,465 men (5.4%) died of the disease.
The review found that annual prostate-specific antigen (PSA) screening significantly reduced the risk of dying from prostate cancer among Black men but not White men.
The study was published online in JAMA Oncology.
“These results may be biologically plausible because a shorter screening interval may be valuable for detecting aggressive disease, which is more common in Black men,” say investigators, led by University of California, San Diego, radiation oncology resident Michael Sherer, MD.
“Given that Black men are younger at diagnosis and have worse prostate cancer survival compared with White men,” more intensive screening recommendations “may benefit Black patients,” they write.
The study “conclusions are reasonable,” said Christopher Wallis, MD, PhD, a urologic oncologist at Mount Sinai Hospital in Toronto, when asked for comment.
Annual screening may well have “a greater potential to benefit” Black men, he said. “While we would ideally see randomized data supporting this, those data are unlikely to ever be forthcoming. Thus, this study provides a strong rationale to support the recommendations from many guideline panels (including those from the American Urological Association) that Black men, in the context of shared decision-making, may benefit more from PSA-based prostate cancer screening than the population at large,” he added.
Overall, the findings could help inform screening discussions with Black men, the investigators comments. In its most recent guidance, the U.S. Preventive Services Task Force recommends shared decision-making regarding PSA screening for men aged 55-69 years.
Similar screening frequency
For their study, the team reviewed Veterans Health Administration data to assess PSA screening patterns – which they categorized as no screening, less than annual screening, or annual screening – in the 5 years leading up to diagnosis.
They then correlated screening behaviors with the subsequent risk of dying from prostate cancer.
Overall, the reduction in risk of prostate cancer–specific mortality (PCSM) associated with screening was similar among Black men (subdistribution hazard ratio, 0.56; P = .001) and White men (sHR, 0.58; P = .001).
However, on multivariable regression, annual screening, in comparison with some screening, was associated with a significant reduction in the risk of dying from prostate cancer only among Black men (sHR, 0.65; P = .02), not among White men (sHR, 0.91; P = .35).
The cumulative incidence of PCSM among Black men was 4.7% with annual screening but 7.3% with only some screening.
Among White men, the cumulative incidence of PCSM with annual screening was 5.9% vs. 6.9% with less than annual screening.
Screening frequency was similar between Black men and White men. Black men were younger on average (61.8 vs. 63.1 years) and had slightly higher PSA levels at diagnosis but were not more likely to have regional or metastatic disease.
No funding was reported for this study. The investigators have disclosed no relevant financial relationships. Dr. Wallis has received personal fees from Janssen Canada.
A version of this article first appeared on Medscape.com.
, new data suggest.
The data come from a review of 45,834 veterans (aged 55-69 years) who had been diagnosed with prostate cancer. About one-third of these men self-identified as non-Hispanic Black, and the rest were White.
During the study period (2004-2017), 2,465 men (5.4%) died of the disease.
The review found that annual prostate-specific antigen (PSA) screening significantly reduced the risk of dying from prostate cancer among Black men but not White men.
The study was published online in JAMA Oncology.
“These results may be biologically plausible because a shorter screening interval may be valuable for detecting aggressive disease, which is more common in Black men,” say investigators, led by University of California, San Diego, radiation oncology resident Michael Sherer, MD.
“Given that Black men are younger at diagnosis and have worse prostate cancer survival compared with White men,” more intensive screening recommendations “may benefit Black patients,” they write.
The study “conclusions are reasonable,” said Christopher Wallis, MD, PhD, a urologic oncologist at Mount Sinai Hospital in Toronto, when asked for comment.
Annual screening may well have “a greater potential to benefit” Black men, he said. “While we would ideally see randomized data supporting this, those data are unlikely to ever be forthcoming. Thus, this study provides a strong rationale to support the recommendations from many guideline panels (including those from the American Urological Association) that Black men, in the context of shared decision-making, may benefit more from PSA-based prostate cancer screening than the population at large,” he added.
Overall, the findings could help inform screening discussions with Black men, the investigators comments. In its most recent guidance, the U.S. Preventive Services Task Force recommends shared decision-making regarding PSA screening for men aged 55-69 years.
Similar screening frequency
For their study, the team reviewed Veterans Health Administration data to assess PSA screening patterns – which they categorized as no screening, less than annual screening, or annual screening – in the 5 years leading up to diagnosis.
They then correlated screening behaviors with the subsequent risk of dying from prostate cancer.
Overall, the reduction in risk of prostate cancer–specific mortality (PCSM) associated with screening was similar among Black men (subdistribution hazard ratio, 0.56; P = .001) and White men (sHR, 0.58; P = .001).
However, on multivariable regression, annual screening, in comparison with some screening, was associated with a significant reduction in the risk of dying from prostate cancer only among Black men (sHR, 0.65; P = .02), not among White men (sHR, 0.91; P = .35).
The cumulative incidence of PCSM among Black men was 4.7% with annual screening but 7.3% with only some screening.
Among White men, the cumulative incidence of PCSM with annual screening was 5.9% vs. 6.9% with less than annual screening.
Screening frequency was similar between Black men and White men. Black men were younger on average (61.8 vs. 63.1 years) and had slightly higher PSA levels at diagnosis but were not more likely to have regional or metastatic disease.
No funding was reported for this study. The investigators have disclosed no relevant financial relationships. Dr. Wallis has received personal fees from Janssen Canada.
A version of this article first appeared on Medscape.com.
FROM JAMA ONCOLOGY
Mechanistic link between herpes virus, Alzheimer’s revealed?
, new research suggests.
“Our results suggest one pathway to Alzheimer’s disease, caused by a VZV infection which creates inflammatory triggers that awaken HSV in the brain,” lead author Dana Cairns, PhD, research associate, department of biomedical engineering at Tufts University, Boston, said in a news release.
The findings were published online in Journal of Alzheimer’s Disease.
‘One-two punch’
Previous research has suggested a correlation between HSV-1 and AD and involvement of VZV. However, the sequence of events that the viruses create to set the disease in motion has been unclear.
“We think we now have evidence of those events,” co–senior author David Kaplan, PhD, chair of the department of biomedical engineering at Tufts, said in the release.
Working with co–senior author Ruth Itzhaki, PhD, University of Oxford, United Kingdom, the researchers infected human-induced neural stem cells (hiNSCs) and 3D brain tissue models with HSV-1 and/or VZV. Dr. Itzhaki was one of the first to hypothesize a connection between herpes virus and AD.
The investigators found that HSV-1 infection of hiNSCs induces amyloid-beta and P-tau accumulation: the main components of AD plaques and neurofibrillary tangles, respectively.
On the other hand, VZV infection of cultured hiNSCs did not lead to amyloid-beta and P-tau accumulation but instead resulted in gliosis and increased levels of proinflammatory cytokines.
“Strikingly,” VZV infection of cells quiescently infected with HSV-1 caused reactivation of HSV-1, leading to AD-like changes, including amyloid-beta and P-tau accumulation, the investigators report.
This suggests that VZV is unlikely to be a direct cause of AD but rather acts indirectly via reactivation of HSV-1, they add.
Similar findings emerged in similar experiments using 3D human brain tissue models.
“It’s a one-two punch of two viruses that are very common and usually harmless, but the lab studies suggest that if a new exposure to VZV wakes up dormant HSV-1, they could cause trouble,” Dr. Cairns said.
The researchers note that vaccination against VZV has been shown previously to reduce risk for dementia. It is possible, they add, that the vaccine is helping to stop the cycle of viral reactivation, inflammation, and neuronal damage.
‘A first step’
Heather M. Snyder, PhD, vice president of Medical & Scientific Relations at the Alzheimer’s Association, said that the study “is using artificial systems with the goal of more clearly and more deeply understanding” the assessed associations.
She added that although it is a first step, it may provide valuable direction for follow-up research.
“This is preliminary work that first needs replication, validation, and further development to understand if any association that is uncovered between viruses and Alzheimer’s/dementia has a mechanistic link,” said Dr. Snyder.
She noted that several past studies have sought to help the research field better understand the links between different viruses and Alzheimer’s and other forms of dementia.
“There have been some challenges in evaluating these associations in our current model systems or in individuals for a number of reasons,” said Dr. Snyder.
However, “the COVID-19 pandemic has created an opportunity to examine and investigate the relationships between different viruses and Alzheimer’s and other dementias by following individuals in more common and well-established ways,” she added.
She reported that her organization is “leading and working with a large global network of studies and investigators to address some of these questions” from during and after the COVID pandemic.
“The lessons we learn and share may inform our understanding of how other viruses are, or are not, connected to Alzheimer’s and other dementia,” Dr. Snyder said.
More information on the Alzheimer’s Association International Cohort Study of Chronic Neurological Sequelae of SARS-CoV-2 is available online.
The study was funded by the National Institutes of Health. Dr. Cairns, Dr. Kaplan, Dr. Itzhaki, and Dr. Snyder have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
“Our results suggest one pathway to Alzheimer’s disease, caused by a VZV infection which creates inflammatory triggers that awaken HSV in the brain,” lead author Dana Cairns, PhD, research associate, department of biomedical engineering at Tufts University, Boston, said in a news release.
The findings were published online in Journal of Alzheimer’s Disease.
‘One-two punch’
Previous research has suggested a correlation between HSV-1 and AD and involvement of VZV. However, the sequence of events that the viruses create to set the disease in motion has been unclear.
“We think we now have evidence of those events,” co–senior author David Kaplan, PhD, chair of the department of biomedical engineering at Tufts, said in the release.
Working with co–senior author Ruth Itzhaki, PhD, University of Oxford, United Kingdom, the researchers infected human-induced neural stem cells (hiNSCs) and 3D brain tissue models with HSV-1 and/or VZV. Dr. Itzhaki was one of the first to hypothesize a connection between herpes virus and AD.
The investigators found that HSV-1 infection of hiNSCs induces amyloid-beta and P-tau accumulation: the main components of AD plaques and neurofibrillary tangles, respectively.
On the other hand, VZV infection of cultured hiNSCs did not lead to amyloid-beta and P-tau accumulation but instead resulted in gliosis and increased levels of proinflammatory cytokines.
“Strikingly,” VZV infection of cells quiescently infected with HSV-1 caused reactivation of HSV-1, leading to AD-like changes, including amyloid-beta and P-tau accumulation, the investigators report.
This suggests that VZV is unlikely to be a direct cause of AD but rather acts indirectly via reactivation of HSV-1, they add.
Similar findings emerged in similar experiments using 3D human brain tissue models.
“It’s a one-two punch of two viruses that are very common and usually harmless, but the lab studies suggest that if a new exposure to VZV wakes up dormant HSV-1, they could cause trouble,” Dr. Cairns said.
The researchers note that vaccination against VZV has been shown previously to reduce risk for dementia. It is possible, they add, that the vaccine is helping to stop the cycle of viral reactivation, inflammation, and neuronal damage.
‘A first step’
Heather M. Snyder, PhD, vice president of Medical & Scientific Relations at the Alzheimer’s Association, said that the study “is using artificial systems with the goal of more clearly and more deeply understanding” the assessed associations.
She added that although it is a first step, it may provide valuable direction for follow-up research.
“This is preliminary work that first needs replication, validation, and further development to understand if any association that is uncovered between viruses and Alzheimer’s/dementia has a mechanistic link,” said Dr. Snyder.
She noted that several past studies have sought to help the research field better understand the links between different viruses and Alzheimer’s and other forms of dementia.
“There have been some challenges in evaluating these associations in our current model systems or in individuals for a number of reasons,” said Dr. Snyder.
However, “the COVID-19 pandemic has created an opportunity to examine and investigate the relationships between different viruses and Alzheimer’s and other dementias by following individuals in more common and well-established ways,” she added.
She reported that her organization is “leading and working with a large global network of studies and investigators to address some of these questions” from during and after the COVID pandemic.
“The lessons we learn and share may inform our understanding of how other viruses are, or are not, connected to Alzheimer’s and other dementia,” Dr. Snyder said.
More information on the Alzheimer’s Association International Cohort Study of Chronic Neurological Sequelae of SARS-CoV-2 is available online.
The study was funded by the National Institutes of Health. Dr. Cairns, Dr. Kaplan, Dr. Itzhaki, and Dr. Snyder have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
“Our results suggest one pathway to Alzheimer’s disease, caused by a VZV infection which creates inflammatory triggers that awaken HSV in the brain,” lead author Dana Cairns, PhD, research associate, department of biomedical engineering at Tufts University, Boston, said in a news release.
The findings were published online in Journal of Alzheimer’s Disease.
‘One-two punch’
Previous research has suggested a correlation between HSV-1 and AD and involvement of VZV. However, the sequence of events that the viruses create to set the disease in motion has been unclear.
“We think we now have evidence of those events,” co–senior author David Kaplan, PhD, chair of the department of biomedical engineering at Tufts, said in the release.
Working with co–senior author Ruth Itzhaki, PhD, University of Oxford, United Kingdom, the researchers infected human-induced neural stem cells (hiNSCs) and 3D brain tissue models with HSV-1 and/or VZV. Dr. Itzhaki was one of the first to hypothesize a connection between herpes virus and AD.
The investigators found that HSV-1 infection of hiNSCs induces amyloid-beta and P-tau accumulation: the main components of AD plaques and neurofibrillary tangles, respectively.
On the other hand, VZV infection of cultured hiNSCs did not lead to amyloid-beta and P-tau accumulation but instead resulted in gliosis and increased levels of proinflammatory cytokines.
“Strikingly,” VZV infection of cells quiescently infected with HSV-1 caused reactivation of HSV-1, leading to AD-like changes, including amyloid-beta and P-tau accumulation, the investigators report.
This suggests that VZV is unlikely to be a direct cause of AD but rather acts indirectly via reactivation of HSV-1, they add.
Similar findings emerged in similar experiments using 3D human brain tissue models.
“It’s a one-two punch of two viruses that are very common and usually harmless, but the lab studies suggest that if a new exposure to VZV wakes up dormant HSV-1, they could cause trouble,” Dr. Cairns said.
The researchers note that vaccination against VZV has been shown previously to reduce risk for dementia. It is possible, they add, that the vaccine is helping to stop the cycle of viral reactivation, inflammation, and neuronal damage.
‘A first step’
Heather M. Snyder, PhD, vice president of Medical & Scientific Relations at the Alzheimer’s Association, said that the study “is using artificial systems with the goal of more clearly and more deeply understanding” the assessed associations.
She added that although it is a first step, it may provide valuable direction for follow-up research.
“This is preliminary work that first needs replication, validation, and further development to understand if any association that is uncovered between viruses and Alzheimer’s/dementia has a mechanistic link,” said Dr. Snyder.
She noted that several past studies have sought to help the research field better understand the links between different viruses and Alzheimer’s and other forms of dementia.
“There have been some challenges in evaluating these associations in our current model systems or in individuals for a number of reasons,” said Dr. Snyder.
However, “the COVID-19 pandemic has created an opportunity to examine and investigate the relationships between different viruses and Alzheimer’s and other dementias by following individuals in more common and well-established ways,” she added.
She reported that her organization is “leading and working with a large global network of studies and investigators to address some of these questions” from during and after the COVID pandemic.
“The lessons we learn and share may inform our understanding of how other viruses are, or are not, connected to Alzheimer’s and other dementia,” Dr. Snyder said.
More information on the Alzheimer’s Association International Cohort Study of Chronic Neurological Sequelae of SARS-CoV-2 is available online.
The study was funded by the National Institutes of Health. Dr. Cairns, Dr. Kaplan, Dr. Itzhaki, and Dr. Snyder have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF ALZHEIMER’S DISEASE