User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Sexual assault in women tied to increased stroke, dementia risk
Traumatic experiences, especially sexual assault, may put women at greater risk for poor brain health.
In the Ms Brain study, middle-aged women with trauma exposure had a greater volume of white matter hyperintensities (WMHs) than those without trauma. In addition, the differences persisted even after adjusting for depressive or post-traumatic stress symptoms.
WMHs are “an important indicator of small vessel disease in the brain and have been linked to future stroke risk, dementia risk, and mortality,” lead investigator Rebecca Thurston, PhD, from the University of Pittsburgh, told this news organization.
“What I take from this is, really, that sexual assault has implications for women’s health, far beyond exclusively mental health outcomes, but also for their cardiovascular health, as we have shown in other work and for their stroke and dementia risk as we are seeing in the present work,” Dr. Thurston added.
The study was presented at the North American Menopause Society (NAMS) Annual Meeting in Washington, D.C., and has been accepted for publication in the journal Brain Imaging and Behavior.
Beyond the usual suspects
As part of the study, 145 women (mean age, 59 years) free of clinical cardiovascular disease, stroke, or dementia provided their medical history, including history of traumatic experiences, depression, and post-traumatic stress disorder and underwent magnetic resonance brain imaging for WMHs.
More than two-thirds (68%) of the women reported at least one trauma, most commonly sexual assault (23%).
In multivariate analysis, women with trauma exposure had greater WMH volume than women without trauma (P = .01), with sexual assault most strongly associated with greater WMH volume (P = .02).
The associations persisted after adjusting for depressive or post-traumatic stress symptoms.
“A history of sexual assault was particularly related to white matter hyperintensities in the parietal lobe, and these kinds of white matter hyperintensities have been linked to Alzheimer’s disease in a fairly pronounced way,” Dr. Thurston said.
“When we think about risk factors for stroke, dementia, we need to think beyond exclusively our usual suspects and also think about women [who experienced] psychological trauma and experienced sexual assault in particular. So ask about it and consider it part of your screening regimen,” she added.
‘Burgeoning’ literature
Commenting on the findings, Charles Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, and director of its Institute for Early Life Adversity Research, said the research adds to the “burgeoning literature on the long term neurobiological consequences of trauma and more specifically, sexual abuse, on brain imaging measures.”
“Our group and others reported several years ago that patients with mood disorders, more specifically bipolar disorder and major depression, had higher rates of WMH than matched controls. Those older studies did not control for a history of early life adversity such as childhood maltreatment,” Dr. Nemeroff said.
“In addition to this finding of increased WMH in subjects exposed to trauma is a very large literature documenting other central nervous system (CNS) changes in this population, including cortical thinning in certain brain areas and clearly an emerging finding that different forms of childhood maltreatment are associated with quite distinct structural brain alterations in adulthood,” he noted.
The study was supported by grants from the National Institutes of Health. Dr. Thurston and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Traumatic experiences, especially sexual assault, may put women at greater risk for poor brain health.
In the Ms Brain study, middle-aged women with trauma exposure had a greater volume of white matter hyperintensities (WMHs) than those without trauma. In addition, the differences persisted even after adjusting for depressive or post-traumatic stress symptoms.
WMHs are “an important indicator of small vessel disease in the brain and have been linked to future stroke risk, dementia risk, and mortality,” lead investigator Rebecca Thurston, PhD, from the University of Pittsburgh, told this news organization.
“What I take from this is, really, that sexual assault has implications for women’s health, far beyond exclusively mental health outcomes, but also for their cardiovascular health, as we have shown in other work and for their stroke and dementia risk as we are seeing in the present work,” Dr. Thurston added.
The study was presented at the North American Menopause Society (NAMS) Annual Meeting in Washington, D.C., and has been accepted for publication in the journal Brain Imaging and Behavior.
Beyond the usual suspects
As part of the study, 145 women (mean age, 59 years) free of clinical cardiovascular disease, stroke, or dementia provided their medical history, including history of traumatic experiences, depression, and post-traumatic stress disorder and underwent magnetic resonance brain imaging for WMHs.
More than two-thirds (68%) of the women reported at least one trauma, most commonly sexual assault (23%).
In multivariate analysis, women with trauma exposure had greater WMH volume than women without trauma (P = .01), with sexual assault most strongly associated with greater WMH volume (P = .02).
The associations persisted after adjusting for depressive or post-traumatic stress symptoms.
“A history of sexual assault was particularly related to white matter hyperintensities in the parietal lobe, and these kinds of white matter hyperintensities have been linked to Alzheimer’s disease in a fairly pronounced way,” Dr. Thurston said.
“When we think about risk factors for stroke, dementia, we need to think beyond exclusively our usual suspects and also think about women [who experienced] psychological trauma and experienced sexual assault in particular. So ask about it and consider it part of your screening regimen,” she added.
‘Burgeoning’ literature
Commenting on the findings, Charles Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, and director of its Institute for Early Life Adversity Research, said the research adds to the “burgeoning literature on the long term neurobiological consequences of trauma and more specifically, sexual abuse, on brain imaging measures.”
“Our group and others reported several years ago that patients with mood disorders, more specifically bipolar disorder and major depression, had higher rates of WMH than matched controls. Those older studies did not control for a history of early life adversity such as childhood maltreatment,” Dr. Nemeroff said.
“In addition to this finding of increased WMH in subjects exposed to trauma is a very large literature documenting other central nervous system (CNS) changes in this population, including cortical thinning in certain brain areas and clearly an emerging finding that different forms of childhood maltreatment are associated with quite distinct structural brain alterations in adulthood,” he noted.
The study was supported by grants from the National Institutes of Health. Dr. Thurston and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Traumatic experiences, especially sexual assault, may put women at greater risk for poor brain health.
In the Ms Brain study, middle-aged women with trauma exposure had a greater volume of white matter hyperintensities (WMHs) than those without trauma. In addition, the differences persisted even after adjusting for depressive or post-traumatic stress symptoms.
WMHs are “an important indicator of small vessel disease in the brain and have been linked to future stroke risk, dementia risk, and mortality,” lead investigator Rebecca Thurston, PhD, from the University of Pittsburgh, told this news organization.
“What I take from this is, really, that sexual assault has implications for women’s health, far beyond exclusively mental health outcomes, but also for their cardiovascular health, as we have shown in other work and for their stroke and dementia risk as we are seeing in the present work,” Dr. Thurston added.
The study was presented at the North American Menopause Society (NAMS) Annual Meeting in Washington, D.C., and has been accepted for publication in the journal Brain Imaging and Behavior.
Beyond the usual suspects
As part of the study, 145 women (mean age, 59 years) free of clinical cardiovascular disease, stroke, or dementia provided their medical history, including history of traumatic experiences, depression, and post-traumatic stress disorder and underwent magnetic resonance brain imaging for WMHs.
More than two-thirds (68%) of the women reported at least one trauma, most commonly sexual assault (23%).
In multivariate analysis, women with trauma exposure had greater WMH volume than women without trauma (P = .01), with sexual assault most strongly associated with greater WMH volume (P = .02).
The associations persisted after adjusting for depressive or post-traumatic stress symptoms.
“A history of sexual assault was particularly related to white matter hyperintensities in the parietal lobe, and these kinds of white matter hyperintensities have been linked to Alzheimer’s disease in a fairly pronounced way,” Dr. Thurston said.
“When we think about risk factors for stroke, dementia, we need to think beyond exclusively our usual suspects and also think about women [who experienced] psychological trauma and experienced sexual assault in particular. So ask about it and consider it part of your screening regimen,” she added.
‘Burgeoning’ literature
Commenting on the findings, Charles Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, and director of its Institute for Early Life Adversity Research, said the research adds to the “burgeoning literature on the long term neurobiological consequences of trauma and more specifically, sexual abuse, on brain imaging measures.”
“Our group and others reported several years ago that patients with mood disorders, more specifically bipolar disorder and major depression, had higher rates of WMH than matched controls. Those older studies did not control for a history of early life adversity such as childhood maltreatment,” Dr. Nemeroff said.
“In addition to this finding of increased WMH in subjects exposed to trauma is a very large literature documenting other central nervous system (CNS) changes in this population, including cortical thinning in certain brain areas and clearly an emerging finding that different forms of childhood maltreatment are associated with quite distinct structural brain alterations in adulthood,” he noted.
The study was supported by grants from the National Institutes of Health. Dr. Thurston and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New finasteride lawsuit brings renewed attention to psychiatric, ED adverse event reports
A new merit a closer look and, potentially, better counseling and monitoring from clinicians.
The nonprofit advocacy group Public Citizen filed the suit on behalf of the Post-Finasteride Syndrome Foundation (PFSF) in the U.S. District Court for the District of Columbia. The PFSF had filed a citizen’s petition in 2017 that requested that the FDA either take the 1-mg formulation off the market, or add warnings about the potential for erectile dysfunction, depression, and suicidal ideation, among other adverse reactions.
The PFSF has alleged that long-term use of Propecia (and its generic equivalents) can lead to postfinasteride syndrome (PFS), characterized by sexual dysfunction and psycho-neurocognitive symptoms. The symptoms may continue long after men stop taking the drug, according to PFSF.
Public Citizen said the FDA needs to take action in part because U.S. prescriptions of the hair loss formulation “more than doubled from 2015 to 2020,” and online and telemedicine companies such as Hims, Roman, and Keeps “aggressively market and sell generic finasteride for hair loss.” According to GoodRx, a 1-month supply of generic 1-mg tablets costs as little as $8-$10.
Both Canadian and British regulatory authorities have added warnings about depression and suicide to the Propecia label but the FDA has not changed its labeling. An agency spokesperson told this news organization that the “FDA does not comment on the status of pending citizen petitions or on pending litigation.”
Propecia’s developer, Merck, has not responded to several requests for comment from this news organization.
Why some patients develop PFS and others do not is still not understood, but some clinicians said they counsel all patients on the risks of severe and persistent side effects that have been associated with Propecia.
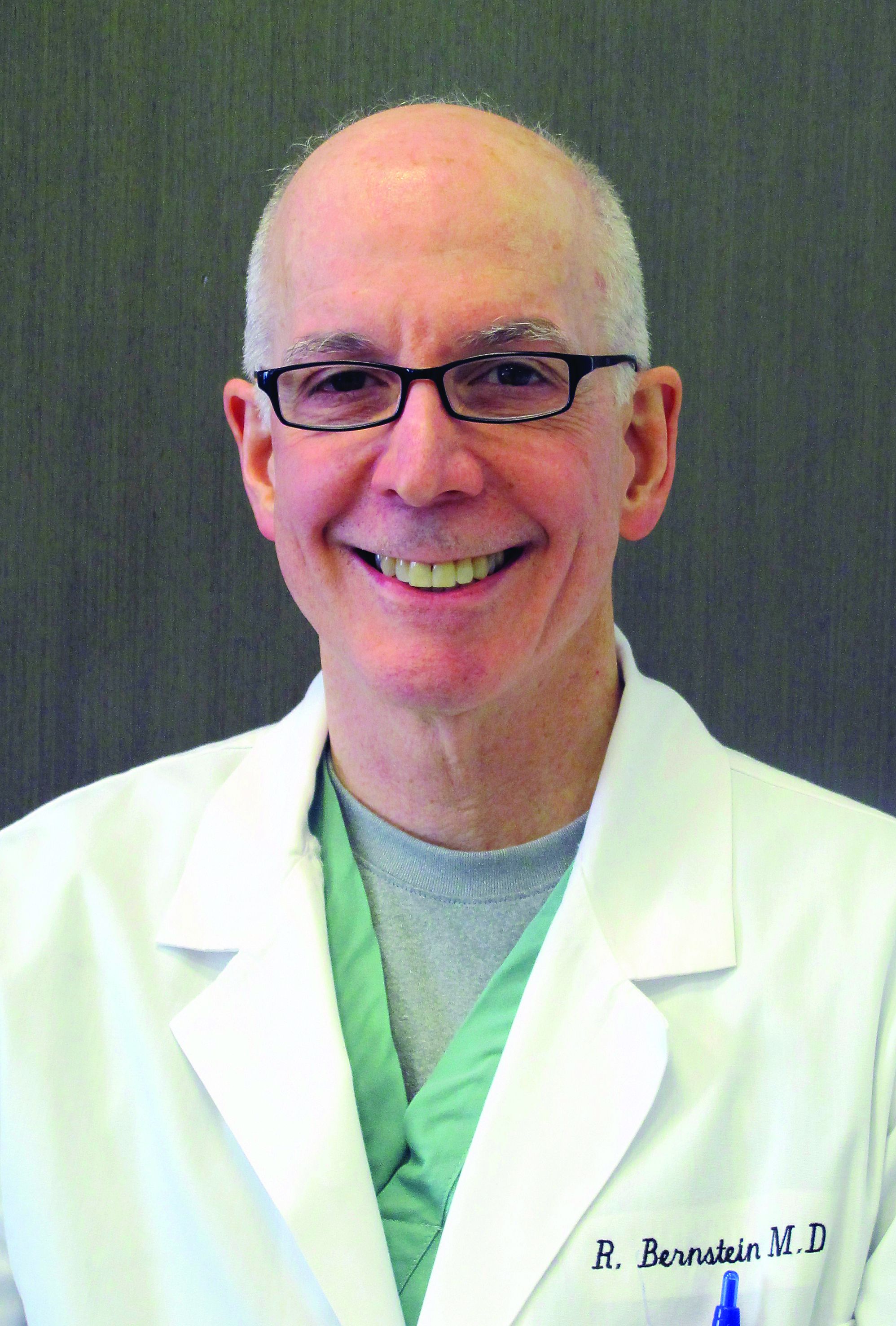
Robert M. Bernstein, MD, of the department of dermatology at Columbia University, New York, and a fellow of the International Society of Hair Restoration Surgery, said that 2%-4% of his patients have some side effects, similar to the original reported incidence, with sexual dysfunction being the most common.
If a man experiences an adverse effect, the drug should be stopped, Dr. Bernstein said in an interview. He noted that “there seems to be a significant increased risk of persistent side effects in people with certain psychiatric conditions, and those people should be counseled carefully before considering the medication.”
“Everybody should be warned that the risk of persistent side effects is real but in the average person it is quite uncommon,” added Dr. Bernstein, founder of Bernstein Medical, a division of Schweiger Dermatology Group focusing on the diagnosis and treatment of hair loss. “I don’t think it should be withdrawn from the market,” he said.
Alan Jacobs, MD, a Manhattan-based neuroendocrinologist and behavioral neurologist in private practice who said he has treated hundreds of men for PFS, and who is an expert witness for the plaintiff in a suit alleging that finasteride led to a man’s suicide, said that taking the drug off the market would be unfortunate because it helps so many men. “I don’t think you need to get rid of the drug per se,” he said in an interview. “But very rapidly, people need to do clinical research to find out how to predict who’s more at risk,” he added.
Michael S. Irwig, MD, associate professor of medicine at Harvard Medical School, Boston, who has studied the persistent sexual and nonsexual side effects of finasteride, said he believes there should be a boxed warning on the finasteride label to let the men who take it “know that they can have permanent persistent sexual dysfunction, and/or depression and suicide have been noted with this medicine.
“Those who prescribe it should be having a conversation with patients about the potential risks and benefits so that everybody knows about the potential before they get on the medicine,” said Dr. Irwig, who also is an endocrinologist at Beth Israel Deaconess Medical Center in Boston.
Other countries warn of psychiatric effects
The FDA approved the 1-mg form of finasteride for male pattern hair loss in 1997.
In 2012, the label and the patient insert were updated to state that side effects included less desire for sex, erectile dysfunction, and a decrease in the amount of semen produced, but that those adverse events occurred in less than 2% of men and generally went away in most men who stopped taking the drug.
That label change unleashed a flood of more than 1,000 lawsuits against Merck. The company reportedly settled at least half of them for $4.3 million in 2018. The Superior Court of New Jersey closed out the consolidated class action against Merck in May 2021, noting that all of the cases had been settled or dismissed.
The suits generally accused Merck of not giving adequate warning about sexual side effects, according to an investigation by Reuters. That 2019 special report found that Merck had understated the number of men who experienced sexual side effects and the duration of those symptoms. The news organization also reported that from 2009 to 2018, the FDA received 5,000 reports of sexual or mental health side effects – and sometimes both – in men who took finasteride. Some 350 of the men reported suicidal thoughts, and there were 50 reports of suicide.
Public Citizen’s lawsuit alleges that VigiBase, which is managed by the World Health Organization Collaborating Centre for International Drug Monitoring, lists 378 cases of suicidal ideation, 39 cases of suicide attempt, and 88 cases of completed suicide associated with finasteride use. VigiBase collects data from 153 countries on adverse reactions to medications.
In February 2021, more documents from the class action lawsuits were unsealed in response to a Reuters request. According to the news organization, the documents showed that Merck knew of reports of depression, including suicidal thoughts, as early as 2009.
However, according to Reuters, the FDA in 2011 granted Merck’s request to only note depression as a potential side effect, without including the risk of suicidal ideation.
The current FDA label notes a small incidence of sexual dysfunction, including decreased libido (1.8% in trials) and erectile dysfunction (1.3%) and mentions depression as a side effect observed during the postmarketing period.
The Canadian label has the same statistics on sexual side effects but is much stronger on mental adverse effects: “Psychiatric disorders: mood alterations and depression, decreased libido that continued after discontinuation of treatment. Mood alterations including depressed mood and, less frequently, suicidal ideation have been reported in patients treated with finasteride 1 mg. Patients should be monitored for psychiatric symptoms, and if these occur, the patient should be advised to seek medical advice.”
In the United Kingdom, patients prescribed the drug are given a leaflet, which notes that “Mood alterations such as depressed mood, depression and, less frequently, suicidal thoughts have been reported in patients treated with Propecia,” and advises patients to stop taking the drug if they experience any of those symptoms and to discuss it with their physician.
Public Citizen noted in its lawsuit that French and German drug regulators have sent letters to clinicians advising them to inform patients of the risk of suicidal thoughts and anxiety.
Is there biological plausibility?
To bolster its argument that finasteride has dangerous psychiatric side effects, the advocacy organization cited a study first published in JAMA Dermatology in late 2020 that investigated suicidality and psychological adverse events in patients taking finasteride.
David-Dan Nguyen, MPH, and his colleagues at Brigham and Women’s Hospital in Boston, McGill University, Montreal, and the University of Montreal, examined the VigiBase database and found 356 cases of suicidality and 2,926 psychological adverse events; cases were highest from 2015 to 2019.
They documented what they called a “significant disproportionality signal for suicidality (reporting odds ratio, 1.63; 95% confidence interval, 2.90-4.15) and psychological adverse events (ROR, 4.33; 95% CI, 4.17-4.49) with finasteride, especially in younger men and those with alopecia, but not in older men or those with benign prostatic hyperplasia.
The study authors noted that some studies have suggested that men with depression have low levels of the neurosteroid allopregnanolone, which is produced by the 5-alpha reductase enzyme. Finasteride is a 5-alpha reductase inhibitor.
According to Public Citizen’s lawsuit, “The product labeling does not disclose important information about finasteride’s mechanism of action,” and “the drug inhibits multiple steroid hormone pathways that are responsible for the formation of brain neurosteroids that regulate many critical functions in the central nervous system, like sexual function, mood, sleep, cognitive function, the stress response, and motivation.”
Dr. Jacobs said that “there’s a lot of good solid high-quality research, mostly in animals, but also some on humans, showing a plausible link between blocking 5-alpha reductase in the brain, deficiency of neuroactive steroids, and depression.”
The author of an accompanying editorial, Roger S. Ho, MD, MPH, an associate professor in the department of dermatology, New York University, was skeptical. “Without a plausible biological hypothesis pharmacodynamically linking the drug and the reported adverse event, this kind of analysis may lead to false findings,” Dr. Ho said in the editorial about the Nguyen study.
Dr. Ho also wrote that he believed that the lack of a suicidality signal for dutasteride, a drug with a similar mechanism of action, but without as much media attention, “hints at a potential reporting bias unique to finasteride.”
He recommended that clinicians “conduct a full evaluation and a detailed, personalized risk-benefit assessment for patients before each prescription of finasteride.”
Important medicine, important caveats
Dr. Jacobs said that many of the men who come to him with side effects after taking finasteride have “been blown off by most of the doctors they go to see.”
Urologists dismiss them because their sexual dysfunction is not a gonad issue. They are told that it’s in their head, said Dr. Jacobs, adding that, “it is in their head, but it’s biological.”
The drug’s label advises that sexual side effects disappear when the drug is stopped. “That’s only true most of the time, not all of the time,” said Dr. Jacobs, adding that the persistence of any side effects impacts what he calls a “small subset” of men who take the drug.
“We have treated tens of thousands of patients who have benefited from the medicine and had no side effects,” said Dr. Bernstein. “But there is a lot that’s still not known about it.”
Even so, “baldness in young people is not a benign condition,” he said, adding that it can be socially debilitating. “An 18-year-old with a full head of thick hair who’s totally bald in 3 or 4 years – that can totally change his psyche,” Dr. Bernstein said. Finasteride may be the best option for those young men, and it is an important medication, he said. Does it need to be used more carefully? “Certainly you can’t argue with that,” he commented.
Dr. Bernstein and Dr. Irwig reported no conflicts. Dr. Jacobs disclosed that he is an expert witness for the plaintiffs in a suit against Propecia maker Merck.
A new merit a closer look and, potentially, better counseling and monitoring from clinicians.
The nonprofit advocacy group Public Citizen filed the suit on behalf of the Post-Finasteride Syndrome Foundation (PFSF) in the U.S. District Court for the District of Columbia. The PFSF had filed a citizen’s petition in 2017 that requested that the FDA either take the 1-mg formulation off the market, or add warnings about the potential for erectile dysfunction, depression, and suicidal ideation, among other adverse reactions.
The PFSF has alleged that long-term use of Propecia (and its generic equivalents) can lead to postfinasteride syndrome (PFS), characterized by sexual dysfunction and psycho-neurocognitive symptoms. The symptoms may continue long after men stop taking the drug, according to PFSF.
Public Citizen said the FDA needs to take action in part because U.S. prescriptions of the hair loss formulation “more than doubled from 2015 to 2020,” and online and telemedicine companies such as Hims, Roman, and Keeps “aggressively market and sell generic finasteride for hair loss.” According to GoodRx, a 1-month supply of generic 1-mg tablets costs as little as $8-$10.
Both Canadian and British regulatory authorities have added warnings about depression and suicide to the Propecia label but the FDA has not changed its labeling. An agency spokesperson told this news organization that the “FDA does not comment on the status of pending citizen petitions or on pending litigation.”
Propecia’s developer, Merck, has not responded to several requests for comment from this news organization.
Why some patients develop PFS and others do not is still not understood, but some clinicians said they counsel all patients on the risks of severe and persistent side effects that have been associated with Propecia.
Robert M. Bernstein, MD, of the department of dermatology at Columbia University, New York, and a fellow of the International Society of Hair Restoration Surgery, said that 2%-4% of his patients have some side effects, similar to the original reported incidence, with sexual dysfunction being the most common.
If a man experiences an adverse effect, the drug should be stopped, Dr. Bernstein said in an interview. He noted that “there seems to be a significant increased risk of persistent side effects in people with certain psychiatric conditions, and those people should be counseled carefully before considering the medication.”
“Everybody should be warned that the risk of persistent side effects is real but in the average person it is quite uncommon,” added Dr. Bernstein, founder of Bernstein Medical, a division of Schweiger Dermatology Group focusing on the diagnosis and treatment of hair loss. “I don’t think it should be withdrawn from the market,” he said.
Alan Jacobs, MD, a Manhattan-based neuroendocrinologist and behavioral neurologist in private practice who said he has treated hundreds of men for PFS, and who is an expert witness for the plaintiff in a suit alleging that finasteride led to a man’s suicide, said that taking the drug off the market would be unfortunate because it helps so many men. “I don’t think you need to get rid of the drug per se,” he said in an interview. “But very rapidly, people need to do clinical research to find out how to predict who’s more at risk,” he added.
Michael S. Irwig, MD, associate professor of medicine at Harvard Medical School, Boston, who has studied the persistent sexual and nonsexual side effects of finasteride, said he believes there should be a boxed warning on the finasteride label to let the men who take it “know that they can have permanent persistent sexual dysfunction, and/or depression and suicide have been noted with this medicine.
“Those who prescribe it should be having a conversation with patients about the potential risks and benefits so that everybody knows about the potential before they get on the medicine,” said Dr. Irwig, who also is an endocrinologist at Beth Israel Deaconess Medical Center in Boston.
Other countries warn of psychiatric effects
The FDA approved the 1-mg form of finasteride for male pattern hair loss in 1997.
In 2012, the label and the patient insert were updated to state that side effects included less desire for sex, erectile dysfunction, and a decrease in the amount of semen produced, but that those adverse events occurred in less than 2% of men and generally went away in most men who stopped taking the drug.
That label change unleashed a flood of more than 1,000 lawsuits against Merck. The company reportedly settled at least half of them for $4.3 million in 2018. The Superior Court of New Jersey closed out the consolidated class action against Merck in May 2021, noting that all of the cases had been settled or dismissed.
The suits generally accused Merck of not giving adequate warning about sexual side effects, according to an investigation by Reuters. That 2019 special report found that Merck had understated the number of men who experienced sexual side effects and the duration of those symptoms. The news organization also reported that from 2009 to 2018, the FDA received 5,000 reports of sexual or mental health side effects – and sometimes both – in men who took finasteride. Some 350 of the men reported suicidal thoughts, and there were 50 reports of suicide.
Public Citizen’s lawsuit alleges that VigiBase, which is managed by the World Health Organization Collaborating Centre for International Drug Monitoring, lists 378 cases of suicidal ideation, 39 cases of suicide attempt, and 88 cases of completed suicide associated with finasteride use. VigiBase collects data from 153 countries on adverse reactions to medications.
In February 2021, more documents from the class action lawsuits were unsealed in response to a Reuters request. According to the news organization, the documents showed that Merck knew of reports of depression, including suicidal thoughts, as early as 2009.
However, according to Reuters, the FDA in 2011 granted Merck’s request to only note depression as a potential side effect, without including the risk of suicidal ideation.
The current FDA label notes a small incidence of sexual dysfunction, including decreased libido (1.8% in trials) and erectile dysfunction (1.3%) and mentions depression as a side effect observed during the postmarketing period.
The Canadian label has the same statistics on sexual side effects but is much stronger on mental adverse effects: “Psychiatric disorders: mood alterations and depression, decreased libido that continued after discontinuation of treatment. Mood alterations including depressed mood and, less frequently, suicidal ideation have been reported in patients treated with finasteride 1 mg. Patients should be monitored for psychiatric symptoms, and if these occur, the patient should be advised to seek medical advice.”
In the United Kingdom, patients prescribed the drug are given a leaflet, which notes that “Mood alterations such as depressed mood, depression and, less frequently, suicidal thoughts have been reported in patients treated with Propecia,” and advises patients to stop taking the drug if they experience any of those symptoms and to discuss it with their physician.
Public Citizen noted in its lawsuit that French and German drug regulators have sent letters to clinicians advising them to inform patients of the risk of suicidal thoughts and anxiety.
Is there biological plausibility?
To bolster its argument that finasteride has dangerous psychiatric side effects, the advocacy organization cited a study first published in JAMA Dermatology in late 2020 that investigated suicidality and psychological adverse events in patients taking finasteride.
David-Dan Nguyen, MPH, and his colleagues at Brigham and Women’s Hospital in Boston, McGill University, Montreal, and the University of Montreal, examined the VigiBase database and found 356 cases of suicidality and 2,926 psychological adverse events; cases were highest from 2015 to 2019.
They documented what they called a “significant disproportionality signal for suicidality (reporting odds ratio, 1.63; 95% confidence interval, 2.90-4.15) and psychological adverse events (ROR, 4.33; 95% CI, 4.17-4.49) with finasteride, especially in younger men and those with alopecia, but not in older men or those with benign prostatic hyperplasia.
The study authors noted that some studies have suggested that men with depression have low levels of the neurosteroid allopregnanolone, which is produced by the 5-alpha reductase enzyme. Finasteride is a 5-alpha reductase inhibitor.
According to Public Citizen’s lawsuit, “The product labeling does not disclose important information about finasteride’s mechanism of action,” and “the drug inhibits multiple steroid hormone pathways that are responsible for the formation of brain neurosteroids that regulate many critical functions in the central nervous system, like sexual function, mood, sleep, cognitive function, the stress response, and motivation.”
Dr. Jacobs said that “there’s a lot of good solid high-quality research, mostly in animals, but also some on humans, showing a plausible link between blocking 5-alpha reductase in the brain, deficiency of neuroactive steroids, and depression.”
The author of an accompanying editorial, Roger S. Ho, MD, MPH, an associate professor in the department of dermatology, New York University, was skeptical. “Without a plausible biological hypothesis pharmacodynamically linking the drug and the reported adverse event, this kind of analysis may lead to false findings,” Dr. Ho said in the editorial about the Nguyen study.
Dr. Ho also wrote that he believed that the lack of a suicidality signal for dutasteride, a drug with a similar mechanism of action, but without as much media attention, “hints at a potential reporting bias unique to finasteride.”
He recommended that clinicians “conduct a full evaluation and a detailed, personalized risk-benefit assessment for patients before each prescription of finasteride.”
Important medicine, important caveats
Dr. Jacobs said that many of the men who come to him with side effects after taking finasteride have “been blown off by most of the doctors they go to see.”
Urologists dismiss them because their sexual dysfunction is not a gonad issue. They are told that it’s in their head, said Dr. Jacobs, adding that, “it is in their head, but it’s biological.”
The drug’s label advises that sexual side effects disappear when the drug is stopped. “That’s only true most of the time, not all of the time,” said Dr. Jacobs, adding that the persistence of any side effects impacts what he calls a “small subset” of men who take the drug.
“We have treated tens of thousands of patients who have benefited from the medicine and had no side effects,” said Dr. Bernstein. “But there is a lot that’s still not known about it.”
Even so, “baldness in young people is not a benign condition,” he said, adding that it can be socially debilitating. “An 18-year-old with a full head of thick hair who’s totally bald in 3 or 4 years – that can totally change his psyche,” Dr. Bernstein said. Finasteride may be the best option for those young men, and it is an important medication, he said. Does it need to be used more carefully? “Certainly you can’t argue with that,” he commented.
Dr. Bernstein and Dr. Irwig reported no conflicts. Dr. Jacobs disclosed that he is an expert witness for the plaintiffs in a suit against Propecia maker Merck.
A new merit a closer look and, potentially, better counseling and monitoring from clinicians.
The nonprofit advocacy group Public Citizen filed the suit on behalf of the Post-Finasteride Syndrome Foundation (PFSF) in the U.S. District Court for the District of Columbia. The PFSF had filed a citizen’s petition in 2017 that requested that the FDA either take the 1-mg formulation off the market, or add warnings about the potential for erectile dysfunction, depression, and suicidal ideation, among other adverse reactions.
The PFSF has alleged that long-term use of Propecia (and its generic equivalents) can lead to postfinasteride syndrome (PFS), characterized by sexual dysfunction and psycho-neurocognitive symptoms. The symptoms may continue long after men stop taking the drug, according to PFSF.
Public Citizen said the FDA needs to take action in part because U.S. prescriptions of the hair loss formulation “more than doubled from 2015 to 2020,” and online and telemedicine companies such as Hims, Roman, and Keeps “aggressively market and sell generic finasteride for hair loss.” According to GoodRx, a 1-month supply of generic 1-mg tablets costs as little as $8-$10.
Both Canadian and British regulatory authorities have added warnings about depression and suicide to the Propecia label but the FDA has not changed its labeling. An agency spokesperson told this news organization that the “FDA does not comment on the status of pending citizen petitions or on pending litigation.”
Propecia’s developer, Merck, has not responded to several requests for comment from this news organization.
Why some patients develop PFS and others do not is still not understood, but some clinicians said they counsel all patients on the risks of severe and persistent side effects that have been associated with Propecia.
Robert M. Bernstein, MD, of the department of dermatology at Columbia University, New York, and a fellow of the International Society of Hair Restoration Surgery, said that 2%-4% of his patients have some side effects, similar to the original reported incidence, with sexual dysfunction being the most common.
If a man experiences an adverse effect, the drug should be stopped, Dr. Bernstein said in an interview. He noted that “there seems to be a significant increased risk of persistent side effects in people with certain psychiatric conditions, and those people should be counseled carefully before considering the medication.”
“Everybody should be warned that the risk of persistent side effects is real but in the average person it is quite uncommon,” added Dr. Bernstein, founder of Bernstein Medical, a division of Schweiger Dermatology Group focusing on the diagnosis and treatment of hair loss. “I don’t think it should be withdrawn from the market,” he said.
Alan Jacobs, MD, a Manhattan-based neuroendocrinologist and behavioral neurologist in private practice who said he has treated hundreds of men for PFS, and who is an expert witness for the plaintiff in a suit alleging that finasteride led to a man’s suicide, said that taking the drug off the market would be unfortunate because it helps so many men. “I don’t think you need to get rid of the drug per se,” he said in an interview. “But very rapidly, people need to do clinical research to find out how to predict who’s more at risk,” he added.
Michael S. Irwig, MD, associate professor of medicine at Harvard Medical School, Boston, who has studied the persistent sexual and nonsexual side effects of finasteride, said he believes there should be a boxed warning on the finasteride label to let the men who take it “know that they can have permanent persistent sexual dysfunction, and/or depression and suicide have been noted with this medicine.
“Those who prescribe it should be having a conversation with patients about the potential risks and benefits so that everybody knows about the potential before they get on the medicine,” said Dr. Irwig, who also is an endocrinologist at Beth Israel Deaconess Medical Center in Boston.
Other countries warn of psychiatric effects
The FDA approved the 1-mg form of finasteride for male pattern hair loss in 1997.
In 2012, the label and the patient insert were updated to state that side effects included less desire for sex, erectile dysfunction, and a decrease in the amount of semen produced, but that those adverse events occurred in less than 2% of men and generally went away in most men who stopped taking the drug.
That label change unleashed a flood of more than 1,000 lawsuits against Merck. The company reportedly settled at least half of them for $4.3 million in 2018. The Superior Court of New Jersey closed out the consolidated class action against Merck in May 2021, noting that all of the cases had been settled or dismissed.
The suits generally accused Merck of not giving adequate warning about sexual side effects, according to an investigation by Reuters. That 2019 special report found that Merck had understated the number of men who experienced sexual side effects and the duration of those symptoms. The news organization also reported that from 2009 to 2018, the FDA received 5,000 reports of sexual or mental health side effects – and sometimes both – in men who took finasteride. Some 350 of the men reported suicidal thoughts, and there were 50 reports of suicide.
Public Citizen’s lawsuit alleges that VigiBase, which is managed by the World Health Organization Collaborating Centre for International Drug Monitoring, lists 378 cases of suicidal ideation, 39 cases of suicide attempt, and 88 cases of completed suicide associated with finasteride use. VigiBase collects data from 153 countries on adverse reactions to medications.
In February 2021, more documents from the class action lawsuits were unsealed in response to a Reuters request. According to the news organization, the documents showed that Merck knew of reports of depression, including suicidal thoughts, as early as 2009.
However, according to Reuters, the FDA in 2011 granted Merck’s request to only note depression as a potential side effect, without including the risk of suicidal ideation.
The current FDA label notes a small incidence of sexual dysfunction, including decreased libido (1.8% in trials) and erectile dysfunction (1.3%) and mentions depression as a side effect observed during the postmarketing period.
The Canadian label has the same statistics on sexual side effects but is much stronger on mental adverse effects: “Psychiatric disorders: mood alterations and depression, decreased libido that continued after discontinuation of treatment. Mood alterations including depressed mood and, less frequently, suicidal ideation have been reported in patients treated with finasteride 1 mg. Patients should be monitored for psychiatric symptoms, and if these occur, the patient should be advised to seek medical advice.”
In the United Kingdom, patients prescribed the drug are given a leaflet, which notes that “Mood alterations such as depressed mood, depression and, less frequently, suicidal thoughts have been reported in patients treated with Propecia,” and advises patients to stop taking the drug if they experience any of those symptoms and to discuss it with their physician.
Public Citizen noted in its lawsuit that French and German drug regulators have sent letters to clinicians advising them to inform patients of the risk of suicidal thoughts and anxiety.
Is there biological plausibility?
To bolster its argument that finasteride has dangerous psychiatric side effects, the advocacy organization cited a study first published in JAMA Dermatology in late 2020 that investigated suicidality and psychological adverse events in patients taking finasteride.
David-Dan Nguyen, MPH, and his colleagues at Brigham and Women’s Hospital in Boston, McGill University, Montreal, and the University of Montreal, examined the VigiBase database and found 356 cases of suicidality and 2,926 psychological adverse events; cases were highest from 2015 to 2019.
They documented what they called a “significant disproportionality signal for suicidality (reporting odds ratio, 1.63; 95% confidence interval, 2.90-4.15) and psychological adverse events (ROR, 4.33; 95% CI, 4.17-4.49) with finasteride, especially in younger men and those with alopecia, but not in older men or those with benign prostatic hyperplasia.
The study authors noted that some studies have suggested that men with depression have low levels of the neurosteroid allopregnanolone, which is produced by the 5-alpha reductase enzyme. Finasteride is a 5-alpha reductase inhibitor.
According to Public Citizen’s lawsuit, “The product labeling does not disclose important information about finasteride’s mechanism of action,” and “the drug inhibits multiple steroid hormone pathways that are responsible for the formation of brain neurosteroids that regulate many critical functions in the central nervous system, like sexual function, mood, sleep, cognitive function, the stress response, and motivation.”
Dr. Jacobs said that “there’s a lot of good solid high-quality research, mostly in animals, but also some on humans, showing a plausible link between blocking 5-alpha reductase in the brain, deficiency of neuroactive steroids, and depression.”
The author of an accompanying editorial, Roger S. Ho, MD, MPH, an associate professor in the department of dermatology, New York University, was skeptical. “Without a plausible biological hypothesis pharmacodynamically linking the drug and the reported adverse event, this kind of analysis may lead to false findings,” Dr. Ho said in the editorial about the Nguyen study.
Dr. Ho also wrote that he believed that the lack of a suicidality signal for dutasteride, a drug with a similar mechanism of action, but without as much media attention, “hints at a potential reporting bias unique to finasteride.”
He recommended that clinicians “conduct a full evaluation and a detailed, personalized risk-benefit assessment for patients before each prescription of finasteride.”
Important medicine, important caveats
Dr. Jacobs said that many of the men who come to him with side effects after taking finasteride have “been blown off by most of the doctors they go to see.”
Urologists dismiss them because their sexual dysfunction is not a gonad issue. They are told that it’s in their head, said Dr. Jacobs, adding that, “it is in their head, but it’s biological.”
The drug’s label advises that sexual side effects disappear when the drug is stopped. “That’s only true most of the time, not all of the time,” said Dr. Jacobs, adding that the persistence of any side effects impacts what he calls a “small subset” of men who take the drug.
“We have treated tens of thousands of patients who have benefited from the medicine and had no side effects,” said Dr. Bernstein. “But there is a lot that’s still not known about it.”
Even so, “baldness in young people is not a benign condition,” he said, adding that it can be socially debilitating. “An 18-year-old with a full head of thick hair who’s totally bald in 3 or 4 years – that can totally change his psyche,” Dr. Bernstein said. Finasteride may be the best option for those young men, and it is an important medication, he said. Does it need to be used more carefully? “Certainly you can’t argue with that,” he commented.
Dr. Bernstein and Dr. Irwig reported no conflicts. Dr. Jacobs disclosed that he is an expert witness for the plaintiffs in a suit against Propecia maker Merck.
Marijuana and LSD guidance for pediatricians
Seeking novelty is central to adolescence; experimentation is how they explore their identity, exert independence, and establish deep and connected relationships outside of the family. Research over the past 2 decades has demonstrated the neurobiological changes that underpin this increase in sensation seeking. Most adolescents are very good at assessing risk but are willing to tolerate higher levels of risk than adults in the pursuit of novelty.1 If their knowledge base is limited or inaccurate, as is often the case with drugs and alcohol, accepting higher risk becomes more dangerous. Adolescents are more likely to trust their peers than their parents, but their pediatricians still have authority and credibility.
While there is ample credible information online (from the National Institute on Drug Abuse and the Substance Abuse and Mental Health Services Administration’s excellent websites, which can be recommended to teens), marijuana and hallucinogens (LSD and psilocybin) bear special discussion here because of changing legality and their potential medical utility. There is an emerging impression of safety with both; however, policy changes and for-profit marketing may not reflect the actual scientific evidence. You have the opportunity and authority to complicate your patient’s thinking by discussing the evidence supporting their medical utility, and the emerging evidence that both types of drugs may pose special risks for their developing brains.
By June 2021, marijuana was legal for recreational use in 19 states; Washington, D.C.; and Guam, and for “medical use” in 36 states and four territories. Entrepreneurs and activists have made spectacular claims that marijuana is effective for the treatment of everything from insomnia to PTSD, but the reality is less impressive. Of course, marijuana remains a schedule I drug under the federal Controlled Substances Act (1970), which has made it difficult for researchers to perform randomized controlled studies concerning treatment or risks.
However, there are a growing number of randomized controlled trials with synthetic cannabinoids (dronabinol and nabilone) and a (legal) drug derived from cannabis (cannabidiol or CBD, as distinct from the other active ingredient, tetrahydrocannabinol). There is Food and Drug Administration approval for CBD for the treatment of epilepsy in Lennox-Gastaut or Dravet syndrome in patients aged 2 years or younger, and for the synthetic agents for the treatment of chemotherapy-related nausea and vomiting in cancer patients and for the treatment of weight loss and muscle wasting related to HIV/AIDS. That’s it. There is some evidence that these agents may be effective for the treatment of muscle spasticity in multiple sclerosis, chronic pain of many etiologies, Tourette syndrome, insomnia related to multiple sclerosis and chronic pain, and possibly PTSD. But there have been multiple studies that have failed to demonstrate efficacy (or have demonstrated exacerbation) for a host of other medical and psychiatric problems.
While the evidence for marijuana’s medicinal uses is modest, there is substantial evidence that its use in adolescence carries risks. It is an addictive substance and regular use is associated with sustained modest cognitive impairment (a loss of up to eight IQ points in the clinically dependent) and higher rates of anxiety and depressive disorders. As with other substances, use before the age of 18 substantially raises the risk (as much as sevenfold) of developing addiction than the same rate of use in adulthood. The rate of schizophrenia in adolescents with heavy marijuana use is between six and seven times greater than in the general population, whereas similar adult use does not have this association.2,3 Studies in rats have demonstrated that use during adolescence delays and permanently changes the maturation of the prefrontal cortex, an area of the brain that is essential for complex decision-making, sustaining attention, abstract reasoning, and impulse control.4 While we do not fully understand the exact nature of these changes, there is good reason to believe that regular marijuana use in adolescence leads to disruption of critical brain development and cognitive or even psychotic consequences. It is worth noting that the potency of many commercially available marijuana products is much higher than those that were studied, raising the risk and uncertainty further.
Hallucinogens, or “psychedelics” (from Greek for “mind manifesting”) are a class that includes LSD and psilocybin (a chemical found in over 200 species of mushrooms). They precipitate visual and auditory “hallucinations,” a loss of sense of self, and a sense of awe that may be transcendent or frightening. While psilocybin was used by many indigenous cultures in religious ceremonies, LSD was synthesized by a chemist at Sandoz in 1938 and made widely available for study until it was classified as a schedule I drug by the 1970 Controlled Substances Act. They are not addictive. Early research demonstrated promise in the treatment of alcohol dependence and several psychiatric conditions (including other addictions and treatment-resistant depression). Research resumed in 2018, demonstrating promise in the treatment of depression related to terminal illness. Research has also concerned the nature of consciousness and spiritual experiences. Hallucinogens have become popular in certain fields (high tech) as a means of optimizing creativity and performance (“microdosing”). There is modest evidence that use in people with a family history of psychotic illness may precipitate sustained psychotic symptoms. Regular use may further increase the risk of persistent psychosis and adolescent users of multiple substances are at high risk for regular hallucinogen use. Adolescents may think that ketamine, phencyclidine , and 3,4-methylenedioxymethamphetamine are also in this category, although they are different and considerably more risky drugs. Overall, these agents show therapeutic promise, but unless your young patients are facing depression related to a terminal illness and until we learn more from studies, the potential risk to their developing brains outweighs any potential benefits.
Aware of this information, you are ready to ask your adolescent patients about their drug and alcohol use and knowledge. Using phrases like “when did you first try ...” can increase the likelihood that your patients will be forthright with you. Or start by asking about what their friends are trying and talking about. Be curious about any drug and alcohol use at home. Find out what they are curious about, whom they trust, and where they get their information. Then you can offer your information about the dramatic changes happening in their brains (just like the rest of their bodies) and the special risks of drug use during this window of brain development. Acknowledge that the risks of marijuana use in adults may very well be lower than the risks of regular alcohol use but remind them about how their brains are different than those of adults. Delaying use until they are 18 (or ideally in their mid-20s when most brain development is complete), can dramatically lower these risks. For adolescents with a family history of addiction, psychosis, or mood and anxiety disorders, discuss the additional risks that drugs may present to them. And for those adolescents who acknowledge very early (before 13) or heavy use, be curious with them about whether they might be trying to “feel better” and not just “feel good.” Screen them for depression, suicidality, and anxiety disorders. Those underlying problems are treatable, but their course will only worsen with drug and alcohol use. You are in a unique position to help your adolescent patients make wise and well-informed choices and to get them assistance if they need it.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. Romer D. Dev Psychobiol. 2010 Apr;52(3):263-76.
2. Szczepanski SM and Knight TR. Neuron. 2014;83:1002-18.
3. Renard J et al. Front Psychiatry. 2018;9:281.
4. Shen H. Proc Natl Acad Sci U S A. 2020 Jan 7;117(1):7-11.
Seeking novelty is central to adolescence; experimentation is how they explore their identity, exert independence, and establish deep and connected relationships outside of the family. Research over the past 2 decades has demonstrated the neurobiological changes that underpin this increase in sensation seeking. Most adolescents are very good at assessing risk but are willing to tolerate higher levels of risk than adults in the pursuit of novelty.1 If their knowledge base is limited or inaccurate, as is often the case with drugs and alcohol, accepting higher risk becomes more dangerous. Adolescents are more likely to trust their peers than their parents, but their pediatricians still have authority and credibility.
While there is ample credible information online (from the National Institute on Drug Abuse and the Substance Abuse and Mental Health Services Administration’s excellent websites, which can be recommended to teens), marijuana and hallucinogens (LSD and psilocybin) bear special discussion here because of changing legality and their potential medical utility. There is an emerging impression of safety with both; however, policy changes and for-profit marketing may not reflect the actual scientific evidence. You have the opportunity and authority to complicate your patient’s thinking by discussing the evidence supporting their medical utility, and the emerging evidence that both types of drugs may pose special risks for their developing brains.
By June 2021, marijuana was legal for recreational use in 19 states; Washington, D.C.; and Guam, and for “medical use” in 36 states and four territories. Entrepreneurs and activists have made spectacular claims that marijuana is effective for the treatment of everything from insomnia to PTSD, but the reality is less impressive. Of course, marijuana remains a schedule I drug under the federal Controlled Substances Act (1970), which has made it difficult for researchers to perform randomized controlled studies concerning treatment or risks.
However, there are a growing number of randomized controlled trials with synthetic cannabinoids (dronabinol and nabilone) and a (legal) drug derived from cannabis (cannabidiol or CBD, as distinct from the other active ingredient, tetrahydrocannabinol). There is Food and Drug Administration approval for CBD for the treatment of epilepsy in Lennox-Gastaut or Dravet syndrome in patients aged 2 years or younger, and for the synthetic agents for the treatment of chemotherapy-related nausea and vomiting in cancer patients and for the treatment of weight loss and muscle wasting related to HIV/AIDS. That’s it. There is some evidence that these agents may be effective for the treatment of muscle spasticity in multiple sclerosis, chronic pain of many etiologies, Tourette syndrome, insomnia related to multiple sclerosis and chronic pain, and possibly PTSD. But there have been multiple studies that have failed to demonstrate efficacy (or have demonstrated exacerbation) for a host of other medical and psychiatric problems.
While the evidence for marijuana’s medicinal uses is modest, there is substantial evidence that its use in adolescence carries risks. It is an addictive substance and regular use is associated with sustained modest cognitive impairment (a loss of up to eight IQ points in the clinically dependent) and higher rates of anxiety and depressive disorders. As with other substances, use before the age of 18 substantially raises the risk (as much as sevenfold) of developing addiction than the same rate of use in adulthood. The rate of schizophrenia in adolescents with heavy marijuana use is between six and seven times greater than in the general population, whereas similar adult use does not have this association.2,3 Studies in rats have demonstrated that use during adolescence delays and permanently changes the maturation of the prefrontal cortex, an area of the brain that is essential for complex decision-making, sustaining attention, abstract reasoning, and impulse control.4 While we do not fully understand the exact nature of these changes, there is good reason to believe that regular marijuana use in adolescence leads to disruption of critical brain development and cognitive or even psychotic consequences. It is worth noting that the potency of many commercially available marijuana products is much higher than those that were studied, raising the risk and uncertainty further.
Hallucinogens, or “psychedelics” (from Greek for “mind manifesting”) are a class that includes LSD and psilocybin (a chemical found in over 200 species of mushrooms). They precipitate visual and auditory “hallucinations,” a loss of sense of self, and a sense of awe that may be transcendent or frightening. While psilocybin was used by many indigenous cultures in religious ceremonies, LSD was synthesized by a chemist at Sandoz in 1938 and made widely available for study until it was classified as a schedule I drug by the 1970 Controlled Substances Act. They are not addictive. Early research demonstrated promise in the treatment of alcohol dependence and several psychiatric conditions (including other addictions and treatment-resistant depression). Research resumed in 2018, demonstrating promise in the treatment of depression related to terminal illness. Research has also concerned the nature of consciousness and spiritual experiences. Hallucinogens have become popular in certain fields (high tech) as a means of optimizing creativity and performance (“microdosing”). There is modest evidence that use in people with a family history of psychotic illness may precipitate sustained psychotic symptoms. Regular use may further increase the risk of persistent psychosis and adolescent users of multiple substances are at high risk for regular hallucinogen use. Adolescents may think that ketamine, phencyclidine , and 3,4-methylenedioxymethamphetamine are also in this category, although they are different and considerably more risky drugs. Overall, these agents show therapeutic promise, but unless your young patients are facing depression related to a terminal illness and until we learn more from studies, the potential risk to their developing brains outweighs any potential benefits.
Aware of this information, you are ready to ask your adolescent patients about their drug and alcohol use and knowledge. Using phrases like “when did you first try ...” can increase the likelihood that your patients will be forthright with you. Or start by asking about what their friends are trying and talking about. Be curious about any drug and alcohol use at home. Find out what they are curious about, whom they trust, and where they get their information. Then you can offer your information about the dramatic changes happening in their brains (just like the rest of their bodies) and the special risks of drug use during this window of brain development. Acknowledge that the risks of marijuana use in adults may very well be lower than the risks of regular alcohol use but remind them about how their brains are different than those of adults. Delaying use until they are 18 (or ideally in their mid-20s when most brain development is complete), can dramatically lower these risks. For adolescents with a family history of addiction, psychosis, or mood and anxiety disorders, discuss the additional risks that drugs may present to them. And for those adolescents who acknowledge very early (before 13) or heavy use, be curious with them about whether they might be trying to “feel better” and not just “feel good.” Screen them for depression, suicidality, and anxiety disorders. Those underlying problems are treatable, but their course will only worsen with drug and alcohol use. You are in a unique position to help your adolescent patients make wise and well-informed choices and to get them assistance if they need it.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. Romer D. Dev Psychobiol. 2010 Apr;52(3):263-76.
2. Szczepanski SM and Knight TR. Neuron. 2014;83:1002-18.
3. Renard J et al. Front Psychiatry. 2018;9:281.
4. Shen H. Proc Natl Acad Sci U S A. 2020 Jan 7;117(1):7-11.
Seeking novelty is central to adolescence; experimentation is how they explore their identity, exert independence, and establish deep and connected relationships outside of the family. Research over the past 2 decades has demonstrated the neurobiological changes that underpin this increase in sensation seeking. Most adolescents are very good at assessing risk but are willing to tolerate higher levels of risk than adults in the pursuit of novelty.1 If their knowledge base is limited or inaccurate, as is often the case with drugs and alcohol, accepting higher risk becomes more dangerous. Adolescents are more likely to trust their peers than their parents, but their pediatricians still have authority and credibility.
While there is ample credible information online (from the National Institute on Drug Abuse and the Substance Abuse and Mental Health Services Administration’s excellent websites, which can be recommended to teens), marijuana and hallucinogens (LSD and psilocybin) bear special discussion here because of changing legality and their potential medical utility. There is an emerging impression of safety with both; however, policy changes and for-profit marketing may not reflect the actual scientific evidence. You have the opportunity and authority to complicate your patient’s thinking by discussing the evidence supporting their medical utility, and the emerging evidence that both types of drugs may pose special risks for their developing brains.
By June 2021, marijuana was legal for recreational use in 19 states; Washington, D.C.; and Guam, and for “medical use” in 36 states and four territories. Entrepreneurs and activists have made spectacular claims that marijuana is effective for the treatment of everything from insomnia to PTSD, but the reality is less impressive. Of course, marijuana remains a schedule I drug under the federal Controlled Substances Act (1970), which has made it difficult for researchers to perform randomized controlled studies concerning treatment or risks.
However, there are a growing number of randomized controlled trials with synthetic cannabinoids (dronabinol and nabilone) and a (legal) drug derived from cannabis (cannabidiol or CBD, as distinct from the other active ingredient, tetrahydrocannabinol). There is Food and Drug Administration approval for CBD for the treatment of epilepsy in Lennox-Gastaut or Dravet syndrome in patients aged 2 years or younger, and for the synthetic agents for the treatment of chemotherapy-related nausea and vomiting in cancer patients and for the treatment of weight loss and muscle wasting related to HIV/AIDS. That’s it. There is some evidence that these agents may be effective for the treatment of muscle spasticity in multiple sclerosis, chronic pain of many etiologies, Tourette syndrome, insomnia related to multiple sclerosis and chronic pain, and possibly PTSD. But there have been multiple studies that have failed to demonstrate efficacy (or have demonstrated exacerbation) for a host of other medical and psychiatric problems.
While the evidence for marijuana’s medicinal uses is modest, there is substantial evidence that its use in adolescence carries risks. It is an addictive substance and regular use is associated with sustained modest cognitive impairment (a loss of up to eight IQ points in the clinically dependent) and higher rates of anxiety and depressive disorders. As with other substances, use before the age of 18 substantially raises the risk (as much as sevenfold) of developing addiction than the same rate of use in adulthood. The rate of schizophrenia in adolescents with heavy marijuana use is between six and seven times greater than in the general population, whereas similar adult use does not have this association.2,3 Studies in rats have demonstrated that use during adolescence delays and permanently changes the maturation of the prefrontal cortex, an area of the brain that is essential for complex decision-making, sustaining attention, abstract reasoning, and impulse control.4 While we do not fully understand the exact nature of these changes, there is good reason to believe that regular marijuana use in adolescence leads to disruption of critical brain development and cognitive or even psychotic consequences. It is worth noting that the potency of many commercially available marijuana products is much higher than those that were studied, raising the risk and uncertainty further.
Hallucinogens, or “psychedelics” (from Greek for “mind manifesting”) are a class that includes LSD and psilocybin (a chemical found in over 200 species of mushrooms). They precipitate visual and auditory “hallucinations,” a loss of sense of self, and a sense of awe that may be transcendent or frightening. While psilocybin was used by many indigenous cultures in religious ceremonies, LSD was synthesized by a chemist at Sandoz in 1938 and made widely available for study until it was classified as a schedule I drug by the 1970 Controlled Substances Act. They are not addictive. Early research demonstrated promise in the treatment of alcohol dependence and several psychiatric conditions (including other addictions and treatment-resistant depression). Research resumed in 2018, demonstrating promise in the treatment of depression related to terminal illness. Research has also concerned the nature of consciousness and spiritual experiences. Hallucinogens have become popular in certain fields (high tech) as a means of optimizing creativity and performance (“microdosing”). There is modest evidence that use in people with a family history of psychotic illness may precipitate sustained psychotic symptoms. Regular use may further increase the risk of persistent psychosis and adolescent users of multiple substances are at high risk for regular hallucinogen use. Adolescents may think that ketamine, phencyclidine , and 3,4-methylenedioxymethamphetamine are also in this category, although they are different and considerably more risky drugs. Overall, these agents show therapeutic promise, but unless your young patients are facing depression related to a terminal illness and until we learn more from studies, the potential risk to their developing brains outweighs any potential benefits.
Aware of this information, you are ready to ask your adolescent patients about their drug and alcohol use and knowledge. Using phrases like “when did you first try ...” can increase the likelihood that your patients will be forthright with you. Or start by asking about what their friends are trying and talking about. Be curious about any drug and alcohol use at home. Find out what they are curious about, whom they trust, and where they get their information. Then you can offer your information about the dramatic changes happening in their brains (just like the rest of their bodies) and the special risks of drug use during this window of brain development. Acknowledge that the risks of marijuana use in adults may very well be lower than the risks of regular alcohol use but remind them about how their brains are different than those of adults. Delaying use until they are 18 (or ideally in their mid-20s when most brain development is complete), can dramatically lower these risks. For adolescents with a family history of addiction, psychosis, or mood and anxiety disorders, discuss the additional risks that drugs may present to them. And for those adolescents who acknowledge very early (before 13) or heavy use, be curious with them about whether they might be trying to “feel better” and not just “feel good.” Screen them for depression, suicidality, and anxiety disorders. Those underlying problems are treatable, but their course will only worsen with drug and alcohol use. You are in a unique position to help your adolescent patients make wise and well-informed choices and to get them assistance if they need it.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. Romer D. Dev Psychobiol. 2010 Apr;52(3):263-76.
2. Szczepanski SM and Knight TR. Neuron. 2014;83:1002-18.
3. Renard J et al. Front Psychiatry. 2018;9:281.
4. Shen H. Proc Natl Acad Sci U S A. 2020 Jan 7;117(1):7-11.
CDC panel unanimously backs Pfizer vax, fortifying FDA approval
An independent expert panel within the Centers for Disease Control and Prevention (CDC) has studied the potential benefits and risks of the Pfizer-BioNTech COVID-19 vaccine and voted unanimously to recommend the shots for all Americans ages 16 and older.
The vaccine was fully approved by the U.S. Food and Drug Administration (FDA) last week.
The inoculation is still available to teens ages 12 to 15 under an emergency use authorization from the FDA.
ACIP now sends its recommendation to the CDC Director Rochelle Walensky, MD, for her sign off.
After reviewing the evidence behind the vaccine, panel member Sarah Long, MD, a professor of pediatrics at Drexel University College of Medicine, Philadelphia, said she couldn’t recall another instance where panelists had so much data on which to base their recommendation.
“This vaccine is worthy of the trust of the American people,” she said.
Doctors across the country use vaccines in line with the recommendations made by the ACIP. Their approval typically means that private and government insurers will cover the cost of the shots. In the case of the COVID-19 vaccines, the government is already picking up the tab.
Few surprises
The panel’s independent review of the vaccine’s effectiveness from nine studies held few surprises.
They found the Pfizer vaccine prevented a COVID infection with symptoms about 90%–92% of the time, at least for the first 4 months after the second shot. Protection against hospitalization and death was even higher.
The vaccine was about 89% effective at preventing a COVID infection without symptoms, according to a pooled estimate of five studies.
The data included in the review was updated only through March 13 of this year, however, and does not reflect the impact of further waning of immunity or the impact of the Delta variant.
In making their recommendation, the panel got an update on the safety of the vaccines, which have now been used in the United States for about 9 months.
The rate of anaphylaxis has settled at around five cases for every million shots given, according to the ACIP’s review of the evidence.
Cases of myocarditis and pericarditis were more common after getting a Pfizer-BioNTech vaccine than would be expected to happen naturally in the general population, but the risk was still very rare, and elevated primarily for men younger than age 30.
Out of 17 million second doses of Pfizer-BioNTech vaccines in the United States, there have been 327 confirmed cases of myocarditis reported to the Vaccine Adverse Event Reporting System in people who are younger than age 30. The average hospital stay for a myocarditis cases is 1 to 2 days.
So far, no one in the United States diagnosed with myocarditis after vaccination has died.
What’s more, the risk of myocarditis after vaccination was dwarfed by the risk of myocarditis after a COVID infection. The risk of myocarditis after a COVID infection was 6 to 34 times higher than the risk after receiving an mRNA vaccine.
About 11% of people who get the vaccine experience a serious reaction to the shot, compared with about 3% in the placebo group. Serious reactions were defined as pain; swelling or redness at the injection site that interferes with activity; needing to visit the hospital or ER for pain; tissue necrosis, or having skin slough off; high fever; vomiting that requires hydration; persistent diarrhea; severe headache; or muscle pain/severe joint pain.
“Safe and effective”
After hearing a presentation on the state of the pandemic in the US, some panel members were struck and shaken that 38% of Americans who are eligible are still not fully vaccinated.
Pablo Sanchez, MD, a pediatrician at Nationwide Children’s Hospital in Columbus, Ohio, said, “We’re doing an abysmal job vaccinating the American people. The message has to go out that the vaccines are safe and effective.”
A version of this story first appeared on Medscape.com.
An independent expert panel within the Centers for Disease Control and Prevention (CDC) has studied the potential benefits and risks of the Pfizer-BioNTech COVID-19 vaccine and voted unanimously to recommend the shots for all Americans ages 16 and older.
The vaccine was fully approved by the U.S. Food and Drug Administration (FDA) last week.
The inoculation is still available to teens ages 12 to 15 under an emergency use authorization from the FDA.
ACIP now sends its recommendation to the CDC Director Rochelle Walensky, MD, for her sign off.
After reviewing the evidence behind the vaccine, panel member Sarah Long, MD, a professor of pediatrics at Drexel University College of Medicine, Philadelphia, said she couldn’t recall another instance where panelists had so much data on which to base their recommendation.
“This vaccine is worthy of the trust of the American people,” she said.
Doctors across the country use vaccines in line with the recommendations made by the ACIP. Their approval typically means that private and government insurers will cover the cost of the shots. In the case of the COVID-19 vaccines, the government is already picking up the tab.
Few surprises
The panel’s independent review of the vaccine’s effectiveness from nine studies held few surprises.
They found the Pfizer vaccine prevented a COVID infection with symptoms about 90%–92% of the time, at least for the first 4 months after the second shot. Protection against hospitalization and death was even higher.
The vaccine was about 89% effective at preventing a COVID infection without symptoms, according to a pooled estimate of five studies.
The data included in the review was updated only through March 13 of this year, however, and does not reflect the impact of further waning of immunity or the impact of the Delta variant.
In making their recommendation, the panel got an update on the safety of the vaccines, which have now been used in the United States for about 9 months.
The rate of anaphylaxis has settled at around five cases for every million shots given, according to the ACIP’s review of the evidence.
Cases of myocarditis and pericarditis were more common after getting a Pfizer-BioNTech vaccine than would be expected to happen naturally in the general population, but the risk was still very rare, and elevated primarily for men younger than age 30.
Out of 17 million second doses of Pfizer-BioNTech vaccines in the United States, there have been 327 confirmed cases of myocarditis reported to the Vaccine Adverse Event Reporting System in people who are younger than age 30. The average hospital stay for a myocarditis cases is 1 to 2 days.
So far, no one in the United States diagnosed with myocarditis after vaccination has died.
What’s more, the risk of myocarditis after vaccination was dwarfed by the risk of myocarditis after a COVID infection. The risk of myocarditis after a COVID infection was 6 to 34 times higher than the risk after receiving an mRNA vaccine.
About 11% of people who get the vaccine experience a serious reaction to the shot, compared with about 3% in the placebo group. Serious reactions were defined as pain; swelling or redness at the injection site that interferes with activity; needing to visit the hospital or ER for pain; tissue necrosis, or having skin slough off; high fever; vomiting that requires hydration; persistent diarrhea; severe headache; or muscle pain/severe joint pain.
“Safe and effective”
After hearing a presentation on the state of the pandemic in the US, some panel members were struck and shaken that 38% of Americans who are eligible are still not fully vaccinated.
Pablo Sanchez, MD, a pediatrician at Nationwide Children’s Hospital in Columbus, Ohio, said, “We’re doing an abysmal job vaccinating the American people. The message has to go out that the vaccines are safe and effective.”
A version of this story first appeared on Medscape.com.
An independent expert panel within the Centers for Disease Control and Prevention (CDC) has studied the potential benefits and risks of the Pfizer-BioNTech COVID-19 vaccine and voted unanimously to recommend the shots for all Americans ages 16 and older.
The vaccine was fully approved by the U.S. Food and Drug Administration (FDA) last week.
The inoculation is still available to teens ages 12 to 15 under an emergency use authorization from the FDA.
ACIP now sends its recommendation to the CDC Director Rochelle Walensky, MD, for her sign off.
After reviewing the evidence behind the vaccine, panel member Sarah Long, MD, a professor of pediatrics at Drexel University College of Medicine, Philadelphia, said she couldn’t recall another instance where panelists had so much data on which to base their recommendation.
“This vaccine is worthy of the trust of the American people,” she said.
Doctors across the country use vaccines in line with the recommendations made by the ACIP. Their approval typically means that private and government insurers will cover the cost of the shots. In the case of the COVID-19 vaccines, the government is already picking up the tab.
Few surprises
The panel’s independent review of the vaccine’s effectiveness from nine studies held few surprises.
They found the Pfizer vaccine prevented a COVID infection with symptoms about 90%–92% of the time, at least for the first 4 months after the second shot. Protection against hospitalization and death was even higher.
The vaccine was about 89% effective at preventing a COVID infection without symptoms, according to a pooled estimate of five studies.
The data included in the review was updated only through March 13 of this year, however, and does not reflect the impact of further waning of immunity or the impact of the Delta variant.
In making their recommendation, the panel got an update on the safety of the vaccines, which have now been used in the United States for about 9 months.
The rate of anaphylaxis has settled at around five cases for every million shots given, according to the ACIP’s review of the evidence.
Cases of myocarditis and pericarditis were more common after getting a Pfizer-BioNTech vaccine than would be expected to happen naturally in the general population, but the risk was still very rare, and elevated primarily for men younger than age 30.
Out of 17 million second doses of Pfizer-BioNTech vaccines in the United States, there have been 327 confirmed cases of myocarditis reported to the Vaccine Adverse Event Reporting System in people who are younger than age 30. The average hospital stay for a myocarditis cases is 1 to 2 days.
So far, no one in the United States diagnosed with myocarditis after vaccination has died.
What’s more, the risk of myocarditis after vaccination was dwarfed by the risk of myocarditis after a COVID infection. The risk of myocarditis after a COVID infection was 6 to 34 times higher than the risk after receiving an mRNA vaccine.
About 11% of people who get the vaccine experience a serious reaction to the shot, compared with about 3% in the placebo group. Serious reactions were defined as pain; swelling or redness at the injection site that interferes with activity; needing to visit the hospital or ER for pain; tissue necrosis, or having skin slough off; high fever; vomiting that requires hydration; persistent diarrhea; severe headache; or muscle pain/severe joint pain.
“Safe and effective”
After hearing a presentation on the state of the pandemic in the US, some panel members were struck and shaken that 38% of Americans who are eligible are still not fully vaccinated.
Pablo Sanchez, MD, a pediatrician at Nationwide Children’s Hospital in Columbus, Ohio, said, “We’re doing an abysmal job vaccinating the American people. The message has to go out that the vaccines are safe and effective.”
A version of this story first appeared on Medscape.com.
Outstanding medical bills: Dealing with deadbeats
Since the COVID-19 pandemic began, I have received a growing number of inquiries about collection issues. For a variety of reasons, many patients seem increasingly reluctant to pay their medical bills. I’ve written many columns on keeping credit card numbers on file, and other techniques for keeping your accounts receivable in check; but despite your best efforts, there will always be a few deadbeats that you will need to pursue.
For the record, I am not speaking about patients who lost income due to the pandemic and are now struggling with debts, or otherwise have fallen on hard times and are unable to pay.
The worst kinds of deadbeats are the ones who rob you twice; they accept payments from insurance companies and keep them. Such crooks must be pursued aggressively, with all the means at your disposal; but to reiterate the point I’ve tried to drive home repeatedly, the best cure is prevention.
You already know that you should collect as many fees as possible at the time of service. For cosmetic procedures you should require a substantial deposit in advance, with the balance due at the time of service. When that is impossible, maximize the chances you will be paid by making sure all available payment mechanisms are in place.
With my credit-card-on-file system that I’ve described many times, patients who fail to pay their credit card bill are the credit card company’s problem, not yours. In cases where you suspect fees might exceed credit card limits, you can arrange a realistic payment schedule in advance and have the patient fill out a credit application. You can find forms for this online at formswift.com, templates.office.com, and many other websites.
In some cases, it may be worth the trouble to run a background check. There are easy and affordable ways to do this. Dunn & Bradstreet, for example, will furnish a report containing payment records and details of any lawsuits, liens, and other legal actions for a nominal fee. The more financial information you have on file, the more leverage you have if a patient later balks at paying his or her balance.
For cosmetic work, always take before and after photos, and have all patients sign a written consent giving permission for the procedure, assuming full financial responsibility, and acknowledging that no guarantees have been given or implied. This defuses the common deadbeat tactics of claiming ignorance of personal financial obligations and professing dissatisfaction with the results.
Despite all your precautions, a deadbeat will inevitably slip through on occasion; but even then, you have options for extracting payment. Collection agencies are the traditional first line of attack for most medical practices. Ideally, your agency should specialize in handling medical accounts, so it will know exactly how much pressure to exert to avoid charges of harassment. Delinquent accounts should be submitted earlier rather than later to maximize the chances of success; my manager never allows an account to age more than 90 days, and if circumstances dictate, she refers them sooner than that.
When collection agencies fail, think about small claims court. You will need to learn the rules in your state, but in most states there is a small filing fee and a limit of $5,000 or so on claims. No attorneys are involved. If your paperwork is in order, the court will nearly always rule in your favor, but it will not provide the means for actual collection. In other words, you will still have to persuade the deadbeat to pay up. However, in many states a court order will give you the authority to attach a lien to property, or garnish wages, which often provides enough leverage to force payment.
What about those double-deadbeats who keep the insurance checks for themselves? First, check your third-party contract; sometimes the insurance company or HMO will be compelled to pay you directly and then go after the patient to get back its money. (They won’t volunteer this service, however – you’ll have to ask for it.)
If that’s not an option, consider reporting the misdirected payment to the Internal Revenue Service as income to the patient, by submitting a 1099 Miscellaneous Income form. Be sure to notify the deadbeat that you will be doing this. Sometimes the threat of such action will convince the individual to pay up; if not, at least you’ll have the satisfaction of knowing he or she will have to pay taxes on the money.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Since the COVID-19 pandemic began, I have received a growing number of inquiries about collection issues. For a variety of reasons, many patients seem increasingly reluctant to pay their medical bills. I’ve written many columns on keeping credit card numbers on file, and other techniques for keeping your accounts receivable in check; but despite your best efforts, there will always be a few deadbeats that you will need to pursue.
For the record, I am not speaking about patients who lost income due to the pandemic and are now struggling with debts, or otherwise have fallen on hard times and are unable to pay.
The worst kinds of deadbeats are the ones who rob you twice; they accept payments from insurance companies and keep them. Such crooks must be pursued aggressively, with all the means at your disposal; but to reiterate the point I’ve tried to drive home repeatedly, the best cure is prevention.
You already know that you should collect as many fees as possible at the time of service. For cosmetic procedures you should require a substantial deposit in advance, with the balance due at the time of service. When that is impossible, maximize the chances you will be paid by making sure all available payment mechanisms are in place.
With my credit-card-on-file system that I’ve described many times, patients who fail to pay their credit card bill are the credit card company’s problem, not yours. In cases where you suspect fees might exceed credit card limits, you can arrange a realistic payment schedule in advance and have the patient fill out a credit application. You can find forms for this online at formswift.com, templates.office.com, and many other websites.
In some cases, it may be worth the trouble to run a background check. There are easy and affordable ways to do this. Dunn & Bradstreet, for example, will furnish a report containing payment records and details of any lawsuits, liens, and other legal actions for a nominal fee. The more financial information you have on file, the more leverage you have if a patient later balks at paying his or her balance.
For cosmetic work, always take before and after photos, and have all patients sign a written consent giving permission for the procedure, assuming full financial responsibility, and acknowledging that no guarantees have been given or implied. This defuses the common deadbeat tactics of claiming ignorance of personal financial obligations and professing dissatisfaction with the results.
Despite all your precautions, a deadbeat will inevitably slip through on occasion; but even then, you have options for extracting payment. Collection agencies are the traditional first line of attack for most medical practices. Ideally, your agency should specialize in handling medical accounts, so it will know exactly how much pressure to exert to avoid charges of harassment. Delinquent accounts should be submitted earlier rather than later to maximize the chances of success; my manager never allows an account to age more than 90 days, and if circumstances dictate, she refers them sooner than that.
When collection agencies fail, think about small claims court. You will need to learn the rules in your state, but in most states there is a small filing fee and a limit of $5,000 or so on claims. No attorneys are involved. If your paperwork is in order, the court will nearly always rule in your favor, but it will not provide the means for actual collection. In other words, you will still have to persuade the deadbeat to pay up. However, in many states a court order will give you the authority to attach a lien to property, or garnish wages, which often provides enough leverage to force payment.
What about those double-deadbeats who keep the insurance checks for themselves? First, check your third-party contract; sometimes the insurance company or HMO will be compelled to pay you directly and then go after the patient to get back its money. (They won’t volunteer this service, however – you’ll have to ask for it.)
If that’s not an option, consider reporting the misdirected payment to the Internal Revenue Service as income to the patient, by submitting a 1099 Miscellaneous Income form. Be sure to notify the deadbeat that you will be doing this. Sometimes the threat of such action will convince the individual to pay up; if not, at least you’ll have the satisfaction of knowing he or she will have to pay taxes on the money.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Since the COVID-19 pandemic began, I have received a growing number of inquiries about collection issues. For a variety of reasons, many patients seem increasingly reluctant to pay their medical bills. I’ve written many columns on keeping credit card numbers on file, and other techniques for keeping your accounts receivable in check; but despite your best efforts, there will always be a few deadbeats that you will need to pursue.
For the record, I am not speaking about patients who lost income due to the pandemic and are now struggling with debts, or otherwise have fallen on hard times and are unable to pay.
The worst kinds of deadbeats are the ones who rob you twice; they accept payments from insurance companies and keep them. Such crooks must be pursued aggressively, with all the means at your disposal; but to reiterate the point I’ve tried to drive home repeatedly, the best cure is prevention.
You already know that you should collect as many fees as possible at the time of service. For cosmetic procedures you should require a substantial deposit in advance, with the balance due at the time of service. When that is impossible, maximize the chances you will be paid by making sure all available payment mechanisms are in place.
With my credit-card-on-file system that I’ve described many times, patients who fail to pay their credit card bill are the credit card company’s problem, not yours. In cases where you suspect fees might exceed credit card limits, you can arrange a realistic payment schedule in advance and have the patient fill out a credit application. You can find forms for this online at formswift.com, templates.office.com, and many other websites.
In some cases, it may be worth the trouble to run a background check. There are easy and affordable ways to do this. Dunn & Bradstreet, for example, will furnish a report containing payment records and details of any lawsuits, liens, and other legal actions for a nominal fee. The more financial information you have on file, the more leverage you have if a patient later balks at paying his or her balance.
For cosmetic work, always take before and after photos, and have all patients sign a written consent giving permission for the procedure, assuming full financial responsibility, and acknowledging that no guarantees have been given or implied. This defuses the common deadbeat tactics of claiming ignorance of personal financial obligations and professing dissatisfaction with the results.
Despite all your precautions, a deadbeat will inevitably slip through on occasion; but even then, you have options for extracting payment. Collection agencies are the traditional first line of attack for most medical practices. Ideally, your agency should specialize in handling medical accounts, so it will know exactly how much pressure to exert to avoid charges of harassment. Delinquent accounts should be submitted earlier rather than later to maximize the chances of success; my manager never allows an account to age more than 90 days, and if circumstances dictate, she refers them sooner than that.
When collection agencies fail, think about small claims court. You will need to learn the rules in your state, but in most states there is a small filing fee and a limit of $5,000 or so on claims. No attorneys are involved. If your paperwork is in order, the court will nearly always rule in your favor, but it will not provide the means for actual collection. In other words, you will still have to persuade the deadbeat to pay up. However, in many states a court order will give you the authority to attach a lien to property, or garnish wages, which often provides enough leverage to force payment.
What about those double-deadbeats who keep the insurance checks for themselves? First, check your third-party contract; sometimes the insurance company or HMO will be compelled to pay you directly and then go after the patient to get back its money. (They won’t volunteer this service, however – you’ll have to ask for it.)
If that’s not an option, consider reporting the misdirected payment to the Internal Revenue Service as income to the patient, by submitting a 1099 Miscellaneous Income form. Be sure to notify the deadbeat that you will be doing this. Sometimes the threat of such action will convince the individual to pay up; if not, at least you’ll have the satisfaction of knowing he or she will have to pay taxes on the money.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Hospitals struggle to find nurses, beds, even oxygen as Delta surges
The state of Mississippi is out of intensive care unit beds. The University of Mississippi Medical Center in Jackson – the state’s largest health system – is converting part of a parking garage into a field hospital to make more room.
“Hospitals are full from Memphis to Gulfport, Natchez to Meridian. Everything’s full,” said Alan Jones, MD, the hospital’s COVID-19 response leader, in a press briefing Aug. 11.
The state has requested the help of a federal disaster medical assistance team of physicians, nurses, respiratory therapists, pharmacists, and paramedics to staff the extra beds. The goal is to open the field hospital on Aug. 13.
Arkansas hospitals have as little as eight ICU beds left to serve a population of 3 million people. Alabama isn’t far behind.
As of Aug. 10, several large metro Atlanta hospitals were diverting patients because they were full.
Hospitals in Alabama, Florida, Tennessee, and Texas are canceling elective surgeries, as they are flooded with COVID patients.
Florida has ordered more ventilators from the federal government. Some hospitals in that state have so many patients on high-flow medical oxygen that it is taxing the building supply lines.
“Most hospitals were not designed for this type of volume distribution in their facilities,” said Mary Mayhew, president of the Florida Hospital Association.
That’s when they can get it. Oxygen deliveries have been disrupted because of a shortage of drivers who are trained to transport it.
“Any disruption in the timing of a delivery can be hugely problematic because of the volume of oxygen they’re going through,” Ms. Mayhew said.
Hospitals ‘under great stress’
Over the month of June, the number of COVID patients in Florida hospitals soared from 2,000 to 10,000. Ms. Mayhew says it took twice as long during the last surge for the state to reach those numbers. And they’re still climbing. The state had 15,000 hospitalized COVID patients as of Aug. 11.
COVID hospitalizations tripled in 3 weeks in South Carolina, said state epidemiologist Linda Bell, MD, in a news conference Aug. 11.
“These hospitals are under great stress,” says Eric Toner, MD, a senior scientist at the Johns Hopkins Center for Health Security in Baltimore
The Delta variant has swept through the unvaccinated South with such veracity that hospitals in the region are unable to keep up. Patients with non-COVID health conditions are in jeopardy too.
Lee Owens, age 56, said he was supposed to have triple bypass surgery on Aug. 12 at St. Thomas West Hospital in Nashville, Tenn. Three of the arteries around his heart are 100%, 90%, and 70% blocked. Mr. Owens said the hospital called him Aug. 10 to postpone his surgery because they’ve cut back elective procedures to just one each day because the ICU beds there are full.
“I’m okay with having to wait a few days (my family isn’t!), especially if there are people worse than me, but so much anger at the reason,” he said. “These idiots that refused health care are now taking up my slot for heart surgery. It’s really aggravating.”
Anjali Bright, a spokesperson for St. Thomas West, provided a statement to this news organization saying they are not suspending elective procedures, but they are reviewing those “requiring an inpatient stay on a case-by-case basis.”
She emphasized, though, that “we will never delay care if the patient’s status changes to ‘urgent.’ ”
“Because of how infectious this variant is, this has the potential to be so much worse than what we saw in January,” said Donald Williamson, MD, president of the Alabama Hospital Association.
Dr. Williamson said they have modeled three possible scenarios for spread in the state, which ranks dead last in the United States for vaccination, with just 35% of its population fully protected. If the Delta variant spreads as it did in the United Kingdom, Alabama could see it hospitalize up to 3,000 people.
“That’s the best scenario,” he said.
If it sweeps through the state as it did in India, Alabama is looking at up to 4,500 patients hospitalized, a number that would require more beds and more staff to care for patients.
Then, there is what Dr. Williamson calls his “nightmare scenario.” If the entire state begins to see transmission rates as high as they’re currently seeing in coastal Mobile and Baldwin counties, that could mean up to 8,000 people in the hospital.
“If we see R-naughts of 5-8 statewide, we’re in real trouble,” he said. The R-naught is the basic rate of reproduction, and it means that each infected person would go on to infect 5-8 others. Dr. Williamson said the federal government would have to send them more staff to handle that kind of a surge.
‘Sense of betrayal’
Unlike the surges of last winter and spring, which sent hospitals scrambling for beds and supplies, the biggest pain point for hospitals now is staffing.
In Mississippi, where 200 patients are parked in emergency departments waiting for available and staffed ICU beds, the state is facing Delta with 2,000 fewer registered nurses than it had during its winter surge.
Some have left because of stress and burnout. Others have taken higher-paying jobs with travel nursing companies. To stop the exodus, hospitals are offering better pay, easier schedules, and sign-on and stay-on bonuses.
Doctors say the incentives are nice, but they don’t help with the anguish and anger many feel after months of battling COVID.
“There’s a big sense of betrayal,” said Sarah Nafziger, MD, vice president of clinical support services at the University of Alabama at Birmingham Hospital. “Our staff and health care workers, in general, feel like we’ve been betrayed by the community.”
“We have a vaccine, which is the key to ending this pandemic and people just refuse to take it, and so I think we’re very frustrated. We feel that our communities have let us down by not taking advantage of the vaccine,” Dr. Nafziger said. “It’s just baffling to me and it’s broken my heart every single day.”
Dr. Nafziger said she met with several surgeons at UAB on Aug. 11 and began making decisions about which surgeries would need to be canceled the following week. “We’re talking about cancer surgery. We’re talking about heart surgery. We’re talking about things that are critical to people.”
Compounding the staffing problems, about half of hospital workers in Alabama are still unvaccinated. Dr. Williamson says they’re now starting to see these unvaccinated health care workers come down with COVID too. He says that will exacerbate their surge even further as health care workers become too sick to help care for patients and some will end up needing hospital beds themselves.
At the University of Mississippi Medical Center, 70 hospital employees and another 20 clinic employees are now being quarantined or have COVID, Dr. Jones said.
“The situation is bleak for Mississippi hospitals,” said Timothy Moore, president and CEO of the Mississippi Hospital Association. He said he doesn’t expect it to get better anytime soon.
Mississippi has more patients hospitalized now than at any other point in the pandemic, said Thomas Dobbs, MD, MPH, the state epidemiologist.
“If we look at the rapidity of this rise, it’s really kind of terrifying and awe-inspiring,” Dr. Dobbs said in a news conference Aug. 11.
Schools are just starting back, and, in many parts of the South, districts are operating under a patchwork of policies – some require masks, while others have made them voluntary. Physicians say they are bracing for what these half measures could mean for pediatric cases and community transmission.
The only sure way for people to help themselves and their hospitals and schools, experts said, is vaccination.
“State data show that in this latest COVID surge, 97% of new COVID-19 infections, 89% of hospitalizations, and 82% of deaths occur in unvaccinated residents,” Mr. Moore said.
“To relieve pressure on hospitals, we need Mississippians – even those who have previously had COVID – to get vaccinated and wear a mask in public. The Delta variant is highly contagious and we need to do all we can to stop the spread,” he said.
A version of this article first appeared on Medscape.com.
The state of Mississippi is out of intensive care unit beds. The University of Mississippi Medical Center in Jackson – the state’s largest health system – is converting part of a parking garage into a field hospital to make more room.
“Hospitals are full from Memphis to Gulfport, Natchez to Meridian. Everything’s full,” said Alan Jones, MD, the hospital’s COVID-19 response leader, in a press briefing Aug. 11.
The state has requested the help of a federal disaster medical assistance team of physicians, nurses, respiratory therapists, pharmacists, and paramedics to staff the extra beds. The goal is to open the field hospital on Aug. 13.
Arkansas hospitals have as little as eight ICU beds left to serve a population of 3 million people. Alabama isn’t far behind.
As of Aug. 10, several large metro Atlanta hospitals were diverting patients because they were full.
Hospitals in Alabama, Florida, Tennessee, and Texas are canceling elective surgeries, as they are flooded with COVID patients.
Florida has ordered more ventilators from the federal government. Some hospitals in that state have so many patients on high-flow medical oxygen that it is taxing the building supply lines.
“Most hospitals were not designed for this type of volume distribution in their facilities,” said Mary Mayhew, president of the Florida Hospital Association.
That’s when they can get it. Oxygen deliveries have been disrupted because of a shortage of drivers who are trained to transport it.
“Any disruption in the timing of a delivery can be hugely problematic because of the volume of oxygen they’re going through,” Ms. Mayhew said.
Hospitals ‘under great stress’
Over the month of June, the number of COVID patients in Florida hospitals soared from 2,000 to 10,000. Ms. Mayhew says it took twice as long during the last surge for the state to reach those numbers. And they’re still climbing. The state had 15,000 hospitalized COVID patients as of Aug. 11.
COVID hospitalizations tripled in 3 weeks in South Carolina, said state epidemiologist Linda Bell, MD, in a news conference Aug. 11.
“These hospitals are under great stress,” says Eric Toner, MD, a senior scientist at the Johns Hopkins Center for Health Security in Baltimore
The Delta variant has swept through the unvaccinated South with such veracity that hospitals in the region are unable to keep up. Patients with non-COVID health conditions are in jeopardy too.
Lee Owens, age 56, said he was supposed to have triple bypass surgery on Aug. 12 at St. Thomas West Hospital in Nashville, Tenn. Three of the arteries around his heart are 100%, 90%, and 70% blocked. Mr. Owens said the hospital called him Aug. 10 to postpone his surgery because they’ve cut back elective procedures to just one each day because the ICU beds there are full.
“I’m okay with having to wait a few days (my family isn’t!), especially if there are people worse than me, but so much anger at the reason,” he said. “These idiots that refused health care are now taking up my slot for heart surgery. It’s really aggravating.”
Anjali Bright, a spokesperson for St. Thomas West, provided a statement to this news organization saying they are not suspending elective procedures, but they are reviewing those “requiring an inpatient stay on a case-by-case basis.”
She emphasized, though, that “we will never delay care if the patient’s status changes to ‘urgent.’ ”
“Because of how infectious this variant is, this has the potential to be so much worse than what we saw in January,” said Donald Williamson, MD, president of the Alabama Hospital Association.
Dr. Williamson said they have modeled three possible scenarios for spread in the state, which ranks dead last in the United States for vaccination, with just 35% of its population fully protected. If the Delta variant spreads as it did in the United Kingdom, Alabama could see it hospitalize up to 3,000 people.
“That’s the best scenario,” he said.
If it sweeps through the state as it did in India, Alabama is looking at up to 4,500 patients hospitalized, a number that would require more beds and more staff to care for patients.
Then, there is what Dr. Williamson calls his “nightmare scenario.” If the entire state begins to see transmission rates as high as they’re currently seeing in coastal Mobile and Baldwin counties, that could mean up to 8,000 people in the hospital.
“If we see R-naughts of 5-8 statewide, we’re in real trouble,” he said. The R-naught is the basic rate of reproduction, and it means that each infected person would go on to infect 5-8 others. Dr. Williamson said the federal government would have to send them more staff to handle that kind of a surge.
‘Sense of betrayal’
Unlike the surges of last winter and spring, which sent hospitals scrambling for beds and supplies, the biggest pain point for hospitals now is staffing.
In Mississippi, where 200 patients are parked in emergency departments waiting for available and staffed ICU beds, the state is facing Delta with 2,000 fewer registered nurses than it had during its winter surge.
Some have left because of stress and burnout. Others have taken higher-paying jobs with travel nursing companies. To stop the exodus, hospitals are offering better pay, easier schedules, and sign-on and stay-on bonuses.
Doctors say the incentives are nice, but they don’t help with the anguish and anger many feel after months of battling COVID.
“There’s a big sense of betrayal,” said Sarah Nafziger, MD, vice president of clinical support services at the University of Alabama at Birmingham Hospital. “Our staff and health care workers, in general, feel like we’ve been betrayed by the community.”
“We have a vaccine, which is the key to ending this pandemic and people just refuse to take it, and so I think we’re very frustrated. We feel that our communities have let us down by not taking advantage of the vaccine,” Dr. Nafziger said. “It’s just baffling to me and it’s broken my heart every single day.”
Dr. Nafziger said she met with several surgeons at UAB on Aug. 11 and began making decisions about which surgeries would need to be canceled the following week. “We’re talking about cancer surgery. We’re talking about heart surgery. We’re talking about things that are critical to people.”
Compounding the staffing problems, about half of hospital workers in Alabama are still unvaccinated. Dr. Williamson says they’re now starting to see these unvaccinated health care workers come down with COVID too. He says that will exacerbate their surge even further as health care workers become too sick to help care for patients and some will end up needing hospital beds themselves.
At the University of Mississippi Medical Center, 70 hospital employees and another 20 clinic employees are now being quarantined or have COVID, Dr. Jones said.
“The situation is bleak for Mississippi hospitals,” said Timothy Moore, president and CEO of the Mississippi Hospital Association. He said he doesn’t expect it to get better anytime soon.
Mississippi has more patients hospitalized now than at any other point in the pandemic, said Thomas Dobbs, MD, MPH, the state epidemiologist.
“If we look at the rapidity of this rise, it’s really kind of terrifying and awe-inspiring,” Dr. Dobbs said in a news conference Aug. 11.
Schools are just starting back, and, in many parts of the South, districts are operating under a patchwork of policies – some require masks, while others have made them voluntary. Physicians say they are bracing for what these half measures could mean for pediatric cases and community transmission.
The only sure way for people to help themselves and their hospitals and schools, experts said, is vaccination.
“State data show that in this latest COVID surge, 97% of new COVID-19 infections, 89% of hospitalizations, and 82% of deaths occur in unvaccinated residents,” Mr. Moore said.
“To relieve pressure on hospitals, we need Mississippians – even those who have previously had COVID – to get vaccinated and wear a mask in public. The Delta variant is highly contagious and we need to do all we can to stop the spread,” he said.
A version of this article first appeared on Medscape.com.
The state of Mississippi is out of intensive care unit beds. The University of Mississippi Medical Center in Jackson – the state’s largest health system – is converting part of a parking garage into a field hospital to make more room.
“Hospitals are full from Memphis to Gulfport, Natchez to Meridian. Everything’s full,” said Alan Jones, MD, the hospital’s COVID-19 response leader, in a press briefing Aug. 11.
The state has requested the help of a federal disaster medical assistance team of physicians, nurses, respiratory therapists, pharmacists, and paramedics to staff the extra beds. The goal is to open the field hospital on Aug. 13.
Arkansas hospitals have as little as eight ICU beds left to serve a population of 3 million people. Alabama isn’t far behind.
As of Aug. 10, several large metro Atlanta hospitals were diverting patients because they were full.
Hospitals in Alabama, Florida, Tennessee, and Texas are canceling elective surgeries, as they are flooded with COVID patients.
Florida has ordered more ventilators from the federal government. Some hospitals in that state have so many patients on high-flow medical oxygen that it is taxing the building supply lines.
“Most hospitals were not designed for this type of volume distribution in their facilities,” said Mary Mayhew, president of the Florida Hospital Association.
That’s when they can get it. Oxygen deliveries have been disrupted because of a shortage of drivers who are trained to transport it.
“Any disruption in the timing of a delivery can be hugely problematic because of the volume of oxygen they’re going through,” Ms. Mayhew said.
Hospitals ‘under great stress’
Over the month of June, the number of COVID patients in Florida hospitals soared from 2,000 to 10,000. Ms. Mayhew says it took twice as long during the last surge for the state to reach those numbers. And they’re still climbing. The state had 15,000 hospitalized COVID patients as of Aug. 11.
COVID hospitalizations tripled in 3 weeks in South Carolina, said state epidemiologist Linda Bell, MD, in a news conference Aug. 11.
“These hospitals are under great stress,” says Eric Toner, MD, a senior scientist at the Johns Hopkins Center for Health Security in Baltimore
The Delta variant has swept through the unvaccinated South with such veracity that hospitals in the region are unable to keep up. Patients with non-COVID health conditions are in jeopardy too.
Lee Owens, age 56, said he was supposed to have triple bypass surgery on Aug. 12 at St. Thomas West Hospital in Nashville, Tenn. Three of the arteries around his heart are 100%, 90%, and 70% blocked. Mr. Owens said the hospital called him Aug. 10 to postpone his surgery because they’ve cut back elective procedures to just one each day because the ICU beds there are full.
“I’m okay with having to wait a few days (my family isn’t!), especially if there are people worse than me, but so much anger at the reason,” he said. “These idiots that refused health care are now taking up my slot for heart surgery. It’s really aggravating.”
Anjali Bright, a spokesperson for St. Thomas West, provided a statement to this news organization saying they are not suspending elective procedures, but they are reviewing those “requiring an inpatient stay on a case-by-case basis.”
She emphasized, though, that “we will never delay care if the patient’s status changes to ‘urgent.’ ”
“Because of how infectious this variant is, this has the potential to be so much worse than what we saw in January,” said Donald Williamson, MD, president of the Alabama Hospital Association.
Dr. Williamson said they have modeled three possible scenarios for spread in the state, which ranks dead last in the United States for vaccination, with just 35% of its population fully protected. If the Delta variant spreads as it did in the United Kingdom, Alabama could see it hospitalize up to 3,000 people.
“That’s the best scenario,” he said.
If it sweeps through the state as it did in India, Alabama is looking at up to 4,500 patients hospitalized, a number that would require more beds and more staff to care for patients.
Then, there is what Dr. Williamson calls his “nightmare scenario.” If the entire state begins to see transmission rates as high as they’re currently seeing in coastal Mobile and Baldwin counties, that could mean up to 8,000 people in the hospital.
“If we see R-naughts of 5-8 statewide, we’re in real trouble,” he said. The R-naught is the basic rate of reproduction, and it means that each infected person would go on to infect 5-8 others. Dr. Williamson said the federal government would have to send them more staff to handle that kind of a surge.
‘Sense of betrayal’
Unlike the surges of last winter and spring, which sent hospitals scrambling for beds and supplies, the biggest pain point for hospitals now is staffing.
In Mississippi, where 200 patients are parked in emergency departments waiting for available and staffed ICU beds, the state is facing Delta with 2,000 fewer registered nurses than it had during its winter surge.
Some have left because of stress and burnout. Others have taken higher-paying jobs with travel nursing companies. To stop the exodus, hospitals are offering better pay, easier schedules, and sign-on and stay-on bonuses.
Doctors say the incentives are nice, but they don’t help with the anguish and anger many feel after months of battling COVID.
“There’s a big sense of betrayal,” said Sarah Nafziger, MD, vice president of clinical support services at the University of Alabama at Birmingham Hospital. “Our staff and health care workers, in general, feel like we’ve been betrayed by the community.”
“We have a vaccine, which is the key to ending this pandemic and people just refuse to take it, and so I think we’re very frustrated. We feel that our communities have let us down by not taking advantage of the vaccine,” Dr. Nafziger said. “It’s just baffling to me and it’s broken my heart every single day.”
Dr. Nafziger said she met with several surgeons at UAB on Aug. 11 and began making decisions about which surgeries would need to be canceled the following week. “We’re talking about cancer surgery. We’re talking about heart surgery. We’re talking about things that are critical to people.”
Compounding the staffing problems, about half of hospital workers in Alabama are still unvaccinated. Dr. Williamson says they’re now starting to see these unvaccinated health care workers come down with COVID too. He says that will exacerbate their surge even further as health care workers become too sick to help care for patients and some will end up needing hospital beds themselves.
At the University of Mississippi Medical Center, 70 hospital employees and another 20 clinic employees are now being quarantined or have COVID, Dr. Jones said.
“The situation is bleak for Mississippi hospitals,” said Timothy Moore, president and CEO of the Mississippi Hospital Association. He said he doesn’t expect it to get better anytime soon.
Mississippi has more patients hospitalized now than at any other point in the pandemic, said Thomas Dobbs, MD, MPH, the state epidemiologist.
“If we look at the rapidity of this rise, it’s really kind of terrifying and awe-inspiring,” Dr. Dobbs said in a news conference Aug. 11.
Schools are just starting back, and, in many parts of the South, districts are operating under a patchwork of policies – some require masks, while others have made them voluntary. Physicians say they are bracing for what these half measures could mean for pediatric cases and community transmission.
The only sure way for people to help themselves and their hospitals and schools, experts said, is vaccination.
“State data show that in this latest COVID surge, 97% of new COVID-19 infections, 89% of hospitalizations, and 82% of deaths occur in unvaccinated residents,” Mr. Moore said.
“To relieve pressure on hospitals, we need Mississippians – even those who have previously had COVID – to get vaccinated and wear a mask in public. The Delta variant is highly contagious and we need to do all we can to stop the spread,” he said.
A version of this article first appeared on Medscape.com.
Pandemic demand for NPs soars, softens for primary care: Report
The COVID-19 pandemic has fueled a growing demand for nurse practitioners (NPs), while demand for primary care physicians has cooled, according to Merritt Hawkins’ annual review of physician and advanced practitioner recruiting trends.
according to the medical search firm. In the 27 prior years, physicians held the top spot. For the previous 14 years, the No. 1 position was held by family physicians.
“COVID-19 and other market forces are changing the dynamics of physician and advanced practitioner recruiting. NPs are coming into their own in a market that puts a premium on easy access to care and cost containment,” Tom Florence, president of Merritt Hawkins, said in a statement.
Primary care ‘recruiting frenzy’ over
Mr. Florence said primary care physicians remain a “vital part of team-based care and will be increasingly responsible for coordinating the care of older patients with multiple chronic conditions. But the recruiting frenzy in primary care is over.”
Merritt Hawkins says that overall COVID-19 has had a “severely inhibiting” effect on demand for physicians. The number of searches the company conducted dropped 25%, compared with 2020, and many hospitals and medical groups shut down or lost money during the pandemic.
But the drop-off in demand for physicians is likely to be temporary because the underlying dynamics driving physician supply and demand remain in place, according to the report. These include a growing and aging population, a limited supply of newly trained physicians, and an aging physician workforce.
COVID-19 will not permanently change these market conditions, and demand for physicians already is rebounding, the company said.
The 2021 review of physician and advanced practitioner recruiting is based on a representative sample of 2,458 permanent search engagements that Merritt Hawkins/AMN Healthcare’s physician staffing companies conducted or were in the process of conducting during the 12-month period from April 1, 2020, to March 31, 2021.
Among the key findings:
- 18% of Merritt Hawkins’ recruiting searches were for advanced practitioners, including NPs, physician assistants (PAs), and certified registered nurse anesthetists, up from 13% in the 2020 review. This represents the highest percentage in the 28 years the review has been conducted.
- About two-thirds (64%) of Merritt Hawkins’ search engagements were for physician specialists, including radiologists, psychiatrists, gastroenterologists, and others, “highlighting the robust demand for specialty physicians.”
- In 2021, 18% of Merritt Hawkins’ search engagements were for primary care physicians, down from 20% in 2020 and 22% in 2019, “signaling a relative decline in demand for primary care doctors.”
- Psychiatrists placed fourth on the list of most requested search engagements, a sign of continued strong demand for mental health professionals that is likely to accelerate because of COVID-19.
Starting salaries take a pandemic hit
Owing to the reduced demand for practitioners, starting salaries decreased for many types of health care professions, with the exception of NPs and PAs.
Average starting salaries for NPs showed strong growth, increasing 12% year over year, from $125,000 to $140,000. The average starting salaries for PAs also showed strong growth, increasing by 14% year over year, from $112,000 to $128,000.
Among physicians, interventional cardiologists were offered the highest average starting salaries, at $611,000, followed by orthopedic surgeons, at $546,000. Pediatricians were offered the lowest average starting salaries, at $236,000.
Merritt Hawkins said only 3% of their search engagements were for solo practice or partnership settings, “underscoring the decline of physician private practice.”
Roughly two-thirds (67%) of Merritt Hawkins’ search engagements were in communities of 100,000 people or more, indicating that demand for physicians and advanced practitioners is not limited to small or rural communities.
A version of this article first appeared on Medscape.com.
The COVID-19 pandemic has fueled a growing demand for nurse practitioners (NPs), while demand for primary care physicians has cooled, according to Merritt Hawkins’ annual review of physician and advanced practitioner recruiting trends.
according to the medical search firm. In the 27 prior years, physicians held the top spot. For the previous 14 years, the No. 1 position was held by family physicians.
“COVID-19 and other market forces are changing the dynamics of physician and advanced practitioner recruiting. NPs are coming into their own in a market that puts a premium on easy access to care and cost containment,” Tom Florence, president of Merritt Hawkins, said in a statement.
Primary care ‘recruiting frenzy’ over
Mr. Florence said primary care physicians remain a “vital part of team-based care and will be increasingly responsible for coordinating the care of older patients with multiple chronic conditions. But the recruiting frenzy in primary care is over.”
Merritt Hawkins says that overall COVID-19 has had a “severely inhibiting” effect on demand for physicians. The number of searches the company conducted dropped 25%, compared with 2020, and many hospitals and medical groups shut down or lost money during the pandemic.
But the drop-off in demand for physicians is likely to be temporary because the underlying dynamics driving physician supply and demand remain in place, according to the report. These include a growing and aging population, a limited supply of newly trained physicians, and an aging physician workforce.
COVID-19 will not permanently change these market conditions, and demand for physicians already is rebounding, the company said.
The 2021 review of physician and advanced practitioner recruiting is based on a representative sample of 2,458 permanent search engagements that Merritt Hawkins/AMN Healthcare’s physician staffing companies conducted or were in the process of conducting during the 12-month period from April 1, 2020, to March 31, 2021.
Among the key findings:
- 18% of Merritt Hawkins’ recruiting searches were for advanced practitioners, including NPs, physician assistants (PAs), and certified registered nurse anesthetists, up from 13% in the 2020 review. This represents the highest percentage in the 28 years the review has been conducted.
- About two-thirds (64%) of Merritt Hawkins’ search engagements were for physician specialists, including radiologists, psychiatrists, gastroenterologists, and others, “highlighting the robust demand for specialty physicians.”
- In 2021, 18% of Merritt Hawkins’ search engagements were for primary care physicians, down from 20% in 2020 and 22% in 2019, “signaling a relative decline in demand for primary care doctors.”
- Psychiatrists placed fourth on the list of most requested search engagements, a sign of continued strong demand for mental health professionals that is likely to accelerate because of COVID-19.
Starting salaries take a pandemic hit
Owing to the reduced demand for practitioners, starting salaries decreased for many types of health care professions, with the exception of NPs and PAs.
Average starting salaries for NPs showed strong growth, increasing 12% year over year, from $125,000 to $140,000. The average starting salaries for PAs also showed strong growth, increasing by 14% year over year, from $112,000 to $128,000.
Among physicians, interventional cardiologists were offered the highest average starting salaries, at $611,000, followed by orthopedic surgeons, at $546,000. Pediatricians were offered the lowest average starting salaries, at $236,000.
Merritt Hawkins said only 3% of their search engagements were for solo practice or partnership settings, “underscoring the decline of physician private practice.”
Roughly two-thirds (67%) of Merritt Hawkins’ search engagements were in communities of 100,000 people or more, indicating that demand for physicians and advanced practitioners is not limited to small or rural communities.
A version of this article first appeared on Medscape.com.
The COVID-19 pandemic has fueled a growing demand for nurse practitioners (NPs), while demand for primary care physicians has cooled, according to Merritt Hawkins’ annual review of physician and advanced practitioner recruiting trends.
according to the medical search firm. In the 27 prior years, physicians held the top spot. For the previous 14 years, the No. 1 position was held by family physicians.
“COVID-19 and other market forces are changing the dynamics of physician and advanced practitioner recruiting. NPs are coming into their own in a market that puts a premium on easy access to care and cost containment,” Tom Florence, president of Merritt Hawkins, said in a statement.
Primary care ‘recruiting frenzy’ over
Mr. Florence said primary care physicians remain a “vital part of team-based care and will be increasingly responsible for coordinating the care of older patients with multiple chronic conditions. But the recruiting frenzy in primary care is over.”
Merritt Hawkins says that overall COVID-19 has had a “severely inhibiting” effect on demand for physicians. The number of searches the company conducted dropped 25%, compared with 2020, and many hospitals and medical groups shut down or lost money during the pandemic.
But the drop-off in demand for physicians is likely to be temporary because the underlying dynamics driving physician supply and demand remain in place, according to the report. These include a growing and aging population, a limited supply of newly trained physicians, and an aging physician workforce.
COVID-19 will not permanently change these market conditions, and demand for physicians already is rebounding, the company said.
The 2021 review of physician and advanced practitioner recruiting is based on a representative sample of 2,458 permanent search engagements that Merritt Hawkins/AMN Healthcare’s physician staffing companies conducted or were in the process of conducting during the 12-month period from April 1, 2020, to March 31, 2021.
Among the key findings:
- 18% of Merritt Hawkins’ recruiting searches were for advanced practitioners, including NPs, physician assistants (PAs), and certified registered nurse anesthetists, up from 13% in the 2020 review. This represents the highest percentage in the 28 years the review has been conducted.
- About two-thirds (64%) of Merritt Hawkins’ search engagements were for physician specialists, including radiologists, psychiatrists, gastroenterologists, and others, “highlighting the robust demand for specialty physicians.”
- In 2021, 18% of Merritt Hawkins’ search engagements were for primary care physicians, down from 20% in 2020 and 22% in 2019, “signaling a relative decline in demand for primary care doctors.”
- Psychiatrists placed fourth on the list of most requested search engagements, a sign of continued strong demand for mental health professionals that is likely to accelerate because of COVID-19.
Starting salaries take a pandemic hit
Owing to the reduced demand for practitioners, starting salaries decreased for many types of health care professions, with the exception of NPs and PAs.
Average starting salaries for NPs showed strong growth, increasing 12% year over year, from $125,000 to $140,000. The average starting salaries for PAs also showed strong growth, increasing by 14% year over year, from $112,000 to $128,000.
Among physicians, interventional cardiologists were offered the highest average starting salaries, at $611,000, followed by orthopedic surgeons, at $546,000. Pediatricians were offered the lowest average starting salaries, at $236,000.
Merritt Hawkins said only 3% of their search engagements were for solo practice or partnership settings, “underscoring the decline of physician private practice.”
Roughly two-thirds (67%) of Merritt Hawkins’ search engagements were in communities of 100,000 people or more, indicating that demand for physicians and advanced practitioners is not limited to small or rural communities.
A version of this article first appeared on Medscape.com.
FDA may okay COVID booster for vulnerable adults before weekend: Media
according to multiple media reports.
The agency, along with the Centers for Disease Control and Prevention (CDC) and the National Institutes of Health, is working through the details of how booster doses for this population would work, and could authorize a third dose of both the Pfizer and Moderna vaccines as early as Aug. 12, Politico reports.
About 2.7% of adults in the United States are immunocompromised, according to the CDC. This group includes people who have cancer, have received solid organ or stem cell transplants, have genetic conditions that weaken the immune function, have HIV, or are people with health conditions that require treatment with medications that turn down immune function, such as rheumatoid arthritis.
Immune function also wanes with age, so the FDA could consider boosters for the elderly.
New research shows that between one-third and one-half of immunocompromised patients who didn’t develop detectable levels of virus-fighting antibodies after two doses of a COVID vaccine will respond to a third dose.
A committee of independent experts that advises the CDC on the use of vaccines in the United States had previously signaled its support for giving boosters to those who are immunocompromised, but noted that it couldn’t officially recommend the strategy until the FDA had updated its emergency-use authorization for the shots or granted them a full biologics license, or “full approval.”
It’s unclear which mechanism the FDA might use, or exactly who will be eligible for the shots.
The United States would follow other nations such as Israel, France, the United Kingdom, and Germany in planning for or authorizing boosters for some vulnerable individuals.
The World Health Organization (WHO) has voiced strong opposition to the use of boosters in wealthy countries while much of the world still doesn’t have access to these lifesaving therapies. The WHO has asked wealthy nations to hold off on giving boosters until at least the end of September to give more people the opportunity to get a first dose.
The CDC’s Advisory Committee on Immunization Practices (ACIP) meets again on Aug. 13 and is expected to discuss booster doses for this population of patients. The ACIP officially makes recommendations on the use of vaccines to the nation’s doctors.
The committee’s recommendation ensures that a vaccine will be covered by public and private insurers. Statutory vaccination requirements are also made based on the ACIP’s recommendations.
A version of this article first appeared on Medscape.com.
according to multiple media reports.
The agency, along with the Centers for Disease Control and Prevention (CDC) and the National Institutes of Health, is working through the details of how booster doses for this population would work, and could authorize a third dose of both the Pfizer and Moderna vaccines as early as Aug. 12, Politico reports.
About 2.7% of adults in the United States are immunocompromised, according to the CDC. This group includes people who have cancer, have received solid organ or stem cell transplants, have genetic conditions that weaken the immune function, have HIV, or are people with health conditions that require treatment with medications that turn down immune function, such as rheumatoid arthritis.
Immune function also wanes with age, so the FDA could consider boosters for the elderly.
New research shows that between one-third and one-half of immunocompromised patients who didn’t develop detectable levels of virus-fighting antibodies after two doses of a COVID vaccine will respond to a third dose.
A committee of independent experts that advises the CDC on the use of vaccines in the United States had previously signaled its support for giving boosters to those who are immunocompromised, but noted that it couldn’t officially recommend the strategy until the FDA had updated its emergency-use authorization for the shots or granted them a full biologics license, or “full approval.”
It’s unclear which mechanism the FDA might use, or exactly who will be eligible for the shots.
The United States would follow other nations such as Israel, France, the United Kingdom, and Germany in planning for or authorizing boosters for some vulnerable individuals.
The World Health Organization (WHO) has voiced strong opposition to the use of boosters in wealthy countries while much of the world still doesn’t have access to these lifesaving therapies. The WHO has asked wealthy nations to hold off on giving boosters until at least the end of September to give more people the opportunity to get a first dose.
The CDC’s Advisory Committee on Immunization Practices (ACIP) meets again on Aug. 13 and is expected to discuss booster doses for this population of patients. The ACIP officially makes recommendations on the use of vaccines to the nation’s doctors.
The committee’s recommendation ensures that a vaccine will be covered by public and private insurers. Statutory vaccination requirements are also made based on the ACIP’s recommendations.
A version of this article first appeared on Medscape.com.
according to multiple media reports.
The agency, along with the Centers for Disease Control and Prevention (CDC) and the National Institutes of Health, is working through the details of how booster doses for this population would work, and could authorize a third dose of both the Pfizer and Moderna vaccines as early as Aug. 12, Politico reports.
About 2.7% of adults in the United States are immunocompromised, according to the CDC. This group includes people who have cancer, have received solid organ or stem cell transplants, have genetic conditions that weaken the immune function, have HIV, or are people with health conditions that require treatment with medications that turn down immune function, such as rheumatoid arthritis.
Immune function also wanes with age, so the FDA could consider boosters for the elderly.
New research shows that between one-third and one-half of immunocompromised patients who didn’t develop detectable levels of virus-fighting antibodies after two doses of a COVID vaccine will respond to a third dose.
A committee of independent experts that advises the CDC on the use of vaccines in the United States had previously signaled its support for giving boosters to those who are immunocompromised, but noted that it couldn’t officially recommend the strategy until the FDA had updated its emergency-use authorization for the shots or granted them a full biologics license, or “full approval.”
It’s unclear which mechanism the FDA might use, or exactly who will be eligible for the shots.
The United States would follow other nations such as Israel, France, the United Kingdom, and Germany in planning for or authorizing boosters for some vulnerable individuals.
The World Health Organization (WHO) has voiced strong opposition to the use of boosters in wealthy countries while much of the world still doesn’t have access to these lifesaving therapies. The WHO has asked wealthy nations to hold off on giving boosters until at least the end of September to give more people the opportunity to get a first dose.
The CDC’s Advisory Committee on Immunization Practices (ACIP) meets again on Aug. 13 and is expected to discuss booster doses for this population of patients. The ACIP officially makes recommendations on the use of vaccines to the nation’s doctors.
The committee’s recommendation ensures that a vaccine will be covered by public and private insurers. Statutory vaccination requirements are also made based on the ACIP’s recommendations.
A version of this article first appeared on Medscape.com.
U.S. health system ranks last among 11 high-income countries
The U.S. health care system ranked last overall among 11 high-income countries in an analysis by the nonprofit Commonwealth Fund, according to a report released on Aug. 4.
The report is the seventh international comparison of countries’ health systems by the Commonwealth Fund since 2004, and the United States has ranked last in every edition, David Blumenthal, MD, president of the Commonwealth Fund, told reporters during a press briefing.
Researchers analyzed survey answers from tens of thousands of patients and physicians in 11 countries. They analyzed performance on 71 measures across five categories – access to care, care process, administrative efficiency, equity, and health care outcomes. Administrative data were gathered from the Organisation for Economic Cooperation and Development and the World Health Organization.
Among contributors to the poor showing by the United States is that half (50%) of lower-income U.S. adults and 27% of higher-income U.S. adults say costs keep them from getting needed health care.
“In no other country does income inequality so profoundly limit access to care,” Dr. Blumenthal said.
In the United Kingdom, only 12% with lower incomes and 7% with higher incomes said costs kept them from care.
In a stark comparison, the researchers found that “a high-income person in the U.S. was more likely to report financial barriers than a low-income person in nearly all the other countries surveyed: Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the U.K.”
Norway, the Netherlands, and Australia were ranked at the top overall in that order. Rounding out the 11 in overall ranking were the U.K., Germany, New Zealand, Sweden, France, Switzerland, Canada, and the United States.
“What this report tells us is that our health care system is not working for Americans, particularly those with lower incomes, who are at a severe disadvantage compared to citizens of other countries. And they are paying the price with their health and their lives,” Dr. Blumenthal said in a press release.
“To catch up with other high-income countries, the administration and Congress would have to expand access to health care, equitably, to all Americans, act aggressively to control costs, and invest in the social services we know can lead to a healthier population.”
High infant mortality, low life expectancy in U.S.
Several factors contributed to the U.S. ranking at the bottom of the outcomes category. Among them are that the United States has the highest infant mortality rate (5.7 deaths per 1,000 live births) and lowest life expectancy at age 60 (living on average 23.1 years after age 60), compared with the other countries surveyed. The U.S. rate of preventable mortality (177 deaths per 100,000 population) is more than double that of the best-performing country, Switzerland.
Lead author Eric Schneider, MD, senior vice president for policy and research at the Commonwealth Fund, pointed out that, in terms of the change in avoidable mortality over a decade, not only did the United States have the highest rate, compared with the other countries surveyed, “it also experienced the smallest decline in avoidable mortality over that 10-year period.”
The U.S. maternal mortality rate of 17.4 deaths per 100,000 live births is twice that of France, the country with the next-highest rate (7.6 deaths per 100,000 live births).
U.S. excelled in only one category
The only category in which the United States did not rank last was in “care process,” where it ranked second behind only New Zealand.
The care process category combines preventive care, safe care, coordinated care, and patient engagement and preferences. The category includes indicators such as mammography screening and influenza vaccination for older adults as well as the percentage of adults counseled by a health care provider about nutrition, smoking, or alcohol use.
The United States and Germany performed best on engagement and patient preferences, although U.S. adults have the lowest rates of continuity with the same doctor.
New Zealand and the United States ranked highest in the safe care category, with higher reported use of computerized alerts and routine review of medications.
‘Too little, too late’: Key recommendations for U.S. to improve
Reginald Williams, vice president of International Health Policy and Practice Innovations at the Commonwealth Fund, pointed out that the U.S. shortcomings in health care come despite spending more than twice as much of its GDP (17% in 2019) as the average OECD country.
“It appears that the US delivers too little of the care that is most needed and often delivers that care too late, especially for people with chronic illnesses,” he said.
He then summarized the team’s recommendations on how the United States can change course.
First is expanding insurance coverage, he said, noting that the United States is the only one of the 11 countries that lacks universal coverage and nearly 30 million people remain uninsured.
Top-performing countries in the survey have universal coverage, annual out-of-pocket caps on covered benefits, and full coverage for primary care and treatment for chronic conditions, he said.
The United States must also improve access to care, he said.
“Top-ranking countries like the Netherlands and Norway ensure timely availability to care by telephone on nights and weekends, and in-person follow-up at home, if needed,” he said.
Mr. Williams said reducing administrative burdens is also critical to free up resources for improving health. He gave an example: “Norway determines patient copayments or physician fees on a regional basis, applying standardized copayments to all physicians within a specialty in a geographic area.”
Reducing income-related barriers is important as well, he said.
The fear of unpredictably high bills and other issues prevent people in the United States from getting the care they ultimately need, he said, adding that top-performing countries invest more in social services to reduce health risks.
That could have implications for the COVID-19 response.
Responding effectively to COVID-19 requires that patients can access affordable health care services, Mr. Williams noted.
“We know from our research that more than two-thirds of U.S. adults say their potential out-of-pocket costs would figure prominently in their decisions to get care if they had coronavirus symptoms,” he said.
Dr. Schneider summed up in the press release: “This study makes clear that higher U.S. spending on health care is not producing better health especially as the U.S. continues on a path of deepening inequality. A country that spends as much as we do should have the best health system in the world. We should adapt what works in other high-income countries to build a better health care system that provides affordable, high-quality health care for everyone.”
Dr. Blumenthal, Dr. Schneider, and Mr. Williams reported no relevant financial relationships outside their employment with the Commonwealth Fund.
A version of this article first appeared on Medscape.com.
The U.S. health care system ranked last overall among 11 high-income countries in an analysis by the nonprofit Commonwealth Fund, according to a report released on Aug. 4.
The report is the seventh international comparison of countries’ health systems by the Commonwealth Fund since 2004, and the United States has ranked last in every edition, David Blumenthal, MD, president of the Commonwealth Fund, told reporters during a press briefing.
Researchers analyzed survey answers from tens of thousands of patients and physicians in 11 countries. They analyzed performance on 71 measures across five categories – access to care, care process, administrative efficiency, equity, and health care outcomes. Administrative data were gathered from the Organisation for Economic Cooperation and Development and the World Health Organization.
Among contributors to the poor showing by the United States is that half (50%) of lower-income U.S. adults and 27% of higher-income U.S. adults say costs keep them from getting needed health care.
“In no other country does income inequality so profoundly limit access to care,” Dr. Blumenthal said.
In the United Kingdom, only 12% with lower incomes and 7% with higher incomes said costs kept them from care.
In a stark comparison, the researchers found that “a high-income person in the U.S. was more likely to report financial barriers than a low-income person in nearly all the other countries surveyed: Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the U.K.”
Norway, the Netherlands, and Australia were ranked at the top overall in that order. Rounding out the 11 in overall ranking were the U.K., Germany, New Zealand, Sweden, France, Switzerland, Canada, and the United States.
“What this report tells us is that our health care system is not working for Americans, particularly those with lower incomes, who are at a severe disadvantage compared to citizens of other countries. And they are paying the price with their health and their lives,” Dr. Blumenthal said in a press release.
“To catch up with other high-income countries, the administration and Congress would have to expand access to health care, equitably, to all Americans, act aggressively to control costs, and invest in the social services we know can lead to a healthier population.”
High infant mortality, low life expectancy in U.S.
Several factors contributed to the U.S. ranking at the bottom of the outcomes category. Among them are that the United States has the highest infant mortality rate (5.7 deaths per 1,000 live births) and lowest life expectancy at age 60 (living on average 23.1 years after age 60), compared with the other countries surveyed. The U.S. rate of preventable mortality (177 deaths per 100,000 population) is more than double that of the best-performing country, Switzerland.
Lead author Eric Schneider, MD, senior vice president for policy and research at the Commonwealth Fund, pointed out that, in terms of the change in avoidable mortality over a decade, not only did the United States have the highest rate, compared with the other countries surveyed, “it also experienced the smallest decline in avoidable mortality over that 10-year period.”
The U.S. maternal mortality rate of 17.4 deaths per 100,000 live births is twice that of France, the country with the next-highest rate (7.6 deaths per 100,000 live births).
U.S. excelled in only one category
The only category in which the United States did not rank last was in “care process,” where it ranked second behind only New Zealand.
The care process category combines preventive care, safe care, coordinated care, and patient engagement and preferences. The category includes indicators such as mammography screening and influenza vaccination for older adults as well as the percentage of adults counseled by a health care provider about nutrition, smoking, or alcohol use.
The United States and Germany performed best on engagement and patient preferences, although U.S. adults have the lowest rates of continuity with the same doctor.
New Zealand and the United States ranked highest in the safe care category, with higher reported use of computerized alerts and routine review of medications.
‘Too little, too late’: Key recommendations for U.S. to improve
Reginald Williams, vice president of International Health Policy and Practice Innovations at the Commonwealth Fund, pointed out that the U.S. shortcomings in health care come despite spending more than twice as much of its GDP (17% in 2019) as the average OECD country.
“It appears that the US delivers too little of the care that is most needed and often delivers that care too late, especially for people with chronic illnesses,” he said.
He then summarized the team’s recommendations on how the United States can change course.
First is expanding insurance coverage, he said, noting that the United States is the only one of the 11 countries that lacks universal coverage and nearly 30 million people remain uninsured.
Top-performing countries in the survey have universal coverage, annual out-of-pocket caps on covered benefits, and full coverage for primary care and treatment for chronic conditions, he said.
The United States must also improve access to care, he said.
“Top-ranking countries like the Netherlands and Norway ensure timely availability to care by telephone on nights and weekends, and in-person follow-up at home, if needed,” he said.
Mr. Williams said reducing administrative burdens is also critical to free up resources for improving health. He gave an example: “Norway determines patient copayments or physician fees on a regional basis, applying standardized copayments to all physicians within a specialty in a geographic area.”
Reducing income-related barriers is important as well, he said.
The fear of unpredictably high bills and other issues prevent people in the United States from getting the care they ultimately need, he said, adding that top-performing countries invest more in social services to reduce health risks.
That could have implications for the COVID-19 response.
Responding effectively to COVID-19 requires that patients can access affordable health care services, Mr. Williams noted.
“We know from our research that more than two-thirds of U.S. adults say their potential out-of-pocket costs would figure prominently in their decisions to get care if they had coronavirus symptoms,” he said.
Dr. Schneider summed up in the press release: “This study makes clear that higher U.S. spending on health care is not producing better health especially as the U.S. continues on a path of deepening inequality. A country that spends as much as we do should have the best health system in the world. We should adapt what works in other high-income countries to build a better health care system that provides affordable, high-quality health care for everyone.”
Dr. Blumenthal, Dr. Schneider, and Mr. Williams reported no relevant financial relationships outside their employment with the Commonwealth Fund.
A version of this article first appeared on Medscape.com.
The U.S. health care system ranked last overall among 11 high-income countries in an analysis by the nonprofit Commonwealth Fund, according to a report released on Aug. 4.
The report is the seventh international comparison of countries’ health systems by the Commonwealth Fund since 2004, and the United States has ranked last in every edition, David Blumenthal, MD, president of the Commonwealth Fund, told reporters during a press briefing.
Researchers analyzed survey answers from tens of thousands of patients and physicians in 11 countries. They analyzed performance on 71 measures across five categories – access to care, care process, administrative efficiency, equity, and health care outcomes. Administrative data were gathered from the Organisation for Economic Cooperation and Development and the World Health Organization.
Among contributors to the poor showing by the United States is that half (50%) of lower-income U.S. adults and 27% of higher-income U.S. adults say costs keep them from getting needed health care.
“In no other country does income inequality so profoundly limit access to care,” Dr. Blumenthal said.
In the United Kingdom, only 12% with lower incomes and 7% with higher incomes said costs kept them from care.
In a stark comparison, the researchers found that “a high-income person in the U.S. was more likely to report financial barriers than a low-income person in nearly all the other countries surveyed: Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the U.K.”
Norway, the Netherlands, and Australia were ranked at the top overall in that order. Rounding out the 11 in overall ranking were the U.K., Germany, New Zealand, Sweden, France, Switzerland, Canada, and the United States.
“What this report tells us is that our health care system is not working for Americans, particularly those with lower incomes, who are at a severe disadvantage compared to citizens of other countries. And they are paying the price with their health and their lives,” Dr. Blumenthal said in a press release.
“To catch up with other high-income countries, the administration and Congress would have to expand access to health care, equitably, to all Americans, act aggressively to control costs, and invest in the social services we know can lead to a healthier population.”
High infant mortality, low life expectancy in U.S.
Several factors contributed to the U.S. ranking at the bottom of the outcomes category. Among them are that the United States has the highest infant mortality rate (5.7 deaths per 1,000 live births) and lowest life expectancy at age 60 (living on average 23.1 years after age 60), compared with the other countries surveyed. The U.S. rate of preventable mortality (177 deaths per 100,000 population) is more than double that of the best-performing country, Switzerland.
Lead author Eric Schneider, MD, senior vice president for policy and research at the Commonwealth Fund, pointed out that, in terms of the change in avoidable mortality over a decade, not only did the United States have the highest rate, compared with the other countries surveyed, “it also experienced the smallest decline in avoidable mortality over that 10-year period.”
The U.S. maternal mortality rate of 17.4 deaths per 100,000 live births is twice that of France, the country with the next-highest rate (7.6 deaths per 100,000 live births).
U.S. excelled in only one category
The only category in which the United States did not rank last was in “care process,” where it ranked second behind only New Zealand.
The care process category combines preventive care, safe care, coordinated care, and patient engagement and preferences. The category includes indicators such as mammography screening and influenza vaccination for older adults as well as the percentage of adults counseled by a health care provider about nutrition, smoking, or alcohol use.
The United States and Germany performed best on engagement and patient preferences, although U.S. adults have the lowest rates of continuity with the same doctor.
New Zealand and the United States ranked highest in the safe care category, with higher reported use of computerized alerts and routine review of medications.
‘Too little, too late’: Key recommendations for U.S. to improve
Reginald Williams, vice president of International Health Policy and Practice Innovations at the Commonwealth Fund, pointed out that the U.S. shortcomings in health care come despite spending more than twice as much of its GDP (17% in 2019) as the average OECD country.
“It appears that the US delivers too little of the care that is most needed and often delivers that care too late, especially for people with chronic illnesses,” he said.
He then summarized the team’s recommendations on how the United States can change course.
First is expanding insurance coverage, he said, noting that the United States is the only one of the 11 countries that lacks universal coverage and nearly 30 million people remain uninsured.
Top-performing countries in the survey have universal coverage, annual out-of-pocket caps on covered benefits, and full coverage for primary care and treatment for chronic conditions, he said.
The United States must also improve access to care, he said.
“Top-ranking countries like the Netherlands and Norway ensure timely availability to care by telephone on nights and weekends, and in-person follow-up at home, if needed,” he said.
Mr. Williams said reducing administrative burdens is also critical to free up resources for improving health. He gave an example: “Norway determines patient copayments or physician fees on a regional basis, applying standardized copayments to all physicians within a specialty in a geographic area.”
Reducing income-related barriers is important as well, he said.
The fear of unpredictably high bills and other issues prevent people in the United States from getting the care they ultimately need, he said, adding that top-performing countries invest more in social services to reduce health risks.
That could have implications for the COVID-19 response.
Responding effectively to COVID-19 requires that patients can access affordable health care services, Mr. Williams noted.
“We know from our research that more than two-thirds of U.S. adults say their potential out-of-pocket costs would figure prominently in their decisions to get care if they had coronavirus symptoms,” he said.
Dr. Schneider summed up in the press release: “This study makes clear that higher U.S. spending on health care is not producing better health especially as the U.S. continues on a path of deepening inequality. A country that spends as much as we do should have the best health system in the world. We should adapt what works in other high-income countries to build a better health care system that provides affordable, high-quality health care for everyone.”
Dr. Blumenthal, Dr. Schneider, and Mr. Williams reported no relevant financial relationships outside their employment with the Commonwealth Fund.
A version of this article first appeared on Medscape.com.
Physicians wearing white coats rated more experienced
Physicians wearing white coats were rated as significantly more experienced and professional than peers wearing casual attire. Regardless of their attire, however, female physicians were more likely to be judged as appearing less professional and were more likely to be misidentified as medical technicians, physician assistants, or nurses, found research published in JAMA Network Open.
“A white coat with scrubs attire was most preferred for surgeons (mean preference index, 1.3), whereas a white coat with business attire was preferred for family physicians and dermatologists (mean preference indexes, 1.6 and 1.2, respectively; P < .001),” Helen Xun, MD, Johns Hopkins University, Baltimore, and colleagues wrote. “A male model wearing business inner wear with a white coat, fleece jacket, or softshell jacket was perceived as significantly more professional than a female model wearing the same attire (mean professionalism score: male, 65.8; female, 56.2; mean difference in professionalism score: white coat, 12.06; fleece, 7.89; softshell, 8.82; P < .001). ... A male model wearing hospital scrubs or fashion scrubs alone was also perceived as more professional than a female model in the same attire.”
While casual attire, such as fleece or softshell jackets emblazoned with the names of the institution and wearer, has become more popular attire for physicians in recent years, the researchers noted theirs is the first published research to identify associations between gender, attire, and how people distinguish between various health care roles. The study authors launched their web-based survey from May to June 2020 and asked people aged 18 years and older to rate a series of photographs of deidentified models wearing health care attire. Inner wear choices were business attire versus scrubs with and without outer wear options of a long white coat, gray fleece jacket, or black softshell jackets. Survey respondents ranked the images on a 6-point Likert scale with 1 being the least experienced, professional, and friendly and 6 being the most experienced, professional, and friendly. Survey respondents also viewed individual images of male or female models and were asked to rate their professionalism on a scale of 0-100 – with 100 as the “most professional” as well as to identify their profession as either physician, surgeon, nurse, medical technician, or physician assistant.
The study team included 487 (93.3%) of 522 completed surveys in their analyses. Respondents’ mean age was 36.2 years; 260 (53.4%) were female; 372 (76.4%) were White; 33 (6.8%) were Black or African American. Younger respondents and those living in the Western United States who had more exposure to physician casual attire appeared more accepting of it, the authors wrote.
“I remember attending my white-coat ceremony as a medical student, and the symbolism of it all representing me entering the profession. It felt very emotional and heavy and I felt very proud to be there. I also remember taking a ‘selfie’ in my long white coat as a doctor for the first time before my first shift as a resident. But, I’ve also been wearing that same white coat, and a large badge with a ‘DOCTOR’ label on it, and been mistaken by a patient or parent for something other than the physician,” Alexandra M. Sims, a pediatrician and health equity researcher in Cincinnati, said in an interview. “So, I’d really hope that the take-home here is not simply that we must wear our white coats to be considered more professional. I think we have to unpack and dismantle how we’ve even built this notion of ‘professionalism’ in the first place. Women, people of color, and other marginalized groups were certainly not a part of the defining, but we must be a part of the reimagining of an equitable health care profession in this new era.”
As sartorial trends usher in more casual attire, clinicians should redouble efforts to build rapport and enhance communication with patients, such as clarifying team members’ roles when introducing themselves. Dr. Xun and coauthors noted that addressing gender bias is important for all clinicians – not just women – and point to the need for institutional and organizational support for disciplines where gender bias is “especially prevalent,” like surgery. “This responsibility should not be undertaken only by the individuals that experience the biases, which may result in additional cumulative career disadvantages. The promotion of equality and diversity begins with recognition, characterization, and evidence-supported interventions and is a community operation,” Dr. Xun and colleagues concluded.
“I do not equate attire to professionalism or experience, nor is it connected to my satisfaction with the physician. For myself and my daughter, it is the experience of care that ultimately influences our perceptions regarding the professionalism of the physician,” Hala H. Durrah, MTA, parent to a chronically ill child with special health care needs and a Patient and Family Engagement Consultant, said in an interview. “My respect for a physician will ultimately be determined by how my daughter and I were treated, not just from a clinical perspective, but how we felt during those interactions.”
Physicians wearing white coats were rated as significantly more experienced and professional than peers wearing casual attire. Regardless of their attire, however, female physicians were more likely to be judged as appearing less professional and were more likely to be misidentified as medical technicians, physician assistants, or nurses, found research published in JAMA Network Open.
“A white coat with scrubs attire was most preferred for surgeons (mean preference index, 1.3), whereas a white coat with business attire was preferred for family physicians and dermatologists (mean preference indexes, 1.6 and 1.2, respectively; P < .001),” Helen Xun, MD, Johns Hopkins University, Baltimore, and colleagues wrote. “A male model wearing business inner wear with a white coat, fleece jacket, or softshell jacket was perceived as significantly more professional than a female model wearing the same attire (mean professionalism score: male, 65.8; female, 56.2; mean difference in professionalism score: white coat, 12.06; fleece, 7.89; softshell, 8.82; P < .001). ... A male model wearing hospital scrubs or fashion scrubs alone was also perceived as more professional than a female model in the same attire.”
While casual attire, such as fleece or softshell jackets emblazoned with the names of the institution and wearer, has become more popular attire for physicians in recent years, the researchers noted theirs is the first published research to identify associations between gender, attire, and how people distinguish between various health care roles. The study authors launched their web-based survey from May to June 2020 and asked people aged 18 years and older to rate a series of photographs of deidentified models wearing health care attire. Inner wear choices were business attire versus scrubs with and without outer wear options of a long white coat, gray fleece jacket, or black softshell jackets. Survey respondents ranked the images on a 6-point Likert scale with 1 being the least experienced, professional, and friendly and 6 being the most experienced, professional, and friendly. Survey respondents also viewed individual images of male or female models and were asked to rate their professionalism on a scale of 0-100 – with 100 as the “most professional” as well as to identify their profession as either physician, surgeon, nurse, medical technician, or physician assistant.
The study team included 487 (93.3%) of 522 completed surveys in their analyses. Respondents’ mean age was 36.2 years; 260 (53.4%) were female; 372 (76.4%) were White; 33 (6.8%) were Black or African American. Younger respondents and those living in the Western United States who had more exposure to physician casual attire appeared more accepting of it, the authors wrote.
“I remember attending my white-coat ceremony as a medical student, and the symbolism of it all representing me entering the profession. It felt very emotional and heavy and I felt very proud to be there. I also remember taking a ‘selfie’ in my long white coat as a doctor for the first time before my first shift as a resident. But, I’ve also been wearing that same white coat, and a large badge with a ‘DOCTOR’ label on it, and been mistaken by a patient or parent for something other than the physician,” Alexandra M. Sims, a pediatrician and health equity researcher in Cincinnati, said in an interview. “So, I’d really hope that the take-home here is not simply that we must wear our white coats to be considered more professional. I think we have to unpack and dismantle how we’ve even built this notion of ‘professionalism’ in the first place. Women, people of color, and other marginalized groups were certainly not a part of the defining, but we must be a part of the reimagining of an equitable health care profession in this new era.”
As sartorial trends usher in more casual attire, clinicians should redouble efforts to build rapport and enhance communication with patients, such as clarifying team members’ roles when introducing themselves. Dr. Xun and coauthors noted that addressing gender bias is important for all clinicians – not just women – and point to the need for institutional and organizational support for disciplines where gender bias is “especially prevalent,” like surgery. “This responsibility should not be undertaken only by the individuals that experience the biases, which may result in additional cumulative career disadvantages. The promotion of equality and diversity begins with recognition, characterization, and evidence-supported interventions and is a community operation,” Dr. Xun and colleagues concluded.
“I do not equate attire to professionalism or experience, nor is it connected to my satisfaction with the physician. For myself and my daughter, it is the experience of care that ultimately influences our perceptions regarding the professionalism of the physician,” Hala H. Durrah, MTA, parent to a chronically ill child with special health care needs and a Patient and Family Engagement Consultant, said in an interview. “My respect for a physician will ultimately be determined by how my daughter and I were treated, not just from a clinical perspective, but how we felt during those interactions.”
Physicians wearing white coats were rated as significantly more experienced and professional than peers wearing casual attire. Regardless of their attire, however, female physicians were more likely to be judged as appearing less professional and were more likely to be misidentified as medical technicians, physician assistants, or nurses, found research published in JAMA Network Open.
“A white coat with scrubs attire was most preferred for surgeons (mean preference index, 1.3), whereas a white coat with business attire was preferred for family physicians and dermatologists (mean preference indexes, 1.6 and 1.2, respectively; P < .001),” Helen Xun, MD, Johns Hopkins University, Baltimore, and colleagues wrote. “A male model wearing business inner wear with a white coat, fleece jacket, or softshell jacket was perceived as significantly more professional than a female model wearing the same attire (mean professionalism score: male, 65.8; female, 56.2; mean difference in professionalism score: white coat, 12.06; fleece, 7.89; softshell, 8.82; P < .001). ... A male model wearing hospital scrubs or fashion scrubs alone was also perceived as more professional than a female model in the same attire.”
While casual attire, such as fleece or softshell jackets emblazoned with the names of the institution and wearer, has become more popular attire for physicians in recent years, the researchers noted theirs is the first published research to identify associations between gender, attire, and how people distinguish between various health care roles. The study authors launched their web-based survey from May to June 2020 and asked people aged 18 years and older to rate a series of photographs of deidentified models wearing health care attire. Inner wear choices were business attire versus scrubs with and without outer wear options of a long white coat, gray fleece jacket, or black softshell jackets. Survey respondents ranked the images on a 6-point Likert scale with 1 being the least experienced, professional, and friendly and 6 being the most experienced, professional, and friendly. Survey respondents also viewed individual images of male or female models and were asked to rate their professionalism on a scale of 0-100 – with 100 as the “most professional” as well as to identify their profession as either physician, surgeon, nurse, medical technician, or physician assistant.
The study team included 487 (93.3%) of 522 completed surveys in their analyses. Respondents’ mean age was 36.2 years; 260 (53.4%) were female; 372 (76.4%) were White; 33 (6.8%) were Black or African American. Younger respondents and those living in the Western United States who had more exposure to physician casual attire appeared more accepting of it, the authors wrote.
“I remember attending my white-coat ceremony as a medical student, and the symbolism of it all representing me entering the profession. It felt very emotional and heavy and I felt very proud to be there. I also remember taking a ‘selfie’ in my long white coat as a doctor for the first time before my first shift as a resident. But, I’ve also been wearing that same white coat, and a large badge with a ‘DOCTOR’ label on it, and been mistaken by a patient or parent for something other than the physician,” Alexandra M. Sims, a pediatrician and health equity researcher in Cincinnati, said in an interview. “So, I’d really hope that the take-home here is not simply that we must wear our white coats to be considered more professional. I think we have to unpack and dismantle how we’ve even built this notion of ‘professionalism’ in the first place. Women, people of color, and other marginalized groups were certainly not a part of the defining, but we must be a part of the reimagining of an equitable health care profession in this new era.”
As sartorial trends usher in more casual attire, clinicians should redouble efforts to build rapport and enhance communication with patients, such as clarifying team members’ roles when introducing themselves. Dr. Xun and coauthors noted that addressing gender bias is important for all clinicians – not just women – and point to the need for institutional and organizational support for disciplines where gender bias is “especially prevalent,” like surgery. “This responsibility should not be undertaken only by the individuals that experience the biases, which may result in additional cumulative career disadvantages. The promotion of equality and diversity begins with recognition, characterization, and evidence-supported interventions and is a community operation,” Dr. Xun and colleagues concluded.
“I do not equate attire to professionalism or experience, nor is it connected to my satisfaction with the physician. For myself and my daughter, it is the experience of care that ultimately influences our perceptions regarding the professionalism of the physician,” Hala H. Durrah, MTA, parent to a chronically ill child with special health care needs and a Patient and Family Engagement Consultant, said in an interview. “My respect for a physician will ultimately be determined by how my daughter and I were treated, not just from a clinical perspective, but how we felt during those interactions.”
FROM JAMA NETWORK OPEN