User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Seeking new vaccines against whooping cough: The PERISCOPE project
Although there is an effective vaccine against Bordetella pertussis, whooping cough remains a leading cause of death. Cases are increasing, and scientists face challenges in developing new vaccines.
In a key research session at the start of the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Dimitri Diavatopoulos, PhD, associate professor at the Radboud University Medical Centre Nijmegen, the Netherlands, summarized the pertussis vaccination problem and what the Pertussis Correlates of Protection Europe (PERISCOPE) project seeks to achieve. Dr. Diavatopoulos has a longstanding interest in pertussis and immunity and will soon take over as the scientific coordinator of PERISCOPE.
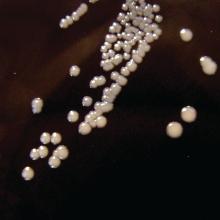
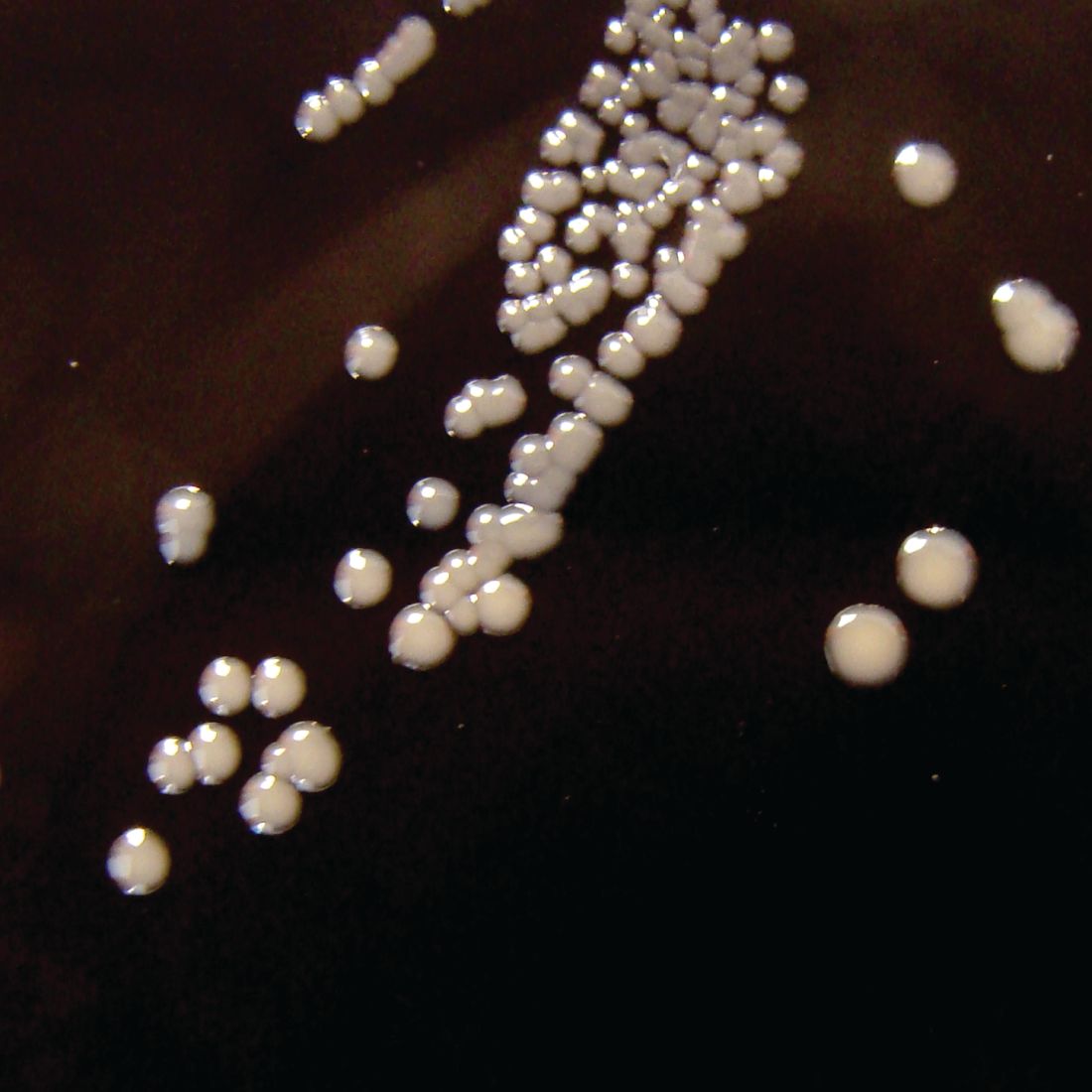
Pertussis is a highly contagious infectious disease that causes uncontrollable coughing. The disease begins with an atypical cough and rhinorrhea before entering a paroxysmal stage characterized by cyanosis, lymphocytosis, vomiting, and whoops. Generally, fever is absent and coughing increases at night. Finally, after weeks to months, the patient enters a convalescent stage. The World Health Organization estimates that there are 16 million pertussis cases annually and approximately 195,000 deaths in children. Most cases are caused by Bordetella pertussis and are preventable by vaccination.
In the United States, following the introduction of a national immunization program using a whole-cell vaccine in the 1950s, cases fell significantly. After a lag phase, the adoption of an acellular vaccine in the United States in 1997 and the Netherlands in 2005 – usually in combination with diphtheria and tetanus via DTaP – saw an increase in case numbers. Dr. Diavatopoulos stated that control is no longer as good, compared with other infectious diseases prevented by the MMR vaccine, such as mumps, measles, and rubella.
In the face of increasing numbers, how do we move to the next generation of vaccines to improve control? There are several barriers to licensure, including the following:
• Universal recommendation for pertussis prevention means that more than 90% of the population will have received DTaP (usually in combination with polio and Haemophilus influenzae B) and be protected for several years after vaccination.
• Because DTaP vaccines are only efficacious for a limited time, the problem is not immediately apparent.
• Pertussis epidemics are cyclical, occurring every 3-5 years. These peaks and troughs complicate the development of epidemiological studies.
What this means is that large-scale Phase III efficacy studies, in which disease is used as the endpoint, are not feasible. Also, formal correlates of protection have not been identified.
The PERISCOPE Project started in March 2016 and is designed to respond to some of these issues. Funding is made available by a public private consortium involving the Bill & Melinda Gates foundation, the European Union, and European Federation of Pharmaceutical Industries and Associations (EFPIA) partners, and in this case, GlaxoSmithKline and Sanofi Pasteur. In total, there are 22 partners in this project.
The strategic objectives of this partnership include the following:
• Foster expertise and increase capacity in Europe to evaluate new pertussis vaccines both in clinical and preclinical models.
• Identify early biomarkers of long-lasting protective immunity to pertussis in humans. (This step will accelerate and de-risk clinical development of next generation pertussis vaccines.)
• Investigate the impact of maternal vaccination on infant response to pertussis vaccination.
The problem is that there is no one single study design that addresses all questions about the pertussis vaccine. For example, in PERISCOPE, the results of preclinical studies using the baboon or mouse models and addressing disease and colonization endpoints or immunogenicity do not perfectly model human infection and disease.
By comparison, controlled human infection studies provide information on colonization but not disease endpoints. Such studies, however, do provide information on immunogenicity endpoints. Also available are booster vaccination studies and infant vaccination studies providing data on immunogenicity, as well as safety information.
Finally, there are patient studies, such as household contact studies where immunogenicity can be correlated to disease endpoints. From these studies, it will be seen that what is needed is integration of evidence from clinical and preclinical studies to support a new vaccine registration.
PERISCOPE addresses these issues by developing novel, functional antibody and cellular assays and employing cutting-edge methods to characterize innate immune responses and cell-mediated systemic and mucosal immunity. PERISCOPE combines two major industrial partners with public researchers from academic and public health institutes and small and medium-sized enterprises with expertise in clinical trials, vaccinology, immunology, molecular microbiology, challenge models, and bioinformatics.
Andrew Gorringe, PhD, from Public Health England and the Research and Development Institute at Porton Down, Wiltshire, England, said, “Vaccines have greatly reduced the incidence of pertussis, but it remains the most prevalent ‘vaccine preventable’ disease. This is an exciting period for pertussis vaccine research as we find new ways to understand the immunity that protects from both infection and disease. The PERISCOPE project provides a collaborative environment that combines expertise across Europe to provide a route to the development of new, more effective vaccines.”
GSK and Sanofi Pasteur have cofunded the PERISCOPE Project. Dr. Diavatopoulos made no other financial disclosures.
Although there is an effective vaccine against Bordetella pertussis, whooping cough remains a leading cause of death. Cases are increasing, and scientists face challenges in developing new vaccines.
In a key research session at the start of the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Dimitri Diavatopoulos, PhD, associate professor at the Radboud University Medical Centre Nijmegen, the Netherlands, summarized the pertussis vaccination problem and what the Pertussis Correlates of Protection Europe (PERISCOPE) project seeks to achieve. Dr. Diavatopoulos has a longstanding interest in pertussis and immunity and will soon take over as the scientific coordinator of PERISCOPE.
Pertussis is a highly contagious infectious disease that causes uncontrollable coughing. The disease begins with an atypical cough and rhinorrhea before entering a paroxysmal stage characterized by cyanosis, lymphocytosis, vomiting, and whoops. Generally, fever is absent and coughing increases at night. Finally, after weeks to months, the patient enters a convalescent stage. The World Health Organization estimates that there are 16 million pertussis cases annually and approximately 195,000 deaths in children. Most cases are caused by Bordetella pertussis and are preventable by vaccination.
In the United States, following the introduction of a national immunization program using a whole-cell vaccine in the 1950s, cases fell significantly. After a lag phase, the adoption of an acellular vaccine in the United States in 1997 and the Netherlands in 2005 – usually in combination with diphtheria and tetanus via DTaP – saw an increase in case numbers. Dr. Diavatopoulos stated that control is no longer as good, compared with other infectious diseases prevented by the MMR vaccine, such as mumps, measles, and rubella.
In the face of increasing numbers, how do we move to the next generation of vaccines to improve control? There are several barriers to licensure, including the following:
• Universal recommendation for pertussis prevention means that more than 90% of the population will have received DTaP (usually in combination with polio and Haemophilus influenzae B) and be protected for several years after vaccination.
• Because DTaP vaccines are only efficacious for a limited time, the problem is not immediately apparent.
• Pertussis epidemics are cyclical, occurring every 3-5 years. These peaks and troughs complicate the development of epidemiological studies.
What this means is that large-scale Phase III efficacy studies, in which disease is used as the endpoint, are not feasible. Also, formal correlates of protection have not been identified.
The PERISCOPE Project started in March 2016 and is designed to respond to some of these issues. Funding is made available by a public private consortium involving the Bill & Melinda Gates foundation, the European Union, and European Federation of Pharmaceutical Industries and Associations (EFPIA) partners, and in this case, GlaxoSmithKline and Sanofi Pasteur. In total, there are 22 partners in this project.
The strategic objectives of this partnership include the following:
• Foster expertise and increase capacity in Europe to evaluate new pertussis vaccines both in clinical and preclinical models.
• Identify early biomarkers of long-lasting protective immunity to pertussis in humans. (This step will accelerate and de-risk clinical development of next generation pertussis vaccines.)
• Investigate the impact of maternal vaccination on infant response to pertussis vaccination.
The problem is that there is no one single study design that addresses all questions about the pertussis vaccine. For example, in PERISCOPE, the results of preclinical studies using the baboon or mouse models and addressing disease and colonization endpoints or immunogenicity do not perfectly model human infection and disease.
By comparison, controlled human infection studies provide information on colonization but not disease endpoints. Such studies, however, do provide information on immunogenicity endpoints. Also available are booster vaccination studies and infant vaccination studies providing data on immunogenicity, as well as safety information.
Finally, there are patient studies, such as household contact studies where immunogenicity can be correlated to disease endpoints. From these studies, it will be seen that what is needed is integration of evidence from clinical and preclinical studies to support a new vaccine registration.
PERISCOPE addresses these issues by developing novel, functional antibody and cellular assays and employing cutting-edge methods to characterize innate immune responses and cell-mediated systemic and mucosal immunity. PERISCOPE combines two major industrial partners with public researchers from academic and public health institutes and small and medium-sized enterprises with expertise in clinical trials, vaccinology, immunology, molecular microbiology, challenge models, and bioinformatics.
Andrew Gorringe, PhD, from Public Health England and the Research and Development Institute at Porton Down, Wiltshire, England, said, “Vaccines have greatly reduced the incidence of pertussis, but it remains the most prevalent ‘vaccine preventable’ disease. This is an exciting period for pertussis vaccine research as we find new ways to understand the immunity that protects from both infection and disease. The PERISCOPE project provides a collaborative environment that combines expertise across Europe to provide a route to the development of new, more effective vaccines.”
GSK and Sanofi Pasteur have cofunded the PERISCOPE Project. Dr. Diavatopoulos made no other financial disclosures.
Although there is an effective vaccine against Bordetella pertussis, whooping cough remains a leading cause of death. Cases are increasing, and scientists face challenges in developing new vaccines.
In a key research session at the start of the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Dimitri Diavatopoulos, PhD, associate professor at the Radboud University Medical Centre Nijmegen, the Netherlands, summarized the pertussis vaccination problem and what the Pertussis Correlates of Protection Europe (PERISCOPE) project seeks to achieve. Dr. Diavatopoulos has a longstanding interest in pertussis and immunity and will soon take over as the scientific coordinator of PERISCOPE.
Pertussis is a highly contagious infectious disease that causes uncontrollable coughing. The disease begins with an atypical cough and rhinorrhea before entering a paroxysmal stage characterized by cyanosis, lymphocytosis, vomiting, and whoops. Generally, fever is absent and coughing increases at night. Finally, after weeks to months, the patient enters a convalescent stage. The World Health Organization estimates that there are 16 million pertussis cases annually and approximately 195,000 deaths in children. Most cases are caused by Bordetella pertussis and are preventable by vaccination.
In the United States, following the introduction of a national immunization program using a whole-cell vaccine in the 1950s, cases fell significantly. After a lag phase, the adoption of an acellular vaccine in the United States in 1997 and the Netherlands in 2005 – usually in combination with diphtheria and tetanus via DTaP – saw an increase in case numbers. Dr. Diavatopoulos stated that control is no longer as good, compared with other infectious diseases prevented by the MMR vaccine, such as mumps, measles, and rubella.
In the face of increasing numbers, how do we move to the next generation of vaccines to improve control? There are several barriers to licensure, including the following:
• Universal recommendation for pertussis prevention means that more than 90% of the population will have received DTaP (usually in combination with polio and Haemophilus influenzae B) and be protected for several years after vaccination.
• Because DTaP vaccines are only efficacious for a limited time, the problem is not immediately apparent.
• Pertussis epidemics are cyclical, occurring every 3-5 years. These peaks and troughs complicate the development of epidemiological studies.
What this means is that large-scale Phase III efficacy studies, in which disease is used as the endpoint, are not feasible. Also, formal correlates of protection have not been identified.
The PERISCOPE Project started in March 2016 and is designed to respond to some of these issues. Funding is made available by a public private consortium involving the Bill & Melinda Gates foundation, the European Union, and European Federation of Pharmaceutical Industries and Associations (EFPIA) partners, and in this case, GlaxoSmithKline and Sanofi Pasteur. In total, there are 22 partners in this project.
The strategic objectives of this partnership include the following:
• Foster expertise and increase capacity in Europe to evaluate new pertussis vaccines both in clinical and preclinical models.
• Identify early biomarkers of long-lasting protective immunity to pertussis in humans. (This step will accelerate and de-risk clinical development of next generation pertussis vaccines.)
• Investigate the impact of maternal vaccination on infant response to pertussis vaccination.
The problem is that there is no one single study design that addresses all questions about the pertussis vaccine. For example, in PERISCOPE, the results of preclinical studies using the baboon or mouse models and addressing disease and colonization endpoints or immunogenicity do not perfectly model human infection and disease.
By comparison, controlled human infection studies provide information on colonization but not disease endpoints. Such studies, however, do provide information on immunogenicity endpoints. Also available are booster vaccination studies and infant vaccination studies providing data on immunogenicity, as well as safety information.
Finally, there are patient studies, such as household contact studies where immunogenicity can be correlated to disease endpoints. From these studies, it will be seen that what is needed is integration of evidence from clinical and preclinical studies to support a new vaccine registration.
PERISCOPE addresses these issues by developing novel, functional antibody and cellular assays and employing cutting-edge methods to characterize innate immune responses and cell-mediated systemic and mucosal immunity. PERISCOPE combines two major industrial partners with public researchers from academic and public health institutes and small and medium-sized enterprises with expertise in clinical trials, vaccinology, immunology, molecular microbiology, challenge models, and bioinformatics.
Andrew Gorringe, PhD, from Public Health England and the Research and Development Institute at Porton Down, Wiltshire, England, said, “Vaccines have greatly reduced the incidence of pertussis, but it remains the most prevalent ‘vaccine preventable’ disease. This is an exciting period for pertussis vaccine research as we find new ways to understand the immunity that protects from both infection and disease. The PERISCOPE project provides a collaborative environment that combines expertise across Europe to provide a route to the development of new, more effective vaccines.”
GSK and Sanofi Pasteur have cofunded the PERISCOPE Project. Dr. Diavatopoulos made no other financial disclosures.
FROM ESPID 2020
Current PERISCOPE vaccine studies: Toward better pertussis prevention?
With increasing whooping cough numbers, developing an effective new vaccine against Bordetella pertussis is a priority. Results from the multifactorial PERISCOPE Project will help scientists and clinicians move forward.
Dominic Kelly, PhD, talked about vaccine-induced immunity and provided an overview of ongoing clinical trials in the PERISCOPE (Pertussis Correlates of Protection Europe) project in a key research session at the start of the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. Dr. Kelly, a pediatrician at the Children’s Hospital in Oxford and a member of the Oxford Vaccines Group, leads one of the studies in the project looking at infant vaccination.
Dr. Kelly began his presentation by showing a figure depicting where vaccine-induced immunity fits into the larger suite of clinical studies. These studies involve mouse models, human challenge models, and infection patients. A key theme is the use of a core group of immunoassays across all studies, with the hope that they will allow effective cross comparisons.
Dr. Kelly stated, “If we find a correlate of protection in the challenge model, we can then interpret the vaccine studies in the light of that because we are using standardized constant immunoassays.”
The assays being used depend in part on the specific study and the volume of blood available. They will generally include Bordetella-specific antibody and functional antibody assays, as well as interesting studies collecting mucosal samples from infants and adults to look at serological responses. Also under examination are a range of enzyme-linked immune absorbent spot, flow cytometry, and culture techniques looking at Memory B cells, T cells, and gene expression.
Complementing these assay studies, PERISCOPE includes a series of clinical investigations designed to throw light on three areas of interest, described below:
First, researchers hope to gain a better understanding regarding the effects of the original whole cell vaccine versus the current acellular variety. The former uses an inactivated version of the whole organism. Epidemiological studies, animal data, and experience in the field demonstrate that whole-cell vaccination results in a broad, long-lasting, and effective immune response.
By comparison, the acellular pertussis vaccine consists of between three and five protein components, which are purified from cultured Bordetella pertussis. While it is an effective vaccine, its effects are less durable; routine use in some countries is associated with cyclical outbreaks of increasing severity.
A second issue for researchers involved in the PERISCOPE project concerns the effects of maternal immunization. In the United Kingdom in 2012, for example, an increasing number of cases were noted 6-7 years after adoption of an acellular vaccine for routine vaccination in the 2nd-3rd trimester of pregnancy. Vaccination appears to effectively control neonatal disease, but whether this influences infant immune responses and long-term control of pertussis for a population is unknown.
Finally, the group is interested in the effects of an acellular booster across all age groups. While the effects may be short-lived, the booster is a potential strategy for controlling a population by repeated boosting of immunity. This is another area where using novel immunoassays may aid better understanding.
To find answers, the consortium has established four studies: the Gambia Pertussis study (GaPs) in Gambia and AWARE, the sister study to GaPs in the United Kingdom, addressing the acellular pertussis versus cellular pertussis question; the Pertussis Maternal Immunization Study in Finland (MIFI) addressing maternal immunization; and the Booster against Pertussis (BERT) study across three countries (U.K., the Netherlands, and Finland) looking at acellular booster across age groups.
Gambia pertussis study
GaPs is the largest single study in the project and is being run at the Medical Research Council–funded London School of Tropical Medicine center in Gambia. Beate Kampmann, MD, PhD, of Imperial College London, England, is the project lead. It is due to complete in 2022. GaPs seeks to enroll 600 mother/infant pairs and randomize the mothers to either an acellular pertussis booster in pregnancy or a tetanus toxoid control vaccine. Infants are subsequently randomized to an acellular or whole-cell pertussis schedule of primary immunization. The vaccine doses are being given at 2, 3, and 4 months. The primary endpoint is a serological finding being measured at 9 months of age, when the infant would usually receive yellow fever, measles, and rubella vaccination.
GaPs has a number of pathways. Within each of the four arms generated by the two randomizations, the maternal randomization and the infant randomization, there are five subgroups. They are designed to study time points in subgroups A and B after the first dose in more detail, looking at the innate immune responses using gene expression. It will enable researchers to study adaptive immune responses to T cells and B cells after the second dose of vaccine. By employing a range of subgroups, the team can explore the immune profile using the assays referred to above. Such information should provide new insights into the differences between acellular and whole-cell vaccines.
The AWARE study
AWARE is the sister study to GaPs and looks at the acellular/whole pertussis issue. Because many developed countries, such as the United Kingdom, have established maternal immunization programs, it is not possible to randomize mothers. Consequently, researchers have opted to recruit infants of mothers who have received an acellular vaccine in pregnancy and randomize them to either an acellular schedule of primary immunization or a whole-cell schedule.
The selected vaccine is ComVac5 from Bharat Biotech. This whole-cell vaccine differs from that used in Gambia. An early obstacle for AWARE has been seeking permission to import a non-conventional vaccine into Europe. It has delayed the anticipated end date to 2023. Participating infants will receive a two-dose schedule at 2 and 4 months of age per their randomization; then, both groups will go on to receive an acellular pertussis booster at 12 months. At all time points, the team will sample blood for cells and serum, as well as mucosal fluid from the nose. Because the mucosal surface is where the action is, this approach will likely generate new data around antibody responses.
The MIFI
The Pertussis Maternal Immunization Study in Finland is being run by Jussi Mertsola, of the University of Turku, Finland, and Qiushui He, of the National Public Health Institute, Turku. It is due to complete in late 2021. Where, in the United Kingdom, researchers are unable to randomize mothers because of the current guidelines, researchers in Finland do not have a maternal immunization program to consider. MIFI will randomize 80 mothers, 40 to immunization with acellular pertussis and 40 to a control group. Dr. Kelly stated that whole cell vaccines are not available for use in Finland. Participants will receive a two-dose schedule at 3 and 5 months. Blood samples will then be taken to compare the serological and cellular responses, which will help researchers understand the effects of maternal immunization. In addition, there will be sampling of mucosal fluid using a device that collects a standardized aliquot of fluid.
The BERT study
The final clinical element of PERISCOPE presented by Dr. Kelly was the Booster against Pertussis study. This study is near completion. It seeks to examine the use of an acellular booster across different age groups and three countries: the United Kingdom, the Netherlands, and Finland. The study is being coordinated by Guy Berbers, PhD, at the National Institute for Public Health and the Environment in the Netherlands.
BERT comprises four cohorts (A, B, C, D) of different ages: 7-10 years (36 participants), 11-15 years (36 participants), mid-adult (25 participants), and older age (25 participants). After receiving an acellular booster, participants will undergo intense sampling. Sampling will take place immediately after immunization at day 7 and look at adaptive effects, then again at day 28 and day 365.
Because some participants will have already received whole cell or acellular vaccination, this approach will allow researchers to look at the effects of priming (i.e., how long the B cell/T cell antibody responses last).
Involving different countries across Europe ensures wide applicability of results, but also allows researchers to compare the effects of very different immunization histories.
At the end of this ESPID session, Dimitri Diavatopoulos, PhD, assistant professor at the Radboud University Medical Centre Nijmegen, the Netherlands, commented that a future problem in studying pertussis vaccines and their potential clinical application is that most vaccination schedules now involve combination products. Obtaining a stand-alone vaccination may prove difficult, and there may be resistance if it complicates current vaccination programs.
Dr. Kelly acknowledged funding for the PERISCOPE project from GlaxoSmithKline and Pasteur Sanofi.
With increasing whooping cough numbers, developing an effective new vaccine against Bordetella pertussis is a priority. Results from the multifactorial PERISCOPE Project will help scientists and clinicians move forward.
Dominic Kelly, PhD, talked about vaccine-induced immunity and provided an overview of ongoing clinical trials in the PERISCOPE (Pertussis Correlates of Protection Europe) project in a key research session at the start of the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. Dr. Kelly, a pediatrician at the Children’s Hospital in Oxford and a member of the Oxford Vaccines Group, leads one of the studies in the project looking at infant vaccination.
Dr. Kelly began his presentation by showing a figure depicting where vaccine-induced immunity fits into the larger suite of clinical studies. These studies involve mouse models, human challenge models, and infection patients. A key theme is the use of a core group of immunoassays across all studies, with the hope that they will allow effective cross comparisons.
Dr. Kelly stated, “If we find a correlate of protection in the challenge model, we can then interpret the vaccine studies in the light of that because we are using standardized constant immunoassays.”
The assays being used depend in part on the specific study and the volume of blood available. They will generally include Bordetella-specific antibody and functional antibody assays, as well as interesting studies collecting mucosal samples from infants and adults to look at serological responses. Also under examination are a range of enzyme-linked immune absorbent spot, flow cytometry, and culture techniques looking at Memory B cells, T cells, and gene expression.
Complementing these assay studies, PERISCOPE includes a series of clinical investigations designed to throw light on three areas of interest, described below:
First, researchers hope to gain a better understanding regarding the effects of the original whole cell vaccine versus the current acellular variety. The former uses an inactivated version of the whole organism. Epidemiological studies, animal data, and experience in the field demonstrate that whole-cell vaccination results in a broad, long-lasting, and effective immune response.
By comparison, the acellular pertussis vaccine consists of between three and five protein components, which are purified from cultured Bordetella pertussis. While it is an effective vaccine, its effects are less durable; routine use in some countries is associated with cyclical outbreaks of increasing severity.
A second issue for researchers involved in the PERISCOPE project concerns the effects of maternal immunization. In the United Kingdom in 2012, for example, an increasing number of cases were noted 6-7 years after adoption of an acellular vaccine for routine vaccination in the 2nd-3rd trimester of pregnancy. Vaccination appears to effectively control neonatal disease, but whether this influences infant immune responses and long-term control of pertussis for a population is unknown.
Finally, the group is interested in the effects of an acellular booster across all age groups. While the effects may be short-lived, the booster is a potential strategy for controlling a population by repeated boosting of immunity. This is another area where using novel immunoassays may aid better understanding.
To find answers, the consortium has established four studies: the Gambia Pertussis study (GaPs) in Gambia and AWARE, the sister study to GaPs in the United Kingdom, addressing the acellular pertussis versus cellular pertussis question; the Pertussis Maternal Immunization Study in Finland (MIFI) addressing maternal immunization; and the Booster against Pertussis (BERT) study across three countries (U.K., the Netherlands, and Finland) looking at acellular booster across age groups.
Gambia pertussis study
GaPs is the largest single study in the project and is being run at the Medical Research Council–funded London School of Tropical Medicine center in Gambia. Beate Kampmann, MD, PhD, of Imperial College London, England, is the project lead. It is due to complete in 2022. GaPs seeks to enroll 600 mother/infant pairs and randomize the mothers to either an acellular pertussis booster in pregnancy or a tetanus toxoid control vaccine. Infants are subsequently randomized to an acellular or whole-cell pertussis schedule of primary immunization. The vaccine doses are being given at 2, 3, and 4 months. The primary endpoint is a serological finding being measured at 9 months of age, when the infant would usually receive yellow fever, measles, and rubella vaccination.
GaPs has a number of pathways. Within each of the four arms generated by the two randomizations, the maternal randomization and the infant randomization, there are five subgroups. They are designed to study time points in subgroups A and B after the first dose in more detail, looking at the innate immune responses using gene expression. It will enable researchers to study adaptive immune responses to T cells and B cells after the second dose of vaccine. By employing a range of subgroups, the team can explore the immune profile using the assays referred to above. Such information should provide new insights into the differences between acellular and whole-cell vaccines.
The AWARE study
AWARE is the sister study to GaPs and looks at the acellular/whole pertussis issue. Because many developed countries, such as the United Kingdom, have established maternal immunization programs, it is not possible to randomize mothers. Consequently, researchers have opted to recruit infants of mothers who have received an acellular vaccine in pregnancy and randomize them to either an acellular schedule of primary immunization or a whole-cell schedule.
The selected vaccine is ComVac5 from Bharat Biotech. This whole-cell vaccine differs from that used in Gambia. An early obstacle for AWARE has been seeking permission to import a non-conventional vaccine into Europe. It has delayed the anticipated end date to 2023. Participating infants will receive a two-dose schedule at 2 and 4 months of age per their randomization; then, both groups will go on to receive an acellular pertussis booster at 12 months. At all time points, the team will sample blood for cells and serum, as well as mucosal fluid from the nose. Because the mucosal surface is where the action is, this approach will likely generate new data around antibody responses.
The MIFI
The Pertussis Maternal Immunization Study in Finland is being run by Jussi Mertsola, of the University of Turku, Finland, and Qiushui He, of the National Public Health Institute, Turku. It is due to complete in late 2021. Where, in the United Kingdom, researchers are unable to randomize mothers because of the current guidelines, researchers in Finland do not have a maternal immunization program to consider. MIFI will randomize 80 mothers, 40 to immunization with acellular pertussis and 40 to a control group. Dr. Kelly stated that whole cell vaccines are not available for use in Finland. Participants will receive a two-dose schedule at 3 and 5 months. Blood samples will then be taken to compare the serological and cellular responses, which will help researchers understand the effects of maternal immunization. In addition, there will be sampling of mucosal fluid using a device that collects a standardized aliquot of fluid.
The BERT study
The final clinical element of PERISCOPE presented by Dr. Kelly was the Booster against Pertussis study. This study is near completion. It seeks to examine the use of an acellular booster across different age groups and three countries: the United Kingdom, the Netherlands, and Finland. The study is being coordinated by Guy Berbers, PhD, at the National Institute for Public Health and the Environment in the Netherlands.
BERT comprises four cohorts (A, B, C, D) of different ages: 7-10 years (36 participants), 11-15 years (36 participants), mid-adult (25 participants), and older age (25 participants). After receiving an acellular booster, participants will undergo intense sampling. Sampling will take place immediately after immunization at day 7 and look at adaptive effects, then again at day 28 and day 365.
Because some participants will have already received whole cell or acellular vaccination, this approach will allow researchers to look at the effects of priming (i.e., how long the B cell/T cell antibody responses last).
Involving different countries across Europe ensures wide applicability of results, but also allows researchers to compare the effects of very different immunization histories.
At the end of this ESPID session, Dimitri Diavatopoulos, PhD, assistant professor at the Radboud University Medical Centre Nijmegen, the Netherlands, commented that a future problem in studying pertussis vaccines and their potential clinical application is that most vaccination schedules now involve combination products. Obtaining a stand-alone vaccination may prove difficult, and there may be resistance if it complicates current vaccination programs.
Dr. Kelly acknowledged funding for the PERISCOPE project from GlaxoSmithKline and Pasteur Sanofi.
With increasing whooping cough numbers, developing an effective new vaccine against Bordetella pertussis is a priority. Results from the multifactorial PERISCOPE Project will help scientists and clinicians move forward.
Dominic Kelly, PhD, talked about vaccine-induced immunity and provided an overview of ongoing clinical trials in the PERISCOPE (Pertussis Correlates of Protection Europe) project in a key research session at the start of the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. Dr. Kelly, a pediatrician at the Children’s Hospital in Oxford and a member of the Oxford Vaccines Group, leads one of the studies in the project looking at infant vaccination.
Dr. Kelly began his presentation by showing a figure depicting where vaccine-induced immunity fits into the larger suite of clinical studies. These studies involve mouse models, human challenge models, and infection patients. A key theme is the use of a core group of immunoassays across all studies, with the hope that they will allow effective cross comparisons.
Dr. Kelly stated, “If we find a correlate of protection in the challenge model, we can then interpret the vaccine studies in the light of that because we are using standardized constant immunoassays.”
The assays being used depend in part on the specific study and the volume of blood available. They will generally include Bordetella-specific antibody and functional antibody assays, as well as interesting studies collecting mucosal samples from infants and adults to look at serological responses. Also under examination are a range of enzyme-linked immune absorbent spot, flow cytometry, and culture techniques looking at Memory B cells, T cells, and gene expression.
Complementing these assay studies, PERISCOPE includes a series of clinical investigations designed to throw light on three areas of interest, described below:
First, researchers hope to gain a better understanding regarding the effects of the original whole cell vaccine versus the current acellular variety. The former uses an inactivated version of the whole organism. Epidemiological studies, animal data, and experience in the field demonstrate that whole-cell vaccination results in a broad, long-lasting, and effective immune response.
By comparison, the acellular pertussis vaccine consists of between three and five protein components, which are purified from cultured Bordetella pertussis. While it is an effective vaccine, its effects are less durable; routine use in some countries is associated with cyclical outbreaks of increasing severity.
A second issue for researchers involved in the PERISCOPE project concerns the effects of maternal immunization. In the United Kingdom in 2012, for example, an increasing number of cases were noted 6-7 years after adoption of an acellular vaccine for routine vaccination in the 2nd-3rd trimester of pregnancy. Vaccination appears to effectively control neonatal disease, but whether this influences infant immune responses and long-term control of pertussis for a population is unknown.
Finally, the group is interested in the effects of an acellular booster across all age groups. While the effects may be short-lived, the booster is a potential strategy for controlling a population by repeated boosting of immunity. This is another area where using novel immunoassays may aid better understanding.
To find answers, the consortium has established four studies: the Gambia Pertussis study (GaPs) in Gambia and AWARE, the sister study to GaPs in the United Kingdom, addressing the acellular pertussis versus cellular pertussis question; the Pertussis Maternal Immunization Study in Finland (MIFI) addressing maternal immunization; and the Booster against Pertussis (BERT) study across three countries (U.K., the Netherlands, and Finland) looking at acellular booster across age groups.
Gambia pertussis study
GaPs is the largest single study in the project and is being run at the Medical Research Council–funded London School of Tropical Medicine center in Gambia. Beate Kampmann, MD, PhD, of Imperial College London, England, is the project lead. It is due to complete in 2022. GaPs seeks to enroll 600 mother/infant pairs and randomize the mothers to either an acellular pertussis booster in pregnancy or a tetanus toxoid control vaccine. Infants are subsequently randomized to an acellular or whole-cell pertussis schedule of primary immunization. The vaccine doses are being given at 2, 3, and 4 months. The primary endpoint is a serological finding being measured at 9 months of age, when the infant would usually receive yellow fever, measles, and rubella vaccination.
GaPs has a number of pathways. Within each of the four arms generated by the two randomizations, the maternal randomization and the infant randomization, there are five subgroups. They are designed to study time points in subgroups A and B after the first dose in more detail, looking at the innate immune responses using gene expression. It will enable researchers to study adaptive immune responses to T cells and B cells after the second dose of vaccine. By employing a range of subgroups, the team can explore the immune profile using the assays referred to above. Such information should provide new insights into the differences between acellular and whole-cell vaccines.
The AWARE study
AWARE is the sister study to GaPs and looks at the acellular/whole pertussis issue. Because many developed countries, such as the United Kingdom, have established maternal immunization programs, it is not possible to randomize mothers. Consequently, researchers have opted to recruit infants of mothers who have received an acellular vaccine in pregnancy and randomize them to either an acellular schedule of primary immunization or a whole-cell schedule.
The selected vaccine is ComVac5 from Bharat Biotech. This whole-cell vaccine differs from that used in Gambia. An early obstacle for AWARE has been seeking permission to import a non-conventional vaccine into Europe. It has delayed the anticipated end date to 2023. Participating infants will receive a two-dose schedule at 2 and 4 months of age per their randomization; then, both groups will go on to receive an acellular pertussis booster at 12 months. At all time points, the team will sample blood for cells and serum, as well as mucosal fluid from the nose. Because the mucosal surface is where the action is, this approach will likely generate new data around antibody responses.
The MIFI
The Pertussis Maternal Immunization Study in Finland is being run by Jussi Mertsola, of the University of Turku, Finland, and Qiushui He, of the National Public Health Institute, Turku. It is due to complete in late 2021. Where, in the United Kingdom, researchers are unable to randomize mothers because of the current guidelines, researchers in Finland do not have a maternal immunization program to consider. MIFI will randomize 80 mothers, 40 to immunization with acellular pertussis and 40 to a control group. Dr. Kelly stated that whole cell vaccines are not available for use in Finland. Participants will receive a two-dose schedule at 3 and 5 months. Blood samples will then be taken to compare the serological and cellular responses, which will help researchers understand the effects of maternal immunization. In addition, there will be sampling of mucosal fluid using a device that collects a standardized aliquot of fluid.
The BERT study
The final clinical element of PERISCOPE presented by Dr. Kelly was the Booster against Pertussis study. This study is near completion. It seeks to examine the use of an acellular booster across different age groups and three countries: the United Kingdom, the Netherlands, and Finland. The study is being coordinated by Guy Berbers, PhD, at the National Institute for Public Health and the Environment in the Netherlands.
BERT comprises four cohorts (A, B, C, D) of different ages: 7-10 years (36 participants), 11-15 years (36 participants), mid-adult (25 participants), and older age (25 participants). After receiving an acellular booster, participants will undergo intense sampling. Sampling will take place immediately after immunization at day 7 and look at adaptive effects, then again at day 28 and day 365.
Because some participants will have already received whole cell or acellular vaccination, this approach will allow researchers to look at the effects of priming (i.e., how long the B cell/T cell antibody responses last).
Involving different countries across Europe ensures wide applicability of results, but also allows researchers to compare the effects of very different immunization histories.
At the end of this ESPID session, Dimitri Diavatopoulos, PhD, assistant professor at the Radboud University Medical Centre Nijmegen, the Netherlands, commented that a future problem in studying pertussis vaccines and their potential clinical application is that most vaccination schedules now involve combination products. Obtaining a stand-alone vaccination may prove difficult, and there may be resistance if it complicates current vaccination programs.
Dr. Kelly acknowledged funding for the PERISCOPE project from GlaxoSmithKline and Pasteur Sanofi.
FROM ESPID 2020
Is diagnostic hysteroscopy safe in patients with type 2 endometrial cancer?
Among women with type 2 endometrial cancer, diagnostic hysteroscopy may not be associated with increased odds of positive peritoneal cytology at the time of surgical staging or with decreased survival, according to a retrospective study of 127 patients.
a researcher said at the meeting sponsored by AAGL, held virtually this year.
Possible associations between cytology and procedures
Prior research has found that positive peritoneal cytology may correlate with greater likelihood of death among patients with endometrial cancer, and researchers have wondered whether pressure on the uterine cavity during hysteroscopy increases the presence of positive peritoneal cytology. “According to some systematic reviews ... it seems that it does,” said study author Luiz Brito, MD, PhD, associate professor of obstetrics and gynecology at the University of Campinas in Brazil.
Nevertheless, research suggests that “most of the time hysteroscopy does not have a powerful impact on the prognosis of these patients,” he said.
Studies have tended to focus on patients with type 1 endometrial cancer, however. Type 2 endometrial cancer, which is more aggressive, “is scarcely studied,” Dr. Brito said. One retrospective study that focused on type 2 endometrial cancer included 140 patients. Among patients who underwent hysteroscopy, 30% had positive cytology. In comparison, 12% of patients in the curettage group had positive cytology. But the difference in disease-specific survival between groups was not statistically significant, and about 33% of the patients in each group developed a recurrence.
To examine associations between diagnostic methods and outcomes in another group of patients with type 2 endometrial cancer, Dr. Brito and colleagues analyzed data from a hospital registry in Brazil.
The database included 1,183 patients with endometrial cancer between 2002 and 2017, including 235 patients with type 2 endometrial cancer. After excluding patients with synchronous tumor and those who did not undergo surgery or did not have peritoneal cytology performed, 127 patients remained for the analysis. The study included follow-up to December 2019.
The researchers compared the prevalence of positive peritoneal cytology among 43 patients who underwent hysteroscopy with that among 84 patients who underwent curettage. The groups had similar baseline characteristics.
Positive peritoneal cytology was more common in the curettage group than in the hysteroscopy group (10.7% vs. 4.6%), although the difference was not statistically significant. Lymphovascular invasion and advanced surgical staging were more common in the curettage group.
In a multivariate analysis, older age and advanced cancer staging were the only factors associated with decreased disease-free survival. Age, advanced cancer staging, and vascular invasion were associated with decreased disease-specific survival.
The researchers also had considered factors such as peritoneal cytology, diagnostic method, age of menarche, menopause time, parity, comorbidities, smoking status, body mass index, abnormal uterine bleeding, histological type, and adjuvant treatment.
A limitation of the study is that it relied on data from a public health system that often has long wait times for diagnosis and treatment, Dr. Brito noted.
Some doctors may forgo cytology
The available research raises questions about the role and relevance of peritoneal cytology in caring for patients with endometrial cancer, René Pareja, MD, a gynecologic oncologist at Instituto Nacional de Cancerología, Bogotá, Colombia, said in a discussion following the presentation.
Peritoneal cytology has not been part of endometrial cancer staging since 2009, Dr. Pareja said. Still, guidelines recommend that surgeons collect cytology during surgical staging, with the idea that the results could inform adjuvant treatment decisions.
“Peritoneal cytology is recommended in the guidelines, but there are no recommendations on how to proceed if it is positive,” Dr. Pareja said. “While some gynecologic oncologists continue to take cytology during endometrial cancer staging, some have stopped doing so. And in Colombia, most of us are not performing pelvic cytology.”
Although some studies indicate that hysteroscopy may increase the rate of positive cytology, positive cytology may not be associated with worse oncological outcomes independent of other risk factors for recurrence, said Dr. Pareja.
So far, studies have been retrospective. Furthermore, the sensitivity and specificity of pelvic cytology tests are not 100%. “Should we continue performing pelvic cytology given the results of this and other studies?” Dr. Pareja asked.
Despite limited knowledge about this variable, physicians may want to be aware if a patient has positive cytology, Dr. Brito suggested. “At least it will give us some red flags so we can be attentive to these patients.”
If researchers were to design a prospective study that incorporates hysteroscopic variables, it could provide more complete answers about the relationship between hysteroscopy and peritoneal cytology and clarify the importance of positive cytology, Dr. Brito said.
Dr. Brito had no relevant disclosures. Dr. Pareja disclosed consulting for Johnson & Johnson.
SOURCE: Oliveira Brito LG et al. J Minim Invasive Gynecol. 2020 Nov. doi: 10.1016/j.jmig.2020.08.356.
Among women with type 2 endometrial cancer, diagnostic hysteroscopy may not be associated with increased odds of positive peritoneal cytology at the time of surgical staging or with decreased survival, according to a retrospective study of 127 patients.
a researcher said at the meeting sponsored by AAGL, held virtually this year.
Possible associations between cytology and procedures
Prior research has found that positive peritoneal cytology may correlate with greater likelihood of death among patients with endometrial cancer, and researchers have wondered whether pressure on the uterine cavity during hysteroscopy increases the presence of positive peritoneal cytology. “According to some systematic reviews ... it seems that it does,” said study author Luiz Brito, MD, PhD, associate professor of obstetrics and gynecology at the University of Campinas in Brazil.
Nevertheless, research suggests that “most of the time hysteroscopy does not have a powerful impact on the prognosis of these patients,” he said.
Studies have tended to focus on patients with type 1 endometrial cancer, however. Type 2 endometrial cancer, which is more aggressive, “is scarcely studied,” Dr. Brito said. One retrospective study that focused on type 2 endometrial cancer included 140 patients. Among patients who underwent hysteroscopy, 30% had positive cytology. In comparison, 12% of patients in the curettage group had positive cytology. But the difference in disease-specific survival between groups was not statistically significant, and about 33% of the patients in each group developed a recurrence.
To examine associations between diagnostic methods and outcomes in another group of patients with type 2 endometrial cancer, Dr. Brito and colleagues analyzed data from a hospital registry in Brazil.
The database included 1,183 patients with endometrial cancer between 2002 and 2017, including 235 patients with type 2 endometrial cancer. After excluding patients with synchronous tumor and those who did not undergo surgery or did not have peritoneal cytology performed, 127 patients remained for the analysis. The study included follow-up to December 2019.
The researchers compared the prevalence of positive peritoneal cytology among 43 patients who underwent hysteroscopy with that among 84 patients who underwent curettage. The groups had similar baseline characteristics.
Positive peritoneal cytology was more common in the curettage group than in the hysteroscopy group (10.7% vs. 4.6%), although the difference was not statistically significant. Lymphovascular invasion and advanced surgical staging were more common in the curettage group.
In a multivariate analysis, older age and advanced cancer staging were the only factors associated with decreased disease-free survival. Age, advanced cancer staging, and vascular invasion were associated with decreased disease-specific survival.
The researchers also had considered factors such as peritoneal cytology, diagnostic method, age of menarche, menopause time, parity, comorbidities, smoking status, body mass index, abnormal uterine bleeding, histological type, and adjuvant treatment.
A limitation of the study is that it relied on data from a public health system that often has long wait times for diagnosis and treatment, Dr. Brito noted.
Some doctors may forgo cytology
The available research raises questions about the role and relevance of peritoneal cytology in caring for patients with endometrial cancer, René Pareja, MD, a gynecologic oncologist at Instituto Nacional de Cancerología, Bogotá, Colombia, said in a discussion following the presentation.
Peritoneal cytology has not been part of endometrial cancer staging since 2009, Dr. Pareja said. Still, guidelines recommend that surgeons collect cytology during surgical staging, with the idea that the results could inform adjuvant treatment decisions.
“Peritoneal cytology is recommended in the guidelines, but there are no recommendations on how to proceed if it is positive,” Dr. Pareja said. “While some gynecologic oncologists continue to take cytology during endometrial cancer staging, some have stopped doing so. And in Colombia, most of us are not performing pelvic cytology.”
Although some studies indicate that hysteroscopy may increase the rate of positive cytology, positive cytology may not be associated with worse oncological outcomes independent of other risk factors for recurrence, said Dr. Pareja.
So far, studies have been retrospective. Furthermore, the sensitivity and specificity of pelvic cytology tests are not 100%. “Should we continue performing pelvic cytology given the results of this and other studies?” Dr. Pareja asked.
Despite limited knowledge about this variable, physicians may want to be aware if a patient has positive cytology, Dr. Brito suggested. “At least it will give us some red flags so we can be attentive to these patients.”
If researchers were to design a prospective study that incorporates hysteroscopic variables, it could provide more complete answers about the relationship between hysteroscopy and peritoneal cytology and clarify the importance of positive cytology, Dr. Brito said.
Dr. Brito had no relevant disclosures. Dr. Pareja disclosed consulting for Johnson & Johnson.
SOURCE: Oliveira Brito LG et al. J Minim Invasive Gynecol. 2020 Nov. doi: 10.1016/j.jmig.2020.08.356.
Among women with type 2 endometrial cancer, diagnostic hysteroscopy may not be associated with increased odds of positive peritoneal cytology at the time of surgical staging or with decreased survival, according to a retrospective study of 127 patients.
a researcher said at the meeting sponsored by AAGL, held virtually this year.
Possible associations between cytology and procedures
Prior research has found that positive peritoneal cytology may correlate with greater likelihood of death among patients with endometrial cancer, and researchers have wondered whether pressure on the uterine cavity during hysteroscopy increases the presence of positive peritoneal cytology. “According to some systematic reviews ... it seems that it does,” said study author Luiz Brito, MD, PhD, associate professor of obstetrics and gynecology at the University of Campinas in Brazil.
Nevertheless, research suggests that “most of the time hysteroscopy does not have a powerful impact on the prognosis of these patients,” he said.
Studies have tended to focus on patients with type 1 endometrial cancer, however. Type 2 endometrial cancer, which is more aggressive, “is scarcely studied,” Dr. Brito said. One retrospective study that focused on type 2 endometrial cancer included 140 patients. Among patients who underwent hysteroscopy, 30% had positive cytology. In comparison, 12% of patients in the curettage group had positive cytology. But the difference in disease-specific survival between groups was not statistically significant, and about 33% of the patients in each group developed a recurrence.
To examine associations between diagnostic methods and outcomes in another group of patients with type 2 endometrial cancer, Dr. Brito and colleagues analyzed data from a hospital registry in Brazil.
The database included 1,183 patients with endometrial cancer between 2002 and 2017, including 235 patients with type 2 endometrial cancer. After excluding patients with synchronous tumor and those who did not undergo surgery or did not have peritoneal cytology performed, 127 patients remained for the analysis. The study included follow-up to December 2019.
The researchers compared the prevalence of positive peritoneal cytology among 43 patients who underwent hysteroscopy with that among 84 patients who underwent curettage. The groups had similar baseline characteristics.
Positive peritoneal cytology was more common in the curettage group than in the hysteroscopy group (10.7% vs. 4.6%), although the difference was not statistically significant. Lymphovascular invasion and advanced surgical staging were more common in the curettage group.
In a multivariate analysis, older age and advanced cancer staging were the only factors associated with decreased disease-free survival. Age, advanced cancer staging, and vascular invasion were associated with decreased disease-specific survival.
The researchers also had considered factors such as peritoneal cytology, diagnostic method, age of menarche, menopause time, parity, comorbidities, smoking status, body mass index, abnormal uterine bleeding, histological type, and adjuvant treatment.
A limitation of the study is that it relied on data from a public health system that often has long wait times for diagnosis and treatment, Dr. Brito noted.
Some doctors may forgo cytology
The available research raises questions about the role and relevance of peritoneal cytology in caring for patients with endometrial cancer, René Pareja, MD, a gynecologic oncologist at Instituto Nacional de Cancerología, Bogotá, Colombia, said in a discussion following the presentation.
Peritoneal cytology has not been part of endometrial cancer staging since 2009, Dr. Pareja said. Still, guidelines recommend that surgeons collect cytology during surgical staging, with the idea that the results could inform adjuvant treatment decisions.
“Peritoneal cytology is recommended in the guidelines, but there are no recommendations on how to proceed if it is positive,” Dr. Pareja said. “While some gynecologic oncologists continue to take cytology during endometrial cancer staging, some have stopped doing so. And in Colombia, most of us are not performing pelvic cytology.”
Although some studies indicate that hysteroscopy may increase the rate of positive cytology, positive cytology may not be associated with worse oncological outcomes independent of other risk factors for recurrence, said Dr. Pareja.
So far, studies have been retrospective. Furthermore, the sensitivity and specificity of pelvic cytology tests are not 100%. “Should we continue performing pelvic cytology given the results of this and other studies?” Dr. Pareja asked.
Despite limited knowledge about this variable, physicians may want to be aware if a patient has positive cytology, Dr. Brito suggested. “At least it will give us some red flags so we can be attentive to these patients.”
If researchers were to design a prospective study that incorporates hysteroscopic variables, it could provide more complete answers about the relationship between hysteroscopy and peritoneal cytology and clarify the importance of positive cytology, Dr. Brito said.
Dr. Brito had no relevant disclosures. Dr. Pareja disclosed consulting for Johnson & Johnson.
SOURCE: Oliveira Brito LG et al. J Minim Invasive Gynecol. 2020 Nov. doi: 10.1016/j.jmig.2020.08.356.
FROM AAGL GLOBAL CONGRESS
COVID-19–induced drop in first measles vaccinations sparks resurgence concerns
Widespread use of the MMR vaccine is not only crucial for protecting the community against infectious outbreaks, but also serves as the overall pacesetter for preventive services, said Sara M. Bode, MD and colleagues at Nationwide Children’s Hospital in Columbus.
As part of a bivariate logistic regression analysis, Dr. Bode and colleagues sought to evaluate changes in measles vaccination rates across 12 clinic sites of the Nationwide Children’s Hospital pediatric primary care network in Columbus among 23,534 children aged 16 months. The study period targeted the time between April and May 2020, when clinic access and appointment attendance declined following the start of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, until the June-to-August 2020 time period, when clinical care was allowed to return.
The need for the study was prompted by Centers for Disease Control and Prevention reporting on a state-specific precipitous decline in MMR vaccination rates shortly after the onset of COVID-19 in May 2020. Citing the results of one study, such reductions in vaccination have raised concerns over the possibility of a measles resurgence, noted Dr. Bode and associates.
MMR vaccination rates begin to drop with onset of COVID-19 pandemic.
From March 2017 to March 2020, the average rate of MMR vaccination in 16-month-olds was 72%. It subsequently decreased to 67% from April to May 2020, and then dropped further to 62% during the period June to August, 2020 (P = .001). Those without insurance were less likely to be vaccinated than were those carrying private insurance or Medicaid.
Among patients who had not attended a preventive care visit after 12 months of age, the proportion who received vaccines declined during the same time periods, from 10% before the pandemic to 6% at the start of the pandemic and 3% during the summer months of 2020.
“Given the baseline low vaccination rates even before the pandemic and the subsequent decline, we face a critical need to improve timely vaccination and provide catch-up opportunities” in areas with the highest incidence of COVID-19, observed Dr. Bode and colleagues.
Innovative approaches are needed to encourage families to seek preventive care.
In response, the researchers announced the implementation of new community-based vaccination approaches in Ohio, including pop-up vaccine clinics, mobile clinics, and school-based clinics to provide families, who are reluctant to visit health care facilities over COVID-19 related concerns, with safe alternatives. “We believe that it is critical to develop innovative approaches to have families return for preventive care,” they added.
In a separate interview, Herschel Lessin, MD, a private practice pediatrician in Poughkeepsie, N.Y., noted: “This study confirms the anecdotal experience of pediatricians around the country, and our greatest fear that the pandemic will interfere with herd immunity of children for vaccine-preventable illness. Although the study was of urban offices with a primarily Medicaid population, I believe the results to be very worrisome should they prove to be generalizable to the country, as a whole. The significant reduction of well-child visits due to COVID-19 (and fear of COVID-19) seriously impaired the vaccination status of a standard required vaccine in a large population. What is even more worrisome is that the rates continued to fall even after the initial closure of many offices and well into their reopening, despite concerted efforts to try to catch up these missed visits and immunizations.”
Measles is an intensely contagious illness that has not been eradicated, as evidenced by the enormous measles outbreak stemming from Disneyland in 2014-2015, and again with the possible exposure of hundreds to an infected Disneyland visitor last fall, where coverage rates were even higher than in this study, added Dr. Lessin. “This phenomenon, unless forcefully remedied, could easily result in large outbreaks of other vaccine-preventable illness besides COVID-19,” he cautioned.
Dr. Bode and colleagues as well as Dr. Lessin had no conflicts of interest and no relevant financial disclosures.
SOURCE: Bode SM et al. Pediatrics. 2021. doi: 10.1542/peds.2020-035576.
Widespread use of the MMR vaccine is not only crucial for protecting the community against infectious outbreaks, but also serves as the overall pacesetter for preventive services, said Sara M. Bode, MD and colleagues at Nationwide Children’s Hospital in Columbus.
As part of a bivariate logistic regression analysis, Dr. Bode and colleagues sought to evaluate changes in measles vaccination rates across 12 clinic sites of the Nationwide Children’s Hospital pediatric primary care network in Columbus among 23,534 children aged 16 months. The study period targeted the time between April and May 2020, when clinic access and appointment attendance declined following the start of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, until the June-to-August 2020 time period, when clinical care was allowed to return.
The need for the study was prompted by Centers for Disease Control and Prevention reporting on a state-specific precipitous decline in MMR vaccination rates shortly after the onset of COVID-19 in May 2020. Citing the results of one study, such reductions in vaccination have raised concerns over the possibility of a measles resurgence, noted Dr. Bode and associates.
MMR vaccination rates begin to drop with onset of COVID-19 pandemic.
From March 2017 to March 2020, the average rate of MMR vaccination in 16-month-olds was 72%. It subsequently decreased to 67% from April to May 2020, and then dropped further to 62% during the period June to August, 2020 (P = .001). Those without insurance were less likely to be vaccinated than were those carrying private insurance or Medicaid.
Among patients who had not attended a preventive care visit after 12 months of age, the proportion who received vaccines declined during the same time periods, from 10% before the pandemic to 6% at the start of the pandemic and 3% during the summer months of 2020.
“Given the baseline low vaccination rates even before the pandemic and the subsequent decline, we face a critical need to improve timely vaccination and provide catch-up opportunities” in areas with the highest incidence of COVID-19, observed Dr. Bode and colleagues.
Innovative approaches are needed to encourage families to seek preventive care.
In response, the researchers announced the implementation of new community-based vaccination approaches in Ohio, including pop-up vaccine clinics, mobile clinics, and school-based clinics to provide families, who are reluctant to visit health care facilities over COVID-19 related concerns, with safe alternatives. “We believe that it is critical to develop innovative approaches to have families return for preventive care,” they added.
In a separate interview, Herschel Lessin, MD, a private practice pediatrician in Poughkeepsie, N.Y., noted: “This study confirms the anecdotal experience of pediatricians around the country, and our greatest fear that the pandemic will interfere with herd immunity of children for vaccine-preventable illness. Although the study was of urban offices with a primarily Medicaid population, I believe the results to be very worrisome should they prove to be generalizable to the country, as a whole. The significant reduction of well-child visits due to COVID-19 (and fear of COVID-19) seriously impaired the vaccination status of a standard required vaccine in a large population. What is even more worrisome is that the rates continued to fall even after the initial closure of many offices and well into their reopening, despite concerted efforts to try to catch up these missed visits and immunizations.”
Measles is an intensely contagious illness that has not been eradicated, as evidenced by the enormous measles outbreak stemming from Disneyland in 2014-2015, and again with the possible exposure of hundreds to an infected Disneyland visitor last fall, where coverage rates were even higher than in this study, added Dr. Lessin. “This phenomenon, unless forcefully remedied, could easily result in large outbreaks of other vaccine-preventable illness besides COVID-19,” he cautioned.
Dr. Bode and colleagues as well as Dr. Lessin had no conflicts of interest and no relevant financial disclosures.
SOURCE: Bode SM et al. Pediatrics. 2021. doi: 10.1542/peds.2020-035576.
Widespread use of the MMR vaccine is not only crucial for protecting the community against infectious outbreaks, but also serves as the overall pacesetter for preventive services, said Sara M. Bode, MD and colleagues at Nationwide Children’s Hospital in Columbus.
As part of a bivariate logistic regression analysis, Dr. Bode and colleagues sought to evaluate changes in measles vaccination rates across 12 clinic sites of the Nationwide Children’s Hospital pediatric primary care network in Columbus among 23,534 children aged 16 months. The study period targeted the time between April and May 2020, when clinic access and appointment attendance declined following the start of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, until the June-to-August 2020 time period, when clinical care was allowed to return.
The need for the study was prompted by Centers for Disease Control and Prevention reporting on a state-specific precipitous decline in MMR vaccination rates shortly after the onset of COVID-19 in May 2020. Citing the results of one study, such reductions in vaccination have raised concerns over the possibility of a measles resurgence, noted Dr. Bode and associates.
MMR vaccination rates begin to drop with onset of COVID-19 pandemic.
From March 2017 to March 2020, the average rate of MMR vaccination in 16-month-olds was 72%. It subsequently decreased to 67% from April to May 2020, and then dropped further to 62% during the period June to August, 2020 (P = .001). Those without insurance were less likely to be vaccinated than were those carrying private insurance or Medicaid.
Among patients who had not attended a preventive care visit after 12 months of age, the proportion who received vaccines declined during the same time periods, from 10% before the pandemic to 6% at the start of the pandemic and 3% during the summer months of 2020.
“Given the baseline low vaccination rates even before the pandemic and the subsequent decline, we face a critical need to improve timely vaccination and provide catch-up opportunities” in areas with the highest incidence of COVID-19, observed Dr. Bode and colleagues.
Innovative approaches are needed to encourage families to seek preventive care.
In response, the researchers announced the implementation of new community-based vaccination approaches in Ohio, including pop-up vaccine clinics, mobile clinics, and school-based clinics to provide families, who are reluctant to visit health care facilities over COVID-19 related concerns, with safe alternatives. “We believe that it is critical to develop innovative approaches to have families return for preventive care,” they added.
In a separate interview, Herschel Lessin, MD, a private practice pediatrician in Poughkeepsie, N.Y., noted: “This study confirms the anecdotal experience of pediatricians around the country, and our greatest fear that the pandemic will interfere with herd immunity of children for vaccine-preventable illness. Although the study was of urban offices with a primarily Medicaid population, I believe the results to be very worrisome should they prove to be generalizable to the country, as a whole. The significant reduction of well-child visits due to COVID-19 (and fear of COVID-19) seriously impaired the vaccination status of a standard required vaccine in a large population. What is even more worrisome is that the rates continued to fall even after the initial closure of many offices and well into their reopening, despite concerted efforts to try to catch up these missed visits and immunizations.”
Measles is an intensely contagious illness that has not been eradicated, as evidenced by the enormous measles outbreak stemming from Disneyland in 2014-2015, and again with the possible exposure of hundreds to an infected Disneyland visitor last fall, where coverage rates were even higher than in this study, added Dr. Lessin. “This phenomenon, unless forcefully remedied, could easily result in large outbreaks of other vaccine-preventable illness besides COVID-19,” he cautioned.
Dr. Bode and colleagues as well as Dr. Lessin had no conflicts of interest and no relevant financial disclosures.
SOURCE: Bode SM et al. Pediatrics. 2021. doi: 10.1542/peds.2020-035576.
FROM PEDIATRICS
Shortcomings identified in study of acne videos on TikTok
, according to an analysis of the top 100 videos using a consumer health validation tool.
The popularity of TikTok among adolescents in particular has implications for the dissemination of acne information, as some teens become “skinfluencers” and receive sponsorship from skin care brands in exchange for social media promotion, wrote David X. Zheng, BA, of the department of dermatology, Case Western Reserve University, Cleveland, and colleagues.
“However, the quality of dermatologic information found on TikTok is largely unknown,” they said.
In a brief report published in Pediatric Dermatology, the researchers identified the top 100 videos on TikTok on May 1, 2020, that were tagged with “#acne.” The information on each video included date of upload, type and gender of the individual uploading the video, physician specialty if applicable, and video category. These top 100 videos had 13,470,501 likes and 64,775 comments over a 7.6-month time period.
The researchers used the DISCERN criteria, a validated 1-5 scale designed to assess consumer health information, to evaluate the video content, with 1 (having “serious” or “extensive shortcomings”) and 5 (having “minimal shortcomings.”)
Overall, the average quality rating of the TikTok acne videos was 2.03. A total of 9 videos were produced by board-certified physicians in the United States, with an average DISCERN score of 2.41.
“Analysis of the DISCERN criteria dimensions suggested that major shortcomings common to both physician and nonphysician uploaders included failure to cite information sources, discuss treatment risks, and provide support for shared decision-making,” the researchers said.
Approximately one-third (34%) of the videos fell into the treatment-product advertisement category, while 26% were personal anecdotes, 20% presented information related to acne, 13% featured home remedy treatments, and 7% were classified as “other.” The researchers also identified the top 200 “#acne” videos on TikTok once a week from May 8, 2020 to June 5, 2020, to determine the evolution of acne content on the app and found a turnover rate of 10.9% per week.
Based on the high turnover and low quality based on DISCERN ratings, the authors suggested that patients seeking acne information should “view acne-related TikTok videos with caution and consult evidence-based resources whenever possible.”
The study findings were limited by several factors including the small sample size of physicians uploading videos, lack of information about the number of nonphysician medical professionals who uploaded videos, and lack of information about the number of video views and country of origin, the researchers noted. However, the results highlight the need for dermatologists to be aware that patients, especially teens, may be using TikTok for acne information that may be of poor quality, they said.
“Conversely, we understand that social media can be a powerful tool for advancing health literacy,” the researchers noted. “Therefore, we also recommend that health care professionals engaging on TikTok create thorough and perhaps standardized educational videos regarding acne, as well as correct any acne-related misinformation that may be present,” they concluded.
The other authors of the study were from the departments of dermatology at Case Western Reserve, University Hospitals Cleveland, and Johns Hopkins University, Baltimore.
The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Zheng DX et al. Pediatr Dermatol. 2020 Nov 28. doi: 10.1111/pde.14471.
, according to an analysis of the top 100 videos using a consumer health validation tool.
The popularity of TikTok among adolescents in particular has implications for the dissemination of acne information, as some teens become “skinfluencers” and receive sponsorship from skin care brands in exchange for social media promotion, wrote David X. Zheng, BA, of the department of dermatology, Case Western Reserve University, Cleveland, and colleagues.
“However, the quality of dermatologic information found on TikTok is largely unknown,” they said.
In a brief report published in Pediatric Dermatology, the researchers identified the top 100 videos on TikTok on May 1, 2020, that were tagged with “#acne.” The information on each video included date of upload, type and gender of the individual uploading the video, physician specialty if applicable, and video category. These top 100 videos had 13,470,501 likes and 64,775 comments over a 7.6-month time period.
The researchers used the DISCERN criteria, a validated 1-5 scale designed to assess consumer health information, to evaluate the video content, with 1 (having “serious” or “extensive shortcomings”) and 5 (having “minimal shortcomings.”)
Overall, the average quality rating of the TikTok acne videos was 2.03. A total of 9 videos were produced by board-certified physicians in the United States, with an average DISCERN score of 2.41.
“Analysis of the DISCERN criteria dimensions suggested that major shortcomings common to both physician and nonphysician uploaders included failure to cite information sources, discuss treatment risks, and provide support for shared decision-making,” the researchers said.
Approximately one-third (34%) of the videos fell into the treatment-product advertisement category, while 26% were personal anecdotes, 20% presented information related to acne, 13% featured home remedy treatments, and 7% were classified as “other.” The researchers also identified the top 200 “#acne” videos on TikTok once a week from May 8, 2020 to June 5, 2020, to determine the evolution of acne content on the app and found a turnover rate of 10.9% per week.
Based on the high turnover and low quality based on DISCERN ratings, the authors suggested that patients seeking acne information should “view acne-related TikTok videos with caution and consult evidence-based resources whenever possible.”
The study findings were limited by several factors including the small sample size of physicians uploading videos, lack of information about the number of nonphysician medical professionals who uploaded videos, and lack of information about the number of video views and country of origin, the researchers noted. However, the results highlight the need for dermatologists to be aware that patients, especially teens, may be using TikTok for acne information that may be of poor quality, they said.
“Conversely, we understand that social media can be a powerful tool for advancing health literacy,” the researchers noted. “Therefore, we also recommend that health care professionals engaging on TikTok create thorough and perhaps standardized educational videos regarding acne, as well as correct any acne-related misinformation that may be present,” they concluded.
The other authors of the study were from the departments of dermatology at Case Western Reserve, University Hospitals Cleveland, and Johns Hopkins University, Baltimore.
The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Zheng DX et al. Pediatr Dermatol. 2020 Nov 28. doi: 10.1111/pde.14471.
, according to an analysis of the top 100 videos using a consumer health validation tool.
The popularity of TikTok among adolescents in particular has implications for the dissemination of acne information, as some teens become “skinfluencers” and receive sponsorship from skin care brands in exchange for social media promotion, wrote David X. Zheng, BA, of the department of dermatology, Case Western Reserve University, Cleveland, and colleagues.
“However, the quality of dermatologic information found on TikTok is largely unknown,” they said.
In a brief report published in Pediatric Dermatology, the researchers identified the top 100 videos on TikTok on May 1, 2020, that were tagged with “#acne.” The information on each video included date of upload, type and gender of the individual uploading the video, physician specialty if applicable, and video category. These top 100 videos had 13,470,501 likes and 64,775 comments over a 7.6-month time period.
The researchers used the DISCERN criteria, a validated 1-5 scale designed to assess consumer health information, to evaluate the video content, with 1 (having “serious” or “extensive shortcomings”) and 5 (having “minimal shortcomings.”)
Overall, the average quality rating of the TikTok acne videos was 2.03. A total of 9 videos were produced by board-certified physicians in the United States, with an average DISCERN score of 2.41.
“Analysis of the DISCERN criteria dimensions suggested that major shortcomings common to both physician and nonphysician uploaders included failure to cite information sources, discuss treatment risks, and provide support for shared decision-making,” the researchers said.
Approximately one-third (34%) of the videos fell into the treatment-product advertisement category, while 26% were personal anecdotes, 20% presented information related to acne, 13% featured home remedy treatments, and 7% were classified as “other.” The researchers also identified the top 200 “#acne” videos on TikTok once a week from May 8, 2020 to June 5, 2020, to determine the evolution of acne content on the app and found a turnover rate of 10.9% per week.
Based on the high turnover and low quality based on DISCERN ratings, the authors suggested that patients seeking acne information should “view acne-related TikTok videos with caution and consult evidence-based resources whenever possible.”
The study findings were limited by several factors including the small sample size of physicians uploading videos, lack of information about the number of nonphysician medical professionals who uploaded videos, and lack of information about the number of video views and country of origin, the researchers noted. However, the results highlight the need for dermatologists to be aware that patients, especially teens, may be using TikTok for acne information that may be of poor quality, they said.
“Conversely, we understand that social media can be a powerful tool for advancing health literacy,” the researchers noted. “Therefore, we also recommend that health care professionals engaging on TikTok create thorough and perhaps standardized educational videos regarding acne, as well as correct any acne-related misinformation that may be present,” they concluded.
The other authors of the study were from the departments of dermatology at Case Western Reserve, University Hospitals Cleveland, and Johns Hopkins University, Baltimore.
The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Zheng DX et al. Pediatr Dermatol. 2020 Nov 28. doi: 10.1111/pde.14471.
FROM PEDIATRIC DERMATOLOGY
Weight loss may be paramount lifestyle change in preventing gout
A recent analysis of the incidence of gout in men, published in JAMA Network Open, offers new insights on the role of lifestyle changes in preventing gout, particularly the importance of obesity and its modification.
Prior gout research, although it addressed lifestyle issues, had not quantified the impact of obesity on incident gout cases, noted first author Natalie McCormick, PhD, and colleagues at Harvard Medical School and Massachusetts General Hospital in Boston. “To date the proportion of actual gout itself that could potentially be prevented by modifying such risk factors remains unknown.” To address that lack of data, they set out to estimate the proportion of avoidable incident gout in a large database in the Health Professionals Follow-up Study, initially of some 51,529 male health professionals who have completed a biannual personal health questionnaire since 1986. The follow-up rate for completing these questionnaires exceeds 90%.
For their analysis, the researchers tracked 44,654 of these men, with an average age of 54 at the 1986 baseline and no history of gout, through the year 2012. They looked at four lifestyle risk factors attributed to gout: body mass index; alcohol intake; adherence to a Dietary Approach to Stop Hypertension (DASH)-style diet, which recommends less red meat and sweetened beverages and more fruits, vegetables, and low-fat dairy products; and the absence of diuretic drugs, which are used to treat blood pressure or heart failure, in order to observe and compare their effects on new reports of gout. Over the subsequent 26 years, nearly 4% of the men developed gout, the most common inflammatory arthritis. Obese men had 2.65 times greater risk for developing gout than did those with a normal body mass index.
If one addressed all four risk factors – modifying obesity, having no alcohol intake, not taking diuretic drugs, and following a DASH-style, lower-fat diet – 77% of new gout cases would disappear, the study’s corresponding author, Hyon K. Choi, MD, DrPH, of the division of rheumatology, allergy, and immunology at Massachusetts General Hospital, said in an interview. “But we learned that if you don’t include modifying obesity as a targetable risk factor, none of the other factors alone reaches significance. We can’t make firm conclusions about cause and effect, but modifying obesity seems to be a prerequisite to preventing gout through lifestyle. It’s a very interesting finding that needs to be confirmed in further research,” he said.
Of course, identifying the importance of lifestyle risk factors is not the same as actually achieving modifications of those factors. Changing lifestyle is difficult, Dr. Choi acknowledged. “But there’s not much potential for achieving the goal if the clinician doesn’t understand the target. Now we know obesity has a lot to do with gout. We can see it as a public health issue, especially since gout increases risks for comorbidities and mortality. All of these risk factors deserve intervention by the physician.”
A worldwide gout epidemic
Currently, there is a kind of worldwide gout epidemic linked to obesity, Dr. Choi said. The disease burden of gout is increasing worldwide. “This may be more of an issue for family practice or primary care physicians, who see 80%-90% of gout cases, rather than for rheumatologists, who are more likely to see advanced cases in need of drug therapy. But we would say: Don’t lose sight of the lifestyle risk factors, which are interrelated. This is not only the responsibility of one doctor or the other.”
The new findings should give practicing rheumatologists more confidence in addressing lifestyle issues, particularly weight loss, with their patients, said Angelo Gaffo, MD, section chief of rheumatology at the Birmingham VA Medical Center and associate professor of medicine in the division of rheumatology at the University of Alabama at Birmingham.
“Our patients with gout are interested in what they can do in their lives that might help with their gout. In the past, we’ve had generic advice about changing their diet. But in general, the evidence for the impact of dietary changes has not been strong.”
Doctors can now recommend a DASH-style diet, allowing room for moderate consumption of red meat, so long as patients are working on their weight loss – and showing results. “Now we have the information to give advice that’s more evidence-based,” Dr. Gaffo said. “You can ask the question whether this study is applicable to patients who already have gout. It doesn’t directly address them. But it mainly builds on the narrative that weight loss is important.”
Other studies have also looked at how weight loss led to serum urate reduction. This study adds to a growing body of literature emphasizing that the most important lifestyle factor relative to gout risk is weight gain, and the simplest, most effective intervention is counseling patients about weight loss, he said.
This research was supported by grants from the National Institutes of Health. Dr. Choi reported receiving research support from Ironwood and Horizon and consulting fees from Ironwood, Selecta, Horizon, Takeda, Kowa, and Vaxart. No other relevant financial disclosures were reported.
SOURCE: McCormick N et al. JAMA Netw Open. 2020;3(11):e2027421. doi: 10.1001/jamanetworkopen.2020.27421.
A recent analysis of the incidence of gout in men, published in JAMA Network Open, offers new insights on the role of lifestyle changes in preventing gout, particularly the importance of obesity and its modification.
Prior gout research, although it addressed lifestyle issues, had not quantified the impact of obesity on incident gout cases, noted first author Natalie McCormick, PhD, and colleagues at Harvard Medical School and Massachusetts General Hospital in Boston. “To date the proportion of actual gout itself that could potentially be prevented by modifying such risk factors remains unknown.” To address that lack of data, they set out to estimate the proportion of avoidable incident gout in a large database in the Health Professionals Follow-up Study, initially of some 51,529 male health professionals who have completed a biannual personal health questionnaire since 1986. The follow-up rate for completing these questionnaires exceeds 90%.
For their analysis, the researchers tracked 44,654 of these men, with an average age of 54 at the 1986 baseline and no history of gout, through the year 2012. They looked at four lifestyle risk factors attributed to gout: body mass index; alcohol intake; adherence to a Dietary Approach to Stop Hypertension (DASH)-style diet, which recommends less red meat and sweetened beverages and more fruits, vegetables, and low-fat dairy products; and the absence of diuretic drugs, which are used to treat blood pressure or heart failure, in order to observe and compare their effects on new reports of gout. Over the subsequent 26 years, nearly 4% of the men developed gout, the most common inflammatory arthritis. Obese men had 2.65 times greater risk for developing gout than did those with a normal body mass index.
If one addressed all four risk factors – modifying obesity, having no alcohol intake, not taking diuretic drugs, and following a DASH-style, lower-fat diet – 77% of new gout cases would disappear, the study’s corresponding author, Hyon K. Choi, MD, DrPH, of the division of rheumatology, allergy, and immunology at Massachusetts General Hospital, said in an interview. “But we learned that if you don’t include modifying obesity as a targetable risk factor, none of the other factors alone reaches significance. We can’t make firm conclusions about cause and effect, but modifying obesity seems to be a prerequisite to preventing gout through lifestyle. It’s a very interesting finding that needs to be confirmed in further research,” he said.
Of course, identifying the importance of lifestyle risk factors is not the same as actually achieving modifications of those factors. Changing lifestyle is difficult, Dr. Choi acknowledged. “But there’s not much potential for achieving the goal if the clinician doesn’t understand the target. Now we know obesity has a lot to do with gout. We can see it as a public health issue, especially since gout increases risks for comorbidities and mortality. All of these risk factors deserve intervention by the physician.”
A worldwide gout epidemic
Currently, there is a kind of worldwide gout epidemic linked to obesity, Dr. Choi said. The disease burden of gout is increasing worldwide. “This may be more of an issue for family practice or primary care physicians, who see 80%-90% of gout cases, rather than for rheumatologists, who are more likely to see advanced cases in need of drug therapy. But we would say: Don’t lose sight of the lifestyle risk factors, which are interrelated. This is not only the responsibility of one doctor or the other.”
The new findings should give practicing rheumatologists more confidence in addressing lifestyle issues, particularly weight loss, with their patients, said Angelo Gaffo, MD, section chief of rheumatology at the Birmingham VA Medical Center and associate professor of medicine in the division of rheumatology at the University of Alabama at Birmingham.
“Our patients with gout are interested in what they can do in their lives that might help with their gout. In the past, we’ve had generic advice about changing their diet. But in general, the evidence for the impact of dietary changes has not been strong.”
Doctors can now recommend a DASH-style diet, allowing room for moderate consumption of red meat, so long as patients are working on their weight loss – and showing results. “Now we have the information to give advice that’s more evidence-based,” Dr. Gaffo said. “You can ask the question whether this study is applicable to patients who already have gout. It doesn’t directly address them. But it mainly builds on the narrative that weight loss is important.”
Other studies have also looked at how weight loss led to serum urate reduction. This study adds to a growing body of literature emphasizing that the most important lifestyle factor relative to gout risk is weight gain, and the simplest, most effective intervention is counseling patients about weight loss, he said.
This research was supported by grants from the National Institutes of Health. Dr. Choi reported receiving research support from Ironwood and Horizon and consulting fees from Ironwood, Selecta, Horizon, Takeda, Kowa, and Vaxart. No other relevant financial disclosures were reported.
SOURCE: McCormick N et al. JAMA Netw Open. 2020;3(11):e2027421. doi: 10.1001/jamanetworkopen.2020.27421.
A recent analysis of the incidence of gout in men, published in JAMA Network Open, offers new insights on the role of lifestyle changes in preventing gout, particularly the importance of obesity and its modification.
Prior gout research, although it addressed lifestyle issues, had not quantified the impact of obesity on incident gout cases, noted first author Natalie McCormick, PhD, and colleagues at Harvard Medical School and Massachusetts General Hospital in Boston. “To date the proportion of actual gout itself that could potentially be prevented by modifying such risk factors remains unknown.” To address that lack of data, they set out to estimate the proportion of avoidable incident gout in a large database in the Health Professionals Follow-up Study, initially of some 51,529 male health professionals who have completed a biannual personal health questionnaire since 1986. The follow-up rate for completing these questionnaires exceeds 90%.
For their analysis, the researchers tracked 44,654 of these men, with an average age of 54 at the 1986 baseline and no history of gout, through the year 2012. They looked at four lifestyle risk factors attributed to gout: body mass index; alcohol intake; adherence to a Dietary Approach to Stop Hypertension (DASH)-style diet, which recommends less red meat and sweetened beverages and more fruits, vegetables, and low-fat dairy products; and the absence of diuretic drugs, which are used to treat blood pressure or heart failure, in order to observe and compare their effects on new reports of gout. Over the subsequent 26 years, nearly 4% of the men developed gout, the most common inflammatory arthritis. Obese men had 2.65 times greater risk for developing gout than did those with a normal body mass index.
If one addressed all four risk factors – modifying obesity, having no alcohol intake, not taking diuretic drugs, and following a DASH-style, lower-fat diet – 77% of new gout cases would disappear, the study’s corresponding author, Hyon K. Choi, MD, DrPH, of the division of rheumatology, allergy, and immunology at Massachusetts General Hospital, said in an interview. “But we learned that if you don’t include modifying obesity as a targetable risk factor, none of the other factors alone reaches significance. We can’t make firm conclusions about cause and effect, but modifying obesity seems to be a prerequisite to preventing gout through lifestyle. It’s a very interesting finding that needs to be confirmed in further research,” he said.
Of course, identifying the importance of lifestyle risk factors is not the same as actually achieving modifications of those factors. Changing lifestyle is difficult, Dr. Choi acknowledged. “But there’s not much potential for achieving the goal if the clinician doesn’t understand the target. Now we know obesity has a lot to do with gout. We can see it as a public health issue, especially since gout increases risks for comorbidities and mortality. All of these risk factors deserve intervention by the physician.”
A worldwide gout epidemic
Currently, there is a kind of worldwide gout epidemic linked to obesity, Dr. Choi said. The disease burden of gout is increasing worldwide. “This may be more of an issue for family practice or primary care physicians, who see 80%-90% of gout cases, rather than for rheumatologists, who are more likely to see advanced cases in need of drug therapy. But we would say: Don’t lose sight of the lifestyle risk factors, which are interrelated. This is not only the responsibility of one doctor or the other.”
The new findings should give practicing rheumatologists more confidence in addressing lifestyle issues, particularly weight loss, with their patients, said Angelo Gaffo, MD, section chief of rheumatology at the Birmingham VA Medical Center and associate professor of medicine in the division of rheumatology at the University of Alabama at Birmingham.
“Our patients with gout are interested in what they can do in their lives that might help with their gout. In the past, we’ve had generic advice about changing their diet. But in general, the evidence for the impact of dietary changes has not been strong.”
Doctors can now recommend a DASH-style diet, allowing room for moderate consumption of red meat, so long as patients are working on their weight loss – and showing results. “Now we have the information to give advice that’s more evidence-based,” Dr. Gaffo said. “You can ask the question whether this study is applicable to patients who already have gout. It doesn’t directly address them. But it mainly builds on the narrative that weight loss is important.”
Other studies have also looked at how weight loss led to serum urate reduction. This study adds to a growing body of literature emphasizing that the most important lifestyle factor relative to gout risk is weight gain, and the simplest, most effective intervention is counseling patients about weight loss, he said.
This research was supported by grants from the National Institutes of Health. Dr. Choi reported receiving research support from Ironwood and Horizon and consulting fees from Ironwood, Selecta, Horizon, Takeda, Kowa, and Vaxart. No other relevant financial disclosures were reported.
SOURCE: McCormick N et al. JAMA Netw Open. 2020;3(11):e2027421. doi: 10.1001/jamanetworkopen.2020.27421.
FROM JAMA NETWORK OPEN
COVID-19 variant sparks U.K. travel restrictions
Researchers have detected a highly contagious coronavirus variant in the United Kingdom, leading Prime Minister Boris Johnson to shut down parts of the country and triggering other nations to impose travel and shipping restrictions on England.
Mr. Johnson held a crisis meeting with ministers Monday after Saturday’s shutdown announcement. The prime minister said in a nationally televised address that this coronavirus variant may be “up to 70% more transmissible than the old variant” and was probably responsible for an increase in cases in southeastern England.
“There is still much we don’t know. While we are fairly certain the variant is transmitted more quickly, there is no evidence to suggest that it is more lethal or causes more severe illness. Equally there is no evidence to suggest the vaccine will be any less effective against the new variant,” he said.
Public Health England says it is working to learn as much about the variant as possible. “We know that mortality is a lagging indicator, and we will need to continually monitor this over the coming weeks,” the agency says.
That scientific uncertainty about the variant’s threat shook European nations that were rushing to ship goods to England in advance of a Dec. 31 Brexit deadline. Under Brexit, which is short for “British exit,” the United Kingdom will leave the European Union on Jan. 31, 2020. Until then, the two sides will come up with new trade and security relationships.
European Union members Austria, Belgium, Bulgaria, France, Germany, Ireland, Italy, and the Netherlands announced travel restrictions hours after Johnson’s speech.
Those restrictions created food uncertainty across the U.K., which imports about a quarter of its food from the EU, according to The New York Times. Long lines of trucks heading to ports in the U.K. came to a standstill on major roads such as the M20 near Kent and the Port of Dover.
Outside Europe, Canada, India, Iran, Israel, Hong Kong, Saudi Arabia, and Turkey banned all incoming flights from the U.K. And more bans could come.
The U.S. reaction
The United States has not imposed any new limits on travel with the United Kingdom, although New York Gov. Andrew Cuomo (D) has requested all passengers bound for John F. Kennedy International Airport from the U.K. be tested before boarding and a new travel ban be placed for Europe. He says the federal government must take action now to avoid a crisis situation like the one New York experienced in March and April.
“The United States has a number of flights coming in from the U.K. each day, and we have done absolutely nothing,” Mr. Cuomo said in a statement on the governor’s webpage. “To me, this is reprehensible because this is what happened in the spring. How many times in life do you have to make the same mistake before you learn?”
Leading U.S. health officials have downplayed the dangers of the virus.
“We don’t know that it’s more dangerous, and very importantly, we have not seen a single mutation yet that would make it evade the vaccine,” U.S. Assistant Secretary of Health and Human Services Adm. Brett Giroir, MD, said Sunday on ABC’s This Week with George Stephanopoulos. “I can’t say that won’t happen in the future, but right now it looks like the vaccine will cover everything that we see.”
Dr. Giroir said the HHS and other U.S. government agencies will monitor the variant.
“Viruses mutate,” he said. “We’ve seen almost 4,000 different mutations among this virus. There is no indication that the mutation right now that they’re talking about is overcoming England.”
Where did the variant come from?
Public Health England says the coronavirus variant had existed in the U.K. since September and circulated at very low levels until mid-November.
“The increase in cases linked to the new variant first came to light in late November when PHE was investigating why infection rates in Kent were not falling despite national restrictions. We then discovered a cluster linked to this variant spreading rapidly into London and Essex,” the agency said.
Public Health England says there’s no evidence the new variant is resistant to the Pfizer-BioNTech vaccine, which is now being given across the country to high-priority groups such as health care workers.
An article in The BMJ, a British medical journal, says the variant was first detected by Covid-19 Genomics UK, a consortium that tests the random genetic sequencing of positive COVID-19 samples around the U.K. The variant cases were mostly in the southeast of England.
A University of Birmingham professor said in a Dec. 15 briefing that the variant accounts for 20% of viruses sequenced in Norfolk, 10% in Essex, and 3% in Suffolk. “There are no data to suggest it had been imported from abroad, so it is likely to have evolved in the U.K.,” he said.
The variant is named VUI-202012/01, for the first “variant under investigation” in December 2020, BMJ says. It’s defined by a set of 17 mutations, with the most significant mutation in the spike protein the virus uses to bind to the human ACE2 receptor.
“Changes in this part of spike protein may, in theory, result in the virus becoming more infectious and spreading more easily between people,” the article says.
The European Centre for Disease Prevention and Control says the variant emerged during the time of year when people usually socialize more.
“There is no indication at this point of increased infection severity associated with the new variant,” the agency said. “A few cases with the new variant have to date been reported by Denmark and the Netherlands and, according to media reports, in Belgium.”
Mr. Johnson announced tighter restrictions on England’s hardest-hit areas, such as the southeast and east of England, where new coronavirus cases have continued to rise. And he said people must cut back on their Christmas socializing.
“In England, those living in tier 4 areas should not mix with anyone outside their own household at Christmas, though support bubbles will remain in place for those at particular risk of loneliness or isolation,” he said.
A version of this article first appeared on WebMD.com.
Researchers have detected a highly contagious coronavirus variant in the United Kingdom, leading Prime Minister Boris Johnson to shut down parts of the country and triggering other nations to impose travel and shipping restrictions on England.
Mr. Johnson held a crisis meeting with ministers Monday after Saturday’s shutdown announcement. The prime minister said in a nationally televised address that this coronavirus variant may be “up to 70% more transmissible than the old variant” and was probably responsible for an increase in cases in southeastern England.
“There is still much we don’t know. While we are fairly certain the variant is transmitted more quickly, there is no evidence to suggest that it is more lethal or causes more severe illness. Equally there is no evidence to suggest the vaccine will be any less effective against the new variant,” he said.
Public Health England says it is working to learn as much about the variant as possible. “We know that mortality is a lagging indicator, and we will need to continually monitor this over the coming weeks,” the agency says.
That scientific uncertainty about the variant’s threat shook European nations that were rushing to ship goods to England in advance of a Dec. 31 Brexit deadline. Under Brexit, which is short for “British exit,” the United Kingdom will leave the European Union on Jan. 31, 2020. Until then, the two sides will come up with new trade and security relationships.
European Union members Austria, Belgium, Bulgaria, France, Germany, Ireland, Italy, and the Netherlands announced travel restrictions hours after Johnson’s speech.
Those restrictions created food uncertainty across the U.K., which imports about a quarter of its food from the EU, according to The New York Times. Long lines of trucks heading to ports in the U.K. came to a standstill on major roads such as the M20 near Kent and the Port of Dover.
Outside Europe, Canada, India, Iran, Israel, Hong Kong, Saudi Arabia, and Turkey banned all incoming flights from the U.K. And more bans could come.
The U.S. reaction
The United States has not imposed any new limits on travel with the United Kingdom, although New York Gov. Andrew Cuomo (D) has requested all passengers bound for John F. Kennedy International Airport from the U.K. be tested before boarding and a new travel ban be placed for Europe. He says the federal government must take action now to avoid a crisis situation like the one New York experienced in March and April.
“The United States has a number of flights coming in from the U.K. each day, and we have done absolutely nothing,” Mr. Cuomo said in a statement on the governor’s webpage. “To me, this is reprehensible because this is what happened in the spring. How many times in life do you have to make the same mistake before you learn?”
Leading U.S. health officials have downplayed the dangers of the virus.
“We don’t know that it’s more dangerous, and very importantly, we have not seen a single mutation yet that would make it evade the vaccine,” U.S. Assistant Secretary of Health and Human Services Adm. Brett Giroir, MD, said Sunday on ABC’s This Week with George Stephanopoulos. “I can’t say that won’t happen in the future, but right now it looks like the vaccine will cover everything that we see.”
Dr. Giroir said the HHS and other U.S. government agencies will monitor the variant.
“Viruses mutate,” he said. “We’ve seen almost 4,000 different mutations among this virus. There is no indication that the mutation right now that they’re talking about is overcoming England.”
Where did the variant come from?
Public Health England says the coronavirus variant had existed in the U.K. since September and circulated at very low levels until mid-November.
“The increase in cases linked to the new variant first came to light in late November when PHE was investigating why infection rates in Kent were not falling despite national restrictions. We then discovered a cluster linked to this variant spreading rapidly into London and Essex,” the agency said.
Public Health England says there’s no evidence the new variant is resistant to the Pfizer-BioNTech vaccine, which is now being given across the country to high-priority groups such as health care workers.
An article in The BMJ, a British medical journal, says the variant was first detected by Covid-19 Genomics UK, a consortium that tests the random genetic sequencing of positive COVID-19 samples around the U.K. The variant cases were mostly in the southeast of England.
A University of Birmingham professor said in a Dec. 15 briefing that the variant accounts for 20% of viruses sequenced in Norfolk, 10% in Essex, and 3% in Suffolk. “There are no data to suggest it had been imported from abroad, so it is likely to have evolved in the U.K.,” he said.
The variant is named VUI-202012/01, for the first “variant under investigation” in December 2020, BMJ says. It’s defined by a set of 17 mutations, with the most significant mutation in the spike protein the virus uses to bind to the human ACE2 receptor.
“Changes in this part of spike protein may, in theory, result in the virus becoming more infectious and spreading more easily between people,” the article says.
The European Centre for Disease Prevention and Control says the variant emerged during the time of year when people usually socialize more.
“There is no indication at this point of increased infection severity associated with the new variant,” the agency said. “A few cases with the new variant have to date been reported by Denmark and the Netherlands and, according to media reports, in Belgium.”
Mr. Johnson announced tighter restrictions on England’s hardest-hit areas, such as the southeast and east of England, where new coronavirus cases have continued to rise. And he said people must cut back on their Christmas socializing.
“In England, those living in tier 4 areas should not mix with anyone outside their own household at Christmas, though support bubbles will remain in place for those at particular risk of loneliness or isolation,” he said.
A version of this article first appeared on WebMD.com.
Researchers have detected a highly contagious coronavirus variant in the United Kingdom, leading Prime Minister Boris Johnson to shut down parts of the country and triggering other nations to impose travel and shipping restrictions on England.
Mr. Johnson held a crisis meeting with ministers Monday after Saturday’s shutdown announcement. The prime minister said in a nationally televised address that this coronavirus variant may be “up to 70% more transmissible than the old variant” and was probably responsible for an increase in cases in southeastern England.
“There is still much we don’t know. While we are fairly certain the variant is transmitted more quickly, there is no evidence to suggest that it is more lethal or causes more severe illness. Equally there is no evidence to suggest the vaccine will be any less effective against the new variant,” he said.
Public Health England says it is working to learn as much about the variant as possible. “We know that mortality is a lagging indicator, and we will need to continually monitor this over the coming weeks,” the agency says.
That scientific uncertainty about the variant’s threat shook European nations that were rushing to ship goods to England in advance of a Dec. 31 Brexit deadline. Under Brexit, which is short for “British exit,” the United Kingdom will leave the European Union on Jan. 31, 2020. Until then, the two sides will come up with new trade and security relationships.
European Union members Austria, Belgium, Bulgaria, France, Germany, Ireland, Italy, and the Netherlands announced travel restrictions hours after Johnson’s speech.
Those restrictions created food uncertainty across the U.K., which imports about a quarter of its food from the EU, according to The New York Times. Long lines of trucks heading to ports in the U.K. came to a standstill on major roads such as the M20 near Kent and the Port of Dover.
Outside Europe, Canada, India, Iran, Israel, Hong Kong, Saudi Arabia, and Turkey banned all incoming flights from the U.K. And more bans could come.
The U.S. reaction
The United States has not imposed any new limits on travel with the United Kingdom, although New York Gov. Andrew Cuomo (D) has requested all passengers bound for John F. Kennedy International Airport from the U.K. be tested before boarding and a new travel ban be placed for Europe. He says the federal government must take action now to avoid a crisis situation like the one New York experienced in March and April.
“The United States has a number of flights coming in from the U.K. each day, and we have done absolutely nothing,” Mr. Cuomo said in a statement on the governor’s webpage. “To me, this is reprehensible because this is what happened in the spring. How many times in life do you have to make the same mistake before you learn?”
Leading U.S. health officials have downplayed the dangers of the virus.
“We don’t know that it’s more dangerous, and very importantly, we have not seen a single mutation yet that would make it evade the vaccine,” U.S. Assistant Secretary of Health and Human Services Adm. Brett Giroir, MD, said Sunday on ABC’s This Week with George Stephanopoulos. “I can’t say that won’t happen in the future, but right now it looks like the vaccine will cover everything that we see.”
Dr. Giroir said the HHS and other U.S. government agencies will monitor the variant.
“Viruses mutate,” he said. “We’ve seen almost 4,000 different mutations among this virus. There is no indication that the mutation right now that they’re talking about is overcoming England.”
Where did the variant come from?
Public Health England says the coronavirus variant had existed in the U.K. since September and circulated at very low levels until mid-November.
“The increase in cases linked to the new variant first came to light in late November when PHE was investigating why infection rates in Kent were not falling despite national restrictions. We then discovered a cluster linked to this variant spreading rapidly into London and Essex,” the agency said.
Public Health England says there’s no evidence the new variant is resistant to the Pfizer-BioNTech vaccine, which is now being given across the country to high-priority groups such as health care workers.
An article in The BMJ, a British medical journal, says the variant was first detected by Covid-19 Genomics UK, a consortium that tests the random genetic sequencing of positive COVID-19 samples around the U.K. The variant cases were mostly in the southeast of England.
A University of Birmingham professor said in a Dec. 15 briefing that the variant accounts for 20% of viruses sequenced in Norfolk, 10% in Essex, and 3% in Suffolk. “There are no data to suggest it had been imported from abroad, so it is likely to have evolved in the U.K.,” he said.
The variant is named VUI-202012/01, for the first “variant under investigation” in December 2020, BMJ says. It’s defined by a set of 17 mutations, with the most significant mutation in the spike protein the virus uses to bind to the human ACE2 receptor.
“Changes in this part of spike protein may, in theory, result in the virus becoming more infectious and spreading more easily between people,” the article says.
The European Centre for Disease Prevention and Control says the variant emerged during the time of year when people usually socialize more.
“There is no indication at this point of increased infection severity associated with the new variant,” the agency said. “A few cases with the new variant have to date been reported by Denmark and the Netherlands and, according to media reports, in Belgium.”
Mr. Johnson announced tighter restrictions on England’s hardest-hit areas, such as the southeast and east of England, where new coronavirus cases have continued to rise. And he said people must cut back on their Christmas socializing.
“In England, those living in tier 4 areas should not mix with anyone outside their own household at Christmas, though support bubbles will remain in place for those at particular risk of loneliness or isolation,” he said.
A version of this article first appeared on WebMD.com.
Food allergy testing for eczema in kids varies by specialty
Specialists vary on their opinion about the ordering of food allergy tests for children with eczema, a recent survey reveals.
A child with eczema is more likely to be given food allergy tests if seen by an allergist or a pediatrician and less likely to be given these tests if seen by a general practitioner or dermatologist.
“In our survey, we found evidence of variation in practice and a spectrum of opinion on what to do to treat eczema in children,” Matthew Ridd, MD, University of Bristol (England) said in an interview.
His clinician survey was sent to 155 health care providers. Findings were presented at the Food Allergy and Anaphylaxis Meeting–European Consortium on Application of Flow Cytometry in Allergy Congress, held virtually. They revealed big differences in the way physicians follow up on eczema. For a child with eczema with reported reactions to food, 20 of 22 (91%) allergists and 22 of 30 (73%) pediatricians always order food allergy tests.
But only 16 of 65 (25%) general practitioners and 3 of 12 (25%) dermatologists always order tests in the same situation.
A total of 155 health care practitioners responded to the survey, sent by a U.K. research team. Of those, 26 were unable to order allergy tests. Of the remaining 129, 65 (50%) specialized in general practice, 30 (23%) in pediatrics, 22 (17%) in the treatment of allergies, and 12 (9%) in dermatology.
Their opinions varied on when to order food allergy tests. For children with severe eczema who had no prior reaction to food, 8 of 22 (36%) practitioners specializing in allergy said they would order food allergy tests, as did 9 of 30 (30%) in pediatrics.
Of those surveyed, only 6 of 65 in general practice (9%) said they would request an allergy test for severe eczema for a patient with no allergy history, and no dermatologists (0%) would order the tests.
Only if a parent specifically requested a food allergy test would practitioners respond in a similar way. About two-thirds of all respondents said they would sometimes order the test if a parent asked (general practice, 75%; pediatrics, 63%; allergy, 68%; dermatology, 75%).
Dr. Ridd said in an interview that it’s not surprising there’s a wide variation in practice, inasmuch as the guidelines are quite convoluted and complex. “Eczema is a common problem, but we don’t have any good evidence to guide clinicians on when to consider food allergy as a possible cause.”
Current guidelines advise calling for allergy tests only when eczema is difficult to treat. “But this is a complex decision. We know that a third of children with eczema are at higher risk for food allergy,” Dr. Ridd said. A 2014 study published in Clinical and Experimental Allergy showed that infants with eczema are six times more likely to have egg allergy and 11 times more likely to have peanut allergy by 12 months than infants without eczema (Clin Exp Allergy. 2014;45:255-64).
Food allergy is a sticky subject, he said. “So we have to wonder, are general practitioners frightened to raise the question?
“We definitely see uncertainty around it.”
He suspects that parents may also be hesitant to bring it up. “They are likely thinking about it even if they don’t ask,” Dr. Ridd said. “I think it’s important to test for food allergy, to provide reassurance. Once we show it’s not an allergy, we can focus on topical treatment.”
Treating eczema with emollients may increase likelihood of food allergy
In a separate presentation at the FAAM-EUROBAT congress, Maeve Kelleher, MD, Imperial College London, said that, rather than help reduce eczema, emollients in infants probably cause an increase in the risk for skin infection and food allergy. Her research team performed a systematic review of 25,827 participants in randomized controlled trials of the use of skin care interventions in term infants for primary prevention of eczema and food allergy. The study focused especially on topical creams.
Dr. Kelleher reported that skin care interventions “probably don’t prevent eczema. They probably increase local skin infections and may increase food allergy.”
Other interventions need to be explored, she said. “Maybe prevention should be along the line of looking at the microbiome, or exposures on the skin when you’re younger.”
Dr. Ridd and Dr. Kelleher have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Specialists vary on their opinion about the ordering of food allergy tests for children with eczema, a recent survey reveals.
A child with eczema is more likely to be given food allergy tests if seen by an allergist or a pediatrician and less likely to be given these tests if seen by a general practitioner or dermatologist.
“In our survey, we found evidence of variation in practice and a spectrum of opinion on what to do to treat eczema in children,” Matthew Ridd, MD, University of Bristol (England) said in an interview.
His clinician survey was sent to 155 health care providers. Findings were presented at the Food Allergy and Anaphylaxis Meeting–European Consortium on Application of Flow Cytometry in Allergy Congress, held virtually. They revealed big differences in the way physicians follow up on eczema. For a child with eczema with reported reactions to food, 20 of 22 (91%) allergists and 22 of 30 (73%) pediatricians always order food allergy tests.
But only 16 of 65 (25%) general practitioners and 3 of 12 (25%) dermatologists always order tests in the same situation.
A total of 155 health care practitioners responded to the survey, sent by a U.K. research team. Of those, 26 were unable to order allergy tests. Of the remaining 129, 65 (50%) specialized in general practice, 30 (23%) in pediatrics, 22 (17%) in the treatment of allergies, and 12 (9%) in dermatology.
Their opinions varied on when to order food allergy tests. For children with severe eczema who had no prior reaction to food, 8 of 22 (36%) practitioners specializing in allergy said they would order food allergy tests, as did 9 of 30 (30%) in pediatrics.
Of those surveyed, only 6 of 65 in general practice (9%) said they would request an allergy test for severe eczema for a patient with no allergy history, and no dermatologists (0%) would order the tests.
Only if a parent specifically requested a food allergy test would practitioners respond in a similar way. About two-thirds of all respondents said they would sometimes order the test if a parent asked (general practice, 75%; pediatrics, 63%; allergy, 68%; dermatology, 75%).
Dr. Ridd said in an interview that it’s not surprising there’s a wide variation in practice, inasmuch as the guidelines are quite convoluted and complex. “Eczema is a common problem, but we don’t have any good evidence to guide clinicians on when to consider food allergy as a possible cause.”
Current guidelines advise calling for allergy tests only when eczema is difficult to treat. “But this is a complex decision. We know that a third of children with eczema are at higher risk for food allergy,” Dr. Ridd said. A 2014 study published in Clinical and Experimental Allergy showed that infants with eczema are six times more likely to have egg allergy and 11 times more likely to have peanut allergy by 12 months than infants without eczema (Clin Exp Allergy. 2014;45:255-64).
Food allergy is a sticky subject, he said. “So we have to wonder, are general practitioners frightened to raise the question?
“We definitely see uncertainty around it.”
He suspects that parents may also be hesitant to bring it up. “They are likely thinking about it even if they don’t ask,” Dr. Ridd said. “I think it’s important to test for food allergy, to provide reassurance. Once we show it’s not an allergy, we can focus on topical treatment.”
Treating eczema with emollients may increase likelihood of food allergy
In a separate presentation at the FAAM-EUROBAT congress, Maeve Kelleher, MD, Imperial College London, said that, rather than help reduce eczema, emollients in infants probably cause an increase in the risk for skin infection and food allergy. Her research team performed a systematic review of 25,827 participants in randomized controlled trials of the use of skin care interventions in term infants for primary prevention of eczema and food allergy. The study focused especially on topical creams.
Dr. Kelleher reported that skin care interventions “probably don’t prevent eczema. They probably increase local skin infections and may increase food allergy.”
Other interventions need to be explored, she said. “Maybe prevention should be along the line of looking at the microbiome, or exposures on the skin when you’re younger.”
Dr. Ridd and Dr. Kelleher have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Specialists vary on their opinion about the ordering of food allergy tests for children with eczema, a recent survey reveals.
A child with eczema is more likely to be given food allergy tests if seen by an allergist or a pediatrician and less likely to be given these tests if seen by a general practitioner or dermatologist.
“In our survey, we found evidence of variation in practice and a spectrum of opinion on what to do to treat eczema in children,” Matthew Ridd, MD, University of Bristol (England) said in an interview.
His clinician survey was sent to 155 health care providers. Findings were presented at the Food Allergy and Anaphylaxis Meeting–European Consortium on Application of Flow Cytometry in Allergy Congress, held virtually. They revealed big differences in the way physicians follow up on eczema. For a child with eczema with reported reactions to food, 20 of 22 (91%) allergists and 22 of 30 (73%) pediatricians always order food allergy tests.
But only 16 of 65 (25%) general practitioners and 3 of 12 (25%) dermatologists always order tests in the same situation.
A total of 155 health care practitioners responded to the survey, sent by a U.K. research team. Of those, 26 were unable to order allergy tests. Of the remaining 129, 65 (50%) specialized in general practice, 30 (23%) in pediatrics, 22 (17%) in the treatment of allergies, and 12 (9%) in dermatology.
Their opinions varied on when to order food allergy tests. For children with severe eczema who had no prior reaction to food, 8 of 22 (36%) practitioners specializing in allergy said they would order food allergy tests, as did 9 of 30 (30%) in pediatrics.
Of those surveyed, only 6 of 65 in general practice (9%) said they would request an allergy test for severe eczema for a patient with no allergy history, and no dermatologists (0%) would order the tests.
Only if a parent specifically requested a food allergy test would practitioners respond in a similar way. About two-thirds of all respondents said they would sometimes order the test if a parent asked (general practice, 75%; pediatrics, 63%; allergy, 68%; dermatology, 75%).
Dr. Ridd said in an interview that it’s not surprising there’s a wide variation in practice, inasmuch as the guidelines are quite convoluted and complex. “Eczema is a common problem, but we don’t have any good evidence to guide clinicians on when to consider food allergy as a possible cause.”
Current guidelines advise calling for allergy tests only when eczema is difficult to treat. “But this is a complex decision. We know that a third of children with eczema are at higher risk for food allergy,” Dr. Ridd said. A 2014 study published in Clinical and Experimental Allergy showed that infants with eczema are six times more likely to have egg allergy and 11 times more likely to have peanut allergy by 12 months than infants without eczema (Clin Exp Allergy. 2014;45:255-64).
Food allergy is a sticky subject, he said. “So we have to wonder, are general practitioners frightened to raise the question?
“We definitely see uncertainty around it.”
He suspects that parents may also be hesitant to bring it up. “They are likely thinking about it even if they don’t ask,” Dr. Ridd said. “I think it’s important to test for food allergy, to provide reassurance. Once we show it’s not an allergy, we can focus on topical treatment.”
Treating eczema with emollients may increase likelihood of food allergy
In a separate presentation at the FAAM-EUROBAT congress, Maeve Kelleher, MD, Imperial College London, said that, rather than help reduce eczema, emollients in infants probably cause an increase in the risk for skin infection and food allergy. Her research team performed a systematic review of 25,827 participants in randomized controlled trials of the use of skin care interventions in term infants for primary prevention of eczema and food allergy. The study focused especially on topical creams.
Dr. Kelleher reported that skin care interventions “probably don’t prevent eczema. They probably increase local skin infections and may increase food allergy.”
Other interventions need to be explored, she said. “Maybe prevention should be along the line of looking at the microbiome, or exposures on the skin when you’re younger.”
Dr. Ridd and Dr. Kelleher have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Gut microbiome influences response to methotrexate in new-onset RA patients
The pretreatment gut microbiome can determine response to methotrexate therapy in patients with newly diagnosed rheumatoid arthritis, according to recent research published in Arthritis & Rheumatology.
About half of patients do not respond to methotrexate (MTX), despite it being a first-line therapy for RA, according to Alejandro Artacho of the Centro Superior de Investigación en Salud Pública in Valencia, Spain, and colleagues. In addition, there is currently no way to predict which patients will respond to MTX.
The role of the microbiome in drug response for patients with RA “has been known since it was discovered in 1972 that sulfasalazine requires gut bacteria for its activity,” Veena Taneja, PhD, a researcher and associate professor of immunology at the Mayo Clinic in Rochester, Minn., said in an interview. The microbiome and how it functions “needs to be explored as biomarkers as well as for treatment options for RA and other diseases,” added Dr. Taneja, who was not involved with the study.
Using 16S rRNA gene and shotgun metagenomic sequencing, the researchers evaluated whether the gut microbiome of a patient newly diagnosed with RA (NORA) influenced their response to MTX. The researchers extracted DNA from fecal samples in 26 patients from New York University Langone Medical Center, Lutheran Hospital, Staten Island, and Mount Sinai School of Medicine rheumatology clinics 48 hours prior to treatment with MTX and determined the bacterial taxa, operational taxonomic units (OTUs), and ribosomal sequence variants in each sample. These patients then received oral MTX with an average dose of 20 mg per week (range, 15-25 mg). The patients were grouped based on whether they responded (39%) or did not respond (61%) to MTX based on improvement of at least 1.8 in their Disease Activity Score in 28 joints (DAS28) after 4 months and no need to add a biologic.
Patients with a statistically significantly lower level of microbial diversity (P < .05) as measured by OTU level tended to respond better to MTX therapy. In patients who did not respond to MTX, there was a significantly higher abundance of Firmicutes, a significantly lower abundance of Bacteroidetes (P < .05), and a higher ratio of Firmicutes to Bacteroidetes.
There was also a consistent difference between abundance of gut microbial genes in patients who did not respond to MTX. “Taken together, these results indicate that the gut microbiome of NORA patients that respond favorably to MTX is distinct from that of MTX-NR, prompting us to hypothesize that the pretreatment microbiome could be used to predict clinical nonresponse,” the researchers said.
Using machine learning, Mr. Artacho and colleagues developed a predictive model based on the initial training cohort of 26 patients to assess MTX response. When the researchers tested the model in a validation cohort of 21 patients, they found it correctly predicted 78% of MTX responders and 83.3% of patients who did not respond to MTX, with the percentage of correct predictions increasing “when considering only those patients with the highest probability score of belonging to either group.”
In a separate set of 20 patients with RA who were prescribed either different conventional synthetic disease-modifying antirheumatic drugs or biologics or had not started any medications, the researchers’ model could not predict clinical response, “suggesting that the potential clinical utility of the model is restricted to RA patients that are both drug naive and exposed directly to MTX, but not to other drugs.”
“Our results open the possibility to rationally design microbiome-modulating strategies to improve oral absorption of MTX and its downstream immune effects, inform clinical decision-making or both,” they said.
Clinical application
Dr. Taneja said the findings of the study are novel and intriguing. “The observations suggest a strong influence of [the] host’s microbiome in response to MTX and in future may inform best treatment options for patients. The study speculates that certain microbial clades or microbes can be used to derive a favorable response in patients. This could explain why “one drug fits all” does not apply in treatment for RA,” she said.
The study is also a “step forward” in using the microbiome in regular clinical practice, she noted. “Since MTX is used as a first line of treatment and is one of the most affordable treatments for RA, the observations are definitely exciting.”
In an interview, Martin Kriegel, MD, PhD, of the department of immunobiology at Yale University, New Haven, Conn., and chair of rheumatology and clinical immunology at the University of Münster (Germany), explained that the prediction model has the potential to one day be a tool for clinicians to predict MTX response in patients with RA. However, he noted the researchers did not test a functional link between MTX and gut microbes in vivo.
“It would be useful to test mechanistic effects of MTX on gut microbial communities in vitro and in vivo,” he said. “In addition, it would be informative to apply the prediction model in other cohorts of RA with a different geographic background, possibly also a different duration of disease. If confirmed in a more heterogeneous group of patients, the tool could potentially be used in the clinic to tell some patients that they might not respond to MTX and therefore start therapy with another agent.”
This study was funded by the National Institutes of Health, the Rheumatology Research Foundation, the Searle Scholars Program, various funds from the Spanish government, the UCSF Breakthrough Program for Rheumatoid Arthritis-related Research, and the Arthritis Foundation Center for Excellence. Four authors report consultancies and memberships on scientific advisory boards with pharmaceutical and biotechnology companies that do not overlap with the current study.
Dr. Taneja reported that her institution holds a patent for developing Prevotella histicola as an anti-inflammatory treatment, of which she is a coinventor. Evelo Biosciences is a licensee for the patent, and Dr. Taneja reported receiving research support from the company. Dr. Kriegel reported receiving salary, consulting fees, honoraria, or research funds from AbbVie, Bristol-Myers Squibb, Cell Applications, Eligo Bioscience, and Roche. He also holds a patent on the use of antibiotics and commensal vaccination to treat autoimmunity.
SOURCE: Artacho A et al. Arthritis Rheumatol. 2020 Dec 13. doi: 10.1002/art.41622.
The pretreatment gut microbiome can determine response to methotrexate therapy in patients with newly diagnosed rheumatoid arthritis, according to recent research published in Arthritis & Rheumatology.
About half of patients do not respond to methotrexate (MTX), despite it being a first-line therapy for RA, according to Alejandro Artacho of the Centro Superior de Investigación en Salud Pública in Valencia, Spain, and colleagues. In addition, there is currently no way to predict which patients will respond to MTX.
The role of the microbiome in drug response for patients with RA “has been known since it was discovered in 1972 that sulfasalazine requires gut bacteria for its activity,” Veena Taneja, PhD, a researcher and associate professor of immunology at the Mayo Clinic in Rochester, Minn., said in an interview. The microbiome and how it functions “needs to be explored as biomarkers as well as for treatment options for RA and other diseases,” added Dr. Taneja, who was not involved with the study.
Using 16S rRNA gene and shotgun metagenomic sequencing, the researchers evaluated whether the gut microbiome of a patient newly diagnosed with RA (NORA) influenced their response to MTX. The researchers extracted DNA from fecal samples in 26 patients from New York University Langone Medical Center, Lutheran Hospital, Staten Island, and Mount Sinai School of Medicine rheumatology clinics 48 hours prior to treatment with MTX and determined the bacterial taxa, operational taxonomic units (OTUs), and ribosomal sequence variants in each sample. These patients then received oral MTX with an average dose of 20 mg per week (range, 15-25 mg). The patients were grouped based on whether they responded (39%) or did not respond (61%) to MTX based on improvement of at least 1.8 in their Disease Activity Score in 28 joints (DAS28) after 4 months and no need to add a biologic.
Patients with a statistically significantly lower level of microbial diversity (P < .05) as measured by OTU level tended to respond better to MTX therapy. In patients who did not respond to MTX, there was a significantly higher abundance of Firmicutes, a significantly lower abundance of Bacteroidetes (P < .05), and a higher ratio of Firmicutes to Bacteroidetes.
There was also a consistent difference between abundance of gut microbial genes in patients who did not respond to MTX. “Taken together, these results indicate that the gut microbiome of NORA patients that respond favorably to MTX is distinct from that of MTX-NR, prompting us to hypothesize that the pretreatment microbiome could be used to predict clinical nonresponse,” the researchers said.
Using machine learning, Mr. Artacho and colleagues developed a predictive model based on the initial training cohort of 26 patients to assess MTX response. When the researchers tested the model in a validation cohort of 21 patients, they found it correctly predicted 78% of MTX responders and 83.3% of patients who did not respond to MTX, with the percentage of correct predictions increasing “when considering only those patients with the highest probability score of belonging to either group.”
In a separate set of 20 patients with RA who were prescribed either different conventional synthetic disease-modifying antirheumatic drugs or biologics or had not started any medications, the researchers’ model could not predict clinical response, “suggesting that the potential clinical utility of the model is restricted to RA patients that are both drug naive and exposed directly to MTX, but not to other drugs.”
“Our results open the possibility to rationally design microbiome-modulating strategies to improve oral absorption of MTX and its downstream immune effects, inform clinical decision-making or both,” they said.
Clinical application
Dr. Taneja said the findings of the study are novel and intriguing. “The observations suggest a strong influence of [the] host’s microbiome in response to MTX and in future may inform best treatment options for patients. The study speculates that certain microbial clades or microbes can be used to derive a favorable response in patients. This could explain why “one drug fits all” does not apply in treatment for RA,” she said.
The study is also a “step forward” in using the microbiome in regular clinical practice, she noted. “Since MTX is used as a first line of treatment and is one of the most affordable treatments for RA, the observations are definitely exciting.”
In an interview, Martin Kriegel, MD, PhD, of the department of immunobiology at Yale University, New Haven, Conn., and chair of rheumatology and clinical immunology at the University of Münster (Germany), explained that the prediction model has the potential to one day be a tool for clinicians to predict MTX response in patients with RA. However, he noted the researchers did not test a functional link between MTX and gut microbes in vivo.
“It would be useful to test mechanistic effects of MTX on gut microbial communities in vitro and in vivo,” he said. “In addition, it would be informative to apply the prediction model in other cohorts of RA with a different geographic background, possibly also a different duration of disease. If confirmed in a more heterogeneous group of patients, the tool could potentially be used in the clinic to tell some patients that they might not respond to MTX and therefore start therapy with another agent.”
This study was funded by the National Institutes of Health, the Rheumatology Research Foundation, the Searle Scholars Program, various funds from the Spanish government, the UCSF Breakthrough Program for Rheumatoid Arthritis-related Research, and the Arthritis Foundation Center for Excellence. Four authors report consultancies and memberships on scientific advisory boards with pharmaceutical and biotechnology companies that do not overlap with the current study.
Dr. Taneja reported that her institution holds a patent for developing Prevotella histicola as an anti-inflammatory treatment, of which she is a coinventor. Evelo Biosciences is a licensee for the patent, and Dr. Taneja reported receiving research support from the company. Dr. Kriegel reported receiving salary, consulting fees, honoraria, or research funds from AbbVie, Bristol-Myers Squibb, Cell Applications, Eligo Bioscience, and Roche. He also holds a patent on the use of antibiotics and commensal vaccination to treat autoimmunity.
SOURCE: Artacho A et al. Arthritis Rheumatol. 2020 Dec 13. doi: 10.1002/art.41622.
The pretreatment gut microbiome can determine response to methotrexate therapy in patients with newly diagnosed rheumatoid arthritis, according to recent research published in Arthritis & Rheumatology.
About half of patients do not respond to methotrexate (MTX), despite it being a first-line therapy for RA, according to Alejandro Artacho of the Centro Superior de Investigación en Salud Pública in Valencia, Spain, and colleagues. In addition, there is currently no way to predict which patients will respond to MTX.
The role of the microbiome in drug response for patients with RA “has been known since it was discovered in 1972 that sulfasalazine requires gut bacteria for its activity,” Veena Taneja, PhD, a researcher and associate professor of immunology at the Mayo Clinic in Rochester, Minn., said in an interview. The microbiome and how it functions “needs to be explored as biomarkers as well as for treatment options for RA and other diseases,” added Dr. Taneja, who was not involved with the study.
Using 16S rRNA gene and shotgun metagenomic sequencing, the researchers evaluated whether the gut microbiome of a patient newly diagnosed with RA (NORA) influenced their response to MTX. The researchers extracted DNA from fecal samples in 26 patients from New York University Langone Medical Center, Lutheran Hospital, Staten Island, and Mount Sinai School of Medicine rheumatology clinics 48 hours prior to treatment with MTX and determined the bacterial taxa, operational taxonomic units (OTUs), and ribosomal sequence variants in each sample. These patients then received oral MTX with an average dose of 20 mg per week (range, 15-25 mg). The patients were grouped based on whether they responded (39%) or did not respond (61%) to MTX based on improvement of at least 1.8 in their Disease Activity Score in 28 joints (DAS28) after 4 months and no need to add a biologic.
Patients with a statistically significantly lower level of microbial diversity (P < .05) as measured by OTU level tended to respond better to MTX therapy. In patients who did not respond to MTX, there was a significantly higher abundance of Firmicutes, a significantly lower abundance of Bacteroidetes (P < .05), and a higher ratio of Firmicutes to Bacteroidetes.
There was also a consistent difference between abundance of gut microbial genes in patients who did not respond to MTX. “Taken together, these results indicate that the gut microbiome of NORA patients that respond favorably to MTX is distinct from that of MTX-NR, prompting us to hypothesize that the pretreatment microbiome could be used to predict clinical nonresponse,” the researchers said.
Using machine learning, Mr. Artacho and colleagues developed a predictive model based on the initial training cohort of 26 patients to assess MTX response. When the researchers tested the model in a validation cohort of 21 patients, they found it correctly predicted 78% of MTX responders and 83.3% of patients who did not respond to MTX, with the percentage of correct predictions increasing “when considering only those patients with the highest probability score of belonging to either group.”
In a separate set of 20 patients with RA who were prescribed either different conventional synthetic disease-modifying antirheumatic drugs or biologics or had not started any medications, the researchers’ model could not predict clinical response, “suggesting that the potential clinical utility of the model is restricted to RA patients that are both drug naive and exposed directly to MTX, but not to other drugs.”
“Our results open the possibility to rationally design microbiome-modulating strategies to improve oral absorption of MTX and its downstream immune effects, inform clinical decision-making or both,” they said.
Clinical application
Dr. Taneja said the findings of the study are novel and intriguing. “The observations suggest a strong influence of [the] host’s microbiome in response to MTX and in future may inform best treatment options for patients. The study speculates that certain microbial clades or microbes can be used to derive a favorable response in patients. This could explain why “one drug fits all” does not apply in treatment for RA,” she said.
The study is also a “step forward” in using the microbiome in regular clinical practice, she noted. “Since MTX is used as a first line of treatment and is one of the most affordable treatments for RA, the observations are definitely exciting.”
In an interview, Martin Kriegel, MD, PhD, of the department of immunobiology at Yale University, New Haven, Conn., and chair of rheumatology and clinical immunology at the University of Münster (Germany), explained that the prediction model has the potential to one day be a tool for clinicians to predict MTX response in patients with RA. However, he noted the researchers did not test a functional link between MTX and gut microbes in vivo.
“It would be useful to test mechanistic effects of MTX on gut microbial communities in vitro and in vivo,” he said. “In addition, it would be informative to apply the prediction model in other cohorts of RA with a different geographic background, possibly also a different duration of disease. If confirmed in a more heterogeneous group of patients, the tool could potentially be used in the clinic to tell some patients that they might not respond to MTX and therefore start therapy with another agent.”
This study was funded by the National Institutes of Health, the Rheumatology Research Foundation, the Searle Scholars Program, various funds from the Spanish government, the UCSF Breakthrough Program for Rheumatoid Arthritis-related Research, and the Arthritis Foundation Center for Excellence. Four authors report consultancies and memberships on scientific advisory boards with pharmaceutical and biotechnology companies that do not overlap with the current study.
Dr. Taneja reported that her institution holds a patent for developing Prevotella histicola as an anti-inflammatory treatment, of which she is a coinventor. Evelo Biosciences is a licensee for the patent, and Dr. Taneja reported receiving research support from the company. Dr. Kriegel reported receiving salary, consulting fees, honoraria, or research funds from AbbVie, Bristol-Myers Squibb, Cell Applications, Eligo Bioscience, and Roche. He also holds a patent on the use of antibiotics and commensal vaccination to treat autoimmunity.
SOURCE: Artacho A et al. Arthritis Rheumatol. 2020 Dec 13. doi: 10.1002/art.41622.
FROM ARTHRITIS & RHEUMATOLOGY
CDC identifies next priority groups for COVID-19 vaccine
The Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention voted 13-1 for the recommendation. This builds on ACIP’s initial recommendation about which groups should be in the first wave of vaccinations, described as Phase 1a.
ACIP earlier recommended that Phase 1a include U.S. health care workers, a group of about 21 million people, and residents of long-term care facilities, a group of about 3 million.
On Dec. 20, ACIP said the next priority group, Phase 1b, should consist of what it called frontline essential workers, a group of about 30 million, and adults aged 75 years and older, a group of about 21 million. When overlap between the groups is taken into account, Phase 1b covers about 49 million people, according to the CDC.
Phase 1c then would include adults aged 65-74 years (a group of about 32 million), adults aged 16-64 years with high-risk medical conditions (a group of about 110 million), and essential workers who did not qualify for inclusion in Phase 1b (a group of about 57 million). With the overlap, Phase 1c would cover about 129 million.
The Food and Drug Administration recently granted emergency use authorizations for two COVID-19 vaccines, one developed by Pfizer-BioNTech and another from Moderna. Other companies, including Johnson & Johnson, have advanced their potential rival COVID-19 vaccines into late-stages of testing. To date, about 2.83 million doses of Pfizer’s COVID-19 vaccine have been distributed and 556,208 doses have been administered, according to the CDC.
But there will likely still be a period of months when competition for limited doses of COVID-19 vaccine will trigger difficult decisions. Current estimates indicate there will be enough supply to provide COVID-19 vaccines for 20 million people in December, 30 million people in January, and 50 million people in February, said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases.
State governments and health systems will take ACIP’s recommendations into account as they roll out the initial supplies of COVID-19 vaccines.
There’s clearly wide latitude in these decisions. Recently, for example, many members of Congress tweeted photos of themselves getting COVID-19 vaccines, despite not falling into ACIP’s description of the Phase 1 group.
Difficult choices
All ACIP members described the Dec. 20 vote as a difficult decision. It forced them to choose among segments of the U.S. population that could benefit from early access to the limited supply of COVID-19 vaccines.
“For every group we add, it means we subtract a group. For every group we subtract, it means they don’t get the vaccine” for some months, said ACIP member Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn. “It’s incredibly humbling and heartbreaking.”
ACIP member Henry Bernstein, DO, who cast the lone dissenting vote, said he agreed with most of the panel’s recommendation. He said he fully supported the inclusion of adults aged 75 years and older and essential frontline workers in the second wave, Phase 1b. But he voted no because the data on COVID-19 morbidity and mortality for adults aged 65-74 years is similar enough to the older group to warrant their inclusion in the first wave.
“Therefore, inclusion of the 65- to 74-year-old group in Phase 1b made more sense to me,” said Dr. Bernstein, professor of pediatrics at the Zucker School of Medicine at Hofstra/Northwell in New York.
As defined by the CDC, frontline essential workers included in phase 1b will be those commonly called “first responders,” such as firefighters and police officers. Also in this group are teachers, support staff, daycare providers, and those employed in grocery and agriculture industries. Others in this group would include U.S. Postal Service employees and transit workers.
ACIP panelists noted the difficulties that will emerge as government officials and leaders of health care organizations move to apply their guidance to real-world decisions about distributing a limited supply of COVID-19 vaccine. There’s a potential to worsen existing disparities in access to health care, as people with more income may find it easier to obtain proof that they qualify as having a high-risk condition, said José Romero, MD, the chair of ACIP.
Many people “don’t have access to medical care and can’t come up with a doctor’s note that says, ‘I have diabetes,’ ” he said.
ACIP panelists also noted in their deliberations that people may technically qualify for a priority group but have little risk, such as someone with a chronic medical condition who works from home.
And the risk for COVID-19 remains serious even for those who will ultimately fall into the phase 2 for vaccination. Young adults have suffered serious complications following COVID-19, such as stroke, that may alter their lives dramatically, ACIP member Dr. Talbot said, adding that she is reminded of this in her work.
“We need to be very cautious about saying, ‘Young adults will be fine,’ ” she said. “I spent the past week on back-up clinical call and have read these charts and have cried every day.”
The three ACIP members who had conflicts that prevented their voting were Robert L. Atmar, MD, who said he had participated in COVID-19 trials, including research on the Moderna vaccine; Sharon E. Frey, MD, who said that she had been involved with research on COVID-19 vaccines, including Moderna’s; and Paul Hunter, MD, who said he has received a grant from Pfizer for pneumococcal vaccines. The other panel members have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention voted 13-1 for the recommendation. This builds on ACIP’s initial recommendation about which groups should be in the first wave of vaccinations, described as Phase 1a.
ACIP earlier recommended that Phase 1a include U.S. health care workers, a group of about 21 million people, and residents of long-term care facilities, a group of about 3 million.
On Dec. 20, ACIP said the next priority group, Phase 1b, should consist of what it called frontline essential workers, a group of about 30 million, and adults aged 75 years and older, a group of about 21 million. When overlap between the groups is taken into account, Phase 1b covers about 49 million people, according to the CDC.
Phase 1c then would include adults aged 65-74 years (a group of about 32 million), adults aged 16-64 years with high-risk medical conditions (a group of about 110 million), and essential workers who did not qualify for inclusion in Phase 1b (a group of about 57 million). With the overlap, Phase 1c would cover about 129 million.
The Food and Drug Administration recently granted emergency use authorizations for two COVID-19 vaccines, one developed by Pfizer-BioNTech and another from Moderna. Other companies, including Johnson & Johnson, have advanced their potential rival COVID-19 vaccines into late-stages of testing. To date, about 2.83 million doses of Pfizer’s COVID-19 vaccine have been distributed and 556,208 doses have been administered, according to the CDC.
But there will likely still be a period of months when competition for limited doses of COVID-19 vaccine will trigger difficult decisions. Current estimates indicate there will be enough supply to provide COVID-19 vaccines for 20 million people in December, 30 million people in January, and 50 million people in February, said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases.
State governments and health systems will take ACIP’s recommendations into account as they roll out the initial supplies of COVID-19 vaccines.
There’s clearly wide latitude in these decisions. Recently, for example, many members of Congress tweeted photos of themselves getting COVID-19 vaccines, despite not falling into ACIP’s description of the Phase 1 group.
Difficult choices
All ACIP members described the Dec. 20 vote as a difficult decision. It forced them to choose among segments of the U.S. population that could benefit from early access to the limited supply of COVID-19 vaccines.
“For every group we add, it means we subtract a group. For every group we subtract, it means they don’t get the vaccine” for some months, said ACIP member Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn. “It’s incredibly humbling and heartbreaking.”
ACIP member Henry Bernstein, DO, who cast the lone dissenting vote, said he agreed with most of the panel’s recommendation. He said he fully supported the inclusion of adults aged 75 years and older and essential frontline workers in the second wave, Phase 1b. But he voted no because the data on COVID-19 morbidity and mortality for adults aged 65-74 years is similar enough to the older group to warrant their inclusion in the first wave.
“Therefore, inclusion of the 65- to 74-year-old group in Phase 1b made more sense to me,” said Dr. Bernstein, professor of pediatrics at the Zucker School of Medicine at Hofstra/Northwell in New York.
As defined by the CDC, frontline essential workers included in phase 1b will be those commonly called “first responders,” such as firefighters and police officers. Also in this group are teachers, support staff, daycare providers, and those employed in grocery and agriculture industries. Others in this group would include U.S. Postal Service employees and transit workers.
ACIP panelists noted the difficulties that will emerge as government officials and leaders of health care organizations move to apply their guidance to real-world decisions about distributing a limited supply of COVID-19 vaccine. There’s a potential to worsen existing disparities in access to health care, as people with more income may find it easier to obtain proof that they qualify as having a high-risk condition, said José Romero, MD, the chair of ACIP.
Many people “don’t have access to medical care and can’t come up with a doctor’s note that says, ‘I have diabetes,’ ” he said.
ACIP panelists also noted in their deliberations that people may technically qualify for a priority group but have little risk, such as someone with a chronic medical condition who works from home.
And the risk for COVID-19 remains serious even for those who will ultimately fall into the phase 2 for vaccination. Young adults have suffered serious complications following COVID-19, such as stroke, that may alter their lives dramatically, ACIP member Dr. Talbot said, adding that she is reminded of this in her work.
“We need to be very cautious about saying, ‘Young adults will be fine,’ ” she said. “I spent the past week on back-up clinical call and have read these charts and have cried every day.”
The three ACIP members who had conflicts that prevented their voting were Robert L. Atmar, MD, who said he had participated in COVID-19 trials, including research on the Moderna vaccine; Sharon E. Frey, MD, who said that she had been involved with research on COVID-19 vaccines, including Moderna’s; and Paul Hunter, MD, who said he has received a grant from Pfizer for pneumococcal vaccines. The other panel members have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention voted 13-1 for the recommendation. This builds on ACIP’s initial recommendation about which groups should be in the first wave of vaccinations, described as Phase 1a.
ACIP earlier recommended that Phase 1a include U.S. health care workers, a group of about 21 million people, and residents of long-term care facilities, a group of about 3 million.
On Dec. 20, ACIP said the next priority group, Phase 1b, should consist of what it called frontline essential workers, a group of about 30 million, and adults aged 75 years and older, a group of about 21 million. When overlap between the groups is taken into account, Phase 1b covers about 49 million people, according to the CDC.
Phase 1c then would include adults aged 65-74 years (a group of about 32 million), adults aged 16-64 years with high-risk medical conditions (a group of about 110 million), and essential workers who did not qualify for inclusion in Phase 1b (a group of about 57 million). With the overlap, Phase 1c would cover about 129 million.
The Food and Drug Administration recently granted emergency use authorizations for two COVID-19 vaccines, one developed by Pfizer-BioNTech and another from Moderna. Other companies, including Johnson & Johnson, have advanced their potential rival COVID-19 vaccines into late-stages of testing. To date, about 2.83 million doses of Pfizer’s COVID-19 vaccine have been distributed and 556,208 doses have been administered, according to the CDC.
But there will likely still be a period of months when competition for limited doses of COVID-19 vaccine will trigger difficult decisions. Current estimates indicate there will be enough supply to provide COVID-19 vaccines for 20 million people in December, 30 million people in January, and 50 million people in February, said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases.
State governments and health systems will take ACIP’s recommendations into account as they roll out the initial supplies of COVID-19 vaccines.
There’s clearly wide latitude in these decisions. Recently, for example, many members of Congress tweeted photos of themselves getting COVID-19 vaccines, despite not falling into ACIP’s description of the Phase 1 group.
Difficult choices
All ACIP members described the Dec. 20 vote as a difficult decision. It forced them to choose among segments of the U.S. population that could benefit from early access to the limited supply of COVID-19 vaccines.
“For every group we add, it means we subtract a group. For every group we subtract, it means they don’t get the vaccine” for some months, said ACIP member Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn. “It’s incredibly humbling and heartbreaking.”
ACIP member Henry Bernstein, DO, who cast the lone dissenting vote, said he agreed with most of the panel’s recommendation. He said he fully supported the inclusion of adults aged 75 years and older and essential frontline workers in the second wave, Phase 1b. But he voted no because the data on COVID-19 morbidity and mortality for adults aged 65-74 years is similar enough to the older group to warrant their inclusion in the first wave.
“Therefore, inclusion of the 65- to 74-year-old group in Phase 1b made more sense to me,” said Dr. Bernstein, professor of pediatrics at the Zucker School of Medicine at Hofstra/Northwell in New York.
As defined by the CDC, frontline essential workers included in phase 1b will be those commonly called “first responders,” such as firefighters and police officers. Also in this group are teachers, support staff, daycare providers, and those employed in grocery and agriculture industries. Others in this group would include U.S. Postal Service employees and transit workers.
ACIP panelists noted the difficulties that will emerge as government officials and leaders of health care organizations move to apply their guidance to real-world decisions about distributing a limited supply of COVID-19 vaccine. There’s a potential to worsen existing disparities in access to health care, as people with more income may find it easier to obtain proof that they qualify as having a high-risk condition, said José Romero, MD, the chair of ACIP.
Many people “don’t have access to medical care and can’t come up with a doctor’s note that says, ‘I have diabetes,’ ” he said.
ACIP panelists also noted in their deliberations that people may technically qualify for a priority group but have little risk, such as someone with a chronic medical condition who works from home.
And the risk for COVID-19 remains serious even for those who will ultimately fall into the phase 2 for vaccination. Young adults have suffered serious complications following COVID-19, such as stroke, that may alter their lives dramatically, ACIP member Dr. Talbot said, adding that she is reminded of this in her work.
“We need to be very cautious about saying, ‘Young adults will be fine,’ ” she said. “I spent the past week on back-up clinical call and have read these charts and have cried every day.”
The three ACIP members who had conflicts that prevented their voting were Robert L. Atmar, MD, who said he had participated in COVID-19 trials, including research on the Moderna vaccine; Sharon E. Frey, MD, who said that she had been involved with research on COVID-19 vaccines, including Moderna’s; and Paul Hunter, MD, who said he has received a grant from Pfizer for pneumococcal vaccines. The other panel members have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.