User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


CMS loosens clinician scope-of-practice, telehealth rules for COVID-19 crisis
To boost the capacity of frontline clinicians and facilities to fight COVID-19, the Centers for Medicare & Medicaid Services (CMS) on Thursday announced it is temporarily suspending rules to allow physicians to provide telehealth services across state lines, and will permit midlevel practitioners to provide as much care as their state licenses allow.
Physicians can now care for patients at rural hospitals across state lines via phone, radio, or online communications without having to be physically present.
“Remotely located physicians, coordinating with nurse practitioners at rural hospitals, will provide staffs at such facilities additional flexibility to meet the needs of their patients,” a CMS news release said.
At skilled nursing facilities, nurse practitioners will now be able to perform some medical exams that doctors normally conduct on Medicare patients, whether they are COVID-19-related or not, CMS said.
Occupational therapists from home health agencies can now perform initial assessments on certain homebound patients, allowing home health services to start sooner and freeing home health nurses to do more direct patient care.
In addition, hospice nurses will be relieved of hospice aide in-service training tasks so they can spend more time with patients.
“It’s all hands on deck during this crisis,” said CMS Administrator Seema Verma in the press release. “All frontline medical professionals need to be able to work at the highest level they were trained for. CMS is making sure there are no regulatory obstacles to increasing the medical workforce to handle the patient surge during the COVID-19 pandemic.”
The announcement did not directly address the question of whether CMS’ new telemedicine and scope-of-practice policies override state laws. The agency said, “CMS sets and enforces essential quality and safety standards that supplement state scope-of-practice and licensure laws for healthcare workers. CMS has continuously examined its regulations to identify areas where federal requirements may be more stringent than state laws and requirements.”
On March 20, Vice President Pence announced that physicians would be allowed to practice across state lines during the COVID-19 crisis, as reported by Medscape Medical News. Until now, however, CMS had not changed its regulations to allow doctors to conduct telehealth consultations in states other than the ones in which they are licensed.
Other Changes
As part of other rule changes to support the healthcare workforce, CMS said on March 30 that it will pay for more than 80 additional services when furnished via telehealth.
These include emergency department visits, initial skilled nursing facility and discharge visits, and home visits. In addition, the agency said it would cover phone visits with Medicare beneficiaries.
Moreover, while virtual “check-in” visits had previously been limited to established patients, CMS said that doctors would be able to provide these services to both new and established patients.
Among its other regulatory changes in recent weeks, CMS has also temporarily:
- Permitted physicians whose privileges will expire to continue practicing at a hospital, and allowed new physicians to begin working prior to full hospital medical staff/governing body review and approval
- Lifted regulatory requirements regarding hospital personnel qualified to perform specific respiratory care procedures, allowing these professionals to operate to the fullest extent of their licensure
- Waived federal minimum personnel qualifications for clinical nurse specialists, nurse practitioners, and physician assistants so they can work at rural hospitals as long as they meet state licensure requirements
- Allowed physicians and nonphysician practitioners to use telehealth to care for patients at long-term care facilities, rather than having to treat patients at those facilities in person
This article first appeared on Medscape.com.
To boost the capacity of frontline clinicians and facilities to fight COVID-19, the Centers for Medicare & Medicaid Services (CMS) on Thursday announced it is temporarily suspending rules to allow physicians to provide telehealth services across state lines, and will permit midlevel practitioners to provide as much care as their state licenses allow.
Physicians can now care for patients at rural hospitals across state lines via phone, radio, or online communications without having to be physically present.
“Remotely located physicians, coordinating with nurse practitioners at rural hospitals, will provide staffs at such facilities additional flexibility to meet the needs of their patients,” a CMS news release said.
At skilled nursing facilities, nurse practitioners will now be able to perform some medical exams that doctors normally conduct on Medicare patients, whether they are COVID-19-related or not, CMS said.
Occupational therapists from home health agencies can now perform initial assessments on certain homebound patients, allowing home health services to start sooner and freeing home health nurses to do more direct patient care.
In addition, hospice nurses will be relieved of hospice aide in-service training tasks so they can spend more time with patients.
“It’s all hands on deck during this crisis,” said CMS Administrator Seema Verma in the press release. “All frontline medical professionals need to be able to work at the highest level they were trained for. CMS is making sure there are no regulatory obstacles to increasing the medical workforce to handle the patient surge during the COVID-19 pandemic.”
The announcement did not directly address the question of whether CMS’ new telemedicine and scope-of-practice policies override state laws. The agency said, “CMS sets and enforces essential quality and safety standards that supplement state scope-of-practice and licensure laws for healthcare workers. CMS has continuously examined its regulations to identify areas where federal requirements may be more stringent than state laws and requirements.”
On March 20, Vice President Pence announced that physicians would be allowed to practice across state lines during the COVID-19 crisis, as reported by Medscape Medical News. Until now, however, CMS had not changed its regulations to allow doctors to conduct telehealth consultations in states other than the ones in which they are licensed.
Other Changes
As part of other rule changes to support the healthcare workforce, CMS said on March 30 that it will pay for more than 80 additional services when furnished via telehealth.
These include emergency department visits, initial skilled nursing facility and discharge visits, and home visits. In addition, the agency said it would cover phone visits with Medicare beneficiaries.
Moreover, while virtual “check-in” visits had previously been limited to established patients, CMS said that doctors would be able to provide these services to both new and established patients.
Among its other regulatory changes in recent weeks, CMS has also temporarily:
- Permitted physicians whose privileges will expire to continue practicing at a hospital, and allowed new physicians to begin working prior to full hospital medical staff/governing body review and approval
- Lifted regulatory requirements regarding hospital personnel qualified to perform specific respiratory care procedures, allowing these professionals to operate to the fullest extent of their licensure
- Waived federal minimum personnel qualifications for clinical nurse specialists, nurse practitioners, and physician assistants so they can work at rural hospitals as long as they meet state licensure requirements
- Allowed physicians and nonphysician practitioners to use telehealth to care for patients at long-term care facilities, rather than having to treat patients at those facilities in person
This article first appeared on Medscape.com.
To boost the capacity of frontline clinicians and facilities to fight COVID-19, the Centers for Medicare & Medicaid Services (CMS) on Thursday announced it is temporarily suspending rules to allow physicians to provide telehealth services across state lines, and will permit midlevel practitioners to provide as much care as their state licenses allow.
Physicians can now care for patients at rural hospitals across state lines via phone, radio, or online communications without having to be physically present.
“Remotely located physicians, coordinating with nurse practitioners at rural hospitals, will provide staffs at such facilities additional flexibility to meet the needs of their patients,” a CMS news release said.
At skilled nursing facilities, nurse practitioners will now be able to perform some medical exams that doctors normally conduct on Medicare patients, whether they are COVID-19-related or not, CMS said.
Occupational therapists from home health agencies can now perform initial assessments on certain homebound patients, allowing home health services to start sooner and freeing home health nurses to do more direct patient care.
In addition, hospice nurses will be relieved of hospice aide in-service training tasks so they can spend more time with patients.
“It’s all hands on deck during this crisis,” said CMS Administrator Seema Verma in the press release. “All frontline medical professionals need to be able to work at the highest level they were trained for. CMS is making sure there are no regulatory obstacles to increasing the medical workforce to handle the patient surge during the COVID-19 pandemic.”
The announcement did not directly address the question of whether CMS’ new telemedicine and scope-of-practice policies override state laws. The agency said, “CMS sets and enforces essential quality and safety standards that supplement state scope-of-practice and licensure laws for healthcare workers. CMS has continuously examined its regulations to identify areas where federal requirements may be more stringent than state laws and requirements.”
On March 20, Vice President Pence announced that physicians would be allowed to practice across state lines during the COVID-19 crisis, as reported by Medscape Medical News. Until now, however, CMS had not changed its regulations to allow doctors to conduct telehealth consultations in states other than the ones in which they are licensed.
Other Changes
As part of other rule changes to support the healthcare workforce, CMS said on March 30 that it will pay for more than 80 additional services when furnished via telehealth.
These include emergency department visits, initial skilled nursing facility and discharge visits, and home visits. In addition, the agency said it would cover phone visits with Medicare beneficiaries.
Moreover, while virtual “check-in” visits had previously been limited to established patients, CMS said that doctors would be able to provide these services to both new and established patients.
Among its other regulatory changes in recent weeks, CMS has also temporarily:
- Permitted physicians whose privileges will expire to continue practicing at a hospital, and allowed new physicians to begin working prior to full hospital medical staff/governing body review and approval
- Lifted regulatory requirements regarding hospital personnel qualified to perform specific respiratory care procedures, allowing these professionals to operate to the fullest extent of their licensure
- Waived federal minimum personnel qualifications for clinical nurse specialists, nurse practitioners, and physician assistants so they can work at rural hospitals as long as they meet state licensure requirements
- Allowed physicians and nonphysician practitioners to use telehealth to care for patients at long-term care facilities, rather than having to treat patients at those facilities in person
This article first appeared on Medscape.com.
Remdesivir tops list of promising COVID-19 treatments in review of nearly 300 trials
, according to authors of a recent review covering nearly 300 active clinical treatment trials underway for the disease.
Remdesivir, which has potent in vitro activity against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is not approved by the Food and Drug Administration and is currently being tested in randomized trials, according to the review authors, led by James M. Sanders, PhD, of the department of pharmacy at University of Texas Southwestern Medical Center in Dallas.
By contrast, oseltamivir has not demonstrated efficacy against the virus, corticosteroids are not recommended, and promising data from a small French hydroxychloroquine study are balanced by “several major limitations” including small sample size and exclusion of early dropouts from the analysis, among others, Dr. Sanders and coauthors said in their report.
“These limitations coupled with concerns of additive cardiotoxicity with combination therapy [i.e., hydroxychloroquine with azithromycin] do not support adoption of this regimen without additional studies,” the researchers wrote. Their report is in JAMA.
Dr. Sanders and colleagues identified 291 COVID-19–specific studies listed in ClinicalTrials.gov through April 2, including 29 placebo-controlled trials.
This might represent just a sliver of the treatments that could combat COVID-19, according to the researchers, who said more than 3,000 small-molecule drug candidates with potential activity against human coronaviruses have been identified.
“This large amount of potential agents will hopefully yield more candidate therapeutics in the race to find effective treatments or preventive strategies against COVID-19,” said Dr. Sanders and coauthors.
Remdesivir for COVID-19
Remdesivir, an investigational nucleotide analog, is one promising agent because of its broad-spectrum and potent activity against SARS-CoV-2 and other novel coronaviruses, they said, adding that phase 1 trials demonstrated the drug was well tolerated without observed liver or kidney toxicity.
There have been “successful” case reports of remdesivir use in COVID-19, and at least five ongoing clinical trials are evaluating the drug’s safety and antiviral activity in this disease. Among those studies is a National Institutes of Health–sponsored adaptive, randomized, placebo-controlled trial that will provide data on the use of remdesivir versus supportive care.
“As the results from randomized controlled trials are anticipated, inclusion of this agent for treatment of COVID-19 may be considered,” Dr. Sanders and colleagues wrote in their report. To date, remdesivir remains investigational and needs to be obtained via compassionate use, through expanded access, or by participating in a clinical trial, they added.
Hydroxychloroquine and chloroquine
Among the published hydroxychloroquine studies is a “promising” 36-patient open-label nonrandomized French study, in which the antimalarial agent given every 8 hours improved virologic clearance by day 6 versus controls (70% vs. 12.5%, respectively), the review authors said. Moreover, viral clearance was 100% for 6 patients who received hydroxychloroquine plus azithromycin, compared to 57% (8 of 14) for patients treated with hydroxychloroquine alone. However, that study had several important limitations, including the small sample size, variable viral loads at baseline between groups, and a lack of safety and clinical outcomes reporting, according to the investigators. Moreover, six patients in the hydroxychloroquine group were taken out of the analysis because of early treatment stoppage due to medical intolerance or critical illness, the authors noted.
One prospective study including 30 patients in China demonstrated no difference in virologic outcomes for patients randomized to hydroxychloroquine plus standard of care versus standard of care alone, they added. There is also a case series of more than 100 patients with COVID-19 that reportedly improved viral clearance and reduced disease progression, though they said results haven’t been published or presented beyond a news briefing in China.
Randomized, controlled trials of chloroquine and hydroxychloroquine for COVID-19 treatment are underway, and studies are planned or enrolling to look at chloroquine prophylaxis in health care personnel and hydroxychloroquine for postexposure prophylaxis, authors said.
In results from one of those randomized trials, just reported, a higher dose of chloroquine was associated with a cardiac adverse event and an increased mortality risk, leading to the closure of that study arm. In the parallel, double-blinded, phase IIb clinical trial, patients in Brazil with SARS-CoV-2 infection received low or high doses of chloroquine plus ceftriaxone and azithromycin. According to the preprint publication, a higher rate of heart rate–corrected QT interval (QTc) prolongation and a “trend toward higher lethality” was observed in the high-dose group, leading investigators to “strongly recommend” the higher dose be abandoned.
“No apparent benefit of chloroquine was seen regarding lethality in our patients so far, but we will still enroll patients in the low chloroquine dose group to complete the originally planned sample size,” said investigators of the study, which at the time of the report had enrolled 81 out of an anticipated 440 patients.
Other COVID-19 pharmacologic therapies under study
Treatments of note in the review included the following:
- Tocilizumab. This monoclonal antibody IL-6 receptor antagonist, approved by the FDA for treatment of rheumatoid arthritis and for cytokine release syndrome related to chimeric antigen receptor (CAR) T-cell therapy, has yielded success in small series of patients with severe cases of COVID-19, according to authors. In one 21-patient report, 91% had clinical improvement, usually after a single dose. In China, tocilizumab is included in COVID-19 treatment guidelines, and several randomized clinical trials are underway in China including patients with COVID-19 with severe pneumonia.
- Immunoglobulin therapy. Antibodies from recovered COVID-19 patients could help with free virus and infected cell immune clearance, the authors said, adding that further studies are warranted beyond a few small published case series that suggest promise. Furthermore, on March 24 the FDA released guidance for screening donors for COVID-19 convalescent plasma and on emergency investigational new drug applications based on this modality.
- Lopinavir/ritonavir. Despite demonstrated in vitro activity against other novel coronaviruses, there is no published in vitro data for lopinavir/ritonavir in SARS-CoV-2, and likely a “limited role” for this combination anticipated in treating COVID-19, according to the review authors. In an open-label randomized clinical trial published in the New England Journal of Medicine (2020 Mar 18. doi: 10.1056/NEJMoa2001282), there were no differences in clinical improvement, viral clearance, or mortality for antiviral treatment versus standard care. Delayed treatment initiation may explain the ineffectiveness, though a subgroup analysis didn’t show a shorter time to clinical improvement for those who got the treatment earlier.
- Ribavirin. Likewise, this antiviral medication has efficacy and safety data suggesting “limited value” for treatment of COVID-19. Treatment of SARS yielded “inconclusive results” for ribavirin, which was also associated with substantial toxicity that included hemolytic anemia in 60% of SARS patients.
- Oseltamivir. While it may treat influenza, it has no documented activity against SARS-CoV-2 in vitro: “This agent has no role in the management of COVID-19 once influenza has been excluded,” said Dr. Sanders and coauthors.
- Corticosteroids. They could decrease inflammatory responses in the lung, but they could also lead to delays in viral clearance and increases in secondary infection risk. Guidelines for COVID-19 say to avoid corticosteroids, and the authors of the review concur, saying that potential harms and lack of proven benefit mean they usually should not be used outside of a randomized clinical trial setting.
- Vaccines. Clearly, vaccines represent the “most effective long-term strategy” to prevent future COVID-19 outbreaks, though at least 12-18 months would be required until vaccines can be widely deployed, authors said.
Dr. Sanders reported no potential conflicts. Senior author James B. Cutrell, MD, also of the University of Texas Southwestern Medical Center, reported nonfinancial support from Gilead and Regeneron outside of the study. No other authors reported disclosures.
, according to authors of a recent review covering nearly 300 active clinical treatment trials underway for the disease.
Remdesivir, which has potent in vitro activity against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is not approved by the Food and Drug Administration and is currently being tested in randomized trials, according to the review authors, led by James M. Sanders, PhD, of the department of pharmacy at University of Texas Southwestern Medical Center in Dallas.
By contrast, oseltamivir has not demonstrated efficacy against the virus, corticosteroids are not recommended, and promising data from a small French hydroxychloroquine study are balanced by “several major limitations” including small sample size and exclusion of early dropouts from the analysis, among others, Dr. Sanders and coauthors said in their report.
“These limitations coupled with concerns of additive cardiotoxicity with combination therapy [i.e., hydroxychloroquine with azithromycin] do not support adoption of this regimen without additional studies,” the researchers wrote. Their report is in JAMA.
Dr. Sanders and colleagues identified 291 COVID-19–specific studies listed in ClinicalTrials.gov through April 2, including 29 placebo-controlled trials.
This might represent just a sliver of the treatments that could combat COVID-19, according to the researchers, who said more than 3,000 small-molecule drug candidates with potential activity against human coronaviruses have been identified.
“This large amount of potential agents will hopefully yield more candidate therapeutics in the race to find effective treatments or preventive strategies against COVID-19,” said Dr. Sanders and coauthors.
Remdesivir for COVID-19
Remdesivir, an investigational nucleotide analog, is one promising agent because of its broad-spectrum and potent activity against SARS-CoV-2 and other novel coronaviruses, they said, adding that phase 1 trials demonstrated the drug was well tolerated without observed liver or kidney toxicity.
There have been “successful” case reports of remdesivir use in COVID-19, and at least five ongoing clinical trials are evaluating the drug’s safety and antiviral activity in this disease. Among those studies is a National Institutes of Health–sponsored adaptive, randomized, placebo-controlled trial that will provide data on the use of remdesivir versus supportive care.
“As the results from randomized controlled trials are anticipated, inclusion of this agent for treatment of COVID-19 may be considered,” Dr. Sanders and colleagues wrote in their report. To date, remdesivir remains investigational and needs to be obtained via compassionate use, through expanded access, or by participating in a clinical trial, they added.
Hydroxychloroquine and chloroquine
Among the published hydroxychloroquine studies is a “promising” 36-patient open-label nonrandomized French study, in which the antimalarial agent given every 8 hours improved virologic clearance by day 6 versus controls (70% vs. 12.5%, respectively), the review authors said. Moreover, viral clearance was 100% for 6 patients who received hydroxychloroquine plus azithromycin, compared to 57% (8 of 14) for patients treated with hydroxychloroquine alone. However, that study had several important limitations, including the small sample size, variable viral loads at baseline between groups, and a lack of safety and clinical outcomes reporting, according to the investigators. Moreover, six patients in the hydroxychloroquine group were taken out of the analysis because of early treatment stoppage due to medical intolerance or critical illness, the authors noted.
One prospective study including 30 patients in China demonstrated no difference in virologic outcomes for patients randomized to hydroxychloroquine plus standard of care versus standard of care alone, they added. There is also a case series of more than 100 patients with COVID-19 that reportedly improved viral clearance and reduced disease progression, though they said results haven’t been published or presented beyond a news briefing in China.
Randomized, controlled trials of chloroquine and hydroxychloroquine for COVID-19 treatment are underway, and studies are planned or enrolling to look at chloroquine prophylaxis in health care personnel and hydroxychloroquine for postexposure prophylaxis, authors said.
In results from one of those randomized trials, just reported, a higher dose of chloroquine was associated with a cardiac adverse event and an increased mortality risk, leading to the closure of that study arm. In the parallel, double-blinded, phase IIb clinical trial, patients in Brazil with SARS-CoV-2 infection received low or high doses of chloroquine plus ceftriaxone and azithromycin. According to the preprint publication, a higher rate of heart rate–corrected QT interval (QTc) prolongation and a “trend toward higher lethality” was observed in the high-dose group, leading investigators to “strongly recommend” the higher dose be abandoned.
“No apparent benefit of chloroquine was seen regarding lethality in our patients so far, but we will still enroll patients in the low chloroquine dose group to complete the originally planned sample size,” said investigators of the study, which at the time of the report had enrolled 81 out of an anticipated 440 patients.
Other COVID-19 pharmacologic therapies under study
Treatments of note in the review included the following:
- Tocilizumab. This monoclonal antibody IL-6 receptor antagonist, approved by the FDA for treatment of rheumatoid arthritis and for cytokine release syndrome related to chimeric antigen receptor (CAR) T-cell therapy, has yielded success in small series of patients with severe cases of COVID-19, according to authors. In one 21-patient report, 91% had clinical improvement, usually after a single dose. In China, tocilizumab is included in COVID-19 treatment guidelines, and several randomized clinical trials are underway in China including patients with COVID-19 with severe pneumonia.
- Immunoglobulin therapy. Antibodies from recovered COVID-19 patients could help with free virus and infected cell immune clearance, the authors said, adding that further studies are warranted beyond a few small published case series that suggest promise. Furthermore, on March 24 the FDA released guidance for screening donors for COVID-19 convalescent plasma and on emergency investigational new drug applications based on this modality.
- Lopinavir/ritonavir. Despite demonstrated in vitro activity against other novel coronaviruses, there is no published in vitro data for lopinavir/ritonavir in SARS-CoV-2, and likely a “limited role” for this combination anticipated in treating COVID-19, according to the review authors. In an open-label randomized clinical trial published in the New England Journal of Medicine (2020 Mar 18. doi: 10.1056/NEJMoa2001282), there were no differences in clinical improvement, viral clearance, or mortality for antiviral treatment versus standard care. Delayed treatment initiation may explain the ineffectiveness, though a subgroup analysis didn’t show a shorter time to clinical improvement for those who got the treatment earlier.
- Ribavirin. Likewise, this antiviral medication has efficacy and safety data suggesting “limited value” for treatment of COVID-19. Treatment of SARS yielded “inconclusive results” for ribavirin, which was also associated with substantial toxicity that included hemolytic anemia in 60% of SARS patients.
- Oseltamivir. While it may treat influenza, it has no documented activity against SARS-CoV-2 in vitro: “This agent has no role in the management of COVID-19 once influenza has been excluded,” said Dr. Sanders and coauthors.
- Corticosteroids. They could decrease inflammatory responses in the lung, but they could also lead to delays in viral clearance and increases in secondary infection risk. Guidelines for COVID-19 say to avoid corticosteroids, and the authors of the review concur, saying that potential harms and lack of proven benefit mean they usually should not be used outside of a randomized clinical trial setting.
- Vaccines. Clearly, vaccines represent the “most effective long-term strategy” to prevent future COVID-19 outbreaks, though at least 12-18 months would be required until vaccines can be widely deployed, authors said.
Dr. Sanders reported no potential conflicts. Senior author James B. Cutrell, MD, also of the University of Texas Southwestern Medical Center, reported nonfinancial support from Gilead and Regeneron outside of the study. No other authors reported disclosures.
, according to authors of a recent review covering nearly 300 active clinical treatment trials underway for the disease.
Remdesivir, which has potent in vitro activity against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is not approved by the Food and Drug Administration and is currently being tested in randomized trials, according to the review authors, led by James M. Sanders, PhD, of the department of pharmacy at University of Texas Southwestern Medical Center in Dallas.
By contrast, oseltamivir has not demonstrated efficacy against the virus, corticosteroids are not recommended, and promising data from a small French hydroxychloroquine study are balanced by “several major limitations” including small sample size and exclusion of early dropouts from the analysis, among others, Dr. Sanders and coauthors said in their report.
“These limitations coupled with concerns of additive cardiotoxicity with combination therapy [i.e., hydroxychloroquine with azithromycin] do not support adoption of this regimen without additional studies,” the researchers wrote. Their report is in JAMA.
Dr. Sanders and colleagues identified 291 COVID-19–specific studies listed in ClinicalTrials.gov through April 2, including 29 placebo-controlled trials.
This might represent just a sliver of the treatments that could combat COVID-19, according to the researchers, who said more than 3,000 small-molecule drug candidates with potential activity against human coronaviruses have been identified.
“This large amount of potential agents will hopefully yield more candidate therapeutics in the race to find effective treatments or preventive strategies against COVID-19,” said Dr. Sanders and coauthors.
Remdesivir for COVID-19
Remdesivir, an investigational nucleotide analog, is one promising agent because of its broad-spectrum and potent activity against SARS-CoV-2 and other novel coronaviruses, they said, adding that phase 1 trials demonstrated the drug was well tolerated without observed liver or kidney toxicity.
There have been “successful” case reports of remdesivir use in COVID-19, and at least five ongoing clinical trials are evaluating the drug’s safety and antiviral activity in this disease. Among those studies is a National Institutes of Health–sponsored adaptive, randomized, placebo-controlled trial that will provide data on the use of remdesivir versus supportive care.
“As the results from randomized controlled trials are anticipated, inclusion of this agent for treatment of COVID-19 may be considered,” Dr. Sanders and colleagues wrote in their report. To date, remdesivir remains investigational and needs to be obtained via compassionate use, through expanded access, or by participating in a clinical trial, they added.
Hydroxychloroquine and chloroquine
Among the published hydroxychloroquine studies is a “promising” 36-patient open-label nonrandomized French study, in which the antimalarial agent given every 8 hours improved virologic clearance by day 6 versus controls (70% vs. 12.5%, respectively), the review authors said. Moreover, viral clearance was 100% for 6 patients who received hydroxychloroquine plus azithromycin, compared to 57% (8 of 14) for patients treated with hydroxychloroquine alone. However, that study had several important limitations, including the small sample size, variable viral loads at baseline between groups, and a lack of safety and clinical outcomes reporting, according to the investigators. Moreover, six patients in the hydroxychloroquine group were taken out of the analysis because of early treatment stoppage due to medical intolerance or critical illness, the authors noted.
One prospective study including 30 patients in China demonstrated no difference in virologic outcomes for patients randomized to hydroxychloroquine plus standard of care versus standard of care alone, they added. There is also a case series of more than 100 patients with COVID-19 that reportedly improved viral clearance and reduced disease progression, though they said results haven’t been published or presented beyond a news briefing in China.
Randomized, controlled trials of chloroquine and hydroxychloroquine for COVID-19 treatment are underway, and studies are planned or enrolling to look at chloroquine prophylaxis in health care personnel and hydroxychloroquine for postexposure prophylaxis, authors said.
In results from one of those randomized trials, just reported, a higher dose of chloroquine was associated with a cardiac adverse event and an increased mortality risk, leading to the closure of that study arm. In the parallel, double-blinded, phase IIb clinical trial, patients in Brazil with SARS-CoV-2 infection received low or high doses of chloroquine plus ceftriaxone and azithromycin. According to the preprint publication, a higher rate of heart rate–corrected QT interval (QTc) prolongation and a “trend toward higher lethality” was observed in the high-dose group, leading investigators to “strongly recommend” the higher dose be abandoned.
“No apparent benefit of chloroquine was seen regarding lethality in our patients so far, but we will still enroll patients in the low chloroquine dose group to complete the originally planned sample size,” said investigators of the study, which at the time of the report had enrolled 81 out of an anticipated 440 patients.
Other COVID-19 pharmacologic therapies under study
Treatments of note in the review included the following:
- Tocilizumab. This monoclonal antibody IL-6 receptor antagonist, approved by the FDA for treatment of rheumatoid arthritis and for cytokine release syndrome related to chimeric antigen receptor (CAR) T-cell therapy, has yielded success in small series of patients with severe cases of COVID-19, according to authors. In one 21-patient report, 91% had clinical improvement, usually after a single dose. In China, tocilizumab is included in COVID-19 treatment guidelines, and several randomized clinical trials are underway in China including patients with COVID-19 with severe pneumonia.
- Immunoglobulin therapy. Antibodies from recovered COVID-19 patients could help with free virus and infected cell immune clearance, the authors said, adding that further studies are warranted beyond a few small published case series that suggest promise. Furthermore, on March 24 the FDA released guidance for screening donors for COVID-19 convalescent plasma and on emergency investigational new drug applications based on this modality.
- Lopinavir/ritonavir. Despite demonstrated in vitro activity against other novel coronaviruses, there is no published in vitro data for lopinavir/ritonavir in SARS-CoV-2, and likely a “limited role” for this combination anticipated in treating COVID-19, according to the review authors. In an open-label randomized clinical trial published in the New England Journal of Medicine (2020 Mar 18. doi: 10.1056/NEJMoa2001282), there were no differences in clinical improvement, viral clearance, or mortality for antiviral treatment versus standard care. Delayed treatment initiation may explain the ineffectiveness, though a subgroup analysis didn’t show a shorter time to clinical improvement for those who got the treatment earlier.
- Ribavirin. Likewise, this antiviral medication has efficacy and safety data suggesting “limited value” for treatment of COVID-19. Treatment of SARS yielded “inconclusive results” for ribavirin, which was also associated with substantial toxicity that included hemolytic anemia in 60% of SARS patients.
- Oseltamivir. While it may treat influenza, it has no documented activity against SARS-CoV-2 in vitro: “This agent has no role in the management of COVID-19 once influenza has been excluded,” said Dr. Sanders and coauthors.
- Corticosteroids. They could decrease inflammatory responses in the lung, but they could also lead to delays in viral clearance and increases in secondary infection risk. Guidelines for COVID-19 say to avoid corticosteroids, and the authors of the review concur, saying that potential harms and lack of proven benefit mean they usually should not be used outside of a randomized clinical trial setting.
- Vaccines. Clearly, vaccines represent the “most effective long-term strategy” to prevent future COVID-19 outbreaks, though at least 12-18 months would be required until vaccines can be widely deployed, authors said.
Dr. Sanders reported no potential conflicts. Senior author James B. Cutrell, MD, also of the University of Texas Southwestern Medical Center, reported nonfinancial support from Gilead and Regeneron outside of the study. No other authors reported disclosures.
FROM JAMA
Troponins touted as ‘ally’ in COVID-19 triage, but message is nuanced
, cardiologists in the United Kingdom advise in a recently published viewpoint.
The tests can be used to “inform the triage of patients to critical care, guide the use of supportive treatments, and facilitate targeted cardiac investigations in those most likely to benefit,” Nicholas Mills, MD, PhD, University of Edinburgh, United Kingdom, told theheart.org | Medscape Cardiology. He is senior author on the viewpoint published online April 6 in the journal Circulation.
Older adults and those with a history of underlying cardiovascular disease appear to be at greatest risk of dying from COVID-19. “From early reports it is clear that elevated cardiac troponin concentrations predict in-hospital mortality,” said Mills.
In a recent report on hospitalized patients with COVID-19 in Wuhan, China, for example, cardiac injury (hs-cTn above the 99th-percentile upper reference limit) was seen in 1 in 5 patients and was an independent predictor of dying in the hospital. Mortality was 10-fold higher in those with cardiac injury on presentation.
Elevated cardiac troponin in the setting of COVID-19, Mills said, “may reflect illness severity with myocardial injury arising due to myocardial oxygen supply–demand imbalance. Or it may be due to direct cardiac involvement through viral myocarditis or stress cardiomyopathy, or where the prothrombotic and proinflammatory state is precipitating acute coronary syndromes.”
In their viewpoint, the authors note that circulating cTn is a marker of myocardial injury, “including but not limited to myocardial infarction or myocarditis, and the clinical relevance of this distinction has never been so clear.”
Therefore, the consequence of not measuring cardiac troponin may be to “ignore the plethora of ischemic and nonischemic causes” of myocardial injury related to COVID-19. “Clinicians who have used troponin measurement as a binary test for myocardial infarction independent of clinical context and those who consider an elevated cardiac troponin concentration to be a mandate for invasive coronary angiography must recalibrate,” they write.
“Rather than encouraging avoidance of troponin testing, we must harness the unheralded engagement from the cardiovascular community due to COVID-19 to better understand the utility of this essential biomarker and to educate clinicians on its interpretation and implications for prognosis and clinical decision making.”
Based on “same logic” as recent ACC guidance
The viewpoint was to some extent a response to a recent informal guidance from the American College of Cardiology (ACC) that advised caution in use of troponin and natriuretic peptide tests in patients with COVID-19.
Even so, that ACC guidance and the new viewpoint in Circulation are based on the “same logic,” James Januzzi Jr, MD, Massachusetts General Hospital, Boston, told theheart.org | Medscape Cardiology. Both documents:
- Point out that troponins are frequently abnormal in patients with severe cases of COVID-19
- Caution that clinicians should not equate an abnormal hs-cTn with acute myocardial infarction
- Note that, in most cases, hs-cTn elevations are a result of noncoronary mechanisms
- Recognize the potential risk to caregivers and the continued unchecked spread of SARS-CoV-2 related to downstream testing that might not be needed
“The Circulation opinion piece states that clinicians often use troponin as a binary test for myocardial infarction and a mandate for downstream testing, suggesting clinicians will need to recalibrate that approach, something I agree with and which is the central message of the ACC position,” Januzzi said.
Probably the biggest difference between the two documents, he said, is in the Circulation authors’ apparent enthusiasm to use hs-cTn as a tool to judge disease severity in patients with COVID-19.
It’s been known for more than a decade that myocardial injury is “an important risk predictor” in critical illness, Januzzi explained. “So the link between cardiac injury and outcomes in critical illness is nothing new. The difference is the fact we are seeing so many patients with COVID-19 all at once, and the authors suggest that using troponin might help in triage decision making.”
“There may be [such] a role here, but the data have not been systematically collected, and whether troponin truly adds something beyond information already available at the bedside — for example, does it add anything not already obvious at the bedside? — has not yet been conclusively proven,” Januzzi cautioned.
“As well, there are no prospective data supporting troponin as a trigger for ICU triage or for deciding on specific treatments.”
Positive cTn status “common” in COVID-19 patients
In his experience, Barry Cohen, MD, Morristown Medical Center, New Jersey, told theheart.org | Medscape Cardiology, that positive cTn status is “common in COVID-19 patients and appears to have prognostic value, not only in type 1 MI due to atherothrombotic disease (related to a proinflammatory and prothrombotic state), but more frequently type 2 MI (supply–demand mismatch), viral myocarditis, coronary microvascular ischemia, stress cardiomyopathy or tachyarrhythmias.”
Moreover, Cohen said, hs-cTn “has identified patients at increased risk for ventilation support (invasive and noninvasive), acute respiratory distress syndrome, acute kidney injury, and mortality.”
Echoing both the ACC document and the Circulation report, Cohen also said hs-cTn measurements “appear to help risk stratify COVID-19 patients, but clearly do not mean that a troponin-positive patient needs to go to the cath lab and be treated as having acute coronary syndrome. Only a minority of these patients require this intervention.”
Mills discloses receiving honoraria from Abbott Diagnostics, Roche Diagnostics, Siemens Healthineers, and LumiraDx. Januzzi has previously disclosed receiving personal fees from the American College of Cardiology, Pfizer, Merck, AbbVie, Amgen, Boehringer Ingelheim, and Takeda; grants and personal fees from Novartis, Roche, Abbott, and Janssen; and grants from Singulex and Prevencio. Cohen has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
, cardiologists in the United Kingdom advise in a recently published viewpoint.
The tests can be used to “inform the triage of patients to critical care, guide the use of supportive treatments, and facilitate targeted cardiac investigations in those most likely to benefit,” Nicholas Mills, MD, PhD, University of Edinburgh, United Kingdom, told theheart.org | Medscape Cardiology. He is senior author on the viewpoint published online April 6 in the journal Circulation.
Older adults and those with a history of underlying cardiovascular disease appear to be at greatest risk of dying from COVID-19. “From early reports it is clear that elevated cardiac troponin concentrations predict in-hospital mortality,” said Mills.
In a recent report on hospitalized patients with COVID-19 in Wuhan, China, for example, cardiac injury (hs-cTn above the 99th-percentile upper reference limit) was seen in 1 in 5 patients and was an independent predictor of dying in the hospital. Mortality was 10-fold higher in those with cardiac injury on presentation.
Elevated cardiac troponin in the setting of COVID-19, Mills said, “may reflect illness severity with myocardial injury arising due to myocardial oxygen supply–demand imbalance. Or it may be due to direct cardiac involvement through viral myocarditis or stress cardiomyopathy, or where the prothrombotic and proinflammatory state is precipitating acute coronary syndromes.”
In their viewpoint, the authors note that circulating cTn is a marker of myocardial injury, “including but not limited to myocardial infarction or myocarditis, and the clinical relevance of this distinction has never been so clear.”
Therefore, the consequence of not measuring cardiac troponin may be to “ignore the plethora of ischemic and nonischemic causes” of myocardial injury related to COVID-19. “Clinicians who have used troponin measurement as a binary test for myocardial infarction independent of clinical context and those who consider an elevated cardiac troponin concentration to be a mandate for invasive coronary angiography must recalibrate,” they write.
“Rather than encouraging avoidance of troponin testing, we must harness the unheralded engagement from the cardiovascular community due to COVID-19 to better understand the utility of this essential biomarker and to educate clinicians on its interpretation and implications for prognosis and clinical decision making.”
Based on “same logic” as recent ACC guidance
The viewpoint was to some extent a response to a recent informal guidance from the American College of Cardiology (ACC) that advised caution in use of troponin and natriuretic peptide tests in patients with COVID-19.
Even so, that ACC guidance and the new viewpoint in Circulation are based on the “same logic,” James Januzzi Jr, MD, Massachusetts General Hospital, Boston, told theheart.org | Medscape Cardiology. Both documents:
- Point out that troponins are frequently abnormal in patients with severe cases of COVID-19
- Caution that clinicians should not equate an abnormal hs-cTn with acute myocardial infarction
- Note that, in most cases, hs-cTn elevations are a result of noncoronary mechanisms
- Recognize the potential risk to caregivers and the continued unchecked spread of SARS-CoV-2 related to downstream testing that might not be needed
“The Circulation opinion piece states that clinicians often use troponin as a binary test for myocardial infarction and a mandate for downstream testing, suggesting clinicians will need to recalibrate that approach, something I agree with and which is the central message of the ACC position,” Januzzi said.
Probably the biggest difference between the two documents, he said, is in the Circulation authors’ apparent enthusiasm to use hs-cTn as a tool to judge disease severity in patients with COVID-19.
It’s been known for more than a decade that myocardial injury is “an important risk predictor” in critical illness, Januzzi explained. “So the link between cardiac injury and outcomes in critical illness is nothing new. The difference is the fact we are seeing so many patients with COVID-19 all at once, and the authors suggest that using troponin might help in triage decision making.”
“There may be [such] a role here, but the data have not been systematically collected, and whether troponin truly adds something beyond information already available at the bedside — for example, does it add anything not already obvious at the bedside? — has not yet been conclusively proven,” Januzzi cautioned.
“As well, there are no prospective data supporting troponin as a trigger for ICU triage or for deciding on specific treatments.”
Positive cTn status “common” in COVID-19 patients
In his experience, Barry Cohen, MD, Morristown Medical Center, New Jersey, told theheart.org | Medscape Cardiology, that positive cTn status is “common in COVID-19 patients and appears to have prognostic value, not only in type 1 MI due to atherothrombotic disease (related to a proinflammatory and prothrombotic state), but more frequently type 2 MI (supply–demand mismatch), viral myocarditis, coronary microvascular ischemia, stress cardiomyopathy or tachyarrhythmias.”
Moreover, Cohen said, hs-cTn “has identified patients at increased risk for ventilation support (invasive and noninvasive), acute respiratory distress syndrome, acute kidney injury, and mortality.”
Echoing both the ACC document and the Circulation report, Cohen also said hs-cTn measurements “appear to help risk stratify COVID-19 patients, but clearly do not mean that a troponin-positive patient needs to go to the cath lab and be treated as having acute coronary syndrome. Only a minority of these patients require this intervention.”
Mills discloses receiving honoraria from Abbott Diagnostics, Roche Diagnostics, Siemens Healthineers, and LumiraDx. Januzzi has previously disclosed receiving personal fees from the American College of Cardiology, Pfizer, Merck, AbbVie, Amgen, Boehringer Ingelheim, and Takeda; grants and personal fees from Novartis, Roche, Abbott, and Janssen; and grants from Singulex and Prevencio. Cohen has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
, cardiologists in the United Kingdom advise in a recently published viewpoint.
The tests can be used to “inform the triage of patients to critical care, guide the use of supportive treatments, and facilitate targeted cardiac investigations in those most likely to benefit,” Nicholas Mills, MD, PhD, University of Edinburgh, United Kingdom, told theheart.org | Medscape Cardiology. He is senior author on the viewpoint published online April 6 in the journal Circulation.
Older adults and those with a history of underlying cardiovascular disease appear to be at greatest risk of dying from COVID-19. “From early reports it is clear that elevated cardiac troponin concentrations predict in-hospital mortality,” said Mills.
In a recent report on hospitalized patients with COVID-19 in Wuhan, China, for example, cardiac injury (hs-cTn above the 99th-percentile upper reference limit) was seen in 1 in 5 patients and was an independent predictor of dying in the hospital. Mortality was 10-fold higher in those with cardiac injury on presentation.
Elevated cardiac troponin in the setting of COVID-19, Mills said, “may reflect illness severity with myocardial injury arising due to myocardial oxygen supply–demand imbalance. Or it may be due to direct cardiac involvement through viral myocarditis or stress cardiomyopathy, or where the prothrombotic and proinflammatory state is precipitating acute coronary syndromes.”
In their viewpoint, the authors note that circulating cTn is a marker of myocardial injury, “including but not limited to myocardial infarction or myocarditis, and the clinical relevance of this distinction has never been so clear.”
Therefore, the consequence of not measuring cardiac troponin may be to “ignore the plethora of ischemic and nonischemic causes” of myocardial injury related to COVID-19. “Clinicians who have used troponin measurement as a binary test for myocardial infarction independent of clinical context and those who consider an elevated cardiac troponin concentration to be a mandate for invasive coronary angiography must recalibrate,” they write.
“Rather than encouraging avoidance of troponin testing, we must harness the unheralded engagement from the cardiovascular community due to COVID-19 to better understand the utility of this essential biomarker and to educate clinicians on its interpretation and implications for prognosis and clinical decision making.”
Based on “same logic” as recent ACC guidance
The viewpoint was to some extent a response to a recent informal guidance from the American College of Cardiology (ACC) that advised caution in use of troponin and natriuretic peptide tests in patients with COVID-19.
Even so, that ACC guidance and the new viewpoint in Circulation are based on the “same logic,” James Januzzi Jr, MD, Massachusetts General Hospital, Boston, told theheart.org | Medscape Cardiology. Both documents:
- Point out that troponins are frequently abnormal in patients with severe cases of COVID-19
- Caution that clinicians should not equate an abnormal hs-cTn with acute myocardial infarction
- Note that, in most cases, hs-cTn elevations are a result of noncoronary mechanisms
- Recognize the potential risk to caregivers and the continued unchecked spread of SARS-CoV-2 related to downstream testing that might not be needed
“The Circulation opinion piece states that clinicians often use troponin as a binary test for myocardial infarction and a mandate for downstream testing, suggesting clinicians will need to recalibrate that approach, something I agree with and which is the central message of the ACC position,” Januzzi said.
Probably the biggest difference between the two documents, he said, is in the Circulation authors’ apparent enthusiasm to use hs-cTn as a tool to judge disease severity in patients with COVID-19.
It’s been known for more than a decade that myocardial injury is “an important risk predictor” in critical illness, Januzzi explained. “So the link between cardiac injury and outcomes in critical illness is nothing new. The difference is the fact we are seeing so many patients with COVID-19 all at once, and the authors suggest that using troponin might help in triage decision making.”
“There may be [such] a role here, but the data have not been systematically collected, and whether troponin truly adds something beyond information already available at the bedside — for example, does it add anything not already obvious at the bedside? — has not yet been conclusively proven,” Januzzi cautioned.
“As well, there are no prospective data supporting troponin as a trigger for ICU triage or for deciding on specific treatments.”
Positive cTn status “common” in COVID-19 patients
In his experience, Barry Cohen, MD, Morristown Medical Center, New Jersey, told theheart.org | Medscape Cardiology, that positive cTn status is “common in COVID-19 patients and appears to have prognostic value, not only in type 1 MI due to atherothrombotic disease (related to a proinflammatory and prothrombotic state), but more frequently type 2 MI (supply–demand mismatch), viral myocarditis, coronary microvascular ischemia, stress cardiomyopathy or tachyarrhythmias.”
Moreover, Cohen said, hs-cTn “has identified patients at increased risk for ventilation support (invasive and noninvasive), acute respiratory distress syndrome, acute kidney injury, and mortality.”
Echoing both the ACC document and the Circulation report, Cohen also said hs-cTn measurements “appear to help risk stratify COVID-19 patients, but clearly do not mean that a troponin-positive patient needs to go to the cath lab and be treated as having acute coronary syndrome. Only a minority of these patients require this intervention.”
Mills discloses receiving honoraria from Abbott Diagnostics, Roche Diagnostics, Siemens Healthineers, and LumiraDx. Januzzi has previously disclosed receiving personal fees from the American College of Cardiology, Pfizer, Merck, AbbVie, Amgen, Boehringer Ingelheim, and Takeda; grants and personal fees from Novartis, Roche, Abbott, and Janssen; and grants from Singulex and Prevencio. Cohen has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
COVID-19 pandemic brings unexpected pediatric consequences
As physicians and advanced practitioners, we have been preparing to face COVID-19 – anticipating increasing volumes of patients with fevers, cough, and shortness of breath, and potential surges in emergency departments (EDs) and primary care offices. Fortunately, while COVID-19 has demonstrated more mild symptoms in pediatric patients, the heightened public health fears and mandated social isolation have created some unforeseen consequences for pediatric patients. This article presents cases encountered over the course of 2 weeks in our ED that shed light on the unexpected ramifications of living in the time of a pandemic. These encounters should remind us as providers to be diligent and thorough in giving guidance to families during a time when face-to-face medicine has become increasingly difficult and limited.
These stories have been modified to protect patient confidentiality.
Case 1
A 2-week-old full-term infant arrived in the ED after having a fever for 48 hours. The patient’s mother reported that she had called the pediatrician yesterday to ask for advice on treating the fever and was instructed to give acetaminophen and bring the infant into the ED for testing.
When we asked mom why she did not bring the infant in yesterday, she stated that the fever went down with acetaminophen, and the baby was drinking well and urinating normally. Mostly, she was afraid to bring the child into the ED given concern for COVID-19; however, when the fever persisted today, she came in. During the work-up, the infant was noted to have focal seizures and was ultimately diagnosed with bacterial meningitis.
Takeaway: Families may be hesitant to follow pediatrician’s advice to seek medical attention at an ED or doctor’s office because of the fear of being exposed to COVID-19.
- If something is urgent or emergent, be sure to stress the importance to families that the advice is non-negotiable for their child’s health.
- Attempt to call ahead for patients who might be more vulnerable in waiting rooms or overcrowded hospitals.
Case 2
A 5-month-old baby presented to the ED with new-onset seizures. Immediate bedside blood work performed demonstrated a normal blood glucose, but the baby was profoundly hyponatremic. Upon asking the mother if the baby has had any vomiting, diarrhea, or difficulty tolerating feeds, she says that she has been diluting formula because all the stores were out of formula. Today, she gave the baby plain water because they were completely out of formula.
Takeaway: With economists estimating unemployment rates in the United States at 13% at press time (the worst since the Great Depression), many families may lack resources to purchase necessities.
- Even if families have the ability to purchase necessities, they may be difficult to find or unavailable (e.g., formula, medications, diapers).
- Consider reaching out to patients in your practice to ask about their ability to find essentials and with advice on what to do if they run out of formula or diapers, or who they should contact if they cannot refill a medication.
- Are you in a position to speak with your mayor or local council to ensure there are regulations on the hoarding of essential items?
- In a time when breast milk or formula is not available for children younger than 1 year of age, what will you recommend for families? There are no current American Academy of Pediatrics’ guidelines.
Case 3
A school-aged girl was helping her mother sanitize the home during the COVID-19 pandemic. She had her gloves on, her commercial antiseptic cleaner ready to go, but it was not spraying. She turned the bottle around to check the nozzle and sprayed herself in the eyes. The family presented to the ED for alkaline burn to her eyes, which required copious irrigation.
Takeaway: Children are spending more time in the house with access to button batteries, choking hazards, and cleaning supplies.
- Cleaning products can cause chemical burns. These products should not be used by young children.
Case 4
A school-aged boy arrived via emergency medical services (EMS) for altered mental status. He told his father he was feeling dizzy and then lost consciousness. EMS noticed that he had some tonic movements of his lower extremities, and when he arrived in the ED, he had eye deviation and was unresponsive.
Work-up ultimately demonstrated that this patient had a seizure and a dangerously elevated ethanol level from drinking an entire bottle of hand sanitizer. Hand sanitizer may contain high concentrations of ethyl alcohol or isopropyl alcohol, which when ingested can cause intoxication or poisoning.
Takeaway: Many products that we may view as harmless can be toxic if ingested in large amounts.
- Consider making a list of products that families may have acquired and have around the home during this COVID-19 pandemic and instruct families to make sure dangerous items (e.g., acetaminophen, aspirin, hand sanitizer, lighters, firearms, batteries) are locked up and/or out of reach of children.
- Make sure families know the Poison Control phone number (800-222-1222).
Case 5
An adolescent female currently being treated with immunosuppressants arrived from home with fever. Her medical history revealed that the patient’s guardian recently passed away from suspected COVID-19. The patient was tested and is herself found to be positive for COVID-19. The patient is currently being cared for by relatives who also live in the same home. They require extensive education and teaching regarding the patient’s medication regimen, while also dealing with the loss of their loved one and the fear of personal exposure.
Takeaway: Communicate with families – especially those with special health care needs – about issues of guardianship in case a child’s primary caretaker falls ill.
- Discuss with families about having easily accessible lists of medications and medical conditions.
- Involve social work and child life specialists to help children and their families deal with life-altering changes and losses suffered during this time, as well as fears related to mortality and exposure.
Case 6
A 3-year-old boy arrived covered in bruises and complaining of stomachache. While the mother denies any known abuse, she states that her significant other has been getting more and more “worked up having to deal with the child’s behavior all day every day.” The preschool the child previously attended has closed due to the pandemic.
Takeaway: Abuse is more common when the parents perceive that there is little community support and when families feel a lack of connection to the community.1 Huang et al. examined the relationship between the economy and nonaccidental trauma, showing a doubling in the rate of nonaccidental head trauma during economic recession.2
- Allow families to know that they are not alone and that child care is difficult
- Offer advice on what caretakers can do if they feel alone or at their mental or physical limit.
- Provide strategies on your practice’s website if a situation at home becomes tense and strained.
Case 7
An adolescent female arrived to the ED with increased suicidality. She normally follows with her psychiatrist once a month and her therapist once a week. Since the beginning of COVID-19 restrictions, she has been using telemedicine for her therapy visits. While previously doing well, she reports that her suicidal ideations have worsened because of feeling isolated from her friends now that school is out and she is not allowed to see them. Although compliant with her medications, her thoughts have increased to the point where she has to be admitted to inpatient psychiatry.
Takeaway: Anxiety, depression, and suicide may increase in a down economy. After the 2008 global economic crisis, rates of suicide drastically increased.3
- Recognize the limitations of telemedicine (technology limitations, patient cooperation, etc.)
- Social isolation may contribute to worsening mental health
- Know when to advise patients to seek in-person evaluation and care for medical and mental health concerns.
Pediatricians are at the forefront of preventative medicine. Families rely on pediatricians for trustworthy and accurate anticipatory guidance, a need that is only heightened during times of local and national stress. The social isolation, fear, and lack of resources accompanying this pandemic have serious consequences for our families. What can you and your practice do to keep children safe in the time of COVID-19?
Dr. Angelica DesPain is a pediatric emergency medicine fellow at Children’s National Hospital in Washington. Dr. Rachel Hatcliffe is an attending physician at the hospital. Neither physician had any relevant financial disclosures. Email Dr. DesPain and/or Dr. Hatcliffe at [email protected].
References
1. Child Dev. 1978;49:604-16.
2. J Neurosurg Pediatr 2011 Aug;8(2):171-6.
3. BMJ 2013;347:f5239.
As physicians and advanced practitioners, we have been preparing to face COVID-19 – anticipating increasing volumes of patients with fevers, cough, and shortness of breath, and potential surges in emergency departments (EDs) and primary care offices. Fortunately, while COVID-19 has demonstrated more mild symptoms in pediatric patients, the heightened public health fears and mandated social isolation have created some unforeseen consequences for pediatric patients. This article presents cases encountered over the course of 2 weeks in our ED that shed light on the unexpected ramifications of living in the time of a pandemic. These encounters should remind us as providers to be diligent and thorough in giving guidance to families during a time when face-to-face medicine has become increasingly difficult and limited.
These stories have been modified to protect patient confidentiality.
Case 1
A 2-week-old full-term infant arrived in the ED after having a fever for 48 hours. The patient’s mother reported that she had called the pediatrician yesterday to ask for advice on treating the fever and was instructed to give acetaminophen and bring the infant into the ED for testing.
When we asked mom why she did not bring the infant in yesterday, she stated that the fever went down with acetaminophen, and the baby was drinking well and urinating normally. Mostly, she was afraid to bring the child into the ED given concern for COVID-19; however, when the fever persisted today, she came in. During the work-up, the infant was noted to have focal seizures and was ultimately diagnosed with bacterial meningitis.
Takeaway: Families may be hesitant to follow pediatrician’s advice to seek medical attention at an ED or doctor’s office because of the fear of being exposed to COVID-19.
- If something is urgent or emergent, be sure to stress the importance to families that the advice is non-negotiable for their child’s health.
- Attempt to call ahead for patients who might be more vulnerable in waiting rooms or overcrowded hospitals.
Case 2
A 5-month-old baby presented to the ED with new-onset seizures. Immediate bedside blood work performed demonstrated a normal blood glucose, but the baby was profoundly hyponatremic. Upon asking the mother if the baby has had any vomiting, diarrhea, or difficulty tolerating feeds, she says that she has been diluting formula because all the stores were out of formula. Today, she gave the baby plain water because they were completely out of formula.
Takeaway: With economists estimating unemployment rates in the United States at 13% at press time (the worst since the Great Depression), many families may lack resources to purchase necessities.
- Even if families have the ability to purchase necessities, they may be difficult to find or unavailable (e.g., formula, medications, diapers).
- Consider reaching out to patients in your practice to ask about their ability to find essentials and with advice on what to do if they run out of formula or diapers, or who they should contact if they cannot refill a medication.
- Are you in a position to speak with your mayor or local council to ensure there are regulations on the hoarding of essential items?
- In a time when breast milk or formula is not available for children younger than 1 year of age, what will you recommend for families? There are no current American Academy of Pediatrics’ guidelines.
Case 3
A school-aged girl was helping her mother sanitize the home during the COVID-19 pandemic. She had her gloves on, her commercial antiseptic cleaner ready to go, but it was not spraying. She turned the bottle around to check the nozzle and sprayed herself in the eyes. The family presented to the ED for alkaline burn to her eyes, which required copious irrigation.
Takeaway: Children are spending more time in the house with access to button batteries, choking hazards, and cleaning supplies.
- Cleaning products can cause chemical burns. These products should not be used by young children.
Case 4
A school-aged boy arrived via emergency medical services (EMS) for altered mental status. He told his father he was feeling dizzy and then lost consciousness. EMS noticed that he had some tonic movements of his lower extremities, and when he arrived in the ED, he had eye deviation and was unresponsive.
Work-up ultimately demonstrated that this patient had a seizure and a dangerously elevated ethanol level from drinking an entire bottle of hand sanitizer. Hand sanitizer may contain high concentrations of ethyl alcohol or isopropyl alcohol, which when ingested can cause intoxication or poisoning.
Takeaway: Many products that we may view as harmless can be toxic if ingested in large amounts.
- Consider making a list of products that families may have acquired and have around the home during this COVID-19 pandemic and instruct families to make sure dangerous items (e.g., acetaminophen, aspirin, hand sanitizer, lighters, firearms, batteries) are locked up and/or out of reach of children.
- Make sure families know the Poison Control phone number (800-222-1222).
Case 5
An adolescent female currently being treated with immunosuppressants arrived from home with fever. Her medical history revealed that the patient’s guardian recently passed away from suspected COVID-19. The patient was tested and is herself found to be positive for COVID-19. The patient is currently being cared for by relatives who also live in the same home. They require extensive education and teaching regarding the patient’s medication regimen, while also dealing with the loss of their loved one and the fear of personal exposure.
Takeaway: Communicate with families – especially those with special health care needs – about issues of guardianship in case a child’s primary caretaker falls ill.
- Discuss with families about having easily accessible lists of medications and medical conditions.
- Involve social work and child life specialists to help children and their families deal with life-altering changes and losses suffered during this time, as well as fears related to mortality and exposure.
Case 6
A 3-year-old boy arrived covered in bruises and complaining of stomachache. While the mother denies any known abuse, she states that her significant other has been getting more and more “worked up having to deal with the child’s behavior all day every day.” The preschool the child previously attended has closed due to the pandemic.
Takeaway: Abuse is more common when the parents perceive that there is little community support and when families feel a lack of connection to the community.1 Huang et al. examined the relationship between the economy and nonaccidental trauma, showing a doubling in the rate of nonaccidental head trauma during economic recession.2
- Allow families to know that they are not alone and that child care is difficult
- Offer advice on what caretakers can do if they feel alone or at their mental or physical limit.
- Provide strategies on your practice’s website if a situation at home becomes tense and strained.
Case 7
An adolescent female arrived to the ED with increased suicidality. She normally follows with her psychiatrist once a month and her therapist once a week. Since the beginning of COVID-19 restrictions, she has been using telemedicine for her therapy visits. While previously doing well, she reports that her suicidal ideations have worsened because of feeling isolated from her friends now that school is out and she is not allowed to see them. Although compliant with her medications, her thoughts have increased to the point where she has to be admitted to inpatient psychiatry.
Takeaway: Anxiety, depression, and suicide may increase in a down economy. After the 2008 global economic crisis, rates of suicide drastically increased.3
- Recognize the limitations of telemedicine (technology limitations, patient cooperation, etc.)
- Social isolation may contribute to worsening mental health
- Know when to advise patients to seek in-person evaluation and care for medical and mental health concerns.
Pediatricians are at the forefront of preventative medicine. Families rely on pediatricians for trustworthy and accurate anticipatory guidance, a need that is only heightened during times of local and national stress. The social isolation, fear, and lack of resources accompanying this pandemic have serious consequences for our families. What can you and your practice do to keep children safe in the time of COVID-19?
Dr. Angelica DesPain is a pediatric emergency medicine fellow at Children’s National Hospital in Washington. Dr. Rachel Hatcliffe is an attending physician at the hospital. Neither physician had any relevant financial disclosures. Email Dr. DesPain and/or Dr. Hatcliffe at [email protected].
References
1. Child Dev. 1978;49:604-16.
2. J Neurosurg Pediatr 2011 Aug;8(2):171-6.
3. BMJ 2013;347:f5239.
As physicians and advanced practitioners, we have been preparing to face COVID-19 – anticipating increasing volumes of patients with fevers, cough, and shortness of breath, and potential surges in emergency departments (EDs) and primary care offices. Fortunately, while COVID-19 has demonstrated more mild symptoms in pediatric patients, the heightened public health fears and mandated social isolation have created some unforeseen consequences for pediatric patients. This article presents cases encountered over the course of 2 weeks in our ED that shed light on the unexpected ramifications of living in the time of a pandemic. These encounters should remind us as providers to be diligent and thorough in giving guidance to families during a time when face-to-face medicine has become increasingly difficult and limited.
These stories have been modified to protect patient confidentiality.
Case 1
A 2-week-old full-term infant arrived in the ED after having a fever for 48 hours. The patient’s mother reported that she had called the pediatrician yesterday to ask for advice on treating the fever and was instructed to give acetaminophen and bring the infant into the ED for testing.
When we asked mom why she did not bring the infant in yesterday, she stated that the fever went down with acetaminophen, and the baby was drinking well and urinating normally. Mostly, she was afraid to bring the child into the ED given concern for COVID-19; however, when the fever persisted today, she came in. During the work-up, the infant was noted to have focal seizures and was ultimately diagnosed with bacterial meningitis.
Takeaway: Families may be hesitant to follow pediatrician’s advice to seek medical attention at an ED or doctor’s office because of the fear of being exposed to COVID-19.
- If something is urgent or emergent, be sure to stress the importance to families that the advice is non-negotiable for their child’s health.
- Attempt to call ahead for patients who might be more vulnerable in waiting rooms or overcrowded hospitals.
Case 2
A 5-month-old baby presented to the ED with new-onset seizures. Immediate bedside blood work performed demonstrated a normal blood glucose, but the baby was profoundly hyponatremic. Upon asking the mother if the baby has had any vomiting, diarrhea, or difficulty tolerating feeds, she says that she has been diluting formula because all the stores were out of formula. Today, she gave the baby plain water because they were completely out of formula.
Takeaway: With economists estimating unemployment rates in the United States at 13% at press time (the worst since the Great Depression), many families may lack resources to purchase necessities.
- Even if families have the ability to purchase necessities, they may be difficult to find or unavailable (e.g., formula, medications, diapers).
- Consider reaching out to patients in your practice to ask about their ability to find essentials and with advice on what to do if they run out of formula or diapers, or who they should contact if they cannot refill a medication.
- Are you in a position to speak with your mayor or local council to ensure there are regulations on the hoarding of essential items?
- In a time when breast milk or formula is not available for children younger than 1 year of age, what will you recommend for families? There are no current American Academy of Pediatrics’ guidelines.
Case 3
A school-aged girl was helping her mother sanitize the home during the COVID-19 pandemic. She had her gloves on, her commercial antiseptic cleaner ready to go, but it was not spraying. She turned the bottle around to check the nozzle and sprayed herself in the eyes. The family presented to the ED for alkaline burn to her eyes, which required copious irrigation.
Takeaway: Children are spending more time in the house with access to button batteries, choking hazards, and cleaning supplies.
- Cleaning products can cause chemical burns. These products should not be used by young children.
Case 4
A school-aged boy arrived via emergency medical services (EMS) for altered mental status. He told his father he was feeling dizzy and then lost consciousness. EMS noticed that he had some tonic movements of his lower extremities, and when he arrived in the ED, he had eye deviation and was unresponsive.
Work-up ultimately demonstrated that this patient had a seizure and a dangerously elevated ethanol level from drinking an entire bottle of hand sanitizer. Hand sanitizer may contain high concentrations of ethyl alcohol or isopropyl alcohol, which when ingested can cause intoxication or poisoning.
Takeaway: Many products that we may view as harmless can be toxic if ingested in large amounts.
- Consider making a list of products that families may have acquired and have around the home during this COVID-19 pandemic and instruct families to make sure dangerous items (e.g., acetaminophen, aspirin, hand sanitizer, lighters, firearms, batteries) are locked up and/or out of reach of children.
- Make sure families know the Poison Control phone number (800-222-1222).
Case 5
An adolescent female currently being treated with immunosuppressants arrived from home with fever. Her medical history revealed that the patient’s guardian recently passed away from suspected COVID-19. The patient was tested and is herself found to be positive for COVID-19. The patient is currently being cared for by relatives who also live in the same home. They require extensive education and teaching regarding the patient’s medication regimen, while also dealing with the loss of their loved one and the fear of personal exposure.
Takeaway: Communicate with families – especially those with special health care needs – about issues of guardianship in case a child’s primary caretaker falls ill.
- Discuss with families about having easily accessible lists of medications and medical conditions.
- Involve social work and child life specialists to help children and their families deal with life-altering changes and losses suffered during this time, as well as fears related to mortality and exposure.
Case 6
A 3-year-old boy arrived covered in bruises and complaining of stomachache. While the mother denies any known abuse, she states that her significant other has been getting more and more “worked up having to deal with the child’s behavior all day every day.” The preschool the child previously attended has closed due to the pandemic.
Takeaway: Abuse is more common when the parents perceive that there is little community support and when families feel a lack of connection to the community.1 Huang et al. examined the relationship between the economy and nonaccidental trauma, showing a doubling in the rate of nonaccidental head trauma during economic recession.2
- Allow families to know that they are not alone and that child care is difficult
- Offer advice on what caretakers can do if they feel alone or at their mental or physical limit.
- Provide strategies on your practice’s website if a situation at home becomes tense and strained.
Case 7
An adolescent female arrived to the ED with increased suicidality. She normally follows with her psychiatrist once a month and her therapist once a week. Since the beginning of COVID-19 restrictions, she has been using telemedicine for her therapy visits. While previously doing well, she reports that her suicidal ideations have worsened because of feeling isolated from her friends now that school is out and she is not allowed to see them. Although compliant with her medications, her thoughts have increased to the point where she has to be admitted to inpatient psychiatry.
Takeaway: Anxiety, depression, and suicide may increase in a down economy. After the 2008 global economic crisis, rates of suicide drastically increased.3
- Recognize the limitations of telemedicine (technology limitations, patient cooperation, etc.)
- Social isolation may contribute to worsening mental health
- Know when to advise patients to seek in-person evaluation and care for medical and mental health concerns.
Pediatricians are at the forefront of preventative medicine. Families rely on pediatricians for trustworthy and accurate anticipatory guidance, a need that is only heightened during times of local and national stress. The social isolation, fear, and lack of resources accompanying this pandemic have serious consequences for our families. What can you and your practice do to keep children safe in the time of COVID-19?
Dr. Angelica DesPain is a pediatric emergency medicine fellow at Children’s National Hospital in Washington. Dr. Rachel Hatcliffe is an attending physician at the hospital. Neither physician had any relevant financial disclosures. Email Dr. DesPain and/or Dr. Hatcliffe at [email protected].
References
1. Child Dev. 1978;49:604-16.
2. J Neurosurg Pediatr 2011 Aug;8(2):171-6.
3. BMJ 2013;347:f5239.
ASH tackles COVID-19 with hematology-related FAQ, promotes new registries
The American Society of Hematology has committed a portion of its website to providing continually updated information addressing specific hematologic disorders in relation to COVID-19.
“As the world grapples with the novel coronavirus, ASH believes that we can help each other be as knowledgeable and prepared as possible,” wrote the society’s president, Stephanie J. Lee, MD, MPH.
On its website, ASH provides relevant COVID-19 information in a series of FAQ divided into malignant and nonmalignant hematologic diseases and disorders. In the malignant category, the various lymphomas and leukemias are individually addressed, as well as other conditions such as myelodysplastic syndromes, myeloproliferative neoplasms, and multiple myeloma. In the nonmalignant category, ASH has provided FAQ on aplastic anemia, thalassemia, sickle cell disease, pulmonary embolism, venous thromboembolism/anticoagulation, coagulopathy, and immune as well as thrombotic thrombocytopenic purpura.
In addition to the continually updated series of relevant FAQ, as part of its response to the pandemic ASH is promoting two unique COVID-19 registries for physicians: the ASH Research Collaborative’s (ASH RC) Data Hub COVID-19 Registry and the Surveillance Epidemiology of Coronavirus (COVID-19) Under Research Exclusion Sickle Cell Disease (SECURE-SCD) Registry.
“The ASH Research Collaborative’s (ASH RC) Data Hub launched the COVID-19 Registry and is currently capturing data on people who test positive for COVID-19 and have been or are currently being treated for hematologic malignancy,” according to the website. The intention is to provide “near real-time observational data summaries,” which will hopefully provide useful information to clinicians treating hematologic malignancies in patients in the midst of the COVID-19 pandemic.
The registry allows clinicians to enter their own cases in a specified format to allow data analysis on clinical practice and patient outcomes that will be aggregated to provide rapid insights for clinicians to help them care for their patients, according to ASH.
The second registry specifically deals with COVID-19 cases in patients with sickle cell disease. It also allows clinicians to add cases with a similar intention of aggregating data to provide near real-time insights into patient care. “We are asking providers caring for these patients to report all of their cases of COVID-19 to this registry,” according to the registry website. The registry is for reporting COVID-19 cases in sickle cell disease patients “after sufficient time has passed to observe the disease course through resolution of acute illness and/or death.”
ASH also provides more generalized information for hematology practitioners dealing with COVID-19 on the topics of conducting their practice and using telemedicine, among others.
Correction, April 15, 2020: This story originally said incorrectly that ASH developed the 2 new registries. The registries are merely being promoted on the ASH website.
The American Society of Hematology has committed a portion of its website to providing continually updated information addressing specific hematologic disorders in relation to COVID-19.
“As the world grapples with the novel coronavirus, ASH believes that we can help each other be as knowledgeable and prepared as possible,” wrote the society’s president, Stephanie J. Lee, MD, MPH.
On its website, ASH provides relevant COVID-19 information in a series of FAQ divided into malignant and nonmalignant hematologic diseases and disorders. In the malignant category, the various lymphomas and leukemias are individually addressed, as well as other conditions such as myelodysplastic syndromes, myeloproliferative neoplasms, and multiple myeloma. In the nonmalignant category, ASH has provided FAQ on aplastic anemia, thalassemia, sickle cell disease, pulmonary embolism, venous thromboembolism/anticoagulation, coagulopathy, and immune as well as thrombotic thrombocytopenic purpura.
In addition to the continually updated series of relevant FAQ, as part of its response to the pandemic ASH is promoting two unique COVID-19 registries for physicians: the ASH Research Collaborative’s (ASH RC) Data Hub COVID-19 Registry and the Surveillance Epidemiology of Coronavirus (COVID-19) Under Research Exclusion Sickle Cell Disease (SECURE-SCD) Registry.
“The ASH Research Collaborative’s (ASH RC) Data Hub launched the COVID-19 Registry and is currently capturing data on people who test positive for COVID-19 and have been or are currently being treated for hematologic malignancy,” according to the website. The intention is to provide “near real-time observational data summaries,” which will hopefully provide useful information to clinicians treating hematologic malignancies in patients in the midst of the COVID-19 pandemic.
The registry allows clinicians to enter their own cases in a specified format to allow data analysis on clinical practice and patient outcomes that will be aggregated to provide rapid insights for clinicians to help them care for their patients, according to ASH.
The second registry specifically deals with COVID-19 cases in patients with sickle cell disease. It also allows clinicians to add cases with a similar intention of aggregating data to provide near real-time insights into patient care. “We are asking providers caring for these patients to report all of their cases of COVID-19 to this registry,” according to the registry website. The registry is for reporting COVID-19 cases in sickle cell disease patients “after sufficient time has passed to observe the disease course through resolution of acute illness and/or death.”
ASH also provides more generalized information for hematology practitioners dealing with COVID-19 on the topics of conducting their practice and using telemedicine, among others.
Correction, April 15, 2020: This story originally said incorrectly that ASH developed the 2 new registries. The registries are merely being promoted on the ASH website.
The American Society of Hematology has committed a portion of its website to providing continually updated information addressing specific hematologic disorders in relation to COVID-19.
“As the world grapples with the novel coronavirus, ASH believes that we can help each other be as knowledgeable and prepared as possible,” wrote the society’s president, Stephanie J. Lee, MD, MPH.
On its website, ASH provides relevant COVID-19 information in a series of FAQ divided into malignant and nonmalignant hematologic diseases and disorders. In the malignant category, the various lymphomas and leukemias are individually addressed, as well as other conditions such as myelodysplastic syndromes, myeloproliferative neoplasms, and multiple myeloma. In the nonmalignant category, ASH has provided FAQ on aplastic anemia, thalassemia, sickle cell disease, pulmonary embolism, venous thromboembolism/anticoagulation, coagulopathy, and immune as well as thrombotic thrombocytopenic purpura.
In addition to the continually updated series of relevant FAQ, as part of its response to the pandemic ASH is promoting two unique COVID-19 registries for physicians: the ASH Research Collaborative’s (ASH RC) Data Hub COVID-19 Registry and the Surveillance Epidemiology of Coronavirus (COVID-19) Under Research Exclusion Sickle Cell Disease (SECURE-SCD) Registry.
“The ASH Research Collaborative’s (ASH RC) Data Hub launched the COVID-19 Registry and is currently capturing data on people who test positive for COVID-19 and have been or are currently being treated for hematologic malignancy,” according to the website. The intention is to provide “near real-time observational data summaries,” which will hopefully provide useful information to clinicians treating hematologic malignancies in patients in the midst of the COVID-19 pandemic.
The registry allows clinicians to enter their own cases in a specified format to allow data analysis on clinical practice and patient outcomes that will be aggregated to provide rapid insights for clinicians to help them care for their patients, according to ASH.
The second registry specifically deals with COVID-19 cases in patients with sickle cell disease. It also allows clinicians to add cases with a similar intention of aggregating data to provide near real-time insights into patient care. “We are asking providers caring for these patients to report all of their cases of COVID-19 to this registry,” according to the registry website. The registry is for reporting COVID-19 cases in sickle cell disease patients “after sufficient time has passed to observe the disease course through resolution of acute illness and/or death.”
ASH also provides more generalized information for hematology practitioners dealing with COVID-19 on the topics of conducting their practice and using telemedicine, among others.
Correction, April 15, 2020: This story originally said incorrectly that ASH developed the 2 new registries. The registries are merely being promoted on the ASH website.
COVID-19: Managing resource crunch and ethical challenges
COVID-19 has been a watershed event in medical history of epic proportions. With this fast-spreading pandemic stretching resources at health care institutions, practical considerations for management of a disease about which we are still learning has been a huge challenge.
Although many guidelines have been made available by medical societies and experts worldwide, there appear to be very few which throw light on management in a resource-poor setup. The hospitalist, as a front-line provider, is likely expected to lead the planning and management of resources in order to deliver appropriate care.
As per American Hospital Association data, there are 2,704 community hospitals that can deliver ICU care in the United States. There are 534,964 acute care beds with 96,596 ICU beds. Additionally, there are 25,157 step-down beds and 1,183 burn unit beds. Of the 2,704 hospitals, 74% are in metropolitan areas (> 50,000 population), 17% (464) are in micropolitan areas (10,000-49,999 population), and the remaining 9% (244) are in rural areas. Only 7% (36,453) of hospital beds and 5% (4715) of ICU beds are in micropolitan areas. Two percent of acute care hospital beds and 1% of ICU beds are in rural areas. Although the US has the highest per capita number of ICU beds in the world, this may not be sufficient as these are concentrated in highly populated metropolitan areas.
Infrastructure and human power resource augmentation will be important. Infrastructure can be ramped up by:
- Canceling elective procedures
- Using the operating room and perioperative room ventilators and beds
- Servicing and using older functioning hospitals, medical wards, and ventilators.
As ventilators are expected to be in short supply, while far from ideal, other resources may include using ventilators from the Strategic National Stockpile, renting from vendors, and using state-owned stockpiles. Use of non-invasive ventilators, such as CPAP (continuous positive airway pressure), BiPAP (bi-level positive airway pressure), and HFNC (high-flow nasal cannula) may be considered in addition to full-featured ventilators. Rapidly manufacturing new ventilators with government direction is also being undertaken.
Although estimates vary based on the model used, about 1 million people are expected to need ventilatory support. However, in addition to infrastructural shortcomings, trained persons to care for these patients are lacking. Approximately 48% of acute care hospitals have no intensivists, and there are only 28,808 intensivists as per 2015 AHA data. In order to increase the amount of skilled manpower needed to staff ICUs, a model from the Society of Critical Care Medicine’s Fundamental Disaster Management Program can be adopted. This involves an intensivist overseeing four different teams, with each team caring for 24 patients. Each team is led by a non-ICU physician or an ICU advanced practice provider (APP) who in turn cares for the patient with respiratory therapists, pharmacists, ICU nurses, and other non-ICU health professionals.
It is essential that infrastructure and human power be augmented and optimized, as well as contingency plans, including triage based on ethical and legal considerations, put in place if demand overwhelms capacity.
Lack of PPE and fear among health care staff
There have been widespread reports in the media, and several anecdotal reports, about severe shortages of personal protective equipment (PPE), and as a result, an increase in fear and anxiety among frontline health care workers.
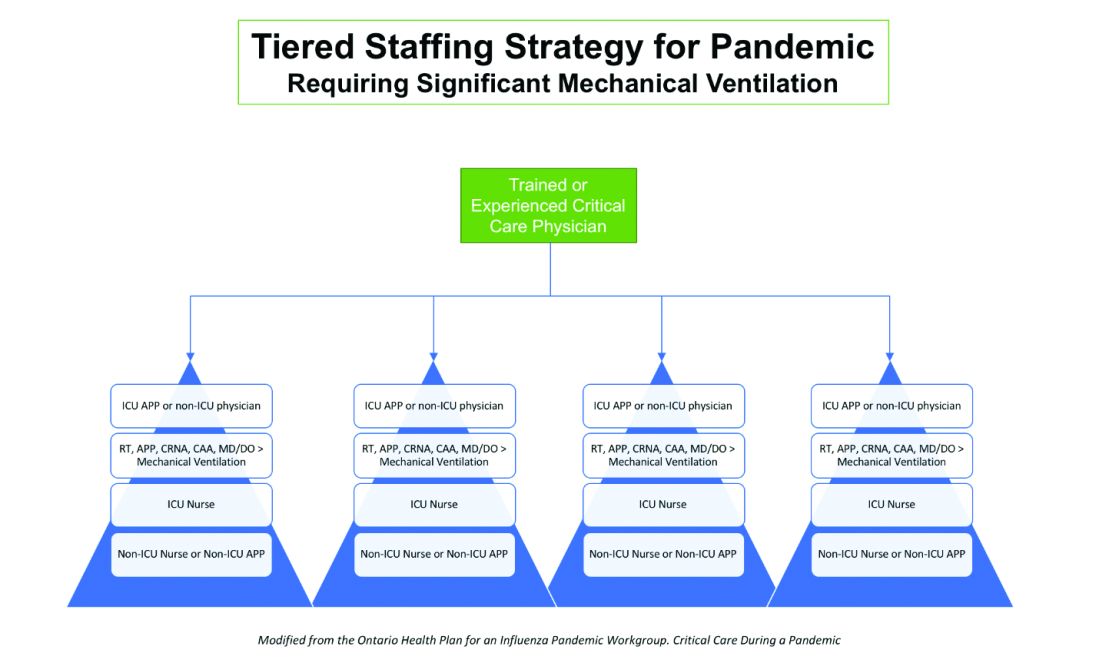
In addition, there also have been reports about hospital administrators disciplining medical and nursing staff for voicing their concerns about PPE shortages to the general public and the media. This likely stems from the narrow “optics” and public relations concerns of health care facilities.
It is evident that the size and magnitude of the COVID-19 pandemic was grossly underestimated, and preparations were inadequate. But according to past surveys of health care workers, a good number of them believe that medical and nursing staff have a duty to deliver care to sick people even if it exposes them to personal danger.
Given the special skills and privileges that health care professionals possess, they do have a moral and ethical responsibility to take care of sick patients even if a danger to themselves exists. However, society also has a responsibility to provide for the safety of these health care workers by supplying them with appropriate safety gear. Given the unprecedented nature of this pandemic, it is obvious that federal and state governments, public health officials, and hospital administrators (along with health care professionals) are still learning how to appropriately respond to the challenge.
It would be reasonable and appropriate for everyone concerned to understand and acknowledge that there is a shortage of PPE, and while arranging for this to be replenished, undertake and implement measures that maximize the safety of all health care workers. An open forum, mutually agreed-upon policy and procedures, along with mechanisms to address concerns should be formulated.
In addition, health care workers who test positive for COVID-19 can be a source of infection for other health care workers and non-infected patients. Therefore, health care workers have the responsibility of reporting their symptoms, the right to have themselves tested, and they must follow agreed-upon procedures that would limit their ability to infect other people, including mandated absenteeism from work. Every individual has a right to safety at the workplace and this right cannot be compromised, as otherwise this will lead to a suboptimal response to the pandemic. The government, hospital administrators, and health care workers will need to come together and work cohesively.
Ethical issues surrounding resource allocation
At the time of hospital admission, any suspected or confirmed COVID-19 patient should have his or her wishes recorded with the admitting team regarding the goals of care and code status. During any critical illness, goals evolve depending on discussions, reflections of the patient with family, and clinical response to therapy. A patient who does not want any kind of life support obviously should not be offered an ICU level of care.
On the other hand, in the event of resources becoming overwhelmed by demand as can be expected during this pandemic, careful ethical considerations will need to be applied.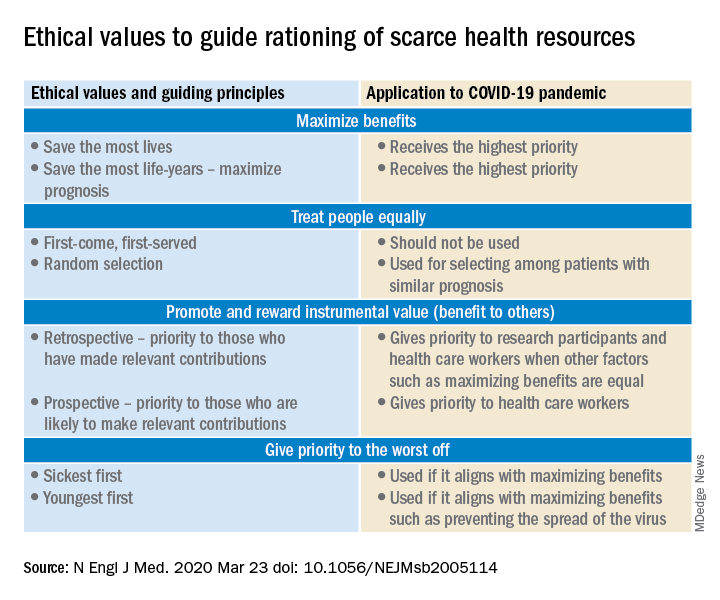
A carefully crafted transparent ethical framework, with a clear understanding of the decision-making process, that involves all stakeholders – including government entities, public health officials, health care workers, ethics specialists, and members of the community – is essential. Ideally, allocation of resources should be made according to a well-written plan, by a triage team that can include a nontreating physician, bioethicists, legal personnel, and religious representatives. It should not be left to the front-line treating physician, who is unlikely to be trained to make these decisions and who has an ethical responsibility to advocate for the patient under his care.
Ethical principles that deserve consideration
The “principle of utility” provides the maximum possible benefit to the maximum number of people. It should not only save the greatest number of lives but also maximize improvements in individuals’ posttreatment length of life.
The “principle of equity” requires that resources are allocated on a nondiscriminatory basis with a fair distribution of benefits and burdens. When conflicts arise between these two principles, a balanced approach likely will help when handled with a transparent decision-making process, with decisions to be applied consistently. Most experts would agree on not only saving more lives but also in preserving more years of life.
The distribution of medical resources should not be based on age or disability. Frailty and functional status are important considerations; however, priority is to be given to sicker patients who have lesser comorbidities and are also likely to survive longer. This could entail that younger, healthier patients will access scarce resources based on the principle of maximizing benefits.
Another consideration is “preservation of functioning of the society.” Those individuals who are important for providing important public services, health care services, and the functioning of other key aspects of society can be considered for prioritization of resources. While this may not satisfy the classic utilitarian principle of doing maximum good to the maximum number of people, it will help to continue augmenting the fight against the pandemic because of the critical role that such individuals play.
For patients with a similar prognosis, the principle of equality comes into play, and distribution should be done by way of random allocation, like a lottery. Distribution based on the principle of “first come, first served” is unlikely to be a fair process, as it would likely discriminate against patients based on their ability to access care.
Care should also be taken not to discriminate among people who have COVID-19 and non–COVID-19 health conditions that require medical care. Distribution should never be done based on an individual’s political influence, celebrity, or financial status, as occurred in the early days of the pandemic regarding access to testing.
Resuscitation or not?
Should a COVID-19 positive patient be offered CPR in case of cardiac arrest? The concern is that CPR is a high-level aerosolizing procedure and PPE is in short supply with the worsening of the pandemic. This will depend more on local policies and resource availability, along with goals of care that have to be determined at the time of admission and subsequent conversations.
The American Hospital Association has issued a general guideline and as more data become available, we can have more informed discussions with patients and families. At this point, all due precautions that prevent the infection of health care personnel are applicable.
Ethical considerations often do not have answers that are a universal fit, and the challenge is always to promote the best interest of the patient with a balance of judiciously utilizing scarce community resources.
Although many states have had discussions and some even have written policies, they have never been implemented. The organization and application of a judicious ethical “crisis level of care” is extremely challenging and likely to test the foundation and fabric of the society.
Dr. Jain is senior associate consultant, hospital & critical care medicine, at Mayo Clinic in Mankato, Minn. He is a board-certified internal medicine, pulmonary, and critical care physician, and has special interests in rural medicine and ethical issues involving critical care medicine. Dr. Tirupathi is the medical director of keystone infectious diseases/HIV in Chambersburg and is currently chair of infection prevention at Wellspan Chambersburg and Waynesboro Hospitals, all in Pennsylvania. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson, and a member of the editorial advisory board for The Hospitalist.
Sources
1. United States Resource Availability for COVID-19. SCCM Blog.
2. Intensive care medicine: Triage in case of bottlenecks. l
3. Interim Guidance for Healthcare Providers during COVID-19 Outbreak.
4. Emanuel EJ et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020 Mar 23.doi: 10.1056/NEJMsb2005114.
5. Devnani M et al. Planning and response to the influenza A (H1N1) pandemic: Ethics, equity and justice. Indian J Med Ethics. 2011 Oct-Dec;8(4):237-40.
6. Alexander C and Wynia M. Ready and willing? Physicians’ sense of preparedness for bioterrorism. Health Aff (Millwood). 2003 Sep-Oct;22(5):189-97.
7. Damery S et al. Healthcare workers’ perceptions of the duty to work during an influenza pandemic. J Med Ethics. 2010 Jan;36(1):12-8.
COVID-19 has been a watershed event in medical history of epic proportions. With this fast-spreading pandemic stretching resources at health care institutions, practical considerations for management of a disease about which we are still learning has been a huge challenge.
Although many guidelines have been made available by medical societies and experts worldwide, there appear to be very few which throw light on management in a resource-poor setup. The hospitalist, as a front-line provider, is likely expected to lead the planning and management of resources in order to deliver appropriate care.
As per American Hospital Association data, there are 2,704 community hospitals that can deliver ICU care in the United States. There are 534,964 acute care beds with 96,596 ICU beds. Additionally, there are 25,157 step-down beds and 1,183 burn unit beds. Of the 2,704 hospitals, 74% are in metropolitan areas (> 50,000 population), 17% (464) are in micropolitan areas (10,000-49,999 population), and the remaining 9% (244) are in rural areas. Only 7% (36,453) of hospital beds and 5% (4715) of ICU beds are in micropolitan areas. Two percent of acute care hospital beds and 1% of ICU beds are in rural areas. Although the US has the highest per capita number of ICU beds in the world, this may not be sufficient as these are concentrated in highly populated metropolitan areas.
Infrastructure and human power resource augmentation will be important. Infrastructure can be ramped up by:
- Canceling elective procedures
- Using the operating room and perioperative room ventilators and beds
- Servicing and using older functioning hospitals, medical wards, and ventilators.
As ventilators are expected to be in short supply, while far from ideal, other resources may include using ventilators from the Strategic National Stockpile, renting from vendors, and using state-owned stockpiles. Use of non-invasive ventilators, such as CPAP (continuous positive airway pressure), BiPAP (bi-level positive airway pressure), and HFNC (high-flow nasal cannula) may be considered in addition to full-featured ventilators. Rapidly manufacturing new ventilators with government direction is also being undertaken.
Although estimates vary based on the model used, about 1 million people are expected to need ventilatory support. However, in addition to infrastructural shortcomings, trained persons to care for these patients are lacking. Approximately 48% of acute care hospitals have no intensivists, and there are only 28,808 intensivists as per 2015 AHA data. In order to increase the amount of skilled manpower needed to staff ICUs, a model from the Society of Critical Care Medicine’s Fundamental Disaster Management Program can be adopted. This involves an intensivist overseeing four different teams, with each team caring for 24 patients. Each team is led by a non-ICU physician or an ICU advanced practice provider (APP) who in turn cares for the patient with respiratory therapists, pharmacists, ICU nurses, and other non-ICU health professionals.
It is essential that infrastructure and human power be augmented and optimized, as well as contingency plans, including triage based on ethical and legal considerations, put in place if demand overwhelms capacity.
Lack of PPE and fear among health care staff
There have been widespread reports in the media, and several anecdotal reports, about severe shortages of personal protective equipment (PPE), and as a result, an increase in fear and anxiety among frontline health care workers.
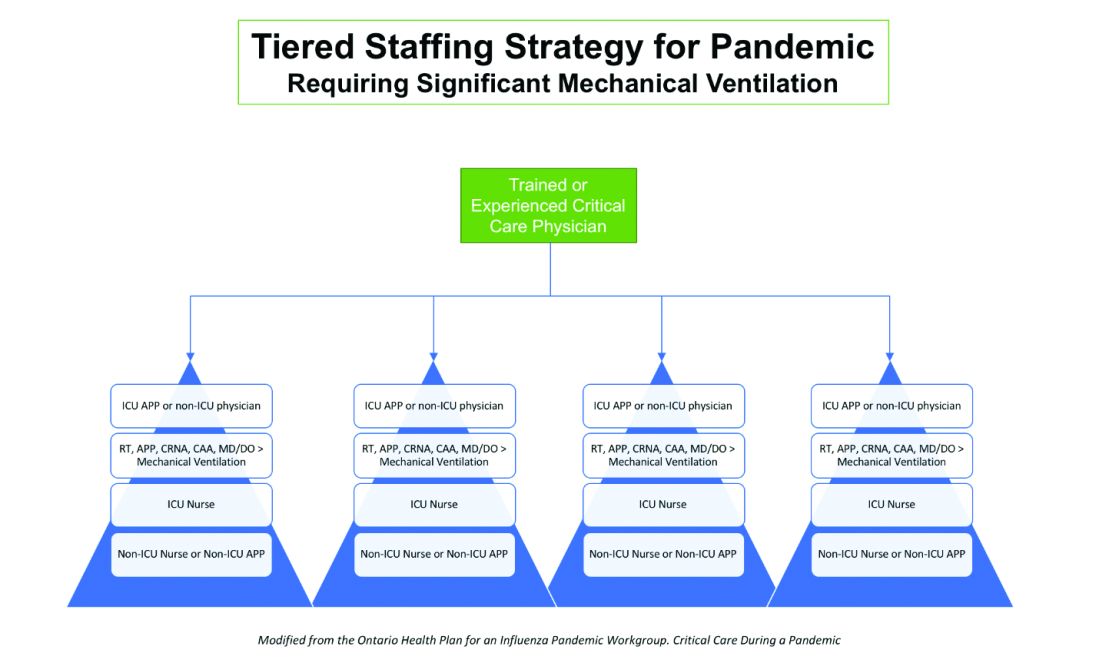
In addition, there also have been reports about hospital administrators disciplining medical and nursing staff for voicing their concerns about PPE shortages to the general public and the media. This likely stems from the narrow “optics” and public relations concerns of health care facilities.
It is evident that the size and magnitude of the COVID-19 pandemic was grossly underestimated, and preparations were inadequate. But according to past surveys of health care workers, a good number of them believe that medical and nursing staff have a duty to deliver care to sick people even if it exposes them to personal danger.
Given the special skills and privileges that health care professionals possess, they do have a moral and ethical responsibility to take care of sick patients even if a danger to themselves exists. However, society also has a responsibility to provide for the safety of these health care workers by supplying them with appropriate safety gear. Given the unprecedented nature of this pandemic, it is obvious that federal and state governments, public health officials, and hospital administrators (along with health care professionals) are still learning how to appropriately respond to the challenge.
It would be reasonable and appropriate for everyone concerned to understand and acknowledge that there is a shortage of PPE, and while arranging for this to be replenished, undertake and implement measures that maximize the safety of all health care workers. An open forum, mutually agreed-upon policy and procedures, along with mechanisms to address concerns should be formulated.
In addition, health care workers who test positive for COVID-19 can be a source of infection for other health care workers and non-infected patients. Therefore, health care workers have the responsibility of reporting their symptoms, the right to have themselves tested, and they must follow agreed-upon procedures that would limit their ability to infect other people, including mandated absenteeism from work. Every individual has a right to safety at the workplace and this right cannot be compromised, as otherwise this will lead to a suboptimal response to the pandemic. The government, hospital administrators, and health care workers will need to come together and work cohesively.
Ethical issues surrounding resource allocation
At the time of hospital admission, any suspected or confirmed COVID-19 patient should have his or her wishes recorded with the admitting team regarding the goals of care and code status. During any critical illness, goals evolve depending on discussions, reflections of the patient with family, and clinical response to therapy. A patient who does not want any kind of life support obviously should not be offered an ICU level of care.
On the other hand, in the event of resources becoming overwhelmed by demand as can be expected during this pandemic, careful ethical considerations will need to be applied.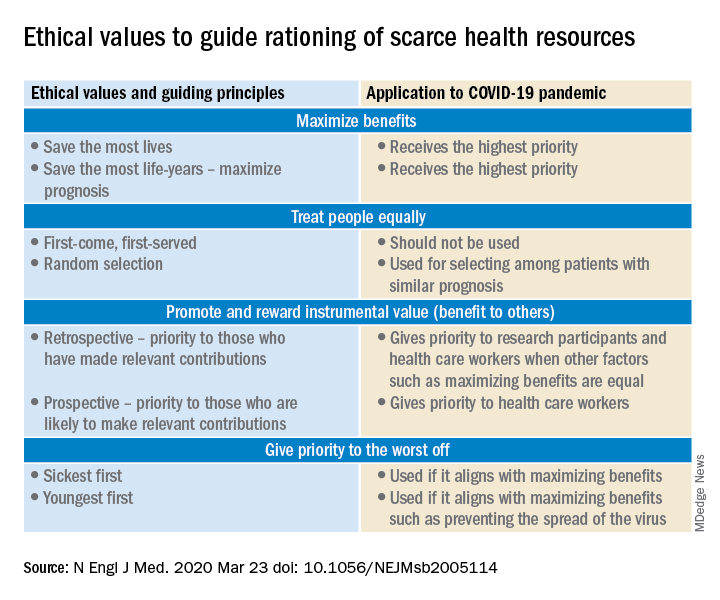
A carefully crafted transparent ethical framework, with a clear understanding of the decision-making process, that involves all stakeholders – including government entities, public health officials, health care workers, ethics specialists, and members of the community – is essential. Ideally, allocation of resources should be made according to a well-written plan, by a triage team that can include a nontreating physician, bioethicists, legal personnel, and religious representatives. It should not be left to the front-line treating physician, who is unlikely to be trained to make these decisions and who has an ethical responsibility to advocate for the patient under his care.
Ethical principles that deserve consideration
The “principle of utility” provides the maximum possible benefit to the maximum number of people. It should not only save the greatest number of lives but also maximize improvements in individuals’ posttreatment length of life.
The “principle of equity” requires that resources are allocated on a nondiscriminatory basis with a fair distribution of benefits and burdens. When conflicts arise between these two principles, a balanced approach likely will help when handled with a transparent decision-making process, with decisions to be applied consistently. Most experts would agree on not only saving more lives but also in preserving more years of life.
The distribution of medical resources should not be based on age or disability. Frailty and functional status are important considerations; however, priority is to be given to sicker patients who have lesser comorbidities and are also likely to survive longer. This could entail that younger, healthier patients will access scarce resources based on the principle of maximizing benefits.
Another consideration is “preservation of functioning of the society.” Those individuals who are important for providing important public services, health care services, and the functioning of other key aspects of society can be considered for prioritization of resources. While this may not satisfy the classic utilitarian principle of doing maximum good to the maximum number of people, it will help to continue augmenting the fight against the pandemic because of the critical role that such individuals play.
For patients with a similar prognosis, the principle of equality comes into play, and distribution should be done by way of random allocation, like a lottery. Distribution based on the principle of “first come, first served” is unlikely to be a fair process, as it would likely discriminate against patients based on their ability to access care.
Care should also be taken not to discriminate among people who have COVID-19 and non–COVID-19 health conditions that require medical care. Distribution should never be done based on an individual’s political influence, celebrity, or financial status, as occurred in the early days of the pandemic regarding access to testing.
Resuscitation or not?
Should a COVID-19 positive patient be offered CPR in case of cardiac arrest? The concern is that CPR is a high-level aerosolizing procedure and PPE is in short supply with the worsening of the pandemic. This will depend more on local policies and resource availability, along with goals of care that have to be determined at the time of admission and subsequent conversations.
The American Hospital Association has issued a general guideline and as more data become available, we can have more informed discussions with patients and families. At this point, all due precautions that prevent the infection of health care personnel are applicable.
Ethical considerations often do not have answers that are a universal fit, and the challenge is always to promote the best interest of the patient with a balance of judiciously utilizing scarce community resources.
Although many states have had discussions and some even have written policies, they have never been implemented. The organization and application of a judicious ethical “crisis level of care” is extremely challenging and likely to test the foundation and fabric of the society.
Dr. Jain is senior associate consultant, hospital & critical care medicine, at Mayo Clinic in Mankato, Minn. He is a board-certified internal medicine, pulmonary, and critical care physician, and has special interests in rural medicine and ethical issues involving critical care medicine. Dr. Tirupathi is the medical director of keystone infectious diseases/HIV in Chambersburg and is currently chair of infection prevention at Wellspan Chambersburg and Waynesboro Hospitals, all in Pennsylvania. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson, and a member of the editorial advisory board for The Hospitalist.
Sources
1. United States Resource Availability for COVID-19. SCCM Blog.
2. Intensive care medicine: Triage in case of bottlenecks. l
3. Interim Guidance for Healthcare Providers during COVID-19 Outbreak.
4. Emanuel EJ et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020 Mar 23.doi: 10.1056/NEJMsb2005114.
5. Devnani M et al. Planning and response to the influenza A (H1N1) pandemic: Ethics, equity and justice. Indian J Med Ethics. 2011 Oct-Dec;8(4):237-40.
6. Alexander C and Wynia M. Ready and willing? Physicians’ sense of preparedness for bioterrorism. Health Aff (Millwood). 2003 Sep-Oct;22(5):189-97.
7. Damery S et al. Healthcare workers’ perceptions of the duty to work during an influenza pandemic. J Med Ethics. 2010 Jan;36(1):12-8.
COVID-19 has been a watershed event in medical history of epic proportions. With this fast-spreading pandemic stretching resources at health care institutions, practical considerations for management of a disease about which we are still learning has been a huge challenge.
Although many guidelines have been made available by medical societies and experts worldwide, there appear to be very few which throw light on management in a resource-poor setup. The hospitalist, as a front-line provider, is likely expected to lead the planning and management of resources in order to deliver appropriate care.
As per American Hospital Association data, there are 2,704 community hospitals that can deliver ICU care in the United States. There are 534,964 acute care beds with 96,596 ICU beds. Additionally, there are 25,157 step-down beds and 1,183 burn unit beds. Of the 2,704 hospitals, 74% are in metropolitan areas (> 50,000 population), 17% (464) are in micropolitan areas (10,000-49,999 population), and the remaining 9% (244) are in rural areas. Only 7% (36,453) of hospital beds and 5% (4715) of ICU beds are in micropolitan areas. Two percent of acute care hospital beds and 1% of ICU beds are in rural areas. Although the US has the highest per capita number of ICU beds in the world, this may not be sufficient as these are concentrated in highly populated metropolitan areas.
Infrastructure and human power resource augmentation will be important. Infrastructure can be ramped up by:
- Canceling elective procedures
- Using the operating room and perioperative room ventilators and beds
- Servicing and using older functioning hospitals, medical wards, and ventilators.
As ventilators are expected to be in short supply, while far from ideal, other resources may include using ventilators from the Strategic National Stockpile, renting from vendors, and using state-owned stockpiles. Use of non-invasive ventilators, such as CPAP (continuous positive airway pressure), BiPAP (bi-level positive airway pressure), and HFNC (high-flow nasal cannula) may be considered in addition to full-featured ventilators. Rapidly manufacturing new ventilators with government direction is also being undertaken.
Although estimates vary based on the model used, about 1 million people are expected to need ventilatory support. However, in addition to infrastructural shortcomings, trained persons to care for these patients are lacking. Approximately 48% of acute care hospitals have no intensivists, and there are only 28,808 intensivists as per 2015 AHA data. In order to increase the amount of skilled manpower needed to staff ICUs, a model from the Society of Critical Care Medicine’s Fundamental Disaster Management Program can be adopted. This involves an intensivist overseeing four different teams, with each team caring for 24 patients. Each team is led by a non-ICU physician or an ICU advanced practice provider (APP) who in turn cares for the patient with respiratory therapists, pharmacists, ICU nurses, and other non-ICU health professionals.
It is essential that infrastructure and human power be augmented and optimized, as well as contingency plans, including triage based on ethical and legal considerations, put in place if demand overwhelms capacity.
Lack of PPE and fear among health care staff
There have been widespread reports in the media, and several anecdotal reports, about severe shortages of personal protective equipment (PPE), and as a result, an increase in fear and anxiety among frontline health care workers.
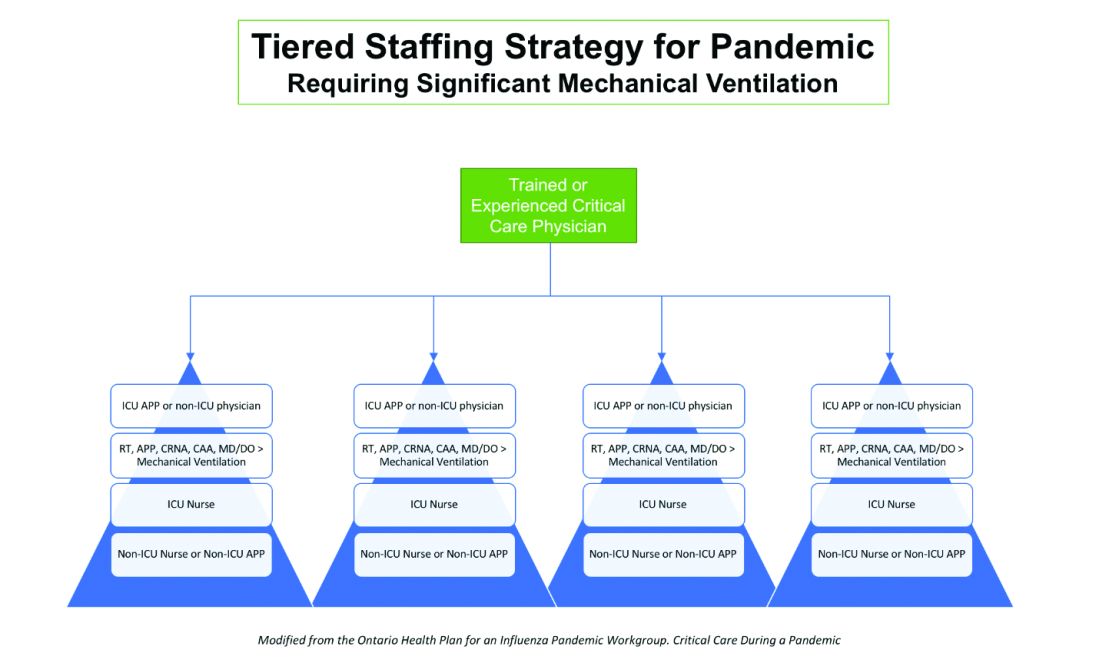
In addition, there also have been reports about hospital administrators disciplining medical and nursing staff for voicing their concerns about PPE shortages to the general public and the media. This likely stems from the narrow “optics” and public relations concerns of health care facilities.
It is evident that the size and magnitude of the COVID-19 pandemic was grossly underestimated, and preparations were inadequate. But according to past surveys of health care workers, a good number of them believe that medical and nursing staff have a duty to deliver care to sick people even if it exposes them to personal danger.
Given the special skills and privileges that health care professionals possess, they do have a moral and ethical responsibility to take care of sick patients even if a danger to themselves exists. However, society also has a responsibility to provide for the safety of these health care workers by supplying them with appropriate safety gear. Given the unprecedented nature of this pandemic, it is obvious that federal and state governments, public health officials, and hospital administrators (along with health care professionals) are still learning how to appropriately respond to the challenge.
It would be reasonable and appropriate for everyone concerned to understand and acknowledge that there is a shortage of PPE, and while arranging for this to be replenished, undertake and implement measures that maximize the safety of all health care workers. An open forum, mutually agreed-upon policy and procedures, along with mechanisms to address concerns should be formulated.
In addition, health care workers who test positive for COVID-19 can be a source of infection for other health care workers and non-infected patients. Therefore, health care workers have the responsibility of reporting their symptoms, the right to have themselves tested, and they must follow agreed-upon procedures that would limit their ability to infect other people, including mandated absenteeism from work. Every individual has a right to safety at the workplace and this right cannot be compromised, as otherwise this will lead to a suboptimal response to the pandemic. The government, hospital administrators, and health care workers will need to come together and work cohesively.
Ethical issues surrounding resource allocation
At the time of hospital admission, any suspected or confirmed COVID-19 patient should have his or her wishes recorded with the admitting team regarding the goals of care and code status. During any critical illness, goals evolve depending on discussions, reflections of the patient with family, and clinical response to therapy. A patient who does not want any kind of life support obviously should not be offered an ICU level of care.
On the other hand, in the event of resources becoming overwhelmed by demand as can be expected during this pandemic, careful ethical considerations will need to be applied.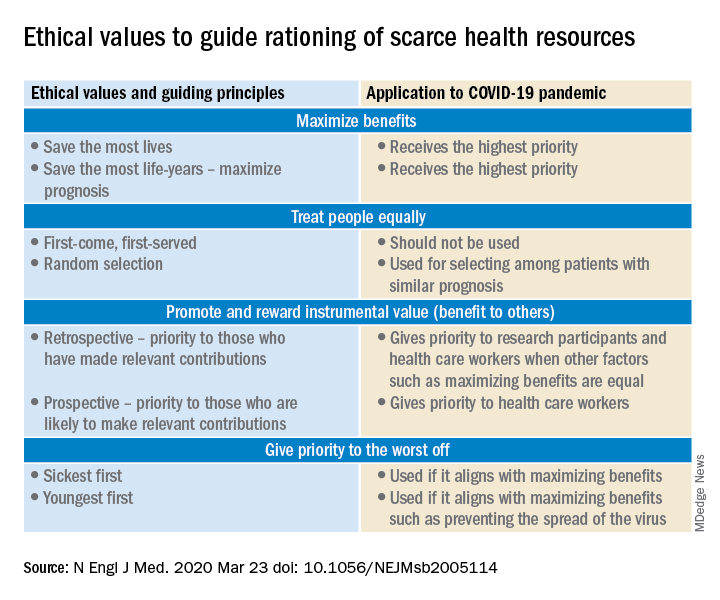
A carefully crafted transparent ethical framework, with a clear understanding of the decision-making process, that involves all stakeholders – including government entities, public health officials, health care workers, ethics specialists, and members of the community – is essential. Ideally, allocation of resources should be made according to a well-written plan, by a triage team that can include a nontreating physician, bioethicists, legal personnel, and religious representatives. It should not be left to the front-line treating physician, who is unlikely to be trained to make these decisions and who has an ethical responsibility to advocate for the patient under his care.
Ethical principles that deserve consideration
The “principle of utility” provides the maximum possible benefit to the maximum number of people. It should not only save the greatest number of lives but also maximize improvements in individuals’ posttreatment length of life.
The “principle of equity” requires that resources are allocated on a nondiscriminatory basis with a fair distribution of benefits and burdens. When conflicts arise between these two principles, a balanced approach likely will help when handled with a transparent decision-making process, with decisions to be applied consistently. Most experts would agree on not only saving more lives but also in preserving more years of life.
The distribution of medical resources should not be based on age or disability. Frailty and functional status are important considerations; however, priority is to be given to sicker patients who have lesser comorbidities and are also likely to survive longer. This could entail that younger, healthier patients will access scarce resources based on the principle of maximizing benefits.
Another consideration is “preservation of functioning of the society.” Those individuals who are important for providing important public services, health care services, and the functioning of other key aspects of society can be considered for prioritization of resources. While this may not satisfy the classic utilitarian principle of doing maximum good to the maximum number of people, it will help to continue augmenting the fight against the pandemic because of the critical role that such individuals play.
For patients with a similar prognosis, the principle of equality comes into play, and distribution should be done by way of random allocation, like a lottery. Distribution based on the principle of “first come, first served” is unlikely to be a fair process, as it would likely discriminate against patients based on their ability to access care.
Care should also be taken not to discriminate among people who have COVID-19 and non–COVID-19 health conditions that require medical care. Distribution should never be done based on an individual’s political influence, celebrity, or financial status, as occurred in the early days of the pandemic regarding access to testing.
Resuscitation or not?
Should a COVID-19 positive patient be offered CPR in case of cardiac arrest? The concern is that CPR is a high-level aerosolizing procedure and PPE is in short supply with the worsening of the pandemic. This will depend more on local policies and resource availability, along with goals of care that have to be determined at the time of admission and subsequent conversations.
The American Hospital Association has issued a general guideline and as more data become available, we can have more informed discussions with patients and families. At this point, all due precautions that prevent the infection of health care personnel are applicable.
Ethical considerations often do not have answers that are a universal fit, and the challenge is always to promote the best interest of the patient with a balance of judiciously utilizing scarce community resources.
Although many states have had discussions and some even have written policies, they have never been implemented. The organization and application of a judicious ethical “crisis level of care” is extremely challenging and likely to test the foundation and fabric of the society.
Dr. Jain is senior associate consultant, hospital & critical care medicine, at Mayo Clinic in Mankato, Minn. He is a board-certified internal medicine, pulmonary, and critical care physician, and has special interests in rural medicine and ethical issues involving critical care medicine. Dr. Tirupathi is the medical director of keystone infectious diseases/HIV in Chambersburg and is currently chair of infection prevention at Wellspan Chambersburg and Waynesboro Hospitals, all in Pennsylvania. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson, and a member of the editorial advisory board for The Hospitalist.
Sources
1. United States Resource Availability for COVID-19. SCCM Blog.
2. Intensive care medicine: Triage in case of bottlenecks. l
3. Interim Guidance for Healthcare Providers during COVID-19 Outbreak.
4. Emanuel EJ et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020 Mar 23.doi: 10.1056/NEJMsb2005114.
5. Devnani M et al. Planning and response to the influenza A (H1N1) pandemic: Ethics, equity and justice. Indian J Med Ethics. 2011 Oct-Dec;8(4):237-40.
6. Alexander C and Wynia M. Ready and willing? Physicians’ sense of preparedness for bioterrorism. Health Aff (Millwood). 2003 Sep-Oct;22(5):189-97.
7. Damery S et al. Healthcare workers’ perceptions of the duty to work during an influenza pandemic. J Med Ethics. 2010 Jan;36(1):12-8.
ABIM grants MOC extension
Physicians will not lose their certification if they are unable to complete maintenance of certification requirements in 2020, the American Board of Internal Medicine announced.
ABIM President Richard Baron, MD, said in a letter sent to all diplomates.
Additionally, physicians “currently in their grace year will also be afforded an additional grace year in 2021,” the letter continued.
ABIM noted that many assessments were planned for the fall of 2020 and the organization will continue to offer them as planned for physicians who are able to take them. It added that more assessment dates for 2020 and 2021 will be sent out later this year.
“The next few weeks and months will challenge our health care system and country like never before,” Dr. Baron stated. “Our many internal medicine colleagues – and the clinical teams that support them – have been heroic in their response, often selflessly putting their own personal safety at risk while using their superb skills to provide care for others. They have inspired all of us.”
Physicians will not lose their certification if they are unable to complete maintenance of certification requirements in 2020, the American Board of Internal Medicine announced.
ABIM President Richard Baron, MD, said in a letter sent to all diplomates.
Additionally, physicians “currently in their grace year will also be afforded an additional grace year in 2021,” the letter continued.
ABIM noted that many assessments were planned for the fall of 2020 and the organization will continue to offer them as planned for physicians who are able to take them. It added that more assessment dates for 2020 and 2021 will be sent out later this year.
“The next few weeks and months will challenge our health care system and country like never before,” Dr. Baron stated. “Our many internal medicine colleagues – and the clinical teams that support them – have been heroic in their response, often selflessly putting their own personal safety at risk while using their superb skills to provide care for others. They have inspired all of us.”
Physicians will not lose their certification if they are unable to complete maintenance of certification requirements in 2020, the American Board of Internal Medicine announced.
ABIM President Richard Baron, MD, said in a letter sent to all diplomates.
Additionally, physicians “currently in their grace year will also be afforded an additional grace year in 2021,” the letter continued.
ABIM noted that many assessments were planned for the fall of 2020 and the organization will continue to offer them as planned for physicians who are able to take them. It added that more assessment dates for 2020 and 2021 will be sent out later this year.
“The next few weeks and months will challenge our health care system and country like never before,” Dr. Baron stated. “Our many internal medicine colleagues – and the clinical teams that support them – have been heroic in their response, often selflessly putting their own personal safety at risk while using their superb skills to provide care for others. They have inspired all of us.”
Presymptomatic or asymptomatic? ID experts on shifting terminology
They also addressed racial disparities surrounding COVID-19, and announced new IDSA guidelines for diagnosis and treatment of the illness.
Regarding the shifting thinking on symptoms and transmission of the novel coronavirus, when it comes to presymptomatic or asymptomatic, “pre” is really the right terminology, Carlos del Rio, MD, professor of medicine, Division of Infectious Diseases, Emory University School of Medicine, Atlanta, Georgia, said during the briefing, because it’s not that people are asymptomatic but that they develop symptoms later and start transmitting the virus 24 to 48 hours before they develop symptoms.
“Clearly, this plays a role in transmission,” with some studies suggesting that 6% to 12% of transmissions occur during this presymptomatic stage, he explained.
Jeanne Marrazzo, MD, MPH, director of the Division of Infectious Diseases at University of Alabama at Birmingham, noted that early in the COVID-19 pandemic, the presymptomatic phase “could have been missed because we didn’t realize the wide ranging symptoms this disease has.”
This is turning out to be a “very interesting” virus with “fascinating” symptoms, she told reporters on the call.
The virus seems to have capacity to affect far more than just the respiratory tract. Initially, however, it was viewed “very much like a classic respiratory viral infection. As a result, a lot of people were refused testing because they were not showing the classic signs” of respiratory infection, Marrazzo noted.
It’s now clear that the range of symptoms is quite different, she said.
Notably, loss of smell seems to be “very characteristic and very specific to this infection. I can’t think of another common viral infection that causes loss of smell before you start to see other things,” Marrazzo said.
Data also suggest that gastrointestinal symptoms are common with COVID-19. Early data suggest that diarrhea probably occurs in about one third of patients. Some people have reported abdominal pain as the first sign, she said.
“Now that we know about the more wide range of symptoms associated [with COVID-19], we are being much more open to considering people perhaps having this infection. There is a lower index of suspicion and much lower threshold for diagnostic testing,” Marrazzo said, adding that there are still many barriers to testing and getting test results.
Stark Racial Disparities Need Greater Understanding
The second major topic of discussion at the briefing was the growing realization of racial disparities in COVID-19.
“Racial disparities in our country are not new but racial disparities in this disease are pretty stark,” del Rio said. “We live in a country where disparities have really colored a lot of what our diseases are, from HIV to diabetes to hypertension, and it’s not surprising that we are seeing this now with COVID-19.”
Marrazzo noted that, in Alabama, around 20% of the population is African American, yet almost 40% of COVID-19 deaths are occurring in this population. “The most stark statistics are coming out of Illinois and Michigan, where less than around 15% of the population is African American and yet 70% of the deaths are occurring in that group,” she said.
Both del Rio and Marrazzo agreed that understanding the racial differences in COVID-19 deaths is going to require a lot of analysis in the coming months.
Part of it likely reflects the challenge of social distancing in urban areas, Marrazzo said. “Social distancing is a luxury afforded by having a really big space, and space is money.”
The other long-standing challenge of unequal access to healthcare also likely plays a role, she said. This includes missing out on preventive health appointments and screenings, which can translate into more comorbidities, particularly hypertension.
The evolving evidence about the virus, and the stark conditions that frontline clinicians face, make this an especially challenging public health crisis, del Rio said.
“Taking care of these patients is incredibly taxing and my hat is off to physicians, residents, nurses, everybody working on this in the hospitals because they are really doing a yeoman’s work,” he said.
“These are not easy patients to take care of. Not only are [the frontline clinicians] providing care, they are caring for the patient and providing a comfort and someone to listen to when family can’t be present,” del Rio emphasized.
New Guidelines
The IDSA just released new guidelines for diagnosis and treatment of COVID-19.
“We are learning new things every day about this virus. Things are rapidly changing, and as we learn new things we have to adapt and make changes,” del Rio said.
del Rio noted that the guildelines “will evolve and change as more information comes out.”
This article first appeared on Medscape.com.
They also addressed racial disparities surrounding COVID-19, and announced new IDSA guidelines for diagnosis and treatment of the illness.
Regarding the shifting thinking on symptoms and transmission of the novel coronavirus, when it comes to presymptomatic or asymptomatic, “pre” is really the right terminology, Carlos del Rio, MD, professor of medicine, Division of Infectious Diseases, Emory University School of Medicine, Atlanta, Georgia, said during the briefing, because it’s not that people are asymptomatic but that they develop symptoms later and start transmitting the virus 24 to 48 hours before they develop symptoms.
“Clearly, this plays a role in transmission,” with some studies suggesting that 6% to 12% of transmissions occur during this presymptomatic stage, he explained.
Jeanne Marrazzo, MD, MPH, director of the Division of Infectious Diseases at University of Alabama at Birmingham, noted that early in the COVID-19 pandemic, the presymptomatic phase “could have been missed because we didn’t realize the wide ranging symptoms this disease has.”
This is turning out to be a “very interesting” virus with “fascinating” symptoms, she told reporters on the call.
The virus seems to have capacity to affect far more than just the respiratory tract. Initially, however, it was viewed “very much like a classic respiratory viral infection. As a result, a lot of people were refused testing because they were not showing the classic signs” of respiratory infection, Marrazzo noted.
It’s now clear that the range of symptoms is quite different, she said.
Notably, loss of smell seems to be “very characteristic and very specific to this infection. I can’t think of another common viral infection that causes loss of smell before you start to see other things,” Marrazzo said.
Data also suggest that gastrointestinal symptoms are common with COVID-19. Early data suggest that diarrhea probably occurs in about one third of patients. Some people have reported abdominal pain as the first sign, she said.
“Now that we know about the more wide range of symptoms associated [with COVID-19], we are being much more open to considering people perhaps having this infection. There is a lower index of suspicion and much lower threshold for diagnostic testing,” Marrazzo said, adding that there are still many barriers to testing and getting test results.
Stark Racial Disparities Need Greater Understanding
The second major topic of discussion at the briefing was the growing realization of racial disparities in COVID-19.
“Racial disparities in our country are not new but racial disparities in this disease are pretty stark,” del Rio said. “We live in a country where disparities have really colored a lot of what our diseases are, from HIV to diabetes to hypertension, and it’s not surprising that we are seeing this now with COVID-19.”
Marrazzo noted that, in Alabama, around 20% of the population is African American, yet almost 40% of COVID-19 deaths are occurring in this population. “The most stark statistics are coming out of Illinois and Michigan, where less than around 15% of the population is African American and yet 70% of the deaths are occurring in that group,” she said.
Both del Rio and Marrazzo agreed that understanding the racial differences in COVID-19 deaths is going to require a lot of analysis in the coming months.
Part of it likely reflects the challenge of social distancing in urban areas, Marrazzo said. “Social distancing is a luxury afforded by having a really big space, and space is money.”
The other long-standing challenge of unequal access to healthcare also likely plays a role, she said. This includes missing out on preventive health appointments and screenings, which can translate into more comorbidities, particularly hypertension.
The evolving evidence about the virus, and the stark conditions that frontline clinicians face, make this an especially challenging public health crisis, del Rio said.
“Taking care of these patients is incredibly taxing and my hat is off to physicians, residents, nurses, everybody working on this in the hospitals because they are really doing a yeoman’s work,” he said.
“These are not easy patients to take care of. Not only are [the frontline clinicians] providing care, they are caring for the patient and providing a comfort and someone to listen to when family can’t be present,” del Rio emphasized.
New Guidelines
The IDSA just released new guidelines for diagnosis and treatment of COVID-19.
“We are learning new things every day about this virus. Things are rapidly changing, and as we learn new things we have to adapt and make changes,” del Rio said.
del Rio noted that the guildelines “will evolve and change as more information comes out.”
This article first appeared on Medscape.com.
They also addressed racial disparities surrounding COVID-19, and announced new IDSA guidelines for diagnosis and treatment of the illness.
Regarding the shifting thinking on symptoms and transmission of the novel coronavirus, when it comes to presymptomatic or asymptomatic, “pre” is really the right terminology, Carlos del Rio, MD, professor of medicine, Division of Infectious Diseases, Emory University School of Medicine, Atlanta, Georgia, said during the briefing, because it’s not that people are asymptomatic but that they develop symptoms later and start transmitting the virus 24 to 48 hours before they develop symptoms.
“Clearly, this plays a role in transmission,” with some studies suggesting that 6% to 12% of transmissions occur during this presymptomatic stage, he explained.
Jeanne Marrazzo, MD, MPH, director of the Division of Infectious Diseases at University of Alabama at Birmingham, noted that early in the COVID-19 pandemic, the presymptomatic phase “could have been missed because we didn’t realize the wide ranging symptoms this disease has.”
This is turning out to be a “very interesting” virus with “fascinating” symptoms, she told reporters on the call.
The virus seems to have capacity to affect far more than just the respiratory tract. Initially, however, it was viewed “very much like a classic respiratory viral infection. As a result, a lot of people were refused testing because they were not showing the classic signs” of respiratory infection, Marrazzo noted.
It’s now clear that the range of symptoms is quite different, she said.
Notably, loss of smell seems to be “very characteristic and very specific to this infection. I can’t think of another common viral infection that causes loss of smell before you start to see other things,” Marrazzo said.
Data also suggest that gastrointestinal symptoms are common with COVID-19. Early data suggest that diarrhea probably occurs in about one third of patients. Some people have reported abdominal pain as the first sign, she said.
“Now that we know about the more wide range of symptoms associated [with COVID-19], we are being much more open to considering people perhaps having this infection. There is a lower index of suspicion and much lower threshold for diagnostic testing,” Marrazzo said, adding that there are still many barriers to testing and getting test results.
Stark Racial Disparities Need Greater Understanding
The second major topic of discussion at the briefing was the growing realization of racial disparities in COVID-19.
“Racial disparities in our country are not new but racial disparities in this disease are pretty stark,” del Rio said. “We live in a country where disparities have really colored a lot of what our diseases are, from HIV to diabetes to hypertension, and it’s not surprising that we are seeing this now with COVID-19.”
Marrazzo noted that, in Alabama, around 20% of the population is African American, yet almost 40% of COVID-19 deaths are occurring in this population. “The most stark statistics are coming out of Illinois and Michigan, where less than around 15% of the population is African American and yet 70% of the deaths are occurring in that group,” she said.
Both del Rio and Marrazzo agreed that understanding the racial differences in COVID-19 deaths is going to require a lot of analysis in the coming months.
Part of it likely reflects the challenge of social distancing in urban areas, Marrazzo said. “Social distancing is a luxury afforded by having a really big space, and space is money.”
The other long-standing challenge of unequal access to healthcare also likely plays a role, she said. This includes missing out on preventive health appointments and screenings, which can translate into more comorbidities, particularly hypertension.
The evolving evidence about the virus, and the stark conditions that frontline clinicians face, make this an especially challenging public health crisis, del Rio said.
“Taking care of these patients is incredibly taxing and my hat is off to physicians, residents, nurses, everybody working on this in the hospitals because they are really doing a yeoman’s work,” he said.
“These are not easy patients to take care of. Not only are [the frontline clinicians] providing care, they are caring for the patient and providing a comfort and someone to listen to when family can’t be present,” del Rio emphasized.
New Guidelines
The IDSA just released new guidelines for diagnosis and treatment of COVID-19.
“We are learning new things every day about this virus. Things are rapidly changing, and as we learn new things we have to adapt and make changes,” del Rio said.
del Rio noted that the guildelines “will evolve and change as more information comes out.”
This article first appeared on Medscape.com.
COVID-19 hits physician couple: Dramatically different responses
A physician couple who both had COVID-19 had very different responses — one ending up in intensive care, the other asymptomatic.
Their story, one of two people living together but with such different responses to the infection, illustrates how much is still to be learned about COVID-19, says Noopur Raje, MD, professor of medicine at Harvard Medical School and director of the Center for Multiple Myeloma at Massachusetts General Hospital (MGH) in Boston.
“After experiencing #Covid_19 from the patient/caregiver end despite both of us being physicians at a major academic medical center, this has been a challenge like no other I have experienced,” Raje (@NoopurRajeMD) wrote on Twitter.
She outlined their experiences in a Twitter thread and elaborated in an interview with Medscape Medical News.
Raje says that she wants clinicians to know how symptoms can evolve both quickly and suddenly.
She recalls how for 10 days, she cared for her COVID-19–positive husband at home, separated from him by a floor in their Boston townhouse and wearing a surgical mask and gloves to bring him food and fluids, as he was too weak to help himself.
Despite the high fevers, chills, extreme fatigue, and dramatic weight loss, Raje says she felt reasonably confident that her husband was getting better. His temperature had dropped from around 103 to 101, his heart rate was in the 80s, and his blood pressure was “OK,” she recalls.
But then Jag Singh, MD, an otherwise healthy 55-year-old Harvard professor and cardiologist, started to cough — and everything suddenly changed.
The cough sounded chesty, and he was weak and unwell. They decided that he needed medical help.
“I was planning on driving him to the hospital, but I ended up having to call 911, although we literally live across the street,” she said.
“We have stairs here and I wasn’t sure that he would be able to make it coming down with me trying to help him, so the safest thing was for me to call for help.”
Singh was admitted straight to the medical intensive care unit (MICU) while his wife waited at home.
“I was blown away when I saw Jag’s x-ray and CT scan and the bilateral pneumonia he had developed,” she commented. “I would not have believed it, the way he was clinically — and seeing that x-ray.
“Honestly, when I took him in to hospital, I thought he’d be there a couple of days — over the weekend — and I’d get him back Monday. But it didn’t turn out that way. He was there for about 9 days.”
That first night in the hospital, Singh consented to intubation — should he need it. “He called me then,” said Raje. “I said we’ve got to do what we’ve got to do, it’s OK — it is what it is, and we’ll do whatever it takes.”
He remained in the MICU overnight and through the next day, still breathing on his own, but with the looming prospect of mechanical ventilation.
“The good news is he maintained his oxygen saturations throughout,” said Raje. “I was able to see his vitals with EPIC [remote monitoring] ... It was crazy,” she recalls. “Seeing a respiratory rate of 26 was difficult. When you see that, you worry about somebody tiring with the breathing. His inflammatory markers kept climbing, his fevers persisted.”
Thankfully, he never needed the ventilator.
But by this time Raje had another worry: She, too, had tested positive and was now alone at home.
“I was unable to talk to my extended family as they all looked to us as physicians for support,” she tweeted. Both children came to Boston to see her, but she saw them only through a window.
Alone, she waited for the same symptoms that had slammed her husband; but they never came — something she wants caregivers to know.
“The fear and anxiety of taking care of somebody who’s COVID positive ... I am hoping that can be alleviated a little bit at least,” she said. “If you’ve been taking care of someone, chances are you’re probably positive already and if you’re not sick, the chances of you getting sick are really low, so don’t be afraid to take care of that person.”
Singh is recovering well at home now, almost a month into his illness. During the interview, conducted via Zoom, he could be heard coughing in the background.
While in the MICU, Singh was treated with azithromycin and hydroxychloroquine — standard at MGH for critically ill COVID-19 patients — and he was also enrolled into a double-blind, randomized, placebo-controlled trial of the investigational agent remdesivir (Gilead).
Raje is not sure what, if anything, helped him turn the corner.
“I saw his inflammatory markers get worse actually — I don’t think we can know if the drugs made a difference,” she says. “His first dose of hydroxychloroquine was Friday night when he was admitted, and the markers continued to climb until the next Thursday.”
In particular, his C-reactive protein (CRP) kept rising, reaching the 260 to 270 mg/dL range, “which to me was scary,” she said. “I do think he had a cytokine storm going, but I didn’t see those results.”
“Understanding the immune compartment is going to be so, so critically important and what it is that we can do to boost folks’ immune systems,” she said.
“If you have a very high viral load and your immune system is not 100% even though you’re otherwise healthy, you might be the person who ends up with that more serious response to this virus. Trying to study this in a focused way, looking at the immune compartment, looking at the antibody status, looking at the viral load — there’s so much more we need to look at. Until we get the vaccine, which is probably a year-and-a-half away, we need to look at how can we develop that herd immunity so we don’t have folks getting as critically ill as they do.”
Despite feeling perfectly healthy, Raje is still at home. Three weeks after her first test, she is still testing positive for COVID-19, waiting for two consecutive negative results 72 hours apart before she is allowed back to work at the hospital.
When she gets the green light, she plans to go work on the COVID-19 floor, if needed. “It’s people like us [who have had COVID-19] who have to get back in the trenches and do the work now,” she says.
“My biggest concern is that it’s a very isolating experience for the COVID-positive patient. We are doing complete-barrier nursing — they are completely alone. The only person who ever walks into the room is the nurse — and the physician goes in once a day. It’s so important that we don’t lose sight of compassion,” she says.
“That’s why, in terms of alleviating anxiety, it is so important we do antibody testing so that people can actually go in and take care of these folks.”
‘Look for red flag’
Raje wants physicians to warn their self-isolating patients and caregivers to look for red flags. “There are primary care physicians who reached out to me [after my tweets] and said ‘when someone calls me and says it’s been 5-7 days and I am still not feeling well, I am going to look at that more seriously.’
“Part of me wanting to share this experience was basically to dispel the notion that 2 weeks into this you’re going to be fine,” she said, because it is not widely appreciated, she feels that “in week 2, you could become pretty sick.”
This article first appeared on Medscape.com.
A physician couple who both had COVID-19 had very different responses — one ending up in intensive care, the other asymptomatic.
Their story, one of two people living together but with such different responses to the infection, illustrates how much is still to be learned about COVID-19, says Noopur Raje, MD, professor of medicine at Harvard Medical School and director of the Center for Multiple Myeloma at Massachusetts General Hospital (MGH) in Boston.
“After experiencing #Covid_19 from the patient/caregiver end despite both of us being physicians at a major academic medical center, this has been a challenge like no other I have experienced,” Raje (@NoopurRajeMD) wrote on Twitter.
She outlined their experiences in a Twitter thread and elaborated in an interview with Medscape Medical News.
Raje says that she wants clinicians to know how symptoms can evolve both quickly and suddenly.
She recalls how for 10 days, she cared for her COVID-19–positive husband at home, separated from him by a floor in their Boston townhouse and wearing a surgical mask and gloves to bring him food and fluids, as he was too weak to help himself.
Despite the high fevers, chills, extreme fatigue, and dramatic weight loss, Raje says she felt reasonably confident that her husband was getting better. His temperature had dropped from around 103 to 101, his heart rate was in the 80s, and his blood pressure was “OK,” she recalls.
But then Jag Singh, MD, an otherwise healthy 55-year-old Harvard professor and cardiologist, started to cough — and everything suddenly changed.
The cough sounded chesty, and he was weak and unwell. They decided that he needed medical help.
“I was planning on driving him to the hospital, but I ended up having to call 911, although we literally live across the street,” she said.
“We have stairs here and I wasn’t sure that he would be able to make it coming down with me trying to help him, so the safest thing was for me to call for help.”
Singh was admitted straight to the medical intensive care unit (MICU) while his wife waited at home.
“I was blown away when I saw Jag’s x-ray and CT scan and the bilateral pneumonia he had developed,” she commented. “I would not have believed it, the way he was clinically — and seeing that x-ray.
“Honestly, when I took him in to hospital, I thought he’d be there a couple of days — over the weekend — and I’d get him back Monday. But it didn’t turn out that way. He was there for about 9 days.”
That first night in the hospital, Singh consented to intubation — should he need it. “He called me then,” said Raje. “I said we’ve got to do what we’ve got to do, it’s OK — it is what it is, and we’ll do whatever it takes.”
He remained in the MICU overnight and through the next day, still breathing on his own, but with the looming prospect of mechanical ventilation.
“The good news is he maintained his oxygen saturations throughout,” said Raje. “I was able to see his vitals with EPIC [remote monitoring] ... It was crazy,” she recalls. “Seeing a respiratory rate of 26 was difficult. When you see that, you worry about somebody tiring with the breathing. His inflammatory markers kept climbing, his fevers persisted.”
Thankfully, he never needed the ventilator.
But by this time Raje had another worry: She, too, had tested positive and was now alone at home.
“I was unable to talk to my extended family as they all looked to us as physicians for support,” she tweeted. Both children came to Boston to see her, but she saw them only through a window.
Alone, she waited for the same symptoms that had slammed her husband; but they never came — something she wants caregivers to know.
“The fear and anxiety of taking care of somebody who’s COVID positive ... I am hoping that can be alleviated a little bit at least,” she said. “If you’ve been taking care of someone, chances are you’re probably positive already and if you’re not sick, the chances of you getting sick are really low, so don’t be afraid to take care of that person.”
Singh is recovering well at home now, almost a month into his illness. During the interview, conducted via Zoom, he could be heard coughing in the background.
While in the MICU, Singh was treated with azithromycin and hydroxychloroquine — standard at MGH for critically ill COVID-19 patients — and he was also enrolled into a double-blind, randomized, placebo-controlled trial of the investigational agent remdesivir (Gilead).
Raje is not sure what, if anything, helped him turn the corner.
“I saw his inflammatory markers get worse actually — I don’t think we can know if the drugs made a difference,” she says. “His first dose of hydroxychloroquine was Friday night when he was admitted, and the markers continued to climb until the next Thursday.”
In particular, his C-reactive protein (CRP) kept rising, reaching the 260 to 270 mg/dL range, “which to me was scary,” she said. “I do think he had a cytokine storm going, but I didn’t see those results.”
“Understanding the immune compartment is going to be so, so critically important and what it is that we can do to boost folks’ immune systems,” she said.
“If you have a very high viral load and your immune system is not 100% even though you’re otherwise healthy, you might be the person who ends up with that more serious response to this virus. Trying to study this in a focused way, looking at the immune compartment, looking at the antibody status, looking at the viral load — there’s so much more we need to look at. Until we get the vaccine, which is probably a year-and-a-half away, we need to look at how can we develop that herd immunity so we don’t have folks getting as critically ill as they do.”
Despite feeling perfectly healthy, Raje is still at home. Three weeks after her first test, she is still testing positive for COVID-19, waiting for two consecutive negative results 72 hours apart before she is allowed back to work at the hospital.
When she gets the green light, she plans to go work on the COVID-19 floor, if needed. “It’s people like us [who have had COVID-19] who have to get back in the trenches and do the work now,” she says.
“My biggest concern is that it’s a very isolating experience for the COVID-positive patient. We are doing complete-barrier nursing — they are completely alone. The only person who ever walks into the room is the nurse — and the physician goes in once a day. It’s so important that we don’t lose sight of compassion,” she says.
“That’s why, in terms of alleviating anxiety, it is so important we do antibody testing so that people can actually go in and take care of these folks.”
‘Look for red flag’
Raje wants physicians to warn their self-isolating patients and caregivers to look for red flags. “There are primary care physicians who reached out to me [after my tweets] and said ‘when someone calls me and says it’s been 5-7 days and I am still not feeling well, I am going to look at that more seriously.’
“Part of me wanting to share this experience was basically to dispel the notion that 2 weeks into this you’re going to be fine,” she said, because it is not widely appreciated, she feels that “in week 2, you could become pretty sick.”
This article first appeared on Medscape.com.
A physician couple who both had COVID-19 had very different responses — one ending up in intensive care, the other asymptomatic.
Their story, one of two people living together but with such different responses to the infection, illustrates how much is still to be learned about COVID-19, says Noopur Raje, MD, professor of medicine at Harvard Medical School and director of the Center for Multiple Myeloma at Massachusetts General Hospital (MGH) in Boston.
“After experiencing #Covid_19 from the patient/caregiver end despite both of us being physicians at a major academic medical center, this has been a challenge like no other I have experienced,” Raje (@NoopurRajeMD) wrote on Twitter.
She outlined their experiences in a Twitter thread and elaborated in an interview with Medscape Medical News.
Raje says that she wants clinicians to know how symptoms can evolve both quickly and suddenly.
She recalls how for 10 days, she cared for her COVID-19–positive husband at home, separated from him by a floor in their Boston townhouse and wearing a surgical mask and gloves to bring him food and fluids, as he was too weak to help himself.
Despite the high fevers, chills, extreme fatigue, and dramatic weight loss, Raje says she felt reasonably confident that her husband was getting better. His temperature had dropped from around 103 to 101, his heart rate was in the 80s, and his blood pressure was “OK,” she recalls.
But then Jag Singh, MD, an otherwise healthy 55-year-old Harvard professor and cardiologist, started to cough — and everything suddenly changed.
The cough sounded chesty, and he was weak and unwell. They decided that he needed medical help.
“I was planning on driving him to the hospital, but I ended up having to call 911, although we literally live across the street,” she said.
“We have stairs here and I wasn’t sure that he would be able to make it coming down with me trying to help him, so the safest thing was for me to call for help.”
Singh was admitted straight to the medical intensive care unit (MICU) while his wife waited at home.
“I was blown away when I saw Jag’s x-ray and CT scan and the bilateral pneumonia he had developed,” she commented. “I would not have believed it, the way he was clinically — and seeing that x-ray.
“Honestly, when I took him in to hospital, I thought he’d be there a couple of days — over the weekend — and I’d get him back Monday. But it didn’t turn out that way. He was there for about 9 days.”
That first night in the hospital, Singh consented to intubation — should he need it. “He called me then,” said Raje. “I said we’ve got to do what we’ve got to do, it’s OK — it is what it is, and we’ll do whatever it takes.”
He remained in the MICU overnight and through the next day, still breathing on his own, but with the looming prospect of mechanical ventilation.
“The good news is he maintained his oxygen saturations throughout,” said Raje. “I was able to see his vitals with EPIC [remote monitoring] ... It was crazy,” she recalls. “Seeing a respiratory rate of 26 was difficult. When you see that, you worry about somebody tiring with the breathing. His inflammatory markers kept climbing, his fevers persisted.”
Thankfully, he never needed the ventilator.
But by this time Raje had another worry: She, too, had tested positive and was now alone at home.
“I was unable to talk to my extended family as they all looked to us as physicians for support,” she tweeted. Both children came to Boston to see her, but she saw them only through a window.
Alone, she waited for the same symptoms that had slammed her husband; but they never came — something she wants caregivers to know.
“The fear and anxiety of taking care of somebody who’s COVID positive ... I am hoping that can be alleviated a little bit at least,” she said. “If you’ve been taking care of someone, chances are you’re probably positive already and if you’re not sick, the chances of you getting sick are really low, so don’t be afraid to take care of that person.”
Singh is recovering well at home now, almost a month into his illness. During the interview, conducted via Zoom, he could be heard coughing in the background.
While in the MICU, Singh was treated with azithromycin and hydroxychloroquine — standard at MGH for critically ill COVID-19 patients — and he was also enrolled into a double-blind, randomized, placebo-controlled trial of the investigational agent remdesivir (Gilead).
Raje is not sure what, if anything, helped him turn the corner.
“I saw his inflammatory markers get worse actually — I don’t think we can know if the drugs made a difference,” she says. “His first dose of hydroxychloroquine was Friday night when he was admitted, and the markers continued to climb until the next Thursday.”
In particular, his C-reactive protein (CRP) kept rising, reaching the 260 to 270 mg/dL range, “which to me was scary,” she said. “I do think he had a cytokine storm going, but I didn’t see those results.”
“Understanding the immune compartment is going to be so, so critically important and what it is that we can do to boost folks’ immune systems,” she said.
“If you have a very high viral load and your immune system is not 100% even though you’re otherwise healthy, you might be the person who ends up with that more serious response to this virus. Trying to study this in a focused way, looking at the immune compartment, looking at the antibody status, looking at the viral load — there’s so much more we need to look at. Until we get the vaccine, which is probably a year-and-a-half away, we need to look at how can we develop that herd immunity so we don’t have folks getting as critically ill as they do.”
Despite feeling perfectly healthy, Raje is still at home. Three weeks after her first test, she is still testing positive for COVID-19, waiting for two consecutive negative results 72 hours apart before she is allowed back to work at the hospital.
When she gets the green light, she plans to go work on the COVID-19 floor, if needed. “It’s people like us [who have had COVID-19] who have to get back in the trenches and do the work now,” she says.
“My biggest concern is that it’s a very isolating experience for the COVID-positive patient. We are doing complete-barrier nursing — they are completely alone. The only person who ever walks into the room is the nurse — and the physician goes in once a day. It’s so important that we don’t lose sight of compassion,” she says.
“That’s why, in terms of alleviating anxiety, it is so important we do antibody testing so that people can actually go in and take care of these folks.”
‘Look for red flag’
Raje wants physicians to warn their self-isolating patients and caregivers to look for red flags. “There are primary care physicians who reached out to me [after my tweets] and said ‘when someone calls me and says it’s been 5-7 days and I am still not feeling well, I am going to look at that more seriously.’
“Part of me wanting to share this experience was basically to dispel the notion that 2 weeks into this you’re going to be fine,” she said, because it is not widely appreciated, she feels that “in week 2, you could become pretty sick.”
This article first appeared on Medscape.com.
NYC hospitals require health care workers to report in person, even for phone and telehealth work
A social worker in New York City was home, caring for his sick son, when the hospital at which he works ordered him to report back to work. His son had COVID-19, yet his hospital told him he had to show up in person.
The social worker’s situation is just one of many NYC Health + Hospitals employees who could work remotely yet are required to report in person. His circumstances were described in a letter sent by Lichten & Bright, a law firm representing the New York City Health Services Employees Union, Local 768.
“Despite the fact that all or virtually all of the work social workers perform can be done remotely, only a handful…are being permitted to work from home,” said the letter, which was written on behalf of about 1000 social workers and 150 medical records specialists and addressed to NYC H+H CEO Mitchell Katz, MD.
Most social workers stopped seeing patients in person in early March. But many still face crowded conditions at several points during their work day. They take public transportation to work, come face-to-face with other health care workers and patients in elevators, and some attend daily meetings with up to 10 employees in conference rooms too small to stay six feet apart, the letter says.
“The social workers are scared to go to work,” said Daniel Bright, the letter’s author. “They’re baffled by the lack of any management response that would allow them to work from home. They are worried about getting exposed to the coronavirus while riding the subway or the bus to work or at work from a doctor or nurse or patient, and getting sick themselves or taking it home to their families.”
There is no good reason that the social workers should be compelled to be physically at work during the COVID-19 pandemic, Bright said. The handful of social workers at NYC H+H’s World Trade Center Environmental Health Center clinic at Bellevue who have been allowed to work from home on an ad hoc basis, he said, have done so successfully.
In response to Bright’s letter, the hospital system issued a statement that seemed to downplay workers’ assessment of the situation, and included the following: “NYC Health + Hospital social workers…play different roles in our system, from acting as front-line providers to navigating safe discharges and helping patients and families with important health care decisions. Depending on the facility, the department, and the role they play, decisions are made by our hospital leaders on whether their critical work could be done remotely.”
Recently, many medical associations have issued statements supporting the rights of health care workers to speak up without fear of repercussion. But NYC H+H social workers have been complying with the orders because they say they’re scared of retaliation: In daily video conference calls, an administrator at one of NYC H+H’s hospitals has shown exasperation when asked about working from home, multiple employees told Medscape Medical News. And other questions, they said, such as whether staff could receive hazard pay, were scoffed at. Instead, the administration mentioned disciplinary action for those who didn’t show up to work.
During Thursday’s call, a recording of which was obtained by Medscape, the CEO of one NYC H+H hospital chastised his employees for taking their concerns to the press.
“People are just taking things and you know, using things for their benefit to be able to create problems for us who are trying to do our jobs,” he said, adding that he refuses to be bullied or blackmailed and that he’ll continue to do what he needs to do as CEO — but he wanted people to know “some of the garbage I have to deal with.”
He also reminded employees of documentation people need to provide if they don’t come in to work for being sick or taking a personal leave so the hospital can verify that “you have a condition that warrants you being out.”
Christopher Miller, a spokesperson for the hospital system, said that “some employees in certain functions may be approved to telecommute.” But employees contacted by Medscape who see all of their clients remotely said their requests to telecommute have not been approved.
At this point, it’s no longer a theoretical problem. COVID-19 appears to have spread among a cluster of people reporting to work in one of the H+H hospitals, employees said. In some cases, employees’ family members also became ill.
This article first appeared on Medscape.com.
A social worker in New York City was home, caring for his sick son, when the hospital at which he works ordered him to report back to work. His son had COVID-19, yet his hospital told him he had to show up in person.
The social worker’s situation is just one of many NYC Health + Hospitals employees who could work remotely yet are required to report in person. His circumstances were described in a letter sent by Lichten & Bright, a law firm representing the New York City Health Services Employees Union, Local 768.
“Despite the fact that all or virtually all of the work social workers perform can be done remotely, only a handful…are being permitted to work from home,” said the letter, which was written on behalf of about 1000 social workers and 150 medical records specialists and addressed to NYC H+H CEO Mitchell Katz, MD.
Most social workers stopped seeing patients in person in early March. But many still face crowded conditions at several points during their work day. They take public transportation to work, come face-to-face with other health care workers and patients in elevators, and some attend daily meetings with up to 10 employees in conference rooms too small to stay six feet apart, the letter says.
“The social workers are scared to go to work,” said Daniel Bright, the letter’s author. “They’re baffled by the lack of any management response that would allow them to work from home. They are worried about getting exposed to the coronavirus while riding the subway or the bus to work or at work from a doctor or nurse or patient, and getting sick themselves or taking it home to their families.”
There is no good reason that the social workers should be compelled to be physically at work during the COVID-19 pandemic, Bright said. The handful of social workers at NYC H+H’s World Trade Center Environmental Health Center clinic at Bellevue who have been allowed to work from home on an ad hoc basis, he said, have done so successfully.
In response to Bright’s letter, the hospital system issued a statement that seemed to downplay workers’ assessment of the situation, and included the following: “NYC Health + Hospital social workers…play different roles in our system, from acting as front-line providers to navigating safe discharges and helping patients and families with important health care decisions. Depending on the facility, the department, and the role they play, decisions are made by our hospital leaders on whether their critical work could be done remotely.”
Recently, many medical associations have issued statements supporting the rights of health care workers to speak up without fear of repercussion. But NYC H+H social workers have been complying with the orders because they say they’re scared of retaliation: In daily video conference calls, an administrator at one of NYC H+H’s hospitals has shown exasperation when asked about working from home, multiple employees told Medscape Medical News. And other questions, they said, such as whether staff could receive hazard pay, were scoffed at. Instead, the administration mentioned disciplinary action for those who didn’t show up to work.
During Thursday’s call, a recording of which was obtained by Medscape, the CEO of one NYC H+H hospital chastised his employees for taking their concerns to the press.
“People are just taking things and you know, using things for their benefit to be able to create problems for us who are trying to do our jobs,” he said, adding that he refuses to be bullied or blackmailed and that he’ll continue to do what he needs to do as CEO — but he wanted people to know “some of the garbage I have to deal with.”
He also reminded employees of documentation people need to provide if they don’t come in to work for being sick or taking a personal leave so the hospital can verify that “you have a condition that warrants you being out.”
Christopher Miller, a spokesperson for the hospital system, said that “some employees in certain functions may be approved to telecommute.” But employees contacted by Medscape who see all of their clients remotely said their requests to telecommute have not been approved.
At this point, it’s no longer a theoretical problem. COVID-19 appears to have spread among a cluster of people reporting to work in one of the H+H hospitals, employees said. In some cases, employees’ family members also became ill.
This article first appeared on Medscape.com.
A social worker in New York City was home, caring for his sick son, when the hospital at which he works ordered him to report back to work. His son had COVID-19, yet his hospital told him he had to show up in person.
The social worker’s situation is just one of many NYC Health + Hospitals employees who could work remotely yet are required to report in person. His circumstances were described in a letter sent by Lichten & Bright, a law firm representing the New York City Health Services Employees Union, Local 768.
“Despite the fact that all or virtually all of the work social workers perform can be done remotely, only a handful…are being permitted to work from home,” said the letter, which was written on behalf of about 1000 social workers and 150 medical records specialists and addressed to NYC H+H CEO Mitchell Katz, MD.
Most social workers stopped seeing patients in person in early March. But many still face crowded conditions at several points during their work day. They take public transportation to work, come face-to-face with other health care workers and patients in elevators, and some attend daily meetings with up to 10 employees in conference rooms too small to stay six feet apart, the letter says.
“The social workers are scared to go to work,” said Daniel Bright, the letter’s author. “They’re baffled by the lack of any management response that would allow them to work from home. They are worried about getting exposed to the coronavirus while riding the subway or the bus to work or at work from a doctor or nurse or patient, and getting sick themselves or taking it home to their families.”
There is no good reason that the social workers should be compelled to be physically at work during the COVID-19 pandemic, Bright said. The handful of social workers at NYC H+H’s World Trade Center Environmental Health Center clinic at Bellevue who have been allowed to work from home on an ad hoc basis, he said, have done so successfully.
In response to Bright’s letter, the hospital system issued a statement that seemed to downplay workers’ assessment of the situation, and included the following: “NYC Health + Hospital social workers…play different roles in our system, from acting as front-line providers to navigating safe discharges and helping patients and families with important health care decisions. Depending on the facility, the department, and the role they play, decisions are made by our hospital leaders on whether their critical work could be done remotely.”
Recently, many medical associations have issued statements supporting the rights of health care workers to speak up without fear of repercussion. But NYC H+H social workers have been complying with the orders because they say they’re scared of retaliation: In daily video conference calls, an administrator at one of NYC H+H’s hospitals has shown exasperation when asked about working from home, multiple employees told Medscape Medical News. And other questions, they said, such as whether staff could receive hazard pay, were scoffed at. Instead, the administration mentioned disciplinary action for those who didn’t show up to work.
During Thursday’s call, a recording of which was obtained by Medscape, the CEO of one NYC H+H hospital chastised his employees for taking their concerns to the press.
“People are just taking things and you know, using things for their benefit to be able to create problems for us who are trying to do our jobs,” he said, adding that he refuses to be bullied or blackmailed and that he’ll continue to do what he needs to do as CEO — but he wanted people to know “some of the garbage I have to deal with.”
He also reminded employees of documentation people need to provide if they don’t come in to work for being sick or taking a personal leave so the hospital can verify that “you have a condition that warrants you being out.”
Christopher Miller, a spokesperson for the hospital system, said that “some employees in certain functions may be approved to telecommute.” But employees contacted by Medscape who see all of their clients remotely said their requests to telecommute have not been approved.
At this point, it’s no longer a theoretical problem. COVID-19 appears to have spread among a cluster of people reporting to work in one of the H+H hospitals, employees said. In some cases, employees’ family members also became ill.
This article first appeared on Medscape.com.







