User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Hospitalists deal with patient discrimination
Encounters with bias are underreported
In the fall of 2016, Hyma Polimera, MD, a hospitalist at Penn State Health in Hershey, Pa., approached the bedside of a patient with dementia and several other chronic conditions, and introduced herself to him and his family.
The patient’s daughter, who had power of attorney, took one look at Dr. Polimera and told her, “I’d like to see an American doctor.” Dr. Polimera is originally from India, but moved to Europe in 2005 and did her residency in Pennsylvania. She stayed calm and confident – she understood that she had done nothing wrong – but didn’t really know what to do next. All of the other hospitalists on the ward at the time were nonwhite and were also rejected by the patient’s daughter.
“I was wondering what was going to happen and who would provide care to this patient?” she said.
Dr. Polimera is far from alone. Nonwhite physicians, nurses, and other health care providers say they increasingly encounter patients who demand that only “white” health professionals take care of them. The number of these reassignment requests has ticked upward in the last few years, they say, coinciding with the 2016 U.S. presidential campaign and the subsequent election of Donald Trump.
The requests often come at medical centers with no policy in place for how to deal with them. And the unpleasant encounters find providers unprepared for how to respond, not knowing whether or how to resolve the situation with patients and their families. Clinicians sometimes wonder whether they are allowed to care for a patient even if they are willing to do so, and how to go about reassigning a patient to another clinician if that is the choice that the family makes.
To many hospitalists working in the field, it seems obvious that such situations are encouraged by a political environment in which discriminatory beliefs – once considered shameful to express publicly – are now deemed acceptable, even in health care encounters. Indeed, the health care encounter is perhaps the only time some patients will find themselves in intimate interactions with people of other ethnicities.
Responding to discrimination
A workshop at the 2019 Society of Hospital Medicine Annual Conference offered hospitalists an opportunity to discuss encounters with patients who expressed discriminatory attitudes. One physician, of South Asian descent, said that she had encountered no reassignment requests rooted in racial intolerance over more than a decade of work, but has encountered several in the last year or two.
Sabrina Chaklos, MD, a hospitalist at Burlington, Mass.–based Lahey Hospital & Medical Center and clinical assistant professor at Tufts University, said she has had a similar experience.
“It was blatantly bad behavior for 2018,” she said. Dr. Chaklos said she and other clinicians of color have been told, “I want an American doctor,” and that some patients see her darker complexion and conclude, “You must not be an American.”
Given the charged political environment since 2016, some medical facilities have been adapting how they respond to these comments and requests.
“The policy of the organization prior to 2016 was to give patients a new doctor,” Dr. Chaklos said. “Within the past year or so, they’re finally allowing people to say, ‘Look, you cannot just pick and choose your doctor,’ based on arbitrary reasons that are discriminatory in nature.”
Emily Whitgob, MD, MEd, a developmental-behavioral pediatrician at Santa Clara Valley Medical Center in San Jose, Calif., said that, several years ago, a scenario unfolded that led her to study the issue. An intern she was overseeing told her that the father of a pediatric patient had scrutinized the intern’s name tag and said, “Is that a Jewish last name? I don’t want a Jewish doctor.”
“I didn’t know what to do,” Dr. Whitgob said. Later, she brought up the situation at a meeting of 30 staff members. It led to an outpouring of sharing about similar incidents that other clinicians had experienced but had never talked about with colleagues.
“Half the room, by the end, was in tears talking about their experiences,” Dr. Whitgob said.
Since then, she has led research into how physicians typically handle such situations, performing semistructured interviews to survey pediatricians about their experiences with patients who discriminate on racial and ethnic grounds.
One important step, she said, is assessing the acuity of the illness involved to help determine whether the transfer of a patient from one provider to another should even be considered. In a dire situation, or when the physician involved is the foremost expert on a given condition, it might not be realistic.
Dr. Whitgob said some clinicians advocated cultivating a kind of alliance with the parents of pediatric patients, informing them that they’re part of a team that interacts with many types of providers, and redirecting them to focus on their child’s care.
“This takes time, and in a busy setting, that might not happen,” she acknowledged.
Physicians surveyed also said they try to depersonalize the uncomfortable encounter, remembering that discrimination is often motivated by a patient’s fears and a lack of control.
An important consideration, researchers found, was ensuring a safe learning environment for trainees, telling patients they would trust the physician with the care of their own children, escalating a complaint to hospital administration when appropriate, and empowering trainees to choose the next step in a situation.
Dr. Whitgob said that handling a reassignment request based on discriminatory sentiments is not as easy as “calling out ‘Code Bigotry.’ ”
“It’s not that simple,” Dr. Whitgob said. “There’s not going to be a one-size-fits-all or even a one-size-fits-most solution. Each case is an individual case.”
Taking action
Penn State Health is based in Hershey, Pa., a city that tends to vote Democratic in local and national elections but is encircled by Republican-leaning counties. Dr. Polimera’s encounter with her patient’s daughter led to changes in the way the health system handles encounters like hers.
When Dr. Polimera explained the situation to physician leadership, she was asked whether she was still comfortable taking care of the patient, and she said yes. The physician leaders informed the family that they could not change providers simply because of ethnicity. But that was just the first step.
Ultimately, the health system undertook a survey of all its health care providers, to determine whether others had similar experiences with patients or families, and had to deal with rude comments or were rejected as caregivers based on their race, gender, or religion.
“The feedback we received was massive and detailed,” Dr. Polimera said.
Brian McGillen, MD, section chief of hospital medicine and associate professor in the department of medicine at Penn State Health, said physician leaders took the survey results to the dean’s executive council, a who’s-who of medical leadership at the health system.
“I read aloud to the executive council what our folks were facing out on the floors,” Dr. McGillen said. “And I was halfway through my third story when the dean threw his hands up in the air and said, ‘We have to do something.’ ”
As a result, the health system’s policy on patient responsibility was changed to protect all health care providers from threats, violence, disrespectful communication, or harassment by patients, families, and other visitors. Before the change, the policy covered only discriminatory acts by patients themselves.
Penn State Health is now embarking on a training program for faculty, residents, and students that uses simulations of common hospital encounters. The health system also is engaging its patient relations staff to help mediate patient reassignment requests, and is trying to increase real-time debriefing of these events to further improve awareness and training.
Dr. McGillen noted that researchers at the University of North Texas, using data from the Anti-Defamation League, found that counties in which President Trump held campaign rallies – such as Dauphin County, Pa., where Hershey is located – had a 226% increase in hate crimes in the months after the rallies.
“This isn’t to say that every county and every person in these counties that voted for Mr. Trump is racist, but we surely know that his campaign unlocked an undercurrent of political incorrectness that has existed for ages,” he said. “We had to do something as an organization.”
Adapting to change
While some health systems are acting to limit the harm caused by discrimination, there is still much awareness to be raised and work to be done on this issue nationally. Some hospitalists at the 2019 SHM Annual Conference said they suspect that discriminatory incidents involving patients are still so underreported that the C-suite leaders at their hospitals do not recognize how serious a problem it is. Attendees at the HM19 workshop said discriminatory behavior by patients could affect hospitalist turnover and lead to burnout.
Multiple hospitalists at the workshop said that if a transfer of a patient is going to take place – if the patient requests a “white” doctor and there is not one available where the patient is admitted – they are unsure whether it is their responsibility to make the necessary phone calls. Some hospitalists say that if that job does fall to them, it interrupts work flow.
Susan Hakes, MHA, director of hospital administration at the Guthrie Clinic in Ithaca, N.Y., said that when a patient recently asked for a “white” doctor and there was not one available at the time of the request, the patient changed her mind when costs were considered.
“I was willing to have this patient transferred to another one of our hospitals that did have a white doctor, but it would have been at her expense since insurance wouldn’t cover the ambulance ride,” Ms. Hakes said. “She had second thoughts after learning that.”
Ms. Hakes said that the broader community in her region – which is predominantly white – needs to adapt to a changing health care scene.
“We’re recruiting international nurses now, due to the nursing shortage,” she said. “It will serve our community well to be receptive and welcome this additional resource.”
Kunal P. Bhagat, MD, chief of hospital medicine at Christiana Care Health System in Newark, Del., said that medical centers should set parameters for action when a patient discriminates, but that clinicians should not expect to fundamentally change a patient’s mindset.
“I think it is important to set limits,” Dr. Bhagat said. “It’s like with your kids. Your children may behave in certain ways, at certain times, that you don’t like. You can tell them, ‘You know, you may not like behaving the way I want you to behave, but the way you’re behaving now is not acceptable.’ If our goal is to try to completely change their world-view at that moment, I think we’re going to be set up for failure. That’s more of a long-term issue for society to address.”
Encounters with bias are underreported
Encounters with bias are underreported
In the fall of 2016, Hyma Polimera, MD, a hospitalist at Penn State Health in Hershey, Pa., approached the bedside of a patient with dementia and several other chronic conditions, and introduced herself to him and his family.
The patient’s daughter, who had power of attorney, took one look at Dr. Polimera and told her, “I’d like to see an American doctor.” Dr. Polimera is originally from India, but moved to Europe in 2005 and did her residency in Pennsylvania. She stayed calm and confident – she understood that she had done nothing wrong – but didn’t really know what to do next. All of the other hospitalists on the ward at the time were nonwhite and were also rejected by the patient’s daughter.
“I was wondering what was going to happen and who would provide care to this patient?” she said.
Dr. Polimera is far from alone. Nonwhite physicians, nurses, and other health care providers say they increasingly encounter patients who demand that only “white” health professionals take care of them. The number of these reassignment requests has ticked upward in the last few years, they say, coinciding with the 2016 U.S. presidential campaign and the subsequent election of Donald Trump.
The requests often come at medical centers with no policy in place for how to deal with them. And the unpleasant encounters find providers unprepared for how to respond, not knowing whether or how to resolve the situation with patients and their families. Clinicians sometimes wonder whether they are allowed to care for a patient even if they are willing to do so, and how to go about reassigning a patient to another clinician if that is the choice that the family makes.
To many hospitalists working in the field, it seems obvious that such situations are encouraged by a political environment in which discriminatory beliefs – once considered shameful to express publicly – are now deemed acceptable, even in health care encounters. Indeed, the health care encounter is perhaps the only time some patients will find themselves in intimate interactions with people of other ethnicities.
Responding to discrimination
A workshop at the 2019 Society of Hospital Medicine Annual Conference offered hospitalists an opportunity to discuss encounters with patients who expressed discriminatory attitudes. One physician, of South Asian descent, said that she had encountered no reassignment requests rooted in racial intolerance over more than a decade of work, but has encountered several in the last year or two.
Sabrina Chaklos, MD, a hospitalist at Burlington, Mass.–based Lahey Hospital & Medical Center and clinical assistant professor at Tufts University, said she has had a similar experience.
“It was blatantly bad behavior for 2018,” she said. Dr. Chaklos said she and other clinicians of color have been told, “I want an American doctor,” and that some patients see her darker complexion and conclude, “You must not be an American.”
Given the charged political environment since 2016, some medical facilities have been adapting how they respond to these comments and requests.
“The policy of the organization prior to 2016 was to give patients a new doctor,” Dr. Chaklos said. “Within the past year or so, they’re finally allowing people to say, ‘Look, you cannot just pick and choose your doctor,’ based on arbitrary reasons that are discriminatory in nature.”
Emily Whitgob, MD, MEd, a developmental-behavioral pediatrician at Santa Clara Valley Medical Center in San Jose, Calif., said that, several years ago, a scenario unfolded that led her to study the issue. An intern she was overseeing told her that the father of a pediatric patient had scrutinized the intern’s name tag and said, “Is that a Jewish last name? I don’t want a Jewish doctor.”
“I didn’t know what to do,” Dr. Whitgob said. Later, she brought up the situation at a meeting of 30 staff members. It led to an outpouring of sharing about similar incidents that other clinicians had experienced but had never talked about with colleagues.
“Half the room, by the end, was in tears talking about their experiences,” Dr. Whitgob said.
Since then, she has led research into how physicians typically handle such situations, performing semistructured interviews to survey pediatricians about their experiences with patients who discriminate on racial and ethnic grounds.
One important step, she said, is assessing the acuity of the illness involved to help determine whether the transfer of a patient from one provider to another should even be considered. In a dire situation, or when the physician involved is the foremost expert on a given condition, it might not be realistic.
Dr. Whitgob said some clinicians advocated cultivating a kind of alliance with the parents of pediatric patients, informing them that they’re part of a team that interacts with many types of providers, and redirecting them to focus on their child’s care.
“This takes time, and in a busy setting, that might not happen,” she acknowledged.
Physicians surveyed also said they try to depersonalize the uncomfortable encounter, remembering that discrimination is often motivated by a patient’s fears and a lack of control.
An important consideration, researchers found, was ensuring a safe learning environment for trainees, telling patients they would trust the physician with the care of their own children, escalating a complaint to hospital administration when appropriate, and empowering trainees to choose the next step in a situation.
Dr. Whitgob said that handling a reassignment request based on discriminatory sentiments is not as easy as “calling out ‘Code Bigotry.’ ”
“It’s not that simple,” Dr. Whitgob said. “There’s not going to be a one-size-fits-all or even a one-size-fits-most solution. Each case is an individual case.”
Taking action
Penn State Health is based in Hershey, Pa., a city that tends to vote Democratic in local and national elections but is encircled by Republican-leaning counties. Dr. Polimera’s encounter with her patient’s daughter led to changes in the way the health system handles encounters like hers.
When Dr. Polimera explained the situation to physician leadership, she was asked whether she was still comfortable taking care of the patient, and she said yes. The physician leaders informed the family that they could not change providers simply because of ethnicity. But that was just the first step.
Ultimately, the health system undertook a survey of all its health care providers, to determine whether others had similar experiences with patients or families, and had to deal with rude comments or were rejected as caregivers based on their race, gender, or religion.
“The feedback we received was massive and detailed,” Dr. Polimera said.
Brian McGillen, MD, section chief of hospital medicine and associate professor in the department of medicine at Penn State Health, said physician leaders took the survey results to the dean’s executive council, a who’s-who of medical leadership at the health system.
“I read aloud to the executive council what our folks were facing out on the floors,” Dr. McGillen said. “And I was halfway through my third story when the dean threw his hands up in the air and said, ‘We have to do something.’ ”
As a result, the health system’s policy on patient responsibility was changed to protect all health care providers from threats, violence, disrespectful communication, or harassment by patients, families, and other visitors. Before the change, the policy covered only discriminatory acts by patients themselves.
Penn State Health is now embarking on a training program for faculty, residents, and students that uses simulations of common hospital encounters. The health system also is engaging its patient relations staff to help mediate patient reassignment requests, and is trying to increase real-time debriefing of these events to further improve awareness and training.
Dr. McGillen noted that researchers at the University of North Texas, using data from the Anti-Defamation League, found that counties in which President Trump held campaign rallies – such as Dauphin County, Pa., where Hershey is located – had a 226% increase in hate crimes in the months after the rallies.
“This isn’t to say that every county and every person in these counties that voted for Mr. Trump is racist, but we surely know that his campaign unlocked an undercurrent of political incorrectness that has existed for ages,” he said. “We had to do something as an organization.”
Adapting to change
While some health systems are acting to limit the harm caused by discrimination, there is still much awareness to be raised and work to be done on this issue nationally. Some hospitalists at the 2019 SHM Annual Conference said they suspect that discriminatory incidents involving patients are still so underreported that the C-suite leaders at their hospitals do not recognize how serious a problem it is. Attendees at the HM19 workshop said discriminatory behavior by patients could affect hospitalist turnover and lead to burnout.
Multiple hospitalists at the workshop said that if a transfer of a patient is going to take place – if the patient requests a “white” doctor and there is not one available where the patient is admitted – they are unsure whether it is their responsibility to make the necessary phone calls. Some hospitalists say that if that job does fall to them, it interrupts work flow.
Susan Hakes, MHA, director of hospital administration at the Guthrie Clinic in Ithaca, N.Y., said that when a patient recently asked for a “white” doctor and there was not one available at the time of the request, the patient changed her mind when costs were considered.
“I was willing to have this patient transferred to another one of our hospitals that did have a white doctor, but it would have been at her expense since insurance wouldn’t cover the ambulance ride,” Ms. Hakes said. “She had second thoughts after learning that.”
Ms. Hakes said that the broader community in her region – which is predominantly white – needs to adapt to a changing health care scene.
“We’re recruiting international nurses now, due to the nursing shortage,” she said. “It will serve our community well to be receptive and welcome this additional resource.”
Kunal P. Bhagat, MD, chief of hospital medicine at Christiana Care Health System in Newark, Del., said that medical centers should set parameters for action when a patient discriminates, but that clinicians should not expect to fundamentally change a patient’s mindset.
“I think it is important to set limits,” Dr. Bhagat said. “It’s like with your kids. Your children may behave in certain ways, at certain times, that you don’t like. You can tell them, ‘You know, you may not like behaving the way I want you to behave, but the way you’re behaving now is not acceptable.’ If our goal is to try to completely change their world-view at that moment, I think we’re going to be set up for failure. That’s more of a long-term issue for society to address.”
In the fall of 2016, Hyma Polimera, MD, a hospitalist at Penn State Health in Hershey, Pa., approached the bedside of a patient with dementia and several other chronic conditions, and introduced herself to him and his family.
The patient’s daughter, who had power of attorney, took one look at Dr. Polimera and told her, “I’d like to see an American doctor.” Dr. Polimera is originally from India, but moved to Europe in 2005 and did her residency in Pennsylvania. She stayed calm and confident – she understood that she had done nothing wrong – but didn’t really know what to do next. All of the other hospitalists on the ward at the time were nonwhite and were also rejected by the patient’s daughter.
“I was wondering what was going to happen and who would provide care to this patient?” she said.
Dr. Polimera is far from alone. Nonwhite physicians, nurses, and other health care providers say they increasingly encounter patients who demand that only “white” health professionals take care of them. The number of these reassignment requests has ticked upward in the last few years, they say, coinciding with the 2016 U.S. presidential campaign and the subsequent election of Donald Trump.
The requests often come at medical centers with no policy in place for how to deal with them. And the unpleasant encounters find providers unprepared for how to respond, not knowing whether or how to resolve the situation with patients and their families. Clinicians sometimes wonder whether they are allowed to care for a patient even if they are willing to do so, and how to go about reassigning a patient to another clinician if that is the choice that the family makes.
To many hospitalists working in the field, it seems obvious that such situations are encouraged by a political environment in which discriminatory beliefs – once considered shameful to express publicly – are now deemed acceptable, even in health care encounters. Indeed, the health care encounter is perhaps the only time some patients will find themselves in intimate interactions with people of other ethnicities.
Responding to discrimination
A workshop at the 2019 Society of Hospital Medicine Annual Conference offered hospitalists an opportunity to discuss encounters with patients who expressed discriminatory attitudes. One physician, of South Asian descent, said that she had encountered no reassignment requests rooted in racial intolerance over more than a decade of work, but has encountered several in the last year or two.
Sabrina Chaklos, MD, a hospitalist at Burlington, Mass.–based Lahey Hospital & Medical Center and clinical assistant professor at Tufts University, said she has had a similar experience.
“It was blatantly bad behavior for 2018,” she said. Dr. Chaklos said she and other clinicians of color have been told, “I want an American doctor,” and that some patients see her darker complexion and conclude, “You must not be an American.”
Given the charged political environment since 2016, some medical facilities have been adapting how they respond to these comments and requests.
“The policy of the organization prior to 2016 was to give patients a new doctor,” Dr. Chaklos said. “Within the past year or so, they’re finally allowing people to say, ‘Look, you cannot just pick and choose your doctor,’ based on arbitrary reasons that are discriminatory in nature.”
Emily Whitgob, MD, MEd, a developmental-behavioral pediatrician at Santa Clara Valley Medical Center in San Jose, Calif., said that, several years ago, a scenario unfolded that led her to study the issue. An intern she was overseeing told her that the father of a pediatric patient had scrutinized the intern’s name tag and said, “Is that a Jewish last name? I don’t want a Jewish doctor.”
“I didn’t know what to do,” Dr. Whitgob said. Later, she brought up the situation at a meeting of 30 staff members. It led to an outpouring of sharing about similar incidents that other clinicians had experienced but had never talked about with colleagues.
“Half the room, by the end, was in tears talking about their experiences,” Dr. Whitgob said.
Since then, she has led research into how physicians typically handle such situations, performing semistructured interviews to survey pediatricians about their experiences with patients who discriminate on racial and ethnic grounds.
One important step, she said, is assessing the acuity of the illness involved to help determine whether the transfer of a patient from one provider to another should even be considered. In a dire situation, or when the physician involved is the foremost expert on a given condition, it might not be realistic.
Dr. Whitgob said some clinicians advocated cultivating a kind of alliance with the parents of pediatric patients, informing them that they’re part of a team that interacts with many types of providers, and redirecting them to focus on their child’s care.
“This takes time, and in a busy setting, that might not happen,” she acknowledged.
Physicians surveyed also said they try to depersonalize the uncomfortable encounter, remembering that discrimination is often motivated by a patient’s fears and a lack of control.
An important consideration, researchers found, was ensuring a safe learning environment for trainees, telling patients they would trust the physician with the care of their own children, escalating a complaint to hospital administration when appropriate, and empowering trainees to choose the next step in a situation.
Dr. Whitgob said that handling a reassignment request based on discriminatory sentiments is not as easy as “calling out ‘Code Bigotry.’ ”
“It’s not that simple,” Dr. Whitgob said. “There’s not going to be a one-size-fits-all or even a one-size-fits-most solution. Each case is an individual case.”
Taking action
Penn State Health is based in Hershey, Pa., a city that tends to vote Democratic in local and national elections but is encircled by Republican-leaning counties. Dr. Polimera’s encounter with her patient’s daughter led to changes in the way the health system handles encounters like hers.
When Dr. Polimera explained the situation to physician leadership, she was asked whether she was still comfortable taking care of the patient, and she said yes. The physician leaders informed the family that they could not change providers simply because of ethnicity. But that was just the first step.
Ultimately, the health system undertook a survey of all its health care providers, to determine whether others had similar experiences with patients or families, and had to deal with rude comments or were rejected as caregivers based on their race, gender, or religion.
“The feedback we received was massive and detailed,” Dr. Polimera said.
Brian McGillen, MD, section chief of hospital medicine and associate professor in the department of medicine at Penn State Health, said physician leaders took the survey results to the dean’s executive council, a who’s-who of medical leadership at the health system.
“I read aloud to the executive council what our folks were facing out on the floors,” Dr. McGillen said. “And I was halfway through my third story when the dean threw his hands up in the air and said, ‘We have to do something.’ ”
As a result, the health system’s policy on patient responsibility was changed to protect all health care providers from threats, violence, disrespectful communication, or harassment by patients, families, and other visitors. Before the change, the policy covered only discriminatory acts by patients themselves.
Penn State Health is now embarking on a training program for faculty, residents, and students that uses simulations of common hospital encounters. The health system also is engaging its patient relations staff to help mediate patient reassignment requests, and is trying to increase real-time debriefing of these events to further improve awareness and training.
Dr. McGillen noted that researchers at the University of North Texas, using data from the Anti-Defamation League, found that counties in which President Trump held campaign rallies – such as Dauphin County, Pa., where Hershey is located – had a 226% increase in hate crimes in the months after the rallies.
“This isn’t to say that every county and every person in these counties that voted for Mr. Trump is racist, but we surely know that his campaign unlocked an undercurrent of political incorrectness that has existed for ages,” he said. “We had to do something as an organization.”
Adapting to change
While some health systems are acting to limit the harm caused by discrimination, there is still much awareness to be raised and work to be done on this issue nationally. Some hospitalists at the 2019 SHM Annual Conference said they suspect that discriminatory incidents involving patients are still so underreported that the C-suite leaders at their hospitals do not recognize how serious a problem it is. Attendees at the HM19 workshop said discriminatory behavior by patients could affect hospitalist turnover and lead to burnout.
Multiple hospitalists at the workshop said that if a transfer of a patient is going to take place – if the patient requests a “white” doctor and there is not one available where the patient is admitted – they are unsure whether it is their responsibility to make the necessary phone calls. Some hospitalists say that if that job does fall to them, it interrupts work flow.
Susan Hakes, MHA, director of hospital administration at the Guthrie Clinic in Ithaca, N.Y., said that when a patient recently asked for a “white” doctor and there was not one available at the time of the request, the patient changed her mind when costs were considered.
“I was willing to have this patient transferred to another one of our hospitals that did have a white doctor, but it would have been at her expense since insurance wouldn’t cover the ambulance ride,” Ms. Hakes said. “She had second thoughts after learning that.”
Ms. Hakes said that the broader community in her region – which is predominantly white – needs to adapt to a changing health care scene.
“We’re recruiting international nurses now, due to the nursing shortage,” she said. “It will serve our community well to be receptive and welcome this additional resource.”
Kunal P. Bhagat, MD, chief of hospital medicine at Christiana Care Health System in Newark, Del., said that medical centers should set parameters for action when a patient discriminates, but that clinicians should not expect to fundamentally change a patient’s mindset.
“I think it is important to set limits,” Dr. Bhagat said. “It’s like with your kids. Your children may behave in certain ways, at certain times, that you don’t like. You can tell them, ‘You know, you may not like behaving the way I want you to behave, but the way you’re behaving now is not acceptable.’ If our goal is to try to completely change their world-view at that moment, I think we’re going to be set up for failure. That’s more of a long-term issue for society to address.”
Treating pain with virtual reality
Pilot studies are underway
Physicians may soon have another tool to help patients deal with pain: virtual reality (VR) therapy. A New York Times article earlier this year described this new treatment option and the way immersive VR experiences seem to crowd pain sensations out of the brain.
Jeffrey I. Gold, PhD, director of the Children’s Outcomes, Research, and Evaluation program at Children’s Hospital Los Angeles, told the newspaper that VR was “like an endogenous narcotic providing a physiological and chemical burst that causes you to feel good.”
So far, VR has been most successfully used in cases of acute pain. “But it can also enhance the effectiveness of established techniques like physical therapy, hypnosis and cognitive behavioral therapy to treat debilitating chronic pain,” the New York Times reported.
“Using VR as an adjunct, we can teach coping skills, techniques patients can use on their own that will help diminish chronic pain,” said Hunter Hoffman, PhD, principal investigator at the Human Photonics Laboratory of the University of Washington, Seattle. “Learning changes the brain and gives patients something that continues to work when they take the helmet off. When patients realize their pain isn’t inevitable, they’re more receptive to doing physical therapy exercises and more likely to move on their own.”
Others with experience in VR say the technique can foster mindfulness, which teaches the mind how to quiet the body and nervous system through breathing.
Pilot studies of VR and pain management are underway, and software companies are developing programs that create therapeutic VR environments.
Reference
1. “Virtual Reality as Therapy for Pain.” Jane E. Brody, New York Times. 2019 Apr 29. https://www.nytimes.com/2019/04/29/well/live/virtual-reality-as-therapy-for-pain.html.
Pilot studies are underway
Pilot studies are underway
Physicians may soon have another tool to help patients deal with pain: virtual reality (VR) therapy. A New York Times article earlier this year described this new treatment option and the way immersive VR experiences seem to crowd pain sensations out of the brain.
Jeffrey I. Gold, PhD, director of the Children’s Outcomes, Research, and Evaluation program at Children’s Hospital Los Angeles, told the newspaper that VR was “like an endogenous narcotic providing a physiological and chemical burst that causes you to feel good.”
So far, VR has been most successfully used in cases of acute pain. “But it can also enhance the effectiveness of established techniques like physical therapy, hypnosis and cognitive behavioral therapy to treat debilitating chronic pain,” the New York Times reported.
“Using VR as an adjunct, we can teach coping skills, techniques patients can use on their own that will help diminish chronic pain,” said Hunter Hoffman, PhD, principal investigator at the Human Photonics Laboratory of the University of Washington, Seattle. “Learning changes the brain and gives patients something that continues to work when they take the helmet off. When patients realize their pain isn’t inevitable, they’re more receptive to doing physical therapy exercises and more likely to move on their own.”
Others with experience in VR say the technique can foster mindfulness, which teaches the mind how to quiet the body and nervous system through breathing.
Pilot studies of VR and pain management are underway, and software companies are developing programs that create therapeutic VR environments.
Reference
1. “Virtual Reality as Therapy for Pain.” Jane E. Brody, New York Times. 2019 Apr 29. https://www.nytimes.com/2019/04/29/well/live/virtual-reality-as-therapy-for-pain.html.
Physicians may soon have another tool to help patients deal with pain: virtual reality (VR) therapy. A New York Times article earlier this year described this new treatment option and the way immersive VR experiences seem to crowd pain sensations out of the brain.
Jeffrey I. Gold, PhD, director of the Children’s Outcomes, Research, and Evaluation program at Children’s Hospital Los Angeles, told the newspaper that VR was “like an endogenous narcotic providing a physiological and chemical burst that causes you to feel good.”
So far, VR has been most successfully used in cases of acute pain. “But it can also enhance the effectiveness of established techniques like physical therapy, hypnosis and cognitive behavioral therapy to treat debilitating chronic pain,” the New York Times reported.
“Using VR as an adjunct, we can teach coping skills, techniques patients can use on their own that will help diminish chronic pain,” said Hunter Hoffman, PhD, principal investigator at the Human Photonics Laboratory of the University of Washington, Seattle. “Learning changes the brain and gives patients something that continues to work when they take the helmet off. When patients realize their pain isn’t inevitable, they’re more receptive to doing physical therapy exercises and more likely to move on their own.”
Others with experience in VR say the technique can foster mindfulness, which teaches the mind how to quiet the body and nervous system through breathing.
Pilot studies of VR and pain management are underway, and software companies are developing programs that create therapeutic VR environments.
Reference
1. “Virtual Reality as Therapy for Pain.” Jane E. Brody, New York Times. 2019 Apr 29. https://www.nytimes.com/2019/04/29/well/live/virtual-reality-as-therapy-for-pain.html.
New hypertension performance measures boost 130/80 mm Hg target
PHILADELPHIA – The American Heart Association and American College of Cardiology took a big step toward facilitating widespread U.S. application of the hypertension management guideline that the societies issued in 2017 by releasing a set of performance and quality measures for adults with high blood pressure based on the 2017 guideline.
This guideline notably set a treatment target for patients diagnosed with hypertension of less than 130/80 mg/dL, and also lowered the threshold for diagnosing stage 1 hypertension to a blood pressure at or above 130/80 mm Hg, adding in a stroke about 31 million adults with hypertension to the U.S. total.
Having performance and quality measures based on the guideline is “critical, because how else would you know whether you’re having an effect on accurately diagnosing and properly controlling hypertension?” said Donald E. Casey Jr., MD, chair of the performance measures writing committee. The next step is field testing of the measures “to show they are reliable and effective,” as well as other steps to encourage widespread U.S. uptake of the performance and quality measures and the specifics of the 2017 guideline, Dr. Casey said during a presentation of the revised measures at the American Heart Association scientific sessions.
He especially highlighted the important role of Target: BP, an education, recognition, and quality improvement program run by the AHA and American Medical Association, as a tool that medical practices, health systems, and even payers and employers can use to begin to apply the new performance and quality measures (J Am Coll Cardiol. 2019 Nov 26;74[21]:2661-706) and better align with the recommendations of the 2017 high blood pressure guideline (J Am Coll Cardiol. 2018 May;71[19]:e127-248).
“We’re trying now to promote Target: BP; it’s something you can take off the shelf and get going if it’s embedded in a real-life delivery model. I think Target: BP is the secret sauce. It will be the way we’ll convince people to adopt this,” said Dr. Casey, principal and founder of IPO 4 Health, a Chicago-based health care consulting firm.
He also advised practices and health systems not to feel compelled to introduce all of the specific performance and quality measures at once. “We don’t believe everyone has the resources to do all of it at once; the point is to move toward this system of care. We understand that people don’t have the resources to get it all done” immediately, Dr. Casey said in an interview.
A report during another session at the meeting documented the potential impact that Target: BP can have on blood pressure control within a health system. The Trinity Health of New England medical group based in Springfield, Mass., a system with about 140,000 patients – including 20,000 adults diagnosed with hypertension – and served by 230 health care providers in 13 offices in western Massachusetts, began using Target: BP’s MAP improvement program in its practices in November 2018. (MAP stands for measure accurately, act rapidly, and partner with patients.) Just before the MAP program began, 72% of patients diagnosed with hypertension in the medical group were at their goal blood pressure. Less than a year later, in September 2019, the hypertension control rate had jumped to 84%, a 12 percentage point improvement in control in practices that already had been doing a relatively good job, said Daniel W. Weiswasser, MD, director of quality and clinical informatics at Trinity Health of New England. Based on this success, Trinity Health plans to next involve the remaining regions of Trinity Health of New England in Target: BP, followed by the other regions of Trinity’s national organization, which operates in 21 states with nearly 4,000 staff physicians and about half a million patients diagnosed with hypertension, Dr. Weiswasser said.
“If clinicians do the three steps of the MAP then we will see substantial drops in blood pressures. It will occur,” declared Brent M. Egan, MD, vice president for cardiovascular disease prevention of the AMA in Greenville, S.C.
The new report includes six performance measures based on the strongest guideline recommendations and designed to document adherence levels for the purposes of public reporting and pay-for-performance programs. It also includes 16 quality measures designed for local quality review purposes, with 6 process quality measures and 10 structural quality measures. The report spells out that the authors designed the performance measures for use by major national organizations such as the Centers for Medicare & Medicaid Services and the National Committee for Quality Assurance (NCQA), while the quality measures are designed to support quality improvement efforts in any care-delivery setting.
The authors said that the writing committee is sensitive to the fact that the 2019 performance measures for controlling high blood pressure developed by the NCQA for the Healthcare Effectiveness Data and Information Set and currently in use in 2019 by CMS also does not incorporate the 2017 Hypertension Clinical Practice Guidelines classification scheme. “It is well understood that these measures are already in widespread use, especially for quality-related payment programs promulgated by CMS, such as the Medicare Advantage ‘Stars’ ratings, the Medicare Shared Savings Program, and the Physician Quality Payment Program, as well as many other programs promoted by commercial health insurers. In particular, the widespread use of the 2017 Hypertension Clinical Practice Guidelines classification scheme will also help to guide decision making about when to prescribe antihypertensive medications in accordance with its current recommendations for the ACC/AHA “stages” of stage 1 and stage 2 hypertension and elevated blood pressure,” they added.
The report also says that “the writing committee was sensitive to the fact that there is currently not complete consensus among other guidelines from the American College of Physicians and the American Academy of Family Physicians, and also the European Society of Cardiology and the European Society of Hypertension. Nonetheless, despite this ongoing debate, the writing committee felt strongly that it is now time to move the U.S. health care system ahead to reflect these differing points of view and expects that widespread use of this new measure set will help to achieve this goal.” The new report revises hypertension performance measures developed by the ACC and AHA in 2011 (J Am Coll Cardiol. 2011 Jul 12;58[3]: 316-36).
In short, the performance and quality measures give all the diverse components of the U.S. health care delivery system a road map for implementing the 2017 High Blood Pressure Guideline in a format that depends on those components electing to adopt and adhere to the 2017 guideline. (Although one of the new performance measures, 1a, harmonizes with an existing and widely applied performance measure.)
“Who is the audience for this, and how will they respond? These performance measures need to be appropriated” by health systems and by performance-assessment groups. “I hope the NCQA will adopt it,” said William C. Cushman, MD, professor of preventive medicine at the University of Tennessee Health Science Center in Memphis, and chief of preventive medicine at the Memphis Veterans Affairs Medical Center. “There are some negatives to performance measures, but on balance they have done good things and led to better care.” Dr. Cushman also approved of several specific performance and quality measures included in the report. “Most of what they emphasized is good,” particularly the importance of accurate pressure measurement, he said in an interview.
“Process drives outcomes” in hypertension management, and the new performance and quality measures “have some very good process metrics,” commented Dr. Egan. “I’d encourage health systems to select two or three measures that are key to what they do and make sense in their setting rather than try to implement it all at once,” he advised, echoing what Dr. Casey had suggested. “It’s ideal to do everything, but we know that if you give physicians a long list of performance measures they just get overwhelmed. The nice thing about hypertension is that we know that process drives outcomes. In the past, we’ve had some process metrics that did not drive outcomes. Getting these processes implemented will lead to better patient outcomes and save a ton of money.”
“We have introduced the 2017 guideline recommendations throughout Target: BP, but like any quality improvement program there is a question of how does it spread,” said Gregory Wozniak, PhD, director of outcomes analytics for the AMA in Chicago. “Our goal for Target: BP is to be impacting 20 million patients by 2021.”
Dr. Casey, Dr. Weiswasser, and Dr. Wozniak had no disclosures. Dr. Cushman has received honoraria as a speaker from Arbor and Sanofi-Aventis, and travel and research support from Eli Lilly. Dr. Egan has been a consultant to and speaker on behalf of Merck and a speaker for Emcure.
SOURCE: Casey DE et al. J Am Coll Cardiol. 2019 Nov 26;74[21]: 2661-706.
PHILADELPHIA – The American Heart Association and American College of Cardiology took a big step toward facilitating widespread U.S. application of the hypertension management guideline that the societies issued in 2017 by releasing a set of performance and quality measures for adults with high blood pressure based on the 2017 guideline.
This guideline notably set a treatment target for patients diagnosed with hypertension of less than 130/80 mg/dL, and also lowered the threshold for diagnosing stage 1 hypertension to a blood pressure at or above 130/80 mm Hg, adding in a stroke about 31 million adults with hypertension to the U.S. total.
Having performance and quality measures based on the guideline is “critical, because how else would you know whether you’re having an effect on accurately diagnosing and properly controlling hypertension?” said Donald E. Casey Jr., MD, chair of the performance measures writing committee. The next step is field testing of the measures “to show they are reliable and effective,” as well as other steps to encourage widespread U.S. uptake of the performance and quality measures and the specifics of the 2017 guideline, Dr. Casey said during a presentation of the revised measures at the American Heart Association scientific sessions.
He especially highlighted the important role of Target: BP, an education, recognition, and quality improvement program run by the AHA and American Medical Association, as a tool that medical practices, health systems, and even payers and employers can use to begin to apply the new performance and quality measures (J Am Coll Cardiol. 2019 Nov 26;74[21]:2661-706) and better align with the recommendations of the 2017 high blood pressure guideline (J Am Coll Cardiol. 2018 May;71[19]:e127-248).
“We’re trying now to promote Target: BP; it’s something you can take off the shelf and get going if it’s embedded in a real-life delivery model. I think Target: BP is the secret sauce. It will be the way we’ll convince people to adopt this,” said Dr. Casey, principal and founder of IPO 4 Health, a Chicago-based health care consulting firm.
He also advised practices and health systems not to feel compelled to introduce all of the specific performance and quality measures at once. “We don’t believe everyone has the resources to do all of it at once; the point is to move toward this system of care. We understand that people don’t have the resources to get it all done” immediately, Dr. Casey said in an interview.
A report during another session at the meeting documented the potential impact that Target: BP can have on blood pressure control within a health system. The Trinity Health of New England medical group based in Springfield, Mass., a system with about 140,000 patients – including 20,000 adults diagnosed with hypertension – and served by 230 health care providers in 13 offices in western Massachusetts, began using Target: BP’s MAP improvement program in its practices in November 2018. (MAP stands for measure accurately, act rapidly, and partner with patients.) Just before the MAP program began, 72% of patients diagnosed with hypertension in the medical group were at their goal blood pressure. Less than a year later, in September 2019, the hypertension control rate had jumped to 84%, a 12 percentage point improvement in control in practices that already had been doing a relatively good job, said Daniel W. Weiswasser, MD, director of quality and clinical informatics at Trinity Health of New England. Based on this success, Trinity Health plans to next involve the remaining regions of Trinity Health of New England in Target: BP, followed by the other regions of Trinity’s national organization, which operates in 21 states with nearly 4,000 staff physicians and about half a million patients diagnosed with hypertension, Dr. Weiswasser said.
“If clinicians do the three steps of the MAP then we will see substantial drops in blood pressures. It will occur,” declared Brent M. Egan, MD, vice president for cardiovascular disease prevention of the AMA in Greenville, S.C.
The new report includes six performance measures based on the strongest guideline recommendations and designed to document adherence levels for the purposes of public reporting and pay-for-performance programs. It also includes 16 quality measures designed for local quality review purposes, with 6 process quality measures and 10 structural quality measures. The report spells out that the authors designed the performance measures for use by major national organizations such as the Centers for Medicare & Medicaid Services and the National Committee for Quality Assurance (NCQA), while the quality measures are designed to support quality improvement efforts in any care-delivery setting.
The authors said that the writing committee is sensitive to the fact that the 2019 performance measures for controlling high blood pressure developed by the NCQA for the Healthcare Effectiveness Data and Information Set and currently in use in 2019 by CMS also does not incorporate the 2017 Hypertension Clinical Practice Guidelines classification scheme. “It is well understood that these measures are already in widespread use, especially for quality-related payment programs promulgated by CMS, such as the Medicare Advantage ‘Stars’ ratings, the Medicare Shared Savings Program, and the Physician Quality Payment Program, as well as many other programs promoted by commercial health insurers. In particular, the widespread use of the 2017 Hypertension Clinical Practice Guidelines classification scheme will also help to guide decision making about when to prescribe antihypertensive medications in accordance with its current recommendations for the ACC/AHA “stages” of stage 1 and stage 2 hypertension and elevated blood pressure,” they added.
The report also says that “the writing committee was sensitive to the fact that there is currently not complete consensus among other guidelines from the American College of Physicians and the American Academy of Family Physicians, and also the European Society of Cardiology and the European Society of Hypertension. Nonetheless, despite this ongoing debate, the writing committee felt strongly that it is now time to move the U.S. health care system ahead to reflect these differing points of view and expects that widespread use of this new measure set will help to achieve this goal.” The new report revises hypertension performance measures developed by the ACC and AHA in 2011 (J Am Coll Cardiol. 2011 Jul 12;58[3]: 316-36).
In short, the performance and quality measures give all the diverse components of the U.S. health care delivery system a road map for implementing the 2017 High Blood Pressure Guideline in a format that depends on those components electing to adopt and adhere to the 2017 guideline. (Although one of the new performance measures, 1a, harmonizes with an existing and widely applied performance measure.)
“Who is the audience for this, and how will they respond? These performance measures need to be appropriated” by health systems and by performance-assessment groups. “I hope the NCQA will adopt it,” said William C. Cushman, MD, professor of preventive medicine at the University of Tennessee Health Science Center in Memphis, and chief of preventive medicine at the Memphis Veterans Affairs Medical Center. “There are some negatives to performance measures, but on balance they have done good things and led to better care.” Dr. Cushman also approved of several specific performance and quality measures included in the report. “Most of what they emphasized is good,” particularly the importance of accurate pressure measurement, he said in an interview.
“Process drives outcomes” in hypertension management, and the new performance and quality measures “have some very good process metrics,” commented Dr. Egan. “I’d encourage health systems to select two or three measures that are key to what they do and make sense in their setting rather than try to implement it all at once,” he advised, echoing what Dr. Casey had suggested. “It’s ideal to do everything, but we know that if you give physicians a long list of performance measures they just get overwhelmed. The nice thing about hypertension is that we know that process drives outcomes. In the past, we’ve had some process metrics that did not drive outcomes. Getting these processes implemented will lead to better patient outcomes and save a ton of money.”
“We have introduced the 2017 guideline recommendations throughout Target: BP, but like any quality improvement program there is a question of how does it spread,” said Gregory Wozniak, PhD, director of outcomes analytics for the AMA in Chicago. “Our goal for Target: BP is to be impacting 20 million patients by 2021.”
Dr. Casey, Dr. Weiswasser, and Dr. Wozniak had no disclosures. Dr. Cushman has received honoraria as a speaker from Arbor and Sanofi-Aventis, and travel and research support from Eli Lilly. Dr. Egan has been a consultant to and speaker on behalf of Merck and a speaker for Emcure.
SOURCE: Casey DE et al. J Am Coll Cardiol. 2019 Nov 26;74[21]: 2661-706.
PHILADELPHIA – The American Heart Association and American College of Cardiology took a big step toward facilitating widespread U.S. application of the hypertension management guideline that the societies issued in 2017 by releasing a set of performance and quality measures for adults with high blood pressure based on the 2017 guideline.
This guideline notably set a treatment target for patients diagnosed with hypertension of less than 130/80 mg/dL, and also lowered the threshold for diagnosing stage 1 hypertension to a blood pressure at or above 130/80 mm Hg, adding in a stroke about 31 million adults with hypertension to the U.S. total.
Having performance and quality measures based on the guideline is “critical, because how else would you know whether you’re having an effect on accurately diagnosing and properly controlling hypertension?” said Donald E. Casey Jr., MD, chair of the performance measures writing committee. The next step is field testing of the measures “to show they are reliable and effective,” as well as other steps to encourage widespread U.S. uptake of the performance and quality measures and the specifics of the 2017 guideline, Dr. Casey said during a presentation of the revised measures at the American Heart Association scientific sessions.
He especially highlighted the important role of Target: BP, an education, recognition, and quality improvement program run by the AHA and American Medical Association, as a tool that medical practices, health systems, and even payers and employers can use to begin to apply the new performance and quality measures (J Am Coll Cardiol. 2019 Nov 26;74[21]:2661-706) and better align with the recommendations of the 2017 high blood pressure guideline (J Am Coll Cardiol. 2018 May;71[19]:e127-248).
“We’re trying now to promote Target: BP; it’s something you can take off the shelf and get going if it’s embedded in a real-life delivery model. I think Target: BP is the secret sauce. It will be the way we’ll convince people to adopt this,” said Dr. Casey, principal and founder of IPO 4 Health, a Chicago-based health care consulting firm.
He also advised practices and health systems not to feel compelled to introduce all of the specific performance and quality measures at once. “We don’t believe everyone has the resources to do all of it at once; the point is to move toward this system of care. We understand that people don’t have the resources to get it all done” immediately, Dr. Casey said in an interview.
A report during another session at the meeting documented the potential impact that Target: BP can have on blood pressure control within a health system. The Trinity Health of New England medical group based in Springfield, Mass., a system with about 140,000 patients – including 20,000 adults diagnosed with hypertension – and served by 230 health care providers in 13 offices in western Massachusetts, began using Target: BP’s MAP improvement program in its practices in November 2018. (MAP stands for measure accurately, act rapidly, and partner with patients.) Just before the MAP program began, 72% of patients diagnosed with hypertension in the medical group were at their goal blood pressure. Less than a year later, in September 2019, the hypertension control rate had jumped to 84%, a 12 percentage point improvement in control in practices that already had been doing a relatively good job, said Daniel W. Weiswasser, MD, director of quality and clinical informatics at Trinity Health of New England. Based on this success, Trinity Health plans to next involve the remaining regions of Trinity Health of New England in Target: BP, followed by the other regions of Trinity’s national organization, which operates in 21 states with nearly 4,000 staff physicians and about half a million patients diagnosed with hypertension, Dr. Weiswasser said.
“If clinicians do the three steps of the MAP then we will see substantial drops in blood pressures. It will occur,” declared Brent M. Egan, MD, vice president for cardiovascular disease prevention of the AMA in Greenville, S.C.
The new report includes six performance measures based on the strongest guideline recommendations and designed to document adherence levels for the purposes of public reporting and pay-for-performance programs. It also includes 16 quality measures designed for local quality review purposes, with 6 process quality measures and 10 structural quality measures. The report spells out that the authors designed the performance measures for use by major national organizations such as the Centers for Medicare & Medicaid Services and the National Committee for Quality Assurance (NCQA), while the quality measures are designed to support quality improvement efforts in any care-delivery setting.
The authors said that the writing committee is sensitive to the fact that the 2019 performance measures for controlling high blood pressure developed by the NCQA for the Healthcare Effectiveness Data and Information Set and currently in use in 2019 by CMS also does not incorporate the 2017 Hypertension Clinical Practice Guidelines classification scheme. “It is well understood that these measures are already in widespread use, especially for quality-related payment programs promulgated by CMS, such as the Medicare Advantage ‘Stars’ ratings, the Medicare Shared Savings Program, and the Physician Quality Payment Program, as well as many other programs promoted by commercial health insurers. In particular, the widespread use of the 2017 Hypertension Clinical Practice Guidelines classification scheme will also help to guide decision making about when to prescribe antihypertensive medications in accordance with its current recommendations for the ACC/AHA “stages” of stage 1 and stage 2 hypertension and elevated blood pressure,” they added.
The report also says that “the writing committee was sensitive to the fact that there is currently not complete consensus among other guidelines from the American College of Physicians and the American Academy of Family Physicians, and also the European Society of Cardiology and the European Society of Hypertension. Nonetheless, despite this ongoing debate, the writing committee felt strongly that it is now time to move the U.S. health care system ahead to reflect these differing points of view and expects that widespread use of this new measure set will help to achieve this goal.” The new report revises hypertension performance measures developed by the ACC and AHA in 2011 (J Am Coll Cardiol. 2011 Jul 12;58[3]: 316-36).
In short, the performance and quality measures give all the diverse components of the U.S. health care delivery system a road map for implementing the 2017 High Blood Pressure Guideline in a format that depends on those components electing to adopt and adhere to the 2017 guideline. (Although one of the new performance measures, 1a, harmonizes with an existing and widely applied performance measure.)
“Who is the audience for this, and how will they respond? These performance measures need to be appropriated” by health systems and by performance-assessment groups. “I hope the NCQA will adopt it,” said William C. Cushman, MD, professor of preventive medicine at the University of Tennessee Health Science Center in Memphis, and chief of preventive medicine at the Memphis Veterans Affairs Medical Center. “There are some negatives to performance measures, but on balance they have done good things and led to better care.” Dr. Cushman also approved of several specific performance and quality measures included in the report. “Most of what they emphasized is good,” particularly the importance of accurate pressure measurement, he said in an interview.
“Process drives outcomes” in hypertension management, and the new performance and quality measures “have some very good process metrics,” commented Dr. Egan. “I’d encourage health systems to select two or three measures that are key to what they do and make sense in their setting rather than try to implement it all at once,” he advised, echoing what Dr. Casey had suggested. “It’s ideal to do everything, but we know that if you give physicians a long list of performance measures they just get overwhelmed. The nice thing about hypertension is that we know that process drives outcomes. In the past, we’ve had some process metrics that did not drive outcomes. Getting these processes implemented will lead to better patient outcomes and save a ton of money.”
“We have introduced the 2017 guideline recommendations throughout Target: BP, but like any quality improvement program there is a question of how does it spread,” said Gregory Wozniak, PhD, director of outcomes analytics for the AMA in Chicago. “Our goal for Target: BP is to be impacting 20 million patients by 2021.”
Dr. Casey, Dr. Weiswasser, and Dr. Wozniak had no disclosures. Dr. Cushman has received honoraria as a speaker from Arbor and Sanofi-Aventis, and travel and research support from Eli Lilly. Dr. Egan has been a consultant to and speaker on behalf of Merck and a speaker for Emcure.
SOURCE: Casey DE et al. J Am Coll Cardiol. 2019 Nov 26;74[21]: 2661-706.
REPORTING FROM AHA 2019
Farxiga granted Priority Review for treatment of adults with HFrEF
The Food and Drug Administration has accepted a supplemental New Drug Application and granted Priority Review for dapagliflozin (Farxiga) for the reduction of risk of cardiovascular death or worsening of heart failure in adult patients with heart failure with reduced ejection fraction (HFrEF).
The application was based on results from the landmark, phase 3 DAPA-HF trial, published in September 2019 in the New England Journal of Medicine. The study showed that dapagliflozin plus standard care reduced the incidence of cardiovascular death and worsening of heart failure versus placebo in patients with HFrEF.
Dapagliflozin was granted Fast Track designation for heart failure by the FDA in September 2019. In August 2019, the FDA also granted Fast Track designation to dapagliflozin for the delayed progression of renal failure and prevention of cardiovascular and renal death in patients with chronic kidney disease.
The drug is currently indicated for the improvement of glycemic control in adults with type 2 diabetes as either monotherapy or in combination. The FDA approved dapagliflozin in October 2019 for the reduction of heart failure hospitalization risk in patients with type 2 diabetes and cardiovascular risk factors.
“Farxiga is well established in the treatment of type 2 diabetes and this Priority Review shows its potential to also impact millions of patients with heart failure. If approved, Farxiga will be the first and only medicine of its kind indicated to treat patients with heart failure,” said Mene Pangalos, executive vice president of biopharmaceutical research and development at AstraZeneca.
Find the full press release on the AstraZeneca website.
The Food and Drug Administration has accepted a supplemental New Drug Application and granted Priority Review for dapagliflozin (Farxiga) for the reduction of risk of cardiovascular death or worsening of heart failure in adult patients with heart failure with reduced ejection fraction (HFrEF).
The application was based on results from the landmark, phase 3 DAPA-HF trial, published in September 2019 in the New England Journal of Medicine. The study showed that dapagliflozin plus standard care reduced the incidence of cardiovascular death and worsening of heart failure versus placebo in patients with HFrEF.
Dapagliflozin was granted Fast Track designation for heart failure by the FDA in September 2019. In August 2019, the FDA also granted Fast Track designation to dapagliflozin for the delayed progression of renal failure and prevention of cardiovascular and renal death in patients with chronic kidney disease.
The drug is currently indicated for the improvement of glycemic control in adults with type 2 diabetes as either monotherapy or in combination. The FDA approved dapagliflozin in October 2019 for the reduction of heart failure hospitalization risk in patients with type 2 diabetes and cardiovascular risk factors.
“Farxiga is well established in the treatment of type 2 diabetes and this Priority Review shows its potential to also impact millions of patients with heart failure. If approved, Farxiga will be the first and only medicine of its kind indicated to treat patients with heart failure,” said Mene Pangalos, executive vice president of biopharmaceutical research and development at AstraZeneca.
Find the full press release on the AstraZeneca website.
The Food and Drug Administration has accepted a supplemental New Drug Application and granted Priority Review for dapagliflozin (Farxiga) for the reduction of risk of cardiovascular death or worsening of heart failure in adult patients with heart failure with reduced ejection fraction (HFrEF).
The application was based on results from the landmark, phase 3 DAPA-HF trial, published in September 2019 in the New England Journal of Medicine. The study showed that dapagliflozin plus standard care reduced the incidence of cardiovascular death and worsening of heart failure versus placebo in patients with HFrEF.
Dapagliflozin was granted Fast Track designation for heart failure by the FDA in September 2019. In August 2019, the FDA also granted Fast Track designation to dapagliflozin for the delayed progression of renal failure and prevention of cardiovascular and renal death in patients with chronic kidney disease.
The drug is currently indicated for the improvement of glycemic control in adults with type 2 diabetes as either monotherapy or in combination. The FDA approved dapagliflozin in October 2019 for the reduction of heart failure hospitalization risk in patients with type 2 diabetes and cardiovascular risk factors.
“Farxiga is well established in the treatment of type 2 diabetes and this Priority Review shows its potential to also impact millions of patients with heart failure. If approved, Farxiga will be the first and only medicine of its kind indicated to treat patients with heart failure,” said Mene Pangalos, executive vice president of biopharmaceutical research and development at AstraZeneca.
Find the full press release on the AstraZeneca website.
Flu records most active December since 2003
The 2019-2020 flu season took a big jump in severity during the last full week of 2019, according to the Centers for Disease Control and Prevention.
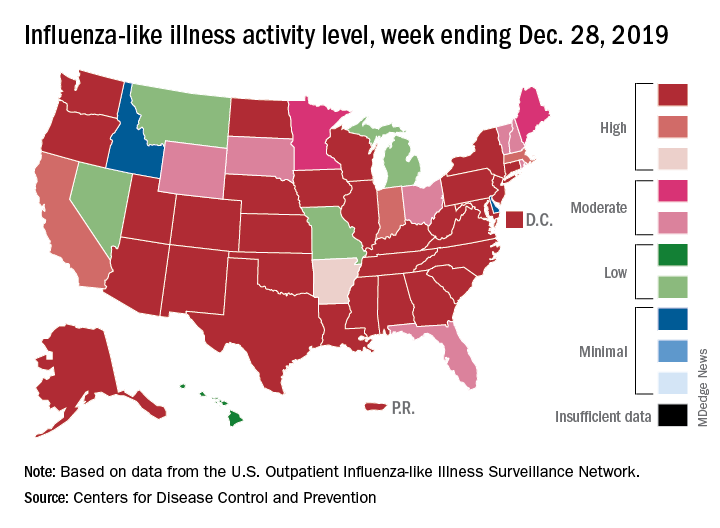
For the week ending Dec. 28, 6.9% of all outpatient visits to health care providers were for influenza-like illness (ILI), the CDC’s influenza division reported Jan. 3. That is up from 5.1% the previous week and is the highest rate recorded in December since 2003. During the flu pandemic season of 2009-2010, the rate peaked in October and dropped to relatively normal levels by the end of November, CDC data show.
This marks the eighth consecutive week that the outpatient visit rate has been at or above the nation’s baseline level of 2.4%, but the data for this week “may in part be influenced by changes in healthcare-seeking behavior that can occur during the holidays,” the CDC suggested.
All those outpatient visits mean that the ILI activity map is getting quite red. Thirty states, as well as the District of Columbia and Puerto Rico, were at the highest level on the CDC’s 1-10 activity scale during the week ending Dec. 28, compared with 20 the week before. Four states were categorized in the “high” range with activity levels of 8 and 9.
There have been approximately 6.4 million flu illnesses so far this season, the CDC estimated, along with 55,000 hospitalizations, although the ILI admission rate of 9.2 per 100,000 population is fairly typical for this time of year.
The week of Dec. 28 also brought reports of five more ILI-related pediatric deaths, which all occurred in the two previous weeks. A total of 27 children have died from the flu so far during the 2019-2020 season, the CDC said.
The 2019-2020 flu season took a big jump in severity during the last full week of 2019, according to the Centers for Disease Control and Prevention.
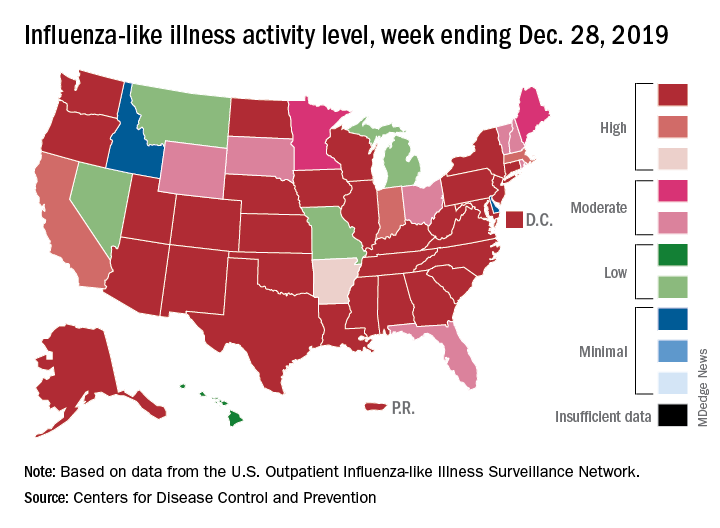
For the week ending Dec. 28, 6.9% of all outpatient visits to health care providers were for influenza-like illness (ILI), the CDC’s influenza division reported Jan. 3. That is up from 5.1% the previous week and is the highest rate recorded in December since 2003. During the flu pandemic season of 2009-2010, the rate peaked in October and dropped to relatively normal levels by the end of November, CDC data show.
This marks the eighth consecutive week that the outpatient visit rate has been at or above the nation’s baseline level of 2.4%, but the data for this week “may in part be influenced by changes in healthcare-seeking behavior that can occur during the holidays,” the CDC suggested.
All those outpatient visits mean that the ILI activity map is getting quite red. Thirty states, as well as the District of Columbia and Puerto Rico, were at the highest level on the CDC’s 1-10 activity scale during the week ending Dec. 28, compared with 20 the week before. Four states were categorized in the “high” range with activity levels of 8 and 9.
There have been approximately 6.4 million flu illnesses so far this season, the CDC estimated, along with 55,000 hospitalizations, although the ILI admission rate of 9.2 per 100,000 population is fairly typical for this time of year.
The week of Dec. 28 also brought reports of five more ILI-related pediatric deaths, which all occurred in the two previous weeks. A total of 27 children have died from the flu so far during the 2019-2020 season, the CDC said.
The 2019-2020 flu season took a big jump in severity during the last full week of 2019, according to the Centers for Disease Control and Prevention.
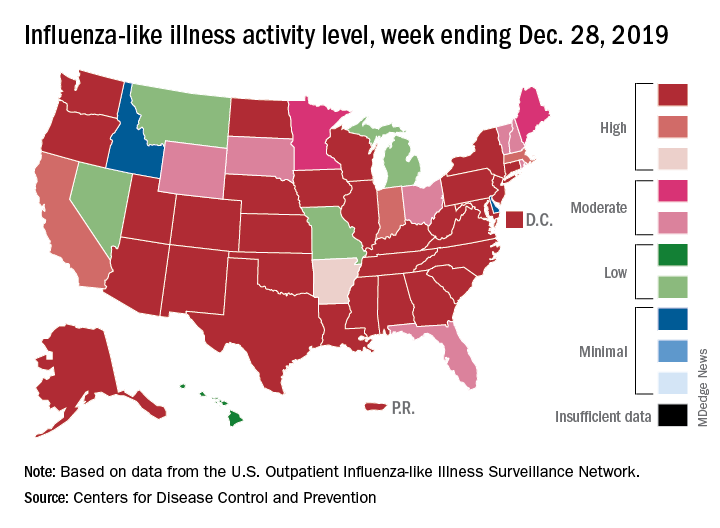
For the week ending Dec. 28, 6.9% of all outpatient visits to health care providers were for influenza-like illness (ILI), the CDC’s influenza division reported Jan. 3. That is up from 5.1% the previous week and is the highest rate recorded in December since 2003. During the flu pandemic season of 2009-2010, the rate peaked in October and dropped to relatively normal levels by the end of November, CDC data show.
This marks the eighth consecutive week that the outpatient visit rate has been at or above the nation’s baseline level of 2.4%, but the data for this week “may in part be influenced by changes in healthcare-seeking behavior that can occur during the holidays,” the CDC suggested.
All those outpatient visits mean that the ILI activity map is getting quite red. Thirty states, as well as the District of Columbia and Puerto Rico, were at the highest level on the CDC’s 1-10 activity scale during the week ending Dec. 28, compared with 20 the week before. Four states were categorized in the “high” range with activity levels of 8 and 9.
There have been approximately 6.4 million flu illnesses so far this season, the CDC estimated, along with 55,000 hospitalizations, although the ILI admission rate of 9.2 per 100,000 population is fairly typical for this time of year.
The week of Dec. 28 also brought reports of five more ILI-related pediatric deaths, which all occurred in the two previous weeks. A total of 27 children have died from the flu so far during the 2019-2020 season, the CDC said.
Cultivating patient activation through technology
Tech alone is not enough
Patient activation refers to an individual’s knowledge, skill, and confidence in managing their health and health care, according to a recent BMJ editorial. It’s recognized as a critical aspect of high-quality, patient-centered health care – patient activation has the potential to improve patient outcomes while reducing costs.
Total knee replacement offers a great opportunity to study patient activation, said editorial lead author Jesse I. Wolfstadt, MD, MS, FRCSC, of the University of Toronto. “It may help address the one in five patients who are unsatisfied with their knee replacement despite an otherwise technically sound procedure.”
The authors considered some patient activation studies that have shown positive results for cultivating activation through technology. In one, patients engaging with a bedside multimedia intervention on a tablet after undergoing knee replacement reported better pain scores, length of stay, knee function, and satisfaction with care. Another study showed patients who received automated text messages after joint replacement improved time spent on home exercises, decreased their use of narcotics, and had fewer calls to the surgeon’s office.
But “negative mobile app studies seem to suggest that when technologies are used as a passive educational intervention, patient activation may suffer,” according to the editorial. “One possible key ingredient to successful patient activation is the engagement of the health care team that is facilitated through mobile technology. ... Mobile apps and other technological interventions also must have clear goals if they are to be used successfully; and these goals are likely to differ for different patient populations and disease processes.”
Technology alone is not enough to affect patient activation, Dr. Wolfstadt said. “The key to success will likely involve tailoring interventions to individual patients and facilitating increased engagement with the health care team. You can’t just give a patient an app or other form of technology and expect it to replace the function of patient-clinician communication/interaction.”
Reference
1. Wolfstadt JI et ak. Improving patient outcomes following total joint arthroplasty: Is there an app for that? BMJ Qual Saf. 2019 May 2019. doi: 10.1136/bmjqs-2019-009571.
Tech alone is not enough
Tech alone is not enough
Patient activation refers to an individual’s knowledge, skill, and confidence in managing their health and health care, according to a recent BMJ editorial. It’s recognized as a critical aspect of high-quality, patient-centered health care – patient activation has the potential to improve patient outcomes while reducing costs.
Total knee replacement offers a great opportunity to study patient activation, said editorial lead author Jesse I. Wolfstadt, MD, MS, FRCSC, of the University of Toronto. “It may help address the one in five patients who are unsatisfied with their knee replacement despite an otherwise technically sound procedure.”
The authors considered some patient activation studies that have shown positive results for cultivating activation through technology. In one, patients engaging with a bedside multimedia intervention on a tablet after undergoing knee replacement reported better pain scores, length of stay, knee function, and satisfaction with care. Another study showed patients who received automated text messages after joint replacement improved time spent on home exercises, decreased their use of narcotics, and had fewer calls to the surgeon’s office.
But “negative mobile app studies seem to suggest that when technologies are used as a passive educational intervention, patient activation may suffer,” according to the editorial. “One possible key ingredient to successful patient activation is the engagement of the health care team that is facilitated through mobile technology. ... Mobile apps and other technological interventions also must have clear goals if they are to be used successfully; and these goals are likely to differ for different patient populations and disease processes.”
Technology alone is not enough to affect patient activation, Dr. Wolfstadt said. “The key to success will likely involve tailoring interventions to individual patients and facilitating increased engagement with the health care team. You can’t just give a patient an app or other form of technology and expect it to replace the function of patient-clinician communication/interaction.”
Reference
1. Wolfstadt JI et ak. Improving patient outcomes following total joint arthroplasty: Is there an app for that? BMJ Qual Saf. 2019 May 2019. doi: 10.1136/bmjqs-2019-009571.
Patient activation refers to an individual’s knowledge, skill, and confidence in managing their health and health care, according to a recent BMJ editorial. It’s recognized as a critical aspect of high-quality, patient-centered health care – patient activation has the potential to improve patient outcomes while reducing costs.
Total knee replacement offers a great opportunity to study patient activation, said editorial lead author Jesse I. Wolfstadt, MD, MS, FRCSC, of the University of Toronto. “It may help address the one in five patients who are unsatisfied with their knee replacement despite an otherwise technically sound procedure.”
The authors considered some patient activation studies that have shown positive results for cultivating activation through technology. In one, patients engaging with a bedside multimedia intervention on a tablet after undergoing knee replacement reported better pain scores, length of stay, knee function, and satisfaction with care. Another study showed patients who received automated text messages after joint replacement improved time spent on home exercises, decreased their use of narcotics, and had fewer calls to the surgeon’s office.
But “negative mobile app studies seem to suggest that when technologies are used as a passive educational intervention, patient activation may suffer,” according to the editorial. “One possible key ingredient to successful patient activation is the engagement of the health care team that is facilitated through mobile technology. ... Mobile apps and other technological interventions also must have clear goals if they are to be used successfully; and these goals are likely to differ for different patient populations and disease processes.”
Technology alone is not enough to affect patient activation, Dr. Wolfstadt said. “The key to success will likely involve tailoring interventions to individual patients and facilitating increased engagement with the health care team. You can’t just give a patient an app or other form of technology and expect it to replace the function of patient-clinician communication/interaction.”
Reference
1. Wolfstadt JI et ak. Improving patient outcomes following total joint arthroplasty: Is there an app for that? BMJ Qual Saf. 2019 May 2019. doi: 10.1136/bmjqs-2019-009571.
Experts call to revise the Uniform Determination of Death Act
, according to an editorial published online Dec. 24, 2019, in Annals of Internal Medicine. Proposed revisions would identify the standards for determining death by neurologic criteria and address the question of whether consent is required to make this determination. If accepted, the revisions would enhance public trust in the determination of death by neurologic criteria, the authors said.
“There is a disconnect between the medical and legal standards for brain death,” said Ariane K. Lewis, MD, associate professor of neurology and neurosurgery at New York University and lead author of the editorial. The discrepancy must be remedied because it has led to lawsuits and has proved to be problematic from a societal standpoint, she added.
“We defend changing the law to match medical practice, rather than changing medical practice to match the law,” said Thaddeus Mason Pope, JD, PhD, director of the Health Law Institute at Mitchell Hamline School of Law in Saint Paul, Minnesota, and an author of the editorial.
Accepted medical standards are unclear
The UDDA was drafted in 1981 to establish a uniform legal standard for death by neurologic criteria. A person with “irreversible cessation of all functions of the entire brain, including the brainstem,” is dead, according to the statute. A determination of death, it adds, “must be made in accordance with accepted medical standards.”
But the medical standards used to determine death by neurologic cause have not been uniform. In 2015, the Supreme Court of Nevada ruled that it was not clear that the standard published by the American Academy of Neurology (AAN), which had been used in the case at issue, was the “accepted medical standard.” An AAN summit later affirmed that the accepted medical standards for determination of death by neurologic cause are the 2010 AAN standard for determination of brain death in adults and the 2011 Society of Critical Care Medicine (SCCM), American Academy of Pediatrics (AAP), and Child Neurology Society (CNS) standard for determination of brain death in children. The Nevada legislature amended the state UDDA to identify these standards as the accepted standards. A revised UDDA also should identify these standards and grant an administrative agency (i.e., the board of medicine) the power to review and update the accepted medical standards as needed, according to the editorial.
To the extent that hospitals are not following the AAN or SCCM/AAP/CNS standards for determining death by neurologic cause, “enshrining” these standards in a revised UDDA “should increase uniformity and consistency” in hospitals’ policies on brain death, Dr. Pope said.
The question of hormonal function
Lawsuits in California and Nevada raised the question of whether the pituitary gland and hypothalamus are parts of the brain. If so, then the accepted medical standards for death by neurologic cause are not consistent with the statutory requirements for the determination of death, since the former do not test for cessation of hormonal function.
The current edition of the adult standards for determining death by neurologic cause were published in 2010. “Whenever we measure brain death, we’re not measuring the cessation of all functions of the entire brain,” Dr. Pope said. “That’s not a new thing; that’s been the case for a long time.”
To address the discrepancy between medical practice and the legal statute, Dr. Lewis and colleagues proposed that the UDDA’s reference to “irreversible cessation of functions of the entire brain” be followed by the following clause: “including the brainstem, leading to unresponsive coma with loss of capacity for consciousness, brainstem areflexia, and the inability to breathe spontaneously.” An alternative revision would be to add the briefer phrase “... with the exception of hormonal function.”
Authors say consent is not required for testing
Other complications have arisen from the UDDA’s failure to specify whether consent is required for a determination of death by neurologic cause. Court rulings on this question have not been consistent. Dr. Lewis and colleagues propose adding the following text to the UDDA: “Reasonable efforts should be made to notify a patient’s legally authorized decision-maker before performing a determination of death by neurologic criteria, but consent is not required to initiate such an evaluation.”
The proposed revisions to the UDDA “might give [clinicians] more confidence to proceed with brain death testing, because it would clarify that they don’t need the parents’ [or the patient’s legally authorized decision-maker] consent to do the tests,” said Dr. Pope. “If anything, they might even have a duty to do the tests.”
The final problem with the UDDA that Dr. Lewis and colleagues cited is that it does not provide clear guidance about how to respond to religious objections to discontinuation of organ support after a determination of death by neurologic cause. “Because the issue is rather complicated, we have not advocated for a singular position related to this [question] in our revised UDDA,” Dr. Lewis said. “Rather, we recommended the need for a multidisciplinary group to come together to determine what is the best approach. In an ideal world, this [approach] would be universal throughout the country.”
Although a revised UDDA would provide greater clarity to physicians and promote uniformity of practice, it would not resolve ongoing theological and philosophical debates about whether brain death is biological death, Dr. Pope said. “The key thing is that it would give clinicians a green light or certainty and clarity that they may proceed to do the test in the first place. If the tests are positive and the patient really is dead, then they could proceed to organ procurement or to move to the morgue.”
Dr. Lewis is a member of various AAN committees and working groups but receives no compensation for her role. A coauthor received personal fees from the AAN that were unrelated to the editorial.
SOURCE: Lewis A et al. Ann Intern Med. 2019 Dec 24. doi: 10.7326/M19-2731.
, according to an editorial published online Dec. 24, 2019, in Annals of Internal Medicine. Proposed revisions would identify the standards for determining death by neurologic criteria and address the question of whether consent is required to make this determination. If accepted, the revisions would enhance public trust in the determination of death by neurologic criteria, the authors said.
“There is a disconnect between the medical and legal standards for brain death,” said Ariane K. Lewis, MD, associate professor of neurology and neurosurgery at New York University and lead author of the editorial. The discrepancy must be remedied because it has led to lawsuits and has proved to be problematic from a societal standpoint, she added.
“We defend changing the law to match medical practice, rather than changing medical practice to match the law,” said Thaddeus Mason Pope, JD, PhD, director of the Health Law Institute at Mitchell Hamline School of Law in Saint Paul, Minnesota, and an author of the editorial.
Accepted medical standards are unclear
The UDDA was drafted in 1981 to establish a uniform legal standard for death by neurologic criteria. A person with “irreversible cessation of all functions of the entire brain, including the brainstem,” is dead, according to the statute. A determination of death, it adds, “must be made in accordance with accepted medical standards.”
But the medical standards used to determine death by neurologic cause have not been uniform. In 2015, the Supreme Court of Nevada ruled that it was not clear that the standard published by the American Academy of Neurology (AAN), which had been used in the case at issue, was the “accepted medical standard.” An AAN summit later affirmed that the accepted medical standards for determination of death by neurologic cause are the 2010 AAN standard for determination of brain death in adults and the 2011 Society of Critical Care Medicine (SCCM), American Academy of Pediatrics (AAP), and Child Neurology Society (CNS) standard for determination of brain death in children. The Nevada legislature amended the state UDDA to identify these standards as the accepted standards. A revised UDDA also should identify these standards and grant an administrative agency (i.e., the board of medicine) the power to review and update the accepted medical standards as needed, according to the editorial.
To the extent that hospitals are not following the AAN or SCCM/AAP/CNS standards for determining death by neurologic cause, “enshrining” these standards in a revised UDDA “should increase uniformity and consistency” in hospitals’ policies on brain death, Dr. Pope said.
The question of hormonal function
Lawsuits in California and Nevada raised the question of whether the pituitary gland and hypothalamus are parts of the brain. If so, then the accepted medical standards for death by neurologic cause are not consistent with the statutory requirements for the determination of death, since the former do not test for cessation of hormonal function.
The current edition of the adult standards for determining death by neurologic cause were published in 2010. “Whenever we measure brain death, we’re not measuring the cessation of all functions of the entire brain,” Dr. Pope said. “That’s not a new thing; that’s been the case for a long time.”
To address the discrepancy between medical practice and the legal statute, Dr. Lewis and colleagues proposed that the UDDA’s reference to “irreversible cessation of functions of the entire brain” be followed by the following clause: “including the brainstem, leading to unresponsive coma with loss of capacity for consciousness, brainstem areflexia, and the inability to breathe spontaneously.” An alternative revision would be to add the briefer phrase “... with the exception of hormonal function.”
Authors say consent is not required for testing
Other complications have arisen from the UDDA’s failure to specify whether consent is required for a determination of death by neurologic cause. Court rulings on this question have not been consistent. Dr. Lewis and colleagues propose adding the following text to the UDDA: “Reasonable efforts should be made to notify a patient’s legally authorized decision-maker before performing a determination of death by neurologic criteria, but consent is not required to initiate such an evaluation.”
The proposed revisions to the UDDA “might give [clinicians] more confidence to proceed with brain death testing, because it would clarify that they don’t need the parents’ [or the patient’s legally authorized decision-maker] consent to do the tests,” said Dr. Pope. “If anything, they might even have a duty to do the tests.”
The final problem with the UDDA that Dr. Lewis and colleagues cited is that it does not provide clear guidance about how to respond to religious objections to discontinuation of organ support after a determination of death by neurologic cause. “Because the issue is rather complicated, we have not advocated for a singular position related to this [question] in our revised UDDA,” Dr. Lewis said. “Rather, we recommended the need for a multidisciplinary group to come together to determine what is the best approach. In an ideal world, this [approach] would be universal throughout the country.”
Although a revised UDDA would provide greater clarity to physicians and promote uniformity of practice, it would not resolve ongoing theological and philosophical debates about whether brain death is biological death, Dr. Pope said. “The key thing is that it would give clinicians a green light or certainty and clarity that they may proceed to do the test in the first place. If the tests are positive and the patient really is dead, then they could proceed to organ procurement or to move to the morgue.”
Dr. Lewis is a member of various AAN committees and working groups but receives no compensation for her role. A coauthor received personal fees from the AAN that were unrelated to the editorial.
SOURCE: Lewis A et al. Ann Intern Med. 2019 Dec 24. doi: 10.7326/M19-2731.
, according to an editorial published online Dec. 24, 2019, in Annals of Internal Medicine. Proposed revisions would identify the standards for determining death by neurologic criteria and address the question of whether consent is required to make this determination. If accepted, the revisions would enhance public trust in the determination of death by neurologic criteria, the authors said.
“There is a disconnect between the medical and legal standards for brain death,” said Ariane K. Lewis, MD, associate professor of neurology and neurosurgery at New York University and lead author of the editorial. The discrepancy must be remedied because it has led to lawsuits and has proved to be problematic from a societal standpoint, she added.
“We defend changing the law to match medical practice, rather than changing medical practice to match the law,” said Thaddeus Mason Pope, JD, PhD, director of the Health Law Institute at Mitchell Hamline School of Law in Saint Paul, Minnesota, and an author of the editorial.
Accepted medical standards are unclear
The UDDA was drafted in 1981 to establish a uniform legal standard for death by neurologic criteria. A person with “irreversible cessation of all functions of the entire brain, including the brainstem,” is dead, according to the statute. A determination of death, it adds, “must be made in accordance with accepted medical standards.”
But the medical standards used to determine death by neurologic cause have not been uniform. In 2015, the Supreme Court of Nevada ruled that it was not clear that the standard published by the American Academy of Neurology (AAN), which had been used in the case at issue, was the “accepted medical standard.” An AAN summit later affirmed that the accepted medical standards for determination of death by neurologic cause are the 2010 AAN standard for determination of brain death in adults and the 2011 Society of Critical Care Medicine (SCCM), American Academy of Pediatrics (AAP), and Child Neurology Society (CNS) standard for determination of brain death in children. The Nevada legislature amended the state UDDA to identify these standards as the accepted standards. A revised UDDA also should identify these standards and grant an administrative agency (i.e., the board of medicine) the power to review and update the accepted medical standards as needed, according to the editorial.
To the extent that hospitals are not following the AAN or SCCM/AAP/CNS standards for determining death by neurologic cause, “enshrining” these standards in a revised UDDA “should increase uniformity and consistency” in hospitals’ policies on brain death, Dr. Pope said.
The question of hormonal function
Lawsuits in California and Nevada raised the question of whether the pituitary gland and hypothalamus are parts of the brain. If so, then the accepted medical standards for death by neurologic cause are not consistent with the statutory requirements for the determination of death, since the former do not test for cessation of hormonal function.
The current edition of the adult standards for determining death by neurologic cause were published in 2010. “Whenever we measure brain death, we’re not measuring the cessation of all functions of the entire brain,” Dr. Pope said. “That’s not a new thing; that’s been the case for a long time.”
To address the discrepancy between medical practice and the legal statute, Dr. Lewis and colleagues proposed that the UDDA’s reference to “irreversible cessation of functions of the entire brain” be followed by the following clause: “including the brainstem, leading to unresponsive coma with loss of capacity for consciousness, brainstem areflexia, and the inability to breathe spontaneously.” An alternative revision would be to add the briefer phrase “... with the exception of hormonal function.”
Authors say consent is not required for testing
Other complications have arisen from the UDDA’s failure to specify whether consent is required for a determination of death by neurologic cause. Court rulings on this question have not been consistent. Dr. Lewis and colleagues propose adding the following text to the UDDA: “Reasonable efforts should be made to notify a patient’s legally authorized decision-maker before performing a determination of death by neurologic criteria, but consent is not required to initiate such an evaluation.”
The proposed revisions to the UDDA “might give [clinicians] more confidence to proceed with brain death testing, because it would clarify that they don’t need the parents’ [or the patient’s legally authorized decision-maker] consent to do the tests,” said Dr. Pope. “If anything, they might even have a duty to do the tests.”
The final problem with the UDDA that Dr. Lewis and colleagues cited is that it does not provide clear guidance about how to respond to religious objections to discontinuation of organ support after a determination of death by neurologic cause. “Because the issue is rather complicated, we have not advocated for a singular position related to this [question] in our revised UDDA,” Dr. Lewis said. “Rather, we recommended the need for a multidisciplinary group to come together to determine what is the best approach. In an ideal world, this [approach] would be universal throughout the country.”
Although a revised UDDA would provide greater clarity to physicians and promote uniformity of practice, it would not resolve ongoing theological and philosophical debates about whether brain death is biological death, Dr. Pope said. “The key thing is that it would give clinicians a green light or certainty and clarity that they may proceed to do the test in the first place. If the tests are positive and the patient really is dead, then they could proceed to organ procurement or to move to the morgue.”
Dr. Lewis is a member of various AAN committees and working groups but receives no compensation for her role. A coauthor received personal fees from the AAN that were unrelated to the editorial.
SOURCE: Lewis A et al. Ann Intern Med. 2019 Dec 24. doi: 10.7326/M19-2731.
FROM ANNALS OF INTERNAL MEDICINE
Aligning scheduling and satisfaction
Research reveals counterintuitive results
Hospitalist work schedules have been the subject of much reporting – and recent research. Studies have shown that control over work hours and schedule flexibility are predictors of clinicians’ career satisfaction and burnout, factors linked to quality of patient care and retention.
Starting in January 2017, an academic hospital medicine group at the University of Colorado at Denver, Aurora, undertook a scheduling redesign using improvement methodology, combined with purchased scheduling software. Tyler Anstett, DO, a hospitalist and assistant professor at the university, and colleagues presented the results in an abstract published during the SHM 2019 annual conference last March.
“We wrote this abstract as a report of the work that we did over several years in our hospital medicine group to improve hospitalist satisfaction with their schedules,” said Dr. Anstett. “We identified that, despite not following the traditional seven-on, seven-off model and 100% fulfillment of individual schedule requests, the majority of clinicians were dissatisfied with the scheduling process and their overall clinical schedules. Further, building these complex, individualized schedules resulted in a heavy administrative burden. We strove to provide better alignment of schedule satisfaction and the administrative burden of incorporating individualized schedule requests.”
Prior to January 2017, service stretches had ranged from 5 to 9 days, and there were few limits on time-off requests.
“Through sequential interventions, we standardized service stretches to 7 days (Tuesday-Monday), introduced a limited number of guaranteed 7-day time-off requests (Tuesday-Monday), and added a limited number of nonguaranteed 3-day flexible time-off requests,” according to the authors. “This simplification improved the automation of the scheduling software, which increased the schedule release lead time to an average of 16 weeks. Further, despite standardizing service stretches to 7 days and limiting time-off requests, physicians surveyed reported improved satisfaction with both their scheduling process (34% of participants ‘satisfied’ in 2017 to 67% in 2018) and their overall clinical schedules (50% of participants ‘satisfied’ in 2017 to 75% in 2018).”So counterintuitively, creating individualized schedules may not result in improved satisfaction and likely results in heavy administrative burden, Dr. Anstett said. “Standardization of schedule creation with allowance of a ‘free-market’ system, allowing clinicians to self-individualize their schedules may also result in less administrative burden and improved satisfaction.”
Reference
1. Anstett T et al. K.I.S.S. (Keep It Simple … Schedules): How Standardization and Simplification Can Improve Scheduling and Physician Satisfaction. SHM 2019, Abstract 112. Accessed June 4, 2019.
Research reveals counterintuitive results
Research reveals counterintuitive results
Hospitalist work schedules have been the subject of much reporting – and recent research. Studies have shown that control over work hours and schedule flexibility are predictors of clinicians’ career satisfaction and burnout, factors linked to quality of patient care and retention.
Starting in January 2017, an academic hospital medicine group at the University of Colorado at Denver, Aurora, undertook a scheduling redesign using improvement methodology, combined with purchased scheduling software. Tyler Anstett, DO, a hospitalist and assistant professor at the university, and colleagues presented the results in an abstract published during the SHM 2019 annual conference last March.
“We wrote this abstract as a report of the work that we did over several years in our hospital medicine group to improve hospitalist satisfaction with their schedules,” said Dr. Anstett. “We identified that, despite not following the traditional seven-on, seven-off model and 100% fulfillment of individual schedule requests, the majority of clinicians were dissatisfied with the scheduling process and their overall clinical schedules. Further, building these complex, individualized schedules resulted in a heavy administrative burden. We strove to provide better alignment of schedule satisfaction and the administrative burden of incorporating individualized schedule requests.”
Prior to January 2017, service stretches had ranged from 5 to 9 days, and there were few limits on time-off requests.
“Through sequential interventions, we standardized service stretches to 7 days (Tuesday-Monday), introduced a limited number of guaranteed 7-day time-off requests (Tuesday-Monday), and added a limited number of nonguaranteed 3-day flexible time-off requests,” according to the authors. “This simplification improved the automation of the scheduling software, which increased the schedule release lead time to an average of 16 weeks. Further, despite standardizing service stretches to 7 days and limiting time-off requests, physicians surveyed reported improved satisfaction with both their scheduling process (34% of participants ‘satisfied’ in 2017 to 67% in 2018) and their overall clinical schedules (50% of participants ‘satisfied’ in 2017 to 75% in 2018).”So counterintuitively, creating individualized schedules may not result in improved satisfaction and likely results in heavy administrative burden, Dr. Anstett said. “Standardization of schedule creation with allowance of a ‘free-market’ system, allowing clinicians to self-individualize their schedules may also result in less administrative burden and improved satisfaction.”
Reference
1. Anstett T et al. K.I.S.S. (Keep It Simple … Schedules): How Standardization and Simplification Can Improve Scheduling and Physician Satisfaction. SHM 2019, Abstract 112. Accessed June 4, 2019.
Hospitalist work schedules have been the subject of much reporting – and recent research. Studies have shown that control over work hours and schedule flexibility are predictors of clinicians’ career satisfaction and burnout, factors linked to quality of patient care and retention.
Starting in January 2017, an academic hospital medicine group at the University of Colorado at Denver, Aurora, undertook a scheduling redesign using improvement methodology, combined with purchased scheduling software. Tyler Anstett, DO, a hospitalist and assistant professor at the university, and colleagues presented the results in an abstract published during the SHM 2019 annual conference last March.
“We wrote this abstract as a report of the work that we did over several years in our hospital medicine group to improve hospitalist satisfaction with their schedules,” said Dr. Anstett. “We identified that, despite not following the traditional seven-on, seven-off model and 100% fulfillment of individual schedule requests, the majority of clinicians were dissatisfied with the scheduling process and their overall clinical schedules. Further, building these complex, individualized schedules resulted in a heavy administrative burden. We strove to provide better alignment of schedule satisfaction and the administrative burden of incorporating individualized schedule requests.”
Prior to January 2017, service stretches had ranged from 5 to 9 days, and there were few limits on time-off requests.
“Through sequential interventions, we standardized service stretches to 7 days (Tuesday-Monday), introduced a limited number of guaranteed 7-day time-off requests (Tuesday-Monday), and added a limited number of nonguaranteed 3-day flexible time-off requests,” according to the authors. “This simplification improved the automation of the scheduling software, which increased the schedule release lead time to an average of 16 weeks. Further, despite standardizing service stretches to 7 days and limiting time-off requests, physicians surveyed reported improved satisfaction with both their scheduling process (34% of participants ‘satisfied’ in 2017 to 67% in 2018) and their overall clinical schedules (50% of participants ‘satisfied’ in 2017 to 75% in 2018).”So counterintuitively, creating individualized schedules may not result in improved satisfaction and likely results in heavy administrative burden, Dr. Anstett said. “Standardization of schedule creation with allowance of a ‘free-market’ system, allowing clinicians to self-individualize their schedules may also result in less administrative burden and improved satisfaction.”
Reference
1. Anstett T et al. K.I.S.S. (Keep It Simple … Schedules): How Standardization and Simplification Can Improve Scheduling and Physician Satisfaction. SHM 2019, Abstract 112. Accessed June 4, 2019.
Early increase in flu activity shows no signs of slowing
An important measure of U.S. flu activity for the 2019-2020 season has already surpassed last season’s high, and more than half the states are experiencing high levels of activity, according to the Centers for Disease Control and Prevention.
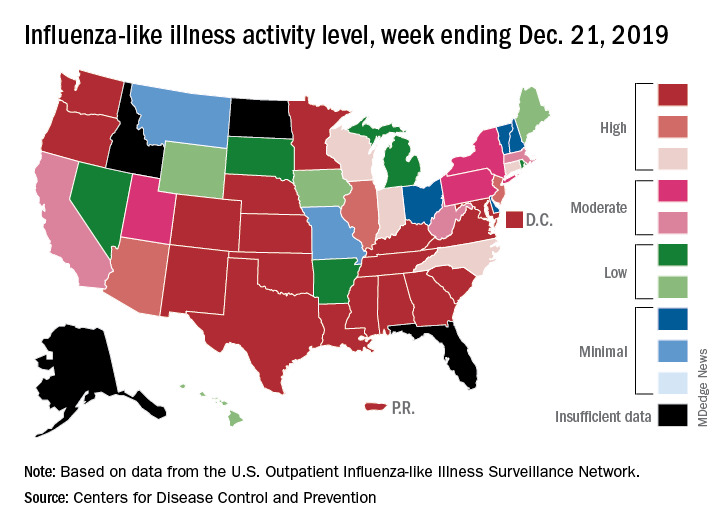
reported Dec. 27.
The last time the outpatient visit rate was higher than that was in February of the 2017-2018 season, when it peaked at 7.5%. The peak month of flu activity occurs most often – about once every 3 years – in February, and the odds of a December peak are about one in five, the CDC has said.
Outpatient illness activity also increased at the state level during the week ending Dec. 21. There were 20 jurisdictions – 18 states, the District of Columbia, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of activity, compared with 13 the previous week, and the number of jurisdictions in the “high” range (levels 8-10) jumped from 21 to 28, the CDC data show.
The influenza division estimated that there have been 4.6 million flu illnesses so far this season, nearly a million more than the total after last week, along with 39,000 hospitalizations. The overall hospitalization rate for the season is up to 6.6 per 100,000 population, which is about average at this point. The proportion of deaths attributed to pneumonia and influenza increased to 5.7%, which is below the epidemic threshold, the CDC said.
Three pediatric deaths related to influenza-like illness were reported during the week ending Dec. 21, two of which occurred in an earlier week. For the 2019-2020 season so far, a total of 22 pediatric deaths have been reported to the CDC.
An important measure of U.S. flu activity for the 2019-2020 season has already surpassed last season’s high, and more than half the states are experiencing high levels of activity, according to the Centers for Disease Control and Prevention.
reported Dec. 27.
The last time the outpatient visit rate was higher than that was in February of the 2017-2018 season, when it peaked at 7.5%. The peak month of flu activity occurs most often – about once every 3 years – in February, and the odds of a December peak are about one in five, the CDC has said.
Outpatient illness activity also increased at the state level during the week ending Dec. 21. There were 20 jurisdictions – 18 states, the District of Columbia, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of activity, compared with 13 the previous week, and the number of jurisdictions in the “high” range (levels 8-10) jumped from 21 to 28, the CDC data show.
The influenza division estimated that there have been 4.6 million flu illnesses so far this season, nearly a million more than the total after last week, along with 39,000 hospitalizations. The overall hospitalization rate for the season is up to 6.6 per 100,000 population, which is about average at this point. The proportion of deaths attributed to pneumonia and influenza increased to 5.7%, which is below the epidemic threshold, the CDC said.
Three pediatric deaths related to influenza-like illness were reported during the week ending Dec. 21, two of which occurred in an earlier week. For the 2019-2020 season so far, a total of 22 pediatric deaths have been reported to the CDC.
An important measure of U.S. flu activity for the 2019-2020 season has already surpassed last season’s high, and more than half the states are experiencing high levels of activity, according to the Centers for Disease Control and Prevention.
reported Dec. 27.
The last time the outpatient visit rate was higher than that was in February of the 2017-2018 season, when it peaked at 7.5%. The peak month of flu activity occurs most often – about once every 3 years – in February, and the odds of a December peak are about one in five, the CDC has said.
Outpatient illness activity also increased at the state level during the week ending Dec. 21. There were 20 jurisdictions – 18 states, the District of Columbia, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of activity, compared with 13 the previous week, and the number of jurisdictions in the “high” range (levels 8-10) jumped from 21 to 28, the CDC data show.
The influenza division estimated that there have been 4.6 million flu illnesses so far this season, nearly a million more than the total after last week, along with 39,000 hospitalizations. The overall hospitalization rate for the season is up to 6.6 per 100,000 population, which is about average at this point. The proportion of deaths attributed to pneumonia and influenza increased to 5.7%, which is below the epidemic threshold, the CDC said.
Three pediatric deaths related to influenza-like illness were reported during the week ending Dec. 21, two of which occurred in an earlier week. For the 2019-2020 season so far, a total of 22 pediatric deaths have been reported to the CDC.