User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Administrative burden and burnout
In May 2019, SHM sent a letter to U.S. Senators Tina Smith and Bill Cassidy in support of the Reducing Administrative Costs and Burdens in Health Care Act of 2019. In excerpts from the letter below, the society details the link between administrative burdens and physician burnout.
Providers and hospital systems expend countless resources, both time and dollars, adhering to unnecessary and excessive administrative burdens instead of investing those resources in providing quality patient care. National data suggests that more than 50 percent of the physician workforce is burned out. Excessive administrative burden is a major contributor to physician burnout, which negatively affects quality and safety within the hospital and further increases health care costs. Notably, the Reducing Administrative Costs and Burdens in Health Care Act calls for a 50% reduction of unnecessary administrative costs from the Department of Health and Human Services within the next ten years.
Hospitalists are front-line clinicians in America's acute care hospitals whose professional focus is the general medical care of hospitalized patients. Their unique position in the healthcare system affords hospitalists a distinct perspective and systems-based approach to confronting and solving challenges at the individual provider and overall institutional level of the hospital. In this capacity, hospitalists experience multiple examples of administrative requirements directly detracting from patient care and redirecting finite resources away from care to meet compliance demands.
By way of example, navigating the administrative rules around inpatient admissions and outpatient observation care, for example, requires a significant shift of healthcare resources away from patient care. While patients admitted under observation receive nearly identical care to those admitted as an inpatient, hospitalists report that, in addition to themselves as the direct healthcare provider, status determinations between inpatient admissions and outpatient observation care require the input of a myriad of staff including nursing, coding/compliance teams, utilization review, case managers and external review organizations. A recent study in the Journal of Hospital Medicine indicated that an average of 5.1 full time employees, not including case managers, are required to navigate the audit and appeals process associated with hospital stay status determinations. These are resources that should be directly used for patient care, but are redirected towards regulation compliance, increasing cost of care without increasing quality.
To read the entire letter, visit https://www.hospitalmedicine.org/policy--advocacy/letters/shm-supports-the-reducing-administrative-costs-and-burdens-in-health-care-act-of-2019/.
In May 2019, SHM sent a letter to U.S. Senators Tina Smith and Bill Cassidy in support of the Reducing Administrative Costs and Burdens in Health Care Act of 2019. In excerpts from the letter below, the society details the link between administrative burdens and physician burnout.
Providers and hospital systems expend countless resources, both time and dollars, adhering to unnecessary and excessive administrative burdens instead of investing those resources in providing quality patient care. National data suggests that more than 50 percent of the physician workforce is burned out. Excessive administrative burden is a major contributor to physician burnout, which negatively affects quality and safety within the hospital and further increases health care costs. Notably, the Reducing Administrative Costs and Burdens in Health Care Act calls for a 50% reduction of unnecessary administrative costs from the Department of Health and Human Services within the next ten years.
Hospitalists are front-line clinicians in America's acute care hospitals whose professional focus is the general medical care of hospitalized patients. Their unique position in the healthcare system affords hospitalists a distinct perspective and systems-based approach to confronting and solving challenges at the individual provider and overall institutional level of the hospital. In this capacity, hospitalists experience multiple examples of administrative requirements directly detracting from patient care and redirecting finite resources away from care to meet compliance demands.
By way of example, navigating the administrative rules around inpatient admissions and outpatient observation care, for example, requires a significant shift of healthcare resources away from patient care. While patients admitted under observation receive nearly identical care to those admitted as an inpatient, hospitalists report that, in addition to themselves as the direct healthcare provider, status determinations between inpatient admissions and outpatient observation care require the input of a myriad of staff including nursing, coding/compliance teams, utilization review, case managers and external review organizations. A recent study in the Journal of Hospital Medicine indicated that an average of 5.1 full time employees, not including case managers, are required to navigate the audit and appeals process associated with hospital stay status determinations. These are resources that should be directly used for patient care, but are redirected towards regulation compliance, increasing cost of care without increasing quality.
To read the entire letter, visit https://www.hospitalmedicine.org/policy--advocacy/letters/shm-supports-the-reducing-administrative-costs-and-burdens-in-health-care-act-of-2019/.
In May 2019, SHM sent a letter to U.S. Senators Tina Smith and Bill Cassidy in support of the Reducing Administrative Costs and Burdens in Health Care Act of 2019. In excerpts from the letter below, the society details the link between administrative burdens and physician burnout.
Providers and hospital systems expend countless resources, both time and dollars, adhering to unnecessary and excessive administrative burdens instead of investing those resources in providing quality patient care. National data suggests that more than 50 percent of the physician workforce is burned out. Excessive administrative burden is a major contributor to physician burnout, which negatively affects quality and safety within the hospital and further increases health care costs. Notably, the Reducing Administrative Costs and Burdens in Health Care Act calls for a 50% reduction of unnecessary administrative costs from the Department of Health and Human Services within the next ten years.
Hospitalists are front-line clinicians in America's acute care hospitals whose professional focus is the general medical care of hospitalized patients. Their unique position in the healthcare system affords hospitalists a distinct perspective and systems-based approach to confronting and solving challenges at the individual provider and overall institutional level of the hospital. In this capacity, hospitalists experience multiple examples of administrative requirements directly detracting from patient care and redirecting finite resources away from care to meet compliance demands.
By way of example, navigating the administrative rules around inpatient admissions and outpatient observation care, for example, requires a significant shift of healthcare resources away from patient care. While patients admitted under observation receive nearly identical care to those admitted as an inpatient, hospitalists report that, in addition to themselves as the direct healthcare provider, status determinations between inpatient admissions and outpatient observation care require the input of a myriad of staff including nursing, coding/compliance teams, utilization review, case managers and external review organizations. A recent study in the Journal of Hospital Medicine indicated that an average of 5.1 full time employees, not including case managers, are required to navigate the audit and appeals process associated with hospital stay status determinations. These are resources that should be directly used for patient care, but are redirected towards regulation compliance, increasing cost of care without increasing quality.
To read the entire letter, visit https://www.hospitalmedicine.org/policy--advocacy/letters/shm-supports-the-reducing-administrative-costs-and-burdens-in-health-care-act-of-2019/.
Community pediatric care is diminishing
The mantra of community hospital administrators is that pediatric care does not pay. Neonatal intensive care pays. For pediatrics, it is similar to how football programs (Medicare patients) support minor sports (pediatrics and obstetrics) at colleges. However, fewer even mildly sick newborns are cared for at community hospitals, which has led to a centralization of neonatal and pediatric care and a loss of pediatric expertise at the affected hospitals.
Pediatric hospitalists are hired to cover the pediatric floor, the emergency department, and labor and delivery, then fired over empty pediatric beds. The rationale expressed is that pediatricians have done such a good job in preventive care that children rarely need hospitalization, so why have a pediatric inpatient unit? It is true that preventive care has been an integral part of primary care for children. Significantly less that 1% of child office visits result in hospitalization.
Advocate Health Care has closed inpatient pediatric units at Illinois Masonic, on Chicago’s North Side, Good Samaritan in Downers Grove, and Good Shepherd in Barrington. Units also have been closed at Mount Sinai in North Lawndale, Norwegian American on Chicago’s West Side, Little Company of Mary in Evergreen Park, and Alexian Brothers in Elk Grove.
As a Chicago-area pediatrician for more than 30 years, I have learned several things about community-based pediatric care:
1. Pediatrics is a geographic specialty. Parents will travel to shop, but would rather walk or have a short ride to their children’s medical providers. Secondary care should be community based, and hospitalization, if necessary, should be close by as well.
2. Hospitals that ceased delivering pediatric inpatient care lost their child-friendliness and pediatric competence, becoming uncomfortable delivering almost any care for children (e.g., sedated MRIs and EEGs, x-rays and ultrasounds, ECGs and echocardiograms, and emergency care).
3. In almost all hospitals, after pediatrics was gone eventually so passed obstetrics (another less remunerative specialty). Sick newborns need immediate, competent care. Most pediatric hospitalizations are short term, often overnight. Delaying newborn care is a medicolegal nightmare. and exposes the child and his or her family to a potentially dangerous drive or helicopter ride.
4. As pediatric subspecialty care becomes more centralized, parents are asked to travel for hours to see a pediatric specialist. There are times when that is necessary (e.g., cardiovascular surgery). Pediatric subspecialists, such as pediatric otolaryngologists, then leave community hospitals, forcing even minor surgeries (e.g., ear ventilation tubes) to be done at a center. In rural areas, this could mean hours of travel, lost work days, and family disruption.
5. Children’s hospitals get uninsured and publicly insured children sent hundreds of miles, because there were no subspecialists in the community who would care for these children.
What is the solution, in our profit-focused health care system?
1. Hospitals’ Certificates of Need could include a mandate for pediatric care.
2. Children’s hospitals could be made responsible for community-based care within their geographic catchment areas.
3. The state or the federal government could mandate and financially support community-based hospital care.
4. Deciding what level of care might be appropriate for each community could depend upon closeness to a pediatric hospital, health problems in the community, and the availability of pediatric specialists.
5. A condition for medical licensure might be that a community-based pediatric subspecialist is required to care for a proportion of the uninsured or publicly insured children in his or her area.
6. Reimbursements for pediatric care need to rise enough to make caring for children worth it.
The major decision point regarding care for children cannot be financial, but must instead embrace the needs of each affected community. If quality health care is a right, and not a privilege, then it is time to stop closing pediatric inpatient units, and, instead, look for creative ways to better care for our children.
This process has led to pediatric care being available only in designated centers. The centralization of pediatric care has progressed from 30 years ago, when most community hospitals had inpatient pediatric units, to the search for innovative ways to fill pediatric beds in the mid-90s (sick day care, flex- or shared pediatric units), to the wholesale closure of community pediatric inpatient beds, from 2000 to the present. I have, unfortunately, seen this firsthand, watching the rise of pediatric mega-hospitals and the demise of community pediatrics. It is a simple financial argument. Care for children simply does not pay nearly as well as does care for adults, especially Medicaid patients. Pediatricians are the poorest paid practicing doctors (public health doctors are paid less).
It is true that pediatricians always have been at the forefront of preventive medicine, and that pediatric patients almost always get better, in spite of our best-intentioned interventions. So community-based pediatricians admit very few patients.
With the loss of pediatric units, community hospitals lose their comfort caring for children. This includes phlebotomy, x-ray, trauma, surgery, and behavioral health. And eroding community hospital pediatric expertise has catastrophic implications for rural hospitals, where parents may have to drive for hours to find a child-friendly emergency department.
Is there an answer?
1. Hospitals are responsible for the patients they serve, including children. Why should a hospital be able to close pediatric services so easily?
2. Every hospital that sees children, through the emergency department, needs to have a pediatrician available to evaluate a child, 24/7.
3. There needs to be an observation unit for children, with pediatric staffing, for overnight stays.
4. Pediatric hospitalists should be staffing community hospitals.
5. Pediatric behavioral health resources need to be available, e.g., inpatient psychiatry, partial hospitalization programs, intensive outpatient programs.
6. Telehealth communication is not adequate to address acute care problems, because the hospital caring for the child has to have the proper equipment and adequate expertise to carry out the recommendations of the teleconsultant.
If we accept that our children will shape the future, we must allow them to survive and thrive. Is health care a right or a privilege, and is it just for adults or for children, too?
Dr. Ochs is in private practice at Ravenswood Pediatrics in Chicago. He said he had no relevant financial disclosures. Email him at [email protected].
The mantra of community hospital administrators is that pediatric care does not pay. Neonatal intensive care pays. For pediatrics, it is similar to how football programs (Medicare patients) support minor sports (pediatrics and obstetrics) at colleges. However, fewer even mildly sick newborns are cared for at community hospitals, which has led to a centralization of neonatal and pediatric care and a loss of pediatric expertise at the affected hospitals.
Pediatric hospitalists are hired to cover the pediatric floor, the emergency department, and labor and delivery, then fired over empty pediatric beds. The rationale expressed is that pediatricians have done such a good job in preventive care that children rarely need hospitalization, so why have a pediatric inpatient unit? It is true that preventive care has been an integral part of primary care for children. Significantly less that 1% of child office visits result in hospitalization.
Advocate Health Care has closed inpatient pediatric units at Illinois Masonic, on Chicago’s North Side, Good Samaritan in Downers Grove, and Good Shepherd in Barrington. Units also have been closed at Mount Sinai in North Lawndale, Norwegian American on Chicago’s West Side, Little Company of Mary in Evergreen Park, and Alexian Brothers in Elk Grove.
As a Chicago-area pediatrician for more than 30 years, I have learned several things about community-based pediatric care:
1. Pediatrics is a geographic specialty. Parents will travel to shop, but would rather walk or have a short ride to their children’s medical providers. Secondary care should be community based, and hospitalization, if necessary, should be close by as well.
2. Hospitals that ceased delivering pediatric inpatient care lost their child-friendliness and pediatric competence, becoming uncomfortable delivering almost any care for children (e.g., sedated MRIs and EEGs, x-rays and ultrasounds, ECGs and echocardiograms, and emergency care).
3. In almost all hospitals, after pediatrics was gone eventually so passed obstetrics (another less remunerative specialty). Sick newborns need immediate, competent care. Most pediatric hospitalizations are short term, often overnight. Delaying newborn care is a medicolegal nightmare. and exposes the child and his or her family to a potentially dangerous drive or helicopter ride.
4. As pediatric subspecialty care becomes more centralized, parents are asked to travel for hours to see a pediatric specialist. There are times when that is necessary (e.g., cardiovascular surgery). Pediatric subspecialists, such as pediatric otolaryngologists, then leave community hospitals, forcing even minor surgeries (e.g., ear ventilation tubes) to be done at a center. In rural areas, this could mean hours of travel, lost work days, and family disruption.
5. Children’s hospitals get uninsured and publicly insured children sent hundreds of miles, because there were no subspecialists in the community who would care for these children.
What is the solution, in our profit-focused health care system?
1. Hospitals’ Certificates of Need could include a mandate for pediatric care.
2. Children’s hospitals could be made responsible for community-based care within their geographic catchment areas.
3. The state or the federal government could mandate and financially support community-based hospital care.
4. Deciding what level of care might be appropriate for each community could depend upon closeness to a pediatric hospital, health problems in the community, and the availability of pediatric specialists.
5. A condition for medical licensure might be that a community-based pediatric subspecialist is required to care for a proportion of the uninsured or publicly insured children in his or her area.
6. Reimbursements for pediatric care need to rise enough to make caring for children worth it.
The major decision point regarding care for children cannot be financial, but must instead embrace the needs of each affected community. If quality health care is a right, and not a privilege, then it is time to stop closing pediatric inpatient units, and, instead, look for creative ways to better care for our children.
This process has led to pediatric care being available only in designated centers. The centralization of pediatric care has progressed from 30 years ago, when most community hospitals had inpatient pediatric units, to the search for innovative ways to fill pediatric beds in the mid-90s (sick day care, flex- or shared pediatric units), to the wholesale closure of community pediatric inpatient beds, from 2000 to the present. I have, unfortunately, seen this firsthand, watching the rise of pediatric mega-hospitals and the demise of community pediatrics. It is a simple financial argument. Care for children simply does not pay nearly as well as does care for adults, especially Medicaid patients. Pediatricians are the poorest paid practicing doctors (public health doctors are paid less).
It is true that pediatricians always have been at the forefront of preventive medicine, and that pediatric patients almost always get better, in spite of our best-intentioned interventions. So community-based pediatricians admit very few patients.
With the loss of pediatric units, community hospitals lose their comfort caring for children. This includes phlebotomy, x-ray, trauma, surgery, and behavioral health. And eroding community hospital pediatric expertise has catastrophic implications for rural hospitals, where parents may have to drive for hours to find a child-friendly emergency department.
Is there an answer?
1. Hospitals are responsible for the patients they serve, including children. Why should a hospital be able to close pediatric services so easily?
2. Every hospital that sees children, through the emergency department, needs to have a pediatrician available to evaluate a child, 24/7.
3. There needs to be an observation unit for children, with pediatric staffing, for overnight stays.
4. Pediatric hospitalists should be staffing community hospitals.
5. Pediatric behavioral health resources need to be available, e.g., inpatient psychiatry, partial hospitalization programs, intensive outpatient programs.
6. Telehealth communication is not adequate to address acute care problems, because the hospital caring for the child has to have the proper equipment and adequate expertise to carry out the recommendations of the teleconsultant.
If we accept that our children will shape the future, we must allow them to survive and thrive. Is health care a right or a privilege, and is it just for adults or for children, too?
Dr. Ochs is in private practice at Ravenswood Pediatrics in Chicago. He said he had no relevant financial disclosures. Email him at [email protected].
The mantra of community hospital administrators is that pediatric care does not pay. Neonatal intensive care pays. For pediatrics, it is similar to how football programs (Medicare patients) support minor sports (pediatrics and obstetrics) at colleges. However, fewer even mildly sick newborns are cared for at community hospitals, which has led to a centralization of neonatal and pediatric care and a loss of pediatric expertise at the affected hospitals.
Pediatric hospitalists are hired to cover the pediatric floor, the emergency department, and labor and delivery, then fired over empty pediatric beds. The rationale expressed is that pediatricians have done such a good job in preventive care that children rarely need hospitalization, so why have a pediatric inpatient unit? It is true that preventive care has been an integral part of primary care for children. Significantly less that 1% of child office visits result in hospitalization.
Advocate Health Care has closed inpatient pediatric units at Illinois Masonic, on Chicago’s North Side, Good Samaritan in Downers Grove, and Good Shepherd in Barrington. Units also have been closed at Mount Sinai in North Lawndale, Norwegian American on Chicago’s West Side, Little Company of Mary in Evergreen Park, and Alexian Brothers in Elk Grove.
As a Chicago-area pediatrician for more than 30 years, I have learned several things about community-based pediatric care:
1. Pediatrics is a geographic specialty. Parents will travel to shop, but would rather walk or have a short ride to their children’s medical providers. Secondary care should be community based, and hospitalization, if necessary, should be close by as well.
2. Hospitals that ceased delivering pediatric inpatient care lost their child-friendliness and pediatric competence, becoming uncomfortable delivering almost any care for children (e.g., sedated MRIs and EEGs, x-rays and ultrasounds, ECGs and echocardiograms, and emergency care).
3. In almost all hospitals, after pediatrics was gone eventually so passed obstetrics (another less remunerative specialty). Sick newborns need immediate, competent care. Most pediatric hospitalizations are short term, often overnight. Delaying newborn care is a medicolegal nightmare. and exposes the child and his or her family to a potentially dangerous drive or helicopter ride.
4. As pediatric subspecialty care becomes more centralized, parents are asked to travel for hours to see a pediatric specialist. There are times when that is necessary (e.g., cardiovascular surgery). Pediatric subspecialists, such as pediatric otolaryngologists, then leave community hospitals, forcing even minor surgeries (e.g., ear ventilation tubes) to be done at a center. In rural areas, this could mean hours of travel, lost work days, and family disruption.
5. Children’s hospitals get uninsured and publicly insured children sent hundreds of miles, because there were no subspecialists in the community who would care for these children.
What is the solution, in our profit-focused health care system?
1. Hospitals’ Certificates of Need could include a mandate for pediatric care.
2. Children’s hospitals could be made responsible for community-based care within their geographic catchment areas.
3. The state or the federal government could mandate and financially support community-based hospital care.
4. Deciding what level of care might be appropriate for each community could depend upon closeness to a pediatric hospital, health problems in the community, and the availability of pediatric specialists.
5. A condition for medical licensure might be that a community-based pediatric subspecialist is required to care for a proportion of the uninsured or publicly insured children in his or her area.
6. Reimbursements for pediatric care need to rise enough to make caring for children worth it.
The major decision point regarding care for children cannot be financial, but must instead embrace the needs of each affected community. If quality health care is a right, and not a privilege, then it is time to stop closing pediatric inpatient units, and, instead, look for creative ways to better care for our children.
This process has led to pediatric care being available only in designated centers. The centralization of pediatric care has progressed from 30 years ago, when most community hospitals had inpatient pediatric units, to the search for innovative ways to fill pediatric beds in the mid-90s (sick day care, flex- or shared pediatric units), to the wholesale closure of community pediatric inpatient beds, from 2000 to the present. I have, unfortunately, seen this firsthand, watching the rise of pediatric mega-hospitals and the demise of community pediatrics. It is a simple financial argument. Care for children simply does not pay nearly as well as does care for adults, especially Medicaid patients. Pediatricians are the poorest paid practicing doctors (public health doctors are paid less).
It is true that pediatricians always have been at the forefront of preventive medicine, and that pediatric patients almost always get better, in spite of our best-intentioned interventions. So community-based pediatricians admit very few patients.
With the loss of pediatric units, community hospitals lose their comfort caring for children. This includes phlebotomy, x-ray, trauma, surgery, and behavioral health. And eroding community hospital pediatric expertise has catastrophic implications for rural hospitals, where parents may have to drive for hours to find a child-friendly emergency department.
Is there an answer?
1. Hospitals are responsible for the patients they serve, including children. Why should a hospital be able to close pediatric services so easily?
2. Every hospital that sees children, through the emergency department, needs to have a pediatrician available to evaluate a child, 24/7.
3. There needs to be an observation unit for children, with pediatric staffing, for overnight stays.
4. Pediatric hospitalists should be staffing community hospitals.
5. Pediatric behavioral health resources need to be available, e.g., inpatient psychiatry, partial hospitalization programs, intensive outpatient programs.
6. Telehealth communication is not adequate to address acute care problems, because the hospital caring for the child has to have the proper equipment and adequate expertise to carry out the recommendations of the teleconsultant.
If we accept that our children will shape the future, we must allow them to survive and thrive. Is health care a right or a privilege, and is it just for adults or for children, too?
Dr. Ochs is in private practice at Ravenswood Pediatrics in Chicago. He said he had no relevant financial disclosures. Email him at [email protected].
SPRINT-type BP control provides up to 3 years of additional life
PHILADELPHIA – in age-dependent fashion, compared with the older target standard BP, according to a novel analysis of data from the landmark SPRINT trial.
SPRINT randomized 9,361 hypertensive patients aged 50 years or older with at least one additional cardiovascular risk factor to intensive control with a target systolic BP of less than 120 mm Hg or to the then-standard target of less than 140 mm Hg. The trial was stopped early for ethical reasons when an interim analysis showed intensive control was associated with a 27% reduction in mortality. But that 27% reduction in mortality risk is a tough concept for many patients to interpret in practical terms, Muthiah Vaduganathan, MD, observed at the American Heart Association scientific sessions.
So he and his coinvestigators sliced and diced the mountainous SPRINT data in a novel way, using an actuarial statistical analysis.
“These actuarial data from SPRINT support the survival benefits of intensive blood pressure control, especially when initiated in middle-aged, high-risk adults. Our analysis really reaffirms the original SPRINT trial results [N Engl J Med. 2015 Nov 26;373(22):2103-16] and helps present them in an alternative format that can potentially be more easily communicated to clinicians, patients, and the public at large,” explained Dr. Vaduganathan, a cardiologist at Brigham and Women’s Hospital and Harvard Medical School, both in Boston.
The impact of intensive BP control on residual survival was magnified in patients who were younger, since they intrinsically have a longer expected survival and will apply the antihypertensive regimen over a longer period. For example, the actuarial analysis concluded that the mean survival benefit of starting intensive BP lowering, rather than settling for a target systolic BP of less than 140 mm Hg starting at age 50 years, was 3 additional years of life, as compared with 1.1 additional years in 65-year-olds and 0.5 years in patients aged 85 years or older. The same approach can be applied to patients at any individual age from 50 to 95 years at the time of enrollment.
“This is very helpful in conveying messages to individual patients. Often if you tell a patient: ‘Your risk is going to go down by 27%,’ it’s tough for them to recognize what the baseline is and if that actually applied to them. So this may personalize that decision-making conversation,” according to the cardiologist.
One audience member commented that this SPRINT analysis might actually underestimate the true survival advantage of intensive BP lowering. He noted that SPRINT, which was halted after an average of 3.3 years, didn’t show a significant benefit for intensive BP lowering in terms of stroke reduction, whereas the ACCORD trial did, but that benefit didn’t occur until after 3 years into the study (Hypertension. 2018 Aug;72[2]:323-30).
Dr. Vaduganathan conceded that’s a limitation of his analysis.
“The assumption we’ve used is that long-term cardiovascular benefits are going to be as seen in the trial, but since SPRINT was stopped early, some benefits may be exaggerated and some may not have been observed yet,” he agreed.
Another audience member observed, “I think a lot of patients will think: ‘Okay, you’re tacking on a year at the end, when I’m going to be 89 and demented.’ The National Institute on Aging is focusing a lot more now on nondisabled life expectancy or healthy life expectancy.’”
Dr. Vaduganathan offered a degree of reassurance on this score. Because of time limitations, he said, he only presented the life expectancy results. But he and his coworkers have performed the same actuarial analysis of the SPRINT data for other endpoints related to freedom from various forms of disease or disability and found a consistent effect: Intensive BP control was associated with a longer time to onset of morbidity.
SPRINT was sponsored primarily by the National Heart, Lung, and Blood Institute. Dr. Vaduganathan reported that he receives research support from/and or serves on advisory boards for Amgen, AstraZeneca, Baxter Healthcare, Bayer, Boehringer Ingelheim, and Relypsa.
SOURCE: Vaduganathan M et al. AHA 2019, Abstract MDP233.
PHILADELPHIA – in age-dependent fashion, compared with the older target standard BP, according to a novel analysis of data from the landmark SPRINT trial.
SPRINT randomized 9,361 hypertensive patients aged 50 years or older with at least one additional cardiovascular risk factor to intensive control with a target systolic BP of less than 120 mm Hg or to the then-standard target of less than 140 mm Hg. The trial was stopped early for ethical reasons when an interim analysis showed intensive control was associated with a 27% reduction in mortality. But that 27% reduction in mortality risk is a tough concept for many patients to interpret in practical terms, Muthiah Vaduganathan, MD, observed at the American Heart Association scientific sessions.
So he and his coinvestigators sliced and diced the mountainous SPRINT data in a novel way, using an actuarial statistical analysis.
“These actuarial data from SPRINT support the survival benefits of intensive blood pressure control, especially when initiated in middle-aged, high-risk adults. Our analysis really reaffirms the original SPRINT trial results [N Engl J Med. 2015 Nov 26;373(22):2103-16] and helps present them in an alternative format that can potentially be more easily communicated to clinicians, patients, and the public at large,” explained Dr. Vaduganathan, a cardiologist at Brigham and Women’s Hospital and Harvard Medical School, both in Boston.
The impact of intensive BP control on residual survival was magnified in patients who were younger, since they intrinsically have a longer expected survival and will apply the antihypertensive regimen over a longer period. For example, the actuarial analysis concluded that the mean survival benefit of starting intensive BP lowering, rather than settling for a target systolic BP of less than 140 mm Hg starting at age 50 years, was 3 additional years of life, as compared with 1.1 additional years in 65-year-olds and 0.5 years in patients aged 85 years or older. The same approach can be applied to patients at any individual age from 50 to 95 years at the time of enrollment.
“This is very helpful in conveying messages to individual patients. Often if you tell a patient: ‘Your risk is going to go down by 27%,’ it’s tough for them to recognize what the baseline is and if that actually applied to them. So this may personalize that decision-making conversation,” according to the cardiologist.
One audience member commented that this SPRINT analysis might actually underestimate the true survival advantage of intensive BP lowering. He noted that SPRINT, which was halted after an average of 3.3 years, didn’t show a significant benefit for intensive BP lowering in terms of stroke reduction, whereas the ACCORD trial did, but that benefit didn’t occur until after 3 years into the study (Hypertension. 2018 Aug;72[2]:323-30).
Dr. Vaduganathan conceded that’s a limitation of his analysis.
“The assumption we’ve used is that long-term cardiovascular benefits are going to be as seen in the trial, but since SPRINT was stopped early, some benefits may be exaggerated and some may not have been observed yet,” he agreed.
Another audience member observed, “I think a lot of patients will think: ‘Okay, you’re tacking on a year at the end, when I’m going to be 89 and demented.’ The National Institute on Aging is focusing a lot more now on nondisabled life expectancy or healthy life expectancy.’”
Dr. Vaduganathan offered a degree of reassurance on this score. Because of time limitations, he said, he only presented the life expectancy results. But he and his coworkers have performed the same actuarial analysis of the SPRINT data for other endpoints related to freedom from various forms of disease or disability and found a consistent effect: Intensive BP control was associated with a longer time to onset of morbidity.
SPRINT was sponsored primarily by the National Heart, Lung, and Blood Institute. Dr. Vaduganathan reported that he receives research support from/and or serves on advisory boards for Amgen, AstraZeneca, Baxter Healthcare, Bayer, Boehringer Ingelheim, and Relypsa.
SOURCE: Vaduganathan M et al. AHA 2019, Abstract MDP233.
PHILADELPHIA – in age-dependent fashion, compared with the older target standard BP, according to a novel analysis of data from the landmark SPRINT trial.
SPRINT randomized 9,361 hypertensive patients aged 50 years or older with at least one additional cardiovascular risk factor to intensive control with a target systolic BP of less than 120 mm Hg or to the then-standard target of less than 140 mm Hg. The trial was stopped early for ethical reasons when an interim analysis showed intensive control was associated with a 27% reduction in mortality. But that 27% reduction in mortality risk is a tough concept for many patients to interpret in practical terms, Muthiah Vaduganathan, MD, observed at the American Heart Association scientific sessions.
So he and his coinvestigators sliced and diced the mountainous SPRINT data in a novel way, using an actuarial statistical analysis.
“These actuarial data from SPRINT support the survival benefits of intensive blood pressure control, especially when initiated in middle-aged, high-risk adults. Our analysis really reaffirms the original SPRINT trial results [N Engl J Med. 2015 Nov 26;373(22):2103-16] and helps present them in an alternative format that can potentially be more easily communicated to clinicians, patients, and the public at large,” explained Dr. Vaduganathan, a cardiologist at Brigham and Women’s Hospital and Harvard Medical School, both in Boston.
The impact of intensive BP control on residual survival was magnified in patients who were younger, since they intrinsically have a longer expected survival and will apply the antihypertensive regimen over a longer period. For example, the actuarial analysis concluded that the mean survival benefit of starting intensive BP lowering, rather than settling for a target systolic BP of less than 140 mm Hg starting at age 50 years, was 3 additional years of life, as compared with 1.1 additional years in 65-year-olds and 0.5 years in patients aged 85 years or older. The same approach can be applied to patients at any individual age from 50 to 95 years at the time of enrollment.
“This is very helpful in conveying messages to individual patients. Often if you tell a patient: ‘Your risk is going to go down by 27%,’ it’s tough for them to recognize what the baseline is and if that actually applied to them. So this may personalize that decision-making conversation,” according to the cardiologist.
One audience member commented that this SPRINT analysis might actually underestimate the true survival advantage of intensive BP lowering. He noted that SPRINT, which was halted after an average of 3.3 years, didn’t show a significant benefit for intensive BP lowering in terms of stroke reduction, whereas the ACCORD trial did, but that benefit didn’t occur until after 3 years into the study (Hypertension. 2018 Aug;72[2]:323-30).
Dr. Vaduganathan conceded that’s a limitation of his analysis.
“The assumption we’ve used is that long-term cardiovascular benefits are going to be as seen in the trial, but since SPRINT was stopped early, some benefits may be exaggerated and some may not have been observed yet,” he agreed.
Another audience member observed, “I think a lot of patients will think: ‘Okay, you’re tacking on a year at the end, when I’m going to be 89 and demented.’ The National Institute on Aging is focusing a lot more now on nondisabled life expectancy or healthy life expectancy.’”
Dr. Vaduganathan offered a degree of reassurance on this score. Because of time limitations, he said, he only presented the life expectancy results. But he and his coworkers have performed the same actuarial analysis of the SPRINT data for other endpoints related to freedom from various forms of disease or disability and found a consistent effect: Intensive BP control was associated with a longer time to onset of morbidity.
SPRINT was sponsored primarily by the National Heart, Lung, and Blood Institute. Dr. Vaduganathan reported that he receives research support from/and or serves on advisory boards for Amgen, AstraZeneca, Baxter Healthcare, Bayer, Boehringer Ingelheim, and Relypsa.
SOURCE: Vaduganathan M et al. AHA 2019, Abstract MDP233.
REPORTING FROM AHA 2019
Drop in flu activity may not signal seasonal peak
A key indicator of flu activity dropped but remains high, but measures of severity have not yet shown any unusual increases, according to the Centers for Disease Control and Prevention.
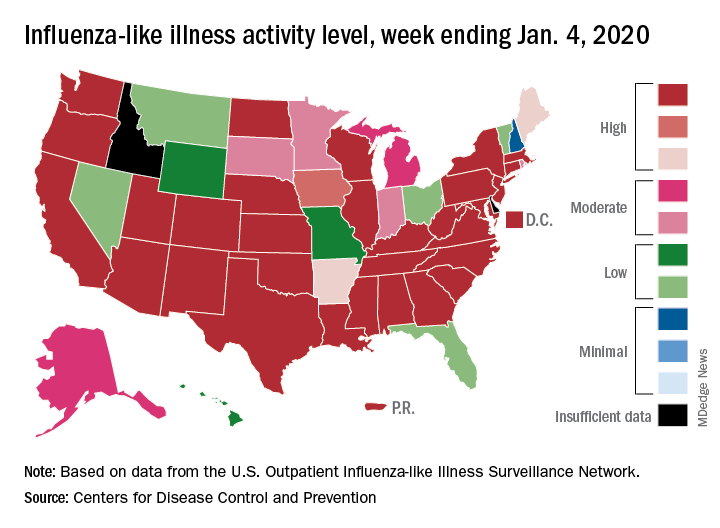
Patients with influenza-like illness (ILI) made up an estimated 5.8% of the visits to outpatient providers during the week ending Jan. 4, and that’s a decline from 7.0% for the last full week of 2019, the CDC’s influenza division reported.
That 7.0% outpatient ILI visit rate was the highest seen in December since 2003, but “hospitalization rates and percent of deaths due to pneumonia and influenza remain low,” the influenza division said in its weekly report.
Influenza B/Victoria and influenza A(H1N1)pdm09 viruses have been the predominant strains so far this season, and they “are more likely to affect children and younger adults than the elderly. Because the majority of hospitalizations and deaths occur among people age 65 and older, with fewer illnesses among that group, we expect, on a population level, to see less impact in flu-related hospitalizations and deaths,” the CDC said.
Last year, there was a similar drop in the outpatient ILI rate in early January after visits rose through December. The rate then increased for another 5 weeks before peaking at 5.0% in February. A similar pattern also occurred during the 2016-2017 and 2015-2016 seasons, CDC data show.
The nationwide ILI hospitalization rate, which is cumulative through the season, was up to 14.6 per 100,000 population for the week ending Jan. 4, the CDC said. Here are the corresponding rates for each of the last five seasons:
- 11.6 (2018-2019).
- 30.5 (2017-2018).
- 12.2 (2016-2017).
- 1.8 (2015-2016).
- 38.3 (2014-2015).
There were five new ILI-related pediatric deaths reported for the week ending Jan. 4, two of which occurred the week before. The total is now up to 32 for the 2019-2020 season, the CDC said in the weekly report. Last season, there were 21 pediatric deaths through the first January report, compared with 42 during the 2017-2018 season and 13 in 2016-2017.
A key indicator of flu activity dropped but remains high, but measures of severity have not yet shown any unusual increases, according to the Centers for Disease Control and Prevention.
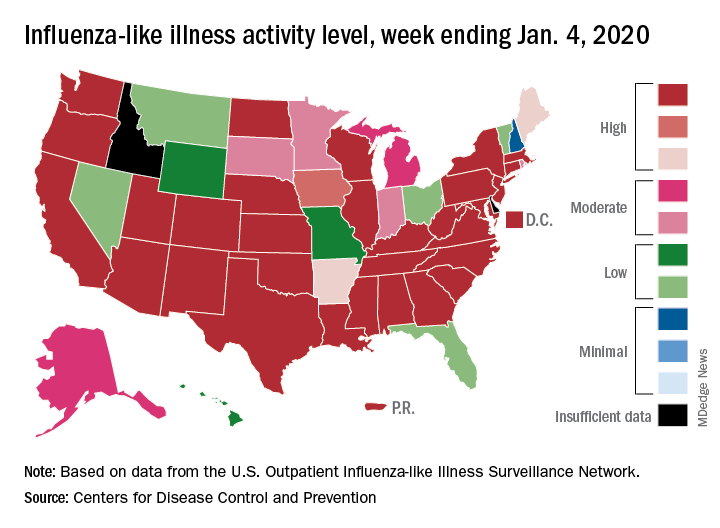
Patients with influenza-like illness (ILI) made up an estimated 5.8% of the visits to outpatient providers during the week ending Jan. 4, and that’s a decline from 7.0% for the last full week of 2019, the CDC’s influenza division reported.
That 7.0% outpatient ILI visit rate was the highest seen in December since 2003, but “hospitalization rates and percent of deaths due to pneumonia and influenza remain low,” the influenza division said in its weekly report.
Influenza B/Victoria and influenza A(H1N1)pdm09 viruses have been the predominant strains so far this season, and they “are more likely to affect children and younger adults than the elderly. Because the majority of hospitalizations and deaths occur among people age 65 and older, with fewer illnesses among that group, we expect, on a population level, to see less impact in flu-related hospitalizations and deaths,” the CDC said.
Last year, there was a similar drop in the outpatient ILI rate in early January after visits rose through December. The rate then increased for another 5 weeks before peaking at 5.0% in February. A similar pattern also occurred during the 2016-2017 and 2015-2016 seasons, CDC data show.
The nationwide ILI hospitalization rate, which is cumulative through the season, was up to 14.6 per 100,000 population for the week ending Jan. 4, the CDC said. Here are the corresponding rates for each of the last five seasons:
- 11.6 (2018-2019).
- 30.5 (2017-2018).
- 12.2 (2016-2017).
- 1.8 (2015-2016).
- 38.3 (2014-2015).
There were five new ILI-related pediatric deaths reported for the week ending Jan. 4, two of which occurred the week before. The total is now up to 32 for the 2019-2020 season, the CDC said in the weekly report. Last season, there were 21 pediatric deaths through the first January report, compared with 42 during the 2017-2018 season and 13 in 2016-2017.
A key indicator of flu activity dropped but remains high, but measures of severity have not yet shown any unusual increases, according to the Centers for Disease Control and Prevention.
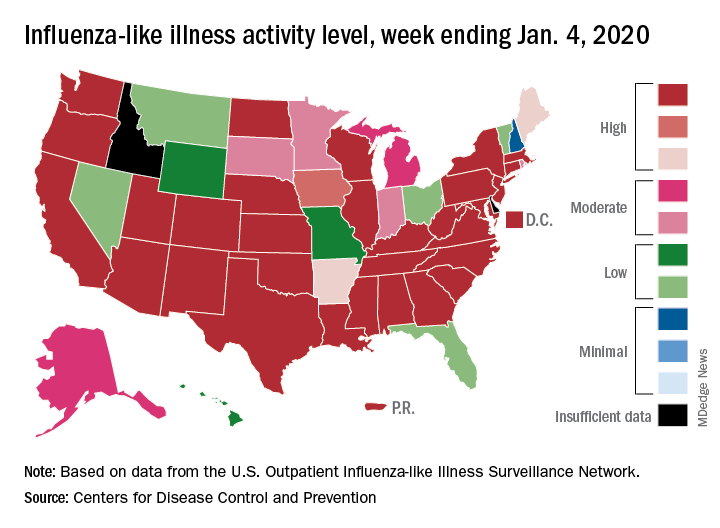
Patients with influenza-like illness (ILI) made up an estimated 5.8% of the visits to outpatient providers during the week ending Jan. 4, and that’s a decline from 7.0% for the last full week of 2019, the CDC’s influenza division reported.
That 7.0% outpatient ILI visit rate was the highest seen in December since 2003, but “hospitalization rates and percent of deaths due to pneumonia and influenza remain low,” the influenza division said in its weekly report.
Influenza B/Victoria and influenza A(H1N1)pdm09 viruses have been the predominant strains so far this season, and they “are more likely to affect children and younger adults than the elderly. Because the majority of hospitalizations and deaths occur among people age 65 and older, with fewer illnesses among that group, we expect, on a population level, to see less impact in flu-related hospitalizations and deaths,” the CDC said.
Last year, there was a similar drop in the outpatient ILI rate in early January after visits rose through December. The rate then increased for another 5 weeks before peaking at 5.0% in February. A similar pattern also occurred during the 2016-2017 and 2015-2016 seasons, CDC data show.
The nationwide ILI hospitalization rate, which is cumulative through the season, was up to 14.6 per 100,000 population for the week ending Jan. 4, the CDC said. Here are the corresponding rates for each of the last five seasons:
- 11.6 (2018-2019).
- 30.5 (2017-2018).
- 12.2 (2016-2017).
- 1.8 (2015-2016).
- 38.3 (2014-2015).
There were five new ILI-related pediatric deaths reported for the week ending Jan. 4, two of which occurred the week before. The total is now up to 32 for the 2019-2020 season, the CDC said in the weekly report. Last season, there were 21 pediatric deaths through the first January report, compared with 42 during the 2017-2018 season and 13 in 2016-2017.
For everything there is a season
2020 SoHM Survey ready to launch
Wow, the last 2 years have just flown by! I can’t believe it’s already time to launch the Society of Hospital Medicine State of Hospital Medicine survey again! Right now is the season for you to roll up your sleeves and get to work helping SHM develop the nation’s definitive resource on the current state of hospital medicine practice.
I’m really excited about this year’s survey. SHM’s Practice Analysis Committee has redesigned it to eliminate some out-of-date or little-used questions and to add a few new, more relevant questions. Even more exciting, we have a new survey platform that should massively improve your experience of submitting data for the survey and also make the back-end data tabulation and analysis much quicker and more accurate. Multisite groups will now have two options for submitting data – a redesigned, more user-friendly Excel tool, or a new pathway to submit data in the reporting platform by replicating responses.
In addition, our new survey platform should help us produce the final report a little more quickly and improve its usability.
New-for-2020 survey topics will include:
- Expanded information on nurse practitioner/physician assistant roles
- Diversity in hospital medicine physician leadership
- Specific questions for hospital medicine groups (HMGs) serving children that will better capture unique attributes of these hospital medicine practices
Why participate?
I can’t emphasize enough that each and every survey submission matters a lot. The State of Hospital Medicine report claims to be the authoritative resource for information about the specialty of hospital medicine. But the report can’t fulfill this claim if the underlying data is skimpy because people were too busy, couldn’t be bothered to participate, or if participation is not broadly representative of the amazing diversity of hospital medicine practices out there.
Your participation will help ensure that you are contributing to a robust hospital medicine database, and that your own group’s information is represented in the survey results. By doing so you will be helping to ensure hospital medicine’s place as perhaps the crucial specialty for U.S. health care in the coming decade.
In addition, participants will receive free access to the survey results, so there’s a direct benefit to you and your HMG as well.
How can you participate?
Here’s what you need to know:
1. The survey opens on Jan.6, 2020, and closes on Feb. 14, 2020.
2. You can find general information about the survey at this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/, and register to participate by using this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/sohm-survey/.
3. To participate, you’ll want to collect the following general types of information for your hospital medicine group:
- Basic group descriptive information (for example, types of patients seen, number of hospitals covered, teaching status, etc.)
- Scope of clinical services
- Nurse practitioners and physician assistants in the HMG
- Full-time equivalent (FTE) information
- Information about the physician leader(s)
- Staffing/scheduling arrangements, including backup plans, paid time off, unfilled positions, predominant scheduling pattern, night coverage arrangements, dedicated admitters, unit-based assignments, etc.
- Compensation model (but not specific amounts)
- Value of employee benefits and CME
- Total work relative value units generated by the HMG, and number of times the following CPT codes were billed: 99221, 99222, 99223, 99231, 99232, 99233, 99238, 99239
- Information about financial support provided to the HMG
- Specific questions for academic HMGs, including financial support for nonclinical work, and allocation of FTEs
- Specific questions for HMGs serving children, including the hospital settings served, proportion of part-time staff, FTE definition, and information about board certification in pediatric hospital medicine
I’m hoping that all of you will join me in working to make the 2020 State of Hospital Medicine survey and report the best one yet!
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
2020 SoHM Survey ready to launch
2020 SoHM Survey ready to launch
Wow, the last 2 years have just flown by! I can’t believe it’s already time to launch the Society of Hospital Medicine State of Hospital Medicine survey again! Right now is the season for you to roll up your sleeves and get to work helping SHM develop the nation’s definitive resource on the current state of hospital medicine practice.
I’m really excited about this year’s survey. SHM’s Practice Analysis Committee has redesigned it to eliminate some out-of-date or little-used questions and to add a few new, more relevant questions. Even more exciting, we have a new survey platform that should massively improve your experience of submitting data for the survey and also make the back-end data tabulation and analysis much quicker and more accurate. Multisite groups will now have two options for submitting data – a redesigned, more user-friendly Excel tool, or a new pathway to submit data in the reporting platform by replicating responses.
In addition, our new survey platform should help us produce the final report a little more quickly and improve its usability.
New-for-2020 survey topics will include:
- Expanded information on nurse practitioner/physician assistant roles
- Diversity in hospital medicine physician leadership
- Specific questions for hospital medicine groups (HMGs) serving children that will better capture unique attributes of these hospital medicine practices
Why participate?
I can’t emphasize enough that each and every survey submission matters a lot. The State of Hospital Medicine report claims to be the authoritative resource for information about the specialty of hospital medicine. But the report can’t fulfill this claim if the underlying data is skimpy because people were too busy, couldn’t be bothered to participate, or if participation is not broadly representative of the amazing diversity of hospital medicine practices out there.
Your participation will help ensure that you are contributing to a robust hospital medicine database, and that your own group’s information is represented in the survey results. By doing so you will be helping to ensure hospital medicine’s place as perhaps the crucial specialty for U.S. health care in the coming decade.
In addition, participants will receive free access to the survey results, so there’s a direct benefit to you and your HMG as well.
How can you participate?
Here’s what you need to know:
1. The survey opens on Jan.6, 2020, and closes on Feb. 14, 2020.
2. You can find general information about the survey at this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/, and register to participate by using this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/sohm-survey/.
3. To participate, you’ll want to collect the following general types of information for your hospital medicine group:
- Basic group descriptive information (for example, types of patients seen, number of hospitals covered, teaching status, etc.)
- Scope of clinical services
- Nurse practitioners and physician assistants in the HMG
- Full-time equivalent (FTE) information
- Information about the physician leader(s)
- Staffing/scheduling arrangements, including backup plans, paid time off, unfilled positions, predominant scheduling pattern, night coverage arrangements, dedicated admitters, unit-based assignments, etc.
- Compensation model (but not specific amounts)
- Value of employee benefits and CME
- Total work relative value units generated by the HMG, and number of times the following CPT codes were billed: 99221, 99222, 99223, 99231, 99232, 99233, 99238, 99239
- Information about financial support provided to the HMG
- Specific questions for academic HMGs, including financial support for nonclinical work, and allocation of FTEs
- Specific questions for HMGs serving children, including the hospital settings served, proportion of part-time staff, FTE definition, and information about board certification in pediatric hospital medicine
I’m hoping that all of you will join me in working to make the 2020 State of Hospital Medicine survey and report the best one yet!
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Wow, the last 2 years have just flown by! I can’t believe it’s already time to launch the Society of Hospital Medicine State of Hospital Medicine survey again! Right now is the season for you to roll up your sleeves and get to work helping SHM develop the nation’s definitive resource on the current state of hospital medicine practice.
I’m really excited about this year’s survey. SHM’s Practice Analysis Committee has redesigned it to eliminate some out-of-date or little-used questions and to add a few new, more relevant questions. Even more exciting, we have a new survey platform that should massively improve your experience of submitting data for the survey and also make the back-end data tabulation and analysis much quicker and more accurate. Multisite groups will now have two options for submitting data – a redesigned, more user-friendly Excel tool, or a new pathway to submit data in the reporting platform by replicating responses.
In addition, our new survey platform should help us produce the final report a little more quickly and improve its usability.
New-for-2020 survey topics will include:
- Expanded information on nurse practitioner/physician assistant roles
- Diversity in hospital medicine physician leadership
- Specific questions for hospital medicine groups (HMGs) serving children that will better capture unique attributes of these hospital medicine practices
Why participate?
I can’t emphasize enough that each and every survey submission matters a lot. The State of Hospital Medicine report claims to be the authoritative resource for information about the specialty of hospital medicine. But the report can’t fulfill this claim if the underlying data is skimpy because people were too busy, couldn’t be bothered to participate, or if participation is not broadly representative of the amazing diversity of hospital medicine practices out there.
Your participation will help ensure that you are contributing to a robust hospital medicine database, and that your own group’s information is represented in the survey results. By doing so you will be helping to ensure hospital medicine’s place as perhaps the crucial specialty for U.S. health care in the coming decade.
In addition, participants will receive free access to the survey results, so there’s a direct benefit to you and your HMG as well.
How can you participate?
Here’s what you need to know:
1. The survey opens on Jan.6, 2020, and closes on Feb. 14, 2020.
2. You can find general information about the survey at this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/, and register to participate by using this link: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/sohm-survey/.
3. To participate, you’ll want to collect the following general types of information for your hospital medicine group:
- Basic group descriptive information (for example, types of patients seen, number of hospitals covered, teaching status, etc.)
- Scope of clinical services
- Nurse practitioners and physician assistants in the HMG
- Full-time equivalent (FTE) information
- Information about the physician leader(s)
- Staffing/scheduling arrangements, including backup plans, paid time off, unfilled positions, predominant scheduling pattern, night coverage arrangements, dedicated admitters, unit-based assignments, etc.
- Compensation model (but not specific amounts)
- Value of employee benefits and CME
- Total work relative value units generated by the HMG, and number of times the following CPT codes were billed: 99221, 99222, 99223, 99231, 99232, 99233, 99238, 99239
- Information about financial support provided to the HMG
- Specific questions for academic HMGs, including financial support for nonclinical work, and allocation of FTEs
- Specific questions for HMGs serving children, including the hospital settings served, proportion of part-time staff, FTE definition, and information about board certification in pediatric hospital medicine
I’m hoping that all of you will join me in working to make the 2020 State of Hospital Medicine survey and report the best one yet!
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Treatment of heart failure with preserved ejection fraction is a work in progress
LOS ANGELES – When it comes to the optimal treatment of patients with heart failure with preserved ejection fraction and diabetes, cardiologists like Mark T. Kearney, MB ChB, MD, remain stumped.
“Over the years, the diagnosis of heart failure with preserved ejection fraction has been notoriously difficult [to treat], controversial, and ultimately involves aggressive catheterization of the heart to assess diastolic dysfunction, complex echocardiography, and invasive tests,” Dr. Kearney said at the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease. “These patients have an ejection fraction of over 50% and classic signs and symptoms of heart failure. Studies of beta-blockers, angiotensin-converting enzyme inhibitors, and angiotensin II receptor blockers have been unsuccessful in this group of patients. We’re at the beginning of a journey in understanding this disorder, and it’s important, because more and more patients present to us with signs and symptoms of heart failure with an ejection fraction greater than 50%.”
In a recent analysis of 1,797 patients with chronic heart failure, Dr. Kearney, British Heart Foundation Professor of Cardiovascular and Diabetes Research at the Leeds (England) Institute of Cardiovascular and Metabolic Medicine, and colleagues examined whether beta-blockers and ACE inhibitors were associated with differential effects on mortality in patients with and without diabetes (Diabetes Care. 2018;41:136-42). Mean follow-up was 4 years.
For the ACE inhibitor component of the trial, the researchers correlated the dose of ramipril to outcomes and found that each milligram increase of ramipril reduced the risk of death by about 3%. “In the nondiabetic patients who did not receive an ACE inhibitor, mortality was about 60% – worse than most cancers,” Dr. Kearney said. “In patients with diabetes, there was a similar pattern. If you didn’t get an ACE inhibitor, mortality was 70%. So, if you get patients on an optimal dose of an ACE inhibitor, you improve their mortality substantially, whether they have diabetes or not.”
The beta-blocker component of the trial yielded similar results. “Among patients who did not receive a beta-blocker, the mortality was about 70% at 5 years – really terrible,” he said. “Every milligram of bisoprolol was associated with a reduction in mortality of about 9%. So, if a patient gets on an optimal dose of a beta-blocker and they have diabetes, it’s associated with prolongation of life over a year.”
Dr. Kearney said that patients often do not want to take an increased dose of a beta-blocker because of concerns about side effects, such as tiredness. “They ask me what the side effects of an increased dose would be. My answer is: ‘It will make you live longer.’ Usually, they’ll respond by agreeing to have a little bit more of the beta-blocker. The message here is, if you have a patient with ejection fraction heart failure and diabetes, get them on the optimal dose of a beta-blocker, even at the expense of an ACE inhibitor.”
In 2016, the European Society of Cardiology introduced guidelines for physicians to make a diagnosis of heart failure with preserved ejection fraction. The guidelines mandate that a diagnosis requires signs and symptoms of heart failure, elevated levels of natriuretic peptide, and echocardiographic abnormalities of cardiac structure and/or function in the presence of a left ventricular ejection fraction of 50% or more (Eur J Heart Fail. 2016;18[8]:891-975).
“Signs and symptoms of heart failure, elevated BNP [brain natriuretic peptide], and echocardiography allow us to make a diagnosis of heart failure with preserved ejection fraction,” Dr. Kearney, who is also dean of the Leeds University School of Medicine. “But we don’t know the outcome of these patients, we don’t know how to treat them, and we don’t know the impact on hospitalizations.”
In a large, unpublished cohort study conducted at Leeds, Dr. Kearney and colleagues evaluated how many patients met criteria for heart failure with reduced ejection fraction or heart failure with preserved ejection fraction after undergoing a BNP measurement. Ultimately, 959 patients met criteria. After assessment, 23% had no heart failure, 44% had heart failure with preserved ejection fraction, and 33% had heart failure with reduced ejection fraction. They found that patients with preserved ejection fraction were older (mean age, 84 years); were more likely to be female; and had less ischemia, less diabetes, and more hypertension. In addition, patients with preserved ejection fraction had significantly better survival than patients with reduced ejection fraction over 5 years follow-up.
“What was really interesting were the findings related to hospitalization,” he said. “All 959 patients accounted for 20,517 days in the hospital over 5 years, which is the equivalent of 1 patient occupying a hospital bed for 56 years. This disorder [heart failure with preserved ejection fraction], despite having a lower mortality than heart failure with reduced ejection fraction, leads to a significant burden on health care systems.”
Among patients with preserved ejection fraction, 82% were hospitalized for a noncardiovascular cause, 6.9% because of heart failure, and 11% were caused by other cardiovascular causes. Most of the hospital admissions were because of chest infections, falls, and other frailty-linked causes. “This link between systemic frailty and heart failure with preserved ejection fraction warrants further investigation,” Dr. Kearney said. “This is a major burden on patient hospital care.”
When the researchers examined outcomes in patients with and without diabetes, those with diabetes were younger, more likely to be male, and have a higher body mass index. They found that, in the presence of diabetes, mortality was increased in heart failure with preserved and reduced ejection fraction. “So, even at the age of 81 or 82, diabetes changes the pathophysiology of mortality in what was previously believed to be a benign disease,” he said.
In a subset analysis of patients with and without diabetes who were not taking a beta-blocker, there did not seem to be increased sympathetic activation in the patients with diabetes and heart failure with preserved ejection fraction, nor a difference in heart rate between the nondiabetic patients and patients with diabetes. However, among patients with heart failure with reduced ejection fraction, those with diabetes had an increased heart rate.
“Is heart failure with preserved ejection fraction in diabetes benign? I think the answer is no,” Dr. Kearney said. “It increases hospitalization and is a major burden on health care systems. What should we do? We deal with comorbidity and fall risk. It’s good old-fashioned doctoring, really. We address frailty and respiratory tract infections, but the key thing here is that we need more research.”
Dr. Kearney reported having no relevant financial disclosures.
LOS ANGELES – When it comes to the optimal treatment of patients with heart failure with preserved ejection fraction and diabetes, cardiologists like Mark T. Kearney, MB ChB, MD, remain stumped.
“Over the years, the diagnosis of heart failure with preserved ejection fraction has been notoriously difficult [to treat], controversial, and ultimately involves aggressive catheterization of the heart to assess diastolic dysfunction, complex echocardiography, and invasive tests,” Dr. Kearney said at the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease. “These patients have an ejection fraction of over 50% and classic signs and symptoms of heart failure. Studies of beta-blockers, angiotensin-converting enzyme inhibitors, and angiotensin II receptor blockers have been unsuccessful in this group of patients. We’re at the beginning of a journey in understanding this disorder, and it’s important, because more and more patients present to us with signs and symptoms of heart failure with an ejection fraction greater than 50%.”
In a recent analysis of 1,797 patients with chronic heart failure, Dr. Kearney, British Heart Foundation Professor of Cardiovascular and Diabetes Research at the Leeds (England) Institute of Cardiovascular and Metabolic Medicine, and colleagues examined whether beta-blockers and ACE inhibitors were associated with differential effects on mortality in patients with and without diabetes (Diabetes Care. 2018;41:136-42). Mean follow-up was 4 years.
For the ACE inhibitor component of the trial, the researchers correlated the dose of ramipril to outcomes and found that each milligram increase of ramipril reduced the risk of death by about 3%. “In the nondiabetic patients who did not receive an ACE inhibitor, mortality was about 60% – worse than most cancers,” Dr. Kearney said. “In patients with diabetes, there was a similar pattern. If you didn’t get an ACE inhibitor, mortality was 70%. So, if you get patients on an optimal dose of an ACE inhibitor, you improve their mortality substantially, whether they have diabetes or not.”
The beta-blocker component of the trial yielded similar results. “Among patients who did not receive a beta-blocker, the mortality was about 70% at 5 years – really terrible,” he said. “Every milligram of bisoprolol was associated with a reduction in mortality of about 9%. So, if a patient gets on an optimal dose of a beta-blocker and they have diabetes, it’s associated with prolongation of life over a year.”
Dr. Kearney said that patients often do not want to take an increased dose of a beta-blocker because of concerns about side effects, such as tiredness. “They ask me what the side effects of an increased dose would be. My answer is: ‘It will make you live longer.’ Usually, they’ll respond by agreeing to have a little bit more of the beta-blocker. The message here is, if you have a patient with ejection fraction heart failure and diabetes, get them on the optimal dose of a beta-blocker, even at the expense of an ACE inhibitor.”
In 2016, the European Society of Cardiology introduced guidelines for physicians to make a diagnosis of heart failure with preserved ejection fraction. The guidelines mandate that a diagnosis requires signs and symptoms of heart failure, elevated levels of natriuretic peptide, and echocardiographic abnormalities of cardiac structure and/or function in the presence of a left ventricular ejection fraction of 50% or more (Eur J Heart Fail. 2016;18[8]:891-975).
“Signs and symptoms of heart failure, elevated BNP [brain natriuretic peptide], and echocardiography allow us to make a diagnosis of heart failure with preserved ejection fraction,” Dr. Kearney, who is also dean of the Leeds University School of Medicine. “But we don’t know the outcome of these patients, we don’t know how to treat them, and we don’t know the impact on hospitalizations.”
In a large, unpublished cohort study conducted at Leeds, Dr. Kearney and colleagues evaluated how many patients met criteria for heart failure with reduced ejection fraction or heart failure with preserved ejection fraction after undergoing a BNP measurement. Ultimately, 959 patients met criteria. After assessment, 23% had no heart failure, 44% had heart failure with preserved ejection fraction, and 33% had heart failure with reduced ejection fraction. They found that patients with preserved ejection fraction were older (mean age, 84 years); were more likely to be female; and had less ischemia, less diabetes, and more hypertension. In addition, patients with preserved ejection fraction had significantly better survival than patients with reduced ejection fraction over 5 years follow-up.
“What was really interesting were the findings related to hospitalization,” he said. “All 959 patients accounted for 20,517 days in the hospital over 5 years, which is the equivalent of 1 patient occupying a hospital bed for 56 years. This disorder [heart failure with preserved ejection fraction], despite having a lower mortality than heart failure with reduced ejection fraction, leads to a significant burden on health care systems.”
Among patients with preserved ejection fraction, 82% were hospitalized for a noncardiovascular cause, 6.9% because of heart failure, and 11% were caused by other cardiovascular causes. Most of the hospital admissions were because of chest infections, falls, and other frailty-linked causes. “This link between systemic frailty and heart failure with preserved ejection fraction warrants further investigation,” Dr. Kearney said. “This is a major burden on patient hospital care.”
When the researchers examined outcomes in patients with and without diabetes, those with diabetes were younger, more likely to be male, and have a higher body mass index. They found that, in the presence of diabetes, mortality was increased in heart failure with preserved and reduced ejection fraction. “So, even at the age of 81 or 82, diabetes changes the pathophysiology of mortality in what was previously believed to be a benign disease,” he said.
In a subset analysis of patients with and without diabetes who were not taking a beta-blocker, there did not seem to be increased sympathetic activation in the patients with diabetes and heart failure with preserved ejection fraction, nor a difference in heart rate between the nondiabetic patients and patients with diabetes. However, among patients with heart failure with reduced ejection fraction, those with diabetes had an increased heart rate.
“Is heart failure with preserved ejection fraction in diabetes benign? I think the answer is no,” Dr. Kearney said. “It increases hospitalization and is a major burden on health care systems. What should we do? We deal with comorbidity and fall risk. It’s good old-fashioned doctoring, really. We address frailty and respiratory tract infections, but the key thing here is that we need more research.”
Dr. Kearney reported having no relevant financial disclosures.
LOS ANGELES – When it comes to the optimal treatment of patients with heart failure with preserved ejection fraction and diabetes, cardiologists like Mark T. Kearney, MB ChB, MD, remain stumped.
“Over the years, the diagnosis of heart failure with preserved ejection fraction has been notoriously difficult [to treat], controversial, and ultimately involves aggressive catheterization of the heart to assess diastolic dysfunction, complex echocardiography, and invasive tests,” Dr. Kearney said at the World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease. “These patients have an ejection fraction of over 50% and classic signs and symptoms of heart failure. Studies of beta-blockers, angiotensin-converting enzyme inhibitors, and angiotensin II receptor blockers have been unsuccessful in this group of patients. We’re at the beginning of a journey in understanding this disorder, and it’s important, because more and more patients present to us with signs and symptoms of heart failure with an ejection fraction greater than 50%.”
In a recent analysis of 1,797 patients with chronic heart failure, Dr. Kearney, British Heart Foundation Professor of Cardiovascular and Diabetes Research at the Leeds (England) Institute of Cardiovascular and Metabolic Medicine, and colleagues examined whether beta-blockers and ACE inhibitors were associated with differential effects on mortality in patients with and without diabetes (Diabetes Care. 2018;41:136-42). Mean follow-up was 4 years.
For the ACE inhibitor component of the trial, the researchers correlated the dose of ramipril to outcomes and found that each milligram increase of ramipril reduced the risk of death by about 3%. “In the nondiabetic patients who did not receive an ACE inhibitor, mortality was about 60% – worse than most cancers,” Dr. Kearney said. “In patients with diabetes, there was a similar pattern. If you didn’t get an ACE inhibitor, mortality was 70%. So, if you get patients on an optimal dose of an ACE inhibitor, you improve their mortality substantially, whether they have diabetes or not.”
The beta-blocker component of the trial yielded similar results. “Among patients who did not receive a beta-blocker, the mortality was about 70% at 5 years – really terrible,” he said. “Every milligram of bisoprolol was associated with a reduction in mortality of about 9%. So, if a patient gets on an optimal dose of a beta-blocker and they have diabetes, it’s associated with prolongation of life over a year.”
Dr. Kearney said that patients often do not want to take an increased dose of a beta-blocker because of concerns about side effects, such as tiredness. “They ask me what the side effects of an increased dose would be. My answer is: ‘It will make you live longer.’ Usually, they’ll respond by agreeing to have a little bit more of the beta-blocker. The message here is, if you have a patient with ejection fraction heart failure and diabetes, get them on the optimal dose of a beta-blocker, even at the expense of an ACE inhibitor.”
In 2016, the European Society of Cardiology introduced guidelines for physicians to make a diagnosis of heart failure with preserved ejection fraction. The guidelines mandate that a diagnosis requires signs and symptoms of heart failure, elevated levels of natriuretic peptide, and echocardiographic abnormalities of cardiac structure and/or function in the presence of a left ventricular ejection fraction of 50% or more (Eur J Heart Fail. 2016;18[8]:891-975).
“Signs and symptoms of heart failure, elevated BNP [brain natriuretic peptide], and echocardiography allow us to make a diagnosis of heart failure with preserved ejection fraction,” Dr. Kearney, who is also dean of the Leeds University School of Medicine. “But we don’t know the outcome of these patients, we don’t know how to treat them, and we don’t know the impact on hospitalizations.”
In a large, unpublished cohort study conducted at Leeds, Dr. Kearney and colleagues evaluated how many patients met criteria for heart failure with reduced ejection fraction or heart failure with preserved ejection fraction after undergoing a BNP measurement. Ultimately, 959 patients met criteria. After assessment, 23% had no heart failure, 44% had heart failure with preserved ejection fraction, and 33% had heart failure with reduced ejection fraction. They found that patients with preserved ejection fraction were older (mean age, 84 years); were more likely to be female; and had less ischemia, less diabetes, and more hypertension. In addition, patients with preserved ejection fraction had significantly better survival than patients with reduced ejection fraction over 5 years follow-up.
“What was really interesting were the findings related to hospitalization,” he said. “All 959 patients accounted for 20,517 days in the hospital over 5 years, which is the equivalent of 1 patient occupying a hospital bed for 56 years. This disorder [heart failure with preserved ejection fraction], despite having a lower mortality than heart failure with reduced ejection fraction, leads to a significant burden on health care systems.”
Among patients with preserved ejection fraction, 82% were hospitalized for a noncardiovascular cause, 6.9% because of heart failure, and 11% were caused by other cardiovascular causes. Most of the hospital admissions were because of chest infections, falls, and other frailty-linked causes. “This link between systemic frailty and heart failure with preserved ejection fraction warrants further investigation,” Dr. Kearney said. “This is a major burden on patient hospital care.”
When the researchers examined outcomes in patients with and without diabetes, those with diabetes were younger, more likely to be male, and have a higher body mass index. They found that, in the presence of diabetes, mortality was increased in heart failure with preserved and reduced ejection fraction. “So, even at the age of 81 or 82, diabetes changes the pathophysiology of mortality in what was previously believed to be a benign disease,” he said.
In a subset analysis of patients with and without diabetes who were not taking a beta-blocker, there did not seem to be increased sympathetic activation in the patients with diabetes and heart failure with preserved ejection fraction, nor a difference in heart rate between the nondiabetic patients and patients with diabetes. However, among patients with heart failure with reduced ejection fraction, those with diabetes had an increased heart rate.
“Is heart failure with preserved ejection fraction in diabetes benign? I think the answer is no,” Dr. Kearney said. “It increases hospitalization and is a major burden on health care systems. What should we do? We deal with comorbidity and fall risk. It’s good old-fashioned doctoring, really. We address frailty and respiratory tract infections, but the key thing here is that we need more research.”
Dr. Kearney reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM WCIRDC 2019
ID consult for Candida bloodstream infections can reduce mortality risk
findings from a large retrospective study suggest.
Mortality attributable to Candida bloodstream infection ranges between 15% and 47%, and delay in initiation of appropriate treatment has been associated with increased mortality. Previous small studies showed that ID consultation has conferred benefits to patients with Candida bloodstream infections. Carlos Mejia-Chew, MD, and colleagues from Washington University, St. Louis, sought to explore this further by performing a retrospective, single-center cohort study of 1,691 patients aged 18 years or older with Candida bloodstream infection from 2002 to 2015. They analyzed demographics, comorbidities, predisposing factors, all-cause mortality, antifungal use, central-line removal, and ophthalmological and echocardiographic evaluation in order to compare 90-day all-cause mortality between individuals with and without an ID consultation.
They found that those patients who received an ID consult for a Candida bloodstream infection had a significantly lower 90-day mortality rate than did those who did not (29% vs. 51%).
With a model using inverse weighting by the propensity score, they found that ID consultation was associated with a hazard ratio of 0.81 for mortality (95% confidence interval, 0.73-0.91; P less than .0001). In the ID consultation group, the median duration of antifungal therapy was significantly longer (18 vs. 14 days; P less than .0001); central-line removal was significantly more common (76% vs. 59%; P less than .0001); echocardiography use was more frequent (57% vs. 33%; P less than .0001); and ophthalmological examinations were performed more often (53% vs. 17%; P less than .0001). Importantly, fewer patients in the ID consultation group were untreated (2% vs. 14%; P less than .0001).
In an accompanying commentary, Katrien Lagrou, MD, and Eric Van Wijngaerden, MD, of the department of microbiology, immunology and transplantation, University Hospitals Leuven (Belgium) stated: “We think that the high proportion of patients (14%) with a Candida bloodstream infection who did not receive any antifungal treatment and did not have an infectious disease consultation is a particularly alarming finding. ... Ninety-day mortality in these untreated patients was high (67%).”
“We believe every hospital should have an expert management strategy addressing all individual cases of candidaemia. The need for such expert management should be incorporated in all future candidaemia management guidelines,” they concluded.
The study was funded by the Astellas Global Development Pharma, the Washington University Institute of Clinical and Translational Sciences, and the Agency for Healthcare Research and Quality. Several of the authors had financial connections to Astellas Global Development or other pharmaceutical companies. Dr. Lagrou and Dr. Van Wijngaerden both reported receiving personal fees and nonfinancial support from a number of pharmaceutical companies, but all outside the scope of the study.
SOURCE: Mejia-Chew C et al. Lancet Infect Dis. 2019;19:1336-44.
findings from a large retrospective study suggest.
Mortality attributable to Candida bloodstream infection ranges between 15% and 47%, and delay in initiation of appropriate treatment has been associated with increased mortality. Previous small studies showed that ID consultation has conferred benefits to patients with Candida bloodstream infections. Carlos Mejia-Chew, MD, and colleagues from Washington University, St. Louis, sought to explore this further by performing a retrospective, single-center cohort study of 1,691 patients aged 18 years or older with Candida bloodstream infection from 2002 to 2015. They analyzed demographics, comorbidities, predisposing factors, all-cause mortality, antifungal use, central-line removal, and ophthalmological and echocardiographic evaluation in order to compare 90-day all-cause mortality between individuals with and without an ID consultation.
They found that those patients who received an ID consult for a Candida bloodstream infection had a significantly lower 90-day mortality rate than did those who did not (29% vs. 51%).
With a model using inverse weighting by the propensity score, they found that ID consultation was associated with a hazard ratio of 0.81 for mortality (95% confidence interval, 0.73-0.91; P less than .0001). In the ID consultation group, the median duration of antifungal therapy was significantly longer (18 vs. 14 days; P less than .0001); central-line removal was significantly more common (76% vs. 59%; P less than .0001); echocardiography use was more frequent (57% vs. 33%; P less than .0001); and ophthalmological examinations were performed more often (53% vs. 17%; P less than .0001). Importantly, fewer patients in the ID consultation group were untreated (2% vs. 14%; P less than .0001).
In an accompanying commentary, Katrien Lagrou, MD, and Eric Van Wijngaerden, MD, of the department of microbiology, immunology and transplantation, University Hospitals Leuven (Belgium) stated: “We think that the high proportion of patients (14%) with a Candida bloodstream infection who did not receive any antifungal treatment and did not have an infectious disease consultation is a particularly alarming finding. ... Ninety-day mortality in these untreated patients was high (67%).”
“We believe every hospital should have an expert management strategy addressing all individual cases of candidaemia. The need for such expert management should be incorporated in all future candidaemia management guidelines,” they concluded.
The study was funded by the Astellas Global Development Pharma, the Washington University Institute of Clinical and Translational Sciences, and the Agency for Healthcare Research and Quality. Several of the authors had financial connections to Astellas Global Development or other pharmaceutical companies. Dr. Lagrou and Dr. Van Wijngaerden both reported receiving personal fees and nonfinancial support from a number of pharmaceutical companies, but all outside the scope of the study.
SOURCE: Mejia-Chew C et al. Lancet Infect Dis. 2019;19:1336-44.
findings from a large retrospective study suggest.
Mortality attributable to Candida bloodstream infection ranges between 15% and 47%, and delay in initiation of appropriate treatment has been associated with increased mortality. Previous small studies showed that ID consultation has conferred benefits to patients with Candida bloodstream infections. Carlos Mejia-Chew, MD, and colleagues from Washington University, St. Louis, sought to explore this further by performing a retrospective, single-center cohort study of 1,691 patients aged 18 years or older with Candida bloodstream infection from 2002 to 2015. They analyzed demographics, comorbidities, predisposing factors, all-cause mortality, antifungal use, central-line removal, and ophthalmological and echocardiographic evaluation in order to compare 90-day all-cause mortality between individuals with and without an ID consultation.
They found that those patients who received an ID consult for a Candida bloodstream infection had a significantly lower 90-day mortality rate than did those who did not (29% vs. 51%).
With a model using inverse weighting by the propensity score, they found that ID consultation was associated with a hazard ratio of 0.81 for mortality (95% confidence interval, 0.73-0.91; P less than .0001). In the ID consultation group, the median duration of antifungal therapy was significantly longer (18 vs. 14 days; P less than .0001); central-line removal was significantly more common (76% vs. 59%; P less than .0001); echocardiography use was more frequent (57% vs. 33%; P less than .0001); and ophthalmological examinations were performed more often (53% vs. 17%; P less than .0001). Importantly, fewer patients in the ID consultation group were untreated (2% vs. 14%; P less than .0001).
In an accompanying commentary, Katrien Lagrou, MD, and Eric Van Wijngaerden, MD, of the department of microbiology, immunology and transplantation, University Hospitals Leuven (Belgium) stated: “We think that the high proportion of patients (14%) with a Candida bloodstream infection who did not receive any antifungal treatment and did not have an infectious disease consultation is a particularly alarming finding. ... Ninety-day mortality in these untreated patients was high (67%).”
“We believe every hospital should have an expert management strategy addressing all individual cases of candidaemia. The need for such expert management should be incorporated in all future candidaemia management guidelines,” they concluded.
The study was funded by the Astellas Global Development Pharma, the Washington University Institute of Clinical and Translational Sciences, and the Agency for Healthcare Research and Quality. Several of the authors had financial connections to Astellas Global Development or other pharmaceutical companies. Dr. Lagrou and Dr. Van Wijngaerden both reported receiving personal fees and nonfinancial support from a number of pharmaceutical companies, but all outside the scope of the study.
SOURCE: Mejia-Chew C et al. Lancet Infect Dis. 2019;19:1336-44.
FROM LANCET: INFECTIOUS DISEASES
Accelerating the careers of future hospitalists
Grant program provides funding, research support
When it comes to what future hospitalists should be doing to accelerate their careers, is there such a thing as a “no-brainer” opportunity? Aram Namavar, MD, MS, thinks so.
Dr. Namavar is a first-year internal medicine resident at UC San Diego pursuing a career as an academic hospitalist. He is passionate about building interdisciplinary platforms for patient care enhancement and serving disadvantaged and underserved communities.
Membership in the Society of Hospital Medicine is free for medical students and offers a diverse array of resources specifically curated for the ever-expanding needs of the specialty and its aspiring leaders. An active member of SHM since 2015, Dr. Namavar has looked to the organization for leading career-enhancing opportunities and resources in hospital medicine to help him achieve his altruistic career goals.
For Dr. Namavar, a few of these professional development–focused opportunities include becoming an active member of the Physicians-in-Training Committee, a founding member of the Resident and Student Special Interest Group, and a recipient of the Student Hospitalist Scholar Grant.
“I applied for the Student Hospitalist Scholar Grant to have a dedicated summer of learning quality improvement through being in meetings with hospital medicine leaders and leading my research initiatives alongside my team,” Dr. Namavar said. He described the experience as pivotal to his growth within hospital medicine and as a medical student.
The key component to SHM’s Student Hospitalist Scholar Grant opportunity is the ability for first- and second-year medical students to work alongside leading hospital medicine professionals in scholarly projects to help interested students gain perspective on working within the specialty.
“As a young, interested trainee in hospital medicine, working with a mentor who is established in the field allows one to learn what steps to take in the future to become a leader,” he said. “[It allowed me to] gain insight into leadership style and develop a strong network for the future.”
In addition to the program’s mentorship benefits, grant recipients also receive complimentary registration to SHM’s Annual Conference with the added perks of funding and research support, accommodation expenses, and acceptance into SHM’s RIV Poster Competition.
“I attended the SHM Annual Conference previously,” Dr. Namavar said. “However, as a grant recipient, you have the chance to connect with faculty who will come to your poster presentation and want to learn about your project. This platform allows you to meet individuals from across the nation and connect with those interested in helping trainees thrive within hospital medicine.”
With the grant funding, Dr. Namavar completed his project, “Evaluation of Decisional Conflict as a Simple Tool to Assess Risk of Readmission.” He described this endeavor as a multidimensional project that took on a holistic view of patient-centered readmissions. “We evaluated patient conflict in posthospitalization resources as a marker of readmission, social determinants of health, and health literacy as risk factors for hospital readmission.”
Described by Dr. Namavar as a “no-brainer” opportunity, SHM’s Student Hospitalist Scholar Grant “offers some of the best benefits overall – funding for your project, automatic acceptance at the Annual Conference, the chance to have your work highlighted in blog posts, networking opportunities with faculty across the nation, and travel reimbursement for the conference.”
Building your networks or establishing your professional career path does not stop at individual networking events or scholarship programs, Dr. Namavar said. It’s about piecing together the building blocks to set yourself up for success.
“My long-term involvement in SHM through working on a committee, leading a special interest group, attending annual meetings, and receiving the grant from SHM has helped me to build new, long-lasting connections in the field,” he said. “Because of this, I plan to continue to serve within SHM in multiple capacities throughout my career in hospital medicine.”
Are you a first- or second-year medical student interested in taking the next step in your hospital medicine career? Apply to SHM’s Student Hospitalist Scholar Grant program through late January 2020 at hospitalmedicine.org/scholargrant.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
Grant program provides funding, research support
Grant program provides funding, research support
When it comes to what future hospitalists should be doing to accelerate their careers, is there such a thing as a “no-brainer” opportunity? Aram Namavar, MD, MS, thinks so.
Dr. Namavar is a first-year internal medicine resident at UC San Diego pursuing a career as an academic hospitalist. He is passionate about building interdisciplinary platforms for patient care enhancement and serving disadvantaged and underserved communities.
Membership in the Society of Hospital Medicine is free for medical students and offers a diverse array of resources specifically curated for the ever-expanding needs of the specialty and its aspiring leaders. An active member of SHM since 2015, Dr. Namavar has looked to the organization for leading career-enhancing opportunities and resources in hospital medicine to help him achieve his altruistic career goals.
For Dr. Namavar, a few of these professional development–focused opportunities include becoming an active member of the Physicians-in-Training Committee, a founding member of the Resident and Student Special Interest Group, and a recipient of the Student Hospitalist Scholar Grant.
“I applied for the Student Hospitalist Scholar Grant to have a dedicated summer of learning quality improvement through being in meetings with hospital medicine leaders and leading my research initiatives alongside my team,” Dr. Namavar said. He described the experience as pivotal to his growth within hospital medicine and as a medical student.
The key component to SHM’s Student Hospitalist Scholar Grant opportunity is the ability for first- and second-year medical students to work alongside leading hospital medicine professionals in scholarly projects to help interested students gain perspective on working within the specialty.
“As a young, interested trainee in hospital medicine, working with a mentor who is established in the field allows one to learn what steps to take in the future to become a leader,” he said. “[It allowed me to] gain insight into leadership style and develop a strong network for the future.”
In addition to the program’s mentorship benefits, grant recipients also receive complimentary registration to SHM’s Annual Conference with the added perks of funding and research support, accommodation expenses, and acceptance into SHM’s RIV Poster Competition.
“I attended the SHM Annual Conference previously,” Dr. Namavar said. “However, as a grant recipient, you have the chance to connect with faculty who will come to your poster presentation and want to learn about your project. This platform allows you to meet individuals from across the nation and connect with those interested in helping trainees thrive within hospital medicine.”
With the grant funding, Dr. Namavar completed his project, “Evaluation of Decisional Conflict as a Simple Tool to Assess Risk of Readmission.” He described this endeavor as a multidimensional project that took on a holistic view of patient-centered readmissions. “We evaluated patient conflict in posthospitalization resources as a marker of readmission, social determinants of health, and health literacy as risk factors for hospital readmission.”
Described by Dr. Namavar as a “no-brainer” opportunity, SHM’s Student Hospitalist Scholar Grant “offers some of the best benefits overall – funding for your project, automatic acceptance at the Annual Conference, the chance to have your work highlighted in blog posts, networking opportunities with faculty across the nation, and travel reimbursement for the conference.”
Building your networks or establishing your professional career path does not stop at individual networking events or scholarship programs, Dr. Namavar said. It’s about piecing together the building blocks to set yourself up for success.
“My long-term involvement in SHM through working on a committee, leading a special interest group, attending annual meetings, and receiving the grant from SHM has helped me to build new, long-lasting connections in the field,” he said. “Because of this, I plan to continue to serve within SHM in multiple capacities throughout my career in hospital medicine.”
Are you a first- or second-year medical student interested in taking the next step in your hospital medicine career? Apply to SHM’s Student Hospitalist Scholar Grant program through late January 2020 at hospitalmedicine.org/scholargrant.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
When it comes to what future hospitalists should be doing to accelerate their careers, is there such a thing as a “no-brainer” opportunity? Aram Namavar, MD, MS, thinks so.
Dr. Namavar is a first-year internal medicine resident at UC San Diego pursuing a career as an academic hospitalist. He is passionate about building interdisciplinary platforms for patient care enhancement and serving disadvantaged and underserved communities.
Membership in the Society of Hospital Medicine is free for medical students and offers a diverse array of resources specifically curated for the ever-expanding needs of the specialty and its aspiring leaders. An active member of SHM since 2015, Dr. Namavar has looked to the organization for leading career-enhancing opportunities and resources in hospital medicine to help him achieve his altruistic career goals.
For Dr. Namavar, a few of these professional development–focused opportunities include becoming an active member of the Physicians-in-Training Committee, a founding member of the Resident and Student Special Interest Group, and a recipient of the Student Hospitalist Scholar Grant.
“I applied for the Student Hospitalist Scholar Grant to have a dedicated summer of learning quality improvement through being in meetings with hospital medicine leaders and leading my research initiatives alongside my team,” Dr. Namavar said. He described the experience as pivotal to his growth within hospital medicine and as a medical student.
The key component to SHM’s Student Hospitalist Scholar Grant opportunity is the ability for first- and second-year medical students to work alongside leading hospital medicine professionals in scholarly projects to help interested students gain perspective on working within the specialty.
“As a young, interested trainee in hospital medicine, working with a mentor who is established in the field allows one to learn what steps to take in the future to become a leader,” he said. “[It allowed me to] gain insight into leadership style and develop a strong network for the future.”
In addition to the program’s mentorship benefits, grant recipients also receive complimentary registration to SHM’s Annual Conference with the added perks of funding and research support, accommodation expenses, and acceptance into SHM’s RIV Poster Competition.
“I attended the SHM Annual Conference previously,” Dr. Namavar said. “However, as a grant recipient, you have the chance to connect with faculty who will come to your poster presentation and want to learn about your project. This platform allows you to meet individuals from across the nation and connect with those interested in helping trainees thrive within hospital medicine.”
With the grant funding, Dr. Namavar completed his project, “Evaluation of Decisional Conflict as a Simple Tool to Assess Risk of Readmission.” He described this endeavor as a multidimensional project that took on a holistic view of patient-centered readmissions. “We evaluated patient conflict in posthospitalization resources as a marker of readmission, social determinants of health, and health literacy as risk factors for hospital readmission.”
Described by Dr. Namavar as a “no-brainer” opportunity, SHM’s Student Hospitalist Scholar Grant “offers some of the best benefits overall – funding for your project, automatic acceptance at the Annual Conference, the chance to have your work highlighted in blog posts, networking opportunities with faculty across the nation, and travel reimbursement for the conference.”
Building your networks or establishing your professional career path does not stop at individual networking events or scholarship programs, Dr. Namavar said. It’s about piecing together the building blocks to set yourself up for success.
“My long-term involvement in SHM through working on a committee, leading a special interest group, attending annual meetings, and receiving the grant from SHM has helped me to build new, long-lasting connections in the field,” he said. “Because of this, I plan to continue to serve within SHM in multiple capacities throughout my career in hospital medicine.”
Are you a first- or second-year medical student interested in taking the next step in your hospital medicine career? Apply to SHM’s Student Hospitalist Scholar Grant program through late January 2020 at hospitalmedicine.org/scholargrant.
Ms. Cowan is a marketing communications specialist at the Society of Hospital Medicine.
PACT-HF: Transitional care derives no overall benefit
Women respond more to intervention
PHILADELPHIA – A clinical trial of a program that transitions heart failure patients after they’re discharged from the hospital didn’t result in any appreciable improvement in all-cause death, readmissions or emergency department visits after 6 months overall, but it did show that women responded more favorably than men.
Harriette G.C. Van Spall, MD, MPH, reported 6-month results of the Patient-Centered Transitional Care Services in Heart Failure (PACT-HF) trial of 2,494 HF patients at 10 hospitals in Ontario during February 2015 to March 2016. They were randomized to the care-transition program or usual care. The findings, she said at the American Heart Association scientific sessions, “highlight the gap between efficacy that’s often demonstrated in mechanistic clinical trials and effectiveness when we aim to implement these results in real-world settings.” Three-month PACT-HF results were reported previously (JAMA. 2019 Feb 26;321:753-61).
The transitional-care model consisted of a comprehensive needs assessment by a nurse who also provided self-care education, a patient-centered discharge summary, and follow-up with a family physician within 7 days of discharge, which Dr. Van Spall noted “is not current practice in our health care system.”
Patients deemed high risk for readmission or death also received nurse home visits and scheduled visits to a multidisciplinary heart function clinic within 2-4 weeks of discharge and continuing as long as clinically suitable, said Dr. Van Spall, a principal investigator at the Population Health Research Institute, Hamilton, Ont., and assistant professor in cardiology at McMaster University in Hamilton.
The trial found no difference between the intervention and usual-care groups in the two composite endpoints at 6 months, Dr. Van Spall said: all-cause death, readmissions, or ED visits (63.1% and 64.5%, respectively; P = .50); or all-cause readmissions or ED visits (60.8% and 62.4%; P = .36).
“Despite the mutual overall clinical outcomes, we noted specific differences in response to treatment,” she said. With regard to the composite endpoint that included all-cause death, “Men had an attenuated response to the treatment with a hazard ratio of 1.05 (95% confidence interval, 0.87-1.26), whereas women had a hazard ratio of 0.85 (95% CI, 0.71-1.03), demonstrating that women have more of a treatment response to this health care service,” she said.
In men, rates for the first primary composite outcome were 66.3% and 64.1% in the intervention and usual-care groups, whereas in women those rates were 59.9% and 64.8% (P = .04 for sex interaction).
In the second composite endpoint, all-cause readmission or ED visit, “again, men had an attenuated response” with a HR of 1.03, whereas women had a HR of 0.83. Results were similar to those for the first primary composite outcome: 63.4% and 61.7% for intervention and usual care in men and 57.7% and 63% in women (P = .03 for sex interaction).
In putting the findings into context, Dr. Van Spall said tailoring services to risk in HF patients may be fraught with pitfalls. “We delivered intensive services to those patients at high risk of readmission or death, but it is quite possible they are the least likely to derive benefit by virtue of their advanced heart failure,” she said. “It may be that more benefit would have been derived had we chosen low- or moderate-risk patients to receive the intervention.”
She also said the sex-specific outcomes must be interpreted with caution. “But they do give us pause to consider that services could be titrated more effectively if delivered to patients who are more likely to derive benefit,” Dr. Van Spall said. The finding that women derived more of a benefit is in line with other prospective and observational studies that have found that women have a higher sense of self-care, self-efficacy, and confidence in managing their own health care needs than men.
Dr. Van Spall has no financial relationships to disclose.
Women respond more to intervention
Women respond more to intervention
PHILADELPHIA – A clinical trial of a program that transitions heart failure patients after they’re discharged from the hospital didn’t result in any appreciable improvement in all-cause death, readmissions or emergency department visits after 6 months overall, but it did show that women responded more favorably than men.
Harriette G.C. Van Spall, MD, MPH, reported 6-month results of the Patient-Centered Transitional Care Services in Heart Failure (PACT-HF) trial of 2,494 HF patients at 10 hospitals in Ontario during February 2015 to March 2016. They were randomized to the care-transition program or usual care. The findings, she said at the American Heart Association scientific sessions, “highlight the gap between efficacy that’s often demonstrated in mechanistic clinical trials and effectiveness when we aim to implement these results in real-world settings.” Three-month PACT-HF results were reported previously (JAMA. 2019 Feb 26;321:753-61).
The transitional-care model consisted of a comprehensive needs assessment by a nurse who also provided self-care education, a patient-centered discharge summary, and follow-up with a family physician within 7 days of discharge, which Dr. Van Spall noted “is not current practice in our health care system.”
Patients deemed high risk for readmission or death also received nurse home visits and scheduled visits to a multidisciplinary heart function clinic within 2-4 weeks of discharge and continuing as long as clinically suitable, said Dr. Van Spall, a principal investigator at the Population Health Research Institute, Hamilton, Ont., and assistant professor in cardiology at McMaster University in Hamilton.
The trial found no difference between the intervention and usual-care groups in the two composite endpoints at 6 months, Dr. Van Spall said: all-cause death, readmissions, or ED visits (63.1% and 64.5%, respectively; P = .50); or all-cause readmissions or ED visits (60.8% and 62.4%; P = .36).
“Despite the mutual overall clinical outcomes, we noted specific differences in response to treatment,” she said. With regard to the composite endpoint that included all-cause death, “Men had an attenuated response to the treatment with a hazard ratio of 1.05 (95% confidence interval, 0.87-1.26), whereas women had a hazard ratio of 0.85 (95% CI, 0.71-1.03), demonstrating that women have more of a treatment response to this health care service,” she said.
In men, rates for the first primary composite outcome were 66.3% and 64.1% in the intervention and usual-care groups, whereas in women those rates were 59.9% and 64.8% (P = .04 for sex interaction).
In the second composite endpoint, all-cause readmission or ED visit, “again, men had an attenuated response” with a HR of 1.03, whereas women had a HR of 0.83. Results were similar to those for the first primary composite outcome: 63.4% and 61.7% for intervention and usual care in men and 57.7% and 63% in women (P = .03 for sex interaction).
In putting the findings into context, Dr. Van Spall said tailoring services to risk in HF patients may be fraught with pitfalls. “We delivered intensive services to those patients at high risk of readmission or death, but it is quite possible they are the least likely to derive benefit by virtue of their advanced heart failure,” she said. “It may be that more benefit would have been derived had we chosen low- or moderate-risk patients to receive the intervention.”
She also said the sex-specific outcomes must be interpreted with caution. “But they do give us pause to consider that services could be titrated more effectively if delivered to patients who are more likely to derive benefit,” Dr. Van Spall said. The finding that women derived more of a benefit is in line with other prospective and observational studies that have found that women have a higher sense of self-care, self-efficacy, and confidence in managing their own health care needs than men.
Dr. Van Spall has no financial relationships to disclose.
PHILADELPHIA – A clinical trial of a program that transitions heart failure patients after they’re discharged from the hospital didn’t result in any appreciable improvement in all-cause death, readmissions or emergency department visits after 6 months overall, but it did show that women responded more favorably than men.
Harriette G.C. Van Spall, MD, MPH, reported 6-month results of the Patient-Centered Transitional Care Services in Heart Failure (PACT-HF) trial of 2,494 HF patients at 10 hospitals in Ontario during February 2015 to March 2016. They were randomized to the care-transition program or usual care. The findings, she said at the American Heart Association scientific sessions, “highlight the gap between efficacy that’s often demonstrated in mechanistic clinical trials and effectiveness when we aim to implement these results in real-world settings.” Three-month PACT-HF results were reported previously (JAMA. 2019 Feb 26;321:753-61).
The transitional-care model consisted of a comprehensive needs assessment by a nurse who also provided self-care education, a patient-centered discharge summary, and follow-up with a family physician within 7 days of discharge, which Dr. Van Spall noted “is not current practice in our health care system.”
Patients deemed high risk for readmission or death also received nurse home visits and scheduled visits to a multidisciplinary heart function clinic within 2-4 weeks of discharge and continuing as long as clinically suitable, said Dr. Van Spall, a principal investigator at the Population Health Research Institute, Hamilton, Ont., and assistant professor in cardiology at McMaster University in Hamilton.
The trial found no difference between the intervention and usual-care groups in the two composite endpoints at 6 months, Dr. Van Spall said: all-cause death, readmissions, or ED visits (63.1% and 64.5%, respectively; P = .50); or all-cause readmissions or ED visits (60.8% and 62.4%; P = .36).
“Despite the mutual overall clinical outcomes, we noted specific differences in response to treatment,” she said. With regard to the composite endpoint that included all-cause death, “Men had an attenuated response to the treatment with a hazard ratio of 1.05 (95% confidence interval, 0.87-1.26), whereas women had a hazard ratio of 0.85 (95% CI, 0.71-1.03), demonstrating that women have more of a treatment response to this health care service,” she said.
In men, rates for the first primary composite outcome were 66.3% and 64.1% in the intervention and usual-care groups, whereas in women those rates were 59.9% and 64.8% (P = .04 for sex interaction).
In the second composite endpoint, all-cause readmission or ED visit, “again, men had an attenuated response” with a HR of 1.03, whereas women had a HR of 0.83. Results were similar to those for the first primary composite outcome: 63.4% and 61.7% for intervention and usual care in men and 57.7% and 63% in women (P = .03 for sex interaction).
In putting the findings into context, Dr. Van Spall said tailoring services to risk in HF patients may be fraught with pitfalls. “We delivered intensive services to those patients at high risk of readmission or death, but it is quite possible they are the least likely to derive benefit by virtue of their advanced heart failure,” she said. “It may be that more benefit would have been derived had we chosen low- or moderate-risk patients to receive the intervention.”
She also said the sex-specific outcomes must be interpreted with caution. “But they do give us pause to consider that services could be titrated more effectively if delivered to patients who are more likely to derive benefit,” Dr. Van Spall said. The finding that women derived more of a benefit is in line with other prospective and observational studies that have found that women have a higher sense of self-care, self-efficacy, and confidence in managing their own health care needs than men.
Dr. Van Spall has no financial relationships to disclose.
REPORTING FROM AHA 2019
State of Hospital Medicine Survey plays key role in operational decision making
Results help establish hospitalist benchmarks
The Hospitalist recently spoke with Brian Schroeder, MHA, FACHE, FHM, assistant vice president, Hospital & Emergency Medicine, at Atrium Health Medical Group in Charlotte, N.C., to discuss his participation in the State of Hospital Medicine Survey, which is distributed every other year, and how he uses the resulting report to guide important operational decisions.
Please describe your current role.
At Carolinas Hospitalist Group, we have approximately 250 providers at nearly 20 care locations across North Carolina. Along with my specialty medical director, I am responsible for the strategic growth, program development, and financial performance for our practice.
How did you first become involved with the Society of Hospital Medicine?
When I first entered the hospital medicine world in 2008, I was looking for an organization that supported our specialty. My physician leaders at the time pointed me to SHM. Since the beginning of my time as a member, I have attended the Annual Conference each year, the SHM Leadership Academy, served on an SHM committee, and participate in SHM’s multisite Leaders group. Additionally, I have served as faculty at SHM’s annual conference for 3 years – and will be presenting for the third time at HM20.
Why is it important that people participate in the State of Hospital Medicine Survey?
Participation in the survey is key for establishing benchmarks for our specialty. The more people participate (from various arenas like private groups, health system employees, and vendors), the more accurate the data. Over the past 4 years, SHM has improved the submission process of survey data – especially for practices with multiple locations.
How has the data in the report impacted important business decisions for your group?
We rely heavily on the investment/provider benchmark within the survey data. Over the years, as the investment/provider was decreasing nationally, our own investment/provider was increasing. Based on the survey, we were able to closely evaluate our staffing models at each location and determine the appropriate skill mix-to-volume ratio. Through turnover and growth, we have strategically hired advanced practice providers to align our investment more closely with the benchmark. Over the past 2 years, our investment/provider metric has decreased significantly. We were able to accomplish this while continuing to provide appropriate care to our patients. We also utilize the Report to monitor performance incentive metrics, staffing model trends, and encounter/provider ratios.
What would you tell people who are on the fence about participating in the survey – and ultimately, purchasing the finished product?
Do it! Our practice would never skip a submission year. The data produced from the survey helps us improve our clinical operations and maximize our financial affordability. The data also assists in defending staffing decisions and clinical operations change with senior leadership within the organization.
Don’t miss your chance to submit data that will build the latest snapshot of the hospital medicine specialty. The State of Hospital Medicine Survey is open now and runs through February 16, 2020. Learn more and register to participate at hospitalmedicine.org/survey.
Results help establish hospitalist benchmarks
Results help establish hospitalist benchmarks
The Hospitalist recently spoke with Brian Schroeder, MHA, FACHE, FHM, assistant vice president, Hospital & Emergency Medicine, at Atrium Health Medical Group in Charlotte, N.C., to discuss his participation in the State of Hospital Medicine Survey, which is distributed every other year, and how he uses the resulting report to guide important operational decisions.
Please describe your current role.
At Carolinas Hospitalist Group, we have approximately 250 providers at nearly 20 care locations across North Carolina. Along with my specialty medical director, I am responsible for the strategic growth, program development, and financial performance for our practice.
How did you first become involved with the Society of Hospital Medicine?
When I first entered the hospital medicine world in 2008, I was looking for an organization that supported our specialty. My physician leaders at the time pointed me to SHM. Since the beginning of my time as a member, I have attended the Annual Conference each year, the SHM Leadership Academy, served on an SHM committee, and participate in SHM’s multisite Leaders group. Additionally, I have served as faculty at SHM’s annual conference for 3 years – and will be presenting for the third time at HM20.
Why is it important that people participate in the State of Hospital Medicine Survey?
Participation in the survey is key for establishing benchmarks for our specialty. The more people participate (from various arenas like private groups, health system employees, and vendors), the more accurate the data. Over the past 4 years, SHM has improved the submission process of survey data – especially for practices with multiple locations.
How has the data in the report impacted important business decisions for your group?
We rely heavily on the investment/provider benchmark within the survey data. Over the years, as the investment/provider was decreasing nationally, our own investment/provider was increasing. Based on the survey, we were able to closely evaluate our staffing models at each location and determine the appropriate skill mix-to-volume ratio. Through turnover and growth, we have strategically hired advanced practice providers to align our investment more closely with the benchmark. Over the past 2 years, our investment/provider metric has decreased significantly. We were able to accomplish this while continuing to provide appropriate care to our patients. We also utilize the Report to monitor performance incentive metrics, staffing model trends, and encounter/provider ratios.
What would you tell people who are on the fence about participating in the survey – and ultimately, purchasing the finished product?
Do it! Our practice would never skip a submission year. The data produced from the survey helps us improve our clinical operations and maximize our financial affordability. The data also assists in defending staffing decisions and clinical operations change with senior leadership within the organization.
Don’t miss your chance to submit data that will build the latest snapshot of the hospital medicine specialty. The State of Hospital Medicine Survey is open now and runs through February 16, 2020. Learn more and register to participate at hospitalmedicine.org/survey.
The Hospitalist recently spoke with Brian Schroeder, MHA, FACHE, FHM, assistant vice president, Hospital & Emergency Medicine, at Atrium Health Medical Group in Charlotte, N.C., to discuss his participation in the State of Hospital Medicine Survey, which is distributed every other year, and how he uses the resulting report to guide important operational decisions.
Please describe your current role.
At Carolinas Hospitalist Group, we have approximately 250 providers at nearly 20 care locations across North Carolina. Along with my specialty medical director, I am responsible for the strategic growth, program development, and financial performance for our practice.
How did you first become involved with the Society of Hospital Medicine?
When I first entered the hospital medicine world in 2008, I was looking for an organization that supported our specialty. My physician leaders at the time pointed me to SHM. Since the beginning of my time as a member, I have attended the Annual Conference each year, the SHM Leadership Academy, served on an SHM committee, and participate in SHM’s multisite Leaders group. Additionally, I have served as faculty at SHM’s annual conference for 3 years – and will be presenting for the third time at HM20.
Why is it important that people participate in the State of Hospital Medicine Survey?
Participation in the survey is key for establishing benchmarks for our specialty. The more people participate (from various arenas like private groups, health system employees, and vendors), the more accurate the data. Over the past 4 years, SHM has improved the submission process of survey data – especially for practices with multiple locations.
How has the data in the report impacted important business decisions for your group?
We rely heavily on the investment/provider benchmark within the survey data. Over the years, as the investment/provider was decreasing nationally, our own investment/provider was increasing. Based on the survey, we were able to closely evaluate our staffing models at each location and determine the appropriate skill mix-to-volume ratio. Through turnover and growth, we have strategically hired advanced practice providers to align our investment more closely with the benchmark. Over the past 2 years, our investment/provider metric has decreased significantly. We were able to accomplish this while continuing to provide appropriate care to our patients. We also utilize the Report to monitor performance incentive metrics, staffing model trends, and encounter/provider ratios.
What would you tell people who are on the fence about participating in the survey – and ultimately, purchasing the finished product?
Do it! Our practice would never skip a submission year. The data produced from the survey helps us improve our clinical operations and maximize our financial affordability. The data also assists in defending staffing decisions and clinical operations change with senior leadership within the organization.
Don’t miss your chance to submit data that will build the latest snapshot of the hospital medicine specialty. The State of Hospital Medicine Survey is open now and runs through February 16, 2020. Learn more and register to participate at hospitalmedicine.org/survey.