User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


The measles comeback of 2019
Measles made a comeback in 2019.
The Centers for Disease Control and Prevention reported that, as of Dec. 5, 2019, 1,276 individual cases of measles of measles were confirmed in 31 states, the largest number since 1992. This number is a major uptick in cases, compared with previous years since 2000 when the CDC declared measles eliminated from the United States. No deaths have been reported for 2019.
Three-quarters of these cases in 2019 were linked to recent outbreaks in New York and occurred in primarily in underimmunized, close-knit communities and in patients with links to international travel. A total of 124 of the people who got measles this year were hospitalized, and 61 reported having complications, including pneumonia and encephalitis. The overall median patient age was 6 years (31% aged 1-4 years, 27% aged 5-17 years, and 29% aged at least 18 years).
The good news is that most of these cases occurred in unvaccinated patients. The national vaccination rate for the almost 4 million kindergartners reported as enrolled in 2018-2019 was 94.7% for two doses of the MMR vaccine, falling just short of the CDC recommended 95% vaccination rate threshold. The CDC reported an approximate 2.5% rate of vaccination exemptions among school-age children.
The bad news is that, despite the high rate of MMR vaccination rates among U.S. children, there are gaps in measles protection in the U.S. population because of factors leaving patients immunocompromised and antivaccination sentiment that has led some parents to defer or refuse the MMR.
In addition, adults who were vaccinated prior to 1968 with either inactivated measles vaccine or measles vaccine of unknown type may have limited immunity. The inactivated measles vaccine, which was available in 1963-1967, did not achieve effective measles protection.
A global measles surge
While antivaccination sentiment contributed to the 2019 measles cases, a more significant factor may be the global surge of measles. More than 140,000 people worldwide died from measles in 2018, according to the World Health Organization and the CDC.
“[Recent data on measles] indicates that during the first 6 months of the year there have been more measles cases reported worldwide than in any year since 2006. From Jan. 1 to July 31, 2019, 182 countries reported 364,808 measles cases to the WHO. This surpasses the 129,239 reported during the same time period in 2018. WHO regions with the biggest increases in cases include the African region (900%), the Western Pacific region (230%), and the European region (150%),” according to a CDC report.
Studies on hospitalization and complications linked to measles in the United States are scarce, but two outbreaks in Minnesota (2011 and 2017) provided some data on what to expect if the measles surge continues into 2020. The investigators found that poor feeding was a primary reason for admission (97%); additional complications included otitis media (42%), pneumonia (30%), and tracheitis (6%). Three-quarters received antibiotics, 30% required oxygen, and 21% received vitamin A. Median length of stay was 3.7 days (range, 1.1-26.2 days) (Pediatr Infect Dis J. 2019 Jun;38[6]:547-52. doi: 10.1097/INF.0000000000002221).
‘Immunological amnesia’
Infection with the measles virus appears to reduce immunity to other pathogens, according to a paper published in Science (2019 Nov 1;366[6465]599-606).
The hypothesis that the measles virus could cause “immunological amnesia” by impairing immune memory is supported by early research showing children with measles had negative cutaneous tuberculin reactions after having previously tested positive.
“Subsequent studies have shown decreased interferon signaling, skewed cytokine responses, lymphopenia, and suppression of lymphocyte proliferation shortly after infection,” wrote Michael Mina, MD, from Brigham and Women’s Hospital in Boston, and coauthors.
“Given the variation in the degree of immune repertoire modulation we observed, we anticipate that future risk of morbidity and mortality after measles would not be homogeneous but would be skewed toward individuals with the most severe elimination of immunological memory,” they wrote. “These findings underscore the crucial need for continued widespread vaccination.”
In this study, researchers compared the levels of around 400 pathogen-specific antibodies in blood samples from 77 unvaccinated children, taken before and 2 months after natural measles infection, with 5 unvaccinated children who did not contract measles. A total of 34 children experienced mild measles, and 43 had severe measles.
They found that the samples taken after measles infection showed “substantial” reductions in the number of pathogen epitopes, compared with the samples from children who did not get infected with measles.
This amounted to approximately a 20% mean reduction in overall diversity or size of the antibody repertoire. However, in children who experienced severe measles, there was a median loss of 40% (range, 11%-62%) of antibody repertoire, compared with a median of 33% (range, 12%-73%) range in children who experienced mild infection. Meanwhile, the control subjects retained approximately 90% of their antibody repertoire over a similar or longer time period. Some children lost up to 70% of antibodies for specific pathogens.
Maternal-acquired immunity fades
In another study of measles immunity, maternal antibodies were found to be insufficient to provide immunity to infants after 6 months.
The study of 196 infants showed that maternal measles antibodies had dropped below the protective threshold by 3 months of age – well before the recommended age of 12-15 months for the first dose of MMR vaccine.
The odds of inadequate protection doubled for each additional month of age, Michelle Science, MD, of the University of Toronto and associates reported in Pediatrics (2019 Dec 1. doi 10.1542/peds.2019-0630).
“The widening gap between loss of maternal antibodies and measles vaccination described in our study leaves infants vulnerable to measles for much of their infancy and highlights the need for further research to support public health policy,” Dr. Science and colleagues wrote.
The researchers randomly selected 25 samples for each of eight different age groups: up to 30 days old; 1 month (31-60 days), 2 months (61-89 days), 3 months (90-119 days), 4 months, 5 months, 6-9 months, and 9-11 months.
Just over half the babies (56%) were male, and 35% had an underlying condition, but none had conditions that might affect antibody levels. The conditions were primarily a developmental delay or otherwise affecting the central nervous system, liver, or gastrointestinal function. Mean maternal age was 32 years.
To ensure high test sensitivity, the researchers used the plaque-reduction neutralization test to test for measles-neutralizing antibodies instead of using enzyme-linked immunosorbent assay, because “ELISA sensitivity decreases as antibody titers decrease,” Dr. Science and colleagues wrote. They used a neutralization titer of less than 192 mIU/mL as the threshold for protection against measles.
When the researchers calculated the predicted standardized mean antibody titer for infants with a mother aged 32 years, they determined their mean to be 541 mIU/mL at 1 month, 142 mIU/mL at 3 months (below the measles threshold of susceptibility of 192 mIU/mL), and 64 mIU/mL at 6 months. None of the infants had measles antibodies above the protective threshold at 6 months old, the authors noted.
Children’s odds of susceptibility to measles doubled for each additional month of age, after adjustment for infant sex and maternal age (odds ratio, 2.13). Children’s likelihood of susceptibility to measles modestly increased as maternal age increased in 5-year increments from 25 to 40 years.
Children with an underlying conditions had greater susceptibility to measles (83%), compared with those without a comorbidity (68%, P = .03). No difference in susceptibility existed between males and females or based on gestational age at birth (ranging from 37 to 41 weeks).
The Advisory Committee on Immunization Practices permits measles vaccination “as early as 6 months for infants who plan to travel internationally, infants with ongoing risk for exposure during measles outbreaks and as postexposure prophylaxis,” Huong Q. McLean, PhD, of Marshfield (Wisc.) Clinic Research Institute, and Walter A. Orenstein, MD, of Emory University, Atlanta, noted in an editorial.
The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures.
Bianca Nogrady and Tara Haelle contributed to this story.
Measles made a comeback in 2019.
The Centers for Disease Control and Prevention reported that, as of Dec. 5, 2019, 1,276 individual cases of measles of measles were confirmed in 31 states, the largest number since 1992. This number is a major uptick in cases, compared with previous years since 2000 when the CDC declared measles eliminated from the United States. No deaths have been reported for 2019.
Three-quarters of these cases in 2019 were linked to recent outbreaks in New York and occurred in primarily in underimmunized, close-knit communities and in patients with links to international travel. A total of 124 of the people who got measles this year were hospitalized, and 61 reported having complications, including pneumonia and encephalitis. The overall median patient age was 6 years (31% aged 1-4 years, 27% aged 5-17 years, and 29% aged at least 18 years).
The good news is that most of these cases occurred in unvaccinated patients. The national vaccination rate for the almost 4 million kindergartners reported as enrolled in 2018-2019 was 94.7% for two doses of the MMR vaccine, falling just short of the CDC recommended 95% vaccination rate threshold. The CDC reported an approximate 2.5% rate of vaccination exemptions among school-age children.
The bad news is that, despite the high rate of MMR vaccination rates among U.S. children, there are gaps in measles protection in the U.S. population because of factors leaving patients immunocompromised and antivaccination sentiment that has led some parents to defer or refuse the MMR.
In addition, adults who were vaccinated prior to 1968 with either inactivated measles vaccine or measles vaccine of unknown type may have limited immunity. The inactivated measles vaccine, which was available in 1963-1967, did not achieve effective measles protection.
A global measles surge
While antivaccination sentiment contributed to the 2019 measles cases, a more significant factor may be the global surge of measles. More than 140,000 people worldwide died from measles in 2018, according to the World Health Organization and the CDC.
“[Recent data on measles] indicates that during the first 6 months of the year there have been more measles cases reported worldwide than in any year since 2006. From Jan. 1 to July 31, 2019, 182 countries reported 364,808 measles cases to the WHO. This surpasses the 129,239 reported during the same time period in 2018. WHO regions with the biggest increases in cases include the African region (900%), the Western Pacific region (230%), and the European region (150%),” according to a CDC report.
Studies on hospitalization and complications linked to measles in the United States are scarce, but two outbreaks in Minnesota (2011 and 2017) provided some data on what to expect if the measles surge continues into 2020. The investigators found that poor feeding was a primary reason for admission (97%); additional complications included otitis media (42%), pneumonia (30%), and tracheitis (6%). Three-quarters received antibiotics, 30% required oxygen, and 21% received vitamin A. Median length of stay was 3.7 days (range, 1.1-26.2 days) (Pediatr Infect Dis J. 2019 Jun;38[6]:547-52. doi: 10.1097/INF.0000000000002221).
‘Immunological amnesia’
Infection with the measles virus appears to reduce immunity to other pathogens, according to a paper published in Science (2019 Nov 1;366[6465]599-606).
The hypothesis that the measles virus could cause “immunological amnesia” by impairing immune memory is supported by early research showing children with measles had negative cutaneous tuberculin reactions after having previously tested positive.
“Subsequent studies have shown decreased interferon signaling, skewed cytokine responses, lymphopenia, and suppression of lymphocyte proliferation shortly after infection,” wrote Michael Mina, MD, from Brigham and Women’s Hospital in Boston, and coauthors.
“Given the variation in the degree of immune repertoire modulation we observed, we anticipate that future risk of morbidity and mortality after measles would not be homogeneous but would be skewed toward individuals with the most severe elimination of immunological memory,” they wrote. “These findings underscore the crucial need for continued widespread vaccination.”
In this study, researchers compared the levels of around 400 pathogen-specific antibodies in blood samples from 77 unvaccinated children, taken before and 2 months after natural measles infection, with 5 unvaccinated children who did not contract measles. A total of 34 children experienced mild measles, and 43 had severe measles.
They found that the samples taken after measles infection showed “substantial” reductions in the number of pathogen epitopes, compared with the samples from children who did not get infected with measles.
This amounted to approximately a 20% mean reduction in overall diversity or size of the antibody repertoire. However, in children who experienced severe measles, there was a median loss of 40% (range, 11%-62%) of antibody repertoire, compared with a median of 33% (range, 12%-73%) range in children who experienced mild infection. Meanwhile, the control subjects retained approximately 90% of their antibody repertoire over a similar or longer time period. Some children lost up to 70% of antibodies for specific pathogens.
Maternal-acquired immunity fades
In another study of measles immunity, maternal antibodies were found to be insufficient to provide immunity to infants after 6 months.
The study of 196 infants showed that maternal measles antibodies had dropped below the protective threshold by 3 months of age – well before the recommended age of 12-15 months for the first dose of MMR vaccine.
The odds of inadequate protection doubled for each additional month of age, Michelle Science, MD, of the University of Toronto and associates reported in Pediatrics (2019 Dec 1. doi 10.1542/peds.2019-0630).
“The widening gap between loss of maternal antibodies and measles vaccination described in our study leaves infants vulnerable to measles for much of their infancy and highlights the need for further research to support public health policy,” Dr. Science and colleagues wrote.
The researchers randomly selected 25 samples for each of eight different age groups: up to 30 days old; 1 month (31-60 days), 2 months (61-89 days), 3 months (90-119 days), 4 months, 5 months, 6-9 months, and 9-11 months.
Just over half the babies (56%) were male, and 35% had an underlying condition, but none had conditions that might affect antibody levels. The conditions were primarily a developmental delay or otherwise affecting the central nervous system, liver, or gastrointestinal function. Mean maternal age was 32 years.
To ensure high test sensitivity, the researchers used the plaque-reduction neutralization test to test for measles-neutralizing antibodies instead of using enzyme-linked immunosorbent assay, because “ELISA sensitivity decreases as antibody titers decrease,” Dr. Science and colleagues wrote. They used a neutralization titer of less than 192 mIU/mL as the threshold for protection against measles.
When the researchers calculated the predicted standardized mean antibody titer for infants with a mother aged 32 years, they determined their mean to be 541 mIU/mL at 1 month, 142 mIU/mL at 3 months (below the measles threshold of susceptibility of 192 mIU/mL), and 64 mIU/mL at 6 months. None of the infants had measles antibodies above the protective threshold at 6 months old, the authors noted.
Children’s odds of susceptibility to measles doubled for each additional month of age, after adjustment for infant sex and maternal age (odds ratio, 2.13). Children’s likelihood of susceptibility to measles modestly increased as maternal age increased in 5-year increments from 25 to 40 years.
Children with an underlying conditions had greater susceptibility to measles (83%), compared with those without a comorbidity (68%, P = .03). No difference in susceptibility existed between males and females or based on gestational age at birth (ranging from 37 to 41 weeks).
The Advisory Committee on Immunization Practices permits measles vaccination “as early as 6 months for infants who plan to travel internationally, infants with ongoing risk for exposure during measles outbreaks and as postexposure prophylaxis,” Huong Q. McLean, PhD, of Marshfield (Wisc.) Clinic Research Institute, and Walter A. Orenstein, MD, of Emory University, Atlanta, noted in an editorial.
The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures.
Bianca Nogrady and Tara Haelle contributed to this story.
Measles made a comeback in 2019.
The Centers for Disease Control and Prevention reported that, as of Dec. 5, 2019, 1,276 individual cases of measles of measles were confirmed in 31 states, the largest number since 1992. This number is a major uptick in cases, compared with previous years since 2000 when the CDC declared measles eliminated from the United States. No deaths have been reported for 2019.
Three-quarters of these cases in 2019 were linked to recent outbreaks in New York and occurred in primarily in underimmunized, close-knit communities and in patients with links to international travel. A total of 124 of the people who got measles this year were hospitalized, and 61 reported having complications, including pneumonia and encephalitis. The overall median patient age was 6 years (31% aged 1-4 years, 27% aged 5-17 years, and 29% aged at least 18 years).
The good news is that most of these cases occurred in unvaccinated patients. The national vaccination rate for the almost 4 million kindergartners reported as enrolled in 2018-2019 was 94.7% for two doses of the MMR vaccine, falling just short of the CDC recommended 95% vaccination rate threshold. The CDC reported an approximate 2.5% rate of vaccination exemptions among school-age children.
The bad news is that, despite the high rate of MMR vaccination rates among U.S. children, there are gaps in measles protection in the U.S. population because of factors leaving patients immunocompromised and antivaccination sentiment that has led some parents to defer or refuse the MMR.
In addition, adults who were vaccinated prior to 1968 with either inactivated measles vaccine or measles vaccine of unknown type may have limited immunity. The inactivated measles vaccine, which was available in 1963-1967, did not achieve effective measles protection.
A global measles surge
While antivaccination sentiment contributed to the 2019 measles cases, a more significant factor may be the global surge of measles. More than 140,000 people worldwide died from measles in 2018, according to the World Health Organization and the CDC.
“[Recent data on measles] indicates that during the first 6 months of the year there have been more measles cases reported worldwide than in any year since 2006. From Jan. 1 to July 31, 2019, 182 countries reported 364,808 measles cases to the WHO. This surpasses the 129,239 reported during the same time period in 2018. WHO regions with the biggest increases in cases include the African region (900%), the Western Pacific region (230%), and the European region (150%),” according to a CDC report.
Studies on hospitalization and complications linked to measles in the United States are scarce, but two outbreaks in Minnesota (2011 and 2017) provided some data on what to expect if the measles surge continues into 2020. The investigators found that poor feeding was a primary reason for admission (97%); additional complications included otitis media (42%), pneumonia (30%), and tracheitis (6%). Three-quarters received antibiotics, 30% required oxygen, and 21% received vitamin A. Median length of stay was 3.7 days (range, 1.1-26.2 days) (Pediatr Infect Dis J. 2019 Jun;38[6]:547-52. doi: 10.1097/INF.0000000000002221).
‘Immunological amnesia’
Infection with the measles virus appears to reduce immunity to other pathogens, according to a paper published in Science (2019 Nov 1;366[6465]599-606).
The hypothesis that the measles virus could cause “immunological amnesia” by impairing immune memory is supported by early research showing children with measles had negative cutaneous tuberculin reactions after having previously tested positive.
“Subsequent studies have shown decreased interferon signaling, skewed cytokine responses, lymphopenia, and suppression of lymphocyte proliferation shortly after infection,” wrote Michael Mina, MD, from Brigham and Women’s Hospital in Boston, and coauthors.
“Given the variation in the degree of immune repertoire modulation we observed, we anticipate that future risk of morbidity and mortality after measles would not be homogeneous but would be skewed toward individuals with the most severe elimination of immunological memory,” they wrote. “These findings underscore the crucial need for continued widespread vaccination.”
In this study, researchers compared the levels of around 400 pathogen-specific antibodies in blood samples from 77 unvaccinated children, taken before and 2 months after natural measles infection, with 5 unvaccinated children who did not contract measles. A total of 34 children experienced mild measles, and 43 had severe measles.
They found that the samples taken after measles infection showed “substantial” reductions in the number of pathogen epitopes, compared with the samples from children who did not get infected with measles.
This amounted to approximately a 20% mean reduction in overall diversity or size of the antibody repertoire. However, in children who experienced severe measles, there was a median loss of 40% (range, 11%-62%) of antibody repertoire, compared with a median of 33% (range, 12%-73%) range in children who experienced mild infection. Meanwhile, the control subjects retained approximately 90% of their antibody repertoire over a similar or longer time period. Some children lost up to 70% of antibodies for specific pathogens.
Maternal-acquired immunity fades
In another study of measles immunity, maternal antibodies were found to be insufficient to provide immunity to infants after 6 months.
The study of 196 infants showed that maternal measles antibodies had dropped below the protective threshold by 3 months of age – well before the recommended age of 12-15 months for the first dose of MMR vaccine.
The odds of inadequate protection doubled for each additional month of age, Michelle Science, MD, of the University of Toronto and associates reported in Pediatrics (2019 Dec 1. doi 10.1542/peds.2019-0630).
“The widening gap between loss of maternal antibodies and measles vaccination described in our study leaves infants vulnerable to measles for much of their infancy and highlights the need for further research to support public health policy,” Dr. Science and colleagues wrote.
The researchers randomly selected 25 samples for each of eight different age groups: up to 30 days old; 1 month (31-60 days), 2 months (61-89 days), 3 months (90-119 days), 4 months, 5 months, 6-9 months, and 9-11 months.
Just over half the babies (56%) were male, and 35% had an underlying condition, but none had conditions that might affect antibody levels. The conditions were primarily a developmental delay or otherwise affecting the central nervous system, liver, or gastrointestinal function. Mean maternal age was 32 years.
To ensure high test sensitivity, the researchers used the plaque-reduction neutralization test to test for measles-neutralizing antibodies instead of using enzyme-linked immunosorbent assay, because “ELISA sensitivity decreases as antibody titers decrease,” Dr. Science and colleagues wrote. They used a neutralization titer of less than 192 mIU/mL as the threshold for protection against measles.
When the researchers calculated the predicted standardized mean antibody titer for infants with a mother aged 32 years, they determined their mean to be 541 mIU/mL at 1 month, 142 mIU/mL at 3 months (below the measles threshold of susceptibility of 192 mIU/mL), and 64 mIU/mL at 6 months. None of the infants had measles antibodies above the protective threshold at 6 months old, the authors noted.
Children’s odds of susceptibility to measles doubled for each additional month of age, after adjustment for infant sex and maternal age (odds ratio, 2.13). Children’s likelihood of susceptibility to measles modestly increased as maternal age increased in 5-year increments from 25 to 40 years.
Children with an underlying conditions had greater susceptibility to measles (83%), compared with those without a comorbidity (68%, P = .03). No difference in susceptibility existed between males and females or based on gestational age at birth (ranging from 37 to 41 weeks).
The Advisory Committee on Immunization Practices permits measles vaccination “as early as 6 months for infants who plan to travel internationally, infants with ongoing risk for exposure during measles outbreaks and as postexposure prophylaxis,” Huong Q. McLean, PhD, of Marshfield (Wisc.) Clinic Research Institute, and Walter A. Orenstein, MD, of Emory University, Atlanta, noted in an editorial.
The research was funded by the Public Health Ontario Project Initiation Fund. The authors had no relevant financial disclosures.
Bianca Nogrady and Tara Haelle contributed to this story.
EVALI readmissions and deaths prompt guideline change
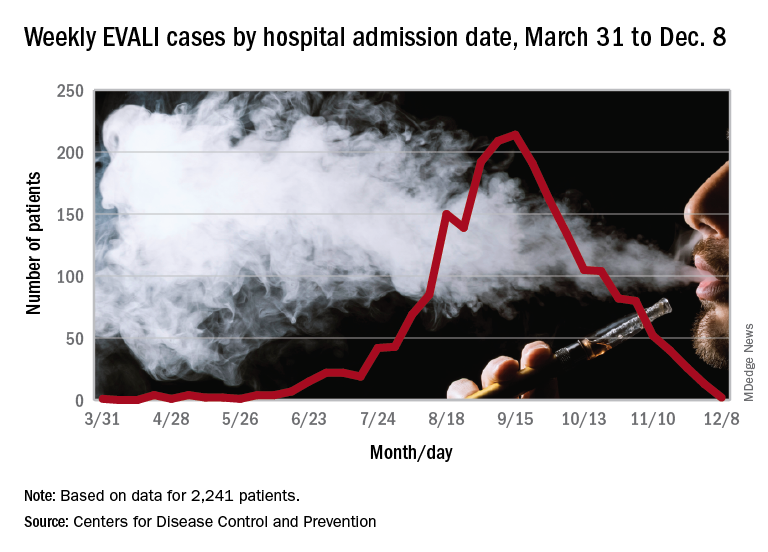
Those who required rehospitalization for e-cigarette or vaping product use–associated lung injury (EVALI) and those who died after discharge were more likely to have one or more chronic conditions than were other EVALI patients, and those “who died also were more likely to have been admitted to an intensive care unit, experienced respiratory failure necessitating intubation and mechanical ventilation, and were significantly older,” Christina A. Mikosz, MD, and associates wrote in the Morbidity and Mortality Weekly Report.
Their analysis included the 1,139 EVALI patients who were discharged on or after Oct. 31, 2019. Of that group, 31 (2.7%) patients were rehospitalized and subsequently discharged and another 7 died after the initial discharge. The median age was 54 years for those who died, 27 years for those who were rehospitalized, and 23 for those who survived without rehospitalization, said Dr. Mikosz of the CDC National Center for Injury Prevention and Control, Atlanta, and associates.
Those findings, along with the rates of one or more comorbidities – 83% for those who died, 71% for those who were rehospitalized, and 26% for those who did not die or get readmitted – prompted the CDC to update its guidance for postdischarge follow-up of EVALI patients.
That update involves six specific recommendations to determine readiness for discharge, which include “confirming no clinically significant fluctuations in vital signs for at least 24-48 hours before discharge [and] preparation for hospital discharge and postdischarge care coordination to reduce risk of rehospitalization and death,” Mary E. Evans, MD, and associates said in a separate CDC communication (MMWR. 2019 Dec. 20. 68[early release]:1-6).
As of Dec. 17, the CDC reports that 2,506 patients have been hospitalized with EVALI since March 31, 2019, and 54 deaths have been confirmed in 27 states and the District of Columbia. The outbreak appears to have peaked in September, but cases are still being reported: 13 during the week of Dec. 1-7 and one case for the week of Dec. 8-14.
SOURCE: Mikosz CA et al. MMWR. 2019 Dec. 20. 68[early release]:1-7.
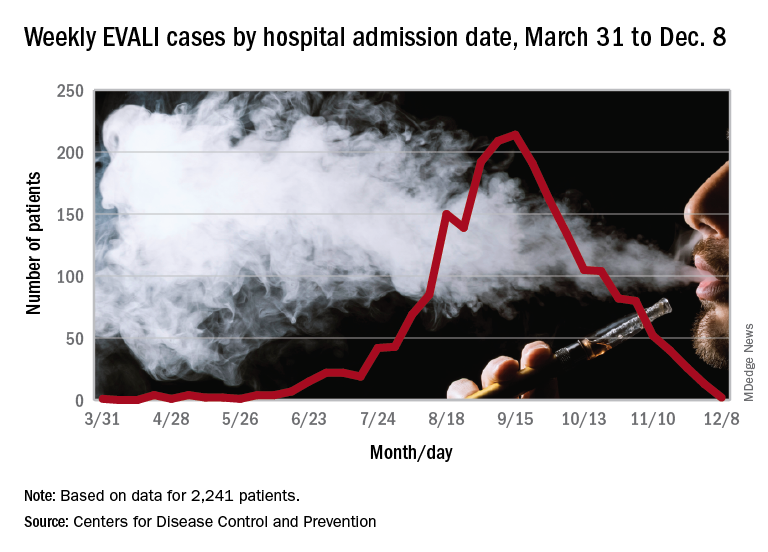
Those who required rehospitalization for e-cigarette or vaping product use–associated lung injury (EVALI) and those who died after discharge were more likely to have one or more chronic conditions than were other EVALI patients, and those “who died also were more likely to have been admitted to an intensive care unit, experienced respiratory failure necessitating intubation and mechanical ventilation, and were significantly older,” Christina A. Mikosz, MD, and associates wrote in the Morbidity and Mortality Weekly Report.
Their analysis included the 1,139 EVALI patients who were discharged on or after Oct. 31, 2019. Of that group, 31 (2.7%) patients were rehospitalized and subsequently discharged and another 7 died after the initial discharge. The median age was 54 years for those who died, 27 years for those who were rehospitalized, and 23 for those who survived without rehospitalization, said Dr. Mikosz of the CDC National Center for Injury Prevention and Control, Atlanta, and associates.
Those findings, along with the rates of one or more comorbidities – 83% for those who died, 71% for those who were rehospitalized, and 26% for those who did not die or get readmitted – prompted the CDC to update its guidance for postdischarge follow-up of EVALI patients.
That update involves six specific recommendations to determine readiness for discharge, which include “confirming no clinically significant fluctuations in vital signs for at least 24-48 hours before discharge [and] preparation for hospital discharge and postdischarge care coordination to reduce risk of rehospitalization and death,” Mary E. Evans, MD, and associates said in a separate CDC communication (MMWR. 2019 Dec. 20. 68[early release]:1-6).
As of Dec. 17, the CDC reports that 2,506 patients have been hospitalized with EVALI since March 31, 2019, and 54 deaths have been confirmed in 27 states and the District of Columbia. The outbreak appears to have peaked in September, but cases are still being reported: 13 during the week of Dec. 1-7 and one case for the week of Dec. 8-14.
SOURCE: Mikosz CA et al. MMWR. 2019 Dec. 20. 68[early release]:1-7.
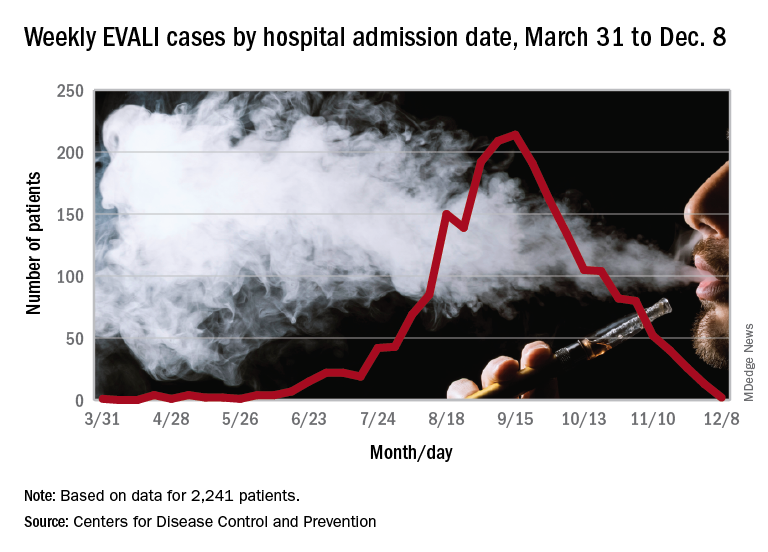
Those who required rehospitalization for e-cigarette or vaping product use–associated lung injury (EVALI) and those who died after discharge were more likely to have one or more chronic conditions than were other EVALI patients, and those “who died also were more likely to have been admitted to an intensive care unit, experienced respiratory failure necessitating intubation and mechanical ventilation, and were significantly older,” Christina A. Mikosz, MD, and associates wrote in the Morbidity and Mortality Weekly Report.
Their analysis included the 1,139 EVALI patients who were discharged on or after Oct. 31, 2019. Of that group, 31 (2.7%) patients were rehospitalized and subsequently discharged and another 7 died after the initial discharge. The median age was 54 years for those who died, 27 years for those who were rehospitalized, and 23 for those who survived without rehospitalization, said Dr. Mikosz of the CDC National Center for Injury Prevention and Control, Atlanta, and associates.
Those findings, along with the rates of one or more comorbidities – 83% for those who died, 71% for those who were rehospitalized, and 26% for those who did not die or get readmitted – prompted the CDC to update its guidance for postdischarge follow-up of EVALI patients.
That update involves six specific recommendations to determine readiness for discharge, which include “confirming no clinically significant fluctuations in vital signs for at least 24-48 hours before discharge [and] preparation for hospital discharge and postdischarge care coordination to reduce risk of rehospitalization and death,” Mary E. Evans, MD, and associates said in a separate CDC communication (MMWR. 2019 Dec. 20. 68[early release]:1-6).
As of Dec. 17, the CDC reports that 2,506 patients have been hospitalized with EVALI since March 31, 2019, and 54 deaths have been confirmed in 27 states and the District of Columbia. The outbreak appears to have peaked in September, but cases are still being reported: 13 during the week of Dec. 1-7 and one case for the week of Dec. 8-14.
SOURCE: Mikosz CA et al. MMWR. 2019 Dec. 20. 68[early release]:1-7.
FROM MMWR
Vitamin E acetate confirmed as likely source of EVALI
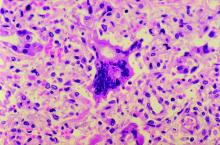
Vitamin E acetate was found in fluid from the lungs of 94% of patients with electronic cigarette, or vaping, product use–associated lung injury, data from a convenience sample of 51 patients indicate. The findings were published in the New England Journal of Medicine.
Cases of electronic cigarette, or vaping, product use–associated lung injury (EVALI) were reported to the Centers for Disease Control and Prevention starting in early 2019, and numbers rose throughout the year, “which suggests new or increased exposure to one or more toxicants from the use of e-cigarette products,” wrote Benjamin C. Blount, PhD, of the National Center for Environmental Health at the CDC, and colleagues.
To further investigate potential toxins in patients with EVALI, the researchers examined bronchoalveolar-lavage (BAL) fluid from 51 EVALI patients and 99 healthy controls.
After the researchers used isotope dilution mass spectrometry on the samples, 48 of the 51 patients (94%) showed vitamin E acetate in their BAL samples. No other potential toxins – including plant oils, medium-chain triglyceride oil, petroleum distillates, and diluent terpenes – were identified. The samples of one patient each showed coconut oil and limonene.
A total of 47 of 51 patients for whom complete laboratory data were available either reported vaping tetrahydrocannabinol products within 90 days of becoming ill, or showed tetrahydrocannabinol or its metabolites in their BAL fluid. In addition, 30 of 47 patients showed nicotine or nicotine metabolites in their BAL fluid.
The average age of the patients was 23 years, 69% were male. Overall, 25 were confirmed EVALI cases and 26 were probable cases, and probable cases included the three patients who showed no vitamin E acetate.
The safety of inhaling vitamin E acetate, which is a common ingredient in dietary supplements and skin care creams, has not been well studied. It could contribute to lung injury when heated in e-cigarette products by splitting the acetate to create the reactive compound and potential lung irritant ketene, the researchers said.
The study findings were limited by several factors including the possibility that vitamin E acetate is a marker for exposure to other toxicants, a lack of data on the impact of heating vitamin e acetate, and the inability to assess the timing of the vitamin E acetate exposure compared to BAL sample collection, the researchers noted.
However, the results suggest that vitamin E acetate may play a role in EVALI because of the high detection rate in patients from across the United States, the biologically possible potential for lung injury from vitamin e acetate, and the timing of the rise of EVALI and the use of vitamin E acetate in vaping products, they concluded.
The research was supported by the National Cancer Institute, the FDA Center for Tobacco Products, and The Ohio State University Pelotonia intramural research program. The authors had no financial conflicts to disclose.
SOURCE: Blount BC et al. N Engl J Med. 2019 Dec 20. doi: 10.1056/NEJMoa1916433.
Vitamin E acetate was found in fluid from the lungs of 94% of patients with electronic cigarette, or vaping, product use–associated lung injury, data from a convenience sample of 51 patients indicate. The findings were published in the New England Journal of Medicine.
Cases of electronic cigarette, or vaping, product use–associated lung injury (EVALI) were reported to the Centers for Disease Control and Prevention starting in early 2019, and numbers rose throughout the year, “which suggests new or increased exposure to one or more toxicants from the use of e-cigarette products,” wrote Benjamin C. Blount, PhD, of the National Center for Environmental Health at the CDC, and colleagues.
To further investigate potential toxins in patients with EVALI, the researchers examined bronchoalveolar-lavage (BAL) fluid from 51 EVALI patients and 99 healthy controls.
After the researchers used isotope dilution mass spectrometry on the samples, 48 of the 51 patients (94%) showed vitamin E acetate in their BAL samples. No other potential toxins – including plant oils, medium-chain triglyceride oil, petroleum distillates, and diluent terpenes – were identified. The samples of one patient each showed coconut oil and limonene.
A total of 47 of 51 patients for whom complete laboratory data were available either reported vaping tetrahydrocannabinol products within 90 days of becoming ill, or showed tetrahydrocannabinol or its metabolites in their BAL fluid. In addition, 30 of 47 patients showed nicotine or nicotine metabolites in their BAL fluid.
The average age of the patients was 23 years, 69% were male. Overall, 25 were confirmed EVALI cases and 26 were probable cases, and probable cases included the three patients who showed no vitamin E acetate.
The safety of inhaling vitamin E acetate, which is a common ingredient in dietary supplements and skin care creams, has not been well studied. It could contribute to lung injury when heated in e-cigarette products by splitting the acetate to create the reactive compound and potential lung irritant ketene, the researchers said.
The study findings were limited by several factors including the possibility that vitamin E acetate is a marker for exposure to other toxicants, a lack of data on the impact of heating vitamin e acetate, and the inability to assess the timing of the vitamin E acetate exposure compared to BAL sample collection, the researchers noted.
However, the results suggest that vitamin E acetate may play a role in EVALI because of the high detection rate in patients from across the United States, the biologically possible potential for lung injury from vitamin e acetate, and the timing of the rise of EVALI and the use of vitamin E acetate in vaping products, they concluded.
The research was supported by the National Cancer Institute, the FDA Center for Tobacco Products, and The Ohio State University Pelotonia intramural research program. The authors had no financial conflicts to disclose.
SOURCE: Blount BC et al. N Engl J Med. 2019 Dec 20. doi: 10.1056/NEJMoa1916433.
Vitamin E acetate was found in fluid from the lungs of 94% of patients with electronic cigarette, or vaping, product use–associated lung injury, data from a convenience sample of 51 patients indicate. The findings were published in the New England Journal of Medicine.
Cases of electronic cigarette, or vaping, product use–associated lung injury (EVALI) were reported to the Centers for Disease Control and Prevention starting in early 2019, and numbers rose throughout the year, “which suggests new or increased exposure to one or more toxicants from the use of e-cigarette products,” wrote Benjamin C. Blount, PhD, of the National Center for Environmental Health at the CDC, and colleagues.
To further investigate potential toxins in patients with EVALI, the researchers examined bronchoalveolar-lavage (BAL) fluid from 51 EVALI patients and 99 healthy controls.
After the researchers used isotope dilution mass spectrometry on the samples, 48 of the 51 patients (94%) showed vitamin E acetate in their BAL samples. No other potential toxins – including plant oils, medium-chain triglyceride oil, petroleum distillates, and diluent terpenes – were identified. The samples of one patient each showed coconut oil and limonene.
A total of 47 of 51 patients for whom complete laboratory data were available either reported vaping tetrahydrocannabinol products within 90 days of becoming ill, or showed tetrahydrocannabinol or its metabolites in their BAL fluid. In addition, 30 of 47 patients showed nicotine or nicotine metabolites in their BAL fluid.
The average age of the patients was 23 years, 69% were male. Overall, 25 were confirmed EVALI cases and 26 were probable cases, and probable cases included the three patients who showed no vitamin E acetate.
The safety of inhaling vitamin E acetate, which is a common ingredient in dietary supplements and skin care creams, has not been well studied. It could contribute to lung injury when heated in e-cigarette products by splitting the acetate to create the reactive compound and potential lung irritant ketene, the researchers said.
The study findings were limited by several factors including the possibility that vitamin E acetate is a marker for exposure to other toxicants, a lack of data on the impact of heating vitamin e acetate, and the inability to assess the timing of the vitamin E acetate exposure compared to BAL sample collection, the researchers noted.
However, the results suggest that vitamin E acetate may play a role in EVALI because of the high detection rate in patients from across the United States, the biologically possible potential for lung injury from vitamin e acetate, and the timing of the rise of EVALI and the use of vitamin E acetate in vaping products, they concluded.
The research was supported by the National Cancer Institute, the FDA Center for Tobacco Products, and The Ohio State University Pelotonia intramural research program. The authors had no financial conflicts to disclose.
SOURCE: Blount BC et al. N Engl J Med. 2019 Dec 20. doi: 10.1056/NEJMoa1916433.
FROM NEW ENGLAND JOURNAL OF MEDICINE
A novel communication framework for inpatient pain management
Introducing the VIEW Framework
Case
A 55-year-old male with a history of diabetes mellitus, lumbar degenerative disc disease, and chronic low back pain was admitted overnight with right lower extremity cellulitis. He reported taking oral hydromorphone for chronic pain, but review of the Prescription Drug Monitoring Program (PDMP) revealed multiple short-term prescriptions from various ED providers, as well as monthly prescriptions from a variety of primary care providers.
Throughout the EHR, he is described as manipulative and narcotic-seeking with notation of multiple ED visits for pain. Multiple discharges against medical advice were noted. He was given two doses of IV hydromorphone in the ED and requested that this be continued. He was admitted for IV antibiotics for severe leg pain that he rated 15/10.
Background
The Society of Hospital Medicine published a consensus statement in the Journal of Hospital Medicine in 2018 that included 16 clinical recommendations on the safe use of opioids for the treatment of acute pain in hospitalized adults.1 In regard to communication about pain, clinicians are encouraged to set realistic goals and expectations of opioid therapy, closely monitor response to opioid therapy, and provide education about the side effects and potential risks of opioid therapy for patients and their families.
However, even when these strategies are employed, the social and behavioral complexities of individual patients can contribute to unsatisfactory interactions with health care staff. Because difficult encounters have been linked to provider burnout, enhanced communication strategies can benefit both the patient and physician.2
SHM’s Patient Experience Committee saw an opportunity to provide complementary evidence-based best-practice tips for communication about pain. Specifically, the committee worked collectively to develop a framework that can be applied to more challenging encounters.
The VIEW Framework
VISIT the patient’s chart and your own mental state.
First, visit the patient’s chart to review information relevant to the patient’s pain history. The EHR can be leveraged through filters and search functions to identify encounters, consultations, and notes relevant to pain management.
Look at the prior to admission medication list and active medication list and see if there are discrepancies. The medication administration record (MAR) can help identify adjunctive medications that the patient may be refusing. PDMP data should be screened for signs of aberrant use, including multiple pharmacies, multiple prescribers, short intervals between prescriptions, and serially prescribed, multiple, low-quantity prescriptions.
While documented pain scores can be a marker of patient distress, objective aspects of the patient’s functional status can shed light on how much his/her discomfort impairs day-to-day living. Examples of these measures include nutritional intake, sleep cycle, out of bed activity, and participation with therapy. Lastly, assess for opioid-related side-effects including constipation, decreased respiratory rate, and any notation of over sedation in narrative documentation from ancillary services.
Once this information has been accrued, it is important to take a moment of mindfulness before meeting with the patient. Take steps to minimize interruptions with electronic devices by silencing your pager/cell phone and disengaging from computers/tablets. Some examples of mindfulness-based practices include taking cycles of deep breathing, going for a short walk to appreciate hospital artwork or view points, or focusing on the sensory aspects of washing your hands prior to seeing the patient. Self-reflection on prior meaningful encounters can also help reset your state of mind. These activities can help clear prior subconscious thoughts and frustrations and prepare for the task ahead of you.3
Intense focus and awareness can enhance your recognition of patient distress, increase your ability to engage in active listening, and enable you to be more receptive to verbal and nonverbal cues.2 Additionally, mindful behaviors have been shown to contribute to decreased burnout and improved empathy.4,5
INTERVIEW the patient.
Once you enter the room, introduce yourself to the patient and others who are present. Interview the patient by eliciting subjective information. Use open-ended and nonjudgmental language, and take moments to summarize the patient’s perspective.
Inquire about the patient’s home baseline pain scores and past levels of acceptable function. Further explore the patient’s performance goals related to activities of daily living and quality of life. Ask about any prior history of addiction to any substance, and if needed, discuss your specific concerns related to substance misuse and abuse.
EMPATHIZE with the patient.
Integrate empathy into your interview by validating any frustrations and experience of pain. Identifying with loss of function and quality of life can help you connect with the patient and initiate a therapeutic relationship. Observe both verbal and nonverbal behaviors that reveal signs of emotional discomfort.6 Use open-ended questions to create space and trust for patients to share their feelings.
Pause to summarize the patient’s perspective while acknowledging and validating emotions that he or she may be experiencing such as anxiety, fear, frustration and anger.6 Statements such as “ I know it is frustrating to ... ” or “I can’t imagine what it must feel like to ... ” can help convey empathy. Multiple studies have suggested that enhanced provider empathy and positive messaging can also reduce patient pain and anxiety and increase quality of life.7,8 Empathic responses to negative emotional expressions from patients have also been associated with higher ratings of communication.9
WRAP UP.
Finally, wrap up by aligning expectations with the patient for pain control and summarize your management recommendations. Educate the patient and his/her family on the risks and benefits of recommended therapy as well as the expected course of recovery. Setting shared goals for functionality relevant to the patient’s personal values and quality of life can build connection between you and your patient.
While handing over the patient to the next provider, refrain from using stereotypical language such as “narcotic-seeking patient.” Clearly communicate the management plan and milestones to other team members, such as nurses, physical therapists, and oncoming hospitalists, to maintain consistency. This will help align patients and their care team and may stave off maladaptive patient behaviors such as splitting.
Applying the VIEW framework to the case
Visit
Upon visiting the medical chart, the physician realized that the patient’s opioid use began in his 20s when he injured his back in a traumatic motor vehicle accident. His successful athletic career came to a halt after this injury and opioid dependence ensued.
While reviewing past notes and prescription data via the PDMP, the physician noted that the patient had been visiting many different providers in order to get more pain medications. The most recent prescription was for oral hydromorphone 4 mg every 4 hours as needed, filled 1 week prior to this presentation.
She reviewed his vital signs and found that he had been persistently hypertensive and tachycardic. His nurse mentioned that he appeared to be in severe pain because of facial grimacing with standing and walking.
Prior to entering the patient’s room, the physician took a moment of mindfulness to become aware of her emotional state because she recognized that she was worried this could be a difficult encounter. She considered how hard his life has been and how much emotional and physical pain he might be experiencing. She took a deep breath, silenced her phone, and entered the room.
Interview
The physician sat at the bedside and interviewed the patient using a calm and nonjudgmental tone. It was quickly obvious to her that he was experiencing real pain. His cellulitis appeared severe and was tender to even minimal palpation. She learned that the pain in his leg had been worsening over the past week to the point that it was becoming difficult to ambulate, sleep and perform his daily hygiene routine. He was taking 4 mg tablets of hydromorphone every 2 hours, and he had run out a few days ago. He added that his mood was increasingly depressed, and he had even admitted to occasional suicidal thoughts because the pain was so unbearable.
When asked directly, he admitted that he was worried he was addicted to hydromorphone. He had first received it for low back pain after the motor vehicle accident, and it been refilled multiple times for ongoing pain over the course of a year. Importantly, she also learned that he felt he was often treated as an addict by medical professionals and felt that doctors no longer listened to him or believed him.
Empathize
As the conversation went on, the physician offered empathetic statements, recognizing the way it might feel to have your pain ignored or minimized by doctors. She expressed how frustrating it is to not be able to perform basic functions and how difficult it must be to constantly live in pain.
She said, “I don’t want you to suffer in pain. I care about you and my goal is to treat your pain so that you can return to doing the things in life that you find meaningful.” She also recognized the severity of his depression and discussed with him the role and importance of psychiatric consultation.
Wrap Up
The physician wrapped up the encounter by summarizing her plan to treat the infection and work together with him to treat his pain with the goal that he could ambulate and perform activities of daily living.
She reviewed the side effects of both acute and long-term use of opioids and discussed the risks and benefits. Given the fact that patient was on chronic baseline opioids and also had objective signs of acute pain, she started an initial regimen of hydromorphone 6 mg tablets every 4 hours as needed (a 50% increase over his home dose) and added acetaminophen 1000 mg every 6 hours and ibuprofen 600 mg every 8 hours.
She informed him that she would check on him in the afternoon and that the ultimate plan would be to taper down on his hydromorphone dose each day as his cellulitis improved. She also communicated that bidirectional respect between the patient and care team members was critical to a successful pain management.
Finally, she explained that there was going to be a different doctor covering at night and major changes to the prescription regimen would be deferred to daytime hours.
When she left the room, she summarized the plan with the patient’s nurse and shared a few details about the patient’s difficult past. At the end of the shift, the physician signed out to the overnight team that the patient had objective signs of pain and recommended a visit to the bedside if the patient’s symptoms were reported as worsening.
During his hospital stay, she monitored the patient’s nonverbal responses to movement, participation in physical therapy, and ability to sleep. She tapered the hydromorphone down each day as the patient’s cellulitis improved. At discharge, he was prescribed a 3-day supply of his home dose of hydromorphone and the same acetaminophen and ibuprofen regimen he had been on in the hospital with instructions for tapering. Finally, after coming to an agreement with the patient, she arranged for follow-up in the opioid taper clinic and communicated the plan with the patient’s primary care provider.
Dr. Horman is a hospitalist and assistant professor of medicine at UC San Diego Health. Dr. Richards is a hospitalist and assistant professor of medicine at the University of Nebraska Medical Center in Omaha. Dr. Horman and Dr. Richards note that they wrote this article in collaboration with the Society of Hospital Medicine Patient Experience Committee.
Key points
- Spend adequate time to fully visit patients’ history as it relates to their current pain complaints.
- Review notes and prescription data to better understand past and current pain regimen.
- Be vigilant about taking a mindful moment to visit your thoughts and potential biases.
- Interview patients using a calm tone and nonjudgmental, reassuring words.
- Empathize with patients and validate any frustrations and experience of pain.
- Wrap-up by summarizing your recommendations with patients, their families, the care team, and subsequent providers.
References
1. Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: A Systematic Review of Existing Guidelines. J Hosp Med. 2018;13(4):256-62.
2. An PG et al. (MEM Investigators). Burden of difficult encounters in primary care: data from the minimizing error, maximizing outcomes study. Arch Intern Med. 2009;169(4):410-4.
3. Sanyer O, Fortenberry K. Using Mindfulness Techniques to improve difficult clinical encounters. Am Fam Physician. 2013;87(6):402.
4. Beckman HB et al. The impact of a program in mindful communication on primary care physicians. Acad Med. 2012;87(6):815-8.
5. Krasner MS et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302(12):1284-93.
6. Dean M, Street R. A 3-Stage model of patient centered communication for addressing cancer patients’ emotional distress. Patient Educ Couns. 2014;94(2):143-8.
7. Howick J et al. Effects of empathic and positive communication in healthcare consultations: A systematic review and meta-analysis. J R Soc Med. 2018;111(7):240-52.
8. Mistiaen P et al. The effect of patient-practitioner communication on pain: A systematic review. Eur J Pain. 2016;20:675-88.
9. Weiss R et al. Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters. J Hosp Med. 2017;12(10):805-10.
Introducing the VIEW Framework
Introducing the VIEW Framework
Case
A 55-year-old male with a history of diabetes mellitus, lumbar degenerative disc disease, and chronic low back pain was admitted overnight with right lower extremity cellulitis. He reported taking oral hydromorphone for chronic pain, but review of the Prescription Drug Monitoring Program (PDMP) revealed multiple short-term prescriptions from various ED providers, as well as monthly prescriptions from a variety of primary care providers.
Throughout the EHR, he is described as manipulative and narcotic-seeking with notation of multiple ED visits for pain. Multiple discharges against medical advice were noted. He was given two doses of IV hydromorphone in the ED and requested that this be continued. He was admitted for IV antibiotics for severe leg pain that he rated 15/10.
Background
The Society of Hospital Medicine published a consensus statement in the Journal of Hospital Medicine in 2018 that included 16 clinical recommendations on the safe use of opioids for the treatment of acute pain in hospitalized adults.1 In regard to communication about pain, clinicians are encouraged to set realistic goals and expectations of opioid therapy, closely monitor response to opioid therapy, and provide education about the side effects and potential risks of opioid therapy for patients and their families.
However, even when these strategies are employed, the social and behavioral complexities of individual patients can contribute to unsatisfactory interactions with health care staff. Because difficult encounters have been linked to provider burnout, enhanced communication strategies can benefit both the patient and physician.2
SHM’s Patient Experience Committee saw an opportunity to provide complementary evidence-based best-practice tips for communication about pain. Specifically, the committee worked collectively to develop a framework that can be applied to more challenging encounters.
The VIEW Framework
VISIT the patient’s chart and your own mental state.
First, visit the patient’s chart to review information relevant to the patient’s pain history. The EHR can be leveraged through filters and search functions to identify encounters, consultations, and notes relevant to pain management.
Look at the prior to admission medication list and active medication list and see if there are discrepancies. The medication administration record (MAR) can help identify adjunctive medications that the patient may be refusing. PDMP data should be screened for signs of aberrant use, including multiple pharmacies, multiple prescribers, short intervals between prescriptions, and serially prescribed, multiple, low-quantity prescriptions.
While documented pain scores can be a marker of patient distress, objective aspects of the patient’s functional status can shed light on how much his/her discomfort impairs day-to-day living. Examples of these measures include nutritional intake, sleep cycle, out of bed activity, and participation with therapy. Lastly, assess for opioid-related side-effects including constipation, decreased respiratory rate, and any notation of over sedation in narrative documentation from ancillary services.
Once this information has been accrued, it is important to take a moment of mindfulness before meeting with the patient. Take steps to minimize interruptions with electronic devices by silencing your pager/cell phone and disengaging from computers/tablets. Some examples of mindfulness-based practices include taking cycles of deep breathing, going for a short walk to appreciate hospital artwork or view points, or focusing on the sensory aspects of washing your hands prior to seeing the patient. Self-reflection on prior meaningful encounters can also help reset your state of mind. These activities can help clear prior subconscious thoughts and frustrations and prepare for the task ahead of you.3
Intense focus and awareness can enhance your recognition of patient distress, increase your ability to engage in active listening, and enable you to be more receptive to verbal and nonverbal cues.2 Additionally, mindful behaviors have been shown to contribute to decreased burnout and improved empathy.4,5
INTERVIEW the patient.
Once you enter the room, introduce yourself to the patient and others who are present. Interview the patient by eliciting subjective information. Use open-ended and nonjudgmental language, and take moments to summarize the patient’s perspective.
Inquire about the patient’s home baseline pain scores and past levels of acceptable function. Further explore the patient’s performance goals related to activities of daily living and quality of life. Ask about any prior history of addiction to any substance, and if needed, discuss your specific concerns related to substance misuse and abuse.
EMPATHIZE with the patient.
Integrate empathy into your interview by validating any frustrations and experience of pain. Identifying with loss of function and quality of life can help you connect with the patient and initiate a therapeutic relationship. Observe both verbal and nonverbal behaviors that reveal signs of emotional discomfort.6 Use open-ended questions to create space and trust for patients to share their feelings.
Pause to summarize the patient’s perspective while acknowledging and validating emotions that he or she may be experiencing such as anxiety, fear, frustration and anger.6 Statements such as “ I know it is frustrating to ... ” or “I can’t imagine what it must feel like to ... ” can help convey empathy. Multiple studies have suggested that enhanced provider empathy and positive messaging can also reduce patient pain and anxiety and increase quality of life.7,8 Empathic responses to negative emotional expressions from patients have also been associated with higher ratings of communication.9
WRAP UP.
Finally, wrap up by aligning expectations with the patient for pain control and summarize your management recommendations. Educate the patient and his/her family on the risks and benefits of recommended therapy as well as the expected course of recovery. Setting shared goals for functionality relevant to the patient’s personal values and quality of life can build connection between you and your patient.
While handing over the patient to the next provider, refrain from using stereotypical language such as “narcotic-seeking patient.” Clearly communicate the management plan and milestones to other team members, such as nurses, physical therapists, and oncoming hospitalists, to maintain consistency. This will help align patients and their care team and may stave off maladaptive patient behaviors such as splitting.
Applying the VIEW framework to the case
Visit
Upon visiting the medical chart, the physician realized that the patient’s opioid use began in his 20s when he injured his back in a traumatic motor vehicle accident. His successful athletic career came to a halt after this injury and opioid dependence ensued.
While reviewing past notes and prescription data via the PDMP, the physician noted that the patient had been visiting many different providers in order to get more pain medications. The most recent prescription was for oral hydromorphone 4 mg every 4 hours as needed, filled 1 week prior to this presentation.
She reviewed his vital signs and found that he had been persistently hypertensive and tachycardic. His nurse mentioned that he appeared to be in severe pain because of facial grimacing with standing and walking.
Prior to entering the patient’s room, the physician took a moment of mindfulness to become aware of her emotional state because she recognized that she was worried this could be a difficult encounter. She considered how hard his life has been and how much emotional and physical pain he might be experiencing. She took a deep breath, silenced her phone, and entered the room.
Interview
The physician sat at the bedside and interviewed the patient using a calm and nonjudgmental tone. It was quickly obvious to her that he was experiencing real pain. His cellulitis appeared severe and was tender to even minimal palpation. She learned that the pain in his leg had been worsening over the past week to the point that it was becoming difficult to ambulate, sleep and perform his daily hygiene routine. He was taking 4 mg tablets of hydromorphone every 2 hours, and he had run out a few days ago. He added that his mood was increasingly depressed, and he had even admitted to occasional suicidal thoughts because the pain was so unbearable.
When asked directly, he admitted that he was worried he was addicted to hydromorphone. He had first received it for low back pain after the motor vehicle accident, and it been refilled multiple times for ongoing pain over the course of a year. Importantly, she also learned that he felt he was often treated as an addict by medical professionals and felt that doctors no longer listened to him or believed him.
Empathize
As the conversation went on, the physician offered empathetic statements, recognizing the way it might feel to have your pain ignored or minimized by doctors. She expressed how frustrating it is to not be able to perform basic functions and how difficult it must be to constantly live in pain.
She said, “I don’t want you to suffer in pain. I care about you and my goal is to treat your pain so that you can return to doing the things in life that you find meaningful.” She also recognized the severity of his depression and discussed with him the role and importance of psychiatric consultation.
Wrap Up
The physician wrapped up the encounter by summarizing her plan to treat the infection and work together with him to treat his pain with the goal that he could ambulate and perform activities of daily living.
She reviewed the side effects of both acute and long-term use of opioids and discussed the risks and benefits. Given the fact that patient was on chronic baseline opioids and also had objective signs of acute pain, she started an initial regimen of hydromorphone 6 mg tablets every 4 hours as needed (a 50% increase over his home dose) and added acetaminophen 1000 mg every 6 hours and ibuprofen 600 mg every 8 hours.
She informed him that she would check on him in the afternoon and that the ultimate plan would be to taper down on his hydromorphone dose each day as his cellulitis improved. She also communicated that bidirectional respect between the patient and care team members was critical to a successful pain management.
Finally, she explained that there was going to be a different doctor covering at night and major changes to the prescription regimen would be deferred to daytime hours.
When she left the room, she summarized the plan with the patient’s nurse and shared a few details about the patient’s difficult past. At the end of the shift, the physician signed out to the overnight team that the patient had objective signs of pain and recommended a visit to the bedside if the patient’s symptoms were reported as worsening.
During his hospital stay, she monitored the patient’s nonverbal responses to movement, participation in physical therapy, and ability to sleep. She tapered the hydromorphone down each day as the patient’s cellulitis improved. At discharge, he was prescribed a 3-day supply of his home dose of hydromorphone and the same acetaminophen and ibuprofen regimen he had been on in the hospital with instructions for tapering. Finally, after coming to an agreement with the patient, she arranged for follow-up in the opioid taper clinic and communicated the plan with the patient’s primary care provider.
Dr. Horman is a hospitalist and assistant professor of medicine at UC San Diego Health. Dr. Richards is a hospitalist and assistant professor of medicine at the University of Nebraska Medical Center in Omaha. Dr. Horman and Dr. Richards note that they wrote this article in collaboration with the Society of Hospital Medicine Patient Experience Committee.
Key points
- Spend adequate time to fully visit patients’ history as it relates to their current pain complaints.
- Review notes and prescription data to better understand past and current pain regimen.
- Be vigilant about taking a mindful moment to visit your thoughts and potential biases.
- Interview patients using a calm tone and nonjudgmental, reassuring words.
- Empathize with patients and validate any frustrations and experience of pain.
- Wrap-up by summarizing your recommendations with patients, their families, the care team, and subsequent providers.
References
1. Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: A Systematic Review of Existing Guidelines. J Hosp Med. 2018;13(4):256-62.
2. An PG et al. (MEM Investigators). Burden of difficult encounters in primary care: data from the minimizing error, maximizing outcomes study. Arch Intern Med. 2009;169(4):410-4.
3. Sanyer O, Fortenberry K. Using Mindfulness Techniques to improve difficult clinical encounters. Am Fam Physician. 2013;87(6):402.
4. Beckman HB et al. The impact of a program in mindful communication on primary care physicians. Acad Med. 2012;87(6):815-8.
5. Krasner MS et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302(12):1284-93.
6. Dean M, Street R. A 3-Stage model of patient centered communication for addressing cancer patients’ emotional distress. Patient Educ Couns. 2014;94(2):143-8.
7. Howick J et al. Effects of empathic and positive communication in healthcare consultations: A systematic review and meta-analysis. J R Soc Med. 2018;111(7):240-52.
8. Mistiaen P et al. The effect of patient-practitioner communication on pain: A systematic review. Eur J Pain. 2016;20:675-88.
9. Weiss R et al. Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters. J Hosp Med. 2017;12(10):805-10.
Case
A 55-year-old male with a history of diabetes mellitus, lumbar degenerative disc disease, and chronic low back pain was admitted overnight with right lower extremity cellulitis. He reported taking oral hydromorphone for chronic pain, but review of the Prescription Drug Monitoring Program (PDMP) revealed multiple short-term prescriptions from various ED providers, as well as monthly prescriptions from a variety of primary care providers.
Throughout the EHR, he is described as manipulative and narcotic-seeking with notation of multiple ED visits for pain. Multiple discharges against medical advice were noted. He was given two doses of IV hydromorphone in the ED and requested that this be continued. He was admitted for IV antibiotics for severe leg pain that he rated 15/10.
Background
The Society of Hospital Medicine published a consensus statement in the Journal of Hospital Medicine in 2018 that included 16 clinical recommendations on the safe use of opioids for the treatment of acute pain in hospitalized adults.1 In regard to communication about pain, clinicians are encouraged to set realistic goals and expectations of opioid therapy, closely monitor response to opioid therapy, and provide education about the side effects and potential risks of opioid therapy for patients and their families.
However, even when these strategies are employed, the social and behavioral complexities of individual patients can contribute to unsatisfactory interactions with health care staff. Because difficult encounters have been linked to provider burnout, enhanced communication strategies can benefit both the patient and physician.2
SHM’s Patient Experience Committee saw an opportunity to provide complementary evidence-based best-practice tips for communication about pain. Specifically, the committee worked collectively to develop a framework that can be applied to more challenging encounters.
The VIEW Framework
VISIT the patient’s chart and your own mental state.
First, visit the patient’s chart to review information relevant to the patient’s pain history. The EHR can be leveraged through filters and search functions to identify encounters, consultations, and notes relevant to pain management.
Look at the prior to admission medication list and active medication list and see if there are discrepancies. The medication administration record (MAR) can help identify adjunctive medications that the patient may be refusing. PDMP data should be screened for signs of aberrant use, including multiple pharmacies, multiple prescribers, short intervals between prescriptions, and serially prescribed, multiple, low-quantity prescriptions.
While documented pain scores can be a marker of patient distress, objective aspects of the patient’s functional status can shed light on how much his/her discomfort impairs day-to-day living. Examples of these measures include nutritional intake, sleep cycle, out of bed activity, and participation with therapy. Lastly, assess for opioid-related side-effects including constipation, decreased respiratory rate, and any notation of over sedation in narrative documentation from ancillary services.
Once this information has been accrued, it is important to take a moment of mindfulness before meeting with the patient. Take steps to minimize interruptions with electronic devices by silencing your pager/cell phone and disengaging from computers/tablets. Some examples of mindfulness-based practices include taking cycles of deep breathing, going for a short walk to appreciate hospital artwork or view points, or focusing on the sensory aspects of washing your hands prior to seeing the patient. Self-reflection on prior meaningful encounters can also help reset your state of mind. These activities can help clear prior subconscious thoughts and frustrations and prepare for the task ahead of you.3
Intense focus and awareness can enhance your recognition of patient distress, increase your ability to engage in active listening, and enable you to be more receptive to verbal and nonverbal cues.2 Additionally, mindful behaviors have been shown to contribute to decreased burnout and improved empathy.4,5
INTERVIEW the patient.
Once you enter the room, introduce yourself to the patient and others who are present. Interview the patient by eliciting subjective information. Use open-ended and nonjudgmental language, and take moments to summarize the patient’s perspective.
Inquire about the patient’s home baseline pain scores and past levels of acceptable function. Further explore the patient’s performance goals related to activities of daily living and quality of life. Ask about any prior history of addiction to any substance, and if needed, discuss your specific concerns related to substance misuse and abuse.
EMPATHIZE with the patient.
Integrate empathy into your interview by validating any frustrations and experience of pain. Identifying with loss of function and quality of life can help you connect with the patient and initiate a therapeutic relationship. Observe both verbal and nonverbal behaviors that reveal signs of emotional discomfort.6 Use open-ended questions to create space and trust for patients to share their feelings.
Pause to summarize the patient’s perspective while acknowledging and validating emotions that he or she may be experiencing such as anxiety, fear, frustration and anger.6 Statements such as “ I know it is frustrating to ... ” or “I can’t imagine what it must feel like to ... ” can help convey empathy. Multiple studies have suggested that enhanced provider empathy and positive messaging can also reduce patient pain and anxiety and increase quality of life.7,8 Empathic responses to negative emotional expressions from patients have also been associated with higher ratings of communication.9
WRAP UP.
Finally, wrap up by aligning expectations with the patient for pain control and summarize your management recommendations. Educate the patient and his/her family on the risks and benefits of recommended therapy as well as the expected course of recovery. Setting shared goals for functionality relevant to the patient’s personal values and quality of life can build connection between you and your patient.
While handing over the patient to the next provider, refrain from using stereotypical language such as “narcotic-seeking patient.” Clearly communicate the management plan and milestones to other team members, such as nurses, physical therapists, and oncoming hospitalists, to maintain consistency. This will help align patients and their care team and may stave off maladaptive patient behaviors such as splitting.
Applying the VIEW framework to the case
Visit
Upon visiting the medical chart, the physician realized that the patient’s opioid use began in his 20s when he injured his back in a traumatic motor vehicle accident. His successful athletic career came to a halt after this injury and opioid dependence ensued.
While reviewing past notes and prescription data via the PDMP, the physician noted that the patient had been visiting many different providers in order to get more pain medications. The most recent prescription was for oral hydromorphone 4 mg every 4 hours as needed, filled 1 week prior to this presentation.
She reviewed his vital signs and found that he had been persistently hypertensive and tachycardic. His nurse mentioned that he appeared to be in severe pain because of facial grimacing with standing and walking.
Prior to entering the patient’s room, the physician took a moment of mindfulness to become aware of her emotional state because she recognized that she was worried this could be a difficult encounter. She considered how hard his life has been and how much emotional and physical pain he might be experiencing. She took a deep breath, silenced her phone, and entered the room.
Interview
The physician sat at the bedside and interviewed the patient using a calm and nonjudgmental tone. It was quickly obvious to her that he was experiencing real pain. His cellulitis appeared severe and was tender to even minimal palpation. She learned that the pain in his leg had been worsening over the past week to the point that it was becoming difficult to ambulate, sleep and perform his daily hygiene routine. He was taking 4 mg tablets of hydromorphone every 2 hours, and he had run out a few days ago. He added that his mood was increasingly depressed, and he had even admitted to occasional suicidal thoughts because the pain was so unbearable.
When asked directly, he admitted that he was worried he was addicted to hydromorphone. He had first received it for low back pain after the motor vehicle accident, and it been refilled multiple times for ongoing pain over the course of a year. Importantly, she also learned that he felt he was often treated as an addict by medical professionals and felt that doctors no longer listened to him or believed him.
Empathize
As the conversation went on, the physician offered empathetic statements, recognizing the way it might feel to have your pain ignored or minimized by doctors. She expressed how frustrating it is to not be able to perform basic functions and how difficult it must be to constantly live in pain.
She said, “I don’t want you to suffer in pain. I care about you and my goal is to treat your pain so that you can return to doing the things in life that you find meaningful.” She also recognized the severity of his depression and discussed with him the role and importance of psychiatric consultation.
Wrap Up
The physician wrapped up the encounter by summarizing her plan to treat the infection and work together with him to treat his pain with the goal that he could ambulate and perform activities of daily living.
She reviewed the side effects of both acute and long-term use of opioids and discussed the risks and benefits. Given the fact that patient was on chronic baseline opioids and also had objective signs of acute pain, she started an initial regimen of hydromorphone 6 mg tablets every 4 hours as needed (a 50% increase over his home dose) and added acetaminophen 1000 mg every 6 hours and ibuprofen 600 mg every 8 hours.
She informed him that she would check on him in the afternoon and that the ultimate plan would be to taper down on his hydromorphone dose each day as his cellulitis improved. She also communicated that bidirectional respect between the patient and care team members was critical to a successful pain management.
Finally, she explained that there was going to be a different doctor covering at night and major changes to the prescription regimen would be deferred to daytime hours.
When she left the room, she summarized the plan with the patient’s nurse and shared a few details about the patient’s difficult past. At the end of the shift, the physician signed out to the overnight team that the patient had objective signs of pain and recommended a visit to the bedside if the patient’s symptoms were reported as worsening.
During his hospital stay, she monitored the patient’s nonverbal responses to movement, participation in physical therapy, and ability to sleep. She tapered the hydromorphone down each day as the patient’s cellulitis improved. At discharge, he was prescribed a 3-day supply of his home dose of hydromorphone and the same acetaminophen and ibuprofen regimen he had been on in the hospital with instructions for tapering. Finally, after coming to an agreement with the patient, she arranged for follow-up in the opioid taper clinic and communicated the plan with the patient’s primary care provider.
Dr. Horman is a hospitalist and assistant professor of medicine at UC San Diego Health. Dr. Richards is a hospitalist and assistant professor of medicine at the University of Nebraska Medical Center in Omaha. Dr. Horman and Dr. Richards note that they wrote this article in collaboration with the Society of Hospital Medicine Patient Experience Committee.
Key points
- Spend adequate time to fully visit patients’ history as it relates to their current pain complaints.
- Review notes and prescription data to better understand past and current pain regimen.
- Be vigilant about taking a mindful moment to visit your thoughts and potential biases.
- Interview patients using a calm tone and nonjudgmental, reassuring words.
- Empathize with patients and validate any frustrations and experience of pain.
- Wrap-up by summarizing your recommendations with patients, their families, the care team, and subsequent providers.
References
1. Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: A Systematic Review of Existing Guidelines. J Hosp Med. 2018;13(4):256-62.
2. An PG et al. (MEM Investigators). Burden of difficult encounters in primary care: data from the minimizing error, maximizing outcomes study. Arch Intern Med. 2009;169(4):410-4.
3. Sanyer O, Fortenberry K. Using Mindfulness Techniques to improve difficult clinical encounters. Am Fam Physician. 2013;87(6):402.
4. Beckman HB et al. The impact of a program in mindful communication on primary care physicians. Acad Med. 2012;87(6):815-8.
5. Krasner MS et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302(12):1284-93.
6. Dean M, Street R. A 3-Stage model of patient centered communication for addressing cancer patients’ emotional distress. Patient Educ Couns. 2014;94(2):143-8.
7. Howick J et al. Effects of empathic and positive communication in healthcare consultations: A systematic review and meta-analysis. J R Soc Med. 2018;111(7):240-52.
8. Mistiaen P et al. The effect of patient-practitioner communication on pain: A systematic review. Eur J Pain. 2016;20:675-88.
9. Weiss R et al. Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters. J Hosp Med. 2017;12(10):805-10.
FDA warns gabapentin, pregabalin may cause serious breathing problems
Elderly patients who take these drugs also are at increased risk of breathing problems, the announcement said.
Gabapentin (marketed as Neurontin, Gralise, and Horizant) and pregabalin (Lyrica and Lyrica CR) are used to treat seizures, nerve pain, and restless legs syndrome. Physicians increasingly are prescribing these medications, and people are misusing and abusing these drugs more frequently, the agency said. Gabapentin and pregabalin often are combined with central nervous system depressants such as opioids, antianxiety medicines, antidepressants, and antihistamines, which increases the risk of respiratory depression.
Conditions that reduce lung function, including chronic obstructive pulmonary disease (COPD), also increase the likelihood of breathing problems when taking gabapentin and pregabalin.
“There is less evidence supporting the risk of serious breathing difficulties in healthy individuals taking gabapentinoids alone. We will continue to monitor these medicines as part of our routine monitoring of all FDA-approved drugs,” the announcement said.
The FDA is requiring new warnings about the risk of respiratory depression in the prescribing information of gabapentinoids. In addition, drug manufacturers must further assess the abuse potential of these drugs, particularly in combination with opioids.
Patients and caregivers should seek immediate medical attention for respiratory problems, which can be life threatening. Symptoms include confusion or disorientation; unusual dizziness or lightheadedness; extreme sleepiness or lethargy; slowed, shallow, or difficult breathing; unresponsiveness; and bluish-colored or tinted skin, especially on the lips, fingers, and toes.
Physicians should start gabapentinoids at the lowest dose and monitor patients for symptoms of respiratory depression and sedation when coprescribing these drugs with an opioid or other central nervous system depressant such as a benzodiazepine, according to the FDA.
The agency reviewed 49 case reports that were submitted between 2012 and 2017. Among these cases, 12 people died from respiratory depression with gabapentinoids. All of the patients who died had at least one risk factor.
Gabapentin first was approved in 1993, and pregabalin was approved in 2004. Drug adverse events and side effects can be reported online, the agency noted.
Elderly patients who take these drugs also are at increased risk of breathing problems, the announcement said.
Gabapentin (marketed as Neurontin, Gralise, and Horizant) and pregabalin (Lyrica and Lyrica CR) are used to treat seizures, nerve pain, and restless legs syndrome. Physicians increasingly are prescribing these medications, and people are misusing and abusing these drugs more frequently, the agency said. Gabapentin and pregabalin often are combined with central nervous system depressants such as opioids, antianxiety medicines, antidepressants, and antihistamines, which increases the risk of respiratory depression.
Conditions that reduce lung function, including chronic obstructive pulmonary disease (COPD), also increase the likelihood of breathing problems when taking gabapentin and pregabalin.
“There is less evidence supporting the risk of serious breathing difficulties in healthy individuals taking gabapentinoids alone. We will continue to monitor these medicines as part of our routine monitoring of all FDA-approved drugs,” the announcement said.
The FDA is requiring new warnings about the risk of respiratory depression in the prescribing information of gabapentinoids. In addition, drug manufacturers must further assess the abuse potential of these drugs, particularly in combination with opioids.
Patients and caregivers should seek immediate medical attention for respiratory problems, which can be life threatening. Symptoms include confusion or disorientation; unusual dizziness or lightheadedness; extreme sleepiness or lethargy; slowed, shallow, or difficult breathing; unresponsiveness; and bluish-colored or tinted skin, especially on the lips, fingers, and toes.
Physicians should start gabapentinoids at the lowest dose and monitor patients for symptoms of respiratory depression and sedation when coprescribing these drugs with an opioid or other central nervous system depressant such as a benzodiazepine, according to the FDA.
The agency reviewed 49 case reports that were submitted between 2012 and 2017. Among these cases, 12 people died from respiratory depression with gabapentinoids. All of the patients who died had at least one risk factor.
Gabapentin first was approved in 1993, and pregabalin was approved in 2004. Drug adverse events and side effects can be reported online, the agency noted.
Elderly patients who take these drugs also are at increased risk of breathing problems, the announcement said.
Gabapentin (marketed as Neurontin, Gralise, and Horizant) and pregabalin (Lyrica and Lyrica CR) are used to treat seizures, nerve pain, and restless legs syndrome. Physicians increasingly are prescribing these medications, and people are misusing and abusing these drugs more frequently, the agency said. Gabapentin and pregabalin often are combined with central nervous system depressants such as opioids, antianxiety medicines, antidepressants, and antihistamines, which increases the risk of respiratory depression.
Conditions that reduce lung function, including chronic obstructive pulmonary disease (COPD), also increase the likelihood of breathing problems when taking gabapentin and pregabalin.
“There is less evidence supporting the risk of serious breathing difficulties in healthy individuals taking gabapentinoids alone. We will continue to monitor these medicines as part of our routine monitoring of all FDA-approved drugs,” the announcement said.
The FDA is requiring new warnings about the risk of respiratory depression in the prescribing information of gabapentinoids. In addition, drug manufacturers must further assess the abuse potential of these drugs, particularly in combination with opioids.
Patients and caregivers should seek immediate medical attention for respiratory problems, which can be life threatening. Symptoms include confusion or disorientation; unusual dizziness or lightheadedness; extreme sleepiness or lethargy; slowed, shallow, or difficult breathing; unresponsiveness; and bluish-colored or tinted skin, especially on the lips, fingers, and toes.
Physicians should start gabapentinoids at the lowest dose and monitor patients for symptoms of respiratory depression and sedation when coprescribing these drugs with an opioid or other central nervous system depressant such as a benzodiazepine, according to the FDA.
The agency reviewed 49 case reports that were submitted between 2012 and 2017. Among these cases, 12 people died from respiratory depression with gabapentinoids. All of the patients who died had at least one risk factor.
Gabapentin first was approved in 1993, and pregabalin was approved in 2004. Drug adverse events and side effects can be reported online, the agency noted.
Out-of-network billing in in-network hospitals adds $40 billion in spending
As the debate over how best to address surprise billing continues, new research shows that billing from out-of-network physicians at in-network facilities is adding $40 billion in costs.
Researchers focused on four different types of physicians that account for out-of-network billing: anesthesiologists, pathologists, radiologists, and cases involving an assistant surgeon, which had out-of-network bills in about 10% of claims that were examined as part of the research.
“To give a rough estimate of the savings that could be achieved by eliminating the ability of these four types of specialists to readily bill out of network, we simulated what would happen if all of these specialists received the same average payments as orthopedic surgeons did (164% of Medicare rates),” Zack Cooper, PhD, associate professor of health policy at Yale University, New Haven, Conn., and colleagues wrote in a research report published in Health Affairs.
“We estimated that if these physicians were paid the same average rate as orthopedists for all of the services that they delivered in our sample, spending would be lowered on anesthesiologists by 53.5%, on pathologists by 47.4%, on radiologists by 16.3%, and on assistant surgeons by 46.2%,” the authors wrote.
Researchers said that physician spending for these four specialties would be lowered by 13.4% and would lower total spending for people with employer-sponsored insurance by about 3.4%, or $40 billion. If spending on these four specialties were lowered to 150% of Medicare rates, it would lower spending on physicians by 15.3%.
To help combat the issues of surprise billing in a way that lowers total commercial health care spending and helps to preserve a competitive price for physician services, Dr. Cooper and colleagues recommended an approach that would regulate the contracts of physicians who work in hospitals and are not chosen by patients. It would establish a bundled package for services that include the emergency department physicians and the four specialists examined as part of the research and would use the fee associated with the package of services to recruit specialists to work at the hospital.
The authors said this kind of policy would eliminate the possibility of patients seeing out-of-network providers at in-network hospitals and, unlike arbitration (a favored solution among physician groups if it is set up in an agreeable manner), patients are protected without being required to take any action. The policy also sets a competitive rate for these services.
“Under this bundled care approach, physicians would compete to offer their services on the basis of price and quality,” Dr. Cooper and colleagues stated. “Hospitals would compete with one another on the price and quality of their care, including the services provided by the physicians they recruited. Hospitals would also need to compete to retain physicians.”
This approach is not included in any current surprise billing legislation. There was hope that surprise billing would be addressed in a government spending bill that would be signed before year’s end. But a second bipartisan plan was introduced in the House Ways and Means Committee after a bipartisan compromise was reached by the House Energy and Commerce and the Senate Health, Education, Labor, and Pensions committees. This has postponed a decision on surprise billing legislation into the coming year.
[email protected]
SOURCE: Cooper Z et al. Health Aff. 2019 Dec 16. doi: 10.1377/hlthaff.2019.00507.
As the debate over how best to address surprise billing continues, new research shows that billing from out-of-network physicians at in-network facilities is adding $40 billion in costs.
Researchers focused on four different types of physicians that account for out-of-network billing: anesthesiologists, pathologists, radiologists, and cases involving an assistant surgeon, which had out-of-network bills in about 10% of claims that were examined as part of the research.
“To give a rough estimate of the savings that could be achieved by eliminating the ability of these four types of specialists to readily bill out of network, we simulated what would happen if all of these specialists received the same average payments as orthopedic surgeons did (164% of Medicare rates),” Zack Cooper, PhD, associate professor of health policy at Yale University, New Haven, Conn., and colleagues wrote in a research report published in Health Affairs.
“We estimated that if these physicians were paid the same average rate as orthopedists for all of the services that they delivered in our sample, spending would be lowered on anesthesiologists by 53.5%, on pathologists by 47.4%, on radiologists by 16.3%, and on assistant surgeons by 46.2%,” the authors wrote.
Researchers said that physician spending for these four specialties would be lowered by 13.4% and would lower total spending for people with employer-sponsored insurance by about 3.4%, or $40 billion. If spending on these four specialties were lowered to 150% of Medicare rates, it would lower spending on physicians by 15.3%.
To help combat the issues of surprise billing in a way that lowers total commercial health care spending and helps to preserve a competitive price for physician services, Dr. Cooper and colleagues recommended an approach that would regulate the contracts of physicians who work in hospitals and are not chosen by patients. It would establish a bundled package for services that include the emergency department physicians and the four specialists examined as part of the research and would use the fee associated with the package of services to recruit specialists to work at the hospital.
The authors said this kind of policy would eliminate the possibility of patients seeing out-of-network providers at in-network hospitals and, unlike arbitration (a favored solution among physician groups if it is set up in an agreeable manner), patients are protected without being required to take any action. The policy also sets a competitive rate for these services.
“Under this bundled care approach, physicians would compete to offer their services on the basis of price and quality,” Dr. Cooper and colleagues stated. “Hospitals would compete with one another on the price and quality of their care, including the services provided by the physicians they recruited. Hospitals would also need to compete to retain physicians.”
This approach is not included in any current surprise billing legislation. There was hope that surprise billing would be addressed in a government spending bill that would be signed before year’s end. But a second bipartisan plan was introduced in the House Ways and Means Committee after a bipartisan compromise was reached by the House Energy and Commerce and the Senate Health, Education, Labor, and Pensions committees. This has postponed a decision on surprise billing legislation into the coming year.
[email protected]
SOURCE: Cooper Z et al. Health Aff. 2019 Dec 16. doi: 10.1377/hlthaff.2019.00507.
As the debate over how best to address surprise billing continues, new research shows that billing from out-of-network physicians at in-network facilities is adding $40 billion in costs.
Researchers focused on four different types of physicians that account for out-of-network billing: anesthesiologists, pathologists, radiologists, and cases involving an assistant surgeon, which had out-of-network bills in about 10% of claims that were examined as part of the research.
“To give a rough estimate of the savings that could be achieved by eliminating the ability of these four types of specialists to readily bill out of network, we simulated what would happen if all of these specialists received the same average payments as orthopedic surgeons did (164% of Medicare rates),” Zack Cooper, PhD, associate professor of health policy at Yale University, New Haven, Conn., and colleagues wrote in a research report published in Health Affairs.
“We estimated that if these physicians were paid the same average rate as orthopedists for all of the services that they delivered in our sample, spending would be lowered on anesthesiologists by 53.5%, on pathologists by 47.4%, on radiologists by 16.3%, and on assistant surgeons by 46.2%,” the authors wrote.
Researchers said that physician spending for these four specialties would be lowered by 13.4% and would lower total spending for people with employer-sponsored insurance by about 3.4%, or $40 billion. If spending on these four specialties were lowered to 150% of Medicare rates, it would lower spending on physicians by 15.3%.
To help combat the issues of surprise billing in a way that lowers total commercial health care spending and helps to preserve a competitive price for physician services, Dr. Cooper and colleagues recommended an approach that would regulate the contracts of physicians who work in hospitals and are not chosen by patients. It would establish a bundled package for services that include the emergency department physicians and the four specialists examined as part of the research and would use the fee associated with the package of services to recruit specialists to work at the hospital.
The authors said this kind of policy would eliminate the possibility of patients seeing out-of-network providers at in-network hospitals and, unlike arbitration (a favored solution among physician groups if it is set up in an agreeable manner), patients are protected without being required to take any action. The policy also sets a competitive rate for these services.
“Under this bundled care approach, physicians would compete to offer their services on the basis of price and quality,” Dr. Cooper and colleagues stated. “Hospitals would compete with one another on the price and quality of their care, including the services provided by the physicians they recruited. Hospitals would also need to compete to retain physicians.”
This approach is not included in any current surprise billing legislation. There was hope that surprise billing would be addressed in a government spending bill that would be signed before year’s end. But a second bipartisan plan was introduced in the House Ways and Means Committee after a bipartisan compromise was reached by the House Energy and Commerce and the Senate Health, Education, Labor, and Pensions committees. This has postponed a decision on surprise billing legislation into the coming year.
[email protected]
SOURCE: Cooper Z et al. Health Aff. 2019 Dec 16. doi: 10.1377/hlthaff.2019.00507.
FROM HEALTH AFFAIRS
Envisioning the future of hospital medicine
I have written frequently over the last few years on topics related to the sustainability of the hospital medicine practice model. I continue to be concerned by what I see as a confluence of significant trends that are conspiring to challenge hospital medicine’s status quo.
On one hand, the financial pressures on U.S. hospitals are unrelenting, and their willingness or even ability to continue providing significant funding to support their hospital medicine groups is in question. Combine this with hospitalists’ rapidly evolving clinical scope and the ever-increasing demands of physicians in other specialties for hospitalist support, and the result is hospital medicine groups that will continue to grow in size, complexity, and the demand for ever more financial support.
On the other hand, the hospitalists I interact with in my work all over the country seem more stressed out than ever, and many are questioning whether this is a job that can be satisfying and sustainable for a career. Increasing patient complexity, productivity pressures, a lack of resources to address patients’ social issues, a systole-diastole schedule, the frustration of EHRs and other documentation responsibilities, and feeling “dumped on” by physicians in other specialties all contribute to hospitalist job stress.
A quick look at the literature confirms that in 2019 hospitalist burnout is definitely “a thing.” Interestingly, it’s been a thing for a while; the risk of hospitalist burnout was first identified by Hoff, et al., in 2002 (doi: 10.2307/30902462002). My colleague, John Nelson, MD, MHM, has written a number of times about strategies for preventing or mitigating hospitalist burnout.
As these trends converge, the hospital medicine practice model as we know it may be facing an existential crisis. If that sounds overly dramatic, let me say instead that the hospital medicine practice model will need to evolve significantly over the next decade in order to continue to meet patient and institutional needs while remaining both affordable and sustainable for the clinicians who work in it.
In September 2019, SHM’s Multi-Site Leaders Special Interest Group met in Chicago for their second annual Multi-Site Leaders Summit to explore the theme of sustainability in hospital medicine. The participants held robust discussions about coping with our changing practice environment, issues relating to hospitalist burnout and resiliency, innovative staffing models, the role of technology in HM sustainability, and financial sustainability
At the end of the meeting, the group engaged in a visioning exercise designed to move beyond what we are doing today by envisioning what the future of hospital medicine will look like and what interventions will be necessary for us to get from here to there. I’d like to share this visioning exercise with you and encourage you to “play along” by thinking seriously about the questions it poses.
Visioning exercise
Feel free to jot down some thoughts as we go through this exercise. But otherwise, just close your eyes and come along for the ride. Imagine yourself sitting at your desk looking at a desk calendar showing today’s date. Watch the pages flip from today, to tomorrow, to the next day, then to next month, and the next, and then to the next year and so on, until we arrive at December 2029.
Imagine that you look up from your desk, and suddenly realize that you aren’t in your office at all, but instead in a huge auditorium where someone is speaking about an award that is going to be announced. It’s crowded and a little stuffy in the auditorium, but people around you are whispering to each other with an air of eager anticipation, their eyes glued to the stage. You realize that the person being introduced up on the podium is the President of the United States, and the award is the Presidential Medal of Freedom, which is only awarded to people or groups who have made “an especially meritorious contribution to the security or national interests of the United States, world peace, cultural, or other significant public or private endeavors.”
Today, the Medal is being awarded to the Society of Hospital Medicine on behalf of all hospital medicine leaders nationally, for their collective accomplishments in saving the specialty of hospital medicine and, by doing so, ensuring that sick people are able to continue receiving the care they need in our nation’s hospitals – and that the hospitals themselves have become reliably safe, efficient, and effective in achieving high quality outcomes.
The President says, “At no time in the history of this award until now have we given this, the highest civilian award in the land, to a whole group of physician leaders across an entire specialty. But the achievements of this group of people in preserving and even enhancing the presence of highly energized, dedicated, capable clinicians in our nation’s hospitals against the significant odds they have faced over the last 10 years is nothing short of extraordinary.” There is a standing ovation, as people jump up out of their chairs to cheer and applaud. When the applause finally dies down, the President goes on to list all the accomplishments that made this group of leaders deserving. Listen to what she is saying. Fill it in in your own mind. What is it that this group has accomplished?
[Brief silence]
Up on a huge screen beside the stage, a video starts. In it, there are several hospital and physician executives in a focus group, and one exec says, “The thing that is great about what these leaders have accomplished in the field of hospital medicine is…” Fill it in – what did that executive say? Another leader jumps in: “That’s all fine and wonderful, but the thing that really makes hospital medicine stand out today compared to where they were 10 years ago is…” Listen to what these executives are saying. What accomplishments are they praising?
The video then moves on to show a focus group of recent hospital patients. One patient says, “10 years ago when my mom was in the hospital, the poor hospitalists caring for her seemed completely overwhelmed and burnt out, and the whole care system seemed fragmented and inefficient; but my own recent hospital experience was so different because…” Additional patients chime in, talking about how confident they felt about the care they received in the hospital and the reasons for that. What is it these patients are describing?
SHM’s CEO gets up to accept the award and explains that 10 years ago, a group of multi-site hospital medicine leaders from across the country came together to begin addressing the issue of sustainability; this led to a formal process for developing a vision and a plan for the future of hospital medicine, and the execution of that plan eventually resulted in the outcomes recognized by this award. She acknowledges that over the years many people questioned whether the hospital medicine model should even continue to exist or whether some other model for inpatient care should be adopted. She talks about all the compelling reasons that supported the continued existence of the specialty of hospital medicine. What are some of the reasons she listed? The SHM CEO goes on to describe some of the key things that were done to address the issues associated with sustainability of the hospital medicine practice model. Listen to what she says; what was it that SHM and the hospital leaders it represents did?
As you are leaving the auditorium, you overhear a group of mid-career staff hospitalists talking. They are saying that they didn’t originally believe the specialty would actually change, and they weren’t sure if they could do this job for a career – but that it did change. They begin talking about what it feels like to work as a hospitalist now, and how these changes have improved their lives. Listen to what they are saying. How does it feel to work as a hospitalist?
As you leave the auditorium and go back to your desk, you sit down to record some of the things you heard. What was it the President of the US said as she presented the Presidential Medal of Freedom? Why did SHM and the hospital medicine leaders it represents deserve the award? What was it that the SHM CEO said was done to bring about the successful changes? What did the staff hospitalists say about working in the specialty?
Whenever you are ready, take a minute to jot down the specifics that came to mind as you read through this exercise. If you are willing to share your thoughts about sustainability in hospital medicine, I’d love to hear from you. Feel free to email me directly at [email protected].
Let’s build the foundation for a sustainable future for our specialty.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif. She serves on SHM’s Practice Analysis Committee, and helps to coordinate SHM’s bi-annual State of Hospital Medicine Survey. This article appeared originally in SHM’s official blog The Hospital Leader.
I have written frequently over the last few years on topics related to the sustainability of the hospital medicine practice model. I continue to be concerned by what I see as a confluence of significant trends that are conspiring to challenge hospital medicine’s status quo.
On one hand, the financial pressures on U.S. hospitals are unrelenting, and their willingness or even ability to continue providing significant funding to support their hospital medicine groups is in question. Combine this with hospitalists’ rapidly evolving clinical scope and the ever-increasing demands of physicians in other specialties for hospitalist support, and the result is hospital medicine groups that will continue to grow in size, complexity, and the demand for ever more financial support.
On the other hand, the hospitalists I interact with in my work all over the country seem more stressed out than ever, and many are questioning whether this is a job that can be satisfying and sustainable for a career. Increasing patient complexity, productivity pressures, a lack of resources to address patients’ social issues, a systole-diastole schedule, the frustration of EHRs and other documentation responsibilities, and feeling “dumped on” by physicians in other specialties all contribute to hospitalist job stress.
A quick look at the literature confirms that in 2019 hospitalist burnout is definitely “a thing.” Interestingly, it’s been a thing for a while; the risk of hospitalist burnout was first identified by Hoff, et al., in 2002 (doi: 10.2307/30902462002). My colleague, John Nelson, MD, MHM, has written a number of times about strategies for preventing or mitigating hospitalist burnout.
As these trends converge, the hospital medicine practice model as we know it may be facing an existential crisis. If that sounds overly dramatic, let me say instead that the hospital medicine practice model will need to evolve significantly over the next decade in order to continue to meet patient and institutional needs while remaining both affordable and sustainable for the clinicians who work in it.
In September 2019, SHM’s Multi-Site Leaders Special Interest Group met in Chicago for their second annual Multi-Site Leaders Summit to explore the theme of sustainability in hospital medicine. The participants held robust discussions about coping with our changing practice environment, issues relating to hospitalist burnout and resiliency, innovative staffing models, the role of technology in HM sustainability, and financial sustainability
At the end of the meeting, the group engaged in a visioning exercise designed to move beyond what we are doing today by envisioning what the future of hospital medicine will look like and what interventions will be necessary for us to get from here to there. I’d like to share this visioning exercise with you and encourage you to “play along” by thinking seriously about the questions it poses.
Visioning exercise
Feel free to jot down some thoughts as we go through this exercise. But otherwise, just close your eyes and come along for the ride. Imagine yourself sitting at your desk looking at a desk calendar showing today’s date. Watch the pages flip from today, to tomorrow, to the next day, then to next month, and the next, and then to the next year and so on, until we arrive at December 2029.
Imagine that you look up from your desk, and suddenly realize that you aren’t in your office at all, but instead in a huge auditorium where someone is speaking about an award that is going to be announced. It’s crowded and a little stuffy in the auditorium, but people around you are whispering to each other with an air of eager anticipation, their eyes glued to the stage. You realize that the person being introduced up on the podium is the President of the United States, and the award is the Presidential Medal of Freedom, which is only awarded to people or groups who have made “an especially meritorious contribution to the security or national interests of the United States, world peace, cultural, or other significant public or private endeavors.”
Today, the Medal is being awarded to the Society of Hospital Medicine on behalf of all hospital medicine leaders nationally, for their collective accomplishments in saving the specialty of hospital medicine and, by doing so, ensuring that sick people are able to continue receiving the care they need in our nation’s hospitals – and that the hospitals themselves have become reliably safe, efficient, and effective in achieving high quality outcomes.
The President says, “At no time in the history of this award until now have we given this, the highest civilian award in the land, to a whole group of physician leaders across an entire specialty. But the achievements of this group of people in preserving and even enhancing the presence of highly energized, dedicated, capable clinicians in our nation’s hospitals against the significant odds they have faced over the last 10 years is nothing short of extraordinary.” There is a standing ovation, as people jump up out of their chairs to cheer and applaud. When the applause finally dies down, the President goes on to list all the accomplishments that made this group of leaders deserving. Listen to what she is saying. Fill it in in your own mind. What is it that this group has accomplished?
[Brief silence]
Up on a huge screen beside the stage, a video starts. In it, there are several hospital and physician executives in a focus group, and one exec says, “The thing that is great about what these leaders have accomplished in the field of hospital medicine is…” Fill it in – what did that executive say? Another leader jumps in: “That’s all fine and wonderful, but the thing that really makes hospital medicine stand out today compared to where they were 10 years ago is…” Listen to what these executives are saying. What accomplishments are they praising?
The video then moves on to show a focus group of recent hospital patients. One patient says, “10 years ago when my mom was in the hospital, the poor hospitalists caring for her seemed completely overwhelmed and burnt out, and the whole care system seemed fragmented and inefficient; but my own recent hospital experience was so different because…” Additional patients chime in, talking about how confident they felt about the care they received in the hospital and the reasons for that. What is it these patients are describing?
SHM’s CEO gets up to accept the award and explains that 10 years ago, a group of multi-site hospital medicine leaders from across the country came together to begin addressing the issue of sustainability; this led to a formal process for developing a vision and a plan for the future of hospital medicine, and the execution of that plan eventually resulted in the outcomes recognized by this award. She acknowledges that over the years many people questioned whether the hospital medicine model should even continue to exist or whether some other model for inpatient care should be adopted. She talks about all the compelling reasons that supported the continued existence of the specialty of hospital medicine. What are some of the reasons she listed? The SHM CEO goes on to describe some of the key things that were done to address the issues associated with sustainability of the hospital medicine practice model. Listen to what she says; what was it that SHM and the hospital leaders it represents did?
As you are leaving the auditorium, you overhear a group of mid-career staff hospitalists talking. They are saying that they didn’t originally believe the specialty would actually change, and they weren’t sure if they could do this job for a career – but that it did change. They begin talking about what it feels like to work as a hospitalist now, and how these changes have improved their lives. Listen to what they are saying. How does it feel to work as a hospitalist?
As you leave the auditorium and go back to your desk, you sit down to record some of the things you heard. What was it the President of the US said as she presented the Presidential Medal of Freedom? Why did SHM and the hospital medicine leaders it represents deserve the award? What was it that the SHM CEO said was done to bring about the successful changes? What did the staff hospitalists say about working in the specialty?
Whenever you are ready, take a minute to jot down the specifics that came to mind as you read through this exercise. If you are willing to share your thoughts about sustainability in hospital medicine, I’d love to hear from you. Feel free to email me directly at [email protected].
Let’s build the foundation for a sustainable future for our specialty.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif. She serves on SHM’s Practice Analysis Committee, and helps to coordinate SHM’s bi-annual State of Hospital Medicine Survey. This article appeared originally in SHM’s official blog The Hospital Leader.
I have written frequently over the last few years on topics related to the sustainability of the hospital medicine practice model. I continue to be concerned by what I see as a confluence of significant trends that are conspiring to challenge hospital medicine’s status quo.
On one hand, the financial pressures on U.S. hospitals are unrelenting, and their willingness or even ability to continue providing significant funding to support their hospital medicine groups is in question. Combine this with hospitalists’ rapidly evolving clinical scope and the ever-increasing demands of physicians in other specialties for hospitalist support, and the result is hospital medicine groups that will continue to grow in size, complexity, and the demand for ever more financial support.
On the other hand, the hospitalists I interact with in my work all over the country seem more stressed out than ever, and many are questioning whether this is a job that can be satisfying and sustainable for a career. Increasing patient complexity, productivity pressures, a lack of resources to address patients’ social issues, a systole-diastole schedule, the frustration of EHRs and other documentation responsibilities, and feeling “dumped on” by physicians in other specialties all contribute to hospitalist job stress.
A quick look at the literature confirms that in 2019 hospitalist burnout is definitely “a thing.” Interestingly, it’s been a thing for a while; the risk of hospitalist burnout was first identified by Hoff, et al., in 2002 (doi: 10.2307/30902462002). My colleague, John Nelson, MD, MHM, has written a number of times about strategies for preventing or mitigating hospitalist burnout.
As these trends converge, the hospital medicine practice model as we know it may be facing an existential crisis. If that sounds overly dramatic, let me say instead that the hospital medicine practice model will need to evolve significantly over the next decade in order to continue to meet patient and institutional needs while remaining both affordable and sustainable for the clinicians who work in it.
In September 2019, SHM’s Multi-Site Leaders Special Interest Group met in Chicago for their second annual Multi-Site Leaders Summit to explore the theme of sustainability in hospital medicine. The participants held robust discussions about coping with our changing practice environment, issues relating to hospitalist burnout and resiliency, innovative staffing models, the role of technology in HM sustainability, and financial sustainability
At the end of the meeting, the group engaged in a visioning exercise designed to move beyond what we are doing today by envisioning what the future of hospital medicine will look like and what interventions will be necessary for us to get from here to there. I’d like to share this visioning exercise with you and encourage you to “play along” by thinking seriously about the questions it poses.
Visioning exercise
Feel free to jot down some thoughts as we go through this exercise. But otherwise, just close your eyes and come along for the ride. Imagine yourself sitting at your desk looking at a desk calendar showing today’s date. Watch the pages flip from today, to tomorrow, to the next day, then to next month, and the next, and then to the next year and so on, until we arrive at December 2029.
Imagine that you look up from your desk, and suddenly realize that you aren’t in your office at all, but instead in a huge auditorium where someone is speaking about an award that is going to be announced. It’s crowded and a little stuffy in the auditorium, but people around you are whispering to each other with an air of eager anticipation, their eyes glued to the stage. You realize that the person being introduced up on the podium is the President of the United States, and the award is the Presidential Medal of Freedom, which is only awarded to people or groups who have made “an especially meritorious contribution to the security or national interests of the United States, world peace, cultural, or other significant public or private endeavors.”
Today, the Medal is being awarded to the Society of Hospital Medicine on behalf of all hospital medicine leaders nationally, for their collective accomplishments in saving the specialty of hospital medicine and, by doing so, ensuring that sick people are able to continue receiving the care they need in our nation’s hospitals – and that the hospitals themselves have become reliably safe, efficient, and effective in achieving high quality outcomes.
The President says, “At no time in the history of this award until now have we given this, the highest civilian award in the land, to a whole group of physician leaders across an entire specialty. But the achievements of this group of people in preserving and even enhancing the presence of highly energized, dedicated, capable clinicians in our nation’s hospitals against the significant odds they have faced over the last 10 years is nothing short of extraordinary.” There is a standing ovation, as people jump up out of their chairs to cheer and applaud. When the applause finally dies down, the President goes on to list all the accomplishments that made this group of leaders deserving. Listen to what she is saying. Fill it in in your own mind. What is it that this group has accomplished?
[Brief silence]
Up on a huge screen beside the stage, a video starts. In it, there are several hospital and physician executives in a focus group, and one exec says, “The thing that is great about what these leaders have accomplished in the field of hospital medicine is…” Fill it in – what did that executive say? Another leader jumps in: “That’s all fine and wonderful, but the thing that really makes hospital medicine stand out today compared to where they were 10 years ago is…” Listen to what these executives are saying. What accomplishments are they praising?
The video then moves on to show a focus group of recent hospital patients. One patient says, “10 years ago when my mom was in the hospital, the poor hospitalists caring for her seemed completely overwhelmed and burnt out, and the whole care system seemed fragmented and inefficient; but my own recent hospital experience was so different because…” Additional patients chime in, talking about how confident they felt about the care they received in the hospital and the reasons for that. What is it these patients are describing?
SHM’s CEO gets up to accept the award and explains that 10 years ago, a group of multi-site hospital medicine leaders from across the country came together to begin addressing the issue of sustainability; this led to a formal process for developing a vision and a plan for the future of hospital medicine, and the execution of that plan eventually resulted in the outcomes recognized by this award. She acknowledges that over the years many people questioned whether the hospital medicine model should even continue to exist or whether some other model for inpatient care should be adopted. She talks about all the compelling reasons that supported the continued existence of the specialty of hospital medicine. What are some of the reasons she listed? The SHM CEO goes on to describe some of the key things that were done to address the issues associated with sustainability of the hospital medicine practice model. Listen to what she says; what was it that SHM and the hospital leaders it represents did?
As you are leaving the auditorium, you overhear a group of mid-career staff hospitalists talking. They are saying that they didn’t originally believe the specialty would actually change, and they weren’t sure if they could do this job for a career – but that it did change. They begin talking about what it feels like to work as a hospitalist now, and how these changes have improved their lives. Listen to what they are saying. How does it feel to work as a hospitalist?
As you leave the auditorium and go back to your desk, you sit down to record some of the things you heard. What was it the President of the US said as she presented the Presidential Medal of Freedom? Why did SHM and the hospital medicine leaders it represents deserve the award? What was it that the SHM CEO said was done to bring about the successful changes? What did the staff hospitalists say about working in the specialty?
Whenever you are ready, take a minute to jot down the specifics that came to mind as you read through this exercise. If you are willing to share your thoughts about sustainability in hospital medicine, I’d love to hear from you. Feel free to email me directly at [email protected].
Let’s build the foundation for a sustainable future for our specialty.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif. She serves on SHM’s Practice Analysis Committee, and helps to coordinate SHM’s bi-annual State of Hospital Medicine Survey. This article appeared originally in SHM’s official blog The Hospital Leader.
Quick Byte: Act locally
To solve our most pressing national health issues, we must start locally, according to a Health Affairs blog post.
“For example, in [Mecklenburg County] North Carolina, African Americans face rates of cardiovascular disease 22% higher than their white counterparts do. To fight this, an organization called Village HeartBEAT joined forces with more than 60 faith-based groups to reach more than 20,000 people – connecting them with health resources to reduce their cardiovascular risk. As a direct result, rates of smoking decreased from 17.4% to 13.9%, and obesity rates fell from 70% to 64.7%.”
Mecklenburg County is a winner of the Healthiest Cities & Counties Challenge, a collaboration between the Aetna Foundation, the American Public Health Association, and the National Association of Counties, which has awarded more than $1.5 million in grants and prizes over the last 2 years.
Reference
1. Graham G, Benjamin G. “Winning Local Solutions to Our Most Pressing Public Health Needs.” Health Affairs. https://www.healthaffairs.org/do/10.1377/hblog20190423.202497/full/. Published April 25, 2019.
To solve our most pressing national health issues, we must start locally, according to a Health Affairs blog post.
“For example, in [Mecklenburg County] North Carolina, African Americans face rates of cardiovascular disease 22% higher than their white counterparts do. To fight this, an organization called Village HeartBEAT joined forces with more than 60 faith-based groups to reach more than 20,000 people – connecting them with health resources to reduce their cardiovascular risk. As a direct result, rates of smoking decreased from 17.4% to 13.9%, and obesity rates fell from 70% to 64.7%.”
Mecklenburg County is a winner of the Healthiest Cities & Counties Challenge, a collaboration between the Aetna Foundation, the American Public Health Association, and the National Association of Counties, which has awarded more than $1.5 million in grants and prizes over the last 2 years.
Reference
1. Graham G, Benjamin G. “Winning Local Solutions to Our Most Pressing Public Health Needs.” Health Affairs. https://www.healthaffairs.org/do/10.1377/hblog20190423.202497/full/. Published April 25, 2019.
To solve our most pressing national health issues, we must start locally, according to a Health Affairs blog post.
“For example, in [Mecklenburg County] North Carolina, African Americans face rates of cardiovascular disease 22% higher than their white counterparts do. To fight this, an organization called Village HeartBEAT joined forces with more than 60 faith-based groups to reach more than 20,000 people – connecting them with health resources to reduce their cardiovascular risk. As a direct result, rates of smoking decreased from 17.4% to 13.9%, and obesity rates fell from 70% to 64.7%.”
Mecklenburg County is a winner of the Healthiest Cities & Counties Challenge, a collaboration between the Aetna Foundation, the American Public Health Association, and the National Association of Counties, which has awarded more than $1.5 million in grants and prizes over the last 2 years.
Reference
1. Graham G, Benjamin G. “Winning Local Solutions to Our Most Pressing Public Health Needs.” Health Affairs. https://www.healthaffairs.org/do/10.1377/hblog20190423.202497/full/. Published April 25, 2019.
ENGAGE AF-TIMI: Insulin linked to greater risk for stroke, CV death, bleeding
LOS ANGELES – Patients with diabetes had significantly higher adjusted risk of bleeding, cardiovascular-related death, and poorer net outcomes, particularly those treated with insulin, a subanalysis of the ENGAGE AF-TIMI 48 trial has shown.
In addition, the pharmacokinetic and pharmacodynamic profile of the study drug, edoxaban – a novel oral anticoagulant drug and a direct factor Xa inhibitor – was generally similar in patients with and without diabetes.
“We know that atrial fibrillation is associated with a fivefold increased risk of stroke,” Anna Plitt, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “Type 2 diabetes is associated with a twofold increased risk of stroke, and longer duration of diabetes is associated with even higher ischemic event rates. The coexistence of [atrial fibrillation] and type 2 diabetes further increases thromboembolic risk.”
Dr. Plitt, a cardiology fellow at Mount Sinai Hospital, New York, noted that, although type 2 diabetes is characterized by a prothrombotic and inflammatory state, the mechanism of action by which hyperglycemia and/or insulin resistance leads to the development of atrial fibrillation (AFib) remains unknown. “Given the complex clinical interactions between AFib and type 2 diabetes, care for these patients remains challenging,” she said. “Recommendations for anticoagulation managements vary based on the presence of additional risk factors and which guidelines are followed.”
In the ENGAGE AF-TIMI 48 trial, 21,105 patients with documented AFib within the previous 12 months were randomized to standard-care warfarin or high-dose edoxaban (60 mg daily) or low-dose edoxaban (30 mg daily). The edoxaban dose was reduced by 50% if creatinine clearance reached 30-50 mL/min, patient weight reached 60 kg or less, or there was concomitant use of a P-glycoprotein inhibitor (N Engl J Med. 2013;369:2093-104). The median follow-up was 2.8 years, and the primary efficacy endpoint was stroke or systemic embolic events (SEEs). The primary safety endpoint was major bleeding, as defined by the International Society on Thrombosis and Haemostasis criteria.
The findings showed that edoxaban was noninferior to warfarin in preventing stroke/SEEs. It also significantly reduced major bleeding, cardiovascular death, and net outcomes. “Therefore, the higher dose of edoxaban was approved globally for treating patients with AFib,” Dr. Plitt said. “The lower-dose regimen was not approved because there was less protection from ischemic stroke, compared with warfarin.”
For the current subanalysis, Dr. Plitt and colleagues set out to further evaluate outcomes of patients enrolled in the ENGAGE AF-TIMI 48 trial, excluding those who were in the low-dose edoxaban group. The presence or absence of diabetes was determined by the local investigator at randomization. The investigators further stratified patients into insulin-treated and non–insulin treated groups and used multivariate Cox regression models to adjust for baseline characteristics across the groups stratified by diabetes status. Next, they analyzed edoxaban concentration, anti–factor Xa activity, and international normalized ratio data and compared outcomes of high-dose edoxaban with those of warfarin.
The primary endpoint and the primary safety endpoint of interest were the same as in the main ENGAGE AF-TIMI 48 trial. Key secondary endpoints included in the subanalysis were cardiovascular death, stroke/SEE, major adverse cardiovascular events (MACE, a composite of myocardial infarction, stroke, SEE, or death because of cardiovascular cause or bleeding), and all-cause death.
In all, 7,624 of the 21,105 patients in the ENGAGE AF-TIMI 48 trial had diabetes, for a rate of 36%. Most of the patients with diabetes did not require insulin (30%), while 6% did. There were fewer female patients with diabetes than without (37% vs. 39%, respectively). Of note was that history of prior stroke/transient ischemic attack was higher in the no-diabetes group than in the diabetes group (33% vs. 21%), as was congestive heart failure (63% vs. 48%).
The mean CHA2DS2-VASc score for predicting thromboembolic risk (0, low risk; greater than 1, high risk) was 4.6 in the diabetes group and 4.2 in the no-diabetes group. When diabetes was not included in the score, the mean CHA2DS2-VASc score was 3.6 in the diabetes group. “Because the trial entry criteria required a minimum CHADS2 score of 2, patients without diabetes were enriched with stroke risk factors other than diabetes,” Dr. Plitt said.
Adjusted outcomes from the subanalysis showed that the risk of stroke/SEE was similar between patients with and without diabetes (hazard ratio, 1.08). However, patients with diabetes were at higher adjusted risk for cardiovascular death than patients without diabetes (HR, 1.29), MACE (HR, 1.28), major bleed (HR, 1.28), and the net outcome of stroke, SEE, major bleed, or all-cause death (HR, 1.25).
The researchers also analyzed the pharmacodynamic and pharmacokinetic data of high-dose edoxaban, stratified by diabetes status. They found that the parameters were generally similar between patients with and without diabetes, including trough concentrations of edoxaban (34.3 and 37.2 ng/mL, respectively; P = .04), trough exogenous anti–factor Xa activity (0.59 and 0.68 IU/mL; P = .11), and the percentage change from baseline in the peak endogenous anti–factor Xa activity (P = .66). The percentage changes from baseline of the trough endogenous anti–factor Xa activity was slightly lower in patients with diabetes, compared with patients without diabetes (P less than .001). “However, these modest differences between the two groups are of unclear clinical significance,” Dr. Plitt said.
Results from the main ENGAGE AF-TIMI 48 showed that the rates of stroke/SEE were reduced by 13% on high-dose edoxaban. However, the subanalysis found no significant effect modification in the reduction in stroke/SEE with edoxaban, compared with warfarin, when stratified by diabetes status (reductions of 16% vs. 7% in the no-diabetes and diabetes groups, respectively; P for interaction = .54). The researchers also observed similar reductions with edoxaban in the risks of secondary outcomes when patients were stratified by diabetes status.
In another finding, patients with diabetes who were treated with insulin were at a higher adjusted risk for all outcomes, compared with those with diabetes who were not treated with insulin. This included stroke/SEE (HR, 1.44), cardiovascular-related death (HR, 1.83), MACE (HR, 1.78), major bleed (HR, 1.31), and net outcome (HR, 1.57).
Next, the researchers compared the study endpoints of high-dose edoxaban and warfarin, with and without insulin. “None of the efficacy, safety, or net outcomes demonstrated evidence of treatment effect modification related to the use of insulin among [patients with diabetes],” she said.
Dr. Plitt disclosed having received honoraria for educational activities from Bristol-Myers Squibb.
LOS ANGELES – Patients with diabetes had significantly higher adjusted risk of bleeding, cardiovascular-related death, and poorer net outcomes, particularly those treated with insulin, a subanalysis of the ENGAGE AF-TIMI 48 trial has shown.
In addition, the pharmacokinetic and pharmacodynamic profile of the study drug, edoxaban – a novel oral anticoagulant drug and a direct factor Xa inhibitor – was generally similar in patients with and without diabetes.
“We know that atrial fibrillation is associated with a fivefold increased risk of stroke,” Anna Plitt, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “Type 2 diabetes is associated with a twofold increased risk of stroke, and longer duration of diabetes is associated with even higher ischemic event rates. The coexistence of [atrial fibrillation] and type 2 diabetes further increases thromboembolic risk.”
Dr. Plitt, a cardiology fellow at Mount Sinai Hospital, New York, noted that, although type 2 diabetes is characterized by a prothrombotic and inflammatory state, the mechanism of action by which hyperglycemia and/or insulin resistance leads to the development of atrial fibrillation (AFib) remains unknown. “Given the complex clinical interactions between AFib and type 2 diabetes, care for these patients remains challenging,” she said. “Recommendations for anticoagulation managements vary based on the presence of additional risk factors and which guidelines are followed.”
In the ENGAGE AF-TIMI 48 trial, 21,105 patients with documented AFib within the previous 12 months were randomized to standard-care warfarin or high-dose edoxaban (60 mg daily) or low-dose edoxaban (30 mg daily). The edoxaban dose was reduced by 50% if creatinine clearance reached 30-50 mL/min, patient weight reached 60 kg or less, or there was concomitant use of a P-glycoprotein inhibitor (N Engl J Med. 2013;369:2093-104). The median follow-up was 2.8 years, and the primary efficacy endpoint was stroke or systemic embolic events (SEEs). The primary safety endpoint was major bleeding, as defined by the International Society on Thrombosis and Haemostasis criteria.
The findings showed that edoxaban was noninferior to warfarin in preventing stroke/SEEs. It also significantly reduced major bleeding, cardiovascular death, and net outcomes. “Therefore, the higher dose of edoxaban was approved globally for treating patients with AFib,” Dr. Plitt said. “The lower-dose regimen was not approved because there was less protection from ischemic stroke, compared with warfarin.”
For the current subanalysis, Dr. Plitt and colleagues set out to further evaluate outcomes of patients enrolled in the ENGAGE AF-TIMI 48 trial, excluding those who were in the low-dose edoxaban group. The presence or absence of diabetes was determined by the local investigator at randomization. The investigators further stratified patients into insulin-treated and non–insulin treated groups and used multivariate Cox regression models to adjust for baseline characteristics across the groups stratified by diabetes status. Next, they analyzed edoxaban concentration, anti–factor Xa activity, and international normalized ratio data and compared outcomes of high-dose edoxaban with those of warfarin.
The primary endpoint and the primary safety endpoint of interest were the same as in the main ENGAGE AF-TIMI 48 trial. Key secondary endpoints included in the subanalysis were cardiovascular death, stroke/SEE, major adverse cardiovascular events (MACE, a composite of myocardial infarction, stroke, SEE, or death because of cardiovascular cause or bleeding), and all-cause death.
In all, 7,624 of the 21,105 patients in the ENGAGE AF-TIMI 48 trial had diabetes, for a rate of 36%. Most of the patients with diabetes did not require insulin (30%), while 6% did. There were fewer female patients with diabetes than without (37% vs. 39%, respectively). Of note was that history of prior stroke/transient ischemic attack was higher in the no-diabetes group than in the diabetes group (33% vs. 21%), as was congestive heart failure (63% vs. 48%).
The mean CHA2DS2-VASc score for predicting thromboembolic risk (0, low risk; greater than 1, high risk) was 4.6 in the diabetes group and 4.2 in the no-diabetes group. When diabetes was not included in the score, the mean CHA2DS2-VASc score was 3.6 in the diabetes group. “Because the trial entry criteria required a minimum CHADS2 score of 2, patients without diabetes were enriched with stroke risk factors other than diabetes,” Dr. Plitt said.
Adjusted outcomes from the subanalysis showed that the risk of stroke/SEE was similar between patients with and without diabetes (hazard ratio, 1.08). However, patients with diabetes were at higher adjusted risk for cardiovascular death than patients without diabetes (HR, 1.29), MACE (HR, 1.28), major bleed (HR, 1.28), and the net outcome of stroke, SEE, major bleed, or all-cause death (HR, 1.25).
The researchers also analyzed the pharmacodynamic and pharmacokinetic data of high-dose edoxaban, stratified by diabetes status. They found that the parameters were generally similar between patients with and without diabetes, including trough concentrations of edoxaban (34.3 and 37.2 ng/mL, respectively; P = .04), trough exogenous anti–factor Xa activity (0.59 and 0.68 IU/mL; P = .11), and the percentage change from baseline in the peak endogenous anti–factor Xa activity (P = .66). The percentage changes from baseline of the trough endogenous anti–factor Xa activity was slightly lower in patients with diabetes, compared with patients without diabetes (P less than .001). “However, these modest differences between the two groups are of unclear clinical significance,” Dr. Plitt said.
Results from the main ENGAGE AF-TIMI 48 showed that the rates of stroke/SEE were reduced by 13% on high-dose edoxaban. However, the subanalysis found no significant effect modification in the reduction in stroke/SEE with edoxaban, compared with warfarin, when stratified by diabetes status (reductions of 16% vs. 7% in the no-diabetes and diabetes groups, respectively; P for interaction = .54). The researchers also observed similar reductions with edoxaban in the risks of secondary outcomes when patients were stratified by diabetes status.
In another finding, patients with diabetes who were treated with insulin were at a higher adjusted risk for all outcomes, compared with those with diabetes who were not treated with insulin. This included stroke/SEE (HR, 1.44), cardiovascular-related death (HR, 1.83), MACE (HR, 1.78), major bleed (HR, 1.31), and net outcome (HR, 1.57).
Next, the researchers compared the study endpoints of high-dose edoxaban and warfarin, with and without insulin. “None of the efficacy, safety, or net outcomes demonstrated evidence of treatment effect modification related to the use of insulin among [patients with diabetes],” she said.
Dr. Plitt disclosed having received honoraria for educational activities from Bristol-Myers Squibb.
LOS ANGELES – Patients with diabetes had significantly higher adjusted risk of bleeding, cardiovascular-related death, and poorer net outcomes, particularly those treated with insulin, a subanalysis of the ENGAGE AF-TIMI 48 trial has shown.
In addition, the pharmacokinetic and pharmacodynamic profile of the study drug, edoxaban – a novel oral anticoagulant drug and a direct factor Xa inhibitor – was generally similar in patients with and without diabetes.
“We know that atrial fibrillation is associated with a fivefold increased risk of stroke,” Anna Plitt, MD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “Type 2 diabetes is associated with a twofold increased risk of stroke, and longer duration of diabetes is associated with even higher ischemic event rates. The coexistence of [atrial fibrillation] and type 2 diabetes further increases thromboembolic risk.”
Dr. Plitt, a cardiology fellow at Mount Sinai Hospital, New York, noted that, although type 2 diabetes is characterized by a prothrombotic and inflammatory state, the mechanism of action by which hyperglycemia and/or insulin resistance leads to the development of atrial fibrillation (AFib) remains unknown. “Given the complex clinical interactions between AFib and type 2 diabetes, care for these patients remains challenging,” she said. “Recommendations for anticoagulation managements vary based on the presence of additional risk factors and which guidelines are followed.”
In the ENGAGE AF-TIMI 48 trial, 21,105 patients with documented AFib within the previous 12 months were randomized to standard-care warfarin or high-dose edoxaban (60 mg daily) or low-dose edoxaban (30 mg daily). The edoxaban dose was reduced by 50% if creatinine clearance reached 30-50 mL/min, patient weight reached 60 kg or less, or there was concomitant use of a P-glycoprotein inhibitor (N Engl J Med. 2013;369:2093-104). The median follow-up was 2.8 years, and the primary efficacy endpoint was stroke or systemic embolic events (SEEs). The primary safety endpoint was major bleeding, as defined by the International Society on Thrombosis and Haemostasis criteria.
The findings showed that edoxaban was noninferior to warfarin in preventing stroke/SEEs. It also significantly reduced major bleeding, cardiovascular death, and net outcomes. “Therefore, the higher dose of edoxaban was approved globally for treating patients with AFib,” Dr. Plitt said. “The lower-dose regimen was not approved because there was less protection from ischemic stroke, compared with warfarin.”
For the current subanalysis, Dr. Plitt and colleagues set out to further evaluate outcomes of patients enrolled in the ENGAGE AF-TIMI 48 trial, excluding those who were in the low-dose edoxaban group. The presence or absence of diabetes was determined by the local investigator at randomization. The investigators further stratified patients into insulin-treated and non–insulin treated groups and used multivariate Cox regression models to adjust for baseline characteristics across the groups stratified by diabetes status. Next, they analyzed edoxaban concentration, anti–factor Xa activity, and international normalized ratio data and compared outcomes of high-dose edoxaban with those of warfarin.
The primary endpoint and the primary safety endpoint of interest were the same as in the main ENGAGE AF-TIMI 48 trial. Key secondary endpoints included in the subanalysis were cardiovascular death, stroke/SEE, major adverse cardiovascular events (MACE, a composite of myocardial infarction, stroke, SEE, or death because of cardiovascular cause or bleeding), and all-cause death.
In all, 7,624 of the 21,105 patients in the ENGAGE AF-TIMI 48 trial had diabetes, for a rate of 36%. Most of the patients with diabetes did not require insulin (30%), while 6% did. There were fewer female patients with diabetes than without (37% vs. 39%, respectively). Of note was that history of prior stroke/transient ischemic attack was higher in the no-diabetes group than in the diabetes group (33% vs. 21%), as was congestive heart failure (63% vs. 48%).
The mean CHA2DS2-VASc score for predicting thromboembolic risk (0, low risk; greater than 1, high risk) was 4.6 in the diabetes group and 4.2 in the no-diabetes group. When diabetes was not included in the score, the mean CHA2DS2-VASc score was 3.6 in the diabetes group. “Because the trial entry criteria required a minimum CHADS2 score of 2, patients without diabetes were enriched with stroke risk factors other than diabetes,” Dr. Plitt said.
Adjusted outcomes from the subanalysis showed that the risk of stroke/SEE was similar between patients with and without diabetes (hazard ratio, 1.08). However, patients with diabetes were at higher adjusted risk for cardiovascular death than patients without diabetes (HR, 1.29), MACE (HR, 1.28), major bleed (HR, 1.28), and the net outcome of stroke, SEE, major bleed, or all-cause death (HR, 1.25).
The researchers also analyzed the pharmacodynamic and pharmacokinetic data of high-dose edoxaban, stratified by diabetes status. They found that the parameters were generally similar between patients with and without diabetes, including trough concentrations of edoxaban (34.3 and 37.2 ng/mL, respectively; P = .04), trough exogenous anti–factor Xa activity (0.59 and 0.68 IU/mL; P = .11), and the percentage change from baseline in the peak endogenous anti–factor Xa activity (P = .66). The percentage changes from baseline of the trough endogenous anti–factor Xa activity was slightly lower in patients with diabetes, compared with patients without diabetes (P less than .001). “However, these modest differences between the two groups are of unclear clinical significance,” Dr. Plitt said.
Results from the main ENGAGE AF-TIMI 48 showed that the rates of stroke/SEE were reduced by 13% on high-dose edoxaban. However, the subanalysis found no significant effect modification in the reduction in stroke/SEE with edoxaban, compared with warfarin, when stratified by diabetes status (reductions of 16% vs. 7% in the no-diabetes and diabetes groups, respectively; P for interaction = .54). The researchers also observed similar reductions with edoxaban in the risks of secondary outcomes when patients were stratified by diabetes status.
In another finding, patients with diabetes who were treated with insulin were at a higher adjusted risk for all outcomes, compared with those with diabetes who were not treated with insulin. This included stroke/SEE (HR, 1.44), cardiovascular-related death (HR, 1.83), MACE (HR, 1.78), major bleed (HR, 1.31), and net outcome (HR, 1.57).
Next, the researchers compared the study endpoints of high-dose edoxaban and warfarin, with and without insulin. “None of the efficacy, safety, or net outcomes demonstrated evidence of treatment effect modification related to the use of insulin among [patients with diabetes],” she said.
Dr. Plitt disclosed having received honoraria for educational activities from Bristol-Myers Squibb.
REPORTING FROM THE WCIRDC 2019
Choosing Wisely® and its impact on low-value care
Focus energy on ‘low-hanging fruit’
It is a well-known fact that health care expenditure in the United States occupies a large proportion of its gross domestic product. In fact, it was 17.8% in 2016, almost twice what is expended in other advanced countries. However, this expenditure does not necessarily translate into optimal patient outcomes.
In 2012, the Institute of Medicine reported that the U.S. health care system wastes $750 billion per year in spending that does not provide any meaningful outcome to patients or the system; and patients can also suffer a financial impact from the delivery of low-value care.
In 2013, the Pediatrics Committee of the Society of Hospital Medicine published five recommendations through the Choosing Wisely® campaign aimed to decrease the use of low-value interventions. These recommendations were:
1. Do not order chest radiographs (CXR) in children with asthma or bronchiolitis.
2. Do not use systemic corticosteroids in children aged under 2 years with a lower respiratory tract infection.
3. Do not use bronchodilators in children with bronchiolitis.
4. Do not treat gastroesophageal reflux in infants routinely with acid suppression therapy.
5. Do not use continuous pulse oximetry routinely in children with acute respiratory illness unless they are on supplemental oxygen.
This publication led to the implementation of quality improvement initiatives across different hospitals and institutions nationally. Eventually, a team of hospitalists developed a report card that could help measure the utilization of these interventions in hospitals that were part of the Children’s Hospital Association (CHA). The data stemming from the report card analysis would allow for benchmarking and comparing performance, as well as determining the secular trend in utilization of these procedures across the different institutions of the CHA.
Reyes et al. recently published the impact of utilization of these scorecards among all hospital members of the CHA in the Journal of Hospital Medicine, noting a positive impact of the SHM Choosing Wisely® recommendation in decreasing the utilization of low-value interventions. The authors compared the performance before and after the publication of the recommendations for a 9-year period (2008-2017). The most relevant impact occurred in children with bronchiolitis, with a decrease of 36% of bronchodilator use and of 31% in CXR utilization. In children with asthma, CXR utilization decreased by 20.8%. The authors found that, although there was a steady decrease in the utilization of low-value services, this was still limited.
What factors could impact the effectiveness of high-value quality initiatives? First of all, quality improvement requires a substantial investment of collective effort and time. It requires a change in culture that often involves changing longstanding paradigms. The Choosing Wisely® recommendations target a very specific, low-clinical-severity population – the focus is on “uncomplicated” disease. This is important as you don’t want to pursue aggressive unnecessary intervention in children and potentially cause harm – for example, unnecessary use of steroids in a child with uncomplicated bronchiolitis who may improve with nasal suctioning alone. There is a need to appraise patients with more complex presentation of these diseases (for example, patients that require escalation of care to ICU), and this is beyond the scope of Choosing Wisely®. Further research is needed to see if higher-value care interventions can be implemented among these higher acuity and severity patients.
In our institution, we have created specific care paths that facilitate following these recommendations. Essentially, we have leveraged the EHR order sets to avoid the inclusion of low-value interventions; all stakeholders (respiratory therapy, nursing, etc.) are aware of the care path and ensure compliance. Even further, as a consequence of the change in culture toward high-value care, we have identified low-value interventions in settings where high-value quality improvement can be implemented – for example, we found that at least 20% of noncritically ill children undergoing an appendectomy receive unnecessary antacid prophylaxis treatment.
Changes always start small; quality improvement requires a lot of effort, and we must focus our energy on “low-hanging fruit,” and also begin tackling higher complexity tasks. In the Choosing Wisely® manuscript cited above, the authors found that there was a change in performance with a tendency toward higher-value care, yet the change was not as substantial as originally thought.
How can we tackle higher complexity tasks if we find it difficult to implement solutions for those of lower complexity? My answer is simple. Maintain a consistent and continuous focus on high value, and ensure the message is iterative and redundant with feedback on performance, decrease in costs, and enhanced patient outcomes.
Dr. Auron is the quality improvement and patient safety officer in the department of hospital medicine at the Cleveland Clinic. He also serves as associate professor of medicine and pediatrics in the staff department of hospital medicine and department of pediatric hospital medicine. This article first appeared on the Hospital Leader, SHM’s official blog, at hospitalleader.org.
Focus energy on ‘low-hanging fruit’
Focus energy on ‘low-hanging fruit’
It is a well-known fact that health care expenditure in the United States occupies a large proportion of its gross domestic product. In fact, it was 17.8% in 2016, almost twice what is expended in other advanced countries. However, this expenditure does not necessarily translate into optimal patient outcomes.
In 2012, the Institute of Medicine reported that the U.S. health care system wastes $750 billion per year in spending that does not provide any meaningful outcome to patients or the system; and patients can also suffer a financial impact from the delivery of low-value care.
In 2013, the Pediatrics Committee of the Society of Hospital Medicine published five recommendations through the Choosing Wisely® campaign aimed to decrease the use of low-value interventions. These recommendations were:
1. Do not order chest radiographs (CXR) in children with asthma or bronchiolitis.
2. Do not use systemic corticosteroids in children aged under 2 years with a lower respiratory tract infection.
3. Do not use bronchodilators in children with bronchiolitis.
4. Do not treat gastroesophageal reflux in infants routinely with acid suppression therapy.
5. Do not use continuous pulse oximetry routinely in children with acute respiratory illness unless they are on supplemental oxygen.
This publication led to the implementation of quality improvement initiatives across different hospitals and institutions nationally. Eventually, a team of hospitalists developed a report card that could help measure the utilization of these interventions in hospitals that were part of the Children’s Hospital Association (CHA). The data stemming from the report card analysis would allow for benchmarking and comparing performance, as well as determining the secular trend in utilization of these procedures across the different institutions of the CHA.
Reyes et al. recently published the impact of utilization of these scorecards among all hospital members of the CHA in the Journal of Hospital Medicine, noting a positive impact of the SHM Choosing Wisely® recommendation in decreasing the utilization of low-value interventions. The authors compared the performance before and after the publication of the recommendations for a 9-year period (2008-2017). The most relevant impact occurred in children with bronchiolitis, with a decrease of 36% of bronchodilator use and of 31% in CXR utilization. In children with asthma, CXR utilization decreased by 20.8%. The authors found that, although there was a steady decrease in the utilization of low-value services, this was still limited.
What factors could impact the effectiveness of high-value quality initiatives? First of all, quality improvement requires a substantial investment of collective effort and time. It requires a change in culture that often involves changing longstanding paradigms. The Choosing Wisely® recommendations target a very specific, low-clinical-severity population – the focus is on “uncomplicated” disease. This is important as you don’t want to pursue aggressive unnecessary intervention in children and potentially cause harm – for example, unnecessary use of steroids in a child with uncomplicated bronchiolitis who may improve with nasal suctioning alone. There is a need to appraise patients with more complex presentation of these diseases (for example, patients that require escalation of care to ICU), and this is beyond the scope of Choosing Wisely®. Further research is needed to see if higher-value care interventions can be implemented among these higher acuity and severity patients.
In our institution, we have created specific care paths that facilitate following these recommendations. Essentially, we have leveraged the EHR order sets to avoid the inclusion of low-value interventions; all stakeholders (respiratory therapy, nursing, etc.) are aware of the care path and ensure compliance. Even further, as a consequence of the change in culture toward high-value care, we have identified low-value interventions in settings where high-value quality improvement can be implemented – for example, we found that at least 20% of noncritically ill children undergoing an appendectomy receive unnecessary antacid prophylaxis treatment.
Changes always start small; quality improvement requires a lot of effort, and we must focus our energy on “low-hanging fruit,” and also begin tackling higher complexity tasks. In the Choosing Wisely® manuscript cited above, the authors found that there was a change in performance with a tendency toward higher-value care, yet the change was not as substantial as originally thought.
How can we tackle higher complexity tasks if we find it difficult to implement solutions for those of lower complexity? My answer is simple. Maintain a consistent and continuous focus on high value, and ensure the message is iterative and redundant with feedback on performance, decrease in costs, and enhanced patient outcomes.
Dr. Auron is the quality improvement and patient safety officer in the department of hospital medicine at the Cleveland Clinic. He also serves as associate professor of medicine and pediatrics in the staff department of hospital medicine and department of pediatric hospital medicine. This article first appeared on the Hospital Leader, SHM’s official blog, at hospitalleader.org.
It is a well-known fact that health care expenditure in the United States occupies a large proportion of its gross domestic product. In fact, it was 17.8% in 2016, almost twice what is expended in other advanced countries. However, this expenditure does not necessarily translate into optimal patient outcomes.
In 2012, the Institute of Medicine reported that the U.S. health care system wastes $750 billion per year in spending that does not provide any meaningful outcome to patients or the system; and patients can also suffer a financial impact from the delivery of low-value care.
In 2013, the Pediatrics Committee of the Society of Hospital Medicine published five recommendations through the Choosing Wisely® campaign aimed to decrease the use of low-value interventions. These recommendations were:
1. Do not order chest radiographs (CXR) in children with asthma or bronchiolitis.
2. Do not use systemic corticosteroids in children aged under 2 years with a lower respiratory tract infection.
3. Do not use bronchodilators in children with bronchiolitis.
4. Do not treat gastroesophageal reflux in infants routinely with acid suppression therapy.
5. Do not use continuous pulse oximetry routinely in children with acute respiratory illness unless they are on supplemental oxygen.
This publication led to the implementation of quality improvement initiatives across different hospitals and institutions nationally. Eventually, a team of hospitalists developed a report card that could help measure the utilization of these interventions in hospitals that were part of the Children’s Hospital Association (CHA). The data stemming from the report card analysis would allow for benchmarking and comparing performance, as well as determining the secular trend in utilization of these procedures across the different institutions of the CHA.
Reyes et al. recently published the impact of utilization of these scorecards among all hospital members of the CHA in the Journal of Hospital Medicine, noting a positive impact of the SHM Choosing Wisely® recommendation in decreasing the utilization of low-value interventions. The authors compared the performance before and after the publication of the recommendations for a 9-year period (2008-2017). The most relevant impact occurred in children with bronchiolitis, with a decrease of 36% of bronchodilator use and of 31% in CXR utilization. In children with asthma, CXR utilization decreased by 20.8%. The authors found that, although there was a steady decrease in the utilization of low-value services, this was still limited.
What factors could impact the effectiveness of high-value quality initiatives? First of all, quality improvement requires a substantial investment of collective effort and time. It requires a change in culture that often involves changing longstanding paradigms. The Choosing Wisely® recommendations target a very specific, low-clinical-severity population – the focus is on “uncomplicated” disease. This is important as you don’t want to pursue aggressive unnecessary intervention in children and potentially cause harm – for example, unnecessary use of steroids in a child with uncomplicated bronchiolitis who may improve with nasal suctioning alone. There is a need to appraise patients with more complex presentation of these diseases (for example, patients that require escalation of care to ICU), and this is beyond the scope of Choosing Wisely®. Further research is needed to see if higher-value care interventions can be implemented among these higher acuity and severity patients.
In our institution, we have created specific care paths that facilitate following these recommendations. Essentially, we have leveraged the EHR order sets to avoid the inclusion of low-value interventions; all stakeholders (respiratory therapy, nursing, etc.) are aware of the care path and ensure compliance. Even further, as a consequence of the change in culture toward high-value care, we have identified low-value interventions in settings where high-value quality improvement can be implemented – for example, we found that at least 20% of noncritically ill children undergoing an appendectomy receive unnecessary antacid prophylaxis treatment.
Changes always start small; quality improvement requires a lot of effort, and we must focus our energy on “low-hanging fruit,” and also begin tackling higher complexity tasks. In the Choosing Wisely® manuscript cited above, the authors found that there was a change in performance with a tendency toward higher-value care, yet the change was not as substantial as originally thought.
How can we tackle higher complexity tasks if we find it difficult to implement solutions for those of lower complexity? My answer is simple. Maintain a consistent and continuous focus on high value, and ensure the message is iterative and redundant with feedback on performance, decrease in costs, and enhanced patient outcomes.
Dr. Auron is the quality improvement and patient safety officer in the department of hospital medicine at the Cleveland Clinic. He also serves as associate professor of medicine and pediatrics in the staff department of hospital medicine and department of pediatric hospital medicine. This article first appeared on the Hospital Leader, SHM’s official blog, at hospitalleader.org.