User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Laurence Wellikson, MD, MHM, announces retirement as CEO of Society of Hospital Medicine
Society recognizes Dr. Wellikson’s leadership, retains Spencer Stuart for successor search
Philadelphia – After serving as the first and only chief executive officer of the Society of Hospital Medicine since January of 2000, Laurence Wellikson, MD, MHM, has announced his retirement effective on Dec. 31, 2020. In parallel, the SHM Board of Directors have commenced a search for his successor.
“When I began as CEO 20 years ago, SHM – then known as the National Association of Inpatient Physicians – was a young national organization with approximately 500 members, and there was minimal understanding as to the value that hospitalists could add to their health communities,” Dr. Wellikson said. “I am proud to say that, nearly 20 years later, SHM boasts a growing membership of more than 17,000, and hospitalists are on the front line of innovation as a driving force in improving patient care.”
SHM has not only grown its membership but also its diverse portfolio of offerings for hospital medicine professionals under Dr. Wellikson’s leadership. Its first annual conference welcomed approximately 300 attendees; the most recent conference, Hospital Medicine 2019, saw that number increase more than tenfold to nearly 4,000. Its conferences, publications, online education, chapter program, advocacy efforts, quality improvement programs, and more have evolved significantly to ensure hospitalists at all stages of their careers – and those who support them – have access to resources to keep them up to date and demonstrate their value in America’s health care system.
During Dr. Wellikson’s tenure, SHM launched its peer-reviewed Journal of Hospital Medicine, the premier, ISI-indexed publication for the specialty, successfully advocated for a Focused Practice in Hospital Medicine certification option and C6 hospitalist specialty code, and earned the John M. Eisenberg Patient Safety and Quality Award for its quality improvement programs. These are just a few of the noteworthy accomplishments that have elevated SHM as a key partner for hospitalists and their institutions.
To assist with the search for SHM’s next CEO, the society has retained Spencer Stuart, a leading global executive and leadership advisory firm. The search process is being overseen by a diverse search committee led by the president-elect of SHM’s Board of Directors, Danielle Scheurer, MD, MSCR, SFHM.
“On behalf of the society and its members, I want to extend a sincere thank you to Larry for his years of dedication and service to SHM, its staff, and the hospital medicine professionals we serve,” said Christopher Frost, MD, SFHM, president of SHM’s Board of Directors. “His legacy will allow SHM to continue its growth trajectory through key programs and services supporting members’ needs for years to come. Larry has taken the specialty of hospital medicine and created a movement in SHM, where the entire hospital medicine team can come for education, community, and betterment of the care we provide to our patients. We are indebted to him beyond words.”
Those who are interested in leading SHM into the future as its next CEO are encouraged to contact either Jennifer P. Heenan ([email protected]) or Mark Furman, MD ([email protected]).
Society recognizes Dr. Wellikson’s leadership, retains Spencer Stuart for successor search
Society recognizes Dr. Wellikson’s leadership, retains Spencer Stuart for successor search
Philadelphia – After serving as the first and only chief executive officer of the Society of Hospital Medicine since January of 2000, Laurence Wellikson, MD, MHM, has announced his retirement effective on Dec. 31, 2020. In parallel, the SHM Board of Directors have commenced a search for his successor.
“When I began as CEO 20 years ago, SHM – then known as the National Association of Inpatient Physicians – was a young national organization with approximately 500 members, and there was minimal understanding as to the value that hospitalists could add to their health communities,” Dr. Wellikson said. “I am proud to say that, nearly 20 years later, SHM boasts a growing membership of more than 17,000, and hospitalists are on the front line of innovation as a driving force in improving patient care.”
SHM has not only grown its membership but also its diverse portfolio of offerings for hospital medicine professionals under Dr. Wellikson’s leadership. Its first annual conference welcomed approximately 300 attendees; the most recent conference, Hospital Medicine 2019, saw that number increase more than tenfold to nearly 4,000. Its conferences, publications, online education, chapter program, advocacy efforts, quality improvement programs, and more have evolved significantly to ensure hospitalists at all stages of their careers – and those who support them – have access to resources to keep them up to date and demonstrate their value in America’s health care system.
During Dr. Wellikson’s tenure, SHM launched its peer-reviewed Journal of Hospital Medicine, the premier, ISI-indexed publication for the specialty, successfully advocated for a Focused Practice in Hospital Medicine certification option and C6 hospitalist specialty code, and earned the John M. Eisenberg Patient Safety and Quality Award for its quality improvement programs. These are just a few of the noteworthy accomplishments that have elevated SHM as a key partner for hospitalists and their institutions.
To assist with the search for SHM’s next CEO, the society has retained Spencer Stuart, a leading global executive and leadership advisory firm. The search process is being overseen by a diverse search committee led by the president-elect of SHM’s Board of Directors, Danielle Scheurer, MD, MSCR, SFHM.
“On behalf of the society and its members, I want to extend a sincere thank you to Larry for his years of dedication and service to SHM, its staff, and the hospital medicine professionals we serve,” said Christopher Frost, MD, SFHM, president of SHM’s Board of Directors. “His legacy will allow SHM to continue its growth trajectory through key programs and services supporting members’ needs for years to come. Larry has taken the specialty of hospital medicine and created a movement in SHM, where the entire hospital medicine team can come for education, community, and betterment of the care we provide to our patients. We are indebted to him beyond words.”
Those who are interested in leading SHM into the future as its next CEO are encouraged to contact either Jennifer P. Heenan ([email protected]) or Mark Furman, MD ([email protected]).
Philadelphia – After serving as the first and only chief executive officer of the Society of Hospital Medicine since January of 2000, Laurence Wellikson, MD, MHM, has announced his retirement effective on Dec. 31, 2020. In parallel, the SHM Board of Directors have commenced a search for his successor.
“When I began as CEO 20 years ago, SHM – then known as the National Association of Inpatient Physicians – was a young national organization with approximately 500 members, and there was minimal understanding as to the value that hospitalists could add to their health communities,” Dr. Wellikson said. “I am proud to say that, nearly 20 years later, SHM boasts a growing membership of more than 17,000, and hospitalists are on the front line of innovation as a driving force in improving patient care.”
SHM has not only grown its membership but also its diverse portfolio of offerings for hospital medicine professionals under Dr. Wellikson’s leadership. Its first annual conference welcomed approximately 300 attendees; the most recent conference, Hospital Medicine 2019, saw that number increase more than tenfold to nearly 4,000. Its conferences, publications, online education, chapter program, advocacy efforts, quality improvement programs, and more have evolved significantly to ensure hospitalists at all stages of their careers – and those who support them – have access to resources to keep them up to date and demonstrate their value in America’s health care system.
During Dr. Wellikson’s tenure, SHM launched its peer-reviewed Journal of Hospital Medicine, the premier, ISI-indexed publication for the specialty, successfully advocated for a Focused Practice in Hospital Medicine certification option and C6 hospitalist specialty code, and earned the John M. Eisenberg Patient Safety and Quality Award for its quality improvement programs. These are just a few of the noteworthy accomplishments that have elevated SHM as a key partner for hospitalists and their institutions.
To assist with the search for SHM’s next CEO, the society has retained Spencer Stuart, a leading global executive and leadership advisory firm. The search process is being overseen by a diverse search committee led by the president-elect of SHM’s Board of Directors, Danielle Scheurer, MD, MSCR, SFHM.
“On behalf of the society and its members, I want to extend a sincere thank you to Larry for his years of dedication and service to SHM, its staff, and the hospital medicine professionals we serve,” said Christopher Frost, MD, SFHM, president of SHM’s Board of Directors. “His legacy will allow SHM to continue its growth trajectory through key programs and services supporting members’ needs for years to come. Larry has taken the specialty of hospital medicine and created a movement in SHM, where the entire hospital medicine team can come for education, community, and betterment of the care we provide to our patients. We are indebted to him beyond words.”
Those who are interested in leading SHM into the future as its next CEO are encouraged to contact either Jennifer P. Heenan ([email protected]) or Mark Furman, MD ([email protected]).
In newborns, concentrated urine helps rule out UTI
SEATTLE – according to investigators at the University of Texas Health Science Center, Houston.
The researchers found that urine testing negative for nitrites with a specific gravity above 1.015 in children up to 2 months old had a sensitivity of 53% for ruling out UTIs, but that urine with a specific gravity below that mark had a sensitivity of just 14%. The finding “should be taken into account when interpreting nitrite results ... in this high-risk population,” they concluded.
Bacteria in the bladder convert nitrates to nitrites, so positive results are pretty much pathognomonic for UTIs, with a specificity of nearly 100%, according to the researchers.
Negative results, however, don’t reliably rule out infection, and are even less reliable in infants because they urinate frequently, which means they usually flush out bacteria before they have enough time to make the conversion, which takes several hours, they said.
The lead investigator Raymond Parlar-Chun, MD, an assistant professor of pediatrics at the University of Texas McGovern Medical School in Houston, said he had a hunch that negative results might be more reliable when newborns urinate less frequently and have more concentrated urine.
He and his team reviewed data collected on 413 infants up to 2 months old who were admitted for fever workup and treated for UTIs both in the hospital and after discharge. Nitrite results were stratified by urine concentration. A specific gravity of 1.015 was used as the cutoff between concentrated and dilute urine, which was “midway between the parameters reported” in every urinalysis, Dr. Parlar-Chun said.
Although the sensitivity of concentrated urine was only 53%, “it’s a stark difference from” the 14% in dilute urine, he said.“You should take a look at specific gravity to interpret nitrites. If urine is concentrated, you have [more confidence] that you don’t have a UTI if you’re negative. It’s better than taking [nitrites] at face value.”
The subjects were 31 days old, on average, and 62% were boys; 112 had a specific gravity above 1.015, and 301 below.
There was no external funding, and Dr. Parlar-Chun didn’t have any disclosures.
SEATTLE – according to investigators at the University of Texas Health Science Center, Houston.
The researchers found that urine testing negative for nitrites with a specific gravity above 1.015 in children up to 2 months old had a sensitivity of 53% for ruling out UTIs, but that urine with a specific gravity below that mark had a sensitivity of just 14%. The finding “should be taken into account when interpreting nitrite results ... in this high-risk population,” they concluded.
Bacteria in the bladder convert nitrates to nitrites, so positive results are pretty much pathognomonic for UTIs, with a specificity of nearly 100%, according to the researchers.
Negative results, however, don’t reliably rule out infection, and are even less reliable in infants because they urinate frequently, which means they usually flush out bacteria before they have enough time to make the conversion, which takes several hours, they said.
The lead investigator Raymond Parlar-Chun, MD, an assistant professor of pediatrics at the University of Texas McGovern Medical School in Houston, said he had a hunch that negative results might be more reliable when newborns urinate less frequently and have more concentrated urine.
He and his team reviewed data collected on 413 infants up to 2 months old who were admitted for fever workup and treated for UTIs both in the hospital and after discharge. Nitrite results were stratified by urine concentration. A specific gravity of 1.015 was used as the cutoff between concentrated and dilute urine, which was “midway between the parameters reported” in every urinalysis, Dr. Parlar-Chun said.
Although the sensitivity of concentrated urine was only 53%, “it’s a stark difference from” the 14% in dilute urine, he said.“You should take a look at specific gravity to interpret nitrites. If urine is concentrated, you have [more confidence] that you don’t have a UTI if you’re negative. It’s better than taking [nitrites] at face value.”
The subjects were 31 days old, on average, and 62% were boys; 112 had a specific gravity above 1.015, and 301 below.
There was no external funding, and Dr. Parlar-Chun didn’t have any disclosures.
SEATTLE – according to investigators at the University of Texas Health Science Center, Houston.
The researchers found that urine testing negative for nitrites with a specific gravity above 1.015 in children up to 2 months old had a sensitivity of 53% for ruling out UTIs, but that urine with a specific gravity below that mark had a sensitivity of just 14%. The finding “should be taken into account when interpreting nitrite results ... in this high-risk population,” they concluded.
Bacteria in the bladder convert nitrates to nitrites, so positive results are pretty much pathognomonic for UTIs, with a specificity of nearly 100%, according to the researchers.
Negative results, however, don’t reliably rule out infection, and are even less reliable in infants because they urinate frequently, which means they usually flush out bacteria before they have enough time to make the conversion, which takes several hours, they said.
The lead investigator Raymond Parlar-Chun, MD, an assistant professor of pediatrics at the University of Texas McGovern Medical School in Houston, said he had a hunch that negative results might be more reliable when newborns urinate less frequently and have more concentrated urine.
He and his team reviewed data collected on 413 infants up to 2 months old who were admitted for fever workup and treated for UTIs both in the hospital and after discharge. Nitrite results were stratified by urine concentration. A specific gravity of 1.015 was used as the cutoff between concentrated and dilute urine, which was “midway between the parameters reported” in every urinalysis, Dr. Parlar-Chun said.
Although the sensitivity of concentrated urine was only 53%, “it’s a stark difference from” the 14% in dilute urine, he said.“You should take a look at specific gravity to interpret nitrites. If urine is concentrated, you have [more confidence] that you don’t have a UTI if you’re negative. It’s better than taking [nitrites] at face value.”
The subjects were 31 days old, on average, and 62% were boys; 112 had a specific gravity above 1.015, and 301 below.
There was no external funding, and Dr. Parlar-Chun didn’t have any disclosures.
REPORTING FROM PHM 2019
Sepsis survivors’ persistent immunosuppression raises mortality risk
readmission after discharge, and mortality, according to a study published in JAMA Network Open.
“Individuals with persistent biomarkers of inflammation and immunosuppression had a higher risk of readmission and death due to cardiovascular disease and cancer compared with those with normal circulating biomarkers,” Sachin Yende, MD, of the VA Pittsburgh Healthcare System and the University of Pittsburgh and colleagues wrote in their study. “Our findings suggest that long-term immunomodulation strategies should be explored in patients hospitalized with sepsis.”
Dr. Yende and colleagues performed a multicenter, prospective cohort study of 483 patients who were hospitalized for sepsis at 12 different sites between January 2012 and May 2017. They measured inflammation using interleukin-6, high-sensitivity C-reactive protein (hs-CRP), and soluble programmed death-ligand 1 (sPD-L1); hemostasis using plasminogen activator inhibitor 1 and D-dimer; and endothelial dysfunction using intercellular adhesion molecule 1, vascular cell adhesion molecule 1, and E-selectin. The patients included were mean age 60.5 years, 54.9% were male, the mean Sequential Organ Failure Assessment score was 4.2, and a total of 376 patients (77.8%) had one or more chronic diseases.
Overall, there were 485 readmissions in 205 patients (42.5%). The mortality rate was 43 patients (8.9%) at 3 months, 56 patients (11.6%) at 6 months, and 85 patients (17.6%) at 12 months. At 3 months, 23 patients (25.8%) had elevated hs-CRP levels, which increased to 26 patients (30.2%) at 6 months and 40 patients (44.9%) at 12 months. sPD-L1 levels were elevated in 45 patients (46.4%) at 3 months, but the number of patients with elevated sPD-L1 did not appear to significantly increase at 6 months (40 patients; 44.9%) or 12 months (44 patients; 49.4%).
From these results, researchers developed a phenotype of hyperinflammation and immunosuppression that consisted of 326 of 477 (68.3%) patients with high hs-CRP and elevated sPD-L1 levels. Patients with this phenotype of hyperinflammation and immunosuppression had more than eight times the risk of 1-year mortality (odds ratio, 8.26; 95% confidence interval, 3.45-21.69; P less than .001) and more than five times the risk of readmission or mortality at 6 months related to cardiovascular disease (hazard ratio, 5.07; 95% CI, 1.18-21.84; P = .02) or cancer (hazard ratio, 5.15; 95% CI, 1.25-21.18; P = .02), compared with patients who had normal hs-CRP and sPD-L1 levels. This hyperinflammation and immunosuppression phenotype also was associated with greater risk of 6-month all-cause readmission or mortality (HR, 1.53; 95% CI, 1.10-2.13; P = .01), compared with patients who had the normal phenotype.
“The persistence of hyperinflammation in a large number of sepsis survivors and the increased risk of cardiovascular events among these patients may explain the association between infection and cardiovascular disease in a prior study,” the authors said. “Although prior trials tested immunomodulation strategies during only the early phase of hospitalization for sepsis, immunomodulation may be needed after hospital discharge,” and suggest points of future study for patients who survive sepsis and develop long-term sequelae.
This study was funded by grants from National Institutes of Health and resources from the VA Pittsburgh Healthcare System. The authors reported personal and institutional relationships in the form of personal fees, grants, and patents for Alung Technologies, Atox Bio, Bayer AG, Beckman Coulter, BristolMyers Squibb, Ferring, NIH, Roche, Selepressin, and the University of Pittsburgh.
SOURCE: Yende S et al. JAMA Netw Open. 2019 Aug 7. doi: 10.1001/jamanetworkopen.2019.8686.
readmission after discharge, and mortality, according to a study published in JAMA Network Open.
“Individuals with persistent biomarkers of inflammation and immunosuppression had a higher risk of readmission and death due to cardiovascular disease and cancer compared with those with normal circulating biomarkers,” Sachin Yende, MD, of the VA Pittsburgh Healthcare System and the University of Pittsburgh and colleagues wrote in their study. “Our findings suggest that long-term immunomodulation strategies should be explored in patients hospitalized with sepsis.”
Dr. Yende and colleagues performed a multicenter, prospective cohort study of 483 patients who were hospitalized for sepsis at 12 different sites between January 2012 and May 2017. They measured inflammation using interleukin-6, high-sensitivity C-reactive protein (hs-CRP), and soluble programmed death-ligand 1 (sPD-L1); hemostasis using plasminogen activator inhibitor 1 and D-dimer; and endothelial dysfunction using intercellular adhesion molecule 1, vascular cell adhesion molecule 1, and E-selectin. The patients included were mean age 60.5 years, 54.9% were male, the mean Sequential Organ Failure Assessment score was 4.2, and a total of 376 patients (77.8%) had one or more chronic diseases.
Overall, there were 485 readmissions in 205 patients (42.5%). The mortality rate was 43 patients (8.9%) at 3 months, 56 patients (11.6%) at 6 months, and 85 patients (17.6%) at 12 months. At 3 months, 23 patients (25.8%) had elevated hs-CRP levels, which increased to 26 patients (30.2%) at 6 months and 40 patients (44.9%) at 12 months. sPD-L1 levels were elevated in 45 patients (46.4%) at 3 months, but the number of patients with elevated sPD-L1 did not appear to significantly increase at 6 months (40 patients; 44.9%) or 12 months (44 patients; 49.4%).
From these results, researchers developed a phenotype of hyperinflammation and immunosuppression that consisted of 326 of 477 (68.3%) patients with high hs-CRP and elevated sPD-L1 levels. Patients with this phenotype of hyperinflammation and immunosuppression had more than eight times the risk of 1-year mortality (odds ratio, 8.26; 95% confidence interval, 3.45-21.69; P less than .001) and more than five times the risk of readmission or mortality at 6 months related to cardiovascular disease (hazard ratio, 5.07; 95% CI, 1.18-21.84; P = .02) or cancer (hazard ratio, 5.15; 95% CI, 1.25-21.18; P = .02), compared with patients who had normal hs-CRP and sPD-L1 levels. This hyperinflammation and immunosuppression phenotype also was associated with greater risk of 6-month all-cause readmission or mortality (HR, 1.53; 95% CI, 1.10-2.13; P = .01), compared with patients who had the normal phenotype.
“The persistence of hyperinflammation in a large number of sepsis survivors and the increased risk of cardiovascular events among these patients may explain the association between infection and cardiovascular disease in a prior study,” the authors said. “Although prior trials tested immunomodulation strategies during only the early phase of hospitalization for sepsis, immunomodulation may be needed after hospital discharge,” and suggest points of future study for patients who survive sepsis and develop long-term sequelae.
This study was funded by grants from National Institutes of Health and resources from the VA Pittsburgh Healthcare System. The authors reported personal and institutional relationships in the form of personal fees, grants, and patents for Alung Technologies, Atox Bio, Bayer AG, Beckman Coulter, BristolMyers Squibb, Ferring, NIH, Roche, Selepressin, and the University of Pittsburgh.
SOURCE: Yende S et al. JAMA Netw Open. 2019 Aug 7. doi: 10.1001/jamanetworkopen.2019.8686.
readmission after discharge, and mortality, according to a study published in JAMA Network Open.
“Individuals with persistent biomarkers of inflammation and immunosuppression had a higher risk of readmission and death due to cardiovascular disease and cancer compared with those with normal circulating biomarkers,” Sachin Yende, MD, of the VA Pittsburgh Healthcare System and the University of Pittsburgh and colleagues wrote in their study. “Our findings suggest that long-term immunomodulation strategies should be explored in patients hospitalized with sepsis.”
Dr. Yende and colleagues performed a multicenter, prospective cohort study of 483 patients who were hospitalized for sepsis at 12 different sites between January 2012 and May 2017. They measured inflammation using interleukin-6, high-sensitivity C-reactive protein (hs-CRP), and soluble programmed death-ligand 1 (sPD-L1); hemostasis using plasminogen activator inhibitor 1 and D-dimer; and endothelial dysfunction using intercellular adhesion molecule 1, vascular cell adhesion molecule 1, and E-selectin. The patients included were mean age 60.5 years, 54.9% were male, the mean Sequential Organ Failure Assessment score was 4.2, and a total of 376 patients (77.8%) had one or more chronic diseases.
Overall, there were 485 readmissions in 205 patients (42.5%). The mortality rate was 43 patients (8.9%) at 3 months, 56 patients (11.6%) at 6 months, and 85 patients (17.6%) at 12 months. At 3 months, 23 patients (25.8%) had elevated hs-CRP levels, which increased to 26 patients (30.2%) at 6 months and 40 patients (44.9%) at 12 months. sPD-L1 levels were elevated in 45 patients (46.4%) at 3 months, but the number of patients with elevated sPD-L1 did not appear to significantly increase at 6 months (40 patients; 44.9%) or 12 months (44 patients; 49.4%).
From these results, researchers developed a phenotype of hyperinflammation and immunosuppression that consisted of 326 of 477 (68.3%) patients with high hs-CRP and elevated sPD-L1 levels. Patients with this phenotype of hyperinflammation and immunosuppression had more than eight times the risk of 1-year mortality (odds ratio, 8.26; 95% confidence interval, 3.45-21.69; P less than .001) and more than five times the risk of readmission or mortality at 6 months related to cardiovascular disease (hazard ratio, 5.07; 95% CI, 1.18-21.84; P = .02) or cancer (hazard ratio, 5.15; 95% CI, 1.25-21.18; P = .02), compared with patients who had normal hs-CRP and sPD-L1 levels. This hyperinflammation and immunosuppression phenotype also was associated with greater risk of 6-month all-cause readmission or mortality (HR, 1.53; 95% CI, 1.10-2.13; P = .01), compared with patients who had the normal phenotype.
“The persistence of hyperinflammation in a large number of sepsis survivors and the increased risk of cardiovascular events among these patients may explain the association between infection and cardiovascular disease in a prior study,” the authors said. “Although prior trials tested immunomodulation strategies during only the early phase of hospitalization for sepsis, immunomodulation may be needed after hospital discharge,” and suggest points of future study for patients who survive sepsis and develop long-term sequelae.
This study was funded by grants from National Institutes of Health and resources from the VA Pittsburgh Healthcare System. The authors reported personal and institutional relationships in the form of personal fees, grants, and patents for Alung Technologies, Atox Bio, Bayer AG, Beckman Coulter, BristolMyers Squibb, Ferring, NIH, Roche, Selepressin, and the University of Pittsburgh.
SOURCE: Yende S et al. JAMA Netw Open. 2019 Aug 7. doi: 10.1001/jamanetworkopen.2019.8686.
FROM JAMA NETWORK OPEN
Key clinical point: Markers of inflammation and immunosuppression persist in over two-thirds of patients hospitalized for sepsis, which could explain worsened outcomes and mortality up to 1 year after hospitalization.
Major finding: Patients with signs of hyperinflammation and immunosuppression had significantly increased mortality after 1 year and were significantly more likely to be readmitted or die because of cardiovascular disease or cancer.
Study details: A prospective cohort study of 483 patients who were hospitalized because of sepsis at 12 different centers between January 2012 and May 2017.
Disclosures: This study was funded by grants from National Institutes of Health and resources from the Veterans Affairs Pittsburgh Healthcare System. The authors reported personal and institutional relationships in the form of personal fees, grants, and patents for Alung Technologies, Atox Bio, Bayer AG, Beckman Coulter, BristolMyers Squibb, Ferring, NIH, Roche, Selepressin, and the University of Pittsburgh.
Source: Yende S et al. JAMA Netw Open. 2019 Aug 7. doi: 10.1001/jamanetworkopen.2019.8686.
Hospital slashes S. aureus vancomycin resistance
LJUBLJANA, SLOVENIA – , Johannes Huebner, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented a retrospective analysis of S. aureus isolates obtained from 540 patients at the Dr. von Hauner Children’s Hospital, Munich, from 2002 to 2017. All were either newly identified methicillin-resistant S. aureus (MRSA) or specimens from bacteremic children with invasive MRSA or methicillin-sensitive S. aureus (MSSA). The strains were tested for vancomycin resistance and minimum inhibitory concentration (MIC). The results from the 200 isolates obtained from 2002 to 2009 were then compared to the 340 specimens from 2010 to 2017, when antibiotic stewardship programs rose to the fore at the pediatric hospital.
All samples proved to be vancomycin sensitive. The further good news was there was absolutely no evidence of the worrisome vancomycin MIC creep that has been described at some centers. On the contrary, the MIC was significantly lower in the later samples, at 0.99 mcg/mL, compared with 1.11 mcg/mL in the earlier period. Moreover, the prevalence of heterogeneous glycopeptide-intermediate S. aureus (hGISA) – a phenotype that has been associated with increased rates of treatment failure – improved from 25% in the earlier period to 6% during the later period, reported Dr. Huebner, head of the division of pediatric infectious diseases at the children’s hospital, part of the University of Munich.
Vancomycin MICs weren’t significantly different between the MRSA and MSSA samples.
Based upon this favorable institutional experience, vancomycin remains the first-line treatment for suspected severe gram-positive cocci infections as well as proven infections involving MRSA at Dr. von Hauner Children’s Hospital.
These vancomycin MIC and hGISA data underscore the importance of periodically monitoring local S. aureus antimicrobial susceptibilities, which, as in this case, can differ from the broader global trends. The vancomycin MIC creep issue hadn’t been studied previously in German hospitals, according to Dr. Huebner.
He and his coworkers have published details of the elements of pediatric antibiotic stewardship programs they have found to be most effective (Infection. 2017 Aug;45[4]:493-504) as well as a systematic review of studies on the favorable economic impact of such programs (J Hosp Infect. 2019 Aug;102[4]:369-376).
Dr. Huebner reported having no financial conflicts regarding his study, which was conducted free of commercial support.
LJUBLJANA, SLOVENIA – , Johannes Huebner, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented a retrospective analysis of S. aureus isolates obtained from 540 patients at the Dr. von Hauner Children’s Hospital, Munich, from 2002 to 2017. All were either newly identified methicillin-resistant S. aureus (MRSA) or specimens from bacteremic children with invasive MRSA or methicillin-sensitive S. aureus (MSSA). The strains were tested for vancomycin resistance and minimum inhibitory concentration (MIC). The results from the 200 isolates obtained from 2002 to 2009 were then compared to the 340 specimens from 2010 to 2017, when antibiotic stewardship programs rose to the fore at the pediatric hospital.
All samples proved to be vancomycin sensitive. The further good news was there was absolutely no evidence of the worrisome vancomycin MIC creep that has been described at some centers. On the contrary, the MIC was significantly lower in the later samples, at 0.99 mcg/mL, compared with 1.11 mcg/mL in the earlier period. Moreover, the prevalence of heterogeneous glycopeptide-intermediate S. aureus (hGISA) – a phenotype that has been associated with increased rates of treatment failure – improved from 25% in the earlier period to 6% during the later period, reported Dr. Huebner, head of the division of pediatric infectious diseases at the children’s hospital, part of the University of Munich.
Vancomycin MICs weren’t significantly different between the MRSA and MSSA samples.
Based upon this favorable institutional experience, vancomycin remains the first-line treatment for suspected severe gram-positive cocci infections as well as proven infections involving MRSA at Dr. von Hauner Children’s Hospital.
These vancomycin MIC and hGISA data underscore the importance of periodically monitoring local S. aureus antimicrobial susceptibilities, which, as in this case, can differ from the broader global trends. The vancomycin MIC creep issue hadn’t been studied previously in German hospitals, according to Dr. Huebner.
He and his coworkers have published details of the elements of pediatric antibiotic stewardship programs they have found to be most effective (Infection. 2017 Aug;45[4]:493-504) as well as a systematic review of studies on the favorable economic impact of such programs (J Hosp Infect. 2019 Aug;102[4]:369-376).
Dr. Huebner reported having no financial conflicts regarding his study, which was conducted free of commercial support.
LJUBLJANA, SLOVENIA – , Johannes Huebner, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
He presented a retrospective analysis of S. aureus isolates obtained from 540 patients at the Dr. von Hauner Children’s Hospital, Munich, from 2002 to 2017. All were either newly identified methicillin-resistant S. aureus (MRSA) or specimens from bacteremic children with invasive MRSA or methicillin-sensitive S. aureus (MSSA). The strains were tested for vancomycin resistance and minimum inhibitory concentration (MIC). The results from the 200 isolates obtained from 2002 to 2009 were then compared to the 340 specimens from 2010 to 2017, when antibiotic stewardship programs rose to the fore at the pediatric hospital.
All samples proved to be vancomycin sensitive. The further good news was there was absolutely no evidence of the worrisome vancomycin MIC creep that has been described at some centers. On the contrary, the MIC was significantly lower in the later samples, at 0.99 mcg/mL, compared with 1.11 mcg/mL in the earlier period. Moreover, the prevalence of heterogeneous glycopeptide-intermediate S. aureus (hGISA) – a phenotype that has been associated with increased rates of treatment failure – improved from 25% in the earlier period to 6% during the later period, reported Dr. Huebner, head of the division of pediatric infectious diseases at the children’s hospital, part of the University of Munich.
Vancomycin MICs weren’t significantly different between the MRSA and MSSA samples.
Based upon this favorable institutional experience, vancomycin remains the first-line treatment for suspected severe gram-positive cocci infections as well as proven infections involving MRSA at Dr. von Hauner Children’s Hospital.
These vancomycin MIC and hGISA data underscore the importance of periodically monitoring local S. aureus antimicrobial susceptibilities, which, as in this case, can differ from the broader global trends. The vancomycin MIC creep issue hadn’t been studied previously in German hospitals, according to Dr. Huebner.
He and his coworkers have published details of the elements of pediatric antibiotic stewardship programs they have found to be most effective (Infection. 2017 Aug;45[4]:493-504) as well as a systematic review of studies on the favorable economic impact of such programs (J Hosp Infect. 2019 Aug;102[4]:369-376).
Dr. Huebner reported having no financial conflicts regarding his study, which was conducted free of commercial support.
REPORTING FROM ESPID 2019
Key clinical point: Staphylococcus aureus vancomycin MIC creep is reversible through dedicated antimicrobial stewardship.
Major finding: The prevalence of hGISA in MRSA and MSSA specimens improved from 25% during 2002-2009 to 6% during 2010-2017 at one German tertiary children’s hospital.
Study details: This was a retrospective single-center analysis of vancomycin resistance trends over time in 540 S. aureus specimens gathered in 2002-2017.
Disclosures: The presenter reported having no financial conflicts regarding this study, which was conducted free of commercial support.
Maximize your leadership in academic hospital medicine
AHA Level 2 course now available
Over the past 2 decades, hospital medicine has grown from a nascent collection of hospitalists to one of the fastest growing specialties, with more than 60,000 active practitioners today.
Ten years ago, the need for mentoring and growth of a new generation of young academic faculty led to the development of the first Academic Hospitalist Academy (AHA) through the coordinated efforts of the Society of Hospital Medicine, the Society of General Internal Medicine, and the Association of Clinical Leaders of General Internal Medicine.
As modern medicine moves at an increasing pace, the intersection of patient care, research, and education has opened further opportunities for fostering the expertise of hospital medicine practitioners. The next level of training is now available with the advent of AHA’s Level 2 course.
Ever wonder why the new clinical service you’ve designed to improve physician and patient efficiency isn’t functioning like it did in the beginning? Patients are staying longer in the hospital, and physicians are working harder. The principles of change management, personal leadership styles, and adult learning will be covered in the AHA Level 2 course. How do I get my project funded and then what do I do with the results? Keys to negotiating for time and resources as well as the skills to write and disseminate your work are integrated into the curriculum.
Participants will be engaged in an interactive course designed around the challenges of practicing and leading in an academic environment. AHA Level 2 aims to help attendees – regardless of their areas of interest – identify and acquire the skills necessary to advance their career, describe the business and cultural landscape of academic health systems, and learn how to leverage that knowledge; to list resources and techniques to continue to further build their skills, and identify and pursue their unique scholarly niche.
Based on the success of AHA’s Level 1 course and the feedback from the almost 1,000 participants who have attended, AHA Level 2 is a 2.5-day course that will allow for the exchange of ideas and skills from nationally regarded faculty and fellow attendees. Through plenary sessions, workshops, small groups, and networking opportunities, attendees will be immersed in the realm of modern academic hospital medicine. The new course is offered in parallel with AHA Level 1 at the Inverness Resort, outside of Denver, on Sept. 10-12, 2019.
The course will leave attendees with an individualized career plan and enhance their area of expertise. The lessons learned and shared will allow participants to return to their institutions and continue to lead in the areas of patient care, financial resourcefulness, and the education of current and future generations of hospital medicine specialists.
Dr. O’Dorisio is a Med-Peds hospitalist at the Ohio State University, Columbus.
AHA Level 2 course now available
AHA Level 2 course now available
Over the past 2 decades, hospital medicine has grown from a nascent collection of hospitalists to one of the fastest growing specialties, with more than 60,000 active practitioners today.
Ten years ago, the need for mentoring and growth of a new generation of young academic faculty led to the development of the first Academic Hospitalist Academy (AHA) through the coordinated efforts of the Society of Hospital Medicine, the Society of General Internal Medicine, and the Association of Clinical Leaders of General Internal Medicine.
As modern medicine moves at an increasing pace, the intersection of patient care, research, and education has opened further opportunities for fostering the expertise of hospital medicine practitioners. The next level of training is now available with the advent of AHA’s Level 2 course.
Ever wonder why the new clinical service you’ve designed to improve physician and patient efficiency isn’t functioning like it did in the beginning? Patients are staying longer in the hospital, and physicians are working harder. The principles of change management, personal leadership styles, and adult learning will be covered in the AHA Level 2 course. How do I get my project funded and then what do I do with the results? Keys to negotiating for time and resources as well as the skills to write and disseminate your work are integrated into the curriculum.
Participants will be engaged in an interactive course designed around the challenges of practicing and leading in an academic environment. AHA Level 2 aims to help attendees – regardless of their areas of interest – identify and acquire the skills necessary to advance their career, describe the business and cultural landscape of academic health systems, and learn how to leverage that knowledge; to list resources and techniques to continue to further build their skills, and identify and pursue their unique scholarly niche.
Based on the success of AHA’s Level 1 course and the feedback from the almost 1,000 participants who have attended, AHA Level 2 is a 2.5-day course that will allow for the exchange of ideas and skills from nationally regarded faculty and fellow attendees. Through plenary sessions, workshops, small groups, and networking opportunities, attendees will be immersed in the realm of modern academic hospital medicine. The new course is offered in parallel with AHA Level 1 at the Inverness Resort, outside of Denver, on Sept. 10-12, 2019.
The course will leave attendees with an individualized career plan and enhance their area of expertise. The lessons learned and shared will allow participants to return to their institutions and continue to lead in the areas of patient care, financial resourcefulness, and the education of current and future generations of hospital medicine specialists.
Dr. O’Dorisio is a Med-Peds hospitalist at the Ohio State University, Columbus.
Over the past 2 decades, hospital medicine has grown from a nascent collection of hospitalists to one of the fastest growing specialties, with more than 60,000 active practitioners today.
Ten years ago, the need for mentoring and growth of a new generation of young academic faculty led to the development of the first Academic Hospitalist Academy (AHA) through the coordinated efforts of the Society of Hospital Medicine, the Society of General Internal Medicine, and the Association of Clinical Leaders of General Internal Medicine.
As modern medicine moves at an increasing pace, the intersection of patient care, research, and education has opened further opportunities for fostering the expertise of hospital medicine practitioners. The next level of training is now available with the advent of AHA’s Level 2 course.
Ever wonder why the new clinical service you’ve designed to improve physician and patient efficiency isn’t functioning like it did in the beginning? Patients are staying longer in the hospital, and physicians are working harder. The principles of change management, personal leadership styles, and adult learning will be covered in the AHA Level 2 course. How do I get my project funded and then what do I do with the results? Keys to negotiating for time and resources as well as the skills to write and disseminate your work are integrated into the curriculum.
Participants will be engaged in an interactive course designed around the challenges of practicing and leading in an academic environment. AHA Level 2 aims to help attendees – regardless of their areas of interest – identify and acquire the skills necessary to advance their career, describe the business and cultural landscape of academic health systems, and learn how to leverage that knowledge; to list resources and techniques to continue to further build their skills, and identify and pursue their unique scholarly niche.
Based on the success of AHA’s Level 1 course and the feedback from the almost 1,000 participants who have attended, AHA Level 2 is a 2.5-day course that will allow for the exchange of ideas and skills from nationally regarded faculty and fellow attendees. Through plenary sessions, workshops, small groups, and networking opportunities, attendees will be immersed in the realm of modern academic hospital medicine. The new course is offered in parallel with AHA Level 1 at the Inverness Resort, outside of Denver, on Sept. 10-12, 2019.
The course will leave attendees with an individualized career plan and enhance their area of expertise. The lessons learned and shared will allow participants to return to their institutions and continue to lead in the areas of patient care, financial resourcefulness, and the education of current and future generations of hospital medicine specialists.
Dr. O’Dorisio is a Med-Peds hospitalist at the Ohio State University, Columbus.
CDC finds that too little naloxone is dispensed
Although the CDC recommends that clinicians consider prescribing naloxone, which can reverse the effects of an opioid overdose, to patients who receive high-dose opioid prescriptions, one naloxone prescription was dispensed in 2018 for every 69 such patients, according to a Vital Signs investigation published Aug. 6 in the Morbidity and Mortality Weekly Report.
Approximately 9 million more naloxone prescriptions could have been dispensed in 2018 if every patient with a high-dose opioid prescription were offered the drug, according to the agency. In addition, the rate at which naloxone is dispensed varies significantly according to region.
“Thousands of Americans are alive today thanks to the use of naloxone,” said Alex M. Azar, secretary of Health and Human Services, in a press release. “Giving people a chance to survive an opioid overdose and safely enter recovery is one of the five key pillars of our HHS strategy for ending the overdose epidemic. With help from Congress, the private sector, state, and local governments and communities, targeted access to naloxone has expanded dramatically over the last several years, but today’s CDC report is a reminder that there is much more all of us need to do to save lives.”
Investigators examined retail pharmacy data
In 2017, 47,600 (67.8%) drug overdose deaths in the United States involved opioids. For decades, emergency medical service providers have administered naloxone to patients with suspected drug overdose. A major focus of public health initiatives intended to address the opioid overdose crisis has been to increase access to naloxone through clinician prescribing and pharmacy dispensing. The CDC recommends considering prescribing naloxone to patients with a history of overdose or substance use disorder, those receiving opioid dosages of 50 morphine milligram equivalents per day or greater (that is, high-dose prescriptions), and those who are using benzodiazepines concurrently.
Investigators at the CDC examined retail pharmacy data from IQVIA, a company that maintains information on prescriptions from approximately 50,400 retail pharmacies. They extracted data from 2012 through 2018 to analyze naloxone dispensing by region, urban versus rural status, prescriber specialty, and recipient characteristics (for example, age group, sex, out-of-pocket costs, and method of payment).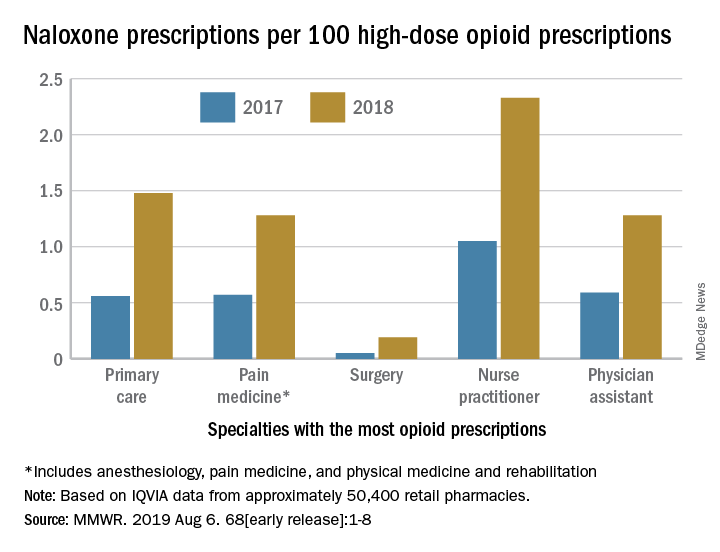
Dispensations doubled from 2017 to 2018
Naloxone dispensing from retail pharmacies increased from 0.4 prescriptions per 100,000 in 2012 to 170.2 prescriptions per 100,000 in 2018. From 2017 to 2018 alone, the number of prescriptions dispensed increased by 106%.
Despite consistency among state laws, naloxone dispensation varied by region. The average rate of naloxone prescriptions per 100 high-dose opioid prescriptions ranged from 0.2 in the lowest quartile to 2.9 in the highest quartile. In 2018, the rate of naloxone prescriptions per 100 high-dose opioid prescriptions ranged from 1.5 in metropolitan counties and 1.6 in the Northeast to 1.2 in rural counties and 1.3 in the Midwest. Rural counties were nearly three times more likely to be low-dispensing counties, compared with metropolitan counties.
The rate of naloxone prescriptions per 100 high-dose opioid prescriptions also varied by provider specialty. This rate was lowest among surgeons (0.2) and highest among psychiatrists (12.9).
Most naloxone prescriptions entailed out-of-pocket costs. About 71% of prescriptions paid for by Medicare entailed out-of-pocket costs, compared with 43.8% of prescriptions paid for by Medicaid, and 41.5% of prescriptions paid for by commercial insurance.
 Centers for Disease Control and Prevention
Centers for Disease Control and Prevention
More can be done

“It is clear from the data that there is still much needed education around the important role naloxone plays in reducing overdose deaths,” said Robert R. Redfield, MD, director of the CDC, in a press release. “The time is now to ensure all individuals who are prescribed high-dose opioids also receive naloxone as a potential life-saving intervention. As we aggressively confront what is the public health crisis of our time, CDC will continue to stress with health care providers the benefit of making this overdose-reversing medicine available to patients.”
“While we’ve seen these important increases [in naloxone prescriptions], we are not as far along as we’d like to be,” said Anne Schuchat, MD, principal deputy director of the CDC, during a press conference. “Cost is one of the issues, but I think awareness is another.” These data should prompt pharmacies to make sure that they stock naloxone and remind clinicians to consider naloxone when they prescribe opioids, she added. Patients and their family members should be aware of naloxone and ask their health care providers about it. “We’d really like to see the increase [in naloxone prescriptions] move much more rapidly,” she concluded.
The investigators disclosed no potential conflicts of interest.
SOURCE: Guy GP et al. MMWR Morb Mortal Wkly Rep. 2019 Aug 6.
Although the CDC recommends that clinicians consider prescribing naloxone, which can reverse the effects of an opioid overdose, to patients who receive high-dose opioid prescriptions, one naloxone prescription was dispensed in 2018 for every 69 such patients, according to a Vital Signs investigation published Aug. 6 in the Morbidity and Mortality Weekly Report.
Approximately 9 million more naloxone prescriptions could have been dispensed in 2018 if every patient with a high-dose opioid prescription were offered the drug, according to the agency. In addition, the rate at which naloxone is dispensed varies significantly according to region.
“Thousands of Americans are alive today thanks to the use of naloxone,” said Alex M. Azar, secretary of Health and Human Services, in a press release. “Giving people a chance to survive an opioid overdose and safely enter recovery is one of the five key pillars of our HHS strategy for ending the overdose epidemic. With help from Congress, the private sector, state, and local governments and communities, targeted access to naloxone has expanded dramatically over the last several years, but today’s CDC report is a reminder that there is much more all of us need to do to save lives.”
Investigators examined retail pharmacy data
In 2017, 47,600 (67.8%) drug overdose deaths in the United States involved opioids. For decades, emergency medical service providers have administered naloxone to patients with suspected drug overdose. A major focus of public health initiatives intended to address the opioid overdose crisis has been to increase access to naloxone through clinician prescribing and pharmacy dispensing. The CDC recommends considering prescribing naloxone to patients with a history of overdose or substance use disorder, those receiving opioid dosages of 50 morphine milligram equivalents per day or greater (that is, high-dose prescriptions), and those who are using benzodiazepines concurrently.
Investigators at the CDC examined retail pharmacy data from IQVIA, a company that maintains information on prescriptions from approximately 50,400 retail pharmacies. They extracted data from 2012 through 2018 to analyze naloxone dispensing by region, urban versus rural status, prescriber specialty, and recipient characteristics (for example, age group, sex, out-of-pocket costs, and method of payment).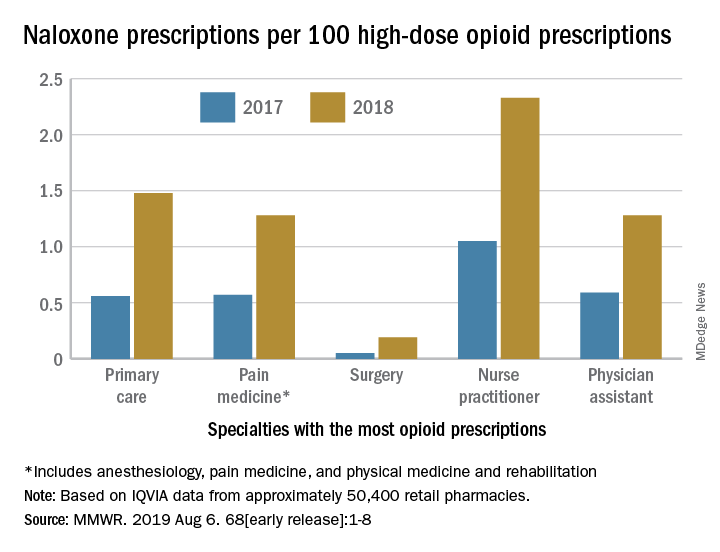
Dispensations doubled from 2017 to 2018
Naloxone dispensing from retail pharmacies increased from 0.4 prescriptions per 100,000 in 2012 to 170.2 prescriptions per 100,000 in 2018. From 2017 to 2018 alone, the number of prescriptions dispensed increased by 106%.
Despite consistency among state laws, naloxone dispensation varied by region. The average rate of naloxone prescriptions per 100 high-dose opioid prescriptions ranged from 0.2 in the lowest quartile to 2.9 in the highest quartile. In 2018, the rate of naloxone prescriptions per 100 high-dose opioid prescriptions ranged from 1.5 in metropolitan counties and 1.6 in the Northeast to 1.2 in rural counties and 1.3 in the Midwest. Rural counties were nearly three times more likely to be low-dispensing counties, compared with metropolitan counties.
The rate of naloxone prescriptions per 100 high-dose opioid prescriptions also varied by provider specialty. This rate was lowest among surgeons (0.2) and highest among psychiatrists (12.9).
Most naloxone prescriptions entailed out-of-pocket costs. About 71% of prescriptions paid for by Medicare entailed out-of-pocket costs, compared with 43.8% of prescriptions paid for by Medicaid, and 41.5% of prescriptions paid for by commercial insurance.
 Centers for Disease Control and Prevention
Centers for Disease Control and Prevention
More can be done

“It is clear from the data that there is still much needed education around the important role naloxone plays in reducing overdose deaths,” said Robert R. Redfield, MD, director of the CDC, in a press release. “The time is now to ensure all individuals who are prescribed high-dose opioids also receive naloxone as a potential life-saving intervention. As we aggressively confront what is the public health crisis of our time, CDC will continue to stress with health care providers the benefit of making this overdose-reversing medicine available to patients.”
“While we’ve seen these important increases [in naloxone prescriptions], we are not as far along as we’d like to be,” said Anne Schuchat, MD, principal deputy director of the CDC, during a press conference. “Cost is one of the issues, but I think awareness is another.” These data should prompt pharmacies to make sure that they stock naloxone and remind clinicians to consider naloxone when they prescribe opioids, she added. Patients and their family members should be aware of naloxone and ask their health care providers about it. “We’d really like to see the increase [in naloxone prescriptions] move much more rapidly,” she concluded.
The investigators disclosed no potential conflicts of interest.
SOURCE: Guy GP et al. MMWR Morb Mortal Wkly Rep. 2019 Aug 6.
Although the CDC recommends that clinicians consider prescribing naloxone, which can reverse the effects of an opioid overdose, to patients who receive high-dose opioid prescriptions, one naloxone prescription was dispensed in 2018 for every 69 such patients, according to a Vital Signs investigation published Aug. 6 in the Morbidity and Mortality Weekly Report.
Approximately 9 million more naloxone prescriptions could have been dispensed in 2018 if every patient with a high-dose opioid prescription were offered the drug, according to the agency. In addition, the rate at which naloxone is dispensed varies significantly according to region.
“Thousands of Americans are alive today thanks to the use of naloxone,” said Alex M. Azar, secretary of Health and Human Services, in a press release. “Giving people a chance to survive an opioid overdose and safely enter recovery is one of the five key pillars of our HHS strategy for ending the overdose epidemic. With help from Congress, the private sector, state, and local governments and communities, targeted access to naloxone has expanded dramatically over the last several years, but today’s CDC report is a reminder that there is much more all of us need to do to save lives.”
Investigators examined retail pharmacy data
In 2017, 47,600 (67.8%) drug overdose deaths in the United States involved opioids. For decades, emergency medical service providers have administered naloxone to patients with suspected drug overdose. A major focus of public health initiatives intended to address the opioid overdose crisis has been to increase access to naloxone through clinician prescribing and pharmacy dispensing. The CDC recommends considering prescribing naloxone to patients with a history of overdose or substance use disorder, those receiving opioid dosages of 50 morphine milligram equivalents per day or greater (that is, high-dose prescriptions), and those who are using benzodiazepines concurrently.
Investigators at the CDC examined retail pharmacy data from IQVIA, a company that maintains information on prescriptions from approximately 50,400 retail pharmacies. They extracted data from 2012 through 2018 to analyze naloxone dispensing by region, urban versus rural status, prescriber specialty, and recipient characteristics (for example, age group, sex, out-of-pocket costs, and method of payment).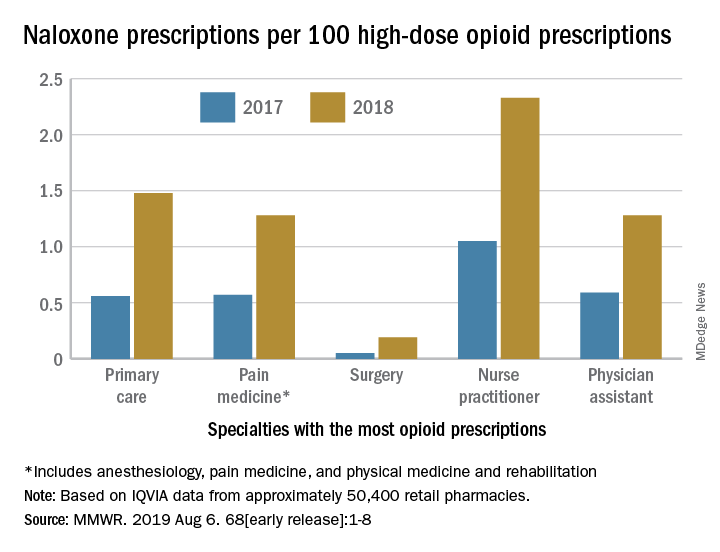
Dispensations doubled from 2017 to 2018
Naloxone dispensing from retail pharmacies increased from 0.4 prescriptions per 100,000 in 2012 to 170.2 prescriptions per 100,000 in 2018. From 2017 to 2018 alone, the number of prescriptions dispensed increased by 106%.
Despite consistency among state laws, naloxone dispensation varied by region. The average rate of naloxone prescriptions per 100 high-dose opioid prescriptions ranged from 0.2 in the lowest quartile to 2.9 in the highest quartile. In 2018, the rate of naloxone prescriptions per 100 high-dose opioid prescriptions ranged from 1.5 in metropolitan counties and 1.6 in the Northeast to 1.2 in rural counties and 1.3 in the Midwest. Rural counties were nearly three times more likely to be low-dispensing counties, compared with metropolitan counties.
The rate of naloxone prescriptions per 100 high-dose opioid prescriptions also varied by provider specialty. This rate was lowest among surgeons (0.2) and highest among psychiatrists (12.9).
Most naloxone prescriptions entailed out-of-pocket costs. About 71% of prescriptions paid for by Medicare entailed out-of-pocket costs, compared with 43.8% of prescriptions paid for by Medicaid, and 41.5% of prescriptions paid for by commercial insurance.
 Centers for Disease Control and Prevention
Centers for Disease Control and Prevention
More can be done

“It is clear from the data that there is still much needed education around the important role naloxone plays in reducing overdose deaths,” said Robert R. Redfield, MD, director of the CDC, in a press release. “The time is now to ensure all individuals who are prescribed high-dose opioids also receive naloxone as a potential life-saving intervention. As we aggressively confront what is the public health crisis of our time, CDC will continue to stress with health care providers the benefit of making this overdose-reversing medicine available to patients.”
“While we’ve seen these important increases [in naloxone prescriptions], we are not as far along as we’d like to be,” said Anne Schuchat, MD, principal deputy director of the CDC, during a press conference. “Cost is one of the issues, but I think awareness is another.” These data should prompt pharmacies to make sure that they stock naloxone and remind clinicians to consider naloxone when they prescribe opioids, she added. Patients and their family members should be aware of naloxone and ask their health care providers about it. “We’d really like to see the increase [in naloxone prescriptions] move much more rapidly,” she concluded.
The investigators disclosed no potential conflicts of interest.
SOURCE: Guy GP et al. MMWR Morb Mortal Wkly Rep. 2019 Aug 6.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
IV fluid weaning unnecessary after gastroenteritis rehydration
SEATTLE – Intravenous fluids can simply be stopped after children with acute viral gastroenteritis are rehydrated in the hospital; there’s no need for a slow wean, according to a review at the Connecticut Children’s Medical Center, Hartford.
Researchers found that children leave the hospital hours sooner, with no ill effects. “This study suggests that slowly weaning IV fluids may not be necessary,” said lead investigator Danielle Klima, DO, a University of Connecticut pediatrics resident.
The team at Connecticut Children’s noticed that weaning practices after gastroenteritis rehydration varied widely on the pediatric floors, and appeared to be largely provider dependent, with “much subjective decision making.” The team wanted to see if it made a difference one way or the other, Dr. Klima said at Pediatric Hospital Medicine.
During respiratory season, “our pediatric floors are surging. Saving even a couple hours to get these kids out” quicker matters, she said, noting that it’s likely the first time the issue has been studied.
The team reviewed 153 children aged 2 months to 18 years, 95 of whom had IV fluids stopped once physicians deemed they were fluid resuscitated and ready for an oral feeding trial; the other 58 were weaned, with at least two reductions by half before final discontinuation.
There were no significant differences in age, gender, race, or insurance type between the two groups. The mean age was 2.6 years, and there were slightly more boys. The ED triage level was a mean of 3.2 points in both groups on a scale of 1-5, with 1 being the most urgent. Children with serious comorbidities, chronic diarrhea, feeding tubes, severe electrolyte abnormalities, or feeding problems were among those excluded.
Overall length of stay was 36 hours in the stop group versus 40.5 hours in the weaning group (P = .004). Children left the hospital about 6 hours after IV fluids were discontinued, versus 26 hours after weaning was started (P less than .001).
Electrolyte abnormalities on admission were more common in the weaning group (65% versus 57%), but not significantly so (P = .541). Electrolyte abnormalities were also more common at the end of fluid resuscitation in the weaning arm, but again not significantly (65% 42%, P = .077).
Fluid resuscitation needed to be restarted in 15 children in the stop group (16%), versus 11 (19%) in the wean arm (P = .459). One child in the stop group (1%) versus four (7%) who were weaned were readmitted to the hospital within a week for acute viral gastroenteritis (P = .067).
“I expected we were taking a more conservative weaning approach in younger infants,” but age didn’t seem to affect whether patients were weaned or not, Dr. Klima said.
With the results in hand, “our group is taking a closer look at exactly what we are doing,” perhaps with an eye toward standardization or even a randomized trial, she said.
She noted that weaning still makes sense for a fussy toddler who refuses to take anything by mouth.
There was no external funding, and Dr. Klima had no disclosures. The conference was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
SEATTLE – Intravenous fluids can simply be stopped after children with acute viral gastroenteritis are rehydrated in the hospital; there’s no need for a slow wean, according to a review at the Connecticut Children’s Medical Center, Hartford.
Researchers found that children leave the hospital hours sooner, with no ill effects. “This study suggests that slowly weaning IV fluids may not be necessary,” said lead investigator Danielle Klima, DO, a University of Connecticut pediatrics resident.
The team at Connecticut Children’s noticed that weaning practices after gastroenteritis rehydration varied widely on the pediatric floors, and appeared to be largely provider dependent, with “much subjective decision making.” The team wanted to see if it made a difference one way or the other, Dr. Klima said at Pediatric Hospital Medicine.
During respiratory season, “our pediatric floors are surging. Saving even a couple hours to get these kids out” quicker matters, she said, noting that it’s likely the first time the issue has been studied.
The team reviewed 153 children aged 2 months to 18 years, 95 of whom had IV fluids stopped once physicians deemed they were fluid resuscitated and ready for an oral feeding trial; the other 58 were weaned, with at least two reductions by half before final discontinuation.
There were no significant differences in age, gender, race, or insurance type between the two groups. The mean age was 2.6 years, and there were slightly more boys. The ED triage level was a mean of 3.2 points in both groups on a scale of 1-5, with 1 being the most urgent. Children with serious comorbidities, chronic diarrhea, feeding tubes, severe electrolyte abnormalities, or feeding problems were among those excluded.
Overall length of stay was 36 hours in the stop group versus 40.5 hours in the weaning group (P = .004). Children left the hospital about 6 hours after IV fluids were discontinued, versus 26 hours after weaning was started (P less than .001).
Electrolyte abnormalities on admission were more common in the weaning group (65% versus 57%), but not significantly so (P = .541). Electrolyte abnormalities were also more common at the end of fluid resuscitation in the weaning arm, but again not significantly (65% 42%, P = .077).
Fluid resuscitation needed to be restarted in 15 children in the stop group (16%), versus 11 (19%) in the wean arm (P = .459). One child in the stop group (1%) versus four (7%) who were weaned were readmitted to the hospital within a week for acute viral gastroenteritis (P = .067).
“I expected we were taking a more conservative weaning approach in younger infants,” but age didn’t seem to affect whether patients were weaned or not, Dr. Klima said.
With the results in hand, “our group is taking a closer look at exactly what we are doing,” perhaps with an eye toward standardization or even a randomized trial, she said.
She noted that weaning still makes sense for a fussy toddler who refuses to take anything by mouth.
There was no external funding, and Dr. Klima had no disclosures. The conference was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
SEATTLE – Intravenous fluids can simply be stopped after children with acute viral gastroenteritis are rehydrated in the hospital; there’s no need for a slow wean, according to a review at the Connecticut Children’s Medical Center, Hartford.
Researchers found that children leave the hospital hours sooner, with no ill effects. “This study suggests that slowly weaning IV fluids may not be necessary,” said lead investigator Danielle Klima, DO, a University of Connecticut pediatrics resident.
The team at Connecticut Children’s noticed that weaning practices after gastroenteritis rehydration varied widely on the pediatric floors, and appeared to be largely provider dependent, with “much subjective decision making.” The team wanted to see if it made a difference one way or the other, Dr. Klima said at Pediatric Hospital Medicine.
During respiratory season, “our pediatric floors are surging. Saving even a couple hours to get these kids out” quicker matters, she said, noting that it’s likely the first time the issue has been studied.
The team reviewed 153 children aged 2 months to 18 years, 95 of whom had IV fluids stopped once physicians deemed they were fluid resuscitated and ready for an oral feeding trial; the other 58 were weaned, with at least two reductions by half before final discontinuation.
There were no significant differences in age, gender, race, or insurance type between the two groups. The mean age was 2.6 years, and there were slightly more boys. The ED triage level was a mean of 3.2 points in both groups on a scale of 1-5, with 1 being the most urgent. Children with serious comorbidities, chronic diarrhea, feeding tubes, severe electrolyte abnormalities, or feeding problems were among those excluded.
Overall length of stay was 36 hours in the stop group versus 40.5 hours in the weaning group (P = .004). Children left the hospital about 6 hours after IV fluids were discontinued, versus 26 hours after weaning was started (P less than .001).
Electrolyte abnormalities on admission were more common in the weaning group (65% versus 57%), but not significantly so (P = .541). Electrolyte abnormalities were also more common at the end of fluid resuscitation in the weaning arm, but again not significantly (65% 42%, P = .077).
Fluid resuscitation needed to be restarted in 15 children in the stop group (16%), versus 11 (19%) in the wean arm (P = .459). One child in the stop group (1%) versus four (7%) who were weaned were readmitted to the hospital within a week for acute viral gastroenteritis (P = .067).
“I expected we were taking a more conservative weaning approach in younger infants,” but age didn’t seem to affect whether patients were weaned or not, Dr. Klima said.
With the results in hand, “our group is taking a closer look at exactly what we are doing,” perhaps with an eye toward standardization or even a randomized trial, she said.
She noted that weaning still makes sense for a fussy toddler who refuses to take anything by mouth.
There was no external funding, and Dr. Klima had no disclosures. The conference was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, and the Academic Pediatric Association.
REPORTING FROM PHM 2019
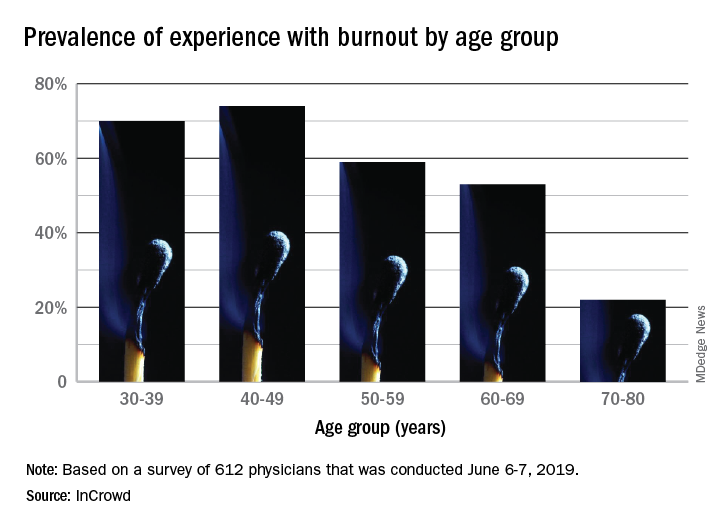
Burnout gets personal for 68% of physicians
by real-time market insights technology firm InCrowd.
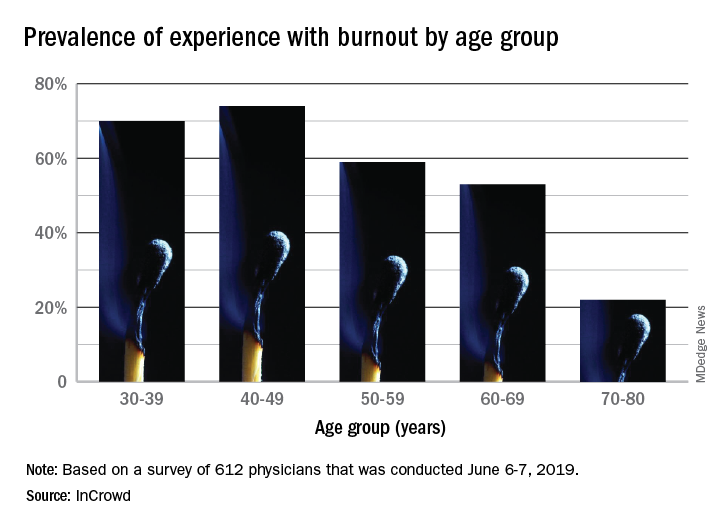
The overall prevalence of personal burnout experience was 68% among respondents, and another 28% said that they had not felt burned out but knew other physicians who had, InCrowd reported Aug. 6.
Specialty appeared to play a part given that 79% of primary care physicians reported experiencing burnout versus 57% of specialists. In response to an open-ended question about ability to manage burnout, the most common answer (23%) was that specialty played a large role, with “no role/all specialties affected equally” next at 13%. Equal proportions of respondents, however, said that specialists (24%) and primary care physicians (24%) were the group most affected, InCrowd said.
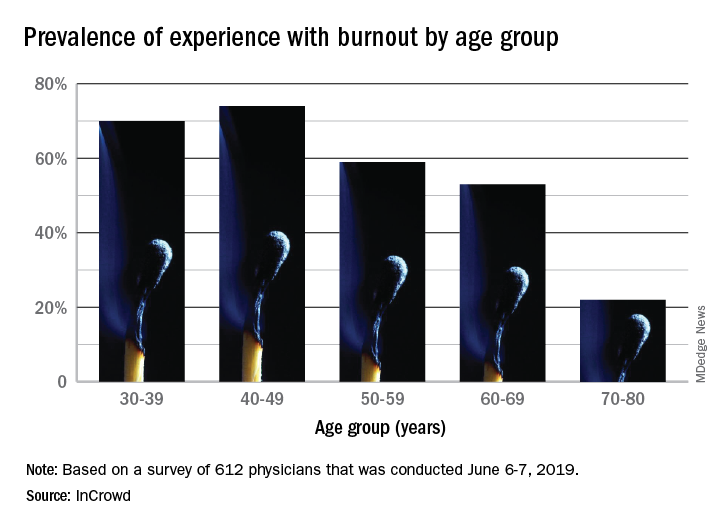
There was also a disconnect regarding age. When answering another open-ended question about the effects of age, 23% of those surveyed said that older physicians are more affected, compared with 9% who put the greater burden on younger physicians. The self-reporting of burnout, however, showed that younger physicians were much more likely to experience its effects than their older counterparts: 70% of those aged 30-39 years and 74% of those 40-49 versus 22% of those aged 70-80, InCrowd reported.
InCrowd noted that its results fall within the range of other recent surveys involving burnout in physicians that have shown levels that were lower, at 44% (MedScape, 2019) or 43.9% (American Academy of Family Physicians, 2019), and those that were higher, at 77.8% (The Physicians Foundation/Merritt Hawkins, 2018).
“The alarming persistence of physician burnout over the years and across multiple studies unfortunately demonstrates that we have not yet turned the tide on this problematic issue,” Diane Hayes, PhD, president of InCrowd, said in a statement accompanying the survey results. “Since we last looked at this in 2016, there really haven’t been any notable improvements. The healthcare industry would benefit from refining and expanding current initiatives to assure adequate staffing levels needed to deliver the quality care patients deserve.”
The survey was conducted June 6-7, 2019, and involved responses from 612 physicians (51% primary care providers, 49% specialists).
by real-time market insights technology firm InCrowd.
The overall prevalence of personal burnout experience was 68% among respondents, and another 28% said that they had not felt burned out but knew other physicians who had, InCrowd reported Aug. 6.
Specialty appeared to play a part given that 79% of primary care physicians reported experiencing burnout versus 57% of specialists. In response to an open-ended question about ability to manage burnout, the most common answer (23%) was that specialty played a large role, with “no role/all specialties affected equally” next at 13%. Equal proportions of respondents, however, said that specialists (24%) and primary care physicians (24%) were the group most affected, InCrowd said.
There was also a disconnect regarding age. When answering another open-ended question about the effects of age, 23% of those surveyed said that older physicians are more affected, compared with 9% who put the greater burden on younger physicians. The self-reporting of burnout, however, showed that younger physicians were much more likely to experience its effects than their older counterparts: 70% of those aged 30-39 years and 74% of those 40-49 versus 22% of those aged 70-80, InCrowd reported.
InCrowd noted that its results fall within the range of other recent surveys involving burnout in physicians that have shown levels that were lower, at 44% (MedScape, 2019) or 43.9% (American Academy of Family Physicians, 2019), and those that were higher, at 77.8% (The Physicians Foundation/Merritt Hawkins, 2018).
“The alarming persistence of physician burnout over the years and across multiple studies unfortunately demonstrates that we have not yet turned the tide on this problematic issue,” Diane Hayes, PhD, president of InCrowd, said in a statement accompanying the survey results. “Since we last looked at this in 2016, there really haven’t been any notable improvements. The healthcare industry would benefit from refining and expanding current initiatives to assure adequate staffing levels needed to deliver the quality care patients deserve.”
The survey was conducted June 6-7, 2019, and involved responses from 612 physicians (51% primary care providers, 49% specialists).
by real-time market insights technology firm InCrowd.
The overall prevalence of personal burnout experience was 68% among respondents, and another 28% said that they had not felt burned out but knew other physicians who had, InCrowd reported Aug. 6.
Specialty appeared to play a part given that 79% of primary care physicians reported experiencing burnout versus 57% of specialists. In response to an open-ended question about ability to manage burnout, the most common answer (23%) was that specialty played a large role, with “no role/all specialties affected equally” next at 13%. Equal proportions of respondents, however, said that specialists (24%) and primary care physicians (24%) were the group most affected, InCrowd said.
There was also a disconnect regarding age. When answering another open-ended question about the effects of age, 23% of those surveyed said that older physicians are more affected, compared with 9% who put the greater burden on younger physicians. The self-reporting of burnout, however, showed that younger physicians were much more likely to experience its effects than their older counterparts: 70% of those aged 30-39 years and 74% of those 40-49 versus 22% of those aged 70-80, InCrowd reported.
InCrowd noted that its results fall within the range of other recent surveys involving burnout in physicians that have shown levels that were lower, at 44% (MedScape, 2019) or 43.9% (American Academy of Family Physicians, 2019), and those that were higher, at 77.8% (The Physicians Foundation/Merritt Hawkins, 2018).
“The alarming persistence of physician burnout over the years and across multiple studies unfortunately demonstrates that we have not yet turned the tide on this problematic issue,” Diane Hayes, PhD, president of InCrowd, said in a statement accompanying the survey results. “Since we last looked at this in 2016, there really haven’t been any notable improvements. The healthcare industry would benefit from refining and expanding current initiatives to assure adequate staffing levels needed to deliver the quality care patients deserve.”
The survey was conducted June 6-7, 2019, and involved responses from 612 physicians (51% primary care providers, 49% specialists).
Professional coaching keeps doctors in the game
Physicians who receive professional coaching are less emotionally exhausted and less vulnerable to burnout, according to the results of a pilot study.
“This intervention adds to the growing literature of evidence-based approaches to promote physician well-being and should be considered a complementary strategy to be deployed in combination with other organizational approaches to improve system-level drivers of work-related stressors,” wrote Liselotte N. Dyrbye, MD, of the Mayo Clinic in Rochester, Minn., and coauthors in JAMA Internal Medicine.
Dr. Dyrbye and colleagues conducted a randomized pilot study of 88 Mayo Clinic physicians in the departments of medicine, family medicine, and pediatrics. Half (n = 44) received 3.5 hours of sessions facilitated by a professional coach. The other half (n = 44) served as controls. Participants’ well-being – in regard to burnout, quality of life, resilience, job satisfaction, engagement, and meaning at work – was surveyed at baseline and the study’s completion.
Physicians in the coaching group participated in a 1-hour initial telephone session, designed to establish a relationship between the physician and coach, as well as to assess needs, set goals, identify values, and create an action plan. During follow-up sessions, coaches would check in, help plan and set goals, and suggest strategies/changes to incorporate into daily life. Physicians were permitted to ask for support on any issue, but also were expected to see as many patients as their colleagues outside of the study.
After 6 months, physicians in the coaching group saw a significant decrease in emotional exhaustion by a mean of 5.2 points, compared with an increase of 1.5 points in the control group. At 5 months, absolute rates of high emotional exhaustion decreased by 19.5% in the coaching group and increased by 9.8% in the control group and absolute rates of overall burnout decreased by 17.1% in the coaching group and increased by 4.9% in the control group. Quality of life and resilience scores also improved, though there were no notable differences between groups in measures of job satisfaction, engagement, and meaning at work.
The authors noted their study’s limitations, which included a modest sample size and a volunteer group of participants.
In addition, the lower percentage of men in the study – 48 of 88 participants were women – may be a result of factors that deserve further investigation. Finally, burnout rates among volunteers were higher than those among other physicians, suggesting that “the study appealed to those in greatest need of the intervention.”
The study was funded by the Mayo Clinic department of medicine’s Program on Physician Well-Being and the Physician Foundation. Two of the authors – Dr. Dyrbye and Tait D. Shanafelt, MD, of Stanford (Calif.) University – reported being the coinventors of, and receiving royalties for, the Physician Well-Being Index, Medical Student Well-Being Index, Nurse Well-Being Index, and the Well-Being Index.
SOURCE: Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5. doi: 10.1001/jamainternmed.2019.2425.
Physicians who receive professional coaching are less emotionally exhausted and less vulnerable to burnout, according to the results of a pilot study.
“This intervention adds to the growing literature of evidence-based approaches to promote physician well-being and should be considered a complementary strategy to be deployed in combination with other organizational approaches to improve system-level drivers of work-related stressors,” wrote Liselotte N. Dyrbye, MD, of the Mayo Clinic in Rochester, Minn., and coauthors in JAMA Internal Medicine.
Dr. Dyrbye and colleagues conducted a randomized pilot study of 88 Mayo Clinic physicians in the departments of medicine, family medicine, and pediatrics. Half (n = 44) received 3.5 hours of sessions facilitated by a professional coach. The other half (n = 44) served as controls. Participants’ well-being – in regard to burnout, quality of life, resilience, job satisfaction, engagement, and meaning at work – was surveyed at baseline and the study’s completion.
Physicians in the coaching group participated in a 1-hour initial telephone session, designed to establish a relationship between the physician and coach, as well as to assess needs, set goals, identify values, and create an action plan. During follow-up sessions, coaches would check in, help plan and set goals, and suggest strategies/changes to incorporate into daily life. Physicians were permitted to ask for support on any issue, but also were expected to see as many patients as their colleagues outside of the study.
After 6 months, physicians in the coaching group saw a significant decrease in emotional exhaustion by a mean of 5.2 points, compared with an increase of 1.5 points in the control group. At 5 months, absolute rates of high emotional exhaustion decreased by 19.5% in the coaching group and increased by 9.8% in the control group and absolute rates of overall burnout decreased by 17.1% in the coaching group and increased by 4.9% in the control group. Quality of life and resilience scores also improved, though there were no notable differences between groups in measures of job satisfaction, engagement, and meaning at work.
The authors noted their study’s limitations, which included a modest sample size and a volunteer group of participants.
In addition, the lower percentage of men in the study – 48 of 88 participants were women – may be a result of factors that deserve further investigation. Finally, burnout rates among volunteers were higher than those among other physicians, suggesting that “the study appealed to those in greatest need of the intervention.”
The study was funded by the Mayo Clinic department of medicine’s Program on Physician Well-Being and the Physician Foundation. Two of the authors – Dr. Dyrbye and Tait D. Shanafelt, MD, of Stanford (Calif.) University – reported being the coinventors of, and receiving royalties for, the Physician Well-Being Index, Medical Student Well-Being Index, Nurse Well-Being Index, and the Well-Being Index.
SOURCE: Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5. doi: 10.1001/jamainternmed.2019.2425.
Physicians who receive professional coaching are less emotionally exhausted and less vulnerable to burnout, according to the results of a pilot study.
“This intervention adds to the growing literature of evidence-based approaches to promote physician well-being and should be considered a complementary strategy to be deployed in combination with other organizational approaches to improve system-level drivers of work-related stressors,” wrote Liselotte N. Dyrbye, MD, of the Mayo Clinic in Rochester, Minn., and coauthors in JAMA Internal Medicine.
Dr. Dyrbye and colleagues conducted a randomized pilot study of 88 Mayo Clinic physicians in the departments of medicine, family medicine, and pediatrics. Half (n = 44) received 3.5 hours of sessions facilitated by a professional coach. The other half (n = 44) served as controls. Participants’ well-being – in regard to burnout, quality of life, resilience, job satisfaction, engagement, and meaning at work – was surveyed at baseline and the study’s completion.
Physicians in the coaching group participated in a 1-hour initial telephone session, designed to establish a relationship between the physician and coach, as well as to assess needs, set goals, identify values, and create an action plan. During follow-up sessions, coaches would check in, help plan and set goals, and suggest strategies/changes to incorporate into daily life. Physicians were permitted to ask for support on any issue, but also were expected to see as many patients as their colleagues outside of the study.
After 6 months, physicians in the coaching group saw a significant decrease in emotional exhaustion by a mean of 5.2 points, compared with an increase of 1.5 points in the control group. At 5 months, absolute rates of high emotional exhaustion decreased by 19.5% in the coaching group and increased by 9.8% in the control group and absolute rates of overall burnout decreased by 17.1% in the coaching group and increased by 4.9% in the control group. Quality of life and resilience scores also improved, though there were no notable differences between groups in measures of job satisfaction, engagement, and meaning at work.
The authors noted their study’s limitations, which included a modest sample size and a volunteer group of participants.
In addition, the lower percentage of men in the study – 48 of 88 participants were women – may be a result of factors that deserve further investigation. Finally, burnout rates among volunteers were higher than those among other physicians, suggesting that “the study appealed to those in greatest need of the intervention.”
The study was funded by the Mayo Clinic department of medicine’s Program on Physician Well-Being and the Physician Foundation. Two of the authors – Dr. Dyrbye and Tait D. Shanafelt, MD, of Stanford (Calif.) University – reported being the coinventors of, and receiving royalties for, the Physician Well-Being Index, Medical Student Well-Being Index, Nurse Well-Being Index, and the Well-Being Index.
SOURCE: Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5. doi: 10.1001/jamainternmed.2019.2425.
FROM JAMA INTERNAL MEDICINE
Generalist knowledge is an asset
Hospitalists trained in family medicine
Lori J. Heim, MD, FAAFP, a hospitalist in practice at Scotland Memorial Hospital in Laurinburg, N.C., for the past 10 years, recalls when she first decided to pursue hospital medicine as a career. As a family physician in private practice who admitted patients to the local hospital in Pinehurst, N.C., and even followed them into the ICU, she needed a more flexible schedule when she became president-elect of the American Academy of Family Physicians (AAFP).
“My local hospital told me they had a policy against hiring family physicians as hospitalists. They didn’t consider us qualified,” Dr. Heim said. “I was incredulous when I first heard that because I already had full admitting privileges at the hospital. It made no sense, since they allowed me to manage my patients in the ICU.”
Then an opportunity opened at Scotland Memorial, located an hour away. “That has been a fabulous experience for me,” she said. The transition was relatively easy, following more than 2 decades of office practice. Dr. Heim’s hospitalist group now includes eight full-time clinicians who have a mix of family medicine and internal medicine backgrounds.
“I’ve never felt anything other than collegial support here. We go to the ER to evaluate patients and decide whether to admit them, and we do a lot of medical procedures. I’m not practicing pediatrics currently, but I have no problem conducting a gynecological exam. I think my experience in family medicine and primary care has been an asset,” Dr. Heim said. “I’m not sure I would be a hospitalist today if I had not been elected president of AAFP, but it was fortuitous.”
Respect for HTFMs is growing
Hospitalists trained in family medicine (HTFM) are a small but important segment of this field and of the membership of the Society of Hospital Medicine. The board specialties of physicians who work in the hospital are not always broken out in existing databases, but HTFMs are believed to represent about 8% of SHM members, and somewhere around 10%-15% of the total hospitalist workforce. According to SHM’s 2018 State of Hospital Medicine Report, 65% of hospital medicine groups employed at least one family medicine–trained provider in their group.1
SHM’s Special Interest Group (SIG) for HTFMs reports to the society’s Board of Directors. The American Academy of Family Medicine, with 131,400 members, also has a Member Interest Group (MIG) for HTFMs. When AAFP recently surveyed its members to identify their primary patient care practice location, only 4% named the hospital (not including the emergency department), while 3% said the hospital emergency department.2
Among 32,450 adult primary care-trained hospitalists surveyed for the June 2016 AAMC In Brief of the American Association of Medical Colleges, 81.9% of the hospitalists identified internal medicine as their specialty, while 5.2% identified themselves as family physicians.3 A 2014 Medical Group Management Association survey, which reported data for 4,200 hospitalists working in community hospitals, found that 82% were internal medicine trained, versus 10% in family medicine and 7% in pediatrics.
Family medicine hospitalists may be more common in rural areas or in small hospitals – where a clinician is often expected to wear more hats, said hospitalist David Goldstein, MD, FHM, assistant director of the family medicine residency program at Natividad Medical Center, Salinas, Calif., and cochair of SHM’s family medicine SIG. “In a smaller hospital, if there’s not sufficient volume to support full-time pediatric and adult hospital medicine services, a family medicine hospitalist might do both – and even help staff the ICU.”
A decade or so ago, much of the professional literature about the role of HTFMs suggested that some had experienced a lack of respect or of equal job opportunities, while others faced pay differentials.3-5 Since then, the field of hospital medicine has come a long way toward recognizing their contributions, although there are still hurdles to overcome, mainly involving issues of credentialing, to allow HTFMs to play equal roles in the hospital, the ICU, or in residency training. The SHM 2018 State of Hospital Medicine Report reveals that HTFMs actually made slightly higher salaries on average than their internist colleagues, $301,833 versus $300,030.
Prior to the advent of hospital medicine, both family medicine and internal medicine physicians practiced in much the same way in their medical offices, and visited their patients in the hospital, said Claudia Geyer, MD, SFHM, system chief of hospital medicine at Central Maine Healthcare in Lewiston. She is trained and boarded in both family and internal medicine. “When hospital medicine launched, its heavy academic emphasis on internists led to underrecognition of the continued contributions of family medicine. Family physicians never left the hospital setting and – in certain locales – were the predominant hospitalists. We just waited for the recognition to catch up with the reality,” Dr. Geyer said.
“I don’t feel family medicine for hospitalists is nearly the stepchild of internal medicine that it was when I first started,” Dr. Heim said. “In my multihospital hospitalist group, I haven’t seen anything to suggest that they treat family medicine hospitalists as second class.” The demand for hospitalists is greater than internists can fill, while clearly the public is not concerned about these distinctions, she said.
Whether clinicians are board certified in family medicine or internal medicine may be less important to their skills for practicing in the hospital than which residency program they completed, what emphasis it placed on working in the hospital or ICU, electives completed, and other past experience. “Some family medicine residencies offer more or less hospital experience,” Dr. Heim said.
Jasen Gundersen, MD, MBA, CPE, SFHM, president of acute and post-acute services for the national hospital services company TeamHealth, agreed that there has been dramatic improvement in the status of HTFMs. He is one, and still practices as a hospitalist at Boca Raton (Fla.) Regional Hospital when administrative responsibilities permit.
TeamHealth has long been open to family medicine doctors, Dr. Gundersen added, although some of the medical staff at hospitals that contract with TeamHealth have issues with it. “We will talk to them about it,” he said. “We hire hospitalists who can do the work, and we evaluate them based on their background and skill set, where they’ve practiced and for how long. We want people who are experienced and good at managing hospitalized patients. For new residency grads, we look at their electives and the focus of their training.”
What is home for HTFMs?
Where are HTFMs most likely to find their professional home? “That’s hard to answer,” said Patricia Seymour, MD, FHM, FAAFP, an academic hospitalist at the University of Massachusetts-Worcester. “In the last 4-5 years, SHM has worked very hard to create a space for HTFMs. AAFP has a hospital medicine track at their annual meeting, and that’s a good thing. But they also need to protect family physicians’ right to practice in any setting they choose. For those pursuing hospital medicine, there’s a different career trajectory, different CME needs, and different recertification needs.”
Dr. Seymour is the executive cochair of SHM’s family medicine SIG and serves as interim chief of a family medicine hospitalist group that provides inpatient training for a family practice residency, where up to a third of the 12 residents each year go on to pursue hospital medicine as a career. “We have the second-oldest family medicine–specific hospitalist group in the country, so our residency training has an emphasis on hospital medicine,” she explained.
“Because I’m a practicing hospitalist, the residents come to me seeking advice. I appreciate the training I received as a family physician in communication science, palliative care, geriatrics, family systems theory, and public health. I wouldn’t have done it any other way, and that’s how I counsel our students and residents,” she said. Others suggest that the generalist training and diverse experiences of family medicine can be a gift for a doctor who later chooses hospital medicine.
AAFP is a large umbrella organization and the majority of its members practice primary care, Dr. Heim said. “I don’t know the percentage of HTFMs who are members of AAFP. Some no doubt belong to both AAFP and SHM.” Even though both groups have recognized this important subset of their members who chose the field of hospital medicine and its status as a career track, it can be a stretch for family medicine to embrace hospitalists.
“It inherently goes against our training, which is to work in outpatient, inpatient, obstetric, pediatric, and adult settings,” Dr. Heim said. “It’s difficult to reconcile giving up a big part of what defined your training – that range of settings. I remember feeling like I should apologize to other family medicine doctors for choosing this path.”
Credentialing opportunities and barriers
For the diverse group of practicing HTFMs, credentialing and scope of practice represent their biggest current issues. A designation of Focused Practice in Hospital Medicine (FPHM) has been offered jointly since 2010 by the American Board of Family Medicine (ABFM) and the American Board of Internal Medicine (ABIM), although their specific requirements vary.
Eligible hospitalist candidates for the focused practice exam must have an unrestricted medical license, maintenance of current primary certification, and verification of three years of unsupervised hospital medicine practice experience. ABIM views FPHM not as a subspecialty, but as a variation of internal medicine certification, identifying diplomates who are board-certified in internal medicine with a hospital medicine specialization. They do not have to take the general internal medicine recertification exam if they qualify for FPHM.
ABFM-certified family physicians who work primarily in a hospital setting can take the same test for FPHM, with the same eligibility requirements. But ABFM does not consider focused practice a subspecialty, or the Certificate of Added Qualifications in Family Medicine as sufficient for board certification. That means family physicians also need to take its general board exam in order to maintain their ABFM board certification.
ABFM’s decision not to accept the focused practice designation as sufficient for boarding was disappointing to a lot of hospitalists, said Laura “Nell” Hodo, MD, FAAFP, chair of AAFP’s hospital medicine MIG, and a pediatric academic hospitalist at Icahn School of Medicine at Mount Sinai, New York. “Many family physicians practice hospital medicine exclusively and would prefer to take one boarding exam instead of two, and not have to do CME and board review in areas where we don’t practice anymore,” Dr. Hodo said, adding that she hopes that this decision could be revisited in the future.
A number of 1-year hospital medicine fellowships across the country provide additional training opportunities for both family practice and internal medicine residency graduates. These fellowships do not offer board certification or designated specialty credentialing for hospitalists and are not recognized by the American College of Graduate Medical Education (ACGME), which sets standards for residency and fellowship training. “But they reflect a need and an interest in optimizing the knowledge of hospital medicine and developing the specific skills needed to practice it well,” Dr. Geyer noted.
She directs a program for one to three fellows per year out of the Central Maine Family Medicine Residency program and Central Maine Medical Center in Lewiston, and is now recruiting her tenth class. At least 13 other hospital medicine fellowships, out of about 40 nationwide, are family medicine based. “We rely heavily on the Core Competencies in Hospital Medicine developed by SHM, which emphasize clinical conditions, medical procedures, and health care systems. Gaining fluency in the latter is really what makes hospital medicine unique,” Dr. Geyer said.
Often residency graduates seeking work in hospital medicine are insufficiently prepared for hospital billing and coding, enacting safe transitions of care, providing palliative care, and understanding how to impact their health care systems for quality improvement, patient safety and the like, she added.
Dr. Geyer said her fellowship does not mean just being a poorly paid hospitalist for a year. “The fellows are clearly trainees, getting the full benefit of our supervision and supplemental training focused on enhanced clinical and procedural exposure, but also on academics, quality improvement, leadership, and efficiency,” she said. “All of our fellows join SHM, go to the Annual Conference, propose case studies, do longitudinal quality or safety projects, and learn the other aspects of hospital medicine not well-taught in residency. We train them to be highly functional hospitalists right out of the gate.”
Until recently, another barrier for HTFMs was their ability to be on the faculty of internal medicine residency programs. Previous language from ACGME indicated that family medicine-trained physicians could not serve as faculty for these programs, Dr. Goldstein said. SHM has lobbied ACGME to change that rule, which could enable family medicine hospitalists who had achieved FPHM designation to be attendings and to teach internal medicine residents.
Needed in critical care – but not credentialed
One of the biggest frustrations for family medicine hospitalists is clarifying their role in the ICU. SHM’s Education Committee recently surveyed hospitalist members who practice in the ICU, finding that at least half felt obliged to practice beyond their scope, 90 percent occasionally perceived insufficient support from intensivists, and two-thirds reported moderate difficulty transferring patients to higher levels of intensive care.7 The respondents overwhelmingly indicated that they wanted more training and education in critical care medicine.
“I want to highlight the fact that in some settings family physicians are the sole providers of critical care,” Dr. Goldstein said. Meanwhile, the standards of the Leapfrog Group, a coalition of health care purchasers, call for ICUs to be staffed by physicians certified in critical care, even though there is a growing shortage of credentialed intensivists to treat an increasing number of older, sicker, critically ill patients.
Some internal medicine physicians don’t want to have anything to do with the ICU because of the medical and legal risks, said David Aymond, MD, a family physician and hospitalist at Byrd Regional Hospital in Leesville, La. “There’s a bunch of sick people in the ICU, and when some doctors like me started doing critical care, we realized we liked it. Depending on your locale, if you are doing hospital medicine, critically ill patients are going to fall in your lap,” he said. “But if you don’t have the skills, that could lead to poor outcomes and unnecessary transfers.”
Dr. Aymond started his career in family medicine. “When I got into residency, I saw how much critical care was needed in rural communities. I decided I would learn everything I could about it. I did a hospital medicine fellowship at the University of Alabama, which included considerable involvement in the ICU. When I went to Byrd Regional, a 60-bed facility with eight ICU beds, we did all of the critical care, and word started to spread in the community. My hospitalist partner and I are now on call 24/7 alternating weeks, doing the majority of the critical care and taking care of anything that goes on in an ICU at a larger center, although we often lack access to consultation services,” he explained.
“We needed to get the attention of the Society of Critical Care Medicine (SCCM) to communicate the scope of this problem. These doctors are doing critical care but there is no official medical training or recognition for them. So they’re legally out on a limb, even though often they are literally the only person available to do it,” Dr. Aymond said. “Certainly there’s a skills gap between HTFMs and board-certified intensivists, but some of that gap has to do with the volume of patients they have seen in the ICU and their comfort level,” he said.
SHM is pursuing initiatives to help address this gap, including collaborating with SCCM on developing a rigorous critical care training curriculum for internal medicine and family medicine hospitalists, with coursework drawn from existing sources, said Eric Siegal, MD, SFHM, a critical care physician in Milwaukee. “It doesn’t replace a 2-year critical care fellowship, but it will be a lot more than what’s currently out there for the nonintensivist who practices in the ICU.” SCCM has approved moving forward with the advanced training curriculum, he said.
Another priority is to try to create a pathway that could permit family medicine–trained hospitalists to apply for existing critical care fellowships, as internal medicine doctors are now able to do. SHM has lobbied ABFM to create a pathway to subspecialty certification in critical care medicine, similar to those that exist for internists and emergency physicians, Dr. Goldstein said, adding that ACGME, which controls access to fellowships, will be the next step. Dr. Aymond expects that there will be a lot of hoops to jump through.
“David Aymond is an exceptional hospitalist,” Dr. Siegal added. “He thinks and talks like an intensivist, but it took concerted and self-directed effort for him to get there. Family practitioners are a significant part of the rural critical care workforce, but their training generally does not adequately prepare them for this role – unless they have made a conscious effort to pursue additional training,” he said.
“My message to family practitioners is not that they’re not good enough to do this, but rather that they are being asked to do something they weren’t trained for. How can we help them do it well?”
References
1. Society of Hospital Medicine (SHM) Practice Analysis Committee. 2018 State of Hospital Medicine Report; Oct 2018.
2. American Academy of Family Physicians Member Census, Dec 31, 2017.
3. Jones KC et al. Hospitalists: A growing part of the primary care workforce. AAMC Analysis in Brief; June 2016; 16(5):1.
4. Berczuk C. Uniquely positioned. The Hospitalist; July 2009.
5. Iqbal Y. Family medicine hospitalists: Separate and unequal? Today’s Hospitalist; May 2007.
6. Kinnan JP. The family way. The Hospitalist; Nov 2007.
7. Sweigart JR et al. Characterizing hospitalist practice and perceptions of critical care delivery. J Hosp Med. 2018 Jan 1;13(1):6-12.
Hospitalists trained in family medicine
Hospitalists trained in family medicine
Lori J. Heim, MD, FAAFP, a hospitalist in practice at Scotland Memorial Hospital in Laurinburg, N.C., for the past 10 years, recalls when she first decided to pursue hospital medicine as a career. As a family physician in private practice who admitted patients to the local hospital in Pinehurst, N.C., and even followed them into the ICU, she needed a more flexible schedule when she became president-elect of the American Academy of Family Physicians (AAFP).
“My local hospital told me they had a policy against hiring family physicians as hospitalists. They didn’t consider us qualified,” Dr. Heim said. “I was incredulous when I first heard that because I already had full admitting privileges at the hospital. It made no sense, since they allowed me to manage my patients in the ICU.”
Then an opportunity opened at Scotland Memorial, located an hour away. “That has been a fabulous experience for me,” she said. The transition was relatively easy, following more than 2 decades of office practice. Dr. Heim’s hospitalist group now includes eight full-time clinicians who have a mix of family medicine and internal medicine backgrounds.
“I’ve never felt anything other than collegial support here. We go to the ER to evaluate patients and decide whether to admit them, and we do a lot of medical procedures. I’m not practicing pediatrics currently, but I have no problem conducting a gynecological exam. I think my experience in family medicine and primary care has been an asset,” Dr. Heim said. “I’m not sure I would be a hospitalist today if I had not been elected president of AAFP, but it was fortuitous.”
Respect for HTFMs is growing
Hospitalists trained in family medicine (HTFM) are a small but important segment of this field and of the membership of the Society of Hospital Medicine. The board specialties of physicians who work in the hospital are not always broken out in existing databases, but HTFMs are believed to represent about 8% of SHM members, and somewhere around 10%-15% of the total hospitalist workforce. According to SHM’s 2018 State of Hospital Medicine Report, 65% of hospital medicine groups employed at least one family medicine–trained provider in their group.1
SHM’s Special Interest Group (SIG) for HTFMs reports to the society’s Board of Directors. The American Academy of Family Medicine, with 131,400 members, also has a Member Interest Group (MIG) for HTFMs. When AAFP recently surveyed its members to identify their primary patient care practice location, only 4% named the hospital (not including the emergency department), while 3% said the hospital emergency department.2
Among 32,450 adult primary care-trained hospitalists surveyed for the June 2016 AAMC In Brief of the American Association of Medical Colleges, 81.9% of the hospitalists identified internal medicine as their specialty, while 5.2% identified themselves as family physicians.3 A 2014 Medical Group Management Association survey, which reported data for 4,200 hospitalists working in community hospitals, found that 82% were internal medicine trained, versus 10% in family medicine and 7% in pediatrics.
Family medicine hospitalists may be more common in rural areas or in small hospitals – where a clinician is often expected to wear more hats, said hospitalist David Goldstein, MD, FHM, assistant director of the family medicine residency program at Natividad Medical Center, Salinas, Calif., and cochair of SHM’s family medicine SIG. “In a smaller hospital, if there’s not sufficient volume to support full-time pediatric and adult hospital medicine services, a family medicine hospitalist might do both – and even help staff the ICU.”
A decade or so ago, much of the professional literature about the role of HTFMs suggested that some had experienced a lack of respect or of equal job opportunities, while others faced pay differentials.3-5 Since then, the field of hospital medicine has come a long way toward recognizing their contributions, although there are still hurdles to overcome, mainly involving issues of credentialing, to allow HTFMs to play equal roles in the hospital, the ICU, or in residency training. The SHM 2018 State of Hospital Medicine Report reveals that HTFMs actually made slightly higher salaries on average than their internist colleagues, $301,833 versus $300,030.
Prior to the advent of hospital medicine, both family medicine and internal medicine physicians practiced in much the same way in their medical offices, and visited their patients in the hospital, said Claudia Geyer, MD, SFHM, system chief of hospital medicine at Central Maine Healthcare in Lewiston. She is trained and boarded in both family and internal medicine. “When hospital medicine launched, its heavy academic emphasis on internists led to underrecognition of the continued contributions of family medicine. Family physicians never left the hospital setting and – in certain locales – were the predominant hospitalists. We just waited for the recognition to catch up with the reality,” Dr. Geyer said.
“I don’t feel family medicine for hospitalists is nearly the stepchild of internal medicine that it was when I first started,” Dr. Heim said. “In my multihospital hospitalist group, I haven’t seen anything to suggest that they treat family medicine hospitalists as second class.” The demand for hospitalists is greater than internists can fill, while clearly the public is not concerned about these distinctions, she said.
Whether clinicians are board certified in family medicine or internal medicine may be less important to their skills for practicing in the hospital than which residency program they completed, what emphasis it placed on working in the hospital or ICU, electives completed, and other past experience. “Some family medicine residencies offer more or less hospital experience,” Dr. Heim said.
Jasen Gundersen, MD, MBA, CPE, SFHM, president of acute and post-acute services for the national hospital services company TeamHealth, agreed that there has been dramatic improvement in the status of HTFMs. He is one, and still practices as a hospitalist at Boca Raton (Fla.) Regional Hospital when administrative responsibilities permit.
TeamHealth has long been open to family medicine doctors, Dr. Gundersen added, although some of the medical staff at hospitals that contract with TeamHealth have issues with it. “We will talk to them about it,” he said. “We hire hospitalists who can do the work, and we evaluate them based on their background and skill set, where they’ve practiced and for how long. We want people who are experienced and good at managing hospitalized patients. For new residency grads, we look at their electives and the focus of their training.”
What is home for HTFMs?
Where are HTFMs most likely to find their professional home? “That’s hard to answer,” said Patricia Seymour, MD, FHM, FAAFP, an academic hospitalist at the University of Massachusetts-Worcester. “In the last 4-5 years, SHM has worked very hard to create a space for HTFMs. AAFP has a hospital medicine track at their annual meeting, and that’s a good thing. But they also need to protect family physicians’ right to practice in any setting they choose. For those pursuing hospital medicine, there’s a different career trajectory, different CME needs, and different recertification needs.”
Dr. Seymour is the executive cochair of SHM’s family medicine SIG and serves as interim chief of a family medicine hospitalist group that provides inpatient training for a family practice residency, where up to a third of the 12 residents each year go on to pursue hospital medicine as a career. “We have the second-oldest family medicine–specific hospitalist group in the country, so our residency training has an emphasis on hospital medicine,” she explained.
“Because I’m a practicing hospitalist, the residents come to me seeking advice. I appreciate the training I received as a family physician in communication science, palliative care, geriatrics, family systems theory, and public health. I wouldn’t have done it any other way, and that’s how I counsel our students and residents,” she said. Others suggest that the generalist training and diverse experiences of family medicine can be a gift for a doctor who later chooses hospital medicine.
AAFP is a large umbrella organization and the majority of its members practice primary care, Dr. Heim said. “I don’t know the percentage of HTFMs who are members of AAFP. Some no doubt belong to both AAFP and SHM.” Even though both groups have recognized this important subset of their members who chose the field of hospital medicine and its status as a career track, it can be a stretch for family medicine to embrace hospitalists.
“It inherently goes against our training, which is to work in outpatient, inpatient, obstetric, pediatric, and adult settings,” Dr. Heim said. “It’s difficult to reconcile giving up a big part of what defined your training – that range of settings. I remember feeling like I should apologize to other family medicine doctors for choosing this path.”
Credentialing opportunities and barriers
For the diverse group of practicing HTFMs, credentialing and scope of practice represent their biggest current issues. A designation of Focused Practice in Hospital Medicine (FPHM) has been offered jointly since 2010 by the American Board of Family Medicine (ABFM) and the American Board of Internal Medicine (ABIM), although their specific requirements vary.
Eligible hospitalist candidates for the focused practice exam must have an unrestricted medical license, maintenance of current primary certification, and verification of three years of unsupervised hospital medicine practice experience. ABIM views FPHM not as a subspecialty, but as a variation of internal medicine certification, identifying diplomates who are board-certified in internal medicine with a hospital medicine specialization. They do not have to take the general internal medicine recertification exam if they qualify for FPHM.
ABFM-certified family physicians who work primarily in a hospital setting can take the same test for FPHM, with the same eligibility requirements. But ABFM does not consider focused practice a subspecialty, or the Certificate of Added Qualifications in Family Medicine as sufficient for board certification. That means family physicians also need to take its general board exam in order to maintain their ABFM board certification.
ABFM’s decision not to accept the focused practice designation as sufficient for boarding was disappointing to a lot of hospitalists, said Laura “Nell” Hodo, MD, FAAFP, chair of AAFP’s hospital medicine MIG, and a pediatric academic hospitalist at Icahn School of Medicine at Mount Sinai, New York. “Many family physicians practice hospital medicine exclusively and would prefer to take one boarding exam instead of two, and not have to do CME and board review in areas where we don’t practice anymore,” Dr. Hodo said, adding that she hopes that this decision could be revisited in the future.
A number of 1-year hospital medicine fellowships across the country provide additional training opportunities for both family practice and internal medicine residency graduates. These fellowships do not offer board certification or designated specialty credentialing for hospitalists and are not recognized by the American College of Graduate Medical Education (ACGME), which sets standards for residency and fellowship training. “But they reflect a need and an interest in optimizing the knowledge of hospital medicine and developing the specific skills needed to practice it well,” Dr. Geyer noted.
She directs a program for one to three fellows per year out of the Central Maine Family Medicine Residency program and Central Maine Medical Center in Lewiston, and is now recruiting her tenth class. At least 13 other hospital medicine fellowships, out of about 40 nationwide, are family medicine based. “We rely heavily on the Core Competencies in Hospital Medicine developed by SHM, which emphasize clinical conditions, medical procedures, and health care systems. Gaining fluency in the latter is really what makes hospital medicine unique,” Dr. Geyer said.
Often residency graduates seeking work in hospital medicine are insufficiently prepared for hospital billing and coding, enacting safe transitions of care, providing palliative care, and understanding how to impact their health care systems for quality improvement, patient safety and the like, she added.
Dr. Geyer said her fellowship does not mean just being a poorly paid hospitalist for a year. “The fellows are clearly trainees, getting the full benefit of our supervision and supplemental training focused on enhanced clinical and procedural exposure, but also on academics, quality improvement, leadership, and efficiency,” she said. “All of our fellows join SHM, go to the Annual Conference, propose case studies, do longitudinal quality or safety projects, and learn the other aspects of hospital medicine not well-taught in residency. We train them to be highly functional hospitalists right out of the gate.”
Until recently, another barrier for HTFMs was their ability to be on the faculty of internal medicine residency programs. Previous language from ACGME indicated that family medicine-trained physicians could not serve as faculty for these programs, Dr. Goldstein said. SHM has lobbied ACGME to change that rule, which could enable family medicine hospitalists who had achieved FPHM designation to be attendings and to teach internal medicine residents.
Needed in critical care – but not credentialed
One of the biggest frustrations for family medicine hospitalists is clarifying their role in the ICU. SHM’s Education Committee recently surveyed hospitalist members who practice in the ICU, finding that at least half felt obliged to practice beyond their scope, 90 percent occasionally perceived insufficient support from intensivists, and two-thirds reported moderate difficulty transferring patients to higher levels of intensive care.7 The respondents overwhelmingly indicated that they wanted more training and education in critical care medicine.
“I want to highlight the fact that in some settings family physicians are the sole providers of critical care,” Dr. Goldstein said. Meanwhile, the standards of the Leapfrog Group, a coalition of health care purchasers, call for ICUs to be staffed by physicians certified in critical care, even though there is a growing shortage of credentialed intensivists to treat an increasing number of older, sicker, critically ill patients.
Some internal medicine physicians don’t want to have anything to do with the ICU because of the medical and legal risks, said David Aymond, MD, a family physician and hospitalist at Byrd Regional Hospital in Leesville, La. “There’s a bunch of sick people in the ICU, and when some doctors like me started doing critical care, we realized we liked it. Depending on your locale, if you are doing hospital medicine, critically ill patients are going to fall in your lap,” he said. “But if you don’t have the skills, that could lead to poor outcomes and unnecessary transfers.”
Dr. Aymond started his career in family medicine. “When I got into residency, I saw how much critical care was needed in rural communities. I decided I would learn everything I could about it. I did a hospital medicine fellowship at the University of Alabama, which included considerable involvement in the ICU. When I went to Byrd Regional, a 60-bed facility with eight ICU beds, we did all of the critical care, and word started to spread in the community. My hospitalist partner and I are now on call 24/7 alternating weeks, doing the majority of the critical care and taking care of anything that goes on in an ICU at a larger center, although we often lack access to consultation services,” he explained.
“We needed to get the attention of the Society of Critical Care Medicine (SCCM) to communicate the scope of this problem. These doctors are doing critical care but there is no official medical training or recognition for them. So they’re legally out on a limb, even though often they are literally the only person available to do it,” Dr. Aymond said. “Certainly there’s a skills gap between HTFMs and board-certified intensivists, but some of that gap has to do with the volume of patients they have seen in the ICU and their comfort level,” he said.
SHM is pursuing initiatives to help address this gap, including collaborating with SCCM on developing a rigorous critical care training curriculum for internal medicine and family medicine hospitalists, with coursework drawn from existing sources, said Eric Siegal, MD, SFHM, a critical care physician in Milwaukee. “It doesn’t replace a 2-year critical care fellowship, but it will be a lot more than what’s currently out there for the nonintensivist who practices in the ICU.” SCCM has approved moving forward with the advanced training curriculum, he said.
Another priority is to try to create a pathway that could permit family medicine–trained hospitalists to apply for existing critical care fellowships, as internal medicine doctors are now able to do. SHM has lobbied ABFM to create a pathway to subspecialty certification in critical care medicine, similar to those that exist for internists and emergency physicians, Dr. Goldstein said, adding that ACGME, which controls access to fellowships, will be the next step. Dr. Aymond expects that there will be a lot of hoops to jump through.
“David Aymond is an exceptional hospitalist,” Dr. Siegal added. “He thinks and talks like an intensivist, but it took concerted and self-directed effort for him to get there. Family practitioners are a significant part of the rural critical care workforce, but their training generally does not adequately prepare them for this role – unless they have made a conscious effort to pursue additional training,” he said.
“My message to family practitioners is not that they’re not good enough to do this, but rather that they are being asked to do something they weren’t trained for. How can we help them do it well?”
References
1. Society of Hospital Medicine (SHM) Practice Analysis Committee. 2018 State of Hospital Medicine Report; Oct 2018.
2. American Academy of Family Physicians Member Census, Dec 31, 2017.
3. Jones KC et al. Hospitalists: A growing part of the primary care workforce. AAMC Analysis in Brief; June 2016; 16(5):1.
4. Berczuk C. Uniquely positioned. The Hospitalist; July 2009.
5. Iqbal Y. Family medicine hospitalists: Separate and unequal? Today’s Hospitalist; May 2007.
6. Kinnan JP. The family way. The Hospitalist; Nov 2007.
7. Sweigart JR et al. Characterizing hospitalist practice and perceptions of critical care delivery. J Hosp Med. 2018 Jan 1;13(1):6-12.
Lori J. Heim, MD, FAAFP, a hospitalist in practice at Scotland Memorial Hospital in Laurinburg, N.C., for the past 10 years, recalls when she first decided to pursue hospital medicine as a career. As a family physician in private practice who admitted patients to the local hospital in Pinehurst, N.C., and even followed them into the ICU, she needed a more flexible schedule when she became president-elect of the American Academy of Family Physicians (AAFP).
“My local hospital told me they had a policy against hiring family physicians as hospitalists. They didn’t consider us qualified,” Dr. Heim said. “I was incredulous when I first heard that because I already had full admitting privileges at the hospital. It made no sense, since they allowed me to manage my patients in the ICU.”
Then an opportunity opened at Scotland Memorial, located an hour away. “That has been a fabulous experience for me,” she said. The transition was relatively easy, following more than 2 decades of office practice. Dr. Heim’s hospitalist group now includes eight full-time clinicians who have a mix of family medicine and internal medicine backgrounds.
“I’ve never felt anything other than collegial support here. We go to the ER to evaluate patients and decide whether to admit them, and we do a lot of medical procedures. I’m not practicing pediatrics currently, but I have no problem conducting a gynecological exam. I think my experience in family medicine and primary care has been an asset,” Dr. Heim said. “I’m not sure I would be a hospitalist today if I had not been elected president of AAFP, but it was fortuitous.”
Respect for HTFMs is growing
Hospitalists trained in family medicine (HTFM) are a small but important segment of this field and of the membership of the Society of Hospital Medicine. The board specialties of physicians who work in the hospital are not always broken out in existing databases, but HTFMs are believed to represent about 8% of SHM members, and somewhere around 10%-15% of the total hospitalist workforce. According to SHM’s 2018 State of Hospital Medicine Report, 65% of hospital medicine groups employed at least one family medicine–trained provider in their group.1
SHM’s Special Interest Group (SIG) for HTFMs reports to the society’s Board of Directors. The American Academy of Family Medicine, with 131,400 members, also has a Member Interest Group (MIG) for HTFMs. When AAFP recently surveyed its members to identify their primary patient care practice location, only 4% named the hospital (not including the emergency department), while 3% said the hospital emergency department.2
Among 32,450 adult primary care-trained hospitalists surveyed for the June 2016 AAMC In Brief of the American Association of Medical Colleges, 81.9% of the hospitalists identified internal medicine as their specialty, while 5.2% identified themselves as family physicians.3 A 2014 Medical Group Management Association survey, which reported data for 4,200 hospitalists working in community hospitals, found that 82% were internal medicine trained, versus 10% in family medicine and 7% in pediatrics.
Family medicine hospitalists may be more common in rural areas or in small hospitals – where a clinician is often expected to wear more hats, said hospitalist David Goldstein, MD, FHM, assistant director of the family medicine residency program at Natividad Medical Center, Salinas, Calif., and cochair of SHM’s family medicine SIG. “In a smaller hospital, if there’s not sufficient volume to support full-time pediatric and adult hospital medicine services, a family medicine hospitalist might do both – and even help staff the ICU.”
A decade or so ago, much of the professional literature about the role of HTFMs suggested that some had experienced a lack of respect or of equal job opportunities, while others faced pay differentials.3-5 Since then, the field of hospital medicine has come a long way toward recognizing their contributions, although there are still hurdles to overcome, mainly involving issues of credentialing, to allow HTFMs to play equal roles in the hospital, the ICU, or in residency training. The SHM 2018 State of Hospital Medicine Report reveals that HTFMs actually made slightly higher salaries on average than their internist colleagues, $301,833 versus $300,030.
Prior to the advent of hospital medicine, both family medicine and internal medicine physicians practiced in much the same way in their medical offices, and visited their patients in the hospital, said Claudia Geyer, MD, SFHM, system chief of hospital medicine at Central Maine Healthcare in Lewiston. She is trained and boarded in both family and internal medicine. “When hospital medicine launched, its heavy academic emphasis on internists led to underrecognition of the continued contributions of family medicine. Family physicians never left the hospital setting and – in certain locales – were the predominant hospitalists. We just waited for the recognition to catch up with the reality,” Dr. Geyer said.
“I don’t feel family medicine for hospitalists is nearly the stepchild of internal medicine that it was when I first started,” Dr. Heim said. “In my multihospital hospitalist group, I haven’t seen anything to suggest that they treat family medicine hospitalists as second class.” The demand for hospitalists is greater than internists can fill, while clearly the public is not concerned about these distinctions, she said.
Whether clinicians are board certified in family medicine or internal medicine may be less important to their skills for practicing in the hospital than which residency program they completed, what emphasis it placed on working in the hospital or ICU, electives completed, and other past experience. “Some family medicine residencies offer more or less hospital experience,” Dr. Heim said.
Jasen Gundersen, MD, MBA, CPE, SFHM, president of acute and post-acute services for the national hospital services company TeamHealth, agreed that there has been dramatic improvement in the status of HTFMs. He is one, and still practices as a hospitalist at Boca Raton (Fla.) Regional Hospital when administrative responsibilities permit.
TeamHealth has long been open to family medicine doctors, Dr. Gundersen added, although some of the medical staff at hospitals that contract with TeamHealth have issues with it. “We will talk to them about it,” he said. “We hire hospitalists who can do the work, and we evaluate them based on their background and skill set, where they’ve practiced and for how long. We want people who are experienced and good at managing hospitalized patients. For new residency grads, we look at their electives and the focus of their training.”
What is home for HTFMs?
Where are HTFMs most likely to find their professional home? “That’s hard to answer,” said Patricia Seymour, MD, FHM, FAAFP, an academic hospitalist at the University of Massachusetts-Worcester. “In the last 4-5 years, SHM has worked very hard to create a space for HTFMs. AAFP has a hospital medicine track at their annual meeting, and that’s a good thing. But they also need to protect family physicians’ right to practice in any setting they choose. For those pursuing hospital medicine, there’s a different career trajectory, different CME needs, and different recertification needs.”
Dr. Seymour is the executive cochair of SHM’s family medicine SIG and serves as interim chief of a family medicine hospitalist group that provides inpatient training for a family practice residency, where up to a third of the 12 residents each year go on to pursue hospital medicine as a career. “We have the second-oldest family medicine–specific hospitalist group in the country, so our residency training has an emphasis on hospital medicine,” she explained.
“Because I’m a practicing hospitalist, the residents come to me seeking advice. I appreciate the training I received as a family physician in communication science, palliative care, geriatrics, family systems theory, and public health. I wouldn’t have done it any other way, and that’s how I counsel our students and residents,” she said. Others suggest that the generalist training and diverse experiences of family medicine can be a gift for a doctor who later chooses hospital medicine.
AAFP is a large umbrella organization and the majority of its members practice primary care, Dr. Heim said. “I don’t know the percentage of HTFMs who are members of AAFP. Some no doubt belong to both AAFP and SHM.” Even though both groups have recognized this important subset of their members who chose the field of hospital medicine and its status as a career track, it can be a stretch for family medicine to embrace hospitalists.
“It inherently goes against our training, which is to work in outpatient, inpatient, obstetric, pediatric, and adult settings,” Dr. Heim said. “It’s difficult to reconcile giving up a big part of what defined your training – that range of settings. I remember feeling like I should apologize to other family medicine doctors for choosing this path.”
Credentialing opportunities and barriers
For the diverse group of practicing HTFMs, credentialing and scope of practice represent their biggest current issues. A designation of Focused Practice in Hospital Medicine (FPHM) has been offered jointly since 2010 by the American Board of Family Medicine (ABFM) and the American Board of Internal Medicine (ABIM), although their specific requirements vary.
Eligible hospitalist candidates for the focused practice exam must have an unrestricted medical license, maintenance of current primary certification, and verification of three years of unsupervised hospital medicine practice experience. ABIM views FPHM not as a subspecialty, but as a variation of internal medicine certification, identifying diplomates who are board-certified in internal medicine with a hospital medicine specialization. They do not have to take the general internal medicine recertification exam if they qualify for FPHM.
ABFM-certified family physicians who work primarily in a hospital setting can take the same test for FPHM, with the same eligibility requirements. But ABFM does not consider focused practice a subspecialty, or the Certificate of Added Qualifications in Family Medicine as sufficient for board certification. That means family physicians also need to take its general board exam in order to maintain their ABFM board certification.
ABFM’s decision not to accept the focused practice designation as sufficient for boarding was disappointing to a lot of hospitalists, said Laura “Nell” Hodo, MD, FAAFP, chair of AAFP’s hospital medicine MIG, and a pediatric academic hospitalist at Icahn School of Medicine at Mount Sinai, New York. “Many family physicians practice hospital medicine exclusively and would prefer to take one boarding exam instead of two, and not have to do CME and board review in areas where we don’t practice anymore,” Dr. Hodo said, adding that she hopes that this decision could be revisited in the future.
A number of 1-year hospital medicine fellowships across the country provide additional training opportunities for both family practice and internal medicine residency graduates. These fellowships do not offer board certification or designated specialty credentialing for hospitalists and are not recognized by the American College of Graduate Medical Education (ACGME), which sets standards for residency and fellowship training. “But they reflect a need and an interest in optimizing the knowledge of hospital medicine and developing the specific skills needed to practice it well,” Dr. Geyer noted.
She directs a program for one to three fellows per year out of the Central Maine Family Medicine Residency program and Central Maine Medical Center in Lewiston, and is now recruiting her tenth class. At least 13 other hospital medicine fellowships, out of about 40 nationwide, are family medicine based. “We rely heavily on the Core Competencies in Hospital Medicine developed by SHM, which emphasize clinical conditions, medical procedures, and health care systems. Gaining fluency in the latter is really what makes hospital medicine unique,” Dr. Geyer said.
Often residency graduates seeking work in hospital medicine are insufficiently prepared for hospital billing and coding, enacting safe transitions of care, providing palliative care, and understanding how to impact their health care systems for quality improvement, patient safety and the like, she added.
Dr. Geyer said her fellowship does not mean just being a poorly paid hospitalist for a year. “The fellows are clearly trainees, getting the full benefit of our supervision and supplemental training focused on enhanced clinical and procedural exposure, but also on academics, quality improvement, leadership, and efficiency,” she said. “All of our fellows join SHM, go to the Annual Conference, propose case studies, do longitudinal quality or safety projects, and learn the other aspects of hospital medicine not well-taught in residency. We train them to be highly functional hospitalists right out of the gate.”
Until recently, another barrier for HTFMs was their ability to be on the faculty of internal medicine residency programs. Previous language from ACGME indicated that family medicine-trained physicians could not serve as faculty for these programs, Dr. Goldstein said. SHM has lobbied ACGME to change that rule, which could enable family medicine hospitalists who had achieved FPHM designation to be attendings and to teach internal medicine residents.
Needed in critical care – but not credentialed
One of the biggest frustrations for family medicine hospitalists is clarifying their role in the ICU. SHM’s Education Committee recently surveyed hospitalist members who practice in the ICU, finding that at least half felt obliged to practice beyond their scope, 90 percent occasionally perceived insufficient support from intensivists, and two-thirds reported moderate difficulty transferring patients to higher levels of intensive care.7 The respondents overwhelmingly indicated that they wanted more training and education in critical care medicine.
“I want to highlight the fact that in some settings family physicians are the sole providers of critical care,” Dr. Goldstein said. Meanwhile, the standards of the Leapfrog Group, a coalition of health care purchasers, call for ICUs to be staffed by physicians certified in critical care, even though there is a growing shortage of credentialed intensivists to treat an increasing number of older, sicker, critically ill patients.
Some internal medicine physicians don’t want to have anything to do with the ICU because of the medical and legal risks, said David Aymond, MD, a family physician and hospitalist at Byrd Regional Hospital in Leesville, La. “There’s a bunch of sick people in the ICU, and when some doctors like me started doing critical care, we realized we liked it. Depending on your locale, if you are doing hospital medicine, critically ill patients are going to fall in your lap,” he said. “But if you don’t have the skills, that could lead to poor outcomes and unnecessary transfers.”
Dr. Aymond started his career in family medicine. “When I got into residency, I saw how much critical care was needed in rural communities. I decided I would learn everything I could about it. I did a hospital medicine fellowship at the University of Alabama, which included considerable involvement in the ICU. When I went to Byrd Regional, a 60-bed facility with eight ICU beds, we did all of the critical care, and word started to spread in the community. My hospitalist partner and I are now on call 24/7 alternating weeks, doing the majority of the critical care and taking care of anything that goes on in an ICU at a larger center, although we often lack access to consultation services,” he explained.
“We needed to get the attention of the Society of Critical Care Medicine (SCCM) to communicate the scope of this problem. These doctors are doing critical care but there is no official medical training or recognition for them. So they’re legally out on a limb, even though often they are literally the only person available to do it,” Dr. Aymond said. “Certainly there’s a skills gap between HTFMs and board-certified intensivists, but some of that gap has to do with the volume of patients they have seen in the ICU and their comfort level,” he said.
SHM is pursuing initiatives to help address this gap, including collaborating with SCCM on developing a rigorous critical care training curriculum for internal medicine and family medicine hospitalists, with coursework drawn from existing sources, said Eric Siegal, MD, SFHM, a critical care physician in Milwaukee. “It doesn’t replace a 2-year critical care fellowship, but it will be a lot more than what’s currently out there for the nonintensivist who practices in the ICU.” SCCM has approved moving forward with the advanced training curriculum, he said.
Another priority is to try to create a pathway that could permit family medicine–trained hospitalists to apply for existing critical care fellowships, as internal medicine doctors are now able to do. SHM has lobbied ABFM to create a pathway to subspecialty certification in critical care medicine, similar to those that exist for internists and emergency physicians, Dr. Goldstein said, adding that ACGME, which controls access to fellowships, will be the next step. Dr. Aymond expects that there will be a lot of hoops to jump through.
“David Aymond is an exceptional hospitalist,” Dr. Siegal added. “He thinks and talks like an intensivist, but it took concerted and self-directed effort for him to get there. Family practitioners are a significant part of the rural critical care workforce, but their training generally does not adequately prepare them for this role – unless they have made a conscious effort to pursue additional training,” he said.
“My message to family practitioners is not that they’re not good enough to do this, but rather that they are being asked to do something they weren’t trained for. How can we help them do it well?”
References
1. Society of Hospital Medicine (SHM) Practice Analysis Committee. 2018 State of Hospital Medicine Report; Oct 2018.
2. American Academy of Family Physicians Member Census, Dec 31, 2017.
3. Jones KC et al. Hospitalists: A growing part of the primary care workforce. AAMC Analysis in Brief; June 2016; 16(5):1.
4. Berczuk C. Uniquely positioned. The Hospitalist; July 2009.
5. Iqbal Y. Family medicine hospitalists: Separate and unequal? Today’s Hospitalist; May 2007.
6. Kinnan JP. The family way. The Hospitalist; Nov 2007.
7. Sweigart JR et al. Characterizing hospitalist practice and perceptions of critical care delivery. J Hosp Med. 2018 Jan 1;13(1):6-12.