User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Non-TB mycobacteria infections rising in COPD patients
Veterans with chronic obstructive pulmonary disease (COPD) have seen a sharp increase since 2012 in rates of non-TB mycobacteria infections, which carry a significantly higher risk of death in COPD patients, according to findings from a nationwide study.
For their research, published in Frontiers of Medicine, Fahim Pyarali, MD, and colleagues at the University of Miami, reviewed data from Veterans Affairs hospitals to identify non-TB mycobacteria (NTM) infections among more than 2 million COPD patients seen between 2000 and 2015. Incidence of NTM infections was 34.2 per 100,000 COPD patients in 2001, a rate that remained steady until 2012, when it began climbing sharply through 2015 to reach 70.3 per 100,000 (P = .035). Dr. Pyarali and colleagues also found that, during the study period, prevalence of NTM climbed from 93.1 infections per 100,000 population in 2001 to 277.6 per 100,000 in 2015.
Hotspots for NTM infections included Puerto Rico, which had the highest prevalence seen in the study at 370 infections per 100,000 COPD population; Florida, with 351 per 100,000; and Washington, D.C., with 309 per 100,000. Additional hotspots were identified around Lake Michigan, in coastal Louisiana, and in parts of the Southwest.
Dr. Pyarali and colleagues noted that the geographical concentration of cases near oceans and lakes was “supported by previous findings that warmer temperatures, lower dissolved oxygen, and lower pH in the soils and waters provide a major environmental source for NTM organisms;” however, the study is the first to identify Puerto Rico as having exceptionally high prevalence. The reasons for this should be extensively investigated, the investigators argued.
The mortality risk was 43% higher among NTM-infected patients than in COPD patients without an NTM diagnosis (95% confidence interval, 1.31-1.58; P less than .001), independent of other comorbidities.
Though rates of NTM infection were seen rising steeply in men and women alike, Dr. Pyarali and colleagues noted as a limitation of their study its use of an overwhelmingly male population, writing that this may obscure “the true reach of NTM disease and mortality” in the general population. The average age of NTM diagnosis remained steady throughout the study period, suggesting that rising incidence is not attributable to earlier diagnosis.
Dr. Pyarali and colleagues reported no outside sources of funding or financial conflicts of interest.
SOURCE: Pyarali F et al. Front Med. 2018 Nov 6. doi: 10.3389/fmed2018.00311.
Veterans with chronic obstructive pulmonary disease (COPD) have seen a sharp increase since 2012 in rates of non-TB mycobacteria infections, which carry a significantly higher risk of death in COPD patients, according to findings from a nationwide study.
For their research, published in Frontiers of Medicine, Fahim Pyarali, MD, and colleagues at the University of Miami, reviewed data from Veterans Affairs hospitals to identify non-TB mycobacteria (NTM) infections among more than 2 million COPD patients seen between 2000 and 2015. Incidence of NTM infections was 34.2 per 100,000 COPD patients in 2001, a rate that remained steady until 2012, when it began climbing sharply through 2015 to reach 70.3 per 100,000 (P = .035). Dr. Pyarali and colleagues also found that, during the study period, prevalence of NTM climbed from 93.1 infections per 100,000 population in 2001 to 277.6 per 100,000 in 2015.
Hotspots for NTM infections included Puerto Rico, which had the highest prevalence seen in the study at 370 infections per 100,000 COPD population; Florida, with 351 per 100,000; and Washington, D.C., with 309 per 100,000. Additional hotspots were identified around Lake Michigan, in coastal Louisiana, and in parts of the Southwest.
Dr. Pyarali and colleagues noted that the geographical concentration of cases near oceans and lakes was “supported by previous findings that warmer temperatures, lower dissolved oxygen, and lower pH in the soils and waters provide a major environmental source for NTM organisms;” however, the study is the first to identify Puerto Rico as having exceptionally high prevalence. The reasons for this should be extensively investigated, the investigators argued.
The mortality risk was 43% higher among NTM-infected patients than in COPD patients without an NTM diagnosis (95% confidence interval, 1.31-1.58; P less than .001), independent of other comorbidities.
Though rates of NTM infection were seen rising steeply in men and women alike, Dr. Pyarali and colleagues noted as a limitation of their study its use of an overwhelmingly male population, writing that this may obscure “the true reach of NTM disease and mortality” in the general population. The average age of NTM diagnosis remained steady throughout the study period, suggesting that rising incidence is not attributable to earlier diagnosis.
Dr. Pyarali and colleagues reported no outside sources of funding or financial conflicts of interest.
SOURCE: Pyarali F et al. Front Med. 2018 Nov 6. doi: 10.3389/fmed2018.00311.
Veterans with chronic obstructive pulmonary disease (COPD) have seen a sharp increase since 2012 in rates of non-TB mycobacteria infections, which carry a significantly higher risk of death in COPD patients, according to findings from a nationwide study.
For their research, published in Frontiers of Medicine, Fahim Pyarali, MD, and colleagues at the University of Miami, reviewed data from Veterans Affairs hospitals to identify non-TB mycobacteria (NTM) infections among more than 2 million COPD patients seen between 2000 and 2015. Incidence of NTM infections was 34.2 per 100,000 COPD patients in 2001, a rate that remained steady until 2012, when it began climbing sharply through 2015 to reach 70.3 per 100,000 (P = .035). Dr. Pyarali and colleagues also found that, during the study period, prevalence of NTM climbed from 93.1 infections per 100,000 population in 2001 to 277.6 per 100,000 in 2015.
Hotspots for NTM infections included Puerto Rico, which had the highest prevalence seen in the study at 370 infections per 100,000 COPD population; Florida, with 351 per 100,000; and Washington, D.C., with 309 per 100,000. Additional hotspots were identified around Lake Michigan, in coastal Louisiana, and in parts of the Southwest.
Dr. Pyarali and colleagues noted that the geographical concentration of cases near oceans and lakes was “supported by previous findings that warmer temperatures, lower dissolved oxygen, and lower pH in the soils and waters provide a major environmental source for NTM organisms;” however, the study is the first to identify Puerto Rico as having exceptionally high prevalence. The reasons for this should be extensively investigated, the investigators argued.
The mortality risk was 43% higher among NTM-infected patients than in COPD patients without an NTM diagnosis (95% confidence interval, 1.31-1.58; P less than .001), independent of other comorbidities.
Though rates of NTM infection were seen rising steeply in men and women alike, Dr. Pyarali and colleagues noted as a limitation of their study its use of an overwhelmingly male population, writing that this may obscure “the true reach of NTM disease and mortality” in the general population. The average age of NTM diagnosis remained steady throughout the study period, suggesting that rising incidence is not attributable to earlier diagnosis.
Dr. Pyarali and colleagues reported no outside sources of funding or financial conflicts of interest.
SOURCE: Pyarali F et al. Front Med. 2018 Nov 6. doi: 10.3389/fmed2018.00311.
FROM FRONTIERS IN MEDICINE
Key clinical point: Incidence and prevalence of non-TB mycobacteria infections rose sharply in a national veterans population with chronic obstructive pulmonary disease after 2012.
Major finding: Incidence of non-TB mycobacteria infections doubled in chronic obstructive pulmonary disease patients between 2001 and 2015, with most of the increase seen after 2012
Study details: A retrospective, cross-sectional study using records from over 2 million, mostly male chronic obstructive pulmonary disease patients in a Veterans Affairs database.
Disclosures: The study authors reported no outside sources of funding or financial conflicts of interest.
Source: Pyarali F et al. Front Med. 2018 Nov 6. doi: 10.3389/fmed2018.00311.
Developing essential skills at all career stages
SHM Leadership Academy continues to grow
This fall I attended the 2018 Society of Hospital Medicine Leadership Academy, held in Vancouver. Once again, this conference sold out weeks ahead of time, and 300 hospitalists took time out of their busy schedules for learning and fun. There have been about 18 Leadership Academies over the years, with approximately 3,000 total participants, but this one may have been the best to date.
Why was it so good? Here are my top four reasons that Leadership Academy 2018 was the best ever:
Setting: Vancouver is just beautiful. My family has a strong maritime background, and I am a water person with saltwater in my veins. My inner sailor was overjoyed with the hotel’s views of False Creek and Vancouver Harbor, and I loved the mix of yachts and working boats. I even saw a seaplane! The hotel was a great match for the 300 hospitalists who traveled to the JW Marriott for 4 days of learning and relaxing. It was the perfect blend, whether for work or play; the hotel and city did not disappoint.
Networking: What’s more fun than getting to know 300 like-minded, leadership-oriented hospitalists for a few days? I am always energized by seeing old friends and making new ones. I really enjoy hearing about the professional adventures hospitalists at all career points are going through. Plus, I get really good advice on my own career! I also appreciate that a number of hospital medicine leaders (and even giants) come to SHM’s Leadership Academy. Over half of the SHM Board of Directors were there, as were a number of current and previous SHM presidents (Mark Williams, Jeff Wiese, Burke Kealey, Bob Harrington, Nasim Afsar, Rusty Holman, Ron Greeno, Chris Frost, and John Nelson), as well as Larry Wellikson, the CEO who has led our society through its many successes. All of these hospitalist leaders are there, having fun and networking, alongside everyone else.
Faculty: The faculty for all four courses (yes, Leadership Academy junkies, we’ve added a fourth course!) are absolutely phenomenal. I think the faculty are just the right blend of expert hospitalists (Jeff Glasheen, Rusty Holman, Jeff Wiese, Mark Williams, John Nelson) and national experts outside of hospital medicine. For example, Lenny Marcus of Harvard T.H. Chan School of Public Health, Boston, brings his experience coaching the Department of Defense, the White House, the Department of Homeland Security, and many others to the Influential Management and Mastering Teamwork courses. Lenny’s experience working with national leaders through disasters like the Boston Marathon bombing, Hurricane Katrina, and the Ebola outbreak make for more than riveting stories; there are real, tangible lessons for hospitalist leaders trying to improve clinical care. Nancy Spector is a pediatrician, nationally recognized for her work in mentoring, and is the executive director of Drexel University’s Executive Leadership in Academic Medicine. We have been fortunate to have her join the Academies, and Nancy successfully led the first group of hospitalists through the launch of SHM’s fourth leadership course, which I will describe in more detail below.
High energy & continued growth: There continues to be an enormous amount of energy around the Leadership Academy. The Vancouver courses sold out months ahead of the actual meeting! Hospitalists across the country continue to take on leadership roles and have told us that they value the skills they have learned from the courses.
Hospitalist leaders want more
In addition to the current 4-day courses (Strategic Essentials, Influential Management, and Mastering Teamwork), hospitalists are looking for a course that continues skill building once they return home.
That’s why SHM has developed a fourth Leadership Academy course. This course, called the Capstone Course, was launched in Vancouver and consists of 2 days of on-site skill development and team building (during the first 2 days of the traditional Leadership Academy) and 6 months of a longitudinal learning collaborative. The six-month learning collaborative component consists of a learning “pod” of five or six fellow hospitalists and monthly virtual meetings around crucial leadership topics. They are facilitated by an experienced Leadership Academy facilitator.
Dr. Spector is the lead faculty; her expertise made the Capstone launch a huge success. She will work with SHM and the Capstone participants throughout the entire 6 months to ensure the Capstone course is as high-quality as the previous three Academy courses.
If you haven’t been, I invite you to attend our next Leadership Academy. Over the years, despite being course director, I have learned many take-home skills from colleagues and leaders in the field that I use often. Just to name a few:
- Flexing my communications style: Tim Keogh’s lecture opened my eyes to the fact that not everyone is a data-driven introvert. I now know that some people need a social warm up, while others just want the facts, and that there are “huggers and shakers.” (In summary, it’s fine to shake hands with a hugger, but be wary of hugging a shaker.)
- I send birthday emails after I heard Jeff Wiese’s talk.
- Lenny Marcus taught me to be aware when I am “in the basement” emotionally. I now know to wait to send emails or confront others until I can get out of the basement.
And that’s just scratching the surface!
In closing, the Vancouver Leadership Academy was fantastic. Good friends, great professional development, a setting that was amazing, and an Academy that remains relevant and dynamic to our specialty. I can’t wait to see how the 2019 Leadership Academy shapes up for its debut in Nashville. My inner sailor may have to give way to my inner musician! I hope to see you and 300 of my closest friends there.
Learn more about SHM’s Leadership Academy at shmleadershipacademy.org.
Dr. Howell is a professor of medicine at Johns Hopkins University, Baltimore, and chief of the division of hospital medicine at Johns Hopkins Bayview Medical Center. He is also chief operating officer at the Society of Hospital Medicine and course director of the SHM Leadership Academy.
SHM Leadership Academy continues to grow
SHM Leadership Academy continues to grow
This fall I attended the 2018 Society of Hospital Medicine Leadership Academy, held in Vancouver. Once again, this conference sold out weeks ahead of time, and 300 hospitalists took time out of their busy schedules for learning and fun. There have been about 18 Leadership Academies over the years, with approximately 3,000 total participants, but this one may have been the best to date.
Why was it so good? Here are my top four reasons that Leadership Academy 2018 was the best ever:
Setting: Vancouver is just beautiful. My family has a strong maritime background, and I am a water person with saltwater in my veins. My inner sailor was overjoyed with the hotel’s views of False Creek and Vancouver Harbor, and I loved the mix of yachts and working boats. I even saw a seaplane! The hotel was a great match for the 300 hospitalists who traveled to the JW Marriott for 4 days of learning and relaxing. It was the perfect blend, whether for work or play; the hotel and city did not disappoint.
Networking: What’s more fun than getting to know 300 like-minded, leadership-oriented hospitalists for a few days? I am always energized by seeing old friends and making new ones. I really enjoy hearing about the professional adventures hospitalists at all career points are going through. Plus, I get really good advice on my own career! I also appreciate that a number of hospital medicine leaders (and even giants) come to SHM’s Leadership Academy. Over half of the SHM Board of Directors were there, as were a number of current and previous SHM presidents (Mark Williams, Jeff Wiese, Burke Kealey, Bob Harrington, Nasim Afsar, Rusty Holman, Ron Greeno, Chris Frost, and John Nelson), as well as Larry Wellikson, the CEO who has led our society through its many successes. All of these hospitalist leaders are there, having fun and networking, alongside everyone else.
Faculty: The faculty for all four courses (yes, Leadership Academy junkies, we’ve added a fourth course!) are absolutely phenomenal. I think the faculty are just the right blend of expert hospitalists (Jeff Glasheen, Rusty Holman, Jeff Wiese, Mark Williams, John Nelson) and national experts outside of hospital medicine. For example, Lenny Marcus of Harvard T.H. Chan School of Public Health, Boston, brings his experience coaching the Department of Defense, the White House, the Department of Homeland Security, and many others to the Influential Management and Mastering Teamwork courses. Lenny’s experience working with national leaders through disasters like the Boston Marathon bombing, Hurricane Katrina, and the Ebola outbreak make for more than riveting stories; there are real, tangible lessons for hospitalist leaders trying to improve clinical care. Nancy Spector is a pediatrician, nationally recognized for her work in mentoring, and is the executive director of Drexel University’s Executive Leadership in Academic Medicine. We have been fortunate to have her join the Academies, and Nancy successfully led the first group of hospitalists through the launch of SHM’s fourth leadership course, which I will describe in more detail below.
High energy & continued growth: There continues to be an enormous amount of energy around the Leadership Academy. The Vancouver courses sold out months ahead of the actual meeting! Hospitalists across the country continue to take on leadership roles and have told us that they value the skills they have learned from the courses.
Hospitalist leaders want more
In addition to the current 4-day courses (Strategic Essentials, Influential Management, and Mastering Teamwork), hospitalists are looking for a course that continues skill building once they return home.
That’s why SHM has developed a fourth Leadership Academy course. This course, called the Capstone Course, was launched in Vancouver and consists of 2 days of on-site skill development and team building (during the first 2 days of the traditional Leadership Academy) and 6 months of a longitudinal learning collaborative. The six-month learning collaborative component consists of a learning “pod” of five or six fellow hospitalists and monthly virtual meetings around crucial leadership topics. They are facilitated by an experienced Leadership Academy facilitator.
Dr. Spector is the lead faculty; her expertise made the Capstone launch a huge success. She will work with SHM and the Capstone participants throughout the entire 6 months to ensure the Capstone course is as high-quality as the previous three Academy courses.
If you haven’t been, I invite you to attend our next Leadership Academy. Over the years, despite being course director, I have learned many take-home skills from colleagues and leaders in the field that I use often. Just to name a few:
- Flexing my communications style: Tim Keogh’s lecture opened my eyes to the fact that not everyone is a data-driven introvert. I now know that some people need a social warm up, while others just want the facts, and that there are “huggers and shakers.” (In summary, it’s fine to shake hands with a hugger, but be wary of hugging a shaker.)
- I send birthday emails after I heard Jeff Wiese’s talk.
- Lenny Marcus taught me to be aware when I am “in the basement” emotionally. I now know to wait to send emails or confront others until I can get out of the basement.
And that’s just scratching the surface!
In closing, the Vancouver Leadership Academy was fantastic. Good friends, great professional development, a setting that was amazing, and an Academy that remains relevant and dynamic to our specialty. I can’t wait to see how the 2019 Leadership Academy shapes up for its debut in Nashville. My inner sailor may have to give way to my inner musician! I hope to see you and 300 of my closest friends there.
Learn more about SHM’s Leadership Academy at shmleadershipacademy.org.
Dr. Howell is a professor of medicine at Johns Hopkins University, Baltimore, and chief of the division of hospital medicine at Johns Hopkins Bayview Medical Center. He is also chief operating officer at the Society of Hospital Medicine and course director of the SHM Leadership Academy.
This fall I attended the 2018 Society of Hospital Medicine Leadership Academy, held in Vancouver. Once again, this conference sold out weeks ahead of time, and 300 hospitalists took time out of their busy schedules for learning and fun. There have been about 18 Leadership Academies over the years, with approximately 3,000 total participants, but this one may have been the best to date.
Why was it so good? Here are my top four reasons that Leadership Academy 2018 was the best ever:
Setting: Vancouver is just beautiful. My family has a strong maritime background, and I am a water person with saltwater in my veins. My inner sailor was overjoyed with the hotel’s views of False Creek and Vancouver Harbor, and I loved the mix of yachts and working boats. I even saw a seaplane! The hotel was a great match for the 300 hospitalists who traveled to the JW Marriott for 4 days of learning and relaxing. It was the perfect blend, whether for work or play; the hotel and city did not disappoint.
Networking: What’s more fun than getting to know 300 like-minded, leadership-oriented hospitalists for a few days? I am always energized by seeing old friends and making new ones. I really enjoy hearing about the professional adventures hospitalists at all career points are going through. Plus, I get really good advice on my own career! I also appreciate that a number of hospital medicine leaders (and even giants) come to SHM’s Leadership Academy. Over half of the SHM Board of Directors were there, as were a number of current and previous SHM presidents (Mark Williams, Jeff Wiese, Burke Kealey, Bob Harrington, Nasim Afsar, Rusty Holman, Ron Greeno, Chris Frost, and John Nelson), as well as Larry Wellikson, the CEO who has led our society through its many successes. All of these hospitalist leaders are there, having fun and networking, alongside everyone else.
Faculty: The faculty for all four courses (yes, Leadership Academy junkies, we’ve added a fourth course!) are absolutely phenomenal. I think the faculty are just the right blend of expert hospitalists (Jeff Glasheen, Rusty Holman, Jeff Wiese, Mark Williams, John Nelson) and national experts outside of hospital medicine. For example, Lenny Marcus of Harvard T.H. Chan School of Public Health, Boston, brings his experience coaching the Department of Defense, the White House, the Department of Homeland Security, and many others to the Influential Management and Mastering Teamwork courses. Lenny’s experience working with national leaders through disasters like the Boston Marathon bombing, Hurricane Katrina, and the Ebola outbreak make for more than riveting stories; there are real, tangible lessons for hospitalist leaders trying to improve clinical care. Nancy Spector is a pediatrician, nationally recognized for her work in mentoring, and is the executive director of Drexel University’s Executive Leadership in Academic Medicine. We have been fortunate to have her join the Academies, and Nancy successfully led the first group of hospitalists through the launch of SHM’s fourth leadership course, which I will describe in more detail below.
High energy & continued growth: There continues to be an enormous amount of energy around the Leadership Academy. The Vancouver courses sold out months ahead of the actual meeting! Hospitalists across the country continue to take on leadership roles and have told us that they value the skills they have learned from the courses.
Hospitalist leaders want more
In addition to the current 4-day courses (Strategic Essentials, Influential Management, and Mastering Teamwork), hospitalists are looking for a course that continues skill building once they return home.
That’s why SHM has developed a fourth Leadership Academy course. This course, called the Capstone Course, was launched in Vancouver and consists of 2 days of on-site skill development and team building (during the first 2 days of the traditional Leadership Academy) and 6 months of a longitudinal learning collaborative. The six-month learning collaborative component consists of a learning “pod” of five or six fellow hospitalists and monthly virtual meetings around crucial leadership topics. They are facilitated by an experienced Leadership Academy facilitator.
Dr. Spector is the lead faculty; her expertise made the Capstone launch a huge success. She will work with SHM and the Capstone participants throughout the entire 6 months to ensure the Capstone course is as high-quality as the previous three Academy courses.
If you haven’t been, I invite you to attend our next Leadership Academy. Over the years, despite being course director, I have learned many take-home skills from colleagues and leaders in the field that I use often. Just to name a few:
- Flexing my communications style: Tim Keogh’s lecture opened my eyes to the fact that not everyone is a data-driven introvert. I now know that some people need a social warm up, while others just want the facts, and that there are “huggers and shakers.” (In summary, it’s fine to shake hands with a hugger, but be wary of hugging a shaker.)
- I send birthday emails after I heard Jeff Wiese’s talk.
- Lenny Marcus taught me to be aware when I am “in the basement” emotionally. I now know to wait to send emails or confront others until I can get out of the basement.
And that’s just scratching the surface!
In closing, the Vancouver Leadership Academy was fantastic. Good friends, great professional development, a setting that was amazing, and an Academy that remains relevant and dynamic to our specialty. I can’t wait to see how the 2019 Leadership Academy shapes up for its debut in Nashville. My inner sailor may have to give way to my inner musician! I hope to see you and 300 of my closest friends there.
Learn more about SHM’s Leadership Academy at shmleadershipacademy.org.
Dr. Howell is a professor of medicine at Johns Hopkins University, Baltimore, and chief of the division of hospital medicine at Johns Hopkins Bayview Medical Center. He is also chief operating officer at the Society of Hospital Medicine and course director of the SHM Leadership Academy.
Parental leave for residents pales in comparison to that of faculty physicians
Leave policies for residents who become new parents are uneven, oft-ignored by training boards, and provide less time off than similar policies for faculty physicians. Those were the findings of a pair of research letters published in JAMA.
Kirti Magudia, MD, of the department of radiology at Brigham and Women’s Hospital in Boston and her colleagues reviewed childbearing and family leave policies for 15 graduate medical education (GME)–sponsoring institutions, all of which were affiliated with the top 12 U.S. medical schools. Though all 12 schools provided paid childbearing or family leave for faculty physicians, only 8 of the 15 did so for residents (JAMA. 2018 Dec 11;320[22)]:2372-4).
In programs that did provide leave, the average of 6.6 weeks of paid total maternity leave for residents was less than the 8.6 weeks faculty receive. Both are considerably less than proscribed by the Family and Medical Leave Act, which requires large employers to provide 12 weeks of unpaid leave, but only after 12 months of employment.
The research focused on only institutional policies for paid leave; unpaid leave and state policies may extend the average, and departments may offer leave that goes beyond specific policies, Dr. Magudia and her colleagues noted.
Changes in the residency population make now the right time for establishing consistent family leave policies, Dr. Magudia said in an interview. “We have people starting training later; we have more female trainees. And with the Match system, you’re not in control of exactly where you’re going. You may not have a support system where you end up, and a lot of the top training institutions are in high cost-of-living areas. All of those things together can make trainees especially vulnerable, and because trainees are temporary employees, changing policies to benefit them is very challenging.
“Wellness is a huge issue in medicine, and at large in society,” she said. “Making sure people have adequate parental leave goes a long way toward reducing stress levels and helping them cope with normal life transitions. We want to take steps that promote success among a diverse community of physicians; we want to retain as many people in the field as possible, and we want them to feel supported.”
Beyond asking all GME-sponsoring institutions to adopt parental leave policies, Dr. Magudia believes trainees must be better informed. “It should be clear to training program applicants what the policies are at those institutions,” she said. “That information is extremely difficult to obtain, as we’ve discovered. You can imagine that, if you are the applicant, it can be difficult to ask about those policies during the interview process because it may affect how things turn out.”
“If we can see changes like these made in the near future,” she added, “we will be in a good place.”
In the second study, Briony K. Varda, MD, of the department of urology at Boston Children’s Hospital, and her colleagues also noted the complications of balancing parental leave with training requirements from specialty boards. They compared leave policies among American Board of Medical Specialty member organizations and found that less than half specifically mentioned parental leave for resident physicians (JAMA. 2018 Dec 11;320[22]:2374-7).
Dr. Varda and her colleagues reviewed the websites of 24 ABMS boards to determine their leave policies; 22 had policies but only 11 cited parental leave as an option for residents. Twenty boards have time-based training requirements and allow for a median of 6 weeks leave for any reason; none of the boards had a specific policy for parental leave. In addition, only eight boards had “explicit and clear clarifying language” that would allow program directors to seek exemptions for their residents.
Though limitations like not detecting all available policies – and a subjective evaluation of the policies that were reviewed – could have impacted their study, the coauthors reiterated that the median of 6 weeks leave is less than the average leave for faculty physicians. They also emphasized the detriments associated with inadequate parental leave, including delayed childbearing, use of assisted reproduction technology, and difficulty breastfeeding.
Dr. Varda underlined the issues that arise for program directors, who “must weigh potentially conflicting factors such as adhering to board and institutional policies, maintaining adequate clinical service coverage, considering precedent within the program, and ensuring that resident physicians are well trained.” To balance the needs of all involved “novel approaches such as use of competency-based rather than time-based training milestones” to determine certification eligibility and, in return, lessen the stresses for new-parent residents, she noted.
The researchers disclosed no relevant conflicts of interest.
SOURCE: Magudia K et al. JAMA. 2018 Dec 11;320[22)]:2372-4; Varda B et al. JAMA. 2018 Dec 11;320[22]:2374-7.
Recent data by Magudia et al. have highlighted the fact that family leave policies supporting parents during medical training are widely inconsistent and in many instances do not exist. Where trainee policies do exist, benefits are routinely less robust than those of permanent faculty who receive on average 30% more paid leave time. Stratifying physician wellness needs by training status seems to be a misplaced approach.
It is not only the medical field which sees inconsistencies in the way family leave is allocated for different types of jobs. Millions of Americans receive no time off after birth or adoption, at a time when corporate America offers elite benefits for child care. In medicine, however, there is an expectation that paid family leave should be the norm, perhaps because of our mission to improve the quality of health care.
Of course, there are valid distinctions between faculty and trainees: faculty are more permanent, are more professionally differentiated and accomplished than trainees, have greater responsibilities, and are recruited for their expertise. Arguably, faculty deserve better compensation than trainees.
But the importance of parental leave transcends the routine benefits arguments. There is something more universal about how we value parenting. Parental leave policies benefit the health of parent and child, increase career satisfaction, and improve retention. The process of birth or adoption, ensuing fatigue, family bonding needs, and life-restructuring will challenge all parents regardless of career status.
Awareness of the inadequacies of parental leave policies is the first step in remedying the disparities in support for our trainees. Establishing an equal and adequate family leave policy for physicians at any stage is consistent with the goal of success and well-being for us all.
Laurel Fisher, MD, AGAF, professor of clinical internal medicine, division of gastroenterology, University of Pennsylvania, Philadelphia. She reports no conflicts of interest.
Recent data by Magudia et al. have highlighted the fact that family leave policies supporting parents during medical training are widely inconsistent and in many instances do not exist. Where trainee policies do exist, benefits are routinely less robust than those of permanent faculty who receive on average 30% more paid leave time. Stratifying physician wellness needs by training status seems to be a misplaced approach.
It is not only the medical field which sees inconsistencies in the way family leave is allocated for different types of jobs. Millions of Americans receive no time off after birth or adoption, at a time when corporate America offers elite benefits for child care. In medicine, however, there is an expectation that paid family leave should be the norm, perhaps because of our mission to improve the quality of health care.
Of course, there are valid distinctions between faculty and trainees: faculty are more permanent, are more professionally differentiated and accomplished than trainees, have greater responsibilities, and are recruited for their expertise. Arguably, faculty deserve better compensation than trainees.
But the importance of parental leave transcends the routine benefits arguments. There is something more universal about how we value parenting. Parental leave policies benefit the health of parent and child, increase career satisfaction, and improve retention. The process of birth or adoption, ensuing fatigue, family bonding needs, and life-restructuring will challenge all parents regardless of career status.
Awareness of the inadequacies of parental leave policies is the first step in remedying the disparities in support for our trainees. Establishing an equal and adequate family leave policy for physicians at any stage is consistent with the goal of success and well-being for us all.
Laurel Fisher, MD, AGAF, professor of clinical internal medicine, division of gastroenterology, University of Pennsylvania, Philadelphia. She reports no conflicts of interest.
Recent data by Magudia et al. have highlighted the fact that family leave policies supporting parents during medical training are widely inconsistent and in many instances do not exist. Where trainee policies do exist, benefits are routinely less robust than those of permanent faculty who receive on average 30% more paid leave time. Stratifying physician wellness needs by training status seems to be a misplaced approach.
It is not only the medical field which sees inconsistencies in the way family leave is allocated for different types of jobs. Millions of Americans receive no time off after birth or adoption, at a time when corporate America offers elite benefits for child care. In medicine, however, there is an expectation that paid family leave should be the norm, perhaps because of our mission to improve the quality of health care.
Of course, there are valid distinctions between faculty and trainees: faculty are more permanent, are more professionally differentiated and accomplished than trainees, have greater responsibilities, and are recruited for their expertise. Arguably, faculty deserve better compensation than trainees.
But the importance of parental leave transcends the routine benefits arguments. There is something more universal about how we value parenting. Parental leave policies benefit the health of parent and child, increase career satisfaction, and improve retention. The process of birth or adoption, ensuing fatigue, family bonding needs, and life-restructuring will challenge all parents regardless of career status.
Awareness of the inadequacies of parental leave policies is the first step in remedying the disparities in support for our trainees. Establishing an equal and adequate family leave policy for physicians at any stage is consistent with the goal of success and well-being for us all.
Laurel Fisher, MD, AGAF, professor of clinical internal medicine, division of gastroenterology, University of Pennsylvania, Philadelphia. She reports no conflicts of interest.
Leave policies for residents who become new parents are uneven, oft-ignored by training boards, and provide less time off than similar policies for faculty physicians. Those were the findings of a pair of research letters published in JAMA.
Kirti Magudia, MD, of the department of radiology at Brigham and Women’s Hospital in Boston and her colleagues reviewed childbearing and family leave policies for 15 graduate medical education (GME)–sponsoring institutions, all of which were affiliated with the top 12 U.S. medical schools. Though all 12 schools provided paid childbearing or family leave for faculty physicians, only 8 of the 15 did so for residents (JAMA. 2018 Dec 11;320[22)]:2372-4).
In programs that did provide leave, the average of 6.6 weeks of paid total maternity leave for residents was less than the 8.6 weeks faculty receive. Both are considerably less than proscribed by the Family and Medical Leave Act, which requires large employers to provide 12 weeks of unpaid leave, but only after 12 months of employment.
The research focused on only institutional policies for paid leave; unpaid leave and state policies may extend the average, and departments may offer leave that goes beyond specific policies, Dr. Magudia and her colleagues noted.
Changes in the residency population make now the right time for establishing consistent family leave policies, Dr. Magudia said in an interview. “We have people starting training later; we have more female trainees. And with the Match system, you’re not in control of exactly where you’re going. You may not have a support system where you end up, and a lot of the top training institutions are in high cost-of-living areas. All of those things together can make trainees especially vulnerable, and because trainees are temporary employees, changing policies to benefit them is very challenging.
“Wellness is a huge issue in medicine, and at large in society,” she said. “Making sure people have adequate parental leave goes a long way toward reducing stress levels and helping them cope with normal life transitions. We want to take steps that promote success among a diverse community of physicians; we want to retain as many people in the field as possible, and we want them to feel supported.”
Beyond asking all GME-sponsoring institutions to adopt parental leave policies, Dr. Magudia believes trainees must be better informed. “It should be clear to training program applicants what the policies are at those institutions,” she said. “That information is extremely difficult to obtain, as we’ve discovered. You can imagine that, if you are the applicant, it can be difficult to ask about those policies during the interview process because it may affect how things turn out.”
“If we can see changes like these made in the near future,” she added, “we will be in a good place.”
In the second study, Briony K. Varda, MD, of the department of urology at Boston Children’s Hospital, and her colleagues also noted the complications of balancing parental leave with training requirements from specialty boards. They compared leave policies among American Board of Medical Specialty member organizations and found that less than half specifically mentioned parental leave for resident physicians (JAMA. 2018 Dec 11;320[22]:2374-7).
Dr. Varda and her colleagues reviewed the websites of 24 ABMS boards to determine their leave policies; 22 had policies but only 11 cited parental leave as an option for residents. Twenty boards have time-based training requirements and allow for a median of 6 weeks leave for any reason; none of the boards had a specific policy for parental leave. In addition, only eight boards had “explicit and clear clarifying language” that would allow program directors to seek exemptions for their residents.
Though limitations like not detecting all available policies – and a subjective evaluation of the policies that were reviewed – could have impacted their study, the coauthors reiterated that the median of 6 weeks leave is less than the average leave for faculty physicians. They also emphasized the detriments associated with inadequate parental leave, including delayed childbearing, use of assisted reproduction technology, and difficulty breastfeeding.
Dr. Varda underlined the issues that arise for program directors, who “must weigh potentially conflicting factors such as adhering to board and institutional policies, maintaining adequate clinical service coverage, considering precedent within the program, and ensuring that resident physicians are well trained.” To balance the needs of all involved “novel approaches such as use of competency-based rather than time-based training milestones” to determine certification eligibility and, in return, lessen the stresses for new-parent residents, she noted.
The researchers disclosed no relevant conflicts of interest.
SOURCE: Magudia K et al. JAMA. 2018 Dec 11;320[22)]:2372-4; Varda B et al. JAMA. 2018 Dec 11;320[22]:2374-7.
Leave policies for residents who become new parents are uneven, oft-ignored by training boards, and provide less time off than similar policies for faculty physicians. Those were the findings of a pair of research letters published in JAMA.
Kirti Magudia, MD, of the department of radiology at Brigham and Women’s Hospital in Boston and her colleagues reviewed childbearing and family leave policies for 15 graduate medical education (GME)–sponsoring institutions, all of which were affiliated with the top 12 U.S. medical schools. Though all 12 schools provided paid childbearing or family leave for faculty physicians, only 8 of the 15 did so for residents (JAMA. 2018 Dec 11;320[22)]:2372-4).
In programs that did provide leave, the average of 6.6 weeks of paid total maternity leave for residents was less than the 8.6 weeks faculty receive. Both are considerably less than proscribed by the Family and Medical Leave Act, which requires large employers to provide 12 weeks of unpaid leave, but only after 12 months of employment.
The research focused on only institutional policies for paid leave; unpaid leave and state policies may extend the average, and departments may offer leave that goes beyond specific policies, Dr. Magudia and her colleagues noted.
Changes in the residency population make now the right time for establishing consistent family leave policies, Dr. Magudia said in an interview. “We have people starting training later; we have more female trainees. And with the Match system, you’re not in control of exactly where you’re going. You may not have a support system where you end up, and a lot of the top training institutions are in high cost-of-living areas. All of those things together can make trainees especially vulnerable, and because trainees are temporary employees, changing policies to benefit them is very challenging.
“Wellness is a huge issue in medicine, and at large in society,” she said. “Making sure people have adequate parental leave goes a long way toward reducing stress levels and helping them cope with normal life transitions. We want to take steps that promote success among a diverse community of physicians; we want to retain as many people in the field as possible, and we want them to feel supported.”
Beyond asking all GME-sponsoring institutions to adopt parental leave policies, Dr. Magudia believes trainees must be better informed. “It should be clear to training program applicants what the policies are at those institutions,” she said. “That information is extremely difficult to obtain, as we’ve discovered. You can imagine that, if you are the applicant, it can be difficult to ask about those policies during the interview process because it may affect how things turn out.”
“If we can see changes like these made in the near future,” she added, “we will be in a good place.”
In the second study, Briony K. Varda, MD, of the department of urology at Boston Children’s Hospital, and her colleagues also noted the complications of balancing parental leave with training requirements from specialty boards. They compared leave policies among American Board of Medical Specialty member organizations and found that less than half specifically mentioned parental leave for resident physicians (JAMA. 2018 Dec 11;320[22]:2374-7).
Dr. Varda and her colleagues reviewed the websites of 24 ABMS boards to determine their leave policies; 22 had policies but only 11 cited parental leave as an option for residents. Twenty boards have time-based training requirements and allow for a median of 6 weeks leave for any reason; none of the boards had a specific policy for parental leave. In addition, only eight boards had “explicit and clear clarifying language” that would allow program directors to seek exemptions for their residents.
Though limitations like not detecting all available policies – and a subjective evaluation of the policies that were reviewed – could have impacted their study, the coauthors reiterated that the median of 6 weeks leave is less than the average leave for faculty physicians. They also emphasized the detriments associated with inadequate parental leave, including delayed childbearing, use of assisted reproduction technology, and difficulty breastfeeding.
Dr. Varda underlined the issues that arise for program directors, who “must weigh potentially conflicting factors such as adhering to board and institutional policies, maintaining adequate clinical service coverage, considering precedent within the program, and ensuring that resident physicians are well trained.” To balance the needs of all involved “novel approaches such as use of competency-based rather than time-based training milestones” to determine certification eligibility and, in return, lessen the stresses for new-parent residents, she noted.
The researchers disclosed no relevant conflicts of interest.
SOURCE: Magudia K et al. JAMA. 2018 Dec 11;320[22)]:2372-4; Varda B et al. JAMA. 2018 Dec 11;320[22]:2374-7.
FROM JAMA
Social media can help doctors stay up to date
SAN DIEGO –
“People want to see that you’re a person and not strictly a physician,” said Dr. Yates, a pediatric hematologist at Texas Children’s Hospital in Houston, who has had an active Twitter presence for the last few years.
Dr. Yates – whose Twitter handle is @sicklecelldoc – said she dipped a toe in the social media waters because she wanted to bring accurate medical information to patients in the arena where they are seeking information.
“I want families to understand their condition as well as they can on whatever level they can, and so I just found this to be another way to do that ... outside of my clinic,” she said during an interview at the annual meeting of the American Society of Hematology.
But beyond correcting misinformation and serving as an advocate for patients, Dr. Yates said she gets professional benefits from being on Twitter. For instance, she uses the platform to find relevant articles as soon as they publish, without wading through all the journals.
“It’s allowed me to kind of streamline what I read,” she said.
Dr. Yates said Twitter is her social media platform of choice because it provides a simple, succinct way to communicate and provide links to more in-depth resources.
While social media can be fun and rewarding for physicians, Dr. Yates said think before you post. Ask yourself, “would you tell your chairperson this?”
Dr. Yates reported having no relevant financial disclosures.
SAN DIEGO –
“People want to see that you’re a person and not strictly a physician,” said Dr. Yates, a pediatric hematologist at Texas Children’s Hospital in Houston, who has had an active Twitter presence for the last few years.
Dr. Yates – whose Twitter handle is @sicklecelldoc – said she dipped a toe in the social media waters because she wanted to bring accurate medical information to patients in the arena where they are seeking information.
“I want families to understand their condition as well as they can on whatever level they can, and so I just found this to be another way to do that ... outside of my clinic,” she said during an interview at the annual meeting of the American Society of Hematology.
But beyond correcting misinformation and serving as an advocate for patients, Dr. Yates said she gets professional benefits from being on Twitter. For instance, she uses the platform to find relevant articles as soon as they publish, without wading through all the journals.
“It’s allowed me to kind of streamline what I read,” she said.
Dr. Yates said Twitter is her social media platform of choice because it provides a simple, succinct way to communicate and provide links to more in-depth resources.
While social media can be fun and rewarding for physicians, Dr. Yates said think before you post. Ask yourself, “would you tell your chairperson this?”
Dr. Yates reported having no relevant financial disclosures.
SAN DIEGO –
“People want to see that you’re a person and not strictly a physician,” said Dr. Yates, a pediatric hematologist at Texas Children’s Hospital in Houston, who has had an active Twitter presence for the last few years.
Dr. Yates – whose Twitter handle is @sicklecelldoc – said she dipped a toe in the social media waters because she wanted to bring accurate medical information to patients in the arena where they are seeking information.
“I want families to understand their condition as well as they can on whatever level they can, and so I just found this to be another way to do that ... outside of my clinic,” she said during an interview at the annual meeting of the American Society of Hematology.
But beyond correcting misinformation and serving as an advocate for patients, Dr. Yates said she gets professional benefits from being on Twitter. For instance, she uses the platform to find relevant articles as soon as they publish, without wading through all the journals.
“It’s allowed me to kind of streamline what I read,” she said.
Dr. Yates said Twitter is her social media platform of choice because it provides a simple, succinct way to communicate and provide links to more in-depth resources.
While social media can be fun and rewarding for physicians, Dr. Yates said think before you post. Ask yourself, “would you tell your chairperson this?”
Dr. Yates reported having no relevant financial disclosures.
REPORTING FROM ASH 2018
AHA: Statins associated with high degree of safety
The benefits of statins highly offset the associated risks in appropriate patients, according to a scientific statement issued by the American Heart Association.
“The review covers the general patient population, as well as demographic subgroups, including the elderly, children, pregnant women, East Asians, and patients with specific conditions.” wrote Connie B. Newman, MD, of New York University, together with her colleagues. The report is in Arteriosclerosis, Thrombosis, and Vascular Biology.
After an extensive review of the literature pertaining to statin safety and tolerability, Dr. Newman and her colleagues reported the compiled findings from several randomized controlled trials, in addition to observational data, where required. They found that the risk of serious muscle complications, such as rhabdomyolysis, attributable to statin use was less than 0.1%. Furthermore, they noted that the risk of serious hepatotoxicity was even less likely, occurring in about 1 in 10,000 patients treated with therapy.
“There is no convincing evidence for a causal relationship between statins and cancer, cataracts, cognitive dysfunction, peripheral neuropathy, erectile dysfunction, or tendinitis,” the experts wrote. “In U.S. clinical practices, roughly 10% of patients stop taking a statin because of subjective complaints, most commonly muscle symptoms without raised creatine kinase,” they further reported.
Contrastingly, data from randomized trials have shown that the change in the incidence of muscle-related symptoms in patients treated with statins versus placebo is less than 1%. Moreover, the incidence is even lower, with an estimated rate of 0.1%, in those who stopped statin therapy because of these symptoms. Given these results, Dr. Newman and her colleagues said that muscle-related symptoms among statin-treated patients are not due to the pharmacological activity of the statin.
“Restarting statin therapy in these patients can be challenging, but it is important, especially in patients at high risk of cardiovascular events, for whom prevention of these events is a priority,” they added.
A large proportion of the population takes statin therapy to lower the risk of major cardiovascular events, including ischemic stroke, myocardial infarction, and other adverse effects of cardiovascular disease. At maximal doses, statins may decrease LDL-cholesterol levels by roughly 55%-60%. In addition, given the multitude of available generics, statins are an economical treatment option for most patients.
However, Dr. Newman and her colleagues suggested that, when considering statin therapy in special populations, particularly in patients with end-stage renal failure or severe hepatic disease, commencing treatment is not recommended.
“The lack of proof of cardiovascular benefit in patients with end-stage renal disease suggests that initiating statin treatment in these patients is generally not warranted,” the experts wrote. “Data on safety in people with more serious liver disease are insufficient, and statin treatment is generally discouraged,” they added.
With respect to statin-induced adverse effects, they are usually reversible upon discontinuation of therapy, with the exception of hemorrhagic stroke. However, damage from an ischemic stroke or myocardial infarction may result in death. As a result, in patients who would benefit from statin therapy, based on most recent guidelines, cardiovascular benefits greatly exceed potential safety concerns.
Dr. Newman and her coauthors disclosed financial affiliations with Amgen, Kowa, Regeneron, Sanofi, and others.
SOURCE: Newman CB et al. Arterioscler Thromb Vasc Biol. 2018 Dec 10. doi: 10.1161/ATV.0000000000000073
The benefits of statins highly offset the associated risks in appropriate patients, according to a scientific statement issued by the American Heart Association.
“The review covers the general patient population, as well as demographic subgroups, including the elderly, children, pregnant women, East Asians, and patients with specific conditions.” wrote Connie B. Newman, MD, of New York University, together with her colleagues. The report is in Arteriosclerosis, Thrombosis, and Vascular Biology.
After an extensive review of the literature pertaining to statin safety and tolerability, Dr. Newman and her colleagues reported the compiled findings from several randomized controlled trials, in addition to observational data, where required. They found that the risk of serious muscle complications, such as rhabdomyolysis, attributable to statin use was less than 0.1%. Furthermore, they noted that the risk of serious hepatotoxicity was even less likely, occurring in about 1 in 10,000 patients treated with therapy.
“There is no convincing evidence for a causal relationship between statins and cancer, cataracts, cognitive dysfunction, peripheral neuropathy, erectile dysfunction, or tendinitis,” the experts wrote. “In U.S. clinical practices, roughly 10% of patients stop taking a statin because of subjective complaints, most commonly muscle symptoms without raised creatine kinase,” they further reported.
Contrastingly, data from randomized trials have shown that the change in the incidence of muscle-related symptoms in patients treated with statins versus placebo is less than 1%. Moreover, the incidence is even lower, with an estimated rate of 0.1%, in those who stopped statin therapy because of these symptoms. Given these results, Dr. Newman and her colleagues said that muscle-related symptoms among statin-treated patients are not due to the pharmacological activity of the statin.
“Restarting statin therapy in these patients can be challenging, but it is important, especially in patients at high risk of cardiovascular events, for whom prevention of these events is a priority,” they added.
A large proportion of the population takes statin therapy to lower the risk of major cardiovascular events, including ischemic stroke, myocardial infarction, and other adverse effects of cardiovascular disease. At maximal doses, statins may decrease LDL-cholesterol levels by roughly 55%-60%. In addition, given the multitude of available generics, statins are an economical treatment option for most patients.
However, Dr. Newman and her colleagues suggested that, when considering statin therapy in special populations, particularly in patients with end-stage renal failure or severe hepatic disease, commencing treatment is not recommended.
“The lack of proof of cardiovascular benefit in patients with end-stage renal disease suggests that initiating statin treatment in these patients is generally not warranted,” the experts wrote. “Data on safety in people with more serious liver disease are insufficient, and statin treatment is generally discouraged,” they added.
With respect to statin-induced adverse effects, they are usually reversible upon discontinuation of therapy, with the exception of hemorrhagic stroke. However, damage from an ischemic stroke or myocardial infarction may result in death. As a result, in patients who would benefit from statin therapy, based on most recent guidelines, cardiovascular benefits greatly exceed potential safety concerns.
Dr. Newman and her coauthors disclosed financial affiliations with Amgen, Kowa, Regeneron, Sanofi, and others.
SOURCE: Newman CB et al. Arterioscler Thromb Vasc Biol. 2018 Dec 10. doi: 10.1161/ATV.0000000000000073
The benefits of statins highly offset the associated risks in appropriate patients, according to a scientific statement issued by the American Heart Association.
“The review covers the general patient population, as well as demographic subgroups, including the elderly, children, pregnant women, East Asians, and patients with specific conditions.” wrote Connie B. Newman, MD, of New York University, together with her colleagues. The report is in Arteriosclerosis, Thrombosis, and Vascular Biology.
After an extensive review of the literature pertaining to statin safety and tolerability, Dr. Newman and her colleagues reported the compiled findings from several randomized controlled trials, in addition to observational data, where required. They found that the risk of serious muscle complications, such as rhabdomyolysis, attributable to statin use was less than 0.1%. Furthermore, they noted that the risk of serious hepatotoxicity was even less likely, occurring in about 1 in 10,000 patients treated with therapy.
“There is no convincing evidence for a causal relationship between statins and cancer, cataracts, cognitive dysfunction, peripheral neuropathy, erectile dysfunction, or tendinitis,” the experts wrote. “In U.S. clinical practices, roughly 10% of patients stop taking a statin because of subjective complaints, most commonly muscle symptoms without raised creatine kinase,” they further reported.
Contrastingly, data from randomized trials have shown that the change in the incidence of muscle-related symptoms in patients treated with statins versus placebo is less than 1%. Moreover, the incidence is even lower, with an estimated rate of 0.1%, in those who stopped statin therapy because of these symptoms. Given these results, Dr. Newman and her colleagues said that muscle-related symptoms among statin-treated patients are not due to the pharmacological activity of the statin.
“Restarting statin therapy in these patients can be challenging, but it is important, especially in patients at high risk of cardiovascular events, for whom prevention of these events is a priority,” they added.
A large proportion of the population takes statin therapy to lower the risk of major cardiovascular events, including ischemic stroke, myocardial infarction, and other adverse effects of cardiovascular disease. At maximal doses, statins may decrease LDL-cholesterol levels by roughly 55%-60%. In addition, given the multitude of available generics, statins are an economical treatment option for most patients.
However, Dr. Newman and her colleagues suggested that, when considering statin therapy in special populations, particularly in patients with end-stage renal failure or severe hepatic disease, commencing treatment is not recommended.
“The lack of proof of cardiovascular benefit in patients with end-stage renal disease suggests that initiating statin treatment in these patients is generally not warranted,” the experts wrote. “Data on safety in people with more serious liver disease are insufficient, and statin treatment is generally discouraged,” they added.
With respect to statin-induced adverse effects, they are usually reversible upon discontinuation of therapy, with the exception of hemorrhagic stroke. However, damage from an ischemic stroke or myocardial infarction may result in death. As a result, in patients who would benefit from statin therapy, based on most recent guidelines, cardiovascular benefits greatly exceed potential safety concerns.
Dr. Newman and her coauthors disclosed financial affiliations with Amgen, Kowa, Regeneron, Sanofi, and others.
SOURCE: Newman CB et al. Arterioscler Thromb Vasc Biol. 2018 Dec 10. doi: 10.1161/ATV.0000000000000073
FROM ARTERIOSCLEROSIS, THROMBOSIS, AND VASCULAR BIOLOGY
Key clinical point: After rigorous review, the benefits of statin therapy were found to markedly exceed associated risks.
Major finding: .
Study details: A scientific statement on statin safety and associated adverse events from the American Heart Association.
Disclosures: Several writing group members disclosed financial affiliations with Amgen, Kowa, Regeneron, Sanofi, and others.
Source: Newman CB et al. Arterioscler Thromb Vasc Biol. 2018 Dec 10. doi: 10.1161/ATV.0000000000000073.
Phone app diagnoses STEMI nearly as well as ECG
CHICAGO – A novel smartphone app performed nearly as well as a standard 12-lead ECG for diagnosis of ST-segment elevation MI (STEMI) in patients presenting with chest pain in ST LEUIS, an international, multicenter study.
“This study demonstrates that a 12-lead-equivalent ECG obtained using a smartphone coupled with a software application and inexpensive two-wire attachment can identify STEMI versus non-STEMI with an excellent correlation to a traditional 12-lead ECG. This technology holds substantial promise to improve outcomes in STEMI by enabling more rapid diagnosis and treatment anywhere in the world for inexpensive cost,” J. Brent Muhlestein, MD, said while presenting the ST LEUIS results at the American Heart Association scientific sessions.
This technology could provide a long-sought breakthrough in overcoming patient denial and motivating hard-headed individuals with a life-threatening MI to get to the hospital more quickly after symptom onset, instead of initially shrugging off the matter as indigestion or another nuisance. If individuals can use their handy cell phone or smartwatch to quickly obtain an ECG that shows they’re having a STEMI, they’re going to seek medical attention much sooner, with resultant greater salvage of heart muscle, noted Dr. Muhlestein of Intermountain Healthcare in Salt Lake City.
ST LEUIS tested whether a smartphone ECG app developed by AliveCor can accurately diagnose STEMI in patients with chest pain. The study, which took place at Intermountain Medical Center and a handful of other sites associated with the Duke University Cooperative Cardiovascular Society, included 204 patients who presented to EDs with chest pain. They simultaneously received both a standard 12-lead ECG and an ECG obtained using the AliveCor smartphone app. The matched ECG pairs were evaluated separately, both quantitatively and qualitatively, by a blinded panel of experienced cardiologists and classified as STEMI, left bundle branch block, non-STEMI, or uninterpretable. The study population included 92 patients with chest pain and activation of a STEMI protocol and 112 who came through the ED chest pain protocol.
Side-by-side ECG comparisons weren’t attempted in 14 pairs deemed not interpretable. In 13 cases this was because of technical problems with the smartphone ECG, and in the 14th because of ventricular pacing in the standard 12-lead ECG.
STEMI was diagnosed in 22.5% of the study population by 12-lead ECG and in 29.4% by smartphone app. The discrepancy was explained by small voltage differences in the ST-segment elevation which met criteria for STEMI by smartphone but not standard 12-lead ECG in 15 cases.
“It appears that the ST elevation was a little bit more obvious in the smartphone ECG,” Dr. Muhlestein observed.
Left bundle branch block was identified in 5.4% of patients by both methods.
The key performance numbers: The smartphone ECG had a sensitivity of 89%, specificity of 84%, positive predictive value of 70%, and negative predictive value of 95% for diagnosis of STEMI or left bundle branch block. The positive predictive value was diminished by the increased likelihood that the smartphone would call STEMI in discordant cases.
Dr. Muhlestein said that, despite the AliveCor device’s very good correlation with the standard 12-lead ECG, the system needs further tweaking.
“We definitely think this is not ready for prime time. Further refinements of the software and hardware may improve on our study results and broaden potential applications through increased ease of use and reliability. I’m sure smart engineers can make a much more simple, really user-friendly device now that we know it’s actually feasible. I envision a time when you turn it on and it speaks loud and tells you what to do and how to do it – like an AED [automated external defibrillator] – then uploads the ECG to the cloud, interprets it, and tells you whether you should go to the emergency department or not,” Dr. Muhlestein said.
This is a device that’s going to be a boon not only in the United States but also in developing countries, where even people living without electricity or running water often have cell phones, the cardiologist noted.
Dr. Muhlestein reported having no financial conflicts of interest regarding the study, which was sponsored by the participating medical institutions.
CHICAGO – A novel smartphone app performed nearly as well as a standard 12-lead ECG for diagnosis of ST-segment elevation MI (STEMI) in patients presenting with chest pain in ST LEUIS, an international, multicenter study.
“This study demonstrates that a 12-lead-equivalent ECG obtained using a smartphone coupled with a software application and inexpensive two-wire attachment can identify STEMI versus non-STEMI with an excellent correlation to a traditional 12-lead ECG. This technology holds substantial promise to improve outcomes in STEMI by enabling more rapid diagnosis and treatment anywhere in the world for inexpensive cost,” J. Brent Muhlestein, MD, said while presenting the ST LEUIS results at the American Heart Association scientific sessions.
This technology could provide a long-sought breakthrough in overcoming patient denial and motivating hard-headed individuals with a life-threatening MI to get to the hospital more quickly after symptom onset, instead of initially shrugging off the matter as indigestion or another nuisance. If individuals can use their handy cell phone or smartwatch to quickly obtain an ECG that shows they’re having a STEMI, they’re going to seek medical attention much sooner, with resultant greater salvage of heart muscle, noted Dr. Muhlestein of Intermountain Healthcare in Salt Lake City.
ST LEUIS tested whether a smartphone ECG app developed by AliveCor can accurately diagnose STEMI in patients with chest pain. The study, which took place at Intermountain Medical Center and a handful of other sites associated with the Duke University Cooperative Cardiovascular Society, included 204 patients who presented to EDs with chest pain. They simultaneously received both a standard 12-lead ECG and an ECG obtained using the AliveCor smartphone app. The matched ECG pairs were evaluated separately, both quantitatively and qualitatively, by a blinded panel of experienced cardiologists and classified as STEMI, left bundle branch block, non-STEMI, or uninterpretable. The study population included 92 patients with chest pain and activation of a STEMI protocol and 112 who came through the ED chest pain protocol.
Side-by-side ECG comparisons weren’t attempted in 14 pairs deemed not interpretable. In 13 cases this was because of technical problems with the smartphone ECG, and in the 14th because of ventricular pacing in the standard 12-lead ECG.
STEMI was diagnosed in 22.5% of the study population by 12-lead ECG and in 29.4% by smartphone app. The discrepancy was explained by small voltage differences in the ST-segment elevation which met criteria for STEMI by smartphone but not standard 12-lead ECG in 15 cases.
“It appears that the ST elevation was a little bit more obvious in the smartphone ECG,” Dr. Muhlestein observed.
Left bundle branch block was identified in 5.4% of patients by both methods.
The key performance numbers: The smartphone ECG had a sensitivity of 89%, specificity of 84%, positive predictive value of 70%, and negative predictive value of 95% for diagnosis of STEMI or left bundle branch block. The positive predictive value was diminished by the increased likelihood that the smartphone would call STEMI in discordant cases.
Dr. Muhlestein said that, despite the AliveCor device’s very good correlation with the standard 12-lead ECG, the system needs further tweaking.
“We definitely think this is not ready for prime time. Further refinements of the software and hardware may improve on our study results and broaden potential applications through increased ease of use and reliability. I’m sure smart engineers can make a much more simple, really user-friendly device now that we know it’s actually feasible. I envision a time when you turn it on and it speaks loud and tells you what to do and how to do it – like an AED [automated external defibrillator] – then uploads the ECG to the cloud, interprets it, and tells you whether you should go to the emergency department or not,” Dr. Muhlestein said.
This is a device that’s going to be a boon not only in the United States but also in developing countries, where even people living without electricity or running water often have cell phones, the cardiologist noted.
Dr. Muhlestein reported having no financial conflicts of interest regarding the study, which was sponsored by the participating medical institutions.
CHICAGO – A novel smartphone app performed nearly as well as a standard 12-lead ECG for diagnosis of ST-segment elevation MI (STEMI) in patients presenting with chest pain in ST LEUIS, an international, multicenter study.
“This study demonstrates that a 12-lead-equivalent ECG obtained using a smartphone coupled with a software application and inexpensive two-wire attachment can identify STEMI versus non-STEMI with an excellent correlation to a traditional 12-lead ECG. This technology holds substantial promise to improve outcomes in STEMI by enabling more rapid diagnosis and treatment anywhere in the world for inexpensive cost,” J. Brent Muhlestein, MD, said while presenting the ST LEUIS results at the American Heart Association scientific sessions.
This technology could provide a long-sought breakthrough in overcoming patient denial and motivating hard-headed individuals with a life-threatening MI to get to the hospital more quickly after symptom onset, instead of initially shrugging off the matter as indigestion or another nuisance. If individuals can use their handy cell phone or smartwatch to quickly obtain an ECG that shows they’re having a STEMI, they’re going to seek medical attention much sooner, with resultant greater salvage of heart muscle, noted Dr. Muhlestein of Intermountain Healthcare in Salt Lake City.
ST LEUIS tested whether a smartphone ECG app developed by AliveCor can accurately diagnose STEMI in patients with chest pain. The study, which took place at Intermountain Medical Center and a handful of other sites associated with the Duke University Cooperative Cardiovascular Society, included 204 patients who presented to EDs with chest pain. They simultaneously received both a standard 12-lead ECG and an ECG obtained using the AliveCor smartphone app. The matched ECG pairs were evaluated separately, both quantitatively and qualitatively, by a blinded panel of experienced cardiologists and classified as STEMI, left bundle branch block, non-STEMI, or uninterpretable. The study population included 92 patients with chest pain and activation of a STEMI protocol and 112 who came through the ED chest pain protocol.
Side-by-side ECG comparisons weren’t attempted in 14 pairs deemed not interpretable. In 13 cases this was because of technical problems with the smartphone ECG, and in the 14th because of ventricular pacing in the standard 12-lead ECG.
STEMI was diagnosed in 22.5% of the study population by 12-lead ECG and in 29.4% by smartphone app. The discrepancy was explained by small voltage differences in the ST-segment elevation which met criteria for STEMI by smartphone but not standard 12-lead ECG in 15 cases.
“It appears that the ST elevation was a little bit more obvious in the smartphone ECG,” Dr. Muhlestein observed.
Left bundle branch block was identified in 5.4% of patients by both methods.
The key performance numbers: The smartphone ECG had a sensitivity of 89%, specificity of 84%, positive predictive value of 70%, and negative predictive value of 95% for diagnosis of STEMI or left bundle branch block. The positive predictive value was diminished by the increased likelihood that the smartphone would call STEMI in discordant cases.
Dr. Muhlestein said that, despite the AliveCor device’s very good correlation with the standard 12-lead ECG, the system needs further tweaking.
“We definitely think this is not ready for prime time. Further refinements of the software and hardware may improve on our study results and broaden potential applications through increased ease of use and reliability. I’m sure smart engineers can make a much more simple, really user-friendly device now that we know it’s actually feasible. I envision a time when you turn it on and it speaks loud and tells you what to do and how to do it – like an AED [automated external defibrillator] – then uploads the ECG to the cloud, interprets it, and tells you whether you should go to the emergency department or not,” Dr. Muhlestein said.
This is a device that’s going to be a boon not only in the United States but also in developing countries, where even people living without electricity or running water often have cell phones, the cardiologist noted.
Dr. Muhlestein reported having no financial conflicts of interest regarding the study, which was sponsored by the participating medical institutions.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: The app, designed to diagnose ST-segment elevation MI, had a sensitivity of 89%, specificity of 84%, and negative predictive value of 95% for this purpose.
Study details: This multicenter, international study featured blinded expert side-by-side comparisons of standard 12-lead ECGs and ECGs obtained via a smartphone app in 204 patients who presented with chest pain.
Disclosures: The presenter reported having no financial conflicts of interest regarding the study, which was fully sponsored by the participating medical institutions.
Bring Schwartz Rounds to your hospital
A more emotional approach to rounds
If you are not doing Schwartz Rounds, get them started. ASAP.
I recently completed a 4-year tenure as physician moderator for our hospital’s Schwartz Rounds. An amazing team at my hospital helped pull the bimonthly sessions together. These compassionate care rounds are a national initiative to help foster empathy and compassion in the health care setting.
We gather a panel of two to three people involved in our patient presentation who share and move quickly through the clinical details, and head on toward the thornier ethical issues, emotional triggers, and responses. The best sessions are when the audience’s voice is heard for the bulk of the time.
The emotional cadence flows from boiling in frustration, drowning in tears, followed by comfort, and ending in thoughts for the next session. It is a more powerful arc than an episode of the television program “This is Us.” Largely, because this was us. This was real life. Real-time catharsis in the hospital.
In the daily grind, we often skip the step of processing our frustration, sadness, and anger, moving right on to the next patient and walking into the next room with that stoic layer of equanimity. I walk the hallways and find I grab my phone to catch up on emails, walking to the wrong floor because I’m not paying attention. Always something to do, someone to talk to, a family to call, pagers going off, phone calls. When do we sit and reflect?
These Schwartz Rounds are those moments of reflection – a slowdown in the day to think more deeply about the case. We talk about everything and anything. We have discussions with opposing views:
“Everything should have been done!”
“How did you not stop care?!”
“I agree with the doctors.”
“I can see the patient’s view more clearly now.”
Our first Schwartz Rounds tended to be end-of-life stories, particularly regarding the family mantra of “Do everything.” The health care team watches the suffering of a patient, a family, in a seemingly futile situation. Conversations around the end of life, choices, and quality of life are cut short daily by family members who simply recite, “Do everything.”
After several of these sessions, a case swings us in the other direction. The elderly gentleman with treatable cancer, who could easily survive another 20 years, declines treatment. “I’m fine, doc; I’ve lived long enough.” His wife at his bedside, shaking her head, tells us, “I don’t know why he wants to give up. He’s been as stubborn as a mule since the day I met him.” I spend 30 minutes convincing him to stay. The nurse does the same. Now we have a patient with a “Do nothing.” The patient’s decisions conflict with the family and the health care team.
Every day in the hospital provides a new ethical dilemma, a frustrating case, a challenging patient. Fodder for rounds.
Read the full post at hospitalleader.org.
Dr. Messler is a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. He previously chaired SHM’s Quality and Patient Safety Committee and has been active in several SHM mentoring programs, most recently with Project BOOST and Glycemic Control.
Also on The Hospital Leader
- Incubating Success: How We Used Structured Feedback to Reduce A Dangerous Practice by Rich Bottner, PA-C & Victoria Valencia, MPH
- New SoHM Report Provides Unique Window into Hospital Medicine Practice Trends by Leslie Flores, MHA, SFHM
- IGNITE Change: Improving Care via Interprofessional Clinical Learning Environments by Vineet Arora, MD, MAPP, MHM
A more emotional approach to rounds
A more emotional approach to rounds
If you are not doing Schwartz Rounds, get them started. ASAP.
I recently completed a 4-year tenure as physician moderator for our hospital’s Schwartz Rounds. An amazing team at my hospital helped pull the bimonthly sessions together. These compassionate care rounds are a national initiative to help foster empathy and compassion in the health care setting.
We gather a panel of two to three people involved in our patient presentation who share and move quickly through the clinical details, and head on toward the thornier ethical issues, emotional triggers, and responses. The best sessions are when the audience’s voice is heard for the bulk of the time.
The emotional cadence flows from boiling in frustration, drowning in tears, followed by comfort, and ending in thoughts for the next session. It is a more powerful arc than an episode of the television program “This is Us.” Largely, because this was us. This was real life. Real-time catharsis in the hospital.
In the daily grind, we often skip the step of processing our frustration, sadness, and anger, moving right on to the next patient and walking into the next room with that stoic layer of equanimity. I walk the hallways and find I grab my phone to catch up on emails, walking to the wrong floor because I’m not paying attention. Always something to do, someone to talk to, a family to call, pagers going off, phone calls. When do we sit and reflect?
These Schwartz Rounds are those moments of reflection – a slowdown in the day to think more deeply about the case. We talk about everything and anything. We have discussions with opposing views:
“Everything should have been done!”
“How did you not stop care?!”
“I agree with the doctors.”
“I can see the patient’s view more clearly now.”
Our first Schwartz Rounds tended to be end-of-life stories, particularly regarding the family mantra of “Do everything.” The health care team watches the suffering of a patient, a family, in a seemingly futile situation. Conversations around the end of life, choices, and quality of life are cut short daily by family members who simply recite, “Do everything.”
After several of these sessions, a case swings us in the other direction. The elderly gentleman with treatable cancer, who could easily survive another 20 years, declines treatment. “I’m fine, doc; I’ve lived long enough.” His wife at his bedside, shaking her head, tells us, “I don’t know why he wants to give up. He’s been as stubborn as a mule since the day I met him.” I spend 30 minutes convincing him to stay. The nurse does the same. Now we have a patient with a “Do nothing.” The patient’s decisions conflict with the family and the health care team.
Every day in the hospital provides a new ethical dilemma, a frustrating case, a challenging patient. Fodder for rounds.
Read the full post at hospitalleader.org.
Dr. Messler is a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. He previously chaired SHM’s Quality and Patient Safety Committee and has been active in several SHM mentoring programs, most recently with Project BOOST and Glycemic Control.
Also on The Hospital Leader
- Incubating Success: How We Used Structured Feedback to Reduce A Dangerous Practice by Rich Bottner, PA-C & Victoria Valencia, MPH
- New SoHM Report Provides Unique Window into Hospital Medicine Practice Trends by Leslie Flores, MHA, SFHM
- IGNITE Change: Improving Care via Interprofessional Clinical Learning Environments by Vineet Arora, MD, MAPP, MHM
If you are not doing Schwartz Rounds, get them started. ASAP.
I recently completed a 4-year tenure as physician moderator for our hospital’s Schwartz Rounds. An amazing team at my hospital helped pull the bimonthly sessions together. These compassionate care rounds are a national initiative to help foster empathy and compassion in the health care setting.
We gather a panel of two to three people involved in our patient presentation who share and move quickly through the clinical details, and head on toward the thornier ethical issues, emotional triggers, and responses. The best sessions are when the audience’s voice is heard for the bulk of the time.
The emotional cadence flows from boiling in frustration, drowning in tears, followed by comfort, and ending in thoughts for the next session. It is a more powerful arc than an episode of the television program “This is Us.” Largely, because this was us. This was real life. Real-time catharsis in the hospital.
In the daily grind, we often skip the step of processing our frustration, sadness, and anger, moving right on to the next patient and walking into the next room with that stoic layer of equanimity. I walk the hallways and find I grab my phone to catch up on emails, walking to the wrong floor because I’m not paying attention. Always something to do, someone to talk to, a family to call, pagers going off, phone calls. When do we sit and reflect?
These Schwartz Rounds are those moments of reflection – a slowdown in the day to think more deeply about the case. We talk about everything and anything. We have discussions with opposing views:
“Everything should have been done!”
“How did you not stop care?!”
“I agree with the doctors.”
“I can see the patient’s view more clearly now.”
Our first Schwartz Rounds tended to be end-of-life stories, particularly regarding the family mantra of “Do everything.” The health care team watches the suffering of a patient, a family, in a seemingly futile situation. Conversations around the end of life, choices, and quality of life are cut short daily by family members who simply recite, “Do everything.”
After several of these sessions, a case swings us in the other direction. The elderly gentleman with treatable cancer, who could easily survive another 20 years, declines treatment. “I’m fine, doc; I’ve lived long enough.” His wife at his bedside, shaking her head, tells us, “I don’t know why he wants to give up. He’s been as stubborn as a mule since the day I met him.” I spend 30 minutes convincing him to stay. The nurse does the same. Now we have a patient with a “Do nothing.” The patient’s decisions conflict with the family and the health care team.
Every day in the hospital provides a new ethical dilemma, a frustrating case, a challenging patient. Fodder for rounds.
Read the full post at hospitalleader.org.
Dr. Messler is a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. He previously chaired SHM’s Quality and Patient Safety Committee and has been active in several SHM mentoring programs, most recently with Project BOOST and Glycemic Control.
Also on The Hospital Leader
- Incubating Success: How We Used Structured Feedback to Reduce A Dangerous Practice by Rich Bottner, PA-C & Victoria Valencia, MPH
- New SoHM Report Provides Unique Window into Hospital Medicine Practice Trends by Leslie Flores, MHA, SFHM
- IGNITE Change: Improving Care via Interprofessional Clinical Learning Environments by Vineet Arora, MD, MAPP, MHM
Acute stroke thrombolysis worked safely despite GI bleed or malignancy
CHICAGO – A recent history of GI bleeding or malignancy may not be a valid contraindication to thrombolytic therapy in patients with an acute ischemic stroke, based on a review of outcomes from more than 40,000 U.S. stroke patients.
The analysis showed that, among 40,396 U.S. patients who had an acute ischemic stroke during 2009-2015 and received timely treatment with alteplase, “we did not find statistically significant increased rates of in-hospital mortality or bleeding” in the small number of patients who received alteplase (Activase) despite a recent GI bleed or diagnosed GI malignancy, Taku Inohara, MD, said at the American Heart Association scientific sessions. The 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke deemed thrombolytic therapy with alteplase in these types of patients contraindicated, based on consensus expert opinion (Stroke. 2018 March;49[3]:e66-e110).
“Further study is needed to evaluate the safety of recombinant tissue–type plasminogen activator [alteplase] in this specific population,” suggested Dr. Inohara, a cardiologist and research fellow at Duke University, Durham, N.C.
His analysis used data collected by the Get With the Guidelines–Stroke program, a voluntary quality promotion and improvement program that during 2009-2015 included records for more than 633,000 U.S. stroke patients that could be linked with records kept by the Centers for Medicare & Medicaid Services. From this database, 40,396 patients (6%) treated with alteplase within 4.5 hours of stroke onset were identified. The alteplase-treated patients included 93 with a diagnosis code during the prior year for a GI malignancy and 43 with a diagnostic code within the prior 21 days for a GI bleed.
Dr. Inohara and his associates determined patients’ mortality during their stroke hospitalization, as well as several measures of functional recovery at hospital discharge and thrombolysis-related complications. For each of these endpoints, the rate among patients with a GI malignancy, a GI bleed, or the rate among a combined group of both patients showed no statistically significant differences, compared with the more than 40,000 other patients without a GI complication after adjustment for several demographic and clinical between-group differences. However, Dr. Inohara cautioned that residual or unmeasured confounding may exist that distorts these findings. The rate of in-hospital mortality, the prespecified primary endpoint for the analysis, was 10% among patients with either type of GI complication and 9% in those without. The rate of serious thrombolysis-related complications was 7% in the patients with GI disease and 9% in those without.
In a separate analysis of the complete database of more than 633,000 patients, Dr. Inohara and his associates found 148 patients who had either a GI bleed or malignancy and otherwise qualified for thrombolytic therapy but did not receive this treatment. This meant that overall, in this large U.S. experience, 136 of 284 (48%) acute ischemic stroke patients who qualified for thrombolysis but had a GI complication nonetheless received thrombolysis. Further analysis showed that the patients not treated with thrombolysis had at admission an average National Institutes of Health Stroke Scale score of 11, compared with an average score of 14 among patients who received thrombolysis.
This apparent selection for thrombolytic treatment of patients with more severe strokes “may have overestimated risk in the patients with GI disease,” Dr. Inohara said.
Dr. Inohara reported receiving research funding from Boston Scientific.
SOURCE: Inohara T et al. Circulation. 2018 Nov 6;138[suppl 1], Abstract 12291.
CHICAGO – A recent history of GI bleeding or malignancy may not be a valid contraindication to thrombolytic therapy in patients with an acute ischemic stroke, based on a review of outcomes from more than 40,000 U.S. stroke patients.
The analysis showed that, among 40,396 U.S. patients who had an acute ischemic stroke during 2009-2015 and received timely treatment with alteplase, “we did not find statistically significant increased rates of in-hospital mortality or bleeding” in the small number of patients who received alteplase (Activase) despite a recent GI bleed or diagnosed GI malignancy, Taku Inohara, MD, said at the American Heart Association scientific sessions. The 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke deemed thrombolytic therapy with alteplase in these types of patients contraindicated, based on consensus expert opinion (Stroke. 2018 March;49[3]:e66-e110).
“Further study is needed to evaluate the safety of recombinant tissue–type plasminogen activator [alteplase] in this specific population,” suggested Dr. Inohara, a cardiologist and research fellow at Duke University, Durham, N.C.
His analysis used data collected by the Get With the Guidelines–Stroke program, a voluntary quality promotion and improvement program that during 2009-2015 included records for more than 633,000 U.S. stroke patients that could be linked with records kept by the Centers for Medicare & Medicaid Services. From this database, 40,396 patients (6%) treated with alteplase within 4.5 hours of stroke onset were identified. The alteplase-treated patients included 93 with a diagnosis code during the prior year for a GI malignancy and 43 with a diagnostic code within the prior 21 days for a GI bleed.
Dr. Inohara and his associates determined patients’ mortality during their stroke hospitalization, as well as several measures of functional recovery at hospital discharge and thrombolysis-related complications. For each of these endpoints, the rate among patients with a GI malignancy, a GI bleed, or the rate among a combined group of both patients showed no statistically significant differences, compared with the more than 40,000 other patients without a GI complication after adjustment for several demographic and clinical between-group differences. However, Dr. Inohara cautioned that residual or unmeasured confounding may exist that distorts these findings. The rate of in-hospital mortality, the prespecified primary endpoint for the analysis, was 10% among patients with either type of GI complication and 9% in those without. The rate of serious thrombolysis-related complications was 7% in the patients with GI disease and 9% in those without.
In a separate analysis of the complete database of more than 633,000 patients, Dr. Inohara and his associates found 148 patients who had either a GI bleed or malignancy and otherwise qualified for thrombolytic therapy but did not receive this treatment. This meant that overall, in this large U.S. experience, 136 of 284 (48%) acute ischemic stroke patients who qualified for thrombolysis but had a GI complication nonetheless received thrombolysis. Further analysis showed that the patients not treated with thrombolysis had at admission an average National Institutes of Health Stroke Scale score of 11, compared with an average score of 14 among patients who received thrombolysis.
This apparent selection for thrombolytic treatment of patients with more severe strokes “may have overestimated risk in the patients with GI disease,” Dr. Inohara said.
Dr. Inohara reported receiving research funding from Boston Scientific.
SOURCE: Inohara T et al. Circulation. 2018 Nov 6;138[suppl 1], Abstract 12291.
CHICAGO – A recent history of GI bleeding or malignancy may not be a valid contraindication to thrombolytic therapy in patients with an acute ischemic stroke, based on a review of outcomes from more than 40,000 U.S. stroke patients.
The analysis showed that, among 40,396 U.S. patients who had an acute ischemic stroke during 2009-2015 and received timely treatment with alteplase, “we did not find statistically significant increased rates of in-hospital mortality or bleeding” in the small number of patients who received alteplase (Activase) despite a recent GI bleed or diagnosed GI malignancy, Taku Inohara, MD, said at the American Heart Association scientific sessions. The 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke deemed thrombolytic therapy with alteplase in these types of patients contraindicated, based on consensus expert opinion (Stroke. 2018 March;49[3]:e66-e110).
“Further study is needed to evaluate the safety of recombinant tissue–type plasminogen activator [alteplase] in this specific population,” suggested Dr. Inohara, a cardiologist and research fellow at Duke University, Durham, N.C.
His analysis used data collected by the Get With the Guidelines–Stroke program, a voluntary quality promotion and improvement program that during 2009-2015 included records for more than 633,000 U.S. stroke patients that could be linked with records kept by the Centers for Medicare & Medicaid Services. From this database, 40,396 patients (6%) treated with alteplase within 4.5 hours of stroke onset were identified. The alteplase-treated patients included 93 with a diagnosis code during the prior year for a GI malignancy and 43 with a diagnostic code within the prior 21 days for a GI bleed.
Dr. Inohara and his associates determined patients’ mortality during their stroke hospitalization, as well as several measures of functional recovery at hospital discharge and thrombolysis-related complications. For each of these endpoints, the rate among patients with a GI malignancy, a GI bleed, or the rate among a combined group of both patients showed no statistically significant differences, compared with the more than 40,000 other patients without a GI complication after adjustment for several demographic and clinical between-group differences. However, Dr. Inohara cautioned that residual or unmeasured confounding may exist that distorts these findings. The rate of in-hospital mortality, the prespecified primary endpoint for the analysis, was 10% among patients with either type of GI complication and 9% in those without. The rate of serious thrombolysis-related complications was 7% in the patients with GI disease and 9% in those without.
In a separate analysis of the complete database of more than 633,000 patients, Dr. Inohara and his associates found 148 patients who had either a GI bleed or malignancy and otherwise qualified for thrombolytic therapy but did not receive this treatment. This meant that overall, in this large U.S. experience, 136 of 284 (48%) acute ischemic stroke patients who qualified for thrombolysis but had a GI complication nonetheless received thrombolysis. Further analysis showed that the patients not treated with thrombolysis had at admission an average National Institutes of Health Stroke Scale score of 11, compared with an average score of 14 among patients who received thrombolysis.
This apparent selection for thrombolytic treatment of patients with more severe strokes “may have overestimated risk in the patients with GI disease,” Dr. Inohara said.
Dr. Inohara reported receiving research funding from Boston Scientific.
SOURCE: Inohara T et al. Circulation. 2018 Nov 6;138[suppl 1], Abstract 12291.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: In-hospital mortality after thrombolysis was 10% in those with a GI bleed or malignancy and 9% in those without.
Study details: A review of Medicare records for 40,396 acute ischemic stroke patients treated with thrombolysis during 2009-2015.
Disclosures: Dr. Inohara reported receiving research funding from Boston Scientific.
Source: Inohara T et al. Circulation. 2018 Nov 6;138[suppl 1], Abstract A12291.
ICU-acquired pneumonia mortality risk may be underestimated
In a large prospectively collected database, the risk of death at 30 days in ICU patients was far greater in those with hospital-acquired pneumonia (HAP) than in those with ventilator-associated pneumonia (VAP) even after adjustment for prognostic factors, according to a large study that compared mortality risk for these complications.
The data for this newly published study were drawn from an evaluation of 14,212 patients treated at 23 ICUs participating in a collaborative French network OUTCOMEREA and published Critical Care Medicine.
HAP in ICU patients “was associated with an 82% increase in the risk of death at day 30,” reported a team of investigators led by Wafa Ibn Saied, MD, of the Université Paris Diderot. Although VAP and HAP were independent risk factors (P both less than .0001) for death at 30 days, VAP increased risk by 38%, less than half of HAP, which increased risk by 82%.
From an observational but prospective database initiated in 1997, this study evaluated 7,735 ICU patients at risk for VAP and 9,747 at risk for HAP. Of those at risk, defined by several factors including an ICU stay of more than 48 hours, HAP developed in 8% and VAP developed in 1%.
The 30-day mortality rates at 30 days after pneumonia were 23.9% for HAP and 28.4% for VAP. The greater risk of death by HR was identified after an analysis that adjusted for mortality risk factors, the adequacy of initial treatment, and other factors, such as prior history of pneumonia.
In HAP patients, the rate of mortality at 30 days was 32% in the 75 who were reintubated but only 16% in the 101 who were not. Adequate empirical therapy within the first 24 hours for HAP was not associated with a reduction in the risk of death.
As in the HAP patients, mortality was not significantly higher in VAP patients who received inadequate empirical therapy, compared with those who did, according to the authors.
Previous studies have suggested that both HAP and VAP increase risk of death in ICU patients, but the authors of this study believe that the relative risk of HAP “is underappreciated.” They asserted, based on these most recent data as well as on previously published analyses, that nonventilated HAP results in “significant increases in cost, length of stay, and mortality.”
The researchers had no disclosures.
SOURCE: Saied WI et al. Crit Care Med. 2018 Nov 7. doi: 10.1097/CCM.0000000000003553.
In a large prospectively collected database, the risk of death at 30 days in ICU patients was far greater in those with hospital-acquired pneumonia (HAP) than in those with ventilator-associated pneumonia (VAP) even after adjustment for prognostic factors, according to a large study that compared mortality risk for these complications.
The data for this newly published study were drawn from an evaluation of 14,212 patients treated at 23 ICUs participating in a collaborative French network OUTCOMEREA and published Critical Care Medicine.
HAP in ICU patients “was associated with an 82% increase in the risk of death at day 30,” reported a team of investigators led by Wafa Ibn Saied, MD, of the Université Paris Diderot. Although VAP and HAP were independent risk factors (P both less than .0001) for death at 30 days, VAP increased risk by 38%, less than half of HAP, which increased risk by 82%.
From an observational but prospective database initiated in 1997, this study evaluated 7,735 ICU patients at risk for VAP and 9,747 at risk for HAP. Of those at risk, defined by several factors including an ICU stay of more than 48 hours, HAP developed in 8% and VAP developed in 1%.
The 30-day mortality rates at 30 days after pneumonia were 23.9% for HAP and 28.4% for VAP. The greater risk of death by HR was identified after an analysis that adjusted for mortality risk factors, the adequacy of initial treatment, and other factors, such as prior history of pneumonia.
In HAP patients, the rate of mortality at 30 days was 32% in the 75 who were reintubated but only 16% in the 101 who were not. Adequate empirical therapy within the first 24 hours for HAP was not associated with a reduction in the risk of death.
As in the HAP patients, mortality was not significantly higher in VAP patients who received inadequate empirical therapy, compared with those who did, according to the authors.
Previous studies have suggested that both HAP and VAP increase risk of death in ICU patients, but the authors of this study believe that the relative risk of HAP “is underappreciated.” They asserted, based on these most recent data as well as on previously published analyses, that nonventilated HAP results in “significant increases in cost, length of stay, and mortality.”
The researchers had no disclosures.
SOURCE: Saied WI et al. Crit Care Med. 2018 Nov 7. doi: 10.1097/CCM.0000000000003553.
In a large prospectively collected database, the risk of death at 30 days in ICU patients was far greater in those with hospital-acquired pneumonia (HAP) than in those with ventilator-associated pneumonia (VAP) even after adjustment for prognostic factors, according to a large study that compared mortality risk for these complications.
The data for this newly published study were drawn from an evaluation of 14,212 patients treated at 23 ICUs participating in a collaborative French network OUTCOMEREA and published Critical Care Medicine.
HAP in ICU patients “was associated with an 82% increase in the risk of death at day 30,” reported a team of investigators led by Wafa Ibn Saied, MD, of the Université Paris Diderot. Although VAP and HAP were independent risk factors (P both less than .0001) for death at 30 days, VAP increased risk by 38%, less than half of HAP, which increased risk by 82%.
From an observational but prospective database initiated in 1997, this study evaluated 7,735 ICU patients at risk for VAP and 9,747 at risk for HAP. Of those at risk, defined by several factors including an ICU stay of more than 48 hours, HAP developed in 8% and VAP developed in 1%.
The 30-day mortality rates at 30 days after pneumonia were 23.9% for HAP and 28.4% for VAP. The greater risk of death by HR was identified after an analysis that adjusted for mortality risk factors, the adequacy of initial treatment, and other factors, such as prior history of pneumonia.
In HAP patients, the rate of mortality at 30 days was 32% in the 75 who were reintubated but only 16% in the 101 who were not. Adequate empirical therapy within the first 24 hours for HAP was not associated with a reduction in the risk of death.
As in the HAP patients, mortality was not significantly higher in VAP patients who received inadequate empirical therapy, compared with those who did, according to the authors.
Previous studies have suggested that both HAP and VAP increase risk of death in ICU patients, but the authors of this study believe that the relative risk of HAP “is underappreciated.” They asserted, based on these most recent data as well as on previously published analyses, that nonventilated HAP results in “significant increases in cost, length of stay, and mortality.”
The researchers had no disclosures.
SOURCE: Saied WI et al. Crit Care Med. 2018 Nov 7. doi: 10.1097/CCM.0000000000003553.
FROM CRITICAL CARE MEDICINE
Key clinical point: Hospital-acquired pneumonia poses a greater risk of death in the ICU than ventilator-associated pneumonia.
Major finding: After prognostic adjustment, the mortality hazard ratios were 1.82 and 1.38 for HAP and VAP, respectively.
Study details: Observational cohort study.
Disclosures: The researchers had no disclosures.
Source: Saied WI et al. Crit Care Med. 2018 Nov 7; doi: 10.1097/CCM.0000000000003553.
Unit-based assignments: Pros and cons
Geographic cohorting shows ‘varying success’
A relatively recent practice catching on in many different hospitalist groups is geographic cohorting, or unit-based assignments. Traditionally, most hospitalists have had patients assigned on multiple different units. Unit-based assignments have been touted as a way of improving interdisciplinary communication and provider and patient satisfaction.1
How frequently are hospital medicine groups using unit-based assignments? SHM sought to quantify this trend in the recently published 2018 State of Hospital Medicine Report. Overall, among hospital medicine groups serving adults only, a little over one-third (36.4%) of groups reported utilizing unit-based assignments. However, there was significant variation, particularly dependent on group size. Geographic cohorting was used only in 7.6% of groups with 4 or fewer full-time equivalents, and in 68.8% of groups with 30 or more FTE. These data seem logical, as the potential gains from cohorting likely increase with group/hospital size, where physicians would otherwise round on an increasingly large number of units.
As has been shared in the hospital medicine literature, groups have experienced variable success with geographic cohorting. Improvements have been achieved in interprofessional collaboration, efficiency, nursing satisfaction,2 and, in some instances, length of stay. Unit-based assignments have allowed some groups to pilot other interventions, such as interdisciplinary rounds.
But geographic cohorting comes with its implementation challenges, too. For example, in many hospitals, some units have differing telemetry or nursing capabilities. And, in other institutions, there are units providing specialized care, such as care for neurology or oncology patients. The workload for hospitalists caring for particular types of patients may vary, and with specialty units, it may be more difficult to keep a similar census assigned to each hospitalist.
While some groups have noted increased professional satisfaction, others have noted decreases in satisfaction. One reason is that, while the frequency of paging may decrease, this is replaced by an increase in face-to-face interruptions. Also, unit-based assignments in some groups have resulted in hospitalists perceiving they are working in silos because of a decrease in interactions and camaraderie among providers in the same hospital medicine group.
At my home institution, University of California, San Diego, geographic cohorting has largely been a successful and positively perceived change. Our efforts have been particularly successful at one of our two campuses where most units have telemetry capabilities and where we have a dedicated daytime admitter (there are data on this in the Report as well, and a dedicated daytime admitter is the topic of a future Survey Insights column). Unit-based assignments have allowed the implementation of what we’ve termed focused interdisciplinary rounds.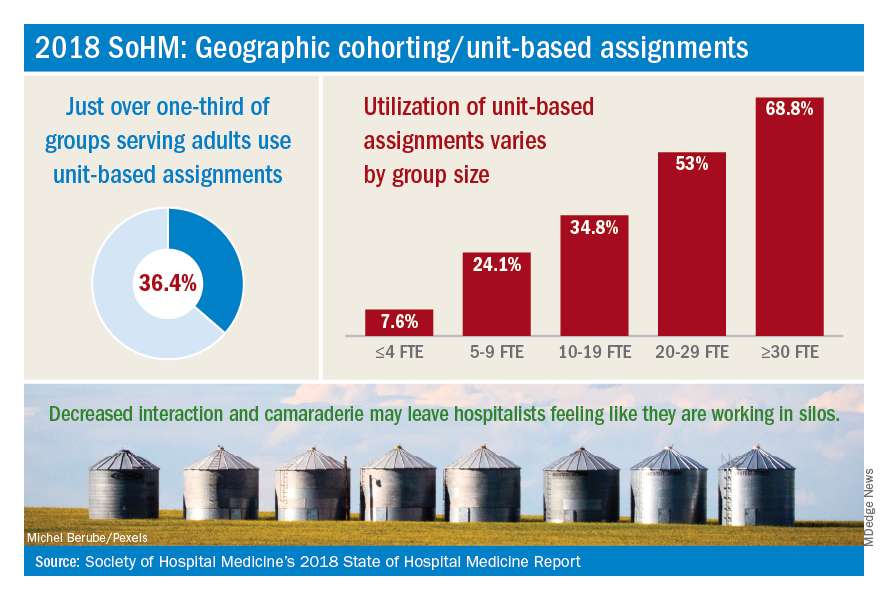
Our unit-based assignments are not perfect – we re-cohort each week when new hospitalists come on service, and some hospitalists are assigned a small number of patients off their home unit. Our internal data have shown a significant increase in patient satisfaction scores, but we have not realized a decrease in length of stay. Despite an overall positive perception, hospitalists have sometimes noted an imbalanced workload – we have a particularly challenging oncology/palliative unit and a daytime admitter that is at times very busy. Our system also requires the use of physician time to assign patients each morning and each week.
In contrast, while we’ve aimed to achieve the same success with unit-based assignments at our other campus, we’ve faced more challenges there. Our other facility is older, and fewer units have telemetry capabilities. A more traditional teaching structure also means that teams take turns with on-call admitting days, as opposed to a daytime admitter structure, and there may not be beds available in the unit assigned to the admitting team of the day.
Overall, geographic cohorting is likely to be considered or implemented in many hospital medicine groups, and efforts have met with varying success. There are certainly pros and cons to every model, and if your group is looking at redesigning services to include unit-based assignments, it’s worth examining the intended outcomes. While unit-based assignments are not for every group, there’s no doubt that this trend has been driven by our specialty’s commitment to outcome-driven process improvement.
Addendum added Feb. 15, 2019: The impact of UC San Diego's efforts discussed in this article are the author's own opinions through limited participation in focused interdisciplinary rounds, and have not been validated with formal data analysis. More study is in progress on the impact of focused interdiscplinary rounds on communication, utilization, and quality metrics. Sarah Horman, MD ([email protected]), Daniel Bouland, MD ([email protected]), and William Frederick, MD ([email protected]), have led efforts at UC San Diego to develop and implement focused interdisciplinary rounds, and may be contacted for further information.
Dr. Huang is physician advisor for care management and associate clinical professor in the division of hospital medicine at the University of California, San Diego. He is a member of SHM’s practice analysis subcommittee.
References
1. O’Leary KJ et al. Interdisciplinary teamwork in hospitals: A review and practical recommendations for improvement. J Hosp Med. 2012 Jan;7(1):48-54.
2. Kara A et al. Hospital-based clinicians’ perceptions of geographic cohorting: Identifying opportunities for improvement. Am J Med Qual. 2018 May/Jun;33(3):303-12.
Geographic cohorting shows ‘varying success’
Geographic cohorting shows ‘varying success’
A relatively recent practice catching on in many different hospitalist groups is geographic cohorting, or unit-based assignments. Traditionally, most hospitalists have had patients assigned on multiple different units. Unit-based assignments have been touted as a way of improving interdisciplinary communication and provider and patient satisfaction.1
How frequently are hospital medicine groups using unit-based assignments? SHM sought to quantify this trend in the recently published 2018 State of Hospital Medicine Report. Overall, among hospital medicine groups serving adults only, a little over one-third (36.4%) of groups reported utilizing unit-based assignments. However, there was significant variation, particularly dependent on group size. Geographic cohorting was used only in 7.6% of groups with 4 or fewer full-time equivalents, and in 68.8% of groups with 30 or more FTE. These data seem logical, as the potential gains from cohorting likely increase with group/hospital size, where physicians would otherwise round on an increasingly large number of units.
As has been shared in the hospital medicine literature, groups have experienced variable success with geographic cohorting. Improvements have been achieved in interprofessional collaboration, efficiency, nursing satisfaction,2 and, in some instances, length of stay. Unit-based assignments have allowed some groups to pilot other interventions, such as interdisciplinary rounds.
But geographic cohorting comes with its implementation challenges, too. For example, in many hospitals, some units have differing telemetry or nursing capabilities. And, in other institutions, there are units providing specialized care, such as care for neurology or oncology patients. The workload for hospitalists caring for particular types of patients may vary, and with specialty units, it may be more difficult to keep a similar census assigned to each hospitalist.
While some groups have noted increased professional satisfaction, others have noted decreases in satisfaction. One reason is that, while the frequency of paging may decrease, this is replaced by an increase in face-to-face interruptions. Also, unit-based assignments in some groups have resulted in hospitalists perceiving they are working in silos because of a decrease in interactions and camaraderie among providers in the same hospital medicine group.
At my home institution, University of California, San Diego, geographic cohorting has largely been a successful and positively perceived change. Our efforts have been particularly successful at one of our two campuses where most units have telemetry capabilities and where we have a dedicated daytime admitter (there are data on this in the Report as well, and a dedicated daytime admitter is the topic of a future Survey Insights column). Unit-based assignments have allowed the implementation of what we’ve termed focused interdisciplinary rounds.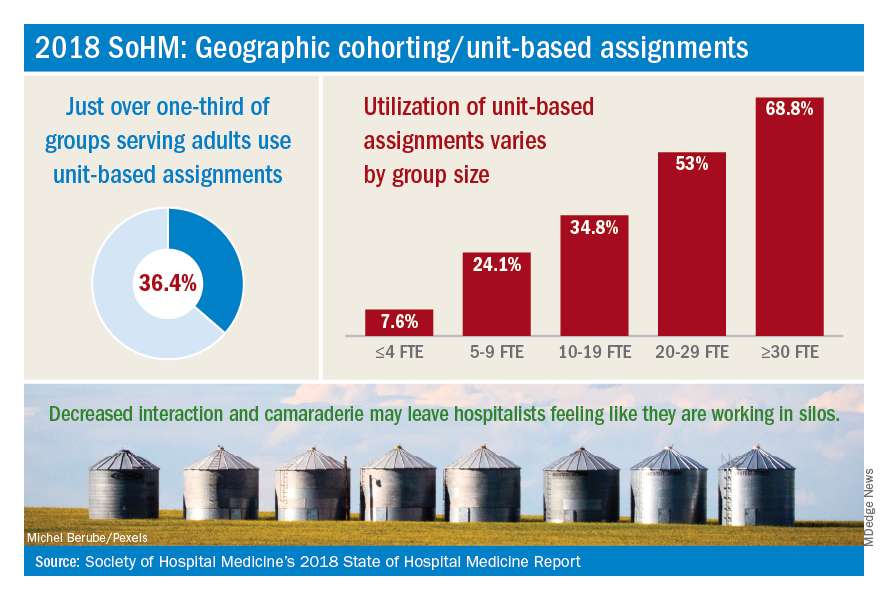
Our unit-based assignments are not perfect – we re-cohort each week when new hospitalists come on service, and some hospitalists are assigned a small number of patients off their home unit. Our internal data have shown a significant increase in patient satisfaction scores, but we have not realized a decrease in length of stay. Despite an overall positive perception, hospitalists have sometimes noted an imbalanced workload – we have a particularly challenging oncology/palliative unit and a daytime admitter that is at times very busy. Our system also requires the use of physician time to assign patients each morning and each week.
In contrast, while we’ve aimed to achieve the same success with unit-based assignments at our other campus, we’ve faced more challenges there. Our other facility is older, and fewer units have telemetry capabilities. A more traditional teaching structure also means that teams take turns with on-call admitting days, as opposed to a daytime admitter structure, and there may not be beds available in the unit assigned to the admitting team of the day.
Overall, geographic cohorting is likely to be considered or implemented in many hospital medicine groups, and efforts have met with varying success. There are certainly pros and cons to every model, and if your group is looking at redesigning services to include unit-based assignments, it’s worth examining the intended outcomes. While unit-based assignments are not for every group, there’s no doubt that this trend has been driven by our specialty’s commitment to outcome-driven process improvement.
Addendum added Feb. 15, 2019: The impact of UC San Diego's efforts discussed in this article are the author's own opinions through limited participation in focused interdisciplinary rounds, and have not been validated with formal data analysis. More study is in progress on the impact of focused interdiscplinary rounds on communication, utilization, and quality metrics. Sarah Horman, MD ([email protected]), Daniel Bouland, MD ([email protected]), and William Frederick, MD ([email protected]), have led efforts at UC San Diego to develop and implement focused interdisciplinary rounds, and may be contacted for further information.
Dr. Huang is physician advisor for care management and associate clinical professor in the division of hospital medicine at the University of California, San Diego. He is a member of SHM’s practice analysis subcommittee.
References
1. O’Leary KJ et al. Interdisciplinary teamwork in hospitals: A review and practical recommendations for improvement. J Hosp Med. 2012 Jan;7(1):48-54.
2. Kara A et al. Hospital-based clinicians’ perceptions of geographic cohorting: Identifying opportunities for improvement. Am J Med Qual. 2018 May/Jun;33(3):303-12.
A relatively recent practice catching on in many different hospitalist groups is geographic cohorting, or unit-based assignments. Traditionally, most hospitalists have had patients assigned on multiple different units. Unit-based assignments have been touted as a way of improving interdisciplinary communication and provider and patient satisfaction.1
How frequently are hospital medicine groups using unit-based assignments? SHM sought to quantify this trend in the recently published 2018 State of Hospital Medicine Report. Overall, among hospital medicine groups serving adults only, a little over one-third (36.4%) of groups reported utilizing unit-based assignments. However, there was significant variation, particularly dependent on group size. Geographic cohorting was used only in 7.6% of groups with 4 or fewer full-time equivalents, and in 68.8% of groups with 30 or more FTE. These data seem logical, as the potential gains from cohorting likely increase with group/hospital size, where physicians would otherwise round on an increasingly large number of units.
As has been shared in the hospital medicine literature, groups have experienced variable success with geographic cohorting. Improvements have been achieved in interprofessional collaboration, efficiency, nursing satisfaction,2 and, in some instances, length of stay. Unit-based assignments have allowed some groups to pilot other interventions, such as interdisciplinary rounds.
But geographic cohorting comes with its implementation challenges, too. For example, in many hospitals, some units have differing telemetry or nursing capabilities. And, in other institutions, there are units providing specialized care, such as care for neurology or oncology patients. The workload for hospitalists caring for particular types of patients may vary, and with specialty units, it may be more difficult to keep a similar census assigned to each hospitalist.
While some groups have noted increased professional satisfaction, others have noted decreases in satisfaction. One reason is that, while the frequency of paging may decrease, this is replaced by an increase in face-to-face interruptions. Also, unit-based assignments in some groups have resulted in hospitalists perceiving they are working in silos because of a decrease in interactions and camaraderie among providers in the same hospital medicine group.
At my home institution, University of California, San Diego, geographic cohorting has largely been a successful and positively perceived change. Our efforts have been particularly successful at one of our two campuses where most units have telemetry capabilities and where we have a dedicated daytime admitter (there are data on this in the Report as well, and a dedicated daytime admitter is the topic of a future Survey Insights column). Unit-based assignments have allowed the implementation of what we’ve termed focused interdisciplinary rounds.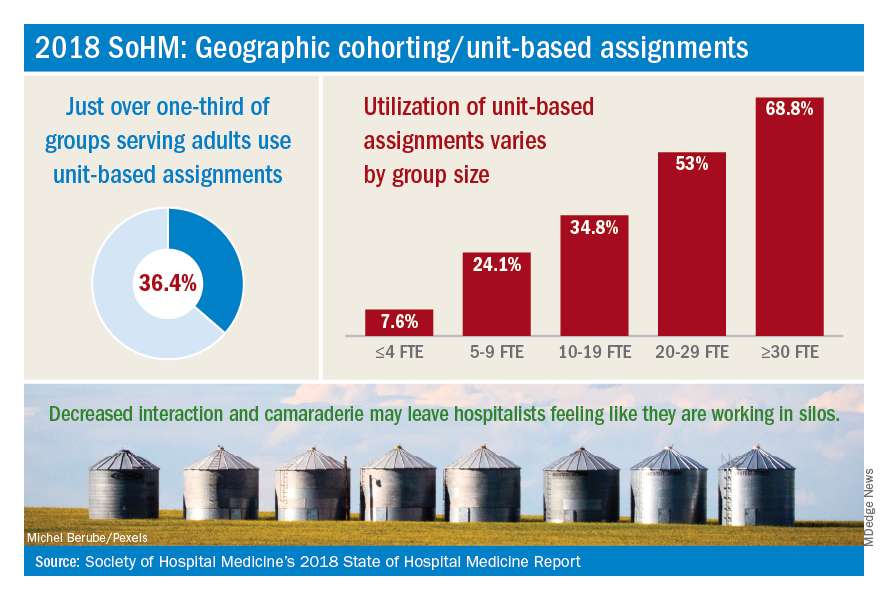
Our unit-based assignments are not perfect – we re-cohort each week when new hospitalists come on service, and some hospitalists are assigned a small number of patients off their home unit. Our internal data have shown a significant increase in patient satisfaction scores, but we have not realized a decrease in length of stay. Despite an overall positive perception, hospitalists have sometimes noted an imbalanced workload – we have a particularly challenging oncology/palliative unit and a daytime admitter that is at times very busy. Our system also requires the use of physician time to assign patients each morning and each week.
In contrast, while we’ve aimed to achieve the same success with unit-based assignments at our other campus, we’ve faced more challenges there. Our other facility is older, and fewer units have telemetry capabilities. A more traditional teaching structure also means that teams take turns with on-call admitting days, as opposed to a daytime admitter structure, and there may not be beds available in the unit assigned to the admitting team of the day.
Overall, geographic cohorting is likely to be considered or implemented in many hospital medicine groups, and efforts have met with varying success. There are certainly pros and cons to every model, and if your group is looking at redesigning services to include unit-based assignments, it’s worth examining the intended outcomes. While unit-based assignments are not for every group, there’s no doubt that this trend has been driven by our specialty’s commitment to outcome-driven process improvement.
Addendum added Feb. 15, 2019: The impact of UC San Diego's efforts discussed in this article are the author's own opinions through limited participation in focused interdisciplinary rounds, and have not been validated with formal data analysis. More study is in progress on the impact of focused interdiscplinary rounds on communication, utilization, and quality metrics. Sarah Horman, MD ([email protected]), Daniel Bouland, MD ([email protected]), and William Frederick, MD ([email protected]), have led efforts at UC San Diego to develop and implement focused interdisciplinary rounds, and may be contacted for further information.
Dr. Huang is physician advisor for care management and associate clinical professor in the division of hospital medicine at the University of California, San Diego. He is a member of SHM’s practice analysis subcommittee.
References
1. O’Leary KJ et al. Interdisciplinary teamwork in hospitals: A review and practical recommendations for improvement. J Hosp Med. 2012 Jan;7(1):48-54.
2. Kara A et al. Hospital-based clinicians’ perceptions of geographic cohorting: Identifying opportunities for improvement. Am J Med Qual. 2018 May/Jun;33(3):303-12.