User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Adding salt to food linked to higher risk of premature death
in a new study.
In the study of more than 500,000 people, compared with those who never or rarely added salt, those who always added salt to their food had a 28% increased risk of dying prematurely (defined as death before the age of 75 years).
Results also showed that adding salt to food was linked to a lower life expectancy. At the age of 50 years, life expectancy was reduced by 1.5 years in women and by 2.28 years in men who always added salt to their food, compared with those who never or rarely did.
However, these increased risks appeared to be attenuated with increasing intakes of high-potassium foods (vegetables and fruits).
The study was published online in the European Heart Journal.
“As far as we are aware, this is the first study to analyze adding salt to meals as a unique measurement for dietary sodium intake. Such a measure is less likely affected by other dietary components, especially potassium intake,” senior author Lu Qi, MD, Tulane University, New Orleans, told this news organization.
“Our study provides supportive evidence from a novel perspective to show the adverse effects of high sodium intake on human health, which is still a controversial topic. Our findings support the advice that reduction of salt intake by reducing the salt added to meals may benefit health and improve life expectancy. Our results also suggest that high intakes of fruits and vegetables are beneficial regarding lowering the adverse effects of salt,” he added.
Link between dietary salt and health is subject of longstanding debate
The researchers explained that the relationship between dietary salt intake and health remains a subject of longstanding debate, with previous studies on the association between sodium intake and mortality having shown conflicting results.
They attributed the inconsistent results to the low accuracy of sodium measurement, noting that sodium intake varies widely from day to day, but the majority of previous studies have largely relied on a single day’s urine collection or dietary survey for estimating the sodium intake, which is inadequate to assess an individual’s usual consumption levels.
They also pointed out that it is difficult to separate the contributions of intakes of sodium and potassium to health based on current methods for measuring dietary sodium and potassium, and this may confound the association between sodium intake and health outcomes.
They noted that the hypothesis that a high-potassium intake may attenuate the adverse association of high-sodium intake with health outcomes has been proposed for many years, but studies assessing the interaction between sodium intake and potassium intake on the risk of mortality are scarce.
Adding salt to food at the table is a common eating behavior directly related to an individual’s long-term preference for salty tasting foods and habitual salt intake, the authors said, adding that commonly used table salt contains 97%-99% sodium chloride, minimizing the potential confounding effects of other dietary factors including potassium. “Therefore, adding salt to foods provides a unique assessment to evaluate the association between habitual sodium intake and mortality.”
UK Biobank study
For the current study Dr. Qi and colleagues analyzed data from 501,379 people taking part in the UK Biobank study. When joining the study between 2006 and 2010, the participants were asked whether they added salt to their foods never/rarely, sometimes, usually or always. Participants were then followed for a median of 9 years.
After adjustment for sex, age, race, smoking, moderate drinking, body mass index, physical activity, Townsend deprivation index, high cholesterol, chronic kidney disease, diabetes, cardiovascular disease, and cancer, results showed an increasing risk of all-cause premature mortality rose with increasing frequency of adding salt to foods.
The adjusted hazard ratios, compared with those who never or rarely added salt, were 1.02 (95% CI, 0.99-1.06) for those who added salt sometimes, 1.07 (95% CI, 1.02-1.11) for those who usually added salt, and 1.28 (95% CI, 1.20-1.35) for those who always added salt.
The researchers also estimated the lower survival time caused by the high frequency of adding salt to foods. At age 50, women who always added salt to foods had an average 1.50 fewer years of life expectancy, and men who always added salt had an average 2.28 fewer years of life expectancy, as compared with their counterparts who never/rarely added salt to foods.
For cause-specific premature mortality, results showed that higher frequency of adding salt to foods was significantly associated with a higher risk of cardiovascular mortality and cancer mortality, but not for dementia mortality or respiratory mortality. For the subtypes of cardiovascular mortality, adding salt to foods was significantly associated with higher risk of stroke mortality but not coronary heart disease mortality.
Other analyses suggested that the association of adding salt to foods with an increased risk of premature mortality appeared to be attenuated with increasing intake of food high in potassium (fruits and vegetables).
The authors point out that the amounts of discretionary sodium intake (the salt used at the table or in home cooking) have been largely overlooked in previous studies, even though adding salt to foods accounts for a considerable proportion of total sodium intake (6%-20%) in Western diets.
“Our findings also support the notion that even a modest reduction in sodium intake is likely to result in substantial health benefits, especially when it is achieved in the general population,” they conclude.
Conflicting information from different studies
But the current findings seem to directly contradict those from another recent study by Messerli and colleagues showing higher sodium intake correlates with improved life expectancy.
Addressing these contradictory results, Dr. Qi commented: “The study of Messerli et al. is based on an ecological design, in which the analysis is performed on country average sodium intake, rather than at the individual level. This type of ecological study has several major limitations, such as the lack of individuals’ sodium intake, uncontrolled confounding, and the cross-sectional nature. Typically, ecological studies are not considered useful for testing hypothesis in epidemiological studies.”
Dr. Qi noted that, in contrast, his current study analyzes individuals’ exposure, and has a prospective design. “Our findings are supported by previous large-scale observational studies and clinical trials which show the high intake of sodium may adversely affect chronic diseases such as cardiovascular disease and hypertension.” =
Lead author of the ecological study, Franz Messerli, MD, Bern (Switzerland) University Hospital, however, was not convinced by the findings from Dr. Qi’s study.
“The difference in 24-hour sodium intake between those who never/rarely added salt and those who always did is a minuscule 0.17 g. It is highly unlikely that such negligible quantity has any impact on blood pressure, not to mention cardiovascular mortality or life expectancy,” he commented in an interview.
He also pointed out that, in Dr. Qi’s study, people who added salt more frequently also consumed more red meat and processed meat, as well as less fish and less fruit and vegetables. “I would suggest that the bad habit of adding salt at the table is simply a powerful marker for an unhealthy diet.”
“There is no question that an excessive salt intake is harmful in hypertensive patients and increases the risk of stroke. But 0.17 g is not going to make any difference,” Dr. Messerli added.
What is the optimum level?
In an editorial accompanying the study by Dr. Qi and colleagues in the European Heart Journal, Annika Rosengren, MD, PhD, Sahlgrenska University Hospital, Gothenburg, Sweden, noted that guidelines recommend a salt intake below 5 g, or about a teaspoon, per day. But few individuals meet this recommendation.
Because several recent studies show a U- or J-shaped association between salt and atherosclerotic cardiovascular disease, reducing salt intake across the whole population may not be universally beneficial, Dr. Rosengren said.
“So far, what the collective evidence about salt seems to indicate is that healthy people consuming what constitutes normal levels of ordinary salt need not worry too much about their salt intake,” she wrote.
Instead, she advised a diet rich in fruit and vegetables should be a priority to counterbalance potentially harmful effects of salt, and for many other reasons.
And she added that people at high risk, such as those with hypertension who have a high salt intake, are probably well advised to cut down, and not adding extra salt to already prepared foods is one way of achieving this. However, at the individual level, the optimal salt consumption range, or the “sweet spot” remains to be determined.
“Not adding extra salt to food is unlikely to be harmful and could contribute to strategies to lower population blood pressure levels,” Dr. Rosengren concluded.
A version of this article first appeared on Medscape.com.
in a new study.
In the study of more than 500,000 people, compared with those who never or rarely added salt, those who always added salt to their food had a 28% increased risk of dying prematurely (defined as death before the age of 75 years).
Results also showed that adding salt to food was linked to a lower life expectancy. At the age of 50 years, life expectancy was reduced by 1.5 years in women and by 2.28 years in men who always added salt to their food, compared with those who never or rarely did.
However, these increased risks appeared to be attenuated with increasing intakes of high-potassium foods (vegetables and fruits).
The study was published online in the European Heart Journal.
“As far as we are aware, this is the first study to analyze adding salt to meals as a unique measurement for dietary sodium intake. Such a measure is less likely affected by other dietary components, especially potassium intake,” senior author Lu Qi, MD, Tulane University, New Orleans, told this news organization.
“Our study provides supportive evidence from a novel perspective to show the adverse effects of high sodium intake on human health, which is still a controversial topic. Our findings support the advice that reduction of salt intake by reducing the salt added to meals may benefit health and improve life expectancy. Our results also suggest that high intakes of fruits and vegetables are beneficial regarding lowering the adverse effects of salt,” he added.
Link between dietary salt and health is subject of longstanding debate
The researchers explained that the relationship between dietary salt intake and health remains a subject of longstanding debate, with previous studies on the association between sodium intake and mortality having shown conflicting results.
They attributed the inconsistent results to the low accuracy of sodium measurement, noting that sodium intake varies widely from day to day, but the majority of previous studies have largely relied on a single day’s urine collection or dietary survey for estimating the sodium intake, which is inadequate to assess an individual’s usual consumption levels.
They also pointed out that it is difficult to separate the contributions of intakes of sodium and potassium to health based on current methods for measuring dietary sodium and potassium, and this may confound the association between sodium intake and health outcomes.
They noted that the hypothesis that a high-potassium intake may attenuate the adverse association of high-sodium intake with health outcomes has been proposed for many years, but studies assessing the interaction between sodium intake and potassium intake on the risk of mortality are scarce.
Adding salt to food at the table is a common eating behavior directly related to an individual’s long-term preference for salty tasting foods and habitual salt intake, the authors said, adding that commonly used table salt contains 97%-99% sodium chloride, minimizing the potential confounding effects of other dietary factors including potassium. “Therefore, adding salt to foods provides a unique assessment to evaluate the association between habitual sodium intake and mortality.”
UK Biobank study
For the current study Dr. Qi and colleagues analyzed data from 501,379 people taking part in the UK Biobank study. When joining the study between 2006 and 2010, the participants were asked whether they added salt to their foods never/rarely, sometimes, usually or always. Participants were then followed for a median of 9 years.
After adjustment for sex, age, race, smoking, moderate drinking, body mass index, physical activity, Townsend deprivation index, high cholesterol, chronic kidney disease, diabetes, cardiovascular disease, and cancer, results showed an increasing risk of all-cause premature mortality rose with increasing frequency of adding salt to foods.
The adjusted hazard ratios, compared with those who never or rarely added salt, were 1.02 (95% CI, 0.99-1.06) for those who added salt sometimes, 1.07 (95% CI, 1.02-1.11) for those who usually added salt, and 1.28 (95% CI, 1.20-1.35) for those who always added salt.
The researchers also estimated the lower survival time caused by the high frequency of adding salt to foods. At age 50, women who always added salt to foods had an average 1.50 fewer years of life expectancy, and men who always added salt had an average 2.28 fewer years of life expectancy, as compared with their counterparts who never/rarely added salt to foods.
For cause-specific premature mortality, results showed that higher frequency of adding salt to foods was significantly associated with a higher risk of cardiovascular mortality and cancer mortality, but not for dementia mortality or respiratory mortality. For the subtypes of cardiovascular mortality, adding salt to foods was significantly associated with higher risk of stroke mortality but not coronary heart disease mortality.
Other analyses suggested that the association of adding salt to foods with an increased risk of premature mortality appeared to be attenuated with increasing intake of food high in potassium (fruits and vegetables).
The authors point out that the amounts of discretionary sodium intake (the salt used at the table or in home cooking) have been largely overlooked in previous studies, even though adding salt to foods accounts for a considerable proportion of total sodium intake (6%-20%) in Western diets.
“Our findings also support the notion that even a modest reduction in sodium intake is likely to result in substantial health benefits, especially when it is achieved in the general population,” they conclude.
Conflicting information from different studies
But the current findings seem to directly contradict those from another recent study by Messerli and colleagues showing higher sodium intake correlates with improved life expectancy.
Addressing these contradictory results, Dr. Qi commented: “The study of Messerli et al. is based on an ecological design, in which the analysis is performed on country average sodium intake, rather than at the individual level. This type of ecological study has several major limitations, such as the lack of individuals’ sodium intake, uncontrolled confounding, and the cross-sectional nature. Typically, ecological studies are not considered useful for testing hypothesis in epidemiological studies.”
Dr. Qi noted that, in contrast, his current study analyzes individuals’ exposure, and has a prospective design. “Our findings are supported by previous large-scale observational studies and clinical trials which show the high intake of sodium may adversely affect chronic diseases such as cardiovascular disease and hypertension.” =
Lead author of the ecological study, Franz Messerli, MD, Bern (Switzerland) University Hospital, however, was not convinced by the findings from Dr. Qi’s study.
“The difference in 24-hour sodium intake between those who never/rarely added salt and those who always did is a minuscule 0.17 g. It is highly unlikely that such negligible quantity has any impact on blood pressure, not to mention cardiovascular mortality or life expectancy,” he commented in an interview.
He also pointed out that, in Dr. Qi’s study, people who added salt more frequently also consumed more red meat and processed meat, as well as less fish and less fruit and vegetables. “I would suggest that the bad habit of adding salt at the table is simply a powerful marker for an unhealthy diet.”
“There is no question that an excessive salt intake is harmful in hypertensive patients and increases the risk of stroke. But 0.17 g is not going to make any difference,” Dr. Messerli added.
What is the optimum level?
In an editorial accompanying the study by Dr. Qi and colleagues in the European Heart Journal, Annika Rosengren, MD, PhD, Sahlgrenska University Hospital, Gothenburg, Sweden, noted that guidelines recommend a salt intake below 5 g, or about a teaspoon, per day. But few individuals meet this recommendation.
Because several recent studies show a U- or J-shaped association between salt and atherosclerotic cardiovascular disease, reducing salt intake across the whole population may not be universally beneficial, Dr. Rosengren said.
“So far, what the collective evidence about salt seems to indicate is that healthy people consuming what constitutes normal levels of ordinary salt need not worry too much about their salt intake,” she wrote.
Instead, she advised a diet rich in fruit and vegetables should be a priority to counterbalance potentially harmful effects of salt, and for many other reasons.
And she added that people at high risk, such as those with hypertension who have a high salt intake, are probably well advised to cut down, and not adding extra salt to already prepared foods is one way of achieving this. However, at the individual level, the optimal salt consumption range, or the “sweet spot” remains to be determined.
“Not adding extra salt to food is unlikely to be harmful and could contribute to strategies to lower population blood pressure levels,” Dr. Rosengren concluded.
A version of this article first appeared on Medscape.com.
in a new study.
In the study of more than 500,000 people, compared with those who never or rarely added salt, those who always added salt to their food had a 28% increased risk of dying prematurely (defined as death before the age of 75 years).
Results also showed that adding salt to food was linked to a lower life expectancy. At the age of 50 years, life expectancy was reduced by 1.5 years in women and by 2.28 years in men who always added salt to their food, compared with those who never or rarely did.
However, these increased risks appeared to be attenuated with increasing intakes of high-potassium foods (vegetables and fruits).
The study was published online in the European Heart Journal.
“As far as we are aware, this is the first study to analyze adding salt to meals as a unique measurement for dietary sodium intake. Such a measure is less likely affected by other dietary components, especially potassium intake,” senior author Lu Qi, MD, Tulane University, New Orleans, told this news organization.
“Our study provides supportive evidence from a novel perspective to show the adverse effects of high sodium intake on human health, which is still a controversial topic. Our findings support the advice that reduction of salt intake by reducing the salt added to meals may benefit health and improve life expectancy. Our results also suggest that high intakes of fruits and vegetables are beneficial regarding lowering the adverse effects of salt,” he added.
Link between dietary salt and health is subject of longstanding debate
The researchers explained that the relationship between dietary salt intake and health remains a subject of longstanding debate, with previous studies on the association between sodium intake and mortality having shown conflicting results.
They attributed the inconsistent results to the low accuracy of sodium measurement, noting that sodium intake varies widely from day to day, but the majority of previous studies have largely relied on a single day’s urine collection or dietary survey for estimating the sodium intake, which is inadequate to assess an individual’s usual consumption levels.
They also pointed out that it is difficult to separate the contributions of intakes of sodium and potassium to health based on current methods for measuring dietary sodium and potassium, and this may confound the association between sodium intake and health outcomes.
They noted that the hypothesis that a high-potassium intake may attenuate the adverse association of high-sodium intake with health outcomes has been proposed for many years, but studies assessing the interaction between sodium intake and potassium intake on the risk of mortality are scarce.
Adding salt to food at the table is a common eating behavior directly related to an individual’s long-term preference for salty tasting foods and habitual salt intake, the authors said, adding that commonly used table salt contains 97%-99% sodium chloride, minimizing the potential confounding effects of other dietary factors including potassium. “Therefore, adding salt to foods provides a unique assessment to evaluate the association between habitual sodium intake and mortality.”
UK Biobank study
For the current study Dr. Qi and colleagues analyzed data from 501,379 people taking part in the UK Biobank study. When joining the study between 2006 and 2010, the participants were asked whether they added salt to their foods never/rarely, sometimes, usually or always. Participants were then followed for a median of 9 years.
After adjustment for sex, age, race, smoking, moderate drinking, body mass index, physical activity, Townsend deprivation index, high cholesterol, chronic kidney disease, diabetes, cardiovascular disease, and cancer, results showed an increasing risk of all-cause premature mortality rose with increasing frequency of adding salt to foods.
The adjusted hazard ratios, compared with those who never or rarely added salt, were 1.02 (95% CI, 0.99-1.06) for those who added salt sometimes, 1.07 (95% CI, 1.02-1.11) for those who usually added salt, and 1.28 (95% CI, 1.20-1.35) for those who always added salt.
The researchers also estimated the lower survival time caused by the high frequency of adding salt to foods. At age 50, women who always added salt to foods had an average 1.50 fewer years of life expectancy, and men who always added salt had an average 2.28 fewer years of life expectancy, as compared with their counterparts who never/rarely added salt to foods.
For cause-specific premature mortality, results showed that higher frequency of adding salt to foods was significantly associated with a higher risk of cardiovascular mortality and cancer mortality, but not for dementia mortality or respiratory mortality. For the subtypes of cardiovascular mortality, adding salt to foods was significantly associated with higher risk of stroke mortality but not coronary heart disease mortality.
Other analyses suggested that the association of adding salt to foods with an increased risk of premature mortality appeared to be attenuated with increasing intake of food high in potassium (fruits and vegetables).
The authors point out that the amounts of discretionary sodium intake (the salt used at the table or in home cooking) have been largely overlooked in previous studies, even though adding salt to foods accounts for a considerable proportion of total sodium intake (6%-20%) in Western diets.
“Our findings also support the notion that even a modest reduction in sodium intake is likely to result in substantial health benefits, especially when it is achieved in the general population,” they conclude.
Conflicting information from different studies
But the current findings seem to directly contradict those from another recent study by Messerli and colleagues showing higher sodium intake correlates with improved life expectancy.
Addressing these contradictory results, Dr. Qi commented: “The study of Messerli et al. is based on an ecological design, in which the analysis is performed on country average sodium intake, rather than at the individual level. This type of ecological study has several major limitations, such as the lack of individuals’ sodium intake, uncontrolled confounding, and the cross-sectional nature. Typically, ecological studies are not considered useful for testing hypothesis in epidemiological studies.”
Dr. Qi noted that, in contrast, his current study analyzes individuals’ exposure, and has a prospective design. “Our findings are supported by previous large-scale observational studies and clinical trials which show the high intake of sodium may adversely affect chronic diseases such as cardiovascular disease and hypertension.” =
Lead author of the ecological study, Franz Messerli, MD, Bern (Switzerland) University Hospital, however, was not convinced by the findings from Dr. Qi’s study.
“The difference in 24-hour sodium intake between those who never/rarely added salt and those who always did is a minuscule 0.17 g. It is highly unlikely that such negligible quantity has any impact on blood pressure, not to mention cardiovascular mortality or life expectancy,” he commented in an interview.
He also pointed out that, in Dr. Qi’s study, people who added salt more frequently also consumed more red meat and processed meat, as well as less fish and less fruit and vegetables. “I would suggest that the bad habit of adding salt at the table is simply a powerful marker for an unhealthy diet.”
“There is no question that an excessive salt intake is harmful in hypertensive patients and increases the risk of stroke. But 0.17 g is not going to make any difference,” Dr. Messerli added.
What is the optimum level?
In an editorial accompanying the study by Dr. Qi and colleagues in the European Heart Journal, Annika Rosengren, MD, PhD, Sahlgrenska University Hospital, Gothenburg, Sweden, noted that guidelines recommend a salt intake below 5 g, or about a teaspoon, per day. But few individuals meet this recommendation.
Because several recent studies show a U- or J-shaped association between salt and atherosclerotic cardiovascular disease, reducing salt intake across the whole population may not be universally beneficial, Dr. Rosengren said.
“So far, what the collective evidence about salt seems to indicate is that healthy people consuming what constitutes normal levels of ordinary salt need not worry too much about their salt intake,” she wrote.
Instead, she advised a diet rich in fruit and vegetables should be a priority to counterbalance potentially harmful effects of salt, and for many other reasons.
And she added that people at high risk, such as those with hypertension who have a high salt intake, are probably well advised to cut down, and not adding extra salt to already prepared foods is one way of achieving this. However, at the individual level, the optimal salt consumption range, or the “sweet spot” remains to be determined.
“Not adding extra salt to food is unlikely to be harmful and could contribute to strategies to lower population blood pressure levels,” Dr. Rosengren concluded.
A version of this article first appeared on Medscape.com.
FROM THE EUROPEAN HEART JOURNAL
Sleep-deprived physicians less empathetic to patient pain?
new research suggests.
In the first of two studies, resident physicians were presented with two hypothetical scenarios involving a patient who complains of pain. They were asked about their likelihood of prescribing pain medication. The test was given to one group of residents who were just starting their day and to another group who were at the end of their night shift after being on call for 26 hours.
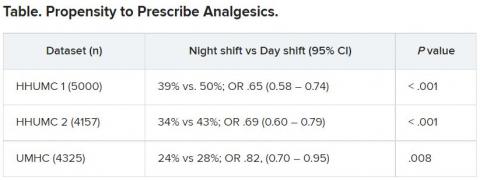
Results showed that the night shift residents were less likely than their daytime counterparts to say they would prescribe pain medication to the patients.
In further analysis of discharge notes from more than 13,000 electronic records of patients presenting with pain complaints at hospitals in Israel and the United States, the likelihood of an analgesic being prescribed during the night shift was 11% lower in Israel and 9% lower in the United States, compared with the day shift.
“Pain management is a major challenge, and a doctor’s perception of a patient’s subjective pain is susceptible to bias,” coinvestigator David Gozal, MD, the Marie M. and Harry L. Smith Endowed Chair of Child Health, University of Missouri–Columbia, said in a press release.
“This study demonstrated that night shift work is an important and previously unrecognized source of bias in pain management, likely stemming from impaired perception of pain,” Dr. Gozal added.
The findings were published online in the Proceedings of the National Academy of Sciences.
‘Directional’ differences
Senior investigator Alex Gileles-Hillel, MD, senior pediatric pulmonologist and sleep researcher at Hadassah University Medical Center, Jerusalem, said in an interview that physicians must make “complex assessments of patients’ subjective pain experience” – and the “subjective nature of pain management decisions can give rise to various biases.”
Dr. Gileles-Hillel has previously researched the cognitive toll of night shift work on physicians.
“It’s pretty established, for example, not to drive when sleep deprived because cognition is impaired,” he said. The current study explored whether sleep deprivation could affect areas other than cognition, including emotions and empathy.
The researchers used “two complementary approaches.” First, they administered tests to measure empathy and pain management decisions in 67 resident physicians at Hadassah Medical Centers either following a 26-hour night shift that began at 8:00 a.m. the day before (n = 36) or immediately before starting the workday (n = 31).
There were no significant differences in demographic, sleep, or burnout measures between the two groups, except that night shift physicians had slept less than those in the daytime group (2.93 vs. 5.96 hours).
Participants completed two tasks. In the empathy-for-pain task, they rated their emotional reactions to pictures of individuals in pain. In the empathy accuracy task, they were asked to assess the feelings of videotaped individuals telling emotional stories.
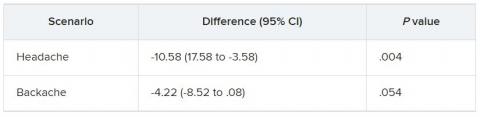
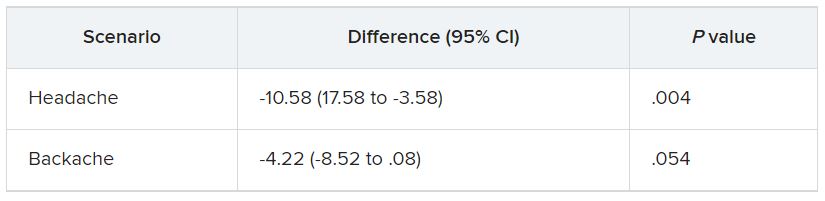
They were then presented with two clinical scenarios: a female patient with a headache and a male patient with a backache. Following that, they were asked to assess the magnitude of the patients’ pain and how likely they would be to prescribe pain medication.
In the empathy-for-pain task, physicians’ empathy scores were significantly lower in the night shift group than in the day group (difference, –0.83; 95% CI, –1.55 to –0.10; P = .026). There were no significant differences between the groups in the empathy accuracy task.
In both scenarios, physicians in the night shift group assessed the patient’s pain as weaker in comparison with physicians in the day group. There was a statistically significant difference in the headache scenario but not the backache scenario.
In the headache scenario, the propensity of the physicians to prescribe analgesics was “directionally lower” but did not reach statistical significance. In the backache scenario, there was no significant difference between the groups’ prescribing propensities.
In both scenarios, pain assessment was positively correlated with the propensity to prescribe analgesics.
Despite the lack of statistical significance, the findings “documented a negative effect of night shift work on physician empathy for pain and a positive association between physician assessment of patient pain and the propensity to prescribe analgesics,” the investigators wrote.
Need for naps?
The researchers then analyzed analgesic prescription patterns drawn from three datasets of discharge notes of patients presenting to the emergency department with pain complaints (n = 13,482) at two branches of Hadassah-Hebrew University Medical Center and the University of Missouri Health Center.
The researchers collected data, including discharge time, medications patients were prescribed upon discharge, and patients’ subjective pain rating on a scale of 0-10 on a visual analogue scale (VAS).
Although patients’ VAS scores did not differ with respect to time or shift, patients were discharged with significantly less prescribed analgesics during the night shift in comparison with the day shift.
No similar differences in prescriptions between night shifts and day shifts were found for nonanalgesic medications, such as for diabetes or blood pressure. This suggests “the effect was specific to pain,” Dr. Gileles-Hillel said.
The pattern remained significant after controlling for potential confounders, including patient and physician variables and emergency department characteristics.
In addition, patients seen during night shifts received fewer analgesics, particularly opioids, than recommended by the World Health Organization for pain management.
“The first study enabled us to measure empathy for pain directly and examine our hypothesis in a controlled environment, while the second enabled us to test the implications by examining real-life pain management decisions,” Dr. Gileles-Hillel said.
“Physicians need to be aware of this,” he noted. “I try to be aware when I’m taking calls [at night] that I’m less empathetic to others and I might be more brief or angry with others.”
On a “house management level, perhaps institutions should try to schedule naps either before or during overnight call. A nap might give a boost and reboot not only to cognitive but also to emotional resources,” Dr. Gileles-Hillel added.
Compromised safety
In a comment, Eti Ben Simon, PhD, a postdoctoral fellow at the Center for Human Sleep Science, University of California, Berkeley, called the study “an important contribution to a growing list of studies that reveal how long night shifts reduce overall safety” for both patients and clinicians.
“It’s time to abandon the notion that the human brain can function as normal after being deprived of sleep for 24 hours,” said Dr. Ben Simon, who was not involved with the research.
“This is especially true in medicine, where we trust others to take care of us and feel our pain. These functions are simply not possible without adequate sleep,” she added.
Also commenting, Kannan Ramar, MD, president of the American Academy of Sleep Medicine, suggested that being cognizant of these findings “may help providers to mitigate this bias” of underprescribing pain medications when treating their patients.
Dr. Ramar, who is also a critical care specialist, pulmonologist, and sleep medicine specialist at Mayo Clinic, Rochester, Minn., was not involved with the research.
He noted that “further studies that systematically evaluate this further in a prospective and blinded way will be important.”
The research was supported in part by grants from the Israel Science Foundation, Joy Ventures, the Recanati Fund at the Jerusalem School of Business at the Hebrew University, and a fellowship from the Azrieli Foundation and received grant support to various investigators from the NIH, the Leda J. Sears Foundation, and the University of Missouri. The investigators, Ramar, and Ben Simon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
In the first of two studies, resident physicians were presented with two hypothetical scenarios involving a patient who complains of pain. They were asked about their likelihood of prescribing pain medication. The test was given to one group of residents who were just starting their day and to another group who were at the end of their night shift after being on call for 26 hours.
Results showed that the night shift residents were less likely than their daytime counterparts to say they would prescribe pain medication to the patients.
In further analysis of discharge notes from more than 13,000 electronic records of patients presenting with pain complaints at hospitals in Israel and the United States, the likelihood of an analgesic being prescribed during the night shift was 11% lower in Israel and 9% lower in the United States, compared with the day shift.
“Pain management is a major challenge, and a doctor’s perception of a patient’s subjective pain is susceptible to bias,” coinvestigator David Gozal, MD, the Marie M. and Harry L. Smith Endowed Chair of Child Health, University of Missouri–Columbia, said in a press release.
“This study demonstrated that night shift work is an important and previously unrecognized source of bias in pain management, likely stemming from impaired perception of pain,” Dr. Gozal added.
The findings were published online in the Proceedings of the National Academy of Sciences.
‘Directional’ differences
Senior investigator Alex Gileles-Hillel, MD, senior pediatric pulmonologist and sleep researcher at Hadassah University Medical Center, Jerusalem, said in an interview that physicians must make “complex assessments of patients’ subjective pain experience” – and the “subjective nature of pain management decisions can give rise to various biases.”
Dr. Gileles-Hillel has previously researched the cognitive toll of night shift work on physicians.
“It’s pretty established, for example, not to drive when sleep deprived because cognition is impaired,” he said. The current study explored whether sleep deprivation could affect areas other than cognition, including emotions and empathy.
The researchers used “two complementary approaches.” First, they administered tests to measure empathy and pain management decisions in 67 resident physicians at Hadassah Medical Centers either following a 26-hour night shift that began at 8:00 a.m. the day before (n = 36) or immediately before starting the workday (n = 31).
There were no significant differences in demographic, sleep, or burnout measures between the two groups, except that night shift physicians had slept less than those in the daytime group (2.93 vs. 5.96 hours).
Participants completed two tasks. In the empathy-for-pain task, they rated their emotional reactions to pictures of individuals in pain. In the empathy accuracy task, they were asked to assess the feelings of videotaped individuals telling emotional stories.
They were then presented with two clinical scenarios: a female patient with a headache and a male patient with a backache. Following that, they were asked to assess the magnitude of the patients’ pain and how likely they would be to prescribe pain medication.
In the empathy-for-pain task, physicians’ empathy scores were significantly lower in the night shift group than in the day group (difference, –0.83; 95% CI, –1.55 to –0.10; P = .026). There were no significant differences between the groups in the empathy accuracy task.
In both scenarios, physicians in the night shift group assessed the patient’s pain as weaker in comparison with physicians in the day group. There was a statistically significant difference in the headache scenario but not the backache scenario.
In the headache scenario, the propensity of the physicians to prescribe analgesics was “directionally lower” but did not reach statistical significance. In the backache scenario, there was no significant difference between the groups’ prescribing propensities.
In both scenarios, pain assessment was positively correlated with the propensity to prescribe analgesics.
Despite the lack of statistical significance, the findings “documented a negative effect of night shift work on physician empathy for pain and a positive association between physician assessment of patient pain and the propensity to prescribe analgesics,” the investigators wrote.
Need for naps?
The researchers then analyzed analgesic prescription patterns drawn from three datasets of discharge notes of patients presenting to the emergency department with pain complaints (n = 13,482) at two branches of Hadassah-Hebrew University Medical Center and the University of Missouri Health Center.
The researchers collected data, including discharge time, medications patients were prescribed upon discharge, and patients’ subjective pain rating on a scale of 0-10 on a visual analogue scale (VAS).
Although patients’ VAS scores did not differ with respect to time or shift, patients were discharged with significantly less prescribed analgesics during the night shift in comparison with the day shift.
No similar differences in prescriptions between night shifts and day shifts were found for nonanalgesic medications, such as for diabetes or blood pressure. This suggests “the effect was specific to pain,” Dr. Gileles-Hillel said.
The pattern remained significant after controlling for potential confounders, including patient and physician variables and emergency department characteristics.
In addition, patients seen during night shifts received fewer analgesics, particularly opioids, than recommended by the World Health Organization for pain management.
“The first study enabled us to measure empathy for pain directly and examine our hypothesis in a controlled environment, while the second enabled us to test the implications by examining real-life pain management decisions,” Dr. Gileles-Hillel said.
“Physicians need to be aware of this,” he noted. “I try to be aware when I’m taking calls [at night] that I’m less empathetic to others and I might be more brief or angry with others.”
On a “house management level, perhaps institutions should try to schedule naps either before or during overnight call. A nap might give a boost and reboot not only to cognitive but also to emotional resources,” Dr. Gileles-Hillel added.
Compromised safety
In a comment, Eti Ben Simon, PhD, a postdoctoral fellow at the Center for Human Sleep Science, University of California, Berkeley, called the study “an important contribution to a growing list of studies that reveal how long night shifts reduce overall safety” for both patients and clinicians.
“It’s time to abandon the notion that the human brain can function as normal after being deprived of sleep for 24 hours,” said Dr. Ben Simon, who was not involved with the research.
“This is especially true in medicine, where we trust others to take care of us and feel our pain. These functions are simply not possible without adequate sleep,” she added.
Also commenting, Kannan Ramar, MD, president of the American Academy of Sleep Medicine, suggested that being cognizant of these findings “may help providers to mitigate this bias” of underprescribing pain medications when treating their patients.
Dr. Ramar, who is also a critical care specialist, pulmonologist, and sleep medicine specialist at Mayo Clinic, Rochester, Minn., was not involved with the research.
He noted that “further studies that systematically evaluate this further in a prospective and blinded way will be important.”
The research was supported in part by grants from the Israel Science Foundation, Joy Ventures, the Recanati Fund at the Jerusalem School of Business at the Hebrew University, and a fellowship from the Azrieli Foundation and received grant support to various investigators from the NIH, the Leda J. Sears Foundation, and the University of Missouri. The investigators, Ramar, and Ben Simon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
In the first of two studies, resident physicians were presented with two hypothetical scenarios involving a patient who complains of pain. They were asked about their likelihood of prescribing pain medication. The test was given to one group of residents who were just starting their day and to another group who were at the end of their night shift after being on call for 26 hours.
Results showed that the night shift residents were less likely than their daytime counterparts to say they would prescribe pain medication to the patients.
In further analysis of discharge notes from more than 13,000 electronic records of patients presenting with pain complaints at hospitals in Israel and the United States, the likelihood of an analgesic being prescribed during the night shift was 11% lower in Israel and 9% lower in the United States, compared with the day shift.
“Pain management is a major challenge, and a doctor’s perception of a patient’s subjective pain is susceptible to bias,” coinvestigator David Gozal, MD, the Marie M. and Harry L. Smith Endowed Chair of Child Health, University of Missouri–Columbia, said in a press release.
“This study demonstrated that night shift work is an important and previously unrecognized source of bias in pain management, likely stemming from impaired perception of pain,” Dr. Gozal added.
The findings were published online in the Proceedings of the National Academy of Sciences.
‘Directional’ differences
Senior investigator Alex Gileles-Hillel, MD, senior pediatric pulmonologist and sleep researcher at Hadassah University Medical Center, Jerusalem, said in an interview that physicians must make “complex assessments of patients’ subjective pain experience” – and the “subjective nature of pain management decisions can give rise to various biases.”
Dr. Gileles-Hillel has previously researched the cognitive toll of night shift work on physicians.
“It’s pretty established, for example, not to drive when sleep deprived because cognition is impaired,” he said. The current study explored whether sleep deprivation could affect areas other than cognition, including emotions and empathy.
The researchers used “two complementary approaches.” First, they administered tests to measure empathy and pain management decisions in 67 resident physicians at Hadassah Medical Centers either following a 26-hour night shift that began at 8:00 a.m. the day before (n = 36) or immediately before starting the workday (n = 31).
There were no significant differences in demographic, sleep, or burnout measures between the two groups, except that night shift physicians had slept less than those in the daytime group (2.93 vs. 5.96 hours).
Participants completed two tasks. In the empathy-for-pain task, they rated their emotional reactions to pictures of individuals in pain. In the empathy accuracy task, they were asked to assess the feelings of videotaped individuals telling emotional stories.
They were then presented with two clinical scenarios: a female patient with a headache and a male patient with a backache. Following that, they were asked to assess the magnitude of the patients’ pain and how likely they would be to prescribe pain medication.
In the empathy-for-pain task, physicians’ empathy scores were significantly lower in the night shift group than in the day group (difference, –0.83; 95% CI, –1.55 to –0.10; P = .026). There were no significant differences between the groups in the empathy accuracy task.
In both scenarios, physicians in the night shift group assessed the patient’s pain as weaker in comparison with physicians in the day group. There was a statistically significant difference in the headache scenario but not the backache scenario.
In the headache scenario, the propensity of the physicians to prescribe analgesics was “directionally lower” but did not reach statistical significance. In the backache scenario, there was no significant difference between the groups’ prescribing propensities.
In both scenarios, pain assessment was positively correlated with the propensity to prescribe analgesics.
Despite the lack of statistical significance, the findings “documented a negative effect of night shift work on physician empathy for pain and a positive association between physician assessment of patient pain and the propensity to prescribe analgesics,” the investigators wrote.
Need for naps?
The researchers then analyzed analgesic prescription patterns drawn from three datasets of discharge notes of patients presenting to the emergency department with pain complaints (n = 13,482) at two branches of Hadassah-Hebrew University Medical Center and the University of Missouri Health Center.
The researchers collected data, including discharge time, medications patients were prescribed upon discharge, and patients’ subjective pain rating on a scale of 0-10 on a visual analogue scale (VAS).
Although patients’ VAS scores did not differ with respect to time or shift, patients were discharged with significantly less prescribed analgesics during the night shift in comparison with the day shift.
No similar differences in prescriptions between night shifts and day shifts were found for nonanalgesic medications, such as for diabetes or blood pressure. This suggests “the effect was specific to pain,” Dr. Gileles-Hillel said.
The pattern remained significant after controlling for potential confounders, including patient and physician variables and emergency department characteristics.
In addition, patients seen during night shifts received fewer analgesics, particularly opioids, than recommended by the World Health Organization for pain management.
“The first study enabled us to measure empathy for pain directly and examine our hypothesis in a controlled environment, while the second enabled us to test the implications by examining real-life pain management decisions,” Dr. Gileles-Hillel said.
“Physicians need to be aware of this,” he noted. “I try to be aware when I’m taking calls [at night] that I’m less empathetic to others and I might be more brief or angry with others.”
On a “house management level, perhaps institutions should try to schedule naps either before or during overnight call. A nap might give a boost and reboot not only to cognitive but also to emotional resources,” Dr. Gileles-Hillel added.
Compromised safety
In a comment, Eti Ben Simon, PhD, a postdoctoral fellow at the Center for Human Sleep Science, University of California, Berkeley, called the study “an important contribution to a growing list of studies that reveal how long night shifts reduce overall safety” for both patients and clinicians.
“It’s time to abandon the notion that the human brain can function as normal after being deprived of sleep for 24 hours,” said Dr. Ben Simon, who was not involved with the research.
“This is especially true in medicine, where we trust others to take care of us and feel our pain. These functions are simply not possible without adequate sleep,” she added.
Also commenting, Kannan Ramar, MD, president of the American Academy of Sleep Medicine, suggested that being cognizant of these findings “may help providers to mitigate this bias” of underprescribing pain medications when treating their patients.
Dr. Ramar, who is also a critical care specialist, pulmonologist, and sleep medicine specialist at Mayo Clinic, Rochester, Minn., was not involved with the research.
He noted that “further studies that systematically evaluate this further in a prospective and blinded way will be important.”
The research was supported in part by grants from the Israel Science Foundation, Joy Ventures, the Recanati Fund at the Jerusalem School of Business at the Hebrew University, and a fellowship from the Azrieli Foundation and received grant support to various investigators from the NIH, the Leda J. Sears Foundation, and the University of Missouri. The investigators, Ramar, and Ben Simon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES
Algorithm method versus spidey sense
One to two times a week I go through my junk mail folder. Usually it’s a collection of, well, junk: ads for CME, office software, car warranties, gift cards, dating sites, eyeglass or razor sellers, etc.
But there are usually a few items I’m glad I found, ones that I’m not sure how they ended up there. Bank notifications, package-tracking updates, a few other things. By the same token, every day a few pieces of junk land in my inbox.
This is, however, what we do for a living in this job.
Some patients are straightforward. The story is clear, the plan obvious.
Some require a bit more thinking.
And some are all over the place. Histories that wander everywhere, a million symptoms and clues. Most are likely red herrings, but which ones isn’t immediately obvious. And it’s up to the doctor to work this out.
With my junk folder, though, it’s usually immediately obvious what the useless things are compared with those of value. In medicine it’s often not so simple. You have to be careful what you discard, and you always need to be ready to change your mind and backtrack.
Artificial intelligence gets better every year but still makes plenty of mistakes. In sorting email my computer has to work out the signal-to-noise ratio of incoming items and decide which ones mean something. If my junk folder is any indication, it still has a ways to go.
This isn’t to say I’m infallible. I’m not. Unlike the algorithms my email program uses, there are no definite rules in medical cases. Picking through the clues is something that comes with training, experience, and a bit of luck. When I realize I’m going in the wrong direction I have to step back and rethink it all.
A lot of chart systems try to incorporate algorithms into medical decision-making. Sometimes they’re helpful, such as pointing out a drug interaction I wasn’t aware of. At other times they’re not, telling me I shouldn’t be ordering a test because such-and-such criteria haven’t been met. The trouble is these algorithms are written to apply to all cases, even though every patient is different. Sometimes the best we can go on is what I call “spidey sense” – realizing that there’s more than meets the eye here. In 24 years it’s served me well, far better than any computer algorithm has.
People talk about a natural fear of being replaced by computers. I agree that there are some things they’re very good at, and they keep getting better. But medicine isn’t a one-size-fits-all field. And the consequences are a lot higher than those from my bank statement being overlooked for a few days.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
One to two times a week I go through my junk mail folder. Usually it’s a collection of, well, junk: ads for CME, office software, car warranties, gift cards, dating sites, eyeglass or razor sellers, etc.
But there are usually a few items I’m glad I found, ones that I’m not sure how they ended up there. Bank notifications, package-tracking updates, a few other things. By the same token, every day a few pieces of junk land in my inbox.
This is, however, what we do for a living in this job.
Some patients are straightforward. The story is clear, the plan obvious.
Some require a bit more thinking.
And some are all over the place. Histories that wander everywhere, a million symptoms and clues. Most are likely red herrings, but which ones isn’t immediately obvious. And it’s up to the doctor to work this out.
With my junk folder, though, it’s usually immediately obvious what the useless things are compared with those of value. In medicine it’s often not so simple. You have to be careful what you discard, and you always need to be ready to change your mind and backtrack.
Artificial intelligence gets better every year but still makes plenty of mistakes. In sorting email my computer has to work out the signal-to-noise ratio of incoming items and decide which ones mean something. If my junk folder is any indication, it still has a ways to go.
This isn’t to say I’m infallible. I’m not. Unlike the algorithms my email program uses, there are no definite rules in medical cases. Picking through the clues is something that comes with training, experience, and a bit of luck. When I realize I’m going in the wrong direction I have to step back and rethink it all.
A lot of chart systems try to incorporate algorithms into medical decision-making. Sometimes they’re helpful, such as pointing out a drug interaction I wasn’t aware of. At other times they’re not, telling me I shouldn’t be ordering a test because such-and-such criteria haven’t been met. The trouble is these algorithms are written to apply to all cases, even though every patient is different. Sometimes the best we can go on is what I call “spidey sense” – realizing that there’s more than meets the eye here. In 24 years it’s served me well, far better than any computer algorithm has.
People talk about a natural fear of being replaced by computers. I agree that there are some things they’re very good at, and they keep getting better. But medicine isn’t a one-size-fits-all field. And the consequences are a lot higher than those from my bank statement being overlooked for a few days.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
One to two times a week I go through my junk mail folder. Usually it’s a collection of, well, junk: ads for CME, office software, car warranties, gift cards, dating sites, eyeglass or razor sellers, etc.
But there are usually a few items I’m glad I found, ones that I’m not sure how they ended up there. Bank notifications, package-tracking updates, a few other things. By the same token, every day a few pieces of junk land in my inbox.
This is, however, what we do for a living in this job.
Some patients are straightforward. The story is clear, the plan obvious.
Some require a bit more thinking.
And some are all over the place. Histories that wander everywhere, a million symptoms and clues. Most are likely red herrings, but which ones isn’t immediately obvious. And it’s up to the doctor to work this out.
With my junk folder, though, it’s usually immediately obvious what the useless things are compared with those of value. In medicine it’s often not so simple. You have to be careful what you discard, and you always need to be ready to change your mind and backtrack.
Artificial intelligence gets better every year but still makes plenty of mistakes. In sorting email my computer has to work out the signal-to-noise ratio of incoming items and decide which ones mean something. If my junk folder is any indication, it still has a ways to go.
This isn’t to say I’m infallible. I’m not. Unlike the algorithms my email program uses, there are no definite rules in medical cases. Picking through the clues is something that comes with training, experience, and a bit of luck. When I realize I’m going in the wrong direction I have to step back and rethink it all.
A lot of chart systems try to incorporate algorithms into medical decision-making. Sometimes they’re helpful, such as pointing out a drug interaction I wasn’t aware of. At other times they’re not, telling me I shouldn’t be ordering a test because such-and-such criteria haven’t been met. The trouble is these algorithms are written to apply to all cases, even though every patient is different. Sometimes the best we can go on is what I call “spidey sense” – realizing that there’s more than meets the eye here. In 24 years it’s served me well, far better than any computer algorithm has.
People talk about a natural fear of being replaced by computers. I agree that there are some things they’re very good at, and they keep getting better. But medicine isn’t a one-size-fits-all field. And the consequences are a lot higher than those from my bank statement being overlooked for a few days.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Cognitive impairment may predict physical disability in MS
, new research suggests. In an analysis of more than 1,600 patients with secondary-progressive MS (SPMS), the likelihood of needing a wheelchair was almost doubled in those who had the worst scores on cognitive testing measures, compared with their counterparts who had the best scores.
“These findings should change our world view of MS,” study investigator Gavin Giovannoni, PhD, professor of neurology, Blizard Institute, Faculty of Medicine and Dentistry, Queen Mary University of London, told attendees at the Congress of the European Academy of Neurology.
On the basis of the results, clinicians should consider testing cognitive processing speed in patients with MS to identify those who are at increased risk for disease progression, Dr. Giovannoni noted. “I urge anybody who runs an MS service to think about putting in place mechanisms in their clinic” to measure cognition of patients over time, he said.
Expand data
Cognitive impairment occurs very early in the course of MS and is part of the disease, although to a greater or lesser degree depending on the patient, Dr. Giovannoni noted. Such impairment has a significant impact on quality of life for patients dealing with this disease, he added.
EXPAND was a phase 3 study of siponimod. Results showed the now-approved oral selective sphingosine 1–phosphate receptor modulator significantly reduced the risk for disability progression in patients with SPMS.
Using the EXPAND clinical trial database, the current researchers assessed 1,628 participants for an association between cognitive processing speed, as measured with the Symbol Digit Modality Test (SDMT), and physical disability progression, as measured with the Expanded Disability Status Scale (EDSS). A score of 7 or more on the EDSS indicates wheelchair dependence.
Dr. Giovannoni noted that cognitive processing speed is considered an indirect measure of thalamic network efficiency and functional brain reserve.
Investigators looked at both the core study, in which all patients continued on treatment or placebo for up to 37 months, and the core plus extension part, in which patients received treatment for up to 5 years.
They separated SDMT scores into quartiles: from worst (n = 435) to two intermediate quartiles (n = 808) to the best quartile (n = 385).
Wheelchair dependence
In addition, the researchers examined the predictive value by baseline SDMT, adjusting for treatment, age, gender, baseline EDSS score, baseline SCMT quartile, and treatment-by-baseline SCMT quartile interaction. On-study SDMT change (month 0-24) was also assessed after adjusting for treatment, age, gender, baseline EDS, baseline SCMT, and on-study change in SCMT quartile.
In the core study, those in the worst SDMT quartile at baseline were numerically more likely to reach deterioration to EDSS 7 or greater (wheelchair dependent), compared with patients in the best SDMT quartile (hazard ratio, 1.31; 95% confidence interval, .72-2.38; P = .371).
The short-term predictive value of baseline SDMT for reaching sustained EDSS of at least 7 was more obvious in the placebo arm than in the treatment arm.
Dr. Giovannoni said this is likely due to the treatment effect of siponimod preventing relatively more events in the worse quartile, and so reducing the risk for wheelchair dependency.
In the core plus extension part, there was an almost twofold increased risk for wheelchair dependence in the worse versus best SDMT groups (HR, 1.81; 95% CI, 1.17-2.78; P = .007).
Both baseline SDMT (HR, 1.81; P = .007) and on-study change in SDMT (HR, 1.73; P = .046) predicted wheelchair dependence in the long-term.
‘More important than a walking stick’
Measuring cognitive change over time “may be a more important predictor than a walking stick in terms of quality of life and outcomes, and it affects clinical decisionmaking,” said Dr. Giovannoni.
The findings are not novel, as post hoc analyses of other studies showed similar results. However, this new analysis adds more evidence to the importance of cognition in MS, Dr. Giovannoni noted.
“I have patients with EDSS of 0 or 1 who are profoundly disabled because of cognition. You shouldn’t just assume someone is not disabled because they don’t have physical disability,” he said.
However, Dr. Giovannoni noted that the study found an association and does not necessarily indicate a cause.
‘Valuable’ insights
Antonia Lefter, MD, of NeuroHope, Monza Oncologic Hospital, Bucharest, Romania, cochaired the session highlighting the research. Commenting on the study, she called this analysis from the “renowned” EXPAND study “valuable.”
In addition, it “underscores” the importance of assessing cognitive processing speed, as it may predict long-term disability progression in patients with SPMS, Dr. Lefter said.
The study was funded by Novartis Pharma AG, Basel, Switzerland. Dr. Giovannoni, a steering committee member of the EXPAND trial, reported receiving consulting fees from AbbVie, Actelion, Atara Bio, Biogen, Celgene, Sanofi-Genzyme, Genentech, GlaxoSmithKline, Merck-Serono, Novartis, Roche, and Reva. He has also received compensation for research from Biogen, Roche, Merck-Serono, Novartis, Sanofi-Genzyme, and Takeda. Dr. Lefter has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests. In an analysis of more than 1,600 patients with secondary-progressive MS (SPMS), the likelihood of needing a wheelchair was almost doubled in those who had the worst scores on cognitive testing measures, compared with their counterparts who had the best scores.
“These findings should change our world view of MS,” study investigator Gavin Giovannoni, PhD, professor of neurology, Blizard Institute, Faculty of Medicine and Dentistry, Queen Mary University of London, told attendees at the Congress of the European Academy of Neurology.
On the basis of the results, clinicians should consider testing cognitive processing speed in patients with MS to identify those who are at increased risk for disease progression, Dr. Giovannoni noted. “I urge anybody who runs an MS service to think about putting in place mechanisms in their clinic” to measure cognition of patients over time, he said.
Expand data
Cognitive impairment occurs very early in the course of MS and is part of the disease, although to a greater or lesser degree depending on the patient, Dr. Giovannoni noted. Such impairment has a significant impact on quality of life for patients dealing with this disease, he added.
EXPAND was a phase 3 study of siponimod. Results showed the now-approved oral selective sphingosine 1–phosphate receptor modulator significantly reduced the risk for disability progression in patients with SPMS.
Using the EXPAND clinical trial database, the current researchers assessed 1,628 participants for an association between cognitive processing speed, as measured with the Symbol Digit Modality Test (SDMT), and physical disability progression, as measured with the Expanded Disability Status Scale (EDSS). A score of 7 or more on the EDSS indicates wheelchair dependence.
Dr. Giovannoni noted that cognitive processing speed is considered an indirect measure of thalamic network efficiency and functional brain reserve.
Investigators looked at both the core study, in which all patients continued on treatment or placebo for up to 37 months, and the core plus extension part, in which patients received treatment for up to 5 years.
They separated SDMT scores into quartiles: from worst (n = 435) to two intermediate quartiles (n = 808) to the best quartile (n = 385).
Wheelchair dependence
In addition, the researchers examined the predictive value by baseline SDMT, adjusting for treatment, age, gender, baseline EDSS score, baseline SCMT quartile, and treatment-by-baseline SCMT quartile interaction. On-study SDMT change (month 0-24) was also assessed after adjusting for treatment, age, gender, baseline EDS, baseline SCMT, and on-study change in SCMT quartile.
In the core study, those in the worst SDMT quartile at baseline were numerically more likely to reach deterioration to EDSS 7 or greater (wheelchair dependent), compared with patients in the best SDMT quartile (hazard ratio, 1.31; 95% confidence interval, .72-2.38; P = .371).
The short-term predictive value of baseline SDMT for reaching sustained EDSS of at least 7 was more obvious in the placebo arm than in the treatment arm.
Dr. Giovannoni said this is likely due to the treatment effect of siponimod preventing relatively more events in the worse quartile, and so reducing the risk for wheelchair dependency.
In the core plus extension part, there was an almost twofold increased risk for wheelchair dependence in the worse versus best SDMT groups (HR, 1.81; 95% CI, 1.17-2.78; P = .007).
Both baseline SDMT (HR, 1.81; P = .007) and on-study change in SDMT (HR, 1.73; P = .046) predicted wheelchair dependence in the long-term.
‘More important than a walking stick’
Measuring cognitive change over time “may be a more important predictor than a walking stick in terms of quality of life and outcomes, and it affects clinical decisionmaking,” said Dr. Giovannoni.
The findings are not novel, as post hoc analyses of other studies showed similar results. However, this new analysis adds more evidence to the importance of cognition in MS, Dr. Giovannoni noted.
“I have patients with EDSS of 0 or 1 who are profoundly disabled because of cognition. You shouldn’t just assume someone is not disabled because they don’t have physical disability,” he said.
However, Dr. Giovannoni noted that the study found an association and does not necessarily indicate a cause.
‘Valuable’ insights
Antonia Lefter, MD, of NeuroHope, Monza Oncologic Hospital, Bucharest, Romania, cochaired the session highlighting the research. Commenting on the study, she called this analysis from the “renowned” EXPAND study “valuable.”
In addition, it “underscores” the importance of assessing cognitive processing speed, as it may predict long-term disability progression in patients with SPMS, Dr. Lefter said.
The study was funded by Novartis Pharma AG, Basel, Switzerland. Dr. Giovannoni, a steering committee member of the EXPAND trial, reported receiving consulting fees from AbbVie, Actelion, Atara Bio, Biogen, Celgene, Sanofi-Genzyme, Genentech, GlaxoSmithKline, Merck-Serono, Novartis, Roche, and Reva. He has also received compensation for research from Biogen, Roche, Merck-Serono, Novartis, Sanofi-Genzyme, and Takeda. Dr. Lefter has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests. In an analysis of more than 1,600 patients with secondary-progressive MS (SPMS), the likelihood of needing a wheelchair was almost doubled in those who had the worst scores on cognitive testing measures, compared with their counterparts who had the best scores.
“These findings should change our world view of MS,” study investigator Gavin Giovannoni, PhD, professor of neurology, Blizard Institute, Faculty of Medicine and Dentistry, Queen Mary University of London, told attendees at the Congress of the European Academy of Neurology.
On the basis of the results, clinicians should consider testing cognitive processing speed in patients with MS to identify those who are at increased risk for disease progression, Dr. Giovannoni noted. “I urge anybody who runs an MS service to think about putting in place mechanisms in their clinic” to measure cognition of patients over time, he said.
Expand data
Cognitive impairment occurs very early in the course of MS and is part of the disease, although to a greater or lesser degree depending on the patient, Dr. Giovannoni noted. Such impairment has a significant impact on quality of life for patients dealing with this disease, he added.
EXPAND was a phase 3 study of siponimod. Results showed the now-approved oral selective sphingosine 1–phosphate receptor modulator significantly reduced the risk for disability progression in patients with SPMS.
Using the EXPAND clinical trial database, the current researchers assessed 1,628 participants for an association between cognitive processing speed, as measured with the Symbol Digit Modality Test (SDMT), and physical disability progression, as measured with the Expanded Disability Status Scale (EDSS). A score of 7 or more on the EDSS indicates wheelchair dependence.
Dr. Giovannoni noted that cognitive processing speed is considered an indirect measure of thalamic network efficiency and functional brain reserve.
Investigators looked at both the core study, in which all patients continued on treatment or placebo for up to 37 months, and the core plus extension part, in which patients received treatment for up to 5 years.
They separated SDMT scores into quartiles: from worst (n = 435) to two intermediate quartiles (n = 808) to the best quartile (n = 385).
Wheelchair dependence
In addition, the researchers examined the predictive value by baseline SDMT, adjusting for treatment, age, gender, baseline EDSS score, baseline SCMT quartile, and treatment-by-baseline SCMT quartile interaction. On-study SDMT change (month 0-24) was also assessed after adjusting for treatment, age, gender, baseline EDS, baseline SCMT, and on-study change in SCMT quartile.
In the core study, those in the worst SDMT quartile at baseline were numerically more likely to reach deterioration to EDSS 7 or greater (wheelchair dependent), compared with patients in the best SDMT quartile (hazard ratio, 1.31; 95% confidence interval, .72-2.38; P = .371).
The short-term predictive value of baseline SDMT for reaching sustained EDSS of at least 7 was more obvious in the placebo arm than in the treatment arm.
Dr. Giovannoni said this is likely due to the treatment effect of siponimod preventing relatively more events in the worse quartile, and so reducing the risk for wheelchair dependency.
In the core plus extension part, there was an almost twofold increased risk for wheelchair dependence in the worse versus best SDMT groups (HR, 1.81; 95% CI, 1.17-2.78; P = .007).
Both baseline SDMT (HR, 1.81; P = .007) and on-study change in SDMT (HR, 1.73; P = .046) predicted wheelchair dependence in the long-term.
‘More important than a walking stick’
Measuring cognitive change over time “may be a more important predictor than a walking stick in terms of quality of life and outcomes, and it affects clinical decisionmaking,” said Dr. Giovannoni.
The findings are not novel, as post hoc analyses of other studies showed similar results. However, this new analysis adds more evidence to the importance of cognition in MS, Dr. Giovannoni noted.
“I have patients with EDSS of 0 or 1 who are profoundly disabled because of cognition. You shouldn’t just assume someone is not disabled because they don’t have physical disability,” he said.
However, Dr. Giovannoni noted that the study found an association and does not necessarily indicate a cause.
‘Valuable’ insights
Antonia Lefter, MD, of NeuroHope, Monza Oncologic Hospital, Bucharest, Romania, cochaired the session highlighting the research. Commenting on the study, she called this analysis from the “renowned” EXPAND study “valuable.”
In addition, it “underscores” the importance of assessing cognitive processing speed, as it may predict long-term disability progression in patients with SPMS, Dr. Lefter said.
The study was funded by Novartis Pharma AG, Basel, Switzerland. Dr. Giovannoni, a steering committee member of the EXPAND trial, reported receiving consulting fees from AbbVie, Actelion, Atara Bio, Biogen, Celgene, Sanofi-Genzyme, Genentech, GlaxoSmithKline, Merck-Serono, Novartis, Roche, and Reva. He has also received compensation for research from Biogen, Roche, Merck-Serono, Novartis, Sanofi-Genzyme, and Takeda. Dr. Lefter has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
From EAN 2022
‘Striking’ jump in cost of brand-name epilepsy meds
, a new analysis shows.
After adjustment for inflation, the cost of a 1-year supply of brand-name ASMs grew 277%, while generics became 42% less expensive.
“Our study makes transparent striking trends in brand name prescribing patterns,” the study team wrote.
Since 2010, the costs for brand-name ASMs have “consistently” increased. Costs were particularly boosted by increases in prescriptions for lacosamide (Vimpat), in addition to a “steep increase in the cost per pill, with brand-name drugs costing 10 times more than their generic counterparts,” first author Samuel Waller Terman, MD, of the University of Michigan, Ann Arbor, added in a news release.
The study was published online in Neurology.
Is a 10-fold increase in cost worth it?
To evaluate trends in ASM prescriptions and costs, the researchers used a random sample of 20% of Medicare beneficiaries with coverage from 2008 to 2018. There were 77,000 to 133,000 patients with epilepsy each year.
Over time, likely because of increasing availability of generics, brand-name ASMs made up a smaller proportion of pills prescribed, from 56% in 2008 to 14% in 2018, but still made up 79% of prescription drug costs in 2018.
The annual cost of brand-name ASMs rose from $2,800 in 2008 to $10,700 in 2018, while the cost of generic drugs decreased from $800 to $460 during that time.
An increased number of prescriptions for lacosamide was responsible for 45% of the total increase in brand-name costs.
As of 2018, lacosamide comprised 30% of all brand-name pill supply (followed by pregabalin, at 15%) and 30% of all brand-name costs (followed by clobazam and pregabalin, both at 9%), the investigators reported.
Brand-name antiepileptic drug costs decreased from 2008 to 2010, but after the introduction of lacosamide, total brand-name costs steadily rose from $72 million in 2010 (in 2018 dollars) to $256 million in 2018, they noted.
Because the dataset consists of a 20% random Medicare sample, total Medicare costs for brand-name ASMs for beneficiaries with epilepsy alone likely rose from roughly $360 million in 2010 to $1.3 billion in 2018, they added.
“Clinicians must remain cognizant of this societal cost magnitude when judging whether the 10-fold increased expense per pill for brand name medications is worth the possible benefits,” they wrote.
“While newer-generation drugs have potential advantages such as limited drug interactions and different side effect profiles, there have been conflicting studies on whether they are cost effective,” Dr. Terman noted in a news release.
A barrier to treatment
The authors of an accompanying editorial propose that the problem of prescription drug costs could be solved through a combination of competition and government regulation of prices. Patients and physicians are the most important stakeholders in this issue.
“When something represents 14% of the total use, but contributes 79% of the cost, it would be wise to consider alternatives, assuming that these alternatives are not of lower quality,” wrote Wyatt Bensken, with Case Western Reserve University, Cleveland, and Iván Sánchez Fernández, MD, with Boston Medical Center.
“When there are several ASMs with a similar mechanism of action, similar efficacy, similar safety and tolerability profile, and different costs, it would be unwise to choose the more expensive alternative just because it is newer,” they said.
This study, they added, provides data to “understand, and begin to act, on the challenging problem of the cost of prescription ASMs. After all, what is the point of having a large number of ASMs if their cost severely limits their use?”
A limitation of the study is that only Medicare prescription claims were included, so the results may not apply to younger patients with private insurance.
The study received no direct funding. The authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new analysis shows.
After adjustment for inflation, the cost of a 1-year supply of brand-name ASMs grew 277%, while generics became 42% less expensive.
“Our study makes transparent striking trends in brand name prescribing patterns,” the study team wrote.
Since 2010, the costs for brand-name ASMs have “consistently” increased. Costs were particularly boosted by increases in prescriptions for lacosamide (Vimpat), in addition to a “steep increase in the cost per pill, with brand-name drugs costing 10 times more than their generic counterparts,” first author Samuel Waller Terman, MD, of the University of Michigan, Ann Arbor, added in a news release.
The study was published online in Neurology.
Is a 10-fold increase in cost worth it?
To evaluate trends in ASM prescriptions and costs, the researchers used a random sample of 20% of Medicare beneficiaries with coverage from 2008 to 2018. There were 77,000 to 133,000 patients with epilepsy each year.
Over time, likely because of increasing availability of generics, brand-name ASMs made up a smaller proportion of pills prescribed, from 56% in 2008 to 14% in 2018, but still made up 79% of prescription drug costs in 2018.
The annual cost of brand-name ASMs rose from $2,800 in 2008 to $10,700 in 2018, while the cost of generic drugs decreased from $800 to $460 during that time.
An increased number of prescriptions for lacosamide was responsible for 45% of the total increase in brand-name costs.
As of 2018, lacosamide comprised 30% of all brand-name pill supply (followed by pregabalin, at 15%) and 30% of all brand-name costs (followed by clobazam and pregabalin, both at 9%), the investigators reported.
Brand-name antiepileptic drug costs decreased from 2008 to 2010, but after the introduction of lacosamide, total brand-name costs steadily rose from $72 million in 2010 (in 2018 dollars) to $256 million in 2018, they noted.
Because the dataset consists of a 20% random Medicare sample, total Medicare costs for brand-name ASMs for beneficiaries with epilepsy alone likely rose from roughly $360 million in 2010 to $1.3 billion in 2018, they added.
“Clinicians must remain cognizant of this societal cost magnitude when judging whether the 10-fold increased expense per pill for brand name medications is worth the possible benefits,” they wrote.
“While newer-generation drugs have potential advantages such as limited drug interactions and different side effect profiles, there have been conflicting studies on whether they are cost effective,” Dr. Terman noted in a news release.
A barrier to treatment
The authors of an accompanying editorial propose that the problem of prescription drug costs could be solved through a combination of competition and government regulation of prices. Patients and physicians are the most important stakeholders in this issue.
“When something represents 14% of the total use, but contributes 79% of the cost, it would be wise to consider alternatives, assuming that these alternatives are not of lower quality,” wrote Wyatt Bensken, with Case Western Reserve University, Cleveland, and Iván Sánchez Fernández, MD, with Boston Medical Center.
“When there are several ASMs with a similar mechanism of action, similar efficacy, similar safety and tolerability profile, and different costs, it would be unwise to choose the more expensive alternative just because it is newer,” they said.
This study, they added, provides data to “understand, and begin to act, on the challenging problem of the cost of prescription ASMs. After all, what is the point of having a large number of ASMs if their cost severely limits their use?”
A limitation of the study is that only Medicare prescription claims were included, so the results may not apply to younger patients with private insurance.
The study received no direct funding. The authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new analysis shows.
After adjustment for inflation, the cost of a 1-year supply of brand-name ASMs grew 277%, while generics became 42% less expensive.
“Our study makes transparent striking trends in brand name prescribing patterns,” the study team wrote.
Since 2010, the costs for brand-name ASMs have “consistently” increased. Costs were particularly boosted by increases in prescriptions for lacosamide (Vimpat), in addition to a “steep increase in the cost per pill, with brand-name drugs costing 10 times more than their generic counterparts,” first author Samuel Waller Terman, MD, of the University of Michigan, Ann Arbor, added in a news release.
The study was published online in Neurology.
Is a 10-fold increase in cost worth it?
To evaluate trends in ASM prescriptions and costs, the researchers used a random sample of 20% of Medicare beneficiaries with coverage from 2008 to 2018. There were 77,000 to 133,000 patients with epilepsy each year.
Over time, likely because of increasing availability of generics, brand-name ASMs made up a smaller proportion of pills prescribed, from 56% in 2008 to 14% in 2018, but still made up 79% of prescription drug costs in 2018.
The annual cost of brand-name ASMs rose from $2,800 in 2008 to $10,700 in 2018, while the cost of generic drugs decreased from $800 to $460 during that time.
An increased number of prescriptions for lacosamide was responsible for 45% of the total increase in brand-name costs.
As of 2018, lacosamide comprised 30% of all brand-name pill supply (followed by pregabalin, at 15%) and 30% of all brand-name costs (followed by clobazam and pregabalin, both at 9%), the investigators reported.
Brand-name antiepileptic drug costs decreased from 2008 to 2010, but after the introduction of lacosamide, total brand-name costs steadily rose from $72 million in 2010 (in 2018 dollars) to $256 million in 2018, they noted.
Because the dataset consists of a 20% random Medicare sample, total Medicare costs for brand-name ASMs for beneficiaries with epilepsy alone likely rose from roughly $360 million in 2010 to $1.3 billion in 2018, they added.
“Clinicians must remain cognizant of this societal cost magnitude when judging whether the 10-fold increased expense per pill for brand name medications is worth the possible benefits,” they wrote.
“While newer-generation drugs have potential advantages such as limited drug interactions and different side effect profiles, there have been conflicting studies on whether they are cost effective,” Dr. Terman noted in a news release.
A barrier to treatment
The authors of an accompanying editorial propose that the problem of prescription drug costs could be solved through a combination of competition and government regulation of prices. Patients and physicians are the most important stakeholders in this issue.
“When something represents 14% of the total use, but contributes 79% of the cost, it would be wise to consider alternatives, assuming that these alternatives are not of lower quality,” wrote Wyatt Bensken, with Case Western Reserve University, Cleveland, and Iván Sánchez Fernández, MD, with Boston Medical Center.
“When there are several ASMs with a similar mechanism of action, similar efficacy, similar safety and tolerability profile, and different costs, it would be unwise to choose the more expensive alternative just because it is newer,” they said.
This study, they added, provides data to “understand, and begin to act, on the challenging problem of the cost of prescription ASMs. After all, what is the point of having a large number of ASMs if their cost severely limits their use?”
A limitation of the study is that only Medicare prescription claims were included, so the results may not apply to younger patients with private insurance.
The study received no direct funding. The authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
WHO tracking new Omicron subvariant in India
The subvariant, a sublineage of BA.2 being called BA.2.75, has been reported in eight countries and hasn’t yet been declared a variant of concern.
“There’s been an emergence of a ‘could be’ subvariant. It’s been not yet officially called, but some people are referring to it as BA.2.75,” Soumya Swaminathan, MD, the WHO’s chief scientist, said in a video posted on Twitter.
The subvariant appears to have mutations similar to other contagious strains, she said, though there are a limited number of sequences available to analyze. How transmissible and severe it is, and how well it can evade our immunity, aren’t yet known.
“We have to wait and see, and of course, we are tracking it,” Dr. Swaminathan said.
The WHO committee responsible for analyzing global coronavirus data will label the subvariant officially and release more information as the situation warrants it, she said.
Public health experts around the world are also talking about the subvariant, which has been nicknamed Centaurus. BA.2.75 was first found in India in May and is now competing with BA.5, which has become dominant in the United States.
BA.2.75 has eight mutations beyond those seen in BA.5, which “could make immune escape worse than what we’re seeing now,” Eric Topol, MD, founder and director of the Scripps Research Translational Institute and editor-in-chief at Medscape, wrote in a Twitter post.
Individually, the extra mutations aren’t too concerning, “but all appearing together at once is another matter,” Tom Peacock, PhD, a virologist at Imperial College London, wrote in a Twitter post.
The “apparent rapid growth and wide geographical spread” are “worth keeping a close eye on,” he said.
BA.2.75 has been found in a handful of cases in the United States, Australia, Canada, Germany, Japan, New Zealand, and the United Kingdom. In India, the sequence accounts for about 23% of recent samples.
“It is really too early to know if BA.2.75 will take over relative to BA.2 or even relative to BA.5,” Ulrich Elling, PhD, a researcher at Australia’s Institute of Molecular Biotechnology, wrote in a Twitter post.
“Just to emphasize it again: While the distribution across Indian regions as well as internationally and the very rapid appearance makes it likely we are dealing with a variant spreading fast and spread widely already, the absolute data points are few,” he said.
Globally, coronavirus cases have increased nearly 30% during the past 2 weeks, the WHO said July 6. Four out of six of the WHO subregions reported an increase in the last week, with BA.4 and BA.5 driving waves in the United States and Europe.
A version of this article first appeared on WebMD.com.
The subvariant, a sublineage of BA.2 being called BA.2.75, has been reported in eight countries and hasn’t yet been declared a variant of concern.
“There’s been an emergence of a ‘could be’ subvariant. It’s been not yet officially called, but some people are referring to it as BA.2.75,” Soumya Swaminathan, MD, the WHO’s chief scientist, said in a video posted on Twitter.
The subvariant appears to have mutations similar to other contagious strains, she said, though there are a limited number of sequences available to analyze. How transmissible and severe it is, and how well it can evade our immunity, aren’t yet known.
“We have to wait and see, and of course, we are tracking it,” Dr. Swaminathan said.
The WHO committee responsible for analyzing global coronavirus data will label the subvariant officially and release more information as the situation warrants it, she said.
Public health experts around the world are also talking about the subvariant, which has been nicknamed Centaurus. BA.2.75 was first found in India in May and is now competing with BA.5, which has become dominant in the United States.
BA.2.75 has eight mutations beyond those seen in BA.5, which “could make immune escape worse than what we’re seeing now,” Eric Topol, MD, founder and director of the Scripps Research Translational Institute and editor-in-chief at Medscape, wrote in a Twitter post.
Individually, the extra mutations aren’t too concerning, “but all appearing together at once is another matter,” Tom Peacock, PhD, a virologist at Imperial College London, wrote in a Twitter post.
The “apparent rapid growth and wide geographical spread” are “worth keeping a close eye on,” he said.
BA.2.75 has been found in a handful of cases in the United States, Australia, Canada, Germany, Japan, New Zealand, and the United Kingdom. In India, the sequence accounts for about 23% of recent samples.
“It is really too early to know if BA.2.75 will take over relative to BA.2 or even relative to BA.5,” Ulrich Elling, PhD, a researcher at Australia’s Institute of Molecular Biotechnology, wrote in a Twitter post.
“Just to emphasize it again: While the distribution across Indian regions as well as internationally and the very rapid appearance makes it likely we are dealing with a variant spreading fast and spread widely already, the absolute data points are few,” he said.
Globally, coronavirus cases have increased nearly 30% during the past 2 weeks, the WHO said July 6. Four out of six of the WHO subregions reported an increase in the last week, with BA.4 and BA.5 driving waves in the United States and Europe.
A version of this article first appeared on WebMD.com.
The subvariant, a sublineage of BA.2 being called BA.2.75, has been reported in eight countries and hasn’t yet been declared a variant of concern.
“There’s been an emergence of a ‘could be’ subvariant. It’s been not yet officially called, but some people are referring to it as BA.2.75,” Soumya Swaminathan, MD, the WHO’s chief scientist, said in a video posted on Twitter.
The subvariant appears to have mutations similar to other contagious strains, she said, though there are a limited number of sequences available to analyze. How transmissible and severe it is, and how well it can evade our immunity, aren’t yet known.
“We have to wait and see, and of course, we are tracking it,” Dr. Swaminathan said.
The WHO committee responsible for analyzing global coronavirus data will label the subvariant officially and release more information as the situation warrants it, she said.
Public health experts around the world are also talking about the subvariant, which has been nicknamed Centaurus. BA.2.75 was first found in India in May and is now competing with BA.5, which has become dominant in the United States.
BA.2.75 has eight mutations beyond those seen in BA.5, which “could make immune escape worse than what we’re seeing now,” Eric Topol, MD, founder and director of the Scripps Research Translational Institute and editor-in-chief at Medscape, wrote in a Twitter post.
Individually, the extra mutations aren’t too concerning, “but all appearing together at once is another matter,” Tom Peacock, PhD, a virologist at Imperial College London, wrote in a Twitter post.
The “apparent rapid growth and wide geographical spread” are “worth keeping a close eye on,” he said.
BA.2.75 has been found in a handful of cases in the United States, Australia, Canada, Germany, Japan, New Zealand, and the United Kingdom. In India, the sequence accounts for about 23% of recent samples.
“It is really too early to know if BA.2.75 will take over relative to BA.2 or even relative to BA.5,” Ulrich Elling, PhD, a researcher at Australia’s Institute of Molecular Biotechnology, wrote in a Twitter post.
“Just to emphasize it again: While the distribution across Indian regions as well as internationally and the very rapid appearance makes it likely we are dealing with a variant spreading fast and spread widely already, the absolute data points are few,” he said.
Globally, coronavirus cases have increased nearly 30% during the past 2 weeks, the WHO said July 6. Four out of six of the WHO subregions reported an increase in the last week, with BA.4 and BA.5 driving waves in the United States and Europe.
A version of this article first appeared on WebMD.com.
Doc releases song after racist massacre in Buffalo
Physician-musician Cleveland Francis, MD, responded to the recent mass shooting in Buffalo, New York, which left 10 dead, in the only way he knew how. He wrote and recorded a song to honor the victims as “a plea to the other side to recognize us as people,” the Black cardiologist told this news organization.
He couldn’t sleep after the shooting, and “this song was just in my head.” In the 1990s, Dr. Francis took a 3-year sabbatical from medicine to perform and tour as a country singer. He leveraged his Nashville connections to get “Buffalo” produced and recorded.
Acclaimed artist James Threalkill created the accompanying art, titled “The Heavenly Escort of the Buffalo 10,” after listening to a scratch demo.
Dr. Francis doesn’t want people to overlook the massacre as just another gun violence incident because this was “overt hate-crime racism,” he said.
According to the affidavit submitted by FBI agent Christopher J. Dlugokinski, the suspect’s “motive for the mass shooting was to prevent Black people from replacing White people and eliminating the White race, and to inspire others to commit similar attacks.”
Dr. Francis views the Buffalo shooting as distinct from cases like the murder of George Floyd that involved crime or police. It immediately made him think of the Mother Emanuel Church shooting in Charleston, South Carolina. “Having a black skin is now a death warrant,” he said.
The song is also an appeal for White people to fight racism. Dr. Francis is concerned about young men caught up in white supremacy and suggests that we be more alert to children or grandchildren who disconnect from their families, spend time on the dark web, and access guns. The lyrics deliberately don’t mention guns because Dr. Francis wanted to stay out of that debate. “I just sang: ‘What else do I have to do to prove to you that I’m human too?’ ”
Despite his country credentials, Dr. Francis wrote “Buffalo” as a Gospel song because that genre “connects with Black people more and because that civil rights movement was through the church with Dr. Martin Luther King,” he explained. Although he sings all styles of music, the song is performed by Nashville-based singer Michael Lusk so that it’s not a “Cleve Francis thing,” he said, referring to his stage name.
Songwriter Norman Kerner collaborated on the song. The music was produced and recorded by David Thein and mixed by Bob Bullock of Nashville, who Dr. Francis had worked with when he was an artist on Capitol Records.
They sent the video and artwork to the Mayor of Buffalo, Byron Brown, but have yet to hear back. Dr. Francis hopes it could be part of their healing, noting that some people used the song in their Juneteenth celebrations.
The Louisiana native grew up during segregation and was one of two Black students in the Medical College of Virginia class of 1973. After completing his cardiology fellowship, no one would hire him, so Dr. Francis set up his own practice in Northern Virginia. He now works at Inova Heart and Vascular Institute in Alexandria, Va. He remains optimistic about race relations in America and would love a Black pop or Gospel star to record “Buffalo” and bring it to a wider audience.
Dr. Francis is a regular blogger for Medscape. His contribution to country music is recognized in the National Museum of African American History and Culture in Washington, DC. You can find more of his music on YouTube.
A version of this article first appeared on Medscape.com.
Physician-musician Cleveland Francis, MD, responded to the recent mass shooting in Buffalo, New York, which left 10 dead, in the only way he knew how. He wrote and recorded a song to honor the victims as “a plea to the other side to recognize us as people,” the Black cardiologist told this news organization.
He couldn’t sleep after the shooting, and “this song was just in my head.” In the 1990s, Dr. Francis took a 3-year sabbatical from medicine to perform and tour as a country singer. He leveraged his Nashville connections to get “Buffalo” produced and recorded.
Acclaimed artist James Threalkill created the accompanying art, titled “The Heavenly Escort of the Buffalo 10,” after listening to a scratch demo.
Dr. Francis doesn’t want people to overlook the massacre as just another gun violence incident because this was “overt hate-crime racism,” he said.
According to the affidavit submitted by FBI agent Christopher J. Dlugokinski, the suspect’s “motive for the mass shooting was to prevent Black people from replacing White people and eliminating the White race, and to inspire others to commit similar attacks.”
Dr. Francis views the Buffalo shooting as distinct from cases like the murder of George Floyd that involved crime or police. It immediately made him think of the Mother Emanuel Church shooting in Charleston, South Carolina. “Having a black skin is now a death warrant,” he said.
The song is also an appeal for White people to fight racism. Dr. Francis is concerned about young men caught up in white supremacy and suggests that we be more alert to children or grandchildren who disconnect from their families, spend time on the dark web, and access guns. The lyrics deliberately don’t mention guns because Dr. Francis wanted to stay out of that debate. “I just sang: ‘What else do I have to do to prove to you that I’m human too?’ ”
Despite his country credentials, Dr. Francis wrote “Buffalo” as a Gospel song because that genre “connects with Black people more and because that civil rights movement was through the church with Dr. Martin Luther King,” he explained. Although he sings all styles of music, the song is performed by Nashville-based singer Michael Lusk so that it’s not a “Cleve Francis thing,” he said, referring to his stage name.
Songwriter Norman Kerner collaborated on the song. The music was produced and recorded by David Thein and mixed by Bob Bullock of Nashville, who Dr. Francis had worked with when he was an artist on Capitol Records.
They sent the video and artwork to the Mayor of Buffalo, Byron Brown, but have yet to hear back. Dr. Francis hopes it could be part of their healing, noting that some people used the song in their Juneteenth celebrations.
The Louisiana native grew up during segregation and was one of two Black students in the Medical College of Virginia class of 1973. After completing his cardiology fellowship, no one would hire him, so Dr. Francis set up his own practice in Northern Virginia. He now works at Inova Heart and Vascular Institute in Alexandria, Va. He remains optimistic about race relations in America and would love a Black pop or Gospel star to record “Buffalo” and bring it to a wider audience.
Dr. Francis is a regular blogger for Medscape. His contribution to country music is recognized in the National Museum of African American History and Culture in Washington, DC. You can find more of his music on YouTube.
A version of this article first appeared on Medscape.com.
Physician-musician Cleveland Francis, MD, responded to the recent mass shooting in Buffalo, New York, which left 10 dead, in the only way he knew how. He wrote and recorded a song to honor the victims as “a plea to the other side to recognize us as people,” the Black cardiologist told this news organization.
He couldn’t sleep after the shooting, and “this song was just in my head.” In the 1990s, Dr. Francis took a 3-year sabbatical from medicine to perform and tour as a country singer. He leveraged his Nashville connections to get “Buffalo” produced and recorded.
Acclaimed artist James Threalkill created the accompanying art, titled “The Heavenly Escort of the Buffalo 10,” after listening to a scratch demo.
Dr. Francis doesn’t want people to overlook the massacre as just another gun violence incident because this was “overt hate-crime racism,” he said.
According to the affidavit submitted by FBI agent Christopher J. Dlugokinski, the suspect’s “motive for the mass shooting was to prevent Black people from replacing White people and eliminating the White race, and to inspire others to commit similar attacks.”
Dr. Francis views the Buffalo shooting as distinct from cases like the murder of George Floyd that involved crime or police. It immediately made him think of the Mother Emanuel Church shooting in Charleston, South Carolina. “Having a black skin is now a death warrant,” he said.
The song is also an appeal for White people to fight racism. Dr. Francis is concerned about young men caught up in white supremacy and suggests that we be more alert to children or grandchildren who disconnect from their families, spend time on the dark web, and access guns. The lyrics deliberately don’t mention guns because Dr. Francis wanted to stay out of that debate. “I just sang: ‘What else do I have to do to prove to you that I’m human too?’ ”
Despite his country credentials, Dr. Francis wrote “Buffalo” as a Gospel song because that genre “connects with Black people more and because that civil rights movement was through the church with Dr. Martin Luther King,” he explained. Although he sings all styles of music, the song is performed by Nashville-based singer Michael Lusk so that it’s not a “Cleve Francis thing,” he said, referring to his stage name.
Songwriter Norman Kerner collaborated on the song. The music was produced and recorded by David Thein and mixed by Bob Bullock of Nashville, who Dr. Francis had worked with when he was an artist on Capitol Records.
They sent the video and artwork to the Mayor of Buffalo, Byron Brown, but have yet to hear back. Dr. Francis hopes it could be part of their healing, noting that some people used the song in their Juneteenth celebrations.
The Louisiana native grew up during segregation and was one of two Black students in the Medical College of Virginia class of 1973. After completing his cardiology fellowship, no one would hire him, so Dr. Francis set up his own practice in Northern Virginia. He now works at Inova Heart and Vascular Institute in Alexandria, Va. He remains optimistic about race relations in America and would love a Black pop or Gospel star to record “Buffalo” and bring it to a wider audience.
Dr. Francis is a regular blogger for Medscape. His contribution to country music is recognized in the National Museum of African American History and Culture in Washington, DC. You can find more of his music on YouTube.
A version of this article first appeared on Medscape.com.
Mosquitoes and the vicious circle that’s gone viral
These viruses want mosquitoes with good taste
Taste can be a pretty subjective sense. Not everyone agrees on what tastes good and what tastes bad. Most people would agree that freshly baked cookies taste good, but what about lima beans? And what about mosquitoes? What tastes good to a mosquito?
The answer? Blood. Blood tastes good to a mosquito. That really wasn’t a very hard question, was it? You did know the answer, didn’t you? They don’t care about cookies, and they certainly don’t care about lima beans. It’s blood that they love.
That brings us back to subjectivity, because it is possible for blood to taste even better. The secret ingredient is dengue … and Zika.
A study just published in Cell demonstrates that mice infected with dengue and Zika viruses release a volatile compound called acetophenone. “We found that flavivirus [like dengue and Zika] can utilize the increased release of acetophenone to help itself achieve its lifecycles more effectively by making their hosts more attractive to mosquito vectors,” senior author Gong Cheng of Tsinghua University, Beijing, said in a written statement.
How do they do it? The viruses, he explained, promote the proliferation of acetophenone-producing skin bacteria. “As a result, some bacteria overreplicate and produce more acetophenone. Suddenly, these sick individuals smell as delicious to mosquitoes as a tray of freshly baked cookies to a group of five-year-old children,” the statement said.
And how do you stop a group of tiny, flying 5-year-olds? That’s right, with acne medication. Really? You knew that one but not the blood one before? The investigators fed isotretinoin to the infected mice, which led to reduced acetophenone release from skin bacteria and made the animals no more attractive to the mosquitoes than their uninfected counterparts.
The investigators are planning to take the next step – feeding isotretinoin to people with dengue and Zika – having gotten the official fictional taste-test approval of celebrity chef Gordon Ramsay, who said, “You’re going to feed this #$^% to sick people? ARE YOU &%*$@#& KIDDING ME?”
Okay, so maybe approval isn’t quite the right word.
Welcome to bladders of the rich and famous!
Don’t you hate it when you’re driving out to your multimillion-dollar second home in the Hamptons and traffic is so bad you absolutely have to find a place to “rest” along the way? But wouldn’t you know it, there just isn’t anywhere to stop! Geez, how do we live?
That’s where David Shusterman, MD, a urologist in New York City and a true American hero, comes in. He’s identified a market and positioned himself as the king of both bladder surgery and “bladder Botox” for the wealthy New Yorkers who regularly make long journeys from the city out to their second homes in the Hamptons. Traffic has increased dramatically on Long Island roads in recent years, and the journey can now taking upward of 4 hours. Some people just can’t make it that long without a bathroom break, and there are very few places to stop along the way.
Dr. Shusterman understands the plight of the Hamptons vacationer, as he told Insider.com: “I can’t tell you how many arguments I personally get into – I’ve lost three friends because I’m the driver and refuse to stop for them.” A tragedy worthy of Shakespeare himself.
During the summer season, Dr. Shusterman performs about 10 prostate artery embolizations a week, an hour-long procedure that shrinks the prostate, which is great for 50- to 60-year-old men with enlarged prostates that cause more frequent bathroom trips. He also performs Botox injections into the bladder once or twice a week for women, which reduces the need to urinate for roughly 6 months. The perfect amount of time to get them through the summer season.
These procedures are sometimes covered by insurance but can cost as much as $20,000 if paid out of pocket. That’s a lot of money to us, but if you’re the sort of person who has a second home in the Hamptons, $20,000 is chump change, especially if it means you won’t have to go 2 entire minutes out of your way to use a gas-station bathroom. Then again, having seen a more than a few gas-station bathrooms in our time, maybe they have a point.
Ditch the apples. Go for the avocados
We’ve all heard about “an apple a day,” but instead of apples you might want to go with avocados.
Avocados are generally thought to be a healthy fat. A study just published in the Journal of the American Heart Association proves that they actually don’t do anything for your waistline but will work wonders on your cholesterol level. The study involved 923 participants who were considered overweight/obese split into two groups: One was asked to consume an avocado a day, and the other continued their usual diets and were asked to consume fewer than two avocados a month.
At the end of the 6 months, the researchers found total cholesterol decreased by an additional 2.9 mg/dL and LDL cholesterol by 2.5 mg/dL in those who ate one avocado every day, compared with the usual-diet group. And even though avocados have a lot of calories, there was no clinical evidence that it impacted weight gain or any cardiometabolic risk factors, according to a statement from Penn State University.
Avocados, then, can be considered a guilt-free food. The findings from this study suggest it can give a substantial boost to your overall quality of diet, in turn lessening your risk of developing type 2 diabetes and some cancers, Kristina Peterson, PhD, assistant professor of nutritional sciences at Texas Tech University, said in the statement.
So get creative with your avocado recipes. You can only eat so much guacamole.
Your nose knows a good friend for you
You’ve probably noticed how dogs sniff other dogs and people before becoming friends. It would be pretty comical if people did the same thing, right? Just walked up to strangers and started sniffing them like dogs?
Well, apparently humans do go by smell when it comes to making friends, and they prefer people who smell like them. Maybe you’ve noticed that your friends look like you, share your values, and think the same way as you. You’re probably right, seeing as previous research has pointed to this.
For the current study, done to show how smell affects human behavior, researchers recruited people who befriended each other quickly, before knowing much about each other. They assumed that the relationships between these same-sex, nonromantic “click friends” relied more on physiological traits, including smell. After collecting samples from the click friends, researchers used an eNose to scan chemical signatures. In another experiment, human volunteers sniffed samples to determine if any were similar. Both experiments showed that click friends had more similar smells than pairs of random people.
“This is not to say that we act like goats or shrews – humans likely rely on other, far more dominant cues in their social decision-making. Nevertheless, our study’s results do suggest that our nose plays a bigger role than previously thought in our choice of friends,” said senior author Noam Sobel, PhD, of the Weizmann Institute of Science in Rehovot, Israel.
Lead author Inbal Ravreby, a graduate student at the institute, put it this way: “These results imply that, as the saying goes, there is chemistry in social chemistry.”
These viruses want mosquitoes with good taste
Taste can be a pretty subjective sense. Not everyone agrees on what tastes good and what tastes bad. Most people would agree that freshly baked cookies taste good, but what about lima beans? And what about mosquitoes? What tastes good to a mosquito?
The answer? Blood. Blood tastes good to a mosquito. That really wasn’t a very hard question, was it? You did know the answer, didn’t you? They don’t care about cookies, and they certainly don’t care about lima beans. It’s blood that they love.
That brings us back to subjectivity, because it is possible for blood to taste even better. The secret ingredient is dengue … and Zika.
A study just published in Cell demonstrates that mice infected with dengue and Zika viruses release a volatile compound called acetophenone. “We found that flavivirus [like dengue and Zika] can utilize the increased release of acetophenone to help itself achieve its lifecycles more effectively by making their hosts more attractive to mosquito vectors,” senior author Gong Cheng of Tsinghua University, Beijing, said in a written statement.
How do they do it? The viruses, he explained, promote the proliferation of acetophenone-producing skin bacteria. “As a result, some bacteria overreplicate and produce more acetophenone. Suddenly, these sick individuals smell as delicious to mosquitoes as a tray of freshly baked cookies to a group of five-year-old children,” the statement said.
And how do you stop a group of tiny, flying 5-year-olds? That’s right, with acne medication. Really? You knew that one but not the blood one before? The investigators fed isotretinoin to the infected mice, which led to reduced acetophenone release from skin bacteria and made the animals no more attractive to the mosquitoes than their uninfected counterparts.
The investigators are planning to take the next step – feeding isotretinoin to people with dengue and Zika – having gotten the official fictional taste-test approval of celebrity chef Gordon Ramsay, who said, “You’re going to feed this #$^% to sick people? ARE YOU &%*$@#& KIDDING ME?”
Okay, so maybe approval isn’t quite the right word.
Welcome to bladders of the rich and famous!
Don’t you hate it when you’re driving out to your multimillion-dollar second home in the Hamptons and traffic is so bad you absolutely have to find a place to “rest” along the way? But wouldn’t you know it, there just isn’t anywhere to stop! Geez, how do we live?
That’s where David Shusterman, MD, a urologist in New York City and a true American hero, comes in. He’s identified a market and positioned himself as the king of both bladder surgery and “bladder Botox” for the wealthy New Yorkers who regularly make long journeys from the city out to their second homes in the Hamptons. Traffic has increased dramatically on Long Island roads in recent years, and the journey can now taking upward of 4 hours. Some people just can’t make it that long without a bathroom break, and there are very few places to stop along the way.
Dr. Shusterman understands the plight of the Hamptons vacationer, as he told Insider.com: “I can’t tell you how many arguments I personally get into – I’ve lost three friends because I’m the driver and refuse to stop for them.” A tragedy worthy of Shakespeare himself.
During the summer season, Dr. Shusterman performs about 10 prostate artery embolizations a week, an hour-long procedure that shrinks the prostate, which is great for 50- to 60-year-old men with enlarged prostates that cause more frequent bathroom trips. He also performs Botox injections into the bladder once or twice a week for women, which reduces the need to urinate for roughly 6 months. The perfect amount of time to get them through the summer season.
These procedures are sometimes covered by insurance but can cost as much as $20,000 if paid out of pocket. That’s a lot of money to us, but if you’re the sort of person who has a second home in the Hamptons, $20,000 is chump change, especially if it means you won’t have to go 2 entire minutes out of your way to use a gas-station bathroom. Then again, having seen a more than a few gas-station bathrooms in our time, maybe they have a point.
Ditch the apples. Go for the avocados
We’ve all heard about “an apple a day,” but instead of apples you might want to go with avocados.
Avocados are generally thought to be a healthy fat. A study just published in the Journal of the American Heart Association proves that they actually don’t do anything for your waistline but will work wonders on your cholesterol level. The study involved 923 participants who were considered overweight/obese split into two groups: One was asked to consume an avocado a day, and the other continued their usual diets and were asked to consume fewer than two avocados a month.
At the end of the 6 months, the researchers found total cholesterol decreased by an additional 2.9 mg/dL and LDL cholesterol by 2.5 mg/dL in those who ate one avocado every day, compared with the usual-diet group. And even though avocados have a lot of calories, there was no clinical evidence that it impacted weight gain or any cardiometabolic risk factors, according to a statement from Penn State University.
Avocados, then, can be considered a guilt-free food. The findings from this study suggest it can give a substantial boost to your overall quality of diet, in turn lessening your risk of developing type 2 diabetes and some cancers, Kristina Peterson, PhD, assistant professor of nutritional sciences at Texas Tech University, said in the statement.
So get creative with your avocado recipes. You can only eat so much guacamole.
Your nose knows a good friend for you
You’ve probably noticed how dogs sniff other dogs and people before becoming friends. It would be pretty comical if people did the same thing, right? Just walked up to strangers and started sniffing them like dogs?
Well, apparently humans do go by smell when it comes to making friends, and they prefer people who smell like them. Maybe you’ve noticed that your friends look like you, share your values, and think the same way as you. You’re probably right, seeing as previous research has pointed to this.
For the current study, done to show how smell affects human behavior, researchers recruited people who befriended each other quickly, before knowing much about each other. They assumed that the relationships between these same-sex, nonromantic “click friends” relied more on physiological traits, including smell. After collecting samples from the click friends, researchers used an eNose to scan chemical signatures. In another experiment, human volunteers sniffed samples to determine if any were similar. Both experiments showed that click friends had more similar smells than pairs of random people.
“This is not to say that we act like goats or shrews – humans likely rely on other, far more dominant cues in their social decision-making. Nevertheless, our study’s results do suggest that our nose plays a bigger role than previously thought in our choice of friends,” said senior author Noam Sobel, PhD, of the Weizmann Institute of Science in Rehovot, Israel.
Lead author Inbal Ravreby, a graduate student at the institute, put it this way: “These results imply that, as the saying goes, there is chemistry in social chemistry.”
These viruses want mosquitoes with good taste
Taste can be a pretty subjective sense. Not everyone agrees on what tastes good and what tastes bad. Most people would agree that freshly baked cookies taste good, but what about lima beans? And what about mosquitoes? What tastes good to a mosquito?
The answer? Blood. Blood tastes good to a mosquito. That really wasn’t a very hard question, was it? You did know the answer, didn’t you? They don’t care about cookies, and they certainly don’t care about lima beans. It’s blood that they love.
That brings us back to subjectivity, because it is possible for blood to taste even better. The secret ingredient is dengue … and Zika.
A study just published in Cell demonstrates that mice infected with dengue and Zika viruses release a volatile compound called acetophenone. “We found that flavivirus [like dengue and Zika] can utilize the increased release of acetophenone to help itself achieve its lifecycles more effectively by making their hosts more attractive to mosquito vectors,” senior author Gong Cheng of Tsinghua University, Beijing, said in a written statement.
How do they do it? The viruses, he explained, promote the proliferation of acetophenone-producing skin bacteria. “As a result, some bacteria overreplicate and produce more acetophenone. Suddenly, these sick individuals smell as delicious to mosquitoes as a tray of freshly baked cookies to a group of five-year-old children,” the statement said.
And how do you stop a group of tiny, flying 5-year-olds? That’s right, with acne medication. Really? You knew that one but not the blood one before? The investigators fed isotretinoin to the infected mice, which led to reduced acetophenone release from skin bacteria and made the animals no more attractive to the mosquitoes than their uninfected counterparts.
The investigators are planning to take the next step – feeding isotretinoin to people with dengue and Zika – having gotten the official fictional taste-test approval of celebrity chef Gordon Ramsay, who said, “You’re going to feed this #$^% to sick people? ARE YOU &%*$@#& KIDDING ME?”
Okay, so maybe approval isn’t quite the right word.
Welcome to bladders of the rich and famous!
Don’t you hate it when you’re driving out to your multimillion-dollar second home in the Hamptons and traffic is so bad you absolutely have to find a place to “rest” along the way? But wouldn’t you know it, there just isn’t anywhere to stop! Geez, how do we live?
That’s where David Shusterman, MD, a urologist in New York City and a true American hero, comes in. He’s identified a market and positioned himself as the king of both bladder surgery and “bladder Botox” for the wealthy New Yorkers who regularly make long journeys from the city out to their second homes in the Hamptons. Traffic has increased dramatically on Long Island roads in recent years, and the journey can now taking upward of 4 hours. Some people just can’t make it that long without a bathroom break, and there are very few places to stop along the way.
Dr. Shusterman understands the plight of the Hamptons vacationer, as he told Insider.com: “I can’t tell you how many arguments I personally get into – I’ve lost three friends because I’m the driver and refuse to stop for them.” A tragedy worthy of Shakespeare himself.
During the summer season, Dr. Shusterman performs about 10 prostate artery embolizations a week, an hour-long procedure that shrinks the prostate, which is great for 50- to 60-year-old men with enlarged prostates that cause more frequent bathroom trips. He also performs Botox injections into the bladder once or twice a week for women, which reduces the need to urinate for roughly 6 months. The perfect amount of time to get them through the summer season.
These procedures are sometimes covered by insurance but can cost as much as $20,000 if paid out of pocket. That’s a lot of money to us, but if you’re the sort of person who has a second home in the Hamptons, $20,000 is chump change, especially if it means you won’t have to go 2 entire minutes out of your way to use a gas-station bathroom. Then again, having seen a more than a few gas-station bathrooms in our time, maybe they have a point.
Ditch the apples. Go for the avocados
We’ve all heard about “an apple a day,” but instead of apples you might want to go with avocados.
Avocados are generally thought to be a healthy fat. A study just published in the Journal of the American Heart Association proves that they actually don’t do anything for your waistline but will work wonders on your cholesterol level. The study involved 923 participants who were considered overweight/obese split into two groups: One was asked to consume an avocado a day, and the other continued their usual diets and were asked to consume fewer than two avocados a month.
At the end of the 6 months, the researchers found total cholesterol decreased by an additional 2.9 mg/dL and LDL cholesterol by 2.5 mg/dL in those who ate one avocado every day, compared with the usual-diet group. And even though avocados have a lot of calories, there was no clinical evidence that it impacted weight gain or any cardiometabolic risk factors, according to a statement from Penn State University.
Avocados, then, can be considered a guilt-free food. The findings from this study suggest it can give a substantial boost to your overall quality of diet, in turn lessening your risk of developing type 2 diabetes and some cancers, Kristina Peterson, PhD, assistant professor of nutritional sciences at Texas Tech University, said in the statement.
So get creative with your avocado recipes. You can only eat so much guacamole.
Your nose knows a good friend for you
You’ve probably noticed how dogs sniff other dogs and people before becoming friends. It would be pretty comical if people did the same thing, right? Just walked up to strangers and started sniffing them like dogs?
Well, apparently humans do go by smell when it comes to making friends, and they prefer people who smell like them. Maybe you’ve noticed that your friends look like you, share your values, and think the same way as you. You’re probably right, seeing as previous research has pointed to this.
For the current study, done to show how smell affects human behavior, researchers recruited people who befriended each other quickly, before knowing much about each other. They assumed that the relationships between these same-sex, nonromantic “click friends” relied more on physiological traits, including smell. After collecting samples from the click friends, researchers used an eNose to scan chemical signatures. In another experiment, human volunteers sniffed samples to determine if any were similar. Both experiments showed that click friends had more similar smells than pairs of random people.
“This is not to say that we act like goats or shrews – humans likely rely on other, far more dominant cues in their social decision-making. Nevertheless, our study’s results do suggest that our nose plays a bigger role than previously thought in our choice of friends,” said senior author Noam Sobel, PhD, of the Weizmann Institute of Science in Rehovot, Israel.
Lead author Inbal Ravreby, a graduate student at the institute, put it this way: “These results imply that, as the saying goes, there is chemistry in social chemistry.”
Will the headache field embrace rofecoxib?
In June, the Concord, Mass.–based company Tremeau Pharmaceuticals announced that the Food and Drug Administration was letting it proceed with a phase 3 clinical trial to test rofecoxib, the once-bestselling painkiller known as Vioxx, in patients with migraine.
The anti-inflammatory drug, a cyclooxygenase-2 (COX-2) inhibitor, received its first FDA approval in 1999 and became widely prescribed for arthritis and acute pain. In 2004 it was withdrawn by its manufacturer, Merck, after being shown to raise the risk of cardiovascular events.
In clinical trials and in real-world epidemiological studies, rofecoxib was associated with elevated heart attack, stroke, and related deaths; one 2005 study estimated that it had been responsible for some 38,000 excess deaths in the United States before being withdrawn. In 2007 Merck, beset with allegations that it had suppressed and mischaracterized rofecoxib’s safety data, paid out nearly $5 billion to settle thousands of lawsuits filed by patients and their families.
, an indication for which it received an orphan drug designation in 2017 and the agency’s green light for trials in 2020.
Brad Sippy, Tremeau’s chief executive officer, said that his company chose the two indications in part because both patient populations have low cardiovascular risk. Migraine patients are generally younger than the arthritis populations formerly treated with rofecoxib and are unlikely to take the drug for more than a day or 2 at time, avoiding the risks associated with extended exposure.
A crowded market
The past several years have seen the emergence of a cornucopia of new migraine treatments, including monoclonal antibodies such as erenumab (Aimovig, Amgen), which help prevent attacks by blocking the vasodilator calcitonin gene-related peptide, or CGRP. In addition to the standard arsenal of triptans and nonsteroidal anti-inflammatory drugs for acute pain relief, migraine patients can now choose among serotonin-blocking agents such as lasmiditan (Reyvow, Eli Lilly), known as “ditans,” and small-molecule CGRP antagonists such as ubrogepant (Ubrelvy, Abbie), known as “gepants.” Some NSAIDs, including one COX inhibitor, have been formulated into rapidly absorbed powders or liquids for migraine.
Mr. Sippy said he sees a role for rofecoxib even in this crowded space. “Migraine as you know is a multimodal situation – few people say that only one drug works for them,” he said. “We think this is an option that would basically be like a high dose of ibuprofen,” but with less frequent dosing and lower gastrointestinal and platelet effects compared with ibuprofen and other NSAIDs.
An improved formulation
Rofecoxib “crosses the blood brain barrier very readily – better than other COX inhibitors on the market,” Mr. Sippy added. “It was well absorbed in its original formulation, and our product is even better absorbed than the original – we estimate it’s probably an hour quicker to [peak concentration].” In addition, he said, “our formulation is more efficient at delivering the drug so we don’t need as much active ingredient – our 17.5 milligrams gets you the same systemic exposure as 25 milligrams of the old product.”
A different mechanism of action
Neurologist Alan M. Rapoport, MD, editor-in-chief of Neurology Reviews and professor of neurology at the University of California, Los Angeles, said that he was “cautiously optimistic” that “if used correctly and not too frequently, [rofecoxib] will find its niche in migraine treatment.”
“Patients liked Vioxx,” said Dr. Rapoport, past president of the International Headache Society. Even people currently on prevention “need to have an acute care drug handy.” While some patients on monoclonal antibodies have had success with gepants for acute care, “these both target the same pathway. It’s always nice to have options with a different mechanism of action.”
One of the arguments Tremeau has cited for reintroducing rofecoxib has been an urgent need for alternatives to opioid painkillers. Indeed some analysts have linked the demise of Vioxx with a subsequent increase in opioid prescribing.
Dr. Rapoport noted that he never prescribes opioids or butalbital, a barbiturate, for migraine, and that most headache specialists avoid them in clinical practice. But in the emergency setting, he said, patients receive them all too frequently.
Mr. Sippy said that opioid prescribing, while not unknown in migraine, was a bigger problem in hemophilic arthropathy, the first indication his company has pursued for rofecoxib. People with hemophilia “have a kind of arthritis that would respond well to an anti-inflammatory drug but they can’t take NSAIDs due to bleeding risk. This is why so many end up on opioids. Rofecoxib, as a COX-2 inhibitor, doesn’t have any effect on platelet aggregation, which would make it another option.”
No unique risks at prescribed doses
The migraine indication originally started out narrower: Patients with both migraine and bleeding disorders. “But in talking with the FDA, they encouraged us to develop it for migraine,” Mr. Sippy said. The company is considering pursuing a third indication: menstrual pain co-occurring with migraine. Tremeau has not ruled out seeking an indication in patients with arthritis who cannot take other painkillers, whether opioids or NSAIDs.
Five years ago, when Tremeau first announced its plans to bring rofecoxib back – indeed the company was set up for that purpose and has only this and another COX-2 inhibitor in development – some experts warned that there is little to prevent the drug from being used off-label, whether in higher doses or for other diseases.
“That’s something else we’re seeking to solve in addition to going for younger populations,” said Mr. Sippy, who worked at Merck during the Vioxx crisis and later headed neurology at Sunovion before starting his own company.
“We’re going for the former middle dose as our high dose and now we know that you don’t want to take more than the prescribed amount. If it doesn’t work you get off it; you don’t want to dose-creep on it. That’s been a key insight: At the appropriate dose, this product has no unique risk relative to the drug class and potentially some unique benefits,” he said.
Risk versus benefit
Joseph Ross, MD, a health policy researcher at Yale University in New Haven, Conn., who in a 2018 editorial expressed concerns about rofecoxib’s revival, said in an email that he felt its use in migraine could be justified, with caveats.
During Vioxx’s original approval and time on the market, “there was a cardiovascular risk associated with use that was not being transparently and clearly reported to patients and clinicians,” Dr. Ross said.
“In terms of testing the product for use in patients with migraine – a population of generally younger patients at lower risk of cardiovascular disease – my only concern is that the risk is clearly communicated and that there is adequate postmarket safety surveillance,” he said. “If patients are making fully informed decisions, the potential benefit of the drug with respect to pain control may be worth the risks.”
Dr. Rapoport serves as an adviser for AbbVie, Amgen, Biohaven, Cala Health, Collegium Pharmaceutical, Satsuma, Teva, Theranica and Xoc; he is on the speakers bureau of AbbVie, Amgen, Biohaven, Impel, Lundbeck, and Teva. Dr. Ross disclosed research support from Johnson and Johnson, the Medical Device Innovation Consortium, and the Laura and John Arnold Foundation, along with government grants; he is also an expert witness in a lawsuit against Biogen.
In June, the Concord, Mass.–based company Tremeau Pharmaceuticals announced that the Food and Drug Administration was letting it proceed with a phase 3 clinical trial to test rofecoxib, the once-bestselling painkiller known as Vioxx, in patients with migraine.
The anti-inflammatory drug, a cyclooxygenase-2 (COX-2) inhibitor, received its first FDA approval in 1999 and became widely prescribed for arthritis and acute pain. In 2004 it was withdrawn by its manufacturer, Merck, after being shown to raise the risk of cardiovascular events.
In clinical trials and in real-world epidemiological studies, rofecoxib was associated with elevated heart attack, stroke, and related deaths; one 2005 study estimated that it had been responsible for some 38,000 excess deaths in the United States before being withdrawn. In 2007 Merck, beset with allegations that it had suppressed and mischaracterized rofecoxib’s safety data, paid out nearly $5 billion to settle thousands of lawsuits filed by patients and their families.
, an indication for which it received an orphan drug designation in 2017 and the agency’s green light for trials in 2020.
Brad Sippy, Tremeau’s chief executive officer, said that his company chose the two indications in part because both patient populations have low cardiovascular risk. Migraine patients are generally younger than the arthritis populations formerly treated with rofecoxib and are unlikely to take the drug for more than a day or 2 at time, avoiding the risks associated with extended exposure.
A crowded market
The past several years have seen the emergence of a cornucopia of new migraine treatments, including monoclonal antibodies such as erenumab (Aimovig, Amgen), which help prevent attacks by blocking the vasodilator calcitonin gene-related peptide, or CGRP. In addition to the standard arsenal of triptans and nonsteroidal anti-inflammatory drugs for acute pain relief, migraine patients can now choose among serotonin-blocking agents such as lasmiditan (Reyvow, Eli Lilly), known as “ditans,” and small-molecule CGRP antagonists such as ubrogepant (Ubrelvy, Abbie), known as “gepants.” Some NSAIDs, including one COX inhibitor, have been formulated into rapidly absorbed powders or liquids for migraine.
Mr. Sippy said he sees a role for rofecoxib even in this crowded space. “Migraine as you know is a multimodal situation – few people say that only one drug works for them,” he said. “We think this is an option that would basically be like a high dose of ibuprofen,” but with less frequent dosing and lower gastrointestinal and platelet effects compared with ibuprofen and other NSAIDs.
An improved formulation
Rofecoxib “crosses the blood brain barrier very readily – better than other COX inhibitors on the market,” Mr. Sippy added. “It was well absorbed in its original formulation, and our product is even better absorbed than the original – we estimate it’s probably an hour quicker to [peak concentration].” In addition, he said, “our formulation is more efficient at delivering the drug so we don’t need as much active ingredient – our 17.5 milligrams gets you the same systemic exposure as 25 milligrams of the old product.”
A different mechanism of action
Neurologist Alan M. Rapoport, MD, editor-in-chief of Neurology Reviews and professor of neurology at the University of California, Los Angeles, said that he was “cautiously optimistic” that “if used correctly and not too frequently, [rofecoxib] will find its niche in migraine treatment.”
“Patients liked Vioxx,” said Dr. Rapoport, past president of the International Headache Society. Even people currently on prevention “need to have an acute care drug handy.” While some patients on monoclonal antibodies have had success with gepants for acute care, “these both target the same pathway. It’s always nice to have options with a different mechanism of action.”
One of the arguments Tremeau has cited for reintroducing rofecoxib has been an urgent need for alternatives to opioid painkillers. Indeed some analysts have linked the demise of Vioxx with a subsequent increase in opioid prescribing.
Dr. Rapoport noted that he never prescribes opioids or butalbital, a barbiturate, for migraine, and that most headache specialists avoid them in clinical practice. But in the emergency setting, he said, patients receive them all too frequently.
Mr. Sippy said that opioid prescribing, while not unknown in migraine, was a bigger problem in hemophilic arthropathy, the first indication his company has pursued for rofecoxib. People with hemophilia “have a kind of arthritis that would respond well to an anti-inflammatory drug but they can’t take NSAIDs due to bleeding risk. This is why so many end up on opioids. Rofecoxib, as a COX-2 inhibitor, doesn’t have any effect on platelet aggregation, which would make it another option.”
No unique risks at prescribed doses
The migraine indication originally started out narrower: Patients with both migraine and bleeding disorders. “But in talking with the FDA, they encouraged us to develop it for migraine,” Mr. Sippy said. The company is considering pursuing a third indication: menstrual pain co-occurring with migraine. Tremeau has not ruled out seeking an indication in patients with arthritis who cannot take other painkillers, whether opioids or NSAIDs.
Five years ago, when Tremeau first announced its plans to bring rofecoxib back – indeed the company was set up for that purpose and has only this and another COX-2 inhibitor in development – some experts warned that there is little to prevent the drug from being used off-label, whether in higher doses or for other diseases.
“That’s something else we’re seeking to solve in addition to going for younger populations,” said Mr. Sippy, who worked at Merck during the Vioxx crisis and later headed neurology at Sunovion before starting his own company.
“We’re going for the former middle dose as our high dose and now we know that you don’t want to take more than the prescribed amount. If it doesn’t work you get off it; you don’t want to dose-creep on it. That’s been a key insight: At the appropriate dose, this product has no unique risk relative to the drug class and potentially some unique benefits,” he said.
Risk versus benefit
Joseph Ross, MD, a health policy researcher at Yale University in New Haven, Conn., who in a 2018 editorial expressed concerns about rofecoxib’s revival, said in an email that he felt its use in migraine could be justified, with caveats.
During Vioxx’s original approval and time on the market, “there was a cardiovascular risk associated with use that was not being transparently and clearly reported to patients and clinicians,” Dr. Ross said.
“In terms of testing the product for use in patients with migraine – a population of generally younger patients at lower risk of cardiovascular disease – my only concern is that the risk is clearly communicated and that there is adequate postmarket safety surveillance,” he said. “If patients are making fully informed decisions, the potential benefit of the drug with respect to pain control may be worth the risks.”
Dr. Rapoport serves as an adviser for AbbVie, Amgen, Biohaven, Cala Health, Collegium Pharmaceutical, Satsuma, Teva, Theranica and Xoc; he is on the speakers bureau of AbbVie, Amgen, Biohaven, Impel, Lundbeck, and Teva. Dr. Ross disclosed research support from Johnson and Johnson, the Medical Device Innovation Consortium, and the Laura and John Arnold Foundation, along with government grants; he is also an expert witness in a lawsuit against Biogen.
In June, the Concord, Mass.–based company Tremeau Pharmaceuticals announced that the Food and Drug Administration was letting it proceed with a phase 3 clinical trial to test rofecoxib, the once-bestselling painkiller known as Vioxx, in patients with migraine.
The anti-inflammatory drug, a cyclooxygenase-2 (COX-2) inhibitor, received its first FDA approval in 1999 and became widely prescribed for arthritis and acute pain. In 2004 it was withdrawn by its manufacturer, Merck, after being shown to raise the risk of cardiovascular events.
In clinical trials and in real-world epidemiological studies, rofecoxib was associated with elevated heart attack, stroke, and related deaths; one 2005 study estimated that it had been responsible for some 38,000 excess deaths in the United States before being withdrawn. In 2007 Merck, beset with allegations that it had suppressed and mischaracterized rofecoxib’s safety data, paid out nearly $5 billion to settle thousands of lawsuits filed by patients and their families.
, an indication for which it received an orphan drug designation in 2017 and the agency’s green light for trials in 2020.
Brad Sippy, Tremeau’s chief executive officer, said that his company chose the two indications in part because both patient populations have low cardiovascular risk. Migraine patients are generally younger than the arthritis populations formerly treated with rofecoxib and are unlikely to take the drug for more than a day or 2 at time, avoiding the risks associated with extended exposure.
A crowded market
The past several years have seen the emergence of a cornucopia of new migraine treatments, including monoclonal antibodies such as erenumab (Aimovig, Amgen), which help prevent attacks by blocking the vasodilator calcitonin gene-related peptide, or CGRP. In addition to the standard arsenal of triptans and nonsteroidal anti-inflammatory drugs for acute pain relief, migraine patients can now choose among serotonin-blocking agents such as lasmiditan (Reyvow, Eli Lilly), known as “ditans,” and small-molecule CGRP antagonists such as ubrogepant (Ubrelvy, Abbie), known as “gepants.” Some NSAIDs, including one COX inhibitor, have been formulated into rapidly absorbed powders or liquids for migraine.
Mr. Sippy said he sees a role for rofecoxib even in this crowded space. “Migraine as you know is a multimodal situation – few people say that only one drug works for them,” he said. “We think this is an option that would basically be like a high dose of ibuprofen,” but with less frequent dosing and lower gastrointestinal and platelet effects compared with ibuprofen and other NSAIDs.
An improved formulation
Rofecoxib “crosses the blood brain barrier very readily – better than other COX inhibitors on the market,” Mr. Sippy added. “It was well absorbed in its original formulation, and our product is even better absorbed than the original – we estimate it’s probably an hour quicker to [peak concentration].” In addition, he said, “our formulation is more efficient at delivering the drug so we don’t need as much active ingredient – our 17.5 milligrams gets you the same systemic exposure as 25 milligrams of the old product.”
A different mechanism of action
Neurologist Alan M. Rapoport, MD, editor-in-chief of Neurology Reviews and professor of neurology at the University of California, Los Angeles, said that he was “cautiously optimistic” that “if used correctly and not too frequently, [rofecoxib] will find its niche in migraine treatment.”
“Patients liked Vioxx,” said Dr. Rapoport, past president of the International Headache Society. Even people currently on prevention “need to have an acute care drug handy.” While some patients on monoclonal antibodies have had success with gepants for acute care, “these both target the same pathway. It’s always nice to have options with a different mechanism of action.”
One of the arguments Tremeau has cited for reintroducing rofecoxib has been an urgent need for alternatives to opioid painkillers. Indeed some analysts have linked the demise of Vioxx with a subsequent increase in opioid prescribing.
Dr. Rapoport noted that he never prescribes opioids or butalbital, a barbiturate, for migraine, and that most headache specialists avoid them in clinical practice. But in the emergency setting, he said, patients receive them all too frequently.
Mr. Sippy said that opioid prescribing, while not unknown in migraine, was a bigger problem in hemophilic arthropathy, the first indication his company has pursued for rofecoxib. People with hemophilia “have a kind of arthritis that would respond well to an anti-inflammatory drug but they can’t take NSAIDs due to bleeding risk. This is why so many end up on opioids. Rofecoxib, as a COX-2 inhibitor, doesn’t have any effect on platelet aggregation, which would make it another option.”
No unique risks at prescribed doses
The migraine indication originally started out narrower: Patients with both migraine and bleeding disorders. “But in talking with the FDA, they encouraged us to develop it for migraine,” Mr. Sippy said. The company is considering pursuing a third indication: menstrual pain co-occurring with migraine. Tremeau has not ruled out seeking an indication in patients with arthritis who cannot take other painkillers, whether opioids or NSAIDs.
Five years ago, when Tremeau first announced its plans to bring rofecoxib back – indeed the company was set up for that purpose and has only this and another COX-2 inhibitor in development – some experts warned that there is little to prevent the drug from being used off-label, whether in higher doses or for other diseases.
“That’s something else we’re seeking to solve in addition to going for younger populations,” said Mr. Sippy, who worked at Merck during the Vioxx crisis and later headed neurology at Sunovion before starting his own company.
“We’re going for the former middle dose as our high dose and now we know that you don’t want to take more than the prescribed amount. If it doesn’t work you get off it; you don’t want to dose-creep on it. That’s been a key insight: At the appropriate dose, this product has no unique risk relative to the drug class and potentially some unique benefits,” he said.
Risk versus benefit
Joseph Ross, MD, a health policy researcher at Yale University in New Haven, Conn., who in a 2018 editorial expressed concerns about rofecoxib’s revival, said in an email that he felt its use in migraine could be justified, with caveats.
During Vioxx’s original approval and time on the market, “there was a cardiovascular risk associated with use that was not being transparently and clearly reported to patients and clinicians,” Dr. Ross said.
“In terms of testing the product for use in patients with migraine – a population of generally younger patients at lower risk of cardiovascular disease – my only concern is that the risk is clearly communicated and that there is adequate postmarket safety surveillance,” he said. “If patients are making fully informed decisions, the potential benefit of the drug with respect to pain control may be worth the risks.”
Dr. Rapoport serves as an adviser for AbbVie, Amgen, Biohaven, Cala Health, Collegium Pharmaceutical, Satsuma, Teva, Theranica and Xoc; he is on the speakers bureau of AbbVie, Amgen, Biohaven, Impel, Lundbeck, and Teva. Dr. Ross disclosed research support from Johnson and Johnson, the Medical Device Innovation Consortium, and the Laura and John Arnold Foundation, along with government grants; he is also an expert witness in a lawsuit against Biogen.
Are headache clinical trials representative of the general patient population?
DENVER – In a debate over whether headache trials are representative of patients, one neurologist declared that they tend to leave out a variety of subjects with many types of headaches – the young, the old, the pregnant, and those without migraines, among others. But her counterpart defended migraine trials in particular, arguing that they’re evolving to become more valuable as researchers address their limitations.
At the core of the debate at the annual meeting of the American Headache Society were sharp divisions over how much the limitations of headache clinical trials matter. Both neurologists – Jan Brandes, MD, of Nashville (Tenn.) Neuroscience Group, and Amy Gelfand, MD, of the University of California at San Francisco, agree that they exist. But they diverged on how much they matter.
Exclusion/inclusion criteria are good
Dr. Brandes argued that randomized controlled trials “remain the single best study design,” and she said migraine headache trials have improved over the past couple of decades.
Eligibility criteria, for example, have expanded to allow patients with more subtypes of migraines to participate, she said. “Another change has been the establishment of guidelines or inclusion criteria that allow patients who have stable and treated hypertension, stable depression, and stable anxiety disorders that are controlled and treated and not interfering with the disease you’re studying.”
In essence, she said, “the exclusion/inclusion criteria are good.”
It’s also a positive change that longer patient-reported outcomes are included in trials, she said.
Exclusion/inclusion criteria are too restrictive
But Dr. Gelfand criticized the inclusion criteria in migraine trials, noting it includes “a lot of amazing complexity.” Trials often will limit participation to subjects aged 18-65, even though people have high rates of headaches, she said, and they frequently overrepresent men. Pregnant and lactating women are often omitted, too, even if a trial is examining a behavioral intervention. In some cases, lactating women may be breastfeeding for a year or two, she noted.
“The vast majority of births in the United States, 92%, are to females who are between the ages of 20 and 39. That is also the age range where migraine is most prevalent,” she said. Yes, certain new agents shouldn’t be tested for the first time in pregnant women because of the risk, she said, “but we need to grapple with the fact that migraine is affecting people who are also going to be pregnant and lactating.”
Many other criteria limit the subjects in headache trials, she said. The studies are “almost exclusively” of drugs for migraines, leaving out many people with other types such as adolescents with new persistent headaches. “Where are the trials for them?” she asked.
Other groups that are left out include those whose headaches that are due to a head injury, a viral infection such as COVID-19, or even vaccination against COVID-19, she said. “There are an infinite number of questions here that we are currently not even attempting to answer.”
Non-Whites are also poorly represented in trials, she said, and studies often don’t include data about non-Whites. “Race data exists. Where do we get off not even reporting it?”
Room for improvement
For her part, Dr. Brandes said less-common headache disorders are best studied in pragmatic trials until they can be better understood. “We need to understand pathophysiology better for some of these other disorders, particularly things like continuous headache and posttraumatic headache. Then we can begin to expand that.”
She added that randomized clinical trials are now underway regarding secondary headache related to COVID-19.
Dr. Brandes did not report disclosures. Dr. Gelfand had no disclosures.
DENVER – In a debate over whether headache trials are representative of patients, one neurologist declared that they tend to leave out a variety of subjects with many types of headaches – the young, the old, the pregnant, and those without migraines, among others. But her counterpart defended migraine trials in particular, arguing that they’re evolving to become more valuable as researchers address their limitations.
At the core of the debate at the annual meeting of the American Headache Society were sharp divisions over how much the limitations of headache clinical trials matter. Both neurologists – Jan Brandes, MD, of Nashville (Tenn.) Neuroscience Group, and Amy Gelfand, MD, of the University of California at San Francisco, agree that they exist. But they diverged on how much they matter.
Exclusion/inclusion criteria are good
Dr. Brandes argued that randomized controlled trials “remain the single best study design,” and she said migraine headache trials have improved over the past couple of decades.
Eligibility criteria, for example, have expanded to allow patients with more subtypes of migraines to participate, she said. “Another change has been the establishment of guidelines or inclusion criteria that allow patients who have stable and treated hypertension, stable depression, and stable anxiety disorders that are controlled and treated and not interfering with the disease you’re studying.”
In essence, she said, “the exclusion/inclusion criteria are good.”
It’s also a positive change that longer patient-reported outcomes are included in trials, she said.
Exclusion/inclusion criteria are too restrictive
But Dr. Gelfand criticized the inclusion criteria in migraine trials, noting it includes “a lot of amazing complexity.” Trials often will limit participation to subjects aged 18-65, even though people have high rates of headaches, she said, and they frequently overrepresent men. Pregnant and lactating women are often omitted, too, even if a trial is examining a behavioral intervention. In some cases, lactating women may be breastfeeding for a year or two, she noted.
“The vast majority of births in the United States, 92%, are to females who are between the ages of 20 and 39. That is also the age range where migraine is most prevalent,” she said. Yes, certain new agents shouldn’t be tested for the first time in pregnant women because of the risk, she said, “but we need to grapple with the fact that migraine is affecting people who are also going to be pregnant and lactating.”
Many other criteria limit the subjects in headache trials, she said. The studies are “almost exclusively” of drugs for migraines, leaving out many people with other types such as adolescents with new persistent headaches. “Where are the trials for them?” she asked.
Other groups that are left out include those whose headaches that are due to a head injury, a viral infection such as COVID-19, or even vaccination against COVID-19, she said. “There are an infinite number of questions here that we are currently not even attempting to answer.”
Non-Whites are also poorly represented in trials, she said, and studies often don’t include data about non-Whites. “Race data exists. Where do we get off not even reporting it?”
Room for improvement
For her part, Dr. Brandes said less-common headache disorders are best studied in pragmatic trials until they can be better understood. “We need to understand pathophysiology better for some of these other disorders, particularly things like continuous headache and posttraumatic headache. Then we can begin to expand that.”
She added that randomized clinical trials are now underway regarding secondary headache related to COVID-19.
Dr. Brandes did not report disclosures. Dr. Gelfand had no disclosures.
DENVER – In a debate over whether headache trials are representative of patients, one neurologist declared that they tend to leave out a variety of subjects with many types of headaches – the young, the old, the pregnant, and those without migraines, among others. But her counterpart defended migraine trials in particular, arguing that they’re evolving to become more valuable as researchers address their limitations.
At the core of the debate at the annual meeting of the American Headache Society were sharp divisions over how much the limitations of headache clinical trials matter. Both neurologists – Jan Brandes, MD, of Nashville (Tenn.) Neuroscience Group, and Amy Gelfand, MD, of the University of California at San Francisco, agree that they exist. But they diverged on how much they matter.
Exclusion/inclusion criteria are good
Dr. Brandes argued that randomized controlled trials “remain the single best study design,” and she said migraine headache trials have improved over the past couple of decades.
Eligibility criteria, for example, have expanded to allow patients with more subtypes of migraines to participate, she said. “Another change has been the establishment of guidelines or inclusion criteria that allow patients who have stable and treated hypertension, stable depression, and stable anxiety disorders that are controlled and treated and not interfering with the disease you’re studying.”
In essence, she said, “the exclusion/inclusion criteria are good.”
It’s also a positive change that longer patient-reported outcomes are included in trials, she said.
Exclusion/inclusion criteria are too restrictive
But Dr. Gelfand criticized the inclusion criteria in migraine trials, noting it includes “a lot of amazing complexity.” Trials often will limit participation to subjects aged 18-65, even though people have high rates of headaches, she said, and they frequently overrepresent men. Pregnant and lactating women are often omitted, too, even if a trial is examining a behavioral intervention. In some cases, lactating women may be breastfeeding for a year or two, she noted.
“The vast majority of births in the United States, 92%, are to females who are between the ages of 20 and 39. That is also the age range where migraine is most prevalent,” she said. Yes, certain new agents shouldn’t be tested for the first time in pregnant women because of the risk, she said, “but we need to grapple with the fact that migraine is affecting people who are also going to be pregnant and lactating.”
Many other criteria limit the subjects in headache trials, she said. The studies are “almost exclusively” of drugs for migraines, leaving out many people with other types such as adolescents with new persistent headaches. “Where are the trials for them?” she asked.
Other groups that are left out include those whose headaches that are due to a head injury, a viral infection such as COVID-19, or even vaccination against COVID-19, she said. “There are an infinite number of questions here that we are currently not even attempting to answer.”
Non-Whites are also poorly represented in trials, she said, and studies often don’t include data about non-Whites. “Race data exists. Where do we get off not even reporting it?”
Room for improvement
For her part, Dr. Brandes said less-common headache disorders are best studied in pragmatic trials until they can be better understood. “We need to understand pathophysiology better for some of these other disorders, particularly things like continuous headache and posttraumatic headache. Then we can begin to expand that.”
She added that randomized clinical trials are now underway regarding secondary headache related to COVID-19.
Dr. Brandes did not report disclosures. Dr. Gelfand had no disclosures.
AT AHS 2022