User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Study finds genetic factor for COVID smell and taste loss
, according to a new study published in the journal Nature Genetics
The finding could eventually help the 1.6 million people in the United States who still can’t smell or have had a change in their ability to smell more than 6 months after getting the coronavirus. The exact cause related to COVID-19 is still unknown, but researchers believe it could be because of damage in a part of the nose called the olfactory epithelium.
“How we get from infection to smell loss remains unclear,” Justin Turner, MD, an associate professor of otolaryngology at Vanderbilt University, Nashville, Tenn., told NBC News. Dr. Turner was not part of the research team.
“Early data suggest that supporting cells of the olfactory epithelium are the ones mostly being infected by the virus, and presumably this leads to the death of the neurons themselves,” he said. “But we don’t really, really know why and when that happens, and why it seems to preferentially happen in certain individuals.”
Researchers at 23andMe, a genomics and biotechnology company, did the study as part of a larger COVID-19 project, which includes people in the United States and the United Kingdom. They analyzed data from nearly 70,000 people who took online surveys after receiving a positive coronavirus test. Among those, 68% reported a loss of smell or taste as a symptom.
The study team compared the genetic differences between those who lost their sense of smell and taste and those who didn’t. They found that a location near two olfactory genes – UGT2A1 and UGT2A2 – is associated with COVID-19 loss of smell and taste. The genetic risk factor makes it 11% more likely for a person with COVID-19 to lose their sense of smell or taste.
The research team also found that women were 11% more likely than men to report a loss of smell and taste. About 73% of those who reported a loss of smell and taste were ages 26-35.
The researchers aren’t sure how the genes are involved, though they suspect that infected cells could lead to smell loss. Typically, the genes are expressed in tissue inside the nose involved with smell and play a role in processing things that have an odor. To use the findings, researchers need to learn more about the genes, how they are expressed, and what their functions are, NBC News reported.
The findings could help lead to treatments. Other research has shown that the loss of taste and smell is related to a “failure to protect the sensory cells of the nose and tongue from viral infection,” Danielle Reed, PhD, associate director of the Monell Chemical Senses Center in Philadelphia, told NBC News. She was not part of the research team but studies person-to-person differences in the loss of these senses because of COVID-19.
“This study suggests a different direction,” she said. “The pathways that break down the chemicals that cause taste and smell in the first place might be over or underactive, reducing or distorting the ability to taste and smell.”
A version of this article first appeared on WebMD.com.
, according to a new study published in the journal Nature Genetics
The finding could eventually help the 1.6 million people in the United States who still can’t smell or have had a change in their ability to smell more than 6 months after getting the coronavirus. The exact cause related to COVID-19 is still unknown, but researchers believe it could be because of damage in a part of the nose called the olfactory epithelium.
“How we get from infection to smell loss remains unclear,” Justin Turner, MD, an associate professor of otolaryngology at Vanderbilt University, Nashville, Tenn., told NBC News. Dr. Turner was not part of the research team.
“Early data suggest that supporting cells of the olfactory epithelium are the ones mostly being infected by the virus, and presumably this leads to the death of the neurons themselves,” he said. “But we don’t really, really know why and when that happens, and why it seems to preferentially happen in certain individuals.”
Researchers at 23andMe, a genomics and biotechnology company, did the study as part of a larger COVID-19 project, which includes people in the United States and the United Kingdom. They analyzed data from nearly 70,000 people who took online surveys after receiving a positive coronavirus test. Among those, 68% reported a loss of smell or taste as a symptom.
The study team compared the genetic differences between those who lost their sense of smell and taste and those who didn’t. They found that a location near two olfactory genes – UGT2A1 and UGT2A2 – is associated with COVID-19 loss of smell and taste. The genetic risk factor makes it 11% more likely for a person with COVID-19 to lose their sense of smell or taste.
The research team also found that women were 11% more likely than men to report a loss of smell and taste. About 73% of those who reported a loss of smell and taste were ages 26-35.
The researchers aren’t sure how the genes are involved, though they suspect that infected cells could lead to smell loss. Typically, the genes are expressed in tissue inside the nose involved with smell and play a role in processing things that have an odor. To use the findings, researchers need to learn more about the genes, how they are expressed, and what their functions are, NBC News reported.
The findings could help lead to treatments. Other research has shown that the loss of taste and smell is related to a “failure to protect the sensory cells of the nose and tongue from viral infection,” Danielle Reed, PhD, associate director of the Monell Chemical Senses Center in Philadelphia, told NBC News. She was not part of the research team but studies person-to-person differences in the loss of these senses because of COVID-19.
“This study suggests a different direction,” she said. “The pathways that break down the chemicals that cause taste and smell in the first place might be over or underactive, reducing or distorting the ability to taste and smell.”
A version of this article first appeared on WebMD.com.
, according to a new study published in the journal Nature Genetics
The finding could eventually help the 1.6 million people in the United States who still can’t smell or have had a change in their ability to smell more than 6 months after getting the coronavirus. The exact cause related to COVID-19 is still unknown, but researchers believe it could be because of damage in a part of the nose called the olfactory epithelium.
“How we get from infection to smell loss remains unclear,” Justin Turner, MD, an associate professor of otolaryngology at Vanderbilt University, Nashville, Tenn., told NBC News. Dr. Turner was not part of the research team.
“Early data suggest that supporting cells of the olfactory epithelium are the ones mostly being infected by the virus, and presumably this leads to the death of the neurons themselves,” he said. “But we don’t really, really know why and when that happens, and why it seems to preferentially happen in certain individuals.”
Researchers at 23andMe, a genomics and biotechnology company, did the study as part of a larger COVID-19 project, which includes people in the United States and the United Kingdom. They analyzed data from nearly 70,000 people who took online surveys after receiving a positive coronavirus test. Among those, 68% reported a loss of smell or taste as a symptom.
The study team compared the genetic differences between those who lost their sense of smell and taste and those who didn’t. They found that a location near two olfactory genes – UGT2A1 and UGT2A2 – is associated with COVID-19 loss of smell and taste. The genetic risk factor makes it 11% more likely for a person with COVID-19 to lose their sense of smell or taste.
The research team also found that women were 11% more likely than men to report a loss of smell and taste. About 73% of those who reported a loss of smell and taste were ages 26-35.
The researchers aren’t sure how the genes are involved, though they suspect that infected cells could lead to smell loss. Typically, the genes are expressed in tissue inside the nose involved with smell and play a role in processing things that have an odor. To use the findings, researchers need to learn more about the genes, how they are expressed, and what their functions are, NBC News reported.
The findings could help lead to treatments. Other research has shown that the loss of taste and smell is related to a “failure to protect the sensory cells of the nose and tongue from viral infection,” Danielle Reed, PhD, associate director of the Monell Chemical Senses Center in Philadelphia, told NBC News. She was not part of the research team but studies person-to-person differences in the loss of these senses because of COVID-19.
“This study suggests a different direction,” she said. “The pathways that break down the chemicals that cause taste and smell in the first place might be over or underactive, reducing or distorting the ability to taste and smell.”
A version of this article first appeared on WebMD.com.
FROM NATURE GENETICS
Fourth vaccine shot less effective against Omicron, Israeli study says
, according to new research at an Israeli hospital.
The preliminary results, released on Jan. 17, challenge the idea of giving a second booster dose to slow the spread of the coronavirus, according to USA Today.
“Despite increased antibody levels, the fourth vaccine only offers a partial defense against the virus,” Gili Regev-Yochay, MD, director of the hospital’s infection prevention and control units, told reporters.
“The vaccines, which were more effective against previous variants, offer less protection versus Omicron,” she said.
In a clinical trial, 274 medical workers at Sheba Medical Center near Tel Aviv received a fourth vaccine dose in December – 154 got the Pfizer vaccine and 120 got the Moderna vaccine – after previously getting three Pfizer shots.
Both groups received a boost in antibodies that was “slightly higher” than after the third shot, Dr. Regev-Yochay said. But when compared with a control group that didn’t receive the fourth dose, the extra boost didn’t prevent the spread of Omicron.
“We see many infected with Omicron who received the fourth dose,” Dr. Regev-Yochay said. “Granted, a bit less than in the control group, but still a lot of infections.”
Some public health officials in Israel say the campaign for fourth doses is still worthwhile, according to The Times of Israel. The vaccine still works well against the Alpha and Delta variants, Dr. Regev-Yochay said, and a fourth shot should go to older adults and those who face higher risks for severe COVID-19.
Hours after releasing the preliminary results, Sheba Medical Center published a statement calling for “continuing the vaccination drive for risk groups at this time, even though the vaccine doesn’t provide optimal protection against getting infected with the variant.” News outlets reported that the hospital was pressured into issuing the statement after Israel’s Health Ministry didn’t like the release of the early study results, The Times of Israel reported.
The second booster “returns the level of antibodies to what it was at the beginning of the third booster,” Nachman Ash, MD, director of Israel’s Health Ministry, told Channel 13 TV in Israel, according to The Associated Press.
“That has great importance, especially among the older population,” he said.
As of Sunday, more than 500,000 people in Israel had received fourth doses since the country began offering them last month to medical workers, immunocompromised patients, and people ages 60 years and older, the AP reported. At the same time, the country has faced a recent coronavirus surge that has led to record-breaking numbers of cases and rising hospitalizations.
On Tuesday, the Israeli government said it would shorten the mandatory quarantine period from 7 days to 5 days, the AP reported.
“This decision will enable us to continue safeguarding public health on the one hand and to keep the economy going at this time on the other, even though it is difficult, so that we can get through this wave safely,” Prime Minister Naftali Bennett said.
A version of this article first appeared on WebMD.com.
, according to new research at an Israeli hospital.
The preliminary results, released on Jan. 17, challenge the idea of giving a second booster dose to slow the spread of the coronavirus, according to USA Today.
“Despite increased antibody levels, the fourth vaccine only offers a partial defense against the virus,” Gili Regev-Yochay, MD, director of the hospital’s infection prevention and control units, told reporters.
“The vaccines, which were more effective against previous variants, offer less protection versus Omicron,” she said.
In a clinical trial, 274 medical workers at Sheba Medical Center near Tel Aviv received a fourth vaccine dose in December – 154 got the Pfizer vaccine and 120 got the Moderna vaccine – after previously getting three Pfizer shots.
Both groups received a boost in antibodies that was “slightly higher” than after the third shot, Dr. Regev-Yochay said. But when compared with a control group that didn’t receive the fourth dose, the extra boost didn’t prevent the spread of Omicron.
“We see many infected with Omicron who received the fourth dose,” Dr. Regev-Yochay said. “Granted, a bit less than in the control group, but still a lot of infections.”
Some public health officials in Israel say the campaign for fourth doses is still worthwhile, according to The Times of Israel. The vaccine still works well against the Alpha and Delta variants, Dr. Regev-Yochay said, and a fourth shot should go to older adults and those who face higher risks for severe COVID-19.
Hours after releasing the preliminary results, Sheba Medical Center published a statement calling for “continuing the vaccination drive for risk groups at this time, even though the vaccine doesn’t provide optimal protection against getting infected with the variant.” News outlets reported that the hospital was pressured into issuing the statement after Israel’s Health Ministry didn’t like the release of the early study results, The Times of Israel reported.
The second booster “returns the level of antibodies to what it was at the beginning of the third booster,” Nachman Ash, MD, director of Israel’s Health Ministry, told Channel 13 TV in Israel, according to The Associated Press.
“That has great importance, especially among the older population,” he said.
As of Sunday, more than 500,000 people in Israel had received fourth doses since the country began offering them last month to medical workers, immunocompromised patients, and people ages 60 years and older, the AP reported. At the same time, the country has faced a recent coronavirus surge that has led to record-breaking numbers of cases and rising hospitalizations.
On Tuesday, the Israeli government said it would shorten the mandatory quarantine period from 7 days to 5 days, the AP reported.
“This decision will enable us to continue safeguarding public health on the one hand and to keep the economy going at this time on the other, even though it is difficult, so that we can get through this wave safely,” Prime Minister Naftali Bennett said.
A version of this article first appeared on WebMD.com.
, according to new research at an Israeli hospital.
The preliminary results, released on Jan. 17, challenge the idea of giving a second booster dose to slow the spread of the coronavirus, according to USA Today.
“Despite increased antibody levels, the fourth vaccine only offers a partial defense against the virus,” Gili Regev-Yochay, MD, director of the hospital’s infection prevention and control units, told reporters.
“The vaccines, which were more effective against previous variants, offer less protection versus Omicron,” she said.
In a clinical trial, 274 medical workers at Sheba Medical Center near Tel Aviv received a fourth vaccine dose in December – 154 got the Pfizer vaccine and 120 got the Moderna vaccine – after previously getting three Pfizer shots.
Both groups received a boost in antibodies that was “slightly higher” than after the third shot, Dr. Regev-Yochay said. But when compared with a control group that didn’t receive the fourth dose, the extra boost didn’t prevent the spread of Omicron.
“We see many infected with Omicron who received the fourth dose,” Dr. Regev-Yochay said. “Granted, a bit less than in the control group, but still a lot of infections.”
Some public health officials in Israel say the campaign for fourth doses is still worthwhile, according to The Times of Israel. The vaccine still works well against the Alpha and Delta variants, Dr. Regev-Yochay said, and a fourth shot should go to older adults and those who face higher risks for severe COVID-19.
Hours after releasing the preliminary results, Sheba Medical Center published a statement calling for “continuing the vaccination drive for risk groups at this time, even though the vaccine doesn’t provide optimal protection against getting infected with the variant.” News outlets reported that the hospital was pressured into issuing the statement after Israel’s Health Ministry didn’t like the release of the early study results, The Times of Israel reported.
The second booster “returns the level of antibodies to what it was at the beginning of the third booster,” Nachman Ash, MD, director of Israel’s Health Ministry, told Channel 13 TV in Israel, according to The Associated Press.
“That has great importance, especially among the older population,” he said.
As of Sunday, more than 500,000 people in Israel had received fourth doses since the country began offering them last month to medical workers, immunocompromised patients, and people ages 60 years and older, the AP reported. At the same time, the country has faced a recent coronavirus surge that has led to record-breaking numbers of cases and rising hospitalizations.
On Tuesday, the Israeli government said it would shorten the mandatory quarantine period from 7 days to 5 days, the AP reported.
“This decision will enable us to continue safeguarding public health on the one hand and to keep the economy going at this time on the other, even though it is difficult, so that we can get through this wave safely,” Prime Minister Naftali Bennett said.
A version of this article first appeared on WebMD.com.
Learning to coexist
There’s another doctor with whom I’ve referred patients, back and forth, for the last 20 years. I think he’s good at his job and assume he feels the same way about me. We aren’t social friends, but chat briefly when we run into each other at the hospital, or store, or local restaurants.
Last week I was at the hospital to read EEGs, and happened to see him in the doctor’s parking lot. We wished each other a happy new year, talked briefly about a few mutual patients, and then went our separate ways.
As he pulled out, I noticed his car had a bumper sticker for a cause I strongly disagree with. I mean, 180 degrees opposed.
Suddenly, I didn’t want to ever refer to him again. Why should I support him? He’s the enemy.
Why should I help him out by referring patients?
But then I had to stop. Isn’t this 2022? Aren’t we supposed to be in a civilized world? This isn’t my tribe versus your tribe, my cave versus your cave. The closest we’re supposed to come to direct conflict with others is the “us versus them” world of professional and college sports.
I hope.
Aren’t I supposed to be better than this? Isn’t learning to coexist the whole point of the playground as a kid (besides burning off energy and giving the teacher a break)? Like Hamilton and Jefferson, or Ronald Reagan and Tip O’Neill?
Refusing to work with another competent physician because I disagree with their personal, religious, or political beliefs is just plain stupid.
Politicians and pundits try to convince us that people who disagree with us are the enemy, but that’s horse hockey. The truth is that the majority of people out there, regardless of personal beliefs, are decent, hardworking, and just trying to support their families like I am mine.
Later that week I had a patient who clearly needed the other doctor’s expertise, and I gave her his name and phone number. She asked if I’d send my own family to him, and I said, unequivocally, “yes” (actually I have).
Because, at the end of the day, we’re all people, along on the same ride. To not send a patient to him wouldn’t be in their best interest, which is what I’m supposed to be watching out for.
Not only that, but if I don’t refer just because I disagree with him as a person, then I’ve become the problem and not the solution.
Because I, and everyone else, have to try to be better than that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
There’s another doctor with whom I’ve referred patients, back and forth, for the last 20 years. I think he’s good at his job and assume he feels the same way about me. We aren’t social friends, but chat briefly when we run into each other at the hospital, or store, or local restaurants.
Last week I was at the hospital to read EEGs, and happened to see him in the doctor’s parking lot. We wished each other a happy new year, talked briefly about a few mutual patients, and then went our separate ways.
As he pulled out, I noticed his car had a bumper sticker for a cause I strongly disagree with. I mean, 180 degrees opposed.
Suddenly, I didn’t want to ever refer to him again. Why should I support him? He’s the enemy.
Why should I help him out by referring patients?
But then I had to stop. Isn’t this 2022? Aren’t we supposed to be in a civilized world? This isn’t my tribe versus your tribe, my cave versus your cave. The closest we’re supposed to come to direct conflict with others is the “us versus them” world of professional and college sports.
I hope.
Aren’t I supposed to be better than this? Isn’t learning to coexist the whole point of the playground as a kid (besides burning off energy and giving the teacher a break)? Like Hamilton and Jefferson, or Ronald Reagan and Tip O’Neill?
Refusing to work with another competent physician because I disagree with their personal, religious, or political beliefs is just plain stupid.
Politicians and pundits try to convince us that people who disagree with us are the enemy, but that’s horse hockey. The truth is that the majority of people out there, regardless of personal beliefs, are decent, hardworking, and just trying to support their families like I am mine.
Later that week I had a patient who clearly needed the other doctor’s expertise, and I gave her his name and phone number. She asked if I’d send my own family to him, and I said, unequivocally, “yes” (actually I have).
Because, at the end of the day, we’re all people, along on the same ride. To not send a patient to him wouldn’t be in their best interest, which is what I’m supposed to be watching out for.
Not only that, but if I don’t refer just because I disagree with him as a person, then I’ve become the problem and not the solution.
Because I, and everyone else, have to try to be better than that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
There’s another doctor with whom I’ve referred patients, back and forth, for the last 20 years. I think he’s good at his job and assume he feels the same way about me. We aren’t social friends, but chat briefly when we run into each other at the hospital, or store, or local restaurants.
Last week I was at the hospital to read EEGs, and happened to see him in the doctor’s parking lot. We wished each other a happy new year, talked briefly about a few mutual patients, and then went our separate ways.
As he pulled out, I noticed his car had a bumper sticker for a cause I strongly disagree with. I mean, 180 degrees opposed.
Suddenly, I didn’t want to ever refer to him again. Why should I support him? He’s the enemy.
Why should I help him out by referring patients?
But then I had to stop. Isn’t this 2022? Aren’t we supposed to be in a civilized world? This isn’t my tribe versus your tribe, my cave versus your cave. The closest we’re supposed to come to direct conflict with others is the “us versus them” world of professional and college sports.
I hope.
Aren’t I supposed to be better than this? Isn’t learning to coexist the whole point of the playground as a kid (besides burning off energy and giving the teacher a break)? Like Hamilton and Jefferson, or Ronald Reagan and Tip O’Neill?
Refusing to work with another competent physician because I disagree with their personal, religious, or political beliefs is just plain stupid.
Politicians and pundits try to convince us that people who disagree with us are the enemy, but that’s horse hockey. The truth is that the majority of people out there, regardless of personal beliefs, are decent, hardworking, and just trying to support their families like I am mine.
Later that week I had a patient who clearly needed the other doctor’s expertise, and I gave her his name and phone number. She asked if I’d send my own family to him, and I said, unequivocally, “yes” (actually I have).
Because, at the end of the day, we’re all people, along on the same ride. To not send a patient to him wouldn’t be in their best interest, which is what I’m supposed to be watching out for.
Not only that, but if I don’t refer just because I disagree with him as a person, then I’ve become the problem and not the solution.
Because I, and everyone else, have to try to be better than that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Feds’ website for free at-home COVID tests launches day early
The Biden administration’s new no-cost, at-home testing program launched Jan. 18, a day ahead of schedule.
The administration said 500 million tests are available to be delivered to homes across the country. This accounts for half of the president’s recent pledge to purchase 1 billion free at-home COVID-19 tests to distribute to the American public.
On a Jan. 14 call with reporters, senior White House officials offered some details about the new program.
Here’s what we know so far.
How do I order my free tests?
Americans can visit COVIDtests.gov to order their rapid at-home tests. You can also order directly from the U.S. Postal Service website. After you order, you’ll receive a confirmation email that promises to send tracking information once your order ships.
What information do I need to order the tests?
You only need your name and home mailing address.
There is also an option to provide your email address to get updates on the status of your order.
What if someone needs help ordering the tests?
There will be a free call-in line for people needing more help, including those having trouble accessing the internet, according to White House officials.
What tests will be available?
There are nine at-home tests available through FDA emergency use authorization. According to the Frequently Asked Questions section of COVIDtests.gov, "You will not be able to choose the brand you order as part of this program.”
How long will it take to get the tests once I order them?
Tests are expected to ship 7 to 12 days after you order them.
But White House officials say that the time frame will likely shorten as the program gains steam.
How many can I order?
There’s a limit of four tests per residential mailing address.
For larger families, White House officials suggest trying other free testing options, like visiting COVID-19 testing sites or your local health center.
Is this a one-time opportunity?
The White House doesn’t say, but officials did mention that if you run out of your four free tests, there are many other ways to access free at-home tests, such as COVID-19 testing sites, pharmacies, and community health centers.
The free tests available through COVIDtests.gov are in addition to an estimated 375 million at-home rapid tests on the market in the U.S. this month.
When should people use a rapid at-home test?
The CDC and experts with other public health groups agree that Americans should consider using at-home rapid tests in the following situations:
- If they begin to have symptoms consistent with COVID-19;
- At least 5 days after close contact with someone who has COVID;
- If someone is indoors with a group of people who are at risk of severe disease or are unvaccinated.
Are at-home rapid tests accurate?
The U.S. Department of Health and Human Services and other federal officials confirmed through studies that all tests distributed through this program can detect the Omicron variant. These agencies also confirmed that their performance is consistent with the FDA’s emergency use authorization.
Is the website designed to handle high demand?
After the original website to sign up for health insurance under the Affordable Care Act crashed repeatedly at launch, the government says it has prepared for high demand for ordering at-home rapid tests.
The U.S. Digital Service (USDS), an organization founded after Healthcare.gov, has partnered with the Postal Service to plan for the launch.
The Postal Service has expanded its staffing, similar to what’s done during the holidays.
All orders in the continental United States will be shipped through first-class mail, with shipments to Alaska, Hawaii, U.S. territories, and military and overseas addresses sent through priority mail.
A version of this article first appeared on WebMD.com.
The Biden administration’s new no-cost, at-home testing program launched Jan. 18, a day ahead of schedule.
The administration said 500 million tests are available to be delivered to homes across the country. This accounts for half of the president’s recent pledge to purchase 1 billion free at-home COVID-19 tests to distribute to the American public.
On a Jan. 14 call with reporters, senior White House officials offered some details about the new program.
Here’s what we know so far.
How do I order my free tests?
Americans can visit COVIDtests.gov to order their rapid at-home tests. You can also order directly from the U.S. Postal Service website. After you order, you’ll receive a confirmation email that promises to send tracking information once your order ships.
What information do I need to order the tests?
You only need your name and home mailing address.
There is also an option to provide your email address to get updates on the status of your order.
What if someone needs help ordering the tests?
There will be a free call-in line for people needing more help, including those having trouble accessing the internet, according to White House officials.
What tests will be available?
There are nine at-home tests available through FDA emergency use authorization. According to the Frequently Asked Questions section of COVIDtests.gov, "You will not be able to choose the brand you order as part of this program.”
How long will it take to get the tests once I order them?
Tests are expected to ship 7 to 12 days after you order them.
But White House officials say that the time frame will likely shorten as the program gains steam.
How many can I order?
There’s a limit of four tests per residential mailing address.
For larger families, White House officials suggest trying other free testing options, like visiting COVID-19 testing sites or your local health center.
Is this a one-time opportunity?
The White House doesn’t say, but officials did mention that if you run out of your four free tests, there are many other ways to access free at-home tests, such as COVID-19 testing sites, pharmacies, and community health centers.
The free tests available through COVIDtests.gov are in addition to an estimated 375 million at-home rapid tests on the market in the U.S. this month.
When should people use a rapid at-home test?
The CDC and experts with other public health groups agree that Americans should consider using at-home rapid tests in the following situations:
- If they begin to have symptoms consistent with COVID-19;
- At least 5 days after close contact with someone who has COVID;
- If someone is indoors with a group of people who are at risk of severe disease or are unvaccinated.
Are at-home rapid tests accurate?
The U.S. Department of Health and Human Services and other federal officials confirmed through studies that all tests distributed through this program can detect the Omicron variant. These agencies also confirmed that their performance is consistent with the FDA’s emergency use authorization.
Is the website designed to handle high demand?
After the original website to sign up for health insurance under the Affordable Care Act crashed repeatedly at launch, the government says it has prepared for high demand for ordering at-home rapid tests.
The U.S. Digital Service (USDS), an organization founded after Healthcare.gov, has partnered with the Postal Service to plan for the launch.
The Postal Service has expanded its staffing, similar to what’s done during the holidays.
All orders in the continental United States will be shipped through first-class mail, with shipments to Alaska, Hawaii, U.S. territories, and military and overseas addresses sent through priority mail.
A version of this article first appeared on WebMD.com.
The Biden administration’s new no-cost, at-home testing program launched Jan. 18, a day ahead of schedule.
The administration said 500 million tests are available to be delivered to homes across the country. This accounts for half of the president’s recent pledge to purchase 1 billion free at-home COVID-19 tests to distribute to the American public.
On a Jan. 14 call with reporters, senior White House officials offered some details about the new program.
Here’s what we know so far.
How do I order my free tests?
Americans can visit COVIDtests.gov to order their rapid at-home tests. You can also order directly from the U.S. Postal Service website. After you order, you’ll receive a confirmation email that promises to send tracking information once your order ships.
What information do I need to order the tests?
You only need your name and home mailing address.
There is also an option to provide your email address to get updates on the status of your order.
What if someone needs help ordering the tests?
There will be a free call-in line for people needing more help, including those having trouble accessing the internet, according to White House officials.
What tests will be available?
There are nine at-home tests available through FDA emergency use authorization. According to the Frequently Asked Questions section of COVIDtests.gov, "You will not be able to choose the brand you order as part of this program.”
How long will it take to get the tests once I order them?
Tests are expected to ship 7 to 12 days after you order them.
But White House officials say that the time frame will likely shorten as the program gains steam.
How many can I order?
There’s a limit of four tests per residential mailing address.
For larger families, White House officials suggest trying other free testing options, like visiting COVID-19 testing sites or your local health center.
Is this a one-time opportunity?
The White House doesn’t say, but officials did mention that if you run out of your four free tests, there are many other ways to access free at-home tests, such as COVID-19 testing sites, pharmacies, and community health centers.
The free tests available through COVIDtests.gov are in addition to an estimated 375 million at-home rapid tests on the market in the U.S. this month.
When should people use a rapid at-home test?
The CDC and experts with other public health groups agree that Americans should consider using at-home rapid tests in the following situations:
- If they begin to have symptoms consistent with COVID-19;
- At least 5 days after close contact with someone who has COVID;
- If someone is indoors with a group of people who are at risk of severe disease or are unvaccinated.
Are at-home rapid tests accurate?
The U.S. Department of Health and Human Services and other federal officials confirmed through studies that all tests distributed through this program can detect the Omicron variant. These agencies also confirmed that their performance is consistent with the FDA’s emergency use authorization.
Is the website designed to handle high demand?
After the original website to sign up for health insurance under the Affordable Care Act crashed repeatedly at launch, the government says it has prepared for high demand for ordering at-home rapid tests.
The U.S. Digital Service (USDS), an organization founded after Healthcare.gov, has partnered with the Postal Service to plan for the launch.
The Postal Service has expanded its staffing, similar to what’s done during the holidays.
All orders in the continental United States will be shipped through first-class mail, with shipments to Alaska, Hawaii, U.S. territories, and military and overseas addresses sent through priority mail.
A version of this article first appeared on WebMD.com.
Survey: Medical cannabis use for skin conditions lags behind interest, acceptance
A , according to the results of a recent survey.
Almost 89% of respondents were in favor of medical cannabis use for dermatologic diseases, and 73% said that they would be comfortable seeing a dermatologist who recommended such products to them, Samuel Yeroushalmi, a 4th-year medical student at George Washington University, Washington, and associates reported.
“Consumers and patients are already using MCPs [medical cannabis products] to treat inflammatory skin conditions, such as acne, rosacea, atopic dermatitis, and psoriasis, even without guidance from a dermatologist. While acceptance was high, there were clear barriers reported limiting use and uptake, such as patient skepticism and a lack of understanding,” Adam Friedman, MD, senior author and chair of the department of dermatology at the university, said in a separate statement.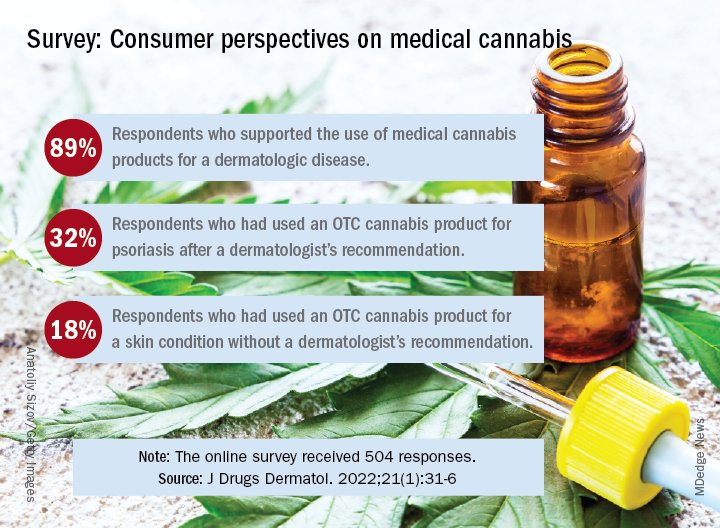
Dermatologic use of OTC cannabis products without the recommendation of a dermatologist was reported by 18% of the 504 of 700 adults who responded in the SurveyMonkey online panel. Of the two-thirds who had seen a dermatologist, 20% received a recommendation for an OTC product and 11% were recommended a product that required a department of health medical card, the investigators said.
Uptake among the patients who did receive a recommendation, however, was high: 76% for OTC products and 72% for those that required a medical card. Among those who had received an OTC recommendation, 32% used the cannabis product for psoriasis and 30% each for acne and rosacea, Mr. Yeroushalmi and his coauthors said.
The most common indication among the respondents with dermatologist recommendations for products requiring a medical card was for acne (68%), followed by psoriasis and rosacea (28% each). Cost was the main deterrent (60%) for those who declined to use the recommended cannabis product, with skepticism, limited understanding, and product illegality in their state each at 50%, the researchers said.
“Though cost and legality concerns are nonmodifiable barriers, dermatologists have an opportunity to educate those who know little in the way of medical cannabis or are skeptic[s],” they wrote. The survey results show that many patients are interested, and “the future should be bright for MCPs; we just need to show and disseminate the science,” Dr. Friedman commented in the statement.
One of the authors was from the University of Maryland, College Park. The authors had no disclosures to report.
A , according to the results of a recent survey.
Almost 89% of respondents were in favor of medical cannabis use for dermatologic diseases, and 73% said that they would be comfortable seeing a dermatologist who recommended such products to them, Samuel Yeroushalmi, a 4th-year medical student at George Washington University, Washington, and associates reported.
“Consumers and patients are already using MCPs [medical cannabis products] to treat inflammatory skin conditions, such as acne, rosacea, atopic dermatitis, and psoriasis, even without guidance from a dermatologist. While acceptance was high, there were clear barriers reported limiting use and uptake, such as patient skepticism and a lack of understanding,” Adam Friedman, MD, senior author and chair of the department of dermatology at the university, said in a separate statement.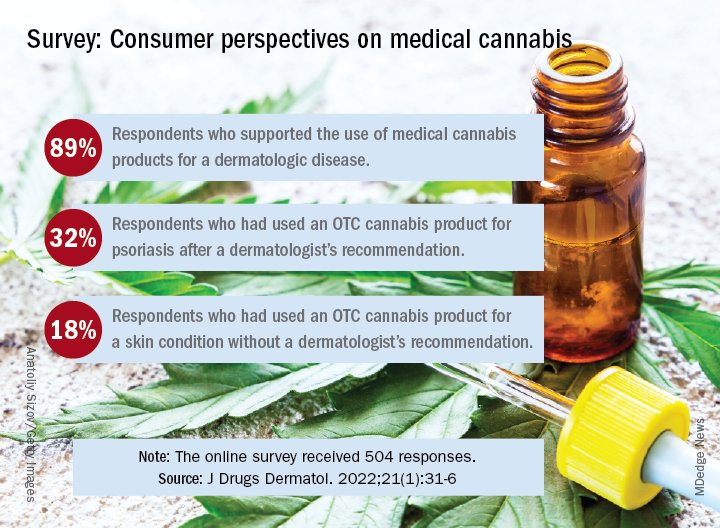
Dermatologic use of OTC cannabis products without the recommendation of a dermatologist was reported by 18% of the 504 of 700 adults who responded in the SurveyMonkey online panel. Of the two-thirds who had seen a dermatologist, 20% received a recommendation for an OTC product and 11% were recommended a product that required a department of health medical card, the investigators said.
Uptake among the patients who did receive a recommendation, however, was high: 76% for OTC products and 72% for those that required a medical card. Among those who had received an OTC recommendation, 32% used the cannabis product for psoriasis and 30% each for acne and rosacea, Mr. Yeroushalmi and his coauthors said.
The most common indication among the respondents with dermatologist recommendations for products requiring a medical card was for acne (68%), followed by psoriasis and rosacea (28% each). Cost was the main deterrent (60%) for those who declined to use the recommended cannabis product, with skepticism, limited understanding, and product illegality in their state each at 50%, the researchers said.
“Though cost and legality concerns are nonmodifiable barriers, dermatologists have an opportunity to educate those who know little in the way of medical cannabis or are skeptic[s],” they wrote. The survey results show that many patients are interested, and “the future should be bright for MCPs; we just need to show and disseminate the science,” Dr. Friedman commented in the statement.
One of the authors was from the University of Maryland, College Park. The authors had no disclosures to report.
A , according to the results of a recent survey.
Almost 89% of respondents were in favor of medical cannabis use for dermatologic diseases, and 73% said that they would be comfortable seeing a dermatologist who recommended such products to them, Samuel Yeroushalmi, a 4th-year medical student at George Washington University, Washington, and associates reported.
“Consumers and patients are already using MCPs [medical cannabis products] to treat inflammatory skin conditions, such as acne, rosacea, atopic dermatitis, and psoriasis, even without guidance from a dermatologist. While acceptance was high, there were clear barriers reported limiting use and uptake, such as patient skepticism and a lack of understanding,” Adam Friedman, MD, senior author and chair of the department of dermatology at the university, said in a separate statement.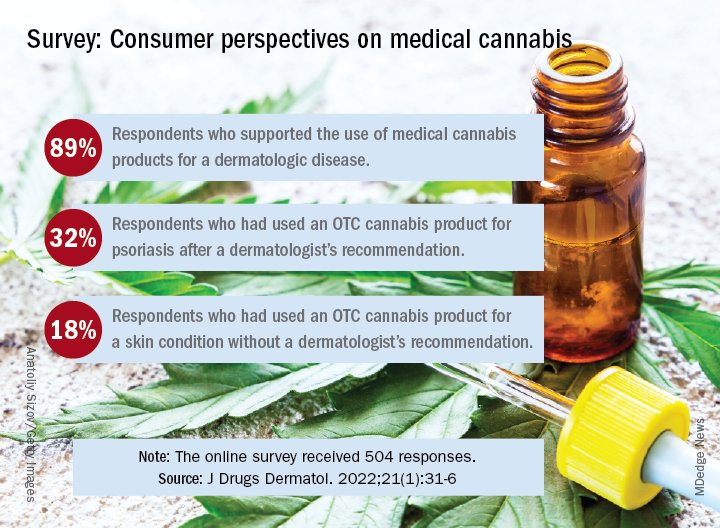
Dermatologic use of OTC cannabis products without the recommendation of a dermatologist was reported by 18% of the 504 of 700 adults who responded in the SurveyMonkey online panel. Of the two-thirds who had seen a dermatologist, 20% received a recommendation for an OTC product and 11% were recommended a product that required a department of health medical card, the investigators said.
Uptake among the patients who did receive a recommendation, however, was high: 76% for OTC products and 72% for those that required a medical card. Among those who had received an OTC recommendation, 32% used the cannabis product for psoriasis and 30% each for acne and rosacea, Mr. Yeroushalmi and his coauthors said.
The most common indication among the respondents with dermatologist recommendations for products requiring a medical card was for acne (68%), followed by psoriasis and rosacea (28% each). Cost was the main deterrent (60%) for those who declined to use the recommended cannabis product, with skepticism, limited understanding, and product illegality in their state each at 50%, the researchers said.
“Though cost and legality concerns are nonmodifiable barriers, dermatologists have an opportunity to educate those who know little in the way of medical cannabis or are skeptic[s],” they wrote. The survey results show that many patients are interested, and “the future should be bright for MCPs; we just need to show and disseminate the science,” Dr. Friedman commented in the statement.
One of the authors was from the University of Maryland, College Park. The authors had no disclosures to report.
FROM JOURNAL OF DRUGS IN DERMATOLOGY
Can supercomputers really keep up with the human brain?
An adult brain contains about 86 billion neurons and even more supercomputing power to closely monitor the entire human brain.
All those neurons have trillions of synapses – or connection points – that make up the circuitry the brain uses to control everything we do from reasoning to breathing to walking. And scientists with the Human Brain Project are trying to build new computing tools that can zoom in on every one of these synapses, peer inside cells, and zoom out to focus on entire regions of the brain at once.
, researchers from the Human Brain Project report in Science. If you have an old smartphone or tablet with 32GB of storage, you’d need more than 31,000 of them to get a single petabyte of storage.
Using an electron microscope to image the entire brain would require more than one exabyte of data, the scientists point out. That’s more than a million petabytes.
Giacomo Indiveri, PhD, professor of neuroinformatics at the University of Zurich, Switzerland, says we need to fundamentally change the way we build computers. Delivering the keynote address at the Human Brain Project Summit in October, he warned we will use 20% of all the world’s electricity on computing by the year 2025.
To meet the computing challenges posed by the quest to map every bit of the human brain, researchers are working to produce the first two exascale supercomputers within the next 5 years. When they’re done, these machines will provide brain scientists with supercomputers powerful enough to explore the human brain in all its complexities.
A version of this article first appeared on Medscape.com.
An adult brain contains about 86 billion neurons and even more supercomputing power to closely monitor the entire human brain.
All those neurons have trillions of synapses – or connection points – that make up the circuitry the brain uses to control everything we do from reasoning to breathing to walking. And scientists with the Human Brain Project are trying to build new computing tools that can zoom in on every one of these synapses, peer inside cells, and zoom out to focus on entire regions of the brain at once.
, researchers from the Human Brain Project report in Science. If you have an old smartphone or tablet with 32GB of storage, you’d need more than 31,000 of them to get a single petabyte of storage.
Using an electron microscope to image the entire brain would require more than one exabyte of data, the scientists point out. That’s more than a million petabytes.
Giacomo Indiveri, PhD, professor of neuroinformatics at the University of Zurich, Switzerland, says we need to fundamentally change the way we build computers. Delivering the keynote address at the Human Brain Project Summit in October, he warned we will use 20% of all the world’s electricity on computing by the year 2025.
To meet the computing challenges posed by the quest to map every bit of the human brain, researchers are working to produce the first two exascale supercomputers within the next 5 years. When they’re done, these machines will provide brain scientists with supercomputers powerful enough to explore the human brain in all its complexities.
A version of this article first appeared on Medscape.com.
An adult brain contains about 86 billion neurons and even more supercomputing power to closely monitor the entire human brain.
All those neurons have trillions of synapses – or connection points – that make up the circuitry the brain uses to control everything we do from reasoning to breathing to walking. And scientists with the Human Brain Project are trying to build new computing tools that can zoom in on every one of these synapses, peer inside cells, and zoom out to focus on entire regions of the brain at once.
, researchers from the Human Brain Project report in Science. If you have an old smartphone or tablet with 32GB of storage, you’d need more than 31,000 of them to get a single petabyte of storage.
Using an electron microscope to image the entire brain would require more than one exabyte of data, the scientists point out. That’s more than a million petabytes.
Giacomo Indiveri, PhD, professor of neuroinformatics at the University of Zurich, Switzerland, says we need to fundamentally change the way we build computers. Delivering the keynote address at the Human Brain Project Summit in October, he warned we will use 20% of all the world’s electricity on computing by the year 2025.
To meet the computing challenges posed by the quest to map every bit of the human brain, researchers are working to produce the first two exascale supercomputers within the next 5 years. When they’re done, these machines will provide brain scientists with supercomputers powerful enough to explore the human brain in all its complexities.
A version of this article first appeared on Medscape.com.
FROM SCIENCE
Federal website for free COVID-19 tests opens Jan. 19
The tests will ship within 7 to 12 days after being ordered, senior officials from President Joe Biden’s administration said Jan. 14. The U.S. Postal Service will handle the shipping and delivery through first-class mail.
People will input their name and mailing address on the website and can share an email address to receive updates on the order, according to NPR. People won’t need to pay shipping costs or enter a credit card number to order tests, according to the website’s homepage.
The website will be offered in both English and Spanish. The Biden administration will also set up a phone number so those without internet access can place orders.
Officials didn’t share a specific time that the website will open, according to he New York Times — simply that it will go live sometime on Jan. 19. Each household will be limited to ordering four tests.
Starting Jan. 15, people with private insurance were able to seek reimbursement for tests they purchase on their own. At the same time, some insurers have said it could take weeks to set up a system for smooth reimbursement, the newspaper reported.
Last week’s announcement is the latest step in the president’s pledge to get coronavirus tests to Americans. In December, Biden said his administration would purchase 500 million tests and distribute them to Americans for free. On Jan. 13, he announced that the administration would buy another 500 million tests, bringing the total to 1 billion.
So far, the administration has signed contracts to produce 420 million tests, the newspaper reported. With the website opening this week and the lag in shipping, the tests will likely arrive by the end of January at the earliest, which could be after the peak of the current coronavirus surge in some parts of the country.
At-home tests have been in high demand, with some pharmacies, retailers, and websites reporting no stock in recent weeks. People have lined up at community testing sites for hours to get tested as the national average of daily cases has climbed above 800,000 last week.
Some consumers have also been confused about how or when to use at-home tests. On Jan. 14, Biden administration officials said that people should use rapid tests for three reasons:
- If they begin to experience COVID-19 symptoms;
- When it has been five or more days after being exposed to someone who tests positive;
- If they are gathering indoors with a high-risk person and want to check if they are negative.
A version of this article first appeared on WebMD.com.
The tests will ship within 7 to 12 days after being ordered, senior officials from President Joe Biden’s administration said Jan. 14. The U.S. Postal Service will handle the shipping and delivery through first-class mail.
People will input their name and mailing address on the website and can share an email address to receive updates on the order, according to NPR. People won’t need to pay shipping costs or enter a credit card number to order tests, according to the website’s homepage.
The website will be offered in both English and Spanish. The Biden administration will also set up a phone number so those without internet access can place orders.
Officials didn’t share a specific time that the website will open, according to he New York Times — simply that it will go live sometime on Jan. 19. Each household will be limited to ordering four tests.
Starting Jan. 15, people with private insurance were able to seek reimbursement for tests they purchase on their own. At the same time, some insurers have said it could take weeks to set up a system for smooth reimbursement, the newspaper reported.
Last week’s announcement is the latest step in the president’s pledge to get coronavirus tests to Americans. In December, Biden said his administration would purchase 500 million tests and distribute them to Americans for free. On Jan. 13, he announced that the administration would buy another 500 million tests, bringing the total to 1 billion.
So far, the administration has signed contracts to produce 420 million tests, the newspaper reported. With the website opening this week and the lag in shipping, the tests will likely arrive by the end of January at the earliest, which could be after the peak of the current coronavirus surge in some parts of the country.
At-home tests have been in high demand, with some pharmacies, retailers, and websites reporting no stock in recent weeks. People have lined up at community testing sites for hours to get tested as the national average of daily cases has climbed above 800,000 last week.
Some consumers have also been confused about how or when to use at-home tests. On Jan. 14, Biden administration officials said that people should use rapid tests for three reasons:
- If they begin to experience COVID-19 symptoms;
- When it has been five or more days after being exposed to someone who tests positive;
- If they are gathering indoors with a high-risk person and want to check if they are negative.
A version of this article first appeared on WebMD.com.
The tests will ship within 7 to 12 days after being ordered, senior officials from President Joe Biden’s administration said Jan. 14. The U.S. Postal Service will handle the shipping and delivery through first-class mail.
People will input their name and mailing address on the website and can share an email address to receive updates on the order, according to NPR. People won’t need to pay shipping costs or enter a credit card number to order tests, according to the website’s homepage.
The website will be offered in both English and Spanish. The Biden administration will also set up a phone number so those without internet access can place orders.
Officials didn’t share a specific time that the website will open, according to he New York Times — simply that it will go live sometime on Jan. 19. Each household will be limited to ordering four tests.
Starting Jan. 15, people with private insurance were able to seek reimbursement for tests they purchase on their own. At the same time, some insurers have said it could take weeks to set up a system for smooth reimbursement, the newspaper reported.
Last week’s announcement is the latest step in the president’s pledge to get coronavirus tests to Americans. In December, Biden said his administration would purchase 500 million tests and distribute them to Americans for free. On Jan. 13, he announced that the administration would buy another 500 million tests, bringing the total to 1 billion.
So far, the administration has signed contracts to produce 420 million tests, the newspaper reported. With the website opening this week and the lag in shipping, the tests will likely arrive by the end of January at the earliest, which could be after the peak of the current coronavirus surge in some parts of the country.
At-home tests have been in high demand, with some pharmacies, retailers, and websites reporting no stock in recent weeks. People have lined up at community testing sites for hours to get tested as the national average of daily cases has climbed above 800,000 last week.
Some consumers have also been confused about how or when to use at-home tests. On Jan. 14, Biden administration officials said that people should use rapid tests for three reasons:
- If they begin to experience COVID-19 symptoms;
- When it has been five or more days after being exposed to someone who tests positive;
- If they are gathering indoors with a high-risk person and want to check if they are negative.
A version of this article first appeared on WebMD.com.
Docs pen open letter to support Fauci against partisan ‘attacks’
“We deplore the personal attacks on Dr. Fauci. The criticism is inaccurate, unscientific, ill-founded in the facts and, increasingly, motivated by partisan politics,” reads the letter of support, initiated by Ezekiel Emanuel, MD, and signed by almost 300 scientists and public health and medical professionals, including Nobel Laureates, a former Republican senator, and leadership of medical societies and institutions.
Dr. Fauci has led the National Institute for Allergy and Infectious Diseases since 1984 and serves as President Biden’s top medical advisor on the pandemic.
“Dr. Anthony Fauci has served the U.S.A. with wisdom and integrity for nearly 40 years. Through HIV, Ebola, and now COVID, he has unswervingly served the United States guiding the country to very successful outcomes. He has our unreserved respect and trust as a scientist and a national leader,” the letter reads.
Dr. Fauci has repeatedly faced harsh criticism from congressional Republicans, especially Sen. Rand Paul (R-Ky.) and Sen. Roger Marshall (R-Kan.).
At a particularly contentious congressional hearing earlier this week on the federal government’s response to Omicron, Dr. Fauci fought back, telling Sen. Marshall, “You’re so misinformed, it’s extraordinary.”
Dr. Fauci, who has received death threats and harassment of his family, told Sen. Rand that his “completely untrue” statements and rhetoric “kindles the crazies out there.”
‘Sagacious counsel’
The personal attacks on Dr. Fauci are a “distraction from what should be the national focus – working together to finally overcome a pandemic that is killing about 500,000 people a year. We are grateful for Dr. Fauci’s dedication and tireless efforts to help the country through this pandemic and other health crises,” the letter reads.
“Throughout the COVID-19 pandemic, Dr. Fauci has provided the American political leadership and the public with sagacious counsel in these most difficult of times. His advice has been as well informed as data and the rapidly evolving circumstances allowed,” it states.
“Importantly,” Dr. Fauci has given his advice with “humility, being clear about what we know and what is unknown, but requires judgment. He has consistently emphasized the importance of mask-wearing, social distancing, and vaccination. These are standard and necessary public health measures that we all support,” the letter states.
“We are grateful that Dr. Fauci has consistently stated the science in a way that represents the facts as they emerge, without unwarranted speculation.”
“Sadly, in these politically polarized times where misinformation contaminates the United States’ response to the pandemic, routine public health measures have become unnecessarily controversial, undermining the effectiveness of our country’s response,” the letter reads.
A version of this article first appeared on Medscape.com.
“We deplore the personal attacks on Dr. Fauci. The criticism is inaccurate, unscientific, ill-founded in the facts and, increasingly, motivated by partisan politics,” reads the letter of support, initiated by Ezekiel Emanuel, MD, and signed by almost 300 scientists and public health and medical professionals, including Nobel Laureates, a former Republican senator, and leadership of medical societies and institutions.
Dr. Fauci has led the National Institute for Allergy and Infectious Diseases since 1984 and serves as President Biden’s top medical advisor on the pandemic.
“Dr. Anthony Fauci has served the U.S.A. with wisdom and integrity for nearly 40 years. Through HIV, Ebola, and now COVID, he has unswervingly served the United States guiding the country to very successful outcomes. He has our unreserved respect and trust as a scientist and a national leader,” the letter reads.
Dr. Fauci has repeatedly faced harsh criticism from congressional Republicans, especially Sen. Rand Paul (R-Ky.) and Sen. Roger Marshall (R-Kan.).
At a particularly contentious congressional hearing earlier this week on the federal government’s response to Omicron, Dr. Fauci fought back, telling Sen. Marshall, “You’re so misinformed, it’s extraordinary.”
Dr. Fauci, who has received death threats and harassment of his family, told Sen. Rand that his “completely untrue” statements and rhetoric “kindles the crazies out there.”
‘Sagacious counsel’
The personal attacks on Dr. Fauci are a “distraction from what should be the national focus – working together to finally overcome a pandemic that is killing about 500,000 people a year. We are grateful for Dr. Fauci’s dedication and tireless efforts to help the country through this pandemic and other health crises,” the letter reads.
“Throughout the COVID-19 pandemic, Dr. Fauci has provided the American political leadership and the public with sagacious counsel in these most difficult of times. His advice has been as well informed as data and the rapidly evolving circumstances allowed,” it states.
“Importantly,” Dr. Fauci has given his advice with “humility, being clear about what we know and what is unknown, but requires judgment. He has consistently emphasized the importance of mask-wearing, social distancing, and vaccination. These are standard and necessary public health measures that we all support,” the letter states.
“We are grateful that Dr. Fauci has consistently stated the science in a way that represents the facts as they emerge, without unwarranted speculation.”
“Sadly, in these politically polarized times where misinformation contaminates the United States’ response to the pandemic, routine public health measures have become unnecessarily controversial, undermining the effectiveness of our country’s response,” the letter reads.
A version of this article first appeared on Medscape.com.
“We deplore the personal attacks on Dr. Fauci. The criticism is inaccurate, unscientific, ill-founded in the facts and, increasingly, motivated by partisan politics,” reads the letter of support, initiated by Ezekiel Emanuel, MD, and signed by almost 300 scientists and public health and medical professionals, including Nobel Laureates, a former Republican senator, and leadership of medical societies and institutions.
Dr. Fauci has led the National Institute for Allergy and Infectious Diseases since 1984 and serves as President Biden’s top medical advisor on the pandemic.
“Dr. Anthony Fauci has served the U.S.A. with wisdom and integrity for nearly 40 years. Through HIV, Ebola, and now COVID, he has unswervingly served the United States guiding the country to very successful outcomes. He has our unreserved respect and trust as a scientist and a national leader,” the letter reads.
Dr. Fauci has repeatedly faced harsh criticism from congressional Republicans, especially Sen. Rand Paul (R-Ky.) and Sen. Roger Marshall (R-Kan.).
At a particularly contentious congressional hearing earlier this week on the federal government’s response to Omicron, Dr. Fauci fought back, telling Sen. Marshall, “You’re so misinformed, it’s extraordinary.”
Dr. Fauci, who has received death threats and harassment of his family, told Sen. Rand that his “completely untrue” statements and rhetoric “kindles the crazies out there.”
‘Sagacious counsel’
The personal attacks on Dr. Fauci are a “distraction from what should be the national focus – working together to finally overcome a pandemic that is killing about 500,000 people a year. We are grateful for Dr. Fauci’s dedication and tireless efforts to help the country through this pandemic and other health crises,” the letter reads.
“Throughout the COVID-19 pandemic, Dr. Fauci has provided the American political leadership and the public with sagacious counsel in these most difficult of times. His advice has been as well informed as data and the rapidly evolving circumstances allowed,” it states.
“Importantly,” Dr. Fauci has given his advice with “humility, being clear about what we know and what is unknown, but requires judgment. He has consistently emphasized the importance of mask-wearing, social distancing, and vaccination. These are standard and necessary public health measures that we all support,” the letter states.
“We are grateful that Dr. Fauci has consistently stated the science in a way that represents the facts as they emerge, without unwarranted speculation.”
“Sadly, in these politically polarized times where misinformation contaminates the United States’ response to the pandemic, routine public health measures have become unnecessarily controversial, undermining the effectiveness of our country’s response,” the letter reads.
A version of this article first appeared on Medscape.com.
Epstein-Barr virus a likely leading cause of multiple sclerosis
This study is the first to provide compelling evidence of a causal link between EBV and MS, principal investigator Alberto Ascherio, MD, DrPH, professor of epidemiology, Harvard T. H. Chan School of Public Health, and professor of medicine, Harvard Medical School, Boston, told this news organization.
The “prevailing” view has been that MS is “an autoimmune disease of unknown etiology,” said Dr. Ascherio. “Now we know MS is a complication of a viral infection.” With this knowledge, he added, “we can redirect research” to find antiviral drugs to treat the disease.
The study was published online Jan. 13 in Science.
Unique dataset
A chronic disease of the central nervous system, MS involves an inflammatory attack on the myelin sheath and the axons it insulates. The disease affects 2.8 million people worldwide.
EBV is a human herpesvirus that can cause infectious mononucleosis. After infection, it persists in latent form in B-lymphocytes.
EBV is common and infects about 95% of adults. Most individuals are already infected with the virus by age 18 or 20 years, making it difficult to study uninfected populations, said Dr. Ascherio.
However, access to a “huge” database of more than 10 million active-duty U.S. service personnel made this possible, he said.
Service members are screened for HIV at the start of their service care and biennially thereafter. The investigators used stored blood samples to determine the relation between EBV infection and MS over a 20-year period from 1993 to 2013.
Researchers examined 801 MS case patients and 1,566 matched controls without MS. Most individuals were under 20 at the time of their first blood collection. Symptom onset for those who developed MS was a median of 10 years after the first sample was obtained.
Only one of the 801 MS case patients had no serologic evidence of EBV. This individual may have been infected with the virus after the last blood collection, failed to seroconvert in response to infection, or was misdiagnosed, the investigators note.
The hazard ratio for MS between EBV seroconversion versus persistent EBV seronegative was 32.4 (95% CI, 4.3-245.3; P < .001).
An MS vaccine?
MS risk was not increased after infection with cytomegalovirus, a herpesvirus that is transmitted through saliva, as is EBV.
Researchers measured serum concentrations of neurofilament light chain (sNflL), a biomarker of neuroaxonal degeneration, in samples from EBV-negative individuals at baseline. There were no signs of neuroaxonal degeneration before EBV seroconversion in subjects who later developed MS.
This indicates that “EBV infection preceded not only symptom onset but also the time of the first detectable pathological mechanisms underlying MS,” the investigators note.
The very magnitude of increased MS risk of MS observed EBV almost completely rules out confounding by known risk factors. Smoking and vitamin D deficiency double the risk, and genetic predisposition and childhood obesity also only raise the risks of MS to a “moderate” degree, said Dr. Ascherio.
It’s not clear why only some people infected with EBV go on to develop MS, he said.
The idea that reverse causation – that immune dysregulation during the preclinical phase of MS increases susceptibility to EBV infection – is unlikely, the investigators note. For instance, EBV seroconversion occurs before elevation of sNfL levels, an early marker of preclinical MS.
Since most MS cases appear to be caused by EBV, a suitable vaccine might thwart the disease. “A vaccine could, in theory, prevent infection and prevent MS,” said Dr. Ascherio, adding that there’s ongoing work to develop such a vaccine.
Another approach is to target the virus driving MS disease progression. Developing appropriate antivirals might treat and even cure MS, said Dr. Ascherio.
‘Compelling data’
In an accompanying commentary, William H. Robinson, MD, PhD, professor, Division of Immunology and Rheumatology, department of medicine, Stanford (Calif.) University, and a colleague said the study findings “provide compelling data that implicate EBV as the trigger for the development of MS.”
The mechanism or mechanisms by which EBV leads to MS “remain elusive,” the commentary authors write.
“Possibilities include molecular mimicry, through which EBV viral protein sequences mimic human myelin proteins and other CNS proteins and thereby induce autoimmunity against myelin and CNS antigens,” they note.
As other factors, including genetic susceptibility, are important to MS, EBV infection is likely necessary but not sufficient to trigger MS, said the commentary. “Infection with EBV is the initial pathogenic step in MS, but additional fuses must be ignited for the full pathophysiology.”
The commentary authors query whether there may be “new opportunities” for therapy with vaccines or antivirals. “Now that the initial trigger for MS has been identified, perhaps MS could be eradicated.”
In a statement from the Science Media Center, an independent venture promoting views from the scientific community, two other experts offered their take on the study.
Paul Farrell, PhD, professor of tumor virology, Imperial College London, said the paper “provides very clear confirmation of a causal role for EBV in most cases of MS.”
While there’s evidence that a vaccine can prevent the EBV disease infectious mononucleosis, no vaccine candidate has yet prevented the virus from infecting and establishing long-term persistence in people, noted Dr. Farrell.
“So, at this stage it is not clear whether a vaccine of the types currently being developed would be able to prevent the long-term effects of EBV in MS,” he said.
Daniel Davis, PhD, professor of immunology, University of Manchester, United Kingdom, commented that the value of this new discovery is not an immediate medical cure or treatment but is “a major step forward” in understanding MS.
The study “sets up new research working out the precise details of how this virus can sometimes lead to an autoimmune disease,” said Dr. Davis. “There is no shortage of ideas in how this might happen in principle and hopefully the correct details will emerge soon.”
The study received funding from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, National Multiple Sclerosis Society, the German Research Foundation, the National Institutes of Health, and the Howard Hughes Medical Institute. Dr. Ascherio reports no relevant financial relaitonships. Dr. Robinson is a coinventor on a patent application filed by Stanford University that includes antibodies to EBV. Dr. Farrell reports serving on an ad hoc review panel for GSK on EBV vaccines in 2019 as a one off. He has a current grant from MRC on EBV biology, including some EBV sequence variation, but the grant is not about MS. Dr. Davis reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This study is the first to provide compelling evidence of a causal link between EBV and MS, principal investigator Alberto Ascherio, MD, DrPH, professor of epidemiology, Harvard T. H. Chan School of Public Health, and professor of medicine, Harvard Medical School, Boston, told this news organization.
The “prevailing” view has been that MS is “an autoimmune disease of unknown etiology,” said Dr. Ascherio. “Now we know MS is a complication of a viral infection.” With this knowledge, he added, “we can redirect research” to find antiviral drugs to treat the disease.
The study was published online Jan. 13 in Science.
Unique dataset
A chronic disease of the central nervous system, MS involves an inflammatory attack on the myelin sheath and the axons it insulates. The disease affects 2.8 million people worldwide.
EBV is a human herpesvirus that can cause infectious mononucleosis. After infection, it persists in latent form in B-lymphocytes.
EBV is common and infects about 95% of adults. Most individuals are already infected with the virus by age 18 or 20 years, making it difficult to study uninfected populations, said Dr. Ascherio.
However, access to a “huge” database of more than 10 million active-duty U.S. service personnel made this possible, he said.
Service members are screened for HIV at the start of their service care and biennially thereafter. The investigators used stored blood samples to determine the relation between EBV infection and MS over a 20-year period from 1993 to 2013.
Researchers examined 801 MS case patients and 1,566 matched controls without MS. Most individuals were under 20 at the time of their first blood collection. Symptom onset for those who developed MS was a median of 10 years after the first sample was obtained.
Only one of the 801 MS case patients had no serologic evidence of EBV. This individual may have been infected with the virus after the last blood collection, failed to seroconvert in response to infection, or was misdiagnosed, the investigators note.
The hazard ratio for MS between EBV seroconversion versus persistent EBV seronegative was 32.4 (95% CI, 4.3-245.3; P < .001).
An MS vaccine?
MS risk was not increased after infection with cytomegalovirus, a herpesvirus that is transmitted through saliva, as is EBV.
Researchers measured serum concentrations of neurofilament light chain (sNflL), a biomarker of neuroaxonal degeneration, in samples from EBV-negative individuals at baseline. There were no signs of neuroaxonal degeneration before EBV seroconversion in subjects who later developed MS.
This indicates that “EBV infection preceded not only symptom onset but also the time of the first detectable pathological mechanisms underlying MS,” the investigators note.
The very magnitude of increased MS risk of MS observed EBV almost completely rules out confounding by known risk factors. Smoking and vitamin D deficiency double the risk, and genetic predisposition and childhood obesity also only raise the risks of MS to a “moderate” degree, said Dr. Ascherio.
It’s not clear why only some people infected with EBV go on to develop MS, he said.
The idea that reverse causation – that immune dysregulation during the preclinical phase of MS increases susceptibility to EBV infection – is unlikely, the investigators note. For instance, EBV seroconversion occurs before elevation of sNfL levels, an early marker of preclinical MS.
Since most MS cases appear to be caused by EBV, a suitable vaccine might thwart the disease. “A vaccine could, in theory, prevent infection and prevent MS,” said Dr. Ascherio, adding that there’s ongoing work to develop such a vaccine.
Another approach is to target the virus driving MS disease progression. Developing appropriate antivirals might treat and even cure MS, said Dr. Ascherio.
‘Compelling data’
In an accompanying commentary, William H. Robinson, MD, PhD, professor, Division of Immunology and Rheumatology, department of medicine, Stanford (Calif.) University, and a colleague said the study findings “provide compelling data that implicate EBV as the trigger for the development of MS.”
The mechanism or mechanisms by which EBV leads to MS “remain elusive,” the commentary authors write.
“Possibilities include molecular mimicry, through which EBV viral protein sequences mimic human myelin proteins and other CNS proteins and thereby induce autoimmunity against myelin and CNS antigens,” they note.
As other factors, including genetic susceptibility, are important to MS, EBV infection is likely necessary but not sufficient to trigger MS, said the commentary. “Infection with EBV is the initial pathogenic step in MS, but additional fuses must be ignited for the full pathophysiology.”
The commentary authors query whether there may be “new opportunities” for therapy with vaccines or antivirals. “Now that the initial trigger for MS has been identified, perhaps MS could be eradicated.”
In a statement from the Science Media Center, an independent venture promoting views from the scientific community, two other experts offered their take on the study.
Paul Farrell, PhD, professor of tumor virology, Imperial College London, said the paper “provides very clear confirmation of a causal role for EBV in most cases of MS.”
While there’s evidence that a vaccine can prevent the EBV disease infectious mononucleosis, no vaccine candidate has yet prevented the virus from infecting and establishing long-term persistence in people, noted Dr. Farrell.
“So, at this stage it is not clear whether a vaccine of the types currently being developed would be able to prevent the long-term effects of EBV in MS,” he said.
Daniel Davis, PhD, professor of immunology, University of Manchester, United Kingdom, commented that the value of this new discovery is not an immediate medical cure or treatment but is “a major step forward” in understanding MS.
The study “sets up new research working out the precise details of how this virus can sometimes lead to an autoimmune disease,” said Dr. Davis. “There is no shortage of ideas in how this might happen in principle and hopefully the correct details will emerge soon.”
The study received funding from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, National Multiple Sclerosis Society, the German Research Foundation, the National Institutes of Health, and the Howard Hughes Medical Institute. Dr. Ascherio reports no relevant financial relaitonships. Dr. Robinson is a coinventor on a patent application filed by Stanford University that includes antibodies to EBV. Dr. Farrell reports serving on an ad hoc review panel for GSK on EBV vaccines in 2019 as a one off. He has a current grant from MRC on EBV biology, including some EBV sequence variation, but the grant is not about MS. Dr. Davis reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This study is the first to provide compelling evidence of a causal link between EBV and MS, principal investigator Alberto Ascherio, MD, DrPH, professor of epidemiology, Harvard T. H. Chan School of Public Health, and professor of medicine, Harvard Medical School, Boston, told this news organization.
The “prevailing” view has been that MS is “an autoimmune disease of unknown etiology,” said Dr. Ascherio. “Now we know MS is a complication of a viral infection.” With this knowledge, he added, “we can redirect research” to find antiviral drugs to treat the disease.
The study was published online Jan. 13 in Science.
Unique dataset
A chronic disease of the central nervous system, MS involves an inflammatory attack on the myelin sheath and the axons it insulates. The disease affects 2.8 million people worldwide.
EBV is a human herpesvirus that can cause infectious mononucleosis. After infection, it persists in latent form in B-lymphocytes.
EBV is common and infects about 95% of adults. Most individuals are already infected with the virus by age 18 or 20 years, making it difficult to study uninfected populations, said Dr. Ascherio.
However, access to a “huge” database of more than 10 million active-duty U.S. service personnel made this possible, he said.
Service members are screened for HIV at the start of their service care and biennially thereafter. The investigators used stored blood samples to determine the relation between EBV infection and MS over a 20-year period from 1993 to 2013.
Researchers examined 801 MS case patients and 1,566 matched controls without MS. Most individuals were under 20 at the time of their first blood collection. Symptom onset for those who developed MS was a median of 10 years after the first sample was obtained.
Only one of the 801 MS case patients had no serologic evidence of EBV. This individual may have been infected with the virus after the last blood collection, failed to seroconvert in response to infection, or was misdiagnosed, the investigators note.
The hazard ratio for MS between EBV seroconversion versus persistent EBV seronegative was 32.4 (95% CI, 4.3-245.3; P < .001).
An MS vaccine?
MS risk was not increased after infection with cytomegalovirus, a herpesvirus that is transmitted through saliva, as is EBV.
Researchers measured serum concentrations of neurofilament light chain (sNflL), a biomarker of neuroaxonal degeneration, in samples from EBV-negative individuals at baseline. There were no signs of neuroaxonal degeneration before EBV seroconversion in subjects who later developed MS.
This indicates that “EBV infection preceded not only symptom onset but also the time of the first detectable pathological mechanisms underlying MS,” the investigators note.
The very magnitude of increased MS risk of MS observed EBV almost completely rules out confounding by known risk factors. Smoking and vitamin D deficiency double the risk, and genetic predisposition and childhood obesity also only raise the risks of MS to a “moderate” degree, said Dr. Ascherio.
It’s not clear why only some people infected with EBV go on to develop MS, he said.
The idea that reverse causation – that immune dysregulation during the preclinical phase of MS increases susceptibility to EBV infection – is unlikely, the investigators note. For instance, EBV seroconversion occurs before elevation of sNfL levels, an early marker of preclinical MS.
Since most MS cases appear to be caused by EBV, a suitable vaccine might thwart the disease. “A vaccine could, in theory, prevent infection and prevent MS,” said Dr. Ascherio, adding that there’s ongoing work to develop such a vaccine.
Another approach is to target the virus driving MS disease progression. Developing appropriate antivirals might treat and even cure MS, said Dr. Ascherio.
‘Compelling data’
In an accompanying commentary, William H. Robinson, MD, PhD, professor, Division of Immunology and Rheumatology, department of medicine, Stanford (Calif.) University, and a colleague said the study findings “provide compelling data that implicate EBV as the trigger for the development of MS.”
The mechanism or mechanisms by which EBV leads to MS “remain elusive,” the commentary authors write.
“Possibilities include molecular mimicry, through which EBV viral protein sequences mimic human myelin proteins and other CNS proteins and thereby induce autoimmunity against myelin and CNS antigens,” they note.
As other factors, including genetic susceptibility, are important to MS, EBV infection is likely necessary but not sufficient to trigger MS, said the commentary. “Infection with EBV is the initial pathogenic step in MS, but additional fuses must be ignited for the full pathophysiology.”
The commentary authors query whether there may be “new opportunities” for therapy with vaccines or antivirals. “Now that the initial trigger for MS has been identified, perhaps MS could be eradicated.”
In a statement from the Science Media Center, an independent venture promoting views from the scientific community, two other experts offered their take on the study.
Paul Farrell, PhD, professor of tumor virology, Imperial College London, said the paper “provides very clear confirmation of a causal role for EBV in most cases of MS.”
While there’s evidence that a vaccine can prevent the EBV disease infectious mononucleosis, no vaccine candidate has yet prevented the virus from infecting and establishing long-term persistence in people, noted Dr. Farrell.
“So, at this stage it is not clear whether a vaccine of the types currently being developed would be able to prevent the long-term effects of EBV in MS,” he said.
Daniel Davis, PhD, professor of immunology, University of Manchester, United Kingdom, commented that the value of this new discovery is not an immediate medical cure or treatment but is “a major step forward” in understanding MS.
The study “sets up new research working out the precise details of how this virus can sometimes lead to an autoimmune disease,” said Dr. Davis. “There is no shortage of ideas in how this might happen in principle and hopefully the correct details will emerge soon.”
The study received funding from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, National Multiple Sclerosis Society, the German Research Foundation, the National Institutes of Health, and the Howard Hughes Medical Institute. Dr. Ascherio reports no relevant financial relaitonships. Dr. Robinson is a coinventor on a patent application filed by Stanford University that includes antibodies to EBV. Dr. Farrell reports serving on an ad hoc review panel for GSK on EBV vaccines in 2019 as a one off. He has a current grant from MRC on EBV biology, including some EBV sequence variation, but the grant is not about MS. Dr. Davis reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM SCIENCE
Cardiac inflammation can be present after mild COVID infection
Myocardial inflammation is present in a small proportion of patients who have recovered from relatively mild cases of COVID-19 infection, a new study shows.
“Our findings suggest that even in patients who have had relatively mild cases of COVID-19, some will have inflammatory changes to the heart, and these changes can be present without any cardiac symptoms,” senior author, Paaladinesh Thavendiranathan, MD, University of Toronto, told this news organization.
“While our data suggest that this inflammation improves over time, and the outcomes seem positive, we don’t know if there will be any long-term consequences,” he added.
Noting that even a short period of inflammation in the heart may be associated with symptoms or arrhythmias in the longer term, Dr. Thavendiranathan said: “I would recommend that it is best to avoid getting the infection if there is any chance of heart inflammation.”
The study was published online in JAMA Cardiology on Jan. 12.
The authors explain that among patients hospitalized with COVID, early studies suggested that approximately one in four experience cardiovascular injury, defined as an elevation in troponin levels, which was associated with a 5- to 10-fold increase in the risk for death. But there is limited information on cardiac injury in patients who do not require hospitalization.
Although a broad range of abnormal myocardial tissue has been reported in several cardiac MRI studies of patients recovered from COVID infection, there is little understanding of persistent changes in myocardial metabolism in recovered patients, which is a potential concern, given that COVID-19 is associated with systemic inflammation during the acute illness, they say.
For the current study, the researchers examined myocardial inflammation measured using two different methods – cardiac MRI and fluorodeoxyglucose–positron emission tomography (FDG-PET) – in individuals who had recovered from COVID-19 infection and looked at how this related to changes in inflammatory blood markers.
Lead author Kate Hanneman, MD, also from the University of Toronto, explained that FDG-PET imaging is more sensitive than MRI in detecting active inflammation. “Inflammatory cells have a higher uptake of glucose, and FDG-PET imaging is used to look for metabolically active inflammatory tissue that takes up glucose. It gives complementary information to MRI. Cardiac MRI shows structural or functional changes, such as scarring or edema, whereas FDG-PET imaging directly measures metabolic activity related to inflammatory cells.”
The study involved 47 individuals, 51% female, with a mean age of 43 years, who had recently recovered from COVID-19 infection. Of these, the majority had had relatively mild COVID disease, with 85% not requiring hospitalization.
Cardiac imaging was performed a mean of 67 days after the diagnosis of COVID-19. At the time of imaging, 19 participants (40%) reported at least one cardiac symptom, including palpitations, chest pain, and shortness of breath.
Results showed that eight patients (17%) had focal FDG uptake on PET consistent with myocardial inflammation. Compared with those without FDG uptake, patients with focal FDG uptake had higher regional T2, T1, and extracellular volume (colocalizing with focal FDG uptake), higher prevalence of late gadolinium enhancement indicating fibrosis, lower left ventricular ejection fraction, worse global longitudinal and circumferential strain, and higher systemic inflammatory blood markers, including interleukin (IL)-6, IL- 8, an high-sensitivity C-reactive protein.
Of the 47 patients in the study, 13 had received at least one dose of a COVID-19 vaccine. There was no significant difference in the proportion of patients who were PET-positive among those who had received a COVID-19 vaccine and those who had not.
There was also no difference in inflammation in patients who had been hospitalized with COVID-19 and those who had managed their infection at home.
Among patients with focal FDG uptake, PET, MRI, and inflammatory blood markers improved at follow-up imaging performed a mean of 52 days after the first imaging. The authors say this suggests that these abnormalities were not related to pre-existing cardiovascular disease.
Of the eight patients with positive FDG-PET results, two did not show any MRI abnormalities. These two patients also had elevated inflammatory biomarkers. “PET is a more sensitive method of measuring cardiac inflammation, and our results show that these changes may not always translate into functional changes seen on MRI,” Dr. Thavendiranathan noted.
The only cardiac risk factor that was more common in participants with FDG uptake was hypertension. Although cardiac symptoms were nearly twice as common in participants with focal FDG uptake, this difference was not statistically significant.
“Given the growing number of survivors with similar symptoms, these interesting findings warrant further investigation,” the authors say.
Noting that FDG uptake correlated with elevations in systemic inflammatory biomarkers, the researchers suggest that “a more intense systemic inflammatory process may be contributing to cardiac inflammation and the consequential alteration to regional and global myocardial function in PET-positive participants.”
On repeat imaging 2 months later, all eight patients who showed FDG uptake showed improvement or resolution of inflammation without any treatment, although two patients still had some signs of inflammation. Blood biomarkers also improved on follow-up.
“This is encouraging information, but we need longer-term data to see if there are any long-term repercussions of this inflammation,” Dr. Hanneman said.
“Overall, the study findings suggest an imaging phenotype that is expected to have good prognosis. However, longer-term follow-up studies are required to understand the need for ongoing cardiac surveillance, relationship to cardiac symptoms, guidance for safe return to exercise and sports participation, and long-term cardiovascular disease risk,” the researchers state.
This study was funded by grants from the Joint Department of Medical Imaging Academic Incentive Fund, Peter Munk Cardiac Center Innovation Committee, and Ted Rogers Center for Heart Research. Dr. Hanneman reports personal fees from Sanofi Genzyme, Amicus, and Medscape outside the submitted work.
A version of this article first appeared on Medscape.com.
Myocardial inflammation is present in a small proportion of patients who have recovered from relatively mild cases of COVID-19 infection, a new study shows.
“Our findings suggest that even in patients who have had relatively mild cases of COVID-19, some will have inflammatory changes to the heart, and these changes can be present without any cardiac symptoms,” senior author, Paaladinesh Thavendiranathan, MD, University of Toronto, told this news organization.
“While our data suggest that this inflammation improves over time, and the outcomes seem positive, we don’t know if there will be any long-term consequences,” he added.
Noting that even a short period of inflammation in the heart may be associated with symptoms or arrhythmias in the longer term, Dr. Thavendiranathan said: “I would recommend that it is best to avoid getting the infection if there is any chance of heart inflammation.”
The study was published online in JAMA Cardiology on Jan. 12.
The authors explain that among patients hospitalized with COVID, early studies suggested that approximately one in four experience cardiovascular injury, defined as an elevation in troponin levels, which was associated with a 5- to 10-fold increase in the risk for death. But there is limited information on cardiac injury in patients who do not require hospitalization.
Although a broad range of abnormal myocardial tissue has been reported in several cardiac MRI studies of patients recovered from COVID infection, there is little understanding of persistent changes in myocardial metabolism in recovered patients, which is a potential concern, given that COVID-19 is associated with systemic inflammation during the acute illness, they say.
For the current study, the researchers examined myocardial inflammation measured using two different methods – cardiac MRI and fluorodeoxyglucose–positron emission tomography (FDG-PET) – in individuals who had recovered from COVID-19 infection and looked at how this related to changes in inflammatory blood markers.
Lead author Kate Hanneman, MD, also from the University of Toronto, explained that FDG-PET imaging is more sensitive than MRI in detecting active inflammation. “Inflammatory cells have a higher uptake of glucose, and FDG-PET imaging is used to look for metabolically active inflammatory tissue that takes up glucose. It gives complementary information to MRI. Cardiac MRI shows structural or functional changes, such as scarring or edema, whereas FDG-PET imaging directly measures metabolic activity related to inflammatory cells.”
The study involved 47 individuals, 51% female, with a mean age of 43 years, who had recently recovered from COVID-19 infection. Of these, the majority had had relatively mild COVID disease, with 85% not requiring hospitalization.
Cardiac imaging was performed a mean of 67 days after the diagnosis of COVID-19. At the time of imaging, 19 participants (40%) reported at least one cardiac symptom, including palpitations, chest pain, and shortness of breath.
Results showed that eight patients (17%) had focal FDG uptake on PET consistent with myocardial inflammation. Compared with those without FDG uptake, patients with focal FDG uptake had higher regional T2, T1, and extracellular volume (colocalizing with focal FDG uptake), higher prevalence of late gadolinium enhancement indicating fibrosis, lower left ventricular ejection fraction, worse global longitudinal and circumferential strain, and higher systemic inflammatory blood markers, including interleukin (IL)-6, IL- 8, an high-sensitivity C-reactive protein.
Of the 47 patients in the study, 13 had received at least one dose of a COVID-19 vaccine. There was no significant difference in the proportion of patients who were PET-positive among those who had received a COVID-19 vaccine and those who had not.
There was also no difference in inflammation in patients who had been hospitalized with COVID-19 and those who had managed their infection at home.
Among patients with focal FDG uptake, PET, MRI, and inflammatory blood markers improved at follow-up imaging performed a mean of 52 days after the first imaging. The authors say this suggests that these abnormalities were not related to pre-existing cardiovascular disease.
Of the eight patients with positive FDG-PET results, two did not show any MRI abnormalities. These two patients also had elevated inflammatory biomarkers. “PET is a more sensitive method of measuring cardiac inflammation, and our results show that these changes may not always translate into functional changes seen on MRI,” Dr. Thavendiranathan noted.
The only cardiac risk factor that was more common in participants with FDG uptake was hypertension. Although cardiac symptoms were nearly twice as common in participants with focal FDG uptake, this difference was not statistically significant.
“Given the growing number of survivors with similar symptoms, these interesting findings warrant further investigation,” the authors say.
Noting that FDG uptake correlated with elevations in systemic inflammatory biomarkers, the researchers suggest that “a more intense systemic inflammatory process may be contributing to cardiac inflammation and the consequential alteration to regional and global myocardial function in PET-positive participants.”
On repeat imaging 2 months later, all eight patients who showed FDG uptake showed improvement or resolution of inflammation without any treatment, although two patients still had some signs of inflammation. Blood biomarkers also improved on follow-up.
“This is encouraging information, but we need longer-term data to see if there are any long-term repercussions of this inflammation,” Dr. Hanneman said.
“Overall, the study findings suggest an imaging phenotype that is expected to have good prognosis. However, longer-term follow-up studies are required to understand the need for ongoing cardiac surveillance, relationship to cardiac symptoms, guidance for safe return to exercise and sports participation, and long-term cardiovascular disease risk,” the researchers state.
This study was funded by grants from the Joint Department of Medical Imaging Academic Incentive Fund, Peter Munk Cardiac Center Innovation Committee, and Ted Rogers Center for Heart Research. Dr. Hanneman reports personal fees from Sanofi Genzyme, Amicus, and Medscape outside the submitted work.
A version of this article first appeared on Medscape.com.
Myocardial inflammation is present in a small proportion of patients who have recovered from relatively mild cases of COVID-19 infection, a new study shows.
“Our findings suggest that even in patients who have had relatively mild cases of COVID-19, some will have inflammatory changes to the heart, and these changes can be present without any cardiac symptoms,” senior author, Paaladinesh Thavendiranathan, MD, University of Toronto, told this news organization.
“While our data suggest that this inflammation improves over time, and the outcomes seem positive, we don’t know if there will be any long-term consequences,” he added.
Noting that even a short period of inflammation in the heart may be associated with symptoms or arrhythmias in the longer term, Dr. Thavendiranathan said: “I would recommend that it is best to avoid getting the infection if there is any chance of heart inflammation.”
The study was published online in JAMA Cardiology on Jan. 12.
The authors explain that among patients hospitalized with COVID, early studies suggested that approximately one in four experience cardiovascular injury, defined as an elevation in troponin levels, which was associated with a 5- to 10-fold increase in the risk for death. But there is limited information on cardiac injury in patients who do not require hospitalization.
Although a broad range of abnormal myocardial tissue has been reported in several cardiac MRI studies of patients recovered from COVID infection, there is little understanding of persistent changes in myocardial metabolism in recovered patients, which is a potential concern, given that COVID-19 is associated with systemic inflammation during the acute illness, they say.
For the current study, the researchers examined myocardial inflammation measured using two different methods – cardiac MRI and fluorodeoxyglucose–positron emission tomography (FDG-PET) – in individuals who had recovered from COVID-19 infection and looked at how this related to changes in inflammatory blood markers.
Lead author Kate Hanneman, MD, also from the University of Toronto, explained that FDG-PET imaging is more sensitive than MRI in detecting active inflammation. “Inflammatory cells have a higher uptake of glucose, and FDG-PET imaging is used to look for metabolically active inflammatory tissue that takes up glucose. It gives complementary information to MRI. Cardiac MRI shows structural or functional changes, such as scarring or edema, whereas FDG-PET imaging directly measures metabolic activity related to inflammatory cells.”
The study involved 47 individuals, 51% female, with a mean age of 43 years, who had recently recovered from COVID-19 infection. Of these, the majority had had relatively mild COVID disease, with 85% not requiring hospitalization.
Cardiac imaging was performed a mean of 67 days after the diagnosis of COVID-19. At the time of imaging, 19 participants (40%) reported at least one cardiac symptom, including palpitations, chest pain, and shortness of breath.
Results showed that eight patients (17%) had focal FDG uptake on PET consistent with myocardial inflammation. Compared with those without FDG uptake, patients with focal FDG uptake had higher regional T2, T1, and extracellular volume (colocalizing with focal FDG uptake), higher prevalence of late gadolinium enhancement indicating fibrosis, lower left ventricular ejection fraction, worse global longitudinal and circumferential strain, and higher systemic inflammatory blood markers, including interleukin (IL)-6, IL- 8, an high-sensitivity C-reactive protein.
Of the 47 patients in the study, 13 had received at least one dose of a COVID-19 vaccine. There was no significant difference in the proportion of patients who were PET-positive among those who had received a COVID-19 vaccine and those who had not.
There was also no difference in inflammation in patients who had been hospitalized with COVID-19 and those who had managed their infection at home.
Among patients with focal FDG uptake, PET, MRI, and inflammatory blood markers improved at follow-up imaging performed a mean of 52 days after the first imaging. The authors say this suggests that these abnormalities were not related to pre-existing cardiovascular disease.
Of the eight patients with positive FDG-PET results, two did not show any MRI abnormalities. These two patients also had elevated inflammatory biomarkers. “PET is a more sensitive method of measuring cardiac inflammation, and our results show that these changes may not always translate into functional changes seen on MRI,” Dr. Thavendiranathan noted.
The only cardiac risk factor that was more common in participants with FDG uptake was hypertension. Although cardiac symptoms were nearly twice as common in participants with focal FDG uptake, this difference was not statistically significant.
“Given the growing number of survivors with similar symptoms, these interesting findings warrant further investigation,” the authors say.
Noting that FDG uptake correlated with elevations in systemic inflammatory biomarkers, the researchers suggest that “a more intense systemic inflammatory process may be contributing to cardiac inflammation and the consequential alteration to regional and global myocardial function in PET-positive participants.”
On repeat imaging 2 months later, all eight patients who showed FDG uptake showed improvement or resolution of inflammation without any treatment, although two patients still had some signs of inflammation. Blood biomarkers also improved on follow-up.
“This is encouraging information, but we need longer-term data to see if there are any long-term repercussions of this inflammation,” Dr. Hanneman said.
“Overall, the study findings suggest an imaging phenotype that is expected to have good prognosis. However, longer-term follow-up studies are required to understand the need for ongoing cardiac surveillance, relationship to cardiac symptoms, guidance for safe return to exercise and sports participation, and long-term cardiovascular disease risk,” the researchers state.
This study was funded by grants from the Joint Department of Medical Imaging Academic Incentive Fund, Peter Munk Cardiac Center Innovation Committee, and Ted Rogers Center for Heart Research. Dr. Hanneman reports personal fees from Sanofi Genzyme, Amicus, and Medscape outside the submitted work.
A version of this article first appeared on Medscape.com.



